User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
MS CONFERENCE NEWS
- Common MS treatment wears off more quickly in Black patients
- A less expensive, more convenient treatment option for MS?
- Investigational drug reduces brain lesions in highly active MS
- Evobrutinib may lower nerve damage biomarker levels
- Disease progression and therapy response vary in MS by ethnicity
- Some MS treatments may heighten COVID risk
- Natalizumab postinfusion reactions
- Common MS treatment wears off more quickly in Black patients
- A less expensive, more convenient treatment option for MS?
- Investigational drug reduces brain lesions in highly active MS
- Evobrutinib may lower nerve damage biomarker levels
- Disease progression and therapy response vary in MS by ethnicity
- Some MS treatments may heighten COVID risk
- Natalizumab postinfusion reactions
- Common MS treatment wears off more quickly in Black patients
- A less expensive, more convenient treatment option for MS?
- Investigational drug reduces brain lesions in highly active MS
- Evobrutinib may lower nerve damage biomarker levels
- Disease progression and therapy response vary in MS by ethnicity
- Some MS treatments may heighten COVID risk
- Natalizumab postinfusion reactions
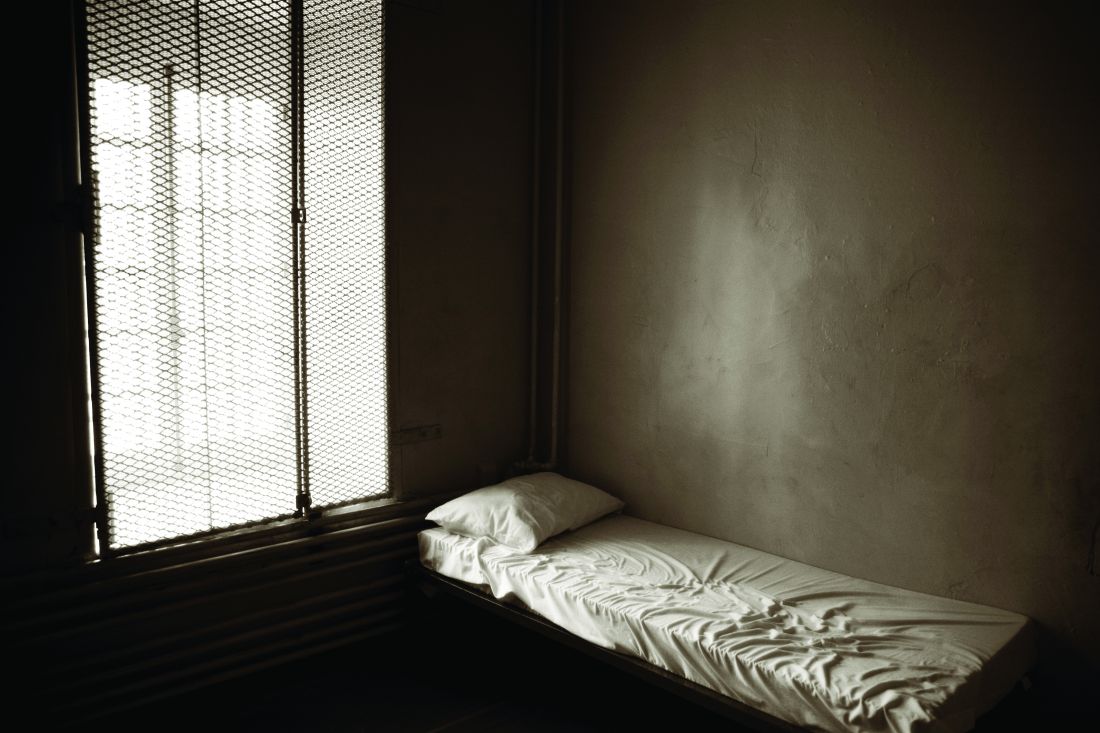
Heart doc offering ‘fountain of youth’ jailed for 6 1/2 years
Cardiologist Samirkumar J. Shah, MD, was sentenced to 78 months in prison after his conviction on two counts of federal health care fraud involving more than $13 million.
As part of his sentence, Dr. Shah, 58, of Fox Chapel, Pa., must pay $1.7 million in restitution and other penalties and undergo 3 years of supervised release after prison.
“Dr. Shah risked the health of his patients so he could make millions of dollars through unnecessary procedures, and lied and fabricated records for years to perpetuate his fraud scheme,” acting U.S. Attorney Stephen R. Kaufman said in an Aug. 5 statement from the Department of Justice.
As previously reported, Dr. Shah was convicted June 14, 2019, of submitting fraudulent claims to private and federal insurance programs between 2008 and 2013 for external counterpulsation (ECP) therapy, a lower limb compression treatment approved for patients with coronary artery disease and refractory angina.
Dr. Shah, however, advertised ECP as the “fountain of youth,” claimed it made patients “younger and smarter,” and offered the treatment for conditions such as obesity, hypertension, hypotension, diabetes, and erectile dysfunction.
Patients were required to undergo diagnostic ultrasounds as a precautionary measure prior to starting ECP, but witness testimony established that Dr. Shah did not review any of the imaging before approving new patients for ECP, placing his patients at risk for serious injury or even death, the DOJ stated.
The evidence also showed that Dr. Shah double-billed insurers, routinely submitted fabricated patient files, and made false statements concerning his practice, patient population, recording keeping, and compliance with coverage guidelines, the government said.
During the scheme, Dr. Shah submitted ECP-related claims for Medicare Part B, UPMC Health Plan, Highmark Blue Cross Blue Shield, and Gateway Health Plan beneficiaries totalling more than $13 million and received reimbursement payments in excess of $3.5 million.
“Rather than upholding the oath he swore and providing care for patients who trusted him, this defendant misled patients and drained critical Medicaid funds from families who needed it,” said Attorney General Josh Shapiro. “We will not let anyone put their patients’ lives at risk for a profit.”
“Today’s sentence holds Mr. Shah accountable for his appalling actions,” said FBI Pittsburgh Special Agent in Charge Mike Nordwall. “Mr. Shah used his position as a doctor to illegally profit from a health care program paid for by taxpayers. Fraud of this magnitude will not be tolerated.”
Dr. Shah has been in custody since July 15, 2021, after skipping out on his original July 14 sentencing date. The Tribune-Review reported that Dr. Shah filed a last-minute request for a continuance, claiming he had an adverse reaction to the Pfizer COVID-19 vaccination and was advised by his doctor that he needed “strict bedrest for at least 6 weeks.”
Dr. Shah reportedly turned himself after presiding U.S. District Judge David S. Cercone denied the motion and issued an arrest warrant.
A version of this article first appeared on Medscape.com.
Cardiologist Samirkumar J. Shah, MD, was sentenced to 78 months in prison after his conviction on two counts of federal health care fraud involving more than $13 million.
As part of his sentence, Dr. Shah, 58, of Fox Chapel, Pa., must pay $1.7 million in restitution and other penalties and undergo 3 years of supervised release after prison.
“Dr. Shah risked the health of his patients so he could make millions of dollars through unnecessary procedures, and lied and fabricated records for years to perpetuate his fraud scheme,” acting U.S. Attorney Stephen R. Kaufman said in an Aug. 5 statement from the Department of Justice.
As previously reported, Dr. Shah was convicted June 14, 2019, of submitting fraudulent claims to private and federal insurance programs between 2008 and 2013 for external counterpulsation (ECP) therapy, a lower limb compression treatment approved for patients with coronary artery disease and refractory angina.
Dr. Shah, however, advertised ECP as the “fountain of youth,” claimed it made patients “younger and smarter,” and offered the treatment for conditions such as obesity, hypertension, hypotension, diabetes, and erectile dysfunction.
Patients were required to undergo diagnostic ultrasounds as a precautionary measure prior to starting ECP, but witness testimony established that Dr. Shah did not review any of the imaging before approving new patients for ECP, placing his patients at risk for serious injury or even death, the DOJ stated.
The evidence also showed that Dr. Shah double-billed insurers, routinely submitted fabricated patient files, and made false statements concerning his practice, patient population, recording keeping, and compliance with coverage guidelines, the government said.
During the scheme, Dr. Shah submitted ECP-related claims for Medicare Part B, UPMC Health Plan, Highmark Blue Cross Blue Shield, and Gateway Health Plan beneficiaries totalling more than $13 million and received reimbursement payments in excess of $3.5 million.
“Rather than upholding the oath he swore and providing care for patients who trusted him, this defendant misled patients and drained critical Medicaid funds from families who needed it,” said Attorney General Josh Shapiro. “We will not let anyone put their patients’ lives at risk for a profit.”
“Today’s sentence holds Mr. Shah accountable for his appalling actions,” said FBI Pittsburgh Special Agent in Charge Mike Nordwall. “Mr. Shah used his position as a doctor to illegally profit from a health care program paid for by taxpayers. Fraud of this magnitude will not be tolerated.”
Dr. Shah has been in custody since July 15, 2021, after skipping out on his original July 14 sentencing date. The Tribune-Review reported that Dr. Shah filed a last-minute request for a continuance, claiming he had an adverse reaction to the Pfizer COVID-19 vaccination and was advised by his doctor that he needed “strict bedrest for at least 6 weeks.”
Dr. Shah reportedly turned himself after presiding U.S. District Judge David S. Cercone denied the motion and issued an arrest warrant.
A version of this article first appeared on Medscape.com.
Cardiologist Samirkumar J. Shah, MD, was sentenced to 78 months in prison after his conviction on two counts of federal health care fraud involving more than $13 million.
As part of his sentence, Dr. Shah, 58, of Fox Chapel, Pa., must pay $1.7 million in restitution and other penalties and undergo 3 years of supervised release after prison.
“Dr. Shah risked the health of his patients so he could make millions of dollars through unnecessary procedures, and lied and fabricated records for years to perpetuate his fraud scheme,” acting U.S. Attorney Stephen R. Kaufman said in an Aug. 5 statement from the Department of Justice.
As previously reported, Dr. Shah was convicted June 14, 2019, of submitting fraudulent claims to private and federal insurance programs between 2008 and 2013 for external counterpulsation (ECP) therapy, a lower limb compression treatment approved for patients with coronary artery disease and refractory angina.
Dr. Shah, however, advertised ECP as the “fountain of youth,” claimed it made patients “younger and smarter,” and offered the treatment for conditions such as obesity, hypertension, hypotension, diabetes, and erectile dysfunction.
Patients were required to undergo diagnostic ultrasounds as a precautionary measure prior to starting ECP, but witness testimony established that Dr. Shah did not review any of the imaging before approving new patients for ECP, placing his patients at risk for serious injury or even death, the DOJ stated.
The evidence also showed that Dr. Shah double-billed insurers, routinely submitted fabricated patient files, and made false statements concerning his practice, patient population, recording keeping, and compliance with coverage guidelines, the government said.
During the scheme, Dr. Shah submitted ECP-related claims for Medicare Part B, UPMC Health Plan, Highmark Blue Cross Blue Shield, and Gateway Health Plan beneficiaries totalling more than $13 million and received reimbursement payments in excess of $3.5 million.
“Rather than upholding the oath he swore and providing care for patients who trusted him, this defendant misled patients and drained critical Medicaid funds from families who needed it,” said Attorney General Josh Shapiro. “We will not let anyone put their patients’ lives at risk for a profit.”
“Today’s sentence holds Mr. Shah accountable for his appalling actions,” said FBI Pittsburgh Special Agent in Charge Mike Nordwall. “Mr. Shah used his position as a doctor to illegally profit from a health care program paid for by taxpayers. Fraud of this magnitude will not be tolerated.”
Dr. Shah has been in custody since July 15, 2021, after skipping out on his original July 14 sentencing date. The Tribune-Review reported that Dr. Shah filed a last-minute request for a continuance, claiming he had an adverse reaction to the Pfizer COVID-19 vaccination and was advised by his doctor that he needed “strict bedrest for at least 6 weeks.”
Dr. Shah reportedly turned himself after presiding U.S. District Judge David S. Cercone denied the motion and issued an arrest warrant.
A version of this article first appeared on Medscape.com.
Better CNS control in children with ALL: ‘Goldilocks’ approach
Treatment of central nervous system involvement in pediatric acute lymphoblastic leukemia (ALL) needs to be based on risk, and should no longer be applied in a one-size-fits all approach, say experts writing in an editorial published July 29 in the journal Blood.
“Because cure rates now exceed 90%, using neurotoxic drugs in non–risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required,” write pediatric leukemia researchers Christina Halsey, PhD, of the University of Glasgow and Gabriele Escherich, MD, of the University Medical Center Hamburg-Eppendorf (Germany).
“We want to reach a Goldilocks point: not too much, not too little, but just right for every child,” they write.
The problem is that “the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity,” including long-term cognitive deficits in 20%-40% of them, they point out.
The editorial accompanied a new study in which investigators in China focused on improving CNS control in children with ALL, which the editorialists said was step in the right direction.
In the Chinese Children’s Cancer Group ALL-2015 trial, investigators found that prephase dexamethasone, delayed intrathecal therapy, intravenous anesthesia to reduce traumatic lumbar punctures, and flow cytometry to accurately ascertain initial CNS involvement may improve CNS control.
The trial included 7,640 consecutive children up to age 18 treated from 2015 to 2019 across 20 major medical centers in China. Children received conventional remission induction and subsequent risk-directed therapy, including 16-22 triple intrathecal treatments. Prophylactic cranial irradiation was not used.
The 5-year event-free survival was 80.3% and overall survival 91.1%. The cumulative risk of isolated CNS relapse was 1.9% and of any CNS relapse 2.7%, comparable to reports from other major study groups, both with and without cranial radiation.
“We attributed our relatively good CNS control to the prephase treatment with dexamethasone, which reduced leukemia cells in blood and the CNS, and to the delayed intrathecal therapy until all (or a large proportion) of circulating leukemic blasts were cleared, thus reducing the consequence of traumatic lumbar puncture with blasts,” said the investigators, led by Jingyan Tang, MD, a hematologist/oncologist at the Shanghai (China) Children’s Medical Center.
“This approach of delayed administration of initial intrathecal therapy after prephase steroid treatment, if confirmed successful by additional studies, can be adopted readily,” they say.
The editorialists concur. The low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, “might suggest a potential protective effect of steroids before diagnostic lumbar puncture,” they said.
“However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow, minimal residual disease (MRD) is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy,” Dr. Halsey and Dr. Escherich say.
It’s not surprising that the use of anesthesia led to fewer traumatic lumbar punctures than in “frightened child[ren] undergoing such a painful procedure without anesthesia,” the study team notes. Its correlation with lower CNS relapses is probably because drug delivery was more accurate in sedated children, the editorialists add.
Female sex was also protective against relapse in cases where general anesthesia wasn’t used for lumbar puncture. “One could speculate that it is more difficult to restrict male patients than female patients for successful intrathecal therapy if they were not undergoing anesthesia during the procedure,” the investigators write.
“Unfortunately,” the editorialists add, rapid adoption of anesthesia for lumbar punctures “is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.”
The work was supported by grants from the National Natural Science Foundation of China, National Cancer Institute, and others. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treatment of central nervous system involvement in pediatric acute lymphoblastic leukemia (ALL) needs to be based on risk, and should no longer be applied in a one-size-fits all approach, say experts writing in an editorial published July 29 in the journal Blood.
“Because cure rates now exceed 90%, using neurotoxic drugs in non–risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required,” write pediatric leukemia researchers Christina Halsey, PhD, of the University of Glasgow and Gabriele Escherich, MD, of the University Medical Center Hamburg-Eppendorf (Germany).
“We want to reach a Goldilocks point: not too much, not too little, but just right for every child,” they write.
The problem is that “the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity,” including long-term cognitive deficits in 20%-40% of them, they point out.
The editorial accompanied a new study in which investigators in China focused on improving CNS control in children with ALL, which the editorialists said was step in the right direction.
In the Chinese Children’s Cancer Group ALL-2015 trial, investigators found that prephase dexamethasone, delayed intrathecal therapy, intravenous anesthesia to reduce traumatic lumbar punctures, and flow cytometry to accurately ascertain initial CNS involvement may improve CNS control.
The trial included 7,640 consecutive children up to age 18 treated from 2015 to 2019 across 20 major medical centers in China. Children received conventional remission induction and subsequent risk-directed therapy, including 16-22 triple intrathecal treatments. Prophylactic cranial irradiation was not used.
The 5-year event-free survival was 80.3% and overall survival 91.1%. The cumulative risk of isolated CNS relapse was 1.9% and of any CNS relapse 2.7%, comparable to reports from other major study groups, both with and without cranial radiation.
“We attributed our relatively good CNS control to the prephase treatment with dexamethasone, which reduced leukemia cells in blood and the CNS, and to the delayed intrathecal therapy until all (or a large proportion) of circulating leukemic blasts were cleared, thus reducing the consequence of traumatic lumbar puncture with blasts,” said the investigators, led by Jingyan Tang, MD, a hematologist/oncologist at the Shanghai (China) Children’s Medical Center.
“This approach of delayed administration of initial intrathecal therapy after prephase steroid treatment, if confirmed successful by additional studies, can be adopted readily,” they say.
The editorialists concur. The low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, “might suggest a potential protective effect of steroids before diagnostic lumbar puncture,” they said.
“However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow, minimal residual disease (MRD) is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy,” Dr. Halsey and Dr. Escherich say.
It’s not surprising that the use of anesthesia led to fewer traumatic lumbar punctures than in “frightened child[ren] undergoing such a painful procedure without anesthesia,” the study team notes. Its correlation with lower CNS relapses is probably because drug delivery was more accurate in sedated children, the editorialists add.
Female sex was also protective against relapse in cases where general anesthesia wasn’t used for lumbar puncture. “One could speculate that it is more difficult to restrict male patients than female patients for successful intrathecal therapy if they were not undergoing anesthesia during the procedure,” the investigators write.
“Unfortunately,” the editorialists add, rapid adoption of anesthesia for lumbar punctures “is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.”
The work was supported by grants from the National Natural Science Foundation of China, National Cancer Institute, and others. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treatment of central nervous system involvement in pediatric acute lymphoblastic leukemia (ALL) needs to be based on risk, and should no longer be applied in a one-size-fits all approach, say experts writing in an editorial published July 29 in the journal Blood.
“Because cure rates now exceed 90%, using neurotoxic drugs in non–risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required,” write pediatric leukemia researchers Christina Halsey, PhD, of the University of Glasgow and Gabriele Escherich, MD, of the University Medical Center Hamburg-Eppendorf (Germany).
“We want to reach a Goldilocks point: not too much, not too little, but just right for every child,” they write.
The problem is that “the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity,” including long-term cognitive deficits in 20%-40% of them, they point out.
The editorial accompanied a new study in which investigators in China focused on improving CNS control in children with ALL, which the editorialists said was step in the right direction.
In the Chinese Children’s Cancer Group ALL-2015 trial, investigators found that prephase dexamethasone, delayed intrathecal therapy, intravenous anesthesia to reduce traumatic lumbar punctures, and flow cytometry to accurately ascertain initial CNS involvement may improve CNS control.
The trial included 7,640 consecutive children up to age 18 treated from 2015 to 2019 across 20 major medical centers in China. Children received conventional remission induction and subsequent risk-directed therapy, including 16-22 triple intrathecal treatments. Prophylactic cranial irradiation was not used.
The 5-year event-free survival was 80.3% and overall survival 91.1%. The cumulative risk of isolated CNS relapse was 1.9% and of any CNS relapse 2.7%, comparable to reports from other major study groups, both with and without cranial radiation.
“We attributed our relatively good CNS control to the prephase treatment with dexamethasone, which reduced leukemia cells in blood and the CNS, and to the delayed intrathecal therapy until all (or a large proportion) of circulating leukemic blasts were cleared, thus reducing the consequence of traumatic lumbar puncture with blasts,” said the investigators, led by Jingyan Tang, MD, a hematologist/oncologist at the Shanghai (China) Children’s Medical Center.
“This approach of delayed administration of initial intrathecal therapy after prephase steroid treatment, if confirmed successful by additional studies, can be adopted readily,” they say.
The editorialists concur. The low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, “might suggest a potential protective effect of steroids before diagnostic lumbar puncture,” they said.
“However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow, minimal residual disease (MRD) is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy,” Dr. Halsey and Dr. Escherich say.
It’s not surprising that the use of anesthesia led to fewer traumatic lumbar punctures than in “frightened child[ren] undergoing such a painful procedure without anesthesia,” the study team notes. Its correlation with lower CNS relapses is probably because drug delivery was more accurate in sedated children, the editorialists add.
Female sex was also protective against relapse in cases where general anesthesia wasn’t used for lumbar puncture. “One could speculate that it is more difficult to restrict male patients than female patients for successful intrathecal therapy if they were not undergoing anesthesia during the procedure,” the investigators write.
“Unfortunately,” the editorialists add, rapid adoption of anesthesia for lumbar punctures “is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.”
The work was supported by grants from the National Natural Science Foundation of China, National Cancer Institute, and others. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mobile stroke teams treat patients faster and reduce disability
Having a mobile interventional stroke team (MIST) travel to treat stroke patients soon after stroke onset may improve patient outcomes, according to a new study. A retrospective analysis of a pilot program in New York found that
“The use of a Mobile Interventional Stroke Team (MIST) traveling to Thrombectomy Capable Stroke Centers to perform endovascular thrombectomy has been shown to be significantly faster with improved discharge outcomes,” wrote lead author Jacob Morey, a doctoral Candidate at Icahn School of Medicine at Mount Sinai in New York and coauthors in the paper. Prior to this study, “the effect of the MIST model stratified by time of presentation” had yet to be studied.
The findings were published online on Aug. 5 in Stroke.
MIST model versus drip-and-ship
The researchers analyzed 226 patients who underwent endovascular thrombectomy between January 2017 and February 2020 at four hospitals in the Mount Sinai health system using the NYC MIST Trial and a stroke database. At baseline, all patients were functionally independent as assessed by the modified Rankin Scale (mRS, score of 0-2). 106 patients were treated by a MIST team – staffed by a neurointerventionalist, a fellow or physician assistant, and radiologic technologist – that traveled to the patient’s location. A total of 120 patients were transferred to a comprehensive stroke center (CSC) or a hospital with endovascular thrombectomy expertise. The analysis was stratified based on whether the patient presented in the early time window (≤ 6 hours) or late time window (> 6 hours).
Patients treated in the early time window were significantly more likely to be mobile and able to perform daily tasks (mRS ≤ 2) 90 days after the procedure in the MIST group (54%), compared with the transferred group (28%, P < 0.01). Outcomes did not differ significantly between groups in the late time window (35% vs. 41%, P = 0.77).
Similarly, early-time-window patients in the MIST group were more likely to have higher functionality at discharge, compared with transferred patients, based on the on the National Institutes of Health Stroke Scale (median score of 5.0 vs. 12.0, P < 0.01). There was no significant difference between groups treated in the late time window (median score of 5.0 vs. 11.0, P = 0.11).
“Ischemic strokes often progress rapidly and can cause severe damage because brain tissue dies quickly without oxygen, resulting in serious long-term disabilities or death,“ said Johanna Fifi, MD, of Icahn School of Medicine, said in a statement to the American Heart Association. “Assessing and treating stroke patients in the early window means that a greater number of fast-progressing strokes are identified and treated.”
Time is brain
Endovascular thrombectomy is a time-sensitive surgical procedure to remove large blood clots in acute ischemic stroke that has “historically been limited to comprehensive stroke centers,” the authors wrote in their paper. It is considered the standard of care in ischemic strokes, which make up 90% of all strokes. “Less than 50% of Americans have direct access to endovascular thrombectomy, the others must be transferred to a thrombectomy-capable hospital for treatment, often losing over 2 hours of time to treatment,” said Dr. Fifi. “Every minute is precious in treating stroke, and getting to a center that offers thrombectomy is very important. The MIST model would address this by providing faster access to this potentially life-saving, disability-reducing procedure.”
Access to timely endovascular thrombectomy is gradually improving as “more institutions and cities have implemented the [MIST] model.” Dr. Fifi said.
“This study stresses the importance of ‘time is brain,’ especially for patients in the early time window. Although the study is limited by the observational, retrospective design and was performed at a single integrated center, the findings are provocative,” said Louise McCullough, MD, of the University of Texas Health Science Center at Houston said in a statement to the American Heart Association. “The use of a MIST model highlights the potential benefit of early and urgent treatment for patients with large-vessel stroke. Stroke systems of care need to take advantage of any opportunity to treat patients early, wherever they are.”
The study was partly funded by a Stryker Foundation grant.
Having a mobile interventional stroke team (MIST) travel to treat stroke patients soon after stroke onset may improve patient outcomes, according to a new study. A retrospective analysis of a pilot program in New York found that
“The use of a Mobile Interventional Stroke Team (MIST) traveling to Thrombectomy Capable Stroke Centers to perform endovascular thrombectomy has been shown to be significantly faster with improved discharge outcomes,” wrote lead author Jacob Morey, a doctoral Candidate at Icahn School of Medicine at Mount Sinai in New York and coauthors in the paper. Prior to this study, “the effect of the MIST model stratified by time of presentation” had yet to be studied.
The findings were published online on Aug. 5 in Stroke.
MIST model versus drip-and-ship
The researchers analyzed 226 patients who underwent endovascular thrombectomy between January 2017 and February 2020 at four hospitals in the Mount Sinai health system using the NYC MIST Trial and a stroke database. At baseline, all patients were functionally independent as assessed by the modified Rankin Scale (mRS, score of 0-2). 106 patients were treated by a MIST team – staffed by a neurointerventionalist, a fellow or physician assistant, and radiologic technologist – that traveled to the patient’s location. A total of 120 patients were transferred to a comprehensive stroke center (CSC) or a hospital with endovascular thrombectomy expertise. The analysis was stratified based on whether the patient presented in the early time window (≤ 6 hours) or late time window (> 6 hours).
Patients treated in the early time window were significantly more likely to be mobile and able to perform daily tasks (mRS ≤ 2) 90 days after the procedure in the MIST group (54%), compared with the transferred group (28%, P < 0.01). Outcomes did not differ significantly between groups in the late time window (35% vs. 41%, P = 0.77).
Similarly, early-time-window patients in the MIST group were more likely to have higher functionality at discharge, compared with transferred patients, based on the on the National Institutes of Health Stroke Scale (median score of 5.0 vs. 12.0, P < 0.01). There was no significant difference between groups treated in the late time window (median score of 5.0 vs. 11.0, P = 0.11).
“Ischemic strokes often progress rapidly and can cause severe damage because brain tissue dies quickly without oxygen, resulting in serious long-term disabilities or death,“ said Johanna Fifi, MD, of Icahn School of Medicine, said in a statement to the American Heart Association. “Assessing and treating stroke patients in the early window means that a greater number of fast-progressing strokes are identified and treated.”
Time is brain
Endovascular thrombectomy is a time-sensitive surgical procedure to remove large blood clots in acute ischemic stroke that has “historically been limited to comprehensive stroke centers,” the authors wrote in their paper. It is considered the standard of care in ischemic strokes, which make up 90% of all strokes. “Less than 50% of Americans have direct access to endovascular thrombectomy, the others must be transferred to a thrombectomy-capable hospital for treatment, often losing over 2 hours of time to treatment,” said Dr. Fifi. “Every minute is precious in treating stroke, and getting to a center that offers thrombectomy is very important. The MIST model would address this by providing faster access to this potentially life-saving, disability-reducing procedure.”
Access to timely endovascular thrombectomy is gradually improving as “more institutions and cities have implemented the [MIST] model.” Dr. Fifi said.
“This study stresses the importance of ‘time is brain,’ especially for patients in the early time window. Although the study is limited by the observational, retrospective design and was performed at a single integrated center, the findings are provocative,” said Louise McCullough, MD, of the University of Texas Health Science Center at Houston said in a statement to the American Heart Association. “The use of a MIST model highlights the potential benefit of early and urgent treatment for patients with large-vessel stroke. Stroke systems of care need to take advantage of any opportunity to treat patients early, wherever they are.”
The study was partly funded by a Stryker Foundation grant.
Having a mobile interventional stroke team (MIST) travel to treat stroke patients soon after stroke onset may improve patient outcomes, according to a new study. A retrospective analysis of a pilot program in New York found that
“The use of a Mobile Interventional Stroke Team (MIST) traveling to Thrombectomy Capable Stroke Centers to perform endovascular thrombectomy has been shown to be significantly faster with improved discharge outcomes,” wrote lead author Jacob Morey, a doctoral Candidate at Icahn School of Medicine at Mount Sinai in New York and coauthors in the paper. Prior to this study, “the effect of the MIST model stratified by time of presentation” had yet to be studied.
The findings were published online on Aug. 5 in Stroke.
MIST model versus drip-and-ship
The researchers analyzed 226 patients who underwent endovascular thrombectomy between January 2017 and February 2020 at four hospitals in the Mount Sinai health system using the NYC MIST Trial and a stroke database. At baseline, all patients were functionally independent as assessed by the modified Rankin Scale (mRS, score of 0-2). 106 patients were treated by a MIST team – staffed by a neurointerventionalist, a fellow or physician assistant, and radiologic technologist – that traveled to the patient’s location. A total of 120 patients were transferred to a comprehensive stroke center (CSC) or a hospital with endovascular thrombectomy expertise. The analysis was stratified based on whether the patient presented in the early time window (≤ 6 hours) or late time window (> 6 hours).
Patients treated in the early time window were significantly more likely to be mobile and able to perform daily tasks (mRS ≤ 2) 90 days after the procedure in the MIST group (54%), compared with the transferred group (28%, P < 0.01). Outcomes did not differ significantly between groups in the late time window (35% vs. 41%, P = 0.77).
Similarly, early-time-window patients in the MIST group were more likely to have higher functionality at discharge, compared with transferred patients, based on the on the National Institutes of Health Stroke Scale (median score of 5.0 vs. 12.0, P < 0.01). There was no significant difference between groups treated in the late time window (median score of 5.0 vs. 11.0, P = 0.11).
“Ischemic strokes often progress rapidly and can cause severe damage because brain tissue dies quickly without oxygen, resulting in serious long-term disabilities or death,“ said Johanna Fifi, MD, of Icahn School of Medicine, said in a statement to the American Heart Association. “Assessing and treating stroke patients in the early window means that a greater number of fast-progressing strokes are identified and treated.”
Time is brain
Endovascular thrombectomy is a time-sensitive surgical procedure to remove large blood clots in acute ischemic stroke that has “historically been limited to comprehensive stroke centers,” the authors wrote in their paper. It is considered the standard of care in ischemic strokes, which make up 90% of all strokes. “Less than 50% of Americans have direct access to endovascular thrombectomy, the others must be transferred to a thrombectomy-capable hospital for treatment, often losing over 2 hours of time to treatment,” said Dr. Fifi. “Every minute is precious in treating stroke, and getting to a center that offers thrombectomy is very important. The MIST model would address this by providing faster access to this potentially life-saving, disability-reducing procedure.”
Access to timely endovascular thrombectomy is gradually improving as “more institutions and cities have implemented the [MIST] model.” Dr. Fifi said.
“This study stresses the importance of ‘time is brain,’ especially for patients in the early time window. Although the study is limited by the observational, retrospective design and was performed at a single integrated center, the findings are provocative,” said Louise McCullough, MD, of the University of Texas Health Science Center at Houston said in a statement to the American Heart Association. “The use of a MIST model highlights the potential benefit of early and urgent treatment for patients with large-vessel stroke. Stroke systems of care need to take advantage of any opportunity to treat patients early, wherever they are.”
The study was partly funded by a Stryker Foundation grant.
FROM STROKE
Moderna says boosters may be needed after 6 months
Moderna says neutralizing antibodies generated by its COVID-19 vaccine against three variants of the virus that causes the disease waned substantially 6 months after the second dose.
Because of this, the company expects an increase in breakthrough infections with a need for boosters before winter.
In an experiment, a 50-mg dose of the vaccine, given as a third shot, boosted levels of antibodies in 20 previously vaccinated people by 32 times against the Beta variant, by 44 times against the Gamma variant, and by 42 times against Delta.
The new data was presented in an earnings call to investors and is based on a small study that hasn’t yet been published in medical literature.
The company also said its vaccine remained highly effective at preventing severe COVID outcomes through 6 months.
Last week, Pfizer released early data suggesting a similar drop in protection from its vaccine. The company also showed a third dose substantially boosted protection, including against the Delta variant.
The new results come just 1 day after the World Health Organization implored wealthy nations to hold off on third doses until more of the world’s population could get a first dose.
More than 80% of the 4 billion vaccine doses given around the world have been distributed to high-income countries.
A version of this article first appeared on WebMD.com.
Moderna says neutralizing antibodies generated by its COVID-19 vaccine against three variants of the virus that causes the disease waned substantially 6 months after the second dose.
Because of this, the company expects an increase in breakthrough infections with a need for boosters before winter.
In an experiment, a 50-mg dose of the vaccine, given as a third shot, boosted levels of antibodies in 20 previously vaccinated people by 32 times against the Beta variant, by 44 times against the Gamma variant, and by 42 times against Delta.
The new data was presented in an earnings call to investors and is based on a small study that hasn’t yet been published in medical literature.
The company also said its vaccine remained highly effective at preventing severe COVID outcomes through 6 months.
Last week, Pfizer released early data suggesting a similar drop in protection from its vaccine. The company also showed a third dose substantially boosted protection, including against the Delta variant.
The new results come just 1 day after the World Health Organization implored wealthy nations to hold off on third doses until more of the world’s population could get a first dose.
More than 80% of the 4 billion vaccine doses given around the world have been distributed to high-income countries.
A version of this article first appeared on WebMD.com.
Moderna says neutralizing antibodies generated by its COVID-19 vaccine against three variants of the virus that causes the disease waned substantially 6 months after the second dose.
Because of this, the company expects an increase in breakthrough infections with a need for boosters before winter.
In an experiment, a 50-mg dose of the vaccine, given as a third shot, boosted levels of antibodies in 20 previously vaccinated people by 32 times against the Beta variant, by 44 times against the Gamma variant, and by 42 times against Delta.
The new data was presented in an earnings call to investors and is based on a small study that hasn’t yet been published in medical literature.
The company also said its vaccine remained highly effective at preventing severe COVID outcomes through 6 months.
Last week, Pfizer released early data suggesting a similar drop in protection from its vaccine. The company also showed a third dose substantially boosted protection, including against the Delta variant.
The new results come just 1 day after the World Health Organization implored wealthy nations to hold off on third doses until more of the world’s population could get a first dose.
More than 80% of the 4 billion vaccine doses given around the world have been distributed to high-income countries.
A version of this article first appeared on WebMD.com.
Despite retraction, study using fraudulent Surgisphere data still cited
A retracted study on the safety of blood pressure medications in patients with COVID-19 continues to be cited nearly a year later, new research shows.
The study in question, published on May 1, 2020, in the New England Journal of Medicine, showed no increased risk for in-hospital death with the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) in hospitalized patients with COVID-19.
Concerns about the veracity of the Surgisphere database used for the study, however, led to a June 4 retraction and to the June 13 retraction of a second study, published in the Lancet, that focused on hydroxychloroquine as a COVID-19 treatment.
Although the Surgisphere scandal caused a global reckoning of COVID-19 scientific studies, the new analysis identified 652 citations of the NEJM article as of May 31.
More than a third of the citations occurred in the first 2 months after the retraction, 54% were at least 3 months later, and 2.8% at least 6 months later. In May, 11 months after the article was retracted, it was cited 21 times, senior author Emily G. McDonald, MD, MSc, McGill University, Montreal, and colleagues reported in a research letter in JAMA Internal Medicine.
“In early May and June there were already more than 200 citations in one of the world’s leading scientific journals, so I do believe it was a highly influential article early on and had an impact on different types of studies or research taking place,” she said in an interview.
Dr. McDonald said she’s also “certain that it impacted patient care,” observing that when there are no guidelines available on how to manage patients, physicians will turn to the most recent evidence in the most reputable journals.
“In the case of ACE [inhibitors] and ARBs, although the study was based on fraudulent data, we were lucky that the overall message was in the end probably correct, but that might not have been the case for another study or dataset,” she said.
Early in the pandemic, concerns existed that ACE inhibitors and ARBs could be harmful, increasing the expression of ACE2 receptors, which the SARS-CoV-2 virus uses to gain entry into cells. The first randomized trial to examine the issue, BRACE CORONA, showed no clinical benefit to interrupting use of the agents in hospitalized patients. An observational study suggested ACE inhibitors may even be protective.
Of two high-profile retractions, McDonald said they chose to bypass the hydroxychloroquine study, which had an eye-popping Altmetric attention score of 23,084, compared with 3,727 for the NEJM paper, because it may have been cited for “other” reasons. “We wanted to focus less on the politics and more on the problem of retracted work.”
The team found that researchers across the globe were citing the retracted ACE/ARB paper (18.7% in the United States, 8.1% in Italy, and 44% other countries). Most citations were used to support a statement in the main text of a study, but in nearly 3% of cases, the data were incorporated into new analyses.
Just 17.6% of the studies cited or noted the retraction. “For sure, that was surprising to us. We suspected it, but our study confirmed it,” Dr. McDonald said.
Although retracted articles can be identified by a watermark or line of text, in some cases that can be easily missed, she noted. What’s more, not all citation software points out when a study has been retracted, a fate shared by the copyediting process.
“There are a lot of mechanisms in place and, in general, what’s happening is rare but there isn’t a perfect automated system solution to absolutely prevent this from happening,” she said. “It’s still subject to human error.”
The findings also have to be taken in the context of a rapidly emerging pandemic and the unprecedented torrent of scientific papers released over the past year.
“That might have contributed to why this happened, but the takeaway message is that this can happen despite our best efforts, and we need to challenge ourselves to come up with a system solution to prevent this from happening in the future,” Dr. McDonald said. “Current mechanisms are probably capturing 95% of it, but we need to do better.”
Limitations of the present analysis are that it was limited to the single retracted study; used only a single search engine, Google Scholar, to identify the citing works; and that additional citations may have been missed, the authors noted.
McDonald and coauthor Todd C. Lee, MD, report being signatories on a public letter calling for the retraction of the Surgisphere papers. Dr. Lee also reported receiving research support from Fonds De Recherche du Quebec-Sante during the conduct of the study.
A version of this article first appeared on Medscape.com.
A retracted study on the safety of blood pressure medications in patients with COVID-19 continues to be cited nearly a year later, new research shows.
The study in question, published on May 1, 2020, in the New England Journal of Medicine, showed no increased risk for in-hospital death with the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) in hospitalized patients with COVID-19.
Concerns about the veracity of the Surgisphere database used for the study, however, led to a June 4 retraction and to the June 13 retraction of a second study, published in the Lancet, that focused on hydroxychloroquine as a COVID-19 treatment.
Although the Surgisphere scandal caused a global reckoning of COVID-19 scientific studies, the new analysis identified 652 citations of the NEJM article as of May 31.
More than a third of the citations occurred in the first 2 months after the retraction, 54% were at least 3 months later, and 2.8% at least 6 months later. In May, 11 months after the article was retracted, it was cited 21 times, senior author Emily G. McDonald, MD, MSc, McGill University, Montreal, and colleagues reported in a research letter in JAMA Internal Medicine.
“In early May and June there were already more than 200 citations in one of the world’s leading scientific journals, so I do believe it was a highly influential article early on and had an impact on different types of studies or research taking place,” she said in an interview.
Dr. McDonald said she’s also “certain that it impacted patient care,” observing that when there are no guidelines available on how to manage patients, physicians will turn to the most recent evidence in the most reputable journals.
“In the case of ACE [inhibitors] and ARBs, although the study was based on fraudulent data, we were lucky that the overall message was in the end probably correct, but that might not have been the case for another study or dataset,” she said.
Early in the pandemic, concerns existed that ACE inhibitors and ARBs could be harmful, increasing the expression of ACE2 receptors, which the SARS-CoV-2 virus uses to gain entry into cells. The first randomized trial to examine the issue, BRACE CORONA, showed no clinical benefit to interrupting use of the agents in hospitalized patients. An observational study suggested ACE inhibitors may even be protective.
Of two high-profile retractions, McDonald said they chose to bypass the hydroxychloroquine study, which had an eye-popping Altmetric attention score of 23,084, compared with 3,727 for the NEJM paper, because it may have been cited for “other” reasons. “We wanted to focus less on the politics and more on the problem of retracted work.”
The team found that researchers across the globe were citing the retracted ACE/ARB paper (18.7% in the United States, 8.1% in Italy, and 44% other countries). Most citations were used to support a statement in the main text of a study, but in nearly 3% of cases, the data were incorporated into new analyses.
Just 17.6% of the studies cited or noted the retraction. “For sure, that was surprising to us. We suspected it, but our study confirmed it,” Dr. McDonald said.
Although retracted articles can be identified by a watermark or line of text, in some cases that can be easily missed, she noted. What’s more, not all citation software points out when a study has been retracted, a fate shared by the copyediting process.
“There are a lot of mechanisms in place and, in general, what’s happening is rare but there isn’t a perfect automated system solution to absolutely prevent this from happening,” she said. “It’s still subject to human error.”
The findings also have to be taken in the context of a rapidly emerging pandemic and the unprecedented torrent of scientific papers released over the past year.
“That might have contributed to why this happened, but the takeaway message is that this can happen despite our best efforts, and we need to challenge ourselves to come up with a system solution to prevent this from happening in the future,” Dr. McDonald said. “Current mechanisms are probably capturing 95% of it, but we need to do better.”
Limitations of the present analysis are that it was limited to the single retracted study; used only a single search engine, Google Scholar, to identify the citing works; and that additional citations may have been missed, the authors noted.
McDonald and coauthor Todd C. Lee, MD, report being signatories on a public letter calling for the retraction of the Surgisphere papers. Dr. Lee also reported receiving research support from Fonds De Recherche du Quebec-Sante during the conduct of the study.
A version of this article first appeared on Medscape.com.
A retracted study on the safety of blood pressure medications in patients with COVID-19 continues to be cited nearly a year later, new research shows.
The study in question, published on May 1, 2020, in the New England Journal of Medicine, showed no increased risk for in-hospital death with the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) in hospitalized patients with COVID-19.
Concerns about the veracity of the Surgisphere database used for the study, however, led to a June 4 retraction and to the June 13 retraction of a second study, published in the Lancet, that focused on hydroxychloroquine as a COVID-19 treatment.
Although the Surgisphere scandal caused a global reckoning of COVID-19 scientific studies, the new analysis identified 652 citations of the NEJM article as of May 31.
More than a third of the citations occurred in the first 2 months after the retraction, 54% were at least 3 months later, and 2.8% at least 6 months later. In May, 11 months after the article was retracted, it was cited 21 times, senior author Emily G. McDonald, MD, MSc, McGill University, Montreal, and colleagues reported in a research letter in JAMA Internal Medicine.
“In early May and June there were already more than 200 citations in one of the world’s leading scientific journals, so I do believe it was a highly influential article early on and had an impact on different types of studies or research taking place,” she said in an interview.
Dr. McDonald said she’s also “certain that it impacted patient care,” observing that when there are no guidelines available on how to manage patients, physicians will turn to the most recent evidence in the most reputable journals.
“In the case of ACE [inhibitors] and ARBs, although the study was based on fraudulent data, we were lucky that the overall message was in the end probably correct, but that might not have been the case for another study or dataset,” she said.
Early in the pandemic, concerns existed that ACE inhibitors and ARBs could be harmful, increasing the expression of ACE2 receptors, which the SARS-CoV-2 virus uses to gain entry into cells. The first randomized trial to examine the issue, BRACE CORONA, showed no clinical benefit to interrupting use of the agents in hospitalized patients. An observational study suggested ACE inhibitors may even be protective.
Of two high-profile retractions, McDonald said they chose to bypass the hydroxychloroquine study, which had an eye-popping Altmetric attention score of 23,084, compared with 3,727 for the NEJM paper, because it may have been cited for “other” reasons. “We wanted to focus less on the politics and more on the problem of retracted work.”
The team found that researchers across the globe were citing the retracted ACE/ARB paper (18.7% in the United States, 8.1% in Italy, and 44% other countries). Most citations were used to support a statement in the main text of a study, but in nearly 3% of cases, the data were incorporated into new analyses.
Just 17.6% of the studies cited or noted the retraction. “For sure, that was surprising to us. We suspected it, but our study confirmed it,” Dr. McDonald said.
Although retracted articles can be identified by a watermark or line of text, in some cases that can be easily missed, she noted. What’s more, not all citation software points out when a study has been retracted, a fate shared by the copyediting process.
“There are a lot of mechanisms in place and, in general, what’s happening is rare but there isn’t a perfect automated system solution to absolutely prevent this from happening,” she said. “It’s still subject to human error.”
The findings also have to be taken in the context of a rapidly emerging pandemic and the unprecedented torrent of scientific papers released over the past year.
“That might have contributed to why this happened, but the takeaway message is that this can happen despite our best efforts, and we need to challenge ourselves to come up with a system solution to prevent this from happening in the future,” Dr. McDonald said. “Current mechanisms are probably capturing 95% of it, but we need to do better.”
Limitations of the present analysis are that it was limited to the single retracted study; used only a single search engine, Google Scholar, to identify the citing works; and that additional citations may have been missed, the authors noted.
McDonald and coauthor Todd C. Lee, MD, report being signatories on a public letter calling for the retraction of the Surgisphere papers. Dr. Lee also reported receiving research support from Fonds De Recherche du Quebec-Sante during the conduct of the study.
A version of this article first appeared on Medscape.com.
COVID-19 tied to acceleration of Alzheimer’s disease pathology
, a new study shows.
These results suggest that COVID-19 may accelerate Alzheimer’s disease symptoms and pathology, said study investigator Thomas Wisniewski, MD, professor of neurology, pathology, and psychiatry at New York University.
The findings were presented here at the Alzheimer’s Association International Conference (AAIC) 2021.
Strong correlation
There’s a clear association between SARS-CoV-2 infection and Alzheimer’s disease-related dementia. Patients with Alzheimer’s disease are at threefold higher risk for the infection and have a twofold higher risk for death, Dr. Wisniewski told meeting delegates.
He and his colleagues conducted a prospective study of patients who had tested positive for SARS-CoV-2 and who experienced neurologic sequelae and SARS-CoV-2 patients who were without neurologic sequelae. All patients were hospitalized from March 10 to May 20, 2020. This was during a period when New York City was overwhelmed by COVID: About 35% of hospitalized patients had COVID.
Of those who experienced neurologic events, the most common “by far and away” (51%) was toxic metabolic encephalopathy (TME), said Dr. Wisniewski. Other associations included seizures, hypoxic/anoxic injury, and ischemic stroke.
The most common TMEs were septic and hypoxic ischemia. In most patients (78%), TME had more than one cause.
Researchers followed 196 patients with COVID and neurologic complications (case patients) and 186 matched control patients who had no neurologic complications over a period of 6 months.
“Unfortunately, both groups had poor outcomes,” said Dr. Wisniewski. About 50% had impaired cognition, and 56% experienced limitations in activities of daily living.
However, those patients with COVID-19 who had neurologic sequelae “fared even worse,” said Dr. Wisniewski. Compared with control patients, they had twofold worse Modified Rankin Scale scores and worse scores on activity of daily living, and they were much less likely to return to work.
Mechanisms by which COVID-19 affects longer-term cognitive dysfunction are unclear, but inflammation likely plays a role.
The research team compared a number of Alzheimer’s disease plasma biomarkers in 158 patients with COVID-19 who had neurologic symptoms and 152 COVID patients with COVID but no neurologic symptoms. They found marked elevations of neurofilament light, a marker of neuronal injury, in those with symptoms (P = .0003) as well as increased glial fibrillary acid protein, a marker of neuroinflammation (P = .0098).
Ubiquitin carboxyl-terminal hydrolase L1, another marker of neuronal injury, was also elevated in those with neurologic symptoms. Regarding Alzheimer’s disease pathology, total tau (t-tau) and phosphorylated tau “also tracked with neurological sequelae,” said Dr. Wisniewski.
There was no difference in levels of amyloid beta 40 (A beta 40) between groups. However, A beta 42 plasma levels were significantly lower in those with neurologic effects, suggesting higher levels in the brain. In addition, the ratio of t-tau to A beta 42 “clearly differentiated the two groups,” he said.
“Serum biomarkers of neuroinflammation and neuronal injury and Alzheimer’s disease correlate strongly, perhaps suggesting that folks with COVID infection and neurological sequelae may have an acceleration of Alzheimer’s disease symptoms and pathology,” he said. “That’s something that needs longer follow-up.”
Important differentiation
Commenting on the research, Rebecca Edelmayer, PhD, senior director of scientific engagement, Alzheimer’s Association, said the study provides important information. The inclusion of plasma biomarkers in this research is “really critical to tease out what’s the impact of COVID itself on the brain,” said Dr. Edelmayer.
“We’re in an era of biomarkers when it comes to Alzheimer’s disease and other dementias, and being able to define those changes that are happening in the brain over time is going to be really critical and aid in early detection and accurate diagnoses,” she said.
What is still to be learned is what these biomarkers reveal long term, said Dr. Edelmayer. “Do those biological markers change? Do they go back to normal? A lot of that is still unknown,” she said.
She noted that many diseases that are linked to inflammation produce similar biomarkers in the brain – for example, neurofilament light.
With other viral infections, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), similar associations between the infection and cognition have been reported, said Dr. Edelmayer.
“But there are still a lot of questions around cause and effect. Is it really a direct effect of the virus on the brain itself? Is it an effect of having an enormous amount of inflammation going on in the body? A lot of that still needs to be teased out,” she commented.
The study was supported by the National Institutes of Health, the Alzheimer’s Association, and the State of New York. Dr. Wisniewski has consulted for Grifols, Amylon Pharmaceuticals, and Alzamed Neuro; 30 NYU patents are related to AD therapeutics.
A version of this article first appeared on Medscape.com.
, a new study shows.
These results suggest that COVID-19 may accelerate Alzheimer’s disease symptoms and pathology, said study investigator Thomas Wisniewski, MD, professor of neurology, pathology, and psychiatry at New York University.
The findings were presented here at the Alzheimer’s Association International Conference (AAIC) 2021.
Strong correlation
There’s a clear association between SARS-CoV-2 infection and Alzheimer’s disease-related dementia. Patients with Alzheimer’s disease are at threefold higher risk for the infection and have a twofold higher risk for death, Dr. Wisniewski told meeting delegates.
He and his colleagues conducted a prospective study of patients who had tested positive for SARS-CoV-2 and who experienced neurologic sequelae and SARS-CoV-2 patients who were without neurologic sequelae. All patients were hospitalized from March 10 to May 20, 2020. This was during a period when New York City was overwhelmed by COVID: About 35% of hospitalized patients had COVID.
Of those who experienced neurologic events, the most common “by far and away” (51%) was toxic metabolic encephalopathy (TME), said Dr. Wisniewski. Other associations included seizures, hypoxic/anoxic injury, and ischemic stroke.
The most common TMEs were septic and hypoxic ischemia. In most patients (78%), TME had more than one cause.
Researchers followed 196 patients with COVID and neurologic complications (case patients) and 186 matched control patients who had no neurologic complications over a period of 6 months.
“Unfortunately, both groups had poor outcomes,” said Dr. Wisniewski. About 50% had impaired cognition, and 56% experienced limitations in activities of daily living.
However, those patients with COVID-19 who had neurologic sequelae “fared even worse,” said Dr. Wisniewski. Compared with control patients, they had twofold worse Modified Rankin Scale scores and worse scores on activity of daily living, and they were much less likely to return to work.
Mechanisms by which COVID-19 affects longer-term cognitive dysfunction are unclear, but inflammation likely plays a role.
The research team compared a number of Alzheimer’s disease plasma biomarkers in 158 patients with COVID-19 who had neurologic symptoms and 152 COVID patients with COVID but no neurologic symptoms. They found marked elevations of neurofilament light, a marker of neuronal injury, in those with symptoms (P = .0003) as well as increased glial fibrillary acid protein, a marker of neuroinflammation (P = .0098).
Ubiquitin carboxyl-terminal hydrolase L1, another marker of neuronal injury, was also elevated in those with neurologic symptoms. Regarding Alzheimer’s disease pathology, total tau (t-tau) and phosphorylated tau “also tracked with neurological sequelae,” said Dr. Wisniewski.
There was no difference in levels of amyloid beta 40 (A beta 40) between groups. However, A beta 42 plasma levels were significantly lower in those with neurologic effects, suggesting higher levels in the brain. In addition, the ratio of t-tau to A beta 42 “clearly differentiated the two groups,” he said.
“Serum biomarkers of neuroinflammation and neuronal injury and Alzheimer’s disease correlate strongly, perhaps suggesting that folks with COVID infection and neurological sequelae may have an acceleration of Alzheimer’s disease symptoms and pathology,” he said. “That’s something that needs longer follow-up.”
Important differentiation
Commenting on the research, Rebecca Edelmayer, PhD, senior director of scientific engagement, Alzheimer’s Association, said the study provides important information. The inclusion of plasma biomarkers in this research is “really critical to tease out what’s the impact of COVID itself on the brain,” said Dr. Edelmayer.
“We’re in an era of biomarkers when it comes to Alzheimer’s disease and other dementias, and being able to define those changes that are happening in the brain over time is going to be really critical and aid in early detection and accurate diagnoses,” she said.
What is still to be learned is what these biomarkers reveal long term, said Dr. Edelmayer. “Do those biological markers change? Do they go back to normal? A lot of that is still unknown,” she said.
She noted that many diseases that are linked to inflammation produce similar biomarkers in the brain – for example, neurofilament light.
With other viral infections, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), similar associations between the infection and cognition have been reported, said Dr. Edelmayer.
“But there are still a lot of questions around cause and effect. Is it really a direct effect of the virus on the brain itself? Is it an effect of having an enormous amount of inflammation going on in the body? A lot of that still needs to be teased out,” she commented.
The study was supported by the National Institutes of Health, the Alzheimer’s Association, and the State of New York. Dr. Wisniewski has consulted for Grifols, Amylon Pharmaceuticals, and Alzamed Neuro; 30 NYU patents are related to AD therapeutics.
A version of this article first appeared on Medscape.com.
, a new study shows.
These results suggest that COVID-19 may accelerate Alzheimer’s disease symptoms and pathology, said study investigator Thomas Wisniewski, MD, professor of neurology, pathology, and psychiatry at New York University.
The findings were presented here at the Alzheimer’s Association International Conference (AAIC) 2021.
Strong correlation
There’s a clear association between SARS-CoV-2 infection and Alzheimer’s disease-related dementia. Patients with Alzheimer’s disease are at threefold higher risk for the infection and have a twofold higher risk for death, Dr. Wisniewski told meeting delegates.
He and his colleagues conducted a prospective study of patients who had tested positive for SARS-CoV-2 and who experienced neurologic sequelae and SARS-CoV-2 patients who were without neurologic sequelae. All patients were hospitalized from March 10 to May 20, 2020. This was during a period when New York City was overwhelmed by COVID: About 35% of hospitalized patients had COVID.
Of those who experienced neurologic events, the most common “by far and away” (51%) was toxic metabolic encephalopathy (TME), said Dr. Wisniewski. Other associations included seizures, hypoxic/anoxic injury, and ischemic stroke.
The most common TMEs were septic and hypoxic ischemia. In most patients (78%), TME had more than one cause.
Researchers followed 196 patients with COVID and neurologic complications (case patients) and 186 matched control patients who had no neurologic complications over a period of 6 months.
“Unfortunately, both groups had poor outcomes,” said Dr. Wisniewski. About 50% had impaired cognition, and 56% experienced limitations in activities of daily living.
However, those patients with COVID-19 who had neurologic sequelae “fared even worse,” said Dr. Wisniewski. Compared with control patients, they had twofold worse Modified Rankin Scale scores and worse scores on activity of daily living, and they were much less likely to return to work.
Mechanisms by which COVID-19 affects longer-term cognitive dysfunction are unclear, but inflammation likely plays a role.
The research team compared a number of Alzheimer’s disease plasma biomarkers in 158 patients with COVID-19 who had neurologic symptoms and 152 COVID patients with COVID but no neurologic symptoms. They found marked elevations of neurofilament light, a marker of neuronal injury, in those with symptoms (P = .0003) as well as increased glial fibrillary acid protein, a marker of neuroinflammation (P = .0098).
Ubiquitin carboxyl-terminal hydrolase L1, another marker of neuronal injury, was also elevated in those with neurologic symptoms. Regarding Alzheimer’s disease pathology, total tau (t-tau) and phosphorylated tau “also tracked with neurological sequelae,” said Dr. Wisniewski.
There was no difference in levels of amyloid beta 40 (A beta 40) between groups. However, A beta 42 plasma levels were significantly lower in those with neurologic effects, suggesting higher levels in the brain. In addition, the ratio of t-tau to A beta 42 “clearly differentiated the two groups,” he said.
“Serum biomarkers of neuroinflammation and neuronal injury and Alzheimer’s disease correlate strongly, perhaps suggesting that folks with COVID infection and neurological sequelae may have an acceleration of Alzheimer’s disease symptoms and pathology,” he said. “That’s something that needs longer follow-up.”
Important differentiation
Commenting on the research, Rebecca Edelmayer, PhD, senior director of scientific engagement, Alzheimer’s Association, said the study provides important information. The inclusion of plasma biomarkers in this research is “really critical to tease out what’s the impact of COVID itself on the brain,” said Dr. Edelmayer.
“We’re in an era of biomarkers when it comes to Alzheimer’s disease and other dementias, and being able to define those changes that are happening in the brain over time is going to be really critical and aid in early detection and accurate diagnoses,” she said.
What is still to be learned is what these biomarkers reveal long term, said Dr. Edelmayer. “Do those biological markers change? Do they go back to normal? A lot of that is still unknown,” she said.
She noted that many diseases that are linked to inflammation produce similar biomarkers in the brain – for example, neurofilament light.
With other viral infections, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), similar associations between the infection and cognition have been reported, said Dr. Edelmayer.
“But there are still a lot of questions around cause and effect. Is it really a direct effect of the virus on the brain itself? Is it an effect of having an enormous amount of inflammation going on in the body? A lot of that still needs to be teased out,” she commented.
The study was supported by the National Institutes of Health, the Alzheimer’s Association, and the State of New York. Dr. Wisniewski has consulted for Grifols, Amylon Pharmaceuticals, and Alzamed Neuro; 30 NYU patents are related to AD therapeutics.
A version of this article first appeared on Medscape.com.
From AAIC 2021
‘Alarming’ data on early cognitive decline in transgender adults
, new research shows.
Investigators found transgender adults – individuals who identify with a gender different than the one assigned to them at birth – were nearly twice as likely to report subjective cognitive decline and more than twice as likely to report SCD-related functional limitations – such as reduced ability to work, volunteer, or be social – than cisgender adults.
“Trans populations are disproportionately impacted by health disparities and also risk factors for dementia. Putting these pieces together, I wasn’t surprised by their greater risk of cognitive decline,” said study investigator Ethan Cicero, PhD, RN, an assistant professor at Emory University, Atlanta.
The findings were presented at the 2021 Alzheimer’s Association International Conference.
‘Alarming’ finding
SCD is a self-reported experience of worsening memory or thinking and is one of the first clinical manifestations of Alzheimer’s disease and related dementia (ADRD). Yet there is limited research into cognitive impairment among transgender adults.
The researchers examined SCD and associated functional limitations among transgender and cisgender adults older than age 45 years who provided health and health behavior data as part of the Behavioral Risk Factor Surveillance System (BRFSS) surveys (2015-2019).
The sample included 386,529 adults of whom 1,302 identified as transgender and 385,227 as cisgender.
Roughly 17% of transgender adults reported SCD, which is significantly higher than the 10.6% rate for cisgender adults (P < .001).
Compared with cisgender adults reporting SCD, transgender adults reporting SCD were younger (mean age 61.9 vs. 65.2 years, P = .0005), more likely to be in a racial/ethnic minority group (37.3% vs. 19.5%, P < .0001), have a high school degree or less (59.6% vs. 43.4%, P = .0003), be uninsured (17% vs. 5.5%, P = .0007) and have a depressive disorder (58.8% vs. 45.7%, P = .0028).
The fact that transgender people who reported SCD were about 3 years younger than cisgender people who reported SCD is “somewhat alarming and a red flag to ask middle-aged trans adults about their brain health and not just older or elderly trans adults,” said Dr. Cicero.
The study also showed that transgender adults reporting SCD were 2.3 times more likely to report related social and self-care limitations when compared with cisgender adults reporting SCD.
The findings align with a study reported at AAIC 2019, which showed that sexual or gender minorities (SGM) are almost 30% more likely to report subjective cognitive decline compared with the non-SGM population.
Cause unclear
“We are not certain what may be causing the elevated subjective cognitive decline rates among transgender adults. We postulate that it may be in part due to anti-transgender stigma and prejudice that expose transgender people to high rates of mistreatment and discrimination where they live, work, learn, seek health care, and age,” Dr. Cicero said.
“More research is needed to identify and target preventive intervention strategies, develop culturally relevant screenings, and shape policies to improve the health and well-being of the transgender population,” he added.
Weighing in on the study, Rebecca Edelmayer, PhD, senior director of scientific engagement at the Alzheimer’s Association, said “researchers have only just started to explore the experiences of dementia within the lesbian, gay, and bisexual community, but this is the first time we are seeing some specific research that’s looking at cognition in transgender individuals and gender nonbinary individuals.”
“We don’t know exactly why transgender and gender nonbinary individuals experience greater rates of subjective cognitive decline, but we do know that they have greater rates of health disparities that are considered risk factors for dementia, including higher rates of cardiovascular disease, depression, diabetes, tobacco and alcohol use, and obesity,” Dr. Edelmayer said.
“Alzheimer’s and dementia do not discriminate. Neither can we,” Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association, said in a statement.
“The Alzheimer’s Association advocates for more research to better understand the cognitive and emotional needs of transgender and nonbinary individuals so that our nation’s health care providers can offer them culturally sensitive care,” said Dr. Carrillo.
The study had no specific funding. Dr. Cicero, Dr. Carrillo, and Dr. Edelmayer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
Investigators found transgender adults – individuals who identify with a gender different than the one assigned to them at birth – were nearly twice as likely to report subjective cognitive decline and more than twice as likely to report SCD-related functional limitations – such as reduced ability to work, volunteer, or be social – than cisgender adults.
“Trans populations are disproportionately impacted by health disparities and also risk factors for dementia. Putting these pieces together, I wasn’t surprised by their greater risk of cognitive decline,” said study investigator Ethan Cicero, PhD, RN, an assistant professor at Emory University, Atlanta.
The findings were presented at the 2021 Alzheimer’s Association International Conference.
‘Alarming’ finding
SCD is a self-reported experience of worsening memory or thinking and is one of the first clinical manifestations of Alzheimer’s disease and related dementia (ADRD). Yet there is limited research into cognitive impairment among transgender adults.
The researchers examined SCD and associated functional limitations among transgender and cisgender adults older than age 45 years who provided health and health behavior data as part of the Behavioral Risk Factor Surveillance System (BRFSS) surveys (2015-2019).
The sample included 386,529 adults of whom 1,302 identified as transgender and 385,227 as cisgender.
Roughly 17% of transgender adults reported SCD, which is significantly higher than the 10.6% rate for cisgender adults (P < .001).
Compared with cisgender adults reporting SCD, transgender adults reporting SCD were younger (mean age 61.9 vs. 65.2 years, P = .0005), more likely to be in a racial/ethnic minority group (37.3% vs. 19.5%, P < .0001), have a high school degree or less (59.6% vs. 43.4%, P = .0003), be uninsured (17% vs. 5.5%, P = .0007) and have a depressive disorder (58.8% vs. 45.7%, P = .0028).
The fact that transgender people who reported SCD were about 3 years younger than cisgender people who reported SCD is “somewhat alarming and a red flag to ask middle-aged trans adults about their brain health and not just older or elderly trans adults,” said Dr. Cicero.
The study also showed that transgender adults reporting SCD were 2.3 times more likely to report related social and self-care limitations when compared with cisgender adults reporting SCD.
The findings align with a study reported at AAIC 2019, which showed that sexual or gender minorities (SGM) are almost 30% more likely to report subjective cognitive decline compared with the non-SGM population.
Cause unclear
“We are not certain what may be causing the elevated subjective cognitive decline rates among transgender adults. We postulate that it may be in part due to anti-transgender stigma and prejudice that expose transgender people to high rates of mistreatment and discrimination where they live, work, learn, seek health care, and age,” Dr. Cicero said.
“More research is needed to identify and target preventive intervention strategies, develop culturally relevant screenings, and shape policies to improve the health and well-being of the transgender population,” he added.
Weighing in on the study, Rebecca Edelmayer, PhD, senior director of scientific engagement at the Alzheimer’s Association, said “researchers have only just started to explore the experiences of dementia within the lesbian, gay, and bisexual community, but this is the first time we are seeing some specific research that’s looking at cognition in transgender individuals and gender nonbinary individuals.”
“We don’t know exactly why transgender and gender nonbinary individuals experience greater rates of subjective cognitive decline, but we do know that they have greater rates of health disparities that are considered risk factors for dementia, including higher rates of cardiovascular disease, depression, diabetes, tobacco and alcohol use, and obesity,” Dr. Edelmayer said.
“Alzheimer’s and dementia do not discriminate. Neither can we,” Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association, said in a statement.
“The Alzheimer’s Association advocates for more research to better understand the cognitive and emotional needs of transgender and nonbinary individuals so that our nation’s health care providers can offer them culturally sensitive care,” said Dr. Carrillo.
The study had no specific funding. Dr. Cicero, Dr. Carrillo, and Dr. Edelmayer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
Investigators found transgender adults – individuals who identify with a gender different than the one assigned to them at birth – were nearly twice as likely to report subjective cognitive decline and more than twice as likely to report SCD-related functional limitations – such as reduced ability to work, volunteer, or be social – than cisgender adults.
“Trans populations are disproportionately impacted by health disparities and also risk factors for dementia. Putting these pieces together, I wasn’t surprised by their greater risk of cognitive decline,” said study investigator Ethan Cicero, PhD, RN, an assistant professor at Emory University, Atlanta.
The findings were presented at the 2021 Alzheimer’s Association International Conference.
‘Alarming’ finding
SCD is a self-reported experience of worsening memory or thinking and is one of the first clinical manifestations of Alzheimer’s disease and related dementia (ADRD). Yet there is limited research into cognitive impairment among transgender adults.
The researchers examined SCD and associated functional limitations among transgender and cisgender adults older than age 45 years who provided health and health behavior data as part of the Behavioral Risk Factor Surveillance System (BRFSS) surveys (2015-2019).
The sample included 386,529 adults of whom 1,302 identified as transgender and 385,227 as cisgender.
Roughly 17% of transgender adults reported SCD, which is significantly higher than the 10.6% rate for cisgender adults (P < .001).
Compared with cisgender adults reporting SCD, transgender adults reporting SCD were younger (mean age 61.9 vs. 65.2 years, P = .0005), more likely to be in a racial/ethnic minority group (37.3% vs. 19.5%, P < .0001), have a high school degree or less (59.6% vs. 43.4%, P = .0003), be uninsured (17% vs. 5.5%, P = .0007) and have a depressive disorder (58.8% vs. 45.7%, P = .0028).
The fact that transgender people who reported SCD were about 3 years younger than cisgender people who reported SCD is “somewhat alarming and a red flag to ask middle-aged trans adults about their brain health and not just older or elderly trans adults,” said Dr. Cicero.
The study also showed that transgender adults reporting SCD were 2.3 times more likely to report related social and self-care limitations when compared with cisgender adults reporting SCD.
The findings align with a study reported at AAIC 2019, which showed that sexual or gender minorities (SGM) are almost 30% more likely to report subjective cognitive decline compared with the non-SGM population.
Cause unclear
“We are not certain what may be causing the elevated subjective cognitive decline rates among transgender adults. We postulate that it may be in part due to anti-transgender stigma and prejudice that expose transgender people to high rates of mistreatment and discrimination where they live, work, learn, seek health care, and age,” Dr. Cicero said.
“More research is needed to identify and target preventive intervention strategies, develop culturally relevant screenings, and shape policies to improve the health and well-being of the transgender population,” he added.
Weighing in on the study, Rebecca Edelmayer, PhD, senior director of scientific engagement at the Alzheimer’s Association, said “researchers have only just started to explore the experiences of dementia within the lesbian, gay, and bisexual community, but this is the first time we are seeing some specific research that’s looking at cognition in transgender individuals and gender nonbinary individuals.”
“We don’t know exactly why transgender and gender nonbinary individuals experience greater rates of subjective cognitive decline, but we do know that they have greater rates of health disparities that are considered risk factors for dementia, including higher rates of cardiovascular disease, depression, diabetes, tobacco and alcohol use, and obesity,” Dr. Edelmayer said.
“Alzheimer’s and dementia do not discriminate. Neither can we,” Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association, said in a statement.
“The Alzheimer’s Association advocates for more research to better understand the cognitive and emotional needs of transgender and nonbinary individuals so that our nation’s health care providers can offer them culturally sensitive care,” said Dr. Carrillo.
The study had no specific funding. Dr. Cicero, Dr. Carrillo, and Dr. Edelmayer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From AAIC 2021
Digital therapeutics extends its reach in neurology
In recent years, a new genre of medical intervention has started to emerge – digital therapeutics. In the wake of promising results in a number of conditions, one high-profile approval by the Food and Drug Administration, and several ongoing clinical studies, neurologists (and other doctors) may soon be prescribing video games alongside conventional therapies for several conditions.
“Digital therapeutics refers to a software-based intervention. It’s not just digital information or digital monitoring, it’s an alternative treatment option based on software,” said John Krakauer, MD, professor of neurology, neuroscience, and physical medicine and rehabilitation at The Johns Hopkins University, Baltimore.
Dr. Krakauer explained that the nervous system is especially amenable to gamified therapies because of its unique ability to learn. “It’s an experience-dependent plastic system. You really want to have a high-intensity, high-dose behavioral intervention to try and rewire and train the nervous system.
“In other words, digital therapeutics complements what happens in physical and occupational therapy sessions with scientifically-informed behavioral interventions based on technology and software,” he said.
The digital dolphin treating stroke
Dr. Krakauer, chief scientific adviser to the company MindMaze, studies immersive digital therapies to enhance neurorehabilitation following stroke. He works on MindPod Dolphin, a virtual reality game that trains motor control of the upper extremities by having the patient simulate swimming in the ocean like a dolphin.
“Your movement is tracked, there are artificial intelligence algorithms controlling the difficulty, and the whole purpose is to take your nervous system for a ride, outside the context of activities of daily living. Patients are so engaged and immersed that they don’t even realize they’re making high-quality, high-intensity, high-dose movements of their arm.”
In a pilot trial called SMARTS2, his group found that MindPod Dolphin was about twice as effective as regular rehabilitation for upper extremity motor recovery in patients who had had a stroke. A larger trial is currently underway in New Zealand.
Another preliminary study found that MindPod Dolphin had positive effects on the physical and cognitive health of elderly patients in an assisted-living facility. Now, MindPod Dolphin is being studied around the world in patients with multiple sclerosis, Parkinson’s disease, concussion, and traumatic brain injury (TBI). There is even a Department of Defense–funded trial underway for veterans with TBI.
Reaching young patients through virtual play
Isabela Granic, PhD, director of the Games for Emotional and Mental Health Lab, and professor and chair of the developmental psychopathology department in the Behavioural Science Institute at Radboud University in the Netherlands, studies gamified therapy for depression and anxiety.
“We take evidence-based techniques in the mental health clinical world or developmental research, such as cognitive-behavioral therapy (CBT) or exposure therapy, and then embed them in games to use a different engine for delivering something we otherwise know works,” she said.
Data for a game she developed called MindLight are promising so far. “We have randomized controlled trials showing that we can cut young people’s anxiety in half after they have as little as five 1-hour sessions per week. We’ve shown that we can get the same benefits as CBT for these young people, which is huge.” MindLight also has proved effective for treating anxiety in children with autism.
A first for therapeutic video games
In the summer of 2020, EndeavorRx, made by Akili Interactive, became the first prescription video game to be approved by the FDA. The game, which is designed to improve attention function, is currently authorized for children aged 8-12 with attention-deficit/hyperactivity disorder.
Players complete “missions” by steering an aircraft through complex obstacle courses and collecting targets. The prescription directs the child to complete five missions each day for 5 days per week. It is recommended that patients use EndeavorRx for at least 4 weeks. Researchers are hopeful that, moving forward, the game will also prove effective for other cognitive disorders, including dementias and mild cognitive impairment.
EndeavorRx is even being studied for its efficacy in combating brain fog in COVID-19 long-haulers. A team of researchers led by Faith Gunning, PhD, psychologist and vice chair of research in the department of psychiatry at Weill Cornell Medicine, New York, is performing a trial of EndeavorRx for post–COVID-19 cognitive dysfunction.
“This therapeutic game gives repeated stimulation of the cognitive processes and networks that support multitasking and attention. And in doing that, my hypothesis is that there will be a restoration of function to that cognitive control network,” said Dr. Gunning. Gamified interventions, she added, are more fun and engaging for patients compared with more conventional therapies.
The fully remote trial will randomize approximately 100 participants to digital cognitive intervention and control groups. Over 6 weeks, the experimental group will be asked to play EndeavorRx at least 5 days per week, for about 25 minutes per day. Pre- and postintervention cognitive assessments will be compared between the groups.
“As far as digital interventions for mental health and cognitive disorders, the pandemic has just really accelerated the work ... that means that in the future more people can actually access what we’re doing in our labs and clinical research,” said Dr. Gunning. “I hope this is going to lead to more scalable approaches that will have a farther reach in the community.”
Dr. Krakauer said he envisions a future where neurologists prescribe medications, devices, and “immersive, plasticity-enhancing digital interventions.”
Hopefully, the synergy of these treatments will be a game changer for our patients.
Dr. Croll is a fellow in the department of neurology at New York University Langone Health in New York City and has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In recent years, a new genre of medical intervention has started to emerge – digital therapeutics. In the wake of promising results in a number of conditions, one high-profile approval by the Food and Drug Administration, and several ongoing clinical studies, neurologists (and other doctors) may soon be prescribing video games alongside conventional therapies for several conditions.
“Digital therapeutics refers to a software-based intervention. It’s not just digital information or digital monitoring, it’s an alternative treatment option based on software,” said John Krakauer, MD, professor of neurology, neuroscience, and physical medicine and rehabilitation at The Johns Hopkins University, Baltimore.
Dr. Krakauer explained that the nervous system is especially amenable to gamified therapies because of its unique ability to learn. “It’s an experience-dependent plastic system. You really want to have a high-intensity, high-dose behavioral intervention to try and rewire and train the nervous system.
“In other words, digital therapeutics complements what happens in physical and occupational therapy sessions with scientifically-informed behavioral interventions based on technology and software,” he said.
The digital dolphin treating stroke
Dr. Krakauer, chief scientific adviser to the company MindMaze, studies immersive digital therapies to enhance neurorehabilitation following stroke. He works on MindPod Dolphin, a virtual reality game that trains motor control of the upper extremities by having the patient simulate swimming in the ocean like a dolphin.
“Your movement is tracked, there are artificial intelligence algorithms controlling the difficulty, and the whole purpose is to take your nervous system for a ride, outside the context of activities of daily living. Patients are so engaged and immersed that they don’t even realize they’re making high-quality, high-intensity, high-dose movements of their arm.”
In a pilot trial called SMARTS2, his group found that MindPod Dolphin was about twice as effective as regular rehabilitation for upper extremity motor recovery in patients who had had a stroke. A larger trial is currently underway in New Zealand.
Another preliminary study found that MindPod Dolphin had positive effects on the physical and cognitive health of elderly patients in an assisted-living facility. Now, MindPod Dolphin is being studied around the world in patients with multiple sclerosis, Parkinson’s disease, concussion, and traumatic brain injury (TBI). There is even a Department of Defense–funded trial underway for veterans with TBI.
Reaching young patients through virtual play
Isabela Granic, PhD, director of the Games for Emotional and Mental Health Lab, and professor and chair of the developmental psychopathology department in the Behavioural Science Institute at Radboud University in the Netherlands, studies gamified therapy for depression and anxiety.
“We take evidence-based techniques in the mental health clinical world or developmental research, such as cognitive-behavioral therapy (CBT) or exposure therapy, and then embed them in games to use a different engine for delivering something we otherwise know works,” she said.
Data for a game she developed called MindLight are promising so far. “We have randomized controlled trials showing that we can cut young people’s anxiety in half after they have as little as five 1-hour sessions per week. We’ve shown that we can get the same benefits as CBT for these young people, which is huge.” MindLight also has proved effective for treating anxiety in children with autism.
A first for therapeutic video games
In the summer of 2020, EndeavorRx, made by Akili Interactive, became the first prescription video game to be approved by the FDA. The game, which is designed to improve attention function, is currently authorized for children aged 8-12 with attention-deficit/hyperactivity disorder.
Players complete “missions” by steering an aircraft through complex obstacle courses and collecting targets. The prescription directs the child to complete five missions each day for 5 days per week. It is recommended that patients use EndeavorRx for at least 4 weeks. Researchers are hopeful that, moving forward, the game will also prove effective for other cognitive disorders, including dementias and mild cognitive impairment.
EndeavorRx is even being studied for its efficacy in combating brain fog in COVID-19 long-haulers. A team of researchers led by Faith Gunning, PhD, psychologist and vice chair of research in the department of psychiatry at Weill Cornell Medicine, New York, is performing a trial of EndeavorRx for post–COVID-19 cognitive dysfunction.
“This therapeutic game gives repeated stimulation of the cognitive processes and networks that support multitasking and attention. And in doing that, my hypothesis is that there will be a restoration of function to that cognitive control network,” said Dr. Gunning. Gamified interventions, she added, are more fun and engaging for patients compared with more conventional therapies.
The fully remote trial will randomize approximately 100 participants to digital cognitive intervention and control groups. Over 6 weeks, the experimental group will be asked to play EndeavorRx at least 5 days per week, for about 25 minutes per day. Pre- and postintervention cognitive assessments will be compared between the groups.
“As far as digital interventions for mental health and cognitive disorders, the pandemic has just really accelerated the work ... that means that in the future more people can actually access what we’re doing in our labs and clinical research,” said Dr. Gunning. “I hope this is going to lead to more scalable approaches that will have a farther reach in the community.”
Dr. Krakauer said he envisions a future where neurologists prescribe medications, devices, and “immersive, plasticity-enhancing digital interventions.”
Hopefully, the synergy of these treatments will be a game changer for our patients.
Dr. Croll is a fellow in the department of neurology at New York University Langone Health in New York City and has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In recent years, a new genre of medical intervention has started to emerge – digital therapeutics. In the wake of promising results in a number of conditions, one high-profile approval by the Food and Drug Administration, and several ongoing clinical studies, neurologists (and other doctors) may soon be prescribing video games alongside conventional therapies for several conditions.
“Digital therapeutics refers to a software-based intervention. It’s not just digital information or digital monitoring, it’s an alternative treatment option based on software,” said John Krakauer, MD, professor of neurology, neuroscience, and physical medicine and rehabilitation at The Johns Hopkins University, Baltimore.
Dr. Krakauer explained that the nervous system is especially amenable to gamified therapies because of its unique ability to learn. “It’s an experience-dependent plastic system. You really want to have a high-intensity, high-dose behavioral intervention to try and rewire and train the nervous system.
“In other words, digital therapeutics complements what happens in physical and occupational therapy sessions with scientifically-informed behavioral interventions based on technology and software,” he said.
The digital dolphin treating stroke
Dr. Krakauer, chief scientific adviser to the company MindMaze, studies immersive digital therapies to enhance neurorehabilitation following stroke. He works on MindPod Dolphin, a virtual reality game that trains motor control of the upper extremities by having the patient simulate swimming in the ocean like a dolphin.
“Your movement is tracked, there are artificial intelligence algorithms controlling the difficulty, and the whole purpose is to take your nervous system for a ride, outside the context of activities of daily living. Patients are so engaged and immersed that they don’t even realize they’re making high-quality, high-intensity, high-dose movements of their arm.”
In a pilot trial called SMARTS2, his group found that MindPod Dolphin was about twice as effective as regular rehabilitation for upper extremity motor recovery in patients who had had a stroke. A larger trial is currently underway in New Zealand.
Another preliminary study found that MindPod Dolphin had positive effects on the physical and cognitive health of elderly patients in an assisted-living facility. Now, MindPod Dolphin is being studied around the world in patients with multiple sclerosis, Parkinson’s disease, concussion, and traumatic brain injury (TBI). There is even a Department of Defense–funded trial underway for veterans with TBI.
Reaching young patients through virtual play
Isabela Granic, PhD, director of the Games for Emotional and Mental Health Lab, and professor and chair of the developmental psychopathology department in the Behavioural Science Institute at Radboud University in the Netherlands, studies gamified therapy for depression and anxiety.
“We take evidence-based techniques in the mental health clinical world or developmental research, such as cognitive-behavioral therapy (CBT) or exposure therapy, and then embed them in games to use a different engine for delivering something we otherwise know works,” she said.
Data for a game she developed called MindLight are promising so far. “We have randomized controlled trials showing that we can cut young people’s anxiety in half after they have as little as five 1-hour sessions per week. We’ve shown that we can get the same benefits as CBT for these young people, which is huge.” MindLight also has proved effective for treating anxiety in children with autism.
A first for therapeutic video games
In the summer of 2020, EndeavorRx, made by Akili Interactive, became the first prescription video game to be approved by the FDA. The game, which is designed to improve attention function, is currently authorized for children aged 8-12 with attention-deficit/hyperactivity disorder.
Players complete “missions” by steering an aircraft through complex obstacle courses and collecting targets. The prescription directs the child to complete five missions each day for 5 days per week. It is recommended that patients use EndeavorRx for at least 4 weeks. Researchers are hopeful that, moving forward, the game will also prove effective for other cognitive disorders, including dementias and mild cognitive impairment.
EndeavorRx is even being studied for its efficacy in combating brain fog in COVID-19 long-haulers. A team of researchers led by Faith Gunning, PhD, psychologist and vice chair of research in the department of psychiatry at Weill Cornell Medicine, New York, is performing a trial of EndeavorRx for post–COVID-19 cognitive dysfunction.
“This therapeutic game gives repeated stimulation of the cognitive processes and networks that support multitasking and attention. And in doing that, my hypothesis is that there will be a restoration of function to that cognitive control network,” said Dr. Gunning. Gamified interventions, she added, are more fun and engaging for patients compared with more conventional therapies.
The fully remote trial will randomize approximately 100 participants to digital cognitive intervention and control groups. Over 6 weeks, the experimental group will be asked to play EndeavorRx at least 5 days per week, for about 25 minutes per day. Pre- and postintervention cognitive assessments will be compared between the groups.
“As far as digital interventions for mental health and cognitive disorders, the pandemic has just really accelerated the work ... that means that in the future more people can actually access what we’re doing in our labs and clinical research,” said Dr. Gunning. “I hope this is going to lead to more scalable approaches that will have a farther reach in the community.”
Dr. Krakauer said he envisions a future where neurologists prescribe medications, devices, and “immersive, plasticity-enhancing digital interventions.”
Hopefully, the synergy of these treatments will be a game changer for our patients.
Dr. Croll is a fellow in the department of neurology at New York University Langone Health in New York City and has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
U.S. health system ranks last among 11 high-income countries
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.