User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
We asked doctors using AI scribes: Just how good are they?
Andrea Partida, DO, an obstetrician and gynecologist in Enid, Okla., loves her new assistant.
The 15 or 20 minutes she used to spend on documentation for each patient visit is now 3. The 2-3 hours she’d spend charting outside clinic hours is maybe 1.
All that time saved allows her to see two to five more patients a day, provide better care to each patient, and get more involved in hospital leadership at Integris Health, where she works.
“I have a better work-life balance with my family,” Dr. Partida said. “I leave work at work and get home earlier.”
You’ve probably figured out the plot twist: Dr. Partida’s assistant is not a person – it’s artificial intelligence (AI).
Dr. Partida uses IRIS, a tool from OnPoint Healthcare Partners, part of a fast-growing niche of AI medical scribes designed to automate onerous data entry. The evolution of generative AI – specifically, large language models, such as ChatGPT – has led to a rapid explosion of these tools. Other companies in the space include Abridge, Ambience Healthcare, Augmedix, DeepScribe, Nuance (part of Microsoft), and Suki. The newest kid on the block, Amazon Web Services, announced the launch of HealthScribe in July.
These tools – some of which are already on the market, with more on the way – record patient visits and generate notes for treatment and billing. Earlier iterations combine AI with offsite human scribes who provide quality control. But more and more are fully automated, no human required. Some also offer video recording and foreign language translation.
The promise is alluring: Ease your workload and reclaim hours in your day so you can spend more time with patients or try that “work-life balance” thing you’ve heard so much about.
But do these tools fulfill that promise?
According to Dr. Partida and other doctors who spoke with this news organization, the answer is a resounding yes.
A tech solution for a tech problem
“I believe a lot of doctors see patients for free. They get paid to do paperwork,” said Anthony J. Mazzarelli, MD, JD, MBE, co-president and CEO of Cooper University Health Care, in Camden, N.J.
Indeed, for every hour U.S. clinicians spend with their patients, they may spend 2 more hours documenting in electronic health records (EHRs), estimates show. About half of doctors, especially those in primary care, report feeling burned out, and some 42% say they want to quit clinical practice.
Enter AI scribes.
“The holy grail in medicine right now is improving burnout while also maintaining or improving productivity and quality,” said Patricia Garcia, MD, associate clinical information officer for ambulatory care at Stanford (Calif.) Health Care. “These ambient digital scribes have the potential to do just that.”
While anyone can buy these products, their use has been mostly limited to pilot programs and early adopters so far, said Dr. Garcia, who has been helping to pilot Nuance’s digital scribe, DAX, at Stanford.
But that’s expected to change quickly. “I don’t think the time horizon is a decade,” Dr. Garcia said. “I think within a matter of 2 or 3 years, these tools will be pervasive throughout health care.”
Since introducing these tools at Cooper, “our doctors’ paperwork burden is significantly lighter,” said Dr. Mazzarelli, who decides which technologies Cooper should invest in and who monitors their results. In Cooper studies, physicians who used DAX more than half the time spent 43% less time working on notes.
“They spend more time connecting with their patients, talking with them, and looking them in the eye,” Dr. Mazzarelli said. That, in turn, seems to improve patient outcomes, reduce doctor burnout and turnover, and lower costs.
The AI scribes, by virtue of eliminating the distraction of note taking, also allow doctors to give their full attention to the patient. “The patient relationship is the most important aspect of medicine,” said Raul Ayala, MD, MHCM, a family medicine physician at Adventist Health, in Hanford, Calif., who uses Augmedix. The digital scribe “helps us strengthen that relationship.”
What’s it like to use an AI medical scribe?
The scribes feature hardware (typically a smartphone or tablet) and software built on automatic speech recognition, natural language processing, and machine learning. Download an app to your device, and you’re ready to go. Use it to record in-person or telehealth visits.
In the first week, a company may help train you to use the hardware and software. You’ll likely start by using it for a few patient visits per day, ramping up gradually. Dr. Partida said she was comfortable using the system for all her patients in 6 weeks.
Each day, Dr. Partida logs in to a dedicated smartphone or tablet, opens the app, and reviews her schedule, including details she needs to prepare for each patient.
At the start of each patient visit, Dr. Partida taps the app icon to begin recording and lays the device nearby. She can pause as needed. At the end of the visit, she taps the icon again to stop recording.
The AI listens, creates the note, and updates relevant data in the EHR. The note includes patient problems, assessment, treatment plan, patient history, orders, and tasks for staff, along with medications, referrals, and preauthorizations. A human scribe, who is also a physician, reviews the information for accuracy and edits it as needed. By the next morning, the data are ready for Dr. Partida to review.
Fully automated versions can generate notes much faster. Jack Shilling, MD, MBA, an orthopedic surgeon at Cooper University Health Care, in Voorhees, N.J., uses DAX. A new feature called DAX Express – which uses OpenAI’s GPT-4 but no humans – provides him with a draft of his clinical notes in just seconds.
How accurate are AI notes?
The accuracy of those notes remains an open question, Dr. Garcia said – mostly because accuracy can be hard to define.
“If you asked five docs to write a note based on the same patient encounter, you’d get five different notes,” Dr. Garcia said. “That makes it hard to assess these technologies in a scientifically rigorous way.”
Still, the onus is on the physician to review the notes and edit them as needed, Dr. Garcia said. How light or heavy those edits are can depend on your unique preferences.
Dr. Shilling said he may need to lightly edit transcripts of his conversations with patients. “When someone tells me how long their knee hurts, slight variability in their transcribed words is tolerable,” he said. But for some things – such as physical exam notes and x-ray readings – he dictates directly into the device, speaking at a closer range and being less conversational, more exact in his speech.
Should you let patients know they’re being recorded?
The federal Health Insurance Portability and Accountability Act (HIPAA) does not require providers to inform patients that their face-to-face conversations are being recorded, said Daniel Lebovic, JD, corporate legal counsel at Compliancy Group, in Greenlawn, N.Y., a company that helps providers adhere to HIPAA rules.
But make sure you know the laws in your state and the policies at your health care practice. State laws may require providers to inform patients and to get patients’ consent in advance of being recorded.
All the doctors who spoke to this news organization said their patients are informed that they’ll be recorded and that they can opt out if they wish.
How much do AI scribes cost?
As the marketplace for these tools expands, companies are offering more products and services at different price points that target a range of organizations, from large health care systems to small private practices.
Price models vary, said Dr. Garcia. Some are based on the number of users, others on the number of notes, and still others on minutes.
Amazon’s HealthScribe is priced at 10 cents per minute. For 1,000 consultation transcripts per month, with each call averaging 15 minutes, it would take 15,000 minutes at a total cost of $1,500 for the month.
In general, the rapidly growing competition in this space could mean prices become more affordable, Dr. Garcia said. “It’s good that so many are getting into this game, because that means the price will come down and it will be a lot more accessible to everybody.”
A version of this article appeared on Medscape.com.
Andrea Partida, DO, an obstetrician and gynecologist in Enid, Okla., loves her new assistant.
The 15 or 20 minutes she used to spend on documentation for each patient visit is now 3. The 2-3 hours she’d spend charting outside clinic hours is maybe 1.
All that time saved allows her to see two to five more patients a day, provide better care to each patient, and get more involved in hospital leadership at Integris Health, where she works.
“I have a better work-life balance with my family,” Dr. Partida said. “I leave work at work and get home earlier.”
You’ve probably figured out the plot twist: Dr. Partida’s assistant is not a person – it’s artificial intelligence (AI).
Dr. Partida uses IRIS, a tool from OnPoint Healthcare Partners, part of a fast-growing niche of AI medical scribes designed to automate onerous data entry. The evolution of generative AI – specifically, large language models, such as ChatGPT – has led to a rapid explosion of these tools. Other companies in the space include Abridge, Ambience Healthcare, Augmedix, DeepScribe, Nuance (part of Microsoft), and Suki. The newest kid on the block, Amazon Web Services, announced the launch of HealthScribe in July.
These tools – some of which are already on the market, with more on the way – record patient visits and generate notes for treatment and billing. Earlier iterations combine AI with offsite human scribes who provide quality control. But more and more are fully automated, no human required. Some also offer video recording and foreign language translation.
The promise is alluring: Ease your workload and reclaim hours in your day so you can spend more time with patients or try that “work-life balance” thing you’ve heard so much about.
But do these tools fulfill that promise?
According to Dr. Partida and other doctors who spoke with this news organization, the answer is a resounding yes.
A tech solution for a tech problem
“I believe a lot of doctors see patients for free. They get paid to do paperwork,” said Anthony J. Mazzarelli, MD, JD, MBE, co-president and CEO of Cooper University Health Care, in Camden, N.J.
Indeed, for every hour U.S. clinicians spend with their patients, they may spend 2 more hours documenting in electronic health records (EHRs), estimates show. About half of doctors, especially those in primary care, report feeling burned out, and some 42% say they want to quit clinical practice.
Enter AI scribes.
“The holy grail in medicine right now is improving burnout while also maintaining or improving productivity and quality,” said Patricia Garcia, MD, associate clinical information officer for ambulatory care at Stanford (Calif.) Health Care. “These ambient digital scribes have the potential to do just that.”
While anyone can buy these products, their use has been mostly limited to pilot programs and early adopters so far, said Dr. Garcia, who has been helping to pilot Nuance’s digital scribe, DAX, at Stanford.
But that’s expected to change quickly. “I don’t think the time horizon is a decade,” Dr. Garcia said. “I think within a matter of 2 or 3 years, these tools will be pervasive throughout health care.”
Since introducing these tools at Cooper, “our doctors’ paperwork burden is significantly lighter,” said Dr. Mazzarelli, who decides which technologies Cooper should invest in and who monitors their results. In Cooper studies, physicians who used DAX more than half the time spent 43% less time working on notes.
“They spend more time connecting with their patients, talking with them, and looking them in the eye,” Dr. Mazzarelli said. That, in turn, seems to improve patient outcomes, reduce doctor burnout and turnover, and lower costs.
The AI scribes, by virtue of eliminating the distraction of note taking, also allow doctors to give their full attention to the patient. “The patient relationship is the most important aspect of medicine,” said Raul Ayala, MD, MHCM, a family medicine physician at Adventist Health, in Hanford, Calif., who uses Augmedix. The digital scribe “helps us strengthen that relationship.”
What’s it like to use an AI medical scribe?
The scribes feature hardware (typically a smartphone or tablet) and software built on automatic speech recognition, natural language processing, and machine learning. Download an app to your device, and you’re ready to go. Use it to record in-person or telehealth visits.
In the first week, a company may help train you to use the hardware and software. You’ll likely start by using it for a few patient visits per day, ramping up gradually. Dr. Partida said she was comfortable using the system for all her patients in 6 weeks.
Each day, Dr. Partida logs in to a dedicated smartphone or tablet, opens the app, and reviews her schedule, including details she needs to prepare for each patient.
At the start of each patient visit, Dr. Partida taps the app icon to begin recording and lays the device nearby. She can pause as needed. At the end of the visit, she taps the icon again to stop recording.
The AI listens, creates the note, and updates relevant data in the EHR. The note includes patient problems, assessment, treatment plan, patient history, orders, and tasks for staff, along with medications, referrals, and preauthorizations. A human scribe, who is also a physician, reviews the information for accuracy and edits it as needed. By the next morning, the data are ready for Dr. Partida to review.
Fully automated versions can generate notes much faster. Jack Shilling, MD, MBA, an orthopedic surgeon at Cooper University Health Care, in Voorhees, N.J., uses DAX. A new feature called DAX Express – which uses OpenAI’s GPT-4 but no humans – provides him with a draft of his clinical notes in just seconds.
How accurate are AI notes?
The accuracy of those notes remains an open question, Dr. Garcia said – mostly because accuracy can be hard to define.
“If you asked five docs to write a note based on the same patient encounter, you’d get five different notes,” Dr. Garcia said. “That makes it hard to assess these technologies in a scientifically rigorous way.”
Still, the onus is on the physician to review the notes and edit them as needed, Dr. Garcia said. How light or heavy those edits are can depend on your unique preferences.
Dr. Shilling said he may need to lightly edit transcripts of his conversations with patients. “When someone tells me how long their knee hurts, slight variability in their transcribed words is tolerable,” he said. But for some things – such as physical exam notes and x-ray readings – he dictates directly into the device, speaking at a closer range and being less conversational, more exact in his speech.
Should you let patients know they’re being recorded?
The federal Health Insurance Portability and Accountability Act (HIPAA) does not require providers to inform patients that their face-to-face conversations are being recorded, said Daniel Lebovic, JD, corporate legal counsel at Compliancy Group, in Greenlawn, N.Y., a company that helps providers adhere to HIPAA rules.
But make sure you know the laws in your state and the policies at your health care practice. State laws may require providers to inform patients and to get patients’ consent in advance of being recorded.
All the doctors who spoke to this news organization said their patients are informed that they’ll be recorded and that they can opt out if they wish.
How much do AI scribes cost?
As the marketplace for these tools expands, companies are offering more products and services at different price points that target a range of organizations, from large health care systems to small private practices.
Price models vary, said Dr. Garcia. Some are based on the number of users, others on the number of notes, and still others on minutes.
Amazon’s HealthScribe is priced at 10 cents per minute. For 1,000 consultation transcripts per month, with each call averaging 15 minutes, it would take 15,000 minutes at a total cost of $1,500 for the month.
In general, the rapidly growing competition in this space could mean prices become more affordable, Dr. Garcia said. “It’s good that so many are getting into this game, because that means the price will come down and it will be a lot more accessible to everybody.”
A version of this article appeared on Medscape.com.
Andrea Partida, DO, an obstetrician and gynecologist in Enid, Okla., loves her new assistant.
The 15 or 20 minutes she used to spend on documentation for each patient visit is now 3. The 2-3 hours she’d spend charting outside clinic hours is maybe 1.
All that time saved allows her to see two to five more patients a day, provide better care to each patient, and get more involved in hospital leadership at Integris Health, where she works.
“I have a better work-life balance with my family,” Dr. Partida said. “I leave work at work and get home earlier.”
You’ve probably figured out the plot twist: Dr. Partida’s assistant is not a person – it’s artificial intelligence (AI).
Dr. Partida uses IRIS, a tool from OnPoint Healthcare Partners, part of a fast-growing niche of AI medical scribes designed to automate onerous data entry. The evolution of generative AI – specifically, large language models, such as ChatGPT – has led to a rapid explosion of these tools. Other companies in the space include Abridge, Ambience Healthcare, Augmedix, DeepScribe, Nuance (part of Microsoft), and Suki. The newest kid on the block, Amazon Web Services, announced the launch of HealthScribe in July.
These tools – some of which are already on the market, with more on the way – record patient visits and generate notes for treatment and billing. Earlier iterations combine AI with offsite human scribes who provide quality control. But more and more are fully automated, no human required. Some also offer video recording and foreign language translation.
The promise is alluring: Ease your workload and reclaim hours in your day so you can spend more time with patients or try that “work-life balance” thing you’ve heard so much about.
But do these tools fulfill that promise?
According to Dr. Partida and other doctors who spoke with this news organization, the answer is a resounding yes.
A tech solution for a tech problem
“I believe a lot of doctors see patients for free. They get paid to do paperwork,” said Anthony J. Mazzarelli, MD, JD, MBE, co-president and CEO of Cooper University Health Care, in Camden, N.J.
Indeed, for every hour U.S. clinicians spend with their patients, they may spend 2 more hours documenting in electronic health records (EHRs), estimates show. About half of doctors, especially those in primary care, report feeling burned out, and some 42% say they want to quit clinical practice.
Enter AI scribes.
“The holy grail in medicine right now is improving burnout while also maintaining or improving productivity and quality,” said Patricia Garcia, MD, associate clinical information officer for ambulatory care at Stanford (Calif.) Health Care. “These ambient digital scribes have the potential to do just that.”
While anyone can buy these products, their use has been mostly limited to pilot programs and early adopters so far, said Dr. Garcia, who has been helping to pilot Nuance’s digital scribe, DAX, at Stanford.
But that’s expected to change quickly. “I don’t think the time horizon is a decade,” Dr. Garcia said. “I think within a matter of 2 or 3 years, these tools will be pervasive throughout health care.”
Since introducing these tools at Cooper, “our doctors’ paperwork burden is significantly lighter,” said Dr. Mazzarelli, who decides which technologies Cooper should invest in and who monitors their results. In Cooper studies, physicians who used DAX more than half the time spent 43% less time working on notes.
“They spend more time connecting with their patients, talking with them, and looking them in the eye,” Dr. Mazzarelli said. That, in turn, seems to improve patient outcomes, reduce doctor burnout and turnover, and lower costs.
The AI scribes, by virtue of eliminating the distraction of note taking, also allow doctors to give their full attention to the patient. “The patient relationship is the most important aspect of medicine,” said Raul Ayala, MD, MHCM, a family medicine physician at Adventist Health, in Hanford, Calif., who uses Augmedix. The digital scribe “helps us strengthen that relationship.”
What’s it like to use an AI medical scribe?
The scribes feature hardware (typically a smartphone or tablet) and software built on automatic speech recognition, natural language processing, and machine learning. Download an app to your device, and you’re ready to go. Use it to record in-person or telehealth visits.
In the first week, a company may help train you to use the hardware and software. You’ll likely start by using it for a few patient visits per day, ramping up gradually. Dr. Partida said she was comfortable using the system for all her patients in 6 weeks.
Each day, Dr. Partida logs in to a dedicated smartphone or tablet, opens the app, and reviews her schedule, including details she needs to prepare for each patient.
At the start of each patient visit, Dr. Partida taps the app icon to begin recording and lays the device nearby. She can pause as needed. At the end of the visit, she taps the icon again to stop recording.
The AI listens, creates the note, and updates relevant data in the EHR. The note includes patient problems, assessment, treatment plan, patient history, orders, and tasks for staff, along with medications, referrals, and preauthorizations. A human scribe, who is also a physician, reviews the information for accuracy and edits it as needed. By the next morning, the data are ready for Dr. Partida to review.
Fully automated versions can generate notes much faster. Jack Shilling, MD, MBA, an orthopedic surgeon at Cooper University Health Care, in Voorhees, N.J., uses DAX. A new feature called DAX Express – which uses OpenAI’s GPT-4 but no humans – provides him with a draft of his clinical notes in just seconds.
How accurate are AI notes?
The accuracy of those notes remains an open question, Dr. Garcia said – mostly because accuracy can be hard to define.
“If you asked five docs to write a note based on the same patient encounter, you’d get five different notes,” Dr. Garcia said. “That makes it hard to assess these technologies in a scientifically rigorous way.”
Still, the onus is on the physician to review the notes and edit them as needed, Dr. Garcia said. How light or heavy those edits are can depend on your unique preferences.
Dr. Shilling said he may need to lightly edit transcripts of his conversations with patients. “When someone tells me how long their knee hurts, slight variability in their transcribed words is tolerable,” he said. But for some things – such as physical exam notes and x-ray readings – he dictates directly into the device, speaking at a closer range and being less conversational, more exact in his speech.
Should you let patients know they’re being recorded?
The federal Health Insurance Portability and Accountability Act (HIPAA) does not require providers to inform patients that their face-to-face conversations are being recorded, said Daniel Lebovic, JD, corporate legal counsel at Compliancy Group, in Greenlawn, N.Y., a company that helps providers adhere to HIPAA rules.
But make sure you know the laws in your state and the policies at your health care practice. State laws may require providers to inform patients and to get patients’ consent in advance of being recorded.
All the doctors who spoke to this news organization said their patients are informed that they’ll be recorded and that they can opt out if they wish.
How much do AI scribes cost?
As the marketplace for these tools expands, companies are offering more products and services at different price points that target a range of organizations, from large health care systems to small private practices.
Price models vary, said Dr. Garcia. Some are based on the number of users, others on the number of notes, and still others on minutes.
Amazon’s HealthScribe is priced at 10 cents per minute. For 1,000 consultation transcripts per month, with each call averaging 15 minutes, it would take 15,000 minutes at a total cost of $1,500 for the month.
In general, the rapidly growing competition in this space could mean prices become more affordable, Dr. Garcia said. “It’s good that so many are getting into this game, because that means the price will come down and it will be a lot more accessible to everybody.”
A version of this article appeared on Medscape.com.
Drug name confusion: More than 80 new drug pairs added to the list
Zolpidem (Ambien) is a well-known sedative for sleep. Letairis (Ambrisentan) is a vasodilator for the treatment of pulmonary arterial hypertension. Citalopram (Celexa) is an antidepressant; escitalopram (Lexapro) is prescribed for anxiety and depression.
The aim is to increase awareness about the potential for a serious medication mistake when the wrong drug is given because of drug names that look and sound similar.
Awareness of these drug names, however, is just the first step in preventing medication mistakes. Health care providers should take a number of other steps as well, experts said.
ISMP launched its confusing drug names list, previously called look-alike, sound-alike (LASA) drugs, in 2008. The new list is an update of the 2019 version, said Michael J. Gaunt, PharmD, senior manager of error reporting programs for the ISMP, which focuses on the prevention of medication mistakes. The new entries were chosen on the basis of a number of factors, including ISMP’s analysis of recent medication mishap reports that were submitted to it.
The ISMP list now includes about 528 drug pairs, Dr. Gaunt said. The list is long, he said, partly because each pair is listed twice, so readers can cross reference. For instance, hydralazine and hydroxyzine are listed in one entry in the list, and hydroxyzine and hydralazine are listed in another.
Brand Institute in Miami has named, among other drugs, Entresto, Rybelsus, and Lunesta. The regulatory arm of the company, the Drug Safety Institute, “considers drug names that have been confused as an important part of our comprehensive drug name assessments,” Todd Bridges, global president of the institute, said in an emailed statement. Information on the confusing drug names are incorporated into the company’s proprietary algorithm and is used when developing brand names for drugs. “We continually update this algorithm as new drug names that are often confused are identified,” Mr. Bridges said.
Confusing drug names: Ongoing issue
The length of the list, as well as the latest additions, are not surprising, said Mary Ann Kliethermes, PharmD, director of medication safety and quality for the American Society of Health-System Pharmacists, a membership organization of about 60,000 pharmacists who practice in inpatient and outpatient settings.
“I’ve been in practice over 45 years,” she said, “and this has been a problem ever since I have been in practice.” The sheer volume of new drugs is one reason, she said. From 2013 through 2022, the U.S. Food and Drug Administration approved an average of 43 novel drugs per year, according to a report from its Center for Drug Evaluation and Research. “Since the 90s, this [confusion about similar drug names] has happened,” Dr. Kliethermes said.
According to a 2023 report, about 7,000-9,000 people die each year in the United States as the result of a medication error. However, it’s impossible to say for sure what percentage of those errors involve name confusion, Dr. Gaunt said.
Not all the mistakes are reported. Some that are reported are dramatic and deadly. In 2022, a Tennessee nurse was convicted of gross neglect and negligent homicide. She was sentenced to 3 years’ probation after she mistakenly gave vercuronium, an anesthetic agent, instead of the sedative Versed to a patient, and the woman died.
Updated list: A closer look
Many of the new drug pairs that are listed in the update are cephalosporins, said Dr. Kliethermes, who reviewed the new list for this news organization. In all, 20 of the latest 82 additions are cephalosporins. These include drugs such as cefazolin, which can be confused with cefotetan, and vice versa. These drugs have been around since the 1980s, she said, but “they needed to be on there.” Even in the 1980s, it was becoming difficult to differentiate them, and there were fewer drugs in that class then, she said.
Influenza vaccines made the new list, too. Fluzone High-Dose Quadrivalent can be confused with fluzone quadrivalent. Other new additions: hydrochlorothiazide and hydroxychloroquine, Lasik and Wakix, Pitressin and Pitocin, Remeron and Rozerem.
Beyond the list
While it’s not possible to pinpoint how big a problem name confusion is in causing medication mistakes, “it is certainly still an issue,” Dr. Gaunt said. A variety of practices can reduce that risk substantially, Dr. Gaunt and Dr. Kliethermes agreed.
Tall-man lettering. Both the FDA and the ISMP recommend the use of so-called tall-man lettering (TML), which involves the use of uppercase letters, sometimes in boldface, to distinguish similar names on product labels and elsewhere. Examples include vinBLAStine and vinCRIStine.
Electronic prescribing. “It eliminates the risk of handwriting confusion,” Dr. Gaunt said. However, electronic prescribing can have a downside, Dr. Kliethermes said. When ordering medication, a person may type in a few letters and may then be presented with a prompt that lists several drug names, and it can be easy to click the wrong one. For that reason, ISMP and other experts recommend typing at least five letters when searching for a medication in an electronic system.
Use both brand and generic names on labels and prescriptions.
Write the indication. That can serve as a double check. If a prescription for Ambien says “For sleep,” there’s probably less risk of filling a prescription for ambrisentan, the vasodilator.
Smart formulary additions. When hospitals add medications to their formularies, “part of that formulary assessment should include looking at the potential risk for errors,” Dr. Gaunt said. This involves keeping an eye out for confusing names and similar packaging. “Do that analysis up front and put in strategies to minimize that. Maybe you look for a different drug [for the same use] that has a different name.” Or choose a different manufacturer, so the medication would at least have a different container.
Use bar code scanning. Suppose a pharmacist goes to the shelf and pulls the wrong drug. “Bar code scanning provides the opportunity to catch the error,” Dr. Gaunt said. Many community pharmacies now have bar code scanning. ISMP just issued best practices for community pharmacies, Dr. Gaunt said, and these include the use of bar code scanning and other measures.
Educate consumers. Health care providers can educate consumers on how to minimize the risk of getting the wrong drug, Dr. Gaunt said. When patients are picking up a prescription, suggest they look at the container label; if it looks different from previous prescriptions of the same medicine, ask the pharmacist for an explanation. Some patients just pass it off, Dr. Gaunt said, figuring the pharmacist or health plan switched manufacturers of their medication.
Access the list. The entire list is on the ISMP site and is accessible after free registration.
Goal: Preventing confusion
The FDA has provided guidance for industry on naming drugs not yet approved so that the proposed names are not too similar in sound or appearance to those already on the market. Included in the lengthy document are checklists, such as, “Across a range of dialects, are the names consistently pronounced differently?” and “Are the lengths of the names dissimilar when scripted?” (Lengths are considered different if they differ by two or more letters.)
The FDA also offers the phonetic and orthographic computer analysis (POCA) program, a software tool that employs an advanced algorithm to evaluate similarities between two drug names. The data sources are updated regularly as new drugs are approved.
Liability update
The problem may be decreasing. In a 2020 report, researchers used pharmacists’ professional liability claim data from the Healthcare Providers Service Organization. They compared 2018 data on claims with 2013 data. The percentage of claims associated with wrong drug dispensing errors declined from 43.8% in 2013 to 36.8% in 2018. Wrong dose claims also declined, from 31.5% to 15.3%.
These researchers concluded that technology and automation have contributed to the prevention of medication errors caused by the use of the wrong drug and the wrong dose, but mistakes continue, owing to system and human errors.
A version of this article first appeared on Medscape.com.
Zolpidem (Ambien) is a well-known sedative for sleep. Letairis (Ambrisentan) is a vasodilator for the treatment of pulmonary arterial hypertension. Citalopram (Celexa) is an antidepressant; escitalopram (Lexapro) is prescribed for anxiety and depression.
The aim is to increase awareness about the potential for a serious medication mistake when the wrong drug is given because of drug names that look and sound similar.
Awareness of these drug names, however, is just the first step in preventing medication mistakes. Health care providers should take a number of other steps as well, experts said.
ISMP launched its confusing drug names list, previously called look-alike, sound-alike (LASA) drugs, in 2008. The new list is an update of the 2019 version, said Michael J. Gaunt, PharmD, senior manager of error reporting programs for the ISMP, which focuses on the prevention of medication mistakes. The new entries were chosen on the basis of a number of factors, including ISMP’s analysis of recent medication mishap reports that were submitted to it.
The ISMP list now includes about 528 drug pairs, Dr. Gaunt said. The list is long, he said, partly because each pair is listed twice, so readers can cross reference. For instance, hydralazine and hydroxyzine are listed in one entry in the list, and hydroxyzine and hydralazine are listed in another.
Brand Institute in Miami has named, among other drugs, Entresto, Rybelsus, and Lunesta. The regulatory arm of the company, the Drug Safety Institute, “considers drug names that have been confused as an important part of our comprehensive drug name assessments,” Todd Bridges, global president of the institute, said in an emailed statement. Information on the confusing drug names are incorporated into the company’s proprietary algorithm and is used when developing brand names for drugs. “We continually update this algorithm as new drug names that are often confused are identified,” Mr. Bridges said.
Confusing drug names: Ongoing issue
The length of the list, as well as the latest additions, are not surprising, said Mary Ann Kliethermes, PharmD, director of medication safety and quality for the American Society of Health-System Pharmacists, a membership organization of about 60,000 pharmacists who practice in inpatient and outpatient settings.
“I’ve been in practice over 45 years,” she said, “and this has been a problem ever since I have been in practice.” The sheer volume of new drugs is one reason, she said. From 2013 through 2022, the U.S. Food and Drug Administration approved an average of 43 novel drugs per year, according to a report from its Center for Drug Evaluation and Research. “Since the 90s, this [confusion about similar drug names] has happened,” Dr. Kliethermes said.
According to a 2023 report, about 7,000-9,000 people die each year in the United States as the result of a medication error. However, it’s impossible to say for sure what percentage of those errors involve name confusion, Dr. Gaunt said.
Not all the mistakes are reported. Some that are reported are dramatic and deadly. In 2022, a Tennessee nurse was convicted of gross neglect and negligent homicide. She was sentenced to 3 years’ probation after she mistakenly gave vercuronium, an anesthetic agent, instead of the sedative Versed to a patient, and the woman died.
Updated list: A closer look
Many of the new drug pairs that are listed in the update are cephalosporins, said Dr. Kliethermes, who reviewed the new list for this news organization. In all, 20 of the latest 82 additions are cephalosporins. These include drugs such as cefazolin, which can be confused with cefotetan, and vice versa. These drugs have been around since the 1980s, she said, but “they needed to be on there.” Even in the 1980s, it was becoming difficult to differentiate them, and there were fewer drugs in that class then, she said.
Influenza vaccines made the new list, too. Fluzone High-Dose Quadrivalent can be confused with fluzone quadrivalent. Other new additions: hydrochlorothiazide and hydroxychloroquine, Lasik and Wakix, Pitressin and Pitocin, Remeron and Rozerem.
Beyond the list
While it’s not possible to pinpoint how big a problem name confusion is in causing medication mistakes, “it is certainly still an issue,” Dr. Gaunt said. A variety of practices can reduce that risk substantially, Dr. Gaunt and Dr. Kliethermes agreed.
Tall-man lettering. Both the FDA and the ISMP recommend the use of so-called tall-man lettering (TML), which involves the use of uppercase letters, sometimes in boldface, to distinguish similar names on product labels and elsewhere. Examples include vinBLAStine and vinCRIStine.
Electronic prescribing. “It eliminates the risk of handwriting confusion,” Dr. Gaunt said. However, electronic prescribing can have a downside, Dr. Kliethermes said. When ordering medication, a person may type in a few letters and may then be presented with a prompt that lists several drug names, and it can be easy to click the wrong one. For that reason, ISMP and other experts recommend typing at least five letters when searching for a medication in an electronic system.
Use both brand and generic names on labels and prescriptions.
Write the indication. That can serve as a double check. If a prescription for Ambien says “For sleep,” there’s probably less risk of filling a prescription for ambrisentan, the vasodilator.
Smart formulary additions. When hospitals add medications to their formularies, “part of that formulary assessment should include looking at the potential risk for errors,” Dr. Gaunt said. This involves keeping an eye out for confusing names and similar packaging. “Do that analysis up front and put in strategies to minimize that. Maybe you look for a different drug [for the same use] that has a different name.” Or choose a different manufacturer, so the medication would at least have a different container.
Use bar code scanning. Suppose a pharmacist goes to the shelf and pulls the wrong drug. “Bar code scanning provides the opportunity to catch the error,” Dr. Gaunt said. Many community pharmacies now have bar code scanning. ISMP just issued best practices for community pharmacies, Dr. Gaunt said, and these include the use of bar code scanning and other measures.
Educate consumers. Health care providers can educate consumers on how to minimize the risk of getting the wrong drug, Dr. Gaunt said. When patients are picking up a prescription, suggest they look at the container label; if it looks different from previous prescriptions of the same medicine, ask the pharmacist for an explanation. Some patients just pass it off, Dr. Gaunt said, figuring the pharmacist or health plan switched manufacturers of their medication.
Access the list. The entire list is on the ISMP site and is accessible after free registration.
Goal: Preventing confusion
The FDA has provided guidance for industry on naming drugs not yet approved so that the proposed names are not too similar in sound or appearance to those already on the market. Included in the lengthy document are checklists, such as, “Across a range of dialects, are the names consistently pronounced differently?” and “Are the lengths of the names dissimilar when scripted?” (Lengths are considered different if they differ by two or more letters.)
The FDA also offers the phonetic and orthographic computer analysis (POCA) program, a software tool that employs an advanced algorithm to evaluate similarities between two drug names. The data sources are updated regularly as new drugs are approved.
Liability update
The problem may be decreasing. In a 2020 report, researchers used pharmacists’ professional liability claim data from the Healthcare Providers Service Organization. They compared 2018 data on claims with 2013 data. The percentage of claims associated with wrong drug dispensing errors declined from 43.8% in 2013 to 36.8% in 2018. Wrong dose claims also declined, from 31.5% to 15.3%.
These researchers concluded that technology and automation have contributed to the prevention of medication errors caused by the use of the wrong drug and the wrong dose, but mistakes continue, owing to system and human errors.
A version of this article first appeared on Medscape.com.
Zolpidem (Ambien) is a well-known sedative for sleep. Letairis (Ambrisentan) is a vasodilator for the treatment of pulmonary arterial hypertension. Citalopram (Celexa) is an antidepressant; escitalopram (Lexapro) is prescribed for anxiety and depression.
The aim is to increase awareness about the potential for a serious medication mistake when the wrong drug is given because of drug names that look and sound similar.
Awareness of these drug names, however, is just the first step in preventing medication mistakes. Health care providers should take a number of other steps as well, experts said.
ISMP launched its confusing drug names list, previously called look-alike, sound-alike (LASA) drugs, in 2008. The new list is an update of the 2019 version, said Michael J. Gaunt, PharmD, senior manager of error reporting programs for the ISMP, which focuses on the prevention of medication mistakes. The new entries were chosen on the basis of a number of factors, including ISMP’s analysis of recent medication mishap reports that were submitted to it.
The ISMP list now includes about 528 drug pairs, Dr. Gaunt said. The list is long, he said, partly because each pair is listed twice, so readers can cross reference. For instance, hydralazine and hydroxyzine are listed in one entry in the list, and hydroxyzine and hydralazine are listed in another.
Brand Institute in Miami has named, among other drugs, Entresto, Rybelsus, and Lunesta. The regulatory arm of the company, the Drug Safety Institute, “considers drug names that have been confused as an important part of our comprehensive drug name assessments,” Todd Bridges, global president of the institute, said in an emailed statement. Information on the confusing drug names are incorporated into the company’s proprietary algorithm and is used when developing brand names for drugs. “We continually update this algorithm as new drug names that are often confused are identified,” Mr. Bridges said.
Confusing drug names: Ongoing issue
The length of the list, as well as the latest additions, are not surprising, said Mary Ann Kliethermes, PharmD, director of medication safety and quality for the American Society of Health-System Pharmacists, a membership organization of about 60,000 pharmacists who practice in inpatient and outpatient settings.
“I’ve been in practice over 45 years,” she said, “and this has been a problem ever since I have been in practice.” The sheer volume of new drugs is one reason, she said. From 2013 through 2022, the U.S. Food and Drug Administration approved an average of 43 novel drugs per year, according to a report from its Center for Drug Evaluation and Research. “Since the 90s, this [confusion about similar drug names] has happened,” Dr. Kliethermes said.
According to a 2023 report, about 7,000-9,000 people die each year in the United States as the result of a medication error. However, it’s impossible to say for sure what percentage of those errors involve name confusion, Dr. Gaunt said.
Not all the mistakes are reported. Some that are reported are dramatic and deadly. In 2022, a Tennessee nurse was convicted of gross neglect and negligent homicide. She was sentenced to 3 years’ probation after she mistakenly gave vercuronium, an anesthetic agent, instead of the sedative Versed to a patient, and the woman died.
Updated list: A closer look
Many of the new drug pairs that are listed in the update are cephalosporins, said Dr. Kliethermes, who reviewed the new list for this news organization. In all, 20 of the latest 82 additions are cephalosporins. These include drugs such as cefazolin, which can be confused with cefotetan, and vice versa. These drugs have been around since the 1980s, she said, but “they needed to be on there.” Even in the 1980s, it was becoming difficult to differentiate them, and there were fewer drugs in that class then, she said.
Influenza vaccines made the new list, too. Fluzone High-Dose Quadrivalent can be confused with fluzone quadrivalent. Other new additions: hydrochlorothiazide and hydroxychloroquine, Lasik and Wakix, Pitressin and Pitocin, Remeron and Rozerem.
Beyond the list
While it’s not possible to pinpoint how big a problem name confusion is in causing medication mistakes, “it is certainly still an issue,” Dr. Gaunt said. A variety of practices can reduce that risk substantially, Dr. Gaunt and Dr. Kliethermes agreed.
Tall-man lettering. Both the FDA and the ISMP recommend the use of so-called tall-man lettering (TML), which involves the use of uppercase letters, sometimes in boldface, to distinguish similar names on product labels and elsewhere. Examples include vinBLAStine and vinCRIStine.
Electronic prescribing. “It eliminates the risk of handwriting confusion,” Dr. Gaunt said. However, electronic prescribing can have a downside, Dr. Kliethermes said. When ordering medication, a person may type in a few letters and may then be presented with a prompt that lists several drug names, and it can be easy to click the wrong one. For that reason, ISMP and other experts recommend typing at least five letters when searching for a medication in an electronic system.
Use both brand and generic names on labels and prescriptions.
Write the indication. That can serve as a double check. If a prescription for Ambien says “For sleep,” there’s probably less risk of filling a prescription for ambrisentan, the vasodilator.
Smart formulary additions. When hospitals add medications to their formularies, “part of that formulary assessment should include looking at the potential risk for errors,” Dr. Gaunt said. This involves keeping an eye out for confusing names and similar packaging. “Do that analysis up front and put in strategies to minimize that. Maybe you look for a different drug [for the same use] that has a different name.” Or choose a different manufacturer, so the medication would at least have a different container.
Use bar code scanning. Suppose a pharmacist goes to the shelf and pulls the wrong drug. “Bar code scanning provides the opportunity to catch the error,” Dr. Gaunt said. Many community pharmacies now have bar code scanning. ISMP just issued best practices for community pharmacies, Dr. Gaunt said, and these include the use of bar code scanning and other measures.
Educate consumers. Health care providers can educate consumers on how to minimize the risk of getting the wrong drug, Dr. Gaunt said. When patients are picking up a prescription, suggest they look at the container label; if it looks different from previous prescriptions of the same medicine, ask the pharmacist for an explanation. Some patients just pass it off, Dr. Gaunt said, figuring the pharmacist or health plan switched manufacturers of their medication.
Access the list. The entire list is on the ISMP site and is accessible after free registration.
Goal: Preventing confusion
The FDA has provided guidance for industry on naming drugs not yet approved so that the proposed names are not too similar in sound or appearance to those already on the market. Included in the lengthy document are checklists, such as, “Across a range of dialects, are the names consistently pronounced differently?” and “Are the lengths of the names dissimilar when scripted?” (Lengths are considered different if they differ by two or more letters.)
The FDA also offers the phonetic and orthographic computer analysis (POCA) program, a software tool that employs an advanced algorithm to evaluate similarities between two drug names. The data sources are updated regularly as new drugs are approved.
Liability update
The problem may be decreasing. In a 2020 report, researchers used pharmacists’ professional liability claim data from the Healthcare Providers Service Organization. They compared 2018 data on claims with 2013 data. The percentage of claims associated with wrong drug dispensing errors declined from 43.8% in 2013 to 36.8% in 2018. Wrong dose claims also declined, from 31.5% to 15.3%.
These researchers concluded that technology and automation have contributed to the prevention of medication errors caused by the use of the wrong drug and the wrong dose, but mistakes continue, owing to system and human errors.
A version of this article first appeared on Medscape.com.
Thrombectomy improves outcomes in pediatric stroke
A matched case-control study followed 52 patients in Canada and Australia with acute stroke and assessed functional outcomes at 3 months for those who received thrombectomy, compared with those who did not. Patients receiving the procedure had significantly improved clinical outcomes (odds ratio [OR], 3.76). The procedure is the standard of care for adults with large vessel occlusion (LVO) stroke, but limited data exist for children.
“In the absence of a randomized trial, this case-control study demonstrates better clinical outcomes with thrombectomy than medical management for pediatric patients aged 2 to 18 years with anterior circulation LVO stroke,” the authors concluded. The study was published in JAMA Neurology.
Improved results
Untreated LVO stroke is associated with poor outcomes, indicated in this study with scoring based on the modified Rankin Scale. Based on this scoring, 53.8% of patients who were managed conservatively had poor outcomes (moderate disability or greater) at 3 months, confirming previous findings. The data were drawn from five hospitals in Australia and Canada between January 2011 and April 2022.
Removing blood clots with mechanical thrombectomy resulted in improved outcomes 3 months after stroke for the patients included in the study, compared with the neuroprotective measures of medical therapy alone. The improved outcomes persisted in the final available follow-up (OR, 3.65).
In adults, thrombectomy has previously been demonstrated to be a safe and effective treatment for LVO stroke and is currently the standard of care. This study sought to expand the data for pediatric patients, for whom stroke is rarer and difficult to diagnose.
The authors cautioned, however, that the outcomes are from hospitals with pediatric neurology expertise and should not be generalized to settings without specialists.
Case-control study
While previous population-based studies of children with LVO stroke found that conservative treatment was associated with poor outcomes, these studies may include significant selection bias. The investigators chose to conduct the case-control study as an alternative to a randomized control trial, which would require withholding treatment from some patients and would not be considered ethical.
The study included 26 patients in each cohort, either receiving mechanical thrombectomy or medical treatment alone. The investigators matched patients by site and side of occlusion, age, and sex. Cases that could not be matched by site of occlusion, the primary criterion, were excluded.
With this methodology, the investigators reduced the impact of selection bias with the aim of providing “the next highest level of comparative evidence,” they stated in the study. However, they also noted that, without randomization, there is likely still some selection bias present.
The two cohorts were not significantly different based on factors such as sex or age. All patients in the study presented within 24 hours of symptom onset, with most eligible for thrombectomy by adult standards. There was a difference between the two cohorts in the timing of arrival to a dedicated hospital and imaging. “Our triage, imaging, and decision-making pathways require streamlining,” the authors concluded, regarding the difference.
‘A heterogeneous condition’
In a comment, Ratika Srivastava, MD, a pediatric neurologist at the University of Alberta, Edmonton, said she was glad to see a well-designed study dedicated to pediatric stroke. Neurologists have traditionally extrapolated from research on adult stroke due to the rarity of pediatric stroke and difficulty of diagnosis.
While physicians have previously relied on findings in adults, stroke presents differently in children. “The challenge is that it’s such a heterogeneous condition,” said Dr. Srivastava, who was not involved in the study. In children, stroke may have several different etiologies, such as a lesion in the heart or arterial disease. “Sometimes it’s amenable to taking the clot out and sometimes it’s not. So you have to figure out: Are they a good candidate for thrombectomy?” This study helps demonstrate that thrombectomy is a good option for some children with LVO stroke, she said.
The study was independently supported. Dr. Srivastava reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A matched case-control study followed 52 patients in Canada and Australia with acute stroke and assessed functional outcomes at 3 months for those who received thrombectomy, compared with those who did not. Patients receiving the procedure had significantly improved clinical outcomes (odds ratio [OR], 3.76). The procedure is the standard of care for adults with large vessel occlusion (LVO) stroke, but limited data exist for children.
“In the absence of a randomized trial, this case-control study demonstrates better clinical outcomes with thrombectomy than medical management for pediatric patients aged 2 to 18 years with anterior circulation LVO stroke,” the authors concluded. The study was published in JAMA Neurology.
Improved results
Untreated LVO stroke is associated with poor outcomes, indicated in this study with scoring based on the modified Rankin Scale. Based on this scoring, 53.8% of patients who were managed conservatively had poor outcomes (moderate disability or greater) at 3 months, confirming previous findings. The data were drawn from five hospitals in Australia and Canada between January 2011 and April 2022.
Removing blood clots with mechanical thrombectomy resulted in improved outcomes 3 months after stroke for the patients included in the study, compared with the neuroprotective measures of medical therapy alone. The improved outcomes persisted in the final available follow-up (OR, 3.65).
In adults, thrombectomy has previously been demonstrated to be a safe and effective treatment for LVO stroke and is currently the standard of care. This study sought to expand the data for pediatric patients, for whom stroke is rarer and difficult to diagnose.
The authors cautioned, however, that the outcomes are from hospitals with pediatric neurology expertise and should not be generalized to settings without specialists.
Case-control study
While previous population-based studies of children with LVO stroke found that conservative treatment was associated with poor outcomes, these studies may include significant selection bias. The investigators chose to conduct the case-control study as an alternative to a randomized control trial, which would require withholding treatment from some patients and would not be considered ethical.
The study included 26 patients in each cohort, either receiving mechanical thrombectomy or medical treatment alone. The investigators matched patients by site and side of occlusion, age, and sex. Cases that could not be matched by site of occlusion, the primary criterion, were excluded.
With this methodology, the investigators reduced the impact of selection bias with the aim of providing “the next highest level of comparative evidence,” they stated in the study. However, they also noted that, without randomization, there is likely still some selection bias present.
The two cohorts were not significantly different based on factors such as sex or age. All patients in the study presented within 24 hours of symptom onset, with most eligible for thrombectomy by adult standards. There was a difference between the two cohorts in the timing of arrival to a dedicated hospital and imaging. “Our triage, imaging, and decision-making pathways require streamlining,” the authors concluded, regarding the difference.
‘A heterogeneous condition’
In a comment, Ratika Srivastava, MD, a pediatric neurologist at the University of Alberta, Edmonton, said she was glad to see a well-designed study dedicated to pediatric stroke. Neurologists have traditionally extrapolated from research on adult stroke due to the rarity of pediatric stroke and difficulty of diagnosis.
While physicians have previously relied on findings in adults, stroke presents differently in children. “The challenge is that it’s such a heterogeneous condition,” said Dr. Srivastava, who was not involved in the study. In children, stroke may have several different etiologies, such as a lesion in the heart or arterial disease. “Sometimes it’s amenable to taking the clot out and sometimes it’s not. So you have to figure out: Are they a good candidate for thrombectomy?” This study helps demonstrate that thrombectomy is a good option for some children with LVO stroke, she said.
The study was independently supported. Dr. Srivastava reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A matched case-control study followed 52 patients in Canada and Australia with acute stroke and assessed functional outcomes at 3 months for those who received thrombectomy, compared with those who did not. Patients receiving the procedure had significantly improved clinical outcomes (odds ratio [OR], 3.76). The procedure is the standard of care for adults with large vessel occlusion (LVO) stroke, but limited data exist for children.
“In the absence of a randomized trial, this case-control study demonstrates better clinical outcomes with thrombectomy than medical management for pediatric patients aged 2 to 18 years with anterior circulation LVO stroke,” the authors concluded. The study was published in JAMA Neurology.
Improved results
Untreated LVO stroke is associated with poor outcomes, indicated in this study with scoring based on the modified Rankin Scale. Based on this scoring, 53.8% of patients who were managed conservatively had poor outcomes (moderate disability or greater) at 3 months, confirming previous findings. The data were drawn from five hospitals in Australia and Canada between January 2011 and April 2022.
Removing blood clots with mechanical thrombectomy resulted in improved outcomes 3 months after stroke for the patients included in the study, compared with the neuroprotective measures of medical therapy alone. The improved outcomes persisted in the final available follow-up (OR, 3.65).
In adults, thrombectomy has previously been demonstrated to be a safe and effective treatment for LVO stroke and is currently the standard of care. This study sought to expand the data for pediatric patients, for whom stroke is rarer and difficult to diagnose.
The authors cautioned, however, that the outcomes are from hospitals with pediatric neurology expertise and should not be generalized to settings without specialists.
Case-control study
While previous population-based studies of children with LVO stroke found that conservative treatment was associated with poor outcomes, these studies may include significant selection bias. The investigators chose to conduct the case-control study as an alternative to a randomized control trial, which would require withholding treatment from some patients and would not be considered ethical.
The study included 26 patients in each cohort, either receiving mechanical thrombectomy or medical treatment alone. The investigators matched patients by site and side of occlusion, age, and sex. Cases that could not be matched by site of occlusion, the primary criterion, were excluded.
With this methodology, the investigators reduced the impact of selection bias with the aim of providing “the next highest level of comparative evidence,” they stated in the study. However, they also noted that, without randomization, there is likely still some selection bias present.
The two cohorts were not significantly different based on factors such as sex or age. All patients in the study presented within 24 hours of symptom onset, with most eligible for thrombectomy by adult standards. There was a difference between the two cohorts in the timing of arrival to a dedicated hospital and imaging. “Our triage, imaging, and decision-making pathways require streamlining,” the authors concluded, regarding the difference.
‘A heterogeneous condition’
In a comment, Ratika Srivastava, MD, a pediatric neurologist at the University of Alberta, Edmonton, said she was glad to see a well-designed study dedicated to pediatric stroke. Neurologists have traditionally extrapolated from research on adult stroke due to the rarity of pediatric stroke and difficulty of diagnosis.
While physicians have previously relied on findings in adults, stroke presents differently in children. “The challenge is that it’s such a heterogeneous condition,” said Dr. Srivastava, who was not involved in the study. In children, stroke may have several different etiologies, such as a lesion in the heart or arterial disease. “Sometimes it’s amenable to taking the clot out and sometimes it’s not. So you have to figure out: Are they a good candidate for thrombectomy?” This study helps demonstrate that thrombectomy is a good option for some children with LVO stroke, she said.
The study was independently supported. Dr. Srivastava reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
Cigna accused of using AI, not doctors, to deny claims: Lawsuit
and forcing providers to bill patients in full.
In a complaint filed recently in California’s eastern district court, plaintiffs and Cigna health plan members Suzanne Kisting-Leung and Ayesha Smiley and their attorneys say that Cigna violates state insurance regulations by failing to conduct a “thorough, fair, and objective” review of their and other members’ claims.
The lawsuit says that, instead, Cigna relies on an algorithm, PxDx, to review and frequently deny medically necessary claims. According to court records, the system allows Cigna’s doctors to “instantly reject claims on medical grounds without ever opening patient files.” With use of the system, the average claims processing time is 1.2 seconds.
Cigna says it uses technology to verify coding on standard, low-cost procedures and to expedite physician reimbursement. In a statement to CBS News, the company called the lawsuit “highly questionable.”
The case highlights growing concerns about AI and its ability to replace humans for tasks and interactions in health care, business, and beyond. Public advocacy law firm Clarkson, which is representing the plaintiffs, has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ personal and professional data to train their AI systems.
According to the complaint, Cigna denied the plaintiffs medically necessary tests, including blood work to screen for vitamin D deficiency and ultrasounds for patients suspected of having ovarian cancer. The plaintiffs’ attempts to appeal were unfruitful, and they were forced to pay out of pocket.
The plaintiff’s attorneys argue that the claims do not undergo more detailed reviews by physicians and employees, as mandated by California insurance laws, and that Cigna benefits by saving on labor costs.
Clarkson is demanding a jury trial and has asked the court to certify the Cigna case as a federal class action, potentially allowing the insurer’s other 2 million health plan members in California to join the lawsuit.
I. Glenn Cohen, JD, deputy dean and professor at Harvard Law School, Cambridge, Mass., said in an interview that this is the first lawsuit he’s aware of in which AI was involved in denying health insurance claims and that it is probably an uphill battle for the plaintiffs.
“In the last 25 years, the U.S. Supreme Court’s decisions have made getting a class action approved more difficult. If allowed to go forward as a class action, which Cigna is likely to vigorously oppose, then the pressure on Cigna to settle the case becomes enormous,” he said.
The allegations come after a recent deep dive by the nonprofit ProPublica uncovered similar claim denial issues. One physician who worked for Cigna told the nonprofit that he and other company doctors essentially rubber-stamped the denials in batches, which took “all of 10 seconds to do 50 at a time.”
In 2022, the American Medical Association and two state physician groups joined another class action against Cigna stemming from allegations that the insurer’s intermediary, Multiplan, intentionally underpaid medical claims. And in March, Cigna’s pharmacy benefit manager, Express Scripts, was accused of conspiring with other PBMs to drive up prescription drug prices for Ohio consumers, violating state antitrust laws.
Mr. Cohen said he expects Cigna to push back in court about the California class size, which the plaintiff’s attorneys hope will encompass all Cigna health plan members in the state.
“The injury is primarily to those whose claims were denied by AI, presumably a much smaller set of individuals and harder to identify,” said Mr. Cohen.
A version of this article first appeared on Medscape.com.
and forcing providers to bill patients in full.
In a complaint filed recently in California’s eastern district court, plaintiffs and Cigna health plan members Suzanne Kisting-Leung and Ayesha Smiley and their attorneys say that Cigna violates state insurance regulations by failing to conduct a “thorough, fair, and objective” review of their and other members’ claims.
The lawsuit says that, instead, Cigna relies on an algorithm, PxDx, to review and frequently deny medically necessary claims. According to court records, the system allows Cigna’s doctors to “instantly reject claims on medical grounds without ever opening patient files.” With use of the system, the average claims processing time is 1.2 seconds.
Cigna says it uses technology to verify coding on standard, low-cost procedures and to expedite physician reimbursement. In a statement to CBS News, the company called the lawsuit “highly questionable.”
The case highlights growing concerns about AI and its ability to replace humans for tasks and interactions in health care, business, and beyond. Public advocacy law firm Clarkson, which is representing the plaintiffs, has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ personal and professional data to train their AI systems.
According to the complaint, Cigna denied the plaintiffs medically necessary tests, including blood work to screen for vitamin D deficiency and ultrasounds for patients suspected of having ovarian cancer. The plaintiffs’ attempts to appeal were unfruitful, and they were forced to pay out of pocket.
The plaintiff’s attorneys argue that the claims do not undergo more detailed reviews by physicians and employees, as mandated by California insurance laws, and that Cigna benefits by saving on labor costs.
Clarkson is demanding a jury trial and has asked the court to certify the Cigna case as a federal class action, potentially allowing the insurer’s other 2 million health plan members in California to join the lawsuit.
I. Glenn Cohen, JD, deputy dean and professor at Harvard Law School, Cambridge, Mass., said in an interview that this is the first lawsuit he’s aware of in which AI was involved in denying health insurance claims and that it is probably an uphill battle for the plaintiffs.
“In the last 25 years, the U.S. Supreme Court’s decisions have made getting a class action approved more difficult. If allowed to go forward as a class action, which Cigna is likely to vigorously oppose, then the pressure on Cigna to settle the case becomes enormous,” he said.
The allegations come after a recent deep dive by the nonprofit ProPublica uncovered similar claim denial issues. One physician who worked for Cigna told the nonprofit that he and other company doctors essentially rubber-stamped the denials in batches, which took “all of 10 seconds to do 50 at a time.”
In 2022, the American Medical Association and two state physician groups joined another class action against Cigna stemming from allegations that the insurer’s intermediary, Multiplan, intentionally underpaid medical claims. And in March, Cigna’s pharmacy benefit manager, Express Scripts, was accused of conspiring with other PBMs to drive up prescription drug prices for Ohio consumers, violating state antitrust laws.
Mr. Cohen said he expects Cigna to push back in court about the California class size, which the plaintiff’s attorneys hope will encompass all Cigna health plan members in the state.
“The injury is primarily to those whose claims were denied by AI, presumably a much smaller set of individuals and harder to identify,” said Mr. Cohen.
A version of this article first appeared on Medscape.com.
and forcing providers to bill patients in full.
In a complaint filed recently in California’s eastern district court, plaintiffs and Cigna health plan members Suzanne Kisting-Leung and Ayesha Smiley and their attorneys say that Cigna violates state insurance regulations by failing to conduct a “thorough, fair, and objective” review of their and other members’ claims.
The lawsuit says that, instead, Cigna relies on an algorithm, PxDx, to review and frequently deny medically necessary claims. According to court records, the system allows Cigna’s doctors to “instantly reject claims on medical grounds without ever opening patient files.” With use of the system, the average claims processing time is 1.2 seconds.
Cigna says it uses technology to verify coding on standard, low-cost procedures and to expedite physician reimbursement. In a statement to CBS News, the company called the lawsuit “highly questionable.”
The case highlights growing concerns about AI and its ability to replace humans for tasks and interactions in health care, business, and beyond. Public advocacy law firm Clarkson, which is representing the plaintiffs, has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ personal and professional data to train their AI systems.
According to the complaint, Cigna denied the plaintiffs medically necessary tests, including blood work to screen for vitamin D deficiency and ultrasounds for patients suspected of having ovarian cancer. The plaintiffs’ attempts to appeal were unfruitful, and they were forced to pay out of pocket.
The plaintiff’s attorneys argue that the claims do not undergo more detailed reviews by physicians and employees, as mandated by California insurance laws, and that Cigna benefits by saving on labor costs.
Clarkson is demanding a jury trial and has asked the court to certify the Cigna case as a federal class action, potentially allowing the insurer’s other 2 million health plan members in California to join the lawsuit.
I. Glenn Cohen, JD, deputy dean and professor at Harvard Law School, Cambridge, Mass., said in an interview that this is the first lawsuit he’s aware of in which AI was involved in denying health insurance claims and that it is probably an uphill battle for the plaintiffs.
“In the last 25 years, the U.S. Supreme Court’s decisions have made getting a class action approved more difficult. If allowed to go forward as a class action, which Cigna is likely to vigorously oppose, then the pressure on Cigna to settle the case becomes enormous,” he said.
The allegations come after a recent deep dive by the nonprofit ProPublica uncovered similar claim denial issues. One physician who worked for Cigna told the nonprofit that he and other company doctors essentially rubber-stamped the denials in batches, which took “all of 10 seconds to do 50 at a time.”
In 2022, the American Medical Association and two state physician groups joined another class action against Cigna stemming from allegations that the insurer’s intermediary, Multiplan, intentionally underpaid medical claims. And in March, Cigna’s pharmacy benefit manager, Express Scripts, was accused of conspiring with other PBMs to drive up prescription drug prices for Ohio consumers, violating state antitrust laws.
Mr. Cohen said he expects Cigna to push back in court about the California class size, which the plaintiff’s attorneys hope will encompass all Cigna health plan members in the state.
“The injury is primarily to those whose claims were denied by AI, presumably a much smaller set of individuals and harder to identify,” said Mr. Cohen.
A version of this article first appeared on Medscape.com.
The argument for grip strength as a vital sign
Most people hear “firm handshake” and automatically think “business world.” A cursory search reveals articles with titles like “Seven Super-Revealing Things Your Handshake Said About You” (Forbes) and “How a Handshake Can Tell You Everything You Need to Know About a Person” (Inc).
Those in the know, however, understand what a handshake really reveals: Current health and vitality. The amount of force that can be generated by the hand is a valid proxy for total-body strength. And total-body strength is one key to healthy aging.
Grip-strength testing is easy, fast, and noninvasive. It can be monitored over time. All it requires is a handgrip dynamometer, a tool that may cost less than a stethoscope, and a chair.
“Many studies have looked at strength as a predictor of positive health and weakness as a predictor of negative health outcomes,” said Mark Peterson, PhD, an associate professor at the University of Michigan, Ann Arbor, who’s worked on dozens of those studies.
Among the health risks associated with low grip strength: type 2 diabetes, heart disease, cancer, dementia and Alzheimer’s disease, depression, functional disability, osteoporosis, and premature death from any cause.
The prognostic merits of grip strength have been documented across continents and cultures. Although most of those studies have focused on older adults, they aren’t the only age group researchers have looked at.
“We have several papers on the value of grip strength for predicting diabetes and cardiovascular disease in children and adolescents,” Dr. Peterson said.
Survival of the strongest
The first thing to understand about grip-strength testing is that it’s only partially about grip. It’s mostly about strength. That’s what attracted Dr. Peterson to this line of research.
“I’m a former strength coach, so I wanted to make a case for why strength was important across populations, not just athletes,” he said. “I strongly believe in strength preservation and healthy living as a predictor for longevity.”
Consider a classic study of Swedish army recruits. Because of Sweden’s post–World War II conscription policy, virtually every young male in the country underwent a physical examination to see if they were fit for military service – an exam that included a grip-strength test.
That gave the researchers a database with more than a million participants. They followed up on them decades later through publicly available records.
What they found: The men with the weakest grip strength in their late teens were 20% more likely to have died by their mid-50s, compared with those with moderate to high grip strength. Even suicide rates were 20%-30% higher for the weakest recruits.
There’s a brutal Darwinian logic to the idea that a stronger person with a more powerful grip would enjoy a longer, healthier life. To our ancient ancestors, stronger hands meant they were probably better at everything that aided survival: hunting, fighting, building shelter, as well as bearing, transporting, and rearing children.
Fast forward to the 21st century where we must force ourselves to engage in physical activity. The old rules still apply: Strength aids survival.
Grip strength and the aging process
Some of the earliest grip-strength studies used it as a proxy for nutritional status in elderly men and women. Nourishment, in turn, predicted their ability to survive an illness or surgery.
Which makes sense; if an older person isn’t eating enough to maintain their health and vitality, their strength would decline. Declining strength would make them more susceptible to infections, hospitalizations, and postsurgical complications, leading to longer hospital stays, loss of independence, and ultimately a higher risk of death from any cause.
Along those lines, Dr. Peterson’s research team at the University of Michigan found that low grip strength is correlated with faster aging at the cellular level.
The study looked at DNA methylation, which Peterson describes as “a reflection of someone’s exposure to life events.”
For example, someone who smokes will have altered methylation patterns, compared with someone who doesn’t. Same with someone who’s had more exposure to environmental pollution.
Accelerated DNA methylation “means you’re essentially at higher risk for what are traditionally considered age-related chronic conditions,” Dr. Peterson said. Those conditions include Alzheimer’s, type 2 diabetes, chronic inflammation, and a higher risk for premature mortality.
Those things are also linked to low grip strength, which is linked to higher DNA methylation and faster biological aging.
But there’s still a missing piece of the puzzle: Why, exactly, would the strength of one’s grip be associated with so many health outcomes?
Grip strength and muscle function
“Declining muscle function is the first step of the disabling process,” said Ryan McGrath, PhD, an assistant professor at North Dakota State University, Fargo. “That’s what you can measure with a handgrip test. It helps you identify individuals at risk for the next step of the process, which is declines in physical performance.”
Dr. McGrath got involved in grip-strength research as a postdoctoral fellow at the University of Michigan, where he worked with Peterson. Like his mentor, he’s published multiple studies using data obtained with a handgrip dynamometer.
“It can be a nice tool for assessing muscle function and muscle strength,” he explained. Because the test is so easy to administer – you sit in a chair with your arm at your side and your elbow bent 90 degrees, and squeeze the device as hard as you can – researchers can work with large groups of study participants and come away with statistically powerful data.
“There are a lot of health outcomes it’s associated with,” Dr. McGrath added, “which is one of its greatest strengths and at the same time one of its key limitations.”
He compared the dynamometer with a tire gauge. Just as a tire gauge can alert you to a loss of air pressure without revealing the source of the leak, a dynamometer can’t tell you why your grip strength is deflated.
“It’s hard to specify the prognostic value,” he said. “You don’t know the next steps to take. As a standalone measurement, that’s a concern.”
That’s why his current research goes beyond simple tests of maximum grip strength to more sophisticated measurements of the rate of force development (how fast you can express strength), repeatability (how much your strength declines from your first to your second or third squeeze), and asymmetry (how big a gap there is between your right- and left-hand strength).
Any of those measures could detect a potential neural or neuromuscular issue.
In a 2020 study, for example, Dr. McGrath and his team at NDSU showed that older adults with both weakness and asymmetry in grip-strength tests were nearly four times more likely to experience functional limitations. Those limitations could affect their ability to do anything from routine chores to keeping themselves clean and fed.
Waging war on weakness
Using dynamometer readings, the generally accepted cutoffs for low grip strength are 26 kg for an adult male and 16 kg for a female.
But that’s way too simple, Dr. Peterson said.
For one thing, age matters. Grip strength typically peaks for men in their late 20s and declines rapidly in middle age and beyond. For women, it plateaus in their 20s and gently declines until their 50s. So, at minimum, the age-based standards included with a dynamometer should be consulted.
Another caveat: Dr. Peterson said grip strength tests aren’t very meaningful for people who actively train for strength, though he suggests dedicated athletes make up a relatively small percentage of the population – even as low as 10%.
The size of the person taking the test is also important.
“You absolutely must account for body mass in the context of understanding how grip strength, or any strength measure, is reflective of health and function,” Dr. Peterson said.
To calculate strength-weight ratio, which Dr. Peterson calls “normalized grip strength,” divide grip strength in kilograms by body weight in kilograms. For men, a ratio greater than 0.70 puts them in the higher percentiles. For women it’s 0.50.
And if the results suggest that the person in question is objectively weak? “For me, that’s easy,” Dr. Peterson said. “They need to exercise.”
Common sense suggests doing a lot of forearm exercises for grip strength. Not so, said Dr. Peterson. The strength of hand and forearm muscles reflects what they can do along with all other muscles moving together.
A 2019 study found that, for older adults, a variety of exercise programs can lead to modest but meaningful increases in participants’ grip strength – and they don’t necessarily have to include actual gripping exercises. The programs ranged from tai chi to water aerobics to walking, stretching, and all kinds of resistance training.
Dr. Peterson’s advice to everyone is pretty straightforward: Get stronger. It doesn’t really matter how you do it, or how much strength you ultimately gain. Even a little more strength means a little less weakness, and a little more life.
A version of this article first appeared on Medscape.com.
Most people hear “firm handshake” and automatically think “business world.” A cursory search reveals articles with titles like “Seven Super-Revealing Things Your Handshake Said About You” (Forbes) and “How a Handshake Can Tell You Everything You Need to Know About a Person” (Inc).
Those in the know, however, understand what a handshake really reveals: Current health and vitality. The amount of force that can be generated by the hand is a valid proxy for total-body strength. And total-body strength is one key to healthy aging.
Grip-strength testing is easy, fast, and noninvasive. It can be monitored over time. All it requires is a handgrip dynamometer, a tool that may cost less than a stethoscope, and a chair.
“Many studies have looked at strength as a predictor of positive health and weakness as a predictor of negative health outcomes,” said Mark Peterson, PhD, an associate professor at the University of Michigan, Ann Arbor, who’s worked on dozens of those studies.
Among the health risks associated with low grip strength: type 2 diabetes, heart disease, cancer, dementia and Alzheimer’s disease, depression, functional disability, osteoporosis, and premature death from any cause.
The prognostic merits of grip strength have been documented across continents and cultures. Although most of those studies have focused on older adults, they aren’t the only age group researchers have looked at.
“We have several papers on the value of grip strength for predicting diabetes and cardiovascular disease in children and adolescents,” Dr. Peterson said.
Survival of the strongest
The first thing to understand about grip-strength testing is that it’s only partially about grip. It’s mostly about strength. That’s what attracted Dr. Peterson to this line of research.
“I’m a former strength coach, so I wanted to make a case for why strength was important across populations, not just athletes,” he said. “I strongly believe in strength preservation and healthy living as a predictor for longevity.”
Consider a classic study of Swedish army recruits. Because of Sweden’s post–World War II conscription policy, virtually every young male in the country underwent a physical examination to see if they were fit for military service – an exam that included a grip-strength test.
That gave the researchers a database with more than a million participants. They followed up on them decades later through publicly available records.
What they found: The men with the weakest grip strength in their late teens were 20% more likely to have died by their mid-50s, compared with those with moderate to high grip strength. Even suicide rates were 20%-30% higher for the weakest recruits.
There’s a brutal Darwinian logic to the idea that a stronger person with a more powerful grip would enjoy a longer, healthier life. To our ancient ancestors, stronger hands meant they were probably better at everything that aided survival: hunting, fighting, building shelter, as well as bearing, transporting, and rearing children.
Fast forward to the 21st century where we must force ourselves to engage in physical activity. The old rules still apply: Strength aids survival.
Grip strength and the aging process
Some of the earliest grip-strength studies used it as a proxy for nutritional status in elderly men and women. Nourishment, in turn, predicted their ability to survive an illness or surgery.
Which makes sense; if an older person isn’t eating enough to maintain their health and vitality, their strength would decline. Declining strength would make them more susceptible to infections, hospitalizations, and postsurgical complications, leading to longer hospital stays, loss of independence, and ultimately a higher risk of death from any cause.
Along those lines, Dr. Peterson’s research team at the University of Michigan found that low grip strength is correlated with faster aging at the cellular level.
The study looked at DNA methylation, which Peterson describes as “a reflection of someone’s exposure to life events.”
For example, someone who smokes will have altered methylation patterns, compared with someone who doesn’t. Same with someone who’s had more exposure to environmental pollution.
Accelerated DNA methylation “means you’re essentially at higher risk for what are traditionally considered age-related chronic conditions,” Dr. Peterson said. Those conditions include Alzheimer’s, type 2 diabetes, chronic inflammation, and a higher risk for premature mortality.
Those things are also linked to low grip strength, which is linked to higher DNA methylation and faster biological aging.
But there’s still a missing piece of the puzzle: Why, exactly, would the strength of one’s grip be associated with so many health outcomes?
Grip strength and muscle function
“Declining muscle function is the first step of the disabling process,” said Ryan McGrath, PhD, an assistant professor at North Dakota State University, Fargo. “That’s what you can measure with a handgrip test. It helps you identify individuals at risk for the next step of the process, which is declines in physical performance.”
Dr. McGrath got involved in grip-strength research as a postdoctoral fellow at the University of Michigan, where he worked with Peterson. Like his mentor, he’s published multiple studies using data obtained with a handgrip dynamometer.
“It can be a nice tool for assessing muscle function and muscle strength,” he explained. Because the test is so easy to administer – you sit in a chair with your arm at your side and your elbow bent 90 degrees, and squeeze the device as hard as you can – researchers can work with large groups of study participants and come away with statistically powerful data.
“There are a lot of health outcomes it’s associated with,” Dr. McGrath added, “which is one of its greatest strengths and at the same time one of its key limitations.”
He compared the dynamometer with a tire gauge. Just as a tire gauge can alert you to a loss of air pressure without revealing the source of the leak, a dynamometer can’t tell you why your grip strength is deflated.
“It’s hard to specify the prognostic value,” he said. “You don’t know the next steps to take. As a standalone measurement, that’s a concern.”
That’s why his current research goes beyond simple tests of maximum grip strength to more sophisticated measurements of the rate of force development (how fast you can express strength), repeatability (how much your strength declines from your first to your second or third squeeze), and asymmetry (how big a gap there is between your right- and left-hand strength).
Any of those measures could detect a potential neural or neuromuscular issue.
In a 2020 study, for example, Dr. McGrath and his team at NDSU showed that older adults with both weakness and asymmetry in grip-strength tests were nearly four times more likely to experience functional limitations. Those limitations could affect their ability to do anything from routine chores to keeping themselves clean and fed.
Waging war on weakness
Using dynamometer readings, the generally accepted cutoffs for low grip strength are 26 kg for an adult male and 16 kg for a female.
But that’s way too simple, Dr. Peterson said.
For one thing, age matters. Grip strength typically peaks for men in their late 20s and declines rapidly in middle age and beyond. For women, it plateaus in their 20s and gently declines until their 50s. So, at minimum, the age-based standards included with a dynamometer should be consulted.
Another caveat: Dr. Peterson said grip strength tests aren’t very meaningful for people who actively train for strength, though he suggests dedicated athletes make up a relatively small percentage of the population – even as low as 10%.
The size of the person taking the test is also important.
“You absolutely must account for body mass in the context of understanding how grip strength, or any strength measure, is reflective of health and function,” Dr. Peterson said.
To calculate strength-weight ratio, which Dr. Peterson calls “normalized grip strength,” divide grip strength in kilograms by body weight in kilograms. For men, a ratio greater than 0.70 puts them in the higher percentiles. For women it’s 0.50.
And if the results suggest that the person in question is objectively weak? “For me, that’s easy,” Dr. Peterson said. “They need to exercise.”
Common sense suggests doing a lot of forearm exercises for grip strength. Not so, said Dr. Peterson. The strength of hand and forearm muscles reflects what they can do along with all other muscles moving together.
A 2019 study found that, for older adults, a variety of exercise programs can lead to modest but meaningful increases in participants’ grip strength – and they don’t necessarily have to include actual gripping exercises. The programs ranged from tai chi to water aerobics to walking, stretching, and all kinds of resistance training.
Dr. Peterson’s advice to everyone is pretty straightforward: Get stronger. It doesn’t really matter how you do it, or how much strength you ultimately gain. Even a little more strength means a little less weakness, and a little more life.
A version of this article first appeared on Medscape.com.
Most people hear “firm handshake” and automatically think “business world.” A cursory search reveals articles with titles like “Seven Super-Revealing Things Your Handshake Said About You” (Forbes) and “How a Handshake Can Tell You Everything You Need to Know About a Person” (Inc).
Those in the know, however, understand what a handshake really reveals: Current health and vitality. The amount of force that can be generated by the hand is a valid proxy for total-body strength. And total-body strength is one key to healthy aging.
Grip-strength testing is easy, fast, and noninvasive. It can be monitored over time. All it requires is a handgrip dynamometer, a tool that may cost less than a stethoscope, and a chair.
“Many studies have looked at strength as a predictor of positive health and weakness as a predictor of negative health outcomes,” said Mark Peterson, PhD, an associate professor at the University of Michigan, Ann Arbor, who’s worked on dozens of those studies.
Among the health risks associated with low grip strength: type 2 diabetes, heart disease, cancer, dementia and Alzheimer’s disease, depression, functional disability, osteoporosis, and premature death from any cause.
The prognostic merits of grip strength have been documented across continents and cultures. Although most of those studies have focused on older adults, they aren’t the only age group researchers have looked at.
“We have several papers on the value of grip strength for predicting diabetes and cardiovascular disease in children and adolescents,” Dr. Peterson said.
Survival of the strongest
The first thing to understand about grip-strength testing is that it’s only partially about grip. It’s mostly about strength. That’s what attracted Dr. Peterson to this line of research.
“I’m a former strength coach, so I wanted to make a case for why strength was important across populations, not just athletes,” he said. “I strongly believe in strength preservation and healthy living as a predictor for longevity.”
Consider a classic study of Swedish army recruits. Because of Sweden’s post–World War II conscription policy, virtually every young male in the country underwent a physical examination to see if they were fit for military service – an exam that included a grip-strength test.
That gave the researchers a database with more than a million participants. They followed up on them decades later through publicly available records.
What they found: The men with the weakest grip strength in their late teens were 20% more likely to have died by their mid-50s, compared with those with moderate to high grip strength. Even suicide rates were 20%-30% higher for the weakest recruits.
There’s a brutal Darwinian logic to the idea that a stronger person with a more powerful grip would enjoy a longer, healthier life. To our ancient ancestors, stronger hands meant they were probably better at everything that aided survival: hunting, fighting, building shelter, as well as bearing, transporting, and rearing children.
Fast forward to the 21st century where we must force ourselves to engage in physical activity. The old rules still apply: Strength aids survival.
Grip strength and the aging process
Some of the earliest grip-strength studies used it as a proxy for nutritional status in elderly men and women. Nourishment, in turn, predicted their ability to survive an illness or surgery.
Which makes sense; if an older person isn’t eating enough to maintain their health and vitality, their strength would decline. Declining strength would make them more susceptible to infections, hospitalizations, and postsurgical complications, leading to longer hospital stays, loss of independence, and ultimately a higher risk of death from any cause.
Along those lines, Dr. Peterson’s research team at the University of Michigan found that low grip strength is correlated with faster aging at the cellular level.
The study looked at DNA methylation, which Peterson describes as “a reflection of someone’s exposure to life events.”
For example, someone who smokes will have altered methylation patterns, compared with someone who doesn’t. Same with someone who’s had more exposure to environmental pollution.
Accelerated DNA methylation “means you’re essentially at higher risk for what are traditionally considered age-related chronic conditions,” Dr. Peterson said. Those conditions include Alzheimer’s, type 2 diabetes, chronic inflammation, and a higher risk for premature mortality.
Those things are also linked to low grip strength, which is linked to higher DNA methylation and faster biological aging.
But there’s still a missing piece of the puzzle: Why, exactly, would the strength of one’s grip be associated with so many health outcomes?
Grip strength and muscle function
“Declining muscle function is the first step of the disabling process,” said Ryan McGrath, PhD, an assistant professor at North Dakota State University, Fargo. “That’s what you can measure with a handgrip test. It helps you identify individuals at risk for the next step of the process, which is declines in physical performance.”
Dr. McGrath got involved in grip-strength research as a postdoctoral fellow at the University of Michigan, where he worked with Peterson. Like his mentor, he’s published multiple studies using data obtained with a handgrip dynamometer.
“It can be a nice tool for assessing muscle function and muscle strength,” he explained. Because the test is so easy to administer – you sit in a chair with your arm at your side and your elbow bent 90 degrees, and squeeze the device as hard as you can – researchers can work with large groups of study participants and come away with statistically powerful data.
“There are a lot of health outcomes it’s associated with,” Dr. McGrath added, “which is one of its greatest strengths and at the same time one of its key limitations.”
He compared the dynamometer with a tire gauge. Just as a tire gauge can alert you to a loss of air pressure without revealing the source of the leak, a dynamometer can’t tell you why your grip strength is deflated.
“It’s hard to specify the prognostic value,” he said. “You don’t know the next steps to take. As a standalone measurement, that’s a concern.”
That’s why his current research goes beyond simple tests of maximum grip strength to more sophisticated measurements of the rate of force development (how fast you can express strength), repeatability (how much your strength declines from your first to your second or third squeeze), and asymmetry (how big a gap there is between your right- and left-hand strength).
Any of those measures could detect a potential neural or neuromuscular issue.
In a 2020 study, for example, Dr. McGrath and his team at NDSU showed that older adults with both weakness and asymmetry in grip-strength tests were nearly four times more likely to experience functional limitations. Those limitations could affect their ability to do anything from routine chores to keeping themselves clean and fed.
Waging war on weakness
Using dynamometer readings, the generally accepted cutoffs for low grip strength are 26 kg for an adult male and 16 kg for a female.
But that’s way too simple, Dr. Peterson said.
For one thing, age matters. Grip strength typically peaks for men in their late 20s and declines rapidly in middle age and beyond. For women, it plateaus in their 20s and gently declines until their 50s. So, at minimum, the age-based standards included with a dynamometer should be consulted.
Another caveat: Dr. Peterson said grip strength tests aren’t very meaningful for people who actively train for strength, though he suggests dedicated athletes make up a relatively small percentage of the population – even as low as 10%.
The size of the person taking the test is also important.
“You absolutely must account for body mass in the context of understanding how grip strength, or any strength measure, is reflective of health and function,” Dr. Peterson said.
To calculate strength-weight ratio, which Dr. Peterson calls “normalized grip strength,” divide grip strength in kilograms by body weight in kilograms. For men, a ratio greater than 0.70 puts them in the higher percentiles. For women it’s 0.50.
And if the results suggest that the person in question is objectively weak? “For me, that’s easy,” Dr. Peterson said. “They need to exercise.”
Common sense suggests doing a lot of forearm exercises for grip strength. Not so, said Dr. Peterson. The strength of hand and forearm muscles reflects what they can do along with all other muscles moving together.
A 2019 study found that, for older adults, a variety of exercise programs can lead to modest but meaningful increases in participants’ grip strength – and they don’t necessarily have to include actual gripping exercises. The programs ranged from tai chi to water aerobics to walking, stretching, and all kinds of resistance training.
Dr. Peterson’s advice to everyone is pretty straightforward: Get stronger. It doesn’t really matter how you do it, or how much strength you ultimately gain. Even a little more strength means a little less weakness, and a little more life.
A version of this article first appeared on Medscape.com.
Top U.S. neurology, neurosurgery hospitals ranked
of best hospitals for neurology and neurosurgery.
NYU Langone also claimed the top spot in last year’s ranking.
In the latest rankings, UCSF Health–UCSF Medical Center, San Francisco, holds the No. 2 spot and New York–Presbyterian Hospital–Columbia and Cornell in New York City holds the No. 3 spot for neurology care, with no change from last year.
This year, Mayo Clinic, Rochester, Minn., is ranked No. 4 in neurology and neurosurgery care, up from No. 6 last year, while Cedars-Sinai Medical Center, Los Angeles, ranks fifth this year, rising two spots from No. 7 last year.
Rounding out the top 10 hospitals for neurology and neurosurgery (in order) are UCLA Medical Center, Los Angeles; Johns Hopkins Hospital, Baltimore; Massachusetts General Hospital, Boston; Mount Sinai Hospital, New York; and Northwestern Medicine–Northwestern Memorial Hospital, Chicago.
U.S. News evaluated 1,245 hospitals and ranked the top 50 that treat patients with challenging neurological issues including stroke, conditions affecting the central nervous system, spinal disorders and injuries, seizures, and degenerative nervous system diagnoses such as multiple sclerosis.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News recognized “honor roll” hospitals that have excelled across multiple areas of care. However, this year, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the organization’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the honor roll hospitals have attained the highest standard of care in the nation,” the letter reads.
This year there are 22 honor roll hospitals:
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania-Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York City
- New York–Presbyterian Hospital–Columbia and Cornell, New York City
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York City
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
U.S. News noted that to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles at usnews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
of best hospitals for neurology and neurosurgery.
NYU Langone also claimed the top spot in last year’s ranking.
In the latest rankings, UCSF Health–UCSF Medical Center, San Francisco, holds the No. 2 spot and New York–Presbyterian Hospital–Columbia and Cornell in New York City holds the No. 3 spot for neurology care, with no change from last year.
This year, Mayo Clinic, Rochester, Minn., is ranked No. 4 in neurology and neurosurgery care, up from No. 6 last year, while Cedars-Sinai Medical Center, Los Angeles, ranks fifth this year, rising two spots from No. 7 last year.
Rounding out the top 10 hospitals for neurology and neurosurgery (in order) are UCLA Medical Center, Los Angeles; Johns Hopkins Hospital, Baltimore; Massachusetts General Hospital, Boston; Mount Sinai Hospital, New York; and Northwestern Medicine–Northwestern Memorial Hospital, Chicago.
U.S. News evaluated 1,245 hospitals and ranked the top 50 that treat patients with challenging neurological issues including stroke, conditions affecting the central nervous system, spinal disorders and injuries, seizures, and degenerative nervous system diagnoses such as multiple sclerosis.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News recognized “honor roll” hospitals that have excelled across multiple areas of care. However, this year, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the organization’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the honor roll hospitals have attained the highest standard of care in the nation,” the letter reads.
This year there are 22 honor roll hospitals:
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania-Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York City
- New York–Presbyterian Hospital–Columbia and Cornell, New York City
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York City
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
U.S. News noted that to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles at usnews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
of best hospitals for neurology and neurosurgery.
NYU Langone also claimed the top spot in last year’s ranking.
In the latest rankings, UCSF Health–UCSF Medical Center, San Francisco, holds the No. 2 spot and New York–Presbyterian Hospital–Columbia and Cornell in New York City holds the No. 3 spot for neurology care, with no change from last year.
This year, Mayo Clinic, Rochester, Minn., is ranked No. 4 in neurology and neurosurgery care, up from No. 6 last year, while Cedars-Sinai Medical Center, Los Angeles, ranks fifth this year, rising two spots from No. 7 last year.
Rounding out the top 10 hospitals for neurology and neurosurgery (in order) are UCLA Medical Center, Los Angeles; Johns Hopkins Hospital, Baltimore; Massachusetts General Hospital, Boston; Mount Sinai Hospital, New York; and Northwestern Medicine–Northwestern Memorial Hospital, Chicago.
U.S. News evaluated 1,245 hospitals and ranked the top 50 that treat patients with challenging neurological issues including stroke, conditions affecting the central nervous system, spinal disorders and injuries, seizures, and degenerative nervous system diagnoses such as multiple sclerosis.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News recognized “honor roll” hospitals that have excelled across multiple areas of care. However, this year, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the organization’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the honor roll hospitals have attained the highest standard of care in the nation,” the letter reads.
This year there are 22 honor roll hospitals:
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania-Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York City
- New York–Presbyterian Hospital–Columbia and Cornell, New York City
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York City
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
U.S. News noted that to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles at usnews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
Medical students are skipping class lectures: Does it matter?
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
A new and completely different pain medicine
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.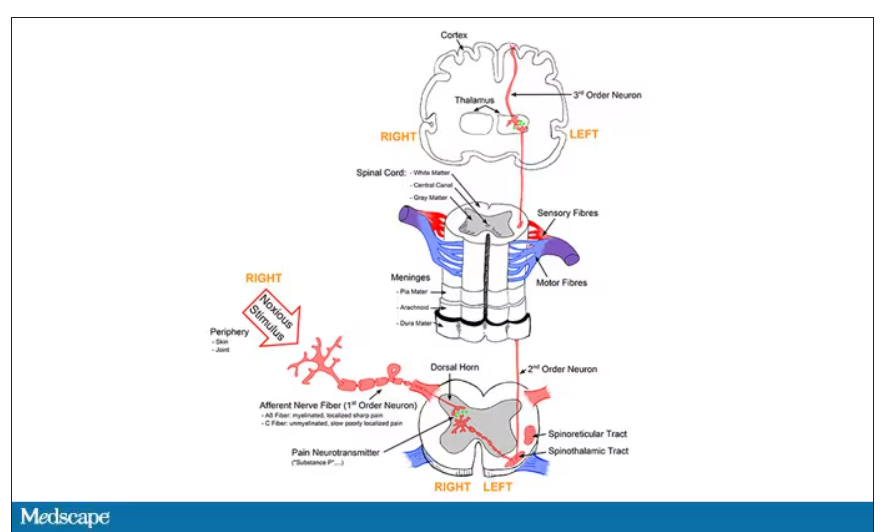
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.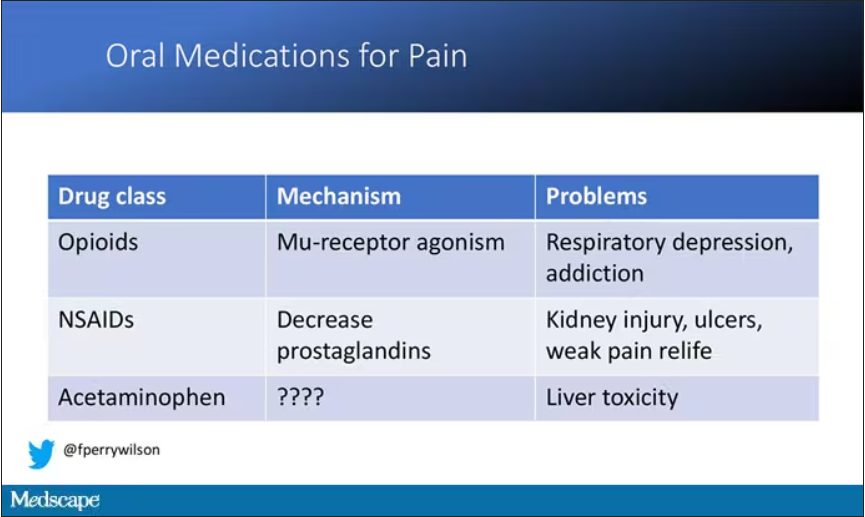
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.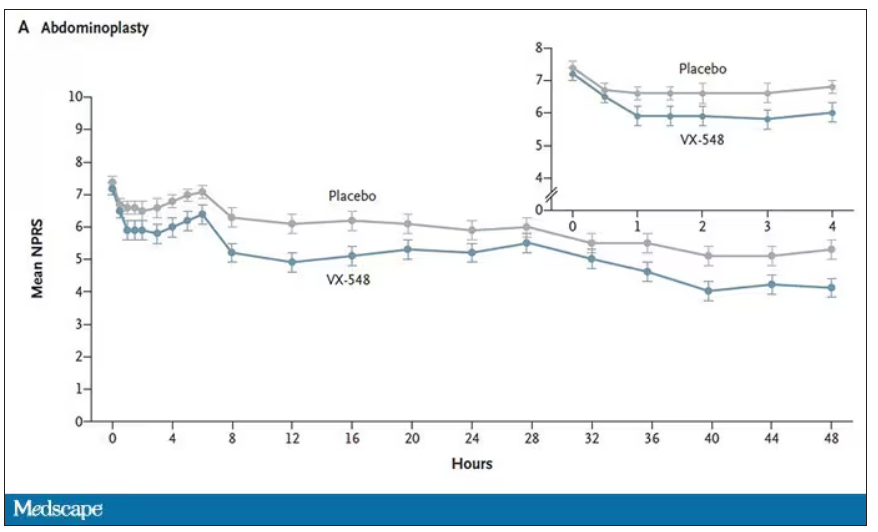
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.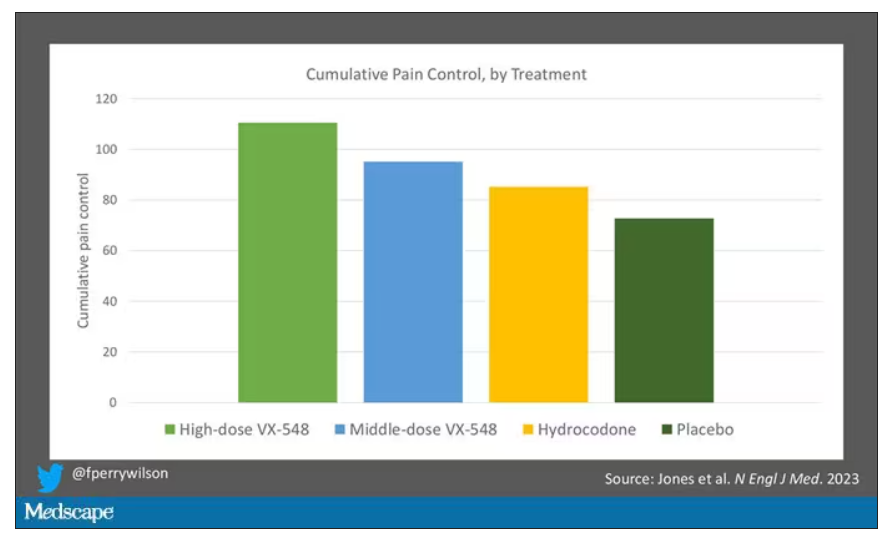
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.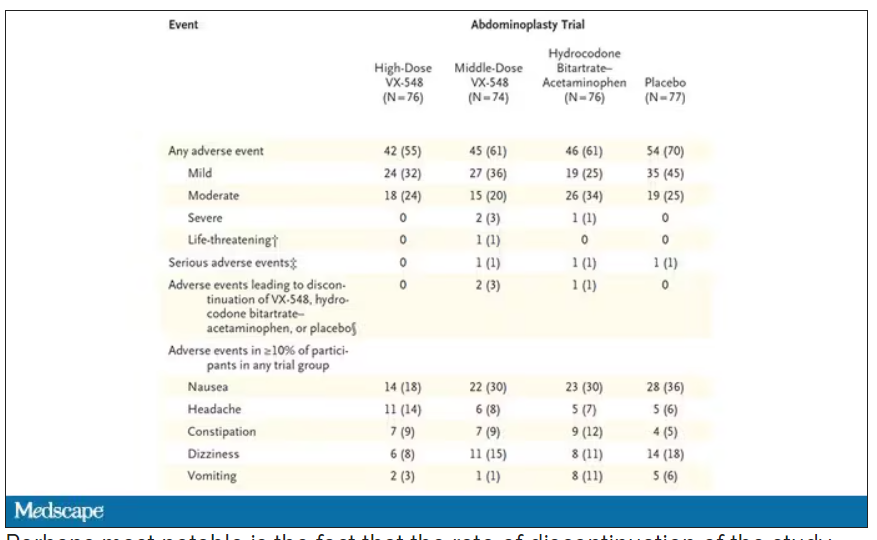
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.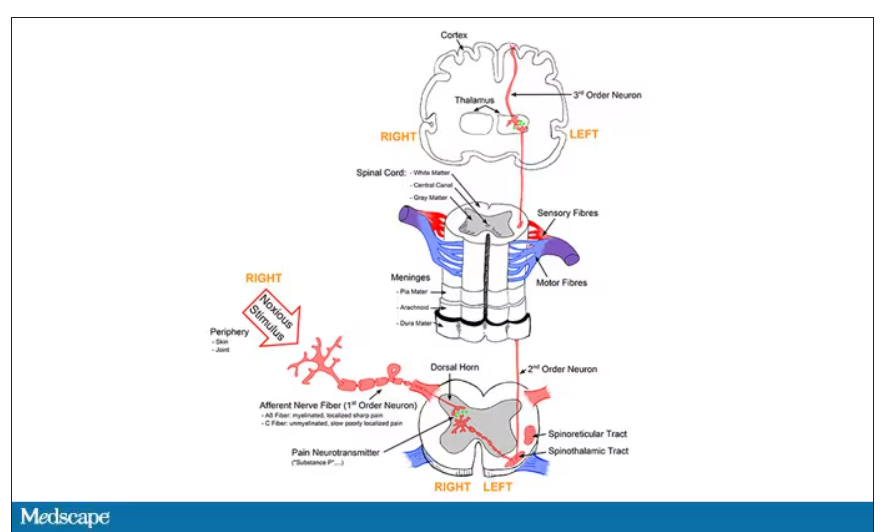
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.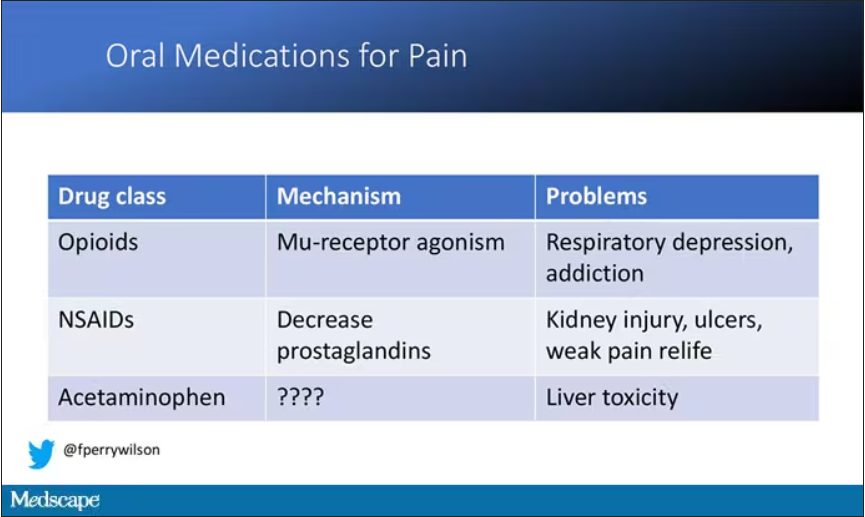
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.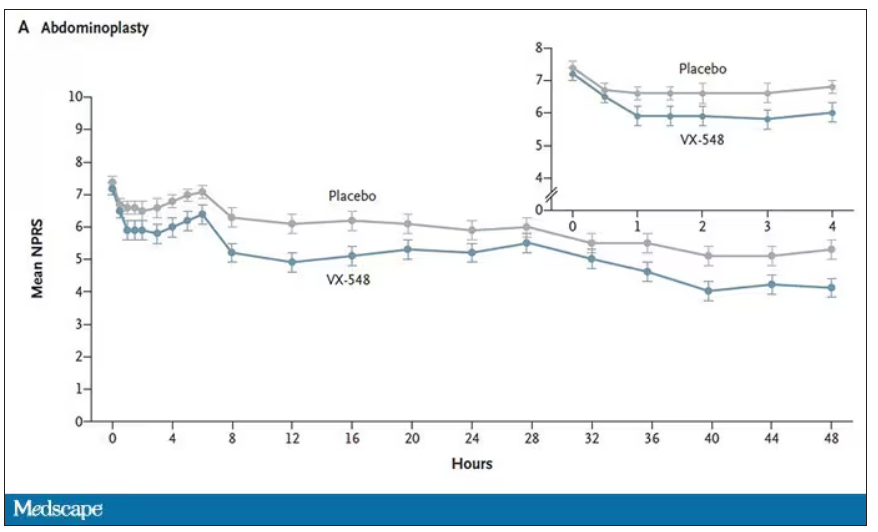
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.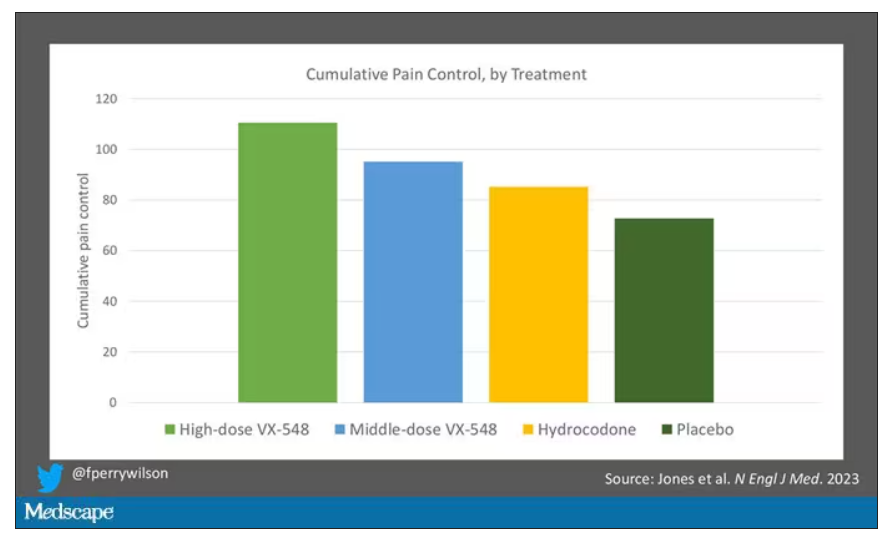
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.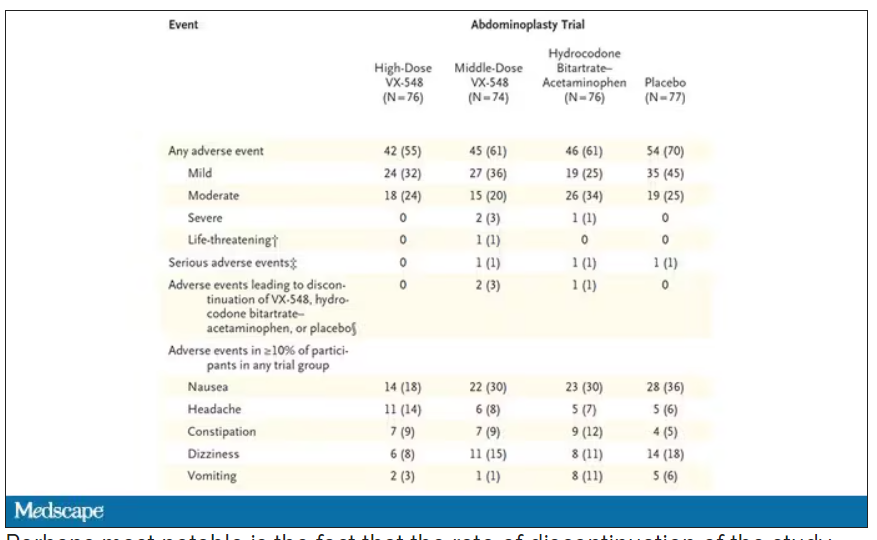
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.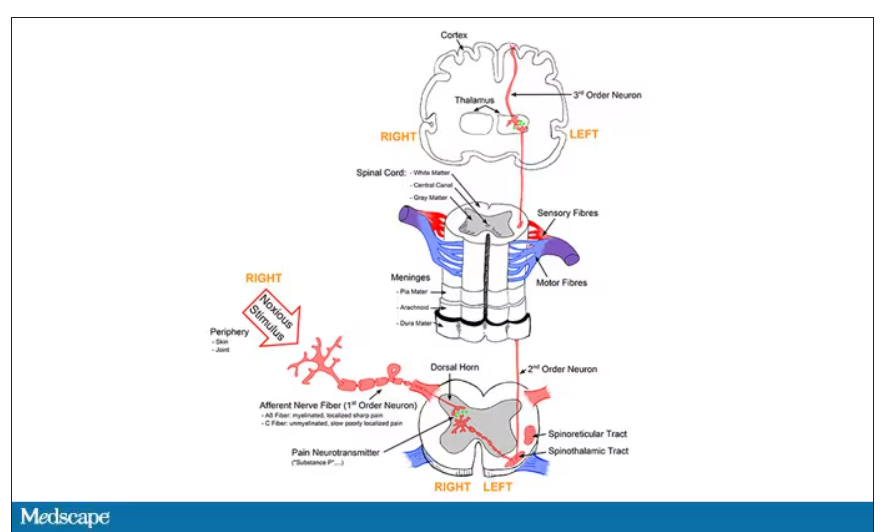
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.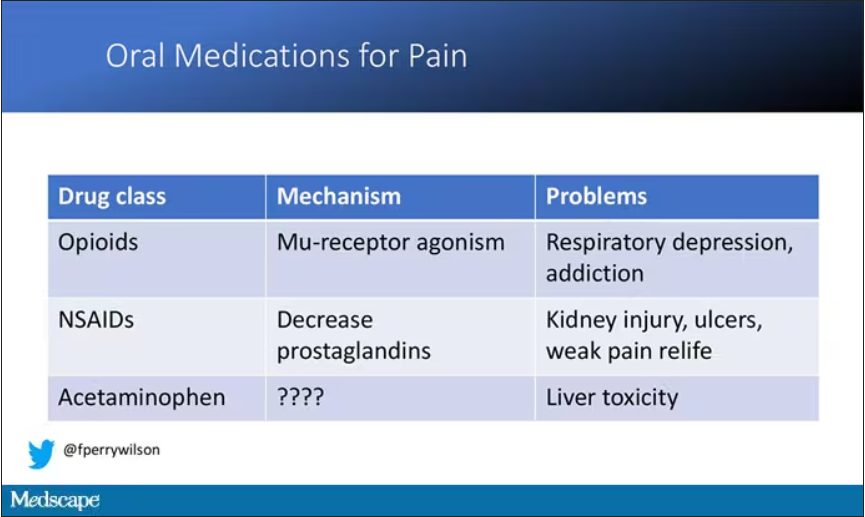
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.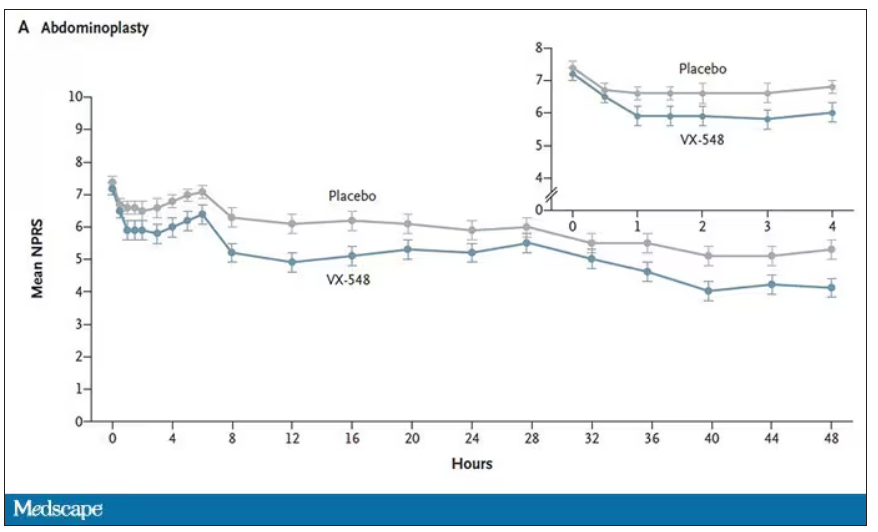
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.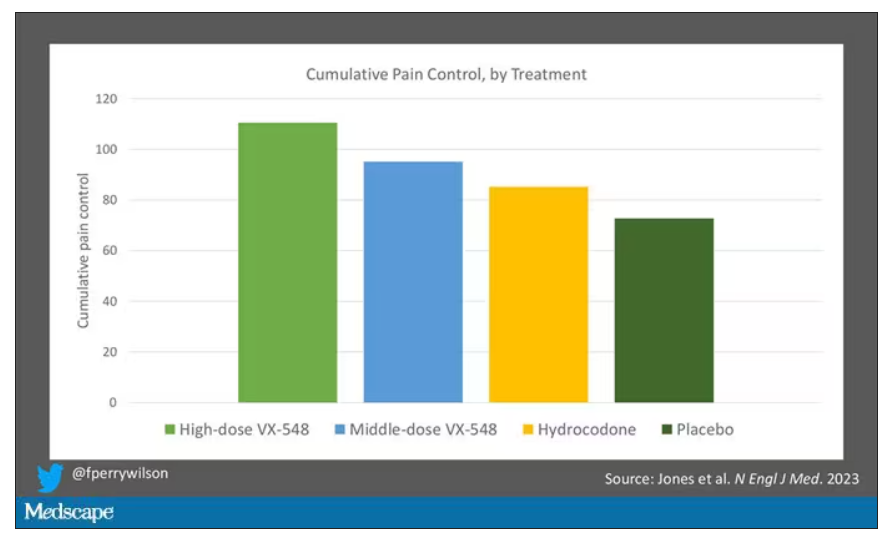
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.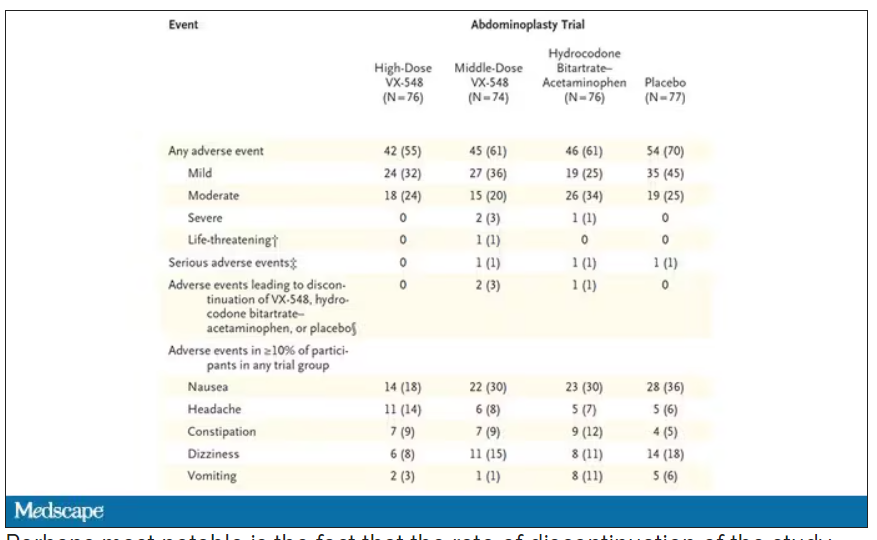
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Long COVID disability court battles just ‘tip of iceberg’
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
Depression at any stage of life tied to increased dementia risk
Adults with depression have more than double the risk of developing dementia and the risk persists regardless of when in life depression is diagnosed, a large population-based study shows.
That the association between depression and dementia persisted even among individuals first diagnosed with depression in early or mid-life provides “strong evidence that depression is not only an early symptom of dementia, but also that depression increases dementia risk,” study investigator Holly Elser, MD, PhD, epidemiologist and resident physician, University of Pennsylvania, Philadelphia, told this news organization.
The study was published online in JAMA Neurology.
Double the risk
Several prior studies that have examined the relationship between depression and dementia over the life course have consistently shown depression later in life is associated with subsequent dementia.
“Late-life depression is generally thought to be an early symptom of dementia or a reaction to subclinical cognitive decline,” said Dr. Elser.
The investigators wanted to examine whether the association between depression and dementia persists even when depression is diagnosed earlier in life, which may suggest it increases the risk of dementia.
“To my knowledge, ours is the largest study on this topic to date, leveraging routinely and prospectively collected data from more than 1.4 million Danish citizens followed from 1977 to 2018,” Dr. Elser noted.
The cohort included 246,499 individuals diagnosed with depression and 1,190,302 individuals without depression.
In both groups, the median age was 50 years and 65% were women. Roughly two-thirds (68%) of those diagnosed with depression were diagnosed before age 60 years.
In Cox proportional hazards regression models, the overall hazard of dementia was more than doubled in those diagnosed with depression (hazard ratio [HR] 2.41). The risk of dementia with depression was more pronounced for men (HR, 2.98) than in women (HR, 2.21).
This association persisted even when the time elapsed from depression diagnosis was between 20 and 39 years (HR, 1.79) and whether depression was diagnosed in early life (18-44 years: HR, 3.08), mid-life (45-59 years: HR, 2.95), or late life (≥ 60 years: HR, 2.31).
It remains unclear whether effective treatment of depression modifies the risk of dementia, as the current study explored the role of antidepressants in a “very limited fashion,” Dr. Elser said.
Specifically, the researchers considered whether an individual was treated with an antidepressant within 6 months of the initial depression diagnosis and found no evidence of a difference in dementia risk between the treated and untreated groups.
“Research that explores implications of the timing and duration of treatment with antidepressants for dementia, treatment with cognitive behavioral therapy, and is able to evaluate the effectiveness of those treatments will be extremely important,” Dr. Elser said.
‘An assault on the brain’
Reached for comment, John Showalter, MD, chief product officer at Linus Health, said one of the most “intriguing” findings of the study is that a depression diagnosis earlier in adulthood conferred a greater risk of developing vascular dementia (HR, 3.28) than did dementia due to Alzheimer’s disease (HR, 1.73).
“The difference in risk for subtypes of dementia is a meaningful addition to our understanding of depression’s connection to dementia,” said Dr. Showalter, who was not involved in the study.
Also weighing in, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the findings from this “far-reaching investigation leave little room for doubt – depression unleashes a devastating storm within the brain, wreaking havoc on the lives of those ensnared by its grip.
“This massive, multi-decade, and high-data quality registry study adds another brick to the growing edifice of evidence attesting to the profound connection between psychiatric health and the very essence of brain health,” said Dr. Lakhan, who was not involved in the study.
“In a resounding declaration, this research underscores that psychiatric health should be perceived as an integral component of overall health – a paradigm shift that challenges long-standing misconceptions and stigmas surrounding mental disorders. Depression, once marginalized, now claims its rightful place on the pedestal of health concerns that must be addressed with unwavering resolve,” said Dr. Lakhan.
He noted that depression is “not just a mental battle, it’s a profound assault on the very fabric of the brain, leaving lives in turmoil and hearts in search of hope. No longer shrouded in silence, depression demands society’s attention.”
The study had no specific funding. Dr. Elser, Dr. Showalter, and Dr. Lakhan have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Adults with depression have more than double the risk of developing dementia and the risk persists regardless of when in life depression is diagnosed, a large population-based study shows.
That the association between depression and dementia persisted even among individuals first diagnosed with depression in early or mid-life provides “strong evidence that depression is not only an early symptom of dementia, but also that depression increases dementia risk,” study investigator Holly Elser, MD, PhD, epidemiologist and resident physician, University of Pennsylvania, Philadelphia, told this news organization.
The study was published online in JAMA Neurology.
Double the risk
Several prior studies that have examined the relationship between depression and dementia over the life course have consistently shown depression later in life is associated with subsequent dementia.
“Late-life depression is generally thought to be an early symptom of dementia or a reaction to subclinical cognitive decline,” said Dr. Elser.
The investigators wanted to examine whether the association between depression and dementia persists even when depression is diagnosed earlier in life, which may suggest it increases the risk of dementia.
“To my knowledge, ours is the largest study on this topic to date, leveraging routinely and prospectively collected data from more than 1.4 million Danish citizens followed from 1977 to 2018,” Dr. Elser noted.
The cohort included 246,499 individuals diagnosed with depression and 1,190,302 individuals without depression.
In both groups, the median age was 50 years and 65% were women. Roughly two-thirds (68%) of those diagnosed with depression were diagnosed before age 60 years.
In Cox proportional hazards regression models, the overall hazard of dementia was more than doubled in those diagnosed with depression (hazard ratio [HR] 2.41). The risk of dementia with depression was more pronounced for men (HR, 2.98) than in women (HR, 2.21).
This association persisted even when the time elapsed from depression diagnosis was between 20 and 39 years (HR, 1.79) and whether depression was diagnosed in early life (18-44 years: HR, 3.08), mid-life (45-59 years: HR, 2.95), or late life (≥ 60 years: HR, 2.31).
It remains unclear whether effective treatment of depression modifies the risk of dementia, as the current study explored the role of antidepressants in a “very limited fashion,” Dr. Elser said.
Specifically, the researchers considered whether an individual was treated with an antidepressant within 6 months of the initial depression diagnosis and found no evidence of a difference in dementia risk between the treated and untreated groups.
“Research that explores implications of the timing and duration of treatment with antidepressants for dementia, treatment with cognitive behavioral therapy, and is able to evaluate the effectiveness of those treatments will be extremely important,” Dr. Elser said.
‘An assault on the brain’
Reached for comment, John Showalter, MD, chief product officer at Linus Health, said one of the most “intriguing” findings of the study is that a depression diagnosis earlier in adulthood conferred a greater risk of developing vascular dementia (HR, 3.28) than did dementia due to Alzheimer’s disease (HR, 1.73).
“The difference in risk for subtypes of dementia is a meaningful addition to our understanding of depression’s connection to dementia,” said Dr. Showalter, who was not involved in the study.
Also weighing in, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the findings from this “far-reaching investigation leave little room for doubt – depression unleashes a devastating storm within the brain, wreaking havoc on the lives of those ensnared by its grip.
“This massive, multi-decade, and high-data quality registry study adds another brick to the growing edifice of evidence attesting to the profound connection between psychiatric health and the very essence of brain health,” said Dr. Lakhan, who was not involved in the study.
“In a resounding declaration, this research underscores that psychiatric health should be perceived as an integral component of overall health – a paradigm shift that challenges long-standing misconceptions and stigmas surrounding mental disorders. Depression, once marginalized, now claims its rightful place on the pedestal of health concerns that must be addressed with unwavering resolve,” said Dr. Lakhan.
He noted that depression is “not just a mental battle, it’s a profound assault on the very fabric of the brain, leaving lives in turmoil and hearts in search of hope. No longer shrouded in silence, depression demands society’s attention.”
The study had no specific funding. Dr. Elser, Dr. Showalter, and Dr. Lakhan have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Adults with depression have more than double the risk of developing dementia and the risk persists regardless of when in life depression is diagnosed, a large population-based study shows.
That the association between depression and dementia persisted even among individuals first diagnosed with depression in early or mid-life provides “strong evidence that depression is not only an early symptom of dementia, but also that depression increases dementia risk,” study investigator Holly Elser, MD, PhD, epidemiologist and resident physician, University of Pennsylvania, Philadelphia, told this news organization.
The study was published online in JAMA Neurology.
Double the risk
Several prior studies that have examined the relationship between depression and dementia over the life course have consistently shown depression later in life is associated with subsequent dementia.
“Late-life depression is generally thought to be an early symptom of dementia or a reaction to subclinical cognitive decline,” said Dr. Elser.
The investigators wanted to examine whether the association between depression and dementia persists even when depression is diagnosed earlier in life, which may suggest it increases the risk of dementia.
“To my knowledge, ours is the largest study on this topic to date, leveraging routinely and prospectively collected data from more than 1.4 million Danish citizens followed from 1977 to 2018,” Dr. Elser noted.
The cohort included 246,499 individuals diagnosed with depression and 1,190,302 individuals without depression.
In both groups, the median age was 50 years and 65% were women. Roughly two-thirds (68%) of those diagnosed with depression were diagnosed before age 60 years.
In Cox proportional hazards regression models, the overall hazard of dementia was more than doubled in those diagnosed with depression (hazard ratio [HR] 2.41). The risk of dementia with depression was more pronounced for men (HR, 2.98) than in women (HR, 2.21).
This association persisted even when the time elapsed from depression diagnosis was between 20 and 39 years (HR, 1.79) and whether depression was diagnosed in early life (18-44 years: HR, 3.08), mid-life (45-59 years: HR, 2.95), or late life (≥ 60 years: HR, 2.31).
It remains unclear whether effective treatment of depression modifies the risk of dementia, as the current study explored the role of antidepressants in a “very limited fashion,” Dr. Elser said.
Specifically, the researchers considered whether an individual was treated with an antidepressant within 6 months of the initial depression diagnosis and found no evidence of a difference in dementia risk between the treated and untreated groups.
“Research that explores implications of the timing and duration of treatment with antidepressants for dementia, treatment with cognitive behavioral therapy, and is able to evaluate the effectiveness of those treatments will be extremely important,” Dr. Elser said.
‘An assault on the brain’
Reached for comment, John Showalter, MD, chief product officer at Linus Health, said one of the most “intriguing” findings of the study is that a depression diagnosis earlier in adulthood conferred a greater risk of developing vascular dementia (HR, 3.28) than did dementia due to Alzheimer’s disease (HR, 1.73).
“The difference in risk for subtypes of dementia is a meaningful addition to our understanding of depression’s connection to dementia,” said Dr. Showalter, who was not involved in the study.
Also weighing in, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said the findings from this “far-reaching investigation leave little room for doubt – depression unleashes a devastating storm within the brain, wreaking havoc on the lives of those ensnared by its grip.
“This massive, multi-decade, and high-data quality registry study adds another brick to the growing edifice of evidence attesting to the profound connection between psychiatric health and the very essence of brain health,” said Dr. Lakhan, who was not involved in the study.
“In a resounding declaration, this research underscores that psychiatric health should be perceived as an integral component of overall health – a paradigm shift that challenges long-standing misconceptions and stigmas surrounding mental disorders. Depression, once marginalized, now claims its rightful place on the pedestal of health concerns that must be addressed with unwavering resolve,” said Dr. Lakhan.
He noted that depression is “not just a mental battle, it’s a profound assault on the very fabric of the brain, leaving lives in turmoil and hearts in search of hope. No longer shrouded in silence, depression demands society’s attention.”
The study had no specific funding. Dr. Elser, Dr. Showalter, and Dr. Lakhan have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.