User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
It’s time for all physicians to have a national medical license
The current pandemic is forcing changes throughout the health care industry. Telehealth is witnessing a surge. Hospitals are struggling without elective care, and remarkably, physicians are being laid off during a time of crisis. While some states have a surplus work force, other states go begging, and they lock the system up with delays in the processing of applications.
Considering the prevalence of noncompete clauses and a schism in state-to-state processing of complaints, patients are suffering and dying under an antiquated system. The Federation of State Medical Boards doesn’t seem to add to the solution, but instead confounds the problem with new directives.
Because physicians’ training requirements don’t vary from state to state, it makes sense. We must take national standardized exams to qualify. Locum tenens physicians must maintain licensure in as many states as they practice; this creates an unnecessary burden and expense, when there is a better alternative. Some states have arranged reciprocity licensure with other states. This is commendable but doesn’t go far enough to manage national shortages in rural areas.
Under a national licensing system, physicians and other health care professionals would not only be free to travel anywhere in the United States to practice, they can count on consistent and equal management of their license. The federal government can track regional overages and shortages and redirect physicians and other medical professionals with incentives to areas in need.
The FSMB claims that there is interstate continuity among state medical boards, but the data don’t support this.
Why is this the case? Each medical board fails to manage their charges equally. Often, action taken by one state board when reported to another state board can cause a review and readjudication. This occasionally results in the overturning of a reprimand or suspension because of differences in legislation.
Yet the physician or health care professional must bear the burden of the notification against their license. Once again, the FSMB claims there is interstate continuity in disciplinary actions, but the data do not support this.
Once someone brings a complaint against a health professional, which in this health care climate is inevitable, the medical board must institute an investigation. Even if it has no merit, the process must go forward. Under a national system, a consistent approach to dismiss and investigate issues and complaints might expedite the process. This eliminates inefficiency and delays in clearance of charges.
A report in 2006 identified fragmentation and discontinuities in the way each state medical board manages a physician or other health care personnel’s complaints. The number of hands involved in the process varies and is often onerous and redundant. Several sources may request the same information, tying it up as it moves through an inefficient and uncooperative system. With the increase in internal politics since then, this only compounds rather than improves the problem.
Yet the benefit of national licensure is not just for the health care personnel but also for insurance companies that must register and screen physicians as they move from region to region. In each state, the physician must repeat the accreditation process, delaying reimbursements and denying care. Hospitals also must repeat the credentialing task as well. This, although the physician or health care worker has a clean record with the same company or the same hospital system in their original state.
Perhaps data from one insurance group or hospital in another state get lost or altered in transfer, but under national licensing, this would not be possible. Furthermore, the current system limits the individual professional’s input. By nationalizing, record corrections would go through a federal database rather than state data banks that don’t sync.
This already partially exists with the National Practitioner Identifier. But we can take it one step further. Through nationalization, we could institute a fairer system of reporting where both the professional’s and the complainant’s summary is included. One might argue the National Physician Data Bank performs this function, but in fact, it merely reflects state assessments – which again vary.
The infrastructure is already in place to transition from a state to national system with facilities and records kept in each state’s medical board. It would simply be a matter of replacing state personnel with federal employees who all work from the same script. A national medical license simply makes sense for all parties. It reduces discontinuity and increases efficiency. A national medical license empowers the individual rather than institutions, yet benefits both.
The time is nigh to nationally certify and set physicians free, reduce paperwork and needless fees, and eliminate state supremacy.
Dr. Raymond is an emergency physician based in Hickory, N.C., and Muckendorf an der Donau, Austria.
A version of this article first appeared on Medscape.com.
The current pandemic is forcing changes throughout the health care industry. Telehealth is witnessing a surge. Hospitals are struggling without elective care, and remarkably, physicians are being laid off during a time of crisis. While some states have a surplus work force, other states go begging, and they lock the system up with delays in the processing of applications.
Considering the prevalence of noncompete clauses and a schism in state-to-state processing of complaints, patients are suffering and dying under an antiquated system. The Federation of State Medical Boards doesn’t seem to add to the solution, but instead confounds the problem with new directives.
Because physicians’ training requirements don’t vary from state to state, it makes sense. We must take national standardized exams to qualify. Locum tenens physicians must maintain licensure in as many states as they practice; this creates an unnecessary burden and expense, when there is a better alternative. Some states have arranged reciprocity licensure with other states. This is commendable but doesn’t go far enough to manage national shortages in rural areas.
Under a national licensing system, physicians and other health care professionals would not only be free to travel anywhere in the United States to practice, they can count on consistent and equal management of their license. The federal government can track regional overages and shortages and redirect physicians and other medical professionals with incentives to areas in need.
The FSMB claims that there is interstate continuity among state medical boards, but the data don’t support this.
Why is this the case? Each medical board fails to manage their charges equally. Often, action taken by one state board when reported to another state board can cause a review and readjudication. This occasionally results in the overturning of a reprimand or suspension because of differences in legislation.
Yet the physician or health care professional must bear the burden of the notification against their license. Once again, the FSMB claims there is interstate continuity in disciplinary actions, but the data do not support this.
Once someone brings a complaint against a health professional, which in this health care climate is inevitable, the medical board must institute an investigation. Even if it has no merit, the process must go forward. Under a national system, a consistent approach to dismiss and investigate issues and complaints might expedite the process. This eliminates inefficiency and delays in clearance of charges.
A report in 2006 identified fragmentation and discontinuities in the way each state medical board manages a physician or other health care personnel’s complaints. The number of hands involved in the process varies and is often onerous and redundant. Several sources may request the same information, tying it up as it moves through an inefficient and uncooperative system. With the increase in internal politics since then, this only compounds rather than improves the problem.
Yet the benefit of national licensure is not just for the health care personnel but also for insurance companies that must register and screen physicians as they move from region to region. In each state, the physician must repeat the accreditation process, delaying reimbursements and denying care. Hospitals also must repeat the credentialing task as well. This, although the physician or health care worker has a clean record with the same company or the same hospital system in their original state.
Perhaps data from one insurance group or hospital in another state get lost or altered in transfer, but under national licensing, this would not be possible. Furthermore, the current system limits the individual professional’s input. By nationalizing, record corrections would go through a federal database rather than state data banks that don’t sync.
This already partially exists with the National Practitioner Identifier. But we can take it one step further. Through nationalization, we could institute a fairer system of reporting where both the professional’s and the complainant’s summary is included. One might argue the National Physician Data Bank performs this function, but in fact, it merely reflects state assessments – which again vary.
The infrastructure is already in place to transition from a state to national system with facilities and records kept in each state’s medical board. It would simply be a matter of replacing state personnel with federal employees who all work from the same script. A national medical license simply makes sense for all parties. It reduces discontinuity and increases efficiency. A national medical license empowers the individual rather than institutions, yet benefits both.
The time is nigh to nationally certify and set physicians free, reduce paperwork and needless fees, and eliminate state supremacy.
Dr. Raymond is an emergency physician based in Hickory, N.C., and Muckendorf an der Donau, Austria.
A version of this article first appeared on Medscape.com.
The current pandemic is forcing changes throughout the health care industry. Telehealth is witnessing a surge. Hospitals are struggling without elective care, and remarkably, physicians are being laid off during a time of crisis. While some states have a surplus work force, other states go begging, and they lock the system up with delays in the processing of applications.
Considering the prevalence of noncompete clauses and a schism in state-to-state processing of complaints, patients are suffering and dying under an antiquated system. The Federation of State Medical Boards doesn’t seem to add to the solution, but instead confounds the problem with new directives.
Because physicians’ training requirements don’t vary from state to state, it makes sense. We must take national standardized exams to qualify. Locum tenens physicians must maintain licensure in as many states as they practice; this creates an unnecessary burden and expense, when there is a better alternative. Some states have arranged reciprocity licensure with other states. This is commendable but doesn’t go far enough to manage national shortages in rural areas.
Under a national licensing system, physicians and other health care professionals would not only be free to travel anywhere in the United States to practice, they can count on consistent and equal management of their license. The federal government can track regional overages and shortages and redirect physicians and other medical professionals with incentives to areas in need.
The FSMB claims that there is interstate continuity among state medical boards, but the data don’t support this.
Why is this the case? Each medical board fails to manage their charges equally. Often, action taken by one state board when reported to another state board can cause a review and readjudication. This occasionally results in the overturning of a reprimand or suspension because of differences in legislation.
Yet the physician or health care professional must bear the burden of the notification against their license. Once again, the FSMB claims there is interstate continuity in disciplinary actions, but the data do not support this.
Once someone brings a complaint against a health professional, which in this health care climate is inevitable, the medical board must institute an investigation. Even if it has no merit, the process must go forward. Under a national system, a consistent approach to dismiss and investigate issues and complaints might expedite the process. This eliminates inefficiency and delays in clearance of charges.
A report in 2006 identified fragmentation and discontinuities in the way each state medical board manages a physician or other health care personnel’s complaints. The number of hands involved in the process varies and is often onerous and redundant. Several sources may request the same information, tying it up as it moves through an inefficient and uncooperative system. With the increase in internal politics since then, this only compounds rather than improves the problem.
Yet the benefit of national licensure is not just for the health care personnel but also for insurance companies that must register and screen physicians as they move from region to region. In each state, the physician must repeat the accreditation process, delaying reimbursements and denying care. Hospitals also must repeat the credentialing task as well. This, although the physician or health care worker has a clean record with the same company or the same hospital system in their original state.
Perhaps data from one insurance group or hospital in another state get lost or altered in transfer, but under national licensing, this would not be possible. Furthermore, the current system limits the individual professional’s input. By nationalizing, record corrections would go through a federal database rather than state data banks that don’t sync.
This already partially exists with the National Practitioner Identifier. But we can take it one step further. Through nationalization, we could institute a fairer system of reporting where both the professional’s and the complainant’s summary is included. One might argue the National Physician Data Bank performs this function, but in fact, it merely reflects state assessments – which again vary.
The infrastructure is already in place to transition from a state to national system with facilities and records kept in each state’s medical board. It would simply be a matter of replacing state personnel with federal employees who all work from the same script. A national medical license simply makes sense for all parties. It reduces discontinuity and increases efficiency. A national medical license empowers the individual rather than institutions, yet benefits both.
The time is nigh to nationally certify and set physicians free, reduce paperwork and needless fees, and eliminate state supremacy.
Dr. Raymond is an emergency physician based in Hickory, N.C., and Muckendorf an der Donau, Austria.
A version of this article first appeared on Medscape.com.
Motherhood can get old fast, and snubbing can become phubbing
Killer babies and their aging mommies
The joys of new parenthood are endless, like the long nights and functioning on 4 hours of sleep. But those babies sure are sweet, and deadly. That’s right, little Johnny junior is shaving years off of your life.
. But hold on, that doesn’t mean mothers need to update their driver licenses. There’s a difference between biological and chronological age.
Biological aging is measured by epigenetics, which analyzes changes in DNA over time by determining whether coding for certain proteins is turned on or off. The process acts as a sort of clock, lead author Judith E. Carroll, PhD, said in a separate statement, allowing scientists to estimate a person’s biological age.
Although loss of sleep may accelerate biological aging and increase health risks, the researchers don’t want people to think that lack of sleep during infant care is going to automatically cause permanent damage. The jury is still out on whether the effects are long lasting. Instead, they emphasized the importance of prioritizing sleep needs and getting some help from others to do it.
“With every hour of additional sleep, the mother’s biological age was younger,” Dr. Carroll said. “I, and many other sleep scientists, consider sleep health to be just as vital to overall health as diet and exercise.”
So, new moms, fix that gourmet dinner after you go for that run because you’re already up at 4 a.m. anyway. It’s all about balance.
Me and my phone-y phriends
It’s been months since you’ve seen your friends in person. You got your vaccine and so, after all this time, you can finally meet with your friends in real life. No more Zoom. It’s a strange dream come true.
The problem is that half your friends barely seem interested, spending much of your time together staring at their phones. Naturally, there’s a clever term for this: You’ve just been the victim of phubbing, specifically friend phubbing or fphubbing (we’re not sure there are enough “f” sounds at the beginning of that word), and it’s been the focus of a new study from the University of Georgia.
So who are these fphubbers? Researchers found that neurotic and depressed individuals are more likely to fphub, as were those with social anxiety, since they may actually prefer online interaction over face-to-face conversation. On the flip side, people with agreeable traits were less likely to fphub, as they felt doing so would be rude and impolite. Quite a bold stance right there, we know.
The researchers noted the complete ordinariness of people pulling their phones out while with friends, and the rapid acceptance of something many people may still consider rude. It could speak to casual smartphone addiction and the urge we all get when we hear that notification in our pocket. Maybe what we need when we see friends is the equivalent of those PSAs before movies telling you to turn off your cell phones. Then you can all go down to the lobby and get yourselves a treat.
Who needs a vaccine when there’s horse paste?
It’s not the first time, and it won’t be the last, that some people think they know best when it comes to COVID-19 safety.
What is the newest “trend” for prevention and treatment? Enter, ivermectin, a Food and Drug Administration–approved drug for treating conditions caused by parasitic worms. The prescription form is hard to find these days, so some folks have been “raiding rural tractor supply stores in search of ivermectin horse paste (packed with ‘apple flavor’!) and [weighing] the benefits of taking ivermectin ‘sheep drench’,” according to the Daily Beast.
The FDA does not condone the use of ivermectin for COVID-19 and warns that the types meant for animals can be harmful to humans if taken in large doses. Facebook has played its part, as groups are forming to share conflicting information about how the drug can be used for COVID-19. The medication often comes from sketchy sources, and it’s seemingly causing more harm than good. Pharmacies are even starting to treat ivermectin as if it’s an opioid.
“My ‘horse’ had no negative side effects, and now he tells me he feels like a million bucks and is now COVID free,” one social media poster wrote in code, according to the Daily Beast.
When the card fits, COVID-19 will take a hit
Good news! We have figured out the problem behind the whole COVID-19 vaccine-denial business.
And by “we,” of course, we mean someone else. But we’re telling you about it, and isn’t that really the important part?
Anyway, back to the problem. It’s not the vaccines themselves, it’s the vaccine cards. They’re the wrong size.
The Atlantic’s Amanda Mull explains: “When I got my first shot, in late February, I sat in the mandatory waiting area, holding my new card in one hand and my wallet in the other, trying to understand why the two objects weren’t compatible.”
She didn’t get very far with the CDC, but Chelsea Cirruzzo, a public-health reporter at U.S. News & World Report who has been tweeting about the vaccine cards, suggested that “someone just printed out a bunch of cards that are easy to write your name and vaccine brand on, without thinking about wallets.”
The evidence does fit the nobody-really-gave-it-any-thought argument. The template was available to the public on some state government websites when the vaccine was approved and can still be found on Florida’s, Ms. Mull notes. “Try to imagine governments freely distributing their templates for driver’s licenses, passports, or other documents intended to certify a particular identity or status.” The FBI, we understand, frowns upon this sort of thing.
Well, there you have it, America. When the card fits in a wallet, the vaccine problem will go away. Just remember where you read it, not where we read it.
Killer babies and their aging mommies
The joys of new parenthood are endless, like the long nights and functioning on 4 hours of sleep. But those babies sure are sweet, and deadly. That’s right, little Johnny junior is shaving years off of your life.
. But hold on, that doesn’t mean mothers need to update their driver licenses. There’s a difference between biological and chronological age.
Biological aging is measured by epigenetics, which analyzes changes in DNA over time by determining whether coding for certain proteins is turned on or off. The process acts as a sort of clock, lead author Judith E. Carroll, PhD, said in a separate statement, allowing scientists to estimate a person’s biological age.
Although loss of sleep may accelerate biological aging and increase health risks, the researchers don’t want people to think that lack of sleep during infant care is going to automatically cause permanent damage. The jury is still out on whether the effects are long lasting. Instead, they emphasized the importance of prioritizing sleep needs and getting some help from others to do it.
“With every hour of additional sleep, the mother’s biological age was younger,” Dr. Carroll said. “I, and many other sleep scientists, consider sleep health to be just as vital to overall health as diet and exercise.”
So, new moms, fix that gourmet dinner after you go for that run because you’re already up at 4 a.m. anyway. It’s all about balance.
Me and my phone-y phriends
It’s been months since you’ve seen your friends in person. You got your vaccine and so, after all this time, you can finally meet with your friends in real life. No more Zoom. It’s a strange dream come true.
The problem is that half your friends barely seem interested, spending much of your time together staring at their phones. Naturally, there’s a clever term for this: You’ve just been the victim of phubbing, specifically friend phubbing or fphubbing (we’re not sure there are enough “f” sounds at the beginning of that word), and it’s been the focus of a new study from the University of Georgia.
So who are these fphubbers? Researchers found that neurotic and depressed individuals are more likely to fphub, as were those with social anxiety, since they may actually prefer online interaction over face-to-face conversation. On the flip side, people with agreeable traits were less likely to fphub, as they felt doing so would be rude and impolite. Quite a bold stance right there, we know.
The researchers noted the complete ordinariness of people pulling their phones out while with friends, and the rapid acceptance of something many people may still consider rude. It could speak to casual smartphone addiction and the urge we all get when we hear that notification in our pocket. Maybe what we need when we see friends is the equivalent of those PSAs before movies telling you to turn off your cell phones. Then you can all go down to the lobby and get yourselves a treat.
Who needs a vaccine when there’s horse paste?
It’s not the first time, and it won’t be the last, that some people think they know best when it comes to COVID-19 safety.
What is the newest “trend” for prevention and treatment? Enter, ivermectin, a Food and Drug Administration–approved drug for treating conditions caused by parasitic worms. The prescription form is hard to find these days, so some folks have been “raiding rural tractor supply stores in search of ivermectin horse paste (packed with ‘apple flavor’!) and [weighing] the benefits of taking ivermectin ‘sheep drench’,” according to the Daily Beast.
The FDA does not condone the use of ivermectin for COVID-19 and warns that the types meant for animals can be harmful to humans if taken in large doses. Facebook has played its part, as groups are forming to share conflicting information about how the drug can be used for COVID-19. The medication often comes from sketchy sources, and it’s seemingly causing more harm than good. Pharmacies are even starting to treat ivermectin as if it’s an opioid.
“My ‘horse’ had no negative side effects, and now he tells me he feels like a million bucks and is now COVID free,” one social media poster wrote in code, according to the Daily Beast.
When the card fits, COVID-19 will take a hit
Good news! We have figured out the problem behind the whole COVID-19 vaccine-denial business.
And by “we,” of course, we mean someone else. But we’re telling you about it, and isn’t that really the important part?
Anyway, back to the problem. It’s not the vaccines themselves, it’s the vaccine cards. They’re the wrong size.
The Atlantic’s Amanda Mull explains: “When I got my first shot, in late February, I sat in the mandatory waiting area, holding my new card in one hand and my wallet in the other, trying to understand why the two objects weren’t compatible.”
She didn’t get very far with the CDC, but Chelsea Cirruzzo, a public-health reporter at U.S. News & World Report who has been tweeting about the vaccine cards, suggested that “someone just printed out a bunch of cards that are easy to write your name and vaccine brand on, without thinking about wallets.”
The evidence does fit the nobody-really-gave-it-any-thought argument. The template was available to the public on some state government websites when the vaccine was approved and can still be found on Florida’s, Ms. Mull notes. “Try to imagine governments freely distributing their templates for driver’s licenses, passports, or other documents intended to certify a particular identity or status.” The FBI, we understand, frowns upon this sort of thing.
Well, there you have it, America. When the card fits in a wallet, the vaccine problem will go away. Just remember where you read it, not where we read it.
Killer babies and their aging mommies
The joys of new parenthood are endless, like the long nights and functioning on 4 hours of sleep. But those babies sure are sweet, and deadly. That’s right, little Johnny junior is shaving years off of your life.
. But hold on, that doesn’t mean mothers need to update their driver licenses. There’s a difference between biological and chronological age.
Biological aging is measured by epigenetics, which analyzes changes in DNA over time by determining whether coding for certain proteins is turned on or off. The process acts as a sort of clock, lead author Judith E. Carroll, PhD, said in a separate statement, allowing scientists to estimate a person’s biological age.
Although loss of sleep may accelerate biological aging and increase health risks, the researchers don’t want people to think that lack of sleep during infant care is going to automatically cause permanent damage. The jury is still out on whether the effects are long lasting. Instead, they emphasized the importance of prioritizing sleep needs and getting some help from others to do it.
“With every hour of additional sleep, the mother’s biological age was younger,” Dr. Carroll said. “I, and many other sleep scientists, consider sleep health to be just as vital to overall health as diet and exercise.”
So, new moms, fix that gourmet dinner after you go for that run because you’re already up at 4 a.m. anyway. It’s all about balance.
Me and my phone-y phriends
It’s been months since you’ve seen your friends in person. You got your vaccine and so, after all this time, you can finally meet with your friends in real life. No more Zoom. It’s a strange dream come true.
The problem is that half your friends barely seem interested, spending much of your time together staring at their phones. Naturally, there’s a clever term for this: You’ve just been the victim of phubbing, specifically friend phubbing or fphubbing (we’re not sure there are enough “f” sounds at the beginning of that word), and it’s been the focus of a new study from the University of Georgia.
So who are these fphubbers? Researchers found that neurotic and depressed individuals are more likely to fphub, as were those with social anxiety, since they may actually prefer online interaction over face-to-face conversation. On the flip side, people with agreeable traits were less likely to fphub, as they felt doing so would be rude and impolite. Quite a bold stance right there, we know.
The researchers noted the complete ordinariness of people pulling their phones out while with friends, and the rapid acceptance of something many people may still consider rude. It could speak to casual smartphone addiction and the urge we all get when we hear that notification in our pocket. Maybe what we need when we see friends is the equivalent of those PSAs before movies telling you to turn off your cell phones. Then you can all go down to the lobby and get yourselves a treat.
Who needs a vaccine when there’s horse paste?
It’s not the first time, and it won’t be the last, that some people think they know best when it comes to COVID-19 safety.
What is the newest “trend” for prevention and treatment? Enter, ivermectin, a Food and Drug Administration–approved drug for treating conditions caused by parasitic worms. The prescription form is hard to find these days, so some folks have been “raiding rural tractor supply stores in search of ivermectin horse paste (packed with ‘apple flavor’!) and [weighing] the benefits of taking ivermectin ‘sheep drench’,” according to the Daily Beast.
The FDA does not condone the use of ivermectin for COVID-19 and warns that the types meant for animals can be harmful to humans if taken in large doses. Facebook has played its part, as groups are forming to share conflicting information about how the drug can be used for COVID-19. The medication often comes from sketchy sources, and it’s seemingly causing more harm than good. Pharmacies are even starting to treat ivermectin as if it’s an opioid.
“My ‘horse’ had no negative side effects, and now he tells me he feels like a million bucks and is now COVID free,” one social media poster wrote in code, according to the Daily Beast.
When the card fits, COVID-19 will take a hit
Good news! We have figured out the problem behind the whole COVID-19 vaccine-denial business.
And by “we,” of course, we mean someone else. But we’re telling you about it, and isn’t that really the important part?
Anyway, back to the problem. It’s not the vaccines themselves, it’s the vaccine cards. They’re the wrong size.
The Atlantic’s Amanda Mull explains: “When I got my first shot, in late February, I sat in the mandatory waiting area, holding my new card in one hand and my wallet in the other, trying to understand why the two objects weren’t compatible.”
She didn’t get very far with the CDC, but Chelsea Cirruzzo, a public-health reporter at U.S. News & World Report who has been tweeting about the vaccine cards, suggested that “someone just printed out a bunch of cards that are easy to write your name and vaccine brand on, without thinking about wallets.”
The evidence does fit the nobody-really-gave-it-any-thought argument. The template was available to the public on some state government websites when the vaccine was approved and can still be found on Florida’s, Ms. Mull notes. “Try to imagine governments freely distributing their templates for driver’s licenses, passports, or other documents intended to certify a particular identity or status.” The FBI, we understand, frowns upon this sort of thing.
Well, there you have it, America. When the card fits in a wallet, the vaccine problem will go away. Just remember where you read it, not where we read it.
Being a good neighbor
My neighbor’s house got burglarized recently.
They were on vacation, and so the thieves were able to take their time inside late at night. The neighborhood wasn’t aware anything was going on until they’d left, with a lot of jewelry and other valuables. As of this writing, they haven’t been caught.
I’m not the kind of person who needs to be close with my neighbors. Some people want a cohesive bunch that does stuff together. That’s not me. I’m fine just being collegial. I wave, I say hi, I let them know if they left a garage door open. I keep to myself and hope they do the same. If we’d been suspicious about a burglary, though, I definitely would have called 911, but all of us were asleep.
I get along with the family that lives there. We occasionally chat about nothing in particular when getting the mail or rolling out the recycling can. I’m pretty sure they don’t vote the way I do, or have the same religious beliefs, but that’s life. I mean, isn’t that the point of America, or even civilization? That we’re all supposed to get along, accept our differences, and work together for the common good? In spite of politicians trying to push the country as an us-against-them narrative, the bottom line is that .
I and the rest of the block offered them any help we could provide in the aftermath. A burglary isn’t as serious as a house fire or medical emergency, but it’s still something that you want to assist with if possible.
A crisis, minor or major, is a good time to step back from the inflammatory rhetoric that television’s talking heads and pundits push. The majority of us live in peace with our neighbors, want to help them if needed, and don’t take any joy in their predicaments – regardless of what we each might believe. After all, next time it could be me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My neighbor’s house got burglarized recently.
They were on vacation, and so the thieves were able to take their time inside late at night. The neighborhood wasn’t aware anything was going on until they’d left, with a lot of jewelry and other valuables. As of this writing, they haven’t been caught.
I’m not the kind of person who needs to be close with my neighbors. Some people want a cohesive bunch that does stuff together. That’s not me. I’m fine just being collegial. I wave, I say hi, I let them know if they left a garage door open. I keep to myself and hope they do the same. If we’d been suspicious about a burglary, though, I definitely would have called 911, but all of us were asleep.
I get along with the family that lives there. We occasionally chat about nothing in particular when getting the mail or rolling out the recycling can. I’m pretty sure they don’t vote the way I do, or have the same religious beliefs, but that’s life. I mean, isn’t that the point of America, or even civilization? That we’re all supposed to get along, accept our differences, and work together for the common good? In spite of politicians trying to push the country as an us-against-them narrative, the bottom line is that .
I and the rest of the block offered them any help we could provide in the aftermath. A burglary isn’t as serious as a house fire or medical emergency, but it’s still something that you want to assist with if possible.
A crisis, minor or major, is a good time to step back from the inflammatory rhetoric that television’s talking heads and pundits push. The majority of us live in peace with our neighbors, want to help them if needed, and don’t take any joy in their predicaments – regardless of what we each might believe. After all, next time it could be me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My neighbor’s house got burglarized recently.
They were on vacation, and so the thieves were able to take their time inside late at night. The neighborhood wasn’t aware anything was going on until they’d left, with a lot of jewelry and other valuables. As of this writing, they haven’t been caught.
I’m not the kind of person who needs to be close with my neighbors. Some people want a cohesive bunch that does stuff together. That’s not me. I’m fine just being collegial. I wave, I say hi, I let them know if they left a garage door open. I keep to myself and hope they do the same. If we’d been suspicious about a burglary, though, I definitely would have called 911, but all of us were asleep.
I get along with the family that lives there. We occasionally chat about nothing in particular when getting the mail or rolling out the recycling can. I’m pretty sure they don’t vote the way I do, or have the same religious beliefs, but that’s life. I mean, isn’t that the point of America, or even civilization? That we’re all supposed to get along, accept our differences, and work together for the common good? In spite of politicians trying to push the country as an us-against-them narrative, the bottom line is that .
I and the rest of the block offered them any help we could provide in the aftermath. A burglary isn’t as serious as a house fire or medical emergency, but it’s still something that you want to assist with if possible.
A crisis, minor or major, is a good time to step back from the inflammatory rhetoric that television’s talking heads and pundits push. The majority of us live in peace with our neighbors, want to help them if needed, and don’t take any joy in their predicaments – regardless of what we each might believe. After all, next time it could be me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Why aren’t more women doctors in the top-paying specialties?
Women compose only 6% of orthopedic surgeons, 8% of interventional cardiologists, 10% of urologists, 17% of plastic surgeons, and 18% of otolaryngologists, according to the 2020 Association of American Medical Colleges Physician Specialty Data Report.
Plastic surgeons earn an average of $526,000 annually, which is the highest-paying specialty. Otolaryngologists earn an average of $417,000 annually, and urologists earn $427,000, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Yet, far more women are practicing in specialties that pay less. Women are the majority in pediatrics (64%), ob.gyn. (59%), internal medicine (53%), and endocrinology (51%), the AAMC data show. The exception is dermatology, which pays well and in which 51% are women. The annual average pay is $394,000.
Why are so many women avoiding the top-paying specialties?
Several physician researchers and leaders in the top-paying specialties point to four main factors: Women are attracted to specialties that have more women in faculty and leadership positions, women prioritize work-life balance over pay, women residents may be deterred from the high-paying specialties because of gender discrimination and sexual harassment, and the longer training periods for surgical specialties may be a deterrent for women who want to have children.
Lack of women leaders
The specialties with the most women tend to have the highest proportion of women in leadership positions. For example, obstetrics and gynecology had the highest proportion of women department chairs (24.1%) and vice chairs (38.8). Pediatrics had the highest proportion of women division directors (31.5%) and residency program directors (64.6%), a study shows.
Surgical specialties, on the other hand, may have a harder time attracting female residents, possibly because of a lack of women in leadership positions. A recent study that examined gender differences in attitudes toward surgery training found that women would be more likely to go into surgery if there were more surgical faculty and residents of their same gender.
An analysis of orthopedic residency programs shows that more trainees were drawn to programs that had more female faculty members, including associate professors and women in leadership positions.
Terri Malcolm, MD, a board-certified ob.gyn. and CEO/founder of Master Physician Leaders, said women need to consider whether they want to be a trailblazer in a specialty that has fewer women. “What support systems are in place to accommodate your goals, whether it’s career advancement, having a family, or mentorship? Where can you show up as your whole self and be supported in that?”
Being the only woman in a residency program can be a challenge, said Dr. Malcolm. If the residents and attendings are predominantly men, for example, they may not think about creating a call schedule that takes into account maternity leave or the fact that women tend to be caretakers for their children and parents.
The study of gender differences toward surgery training shows that 75% of women, in comparison with 46% of men, would be more willing to enter surgery if maternity leave and childcare were made available to female residents and attending physicians.
Women want work-life balance
Although both men and women want families, women still shoulder more family and childcare responsibilities. That may explain why women physicians ranked work-life balance first and compensation second in the Medscape Women Physicians 2020 Report: The Issues They Care About.
“My physician colleagues have been and are supportive of intellectual abilities, but I feel they don’t fully understand the uneven distribution of childcare issues on women,” a woman dermatologist commented.
Women may want to work fewer hours or have a more flexible schedule to take care of children. “I can count on one hand the number of women who have a part-time job in orthopedics. It’s very rare, and working part time absolutely is a barrier for someone who wants to be a surgeon,” said Julie Samora, MD, PhD, a researcher and pediatric hand surgeon at Nationwide Children’s Hospital, in Columbus, Ohio. She is also a spokesperson for the American Association of Orthopedic Surgeons.
Preeti Malani, MD, a professor of medicine who specializes in infectious diseases at the University of Michigan, chose to work full-time in academia while raising two children with her husband. In a decade, she rose through the ranks to full professor. “I took the advice of a woman who wanted to recruit me to have a full-time position with maximum flexibility rather than work part time, often for more hours and less pay. I also have tried to build my career so I was not doing all clinical work.”
Her husband is a surgeon at the University of Michigan. His schedule was not flexible, and he was unable to take on family responsibilities, said Dr. Malani. “I knew someone had to be able to grab the kids from daycare or pick them up at school if they were sick.” She also took work home and worked weekends.
Young women physicians in particular are thinking about combining parenting with work – in the Medscape report, that issue ranked third among the issues women care about. Seeing other women doctors navigate that in their particular specialty can have a positive impact.
“When I chose adolescent medicine, I remember working with a doctor in this field who talked about how much she enjoyed raising her kids even as teenagers and how much she was enjoying them as young adults. She seemed so balanced and happy in her family, and it gave me a nice feeling about the field,” said Nancy Dodson, MD, MPH, a pediatrician specializing in adolescent medicine at Pediatrics on Hudson in New York.
Rachel Zhuk, MD, a reproductive psychiatrist in New York, took a break after medical school to spend time with her newborn son. She met a woman who was also a young parent and a psychiatrist. “We were both figuring out parenting together – it was like looking into my future.” That friendship and her desire to have more time with patients influenced her decision to pursue psychiatry instead of internal medicine.
Discrimination and harassment influence specialty choice
Women doctors in the top-paying surgical and other specialties have reported experiencing more discrimination and harassment than men.
Of 927 orthopedic surgeons who responded to an AAOS survey, 66% said they experienced gender discrimination, bullying, sexual harassment, or harassment in the health care workplace. More than twice as many women (81%) experienced these behaviors as men (35%).
“This study shows that women in orthopedic surgery disproportionately experience these negative behaviors, and only a handful of institutions in the United States provide any type of training to prevent them,” said Dr. Samora, the lead author of the AAOS report.
Radiology is another male-dominated field – women represent 26% of all radiologists, the 2020 AAMC specialty report shows. A systematic review shows that 40% of women radiologists experienced gender discrimination at work, compared with 1% of men, and that 47% of women experienced sexual harassment.
Female trainees in surgery have also reported disproportionate rates of discrimination and harassment. Female general surgical residents have experienced more gender discrimination than male residents (65.1% vs. 10.0%) and more sexual harassment than male residents (19.9% vs. 3.9), a national survey indicates.
When medical students are exposed to these behaviors through personal experience, witnessing, or hearing about them, it can affect which specialty they choose. A survey of fourth-year medical students shows that far more women than men reported that exposure to gender discrimination and sexual harassment influenced their specialty choices (45.3% vs. 16.4%) and residency rankings (25.3% vs. 10.9%). Women who chose general surgery were the most likely to experience gender discrimination and sexual harassment during residency selection; women who chose psychiatry were the least likely to experience such behaviors, the report shows.
“If young trainees witness such behaviors in a specific field, they would naturally migrate toward a different specialty,” said Dr. Samora.
Trainees can also be put off by residency directors asking them inappropriate questions. Of nearly 500 female orthopedic surgeons surveyed, 62% reported that they were asked inappropriate questions during their residency interviews. “Inappropriate questions and comments directed toward women during residency interviews are clearly not conducive to women entering the field,” the authors stated. They found that little changed during the study period from 1971 to 2015.
The most frequent inappropriate questions concerned whether the prospective residents would be getting pregnant or raising children during residency and their marital status. One female orthopedic surgeon reported: “I was asked if I have children and was told that it would be too difficult to complete an orthopedic residency with children.”
The interviewers also made frequent comments about the inferiority of women to men. For example, “I was told by one program interviewer that ‘I don’t have a bias about women in medicine, I have a bias about women in orthopedic surgery,’ ” another female orthopedic surgeon commented.
Longer training
Residency training for the top-paying surgical specialties, including orthopedic surgery, plastic surgery, and otolaryngology, lasts 5-6 years. This compares with 3-4 years for the lower-paying specialties, such as pediatrics, internal medicine, and ob.gyn., according to data from the American Medical Association.
Women doctors are in their prime childbearing years during residency. Women who want to start a family will consider whether they want to get pregnant during residency or wait until they finish their training, said Dr. Malcolm.
The vast majority (84%) of 190 female orthopedic surgery trainees who responded to a survey indicated that they did not have children or were pregnant during residency. Nearly half (48%) reported that they had postponed having children because they were in training.
“The longer training is definitely a concerning issue for women of childbearing age. Many professional women are waiting to have children, for multiple reasons, but one major fear is the stigma due to taking time off from work obligations. There is a risk of irritating your peers because they may have to take on more work and cover more calls for you during your absence,” said Dr. Samora.
That fear is not unfounded. At least half of the 190 female orthopedic residents reported that they encountered bias against becoming pregnant during training from both coresidents (60%) and attendings (50%), according to the study.
Another recent survey suggests that pregnant surgical residents face several barriers during their training, including a lack of salary for extended family leave, resentment from fellow residents who need to cover for them during maternity leave, and a lack of formal lactation policies.
A few policy changes by national board organizations, including those in the surgical specialties, may make life a little easier for female trainees to have children, suggested Dr. Samora.
Residents and fellows are now allowed a minimum of 6 weeks away for medical leave or caregiving once during training, without having to use vacation or sick leave and without having to extend their training, the American Board of Medical Specialties has announced.
In addition, the American Board of Orthopaedic Surgery and the American Board of Surgery have enacted policies that allow lactating women to take a break to pump during their board exams.
A version of this article first appeared on Medscape.com.
Women compose only 6% of orthopedic surgeons, 8% of interventional cardiologists, 10% of urologists, 17% of plastic surgeons, and 18% of otolaryngologists, according to the 2020 Association of American Medical Colleges Physician Specialty Data Report.
Plastic surgeons earn an average of $526,000 annually, which is the highest-paying specialty. Otolaryngologists earn an average of $417,000 annually, and urologists earn $427,000, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Yet, far more women are practicing in specialties that pay less. Women are the majority in pediatrics (64%), ob.gyn. (59%), internal medicine (53%), and endocrinology (51%), the AAMC data show. The exception is dermatology, which pays well and in which 51% are women. The annual average pay is $394,000.
Why are so many women avoiding the top-paying specialties?
Several physician researchers and leaders in the top-paying specialties point to four main factors: Women are attracted to specialties that have more women in faculty and leadership positions, women prioritize work-life balance over pay, women residents may be deterred from the high-paying specialties because of gender discrimination and sexual harassment, and the longer training periods for surgical specialties may be a deterrent for women who want to have children.
Lack of women leaders
The specialties with the most women tend to have the highest proportion of women in leadership positions. For example, obstetrics and gynecology had the highest proportion of women department chairs (24.1%) and vice chairs (38.8). Pediatrics had the highest proportion of women division directors (31.5%) and residency program directors (64.6%), a study shows.
Surgical specialties, on the other hand, may have a harder time attracting female residents, possibly because of a lack of women in leadership positions. A recent study that examined gender differences in attitudes toward surgery training found that women would be more likely to go into surgery if there were more surgical faculty and residents of their same gender.
An analysis of orthopedic residency programs shows that more trainees were drawn to programs that had more female faculty members, including associate professors and women in leadership positions.
Terri Malcolm, MD, a board-certified ob.gyn. and CEO/founder of Master Physician Leaders, said women need to consider whether they want to be a trailblazer in a specialty that has fewer women. “What support systems are in place to accommodate your goals, whether it’s career advancement, having a family, or mentorship? Where can you show up as your whole self and be supported in that?”
Being the only woman in a residency program can be a challenge, said Dr. Malcolm. If the residents and attendings are predominantly men, for example, they may not think about creating a call schedule that takes into account maternity leave or the fact that women tend to be caretakers for their children and parents.
The study of gender differences toward surgery training shows that 75% of women, in comparison with 46% of men, would be more willing to enter surgery if maternity leave and childcare were made available to female residents and attending physicians.
Women want work-life balance
Although both men and women want families, women still shoulder more family and childcare responsibilities. That may explain why women physicians ranked work-life balance first and compensation second in the Medscape Women Physicians 2020 Report: The Issues They Care About.
“My physician colleagues have been and are supportive of intellectual abilities, but I feel they don’t fully understand the uneven distribution of childcare issues on women,” a woman dermatologist commented.
Women may want to work fewer hours or have a more flexible schedule to take care of children. “I can count on one hand the number of women who have a part-time job in orthopedics. It’s very rare, and working part time absolutely is a barrier for someone who wants to be a surgeon,” said Julie Samora, MD, PhD, a researcher and pediatric hand surgeon at Nationwide Children’s Hospital, in Columbus, Ohio. She is also a spokesperson for the American Association of Orthopedic Surgeons.
Preeti Malani, MD, a professor of medicine who specializes in infectious diseases at the University of Michigan, chose to work full-time in academia while raising two children with her husband. In a decade, she rose through the ranks to full professor. “I took the advice of a woman who wanted to recruit me to have a full-time position with maximum flexibility rather than work part time, often for more hours and less pay. I also have tried to build my career so I was not doing all clinical work.”
Her husband is a surgeon at the University of Michigan. His schedule was not flexible, and he was unable to take on family responsibilities, said Dr. Malani. “I knew someone had to be able to grab the kids from daycare or pick them up at school if they were sick.” She also took work home and worked weekends.
Young women physicians in particular are thinking about combining parenting with work – in the Medscape report, that issue ranked third among the issues women care about. Seeing other women doctors navigate that in their particular specialty can have a positive impact.
“When I chose adolescent medicine, I remember working with a doctor in this field who talked about how much she enjoyed raising her kids even as teenagers and how much she was enjoying them as young adults. She seemed so balanced and happy in her family, and it gave me a nice feeling about the field,” said Nancy Dodson, MD, MPH, a pediatrician specializing in adolescent medicine at Pediatrics on Hudson in New York.
Rachel Zhuk, MD, a reproductive psychiatrist in New York, took a break after medical school to spend time with her newborn son. She met a woman who was also a young parent and a psychiatrist. “We were both figuring out parenting together – it was like looking into my future.” That friendship and her desire to have more time with patients influenced her decision to pursue psychiatry instead of internal medicine.
Discrimination and harassment influence specialty choice
Women doctors in the top-paying surgical and other specialties have reported experiencing more discrimination and harassment than men.
Of 927 orthopedic surgeons who responded to an AAOS survey, 66% said they experienced gender discrimination, bullying, sexual harassment, or harassment in the health care workplace. More than twice as many women (81%) experienced these behaviors as men (35%).
“This study shows that women in orthopedic surgery disproportionately experience these negative behaviors, and only a handful of institutions in the United States provide any type of training to prevent them,” said Dr. Samora, the lead author of the AAOS report.
Radiology is another male-dominated field – women represent 26% of all radiologists, the 2020 AAMC specialty report shows. A systematic review shows that 40% of women radiologists experienced gender discrimination at work, compared with 1% of men, and that 47% of women experienced sexual harassment.
Female trainees in surgery have also reported disproportionate rates of discrimination and harassment. Female general surgical residents have experienced more gender discrimination than male residents (65.1% vs. 10.0%) and more sexual harassment than male residents (19.9% vs. 3.9), a national survey indicates.
When medical students are exposed to these behaviors through personal experience, witnessing, or hearing about them, it can affect which specialty they choose. A survey of fourth-year medical students shows that far more women than men reported that exposure to gender discrimination and sexual harassment influenced their specialty choices (45.3% vs. 16.4%) and residency rankings (25.3% vs. 10.9%). Women who chose general surgery were the most likely to experience gender discrimination and sexual harassment during residency selection; women who chose psychiatry were the least likely to experience such behaviors, the report shows.
“If young trainees witness such behaviors in a specific field, they would naturally migrate toward a different specialty,” said Dr. Samora.
Trainees can also be put off by residency directors asking them inappropriate questions. Of nearly 500 female orthopedic surgeons surveyed, 62% reported that they were asked inappropriate questions during their residency interviews. “Inappropriate questions and comments directed toward women during residency interviews are clearly not conducive to women entering the field,” the authors stated. They found that little changed during the study period from 1971 to 2015.
The most frequent inappropriate questions concerned whether the prospective residents would be getting pregnant or raising children during residency and their marital status. One female orthopedic surgeon reported: “I was asked if I have children and was told that it would be too difficult to complete an orthopedic residency with children.”
The interviewers also made frequent comments about the inferiority of women to men. For example, “I was told by one program interviewer that ‘I don’t have a bias about women in medicine, I have a bias about women in orthopedic surgery,’ ” another female orthopedic surgeon commented.
Longer training
Residency training for the top-paying surgical specialties, including orthopedic surgery, plastic surgery, and otolaryngology, lasts 5-6 years. This compares with 3-4 years for the lower-paying specialties, such as pediatrics, internal medicine, and ob.gyn., according to data from the American Medical Association.
Women doctors are in their prime childbearing years during residency. Women who want to start a family will consider whether they want to get pregnant during residency or wait until they finish their training, said Dr. Malcolm.
The vast majority (84%) of 190 female orthopedic surgery trainees who responded to a survey indicated that they did not have children or were pregnant during residency. Nearly half (48%) reported that they had postponed having children because they were in training.
“The longer training is definitely a concerning issue for women of childbearing age. Many professional women are waiting to have children, for multiple reasons, but one major fear is the stigma due to taking time off from work obligations. There is a risk of irritating your peers because they may have to take on more work and cover more calls for you during your absence,” said Dr. Samora.
That fear is not unfounded. At least half of the 190 female orthopedic residents reported that they encountered bias against becoming pregnant during training from both coresidents (60%) and attendings (50%), according to the study.
Another recent survey suggests that pregnant surgical residents face several barriers during their training, including a lack of salary for extended family leave, resentment from fellow residents who need to cover for them during maternity leave, and a lack of formal lactation policies.
A few policy changes by national board organizations, including those in the surgical specialties, may make life a little easier for female trainees to have children, suggested Dr. Samora.
Residents and fellows are now allowed a minimum of 6 weeks away for medical leave or caregiving once during training, without having to use vacation or sick leave and without having to extend their training, the American Board of Medical Specialties has announced.
In addition, the American Board of Orthopaedic Surgery and the American Board of Surgery have enacted policies that allow lactating women to take a break to pump during their board exams.
A version of this article first appeared on Medscape.com.
Women compose only 6% of orthopedic surgeons, 8% of interventional cardiologists, 10% of urologists, 17% of plastic surgeons, and 18% of otolaryngologists, according to the 2020 Association of American Medical Colleges Physician Specialty Data Report.
Plastic surgeons earn an average of $526,000 annually, which is the highest-paying specialty. Otolaryngologists earn an average of $417,000 annually, and urologists earn $427,000, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Yet, far more women are practicing in specialties that pay less. Women are the majority in pediatrics (64%), ob.gyn. (59%), internal medicine (53%), and endocrinology (51%), the AAMC data show. The exception is dermatology, which pays well and in which 51% are women. The annual average pay is $394,000.
Why are so many women avoiding the top-paying specialties?
Several physician researchers and leaders in the top-paying specialties point to four main factors: Women are attracted to specialties that have more women in faculty and leadership positions, women prioritize work-life balance over pay, women residents may be deterred from the high-paying specialties because of gender discrimination and sexual harassment, and the longer training periods for surgical specialties may be a deterrent for women who want to have children.
Lack of women leaders
The specialties with the most women tend to have the highest proportion of women in leadership positions. For example, obstetrics and gynecology had the highest proportion of women department chairs (24.1%) and vice chairs (38.8). Pediatrics had the highest proportion of women division directors (31.5%) and residency program directors (64.6%), a study shows.
Surgical specialties, on the other hand, may have a harder time attracting female residents, possibly because of a lack of women in leadership positions. A recent study that examined gender differences in attitudes toward surgery training found that women would be more likely to go into surgery if there were more surgical faculty and residents of their same gender.
An analysis of orthopedic residency programs shows that more trainees were drawn to programs that had more female faculty members, including associate professors and women in leadership positions.
Terri Malcolm, MD, a board-certified ob.gyn. and CEO/founder of Master Physician Leaders, said women need to consider whether they want to be a trailblazer in a specialty that has fewer women. “What support systems are in place to accommodate your goals, whether it’s career advancement, having a family, or mentorship? Where can you show up as your whole self and be supported in that?”
Being the only woman in a residency program can be a challenge, said Dr. Malcolm. If the residents and attendings are predominantly men, for example, they may not think about creating a call schedule that takes into account maternity leave or the fact that women tend to be caretakers for their children and parents.
The study of gender differences toward surgery training shows that 75% of women, in comparison with 46% of men, would be more willing to enter surgery if maternity leave and childcare were made available to female residents and attending physicians.
Women want work-life balance
Although both men and women want families, women still shoulder more family and childcare responsibilities. That may explain why women physicians ranked work-life balance first and compensation second in the Medscape Women Physicians 2020 Report: The Issues They Care About.
“My physician colleagues have been and are supportive of intellectual abilities, but I feel they don’t fully understand the uneven distribution of childcare issues on women,” a woman dermatologist commented.
Women may want to work fewer hours or have a more flexible schedule to take care of children. “I can count on one hand the number of women who have a part-time job in orthopedics. It’s very rare, and working part time absolutely is a barrier for someone who wants to be a surgeon,” said Julie Samora, MD, PhD, a researcher and pediatric hand surgeon at Nationwide Children’s Hospital, in Columbus, Ohio. She is also a spokesperson for the American Association of Orthopedic Surgeons.
Preeti Malani, MD, a professor of medicine who specializes in infectious diseases at the University of Michigan, chose to work full-time in academia while raising two children with her husband. In a decade, she rose through the ranks to full professor. “I took the advice of a woman who wanted to recruit me to have a full-time position with maximum flexibility rather than work part time, often for more hours and less pay. I also have tried to build my career so I was not doing all clinical work.”
Her husband is a surgeon at the University of Michigan. His schedule was not flexible, and he was unable to take on family responsibilities, said Dr. Malani. “I knew someone had to be able to grab the kids from daycare or pick them up at school if they were sick.” She also took work home and worked weekends.
Young women physicians in particular are thinking about combining parenting with work – in the Medscape report, that issue ranked third among the issues women care about. Seeing other women doctors navigate that in their particular specialty can have a positive impact.
“When I chose adolescent medicine, I remember working with a doctor in this field who talked about how much she enjoyed raising her kids even as teenagers and how much she was enjoying them as young adults. She seemed so balanced and happy in her family, and it gave me a nice feeling about the field,” said Nancy Dodson, MD, MPH, a pediatrician specializing in adolescent medicine at Pediatrics on Hudson in New York.
Rachel Zhuk, MD, a reproductive psychiatrist in New York, took a break after medical school to spend time with her newborn son. She met a woman who was also a young parent and a psychiatrist. “We were both figuring out parenting together – it was like looking into my future.” That friendship and her desire to have more time with patients influenced her decision to pursue psychiatry instead of internal medicine.
Discrimination and harassment influence specialty choice
Women doctors in the top-paying surgical and other specialties have reported experiencing more discrimination and harassment than men.
Of 927 orthopedic surgeons who responded to an AAOS survey, 66% said they experienced gender discrimination, bullying, sexual harassment, or harassment in the health care workplace. More than twice as many women (81%) experienced these behaviors as men (35%).
“This study shows that women in orthopedic surgery disproportionately experience these negative behaviors, and only a handful of institutions in the United States provide any type of training to prevent them,” said Dr. Samora, the lead author of the AAOS report.
Radiology is another male-dominated field – women represent 26% of all radiologists, the 2020 AAMC specialty report shows. A systematic review shows that 40% of women radiologists experienced gender discrimination at work, compared with 1% of men, and that 47% of women experienced sexual harassment.
Female trainees in surgery have also reported disproportionate rates of discrimination and harassment. Female general surgical residents have experienced more gender discrimination than male residents (65.1% vs. 10.0%) and more sexual harassment than male residents (19.9% vs. 3.9), a national survey indicates.
When medical students are exposed to these behaviors through personal experience, witnessing, or hearing about them, it can affect which specialty they choose. A survey of fourth-year medical students shows that far more women than men reported that exposure to gender discrimination and sexual harassment influenced their specialty choices (45.3% vs. 16.4%) and residency rankings (25.3% vs. 10.9%). Women who chose general surgery were the most likely to experience gender discrimination and sexual harassment during residency selection; women who chose psychiatry were the least likely to experience such behaviors, the report shows.
“If young trainees witness such behaviors in a specific field, they would naturally migrate toward a different specialty,” said Dr. Samora.
Trainees can also be put off by residency directors asking them inappropriate questions. Of nearly 500 female orthopedic surgeons surveyed, 62% reported that they were asked inappropriate questions during their residency interviews. “Inappropriate questions and comments directed toward women during residency interviews are clearly not conducive to women entering the field,” the authors stated. They found that little changed during the study period from 1971 to 2015.
The most frequent inappropriate questions concerned whether the prospective residents would be getting pregnant or raising children during residency and their marital status. One female orthopedic surgeon reported: “I was asked if I have children and was told that it would be too difficult to complete an orthopedic residency with children.”
The interviewers also made frequent comments about the inferiority of women to men. For example, “I was told by one program interviewer that ‘I don’t have a bias about women in medicine, I have a bias about women in orthopedic surgery,’ ” another female orthopedic surgeon commented.
Longer training
Residency training for the top-paying surgical specialties, including orthopedic surgery, plastic surgery, and otolaryngology, lasts 5-6 years. This compares with 3-4 years for the lower-paying specialties, such as pediatrics, internal medicine, and ob.gyn., according to data from the American Medical Association.
Women doctors are in their prime childbearing years during residency. Women who want to start a family will consider whether they want to get pregnant during residency or wait until they finish their training, said Dr. Malcolm.
The vast majority (84%) of 190 female orthopedic surgery trainees who responded to a survey indicated that they did not have children or were pregnant during residency. Nearly half (48%) reported that they had postponed having children because they were in training.
“The longer training is definitely a concerning issue for women of childbearing age. Many professional women are waiting to have children, for multiple reasons, but one major fear is the stigma due to taking time off from work obligations. There is a risk of irritating your peers because they may have to take on more work and cover more calls for you during your absence,” said Dr. Samora.
That fear is not unfounded. At least half of the 190 female orthopedic residents reported that they encountered bias against becoming pregnant during training from both coresidents (60%) and attendings (50%), according to the study.
Another recent survey suggests that pregnant surgical residents face several barriers during their training, including a lack of salary for extended family leave, resentment from fellow residents who need to cover for them during maternity leave, and a lack of formal lactation policies.
A few policy changes by national board organizations, including those in the surgical specialties, may make life a little easier for female trainees to have children, suggested Dr. Samora.
Residents and fellows are now allowed a minimum of 6 weeks away for medical leave or caregiving once during training, without having to use vacation or sick leave and without having to extend their training, the American Board of Medical Specialties has announced.
In addition, the American Board of Orthopaedic Surgery and the American Board of Surgery have enacted policies that allow lactating women to take a break to pump during their board exams.
A version of this article first appeared on Medscape.com.
Flavonoids dietary ‘powerhouses’ for cognitive decline prevention
, new research shows.
Among the different types of flavonoids, flavones (found in some spices and yellow or orange fruits and vegetables) and anthocyanins (found in blueberries, blackberries, and cherries) seem to have most protective effect, the researchers report.
“There is mounting evidence suggesting flavonoids are powerhouses when it comes to preventing your thinking skills from declining as you get older,” study investigator Walter Willett, MD, DrPH, Harvard University, Boston, said in a statement.
“Our results are exciting because they show that making simple changes to your diet could help prevent cognitive decline,” said Dr. Willett.
The study was published online July 28 in the journal Neurology.
Antioxidant punch
Flavonoids, naturally occurring phytochemicals found in plants, are strong antioxidants. Considering the likely role of oxidative stress in age-related cognitive decline, flavonoids have been proposed as a potentially important preventive.
For the study, Dr. Willett and colleagues prospectively examined associations between long-term dietary flavonoids (flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, polymeric flavonoids, and proanthocyanidins) and subjective cognitive decline in 49,493 women from the Nurses’ Health Study (1984-2006) and 27,842 men from the Health Professionals Follow-up Study (1986-2002).
Those in the highest quintile of flavonoid consumption consumed about 600 mg daily on average while those in the lowest quintile got only about 150 mg daily.
After adjusting for age, total energy intake, major nondietary factors, and specific dietary factors, a higher intake of total flavonoids was associated with lower likelihood of self-reported subjective cognitive decline during follow up.
Individuals in the highest quintile of daily consumption had about a 20% lower risk of subjective cognitive decline relative to peers in the lowest quintile (pooled multivariable-adjusted odds ratio: 0.81; 95% confidence interval, 0.76-0.89).
The strongest protective associations were found for flavones (OR, 0.62; 95% confidence interval, 0.57-0.68), flavanones (OR, 0.64; 95% CI, 0.58-0.68), and anthocyanins (OR, 0.76; 95% CI, 0.72-0.84) (P trend < .0001 for all groups).
“The people in our study who did the best over time ate an average of at least half a serving per day of foods like orange juice, oranges, peppers, celery, grapefruits, grapefruit juice, apples, and pears,” Dr. Willett said.
“While it is possible other phytochemicals are at work here, a colorful diet rich in flavonoids – and specifically flavones and anthocyanins – seems to be a good bet for promoting long-term brain health,” he added.
A limitation of the study is that participants reported on their diets and may not recall perfectly what they ate or how much.
Healthy diet best bet for brain health
Reached for comment, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, said this study “adds to our understanding of which elements of a healthy diet may be important in reducing dementia risk; flavonols may be one of those elements.”
“However, at this point, people should not put too much stock in specific nutrients – including subsets of flavonols – for reducing dementia risk until more research is done. Rather, they should focus on eating an overall healthy diet,” he said.
“It would be wonderful if a particular food or supplement could delay or prevent Alzheimer’s disease, but we do not have scientific evidence to support such claims. Randomized controlled clinical trials are necessary to evaluate whether any food or supplement has a scientifically proven beneficial effect,” Dr. Weber added.
For now, the Alzheimer’s Association “encourages everyone to eat a healthy and balanced diet as a way to help reduce the risk of cognitive decline,” Dr. Weber said.
“With more than 6 million Americans living with Alzheimer’s disease and other dementia today, there is a pressing need to test the effectiveness of a healthy lifestyle regimen to reduce risk of cognitive decline in a large and diverse population,” he added.
The Alzheimer’s Association has launched a 2-year clinical trial, called the U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER), to do just that.
“While we research that definitive lifestyle ‘recipe,’ there are things we can do today that may decrease our risk of cognitive decline as we age. Eating a heart-healthy diet, exercising regularly, and staying cognitively engaged are just a few,” Dr. Weber added.
Also weighing in, Taylor Wallace, PhD, adjunct professor, department of nutrition and food studies, George Mason University, Fairfax, Va., said the study results are not surprising.
“Scientific data on the ability of flavonoids to prevent age-related chronic diseases, including cognitive decline, has accumulated immensely over the last decade. This epidemiological study reinforces findings from smaller shorter-duration clinical trials and mechanistic studies,” said Dr. Wallace, who was not involved in the study.
“Flavonoids show great potential in reducing inflammation and oxidative stress in the body. They are also vasodilators that help improve blood flow, which is important for the cardiovascular and cerebrovascular systems,” he noted.
“Typically, foods rich in flavonoids are also nutrient-dense in vitamins, minerals, and dietary fiber (eg, fruits and vegetables). Anthocyanins in blueberries have long been known to prevent cognitive decline with age,” Dr. Wallace said.
Dr. Wallace was part of a 14-member panel of nutrition scientists who recently reviewed available evidence around fruit and vegetable intake and health.
“Our findings are consistent with this study in regard to cognitive decline and other disease states. Cruciferous vegetables, dark-green leafy vegetables, citrus fruits, and dark-colored berries seem to have superior effects on health promotion and disease prevention in general,” said Dr. Wallace.
This work was supported by grants from the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Weber has no relevant disclosures. Dr. Wallace is principal and chief executive officer of the Think Healthy Group; editor of the Journal of Dietary Supplements; and deputy editor-in-chief of the Journal of the American College of Nutrition.
A version of this article first appeared on Medscape.com.
, new research shows.
Among the different types of flavonoids, flavones (found in some spices and yellow or orange fruits and vegetables) and anthocyanins (found in blueberries, blackberries, and cherries) seem to have most protective effect, the researchers report.
“There is mounting evidence suggesting flavonoids are powerhouses when it comes to preventing your thinking skills from declining as you get older,” study investigator Walter Willett, MD, DrPH, Harvard University, Boston, said in a statement.
“Our results are exciting because they show that making simple changes to your diet could help prevent cognitive decline,” said Dr. Willett.
The study was published online July 28 in the journal Neurology.
Antioxidant punch
Flavonoids, naturally occurring phytochemicals found in plants, are strong antioxidants. Considering the likely role of oxidative stress in age-related cognitive decline, flavonoids have been proposed as a potentially important preventive.
For the study, Dr. Willett and colleagues prospectively examined associations between long-term dietary flavonoids (flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, polymeric flavonoids, and proanthocyanidins) and subjective cognitive decline in 49,493 women from the Nurses’ Health Study (1984-2006) and 27,842 men from the Health Professionals Follow-up Study (1986-2002).
Those in the highest quintile of flavonoid consumption consumed about 600 mg daily on average while those in the lowest quintile got only about 150 mg daily.
After adjusting for age, total energy intake, major nondietary factors, and specific dietary factors, a higher intake of total flavonoids was associated with lower likelihood of self-reported subjective cognitive decline during follow up.
Individuals in the highest quintile of daily consumption had about a 20% lower risk of subjective cognitive decline relative to peers in the lowest quintile (pooled multivariable-adjusted odds ratio: 0.81; 95% confidence interval, 0.76-0.89).
The strongest protective associations were found for flavones (OR, 0.62; 95% confidence interval, 0.57-0.68), flavanones (OR, 0.64; 95% CI, 0.58-0.68), and anthocyanins (OR, 0.76; 95% CI, 0.72-0.84) (P trend < .0001 for all groups).
“The people in our study who did the best over time ate an average of at least half a serving per day of foods like orange juice, oranges, peppers, celery, grapefruits, grapefruit juice, apples, and pears,” Dr. Willett said.
“While it is possible other phytochemicals are at work here, a colorful diet rich in flavonoids – and specifically flavones and anthocyanins – seems to be a good bet for promoting long-term brain health,” he added.
A limitation of the study is that participants reported on their diets and may not recall perfectly what they ate or how much.
Healthy diet best bet for brain health
Reached for comment, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, said this study “adds to our understanding of which elements of a healthy diet may be important in reducing dementia risk; flavonols may be one of those elements.”
“However, at this point, people should not put too much stock in specific nutrients – including subsets of flavonols – for reducing dementia risk until more research is done. Rather, they should focus on eating an overall healthy diet,” he said.
“It would be wonderful if a particular food or supplement could delay or prevent Alzheimer’s disease, but we do not have scientific evidence to support such claims. Randomized controlled clinical trials are necessary to evaluate whether any food or supplement has a scientifically proven beneficial effect,” Dr. Weber added.
For now, the Alzheimer’s Association “encourages everyone to eat a healthy and balanced diet as a way to help reduce the risk of cognitive decline,” Dr. Weber said.
“With more than 6 million Americans living with Alzheimer’s disease and other dementia today, there is a pressing need to test the effectiveness of a healthy lifestyle regimen to reduce risk of cognitive decline in a large and diverse population,” he added.
The Alzheimer’s Association has launched a 2-year clinical trial, called the U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER), to do just that.
“While we research that definitive lifestyle ‘recipe,’ there are things we can do today that may decrease our risk of cognitive decline as we age. Eating a heart-healthy diet, exercising regularly, and staying cognitively engaged are just a few,” Dr. Weber added.
Also weighing in, Taylor Wallace, PhD, adjunct professor, department of nutrition and food studies, George Mason University, Fairfax, Va., said the study results are not surprising.
“Scientific data on the ability of flavonoids to prevent age-related chronic diseases, including cognitive decline, has accumulated immensely over the last decade. This epidemiological study reinforces findings from smaller shorter-duration clinical trials and mechanistic studies,” said Dr. Wallace, who was not involved in the study.
“Flavonoids show great potential in reducing inflammation and oxidative stress in the body. They are also vasodilators that help improve blood flow, which is important for the cardiovascular and cerebrovascular systems,” he noted.
“Typically, foods rich in flavonoids are also nutrient-dense in vitamins, minerals, and dietary fiber (eg, fruits and vegetables). Anthocyanins in blueberries have long been known to prevent cognitive decline with age,” Dr. Wallace said.
Dr. Wallace was part of a 14-member panel of nutrition scientists who recently reviewed available evidence around fruit and vegetable intake and health.
“Our findings are consistent with this study in regard to cognitive decline and other disease states. Cruciferous vegetables, dark-green leafy vegetables, citrus fruits, and dark-colored berries seem to have superior effects on health promotion and disease prevention in general,” said Dr. Wallace.
This work was supported by grants from the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Weber has no relevant disclosures. Dr. Wallace is principal and chief executive officer of the Think Healthy Group; editor of the Journal of Dietary Supplements; and deputy editor-in-chief of the Journal of the American College of Nutrition.
A version of this article first appeared on Medscape.com.
, new research shows.
Among the different types of flavonoids, flavones (found in some spices and yellow or orange fruits and vegetables) and anthocyanins (found in blueberries, blackberries, and cherries) seem to have most protective effect, the researchers report.
“There is mounting evidence suggesting flavonoids are powerhouses when it comes to preventing your thinking skills from declining as you get older,” study investigator Walter Willett, MD, DrPH, Harvard University, Boston, said in a statement.
“Our results are exciting because they show that making simple changes to your diet could help prevent cognitive decline,” said Dr. Willett.
The study was published online July 28 in the journal Neurology.
Antioxidant punch
Flavonoids, naturally occurring phytochemicals found in plants, are strong antioxidants. Considering the likely role of oxidative stress in age-related cognitive decline, flavonoids have been proposed as a potentially important preventive.
For the study, Dr. Willett and colleagues prospectively examined associations between long-term dietary flavonoids (flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, polymeric flavonoids, and proanthocyanidins) and subjective cognitive decline in 49,493 women from the Nurses’ Health Study (1984-2006) and 27,842 men from the Health Professionals Follow-up Study (1986-2002).
Those in the highest quintile of flavonoid consumption consumed about 600 mg daily on average while those in the lowest quintile got only about 150 mg daily.
After adjusting for age, total energy intake, major nondietary factors, and specific dietary factors, a higher intake of total flavonoids was associated with lower likelihood of self-reported subjective cognitive decline during follow up.
Individuals in the highest quintile of daily consumption had about a 20% lower risk of subjective cognitive decline relative to peers in the lowest quintile (pooled multivariable-adjusted odds ratio: 0.81; 95% confidence interval, 0.76-0.89).
The strongest protective associations were found for flavones (OR, 0.62; 95% confidence interval, 0.57-0.68), flavanones (OR, 0.64; 95% CI, 0.58-0.68), and anthocyanins (OR, 0.76; 95% CI, 0.72-0.84) (P trend < .0001 for all groups).
“The people in our study who did the best over time ate an average of at least half a serving per day of foods like orange juice, oranges, peppers, celery, grapefruits, grapefruit juice, apples, and pears,” Dr. Willett said.
“While it is possible other phytochemicals are at work here, a colorful diet rich in flavonoids – and specifically flavones and anthocyanins – seems to be a good bet for promoting long-term brain health,” he added.
A limitation of the study is that participants reported on their diets and may not recall perfectly what they ate or how much.
Healthy diet best bet for brain health
Reached for comment, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, said this study “adds to our understanding of which elements of a healthy diet may be important in reducing dementia risk; flavonols may be one of those elements.”
“However, at this point, people should not put too much stock in specific nutrients – including subsets of flavonols – for reducing dementia risk until more research is done. Rather, they should focus on eating an overall healthy diet,” he said.
“It would be wonderful if a particular food or supplement could delay or prevent Alzheimer’s disease, but we do not have scientific evidence to support such claims. Randomized controlled clinical trials are necessary to evaluate whether any food or supplement has a scientifically proven beneficial effect,” Dr. Weber added.
For now, the Alzheimer’s Association “encourages everyone to eat a healthy and balanced diet as a way to help reduce the risk of cognitive decline,” Dr. Weber said.
“With more than 6 million Americans living with Alzheimer’s disease and other dementia today, there is a pressing need to test the effectiveness of a healthy lifestyle regimen to reduce risk of cognitive decline in a large and diverse population,” he added.
The Alzheimer’s Association has launched a 2-year clinical trial, called the U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER), to do just that.
“While we research that definitive lifestyle ‘recipe,’ there are things we can do today that may decrease our risk of cognitive decline as we age. Eating a heart-healthy diet, exercising regularly, and staying cognitively engaged are just a few,” Dr. Weber added.
Also weighing in, Taylor Wallace, PhD, adjunct professor, department of nutrition and food studies, George Mason University, Fairfax, Va., said the study results are not surprising.
“Scientific data on the ability of flavonoids to prevent age-related chronic diseases, including cognitive decline, has accumulated immensely over the last decade. This epidemiological study reinforces findings from smaller shorter-duration clinical trials and mechanistic studies,” said Dr. Wallace, who was not involved in the study.
“Flavonoids show great potential in reducing inflammation and oxidative stress in the body. They are also vasodilators that help improve blood flow, which is important for the cardiovascular and cerebrovascular systems,” he noted.
“Typically, foods rich in flavonoids are also nutrient-dense in vitamins, minerals, and dietary fiber (eg, fruits and vegetables). Anthocyanins in blueberries have long been known to prevent cognitive decline with age,” Dr. Wallace said.
Dr. Wallace was part of a 14-member panel of nutrition scientists who recently reviewed available evidence around fruit and vegetable intake and health.
“Our findings are consistent with this study in regard to cognitive decline and other disease states. Cruciferous vegetables, dark-green leafy vegetables, citrus fruits, and dark-colored berries seem to have superior effects on health promotion and disease prevention in general,” said Dr. Wallace.
This work was supported by grants from the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Weber has no relevant disclosures. Dr. Wallace is principal and chief executive officer of the Think Healthy Group; editor of the Journal of Dietary Supplements; and deputy editor-in-chief of the Journal of the American College of Nutrition.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
FDA approves new enzyme replacement therapy for Pompe disease
Pompe disease is a rare genetic disease that occurs in an estimated 1 in 40,000 births. It is caused by a genetic deficiency or dysfunction of the lysosomal enzyme acid alpha-glucosidase (GAA), which leads to a buildup of glycogen in skeletal and cardiac muscle cells, causing muscle weakness and premature death from respiratory failure or heart failure.
Nexviazyme, administered by intravenous infusion every 2 weeks, supplements GAA and helps reduce glycogen accumulation.
The approval of this product “brings patients with Pompe disease another enzyme replacement therapy option for this rare disease,” said Janet Maynard, MD, deputy director, Office of Rare Diseases, Pediatrics, Urologic and Reproductive Medicine, in the FDA’s Center for Drug Evaluation and Research, in a news release.
In 2010, the FDA approved alglucosidase alfa (Lumizyme) for the treatment of late-onset Pompe disease.
“The FDA will continue to work with stakeholders to advance the development of additional new, effective, and safe therapies for rare diseases, including Pompe disease,” said Dr. Maynard.
The approval is based on positive phase 3 data that demonstrated improvements in key disease burden measures, including respiratory function and walking disease, and that established the drug’s safety profile, Genzyme said in a news release.
The most common side effects were headache, fatigue, diarrhea, nausea, joint pain, dizziness, myalgia, pruritus, vomiting, dyspnea, erythema, paresthesia, and urticaria.
Serious reactions included hypersensitivity reactions, such as anaphylaxis, and infusion-associated reactions, including respiratory distress, chills, and pyrexia.
Patients susceptible to fluid volume overload or those with compromised cardiac or respiratory function may be at risk for serious acute cardiorespiratory failure.
The FDA granted Nexviazyme orphan drug designation, priority review, and breakthrough status.
Genzyme expects the new therapy to be available in the United States in the coming weeks and said it will be priced on par with Lumizyme.
A version of this article first appeared on Medscape.com.
Pompe disease is a rare genetic disease that occurs in an estimated 1 in 40,000 births. It is caused by a genetic deficiency or dysfunction of the lysosomal enzyme acid alpha-glucosidase (GAA), which leads to a buildup of glycogen in skeletal and cardiac muscle cells, causing muscle weakness and premature death from respiratory failure or heart failure.
Nexviazyme, administered by intravenous infusion every 2 weeks, supplements GAA and helps reduce glycogen accumulation.
The approval of this product “brings patients with Pompe disease another enzyme replacement therapy option for this rare disease,” said Janet Maynard, MD, deputy director, Office of Rare Diseases, Pediatrics, Urologic and Reproductive Medicine, in the FDA’s Center for Drug Evaluation and Research, in a news release.
In 2010, the FDA approved alglucosidase alfa (Lumizyme) for the treatment of late-onset Pompe disease.
“The FDA will continue to work with stakeholders to advance the development of additional new, effective, and safe therapies for rare diseases, including Pompe disease,” said Dr. Maynard.
The approval is based on positive phase 3 data that demonstrated improvements in key disease burden measures, including respiratory function and walking disease, and that established the drug’s safety profile, Genzyme said in a news release.
The most common side effects were headache, fatigue, diarrhea, nausea, joint pain, dizziness, myalgia, pruritus, vomiting, dyspnea, erythema, paresthesia, and urticaria.
Serious reactions included hypersensitivity reactions, such as anaphylaxis, and infusion-associated reactions, including respiratory distress, chills, and pyrexia.
Patients susceptible to fluid volume overload or those with compromised cardiac or respiratory function may be at risk for serious acute cardiorespiratory failure.
The FDA granted Nexviazyme orphan drug designation, priority review, and breakthrough status.
Genzyme expects the new therapy to be available in the United States in the coming weeks and said it will be priced on par with Lumizyme.
A version of this article first appeared on Medscape.com.
Pompe disease is a rare genetic disease that occurs in an estimated 1 in 40,000 births. It is caused by a genetic deficiency or dysfunction of the lysosomal enzyme acid alpha-glucosidase (GAA), which leads to a buildup of glycogen in skeletal and cardiac muscle cells, causing muscle weakness and premature death from respiratory failure or heart failure.
Nexviazyme, administered by intravenous infusion every 2 weeks, supplements GAA and helps reduce glycogen accumulation.
The approval of this product “brings patients with Pompe disease another enzyme replacement therapy option for this rare disease,” said Janet Maynard, MD, deputy director, Office of Rare Diseases, Pediatrics, Urologic and Reproductive Medicine, in the FDA’s Center for Drug Evaluation and Research, in a news release.
In 2010, the FDA approved alglucosidase alfa (Lumizyme) for the treatment of late-onset Pompe disease.
“The FDA will continue to work with stakeholders to advance the development of additional new, effective, and safe therapies for rare diseases, including Pompe disease,” said Dr. Maynard.
The approval is based on positive phase 3 data that demonstrated improvements in key disease burden measures, including respiratory function and walking disease, and that established the drug’s safety profile, Genzyme said in a news release.
The most common side effects were headache, fatigue, diarrhea, nausea, joint pain, dizziness, myalgia, pruritus, vomiting, dyspnea, erythema, paresthesia, and urticaria.
Serious reactions included hypersensitivity reactions, such as anaphylaxis, and infusion-associated reactions, including respiratory distress, chills, and pyrexia.
Patients susceptible to fluid volume overload or those with compromised cardiac or respiratory function may be at risk for serious acute cardiorespiratory failure.
The FDA granted Nexviazyme orphan drug designation, priority review, and breakthrough status.
Genzyme expects the new therapy to be available in the United States in the coming weeks and said it will be priced on par with Lumizyme.
A version of this article first appeared on Medscape.com.
Short-term approach is best for seizure prevention after intracerebral hemorrhage
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
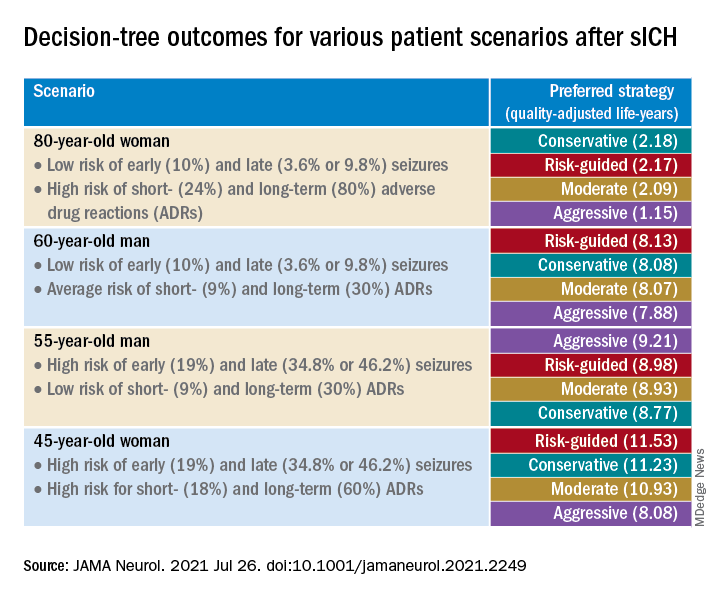
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
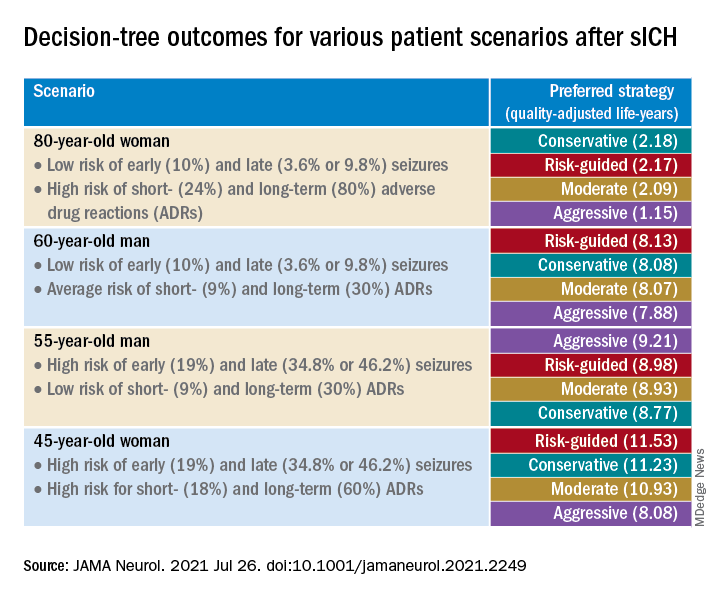
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
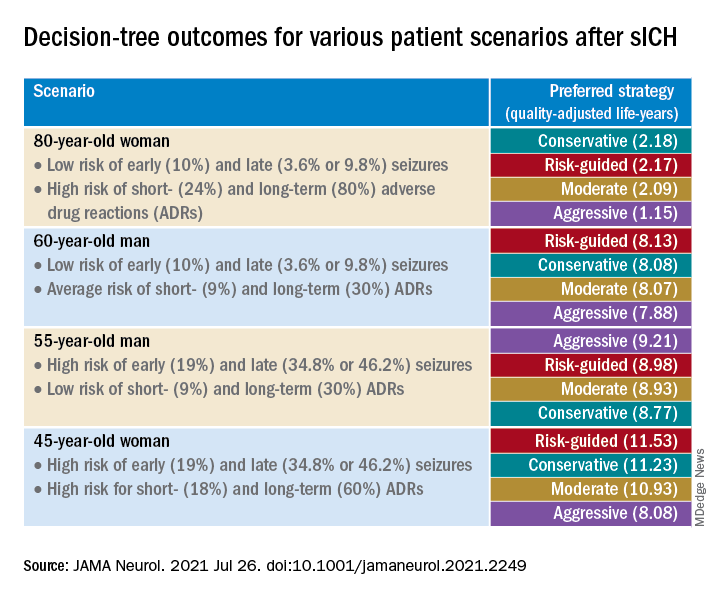
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
Virtual roller-coaster may explain the ups and downs of migraine
and may explain the mechanisms underlying common symptoms and increased activity in certain brain regions in migraine patients.
In a new study, the prevalence of dizziness was 65% among patients with migraine who underwent a virtual roller-coaster ride versus 30% among those without migraine. In addition, imaging showed greater neuronal activity after the simulation in those with migraine.
“Migraine patients reported more dizziness and motion sickness, as well as longer symptom duration and intensity, in a virtual roller-coaster ride,” even though the videos and timing were identical for both groups, said study investigator Arne May, MD, PhD, professor of neurology at the University of Hamburg (Germany).
“We found differences not just in behavioral results but also in specific activations of areas within the cerebellum and the frontal gyrus. Migraine patients process such visual input differently from controls and activate a specific brain network to do so,” he added.
The findings were published online July 21, 2021, in Neurology.
The brain’s response
Nausea, which is among the diagnostic criteria for migraine, is the main symptom of motion sickness. Vestibular symptoms such as dizziness are also components of migraine.
Previous research has examined how the brain processes visual and motion stimuli in migraine, but the reasons patients with migraine are susceptible to motion sickness and dizziness remain unclear.
The researchers used a simulated roller-coaster ride to study the clinical and brain responses to motion among participants with and participants without migraine. They enrolled 20 consecutive patients with migraine who presented to a tertiary headache clinic between January and March 2020 and enrolled 20 healthy participants from a university hospital and the community. The average age of the study population was 30 years, and more than 80% were women.
In response to a questionnaire, participants provided information about demographics and headache features, including onset, frequency, and intensity. They also provided information about their status within the migraine phase and about vestibular symptoms experienced in daily life.
While undergoing functional MRI (fMRI), all participants watched two short videos that provided a first-person perspective of a roller-coaster ride. During the videos, they wore ear buds that conveyed the sound of a car riding over the rails.
The first video included more horizontal perspectives, and the second had more vertical perspectives. Each video was shown three times in random order.
During fMRI, participants reported intensity of nausea and vestibular symptoms using an 11-point Likert scale. After the experiment, they responded to a questionnaire that evaluated intensity and duration of nausea, dizziness, and vertigo experienced during the videos.
Participants also were given the Simulator Sickness Questionnaire (SSQ), which assessed motion sickness. A 100-point visual analog scale (VAS) was used to rate how realistic the roller-coaster experience had been.
There were no differences in sex or age between the migraine group and the healthy control group. Half of the patients with migraine reported aura. The mean number of migraine attacks within the previous month was 3.7. The mean Migraine Disability Assessment score was 21.5, which indicates severe disability.
Nausea, dizziness often neglected
Baseline prevalence of vestibular symptoms was 75% in the migraine group and 5% in the control group (P < .0001). These symptoms included dizziness (60% and 5%, respectively; P < .0001) and postural symptoms (40% and 0%, respectively; P = .003).
At baseline, vestibular symptoms were more frequent (P = .001), more intense (P < .0001), and were associated with greater disability (P = .001) in patients with migraine, compared with participants without migraine. The patients with migraine were also more susceptible to motion sickness (P = .02) and had higher depression scores (P = .001).
During the roller-coaster simulation, dizziness was more prevalent among patients with migraine than among those without migraine (65% vs. 30%; P = .03). Patients with migraine also reported more motion sickness (SSQ score, 47.3 vs. 24.3; P = .004), longer symptom duration (1:19 minutes vs. 00:27 minutes; P = .03), and symptoms of greater intensity (VAS, 22.0 vs. 9.9; P = .03).
Brain activity also differed between groups. Among patients with migraine, neuronal activity was greater in clusters within the right superior and left inferior occipital gyrus, the left pontine nuclei, and the left cerebellar lobules V and VI.
There was a moderately negative correlation of activation of the inferior occipital gyrus with migraine disability (r = –0.46; P = .04). Activation within the pontine nuclei correlated positively with motion sickness scores (r = 0.32; P = .04).
In addition, among patients with migraine, activity in the cerebellar lobule VIIb and in the left middle frontal gyrus was decreased in comparison with persons without migraine. Also among patients with migraine, there was enhanced connectivity between the pontine nuclei, cerebellar areas V and VI, and the interior and superior occipital gyrus and numerous cortical areas.
Clinicians often neglect to treat dizziness and nausea in patients with migraine, said Dr. May. However, these symptoms are part of migraine, even when attacks are not occurring.
“I have learned that if we can explain such symptoms, they are better accepted,” said Dr. May. “We need more and better basic research because we need to understand before we treat.”
Toward faster, more effective treatment
Commenting on the study, Erik Viirre, MD, PhD, professor in the department of neurosciences, University of California, San Diego, said, “we can be excited and celebrate that these researchers are using these news tools to investigate the operation of the migraine brain.
“That will combine with the new therapies and the genomics to give us a powerful approach to this particular condition,” said Dr. Viirre, who was not involved with the research.
The findings provide significant detail about the interconnections between the various brain regions affected by migraine, he noted. These regions include not just the sensory centers but also areas involved in higher executive function and emotional responses.
By identifying these regions, the findings show “some of the underlying mechanisms of these clinically relevant features,” said Dr. Viirre, who is also director of UCSD’s Arthur C. Clarke Center for Human Imagination.
The investigators set up the motion simulation well and used sound fMRI methodology, he added. However, imaging studies of the brain’s response to motion pose several challenges.
“The biggest challenge in any of these circumstances is that you can’t put an actual fMRI scanner on a roller-coaster,” said Dr. Viirre. “The actual acceleration and gravitational sensations delivered by a roller-coaster and gravity, of course, do not occur when you’re lying still in an MRI scanner.” Nevertheless, the pseudoacceleration produced by a visual stimulus is a reasonable proxy.
The findings also suggest that researchers in the future could examine whether any new therapeutic interventions for migraine modulate the brain functions differently for individuals with migraine than for those without migraine, he noted.
“That’s going to lead us to a faster, more effective, more reliable suite of migraine therapies,” said Dr. Viirre.
The study also reminds clinicians to take a broader approach to patients with migraine, and it underscores the value of strategies such as self-calming techniques, which can reduce the number and intensity of headaches, he said.
“Literally demonstrating these functional differences in the migraine brain is a hugely important message of advocacy for people with migraine,” Dr. Viirre concluded.
The study was funded by the German Research Foundation. Drs. May and Viirre have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and may explain the mechanisms underlying common symptoms and increased activity in certain brain regions in migraine patients.
In a new study, the prevalence of dizziness was 65% among patients with migraine who underwent a virtual roller-coaster ride versus 30% among those without migraine. In addition, imaging showed greater neuronal activity after the simulation in those with migraine.
“Migraine patients reported more dizziness and motion sickness, as well as longer symptom duration and intensity, in a virtual roller-coaster ride,” even though the videos and timing were identical for both groups, said study investigator Arne May, MD, PhD, professor of neurology at the University of Hamburg (Germany).
“We found differences not just in behavioral results but also in specific activations of areas within the cerebellum and the frontal gyrus. Migraine patients process such visual input differently from controls and activate a specific brain network to do so,” he added.
The findings were published online July 21, 2021, in Neurology.
The brain’s response
Nausea, which is among the diagnostic criteria for migraine, is the main symptom of motion sickness. Vestibular symptoms such as dizziness are also components of migraine.
Previous research has examined how the brain processes visual and motion stimuli in migraine, but the reasons patients with migraine are susceptible to motion sickness and dizziness remain unclear.
The researchers used a simulated roller-coaster ride to study the clinical and brain responses to motion among participants with and participants without migraine. They enrolled 20 consecutive patients with migraine who presented to a tertiary headache clinic between January and March 2020 and enrolled 20 healthy participants from a university hospital and the community. The average age of the study population was 30 years, and more than 80% were women.
In response to a questionnaire, participants provided information about demographics and headache features, including onset, frequency, and intensity. They also provided information about their status within the migraine phase and about vestibular symptoms experienced in daily life.
While undergoing functional MRI (fMRI), all participants watched two short videos that provided a first-person perspective of a roller-coaster ride. During the videos, they wore ear buds that conveyed the sound of a car riding over the rails.
The first video included more horizontal perspectives, and the second had more vertical perspectives. Each video was shown three times in random order.
During fMRI, participants reported intensity of nausea and vestibular symptoms using an 11-point Likert scale. After the experiment, they responded to a questionnaire that evaluated intensity and duration of nausea, dizziness, and vertigo experienced during the videos.
Participants also were given the Simulator Sickness Questionnaire (SSQ), which assessed motion sickness. A 100-point visual analog scale (VAS) was used to rate how realistic the roller-coaster experience had been.
There were no differences in sex or age between the migraine group and the healthy control group. Half of the patients with migraine reported aura. The mean number of migraine attacks within the previous month was 3.7. The mean Migraine Disability Assessment score was 21.5, which indicates severe disability.
Nausea, dizziness often neglected
Baseline prevalence of vestibular symptoms was 75% in the migraine group and 5% in the control group (P < .0001). These symptoms included dizziness (60% and 5%, respectively; P < .0001) and postural symptoms (40% and 0%, respectively; P = .003).
At baseline, vestibular symptoms were more frequent (P = .001), more intense (P < .0001), and were associated with greater disability (P = .001) in patients with migraine, compared with participants without migraine. The patients with migraine were also more susceptible to motion sickness (P = .02) and had higher depression scores (P = .001).
During the roller-coaster simulation, dizziness was more prevalent among patients with migraine than among those without migraine (65% vs. 30%; P = .03). Patients with migraine also reported more motion sickness (SSQ score, 47.3 vs. 24.3; P = .004), longer symptom duration (1:19 minutes vs. 00:27 minutes; P = .03), and symptoms of greater intensity (VAS, 22.0 vs. 9.9; P = .03).
Brain activity also differed between groups. Among patients with migraine, neuronal activity was greater in clusters within the right superior and left inferior occipital gyrus, the left pontine nuclei, and the left cerebellar lobules V and VI.
There was a moderately negative correlation of activation of the inferior occipital gyrus with migraine disability (r = –0.46; P = .04). Activation within the pontine nuclei correlated positively with motion sickness scores (r = 0.32; P = .04).
In addition, among patients with migraine, activity in the cerebellar lobule VIIb and in the left middle frontal gyrus was decreased in comparison with persons without migraine. Also among patients with migraine, there was enhanced connectivity between the pontine nuclei, cerebellar areas V and VI, and the interior and superior occipital gyrus and numerous cortical areas.
Clinicians often neglect to treat dizziness and nausea in patients with migraine, said Dr. May. However, these symptoms are part of migraine, even when attacks are not occurring.
“I have learned that if we can explain such symptoms, they are better accepted,” said Dr. May. “We need more and better basic research because we need to understand before we treat.”
Toward faster, more effective treatment
Commenting on the study, Erik Viirre, MD, PhD, professor in the department of neurosciences, University of California, San Diego, said, “we can be excited and celebrate that these researchers are using these news tools to investigate the operation of the migraine brain.
“That will combine with the new therapies and the genomics to give us a powerful approach to this particular condition,” said Dr. Viirre, who was not involved with the research.
The findings provide significant detail about the interconnections between the various brain regions affected by migraine, he noted. These regions include not just the sensory centers but also areas involved in higher executive function and emotional responses.
By identifying these regions, the findings show “some of the underlying mechanisms of these clinically relevant features,” said Dr. Viirre, who is also director of UCSD’s Arthur C. Clarke Center for Human Imagination.
The investigators set up the motion simulation well and used sound fMRI methodology, he added. However, imaging studies of the brain’s response to motion pose several challenges.
“The biggest challenge in any of these circumstances is that you can’t put an actual fMRI scanner on a roller-coaster,” said Dr. Viirre. “The actual acceleration and gravitational sensations delivered by a roller-coaster and gravity, of course, do not occur when you’re lying still in an MRI scanner.” Nevertheless, the pseudoacceleration produced by a visual stimulus is a reasonable proxy.
The findings also suggest that researchers in the future could examine whether any new therapeutic interventions for migraine modulate the brain functions differently for individuals with migraine than for those without migraine, he noted.
“That’s going to lead us to a faster, more effective, more reliable suite of migraine therapies,” said Dr. Viirre.
The study also reminds clinicians to take a broader approach to patients with migraine, and it underscores the value of strategies such as self-calming techniques, which can reduce the number and intensity of headaches, he said.
“Literally demonstrating these functional differences in the migraine brain is a hugely important message of advocacy for people with migraine,” Dr. Viirre concluded.
The study was funded by the German Research Foundation. Drs. May and Viirre have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and may explain the mechanisms underlying common symptoms and increased activity in certain brain regions in migraine patients.
In a new study, the prevalence of dizziness was 65% among patients with migraine who underwent a virtual roller-coaster ride versus 30% among those without migraine. In addition, imaging showed greater neuronal activity after the simulation in those with migraine.
“Migraine patients reported more dizziness and motion sickness, as well as longer symptom duration and intensity, in a virtual roller-coaster ride,” even though the videos and timing were identical for both groups, said study investigator Arne May, MD, PhD, professor of neurology at the University of Hamburg (Germany).
“We found differences not just in behavioral results but also in specific activations of areas within the cerebellum and the frontal gyrus. Migraine patients process such visual input differently from controls and activate a specific brain network to do so,” he added.
The findings were published online July 21, 2021, in Neurology.
The brain’s response
Nausea, which is among the diagnostic criteria for migraine, is the main symptom of motion sickness. Vestibular symptoms such as dizziness are also components of migraine.
Previous research has examined how the brain processes visual and motion stimuli in migraine, but the reasons patients with migraine are susceptible to motion sickness and dizziness remain unclear.
The researchers used a simulated roller-coaster ride to study the clinical and brain responses to motion among participants with and participants without migraine. They enrolled 20 consecutive patients with migraine who presented to a tertiary headache clinic between January and March 2020 and enrolled 20 healthy participants from a university hospital and the community. The average age of the study population was 30 years, and more than 80% were women.
In response to a questionnaire, participants provided information about demographics and headache features, including onset, frequency, and intensity. They also provided information about their status within the migraine phase and about vestibular symptoms experienced in daily life.
While undergoing functional MRI (fMRI), all participants watched two short videos that provided a first-person perspective of a roller-coaster ride. During the videos, they wore ear buds that conveyed the sound of a car riding over the rails.
The first video included more horizontal perspectives, and the second had more vertical perspectives. Each video was shown three times in random order.
During fMRI, participants reported intensity of nausea and vestibular symptoms using an 11-point Likert scale. After the experiment, they responded to a questionnaire that evaluated intensity and duration of nausea, dizziness, and vertigo experienced during the videos.
Participants also were given the Simulator Sickness Questionnaire (SSQ), which assessed motion sickness. A 100-point visual analog scale (VAS) was used to rate how realistic the roller-coaster experience had been.
There were no differences in sex or age between the migraine group and the healthy control group. Half of the patients with migraine reported aura. The mean number of migraine attacks within the previous month was 3.7. The mean Migraine Disability Assessment score was 21.5, which indicates severe disability.
Nausea, dizziness often neglected
Baseline prevalence of vestibular symptoms was 75% in the migraine group and 5% in the control group (P < .0001). These symptoms included dizziness (60% and 5%, respectively; P < .0001) and postural symptoms (40% and 0%, respectively; P = .003).
At baseline, vestibular symptoms were more frequent (P = .001), more intense (P < .0001), and were associated with greater disability (P = .001) in patients with migraine, compared with participants without migraine. The patients with migraine were also more susceptible to motion sickness (P = .02) and had higher depression scores (P = .001).
During the roller-coaster simulation, dizziness was more prevalent among patients with migraine than among those without migraine (65% vs. 30%; P = .03). Patients with migraine also reported more motion sickness (SSQ score, 47.3 vs. 24.3; P = .004), longer symptom duration (1:19 minutes vs. 00:27 minutes; P = .03), and symptoms of greater intensity (VAS, 22.0 vs. 9.9; P = .03).
Brain activity also differed between groups. Among patients with migraine, neuronal activity was greater in clusters within the right superior and left inferior occipital gyrus, the left pontine nuclei, and the left cerebellar lobules V and VI.
There was a moderately negative correlation of activation of the inferior occipital gyrus with migraine disability (r = –0.46; P = .04). Activation within the pontine nuclei correlated positively with motion sickness scores (r = 0.32; P = .04).
In addition, among patients with migraine, activity in the cerebellar lobule VIIb and in the left middle frontal gyrus was decreased in comparison with persons without migraine. Also among patients with migraine, there was enhanced connectivity between the pontine nuclei, cerebellar areas V and VI, and the interior and superior occipital gyrus and numerous cortical areas.
Clinicians often neglect to treat dizziness and nausea in patients with migraine, said Dr. May. However, these symptoms are part of migraine, even when attacks are not occurring.
“I have learned that if we can explain such symptoms, they are better accepted,” said Dr. May. “We need more and better basic research because we need to understand before we treat.”
Toward faster, more effective treatment
Commenting on the study, Erik Viirre, MD, PhD, professor in the department of neurosciences, University of California, San Diego, said, “we can be excited and celebrate that these researchers are using these news tools to investigate the operation of the migraine brain.
“That will combine with the new therapies and the genomics to give us a powerful approach to this particular condition,” said Dr. Viirre, who was not involved with the research.
The findings provide significant detail about the interconnections between the various brain regions affected by migraine, he noted. These regions include not just the sensory centers but also areas involved in higher executive function and emotional responses.
By identifying these regions, the findings show “some of the underlying mechanisms of these clinically relevant features,” said Dr. Viirre, who is also director of UCSD’s Arthur C. Clarke Center for Human Imagination.
The investigators set up the motion simulation well and used sound fMRI methodology, he added. However, imaging studies of the brain’s response to motion pose several challenges.
“The biggest challenge in any of these circumstances is that you can’t put an actual fMRI scanner on a roller-coaster,” said Dr. Viirre. “The actual acceleration and gravitational sensations delivered by a roller-coaster and gravity, of course, do not occur when you’re lying still in an MRI scanner.” Nevertheless, the pseudoacceleration produced by a visual stimulus is a reasonable proxy.
The findings also suggest that researchers in the future could examine whether any new therapeutic interventions for migraine modulate the brain functions differently for individuals with migraine than for those without migraine, he noted.
“That’s going to lead us to a faster, more effective, more reliable suite of migraine therapies,” said Dr. Viirre.
The study also reminds clinicians to take a broader approach to patients with migraine, and it underscores the value of strategies such as self-calming techniques, which can reduce the number and intensity of headaches, he said.
“Literally demonstrating these functional differences in the migraine brain is a hugely important message of advocacy for people with migraine,” Dr. Viirre concluded.
The study was funded by the German Research Foundation. Drs. May and Viirre have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physician ‘predator’ sentenced for opioid-related patient death; more
Doctor’s illegal opioid distribution results in patient death
Thomas K. Ballard III, MD, of Jackson, Tenn., pleaded guilty to causing the death of one of his patients in 2015 by illegally prescribing hydrocodone. He faces a minimum of 20 years in prison for one count of illegal drug distribution resulting in death. He will be sentenced in September.
Dr. Ballard, 63, owned and operated the Ballard Clinic, from which he prescribed dangerous and addictive drugs without legitimate medical purpose. according to the U.S. Department of Justice.
Dr. Ballard’s treatment records show that he believed a patient had psychiatric problems and was abusing her medication, evidenced by positive drug screens and prescriptions obtained elsewhere for suboxone, a drug used to treat opioid dependency. However, Dr. Ballard continued to prescribe hydrocodone to the patient, including on May 28, 2015, when the patient fatally overdosed on the drug.
“Ballard has proven himself to be nothing more than a predator in a white lab coat, and he should expect to be punished accordingly,” said Special Agent in Charge J. Todd Scott of the Drug Enforcement Administration’s Louisville Division. “Doctors take an oath to first do no harm, and instead, Ballard chose to put his own licentious interests above his patients’ well-being.”
Clinical researchers falsify drug trial data
Eduardo Navarro, of Miami, and Nayade Varona, of Port St. Lucie, Fla., pleaded guilty to conspiring to falsify clinical trial data. Mr. Navarro, 52, was sentenced to 46 months in prison and Ms. Varona, 50, received 30 months in prison.
The court also ordered the defendants to pay $2,134,503 in restitution.
Mr. Navarro and Ms. Varona both worked for Tellus Clinical Research, where Mr. Navarro was a subinvestigator and nurse practitioner, and Ms. Varona was an assistant study coordinator. They admitted to agreeing with one another and others to falsify data in medical records for two clinical trials that were evaluating a treatment for irritable bowel syndrome. Mr. Navarro and Ms. Varona falsified data to make it appear as though patients were participating in the trials, which never occurred.
Doctor faces decade in prison for $6 million health care fraud
Keyvan Amirikhorheh, MD, a family physician in Seal Beach, Calif., pleaded guilty to conspiring to commit health care fraud. He faces a maximum of 10 years in prison.
While working at Los Angeles Community Clinic, Dr. Amirikhorheh submitted fraudulent claims for family planning services, diagnostic testing, and prescriptions for nonexistent patients, defrauding the Family Planning, Access, Care and Treatment (Family PACT) program administered by Medi-Cal, the California Medicaid program.
Between March 2016 and April 2019, Los Angeles Community Clinic and associated laboratories and pharmacies submitted approximately $8,406,204 in claims to Medi-Cal and were paid approximately $6,660,028. Dr. Amirikhorheh, 61, is the final defendant of five to plead guilty in the case, according to the DOJ.
Dentist office sued for HIV discrimination
Night and Day Dental, of North Carolina, settled with the DOJ to resolve a claim that it discriminated against a woman with HIV in violation of the Americans With Disabilities Act.
Title III of the ADA prohibits health care professionals from discriminating against people with disabilities, including those with HIV. The DOJ found that Night and Day Dental refused to accept a woman as a new patient because of her HIV-positive status. The patient was seeking routine dental care, including a cleaning and check-up. Night and Day Dental additionally requires certain blood work results from patients with HIV before deciding whether to provide dental care, when requiring such results is not medically necessary.
They will pay $30,000 to the victim of the discrimination, train their staff on the ADA, develop an antidiscrimination policy, and report to the DOJ every time they refuse to treat a person with HIV or stop providing treatment after learning of a patient’s HIV-positive status. “Turning away patients with HIV or requiring them to provide information that is not medically recommended creates unfair barriers to health care for people with HIV,” said Kristen Clarke, assistant attorney general in the DOJ’s Civil Rights Division.
A version of this article first appeared on Medscape.com.
This article was updated 8/12/21.
Doctor’s illegal opioid distribution results in patient death
Thomas K. Ballard III, MD, of Jackson, Tenn., pleaded guilty to causing the death of one of his patients in 2015 by illegally prescribing hydrocodone. He faces a minimum of 20 years in prison for one count of illegal drug distribution resulting in death. He will be sentenced in September.
Dr. Ballard, 63, owned and operated the Ballard Clinic, from which he prescribed dangerous and addictive drugs without legitimate medical purpose. according to the U.S. Department of Justice.
Dr. Ballard’s treatment records show that he believed a patient had psychiatric problems and was abusing her medication, evidenced by positive drug screens and prescriptions obtained elsewhere for suboxone, a drug used to treat opioid dependency. However, Dr. Ballard continued to prescribe hydrocodone to the patient, including on May 28, 2015, when the patient fatally overdosed on the drug.
“Ballard has proven himself to be nothing more than a predator in a white lab coat, and he should expect to be punished accordingly,” said Special Agent in Charge J. Todd Scott of the Drug Enforcement Administration’s Louisville Division. “Doctors take an oath to first do no harm, and instead, Ballard chose to put his own licentious interests above his patients’ well-being.”
Clinical researchers falsify drug trial data
Eduardo Navarro, of Miami, and Nayade Varona, of Port St. Lucie, Fla., pleaded guilty to conspiring to falsify clinical trial data. Mr. Navarro, 52, was sentenced to 46 months in prison and Ms. Varona, 50, received 30 months in prison.
The court also ordered the defendants to pay $2,134,503 in restitution.
Mr. Navarro and Ms. Varona both worked for Tellus Clinical Research, where Mr. Navarro was a subinvestigator and nurse practitioner, and Ms. Varona was an assistant study coordinator. They admitted to agreeing with one another and others to falsify data in medical records for two clinical trials that were evaluating a treatment for irritable bowel syndrome. Mr. Navarro and Ms. Varona falsified data to make it appear as though patients were participating in the trials, which never occurred.
Doctor faces decade in prison for $6 million health care fraud
Keyvan Amirikhorheh, MD, a family physician in Seal Beach, Calif., pleaded guilty to conspiring to commit health care fraud. He faces a maximum of 10 years in prison.
While working at Los Angeles Community Clinic, Dr. Amirikhorheh submitted fraudulent claims for family planning services, diagnostic testing, and prescriptions for nonexistent patients, defrauding the Family Planning, Access, Care and Treatment (Family PACT) program administered by Medi-Cal, the California Medicaid program.
Between March 2016 and April 2019, Los Angeles Community Clinic and associated laboratories and pharmacies submitted approximately $8,406,204 in claims to Medi-Cal and were paid approximately $6,660,028. Dr. Amirikhorheh, 61, is the final defendant of five to plead guilty in the case, according to the DOJ.
Dentist office sued for HIV discrimination
Night and Day Dental, of North Carolina, settled with the DOJ to resolve a claim that it discriminated against a woman with HIV in violation of the Americans With Disabilities Act.
Title III of the ADA prohibits health care professionals from discriminating against people with disabilities, including those with HIV. The DOJ found that Night and Day Dental refused to accept a woman as a new patient because of her HIV-positive status. The patient was seeking routine dental care, including a cleaning and check-up. Night and Day Dental additionally requires certain blood work results from patients with HIV before deciding whether to provide dental care, when requiring such results is not medically necessary.
They will pay $30,000 to the victim of the discrimination, train their staff on the ADA, develop an antidiscrimination policy, and report to the DOJ every time they refuse to treat a person with HIV or stop providing treatment after learning of a patient’s HIV-positive status. “Turning away patients with HIV or requiring them to provide information that is not medically recommended creates unfair barriers to health care for people with HIV,” said Kristen Clarke, assistant attorney general in the DOJ’s Civil Rights Division.
A version of this article first appeared on Medscape.com.
This article was updated 8/12/21.
Doctor’s illegal opioid distribution results in patient death
Thomas K. Ballard III, MD, of Jackson, Tenn., pleaded guilty to causing the death of one of his patients in 2015 by illegally prescribing hydrocodone. He faces a minimum of 20 years in prison for one count of illegal drug distribution resulting in death. He will be sentenced in September.
Dr. Ballard, 63, owned and operated the Ballard Clinic, from which he prescribed dangerous and addictive drugs without legitimate medical purpose. according to the U.S. Department of Justice.
Dr. Ballard’s treatment records show that he believed a patient had psychiatric problems and was abusing her medication, evidenced by positive drug screens and prescriptions obtained elsewhere for suboxone, a drug used to treat opioid dependency. However, Dr. Ballard continued to prescribe hydrocodone to the patient, including on May 28, 2015, when the patient fatally overdosed on the drug.
“Ballard has proven himself to be nothing more than a predator in a white lab coat, and he should expect to be punished accordingly,” said Special Agent in Charge J. Todd Scott of the Drug Enforcement Administration’s Louisville Division. “Doctors take an oath to first do no harm, and instead, Ballard chose to put his own licentious interests above his patients’ well-being.”
Clinical researchers falsify drug trial data
Eduardo Navarro, of Miami, and Nayade Varona, of Port St. Lucie, Fla., pleaded guilty to conspiring to falsify clinical trial data. Mr. Navarro, 52, was sentenced to 46 months in prison and Ms. Varona, 50, received 30 months in prison.
The court also ordered the defendants to pay $2,134,503 in restitution.
Mr. Navarro and Ms. Varona both worked for Tellus Clinical Research, where Mr. Navarro was a subinvestigator and nurse practitioner, and Ms. Varona was an assistant study coordinator. They admitted to agreeing with one another and others to falsify data in medical records for two clinical trials that were evaluating a treatment for irritable bowel syndrome. Mr. Navarro and Ms. Varona falsified data to make it appear as though patients were participating in the trials, which never occurred.
Doctor faces decade in prison for $6 million health care fraud
Keyvan Amirikhorheh, MD, a family physician in Seal Beach, Calif., pleaded guilty to conspiring to commit health care fraud. He faces a maximum of 10 years in prison.
While working at Los Angeles Community Clinic, Dr. Amirikhorheh submitted fraudulent claims for family planning services, diagnostic testing, and prescriptions for nonexistent patients, defrauding the Family Planning, Access, Care and Treatment (Family PACT) program administered by Medi-Cal, the California Medicaid program.
Between March 2016 and April 2019, Los Angeles Community Clinic and associated laboratories and pharmacies submitted approximately $8,406,204 in claims to Medi-Cal and were paid approximately $6,660,028. Dr. Amirikhorheh, 61, is the final defendant of five to plead guilty in the case, according to the DOJ.
Dentist office sued for HIV discrimination
Night and Day Dental, of North Carolina, settled with the DOJ to resolve a claim that it discriminated against a woman with HIV in violation of the Americans With Disabilities Act.
Title III of the ADA prohibits health care professionals from discriminating against people with disabilities, including those with HIV. The DOJ found that Night and Day Dental refused to accept a woman as a new patient because of her HIV-positive status. The patient was seeking routine dental care, including a cleaning and check-up. Night and Day Dental additionally requires certain blood work results from patients with HIV before deciding whether to provide dental care, when requiring such results is not medically necessary.
They will pay $30,000 to the victim of the discrimination, train their staff on the ADA, develop an antidiscrimination policy, and report to the DOJ every time they refuse to treat a person with HIV or stop providing treatment after learning of a patient’s HIV-positive status. “Turning away patients with HIV or requiring them to provide information that is not medically recommended creates unfair barriers to health care for people with HIV,” said Kristen Clarke, assistant attorney general in the DOJ’s Civil Rights Division.
A version of this article first appeared on Medscape.com.
This article was updated 8/12/21.
MS CONFERENCE NEWS
- Common MS treatment wears off more quickly in Black patients
- A less expensive, more convenient treatment option for MS?
- Investigational drug reduces brain lesions in highly active MS
- Evobrutinib may lower nerve damage biomarker levels
- Disease progression and therapy response vary in MS by ethnicity
- Some MS treatments may heighten COVID risk
- Natalizumab postinfusion reactions
- Common MS treatment wears off more quickly in Black patients
- A less expensive, more convenient treatment option for MS?
- Investigational drug reduces brain lesions in highly active MS
- Evobrutinib may lower nerve damage biomarker levels
- Disease progression and therapy response vary in MS by ethnicity
- Some MS treatments may heighten COVID risk
- Natalizumab postinfusion reactions
- Common MS treatment wears off more quickly in Black patients
- A less expensive, more convenient treatment option for MS?
- Investigational drug reduces brain lesions in highly active MS
- Evobrutinib may lower nerve damage biomarker levels
- Disease progression and therapy response vary in MS by ethnicity
- Some MS treatments may heighten COVID risk
- Natalizumab postinfusion reactions










