User login
Before you refer for AF ablation
SNOWMASS, COLO. – Appropriate in the way of benefit, along with instilling awareness of the warning signals heralding serious late complications, Samuel J. Asirvatham, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Who to steer toward ablation? You have to have a symptomatic patient – that’s a given. For the ones who are paroxysmal, the ones with a relatively normal heart, there’s a much better chance that you’ll help manage their symptoms with ablation than if they have persistent or permanent A-fib. Notice I do not use the word ‘cure’ for A-fib. We talk about controlling symptoms and decreasing frequency, because the longer follow-up you have with intensive monitoring, the more you realize that patients still tend to have some A-fib,” explained Dr. Asirvatham, an electrophysiologist who is professor of medicine and pediatrics at the Mayo Clinic in Rochester, Minn.
The rationale for early atrial fibrillation (AF) ablation in younger patients with troublesome symptoms of paroxysmal AF despite pharmacologic attempts at rate or rhythm control is that it will arrest the progression from an atrial arrhythmia that has just a few triggers readily neutralized by pulmonary vein isolation to persistent AF with a diseased heart and a multitude of arrhythmia trigger points coming from many directions.
A solid candidate for ablation of paroxysmal AF has about a 75% likelihood of having a successful first ablation procedure, with substantial improvement in symptoms and no need for medication. Another 9%-10% will achieve marked reduction in symptom burden upon addition of antiarrhythmic agents that weren’t effective before ablation.
Late complications can be deceptive
Periprocedural stroke/transient ischemic attack, tamponade, or bleeding on the table are infrequent complications readily recognized by the interventionalist. More problematic are several late complications which are often misinterpreted, with the resultant delay causing major harm.
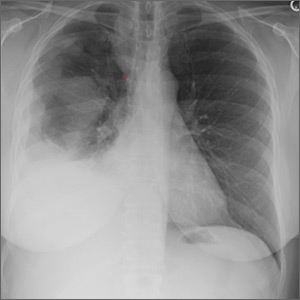
- Pulmonary vein stenosis. This complication of inadvertent ablation inside the pulmonary vein manifests as shortness of breath, typically beginning about 4 weeks post ablation.
“This is very different from the shortness of breath they had with atrial fibrillation. They almost always have a cough that they didn’t have before, and they may have hemoptysis. It’s very important to recognize this promptly, because before it closes completely we can do an angioplasty and stent the vein with good results. But once it closes completely, it becomes an extremely complicated procedure to try to reopen that vein,” according to Dr. Asirvatham.
Very often the patient’s general cardiologist, chest physician, or primary care physician fails to recognize what’s happening. He cited an example: He recently had a patient with a cough who was first referred to an infectious disease specialist, who ordered a bronchoalveolar lavage. The specimen grew atypical actinomycetes. That prompted a referral to thoracic surgery for an open-lung biopsy. But that procedure required cardiac clearance beforehand. It was a cardiologist who said, ‘Wait – all this started after you had an ablation?’
“That patient had pulmonary vein stenosis. And, unfortunately, that complication has not gone away. Being a referral center for pulmonary vein isolation, we see just as many cases of pulmonary vein stenosis today as we did a few years ago,” he said.
- Atrial esophageal fistula. The hallmark of this complication is onset of a plethora of what Dr. Asirvatham called “funny symptoms” more than a month post ablation. These include fever, transient ischemic attacks (TIAs), sepsislike symptoms, discomfort in swallowing, and in some cases hemoptysis.
“The predominant picture is endocarditis/TIA/stroke. If you see this, and the patient has had ablation, immediately refer to surgery to have the fistula between the esophagus and heart fixed. This is not a patient where you say, ‘Nothing by mouth, give some antibiotics, and see what happens.’ I can tell you what will happen: The patient will die,” the cardiologist said.
- Atrial stiffness. This typically occurs about a month after a second or third ablation procedure, when the patient develops shortness of breath that keeps worsening.
“You think ‘pulmonary vein stenosis,’ but the CT scan shows the veins are wide open. Many of these patients will get misdiagnosed as having heart failure with preserved ejection fraction even though they never had it before. The problem here is the atrium has become too stiff from the ablation, and this stiff atrium causes increased pressure, resulting in the shortness of breath. Sometimes patients feel better over time, but sometimes it’s very difficult to treat. But it’s important to recognize atrial stiffness and exclude other causes like pulmonary vein stenosis,” Dr. Asirvatham continued.
- Gastroparesis. This occurs because of injury to the vagus nerve branches located at the top of the esophagus, with resultant delayed gastric emptying.
“It’s an uncomfortable feeling of fullness all the time. The patient will say, ‘It seems like I just ate, even though I ate 8 hours ago,” the electrophysiologist said. “Most of these patients will recover in about 6 months. They may feel better on a gastric motility agent, like a macrolide antibiotic. I personally have not seen a patient who did not feel better within 6-8 months.”
Novel treatment approaches: “A-fib may be an autonomic epilepsy of the heart”
“Patients sometimes will ask you, ‘What is this ablation? What does that mean?’ You have to be truthful and tell them that it’s just a fancy word for burning,” the electrophysiologist said.
Achievement of AF ablation without radiofrequency or cryoablation, instead utilizing nonthermal direct-current pulsed electrical fields, is “the hottest topic in the field of electrophysiology,” according to Dr. Asirvatham.
These electrical fields result in irreversible electroporation of targeted myocardial cell membranes, leading to cell death. It is a tissue-specific intervention, so it’s much less likely than conventional ablation to cause collateral damage to the esophagus and other structures.
“Direct current electroporation has transitioned from proof-of-concept studies to three relatively large patient trials. This is potentially an important breakthrough because if we don’t heat, a lot of the complications of A-fib ablation will probably decrease,” he explained.
Two other promising outside-the-box approaches to the treatment of AF are autonomic nervous system modulation at sites distant from the heart and particle beam ablation without need for cardiac catheters.
“If you put electrodes everywhere in the body to see where A-fib starts, it’s not in the atrium, not in the pulmonary veins, it’s in the nerves behind the pulmonary veins, and before those nerves it’s in some other area of the autonomic nervous system. This has given rise to the notion that A-fib may be an autonomic epilepsy of the heart,” according to the electrophysiologist.
This concept has given rise to a completely different approach to treatment of AF through neurostimulation. That’s how acupuncture works. Also, headphones have been used successfully to terminate and prevent AF by stimulating autonomic nerve centers near the ears. Low-level electrical stimulation of the vagus nerve in order to reduce stellate ganglion activity is under study. So is the application of botulinum toxin at key points in the autonomic nervous system.
“Catheters, drugs, and devices that target these areas, maybe without any ablation in the heart itself, is an exciting area of future management of A-fib,” he said.
Another promising approach is borrowed from radiation oncology: particulate ablation using beams of carbon atoms, protons, or photons.
“The first patients have now been treated for ventricular tachycardia and A-fib. It really is quite amazing how precise the lesion formation is. And with no catheters in the heart, clot can’t form on catheters,” he observed.
Dr. Asirvatham reported having no financial conflicts regarding his presentation, although he serves as a consultant to a handful of medical startup companies and holds patents on intellectual property, the royalties for which go directly to the Mayo Clinic.
SNOWMASS, COLO. – Appropriate in the way of benefit, along with instilling awareness of the warning signals heralding serious late complications, Samuel J. Asirvatham, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Who to steer toward ablation? You have to have a symptomatic patient – that’s a given. For the ones who are paroxysmal, the ones with a relatively normal heart, there’s a much better chance that you’ll help manage their symptoms with ablation than if they have persistent or permanent A-fib. Notice I do not use the word ‘cure’ for A-fib. We talk about controlling symptoms and decreasing frequency, because the longer follow-up you have with intensive monitoring, the more you realize that patients still tend to have some A-fib,” explained Dr. Asirvatham, an electrophysiologist who is professor of medicine and pediatrics at the Mayo Clinic in Rochester, Minn.
The rationale for early atrial fibrillation (AF) ablation in younger patients with troublesome symptoms of paroxysmal AF despite pharmacologic attempts at rate or rhythm control is that it will arrest the progression from an atrial arrhythmia that has just a few triggers readily neutralized by pulmonary vein isolation to persistent AF with a diseased heart and a multitude of arrhythmia trigger points coming from many directions.
A solid candidate for ablation of paroxysmal AF has about a 75% likelihood of having a successful first ablation procedure, with substantial improvement in symptoms and no need for medication. Another 9%-10% will achieve marked reduction in symptom burden upon addition of antiarrhythmic agents that weren’t effective before ablation.
Late complications can be deceptive
Periprocedural stroke/transient ischemic attack, tamponade, or bleeding on the table are infrequent complications readily recognized by the interventionalist. More problematic are several late complications which are often misinterpreted, with the resultant delay causing major harm.
- Pulmonary vein stenosis. This complication of inadvertent ablation inside the pulmonary vein manifests as shortness of breath, typically beginning about 4 weeks post ablation.
“This is very different from the shortness of breath they had with atrial fibrillation. They almost always have a cough that they didn’t have before, and they may have hemoptysis. It’s very important to recognize this promptly, because before it closes completely we can do an angioplasty and stent the vein with good results. But once it closes completely, it becomes an extremely complicated procedure to try to reopen that vein,” according to Dr. Asirvatham.
Very often the patient’s general cardiologist, chest physician, or primary care physician fails to recognize what’s happening. He cited an example: He recently had a patient with a cough who was first referred to an infectious disease specialist, who ordered a bronchoalveolar lavage. The specimen grew atypical actinomycetes. That prompted a referral to thoracic surgery for an open-lung biopsy. But that procedure required cardiac clearance beforehand. It was a cardiologist who said, ‘Wait – all this started after you had an ablation?’
“That patient had pulmonary vein stenosis. And, unfortunately, that complication has not gone away. Being a referral center for pulmonary vein isolation, we see just as many cases of pulmonary vein stenosis today as we did a few years ago,” he said.
- Atrial esophageal fistula. The hallmark of this complication is onset of a plethora of what Dr. Asirvatham called “funny symptoms” more than a month post ablation. These include fever, transient ischemic attacks (TIAs), sepsislike symptoms, discomfort in swallowing, and in some cases hemoptysis.
“The predominant picture is endocarditis/TIA/stroke. If you see this, and the patient has had ablation, immediately refer to surgery to have the fistula between the esophagus and heart fixed. This is not a patient where you say, ‘Nothing by mouth, give some antibiotics, and see what happens.’ I can tell you what will happen: The patient will die,” the cardiologist said.
- Atrial stiffness. This typically occurs about a month after a second or third ablation procedure, when the patient develops shortness of breath that keeps worsening.
“You think ‘pulmonary vein stenosis,’ but the CT scan shows the veins are wide open. Many of these patients will get misdiagnosed as having heart failure with preserved ejection fraction even though they never had it before. The problem here is the atrium has become too stiff from the ablation, and this stiff atrium causes increased pressure, resulting in the shortness of breath. Sometimes patients feel better over time, but sometimes it’s very difficult to treat. But it’s important to recognize atrial stiffness and exclude other causes like pulmonary vein stenosis,” Dr. Asirvatham continued.
- Gastroparesis. This occurs because of injury to the vagus nerve branches located at the top of the esophagus, with resultant delayed gastric emptying.
“It’s an uncomfortable feeling of fullness all the time. The patient will say, ‘It seems like I just ate, even though I ate 8 hours ago,” the electrophysiologist said. “Most of these patients will recover in about 6 months. They may feel better on a gastric motility agent, like a macrolide antibiotic. I personally have not seen a patient who did not feel better within 6-8 months.”
Novel treatment approaches: “A-fib may be an autonomic epilepsy of the heart”
“Patients sometimes will ask you, ‘What is this ablation? What does that mean?’ You have to be truthful and tell them that it’s just a fancy word for burning,” the electrophysiologist said.
Achievement of AF ablation without radiofrequency or cryoablation, instead utilizing nonthermal direct-current pulsed electrical fields, is “the hottest topic in the field of electrophysiology,” according to Dr. Asirvatham.
These electrical fields result in irreversible electroporation of targeted myocardial cell membranes, leading to cell death. It is a tissue-specific intervention, so it’s much less likely than conventional ablation to cause collateral damage to the esophagus and other structures.
“Direct current electroporation has transitioned from proof-of-concept studies to three relatively large patient trials. This is potentially an important breakthrough because if we don’t heat, a lot of the complications of A-fib ablation will probably decrease,” he explained.
Two other promising outside-the-box approaches to the treatment of AF are autonomic nervous system modulation at sites distant from the heart and particle beam ablation without need for cardiac catheters.
“If you put electrodes everywhere in the body to see where A-fib starts, it’s not in the atrium, not in the pulmonary veins, it’s in the nerves behind the pulmonary veins, and before those nerves it’s in some other area of the autonomic nervous system. This has given rise to the notion that A-fib may be an autonomic epilepsy of the heart,” according to the electrophysiologist.
This concept has given rise to a completely different approach to treatment of AF through neurostimulation. That’s how acupuncture works. Also, headphones have been used successfully to terminate and prevent AF by stimulating autonomic nerve centers near the ears. Low-level electrical stimulation of the vagus nerve in order to reduce stellate ganglion activity is under study. So is the application of botulinum toxin at key points in the autonomic nervous system.
“Catheters, drugs, and devices that target these areas, maybe without any ablation in the heart itself, is an exciting area of future management of A-fib,” he said.
Another promising approach is borrowed from radiation oncology: particulate ablation using beams of carbon atoms, protons, or photons.
“The first patients have now been treated for ventricular tachycardia and A-fib. It really is quite amazing how precise the lesion formation is. And with no catheters in the heart, clot can’t form on catheters,” he observed.
Dr. Asirvatham reported having no financial conflicts regarding his presentation, although he serves as a consultant to a handful of medical startup companies and holds patents on intellectual property, the royalties for which go directly to the Mayo Clinic.
SNOWMASS, COLO. – Appropriate in the way of benefit, along with instilling awareness of the warning signals heralding serious late complications, Samuel J. Asirvatham, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Who to steer toward ablation? You have to have a symptomatic patient – that’s a given. For the ones who are paroxysmal, the ones with a relatively normal heart, there’s a much better chance that you’ll help manage their symptoms with ablation than if they have persistent or permanent A-fib. Notice I do not use the word ‘cure’ for A-fib. We talk about controlling symptoms and decreasing frequency, because the longer follow-up you have with intensive monitoring, the more you realize that patients still tend to have some A-fib,” explained Dr. Asirvatham, an electrophysiologist who is professor of medicine and pediatrics at the Mayo Clinic in Rochester, Minn.
The rationale for early atrial fibrillation (AF) ablation in younger patients with troublesome symptoms of paroxysmal AF despite pharmacologic attempts at rate or rhythm control is that it will arrest the progression from an atrial arrhythmia that has just a few triggers readily neutralized by pulmonary vein isolation to persistent AF with a diseased heart and a multitude of arrhythmia trigger points coming from many directions.
A solid candidate for ablation of paroxysmal AF has about a 75% likelihood of having a successful first ablation procedure, with substantial improvement in symptoms and no need for medication. Another 9%-10% will achieve marked reduction in symptom burden upon addition of antiarrhythmic agents that weren’t effective before ablation.
Late complications can be deceptive
Periprocedural stroke/transient ischemic attack, tamponade, or bleeding on the table are infrequent complications readily recognized by the interventionalist. More problematic are several late complications which are often misinterpreted, with the resultant delay causing major harm.
- Pulmonary vein stenosis. This complication of inadvertent ablation inside the pulmonary vein manifests as shortness of breath, typically beginning about 4 weeks post ablation.
“This is very different from the shortness of breath they had with atrial fibrillation. They almost always have a cough that they didn’t have before, and they may have hemoptysis. It’s very important to recognize this promptly, because before it closes completely we can do an angioplasty and stent the vein with good results. But once it closes completely, it becomes an extremely complicated procedure to try to reopen that vein,” according to Dr. Asirvatham.
Very often the patient’s general cardiologist, chest physician, or primary care physician fails to recognize what’s happening. He cited an example: He recently had a patient with a cough who was first referred to an infectious disease specialist, who ordered a bronchoalveolar lavage. The specimen grew atypical actinomycetes. That prompted a referral to thoracic surgery for an open-lung biopsy. But that procedure required cardiac clearance beforehand. It was a cardiologist who said, ‘Wait – all this started after you had an ablation?’
“That patient had pulmonary vein stenosis. And, unfortunately, that complication has not gone away. Being a referral center for pulmonary vein isolation, we see just as many cases of pulmonary vein stenosis today as we did a few years ago,” he said.
- Atrial esophageal fistula. The hallmark of this complication is onset of a plethora of what Dr. Asirvatham called “funny symptoms” more than a month post ablation. These include fever, transient ischemic attacks (TIAs), sepsislike symptoms, discomfort in swallowing, and in some cases hemoptysis.
“The predominant picture is endocarditis/TIA/stroke. If you see this, and the patient has had ablation, immediately refer to surgery to have the fistula between the esophagus and heart fixed. This is not a patient where you say, ‘Nothing by mouth, give some antibiotics, and see what happens.’ I can tell you what will happen: The patient will die,” the cardiologist said.
- Atrial stiffness. This typically occurs about a month after a second or third ablation procedure, when the patient develops shortness of breath that keeps worsening.
“You think ‘pulmonary vein stenosis,’ but the CT scan shows the veins are wide open. Many of these patients will get misdiagnosed as having heart failure with preserved ejection fraction even though they never had it before. The problem here is the atrium has become too stiff from the ablation, and this stiff atrium causes increased pressure, resulting in the shortness of breath. Sometimes patients feel better over time, but sometimes it’s very difficult to treat. But it’s important to recognize atrial stiffness and exclude other causes like pulmonary vein stenosis,” Dr. Asirvatham continued.
- Gastroparesis. This occurs because of injury to the vagus nerve branches located at the top of the esophagus, with resultant delayed gastric emptying.
“It’s an uncomfortable feeling of fullness all the time. The patient will say, ‘It seems like I just ate, even though I ate 8 hours ago,” the electrophysiologist said. “Most of these patients will recover in about 6 months. They may feel better on a gastric motility agent, like a macrolide antibiotic. I personally have not seen a patient who did not feel better within 6-8 months.”
Novel treatment approaches: “A-fib may be an autonomic epilepsy of the heart”
“Patients sometimes will ask you, ‘What is this ablation? What does that mean?’ You have to be truthful and tell them that it’s just a fancy word for burning,” the electrophysiologist said.
Achievement of AF ablation without radiofrequency or cryoablation, instead utilizing nonthermal direct-current pulsed electrical fields, is “the hottest topic in the field of electrophysiology,” according to Dr. Asirvatham.
These electrical fields result in irreversible electroporation of targeted myocardial cell membranes, leading to cell death. It is a tissue-specific intervention, so it’s much less likely than conventional ablation to cause collateral damage to the esophagus and other structures.
“Direct current electroporation has transitioned from proof-of-concept studies to three relatively large patient trials. This is potentially an important breakthrough because if we don’t heat, a lot of the complications of A-fib ablation will probably decrease,” he explained.
Two other promising outside-the-box approaches to the treatment of AF are autonomic nervous system modulation at sites distant from the heart and particle beam ablation without need for cardiac catheters.
“If you put electrodes everywhere in the body to see where A-fib starts, it’s not in the atrium, not in the pulmonary veins, it’s in the nerves behind the pulmonary veins, and before those nerves it’s in some other area of the autonomic nervous system. This has given rise to the notion that A-fib may be an autonomic epilepsy of the heart,” according to the electrophysiologist.
This concept has given rise to a completely different approach to treatment of AF through neurostimulation. That’s how acupuncture works. Also, headphones have been used successfully to terminate and prevent AF by stimulating autonomic nerve centers near the ears. Low-level electrical stimulation of the vagus nerve in order to reduce stellate ganglion activity is under study. So is the application of botulinum toxin at key points in the autonomic nervous system.
“Catheters, drugs, and devices that target these areas, maybe without any ablation in the heart itself, is an exciting area of future management of A-fib,” he said.
Another promising approach is borrowed from radiation oncology: particulate ablation using beams of carbon atoms, protons, or photons.
“The first patients have now been treated for ventricular tachycardia and A-fib. It really is quite amazing how precise the lesion formation is. And with no catheters in the heart, clot can’t form on catheters,” he observed.
Dr. Asirvatham reported having no financial conflicts regarding his presentation, although he serves as a consultant to a handful of medical startup companies and holds patents on intellectual property, the royalties for which go directly to the Mayo Clinic.
REPORTING FROM ACC SNOWMASS 2019
A theory of relativity for rosacea patients
Rosacea has several known comorbidities, but the widespread use of their relative, rather than absolute, risks “may result in overestimation of the clinical importance of exposures,” Leonardo A. Tjahjono and his associates wrote.
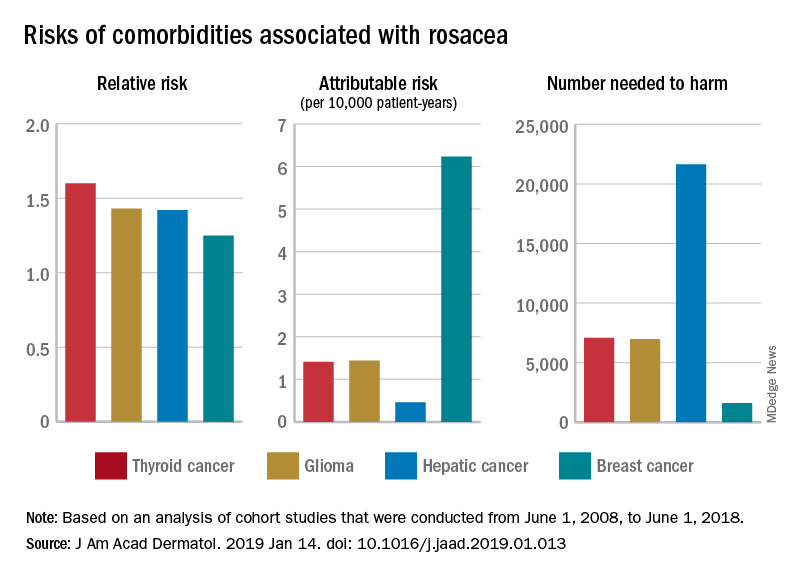
For a patient with rosacea, the relative risk of hepatic cancer is 1.42, but the attributable risk and the number needed to harm (NNH), which provide “a clearer, absolute picture regarding the association” with rosacea, are 0.46 per 10,000 patient-years and 21,645, respectively. The relative risk of comorbid breast cancer is 1.25, compared with an attributable risk of 6.23 per 10,000 patient-years and an NNH of 1,606, Mr. Tjahjono of Wake Forest University in Winston-Salem, N.C., and his associates reported in the Journal of the American Academy of Dermatology.
Physician misconceptions based on patients’ relative risks of comorbidities may lead to increased cancer screenings, which “can provide great benefit in a proper context; however, they are not without consequences. For example, 0.7 % of liver biopsies result in severe intraperitoneal hematoma,” the investigators said.
The absolute risks – calculated by the investigators using cohort studies that were conducted from June 1, 2008, to June 1, 2018 – present “a better understanding regarding rosacea’s impact on public health and clinical settings, “ they wrote.
SOURCE: Tjahjono LA et al. J Am Acad Dermatol. 2019 Jan 14. doi: 10.1016/j.jaad.2019.01.013.
Rosacea has several known comorbidities, but the widespread use of their relative, rather than absolute, risks “may result in overestimation of the clinical importance of exposures,” Leonardo A. Tjahjono and his associates wrote.
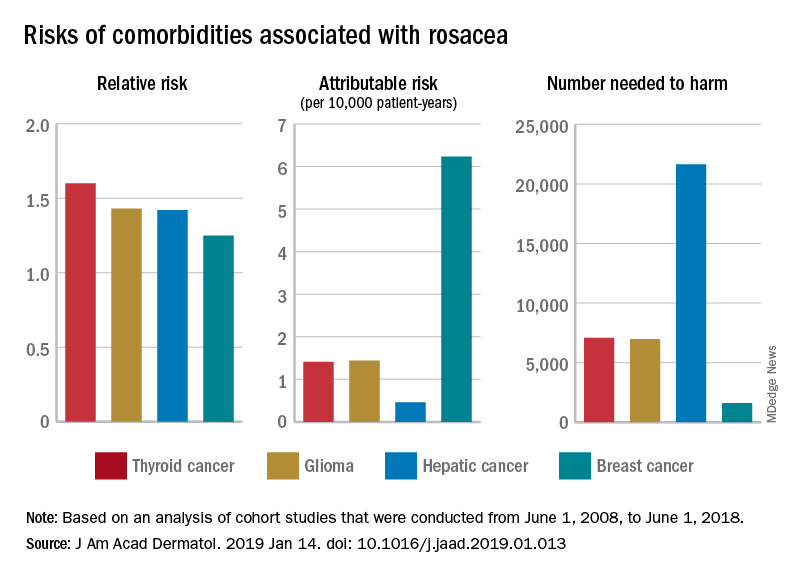
For a patient with rosacea, the relative risk of hepatic cancer is 1.42, but the attributable risk and the number needed to harm (NNH), which provide “a clearer, absolute picture regarding the association” with rosacea, are 0.46 per 10,000 patient-years and 21,645, respectively. The relative risk of comorbid breast cancer is 1.25, compared with an attributable risk of 6.23 per 10,000 patient-years and an NNH of 1,606, Mr. Tjahjono of Wake Forest University in Winston-Salem, N.C., and his associates reported in the Journal of the American Academy of Dermatology.
Physician misconceptions based on patients’ relative risks of comorbidities may lead to increased cancer screenings, which “can provide great benefit in a proper context; however, they are not without consequences. For example, 0.7 % of liver biopsies result in severe intraperitoneal hematoma,” the investigators said.
The absolute risks – calculated by the investigators using cohort studies that were conducted from June 1, 2008, to June 1, 2018 – present “a better understanding regarding rosacea’s impact on public health and clinical settings, “ they wrote.
SOURCE: Tjahjono LA et al. J Am Acad Dermatol. 2019 Jan 14. doi: 10.1016/j.jaad.2019.01.013.
Rosacea has several known comorbidities, but the widespread use of their relative, rather than absolute, risks “may result in overestimation of the clinical importance of exposures,” Leonardo A. Tjahjono and his associates wrote.
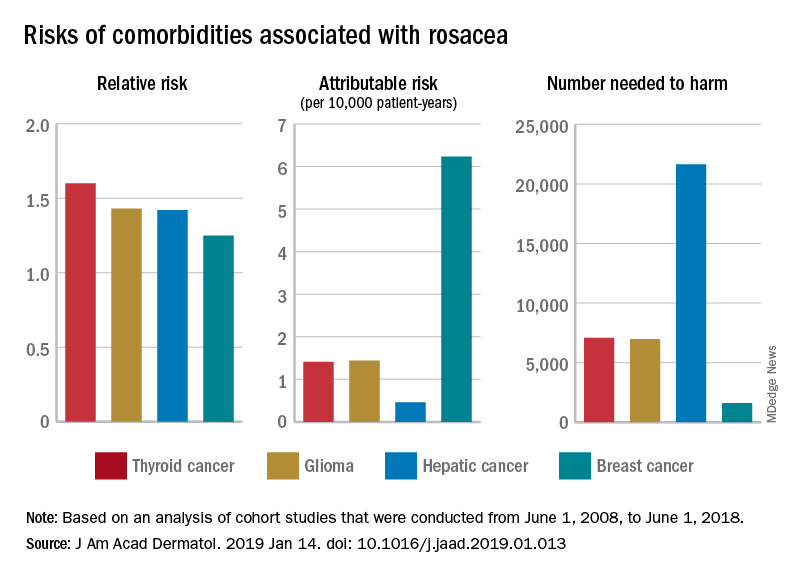
For a patient with rosacea, the relative risk of hepatic cancer is 1.42, but the attributable risk and the number needed to harm (NNH), which provide “a clearer, absolute picture regarding the association” with rosacea, are 0.46 per 10,000 patient-years and 21,645, respectively. The relative risk of comorbid breast cancer is 1.25, compared with an attributable risk of 6.23 per 10,000 patient-years and an NNH of 1,606, Mr. Tjahjono of Wake Forest University in Winston-Salem, N.C., and his associates reported in the Journal of the American Academy of Dermatology.
Physician misconceptions based on patients’ relative risks of comorbidities may lead to increased cancer screenings, which “can provide great benefit in a proper context; however, they are not without consequences. For example, 0.7 % of liver biopsies result in severe intraperitoneal hematoma,” the investigators said.
The absolute risks – calculated by the investigators using cohort studies that were conducted from June 1, 2008, to June 1, 2018 – present “a better understanding regarding rosacea’s impact on public health and clinical settings, “ they wrote.
SOURCE: Tjahjono LA et al. J Am Acad Dermatol. 2019 Jan 14. doi: 10.1016/j.jaad.2019.01.013.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Winter exfoliation: A multicultural approach
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
AAP policy promotes school attendance
Promoting school attendance can have positive effects on children’s health, according to a new policy statement from the American Academy of Pediatrics’ Council on School Health.
School absence can affect not only children’s academic achievement but also their health, and the AAP advises health care providers to promote regular school attendance as preventive medicine, wrote Mandy Allison, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and Elliott Attisha, DO, FAAP, of the Detroit Public Schools Community District.
In the statement, published in Pediatrics, the authors detailed factors associated with chronic absenteeism and provided guidelines for how clinicians can help reduce and prevent the problem. “Regardless of whether absences are unexcused or excused, chronic absenteeism typically results in poor academic outcomes and is linked to poor health outcomes,” they noted.
Factors linked with chronic absenteeism, defined by the U.S. Department of Education as missing 15 or more days of school in a year, include socioeconomic factors such as poverty, domestic violence, and foster care, as well as poorly controlled health conditions, such as asthma and diabetes. Approximately 13% of all students meet criteria for chronic absenteeism, the researchers noted.
Chronic absenteeism has been linked to an increased risk of unhealthy behaviors, including mental health problems in teens and poor health in adulthood, and students who miss school often struggle academically and may be more likely to drop out, they noted.
The AAP statement emphasizes school strategies to improve attendance, including education on hand washing and other infection prevention measures, use of school-based flu vaccination programs, availability of school nurses and counselors, and other school-based health and nutrition services.
The policy statement encourages pediatricians and other health care providers to promote school attendance in the office setting and the community.
The AAP encourages pediatricians and their colleagues caring for children to promote school attendance. In the office setting, the AAP recommends the clinicians stress the importance of school attendance, ask whether children have been absent from school and how often, encourage families to share any health concerns with the school nurse, and provide firm and specific guidance on when children should go to school or stay home. The AAP also recommends encouraging well children to return to school after routine appointments rather than miss a whole day and documenting medical needs for an Individualized Education Program or 504 Plan to maximize learning and promote attendance.
For students who are chronically absent from school (missing 2-3 days/month), the AAP encourages clinicians to identify physical health issues and psychosocial factors that may be contributing to absenteeism and to communicate with school health providers. In rare cases, out-of-school educational services may be justified, but with an established time line for returning to school, according to the statement.
In addition, the AAP encourages clinicians to advocate in the community in support of school attendance by sharing relevant data on chronic absences, working with community leaders to send a consistent message about the value of school attendance, and serving as a school physician or on a school board or wellness committee to promote attendance.
The full statement is available online and includes links to parent handouts, a waiting room video, and a mobile-friendly website for preteens, teens, and parents.
The researchers had no financial conflicts to disclose.
SOURCE: Allison MA et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3648.
“American pediatrics is somewhat unique in that we focus on promoting optimal development in addition to health as our primary mission. Pediatricians and their staffs have a role in promoting both school readiness and diminishing school absenteeism,” Francis Rushton Jr., MD, said in an interview to comment on the AAP statement.
“Sure, pediatric offices already face a tremendous amount of issues to cover at well child visits, but promoting school attendance overlaps with other discussions we already have with families. Sharing care plans with school nurses for asthmatics and medically complex children helps pediatric offices work synergistically with school health staff. Working with schools to identify social factors that contribute to poor school success and screening for social environmental or mental health issues are other ways in which we support attendance at school. These are just some examples of ideas that AAP shares with us in their recent statement, ideas we can work on, ideas that will help us enhance optimal development in our children,” Dr. Rushton added.
Dr. Rushton is affiliated with Beaufort (S.C.) Memorial Hospital, and he serves on the Pediatric News Editorial Advisory Board. He had no relevant financial conflicts to disclose.
“American pediatrics is somewhat unique in that we focus on promoting optimal development in addition to health as our primary mission. Pediatricians and their staffs have a role in promoting both school readiness and diminishing school absenteeism,” Francis Rushton Jr., MD, said in an interview to comment on the AAP statement.
“Sure, pediatric offices already face a tremendous amount of issues to cover at well child visits, but promoting school attendance overlaps with other discussions we already have with families. Sharing care plans with school nurses for asthmatics and medically complex children helps pediatric offices work synergistically with school health staff. Working with schools to identify social factors that contribute to poor school success and screening for social environmental or mental health issues are other ways in which we support attendance at school. These are just some examples of ideas that AAP shares with us in their recent statement, ideas we can work on, ideas that will help us enhance optimal development in our children,” Dr. Rushton added.
Dr. Rushton is affiliated with Beaufort (S.C.) Memorial Hospital, and he serves on the Pediatric News Editorial Advisory Board. He had no relevant financial conflicts to disclose.
“American pediatrics is somewhat unique in that we focus on promoting optimal development in addition to health as our primary mission. Pediatricians and their staffs have a role in promoting both school readiness and diminishing school absenteeism,” Francis Rushton Jr., MD, said in an interview to comment on the AAP statement.
“Sure, pediatric offices already face a tremendous amount of issues to cover at well child visits, but promoting school attendance overlaps with other discussions we already have with families. Sharing care plans with school nurses for asthmatics and medically complex children helps pediatric offices work synergistically with school health staff. Working with schools to identify social factors that contribute to poor school success and screening for social environmental or mental health issues are other ways in which we support attendance at school. These are just some examples of ideas that AAP shares with us in their recent statement, ideas we can work on, ideas that will help us enhance optimal development in our children,” Dr. Rushton added.
Dr. Rushton is affiliated with Beaufort (S.C.) Memorial Hospital, and he serves on the Pediatric News Editorial Advisory Board. He had no relevant financial conflicts to disclose.
Promoting school attendance can have positive effects on children’s health, according to a new policy statement from the American Academy of Pediatrics’ Council on School Health.
School absence can affect not only children’s academic achievement but also their health, and the AAP advises health care providers to promote regular school attendance as preventive medicine, wrote Mandy Allison, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and Elliott Attisha, DO, FAAP, of the Detroit Public Schools Community District.
In the statement, published in Pediatrics, the authors detailed factors associated with chronic absenteeism and provided guidelines for how clinicians can help reduce and prevent the problem. “Regardless of whether absences are unexcused or excused, chronic absenteeism typically results in poor academic outcomes and is linked to poor health outcomes,” they noted.
Factors linked with chronic absenteeism, defined by the U.S. Department of Education as missing 15 or more days of school in a year, include socioeconomic factors such as poverty, domestic violence, and foster care, as well as poorly controlled health conditions, such as asthma and diabetes. Approximately 13% of all students meet criteria for chronic absenteeism, the researchers noted.
Chronic absenteeism has been linked to an increased risk of unhealthy behaviors, including mental health problems in teens and poor health in adulthood, and students who miss school often struggle academically and may be more likely to drop out, they noted.
The AAP statement emphasizes school strategies to improve attendance, including education on hand washing and other infection prevention measures, use of school-based flu vaccination programs, availability of school nurses and counselors, and other school-based health and nutrition services.
The policy statement encourages pediatricians and other health care providers to promote school attendance in the office setting and the community.
The AAP encourages pediatricians and their colleagues caring for children to promote school attendance. In the office setting, the AAP recommends the clinicians stress the importance of school attendance, ask whether children have been absent from school and how often, encourage families to share any health concerns with the school nurse, and provide firm and specific guidance on when children should go to school or stay home. The AAP also recommends encouraging well children to return to school after routine appointments rather than miss a whole day and documenting medical needs for an Individualized Education Program or 504 Plan to maximize learning and promote attendance.
For students who are chronically absent from school (missing 2-3 days/month), the AAP encourages clinicians to identify physical health issues and psychosocial factors that may be contributing to absenteeism and to communicate with school health providers. In rare cases, out-of-school educational services may be justified, but with an established time line for returning to school, according to the statement.
In addition, the AAP encourages clinicians to advocate in the community in support of school attendance by sharing relevant data on chronic absences, working with community leaders to send a consistent message about the value of school attendance, and serving as a school physician or on a school board or wellness committee to promote attendance.
The full statement is available online and includes links to parent handouts, a waiting room video, and a mobile-friendly website for preteens, teens, and parents.
The researchers had no financial conflicts to disclose.
SOURCE: Allison MA et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3648.
Promoting school attendance can have positive effects on children’s health, according to a new policy statement from the American Academy of Pediatrics’ Council on School Health.
School absence can affect not only children’s academic achievement but also their health, and the AAP advises health care providers to promote regular school attendance as preventive medicine, wrote Mandy Allison, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and Elliott Attisha, DO, FAAP, of the Detroit Public Schools Community District.
In the statement, published in Pediatrics, the authors detailed factors associated with chronic absenteeism and provided guidelines for how clinicians can help reduce and prevent the problem. “Regardless of whether absences are unexcused or excused, chronic absenteeism typically results in poor academic outcomes and is linked to poor health outcomes,” they noted.
Factors linked with chronic absenteeism, defined by the U.S. Department of Education as missing 15 or more days of school in a year, include socioeconomic factors such as poverty, domestic violence, and foster care, as well as poorly controlled health conditions, such as asthma and diabetes. Approximately 13% of all students meet criteria for chronic absenteeism, the researchers noted.
Chronic absenteeism has been linked to an increased risk of unhealthy behaviors, including mental health problems in teens and poor health in adulthood, and students who miss school often struggle academically and may be more likely to drop out, they noted.
The AAP statement emphasizes school strategies to improve attendance, including education on hand washing and other infection prevention measures, use of school-based flu vaccination programs, availability of school nurses and counselors, and other school-based health and nutrition services.
The policy statement encourages pediatricians and other health care providers to promote school attendance in the office setting and the community.
The AAP encourages pediatricians and their colleagues caring for children to promote school attendance. In the office setting, the AAP recommends the clinicians stress the importance of school attendance, ask whether children have been absent from school and how often, encourage families to share any health concerns with the school nurse, and provide firm and specific guidance on when children should go to school or stay home. The AAP also recommends encouraging well children to return to school after routine appointments rather than miss a whole day and documenting medical needs for an Individualized Education Program or 504 Plan to maximize learning and promote attendance.
For students who are chronically absent from school (missing 2-3 days/month), the AAP encourages clinicians to identify physical health issues and psychosocial factors that may be contributing to absenteeism and to communicate with school health providers. In rare cases, out-of-school educational services may be justified, but with an established time line for returning to school, according to the statement.
In addition, the AAP encourages clinicians to advocate in the community in support of school attendance by sharing relevant data on chronic absences, working with community leaders to send a consistent message about the value of school attendance, and serving as a school physician or on a school board or wellness committee to promote attendance.
The full statement is available online and includes links to parent handouts, a waiting room video, and a mobile-friendly website for preteens, teens, and parents.
The researchers had no financial conflicts to disclose.
SOURCE: Allison MA et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3648.
FROM PEDIATRICS
Key clinical point: Clinicians can promote school attendance in the office and in the community as part of a preventive health strategy.
Major finding: Approximately 13% of all school age students in the United States miss 15 or more days of school each year, according to the American Academy of Pediatrics.
Study details: Statement by the American Academy of Pediatrics.
Disclosures: The researchers had no financial conflicts to disclose.
Source: Allison MA et al. Pediatrics. 2019; doi: 10.1542/peds.2018-3648.
Family handgun ownership linked to young children’s gun deaths
A recent increase in U.S. handgun ownership among white families tracks with a similar trend of recently rising gun deaths among young white children, a new study found. This association held even after adjustments for multiple sociodemographic variables that research previously had linked to higher gun ownership and higher firearm mortality.
“Indeed, firearm ownership, generally, was positively associated with firearm-related mortality among 1- to 5-year-old white children, but this correlation was primarily driven by changes in the proportion of families who owned handguns: firearms more often stored unsecured and loaded,” wrote Kate C. Prickett, PhD, of the Victoria University of Wellington (New Zealand) and her associates in Pediatrics.
“These findings suggest that ease of access and use may be an important consideration when examining firearm-related fatality risk among young children,” they continued. Given the lack of attenuation in the relationship from controlling for sociodemographic variables, they add, “this finding is in line with research documenting that the presence of a firearm in the home matters above and beyond other risk factors associated with child injury.”
Even though U.S. gun ownership and pediatric firearm mortality overall have been dropping over the past several decades, the latter has stagnated recently, and gun deaths among children aged 1-4 years nearly doubled between 2006-2016, the researchers noted.
Given the counterintuitive increase in young children’s gun deaths while overall gun ownership kept dropping, the researchers took a closer look at the relationship between gun deaths among children aged 1-5 years and specific types of firearm ownership among families with children under age 5 years in the home. They relied on household data from the nationally representative General Social Survey and on fatality statistics from the National Vital Statistics System from 1976-2016.
Over those 4 decades, gun ownership in white families with small children decreased from 50% to 45% and in black families with small children from 38% to 6%.
Simultaneously, however, handgun ownership increased from 25% to 32% among white families with young children. In fact, most firearm-owning white families (72%) owned a handgun in 2016 while rifle ownership had declined substantially.
Meanwhile, “firearm-related mortality rate among young white children declined from historic highs in the late 1970s to early 1980s until 2001,” the authors reported. “After 2004, however, the mortality rate began to rise, reaching mid-1980s levels.” Further, gun deaths constituted 2% of young children’s injury deaths in 1976 but nearly 5% in 2016.
When the researchers compared these findings, they found a positive, significant association between white child firearm mortality and the proportion of white families who owned a handgun but not a rifle or shotgun.
The association remained after the researchers adjusted for several covariates already established in the evidence base to have associations with firearm ownership, child injury risk and/or firearm mortality: living in a rural area, living in the South, neither parent having a college degree, and a household income in the bottom quartile nationally. In addition, “the annual national unemployment rate by race was included as an indicator of the broader economic context,” the authors wrote.
Although young black children die from guns nearly three times more frequently than white children, the authors were unable to present detailed findings on associations with gun ownership because of small sample sizes. They noted, however, that handgun ownership actually declined during the study period from 15% to 6% in black families with young children.
The researchers concluded that the recent increase in young children’s gun deaths may be partly driven by an increase in handgun ownership, even as overall gun ownership (primarily rifles and shotguns) has continued dropping.
“For young children, shootings are more likely to be unintentional, making the ease at which firearms can be accessed and used a more important determinant of mortality than perhaps for older children,” the authors wrote. “Moreover, relative to other firearms like hunting rifles, handguns, because they are more likely to be purchased for personal protection, are more likely to be stored loaded with ammunition, unlocked, and in a more easily accessible place, such as a bedroom drawer.”
The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
SOURCE: Prickett KC et al. Pediatrics. 2019;143(2):e20181171.
The “unique and important approach” used by Prickett et al. to investigate an association between gun ownership and children’s gun deaths is “novel” because of their focus on firearm types and the youngest children, wrote Shilpa J. Patel, MD; Monika K. Goyal, MD; and Kavita Parikh, MD, all with the Children’s National Health System in Washington, DC, in an editorial published with the study (Pediatrics. 2018 Jan 28. doi: 10.1542/peds.2018-3611).
The findings are particularly relevant to pediatricians’ conversations with families about safe firearm storage practices. The American Academy of Pediatrics recommends all firearms are stored locked and unloaded with ammunition stored separately.
For families who find these guidelines difficult because they keep handguns at the ready for protection, “it is important to note that the risk of unintentional or intentional injury from a household firearm is much greater than the likelihood of providing protection for self-defense,” the editorial’s authors wrote. But they advocate for personalized safe storage strategies and shared decision making based on families’ needs and values.
“This study is a loud and compelling call to action for all pediatricians to start open discussions around firearm ownership with all families and to share data on the significant risks associated with unsafe storage,” they wrote. “It is an even louder call to firearm manufacturers to step up and innovate, test, and design smart handguns that are inoperable by young children to prevent unintentional injury.”
Although having no firearms in the home is the most effective way to reduce children’s risk of gun-related injuries and deaths, developing effective safety controls on guns could also substantially curtail young children’s gun deaths. “We as a society should be advocating for continued research to childproof firearms so that if families choose to have firearms in the home, the safety of their children is not compromised,” they wrote.
Dr. Parikh is a hospitalist, Dr. Goyal is assistant division chief or emergency medicine, and Dr. Patel is an emergency medicine specialist, all with Children’s National Health System in Washington, DC. They reported no funding and no disclosures.
The “unique and important approach” used by Prickett et al. to investigate an association between gun ownership and children’s gun deaths is “novel” because of their focus on firearm types and the youngest children, wrote Shilpa J. Patel, MD; Monika K. Goyal, MD; and Kavita Parikh, MD, all with the Children’s National Health System in Washington, DC, in an editorial published with the study (Pediatrics. 2018 Jan 28. doi: 10.1542/peds.2018-3611).
The findings are particularly relevant to pediatricians’ conversations with families about safe firearm storage practices. The American Academy of Pediatrics recommends all firearms are stored locked and unloaded with ammunition stored separately.
For families who find these guidelines difficult because they keep handguns at the ready for protection, “it is important to note that the risk of unintentional or intentional injury from a household firearm is much greater than the likelihood of providing protection for self-defense,” the editorial’s authors wrote. But they advocate for personalized safe storage strategies and shared decision making based on families’ needs and values.
“This study is a loud and compelling call to action for all pediatricians to start open discussions around firearm ownership with all families and to share data on the significant risks associated with unsafe storage,” they wrote. “It is an even louder call to firearm manufacturers to step up and innovate, test, and design smart handguns that are inoperable by young children to prevent unintentional injury.”
Although having no firearms in the home is the most effective way to reduce children’s risk of gun-related injuries and deaths, developing effective safety controls on guns could also substantially curtail young children’s gun deaths. “We as a society should be advocating for continued research to childproof firearms so that if families choose to have firearms in the home, the safety of their children is not compromised,” they wrote.
Dr. Parikh is a hospitalist, Dr. Goyal is assistant division chief or emergency medicine, and Dr. Patel is an emergency medicine specialist, all with Children’s National Health System in Washington, DC. They reported no funding and no disclosures.
The “unique and important approach” used by Prickett et al. to investigate an association between gun ownership and children’s gun deaths is “novel” because of their focus on firearm types and the youngest children, wrote Shilpa J. Patel, MD; Monika K. Goyal, MD; and Kavita Parikh, MD, all with the Children’s National Health System in Washington, DC, in an editorial published with the study (Pediatrics. 2018 Jan 28. doi: 10.1542/peds.2018-3611).
The findings are particularly relevant to pediatricians’ conversations with families about safe firearm storage practices. The American Academy of Pediatrics recommends all firearms are stored locked and unloaded with ammunition stored separately.
For families who find these guidelines difficult because they keep handguns at the ready for protection, “it is important to note that the risk of unintentional or intentional injury from a household firearm is much greater than the likelihood of providing protection for self-defense,” the editorial’s authors wrote. But they advocate for personalized safe storage strategies and shared decision making based on families’ needs and values.
“This study is a loud and compelling call to action for all pediatricians to start open discussions around firearm ownership with all families and to share data on the significant risks associated with unsafe storage,” they wrote. “It is an even louder call to firearm manufacturers to step up and innovate, test, and design smart handguns that are inoperable by young children to prevent unintentional injury.”
Although having no firearms in the home is the most effective way to reduce children’s risk of gun-related injuries and deaths, developing effective safety controls on guns could also substantially curtail young children’s gun deaths. “We as a society should be advocating for continued research to childproof firearms so that if families choose to have firearms in the home, the safety of their children is not compromised,” they wrote.
Dr. Parikh is a hospitalist, Dr. Goyal is assistant division chief or emergency medicine, and Dr. Patel is an emergency medicine specialist, all with Children’s National Health System in Washington, DC. They reported no funding and no disclosures.
A recent increase in U.S. handgun ownership among white families tracks with a similar trend of recently rising gun deaths among young white children, a new study found. This association held even after adjustments for multiple sociodemographic variables that research previously had linked to higher gun ownership and higher firearm mortality.
“Indeed, firearm ownership, generally, was positively associated with firearm-related mortality among 1- to 5-year-old white children, but this correlation was primarily driven by changes in the proportion of families who owned handguns: firearms more often stored unsecured and loaded,” wrote Kate C. Prickett, PhD, of the Victoria University of Wellington (New Zealand) and her associates in Pediatrics.
“These findings suggest that ease of access and use may be an important consideration when examining firearm-related fatality risk among young children,” they continued. Given the lack of attenuation in the relationship from controlling for sociodemographic variables, they add, “this finding is in line with research documenting that the presence of a firearm in the home matters above and beyond other risk factors associated with child injury.”
Even though U.S. gun ownership and pediatric firearm mortality overall have been dropping over the past several decades, the latter has stagnated recently, and gun deaths among children aged 1-4 years nearly doubled between 2006-2016, the researchers noted.
Given the counterintuitive increase in young children’s gun deaths while overall gun ownership kept dropping, the researchers took a closer look at the relationship between gun deaths among children aged 1-5 years and specific types of firearm ownership among families with children under age 5 years in the home. They relied on household data from the nationally representative General Social Survey and on fatality statistics from the National Vital Statistics System from 1976-2016.
Over those 4 decades, gun ownership in white families with small children decreased from 50% to 45% and in black families with small children from 38% to 6%.
Simultaneously, however, handgun ownership increased from 25% to 32% among white families with young children. In fact, most firearm-owning white families (72%) owned a handgun in 2016 while rifle ownership had declined substantially.
Meanwhile, “firearm-related mortality rate among young white children declined from historic highs in the late 1970s to early 1980s until 2001,” the authors reported. “After 2004, however, the mortality rate began to rise, reaching mid-1980s levels.” Further, gun deaths constituted 2% of young children’s injury deaths in 1976 but nearly 5% in 2016.
When the researchers compared these findings, they found a positive, significant association between white child firearm mortality and the proportion of white families who owned a handgun but not a rifle or shotgun.
The association remained after the researchers adjusted for several covariates already established in the evidence base to have associations with firearm ownership, child injury risk and/or firearm mortality: living in a rural area, living in the South, neither parent having a college degree, and a household income in the bottom quartile nationally. In addition, “the annual national unemployment rate by race was included as an indicator of the broader economic context,” the authors wrote.
Although young black children die from guns nearly three times more frequently than white children, the authors were unable to present detailed findings on associations with gun ownership because of small sample sizes. They noted, however, that handgun ownership actually declined during the study period from 15% to 6% in black families with young children.
The researchers concluded that the recent increase in young children’s gun deaths may be partly driven by an increase in handgun ownership, even as overall gun ownership (primarily rifles and shotguns) has continued dropping.
“For young children, shootings are more likely to be unintentional, making the ease at which firearms can be accessed and used a more important determinant of mortality than perhaps for older children,” the authors wrote. “Moreover, relative to other firearms like hunting rifles, handguns, because they are more likely to be purchased for personal protection, are more likely to be stored loaded with ammunition, unlocked, and in a more easily accessible place, such as a bedroom drawer.”
The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
SOURCE: Prickett KC et al. Pediatrics. 2019;143(2):e20181171.
A recent increase in U.S. handgun ownership among white families tracks with a similar trend of recently rising gun deaths among young white children, a new study found. This association held even after adjustments for multiple sociodemographic variables that research previously had linked to higher gun ownership and higher firearm mortality.
“Indeed, firearm ownership, generally, was positively associated with firearm-related mortality among 1- to 5-year-old white children, but this correlation was primarily driven by changes in the proportion of families who owned handguns: firearms more often stored unsecured and loaded,” wrote Kate C. Prickett, PhD, of the Victoria University of Wellington (New Zealand) and her associates in Pediatrics.
“These findings suggest that ease of access and use may be an important consideration when examining firearm-related fatality risk among young children,” they continued. Given the lack of attenuation in the relationship from controlling for sociodemographic variables, they add, “this finding is in line with research documenting that the presence of a firearm in the home matters above and beyond other risk factors associated with child injury.”
Even though U.S. gun ownership and pediatric firearm mortality overall have been dropping over the past several decades, the latter has stagnated recently, and gun deaths among children aged 1-4 years nearly doubled between 2006-2016, the researchers noted.
Given the counterintuitive increase in young children’s gun deaths while overall gun ownership kept dropping, the researchers took a closer look at the relationship between gun deaths among children aged 1-5 years and specific types of firearm ownership among families with children under age 5 years in the home. They relied on household data from the nationally representative General Social Survey and on fatality statistics from the National Vital Statistics System from 1976-2016.
Over those 4 decades, gun ownership in white families with small children decreased from 50% to 45% and in black families with small children from 38% to 6%.
Simultaneously, however, handgun ownership increased from 25% to 32% among white families with young children. In fact, most firearm-owning white families (72%) owned a handgun in 2016 while rifle ownership had declined substantially.
Meanwhile, “firearm-related mortality rate among young white children declined from historic highs in the late 1970s to early 1980s until 2001,” the authors reported. “After 2004, however, the mortality rate began to rise, reaching mid-1980s levels.” Further, gun deaths constituted 2% of young children’s injury deaths in 1976 but nearly 5% in 2016.
When the researchers compared these findings, they found a positive, significant association between white child firearm mortality and the proportion of white families who owned a handgun but not a rifle or shotgun.
The association remained after the researchers adjusted for several covariates already established in the evidence base to have associations with firearm ownership, child injury risk and/or firearm mortality: living in a rural area, living in the South, neither parent having a college degree, and a household income in the bottom quartile nationally. In addition, “the annual national unemployment rate by race was included as an indicator of the broader economic context,” the authors wrote.
Although young black children die from guns nearly three times more frequently than white children, the authors were unable to present detailed findings on associations with gun ownership because of small sample sizes. They noted, however, that handgun ownership actually declined during the study period from 15% to 6% in black families with young children.
The researchers concluded that the recent increase in young children’s gun deaths may be partly driven by an increase in handgun ownership, even as overall gun ownership (primarily rifles and shotguns) has continued dropping.
“For young children, shootings are more likely to be unintentional, making the ease at which firearms can be accessed and used a more important determinant of mortality than perhaps for older children,” the authors wrote. “Moreover, relative to other firearms like hunting rifles, handguns, because they are more likely to be purchased for personal protection, are more likely to be stored loaded with ammunition, unlocked, and in a more easily accessible place, such as a bedroom drawer.”
The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
SOURCE: Prickett KC et al. Pediatrics. 2019;143(2):e20181171.
FROM PEDIATRICS
Key clinical point: Greater handgun ownership in families may increase young children’s risk of gun death.
Major finding: Handgun ownership in white families with young children rose from 25% to 32% during 1976-2016, alongside increasing rates of firearm deaths in young white children.
Study details: The findings are based on analysis of data on U.S. family firearm ownership and pediatric gun deaths in the General Social Study and National Vital Statistics System from 1976-2016.
Disclosures: The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
Source: Prickett KC et al. Pediatrics. 2019 Jan 28;143(2):e20181171.
Pediatricians get more guidance to be proactive on youth e-cig use
The American Academy of Pediatrics is pushing for pediatricians to be more proactive in keeping youth from becoming addicted to nicotine through the use of electronic cigarettes. “E-cigarettes are the most common tobacco product used among youth,” Brian Jenssen, MD, policy chair of the AAP Section on Tobacco Control and Susan Walley, MD, chair of the section, wrote in recommendations for pediatricians and policy makers regarding the use of e-cigarettes and similar devices. These recommendations were published in0 Pediatrics.
“To prevent children, adolescents, and young adults from transitioning from e-cigarettes to traditional cigarettes and to minimize the potential public health harm from e-cigarette use, there is a critical need for e-cigarette legislative action, and counterpromotion to help youth live tobacco-free lives,” the authors continued.
To that end, AAP is making a series of recommended actions by pediatricians. First, they are calling for pediatricians to screen for e-cigarette use and exposure and to provide prevention counseling in clinical practice.
Second, the organization is calling on pediatricians to provide counseling that areas where youth spend time – including homes, cars, schools, and other places – should have “comprehensive tobacco-free bans that include e-cigarettes as well as combustible tobacco products.”
Finally, pediatricians should never recommend e-cigarettes as a tobacco-dependence treatment product.
AAP in the guidance document also made a series of policy recommendations, including calling on the Food and Drug Administration to regulate e-cigarettes as they do traditional tobacco products; ban the sale of e-cigarettes to anyone under 21 years of age; ban all flavored e-cigarettes, including menthol; ban advertising of e-cigarettes that is accessible to youth; tax e-cigarettes similar to traditional cigarettes; and incorporate e-cigarettes into current tobacco-free laws and ordinances.
Dr. Jenssen and Dr. Walley also call for more research to inform public policy and understand health effects.
“Additional research is needed to understand the trajectory of addiction among youth and the progression to combustible tobacco products,” they wrote. “Studies are needed to determine if and how e-cigarettes may be effective for smoking cessation; these trials must be carefully designed and adequately powered. Finally, research is needed to evaluate effective countermessaging and public health interventions.”
SOURCE: Jenssen B et al. Pediatrics. doi: 10.1542/peds.2018-3652.
The American Academy of Pediatrics is pushing for pediatricians to be more proactive in keeping youth from becoming addicted to nicotine through the use of electronic cigarettes. “E-cigarettes are the most common tobacco product used among youth,” Brian Jenssen, MD, policy chair of the AAP Section on Tobacco Control and Susan Walley, MD, chair of the section, wrote in recommendations for pediatricians and policy makers regarding the use of e-cigarettes and similar devices. These recommendations were published in0 Pediatrics.
“To prevent children, adolescents, and young adults from transitioning from e-cigarettes to traditional cigarettes and to minimize the potential public health harm from e-cigarette use, there is a critical need for e-cigarette legislative action, and counterpromotion to help youth live tobacco-free lives,” the authors continued.
To that end, AAP is making a series of recommended actions by pediatricians. First, they are calling for pediatricians to screen for e-cigarette use and exposure and to provide prevention counseling in clinical practice.
Second, the organization is calling on pediatricians to provide counseling that areas where youth spend time – including homes, cars, schools, and other places – should have “comprehensive tobacco-free bans that include e-cigarettes as well as combustible tobacco products.”
Finally, pediatricians should never recommend e-cigarettes as a tobacco-dependence treatment product.
AAP in the guidance document also made a series of policy recommendations, including calling on the Food and Drug Administration to regulate e-cigarettes as they do traditional tobacco products; ban the sale of e-cigarettes to anyone under 21 years of age; ban all flavored e-cigarettes, including menthol; ban advertising of e-cigarettes that is accessible to youth; tax e-cigarettes similar to traditional cigarettes; and incorporate e-cigarettes into current tobacco-free laws and ordinances.
Dr. Jenssen and Dr. Walley also call for more research to inform public policy and understand health effects.
“Additional research is needed to understand the trajectory of addiction among youth and the progression to combustible tobacco products,” they wrote. “Studies are needed to determine if and how e-cigarettes may be effective for smoking cessation; these trials must be carefully designed and adequately powered. Finally, research is needed to evaluate effective countermessaging and public health interventions.”
SOURCE: Jenssen B et al. Pediatrics. doi: 10.1542/peds.2018-3652.
The American Academy of Pediatrics is pushing for pediatricians to be more proactive in keeping youth from becoming addicted to nicotine through the use of electronic cigarettes. “E-cigarettes are the most common tobacco product used among youth,” Brian Jenssen, MD, policy chair of the AAP Section on Tobacco Control and Susan Walley, MD, chair of the section, wrote in recommendations for pediatricians and policy makers regarding the use of e-cigarettes and similar devices. These recommendations were published in0 Pediatrics.
“To prevent children, adolescents, and young adults from transitioning from e-cigarettes to traditional cigarettes and to minimize the potential public health harm from e-cigarette use, there is a critical need for e-cigarette legislative action, and counterpromotion to help youth live tobacco-free lives,” the authors continued.
To that end, AAP is making a series of recommended actions by pediatricians. First, they are calling for pediatricians to screen for e-cigarette use and exposure and to provide prevention counseling in clinical practice.
Second, the organization is calling on pediatricians to provide counseling that areas where youth spend time – including homes, cars, schools, and other places – should have “comprehensive tobacco-free bans that include e-cigarettes as well as combustible tobacco products.”
Finally, pediatricians should never recommend e-cigarettes as a tobacco-dependence treatment product.
AAP in the guidance document also made a series of policy recommendations, including calling on the Food and Drug Administration to regulate e-cigarettes as they do traditional tobacco products; ban the sale of e-cigarettes to anyone under 21 years of age; ban all flavored e-cigarettes, including menthol; ban advertising of e-cigarettes that is accessible to youth; tax e-cigarettes similar to traditional cigarettes; and incorporate e-cigarettes into current tobacco-free laws and ordinances.
Dr. Jenssen and Dr. Walley also call for more research to inform public policy and understand health effects.
“Additional research is needed to understand the trajectory of addiction among youth and the progression to combustible tobacco products,” they wrote. “Studies are needed to determine if and how e-cigarettes may be effective for smoking cessation; these trials must be carefully designed and adequately powered. Finally, research is needed to evaluate effective countermessaging and public health interventions.”
SOURCE: Jenssen B et al. Pediatrics. doi: 10.1542/peds.2018-3652.
FROM PEDIATRICS
Key clinical point: Pediatrics, policy makers need to be more proactive to curb e-cig use in youth
Major finding: There is a critical need for more regulation to protect youth from harmful effects of e-cigs.
Study details: Recommendations by the American Academy of Pediatrics to help minimize youth exposure to e-cigs.
Disclosures: No disclosures were reported by the authors.
Source: Jenssen B et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3652.
Long-term opioid use substantial in elderly adults prior to total joint replacement
In elderly patients with osteoarthritis, long-term opioid use is highly prevalent and varies substantially by state, suggest the results of a large, observational cohort study.
Long term opioid use prior to total joint replacement (TJR) varied somewhat by access to primary care providers, but not by access to rheumatologists, according to authors of the study, led by Rishi J Desai, MS, PhD, of the department of medicine at Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
“These findings suggest that geographically targeted dissemination strategies for safe opioid prescribing guidelines may be required to address the high use observed in certain states,” said Dr. Desai and his colleagues in a report on the study published in Arthritis & Rheumatology.
This study by Dr. Desai and his colleagues looked at long-term use of opioids, which was defined as at least 90 days of use in the year prior to TJR. They analyzed a total of 358,121 Medicare enrollees with advanced osteoarthritis, with a mean age of 74 years.
Geographic areas in the South tended to have higher proportions of long-term opioid users, while the Northeast and Midwest had lower proportions, according to investigators.
Long-term use of opioids ranged from a low of 8.9% in Minnesota to 26.4% in Alabama, they reported. Beyond Alabama, the top 10 states included West Virginia, Georgia, Kentucky, Louisiana, Oklahoma, North Carolina, Virginia, Indiana, and Mississippi, with proportions of long-term opioid users ranging from 17% to 25%, the report shows.
Only modest associations were seen between provider density and opioid use, investigators said. There was a 1.4% mean difference (95% confidence interval, 0.8%-2.0%) in long-term opioid users between primary care service areas (PCSAs) with the highest concentrations of primary care providers versus those with the lowest, and there was just a 0.6% mean difference (95% CI, –0.1% to 1.3%) between PCSAs with the highest concentrations of rheumatologists and those with the lowest.
Among long-term opioid users, almost 20% were using an average daily dose of 50 or more morphine milligram equivalents, a range that potentially imparts a high risk of opioid-related harms, according to investigators.
Funding for the study came from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Desai reported disclosures related to Merck and Vertex. Co-authors provided disclosures related to a number of pharmaceutical companies.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2019. doi: 10.1002/art.40834.
In elderly patients with osteoarthritis, long-term opioid use is highly prevalent and varies substantially by state, suggest the results of a large, observational cohort study.
Long term opioid use prior to total joint replacement (TJR) varied somewhat by access to primary care providers, but not by access to rheumatologists, according to authors of the study, led by Rishi J Desai, MS, PhD, of the department of medicine at Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
“These findings suggest that geographically targeted dissemination strategies for safe opioid prescribing guidelines may be required to address the high use observed in certain states,” said Dr. Desai and his colleagues in a report on the study published in Arthritis & Rheumatology.
This study by Dr. Desai and his colleagues looked at long-term use of opioids, which was defined as at least 90 days of use in the year prior to TJR. They analyzed a total of 358,121 Medicare enrollees with advanced osteoarthritis, with a mean age of 74 years.
Geographic areas in the South tended to have higher proportions of long-term opioid users, while the Northeast and Midwest had lower proportions, according to investigators.
Long-term use of opioids ranged from a low of 8.9% in Minnesota to 26.4% in Alabama, they reported. Beyond Alabama, the top 10 states included West Virginia, Georgia, Kentucky, Louisiana, Oklahoma, North Carolina, Virginia, Indiana, and Mississippi, with proportions of long-term opioid users ranging from 17% to 25%, the report shows.
Only modest associations were seen between provider density and opioid use, investigators said. There was a 1.4% mean difference (95% confidence interval, 0.8%-2.0%) in long-term opioid users between primary care service areas (PCSAs) with the highest concentrations of primary care providers versus those with the lowest, and there was just a 0.6% mean difference (95% CI, –0.1% to 1.3%) between PCSAs with the highest concentrations of rheumatologists and those with the lowest.
Among long-term opioid users, almost 20% were using an average daily dose of 50 or more morphine milligram equivalents, a range that potentially imparts a high risk of opioid-related harms, according to investigators.
Funding for the study came from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Desai reported disclosures related to Merck and Vertex. Co-authors provided disclosures related to a number of pharmaceutical companies.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2019. doi: 10.1002/art.40834.
In elderly patients with osteoarthritis, long-term opioid use is highly prevalent and varies substantially by state, suggest the results of a large, observational cohort study.
Long term opioid use prior to total joint replacement (TJR) varied somewhat by access to primary care providers, but not by access to rheumatologists, according to authors of the study, led by Rishi J Desai, MS, PhD, of the department of medicine at Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
“These findings suggest that geographically targeted dissemination strategies for safe opioid prescribing guidelines may be required to address the high use observed in certain states,” said Dr. Desai and his colleagues in a report on the study published in Arthritis & Rheumatology.
This study by Dr. Desai and his colleagues looked at long-term use of opioids, which was defined as at least 90 days of use in the year prior to TJR. They analyzed a total of 358,121 Medicare enrollees with advanced osteoarthritis, with a mean age of 74 years.
Geographic areas in the South tended to have higher proportions of long-term opioid users, while the Northeast and Midwest had lower proportions, according to investigators.
Long-term use of opioids ranged from a low of 8.9% in Minnesota to 26.4% in Alabama, they reported. Beyond Alabama, the top 10 states included West Virginia, Georgia, Kentucky, Louisiana, Oklahoma, North Carolina, Virginia, Indiana, and Mississippi, with proportions of long-term opioid users ranging from 17% to 25%, the report shows.
Only modest associations were seen between provider density and opioid use, investigators said. There was a 1.4% mean difference (95% confidence interval, 0.8%-2.0%) in long-term opioid users between primary care service areas (PCSAs) with the highest concentrations of primary care providers versus those with the lowest, and there was just a 0.6% mean difference (95% CI, –0.1% to 1.3%) between PCSAs with the highest concentrations of rheumatologists and those with the lowest.
Among long-term opioid users, almost 20% were using an average daily dose of 50 or more morphine milligram equivalents, a range that potentially imparts a high risk of opioid-related harms, according to investigators.
Funding for the study came from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Desai reported disclosures related to Merck and Vertex. Co-authors provided disclosures related to a number of pharmaceutical companies.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2019. doi: 10.1002/art.40834.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Long-term opioid use is highly prevalent among older adults with osteoarthritis who underwent total joint replacement.
Major finding: Long-term use of opioids ranged from a low of 8.9% in Minnesota to 26.4% in Alabama.
Study details: An observational cohort study including 358,121 Medicare enrollees with advanced osteoarthritis.
Disclosures: Funding for the study came from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Desai reported disclosures related to Merck and Vertex. Coauthors provided disclosures related to a number of pharmaceutical companies.
Source: Desai RJ et al. Arthritis Rheumatol. 2019. doi: 10.1002/art.40834.
What are the best treatments for reducing osteoporotic compression fracture pain?
EVIDENCE SUMMARY
A 2015 meta-analysis of 8 RCTs compared pain reduction in adults >50 years with osteoporotic compression fractures who received either vertebral augmentation (vertebroplasty or balloon kyphoplasty; 495 patients) or conservative or sham treatment (492 patients).1 Pain was measured by the visual analog scale (VAS) periodically between 1 week and 1 year.
The study included patients of both sexes who had an acute or chronic osteoporotic vertebral compression fracture that caused pain and functional limitations in daily activities. It excluded patients with neoplasm, pre-existing chronic pain or functional disability unrelated to vertebral fractures, and vertebral fractures unaccompanied by signal changes on magnetic resonance imaging.
Vertebral augmentation resulted in small to moderate reductions in pain scores compared with placebo at 1 to 4 weeks (7 trials, 938 patients; standardized mean difference [SMD]=0.3; 95% confidence interval [CI], 0.1-0.5), 2 to 3 months (7 trials, 953 patients; SMD=0.3; 95% CI, 0.1-0.4), and 1 year (5 trials, 744 patients; SMD=0.3; 95% CI, 0.1-0.4). The study is considered low-quality because of increased heterogeneity.
Calcitonin reduces pain but with some adverse effects
A 2011 meta-analysis of 10 RCTs (467 patients) examined the analgesic effectiveness of calcitonin in adults >60 years, of either sex, with osteoporotic compression fractures who received calcitonin in the acute phase (<10 days after fracture) and chronic phase (>3 months after fracture).2 For acute fractures, pain was measured at 1, 2, 3, and 4 weeks following treatment. For chronic fractures, pain was measured at 1, 3, and 6 months post-treatment.
Continue to: Calcitonin was administered...
Calcitonin was administered in varying doses by various routes (200 IU intranasal, 50-200 IU intramuscular or subcutaneous injection, or 200 IU rectal suppository) and compared with placebo, usual treatment, or other analgesia. The VAS was varied (10 cm, 100 mm, or 5-point) and assessed pain and length of time to mobilization with patients at rest, sitting, standing, and walking by using mean deviation (MD) and SMD.
In the acute phase, calcitonin resulted in greater pain relief 1 week after fracture at rest (4 trials; 260 patients; 10-cm VAS; MD=−3.4; 95% CI, −4 to −2.8) and with walking (4 trials, 228 patients; SMD=2.6; 95% CI, −4.1 to −1.1) compared with the control group. At 6 months, calcitonin had reduced pain in mobile patients more than in the control group (7 trials, 207 patients; SMD=−0.5; 95% CI, −0.9 to −0.1).
Statistically significant adverse effects of calcitonin included gastrointestinal disturbances and flushing compared with placebo. Adverse effects were more predominant in the studies that used injectable calcitonin and in the chronic pain group. The study is considered low-quality because of increased heterogeneity in the acute pain studies.
1. Li L, Ren J, Liu J, et al. Results of vertebral augmentation treatment for patients of painful osteoporotic vertebral compression fractures: a meta-analysis of eight randomized controlled trials. PLoS ONE. 2015;10:e0138126.
2. Knopp-Sihota JA, Newburn-Cook CV, Homik J, et al. Calcitonin for treating acute and chronic pain of recent and remote osteoporotic compression fractures: a systematic review and meta-analysis. Osteoporos Intl. 2012;23:17-38.
EVIDENCE SUMMARY
A 2015 meta-analysis of 8 RCTs compared pain reduction in adults >50 years with osteoporotic compression fractures who received either vertebral augmentation (vertebroplasty or balloon kyphoplasty; 495 patients) or conservative or sham treatment (492 patients).1 Pain was measured by the visual analog scale (VAS) periodically between 1 week and 1 year.
The study included patients of both sexes who had an acute or chronic osteoporotic vertebral compression fracture that caused pain and functional limitations in daily activities. It excluded patients with neoplasm, pre-existing chronic pain or functional disability unrelated to vertebral fractures, and vertebral fractures unaccompanied by signal changes on magnetic resonance imaging.
Vertebral augmentation resulted in small to moderate reductions in pain scores compared with placebo at 1 to 4 weeks (7 trials, 938 patients; standardized mean difference [SMD]=0.3; 95% confidence interval [CI], 0.1-0.5), 2 to 3 months (7 trials, 953 patients; SMD=0.3; 95% CI, 0.1-0.4), and 1 year (5 trials, 744 patients; SMD=0.3; 95% CI, 0.1-0.4). The study is considered low-quality because of increased heterogeneity.
Calcitonin reduces pain but with some adverse effects
A 2011 meta-analysis of 10 RCTs (467 patients) examined the analgesic effectiveness of calcitonin in adults >60 years, of either sex, with osteoporotic compression fractures who received calcitonin in the acute phase (<10 days after fracture) and chronic phase (>3 months after fracture).2 For acute fractures, pain was measured at 1, 2, 3, and 4 weeks following treatment. For chronic fractures, pain was measured at 1, 3, and 6 months post-treatment.
Continue to: Calcitonin was administered...
Calcitonin was administered in varying doses by various routes (200 IU intranasal, 50-200 IU intramuscular or subcutaneous injection, or 200 IU rectal suppository) and compared with placebo, usual treatment, or other analgesia. The VAS was varied (10 cm, 100 mm, or 5-point) and assessed pain and length of time to mobilization with patients at rest, sitting, standing, and walking by using mean deviation (MD) and SMD.
In the acute phase, calcitonin resulted in greater pain relief 1 week after fracture at rest (4 trials; 260 patients; 10-cm VAS; MD=−3.4; 95% CI, −4 to −2.8) and with walking (4 trials, 228 patients; SMD=2.6; 95% CI, −4.1 to −1.1) compared with the control group. At 6 months, calcitonin had reduced pain in mobile patients more than in the control group (7 trials, 207 patients; SMD=−0.5; 95% CI, −0.9 to −0.1).
Statistically significant adverse effects of calcitonin included gastrointestinal disturbances and flushing compared with placebo. Adverse effects were more predominant in the studies that used injectable calcitonin and in the chronic pain group. The study is considered low-quality because of increased heterogeneity in the acute pain studies.
EVIDENCE SUMMARY
A 2015 meta-analysis of 8 RCTs compared pain reduction in adults >50 years with osteoporotic compression fractures who received either vertebral augmentation (vertebroplasty or balloon kyphoplasty; 495 patients) or conservative or sham treatment (492 patients).1 Pain was measured by the visual analog scale (VAS) periodically between 1 week and 1 year.
The study included patients of both sexes who had an acute or chronic osteoporotic vertebral compression fracture that caused pain and functional limitations in daily activities. It excluded patients with neoplasm, pre-existing chronic pain or functional disability unrelated to vertebral fractures, and vertebral fractures unaccompanied by signal changes on magnetic resonance imaging.
Vertebral augmentation resulted in small to moderate reductions in pain scores compared with placebo at 1 to 4 weeks (7 trials, 938 patients; standardized mean difference [SMD]=0.3; 95% confidence interval [CI], 0.1-0.5), 2 to 3 months (7 trials, 953 patients; SMD=0.3; 95% CI, 0.1-0.4), and 1 year (5 trials, 744 patients; SMD=0.3; 95% CI, 0.1-0.4). The study is considered low-quality because of increased heterogeneity.
Calcitonin reduces pain but with some adverse effects
A 2011 meta-analysis of 10 RCTs (467 patients) examined the analgesic effectiveness of calcitonin in adults >60 years, of either sex, with osteoporotic compression fractures who received calcitonin in the acute phase (<10 days after fracture) and chronic phase (>3 months after fracture).2 For acute fractures, pain was measured at 1, 2, 3, and 4 weeks following treatment. For chronic fractures, pain was measured at 1, 3, and 6 months post-treatment.
Continue to: Calcitonin was administered...
Calcitonin was administered in varying doses by various routes (200 IU intranasal, 50-200 IU intramuscular or subcutaneous injection, or 200 IU rectal suppository) and compared with placebo, usual treatment, or other analgesia. The VAS was varied (10 cm, 100 mm, or 5-point) and assessed pain and length of time to mobilization with patients at rest, sitting, standing, and walking by using mean deviation (MD) and SMD.
In the acute phase, calcitonin resulted in greater pain relief 1 week after fracture at rest (4 trials; 260 patients; 10-cm VAS; MD=−3.4; 95% CI, −4 to −2.8) and with walking (4 trials, 228 patients; SMD=2.6; 95% CI, −4.1 to −1.1) compared with the control group. At 6 months, calcitonin had reduced pain in mobile patients more than in the control group (7 trials, 207 patients; SMD=−0.5; 95% CI, −0.9 to −0.1).
Statistically significant adverse effects of calcitonin included gastrointestinal disturbances and flushing compared with placebo. Adverse effects were more predominant in the studies that used injectable calcitonin and in the chronic pain group. The study is considered low-quality because of increased heterogeneity in the acute pain studies.
1. Li L, Ren J, Liu J, et al. Results of vertebral augmentation treatment for patients of painful osteoporotic vertebral compression fractures: a meta-analysis of eight randomized controlled trials. PLoS ONE. 2015;10:e0138126.
2. Knopp-Sihota JA, Newburn-Cook CV, Homik J, et al. Calcitonin for treating acute and chronic pain of recent and remote osteoporotic compression fractures: a systematic review and meta-analysis. Osteoporos Intl. 2012;23:17-38.
1. Li L, Ren J, Liu J, et al. Results of vertebral augmentation treatment for patients of painful osteoporotic vertebral compression fractures: a meta-analysis of eight randomized controlled trials. PLoS ONE. 2015;10:e0138126.
2. Knopp-Sihota JA, Newburn-Cook CV, Homik J, et al. Calcitonin for treating acute and chronic pain of recent and remote osteoporotic compression fractures: a systematic review and meta-analysis. Osteoporos Intl. 2012;23:17-38.
EVIDENCE-BASED ANSWER:
Vertebral augmentation with vertebroplasty or balloon kyphoplasty yields a small reduction in both acute and chronic pain scores in adults with osteoporotic compression fractures compared with conservative therapy or sham treatment (strength of recommendation [SOR]: B, meta-analysis of randomized controlled trials [RCTs]).
When compared with placebo, usual treatment, or other analgesia, calcitonin reduces the severity and duration of pain at rest and with mobility 1 week after an osteoporotic compression fracture and with mobility at 6 months postfracture (SOR: B, meta-analysis of RCTs).
A young girl with a painful rash
A 3-year-old girl presented with a rapidly progressing rash. The rash began the previous day with redness around her lips and nose (FIGURE 1). Twelve hours later, the rash had progressed to involve her neck, trunk, and inguinal area (FIGURE 2). The child’s parents reported that she had no recent illnesses or treatment with antibiotics.
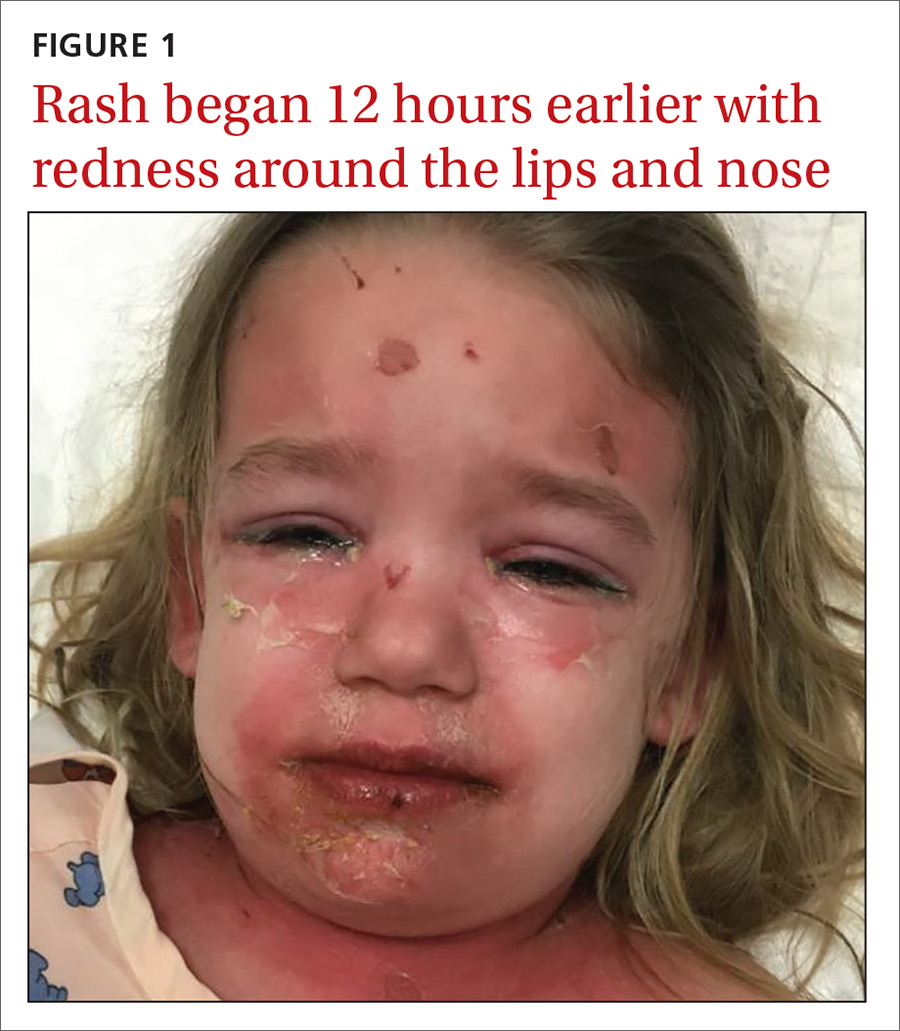
On physical examination, she was febrile (101.8° F) and irritable throughout the encounter. She had perioral and nasolabial erythema and dryness. Her lips were dry with no intraoral mucosal lesions, and her conjunctiva was clear.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Staphylococcal scalded skin syndrome
Based on the patient’s classic presentation and exam findings, the physician suspected staphylococcal scalded skin syndrome. SSSS is a rare but serious condition that progresses quickly with high fevers and diffuse painful erythema. The exact epidemiology of SSSS is unclear; some articles report incidences between 0.09 and 0.13 cases per 1 million people.1 The mortality rate is about 5% due to complications of sepsis, superinfection, and electrolyte disturbances.2
SSSS is caused by Staphylococcus aureus from a localized source that produces exfoliative toxins A and B that spread hematogenously, causing extensive epidermal damage. Exotoxins bind to desmosomes, causing skin cells to lose adherence.3 Histopathology shows intraepidermal cleavage through the stratum granulosum.
Infants and younger children appear more likely to be affected by SSSS, although it may occur in older children or adults who are immunocompromised. It may be that younger children are most susceptible due to a lack of antibodies to the toxin produced or because of a delayed clearance of the toxin-antibody complex from an immature renal system.
What you’ll see. Patients with SSSS may have a prodrome of irritability, malaise, and fever. The rash is first noticeable as erythema in the flexural areas.4 The erythematous tender patches spread and coalesce into a scarlatiniform erythema. Fragile bullae become large sheets of epidermis that slough (a positive Nikolsky’s sign).5 The desquamated areas can exhibit a scalded appearance.3
Differential diagnosis includes TEN and SJS
There is a broad differential for vesiculobullous rashes, ranging from self-limiting conditions to those that are life threatening.
Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), and erythema multiforme major (EMM) are immunological reactions to certain drugs or infections varying in the severity of their presentation. EMM, SJS, and TEN involve the mucosal surfaces, while SSSS does not. The histopathology of these conditions also differs from SSSS as they have keratinocyte necrosis of varying levels of the skin, whereas SSSS only involves the epidermis.
SSSS also may be confused with drug reactions, such as DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. DRESS typically is associated with anticonvulsants and sulfonamides and may have peripheral eosinophilia and a transaminitis.4
Continue to: Other more self-limited vesiculobullous rashes...
Other more self-limited vesiculobullous rashes include human enteroviruses such as coxsackie virus (hand-foot-mouth disease), echovirus, and enterovirus. However, unlike SSSS, which only affects the epidermis, these disorders may produce epidermal necrosis resulting in epidermal-dermal separation and mucocutaneous blistering.4
Making the diagnosis
When a patient has classic SSSS, the diagnosis can be made based on exam findings and the patient’s history. Families will usually report a generalized rash in neonates with desquamation of the entire skin. Fever is often present. Recent exposures to other family members with skin and soft-tissue infections is a possibility. If there is doubt, a skin biopsy can be obtained for histology. Lab work may reveal an elevated white blood cell count; blood culture is often negative.
The primary site of S aureus infection is usually the nasopharynx, causing a mild upper respiratory tract infection; therefore, nasopharyngeal cultures may be positive.4 Cultures can also be drawn from blood, wounds, nares, and ocular exudates if there is suspicion. Cultures from the actual blisters are typically negative, as the toxin—not the actual bacteria—is responsible for the blistering. Unlike adults who experience SSSS, children typically have negative blood cultures.4
Prompt treatment is essential
Swift diagnosis and management of SSSS is important due to the risk of severe disease. It is important to start antibiotics early because methicillin-sensitive S aureus is a predominant cause of SSSS.2 The epidemiology of methicillin-sensitive and methicillin-resistant S aureus (MRSA) continues to shift. A recent study suggests that empiric therapy with penicillinase-resistant penicillins, along with clindamycin, be employed until culture sensitivities are available to guide therapy.2 Local resistance patterns to S aureus should help guide initial empiric antibiotic treatment. Patients should receive intravenous (IV) fluids to compensate for insensible fluid losses similar to an extensive burn wound. Wound dressings placed over sloughed skin can help prevent secondary infection.2 Lastly, the use of anti-inflammatory drugs and opiates often depends upon the extent of pain the patient experiences.
Our patient was immediately started on IV clindamycin 10 mg/kg tid and IV fluids. She was given morphine 0.01 mg/kg for pain control. As expected, cultures of her nasopharynx, blood, and vulva did not grow S aureus. Although no organism was isolated, her rash rapidly improved, and she was discharged home to complete a 10-day oral course of clindamycin 10 mg/kg tid.
CORRESPONDENCE
Nicholas M. Potisek, MD, Wake Forest School of Medicine, Department of Pediatrics, Medical Center Blvd, Winston-Salem, NC 27157; [email protected]
1. Mockenhaupt M, Idzko M, Grosber M, et al. Epidemiology of staphylococcal scalded skin syndrome in Germany. J Invest Dermatol. 2005;124:700-703.
2. Braunstein I, Wanat K, Abuabara K, et al. Antibiotic sensitivity and resistance patterns in pediatric staphylococcal scalded skin syndrome. Pediatr Dermatol. 2014;31:305-308.
3. Mishra AK, Yadav, P, Mishra A. A systemic review on Staphylococcal Scalded Skin Syndrome (SSSS): A rare and critical disease of neonates. Open Microbiol J. 2016;10: 150-159.
4. Handler MZ, Schwarz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014;28:1418-1423.
5. Franco L, Pereira P. Staphylococcal scalded skin syndrome. Indian Pediatr. 2016. 53:939.
A 3-year-old girl presented with a rapidly progressing rash. The rash began the previous day with redness around her lips and nose (FIGURE 1). Twelve hours later, the rash had progressed to involve her neck, trunk, and inguinal area (FIGURE 2). The child’s parents reported that she had no recent illnesses or treatment with antibiotics.
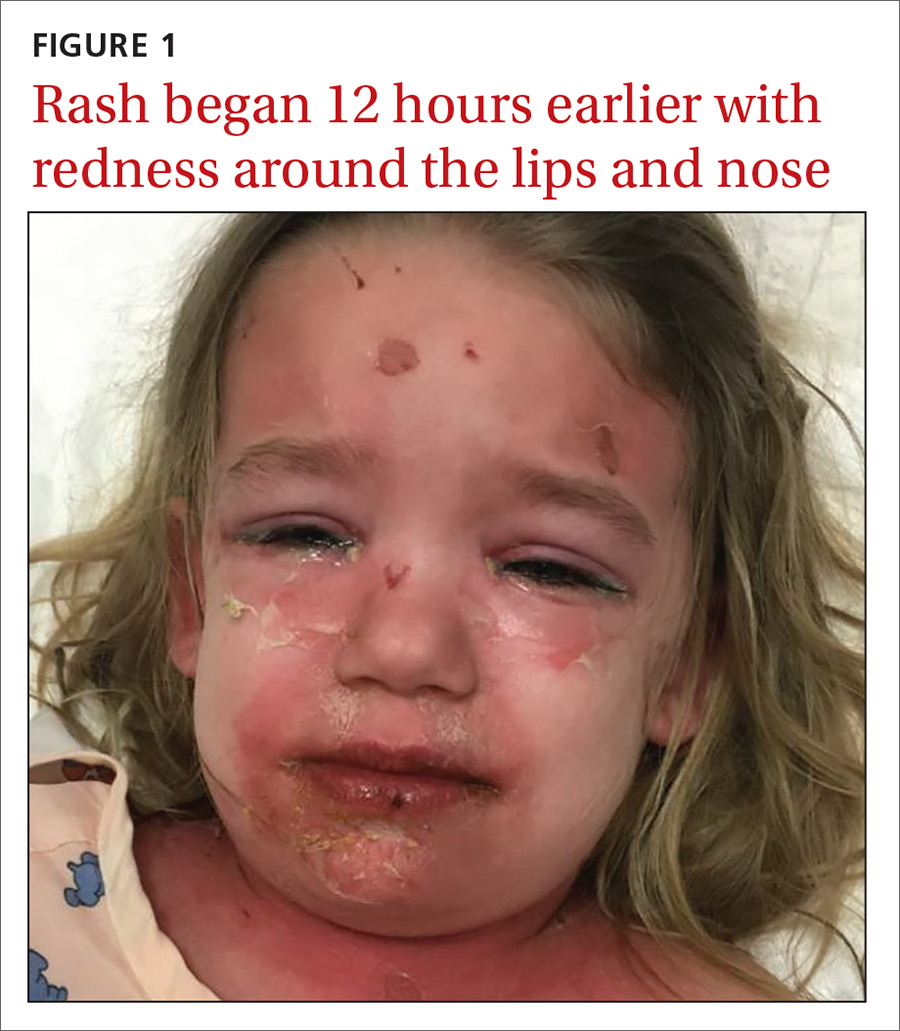
On physical examination, she was febrile (101.8° F) and irritable throughout the encounter. She had perioral and nasolabial erythema and dryness. Her lips were dry with no intraoral mucosal lesions, and her conjunctiva was clear.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Staphylococcal scalded skin syndrome
Based on the patient’s classic presentation and exam findings, the physician suspected staphylococcal scalded skin syndrome. SSSS is a rare but serious condition that progresses quickly with high fevers and diffuse painful erythema. The exact epidemiology of SSSS is unclear; some articles report incidences between 0.09 and 0.13 cases per 1 million people.1 The mortality rate is about 5% due to complications of sepsis, superinfection, and electrolyte disturbances.2
SSSS is caused by Staphylococcus aureus from a localized source that produces exfoliative toxins A and B that spread hematogenously, causing extensive epidermal damage. Exotoxins bind to desmosomes, causing skin cells to lose adherence.3 Histopathology shows intraepidermal cleavage through the stratum granulosum.
Infants and younger children appear more likely to be affected by SSSS, although it may occur in older children or adults who are immunocompromised. It may be that younger children are most susceptible due to a lack of antibodies to the toxin produced or because of a delayed clearance of the toxin-antibody complex from an immature renal system.
What you’ll see. Patients with SSSS may have a prodrome of irritability, malaise, and fever. The rash is first noticeable as erythema in the flexural areas.4 The erythematous tender patches spread and coalesce into a scarlatiniform erythema. Fragile bullae become large sheets of epidermis that slough (a positive Nikolsky’s sign).5 The desquamated areas can exhibit a scalded appearance.3
Differential diagnosis includes TEN and SJS
There is a broad differential for vesiculobullous rashes, ranging from self-limiting conditions to those that are life threatening.
Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), and erythema multiforme major (EMM) are immunological reactions to certain drugs or infections varying in the severity of their presentation. EMM, SJS, and TEN involve the mucosal surfaces, while SSSS does not. The histopathology of these conditions also differs from SSSS as they have keratinocyte necrosis of varying levels of the skin, whereas SSSS only involves the epidermis.
SSSS also may be confused with drug reactions, such as DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. DRESS typically is associated with anticonvulsants and sulfonamides and may have peripheral eosinophilia and a transaminitis.4
Continue to: Other more self-limited vesiculobullous rashes...
Other more self-limited vesiculobullous rashes include human enteroviruses such as coxsackie virus (hand-foot-mouth disease), echovirus, and enterovirus. However, unlike SSSS, which only affects the epidermis, these disorders may produce epidermal necrosis resulting in epidermal-dermal separation and mucocutaneous blistering.4
Making the diagnosis
When a patient has classic SSSS, the diagnosis can be made based on exam findings and the patient’s history. Families will usually report a generalized rash in neonates with desquamation of the entire skin. Fever is often present. Recent exposures to other family members with skin and soft-tissue infections is a possibility. If there is doubt, a skin biopsy can be obtained for histology. Lab work may reveal an elevated white blood cell count; blood culture is often negative.
The primary site of S aureus infection is usually the nasopharynx, causing a mild upper respiratory tract infection; therefore, nasopharyngeal cultures may be positive.4 Cultures can also be drawn from blood, wounds, nares, and ocular exudates if there is suspicion. Cultures from the actual blisters are typically negative, as the toxin—not the actual bacteria—is responsible for the blistering. Unlike adults who experience SSSS, children typically have negative blood cultures.4
Prompt treatment is essential
Swift diagnosis and management of SSSS is important due to the risk of severe disease. It is important to start antibiotics early because methicillin-sensitive S aureus is a predominant cause of SSSS.2 The epidemiology of methicillin-sensitive and methicillin-resistant S aureus (MRSA) continues to shift. A recent study suggests that empiric therapy with penicillinase-resistant penicillins, along with clindamycin, be employed until culture sensitivities are available to guide therapy.2 Local resistance patterns to S aureus should help guide initial empiric antibiotic treatment. Patients should receive intravenous (IV) fluids to compensate for insensible fluid losses similar to an extensive burn wound. Wound dressings placed over sloughed skin can help prevent secondary infection.2 Lastly, the use of anti-inflammatory drugs and opiates often depends upon the extent of pain the patient experiences.
Our patient was immediately started on IV clindamycin 10 mg/kg tid and IV fluids. She was given morphine 0.01 mg/kg for pain control. As expected, cultures of her nasopharynx, blood, and vulva did not grow S aureus. Although no organism was isolated, her rash rapidly improved, and she was discharged home to complete a 10-day oral course of clindamycin 10 mg/kg tid.
CORRESPONDENCE
Nicholas M. Potisek, MD, Wake Forest School of Medicine, Department of Pediatrics, Medical Center Blvd, Winston-Salem, NC 27157; [email protected]
A 3-year-old girl presented with a rapidly progressing rash. The rash began the previous day with redness around her lips and nose (FIGURE 1). Twelve hours later, the rash had progressed to involve her neck, trunk, and inguinal area (FIGURE 2). The child’s parents reported that she had no recent illnesses or treatment with antibiotics.
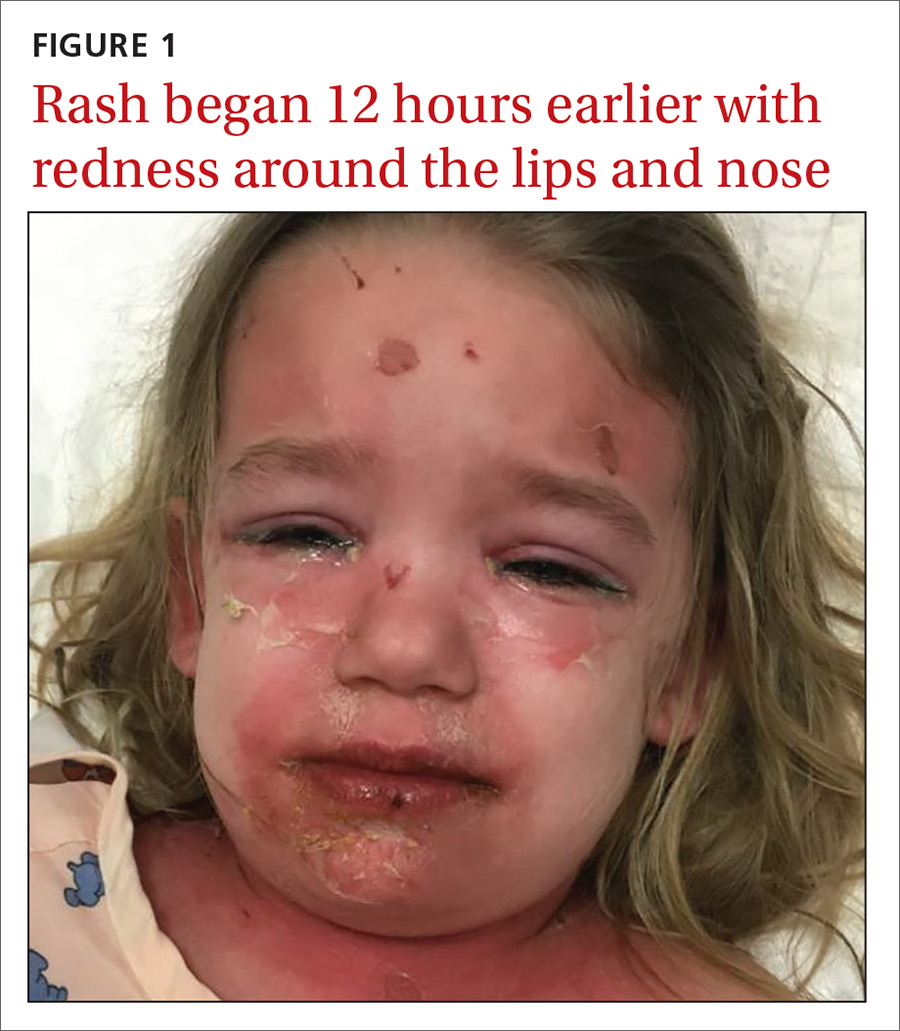
On physical examination, she was febrile (101.8° F) and irritable throughout the encounter. She had perioral and nasolabial erythema and dryness. Her lips were dry with no intraoral mucosal lesions, and her conjunctiva was clear.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Staphylococcal scalded skin syndrome
Based on the patient’s classic presentation and exam findings, the physician suspected staphylococcal scalded skin syndrome. SSSS is a rare but serious condition that progresses quickly with high fevers and diffuse painful erythema. The exact epidemiology of SSSS is unclear; some articles report incidences between 0.09 and 0.13 cases per 1 million people.1 The mortality rate is about 5% due to complications of sepsis, superinfection, and electrolyte disturbances.2
SSSS is caused by Staphylococcus aureus from a localized source that produces exfoliative toxins A and B that spread hematogenously, causing extensive epidermal damage. Exotoxins bind to desmosomes, causing skin cells to lose adherence.3 Histopathology shows intraepidermal cleavage through the stratum granulosum.
Infants and younger children appear more likely to be affected by SSSS, although it may occur in older children or adults who are immunocompromised. It may be that younger children are most susceptible due to a lack of antibodies to the toxin produced or because of a delayed clearance of the toxin-antibody complex from an immature renal system.
What you’ll see. Patients with SSSS may have a prodrome of irritability, malaise, and fever. The rash is first noticeable as erythema in the flexural areas.4 The erythematous tender patches spread and coalesce into a scarlatiniform erythema. Fragile bullae become large sheets of epidermis that slough (a positive Nikolsky’s sign).5 The desquamated areas can exhibit a scalded appearance.3
Differential diagnosis includes TEN and SJS
There is a broad differential for vesiculobullous rashes, ranging from self-limiting conditions to those that are life threatening.
Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), and erythema multiforme major (EMM) are immunological reactions to certain drugs or infections varying in the severity of their presentation. EMM, SJS, and TEN involve the mucosal surfaces, while SSSS does not. The histopathology of these conditions also differs from SSSS as they have keratinocyte necrosis of varying levels of the skin, whereas SSSS only involves the epidermis.
SSSS also may be confused with drug reactions, such as DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. DRESS typically is associated with anticonvulsants and sulfonamides and may have peripheral eosinophilia and a transaminitis.4
Continue to: Other more self-limited vesiculobullous rashes...
Other more self-limited vesiculobullous rashes include human enteroviruses such as coxsackie virus (hand-foot-mouth disease), echovirus, and enterovirus. However, unlike SSSS, which only affects the epidermis, these disorders may produce epidermal necrosis resulting in epidermal-dermal separation and mucocutaneous blistering.4
Making the diagnosis
When a patient has classic SSSS, the diagnosis can be made based on exam findings and the patient’s history. Families will usually report a generalized rash in neonates with desquamation of the entire skin. Fever is often present. Recent exposures to other family members with skin and soft-tissue infections is a possibility. If there is doubt, a skin biopsy can be obtained for histology. Lab work may reveal an elevated white blood cell count; blood culture is often negative.
The primary site of S aureus infection is usually the nasopharynx, causing a mild upper respiratory tract infection; therefore, nasopharyngeal cultures may be positive.4 Cultures can also be drawn from blood, wounds, nares, and ocular exudates if there is suspicion. Cultures from the actual blisters are typically negative, as the toxin—not the actual bacteria—is responsible for the blistering. Unlike adults who experience SSSS, children typically have negative blood cultures.4
Prompt treatment is essential
Swift diagnosis and management of SSSS is important due to the risk of severe disease. It is important to start antibiotics early because methicillin-sensitive S aureus is a predominant cause of SSSS.2 The epidemiology of methicillin-sensitive and methicillin-resistant S aureus (MRSA) continues to shift. A recent study suggests that empiric therapy with penicillinase-resistant penicillins, along with clindamycin, be employed until culture sensitivities are available to guide therapy.2 Local resistance patterns to S aureus should help guide initial empiric antibiotic treatment. Patients should receive intravenous (IV) fluids to compensate for insensible fluid losses similar to an extensive burn wound. Wound dressings placed over sloughed skin can help prevent secondary infection.2 Lastly, the use of anti-inflammatory drugs and opiates often depends upon the extent of pain the patient experiences.
Our patient was immediately started on IV clindamycin 10 mg/kg tid and IV fluids. She was given morphine 0.01 mg/kg for pain control. As expected, cultures of her nasopharynx, blood, and vulva did not grow S aureus. Although no organism was isolated, her rash rapidly improved, and she was discharged home to complete a 10-day oral course of clindamycin 10 mg/kg tid.
CORRESPONDENCE
Nicholas M. Potisek, MD, Wake Forest School of Medicine, Department of Pediatrics, Medical Center Blvd, Winston-Salem, NC 27157; [email protected]
1. Mockenhaupt M, Idzko M, Grosber M, et al. Epidemiology of staphylococcal scalded skin syndrome in Germany. J Invest Dermatol. 2005;124:700-703.
2. Braunstein I, Wanat K, Abuabara K, et al. Antibiotic sensitivity and resistance patterns in pediatric staphylococcal scalded skin syndrome. Pediatr Dermatol. 2014;31:305-308.
3. Mishra AK, Yadav, P, Mishra A. A systemic review on Staphylococcal Scalded Skin Syndrome (SSSS): A rare and critical disease of neonates. Open Microbiol J. 2016;10: 150-159.
4. Handler MZ, Schwarz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014;28:1418-1423.
5. Franco L, Pereira P. Staphylococcal scalded skin syndrome. Indian Pediatr. 2016. 53:939.
1. Mockenhaupt M, Idzko M, Grosber M, et al. Epidemiology of staphylococcal scalded skin syndrome in Germany. J Invest Dermatol. 2005;124:700-703.
2. Braunstein I, Wanat K, Abuabara K, et al. Antibiotic sensitivity and resistance patterns in pediatric staphylococcal scalded skin syndrome. Pediatr Dermatol. 2014;31:305-308.
3. Mishra AK, Yadav, P, Mishra A. A systemic review on Staphylococcal Scalded Skin Syndrome (SSSS): A rare and critical disease of neonates. Open Microbiol J. 2016;10: 150-159.
4. Handler MZ, Schwarz RA. Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol. 2014;28:1418-1423.
5. Franco L, Pereira P. Staphylococcal scalded skin syndrome. Indian Pediatr. 2016. 53:939.
History of melanoma in situ • dyspnea • rib pain • Dx?
THE CASE
A 56-year-old woman with a history of melanoma in situ presented with progressive dyspnea on exertion, cough productive of clear sputum, and right-sided rib pain radiating to the upper back of 5 weeks’ duration.
Twenty-four years earlier, the patient had undergone excision of a skin lesion from the right side of her back. Pathology revealed melanoma in situ with no evidence of invasion of the underlying dermis. Because of close margins, she underwent wider excision 2 weeks later and no residual tumor was found. The patient subsequently underwent routine biannual dermatologic follow-up and transitioned (within the past few years) to annual dermatologic follow-up. At a recent dermatologic visit (9 months earlier), there were no suspicious skin lesions.
At current presentation, she denied fever, chills, night sweats, or unintentional weight loss. On examination, her vital signs were normal. Her pulse oximetry on room air was 95% at rest and 94% with ambulation. She had decreased breath sounds at the right lung base and a fixed 2 × 2-cm nontender, indurated mass in the right upper anterior chest wall, superior to the right breast. A skin examination was not performed at this time.

A complete blood count revealed a white blood cell count of 8220/mcL (reference range, 4500–11,000/mcL), hemoglobin of 13.6 g/dL (reference range, 14–17.5 g/dL), and a platelet count of 162 × 103/mcL (reference range, 150–350 × 103/mcL). The patient’s electrolytes were within normal limits, with a creatinine level of 0.67 mg/dL (reference range, 0.1–1.2 mg/dL) and a calcium level of 9.4 mg/dL (reference range, 8.2–10.2 mg/dL). Lactate dehydrogenase was elevated at 308 U/L (reference range, 100–200 U/L).
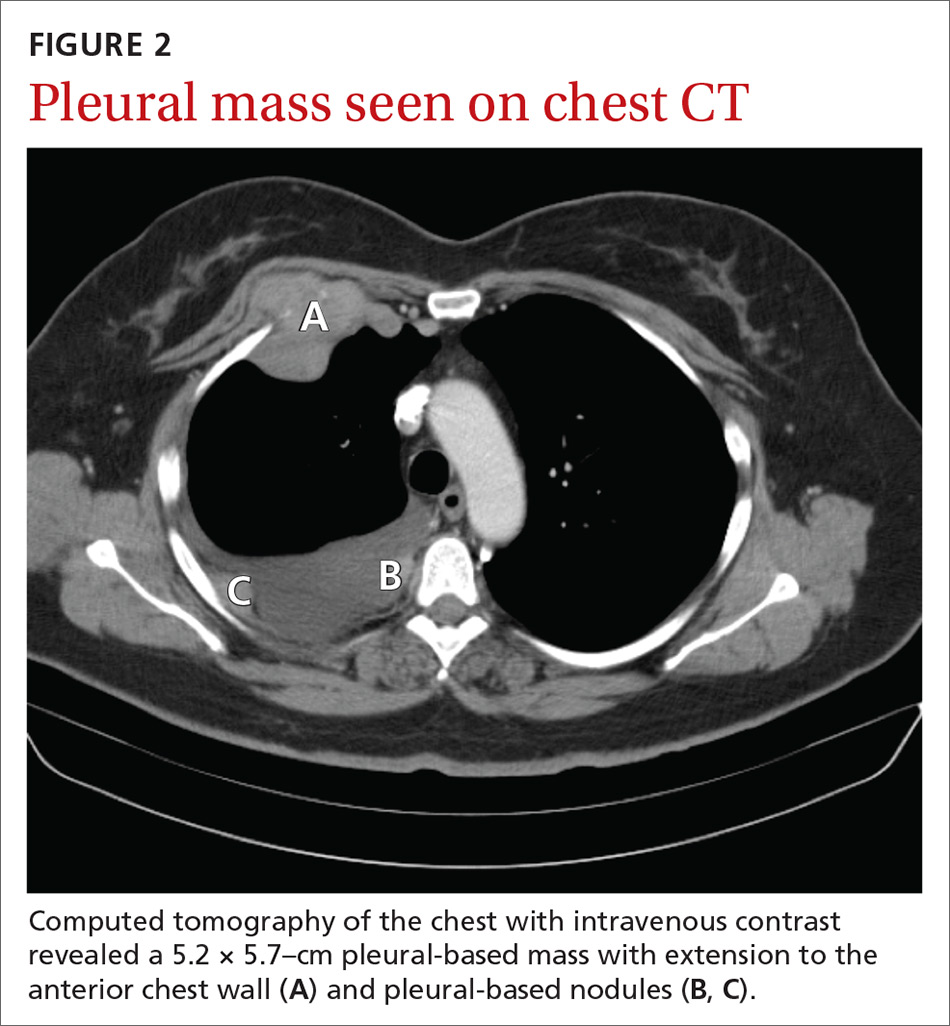
A chest radiograph revealed a right upper lobe mass, right lower lobe consolidation, and a large right-sided pleural effusion (FIGURE 1). Chest computed tomography (CT) with intravenous contrast revealed a 5.2 × 5.7–cm right pleural-based mass with extension to the anterior chest wall, 3 left-sided pulmonary nodules, numerous right-sided pleural-based nodules (FIGURE 2), and multiple low-density liver lesions. An abdominal and pelvic CT scan revealed a 5.6 × 2.5 × 4.8–cm hepatic lesion (FIGURE 3) with scattered hepatic cysts.
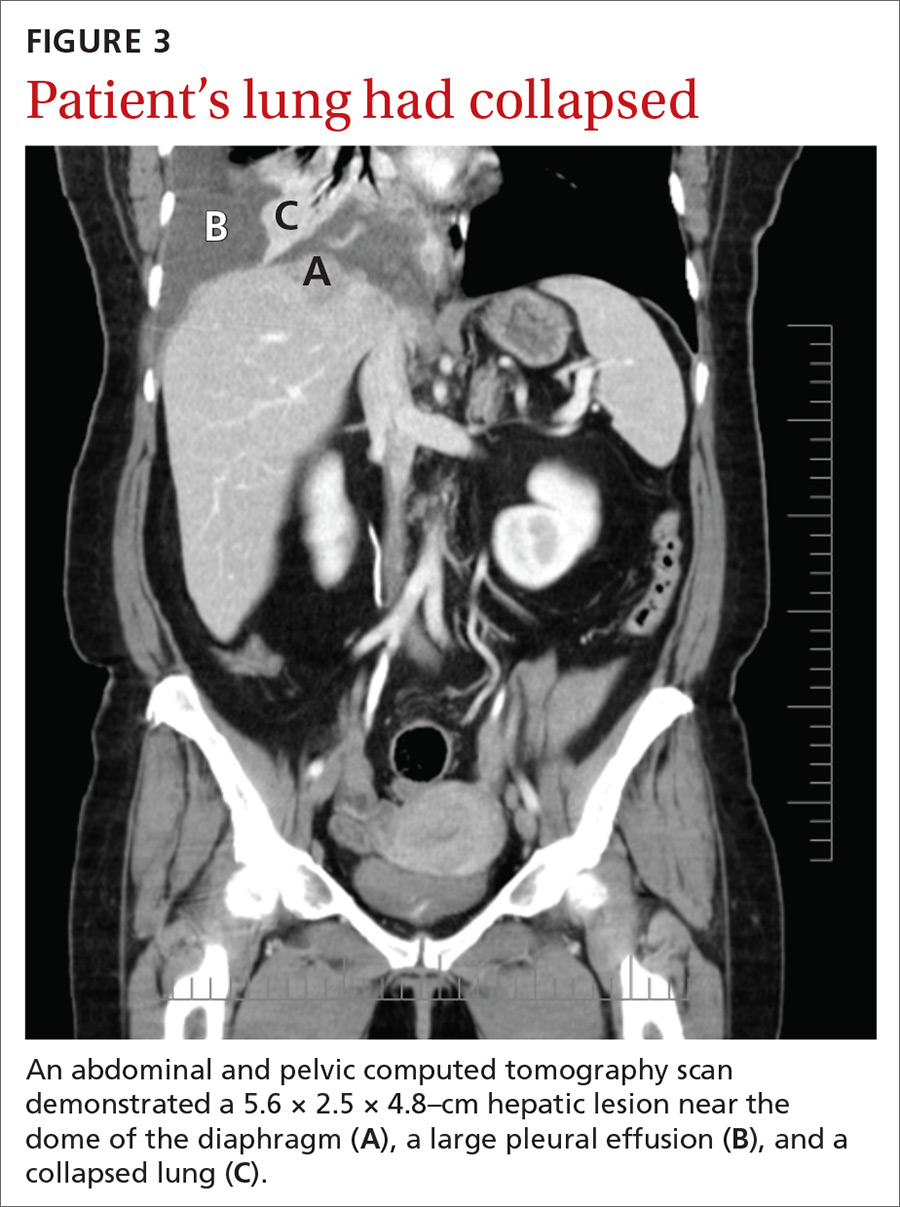
THE DIAGNOSIS
A diagnostic thoracentesis was performed, and pleural fluid cytology results revealed metastatic melanoma. Magnetic resonance imaging (MRI) of the brain showed no evidence of metastases.
After the patient’s initial presentation, her dermatologist performed a biopsy on a pre-existing skin lesion on the patient’s left abdomen, which initially was thought to be a cherry angioma. This left abdominal skin lesion was in a location different from her previous melanoma in situ, which was located on the right side of the back. Biopsy results of the presumed cherry angioma revealed a nodular malignant melanoma (which was partially removed), adjacent to a cherry angioma (which was completely excised).
Continue to: Two primary melanomas
Two primary melanomas. Our patient had 2 different primary melanomas: a melanoma in situ on the right back diagnosed 24 years prior to the current presentation and the more recently identified melanoma on the left abdomen with metastases to the lung and liver.
We referred the patient to Oncology and she was enrolled in a clinical study with ipilimumab and nivolumab, monoclonal antibodies directed against negative regulators of T-cell activation.
DISCUSSION
In the United States, melanoma is the fifth leading cancer in men and the sixth leading cancer in women.1 A prior history of melanoma or melanoma in situ increases the risk for a second melanoma,2-4 and the risk remains elevated for more than 20 years after the initial diagnosis.2 One- and 2-year survival rates for metastatic melanoma are 32% to 65% and 18% to 40%, respectively5; the 5-year survival rate of metastatic melanoma to the lung is approximately 16%.6
Recommendations regarding the appropriate follow-up of patients with a history of melanoma in situ and melanoma vary widely.7 For patients with a history of melanoma in situ, the American Academy of Dermatology and the National Comprehensive Cancer Network recommend annual skin examination indefinitely and self-examination of the skin and lymph nodes monthly.4,7,8
Novel therapies are powerful allies in fight against melanoma
Previous standard treatment of metastatic melanoma included surgery, radiation, and cytotoxic chemotherapy. Resection rarely is curative in distant metastatic melanoma, and cytotoxic chemotherapy has low response rates, has a response duration of 4 to 6 months, and does not improve overall survival in advanced melanoma.9-12
Continue to: Novel therapies...
Novel therapies, such as immunotherapy and molecular-targeted therapies, are dramatically increasing survival rates in metastatic melanoma. Melanoma frequently is associated with somatic mutations, and each patient may have a unique collection of mutations resulting in the expression of antigens that bind to certain T-cell receptors, which serve as targets for inhibitor immunotherapy.
Ipilimumab and nivolumab are monoclonal antibodies directed against negative regulators of T-cell activation. When ipilimumab and nivolumab bind to their receptors, feedback inhibition is prevented, which results in an immune response against the tumor. In a trial of 53 patients with advanced melanoma treated with both drugs, the overall survival rate at 1 and 2 years was 94% and 88%, respectively.13
Dabrafenib and trametinib. Mutations that activate the serine/threonine kinase gene, BRAF, are present in approximately 40% to 60% of advanced melanomas and lead to clonal expansion and tumor progression.14,15 Inhibition of BRAF produces rapid tumor regression—even in extensive disease. Treatment with dabrafenib, a BRAF inhibitor, and trametinib, a mitogen-activated protein kinase inhibitor, has been shown to be superior to a BRAF inhibitor alone and is associated with a survival rate of 72% at 1 year.16
Our patient. Seven months after enrolling in the clinical trial with ipilimumab and nivolumab, our patient developed brain metastases and was withdrawn from the trial. A resection of her brain metastases and radiation therapy followed. The patient was then started on molecular-targeted therapy with dabrafenib and trametinib. Twelve weeks later, a repeat CT scan of the chest, abdomen, and pelvis demonstrated an interval decrease in the size of the majority of the metastatic lesions, and a repeat brain MRI showed no additional metastases.
More than 4 years after her diagnosis, our patient remains on dabrafenib and trametinib therapy and her metastatic lesions to the lung and liver remain stable.
Continue to: THE TAKEAWAY
THE TAKEAWAY
Patients with a prior melanoma in situ or invasive melanoma have a higher risk for a subsequent invasive melanoma, and this risk remains elevated for more than 20 years. While patients with a history of melanoma in situ do not require specific oncologic follow-up, they do require annual dermatologic follow-up indefinitely and should perform monthly self-examination of their skin and lymph nodes.
Heightened awareness of the risk for a second primary melanoma should prompt primary care physicians to conduct ongoing patient surveillance. Family physicians should also keep in mind that novel therapies for metastatic melanoma, such as molecular-targeted therapies and immunotherapy, are associated with a much higher survival rate than previous standard therapy.
CORRESPONDENCE
Iris Tong, MD, Associate Professor, Division of General Internal Medicine, Department of Medicine, Alpert Medical School of Brown University, 146 W River St, Providence, RI 02904; [email protected]
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018 [published online January 4, 2018]. Cancer J Clin. 2018;68:7-30.
2. Bradford PT, Freedman DM, Goldstein AM, et al. Increased risk of second primary cancers after diagnosis of melanoma. Arch Dermatol. 2010;146:265-272.
3. Balamurugan A, Rees JR, Kosary C, et al. Subsequent primary cancers among men and women with in situ and invasive melanoma of the skin. J Am Acad Dermatol. 2011;65(5) (suppl 1):S69-S77.
4. Pomerantz H, Huang D, Weinstock MA. Risk of subsequent melanoma after melanoma in situ and invasive melanoma: a population-based study from 1973 to 2011. J Am Acad Dermatol. 2015;72:794-800.
5. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199-6206.
6. American Cancer Society. Cancer facts & figures 2015. www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/index. Accessed November 26, 2018.
7. Coit DG, Andtbacka R, Anker CJ, et al. Melanoma: clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;3:366-400.
8. Bichakjian CK, Halpern AC, Johnson TM. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 2011;5:1032-1047.
9. Atkins MB. The role of cytotoxic chemotherapeutic agents either alone or in combination with biological response modifiers. In: Kirkwood JK, ed. Molecular Diagnosis, Prevention & Therapy of Melanoma. New York, NY: Marcel Dekker; 1997:219.
10. Patel PM, Suciu S, Mortier L, et al; EORTC Melanoma Group. Extended schedule, escalated dose temozolomide versus dacarbazine in stage IV melanoma: final results of a randomised phase III study (EORTC 18032) [published online May 18, 2011]. Eur J Cancer. 2011;47:1476-1483.
11. Flaherty KT, Lee SJ, Zhao F, et al. Phase III trial of carboplatin and paclitaxel with or without sorafenib in metastatic melanoma [published online December 17, 2012]. J Clin Oncol. 2013;31:373-379.
12. Sosman JA, Moon J, Tuthill RJ, et al. A phase 2 trial of complete resection for stage IV melanoma: results of Southwest Oncology Group Clinical Trial S9430 [published online March 31, 2011]. Cancer. 2011;117:4740-4746.
13. Sznol M, Kluger HM, Callahan MK, et al. Abstract LBA9003. Presented at: 2014 American Society of Clinical Oncology (ASCO) Annual Meeting; May 30–June 3, 2014; Chicago, IL.
14. Omholt K, Platz A, Kanter L, et al. NRAS and BRAF mutations arise early during melanoma pathogenesis and are preserved throughout tumor progression. Clin Cancer Res. 2003;9:6483-6488.
15. Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29:1239-1246.
16. Robert C, Karaszewska B, Schachter J, et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med. 2015;372:30-39.
THE CASE
A 56-year-old woman with a history of melanoma in situ presented with progressive dyspnea on exertion, cough productive of clear sputum, and right-sided rib pain radiating to the upper back of 5 weeks’ duration.
Twenty-four years earlier, the patient had undergone excision of a skin lesion from the right side of her back. Pathology revealed melanoma in situ with no evidence of invasion of the underlying dermis. Because of close margins, she underwent wider excision 2 weeks later and no residual tumor was found. The patient subsequently underwent routine biannual dermatologic follow-up and transitioned (within the past few years) to annual dermatologic follow-up. At a recent dermatologic visit (9 months earlier), there were no suspicious skin lesions.
At current presentation, she denied fever, chills, night sweats, or unintentional weight loss. On examination, her vital signs were normal. Her pulse oximetry on room air was 95% at rest and 94% with ambulation. She had decreased breath sounds at the right lung base and a fixed 2 × 2-cm nontender, indurated mass in the right upper anterior chest wall, superior to the right breast. A skin examination was not performed at this time.

A complete blood count revealed a white blood cell count of 8220/mcL (reference range, 4500–11,000/mcL), hemoglobin of 13.6 g/dL (reference range, 14–17.5 g/dL), and a platelet count of 162 × 103/mcL (reference range, 150–350 × 103/mcL). The patient’s electrolytes were within normal limits, with a creatinine level of 0.67 mg/dL (reference range, 0.1–1.2 mg/dL) and a calcium level of 9.4 mg/dL (reference range, 8.2–10.2 mg/dL). Lactate dehydrogenase was elevated at 308 U/L (reference range, 100–200 U/L).
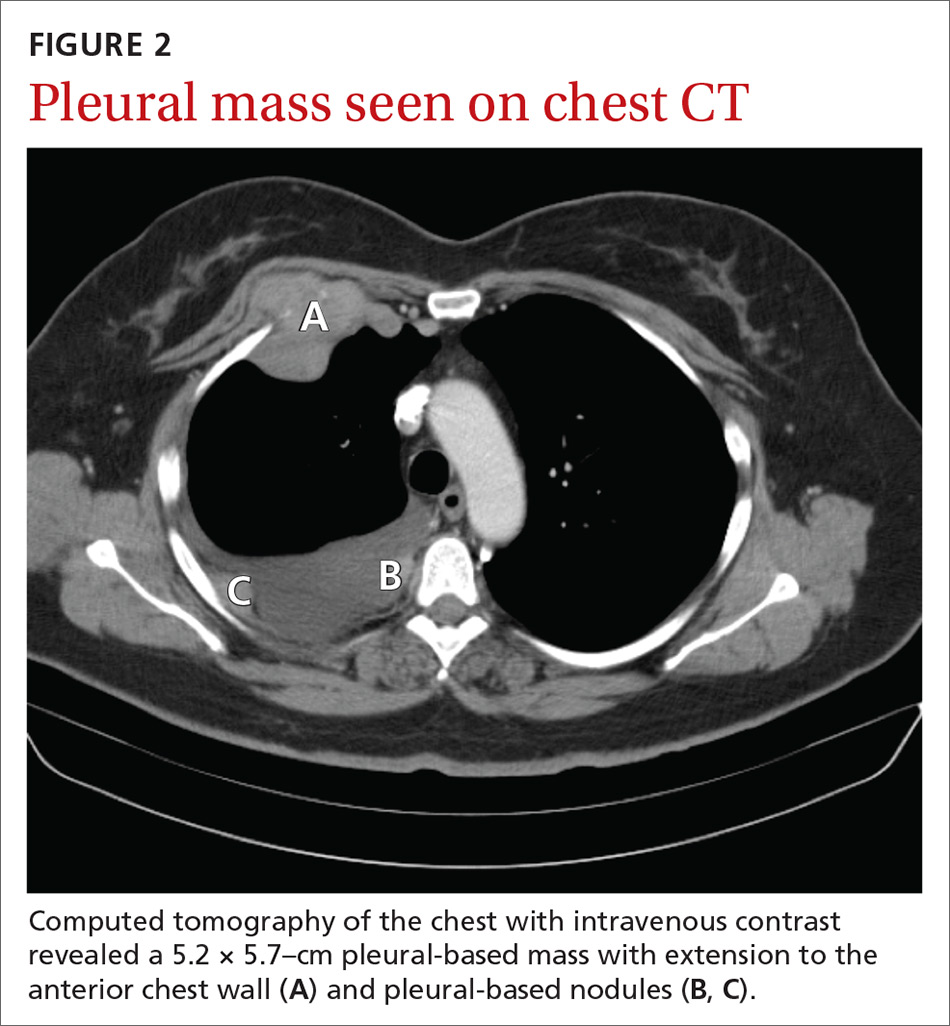
A chest radiograph revealed a right upper lobe mass, right lower lobe consolidation, and a large right-sided pleural effusion (FIGURE 1). Chest computed tomography (CT) with intravenous contrast revealed a 5.2 × 5.7–cm right pleural-based mass with extension to the anterior chest wall, 3 left-sided pulmonary nodules, numerous right-sided pleural-based nodules (FIGURE 2), and multiple low-density liver lesions. An abdominal and pelvic CT scan revealed a 5.6 × 2.5 × 4.8–cm hepatic lesion (FIGURE 3) with scattered hepatic cysts.
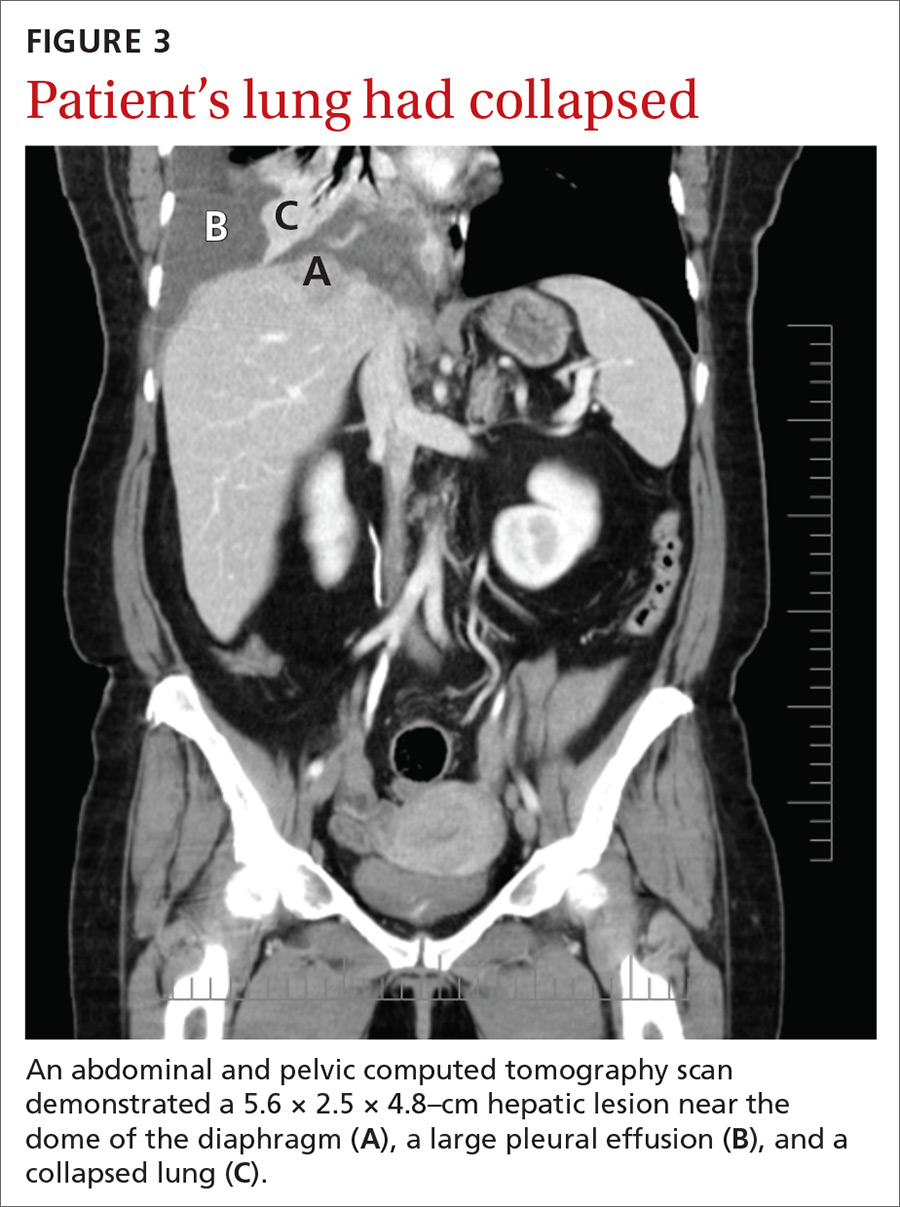
THE DIAGNOSIS
A diagnostic thoracentesis was performed, and pleural fluid cytology results revealed metastatic melanoma. Magnetic resonance imaging (MRI) of the brain showed no evidence of metastases.
After the patient’s initial presentation, her dermatologist performed a biopsy on a pre-existing skin lesion on the patient’s left abdomen, which initially was thought to be a cherry angioma. This left abdominal skin lesion was in a location different from her previous melanoma in situ, which was located on the right side of the back. Biopsy results of the presumed cherry angioma revealed a nodular malignant melanoma (which was partially removed), adjacent to a cherry angioma (which was completely excised).
Continue to: Two primary melanomas
Two primary melanomas. Our patient had 2 different primary melanomas: a melanoma in situ on the right back diagnosed 24 years prior to the current presentation and the more recently identified melanoma on the left abdomen with metastases to the lung and liver.
We referred the patient to Oncology and she was enrolled in a clinical study with ipilimumab and nivolumab, monoclonal antibodies directed against negative regulators of T-cell activation.
DISCUSSION
In the United States, melanoma is the fifth leading cancer in men and the sixth leading cancer in women.1 A prior history of melanoma or melanoma in situ increases the risk for a second melanoma,2-4 and the risk remains elevated for more than 20 years after the initial diagnosis.2 One- and 2-year survival rates for metastatic melanoma are 32% to 65% and 18% to 40%, respectively5; the 5-year survival rate of metastatic melanoma to the lung is approximately 16%.6
Recommendations regarding the appropriate follow-up of patients with a history of melanoma in situ and melanoma vary widely.7 For patients with a history of melanoma in situ, the American Academy of Dermatology and the National Comprehensive Cancer Network recommend annual skin examination indefinitely and self-examination of the skin and lymph nodes monthly.4,7,8
Novel therapies are powerful allies in fight against melanoma
Previous standard treatment of metastatic melanoma included surgery, radiation, and cytotoxic chemotherapy. Resection rarely is curative in distant metastatic melanoma, and cytotoxic chemotherapy has low response rates, has a response duration of 4 to 6 months, and does not improve overall survival in advanced melanoma.9-12
Continue to: Novel therapies...
Novel therapies, such as immunotherapy and molecular-targeted therapies, are dramatically increasing survival rates in metastatic melanoma. Melanoma frequently is associated with somatic mutations, and each patient may have a unique collection of mutations resulting in the expression of antigens that bind to certain T-cell receptors, which serve as targets for inhibitor immunotherapy.
Ipilimumab and nivolumab are monoclonal antibodies directed against negative regulators of T-cell activation. When ipilimumab and nivolumab bind to their receptors, feedback inhibition is prevented, which results in an immune response against the tumor. In a trial of 53 patients with advanced melanoma treated with both drugs, the overall survival rate at 1 and 2 years was 94% and 88%, respectively.13
Dabrafenib and trametinib. Mutations that activate the serine/threonine kinase gene, BRAF, are present in approximately 40% to 60% of advanced melanomas and lead to clonal expansion and tumor progression.14,15 Inhibition of BRAF produces rapid tumor regression—even in extensive disease. Treatment with dabrafenib, a BRAF inhibitor, and trametinib, a mitogen-activated protein kinase inhibitor, has been shown to be superior to a BRAF inhibitor alone and is associated with a survival rate of 72% at 1 year.16
Our patient. Seven months after enrolling in the clinical trial with ipilimumab and nivolumab, our patient developed brain metastases and was withdrawn from the trial. A resection of her brain metastases and radiation therapy followed. The patient was then started on molecular-targeted therapy with dabrafenib and trametinib. Twelve weeks later, a repeat CT scan of the chest, abdomen, and pelvis demonstrated an interval decrease in the size of the majority of the metastatic lesions, and a repeat brain MRI showed no additional metastases.
More than 4 years after her diagnosis, our patient remains on dabrafenib and trametinib therapy and her metastatic lesions to the lung and liver remain stable.
Continue to: THE TAKEAWAY
THE TAKEAWAY
Patients with a prior melanoma in situ or invasive melanoma have a higher risk for a subsequent invasive melanoma, and this risk remains elevated for more than 20 years. While patients with a history of melanoma in situ do not require specific oncologic follow-up, they do require annual dermatologic follow-up indefinitely and should perform monthly self-examination of their skin and lymph nodes.
Heightened awareness of the risk for a second primary melanoma should prompt primary care physicians to conduct ongoing patient surveillance. Family physicians should also keep in mind that novel therapies for metastatic melanoma, such as molecular-targeted therapies and immunotherapy, are associated with a much higher survival rate than previous standard therapy.
CORRESPONDENCE
Iris Tong, MD, Associate Professor, Division of General Internal Medicine, Department of Medicine, Alpert Medical School of Brown University, 146 W River St, Providence, RI 02904; [email protected]
THE CASE
A 56-year-old woman with a history of melanoma in situ presented with progressive dyspnea on exertion, cough productive of clear sputum, and right-sided rib pain radiating to the upper back of 5 weeks’ duration.
Twenty-four years earlier, the patient had undergone excision of a skin lesion from the right side of her back. Pathology revealed melanoma in situ with no evidence of invasion of the underlying dermis. Because of close margins, she underwent wider excision 2 weeks later and no residual tumor was found. The patient subsequently underwent routine biannual dermatologic follow-up and transitioned (within the past few years) to annual dermatologic follow-up. At a recent dermatologic visit (9 months earlier), there were no suspicious skin lesions.
At current presentation, she denied fever, chills, night sweats, or unintentional weight loss. On examination, her vital signs were normal. Her pulse oximetry on room air was 95% at rest and 94% with ambulation. She had decreased breath sounds at the right lung base and a fixed 2 × 2-cm nontender, indurated mass in the right upper anterior chest wall, superior to the right breast. A skin examination was not performed at this time.

A complete blood count revealed a white blood cell count of 8220/mcL (reference range, 4500–11,000/mcL), hemoglobin of 13.6 g/dL (reference range, 14–17.5 g/dL), and a platelet count of 162 × 103/mcL (reference range, 150–350 × 103/mcL). The patient’s electrolytes were within normal limits, with a creatinine level of 0.67 mg/dL (reference range, 0.1–1.2 mg/dL) and a calcium level of 9.4 mg/dL (reference range, 8.2–10.2 mg/dL). Lactate dehydrogenase was elevated at 308 U/L (reference range, 100–200 U/L).
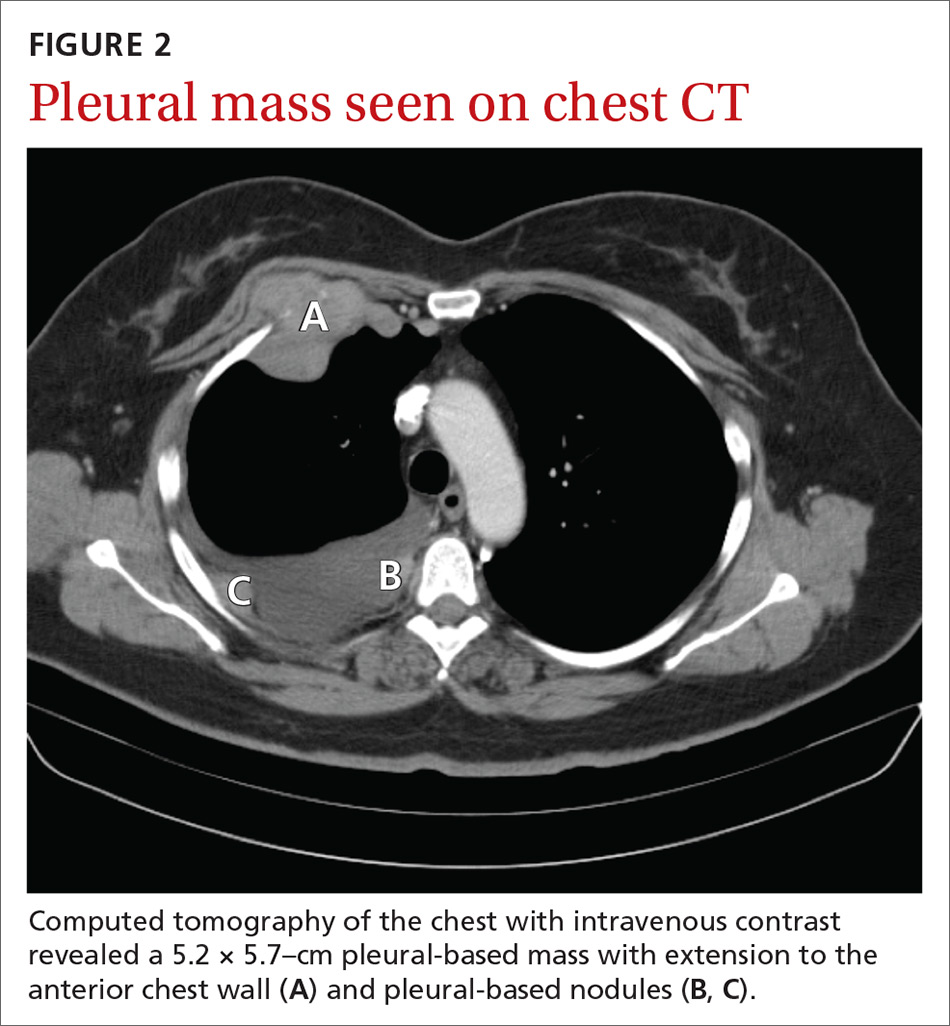
A chest radiograph revealed a right upper lobe mass, right lower lobe consolidation, and a large right-sided pleural effusion (FIGURE 1). Chest computed tomography (CT) with intravenous contrast revealed a 5.2 × 5.7–cm right pleural-based mass with extension to the anterior chest wall, 3 left-sided pulmonary nodules, numerous right-sided pleural-based nodules (FIGURE 2), and multiple low-density liver lesions. An abdominal and pelvic CT scan revealed a 5.6 × 2.5 × 4.8–cm hepatic lesion (FIGURE 3) with scattered hepatic cysts.
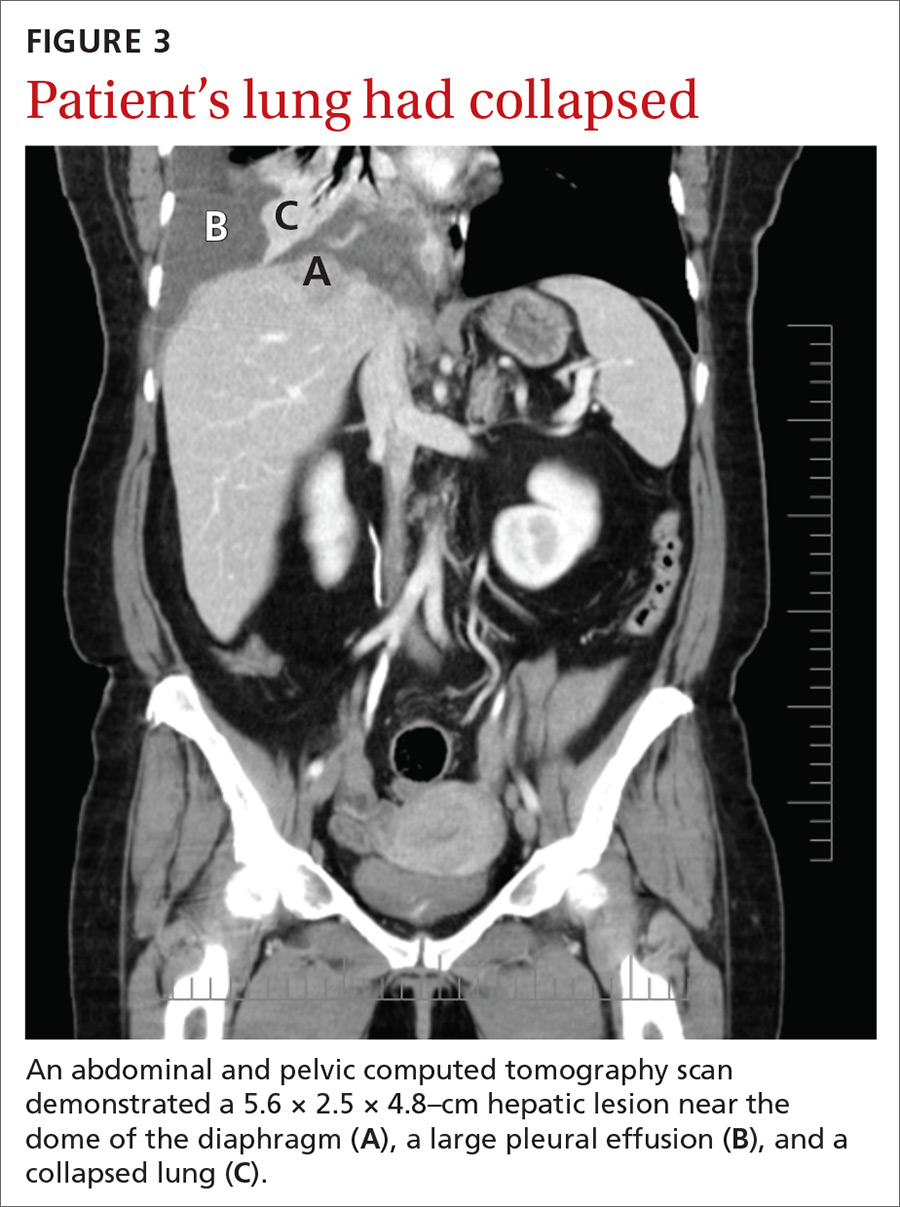
THE DIAGNOSIS
A diagnostic thoracentesis was performed, and pleural fluid cytology results revealed metastatic melanoma. Magnetic resonance imaging (MRI) of the brain showed no evidence of metastases.
After the patient’s initial presentation, her dermatologist performed a biopsy on a pre-existing skin lesion on the patient’s left abdomen, which initially was thought to be a cherry angioma. This left abdominal skin lesion was in a location different from her previous melanoma in situ, which was located on the right side of the back. Biopsy results of the presumed cherry angioma revealed a nodular malignant melanoma (which was partially removed), adjacent to a cherry angioma (which was completely excised).
Continue to: Two primary melanomas
Two primary melanomas. Our patient had 2 different primary melanomas: a melanoma in situ on the right back diagnosed 24 years prior to the current presentation and the more recently identified melanoma on the left abdomen with metastases to the lung and liver.
We referred the patient to Oncology and she was enrolled in a clinical study with ipilimumab and nivolumab, monoclonal antibodies directed against negative regulators of T-cell activation.
DISCUSSION
In the United States, melanoma is the fifth leading cancer in men and the sixth leading cancer in women.1 A prior history of melanoma or melanoma in situ increases the risk for a second melanoma,2-4 and the risk remains elevated for more than 20 years after the initial diagnosis.2 One- and 2-year survival rates for metastatic melanoma are 32% to 65% and 18% to 40%, respectively5; the 5-year survival rate of metastatic melanoma to the lung is approximately 16%.6
Recommendations regarding the appropriate follow-up of patients with a history of melanoma in situ and melanoma vary widely.7 For patients with a history of melanoma in situ, the American Academy of Dermatology and the National Comprehensive Cancer Network recommend annual skin examination indefinitely and self-examination of the skin and lymph nodes monthly.4,7,8
Novel therapies are powerful allies in fight against melanoma
Previous standard treatment of metastatic melanoma included surgery, radiation, and cytotoxic chemotherapy. Resection rarely is curative in distant metastatic melanoma, and cytotoxic chemotherapy has low response rates, has a response duration of 4 to 6 months, and does not improve overall survival in advanced melanoma.9-12
Continue to: Novel therapies...
Novel therapies, such as immunotherapy and molecular-targeted therapies, are dramatically increasing survival rates in metastatic melanoma. Melanoma frequently is associated with somatic mutations, and each patient may have a unique collection of mutations resulting in the expression of antigens that bind to certain T-cell receptors, which serve as targets for inhibitor immunotherapy.
Ipilimumab and nivolumab are monoclonal antibodies directed against negative regulators of T-cell activation. When ipilimumab and nivolumab bind to their receptors, feedback inhibition is prevented, which results in an immune response against the tumor. In a trial of 53 patients with advanced melanoma treated with both drugs, the overall survival rate at 1 and 2 years was 94% and 88%, respectively.13
Dabrafenib and trametinib. Mutations that activate the serine/threonine kinase gene, BRAF, are present in approximately 40% to 60% of advanced melanomas and lead to clonal expansion and tumor progression.14,15 Inhibition of BRAF produces rapid tumor regression—even in extensive disease. Treatment with dabrafenib, a BRAF inhibitor, and trametinib, a mitogen-activated protein kinase inhibitor, has been shown to be superior to a BRAF inhibitor alone and is associated with a survival rate of 72% at 1 year.16
Our patient. Seven months after enrolling in the clinical trial with ipilimumab and nivolumab, our patient developed brain metastases and was withdrawn from the trial. A resection of her brain metastases and radiation therapy followed. The patient was then started on molecular-targeted therapy with dabrafenib and trametinib. Twelve weeks later, a repeat CT scan of the chest, abdomen, and pelvis demonstrated an interval decrease in the size of the majority of the metastatic lesions, and a repeat brain MRI showed no additional metastases.
More than 4 years after her diagnosis, our patient remains on dabrafenib and trametinib therapy and her metastatic lesions to the lung and liver remain stable.
Continue to: THE TAKEAWAY
THE TAKEAWAY
Patients with a prior melanoma in situ or invasive melanoma have a higher risk for a subsequent invasive melanoma, and this risk remains elevated for more than 20 years. While patients with a history of melanoma in situ do not require specific oncologic follow-up, they do require annual dermatologic follow-up indefinitely and should perform monthly self-examination of their skin and lymph nodes.
Heightened awareness of the risk for a second primary melanoma should prompt primary care physicians to conduct ongoing patient surveillance. Family physicians should also keep in mind that novel therapies for metastatic melanoma, such as molecular-targeted therapies and immunotherapy, are associated with a much higher survival rate than previous standard therapy.
CORRESPONDENCE
Iris Tong, MD, Associate Professor, Division of General Internal Medicine, Department of Medicine, Alpert Medical School of Brown University, 146 W River St, Providence, RI 02904; [email protected]
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018 [published online January 4, 2018]. Cancer J Clin. 2018;68:7-30.
2. Bradford PT, Freedman DM, Goldstein AM, et al. Increased risk of second primary cancers after diagnosis of melanoma. Arch Dermatol. 2010;146:265-272.
3. Balamurugan A, Rees JR, Kosary C, et al. Subsequent primary cancers among men and women with in situ and invasive melanoma of the skin. J Am Acad Dermatol. 2011;65(5) (suppl 1):S69-S77.
4. Pomerantz H, Huang D, Weinstock MA. Risk of subsequent melanoma after melanoma in situ and invasive melanoma: a population-based study from 1973 to 2011. J Am Acad Dermatol. 2015;72:794-800.
5. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199-6206.
6. American Cancer Society. Cancer facts & figures 2015. www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/index. Accessed November 26, 2018.
7. Coit DG, Andtbacka R, Anker CJ, et al. Melanoma: clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;3:366-400.
8. Bichakjian CK, Halpern AC, Johnson TM. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 2011;5:1032-1047.
9. Atkins MB. The role of cytotoxic chemotherapeutic agents either alone or in combination with biological response modifiers. In: Kirkwood JK, ed. Molecular Diagnosis, Prevention & Therapy of Melanoma. New York, NY: Marcel Dekker; 1997:219.
10. Patel PM, Suciu S, Mortier L, et al; EORTC Melanoma Group. Extended schedule, escalated dose temozolomide versus dacarbazine in stage IV melanoma: final results of a randomised phase III study (EORTC 18032) [published online May 18, 2011]. Eur J Cancer. 2011;47:1476-1483.
11. Flaherty KT, Lee SJ, Zhao F, et al. Phase III trial of carboplatin and paclitaxel with or without sorafenib in metastatic melanoma [published online December 17, 2012]. J Clin Oncol. 2013;31:373-379.
12. Sosman JA, Moon J, Tuthill RJ, et al. A phase 2 trial of complete resection for stage IV melanoma: results of Southwest Oncology Group Clinical Trial S9430 [published online March 31, 2011]. Cancer. 2011;117:4740-4746.
13. Sznol M, Kluger HM, Callahan MK, et al. Abstract LBA9003. Presented at: 2014 American Society of Clinical Oncology (ASCO) Annual Meeting; May 30–June 3, 2014; Chicago, IL.
14. Omholt K, Platz A, Kanter L, et al. NRAS and BRAF mutations arise early during melanoma pathogenesis and are preserved throughout tumor progression. Clin Cancer Res. 2003;9:6483-6488.
15. Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29:1239-1246.
16. Robert C, Karaszewska B, Schachter J, et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med. 2015;372:30-39.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018 [published online January 4, 2018]. Cancer J Clin. 2018;68:7-30.
2. Bradford PT, Freedman DM, Goldstein AM, et al. Increased risk of second primary cancers after diagnosis of melanoma. Arch Dermatol. 2010;146:265-272.
3. Balamurugan A, Rees JR, Kosary C, et al. Subsequent primary cancers among men and women with in situ and invasive melanoma of the skin. J Am Acad Dermatol. 2011;65(5) (suppl 1):S69-S77.
4. Pomerantz H, Huang D, Weinstock MA. Risk of subsequent melanoma after melanoma in situ and invasive melanoma: a population-based study from 1973 to 2011. J Am Acad Dermatol. 2015;72:794-800.
5. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199-6206.
6. American Cancer Society. Cancer facts & figures 2015. www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/index. Accessed November 26, 2018.
7. Coit DG, Andtbacka R, Anker CJ, et al. Melanoma: clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;3:366-400.
8. Bichakjian CK, Halpern AC, Johnson TM. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 2011;5:1032-1047.
9. Atkins MB. The role of cytotoxic chemotherapeutic agents either alone or in combination with biological response modifiers. In: Kirkwood JK, ed. Molecular Diagnosis, Prevention & Therapy of Melanoma. New York, NY: Marcel Dekker; 1997:219.
10. Patel PM, Suciu S, Mortier L, et al; EORTC Melanoma Group. Extended schedule, escalated dose temozolomide versus dacarbazine in stage IV melanoma: final results of a randomised phase III study (EORTC 18032) [published online May 18, 2011]. Eur J Cancer. 2011;47:1476-1483.
11. Flaherty KT, Lee SJ, Zhao F, et al. Phase III trial of carboplatin and paclitaxel with or without sorafenib in metastatic melanoma [published online December 17, 2012]. J Clin Oncol. 2013;31:373-379.
12. Sosman JA, Moon J, Tuthill RJ, et al. A phase 2 trial of complete resection for stage IV melanoma: results of Southwest Oncology Group Clinical Trial S9430 [published online March 31, 2011]. Cancer. 2011;117:4740-4746.
13. Sznol M, Kluger HM, Callahan MK, et al. Abstract LBA9003. Presented at: 2014 American Society of Clinical Oncology (ASCO) Annual Meeting; May 30–June 3, 2014; Chicago, IL.
14. Omholt K, Platz A, Kanter L, et al. NRAS and BRAF mutations arise early during melanoma pathogenesis and are preserved throughout tumor progression. Clin Cancer Res. 2003;9:6483-6488.
15. Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29:1239-1246.
16. Robert C, Karaszewska B, Schachter J, et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med. 2015;372:30-39.