User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
More on GRADE: Cognitive deficits linked to CV risk factors in T2D
In type 2 diabetes (T2D), a greater degree of hyperlipidemia and hypertension, although not hyperglycemia, was associated with measurable cognitive impairment even among patients with only a 4-year mean disease duration, according to a substudy of the GRADE trial.
The association of these cardiovascular (CV) risk factors with impairments in cognition has been reported before, but the findings are notable because the mean duration of T2D was short in a relatively healthy study population, reported a multicenter team of investigators.
The relative impairments in cognitive function “may not be clinically significant given the very small size of the differences,” conceded the authors of this study, led by José A. Luchsinger, MD, but they are consistent with previous reports of the same association in older patients with a longer duration of diabetes. In other words, the data suggest the risk of cognitive loss from CV risk factors in T2D patients begins early.
“A potential explanation for the small differences, compared with those previously reported, is that the GRADE cohort is relatively young with a healthier cardiovascular profile and shorter diabetes duration compared with other studies,” reported the investigators, whose results were published online July 20, 2021, in Diabetes Care.
99% complete cognitive assessments
In the GRADE (Glycemia Reduction Approaches in Diabetes: Comparative Effectiveness) trial, 5,018 (99.4%) of the 5,047 enrolled patients completed a battery of cognitive assessments at baseline. Patients were excluded from this study if they had any major CV event in the previous year, if they had T2D for more than 10 years, if they had significant renal impairment, and if they had any history of stage 3 or greater heart failure. Their mean age was 56.7 years.
By cross-sectional analysis, cognitive evaluations, including the Digit Symbol Substitution Test (DSST) and the Spanish English Verbal Learning Test, were evaluated in relation to baseline LDL cholesterol levels, systolic and diastolic blood pressure, hemoglobin A1c, and statin use.
Unlike previous studies in T2D patients, no relationship was observed between cognitive function and A1c level at baseline. However, LDL cholesterol greater than 100 mg/dL was associated with cognitive impairment as measured with the DSST after adjustment for age, sex, education, and general health. The mean difference relative to LDL cholesterol below 70 mg/dL was only 1.8 points, but this was highly significant (P < .001).
Similarly, significant but modest cognitive impairment on DSST score after adjustment for variables were seen for those with a systolic BP between 120 mg and <140 mg relative to either <120 mm Hg or at least 140 mm Hg (P = .014). The same was seen for diastolic BPs of 80 to <90 when compared with either <80 mm Hg or to 90 mm Hg or higher (P = .01).
For those taking statins versus no statins at baseline, there was a 1.4-point mean advantage in DSST score after adjusting for variables (P < .001).
Modest cognitive impairments recorded
Again, the absolute mean differences in the DSST cognitive scores, despite their statistical significance, were modest, according to the authors. In general, the mean difference was rarely greater than 2.0 points and often 1.0 point or less. The authors acknowledged that these changes are of an uncertain clinical significance, but they considered the findings consistent with the association of CV risk factors with cognitive deficits in older T2DM patients or T2DM patients with longer duration of disease.
One difference between this GRADE substudy and previous studies was the lack of an association between cognitive impairment and hyperglycemia. In the ACCORD trial for example, increased levels of blood glycemia were associated with lower performance on numerous tests of cognitive function.
In the Diabetes Control and Complications Trial (DCCT), poorer glycemic control was related to poorer performance on tests of executive function.
Both of those studies also linked hypertension and hyperlipidemia with cognitive deficits, but given that patients in ACCORD had T2DM of substantially longer duration and those in DCCT were older, “it seems reasonable to speculate that, in patients with diabetes duration of less than 10 years, the association between hyperglycemia and cognitive performance may not yet be evident,” the GRADE authors reported.
GRADE trial compares drugs in four classes
The GRADE trial was conducted to compare four classes of T2D therapies for long-term glycemic control as expressed by A1c control over time. The results of the trial, presented recently at the 2021 annual scientific sessions of the American Diabetes Association, found that insulin glargine and the glucagonlike peptide–1 receptor agonist liraglutide performed best on the primary endpoint of maintaining A1c below 7.0%. Both performed significantly better than the sulfonylurea glimepiride and the dipeptidyl peptidase–4 inhibitor sitagliptin.
This substudy of baseline cognitive function in the relatively large GRADE trial provided a unique opportunity to evaluate the impact of CV risk factors in patients with T2D of relatively short duration.
While the data support the adverse impact of inadequately controlled modifiable risk factors on cognitive function in T2D patients, David R. Matthews, DPhil, BM, BCh, emeritus professor of diabetes medicine at the University of Oxford (England), noted that the association was weak and advised a cautious interpretation.
“The effect size is very small indeed. The data are found as a subset of multiple testing,” he said in an interview. He suggested the associations might be the result of “data farming,” and he emphasized that the relationships between these risk factors and cognitive deficits are associations that do not imply causation.
Nevertheless, and despite their unclear clinical implications, Dr. Matthews said that these data might still have a message.
“It is another reminder that for many reasons we all need to be alert to the need for lowering hyperlipidemia and hypertension to normal levels – the benefits may not just be limited to cardiovascular outcome,” Dr. Matthews stated.
The lead author of the study, Dr. Luchsinger, also cautioned against overinterpreting the data.
While the data show that “lipid and blood pressure control within recommended guidelines are associated with marginally better cognitive function in patients with type 2 diabetes of less than 5 years duration on average,” he added that “the study is limited by its cross-sectional nature.”
He indicated that further analysis will be helpful in assessing the implications.
“Longitudinal analyses of the same group of individuals will be conducted next year,” noted Dr. Luchsinger, associate professor of medicine and epidemiology, Columbia University Medical Center, New York.
Dr. Luchsinger reported financial relationships with vTv therapeutics. Dr. Matthews reported no potential conflicts of interest.
In type 2 diabetes (T2D), a greater degree of hyperlipidemia and hypertension, although not hyperglycemia, was associated with measurable cognitive impairment even among patients with only a 4-year mean disease duration, according to a substudy of the GRADE trial.
The association of these cardiovascular (CV) risk factors with impairments in cognition has been reported before, but the findings are notable because the mean duration of T2D was short in a relatively healthy study population, reported a multicenter team of investigators.
The relative impairments in cognitive function “may not be clinically significant given the very small size of the differences,” conceded the authors of this study, led by José A. Luchsinger, MD, but they are consistent with previous reports of the same association in older patients with a longer duration of diabetes. In other words, the data suggest the risk of cognitive loss from CV risk factors in T2D patients begins early.
“A potential explanation for the small differences, compared with those previously reported, is that the GRADE cohort is relatively young with a healthier cardiovascular profile and shorter diabetes duration compared with other studies,” reported the investigators, whose results were published online July 20, 2021, in Diabetes Care.
99% complete cognitive assessments
In the GRADE (Glycemia Reduction Approaches in Diabetes: Comparative Effectiveness) trial, 5,018 (99.4%) of the 5,047 enrolled patients completed a battery of cognitive assessments at baseline. Patients were excluded from this study if they had any major CV event in the previous year, if they had T2D for more than 10 years, if they had significant renal impairment, and if they had any history of stage 3 or greater heart failure. Their mean age was 56.7 years.
By cross-sectional analysis, cognitive evaluations, including the Digit Symbol Substitution Test (DSST) and the Spanish English Verbal Learning Test, were evaluated in relation to baseline LDL cholesterol levels, systolic and diastolic blood pressure, hemoglobin A1c, and statin use.
Unlike previous studies in T2D patients, no relationship was observed between cognitive function and A1c level at baseline. However, LDL cholesterol greater than 100 mg/dL was associated with cognitive impairment as measured with the DSST after adjustment for age, sex, education, and general health. The mean difference relative to LDL cholesterol below 70 mg/dL was only 1.8 points, but this was highly significant (P < .001).
Similarly, significant but modest cognitive impairment on DSST score after adjustment for variables were seen for those with a systolic BP between 120 mg and <140 mg relative to either <120 mm Hg or at least 140 mm Hg (P = .014). The same was seen for diastolic BPs of 80 to <90 when compared with either <80 mm Hg or to 90 mm Hg or higher (P = .01).
For those taking statins versus no statins at baseline, there was a 1.4-point mean advantage in DSST score after adjusting for variables (P < .001).
Modest cognitive impairments recorded
Again, the absolute mean differences in the DSST cognitive scores, despite their statistical significance, were modest, according to the authors. In general, the mean difference was rarely greater than 2.0 points and often 1.0 point or less. The authors acknowledged that these changes are of an uncertain clinical significance, but they considered the findings consistent with the association of CV risk factors with cognitive deficits in older T2DM patients or T2DM patients with longer duration of disease.
One difference between this GRADE substudy and previous studies was the lack of an association between cognitive impairment and hyperglycemia. In the ACCORD trial for example, increased levels of blood glycemia were associated with lower performance on numerous tests of cognitive function.
In the Diabetes Control and Complications Trial (DCCT), poorer glycemic control was related to poorer performance on tests of executive function.
Both of those studies also linked hypertension and hyperlipidemia with cognitive deficits, but given that patients in ACCORD had T2DM of substantially longer duration and those in DCCT were older, “it seems reasonable to speculate that, in patients with diabetes duration of less than 10 years, the association between hyperglycemia and cognitive performance may not yet be evident,” the GRADE authors reported.
GRADE trial compares drugs in four classes
The GRADE trial was conducted to compare four classes of T2D therapies for long-term glycemic control as expressed by A1c control over time. The results of the trial, presented recently at the 2021 annual scientific sessions of the American Diabetes Association, found that insulin glargine and the glucagonlike peptide–1 receptor agonist liraglutide performed best on the primary endpoint of maintaining A1c below 7.0%. Both performed significantly better than the sulfonylurea glimepiride and the dipeptidyl peptidase–4 inhibitor sitagliptin.
This substudy of baseline cognitive function in the relatively large GRADE trial provided a unique opportunity to evaluate the impact of CV risk factors in patients with T2D of relatively short duration.
While the data support the adverse impact of inadequately controlled modifiable risk factors on cognitive function in T2D patients, David R. Matthews, DPhil, BM, BCh, emeritus professor of diabetes medicine at the University of Oxford (England), noted that the association was weak and advised a cautious interpretation.
“The effect size is very small indeed. The data are found as a subset of multiple testing,” he said in an interview. He suggested the associations might be the result of “data farming,” and he emphasized that the relationships between these risk factors and cognitive deficits are associations that do not imply causation.
Nevertheless, and despite their unclear clinical implications, Dr. Matthews said that these data might still have a message.
“It is another reminder that for many reasons we all need to be alert to the need for lowering hyperlipidemia and hypertension to normal levels – the benefits may not just be limited to cardiovascular outcome,” Dr. Matthews stated.
The lead author of the study, Dr. Luchsinger, also cautioned against overinterpreting the data.
While the data show that “lipid and blood pressure control within recommended guidelines are associated with marginally better cognitive function in patients with type 2 diabetes of less than 5 years duration on average,” he added that “the study is limited by its cross-sectional nature.”
He indicated that further analysis will be helpful in assessing the implications.
“Longitudinal analyses of the same group of individuals will be conducted next year,” noted Dr. Luchsinger, associate professor of medicine and epidemiology, Columbia University Medical Center, New York.
Dr. Luchsinger reported financial relationships with vTv therapeutics. Dr. Matthews reported no potential conflicts of interest.
In type 2 diabetes (T2D), a greater degree of hyperlipidemia and hypertension, although not hyperglycemia, was associated with measurable cognitive impairment even among patients with only a 4-year mean disease duration, according to a substudy of the GRADE trial.
The association of these cardiovascular (CV) risk factors with impairments in cognition has been reported before, but the findings are notable because the mean duration of T2D was short in a relatively healthy study population, reported a multicenter team of investigators.
The relative impairments in cognitive function “may not be clinically significant given the very small size of the differences,” conceded the authors of this study, led by José A. Luchsinger, MD, but they are consistent with previous reports of the same association in older patients with a longer duration of diabetes. In other words, the data suggest the risk of cognitive loss from CV risk factors in T2D patients begins early.
“A potential explanation for the small differences, compared with those previously reported, is that the GRADE cohort is relatively young with a healthier cardiovascular profile and shorter diabetes duration compared with other studies,” reported the investigators, whose results were published online July 20, 2021, in Diabetes Care.
99% complete cognitive assessments
In the GRADE (Glycemia Reduction Approaches in Diabetes: Comparative Effectiveness) trial, 5,018 (99.4%) of the 5,047 enrolled patients completed a battery of cognitive assessments at baseline. Patients were excluded from this study if they had any major CV event in the previous year, if they had T2D for more than 10 years, if they had significant renal impairment, and if they had any history of stage 3 or greater heart failure. Their mean age was 56.7 years.
By cross-sectional analysis, cognitive evaluations, including the Digit Symbol Substitution Test (DSST) and the Spanish English Verbal Learning Test, were evaluated in relation to baseline LDL cholesterol levels, systolic and diastolic blood pressure, hemoglobin A1c, and statin use.
Unlike previous studies in T2D patients, no relationship was observed between cognitive function and A1c level at baseline. However, LDL cholesterol greater than 100 mg/dL was associated with cognitive impairment as measured with the DSST after adjustment for age, sex, education, and general health. The mean difference relative to LDL cholesterol below 70 mg/dL was only 1.8 points, but this was highly significant (P < .001).
Similarly, significant but modest cognitive impairment on DSST score after adjustment for variables were seen for those with a systolic BP between 120 mg and <140 mg relative to either <120 mm Hg or at least 140 mm Hg (P = .014). The same was seen for diastolic BPs of 80 to <90 when compared with either <80 mm Hg or to 90 mm Hg or higher (P = .01).
For those taking statins versus no statins at baseline, there was a 1.4-point mean advantage in DSST score after adjusting for variables (P < .001).
Modest cognitive impairments recorded
Again, the absolute mean differences in the DSST cognitive scores, despite their statistical significance, were modest, according to the authors. In general, the mean difference was rarely greater than 2.0 points and often 1.0 point or less. The authors acknowledged that these changes are of an uncertain clinical significance, but they considered the findings consistent with the association of CV risk factors with cognitive deficits in older T2DM patients or T2DM patients with longer duration of disease.
One difference between this GRADE substudy and previous studies was the lack of an association between cognitive impairment and hyperglycemia. In the ACCORD trial for example, increased levels of blood glycemia were associated with lower performance on numerous tests of cognitive function.
In the Diabetes Control and Complications Trial (DCCT), poorer glycemic control was related to poorer performance on tests of executive function.
Both of those studies also linked hypertension and hyperlipidemia with cognitive deficits, but given that patients in ACCORD had T2DM of substantially longer duration and those in DCCT were older, “it seems reasonable to speculate that, in patients with diabetes duration of less than 10 years, the association between hyperglycemia and cognitive performance may not yet be evident,” the GRADE authors reported.
GRADE trial compares drugs in four classes
The GRADE trial was conducted to compare four classes of T2D therapies for long-term glycemic control as expressed by A1c control over time. The results of the trial, presented recently at the 2021 annual scientific sessions of the American Diabetes Association, found that insulin glargine and the glucagonlike peptide–1 receptor agonist liraglutide performed best on the primary endpoint of maintaining A1c below 7.0%. Both performed significantly better than the sulfonylurea glimepiride and the dipeptidyl peptidase–4 inhibitor sitagliptin.
This substudy of baseline cognitive function in the relatively large GRADE trial provided a unique opportunity to evaluate the impact of CV risk factors in patients with T2D of relatively short duration.
While the data support the adverse impact of inadequately controlled modifiable risk factors on cognitive function in T2D patients, David R. Matthews, DPhil, BM, BCh, emeritus professor of diabetes medicine at the University of Oxford (England), noted that the association was weak and advised a cautious interpretation.
“The effect size is very small indeed. The data are found as a subset of multiple testing,” he said in an interview. He suggested the associations might be the result of “data farming,” and he emphasized that the relationships between these risk factors and cognitive deficits are associations that do not imply causation.
Nevertheless, and despite their unclear clinical implications, Dr. Matthews said that these data might still have a message.
“It is another reminder that for many reasons we all need to be alert to the need for lowering hyperlipidemia and hypertension to normal levels – the benefits may not just be limited to cardiovascular outcome,” Dr. Matthews stated.
The lead author of the study, Dr. Luchsinger, also cautioned against overinterpreting the data.
While the data show that “lipid and blood pressure control within recommended guidelines are associated with marginally better cognitive function in patients with type 2 diabetes of less than 5 years duration on average,” he added that “the study is limited by its cross-sectional nature.”
He indicated that further analysis will be helpful in assessing the implications.
“Longitudinal analyses of the same group of individuals will be conducted next year,” noted Dr. Luchsinger, associate professor of medicine and epidemiology, Columbia University Medical Center, New York.
Dr. Luchsinger reported financial relationships with vTv therapeutics. Dr. Matthews reported no potential conflicts of interest.
FROM DIABETES CARE
A clarion call for regulating PBMs: Health care groups, states push back on legal challenges
Mark Nelson, PharmD, recalls the anguish when a major pharmacy benefit manager (PBM) moved all veteran patients with prostate cancer at his facility from an effective medication to a pricier alternative therapy. “All of these patients were stable on their therapy and were extremely distraught about their medications being changed,” said Dr. Nelson, CEO of Northwest Medical Specialties in Washington State. While there was no clinical reason to change the medication, “our oncologists had no choice other than to comply,” he said.
It’s unclear why a PBM would switch to a more expensive medication that has no additional clinical benefit, he continued. “Why upset so many veterans? For what reason? We were not given a reason despite our very vocal protest.”
Angus B. Worthing, MD, sees these scenarios unfold every day in his rheumatology practice in the Washington, D.C., area. “In my clinic with 25 doctors, we have three full-time people that only handle PBMs,” he said in an interview. He and others in the medical community, as well as many states, have been pushing back on what they see as efforts by PBMs to raise drug prices and collect the profits at the expense of patients.
PCMA’s challenges against PBM law
The Pharmaceutical Care Management Association (PCMA), a trade group that represents PBMs, has sued at least a half dozen states on their ability to regulate PBMs. However, a landmark case in late 2020 (Pharmaceutical Care Management Association v. Rutledge) set a new precedent. Reversing a lower appeals court decision, the Supreme Court unanimously ruled in favor of allowing states to put in place fair regulation of these entities.
Dr. Worthing and others hope that the medical community and states can leverage this ruling in another lawsuit PCMA brought against North Dakota (PCMA v. Wehbi). PCMA filed this lawsuit in 2017, which challenges two statutes on PBM regulation. The group has issued similar legal challenges in Maine, the District of Columbia, Iowa, Oklahoma, and Arkansas with the Rutledge case.
“PBMs have become massive profit centers while (ironically) increasing patients’ out-of-pocket costs, interfering with doctor-patient relationships, and impairing patient access to appropriate treatment,” according to an amicus brief filed by The Alliance for Transparent & Affordable Prescriptions (ATAP), the Community Oncology Alliance (COA), and American Pharmacies, supporting North Dakota in the Wehbi case.
This is to ensure the case represents the voices of physicians, patients, nurses, and other stakeholders, and underscores PBM abuses, said Dr. Worthing, vice president of ATAP. He also serves as the American College of Rheumatology’s representative on ATAP’s Executive Committee.
PCMA did not respond to requests for comment. Its CEO and president, J.C. Scott, emphasizes that PBMs have a long track record of reducing drug costs for patients and plan sponsors. In 2021, PCMA released 21 policy solutions, a set of industry principles and a three-part policy platform, all with an aim to bring down costs and increase access to pharmaceutical care, according to the organization.
PCMA estimates that the strategies in its platform (updating Medicare Part D, accelerating value-based care, and eliminating anticompetitive ‘pay for delay’ agreements) would save the federal government a maximum of $398.7 billion over 10 years.
According to Wendy Hemmen, senior director with Texas Oncology in Dallas, PBMs do their own unique calculations to arrive at their cost reductions. “Essentially in a PBM, they use things that make their story. Numbers reported to plan sponsors and to the public are not audited and are usually in terms of percentages or a per member per month. Data points are moved around, dropped, or reclassified to make the story that the PBM needs to tell,” Ms. Hemmen said.
Amicus briefs dispute ERISA connection
North Dakota legislation prohibits PBMs from charging copays to patients that exceed the cost of a drug. It also prohibits gag clause provisions that restrict what pharmacists may discuss with patients. PBMs may charge fees based on performance metrics, but they must use nationally recognized metrics. Fees must be disclosed at the point of sale.
In its legal challenges, PCMA has asserted that state laws violate the preemption clause in the Employee Retirement Income Security Act (ERISA). “Federal preemption allows employers flexibility to administer innovative benefit plans in an environment of increasing health care costs. The court’s decision in Rutledge v. PCMA will either uphold or threaten these federal protections,” PCMA asserted in a statement issued in March 2020.
ATAP’s amicus brief, and another one filed by 34 attorneys general that supports the North Dakota statute to regulate PBMs, counter that this isn’t the case.
“First, PBM regulation (in its common and standard form) does not reference ERISA itself. These laws leave all plans on equal footing; they do not single out ERISA plans for preferred or disfavored coverage, and they do not change the playing field for ERISA plans alone ... Second, PBM regulation does not have any prohibited connection with ERISA plans,” noted authors in the ATAP brief.
PCMA has also included Medicare preemption in its arguments against PBM regulation. This is meritless, wrote the state attorneys general. “Medicare preempts state laws only if a Medicare ‘standard’ particularly addresses the subject of state regulation. Because the challenged North Dakota laws do not dictate plan benefits or conflict with a Medicare standard, they are not preempted.”
The auctioning of medications
PBMs in theory could use their market power to drive down costs by extracting discounts from drug makers and pharmacies. In reality, they retain any price concessions and discounts for themselves, ATAP’s brief continued.
A system that PBMs have put into place, called step therapy, is essentially an auction for the preferred spot that will be authorized and covered, Dr. Worthing explained.
PBMs create formularies through this auction. The highest rebate to the PBM earns the top spot in the auction and becomes the preferred drug. “That highest bid gets paid for by passing the cost along to patients and insurance plans, and PBMs pocket the profits. This provides an incentive for pharmaceutical manufacturers to raise prices,” he said.
Dr. Worthing has seen these practices trickle down and affect his patients. “Frequently, the medication I prescribe based on what’s best for the patient based on their disease activity, values, and medical history is often not covered because a different drug or portfolio of drugs has earned the top spot in step therapy. This is an extremely frustrating and cumbersome process that not only delays access to treatments but also provides an incentive for higher drug prices,” he said.
There are other ways in which PBMs get in the way of care, said Ms. Hemmen, whose facility serves complex-care oncology patients.
“PBMs force scripts out of higher-quality pharmacies that preserve unfragmented care. They incentivize plan sponsors to put programs into place that take away patient choice, fragment care, and drive scripts to their own owned pharmacies,” she said.
Rutledge case sets precedent
In the Rutledge case, PCMA had challenged an Arkansas law that forbid PBMs from paying local pharmacies at a lower rate than what the pharmacies were reimbursed to fill prescriptions. Although the 8th Circuit Court of Appeals agreed with PCMA, the Supreme Court ruled in favor of Arkansas in late 2020.
The appeals court also backed PCMA in PCMA v. Wehbi. However, the Supreme Court vacated this decision and remanded it back to the appeals court, asking for a reconsideration in wake of the outcome in Rutledge v. PCMA.
PCMA has argued that Rutledge was a narrow decision, limited to state laws that regulate PBM reimbursements, and that Rutledge has no bearing on North Dakota law.
While it’s unfortunate that PCMA is trying to delay implementation of sensible regulations, “a lot of us are happy that this issue is coming to light,” Dr. Worthing said. “As a rheumatologist and health policy advocate, exposing drug middlemen is the most important bipartisan issue in the country today because it gets at the core of making sure that sick people get access to the medications they need and reducing the budget of insurance carriers, hospitals, and the federal budget.”
The ATAP brief noted that 28 state attorneys general have filed suit against PBMs, “securing settlements compelling PBMs to correct deceptive trade practices.”
Many people at the state and local level were waiting for the Supreme Court to decide on Rutledge before enacting legislation and sensible regulations, and now they can go ahead and do it, said Dr. Worthing. “I expect to see this across the country as states look at budgets, and as patients bring personal stories to light. We look forward to states passing these kinds of laws to regulate PBMs.”
The ACR doesn’t anticipate a ruling in the Wehbi case until the spring of 2022.
Recent laws passed around PBMs and the pharmacy benefit are a good first step in holding PBMs accountable for quality of care and honoring patient choice, Ms. Hemmen said. The laws also begin to address the fiscal manipulations PBMs use to gain advantage and direct scripts to their own coffers, she added. However, this may not have enough teeth. “These state laws are coming from a provider perspective, and they don’t anticipate what PBMs will do in response. The PBMs are going to work around it.”
Mark Nelson, PharmD, recalls the anguish when a major pharmacy benefit manager (PBM) moved all veteran patients with prostate cancer at his facility from an effective medication to a pricier alternative therapy. “All of these patients were stable on their therapy and were extremely distraught about their medications being changed,” said Dr. Nelson, CEO of Northwest Medical Specialties in Washington State. While there was no clinical reason to change the medication, “our oncologists had no choice other than to comply,” he said.
It’s unclear why a PBM would switch to a more expensive medication that has no additional clinical benefit, he continued. “Why upset so many veterans? For what reason? We were not given a reason despite our very vocal protest.”
Angus B. Worthing, MD, sees these scenarios unfold every day in his rheumatology practice in the Washington, D.C., area. “In my clinic with 25 doctors, we have three full-time people that only handle PBMs,” he said in an interview. He and others in the medical community, as well as many states, have been pushing back on what they see as efforts by PBMs to raise drug prices and collect the profits at the expense of patients.
PCMA’s challenges against PBM law
The Pharmaceutical Care Management Association (PCMA), a trade group that represents PBMs, has sued at least a half dozen states on their ability to regulate PBMs. However, a landmark case in late 2020 (Pharmaceutical Care Management Association v. Rutledge) set a new precedent. Reversing a lower appeals court decision, the Supreme Court unanimously ruled in favor of allowing states to put in place fair regulation of these entities.
Dr. Worthing and others hope that the medical community and states can leverage this ruling in another lawsuit PCMA brought against North Dakota (PCMA v. Wehbi). PCMA filed this lawsuit in 2017, which challenges two statutes on PBM regulation. The group has issued similar legal challenges in Maine, the District of Columbia, Iowa, Oklahoma, and Arkansas with the Rutledge case.
“PBMs have become massive profit centers while (ironically) increasing patients’ out-of-pocket costs, interfering with doctor-patient relationships, and impairing patient access to appropriate treatment,” according to an amicus brief filed by The Alliance for Transparent & Affordable Prescriptions (ATAP), the Community Oncology Alliance (COA), and American Pharmacies, supporting North Dakota in the Wehbi case.
This is to ensure the case represents the voices of physicians, patients, nurses, and other stakeholders, and underscores PBM abuses, said Dr. Worthing, vice president of ATAP. He also serves as the American College of Rheumatology’s representative on ATAP’s Executive Committee.
PCMA did not respond to requests for comment. Its CEO and president, J.C. Scott, emphasizes that PBMs have a long track record of reducing drug costs for patients and plan sponsors. In 2021, PCMA released 21 policy solutions, a set of industry principles and a three-part policy platform, all with an aim to bring down costs and increase access to pharmaceutical care, according to the organization.
PCMA estimates that the strategies in its platform (updating Medicare Part D, accelerating value-based care, and eliminating anticompetitive ‘pay for delay’ agreements) would save the federal government a maximum of $398.7 billion over 10 years.
According to Wendy Hemmen, senior director with Texas Oncology in Dallas, PBMs do their own unique calculations to arrive at their cost reductions. “Essentially in a PBM, they use things that make their story. Numbers reported to plan sponsors and to the public are not audited and are usually in terms of percentages or a per member per month. Data points are moved around, dropped, or reclassified to make the story that the PBM needs to tell,” Ms. Hemmen said.
Amicus briefs dispute ERISA connection
North Dakota legislation prohibits PBMs from charging copays to patients that exceed the cost of a drug. It also prohibits gag clause provisions that restrict what pharmacists may discuss with patients. PBMs may charge fees based on performance metrics, but they must use nationally recognized metrics. Fees must be disclosed at the point of sale.
In its legal challenges, PCMA has asserted that state laws violate the preemption clause in the Employee Retirement Income Security Act (ERISA). “Federal preemption allows employers flexibility to administer innovative benefit plans in an environment of increasing health care costs. The court’s decision in Rutledge v. PCMA will either uphold or threaten these federal protections,” PCMA asserted in a statement issued in March 2020.
ATAP’s amicus brief, and another one filed by 34 attorneys general that supports the North Dakota statute to regulate PBMs, counter that this isn’t the case.
“First, PBM regulation (in its common and standard form) does not reference ERISA itself. These laws leave all plans on equal footing; they do not single out ERISA plans for preferred or disfavored coverage, and they do not change the playing field for ERISA plans alone ... Second, PBM regulation does not have any prohibited connection with ERISA plans,” noted authors in the ATAP brief.
PCMA has also included Medicare preemption in its arguments against PBM regulation. This is meritless, wrote the state attorneys general. “Medicare preempts state laws only if a Medicare ‘standard’ particularly addresses the subject of state regulation. Because the challenged North Dakota laws do not dictate plan benefits or conflict with a Medicare standard, they are not preempted.”
The auctioning of medications
PBMs in theory could use their market power to drive down costs by extracting discounts from drug makers and pharmacies. In reality, they retain any price concessions and discounts for themselves, ATAP’s brief continued.
A system that PBMs have put into place, called step therapy, is essentially an auction for the preferred spot that will be authorized and covered, Dr. Worthing explained.
PBMs create formularies through this auction. The highest rebate to the PBM earns the top spot in the auction and becomes the preferred drug. “That highest bid gets paid for by passing the cost along to patients and insurance plans, and PBMs pocket the profits. This provides an incentive for pharmaceutical manufacturers to raise prices,” he said.
Dr. Worthing has seen these practices trickle down and affect his patients. “Frequently, the medication I prescribe based on what’s best for the patient based on their disease activity, values, and medical history is often not covered because a different drug or portfolio of drugs has earned the top spot in step therapy. This is an extremely frustrating and cumbersome process that not only delays access to treatments but also provides an incentive for higher drug prices,” he said.
There are other ways in which PBMs get in the way of care, said Ms. Hemmen, whose facility serves complex-care oncology patients.
“PBMs force scripts out of higher-quality pharmacies that preserve unfragmented care. They incentivize plan sponsors to put programs into place that take away patient choice, fragment care, and drive scripts to their own owned pharmacies,” she said.
Rutledge case sets precedent
In the Rutledge case, PCMA had challenged an Arkansas law that forbid PBMs from paying local pharmacies at a lower rate than what the pharmacies were reimbursed to fill prescriptions. Although the 8th Circuit Court of Appeals agreed with PCMA, the Supreme Court ruled in favor of Arkansas in late 2020.
The appeals court also backed PCMA in PCMA v. Wehbi. However, the Supreme Court vacated this decision and remanded it back to the appeals court, asking for a reconsideration in wake of the outcome in Rutledge v. PCMA.
PCMA has argued that Rutledge was a narrow decision, limited to state laws that regulate PBM reimbursements, and that Rutledge has no bearing on North Dakota law.
While it’s unfortunate that PCMA is trying to delay implementation of sensible regulations, “a lot of us are happy that this issue is coming to light,” Dr. Worthing said. “As a rheumatologist and health policy advocate, exposing drug middlemen is the most important bipartisan issue in the country today because it gets at the core of making sure that sick people get access to the medications they need and reducing the budget of insurance carriers, hospitals, and the federal budget.”
The ATAP brief noted that 28 state attorneys general have filed suit against PBMs, “securing settlements compelling PBMs to correct deceptive trade practices.”
Many people at the state and local level were waiting for the Supreme Court to decide on Rutledge before enacting legislation and sensible regulations, and now they can go ahead and do it, said Dr. Worthing. “I expect to see this across the country as states look at budgets, and as patients bring personal stories to light. We look forward to states passing these kinds of laws to regulate PBMs.”
The ACR doesn’t anticipate a ruling in the Wehbi case until the spring of 2022.
Recent laws passed around PBMs and the pharmacy benefit are a good first step in holding PBMs accountable for quality of care and honoring patient choice, Ms. Hemmen said. The laws also begin to address the fiscal manipulations PBMs use to gain advantage and direct scripts to their own coffers, she added. However, this may not have enough teeth. “These state laws are coming from a provider perspective, and they don’t anticipate what PBMs will do in response. The PBMs are going to work around it.”
Mark Nelson, PharmD, recalls the anguish when a major pharmacy benefit manager (PBM) moved all veteran patients with prostate cancer at his facility from an effective medication to a pricier alternative therapy. “All of these patients were stable on their therapy and were extremely distraught about their medications being changed,” said Dr. Nelson, CEO of Northwest Medical Specialties in Washington State. While there was no clinical reason to change the medication, “our oncologists had no choice other than to comply,” he said.
It’s unclear why a PBM would switch to a more expensive medication that has no additional clinical benefit, he continued. “Why upset so many veterans? For what reason? We were not given a reason despite our very vocal protest.”
Angus B. Worthing, MD, sees these scenarios unfold every day in his rheumatology practice in the Washington, D.C., area. “In my clinic with 25 doctors, we have three full-time people that only handle PBMs,” he said in an interview. He and others in the medical community, as well as many states, have been pushing back on what they see as efforts by PBMs to raise drug prices and collect the profits at the expense of patients.
PCMA’s challenges against PBM law
The Pharmaceutical Care Management Association (PCMA), a trade group that represents PBMs, has sued at least a half dozen states on their ability to regulate PBMs. However, a landmark case in late 2020 (Pharmaceutical Care Management Association v. Rutledge) set a new precedent. Reversing a lower appeals court decision, the Supreme Court unanimously ruled in favor of allowing states to put in place fair regulation of these entities.
Dr. Worthing and others hope that the medical community and states can leverage this ruling in another lawsuit PCMA brought against North Dakota (PCMA v. Wehbi). PCMA filed this lawsuit in 2017, which challenges two statutes on PBM regulation. The group has issued similar legal challenges in Maine, the District of Columbia, Iowa, Oklahoma, and Arkansas with the Rutledge case.
“PBMs have become massive profit centers while (ironically) increasing patients’ out-of-pocket costs, interfering with doctor-patient relationships, and impairing patient access to appropriate treatment,” according to an amicus brief filed by The Alliance for Transparent & Affordable Prescriptions (ATAP), the Community Oncology Alliance (COA), and American Pharmacies, supporting North Dakota in the Wehbi case.
This is to ensure the case represents the voices of physicians, patients, nurses, and other stakeholders, and underscores PBM abuses, said Dr. Worthing, vice president of ATAP. He also serves as the American College of Rheumatology’s representative on ATAP’s Executive Committee.
PCMA did not respond to requests for comment. Its CEO and president, J.C. Scott, emphasizes that PBMs have a long track record of reducing drug costs for patients and plan sponsors. In 2021, PCMA released 21 policy solutions, a set of industry principles and a three-part policy platform, all with an aim to bring down costs and increase access to pharmaceutical care, according to the organization.
PCMA estimates that the strategies in its platform (updating Medicare Part D, accelerating value-based care, and eliminating anticompetitive ‘pay for delay’ agreements) would save the federal government a maximum of $398.7 billion over 10 years.
According to Wendy Hemmen, senior director with Texas Oncology in Dallas, PBMs do their own unique calculations to arrive at their cost reductions. “Essentially in a PBM, they use things that make their story. Numbers reported to plan sponsors and to the public are not audited and are usually in terms of percentages or a per member per month. Data points are moved around, dropped, or reclassified to make the story that the PBM needs to tell,” Ms. Hemmen said.
Amicus briefs dispute ERISA connection
North Dakota legislation prohibits PBMs from charging copays to patients that exceed the cost of a drug. It also prohibits gag clause provisions that restrict what pharmacists may discuss with patients. PBMs may charge fees based on performance metrics, but they must use nationally recognized metrics. Fees must be disclosed at the point of sale.
In its legal challenges, PCMA has asserted that state laws violate the preemption clause in the Employee Retirement Income Security Act (ERISA). “Federal preemption allows employers flexibility to administer innovative benefit plans in an environment of increasing health care costs. The court’s decision in Rutledge v. PCMA will either uphold or threaten these federal protections,” PCMA asserted in a statement issued in March 2020.
ATAP’s amicus brief, and another one filed by 34 attorneys general that supports the North Dakota statute to regulate PBMs, counter that this isn’t the case.
“First, PBM regulation (in its common and standard form) does not reference ERISA itself. These laws leave all plans on equal footing; they do not single out ERISA plans for preferred or disfavored coverage, and they do not change the playing field for ERISA plans alone ... Second, PBM regulation does not have any prohibited connection with ERISA plans,” noted authors in the ATAP brief.
PCMA has also included Medicare preemption in its arguments against PBM regulation. This is meritless, wrote the state attorneys general. “Medicare preempts state laws only if a Medicare ‘standard’ particularly addresses the subject of state regulation. Because the challenged North Dakota laws do not dictate plan benefits or conflict with a Medicare standard, they are not preempted.”
The auctioning of medications
PBMs in theory could use their market power to drive down costs by extracting discounts from drug makers and pharmacies. In reality, they retain any price concessions and discounts for themselves, ATAP’s brief continued.
A system that PBMs have put into place, called step therapy, is essentially an auction for the preferred spot that will be authorized and covered, Dr. Worthing explained.
PBMs create formularies through this auction. The highest rebate to the PBM earns the top spot in the auction and becomes the preferred drug. “That highest bid gets paid for by passing the cost along to patients and insurance plans, and PBMs pocket the profits. This provides an incentive for pharmaceutical manufacturers to raise prices,” he said.
Dr. Worthing has seen these practices trickle down and affect his patients. “Frequently, the medication I prescribe based on what’s best for the patient based on their disease activity, values, and medical history is often not covered because a different drug or portfolio of drugs has earned the top spot in step therapy. This is an extremely frustrating and cumbersome process that not only delays access to treatments but also provides an incentive for higher drug prices,” he said.
There are other ways in which PBMs get in the way of care, said Ms. Hemmen, whose facility serves complex-care oncology patients.
“PBMs force scripts out of higher-quality pharmacies that preserve unfragmented care. They incentivize plan sponsors to put programs into place that take away patient choice, fragment care, and drive scripts to their own owned pharmacies,” she said.
Rutledge case sets precedent
In the Rutledge case, PCMA had challenged an Arkansas law that forbid PBMs from paying local pharmacies at a lower rate than what the pharmacies were reimbursed to fill prescriptions. Although the 8th Circuit Court of Appeals agreed with PCMA, the Supreme Court ruled in favor of Arkansas in late 2020.
The appeals court also backed PCMA in PCMA v. Wehbi. However, the Supreme Court vacated this decision and remanded it back to the appeals court, asking for a reconsideration in wake of the outcome in Rutledge v. PCMA.
PCMA has argued that Rutledge was a narrow decision, limited to state laws that regulate PBM reimbursements, and that Rutledge has no bearing on North Dakota law.
While it’s unfortunate that PCMA is trying to delay implementation of sensible regulations, “a lot of us are happy that this issue is coming to light,” Dr. Worthing said. “As a rheumatologist and health policy advocate, exposing drug middlemen is the most important bipartisan issue in the country today because it gets at the core of making sure that sick people get access to the medications they need and reducing the budget of insurance carriers, hospitals, and the federal budget.”
The ATAP brief noted that 28 state attorneys general have filed suit against PBMs, “securing settlements compelling PBMs to correct deceptive trade practices.”
Many people at the state and local level were waiting for the Supreme Court to decide on Rutledge before enacting legislation and sensible regulations, and now they can go ahead and do it, said Dr. Worthing. “I expect to see this across the country as states look at budgets, and as patients bring personal stories to light. We look forward to states passing these kinds of laws to regulate PBMs.”
The ACR doesn’t anticipate a ruling in the Wehbi case until the spring of 2022.
Recent laws passed around PBMs and the pharmacy benefit are a good first step in holding PBMs accountable for quality of care and honoring patient choice, Ms. Hemmen said. The laws also begin to address the fiscal manipulations PBMs use to gain advantage and direct scripts to their own coffers, she added. However, this may not have enough teeth. “These state laws are coming from a provider perspective, and they don’t anticipate what PBMs will do in response. The PBMs are going to work around it.”
The first signs of elusive dysautonomia may appear on the skin
During the annual meeting of the Society for Pediatric Dermatology, Adelaide A. Hebert, MD, defined dysautonomia as an umbrella term describing conditions that result in a malfunction of the autonomic nervous system. “This encompasses both the sympathetic and the parasympathetic components of the nervous system,” said Dr. Hebert, professor of dermatology and pediatrics, and chief of pediatric dermatology at the University of Texas, Houston. “Clinical findings may be neurometabolic, developmental, and/or degenerative,” representing a “whole constellation of issues” that physicians may encounter in practice, she noted. Of particular interest is postural orthostatic tachycardia syndrome (POTS), which affects between 1 million and 3 million people in the United States. Typical symptoms include lightheadedness, fainting, and a rapid increase in heartbeat after standing up from a seated position. Other conditions associated with dysautonomia include neurocardiogenic syncope and multiple system atrophy.
Dysautonomia can impact the brain, heart, mouth, blood vessels, eyes, immune cells, and bladder, as well as the skin. Patient presentations vary with symptoms that can range from mild to debilitating. The average time from symptom onset to diagnosis of dysautonomia is 7 years. “It is very difficult to put together these mysterious symptoms that patients have unless one really thinks about dysautonomia as a possible diagnosis,” Dr. Hebert said.
One of the common symptoms that she has seen in her clinical practice is joint hypermobility. “There is a known association between dysautonomia and hypermobile-type Ehlers-Danlos syndrome (EDS), and these patients often have hyperhidrosis,” she said. “So, keep in mind that you could see hypermobility, especially in those with EDS, with associated hyperhidrosis and dysautonomia.” Two key references that she recommends to clinicians when evaluating patients with possible dysautonomia are a study on postural tachycardia in hypermobile EDS, and an article on cardiovascular autonomic dysfunction in hypermobile EDS.
The Beighton Scoring System, which measures joint mobility on a 9-point scale, involves assessment of the joint mobility of the knuckle of both pinky fingers, the base of both thumbs, the elbows, knees, and spine. An instructional video on how to perform a joint hypermobility assessment is available on the Ehler-Danlos Society website.
Literature review
In March 2021, Dr. Hebert and colleagues from other medical specialties published a summary of the literature on cutaneous manifestations in dysautonomia, with an emphasis on syndromes of orthostatic intolerance. “We had neurology, cardiology, along with dermatology involved in contributing the findings they had seen in the UTHealth McGovern Dysautonomia Center of Excellence as there was a dearth of literature that taught us about the cutaneous manifestations of orthostatic intolerance syndromes,” Dr. Hebert said.
One study included in the review showed that 23 out of 26 patients with POTS had at least one of the following cutaneous manifestations: flushing, Raynaud’s phenomenon, evanescent hyperemia, livedo reticularis, erythromelalgia, and hypo- or hyperhidrosis. “If you see a patient with any of these findings, you want to think about the possibility of dysautonomia,” she said, adding that urticaria can also be a finding.
To screen for dysautonomia, she advised, “ask patients if they have difficulty sitting or standing upright, if they have indigestion or other gastric symptoms, abnormal blood vessel functioning such as low or high blood pressure, increased or decreased sweating, changes in urinary frequency or urinary incontinence, or challenges with vision.”
If the patient answers yes to two or more of these questions, she said, consider a referral to neurology and/or cardiology or a center of excellence for further evaluation with tilt-table testing and other screening tools. She also recommended a review published in 2015 that describes the dermatological manifestations of postural tachycardia syndrome and includes illustrated cases.
One of Dr. Hebert’s future dermatology residents assembled a composite of data from the Dysautonomia Center of Excellence, and in the study, found that, compared with males, females with dysautonomia suffer more from excessive sweating, paleness of the face, pale extremities, swelling, cyanosis, cold intolerance, flushing, and hot flashes.
Dr. Hebert disclosed that she has been a consultant to and an adviser for several pharmaceutical companies.
During the annual meeting of the Society for Pediatric Dermatology, Adelaide A. Hebert, MD, defined dysautonomia as an umbrella term describing conditions that result in a malfunction of the autonomic nervous system. “This encompasses both the sympathetic and the parasympathetic components of the nervous system,” said Dr. Hebert, professor of dermatology and pediatrics, and chief of pediatric dermatology at the University of Texas, Houston. “Clinical findings may be neurometabolic, developmental, and/or degenerative,” representing a “whole constellation of issues” that physicians may encounter in practice, she noted. Of particular interest is postural orthostatic tachycardia syndrome (POTS), which affects between 1 million and 3 million people in the United States. Typical symptoms include lightheadedness, fainting, and a rapid increase in heartbeat after standing up from a seated position. Other conditions associated with dysautonomia include neurocardiogenic syncope and multiple system atrophy.
Dysautonomia can impact the brain, heart, mouth, blood vessels, eyes, immune cells, and bladder, as well as the skin. Patient presentations vary with symptoms that can range from mild to debilitating. The average time from symptom onset to diagnosis of dysautonomia is 7 years. “It is very difficult to put together these mysterious symptoms that patients have unless one really thinks about dysautonomia as a possible diagnosis,” Dr. Hebert said.
One of the common symptoms that she has seen in her clinical practice is joint hypermobility. “There is a known association between dysautonomia and hypermobile-type Ehlers-Danlos syndrome (EDS), and these patients often have hyperhidrosis,” she said. “So, keep in mind that you could see hypermobility, especially in those with EDS, with associated hyperhidrosis and dysautonomia.” Two key references that she recommends to clinicians when evaluating patients with possible dysautonomia are a study on postural tachycardia in hypermobile EDS, and an article on cardiovascular autonomic dysfunction in hypermobile EDS.
The Beighton Scoring System, which measures joint mobility on a 9-point scale, involves assessment of the joint mobility of the knuckle of both pinky fingers, the base of both thumbs, the elbows, knees, and spine. An instructional video on how to perform a joint hypermobility assessment is available on the Ehler-Danlos Society website.
Literature review
In March 2021, Dr. Hebert and colleagues from other medical specialties published a summary of the literature on cutaneous manifestations in dysautonomia, with an emphasis on syndromes of orthostatic intolerance. “We had neurology, cardiology, along with dermatology involved in contributing the findings they had seen in the UTHealth McGovern Dysautonomia Center of Excellence as there was a dearth of literature that taught us about the cutaneous manifestations of orthostatic intolerance syndromes,” Dr. Hebert said.
One study included in the review showed that 23 out of 26 patients with POTS had at least one of the following cutaneous manifestations: flushing, Raynaud’s phenomenon, evanescent hyperemia, livedo reticularis, erythromelalgia, and hypo- or hyperhidrosis. “If you see a patient with any of these findings, you want to think about the possibility of dysautonomia,” she said, adding that urticaria can also be a finding.
To screen for dysautonomia, she advised, “ask patients if they have difficulty sitting or standing upright, if they have indigestion or other gastric symptoms, abnormal blood vessel functioning such as low or high blood pressure, increased or decreased sweating, changes in urinary frequency or urinary incontinence, or challenges with vision.”
If the patient answers yes to two or more of these questions, she said, consider a referral to neurology and/or cardiology or a center of excellence for further evaluation with tilt-table testing and other screening tools. She also recommended a review published in 2015 that describes the dermatological manifestations of postural tachycardia syndrome and includes illustrated cases.
One of Dr. Hebert’s future dermatology residents assembled a composite of data from the Dysautonomia Center of Excellence, and in the study, found that, compared with males, females with dysautonomia suffer more from excessive sweating, paleness of the face, pale extremities, swelling, cyanosis, cold intolerance, flushing, and hot flashes.
Dr. Hebert disclosed that she has been a consultant to and an adviser for several pharmaceutical companies.
During the annual meeting of the Society for Pediatric Dermatology, Adelaide A. Hebert, MD, defined dysautonomia as an umbrella term describing conditions that result in a malfunction of the autonomic nervous system. “This encompasses both the sympathetic and the parasympathetic components of the nervous system,” said Dr. Hebert, professor of dermatology and pediatrics, and chief of pediatric dermatology at the University of Texas, Houston. “Clinical findings may be neurometabolic, developmental, and/or degenerative,” representing a “whole constellation of issues” that physicians may encounter in practice, she noted. Of particular interest is postural orthostatic tachycardia syndrome (POTS), which affects between 1 million and 3 million people in the United States. Typical symptoms include lightheadedness, fainting, and a rapid increase in heartbeat after standing up from a seated position. Other conditions associated with dysautonomia include neurocardiogenic syncope and multiple system atrophy.
Dysautonomia can impact the brain, heart, mouth, blood vessels, eyes, immune cells, and bladder, as well as the skin. Patient presentations vary with symptoms that can range from mild to debilitating. The average time from symptom onset to diagnosis of dysautonomia is 7 years. “It is very difficult to put together these mysterious symptoms that patients have unless one really thinks about dysautonomia as a possible diagnosis,” Dr. Hebert said.
One of the common symptoms that she has seen in her clinical practice is joint hypermobility. “There is a known association between dysautonomia and hypermobile-type Ehlers-Danlos syndrome (EDS), and these patients often have hyperhidrosis,” she said. “So, keep in mind that you could see hypermobility, especially in those with EDS, with associated hyperhidrosis and dysautonomia.” Two key references that she recommends to clinicians when evaluating patients with possible dysautonomia are a study on postural tachycardia in hypermobile EDS, and an article on cardiovascular autonomic dysfunction in hypermobile EDS.
The Beighton Scoring System, which measures joint mobility on a 9-point scale, involves assessment of the joint mobility of the knuckle of both pinky fingers, the base of both thumbs, the elbows, knees, and spine. An instructional video on how to perform a joint hypermobility assessment is available on the Ehler-Danlos Society website.
Literature review
In March 2021, Dr. Hebert and colleagues from other medical specialties published a summary of the literature on cutaneous manifestations in dysautonomia, with an emphasis on syndromes of orthostatic intolerance. “We had neurology, cardiology, along with dermatology involved in contributing the findings they had seen in the UTHealth McGovern Dysautonomia Center of Excellence as there was a dearth of literature that taught us about the cutaneous manifestations of orthostatic intolerance syndromes,” Dr. Hebert said.
One study included in the review showed that 23 out of 26 patients with POTS had at least one of the following cutaneous manifestations: flushing, Raynaud’s phenomenon, evanescent hyperemia, livedo reticularis, erythromelalgia, and hypo- or hyperhidrosis. “If you see a patient with any of these findings, you want to think about the possibility of dysautonomia,” she said, adding that urticaria can also be a finding.
To screen for dysautonomia, she advised, “ask patients if they have difficulty sitting or standing upright, if they have indigestion or other gastric symptoms, abnormal blood vessel functioning such as low or high blood pressure, increased or decreased sweating, changes in urinary frequency or urinary incontinence, or challenges with vision.”
If the patient answers yes to two or more of these questions, she said, consider a referral to neurology and/or cardiology or a center of excellence for further evaluation with tilt-table testing and other screening tools. She also recommended a review published in 2015 that describes the dermatological manifestations of postural tachycardia syndrome and includes illustrated cases.
One of Dr. Hebert’s future dermatology residents assembled a composite of data from the Dysautonomia Center of Excellence, and in the study, found that, compared with males, females with dysautonomia suffer more from excessive sweating, paleness of the face, pale extremities, swelling, cyanosis, cold intolerance, flushing, and hot flashes.
Dr. Hebert disclosed that she has been a consultant to and an adviser for several pharmaceutical companies.
FROM SPD 2021
CDC panel updates info on rare side effect after J&J vaccine
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Rising meth-related heart failure admissions a ‘crisis,’ costly for society
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of heart failure (HF) caused by methamphetamine abuse are climbing quickly in the western United States, at great financial and societal cost, suggests an analysis that documents the trends in California over a recent decade.
In the new study, methamphetamine-associated HF (meth-HF) admissions in the state rose by 585% between 2008 and 2018, and charges related those hospitalizations jumped 840%. Cases of HF unrelated to meth fell by 6% during the same period.
The recent explosion in meth-HF hospitalizations has also been costly for society in general, because most cases are younger adults in their most productive, prime earning years, Susan X. Zhao, MD, Santa Clara Valley Medical Center, San Jose, Calif., said in an interview.
“Over the past 11 years, especially since 2018, it has really started to take off, with a pretty dramatic rise. And it happened without much attention, because when we think about drugs, we think about acute overdose and not so much about the chronic, smoldering, long-term effects,” said Dr. Zhao, who is lead author on the study published July 13, 2021, in Circulation: Cardiovascular Quality and Outcomes.
“It’s really affecting a section of the population that is not supposed to be having heart failure problems. I think it is going to continue for the next decade until we put a stop to the parent problem, which is methamphetamine,” Dr. Zhao said. “We’re at the beginning, even though the rise has been pretty dramatic. The worst is yet to come.”
Under the radar
Methamphetamine-associated HF has been a growing problem for many years but has largely been “flying under the radar” because HF hospitalization data focus on Medicare-age patients, not the overwhelmingly younger meth-HF population, the report notes.
“We have to get this message out. Many of my patients with meth heart failure had no idea this would happen to them. They didn’t know,” Dr. Zhao said. “Once I tell them that this is what methamphetamines will do to you after years and years of use, they say they wish someone had told them.”
Dr. Zhao and colleagues looked at HF admission data collected by California’s Health and Human Services Agency to assess meth-HF trends and disease burden. They identified 1,033,076 HF hospitalizations during the decade, of which 42,565 (4.12%) were for meth-HF.
Patients hospitalized with meth-HF had a mean age of 49.6 years, compared with 72.2 for the other patients admitted with HF (P < .001). Virtually all of the patients hospitalized for meth-HF were younger than 65 years: 94.5%, compared with 30% for the other HF patients (P < .001).
Hospitalized patients with meth-HF were mostly men, their prevalence of 80% contrasting with 52.4% for patients with non–meth-related HF (P < .001).
Rates of hospitalization for meth-HF steadily increased during the study period. The age-adjusted rate of meth-HF hospitalization per 100,000 rose from 4.1 in 2008 to 28.1 in 2018. The rate of hospitalization for HF unrelated to meth actually declined, going from 342.3 in 2008 to 321.6 in 2018.
Charges for hospitalizations related to meth-HF shot up more than eight times, from $41.5 million in 2008 to $390.2 million in 2018. In contrast, charges for other HF hospitalizations rose by only 82%, from $3.5 billion to $6.3 billion.
Multiple layers of prevention
Dr. Zhao proposed ways that clinicians can communicate with their patients who are using or considering to use meth. “There are multiple layers of prevention. For people who are thinking of using meth, they need to get the message that something really bad can happen to them years down the road. They’re not going to die from it overnight, but it will damage the heart slowly,” she said.
The next layer of prevention can potentially help meth users who have not yet developed heart problems, Dr. Zhao said. “This would be the time to say, ‘you’re so lucky, your heart is still good. It’s time to stop because people like you, a few years from now are going to die prematurely from a very horrible, very suffering kind of death’.”
Importantly, in meth users who have already developed HF, even then it may not be too late to reverse the cardiomyopathy and symptoms. For up to a third of people with established meth-HF, “if they stop using meth, if they take good cardiac medications, and if the heart failure is in an early enough course, their heart can entirely revert to normal,” Dr. Zhao said, citing an earlier work from her and her colleagues.
Currently, methamphetamine abuse has taken especially strong root in rural areas in California and the Midwest. But Dr. Zhao predicts it will soon become prevalent throughout the United States.
Spotlight on an ‘epidemic’
The rapid growth of the methamphetamine “epidemic” has been well-documented in the United States and around the world, observed an accompanying editorial from Pavan Reddy, MD, Icahn School of Medicine at Mount Sinai Morningside, New York, and Uri Elkayam, MD, University of Southern California, Los Angeles.
They contend that more attention has been given to opioid overdose deaths; meth abuse does not seem to command the same attention, likely because meth is not as strongly associated with acute overdose.
But meth, wrote Dr. Reddy and Dr. Elkayam, “is a different drug with its own M.O., equally dangerous and costly to society but more insidious in nature, its effects potentially causing decades of mental and physical debilitation before ending in premature death.”
The current study “has turned a spotlight on a public health crisis that has grown unfettered for over 2 decades,” and is a call for the “medical community to recognize and manage cases of meth-HF with a comprehensive approach that addresses both mental and physical illness,” they concluded. “Only then can we hope to properly help these patients and with that, reduce the socioeconomic burden of meth-HF.”
A quietly building crisis
The sharp rise in meth-HF hospitalizations is an expected reflection of the methamphetamine crisis, which has been quietly building over the last few years, addiction psychiatrist Corneliu N. Stanciu, MD, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview.
“This new version of methamphetamines looks like ice and is more potent and toxic than former versions traditionally made in home-built labs,” he said. Lately the vast majority of methamphetamines in the United States have come from Mexico, are less expensive with higher purity, “and can be manufactured in greater quantities.”
Some patients with opioid use disorder (OUD) also inject methamphetamines, which can make OUD treatment clinics good places to screen for meth abuse and educate about its cardiovascular implications, Dr. Stanciu said.
“Just as addiction treatment centers present an opportunity to implement cardiac screening and referrals,” he said, “cardiology visits and hospitalizations such as those for meth-HF also present a golden opportunity for involvement of substance use disorder interventions and referrals to get patients into treatment and prevent further damage through ongoing use.”
Dr. Zhao, Dr. Reddy, Dr. Eklayam, and Dr. Stanciu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Common parasite now tied to impaired cognitive function
Investigators reviewed and conducted a meta-analysis of 13 studies that encompassed more than 13,000 healthy adults and found a modest but significant association between T. gondii seropositivity and impaired performance on cognitive tests of processing speed, working memory, short-term verbal memory, and executive function. The average age of the persons in the studies was close to 50 years.
“Our findings show that T. gondii could have a negative but small effect on cognition,” study investigator Arjen Sutterland, MD, of the Amsterdam Neuroscience Research Institute and the Amsterdam Institute for Infection and Immunity, University of Amsterdam, said in an interview.
The study was published online July 14, 2021, in JAMA Psychiatry.
Mental illness link
T. gondii is “an intracellular parasite that produces quiescent infection in approximately 30% of humans worldwide,” the authors wrote. The parasite that causes the infection not only settles in muscle and liver tissue but also can cross the blood-brain barrier and settle quiescently in brain tissue. It can be spread through contact with cat feces or by consuming contaminated meat.
Previous research has shown that neurocognitive changes associated with toxoplasmosis can occur in humans, and meta-analyses suggest an association with neuropsychiatric disorders. Some research has also tied T. gondii infection to increased motor vehicle crashes and suicide attempts.
Dr. Sutterland said he had been inspired by the work of E. Fuller Torrey and Bob Yolken, who proposed the connection between T. gondii and schizophrenia.
Some years ago, Dr. Sutterland and his group analyzed the mental health consequences of T. gondii infection and found “several interesting associations,” but they were unable to “rule out reverse causation – i.e., people with mental health disorders more often get these infections – as well as determine the impact on the population of this common infection.”
For the current study, the investigators analyzed studies that examined specifically cognitive functioning in otherwise healthy individuals in relation to T. gondii infection, “because reverse causation would be less likely in this population and a grasp of global impact would become more clear.”
The researchers conducted a literature search of studies conducted through June 7, 2019, that analyzed cognitive function among healthy participants for whom data on T. gondii seropositivity were available.
A total of 13 studies (n = 13,289 participants; mean age, 46.7 years; 49.6% male) were used in the review and meta-analysis. Some of the studies enrolled a healthy population sample; other studies compared participants with and those without psychiatric disorders. From these, the researchers extracted only the data concerning healthy participants.
The studies analyzed four cognitive domains: processing speed, working memory, short-term verbal memory, and executive functioning.
All cognitive domains affected
Of all the participants, 22.6% had antibodies against T. gondii.
Participants who were seropositive for T. gondii had less favorable functioning in all cognitive domains, with “small but significant” differences. 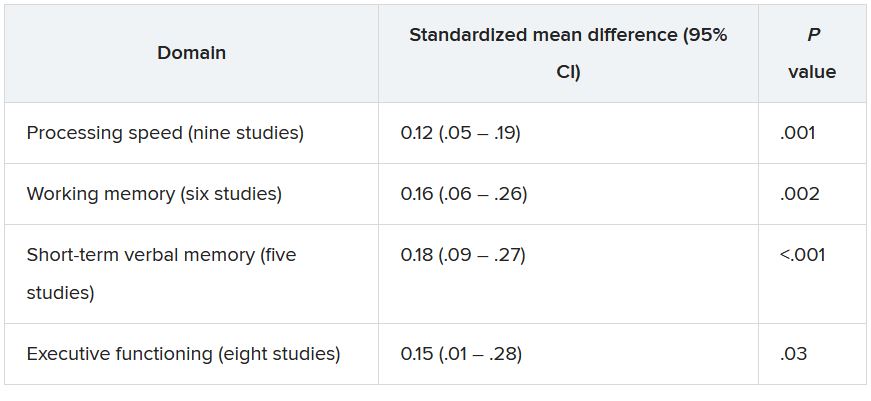
The researchers conducted a meta-regression analysis of mean age in the analysis of executive functioning and found greater effect sizes as age increased (Q = 6.17; R2 = 81%; P = .01).
The studies were of “high quality,” and there was “little suggestion of publication bias was detected,” the authors noted.
“Although the extent of the associations was modest, the ubiquitous prevalence of the quiescent infection worldwide ... suggests that the consequences for cognitive function of the population as a whole may be substantial, although it is difficult to quantify the global impact,” they wrote.
They note that because the studies were cross-sectional in nature, causality cannot be established.
Nevertheless, Dr. Sutterland suggested several possible mechanisms through which T. gondii might affect neurocognition.
“We know the parasite forms cysts in the brain and can influence dopaminergic neurotransmission, which, in turn, affects neurocognition. Alternatively, it is also possible that the immune response to the infection in the brain causes cognitive impairment. This remains an important question to explore further,” he said.
He noted that clinicians can reassure patients who test positive for T. gondii that although the infection can have a negative impact on cognition, the effect is “small.”
Prevention programs warranted
Commenting on the study in an interview, Shawn D. Gale, PhD, associate professor, department of psychology and neuroscience center, Brigham Young University, Provo, Utah, called it a “great meta-analysis.” He noted that his group is researching the subject and has obtained similar findings. A big plus is that the researchers assessed several cognitive domains, not just one.
Although the data showed “mild effects,” the findings could be important on a population level. Because 30% of the world’s population are seropositive for T. gondii, a potentially large number of people are at risk for cognitive impairment, noted Dr. Gale, who was not involved with the study.
“If you look at the United States, perhaps 10%-15% of people might test positive [for T. gondii], but in Germany and France, the number comes closer to 50%, and in other places in the world – especially countries that have a harder time economically – the rates are even higher. So if it can affect cognition, even a small effect is a big deal,” Dr. Gale said.
“I think prevention will be the most important thing, and perhaps down the road, I hope that a vaccine will be considered,” Dr. Gale added.
“These findings indicate that primary prevention of the infection could have substantial global impact on mental health” and that public health programs to prevent T. gondii “are warranted.”
These programs might consist of hygienic measures, especially after human contact with contaminated sources, as well as research into vaccine development.
No source of funding for the study was listed. The authors and Dr. Gale reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators reviewed and conducted a meta-analysis of 13 studies that encompassed more than 13,000 healthy adults and found a modest but significant association between T. gondii seropositivity and impaired performance on cognitive tests of processing speed, working memory, short-term verbal memory, and executive function. The average age of the persons in the studies was close to 50 years.
“Our findings show that T. gondii could have a negative but small effect on cognition,” study investigator Arjen Sutterland, MD, of the Amsterdam Neuroscience Research Institute and the Amsterdam Institute for Infection and Immunity, University of Amsterdam, said in an interview.
The study was published online July 14, 2021, in JAMA Psychiatry.
Mental illness link
T. gondii is “an intracellular parasite that produces quiescent infection in approximately 30% of humans worldwide,” the authors wrote. The parasite that causes the infection not only settles in muscle and liver tissue but also can cross the blood-brain barrier and settle quiescently in brain tissue. It can be spread through contact with cat feces or by consuming contaminated meat.
Previous research has shown that neurocognitive changes associated with toxoplasmosis can occur in humans, and meta-analyses suggest an association with neuropsychiatric disorders. Some research has also tied T. gondii infection to increased motor vehicle crashes and suicide attempts.
Dr. Sutterland said he had been inspired by the work of E. Fuller Torrey and Bob Yolken, who proposed the connection between T. gondii and schizophrenia.
Some years ago, Dr. Sutterland and his group analyzed the mental health consequences of T. gondii infection and found “several interesting associations,” but they were unable to “rule out reverse causation – i.e., people with mental health disorders more often get these infections – as well as determine the impact on the population of this common infection.”
For the current study, the investigators analyzed studies that examined specifically cognitive functioning in otherwise healthy individuals in relation to T. gondii infection, “because reverse causation would be less likely in this population and a grasp of global impact would become more clear.”
The researchers conducted a literature search of studies conducted through June 7, 2019, that analyzed cognitive function among healthy participants for whom data on T. gondii seropositivity were available.
A total of 13 studies (n = 13,289 participants; mean age, 46.7 years; 49.6% male) were used in the review and meta-analysis. Some of the studies enrolled a healthy population sample; other studies compared participants with and those without psychiatric disorders. From these, the researchers extracted only the data concerning healthy participants.
The studies analyzed four cognitive domains: processing speed, working memory, short-term verbal memory, and executive functioning.
All cognitive domains affected
Of all the participants, 22.6% had antibodies against T. gondii.
Participants who were seropositive for T. gondii had less favorable functioning in all cognitive domains, with “small but significant” differences. 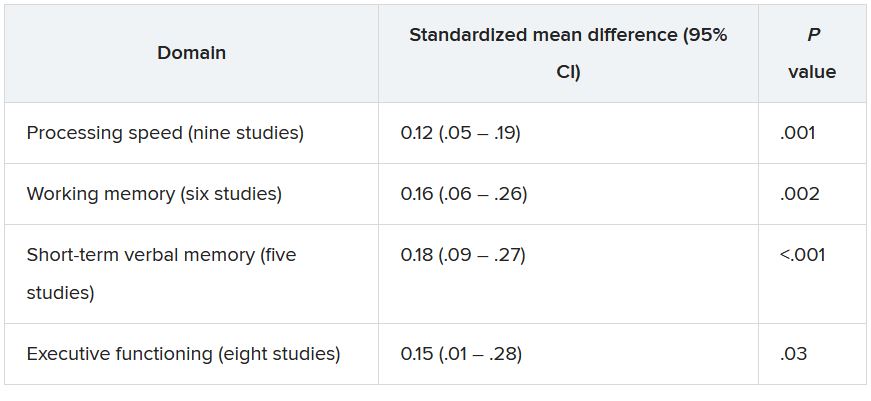
The researchers conducted a meta-regression analysis of mean age in the analysis of executive functioning and found greater effect sizes as age increased (Q = 6.17; R2 = 81%; P = .01).
The studies were of “high quality,” and there was “little suggestion of publication bias was detected,” the authors noted.
“Although the extent of the associations was modest, the ubiquitous prevalence of the quiescent infection worldwide ... suggests that the consequences for cognitive function of the population as a whole may be substantial, although it is difficult to quantify the global impact,” they wrote.
They note that because the studies were cross-sectional in nature, causality cannot be established.
Nevertheless, Dr. Sutterland suggested several possible mechanisms through which T. gondii might affect neurocognition.
“We know the parasite forms cysts in the brain and can influence dopaminergic neurotransmission, which, in turn, affects neurocognition. Alternatively, it is also possible that the immune response to the infection in the brain causes cognitive impairment. This remains an important question to explore further,” he said.
He noted that clinicians can reassure patients who test positive for T. gondii that although the infection can have a negative impact on cognition, the effect is “small.”
Prevention programs warranted
Commenting on the study in an interview, Shawn D. Gale, PhD, associate professor, department of psychology and neuroscience center, Brigham Young University, Provo, Utah, called it a “great meta-analysis.” He noted that his group is researching the subject and has obtained similar findings. A big plus is that the researchers assessed several cognitive domains, not just one.
Although the data showed “mild effects,” the findings could be important on a population level. Because 30% of the world’s population are seropositive for T. gondii, a potentially large number of people are at risk for cognitive impairment, noted Dr. Gale, who was not involved with the study.
“If you look at the United States, perhaps 10%-15% of people might test positive [for T. gondii], but in Germany and France, the number comes closer to 50%, and in other places in the world – especially countries that have a harder time economically – the rates are even higher. So if it can affect cognition, even a small effect is a big deal,” Dr. Gale said.
“I think prevention will be the most important thing, and perhaps down the road, I hope that a vaccine will be considered,” Dr. Gale added.
“These findings indicate that primary prevention of the infection could have substantial global impact on mental health” and that public health programs to prevent T. gondii “are warranted.”
These programs might consist of hygienic measures, especially after human contact with contaminated sources, as well as research into vaccine development.
No source of funding for the study was listed. The authors and Dr. Gale reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators reviewed and conducted a meta-analysis of 13 studies that encompassed more than 13,000 healthy adults and found a modest but significant association between T. gondii seropositivity and impaired performance on cognitive tests of processing speed, working memory, short-term verbal memory, and executive function. The average age of the persons in the studies was close to 50 years.
“Our findings show that T. gondii could have a negative but small effect on cognition,” study investigator Arjen Sutterland, MD, of the Amsterdam Neuroscience Research Institute and the Amsterdam Institute for Infection and Immunity, University of Amsterdam, said in an interview.
The study was published online July 14, 2021, in JAMA Psychiatry.
Mental illness link
T. gondii is “an intracellular parasite that produces quiescent infection in approximately 30% of humans worldwide,” the authors wrote. The parasite that causes the infection not only settles in muscle and liver tissue but also can cross the blood-brain barrier and settle quiescently in brain tissue. It can be spread through contact with cat feces or by consuming contaminated meat.
Previous research has shown that neurocognitive changes associated with toxoplasmosis can occur in humans, and meta-analyses suggest an association with neuropsychiatric disorders. Some research has also tied T. gondii infection to increased motor vehicle crashes and suicide attempts.
Dr. Sutterland said he had been inspired by the work of E. Fuller Torrey and Bob Yolken, who proposed the connection between T. gondii and schizophrenia.
Some years ago, Dr. Sutterland and his group analyzed the mental health consequences of T. gondii infection and found “several interesting associations,” but they were unable to “rule out reverse causation – i.e., people with mental health disorders more often get these infections – as well as determine the impact on the population of this common infection.”
For the current study, the investigators analyzed studies that examined specifically cognitive functioning in otherwise healthy individuals in relation to T. gondii infection, “because reverse causation would be less likely in this population and a grasp of global impact would become more clear.”
The researchers conducted a literature search of studies conducted through June 7, 2019, that analyzed cognitive function among healthy participants for whom data on T. gondii seropositivity were available.
A total of 13 studies (n = 13,289 participants; mean age, 46.7 years; 49.6% male) were used in the review and meta-analysis. Some of the studies enrolled a healthy population sample; other studies compared participants with and those without psychiatric disorders. From these, the researchers extracted only the data concerning healthy participants.
The studies analyzed four cognitive domains: processing speed, working memory, short-term verbal memory, and executive functioning.
All cognitive domains affected
Of all the participants, 22.6% had antibodies against T. gondii.
Participants who were seropositive for T. gondii had less favorable functioning in all cognitive domains, with “small but significant” differences. 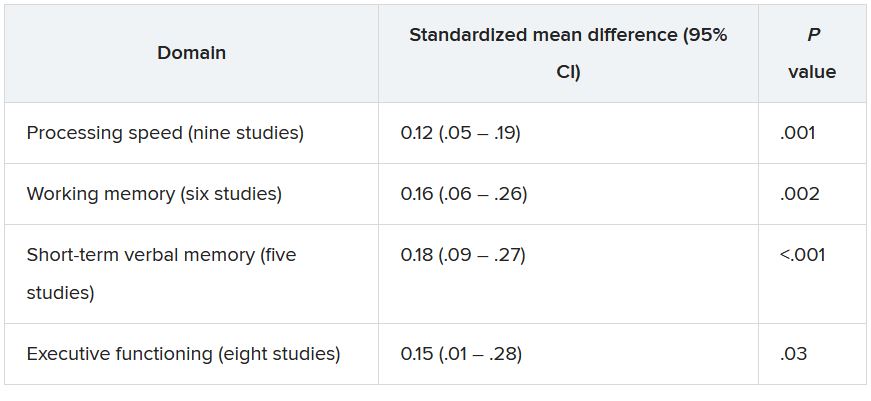
The researchers conducted a meta-regression analysis of mean age in the analysis of executive functioning and found greater effect sizes as age increased (Q = 6.17; R2 = 81%; P = .01).
The studies were of “high quality,” and there was “little suggestion of publication bias was detected,” the authors noted.
“Although the extent of the associations was modest, the ubiquitous prevalence of the quiescent infection worldwide ... suggests that the consequences for cognitive function of the population as a whole may be substantial, although it is difficult to quantify the global impact,” they wrote.
They note that because the studies were cross-sectional in nature, causality cannot be established.
Nevertheless, Dr. Sutterland suggested several possible mechanisms through which T. gondii might affect neurocognition.
“We know the parasite forms cysts in the brain and can influence dopaminergic neurotransmission, which, in turn, affects neurocognition. Alternatively, it is also possible that the immune response to the infection in the brain causes cognitive impairment. This remains an important question to explore further,” he said.
He noted that clinicians can reassure patients who test positive for T. gondii that although the infection can have a negative impact on cognition, the effect is “small.”
Prevention programs warranted
Commenting on the study in an interview, Shawn D. Gale, PhD, associate professor, department of psychology and neuroscience center, Brigham Young University, Provo, Utah, called it a “great meta-analysis.” He noted that his group is researching the subject and has obtained similar findings. A big plus is that the researchers assessed several cognitive domains, not just one.
Although the data showed “mild effects,” the findings could be important on a population level. Because 30% of the world’s population are seropositive for T. gondii, a potentially large number of people are at risk for cognitive impairment, noted Dr. Gale, who was not involved with the study.
“If you look at the United States, perhaps 10%-15% of people might test positive [for T. gondii], but in Germany and France, the number comes closer to 50%, and in other places in the world – especially countries that have a harder time economically – the rates are even higher. So if it can affect cognition, even a small effect is a big deal,” Dr. Gale said.
“I think prevention will be the most important thing, and perhaps down the road, I hope that a vaccine will be considered,” Dr. Gale added.
“These findings indicate that primary prevention of the infection could have substantial global impact on mental health” and that public health programs to prevent T. gondii “are warranted.”
These programs might consist of hygienic measures, especially after human contact with contaminated sources, as well as research into vaccine development.
No source of funding for the study was listed. The authors and Dr. Gale reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Trauma, psychiatric comorbidities tied to functional motor disorders
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
Novel gene therapy ‘reprograms’ cells to reverse neurologic deficits in children with rare disease
An experimental gene therapy produced marked clinical improvement in children with aromatic L-amino acid decarboxylase (AADC) deficiency, a rare genetic disorder that affects the synthesis of key neurotransmitters to cause severe developmental and motor disability.
In an article published July 12, 2021, in Nature Communications, a group of researchers based at the University of California, San Francisco, and Ohio State University, Columbus, described results from seven children ages 4-9 with AADC deficiency who underwent a novel form of surgery to deliver a viral vector expressing the human AADC gene to the midbrain.
Previous trials of this gene therapy in children with AADC deficiency targeted a different region of the brain, the putamen, with only slight clinical improvement. Here, investigators chose two midbrain regions – the substantia nigra pars compacta and the ventral tegmental area – in the hope of restoring healthy AADC enzyme activity in those neurons.
The study’s corresponding author, Krystof Bankiewicz, MD, PhD, professor and vice chair of research at Ohio State University, director of the Brain Health and Performance Center at Ohio State University, and professor emeritus and vice chair for research at UCSF, said in an interview that the brain regions chosen for this trial resulted from years of efforts to identify an ideal target in this disease.
“This particular vector undergoes axonal transport,” he said. “If you inject it into specific regions of the brain it will be transported into the terminals [of the nerve fibers]. And by looking at the imaging of these patients, we found that they still have the wiring in the brain that’s so critical. So we decided to aim at a much more difficult target, going directly to the source of the problem, which is the substantia nigra and the ventral tegmental area. This targets two critical pathways in the brain: one that drives motor responses and another that controls emotions.”
‘Surprising’ improvement seen
The children in the study – four girls and three boys – underwent surgery from 2016 to the end of 2018, and were divided into two dose cohorts, with one receiving three times the amount of vector as the other. Both groups, however, saw similar levels of improvement.
All but one child saw complete resolution of a hallmark symptom of the disease – oculogyric crises, or prolonged spasms of muscles controlling eye movement – within 3 months of surgery. Of the children followed at least 18 months, six attained head control within a year, two became able to eat and drink by mouth, and four gained the ability to sit up unaided in that time. At 18 months one child had learned to speak 50 words using an augmentative communication device.
One child died unexpectedly 7 months after the procedure, Dr. Bankiewicz said in an interview. This death appeared to be caused by cardiac complications of his disease, Dr. Bankiewicz said, which are common in AADC deficiency.
While the investigators are now looking at delivering the AADC gene therapy in younger children – who were excluded from this trial because of safety concerns surrounding the complex procedure – investigators were surprised by the level of improvement seen in older children.
“We initially didn’t believe – at least not all of us – that we could actually make an impact in the older patients, and that is not the case,” said Dr. Bankiewicz, who has since used the same gene therapy on a compassionate-use basis in Europe and seen durable clinical improvement in patients as old as 26. “The fact that we saw a response in that patient tells us something about how incredibly plastic the brain is.”
While the new study does not detail improvements in the children’s social and emotional well-being, Dr. Bankiewicz said these, too, were pronounced. “Kids fall into oculogyric crises in stress-inducing situation. They might be in a stroller being taken for a walk, and something in the environment would stress them. Sometimes they had to be kept in a dark room isolated from stress.” Following the gene therapy, “they’re laughing, they’re social, they can interact with their environment. It’s really touching to see them able to develop a bond now with their caregivers.”
Implication for other disorders
Dr. Bankiewicz and colleagues have previously used the same gene to boost AADC activity in patients with Parkinson’s disease. The group is also in trials to deliver a neuroprotective gene to the brains of people with early-stage Alzheimer’s disease, and a gene-silencing therapy in patients with Huntington’s disease. They will also continue recruiting pediatric patients for trials of the AADC gene therapy.
“We have been developing a method for safely treating younger children, so now we will go to 3 years old and maybe even below,” Dr. Bankiewicz said. “Earlier is probably better, but for technical and safety considerations we needed to be conservative first. It is hugely stressful to go into very sick patients with that type of therapy in that part of the brain. We had to get it right the first time, and it looks like we did.”
The study was funded by the National Institutes of Health, the AADC Research Trust, the Pediatric Neurotransmitter Disease Association, and Ohio State University, with materials and technical support donated by ClearPoint Neuro. Several coauthors disclosed financial relationships with producers of diagnostic tests or biotechnology firms. Dr. Bankiewicz is a founder and shareholder of Brain Neurotherapy Bio, a company that develops gene therapies for Parkinson’s and other diseases.
An experimental gene therapy produced marked clinical improvement in children with aromatic L-amino acid decarboxylase (AADC) deficiency, a rare genetic disorder that affects the synthesis of key neurotransmitters to cause severe developmental and motor disability.
In an article published July 12, 2021, in Nature Communications, a group of researchers based at the University of California, San Francisco, and Ohio State University, Columbus, described results from seven children ages 4-9 with AADC deficiency who underwent a novel form of surgery to deliver a viral vector expressing the human AADC gene to the midbrain.
Previous trials of this gene therapy in children with AADC deficiency targeted a different region of the brain, the putamen, with only slight clinical improvement. Here, investigators chose two midbrain regions – the substantia nigra pars compacta and the ventral tegmental area – in the hope of restoring healthy AADC enzyme activity in those neurons.
The study’s corresponding author, Krystof Bankiewicz, MD, PhD, professor and vice chair of research at Ohio State University, director of the Brain Health and Performance Center at Ohio State University, and professor emeritus and vice chair for research at UCSF, said in an interview that the brain regions chosen for this trial resulted from years of efforts to identify an ideal target in this disease.
“This particular vector undergoes axonal transport,” he said. “If you inject it into specific regions of the brain it will be transported into the terminals [of the nerve fibers]. And by looking at the imaging of these patients, we found that they still have the wiring in the brain that’s so critical. So we decided to aim at a much more difficult target, going directly to the source of the problem, which is the substantia nigra and the ventral tegmental area. This targets two critical pathways in the brain: one that drives motor responses and another that controls emotions.”
‘Surprising’ improvement seen
The children in the study – four girls and three boys – underwent surgery from 2016 to the end of 2018, and were divided into two dose cohorts, with one receiving three times the amount of vector as the other. Both groups, however, saw similar levels of improvement.
All but one child saw complete resolution of a hallmark symptom of the disease – oculogyric crises, or prolonged spasms of muscles controlling eye movement – within 3 months of surgery. Of the children followed at least 18 months, six attained head control within a year, two became able to eat and drink by mouth, and four gained the ability to sit up unaided in that time. At 18 months one child had learned to speak 50 words using an augmentative communication device.
One child died unexpectedly 7 months after the procedure, Dr. Bankiewicz said in an interview. This death appeared to be caused by cardiac complications of his disease, Dr. Bankiewicz said, which are common in AADC deficiency.
While the investigators are now looking at delivering the AADC gene therapy in younger children – who were excluded from this trial because of safety concerns surrounding the complex procedure – investigators were surprised by the level of improvement seen in older children.
“We initially didn’t believe – at least not all of us – that we could actually make an impact in the older patients, and that is not the case,” said Dr. Bankiewicz, who has since used the same gene therapy on a compassionate-use basis in Europe and seen durable clinical improvement in patients as old as 26. “The fact that we saw a response in that patient tells us something about how incredibly plastic the brain is.”
While the new study does not detail improvements in the children’s social and emotional well-being, Dr. Bankiewicz said these, too, were pronounced. “Kids fall into oculogyric crises in stress-inducing situation. They might be in a stroller being taken for a walk, and something in the environment would stress them. Sometimes they had to be kept in a dark room isolated from stress.” Following the gene therapy, “they’re laughing, they’re social, they can interact with their environment. It’s really touching to see them able to develop a bond now with their caregivers.”
Implication for other disorders
Dr. Bankiewicz and colleagues have previously used the same gene to boost AADC activity in patients with Parkinson’s disease. The group is also in trials to deliver a neuroprotective gene to the brains of people with early-stage Alzheimer’s disease, and a gene-silencing therapy in patients with Huntington’s disease. They will also continue recruiting pediatric patients for trials of the AADC gene therapy.
“We have been developing a method for safely treating younger children, so now we will go to 3 years old and maybe even below,” Dr. Bankiewicz said. “Earlier is probably better, but for technical and safety considerations we needed to be conservative first. It is hugely stressful to go into very sick patients with that type of therapy in that part of the brain. We had to get it right the first time, and it looks like we did.”
The study was funded by the National Institutes of Health, the AADC Research Trust, the Pediatric Neurotransmitter Disease Association, and Ohio State University, with materials and technical support donated by ClearPoint Neuro. Several coauthors disclosed financial relationships with producers of diagnostic tests or biotechnology firms. Dr. Bankiewicz is a founder and shareholder of Brain Neurotherapy Bio, a company that develops gene therapies for Parkinson’s and other diseases.
An experimental gene therapy produced marked clinical improvement in children with aromatic L-amino acid decarboxylase (AADC) deficiency, a rare genetic disorder that affects the synthesis of key neurotransmitters to cause severe developmental and motor disability.
In an article published July 12, 2021, in Nature Communications, a group of researchers based at the University of California, San Francisco, and Ohio State University, Columbus, described results from seven children ages 4-9 with AADC deficiency who underwent a novel form of surgery to deliver a viral vector expressing the human AADC gene to the midbrain.
Previous trials of this gene therapy in children with AADC deficiency targeted a different region of the brain, the putamen, with only slight clinical improvement. Here, investigators chose two midbrain regions – the substantia nigra pars compacta and the ventral tegmental area – in the hope of restoring healthy AADC enzyme activity in those neurons.
The study’s corresponding author, Krystof Bankiewicz, MD, PhD, professor and vice chair of research at Ohio State University, director of the Brain Health and Performance Center at Ohio State University, and professor emeritus and vice chair for research at UCSF, said in an interview that the brain regions chosen for this trial resulted from years of efforts to identify an ideal target in this disease.
“This particular vector undergoes axonal transport,” he said. “If you inject it into specific regions of the brain it will be transported into the terminals [of the nerve fibers]. And by looking at the imaging of these patients, we found that they still have the wiring in the brain that’s so critical. So we decided to aim at a much more difficult target, going directly to the source of the problem, which is the substantia nigra and the ventral tegmental area. This targets two critical pathways in the brain: one that drives motor responses and another that controls emotions.”
‘Surprising’ improvement seen
The children in the study – four girls and three boys – underwent surgery from 2016 to the end of 2018, and were divided into two dose cohorts, with one receiving three times the amount of vector as the other. Both groups, however, saw similar levels of improvement.
All but one child saw complete resolution of a hallmark symptom of the disease – oculogyric crises, or prolonged spasms of muscles controlling eye movement – within 3 months of surgery. Of the children followed at least 18 months, six attained head control within a year, two became able to eat and drink by mouth, and four gained the ability to sit up unaided in that time. At 18 months one child had learned to speak 50 words using an augmentative communication device.
One child died unexpectedly 7 months after the procedure, Dr. Bankiewicz said in an interview. This death appeared to be caused by cardiac complications of his disease, Dr. Bankiewicz said, which are common in AADC deficiency.
While the investigators are now looking at delivering the AADC gene therapy in younger children – who were excluded from this trial because of safety concerns surrounding the complex procedure – investigators were surprised by the level of improvement seen in older children.
“We initially didn’t believe – at least not all of us – that we could actually make an impact in the older patients, and that is not the case,” said Dr. Bankiewicz, who has since used the same gene therapy on a compassionate-use basis in Europe and seen durable clinical improvement in patients as old as 26. “The fact that we saw a response in that patient tells us something about how incredibly plastic the brain is.”
While the new study does not detail improvements in the children’s social and emotional well-being, Dr. Bankiewicz said these, too, were pronounced. “Kids fall into oculogyric crises in stress-inducing situation. They might be in a stroller being taken for a walk, and something in the environment would stress them. Sometimes they had to be kept in a dark room isolated from stress.” Following the gene therapy, “they’re laughing, they’re social, they can interact with their environment. It’s really touching to see them able to develop a bond now with their caregivers.”
Implication for other disorders
Dr. Bankiewicz and colleagues have previously used the same gene to boost AADC activity in patients with Parkinson’s disease. The group is also in trials to deliver a neuroprotective gene to the brains of people with early-stage Alzheimer’s disease, and a gene-silencing therapy in patients with Huntington’s disease. They will also continue recruiting pediatric patients for trials of the AADC gene therapy.
“We have been developing a method for safely treating younger children, so now we will go to 3 years old and maybe even below,” Dr. Bankiewicz said. “Earlier is probably better, but for technical and safety considerations we needed to be conservative first. It is hugely stressful to go into very sick patients with that type of therapy in that part of the brain. We had to get it right the first time, and it looks like we did.”
The study was funded by the National Institutes of Health, the AADC Research Trust, the Pediatric Neurotransmitter Disease Association, and Ohio State University, with materials and technical support donated by ClearPoint Neuro. Several coauthors disclosed financial relationships with producers of diagnostic tests or biotechnology firms. Dr. Bankiewicz is a founder and shareholder of Brain Neurotherapy Bio, a company that develops gene therapies for Parkinson’s and other diseases.
FROM NATURE COMMUNICATIONS
On a scale of 1-5 ... How frustrating is this?
Like most American doctors, I take a variety of insurances and insurance plans.
Some of these, particularly HMOs, require a referring physician to send me a written, insurance-approved, referral (AKA authorization) before the visit, to submit with my bill.
Medical visits of all kinds are generally billed on a scale from 1 (brief/simple issue) to 5 (lots of time needed/very complicated).
After 23 years, I’m used to this.
But recently a new wrinkle has emerged.
In the last month I’ve gotten two referrals (both from the same internist), except these state, very clearly, that charges for any visit cannot exceed level 3.
And they’re telling me this before I’ve ever seen the patients, or have any idea how complicated they are, or how long a list of questions they and/or their families will have.
No.
I faxed them back asking for a referral allowing me to bill up to level 5 if needed. I might charge less than that, but none of us know how complicated or long a visit will be until someone comes in. There’s no crystal ball in medicine.
I’m sure someone will say I’m a money-grubbing doctor who couldn’t care less about the patient.
That’s far from the truth. I’m here for the patients. I like helping them. It’s why I do this.
But I can’t help anyone if I can’t afford to keep the office lights on, either.
I never heard back from them. Maybe they decided the patients didn’t need me that much. Maybe they sent them to another neurologist and took my name off their referral list. Maybe they never even noticed my return fax.
What will happen now, I have no idea. Maybe this was something that office tried, to see if I noticed. Maybe it’s the start of the next wave of medical cutbacks. Maybe it was a staff error at the other end.
But either way, This isn’t an amusement park or thrift store. People with problems need time, and time costs money. I need to pay my staff, my rent, and my mortgage. If I can’t do those things, I won’t be able to help anyone.
That’s just, for better or worse, the way it is.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Like most American doctors, I take a variety of insurances and insurance plans.
Some of these, particularly HMOs, require a referring physician to send me a written, insurance-approved, referral (AKA authorization) before the visit, to submit with my bill.
Medical visits of all kinds are generally billed on a scale from 1 (brief/simple issue) to 5 (lots of time needed/very complicated).
After 23 years, I’m used to this.
But recently a new wrinkle has emerged.
In the last month I’ve gotten two referrals (both from the same internist), except these state, very clearly, that charges for any visit cannot exceed level 3.
And they’re telling me this before I’ve ever seen the patients, or have any idea how complicated they are, or how long a list of questions they and/or their families will have.
No.
I faxed them back asking for a referral allowing me to bill up to level 5 if needed. I might charge less than that, but none of us know how complicated or long a visit will be until someone comes in. There’s no crystal ball in medicine.
I’m sure someone will say I’m a money-grubbing doctor who couldn’t care less about the patient.
That’s far from the truth. I’m here for the patients. I like helping them. It’s why I do this.
But I can’t help anyone if I can’t afford to keep the office lights on, either.
I never heard back from them. Maybe they decided the patients didn’t need me that much. Maybe they sent them to another neurologist and took my name off their referral list. Maybe they never even noticed my return fax.
What will happen now, I have no idea. Maybe this was something that office tried, to see if I noticed. Maybe it’s the start of the next wave of medical cutbacks. Maybe it was a staff error at the other end.
But either way, This isn’t an amusement park or thrift store. People with problems need time, and time costs money. I need to pay my staff, my rent, and my mortgage. If I can’t do those things, I won’t be able to help anyone.
That’s just, for better or worse, the way it is.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Like most American doctors, I take a variety of insurances and insurance plans.
Some of these, particularly HMOs, require a referring physician to send me a written, insurance-approved, referral (AKA authorization) before the visit, to submit with my bill.
Medical visits of all kinds are generally billed on a scale from 1 (brief/simple issue) to 5 (lots of time needed/very complicated).
After 23 years, I’m used to this.
But recently a new wrinkle has emerged.
In the last month I’ve gotten two referrals (both from the same internist), except these state, very clearly, that charges for any visit cannot exceed level 3.
And they’re telling me this before I’ve ever seen the patients, or have any idea how complicated they are, or how long a list of questions they and/or their families will have.
No.
I faxed them back asking for a referral allowing me to bill up to level 5 if needed. I might charge less than that, but none of us know how complicated or long a visit will be until someone comes in. There’s no crystal ball in medicine.
I’m sure someone will say I’m a money-grubbing doctor who couldn’t care less about the patient.
That’s far from the truth. I’m here for the patients. I like helping them. It’s why I do this.
But I can’t help anyone if I can’t afford to keep the office lights on, either.
I never heard back from them. Maybe they decided the patients didn’t need me that much. Maybe they sent them to another neurologist and took my name off their referral list. Maybe they never even noticed my return fax.
What will happen now, I have no idea. Maybe this was something that office tried, to see if I noticed. Maybe it’s the start of the next wave of medical cutbacks. Maybe it was a staff error at the other end.
But either way, This isn’t an amusement park or thrift store. People with problems need time, and time costs money. I need to pay my staff, my rent, and my mortgage. If I can’t do those things, I won’t be able to help anyone.
That’s just, for better or worse, the way it is.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Lucid abductions and Candy Crush addiction
I dream of alien abductions
There he goes! It’s lunchtime and your colleague Tom is going on and on again about that time he was abducted by aliens. It sounds ridiculous, but he does make some convincing arguments. Tom thinks it was real, but could it have all just been in his head?
Lucid dreaming may help explain alleged alien abductions. During a lucid dream, people know that they’re dreaming, and can also have some control over how the dreams play out. During some dream states, a person can feel intense sensations, such as terror and paralysis, so it’s no wonder these dreams feel so real.
In a recent study, scientists encouraged 152 participants who had self-identified as lucid dreamers to dream about aliens. Many (75%) of the participants were able to dream about alien encounters, and 15% “achieved relatively realistic experiences,” the investigators reported.
So cut Tom some slack. He’s not crazy, he might just have lucid dreaming privileges. Tell him he should dream about something more fun, like a vacation in the Bahamas.
Follow your heart: Drink more coffee
It seems like the world is divided into coffee drinkers and non–coffee drinkers. Then there’s decaf and regular drinkers. Whichever camp you fall into, know this: The widespread belief that caffeine consumption has an effect on your heart is all beans.
In what is the largest investigation of its kind, researchers from the University of California, San Francisco, looked into whether drinking caffeinated coffee was linked to a risk for heart arrhythmia. They also researched whether patients with genetic variants that affect their metabolism could change that association. Almost 400,000 people with a mean age of 56 years participated in the study. More than half of the participants were women.
The investigators analyzed the participants’ self-reported coffee consumption using a technique called Mendelian randomization to leverage genetic data with the participants’ relationship with caffeine, making it an even field and not relying on the participant consumption self-reporting for outcomes as in previous studies.
What they found, after the 4-year follow up, was nothing short of myth busting.
“We found no evidence that caffeine consumption leads to a greater risk of arrhythmias,” said senior and corresponding author Gregory Marcus, MD. “Our population-based study provides reassurance that common prohibitions against caffeine to reduce arrhythmia risk are likely unwarranted.”
There was no evidence of a heightened risk of arrhythmias in participants who were genetically predisposed to metabolize caffeine differently from those who were not. And, there was a 3% reduction of arrhythmias in patients who consumed higher amounts of coffee.
We are not lobbying for Big Caffeine, but this study adds to the reported health benefits linked to coffee, which already include reduced risk for cancer, diabetes, and Parkinson’s disease, with an added bonus of anti-inflammatory benefits. So, the next time you’re hesitant to pour that second cup of Joe, just go for it. Your heart can take it.
Bored? Feeling down? Don’t play Candy Crush
Now hang on, aren’t those the perfect times to play video games? If there’s nothing else to do, why not open Candy Crush and mindlessly power through the levels?
Because, according to a study by a group of Canadian researchers, it’s actually the worst thing you can do. Well, maybe not literally, but it’s not helpful. Researchers recruited 60 Candy Crush players who were at various levels in the game. They had the participants play early levels that were far too easy or levels balanced with their gameplay abilities.
Players in the easy-level group got bored and quit far earlier than did those in the advanced-level group. The group playing to their abilities were able to access a “flow” state and focus all their attention on the game. While this is all well and good for their gaming performance, according to the researchers, it confirms the theory that playing to escape boredom or negative emotions is more likely to lead to addiction. As with all addictions, the temporary high can give way to a self-repeating loop, causing patients to ignore real life and deepen depression.
The researchers hope their findings will encourage game developers to “consider implementing responsible video gaming tools directly within their games.” Comedy gold. Perhaps Canadians’ idea of capitalism is a little different from that of those south of the border.
Hiccups and vaccine refusal
Tonight, LOTME News dives into the fetid cesspool that is international politics and comes out with … hiccups?
But first, a word from our sponsor, Fearless Boxing Club of South Etobicoke, Ontario.
Are you looking to flout public health restrictions? Do you want to spend time in an enclosed space with other people who haven’t gotten the COVID-19 vaccine? Do you “feel safer waiting until more research is done on the side effects being discovered right now”? (We are not making this up.)
Then join the Fearless Boxing Club, because we “will not be accepting any vaccinated members.” Our founders, Mohammed Abedeen and Krystal Glazier-Roscoe, are working hard to exclude “those who received the experimental COVID vaccine.” (Still not making it up.)
And now, back to the news.
Brazilian president Jair Bolsonaro was hospitalized recently for a severe case of hiccups that may have been related to a stab wound he received in 2018. [Nope, didn’t make that up, either.]
Mr. Bolsonaro had been hiccuping for 10 days, and was experiencing abdominal pain and difficulty speaking, when he entered the hospital on July 14. Since being stabbed while on the campaign trail, he has undergone several operations, which may have led to the partial intestinal obstruction that caused his latest symptoms.
His medical team advised Mr. Bolsonaro to go on a diet to aid his recovery, but when he was released on July 18 he said, “I hope in 10 days I’ll be eating barbecued ribs.” (Maybe this is all just a lucid dream. Probably shouldn’t have had ribs right before bed.)
I dream of alien abductions
There he goes! It’s lunchtime and your colleague Tom is going on and on again about that time he was abducted by aliens. It sounds ridiculous, but he does make some convincing arguments. Tom thinks it was real, but could it have all just been in his head?
Lucid dreaming may help explain alleged alien abductions. During a lucid dream, people know that they’re dreaming, and can also have some control over how the dreams play out. During some dream states, a person can feel intense sensations, such as terror and paralysis, so it’s no wonder these dreams feel so real.
In a recent study, scientists encouraged 152 participants who had self-identified as lucid dreamers to dream about aliens. Many (75%) of the participants were able to dream about alien encounters, and 15% “achieved relatively realistic experiences,” the investigators reported.
So cut Tom some slack. He’s not crazy, he might just have lucid dreaming privileges. Tell him he should dream about something more fun, like a vacation in the Bahamas.
Follow your heart: Drink more coffee
It seems like the world is divided into coffee drinkers and non–coffee drinkers. Then there’s decaf and regular drinkers. Whichever camp you fall into, know this: The widespread belief that caffeine consumption has an effect on your heart is all beans.
In what is the largest investigation of its kind, researchers from the University of California, San Francisco, looked into whether drinking caffeinated coffee was linked to a risk for heart arrhythmia. They also researched whether patients with genetic variants that affect their metabolism could change that association. Almost 400,000 people with a mean age of 56 years participated in the study. More than half of the participants were women.
The investigators analyzed the participants’ self-reported coffee consumption using a technique called Mendelian randomization to leverage genetic data with the participants’ relationship with caffeine, making it an even field and not relying on the participant consumption self-reporting for outcomes as in previous studies.
What they found, after the 4-year follow up, was nothing short of myth busting.
“We found no evidence that caffeine consumption leads to a greater risk of arrhythmias,” said senior and corresponding author Gregory Marcus, MD. “Our population-based study provides reassurance that common prohibitions against caffeine to reduce arrhythmia risk are likely unwarranted.”
There was no evidence of a heightened risk of arrhythmias in participants who were genetically predisposed to metabolize caffeine differently from those who were not. And, there was a 3% reduction of arrhythmias in patients who consumed higher amounts of coffee.
We are not lobbying for Big Caffeine, but this study adds to the reported health benefits linked to coffee, which already include reduced risk for cancer, diabetes, and Parkinson’s disease, with an added bonus of anti-inflammatory benefits. So, the next time you’re hesitant to pour that second cup of Joe, just go for it. Your heart can take it.
Bored? Feeling down? Don’t play Candy Crush
Now hang on, aren’t those the perfect times to play video games? If there’s nothing else to do, why not open Candy Crush and mindlessly power through the levels?
Because, according to a study by a group of Canadian researchers, it’s actually the worst thing you can do. Well, maybe not literally, but it’s not helpful. Researchers recruited 60 Candy Crush players who were at various levels in the game. They had the participants play early levels that were far too easy or levels balanced with their gameplay abilities.
Players in the easy-level group got bored and quit far earlier than did those in the advanced-level group. The group playing to their abilities were able to access a “flow” state and focus all their attention on the game. While this is all well and good for their gaming performance, according to the researchers, it confirms the theory that playing to escape boredom or negative emotions is more likely to lead to addiction. As with all addictions, the temporary high can give way to a self-repeating loop, causing patients to ignore real life and deepen depression.
The researchers hope their findings will encourage game developers to “consider implementing responsible video gaming tools directly within their games.” Comedy gold. Perhaps Canadians’ idea of capitalism is a little different from that of those south of the border.
Hiccups and vaccine refusal
Tonight, LOTME News dives into the fetid cesspool that is international politics and comes out with … hiccups?
But first, a word from our sponsor, Fearless Boxing Club of South Etobicoke, Ontario.
Are you looking to flout public health restrictions? Do you want to spend time in an enclosed space with other people who haven’t gotten the COVID-19 vaccine? Do you “feel safer waiting until more research is done on the side effects being discovered right now”? (We are not making this up.)
Then join the Fearless Boxing Club, because we “will not be accepting any vaccinated members.” Our founders, Mohammed Abedeen and Krystal Glazier-Roscoe, are working hard to exclude “those who received the experimental COVID vaccine.” (Still not making it up.)
And now, back to the news.
Brazilian president Jair Bolsonaro was hospitalized recently for a severe case of hiccups that may have been related to a stab wound he received in 2018. [Nope, didn’t make that up, either.]
Mr. Bolsonaro had been hiccuping for 10 days, and was experiencing abdominal pain and difficulty speaking, when he entered the hospital on July 14. Since being stabbed while on the campaign trail, he has undergone several operations, which may have led to the partial intestinal obstruction that caused his latest symptoms.
His medical team advised Mr. Bolsonaro to go on a diet to aid his recovery, but when he was released on July 18 he said, “I hope in 10 days I’ll be eating barbecued ribs.” (Maybe this is all just a lucid dream. Probably shouldn’t have had ribs right before bed.)
I dream of alien abductions
There he goes! It’s lunchtime and your colleague Tom is going on and on again about that time he was abducted by aliens. It sounds ridiculous, but he does make some convincing arguments. Tom thinks it was real, but could it have all just been in his head?
Lucid dreaming may help explain alleged alien abductions. During a lucid dream, people know that they’re dreaming, and can also have some control over how the dreams play out. During some dream states, a person can feel intense sensations, such as terror and paralysis, so it’s no wonder these dreams feel so real.
In a recent study, scientists encouraged 152 participants who had self-identified as lucid dreamers to dream about aliens. Many (75%) of the participants were able to dream about alien encounters, and 15% “achieved relatively realistic experiences,” the investigators reported.
So cut Tom some slack. He’s not crazy, he might just have lucid dreaming privileges. Tell him he should dream about something more fun, like a vacation in the Bahamas.
Follow your heart: Drink more coffee
It seems like the world is divided into coffee drinkers and non–coffee drinkers. Then there’s decaf and regular drinkers. Whichever camp you fall into, know this: The widespread belief that caffeine consumption has an effect on your heart is all beans.
In what is the largest investigation of its kind, researchers from the University of California, San Francisco, looked into whether drinking caffeinated coffee was linked to a risk for heart arrhythmia. They also researched whether patients with genetic variants that affect their metabolism could change that association. Almost 400,000 people with a mean age of 56 years participated in the study. More than half of the participants were women.
The investigators analyzed the participants’ self-reported coffee consumption using a technique called Mendelian randomization to leverage genetic data with the participants’ relationship with caffeine, making it an even field and not relying on the participant consumption self-reporting for outcomes as in previous studies.
What they found, after the 4-year follow up, was nothing short of myth busting.
“We found no evidence that caffeine consumption leads to a greater risk of arrhythmias,” said senior and corresponding author Gregory Marcus, MD. “Our population-based study provides reassurance that common prohibitions against caffeine to reduce arrhythmia risk are likely unwarranted.”
There was no evidence of a heightened risk of arrhythmias in participants who were genetically predisposed to metabolize caffeine differently from those who were not. And, there was a 3% reduction of arrhythmias in patients who consumed higher amounts of coffee.
We are not lobbying for Big Caffeine, but this study adds to the reported health benefits linked to coffee, which already include reduced risk for cancer, diabetes, and Parkinson’s disease, with an added bonus of anti-inflammatory benefits. So, the next time you’re hesitant to pour that second cup of Joe, just go for it. Your heart can take it.
Bored? Feeling down? Don’t play Candy Crush
Now hang on, aren’t those the perfect times to play video games? If there’s nothing else to do, why not open Candy Crush and mindlessly power through the levels?
Because, according to a study by a group of Canadian researchers, it’s actually the worst thing you can do. Well, maybe not literally, but it’s not helpful. Researchers recruited 60 Candy Crush players who were at various levels in the game. They had the participants play early levels that were far too easy or levels balanced with their gameplay abilities.
Players in the easy-level group got bored and quit far earlier than did those in the advanced-level group. The group playing to their abilities were able to access a “flow” state and focus all their attention on the game. While this is all well and good for their gaming performance, according to the researchers, it confirms the theory that playing to escape boredom or negative emotions is more likely to lead to addiction. As with all addictions, the temporary high can give way to a self-repeating loop, causing patients to ignore real life and deepen depression.
The researchers hope their findings will encourage game developers to “consider implementing responsible video gaming tools directly within their games.” Comedy gold. Perhaps Canadians’ idea of capitalism is a little different from that of those south of the border.
Hiccups and vaccine refusal
Tonight, LOTME News dives into the fetid cesspool that is international politics and comes out with … hiccups?
But first, a word from our sponsor, Fearless Boxing Club of South Etobicoke, Ontario.
Are you looking to flout public health restrictions? Do you want to spend time in an enclosed space with other people who haven’t gotten the COVID-19 vaccine? Do you “feel safer waiting until more research is done on the side effects being discovered right now”? (We are not making this up.)
Then join the Fearless Boxing Club, because we “will not be accepting any vaccinated members.” Our founders, Mohammed Abedeen and Krystal Glazier-Roscoe, are working hard to exclude “those who received the experimental COVID vaccine.” (Still not making it up.)
And now, back to the news.
Brazilian president Jair Bolsonaro was hospitalized recently for a severe case of hiccups that may have been related to a stab wound he received in 2018. [Nope, didn’t make that up, either.]
Mr. Bolsonaro had been hiccuping for 10 days, and was experiencing abdominal pain and difficulty speaking, when he entered the hospital on July 14. Since being stabbed while on the campaign trail, he has undergone several operations, which may have led to the partial intestinal obstruction that caused his latest symptoms.
His medical team advised Mr. Bolsonaro to go on a diet to aid his recovery, but when he was released on July 18 he said, “I hope in 10 days I’ll be eating barbecued ribs.” (Maybe this is all just a lucid dream. Probably shouldn’t have had ribs right before bed.)

















