User login
VIDEO: How to discharge new pediatric diabetes cases in 2 days
NASHVILLE, TENN. – Pediatric endocrinologist Cassandra Brady, MD, caught the attention of her audience at Pediatric Hospital Medicine when she mentioned that children presenting with new-onset diabetes rarely spend more than 2 days at Vanderbilt University’s children’s hospital, even if they present in diabetic ketoacidosis.
In many places, children with new-onset diabetes spend quite a bit longer in the hospital – even if they are medically stable and feeling fine – for diabetes education.
That’s not the case at Vanderbilt, where Dr. Brady is an assistant professor. Once kids are stabilized, they and their parents undergo a 3-hour crash course – sometimes even in the PICU – on diabetes survival skills, and then they’re sent home with insulin. They learn the finer points about carbohydrate counting and tight glucose control at subsequent outpatient visits.
More and more payers are probably going to push for that model, Dr. Brady noted at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
For those interested in making the transition to outpatient eduction, she explained in an interview exactly how Vanderbilt’s been doing it safely for years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NASHVILLE, TENN. – Pediatric endocrinologist Cassandra Brady, MD, caught the attention of her audience at Pediatric Hospital Medicine when she mentioned that children presenting with new-onset diabetes rarely spend more than 2 days at Vanderbilt University’s children’s hospital, even if they present in diabetic ketoacidosis.
In many places, children with new-onset diabetes spend quite a bit longer in the hospital – even if they are medically stable and feeling fine – for diabetes education.
That’s not the case at Vanderbilt, where Dr. Brady is an assistant professor. Once kids are stabilized, they and their parents undergo a 3-hour crash course – sometimes even in the PICU – on diabetes survival skills, and then they’re sent home with insulin. They learn the finer points about carbohydrate counting and tight glucose control at subsequent outpatient visits.
More and more payers are probably going to push for that model, Dr. Brady noted at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
For those interested in making the transition to outpatient eduction, she explained in an interview exactly how Vanderbilt’s been doing it safely for years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NASHVILLE, TENN. – Pediatric endocrinologist Cassandra Brady, MD, caught the attention of her audience at Pediatric Hospital Medicine when she mentioned that children presenting with new-onset diabetes rarely spend more than 2 days at Vanderbilt University’s children’s hospital, even if they present in diabetic ketoacidosis.
In many places, children with new-onset diabetes spend quite a bit longer in the hospital – even if they are medically stable and feeling fine – for diabetes education.
That’s not the case at Vanderbilt, where Dr. Brady is an assistant professor. Once kids are stabilized, they and their parents undergo a 3-hour crash course – sometimes even in the PICU – on diabetes survival skills, and then they’re sent home with insulin. They learn the finer points about carbohydrate counting and tight glucose control at subsequent outpatient visits.
More and more payers are probably going to push for that model, Dr. Brady noted at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
For those interested in making the transition to outpatient eduction, she explained in an interview exactly how Vanderbilt’s been doing it safely for years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT PHM 2017
Treating RLS With Dopamine Agonists May Increase Risk for New-Onset Mental Disorders
BOSTON—Among patients with primary restless legs syndrome (RLS) and without a history of psychiatric disorders, patients who receive de novo dopamine agonist treatment are approximately twice as likely to subsequently develop a mental disorder as those who do not receive dopamine agonist treatment, according to a large-scale retrospective study presented at the 31st Annual Meeting of the Associated Professional Sleep Societies.
Previous research has demonstrated an increased risk of mental disorders among patients with Parkinson’s disease who are treated with dopamine agonists. Many patients with RLS are also treated with dopamine agonists, although at lower doses than patients with Parkinson’s disease. Given these lower doses, clinicians assumed that the risk of dopamine agonist-induced mental disorders in RLS would be small. Clinical case studies suggest a higher-than-anticipated risk, however.
An Examination of Claims Data
To investigate whether dopamine agonists increase the risk of developing mental disorders in patients with RLS, Cheryl Hankin, PhD, President and Chief Scientific Officer of BioMedEcon, a health economics and outcomes research firm in Moss Beach, California, and colleagues examined Truven MarketScan Commercial and Medicare Supplemental databases of claims filed between July 1, 2008, and December 31, 2014. From a pool of 539,399 patients with a diagnosis of RLS, investigators identified adults with two or more years of claims data preceding and following their index RLS diagnosis dates.
Patients were excluded from the analysis if, in the two or more years preceding RLS diagnosis, they received a diagnosis of mental disorder or filled a prescription for an antidepressant or antipsychotic. Also excluded were patients who filled a prescription for a dopamine agonist in the two or more years preceding RLS diagnosis. Patients who were ever diagnosed with Parkinson’s disease, kidney disease, iron deficiency, or pregnancy were assumed to have secondary RLS and were also excluded.
The investigators identified 5,419 eligible participants. Of this group, 1,649 patients received dopamine agonists after RLS diagnosis. Specifically, 571 participants received pramipexole, 915 received ropinirole, and 163 received both. Approximately 65% of patients were female. Patients residing in the Northeast were significantly less likely to receive dopamine agonists, compared with patients residing in the Midwest or the South. The investigators found no significant differences in treatment status by comorbid illness burden or by sex. The investigators also found no significant differences in demographic characteristics between patients receiving pramipexole and those receiving ropinirole.
Risk Was Significantly Greater in Patients Receiving Dopamine Agonist
Next, from this pool of eligible subjects, the researchers matched 1,080 patients treated with dopamine agonists with 1,080 dopamine agonist-naïve patients on sex, age at RLS diagnosis, region, employment, and illness burden. Dr. Hankin and colleagues found a significant increase in mental disorder diagnoses (eg, bipolar disorder, anxiety, depression, and substance abuse) among patients treated with dopamine agonists, compared with dopamine agonist-naïve patients. Among patients receiving dopamine agonists, the odds ratio for severe mental disorder (eg, psychoses and bipolar disorder) was 2.2, the odds ratio for moderate to severe mental disorder (eg, posttraumatic stress disorder and major depression) was 1.8, and the odds ratio for mild mental disorder (eg, anxiety disorders) was 1.9, compared with dopamine agonist-naïve patients.
“This is the first large-scale, real-world, claims-based study to examine the association between treatment of RLS with dopamine agonists and the development of psychiatric adverse events. Our findings are compelling, but need to be replicated in other patient populations,” said Dr. Hankin.
“Our retrospective analysis required careful consideration of matching,” said Daniel On-Fai Lee, MD, Clinical Professor of Neurology at the University of Kentucky College of Medicine in Lexington, who collaborated on the study. Although the investigators took care to match participants and to remove cases of secondary RLS from the analysis, they may have inadvertently overlooked one or more important matching variables that could affect the outcome, he added.
Arbor Pharmaceuticals provided funding for the study, but did not influence its methodology, analysis, results, or conclusion, said Dr. Lee.
—Erik Greb
Suggested Reading
Sierra M, Carnicella S, Strafella AP, et al. Apathy and impulse control disorders: yin & yang of dopamine dependent behaviors. J Parkinsons Dis. 2015;5(3):625-636.
Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496-505.
BOSTON—Among patients with primary restless legs syndrome (RLS) and without a history of psychiatric disorders, patients who receive de novo dopamine agonist treatment are approximately twice as likely to subsequently develop a mental disorder as those who do not receive dopamine agonist treatment, according to a large-scale retrospective study presented at the 31st Annual Meeting of the Associated Professional Sleep Societies.
Previous research has demonstrated an increased risk of mental disorders among patients with Parkinson’s disease who are treated with dopamine agonists. Many patients with RLS are also treated with dopamine agonists, although at lower doses than patients with Parkinson’s disease. Given these lower doses, clinicians assumed that the risk of dopamine agonist-induced mental disorders in RLS would be small. Clinical case studies suggest a higher-than-anticipated risk, however.
An Examination of Claims Data
To investigate whether dopamine agonists increase the risk of developing mental disorders in patients with RLS, Cheryl Hankin, PhD, President and Chief Scientific Officer of BioMedEcon, a health economics and outcomes research firm in Moss Beach, California, and colleagues examined Truven MarketScan Commercial and Medicare Supplemental databases of claims filed between July 1, 2008, and December 31, 2014. From a pool of 539,399 patients with a diagnosis of RLS, investigators identified adults with two or more years of claims data preceding and following their index RLS diagnosis dates.
Patients were excluded from the analysis if, in the two or more years preceding RLS diagnosis, they received a diagnosis of mental disorder or filled a prescription for an antidepressant or antipsychotic. Also excluded were patients who filled a prescription for a dopamine agonist in the two or more years preceding RLS diagnosis. Patients who were ever diagnosed with Parkinson’s disease, kidney disease, iron deficiency, or pregnancy were assumed to have secondary RLS and were also excluded.
The investigators identified 5,419 eligible participants. Of this group, 1,649 patients received dopamine agonists after RLS diagnosis. Specifically, 571 participants received pramipexole, 915 received ropinirole, and 163 received both. Approximately 65% of patients were female. Patients residing in the Northeast were significantly less likely to receive dopamine agonists, compared with patients residing in the Midwest or the South. The investigators found no significant differences in treatment status by comorbid illness burden or by sex. The investigators also found no significant differences in demographic characteristics between patients receiving pramipexole and those receiving ropinirole.
Risk Was Significantly Greater in Patients Receiving Dopamine Agonist
Next, from this pool of eligible subjects, the researchers matched 1,080 patients treated with dopamine agonists with 1,080 dopamine agonist-naïve patients on sex, age at RLS diagnosis, region, employment, and illness burden. Dr. Hankin and colleagues found a significant increase in mental disorder diagnoses (eg, bipolar disorder, anxiety, depression, and substance abuse) among patients treated with dopamine agonists, compared with dopamine agonist-naïve patients. Among patients receiving dopamine agonists, the odds ratio for severe mental disorder (eg, psychoses and bipolar disorder) was 2.2, the odds ratio for moderate to severe mental disorder (eg, posttraumatic stress disorder and major depression) was 1.8, and the odds ratio for mild mental disorder (eg, anxiety disorders) was 1.9, compared with dopamine agonist-naïve patients.
“This is the first large-scale, real-world, claims-based study to examine the association between treatment of RLS with dopamine agonists and the development of psychiatric adverse events. Our findings are compelling, but need to be replicated in other patient populations,” said Dr. Hankin.
“Our retrospective analysis required careful consideration of matching,” said Daniel On-Fai Lee, MD, Clinical Professor of Neurology at the University of Kentucky College of Medicine in Lexington, who collaborated on the study. Although the investigators took care to match participants and to remove cases of secondary RLS from the analysis, they may have inadvertently overlooked one or more important matching variables that could affect the outcome, he added.
Arbor Pharmaceuticals provided funding for the study, but did not influence its methodology, analysis, results, or conclusion, said Dr. Lee.
—Erik Greb
Suggested Reading
Sierra M, Carnicella S, Strafella AP, et al. Apathy and impulse control disorders: yin & yang of dopamine dependent behaviors. J Parkinsons Dis. 2015;5(3):625-636.
Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496-505.
BOSTON—Among patients with primary restless legs syndrome (RLS) and without a history of psychiatric disorders, patients who receive de novo dopamine agonist treatment are approximately twice as likely to subsequently develop a mental disorder as those who do not receive dopamine agonist treatment, according to a large-scale retrospective study presented at the 31st Annual Meeting of the Associated Professional Sleep Societies.
Previous research has demonstrated an increased risk of mental disorders among patients with Parkinson’s disease who are treated with dopamine agonists. Many patients with RLS are also treated with dopamine agonists, although at lower doses than patients with Parkinson’s disease. Given these lower doses, clinicians assumed that the risk of dopamine agonist-induced mental disorders in RLS would be small. Clinical case studies suggest a higher-than-anticipated risk, however.
An Examination of Claims Data
To investigate whether dopamine agonists increase the risk of developing mental disorders in patients with RLS, Cheryl Hankin, PhD, President and Chief Scientific Officer of BioMedEcon, a health economics and outcomes research firm in Moss Beach, California, and colleagues examined Truven MarketScan Commercial and Medicare Supplemental databases of claims filed between July 1, 2008, and December 31, 2014. From a pool of 539,399 patients with a diagnosis of RLS, investigators identified adults with two or more years of claims data preceding and following their index RLS diagnosis dates.
Patients were excluded from the analysis if, in the two or more years preceding RLS diagnosis, they received a diagnosis of mental disorder or filled a prescription for an antidepressant or antipsychotic. Also excluded were patients who filled a prescription for a dopamine agonist in the two or more years preceding RLS diagnosis. Patients who were ever diagnosed with Parkinson’s disease, kidney disease, iron deficiency, or pregnancy were assumed to have secondary RLS and were also excluded.
The investigators identified 5,419 eligible participants. Of this group, 1,649 patients received dopamine agonists after RLS diagnosis. Specifically, 571 participants received pramipexole, 915 received ropinirole, and 163 received both. Approximately 65% of patients were female. Patients residing in the Northeast were significantly less likely to receive dopamine agonists, compared with patients residing in the Midwest or the South. The investigators found no significant differences in treatment status by comorbid illness burden or by sex. The investigators also found no significant differences in demographic characteristics between patients receiving pramipexole and those receiving ropinirole.
Risk Was Significantly Greater in Patients Receiving Dopamine Agonist
Next, from this pool of eligible subjects, the researchers matched 1,080 patients treated with dopamine agonists with 1,080 dopamine agonist-naïve patients on sex, age at RLS diagnosis, region, employment, and illness burden. Dr. Hankin and colleagues found a significant increase in mental disorder diagnoses (eg, bipolar disorder, anxiety, depression, and substance abuse) among patients treated with dopamine agonists, compared with dopamine agonist-naïve patients. Among patients receiving dopamine agonists, the odds ratio for severe mental disorder (eg, psychoses and bipolar disorder) was 2.2, the odds ratio for moderate to severe mental disorder (eg, posttraumatic stress disorder and major depression) was 1.8, and the odds ratio for mild mental disorder (eg, anxiety disorders) was 1.9, compared with dopamine agonist-naïve patients.
“This is the first large-scale, real-world, claims-based study to examine the association between treatment of RLS with dopamine agonists and the development of psychiatric adverse events. Our findings are compelling, but need to be replicated in other patient populations,” said Dr. Hankin.
“Our retrospective analysis required careful consideration of matching,” said Daniel On-Fai Lee, MD, Clinical Professor of Neurology at the University of Kentucky College of Medicine in Lexington, who collaborated on the study. Although the investigators took care to match participants and to remove cases of secondary RLS from the analysis, they may have inadvertently overlooked one or more important matching variables that could affect the outcome, he added.
Arbor Pharmaceuticals provided funding for the study, but did not influence its methodology, analysis, results, or conclusion, said Dr. Lee.
—Erik Greb
Suggested Reading
Sierra M, Carnicella S, Strafella AP, et al. Apathy and impulse control disorders: yin & yang of dopamine dependent behaviors. J Parkinsons Dis. 2015;5(3):625-636.
Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496-505.
First Clinical Trial of a Genetic Therapy for Huntington’s Disease Nears Completion
VANCOUVER—Antisense oligonucleotides hold promise as treatments for Huntington’s disease, according to an overview delivered at the 21st International Congress of Parkinson’s Disease and Movement Disorders. Preclinical evidence suggests that these treatments are safe and will decrease levels of mutant huntingtin in the brain. The first clinical trial of an antisense oligonucleotide for Huntington’s disease is currently under way and fully enrolled. Results will be available in the near future, said Blair R. Leavitt, MDCM, Professor of Medical Genetics at the University of British Columbia in Vancouver.
What Are Antisense Oligonucleotides?
Antisense oligonucleotides are small, artificial units of DNA that are modified chemically to have a long half-life. They can be targeted to bind to any RNA in the body, and when they bind with huntingtin messenger RNA, they prevent production of mutant huntingtin protein. In theory, this action should prevent all subsequent pathology and delay or prevent the onset of Huntington’s disease, said Dr. Leavitt.
Among the advantages of antisense oligonucleotides is that neurons and glia take them up freely. They reach the desired areas of the brain without requiring a vector to introduce them. Antisense oligonucleotides are stable, have a long term of activity, act in a dose-dependent manner, and have reversible effects. “They are much like our classic small-molecule drugs, so we are comfortable bringing these therapies into clinical development,” said Dr. Leavitt.
Preclinical Data Indicate Safety
Kordasiewicz and colleagues infused 75 mg of an antisense oligonucleotide directly into the brain of a mouse model of Huntington’s disease (ie, BACHD mice) over 14 days. They observed a decline in huntingtin RNA that endured for as long as three months. The treated mice had better motor coordination and performed better on the rotorod test. The treatment also slowed the loss of brain mass and improved hypoactivity and anxiety.
The investigators also showed that antisense oligonucleotide reached the brain after intrathecal administration to monkeys. The treatment reduced huntingtin levels by approximately 50% in the cortex, and by between 20% and 25% in deep brain structures.
A Potential Biomarker of Target Engagement
To gauge treatment efficacy in humans, neurologists need a noninvasive way to measure levels of huntingtin in the brain. It is not yet possible to measure brain huntingtin levels directly using imaging, but CSF levels of huntingtin could be a surrogate measure, Dr. Leavitt said.
Dr. Leavitt and colleagues developed an ultrasensitive single-molecule counting immunoassay that successfully quantified mutant huntingtin in the CSF of patients with Huntington’s disease. Mutant huntingtin was undetectable in healthy controls. Patients with manifest Huntington’s disease had three times more mutant huntingtin than asymptomatic mutation carriers did. Huntingtin levels increased as the disease progressed. In addition, huntingtin concentration predicted cognitive and motor dysfunction.
The investigators observed similar findings after they used microbead-based immunoprecipitation and flow cytometry to develop a second highly sensitive assay for detecting mutant huntingtin. They demonstrated that CSF levels of mutant huntingtin reflect brain levels of the protein in mouse models of Huntington’s disease, and in patients with Huntington’s disease, the levels increased with disease stage. They also demonstrated that CSF huntingtin levels decreased following suppression of huntingtin in the brain.
A Clinical Trial Nears Completion
Ionis Pharmaceuticals developed an antisense oligonucleotide that targets both the mutant and normal alleles of huntingtin. Investigators subsequently began a first-in-human phase I/IIa trial of the drug in patients with early Huntington’s disease. Participants were randomized 3:1 to drug or placebo at sites in the United Kingdom, Germany, and Canada. The drug is administered intrathecally, and maximal protein suppression occurs approximately four weeks later. Each study participant will undergo intrathecal injections every month for four months.
The trial’s primary objective is to evaluate the treatment’s safety and tolerability. Its secondary objective is to examine the drug’s CSF pharmacokinetics. Finally, an exploratory objective is to assess the treatment’s effect on pharmacodynamic biomarkers and on clinical end points of Huntington’s disease.
All of the participants have been enrolled in the study, and Dr. Leavitt administered an intrathecal infusion to the first subject at the Vancouver site in September 2015. Participants are generally in good health and have high levels of function. Thus far, the researchers have found no evidence of significant adverse events or safety concerns, and the drug appears tolerable, said Dr. Leavitt. Results of the trial should be available in the coming months, he added. “This is certainly exciting, and it is the first time we have been able to bring a genetic therapy into the clinic for this devastating disorder.”
Other Therapies in Development
Wave Life Sciences also has created an antisense oligonucleotide for Huntington’s disease that is in the late preclinical stages of development. The company uses a type of chemistry that allows it to control the stereoisomer composition of the nucleic acids. The therapy targets specific single-nucleotide polymorphisms on mutant huntingtin and therefore may not be appropriate for every patient with Huntington’s disease. “This [treatment] has at least the potential for allele-specific targeting … and will hopefully be entering the clinic fairly soon,” said Dr. Leavitt.
Other gene-therapy approaches require a vector, most often a nonpathogenic adeno-associated virus (AAV), to bring the treatment into the CNS. Several such therapeutic candidates in preclinical development are close to entering early human trials, said Dr. Leavitt.
UniQure is developing a form of AAV5 that expresses an artificial micro-RNA that targets huntingtin. The drug will require stereotaxic injection directly into the brain. In one study, direct intraparenchymal injection of the drug significantly reduced levels of mutant huntingtin in the putamen, caudate, and thalamus of a minipig model of Huntington’s disease. The drug had less effect in the cortex. Depending on where the virus is injected, viral approaches generally have good local targeting, but not necessarily widespread targeting, said Dr. Leavitt. Spark Therapeutics and Voyager Therapeutics are also developing therapies similar to that of UniQure.
—Erik Greb
Suggested Reading
Kordasiewicz HB, Stanek LM, Wancewicz EV, et al. Sustained therapeutic reversal of Huntington’s disease by transient repression of huntingtin synthesis. Neuron. 2012; 74(6): 1031–1044.
Southwell AL, Smith SE, Davis TR, et al. Ultrasensitive measurement of huntingtin protein in cerebrospinal fluid demonstrates increase with Huntington disease stage and decrease following brain huntingtin suppression. Sci Rep. 2015;5:12166.
Wild EJ, Boggio R, Langbehn D, et al. Quantification of mutant huntingtin protein in cerebrospinal fluid from Huntington’s disease patients. J Clin Invest. 2015;125(5):1979-1986.
VANCOUVER—Antisense oligonucleotides hold promise as treatments for Huntington’s disease, according to an overview delivered at the 21st International Congress of Parkinson’s Disease and Movement Disorders. Preclinical evidence suggests that these treatments are safe and will decrease levels of mutant huntingtin in the brain. The first clinical trial of an antisense oligonucleotide for Huntington’s disease is currently under way and fully enrolled. Results will be available in the near future, said Blair R. Leavitt, MDCM, Professor of Medical Genetics at the University of British Columbia in Vancouver.
What Are Antisense Oligonucleotides?
Antisense oligonucleotides are small, artificial units of DNA that are modified chemically to have a long half-life. They can be targeted to bind to any RNA in the body, and when they bind with huntingtin messenger RNA, they prevent production of mutant huntingtin protein. In theory, this action should prevent all subsequent pathology and delay or prevent the onset of Huntington’s disease, said Dr. Leavitt.
Among the advantages of antisense oligonucleotides is that neurons and glia take them up freely. They reach the desired areas of the brain without requiring a vector to introduce them. Antisense oligonucleotides are stable, have a long term of activity, act in a dose-dependent manner, and have reversible effects. “They are much like our classic small-molecule drugs, so we are comfortable bringing these therapies into clinical development,” said Dr. Leavitt.
Preclinical Data Indicate Safety
Kordasiewicz and colleagues infused 75 mg of an antisense oligonucleotide directly into the brain of a mouse model of Huntington’s disease (ie, BACHD mice) over 14 days. They observed a decline in huntingtin RNA that endured for as long as three months. The treated mice had better motor coordination and performed better on the rotorod test. The treatment also slowed the loss of brain mass and improved hypoactivity and anxiety.
The investigators also showed that antisense oligonucleotide reached the brain after intrathecal administration to monkeys. The treatment reduced huntingtin levels by approximately 50% in the cortex, and by between 20% and 25% in deep brain structures.
A Potential Biomarker of Target Engagement
To gauge treatment efficacy in humans, neurologists need a noninvasive way to measure levels of huntingtin in the brain. It is not yet possible to measure brain huntingtin levels directly using imaging, but CSF levels of huntingtin could be a surrogate measure, Dr. Leavitt said.
Dr. Leavitt and colleagues developed an ultrasensitive single-molecule counting immunoassay that successfully quantified mutant huntingtin in the CSF of patients with Huntington’s disease. Mutant huntingtin was undetectable in healthy controls. Patients with manifest Huntington’s disease had three times more mutant huntingtin than asymptomatic mutation carriers did. Huntingtin levels increased as the disease progressed. In addition, huntingtin concentration predicted cognitive and motor dysfunction.
The investigators observed similar findings after they used microbead-based immunoprecipitation and flow cytometry to develop a second highly sensitive assay for detecting mutant huntingtin. They demonstrated that CSF levels of mutant huntingtin reflect brain levels of the protein in mouse models of Huntington’s disease, and in patients with Huntington’s disease, the levels increased with disease stage. They also demonstrated that CSF huntingtin levels decreased following suppression of huntingtin in the brain.
A Clinical Trial Nears Completion
Ionis Pharmaceuticals developed an antisense oligonucleotide that targets both the mutant and normal alleles of huntingtin. Investigators subsequently began a first-in-human phase I/IIa trial of the drug in patients with early Huntington’s disease. Participants were randomized 3:1 to drug or placebo at sites in the United Kingdom, Germany, and Canada. The drug is administered intrathecally, and maximal protein suppression occurs approximately four weeks later. Each study participant will undergo intrathecal injections every month for four months.
The trial’s primary objective is to evaluate the treatment’s safety and tolerability. Its secondary objective is to examine the drug’s CSF pharmacokinetics. Finally, an exploratory objective is to assess the treatment’s effect on pharmacodynamic biomarkers and on clinical end points of Huntington’s disease.
All of the participants have been enrolled in the study, and Dr. Leavitt administered an intrathecal infusion to the first subject at the Vancouver site in September 2015. Participants are generally in good health and have high levels of function. Thus far, the researchers have found no evidence of significant adverse events or safety concerns, and the drug appears tolerable, said Dr. Leavitt. Results of the trial should be available in the coming months, he added. “This is certainly exciting, and it is the first time we have been able to bring a genetic therapy into the clinic for this devastating disorder.”
Other Therapies in Development
Wave Life Sciences also has created an antisense oligonucleotide for Huntington’s disease that is in the late preclinical stages of development. The company uses a type of chemistry that allows it to control the stereoisomer composition of the nucleic acids. The therapy targets specific single-nucleotide polymorphisms on mutant huntingtin and therefore may not be appropriate for every patient with Huntington’s disease. “This [treatment] has at least the potential for allele-specific targeting … and will hopefully be entering the clinic fairly soon,” said Dr. Leavitt.
Other gene-therapy approaches require a vector, most often a nonpathogenic adeno-associated virus (AAV), to bring the treatment into the CNS. Several such therapeutic candidates in preclinical development are close to entering early human trials, said Dr. Leavitt.
UniQure is developing a form of AAV5 that expresses an artificial micro-RNA that targets huntingtin. The drug will require stereotaxic injection directly into the brain. In one study, direct intraparenchymal injection of the drug significantly reduced levels of mutant huntingtin in the putamen, caudate, and thalamus of a minipig model of Huntington’s disease. The drug had less effect in the cortex. Depending on where the virus is injected, viral approaches generally have good local targeting, but not necessarily widespread targeting, said Dr. Leavitt. Spark Therapeutics and Voyager Therapeutics are also developing therapies similar to that of UniQure.
—Erik Greb
Suggested Reading
Kordasiewicz HB, Stanek LM, Wancewicz EV, et al. Sustained therapeutic reversal of Huntington’s disease by transient repression of huntingtin synthesis. Neuron. 2012; 74(6): 1031–1044.
Southwell AL, Smith SE, Davis TR, et al. Ultrasensitive measurement of huntingtin protein in cerebrospinal fluid demonstrates increase with Huntington disease stage and decrease following brain huntingtin suppression. Sci Rep. 2015;5:12166.
Wild EJ, Boggio R, Langbehn D, et al. Quantification of mutant huntingtin protein in cerebrospinal fluid from Huntington’s disease patients. J Clin Invest. 2015;125(5):1979-1986.
VANCOUVER—Antisense oligonucleotides hold promise as treatments for Huntington’s disease, according to an overview delivered at the 21st International Congress of Parkinson’s Disease and Movement Disorders. Preclinical evidence suggests that these treatments are safe and will decrease levels of mutant huntingtin in the brain. The first clinical trial of an antisense oligonucleotide for Huntington’s disease is currently under way and fully enrolled. Results will be available in the near future, said Blair R. Leavitt, MDCM, Professor of Medical Genetics at the University of British Columbia in Vancouver.
What Are Antisense Oligonucleotides?
Antisense oligonucleotides are small, artificial units of DNA that are modified chemically to have a long half-life. They can be targeted to bind to any RNA in the body, and when they bind with huntingtin messenger RNA, they prevent production of mutant huntingtin protein. In theory, this action should prevent all subsequent pathology and delay or prevent the onset of Huntington’s disease, said Dr. Leavitt.
Among the advantages of antisense oligonucleotides is that neurons and glia take them up freely. They reach the desired areas of the brain without requiring a vector to introduce them. Antisense oligonucleotides are stable, have a long term of activity, act in a dose-dependent manner, and have reversible effects. “They are much like our classic small-molecule drugs, so we are comfortable bringing these therapies into clinical development,” said Dr. Leavitt.
Preclinical Data Indicate Safety
Kordasiewicz and colleagues infused 75 mg of an antisense oligonucleotide directly into the brain of a mouse model of Huntington’s disease (ie, BACHD mice) over 14 days. They observed a decline in huntingtin RNA that endured for as long as three months. The treated mice had better motor coordination and performed better on the rotorod test. The treatment also slowed the loss of brain mass and improved hypoactivity and anxiety.
The investigators also showed that antisense oligonucleotide reached the brain after intrathecal administration to monkeys. The treatment reduced huntingtin levels by approximately 50% in the cortex, and by between 20% and 25% in deep brain structures.
A Potential Biomarker of Target Engagement
To gauge treatment efficacy in humans, neurologists need a noninvasive way to measure levels of huntingtin in the brain. It is not yet possible to measure brain huntingtin levels directly using imaging, but CSF levels of huntingtin could be a surrogate measure, Dr. Leavitt said.
Dr. Leavitt and colleagues developed an ultrasensitive single-molecule counting immunoassay that successfully quantified mutant huntingtin in the CSF of patients with Huntington’s disease. Mutant huntingtin was undetectable in healthy controls. Patients with manifest Huntington’s disease had three times more mutant huntingtin than asymptomatic mutation carriers did. Huntingtin levels increased as the disease progressed. In addition, huntingtin concentration predicted cognitive and motor dysfunction.
The investigators observed similar findings after they used microbead-based immunoprecipitation and flow cytometry to develop a second highly sensitive assay for detecting mutant huntingtin. They demonstrated that CSF levels of mutant huntingtin reflect brain levels of the protein in mouse models of Huntington’s disease, and in patients with Huntington’s disease, the levels increased with disease stage. They also demonstrated that CSF huntingtin levels decreased following suppression of huntingtin in the brain.
A Clinical Trial Nears Completion
Ionis Pharmaceuticals developed an antisense oligonucleotide that targets both the mutant and normal alleles of huntingtin. Investigators subsequently began a first-in-human phase I/IIa trial of the drug in patients with early Huntington’s disease. Participants were randomized 3:1 to drug or placebo at sites in the United Kingdom, Germany, and Canada. The drug is administered intrathecally, and maximal protein suppression occurs approximately four weeks later. Each study participant will undergo intrathecal injections every month for four months.
The trial’s primary objective is to evaluate the treatment’s safety and tolerability. Its secondary objective is to examine the drug’s CSF pharmacokinetics. Finally, an exploratory objective is to assess the treatment’s effect on pharmacodynamic biomarkers and on clinical end points of Huntington’s disease.
All of the participants have been enrolled in the study, and Dr. Leavitt administered an intrathecal infusion to the first subject at the Vancouver site in September 2015. Participants are generally in good health and have high levels of function. Thus far, the researchers have found no evidence of significant adverse events or safety concerns, and the drug appears tolerable, said Dr. Leavitt. Results of the trial should be available in the coming months, he added. “This is certainly exciting, and it is the first time we have been able to bring a genetic therapy into the clinic for this devastating disorder.”
Other Therapies in Development
Wave Life Sciences also has created an antisense oligonucleotide for Huntington’s disease that is in the late preclinical stages of development. The company uses a type of chemistry that allows it to control the stereoisomer composition of the nucleic acids. The therapy targets specific single-nucleotide polymorphisms on mutant huntingtin and therefore may not be appropriate for every patient with Huntington’s disease. “This [treatment] has at least the potential for allele-specific targeting … and will hopefully be entering the clinic fairly soon,” said Dr. Leavitt.
Other gene-therapy approaches require a vector, most often a nonpathogenic adeno-associated virus (AAV), to bring the treatment into the CNS. Several such therapeutic candidates in preclinical development are close to entering early human trials, said Dr. Leavitt.
UniQure is developing a form of AAV5 that expresses an artificial micro-RNA that targets huntingtin. The drug will require stereotaxic injection directly into the brain. In one study, direct intraparenchymal injection of the drug significantly reduced levels of mutant huntingtin in the putamen, caudate, and thalamus of a minipig model of Huntington’s disease. The drug had less effect in the cortex. Depending on where the virus is injected, viral approaches generally have good local targeting, but not necessarily widespread targeting, said Dr. Leavitt. Spark Therapeutics and Voyager Therapeutics are also developing therapies similar to that of UniQure.
—Erik Greb
Suggested Reading
Kordasiewicz HB, Stanek LM, Wancewicz EV, et al. Sustained therapeutic reversal of Huntington’s disease by transient repression of huntingtin synthesis. Neuron. 2012; 74(6): 1031–1044.
Southwell AL, Smith SE, Davis TR, et al. Ultrasensitive measurement of huntingtin protein in cerebrospinal fluid demonstrates increase with Huntington disease stage and decrease following brain huntingtin suppression. Sci Rep. 2015;5:12166.
Wild EJ, Boggio R, Langbehn D, et al. Quantification of mutant huntingtin protein in cerebrospinal fluid from Huntington’s disease patients. J Clin Invest. 2015;125(5):1979-1986.
Fluid protocol takes aim at bariatric surgery readmissions
NEW YORK – With dehydration considered a contributor to hospital readmission after bariatric weight loss surgery, a multidisciplinary team of clinicians searched for a way to get patients to drink up. Specifically,
The project results were presented at a poster session at the American College of Surgeons Quality and Safety Conference.
“Our QI project was to streamline that process to ultimately eliminate or decrease those readmits,” Ms. Melei said.
They used 8-ounce water bottles. To track water consumption, they also numbered the bottles one through six for each patient. One-ounce cups were used during mealtimes. RNs, certified nursing assistants, and food service staff were educated about the fluid intake initiative. Only fluids provided by nursing were permitted and patients also received a clear message about fluid goals.
Another focus was standardizing communication with patients. They were not getting a consistent message from staff on what to expect before, during, and after surgery. “So we had to make sure [we] were all saying the same thing.”
The nurses and the other staff now ask the patients “Did you finish the bottle?” or “Where are you with the bottles?” Ms. Melei said. “At the end of a shift, the nurses document fluid consumption.”
During a 2-month baseline period, 12 patients drank an average 381.5 mL over 24 hours. Since the close of the project, the average daily fluid intake for patients undergoing bariatric surgery is 1,007 mL. In 12 months post implementation, average fluid intake for 39 patients jumped to 1,109.5 mL over 24 hours. “It was just such a hugely successful program. We had buy-in from every department, it worked really well, and we had great results,” said Cheryl Williams, the current bariatric program coordinator at Greenwich Hospital.
Sometimes dehydrated patients present to an emergency department complaining of vomiting, headache, and dizziness if they are not properly hydrated after surgery, Ms. Williams said. “Preventing dehydration helps to improve the patient’s recovery, as well as decrease emergency room visits and hospital admissions.”
Ashutosh Kaul, MD, FACS, medical director of the bariatric surgery program at Greenwich Hospital, said this study shows the importance of team building to improve patient care. “We built a core team that implemented a simple, low-cost, structured, and well-defined water distribution and documentation process, which resulted in better compliance of water intake. This reduced variability and improved postoperative intake progression, and we are presently studying its effect on reduction of readmissions and facilitating early discharge.”
Greenwich Hospital’s bariatric surgery center is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery. Ms. Williams and Ms. Melei had no relevant financial disclosures.
NEW YORK – With dehydration considered a contributor to hospital readmission after bariatric weight loss surgery, a multidisciplinary team of clinicians searched for a way to get patients to drink up. Specifically,
The project results were presented at a poster session at the American College of Surgeons Quality and Safety Conference.
“Our QI project was to streamline that process to ultimately eliminate or decrease those readmits,” Ms. Melei said.
They used 8-ounce water bottles. To track water consumption, they also numbered the bottles one through six for each patient. One-ounce cups were used during mealtimes. RNs, certified nursing assistants, and food service staff were educated about the fluid intake initiative. Only fluids provided by nursing were permitted and patients also received a clear message about fluid goals.
Another focus was standardizing communication with patients. They were not getting a consistent message from staff on what to expect before, during, and after surgery. “So we had to make sure [we] were all saying the same thing.”
The nurses and the other staff now ask the patients “Did you finish the bottle?” or “Where are you with the bottles?” Ms. Melei said. “At the end of a shift, the nurses document fluid consumption.”
During a 2-month baseline period, 12 patients drank an average 381.5 mL over 24 hours. Since the close of the project, the average daily fluid intake for patients undergoing bariatric surgery is 1,007 mL. In 12 months post implementation, average fluid intake for 39 patients jumped to 1,109.5 mL over 24 hours. “It was just such a hugely successful program. We had buy-in from every department, it worked really well, and we had great results,” said Cheryl Williams, the current bariatric program coordinator at Greenwich Hospital.
Sometimes dehydrated patients present to an emergency department complaining of vomiting, headache, and dizziness if they are not properly hydrated after surgery, Ms. Williams said. “Preventing dehydration helps to improve the patient’s recovery, as well as decrease emergency room visits and hospital admissions.”
Ashutosh Kaul, MD, FACS, medical director of the bariatric surgery program at Greenwich Hospital, said this study shows the importance of team building to improve patient care. “We built a core team that implemented a simple, low-cost, structured, and well-defined water distribution and documentation process, which resulted in better compliance of water intake. This reduced variability and improved postoperative intake progression, and we are presently studying its effect on reduction of readmissions and facilitating early discharge.”
Greenwich Hospital’s bariatric surgery center is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery. Ms. Williams and Ms. Melei had no relevant financial disclosures.
NEW YORK – With dehydration considered a contributor to hospital readmission after bariatric weight loss surgery, a multidisciplinary team of clinicians searched for a way to get patients to drink up. Specifically,
The project results were presented at a poster session at the American College of Surgeons Quality and Safety Conference.
“Our QI project was to streamline that process to ultimately eliminate or decrease those readmits,” Ms. Melei said.
They used 8-ounce water bottles. To track water consumption, they also numbered the bottles one through six for each patient. One-ounce cups were used during mealtimes. RNs, certified nursing assistants, and food service staff were educated about the fluid intake initiative. Only fluids provided by nursing were permitted and patients also received a clear message about fluid goals.
Another focus was standardizing communication with patients. They were not getting a consistent message from staff on what to expect before, during, and after surgery. “So we had to make sure [we] were all saying the same thing.”
The nurses and the other staff now ask the patients “Did you finish the bottle?” or “Where are you with the bottles?” Ms. Melei said. “At the end of a shift, the nurses document fluid consumption.”
During a 2-month baseline period, 12 patients drank an average 381.5 mL over 24 hours. Since the close of the project, the average daily fluid intake for patients undergoing bariatric surgery is 1,007 mL. In 12 months post implementation, average fluid intake for 39 patients jumped to 1,109.5 mL over 24 hours. “It was just such a hugely successful program. We had buy-in from every department, it worked really well, and we had great results,” said Cheryl Williams, the current bariatric program coordinator at Greenwich Hospital.
Sometimes dehydrated patients present to an emergency department complaining of vomiting, headache, and dizziness if they are not properly hydrated after surgery, Ms. Williams said. “Preventing dehydration helps to improve the patient’s recovery, as well as decrease emergency room visits and hospital admissions.”
Ashutosh Kaul, MD, FACS, medical director of the bariatric surgery program at Greenwich Hospital, said this study shows the importance of team building to improve patient care. “We built a core team that implemented a simple, low-cost, structured, and well-defined water distribution and documentation process, which resulted in better compliance of water intake. This reduced variability and improved postoperative intake progression, and we are presently studying its effect on reduction of readmissions and facilitating early discharge.”
Greenwich Hospital’s bariatric surgery center is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery. Ms. Williams and Ms. Melei had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
Key clinical point: QI project to increase water intake after bariatric surgery could decrease hospital readmission rates.
Major finding: Multidisciplinary protocol increases 24-hour fluid intake from 382 mL to 1,110 mL on average.
Data source: Comparison of water consumed by 12 patients before versus 39 patients after implementation.
Disclosures: Ms. Williams and Ms. Melei had no relevant financial disclosures.
Meningitis before age 3 months: Consider enterovirus and parechovirus
MADRID – Ninety-five percent of cases of enterovirus and parechovirus meningitis in infants younger than 90 days old in the United Kingdom and Ireland were diagnosed through lumbar puncture and identification of the virus in the CSF by PCR, Seilesh Kadambari, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“We recommend that routine testing of CSF for enterovirus and parechovirus in febrile infants should be promoted, even in the absence of pleocytosis,” said Dr. Kadambari of John Radcliffe Hospital in Oxford, England.
This active enhanced prospective surveillance study was undertaken because an earlier retrospective study concluded that the rate of viral meningitis across all pediatric and adult age groups had increased rapidly during a recent 10-year period in the United Kingdom and Ireland. Infants younger than 3 months of age were especially hard hit by enterovirus, which accounted in the earlier study for 92% of all viral meningitis cases in that age group. Dr. Kadambari and his coinvestigators decided to take a closer prospective look at the sub-3-month age group because it’s such an important time neurodevelopmentally.
During the 13-month period of June 2014 to June 2015, 710 patients younger than 90 days old were hospitalized for enterovirus or parechovirus meningitis across the United Kingdom and Republic of Ireland. Ninety-five percent were due to enterovirus. Only 6% of affected infants were born prematurely.
“One of the take-home messages for me from the study was that 12% of enterovirus cases and 23% of parechovirus meningitis cases required admission to an ICU setting,” the pediatrician observed.
Among the infants admitted to a pediatric ICU, half of those with enterovirus meningitis and all those with parechovirus meningitis required intubation and mechanical ventilation. One-fifth of the enterovirus meningitis patients in pediatric ICUs required inotropic support for cardiovascular stabilization, as did all young infants with parechovirus meningitis.
Among the 710 patients, the three most common clinical presenting features were fever, irritability, and reduced feeding, present in 85%, 66%, and 54%, respectively.
Upon physical examination, two noteworthy common findings were signs of shock, present in 27% of infants with enterovirus meningitis and 43% with parechovirus meningitis, and respiratory distress, seen in 12% and 26%, respectively.
None of the 710 infants had a secondary bacterial infection. “That has implications for antimicrobial stewardship programs,” according to Dr. Kadambari.
The majority of infants had a normal CSF WBC count and a normal-range C-reactive protein level.
“Raised inflammatory markers were not a common feature in our cohort,” he noted.
Two infants died: one of a massive pulmonary hemorrhage and the other as a result of septic shock. Of the remaining 708 patients, however, 699 (98.7%) were discharged without significant neurologic impairment. Seven infants with enterovirus meningitis and two with parechovirus meningitis were discharged with severe delay, including cases of fine motor and gross motor delay, visual abnormalities, and a single case of severe cardiac dysfunction requiring discharge on an ACE inhibitor.
This surveillance study was a collaboration between St. George’s University of London and Public Health England. Dr. Kadambari reported having no financial conflicts.
Future studies need to examine long-term neurodevelopmental outcomes in affected young infants out to age 24 months, he said.
MADRID – Ninety-five percent of cases of enterovirus and parechovirus meningitis in infants younger than 90 days old in the United Kingdom and Ireland were diagnosed through lumbar puncture and identification of the virus in the CSF by PCR, Seilesh Kadambari, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“We recommend that routine testing of CSF for enterovirus and parechovirus in febrile infants should be promoted, even in the absence of pleocytosis,” said Dr. Kadambari of John Radcliffe Hospital in Oxford, England.
This active enhanced prospective surveillance study was undertaken because an earlier retrospective study concluded that the rate of viral meningitis across all pediatric and adult age groups had increased rapidly during a recent 10-year period in the United Kingdom and Ireland. Infants younger than 3 months of age were especially hard hit by enterovirus, which accounted in the earlier study for 92% of all viral meningitis cases in that age group. Dr. Kadambari and his coinvestigators decided to take a closer prospective look at the sub-3-month age group because it’s such an important time neurodevelopmentally.
During the 13-month period of June 2014 to June 2015, 710 patients younger than 90 days old were hospitalized for enterovirus or parechovirus meningitis across the United Kingdom and Republic of Ireland. Ninety-five percent were due to enterovirus. Only 6% of affected infants were born prematurely.
“One of the take-home messages for me from the study was that 12% of enterovirus cases and 23% of parechovirus meningitis cases required admission to an ICU setting,” the pediatrician observed.
Among the infants admitted to a pediatric ICU, half of those with enterovirus meningitis and all those with parechovirus meningitis required intubation and mechanical ventilation. One-fifth of the enterovirus meningitis patients in pediatric ICUs required inotropic support for cardiovascular stabilization, as did all young infants with parechovirus meningitis.
Among the 710 patients, the three most common clinical presenting features were fever, irritability, and reduced feeding, present in 85%, 66%, and 54%, respectively.
Upon physical examination, two noteworthy common findings were signs of shock, present in 27% of infants with enterovirus meningitis and 43% with parechovirus meningitis, and respiratory distress, seen in 12% and 26%, respectively.
None of the 710 infants had a secondary bacterial infection. “That has implications for antimicrobial stewardship programs,” according to Dr. Kadambari.
The majority of infants had a normal CSF WBC count and a normal-range C-reactive protein level.
“Raised inflammatory markers were not a common feature in our cohort,” he noted.
Two infants died: one of a massive pulmonary hemorrhage and the other as a result of septic shock. Of the remaining 708 patients, however, 699 (98.7%) were discharged without significant neurologic impairment. Seven infants with enterovirus meningitis and two with parechovirus meningitis were discharged with severe delay, including cases of fine motor and gross motor delay, visual abnormalities, and a single case of severe cardiac dysfunction requiring discharge on an ACE inhibitor.
This surveillance study was a collaboration between St. George’s University of London and Public Health England. Dr. Kadambari reported having no financial conflicts.
Future studies need to examine long-term neurodevelopmental outcomes in affected young infants out to age 24 months, he said.
MADRID – Ninety-five percent of cases of enterovirus and parechovirus meningitis in infants younger than 90 days old in the United Kingdom and Ireland were diagnosed through lumbar puncture and identification of the virus in the CSF by PCR, Seilesh Kadambari, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“We recommend that routine testing of CSF for enterovirus and parechovirus in febrile infants should be promoted, even in the absence of pleocytosis,” said Dr. Kadambari of John Radcliffe Hospital in Oxford, England.
This active enhanced prospective surveillance study was undertaken because an earlier retrospective study concluded that the rate of viral meningitis across all pediatric and adult age groups had increased rapidly during a recent 10-year period in the United Kingdom and Ireland. Infants younger than 3 months of age were especially hard hit by enterovirus, which accounted in the earlier study for 92% of all viral meningitis cases in that age group. Dr. Kadambari and his coinvestigators decided to take a closer prospective look at the sub-3-month age group because it’s such an important time neurodevelopmentally.
During the 13-month period of June 2014 to June 2015, 710 patients younger than 90 days old were hospitalized for enterovirus or parechovirus meningitis across the United Kingdom and Republic of Ireland. Ninety-five percent were due to enterovirus. Only 6% of affected infants were born prematurely.
“One of the take-home messages for me from the study was that 12% of enterovirus cases and 23% of parechovirus meningitis cases required admission to an ICU setting,” the pediatrician observed.
Among the infants admitted to a pediatric ICU, half of those with enterovirus meningitis and all those with parechovirus meningitis required intubation and mechanical ventilation. One-fifth of the enterovirus meningitis patients in pediatric ICUs required inotropic support for cardiovascular stabilization, as did all young infants with parechovirus meningitis.
Among the 710 patients, the three most common clinical presenting features were fever, irritability, and reduced feeding, present in 85%, 66%, and 54%, respectively.
Upon physical examination, two noteworthy common findings were signs of shock, present in 27% of infants with enterovirus meningitis and 43% with parechovirus meningitis, and respiratory distress, seen in 12% and 26%, respectively.
None of the 710 infants had a secondary bacterial infection. “That has implications for antimicrobial stewardship programs,” according to Dr. Kadambari.
The majority of infants had a normal CSF WBC count and a normal-range C-reactive protein level.
“Raised inflammatory markers were not a common feature in our cohort,” he noted.
Two infants died: one of a massive pulmonary hemorrhage and the other as a result of septic shock. Of the remaining 708 patients, however, 699 (98.7%) were discharged without significant neurologic impairment. Seven infants with enterovirus meningitis and two with parechovirus meningitis were discharged with severe delay, including cases of fine motor and gross motor delay, visual abnormalities, and a single case of severe cardiac dysfunction requiring discharge on an ACE inhibitor.
This surveillance study was a collaboration between St. George’s University of London and Public Health England. Dr. Kadambari reported having no financial conflicts.
Future studies need to examine long-term neurodevelopmental outcomes in affected young infants out to age 24 months, he said.
AT ESPID 2017
Key clinical point:
Major finding: More than 98% of infants in the United Kingdom and Ireland younger than 90 days old with enterovirus or parechovirus meningitis were discharged without significant neurologic impairment.
Data source: A prospective active enhanced surveillance study including all 710 infants younger than 90 days old hospitalized for enterovirus or parechovirus meningitis in the United Kingdom and Ireland in a 13-month period.
Disclosures: The study was jointly sponsored by Public Health England and St. George’s University of London. The presenter reported having no financial conflicts.
New monotherapy approved for partial-onset seizures
The U.S. Food and Drug Administration has approved perampanel (Fycompa) for monotherapy treatment of partial-onset seizures (POS) in patients aged 12 years or older as of July 27. It was approved in 2012 for adjunctive use for POS and primary, generalized tonic-clonic seizures in patients aged 12 years or older.
Three clinical trials showed improvement in seizure control for the patients with POS taking perampanel, compared with placebo.
The drug is available in tablets from 2 mg to 12 mg and as an oral suspension formulation. It is taken once daily.
“Approximately one-third of people living with epilepsy have seizures that are not adequately controlled,” said Robert T. Wechsler, MD, PhD, medical director of the Idaho Comprehensive Epilepsy Center, in Eisai’s press release. “Having a new monotherapy option for partial-onset seizures that is once a day gives physicians and patients an effective treatment option that has the potential to make a difference in patients’ lives.”
The U.S. Food and Drug Administration has approved perampanel (Fycompa) for monotherapy treatment of partial-onset seizures (POS) in patients aged 12 years or older as of July 27. It was approved in 2012 for adjunctive use for POS and primary, generalized tonic-clonic seizures in patients aged 12 years or older.
Three clinical trials showed improvement in seizure control for the patients with POS taking perampanel, compared with placebo.
The drug is available in tablets from 2 mg to 12 mg and as an oral suspension formulation. It is taken once daily.
“Approximately one-third of people living with epilepsy have seizures that are not adequately controlled,” said Robert T. Wechsler, MD, PhD, medical director of the Idaho Comprehensive Epilepsy Center, in Eisai’s press release. “Having a new monotherapy option for partial-onset seizures that is once a day gives physicians and patients an effective treatment option that has the potential to make a difference in patients’ lives.”
The U.S. Food and Drug Administration has approved perampanel (Fycompa) for monotherapy treatment of partial-onset seizures (POS) in patients aged 12 years or older as of July 27. It was approved in 2012 for adjunctive use for POS and primary, generalized tonic-clonic seizures in patients aged 12 years or older.
Three clinical trials showed improvement in seizure control for the patients with POS taking perampanel, compared with placebo.
The drug is available in tablets from 2 mg to 12 mg and as an oral suspension formulation. It is taken once daily.
“Approximately one-third of people living with epilepsy have seizures that are not adequately controlled,” said Robert T. Wechsler, MD, PhD, medical director of the Idaho Comprehensive Epilepsy Center, in Eisai’s press release. “Having a new monotherapy option for partial-onset seizures that is once a day gives physicians and patients an effective treatment option that has the potential to make a difference in patients’ lives.”
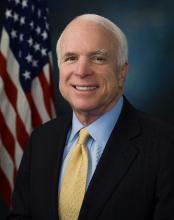
Senate sinks GOP health care reform effort
After casting the deciding vote to begin debate in the Senate on the Republican effort to repeal and replace the Affordable Care Act, Sen. John McCain (R-Ariz.) brought the effort to an end when he voted against the so-called “skinny repeal” bill introduced by Senate Majority Leader Mitch McConnell (R-Ky.).
Sen. McCain crossed the aisle with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) and voted with the 48 members of the chamber’s Democratic caucus to kill the bill. Republicans would have needed 50 votes to pass the measure, with Vice President Mike Pence on hand to cast a tie-breaking vote if necessary. With three senators voting against the measure, however, the 49 votes were not enough.
In the early evening on July 27, however, Sen. McCain made it clear during a press conference that he would not vote for a skinny repeal. Other senators expressed concern over the skinny repeal but said they would vote for it if there were assurances that the House would actually go to conference committee (a procedure used when the House and Senate pass different versions of the same bill to allow a bipartisan group to find consensus and create a unified bill) and work out a final bill and not simply move the skinny repeal straight to the president’s desk.
Speaker of the House Paul Ryan (R-Wisc.) had issued a statement to that effect, but the House was laying a path to simply move any bill passed by the Senate, leaving it up in the air as to whether a conference committee would actually be created.
Despite a reported phone call from Speaker Ryan and conversations directly with Vice President Pence on the Senate floor, Sen. McCain ultimately could not be convinced to vote with the majority of Republicans.
“From the beginning, I have believed that Obamacare should be repealed and replaced with a solution that increases competition, lowers costs, and improves care for the American people,” Sen. McCain said in a statement issued July 28, following the early-morning vote. “The so-called ‘skinny repeal’ amendment the Senate voted on today would not accomplish those goals. While the amendment would have repealed some of Obamacare’s most burdensome regulations, it offered no replacement to actually reform our health care system and deliver affordable, quality health care to our citizens. The Speaker’s statement that the House would be ‘willing’ to go to conference does not ease my concern that this shell of a bill could be taken up and passed at any time.”
The vote brought to an end a few days of minimal activity. Every attempt by the GOP to pass some form of amendment to move the process forward – from the tweaked version of the Better Care Replacement Act to a straight repeal of the ACA – failed. Sen. Steve Daines (R-Mont.) even introduced a single-payer amendment, but that failed to get a single yes vote, with all 52 GOP members and five Democrats voting against it and the remaining 43 Democrats voting “present.”
Very few amendments were proposed, though one did get passed in the process that would have permanently repealed the so-called “Cadillac tax,” which levies a 40% tax on plans that exceed a certain value. That amendment passed along party lines by a 52-48 vote.
The future of the ACA and future reform efforts remain unclear at the moment. Following the vote, a defeated Majority Leader McConnell asked the minority party what plan they have to offer. Senate Minority Leader Charles E. Schumer (D-N.Y.) echoed Sen. McCain’s speech earlier in the week after the vote was cast to start the debate to return to regular and hammer out a bipartisan solution though the committee process.
Meanwhile, President Donald Trump advocated via Twitter to simply let the ACA continue to crumble and when it failed, then to work on a deal.
The American Medical Association called on Congress to continue its work on fixing the health care system. “While we are relieved that the Senate did not adopt legislation that would have harmed patients and critical safety net programs, the status quo is not acceptable,” AMA President David Barbe said in a statement. “We urge Congress to initiate a bipartisan effort to address shortcomings in the Affordable Care Act. The first priority should be to stabilize the individual marketplace to achieve the goal of providing access to quality, affordable health coverage for more Americans.”
After casting the deciding vote to begin debate in the Senate on the Republican effort to repeal and replace the Affordable Care Act, Sen. John McCain (R-Ariz.) brought the effort to an end when he voted against the so-called “skinny repeal” bill introduced by Senate Majority Leader Mitch McConnell (R-Ky.).
Sen. McCain crossed the aisle with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) and voted with the 48 members of the chamber’s Democratic caucus to kill the bill. Republicans would have needed 50 votes to pass the measure, with Vice President Mike Pence on hand to cast a tie-breaking vote if necessary. With three senators voting against the measure, however, the 49 votes were not enough.
In the early evening on July 27, however, Sen. McCain made it clear during a press conference that he would not vote for a skinny repeal. Other senators expressed concern over the skinny repeal but said they would vote for it if there were assurances that the House would actually go to conference committee (a procedure used when the House and Senate pass different versions of the same bill to allow a bipartisan group to find consensus and create a unified bill) and work out a final bill and not simply move the skinny repeal straight to the president’s desk.
Speaker of the House Paul Ryan (R-Wisc.) had issued a statement to that effect, but the House was laying a path to simply move any bill passed by the Senate, leaving it up in the air as to whether a conference committee would actually be created.
Despite a reported phone call from Speaker Ryan and conversations directly with Vice President Pence on the Senate floor, Sen. McCain ultimately could not be convinced to vote with the majority of Republicans.
“From the beginning, I have believed that Obamacare should be repealed and replaced with a solution that increases competition, lowers costs, and improves care for the American people,” Sen. McCain said in a statement issued July 28, following the early-morning vote. “The so-called ‘skinny repeal’ amendment the Senate voted on today would not accomplish those goals. While the amendment would have repealed some of Obamacare’s most burdensome regulations, it offered no replacement to actually reform our health care system and deliver affordable, quality health care to our citizens. The Speaker’s statement that the House would be ‘willing’ to go to conference does not ease my concern that this shell of a bill could be taken up and passed at any time.”
The vote brought to an end a few days of minimal activity. Every attempt by the GOP to pass some form of amendment to move the process forward – from the tweaked version of the Better Care Replacement Act to a straight repeal of the ACA – failed. Sen. Steve Daines (R-Mont.) even introduced a single-payer amendment, but that failed to get a single yes vote, with all 52 GOP members and five Democrats voting against it and the remaining 43 Democrats voting “present.”
Very few amendments were proposed, though one did get passed in the process that would have permanently repealed the so-called “Cadillac tax,” which levies a 40% tax on plans that exceed a certain value. That amendment passed along party lines by a 52-48 vote.
The future of the ACA and future reform efforts remain unclear at the moment. Following the vote, a defeated Majority Leader McConnell asked the minority party what plan they have to offer. Senate Minority Leader Charles E. Schumer (D-N.Y.) echoed Sen. McCain’s speech earlier in the week after the vote was cast to start the debate to return to regular and hammer out a bipartisan solution though the committee process.
Meanwhile, President Donald Trump advocated via Twitter to simply let the ACA continue to crumble and when it failed, then to work on a deal.
The American Medical Association called on Congress to continue its work on fixing the health care system. “While we are relieved that the Senate did not adopt legislation that would have harmed patients and critical safety net programs, the status quo is not acceptable,” AMA President David Barbe said in a statement. “We urge Congress to initiate a bipartisan effort to address shortcomings in the Affordable Care Act. The first priority should be to stabilize the individual marketplace to achieve the goal of providing access to quality, affordable health coverage for more Americans.”
After casting the deciding vote to begin debate in the Senate on the Republican effort to repeal and replace the Affordable Care Act, Sen. John McCain (R-Ariz.) brought the effort to an end when he voted against the so-called “skinny repeal” bill introduced by Senate Majority Leader Mitch McConnell (R-Ky.).
Sen. McCain crossed the aisle with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) and voted with the 48 members of the chamber’s Democratic caucus to kill the bill. Republicans would have needed 50 votes to pass the measure, with Vice President Mike Pence on hand to cast a tie-breaking vote if necessary. With three senators voting against the measure, however, the 49 votes were not enough.
In the early evening on July 27, however, Sen. McCain made it clear during a press conference that he would not vote for a skinny repeal. Other senators expressed concern over the skinny repeal but said they would vote for it if there were assurances that the House would actually go to conference committee (a procedure used when the House and Senate pass different versions of the same bill to allow a bipartisan group to find consensus and create a unified bill) and work out a final bill and not simply move the skinny repeal straight to the president’s desk.
Speaker of the House Paul Ryan (R-Wisc.) had issued a statement to that effect, but the House was laying a path to simply move any bill passed by the Senate, leaving it up in the air as to whether a conference committee would actually be created.
Despite a reported phone call from Speaker Ryan and conversations directly with Vice President Pence on the Senate floor, Sen. McCain ultimately could not be convinced to vote with the majority of Republicans.
“From the beginning, I have believed that Obamacare should be repealed and replaced with a solution that increases competition, lowers costs, and improves care for the American people,” Sen. McCain said in a statement issued July 28, following the early-morning vote. “The so-called ‘skinny repeal’ amendment the Senate voted on today would not accomplish those goals. While the amendment would have repealed some of Obamacare’s most burdensome regulations, it offered no replacement to actually reform our health care system and deliver affordable, quality health care to our citizens. The Speaker’s statement that the House would be ‘willing’ to go to conference does not ease my concern that this shell of a bill could be taken up and passed at any time.”
The vote brought to an end a few days of minimal activity. Every attempt by the GOP to pass some form of amendment to move the process forward – from the tweaked version of the Better Care Replacement Act to a straight repeal of the ACA – failed. Sen. Steve Daines (R-Mont.) even introduced a single-payer amendment, but that failed to get a single yes vote, with all 52 GOP members and five Democrats voting against it and the remaining 43 Democrats voting “present.”
Very few amendments were proposed, though one did get passed in the process that would have permanently repealed the so-called “Cadillac tax,” which levies a 40% tax on plans that exceed a certain value. That amendment passed along party lines by a 52-48 vote.
The future of the ACA and future reform efforts remain unclear at the moment. Following the vote, a defeated Majority Leader McConnell asked the minority party what plan they have to offer. Senate Minority Leader Charles E. Schumer (D-N.Y.) echoed Sen. McCain’s speech earlier in the week after the vote was cast to start the debate to return to regular and hammer out a bipartisan solution though the committee process.
Meanwhile, President Donald Trump advocated via Twitter to simply let the ACA continue to crumble and when it failed, then to work on a deal.
The American Medical Association called on Congress to continue its work on fixing the health care system. “While we are relieved that the Senate did not adopt legislation that would have harmed patients and critical safety net programs, the status quo is not acceptable,” AMA President David Barbe said in a statement. “We urge Congress to initiate a bipartisan effort to address shortcomings in the Affordable Care Act. The first priority should be to stabilize the individual marketplace to achieve the goal of providing access to quality, affordable health coverage for more Americans.”
Leonard Wood: Advocate of Military Preparedness
Unless you have been assigned to the post or the hospital, you have probably never heard of Leonard Wood. Leonard Wood arguably had the most distinguished military-government career of someone who did not become president. Wood was a Harvard-educated physician, pursued the Apache Chief Geronimo, received the Medal of Honor, was physician to 2 U.S. presidents, served as U.S. army chief of staff, was a successful military governor, ran for president, was a colleague of Walter Reed, and was commander-inarms for President Theodore Roosevelt.
Wood was born in 1860 to an established New England family; his father was a Union Army physician during the Civil War and was practicing on Cape Cod when he died unexpectedly in 1880. The family was left destitute, but Wood was able to continue his education when a wealthy family friend agreed to pay for him to attend Harvard Medical School, which at the time did not require any prior college. He graduated in 1883 and was selected for a prized internship at Boston City Hospital; however, he was dismissed for a rule violation that the program director later admitted was a mistake.
Unable to support himself in practice in Boston, Wood turned to the U.S. Army, a decision that would change his life. Assigned to Fort Huachuca in Arizona, Wood participated in the yearlong pursuit and final surrender of Geronimo; for his role he was awarded the Medal of Honor in 1898. His experiences in the wild and rugged terrain of the west triggered a legendary and lifelong pursuit of hard and stressful physical activity. Transferred to California, Wood met Louise Condit-Smith, ward of an associate justice of the U.S. Supreme Court. When they married in November 1890 in Washington, DC, the ceremony was attended by all of the Supreme Court justices.
In 1893 while assigned to Fort McPherson outside Atlanta, Wood, whose duties were not demanding, needed a physical outlet for his unbounded energies. He enrolled at Georgia Tech at age 33 to play football. He was eligible to play because he had not previously attended college. He scored 5 touchdowns, winning the game against rival University of Georgia.
Later, Wood was assigned to Washington, where he quickly became known and sought after as a physician. He served many of the political and military elite, including presidents Grover Cleveland and William McKinley. In 1897, he met Theodore Roosevelt, the 38-year-old assistant secretary of the U.S. Navy who shared his love of outdoor adventure and the military. They became fast friends/companions/competitors; Roosevelt wrote to a friend that he had found a “playmate.”
When the U.S.S. Maine was sunk in Havana Harbor in 1898 and war was declared on Spain, Wood and Roosevelt schemed on how to go to war together. Wood the career soldier and Roosevelt the career politician had excellent connections and became commander and deputy commander of the First Volunteer Calvary, later famously known as the Rough Riders. When a more senior general became ill, Wood was promoted to brigadier general, and Roosevelt became the regiment colonel.
After the war, Wood became military governor of Cuba and major general of volunteers. During the U.S. occupation, Walter Reed was sent to investigate infectious diseases, including yellow fever. Wood provided $10,000 to fund the second phase of Reed’s research and approved the use of human volunteers. When the U.S. occupation ended in 1902, Wood was to revert to captain, medical corps.
Wood’s success in Cuba was obvious and wel l known; President McKinley promoted him to U.S. Army brigadier general. At that time, as a brigadier general, Wood was essentially guaranteed a second star and a rotation through the chief of staff position. He served as chief of staff from 1910 to 1914, the only physician ever to do so. As chief of staff he eliminated the antiquated bureau system, developed the maneuver unit concept, and laid the groundwork for the Reserve Officers’ Training Corps.
Wood stayed on active duty and rotated through other senior-level positions. Because of Wood’s political activity promoting universal service and improving readiness, President Woodrow Wilson passed over him, instead selecting John J. Pershing to command the American Expeditionary Force in World War I. Wood stayed politically active and ran for the Republican presidential nomination in 1920, losing to Warren G. Harding at the convention. Wood was appointed governor general of the Philippines, a position he held until his death in 1927.
While in Cuba, Wood was severely injured by striking his head on a chandelier, most likely resulting in an undiagnosed skull fracture. Over time he developed neurologic symptoms and was seen by neurosurgeon Harvey Cushing, MD, at Johns Hopkins, who removed a meningioma in February 1910. Wood made a dramatic recovery. Over a decade later while in the Philippines, his symptoms returned, and after significant delay he went home to see Cushing who was then at Harvard Medical School. When Wood died after surgery, Cushing admitted that he should not have tackled such a difficult case so quickly after returning from a trip to Europe.
Fort Leonard Wood in Missouri and the on-base General Leonard Wood U.S. Army Community Hospital are named in Wood’s honor.
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual
your facility was named for or to offer a topic suggestion, contact us at [email protected] or on Facebook.
Unless you have been assigned to the post or the hospital, you have probably never heard of Leonard Wood. Leonard Wood arguably had the most distinguished military-government career of someone who did not become president. Wood was a Harvard-educated physician, pursued the Apache Chief Geronimo, received the Medal of Honor, was physician to 2 U.S. presidents, served as U.S. army chief of staff, was a successful military governor, ran for president, was a colleague of Walter Reed, and was commander-inarms for President Theodore Roosevelt.
Wood was born in 1860 to an established New England family; his father was a Union Army physician during the Civil War and was practicing on Cape Cod when he died unexpectedly in 1880. The family was left destitute, but Wood was able to continue his education when a wealthy family friend agreed to pay for him to attend Harvard Medical School, which at the time did not require any prior college. He graduated in 1883 and was selected for a prized internship at Boston City Hospital; however, he was dismissed for a rule violation that the program director later admitted was a mistake.
Unable to support himself in practice in Boston, Wood turned to the U.S. Army, a decision that would change his life. Assigned to Fort Huachuca in Arizona, Wood participated in the yearlong pursuit and final surrender of Geronimo; for his role he was awarded the Medal of Honor in 1898. His experiences in the wild and rugged terrain of the west triggered a legendary and lifelong pursuit of hard and stressful physical activity. Transferred to California, Wood met Louise Condit-Smith, ward of an associate justice of the U.S. Supreme Court. When they married in November 1890 in Washington, DC, the ceremony was attended by all of the Supreme Court justices.
In 1893 while assigned to Fort McPherson outside Atlanta, Wood, whose duties were not demanding, needed a physical outlet for his unbounded energies. He enrolled at Georgia Tech at age 33 to play football. He was eligible to play because he had not previously attended college. He scored 5 touchdowns, winning the game against rival University of Georgia.
Later, Wood was assigned to Washington, where he quickly became known and sought after as a physician. He served many of the political and military elite, including presidents Grover Cleveland and William McKinley. In 1897, he met Theodore Roosevelt, the 38-year-old assistant secretary of the U.S. Navy who shared his love of outdoor adventure and the military. They became fast friends/companions/competitors; Roosevelt wrote to a friend that he had found a “playmate.”
When the U.S.S. Maine was sunk in Havana Harbor in 1898 and war was declared on Spain, Wood and Roosevelt schemed on how to go to war together. Wood the career soldier and Roosevelt the career politician had excellent connections and became commander and deputy commander of the First Volunteer Calvary, later famously known as the Rough Riders. When a more senior general became ill, Wood was promoted to brigadier general, and Roosevelt became the regiment colonel.
After the war, Wood became military governor of Cuba and major general of volunteers. During the U.S. occupation, Walter Reed was sent to investigate infectious diseases, including yellow fever. Wood provided $10,000 to fund the second phase of Reed’s research and approved the use of human volunteers. When the U.S. occupation ended in 1902, Wood was to revert to captain, medical corps.
Wood’s success in Cuba was obvious and wel l known; President McKinley promoted him to U.S. Army brigadier general. At that time, as a brigadier general, Wood was essentially guaranteed a second star and a rotation through the chief of staff position. He served as chief of staff from 1910 to 1914, the only physician ever to do so. As chief of staff he eliminated the antiquated bureau system, developed the maneuver unit concept, and laid the groundwork for the Reserve Officers’ Training Corps.
Wood stayed on active duty and rotated through other senior-level positions. Because of Wood’s political activity promoting universal service and improving readiness, President Woodrow Wilson passed over him, instead selecting John J. Pershing to command the American Expeditionary Force in World War I. Wood stayed politically active and ran for the Republican presidential nomination in 1920, losing to Warren G. Harding at the convention. Wood was appointed governor general of the Philippines, a position he held until his death in 1927.
While in Cuba, Wood was severely injured by striking his head on a chandelier, most likely resulting in an undiagnosed skull fracture. Over time he developed neurologic symptoms and was seen by neurosurgeon Harvey Cushing, MD, at Johns Hopkins, who removed a meningioma in February 1910. Wood made a dramatic recovery. Over a decade later while in the Philippines, his symptoms returned, and after significant delay he went home to see Cushing who was then at Harvard Medical School. When Wood died after surgery, Cushing admitted that he should not have tackled such a difficult case so quickly after returning from a trip to Europe.
Fort Leonard Wood in Missouri and the on-base General Leonard Wood U.S. Army Community Hospital are named in Wood’s honor.
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual
your facility was named for or to offer a topic suggestion, contact us at [email protected] or on Facebook.
Unless you have been assigned to the post or the hospital, you have probably never heard of Leonard Wood. Leonard Wood arguably had the most distinguished military-government career of someone who did not become president. Wood was a Harvard-educated physician, pursued the Apache Chief Geronimo, received the Medal of Honor, was physician to 2 U.S. presidents, served as U.S. army chief of staff, was a successful military governor, ran for president, was a colleague of Walter Reed, and was commander-inarms for President Theodore Roosevelt.
Wood was born in 1860 to an established New England family; his father was a Union Army physician during the Civil War and was practicing on Cape Cod when he died unexpectedly in 1880. The family was left destitute, but Wood was able to continue his education when a wealthy family friend agreed to pay for him to attend Harvard Medical School, which at the time did not require any prior college. He graduated in 1883 and was selected for a prized internship at Boston City Hospital; however, he was dismissed for a rule violation that the program director later admitted was a mistake.
Unable to support himself in practice in Boston, Wood turned to the U.S. Army, a decision that would change his life. Assigned to Fort Huachuca in Arizona, Wood participated in the yearlong pursuit and final surrender of Geronimo; for his role he was awarded the Medal of Honor in 1898. His experiences in the wild and rugged terrain of the west triggered a legendary and lifelong pursuit of hard and stressful physical activity. Transferred to California, Wood met Louise Condit-Smith, ward of an associate justice of the U.S. Supreme Court. When they married in November 1890 in Washington, DC, the ceremony was attended by all of the Supreme Court justices.
In 1893 while assigned to Fort McPherson outside Atlanta, Wood, whose duties were not demanding, needed a physical outlet for his unbounded energies. He enrolled at Georgia Tech at age 33 to play football. He was eligible to play because he had not previously attended college. He scored 5 touchdowns, winning the game against rival University of Georgia.
Later, Wood was assigned to Washington, where he quickly became known and sought after as a physician. He served many of the political and military elite, including presidents Grover Cleveland and William McKinley. In 1897, he met Theodore Roosevelt, the 38-year-old assistant secretary of the U.S. Navy who shared his love of outdoor adventure and the military. They became fast friends/companions/competitors; Roosevelt wrote to a friend that he had found a “playmate.”
When the U.S.S. Maine was sunk in Havana Harbor in 1898 and war was declared on Spain, Wood and Roosevelt schemed on how to go to war together. Wood the career soldier and Roosevelt the career politician had excellent connections and became commander and deputy commander of the First Volunteer Calvary, later famously known as the Rough Riders. When a more senior general became ill, Wood was promoted to brigadier general, and Roosevelt became the regiment colonel.
After the war, Wood became military governor of Cuba and major general of volunteers. During the U.S. occupation, Walter Reed was sent to investigate infectious diseases, including yellow fever. Wood provided $10,000 to fund the second phase of Reed’s research and approved the use of human volunteers. When the U.S. occupation ended in 1902, Wood was to revert to captain, medical corps.
Wood’s success in Cuba was obvious and wel l known; President McKinley promoted him to U.S. Army brigadier general. At that time, as a brigadier general, Wood was essentially guaranteed a second star and a rotation through the chief of staff position. He served as chief of staff from 1910 to 1914, the only physician ever to do so. As chief of staff he eliminated the antiquated bureau system, developed the maneuver unit concept, and laid the groundwork for the Reserve Officers’ Training Corps.
Wood stayed on active duty and rotated through other senior-level positions. Because of Wood’s political activity promoting universal service and improving readiness, President Woodrow Wilson passed over him, instead selecting John J. Pershing to command the American Expeditionary Force in World War I. Wood stayed politically active and ran for the Republican presidential nomination in 1920, losing to Warren G. Harding at the convention. Wood was appointed governor general of the Philippines, a position he held until his death in 1927.
While in Cuba, Wood was severely injured by striking his head on a chandelier, most likely resulting in an undiagnosed skull fracture. Over time he developed neurologic symptoms and was seen by neurosurgeon Harvey Cushing, MD, at Johns Hopkins, who removed a meningioma in February 1910. Wood made a dramatic recovery. Over a decade later while in the Philippines, his symptoms returned, and after significant delay he went home to see Cushing who was then at Harvard Medical School. When Wood died after surgery, Cushing admitted that he should not have tackled such a difficult case so quickly after returning from a trip to Europe.
Fort Leonard Wood in Missouri and the on-base General Leonard Wood U.S. Army Community Hospital are named in Wood’s honor.
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual
your facility was named for or to offer a topic suggestion, contact us at [email protected] or on Facebook.
CRISPR sheds light on dyskeratosis congenita
Gene editing has revealed how dyskeratosis congenita (DC) impairs the formation of blood cells, according to research published in Stem Cell Reports.
The discovery has opened up new lines of investigation into how to treat DC, which is characterized by shortened telomeres.
“Lengthening telomeres seems like a logical way to help these patients, but it could possibly come with its own set of problems,” said study author Luis F.Z. Batista, PhD, of the Washington University School of Medicine in St. Louis, Missouri.
“We would worry about encouraging cancer formation, for example, as high levels of the protein that lengthens telomeres—telomerase—are commonly found with cancer. But if we could find a way to block the signaling pathways that short telomeres activate—that specifically lead to the problems in blood cell formation—it could allow these patients to continue making blood cells.”
With this in mind, Dr Batista and his colleagues used CRISPR to edit into human embryonic stem cells a pair of mutations associated with DC— DKC1_A353V and TERT_P704S. These cells reproduced the telomere-shortening defect seen in patients with DC.
With this model, the researchers showed how the telomere defect leads to the gradual loss of blood cell formation and how blocking the downstream effects of the defect can reverse this loss, leading to normal production of blood cells.
Blocking this signaling pathway did not lengthen telomeres or stop their shortening, but it allowed the manufacturing of different types of blood cells to continue.
The researchers also made a discovery that provides a distinction regarding the detrimental effect of short telomeres during early development. The team found the defect did not hinder primitive hematopoiesis, but it did impair definitive hematopoiesis.
“This was tremendously interesting from a developmental biology perspective as well as from a disease modeling perspective,” said study author Christopher M. Sturgeon, PhD, of the Washington University School of Medicine. “We now have a platform to really dig deeper into understanding the mechanisms behind some forms of bone marrow failure.”
The researchers implicated high levels of the protein p53 as one of the signals that leads to the drop in definitive hematopoiesis.
“P53 is thought of as a guardian of the genome,” Dr Batista noted. “Mutations that disable p53 are associated with different types of cancer. Because of this, we would not consider directly trying to block p53 in these patients.”
“But what this study provides is proof-of-concept that this pathway is involved in this response. So we now are looking for ways to block the pathway further downstream without necessarily blocking p53 directly.”
Drs Batista and Sturgeon recently received a grant from the Department of Defense to investigate the pathway. The pair believes the strategy used in this study could be relevant for other bone marrow failure syndromes as well, such as Fanconi anemia and aplastic anemia. ![]()
Gene editing has revealed how dyskeratosis congenita (DC) impairs the formation of blood cells, according to research published in Stem Cell Reports.
The discovery has opened up new lines of investigation into how to treat DC, which is characterized by shortened telomeres.
“Lengthening telomeres seems like a logical way to help these patients, but it could possibly come with its own set of problems,” said study author Luis F.Z. Batista, PhD, of the Washington University School of Medicine in St. Louis, Missouri.
“We would worry about encouraging cancer formation, for example, as high levels of the protein that lengthens telomeres—telomerase—are commonly found with cancer. But if we could find a way to block the signaling pathways that short telomeres activate—that specifically lead to the problems in blood cell formation—it could allow these patients to continue making blood cells.”
With this in mind, Dr Batista and his colleagues used CRISPR to edit into human embryonic stem cells a pair of mutations associated with DC— DKC1_A353V and TERT_P704S. These cells reproduced the telomere-shortening defect seen in patients with DC.
With this model, the researchers showed how the telomere defect leads to the gradual loss of blood cell formation and how blocking the downstream effects of the defect can reverse this loss, leading to normal production of blood cells.
Blocking this signaling pathway did not lengthen telomeres or stop their shortening, but it allowed the manufacturing of different types of blood cells to continue.
The researchers also made a discovery that provides a distinction regarding the detrimental effect of short telomeres during early development. The team found the defect did not hinder primitive hematopoiesis, but it did impair definitive hematopoiesis.
“This was tremendously interesting from a developmental biology perspective as well as from a disease modeling perspective,” said study author Christopher M. Sturgeon, PhD, of the Washington University School of Medicine. “We now have a platform to really dig deeper into understanding the mechanisms behind some forms of bone marrow failure.”
The researchers implicated high levels of the protein p53 as one of the signals that leads to the drop in definitive hematopoiesis.
“P53 is thought of as a guardian of the genome,” Dr Batista noted. “Mutations that disable p53 are associated with different types of cancer. Because of this, we would not consider directly trying to block p53 in these patients.”
“But what this study provides is proof-of-concept that this pathway is involved in this response. So we now are looking for ways to block the pathway further downstream without necessarily blocking p53 directly.”
Drs Batista and Sturgeon recently received a grant from the Department of Defense to investigate the pathway. The pair believes the strategy used in this study could be relevant for other bone marrow failure syndromes as well, such as Fanconi anemia and aplastic anemia. ![]()
Gene editing has revealed how dyskeratosis congenita (DC) impairs the formation of blood cells, according to research published in Stem Cell Reports.
The discovery has opened up new lines of investigation into how to treat DC, which is characterized by shortened telomeres.
“Lengthening telomeres seems like a logical way to help these patients, but it could possibly come with its own set of problems,” said study author Luis F.Z. Batista, PhD, of the Washington University School of Medicine in St. Louis, Missouri.
“We would worry about encouraging cancer formation, for example, as high levels of the protein that lengthens telomeres—telomerase—are commonly found with cancer. But if we could find a way to block the signaling pathways that short telomeres activate—that specifically lead to the problems in blood cell formation—it could allow these patients to continue making blood cells.”
With this in mind, Dr Batista and his colleagues used CRISPR to edit into human embryonic stem cells a pair of mutations associated with DC— DKC1_A353V and TERT_P704S. These cells reproduced the telomere-shortening defect seen in patients with DC.
With this model, the researchers showed how the telomere defect leads to the gradual loss of blood cell formation and how blocking the downstream effects of the defect can reverse this loss, leading to normal production of blood cells.
Blocking this signaling pathway did not lengthen telomeres or stop their shortening, but it allowed the manufacturing of different types of blood cells to continue.
The researchers also made a discovery that provides a distinction regarding the detrimental effect of short telomeres during early development. The team found the defect did not hinder primitive hematopoiesis, but it did impair definitive hematopoiesis.
“This was tremendously interesting from a developmental biology perspective as well as from a disease modeling perspective,” said study author Christopher M. Sturgeon, PhD, of the Washington University School of Medicine. “We now have a platform to really dig deeper into understanding the mechanisms behind some forms of bone marrow failure.”
The researchers implicated high levels of the protein p53 as one of the signals that leads to the drop in definitive hematopoiesis.
“P53 is thought of as a guardian of the genome,” Dr Batista noted. “Mutations that disable p53 are associated with different types of cancer. Because of this, we would not consider directly trying to block p53 in these patients.”
“But what this study provides is proof-of-concept that this pathway is involved in this response. So we now are looking for ways to block the pathway further downstream without necessarily blocking p53 directly.”
Drs Batista and Sturgeon recently received a grant from the Department of Defense to investigate the pathway. The pair believes the strategy used in this study could be relevant for other bone marrow failure syndromes as well, such as Fanconi anemia and aplastic anemia. ![]()
Developing better mouse models
Researchers say they have developed a new approach to model human immune variation that overcomes the limitations of traditional mouse models.
With this approach, the team identified genetic markers that directly correlate with the outcome of inflammatory and malignant diseases in humans, including chronic lymphocytic leukemia and Burkitt lymphoma.
The findings suggest that accounting for immune diversity is critical to the success of predicting disease outcomes based on immune cell measurements.
The team reported these findings in Nature Communications.
Traditionally, researchers have relied on inbred mouse strains to gain insight into human diseases while reducing experimental noise.
“If you take a black, a brown, or a white mouse, each one will give you a different answer in the same assay,” said Klaus Ley, MD, of La Jolla Institute for Allergy and Immunology in California.
“For example, if you vaccinate them, their responses will be different, which creates a lot of experimental noise. However, when you think about patients, or even healthy people, we are all different.”
To mine those differences for information, the researchers embraced the experimental noise. Instead of analyzing a single inbred mouse strain, they turned to the hybrid mouse diversity panel (HDMP).
The HDMP is a panel of about 100 different inbred mouse strains that mirror the breadth of genetic and immunological diversity found in the human population.
The researchers studied the natural variation in the activation pattern of abdominal macrophages. Macrophages isolated from 83 different mouse strains from the HDMP were exposed to lipopolysaccharide (LPS), a major component of the outer wall of gram-negative bacteria.
“Fundamentally, when the immune system is confronted with gram-negative bacteria, it can deal with the situation in 2 ways—either it gets very angry and tries to kill the bacteria or it can wall them off in an attempt to live with it,” explained Dr Ley. “Both strategies carry a certain risk, but a long evolutionary history has ensured that mice and people can survive with either strategy.”
The LPS-induced reactions of the macrophages covered the whole spectrum—from very aggressive (LPS+) to very tolerant (LPS-), depending on the mouse strain.
Next, the researchers asked which genes were active during each type of response to identify gene signatures that correlated with LPS responsiveness.
The team then ran these gene signatures across various human gene expression data sets and discovered they strongly correlated with human disease outcomes.
For example, macrophages isolated from healthy joints were enriched in LPS-tolerant genes, whereas macrophages from rheumatoid arthritis patients were strongly skewed toward LPS-aggressive.
Since it was known that mice and people with the aggressive phenotype are better at fighting cancer, the researchers specifically asked whether the level of LPS responsiveness could predict tumor survival.
After analyzing data from 18,000 biopsies across 39 different tumor types, the team found the LPS+ gene signature strongly correlated with survival, while the LPS- signature correlated with cancer death.
The pattern was significant across many types of cancer, including chronic lymphocytic leukemia, Burkitt lymphoma, osteosarcoma, melanoma, and large-cell lung carcinoma. ![]()
Researchers say they have developed a new approach to model human immune variation that overcomes the limitations of traditional mouse models.
With this approach, the team identified genetic markers that directly correlate with the outcome of inflammatory and malignant diseases in humans, including chronic lymphocytic leukemia and Burkitt lymphoma.
The findings suggest that accounting for immune diversity is critical to the success of predicting disease outcomes based on immune cell measurements.
The team reported these findings in Nature Communications.
Traditionally, researchers have relied on inbred mouse strains to gain insight into human diseases while reducing experimental noise.
“If you take a black, a brown, or a white mouse, each one will give you a different answer in the same assay,” said Klaus Ley, MD, of La Jolla Institute for Allergy and Immunology in California.
“For example, if you vaccinate them, their responses will be different, which creates a lot of experimental noise. However, when you think about patients, or even healthy people, we are all different.”
To mine those differences for information, the researchers embraced the experimental noise. Instead of analyzing a single inbred mouse strain, they turned to the hybrid mouse diversity panel (HDMP).
The HDMP is a panel of about 100 different inbred mouse strains that mirror the breadth of genetic and immunological diversity found in the human population.
The researchers studied the natural variation in the activation pattern of abdominal macrophages. Macrophages isolated from 83 different mouse strains from the HDMP were exposed to lipopolysaccharide (LPS), a major component of the outer wall of gram-negative bacteria.
“Fundamentally, when the immune system is confronted with gram-negative bacteria, it can deal with the situation in 2 ways—either it gets very angry and tries to kill the bacteria or it can wall them off in an attempt to live with it,” explained Dr Ley. “Both strategies carry a certain risk, but a long evolutionary history has ensured that mice and people can survive with either strategy.”
The LPS-induced reactions of the macrophages covered the whole spectrum—from very aggressive (LPS+) to very tolerant (LPS-), depending on the mouse strain.
Next, the researchers asked which genes were active during each type of response to identify gene signatures that correlated with LPS responsiveness.
The team then ran these gene signatures across various human gene expression data sets and discovered they strongly correlated with human disease outcomes.
For example, macrophages isolated from healthy joints were enriched in LPS-tolerant genes, whereas macrophages from rheumatoid arthritis patients were strongly skewed toward LPS-aggressive.
Since it was known that mice and people with the aggressive phenotype are better at fighting cancer, the researchers specifically asked whether the level of LPS responsiveness could predict tumor survival.
After analyzing data from 18,000 biopsies across 39 different tumor types, the team found the LPS+ gene signature strongly correlated with survival, while the LPS- signature correlated with cancer death.
The pattern was significant across many types of cancer, including chronic lymphocytic leukemia, Burkitt lymphoma, osteosarcoma, melanoma, and large-cell lung carcinoma. ![]()
Researchers say they have developed a new approach to model human immune variation that overcomes the limitations of traditional mouse models.
With this approach, the team identified genetic markers that directly correlate with the outcome of inflammatory and malignant diseases in humans, including chronic lymphocytic leukemia and Burkitt lymphoma.
The findings suggest that accounting for immune diversity is critical to the success of predicting disease outcomes based on immune cell measurements.
The team reported these findings in Nature Communications.
Traditionally, researchers have relied on inbred mouse strains to gain insight into human diseases while reducing experimental noise.
“If you take a black, a brown, or a white mouse, each one will give you a different answer in the same assay,” said Klaus Ley, MD, of La Jolla Institute for Allergy and Immunology in California.
“For example, if you vaccinate them, their responses will be different, which creates a lot of experimental noise. However, when you think about patients, or even healthy people, we are all different.”
To mine those differences for information, the researchers embraced the experimental noise. Instead of analyzing a single inbred mouse strain, they turned to the hybrid mouse diversity panel (HDMP).
The HDMP is a panel of about 100 different inbred mouse strains that mirror the breadth of genetic and immunological diversity found in the human population.
The researchers studied the natural variation in the activation pattern of abdominal macrophages. Macrophages isolated from 83 different mouse strains from the HDMP were exposed to lipopolysaccharide (LPS), a major component of the outer wall of gram-negative bacteria.
“Fundamentally, when the immune system is confronted with gram-negative bacteria, it can deal with the situation in 2 ways—either it gets very angry and tries to kill the bacteria or it can wall them off in an attempt to live with it,” explained Dr Ley. “Both strategies carry a certain risk, but a long evolutionary history has ensured that mice and people can survive with either strategy.”
The LPS-induced reactions of the macrophages covered the whole spectrum—from very aggressive (LPS+) to very tolerant (LPS-), depending on the mouse strain.
Next, the researchers asked which genes were active during each type of response to identify gene signatures that correlated with LPS responsiveness.
The team then ran these gene signatures across various human gene expression data sets and discovered they strongly correlated with human disease outcomes.
For example, macrophages isolated from healthy joints were enriched in LPS-tolerant genes, whereas macrophages from rheumatoid arthritis patients were strongly skewed toward LPS-aggressive.
Since it was known that mice and people with the aggressive phenotype are better at fighting cancer, the researchers specifically asked whether the level of LPS responsiveness could predict tumor survival.
After analyzing data from 18,000 biopsies across 39 different tumor types, the team found the LPS+ gene signature strongly correlated with survival, while the LPS- signature correlated with cancer death.
The pattern was significant across many types of cancer, including chronic lymphocytic leukemia, Burkitt lymphoma, osteosarcoma, melanoma, and large-cell lung carcinoma. ![]()