User login
Borderline personality disorder: Remember empathy and compassion
Oh, great!” a senior resident sardonically remarked with a smirk as they read up on the next patient in the clinic. “A borderline patient. Get ready for a rough one ... Ugh.”
Before ever stepping foot into the patient’s room, this resident had prematurely established and demonstrated an unfortunate dynamic for any student or trainee within earshot. This is an all-too-familiar occurrence when caring for individuals with borderline personality disorder (BPD), or any other patients deemed to be “difficult.” The patient, however, likely walked into the room with a traumatic past that they continue to suffer from, in addition to any other issues for which they were seeking care.
Consider what these patients have experienced
A typical profile of these resilient patients with BPD: They were born emotionally sensitive. They grew up in homes with caretakers who knowingly or unknowingly invalidated their complaints about having their feelings hurt, about being abused emotionally, sexually, or otherwise, or about their worries concerning their interactions with peers at school. These caretakers may have been frightening and unpredictable, randomly showing affection or arbitrarily punishing for any perceived misstep, which led these patients to develop (for their own safety’s sake) a hypersensitivity to the affect of others. Their wariness and distrust of their social surroundings may have led to a skeptical view of kindness from others. Over time, without any guidance from prior demonstrations of healthy coping skills or interpersonal outlets from their caregivers, the emotional pressure builds. This pressure finally erupts in the form of impulsivity, self-harm, desperation, and defensiveness—in other words, survival. This is often followed by these patients’ first experience with receiving some degree of appropriate response to their complaints—their first experience with feeling seen and heard by their caretakers. They learn that their needs are met only when they cry out in desperation.1-3
These patients typically bring these maladaptive coping skills with them into adulthood, which often leads to a series of intense, unhealthy, and short-lived interpersonal and professional connections. They desire healthy, lasting connections with others, but through no fault of their own are unable to appropriately manage the normal stressors therein.1 Often, these patients do not know of their eventual BPD diagnosis, or even reject it due to its ever-negative valence. For other patients, receiving a personality disorder diagnosis is incredibly validating because they are no longer alone regarding this type of suffering, and a doctor—a caretaker—is finally making sense of this tumultuous world.
The countertransference of frustration, anxiety, doubt, and annoyance we may feel when caring for patients with BPD pales in comparison to living in their shoes and carrying the weight of what they have had to endure before presenting to our care. As these resilient patients wait in the exam room for the chance to be heard, let this be a reminder to greet them with the patience, understanding, empathy, and compassion that physicians are known to embody.
Suggestions for working with ‘difficult’ patients
The following tips may be helpful for building rapport with patients with BPD or other “difficult” patients:
- validate their complaints, and the difficulties they cause
- be genuine and honest when discussing their complaints
- acknowledge your own mistakes and misunderstandings in their care
- don’t be defensive—accept criticism with an open mind
- practice listening with intent, and reflective listening
- set ground rules and stick to them (eg, time limits, prescribing expectations, patient-physician relationship boundaries)
- educate and support the patient and their loved ones.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013:947.
2. Porter C, Palmier-Claus J, Branitsky A, et al. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6-20.
3. Sansone RA, Sansone LA. Emotional hyper-reactivity in borderline personality disorder. Psychiatry (Edgmont). 2010;7(9):16-20.
Oh, great!” a senior resident sardonically remarked with a smirk as they read up on the next patient in the clinic. “A borderline patient. Get ready for a rough one ... Ugh.”
Before ever stepping foot into the patient’s room, this resident had prematurely established and demonstrated an unfortunate dynamic for any student or trainee within earshot. This is an all-too-familiar occurrence when caring for individuals with borderline personality disorder (BPD), or any other patients deemed to be “difficult.” The patient, however, likely walked into the room with a traumatic past that they continue to suffer from, in addition to any other issues for which they were seeking care.
Consider what these patients have experienced
A typical profile of these resilient patients with BPD: They were born emotionally sensitive. They grew up in homes with caretakers who knowingly or unknowingly invalidated their complaints about having their feelings hurt, about being abused emotionally, sexually, or otherwise, or about their worries concerning their interactions with peers at school. These caretakers may have been frightening and unpredictable, randomly showing affection or arbitrarily punishing for any perceived misstep, which led these patients to develop (for their own safety’s sake) a hypersensitivity to the affect of others. Their wariness and distrust of their social surroundings may have led to a skeptical view of kindness from others. Over time, without any guidance from prior demonstrations of healthy coping skills or interpersonal outlets from their caregivers, the emotional pressure builds. This pressure finally erupts in the form of impulsivity, self-harm, desperation, and defensiveness—in other words, survival. This is often followed by these patients’ first experience with receiving some degree of appropriate response to their complaints—their first experience with feeling seen and heard by their caretakers. They learn that their needs are met only when they cry out in desperation.1-3
These patients typically bring these maladaptive coping skills with them into adulthood, which often leads to a series of intense, unhealthy, and short-lived interpersonal and professional connections. They desire healthy, lasting connections with others, but through no fault of their own are unable to appropriately manage the normal stressors therein.1 Often, these patients do not know of their eventual BPD diagnosis, or even reject it due to its ever-negative valence. For other patients, receiving a personality disorder diagnosis is incredibly validating because they are no longer alone regarding this type of suffering, and a doctor—a caretaker—is finally making sense of this tumultuous world.
The countertransference of frustration, anxiety, doubt, and annoyance we may feel when caring for patients with BPD pales in comparison to living in their shoes and carrying the weight of what they have had to endure before presenting to our care. As these resilient patients wait in the exam room for the chance to be heard, let this be a reminder to greet them with the patience, understanding, empathy, and compassion that physicians are known to embody.
Suggestions for working with ‘difficult’ patients
The following tips may be helpful for building rapport with patients with BPD or other “difficult” patients:
- validate their complaints, and the difficulties they cause
- be genuine and honest when discussing their complaints
- acknowledge your own mistakes and misunderstandings in their care
- don’t be defensive—accept criticism with an open mind
- practice listening with intent, and reflective listening
- set ground rules and stick to them (eg, time limits, prescribing expectations, patient-physician relationship boundaries)
- educate and support the patient and their loved ones.
Oh, great!” a senior resident sardonically remarked with a smirk as they read up on the next patient in the clinic. “A borderline patient. Get ready for a rough one ... Ugh.”
Before ever stepping foot into the patient’s room, this resident had prematurely established and demonstrated an unfortunate dynamic for any student or trainee within earshot. This is an all-too-familiar occurrence when caring for individuals with borderline personality disorder (BPD), or any other patients deemed to be “difficult.” The patient, however, likely walked into the room with a traumatic past that they continue to suffer from, in addition to any other issues for which they were seeking care.
Consider what these patients have experienced
A typical profile of these resilient patients with BPD: They were born emotionally sensitive. They grew up in homes with caretakers who knowingly or unknowingly invalidated their complaints about having their feelings hurt, about being abused emotionally, sexually, or otherwise, or about their worries concerning their interactions with peers at school. These caretakers may have been frightening and unpredictable, randomly showing affection or arbitrarily punishing for any perceived misstep, which led these patients to develop (for their own safety’s sake) a hypersensitivity to the affect of others. Their wariness and distrust of their social surroundings may have led to a skeptical view of kindness from others. Over time, without any guidance from prior demonstrations of healthy coping skills or interpersonal outlets from their caregivers, the emotional pressure builds. This pressure finally erupts in the form of impulsivity, self-harm, desperation, and defensiveness—in other words, survival. This is often followed by these patients’ first experience with receiving some degree of appropriate response to their complaints—their first experience with feeling seen and heard by their caretakers. They learn that their needs are met only when they cry out in desperation.1-3
These patients typically bring these maladaptive coping skills with them into adulthood, which often leads to a series of intense, unhealthy, and short-lived interpersonal and professional connections. They desire healthy, lasting connections with others, but through no fault of their own are unable to appropriately manage the normal stressors therein.1 Often, these patients do not know of their eventual BPD diagnosis, or even reject it due to its ever-negative valence. For other patients, receiving a personality disorder diagnosis is incredibly validating because they are no longer alone regarding this type of suffering, and a doctor—a caretaker—is finally making sense of this tumultuous world.
The countertransference of frustration, anxiety, doubt, and annoyance we may feel when caring for patients with BPD pales in comparison to living in their shoes and carrying the weight of what they have had to endure before presenting to our care. As these resilient patients wait in the exam room for the chance to be heard, let this be a reminder to greet them with the patience, understanding, empathy, and compassion that physicians are known to embody.
Suggestions for working with ‘difficult’ patients
The following tips may be helpful for building rapport with patients with BPD or other “difficult” patients:
- validate their complaints, and the difficulties they cause
- be genuine and honest when discussing their complaints
- acknowledge your own mistakes and misunderstandings in their care
- don’t be defensive—accept criticism with an open mind
- practice listening with intent, and reflective listening
- set ground rules and stick to them (eg, time limits, prescribing expectations, patient-physician relationship boundaries)
- educate and support the patient and their loved ones.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013:947.
2. Porter C, Palmier-Claus J, Branitsky A, et al. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6-20.
3. Sansone RA, Sansone LA. Emotional hyper-reactivity in borderline personality disorder. Psychiatry (Edgmont). 2010;7(9):16-20.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013:947.
2. Porter C, Palmier-Claus J, Branitsky A, et al. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6-20.
3. Sansone RA, Sansone LA. Emotional hyper-reactivity in borderline personality disorder. Psychiatry (Edgmont). 2010;7(9):16-20.
Vegetarian diet as good for children, with slight risk of underweight
With more families placing their children on vegetarian diets, the results from a Canadian longitudinal cohort study are reassuring: It found no clinically meaningful differences in height, growth, or biochemical measures of nutrition in young children on vegetarian and nonvegetarian diets.
While z scores (the standard deviation above or below the mean) were similar in both dietary groups, there was a weak association between a vegetarian diet and lower mean z height, as well as slightly higher odds of underweight.
No significant associations were identified between vegetarian and nonvegetarian diets for child z body mass index (BMI), serum ferritin, 25(OH)D, and serum lipids, according to Jonathon L. Maguire, MD. MSc, of St. Michael’s Hospital Pediatric Clinic in Toronto.
Moreover, the magnitude of the height and vegetarian diet association was small at just 0.3 cm for a 3-year-old child and unlikely to be clinically meaningful, Dr. Maguire and colleagues wrote online in Pediatrics.
In a secondary study outcome, cow’s milk consumption was associated with higher serum lipid levels for both diets. Serum lipids were similar among those who did or did not consume a vegetarian diet and consumed the recommended 2 cups of cow’s milk per day.
“The vast majority of children with vegetarian diets have similar growth and nutrition as children without vegetarian diets,” said Dr. Maguire, who is also a professor of pediatrics and nutritional sciences at the University of Toronto, in an interview. “But, I think we should be mindful to carefully plan vegetarian diets for children [who are] underweight.”
The study conclusion was based on 8,907 children, 6 months to 8 years of age, including 248 vegetarian and 25 vegan children, at baseline. They were part of theTARGet Kids! practice-based research network in Toronto.
The mean age of children at baseline was 2.2 years (standard deviation, 1.5), and 52.4% were male. Participants were followed for an average of 2.8 years (SD, 1.7).
Those with a vegetarian diet had longer breastfeeding duration: 12.6 months (SD, 9.5) versus 10.0 months (SD, 7.0). They were also more likely to be of Asian ethnicity: 33.8% versus 19.0%. Otherwise, children with and without a vegetarian diet were similar at baseline.
In study outcomes, vegetarian children had higher odds of underweight: body mass index z score less than –2 (odds ratio 1.87; 95% confidence interval, 1.19-2.96, P = .007), while no association with overweight or obesity was found.
In a secondary outcome, cow’s milk consumption was associated with higher levels of non–high-density lipoprotein cholesterol (P = .03), total cholesterol (P = .04), and low-density lipoprotein cholesterol (P = .02) in young children on a vegetarian diet. Levels were similar in children with and without a vegetarian diet who consumed the recommended 2 cups of cow’s milk per day.
Previous studies have found that vegetarian children have normal growth and development but tend to be leaner than their omnivore peers.
As for the potential effect of following a fully vegan diet on these nutritional measures, Dr. Maguire said, “Unfortunately, there were not enough children with vegan diets to make meaningful conclusions.”
Would results likely be similar in older children who have more independence and engage more with their peers?“ I don’t know, but we will be following these children for many years to come through the TARGet Kids! research network, Dr. Maguire said.
Studies such as this are timely as plant-based eating becomes more widespread in the United States. The 2007-2010 National Health and Nutrition Examination Surveys found that 2.1% of American adults followed a vegetarian diet, and that figure appears to have increased, with 5% of American adults self-identifying as vegetarian in a 2019 Gallup poll.
Offering her perspective on the Canadian study but not involved in it, Stephanie Di Figlia-Peck, MS, RDN, agreed the results indicate that “a vegetarian diet is not a negative thing for growth and development.” She is a lead registered dietitian in the division of adolescent medicine at Cohen Children’s Medical Center in New Hyde Park, N.Y. She noted, however, that the study looked only at very young children on average.
She stressed that vegetarian regimens require family commitment and agreed on the need for planning. “For these diets to work, a lot has to go into it. But if they’re carefully planned, there is adequate protein and micro- and macronutrients and there’s a nonnegative effect on growth and development.”
The study results mirror what she sees in clinical practice, with vegetarian children tending to weigh less. “Some obese and overweight children will adopt vegetarian diets to lose weight,” Ms. Di Figlia-Peck said.
And perseverance has rewards. “When people follow a vegetarian diet, they tend to have lower blood pressure and cholesterol. A plant-based diet can favorably impact diseases for an entire lifetime.”
This study was supported by the Canadian Institutes of Health Research and the St. Michael’s Hospital and SickKids Hospital foundations. Dr. Maguire received an unrestricted research grant for a previous investigator-initiated study from Dairy Farmers of Canada, and D drops provided nonfinancial support (vitamin D supplements) for a previous investigator-initiated study on vitamin D and respiratory tract infections. Coauthor David Jenkins, MD, PhD, DSc, reported research support from multiple private-sector and nonprivate organizations; several of his family members are involved in the promotion of vegetarian diets. Ms. Di Figlia-Peck had no competing interests to declare.
With more families placing their children on vegetarian diets, the results from a Canadian longitudinal cohort study are reassuring: It found no clinically meaningful differences in height, growth, or biochemical measures of nutrition in young children on vegetarian and nonvegetarian diets.
While z scores (the standard deviation above or below the mean) were similar in both dietary groups, there was a weak association between a vegetarian diet and lower mean z height, as well as slightly higher odds of underweight.
No significant associations were identified between vegetarian and nonvegetarian diets for child z body mass index (BMI), serum ferritin, 25(OH)D, and serum lipids, according to Jonathon L. Maguire, MD. MSc, of St. Michael’s Hospital Pediatric Clinic in Toronto.
Moreover, the magnitude of the height and vegetarian diet association was small at just 0.3 cm for a 3-year-old child and unlikely to be clinically meaningful, Dr. Maguire and colleagues wrote online in Pediatrics.
In a secondary study outcome, cow’s milk consumption was associated with higher serum lipid levels for both diets. Serum lipids were similar among those who did or did not consume a vegetarian diet and consumed the recommended 2 cups of cow’s milk per day.
“The vast majority of children with vegetarian diets have similar growth and nutrition as children without vegetarian diets,” said Dr. Maguire, who is also a professor of pediatrics and nutritional sciences at the University of Toronto, in an interview. “But, I think we should be mindful to carefully plan vegetarian diets for children [who are] underweight.”
The study conclusion was based on 8,907 children, 6 months to 8 years of age, including 248 vegetarian and 25 vegan children, at baseline. They were part of theTARGet Kids! practice-based research network in Toronto.
The mean age of children at baseline was 2.2 years (standard deviation, 1.5), and 52.4% were male. Participants were followed for an average of 2.8 years (SD, 1.7).
Those with a vegetarian diet had longer breastfeeding duration: 12.6 months (SD, 9.5) versus 10.0 months (SD, 7.0). They were also more likely to be of Asian ethnicity: 33.8% versus 19.0%. Otherwise, children with and without a vegetarian diet were similar at baseline.
In study outcomes, vegetarian children had higher odds of underweight: body mass index z score less than –2 (odds ratio 1.87; 95% confidence interval, 1.19-2.96, P = .007), while no association with overweight or obesity was found.
In a secondary outcome, cow’s milk consumption was associated with higher levels of non–high-density lipoprotein cholesterol (P = .03), total cholesterol (P = .04), and low-density lipoprotein cholesterol (P = .02) in young children on a vegetarian diet. Levels were similar in children with and without a vegetarian diet who consumed the recommended 2 cups of cow’s milk per day.
Previous studies have found that vegetarian children have normal growth and development but tend to be leaner than their omnivore peers.
As for the potential effect of following a fully vegan diet on these nutritional measures, Dr. Maguire said, “Unfortunately, there were not enough children with vegan diets to make meaningful conclusions.”
Would results likely be similar in older children who have more independence and engage more with their peers?“ I don’t know, but we will be following these children for many years to come through the TARGet Kids! research network, Dr. Maguire said.
Studies such as this are timely as plant-based eating becomes more widespread in the United States. The 2007-2010 National Health and Nutrition Examination Surveys found that 2.1% of American adults followed a vegetarian diet, and that figure appears to have increased, with 5% of American adults self-identifying as vegetarian in a 2019 Gallup poll.
Offering her perspective on the Canadian study but not involved in it, Stephanie Di Figlia-Peck, MS, RDN, agreed the results indicate that “a vegetarian diet is not a negative thing for growth and development.” She is a lead registered dietitian in the division of adolescent medicine at Cohen Children’s Medical Center in New Hyde Park, N.Y. She noted, however, that the study looked only at very young children on average.
She stressed that vegetarian regimens require family commitment and agreed on the need for planning. “For these diets to work, a lot has to go into it. But if they’re carefully planned, there is adequate protein and micro- and macronutrients and there’s a nonnegative effect on growth and development.”
The study results mirror what she sees in clinical practice, with vegetarian children tending to weigh less. “Some obese and overweight children will adopt vegetarian diets to lose weight,” Ms. Di Figlia-Peck said.
And perseverance has rewards. “When people follow a vegetarian diet, they tend to have lower blood pressure and cholesterol. A plant-based diet can favorably impact diseases for an entire lifetime.”
This study was supported by the Canadian Institutes of Health Research and the St. Michael’s Hospital and SickKids Hospital foundations. Dr. Maguire received an unrestricted research grant for a previous investigator-initiated study from Dairy Farmers of Canada, and D drops provided nonfinancial support (vitamin D supplements) for a previous investigator-initiated study on vitamin D and respiratory tract infections. Coauthor David Jenkins, MD, PhD, DSc, reported research support from multiple private-sector and nonprivate organizations; several of his family members are involved in the promotion of vegetarian diets. Ms. Di Figlia-Peck had no competing interests to declare.
With more families placing their children on vegetarian diets, the results from a Canadian longitudinal cohort study are reassuring: It found no clinically meaningful differences in height, growth, or biochemical measures of nutrition in young children on vegetarian and nonvegetarian diets.
While z scores (the standard deviation above or below the mean) were similar in both dietary groups, there was a weak association between a vegetarian diet and lower mean z height, as well as slightly higher odds of underweight.
No significant associations were identified between vegetarian and nonvegetarian diets for child z body mass index (BMI), serum ferritin, 25(OH)D, and serum lipids, according to Jonathon L. Maguire, MD. MSc, of St. Michael’s Hospital Pediatric Clinic in Toronto.
Moreover, the magnitude of the height and vegetarian diet association was small at just 0.3 cm for a 3-year-old child and unlikely to be clinically meaningful, Dr. Maguire and colleagues wrote online in Pediatrics.
In a secondary study outcome, cow’s milk consumption was associated with higher serum lipid levels for both diets. Serum lipids were similar among those who did or did not consume a vegetarian diet and consumed the recommended 2 cups of cow’s milk per day.
“The vast majority of children with vegetarian diets have similar growth and nutrition as children without vegetarian diets,” said Dr. Maguire, who is also a professor of pediatrics and nutritional sciences at the University of Toronto, in an interview. “But, I think we should be mindful to carefully plan vegetarian diets for children [who are] underweight.”
The study conclusion was based on 8,907 children, 6 months to 8 years of age, including 248 vegetarian and 25 vegan children, at baseline. They were part of theTARGet Kids! practice-based research network in Toronto.
The mean age of children at baseline was 2.2 years (standard deviation, 1.5), and 52.4% were male. Participants were followed for an average of 2.8 years (SD, 1.7).
Those with a vegetarian diet had longer breastfeeding duration: 12.6 months (SD, 9.5) versus 10.0 months (SD, 7.0). They were also more likely to be of Asian ethnicity: 33.8% versus 19.0%. Otherwise, children with and without a vegetarian diet were similar at baseline.
In study outcomes, vegetarian children had higher odds of underweight: body mass index z score less than –2 (odds ratio 1.87; 95% confidence interval, 1.19-2.96, P = .007), while no association with overweight or obesity was found.
In a secondary outcome, cow’s milk consumption was associated with higher levels of non–high-density lipoprotein cholesterol (P = .03), total cholesterol (P = .04), and low-density lipoprotein cholesterol (P = .02) in young children on a vegetarian diet. Levels were similar in children with and without a vegetarian diet who consumed the recommended 2 cups of cow’s milk per day.
Previous studies have found that vegetarian children have normal growth and development but tend to be leaner than their omnivore peers.
As for the potential effect of following a fully vegan diet on these nutritional measures, Dr. Maguire said, “Unfortunately, there were not enough children with vegan diets to make meaningful conclusions.”
Would results likely be similar in older children who have more independence and engage more with their peers?“ I don’t know, but we will be following these children for many years to come through the TARGet Kids! research network, Dr. Maguire said.
Studies such as this are timely as plant-based eating becomes more widespread in the United States. The 2007-2010 National Health and Nutrition Examination Surveys found that 2.1% of American adults followed a vegetarian diet, and that figure appears to have increased, with 5% of American adults self-identifying as vegetarian in a 2019 Gallup poll.
Offering her perspective on the Canadian study but not involved in it, Stephanie Di Figlia-Peck, MS, RDN, agreed the results indicate that “a vegetarian diet is not a negative thing for growth and development.” She is a lead registered dietitian in the division of adolescent medicine at Cohen Children’s Medical Center in New Hyde Park, N.Y. She noted, however, that the study looked only at very young children on average.
She stressed that vegetarian regimens require family commitment and agreed on the need for planning. “For these diets to work, a lot has to go into it. But if they’re carefully planned, there is adequate protein and micro- and macronutrients and there’s a nonnegative effect on growth and development.”
The study results mirror what she sees in clinical practice, with vegetarian children tending to weigh less. “Some obese and overweight children will adopt vegetarian diets to lose weight,” Ms. Di Figlia-Peck said.
And perseverance has rewards. “When people follow a vegetarian diet, they tend to have lower blood pressure and cholesterol. A plant-based diet can favorably impact diseases for an entire lifetime.”
This study was supported by the Canadian Institutes of Health Research and the St. Michael’s Hospital and SickKids Hospital foundations. Dr. Maguire received an unrestricted research grant for a previous investigator-initiated study from Dairy Farmers of Canada, and D drops provided nonfinancial support (vitamin D supplements) for a previous investigator-initiated study on vitamin D and respiratory tract infections. Coauthor David Jenkins, MD, PhD, DSc, reported research support from multiple private-sector and nonprivate organizations; several of his family members are involved in the promotion of vegetarian diets. Ms. Di Figlia-Peck had no competing interests to declare.
FROM PEDIATRICS
Hepatitis C: Essential Treatment Considerations
Until recently, chronic hepatitis C virus (HCV) treatment had poor efficacy and was provided only by specialists such as hepatologists and gastroenterologists. However, the introduction of safe, effective direct-acting antivirals (DAAs) has revolutionized HCV treatment.
One pivotal transformation has been the expansion of treatment to nonspecialist physicians. Nevertheless, various factors must be considered when initiating treatment for HCV.
Dr Elizabeth Verna, director of hepatology research at Columbia University in New York City, examines the essential treatment considerations for chronic HCV in treatment-naive patients.
First, she outlines recommended first-line therapies and the simplified HCV treatment algorithm recently issued by the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. She then discusses patient-specific factors, such as cirrhosis, co-infections, age, and pregnancy, that can create treatment challenges and change the algorithm.
In closing, she talks about changes in HCV screening recommendations and how diagnosis and treatment of this infectious disease largely rest in the hands of general practitioners who are the first line of defense in controlling HCV spread.
--
Associate Professor of Medicine, Director of Hepatology Research, Associate Physician, Department of Medicine, Columbia University, New York, NY
Elizabeth Verna, MD, has disclosed the following relevant financial relationships:
Received research grant from: Salix
Until recently, chronic hepatitis C virus (HCV) treatment had poor efficacy and was provided only by specialists such as hepatologists and gastroenterologists. However, the introduction of safe, effective direct-acting antivirals (DAAs) has revolutionized HCV treatment.
One pivotal transformation has been the expansion of treatment to nonspecialist physicians. Nevertheless, various factors must be considered when initiating treatment for HCV.
Dr Elizabeth Verna, director of hepatology research at Columbia University in New York City, examines the essential treatment considerations for chronic HCV in treatment-naive patients.
First, she outlines recommended first-line therapies and the simplified HCV treatment algorithm recently issued by the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. She then discusses patient-specific factors, such as cirrhosis, co-infections, age, and pregnancy, that can create treatment challenges and change the algorithm.
In closing, she talks about changes in HCV screening recommendations and how diagnosis and treatment of this infectious disease largely rest in the hands of general practitioners who are the first line of defense in controlling HCV spread.
--
Associate Professor of Medicine, Director of Hepatology Research, Associate Physician, Department of Medicine, Columbia University, New York, NY
Elizabeth Verna, MD, has disclosed the following relevant financial relationships:
Received research grant from: Salix
Until recently, chronic hepatitis C virus (HCV) treatment had poor efficacy and was provided only by specialists such as hepatologists and gastroenterologists. However, the introduction of safe, effective direct-acting antivirals (DAAs) has revolutionized HCV treatment.
One pivotal transformation has been the expansion of treatment to nonspecialist physicians. Nevertheless, various factors must be considered when initiating treatment for HCV.
Dr Elizabeth Verna, director of hepatology research at Columbia University in New York City, examines the essential treatment considerations for chronic HCV in treatment-naive patients.
First, she outlines recommended first-line therapies and the simplified HCV treatment algorithm recently issued by the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. She then discusses patient-specific factors, such as cirrhosis, co-infections, age, and pregnancy, that can create treatment challenges and change the algorithm.
In closing, she talks about changes in HCV screening recommendations and how diagnosis and treatment of this infectious disease largely rest in the hands of general practitioners who are the first line of defense in controlling HCV spread.
--
Associate Professor of Medicine, Director of Hepatology Research, Associate Physician, Department of Medicine, Columbia University, New York, NY
Elizabeth Verna, MD, has disclosed the following relevant financial relationships:
Received research grant from: Salix

Clinical Edge Journal Scan Commentary: Gastric Cancer, May 2022
In early-stage disease, perioperative chemotherapy plays a critical role. The triple-chemotherapy FLOT regimen is now the standard treatment in patients who are able to tolerate it. However, it is associated with significant toxicities, and modifications frequently are needed. In clinical practice, FOLFOX chemotherapy can be used in patients who are not candidates for FLOT. A phase 2 OGSG 1601 study enrolled 37 patients with clinical stage T3/T4a N1-3 M0 gastric cancer who received perioperative doublet chemotherapy with capecitabine and oxaliplatin. At the 3-year follow-up, this study continues to demonstrate good activity of this doublet chemotherapy, with an overall survival rate of 83.8% at 3 years and relapse-free rate of 73%. These results support the use of this doublet in patients who cannot tolerate a more intense chemotherapy regimen. The interpretation of this study is limited by its small size and nonrandomized design. Given what we know about the activity of this regimen in advanced disease, however, these results add to the body of evidence that supports the use of this doublet in select patients.
There have been efforts to augment the activity of perioperative chemotherapy using antiangiogenic agents. In the advanced setting, studies with antiangiogenic agents have had mixed results. Ramucirumab in combination with paclitaxel is FDA-approved in the second-line setting, but a subsequent study in the first line-setting showed no improvement from the addition of ramucirumab.4,7 In the preoperative setting, the role of ramucirumab in combination with chemotherapy was evaluated in a phase 2 study. Although a hint of activity was seen, there was increased toxicity, especially in Siewert type I tumors.8 The phase 2 study by Tang and colleagues enrolled 32 patients with resectable gastric and gastroesophageal juncture adenocarcinoma who received neoadjuvant oxaliplatin, capecitabine, and apatinib. Apatinib is a small-molecule tyrosine kinase inhibitor with highly selective affinity to vascular endothelial growth factor receptor 2. The treatment had manageable toxicity, with hypertension being the most common adverse event, as expected. Early signs of potential clinical efficacy were seen (pathologic complete response and pathologic response were achieved in 6.3% and 34.4% of the patients, respectively), but the true contribution from the addition of apatinib can be established only in a prospective randomized study. For now, chemotherapy alone remains the standard perioperative treatment, although ongoing studies are evaluating the addition of immune checkpoint inhibitors in this setting (NCT03221426, NCT04592913). These types of agents are probably more likely than antiangiogenic agents to become part of standard treatment in the perioperative setting.
Additional References
- Janjigian YY, Shitara K, Moehler M, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): A randomised, open-label, phase 3 trial. Lancet. 2021;398:27-40. Doi: 10.1016/S0140-6736(21)00797-2 Source
- Van Cutsem E, Moiseyenko VM, Tjulandin S, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: A report of the V325 Study Group. J Clin Oncol. 2006;24:4991-4997. Doi: 10.1200/JCO.2006.06.8429 Source
- Al-Batran S-E, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): A randomised, phase 2/3 trial. Lancet. 2019;393:1948-1957. Doi: 10.1016/S0140-6736(18)32557-1 Source0
- Wilke H, Van Cutsem E, Cheul Oh S, et al. RAINBOW: A global, phase 3, randomized, double-blind study of ramucirumab plus paclitaxel versus placebo plus paclitaxel in the treatment of metastatic gastric adenocarcinoma following disease progression on first-line platinum- and fluoropyrimidine-containing combination therapy: Results of a multiple Cox regression analysis adjusting for prognostic factors. J Clin Oncol. 2014;32(15, suppl):1076. Doi: 10.1200/jco.2014.32.15_suppl.4076 Source
- Elimova E, Janjigian YY, Mulcahy M, et al. It is time to stop using epirubicin to treat any patient with gastroesophageal adenocarcinoma. J Clin Oncol. 2017;35:475-477. Doi: 10.1200/JCO.2016.69.7276 Source
- Park H, Jin RU, Wang-Gillam A, et al. FOLFIRINOX for the treatment of advanced gastroesophageal cancers: A phase 2 nonrandomized clinical trial. JAMA Oncol. 2020;6:1231-1240. Doi: 10.1001/jamaoncol.2020.2020 Source
- Fuchs CS, Shitara K, Di Bartolomeo M, et al. RAINFALL: A randomized, double-blind, placebo-controlled phase III study of cisplatin (Cis) plus capecitabine (Cape) or 5FU with or without ramucirumab (RAM) as first-line therapy in patients with metastatic gastric or gastroesophageal junction (G-GEJ) adenocarcinoma. J Clin Oncol. 2018;36(4, suppl):5. Doi: 10.1200/JCO.2018.36.4_suppl.5 Source
- Al-Batran S-E, Hofheinz RD, Schmalenberg H, et al. Perioperative ramucirumab in combination with FLOT versus FLOT alone for resectable esophagogastric adenocarcinoma (RAMSES/FLOT7): Results of the phase II-portion—A multicenter, randomized phase II/III trial of the German AIO and Italian GOIM. J Clin Oncol. 2020;38(15, suppl):4501. Doi: 10.1200/JCO.2020.38.15_suppl.4501 Source
In early-stage disease, perioperative chemotherapy plays a critical role. The triple-chemotherapy FLOT regimen is now the standard treatment in patients who are able to tolerate it. However, it is associated with significant toxicities, and modifications frequently are needed. In clinical practice, FOLFOX chemotherapy can be used in patients who are not candidates for FLOT. A phase 2 OGSG 1601 study enrolled 37 patients with clinical stage T3/T4a N1-3 M0 gastric cancer who received perioperative doublet chemotherapy with capecitabine and oxaliplatin. At the 3-year follow-up, this study continues to demonstrate good activity of this doublet chemotherapy, with an overall survival rate of 83.8% at 3 years and relapse-free rate of 73%. These results support the use of this doublet in patients who cannot tolerate a more intense chemotherapy regimen. The interpretation of this study is limited by its small size and nonrandomized design. Given what we know about the activity of this regimen in advanced disease, however, these results add to the body of evidence that supports the use of this doublet in select patients.
There have been efforts to augment the activity of perioperative chemotherapy using antiangiogenic agents. In the advanced setting, studies with antiangiogenic agents have had mixed results. Ramucirumab in combination with paclitaxel is FDA-approved in the second-line setting, but a subsequent study in the first line-setting showed no improvement from the addition of ramucirumab.4,7 In the preoperative setting, the role of ramucirumab in combination with chemotherapy was evaluated in a phase 2 study. Although a hint of activity was seen, there was increased toxicity, especially in Siewert type I tumors.8 The phase 2 study by Tang and colleagues enrolled 32 patients with resectable gastric and gastroesophageal juncture adenocarcinoma who received neoadjuvant oxaliplatin, capecitabine, and apatinib. Apatinib is a small-molecule tyrosine kinase inhibitor with highly selective affinity to vascular endothelial growth factor receptor 2. The treatment had manageable toxicity, with hypertension being the most common adverse event, as expected. Early signs of potential clinical efficacy were seen (pathologic complete response and pathologic response were achieved in 6.3% and 34.4% of the patients, respectively), but the true contribution from the addition of apatinib can be established only in a prospective randomized study. For now, chemotherapy alone remains the standard perioperative treatment, although ongoing studies are evaluating the addition of immune checkpoint inhibitors in this setting (NCT03221426, NCT04592913). These types of agents are probably more likely than antiangiogenic agents to become part of standard treatment in the perioperative setting.
Additional References
- Janjigian YY, Shitara K, Moehler M, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): A randomised, open-label, phase 3 trial. Lancet. 2021;398:27-40. Doi: 10.1016/S0140-6736(21)00797-2 Source
- Van Cutsem E, Moiseyenko VM, Tjulandin S, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: A report of the V325 Study Group. J Clin Oncol. 2006;24:4991-4997. Doi: 10.1200/JCO.2006.06.8429 Source
- Al-Batran S-E, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): A randomised, phase 2/3 trial. Lancet. 2019;393:1948-1957. Doi: 10.1016/S0140-6736(18)32557-1 Source0
- Wilke H, Van Cutsem E, Cheul Oh S, et al. RAINBOW: A global, phase 3, randomized, double-blind study of ramucirumab plus paclitaxel versus placebo plus paclitaxel in the treatment of metastatic gastric adenocarcinoma following disease progression on first-line platinum- and fluoropyrimidine-containing combination therapy: Results of a multiple Cox regression analysis adjusting for prognostic factors. J Clin Oncol. 2014;32(15, suppl):1076. Doi: 10.1200/jco.2014.32.15_suppl.4076 Source
- Elimova E, Janjigian YY, Mulcahy M, et al. It is time to stop using epirubicin to treat any patient with gastroesophageal adenocarcinoma. J Clin Oncol. 2017;35:475-477. Doi: 10.1200/JCO.2016.69.7276 Source
- Park H, Jin RU, Wang-Gillam A, et al. FOLFIRINOX for the treatment of advanced gastroesophageal cancers: A phase 2 nonrandomized clinical trial. JAMA Oncol. 2020;6:1231-1240. Doi: 10.1001/jamaoncol.2020.2020 Source
- Fuchs CS, Shitara K, Di Bartolomeo M, et al. RAINFALL: A randomized, double-blind, placebo-controlled phase III study of cisplatin (Cis) plus capecitabine (Cape) or 5FU with or without ramucirumab (RAM) as first-line therapy in patients with metastatic gastric or gastroesophageal junction (G-GEJ) adenocarcinoma. J Clin Oncol. 2018;36(4, suppl):5. Doi: 10.1200/JCO.2018.36.4_suppl.5 Source
- Al-Batran S-E, Hofheinz RD, Schmalenberg H, et al. Perioperative ramucirumab in combination with FLOT versus FLOT alone for resectable esophagogastric adenocarcinoma (RAMSES/FLOT7): Results of the phase II-portion—A multicenter, randomized phase II/III trial of the German AIO and Italian GOIM. J Clin Oncol. 2020;38(15, suppl):4501. Doi: 10.1200/JCO.2020.38.15_suppl.4501 Source
In early-stage disease, perioperative chemotherapy plays a critical role. The triple-chemotherapy FLOT regimen is now the standard treatment in patients who are able to tolerate it. However, it is associated with significant toxicities, and modifications frequently are needed. In clinical practice, FOLFOX chemotherapy can be used in patients who are not candidates for FLOT. A phase 2 OGSG 1601 study enrolled 37 patients with clinical stage T3/T4a N1-3 M0 gastric cancer who received perioperative doublet chemotherapy with capecitabine and oxaliplatin. At the 3-year follow-up, this study continues to demonstrate good activity of this doublet chemotherapy, with an overall survival rate of 83.8% at 3 years and relapse-free rate of 73%. These results support the use of this doublet in patients who cannot tolerate a more intense chemotherapy regimen. The interpretation of this study is limited by its small size and nonrandomized design. Given what we know about the activity of this regimen in advanced disease, however, these results add to the body of evidence that supports the use of this doublet in select patients.
There have been efforts to augment the activity of perioperative chemotherapy using antiangiogenic agents. In the advanced setting, studies with antiangiogenic agents have had mixed results. Ramucirumab in combination with paclitaxel is FDA-approved in the second-line setting, but a subsequent study in the first line-setting showed no improvement from the addition of ramucirumab.4,7 In the preoperative setting, the role of ramucirumab in combination with chemotherapy was evaluated in a phase 2 study. Although a hint of activity was seen, there was increased toxicity, especially in Siewert type I tumors.8 The phase 2 study by Tang and colleagues enrolled 32 patients with resectable gastric and gastroesophageal juncture adenocarcinoma who received neoadjuvant oxaliplatin, capecitabine, and apatinib. Apatinib is a small-molecule tyrosine kinase inhibitor with highly selective affinity to vascular endothelial growth factor receptor 2. The treatment had manageable toxicity, with hypertension being the most common adverse event, as expected. Early signs of potential clinical efficacy were seen (pathologic complete response and pathologic response were achieved in 6.3% and 34.4% of the patients, respectively), but the true contribution from the addition of apatinib can be established only in a prospective randomized study. For now, chemotherapy alone remains the standard perioperative treatment, although ongoing studies are evaluating the addition of immune checkpoint inhibitors in this setting (NCT03221426, NCT04592913). These types of agents are probably more likely than antiangiogenic agents to become part of standard treatment in the perioperative setting.
Additional References
- Janjigian YY, Shitara K, Moehler M, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): A randomised, open-label, phase 3 trial. Lancet. 2021;398:27-40. Doi: 10.1016/S0140-6736(21)00797-2 Source
- Van Cutsem E, Moiseyenko VM, Tjulandin S, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: A report of the V325 Study Group. J Clin Oncol. 2006;24:4991-4997. Doi: 10.1200/JCO.2006.06.8429 Source
- Al-Batran S-E, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): A randomised, phase 2/3 trial. Lancet. 2019;393:1948-1957. Doi: 10.1016/S0140-6736(18)32557-1 Source0
- Wilke H, Van Cutsem E, Cheul Oh S, et al. RAINBOW: A global, phase 3, randomized, double-blind study of ramucirumab plus paclitaxel versus placebo plus paclitaxel in the treatment of metastatic gastric adenocarcinoma following disease progression on first-line platinum- and fluoropyrimidine-containing combination therapy: Results of a multiple Cox regression analysis adjusting for prognostic factors. J Clin Oncol. 2014;32(15, suppl):1076. Doi: 10.1200/jco.2014.32.15_suppl.4076 Source
- Elimova E, Janjigian YY, Mulcahy M, et al. It is time to stop using epirubicin to treat any patient with gastroesophageal adenocarcinoma. J Clin Oncol. 2017;35:475-477. Doi: 10.1200/JCO.2016.69.7276 Source
- Park H, Jin RU, Wang-Gillam A, et al. FOLFIRINOX for the treatment of advanced gastroesophageal cancers: A phase 2 nonrandomized clinical trial. JAMA Oncol. 2020;6:1231-1240. Doi: 10.1001/jamaoncol.2020.2020 Source
- Fuchs CS, Shitara K, Di Bartolomeo M, et al. RAINFALL: A randomized, double-blind, placebo-controlled phase III study of cisplatin (Cis) plus capecitabine (Cape) or 5FU with or without ramucirumab (RAM) as first-line therapy in patients with metastatic gastric or gastroesophageal junction (G-GEJ) adenocarcinoma. J Clin Oncol. 2018;36(4, suppl):5. Doi: 10.1200/JCO.2018.36.4_suppl.5 Source
- Al-Batran S-E, Hofheinz RD, Schmalenberg H, et al. Perioperative ramucirumab in combination with FLOT versus FLOT alone for resectable esophagogastric adenocarcinoma (RAMSES/FLOT7): Results of the phase II-portion—A multicenter, randomized phase II/III trial of the German AIO and Italian GOIM. J Clin Oncol. 2020;38(15, suppl):4501. Doi: 10.1200/JCO.2020.38.15_suppl.4501 Source
Clinical Edge Journal Scan Commentary: PsA May 2022
Although most patients with psoriatic arthritis (PsA) have concomitant psoriasis, many with PsA who are enrolled in clinic trials as well as in rheumatology clinic do not have severe psoriasis. Therefore, an unanswered question is how much psoriasis symptoms contribute to impaired quality of life (QOL) in PsA patients. This question was addressed in a recent study by Taylor and colleagues. This post hoc analysis of two phase 3 studies, OPAL Broaden and OPAL Beyond, included 816 patients with active PsA and an inadequate response to previous therapies who received tofacitinib, adalimumab, or placebo. The analyses demonstrated that Itch Severity Item (ISI) scores of 7-10, Physician's Global Assessment of Psoriasis (PGA-PsO) scores of 4, and Patient's Global Joint and Skin Assessment-Visual Analog Scale (PGJS-VAS) scores of 90-100 mm corresponded with Dermatology Life Quality Index (DLQI) scores categorized as having a very large effect on a patient's life. An improvement of ≥ 3 points in ISI, ≥ 2 points in PGA-PsO, and ≥ 40 mm in PGJS-VAS translated to a clinically meaningful improvement in DLQI scores; improvements from baseline of ≥4/≥3/≥40-mm in the above scores, respectively, were also associated with clinically meaningful improvements across SF-36v2 (Short-Form Health Survey) domains. Thus, dermatologic symptoms are substantially associated with QOL in patients with active PsA, and improvements in skin measures could translate to clinically meaningful improvements in their QOL.
There is also increasing scrutiny on sex differences in PsA. Eder and colleagues conducted a post hoc analysis of two phase 3 trials that included 679 patients with active PsA who were either biologic-naive (SPIRIT-P1) or showed an inadequate response to one or two tumor necrosis factor inhibitors (TNFi) (SPIRIT-P2) and were randomly assigned to receive ixekizumab, an IL-17A inhibitor (IL-17Ai), or placebo. They demonstrated that at baseline female vs male patients had significantly higher Health Assessment Questionnaire Disability Index scores (P ≤ .003), with a significantly higher proportion of male vs female patients in the ixekizumab every-4-weeks treatment arm (53.8% vs 38.3%) and ixekizumab every-2-weeks treatment arm(41.2% vs 28.1%) achieving ≥50% and ≥70% improvement in the American College of Rheumatology response criteria, respectively (both P < .05). Thus, female patients with PsA exhibited significantly higher disease activity at baseline and a poorer response to ixekizumab.
Janus kinase (JAK) inhibitors have been shown to improve inflammatory and other types of pain in rheumatoid arthritis. To further evaluate the effect of inhibition of JAK1 on pain, McInnes and colleagues aimed to evaluate the effect of upadacitinib on pain outcomes in patients with active PsA or ankylosing spondylitis across three randomized trials (SELECT-PsA-1 and -2 for PsA; SELECT-AXIS 1 for ankylosing spondylitis). A significantly higher proportion of patients receiving 15 mg upadacitinib vs placebo achieved ≥30%, ≥50%, and ≥70% reductions in pain as early as 2 weeks (P < .05), with improvements sustained up to week 56. Further research on whether improvement in pain is at least partially independent of improvement in musculoskeletal inflammation is required.
Persistence of drug treatment is an important outcome and is a surrogate measure of safety and effectiveness. Vegas and colleagues assessed the long-term persistence of different biologic classes in a nationwide cohort study that included 16,892 adults with psoriasis and 6531 adults with PsA who initiated first-line treatment with a TNFi, IL-12/23 inhibitors (IL-12/23i), or an IL-17i. Treatment persistence was higher with IL-17i than with TNFi (weighted hazard ratio [HR] 0.70; P < .001) or IL-12/23i (weighted HR 0.69; P < .001); however, IL-12/23i and TNFi showed similar persistence (P = .70). Thus, IL-17i may be associated with higher treatment persistence in PsA compared with TNFi.
Although most patients with psoriatic arthritis (PsA) have concomitant psoriasis, many with PsA who are enrolled in clinic trials as well as in rheumatology clinic do not have severe psoriasis. Therefore, an unanswered question is how much psoriasis symptoms contribute to impaired quality of life (QOL) in PsA patients. This question was addressed in a recent study by Taylor and colleagues. This post hoc analysis of two phase 3 studies, OPAL Broaden and OPAL Beyond, included 816 patients with active PsA and an inadequate response to previous therapies who received tofacitinib, adalimumab, or placebo. The analyses demonstrated that Itch Severity Item (ISI) scores of 7-10, Physician's Global Assessment of Psoriasis (PGA-PsO) scores of 4, and Patient's Global Joint and Skin Assessment-Visual Analog Scale (PGJS-VAS) scores of 90-100 mm corresponded with Dermatology Life Quality Index (DLQI) scores categorized as having a very large effect on a patient's life. An improvement of ≥ 3 points in ISI, ≥ 2 points in PGA-PsO, and ≥ 40 mm in PGJS-VAS translated to a clinically meaningful improvement in DLQI scores; improvements from baseline of ≥4/≥3/≥40-mm in the above scores, respectively, were also associated with clinically meaningful improvements across SF-36v2 (Short-Form Health Survey) domains. Thus, dermatologic symptoms are substantially associated with QOL in patients with active PsA, and improvements in skin measures could translate to clinically meaningful improvements in their QOL.
There is also increasing scrutiny on sex differences in PsA. Eder and colleagues conducted a post hoc analysis of two phase 3 trials that included 679 patients with active PsA who were either biologic-naive (SPIRIT-P1) or showed an inadequate response to one or two tumor necrosis factor inhibitors (TNFi) (SPIRIT-P2) and were randomly assigned to receive ixekizumab, an IL-17A inhibitor (IL-17Ai), or placebo. They demonstrated that at baseline female vs male patients had significantly higher Health Assessment Questionnaire Disability Index scores (P ≤ .003), with a significantly higher proportion of male vs female patients in the ixekizumab every-4-weeks treatment arm (53.8% vs 38.3%) and ixekizumab every-2-weeks treatment arm(41.2% vs 28.1%) achieving ≥50% and ≥70% improvement in the American College of Rheumatology response criteria, respectively (both P < .05). Thus, female patients with PsA exhibited significantly higher disease activity at baseline and a poorer response to ixekizumab.
Janus kinase (JAK) inhibitors have been shown to improve inflammatory and other types of pain in rheumatoid arthritis. To further evaluate the effect of inhibition of JAK1 on pain, McInnes and colleagues aimed to evaluate the effect of upadacitinib on pain outcomes in patients with active PsA or ankylosing spondylitis across three randomized trials (SELECT-PsA-1 and -2 for PsA; SELECT-AXIS 1 for ankylosing spondylitis). A significantly higher proportion of patients receiving 15 mg upadacitinib vs placebo achieved ≥30%, ≥50%, and ≥70% reductions in pain as early as 2 weeks (P < .05), with improvements sustained up to week 56. Further research on whether improvement in pain is at least partially independent of improvement in musculoskeletal inflammation is required.
Persistence of drug treatment is an important outcome and is a surrogate measure of safety and effectiveness. Vegas and colleagues assessed the long-term persistence of different biologic classes in a nationwide cohort study that included 16,892 adults with psoriasis and 6531 adults with PsA who initiated first-line treatment with a TNFi, IL-12/23 inhibitors (IL-12/23i), or an IL-17i. Treatment persistence was higher with IL-17i than with TNFi (weighted hazard ratio [HR] 0.70; P < .001) or IL-12/23i (weighted HR 0.69; P < .001); however, IL-12/23i and TNFi showed similar persistence (P = .70). Thus, IL-17i may be associated with higher treatment persistence in PsA compared with TNFi.
Although most patients with psoriatic arthritis (PsA) have concomitant psoriasis, many with PsA who are enrolled in clinic trials as well as in rheumatology clinic do not have severe psoriasis. Therefore, an unanswered question is how much psoriasis symptoms contribute to impaired quality of life (QOL) in PsA patients. This question was addressed in a recent study by Taylor and colleagues. This post hoc analysis of two phase 3 studies, OPAL Broaden and OPAL Beyond, included 816 patients with active PsA and an inadequate response to previous therapies who received tofacitinib, adalimumab, or placebo. The analyses demonstrated that Itch Severity Item (ISI) scores of 7-10, Physician's Global Assessment of Psoriasis (PGA-PsO) scores of 4, and Patient's Global Joint and Skin Assessment-Visual Analog Scale (PGJS-VAS) scores of 90-100 mm corresponded with Dermatology Life Quality Index (DLQI) scores categorized as having a very large effect on a patient's life. An improvement of ≥ 3 points in ISI, ≥ 2 points in PGA-PsO, and ≥ 40 mm in PGJS-VAS translated to a clinically meaningful improvement in DLQI scores; improvements from baseline of ≥4/≥3/≥40-mm in the above scores, respectively, were also associated with clinically meaningful improvements across SF-36v2 (Short-Form Health Survey) domains. Thus, dermatologic symptoms are substantially associated with QOL in patients with active PsA, and improvements in skin measures could translate to clinically meaningful improvements in their QOL.
There is also increasing scrutiny on sex differences in PsA. Eder and colleagues conducted a post hoc analysis of two phase 3 trials that included 679 patients with active PsA who were either biologic-naive (SPIRIT-P1) or showed an inadequate response to one or two tumor necrosis factor inhibitors (TNFi) (SPIRIT-P2) and were randomly assigned to receive ixekizumab, an IL-17A inhibitor (IL-17Ai), or placebo. They demonstrated that at baseline female vs male patients had significantly higher Health Assessment Questionnaire Disability Index scores (P ≤ .003), with a significantly higher proportion of male vs female patients in the ixekizumab every-4-weeks treatment arm (53.8% vs 38.3%) and ixekizumab every-2-weeks treatment arm(41.2% vs 28.1%) achieving ≥50% and ≥70% improvement in the American College of Rheumatology response criteria, respectively (both P < .05). Thus, female patients with PsA exhibited significantly higher disease activity at baseline and a poorer response to ixekizumab.
Janus kinase (JAK) inhibitors have been shown to improve inflammatory and other types of pain in rheumatoid arthritis. To further evaluate the effect of inhibition of JAK1 on pain, McInnes and colleagues aimed to evaluate the effect of upadacitinib on pain outcomes in patients with active PsA or ankylosing spondylitis across three randomized trials (SELECT-PsA-1 and -2 for PsA; SELECT-AXIS 1 for ankylosing spondylitis). A significantly higher proportion of patients receiving 15 mg upadacitinib vs placebo achieved ≥30%, ≥50%, and ≥70% reductions in pain as early as 2 weeks (P < .05), with improvements sustained up to week 56. Further research on whether improvement in pain is at least partially independent of improvement in musculoskeletal inflammation is required.
Persistence of drug treatment is an important outcome and is a surrogate measure of safety and effectiveness. Vegas and colleagues assessed the long-term persistence of different biologic classes in a nationwide cohort study that included 16,892 adults with psoriasis and 6531 adults with PsA who initiated first-line treatment with a TNFi, IL-12/23 inhibitors (IL-12/23i), or an IL-17i. Treatment persistence was higher with IL-17i than with TNFi (weighted hazard ratio [HR] 0.70; P < .001) or IL-12/23i (weighted HR 0.69; P < .001); however, IL-12/23i and TNFi showed similar persistence (P = .70). Thus, IL-17i may be associated with higher treatment persistence in PsA compared with TNFi.
Clinical Edge Journal Scan Commentary: RA May 2022
Despite the improved outcomes in rheumatoid arthritis (RA) observed in clinical trials from early use of biologic disease-modifying antirheumatic drugs (bDMARD) in a treat-to-target strategy, real-world use may be limited by stopping medications for various reasons. Burkard and colleagues used the Swiss RA registry to examine potential reasons for discontinuation of bDMARD and targeted synthetic disease-modifying antirheumatic drugs (tsDMARD) among over 2500 adults with RA who stopped these medications from 1999 through 2018. In this cohort study, patients were followed from date of discontinuation of their medication until restarting a bDMARD or tsDMARD. The most common reasons for discontinuation were nonresponse and adverse events; of these patients, over 80% restarted a bDMARD or tsDMARD. Only 8% of patients stopped due to remission; of these, nearly half restarted. The authors found a higher proportion of fibromyalgia among patients who stopped due to nonresponse and adverse events vs due to remission. Oddly, though 40%-50% of patients stopped for "unknown reasons" between 2002 and 2006, this proportion dropped to close to 0 after 2010; during the first time period, the proportions stopping medication due to adverse events and nonresponse were also low, suggesting possible misattribution of the reason for treatment cessation. As such, drawing further conclusions on association of different patient characteristics with reasons for treatment cessation is difficult.
The gap between control of inflammatory joint pain in RA and overall patient outcomes has come up frequently in recent studies. Gwinnutt and colleagues looked at patients participating in three European RA registries, comprising over 2500 patients followed over 8-10 years, and classified them as having high or low inflammation on the basis of Disease Activity Score (DAS28) and analyzed Health Assessment Questionnaire (HAQ) score trajectories as low vs high as a measure of disability. Overall, patients in the three registries had different trajectory patterns, though it appears clear, in keeping with other studies, that a subset of patients remain with high HAQ scores despite decreases in DAS28 scores. Older age; being a woman; and more pain, fatigue, and depressive symptoms were associated with higher HAQ trajectory in both the high and low inflammation pairs, suggesting that this phenomenon is not quite "excess disability" solely in patients with low inflammation.
An additional factor that increases morbidity as well as mortality in RA is frailty, which is associated with age as well as with RA (including people < 65 years old). Hanlon and colleagues examined the change in the "frailty phenotype" over time and its association with adverse clinical outcomes in people with early RA in the Scottish Early Rheumatoid Arthritis (SERA) and UK Biobank cohorts. Frailty was defined by different measures in the two cohorts, including elements of the HAQ disability index for SERA and self-reported fatigue, depression, and poor health for UK Biobank. The computed frailty index was higher in people with higher DAS28 scores and increased with age. Of note, frailty index values were higher prior to treatment initiation and improved somewhat with lower disease activity over time, though those with higher baseline frailty index values tended to have poorer physical function and disease activity over time. Understanding frailty in RA may allow us to better predict and prevent functional limitation, disease progression, and mortality in people with RA.
Of current interest is an observational study by van der Togt and colleagues on the response to COVID-19 vaccines in people with RA being treated with rituximab. Of patients who had previously been treated with 200, 500, or 1000 mg of rituximab prior to COVID-19 vaccination, those who received 200 mg rituximab as well as those who had longer intervals between rituximab dose and vaccination had a better response to vaccination as defined by immunoglobulins (total, IgG, and IgM) against SARS-CoV-2. Although this study lacked a control arm of people being treated with other disease-modifying antirheumatic drugs and did not evaluate COVID-19 infections or outcomes, its findings do suggest that dosage and timing of rituximab in people with RA should be studied further in regard to vaccine response and infection risk.
Despite the improved outcomes in rheumatoid arthritis (RA) observed in clinical trials from early use of biologic disease-modifying antirheumatic drugs (bDMARD) in a treat-to-target strategy, real-world use may be limited by stopping medications for various reasons. Burkard and colleagues used the Swiss RA registry to examine potential reasons for discontinuation of bDMARD and targeted synthetic disease-modifying antirheumatic drugs (tsDMARD) among over 2500 adults with RA who stopped these medications from 1999 through 2018. In this cohort study, patients were followed from date of discontinuation of their medication until restarting a bDMARD or tsDMARD. The most common reasons for discontinuation were nonresponse and adverse events; of these patients, over 80% restarted a bDMARD or tsDMARD. Only 8% of patients stopped due to remission; of these, nearly half restarted. The authors found a higher proportion of fibromyalgia among patients who stopped due to nonresponse and adverse events vs due to remission. Oddly, though 40%-50% of patients stopped for "unknown reasons" between 2002 and 2006, this proportion dropped to close to 0 after 2010; during the first time period, the proportions stopping medication due to adverse events and nonresponse were also low, suggesting possible misattribution of the reason for treatment cessation. As such, drawing further conclusions on association of different patient characteristics with reasons for treatment cessation is difficult.
The gap between control of inflammatory joint pain in RA and overall patient outcomes has come up frequently in recent studies. Gwinnutt and colleagues looked at patients participating in three European RA registries, comprising over 2500 patients followed over 8-10 years, and classified them as having high or low inflammation on the basis of Disease Activity Score (DAS28) and analyzed Health Assessment Questionnaire (HAQ) score trajectories as low vs high as a measure of disability. Overall, patients in the three registries had different trajectory patterns, though it appears clear, in keeping with other studies, that a subset of patients remain with high HAQ scores despite decreases in DAS28 scores. Older age; being a woman; and more pain, fatigue, and depressive symptoms were associated with higher HAQ trajectory in both the high and low inflammation pairs, suggesting that this phenomenon is not quite "excess disability" solely in patients with low inflammation.
An additional factor that increases morbidity as well as mortality in RA is frailty, which is associated with age as well as with RA (including people < 65 years old). Hanlon and colleagues examined the change in the "frailty phenotype" over time and its association with adverse clinical outcomes in people with early RA in the Scottish Early Rheumatoid Arthritis (SERA) and UK Biobank cohorts. Frailty was defined by different measures in the two cohorts, including elements of the HAQ disability index for SERA and self-reported fatigue, depression, and poor health for UK Biobank. The computed frailty index was higher in people with higher DAS28 scores and increased with age. Of note, frailty index values were higher prior to treatment initiation and improved somewhat with lower disease activity over time, though those with higher baseline frailty index values tended to have poorer physical function and disease activity over time. Understanding frailty in RA may allow us to better predict and prevent functional limitation, disease progression, and mortality in people with RA.
Of current interest is an observational study by van der Togt and colleagues on the response to COVID-19 vaccines in people with RA being treated with rituximab. Of patients who had previously been treated with 200, 500, or 1000 mg of rituximab prior to COVID-19 vaccination, those who received 200 mg rituximab as well as those who had longer intervals between rituximab dose and vaccination had a better response to vaccination as defined by immunoglobulins (total, IgG, and IgM) against SARS-CoV-2. Although this study lacked a control arm of people being treated with other disease-modifying antirheumatic drugs and did not evaluate COVID-19 infections or outcomes, its findings do suggest that dosage and timing of rituximab in people with RA should be studied further in regard to vaccine response and infection risk.
Despite the improved outcomes in rheumatoid arthritis (RA) observed in clinical trials from early use of biologic disease-modifying antirheumatic drugs (bDMARD) in a treat-to-target strategy, real-world use may be limited by stopping medications for various reasons. Burkard and colleagues used the Swiss RA registry to examine potential reasons for discontinuation of bDMARD and targeted synthetic disease-modifying antirheumatic drugs (tsDMARD) among over 2500 adults with RA who stopped these medications from 1999 through 2018. In this cohort study, patients were followed from date of discontinuation of their medication until restarting a bDMARD or tsDMARD. The most common reasons for discontinuation were nonresponse and adverse events; of these patients, over 80% restarted a bDMARD or tsDMARD. Only 8% of patients stopped due to remission; of these, nearly half restarted. The authors found a higher proportion of fibromyalgia among patients who stopped due to nonresponse and adverse events vs due to remission. Oddly, though 40%-50% of patients stopped for "unknown reasons" between 2002 and 2006, this proportion dropped to close to 0 after 2010; during the first time period, the proportions stopping medication due to adverse events and nonresponse were also low, suggesting possible misattribution of the reason for treatment cessation. As such, drawing further conclusions on association of different patient characteristics with reasons for treatment cessation is difficult.
The gap between control of inflammatory joint pain in RA and overall patient outcomes has come up frequently in recent studies. Gwinnutt and colleagues looked at patients participating in three European RA registries, comprising over 2500 patients followed over 8-10 years, and classified them as having high or low inflammation on the basis of Disease Activity Score (DAS28) and analyzed Health Assessment Questionnaire (HAQ) score trajectories as low vs high as a measure of disability. Overall, patients in the three registries had different trajectory patterns, though it appears clear, in keeping with other studies, that a subset of patients remain with high HAQ scores despite decreases in DAS28 scores. Older age; being a woman; and more pain, fatigue, and depressive symptoms were associated with higher HAQ trajectory in both the high and low inflammation pairs, suggesting that this phenomenon is not quite "excess disability" solely in patients with low inflammation.
An additional factor that increases morbidity as well as mortality in RA is frailty, which is associated with age as well as with RA (including people < 65 years old). Hanlon and colleagues examined the change in the "frailty phenotype" over time and its association with adverse clinical outcomes in people with early RA in the Scottish Early Rheumatoid Arthritis (SERA) and UK Biobank cohorts. Frailty was defined by different measures in the two cohorts, including elements of the HAQ disability index for SERA and self-reported fatigue, depression, and poor health for UK Biobank. The computed frailty index was higher in people with higher DAS28 scores and increased with age. Of note, frailty index values were higher prior to treatment initiation and improved somewhat with lower disease activity over time, though those with higher baseline frailty index values tended to have poorer physical function and disease activity over time. Understanding frailty in RA may allow us to better predict and prevent functional limitation, disease progression, and mortality in people with RA.
Of current interest is an observational study by van der Togt and colleagues on the response to COVID-19 vaccines in people with RA being treated with rituximab. Of patients who had previously been treated with 200, 500, or 1000 mg of rituximab prior to COVID-19 vaccination, those who received 200 mg rituximab as well as those who had longer intervals between rituximab dose and vaccination had a better response to vaccination as defined by immunoglobulins (total, IgG, and IgM) against SARS-CoV-2. Although this study lacked a control arm of people being treated with other disease-modifying antirheumatic drugs and did not evaluate COVID-19 infections or outcomes, its findings do suggest that dosage and timing of rituximab in people with RA should be studied further in regard to vaccine response and infection risk.
Clinical Edge Journal Scan Commentary: Prenatal Testing, May 2022
Detection of fetal heart defects is an important aspect of prenatal diagnostic ultrasound. A recent study by Haberer and colleagues in the Journal of the American Society of Echocardiography investigated the diagnostic accuracy of fetal echocardiography. They looked at all of the fetuses with major cardiac anomalies diagnosed at a single institution over an 11-year period and compared the fetal echocardiogram reports with postnatal imaging, surgical reports, and autopsies. Of the almost 600 cases examined, 90% of the diagnoses were accurate. The highest rate of accuracy was for univentricular hearts defects (97.6%) and the lowest was with heterotaxy (71.1%). This article is important because findings show that diagnostic accuracy of fetal echocardiography was high for major fetal cardiac defects.
The ability to accurately diagnose placenta accreta prenatally is important to obstetricians because of the increased risk it poses for maternal morbidity and mortality. This issue is considered in a recent systematic review and meta-analysis by Hong and colleagues in the journal Insights into Imaging. They compared ultrasound to MRI for diagnostic accuracy of placenta accreta spectrum disorder (PAS). In the studies they examined, the diagnostic accuracy of ultrasound for PAS had a sensitivity of 0.9 and a specificity of 0.83, while the diagnostic accuracy of MRI had a sensitivity of 0.89 and a specificity of 0.87. This shows that the diagnostic accuracy of PAS is similar for both ultrasound and MRI. Given the significant expense of an MRI, this raises the question of its importance in the role of evaluating patients suspected of placenta accreta.
Precise prenatal diagnosis of estimated fetal weight (EFW) is central to the care of pregnant patients. It allows for appropriate timing of delivery to decrease the risk for stillbirth. A recent article by Visentin and colleagues evaluates prenatal methods for estimation of fetal weight and prediction of small-for-gestational-age (SGA) fetuses. The researchers performed a retrospective review of singleton gestations that were at increased risk for fetal growth restriction from two hospitals. They found that EFW z-scores derived from either the Hadlock method or the International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) assessment were similar and more accurate than abdominal circumference (AC) z-scores for detecting SGA infants. This study should open the debate again on how to best measure estimated fetal weight: EFW alone or assessment of both EFW and AC.
Detection of fetal heart defects is an important aspect of prenatal diagnostic ultrasound. A recent study by Haberer and colleagues in the Journal of the American Society of Echocardiography investigated the diagnostic accuracy of fetal echocardiography. They looked at all of the fetuses with major cardiac anomalies diagnosed at a single institution over an 11-year period and compared the fetal echocardiogram reports with postnatal imaging, surgical reports, and autopsies. Of the almost 600 cases examined, 90% of the diagnoses were accurate. The highest rate of accuracy was for univentricular hearts defects (97.6%) and the lowest was with heterotaxy (71.1%). This article is important because findings show that diagnostic accuracy of fetal echocardiography was high for major fetal cardiac defects.
The ability to accurately diagnose placenta accreta prenatally is important to obstetricians because of the increased risk it poses for maternal morbidity and mortality. This issue is considered in a recent systematic review and meta-analysis by Hong and colleagues in the journal Insights into Imaging. They compared ultrasound to MRI for diagnostic accuracy of placenta accreta spectrum disorder (PAS). In the studies they examined, the diagnostic accuracy of ultrasound for PAS had a sensitivity of 0.9 and a specificity of 0.83, while the diagnostic accuracy of MRI had a sensitivity of 0.89 and a specificity of 0.87. This shows that the diagnostic accuracy of PAS is similar for both ultrasound and MRI. Given the significant expense of an MRI, this raises the question of its importance in the role of evaluating patients suspected of placenta accreta.
Precise prenatal diagnosis of estimated fetal weight (EFW) is central to the care of pregnant patients. It allows for appropriate timing of delivery to decrease the risk for stillbirth. A recent article by Visentin and colleagues evaluates prenatal methods for estimation of fetal weight and prediction of small-for-gestational-age (SGA) fetuses. The researchers performed a retrospective review of singleton gestations that were at increased risk for fetal growth restriction from two hospitals. They found that EFW z-scores derived from either the Hadlock method or the International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) assessment were similar and more accurate than abdominal circumference (AC) z-scores for detecting SGA infants. This study should open the debate again on how to best measure estimated fetal weight: EFW alone or assessment of both EFW and AC.
Detection of fetal heart defects is an important aspect of prenatal diagnostic ultrasound. A recent study by Haberer and colleagues in the Journal of the American Society of Echocardiography investigated the diagnostic accuracy of fetal echocardiography. They looked at all of the fetuses with major cardiac anomalies diagnosed at a single institution over an 11-year period and compared the fetal echocardiogram reports with postnatal imaging, surgical reports, and autopsies. Of the almost 600 cases examined, 90% of the diagnoses were accurate. The highest rate of accuracy was for univentricular hearts defects (97.6%) and the lowest was with heterotaxy (71.1%). This article is important because findings show that diagnostic accuracy of fetal echocardiography was high for major fetal cardiac defects.
The ability to accurately diagnose placenta accreta prenatally is important to obstetricians because of the increased risk it poses for maternal morbidity and mortality. This issue is considered in a recent systematic review and meta-analysis by Hong and colleagues in the journal Insights into Imaging. They compared ultrasound to MRI for diagnostic accuracy of placenta accreta spectrum disorder (PAS). In the studies they examined, the diagnostic accuracy of ultrasound for PAS had a sensitivity of 0.9 and a specificity of 0.83, while the diagnostic accuracy of MRI had a sensitivity of 0.89 and a specificity of 0.87. This shows that the diagnostic accuracy of PAS is similar for both ultrasound and MRI. Given the significant expense of an MRI, this raises the question of its importance in the role of evaluating patients suspected of placenta accreta.
Precise prenatal diagnosis of estimated fetal weight (EFW) is central to the care of pregnant patients. It allows for appropriate timing of delivery to decrease the risk for stillbirth. A recent article by Visentin and colleagues evaluates prenatal methods for estimation of fetal weight and prediction of small-for-gestational-age (SGA) fetuses. The researchers performed a retrospective review of singleton gestations that were at increased risk for fetal growth restriction from two hospitals. They found that EFW z-scores derived from either the Hadlock method or the International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) assessment were similar and more accurate than abdominal circumference (AC) z-scores for detecting SGA infants. This study should open the debate again on how to best measure estimated fetal weight: EFW alone or assessment of both EFW and AC.
Commentary: Antibiotics use and vaccine antibody levels
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Antibiotics use and vaccine antibody levels
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).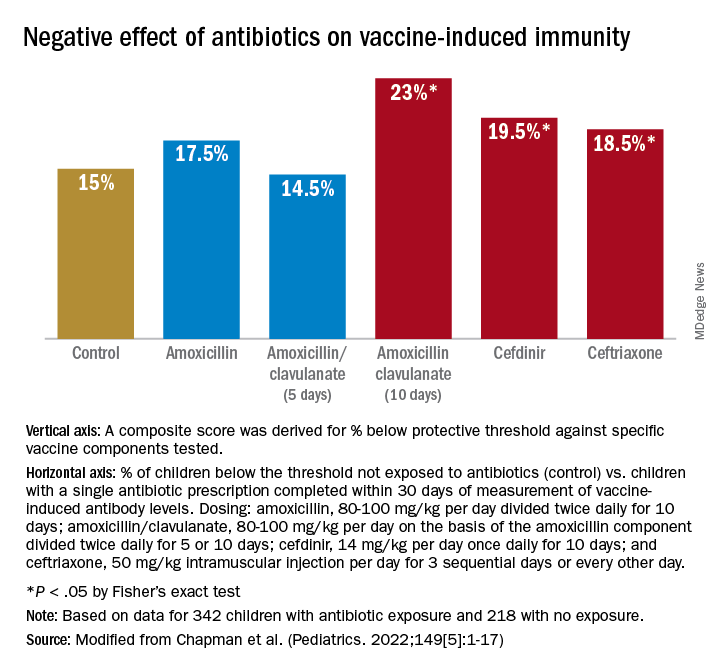
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).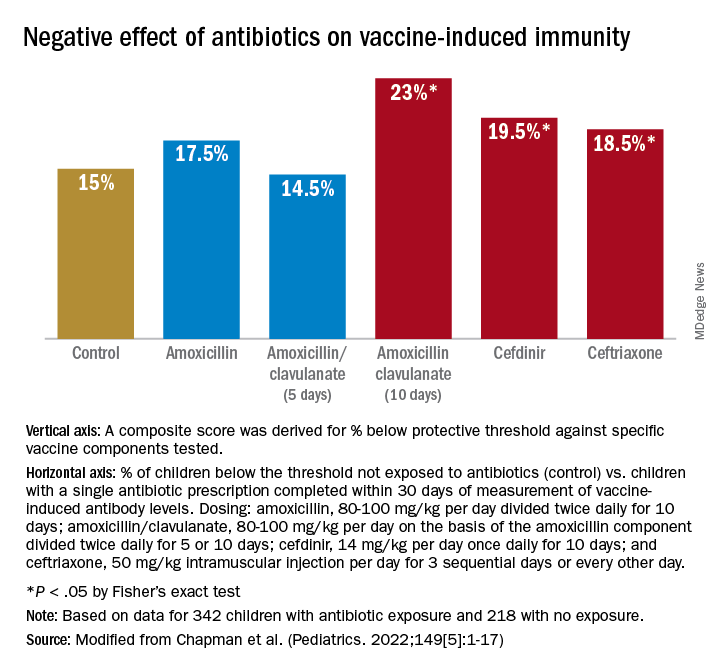
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).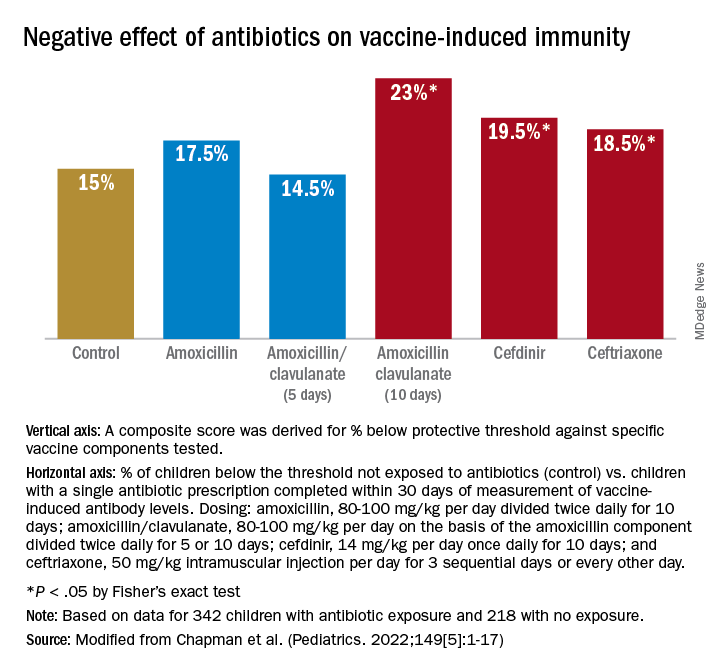
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
San Diego, here we come
I attended my inaugural Digestive Disease Week® (DDW) in Orlando in 2013 as a first-year fellow, both excited and somewhat intimidated to be giving my first oral abstract presentation on an international stage. At that time, the only familiar faces at the conference were my co-fellows and faculty, along with a few welcoming faces from the fellowship interview trail. My attendings, on the other hand, couldn’t walk more than 100 feet in the conference hall without bumping into a smiling colleague! Now nearly a decade later, I am pleased to say that there are many more familiar faces in the crowd as I walk the halls of DDW. Each May, I look forward to meeting up with friends and colleagues across the country and the world while learning from an outstanding group of GI thought-leaders. While the COVID pandemic has disrupted this annual tradition in recent years, for the first time since 2019 those who feel comfortable will convene in San Diego to see old colleagues and meet new ones, learn about exciting, practice-changing innovations in our field, and enjoy the California sunshine. For those who cannot travel, robust DDW virtual offerings are planned as well.
A quick look at the 2022 conference schedule reveals an astonishing 3,300 oral abstract and poster presentations, 400 original lectures, and a variety of professional networking events on the agenda. The conference weekend will open with the AGA Post-Graduate Course, which offers a great opportunity to efficiently brush up on your clinical knowledge, guided by leading experts in the field. Monday, May 23 will feature the AGA Presidential Plenary, with AGA Institute President John Inadomi, MD, AGAF, and an exciting lineup of speakers discussing how best to address health care disparities impacting our patients and outlining AGA’s recent efforts to promote diversity, equity, and inclusion in our field. While it is nearly impossible to attend all sessions of interest during this whirlwind 4-day conference, you can rely on GI & Hepatology News to bring you key conference highlights over the coming months to ensure you don’t miss a beat!
Megan A. Adams, MD, JD, MSc
I attended my inaugural Digestive Disease Week® (DDW) in Orlando in 2013 as a first-year fellow, both excited and somewhat intimidated to be giving my first oral abstract presentation on an international stage. At that time, the only familiar faces at the conference were my co-fellows and faculty, along with a few welcoming faces from the fellowship interview trail. My attendings, on the other hand, couldn’t walk more than 100 feet in the conference hall without bumping into a smiling colleague! Now nearly a decade later, I am pleased to say that there are many more familiar faces in the crowd as I walk the halls of DDW. Each May, I look forward to meeting up with friends and colleagues across the country and the world while learning from an outstanding group of GI thought-leaders. While the COVID pandemic has disrupted this annual tradition in recent years, for the first time since 2019 those who feel comfortable will convene in San Diego to see old colleagues and meet new ones, learn about exciting, practice-changing innovations in our field, and enjoy the California sunshine. For those who cannot travel, robust DDW virtual offerings are planned as well.
A quick look at the 2022 conference schedule reveals an astonishing 3,300 oral abstract and poster presentations, 400 original lectures, and a variety of professional networking events on the agenda. The conference weekend will open with the AGA Post-Graduate Course, which offers a great opportunity to efficiently brush up on your clinical knowledge, guided by leading experts in the field. Monday, May 23 will feature the AGA Presidential Plenary, with AGA Institute President John Inadomi, MD, AGAF, and an exciting lineup of speakers discussing how best to address health care disparities impacting our patients and outlining AGA’s recent efforts to promote diversity, equity, and inclusion in our field. While it is nearly impossible to attend all sessions of interest during this whirlwind 4-day conference, you can rely on GI & Hepatology News to bring you key conference highlights over the coming months to ensure you don’t miss a beat!
Megan A. Adams, MD, JD, MSc
I attended my inaugural Digestive Disease Week® (DDW) in Orlando in 2013 as a first-year fellow, both excited and somewhat intimidated to be giving my first oral abstract presentation on an international stage. At that time, the only familiar faces at the conference were my co-fellows and faculty, along with a few welcoming faces from the fellowship interview trail. My attendings, on the other hand, couldn’t walk more than 100 feet in the conference hall without bumping into a smiling colleague! Now nearly a decade later, I am pleased to say that there are many more familiar faces in the crowd as I walk the halls of DDW. Each May, I look forward to meeting up with friends and colleagues across the country and the world while learning from an outstanding group of GI thought-leaders. While the COVID pandemic has disrupted this annual tradition in recent years, for the first time since 2019 those who feel comfortable will convene in San Diego to see old colleagues and meet new ones, learn about exciting, practice-changing innovations in our field, and enjoy the California sunshine. For those who cannot travel, robust DDW virtual offerings are planned as well.
A quick look at the 2022 conference schedule reveals an astonishing 3,300 oral abstract and poster presentations, 400 original lectures, and a variety of professional networking events on the agenda. The conference weekend will open with the AGA Post-Graduate Course, which offers a great opportunity to efficiently brush up on your clinical knowledge, guided by leading experts in the field. Monday, May 23 will feature the AGA Presidential Plenary, with AGA Institute President John Inadomi, MD, AGAF, and an exciting lineup of speakers discussing how best to address health care disparities impacting our patients and outlining AGA’s recent efforts to promote diversity, equity, and inclusion in our field. While it is nearly impossible to attend all sessions of interest during this whirlwind 4-day conference, you can rely on GI & Hepatology News to bring you key conference highlights over the coming months to ensure you don’t miss a beat!
Megan A. Adams, MD, JD, MSc









