User login
CDC says child vaccination exemptions hit all-time high
– the highest exemption rate ever reported in the United States.
Of the 3% of children who got exemptions, 0.2% were for medical reasons and 2.8% for nonmedical reasons, the CDC report said. The overall exemption rate was 2.6% for the previous school year.
Though more children received exemptions, the overall national vaccination rate remained steady at 93% for children entering kindergarten for the 2022-2023 school year. Before the COVID-19 pandemic, the overall rate was 95%, the CDC said.
“The bad news is that it’s gone down since the pandemic and still hasn’t rebounded,” Sean O’Leary, MD, a University of Colorado pediatric infectious diseases specialist, told The Associated Press. “The good news is that the vast majority of parents are still vaccinating their kids according to the recommended schedule.”
The CDC report did not offer a specific reason for higher vaccine exemptions. But it did note that the increase could be caused by the COVID-19 pandemic and COVID vaccine hesitancy.
“There is a rising distrust in the health care system,” Amna Husain, MD, a pediatrician in private practice in North Carolina and a spokesperson for the American Academy of Pediatrics, told NBC News. Vaccine exemptions “have unfortunately trended upward with it.”
Exemption rates varied across the nation. The CDC said 40 states reported a rise in exemptions and that the exemption rate went over 5% in 10 states: Alaska, Arizona, Hawaii, Idaho, Michigan, Nevada, North Dakota, Oregon, Utah, and Wisconsin. Idaho had the highest exemption rate in 2022 with 12%.
While requirements vary from state to state, most states require students entering kindergarten to receive four vaccines: MMR, DTaP, polio, and chickenpox.
A version of this article first appeared on WebMD.com.
– the highest exemption rate ever reported in the United States.
Of the 3% of children who got exemptions, 0.2% were for medical reasons and 2.8% for nonmedical reasons, the CDC report said. The overall exemption rate was 2.6% for the previous school year.
Though more children received exemptions, the overall national vaccination rate remained steady at 93% for children entering kindergarten for the 2022-2023 school year. Before the COVID-19 pandemic, the overall rate was 95%, the CDC said.
“The bad news is that it’s gone down since the pandemic and still hasn’t rebounded,” Sean O’Leary, MD, a University of Colorado pediatric infectious diseases specialist, told The Associated Press. “The good news is that the vast majority of parents are still vaccinating their kids according to the recommended schedule.”
The CDC report did not offer a specific reason for higher vaccine exemptions. But it did note that the increase could be caused by the COVID-19 pandemic and COVID vaccine hesitancy.
“There is a rising distrust in the health care system,” Amna Husain, MD, a pediatrician in private practice in North Carolina and a spokesperson for the American Academy of Pediatrics, told NBC News. Vaccine exemptions “have unfortunately trended upward with it.”
Exemption rates varied across the nation. The CDC said 40 states reported a rise in exemptions and that the exemption rate went over 5% in 10 states: Alaska, Arizona, Hawaii, Idaho, Michigan, Nevada, North Dakota, Oregon, Utah, and Wisconsin. Idaho had the highest exemption rate in 2022 with 12%.
While requirements vary from state to state, most states require students entering kindergarten to receive four vaccines: MMR, DTaP, polio, and chickenpox.
A version of this article first appeared on WebMD.com.
– the highest exemption rate ever reported in the United States.
Of the 3% of children who got exemptions, 0.2% were for medical reasons and 2.8% for nonmedical reasons, the CDC report said. The overall exemption rate was 2.6% for the previous school year.
Though more children received exemptions, the overall national vaccination rate remained steady at 93% for children entering kindergarten for the 2022-2023 school year. Before the COVID-19 pandemic, the overall rate was 95%, the CDC said.
“The bad news is that it’s gone down since the pandemic and still hasn’t rebounded,” Sean O’Leary, MD, a University of Colorado pediatric infectious diseases specialist, told The Associated Press. “The good news is that the vast majority of parents are still vaccinating their kids according to the recommended schedule.”
The CDC report did not offer a specific reason for higher vaccine exemptions. But it did note that the increase could be caused by the COVID-19 pandemic and COVID vaccine hesitancy.
“There is a rising distrust in the health care system,” Amna Husain, MD, a pediatrician in private practice in North Carolina and a spokesperson for the American Academy of Pediatrics, told NBC News. Vaccine exemptions “have unfortunately trended upward with it.”
Exemption rates varied across the nation. The CDC said 40 states reported a rise in exemptions and that the exemption rate went over 5% in 10 states: Alaska, Arizona, Hawaii, Idaho, Michigan, Nevada, North Dakota, Oregon, Utah, and Wisconsin. Idaho had the highest exemption rate in 2022 with 12%.
While requirements vary from state to state, most states require students entering kindergarten to receive four vaccines: MMR, DTaP, polio, and chickenpox.
A version of this article first appeared on WebMD.com.
Jury still out on whether green tea lowers colon cancer risk
Can green tea lower your risk of colorectal cancer? It depends on who – and what research – you believe.
Some researchers have found little or no significant risk from drinking the popular tea, while others point to a potential benefit. Now add two more studies – one that found no reduced risk and another that seems to strengthen the link between green tea and a lower risk of colon cancer.
Randomized controlled trials – where some people get randomly assigned to drink green tea and others do not – are considered the gold standard of medical research. Combine the findings from several of these trials, the thinking goes, and the findings get even stronger.
Combining random trials so far shows no advantage from green tea. But there may still be a benefit, said lead researcher Vishal Chandel, MD, who is affiliated with Suburban Community Hospital in Norristown, Pa. It could be that there are just not enough randomized controlled trials yet to show green tea has a protective effect.
“Many, many factors contribute to colorectal cancer, and one of them is diet. One thing which struck me was tea, because tea is something that people consume all over the world, and it has shown some stronger effects in Japan and in China,” said Dr. Chandel.
Comparing hundreds of people
Dr. Chandel and colleagues found three randomized controlled trials that looked at the link between green tea and colorectal cancer risk. Combined, the data included 451 people with colorectal cancer and 460 others without cancer who made up a control, or comparison, group.
They found green tea consumption did not reduce the risk of colorectal cancer in a statically significant way.
“There are only three randomized controlled trials from anywhere concerning green tea and colon cancer,” Dr. Chandel said. “We really need more. If we had 7, 8, or 10 … I’m very positive we will have a much stronger association to say that green tea can have a positive effect.”
Comparing thousands of people
Dr. Chandel and colleagues also performed another study where they looked at less rigorous evidence – 10 cohort studies and 15 prospective case-control studies. These studies included 198,488 cancer cases and 581,556 controls. This time, they found a stronger link between green tea and a reduced risk of colorectal cancer.
The “meta-analysis results indicate a lower tendency to develop colorectal cancer with green tea consumption, with reduced risk of colorectal cancer more pronounced in Asia than America or Europe,” the authors note. “Although there is insufficient epidemiological data to conclude at present that green tea can have protective effects in human beings.”
Dr. Chandel presented the findings of both studies in Vancouver at the American College of Gastroenterology annual scientific meeting.
Why green tea?
Dr. Chandel said he studied colorectal cancer because it is the third most diagnosed cancer worldwide, accounting for about 10% of all new cancer cases in 2020, according to the World Health Organization’s Global Cancer Observatory data. It is also a common cause of cancer death globally, second only to lung cancer.
Green tea contains high level of polyphenols known as catechins. The main catechin in green tea believed to provide cancer protective effects is epigallocatechin-3 gallate (EGCG). EGCG “has been shown in some studies to inhibit or prevent colon cancer,” Dr. Chandel said.
EGCG is present in higher amounts in green tea, compared with black or oolong tea, because green tea is made from unfermented, unoxidized tea leaves.
Difficult to read the tea leaves
These studies “add to the literature, which remains undefined regarding the role of green tea in reducing the risk of colorectal cancer,” Catherine Eng, MD, a spokesperson for the American Society of Clinical Oncology, said when asked to comment.
Although combining three trials did not reveal a significant benefit, looking at a greater number of studies did in some populations, said Dr. Eng, codirector of gastrointestinal oncology and chair of surgical and medical oncology at Vanderbilt-Ingram Cancer Center in Nashville.
“Potential benefit for green tea in reducing the risk of colorectal cancer was noted in the Asian cases but was not found to be statistically significant in the European or U.S. studies,” she said. “Currently, the role of dietary consumption of green tea on reducing the risk of colorectal cancer is not well established and requires further investigation.”
A version of this article appeared on WebMD.com.
Can green tea lower your risk of colorectal cancer? It depends on who – and what research – you believe.
Some researchers have found little or no significant risk from drinking the popular tea, while others point to a potential benefit. Now add two more studies – one that found no reduced risk and another that seems to strengthen the link between green tea and a lower risk of colon cancer.
Randomized controlled trials – where some people get randomly assigned to drink green tea and others do not – are considered the gold standard of medical research. Combine the findings from several of these trials, the thinking goes, and the findings get even stronger.
Combining random trials so far shows no advantage from green tea. But there may still be a benefit, said lead researcher Vishal Chandel, MD, who is affiliated with Suburban Community Hospital in Norristown, Pa. It could be that there are just not enough randomized controlled trials yet to show green tea has a protective effect.
“Many, many factors contribute to colorectal cancer, and one of them is diet. One thing which struck me was tea, because tea is something that people consume all over the world, and it has shown some stronger effects in Japan and in China,” said Dr. Chandel.
Comparing hundreds of people
Dr. Chandel and colleagues found three randomized controlled trials that looked at the link between green tea and colorectal cancer risk. Combined, the data included 451 people with colorectal cancer and 460 others without cancer who made up a control, or comparison, group.
They found green tea consumption did not reduce the risk of colorectal cancer in a statically significant way.
“There are only three randomized controlled trials from anywhere concerning green tea and colon cancer,” Dr. Chandel said. “We really need more. If we had 7, 8, or 10 … I’m very positive we will have a much stronger association to say that green tea can have a positive effect.”
Comparing thousands of people
Dr. Chandel and colleagues also performed another study where they looked at less rigorous evidence – 10 cohort studies and 15 prospective case-control studies. These studies included 198,488 cancer cases and 581,556 controls. This time, they found a stronger link between green tea and a reduced risk of colorectal cancer.
The “meta-analysis results indicate a lower tendency to develop colorectal cancer with green tea consumption, with reduced risk of colorectal cancer more pronounced in Asia than America or Europe,” the authors note. “Although there is insufficient epidemiological data to conclude at present that green tea can have protective effects in human beings.”
Dr. Chandel presented the findings of both studies in Vancouver at the American College of Gastroenterology annual scientific meeting.
Why green tea?
Dr. Chandel said he studied colorectal cancer because it is the third most diagnosed cancer worldwide, accounting for about 10% of all new cancer cases in 2020, according to the World Health Organization’s Global Cancer Observatory data. It is also a common cause of cancer death globally, second only to lung cancer.
Green tea contains high level of polyphenols known as catechins. The main catechin in green tea believed to provide cancer protective effects is epigallocatechin-3 gallate (EGCG). EGCG “has been shown in some studies to inhibit or prevent colon cancer,” Dr. Chandel said.
EGCG is present in higher amounts in green tea, compared with black or oolong tea, because green tea is made from unfermented, unoxidized tea leaves.
Difficult to read the tea leaves
These studies “add to the literature, which remains undefined regarding the role of green tea in reducing the risk of colorectal cancer,” Catherine Eng, MD, a spokesperson for the American Society of Clinical Oncology, said when asked to comment.
Although combining three trials did not reveal a significant benefit, looking at a greater number of studies did in some populations, said Dr. Eng, codirector of gastrointestinal oncology and chair of surgical and medical oncology at Vanderbilt-Ingram Cancer Center in Nashville.
“Potential benefit for green tea in reducing the risk of colorectal cancer was noted in the Asian cases but was not found to be statistically significant in the European or U.S. studies,” she said. “Currently, the role of dietary consumption of green tea on reducing the risk of colorectal cancer is not well established and requires further investigation.”
A version of this article appeared on WebMD.com.
Can green tea lower your risk of colorectal cancer? It depends on who – and what research – you believe.
Some researchers have found little or no significant risk from drinking the popular tea, while others point to a potential benefit. Now add two more studies – one that found no reduced risk and another that seems to strengthen the link between green tea and a lower risk of colon cancer.
Randomized controlled trials – where some people get randomly assigned to drink green tea and others do not – are considered the gold standard of medical research. Combine the findings from several of these trials, the thinking goes, and the findings get even stronger.
Combining random trials so far shows no advantage from green tea. But there may still be a benefit, said lead researcher Vishal Chandel, MD, who is affiliated with Suburban Community Hospital in Norristown, Pa. It could be that there are just not enough randomized controlled trials yet to show green tea has a protective effect.
“Many, many factors contribute to colorectal cancer, and one of them is diet. One thing which struck me was tea, because tea is something that people consume all over the world, and it has shown some stronger effects in Japan and in China,” said Dr. Chandel.
Comparing hundreds of people
Dr. Chandel and colleagues found three randomized controlled trials that looked at the link between green tea and colorectal cancer risk. Combined, the data included 451 people with colorectal cancer and 460 others without cancer who made up a control, or comparison, group.
They found green tea consumption did not reduce the risk of colorectal cancer in a statically significant way.
“There are only three randomized controlled trials from anywhere concerning green tea and colon cancer,” Dr. Chandel said. “We really need more. If we had 7, 8, or 10 … I’m very positive we will have a much stronger association to say that green tea can have a positive effect.”
Comparing thousands of people
Dr. Chandel and colleagues also performed another study where they looked at less rigorous evidence – 10 cohort studies and 15 prospective case-control studies. These studies included 198,488 cancer cases and 581,556 controls. This time, they found a stronger link between green tea and a reduced risk of colorectal cancer.
The “meta-analysis results indicate a lower tendency to develop colorectal cancer with green tea consumption, with reduced risk of colorectal cancer more pronounced in Asia than America or Europe,” the authors note. “Although there is insufficient epidemiological data to conclude at present that green tea can have protective effects in human beings.”
Dr. Chandel presented the findings of both studies in Vancouver at the American College of Gastroenterology annual scientific meeting.
Why green tea?
Dr. Chandel said he studied colorectal cancer because it is the third most diagnosed cancer worldwide, accounting for about 10% of all new cancer cases in 2020, according to the World Health Organization’s Global Cancer Observatory data. It is also a common cause of cancer death globally, second only to lung cancer.
Green tea contains high level of polyphenols known as catechins. The main catechin in green tea believed to provide cancer protective effects is epigallocatechin-3 gallate (EGCG). EGCG “has been shown in some studies to inhibit or prevent colon cancer,” Dr. Chandel said.
EGCG is present in higher amounts in green tea, compared with black or oolong tea, because green tea is made from unfermented, unoxidized tea leaves.
Difficult to read the tea leaves
These studies “add to the literature, which remains undefined regarding the role of green tea in reducing the risk of colorectal cancer,” Catherine Eng, MD, a spokesperson for the American Society of Clinical Oncology, said when asked to comment.
Although combining three trials did not reveal a significant benefit, looking at a greater number of studies did in some populations, said Dr. Eng, codirector of gastrointestinal oncology and chair of surgical and medical oncology at Vanderbilt-Ingram Cancer Center in Nashville.
“Potential benefit for green tea in reducing the risk of colorectal cancer was noted in the Asian cases but was not found to be statistically significant in the European or U.S. studies,” she said. “Currently, the role of dietary consumption of green tea on reducing the risk of colorectal cancer is not well established and requires further investigation.”
A version of this article appeared on WebMD.com.
Better postpartum BP control with self-monitoring: POP-HT
, new research suggests.
In a randomized trial of 220 women with preeclampsia or gestational hypertension, those who took daily postpartum BP readings and received clinician-guided advice for titrating antihypertensives had a 5 mm Hg–lower average diastolic BP at 9 months, compared with those receiving usual care.
Jamie Kitt, DPhil, from the University of Oxford (England) presented these findings from the Physicians Optimized Postpartum Hypertension Treatment (POP-HT, NCT04273854) clinical trial at the American Heart Association scientific sessions. The study was simultaneously published online in JAMA, and a cardiac imaging substudy was published online in Circulation.
“This trial identifies a potential need for a paradigm shift in the way women affected by hypertensive pregnancy are managed postnatally,” Dr. Kitt said. “If a 5–mm Hg improvement in BP is maintained longer term, it can result in about a 20% reduction in lifetime cardiovascular risk.”
The imaging substudy suggests that short-term postnatal optimization of BP control following hypertensive pregnancy through self-monitoring and physician-guided antihypertensive titration is linked with better cardiac remodeling changes seen by cardiovascular magnetic resonance and echocardiography.
POP-HT “proves for the first time that the first few weeks after delivery are a critical time that can determine the long-term cardiovascular health of the mother,” senior author Paul Leeson, PhD, also from the University of Oxford, who presented the findings in a press briefing, said in an interview.
“Interventions during this period can have long-term beneficial impacts on cardiovascular health,” he said. “These findings rewrite the textbook on our understanding of how and why hypertensive pregnancies associate with later cardiovascular disease in the mother.”
Next, Dr. Leeson said, “We need to work out the best ways to implement these interventions “at scale. Then we can ensure all women who have hypertensive pregnancies can get access to the long-term cardiovascular benefits we have demonstrated are possible through improving postpartum cardiac care,” he said, adding that “this is entirely achievable using current available technologies.”
Hypertension in pregnancy
About 1 in 10 pregnant women develop hypertension in pregnancy (preeclampsia or gestational hypertension), and 1 in 3 such women go on to develop chronic hypertension within 10 years, “when they are usually still in their 30s or 40s,” Dr. Leeson said.
During pregnancy, the heart remodels to cope with pregnancy, and it undergoes more severe changes if BP is high. Then during the 6 weeks after giving birth, this remodeling rapidly reverses.
Higher blood pressure in young adulthood is associated with a twofold higher risk of subsequent myocardial infarction and stroke. And abnormal cardiac remodeling postpartum is also linked with higher cardiovascular risk.
Self-monitoring blood pressure during the postpartum period may be a “critical window” for intervention.
Previously, the research group performed a pilot study, the Self-Management of Postnatal Antihypertensive Treatment (SNAP-HT) trial and the SNAP-extension trial, which compared a BP self-monitoring intervention with usual care in 91 women with gestational hypertension or preeclampsia requiring postnatal antihypertensive treatment.
Diastolic BP, which drives cardiovascular risk in younger populations, was 4.5–mm Hg lower at 6 months postpartum and 7–mm Hg lower at 4 years post partum in patients randomly assigned to BP self-management vs. usual care – even after they were no longer taking antihypertensives.
Building on these findings, the POP-HT trial enrolled 220 pregnant women seen at Oxford University Hospitals in the United Kingdom who were age 18 years or older, had either gestational hypertension or preeclampsia, and still required antihypertensives when they were being discharged from hospital after giving birth.
Following a baseline visit at day 1-6 after delivery, while in the postnatal ward, the patients were randomly assigned 1:1 to the intervention group (112 women) or usual-care group (108 women).
They had an average age of 32.6 years; 40% had gestational hypertension, and 60% had preeclampsia.
Women in the usual-care group typically received a BP review at 7-10 days after hospital discharge with a community midwife, and another at 6-8 weeks with their general practitioner.
The women in the intervention group were given and taught to use a Bluetooth-enabled OMRON Evolv BP monitor (Omron Healthcare Europe) while on the postnatal ward, and they installed a smartphone app on their mobile phones that transmitted self-monitored BP readings to a National Health Service-hosted, web-based platform.
They were instructed to take daily BP measurements (twice daily if out of target range). Dose titration of antihypertensives after hospital discharge was guided remotely by research clinicians, according to a guideline-based algorithm.
Patients in both groups had four study visits when their BP was measured: visit 1 (baseline) between days 1 and 6 post partum; visit 2 at week 1; visit 3 at week 6; and visit 4 between months 6 and 9 post partum.
Similar antihypertensive classes were prescribed in each group (enalapril 57%, nifedipine 27%, and labetalol 30% for intervention vs. enalapril 43%, nifedipine 30%, and labetalol 27% for control).
At 6 weeks, approximately 30% of participants in each group were still taking medication; this dropped to approximately 12% by visit 4.
The primary outcome – the mean 24-hour diastolic BP at visit 4 (roughly 9 months post partum), adjusted for baseline postnatal diastolic blood pressure – was 5.8–mm Hg lower in the intervention group than in the control group (71.2 mm Hg vs. 76.6 mm Hg; P < .001).
Secondary outcomes – between-group differences in systolic BP at 9 months, BP-related postnatal admission, and cardiac remodeling assessed by cardiac magnetic resonance – were all better in the intervention group.
The mean 24-hour average systolic BP at 9 months post partum, adjusted for baseline postnatal systolic BP was 6.5–mm Hg lower in the intervention group than in the control group (114.0 mm Hg vs. 120.3 mm Hg; P < .001).
There was an absolute risk reduction of 20% and a relative risk reduction of 73.5% in postnatal readmission. The number needed to treat to avoid one postnatal readmission was five, which “has potential for big cost savings,” said Dr. Leeson.
Blood pressure post partum can be improved with self-monitoring and physician-guided medication adjustment, Dr. Leeson summarized. The blood pressure remains low for at least 9 months, even when medication is stopped, and the intervention leads to beneficial cardiac remodeling.
U.S. pilot study
Non-Hispanic Black adults have a high hypertension and cardiovascular disease burden, and a related small U.S. study showed benefits of BP self-monitoring in a population comprising mainly Black women, Keith Ferdinand, MD, discussant of the POP-HT trial in the press briefing, said in an interview.
Dr. Ferdinand, from Tulane University, New Orleans, Louisiana, was lead author of the Text My Hypertension BP Meds NOLA pilot study that was published in February in the American Heart Journal Plus: Cardiology Research and Practice.
The study showed that text-messaging and social support increased hypertension medication adherence.
They enrolled 36 individuals, of whom 32 (89%) were non-Hispanic Black, and 23 (64%) were women. The participants received validated Bluetooth-enabled BP-monitoring devices that were synced to smartphones via a secured cloud-based application. The participants could send and receive messages to health care practitioners.
This intervention significantly improved medication adherence and systolic BP without modifying pharmacotherapy.
‘Need to be passionate about monitoring BP’
“The take-home messages from these exciting findings is that physicians and women who have had high BP during pregnancy need to be passionate about monitoring and controlling their blood pressure and not ignore it,” Anastasia Mihailidou, PhD, Royal North Shore Hospital, Sydney, the assigned discussant in the late-breaking trial session, said in an interview.
“It also resulted in fewer postpartum hospital readmissions for high blood pressure and benefit at 9 months in the structure and function of the heart and blood vessels of the women,” she said.
“While we need to see further studies in ethnically diverse women to see that they are reproducible, there are simple measures that clinicians can implement, and women can ask to have their BP monitored more frequently than the current practice. In the U.K. it is 5-10 days after delivery and then at 6-8 weeks after giving birth when changes in heart structure have already started,” Dr. Mihailidou noted.
“The procedure will need to be modified if there are no telemedicine facilities, but that should not stop having close monitoring of BP and treating it adequately. Monitoring requires an accurate BP monitor. There also has to be monitoring BP for the children.”
The trial was funded by a BHF Clinical Research Training Fellowship to Dr. Kitt, with additional support from the NIHR Oxford Biomedical Research Centre and Oxford BHF Centre for Research Excellence.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a randomized trial of 220 women with preeclampsia or gestational hypertension, those who took daily postpartum BP readings and received clinician-guided advice for titrating antihypertensives had a 5 mm Hg–lower average diastolic BP at 9 months, compared with those receiving usual care.
Jamie Kitt, DPhil, from the University of Oxford (England) presented these findings from the Physicians Optimized Postpartum Hypertension Treatment (POP-HT, NCT04273854) clinical trial at the American Heart Association scientific sessions. The study was simultaneously published online in JAMA, and a cardiac imaging substudy was published online in Circulation.
“This trial identifies a potential need for a paradigm shift in the way women affected by hypertensive pregnancy are managed postnatally,” Dr. Kitt said. “If a 5–mm Hg improvement in BP is maintained longer term, it can result in about a 20% reduction in lifetime cardiovascular risk.”
The imaging substudy suggests that short-term postnatal optimization of BP control following hypertensive pregnancy through self-monitoring and physician-guided antihypertensive titration is linked with better cardiac remodeling changes seen by cardiovascular magnetic resonance and echocardiography.
POP-HT “proves for the first time that the first few weeks after delivery are a critical time that can determine the long-term cardiovascular health of the mother,” senior author Paul Leeson, PhD, also from the University of Oxford, who presented the findings in a press briefing, said in an interview.
“Interventions during this period can have long-term beneficial impacts on cardiovascular health,” he said. “These findings rewrite the textbook on our understanding of how and why hypertensive pregnancies associate with later cardiovascular disease in the mother.”
Next, Dr. Leeson said, “We need to work out the best ways to implement these interventions “at scale. Then we can ensure all women who have hypertensive pregnancies can get access to the long-term cardiovascular benefits we have demonstrated are possible through improving postpartum cardiac care,” he said, adding that “this is entirely achievable using current available technologies.”
Hypertension in pregnancy
About 1 in 10 pregnant women develop hypertension in pregnancy (preeclampsia or gestational hypertension), and 1 in 3 such women go on to develop chronic hypertension within 10 years, “when they are usually still in their 30s or 40s,” Dr. Leeson said.
During pregnancy, the heart remodels to cope with pregnancy, and it undergoes more severe changes if BP is high. Then during the 6 weeks after giving birth, this remodeling rapidly reverses.
Higher blood pressure in young adulthood is associated with a twofold higher risk of subsequent myocardial infarction and stroke. And abnormal cardiac remodeling postpartum is also linked with higher cardiovascular risk.
Self-monitoring blood pressure during the postpartum period may be a “critical window” for intervention.
Previously, the research group performed a pilot study, the Self-Management of Postnatal Antihypertensive Treatment (SNAP-HT) trial and the SNAP-extension trial, which compared a BP self-monitoring intervention with usual care in 91 women with gestational hypertension or preeclampsia requiring postnatal antihypertensive treatment.
Diastolic BP, which drives cardiovascular risk in younger populations, was 4.5–mm Hg lower at 6 months postpartum and 7–mm Hg lower at 4 years post partum in patients randomly assigned to BP self-management vs. usual care – even after they were no longer taking antihypertensives.
Building on these findings, the POP-HT trial enrolled 220 pregnant women seen at Oxford University Hospitals in the United Kingdom who were age 18 years or older, had either gestational hypertension or preeclampsia, and still required antihypertensives when they were being discharged from hospital after giving birth.
Following a baseline visit at day 1-6 after delivery, while in the postnatal ward, the patients were randomly assigned 1:1 to the intervention group (112 women) or usual-care group (108 women).
They had an average age of 32.6 years; 40% had gestational hypertension, and 60% had preeclampsia.
Women in the usual-care group typically received a BP review at 7-10 days after hospital discharge with a community midwife, and another at 6-8 weeks with their general practitioner.
The women in the intervention group were given and taught to use a Bluetooth-enabled OMRON Evolv BP monitor (Omron Healthcare Europe) while on the postnatal ward, and they installed a smartphone app on their mobile phones that transmitted self-monitored BP readings to a National Health Service-hosted, web-based platform.
They were instructed to take daily BP measurements (twice daily if out of target range). Dose titration of antihypertensives after hospital discharge was guided remotely by research clinicians, according to a guideline-based algorithm.
Patients in both groups had four study visits when their BP was measured: visit 1 (baseline) between days 1 and 6 post partum; visit 2 at week 1; visit 3 at week 6; and visit 4 between months 6 and 9 post partum.
Similar antihypertensive classes were prescribed in each group (enalapril 57%, nifedipine 27%, and labetalol 30% for intervention vs. enalapril 43%, nifedipine 30%, and labetalol 27% for control).
At 6 weeks, approximately 30% of participants in each group were still taking medication; this dropped to approximately 12% by visit 4.
The primary outcome – the mean 24-hour diastolic BP at visit 4 (roughly 9 months post partum), adjusted for baseline postnatal diastolic blood pressure – was 5.8–mm Hg lower in the intervention group than in the control group (71.2 mm Hg vs. 76.6 mm Hg; P < .001).
Secondary outcomes – between-group differences in systolic BP at 9 months, BP-related postnatal admission, and cardiac remodeling assessed by cardiac magnetic resonance – were all better in the intervention group.
The mean 24-hour average systolic BP at 9 months post partum, adjusted for baseline postnatal systolic BP was 6.5–mm Hg lower in the intervention group than in the control group (114.0 mm Hg vs. 120.3 mm Hg; P < .001).
There was an absolute risk reduction of 20% and a relative risk reduction of 73.5% in postnatal readmission. The number needed to treat to avoid one postnatal readmission was five, which “has potential for big cost savings,” said Dr. Leeson.
Blood pressure post partum can be improved with self-monitoring and physician-guided medication adjustment, Dr. Leeson summarized. The blood pressure remains low for at least 9 months, even when medication is stopped, and the intervention leads to beneficial cardiac remodeling.
U.S. pilot study
Non-Hispanic Black adults have a high hypertension and cardiovascular disease burden, and a related small U.S. study showed benefits of BP self-monitoring in a population comprising mainly Black women, Keith Ferdinand, MD, discussant of the POP-HT trial in the press briefing, said in an interview.
Dr. Ferdinand, from Tulane University, New Orleans, Louisiana, was lead author of the Text My Hypertension BP Meds NOLA pilot study that was published in February in the American Heart Journal Plus: Cardiology Research and Practice.
The study showed that text-messaging and social support increased hypertension medication adherence.
They enrolled 36 individuals, of whom 32 (89%) were non-Hispanic Black, and 23 (64%) were women. The participants received validated Bluetooth-enabled BP-monitoring devices that were synced to smartphones via a secured cloud-based application. The participants could send and receive messages to health care practitioners.
This intervention significantly improved medication adherence and systolic BP without modifying pharmacotherapy.
‘Need to be passionate about monitoring BP’
“The take-home messages from these exciting findings is that physicians and women who have had high BP during pregnancy need to be passionate about monitoring and controlling their blood pressure and not ignore it,” Anastasia Mihailidou, PhD, Royal North Shore Hospital, Sydney, the assigned discussant in the late-breaking trial session, said in an interview.
“It also resulted in fewer postpartum hospital readmissions for high blood pressure and benefit at 9 months in the structure and function of the heart and blood vessels of the women,” she said.
“While we need to see further studies in ethnically diverse women to see that they are reproducible, there are simple measures that clinicians can implement, and women can ask to have their BP monitored more frequently than the current practice. In the U.K. it is 5-10 days after delivery and then at 6-8 weeks after giving birth when changes in heart structure have already started,” Dr. Mihailidou noted.
“The procedure will need to be modified if there are no telemedicine facilities, but that should not stop having close monitoring of BP and treating it adequately. Monitoring requires an accurate BP monitor. There also has to be monitoring BP for the children.”
The trial was funded by a BHF Clinical Research Training Fellowship to Dr. Kitt, with additional support from the NIHR Oxford Biomedical Research Centre and Oxford BHF Centre for Research Excellence.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a randomized trial of 220 women with preeclampsia or gestational hypertension, those who took daily postpartum BP readings and received clinician-guided advice for titrating antihypertensives had a 5 mm Hg–lower average diastolic BP at 9 months, compared with those receiving usual care.
Jamie Kitt, DPhil, from the University of Oxford (England) presented these findings from the Physicians Optimized Postpartum Hypertension Treatment (POP-HT, NCT04273854) clinical trial at the American Heart Association scientific sessions. The study was simultaneously published online in JAMA, and a cardiac imaging substudy was published online in Circulation.
“This trial identifies a potential need for a paradigm shift in the way women affected by hypertensive pregnancy are managed postnatally,” Dr. Kitt said. “If a 5–mm Hg improvement in BP is maintained longer term, it can result in about a 20% reduction in lifetime cardiovascular risk.”
The imaging substudy suggests that short-term postnatal optimization of BP control following hypertensive pregnancy through self-monitoring and physician-guided antihypertensive titration is linked with better cardiac remodeling changes seen by cardiovascular magnetic resonance and echocardiography.
POP-HT “proves for the first time that the first few weeks after delivery are a critical time that can determine the long-term cardiovascular health of the mother,” senior author Paul Leeson, PhD, also from the University of Oxford, who presented the findings in a press briefing, said in an interview.
“Interventions during this period can have long-term beneficial impacts on cardiovascular health,” he said. “These findings rewrite the textbook on our understanding of how and why hypertensive pregnancies associate with later cardiovascular disease in the mother.”
Next, Dr. Leeson said, “We need to work out the best ways to implement these interventions “at scale. Then we can ensure all women who have hypertensive pregnancies can get access to the long-term cardiovascular benefits we have demonstrated are possible through improving postpartum cardiac care,” he said, adding that “this is entirely achievable using current available technologies.”
Hypertension in pregnancy
About 1 in 10 pregnant women develop hypertension in pregnancy (preeclampsia or gestational hypertension), and 1 in 3 such women go on to develop chronic hypertension within 10 years, “when they are usually still in their 30s or 40s,” Dr. Leeson said.
During pregnancy, the heart remodels to cope with pregnancy, and it undergoes more severe changes if BP is high. Then during the 6 weeks after giving birth, this remodeling rapidly reverses.
Higher blood pressure in young adulthood is associated with a twofold higher risk of subsequent myocardial infarction and stroke. And abnormal cardiac remodeling postpartum is also linked with higher cardiovascular risk.
Self-monitoring blood pressure during the postpartum period may be a “critical window” for intervention.
Previously, the research group performed a pilot study, the Self-Management of Postnatal Antihypertensive Treatment (SNAP-HT) trial and the SNAP-extension trial, which compared a BP self-monitoring intervention with usual care in 91 women with gestational hypertension or preeclampsia requiring postnatal antihypertensive treatment.
Diastolic BP, which drives cardiovascular risk in younger populations, was 4.5–mm Hg lower at 6 months postpartum and 7–mm Hg lower at 4 years post partum in patients randomly assigned to BP self-management vs. usual care – even after they were no longer taking antihypertensives.
Building on these findings, the POP-HT trial enrolled 220 pregnant women seen at Oxford University Hospitals in the United Kingdom who were age 18 years or older, had either gestational hypertension or preeclampsia, and still required antihypertensives when they were being discharged from hospital after giving birth.
Following a baseline visit at day 1-6 after delivery, while in the postnatal ward, the patients were randomly assigned 1:1 to the intervention group (112 women) or usual-care group (108 women).
They had an average age of 32.6 years; 40% had gestational hypertension, and 60% had preeclampsia.
Women in the usual-care group typically received a BP review at 7-10 days after hospital discharge with a community midwife, and another at 6-8 weeks with their general practitioner.
The women in the intervention group were given and taught to use a Bluetooth-enabled OMRON Evolv BP monitor (Omron Healthcare Europe) while on the postnatal ward, and they installed a smartphone app on their mobile phones that transmitted self-monitored BP readings to a National Health Service-hosted, web-based platform.
They were instructed to take daily BP measurements (twice daily if out of target range). Dose titration of antihypertensives after hospital discharge was guided remotely by research clinicians, according to a guideline-based algorithm.
Patients in both groups had four study visits when their BP was measured: visit 1 (baseline) between days 1 and 6 post partum; visit 2 at week 1; visit 3 at week 6; and visit 4 between months 6 and 9 post partum.
Similar antihypertensive classes were prescribed in each group (enalapril 57%, nifedipine 27%, and labetalol 30% for intervention vs. enalapril 43%, nifedipine 30%, and labetalol 27% for control).
At 6 weeks, approximately 30% of participants in each group were still taking medication; this dropped to approximately 12% by visit 4.
The primary outcome – the mean 24-hour diastolic BP at visit 4 (roughly 9 months post partum), adjusted for baseline postnatal diastolic blood pressure – was 5.8–mm Hg lower in the intervention group than in the control group (71.2 mm Hg vs. 76.6 mm Hg; P < .001).
Secondary outcomes – between-group differences in systolic BP at 9 months, BP-related postnatal admission, and cardiac remodeling assessed by cardiac magnetic resonance – were all better in the intervention group.
The mean 24-hour average systolic BP at 9 months post partum, adjusted for baseline postnatal systolic BP was 6.5–mm Hg lower in the intervention group than in the control group (114.0 mm Hg vs. 120.3 mm Hg; P < .001).
There was an absolute risk reduction of 20% and a relative risk reduction of 73.5% in postnatal readmission. The number needed to treat to avoid one postnatal readmission was five, which “has potential for big cost savings,” said Dr. Leeson.
Blood pressure post partum can be improved with self-monitoring and physician-guided medication adjustment, Dr. Leeson summarized. The blood pressure remains low for at least 9 months, even when medication is stopped, and the intervention leads to beneficial cardiac remodeling.
U.S. pilot study
Non-Hispanic Black adults have a high hypertension and cardiovascular disease burden, and a related small U.S. study showed benefits of BP self-monitoring in a population comprising mainly Black women, Keith Ferdinand, MD, discussant of the POP-HT trial in the press briefing, said in an interview.
Dr. Ferdinand, from Tulane University, New Orleans, Louisiana, was lead author of the Text My Hypertension BP Meds NOLA pilot study that was published in February in the American Heart Journal Plus: Cardiology Research and Practice.
The study showed that text-messaging and social support increased hypertension medication adherence.
They enrolled 36 individuals, of whom 32 (89%) were non-Hispanic Black, and 23 (64%) were women. The participants received validated Bluetooth-enabled BP-monitoring devices that were synced to smartphones via a secured cloud-based application. The participants could send and receive messages to health care practitioners.
This intervention significantly improved medication adherence and systolic BP without modifying pharmacotherapy.
‘Need to be passionate about monitoring BP’
“The take-home messages from these exciting findings is that physicians and women who have had high BP during pregnancy need to be passionate about monitoring and controlling their blood pressure and not ignore it,” Anastasia Mihailidou, PhD, Royal North Shore Hospital, Sydney, the assigned discussant in the late-breaking trial session, said in an interview.
“It also resulted in fewer postpartum hospital readmissions for high blood pressure and benefit at 9 months in the structure and function of the heart and blood vessels of the women,” she said.
“While we need to see further studies in ethnically diverse women to see that they are reproducible, there are simple measures that clinicians can implement, and women can ask to have their BP monitored more frequently than the current practice. In the U.K. it is 5-10 days after delivery and then at 6-8 weeks after giving birth when changes in heart structure have already started,” Dr. Mihailidou noted.
“The procedure will need to be modified if there are no telemedicine facilities, but that should not stop having close monitoring of BP and treating it adequately. Monitoring requires an accurate BP monitor. There also has to be monitoring BP for the children.”
The trial was funded by a BHF Clinical Research Training Fellowship to Dr. Kitt, with additional support from the NIHR Oxford Biomedical Research Centre and Oxford BHF Centre for Research Excellence.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Apixaban cuts stroke but ups bleeding in subclinical AFib: ARTESIA
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Chemotherapy-induced peripheral neuropathy tied to compromised executive function
PHOENIX – , a new finding that may increase the risk for compromised mobility and fall risk.
“Among older cancer survivors treated with chemotherapy, the presence of CIPN was independently associated with reduced executive function,” said study investigator Brendan L. McNeish, MD, of the department of physical medicine and rehabilitation, University of Pittsburgh.
“Importantly, given the emerging relationship of executive function with mobility in this population, stakeholders and clinicians are called to acknowledge that chemotherapy-related mobility declines in CIPN survivors are likely due to both neuromuscular and executive dysfunction,” he said.
The findings were presented at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
Research gap
Characterized by numbness, tingling, pain, and motor impairment, CIPN affects up to 50% of all patients with cancer that is treated with taxane-, platinum-, or vinca alkaloid–based chemotherapy. The condition is among the leading dose-limiting toxicities, potentially increasing mortality risk.
Though the effects of chemotherapy on cognitive function are well-established, less is known about a potential relationship between this side effect and CIPN, Dr. McNeish said.
“Chemotherapy can be neurotoxic, but few studies have linked neurotoxicity to the central nervous system and peripheral nervous system,” Dr. McNeish said.
To compare cognitive outcomes in patients treated with chemotherapy who did and did not develop CIPN, the investigators conducted a cross-sectional study that included 50 chemotherapy-treated cancer survivors at a single time point post chemotherapy. The mean age of participants was 65.6 years, and 90% were women.
Twenty-two (44%) patients had CIPN on the basis of patient-reported distal paresthesias or numbness that started when chemotherapy was initiated and was present at the time of study enrollment.
Patients with CIPN had a greater decline in executive function, compared with those without the condition, as measured by the Trail Making Test Part B (TMT-B; CIPN-positive, 84.9 sec vs. 59.1 sec, respectively; P = .01) and the Stroop Color and Word Test (SCWT; CIPN-positive, 178.1 sec vs. CIPN-negative, 152.7 sec; P = .04), as well as lower rapid reaction accuracy (CIPN-positive, 60.3% vs. CIPN-negative, 70.6%; P = .01).
The association between CIPN and decreased executive function remained after multivariate adjusting for age, gender, depression, and benzodiazepine use for TMT-B (beta, 18.7; P = .046) and rapid reaction accuracy (beta, -.088; P = .018) but not SCWT (beta, 9.52; P = .233).
Clinical guidance
A recent study by the same investigators showed a link between executive function and balance in cancer survivors (mean age, 65.6 years; 88% women) treated with chemotherapy.
Another study of 116 patients treated with chemotherapy, including 32 who developed CIPN, showed that those with CIPN were nearly three times more likely to report a fall or near fall than were those without CIPN symptoms. In addition, those with CIPN symptoms were also more likely to have received medical care for falls.
Based on the current findings, the research suggests that “current clinical approaches to caring for this growing population [of cancer patients] should not assume that the well-known increased fall risk is solely related to CIPN.”
Dr. McNeish speculated that two potential hypotheses could explain the association between CIPN and reduced executive function in older cancer survivors.
“First, CIPN is associated with other conditions such as depression and anxiety, which are associated with reduced executive function,” he said.
“The second is that cancer-related cognitive dysfunction and CIPN share pathogenic mechanisms of neuronal injury, inflammation, and advanced aging, and thus some patients are vulnerable to both central (cancer-related cognitive function) and peripheral neurotoxicity.”
Either way, Dr. McNeish noted that “all interventions should measure both CIPN and executive function, as one could confound the other.”
Need for increased awareness
Commenting on the study, Ting Bao, MD, co-director of the Leonard P. Zakim Center for Integrative Therapies & Healthy Living at the Dana-Farber Cancer Institute, Boston, said that the findings underscore that “there is a need for increased awareness of the diverse manifestations of chemotherapy-induced neuropathy.”
These include the fact that “neurotoxic chemotherapy impacts both the peripheral and central nervous systems, affecting balance through distinct mechanisms.”
Although treatments routinely recommended for CIPN include duloxetine, tricyclic antidepressants, or gabapentin as well as topical agents such as lidocaine, evidence also shows benefits of nonpharmacologic approaches including exercise, acupuncture, and yoga. Dr. Bao’s own research has suggested that those benefits can extend improved balance and reduced fall risk.
Dr. Bao and colleagues recently conducted a randomized study that included 41 patients with CIPN to receive either yoga or usual care.
“The findings revealed that after eight biweekly sessions of yoga, there was a notable improvement in the far-reach test, which is a predictor of fall risk,” she said.
To validate these findings, the researchers are currently conducting a larger randomized controlled trial, she said.
In the meantime, “further research into the mechanisms and effective treatments for chemotherapy-induced neurotoxicity is essential,” added Dr. Bao.
Dr. McNeish and Dr. Bao report no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHOENIX – , a new finding that may increase the risk for compromised mobility and fall risk.
“Among older cancer survivors treated with chemotherapy, the presence of CIPN was independently associated with reduced executive function,” said study investigator Brendan L. McNeish, MD, of the department of physical medicine and rehabilitation, University of Pittsburgh.
“Importantly, given the emerging relationship of executive function with mobility in this population, stakeholders and clinicians are called to acknowledge that chemotherapy-related mobility declines in CIPN survivors are likely due to both neuromuscular and executive dysfunction,” he said.
The findings were presented at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
Research gap
Characterized by numbness, tingling, pain, and motor impairment, CIPN affects up to 50% of all patients with cancer that is treated with taxane-, platinum-, or vinca alkaloid–based chemotherapy. The condition is among the leading dose-limiting toxicities, potentially increasing mortality risk.
Though the effects of chemotherapy on cognitive function are well-established, less is known about a potential relationship between this side effect and CIPN, Dr. McNeish said.
“Chemotherapy can be neurotoxic, but few studies have linked neurotoxicity to the central nervous system and peripheral nervous system,” Dr. McNeish said.
To compare cognitive outcomes in patients treated with chemotherapy who did and did not develop CIPN, the investigators conducted a cross-sectional study that included 50 chemotherapy-treated cancer survivors at a single time point post chemotherapy. The mean age of participants was 65.6 years, and 90% were women.
Twenty-two (44%) patients had CIPN on the basis of patient-reported distal paresthesias or numbness that started when chemotherapy was initiated and was present at the time of study enrollment.
Patients with CIPN had a greater decline in executive function, compared with those without the condition, as measured by the Trail Making Test Part B (TMT-B; CIPN-positive, 84.9 sec vs. 59.1 sec, respectively; P = .01) and the Stroop Color and Word Test (SCWT; CIPN-positive, 178.1 sec vs. CIPN-negative, 152.7 sec; P = .04), as well as lower rapid reaction accuracy (CIPN-positive, 60.3% vs. CIPN-negative, 70.6%; P = .01).
The association between CIPN and decreased executive function remained after multivariate adjusting for age, gender, depression, and benzodiazepine use for TMT-B (beta, 18.7; P = .046) and rapid reaction accuracy (beta, -.088; P = .018) but not SCWT (beta, 9.52; P = .233).
Clinical guidance
A recent study by the same investigators showed a link between executive function and balance in cancer survivors (mean age, 65.6 years; 88% women) treated with chemotherapy.
Another study of 116 patients treated with chemotherapy, including 32 who developed CIPN, showed that those with CIPN were nearly three times more likely to report a fall or near fall than were those without CIPN symptoms. In addition, those with CIPN symptoms were also more likely to have received medical care for falls.
Based on the current findings, the research suggests that “current clinical approaches to caring for this growing population [of cancer patients] should not assume that the well-known increased fall risk is solely related to CIPN.”
Dr. McNeish speculated that two potential hypotheses could explain the association between CIPN and reduced executive function in older cancer survivors.
“First, CIPN is associated with other conditions such as depression and anxiety, which are associated with reduced executive function,” he said.
“The second is that cancer-related cognitive dysfunction and CIPN share pathogenic mechanisms of neuronal injury, inflammation, and advanced aging, and thus some patients are vulnerable to both central (cancer-related cognitive function) and peripheral neurotoxicity.”
Either way, Dr. McNeish noted that “all interventions should measure both CIPN and executive function, as one could confound the other.”
Need for increased awareness
Commenting on the study, Ting Bao, MD, co-director of the Leonard P. Zakim Center for Integrative Therapies & Healthy Living at the Dana-Farber Cancer Institute, Boston, said that the findings underscore that “there is a need for increased awareness of the diverse manifestations of chemotherapy-induced neuropathy.”
These include the fact that “neurotoxic chemotherapy impacts both the peripheral and central nervous systems, affecting balance through distinct mechanisms.”
Although treatments routinely recommended for CIPN include duloxetine, tricyclic antidepressants, or gabapentin as well as topical agents such as lidocaine, evidence also shows benefits of nonpharmacologic approaches including exercise, acupuncture, and yoga. Dr. Bao’s own research has suggested that those benefits can extend improved balance and reduced fall risk.
Dr. Bao and colleagues recently conducted a randomized study that included 41 patients with CIPN to receive either yoga or usual care.
“The findings revealed that after eight biweekly sessions of yoga, there was a notable improvement in the far-reach test, which is a predictor of fall risk,” she said.
To validate these findings, the researchers are currently conducting a larger randomized controlled trial, she said.
In the meantime, “further research into the mechanisms and effective treatments for chemotherapy-induced neurotoxicity is essential,” added Dr. Bao.
Dr. McNeish and Dr. Bao report no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHOENIX – , a new finding that may increase the risk for compromised mobility and fall risk.
“Among older cancer survivors treated with chemotherapy, the presence of CIPN was independently associated with reduced executive function,” said study investigator Brendan L. McNeish, MD, of the department of physical medicine and rehabilitation, University of Pittsburgh.
“Importantly, given the emerging relationship of executive function with mobility in this population, stakeholders and clinicians are called to acknowledge that chemotherapy-related mobility declines in CIPN survivors are likely due to both neuromuscular and executive dysfunction,” he said.
The findings were presented at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
Research gap
Characterized by numbness, tingling, pain, and motor impairment, CIPN affects up to 50% of all patients with cancer that is treated with taxane-, platinum-, or vinca alkaloid–based chemotherapy. The condition is among the leading dose-limiting toxicities, potentially increasing mortality risk.
Though the effects of chemotherapy on cognitive function are well-established, less is known about a potential relationship between this side effect and CIPN, Dr. McNeish said.
“Chemotherapy can be neurotoxic, but few studies have linked neurotoxicity to the central nervous system and peripheral nervous system,” Dr. McNeish said.
To compare cognitive outcomes in patients treated with chemotherapy who did and did not develop CIPN, the investigators conducted a cross-sectional study that included 50 chemotherapy-treated cancer survivors at a single time point post chemotherapy. The mean age of participants was 65.6 years, and 90% were women.
Twenty-two (44%) patients had CIPN on the basis of patient-reported distal paresthesias or numbness that started when chemotherapy was initiated and was present at the time of study enrollment.
Patients with CIPN had a greater decline in executive function, compared with those without the condition, as measured by the Trail Making Test Part B (TMT-B; CIPN-positive, 84.9 sec vs. 59.1 sec, respectively; P = .01) and the Stroop Color and Word Test (SCWT; CIPN-positive, 178.1 sec vs. CIPN-negative, 152.7 sec; P = .04), as well as lower rapid reaction accuracy (CIPN-positive, 60.3% vs. CIPN-negative, 70.6%; P = .01).
The association between CIPN and decreased executive function remained after multivariate adjusting for age, gender, depression, and benzodiazepine use for TMT-B (beta, 18.7; P = .046) and rapid reaction accuracy (beta, -.088; P = .018) but not SCWT (beta, 9.52; P = .233).
Clinical guidance
A recent study by the same investigators showed a link between executive function and balance in cancer survivors (mean age, 65.6 years; 88% women) treated with chemotherapy.
Another study of 116 patients treated with chemotherapy, including 32 who developed CIPN, showed that those with CIPN were nearly three times more likely to report a fall or near fall than were those without CIPN symptoms. In addition, those with CIPN symptoms were also more likely to have received medical care for falls.
Based on the current findings, the research suggests that “current clinical approaches to caring for this growing population [of cancer patients] should not assume that the well-known increased fall risk is solely related to CIPN.”
Dr. McNeish speculated that two potential hypotheses could explain the association between CIPN and reduced executive function in older cancer survivors.
“First, CIPN is associated with other conditions such as depression and anxiety, which are associated with reduced executive function,” he said.
“The second is that cancer-related cognitive dysfunction and CIPN share pathogenic mechanisms of neuronal injury, inflammation, and advanced aging, and thus some patients are vulnerable to both central (cancer-related cognitive function) and peripheral neurotoxicity.”
Either way, Dr. McNeish noted that “all interventions should measure both CIPN and executive function, as one could confound the other.”
Need for increased awareness
Commenting on the study, Ting Bao, MD, co-director of the Leonard P. Zakim Center for Integrative Therapies & Healthy Living at the Dana-Farber Cancer Institute, Boston, said that the findings underscore that “there is a need for increased awareness of the diverse manifestations of chemotherapy-induced neuropathy.”
These include the fact that “neurotoxic chemotherapy impacts both the peripheral and central nervous systems, affecting balance through distinct mechanisms.”
Although treatments routinely recommended for CIPN include duloxetine, tricyclic antidepressants, or gabapentin as well as topical agents such as lidocaine, evidence also shows benefits of nonpharmacologic approaches including exercise, acupuncture, and yoga. Dr. Bao’s own research has suggested that those benefits can extend improved balance and reduced fall risk.
Dr. Bao and colleagues recently conducted a randomized study that included 41 patients with CIPN to receive either yoga or usual care.
“The findings revealed that after eight biweekly sessions of yoga, there was a notable improvement in the far-reach test, which is a predictor of fall risk,” she said.
To validate these findings, the researchers are currently conducting a larger randomized controlled trial, she said.
In the meantime, “further research into the mechanisms and effective treatments for chemotherapy-induced neurotoxicity is essential,” added Dr. Bao.
Dr. McNeish and Dr. Bao report no relevant disclosures.
A version of this article first appeared on Medscape.com.
AT AANEM 2023
Preventing RSV in children and adults: A vaccine update
In the past year, there has been significant progress in the availability of interventions to prevent respiratory syncytial virus (RSV) and its complications. Four products have been approved by the US Food and Drug Administration (FDA) and recommended by the Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP). They include 2 vaccines for adults ages 60 years and older, a monoclonal antibody for infants and high-risk children, and a maternal vaccine to prevent RSV infection in newborns.
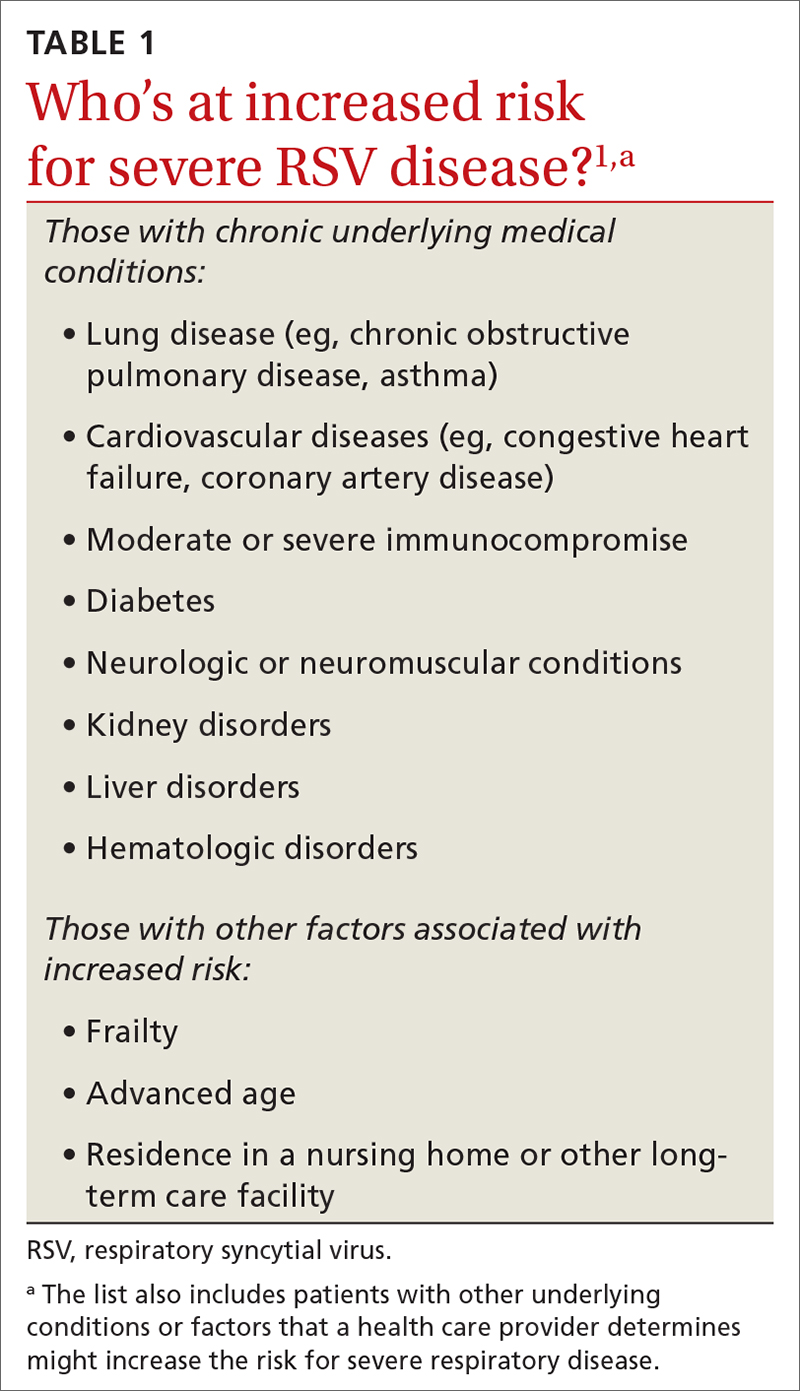
RSV in adults
While there is some uncertainty about the total burden of RSV in adults in the United States, the CDC estimates that each year it causes 0.9 to 1.4 million medical encounters, 60,000 to 160,000 hospitalizations, and 6000 to 10,000 deaths.1 The rate of RSV-caused hospitalization increases with age,2 and the infection is more severe in those with certain chronic medical conditions (TABLE 11). The FIGURE2 demonstrates the outcomes of adults who are hospitalized for RSV. Adults older than 65 years have a 5% mortality rate if hospitalized for RSV infection.2
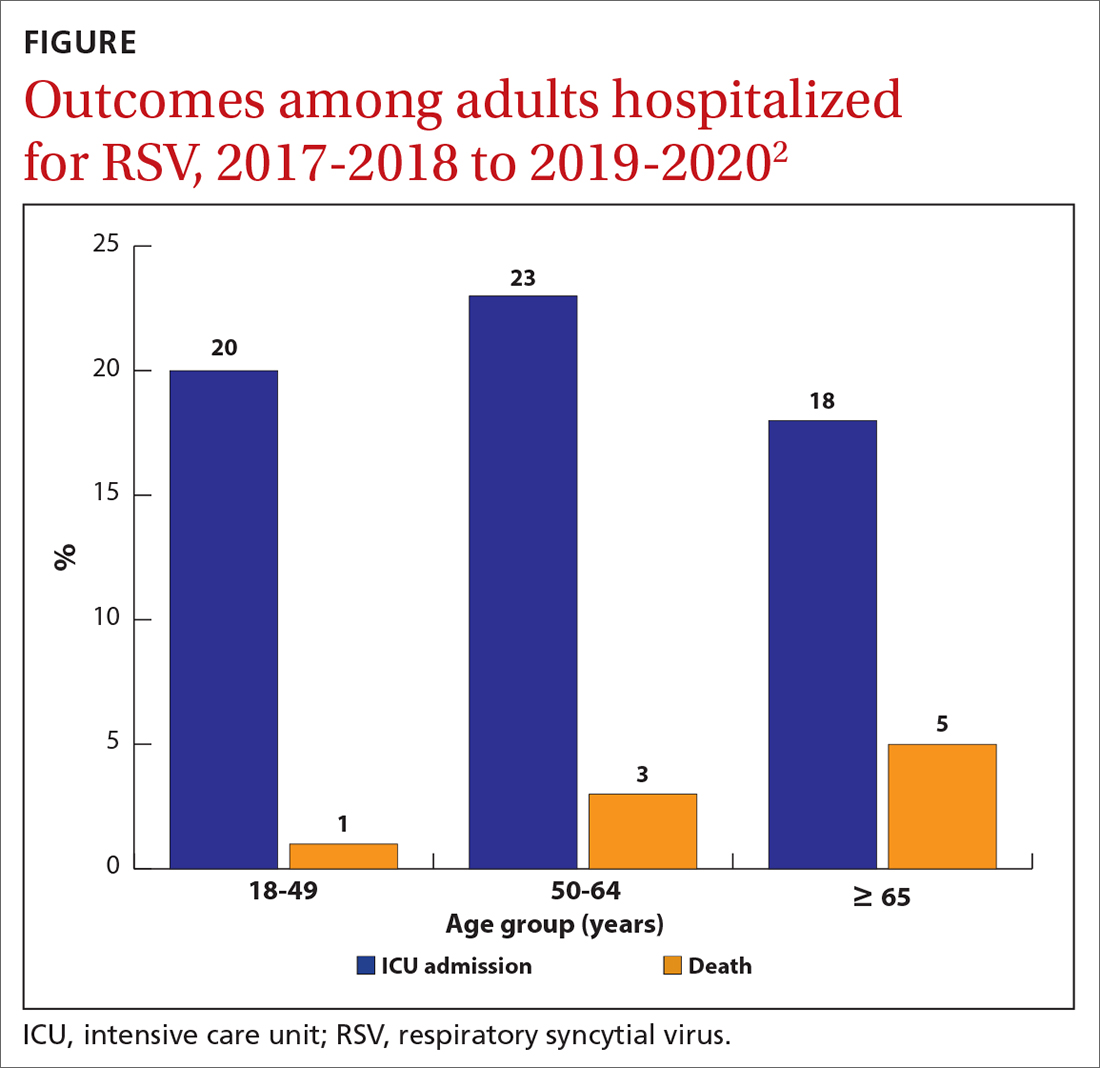
Vaccine options for adults
Two vaccines were recently approved for the prevention of RSV-associated lower respiratory tract disease (LRTD) in those ages 60 years and older: RSVPreF3 (Arexvy, GSK), which is an adjuvanted recombinant F protein vaccine, and RSVpreF (Abrysvo, Pfizer), which is a recombinant stabilized vaccine. Both require only a single dose (0.5 mL IM), which provides protection for 2 years.
The efficacy of the GSK vaccine in preventing laboratory-confirmed, RSV-associated LRTD was 82.6% during the first RSV season and 56.1% during the second season. The efficacy of the Pfizer vaccine in preventing symptomatic, laboratory-confirmed LRTD was 88.9% during the first RSV season and 78.6% during the second season.1 However, the trials leading to licensure of both vaccines were underpowered to show efficacy in the oldest adults and those who are frail or to show efficacy against RSV-caused hospitalization.
Safety of the adult RSV vaccines. The safety trials for both vaccines had a total of 38,177 participants. There were a total of 6 neurologic inflammatory conditions that developed within 42 days of vaccination, including 2 cases of suspected Guillain-Barré syndrome (GBS), 2 cases of possible acute disseminated encephalomyelitis, and 1 case each of chronic inflammatory demyelinating polyneuropathy and undifferentiated motor-sensory axonal polyneuropathy.1 That is a rate of 1 case of a neurologic inflammatory condition for every 6363 people vaccinated. Since the trials were not powered to determine whether the small number of cases were due to chance, postmarketing surveillance will be needed to clarify the true risk for GBS or other neurologic inflammatory events from RSV vaccination.
The lack of efficacy data for the most vulnerable older adults and the lingering questions about safety prompted the ACIP to recommend that adults ages 60 years and older may receive a single dose of RSV vaccine, using shared clinical decision-making—which is different from a routine or risk-based vaccine recommendation. For RSV vaccination, the decision to vaccinate should be based on a risk/benefit discussion between the clinician and the patient. Those most likely to benefit from the vaccine are listed in TABLE 1.1
While data on coadministration of RSV vaccines with other adult vaccines are sparse, the ACIP states that co-administration with other vaccines is acceptable.1 It is not known yet whether boosters will be needed after 2 years.
Continue to: RSV in infants and children
RSV in infants and children
RSV is the most common cause of hospitalization among infants and children in the United States. The CDC estimates that each year in children younger than 5 years, RSV is responsible for 1.5 million outpatient clinic visits, 520,000 emergency department visits, 58,000 to 80,000 hospitalizations, and 100 to 200 deaths.3 The risk for hospitalization from RSV is highest in the second and third months of life and decreases with increasing age.3
There are racial disparities in RSV severity: Intensive care unit admission rates are 1.2 to 1.6 times higher among non-Hispanic Black infants younger than 6 months than among non-Hispanic White infants, and hospitalization rates are up to 5 times higher in American Indian and Alaska Native populations.3
The months of highest RSV transmission in most locations are December through February, but this can vary. For practical purposes, RSV season runs from October through March.
Prevention in infants and children
The monoclonal antibody nirsevimab is now available for use in infants younger than 8 months born during or entering their first RSV season and children ages 8 to 19 months who are at increased risk for severe RSV disease and entering their second RSV season. Details regarding the use of this product were described in a recent Practice Alert Brief.4
Early studies on nirsevimab demonstrated 79% effectiveness in preventing medical-attended LRTD, 80.6% effectiveness in preventing hospitalization, and 90% effectiveness in preventing ICU admission. The number needed to immunize with nirsevimab to prevent an outpatient visit is estimated to be 17; to prevent an ED visit, 48; and to prevent an inpatient admission, 128. Due to the low RSV death rate, the studies were not able to demonstrate reduced mortality.5
Continue to: RSV vaccine in pregnancy
RSV vaccine in pregnancy
In August, the FDA approved Pfizer’s RSVpreF vaccine for use during pregnancy—as a single dose given at 32 to 36 weeks’ gestation—for the prevention of RSV LRTD in infants in the first 6 months of life. In the clinical trials, the vaccine was given at 24 to 36 weeks’ gestation. However, there was a statistically nonsignificant increase in preterm births in the RSVpreF group compared to the placebo group.6 While there were insufficient data to prove or rule out a causal relationship, the FDA advisory committee was more comfortable approving the vaccine for use only later in pregnancy, to avoid the possibility of very early preterm births after vaccination. The ACIP agreed.
From time of maternal vaccination, at least 14 days are needed to develop and transfer maternal antibodies across the placenta to protect the infant. Therefore, infants born less than 14 days after maternal vaccination should be considered unprotected.
Both maternal vaccination with RSVpreF and infant injection with nirsevimab are now options to protect newborns and infants from RSV. However, use of both products is not needed, since combined they do not offer significant added protection compared to either product alone (exceptions to be discussed shortly).6 When the estimated due date will occur in the RSV season, maternity clinicians should provide information on both products and assist the mother in deciding whether to be vaccinated or rely on administration of nirsevimab to the infant after birth. The benefits and risks of these 2 options are listed in TABLE 2.6
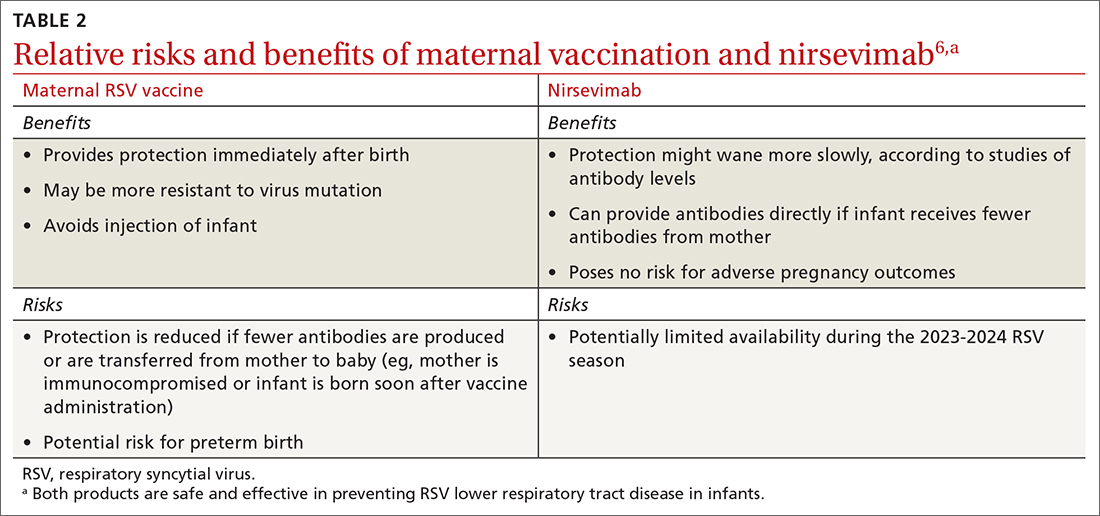
There are some rare situations in which use of both products is recommended, and they include6:
- When the baby is born less than 14 days from the time of maternal vaccination
- When the mother has a condition that could produce an inadequate response to the vaccine
- When the infant has had cardiopulmonary bypass, which would lead to loss of maternal antibodies
- When the infant has severe disease placing them at increased risk for severe RSV.
Conclusion
All of these new RSV preventive products should soon be widely available and covered with no out-of-pocket expense by commercial and government payers. The exception might be nirsevimab—because of the time needed to produce it, it might not be universally available in the 2023-2024 season.
1. Melgar M, Britton A, Roper LE, et al. Use of respiratory syncytial virus vaccine in older adults: recommendation of the Advisory Committee on Immunization Practices—United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:793-801.
2. Melgar M. Evidence to recommendation framework. RSV in adults. Presented to the ACIP on February 23, 2023. Accessed November 7, 2023. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2023-02/slides-02-23/RSV-Adults-04-Melgar-508.pdf
3. Jones JM, Fleming-Dutra KE, Prill MM, et al. Use of nirsevimab for the prevention of respiratory syncytial virus disease among infants and young children: recommendation of the Advisory Committee on Immunization Practices—United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:90-925.
4. Campos-Outcalt D. Are you ready for RSV season? There’s a new preventive option. J Fam Pract. 2023;72. doi: 10.12788/jfp.0663
5. Jones J. Evidence to recommendation framework: nirsevimab updates. Presented to the ACIP on August 3, 2023. Accessed August 23, 2023. https://stacks.cdc.gov/view/cdc/131586
6. Jones J. Clinical considerations for maternal RSVPreF vaccine and nirsevimab. Presented to the ACIP on September 25, 2023. Accessed November 8, 2023. www2.cdc.gov/vaccines/ed/ciinc/archives/23/09/ciiw_RSV2/CIIW%20RSV%20maternal%20vaccine%20mAb%209.27.23.pdf
In the past year, there has been significant progress in the availability of interventions to prevent respiratory syncytial virus (RSV) and its complications. Four products have been approved by the US Food and Drug Administration (FDA) and recommended by the Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP). They include 2 vaccines for adults ages 60 years and older, a monoclonal antibody for infants and high-risk children, and a maternal vaccine to prevent RSV infection in newborns.
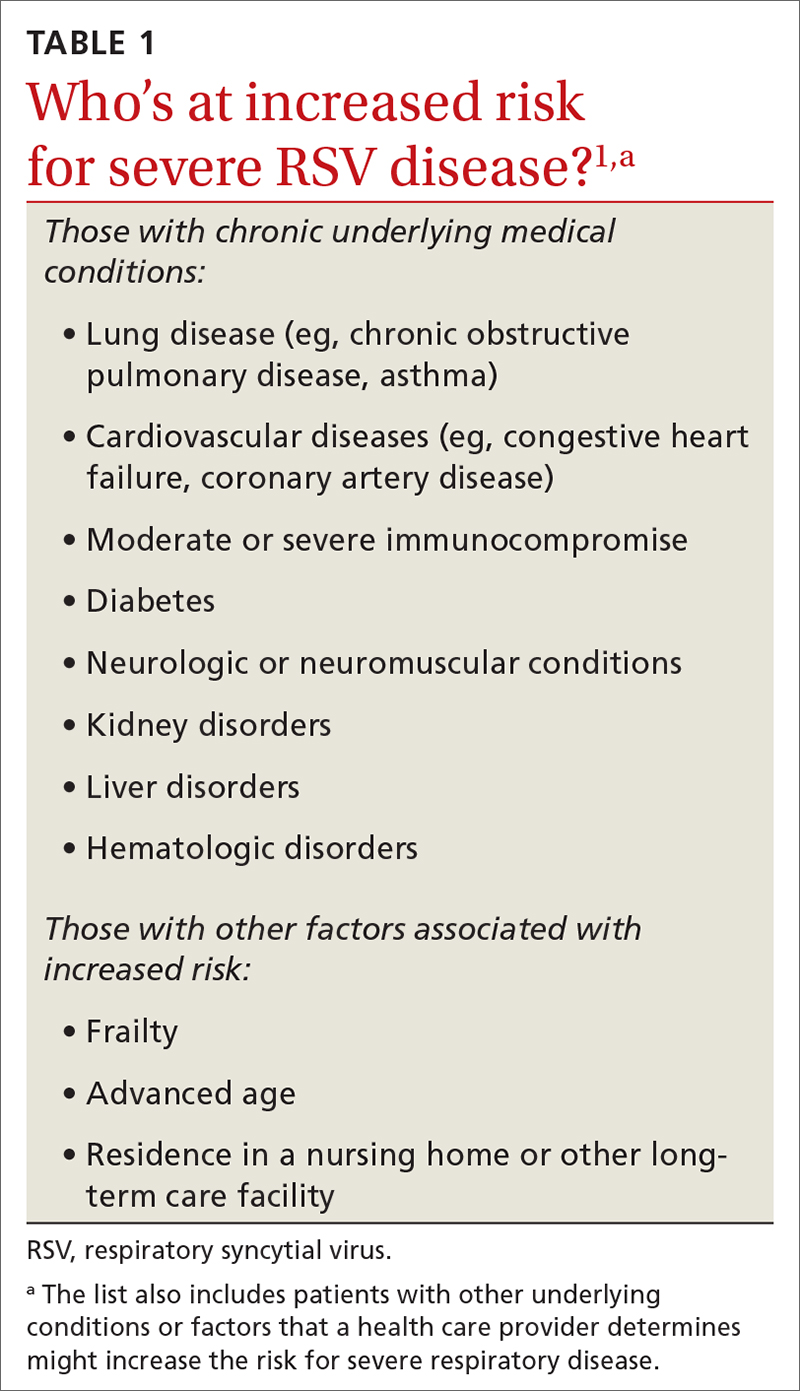
RSV in adults
While there is some uncertainty about the total burden of RSV in adults in the United States, the CDC estimates that each year it causes 0.9 to 1.4 million medical encounters, 60,000 to 160,000 hospitalizations, and 6000 to 10,000 deaths.1 The rate of RSV-caused hospitalization increases with age,2 and the infection is more severe in those with certain chronic medical conditions (TABLE 11). The FIGURE2 demonstrates the outcomes of adults who are hospitalized for RSV. Adults older than 65 years have a 5% mortality rate if hospitalized for RSV infection.2
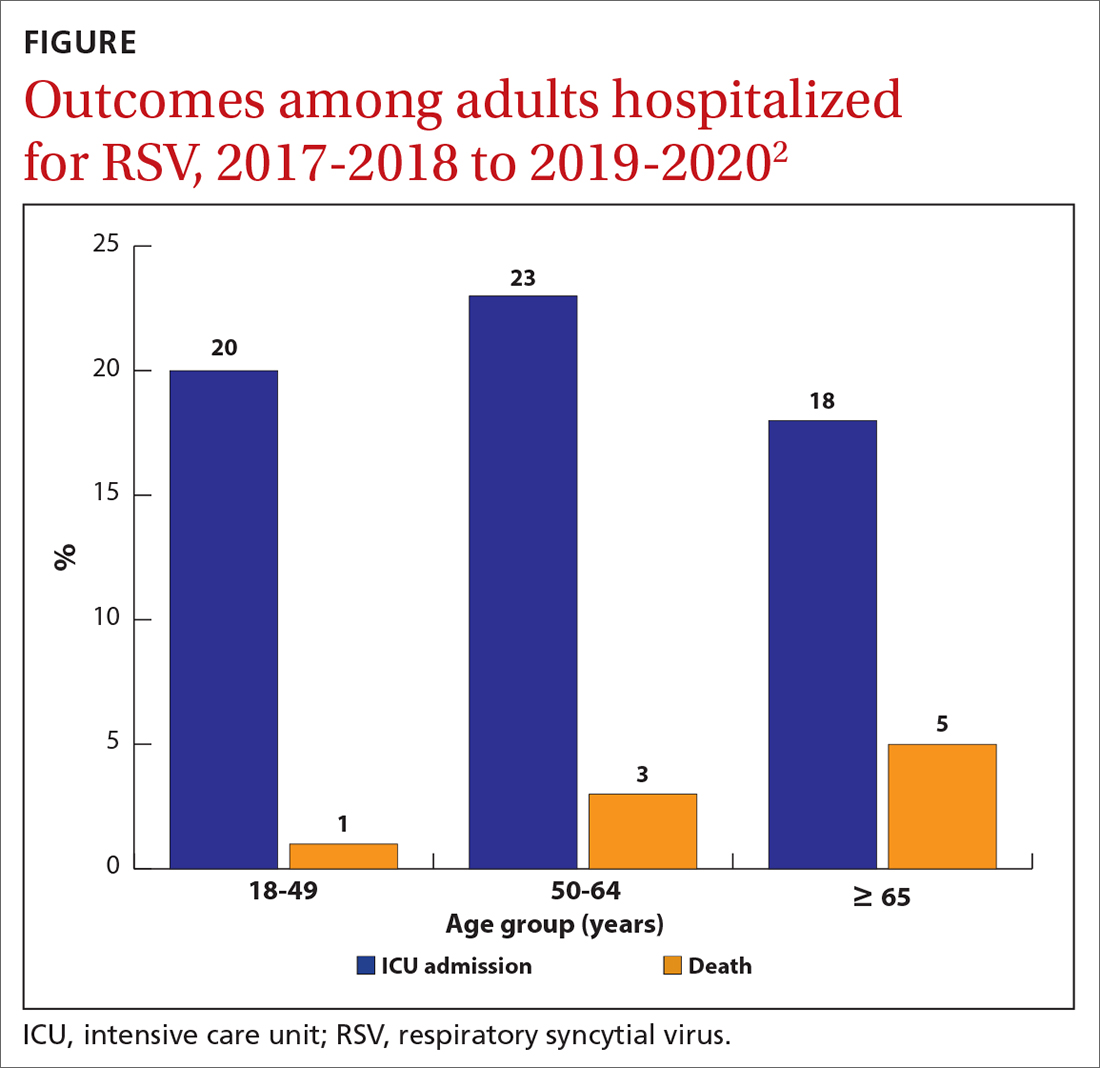
Vaccine options for adults
Two vaccines were recently approved for the prevention of RSV-associated lower respiratory tract disease (LRTD) in those ages 60 years and older: RSVPreF3 (Arexvy, GSK), which is an adjuvanted recombinant F protein vaccine, and RSVpreF (Abrysvo, Pfizer), which is a recombinant stabilized vaccine. Both require only a single dose (0.5 mL IM), which provides protection for 2 years.
The efficacy of the GSK vaccine in preventing laboratory-confirmed, RSV-associated LRTD was 82.6% during the first RSV season and 56.1% during the second season. The efficacy of the Pfizer vaccine in preventing symptomatic, laboratory-confirmed LRTD was 88.9% during the first RSV season and 78.6% during the second season.1 However, the trials leading to licensure of both vaccines were underpowered to show efficacy in the oldest adults and those who are frail or to show efficacy against RSV-caused hospitalization.
Safety of the adult RSV vaccines. The safety trials for both vaccines had a total of 38,177 participants. There were a total of 6 neurologic inflammatory conditions that developed within 42 days of vaccination, including 2 cases of suspected Guillain-Barré syndrome (GBS), 2 cases of possible acute disseminated encephalomyelitis, and 1 case each of chronic inflammatory demyelinating polyneuropathy and undifferentiated motor-sensory axonal polyneuropathy.1 That is a rate of 1 case of a neurologic inflammatory condition for every 6363 people vaccinated. Since the trials were not powered to determine whether the small number of cases were due to chance, postmarketing surveillance will be needed to clarify the true risk for GBS or other neurologic inflammatory events from RSV vaccination.
The lack of efficacy data for the most vulnerable older adults and the lingering questions about safety prompted the ACIP to recommend that adults ages 60 years and older may receive a single dose of RSV vaccine, using shared clinical decision-making—which is different from a routine or risk-based vaccine recommendation. For RSV vaccination, the decision to vaccinate should be based on a risk/benefit discussion between the clinician and the patient. Those most likely to benefit from the vaccine are listed in TABLE 1.1
While data on coadministration of RSV vaccines with other adult vaccines are sparse, the ACIP states that co-administration with other vaccines is acceptable.1 It is not known yet whether boosters will be needed after 2 years.
Continue to: RSV in infants and children
RSV in infants and children
RSV is the most common cause of hospitalization among infants and children in the United States. The CDC estimates that each year in children younger than 5 years, RSV is responsible for 1.5 million outpatient clinic visits, 520,000 emergency department visits, 58,000 to 80,000 hospitalizations, and 100 to 200 deaths.3 The risk for hospitalization from RSV is highest in the second and third months of life and decreases with increasing age.3
There are racial disparities in RSV severity: Intensive care unit admission rates are 1.2 to 1.6 times higher among non-Hispanic Black infants younger than 6 months than among non-Hispanic White infants, and hospitalization rates are up to 5 times higher in American Indian and Alaska Native populations.3
The months of highest RSV transmission in most locations are December through February, but this can vary. For practical purposes, RSV season runs from October through March.
Prevention in infants and children
The monoclonal antibody nirsevimab is now available for use in infants younger than 8 months born during or entering their first RSV season and children ages 8 to 19 months who are at increased risk for severe RSV disease and entering their second RSV season. Details regarding the use of this product were described in a recent Practice Alert Brief.4
Early studies on nirsevimab demonstrated 79% effectiveness in preventing medical-attended LRTD, 80.6% effectiveness in preventing hospitalization, and 90% effectiveness in preventing ICU admission. The number needed to immunize with nirsevimab to prevent an outpatient visit is estimated to be 17; to prevent an ED visit, 48; and to prevent an inpatient admission, 128. Due to the low RSV death rate, the studies were not able to demonstrate reduced mortality.5
Continue to: RSV vaccine in pregnancy
RSV vaccine in pregnancy
In August, the FDA approved Pfizer’s RSVpreF vaccine for use during pregnancy—as a single dose given at 32 to 36 weeks’ gestation—for the prevention of RSV LRTD in infants in the first 6 months of life. In the clinical trials, the vaccine was given at 24 to 36 weeks’ gestation. However, there was a statistically nonsignificant increase in preterm births in the RSVpreF group compared to the placebo group.6 While there were insufficient data to prove or rule out a causal relationship, the FDA advisory committee was more comfortable approving the vaccine for use only later in pregnancy, to avoid the possibility of very early preterm births after vaccination. The ACIP agreed.
From time of maternal vaccination, at least 14 days are needed to develop and transfer maternal antibodies across the placenta to protect the infant. Therefore, infants born less than 14 days after maternal vaccination should be considered unprotected.
Both maternal vaccination with RSVpreF and infant injection with nirsevimab are now options to protect newborns and infants from RSV. However, use of both products is not needed, since combined they do not offer significant added protection compared to either product alone (exceptions to be discussed shortly).6 When the estimated due date will occur in the RSV season, maternity clinicians should provide information on both products and assist the mother in deciding whether to be vaccinated or rely on administration of nirsevimab to the infant after birth. The benefits and risks of these 2 options are listed in TABLE 2.6
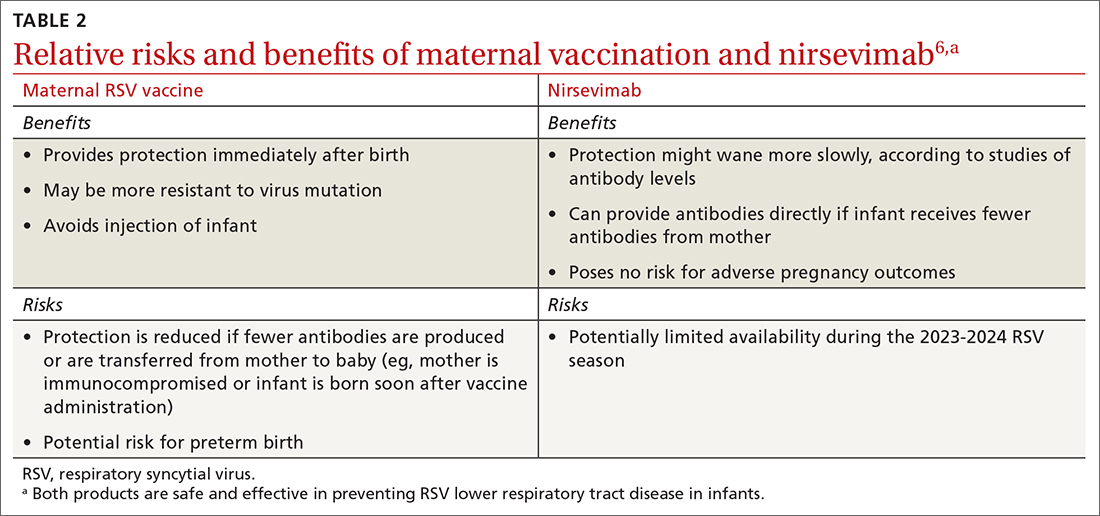
There are some rare situations in which use of both products is recommended, and they include6:
- When the baby is born less than 14 days from the time of maternal vaccination
- When the mother has a condition that could produce an inadequate response to the vaccine
- When the infant has had cardiopulmonary bypass, which would lead to loss of maternal antibodies
- When the infant has severe disease placing them at increased risk for severe RSV.
Conclusion
All of these new RSV preventive products should soon be widely available and covered with no out-of-pocket expense by commercial and government payers. The exception might be nirsevimab—because of the time needed to produce it, it might not be universally available in the 2023-2024 season.
In the past year, there has been significant progress in the availability of interventions to prevent respiratory syncytial virus (RSV) and its complications. Four products have been approved by the US Food and Drug Administration (FDA) and recommended by the Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP). They include 2 vaccines for adults ages 60 years and older, a monoclonal antibody for infants and high-risk children, and a maternal vaccine to prevent RSV infection in newborns.
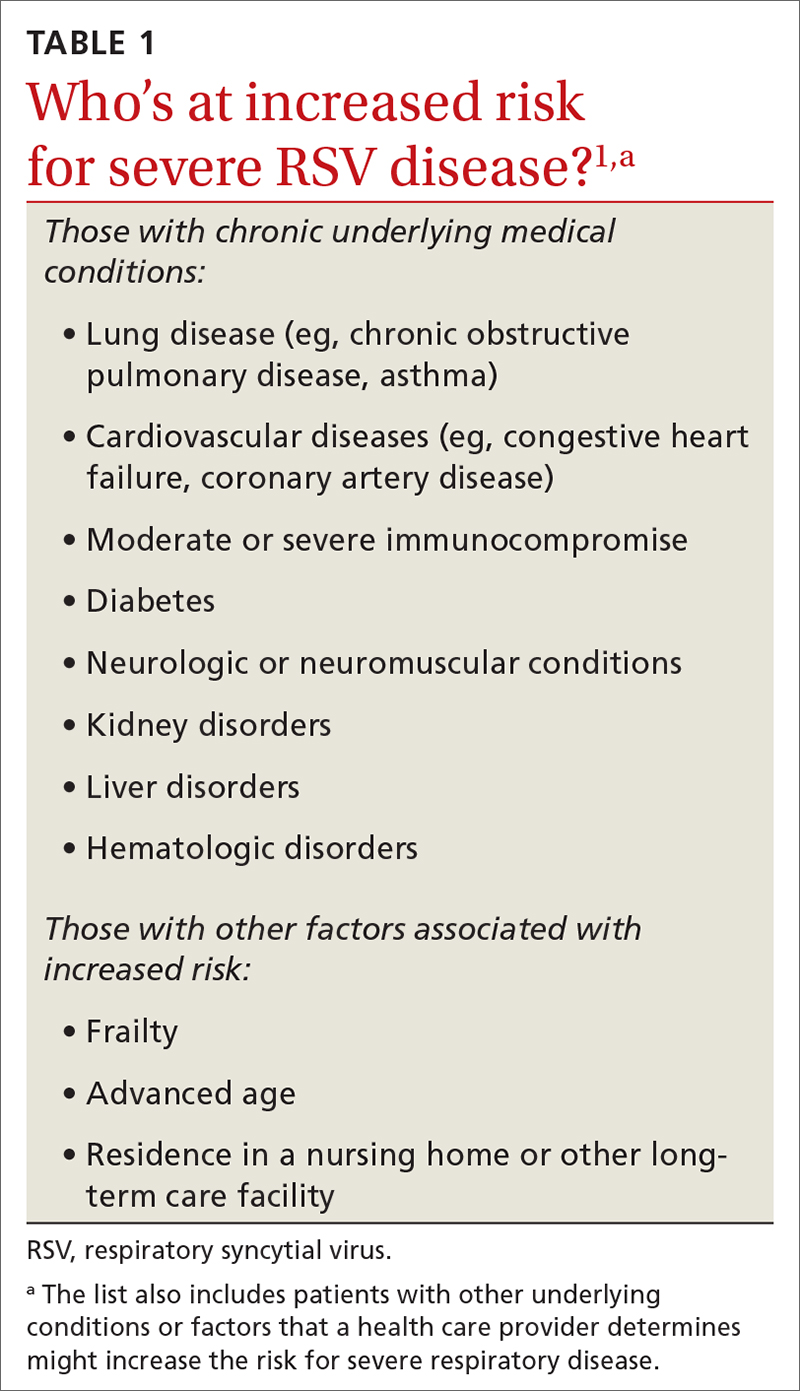
RSV in adults
While there is some uncertainty about the total burden of RSV in adults in the United States, the CDC estimates that each year it causes 0.9 to 1.4 million medical encounters, 60,000 to 160,000 hospitalizations, and 6000 to 10,000 deaths.1 The rate of RSV-caused hospitalization increases with age,2 and the infection is more severe in those with certain chronic medical conditions (TABLE 11). The FIGURE2 demonstrates the outcomes of adults who are hospitalized for RSV. Adults older than 65 years have a 5% mortality rate if hospitalized for RSV infection.2
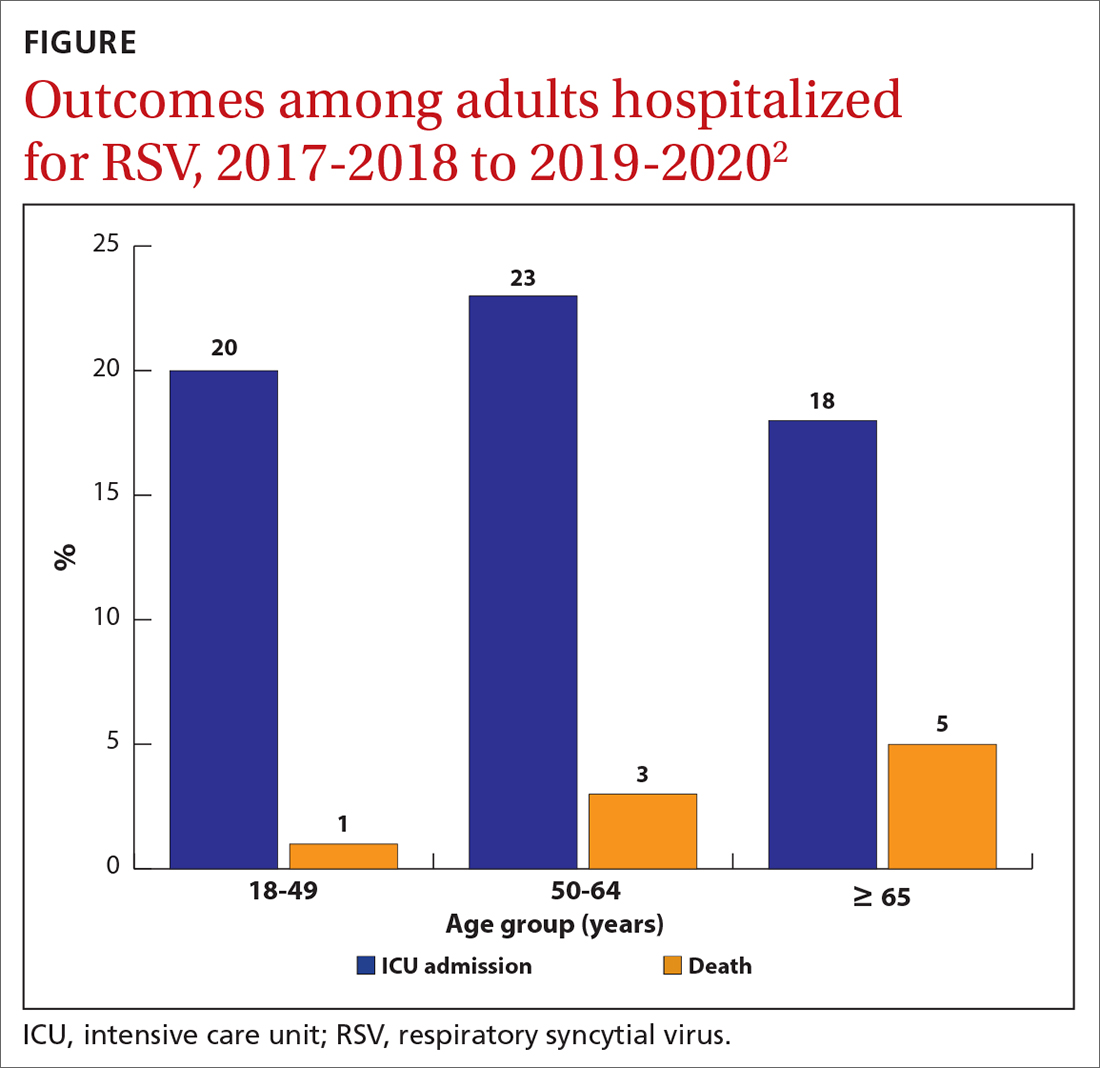
Vaccine options for adults
Two vaccines were recently approved for the prevention of RSV-associated lower respiratory tract disease (LRTD) in those ages 60 years and older: RSVPreF3 (Arexvy, GSK), which is an adjuvanted recombinant F protein vaccine, and RSVpreF (Abrysvo, Pfizer), which is a recombinant stabilized vaccine. Both require only a single dose (0.5 mL IM), which provides protection for 2 years.
The efficacy of the GSK vaccine in preventing laboratory-confirmed, RSV-associated LRTD was 82.6% during the first RSV season and 56.1% during the second season. The efficacy of the Pfizer vaccine in preventing symptomatic, laboratory-confirmed LRTD was 88.9% during the first RSV season and 78.6% during the second season.1 However, the trials leading to licensure of both vaccines were underpowered to show efficacy in the oldest adults and those who are frail or to show efficacy against RSV-caused hospitalization.
Safety of the adult RSV vaccines. The safety trials for both vaccines had a total of 38,177 participants. There were a total of 6 neurologic inflammatory conditions that developed within 42 days of vaccination, including 2 cases of suspected Guillain-Barré syndrome (GBS), 2 cases of possible acute disseminated encephalomyelitis, and 1 case each of chronic inflammatory demyelinating polyneuropathy and undifferentiated motor-sensory axonal polyneuropathy.1 That is a rate of 1 case of a neurologic inflammatory condition for every 6363 people vaccinated. Since the trials were not powered to determine whether the small number of cases were due to chance, postmarketing surveillance will be needed to clarify the true risk for GBS or other neurologic inflammatory events from RSV vaccination.
The lack of efficacy data for the most vulnerable older adults and the lingering questions about safety prompted the ACIP to recommend that adults ages 60 years and older may receive a single dose of RSV vaccine, using shared clinical decision-making—which is different from a routine or risk-based vaccine recommendation. For RSV vaccination, the decision to vaccinate should be based on a risk/benefit discussion between the clinician and the patient. Those most likely to benefit from the vaccine are listed in TABLE 1.1
While data on coadministration of RSV vaccines with other adult vaccines are sparse, the ACIP states that co-administration with other vaccines is acceptable.1 It is not known yet whether boosters will be needed after 2 years.
Continue to: RSV in infants and children
RSV in infants and children
RSV is the most common cause of hospitalization among infants and children in the United States. The CDC estimates that each year in children younger than 5 years, RSV is responsible for 1.5 million outpatient clinic visits, 520,000 emergency department visits, 58,000 to 80,000 hospitalizations, and 100 to 200 deaths.3 The risk for hospitalization from RSV is highest in the second and third months of life and decreases with increasing age.3
There are racial disparities in RSV severity: Intensive care unit admission rates are 1.2 to 1.6 times higher among non-Hispanic Black infants younger than 6 months than among non-Hispanic White infants, and hospitalization rates are up to 5 times higher in American Indian and Alaska Native populations.3
The months of highest RSV transmission in most locations are December through February, but this can vary. For practical purposes, RSV season runs from October through March.
Prevention in infants and children
The monoclonal antibody nirsevimab is now available for use in infants younger than 8 months born during or entering their first RSV season and children ages 8 to 19 months who are at increased risk for severe RSV disease and entering their second RSV season. Details regarding the use of this product were described in a recent Practice Alert Brief.4
Early studies on nirsevimab demonstrated 79% effectiveness in preventing medical-attended LRTD, 80.6% effectiveness in preventing hospitalization, and 90% effectiveness in preventing ICU admission. The number needed to immunize with nirsevimab to prevent an outpatient visit is estimated to be 17; to prevent an ED visit, 48; and to prevent an inpatient admission, 128. Due to the low RSV death rate, the studies were not able to demonstrate reduced mortality.5
Continue to: RSV vaccine in pregnancy
RSV vaccine in pregnancy
In August, the FDA approved Pfizer’s RSVpreF vaccine for use during pregnancy—as a single dose given at 32 to 36 weeks’ gestation—for the prevention of RSV LRTD in infants in the first 6 months of life. In the clinical trials, the vaccine was given at 24 to 36 weeks’ gestation. However, there was a statistically nonsignificant increase in preterm births in the RSVpreF group compared to the placebo group.6 While there were insufficient data to prove or rule out a causal relationship, the FDA advisory committee was more comfortable approving the vaccine for use only later in pregnancy, to avoid the possibility of very early preterm births after vaccination. The ACIP agreed.
From time of maternal vaccination, at least 14 days are needed to develop and transfer maternal antibodies across the placenta to protect the infant. Therefore, infants born less than 14 days after maternal vaccination should be considered unprotected.
Both maternal vaccination with RSVpreF and infant injection with nirsevimab are now options to protect newborns and infants from RSV. However, use of both products is not needed, since combined they do not offer significant added protection compared to either product alone (exceptions to be discussed shortly).6 When the estimated due date will occur in the RSV season, maternity clinicians should provide information on both products and assist the mother in deciding whether to be vaccinated or rely on administration of nirsevimab to the infant after birth. The benefits and risks of these 2 options are listed in TABLE 2.6
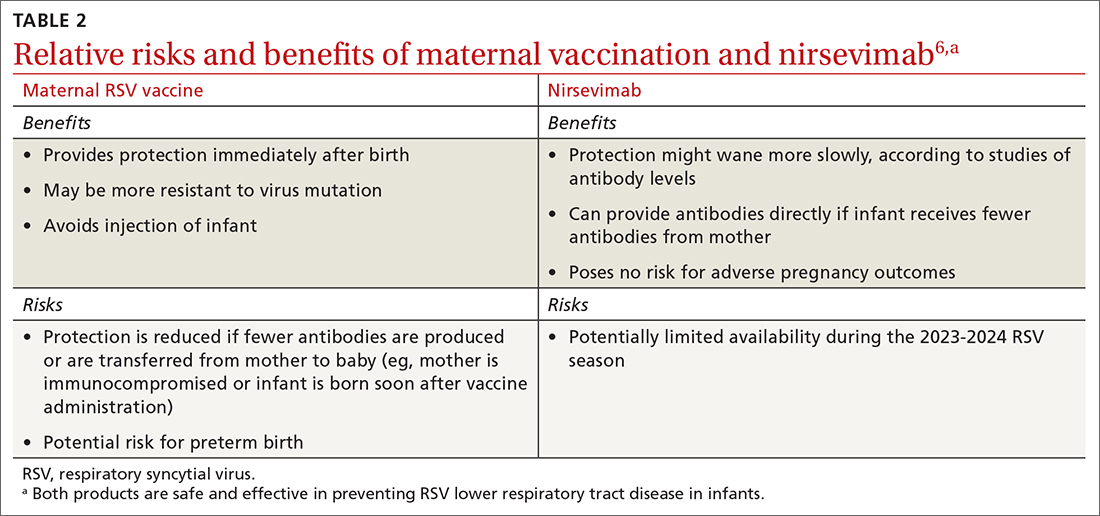
There are some rare situations in which use of both products is recommended, and they include6:
- When the baby is born less than 14 days from the time of maternal vaccination
- When the mother has a condition that could produce an inadequate response to the vaccine
- When the infant has had cardiopulmonary bypass, which would lead to loss of maternal antibodies
- When the infant has severe disease placing them at increased risk for severe RSV.
Conclusion
All of these new RSV preventive products should soon be widely available and covered with no out-of-pocket expense by commercial and government payers. The exception might be nirsevimab—because of the time needed to produce it, it might not be universally available in the 2023-2024 season.
1. Melgar M, Britton A, Roper LE, et al. Use of respiratory syncytial virus vaccine in older adults: recommendation of the Advisory Committee on Immunization Practices—United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:793-801.
2. Melgar M. Evidence to recommendation framework. RSV in adults. Presented to the ACIP on February 23, 2023. Accessed November 7, 2023. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2023-02/slides-02-23/RSV-Adults-04-Melgar-508.pdf
3. Jones JM, Fleming-Dutra KE, Prill MM, et al. Use of nirsevimab for the prevention of respiratory syncytial virus disease among infants and young children: recommendation of the Advisory Committee on Immunization Practices—United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:90-925.
4. Campos-Outcalt D. Are you ready for RSV season? There’s a new preventive option. J Fam Pract. 2023;72. doi: 10.12788/jfp.0663
5. Jones J. Evidence to recommendation framework: nirsevimab updates. Presented to the ACIP on August 3, 2023. Accessed August 23, 2023. https://stacks.cdc.gov/view/cdc/131586
6. Jones J. Clinical considerations for maternal RSVPreF vaccine and nirsevimab. Presented to the ACIP on September 25, 2023. Accessed November 8, 2023. www2.cdc.gov/vaccines/ed/ciinc/archives/23/09/ciiw_RSV2/CIIW%20RSV%20maternal%20vaccine%20mAb%209.27.23.pdf
1. Melgar M, Britton A, Roper LE, et al. Use of respiratory syncytial virus vaccine in older adults: recommendation of the Advisory Committee on Immunization Practices—United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:793-801.
2. Melgar M. Evidence to recommendation framework. RSV in adults. Presented to the ACIP on February 23, 2023. Accessed November 7, 2023. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2023-02/slides-02-23/RSV-Adults-04-Melgar-508.pdf
3. Jones JM, Fleming-Dutra KE, Prill MM, et al. Use of nirsevimab for the prevention of respiratory syncytial virus disease among infants and young children: recommendation of the Advisory Committee on Immunization Practices—United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72:90-925.
4. Campos-Outcalt D. Are you ready for RSV season? There’s a new preventive option. J Fam Pract. 2023;72. doi: 10.12788/jfp.0663
5. Jones J. Evidence to recommendation framework: nirsevimab updates. Presented to the ACIP on August 3, 2023. Accessed August 23, 2023. https://stacks.cdc.gov/view/cdc/131586
6. Jones J. Clinical considerations for maternal RSVPreF vaccine and nirsevimab. Presented to the ACIP on September 25, 2023. Accessed November 8, 2023. www2.cdc.gov/vaccines/ed/ciinc/archives/23/09/ciiw_RSV2/CIIW%20RSV%20maternal%20vaccine%20mAb%209.27.23.pdf
Is low-molecular-weight heparin superior to aspirin for VTE prophylaxis?
ILLUSTRATIVE CASE
A 72-year-old man with well-controlled hypertension and chronic obstructive pulmonary disease is scheduled for right total hip arthroplasty (THA) due to severe arthritis. He will be admitted to the hospital overnight, and his orthopedic surgeon anticipates 2 to 3 days of inpatient recovery time. In addition to medical management of the patient’s comorbid conditions, the surgeon asks if you have any insight regarding VTE prophylaxis for this patient. Specifically, do you think aspirin is equal to LMWH for VTE prophylaxis?
All adults undergoing major orthopedic surgery are considered to be at high risk for postoperative VTE development, with those having lower-limb procedures at highest risk.2 Of the more than 2.2 million THAs and total knee arthroplasties (TKAs) performed in the United States between 2012 and 2020, 55% were primary TKAs and 39% primary THAs.3 The American College of Chest Physicians (ACCP) estimated a baseline 35-day risk for VTE of 4.3% in patients undergoing major orthopedic surgery.4 The highest VTE risk occurs during the first 7 to 14 days post surgery (1.8% for symptomatic deep vein thrombosis [DVT] and 1% for pulmonary embolism [PE]), with a slightly lower risk during the subsequent 15 to 35 days (1% for symptomatic DVT and 0.5% for PE).4
Aspirin’s low cost, availability, and ease of administration make it an attractive choice for VTE prevention in patients post THA and TKA surgery. The Pulmonary Embolism Prevention (PEP) trial evaluated 13,356 patients undergoing hip fracture repair and 4088 patients undergoing arthroplasty and found aspirin to be safe and effective in prevention of VTEs compared with placebo. The investigators concluded that “there is now good evidence for considering aspirin routinely in a wide range of surgical and medical groups at high risk of venous thromboembolism.”5 The PEP study, along with others, led to the emergence of aspirin monotherapy for VTE prophylaxis.
Current guidelines for perioperative VTE prophylaxis are based on American Society of Hematology (ASH) and ACCP recommendations. For patients undergoing THA or TKA, ASH suggests using aspirin or anticoagulants for VTE prophylaxis; when anticoagulants are used, they suggest using a direct oral anticoagulant (DOAC) over LMWH.6 The ASH guidelines are conditional recommendations based on very low certainty of effects, and the ASH panel recognized the need for further investigation with large, high-quality clinical trials.
The ACCP guidelines are clearer in recommending VTE prophylaxis vs no prophylaxis for major orthopedic surgeries and recommend the use of LMWH over other agents, including aspirin, DOACs, warfarin, and intermittent pneumatic compression (IPC) devices.4
Although prophylaxis is widely recommended to mitigate the elevated risk for VTE among patients undergoing orthopedic surgery, aspirin as monotherapy remains controversial.7 Many orthopedic surgeons prescribe aspirin as a sole VTE prophylaxis agent; however, this practice is not well supported by data from large, well-conducted, randomized trials or inferiority trials.2
STUDY SUMMARY
Aspirin did not meet the noninferiority criterion for postoperative VTE
The CRISTAL trial compared the use of aspirin vs LMWH (enoxaparin) for VTE prophylaxis in patients ages 18 years or older undergoing primary THA or TKA for osteoarthritis.1 This Australian study used a cluster-randomized, crossover, registry-nested, noninferiority trial design. Of note, in Australia, aspirin is formulated in 100-mg tablets, equivalent to the standard 81-mg low-dose tablet in the United States.
Continue to: Patients taking prescribed antiplatelet...
Patients taking prescribed antiplatelet medication for preexisting conditions (~20% of patients in each group) were allowed to continue antiplatelet therapy during the trial. Patients were excluded if they were receiving an anticoagulant prior to their procedure or had a medical contraindication to aspirin or enoxaparin.
Thirty-one hospital sites were randomly assigned a treatment protocol using either aspirin or enoxaparin. Once target patient enrollment was met with the initial assigned medication, the site switched to the second/other agent. This resulted in 5675 patients in the aspirin group and 4036 in the enoxaparin group enrolled between April 2019 and December 2020, with final follow-up in August 2021; of these, 259 in the aspirin group and 249 in the enoxaparin group were lost to follow-up, opted out, or died.
The aspirin group was given 100 mg PO daily and the enoxaparin group was given 40 mg SC daily (20 mg daily for patients weighing < 50 kg or with an estimated glomerular filtration rate < 30 mL/min/1.73 m2) for 35 days after THA and 14 days after TKA. Both treatment groups received IPC calf devices intraoperatively and postoperatively, and mobilization was offered on postoperative Day 0 or 1.
The primary outcome—development of symptomatic VTE within 90 days of the procedure—occurred in 187 (3.5%) patients in the aspirin group and 69 (1.8%) patients in the enoxaparin group (estimated difference = 1.97%; 95% CI, 0.54%-3.41%). This did not meet the noninferiority criterion for aspirin, based on an estimated assumed rate of 2% and a noninferiority margin of 1%, and in fact was statistically superior for enoxaparin (P = .007). There were no significant differences between the 2 groups in major bleeding or death within 90 days.1
WHAT’S NEW
Enoxaparin was significantly superior to aspirin for VTE prophylaxis
Although this study was designed as a noninferiority trial, analysis showed enoxaparin to be significantly superior for postoperative VTE prophylaxis compared with aspirin.
Continue to: CAVEATS
CAVEATS
Study aspirin dosing differed from US standard
This study showed significantly lower rates of symptomatic VTE in the enoxaparin group compared with the aspirin group; however, the majority of this difference was driven by rates of below-the-knee DVTs, which are clinically less relevant.8 Also, this trial used a 100-mg aspirin formulation, which is not available in the United States.
CHALLENGES TO IMPLEMENTATION
Aspirin is far cheaper and administered orally
Aspirin is significantly cheaper than enoxaparin, costing about $0.13 per dose (~$4 for 30 tablets at the 81-mg dose) vs roughly $9 per 40 mg/0.4 mL dose for enoxaparin.9 However, a cost-effectiveness analysis may be useful to determine (for example) whether the higher cost of enoxaparin may be offset by fewer DVTs and other sequelae. Lastly, LMWH is an injection, which some patients may refuse.
1. CRISTAL Study Group; Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA. 2022;328:719-727. doi: 10.1001/jama.2022.13416
2. Douketis JD, Mithoowani S. Prevention of venous thromboembolism in adults undergoing hip fracture repair or hip or knee replacement. UpToDate. Updated January 25, 2023. Accessed May 24, 2023. www.uptodate.com/contents/prevention-of-venous-thromboembolism-in-adults-undergoing-hip-fracture-repair-or-hip-or-knee-replacement
3. Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American Joint Replacement Registry annual report. Arthroplast Today. 2022;13:205-207. doi: 10.1016/j.artd.2022.01.020
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S-e325S. doi: 10.1378/chest.11-2404
5. Pulmonary Embolism Prevention (PEP) trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. doi: 10.1016/S0140-6736(00)02110-3
6. Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898-3944. doi: 10.1182/bloodadvances.2019000975
7. Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2020;180:376-384. doi: 10.1001/jamainternmed.2019.6108
8. Brett AS, Friedman RJ. Aspirin vs. enoxaparin for prophylaxis after hip or knee replacement. NEJM Journal Watch. September 15, 2022. Accessed May 24, 2023. www.jwatch.org/na55272/2022/09/15/aspirin-vs-enoxaparin-prophylaxis-after-hip-or-knee
9. Enoxaparin. GoodRx. Accessed August 7, 2023. www.goodrx.com/enoxaparin
ILLUSTRATIVE CASE
A 72-year-old man with well-controlled hypertension and chronic obstructive pulmonary disease is scheduled for right total hip arthroplasty (THA) due to severe arthritis. He will be admitted to the hospital overnight, and his orthopedic surgeon anticipates 2 to 3 days of inpatient recovery time. In addition to medical management of the patient’s comorbid conditions, the surgeon asks if you have any insight regarding VTE prophylaxis for this patient. Specifically, do you think aspirin is equal to LMWH for VTE prophylaxis?
All adults undergoing major orthopedic surgery are considered to be at high risk for postoperative VTE development, with those having lower-limb procedures at highest risk.2 Of the more than 2.2 million THAs and total knee arthroplasties (TKAs) performed in the United States between 2012 and 2020, 55% were primary TKAs and 39% primary THAs.3 The American College of Chest Physicians (ACCP) estimated a baseline 35-day risk for VTE of 4.3% in patients undergoing major orthopedic surgery.4 The highest VTE risk occurs during the first 7 to 14 days post surgery (1.8% for symptomatic deep vein thrombosis [DVT] and 1% for pulmonary embolism [PE]), with a slightly lower risk during the subsequent 15 to 35 days (1% for symptomatic DVT and 0.5% for PE).4
Aspirin’s low cost, availability, and ease of administration make it an attractive choice for VTE prevention in patients post THA and TKA surgery. The Pulmonary Embolism Prevention (PEP) trial evaluated 13,356 patients undergoing hip fracture repair and 4088 patients undergoing arthroplasty and found aspirin to be safe and effective in prevention of VTEs compared with placebo. The investigators concluded that “there is now good evidence for considering aspirin routinely in a wide range of surgical and medical groups at high risk of venous thromboembolism.”5 The PEP study, along with others, led to the emergence of aspirin monotherapy for VTE prophylaxis.
Current guidelines for perioperative VTE prophylaxis are based on American Society of Hematology (ASH) and ACCP recommendations. For patients undergoing THA or TKA, ASH suggests using aspirin or anticoagulants for VTE prophylaxis; when anticoagulants are used, they suggest using a direct oral anticoagulant (DOAC) over LMWH.6 The ASH guidelines are conditional recommendations based on very low certainty of effects, and the ASH panel recognized the need for further investigation with large, high-quality clinical trials.
The ACCP guidelines are clearer in recommending VTE prophylaxis vs no prophylaxis for major orthopedic surgeries and recommend the use of LMWH over other agents, including aspirin, DOACs, warfarin, and intermittent pneumatic compression (IPC) devices.4
Although prophylaxis is widely recommended to mitigate the elevated risk for VTE among patients undergoing orthopedic surgery, aspirin as monotherapy remains controversial.7 Many orthopedic surgeons prescribe aspirin as a sole VTE prophylaxis agent; however, this practice is not well supported by data from large, well-conducted, randomized trials or inferiority trials.2
STUDY SUMMARY
Aspirin did not meet the noninferiority criterion for postoperative VTE
The CRISTAL trial compared the use of aspirin vs LMWH (enoxaparin) for VTE prophylaxis in patients ages 18 years or older undergoing primary THA or TKA for osteoarthritis.1 This Australian study used a cluster-randomized, crossover, registry-nested, noninferiority trial design. Of note, in Australia, aspirin is formulated in 100-mg tablets, equivalent to the standard 81-mg low-dose tablet in the United States.
Continue to: Patients taking prescribed antiplatelet...
Patients taking prescribed antiplatelet medication for preexisting conditions (~20% of patients in each group) were allowed to continue antiplatelet therapy during the trial. Patients were excluded if they were receiving an anticoagulant prior to their procedure or had a medical contraindication to aspirin or enoxaparin.
Thirty-one hospital sites were randomly assigned a treatment protocol using either aspirin or enoxaparin. Once target patient enrollment was met with the initial assigned medication, the site switched to the second/other agent. This resulted in 5675 patients in the aspirin group and 4036 in the enoxaparin group enrolled between April 2019 and December 2020, with final follow-up in August 2021; of these, 259 in the aspirin group and 249 in the enoxaparin group were lost to follow-up, opted out, or died.
The aspirin group was given 100 mg PO daily and the enoxaparin group was given 40 mg SC daily (20 mg daily for patients weighing < 50 kg or with an estimated glomerular filtration rate < 30 mL/min/1.73 m2) for 35 days after THA and 14 days after TKA. Both treatment groups received IPC calf devices intraoperatively and postoperatively, and mobilization was offered on postoperative Day 0 or 1.
The primary outcome—development of symptomatic VTE within 90 days of the procedure—occurred in 187 (3.5%) patients in the aspirin group and 69 (1.8%) patients in the enoxaparin group (estimated difference = 1.97%; 95% CI, 0.54%-3.41%). This did not meet the noninferiority criterion for aspirin, based on an estimated assumed rate of 2% and a noninferiority margin of 1%, and in fact was statistically superior for enoxaparin (P = .007). There were no significant differences between the 2 groups in major bleeding or death within 90 days.1
WHAT’S NEW
Enoxaparin was significantly superior to aspirin for VTE prophylaxis
Although this study was designed as a noninferiority trial, analysis showed enoxaparin to be significantly superior for postoperative VTE prophylaxis compared with aspirin.
Continue to: CAVEATS
CAVEATS
Study aspirin dosing differed from US standard
This study showed significantly lower rates of symptomatic VTE in the enoxaparin group compared with the aspirin group; however, the majority of this difference was driven by rates of below-the-knee DVTs, which are clinically less relevant.8 Also, this trial used a 100-mg aspirin formulation, which is not available in the United States.
CHALLENGES TO IMPLEMENTATION
Aspirin is far cheaper and administered orally
Aspirin is significantly cheaper than enoxaparin, costing about $0.13 per dose (~$4 for 30 tablets at the 81-mg dose) vs roughly $9 per 40 mg/0.4 mL dose for enoxaparin.9 However, a cost-effectiveness analysis may be useful to determine (for example) whether the higher cost of enoxaparin may be offset by fewer DVTs and other sequelae. Lastly, LMWH is an injection, which some patients may refuse.
ILLUSTRATIVE CASE
A 72-year-old man with well-controlled hypertension and chronic obstructive pulmonary disease is scheduled for right total hip arthroplasty (THA) due to severe arthritis. He will be admitted to the hospital overnight, and his orthopedic surgeon anticipates 2 to 3 days of inpatient recovery time. In addition to medical management of the patient’s comorbid conditions, the surgeon asks if you have any insight regarding VTE prophylaxis for this patient. Specifically, do you think aspirin is equal to LMWH for VTE prophylaxis?
All adults undergoing major orthopedic surgery are considered to be at high risk for postoperative VTE development, with those having lower-limb procedures at highest risk.2 Of the more than 2.2 million THAs and total knee arthroplasties (TKAs) performed in the United States between 2012 and 2020, 55% were primary TKAs and 39% primary THAs.3 The American College of Chest Physicians (ACCP) estimated a baseline 35-day risk for VTE of 4.3% in patients undergoing major orthopedic surgery.4 The highest VTE risk occurs during the first 7 to 14 days post surgery (1.8% for symptomatic deep vein thrombosis [DVT] and 1% for pulmonary embolism [PE]), with a slightly lower risk during the subsequent 15 to 35 days (1% for symptomatic DVT and 0.5% for PE).4
Aspirin’s low cost, availability, and ease of administration make it an attractive choice for VTE prevention in patients post THA and TKA surgery. The Pulmonary Embolism Prevention (PEP) trial evaluated 13,356 patients undergoing hip fracture repair and 4088 patients undergoing arthroplasty and found aspirin to be safe and effective in prevention of VTEs compared with placebo. The investigators concluded that “there is now good evidence for considering aspirin routinely in a wide range of surgical and medical groups at high risk of venous thromboembolism.”5 The PEP study, along with others, led to the emergence of aspirin monotherapy for VTE prophylaxis.
Current guidelines for perioperative VTE prophylaxis are based on American Society of Hematology (ASH) and ACCP recommendations. For patients undergoing THA or TKA, ASH suggests using aspirin or anticoagulants for VTE prophylaxis; when anticoagulants are used, they suggest using a direct oral anticoagulant (DOAC) over LMWH.6 The ASH guidelines are conditional recommendations based on very low certainty of effects, and the ASH panel recognized the need for further investigation with large, high-quality clinical trials.
The ACCP guidelines are clearer in recommending VTE prophylaxis vs no prophylaxis for major orthopedic surgeries and recommend the use of LMWH over other agents, including aspirin, DOACs, warfarin, and intermittent pneumatic compression (IPC) devices.4
Although prophylaxis is widely recommended to mitigate the elevated risk for VTE among patients undergoing orthopedic surgery, aspirin as monotherapy remains controversial.7 Many orthopedic surgeons prescribe aspirin as a sole VTE prophylaxis agent; however, this practice is not well supported by data from large, well-conducted, randomized trials or inferiority trials.2
STUDY SUMMARY
Aspirin did not meet the noninferiority criterion for postoperative VTE
The CRISTAL trial compared the use of aspirin vs LMWH (enoxaparin) for VTE prophylaxis in patients ages 18 years or older undergoing primary THA or TKA for osteoarthritis.1 This Australian study used a cluster-randomized, crossover, registry-nested, noninferiority trial design. Of note, in Australia, aspirin is formulated in 100-mg tablets, equivalent to the standard 81-mg low-dose tablet in the United States.
Continue to: Patients taking prescribed antiplatelet...
Patients taking prescribed antiplatelet medication for preexisting conditions (~20% of patients in each group) were allowed to continue antiplatelet therapy during the trial. Patients were excluded if they were receiving an anticoagulant prior to their procedure or had a medical contraindication to aspirin or enoxaparin.
Thirty-one hospital sites were randomly assigned a treatment protocol using either aspirin or enoxaparin. Once target patient enrollment was met with the initial assigned medication, the site switched to the second/other agent. This resulted in 5675 patients in the aspirin group and 4036 in the enoxaparin group enrolled between April 2019 and December 2020, with final follow-up in August 2021; of these, 259 in the aspirin group and 249 in the enoxaparin group were lost to follow-up, opted out, or died.
The aspirin group was given 100 mg PO daily and the enoxaparin group was given 40 mg SC daily (20 mg daily for patients weighing < 50 kg or with an estimated glomerular filtration rate < 30 mL/min/1.73 m2) for 35 days after THA and 14 days after TKA. Both treatment groups received IPC calf devices intraoperatively and postoperatively, and mobilization was offered on postoperative Day 0 or 1.
The primary outcome—development of symptomatic VTE within 90 days of the procedure—occurred in 187 (3.5%) patients in the aspirin group and 69 (1.8%) patients in the enoxaparin group (estimated difference = 1.97%; 95% CI, 0.54%-3.41%). This did not meet the noninferiority criterion for aspirin, based on an estimated assumed rate of 2% and a noninferiority margin of 1%, and in fact was statistically superior for enoxaparin (P = .007). There were no significant differences between the 2 groups in major bleeding or death within 90 days.1
WHAT’S NEW
Enoxaparin was significantly superior to aspirin for VTE prophylaxis
Although this study was designed as a noninferiority trial, analysis showed enoxaparin to be significantly superior for postoperative VTE prophylaxis compared with aspirin.
Continue to: CAVEATS
CAVEATS
Study aspirin dosing differed from US standard
This study showed significantly lower rates of symptomatic VTE in the enoxaparin group compared with the aspirin group; however, the majority of this difference was driven by rates of below-the-knee DVTs, which are clinically less relevant.8 Also, this trial used a 100-mg aspirin formulation, which is not available in the United States.
CHALLENGES TO IMPLEMENTATION
Aspirin is far cheaper and administered orally
Aspirin is significantly cheaper than enoxaparin, costing about $0.13 per dose (~$4 for 30 tablets at the 81-mg dose) vs roughly $9 per 40 mg/0.4 mL dose for enoxaparin.9 However, a cost-effectiveness analysis may be useful to determine (for example) whether the higher cost of enoxaparin may be offset by fewer DVTs and other sequelae. Lastly, LMWH is an injection, which some patients may refuse.
1. CRISTAL Study Group; Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA. 2022;328:719-727. doi: 10.1001/jama.2022.13416
2. Douketis JD, Mithoowani S. Prevention of venous thromboembolism in adults undergoing hip fracture repair or hip or knee replacement. UpToDate. Updated January 25, 2023. Accessed May 24, 2023. www.uptodate.com/contents/prevention-of-venous-thromboembolism-in-adults-undergoing-hip-fracture-repair-or-hip-or-knee-replacement
3. Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American Joint Replacement Registry annual report. Arthroplast Today. 2022;13:205-207. doi: 10.1016/j.artd.2022.01.020
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S-e325S. doi: 10.1378/chest.11-2404
5. Pulmonary Embolism Prevention (PEP) trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. doi: 10.1016/S0140-6736(00)02110-3
6. Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898-3944. doi: 10.1182/bloodadvances.2019000975
7. Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2020;180:376-384. doi: 10.1001/jamainternmed.2019.6108
8. Brett AS, Friedman RJ. Aspirin vs. enoxaparin for prophylaxis after hip or knee replacement. NEJM Journal Watch. September 15, 2022. Accessed May 24, 2023. www.jwatch.org/na55272/2022/09/15/aspirin-vs-enoxaparin-prophylaxis-after-hip-or-knee
9. Enoxaparin. GoodRx. Accessed August 7, 2023. www.goodrx.com/enoxaparin
1. CRISTAL Study Group; Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA. 2022;328:719-727. doi: 10.1001/jama.2022.13416
2. Douketis JD, Mithoowani S. Prevention of venous thromboembolism in adults undergoing hip fracture repair or hip or knee replacement. UpToDate. Updated January 25, 2023. Accessed May 24, 2023. www.uptodate.com/contents/prevention-of-venous-thromboembolism-in-adults-undergoing-hip-fracture-repair-or-hip-or-knee-replacement
3. Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American Joint Replacement Registry annual report. Arthroplast Today. 2022;13:205-207. doi: 10.1016/j.artd.2022.01.020
4. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 suppl):e278S-e325S. doi: 10.1378/chest.11-2404
5. Pulmonary Embolism Prevention (PEP) trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. doi: 10.1016/S0140-6736(00)02110-3
6. Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898-3944. doi: 10.1182/bloodadvances.2019000975
7. Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2020;180:376-384. doi: 10.1001/jamainternmed.2019.6108
8. Brett AS, Friedman RJ. Aspirin vs. enoxaparin for prophylaxis after hip or knee replacement. NEJM Journal Watch. September 15, 2022. Accessed May 24, 2023. www.jwatch.org/na55272/2022/09/15/aspirin-vs-enoxaparin-prophylaxis-after-hip-or-knee
9. Enoxaparin. GoodRx. Accessed August 7, 2023. www.goodrx.com/enoxaparin
PRACTICE CHANGER
Consider low-molecular-weight heparin (LMWH) rather than aspirin to prevent postoperative venous thromboembolism (VTE) in patients undergoing total hip or knee arthroplasty for osteoarthritis.
STRENGTH OF RECOMMENDATION
B: Based on a single cluster-randomized crossover trial.1
Does taking BP medicine at night (vs morning) result in fewer cardiovascular events?
Evidence summary
Recent UK study shows no difference by timing
A 2022 UK prospective, randomized, multicenter trial assigned 21,104 predominantly White adults (58% men) with hypertension to take their usual antihypertensive medication either in the morning (6
All patient baseline characteristics were equivalent between groups. If troubled by nocturia, patients in the evening group taking diuretics were told to take only the diuretic earlier (6
The median follow-up was 5.2 years. Data were collected at regular intervals through patient completion of online questionnaires and researcher analysis of National Health Service data on hospitalization and death. The intention-to-treat analysis showed no difference in the primary outcome (a composite of vascular death, nonfatal myocardial infarction, or nonfatal stroke) between the evening and morning administration groups (0.69 events vs 0.72 events per 100 person-years; hazard ratio [HR] = 0.95; 95% CI, 0.83-1.10; P = .53).
The controversial Hygia Project favored evening
Prior to the UK study was the Hygia Chronotherapy Trial, a prospective, controlled, multicenter study conducted within the primary care setting in Spain. Caucasian Spanish adults (N = 19,168; mean age, 61 years; 56% men) with hypertension were randomly assigned to take all prescribed antihypertensive medication either at bedtime or upon waking.2
The Hygia Project initially sought to establish the value of ambulatory blood pressure monitoring (ABPM) compared to office blood pressure (BP) monitoring and to explore the prognostic value of sleeping BP.3 The study objectives evolved over time. The randomization process was not clearly described,2,3 but multiple randomizations were alluded to. The authors stated that “for any of these chronotherapy trials” randomizations were done separately for “each participating center” and “randomization of participants to treatment-time regimen is done separately for each hypertension medication or combination being tested.”
The baseline characteristics of patients in the evening and morning administration groups were similar, but statistically significant differences existed in BMI (29.6 vs 29.7; P = .030) and sleep-time systolic BP percent decline (9.3 vs 9.0; P < .001). Mean baseline 48-hour BP was 132/77 mm Hg. Hypertension was defined as an awake systolic BP ≥
Prescribers were free to prescribe medicines from 5 classes (diuretic, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, calcium channel blocker, or beta-blocker) as they thought appropriate, were encouraged to use fixed-dose combination pills, and were told not to use split (eg, twice per day) dosing. Annual 48-hour ABPM was completed, and patients’ electronic health records were analyzed by blinded investigators. Median follow-up was 6.3 years, and only 84 participants failed to complete the minimum 1-year participation requirement.
Continue to: The primary outcome...
The primary outcome—a composite of cardiovascular death, myocardial infarction, coronary revascularization, heart failure, or stroke—occurred in 1752 patients, favoring the bedtime group (HR = 0.55; 95% CI, 0.50-0.61; P < .001). The calculated number of events was 1130 in the morning administration group and 622 in the evening administration group; the authors did not explicitly report the event numbers in each group. Each component of the composite outcome also favored evening administration (P < .001 for all): cardiovascular death (HR = 0.44; 95% CI, 0.34-0.56), myocardial infarction (HR = 0.66; 95% CI, 0.52-0.84), coronary revascularization (HR = 0.60; 95% CI, 0.47-0.75), heart failure (HR = 0.58; 95% CI, 0.49-0.70), and stroke (HR = 0.51; 95% CI, 0.41-0.63).
The complicated, layered study design and randomization methods limit the ability to critically appraise the study.
Smaller Spanish study also supported evening administration
A prior, smaller, prospective randomized trial conducted by the same researchers as the Hygia Project found even greater benefits to evening BP medication administration.4 The 2156 Spanish patients (52% men; average age, 55 years) from multiple primary care offices were randomized 1:1 to BP medication administration either upon awakening or at bedtime. Dozens of baseline characteristics were evenly distributed except for age (55.0 vs 56.3; P = .021) and creatinine (0.96 vs 0.98; P = .028), both of which were lower in the evening group.
After a median follow-up of 5.6 years, the bedtime group had significantly lower total events (187 events in the morning group vs 68 in the evening group; relative risk [RR] = 0.39; 95% CI, 0.29-0.51; P < .001). Individual cardiovascular outcomes also dramatically favored the evening group: total deaths (12 vs 28; P = .008), cardiovascular deaths (3 vs 14; P = .006), cardiovascular disease events (30 vs 74; P < .001), stroke (7 vs 24; P = .001), and heart failure (8 vs 33; P < .001).
Limits of both the UK trial and the Hygia Project trial included single countries of study with a lack of racial and ethnic diversity, and greater nonadherence to the evening administration of the medications.
Recommendations from others
A 2022 consensus statement from the International Society of Hypertension, published before the UK trial, recommended against bedtime dosing until more high-quality data became available. They pointed to evidence showing higher medication adherence with morning dosing, risk for asleep BP dropping, and worsening daytime BP control as reasons to continue morning administration.5 Other reviewers have questioned the Hygia Project results due to their reported implausibly large effects on cardiovascular outcomes, noting that independent attempts to verify the methods and the data have proven challenging and are not completed.6
Editor’s takeaway
I confess that I was swayed by the results of the Hygia Project; for a year or so, I advised my patients to take at least 1 BP pill at night. But after the UK study came out, I needed to reconsider. I began to worry that the great outcomes of nocturnal therapy may have been a mirage. I have returned to counseling patients to take their BP medications in whichever way fosters consistency while minimizing adverse effects for them.
1. Mackenzie IS, Rogers A, Poulter NR, et al; TIME Study Group. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial. Lancet. 2022;400:1417-1425. doi: 10.1016/S0140-6736(22)01786-X
2. Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al; Hygia Project Investigators. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2020;41:4565-4576. doi: 10.1093/eurheartj/ehz754
3. Hermida RC. Sleep-time ambulatory blood pressure as a prognostic marker of vascular and other risks and therapeutic target for prevention by hypertension chronotherapy: rationale and design of the Hygia Project. Chronobiol Int. 2016;33:906-936. doi: 10.1080/07420528.2016.1181078
4. Hermida RC, Ayala DE, Mojón A, et al. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629-1651. doi: 10.3109/07420528.2010.510230
5. Stergiou G, Brunström M, MacDonald T, et al. Bedtime dosing of antihypertensive medications: systematic review and consensus statement: International Society of Hypertension position paper endorsed by World Hypertension League and European Society of Hypertension. J Hypertens. 2022;40:1847-1858. doi: 10.1097/HJH.0000000000003240
6. Brunström M, Kjeldsen SE, Kreutz R, et al. Missing verification of source data in hypertension research: The HYGIA PROJECT in Perspective. Hypertension. 2021;78:555-558. doi: 10.1161/HYPERTENSIONAHA.121.17356
Evidence summary
Recent UK study shows no difference by timing
A 2022 UK prospective, randomized, multicenter trial assigned 21,104 predominantly White adults (58% men) with hypertension to take their usual antihypertensive medication either in the morning (6
All patient baseline characteristics were equivalent between groups. If troubled by nocturia, patients in the evening group taking diuretics were told to take only the diuretic earlier (6
The median follow-up was 5.2 years. Data were collected at regular intervals through patient completion of online questionnaires and researcher analysis of National Health Service data on hospitalization and death. The intention-to-treat analysis showed no difference in the primary outcome (a composite of vascular death, nonfatal myocardial infarction, or nonfatal stroke) between the evening and morning administration groups (0.69 events vs 0.72 events per 100 person-years; hazard ratio [HR] = 0.95; 95% CI, 0.83-1.10; P = .53).
The controversial Hygia Project favored evening
Prior to the UK study was the Hygia Chronotherapy Trial, a prospective, controlled, multicenter study conducted within the primary care setting in Spain. Caucasian Spanish adults (N = 19,168; mean age, 61 years; 56% men) with hypertension were randomly assigned to take all prescribed antihypertensive medication either at bedtime or upon waking.2
The Hygia Project initially sought to establish the value of ambulatory blood pressure monitoring (ABPM) compared to office blood pressure (BP) monitoring and to explore the prognostic value of sleeping BP.3 The study objectives evolved over time. The randomization process was not clearly described,2,3 but multiple randomizations were alluded to. The authors stated that “for any of these chronotherapy trials” randomizations were done separately for “each participating center” and “randomization of participants to treatment-time regimen is done separately for each hypertension medication or combination being tested.”
The baseline characteristics of patients in the evening and morning administration groups were similar, but statistically significant differences existed in BMI (29.6 vs 29.7; P = .030) and sleep-time systolic BP percent decline (9.3 vs 9.0; P < .001). Mean baseline 48-hour BP was 132/77 mm Hg. Hypertension was defined as an awake systolic BP ≥
Prescribers were free to prescribe medicines from 5 classes (diuretic, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, calcium channel blocker, or beta-blocker) as they thought appropriate, were encouraged to use fixed-dose combination pills, and were told not to use split (eg, twice per day) dosing. Annual 48-hour ABPM was completed, and patients’ electronic health records were analyzed by blinded investigators. Median follow-up was 6.3 years, and only 84 participants failed to complete the minimum 1-year participation requirement.
Continue to: The primary outcome...
The primary outcome—a composite of cardiovascular death, myocardial infarction, coronary revascularization, heart failure, or stroke—occurred in 1752 patients, favoring the bedtime group (HR = 0.55; 95% CI, 0.50-0.61; P < .001). The calculated number of events was 1130 in the morning administration group and 622 in the evening administration group; the authors did not explicitly report the event numbers in each group. Each component of the composite outcome also favored evening administration (P < .001 for all): cardiovascular death (HR = 0.44; 95% CI, 0.34-0.56), myocardial infarction (HR = 0.66; 95% CI, 0.52-0.84), coronary revascularization (HR = 0.60; 95% CI, 0.47-0.75), heart failure (HR = 0.58; 95% CI, 0.49-0.70), and stroke (HR = 0.51; 95% CI, 0.41-0.63).
The complicated, layered study design and randomization methods limit the ability to critically appraise the study.
Smaller Spanish study also supported evening administration
A prior, smaller, prospective randomized trial conducted by the same researchers as the Hygia Project found even greater benefits to evening BP medication administration.4 The 2156 Spanish patients (52% men; average age, 55 years) from multiple primary care offices were randomized 1:1 to BP medication administration either upon awakening or at bedtime. Dozens of baseline characteristics were evenly distributed except for age (55.0 vs 56.3; P = .021) and creatinine (0.96 vs 0.98; P = .028), both of which were lower in the evening group.
After a median follow-up of 5.6 years, the bedtime group had significantly lower total events (187 events in the morning group vs 68 in the evening group; relative risk [RR] = 0.39; 95% CI, 0.29-0.51; P < .001). Individual cardiovascular outcomes also dramatically favored the evening group: total deaths (12 vs 28; P = .008), cardiovascular deaths (3 vs 14; P = .006), cardiovascular disease events (30 vs 74; P < .001), stroke (7 vs 24; P = .001), and heart failure (8 vs 33; P < .001).
Limits of both the UK trial and the Hygia Project trial included single countries of study with a lack of racial and ethnic diversity, and greater nonadherence to the evening administration of the medications.
Recommendations from others
A 2022 consensus statement from the International Society of Hypertension, published before the UK trial, recommended against bedtime dosing until more high-quality data became available. They pointed to evidence showing higher medication adherence with morning dosing, risk for asleep BP dropping, and worsening daytime BP control as reasons to continue morning administration.5 Other reviewers have questioned the Hygia Project results due to their reported implausibly large effects on cardiovascular outcomes, noting that independent attempts to verify the methods and the data have proven challenging and are not completed.6
Editor’s takeaway
I confess that I was swayed by the results of the Hygia Project; for a year or so, I advised my patients to take at least 1 BP pill at night. But after the UK study came out, I needed to reconsider. I began to worry that the great outcomes of nocturnal therapy may have been a mirage. I have returned to counseling patients to take their BP medications in whichever way fosters consistency while minimizing adverse effects for them.
Evidence summary
Recent UK study shows no difference by timing
A 2022 UK prospective, randomized, multicenter trial assigned 21,104 predominantly White adults (58% men) with hypertension to take their usual antihypertensive medication either in the morning (6
All patient baseline characteristics were equivalent between groups. If troubled by nocturia, patients in the evening group taking diuretics were told to take only the diuretic earlier (6
The median follow-up was 5.2 years. Data were collected at regular intervals through patient completion of online questionnaires and researcher analysis of National Health Service data on hospitalization and death. The intention-to-treat analysis showed no difference in the primary outcome (a composite of vascular death, nonfatal myocardial infarction, or nonfatal stroke) between the evening and morning administration groups (0.69 events vs 0.72 events per 100 person-years; hazard ratio [HR] = 0.95; 95% CI, 0.83-1.10; P = .53).
The controversial Hygia Project favored evening
Prior to the UK study was the Hygia Chronotherapy Trial, a prospective, controlled, multicenter study conducted within the primary care setting in Spain. Caucasian Spanish adults (N = 19,168; mean age, 61 years; 56% men) with hypertension were randomly assigned to take all prescribed antihypertensive medication either at bedtime or upon waking.2
The Hygia Project initially sought to establish the value of ambulatory blood pressure monitoring (ABPM) compared to office blood pressure (BP) monitoring and to explore the prognostic value of sleeping BP.3 The study objectives evolved over time. The randomization process was not clearly described,2,3 but multiple randomizations were alluded to. The authors stated that “for any of these chronotherapy trials” randomizations were done separately for “each participating center” and “randomization of participants to treatment-time regimen is done separately for each hypertension medication or combination being tested.”
The baseline characteristics of patients in the evening and morning administration groups were similar, but statistically significant differences existed in BMI (29.6 vs 29.7; P = .030) and sleep-time systolic BP percent decline (9.3 vs 9.0; P < .001). Mean baseline 48-hour BP was 132/77 mm Hg. Hypertension was defined as an awake systolic BP ≥
Prescribers were free to prescribe medicines from 5 classes (diuretic, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, calcium channel blocker, or beta-blocker) as they thought appropriate, were encouraged to use fixed-dose combination pills, and were told not to use split (eg, twice per day) dosing. Annual 48-hour ABPM was completed, and patients’ electronic health records were analyzed by blinded investigators. Median follow-up was 6.3 years, and only 84 participants failed to complete the minimum 1-year participation requirement.
Continue to: The primary outcome...
The primary outcome—a composite of cardiovascular death, myocardial infarction, coronary revascularization, heart failure, or stroke—occurred in 1752 patients, favoring the bedtime group (HR = 0.55; 95% CI, 0.50-0.61; P < .001). The calculated number of events was 1130 in the morning administration group and 622 in the evening administration group; the authors did not explicitly report the event numbers in each group. Each component of the composite outcome also favored evening administration (P < .001 for all): cardiovascular death (HR = 0.44; 95% CI, 0.34-0.56), myocardial infarction (HR = 0.66; 95% CI, 0.52-0.84), coronary revascularization (HR = 0.60; 95% CI, 0.47-0.75), heart failure (HR = 0.58; 95% CI, 0.49-0.70), and stroke (HR = 0.51; 95% CI, 0.41-0.63).
The complicated, layered study design and randomization methods limit the ability to critically appraise the study.
Smaller Spanish study also supported evening administration
A prior, smaller, prospective randomized trial conducted by the same researchers as the Hygia Project found even greater benefits to evening BP medication administration.4 The 2156 Spanish patients (52% men; average age, 55 years) from multiple primary care offices were randomized 1:1 to BP medication administration either upon awakening or at bedtime. Dozens of baseline characteristics were evenly distributed except for age (55.0 vs 56.3; P = .021) and creatinine (0.96 vs 0.98; P = .028), both of which were lower in the evening group.
After a median follow-up of 5.6 years, the bedtime group had significantly lower total events (187 events in the morning group vs 68 in the evening group; relative risk [RR] = 0.39; 95% CI, 0.29-0.51; P < .001). Individual cardiovascular outcomes also dramatically favored the evening group: total deaths (12 vs 28; P = .008), cardiovascular deaths (3 vs 14; P = .006), cardiovascular disease events (30 vs 74; P < .001), stroke (7 vs 24; P = .001), and heart failure (8 vs 33; P < .001).
Limits of both the UK trial and the Hygia Project trial included single countries of study with a lack of racial and ethnic diversity, and greater nonadherence to the evening administration of the medications.
Recommendations from others
A 2022 consensus statement from the International Society of Hypertension, published before the UK trial, recommended against bedtime dosing until more high-quality data became available. They pointed to evidence showing higher medication adherence with morning dosing, risk for asleep BP dropping, and worsening daytime BP control as reasons to continue morning administration.5 Other reviewers have questioned the Hygia Project results due to their reported implausibly large effects on cardiovascular outcomes, noting that independent attempts to verify the methods and the data have proven challenging and are not completed.6
Editor’s takeaway
I confess that I was swayed by the results of the Hygia Project; for a year or so, I advised my patients to take at least 1 BP pill at night. But after the UK study came out, I needed to reconsider. I began to worry that the great outcomes of nocturnal therapy may have been a mirage. I have returned to counseling patients to take their BP medications in whichever way fosters consistency while minimizing adverse effects for them.
1. Mackenzie IS, Rogers A, Poulter NR, et al; TIME Study Group. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial. Lancet. 2022;400:1417-1425. doi: 10.1016/S0140-6736(22)01786-X
2. Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al; Hygia Project Investigators. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2020;41:4565-4576. doi: 10.1093/eurheartj/ehz754
3. Hermida RC. Sleep-time ambulatory blood pressure as a prognostic marker of vascular and other risks and therapeutic target for prevention by hypertension chronotherapy: rationale and design of the Hygia Project. Chronobiol Int. 2016;33:906-936. doi: 10.1080/07420528.2016.1181078
4. Hermida RC, Ayala DE, Mojón A, et al. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629-1651. doi: 10.3109/07420528.2010.510230
5. Stergiou G, Brunström M, MacDonald T, et al. Bedtime dosing of antihypertensive medications: systematic review and consensus statement: International Society of Hypertension position paper endorsed by World Hypertension League and European Society of Hypertension. J Hypertens. 2022;40:1847-1858. doi: 10.1097/HJH.0000000000003240
6. Brunström M, Kjeldsen SE, Kreutz R, et al. Missing verification of source data in hypertension research: The HYGIA PROJECT in Perspective. Hypertension. 2021;78:555-558. doi: 10.1161/HYPERTENSIONAHA.121.17356
1. Mackenzie IS, Rogers A, Poulter NR, et al; TIME Study Group. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial. Lancet. 2022;400:1417-1425. doi: 10.1016/S0140-6736(22)01786-X
2. Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al; Hygia Project Investigators. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2020;41:4565-4576. doi: 10.1093/eurheartj/ehz754
3. Hermida RC. Sleep-time ambulatory blood pressure as a prognostic marker of vascular and other risks and therapeutic target for prevention by hypertension chronotherapy: rationale and design of the Hygia Project. Chronobiol Int. 2016;33:906-936. doi: 10.1080/07420528.2016.1181078
4. Hermida RC, Ayala DE, Mojón A, et al. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629-1651. doi: 10.3109/07420528.2010.510230
5. Stergiou G, Brunström M, MacDonald T, et al. Bedtime dosing of antihypertensive medications: systematic review and consensus statement: International Society of Hypertension position paper endorsed by World Hypertension League and European Society of Hypertension. J Hypertens. 2022;40:1847-1858. doi: 10.1097/HJH.0000000000003240
6. Brunström M, Kjeldsen SE, Kreutz R, et al. Missing verification of source data in hypertension research: The HYGIA PROJECT in Perspective. Hypertension. 2021;78:555-558. doi: 10.1161/HYPERTENSIONAHA.121.17356
EVIDENCE-BASED ANSWER:
51-year-old woman • history of Graves disease • general fatigue, palpitations, and hand tremors • Dx?
THE CASE
A 51-year-old Japanese woman presented with fever, sore throat, and dyspnea of less than 1 day’s duration. Although she had developed general fatigue, palpitations, and tremors of the hands 2 months earlier, she had not sought medical care.
Her medical history included Graves disease, which had been diagnosed 13 years earlier. She reported that her only medication was methimazole 10 mg/d. She did not have any family history of endocrinopathies or hematologic diseases.
Physical examination revealed a body temperature of 99.7 °F; heart rate, 130 beats/min; blood pressure, 182/62 mm Hg; respiratory rate, 46 breaths/min; and oxygen saturation, 100% on room air. Pharyngeal erythema was seen. Lung sounds were clear. The patient had tremors in her hands, tenderness of the thyroid gland, and exophthalmos. No leg edema or jugular vein distension was seen.
Laboratory tests indicated hyperthyroidism, with a thyroid-stimulating hormone level < 0.01 µIU/mL (normal range, 0.5-5 µIU/mL); free T3 level, 4.87 pg/mL (normal range, 2.3-4.3 pg/mL); and free T4 level, 2.97 ng/dL (normal range, 0.9-1.7 ng/dL). The patient also had a white blood cell (WBC) count of 1020 cells/µL (normal range, 3500-9000 cells/µL) and neutrophil count of 5 cells/µL (normal range, 1500-6500 cells/µL).
Other blood cell counts were normal, and a chest x-ray did not reveal any abnormal findings. In addition, there was no evidence to suggest hematologic malignancies or congenital neutropenia.
THE DIAGNOSIS
Based on the patient’s low WBC and neutrophil counts, agranulocytosis due to antithyroid drug therapy was suspected; however, this diagnosis would be highly unusual in the context of a 13-year history of therapy. Further history taking revealed that, because of her lack of financial means, unstable living conditions, and lack of understanding of the necessity for medication adherence, the patient had not taken methimazole
In consideration of these factors, a diagnosis of exacerbation of hyperthyroidism and agranulocytosis (due to methimazole restart and upper respiratory infection) was made.
Continue to: DISCUSSION
DISCUSSION
Agranulocytosis is a severe adverse event of antithyroid agents and requires prompt diagnosis and treatment. In a 26-year study at one clinic, it occurred in approximately 0.4% of patients taking antithyroid agents.1 The possible mechanisms of agranulocytosis are the direct toxicity of drugs and immune-mediated responses.2 Older age, female sex, and some HLA genotypes are reported to be associated with susceptibility to agranulocytosis.2
Although the development of agranulocytosis tends to be dose related, a small dose of antithyroid agent can sometimes cause the condition.3,4 It usually occurs within the first 3 months of treatment initiation, but occasionally patients develop agranulocytosis after long-term therapy.5 Interruption and subsequent resumption of the same antithyroid drug treatment also can be a risk factor for agranulocytosis, as in this case.5
Treatment includes drug cessation, administration of broad-spectrum antibiotics if infection is suspected, and granulocyte-colony stimulating factor (G-CSF) therapy.5
Our patient was hospitalized, and methimazole was stopped immediately. Administration of potassium iodide 50 mg/d and G-CSF was started. Meropenem 3 g/d also was administered for neutropenic fever.
The patient’s condition improved, and her WBC count increased to 1640 cells/µL on Day 8 and 10,890 cells/µL on Day 9. G-CSF was stopped on Day 12 and meropenem on Day 13. Bone marrow aspiration was not performed because of improvement in lab values and her overall condition. Although monitoring of WBC count during methimazole therapy is controversial,5 we decided to routinely monitor this patient due to the possibility of drug cross-reactivity.
Continue to: Despite repeated explanations...
Despite repeated explanations that it was dangerous for a patient who had developed agranulocytosis to take another antithyroid medication, the patient refused surgical treatment or radioiodine ablation because of her financial situation. (While all Japanese citizens are covered by a national health insurance program, patients ages 6 to 70 years are required to pay approximately 30% of medical and pharmaceutical costs.) On Day 21, potassium iodide was stopped, and propylthiouracil 300 mg/d was administered with careful follow-up. Agranulocytosis did not recur.
Immediate problem solved, but what about the future?
During her hospital stay, the medical team spoke with the patient many times, during which she expressed anxiety about her health conditions and the difficulties that she had experienced in her life. The clinicians acknowledged her concerns and assured the patient of their continuing commitment to her well-being even after discharge. The patient also was advised that she should take her medication as prescribed and that if she had a fever or sore throat, she should stop the medication and seek medical care as soon as possible. The patient accepted the medical team’s advice and expressed hope for the future.
Conversations about medication adherence. In 1 survey, about 60% of patients taking antithyroid drugs were unfamiliar with the symptoms of agranulocytosis.6 To deliver safe and effective treatment and detect conditions such as agranulocytosis at an early stage, clinicians must communicate clearly with patients who have hyperthyroidism, providing sufficient explanation and ensuring understanding on the patient’s part.
Patients may be reluctant to provide the details of medication adherence.7 Although it is common for patients to need services for socioeconomic issues,8 health care professionals sometimes fail to adequately discuss these issues with patients, especially if the patients are marginalized and/or have lower economic status.9 Cases such as ours underscore the importance of improving clinicians’ awareness and sensitivity to patients’ socioeconomic challenges.10,11
Our patient received information about welfare and other government services from a medical social worker during her hospital stay. She also was informed that she could seek assistance from medical social workers in the future if needed.
Continue to: The patient was discharged...
The patient was discharged on Day 28. After discharge, she took propylthiouracil as prescribed (300 mg/d), and her Graves disease was well controlled. Outpatient follow-up visits were performed every 1 or 2 months. No adverse events of propylthiouracil were seen in the ensuing time.
THE TAKEAWAY
Patients with chronic conditions sometimes discontinue medications, and they may not talk about it with their medical team, especially if they have socioeconomic or other difficulties in their lives. Clinicians should consider medication nonadherence and its risk factors when patients with chronic conditions develop unexpected adverse events.
We thank Jane Charbonneau, DVM, from Edanz for doing an English-language review of a draft of this manuscript.
CORRESPONDENCE
Takuya Maejima, MD, Department of General Medicine and Primary Care, University of Tsukuba Hospital, 2-1-1 Amakubo, Tsukuba, Ibaraki 305-8576 Japan; [email protected]
1. Tajiri J, Noguchi S. Antithyroid drug-induced agranulocytosis: special reference to normal white blood cell count agranulocytosis. Thyroid. 2004;14:459-462. doi: 10.1089/105072504323150787
2. Vicente N, Cardoso L, Barros L, et al. Antithyroid drug-induced agranulocytosis: state of the art on diagnosis and management. Drugs R D. 2017;17:91-96. doi: 10.1007/s40268-017-0172-1
3. Takata K, Kubota S, Fukata S, et al. Methimazole-induced agranulocytosis in patients with Graves’ disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid. 2009;19:559-563. doi: 10.1089/thy.2008.0364
4. Tsuboi K, Ueshiba H, Shimojo M, et al. The relation of initial methimazole dose to the incidence of methimazole-induced agranulocytosis in patients with Graves’ disease. Endocr J. 2007;54:39-43. doi: 10.1507/endocrj.k05-068
5. Burch HB, Cooper DS. Management of Graves disease: a review. J Am Med Assoc. 2015;314:2544-2554. doi: 10.1001/jama.2015.16535
6. Robinson J, Richardson M, Hickey J, et al. Patient knowledge of antithyroid drug-induced agranulocytosis. Eur Thyroid J. 2014;3:245-251. doi: https://doi.org/10.1159/000367990
7. Kini V, Ho PM. Interventions to improve medication adherence: a review. J Am Med Assoc. 2018;320:2461-2473. doi: 10.1001/jama.2018.19271
8. Vest JR, Grannis SJ, Haut DP, et al. Using structured and unstructured data to identify patients’ need for services that address the social determinants of health. Int J Med Inform. 2017;107:101-106. doi: 10.1016/j.ijmedinf.2017.09.008
9. Willems S, De Maesschalck S, Deveugele M, et al. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. 2005;56:139-146. doi: 10.1016/j.pec.2004.02.011
10. The College of Family Physicians of Canada. Best advice: social determinants of health. Accessed September 15, 2023. https://patientsmedicalhome.ca/resources/best-advice-guides/best-advice-guide-social-determinants-health/
11. Hunter K, Thomson B. A scoping review of social determinants of health curricula in post-graduate medical education. Can Med Educ J. 2019;10:e61-e71. doi: 10.36834/cmej.61709
THE CASE
A 51-year-old Japanese woman presented with fever, sore throat, and dyspnea of less than 1 day’s duration. Although she had developed general fatigue, palpitations, and tremors of the hands 2 months earlier, she had not sought medical care.
Her medical history included Graves disease, which had been diagnosed 13 years earlier. She reported that her only medication was methimazole 10 mg/d. She did not have any family history of endocrinopathies or hematologic diseases.
Physical examination revealed a body temperature of 99.7 °F; heart rate, 130 beats/min; blood pressure, 182/62 mm Hg; respiratory rate, 46 breaths/min; and oxygen saturation, 100% on room air. Pharyngeal erythema was seen. Lung sounds were clear. The patient had tremors in her hands, tenderness of the thyroid gland, and exophthalmos. No leg edema or jugular vein distension was seen.
Laboratory tests indicated hyperthyroidism, with a thyroid-stimulating hormone level < 0.01 µIU/mL (normal range, 0.5-5 µIU/mL); free T3 level, 4.87 pg/mL (normal range, 2.3-4.3 pg/mL); and free T4 level, 2.97 ng/dL (normal range, 0.9-1.7 ng/dL). The patient also had a white blood cell (WBC) count of 1020 cells/µL (normal range, 3500-9000 cells/µL) and neutrophil count of 5 cells/µL (normal range, 1500-6500 cells/µL).
Other blood cell counts were normal, and a chest x-ray did not reveal any abnormal findings. In addition, there was no evidence to suggest hematologic malignancies or congenital neutropenia.
THE DIAGNOSIS
Based on the patient’s low WBC and neutrophil counts, agranulocytosis due to antithyroid drug therapy was suspected; however, this diagnosis would be highly unusual in the context of a 13-year history of therapy. Further history taking revealed that, because of her lack of financial means, unstable living conditions, and lack of understanding of the necessity for medication adherence, the patient had not taken methimazole
In consideration of these factors, a diagnosis of exacerbation of hyperthyroidism and agranulocytosis (due to methimazole restart and upper respiratory infection) was made.
Continue to: DISCUSSION
DISCUSSION
Agranulocytosis is a severe adverse event of antithyroid agents and requires prompt diagnosis and treatment. In a 26-year study at one clinic, it occurred in approximately 0.4% of patients taking antithyroid agents.1 The possible mechanisms of agranulocytosis are the direct toxicity of drugs and immune-mediated responses.2 Older age, female sex, and some HLA genotypes are reported to be associated with susceptibility to agranulocytosis.2
Although the development of agranulocytosis tends to be dose related, a small dose of antithyroid agent can sometimes cause the condition.3,4 It usually occurs within the first 3 months of treatment initiation, but occasionally patients develop agranulocytosis after long-term therapy.5 Interruption and subsequent resumption of the same antithyroid drug treatment also can be a risk factor for agranulocytosis, as in this case.5
Treatment includes drug cessation, administration of broad-spectrum antibiotics if infection is suspected, and granulocyte-colony stimulating factor (G-CSF) therapy.5
Our patient was hospitalized, and methimazole was stopped immediately. Administration of potassium iodide 50 mg/d and G-CSF was started. Meropenem 3 g/d also was administered for neutropenic fever.
The patient’s condition improved, and her WBC count increased to 1640 cells/µL on Day 8 and 10,890 cells/µL on Day 9. G-CSF was stopped on Day 12 and meropenem on Day 13. Bone marrow aspiration was not performed because of improvement in lab values and her overall condition. Although monitoring of WBC count during methimazole therapy is controversial,5 we decided to routinely monitor this patient due to the possibility of drug cross-reactivity.
Continue to: Despite repeated explanations...
Despite repeated explanations that it was dangerous for a patient who had developed agranulocytosis to take another antithyroid medication, the patient refused surgical treatment or radioiodine ablation because of her financial situation. (While all Japanese citizens are covered by a national health insurance program, patients ages 6 to 70 years are required to pay approximately 30% of medical and pharmaceutical costs.) On Day 21, potassium iodide was stopped, and propylthiouracil 300 mg/d was administered with careful follow-up. Agranulocytosis did not recur.
Immediate problem solved, but what about the future?
During her hospital stay, the medical team spoke with the patient many times, during which she expressed anxiety about her health conditions and the difficulties that she had experienced in her life. The clinicians acknowledged her concerns and assured the patient of their continuing commitment to her well-being even after discharge. The patient also was advised that she should take her medication as prescribed and that if she had a fever or sore throat, she should stop the medication and seek medical care as soon as possible. The patient accepted the medical team’s advice and expressed hope for the future.
Conversations about medication adherence. In 1 survey, about 60% of patients taking antithyroid drugs were unfamiliar with the symptoms of agranulocytosis.6 To deliver safe and effective treatment and detect conditions such as agranulocytosis at an early stage, clinicians must communicate clearly with patients who have hyperthyroidism, providing sufficient explanation and ensuring understanding on the patient’s part.
Patients may be reluctant to provide the details of medication adherence.7 Although it is common for patients to need services for socioeconomic issues,8 health care professionals sometimes fail to adequately discuss these issues with patients, especially if the patients are marginalized and/or have lower economic status.9 Cases such as ours underscore the importance of improving clinicians’ awareness and sensitivity to patients’ socioeconomic challenges.10,11
Our patient received information about welfare and other government services from a medical social worker during her hospital stay. She also was informed that she could seek assistance from medical social workers in the future if needed.
Continue to: The patient was discharged...
The patient was discharged on Day 28. After discharge, she took propylthiouracil as prescribed (300 mg/d), and her Graves disease was well controlled. Outpatient follow-up visits were performed every 1 or 2 months. No adverse events of propylthiouracil were seen in the ensuing time.
THE TAKEAWAY
Patients with chronic conditions sometimes discontinue medications, and they may not talk about it with their medical team, especially if they have socioeconomic or other difficulties in their lives. Clinicians should consider medication nonadherence and its risk factors when patients with chronic conditions develop unexpected adverse events.
We thank Jane Charbonneau, DVM, from Edanz for doing an English-language review of a draft of this manuscript.
CORRESPONDENCE
Takuya Maejima, MD, Department of General Medicine and Primary Care, University of Tsukuba Hospital, 2-1-1 Amakubo, Tsukuba, Ibaraki 305-8576 Japan; [email protected]
THE CASE
A 51-year-old Japanese woman presented with fever, sore throat, and dyspnea of less than 1 day’s duration. Although she had developed general fatigue, palpitations, and tremors of the hands 2 months earlier, she had not sought medical care.
Her medical history included Graves disease, which had been diagnosed 13 years earlier. She reported that her only medication was methimazole 10 mg/d. She did not have any family history of endocrinopathies or hematologic diseases.
Physical examination revealed a body temperature of 99.7 °F; heart rate, 130 beats/min; blood pressure, 182/62 mm Hg; respiratory rate, 46 breaths/min; and oxygen saturation, 100% on room air. Pharyngeal erythema was seen. Lung sounds were clear. The patient had tremors in her hands, tenderness of the thyroid gland, and exophthalmos. No leg edema or jugular vein distension was seen.
Laboratory tests indicated hyperthyroidism, with a thyroid-stimulating hormone level < 0.01 µIU/mL (normal range, 0.5-5 µIU/mL); free T3 level, 4.87 pg/mL (normal range, 2.3-4.3 pg/mL); and free T4 level, 2.97 ng/dL (normal range, 0.9-1.7 ng/dL). The patient also had a white blood cell (WBC) count of 1020 cells/µL (normal range, 3500-9000 cells/µL) and neutrophil count of 5 cells/µL (normal range, 1500-6500 cells/µL).
Other blood cell counts were normal, and a chest x-ray did not reveal any abnormal findings. In addition, there was no evidence to suggest hematologic malignancies or congenital neutropenia.
THE DIAGNOSIS
Based on the patient’s low WBC and neutrophil counts, agranulocytosis due to antithyroid drug therapy was suspected; however, this diagnosis would be highly unusual in the context of a 13-year history of therapy. Further history taking revealed that, because of her lack of financial means, unstable living conditions, and lack of understanding of the necessity for medication adherence, the patient had not taken methimazole
In consideration of these factors, a diagnosis of exacerbation of hyperthyroidism and agranulocytosis (due to methimazole restart and upper respiratory infection) was made.
Continue to: DISCUSSION
DISCUSSION
Agranulocytosis is a severe adverse event of antithyroid agents and requires prompt diagnosis and treatment. In a 26-year study at one clinic, it occurred in approximately 0.4% of patients taking antithyroid agents.1 The possible mechanisms of agranulocytosis are the direct toxicity of drugs and immune-mediated responses.2 Older age, female sex, and some HLA genotypes are reported to be associated with susceptibility to agranulocytosis.2
Although the development of agranulocytosis tends to be dose related, a small dose of antithyroid agent can sometimes cause the condition.3,4 It usually occurs within the first 3 months of treatment initiation, but occasionally patients develop agranulocytosis after long-term therapy.5 Interruption and subsequent resumption of the same antithyroid drug treatment also can be a risk factor for agranulocytosis, as in this case.5
Treatment includes drug cessation, administration of broad-spectrum antibiotics if infection is suspected, and granulocyte-colony stimulating factor (G-CSF) therapy.5
Our patient was hospitalized, and methimazole was stopped immediately. Administration of potassium iodide 50 mg/d and G-CSF was started. Meropenem 3 g/d also was administered for neutropenic fever.
The patient’s condition improved, and her WBC count increased to 1640 cells/µL on Day 8 and 10,890 cells/µL on Day 9. G-CSF was stopped on Day 12 and meropenem on Day 13. Bone marrow aspiration was not performed because of improvement in lab values and her overall condition. Although monitoring of WBC count during methimazole therapy is controversial,5 we decided to routinely monitor this patient due to the possibility of drug cross-reactivity.
Continue to: Despite repeated explanations...
Despite repeated explanations that it was dangerous for a patient who had developed agranulocytosis to take another antithyroid medication, the patient refused surgical treatment or radioiodine ablation because of her financial situation. (While all Japanese citizens are covered by a national health insurance program, patients ages 6 to 70 years are required to pay approximately 30% of medical and pharmaceutical costs.) On Day 21, potassium iodide was stopped, and propylthiouracil 300 mg/d was administered with careful follow-up. Agranulocytosis did not recur.
Immediate problem solved, but what about the future?
During her hospital stay, the medical team spoke with the patient many times, during which she expressed anxiety about her health conditions and the difficulties that she had experienced in her life. The clinicians acknowledged her concerns and assured the patient of their continuing commitment to her well-being even after discharge. The patient also was advised that she should take her medication as prescribed and that if she had a fever or sore throat, she should stop the medication and seek medical care as soon as possible. The patient accepted the medical team’s advice and expressed hope for the future.
Conversations about medication adherence. In 1 survey, about 60% of patients taking antithyroid drugs were unfamiliar with the symptoms of agranulocytosis.6 To deliver safe and effective treatment and detect conditions such as agranulocytosis at an early stage, clinicians must communicate clearly with patients who have hyperthyroidism, providing sufficient explanation and ensuring understanding on the patient’s part.
Patients may be reluctant to provide the details of medication adherence.7 Although it is common for patients to need services for socioeconomic issues,8 health care professionals sometimes fail to adequately discuss these issues with patients, especially if the patients are marginalized and/or have lower economic status.9 Cases such as ours underscore the importance of improving clinicians’ awareness and sensitivity to patients’ socioeconomic challenges.10,11
Our patient received information about welfare and other government services from a medical social worker during her hospital stay. She also was informed that she could seek assistance from medical social workers in the future if needed.
Continue to: The patient was discharged...
The patient was discharged on Day 28. After discharge, she took propylthiouracil as prescribed (300 mg/d), and her Graves disease was well controlled. Outpatient follow-up visits were performed every 1 or 2 months. No adverse events of propylthiouracil were seen in the ensuing time.
THE TAKEAWAY
Patients with chronic conditions sometimes discontinue medications, and they may not talk about it with their medical team, especially if they have socioeconomic or other difficulties in their lives. Clinicians should consider medication nonadherence and its risk factors when patients with chronic conditions develop unexpected adverse events.
We thank Jane Charbonneau, DVM, from Edanz for doing an English-language review of a draft of this manuscript.
CORRESPONDENCE
Takuya Maejima, MD, Department of General Medicine and Primary Care, University of Tsukuba Hospital, 2-1-1 Amakubo, Tsukuba, Ibaraki 305-8576 Japan; [email protected]
1. Tajiri J, Noguchi S. Antithyroid drug-induced agranulocytosis: special reference to normal white blood cell count agranulocytosis. Thyroid. 2004;14:459-462. doi: 10.1089/105072504323150787
2. Vicente N, Cardoso L, Barros L, et al. Antithyroid drug-induced agranulocytosis: state of the art on diagnosis and management. Drugs R D. 2017;17:91-96. doi: 10.1007/s40268-017-0172-1
3. Takata K, Kubota S, Fukata S, et al. Methimazole-induced agranulocytosis in patients with Graves’ disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid. 2009;19:559-563. doi: 10.1089/thy.2008.0364
4. Tsuboi K, Ueshiba H, Shimojo M, et al. The relation of initial methimazole dose to the incidence of methimazole-induced agranulocytosis in patients with Graves’ disease. Endocr J. 2007;54:39-43. doi: 10.1507/endocrj.k05-068
5. Burch HB, Cooper DS. Management of Graves disease: a review. J Am Med Assoc. 2015;314:2544-2554. doi: 10.1001/jama.2015.16535
6. Robinson J, Richardson M, Hickey J, et al. Patient knowledge of antithyroid drug-induced agranulocytosis. Eur Thyroid J. 2014;3:245-251. doi: https://doi.org/10.1159/000367990
7. Kini V, Ho PM. Interventions to improve medication adherence: a review. J Am Med Assoc. 2018;320:2461-2473. doi: 10.1001/jama.2018.19271
8. Vest JR, Grannis SJ, Haut DP, et al. Using structured and unstructured data to identify patients’ need for services that address the social determinants of health. Int J Med Inform. 2017;107:101-106. doi: 10.1016/j.ijmedinf.2017.09.008
9. Willems S, De Maesschalck S, Deveugele M, et al. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. 2005;56:139-146. doi: 10.1016/j.pec.2004.02.011
10. The College of Family Physicians of Canada. Best advice: social determinants of health. Accessed September 15, 2023. https://patientsmedicalhome.ca/resources/best-advice-guides/best-advice-guide-social-determinants-health/
11. Hunter K, Thomson B. A scoping review of social determinants of health curricula in post-graduate medical education. Can Med Educ J. 2019;10:e61-e71. doi: 10.36834/cmej.61709
1. Tajiri J, Noguchi S. Antithyroid drug-induced agranulocytosis: special reference to normal white blood cell count agranulocytosis. Thyroid. 2004;14:459-462. doi: 10.1089/105072504323150787
2. Vicente N, Cardoso L, Barros L, et al. Antithyroid drug-induced agranulocytosis: state of the art on diagnosis and management. Drugs R D. 2017;17:91-96. doi: 10.1007/s40268-017-0172-1
3. Takata K, Kubota S, Fukata S, et al. Methimazole-induced agranulocytosis in patients with Graves’ disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid. 2009;19:559-563. doi: 10.1089/thy.2008.0364
4. Tsuboi K, Ueshiba H, Shimojo M, et al. The relation of initial methimazole dose to the incidence of methimazole-induced agranulocytosis in patients with Graves’ disease. Endocr J. 2007;54:39-43. doi: 10.1507/endocrj.k05-068
5. Burch HB, Cooper DS. Management of Graves disease: a review. J Am Med Assoc. 2015;314:2544-2554. doi: 10.1001/jama.2015.16535
6. Robinson J, Richardson M, Hickey J, et al. Patient knowledge of antithyroid drug-induced agranulocytosis. Eur Thyroid J. 2014;3:245-251. doi: https://doi.org/10.1159/000367990
7. Kini V, Ho PM. Interventions to improve medication adherence: a review. J Am Med Assoc. 2018;320:2461-2473. doi: 10.1001/jama.2018.19271
8. Vest JR, Grannis SJ, Haut DP, et al. Using structured and unstructured data to identify patients’ need for services that address the social determinants of health. Int J Med Inform. 2017;107:101-106. doi: 10.1016/j.ijmedinf.2017.09.008
9. Willems S, De Maesschalck S, Deveugele M, et al. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. 2005;56:139-146. doi: 10.1016/j.pec.2004.02.011
10. The College of Family Physicians of Canada. Best advice: social determinants of health. Accessed September 15, 2023. https://patientsmedicalhome.ca/resources/best-advice-guides/best-advice-guide-social-determinants-health/
11. Hunter K, Thomson B. A scoping review of social determinants of health curricula in post-graduate medical education. Can Med Educ J. 2019;10:e61-e71. doi: 10.36834/cmej.61709
► History of Graves disease
► General fatigue, palpitations, and hand tremors
Getting PrEP to the patients who need it
More than 1.2 million Americans are living with HIV, and more than 30,000 new cases are diagnosed each year. While total incidence has declined since 2016, HIV remains a nationwide epidemic.1
Medications that prevent HIV acquisition, termed preexposure prophylaxis (PrEP), are an important tool to initiate in the primary care setting to reduce HIV transmission. However, while there are an estimated 1.2 million people eligible for PrEP, only 36% have received PrEP prescriptions.2 Several barriers that have impeded its widespread adoption include a lack of clinician knowledge and clinical resources for testing, high medication costs, and stigma around sexual health and intravenous (IV) drug use.
The value of PrEP
PrEP is chemoprophylaxis against the acquisition of HIV infection through the administration of an oral or injectable medication to people at risk for HIV. This practice began in the early 2000s, with the first oral regimen approved in 2012, and since has become an important tool in preventing HIV transmission.
When taken as prescribed, PrEP medications reduce the risk for acquiring HIV through sex by approximately 99% and can reduce the risk for acquiring HIV from injection drug use by approximately 74%.3 The US Preventive Services Task Force issued a Grade “A” recommendation to offer PrEP to people at high risk for HIV acquisition in June 2019 and reaffirmed it in a 2023 update.4
PrEP is notably distinct from postexposure prophylaxis (PEP), which is the administration of medication to prevent HIV infection after a possible exposure.
The available regimens
Regimens for PrEP include oral tablets or intramuscular (IM) injections.5 There are 3 PrEP regimens approved by the US Food and Drug Administration (FDA): tenofovir disoproxil fumarate/emtricitabine (Truvada), tenofovir alafenamide/emtricitabine (Descovy), and cabotegravir (Apretude).
Truvada is once-daily oral PrEP that was approved in 2012 and is now available in a generic formulation. Notable adverse effects of Truvada include a small negative impact on renal function and small reductions in bone mineral density; these have been noted in individual trials, but in meta-analyses such differences were not found to be statistically significant.6-8 The most common adverse effects of Truvada, experienced by up to 6% of patients, are gastrointestinal symptoms, fatigue, headache/dizziness, depression, and insomnia; most symptoms resolve within weeks.
Continue to: Descovy
Descovy is daily oral PrEP that was approved in 2019. Descovy is associated with increases in LDL and triglycerides but has less impact on renal and bone health.9 The most common adverse effect of Descovy, experienced by about 5% of patients, is diarrhea, followed by nausea.
Apretude was approved in 2021 and is a 600-mg IM injection given monthly for 2 months, then every 2 months (± 7 days). The advantages of Apretude are frequency and discreteness of dosing and the ability to use in patients with estimated creatinine clearance (eCrCl) > 15 mL/min. The most common adverse effects of Apretude are injection-site reactions, which occur in 30% to 80% of patients but are rarely significant enough to lead to discontinuation (< 2% of patients discontinue use due to injection-site reactions).10
Who should take PrEP?
The latest Centers for Disease Control and Prevention (CDC) guidelines recommend that all sexually active adults receive information about PrEP.5 Indications for PrEP are broad and summarized in the FIGURE.5
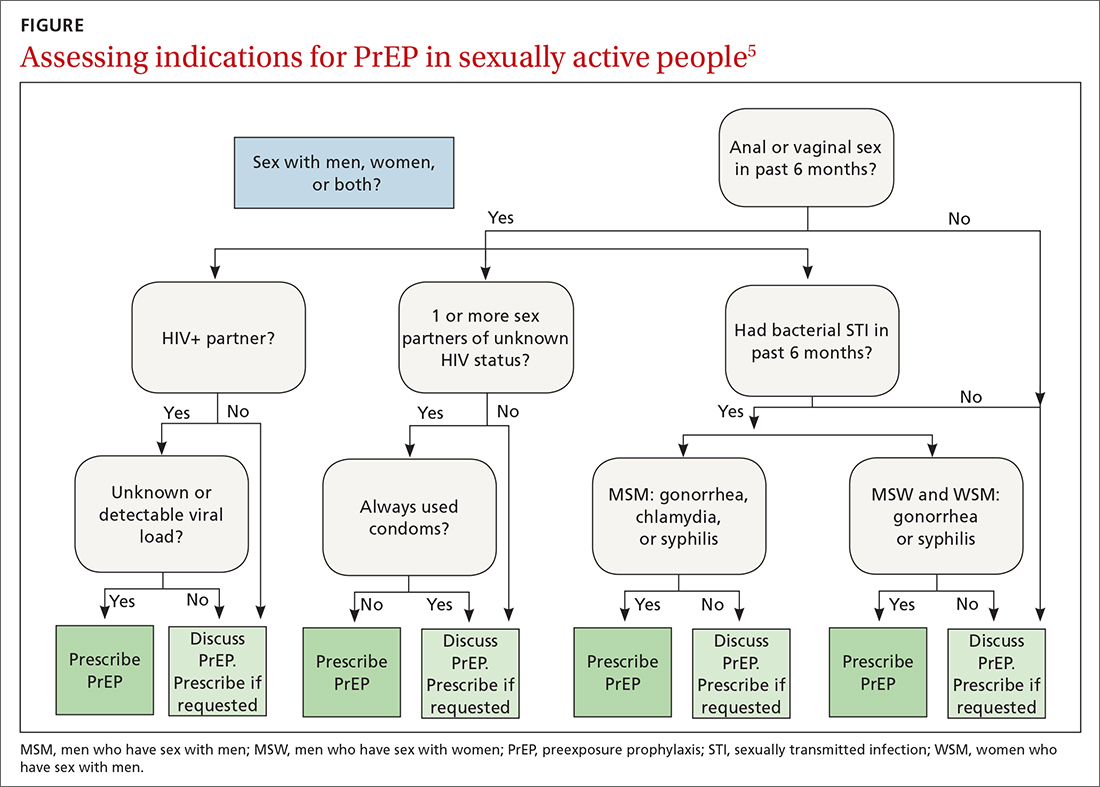
PrEP is indicated in patients who report sexual or injection drug use behaviors that place them at substantial ongoing risk for HIV exposure. Specific indications include patients with sexual partner(s) with unknown HIV status with whom they have inconsistent or no condom use, a history of bacterial sexually transmitted infection (STI) in the past 6 months, an HIV-positive sexual partner, or the sharing of injection drug equipment.
Hepatitis B infection is not a contraindication for PrEP use, but knowledge of infection status is essential. All current oral medications used for PrEP have activity against hepatitis B. Incomplete adherence to or abrupt discontinuation of oral PrEP could precipitate a hepatitis B flare. Hepatitis B surface antigen should be tested at the time of PrEP initiation, although PrEP can begin while testing is in process.
Continue to: How to use PrEP
How to use PrEP
At PrEP initiation, acute or chronic HIV infection must be excluded with a documented negative HIV antigen/antibody test within 1 week of prescribing PrEP.5 The CDC guidelines provide an updated HIV testing algorithm (www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf, p 30-31, Figures 4a and 4b), which considers whether patients have received PrEP recently.
Patients with recent high-risk exposures or symptoms of acute HIV at the time of desired PrEP initiation should have an HIV-1 viral load checked with negative results before PrEP is prescribed. Additional criteria for PrEP include weight > 35 kg; screening for hepatitis B virus infection; screening for drug interactions; and drug-specific eCrCl cutoffs of > 60 mL/min for Truvada, > 30 mL/min for Descovy, and > 15 mL/min for Apretude.5
Studies regarding time to medication effectiveness are limited. Pharmacokinetic studies of Truvada demonstrate sufficient drug concentrations should be present in peripheral blood mononuclear cells and rectal tissue within 7 days of initiation of oral dosing and around 20 days in vaginal tissue.
Of note, while expedited partner therapy is used as a harm-reduction strategy to treat the sexual partners of patients diagnosed with certain STIs, PrEP is not recommended to be used in this way.
Ongoing monitoring with PrEP. Once oral PrEP is started, STI risk assessment and HIV testing via 4th generation antibody/antigen test should be completed at least every 3 months. PrEP oral prescription refills should be limited to 3 months. For patients receiving IM PrEP (Apretude), HIV testing via viral load and antibody/antigen testing should be done at the time of each injection (every 2 months).5
Continue to: With oral PrEP...
With oral PrEP, renal function should be checked every 6 months in patients older than 50 years or those with eCrCl < 90 mL/min at initiation. For patients younger than 50 years with no baseline renal dysfunction, the latest guidelines now recommend monitoring every 12 months instead of 6 months.5
For patients on Descovy, a lipid panel is recommended at PrEP initiation and every 12 months. Testing for other STIs can be considered on this schedule, based on clinical assessment. The TABLE5 summarizes recommended monitoring for patients taking oral PrEP.
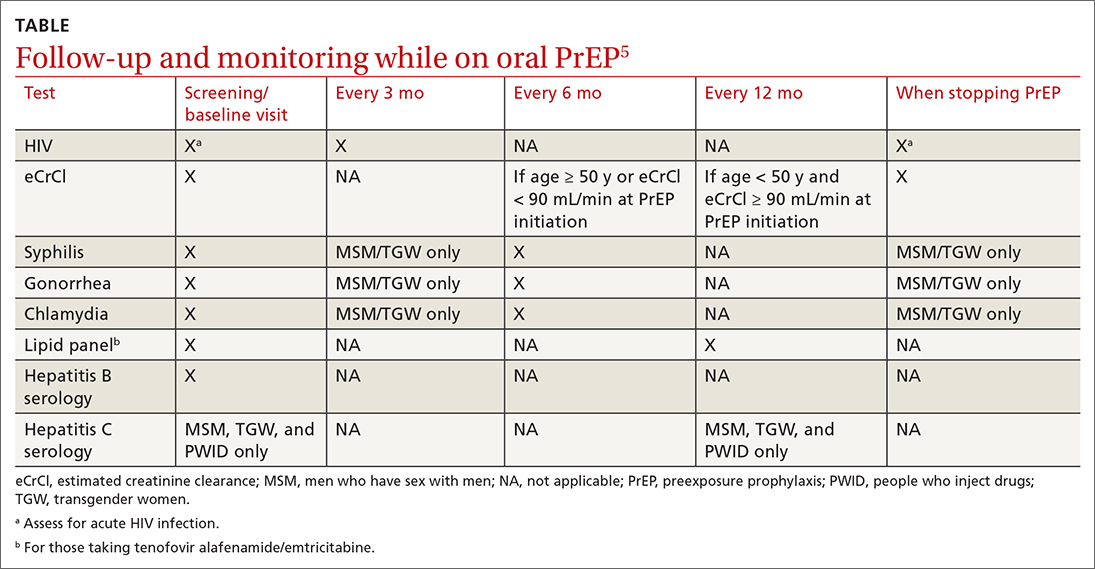
Recommended follow-up provides an opportunity to have frequent contact with a potentially high-risk population, and PrEP should be one part of a comprehensive HIV prevention and risk reduction plan. Many patients at high risk for HIV acquisition may benefit from frequent follow-up to address screening, referral, and treatment of substance use disorders, mental health conditions, and chronic medical conditions (including hepatitis C infection) and provide ongoing preventive health care.
Special uses of PrEP
Same-day PrEP. Starting PrEP on the day of the initial appointment may be appropriate based on patient risk factors and barriers to care, such as a high risk for contracting HIV before the subsequent appointment for a prescription of PrEP or an inability to return to the clinic in a timely fashion due to transportation or work constraints, or clinician availability. For these patients, assuming there is a low concern for acute or chronic HIV infection, PrEP can be initiated on the day of the initial visit.5
In these cases, point-of-care HIV and creatinine testing with same-day results should be completed. Antigen/antibody fingerstick testing or HIV-1 RNA test are preferred; oral fluid HIV testing should not be used for same-day PrEP due to its lower sensitivity for HIV detection. If same-day testing is unavailable, blood should be drawn at the visit so that HIV and creatinine testing can be completed as soon as possible.
Continue to: In addition to initial laboratory testing...
In addition to initial laboratory testing, clinics offering same-day PrEP should be able to provide: (1) assistance for patients to enroll in health insurance or a medication assistance program (eg, Ready, Set, PrEP) for those ineligible for insurance coverage, (2) rapid follow-up on all laboratory results with reliable patient contact information, and (3) follow-up appointments with clinicians able to prescribe and administer PrEP medications.
Off-label “on-demand” PrEP. An off-label treatment regimen for men who have sex with men (MSM) is termed “on-demand” PrEP or “2-1-1 PrEP” and is included in the CDC guidelines for consideration by clinicians.5 This alternative dosing schedule can be used for individuals who have sex less frequently and in a more planned fashion.
On-demand PrEP requires a patient to take 2 tablets of Truvada 2 to 24 hours before sex, followed by 1 tablet 24 hours and 1 tablet 48 hours after sexual activity. If a sexual act occurs at 48 hours, the patient should extend the daily dose for 48 additional hours, such that PrEP is always used daily for 48 hours after the last sex act.
This method has been studied with Truvada in MSM in Europe and Canada through the IPERGAY and PREVENIR trials and shown to have ≥ 86% efficacy in preventing HIV acquisition.11,12 The only US-based study showed lower efficacy; however, based on the currently available data, the International Antiviral Society-USA Panel has recommended it as an alternative regimen.13,14
PrEP via telehealth. Visits for PrEP initiation and continuation can be completed via telehealth.5 Patients then can complete necessary laboratory tests by going to a physical laboratory location or using mailed specimen kits in which they can self-collect urine, oral/rectal swabs, and fingerstick blood samples.
Continue to: PrEP use in specific populations
PrEP use in specific populations
Adolescents
Truvada, Descovy, and Apretude all are now approved for use in adolescents weighing ≥ 35 kg. Two important considerations when prescribing to this population are the effects of Truvada on bone health and the unique barriers to access.
In studies of adolescent MSM using Truvada for PrEP, bone mineral density declined, especially among those ages 15 to 19 years.15 As such, the clinical impact of decreased bone mineral density should be weighed against the risk for HIV acquisition; however, bone mineral density monitoring is not recommended in the current guidelines. CDC guidelines suggest considering Descovy for male adolescents given its potential lower impact on bone mineral density.5
Confidentiality and legal issues exist when prescribing PrEP to minors. In terms of parental/guardian involvement, clinicians who are prescribing PrEP for patients younger than 18 years should consult the CDC website for guidance on local and state regulations that govern prescribing and confidentiality (www.cdc.gov/hiv/policies/law/states/minors.html).
Insurance billing statements may lead to inadvertent disclosure of a minor’s decision to take PrEP to their legal guardian.16 Generic Truvada costs less than $100 for a 3-month supply when using goodrx.com, which may offer an alternative to insurance for medication payment.
Peripartum patients
The increased risk for HIV acquisition in the peripartum period for female patients is well documented.17 Guidelines recommend offering PrEP with Truvada to female patients at risk for conception, currently pregnant, or breastfeeding when that patient’s partner has HIV and the partner’s viral load is unknown or detectable. Descovy is not recommended for pregnant or breastfeeding patients.5 Cabotegravir-containing regimens (Apretude) have not been approved by the FDA for pregnant or breastfeeding patients.5
Continue to: Data on the impact of...
Data on the impact of Truvada for PrEP on fetal health are still emerging. A large study in Kenya showed no significant differences in preterm birth, low birth weight, or early infant growth, and a randomized, noninferiority trial in South Africa showed no association between Truvada for PrEP and preterm birth or the birth of small-for-gestational-age infants.18,19 There are no definitive studies of breastfeeding infants exposed to Truvada, but data from previous trials of breastfeeding mothers who were taking the individual components that are combined in the Truvada pill indicated there is minimal medication exposure to the infant.5
PrEP studies in the peripartum period to date have been conducted exclusively among cisgender women, and data do not yet reflect the experiences of transgender men, genderqueer people, and nonbinary individuals in the peripartum period.5
Transgender people
Transgender women should be strongly considered candidates for PrEP as they are at an extremely high risk for HIV acquisition. The most recent National HIV Behavioral Surveillance survey found that approximately 42% of transgender women were living with HIV.20 The survey revealed stark racial and ethnic disparities among transgender women living with HIV: 62% identified as Black/African American, compared with 35% Hispanic/Latina and 17% White.20
Transgender women report high rates of sexual assault, unprotected receptive anal sex, commercial sex work, homelessness, mental health disorders, and substance use, putting them at increased risk for HIV acquisition.21 However, transgender women are less likely to have discussed PrEP with a clinician, are less likely to be on PrEP even when interested in starting, and have higher rates of medication nonadherence compared with cisgender MSM.21,22 PrEP has not been found to decrease levels of feminizing hormones; however, studies are mixed as to whether feminizing hormones decrease Truvada concentrations in rectal mucosa, so clinicians should emphasize the importance of daily medication adherence.23
Transgender men have not been included in any PrEP trials, so no specific recommendations are available.
Continue to: Disparities in PrEP access and use exist
Disparities in PrEP access and use exist
The lifetime risk for HIV acquisition is 9% among White MSM, 50% among Black MSM, and 20% among Hispanic MSM.24 Despite this large disparity in disease burden, Black and Hispanic individuals are less likely to be aware of PrEP, have discussed PrEP with a health care professional, or used PrEP compared with their White counterparts.25 As a result, in 2020, PrEP coverage for eligible White individuals was 61%, while coverage among eligible Black and Hispanic/Latino individuals was just 8% and 14%, respectively.26
Surveillance data comparing male and female PrEP coverage reveal further disparities between the sexes, with PrEP coverage for eligible female-at-birth patients estimated to be 9% compared with 25.8% for male-at-birth patients.26 The gap between the risk for HIV infection and the access to and uptake of PrEP coverage is most pronounced among Black women, for whom the rate of new HIV diagnosis is > 10 times higher than it is for White women, but who have some of the lowest awareness and utilization rates of all demographics.27
The rural population at risk. Disparities in HIV awareness and PrEP use also exist between rural and urban populations, as well as by health insurance status. Rural areas have been shown to lag behind urban areas in PrEP awareness and use. Two potential explanations for this disparity are differences in HIV- and drug use–associated stigma and health insurance status. Greater stigma against drug use and HIV in rural areas has been associated with lower rates of PrEP use.28
Individuals younger than 65 years in rural areas are less likely to have private health insurance and more likely to be uninsured compared with their urban counterparts, which may impact access to clinicians knowledgeable about PrEP.29 Notably, MSM who live in states that have expanded Medicaid have higher rates of PrEP use compared with MSM living in states that have not expanded Medicaid.30
Health insurers in the United States are required to cover PrEP medication, clinician visits, and associated blood work with no patient cost-sharing, although implementation barriers such as prior authorizations still exist.
Conclusion
Family physicians are well positioned to identify patients at risk for HIV infection, prescribe PrEP, organize comprehensive follow-up care, and partner with their health systems and local communities to reduce barriers to care. Those who can leverage existing relationships with local health departments, school-based health clinics, congregate housing programs, LGBTQIA+ advocacy groups, harm-reduction coalitions, and other community-based organizations to raise PrEP awareness play a critical role in preventing HIV transmission and reducing health care disparities in their communities.
CORRESPONDENCE
Andrew V.A. Foley, MD, MPH, Erie Family Health Centers, 2418 W Division Street, Chicago, IL 60622; [email protected]
1. CDC. Estimated HIV incidence and prevalence in the United States 2017–2021. HIV Surveill Supplemental Rep. 2023;28. Accessed October 23, 2023. https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-28-no-3/index.html
2. CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (preliminary data): National HIV Surveillance System data reported through March 2023; and preexposure prophylaxis (PrEP) data reported through December 2022. HIV Surveill Data Tables. 2023;4. Published June 2023. Accessed October 23, 2023. https://www.cdc.gov/hiv/library/reports/surveillance-data-tables/
3. CDC. Division of HIV Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention. PrEP effectiveness. Updated June 2022. Accessed October 23, 2023. https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html
4. US Preventive Services Task Force. Prevention of acquisition of HIV: preexposure prophylaxis. Final recommendation statement. August 22, 2023. Accessed October 23, 2023. https://uspreventiveservicestaskforce.org/uspstf/recommendation/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis
5. CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update: a clinical practice guideline. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
6. Mugwanya KK, Wyatt C, Celum C, et al. Changes in glomerular kidney function among HIV-1-uninfected men and women receiving emtricitabine-tenofovir disoproxil fumarate preexposure prophylaxis: a randomized clinical trial. JAMA Intern Med. 2015;175:246-254. doi: 10.1001/jamainternmed.2014.6786
7. Havens PL, Stephensen CB, Van Loan MD, et al. Decline in bone mass with tenofovir disoproxil fumarate/emtricitabine is associated with hormonal changes in the absence of renal impairment when used by HIV-uninfected adolescent boys and young men for HIV preexposure prophylaxis. Clin Infect Dis. 2017;64:317-325. doi: 10.1093/cid/ciw765
8. Pilkington V, Hill A, Hughes S, et al. How safe is TDF/FTC as PrEP? A systematic review and meta-analysis of the risk of adverse events in 13 randomised trials of PrEP. J Virus Erad. 2018;4:215-224.
9. Mayer KH, Molina JM, Thompson MA, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020;396:239-254. doi: 10.1016/S0140-6736(20)31065-5
10. Liegeon G, Ghosn, J. Long-acting injectable cabotegravir for PrEP: a game-changer in HIV prevention. HIV Med. 2022;24:653-663. doi: 10.1111/hiv.13451
11. Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246. doi: 10.1056/NEJMoa1506273
12. Molina JM, Ghosn J, Assoumou L, et al. Daily and on-demand HIV pre-exposure prophylaxis with emtricitabine and tenofovir disoproxil (ANRS PREVENIR): a prospective observational cohort study. Lancet HIV. 2022;9:e554-e562. doi: 10.1016/S2352-3018(22)00133-3
13. Dimitrov D, Moore JR, Wood D, et al. Predicted effectiveness of daily and nondaily preexposure prophylaxis for men who have sex with men based on sex and pill-taking patterns from the Human Immuno Virus Prevention Trials Network 067/ADAPT Study. Clin Infect Dis. 2020;71:249-255. doi: 10.1093/cid/ciz799
14. Saag MS, Gandhi RT, Hoy JF, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2020 recommendations of the International Antiviral Society-USA Panel. JAMA. 2020;324:1651-1669. doi: 10.1001/jama.2020.17025
15. Havens PL, Perumean-Chaney SE, Patki A, et al. Changes in bone mass after discontinuation of preexposure prophylaxis with tenofovir disoproxil fumarate/emtricitabine in young men who have sex with men: extension phase results of Adolescent Trials Network Protocols 110 and 113. Clin Infect Dis. 2020;70:687-691. doi: 10.1093/cid/ciz486
16. Neilan AM, Salvant Valentine S, Knopf AS. Case 27-2021: a 16-year-old boy seeking human immunodeficiency virus prophylaxis. N Engl J Med. 2021;385:1034-1041. doi: 10.1056/NEJMcpc1909626
17. Thomson KA, Hughes J, Baeten JM, et al. Increased risk of HIV acquisition among women throughout pregnancy and during the postpartum period: a prospective per-coital-act analysis among women with HIV-infected partners. J Infect Dis. 2018;218:16-25. doi: 10.1093/infdis/jiy113
18. Dettinger JC, Kinuthia J, Pintye J, et al. Perinatal outcomes following maternal pre-exposure prophylaxis (PrEP) use during pregnancy: results from a large PrEP implementation program in Kenya. J Int AIDS Soc. 2019;22:e25378. doi: 10.1002/jia2.25378
19. Moodley D, Lombard C, Govender V, et al. Pregnancy and neonatal safety outcomes of timing of initiation of daily oral tenofovir disoproxil fumarate and emtricitabine pre-exposure prophylaxis for HIV prevention (CAP016): an open-label, randomised, non-inferiority trial. Lancet HIV. 2023;10:e154-e163. doi: 10.1016/S2352-3018(22)00369-1
20. CDC. HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women—National HIV Behavioral Surveillance, 7 U.S. Cities, 2019–2020. HIV Surveillance Special Report 27. April 2021. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-27.pdf
21. Wilson EC, Turner CM, Arayasirikul S, et al. Disparities in the PrEP continuum for trans women compared to MSM in San Francisco, California: results from population-based cross-sectional behavioural surveillance studies. J Int AIDS Soc. 2020;23:e25539. doi: 10.1002/jia2.25539
22. Poteat T, Wirtz A, Malik M, et al. A gap between willingness and uptake: findings from mixed methods research on HIV prevention among Black and Latina transgender women. J Acquir Immune Defic Syndr. 2019;82:131-140. doi: 10.1097/QAI.0000000000002112
23. Cottrell ML, Prince HM, Schauer AP, et al. Decreased tenofovir diphosphate concentrations in a transgender female cohort: implications for human immunodeficiency virus preexposure prophylaxis. Clin Infect Dis. 2019;69:2201-2204. doi: 10.1093/cid/ciz290
24. Hess KL, Hu X, Lansky A, et al. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27:238-243. doi: 10.1016/j.annepidem.2017.02.003
25. Kanny D, Jeffries WL 4th, Chapin-Bardales J, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:801-806. doi: 10.15585/mmwr.mm6837a2
26. CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (early release): National HIV Surveillance System data reported through December 2020; and preexposure prophylaxis (PrEP) data reported through September 2020. HIV Surveill Data Tables. 2021;2. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/library/reports/surveillance-data-tables/vol-2-no-2/cdc-hiv-surveillance-tables-vol-2-no-2.pdf
27. CDC. Diagnoses of HIV infection in the United States and dependent areas 2021: special focus profiles. Updated May 23, 2023. Accessed October 23, 2023. www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-34/content/special-focus-profiles.html
28. Walters SM, Frank D, Van Ham B, et al. PrEP care continuum engagement among persons who inject drugs: rural and urban differences in stigma and social infrastructure. AIDS Behav. 2021;26:1308-1320. doi: 10.1007/s10461-021-03488-2
29. Foutz J, Artiga S, Garfield R. The role of Medicaid in rural America [issue brief]. April 25, 2017. Accessed August 16, 2023. www.kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
30. Baugher AR, Finlayson T, Lewis R, et al. Health care coverage and preexposure prophylaxis (PrEP) use among men who have sex with men living in 22 US cities with vs without Medicaid expansion, 2017. Am J Public Health. 2021;111:743-751. doi: 10.2105/AJPH.2020.306035
More than 1.2 million Americans are living with HIV, and more than 30,000 new cases are diagnosed each year. While total incidence has declined since 2016, HIV remains a nationwide epidemic.1
Medications that prevent HIV acquisition, termed preexposure prophylaxis (PrEP), are an important tool to initiate in the primary care setting to reduce HIV transmission. However, while there are an estimated 1.2 million people eligible for PrEP, only 36% have received PrEP prescriptions.2 Several barriers that have impeded its widespread adoption include a lack of clinician knowledge and clinical resources for testing, high medication costs, and stigma around sexual health and intravenous (IV) drug use.
The value of PrEP
PrEP is chemoprophylaxis against the acquisition of HIV infection through the administration of an oral or injectable medication to people at risk for HIV. This practice began in the early 2000s, with the first oral regimen approved in 2012, and since has become an important tool in preventing HIV transmission.
When taken as prescribed, PrEP medications reduce the risk for acquiring HIV through sex by approximately 99% and can reduce the risk for acquiring HIV from injection drug use by approximately 74%.3 The US Preventive Services Task Force issued a Grade “A” recommendation to offer PrEP to people at high risk for HIV acquisition in June 2019 and reaffirmed it in a 2023 update.4
PrEP is notably distinct from postexposure prophylaxis (PEP), which is the administration of medication to prevent HIV infection after a possible exposure.
The available regimens
Regimens for PrEP include oral tablets or intramuscular (IM) injections.5 There are 3 PrEP regimens approved by the US Food and Drug Administration (FDA): tenofovir disoproxil fumarate/emtricitabine (Truvada), tenofovir alafenamide/emtricitabine (Descovy), and cabotegravir (Apretude).
Truvada is once-daily oral PrEP that was approved in 2012 and is now available in a generic formulation. Notable adverse effects of Truvada include a small negative impact on renal function and small reductions in bone mineral density; these have been noted in individual trials, but in meta-analyses such differences were not found to be statistically significant.6-8 The most common adverse effects of Truvada, experienced by up to 6% of patients, are gastrointestinal symptoms, fatigue, headache/dizziness, depression, and insomnia; most symptoms resolve within weeks.
Continue to: Descovy
Descovy is daily oral PrEP that was approved in 2019. Descovy is associated with increases in LDL and triglycerides but has less impact on renal and bone health.9 The most common adverse effect of Descovy, experienced by about 5% of patients, is diarrhea, followed by nausea.
Apretude was approved in 2021 and is a 600-mg IM injection given monthly for 2 months, then every 2 months (± 7 days). The advantages of Apretude are frequency and discreteness of dosing and the ability to use in patients with estimated creatinine clearance (eCrCl) > 15 mL/min. The most common adverse effects of Apretude are injection-site reactions, which occur in 30% to 80% of patients but are rarely significant enough to lead to discontinuation (< 2% of patients discontinue use due to injection-site reactions).10
Who should take PrEP?
The latest Centers for Disease Control and Prevention (CDC) guidelines recommend that all sexually active adults receive information about PrEP.5 Indications for PrEP are broad and summarized in the FIGURE.5
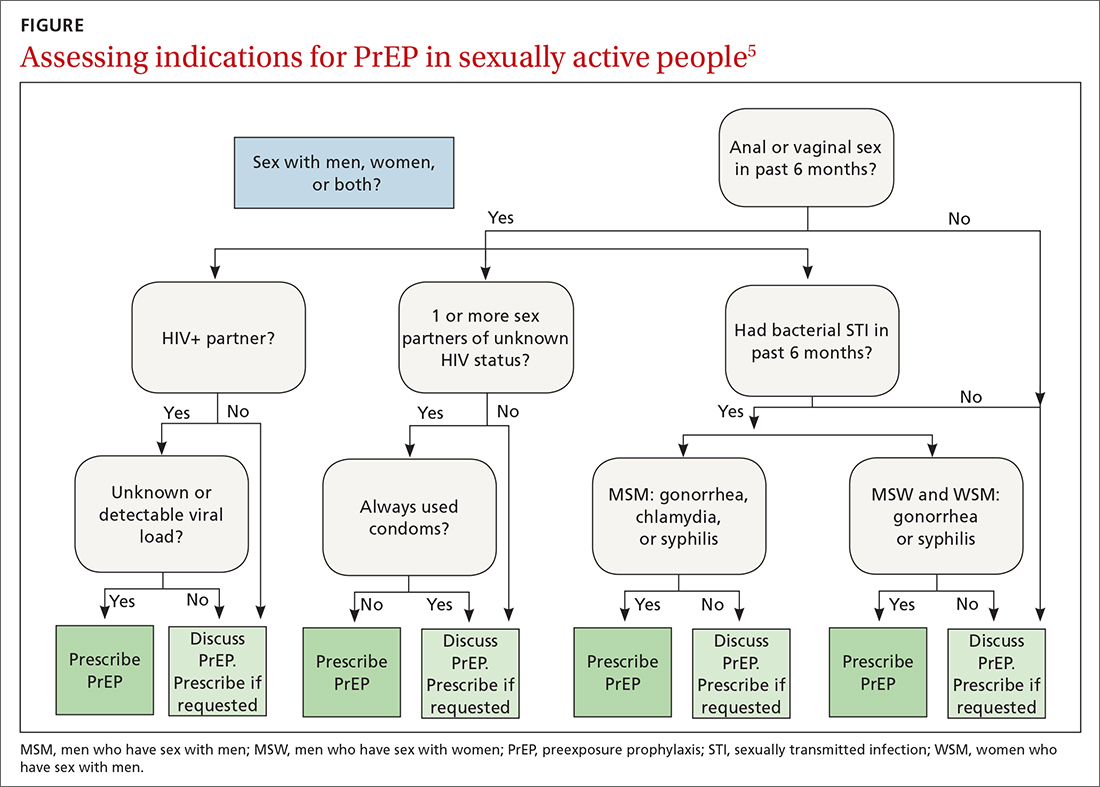
PrEP is indicated in patients who report sexual or injection drug use behaviors that place them at substantial ongoing risk for HIV exposure. Specific indications include patients with sexual partner(s) with unknown HIV status with whom they have inconsistent or no condom use, a history of bacterial sexually transmitted infection (STI) in the past 6 months, an HIV-positive sexual partner, or the sharing of injection drug equipment.
Hepatitis B infection is not a contraindication for PrEP use, but knowledge of infection status is essential. All current oral medications used for PrEP have activity against hepatitis B. Incomplete adherence to or abrupt discontinuation of oral PrEP could precipitate a hepatitis B flare. Hepatitis B surface antigen should be tested at the time of PrEP initiation, although PrEP can begin while testing is in process.
Continue to: How to use PrEP
How to use PrEP
At PrEP initiation, acute or chronic HIV infection must be excluded with a documented negative HIV antigen/antibody test within 1 week of prescribing PrEP.5 The CDC guidelines provide an updated HIV testing algorithm (www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf, p 30-31, Figures 4a and 4b), which considers whether patients have received PrEP recently.
Patients with recent high-risk exposures or symptoms of acute HIV at the time of desired PrEP initiation should have an HIV-1 viral load checked with negative results before PrEP is prescribed. Additional criteria for PrEP include weight > 35 kg; screening for hepatitis B virus infection; screening for drug interactions; and drug-specific eCrCl cutoffs of > 60 mL/min for Truvada, > 30 mL/min for Descovy, and > 15 mL/min for Apretude.5
Studies regarding time to medication effectiveness are limited. Pharmacokinetic studies of Truvada demonstrate sufficient drug concentrations should be present in peripheral blood mononuclear cells and rectal tissue within 7 days of initiation of oral dosing and around 20 days in vaginal tissue.
Of note, while expedited partner therapy is used as a harm-reduction strategy to treat the sexual partners of patients diagnosed with certain STIs, PrEP is not recommended to be used in this way.
Ongoing monitoring with PrEP. Once oral PrEP is started, STI risk assessment and HIV testing via 4th generation antibody/antigen test should be completed at least every 3 months. PrEP oral prescription refills should be limited to 3 months. For patients receiving IM PrEP (Apretude), HIV testing via viral load and antibody/antigen testing should be done at the time of each injection (every 2 months).5
Continue to: With oral PrEP...
With oral PrEP, renal function should be checked every 6 months in patients older than 50 years or those with eCrCl < 90 mL/min at initiation. For patients younger than 50 years with no baseline renal dysfunction, the latest guidelines now recommend monitoring every 12 months instead of 6 months.5
For patients on Descovy, a lipid panel is recommended at PrEP initiation and every 12 months. Testing for other STIs can be considered on this schedule, based on clinical assessment. The TABLE5 summarizes recommended monitoring for patients taking oral PrEP.
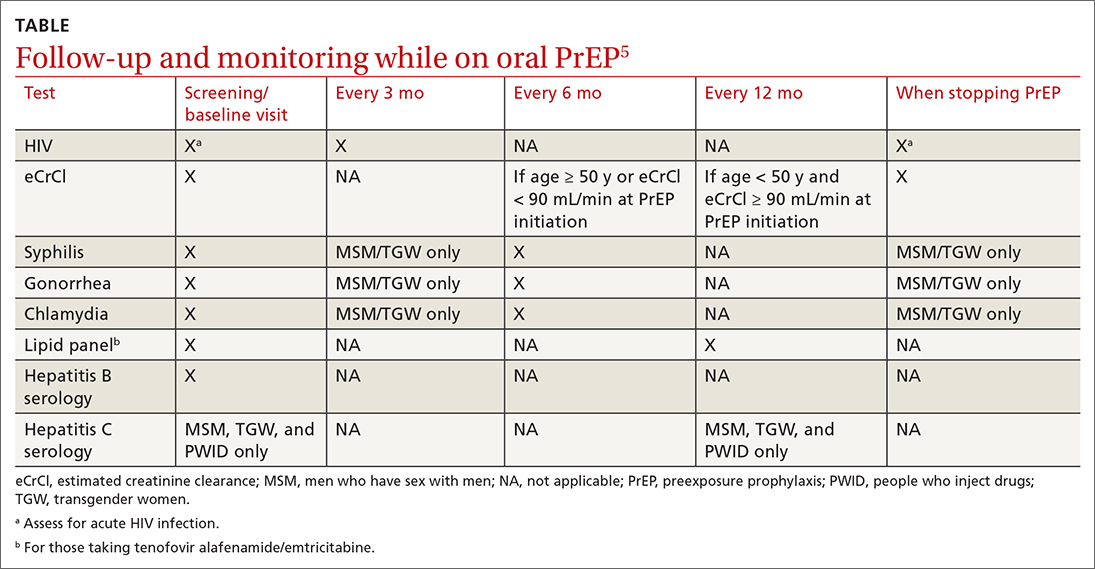
Recommended follow-up provides an opportunity to have frequent contact with a potentially high-risk population, and PrEP should be one part of a comprehensive HIV prevention and risk reduction plan. Many patients at high risk for HIV acquisition may benefit from frequent follow-up to address screening, referral, and treatment of substance use disorders, mental health conditions, and chronic medical conditions (including hepatitis C infection) and provide ongoing preventive health care.
Special uses of PrEP
Same-day PrEP. Starting PrEP on the day of the initial appointment may be appropriate based on patient risk factors and barriers to care, such as a high risk for contracting HIV before the subsequent appointment for a prescription of PrEP or an inability to return to the clinic in a timely fashion due to transportation or work constraints, or clinician availability. For these patients, assuming there is a low concern for acute or chronic HIV infection, PrEP can be initiated on the day of the initial visit.5
In these cases, point-of-care HIV and creatinine testing with same-day results should be completed. Antigen/antibody fingerstick testing or HIV-1 RNA test are preferred; oral fluid HIV testing should not be used for same-day PrEP due to its lower sensitivity for HIV detection. If same-day testing is unavailable, blood should be drawn at the visit so that HIV and creatinine testing can be completed as soon as possible.
Continue to: In addition to initial laboratory testing...
In addition to initial laboratory testing, clinics offering same-day PrEP should be able to provide: (1) assistance for patients to enroll in health insurance or a medication assistance program (eg, Ready, Set, PrEP) for those ineligible for insurance coverage, (2) rapid follow-up on all laboratory results with reliable patient contact information, and (3) follow-up appointments with clinicians able to prescribe and administer PrEP medications.
Off-label “on-demand” PrEP. An off-label treatment regimen for men who have sex with men (MSM) is termed “on-demand” PrEP or “2-1-1 PrEP” and is included in the CDC guidelines for consideration by clinicians.5 This alternative dosing schedule can be used for individuals who have sex less frequently and in a more planned fashion.
On-demand PrEP requires a patient to take 2 tablets of Truvada 2 to 24 hours before sex, followed by 1 tablet 24 hours and 1 tablet 48 hours after sexual activity. If a sexual act occurs at 48 hours, the patient should extend the daily dose for 48 additional hours, such that PrEP is always used daily for 48 hours after the last sex act.
This method has been studied with Truvada in MSM in Europe and Canada through the IPERGAY and PREVENIR trials and shown to have ≥ 86% efficacy in preventing HIV acquisition.11,12 The only US-based study showed lower efficacy; however, based on the currently available data, the International Antiviral Society-USA Panel has recommended it as an alternative regimen.13,14
PrEP via telehealth. Visits for PrEP initiation and continuation can be completed via telehealth.5 Patients then can complete necessary laboratory tests by going to a physical laboratory location or using mailed specimen kits in which they can self-collect urine, oral/rectal swabs, and fingerstick blood samples.
Continue to: PrEP use in specific populations
PrEP use in specific populations
Adolescents
Truvada, Descovy, and Apretude all are now approved for use in adolescents weighing ≥ 35 kg. Two important considerations when prescribing to this population are the effects of Truvada on bone health and the unique barriers to access.
In studies of adolescent MSM using Truvada for PrEP, bone mineral density declined, especially among those ages 15 to 19 years.15 As such, the clinical impact of decreased bone mineral density should be weighed against the risk for HIV acquisition; however, bone mineral density monitoring is not recommended in the current guidelines. CDC guidelines suggest considering Descovy for male adolescents given its potential lower impact on bone mineral density.5
Confidentiality and legal issues exist when prescribing PrEP to minors. In terms of parental/guardian involvement, clinicians who are prescribing PrEP for patients younger than 18 years should consult the CDC website for guidance on local and state regulations that govern prescribing and confidentiality (www.cdc.gov/hiv/policies/law/states/minors.html).
Insurance billing statements may lead to inadvertent disclosure of a minor’s decision to take PrEP to their legal guardian.16 Generic Truvada costs less than $100 for a 3-month supply when using goodrx.com, which may offer an alternative to insurance for medication payment.
Peripartum patients
The increased risk for HIV acquisition in the peripartum period for female patients is well documented.17 Guidelines recommend offering PrEP with Truvada to female patients at risk for conception, currently pregnant, or breastfeeding when that patient’s partner has HIV and the partner’s viral load is unknown or detectable. Descovy is not recommended for pregnant or breastfeeding patients.5 Cabotegravir-containing regimens (Apretude) have not been approved by the FDA for pregnant or breastfeeding patients.5
Continue to: Data on the impact of...
Data on the impact of Truvada for PrEP on fetal health are still emerging. A large study in Kenya showed no significant differences in preterm birth, low birth weight, or early infant growth, and a randomized, noninferiority trial in South Africa showed no association between Truvada for PrEP and preterm birth or the birth of small-for-gestational-age infants.18,19 There are no definitive studies of breastfeeding infants exposed to Truvada, but data from previous trials of breastfeeding mothers who were taking the individual components that are combined in the Truvada pill indicated there is minimal medication exposure to the infant.5
PrEP studies in the peripartum period to date have been conducted exclusively among cisgender women, and data do not yet reflect the experiences of transgender men, genderqueer people, and nonbinary individuals in the peripartum period.5
Transgender people
Transgender women should be strongly considered candidates for PrEP as they are at an extremely high risk for HIV acquisition. The most recent National HIV Behavioral Surveillance survey found that approximately 42% of transgender women were living with HIV.20 The survey revealed stark racial and ethnic disparities among transgender women living with HIV: 62% identified as Black/African American, compared with 35% Hispanic/Latina and 17% White.20
Transgender women report high rates of sexual assault, unprotected receptive anal sex, commercial sex work, homelessness, mental health disorders, and substance use, putting them at increased risk for HIV acquisition.21 However, transgender women are less likely to have discussed PrEP with a clinician, are less likely to be on PrEP even when interested in starting, and have higher rates of medication nonadherence compared with cisgender MSM.21,22 PrEP has not been found to decrease levels of feminizing hormones; however, studies are mixed as to whether feminizing hormones decrease Truvada concentrations in rectal mucosa, so clinicians should emphasize the importance of daily medication adherence.23
Transgender men have not been included in any PrEP trials, so no specific recommendations are available.
Continue to: Disparities in PrEP access and use exist
Disparities in PrEP access and use exist
The lifetime risk for HIV acquisition is 9% among White MSM, 50% among Black MSM, and 20% among Hispanic MSM.24 Despite this large disparity in disease burden, Black and Hispanic individuals are less likely to be aware of PrEP, have discussed PrEP with a health care professional, or used PrEP compared with their White counterparts.25 As a result, in 2020, PrEP coverage for eligible White individuals was 61%, while coverage among eligible Black and Hispanic/Latino individuals was just 8% and 14%, respectively.26
Surveillance data comparing male and female PrEP coverage reveal further disparities between the sexes, with PrEP coverage for eligible female-at-birth patients estimated to be 9% compared with 25.8% for male-at-birth patients.26 The gap between the risk for HIV infection and the access to and uptake of PrEP coverage is most pronounced among Black women, for whom the rate of new HIV diagnosis is > 10 times higher than it is for White women, but who have some of the lowest awareness and utilization rates of all demographics.27
The rural population at risk. Disparities in HIV awareness and PrEP use also exist between rural and urban populations, as well as by health insurance status. Rural areas have been shown to lag behind urban areas in PrEP awareness and use. Two potential explanations for this disparity are differences in HIV- and drug use–associated stigma and health insurance status. Greater stigma against drug use and HIV in rural areas has been associated with lower rates of PrEP use.28
Individuals younger than 65 years in rural areas are less likely to have private health insurance and more likely to be uninsured compared with their urban counterparts, which may impact access to clinicians knowledgeable about PrEP.29 Notably, MSM who live in states that have expanded Medicaid have higher rates of PrEP use compared with MSM living in states that have not expanded Medicaid.30
Health insurers in the United States are required to cover PrEP medication, clinician visits, and associated blood work with no patient cost-sharing, although implementation barriers such as prior authorizations still exist.
Conclusion
Family physicians are well positioned to identify patients at risk for HIV infection, prescribe PrEP, organize comprehensive follow-up care, and partner with their health systems and local communities to reduce barriers to care. Those who can leverage existing relationships with local health departments, school-based health clinics, congregate housing programs, LGBTQIA+ advocacy groups, harm-reduction coalitions, and other community-based organizations to raise PrEP awareness play a critical role in preventing HIV transmission and reducing health care disparities in their communities.
CORRESPONDENCE
Andrew V.A. Foley, MD, MPH, Erie Family Health Centers, 2418 W Division Street, Chicago, IL 60622; [email protected]
More than 1.2 million Americans are living with HIV, and more than 30,000 new cases are diagnosed each year. While total incidence has declined since 2016, HIV remains a nationwide epidemic.1
Medications that prevent HIV acquisition, termed preexposure prophylaxis (PrEP), are an important tool to initiate in the primary care setting to reduce HIV transmission. However, while there are an estimated 1.2 million people eligible for PrEP, only 36% have received PrEP prescriptions.2 Several barriers that have impeded its widespread adoption include a lack of clinician knowledge and clinical resources for testing, high medication costs, and stigma around sexual health and intravenous (IV) drug use.
The value of PrEP
PrEP is chemoprophylaxis against the acquisition of HIV infection through the administration of an oral or injectable medication to people at risk for HIV. This practice began in the early 2000s, with the first oral regimen approved in 2012, and since has become an important tool in preventing HIV transmission.
When taken as prescribed, PrEP medications reduce the risk for acquiring HIV through sex by approximately 99% and can reduce the risk for acquiring HIV from injection drug use by approximately 74%.3 The US Preventive Services Task Force issued a Grade “A” recommendation to offer PrEP to people at high risk for HIV acquisition in June 2019 and reaffirmed it in a 2023 update.4
PrEP is notably distinct from postexposure prophylaxis (PEP), which is the administration of medication to prevent HIV infection after a possible exposure.
The available regimens
Regimens for PrEP include oral tablets or intramuscular (IM) injections.5 There are 3 PrEP regimens approved by the US Food and Drug Administration (FDA): tenofovir disoproxil fumarate/emtricitabine (Truvada), tenofovir alafenamide/emtricitabine (Descovy), and cabotegravir (Apretude).
Truvada is once-daily oral PrEP that was approved in 2012 and is now available in a generic formulation. Notable adverse effects of Truvada include a small negative impact on renal function and small reductions in bone mineral density; these have been noted in individual trials, but in meta-analyses such differences were not found to be statistically significant.6-8 The most common adverse effects of Truvada, experienced by up to 6% of patients, are gastrointestinal symptoms, fatigue, headache/dizziness, depression, and insomnia; most symptoms resolve within weeks.
Continue to: Descovy
Descovy is daily oral PrEP that was approved in 2019. Descovy is associated with increases in LDL and triglycerides but has less impact on renal and bone health.9 The most common adverse effect of Descovy, experienced by about 5% of patients, is diarrhea, followed by nausea.
Apretude was approved in 2021 and is a 600-mg IM injection given monthly for 2 months, then every 2 months (± 7 days). The advantages of Apretude are frequency and discreteness of dosing and the ability to use in patients with estimated creatinine clearance (eCrCl) > 15 mL/min. The most common adverse effects of Apretude are injection-site reactions, which occur in 30% to 80% of patients but are rarely significant enough to lead to discontinuation (< 2% of patients discontinue use due to injection-site reactions).10
Who should take PrEP?
The latest Centers for Disease Control and Prevention (CDC) guidelines recommend that all sexually active adults receive information about PrEP.5 Indications for PrEP are broad and summarized in the FIGURE.5
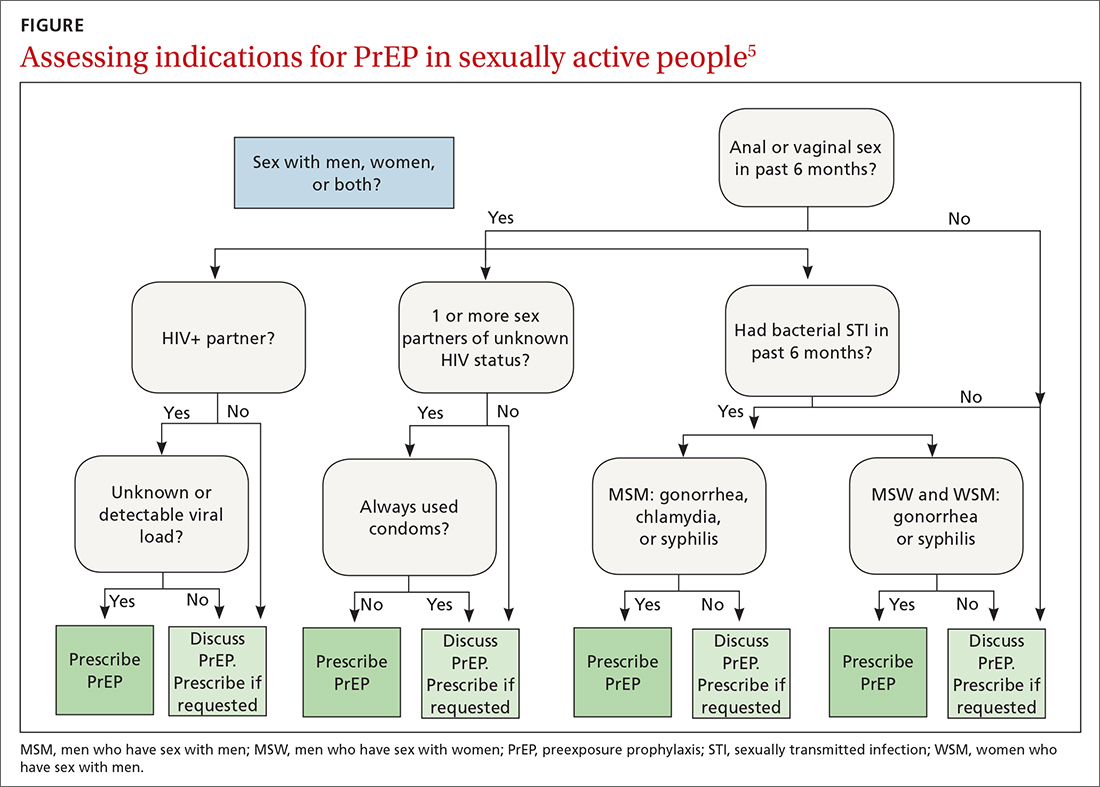
PrEP is indicated in patients who report sexual or injection drug use behaviors that place them at substantial ongoing risk for HIV exposure. Specific indications include patients with sexual partner(s) with unknown HIV status with whom they have inconsistent or no condom use, a history of bacterial sexually transmitted infection (STI) in the past 6 months, an HIV-positive sexual partner, or the sharing of injection drug equipment.
Hepatitis B infection is not a contraindication for PrEP use, but knowledge of infection status is essential. All current oral medications used for PrEP have activity against hepatitis B. Incomplete adherence to or abrupt discontinuation of oral PrEP could precipitate a hepatitis B flare. Hepatitis B surface antigen should be tested at the time of PrEP initiation, although PrEP can begin while testing is in process.
Continue to: How to use PrEP
How to use PrEP
At PrEP initiation, acute or chronic HIV infection must be excluded with a documented negative HIV antigen/antibody test within 1 week of prescribing PrEP.5 The CDC guidelines provide an updated HIV testing algorithm (www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf, p 30-31, Figures 4a and 4b), which considers whether patients have received PrEP recently.
Patients with recent high-risk exposures or symptoms of acute HIV at the time of desired PrEP initiation should have an HIV-1 viral load checked with negative results before PrEP is prescribed. Additional criteria for PrEP include weight > 35 kg; screening for hepatitis B virus infection; screening for drug interactions; and drug-specific eCrCl cutoffs of > 60 mL/min for Truvada, > 30 mL/min for Descovy, and > 15 mL/min for Apretude.5
Studies regarding time to medication effectiveness are limited. Pharmacokinetic studies of Truvada demonstrate sufficient drug concentrations should be present in peripheral blood mononuclear cells and rectal tissue within 7 days of initiation of oral dosing and around 20 days in vaginal tissue.
Of note, while expedited partner therapy is used as a harm-reduction strategy to treat the sexual partners of patients diagnosed with certain STIs, PrEP is not recommended to be used in this way.
Ongoing monitoring with PrEP. Once oral PrEP is started, STI risk assessment and HIV testing via 4th generation antibody/antigen test should be completed at least every 3 months. PrEP oral prescription refills should be limited to 3 months. For patients receiving IM PrEP (Apretude), HIV testing via viral load and antibody/antigen testing should be done at the time of each injection (every 2 months).5
Continue to: With oral PrEP...
With oral PrEP, renal function should be checked every 6 months in patients older than 50 years or those with eCrCl < 90 mL/min at initiation. For patients younger than 50 years with no baseline renal dysfunction, the latest guidelines now recommend monitoring every 12 months instead of 6 months.5
For patients on Descovy, a lipid panel is recommended at PrEP initiation and every 12 months. Testing for other STIs can be considered on this schedule, based on clinical assessment. The TABLE5 summarizes recommended monitoring for patients taking oral PrEP.
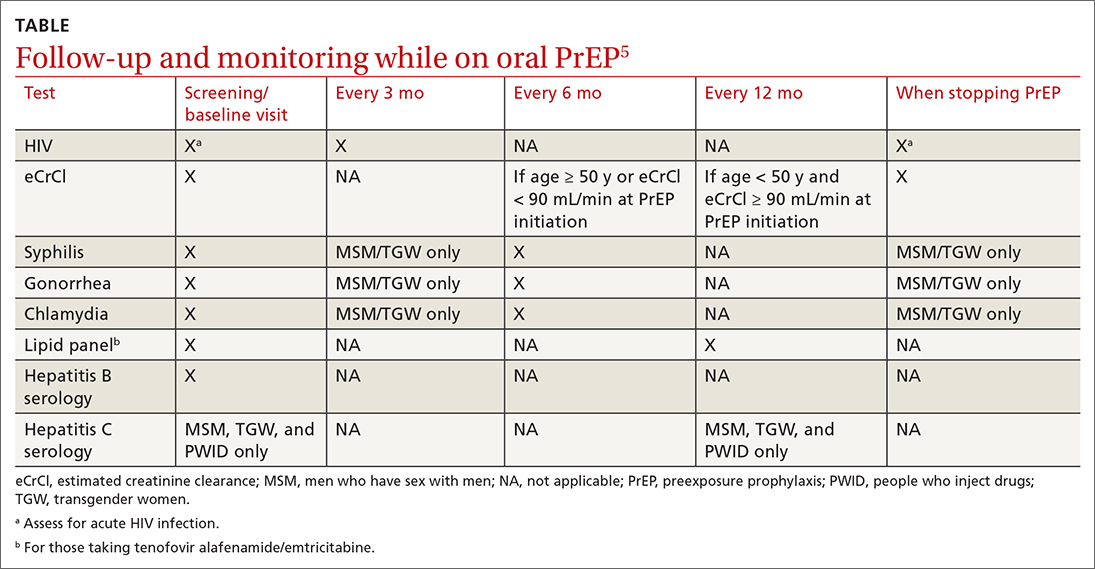
Recommended follow-up provides an opportunity to have frequent contact with a potentially high-risk population, and PrEP should be one part of a comprehensive HIV prevention and risk reduction plan. Many patients at high risk for HIV acquisition may benefit from frequent follow-up to address screening, referral, and treatment of substance use disorders, mental health conditions, and chronic medical conditions (including hepatitis C infection) and provide ongoing preventive health care.
Special uses of PrEP
Same-day PrEP. Starting PrEP on the day of the initial appointment may be appropriate based on patient risk factors and barriers to care, such as a high risk for contracting HIV before the subsequent appointment for a prescription of PrEP or an inability to return to the clinic in a timely fashion due to transportation or work constraints, or clinician availability. For these patients, assuming there is a low concern for acute or chronic HIV infection, PrEP can be initiated on the day of the initial visit.5
In these cases, point-of-care HIV and creatinine testing with same-day results should be completed. Antigen/antibody fingerstick testing or HIV-1 RNA test are preferred; oral fluid HIV testing should not be used for same-day PrEP due to its lower sensitivity for HIV detection. If same-day testing is unavailable, blood should be drawn at the visit so that HIV and creatinine testing can be completed as soon as possible.
Continue to: In addition to initial laboratory testing...
In addition to initial laboratory testing, clinics offering same-day PrEP should be able to provide: (1) assistance for patients to enroll in health insurance or a medication assistance program (eg, Ready, Set, PrEP) for those ineligible for insurance coverage, (2) rapid follow-up on all laboratory results with reliable patient contact information, and (3) follow-up appointments with clinicians able to prescribe and administer PrEP medications.
Off-label “on-demand” PrEP. An off-label treatment regimen for men who have sex with men (MSM) is termed “on-demand” PrEP or “2-1-1 PrEP” and is included in the CDC guidelines for consideration by clinicians.5 This alternative dosing schedule can be used for individuals who have sex less frequently and in a more planned fashion.
On-demand PrEP requires a patient to take 2 tablets of Truvada 2 to 24 hours before sex, followed by 1 tablet 24 hours and 1 tablet 48 hours after sexual activity. If a sexual act occurs at 48 hours, the patient should extend the daily dose for 48 additional hours, such that PrEP is always used daily for 48 hours after the last sex act.
This method has been studied with Truvada in MSM in Europe and Canada through the IPERGAY and PREVENIR trials and shown to have ≥ 86% efficacy in preventing HIV acquisition.11,12 The only US-based study showed lower efficacy; however, based on the currently available data, the International Antiviral Society-USA Panel has recommended it as an alternative regimen.13,14
PrEP via telehealth. Visits for PrEP initiation and continuation can be completed via telehealth.5 Patients then can complete necessary laboratory tests by going to a physical laboratory location or using mailed specimen kits in which they can self-collect urine, oral/rectal swabs, and fingerstick blood samples.
Continue to: PrEP use in specific populations
PrEP use in specific populations
Adolescents
Truvada, Descovy, and Apretude all are now approved for use in adolescents weighing ≥ 35 kg. Two important considerations when prescribing to this population are the effects of Truvada on bone health and the unique barriers to access.
In studies of adolescent MSM using Truvada for PrEP, bone mineral density declined, especially among those ages 15 to 19 years.15 As such, the clinical impact of decreased bone mineral density should be weighed against the risk for HIV acquisition; however, bone mineral density monitoring is not recommended in the current guidelines. CDC guidelines suggest considering Descovy for male adolescents given its potential lower impact on bone mineral density.5
Confidentiality and legal issues exist when prescribing PrEP to minors. In terms of parental/guardian involvement, clinicians who are prescribing PrEP for patients younger than 18 years should consult the CDC website for guidance on local and state regulations that govern prescribing and confidentiality (www.cdc.gov/hiv/policies/law/states/minors.html).
Insurance billing statements may lead to inadvertent disclosure of a minor’s decision to take PrEP to their legal guardian.16 Generic Truvada costs less than $100 for a 3-month supply when using goodrx.com, which may offer an alternative to insurance for medication payment.
Peripartum patients
The increased risk for HIV acquisition in the peripartum period for female patients is well documented.17 Guidelines recommend offering PrEP with Truvada to female patients at risk for conception, currently pregnant, or breastfeeding when that patient’s partner has HIV and the partner’s viral load is unknown or detectable. Descovy is not recommended for pregnant or breastfeeding patients.5 Cabotegravir-containing regimens (Apretude) have not been approved by the FDA for pregnant or breastfeeding patients.5
Continue to: Data on the impact of...
Data on the impact of Truvada for PrEP on fetal health are still emerging. A large study in Kenya showed no significant differences in preterm birth, low birth weight, or early infant growth, and a randomized, noninferiority trial in South Africa showed no association between Truvada for PrEP and preterm birth or the birth of small-for-gestational-age infants.18,19 There are no definitive studies of breastfeeding infants exposed to Truvada, but data from previous trials of breastfeeding mothers who were taking the individual components that are combined in the Truvada pill indicated there is minimal medication exposure to the infant.5
PrEP studies in the peripartum period to date have been conducted exclusively among cisgender women, and data do not yet reflect the experiences of transgender men, genderqueer people, and nonbinary individuals in the peripartum period.5
Transgender people
Transgender women should be strongly considered candidates for PrEP as they are at an extremely high risk for HIV acquisition. The most recent National HIV Behavioral Surveillance survey found that approximately 42% of transgender women were living with HIV.20 The survey revealed stark racial and ethnic disparities among transgender women living with HIV: 62% identified as Black/African American, compared with 35% Hispanic/Latina and 17% White.20
Transgender women report high rates of sexual assault, unprotected receptive anal sex, commercial sex work, homelessness, mental health disorders, and substance use, putting them at increased risk for HIV acquisition.21 However, transgender women are less likely to have discussed PrEP with a clinician, are less likely to be on PrEP even when interested in starting, and have higher rates of medication nonadherence compared with cisgender MSM.21,22 PrEP has not been found to decrease levels of feminizing hormones; however, studies are mixed as to whether feminizing hormones decrease Truvada concentrations in rectal mucosa, so clinicians should emphasize the importance of daily medication adherence.23
Transgender men have not been included in any PrEP trials, so no specific recommendations are available.
Continue to: Disparities in PrEP access and use exist
Disparities in PrEP access and use exist
The lifetime risk for HIV acquisition is 9% among White MSM, 50% among Black MSM, and 20% among Hispanic MSM.24 Despite this large disparity in disease burden, Black and Hispanic individuals are less likely to be aware of PrEP, have discussed PrEP with a health care professional, or used PrEP compared with their White counterparts.25 As a result, in 2020, PrEP coverage for eligible White individuals was 61%, while coverage among eligible Black and Hispanic/Latino individuals was just 8% and 14%, respectively.26
Surveillance data comparing male and female PrEP coverage reveal further disparities between the sexes, with PrEP coverage for eligible female-at-birth patients estimated to be 9% compared with 25.8% for male-at-birth patients.26 The gap between the risk for HIV infection and the access to and uptake of PrEP coverage is most pronounced among Black women, for whom the rate of new HIV diagnosis is > 10 times higher than it is for White women, but who have some of the lowest awareness and utilization rates of all demographics.27
The rural population at risk. Disparities in HIV awareness and PrEP use also exist between rural and urban populations, as well as by health insurance status. Rural areas have been shown to lag behind urban areas in PrEP awareness and use. Two potential explanations for this disparity are differences in HIV- and drug use–associated stigma and health insurance status. Greater stigma against drug use and HIV in rural areas has been associated with lower rates of PrEP use.28
Individuals younger than 65 years in rural areas are less likely to have private health insurance and more likely to be uninsured compared with their urban counterparts, which may impact access to clinicians knowledgeable about PrEP.29 Notably, MSM who live in states that have expanded Medicaid have higher rates of PrEP use compared with MSM living in states that have not expanded Medicaid.30
Health insurers in the United States are required to cover PrEP medication, clinician visits, and associated blood work with no patient cost-sharing, although implementation barriers such as prior authorizations still exist.
Conclusion
Family physicians are well positioned to identify patients at risk for HIV infection, prescribe PrEP, organize comprehensive follow-up care, and partner with their health systems and local communities to reduce barriers to care. Those who can leverage existing relationships with local health departments, school-based health clinics, congregate housing programs, LGBTQIA+ advocacy groups, harm-reduction coalitions, and other community-based organizations to raise PrEP awareness play a critical role in preventing HIV transmission and reducing health care disparities in their communities.
CORRESPONDENCE
Andrew V.A. Foley, MD, MPH, Erie Family Health Centers, 2418 W Division Street, Chicago, IL 60622; [email protected]
1. CDC. Estimated HIV incidence and prevalence in the United States 2017–2021. HIV Surveill Supplemental Rep. 2023;28. Accessed October 23, 2023. https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-28-no-3/index.html
2. CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (preliminary data): National HIV Surveillance System data reported through March 2023; and preexposure prophylaxis (PrEP) data reported through December 2022. HIV Surveill Data Tables. 2023;4. Published June 2023. Accessed October 23, 2023. https://www.cdc.gov/hiv/library/reports/surveillance-data-tables/
3. CDC. Division of HIV Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention. PrEP effectiveness. Updated June 2022. Accessed October 23, 2023. https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html
4. US Preventive Services Task Force. Prevention of acquisition of HIV: preexposure prophylaxis. Final recommendation statement. August 22, 2023. Accessed October 23, 2023. https://uspreventiveservicestaskforce.org/uspstf/recommendation/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis
5. CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update: a clinical practice guideline. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
6. Mugwanya KK, Wyatt C, Celum C, et al. Changes in glomerular kidney function among HIV-1-uninfected men and women receiving emtricitabine-tenofovir disoproxil fumarate preexposure prophylaxis: a randomized clinical trial. JAMA Intern Med. 2015;175:246-254. doi: 10.1001/jamainternmed.2014.6786
7. Havens PL, Stephensen CB, Van Loan MD, et al. Decline in bone mass with tenofovir disoproxil fumarate/emtricitabine is associated with hormonal changes in the absence of renal impairment when used by HIV-uninfected adolescent boys and young men for HIV preexposure prophylaxis. Clin Infect Dis. 2017;64:317-325. doi: 10.1093/cid/ciw765
8. Pilkington V, Hill A, Hughes S, et al. How safe is TDF/FTC as PrEP? A systematic review and meta-analysis of the risk of adverse events in 13 randomised trials of PrEP. J Virus Erad. 2018;4:215-224.
9. Mayer KH, Molina JM, Thompson MA, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020;396:239-254. doi: 10.1016/S0140-6736(20)31065-5
10. Liegeon G, Ghosn, J. Long-acting injectable cabotegravir for PrEP: a game-changer in HIV prevention. HIV Med. 2022;24:653-663. doi: 10.1111/hiv.13451
11. Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246. doi: 10.1056/NEJMoa1506273
12. Molina JM, Ghosn J, Assoumou L, et al. Daily and on-demand HIV pre-exposure prophylaxis with emtricitabine and tenofovir disoproxil (ANRS PREVENIR): a prospective observational cohort study. Lancet HIV. 2022;9:e554-e562. doi: 10.1016/S2352-3018(22)00133-3
13. Dimitrov D, Moore JR, Wood D, et al. Predicted effectiveness of daily and nondaily preexposure prophylaxis for men who have sex with men based on sex and pill-taking patterns from the Human Immuno Virus Prevention Trials Network 067/ADAPT Study. Clin Infect Dis. 2020;71:249-255. doi: 10.1093/cid/ciz799
14. Saag MS, Gandhi RT, Hoy JF, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2020 recommendations of the International Antiviral Society-USA Panel. JAMA. 2020;324:1651-1669. doi: 10.1001/jama.2020.17025
15. Havens PL, Perumean-Chaney SE, Patki A, et al. Changes in bone mass after discontinuation of preexposure prophylaxis with tenofovir disoproxil fumarate/emtricitabine in young men who have sex with men: extension phase results of Adolescent Trials Network Protocols 110 and 113. Clin Infect Dis. 2020;70:687-691. doi: 10.1093/cid/ciz486
16. Neilan AM, Salvant Valentine S, Knopf AS. Case 27-2021: a 16-year-old boy seeking human immunodeficiency virus prophylaxis. N Engl J Med. 2021;385:1034-1041. doi: 10.1056/NEJMcpc1909626
17. Thomson KA, Hughes J, Baeten JM, et al. Increased risk of HIV acquisition among women throughout pregnancy and during the postpartum period: a prospective per-coital-act analysis among women with HIV-infected partners. J Infect Dis. 2018;218:16-25. doi: 10.1093/infdis/jiy113
18. Dettinger JC, Kinuthia J, Pintye J, et al. Perinatal outcomes following maternal pre-exposure prophylaxis (PrEP) use during pregnancy: results from a large PrEP implementation program in Kenya. J Int AIDS Soc. 2019;22:e25378. doi: 10.1002/jia2.25378
19. Moodley D, Lombard C, Govender V, et al. Pregnancy and neonatal safety outcomes of timing of initiation of daily oral tenofovir disoproxil fumarate and emtricitabine pre-exposure prophylaxis for HIV prevention (CAP016): an open-label, randomised, non-inferiority trial. Lancet HIV. 2023;10:e154-e163. doi: 10.1016/S2352-3018(22)00369-1
20. CDC. HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women—National HIV Behavioral Surveillance, 7 U.S. Cities, 2019–2020. HIV Surveillance Special Report 27. April 2021. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-27.pdf
21. Wilson EC, Turner CM, Arayasirikul S, et al. Disparities in the PrEP continuum for trans women compared to MSM in San Francisco, California: results from population-based cross-sectional behavioural surveillance studies. J Int AIDS Soc. 2020;23:e25539. doi: 10.1002/jia2.25539
22. Poteat T, Wirtz A, Malik M, et al. A gap between willingness and uptake: findings from mixed methods research on HIV prevention among Black and Latina transgender women. J Acquir Immune Defic Syndr. 2019;82:131-140. doi: 10.1097/QAI.0000000000002112
23. Cottrell ML, Prince HM, Schauer AP, et al. Decreased tenofovir diphosphate concentrations in a transgender female cohort: implications for human immunodeficiency virus preexposure prophylaxis. Clin Infect Dis. 2019;69:2201-2204. doi: 10.1093/cid/ciz290
24. Hess KL, Hu X, Lansky A, et al. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27:238-243. doi: 10.1016/j.annepidem.2017.02.003
25. Kanny D, Jeffries WL 4th, Chapin-Bardales J, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:801-806. doi: 10.15585/mmwr.mm6837a2
26. CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (early release): National HIV Surveillance System data reported through December 2020; and preexposure prophylaxis (PrEP) data reported through September 2020. HIV Surveill Data Tables. 2021;2. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/library/reports/surveillance-data-tables/vol-2-no-2/cdc-hiv-surveillance-tables-vol-2-no-2.pdf
27. CDC. Diagnoses of HIV infection in the United States and dependent areas 2021: special focus profiles. Updated May 23, 2023. Accessed October 23, 2023. www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-34/content/special-focus-profiles.html
28. Walters SM, Frank D, Van Ham B, et al. PrEP care continuum engagement among persons who inject drugs: rural and urban differences in stigma and social infrastructure. AIDS Behav. 2021;26:1308-1320. doi: 10.1007/s10461-021-03488-2
29. Foutz J, Artiga S, Garfield R. The role of Medicaid in rural America [issue brief]. April 25, 2017. Accessed August 16, 2023. www.kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
30. Baugher AR, Finlayson T, Lewis R, et al. Health care coverage and preexposure prophylaxis (PrEP) use among men who have sex with men living in 22 US cities with vs without Medicaid expansion, 2017. Am J Public Health. 2021;111:743-751. doi: 10.2105/AJPH.2020.306035
1. CDC. Estimated HIV incidence and prevalence in the United States 2017–2021. HIV Surveill Supplemental Rep. 2023;28. Accessed October 23, 2023. https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-28-no-3/index.html
2. CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (preliminary data): National HIV Surveillance System data reported through March 2023; and preexposure prophylaxis (PrEP) data reported through December 2022. HIV Surveill Data Tables. 2023;4. Published June 2023. Accessed October 23, 2023. https://www.cdc.gov/hiv/library/reports/surveillance-data-tables/
3. CDC. Division of HIV Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention. PrEP effectiveness. Updated June 2022. Accessed October 23, 2023. https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html
4. US Preventive Services Task Force. Prevention of acquisition of HIV: preexposure prophylaxis. Final recommendation statement. August 22, 2023. Accessed October 23, 2023. https://uspreventiveservicestaskforce.org/uspstf/recommendation/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis
5. CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update: a clinical practice guideline. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
6. Mugwanya KK, Wyatt C, Celum C, et al. Changes in glomerular kidney function among HIV-1-uninfected men and women receiving emtricitabine-tenofovir disoproxil fumarate preexposure prophylaxis: a randomized clinical trial. JAMA Intern Med. 2015;175:246-254. doi: 10.1001/jamainternmed.2014.6786
7. Havens PL, Stephensen CB, Van Loan MD, et al. Decline in bone mass with tenofovir disoproxil fumarate/emtricitabine is associated with hormonal changes in the absence of renal impairment when used by HIV-uninfected adolescent boys and young men for HIV preexposure prophylaxis. Clin Infect Dis. 2017;64:317-325. doi: 10.1093/cid/ciw765
8. Pilkington V, Hill A, Hughes S, et al. How safe is TDF/FTC as PrEP? A systematic review and meta-analysis of the risk of adverse events in 13 randomised trials of PrEP. J Virus Erad. 2018;4:215-224.
9. Mayer KH, Molina JM, Thompson MA, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020;396:239-254. doi: 10.1016/S0140-6736(20)31065-5
10. Liegeon G, Ghosn, J. Long-acting injectable cabotegravir for PrEP: a game-changer in HIV prevention. HIV Med. 2022;24:653-663. doi: 10.1111/hiv.13451
11. Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237-2246. doi: 10.1056/NEJMoa1506273
12. Molina JM, Ghosn J, Assoumou L, et al. Daily and on-demand HIV pre-exposure prophylaxis with emtricitabine and tenofovir disoproxil (ANRS PREVENIR): a prospective observational cohort study. Lancet HIV. 2022;9:e554-e562. doi: 10.1016/S2352-3018(22)00133-3
13. Dimitrov D, Moore JR, Wood D, et al. Predicted effectiveness of daily and nondaily preexposure prophylaxis for men who have sex with men based on sex and pill-taking patterns from the Human Immuno Virus Prevention Trials Network 067/ADAPT Study. Clin Infect Dis. 2020;71:249-255. doi: 10.1093/cid/ciz799
14. Saag MS, Gandhi RT, Hoy JF, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2020 recommendations of the International Antiviral Society-USA Panel. JAMA. 2020;324:1651-1669. doi: 10.1001/jama.2020.17025
15. Havens PL, Perumean-Chaney SE, Patki A, et al. Changes in bone mass after discontinuation of preexposure prophylaxis with tenofovir disoproxil fumarate/emtricitabine in young men who have sex with men: extension phase results of Adolescent Trials Network Protocols 110 and 113. Clin Infect Dis. 2020;70:687-691. doi: 10.1093/cid/ciz486
16. Neilan AM, Salvant Valentine S, Knopf AS. Case 27-2021: a 16-year-old boy seeking human immunodeficiency virus prophylaxis. N Engl J Med. 2021;385:1034-1041. doi: 10.1056/NEJMcpc1909626
17. Thomson KA, Hughes J, Baeten JM, et al. Increased risk of HIV acquisition among women throughout pregnancy and during the postpartum period: a prospective per-coital-act analysis among women with HIV-infected partners. J Infect Dis. 2018;218:16-25. doi: 10.1093/infdis/jiy113
18. Dettinger JC, Kinuthia J, Pintye J, et al. Perinatal outcomes following maternal pre-exposure prophylaxis (PrEP) use during pregnancy: results from a large PrEP implementation program in Kenya. J Int AIDS Soc. 2019;22:e25378. doi: 10.1002/jia2.25378
19. Moodley D, Lombard C, Govender V, et al. Pregnancy and neonatal safety outcomes of timing of initiation of daily oral tenofovir disoproxil fumarate and emtricitabine pre-exposure prophylaxis for HIV prevention (CAP016): an open-label, randomised, non-inferiority trial. Lancet HIV. 2023;10:e154-e163. doi: 10.1016/S2352-3018(22)00369-1
20. CDC. HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women—National HIV Behavioral Surveillance, 7 U.S. Cities, 2019–2020. HIV Surveillance Special Report 27. April 2021. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-27.pdf
21. Wilson EC, Turner CM, Arayasirikul S, et al. Disparities in the PrEP continuum for trans women compared to MSM in San Francisco, California: results from population-based cross-sectional behavioural surveillance studies. J Int AIDS Soc. 2020;23:e25539. doi: 10.1002/jia2.25539
22. Poteat T, Wirtz A, Malik M, et al. A gap between willingness and uptake: findings from mixed methods research on HIV prevention among Black and Latina transgender women. J Acquir Immune Defic Syndr. 2019;82:131-140. doi: 10.1097/QAI.0000000000002112
23. Cottrell ML, Prince HM, Schauer AP, et al. Decreased tenofovir diphosphate concentrations in a transgender female cohort: implications for human immunodeficiency virus preexposure prophylaxis. Clin Infect Dis. 2019;69:2201-2204. doi: 10.1093/cid/ciz290
24. Hess KL, Hu X, Lansky A, et al. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27:238-243. doi: 10.1016/j.annepidem.2017.02.003
25. Kanny D, Jeffries WL 4th, Chapin-Bardales J, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:801-806. doi: 10.15585/mmwr.mm6837a2
26. CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (early release): National HIV Surveillance System data reported through December 2020; and preexposure prophylaxis (PrEP) data reported through September 2020. HIV Surveill Data Tables. 2021;2. Accessed October 23, 2023. www.cdc.gov/hiv/pdf/library/reports/surveillance-data-tables/vol-2-no-2/cdc-hiv-surveillance-tables-vol-2-no-2.pdf
27. CDC. Diagnoses of HIV infection in the United States and dependent areas 2021: special focus profiles. Updated May 23, 2023. Accessed October 23, 2023. www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-34/content/special-focus-profiles.html
28. Walters SM, Frank D, Van Ham B, et al. PrEP care continuum engagement among persons who inject drugs: rural and urban differences in stigma and social infrastructure. AIDS Behav. 2021;26:1308-1320. doi: 10.1007/s10461-021-03488-2
29. Foutz J, Artiga S, Garfield R. The role of Medicaid in rural America [issue brief]. April 25, 2017. Accessed August 16, 2023. www.kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
30. Baugher AR, Finlayson T, Lewis R, et al. Health care coverage and preexposure prophylaxis (PrEP) use among men who have sex with men living in 22 US cities with vs without Medicaid expansion, 2017. Am J Public Health. 2021;111:743-751. doi: 10.2105/AJPH.2020.306035
PRACTICE RECOMMENDATIONS
› Perform routine screening of patients for preexposure prophylaxis (PrEP) eligibility. B
› Prescribe oral or intramuscular PrEP for eligible patients after screening for HIV, other sexually transmitted infections, and hepatitis B, and establishing baseline renal function. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series