User login
Sulindac-erlotinib as chemoprevention for FAP
Familial adenomatous polyposis (FAP) is an autosomal dominant inherited disorder caused by germline mutations in the APC (adenomatous polyposis coli) gene. The disease is characterized by the formation of hundreds to thousands of adenomatous polyps in the colorectum and a nearly 100% lifetime risk of colorectal cancer, if left untreated.
Six randomized clinical trials explore chemoprevention in FAP, including the use of sulindac, celecoxib, low-dose aspirin, eicosapentaenoic acid, and one ongoing trial using sulindac and difluoromethylornithine. These trials have shown at most a 30% decrease in colorectal adenoma burden over short-term treatment, compared with placebo.
Preclinical studies have shown that inactivation of the APC gene and epidermal growth factor receptor (EGFR) signaling promotes cyclooxygenase (COX)-2 expression and subsequent development of intestinal neoplasia. Our group has previously shown that the combination of COX and EGFR inhibition with sulindac and erlotinib led to a 71% reduction in duodenal polyp burden in patients with FAP.
The hypothesis of this study was that a combination of COX and EGFR inhibition would inhibit colorectal adenoma formation in patient with FAP. We designed a phase 2 double-blind, placebo-controlled randomized trial in FAP patients who received combination therapy with 150 mg sulindac b.i.d. and 75 mg erlotinib daily, or placebo tablets for 6 months and assessed the number of polyps in the colorectum, rectum, or ileal pouch at baseline and at 6 months.
The total colorectal polyp count was significantly different between the placebo and sulindac-erlotinib groups at 6 months in FAP patients with an intact colon (P less than .0001), with a net percentage change of 89.3% between the two groups. Similar reductions were found in the ileal pouch anal anastomosis and ileorectal anastomosis groups. 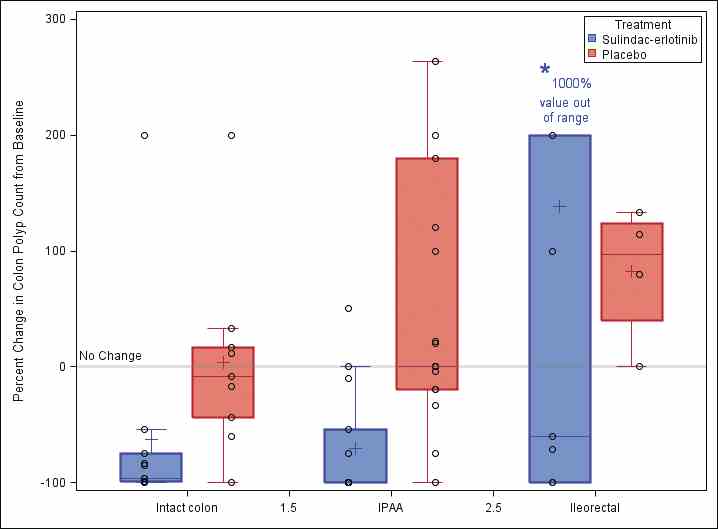
Further research is necessary to evaluate these preliminary findings in a larger study population with longer follow-up to determine whether the observed effects will result in improved long-term clinical outcomes. A new phase 2 multicenter clinical trial (sponsored by the National Cancer Institute) of erlotinib therapy in patients with FAP will be activating this summer across seven U.S. cancer centers and will add further evidence for this chemoprevention strategy.
Dr. Samadder is in the division of gastroenterology and hepatology, Mayo Clinic, Scottsdale, Ariz. His comments were made during the AGA Institute Presidential Plenary at the Annual Digestive Disease Week.
Familial adenomatous polyposis (FAP) is an autosomal dominant inherited disorder caused by germline mutations in the APC (adenomatous polyposis coli) gene. The disease is characterized by the formation of hundreds to thousands of adenomatous polyps in the colorectum and a nearly 100% lifetime risk of colorectal cancer, if left untreated.
Six randomized clinical trials explore chemoprevention in FAP, including the use of sulindac, celecoxib, low-dose aspirin, eicosapentaenoic acid, and one ongoing trial using sulindac and difluoromethylornithine. These trials have shown at most a 30% decrease in colorectal adenoma burden over short-term treatment, compared with placebo.
Preclinical studies have shown that inactivation of the APC gene and epidermal growth factor receptor (EGFR) signaling promotes cyclooxygenase (COX)-2 expression and subsequent development of intestinal neoplasia. Our group has previously shown that the combination of COX and EGFR inhibition with sulindac and erlotinib led to a 71% reduction in duodenal polyp burden in patients with FAP.
The hypothesis of this study was that a combination of COX and EGFR inhibition would inhibit colorectal adenoma formation in patient with FAP. We designed a phase 2 double-blind, placebo-controlled randomized trial in FAP patients who received combination therapy with 150 mg sulindac b.i.d. and 75 mg erlotinib daily, or placebo tablets for 6 months and assessed the number of polyps in the colorectum, rectum, or ileal pouch at baseline and at 6 months.
The total colorectal polyp count was significantly different between the placebo and sulindac-erlotinib groups at 6 months in FAP patients with an intact colon (P less than .0001), with a net percentage change of 89.3% between the two groups. Similar reductions were found in the ileal pouch anal anastomosis and ileorectal anastomosis groups. 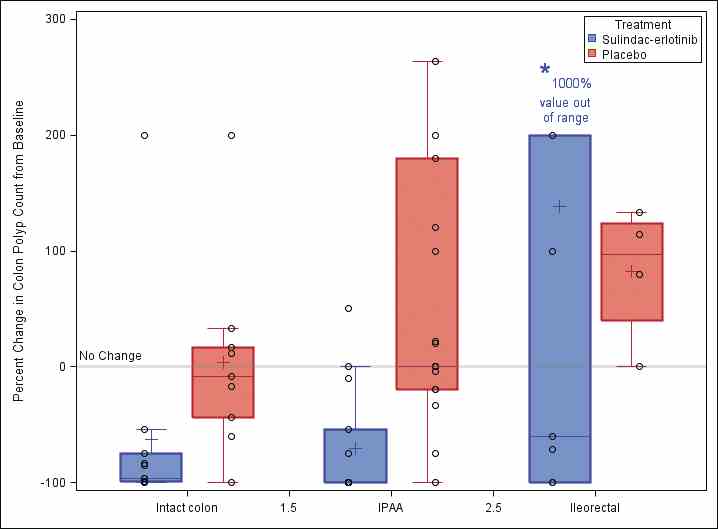
Further research is necessary to evaluate these preliminary findings in a larger study population with longer follow-up to determine whether the observed effects will result in improved long-term clinical outcomes. A new phase 2 multicenter clinical trial (sponsored by the National Cancer Institute) of erlotinib therapy in patients with FAP will be activating this summer across seven U.S. cancer centers and will add further evidence for this chemoprevention strategy.
Dr. Samadder is in the division of gastroenterology and hepatology, Mayo Clinic, Scottsdale, Ariz. His comments were made during the AGA Institute Presidential Plenary at the Annual Digestive Disease Week.
Familial adenomatous polyposis (FAP) is an autosomal dominant inherited disorder caused by germline mutations in the APC (adenomatous polyposis coli) gene. The disease is characterized by the formation of hundreds to thousands of adenomatous polyps in the colorectum and a nearly 100% lifetime risk of colorectal cancer, if left untreated.
Six randomized clinical trials explore chemoprevention in FAP, including the use of sulindac, celecoxib, low-dose aspirin, eicosapentaenoic acid, and one ongoing trial using sulindac and difluoromethylornithine. These trials have shown at most a 30% decrease in colorectal adenoma burden over short-term treatment, compared with placebo.
Preclinical studies have shown that inactivation of the APC gene and epidermal growth factor receptor (EGFR) signaling promotes cyclooxygenase (COX)-2 expression and subsequent development of intestinal neoplasia. Our group has previously shown that the combination of COX and EGFR inhibition with sulindac and erlotinib led to a 71% reduction in duodenal polyp burden in patients with FAP.
The hypothesis of this study was that a combination of COX and EGFR inhibition would inhibit colorectal adenoma formation in patient with FAP. We designed a phase 2 double-blind, placebo-controlled randomized trial in FAP patients who received combination therapy with 150 mg sulindac b.i.d. and 75 mg erlotinib daily, or placebo tablets for 6 months and assessed the number of polyps in the colorectum, rectum, or ileal pouch at baseline and at 6 months.
The total colorectal polyp count was significantly different between the placebo and sulindac-erlotinib groups at 6 months in FAP patients with an intact colon (P less than .0001), with a net percentage change of 89.3% between the two groups. Similar reductions were found in the ileal pouch anal anastomosis and ileorectal anastomosis groups. 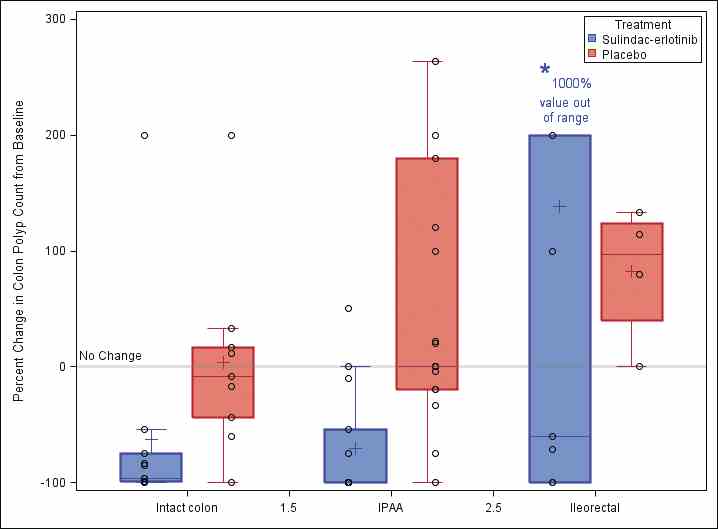
Further research is necessary to evaluate these preliminary findings in a larger study population with longer follow-up to determine whether the observed effects will result in improved long-term clinical outcomes. A new phase 2 multicenter clinical trial (sponsored by the National Cancer Institute) of erlotinib therapy in patients with FAP will be activating this summer across seven U.S. cancer centers and will add further evidence for this chemoprevention strategy.
Dr. Samadder is in the division of gastroenterology and hepatology, Mayo Clinic, Scottsdale, Ariz. His comments were made during the AGA Institute Presidential Plenary at the Annual Digestive Disease Week.
Novel drug-eluting coronary stent looks good in DESSOLVE III
PARIS – A unique drug-eluting coronary stent showed positive interim results in the DESSOLVE III trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
In DESSOLVE III, 1,398 patients undergoing percutaneous coronary intervention were randomized to the widely used Xience everolimus-eluting stent or to MiStent, a novel thin-strut stent with a polymer coating that is quickly absorbed after delivering microcrystalline sirolimus into the vessel wall for prolonged release at a near-linear rate.
At an interim analysis at 12 months of follow-up, the primary endpoint – a composite of cardiac death, target vessel MI, and clinically indicated target lesion revascularization – had occurred in 5.8% of the MiStent group and 6.5% of Xience recipients in the study, which was designed as a noninferiority trial, reported Robbert J. de Winter, MD, professor of clinical cardiology at the Academic Medical Center in Amsterdam.
“The data support the hypothesis that long-term cytostatic inhibition of early neointima could prevent the late neointimal growth seen at medium and long term with conventional drug-eluting stents,” he said.
MiStent is designed to overcome a shortcoming of conventional drug-eluting stents: namely, their durable polymer coating sticks around after the cytostatic drug is finished being released. It is believed that this residual polymer, which may not disappear for 6-9 months, induces inflammation in the vessel wall, eventually leading to intimal growth, restenosis, and new atherosclerosis.
“The unique feature of the MiStent is that the polymer is bioabsorbable and is fully absorbed at 3 months, whereas the drug is present in the vessel wall out to 9 months, well after the coating has disappeared. So in theory you would expect that any inflammatory response caused by the polymer coating will be counteracted by the drug. This was seen in animal models. And in the DESSOLVE I and II studies, angiographic follow-up showed that late luminal loss was flat after 6 months, in contrast to other drug-eluting stents, which show accrual of late neointimal growth after 6 months to a year,” according to the cardiologist.
DESSOLVE III is planned as a 3-year study. Already by 6 months the curves for target lesion revascularization started to separate, with a 12-month rate of 2.6% in the MiStent group versus 3.8% for Xience. And while this difference is not yet statistically significant, Dr. de Winter and his coinvestigators expect that by 3 years the separation will have grown to the point that the difference becomes statistically significant and clinically meaningful.
The MiStent platform is composed of a cobalt/chromium alloy. The stent strut thickness is only 64 microns, in contrast to 81 microns for the Xience stent. Thinner stent struts have previously been shown to be less injurious to the vessel wall.
DESSOLVE III is an all-comers trial conducted at 20 sites in four European countries. Participants had to have a reference vessel diameter of 2.5-3.5 mm. Roughly 60% of patients had an acute coronary syndrome as their indication for PCI. The study population included, among others, patients with left main coronary artery lesions, restenotic lesions, and failed saphenous vein grafts. Dual-antiplatelet therapy was given for 6 months in patients with stable angina and 12 months for those with ACS, in accordance with European Society of Cardiology guidelines.
Discussant Robert A. Byrne, MD, of the German Heart Center in Munich, declared: “For me, this is a potentially interesting device. It’s the only device where we have a drug elution that’s more prolonged than the polymer, and this does offer the potential for later benefit.”
Dr. Byrne was a member of a European Commission–backed task force that developed European regulatory guidance for the evaluation of new coronary stents. “This MiStent trial program ticks off a lot of boxes: We had a successful first human use study, then we had a modest-size angiographic endpoint study where the late lumen loss looked good, and now we have a clinical endpoint study. This is what we want to see in the regulatory space.”
Another discussant, Chaim Lotan, MD, pronounced the MiStent “definitely another good stent on the shelf.”
It’s impossible to say whether the excellent 1-year outcomes seen with MiStent in DESSOLVE III were due to the prolonged-release microcrystalline sirolimus, the ultrathin stent struts, or both. In any case, the major adverse cardiovascular event rates seen in DESSOLVE III are so low by historical standards that it will become extremely difficult to show superiority for one contemporary drug-eluting stent over another, predicted Dr. Lotan of Hadassah Medical Center in Jerusalem.
Dr. de Winter concurred.
“I think we can now say that the benchmark for present day drug-eluting stents is a target lesion failure rate of about 6% at 12 months and a stent thrombosis rate below 1% at 12 months. It’s going to be increasingly more difficult to improve on that,” he said.
The MiStent, manufactured by Micell Technologies, is commercially available in Europe but investigational in the United States.
DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys.
Dr. de Winter reported receiving research grants from OrbusNeich, Abbott Vascular, AstraZeneca, Stentys, and Tryton.
PARIS – A unique drug-eluting coronary stent showed positive interim results in the DESSOLVE III trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
In DESSOLVE III, 1,398 patients undergoing percutaneous coronary intervention were randomized to the widely used Xience everolimus-eluting stent or to MiStent, a novel thin-strut stent with a polymer coating that is quickly absorbed after delivering microcrystalline sirolimus into the vessel wall for prolonged release at a near-linear rate.
At an interim analysis at 12 months of follow-up, the primary endpoint – a composite of cardiac death, target vessel MI, and clinically indicated target lesion revascularization – had occurred in 5.8% of the MiStent group and 6.5% of Xience recipients in the study, which was designed as a noninferiority trial, reported Robbert J. de Winter, MD, professor of clinical cardiology at the Academic Medical Center in Amsterdam.
“The data support the hypothesis that long-term cytostatic inhibition of early neointima could prevent the late neointimal growth seen at medium and long term with conventional drug-eluting stents,” he said.
MiStent is designed to overcome a shortcoming of conventional drug-eluting stents: namely, their durable polymer coating sticks around after the cytostatic drug is finished being released. It is believed that this residual polymer, which may not disappear for 6-9 months, induces inflammation in the vessel wall, eventually leading to intimal growth, restenosis, and new atherosclerosis.
“The unique feature of the MiStent is that the polymer is bioabsorbable and is fully absorbed at 3 months, whereas the drug is present in the vessel wall out to 9 months, well after the coating has disappeared. So in theory you would expect that any inflammatory response caused by the polymer coating will be counteracted by the drug. This was seen in animal models. And in the DESSOLVE I and II studies, angiographic follow-up showed that late luminal loss was flat after 6 months, in contrast to other drug-eluting stents, which show accrual of late neointimal growth after 6 months to a year,” according to the cardiologist.
DESSOLVE III is planned as a 3-year study. Already by 6 months the curves for target lesion revascularization started to separate, with a 12-month rate of 2.6% in the MiStent group versus 3.8% for Xience. And while this difference is not yet statistically significant, Dr. de Winter and his coinvestigators expect that by 3 years the separation will have grown to the point that the difference becomes statistically significant and clinically meaningful.
The MiStent platform is composed of a cobalt/chromium alloy. The stent strut thickness is only 64 microns, in contrast to 81 microns for the Xience stent. Thinner stent struts have previously been shown to be less injurious to the vessel wall.
DESSOLVE III is an all-comers trial conducted at 20 sites in four European countries. Participants had to have a reference vessel diameter of 2.5-3.5 mm. Roughly 60% of patients had an acute coronary syndrome as their indication for PCI. The study population included, among others, patients with left main coronary artery lesions, restenotic lesions, and failed saphenous vein grafts. Dual-antiplatelet therapy was given for 6 months in patients with stable angina and 12 months for those with ACS, in accordance with European Society of Cardiology guidelines.
Discussant Robert A. Byrne, MD, of the German Heart Center in Munich, declared: “For me, this is a potentially interesting device. It’s the only device where we have a drug elution that’s more prolonged than the polymer, and this does offer the potential for later benefit.”
Dr. Byrne was a member of a European Commission–backed task force that developed European regulatory guidance for the evaluation of new coronary stents. “This MiStent trial program ticks off a lot of boxes: We had a successful first human use study, then we had a modest-size angiographic endpoint study where the late lumen loss looked good, and now we have a clinical endpoint study. This is what we want to see in the regulatory space.”
Another discussant, Chaim Lotan, MD, pronounced the MiStent “definitely another good stent on the shelf.”
It’s impossible to say whether the excellent 1-year outcomes seen with MiStent in DESSOLVE III were due to the prolonged-release microcrystalline sirolimus, the ultrathin stent struts, or both. In any case, the major adverse cardiovascular event rates seen in DESSOLVE III are so low by historical standards that it will become extremely difficult to show superiority for one contemporary drug-eluting stent over another, predicted Dr. Lotan of Hadassah Medical Center in Jerusalem.
Dr. de Winter concurred.
“I think we can now say that the benchmark for present day drug-eluting stents is a target lesion failure rate of about 6% at 12 months and a stent thrombosis rate below 1% at 12 months. It’s going to be increasingly more difficult to improve on that,” he said.
The MiStent, manufactured by Micell Technologies, is commercially available in Europe but investigational in the United States.
DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys.
Dr. de Winter reported receiving research grants from OrbusNeich, Abbott Vascular, AstraZeneca, Stentys, and Tryton.
PARIS – A unique drug-eluting coronary stent showed positive interim results in the DESSOLVE III trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
In DESSOLVE III, 1,398 patients undergoing percutaneous coronary intervention were randomized to the widely used Xience everolimus-eluting stent or to MiStent, a novel thin-strut stent with a polymer coating that is quickly absorbed after delivering microcrystalline sirolimus into the vessel wall for prolonged release at a near-linear rate.
At an interim analysis at 12 months of follow-up, the primary endpoint – a composite of cardiac death, target vessel MI, and clinically indicated target lesion revascularization – had occurred in 5.8% of the MiStent group and 6.5% of Xience recipients in the study, which was designed as a noninferiority trial, reported Robbert J. de Winter, MD, professor of clinical cardiology at the Academic Medical Center in Amsterdam.
“The data support the hypothesis that long-term cytostatic inhibition of early neointima could prevent the late neointimal growth seen at medium and long term with conventional drug-eluting stents,” he said.
MiStent is designed to overcome a shortcoming of conventional drug-eluting stents: namely, their durable polymer coating sticks around after the cytostatic drug is finished being released. It is believed that this residual polymer, which may not disappear for 6-9 months, induces inflammation in the vessel wall, eventually leading to intimal growth, restenosis, and new atherosclerosis.
“The unique feature of the MiStent is that the polymer is bioabsorbable and is fully absorbed at 3 months, whereas the drug is present in the vessel wall out to 9 months, well after the coating has disappeared. So in theory you would expect that any inflammatory response caused by the polymer coating will be counteracted by the drug. This was seen in animal models. And in the DESSOLVE I and II studies, angiographic follow-up showed that late luminal loss was flat after 6 months, in contrast to other drug-eluting stents, which show accrual of late neointimal growth after 6 months to a year,” according to the cardiologist.
DESSOLVE III is planned as a 3-year study. Already by 6 months the curves for target lesion revascularization started to separate, with a 12-month rate of 2.6% in the MiStent group versus 3.8% for Xience. And while this difference is not yet statistically significant, Dr. de Winter and his coinvestigators expect that by 3 years the separation will have grown to the point that the difference becomes statistically significant and clinically meaningful.
The MiStent platform is composed of a cobalt/chromium alloy. The stent strut thickness is only 64 microns, in contrast to 81 microns for the Xience stent. Thinner stent struts have previously been shown to be less injurious to the vessel wall.
DESSOLVE III is an all-comers trial conducted at 20 sites in four European countries. Participants had to have a reference vessel diameter of 2.5-3.5 mm. Roughly 60% of patients had an acute coronary syndrome as their indication for PCI. The study population included, among others, patients with left main coronary artery lesions, restenotic lesions, and failed saphenous vein grafts. Dual-antiplatelet therapy was given for 6 months in patients with stable angina and 12 months for those with ACS, in accordance with European Society of Cardiology guidelines.
Discussant Robert A. Byrne, MD, of the German Heart Center in Munich, declared: “For me, this is a potentially interesting device. It’s the only device where we have a drug elution that’s more prolonged than the polymer, and this does offer the potential for later benefit.”
Dr. Byrne was a member of a European Commission–backed task force that developed European regulatory guidance for the evaluation of new coronary stents. “This MiStent trial program ticks off a lot of boxes: We had a successful first human use study, then we had a modest-size angiographic endpoint study where the late lumen loss looked good, and now we have a clinical endpoint study. This is what we want to see in the regulatory space.”
Another discussant, Chaim Lotan, MD, pronounced the MiStent “definitely another good stent on the shelf.”
It’s impossible to say whether the excellent 1-year outcomes seen with MiStent in DESSOLVE III were due to the prolonged-release microcrystalline sirolimus, the ultrathin stent struts, or both. In any case, the major adverse cardiovascular event rates seen in DESSOLVE III are so low by historical standards that it will become extremely difficult to show superiority for one contemporary drug-eluting stent over another, predicted Dr. Lotan of Hadassah Medical Center in Jerusalem.
Dr. de Winter concurred.
“I think we can now say that the benchmark for present day drug-eluting stents is a target lesion failure rate of about 6% at 12 months and a stent thrombosis rate below 1% at 12 months. It’s going to be increasingly more difficult to improve on that,” he said.
The MiStent, manufactured by Micell Technologies, is commercially available in Europe but investigational in the United States.
DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys.
Dr. de Winter reported receiving research grants from OrbusNeich, Abbott Vascular, AstraZeneca, Stentys, and Tryton.
AT EUROPCR
Key clinical point:
Major finding: At an interim 12-month analysis, the composite rate of cardiac death, target vessel MI, and clinically indicated target lesion revascularization was 6.5% in recipients of a Xience everolimus-eluting coronary stent and 5.8% in those randomized to the novel MiStent.
Data source: DESSOLVE III, a prospective, randomized, international trial that randomized 1,398 real-world-type all-comers undergoing PCI to the Xience device or the MiStent.
Disclosures: DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys. The presenter reported receiving research grants from both companies.
Integrated health system builds collegial network of rural surgeons
Recruiting and retaining general surgeons is a longstanding problem for rural hospitals. A regional medical system in the Upper Midwest tackles this challenge by integrating small-town general surgeons into the network and emphasizing professional development, fair compensation, and a sustainable call and leave schedule.
The Gundersen Health System (GHS) is a physician-led, nonprofit health care network that operates in 19 rural counties in parts of Wisconsin, Minnesota, and Iowa, with its main campus in La Crosse, Wis. The network, established over a period of almost 40 years, is a mix of larger GHS medical centers, community hospitals, medical clinics, and GHS-managed and independent critical access hospitals (CAHs).
A sustainable model
“It is clear that the older paradigm of a single rural surgeon providing care 24/7 to an isolated community is vanishing. Design of a more sustainable model involves small groups of rural surgeons working together to provide general surgery and some subspecialty care locally, but who are also part of a larger network for administrative and clinical support,” said Dr. Cogbill in an interview.
Lessons learned
Dr. Cogbill said, “Our 38-year experience with rural surgery in our region has taught us many lessons. The strategy of trying to place a solo general surgeon in every small town with a CAH within our service area was not sustainable nor practical. The development of several rural centers of care within our region has allowed us to be more successful in the recruitment and retention of rural general surgeons who are hired to be part of a small group (optimally three) who provide care to their home community as well as outreach surgical care to several outlying CAHs near their home CAH. This has made it possible to offer a reasonable call schedule, mutual assistance, and the chance to build adequate case volumes. Connectivity to the health system should not mean ‘send all the great cases to the main campus,’ but instead should support the rural surgeons in performing appropriate cases locally.”
The survey respondents were aged 36-55 years, five were male, and all were graduates of U.S. medical schools. Eight are board certified and seven are either fellows or associate members of the American College of Surgeons. Their tenure in the GHS system averaged at least 7 years, ranging from 2 years to more than 20. Their surgical logs for a recent 1-year period show a case mix of endoscopy (63.8%), general surgery (26.7%), and obstetrics (6.1%). Mean annual relative value units for the group were 3,627 (range 2,456-5,846).
One goal of the confidential survey was to explore the reasons behind these surgeons’ choice of a rural practice. Their primary motivations were a preference for a rural lifestyle and a desire for a broad scope of practice. Loan forgiveness motivated some (37.5%), and the influence of a mentor was important for others (25%). The opportunity to join an integrated health system such as GHS was deemed extremely important to seven of the respondents.
Retention of rural surgeons
The most important factors mentioned by survey respondents for remaining in their positions were lifestyle (87.5%), family (75.0%), relationship with patients and colleagues, and scope of practice (75.0%), and compensation (62.6%).
Reasons to consider leaving were call burden (37.5%), relationship with the local hospital (25.0%), and compensation (25.0%).
The survey also looked at potential retention of these general surgeons in the coming 5 years: 37.5% said they were somewhat likely to remain, 25% said they were very likely to remain, and 37.5% said they were extremely likely to stay.
Two successful strategies have been promoting a satisfactory case mix and comanagement of patients who are referred to the main campus. The surgeons from the small towns are encouraged to come to La Crosse to assist in procedures on referred patients, to teach in the surgical residency and the Transition to Practice General Surgery fellowship programs at Gundersen, to participate in clinical research activities, and to engage in a variety of professional activities that strengthen the bonds between GHS and rural surgeons. These interactions help minimize professional isolation, a serious problem for surgeons working on their own in small communities.
Communication is maintained electronically. “Our system includes the use of a common EMR across the entire system allowing mutual access to both inpatient and outpatient records, including full access to digitized diagnostic imaging. GHS has established a number of distance-learning telemedicine links between the main campus and the rural communities that permit real-time patient consultations as well as participation in teaching conferences including Morbidity and Mortality Conferences.”
Reducing burnout in rural surgeons
The GHS model may have some impact on burnout among the rural surgeons in the system, said Dr. Cogbill. “Rural surgeon employment as part of a fully integrated regional network has the potential to reduce the magnitude of burnout by providing administrative assistance to help navigate bureaucratic complexities, easy access for subspecialty consults with colleagues who are known entities, and a model of rural surgery involving pods of three colleagues who can share call, mutual assistance, and case volumes.” Fair and competitive compensation and some degree of loan forgiveness have been in the mix of factors that have helped with recruitment. Administrative assistance from the main campus eases the clerical burden the surgeons face. Guaranteed free time for vacations and educational meetings, as well as a reasonable call schedule, are all built into contracts; this has had a big impact on recruitment. GHS has concluded that three general surgeons in a community is the optimal number to maintain call coverage and mutual assistance. Dr. Cogbill said, “The call schedule is managed by each “pod” of rural general surgeons themselves. With a full complement of three rural surgeons in a pod, they maintain an every third night call schedule. In towns in which there are fewer than three surgeons, the GHS surgeons often share call with surgeons who are not part of GHS to maintain a reasonable/sustainable call schedule.”
The retention track record at GHS is impressive. Since 1978, 19 rural general surgeons have been employed by GHS. Four (21%) rural general surgeons have retired 10 (53%) continue to practice in the network; only 5 (26%) left prior to retirement. Six rural general surgeons practiced in one location for over 20 years.
[email protected]
On Twitter @ThereseBorden
The rural surgeon needs some financial assurance, a reasonable call schedule that allows him/her time away from the job without compromising the care of patients in his/her town, regulatory relief, and a relationship with a “mother ship” referral center that is a true two-way street. The days of the independent private solo practitioner are numbered, and the statistics bear this out. The convergence of declining reimbursement, increasing burden of scrutiny and documentation placed by payers and the government, and an emerging workforce that values work-life balance all contribute to the need to develop programs like this one at Gunderson to maintain the surgical workforce in our small towns. Rural surgery comes with a great deal of intrinsic reward, which makes it an excellent career, if these obstacles can be overcome.
Mark Savarise, MD, FACS, is a general surgeon practicing in South Jordan, Utah, and is clinical associate professor of surgery at the University of Utah, Salt Lake City. He has no disclosures.
The rural surgeon needs some financial assurance, a reasonable call schedule that allows him/her time away from the job without compromising the care of patients in his/her town, regulatory relief, and a relationship with a “mother ship” referral center that is a true two-way street. The days of the independent private solo practitioner are numbered, and the statistics bear this out. The convergence of declining reimbursement, increasing burden of scrutiny and documentation placed by payers and the government, and an emerging workforce that values work-life balance all contribute to the need to develop programs like this one at Gunderson to maintain the surgical workforce in our small towns. Rural surgery comes with a great deal of intrinsic reward, which makes it an excellent career, if these obstacles can be overcome.
Mark Savarise, MD, FACS, is a general surgeon practicing in South Jordan, Utah, and is clinical associate professor of surgery at the University of Utah, Salt Lake City. He has no disclosures.
The rural surgeon needs some financial assurance, a reasonable call schedule that allows him/her time away from the job without compromising the care of patients in his/her town, regulatory relief, and a relationship with a “mother ship” referral center that is a true two-way street. The days of the independent private solo practitioner are numbered, and the statistics bear this out. The convergence of declining reimbursement, increasing burden of scrutiny and documentation placed by payers and the government, and an emerging workforce that values work-life balance all contribute to the need to develop programs like this one at Gunderson to maintain the surgical workforce in our small towns. Rural surgery comes with a great deal of intrinsic reward, which makes it an excellent career, if these obstacles can be overcome.
Mark Savarise, MD, FACS, is a general surgeon practicing in South Jordan, Utah, and is clinical associate professor of surgery at the University of Utah, Salt Lake City. He has no disclosures.
Recruiting and retaining general surgeons is a longstanding problem for rural hospitals. A regional medical system in the Upper Midwest tackles this challenge by integrating small-town general surgeons into the network and emphasizing professional development, fair compensation, and a sustainable call and leave schedule.
The Gundersen Health System (GHS) is a physician-led, nonprofit health care network that operates in 19 rural counties in parts of Wisconsin, Minnesota, and Iowa, with its main campus in La Crosse, Wis. The network, established over a period of almost 40 years, is a mix of larger GHS medical centers, community hospitals, medical clinics, and GHS-managed and independent critical access hospitals (CAHs).
A sustainable model
“It is clear that the older paradigm of a single rural surgeon providing care 24/7 to an isolated community is vanishing. Design of a more sustainable model involves small groups of rural surgeons working together to provide general surgery and some subspecialty care locally, but who are also part of a larger network for administrative and clinical support,” said Dr. Cogbill in an interview.
Lessons learned
Dr. Cogbill said, “Our 38-year experience with rural surgery in our region has taught us many lessons. The strategy of trying to place a solo general surgeon in every small town with a CAH within our service area was not sustainable nor practical. The development of several rural centers of care within our region has allowed us to be more successful in the recruitment and retention of rural general surgeons who are hired to be part of a small group (optimally three) who provide care to their home community as well as outreach surgical care to several outlying CAHs near their home CAH. This has made it possible to offer a reasonable call schedule, mutual assistance, and the chance to build adequate case volumes. Connectivity to the health system should not mean ‘send all the great cases to the main campus,’ but instead should support the rural surgeons in performing appropriate cases locally.”
The survey respondents were aged 36-55 years, five were male, and all were graduates of U.S. medical schools. Eight are board certified and seven are either fellows or associate members of the American College of Surgeons. Their tenure in the GHS system averaged at least 7 years, ranging from 2 years to more than 20. Their surgical logs for a recent 1-year period show a case mix of endoscopy (63.8%), general surgery (26.7%), and obstetrics (6.1%). Mean annual relative value units for the group were 3,627 (range 2,456-5,846).
One goal of the confidential survey was to explore the reasons behind these surgeons’ choice of a rural practice. Their primary motivations were a preference for a rural lifestyle and a desire for a broad scope of practice. Loan forgiveness motivated some (37.5%), and the influence of a mentor was important for others (25%). The opportunity to join an integrated health system such as GHS was deemed extremely important to seven of the respondents.
Retention of rural surgeons
The most important factors mentioned by survey respondents for remaining in their positions were lifestyle (87.5%), family (75.0%), relationship with patients and colleagues, and scope of practice (75.0%), and compensation (62.6%).
Reasons to consider leaving were call burden (37.5%), relationship with the local hospital (25.0%), and compensation (25.0%).
The survey also looked at potential retention of these general surgeons in the coming 5 years: 37.5% said they were somewhat likely to remain, 25% said they were very likely to remain, and 37.5% said they were extremely likely to stay.
Two successful strategies have been promoting a satisfactory case mix and comanagement of patients who are referred to the main campus. The surgeons from the small towns are encouraged to come to La Crosse to assist in procedures on referred patients, to teach in the surgical residency and the Transition to Practice General Surgery fellowship programs at Gundersen, to participate in clinical research activities, and to engage in a variety of professional activities that strengthen the bonds between GHS and rural surgeons. These interactions help minimize professional isolation, a serious problem for surgeons working on their own in small communities.
Communication is maintained electronically. “Our system includes the use of a common EMR across the entire system allowing mutual access to both inpatient and outpatient records, including full access to digitized diagnostic imaging. GHS has established a number of distance-learning telemedicine links between the main campus and the rural communities that permit real-time patient consultations as well as participation in teaching conferences including Morbidity and Mortality Conferences.”
Reducing burnout in rural surgeons
The GHS model may have some impact on burnout among the rural surgeons in the system, said Dr. Cogbill. “Rural surgeon employment as part of a fully integrated regional network has the potential to reduce the magnitude of burnout by providing administrative assistance to help navigate bureaucratic complexities, easy access for subspecialty consults with colleagues who are known entities, and a model of rural surgery involving pods of three colleagues who can share call, mutual assistance, and case volumes.” Fair and competitive compensation and some degree of loan forgiveness have been in the mix of factors that have helped with recruitment. Administrative assistance from the main campus eases the clerical burden the surgeons face. Guaranteed free time for vacations and educational meetings, as well as a reasonable call schedule, are all built into contracts; this has had a big impact on recruitment. GHS has concluded that three general surgeons in a community is the optimal number to maintain call coverage and mutual assistance. Dr. Cogbill said, “The call schedule is managed by each “pod” of rural general surgeons themselves. With a full complement of three rural surgeons in a pod, they maintain an every third night call schedule. In towns in which there are fewer than three surgeons, the GHS surgeons often share call with surgeons who are not part of GHS to maintain a reasonable/sustainable call schedule.”
The retention track record at GHS is impressive. Since 1978, 19 rural general surgeons have been employed by GHS. Four (21%) rural general surgeons have retired 10 (53%) continue to practice in the network; only 5 (26%) left prior to retirement. Six rural general surgeons practiced in one location for over 20 years.
[email protected]
On Twitter @ThereseBorden
Recruiting and retaining general surgeons is a longstanding problem for rural hospitals. A regional medical system in the Upper Midwest tackles this challenge by integrating small-town general surgeons into the network and emphasizing professional development, fair compensation, and a sustainable call and leave schedule.
The Gundersen Health System (GHS) is a physician-led, nonprofit health care network that operates in 19 rural counties in parts of Wisconsin, Minnesota, and Iowa, with its main campus in La Crosse, Wis. The network, established over a period of almost 40 years, is a mix of larger GHS medical centers, community hospitals, medical clinics, and GHS-managed and independent critical access hospitals (CAHs).
A sustainable model
“It is clear that the older paradigm of a single rural surgeon providing care 24/7 to an isolated community is vanishing. Design of a more sustainable model involves small groups of rural surgeons working together to provide general surgery and some subspecialty care locally, but who are also part of a larger network for administrative and clinical support,” said Dr. Cogbill in an interview.
Lessons learned
Dr. Cogbill said, “Our 38-year experience with rural surgery in our region has taught us many lessons. The strategy of trying to place a solo general surgeon in every small town with a CAH within our service area was not sustainable nor practical. The development of several rural centers of care within our region has allowed us to be more successful in the recruitment and retention of rural general surgeons who are hired to be part of a small group (optimally three) who provide care to their home community as well as outreach surgical care to several outlying CAHs near their home CAH. This has made it possible to offer a reasonable call schedule, mutual assistance, and the chance to build adequate case volumes. Connectivity to the health system should not mean ‘send all the great cases to the main campus,’ but instead should support the rural surgeons in performing appropriate cases locally.”
The survey respondents were aged 36-55 years, five were male, and all were graduates of U.S. medical schools. Eight are board certified and seven are either fellows or associate members of the American College of Surgeons. Their tenure in the GHS system averaged at least 7 years, ranging from 2 years to more than 20. Their surgical logs for a recent 1-year period show a case mix of endoscopy (63.8%), general surgery (26.7%), and obstetrics (6.1%). Mean annual relative value units for the group were 3,627 (range 2,456-5,846).
One goal of the confidential survey was to explore the reasons behind these surgeons’ choice of a rural practice. Their primary motivations were a preference for a rural lifestyle and a desire for a broad scope of practice. Loan forgiveness motivated some (37.5%), and the influence of a mentor was important for others (25%). The opportunity to join an integrated health system such as GHS was deemed extremely important to seven of the respondents.
Retention of rural surgeons
The most important factors mentioned by survey respondents for remaining in their positions were lifestyle (87.5%), family (75.0%), relationship with patients and colleagues, and scope of practice (75.0%), and compensation (62.6%).
Reasons to consider leaving were call burden (37.5%), relationship with the local hospital (25.0%), and compensation (25.0%).
The survey also looked at potential retention of these general surgeons in the coming 5 years: 37.5% said they were somewhat likely to remain, 25% said they were very likely to remain, and 37.5% said they were extremely likely to stay.
Two successful strategies have been promoting a satisfactory case mix and comanagement of patients who are referred to the main campus. The surgeons from the small towns are encouraged to come to La Crosse to assist in procedures on referred patients, to teach in the surgical residency and the Transition to Practice General Surgery fellowship programs at Gundersen, to participate in clinical research activities, and to engage in a variety of professional activities that strengthen the bonds between GHS and rural surgeons. These interactions help minimize professional isolation, a serious problem for surgeons working on their own in small communities.
Communication is maintained electronically. “Our system includes the use of a common EMR across the entire system allowing mutual access to both inpatient and outpatient records, including full access to digitized diagnostic imaging. GHS has established a number of distance-learning telemedicine links between the main campus and the rural communities that permit real-time patient consultations as well as participation in teaching conferences including Morbidity and Mortality Conferences.”
Reducing burnout in rural surgeons
The GHS model may have some impact on burnout among the rural surgeons in the system, said Dr. Cogbill. “Rural surgeon employment as part of a fully integrated regional network has the potential to reduce the magnitude of burnout by providing administrative assistance to help navigate bureaucratic complexities, easy access for subspecialty consults with colleagues who are known entities, and a model of rural surgery involving pods of three colleagues who can share call, mutual assistance, and case volumes.” Fair and competitive compensation and some degree of loan forgiveness have been in the mix of factors that have helped with recruitment. Administrative assistance from the main campus eases the clerical burden the surgeons face. Guaranteed free time for vacations and educational meetings, as well as a reasonable call schedule, are all built into contracts; this has had a big impact on recruitment. GHS has concluded that three general surgeons in a community is the optimal number to maintain call coverage and mutual assistance. Dr. Cogbill said, “The call schedule is managed by each “pod” of rural general surgeons themselves. With a full complement of three rural surgeons in a pod, they maintain an every third night call schedule. In towns in which there are fewer than three surgeons, the GHS surgeons often share call with surgeons who are not part of GHS to maintain a reasonable/sustainable call schedule.”
The retention track record at GHS is impressive. Since 1978, 19 rural general surgeons have been employed by GHS. Four (21%) rural general surgeons have retired 10 (53%) continue to practice in the network; only 5 (26%) left prior to retirement. Six rural general surgeons practiced in one location for over 20 years.
[email protected]
On Twitter @ThereseBorden
Comprehensive guidelines released for enhanced colorectal surgery recovery
New guidelines for enhanced recovery from colon and rectal surgery highlight the small steps that can add up to big improvements in patient outcomes.
“I think one of the most surprising aspects” of the guidelines – a joint effort from the American Society of Colon and Rectal Surgeons (ASCRS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – “is how enhanced recovery in many ways involves all the little things,” said senior author Scott Steele, MD, FACS, chairman of the department of colorectal surgery at the Cleveland Clinic (Dis Colon Rectum. 2017 Aug;60[8]:761-84. doi: 10.1097/DCR.0000000000000883). The guideline includes 24 literature-based recommendations covering everything from preoperative stoma counseling to postop chewing gum, all rated by quality of evidence.
“Many are easy to incorporate into day-to-day practice: getting [patients] out of bed, avoiding nasogastric tubes, not giving as much IV fluid as we used to, having patients take oral food and drink right after surgery, and having nursing/anesthesia/surgeons all on the same page and understanding that ... multidisciplinary, multisetting care leads to the best outcomes,” he said.
ASCRS and SAGES joined forces after noting that previous guidelines for enhanced recovery – perhaps better known as enhanced recovery after surgery, or ERAS, protocols – are dated, including studies only up to 2012; much has been published since then.
Preop measures
Some of the new recommendations encourage closer patient involvement with care. For instance, the groups strongly recommend discussing goals and discharge criteria with patients before surgery. Recent work has found that compliance and success go up when patients understand what’s going on, and length of stay and complications go down. For similar reasons, stoma education, stoma marking, and counseling on avoiding dehydration should happen preoperatively.
Meanwhile, “although there appear to be no meaningful benefits of [mechanical bowel prep (MBP)] alone in terms of complications,” the groups made a weak recommendation for MBP plus oral antibiotics before surgery. “A meta-analysis of seven RCTs comparing MBP with [antibiotics] versus MBP alone showed a reduction in total surgical site infection and incisional site infection,” they noted.
ASCRS and SAGES strongly recommended that patients drink clear fluids in the 2 hours before surgery, and also recommended carbohydrate loading – specifically drinks high in complex carbohydrates – in nondiabetic patients to attenuate insulin resistance induced by surgery and starvation.
The groups also recommended preset orders to standardize care, and care bundles to reduce surgical site infections. Measures could include preop chlorhexidine showers, ertapenem (Invanz) within an hour of incision, gown and glove changes before fascial closure, and washing incisions with chlorhexidine during recovery.
Pain control
“A multimodal, opioid-sparing, pain management plan should be ... implemented before the induction of anesthesia” for earlier return of bowel function and shorter lengths of stay, they said in a strong recommendation. “One of the simplest techniques to limit opioid intake is to schedule narcotic alternatives, such as oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and gabapentin, rather than giving them on an as-needed basis.” The risk of anastomotic leaks with NSAIDs appears to be most pronounced when patients are on them for more than 3 days.
Wound infiltration and abdominal trunk blocks with liposomal bupivacaine have shown promising results, as well. “Limited data demonstrate that the (TAP) block with a local anesthetic [is] associated with decreased length of stay ... TAP blocks performed before surgery appear to provide better analgesia than TAP blocks performed at the end,” the groups said.
ASCRS and SAGES strongly recommended thoracic epidural analgesia for open colorectal cases, but not for routine use in laparoscopic cases. “The modest analgesic benefits provided by TEA do not support a faster recovery in laparoscopic surgery,” they said, noting that at least in open cases, infusion of a local anesthetic and a lipophilic opioid seems to work better than either option alone.
They also strongly recommended that surgery teams preempt postop nausea and vomiting. Dexamethasone at anesthesia induction and ondansetron at emergence is a common option for patients at risk. Others include total intravenous anesthesia, intravenous acetaminophen, and gabapentin.
Fluid management
Intraoperative crystalloids have to be managed to avoid volume overload and its bad effects. “A maintenance infusion of 1.5-2 mL/kg/h of balanced crystalloid solution is sufficient to cover the needs derived from salt water homeostasis during major abdominal surgery,” ASCRS and SAGES said in a strong recommendation.
“The neuroendocrine response induced by surgical trauma leads to a physiologic reduction of urine output that, in the absence of other signs of hypovolemia, should not trigger additional fluid administration.” Also, “crystalloid or colloid preloading does not prevent hypotension induced by neuraxial blockade ... hypotension induced by epidural analgesia should be managed by reducing the epidural infusion rate and with small doses of vasopressors” – not IV fluids – “so long at the patient is normovolemic,” they noted.
Intravenous fluids should be stopped after recovery room discharge, and clear fluids encouraged as soon as patients can tolerate them.
Postop care
ASCRS and SAGES made strong recommendations for minimally invasive surgery when possible, and for avoiding intra-abdominal drains and nasogastric tubes, both recommendations that support current practice in many places. NG tubes can push oral intake back 2 days, and there’s no evidence that abdominal drains prevent anastomotic leaks, plus there can be complications with both.
The groups also strongly recommended early and progressive patient mobilization to shorten length of stay, and a regular diet immediately after surgery.
As for the chewing gum, “sham feeding (i.e., chewing sugar-free gum for [at least] 10 minutes 3-4 times per day) after colorectal surgery is safe, results in small improvements in GI recovery” – flatus and bowel moments happen sooner – “and may be associated with a reduction in the length of hospital stay.” The groups strongly recommended it based on high-quality evidence
Alvimopan was also a strong recommendation to reverse increased GI transit time and constipation from opioids after open cases. “Several RCTs and pooled post hoc analyses showed accelerated time to recovery of GI function with 6- and 12-mg doses compared with placebo and a significantly shorter hospital length of stay in the alvimopan 12-mg group.” It’s unclear at this point, however, if alvimopan has a role in laparoscopic cases, the groups said.
To reduce the risk of urinary tract infections, they said urinary catheters should be pulled within 24 hours of elective colonic or upper rectal resection not involving a vesicular fistula, and within 48 hours of midrectal/lower rectal resections, which carry a greater risk of urinary retention.
ASCRS and SAGES funded the work. Seven of the 10 authors, including Dr. Steele, had no financial disclosures. One author is a speaker for Pacira Pharmaceuticals, and her institution has received unrestricted educational grants from the company. Another author reported grant support from Medtronic and Merck, maker of alvimopan and ertapenem, and a third reported collaborations with Medtronic and Johnson & Johnson.
New guidelines for enhanced recovery from colon and rectal surgery highlight the small steps that can add up to big improvements in patient outcomes.
“I think one of the most surprising aspects” of the guidelines – a joint effort from the American Society of Colon and Rectal Surgeons (ASCRS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – “is how enhanced recovery in many ways involves all the little things,” said senior author Scott Steele, MD, FACS, chairman of the department of colorectal surgery at the Cleveland Clinic (Dis Colon Rectum. 2017 Aug;60[8]:761-84. doi: 10.1097/DCR.0000000000000883). The guideline includes 24 literature-based recommendations covering everything from preoperative stoma counseling to postop chewing gum, all rated by quality of evidence.
“Many are easy to incorporate into day-to-day practice: getting [patients] out of bed, avoiding nasogastric tubes, not giving as much IV fluid as we used to, having patients take oral food and drink right after surgery, and having nursing/anesthesia/surgeons all on the same page and understanding that ... multidisciplinary, multisetting care leads to the best outcomes,” he said.
ASCRS and SAGES joined forces after noting that previous guidelines for enhanced recovery – perhaps better known as enhanced recovery after surgery, or ERAS, protocols – are dated, including studies only up to 2012; much has been published since then.
Preop measures
Some of the new recommendations encourage closer patient involvement with care. For instance, the groups strongly recommend discussing goals and discharge criteria with patients before surgery. Recent work has found that compliance and success go up when patients understand what’s going on, and length of stay and complications go down. For similar reasons, stoma education, stoma marking, and counseling on avoiding dehydration should happen preoperatively.
Meanwhile, “although there appear to be no meaningful benefits of [mechanical bowel prep (MBP)] alone in terms of complications,” the groups made a weak recommendation for MBP plus oral antibiotics before surgery. “A meta-analysis of seven RCTs comparing MBP with [antibiotics] versus MBP alone showed a reduction in total surgical site infection and incisional site infection,” they noted.
ASCRS and SAGES strongly recommended that patients drink clear fluids in the 2 hours before surgery, and also recommended carbohydrate loading – specifically drinks high in complex carbohydrates – in nondiabetic patients to attenuate insulin resistance induced by surgery and starvation.
The groups also recommended preset orders to standardize care, and care bundles to reduce surgical site infections. Measures could include preop chlorhexidine showers, ertapenem (Invanz) within an hour of incision, gown and glove changes before fascial closure, and washing incisions with chlorhexidine during recovery.
Pain control
“A multimodal, opioid-sparing, pain management plan should be ... implemented before the induction of anesthesia” for earlier return of bowel function and shorter lengths of stay, they said in a strong recommendation. “One of the simplest techniques to limit opioid intake is to schedule narcotic alternatives, such as oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and gabapentin, rather than giving them on an as-needed basis.” The risk of anastomotic leaks with NSAIDs appears to be most pronounced when patients are on them for more than 3 days.
Wound infiltration and abdominal trunk blocks with liposomal bupivacaine have shown promising results, as well. “Limited data demonstrate that the (TAP) block with a local anesthetic [is] associated with decreased length of stay ... TAP blocks performed before surgery appear to provide better analgesia than TAP blocks performed at the end,” the groups said.
ASCRS and SAGES strongly recommended thoracic epidural analgesia for open colorectal cases, but not for routine use in laparoscopic cases. “The modest analgesic benefits provided by TEA do not support a faster recovery in laparoscopic surgery,” they said, noting that at least in open cases, infusion of a local anesthetic and a lipophilic opioid seems to work better than either option alone.
They also strongly recommended that surgery teams preempt postop nausea and vomiting. Dexamethasone at anesthesia induction and ondansetron at emergence is a common option for patients at risk. Others include total intravenous anesthesia, intravenous acetaminophen, and gabapentin.
Fluid management
Intraoperative crystalloids have to be managed to avoid volume overload and its bad effects. “A maintenance infusion of 1.5-2 mL/kg/h of balanced crystalloid solution is sufficient to cover the needs derived from salt water homeostasis during major abdominal surgery,” ASCRS and SAGES said in a strong recommendation.
“The neuroendocrine response induced by surgical trauma leads to a physiologic reduction of urine output that, in the absence of other signs of hypovolemia, should not trigger additional fluid administration.” Also, “crystalloid or colloid preloading does not prevent hypotension induced by neuraxial blockade ... hypotension induced by epidural analgesia should be managed by reducing the epidural infusion rate and with small doses of vasopressors” – not IV fluids – “so long at the patient is normovolemic,” they noted.
Intravenous fluids should be stopped after recovery room discharge, and clear fluids encouraged as soon as patients can tolerate them.
Postop care
ASCRS and SAGES made strong recommendations for minimally invasive surgery when possible, and for avoiding intra-abdominal drains and nasogastric tubes, both recommendations that support current practice in many places. NG tubes can push oral intake back 2 days, and there’s no evidence that abdominal drains prevent anastomotic leaks, plus there can be complications with both.
The groups also strongly recommended early and progressive patient mobilization to shorten length of stay, and a regular diet immediately after surgery.
As for the chewing gum, “sham feeding (i.e., chewing sugar-free gum for [at least] 10 minutes 3-4 times per day) after colorectal surgery is safe, results in small improvements in GI recovery” – flatus and bowel moments happen sooner – “and may be associated with a reduction in the length of hospital stay.” The groups strongly recommended it based on high-quality evidence
Alvimopan was also a strong recommendation to reverse increased GI transit time and constipation from opioids after open cases. “Several RCTs and pooled post hoc analyses showed accelerated time to recovery of GI function with 6- and 12-mg doses compared with placebo and a significantly shorter hospital length of stay in the alvimopan 12-mg group.” It’s unclear at this point, however, if alvimopan has a role in laparoscopic cases, the groups said.
To reduce the risk of urinary tract infections, they said urinary catheters should be pulled within 24 hours of elective colonic or upper rectal resection not involving a vesicular fistula, and within 48 hours of midrectal/lower rectal resections, which carry a greater risk of urinary retention.
ASCRS and SAGES funded the work. Seven of the 10 authors, including Dr. Steele, had no financial disclosures. One author is a speaker for Pacira Pharmaceuticals, and her institution has received unrestricted educational grants from the company. Another author reported grant support from Medtronic and Merck, maker of alvimopan and ertapenem, and a third reported collaborations with Medtronic and Johnson & Johnson.
New guidelines for enhanced recovery from colon and rectal surgery highlight the small steps that can add up to big improvements in patient outcomes.
“I think one of the most surprising aspects” of the guidelines – a joint effort from the American Society of Colon and Rectal Surgeons (ASCRS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – “is how enhanced recovery in many ways involves all the little things,” said senior author Scott Steele, MD, FACS, chairman of the department of colorectal surgery at the Cleveland Clinic (Dis Colon Rectum. 2017 Aug;60[8]:761-84. doi: 10.1097/DCR.0000000000000883). The guideline includes 24 literature-based recommendations covering everything from preoperative stoma counseling to postop chewing gum, all rated by quality of evidence.
“Many are easy to incorporate into day-to-day practice: getting [patients] out of bed, avoiding nasogastric tubes, not giving as much IV fluid as we used to, having patients take oral food and drink right after surgery, and having nursing/anesthesia/surgeons all on the same page and understanding that ... multidisciplinary, multisetting care leads to the best outcomes,” he said.
ASCRS and SAGES joined forces after noting that previous guidelines for enhanced recovery – perhaps better known as enhanced recovery after surgery, or ERAS, protocols – are dated, including studies only up to 2012; much has been published since then.
Preop measures
Some of the new recommendations encourage closer patient involvement with care. For instance, the groups strongly recommend discussing goals and discharge criteria with patients before surgery. Recent work has found that compliance and success go up when patients understand what’s going on, and length of stay and complications go down. For similar reasons, stoma education, stoma marking, and counseling on avoiding dehydration should happen preoperatively.
Meanwhile, “although there appear to be no meaningful benefits of [mechanical bowel prep (MBP)] alone in terms of complications,” the groups made a weak recommendation for MBP plus oral antibiotics before surgery. “A meta-analysis of seven RCTs comparing MBP with [antibiotics] versus MBP alone showed a reduction in total surgical site infection and incisional site infection,” they noted.
ASCRS and SAGES strongly recommended that patients drink clear fluids in the 2 hours before surgery, and also recommended carbohydrate loading – specifically drinks high in complex carbohydrates – in nondiabetic patients to attenuate insulin resistance induced by surgery and starvation.
The groups also recommended preset orders to standardize care, and care bundles to reduce surgical site infections. Measures could include preop chlorhexidine showers, ertapenem (Invanz) within an hour of incision, gown and glove changes before fascial closure, and washing incisions with chlorhexidine during recovery.
Pain control
“A multimodal, opioid-sparing, pain management plan should be ... implemented before the induction of anesthesia” for earlier return of bowel function and shorter lengths of stay, they said in a strong recommendation. “One of the simplest techniques to limit opioid intake is to schedule narcotic alternatives, such as oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and gabapentin, rather than giving them on an as-needed basis.” The risk of anastomotic leaks with NSAIDs appears to be most pronounced when patients are on them for more than 3 days.
Wound infiltration and abdominal trunk blocks with liposomal bupivacaine have shown promising results, as well. “Limited data demonstrate that the (TAP) block with a local anesthetic [is] associated with decreased length of stay ... TAP blocks performed before surgery appear to provide better analgesia than TAP blocks performed at the end,” the groups said.
ASCRS and SAGES strongly recommended thoracic epidural analgesia for open colorectal cases, but not for routine use in laparoscopic cases. “The modest analgesic benefits provided by TEA do not support a faster recovery in laparoscopic surgery,” they said, noting that at least in open cases, infusion of a local anesthetic and a lipophilic opioid seems to work better than either option alone.
They also strongly recommended that surgery teams preempt postop nausea and vomiting. Dexamethasone at anesthesia induction and ondansetron at emergence is a common option for patients at risk. Others include total intravenous anesthesia, intravenous acetaminophen, and gabapentin.
Fluid management
Intraoperative crystalloids have to be managed to avoid volume overload and its bad effects. “A maintenance infusion of 1.5-2 mL/kg/h of balanced crystalloid solution is sufficient to cover the needs derived from salt water homeostasis during major abdominal surgery,” ASCRS and SAGES said in a strong recommendation.
“The neuroendocrine response induced by surgical trauma leads to a physiologic reduction of urine output that, in the absence of other signs of hypovolemia, should not trigger additional fluid administration.” Also, “crystalloid or colloid preloading does not prevent hypotension induced by neuraxial blockade ... hypotension induced by epidural analgesia should be managed by reducing the epidural infusion rate and with small doses of vasopressors” – not IV fluids – “so long at the patient is normovolemic,” they noted.
Intravenous fluids should be stopped after recovery room discharge, and clear fluids encouraged as soon as patients can tolerate them.
Postop care
ASCRS and SAGES made strong recommendations for minimally invasive surgery when possible, and for avoiding intra-abdominal drains and nasogastric tubes, both recommendations that support current practice in many places. NG tubes can push oral intake back 2 days, and there’s no evidence that abdominal drains prevent anastomotic leaks, plus there can be complications with both.
The groups also strongly recommended early and progressive patient mobilization to shorten length of stay, and a regular diet immediately after surgery.
As for the chewing gum, “sham feeding (i.e., chewing sugar-free gum for [at least] 10 minutes 3-4 times per day) after colorectal surgery is safe, results in small improvements in GI recovery” – flatus and bowel moments happen sooner – “and may be associated with a reduction in the length of hospital stay.” The groups strongly recommended it based on high-quality evidence
Alvimopan was also a strong recommendation to reverse increased GI transit time and constipation from opioids after open cases. “Several RCTs and pooled post hoc analyses showed accelerated time to recovery of GI function with 6- and 12-mg doses compared with placebo and a significantly shorter hospital length of stay in the alvimopan 12-mg group.” It’s unclear at this point, however, if alvimopan has a role in laparoscopic cases, the groups said.
To reduce the risk of urinary tract infections, they said urinary catheters should be pulled within 24 hours of elective colonic or upper rectal resection not involving a vesicular fistula, and within 48 hours of midrectal/lower rectal resections, which carry a greater risk of urinary retention.
ASCRS and SAGES funded the work. Seven of the 10 authors, including Dr. Steele, had no financial disclosures. One author is a speaker for Pacira Pharmaceuticals, and her institution has received unrestricted educational grants from the company. Another author reported grant support from Medtronic and Merck, maker of alvimopan and ertapenem, and a third reported collaborations with Medtronic and Johnson & Johnson.
FROM DISEASES OF THE COLON AND RECTUM
Molecular subtypes predicted outcomes in gastric cancer
Recurrence-free and overall survival in gastric cancer was highest among patients with the Epstein-Barr virus molecular subtype, investigators reported online July 27 in Clinical Cancer Research.
In contrast, the genomically stable subtype had the worst prognosis and was least likely to benefit from adjuvant chemotherapy, Bo Hwa Sohn, PhD, of the University of Texas MD Anderson Cancer Center, Houston, reported with her associates. Their prediction model “successfully stratified patients by survival and adjuvant chemotherapy outcomes,” they concluded.
The MSI subtype was tied to a moderate prognosis. Prognosis for the CIN subtype also was moderate, but was worse in the cohort from South Korea than in the MD Anderson cohort. These results might reflect more heterogeneity within the CIN subtype, the researchers said.
Importantly, adjuvant chemotherapy most benefited CIN patients – 59% were alive without recurrence at 3 years, compared with only 34% of those who received no adjuvant therapy (hazard ratio, 0.39; 95% confidence interval, 0.16-0.94; P = .03). In contrast, adjuvant chemotherapy produced only modest benefits in MSI (HR, 0.55; P = .18), and did not benefit GS patients (P = .66).
Analyses of 24 gastric cancer cell lines from the Genomics of Drug Sensitivity in Cancer project supported that finding, said the researchers. Lines of GS cells had the highest 5-fluorouracil IC50 values, indicating they are resistant to 5-fluorouracil. The activated transcription regulator NUPR1 has been linked to chemoresistance in other cancers and is often altered in the GS subtype, they noted. They only studied adjuvant chemotherapy in the MD Anderson cohort because most South Korean patients did not receive it. Also, all EBV patients received adjuvant chemotherapy, so the researchers could not examine outcomes for this subtype.
The researchers also created a predictive model by pooling probabilities of recurrence. On a scale of 0 to 100, patients who scored under 20 had a 67% chance of recurrence-free survival at 5 years, compared with 52% for patients scoring between 20 and 30 and 38% for patients scoring above 30. Differences between these probabilities were highly statistically significant, and results for overall survival were similar. Score independently predicted recurrence-free survival after other clinicopathologic variables were controlled for in the pooled cohorts and in patients with more heterogeneous stage II cancers.
This prediction model will need to be whittled down to a few genes that adequately represent each subtype before it is useful in the clinic, the researchers acknowledged. “Nevertheless, the validation of our prediction model in two independent patient cohorts and the fact that the model reflects the biological characteristics associated with each subtype indicate that this prediction model could be used to develop rational therapy recommendations,” they concluded.
Funders included the National Institutes of Health, The University of Texas MD Anderson Cancer Center, the Korea National Research Foundation, the Scientific Research Center Program, and the Korean Research Institute of Bioscience and Biotechnology. No investigator declared potential conflicts of interest.
Recurrence-free and overall survival in gastric cancer was highest among patients with the Epstein-Barr virus molecular subtype, investigators reported online July 27 in Clinical Cancer Research.
In contrast, the genomically stable subtype had the worst prognosis and was least likely to benefit from adjuvant chemotherapy, Bo Hwa Sohn, PhD, of the University of Texas MD Anderson Cancer Center, Houston, reported with her associates. Their prediction model “successfully stratified patients by survival and adjuvant chemotherapy outcomes,” they concluded.
The MSI subtype was tied to a moderate prognosis. Prognosis for the CIN subtype also was moderate, but was worse in the cohort from South Korea than in the MD Anderson cohort. These results might reflect more heterogeneity within the CIN subtype, the researchers said.
Importantly, adjuvant chemotherapy most benefited CIN patients – 59% were alive without recurrence at 3 years, compared with only 34% of those who received no adjuvant therapy (hazard ratio, 0.39; 95% confidence interval, 0.16-0.94; P = .03). In contrast, adjuvant chemotherapy produced only modest benefits in MSI (HR, 0.55; P = .18), and did not benefit GS patients (P = .66).
Analyses of 24 gastric cancer cell lines from the Genomics of Drug Sensitivity in Cancer project supported that finding, said the researchers. Lines of GS cells had the highest 5-fluorouracil IC50 values, indicating they are resistant to 5-fluorouracil. The activated transcription regulator NUPR1 has been linked to chemoresistance in other cancers and is often altered in the GS subtype, they noted. They only studied adjuvant chemotherapy in the MD Anderson cohort because most South Korean patients did not receive it. Also, all EBV patients received adjuvant chemotherapy, so the researchers could not examine outcomes for this subtype.
The researchers also created a predictive model by pooling probabilities of recurrence. On a scale of 0 to 100, patients who scored under 20 had a 67% chance of recurrence-free survival at 5 years, compared with 52% for patients scoring between 20 and 30 and 38% for patients scoring above 30. Differences between these probabilities were highly statistically significant, and results for overall survival were similar. Score independently predicted recurrence-free survival after other clinicopathologic variables were controlled for in the pooled cohorts and in patients with more heterogeneous stage II cancers.
This prediction model will need to be whittled down to a few genes that adequately represent each subtype before it is useful in the clinic, the researchers acknowledged. “Nevertheless, the validation of our prediction model in two independent patient cohorts and the fact that the model reflects the biological characteristics associated with each subtype indicate that this prediction model could be used to develop rational therapy recommendations,” they concluded.
Funders included the National Institutes of Health, The University of Texas MD Anderson Cancer Center, the Korea National Research Foundation, the Scientific Research Center Program, and the Korean Research Institute of Bioscience and Biotechnology. No investigator declared potential conflicts of interest.
Recurrence-free and overall survival in gastric cancer was highest among patients with the Epstein-Barr virus molecular subtype, investigators reported online July 27 in Clinical Cancer Research.
In contrast, the genomically stable subtype had the worst prognosis and was least likely to benefit from adjuvant chemotherapy, Bo Hwa Sohn, PhD, of the University of Texas MD Anderson Cancer Center, Houston, reported with her associates. Their prediction model “successfully stratified patients by survival and adjuvant chemotherapy outcomes,” they concluded.
The MSI subtype was tied to a moderate prognosis. Prognosis for the CIN subtype also was moderate, but was worse in the cohort from South Korea than in the MD Anderson cohort. These results might reflect more heterogeneity within the CIN subtype, the researchers said.
Importantly, adjuvant chemotherapy most benefited CIN patients – 59% were alive without recurrence at 3 years, compared with only 34% of those who received no adjuvant therapy (hazard ratio, 0.39; 95% confidence interval, 0.16-0.94; P = .03). In contrast, adjuvant chemotherapy produced only modest benefits in MSI (HR, 0.55; P = .18), and did not benefit GS patients (P = .66).
Analyses of 24 gastric cancer cell lines from the Genomics of Drug Sensitivity in Cancer project supported that finding, said the researchers. Lines of GS cells had the highest 5-fluorouracil IC50 values, indicating they are resistant to 5-fluorouracil. The activated transcription regulator NUPR1 has been linked to chemoresistance in other cancers and is often altered in the GS subtype, they noted. They only studied adjuvant chemotherapy in the MD Anderson cohort because most South Korean patients did not receive it. Also, all EBV patients received adjuvant chemotherapy, so the researchers could not examine outcomes for this subtype.
The researchers also created a predictive model by pooling probabilities of recurrence. On a scale of 0 to 100, patients who scored under 20 had a 67% chance of recurrence-free survival at 5 years, compared with 52% for patients scoring between 20 and 30 and 38% for patients scoring above 30. Differences between these probabilities were highly statistically significant, and results for overall survival were similar. Score independently predicted recurrence-free survival after other clinicopathologic variables were controlled for in the pooled cohorts and in patients with more heterogeneous stage II cancers.
This prediction model will need to be whittled down to a few genes that adequately represent each subtype before it is useful in the clinic, the researchers acknowledged. “Nevertheless, the validation of our prediction model in two independent patient cohorts and the fact that the model reflects the biological characteristics associated with each subtype indicate that this prediction model could be used to develop rational therapy recommendations,” they concluded.
Funders included the National Institutes of Health, The University of Texas MD Anderson Cancer Center, the Korea National Research Foundation, the Scientific Research Center Program, and the Korean Research Institute of Bioscience and Biotechnology. No investigator declared potential conflicts of interest.
FROM CLINICAL CANCER RESEARCH
Key clinical point: In gastric cancer, molecular subtypes predicted survival and response to adjuvant chemotherapy.
Major finding: Epstein-Barr virus subtype was associated with the highest probability of recurrence-free and overall survival. The genomically stable subtype had the worst prognosis and was least likely to benefit from adjuvant chemotherapy.
Data source: A retrospective study of 267 patients from South Korea and 432 patients from MD Anderson with gastric cancer.
Disclosures: Funders included the National Institutes of Health, The University of Texas MD Anderson Cancer Center, the Korea National Research Foundation, the Scientific Research Center Program, and the Korean Research Institute of Bioscience and Biotechnology. No investigator declared potential conflicts of interest.
Religion and LGBTQ identities
JB is a 15-year-old female who presents to your office for a wellness check. Mom is concerned because she has seemed more depressed and withdrawn over the past few months. During the confidential portion of your visit, JB discloses that, while she has had boyfriends in the past, she is realizing that she is romantically and sexually attracted to females. Many members of her religious faith, which she is strongly connected to, believe that homosexuality is a sin. She has been secretly researching therapies to help her “not be gay” and asks you for advice.
Adolescence is a time of rapid growth and development. Two important developmental tasks of adolescence are to establish key aspects of identity and identify meaningful moral standards, values, and belief systems.1 For some LGBTQ adolescents, these tasks can become more complicated when the value system or religious faith in which they were raised views homosexuality or gender nonconformity as a sin.
- Identifying as lesbian, gay, bisexual, or transgender is normal, just different.
- LGBT people exist in almost every faith group across the country.
- Many religious groups have wrestled with homosexuality, gender identity, and religion and decided to be more welcoming to LGBT communities.
- Within most faiths, there are many interpretations of religious texts, such as the Bible and the Koran, on all issues, including homosexuality.
- While every religion has different teachings, almost all religions advocate love and compassion.
- Clergy and other faith leaders can be a source of support. However, every faith community is different and may not always be supportive. Safely investigate your individual community’s approach. You have the right to question and explore your faith, sexuality, and/or gender identity and reconcile these in a way that is true to you.
- Remember this is your journey. You get to decide the path and the pace.
- Recognize that this may involve working for change within your community or it may mean leaving it.
- Referral for “conversion” or “reparative therapy” is never indicated. Such therapy is not effective and may be harmful to LGBTQ individuals by increasing internalized stigma, distress, and depression.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. She has no relevant financial disclosures. Email her at [email protected].
Spirituality resources
- LGBTQ and Religion: Your Relationship with Religion is Completely Up to You, the FAQ Page by the Trevor Project, a national organization that provides crisis intervention and suicide prevention resources to LGBTQ young people ages 13-24 years. www.thetrevorproject.org/pages/lgbtq-and-religion
- Faith in Our Families: Parents, Families and Friends Talk About Religion and Homosexuality, a resource from PFLAG (Parents, Families, and Friends of Lesbians and Gays). www.pflag.org/sites/default/files/Faith%20In%20Our%20Families.pdf
- LGBT Center UNC Chapel Hill: Religion and Spirituality, a page with a link to nondenominational and denomination-specific resources with various religious and spiritual communities’ beliefs regarding faith and LGBTQIA+ (Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual). lgbtq.unc.edu/resources/exploring-identities/religion-and-spirituality
- HRC: Explore Religion and Faith, a Human Rights Campaign page containing links to resources on religion and faith. It also has links to the Coming Home Series, guides aimed at those who hope to lead their faith communities toward a more welcoming stance and those seeking a path back to beloved traditions. www.hrc.org/explore/topic/religion-faith
References
1. Raising teens: A synthesis or research and a foundation for action. (Boston: Center for Health Communication, Harvard School of Public Health, 2001).
2. Faith in Our Families: Parents, Families and Friends Talk About Religion and Homosexuality (Washington, D.C.: Parents, Families and Friends of Lesbians and Gays, 1997)
3. Pediatrics. 2013 Jul;132(1):198-203.
4. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. (Washington, D.C.: National Academies Press, 2011)
5. Coming Home: To Faith, to Spirit, to Self. Pamphlet by the Human Rights Campaign.
JB is a 15-year-old female who presents to your office for a wellness check. Mom is concerned because she has seemed more depressed and withdrawn over the past few months. During the confidential portion of your visit, JB discloses that, while she has had boyfriends in the past, she is realizing that she is romantically and sexually attracted to females. Many members of her religious faith, which she is strongly connected to, believe that homosexuality is a sin. She has been secretly researching therapies to help her “not be gay” and asks you for advice.
Adolescence is a time of rapid growth and development. Two important developmental tasks of adolescence are to establish key aspects of identity and identify meaningful moral standards, values, and belief systems.1 For some LGBTQ adolescents, these tasks can become more complicated when the value system or religious faith in which they were raised views homosexuality or gender nonconformity as a sin.
- Identifying as lesbian, gay, bisexual, or transgender is normal, just different.
- LGBT people exist in almost every faith group across the country.
- Many religious groups have wrestled with homosexuality, gender identity, and religion and decided to be more welcoming to LGBT communities.
- Within most faiths, there are many interpretations of religious texts, such as the Bible and the Koran, on all issues, including homosexuality.
- While every religion has different teachings, almost all religions advocate love and compassion.
- Clergy and other faith leaders can be a source of support. However, every faith community is different and may not always be supportive. Safely investigate your individual community’s approach. You have the right to question and explore your faith, sexuality, and/or gender identity and reconcile these in a way that is true to you.
- Remember this is your journey. You get to decide the path and the pace.
- Recognize that this may involve working for change within your community or it may mean leaving it.
- Referral for “conversion” or “reparative therapy” is never indicated. Such therapy is not effective and may be harmful to LGBTQ individuals by increasing internalized stigma, distress, and depression.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. She has no relevant financial disclosures. Email her at [email protected].
Spirituality resources
- LGBTQ and Religion: Your Relationship with Religion is Completely Up to You, the FAQ Page by the Trevor Project, a national organization that provides crisis intervention and suicide prevention resources to LGBTQ young people ages 13-24 years. www.thetrevorproject.org/pages/lgbtq-and-religion
- Faith in Our Families: Parents, Families and Friends Talk About Religion and Homosexuality, a resource from PFLAG (Parents, Families, and Friends of Lesbians and Gays). www.pflag.org/sites/default/files/Faith%20In%20Our%20Families.pdf
- LGBT Center UNC Chapel Hill: Religion and Spirituality, a page with a link to nondenominational and denomination-specific resources with various religious and spiritual communities’ beliefs regarding faith and LGBTQIA+ (Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual). lgbtq.unc.edu/resources/exploring-identities/religion-and-spirituality
- HRC: Explore Religion and Faith, a Human Rights Campaign page containing links to resources on religion and faith. It also has links to the Coming Home Series, guides aimed at those who hope to lead their faith communities toward a more welcoming stance and those seeking a path back to beloved traditions. www.hrc.org/explore/topic/religion-faith
References
1. Raising teens: A synthesis or research and a foundation for action. (Boston: Center for Health Communication, Harvard School of Public Health, 2001).
2. Faith in Our Families: Parents, Families and Friends Talk About Religion and Homosexuality (Washington, D.C.: Parents, Families and Friends of Lesbians and Gays, 1997)
3. Pediatrics. 2013 Jul;132(1):198-203.
4. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. (Washington, D.C.: National Academies Press, 2011)
5. Coming Home: To Faith, to Spirit, to Self. Pamphlet by the Human Rights Campaign.
JB is a 15-year-old female who presents to your office for a wellness check. Mom is concerned because she has seemed more depressed and withdrawn over the past few months. During the confidential portion of your visit, JB discloses that, while she has had boyfriends in the past, she is realizing that she is romantically and sexually attracted to females. Many members of her religious faith, which she is strongly connected to, believe that homosexuality is a sin. She has been secretly researching therapies to help her “not be gay” and asks you for advice.
Adolescence is a time of rapid growth and development. Two important developmental tasks of adolescence are to establish key aspects of identity and identify meaningful moral standards, values, and belief systems.1 For some LGBTQ adolescents, these tasks can become more complicated when the value system or religious faith in which they were raised views homosexuality or gender nonconformity as a sin.
- Identifying as lesbian, gay, bisexual, or transgender is normal, just different.
- LGBT people exist in almost every faith group across the country.
- Many religious groups have wrestled with homosexuality, gender identity, and religion and decided to be more welcoming to LGBT communities.
- Within most faiths, there are many interpretations of religious texts, such as the Bible and the Koran, on all issues, including homosexuality.
- While every religion has different teachings, almost all religions advocate love and compassion.
- Clergy and other faith leaders can be a source of support. However, every faith community is different and may not always be supportive. Safely investigate your individual community’s approach. You have the right to question and explore your faith, sexuality, and/or gender identity and reconcile these in a way that is true to you.
- Remember this is your journey. You get to decide the path and the pace.
- Recognize that this may involve working for change within your community or it may mean leaving it.
- Referral for “conversion” or “reparative therapy” is never indicated. Such therapy is not effective and may be harmful to LGBTQ individuals by increasing internalized stigma, distress, and depression.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. She has no relevant financial disclosures. Email her at [email protected].
Spirituality resources
- LGBTQ and Religion: Your Relationship with Religion is Completely Up to You, the FAQ Page by the Trevor Project, a national organization that provides crisis intervention and suicide prevention resources to LGBTQ young people ages 13-24 years. www.thetrevorproject.org/pages/lgbtq-and-religion
- Faith in Our Families: Parents, Families and Friends Talk About Religion and Homosexuality, a resource from PFLAG (Parents, Families, and Friends of Lesbians and Gays). www.pflag.org/sites/default/files/Faith%20In%20Our%20Families.pdf
- LGBT Center UNC Chapel Hill: Religion and Spirituality, a page with a link to nondenominational and denomination-specific resources with various religious and spiritual communities’ beliefs regarding faith and LGBTQIA+ (Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual). lgbtq.unc.edu/resources/exploring-identities/religion-and-spirituality
- HRC: Explore Religion and Faith, a Human Rights Campaign page containing links to resources on religion and faith. It also has links to the Coming Home Series, guides aimed at those who hope to lead their faith communities toward a more welcoming stance and those seeking a path back to beloved traditions. www.hrc.org/explore/topic/religion-faith
References
1. Raising teens: A synthesis or research and a foundation for action. (Boston: Center for Health Communication, Harvard School of Public Health, 2001).
2. Faith in Our Families: Parents, Families and Friends Talk About Religion and Homosexuality (Washington, D.C.: Parents, Families and Friends of Lesbians and Gays, 1997)
3. Pediatrics. 2013 Jul;132(1):198-203.
4. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. (Washington, D.C.: National Academies Press, 2011)
5. Coming Home: To Faith, to Spirit, to Self. Pamphlet by the Human Rights Campaign.
Sleep Duration Affects Likelihood of Insomnia and Depression Remission
BOSTON—Objective sleep duration moderates the probability of remission among patients with comorbid depression and insomnia, according to research presented at the 31st Annual Meeting of the Associated Professional Sleep Societies. Sleep durations of greater than five to six hours increase the likelihood that these patients will achieve insomnia remission with cognitive behavioral therapy for insomnia (CBT-I), but do not affect the likelihood of depression remission. Sleep durations of seven or more hours optimize the likelihood of insomnia remission and depression remission in response to CBT-I.
In a 2015 consensus statement, the Sleep Research Society recommended seven or more hours of sleep per night for adults younger than 60. Investigations by Vgontzas and colleagues indicate that sleep durations of less than five hours and less than six hours are associated with increased morbidity and poor treatment response among patients with insomnia. “We wanted to know what [sleep-duration] cutoffs … might be better predictors of eventual insomnia and depression remission through treatment,” said Jack Edinger, PhD, Professor of Medicine at National Jewish Health in Denver.
An Analysis of the TRIAD Study
Dr. Edinger and colleagues conducted a secondary analysis of the TRIAD study, which examined whether combined treatment of depression and insomnia improves depression and sleep outcomes in participants with both disorders. Eligible participants met Diagnostic and Statistical Manual of Mental Disorders (4th ed.) criteria for major depression and primary insomnia, had a Hamilton Rating Scale for Depression (HAMD-17) score of 16 or greater, and had an Insomnia Severity Index (ISI) score of 11 or greater. People who had had psychotherapy in the previous four months, or had failed or could not tolerate previous adequate trials of the study medications, were excluded. Participants completed one night of baseline polysomnography before entering the treatment phase of the study.
The study population included 104 participants (75 women) with a mean age of 47. Mean baseline HAMD-17 score was 22, and mean baseline ISI score was 20.6. All participants received antidepressant medication (ie, citalopram, sertraline, or venlafaxine). Patients were randomized to CBT-I or sham (ie, a pseudo desensitization condition with sleep education). The investigators assessed participants biweekly with the HAMD-17 and the ISI. The treatment period lasted for 16 weeks.
CBT-I Provided Benefits
Participants with five or more hours of sleep were more likely to respond to CBT-I than participants with fewer than five hours of sleep. Among participants with sleep duration of five or more hours, insomnia remission was more likely with CBT-I than with the control condition. The five-hour cutoff had no association with depression remission.
Among participants with six or more hours of sleep, those who received CBT-I were more likely to achieve insomnia remission than controls. The six-hour cutoff did not affect the likelihood of depression remission, however.
Among participants with seven or more hours of sleep, those randomized to CBT-I were more likely to achieve insomnia remission and depression remission than controls.
“More research is needed to determine how best to achieve depression remission in those patients with less than seven hours of objective sleep duration prior to starting treatment,” Dr. Edinger concluded.
—Erik Greb
Suggested Reading
Bathgate CJ, Edinger JD, Krystal AD. Insomnia patients with objective short sleep duration have a blunted response to cognitive behavioral therapy for insomnia. Sleep. 2017;40(1).
Vgontzas AN, Liao D, Bixler EO, et al. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491-497.
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-844.
BOSTON—Objective sleep duration moderates the probability of remission among patients with comorbid depression and insomnia, according to research presented at the 31st Annual Meeting of the Associated Professional Sleep Societies. Sleep durations of greater than five to six hours increase the likelihood that these patients will achieve insomnia remission with cognitive behavioral therapy for insomnia (CBT-I), but do not affect the likelihood of depression remission. Sleep durations of seven or more hours optimize the likelihood of insomnia remission and depression remission in response to CBT-I.
In a 2015 consensus statement, the Sleep Research Society recommended seven or more hours of sleep per night for adults younger than 60. Investigations by Vgontzas and colleagues indicate that sleep durations of less than five hours and less than six hours are associated with increased morbidity and poor treatment response among patients with insomnia. “We wanted to know what [sleep-duration] cutoffs … might be better predictors of eventual insomnia and depression remission through treatment,” said Jack Edinger, PhD, Professor of Medicine at National Jewish Health in Denver.
An Analysis of the TRIAD Study
Dr. Edinger and colleagues conducted a secondary analysis of the TRIAD study, which examined whether combined treatment of depression and insomnia improves depression and sleep outcomes in participants with both disorders. Eligible participants met Diagnostic and Statistical Manual of Mental Disorders (4th ed.) criteria for major depression and primary insomnia, had a Hamilton Rating Scale for Depression (HAMD-17) score of 16 or greater, and had an Insomnia Severity Index (ISI) score of 11 or greater. People who had had psychotherapy in the previous four months, or had failed or could not tolerate previous adequate trials of the study medications, were excluded. Participants completed one night of baseline polysomnography before entering the treatment phase of the study.
The study population included 104 participants (75 women) with a mean age of 47. Mean baseline HAMD-17 score was 22, and mean baseline ISI score was 20.6. All participants received antidepressant medication (ie, citalopram, sertraline, or venlafaxine). Patients were randomized to CBT-I or sham (ie, a pseudo desensitization condition with sleep education). The investigators assessed participants biweekly with the HAMD-17 and the ISI. The treatment period lasted for 16 weeks.
CBT-I Provided Benefits
Participants with five or more hours of sleep were more likely to respond to CBT-I than participants with fewer than five hours of sleep. Among participants with sleep duration of five or more hours, insomnia remission was more likely with CBT-I than with the control condition. The five-hour cutoff had no association with depression remission.
Among participants with six or more hours of sleep, those who received CBT-I were more likely to achieve insomnia remission than controls. The six-hour cutoff did not affect the likelihood of depression remission, however.
Among participants with seven or more hours of sleep, those randomized to CBT-I were more likely to achieve insomnia remission and depression remission than controls.
“More research is needed to determine how best to achieve depression remission in those patients with less than seven hours of objective sleep duration prior to starting treatment,” Dr. Edinger concluded.
—Erik Greb
Suggested Reading
Bathgate CJ, Edinger JD, Krystal AD. Insomnia patients with objective short sleep duration have a blunted response to cognitive behavioral therapy for insomnia. Sleep. 2017;40(1).
Vgontzas AN, Liao D, Bixler EO, et al. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491-497.
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-844.
BOSTON—Objective sleep duration moderates the probability of remission among patients with comorbid depression and insomnia, according to research presented at the 31st Annual Meeting of the Associated Professional Sleep Societies. Sleep durations of greater than five to six hours increase the likelihood that these patients will achieve insomnia remission with cognitive behavioral therapy for insomnia (CBT-I), but do not affect the likelihood of depression remission. Sleep durations of seven or more hours optimize the likelihood of insomnia remission and depression remission in response to CBT-I.
In a 2015 consensus statement, the Sleep Research Society recommended seven or more hours of sleep per night for adults younger than 60. Investigations by Vgontzas and colleagues indicate that sleep durations of less than five hours and less than six hours are associated with increased morbidity and poor treatment response among patients with insomnia. “We wanted to know what [sleep-duration] cutoffs … might be better predictors of eventual insomnia and depression remission through treatment,” said Jack Edinger, PhD, Professor of Medicine at National Jewish Health in Denver.
An Analysis of the TRIAD Study
Dr. Edinger and colleagues conducted a secondary analysis of the TRIAD study, which examined whether combined treatment of depression and insomnia improves depression and sleep outcomes in participants with both disorders. Eligible participants met Diagnostic and Statistical Manual of Mental Disorders (4th ed.) criteria for major depression and primary insomnia, had a Hamilton Rating Scale for Depression (HAMD-17) score of 16 or greater, and had an Insomnia Severity Index (ISI) score of 11 or greater. People who had had psychotherapy in the previous four months, or had failed or could not tolerate previous adequate trials of the study medications, were excluded. Participants completed one night of baseline polysomnography before entering the treatment phase of the study.
The study population included 104 participants (75 women) with a mean age of 47. Mean baseline HAMD-17 score was 22, and mean baseline ISI score was 20.6. All participants received antidepressant medication (ie, citalopram, sertraline, or venlafaxine). Patients were randomized to CBT-I or sham (ie, a pseudo desensitization condition with sleep education). The investigators assessed participants biweekly with the HAMD-17 and the ISI. The treatment period lasted for 16 weeks.
CBT-I Provided Benefits
Participants with five or more hours of sleep were more likely to respond to CBT-I than participants with fewer than five hours of sleep. Among participants with sleep duration of five or more hours, insomnia remission was more likely with CBT-I than with the control condition. The five-hour cutoff had no association with depression remission.
Among participants with six or more hours of sleep, those who received CBT-I were more likely to achieve insomnia remission than controls. The six-hour cutoff did not affect the likelihood of depression remission, however.
Among participants with seven or more hours of sleep, those randomized to CBT-I were more likely to achieve insomnia remission and depression remission than controls.
“More research is needed to determine how best to achieve depression remission in those patients with less than seven hours of objective sleep duration prior to starting treatment,” Dr. Edinger concluded.
—Erik Greb
Suggested Reading
Bathgate CJ, Edinger JD, Krystal AD. Insomnia patients with objective short sleep duration have a blunted response to cognitive behavioral therapy for insomnia. Sleep. 2017;40(1).
Vgontzas AN, Liao D, Bixler EO, et al. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491-497.
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-844.
Topical Timolol May Improve Overall Scar Cosmesis in Acute Surgical Wounds
Timolol is a nonselective β-adrenergic receptor antagonist indicated for treating glaucoma, heart attacks, hypertension, and migraine headaches. It is made in both an oral and ophthalmic form. In dermatology, the beta-blocker propranolol is approved for the treatment of infantile hemangiomas (IHs). The exact mechanism of action of beta-blockers for the treatment of IHs is not yet completely understood, but it is postulated that they inhibit growth by at least 4 distinct mechanisms: (1) vasoconstriction, (2) inhibition of angiogenesis or vasculogenesis, (3) induction of apoptosis, and (4) recruitment of endothelial progenitor cells to the site of the hemangioma.1
Scar cosmesis can be calculated using the visual analog scale (VAS), which is a subjective scar assessment scored from poor to excellent. The multidimensional VAS is a photograph-based scale derived from evaluating standardized digital photographs in 4 dimensions—pigmentation, vascularity, acceptability, and observer comfort—plus contour. It uses the sum of the individual scores to obtain a single overall score ranging from excellent to poor.2 In this study, we sought to determine if the use of topical timolol after excision or Mohs micrographic surgery (MMS) treatment of nonmelanoma skin cancers improved the overall cosmesis of the scar.
Methods
The study protocol was approved by the institutional review board at Roger Williams Medical Center (Providence, Rhode Island). Eligibility criteria included patients who required excision or MMS for their nonmelanoma skin cancer located below the patella and those who agreed to allow their wounds to heal by secondary intention when given options for closure of their wounds. Patients were randomized to either the timolol (study medication) group or the saline (placebo) group. The initial defects were measured and photographed. Patients were educated on how to apply the study medication. All patients were prescribed 40 mm Hg compression stockings to wear following application of the study medication. Patients were asked to return at 1 and 5 weeks postsurgery and then every 1 to 2 weeks for wound assessment and measurement until their wounds had healed or at 13 weeks, depending on which came first. A healed wound was defined as having no exudate, exhibiting complete reepithelialization, and being stable for 1 week.
Healed wounds were assessed by a blinded outside dermatologist who examined photographs of the wounds and then completed the VAS for each participant’s scar.
Results
A total of 9 participants were enrolled in the study. Three participants were lost to follow-up; 6 completed the study (4 females, 2 males). The mean age was 70 years (age range, 46–89 years). The average wound size was 2×2 cm with a depth of 1 mm. Three participants were in the active medication group and 3 were in the control group.
A VAS was completed for each participant’s scar by an outside blinded dermatologist. Based on the VAS, wounds treated with timolol resulted in more cosmetically favorable scars (scored higher on the VAS) compared to control (mean [SD]: 6.5±0.9 vs 2.5±0.7; P<0.05). See Figures 1 and 2 for representative results.
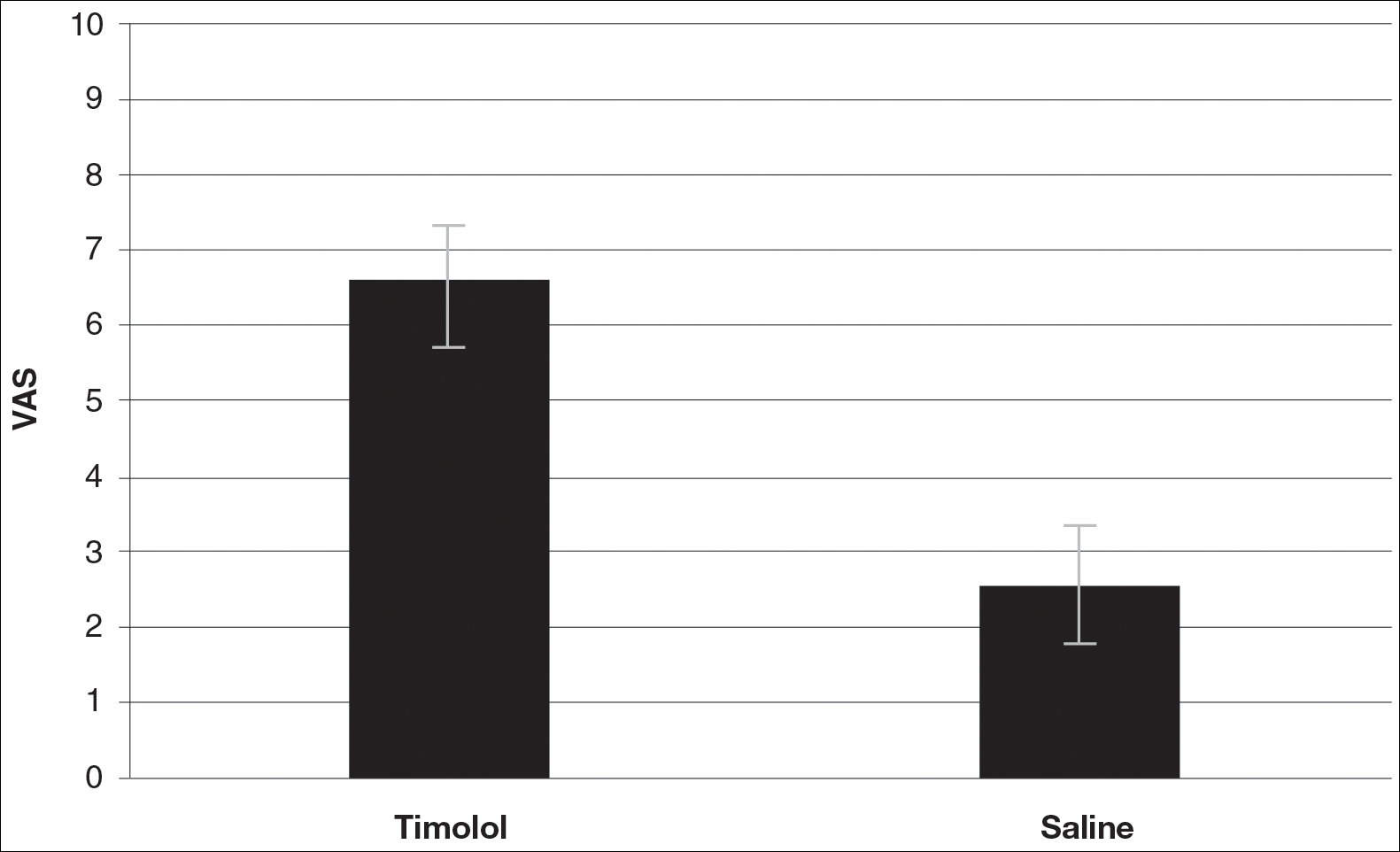
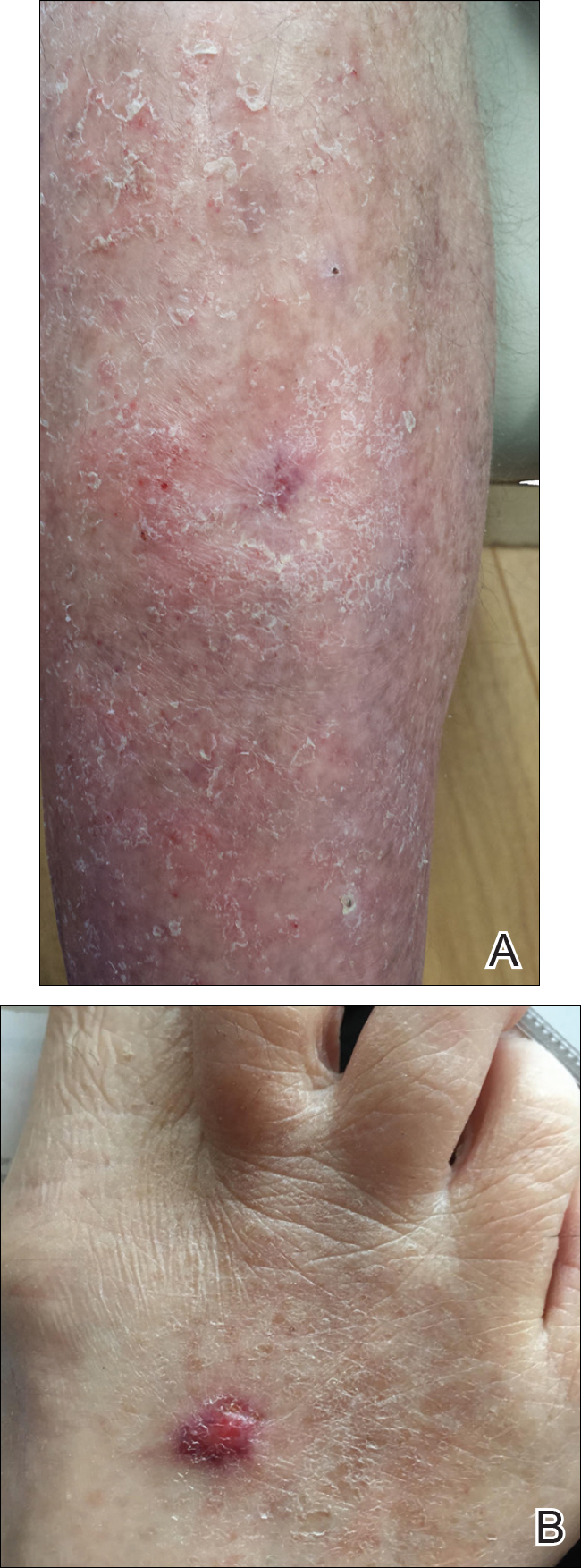
Comment
Dermatologists create acute wounds in patients on a daily basis. Ensuring that patients achieve the most desirable cosmetic outcome is a primary goal for dermatologists and an important component of patient satisfaction. A number of studies have examined patient satisfaction following MMS.3,4 Patient satisfaction is an especially important outcome measure in dermatology, as dermatologic diseases affect cosmetic appearance and are related to quality of life.3,4
Timolol is a nonselective β-adrenergic receptor antagonist that is used in dermatology to treat IHs. In this preliminary study, the authors sought to determine if topical timolol applied to acute wounds following surgical removal of nonmelanoma skin cancers could improve the overall cosmetic outcome of acute surgical scars. The results showed that compared to control, topical timolol resulted in a more cosmetically favorable scar. The results are preliminary, and it would be of future interest to further study the effects of topical timolol on acute surgical wounds from a wound-healing standpoint as well as to further test its effects on the cosmesis of these wounds.
- Chisholm KM, Chang KW, Truong MT, et al. β-Adrenergic receptor expression in vascular tumors [published online June 29, 2012]. Mod Pathol. 2012;25:1446-1451.
- Fearmonti R, Bond J, Erdmann D, et al. A review of scar scales and scar measuring devices. Eplasty. 2010;10:e43.
- Asgari MM, Warton EM, Neugebauer R, et al. Predictors of patient satisfaction with Mohs surgery: analysis of preoperative, intraoperative, and postoperative factors in a prospective cohort. Arch Dermatol. 2011;147:1387-1394.
- Asgari MM, Bertenthal D, Sen S, et al. Patient satisfaction after treatment of nonmelanoma skin cancer. Dermatol Surg. 2009;35:1041-1049.
Timolol is a nonselective β-adrenergic receptor antagonist indicated for treating glaucoma, heart attacks, hypertension, and migraine headaches. It is made in both an oral and ophthalmic form. In dermatology, the beta-blocker propranolol is approved for the treatment of infantile hemangiomas (IHs). The exact mechanism of action of beta-blockers for the treatment of IHs is not yet completely understood, but it is postulated that they inhibit growth by at least 4 distinct mechanisms: (1) vasoconstriction, (2) inhibition of angiogenesis or vasculogenesis, (3) induction of apoptosis, and (4) recruitment of endothelial progenitor cells to the site of the hemangioma.1
Scar cosmesis can be calculated using the visual analog scale (VAS), which is a subjective scar assessment scored from poor to excellent. The multidimensional VAS is a photograph-based scale derived from evaluating standardized digital photographs in 4 dimensions—pigmentation, vascularity, acceptability, and observer comfort—plus contour. It uses the sum of the individual scores to obtain a single overall score ranging from excellent to poor.2 In this study, we sought to determine if the use of topical timolol after excision or Mohs micrographic surgery (MMS) treatment of nonmelanoma skin cancers improved the overall cosmesis of the scar.
Methods
The study protocol was approved by the institutional review board at Roger Williams Medical Center (Providence, Rhode Island). Eligibility criteria included patients who required excision or MMS for their nonmelanoma skin cancer located below the patella and those who agreed to allow their wounds to heal by secondary intention when given options for closure of their wounds. Patients were randomized to either the timolol (study medication) group or the saline (placebo) group. The initial defects were measured and photographed. Patients were educated on how to apply the study medication. All patients were prescribed 40 mm Hg compression stockings to wear following application of the study medication. Patients were asked to return at 1 and 5 weeks postsurgery and then every 1 to 2 weeks for wound assessment and measurement until their wounds had healed or at 13 weeks, depending on which came first. A healed wound was defined as having no exudate, exhibiting complete reepithelialization, and being stable for 1 week.
Healed wounds were assessed by a blinded outside dermatologist who examined photographs of the wounds and then completed the VAS for each participant’s scar.
Results
A total of 9 participants were enrolled in the study. Three participants were lost to follow-up; 6 completed the study (4 females, 2 males). The mean age was 70 years (age range, 46–89 years). The average wound size was 2×2 cm with a depth of 1 mm. Three participants were in the active medication group and 3 were in the control group.
A VAS was completed for each participant’s scar by an outside blinded dermatologist. Based on the VAS, wounds treated with timolol resulted in more cosmetically favorable scars (scored higher on the VAS) compared to control (mean [SD]: 6.5±0.9 vs 2.5±0.7; P<0.05). See Figures 1 and 2 for representative results.
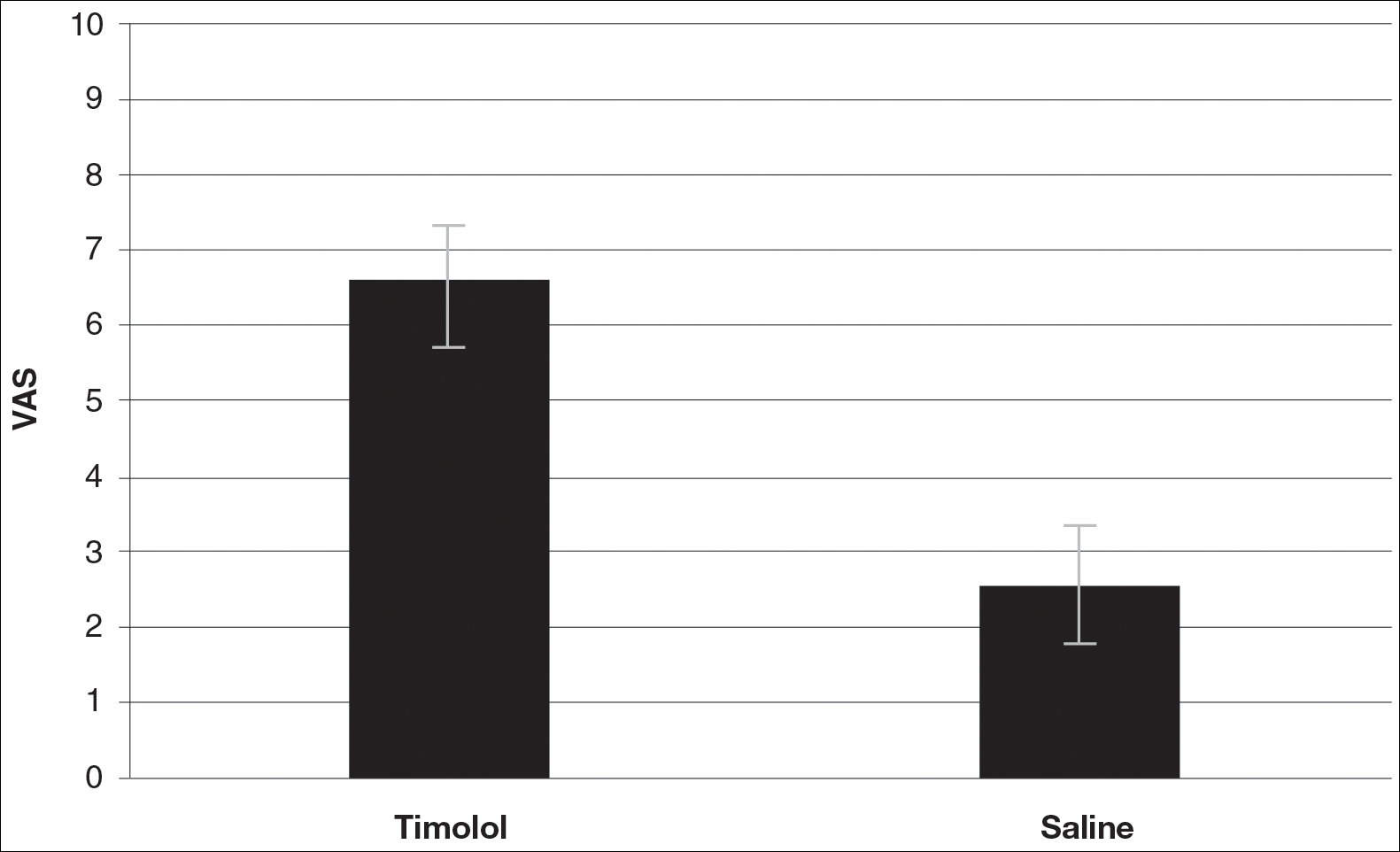
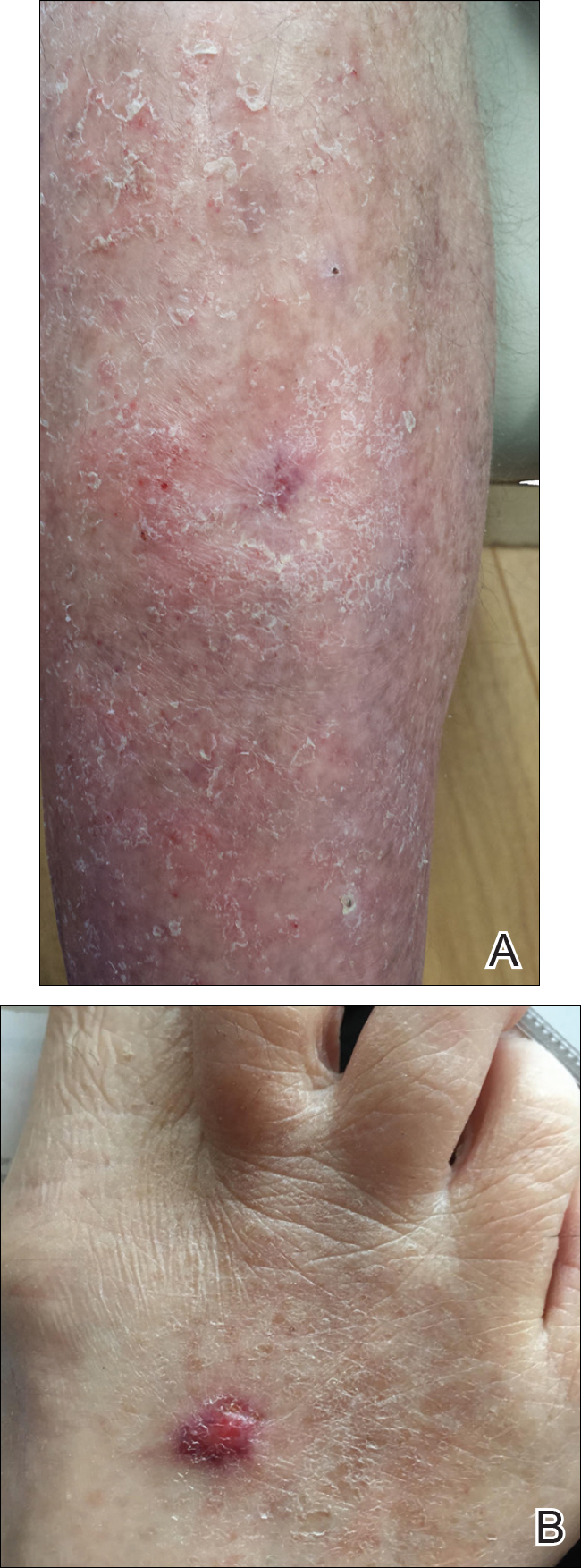
Comment
Dermatologists create acute wounds in patients on a daily basis. Ensuring that patients achieve the most desirable cosmetic outcome is a primary goal for dermatologists and an important component of patient satisfaction. A number of studies have examined patient satisfaction following MMS.3,4 Patient satisfaction is an especially important outcome measure in dermatology, as dermatologic diseases affect cosmetic appearance and are related to quality of life.3,4
Timolol is a nonselective β-adrenergic receptor antagonist that is used in dermatology to treat IHs. In this preliminary study, the authors sought to determine if topical timolol applied to acute wounds following surgical removal of nonmelanoma skin cancers could improve the overall cosmetic outcome of acute surgical scars. The results showed that compared to control, topical timolol resulted in a more cosmetically favorable scar. The results are preliminary, and it would be of future interest to further study the effects of topical timolol on acute surgical wounds from a wound-healing standpoint as well as to further test its effects on the cosmesis of these wounds.
Timolol is a nonselective β-adrenergic receptor antagonist indicated for treating glaucoma, heart attacks, hypertension, and migraine headaches. It is made in both an oral and ophthalmic form. In dermatology, the beta-blocker propranolol is approved for the treatment of infantile hemangiomas (IHs). The exact mechanism of action of beta-blockers for the treatment of IHs is not yet completely understood, but it is postulated that they inhibit growth by at least 4 distinct mechanisms: (1) vasoconstriction, (2) inhibition of angiogenesis or vasculogenesis, (3) induction of apoptosis, and (4) recruitment of endothelial progenitor cells to the site of the hemangioma.1
Scar cosmesis can be calculated using the visual analog scale (VAS), which is a subjective scar assessment scored from poor to excellent. The multidimensional VAS is a photograph-based scale derived from evaluating standardized digital photographs in 4 dimensions—pigmentation, vascularity, acceptability, and observer comfort—plus contour. It uses the sum of the individual scores to obtain a single overall score ranging from excellent to poor.2 In this study, we sought to determine if the use of topical timolol after excision or Mohs micrographic surgery (MMS) treatment of nonmelanoma skin cancers improved the overall cosmesis of the scar.
Methods
The study protocol was approved by the institutional review board at Roger Williams Medical Center (Providence, Rhode Island). Eligibility criteria included patients who required excision or MMS for their nonmelanoma skin cancer located below the patella and those who agreed to allow their wounds to heal by secondary intention when given options for closure of their wounds. Patients were randomized to either the timolol (study medication) group or the saline (placebo) group. The initial defects were measured and photographed. Patients were educated on how to apply the study medication. All patients were prescribed 40 mm Hg compression stockings to wear following application of the study medication. Patients were asked to return at 1 and 5 weeks postsurgery and then every 1 to 2 weeks for wound assessment and measurement until their wounds had healed or at 13 weeks, depending on which came first. A healed wound was defined as having no exudate, exhibiting complete reepithelialization, and being stable for 1 week.
Healed wounds were assessed by a blinded outside dermatologist who examined photographs of the wounds and then completed the VAS for each participant’s scar.
Results
A total of 9 participants were enrolled in the study. Three participants were lost to follow-up; 6 completed the study (4 females, 2 males). The mean age was 70 years (age range, 46–89 years). The average wound size was 2×2 cm with a depth of 1 mm. Three participants were in the active medication group and 3 were in the control group.
A VAS was completed for each participant’s scar by an outside blinded dermatologist. Based on the VAS, wounds treated with timolol resulted in more cosmetically favorable scars (scored higher on the VAS) compared to control (mean [SD]: 6.5±0.9 vs 2.5±0.7; P<0.05). See Figures 1 and 2 for representative results.
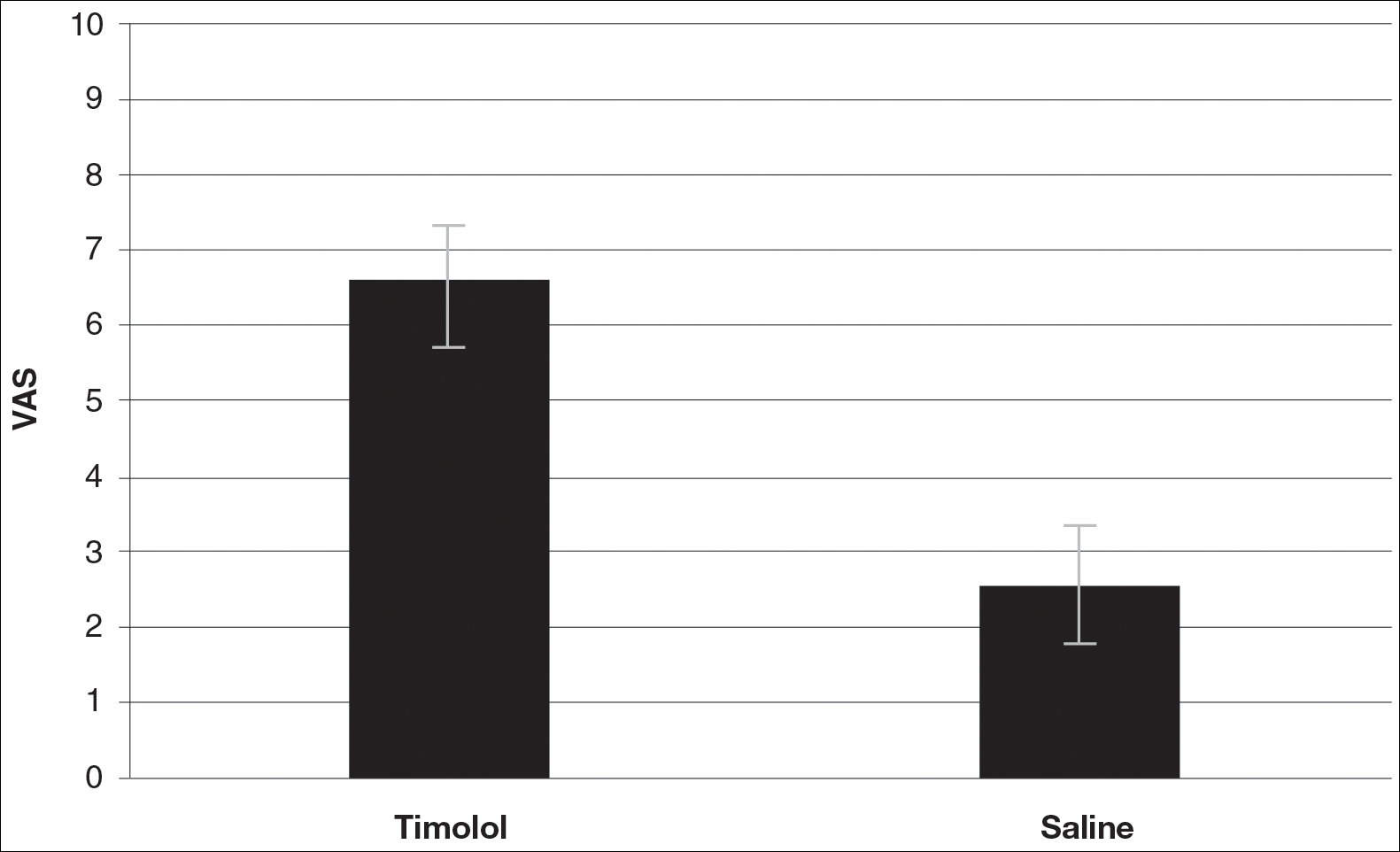
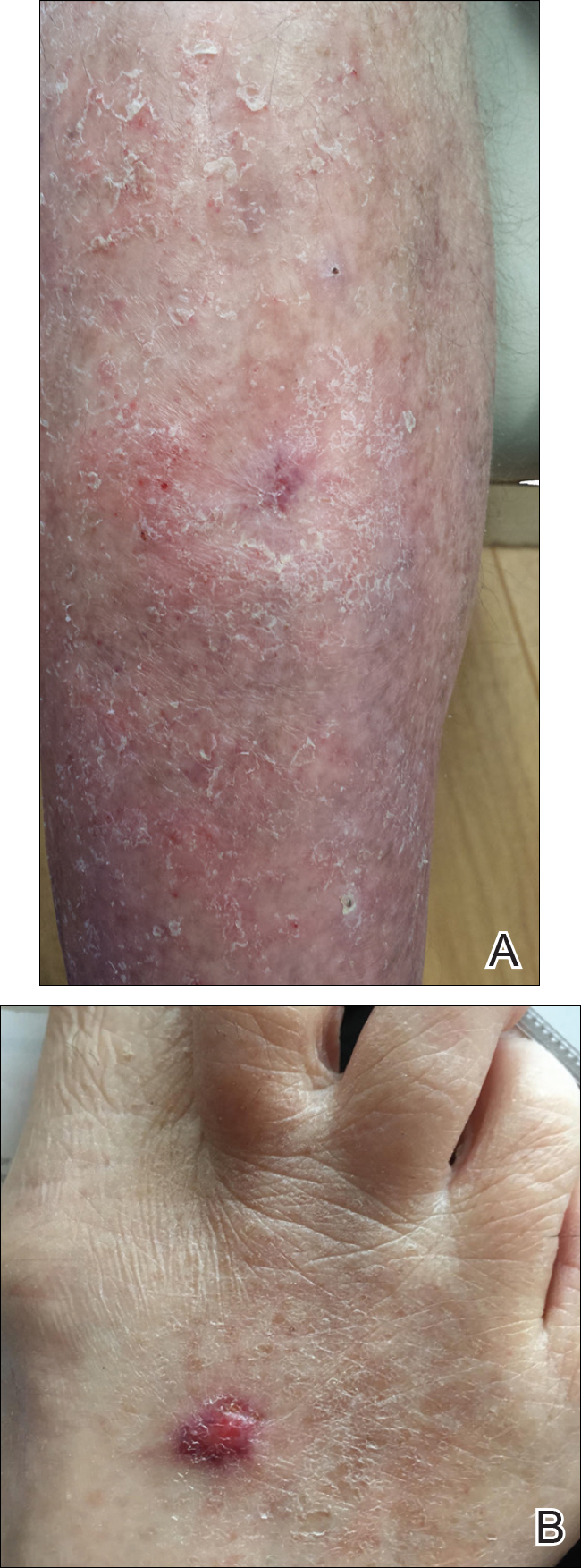
Comment
Dermatologists create acute wounds in patients on a daily basis. Ensuring that patients achieve the most desirable cosmetic outcome is a primary goal for dermatologists and an important component of patient satisfaction. A number of studies have examined patient satisfaction following MMS.3,4 Patient satisfaction is an especially important outcome measure in dermatology, as dermatologic diseases affect cosmetic appearance and are related to quality of life.3,4
Timolol is a nonselective β-adrenergic receptor antagonist that is used in dermatology to treat IHs. In this preliminary study, the authors sought to determine if topical timolol applied to acute wounds following surgical removal of nonmelanoma skin cancers could improve the overall cosmetic outcome of acute surgical scars. The results showed that compared to control, topical timolol resulted in a more cosmetically favorable scar. The results are preliminary, and it would be of future interest to further study the effects of topical timolol on acute surgical wounds from a wound-healing standpoint as well as to further test its effects on the cosmesis of these wounds.
- Chisholm KM, Chang KW, Truong MT, et al. β-Adrenergic receptor expression in vascular tumors [published online June 29, 2012]. Mod Pathol. 2012;25:1446-1451.
- Fearmonti R, Bond J, Erdmann D, et al. A review of scar scales and scar measuring devices. Eplasty. 2010;10:e43.
- Asgari MM, Warton EM, Neugebauer R, et al. Predictors of patient satisfaction with Mohs surgery: analysis of preoperative, intraoperative, and postoperative factors in a prospective cohort. Arch Dermatol. 2011;147:1387-1394.
- Asgari MM, Bertenthal D, Sen S, et al. Patient satisfaction after treatment of nonmelanoma skin cancer. Dermatol Surg. 2009;35:1041-1049.
- Chisholm KM, Chang KW, Truong MT, et al. β-Adrenergic receptor expression in vascular tumors [published online June 29, 2012]. Mod Pathol. 2012;25:1446-1451.
- Fearmonti R, Bond J, Erdmann D, et al. A review of scar scales and scar measuring devices. Eplasty. 2010;10:e43.
- Asgari MM, Warton EM, Neugebauer R, et al. Predictors of patient satisfaction with Mohs surgery: analysis of preoperative, intraoperative, and postoperative factors in a prospective cohort. Arch Dermatol. 2011;147:1387-1394.
- Asgari MM, Bertenthal D, Sen S, et al. Patient satisfaction after treatment of nonmelanoma skin cancer. Dermatol Surg. 2009;35:1041-1049.
Resident Pearl
- Dermatologists create acute surgical wounds on a daily basis. We should strive for excellent patient outcomes as well as the most desirable cosmetic result. This research article points to a possible new application of a longstanding medication to improve the cosmetic outcome in acute surgical wounds.
Better bariatric surgery outcomes with lower preoperative BMI
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according toa paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Patients with obesity need a multidisciplinary approach to achieve a healthy weight, and AGA believes that gastroenterologists are in a unique position to lead the care team.
To provide gastroenterologists with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management, including a model for how to operationalize business issues, AGA has created an Obesity Practice Guide. The program includes an obesity program to help gastroenterologists manage their patients with obesity, as well as a framework focused on the business operational issues related to the management of obese patients. Learn more at www.gastro.org/obesity.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according toa paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Patients with obesity need a multidisciplinary approach to achieve a healthy weight, and AGA believes that gastroenterologists are in a unique position to lead the care team.
To provide gastroenterologists with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management, including a model for how to operationalize business issues, AGA has created an Obesity Practice Guide. The program includes an obesity program to help gastroenterologists manage their patients with obesity, as well as a framework focused on the business operational issues related to the management of obese patients. Learn more at www.gastro.org/obesity.
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according toa paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Patients with obesity need a multidisciplinary approach to achieve a healthy weight, and AGA believes that gastroenterologists are in a unique position to lead the care team.
To provide gastroenterologists with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management, including a model for how to operationalize business issues, AGA has created an Obesity Practice Guide. The program includes an obesity program to help gastroenterologists manage their patients with obesity, as well as a framework focused on the business operational issues related to the management of obese patients. Learn more at www.gastro.org/obesity.
FROM JAMA SURGERY
Key clinical point: A BMI below 40 prior to undergoing bariatric surgery gives patients a significantly better chance of achieving a 1-year postoperative BMI under 30.
Major finding: Obese patients with a BMI less than 40 before undergoing bariatric surgery are more than 12 times more likely to achieve a postoperative BMI of under 30.
Data source: A retrospective study using prospectively gathered clinical data of 27, 320 adults who underwent bariatric surgery.
Disclosures: Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Elective open conversion after failed EVAR safer than emergent
Emergency open conversion after failed endovascular aortic aneurysm repair shows significantly higher mortality and morbidity, compared with elective conversion, according to the results of a retrospective, observational study of 31 patients at a single institution.
The primary endpoints of the study were 30-day and in-hospital mortality. Secondary endpoints included moderate to severe complications, secondary interventions, length of ICU stay, and length of hospital stay (LOS), according to I. Ben Abdallah, MD, of the Hôpital Européen Georges Pompidou and his colleagues.
During the study period, a total of 338 patients received EVAR at the institution. Of these, 31 patients underwent open conversion (19 elective, 12 emergent) after EVAR between August 2008 and September 2016. The median time from the index EVAR to the open conversion was 35 months, with the most common indications for intervention being endoleaks (24 patients, 77%), stent graft infection (3, 10%), thrombosis (3, 10%) and kinking (1, 3%). Stents removed were manufactured by various device makers, according to the report (Eur J Vasc Endovasc Surg. 2017;53:831-6).
The patient population had a mean age of 73 years and comprised 84% men. The two groups, elective and emergent, were highly similar in numerous comorbidities, with the only significant difference between them being a greater incidence of chronic renal disease among the emergent group, as compared with the elective (42% vs. 5%).
Overall in-hospital mortality was 10%, and significantly greater in emergent vs. elective conversion (25% vs. 0%). Renal and pulmonary complications were significantly higher in the emergency group (42% vs. 5% and 42% vs. 0%, respectively). There was no significant difference between elective and emergent hospital stay (14 days vs. 20 days), but ICU stay was significantly shorter for elective conversion (2 days vs. 7 days).
There were no late complications or death seen in either group after a mean follow-up of 18 months.
“In this series, open conversion seems to be significantly safer and more effective when performed electively with no mortality, a lower incidence of morbidity (renal and pulmonary), and shorter ICU stay. These results underline that close surveillance, allowing planned elective open conversion, is the key to better outcomes after failed EVAR,” the researchers concluded.
The authors reported that they had no conflicts of interest, and the study received no outside funding.
Emergency open conversion after failed endovascular aortic aneurysm repair shows significantly higher mortality and morbidity, compared with elective conversion, according to the results of a retrospective, observational study of 31 patients at a single institution.
The primary endpoints of the study were 30-day and in-hospital mortality. Secondary endpoints included moderate to severe complications, secondary interventions, length of ICU stay, and length of hospital stay (LOS), according to I. Ben Abdallah, MD, of the Hôpital Européen Georges Pompidou and his colleagues.
During the study period, a total of 338 patients received EVAR at the institution. Of these, 31 patients underwent open conversion (19 elective, 12 emergent) after EVAR between August 2008 and September 2016. The median time from the index EVAR to the open conversion was 35 months, with the most common indications for intervention being endoleaks (24 patients, 77%), stent graft infection (3, 10%), thrombosis (3, 10%) and kinking (1, 3%). Stents removed were manufactured by various device makers, according to the report (Eur J Vasc Endovasc Surg. 2017;53:831-6).
The patient population had a mean age of 73 years and comprised 84% men. The two groups, elective and emergent, were highly similar in numerous comorbidities, with the only significant difference between them being a greater incidence of chronic renal disease among the emergent group, as compared with the elective (42% vs. 5%).
Overall in-hospital mortality was 10%, and significantly greater in emergent vs. elective conversion (25% vs. 0%). Renal and pulmonary complications were significantly higher in the emergency group (42% vs. 5% and 42% vs. 0%, respectively). There was no significant difference between elective and emergent hospital stay (14 days vs. 20 days), but ICU stay was significantly shorter for elective conversion (2 days vs. 7 days).
There were no late complications or death seen in either group after a mean follow-up of 18 months.
“In this series, open conversion seems to be significantly safer and more effective when performed electively with no mortality, a lower incidence of morbidity (renal and pulmonary), and shorter ICU stay. These results underline that close surveillance, allowing planned elective open conversion, is the key to better outcomes after failed EVAR,” the researchers concluded.
The authors reported that they had no conflicts of interest, and the study received no outside funding.
Emergency open conversion after failed endovascular aortic aneurysm repair shows significantly higher mortality and morbidity, compared with elective conversion, according to the results of a retrospective, observational study of 31 patients at a single institution.
The primary endpoints of the study were 30-day and in-hospital mortality. Secondary endpoints included moderate to severe complications, secondary interventions, length of ICU stay, and length of hospital stay (LOS), according to I. Ben Abdallah, MD, of the Hôpital Européen Georges Pompidou and his colleagues.
During the study period, a total of 338 patients received EVAR at the institution. Of these, 31 patients underwent open conversion (19 elective, 12 emergent) after EVAR between August 2008 and September 2016. The median time from the index EVAR to the open conversion was 35 months, with the most common indications for intervention being endoleaks (24 patients, 77%), stent graft infection (3, 10%), thrombosis (3, 10%) and kinking (1, 3%). Stents removed were manufactured by various device makers, according to the report (Eur J Vasc Endovasc Surg. 2017;53:831-6).
The patient population had a mean age of 73 years and comprised 84% men. The two groups, elective and emergent, were highly similar in numerous comorbidities, with the only significant difference between them being a greater incidence of chronic renal disease among the emergent group, as compared with the elective (42% vs. 5%).
Overall in-hospital mortality was 10%, and significantly greater in emergent vs. elective conversion (25% vs. 0%). Renal and pulmonary complications were significantly higher in the emergency group (42% vs. 5% and 42% vs. 0%, respectively). There was no significant difference between elective and emergent hospital stay (14 days vs. 20 days), but ICU stay was significantly shorter for elective conversion (2 days vs. 7 days).
There were no late complications or death seen in either group after a mean follow-up of 18 months.
“In this series, open conversion seems to be significantly safer and more effective when performed electively with no mortality, a lower incidence of morbidity (renal and pulmonary), and shorter ICU stay. These results underline that close surveillance, allowing planned elective open conversion, is the key to better outcomes after failed EVAR,” the researchers concluded.
The authors reported that they had no conflicts of interest, and the study received no outside funding.
FROM THE EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point:
Major finding: Overall in-hospital mortality was 10% and significantly greater in emergent vs. elective conversion (25% vs. 0%).
Data source: A retrospective database analysis of 31 patients undergoing EVAR open conversion at a single institution.
Disclosures: The authors reported that they had no conflicts of interest, and the study received no outside funding.