User login
In hypoparathyroidism, phosphate, calcium levels may matter
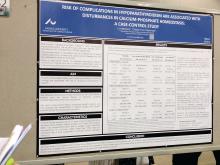
DENVER – Most patients maintained time-weighted serum levels in the normal range in a case-control study of hypoparathyroidism, but serum levels of phosphate and calcium phosphate above median values were associated with a higher mortality and risk of complications.
Patients with calcium levels in the lowest tertile also had an increased risk of cardiovascular disease, while those who experienced episodes of hypercalcemia had a higher risk of mortality and infections.
Denmark has a well-established cohort of patients with hypoparathyroidism, and previous epidemiologic studies have shown that those patients have increased risks of cardiovascular disease, renal diseases, and infections.
“From our epidemiologic study, we did not see increased mortality when we compared patients with hypoparathyroidism to [the] Danish population. So, we were actually a bit surprised that the phosphate and the calcium phosphate product had an influence on mortality,” said Dr. Underbjerg.
To find out if there were any associations between the biochemical findings and complications, the researchers collected biochemical data on 431 patients with hypoparathyroidism (81% of whom were women, with an average age of 41 years and a median disease duration of 12 years); 88% of the patients had the condition as a result of surgery, and 95% of patients received daily calcium and/or activated vitamin D supplements.
The researchers looked at four complications: mortality, cardiovascular disease, renal disease, and any infection. For each complication, they compared patients who had experienced the complication to hypoparathyroidism patients who did not experience the complication.
The subjects had a median time-weighted serum level of ionized calcium of 1.17 mmol/L (interquartile range [IQR], 1.14-1.21), a median of value of 1.21 mmol/L of phosphate (IQR, 1.11-1.32), and a median value of 2.80 mmol2/L2 of the calcium-phosphate product (IQR, 2.51-3.03).
Patients in the lowest tertile of ionized calcium (less than or equal to 1.16) had a greater risk of developing cardiovascular diseases than patients in the midtertile (1.16-1.19; odds ratio [OR], 2.96; 95% confidence interval [CI], 1.02-8.59).
Compared with patients in the midquartile, patients with serum phosphate levels above the median value of 1.21 were at a higher risk of mortality (OR, 2.76; 95% CI, 1.32-5.80) and infections (OR, 1.77; 95% CI, 1.04-3.01).
Calcium-phosphate product levels above the median value of 2.80 were associated with heightened mortality (OR, 2.67; 95% CI, 1.27-5.63) and renal diseases (OR, 1.71; 95% CI, 1.03-2.86).
Hypercalcemia occurred in 41% of patients and was also tied to increased mortality (OR, 1.76; 95% CI, 1.02-3.05) and risk of infections (OR, 1.86; 95% CI, 1.18-2.93).
The results suggest that those values have the potential to be clinically important. “I think you have to be aware that phosphate and calcium phosphate levels have an influence on a patient’s well-being,” said Dr. Underbjerg.
Shire funded the study. Dr. Underbjerg reported having no relevant financial disclosures.
DENVER – Most patients maintained time-weighted serum levels in the normal range in a case-control study of hypoparathyroidism, but serum levels of phosphate and calcium phosphate above median values were associated with a higher mortality and risk of complications.
Patients with calcium levels in the lowest tertile also had an increased risk of cardiovascular disease, while those who experienced episodes of hypercalcemia had a higher risk of mortality and infections.
Denmark has a well-established cohort of patients with hypoparathyroidism, and previous epidemiologic studies have shown that those patients have increased risks of cardiovascular disease, renal diseases, and infections.
“From our epidemiologic study, we did not see increased mortality when we compared patients with hypoparathyroidism to [the] Danish population. So, we were actually a bit surprised that the phosphate and the calcium phosphate product had an influence on mortality,” said Dr. Underbjerg.
To find out if there were any associations between the biochemical findings and complications, the researchers collected biochemical data on 431 patients with hypoparathyroidism (81% of whom were women, with an average age of 41 years and a median disease duration of 12 years); 88% of the patients had the condition as a result of surgery, and 95% of patients received daily calcium and/or activated vitamin D supplements.
The researchers looked at four complications: mortality, cardiovascular disease, renal disease, and any infection. For each complication, they compared patients who had experienced the complication to hypoparathyroidism patients who did not experience the complication.
The subjects had a median time-weighted serum level of ionized calcium of 1.17 mmol/L (interquartile range [IQR], 1.14-1.21), a median of value of 1.21 mmol/L of phosphate (IQR, 1.11-1.32), and a median value of 2.80 mmol2/L2 of the calcium-phosphate product (IQR, 2.51-3.03).
Patients in the lowest tertile of ionized calcium (less than or equal to 1.16) had a greater risk of developing cardiovascular diseases than patients in the midtertile (1.16-1.19; odds ratio [OR], 2.96; 95% confidence interval [CI], 1.02-8.59).
Compared with patients in the midquartile, patients with serum phosphate levels above the median value of 1.21 were at a higher risk of mortality (OR, 2.76; 95% CI, 1.32-5.80) and infections (OR, 1.77; 95% CI, 1.04-3.01).
Calcium-phosphate product levels above the median value of 2.80 were associated with heightened mortality (OR, 2.67; 95% CI, 1.27-5.63) and renal diseases (OR, 1.71; 95% CI, 1.03-2.86).
Hypercalcemia occurred in 41% of patients and was also tied to increased mortality (OR, 1.76; 95% CI, 1.02-3.05) and risk of infections (OR, 1.86; 95% CI, 1.18-2.93).
The results suggest that those values have the potential to be clinically important. “I think you have to be aware that phosphate and calcium phosphate levels have an influence on a patient’s well-being,” said Dr. Underbjerg.
Shire funded the study. Dr. Underbjerg reported having no relevant financial disclosures.
DENVER – Most patients maintained time-weighted serum levels in the normal range in a case-control study of hypoparathyroidism, but serum levels of phosphate and calcium phosphate above median values were associated with a higher mortality and risk of complications.
Patients with calcium levels in the lowest tertile also had an increased risk of cardiovascular disease, while those who experienced episodes of hypercalcemia had a higher risk of mortality and infections.
Denmark has a well-established cohort of patients with hypoparathyroidism, and previous epidemiologic studies have shown that those patients have increased risks of cardiovascular disease, renal diseases, and infections.
“From our epidemiologic study, we did not see increased mortality when we compared patients with hypoparathyroidism to [the] Danish population. So, we were actually a bit surprised that the phosphate and the calcium phosphate product had an influence on mortality,” said Dr. Underbjerg.
To find out if there were any associations between the biochemical findings and complications, the researchers collected biochemical data on 431 patients with hypoparathyroidism (81% of whom were women, with an average age of 41 years and a median disease duration of 12 years); 88% of the patients had the condition as a result of surgery, and 95% of patients received daily calcium and/or activated vitamin D supplements.
The researchers looked at four complications: mortality, cardiovascular disease, renal disease, and any infection. For each complication, they compared patients who had experienced the complication to hypoparathyroidism patients who did not experience the complication.
The subjects had a median time-weighted serum level of ionized calcium of 1.17 mmol/L (interquartile range [IQR], 1.14-1.21), a median of value of 1.21 mmol/L of phosphate (IQR, 1.11-1.32), and a median value of 2.80 mmol2/L2 of the calcium-phosphate product (IQR, 2.51-3.03).
Patients in the lowest tertile of ionized calcium (less than or equal to 1.16) had a greater risk of developing cardiovascular diseases than patients in the midtertile (1.16-1.19; odds ratio [OR], 2.96; 95% confidence interval [CI], 1.02-8.59).
Compared with patients in the midquartile, patients with serum phosphate levels above the median value of 1.21 were at a higher risk of mortality (OR, 2.76; 95% CI, 1.32-5.80) and infections (OR, 1.77; 95% CI, 1.04-3.01).
Calcium-phosphate product levels above the median value of 2.80 were associated with heightened mortality (OR, 2.67; 95% CI, 1.27-5.63) and renal diseases (OR, 1.71; 95% CI, 1.03-2.86).
Hypercalcemia occurred in 41% of patients and was also tied to increased mortality (OR, 1.76; 95% CI, 1.02-3.05) and risk of infections (OR, 1.86; 95% CI, 1.18-2.93).
The results suggest that those values have the potential to be clinically important. “I think you have to be aware that phosphate and calcium phosphate levels have an influence on a patient’s well-being,” said Dr. Underbjerg.
Shire funded the study. Dr. Underbjerg reported having no relevant financial disclosures.
AT ASBMR
Key clinical point: Serum phosphate and calcium-phosphate levels may influence patient outcomes in hypoparathyroidism.
Major finding: Higher phosphate levels are tied to an increased risk of mortality (OR, 2.76) and infections (OR, 1.77).
Data source: A case-control study of 431 patients with hypoparathyroidism.
Disclosures: Shire funded the study. Dr. Underbjerg reported having no relevant financial disclosures.
Laser Interstitial Thermal Ablation: A Promising Approach to TLE
Laser interstitial thermal ablation (LiTT) appears to benefit patients with temporal lobe epilepsy (TLE) according to a recent article published in Epilepsy Research.
- According to the author, LiTT has been found to eliminate seizures in about half of patients with mesial temporal lobe epilepsy who undergo the procedure.
- Neuropsychological side effects of the procedure seem to be less severe, when compared to surgeries that require large resections.
- LiTT involves inserting a probe into the area of the brain responsible for the seizures, including the mesial temporal lobe and hypothalamic hamartoma, and heating the tip of the probe by means of laser energy.
- Advantages include the fact that LiTT is less invasive than open surgery and allows patients to leave the hospital sooner and experience less pain.
- The minimally invasive surgery typically requires a single day of hospitalization and allows patients to return to work in 3 days.
- It remains uncertain whether LiTT is as efficacious as more invasive procedures but appears to be about as efficacious as anterior temporal lobectomy.
Kang JY, Sperling MR. Epileptologist’s view: Laser interstitial thermal ablation for treatment of temporal lobe epilepsy. [Published online ahead of print July 25, 2017] Epilepsy Res. https://doi.org/10.1016/j.eplepsyres.2017.07.007
Laser interstitial thermal ablation (LiTT) appears to benefit patients with temporal lobe epilepsy (TLE) according to a recent article published in Epilepsy Research.
- According to the author, LiTT has been found to eliminate seizures in about half of patients with mesial temporal lobe epilepsy who undergo the procedure.
- Neuropsychological side effects of the procedure seem to be less severe, when compared to surgeries that require large resections.
- LiTT involves inserting a probe into the area of the brain responsible for the seizures, including the mesial temporal lobe and hypothalamic hamartoma, and heating the tip of the probe by means of laser energy.
- Advantages include the fact that LiTT is less invasive than open surgery and allows patients to leave the hospital sooner and experience less pain.
- The minimally invasive surgery typically requires a single day of hospitalization and allows patients to return to work in 3 days.
- It remains uncertain whether LiTT is as efficacious as more invasive procedures but appears to be about as efficacious as anterior temporal lobectomy.
Kang JY, Sperling MR. Epileptologist’s view: Laser interstitial thermal ablation for treatment of temporal lobe epilepsy. [Published online ahead of print July 25, 2017] Epilepsy Res. https://doi.org/10.1016/j.eplepsyres.2017.07.007
Laser interstitial thermal ablation (LiTT) appears to benefit patients with temporal lobe epilepsy (TLE) according to a recent article published in Epilepsy Research.
- According to the author, LiTT has been found to eliminate seizures in about half of patients with mesial temporal lobe epilepsy who undergo the procedure.
- Neuropsychological side effects of the procedure seem to be less severe, when compared to surgeries that require large resections.
- LiTT involves inserting a probe into the area of the brain responsible for the seizures, including the mesial temporal lobe and hypothalamic hamartoma, and heating the tip of the probe by means of laser energy.
- Advantages include the fact that LiTT is less invasive than open surgery and allows patients to leave the hospital sooner and experience less pain.
- The minimally invasive surgery typically requires a single day of hospitalization and allows patients to return to work in 3 days.
- It remains uncertain whether LiTT is as efficacious as more invasive procedures but appears to be about as efficacious as anterior temporal lobectomy.
Kang JY, Sperling MR. Epileptologist’s view: Laser interstitial thermal ablation for treatment of temporal lobe epilepsy. [Published online ahead of print July 25, 2017] Epilepsy Res. https://doi.org/10.1016/j.eplepsyres.2017.07.007
The Link Between Ischemic Stroke and Seizures
The threat of seizures and epilepsy is a significant concern for patients who have had a stroke, according to a review of 41 studies published in Neurology.
- Investigators found 35 studies that reported stroke-related seizures and 6 studies that found details on the effects of antiepileptic drugs.
- Seizures occurred early on in 3.3% of patients who had experienced a stroke.
- Late-onset seizures or epilepsy was reported in 18/1000 person-years.
- Researchers were unable to find any evidence to suggest that a specific drug was more effective among patients who had seizures after a stroke.
- Newer drugs caused fewer side effects than older medications.
- The systematic review and meta-analysis included measurement of I2 statistic to evaluate heterogeneity and sensitivity analyses were also performed.
- Early onset and late onset seizures generated I2 statistics of 92.8% and 94.1%, respectively.
- Sensitivity analyses was unable to explain the high degree of heterogeneity.
Wang JZ, Vyas MV, Saposnik G, Burneo JG. Incidence and management of seizures after ischemic stroke. Neurology. 2017;89:1220-1228.
The threat of seizures and epilepsy is a significant concern for patients who have had a stroke, according to a review of 41 studies published in Neurology.
- Investigators found 35 studies that reported stroke-related seizures and 6 studies that found details on the effects of antiepileptic drugs.
- Seizures occurred early on in 3.3% of patients who had experienced a stroke.
- Late-onset seizures or epilepsy was reported in 18/1000 person-years.
- Researchers were unable to find any evidence to suggest that a specific drug was more effective among patients who had seizures after a stroke.
- Newer drugs caused fewer side effects than older medications.
- The systematic review and meta-analysis included measurement of I2 statistic to evaluate heterogeneity and sensitivity analyses were also performed.
- Early onset and late onset seizures generated I2 statistics of 92.8% and 94.1%, respectively.
- Sensitivity analyses was unable to explain the high degree of heterogeneity.
Wang JZ, Vyas MV, Saposnik G, Burneo JG. Incidence and management of seizures after ischemic stroke. Neurology. 2017;89:1220-1228.
The threat of seizures and epilepsy is a significant concern for patients who have had a stroke, according to a review of 41 studies published in Neurology.
- Investigators found 35 studies that reported stroke-related seizures and 6 studies that found details on the effects of antiepileptic drugs.
- Seizures occurred early on in 3.3% of patients who had experienced a stroke.
- Late-onset seizures or epilepsy was reported in 18/1000 person-years.
- Researchers were unable to find any evidence to suggest that a specific drug was more effective among patients who had seizures after a stroke.
- Newer drugs caused fewer side effects than older medications.
- The systematic review and meta-analysis included measurement of I2 statistic to evaluate heterogeneity and sensitivity analyses were also performed.
- Early onset and late onset seizures generated I2 statistics of 92.8% and 94.1%, respectively.
- Sensitivity analyses was unable to explain the high degree of heterogeneity.
Wang JZ, Vyas MV, Saposnik G, Burneo JG. Incidence and management of seizures after ischemic stroke. Neurology. 2017;89:1220-1228.
Sleep, Age, and Prone Position Linked to SUDEP
Patients are more likely to die of sudden unexpected death in epilepsy (SUDEP) while they are asleep, according to a review of over 1000 SUDEP cases gleaned from 67 studies.
- Among 1025 patients with SUDEP, 880 cases had a circadian pattern.
- Of the 880 cases with a circadian pattern, 69.3% of the deaths occurred during sleep and 30.7% while patients were awake (P<0.001).
- Subgroup analysis found 272 patients in which both circadian pattern and age could be established.
- In this subgroup, patients aged 40 years and younger were more likely to die while asleep, when compared with older patients (odds ratio, 2.0).
- Among patients whose body position could also be verified, prone position was more often associated with death, when compared with those in prone position who were awake (87.6% vs 52.9%).
Ali A, Wu S, Issa NP, et al. Association of sleep with sudden unexpected death in epilepsy. [Published online ahead of print September 13, 2017] Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2017.08.021
Patients are more likely to die of sudden unexpected death in epilepsy (SUDEP) while they are asleep, according to a review of over 1000 SUDEP cases gleaned from 67 studies.
- Among 1025 patients with SUDEP, 880 cases had a circadian pattern.
- Of the 880 cases with a circadian pattern, 69.3% of the deaths occurred during sleep and 30.7% while patients were awake (P<0.001).
- Subgroup analysis found 272 patients in which both circadian pattern and age could be established.
- In this subgroup, patients aged 40 years and younger were more likely to die while asleep, when compared with older patients (odds ratio, 2.0).
- Among patients whose body position could also be verified, prone position was more often associated with death, when compared with those in prone position who were awake (87.6% vs 52.9%).
Ali A, Wu S, Issa NP, et al. Association of sleep with sudden unexpected death in epilepsy. [Published online ahead of print September 13, 2017] Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2017.08.021
Patients are more likely to die of sudden unexpected death in epilepsy (SUDEP) while they are asleep, according to a review of over 1000 SUDEP cases gleaned from 67 studies.
- Among 1025 patients with SUDEP, 880 cases had a circadian pattern.
- Of the 880 cases with a circadian pattern, 69.3% of the deaths occurred during sleep and 30.7% while patients were awake (P<0.001).
- Subgroup analysis found 272 patients in which both circadian pattern and age could be established.
- In this subgroup, patients aged 40 years and younger were more likely to die while asleep, when compared with older patients (odds ratio, 2.0).
- Among patients whose body position could also be verified, prone position was more often associated with death, when compared with those in prone position who were awake (87.6% vs 52.9%).
Ali A, Wu S, Issa NP, et al. Association of sleep with sudden unexpected death in epilepsy. [Published online ahead of print September 13, 2017] Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2017.08.021
Leukocyte activation test–based elimination diet improves IBS symptoms
Elimination diets guided by leukocyte activation tests reduced symptoms in patients with irritable bowel syndrome (IBS) in a parallel-group, double-blind, randomized controlled trial.
Study participants were randomized to a 4-week diet with individualized guidance to either eliminate foods with positive assay results and to allow foods with negative assay results (intervention group), or to eliminate foods with negative assay results and allow foods with positive assay results (comparison group). The 29 patients in the intervention group had significantly greater increases in mean IBS Global Improvement Scale scores at 4 weeks and 8 weeks vs. the 29 patients in the comparison group (mean between-group differences, 0.86 and 1.22 points, respectively), reported Ather Ali, ND, of Yale University, New Haven, Conn., and colleagues (BMJ Open Gastro. 2017;0:e000164. doi: 10.1136/bmjgast-2017-000164).
Improvements were seen in IBS Adequate Relief and Quality of Life scores in the intervention group, but the differences between the groups were not statistically significant. No adverse effects related to the intervention were reported, they said.
Of note, strong responders in the intervention group experienced significant reductions in neutrophil elastase.
IBS is a prevalent, costly, and often disabling condition, but assessing food intolerance in clinical practice is challenging, the investigators said, adding that while a number of commercially available blood tests claim to diagnose food intolerance – including leukocyte activation tests, which are among the most widely used for this purpose – no rigorous studies of the tests have been published.
For the current study, adults aged 18-75 years who met Rome III criteria for any subtype of IBS and had active symptoms were enrolled from an academic health center in Connecticut. The leukocyte activation test was used to culture peripheral blood leukocytes with standardized individual food extracts, producing either a positive or negative result, which then guided the food elimination.
The findings demonstrate that “a diet guided by leukocyte activation testing results in demonstrable clinical improvement in IBS,” they wrote, noting that dietary changes based on a leukocyte activation test may be less restrictive than those associated with a low–fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (low FODMAPs) diet (which has also shown promise as “an efficacious, although burdensome, dietary intervention for IBS”), and may result in better long-term adherence.
“These clinical results, associated with a reduction in plasma neutrophil elastase, have implication for better understanding the role of food intolerance and the pathophysiology of IBS,” they said, adding that “future studies, ideally multisite and in larger samples, can assess comparative effects of other dietary interventions in IBS, the effects of restricting specific foods, and whether dietary changes guided by leukocyte activation testing affect other conditions.”
Cell Science Systems funded the study. The authors reported having no disclosures.
Elimination diets guided by leukocyte activation tests reduced symptoms in patients with irritable bowel syndrome (IBS) in a parallel-group, double-blind, randomized controlled trial.
Study participants were randomized to a 4-week diet with individualized guidance to either eliminate foods with positive assay results and to allow foods with negative assay results (intervention group), or to eliminate foods with negative assay results and allow foods with positive assay results (comparison group). The 29 patients in the intervention group had significantly greater increases in mean IBS Global Improvement Scale scores at 4 weeks and 8 weeks vs. the 29 patients in the comparison group (mean between-group differences, 0.86 and 1.22 points, respectively), reported Ather Ali, ND, of Yale University, New Haven, Conn., and colleagues (BMJ Open Gastro. 2017;0:e000164. doi: 10.1136/bmjgast-2017-000164).
Improvements were seen in IBS Adequate Relief and Quality of Life scores in the intervention group, but the differences between the groups were not statistically significant. No adverse effects related to the intervention were reported, they said.
Of note, strong responders in the intervention group experienced significant reductions in neutrophil elastase.
IBS is a prevalent, costly, and often disabling condition, but assessing food intolerance in clinical practice is challenging, the investigators said, adding that while a number of commercially available blood tests claim to diagnose food intolerance – including leukocyte activation tests, which are among the most widely used for this purpose – no rigorous studies of the tests have been published.
For the current study, adults aged 18-75 years who met Rome III criteria for any subtype of IBS and had active symptoms were enrolled from an academic health center in Connecticut. The leukocyte activation test was used to culture peripheral blood leukocytes with standardized individual food extracts, producing either a positive or negative result, which then guided the food elimination.
The findings demonstrate that “a diet guided by leukocyte activation testing results in demonstrable clinical improvement in IBS,” they wrote, noting that dietary changes based on a leukocyte activation test may be less restrictive than those associated with a low–fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (low FODMAPs) diet (which has also shown promise as “an efficacious, although burdensome, dietary intervention for IBS”), and may result in better long-term adherence.
“These clinical results, associated with a reduction in plasma neutrophil elastase, have implication for better understanding the role of food intolerance and the pathophysiology of IBS,” they said, adding that “future studies, ideally multisite and in larger samples, can assess comparative effects of other dietary interventions in IBS, the effects of restricting specific foods, and whether dietary changes guided by leukocyte activation testing affect other conditions.”
Cell Science Systems funded the study. The authors reported having no disclosures.
Elimination diets guided by leukocyte activation tests reduced symptoms in patients with irritable bowel syndrome (IBS) in a parallel-group, double-blind, randomized controlled trial.
Study participants were randomized to a 4-week diet with individualized guidance to either eliminate foods with positive assay results and to allow foods with negative assay results (intervention group), or to eliminate foods with negative assay results and allow foods with positive assay results (comparison group). The 29 patients in the intervention group had significantly greater increases in mean IBS Global Improvement Scale scores at 4 weeks and 8 weeks vs. the 29 patients in the comparison group (mean between-group differences, 0.86 and 1.22 points, respectively), reported Ather Ali, ND, of Yale University, New Haven, Conn., and colleagues (BMJ Open Gastro. 2017;0:e000164. doi: 10.1136/bmjgast-2017-000164).
Improvements were seen in IBS Adequate Relief and Quality of Life scores in the intervention group, but the differences between the groups were not statistically significant. No adverse effects related to the intervention were reported, they said.
Of note, strong responders in the intervention group experienced significant reductions in neutrophil elastase.
IBS is a prevalent, costly, and often disabling condition, but assessing food intolerance in clinical practice is challenging, the investigators said, adding that while a number of commercially available blood tests claim to diagnose food intolerance – including leukocyte activation tests, which are among the most widely used for this purpose – no rigorous studies of the tests have been published.
For the current study, adults aged 18-75 years who met Rome III criteria for any subtype of IBS and had active symptoms were enrolled from an academic health center in Connecticut. The leukocyte activation test was used to culture peripheral blood leukocytes with standardized individual food extracts, producing either a positive or negative result, which then guided the food elimination.
The findings demonstrate that “a diet guided by leukocyte activation testing results in demonstrable clinical improvement in IBS,” they wrote, noting that dietary changes based on a leukocyte activation test may be less restrictive than those associated with a low–fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (low FODMAPs) diet (which has also shown promise as “an efficacious, although burdensome, dietary intervention for IBS”), and may result in better long-term adherence.
“These clinical results, associated with a reduction in plasma neutrophil elastase, have implication for better understanding the role of food intolerance and the pathophysiology of IBS,” they said, adding that “future studies, ideally multisite and in larger samples, can assess comparative effects of other dietary interventions in IBS, the effects of restricting specific foods, and whether dietary changes guided by leukocyte activation testing affect other conditions.”
Cell Science Systems funded the study. The authors reported having no disclosures.
FROM BMJ OPEN GASTROENTEROLOGY
Key clinical point:
Major finding: Mean IBS Global Improvement Scale scores improved significantly more in the intervention vs. comparison group at 4 weeks and 8 weeks (mean between-group differences of 0.86 and 1.22 points, respectively).
Data source: A parallel-group, double-blind, randomized controlled trial of 58 IBS patients.
Disclosures: Cell Science Systems funded the study. The authors reported having no disclosures.
Benzodiazepines and antidepressants do not impair cognition in midlife schizophrenia
PARIS – Cumulative lifetime exposure to benzodiazepines and antidepressants in the relatively modest amounts typically prescribed in schizophrenia did not appear to adversely affect patients’ cognition in midlife, according to a first-of-its-kind study from Finland.
“These findings are reassuring,” said Anja P. Hulkko, MD, a psychiatric resident at the University of Oulu (Finland).
“Similarly, you don’t need to worry about using benzodiazepines in schizophrenia if you are using small doses or for short periods to treat a specific condition like anxiety or sleeplessness,” Dr. Hulkko said at the annual congress of the European College of Neuropsychopharmacology.
These observations were among the key findings of her analysis from the Northern Finnish Birth Cohort 1966. This ongoing unique and naturalistic observational study – or actually, more than 20 different studies conducted in the same population – was designed to study risk factors involved in preterm birth and intrauterine growth retardation, as well as the consequences of these early adverse events on later morbidity and mortality. Data including maternal health during pregnancy have been prospectively collected from first prenatal contact at weeks 10-16 well into adulthood.
The 1966 cohort included 12,058 live births in the two northernmost provinces of Finland, which was 96% of all births there in that year. DNA samples were obtained from nearly 6,000 subjects in the cohort. After birth and again every 7-15 years, the offspring were examined and underwent clinical evaluation in which a wide range of phenotypic, behavioral, and demographic data were collected. Linkage to Finland’s comprehensive national registries provides investigators with up-to-date information about participants’ education, medication, hospitalizations, significant medical diagnoses, pensions, and death. These prospective data allow investigations of the importance of genetic, biologic, social, and behavioral risk factors in the emergence of various target diseases, one of which is schizophrenia.
Dr. Hulkko’s presentation focused on 60 patients with various schizophrenia spectrum disorders who underwent an extensive battery of neuropsychological tests at age 43, when they averaged 16.5 years of illness.
Lifetime cumulative exposure to benzodiazepines or antidepressants was not significantly associated with a global composite cognition score in a multivariate analysis adjusted for potential confounders including sex, age at schizophrenia onset, and lifetime psychiatric hospital treatment days.
The comprehensive test battery included the California Verbal Learning Test, the Abstraction Inhibition and Working Memory Task, Digit Span and Matrix Reasoning, verbal fluency and vocabulary testing, and the Visual Object Learning Test.
This, she said, is the first report to look at the cognitive impact of these drug classes in midlife schizophrenia. Long-term, high-dose use of benzodiazepines has in recent years been linked to increased risk for cognitive impairment in other populations, but that’s not ordinarily how those drugs are employed in schizophrenia.
In contrast to the new Finnish antidepressant and benzodiazepine findings, higher lifetime antipsychotic dose-years in the study population were recently reported by Dr. Hulkko’s senior coinvestigators to be significantly associated with a worse adjusted cognition score, with no difference between typical and atypical antipsychotics. “It is possible that large antipsychotic doses harm cognition in schizophrenia in the long term,” the researchers concluded (Psychiatry Res. 2017 Jan;247:130-8).
At the meeting, Dr. Hulkko presented new data on the cognitive impact of cumulative exposure to antipsychotics in the midlife schizophrenia cohort. The new finding is that having an antipsychotic-free period of at least 1 year at any point since treatment started an average of more than 16 years earlier was associated with a better adjusted cognitive performance.
The same was true for having an antipsychotic-free interval of at least 11 months directly before administration of the neuropsychological test battery. This is an encouraging finding because it suggests that an antipsychotic drug holiday might promote a measurable degree of cognitive recovery. But this observation must be viewed as hypothesis generating rather than conclusive, given the relatively small size of the study population, the observational nature of the study, and the possibility that the patients on a pretest antipsychotic break had less severe illness.
“Although we have tried to control for many factors, still, it’s possible that we cannot control for everything,” she noted. “It seems likely that both the illness itself and treatment are associated with the course of cognition.”
Kamilla W. Miskowiak, PhD, a neuropsychologist at the University of Copenhagen deemed the Finnish results “highly interesting.”
“This is reassuring, since many patients are worried about taking these medications [antidepressants and benzodiazepines] because of their potential negative effects on cognition. In contrast, long-term high-dose antipsychotic medication was associated with poorer cognitive outcome. This underscores the importance of close dose monitoring of antipsychotic medication for these patients to improve their cognitive outcome,” said Dr. Miskowiak, who was not involved in the study.
The study was supported by the Academy of Finland, the Finnish Cultural Foundation Lapland Regional Fund, and grants from various nonprofit foundations. Dr. Hulkko reported having no financial conflicts of interest.
PARIS – Cumulative lifetime exposure to benzodiazepines and antidepressants in the relatively modest amounts typically prescribed in schizophrenia did not appear to adversely affect patients’ cognition in midlife, according to a first-of-its-kind study from Finland.
“These findings are reassuring,” said Anja P. Hulkko, MD, a psychiatric resident at the University of Oulu (Finland).
“Similarly, you don’t need to worry about using benzodiazepines in schizophrenia if you are using small doses or for short periods to treat a specific condition like anxiety or sleeplessness,” Dr. Hulkko said at the annual congress of the European College of Neuropsychopharmacology.
These observations were among the key findings of her analysis from the Northern Finnish Birth Cohort 1966. This ongoing unique and naturalistic observational study – or actually, more than 20 different studies conducted in the same population – was designed to study risk factors involved in preterm birth and intrauterine growth retardation, as well as the consequences of these early adverse events on later morbidity and mortality. Data including maternal health during pregnancy have been prospectively collected from first prenatal contact at weeks 10-16 well into adulthood.
The 1966 cohort included 12,058 live births in the two northernmost provinces of Finland, which was 96% of all births there in that year. DNA samples were obtained from nearly 6,000 subjects in the cohort. After birth and again every 7-15 years, the offspring were examined and underwent clinical evaluation in which a wide range of phenotypic, behavioral, and demographic data were collected. Linkage to Finland’s comprehensive national registries provides investigators with up-to-date information about participants’ education, medication, hospitalizations, significant medical diagnoses, pensions, and death. These prospective data allow investigations of the importance of genetic, biologic, social, and behavioral risk factors in the emergence of various target diseases, one of which is schizophrenia.
Dr. Hulkko’s presentation focused on 60 patients with various schizophrenia spectrum disorders who underwent an extensive battery of neuropsychological tests at age 43, when they averaged 16.5 years of illness.
Lifetime cumulative exposure to benzodiazepines or antidepressants was not significantly associated with a global composite cognition score in a multivariate analysis adjusted for potential confounders including sex, age at schizophrenia onset, and lifetime psychiatric hospital treatment days.
The comprehensive test battery included the California Verbal Learning Test, the Abstraction Inhibition and Working Memory Task, Digit Span and Matrix Reasoning, verbal fluency and vocabulary testing, and the Visual Object Learning Test.
This, she said, is the first report to look at the cognitive impact of these drug classes in midlife schizophrenia. Long-term, high-dose use of benzodiazepines has in recent years been linked to increased risk for cognitive impairment in other populations, but that’s not ordinarily how those drugs are employed in schizophrenia.
In contrast to the new Finnish antidepressant and benzodiazepine findings, higher lifetime antipsychotic dose-years in the study population were recently reported by Dr. Hulkko’s senior coinvestigators to be significantly associated with a worse adjusted cognition score, with no difference between typical and atypical antipsychotics. “It is possible that large antipsychotic doses harm cognition in schizophrenia in the long term,” the researchers concluded (Psychiatry Res. 2017 Jan;247:130-8).
At the meeting, Dr. Hulkko presented new data on the cognitive impact of cumulative exposure to antipsychotics in the midlife schizophrenia cohort. The new finding is that having an antipsychotic-free period of at least 1 year at any point since treatment started an average of more than 16 years earlier was associated with a better adjusted cognitive performance.
The same was true for having an antipsychotic-free interval of at least 11 months directly before administration of the neuropsychological test battery. This is an encouraging finding because it suggests that an antipsychotic drug holiday might promote a measurable degree of cognitive recovery. But this observation must be viewed as hypothesis generating rather than conclusive, given the relatively small size of the study population, the observational nature of the study, and the possibility that the patients on a pretest antipsychotic break had less severe illness.
“Although we have tried to control for many factors, still, it’s possible that we cannot control for everything,” she noted. “It seems likely that both the illness itself and treatment are associated with the course of cognition.”
Kamilla W. Miskowiak, PhD, a neuropsychologist at the University of Copenhagen deemed the Finnish results “highly interesting.”
“This is reassuring, since many patients are worried about taking these medications [antidepressants and benzodiazepines] because of their potential negative effects on cognition. In contrast, long-term high-dose antipsychotic medication was associated with poorer cognitive outcome. This underscores the importance of close dose monitoring of antipsychotic medication for these patients to improve their cognitive outcome,” said Dr. Miskowiak, who was not involved in the study.
The study was supported by the Academy of Finland, the Finnish Cultural Foundation Lapland Regional Fund, and grants from various nonprofit foundations. Dr. Hulkko reported having no financial conflicts of interest.
PARIS – Cumulative lifetime exposure to benzodiazepines and antidepressants in the relatively modest amounts typically prescribed in schizophrenia did not appear to adversely affect patients’ cognition in midlife, according to a first-of-its-kind study from Finland.
“These findings are reassuring,” said Anja P. Hulkko, MD, a psychiatric resident at the University of Oulu (Finland).
“Similarly, you don’t need to worry about using benzodiazepines in schizophrenia if you are using small doses or for short periods to treat a specific condition like anxiety or sleeplessness,” Dr. Hulkko said at the annual congress of the European College of Neuropsychopharmacology.
These observations were among the key findings of her analysis from the Northern Finnish Birth Cohort 1966. This ongoing unique and naturalistic observational study – or actually, more than 20 different studies conducted in the same population – was designed to study risk factors involved in preterm birth and intrauterine growth retardation, as well as the consequences of these early adverse events on later morbidity and mortality. Data including maternal health during pregnancy have been prospectively collected from first prenatal contact at weeks 10-16 well into adulthood.
The 1966 cohort included 12,058 live births in the two northernmost provinces of Finland, which was 96% of all births there in that year. DNA samples were obtained from nearly 6,000 subjects in the cohort. After birth and again every 7-15 years, the offspring were examined and underwent clinical evaluation in which a wide range of phenotypic, behavioral, and demographic data were collected. Linkage to Finland’s comprehensive national registries provides investigators with up-to-date information about participants’ education, medication, hospitalizations, significant medical diagnoses, pensions, and death. These prospective data allow investigations of the importance of genetic, biologic, social, and behavioral risk factors in the emergence of various target diseases, one of which is schizophrenia.
Dr. Hulkko’s presentation focused on 60 patients with various schizophrenia spectrum disorders who underwent an extensive battery of neuropsychological tests at age 43, when they averaged 16.5 years of illness.
Lifetime cumulative exposure to benzodiazepines or antidepressants was not significantly associated with a global composite cognition score in a multivariate analysis adjusted for potential confounders including sex, age at schizophrenia onset, and lifetime psychiatric hospital treatment days.
The comprehensive test battery included the California Verbal Learning Test, the Abstraction Inhibition and Working Memory Task, Digit Span and Matrix Reasoning, verbal fluency and vocabulary testing, and the Visual Object Learning Test.
This, she said, is the first report to look at the cognitive impact of these drug classes in midlife schizophrenia. Long-term, high-dose use of benzodiazepines has in recent years been linked to increased risk for cognitive impairment in other populations, but that’s not ordinarily how those drugs are employed in schizophrenia.
In contrast to the new Finnish antidepressant and benzodiazepine findings, higher lifetime antipsychotic dose-years in the study population were recently reported by Dr. Hulkko’s senior coinvestigators to be significantly associated with a worse adjusted cognition score, with no difference between typical and atypical antipsychotics. “It is possible that large antipsychotic doses harm cognition in schizophrenia in the long term,” the researchers concluded (Psychiatry Res. 2017 Jan;247:130-8).
At the meeting, Dr. Hulkko presented new data on the cognitive impact of cumulative exposure to antipsychotics in the midlife schizophrenia cohort. The new finding is that having an antipsychotic-free period of at least 1 year at any point since treatment started an average of more than 16 years earlier was associated with a better adjusted cognitive performance.
The same was true for having an antipsychotic-free interval of at least 11 months directly before administration of the neuropsychological test battery. This is an encouraging finding because it suggests that an antipsychotic drug holiday might promote a measurable degree of cognitive recovery. But this observation must be viewed as hypothesis generating rather than conclusive, given the relatively small size of the study population, the observational nature of the study, and the possibility that the patients on a pretest antipsychotic break had less severe illness.
“Although we have tried to control for many factors, still, it’s possible that we cannot control for everything,” she noted. “It seems likely that both the illness itself and treatment are associated with the course of cognition.”
Kamilla W. Miskowiak, PhD, a neuropsychologist at the University of Copenhagen deemed the Finnish results “highly interesting.”
“This is reassuring, since many patients are worried about taking these medications [antidepressants and benzodiazepines] because of their potential negative effects on cognition. In contrast, long-term high-dose antipsychotic medication was associated with poorer cognitive outcome. This underscores the importance of close dose monitoring of antipsychotic medication for these patients to improve their cognitive outcome,” said Dr. Miskowiak, who was not involved in the study.
The study was supported by the Academy of Finland, the Finnish Cultural Foundation Lapland Regional Fund, and grants from various nonprofit foundations. Dr. Hulkko reported having no financial conflicts of interest.
AT THE ECNP CONGRESS
Key clinical point:
Major finding: As-needed prescription of antidepressants and benzodiazepines in the dose typically used in schizophrenia does not impair midlife cognition.
Data source: An ongoing naturalistic, observational, general population-based study of more than 12,000 babies born in Northern Finland in 1966 from fetal life through middle age.
Disclosures: The study was supported by the Academy of Finland, the Finnish Cultural Foundation Lapland Regional Fund, and grants from various nonprofit charitable foundations. The presenter reported having no financial conflicts of interest.
DETOUR system shows early promise for long SFA lesions
A new, percutaneous bypass system appeared safe and effective for treating long-segment blockages in the femoropopliteal artery, a subset of the DETOUR I trial showed. Data at 30 days showed low levels of major adverse events and the results showed that there was promising graft patency at 6 months.
Sean Lyden, MD, chairman of the department of vascular surgery at the Cleveland Clinic, presented the results in a late-breaking clinical trial session at the 2017 Vascular Interventional Advances meeting. The study evaluated the safety and effectiveness of the DETOUR System for treating long-segment (greater than 25 cm) blockages in the femoropopliteal artery.
To address this problem, the PQ Bypass DETOUR System was developed as a fully percutaneous bypass approach designed to achieve comparable end results as open bypass surgery, by using the femoral vein as a pathway for created a modular stent graft bypass.
“The DETOUR procedure creates a pathway around a lesion by placing stent grafts that cross from the superficial femoral artery (SFA) into the femoral vein and back into the artery. The new path through the stent grafts redirects oxygen-rich blood around the blockage and restores blood flow to the lower leg and foot of the patient,” according to a company press release.
The DETOUR 1 trial was a prospective, single-arm study of 77 patients (81 limbs) treated at eight global sites. Dr. Lyden reported on a subset analysis of 50 patients with long lesions (greater than 25 cm). The mean age of the patients was 65 years; 84% were men.
Comorbidities included diabetes (30%), history of renal insufficiency (26%), smoking (90%), and previous peripheral intervention (30%). There were 53 lesions treated in all, with a mean length of 33.5 cm. The percentage of total occlusions was 96% and the percentage of lesions with zero, one, two, or three runoff vessels was 0%, 4%, 26%, and 70%, respectively, according to Dr. Lyden.
The primary safety endpoint of 2% major adverse events defined as death, target vessel revascularization or amputation at 30 days was met, with no deaths or amputations and only one target vessel revascularization.
The primary patency was 89% at 6 months with optimal placement, with an overall primary patency of 77%.
Both the delivery and removal of the device was successful in all the lesions treated.
The Rutherford Class improved at least 2 grades in 92% of the patients, and there was a statistically significant improvement in ankle brachial index from 0.64 to 0.92 (P less than .0001).
“Percutaneous bypass using the femoral vein as a pathway may end up being an important step forward in the treatment of long-segment SFA disease,” Dr. Lyden concluded.
In March 2017, the DETOUR System received CE (Conformité Européenne) Mark approval, but the system is not yet approved by the Food and Drug Administration for sale in the United States.
The DETOUR trial was sponsored by PQ Bypass Inc. Dr. Lyden reported receiving fees Spectranetics Corp and VIVA Physicians. He has no financial conflicts with regard to PQ Bypass.
A new, percutaneous bypass system appeared safe and effective for treating long-segment blockages in the femoropopliteal artery, a subset of the DETOUR I trial showed. Data at 30 days showed low levels of major adverse events and the results showed that there was promising graft patency at 6 months.
Sean Lyden, MD, chairman of the department of vascular surgery at the Cleveland Clinic, presented the results in a late-breaking clinical trial session at the 2017 Vascular Interventional Advances meeting. The study evaluated the safety and effectiveness of the DETOUR System for treating long-segment (greater than 25 cm) blockages in the femoropopliteal artery.
To address this problem, the PQ Bypass DETOUR System was developed as a fully percutaneous bypass approach designed to achieve comparable end results as open bypass surgery, by using the femoral vein as a pathway for created a modular stent graft bypass.
“The DETOUR procedure creates a pathway around a lesion by placing stent grafts that cross from the superficial femoral artery (SFA) into the femoral vein and back into the artery. The new path through the stent grafts redirects oxygen-rich blood around the blockage and restores blood flow to the lower leg and foot of the patient,” according to a company press release.
The DETOUR 1 trial was a prospective, single-arm study of 77 patients (81 limbs) treated at eight global sites. Dr. Lyden reported on a subset analysis of 50 patients with long lesions (greater than 25 cm). The mean age of the patients was 65 years; 84% were men.
Comorbidities included diabetes (30%), history of renal insufficiency (26%), smoking (90%), and previous peripheral intervention (30%). There were 53 lesions treated in all, with a mean length of 33.5 cm. The percentage of total occlusions was 96% and the percentage of lesions with zero, one, two, or three runoff vessels was 0%, 4%, 26%, and 70%, respectively, according to Dr. Lyden.
The primary safety endpoint of 2% major adverse events defined as death, target vessel revascularization or amputation at 30 days was met, with no deaths or amputations and only one target vessel revascularization.
The primary patency was 89% at 6 months with optimal placement, with an overall primary patency of 77%.
Both the delivery and removal of the device was successful in all the lesions treated.
The Rutherford Class improved at least 2 grades in 92% of the patients, and there was a statistically significant improvement in ankle brachial index from 0.64 to 0.92 (P less than .0001).
“Percutaneous bypass using the femoral vein as a pathway may end up being an important step forward in the treatment of long-segment SFA disease,” Dr. Lyden concluded.
In March 2017, the DETOUR System received CE (Conformité Européenne) Mark approval, but the system is not yet approved by the Food and Drug Administration for sale in the United States.
The DETOUR trial was sponsored by PQ Bypass Inc. Dr. Lyden reported receiving fees Spectranetics Corp and VIVA Physicians. He has no financial conflicts with regard to PQ Bypass.
A new, percutaneous bypass system appeared safe and effective for treating long-segment blockages in the femoropopliteal artery, a subset of the DETOUR I trial showed. Data at 30 days showed low levels of major adverse events and the results showed that there was promising graft patency at 6 months.
Sean Lyden, MD, chairman of the department of vascular surgery at the Cleveland Clinic, presented the results in a late-breaking clinical trial session at the 2017 Vascular Interventional Advances meeting. The study evaluated the safety and effectiveness of the DETOUR System for treating long-segment (greater than 25 cm) blockages in the femoropopliteal artery.
To address this problem, the PQ Bypass DETOUR System was developed as a fully percutaneous bypass approach designed to achieve comparable end results as open bypass surgery, by using the femoral vein as a pathway for created a modular stent graft bypass.
“The DETOUR procedure creates a pathway around a lesion by placing stent grafts that cross from the superficial femoral artery (SFA) into the femoral vein and back into the artery. The new path through the stent grafts redirects oxygen-rich blood around the blockage and restores blood flow to the lower leg and foot of the patient,” according to a company press release.
The DETOUR 1 trial was a prospective, single-arm study of 77 patients (81 limbs) treated at eight global sites. Dr. Lyden reported on a subset analysis of 50 patients with long lesions (greater than 25 cm). The mean age of the patients was 65 years; 84% were men.
Comorbidities included diabetes (30%), history of renal insufficiency (26%), smoking (90%), and previous peripheral intervention (30%). There were 53 lesions treated in all, with a mean length of 33.5 cm. The percentage of total occlusions was 96% and the percentage of lesions with zero, one, two, or three runoff vessels was 0%, 4%, 26%, and 70%, respectively, according to Dr. Lyden.
The primary safety endpoint of 2% major adverse events defined as death, target vessel revascularization or amputation at 30 days was met, with no deaths or amputations and only one target vessel revascularization.
The primary patency was 89% at 6 months with optimal placement, with an overall primary patency of 77%.
Both the delivery and removal of the device was successful in all the lesions treated.
The Rutherford Class improved at least 2 grades in 92% of the patients, and there was a statistically significant improvement in ankle brachial index from 0.64 to 0.92 (P less than .0001).
“Percutaneous bypass using the femoral vein as a pathway may end up being an important step forward in the treatment of long-segment SFA disease,” Dr. Lyden concluded.
In March 2017, the DETOUR System received CE (Conformité Européenne) Mark approval, but the system is not yet approved by the Food and Drug Administration for sale in the United States.
The DETOUR trial was sponsored by PQ Bypass Inc. Dr. Lyden reported receiving fees Spectranetics Corp and VIVA Physicians. He has no financial conflicts with regard to PQ Bypass.
FROM VIVA 17
Key clinical point:
Major finding: Primary patency was 89% at 6 months, with low MAE at 30 days.
Data source: Subset analysis of 50 patients with long lesions in the multicenter, prospective, single-arm DETOUR 1 trial.
Disclosures: The DETOUR trial was sponsored by PQ Bypass. Dr. Lyden reported receiving fees from Spectranetics Corp and VIVA Physicians. He has no financial conflicts with regard to PQ Bypass.
Antipsychotics may reduce mortality in schizophrenia
PARIS – All-cause mortality was 46% lower while schizophrenia patients were on antipsychotic agents than when off therapy in a nationwide observational study of nearly 30,000 Swedes with schizophrenia – and the biggest risk reduction occurred in patients on second-generation long-acting injectables, according to Jari Tiihonen, MD, PhD.
“The guidelines say there are special situations where you should consider using depot antipsychotics. I think the guidelines got it wrong. I think the right way to think of it is there are special situations where you might consider oral agents; otherwise you should use long-acting injectables,” said Dr. Tiihonen, who holds joint appointments as professor of psychiatry at the University of Eastern Finland in Kuopio and the Karolinska Institute in Stockholm.

During a mean follow-up of 5.7 years, 8.4% of the patients died. In a multivariate Cox regression analysis adjusted for 20 potential confounding variables, including age, sex, time since diagnosis, education, and comorbid conditions, the all-cause mortality was 46% lower when patients were on an antipsychotic agent than when off therapy.
The lowest mortality was observed in patients on a second-generation long-acting injectable (LAI) antipsychotic agent. Specifically, all-cause mortality was reduced by 89% while patients were on once-monthly palpiperidone palmitate LAI (Invega Sustenna) than during periods when they were not using an antipsychotic. They were 69% less likely to die while on risperidone LAI (Risperdal Consta), and 77% less likely to die while taking oral aripiprazole (Abilify).
In a pairwise comparison between the LAI and oral versions of antipsychotic agents, the LAIs were associated with a 33% lower mortality than the equivalent oral drugs.
Compared with periods of nonuse of any antipsychotic agent, the adjusted risk of mortality was reduced by 85% while patients were on a second-generation LAI, by 47% when on second-generation oral agents, by 36% with first-generation LAIs, and by 34% for first-generation oral antipsychotics.
Also at the ECNP congress, Dr. Tiihonen presented a separate analysis of the same cohort of 29,823 patients, this time examining the real-world effectiveness of various antipsychotic agents in preventing relapse, treatment failure, and rehospitalization. For this purpose, he and his coinvestigators performed a within-individual analysis in which each patient served as his or her own control. The advantage of this analytic strategy is that it corrects for selection bias and other forms of residual confounding inherent in observational studies.
During 7 years of follow-up, 44% of patients were rehospitalized. The risk of psychiatric rehospitalization was lowest when patients were on monotherapy with once-monthly palpiperidone LAI, as evidenced by a 49% reduction, compared with no use of antipsychotic agents. Clozapine (Clozaril) monotherapy and zuclopenthixol LAI (Clopixol) were similarly effective, with each conferring a 47% reduction in rehospitalization risk, compared with periods off therapy. Perphenazine LAI (Trilafon) and olanzapine LAI (Relprevv) each brought a 42% reduction in rehospitalization risk, while the oral version of perphenazine was associated with a 14% risk reduction.
In contrast, the risk of rehospitalization when patients were on oral flupentixol (Depixol) or quetiapine (Seroquel) was not significantly different from when they were off antipsychotic agents altogether.
Collectively, the LAIs were associated with a 22% lower risk of rehospitalization, compared with their equivalent oral versions. And among the 4,603 patients newly diagnosed with schizophrenia in 2006, the LAIs were associated with a more substantial 32% risk reduction, compared with their oral formulations.
Oral clozapine had the lowest treatment failure rate: 42% less than with oral olanzapine (Zyprexa), which served as the reference standard because it was the most commonly used antipsychotic agent. Treatment failure was defined as psychiatric rehospitalization, attempted suicide, treatment discontinuation or a switch to another antipsychotic agent, or death. The various LAIs were associated with 20%-35% lower treatment failure rates than oral olanzapine.
Dr. Tiihonen’s relapse prevention analysis has been published (JAMA Psychiatry. 2017 Jul 1;74[7]:686-93).
The two studies were funded by Janssen-Cilag. Dr. Tiihonen reported serving as a consultant to that pharmaceutical company and a half-dozen others.
PARIS – All-cause mortality was 46% lower while schizophrenia patients were on antipsychotic agents than when off therapy in a nationwide observational study of nearly 30,000 Swedes with schizophrenia – and the biggest risk reduction occurred in patients on second-generation long-acting injectables, according to Jari Tiihonen, MD, PhD.
“The guidelines say there are special situations where you should consider using depot antipsychotics. I think the guidelines got it wrong. I think the right way to think of it is there are special situations where you might consider oral agents; otherwise you should use long-acting injectables,” said Dr. Tiihonen, who holds joint appointments as professor of psychiatry at the University of Eastern Finland in Kuopio and the Karolinska Institute in Stockholm.

During a mean follow-up of 5.7 years, 8.4% of the patients died. In a multivariate Cox regression analysis adjusted for 20 potential confounding variables, including age, sex, time since diagnosis, education, and comorbid conditions, the all-cause mortality was 46% lower when patients were on an antipsychotic agent than when off therapy.
The lowest mortality was observed in patients on a second-generation long-acting injectable (LAI) antipsychotic agent. Specifically, all-cause mortality was reduced by 89% while patients were on once-monthly palpiperidone palmitate LAI (Invega Sustenna) than during periods when they were not using an antipsychotic. They were 69% less likely to die while on risperidone LAI (Risperdal Consta), and 77% less likely to die while taking oral aripiprazole (Abilify).
In a pairwise comparison between the LAI and oral versions of antipsychotic agents, the LAIs were associated with a 33% lower mortality than the equivalent oral drugs.
Compared with periods of nonuse of any antipsychotic agent, the adjusted risk of mortality was reduced by 85% while patients were on a second-generation LAI, by 47% when on second-generation oral agents, by 36% with first-generation LAIs, and by 34% for first-generation oral antipsychotics.
Also at the ECNP congress, Dr. Tiihonen presented a separate analysis of the same cohort of 29,823 patients, this time examining the real-world effectiveness of various antipsychotic agents in preventing relapse, treatment failure, and rehospitalization. For this purpose, he and his coinvestigators performed a within-individual analysis in which each patient served as his or her own control. The advantage of this analytic strategy is that it corrects for selection bias and other forms of residual confounding inherent in observational studies.
During 7 years of follow-up, 44% of patients were rehospitalized. The risk of psychiatric rehospitalization was lowest when patients were on monotherapy with once-monthly palpiperidone LAI, as evidenced by a 49% reduction, compared with no use of antipsychotic agents. Clozapine (Clozaril) monotherapy and zuclopenthixol LAI (Clopixol) were similarly effective, with each conferring a 47% reduction in rehospitalization risk, compared with periods off therapy. Perphenazine LAI (Trilafon) and olanzapine LAI (Relprevv) each brought a 42% reduction in rehospitalization risk, while the oral version of perphenazine was associated with a 14% risk reduction.
In contrast, the risk of rehospitalization when patients were on oral flupentixol (Depixol) or quetiapine (Seroquel) was not significantly different from when they were off antipsychotic agents altogether.
Collectively, the LAIs were associated with a 22% lower risk of rehospitalization, compared with their equivalent oral versions. And among the 4,603 patients newly diagnosed with schizophrenia in 2006, the LAIs were associated with a more substantial 32% risk reduction, compared with their oral formulations.
Oral clozapine had the lowest treatment failure rate: 42% less than with oral olanzapine (Zyprexa), which served as the reference standard because it was the most commonly used antipsychotic agent. Treatment failure was defined as psychiatric rehospitalization, attempted suicide, treatment discontinuation or a switch to another antipsychotic agent, or death. The various LAIs were associated with 20%-35% lower treatment failure rates than oral olanzapine.
Dr. Tiihonen’s relapse prevention analysis has been published (JAMA Psychiatry. 2017 Jul 1;74[7]:686-93).
The two studies were funded by Janssen-Cilag. Dr. Tiihonen reported serving as a consultant to that pharmaceutical company and a half-dozen others.
PARIS – All-cause mortality was 46% lower while schizophrenia patients were on antipsychotic agents than when off therapy in a nationwide observational study of nearly 30,000 Swedes with schizophrenia – and the biggest risk reduction occurred in patients on second-generation long-acting injectables, according to Jari Tiihonen, MD, PhD.
“The guidelines say there are special situations where you should consider using depot antipsychotics. I think the guidelines got it wrong. I think the right way to think of it is there are special situations where you might consider oral agents; otherwise you should use long-acting injectables,” said Dr. Tiihonen, who holds joint appointments as professor of psychiatry at the University of Eastern Finland in Kuopio and the Karolinska Institute in Stockholm.

During a mean follow-up of 5.7 years, 8.4% of the patients died. In a multivariate Cox regression analysis adjusted for 20 potential confounding variables, including age, sex, time since diagnosis, education, and comorbid conditions, the all-cause mortality was 46% lower when patients were on an antipsychotic agent than when off therapy.
The lowest mortality was observed in patients on a second-generation long-acting injectable (LAI) antipsychotic agent. Specifically, all-cause mortality was reduced by 89% while patients were on once-monthly palpiperidone palmitate LAI (Invega Sustenna) than during periods when they were not using an antipsychotic. They were 69% less likely to die while on risperidone LAI (Risperdal Consta), and 77% less likely to die while taking oral aripiprazole (Abilify).
In a pairwise comparison between the LAI and oral versions of antipsychotic agents, the LAIs were associated with a 33% lower mortality than the equivalent oral drugs.
Compared with periods of nonuse of any antipsychotic agent, the adjusted risk of mortality was reduced by 85% while patients were on a second-generation LAI, by 47% when on second-generation oral agents, by 36% with first-generation LAIs, and by 34% for first-generation oral antipsychotics.
Also at the ECNP congress, Dr. Tiihonen presented a separate analysis of the same cohort of 29,823 patients, this time examining the real-world effectiveness of various antipsychotic agents in preventing relapse, treatment failure, and rehospitalization. For this purpose, he and his coinvestigators performed a within-individual analysis in which each patient served as his or her own control. The advantage of this analytic strategy is that it corrects for selection bias and other forms of residual confounding inherent in observational studies.
During 7 years of follow-up, 44% of patients were rehospitalized. The risk of psychiatric rehospitalization was lowest when patients were on monotherapy with once-monthly palpiperidone LAI, as evidenced by a 49% reduction, compared with no use of antipsychotic agents. Clozapine (Clozaril) monotherapy and zuclopenthixol LAI (Clopixol) were similarly effective, with each conferring a 47% reduction in rehospitalization risk, compared with periods off therapy. Perphenazine LAI (Trilafon) and olanzapine LAI (Relprevv) each brought a 42% reduction in rehospitalization risk, while the oral version of perphenazine was associated with a 14% risk reduction.
In contrast, the risk of rehospitalization when patients were on oral flupentixol (Depixol) or quetiapine (Seroquel) was not significantly different from when they were off antipsychotic agents altogether.
Collectively, the LAIs were associated with a 22% lower risk of rehospitalization, compared with their equivalent oral versions. And among the 4,603 patients newly diagnosed with schizophrenia in 2006, the LAIs were associated with a more substantial 32% risk reduction, compared with their oral formulations.
Oral clozapine had the lowest treatment failure rate: 42% less than with oral olanzapine (Zyprexa), which served as the reference standard because it was the most commonly used antipsychotic agent. Treatment failure was defined as psychiatric rehospitalization, attempted suicide, treatment discontinuation or a switch to another antipsychotic agent, or death. The various LAIs were associated with 20%-35% lower treatment failure rates than oral olanzapine.
Dr. Tiihonen’s relapse prevention analysis has been published (JAMA Psychiatry. 2017 Jul 1;74[7]:686-93).
The two studies were funded by Janssen-Cilag. Dr. Tiihonen reported serving as a consultant to that pharmaceutical company and a half-dozen others.
AT THE ECNP CONGRESS
Key clinical point:
Major finding: The all-cause mortality rate was 85% lower when patients with schizophrenia were on a second-generation long-acting injectable antipsychotic than when not taking an antipsychotic.
Data source: An observational study of the association between antipsychotic medication use and all-cause mortality over the course of more than half a decade in nearly 30,000 Swedish schizophrenia patients.
Disclosures: The study was funded by Janssen-Cilag. The presenter reported serving as a consultant to that pharmaceutical company and a half-dozen others.
How Low Can Cholesterol Safely Go?
BARCELONA—Very aggressive reduction of LDL-cholesterol to ultralow levels is associated with progressively fewer cardiovascular events and appears to pose no safety concerns in patients with stable atherosclerotic cardiovascular disease over 2.2 years of follow-up, according to a new analysis. This finding, which was presented at the European Society of Cardiology Congress 2017 and published online ahead of print August 28 in the Lancet, comes from a prespecified secondary analysis of the Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk (FOURIER) trial. “These data support further LDL-cholesterol lowering in patients with cardiovascular disease to well below current recommendations,” said Robert P. Giugliano, MD, Associate Professor of Cardiovascular Medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston, and his research colleagues.
“These findings are unique, in that they represent the first analysis of a large cohort of patients to achieve such very low LDL-cholesterol levels, namely … less than one-third of the most common treatment goal of below 1.8 mmol/L for highest risk patients,” Dr. Giugliano said.
The FOURIER trial randomized patients with stable atherosclerotic cardiovascular disease who were receiving background statin therapy to either placebo or evolocumab, a proprotein convertase subtilisin-kexin type 9 (PCSK9) monoclonal antibody. Initial results from the trial, which was published earlier this year in the New England Journal of Medicine, showed that evolocumab lowered LDL-cholesterol levels to a median of 0.8 mmol/L and significantly reduced the risk of cardiovascular events at a median follow-up of 2.2 years.
The new analysis examined efficacy and safety end points according to degree of LDL-cholesterol reduction at four weeks. In addition, a study known as EBBINGHAUS embedded within the larger analysis explored effects on cognition using a validated tablet-based tool.
A total of 25,982 patients with an LDL-cholesterol assessment at week four who did not experience a primary efficacy or prespecified safety event prior to the week four follow-up visit were included in the analysis. The study showed that the risk of the primary efficacy end point—a composite of cardiovascular death, myocardial infarction, stroke, coronary revascularization, or hospitalization for unstable angina—declined steadily as LDL-cholesterol levels decreased, with no significant association between LDL-cholesterol level and adverse events.
A similar reduction was observed in the key secondary end point, with 2,669 subjects in the lowest LDL-cholesterol category (< 0.5 mmol/L) at four weeks experiencing the lowest rate for cardiovascular death, myocardial infarction, or stroke (adjusted hazard ratio, 0.69), compared with the group with the highest LDL-cholesterol (> 2.6 mmol/L). Exploratory analyses in a subgroup of 504 patients with an LDL-cholesterol level of < 0.25 mmol/L showed further reduction in cardiovascular events with no increase in safety events.
Among 1,154 patients who underwent formal cognitive testing prior to, or on the first day of, study treatment as part of the EBBINGHAUS study, lowered LDL-cholesterol was not associated with adverse effects on memory, executive function, or reaction time.
“Although longer-term follow-up will be important, the totality of evidence to date from trials of intensive lipid lowering supports reduction of LDL-cholesterol in high-risk patients to levels below those currently recommended in cholesterol guidelines,” noted Dr. Giugliano.
This study was sponsored by Amgen.
Important Clinical Implications
The FOURIER secondary analysis, together with a meta-analysis of major statin trials, creates a body of evidence that “heralds the transition from a concept of ‘the lower the better’ towards LDL-cholesterol eradication,” said G. Kees Hovingh, MD, PhD, an internist and vascular medicine specialist at the Academic Medical Center in Amsterdam, and colleagues in an editorial accompanying the published study results.
“For clinicians who prescribe PCSK9 inhibitors, however, the findings from the FOURIER trial, with regard to the potential adverse events, are of even greater importance,” said Dr. Hovingh and colleagues. “Having been trained to first do no harm, many physicians might wonder whether they would infringe on this idea by prescribing PCSK9 inhibitors. Many patients using PCSK9 inhibitors reach extremely low LDL-cholesterol concentrations …, but good safety data for such low LDL-cholesterol values are scarce. In clinical practice, this [situation] often leads to down titration of the dose of conventional lipid-lowering therapy, PCSK9-antibody dose, or both, for fear of potentially unknown side effects.” The results of the FOURIER subanalysis show that “patients achieving very low LDL-cholesterol concentrations are not at increased risk of any of the adverse events assessed.”
—Glenn S. Williams
Suggested Reading
Giugliano RP, Pedersen TR, Park JG, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017 Aug 28 [Ep
Hovingh GK, Boekholdt SM, Stroes ES. Very low LDL-cholesterol concentrations achieved: which target is next? Lancet. 2017 Aug 28 [Epub ahead of print].
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713-1722.
BARCELONA—Very aggressive reduction of LDL-cholesterol to ultralow levels is associated with progressively fewer cardiovascular events and appears to pose no safety concerns in patients with stable atherosclerotic cardiovascular disease over 2.2 years of follow-up, according to a new analysis. This finding, which was presented at the European Society of Cardiology Congress 2017 and published online ahead of print August 28 in the Lancet, comes from a prespecified secondary analysis of the Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk (FOURIER) trial. “These data support further LDL-cholesterol lowering in patients with cardiovascular disease to well below current recommendations,” said Robert P. Giugliano, MD, Associate Professor of Cardiovascular Medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston, and his research colleagues.
“These findings are unique, in that they represent the first analysis of a large cohort of patients to achieve such very low LDL-cholesterol levels, namely … less than one-third of the most common treatment goal of below 1.8 mmol/L for highest risk patients,” Dr. Giugliano said.
The FOURIER trial randomized patients with stable atherosclerotic cardiovascular disease who were receiving background statin therapy to either placebo or evolocumab, a proprotein convertase subtilisin-kexin type 9 (PCSK9) monoclonal antibody. Initial results from the trial, which was published earlier this year in the New England Journal of Medicine, showed that evolocumab lowered LDL-cholesterol levels to a median of 0.8 mmol/L and significantly reduced the risk of cardiovascular events at a median follow-up of 2.2 years.
The new analysis examined efficacy and safety end points according to degree of LDL-cholesterol reduction at four weeks. In addition, a study known as EBBINGHAUS embedded within the larger analysis explored effects on cognition using a validated tablet-based tool.
A total of 25,982 patients with an LDL-cholesterol assessment at week four who did not experience a primary efficacy or prespecified safety event prior to the week four follow-up visit were included in the analysis. The study showed that the risk of the primary efficacy end point—a composite of cardiovascular death, myocardial infarction, stroke, coronary revascularization, or hospitalization for unstable angina—declined steadily as LDL-cholesterol levels decreased, with no significant association between LDL-cholesterol level and adverse events.
A similar reduction was observed in the key secondary end point, with 2,669 subjects in the lowest LDL-cholesterol category (< 0.5 mmol/L) at four weeks experiencing the lowest rate for cardiovascular death, myocardial infarction, or stroke (adjusted hazard ratio, 0.69), compared with the group with the highest LDL-cholesterol (> 2.6 mmol/L). Exploratory analyses in a subgroup of 504 patients with an LDL-cholesterol level of < 0.25 mmol/L showed further reduction in cardiovascular events with no increase in safety events.
Among 1,154 patients who underwent formal cognitive testing prior to, or on the first day of, study treatment as part of the EBBINGHAUS study, lowered LDL-cholesterol was not associated with adverse effects on memory, executive function, or reaction time.
“Although longer-term follow-up will be important, the totality of evidence to date from trials of intensive lipid lowering supports reduction of LDL-cholesterol in high-risk patients to levels below those currently recommended in cholesterol guidelines,” noted Dr. Giugliano.
This study was sponsored by Amgen.
Important Clinical Implications
The FOURIER secondary analysis, together with a meta-analysis of major statin trials, creates a body of evidence that “heralds the transition from a concept of ‘the lower the better’ towards LDL-cholesterol eradication,” said G. Kees Hovingh, MD, PhD, an internist and vascular medicine specialist at the Academic Medical Center in Amsterdam, and colleagues in an editorial accompanying the published study results.
“For clinicians who prescribe PCSK9 inhibitors, however, the findings from the FOURIER trial, with regard to the potential adverse events, are of even greater importance,” said Dr. Hovingh and colleagues. “Having been trained to first do no harm, many physicians might wonder whether they would infringe on this idea by prescribing PCSK9 inhibitors. Many patients using PCSK9 inhibitors reach extremely low LDL-cholesterol concentrations …, but good safety data for such low LDL-cholesterol values are scarce. In clinical practice, this [situation] often leads to down titration of the dose of conventional lipid-lowering therapy, PCSK9-antibody dose, or both, for fear of potentially unknown side effects.” The results of the FOURIER subanalysis show that “patients achieving very low LDL-cholesterol concentrations are not at increased risk of any of the adverse events assessed.”
—Glenn S. Williams
Suggested Reading
Giugliano RP, Pedersen TR, Park JG, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017 Aug 28 [Ep
Hovingh GK, Boekholdt SM, Stroes ES. Very low LDL-cholesterol concentrations achieved: which target is next? Lancet. 2017 Aug 28 [Epub ahead of print].
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713-1722.
BARCELONA—Very aggressive reduction of LDL-cholesterol to ultralow levels is associated with progressively fewer cardiovascular events and appears to pose no safety concerns in patients with stable atherosclerotic cardiovascular disease over 2.2 years of follow-up, according to a new analysis. This finding, which was presented at the European Society of Cardiology Congress 2017 and published online ahead of print August 28 in the Lancet, comes from a prespecified secondary analysis of the Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk (FOURIER) trial. “These data support further LDL-cholesterol lowering in patients with cardiovascular disease to well below current recommendations,” said Robert P. Giugliano, MD, Associate Professor of Cardiovascular Medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston, and his research colleagues.
“These findings are unique, in that they represent the first analysis of a large cohort of patients to achieve such very low LDL-cholesterol levels, namely … less than one-third of the most common treatment goal of below 1.8 mmol/L for highest risk patients,” Dr. Giugliano said.
The FOURIER trial randomized patients with stable atherosclerotic cardiovascular disease who were receiving background statin therapy to either placebo or evolocumab, a proprotein convertase subtilisin-kexin type 9 (PCSK9) monoclonal antibody. Initial results from the trial, which was published earlier this year in the New England Journal of Medicine, showed that evolocumab lowered LDL-cholesterol levels to a median of 0.8 mmol/L and significantly reduced the risk of cardiovascular events at a median follow-up of 2.2 years.
The new analysis examined efficacy and safety end points according to degree of LDL-cholesterol reduction at four weeks. In addition, a study known as EBBINGHAUS embedded within the larger analysis explored effects on cognition using a validated tablet-based tool.
A total of 25,982 patients with an LDL-cholesterol assessment at week four who did not experience a primary efficacy or prespecified safety event prior to the week four follow-up visit were included in the analysis. The study showed that the risk of the primary efficacy end point—a composite of cardiovascular death, myocardial infarction, stroke, coronary revascularization, or hospitalization for unstable angina—declined steadily as LDL-cholesterol levels decreased, with no significant association between LDL-cholesterol level and adverse events.
A similar reduction was observed in the key secondary end point, with 2,669 subjects in the lowest LDL-cholesterol category (< 0.5 mmol/L) at four weeks experiencing the lowest rate for cardiovascular death, myocardial infarction, or stroke (adjusted hazard ratio, 0.69), compared with the group with the highest LDL-cholesterol (> 2.6 mmol/L). Exploratory analyses in a subgroup of 504 patients with an LDL-cholesterol level of < 0.25 mmol/L showed further reduction in cardiovascular events with no increase in safety events.
Among 1,154 patients who underwent formal cognitive testing prior to, or on the first day of, study treatment as part of the EBBINGHAUS study, lowered LDL-cholesterol was not associated with adverse effects on memory, executive function, or reaction time.
“Although longer-term follow-up will be important, the totality of evidence to date from trials of intensive lipid lowering supports reduction of LDL-cholesterol in high-risk patients to levels below those currently recommended in cholesterol guidelines,” noted Dr. Giugliano.
This study was sponsored by Amgen.
Important Clinical Implications
The FOURIER secondary analysis, together with a meta-analysis of major statin trials, creates a body of evidence that “heralds the transition from a concept of ‘the lower the better’ towards LDL-cholesterol eradication,” said G. Kees Hovingh, MD, PhD, an internist and vascular medicine specialist at the Academic Medical Center in Amsterdam, and colleagues in an editorial accompanying the published study results.
“For clinicians who prescribe PCSK9 inhibitors, however, the findings from the FOURIER trial, with regard to the potential adverse events, are of even greater importance,” said Dr. Hovingh and colleagues. “Having been trained to first do no harm, many physicians might wonder whether they would infringe on this idea by prescribing PCSK9 inhibitors. Many patients using PCSK9 inhibitors reach extremely low LDL-cholesterol concentrations …, but good safety data for such low LDL-cholesterol values are scarce. In clinical practice, this [situation] often leads to down titration of the dose of conventional lipid-lowering therapy, PCSK9-antibody dose, or both, for fear of potentially unknown side effects.” The results of the FOURIER subanalysis show that “patients achieving very low LDL-cholesterol concentrations are not at increased risk of any of the adverse events assessed.”
—Glenn S. Williams
Suggested Reading
Giugliano RP, Pedersen TR, Park JG, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017 Aug 28 [Ep
Hovingh GK, Boekholdt SM, Stroes ES. Very low LDL-cholesterol concentrations achieved: which target is next? Lancet. 2017 Aug 28 [Epub ahead of print].
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713-1722.
Empagliflozin’s effects independent of CVD risk factors
LISBON – The mortality reductions that can be achieved with the sodium–glucose cotransporter 2 inhibitor empagliflozin versus placebo in people with type 2 diabetes remained after investigators controlled for traditional cardiovascular (CV) risk factors over time, analyses from the EMPA-REG OUTCOME trial showed.
The 38% reduction in CV deaths and 32% reduction in all-cause mortality that were observed in the main trial (N Engl J Med. 2015;373:2117-28) were “largely unchanged when adjusted for control of blood pressure, LDL cholesterol, and glycated hemoglobin (HbA1c) during the study,” David Fitchett, MD, reported at the annual meeting of the European Association for the Study of Diabetes.
“EMPA-REG OUTCOME was the first diabetes outcome trial to show a reduction in the primary cardiovascular endpoint,” Dr. Fitchett, a cardiologist on the staff of St. Michael’s Hospital, University of Toronto, said. “It was designed as a safety study, but the statistical analysis allowed for an efficacy analysis once safety had been proven.”
EMPA-REG OUTCOME was an international, multicenter, phase 3, randomized, double-blind, placebo-controlled trial set up to look at the effects of a once-daily dose of empagliflozin (Jardiance) versus placebo on CV events in 7,020 adults with type 2 diabetes with established CV disease. Empagliflozin (10 mg or 25 mg) or placebo was given in addition to the standard of care, with the design stipulating that glucose-lowering treatment should be unchanged for the first 3 months.
The trial continued until an adjudicated primary outcome event, defined as a composite of CV death, nonfatal myocardial infarction, or nonfatal stroke, had occurred in at least 691 patients. This three-point major cardiovascular outcome (MACE) occurred in 10.5% of patients treated with empagliflozin and in 12.5% of those who had been given placebo, with a 14% reduction overall (HR, 0.86; 95% CI, 0.74–0.99; P = .04). Almost all of this benefit was due to the reduction in CV deaths, Dr. Fitchett noted, which in turn drove the reduction in all-cause mortality.
The question, then, was how did empagliflozin have this apparent cardiovascular effect? Seeking an answer, the core EMPA-REG OUTCOME investigators looked to see if it could be explained by changes in blood pressure, LDL cholesterol, or HbA1c level, as small reductions had been seen in the main trial. Cox proportional analyses were performed to see how controlling for each of these might affect the results. In these analyses, control of blood pressure was defined as achieving a systolic value of less than 140 mm Hg and a diastolic value of less than 90 mm Hg; control of LDL cholesterol as a value of less than 100 mg/dL, and control of HbA1c level as a value below 7.5%.
Comparing baseline values to the last recorded values, the proportions of patients who achieved control of HbA1c with empagliflozin were a respective 26.7% and 46.7% versus 25.5% and 34% for placebo. LDL cholesterol was controlled in 70.6% and 68.7%, respectively, with empagliflozin and in 72.9% and 70% with placebo. The proportions of patients who achieved control of HbA1c, LDL cholesterol, and blood pressure were 12.6% and 21.8% for empagliflozin and 11.7% and 16.7% for placebo.*
The latest findings “suggest that the mortality reductions in the EMPA-REG OUTCOME trial were not driven by control of these standard cardiovascular risk factors during the trial,” Dr. Fitchett concluded.
In a separate poster presentation at the meeting, EMPA-REG OUTCOME investigators reported that empagliflozin also reduced heart failure outcomes, regardless of blood pressure, LDL cholesterol, or HbA1c control. Hazard ratios for hospitalization for heart failure with or without CV death were 0.64-0.67 (95% CIs, 0.49–0.87). Other subanalyses from the study showed that neither baseline HbA1c nor change in HbA1c predicted the reduction in CV deaths with empagliflozin and that background glucose-lowering treatment – metformin or sulfonylurea use – did not change the results.
The Boehringer Ingelheim and Lilly Diabetes Alliance funded the study. Dr. Fitchett disclosed receiving honoraria from Sanofi, Merck, Amgen, AstraZeneca, Eli Lilly, and Boehringer Ingelheim.
*This article was updated Sept. 28, 2017.
LISBON – The mortality reductions that can be achieved with the sodium–glucose cotransporter 2 inhibitor empagliflozin versus placebo in people with type 2 diabetes remained after investigators controlled for traditional cardiovascular (CV) risk factors over time, analyses from the EMPA-REG OUTCOME trial showed.
The 38% reduction in CV deaths and 32% reduction in all-cause mortality that were observed in the main trial (N Engl J Med. 2015;373:2117-28) were “largely unchanged when adjusted for control of blood pressure, LDL cholesterol, and glycated hemoglobin (HbA1c) during the study,” David Fitchett, MD, reported at the annual meeting of the European Association for the Study of Diabetes.
“EMPA-REG OUTCOME was the first diabetes outcome trial to show a reduction in the primary cardiovascular endpoint,” Dr. Fitchett, a cardiologist on the staff of St. Michael’s Hospital, University of Toronto, said. “It was designed as a safety study, but the statistical analysis allowed for an efficacy analysis once safety had been proven.”
EMPA-REG OUTCOME was an international, multicenter, phase 3, randomized, double-blind, placebo-controlled trial set up to look at the effects of a once-daily dose of empagliflozin (Jardiance) versus placebo on CV events in 7,020 adults with type 2 diabetes with established CV disease. Empagliflozin (10 mg or 25 mg) or placebo was given in addition to the standard of care, with the design stipulating that glucose-lowering treatment should be unchanged for the first 3 months.
The trial continued until an adjudicated primary outcome event, defined as a composite of CV death, nonfatal myocardial infarction, or nonfatal stroke, had occurred in at least 691 patients. This three-point major cardiovascular outcome (MACE) occurred in 10.5% of patients treated with empagliflozin and in 12.5% of those who had been given placebo, with a 14% reduction overall (HR, 0.86; 95% CI, 0.74–0.99; P = .04). Almost all of this benefit was due to the reduction in CV deaths, Dr. Fitchett noted, which in turn drove the reduction in all-cause mortality.
The question, then, was how did empagliflozin have this apparent cardiovascular effect? Seeking an answer, the core EMPA-REG OUTCOME investigators looked to see if it could be explained by changes in blood pressure, LDL cholesterol, or HbA1c level, as small reductions had been seen in the main trial. Cox proportional analyses were performed to see how controlling for each of these might affect the results. In these analyses, control of blood pressure was defined as achieving a systolic value of less than 140 mm Hg and a diastolic value of less than 90 mm Hg; control of LDL cholesterol as a value of less than 100 mg/dL, and control of HbA1c level as a value below 7.5%.
Comparing baseline values to the last recorded values, the proportions of patients who achieved control of HbA1c with empagliflozin were a respective 26.7% and 46.7% versus 25.5% and 34% for placebo. LDL cholesterol was controlled in 70.6% and 68.7%, respectively, with empagliflozin and in 72.9% and 70% with placebo. The proportions of patients who achieved control of HbA1c, LDL cholesterol, and blood pressure were 12.6% and 21.8% for empagliflozin and 11.7% and 16.7% for placebo.*
The latest findings “suggest that the mortality reductions in the EMPA-REG OUTCOME trial were not driven by control of these standard cardiovascular risk factors during the trial,” Dr. Fitchett concluded.
In a separate poster presentation at the meeting, EMPA-REG OUTCOME investigators reported that empagliflozin also reduced heart failure outcomes, regardless of blood pressure, LDL cholesterol, or HbA1c control. Hazard ratios for hospitalization for heart failure with or without CV death were 0.64-0.67 (95% CIs, 0.49–0.87). Other subanalyses from the study showed that neither baseline HbA1c nor change in HbA1c predicted the reduction in CV deaths with empagliflozin and that background glucose-lowering treatment – metformin or sulfonylurea use – did not change the results.
The Boehringer Ingelheim and Lilly Diabetes Alliance funded the study. Dr. Fitchett disclosed receiving honoraria from Sanofi, Merck, Amgen, AstraZeneca, Eli Lilly, and Boehringer Ingelheim.
*This article was updated Sept. 28, 2017.
LISBON – The mortality reductions that can be achieved with the sodium–glucose cotransporter 2 inhibitor empagliflozin versus placebo in people with type 2 diabetes remained after investigators controlled for traditional cardiovascular (CV) risk factors over time, analyses from the EMPA-REG OUTCOME trial showed.
The 38% reduction in CV deaths and 32% reduction in all-cause mortality that were observed in the main trial (N Engl J Med. 2015;373:2117-28) were “largely unchanged when adjusted for control of blood pressure, LDL cholesterol, and glycated hemoglobin (HbA1c) during the study,” David Fitchett, MD, reported at the annual meeting of the European Association for the Study of Diabetes.
“EMPA-REG OUTCOME was the first diabetes outcome trial to show a reduction in the primary cardiovascular endpoint,” Dr. Fitchett, a cardiologist on the staff of St. Michael’s Hospital, University of Toronto, said. “It was designed as a safety study, but the statistical analysis allowed for an efficacy analysis once safety had been proven.”
EMPA-REG OUTCOME was an international, multicenter, phase 3, randomized, double-blind, placebo-controlled trial set up to look at the effects of a once-daily dose of empagliflozin (Jardiance) versus placebo on CV events in 7,020 adults with type 2 diabetes with established CV disease. Empagliflozin (10 mg or 25 mg) or placebo was given in addition to the standard of care, with the design stipulating that glucose-lowering treatment should be unchanged for the first 3 months.
The trial continued until an adjudicated primary outcome event, defined as a composite of CV death, nonfatal myocardial infarction, or nonfatal stroke, had occurred in at least 691 patients. This three-point major cardiovascular outcome (MACE) occurred in 10.5% of patients treated with empagliflozin and in 12.5% of those who had been given placebo, with a 14% reduction overall (HR, 0.86; 95% CI, 0.74–0.99; P = .04). Almost all of this benefit was due to the reduction in CV deaths, Dr. Fitchett noted, which in turn drove the reduction in all-cause mortality.
The question, then, was how did empagliflozin have this apparent cardiovascular effect? Seeking an answer, the core EMPA-REG OUTCOME investigators looked to see if it could be explained by changes in blood pressure, LDL cholesterol, or HbA1c level, as small reductions had been seen in the main trial. Cox proportional analyses were performed to see how controlling for each of these might affect the results. In these analyses, control of blood pressure was defined as achieving a systolic value of less than 140 mm Hg and a diastolic value of less than 90 mm Hg; control of LDL cholesterol as a value of less than 100 mg/dL, and control of HbA1c level as a value below 7.5%.
Comparing baseline values to the last recorded values, the proportions of patients who achieved control of HbA1c with empagliflozin were a respective 26.7% and 46.7% versus 25.5% and 34% for placebo. LDL cholesterol was controlled in 70.6% and 68.7%, respectively, with empagliflozin and in 72.9% and 70% with placebo. The proportions of patients who achieved control of HbA1c, LDL cholesterol, and blood pressure were 12.6% and 21.8% for empagliflozin and 11.7% and 16.7% for placebo.*
The latest findings “suggest that the mortality reductions in the EMPA-REG OUTCOME trial were not driven by control of these standard cardiovascular risk factors during the trial,” Dr. Fitchett concluded.
In a separate poster presentation at the meeting, EMPA-REG OUTCOME investigators reported that empagliflozin also reduced heart failure outcomes, regardless of blood pressure, LDL cholesterol, or HbA1c control. Hazard ratios for hospitalization for heart failure with or without CV death were 0.64-0.67 (95% CIs, 0.49–0.87). Other subanalyses from the study showed that neither baseline HbA1c nor change in HbA1c predicted the reduction in CV deaths with empagliflozin and that background glucose-lowering treatment – metformin or sulfonylurea use – did not change the results.
The Boehringer Ingelheim and Lilly Diabetes Alliance funded the study. Dr. Fitchett disclosed receiving honoraria from Sanofi, Merck, Amgen, AstraZeneca, Eli Lilly, and Boehringer Ingelheim.
*This article was updated Sept. 28, 2017.
AT EASD 2017
Key clinical point:
Major finding: The 38% reduction in CV deaths and 32% reduction in all-cause mortality were largely unchanged after adjustment for blood pressure, LDL cholesterol, and HbA1c at baseline and during the study.
Data source: Secondary analyses of EMPA-REG OUTCOME, a phase 3, randomized controlled trial of 7,020 people with type 2 diabetes at high risk for cardiovascular events who were receiving standard care.
Disclosures: The Boehringer Ingelheim and Lilly Diabetes Alliance funded the study. Dr. Fitchett disclosed receiving honoraria from Sanofi, Merck, Amgen, AstraZeneca, Eli Lilly, and Boehringer Ingelheim.