User login
Pharyngeal reservoir drives gonorrhea epidemic in gay men
VIENNA – , Colm O’Mahony, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“We think pharyngeal gonorrhea is now the most important factor in this continuing epidemic,” according to Dr. O’Mahony, professor of medicine and a venereologist at the University of Chester (England).
Recent studies have shown that men can carry Neisseria gonorrhoeae in their throats for weeks or months without symptoms and can readily spread the infection through unprotected oral sex.
Also, surveys of men who have sex with men (MSM) indicate that saliva is commonly used as a lubricant for anal sex. Australian investigators have estimated that about half of rectal gonorrhea in MSM would be eliminated if they stopped using their partner’s saliva for this purpose (Sex Trans Infect. 2016 Mar 3. pii:sextrans-2015-052502. doi: 10.1136/sextrans-2015-052502).
And then there is French kissing.
“Men don’t go out to a nightclub and have indiscriminate anal sex anymore. It’s not like that,” according to Dr. O’Mahony. “But they do kiss quite a lot of other men over the course of an evening, and it’s deep kissing. They may French kiss 15-20 other young men. And we think there’s actually a significant risk of transmission of gonorrhea from this simple deep kissing.”
Indeed, Australian investigators are now conducting a study examining whether having young gay men take a bottle of mouthwash with them when they go clubbing so they can take a good swish in between kissing will protect against N. gonorrhoeae infection.
“Apparently gonorrhea is quite sensitive to mouthwashes like Listerine. So we await those study results with interest,” he continued.
Dr. O’Mahony warned that the problem of multidrug-resistant gonorrhea is further along than most noninfectious disease experts realize. That’s a frightening prospect, given that an estimated 800,000 cases of gonorrhea occur annually in the United States alone. Because of well-documented treatment failures with cefixime and other oral cephalosporins, the Centers for Disease Control and Prevention now recommends only one regimen for the treatment of gonorrhea: dual treatment with a single intramuscular dose of 250 mg of ceftriaxone (Rocephin) plus 1 g of azithromycin in a single dose.
“There have already been some cases of ceftriaxone-resistant gonorrhea reported in Japan, Spain, and other parts of Europe. And we’re now seeing azithromycin-resistant gonorrhea throughout the U.K., which is a problem. So we are really worried that we will end up with untreatable gonorrhea within a couple of years,” Dr. O’Mahony said.
The evolving antimicrobial resistance scenario is reminiscent of the quinolone experience, he added.
“In 1992, I published the first reported case of quinolone-resistant gonorrhea in Liverpool. Five years later we had to stop using quinolones because more than 10% of gonorrhea was resistant,” the venereologist said.
In mid-2016 the CDC published the first-ever comprehensive data from its Gonococcal Isolate Surveillance Project. An analysis of more than 5,000 N. gonorrhoeae isolates obtained from men with gonococcal urethritis presenting at U.S. STD clinics showed that 25.3% of samples were resistant to tetracycline, 19.2% to ciprofloxacin, and 16.2% to penicillin. The prevalence of reduced azithromycin susceptibility jumped from 0.6% in 2013 to 2.5% in 2014. Reduced ceftriaxone susceptibility doubled from 0.4% in 2013 to 0.8% the following year. Antimicrobial susceptibility patterns varied by geographic region, with the highest rates of reduced susceptibility being seen in the Midwest and among MSM (MMWR Surveill Summ. 2016;65[No. SS-7]:1–19. doi: 10.15585/mmwr.ss6507a1).
Dr. O’Mahony reported having no relevant financial conflicts.
VIENNA – , Colm O’Mahony, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“We think pharyngeal gonorrhea is now the most important factor in this continuing epidemic,” according to Dr. O’Mahony, professor of medicine and a venereologist at the University of Chester (England).
Recent studies have shown that men can carry Neisseria gonorrhoeae in their throats for weeks or months without symptoms and can readily spread the infection through unprotected oral sex.
Also, surveys of men who have sex with men (MSM) indicate that saliva is commonly used as a lubricant for anal sex. Australian investigators have estimated that about half of rectal gonorrhea in MSM would be eliminated if they stopped using their partner’s saliva for this purpose (Sex Trans Infect. 2016 Mar 3. pii:sextrans-2015-052502. doi: 10.1136/sextrans-2015-052502).
And then there is French kissing.
“Men don’t go out to a nightclub and have indiscriminate anal sex anymore. It’s not like that,” according to Dr. O’Mahony. “But they do kiss quite a lot of other men over the course of an evening, and it’s deep kissing. They may French kiss 15-20 other young men. And we think there’s actually a significant risk of transmission of gonorrhea from this simple deep kissing.”
Indeed, Australian investigators are now conducting a study examining whether having young gay men take a bottle of mouthwash with them when they go clubbing so they can take a good swish in between kissing will protect against N. gonorrhoeae infection.
“Apparently gonorrhea is quite sensitive to mouthwashes like Listerine. So we await those study results with interest,” he continued.
Dr. O’Mahony warned that the problem of multidrug-resistant gonorrhea is further along than most noninfectious disease experts realize. That’s a frightening prospect, given that an estimated 800,000 cases of gonorrhea occur annually in the United States alone. Because of well-documented treatment failures with cefixime and other oral cephalosporins, the Centers for Disease Control and Prevention now recommends only one regimen for the treatment of gonorrhea: dual treatment with a single intramuscular dose of 250 mg of ceftriaxone (Rocephin) plus 1 g of azithromycin in a single dose.
“There have already been some cases of ceftriaxone-resistant gonorrhea reported in Japan, Spain, and other parts of Europe. And we’re now seeing azithromycin-resistant gonorrhea throughout the U.K., which is a problem. So we are really worried that we will end up with untreatable gonorrhea within a couple of years,” Dr. O’Mahony said.
The evolving antimicrobial resistance scenario is reminiscent of the quinolone experience, he added.
“In 1992, I published the first reported case of quinolone-resistant gonorrhea in Liverpool. Five years later we had to stop using quinolones because more than 10% of gonorrhea was resistant,” the venereologist said.
In mid-2016 the CDC published the first-ever comprehensive data from its Gonococcal Isolate Surveillance Project. An analysis of more than 5,000 N. gonorrhoeae isolates obtained from men with gonococcal urethritis presenting at U.S. STD clinics showed that 25.3% of samples were resistant to tetracycline, 19.2% to ciprofloxacin, and 16.2% to penicillin. The prevalence of reduced azithromycin susceptibility jumped from 0.6% in 2013 to 2.5% in 2014. Reduced ceftriaxone susceptibility doubled from 0.4% in 2013 to 0.8% the following year. Antimicrobial susceptibility patterns varied by geographic region, with the highest rates of reduced susceptibility being seen in the Midwest and among MSM (MMWR Surveill Summ. 2016;65[No. SS-7]:1–19. doi: 10.15585/mmwr.ss6507a1).
Dr. O’Mahony reported having no relevant financial conflicts.
VIENNA – , Colm O’Mahony, MD, said at the annual congress of the European Academy of Dermatology and Venereology.
“We think pharyngeal gonorrhea is now the most important factor in this continuing epidemic,” according to Dr. O’Mahony, professor of medicine and a venereologist at the University of Chester (England).
Recent studies have shown that men can carry Neisseria gonorrhoeae in their throats for weeks or months without symptoms and can readily spread the infection through unprotected oral sex.
Also, surveys of men who have sex with men (MSM) indicate that saliva is commonly used as a lubricant for anal sex. Australian investigators have estimated that about half of rectal gonorrhea in MSM would be eliminated if they stopped using their partner’s saliva for this purpose (Sex Trans Infect. 2016 Mar 3. pii:sextrans-2015-052502. doi: 10.1136/sextrans-2015-052502).
And then there is French kissing.
“Men don’t go out to a nightclub and have indiscriminate anal sex anymore. It’s not like that,” according to Dr. O’Mahony. “But they do kiss quite a lot of other men over the course of an evening, and it’s deep kissing. They may French kiss 15-20 other young men. And we think there’s actually a significant risk of transmission of gonorrhea from this simple deep kissing.”
Indeed, Australian investigators are now conducting a study examining whether having young gay men take a bottle of mouthwash with them when they go clubbing so they can take a good swish in between kissing will protect against N. gonorrhoeae infection.
“Apparently gonorrhea is quite sensitive to mouthwashes like Listerine. So we await those study results with interest,” he continued.
Dr. O’Mahony warned that the problem of multidrug-resistant gonorrhea is further along than most noninfectious disease experts realize. That’s a frightening prospect, given that an estimated 800,000 cases of gonorrhea occur annually in the United States alone. Because of well-documented treatment failures with cefixime and other oral cephalosporins, the Centers for Disease Control and Prevention now recommends only one regimen for the treatment of gonorrhea: dual treatment with a single intramuscular dose of 250 mg of ceftriaxone (Rocephin) plus 1 g of azithromycin in a single dose.
“There have already been some cases of ceftriaxone-resistant gonorrhea reported in Japan, Spain, and other parts of Europe. And we’re now seeing azithromycin-resistant gonorrhea throughout the U.K., which is a problem. So we are really worried that we will end up with untreatable gonorrhea within a couple of years,” Dr. O’Mahony said.
The evolving antimicrobial resistance scenario is reminiscent of the quinolone experience, he added.
“In 1992, I published the first reported case of quinolone-resistant gonorrhea in Liverpool. Five years later we had to stop using quinolones because more than 10% of gonorrhea was resistant,” the venereologist said.
In mid-2016 the CDC published the first-ever comprehensive data from its Gonococcal Isolate Surveillance Project. An analysis of more than 5,000 N. gonorrhoeae isolates obtained from men with gonococcal urethritis presenting at U.S. STD clinics showed that 25.3% of samples were resistant to tetracycline, 19.2% to ciprofloxacin, and 16.2% to penicillin. The prevalence of reduced azithromycin susceptibility jumped from 0.6% in 2013 to 2.5% in 2014. Reduced ceftriaxone susceptibility doubled from 0.4% in 2013 to 0.8% the following year. Antimicrobial susceptibility patterns varied by geographic region, with the highest rates of reduced susceptibility being seen in the Midwest and among MSM (MMWR Surveill Summ. 2016;65[No. SS-7]:1–19. doi: 10.15585/mmwr.ss6507a1).
Dr. O’Mahony reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM THE EADV CONGRESS
Rate of mosaicism in parents of children with epileptic encephalopathy likely underestimated
HOUSTON – The rate of parental mosaicism in children with sporadic cases of epileptic encephalopathy and an apparent de novo mutation is believed to be at least 10%, which is much higher than previously thought.
The discovery, which was revealed with advanced genetic testing methods, underscores the need to rethink how parents of children with epileptic encephalopathy are counseled with regard to family planning, lead study author Candace T. Myers, PhD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “Generally, families are counseled with a recurrence risk of 1%-3%, but we found that in 10% of our families their recurrence risk is much higher because we’re able to see the genetic mutation in either blood or saliva of an unaffected parent,” said Dr. Myers of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle. “If we’re able to detect it in either of those tissues that means that the level in their gametes is much higher than just a single cell or a handful of cells, which is usually how people think about de novo mutations. What we’re finding is that in 10% of cases these mutations happen during embryonic development of the parent.”
Dr. Myers reported that of the 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers. The fraction of mutant alleles identified ranged from 3%-25%, which are levels that would pass undetected by traditional Sanger sequencing methods. In three families where a mosaic parent was identified, there were multiple affected children. The finding “opens up more questions for families that are thinking about future pregnancies,” she said. “I think we should have more genetic counselors working with pediatric neurologists to facilitate those discussions.”
She acknowledged certain limitations of the study, including the fact that DNA samples were extracted only from blood and saliva. “If the mutation is not present or detected in those particular tissues, it is still possible for the parent to be a germline carrier,” Dr. Myers said. “The most relevant tissue type for us to be testing would be the sex cells. We’ll have to look for families to see if they’re willing to donate [those cells] for future studies.”
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
HOUSTON – The rate of parental mosaicism in children with sporadic cases of epileptic encephalopathy and an apparent de novo mutation is believed to be at least 10%, which is much higher than previously thought.
The discovery, which was revealed with advanced genetic testing methods, underscores the need to rethink how parents of children with epileptic encephalopathy are counseled with regard to family planning, lead study author Candace T. Myers, PhD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “Generally, families are counseled with a recurrence risk of 1%-3%, but we found that in 10% of our families their recurrence risk is much higher because we’re able to see the genetic mutation in either blood or saliva of an unaffected parent,” said Dr. Myers of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle. “If we’re able to detect it in either of those tissues that means that the level in their gametes is much higher than just a single cell or a handful of cells, which is usually how people think about de novo mutations. What we’re finding is that in 10% of cases these mutations happen during embryonic development of the parent.”
Dr. Myers reported that of the 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers. The fraction of mutant alleles identified ranged from 3%-25%, which are levels that would pass undetected by traditional Sanger sequencing methods. In three families where a mosaic parent was identified, there were multiple affected children. The finding “opens up more questions for families that are thinking about future pregnancies,” she said. “I think we should have more genetic counselors working with pediatric neurologists to facilitate those discussions.”
She acknowledged certain limitations of the study, including the fact that DNA samples were extracted only from blood and saliva. “If the mutation is not present or detected in those particular tissues, it is still possible for the parent to be a germline carrier,” Dr. Myers said. “The most relevant tissue type for us to be testing would be the sex cells. We’ll have to look for families to see if they’re willing to donate [those cells] for future studies.”
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
HOUSTON – The rate of parental mosaicism in children with sporadic cases of epileptic encephalopathy and an apparent de novo mutation is believed to be at least 10%, which is much higher than previously thought.
The discovery, which was revealed with advanced genetic testing methods, underscores the need to rethink how parents of children with epileptic encephalopathy are counseled with regard to family planning, lead study author Candace T. Myers, PhD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “Generally, families are counseled with a recurrence risk of 1%-3%, but we found that in 10% of our families their recurrence risk is much higher because we’re able to see the genetic mutation in either blood or saliva of an unaffected parent,” said Dr. Myers of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle. “If we’re able to detect it in either of those tissues that means that the level in their gametes is much higher than just a single cell or a handful of cells, which is usually how people think about de novo mutations. What we’re finding is that in 10% of cases these mutations happen during embryonic development of the parent.”
Dr. Myers reported that of the 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers. The fraction of mutant alleles identified ranged from 3%-25%, which are levels that would pass undetected by traditional Sanger sequencing methods. In three families where a mosaic parent was identified, there were multiple affected children. The finding “opens up more questions for families that are thinking about future pregnancies,” she said. “I think we should have more genetic counselors working with pediatric neurologists to facilitate those discussions.”
She acknowledged certain limitations of the study, including the fact that DNA samples were extracted only from blood and saliva. “If the mutation is not present or detected in those particular tissues, it is still possible for the parent to be a germline carrier,” Dr. Myers said. “The most relevant tissue type for us to be testing would be the sex cells. We’ll have to look for families to see if they’re willing to donate [those cells] for future studies.”
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: Of 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers.
Data source: Screening of 109 families where the affected child’s epileptic encephalopathy was attributed to a substitution or small indel in 1 of 31 established epilepsy genes and reported as “de novo” by either clinical or research analysis of parental DNA.
Disclosures: The study was funded by National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
VIDEO: Addition of antibody drug conjugate produces deep AML remissions
SAN DIEGO – After more than four decades of near stagnation in the treatment of patients with acute myeloid leukemia (AML), investigators are beginning to identify drugs that can produce rapid and deep complete remissions, which recent evidence suggests are associated with prolonged survival.
In this video interview at the annual meeting of the American Society of Hematology, Harry P. Erba, MD, PhD, professor of medicine, University of Alabama, Birmingham, describes the early results of one such agent, a novel antibody drug conjugate called vadastuximab talirine, or 33A for short. In the phase Ib clinical trial of induction therapy for newly diagnosed AML, a combination of standard 7+3 induction chemotherapy with cytarabine and daunorubicin plus 33A was associated with a 76% composite rate of complete remissions or complete remissions with incomplete recovery of platelets.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – After more than four decades of near stagnation in the treatment of patients with acute myeloid leukemia (AML), investigators are beginning to identify drugs that can produce rapid and deep complete remissions, which recent evidence suggests are associated with prolonged survival.
In this video interview at the annual meeting of the American Society of Hematology, Harry P. Erba, MD, PhD, professor of medicine, University of Alabama, Birmingham, describes the early results of one such agent, a novel antibody drug conjugate called vadastuximab talirine, or 33A for short. In the phase Ib clinical trial of induction therapy for newly diagnosed AML, a combination of standard 7+3 induction chemotherapy with cytarabine and daunorubicin plus 33A was associated with a 76% composite rate of complete remissions or complete remissions with incomplete recovery of platelets.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – After more than four decades of near stagnation in the treatment of patients with acute myeloid leukemia (AML), investigators are beginning to identify drugs that can produce rapid and deep complete remissions, which recent evidence suggests are associated with prolonged survival.
In this video interview at the annual meeting of the American Society of Hematology, Harry P. Erba, MD, PhD, professor of medicine, University of Alabama, Birmingham, describes the early results of one such agent, a novel antibody drug conjugate called vadastuximab talirine, or 33A for short. In the phase Ib clinical trial of induction therapy for newly diagnosed AML, a combination of standard 7+3 induction chemotherapy with cytarabine and daunorubicin plus 33A was associated with a 76% composite rate of complete remissions or complete remissions with incomplete recovery of platelets.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2016
Psoriasis and Internal Disease: Report From the Mount Sinai Winter Symposium
At the 19th Annual Mount Sinai Winter Symposium, Dr. Jashin J. Wu spoke about psoriasis and internal disease. He discussed psoriasis and noncardiovascular comorbidities as well as cardiovascular comorbidities. Dr. Wu also addressed if treating psoriasis can improve cardiovascular disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At the 19th Annual Mount Sinai Winter Symposium, Dr. Jashin J. Wu spoke about psoriasis and internal disease. He discussed psoriasis and noncardiovascular comorbidities as well as cardiovascular comorbidities. Dr. Wu also addressed if treating psoriasis can improve cardiovascular disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At the 19th Annual Mount Sinai Winter Symposium, Dr. Jashin J. Wu spoke about psoriasis and internal disease. He discussed psoriasis and noncardiovascular comorbidities as well as cardiovascular comorbidities. Dr. Wu also addressed if treating psoriasis can improve cardiovascular disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Mycotic Septic Arthritis of the Ankle Joint
Septic arthritis is a common orthopedic emergency. The most common causative organism is Staphylococcus aureus. Mycotic infections, such as those involving Candida organisms, are much less common but just as debilitating. Delayed diagnosis of septic arthritis caused by Candida infection may result in increased morbidity, making treatment more challenging. Here we report a case of Candida albicans septic arthritis of the ankle and subtalar joint in a patient with diabetes mellitus (DM) and rheumatoid arthritis (RA). The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 52-year-old woman with type 2 DM (requiring subcutaneous insulin analogue therapy) and RA presented to a local emergency department with a 3-day history of right ankle pain after having the subtalar joint injected with steroid by a rheumatologist 4 weeks earlier. For about 2 weeks, there was purulent discharge from the peroneal sheath. The patient’s RA was being treated with prednisolone (maintenance therapy). Physical examination revealed low-grade pyrexia (37.8°C) and difficulty bearing full weight on the ankle. Clinically, the joint was not erythematous, but active and passive movements were painful. Blood tests revealed a C-reactive protein level of 98 mg/dL and a white blood cell (WBC) count of 11.3 × 109/L. Erythrocyte sedimentation rate (ESR) was not checked. The ankle underwent magnetic resonance imaging (Figures A-D).
Mycotic screening of the fluid was positive for C albicans. The patient was referred to the orthopedic team, which performed urgent arthroscopic surgical débridement, biopsy, and washout of the subtalar joint. After surgery, a 6-week course of antifungal therapy with anidulafungin was started, per specialist microbiology advice.
The septic ankle was successfully managed with arthroscopic surgical débridement followed by treatment with anidulafungin. The patient continued to make good progress and was weight-bearing when discharged home from the orthopedic unit.
Discussion
Worldwide, about 1 in 6 people has arthritis, which affects daily lifestyle and reduces quality of life. Degenerative, inflammatory, and septic arthritis each has its management challenges.1
Septic arthritis is an acute infection of the joint, usually of bacterial etiology. It can present as a polyarticular arthropathy (~15% of cases),2,3 but a monoarthropathy of the hip, knee, or ankle is more common.4The Kocher criteria are often applied to cases of suspected septic arthritis of joints, even though they were initially used to distinguish septic arthritis from transient synovitis in pediatric hip joints.5 Kocher and colleagues5 reported 4 key clinical criteria: inability to bear weight, WBC count over 12 × 109/L, ESR over 40 mm/h, and temperature over 38.5°C. When all 4 criteria are met, the predictive value is 99.6%. These criteria are now widely applied to adult joints, and not only the hips.
In septic arthritis, the most common causative pathogen is S aureus.3,6Streptococcus, Neisseria, and Pseudomonas also are common.7 Although much rarer, Candida variants and other mycotic pathogens have been implicated as well.8C albicans is a well-known fungus that colonizes mucosal surfaces. Research indicates increased oral C albicans colonization in rheumatoid patients.9 Although most Candida septic arthritis cases are caused by C albicans, there is no large body of data showing the true incidence of fungal pathogens in septic arthritis.
Our literature search yielded 2 case reports on Candida septic arthritis involving the ankle, but the causative organisms were Candida parapsilosis and Candida glabrata.9,10 Cases of Candida septic arthritis involving the knee or shoulder have also been reported.11-15 Case reports demonstrate that Candida fungal arthritis is extremely rare.9 Etiology reportedly includes direct intra-articular inoculation by surgery or secondary to hematogenous seeding, particularly in immunocompromised patients.10 Risk factors include immunosuppression and joint suppression. DM and RA are common comorbidities in patients with septic arthritis.6,16 The pathophysiology of RA is inflammatory pannus formation of the periarticular surface with subsequent articular cartilage destruction and erosion, as well as progressive deformity and functional debilitation.1Patients with DM are at increased risk for developing fungal and other infections. Factors increasing this risk include disruption of skin-barrier integrity; reduced peripheral oxygen and blood supply, which also disrupts antibiotic delivery; and hyperglycemia-induced reduction in antibody function and disruption of phagocytosis and chemotaxis.17Fungi are eukaryotic, and infections caused by these organisms are difficult to treat.18 As fungal infections are more prevalent among immunosuppressed patients, they often result in prolonged treatment without guarantee of eradication, as spores may persist subclinically.
Literature on C albicans septic arthritis is lacking in general but especially in rheumatoid patients. Delayed diagnosis and suboptimal treatment may result in fungal osteomyelitis. There is little evidence on treating this rare fungal complication, and outcomes historically have been poor.19In an animal model, Marijnissen and colleagues20 found that C albicans infection can increase destruction in an arthritic joint by cytokine environment modification. The result was advanced destruction of the joint and debilitation. For disease management, the authors considered these essential: early diagnosis, prompt treatment, and, as indicated, surgical débridement.
Treatment of Candida septic arthritis largely involves use of antifungal medication, either with surgical débridement, as in our patient’s case, or without. Which antifungal medication to use should be based on sensitivities, identified from wound aspirate, and microbiology advice about treatment duration. The antibiotic should be a broad-spectrum antifungal cover, in keeping with local antibiotic prescribing guidelines, which can be refined once definitive organism culture and sensitivity results are known. However, early aggressive treatment is essential. Periprosthetic fungal infection is rarely resolved without implant removal.21
Conclusion
This case reflects the complexities of septic arthritis caused by atypical pathogens and highlights the need for clinical vigilance in the setting of comorbidities, such as DM and RA. Failure to consider the diagnosis early on might result in delayed and inadequate treatment, increased joint destruction, and, potentially, osteomyelitis with subsequent increased morbidity. Early diagnosis (based on joint aspirate findings), surgical débridement, and prolonged aggressive treatment with antifungal medication are the mainstays of treatment.
Am J Orthop. 2016;45(7):E478-E480. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Auday BC, Buratovich MA, Marrocco, GF, Moglia P, eds. Magill’s Medical Guide. 7th ed. Ipswich, MA: Salem Press; 2014.
2. Dhaliwal S, LeBel ME. Rapidly progressing polyarticular septic arthritis in a patient with rheumatoid arthritis. Am J Orthop. 2012;41(7):E100-E101.
3. Mateo Soria L, Olivé Marqués A, García Casares E, García Melchor E, Holgado Pérez S, Tena Marsà X. Polyarticular septic arthritis: analysis of 19 cases [in Spanish]. Reumatol Clin. 2009;5(1):18-22.
4. Caksen H, Oztürk MK, Uzüm K, Yüksel S, Ustünbaş HB, Per H. Septic arthritis in childhood. Pediatr Int. 2000;42(5):534-540.
5. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm. J Bone Joint Surg Am. 1999;81(12):1662-1670.
6. Madruga Dias J, Costa MM, Pereira da Silva JA, Viana de Queiroz M. Septic arthritis: patients with or without isolated infectious agents have similar characteristics. Infection. 2014;42(2):385-391.
7. Louthrenoo W, Kasitanon N, Wangkaew S, Hongsongkiat S, Sukitawut W, Wichainun R. Streptococcus agalactiae: an emerging cause of septic arthritis. J Clin Rheumatol. 2014;20(2):74-78.
8. Zmierczak H, Goemaere S, Mielants H, Verbruggen G, Veys EM. Candida glabrata arthritis: case report and review of the literature of Candida arthritis. Clin Rheumatol. 1999;18(5):406-409.
9. Bishu S, Su EW, Wilkerson ER, et al. Rheumatoid arthritis patients exhibit impaired Candida albicans–specific Th17 responses. Arthritis Res Ther. 2014;16(1):R50.
10. Legout L, Assal M, Rohner P, Lew D, Bernard L, Hoffmeyer P. Successful treatment of Candida parapsilosis (fluconazole-resistant) osteomyelitis with caspofungin in a HIV patient. Scand J Infect Dis. 2006;38(8):728-730.
11. Sung J, Chun K. Candida parapsilosis arthritis involving the ankle in a diabetes patient. J Korean Soc Radiol. 2011;64:587-591.
12. Marmor L, Peter JB. Candida arthritis of the knee joint. Clin Orthop Relat Res. 1976;(118):133-135.
13. Turgut B, Vural O, Demir M, Kaldir M. Candida arthritis in a patient with chronic myelogenous leukemia (CML) in blastic transformation, unresponsive to fluconazole, but treated effectively with liposomal amphotericin B. Ann Hematol. 2002;81(9):529-531.
14. Christensson B, Ryd L, Dahlberg L, Lohmander S. Candida albicans arthritis in a nonimmunocompromised patient. Complication of placebo intraarticular injections. Acta Orthop Scand. 1993;64(6):695-698.
15. Jeong YM, Cho HY, Lee SW, Hwang YM, Kim YK. Candida septic arthritis with rice body formation: a case report and review of literature. Korean J Radiol. 2013;14(3):465-469.
16. Favero M, Schiavon R, Riato L, Carraro V, Punzi L. Septic arthritis: a 12 years retrospective study in a rheumatological university clinic [in Italian]. Reumatismo. 2008;60(4):260-267.
17. Leslie D, Lansang C, Coppack S, Kennedy L. Diabetes: Clinician’s Desk Reference. Boca Raton, FL: CRC Press; 2012.
18. Silva PM, Gonçalves S, Santos NC. Defensins: antifungal lesions from eukaryotes. Front Microbiol. 2014;5:97.
19. Bariteau JT, Waryasz GR, McDonnell M, Fischer SA, Hayda RA, Born CT. Fungal osteomyelitis and septic arthritis. J Am Acad Orthop Surg. 2014;22(6):390-401.
20. Marijnissen RJ, Koenders MI, van de Veerdonk FL, et al. Exposure to Candida albicans polarizes a T-cell driven arthritis model towards Th17 responses, resulting in a more destructive arthritis. PLoS One. 2012;7(6):e38889.
21. International Consensus on Periprosthetic Joint Infection. Musculoskeletal Infection Society website. http://www.msis-na.org/international-consensus. Published August 1, 2013. Accessed October 16, 2016.
Septic arthritis is a common orthopedic emergency. The most common causative organism is Staphylococcus aureus. Mycotic infections, such as those involving Candida organisms, are much less common but just as debilitating. Delayed diagnosis of septic arthritis caused by Candida infection may result in increased morbidity, making treatment more challenging. Here we report a case of Candida albicans septic arthritis of the ankle and subtalar joint in a patient with diabetes mellitus (DM) and rheumatoid arthritis (RA). The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 52-year-old woman with type 2 DM (requiring subcutaneous insulin analogue therapy) and RA presented to a local emergency department with a 3-day history of right ankle pain after having the subtalar joint injected with steroid by a rheumatologist 4 weeks earlier. For about 2 weeks, there was purulent discharge from the peroneal sheath. The patient’s RA was being treated with prednisolone (maintenance therapy). Physical examination revealed low-grade pyrexia (37.8°C) and difficulty bearing full weight on the ankle. Clinically, the joint was not erythematous, but active and passive movements were painful. Blood tests revealed a C-reactive protein level of 98 mg/dL and a white blood cell (WBC) count of 11.3 × 109/L. Erythrocyte sedimentation rate (ESR) was not checked. The ankle underwent magnetic resonance imaging (Figures A-D).
Mycotic screening of the fluid was positive for C albicans. The patient was referred to the orthopedic team, which performed urgent arthroscopic surgical débridement, biopsy, and washout of the subtalar joint. After surgery, a 6-week course of antifungal therapy with anidulafungin was started, per specialist microbiology advice.
The septic ankle was successfully managed with arthroscopic surgical débridement followed by treatment with anidulafungin. The patient continued to make good progress and was weight-bearing when discharged home from the orthopedic unit.
Discussion
Worldwide, about 1 in 6 people has arthritis, which affects daily lifestyle and reduces quality of life. Degenerative, inflammatory, and septic arthritis each has its management challenges.1
Septic arthritis is an acute infection of the joint, usually of bacterial etiology. It can present as a polyarticular arthropathy (~15% of cases),2,3 but a monoarthropathy of the hip, knee, or ankle is more common.4The Kocher criteria are often applied to cases of suspected septic arthritis of joints, even though they were initially used to distinguish septic arthritis from transient synovitis in pediatric hip joints.5 Kocher and colleagues5 reported 4 key clinical criteria: inability to bear weight, WBC count over 12 × 109/L, ESR over 40 mm/h, and temperature over 38.5°C. When all 4 criteria are met, the predictive value is 99.6%. These criteria are now widely applied to adult joints, and not only the hips.
In septic arthritis, the most common causative pathogen is S aureus.3,6Streptococcus, Neisseria, and Pseudomonas also are common.7 Although much rarer, Candida variants and other mycotic pathogens have been implicated as well.8C albicans is a well-known fungus that colonizes mucosal surfaces. Research indicates increased oral C albicans colonization in rheumatoid patients.9 Although most Candida septic arthritis cases are caused by C albicans, there is no large body of data showing the true incidence of fungal pathogens in septic arthritis.
Our literature search yielded 2 case reports on Candida septic arthritis involving the ankle, but the causative organisms were Candida parapsilosis and Candida glabrata.9,10 Cases of Candida septic arthritis involving the knee or shoulder have also been reported.11-15 Case reports demonstrate that Candida fungal arthritis is extremely rare.9 Etiology reportedly includes direct intra-articular inoculation by surgery or secondary to hematogenous seeding, particularly in immunocompromised patients.10 Risk factors include immunosuppression and joint suppression. DM and RA are common comorbidities in patients with septic arthritis.6,16 The pathophysiology of RA is inflammatory pannus formation of the periarticular surface with subsequent articular cartilage destruction and erosion, as well as progressive deformity and functional debilitation.1Patients with DM are at increased risk for developing fungal and other infections. Factors increasing this risk include disruption of skin-barrier integrity; reduced peripheral oxygen and blood supply, which also disrupts antibiotic delivery; and hyperglycemia-induced reduction in antibody function and disruption of phagocytosis and chemotaxis.17Fungi are eukaryotic, and infections caused by these organisms are difficult to treat.18 As fungal infections are more prevalent among immunosuppressed patients, they often result in prolonged treatment without guarantee of eradication, as spores may persist subclinically.
Literature on C albicans septic arthritis is lacking in general but especially in rheumatoid patients. Delayed diagnosis and suboptimal treatment may result in fungal osteomyelitis. There is little evidence on treating this rare fungal complication, and outcomes historically have been poor.19In an animal model, Marijnissen and colleagues20 found that C albicans infection can increase destruction in an arthritic joint by cytokine environment modification. The result was advanced destruction of the joint and debilitation. For disease management, the authors considered these essential: early diagnosis, prompt treatment, and, as indicated, surgical débridement.
Treatment of Candida septic arthritis largely involves use of antifungal medication, either with surgical débridement, as in our patient’s case, or without. Which antifungal medication to use should be based on sensitivities, identified from wound aspirate, and microbiology advice about treatment duration. The antibiotic should be a broad-spectrum antifungal cover, in keeping with local antibiotic prescribing guidelines, which can be refined once definitive organism culture and sensitivity results are known. However, early aggressive treatment is essential. Periprosthetic fungal infection is rarely resolved without implant removal.21
Conclusion
This case reflects the complexities of septic arthritis caused by atypical pathogens and highlights the need for clinical vigilance in the setting of comorbidities, such as DM and RA. Failure to consider the diagnosis early on might result in delayed and inadequate treatment, increased joint destruction, and, potentially, osteomyelitis with subsequent increased morbidity. Early diagnosis (based on joint aspirate findings), surgical débridement, and prolonged aggressive treatment with antifungal medication are the mainstays of treatment.
Am J Orthop. 2016;45(7):E478-E480. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Septic arthritis is a common orthopedic emergency. The most common causative organism is Staphylococcus aureus. Mycotic infections, such as those involving Candida organisms, are much less common but just as debilitating. Delayed diagnosis of septic arthritis caused by Candida infection may result in increased morbidity, making treatment more challenging. Here we report a case of Candida albicans septic arthritis of the ankle and subtalar joint in a patient with diabetes mellitus (DM) and rheumatoid arthritis (RA). The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 52-year-old woman with type 2 DM (requiring subcutaneous insulin analogue therapy) and RA presented to a local emergency department with a 3-day history of right ankle pain after having the subtalar joint injected with steroid by a rheumatologist 4 weeks earlier. For about 2 weeks, there was purulent discharge from the peroneal sheath. The patient’s RA was being treated with prednisolone (maintenance therapy). Physical examination revealed low-grade pyrexia (37.8°C) and difficulty bearing full weight on the ankle. Clinically, the joint was not erythematous, but active and passive movements were painful. Blood tests revealed a C-reactive protein level of 98 mg/dL and a white blood cell (WBC) count of 11.3 × 109/L. Erythrocyte sedimentation rate (ESR) was not checked. The ankle underwent magnetic resonance imaging (Figures A-D).
Mycotic screening of the fluid was positive for C albicans. The patient was referred to the orthopedic team, which performed urgent arthroscopic surgical débridement, biopsy, and washout of the subtalar joint. After surgery, a 6-week course of antifungal therapy with anidulafungin was started, per specialist microbiology advice.
The septic ankle was successfully managed with arthroscopic surgical débridement followed by treatment with anidulafungin. The patient continued to make good progress and was weight-bearing when discharged home from the orthopedic unit.
Discussion
Worldwide, about 1 in 6 people has arthritis, which affects daily lifestyle and reduces quality of life. Degenerative, inflammatory, and septic arthritis each has its management challenges.1
Septic arthritis is an acute infection of the joint, usually of bacterial etiology. It can present as a polyarticular arthropathy (~15% of cases),2,3 but a monoarthropathy of the hip, knee, or ankle is more common.4The Kocher criteria are often applied to cases of suspected septic arthritis of joints, even though they were initially used to distinguish septic arthritis from transient synovitis in pediatric hip joints.5 Kocher and colleagues5 reported 4 key clinical criteria: inability to bear weight, WBC count over 12 × 109/L, ESR over 40 mm/h, and temperature over 38.5°C. When all 4 criteria are met, the predictive value is 99.6%. These criteria are now widely applied to adult joints, and not only the hips.
In septic arthritis, the most common causative pathogen is S aureus.3,6Streptococcus, Neisseria, and Pseudomonas also are common.7 Although much rarer, Candida variants and other mycotic pathogens have been implicated as well.8C albicans is a well-known fungus that colonizes mucosal surfaces. Research indicates increased oral C albicans colonization in rheumatoid patients.9 Although most Candida septic arthritis cases are caused by C albicans, there is no large body of data showing the true incidence of fungal pathogens in septic arthritis.
Our literature search yielded 2 case reports on Candida septic arthritis involving the ankle, but the causative organisms were Candida parapsilosis and Candida glabrata.9,10 Cases of Candida septic arthritis involving the knee or shoulder have also been reported.11-15 Case reports demonstrate that Candida fungal arthritis is extremely rare.9 Etiology reportedly includes direct intra-articular inoculation by surgery or secondary to hematogenous seeding, particularly in immunocompromised patients.10 Risk factors include immunosuppression and joint suppression. DM and RA are common comorbidities in patients with septic arthritis.6,16 The pathophysiology of RA is inflammatory pannus formation of the periarticular surface with subsequent articular cartilage destruction and erosion, as well as progressive deformity and functional debilitation.1Patients with DM are at increased risk for developing fungal and other infections. Factors increasing this risk include disruption of skin-barrier integrity; reduced peripheral oxygen and blood supply, which also disrupts antibiotic delivery; and hyperglycemia-induced reduction in antibody function and disruption of phagocytosis and chemotaxis.17Fungi are eukaryotic, and infections caused by these organisms are difficult to treat.18 As fungal infections are more prevalent among immunosuppressed patients, they often result in prolonged treatment without guarantee of eradication, as spores may persist subclinically.
Literature on C albicans septic arthritis is lacking in general but especially in rheumatoid patients. Delayed diagnosis and suboptimal treatment may result in fungal osteomyelitis. There is little evidence on treating this rare fungal complication, and outcomes historically have been poor.19In an animal model, Marijnissen and colleagues20 found that C albicans infection can increase destruction in an arthritic joint by cytokine environment modification. The result was advanced destruction of the joint and debilitation. For disease management, the authors considered these essential: early diagnosis, prompt treatment, and, as indicated, surgical débridement.
Treatment of Candida septic arthritis largely involves use of antifungal medication, either with surgical débridement, as in our patient’s case, or without. Which antifungal medication to use should be based on sensitivities, identified from wound aspirate, and microbiology advice about treatment duration. The antibiotic should be a broad-spectrum antifungal cover, in keeping with local antibiotic prescribing guidelines, which can be refined once definitive organism culture and sensitivity results are known. However, early aggressive treatment is essential. Periprosthetic fungal infection is rarely resolved without implant removal.21
Conclusion
This case reflects the complexities of septic arthritis caused by atypical pathogens and highlights the need for clinical vigilance in the setting of comorbidities, such as DM and RA. Failure to consider the diagnosis early on might result in delayed and inadequate treatment, increased joint destruction, and, potentially, osteomyelitis with subsequent increased morbidity. Early diagnosis (based on joint aspirate findings), surgical débridement, and prolonged aggressive treatment with antifungal medication are the mainstays of treatment.
Am J Orthop. 2016;45(7):E478-E480. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Auday BC, Buratovich MA, Marrocco, GF, Moglia P, eds. Magill’s Medical Guide. 7th ed. Ipswich, MA: Salem Press; 2014.
2. Dhaliwal S, LeBel ME. Rapidly progressing polyarticular septic arthritis in a patient with rheumatoid arthritis. Am J Orthop. 2012;41(7):E100-E101.
3. Mateo Soria L, Olivé Marqués A, García Casares E, García Melchor E, Holgado Pérez S, Tena Marsà X. Polyarticular septic arthritis: analysis of 19 cases [in Spanish]. Reumatol Clin. 2009;5(1):18-22.
4. Caksen H, Oztürk MK, Uzüm K, Yüksel S, Ustünbaş HB, Per H. Septic arthritis in childhood. Pediatr Int. 2000;42(5):534-540.
5. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm. J Bone Joint Surg Am. 1999;81(12):1662-1670.
6. Madruga Dias J, Costa MM, Pereira da Silva JA, Viana de Queiroz M. Septic arthritis: patients with or without isolated infectious agents have similar characteristics. Infection. 2014;42(2):385-391.
7. Louthrenoo W, Kasitanon N, Wangkaew S, Hongsongkiat S, Sukitawut W, Wichainun R. Streptococcus agalactiae: an emerging cause of septic arthritis. J Clin Rheumatol. 2014;20(2):74-78.
8. Zmierczak H, Goemaere S, Mielants H, Verbruggen G, Veys EM. Candida glabrata arthritis: case report and review of the literature of Candida arthritis. Clin Rheumatol. 1999;18(5):406-409.
9. Bishu S, Su EW, Wilkerson ER, et al. Rheumatoid arthritis patients exhibit impaired Candida albicans–specific Th17 responses. Arthritis Res Ther. 2014;16(1):R50.
10. Legout L, Assal M, Rohner P, Lew D, Bernard L, Hoffmeyer P. Successful treatment of Candida parapsilosis (fluconazole-resistant) osteomyelitis with caspofungin in a HIV patient. Scand J Infect Dis. 2006;38(8):728-730.
11. Sung J, Chun K. Candida parapsilosis arthritis involving the ankle in a diabetes patient. J Korean Soc Radiol. 2011;64:587-591.
12. Marmor L, Peter JB. Candida arthritis of the knee joint. Clin Orthop Relat Res. 1976;(118):133-135.
13. Turgut B, Vural O, Demir M, Kaldir M. Candida arthritis in a patient with chronic myelogenous leukemia (CML) in blastic transformation, unresponsive to fluconazole, but treated effectively with liposomal amphotericin B. Ann Hematol. 2002;81(9):529-531.
14. Christensson B, Ryd L, Dahlberg L, Lohmander S. Candida albicans arthritis in a nonimmunocompromised patient. Complication of placebo intraarticular injections. Acta Orthop Scand. 1993;64(6):695-698.
15. Jeong YM, Cho HY, Lee SW, Hwang YM, Kim YK. Candida septic arthritis with rice body formation: a case report and review of literature. Korean J Radiol. 2013;14(3):465-469.
16. Favero M, Schiavon R, Riato L, Carraro V, Punzi L. Septic arthritis: a 12 years retrospective study in a rheumatological university clinic [in Italian]. Reumatismo. 2008;60(4):260-267.
17. Leslie D, Lansang C, Coppack S, Kennedy L. Diabetes: Clinician’s Desk Reference. Boca Raton, FL: CRC Press; 2012.
18. Silva PM, Gonçalves S, Santos NC. Defensins: antifungal lesions from eukaryotes. Front Microbiol. 2014;5:97.
19. Bariteau JT, Waryasz GR, McDonnell M, Fischer SA, Hayda RA, Born CT. Fungal osteomyelitis and septic arthritis. J Am Acad Orthop Surg. 2014;22(6):390-401.
20. Marijnissen RJ, Koenders MI, van de Veerdonk FL, et al. Exposure to Candida albicans polarizes a T-cell driven arthritis model towards Th17 responses, resulting in a more destructive arthritis. PLoS One. 2012;7(6):e38889.
21. International Consensus on Periprosthetic Joint Infection. Musculoskeletal Infection Society website. http://www.msis-na.org/international-consensus. Published August 1, 2013. Accessed October 16, 2016.
1. Auday BC, Buratovich MA, Marrocco, GF, Moglia P, eds. Magill’s Medical Guide. 7th ed. Ipswich, MA: Salem Press; 2014.
2. Dhaliwal S, LeBel ME. Rapidly progressing polyarticular septic arthritis in a patient with rheumatoid arthritis. Am J Orthop. 2012;41(7):E100-E101.
3. Mateo Soria L, Olivé Marqués A, García Casares E, García Melchor E, Holgado Pérez S, Tena Marsà X. Polyarticular septic arthritis: analysis of 19 cases [in Spanish]. Reumatol Clin. 2009;5(1):18-22.
4. Caksen H, Oztürk MK, Uzüm K, Yüksel S, Ustünbaş HB, Per H. Septic arthritis in childhood. Pediatr Int. 2000;42(5):534-540.
5. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm. J Bone Joint Surg Am. 1999;81(12):1662-1670.
6. Madruga Dias J, Costa MM, Pereira da Silva JA, Viana de Queiroz M. Septic arthritis: patients with or without isolated infectious agents have similar characteristics. Infection. 2014;42(2):385-391.
7. Louthrenoo W, Kasitanon N, Wangkaew S, Hongsongkiat S, Sukitawut W, Wichainun R. Streptococcus agalactiae: an emerging cause of septic arthritis. J Clin Rheumatol. 2014;20(2):74-78.
8. Zmierczak H, Goemaere S, Mielants H, Verbruggen G, Veys EM. Candida glabrata arthritis: case report and review of the literature of Candida arthritis. Clin Rheumatol. 1999;18(5):406-409.
9. Bishu S, Su EW, Wilkerson ER, et al. Rheumatoid arthritis patients exhibit impaired Candida albicans–specific Th17 responses. Arthritis Res Ther. 2014;16(1):R50.
10. Legout L, Assal M, Rohner P, Lew D, Bernard L, Hoffmeyer P. Successful treatment of Candida parapsilosis (fluconazole-resistant) osteomyelitis with caspofungin in a HIV patient. Scand J Infect Dis. 2006;38(8):728-730.
11. Sung J, Chun K. Candida parapsilosis arthritis involving the ankle in a diabetes patient. J Korean Soc Radiol. 2011;64:587-591.
12. Marmor L, Peter JB. Candida arthritis of the knee joint. Clin Orthop Relat Res. 1976;(118):133-135.
13. Turgut B, Vural O, Demir M, Kaldir M. Candida arthritis in a patient with chronic myelogenous leukemia (CML) in blastic transformation, unresponsive to fluconazole, but treated effectively with liposomal amphotericin B. Ann Hematol. 2002;81(9):529-531.
14. Christensson B, Ryd L, Dahlberg L, Lohmander S. Candida albicans arthritis in a nonimmunocompromised patient. Complication of placebo intraarticular injections. Acta Orthop Scand. 1993;64(6):695-698.
15. Jeong YM, Cho HY, Lee SW, Hwang YM, Kim YK. Candida septic arthritis with rice body formation: a case report and review of literature. Korean J Radiol. 2013;14(3):465-469.
16. Favero M, Schiavon R, Riato L, Carraro V, Punzi L. Septic arthritis: a 12 years retrospective study in a rheumatological university clinic [in Italian]. Reumatismo. 2008;60(4):260-267.
17. Leslie D, Lansang C, Coppack S, Kennedy L. Diabetes: Clinician’s Desk Reference. Boca Raton, FL: CRC Press; 2012.
18. Silva PM, Gonçalves S, Santos NC. Defensins: antifungal lesions from eukaryotes. Front Microbiol. 2014;5:97.
19. Bariteau JT, Waryasz GR, McDonnell M, Fischer SA, Hayda RA, Born CT. Fungal osteomyelitis and septic arthritis. J Am Acad Orthop Surg. 2014;22(6):390-401.
20. Marijnissen RJ, Koenders MI, van de Veerdonk FL, et al. Exposure to Candida albicans polarizes a T-cell driven arthritis model towards Th17 responses, resulting in a more destructive arthritis. PLoS One. 2012;7(6):e38889.
21. International Consensus on Periprosthetic Joint Infection. Musculoskeletal Infection Society website. http://www.msis-na.org/international-consensus. Published August 1, 2013. Accessed October 16, 2016.
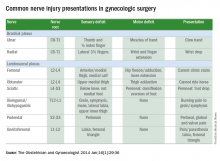
Tips for avoiding nerve injuries in gynecologic surgery
Upper- and lower-extremity injuries can occur during gynecologic surgery. The incidence of lower-extremity injury is 1.1%-1.9% and upper-extremity injuries can occur in 0.16% of cases.1-5 Fortunately, most of the injuries are transient, sensory injuries that resolve spontaneously. However, a small percentage of injuries result in long-term sequelae.
The pathophysiology of the nerve injuries can be mechanistically separated into three categories: neuropraxia, axonotmesis, and neurotmesis. Neuropraxia results from nerve demyelination at the site of injury because of compression and typically resolves within weeks to months as the nerve is remyelinated. Axonotmesis results from severe compression with axon damage. This may take up to a year to resolve as axonal regeneration proceeds at the rate of 1 mm per day. This can be separated into second and third degree and refers to the severity of damage and the resultant persistent deficit. Neurotmesis results from complete transection and is associated with a poor prognosis without reparative surgery.
Brachial plexus
Stretch injury is the most common reason for a brachial plexus injury. This can occur if the arm board is extended to greater than 90 degrees from the patient’s torso or if the patient’s arm falls off of the arm board. Careful positioning and securing the patient’s arm on the arm board before draping can avoid this injury. A brachial plexus injury can also occur if shoulder braces are placed too laterally during minimally invasive surgery. Radial nerve injuries can occur if there is too much pressure on the humerus during positioning. Ulnar injuries arise from pressure placed on the medial aspect of the elbow.
Tip #1: When tucking a patient’s arm for minimally invasive surgery, appropriate padding should be placed around the elbow and wrist, and the arm should be in the “thumbs-up” position.
Tip #2: Shoulder blocks should be placed over the acromioclavicular (AC) joint.
Lumbosacral plexus
The femoral nerve is the nerve most commonly injured during gynecologic surgery and this usually occurs because of compression of the nerve from the lateral blades of self-retaining retractors. One study showed an 8% incidence of injury from self-retaining retractors, compared with less than 1% when the retractors were not used.6 The femoral nerve can also be stretched when patients are placed in the lithotomy position and the hip is hyperflexed.
As with brachial injury prevention, patients should be positioned prior to draping and care must be taken to not hyperflex or externally rotate the hip during minimally invasive surgical procedures. With the introduction of robot-assisted surgery, care must be taken when docking the robot and surgeons must resist excessive movement of the stirrups.
Tip #3: During laparotomy, surgeons should use the shortest blades that allow for adequate visualization and check the blades during the procedure to ensure that excessive pressure is not placed on the psoas muscle. Consider intermittently releasing the pressure on the lateral blades during other portions of the procedure.
Tip #4: Make sure the stirrups are at the same height and that the leg is in line with the patient’s contralateral shoulder.
Obturator nerve injuries can occur during retroperitoneal dissection for pelvic lymphadenectomy (obturator nodes) and can be either a transection or a cautery injury. It can also be injured during urogynecologic procedures including paravaginal defect repairs and during the placement of transobturator tapes.
The sciatic nerve and its branch, the common peroneal, are generally injured because of excessive stretch or pressure. Both nerves can be injured from hyperflexion of the thigh and the common peroneal can suffer a pressure injury as it courses around the lateral head of the fibula. Therefore, care during lithotomy positioning with both candy cane and Allen stirrups is critical during vaginal surgery.
Tip #5: Ensure that the lateral fibula is not touching the stirrup or that padding is placed between the fibular head and the stirrup.
The ilioinguinal and iliohypogastric nerves are typically injured via suture entrapment from low transverse skin incisions, though laparoscopic injury has also been reported. The incidence after a Pfannenstiel incision is about 3.7%.7
Tip #6: Avoid extending the low transverse incision beyond the lateral margin of the rectus muscle, and do not extend the fascial closure suture more than 1.5 cm from the lateral edge of the fascial incision to avoid catching the nerve with the suture.
The pudendal nerve is most commonly injured during vaginal procedures such as sacrospinous fixation. Pain is typically worse when seated.
The genitofemoral nerve is typically injured during retroperitoneal lymph node dissection, particularly the external iliac nodes. The nerve is small and runs lateral to the external iliac artery. It can suffer cautery and transection injuries. Usually, the paresthesias over the mons pubis, labia majora, and medial inner thigh are temporary.
Tip #7: Care should be taken to identify and spare the nerve during retroperitoneal dissection or external iliac node removal.
Nerve injuries during gynecologic surgery are common and are a significant cause of potential morbidity. While occasionally unavoidable and inherent to the surgical procedure, many times the injury could be prevented with proper attention and care to patient positioning and retractor use. Gynecologists should be aware of the risks and have a through understanding of the anatomy. However, should an injury occur, the patient can be reassured that most are self-limited and full recovery is generally expected. In a prospective study, the median time to resolution of symptoms was 31.5 days (range, 1 day to 6 months).5
References
1. The Obstetrician & Gynaecologist 2014;16:29-36.
2. Gynecol Oncol. 1988 Nov;31(3):462-6.
3. Fertil Steril. 1993 Oct;60(4):729-32.
4. J Minim Invasive Gynecol. 2007 Sep-Oct;14(5):664-72.
5. Am J Obstet Gynecol. 2009 Nov;201(5):531.e1-7.
6. Eur J Obstet Gynecol Reprod Biol. 1985 Dec;20(6):385-92.
7. Obstet Gynecol. 2008 Apr;111(4):839-46.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. She reported having no financial disclosures relevant to this column. Email her at [email protected].
Upper- and lower-extremity injuries can occur during gynecologic surgery. The incidence of lower-extremity injury is 1.1%-1.9% and upper-extremity injuries can occur in 0.16% of cases.1-5 Fortunately, most of the injuries are transient, sensory injuries that resolve spontaneously. However, a small percentage of injuries result in long-term sequelae.
The pathophysiology of the nerve injuries can be mechanistically separated into three categories: neuropraxia, axonotmesis, and neurotmesis. Neuropraxia results from nerve demyelination at the site of injury because of compression and typically resolves within weeks to months as the nerve is remyelinated. Axonotmesis results from severe compression with axon damage. This may take up to a year to resolve as axonal regeneration proceeds at the rate of 1 mm per day. This can be separated into second and third degree and refers to the severity of damage and the resultant persistent deficit. Neurotmesis results from complete transection and is associated with a poor prognosis without reparative surgery.
Brachial plexus
Stretch injury is the most common reason for a brachial plexus injury. This can occur if the arm board is extended to greater than 90 degrees from the patient’s torso or if the patient’s arm falls off of the arm board. Careful positioning and securing the patient’s arm on the arm board before draping can avoid this injury. A brachial plexus injury can also occur if shoulder braces are placed too laterally during minimally invasive surgery. Radial nerve injuries can occur if there is too much pressure on the humerus during positioning. Ulnar injuries arise from pressure placed on the medial aspect of the elbow.
Tip #1: When tucking a patient’s arm for minimally invasive surgery, appropriate padding should be placed around the elbow and wrist, and the arm should be in the “thumbs-up” position.
Tip #2: Shoulder blocks should be placed over the acromioclavicular (AC) joint.
Lumbosacral plexus
The femoral nerve is the nerve most commonly injured during gynecologic surgery and this usually occurs because of compression of the nerve from the lateral blades of self-retaining retractors. One study showed an 8% incidence of injury from self-retaining retractors, compared with less than 1% when the retractors were not used.6 The femoral nerve can also be stretched when patients are placed in the lithotomy position and the hip is hyperflexed.
As with brachial injury prevention, patients should be positioned prior to draping and care must be taken to not hyperflex or externally rotate the hip during minimally invasive surgical procedures. With the introduction of robot-assisted surgery, care must be taken when docking the robot and surgeons must resist excessive movement of the stirrups.
Tip #3: During laparotomy, surgeons should use the shortest blades that allow for adequate visualization and check the blades during the procedure to ensure that excessive pressure is not placed on the psoas muscle. Consider intermittently releasing the pressure on the lateral blades during other portions of the procedure.
Tip #4: Make sure the stirrups are at the same height and that the leg is in line with the patient’s contralateral shoulder.
Obturator nerve injuries can occur during retroperitoneal dissection for pelvic lymphadenectomy (obturator nodes) and can be either a transection or a cautery injury. It can also be injured during urogynecologic procedures including paravaginal defect repairs and during the placement of transobturator tapes.
The sciatic nerve and its branch, the common peroneal, are generally injured because of excessive stretch or pressure. Both nerves can be injured from hyperflexion of the thigh and the common peroneal can suffer a pressure injury as it courses around the lateral head of the fibula. Therefore, care during lithotomy positioning with both candy cane and Allen stirrups is critical during vaginal surgery.
Tip #5: Ensure that the lateral fibula is not touching the stirrup or that padding is placed between the fibular head and the stirrup.
The ilioinguinal and iliohypogastric nerves are typically injured via suture entrapment from low transverse skin incisions, though laparoscopic injury has also been reported. The incidence after a Pfannenstiel incision is about 3.7%.7
Tip #6: Avoid extending the low transverse incision beyond the lateral margin of the rectus muscle, and do not extend the fascial closure suture more than 1.5 cm from the lateral edge of the fascial incision to avoid catching the nerve with the suture.
The pudendal nerve is most commonly injured during vaginal procedures such as sacrospinous fixation. Pain is typically worse when seated.
The genitofemoral nerve is typically injured during retroperitoneal lymph node dissection, particularly the external iliac nodes. The nerve is small and runs lateral to the external iliac artery. It can suffer cautery and transection injuries. Usually, the paresthesias over the mons pubis, labia majora, and medial inner thigh are temporary.
Tip #7: Care should be taken to identify and spare the nerve during retroperitoneal dissection or external iliac node removal.
Nerve injuries during gynecologic surgery are common and are a significant cause of potential morbidity. While occasionally unavoidable and inherent to the surgical procedure, many times the injury could be prevented with proper attention and care to patient positioning and retractor use. Gynecologists should be aware of the risks and have a through understanding of the anatomy. However, should an injury occur, the patient can be reassured that most are self-limited and full recovery is generally expected. In a prospective study, the median time to resolution of symptoms was 31.5 days (range, 1 day to 6 months).5
References
1. The Obstetrician & Gynaecologist 2014;16:29-36.
2. Gynecol Oncol. 1988 Nov;31(3):462-6.
3. Fertil Steril. 1993 Oct;60(4):729-32.
4. J Minim Invasive Gynecol. 2007 Sep-Oct;14(5):664-72.
5. Am J Obstet Gynecol. 2009 Nov;201(5):531.e1-7.
6. Eur J Obstet Gynecol Reprod Biol. 1985 Dec;20(6):385-92.
7. Obstet Gynecol. 2008 Apr;111(4):839-46.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. She reported having no financial disclosures relevant to this column. Email her at [email protected].
Upper- and lower-extremity injuries can occur during gynecologic surgery. The incidence of lower-extremity injury is 1.1%-1.9% and upper-extremity injuries can occur in 0.16% of cases.1-5 Fortunately, most of the injuries are transient, sensory injuries that resolve spontaneously. However, a small percentage of injuries result in long-term sequelae.
The pathophysiology of the nerve injuries can be mechanistically separated into three categories: neuropraxia, axonotmesis, and neurotmesis. Neuropraxia results from nerve demyelination at the site of injury because of compression and typically resolves within weeks to months as the nerve is remyelinated. Axonotmesis results from severe compression with axon damage. This may take up to a year to resolve as axonal regeneration proceeds at the rate of 1 mm per day. This can be separated into second and third degree and refers to the severity of damage and the resultant persistent deficit. Neurotmesis results from complete transection and is associated with a poor prognosis without reparative surgery.
Brachial plexus
Stretch injury is the most common reason for a brachial plexus injury. This can occur if the arm board is extended to greater than 90 degrees from the patient’s torso or if the patient’s arm falls off of the arm board. Careful positioning and securing the patient’s arm on the arm board before draping can avoid this injury. A brachial plexus injury can also occur if shoulder braces are placed too laterally during minimally invasive surgery. Radial nerve injuries can occur if there is too much pressure on the humerus during positioning. Ulnar injuries arise from pressure placed on the medial aspect of the elbow.
Tip #1: When tucking a patient’s arm for minimally invasive surgery, appropriate padding should be placed around the elbow and wrist, and the arm should be in the “thumbs-up” position.
Tip #2: Shoulder blocks should be placed over the acromioclavicular (AC) joint.
Lumbosacral plexus
The femoral nerve is the nerve most commonly injured during gynecologic surgery and this usually occurs because of compression of the nerve from the lateral blades of self-retaining retractors. One study showed an 8% incidence of injury from self-retaining retractors, compared with less than 1% when the retractors were not used.6 The femoral nerve can also be stretched when patients are placed in the lithotomy position and the hip is hyperflexed.
As with brachial injury prevention, patients should be positioned prior to draping and care must be taken to not hyperflex or externally rotate the hip during minimally invasive surgical procedures. With the introduction of robot-assisted surgery, care must be taken when docking the robot and surgeons must resist excessive movement of the stirrups.
Tip #3: During laparotomy, surgeons should use the shortest blades that allow for adequate visualization and check the blades during the procedure to ensure that excessive pressure is not placed on the psoas muscle. Consider intermittently releasing the pressure on the lateral blades during other portions of the procedure.
Tip #4: Make sure the stirrups are at the same height and that the leg is in line with the patient’s contralateral shoulder.
Obturator nerve injuries can occur during retroperitoneal dissection for pelvic lymphadenectomy (obturator nodes) and can be either a transection or a cautery injury. It can also be injured during urogynecologic procedures including paravaginal defect repairs and during the placement of transobturator tapes.
The sciatic nerve and its branch, the common peroneal, are generally injured because of excessive stretch or pressure. Both nerves can be injured from hyperflexion of the thigh and the common peroneal can suffer a pressure injury as it courses around the lateral head of the fibula. Therefore, care during lithotomy positioning with both candy cane and Allen stirrups is critical during vaginal surgery.
Tip #5: Ensure that the lateral fibula is not touching the stirrup or that padding is placed between the fibular head and the stirrup.
The ilioinguinal and iliohypogastric nerves are typically injured via suture entrapment from low transverse skin incisions, though laparoscopic injury has also been reported. The incidence after a Pfannenstiel incision is about 3.7%.7
Tip #6: Avoid extending the low transverse incision beyond the lateral margin of the rectus muscle, and do not extend the fascial closure suture more than 1.5 cm from the lateral edge of the fascial incision to avoid catching the nerve with the suture.
The pudendal nerve is most commonly injured during vaginal procedures such as sacrospinous fixation. Pain is typically worse when seated.
The genitofemoral nerve is typically injured during retroperitoneal lymph node dissection, particularly the external iliac nodes. The nerve is small and runs lateral to the external iliac artery. It can suffer cautery and transection injuries. Usually, the paresthesias over the mons pubis, labia majora, and medial inner thigh are temporary.
Tip #7: Care should be taken to identify and spare the nerve during retroperitoneal dissection or external iliac node removal.
Nerve injuries during gynecologic surgery are common and are a significant cause of potential morbidity. While occasionally unavoidable and inherent to the surgical procedure, many times the injury could be prevented with proper attention and care to patient positioning and retractor use. Gynecologists should be aware of the risks and have a through understanding of the anatomy. However, should an injury occur, the patient can be reassured that most are self-limited and full recovery is generally expected. In a prospective study, the median time to resolution of symptoms was 31.5 days (range, 1 day to 6 months).5
References
1. The Obstetrician & Gynaecologist 2014;16:29-36.
2. Gynecol Oncol. 1988 Nov;31(3):462-6.
3. Fertil Steril. 1993 Oct;60(4):729-32.
4. J Minim Invasive Gynecol. 2007 Sep-Oct;14(5):664-72.
5. Am J Obstet Gynecol. 2009 Nov;201(5):531.e1-7.
6. Eur J Obstet Gynecol Reprod Biol. 1985 Dec;20(6):385-92.
7. Obstet Gynecol. 2008 Apr;111(4):839-46.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. She reported having no financial disclosures relevant to this column. Email her at [email protected].
Examining the safety of lipid-lowering drugs in pregnancy
Lipid-lowering medications are some of the most commonly prescribed drugs in the United States. But while much is known about their general safety, the data are limited when it comes to pregnancy and breastfeeding.
Antilipemic agents are a pharmacologic class that contains 18 drugs. The class is divided into eight subclasses: bile acid sequestrants; fibric acid derivatives, HMG-CoA inhibitors; immunoglobulins; monoclonal antibodies; oligonucleotide inhibitors; vitamins; as well as two miscellaneous drugs, ezetimibe (Zetia) and lomitapide (Juxtapid). Another antilipemic – dextrothyroxine – has been removed from the market by the manufacturer.
Bile acid sequestrants
Bile acid sequestrants include cholestyramine (Prevalite, Questran), colesevelam (Welchol), and colestipol (Colestid). These drugs have the potential to cause fetal toxicity. This assessment is based on their mechanism of action. These agents are not absorbed systemically, or absorption is very poor and they bind bile acids into a nonabsorbable complex. This action can reduce intestinal absorption of fat-soluble vitamins A, D, E, and K.
Reports of fetal harm have not been located for the other two agents in this class, but there is only one case report involving five women for colesevelam and no reports for colestipol. Nevertheless, both of these drugs have the potential to cause fetal hemorrhage if they are taken for prolonged periods in pregnancy.
Fibric acid derivatives
The fibric acid derivatives subclass includes fenofibrate (Tricor, Lofibra) and gemfibrozil (Lopid).
Six reports, involving 13 pregnancies, have described the use of gemfibrozil during all phases of pregnancy. No teratogenic effects were observed in these cases. In one woman, similar concentrations of gemfibrozil and its active metabolite were found in the umbilical vein and artery at levels within the normal reference for adults.
Statins
There are seven HMG-CoA inhibitors, known as statins: atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor), and simvastatin (Zocor).
The interruption of cholesterol-lowering therapy during pregnancy should have no effect on the long-term treatment of hyperlipidemia. Moreover, cholesterol and products synthesized by cholesterol are important during fetal development as shown by the rise in maternal cholesterol levels during pregnancy. Although the potential for embryo-fetal harm has not been clearly documented, and that potential may eventually be confirmed as low, the use of these agents in the first trimester are best classified as contraindicated.
One consideration in estimating the embryo-fetal risk of statins is their classification as either lipophilic or hydrophilic. Three of the seven statins are hydrophilic (fluvastatin, pravastatin, and rosuvastatin); the remaining four agents are lipophilic. In a 2004 review of 70 reports, all adverse birth outcomes were reported following exposure to lipophilic statins (atorvastatin, lovastatin, or simvastatin) and none with the hydrophilic pravastatin. The authors stated that the findings were due to the fact that lipophilic agents equilibrate between maternal and embryonic compartments, whereas pravastatin is minimally present in the embryo.3 If this is indeed the case, and a statin must be used during pregnancy, fluvastatin, pravastatin, or rosuvastatin appears to be best.
Pravastatin also has been used for the prevention and treatment of preeclampsia.5,6 Although the teratogenic potential of these agents has not been fully determined, the risk for birth defects, if any, appears to be low even when exposure occurs during organogenesis.7,8,9 Nevertheless, avoiding these products during the first trimester appears to be best.
Immunoglobulins
The only immunoglobulin in the antilipemic class is evolocumab (Repatha), which has no human pregnancy data. It is an immunoglobulin G2 that is indicated as an adjunct to diet and maximally tolerated statin therapy. It is also indicated as an adjunct to diet and other low-density lipoprotein–lowering therapies in patients with homozygous familial hypercholesterolemia who require additional lowering. No adverse embryo-fetal effects were observed in monkeys. Because statins are contraindicated in the first trimester, the drug, if combined with a statin, can also be classified as contraindicated. However, if the drug is used alone, the embryo-fetal risk appears to be low based on the animal data.
Monoclonal antibodies
The protein alirocumab (Praluent) is a human monoclonal antibody. It is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease. There are no human pregnancy data. The animal data in rats and monkeys suggest low embryo-fetal risk. However, suppression of the humoral immune response to keyhole hemocyanin antigen was observed in infant monkeys at 4-6 months of age. The significance of this in human infants is apparently unknown. Because statins are contraindicated in the first trimester, the drug should not be used with these agents during that period.
Oligonucleotide inhibitors
No reports describing the use of mipomersen (Kynamro), an oligonucleotide inhibitor of apolipoprotein B-100 synthesis, in human pregnancy have been located. The drug is indicated as an adjunct to lipid-lowering medications and diet to reduce low-density lipoprotein cholesterol, apolipoprotein B, total cholesterol, and non–high-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. It has a very long (1-2 months) elimination half-life. The drug caused fetal toxicity in rats, but not in mice or rabbits.
Vitamins
Niacin is a water-soluble B complex vitamin that is converted in vivo to niacinamide. Niacin has no known embryo-fetal risk.
Miscellaneous agents
The two agents in the miscellaneous category are ezetimibe and lomitapide. Ezetimibe is indicated, either alone or in combination with a statin, as adjunctive therapy to diet for the reduction of cholesterol and triglycerides. Statins are contraindicated in the first trimester, but ezetimibe alone could be used during that period if treatment of the mother was mandated. The drug caused no problems in rabbits, but in rats, a dose 10 times the human exposure increased the incidence of skeletal abnormalities. In one report, a woman with homozygous familial hypercholesterolemia was treated with direct adsorption of lipoprotein apheresis, ezetimibe, and rosuvastatin. When pregnancy was discovered (gestational age not specified), the two drugs were stopped but biweekly apheresis was continued. At 37 weeks’ gestation, the patient gave birth to a healthy 2,400-g male infant.10
There are no human pregnancy data with lomitapide. It is indicated as an adjunct to a low-fat diet and other lipid-lowering treatments, including low-density lipoprotein apheresis where available, to reduce LDL cholesterol, total cholesterol, apolipoprotein B, and non–high-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. At doses less than 10 times the human dose, the drug caused congenital malformations and embryo-fetal death in rats, rabbits, and ferrets. The manufacturer classifies the drug as contraindicated in pregnancy because of the animal data.
Breastfeeding
Only niacin, pravastatin, and rosuvastatin have data regarding human milk concentrations. Niacin and its active form – niacinamide – are excreted into breast milk.
The average peak milk level in 11 lactating women given pravastatin 20 mg twice daily for 2.5 days was 3.9 mcg/L, whereas the level for the active metabolite was 2.1 mcg/L. Based on these data, a fully breastfed infant would receive daily about 1.4% of the mother’s weight-adjusted dose.11
A 31-year-old woman was treated with rosuvastatin for familial hypercholesterolemia while breastfeeding her infant. The drug was stopped during breastfeeding but was restarted at 33 days post partum. Breast milk concentrations of the drug were 1.2 times serum levels (about 22 ng/mL vs. 18 ng/mL). Unfortunately, no information was provided on the status of the nursing infant.12
Three of the above agents have high molecular weights - alirocumab, evolocumab, and mipomersen - and are probably not excreted into mature breast milk. Moreover, colesevelam is not absorbed, and very small amounts of colestipol are absorbed by mothers. Several antilipemic agents have characteristics (for example, low molecular weight or long elimination half-life) that suggest they will be excreted into breast milk: ezetimibe, fenofibric acid (active metabolite of fenofibrate), gemfibrozil, lomitapide, and all the statins.
Taken in sum, all of the antilipemics, with the exception of niacin, have the potential to cause a deficiency of fat-soluble vitamins (A, D, E, K) in mother’s milk and in the nursing infant. Deficiency is a concern for all of these vitamins, but especially for vitamin K, because it could cause bruising, petechiae, hematomas, and bleeding in the nursing infant. In addition, antilipemics could cause low levels in milk of cholesterol and lipids, which are required by a nursing infant. Consequently, they should not be used by mothers who are breastfeeding an infant.
References
1. Br J Obstet Gynaecol. 1995 Feb;102(2):169-70.
2. J Matern Fetal Neonatal Med. 2015 May;28(8):954-8.
3. Am J Med Genet A. 2004 Dec 15;131(3):287-98.
4. J Clin Invest. 2016 Aug 1;126(8):2933-40.
5. Hypertension. 2015 Sep;66(3):687-97.
6. Am J Obstet Gynecol. 2016 Jun;214(6):720.e1-720.e17.
7. Birth Defects Res A Clin Mol Teratol. 2005 Nov;73(11):888-96.
8. Reprod Toxicol. 2008 Oct;26(2):175-7.
9. Ann Pharmacother. 2012 Oct;46(10):1419-24.
10. Open Cardiovasc Med J. 2015 Dec 29;9:114-7.
11. J Clin Pharmacol. 1988;28:942.
12. Am J Med. 2013 Sep;126(9):e7-e8.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He has no relevant financial disclosures.
Lipid-lowering medications are some of the most commonly prescribed drugs in the United States. But while much is known about their general safety, the data are limited when it comes to pregnancy and breastfeeding.
Antilipemic agents are a pharmacologic class that contains 18 drugs. The class is divided into eight subclasses: bile acid sequestrants; fibric acid derivatives, HMG-CoA inhibitors; immunoglobulins; monoclonal antibodies; oligonucleotide inhibitors; vitamins; as well as two miscellaneous drugs, ezetimibe (Zetia) and lomitapide (Juxtapid). Another antilipemic – dextrothyroxine – has been removed from the market by the manufacturer.
Bile acid sequestrants
Bile acid sequestrants include cholestyramine (Prevalite, Questran), colesevelam (Welchol), and colestipol (Colestid). These drugs have the potential to cause fetal toxicity. This assessment is based on their mechanism of action. These agents are not absorbed systemically, or absorption is very poor and they bind bile acids into a nonabsorbable complex. This action can reduce intestinal absorption of fat-soluble vitamins A, D, E, and K.
Reports of fetal harm have not been located for the other two agents in this class, but there is only one case report involving five women for colesevelam and no reports for colestipol. Nevertheless, both of these drugs have the potential to cause fetal hemorrhage if they are taken for prolonged periods in pregnancy.
Fibric acid derivatives
The fibric acid derivatives subclass includes fenofibrate (Tricor, Lofibra) and gemfibrozil (Lopid).
Six reports, involving 13 pregnancies, have described the use of gemfibrozil during all phases of pregnancy. No teratogenic effects were observed in these cases. In one woman, similar concentrations of gemfibrozil and its active metabolite were found in the umbilical vein and artery at levels within the normal reference for adults.
Statins
There are seven HMG-CoA inhibitors, known as statins: atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor), and simvastatin (Zocor).
The interruption of cholesterol-lowering therapy during pregnancy should have no effect on the long-term treatment of hyperlipidemia. Moreover, cholesterol and products synthesized by cholesterol are important during fetal development as shown by the rise in maternal cholesterol levels during pregnancy. Although the potential for embryo-fetal harm has not been clearly documented, and that potential may eventually be confirmed as low, the use of these agents in the first trimester are best classified as contraindicated.
One consideration in estimating the embryo-fetal risk of statins is their classification as either lipophilic or hydrophilic. Three of the seven statins are hydrophilic (fluvastatin, pravastatin, and rosuvastatin); the remaining four agents are lipophilic. In a 2004 review of 70 reports, all adverse birth outcomes were reported following exposure to lipophilic statins (atorvastatin, lovastatin, or simvastatin) and none with the hydrophilic pravastatin. The authors stated that the findings were due to the fact that lipophilic agents equilibrate between maternal and embryonic compartments, whereas pravastatin is minimally present in the embryo.3 If this is indeed the case, and a statin must be used during pregnancy, fluvastatin, pravastatin, or rosuvastatin appears to be best.
Pravastatin also has been used for the prevention and treatment of preeclampsia.5,6 Although the teratogenic potential of these agents has not been fully determined, the risk for birth defects, if any, appears to be low even when exposure occurs during organogenesis.7,8,9 Nevertheless, avoiding these products during the first trimester appears to be best.
Immunoglobulins
The only immunoglobulin in the antilipemic class is evolocumab (Repatha), which has no human pregnancy data. It is an immunoglobulin G2 that is indicated as an adjunct to diet and maximally tolerated statin therapy. It is also indicated as an adjunct to diet and other low-density lipoprotein–lowering therapies in patients with homozygous familial hypercholesterolemia who require additional lowering. No adverse embryo-fetal effects were observed in monkeys. Because statins are contraindicated in the first trimester, the drug, if combined with a statin, can also be classified as contraindicated. However, if the drug is used alone, the embryo-fetal risk appears to be low based on the animal data.
Monoclonal antibodies
The protein alirocumab (Praluent) is a human monoclonal antibody. It is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease. There are no human pregnancy data. The animal data in rats and monkeys suggest low embryo-fetal risk. However, suppression of the humoral immune response to keyhole hemocyanin antigen was observed in infant monkeys at 4-6 months of age. The significance of this in human infants is apparently unknown. Because statins are contraindicated in the first trimester, the drug should not be used with these agents during that period.
Oligonucleotide inhibitors
No reports describing the use of mipomersen (Kynamro), an oligonucleotide inhibitor of apolipoprotein B-100 synthesis, in human pregnancy have been located. The drug is indicated as an adjunct to lipid-lowering medications and diet to reduce low-density lipoprotein cholesterol, apolipoprotein B, total cholesterol, and non–high-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. It has a very long (1-2 months) elimination half-life. The drug caused fetal toxicity in rats, but not in mice or rabbits.
Vitamins
Niacin is a water-soluble B complex vitamin that is converted in vivo to niacinamide. Niacin has no known embryo-fetal risk.
Miscellaneous agents
The two agents in the miscellaneous category are ezetimibe and lomitapide. Ezetimibe is indicated, either alone or in combination with a statin, as adjunctive therapy to diet for the reduction of cholesterol and triglycerides. Statins are contraindicated in the first trimester, but ezetimibe alone could be used during that period if treatment of the mother was mandated. The drug caused no problems in rabbits, but in rats, a dose 10 times the human exposure increased the incidence of skeletal abnormalities. In one report, a woman with homozygous familial hypercholesterolemia was treated with direct adsorption of lipoprotein apheresis, ezetimibe, and rosuvastatin. When pregnancy was discovered (gestational age not specified), the two drugs were stopped but biweekly apheresis was continued. At 37 weeks’ gestation, the patient gave birth to a healthy 2,400-g male infant.10
There are no human pregnancy data with lomitapide. It is indicated as an adjunct to a low-fat diet and other lipid-lowering treatments, including low-density lipoprotein apheresis where available, to reduce LDL cholesterol, total cholesterol, apolipoprotein B, and non–high-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. At doses less than 10 times the human dose, the drug caused congenital malformations and embryo-fetal death in rats, rabbits, and ferrets. The manufacturer classifies the drug as contraindicated in pregnancy because of the animal data.
Breastfeeding
Only niacin, pravastatin, and rosuvastatin have data regarding human milk concentrations. Niacin and its active form – niacinamide – are excreted into breast milk.
The average peak milk level in 11 lactating women given pravastatin 20 mg twice daily for 2.5 days was 3.9 mcg/L, whereas the level for the active metabolite was 2.1 mcg/L. Based on these data, a fully breastfed infant would receive daily about 1.4% of the mother’s weight-adjusted dose.11
A 31-year-old woman was treated with rosuvastatin for familial hypercholesterolemia while breastfeeding her infant. The drug was stopped during breastfeeding but was restarted at 33 days post partum. Breast milk concentrations of the drug were 1.2 times serum levels (about 22 ng/mL vs. 18 ng/mL). Unfortunately, no information was provided on the status of the nursing infant.12
Three of the above agents have high molecular weights - alirocumab, evolocumab, and mipomersen - and are probably not excreted into mature breast milk. Moreover, colesevelam is not absorbed, and very small amounts of colestipol are absorbed by mothers. Several antilipemic agents have characteristics (for example, low molecular weight or long elimination half-life) that suggest they will be excreted into breast milk: ezetimibe, fenofibric acid (active metabolite of fenofibrate), gemfibrozil, lomitapide, and all the statins.
Taken in sum, all of the antilipemics, with the exception of niacin, have the potential to cause a deficiency of fat-soluble vitamins (A, D, E, K) in mother’s milk and in the nursing infant. Deficiency is a concern for all of these vitamins, but especially for vitamin K, because it could cause bruising, petechiae, hematomas, and bleeding in the nursing infant. In addition, antilipemics could cause low levels in milk of cholesterol and lipids, which are required by a nursing infant. Consequently, they should not be used by mothers who are breastfeeding an infant.
References
1. Br J Obstet Gynaecol. 1995 Feb;102(2):169-70.
2. J Matern Fetal Neonatal Med. 2015 May;28(8):954-8.
3. Am J Med Genet A. 2004 Dec 15;131(3):287-98.
4. J Clin Invest. 2016 Aug 1;126(8):2933-40.
5. Hypertension. 2015 Sep;66(3):687-97.
6. Am J Obstet Gynecol. 2016 Jun;214(6):720.e1-720.e17.
7. Birth Defects Res A Clin Mol Teratol. 2005 Nov;73(11):888-96.
8. Reprod Toxicol. 2008 Oct;26(2):175-7.
9. Ann Pharmacother. 2012 Oct;46(10):1419-24.
10. Open Cardiovasc Med J. 2015 Dec 29;9:114-7.
11. J Clin Pharmacol. 1988;28:942.
12. Am J Med. 2013 Sep;126(9):e7-e8.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He has no relevant financial disclosures.
Lipid-lowering medications are some of the most commonly prescribed drugs in the United States. But while much is known about their general safety, the data are limited when it comes to pregnancy and breastfeeding.
Antilipemic agents are a pharmacologic class that contains 18 drugs. The class is divided into eight subclasses: bile acid sequestrants; fibric acid derivatives, HMG-CoA inhibitors; immunoglobulins; monoclonal antibodies; oligonucleotide inhibitors; vitamins; as well as two miscellaneous drugs, ezetimibe (Zetia) and lomitapide (Juxtapid). Another antilipemic – dextrothyroxine – has been removed from the market by the manufacturer.
Bile acid sequestrants
Bile acid sequestrants include cholestyramine (Prevalite, Questran), colesevelam (Welchol), and colestipol (Colestid). These drugs have the potential to cause fetal toxicity. This assessment is based on their mechanism of action. These agents are not absorbed systemically, or absorption is very poor and they bind bile acids into a nonabsorbable complex. This action can reduce intestinal absorption of fat-soluble vitamins A, D, E, and K.
Reports of fetal harm have not been located for the other two agents in this class, but there is only one case report involving five women for colesevelam and no reports for colestipol. Nevertheless, both of these drugs have the potential to cause fetal hemorrhage if they are taken for prolonged periods in pregnancy.
Fibric acid derivatives
The fibric acid derivatives subclass includes fenofibrate (Tricor, Lofibra) and gemfibrozil (Lopid).
Six reports, involving 13 pregnancies, have described the use of gemfibrozil during all phases of pregnancy. No teratogenic effects were observed in these cases. In one woman, similar concentrations of gemfibrozil and its active metabolite were found in the umbilical vein and artery at levels within the normal reference for adults.
Statins
There are seven HMG-CoA inhibitors, known as statins: atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor), and simvastatin (Zocor).
The interruption of cholesterol-lowering therapy during pregnancy should have no effect on the long-term treatment of hyperlipidemia. Moreover, cholesterol and products synthesized by cholesterol are important during fetal development as shown by the rise in maternal cholesterol levels during pregnancy. Although the potential for embryo-fetal harm has not been clearly documented, and that potential may eventually be confirmed as low, the use of these agents in the first trimester are best classified as contraindicated.
One consideration in estimating the embryo-fetal risk of statins is their classification as either lipophilic or hydrophilic. Three of the seven statins are hydrophilic (fluvastatin, pravastatin, and rosuvastatin); the remaining four agents are lipophilic. In a 2004 review of 70 reports, all adverse birth outcomes were reported following exposure to lipophilic statins (atorvastatin, lovastatin, or simvastatin) and none with the hydrophilic pravastatin. The authors stated that the findings were due to the fact that lipophilic agents equilibrate between maternal and embryonic compartments, whereas pravastatin is minimally present in the embryo.3 If this is indeed the case, and a statin must be used during pregnancy, fluvastatin, pravastatin, or rosuvastatin appears to be best.
Pravastatin also has been used for the prevention and treatment of preeclampsia.5,6 Although the teratogenic potential of these agents has not been fully determined, the risk for birth defects, if any, appears to be low even when exposure occurs during organogenesis.7,8,9 Nevertheless, avoiding these products during the first trimester appears to be best.
Immunoglobulins
The only immunoglobulin in the antilipemic class is evolocumab (Repatha), which has no human pregnancy data. It is an immunoglobulin G2 that is indicated as an adjunct to diet and maximally tolerated statin therapy. It is also indicated as an adjunct to diet and other low-density lipoprotein–lowering therapies in patients with homozygous familial hypercholesterolemia who require additional lowering. No adverse embryo-fetal effects were observed in monkeys. Because statins are contraindicated in the first trimester, the drug, if combined with a statin, can also be classified as contraindicated. However, if the drug is used alone, the embryo-fetal risk appears to be low based on the animal data.
Monoclonal antibodies
The protein alirocumab (Praluent) is a human monoclonal antibody. It is indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease. There are no human pregnancy data. The animal data in rats and monkeys suggest low embryo-fetal risk. However, suppression of the humoral immune response to keyhole hemocyanin antigen was observed in infant monkeys at 4-6 months of age. The significance of this in human infants is apparently unknown. Because statins are contraindicated in the first trimester, the drug should not be used with these agents during that period.
Oligonucleotide inhibitors
No reports describing the use of mipomersen (Kynamro), an oligonucleotide inhibitor of apolipoprotein B-100 synthesis, in human pregnancy have been located. The drug is indicated as an adjunct to lipid-lowering medications and diet to reduce low-density lipoprotein cholesterol, apolipoprotein B, total cholesterol, and non–high-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. It has a very long (1-2 months) elimination half-life. The drug caused fetal toxicity in rats, but not in mice or rabbits.
Vitamins
Niacin is a water-soluble B complex vitamin that is converted in vivo to niacinamide. Niacin has no known embryo-fetal risk.
Miscellaneous agents
The two agents in the miscellaneous category are ezetimibe and lomitapide. Ezetimibe is indicated, either alone or in combination with a statin, as adjunctive therapy to diet for the reduction of cholesterol and triglycerides. Statins are contraindicated in the first trimester, but ezetimibe alone could be used during that period if treatment of the mother was mandated. The drug caused no problems in rabbits, but in rats, a dose 10 times the human exposure increased the incidence of skeletal abnormalities. In one report, a woman with homozygous familial hypercholesterolemia was treated with direct adsorption of lipoprotein apheresis, ezetimibe, and rosuvastatin. When pregnancy was discovered (gestational age not specified), the two drugs were stopped but biweekly apheresis was continued. At 37 weeks’ gestation, the patient gave birth to a healthy 2,400-g male infant.10
There are no human pregnancy data with lomitapide. It is indicated as an adjunct to a low-fat diet and other lipid-lowering treatments, including low-density lipoprotein apheresis where available, to reduce LDL cholesterol, total cholesterol, apolipoprotein B, and non–high-density lipoprotein cholesterol in patients with homozygous familial hypercholesterolemia. At doses less than 10 times the human dose, the drug caused congenital malformations and embryo-fetal death in rats, rabbits, and ferrets. The manufacturer classifies the drug as contraindicated in pregnancy because of the animal data.
Breastfeeding
Only niacin, pravastatin, and rosuvastatin have data regarding human milk concentrations. Niacin and its active form – niacinamide – are excreted into breast milk.
The average peak milk level in 11 lactating women given pravastatin 20 mg twice daily for 2.5 days was 3.9 mcg/L, whereas the level for the active metabolite was 2.1 mcg/L. Based on these data, a fully breastfed infant would receive daily about 1.4% of the mother’s weight-adjusted dose.11
A 31-year-old woman was treated with rosuvastatin for familial hypercholesterolemia while breastfeeding her infant. The drug was stopped during breastfeeding but was restarted at 33 days post partum. Breast milk concentrations of the drug were 1.2 times serum levels (about 22 ng/mL vs. 18 ng/mL). Unfortunately, no information was provided on the status of the nursing infant.12
Three of the above agents have high molecular weights - alirocumab, evolocumab, and mipomersen - and are probably not excreted into mature breast milk. Moreover, colesevelam is not absorbed, and very small amounts of colestipol are absorbed by mothers. Several antilipemic agents have characteristics (for example, low molecular weight or long elimination half-life) that suggest they will be excreted into breast milk: ezetimibe, fenofibric acid (active metabolite of fenofibrate), gemfibrozil, lomitapide, and all the statins.
Taken in sum, all of the antilipemics, with the exception of niacin, have the potential to cause a deficiency of fat-soluble vitamins (A, D, E, K) in mother’s milk and in the nursing infant. Deficiency is a concern for all of these vitamins, but especially for vitamin K, because it could cause bruising, petechiae, hematomas, and bleeding in the nursing infant. In addition, antilipemics could cause low levels in milk of cholesterol and lipids, which are required by a nursing infant. Consequently, they should not be used by mothers who are breastfeeding an infant.
References
1. Br J Obstet Gynaecol. 1995 Feb;102(2):169-70.
2. J Matern Fetal Neonatal Med. 2015 May;28(8):954-8.
3. Am J Med Genet A. 2004 Dec 15;131(3):287-98.
4. J Clin Invest. 2016 Aug 1;126(8):2933-40.
5. Hypertension. 2015 Sep;66(3):687-97.
6. Am J Obstet Gynecol. 2016 Jun;214(6):720.e1-720.e17.
7. Birth Defects Res A Clin Mol Teratol. 2005 Nov;73(11):888-96.
8. Reprod Toxicol. 2008 Oct;26(2):175-7.
9. Ann Pharmacother. 2012 Oct;46(10):1419-24.
10. Open Cardiovasc Med J. 2015 Dec 29;9:114-7.
11. J Clin Pharmacol. 1988;28:942.
12. Am J Med. 2013 Sep;126(9):e7-e8.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, and Washington State University, Spokane. He is coauthor of “Drugs in Pregnancy and Lactation,” and coeditor of “Diseases, Complications, and Drug Therapy in Obstetrics.” He has no relevant financial disclosures.
Alarming gaps in gestational diabetes care
BY E. ALBERT REECE, MD, PhD, MBA
Much attention has been given in the media to the incidence of prediabetes in the general population. The Centers for Disease Control and Prevention estimates that approximately 86 million adults have prediabetes, and that the incidence of this condition is similar across racial and ethnic groups. Indeed, the seriousness of this public health concern prompted the Centers for Medicare & Medicaid Services to expand Medicare coverage for interventions for people with prediabetes, a move that was finalized in November 2016.
Despite a widespread focus on the need to prevent prediabetes from becoming type 2 diabetes, women diagnosed with gestational diabetes mellitus (GDM), which accounts for about 9% of women in the United States, may not be receiving critical advice and care.
The investigators analyzed data collected via the National Health and Nutrition Examination Survey from 2007-2012, and identified 284 women with a history of GDM. Only 67% of these women received diabetes screening, and approximately one-third of women included in the study had undiagnosed prediabetes and diabetes. The authors concluded that prediabetes in women who have had GDM may be underdiagnosed. They argued that women with GDM should be encouraged to have additional health visits and screenings to prevent the development of prediabetes or diabetes. Considering the fact that a number of studies have shown that GDM predisposes a woman to developing type 2 diabetes, the University of Illinois findings are alarming.
As ob.gyns., we have increasingly become a woman’s only health care practitioner. Although individuals may skip annual exams with a primary care physician, during which blood work is typically drawn, many women will see their ob.gyn. for regular check-ups. Therefore, we have a unique role to play in our patients’ lifelong health. This is especially important during pregnancy, when it may be easy to focus only on the mother’s health as it pertains to the health of the baby, rather than her health in pregnancy as it may affect her long-term well-being.
We have invited Robert Ratner, MD, the chief scientific and medical officer at the American Diabetes Association, to discuss the need to carefully follow up with patients who have had GDM and to educate them about their risk for developing type 2 diabetes later in life.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Why postpartum GDM follow-up is so important
BY ROBERT E. RATNER, MD
Much of the attention paid to diagnosing gestational diabetes has focused on the fetus and on babies being born very large. However, it is important to appreciate that the original definitions of the condition were based entirely on the long-term outcomes of the mother.
John O’Sullivan, MD, and statistician Claire Mahan published diagnostic criteria in 1964 after performing 3-hour oral glucose tolerance tests (OGTTs) in more than 500 unselected women during their pregnancies, and then following these women and babies out as far as 23 years. Retrospectively, Dr. O’Sullivan and Ms. Mahan defined gestational diabetes mellitus (GDM) as glucose values exceeding two standard deviations above the mean on two out of four OGTT values.
They came to their conclusions after tracking the later development of diabetes outside of pregnancy. More than 20 years later, 70% of women with the higher OGTT values had developed type 2 diabetes, compared with approximately 10% of women who did not have higher values during pregnancy. The O’Sullivan criteria were established, essentially, based on their association with the development of diabetes after pregnancy. In addition to being a significant predictor of subsequent diabetes, a history of GDM also conferred a three- to fourfold increase in maternal mortality.
Fifty-some years later, these findings have been affirmed through additional research and are the crux of what drives the current recommendations for postpartum follow-up of women with a history of GDM.
Long-term maternal risks
Postpartum, the current recommendation from both the American Diabetes Association and the American College of Obstetricians and Gynecologists is that women with GDM be tested at 6-12 weeks after delivery to ensure that the diabetes has resolved.
This recommendation for initial postpartum testing carries with it a stipulation that’s different from subsequent postpartum testing. It says that postpartum testing at 6-12 weeks should be performed with either a fasting glucose test or a 2-hour OGTT. Since hemoglobin A1c may still be impacted by the rapid red blood cell turnover in pregnancy or blood loss at delivery, A1c testing lacks sensitivity for identifying diabetes during this window of time.
Initial postpartum testing also serves as a way to identify whether the diabetes during pregnancy was preexisting or purely secondary to the hormonal changes associated with the pregnancy.
If this first postpartum test shows diabetes, the patient most likely had preexisting diabetes, and therapy must be initiated immediately. In the case of a normal result, the patient remains at higher risk for the development of type 2 diabetes essentially for the rest of her life and should be tested at least every 3 years for the occurrence of the disease.
Much of the increased risk for different ethnic groups occurs within 5 years of the index pregnancy. This was shown in a systematic review led by Catherine Kim, MD; the review examined more than two dozen studies with follow-up of up to 28 years postpartum. The cumulative incidence of type 2 diabetes increased markedly in the first 5 years and then appeared to plateau after 10 years (Diabetes Care. 2002 Oct;25[10]:1862-8).
The best data on late-occurring diabetes following GDM comes from the multicenter National Institutes of Health–sponsored Diabetes Prevention Program (DPP) trial, which randomized more than 3,000 individuals with baseline impaired glucose tolerance – or prediabetes – to one of two interventions: metformin therapy or intensive lifestyle intervention, or to placebo.
Within this population, there were more than 1,700 women who had a previous live birth. Of these women, 350 reported a history of GDM at a mean of 12 years since the delivery of their first GDM pregnancy. The DPP gave us the opportunity, therefore, to look at a large group of women about 12 years away from their GDM pregnancy who had abnormal glucose levels but had not reached the level of type 2 diabetes, and compare them with women with similarly impaired glucose tolerance who did not have a history of GDM.
There were interesting similarities and differences. Women with a GDM history were on average 8 years younger than women without a GDM history, but they had comparable BMIs. In addition, within the placebo arm, we could observe the natural history of glucose intolerance in women with and without a history of GDM. Despite both groups entering the study with equivalent degrees of impaired glucose tolerance and similar BMI, women with a history of GDM had a 71% higher risk of developing diabetes during the 3-year intervention period than that of parous women without a history of GDM (J Clin Endocrinol Metab. 2008 Dec;93[12]:4774-9).
Clearly, there was something about the history of GDM that puts these women at greater risk for diabetes than women who had the same impaired glucose tolerance, but no GDM. The study demonstrated that GDM is an exceptionally strong predictor of the development of type 2 diabetes, even for those who manage to escape diabetes for the first 10 years.
Postpartum prevention
The DPP demonstrated, moreover, that intensive lifestyle therapy and metformin not only were both effective, but that they were equally effective, in delaying or preventing diabetes in women with impaired glucose tolerance and a history of GDM. Both reduced the risk by about 50% at 3 years. This was striking because in parous women without GDM, the reductions were 49% and 14%, respectively. Metformin thus appeared to be more effective in women with a history of GDM.
The effects of the interventions persisted over a 10-year follow up of the DPP population. In women with a history of GDM, the intensive lifestyle intervention and metformin reduced progression to diabetes by 35% and 40%, respectively, over 10 years (J Clin Endocrinol Metab. 2015 Apr;100[4]:1646-53).
Pregnancy presents a stress test for beta cell function, and gestational diabetes clearly is a harbinger of further deterioration in beta-cell function and metabolic abnormalities in the mother. Because of these risks and because early intervention makes a difference, surveillance is critically important. Most women see their ob.gyn. as their primary care physician in the 10 years following a pregnancy – the time when more than 50% of all cases of subsequent diabetes will occur – and many continue to see their ob.gyns. in the longer term, as their risk continues to linger.
Immediately after a pregnancy with GDM, ob.gyns. can counsel women not only about their risks of developing type 2 diabetes and the importance of screening, but also about the beneficial impact of lifestyle modification, caloric restriction and weight loss if necessary, and increased exercise. Mothers should also know that GDM is a family affair, and that lifestyle changes that are beneficial for the mother will be equally beneficial for the baby.
The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study taught us that there are continuous linear relationships between maternal glucose and adverse fetal outcomes like birth weight and percent body fat greater than the 90th percentile. Longitudinal studies of the Pima Indians showed us that offspring of women who had diabetes during pregnancy were more likely to be obese and more likely to develop diabetes than offspring of women who did not have diabetes during pregnancy. Even when GDM has been well treated and controlled, we should have heightened awareness to the potential risks in the fetus and the growing child and adolescent.
Patients who are found to have subsequent type 2 diabetes should know that aggressive therapy early on in the natural history of the disease reduces the risk of microvascular and macrovascular complications. And as the DPP has demonstrated, lifestyle interventions and metformin may also keep women who are found to have prediabetes outside of pregnancy from progressing on to diabetes.
Dr. Ratner is the chief scientific and medical officer for the American Diabetes Association. He reported having no financial disclosures relevant to this Master Class.
BY E. ALBERT REECE, MD, PhD, MBA
Much attention has been given in the media to the incidence of prediabetes in the general population. The Centers for Disease Control and Prevention estimates that approximately 86 million adults have prediabetes, and that the incidence of this condition is similar across racial and ethnic groups. Indeed, the seriousness of this public health concern prompted the Centers for Medicare & Medicaid Services to expand Medicare coverage for interventions for people with prediabetes, a move that was finalized in November 2016.
Despite a widespread focus on the need to prevent prediabetes from becoming type 2 diabetes, women diagnosed with gestational diabetes mellitus (GDM), which accounts for about 9% of women in the United States, may not be receiving critical advice and care.
The investigators analyzed data collected via the National Health and Nutrition Examination Survey from 2007-2012, and identified 284 women with a history of GDM. Only 67% of these women received diabetes screening, and approximately one-third of women included in the study had undiagnosed prediabetes and diabetes. The authors concluded that prediabetes in women who have had GDM may be underdiagnosed. They argued that women with GDM should be encouraged to have additional health visits and screenings to prevent the development of prediabetes or diabetes. Considering the fact that a number of studies have shown that GDM predisposes a woman to developing type 2 diabetes, the University of Illinois findings are alarming.
As ob.gyns., we have increasingly become a woman’s only health care practitioner. Although individuals may skip annual exams with a primary care physician, during which blood work is typically drawn, many women will see their ob.gyn. for regular check-ups. Therefore, we have a unique role to play in our patients’ lifelong health. This is especially important during pregnancy, when it may be easy to focus only on the mother’s health as it pertains to the health of the baby, rather than her health in pregnancy as it may affect her long-term well-being.
We have invited Robert Ratner, MD, the chief scientific and medical officer at the American Diabetes Association, to discuss the need to carefully follow up with patients who have had GDM and to educate them about their risk for developing type 2 diabetes later in life.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Why postpartum GDM follow-up is so important
BY ROBERT E. RATNER, MD
Much of the attention paid to diagnosing gestational diabetes has focused on the fetus and on babies being born very large. However, it is important to appreciate that the original definitions of the condition were based entirely on the long-term outcomes of the mother.
John O’Sullivan, MD, and statistician Claire Mahan published diagnostic criteria in 1964 after performing 3-hour oral glucose tolerance tests (OGTTs) in more than 500 unselected women during their pregnancies, and then following these women and babies out as far as 23 years. Retrospectively, Dr. O’Sullivan and Ms. Mahan defined gestational diabetes mellitus (GDM) as glucose values exceeding two standard deviations above the mean on two out of four OGTT values.
They came to their conclusions after tracking the later development of diabetes outside of pregnancy. More than 20 years later, 70% of women with the higher OGTT values had developed type 2 diabetes, compared with approximately 10% of women who did not have higher values during pregnancy. The O’Sullivan criteria were established, essentially, based on their association with the development of diabetes after pregnancy. In addition to being a significant predictor of subsequent diabetes, a history of GDM also conferred a three- to fourfold increase in maternal mortality.
Fifty-some years later, these findings have been affirmed through additional research and are the crux of what drives the current recommendations for postpartum follow-up of women with a history of GDM.
Long-term maternal risks
Postpartum, the current recommendation from both the American Diabetes Association and the American College of Obstetricians and Gynecologists is that women with GDM be tested at 6-12 weeks after delivery to ensure that the diabetes has resolved.
This recommendation for initial postpartum testing carries with it a stipulation that’s different from subsequent postpartum testing. It says that postpartum testing at 6-12 weeks should be performed with either a fasting glucose test or a 2-hour OGTT. Since hemoglobin A1c may still be impacted by the rapid red blood cell turnover in pregnancy or blood loss at delivery, A1c testing lacks sensitivity for identifying diabetes during this window of time.
Initial postpartum testing also serves as a way to identify whether the diabetes during pregnancy was preexisting or purely secondary to the hormonal changes associated with the pregnancy.
If this first postpartum test shows diabetes, the patient most likely had preexisting diabetes, and therapy must be initiated immediately. In the case of a normal result, the patient remains at higher risk for the development of type 2 diabetes essentially for the rest of her life and should be tested at least every 3 years for the occurrence of the disease.
Much of the increased risk for different ethnic groups occurs within 5 years of the index pregnancy. This was shown in a systematic review led by Catherine Kim, MD; the review examined more than two dozen studies with follow-up of up to 28 years postpartum. The cumulative incidence of type 2 diabetes increased markedly in the first 5 years and then appeared to plateau after 10 years (Diabetes Care. 2002 Oct;25[10]:1862-8).
The best data on late-occurring diabetes following GDM comes from the multicenter National Institutes of Health–sponsored Diabetes Prevention Program (DPP) trial, which randomized more than 3,000 individuals with baseline impaired glucose tolerance – or prediabetes – to one of two interventions: metformin therapy or intensive lifestyle intervention, or to placebo.
Within this population, there were more than 1,700 women who had a previous live birth. Of these women, 350 reported a history of GDM at a mean of 12 years since the delivery of their first GDM pregnancy. The DPP gave us the opportunity, therefore, to look at a large group of women about 12 years away from their GDM pregnancy who had abnormal glucose levels but had not reached the level of type 2 diabetes, and compare them with women with similarly impaired glucose tolerance who did not have a history of GDM.
There were interesting similarities and differences. Women with a GDM history were on average 8 years younger than women without a GDM history, but they had comparable BMIs. In addition, within the placebo arm, we could observe the natural history of glucose intolerance in women with and without a history of GDM. Despite both groups entering the study with equivalent degrees of impaired glucose tolerance and similar BMI, women with a history of GDM had a 71% higher risk of developing diabetes during the 3-year intervention period than that of parous women without a history of GDM (J Clin Endocrinol Metab. 2008 Dec;93[12]:4774-9).
Clearly, there was something about the history of GDM that puts these women at greater risk for diabetes than women who had the same impaired glucose tolerance, but no GDM. The study demonstrated that GDM is an exceptionally strong predictor of the development of type 2 diabetes, even for those who manage to escape diabetes for the first 10 years.
Postpartum prevention
The DPP demonstrated, moreover, that intensive lifestyle therapy and metformin not only were both effective, but that they were equally effective, in delaying or preventing diabetes in women with impaired glucose tolerance and a history of GDM. Both reduced the risk by about 50% at 3 years. This was striking because in parous women without GDM, the reductions were 49% and 14%, respectively. Metformin thus appeared to be more effective in women with a history of GDM.
The effects of the interventions persisted over a 10-year follow up of the DPP population. In women with a history of GDM, the intensive lifestyle intervention and metformin reduced progression to diabetes by 35% and 40%, respectively, over 10 years (J Clin Endocrinol Metab. 2015 Apr;100[4]:1646-53).
Pregnancy presents a stress test for beta cell function, and gestational diabetes clearly is a harbinger of further deterioration in beta-cell function and metabolic abnormalities in the mother. Because of these risks and because early intervention makes a difference, surveillance is critically important. Most women see their ob.gyn. as their primary care physician in the 10 years following a pregnancy – the time when more than 50% of all cases of subsequent diabetes will occur – and many continue to see their ob.gyns. in the longer term, as their risk continues to linger.
Immediately after a pregnancy with GDM, ob.gyns. can counsel women not only about their risks of developing type 2 diabetes and the importance of screening, but also about the beneficial impact of lifestyle modification, caloric restriction and weight loss if necessary, and increased exercise. Mothers should also know that GDM is a family affair, and that lifestyle changes that are beneficial for the mother will be equally beneficial for the baby.
The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study taught us that there are continuous linear relationships between maternal glucose and adverse fetal outcomes like birth weight and percent body fat greater than the 90th percentile. Longitudinal studies of the Pima Indians showed us that offspring of women who had diabetes during pregnancy were more likely to be obese and more likely to develop diabetes than offspring of women who did not have diabetes during pregnancy. Even when GDM has been well treated and controlled, we should have heightened awareness to the potential risks in the fetus and the growing child and adolescent.
Patients who are found to have subsequent type 2 diabetes should know that aggressive therapy early on in the natural history of the disease reduces the risk of microvascular and macrovascular complications. And as the DPP has demonstrated, lifestyle interventions and metformin may also keep women who are found to have prediabetes outside of pregnancy from progressing on to diabetes.
Dr. Ratner is the chief scientific and medical officer for the American Diabetes Association. He reported having no financial disclosures relevant to this Master Class.
BY E. ALBERT REECE, MD, PhD, MBA
Much attention has been given in the media to the incidence of prediabetes in the general population. The Centers for Disease Control and Prevention estimates that approximately 86 million adults have prediabetes, and that the incidence of this condition is similar across racial and ethnic groups. Indeed, the seriousness of this public health concern prompted the Centers for Medicare & Medicaid Services to expand Medicare coverage for interventions for people with prediabetes, a move that was finalized in November 2016.
Despite a widespread focus on the need to prevent prediabetes from becoming type 2 diabetes, women diagnosed with gestational diabetes mellitus (GDM), which accounts for about 9% of women in the United States, may not be receiving critical advice and care.
The investigators analyzed data collected via the National Health and Nutrition Examination Survey from 2007-2012, and identified 284 women with a history of GDM. Only 67% of these women received diabetes screening, and approximately one-third of women included in the study had undiagnosed prediabetes and diabetes. The authors concluded that prediabetes in women who have had GDM may be underdiagnosed. They argued that women with GDM should be encouraged to have additional health visits and screenings to prevent the development of prediabetes or diabetes. Considering the fact that a number of studies have shown that GDM predisposes a woman to developing type 2 diabetes, the University of Illinois findings are alarming.
As ob.gyns., we have increasingly become a woman’s only health care practitioner. Although individuals may skip annual exams with a primary care physician, during which blood work is typically drawn, many women will see their ob.gyn. for regular check-ups. Therefore, we have a unique role to play in our patients’ lifelong health. This is especially important during pregnancy, when it may be easy to focus only on the mother’s health as it pertains to the health of the baby, rather than her health in pregnancy as it may affect her long-term well-being.
We have invited Robert Ratner, MD, the chief scientific and medical officer at the American Diabetes Association, to discuss the need to carefully follow up with patients who have had GDM and to educate them about their risk for developing type 2 diabetes later in life.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Why postpartum GDM follow-up is so important
BY ROBERT E. RATNER, MD
Much of the attention paid to diagnosing gestational diabetes has focused on the fetus and on babies being born very large. However, it is important to appreciate that the original definitions of the condition were based entirely on the long-term outcomes of the mother.
John O’Sullivan, MD, and statistician Claire Mahan published diagnostic criteria in 1964 after performing 3-hour oral glucose tolerance tests (OGTTs) in more than 500 unselected women during their pregnancies, and then following these women and babies out as far as 23 years. Retrospectively, Dr. O’Sullivan and Ms. Mahan defined gestational diabetes mellitus (GDM) as glucose values exceeding two standard deviations above the mean on two out of four OGTT values.
They came to their conclusions after tracking the later development of diabetes outside of pregnancy. More than 20 years later, 70% of women with the higher OGTT values had developed type 2 diabetes, compared with approximately 10% of women who did not have higher values during pregnancy. The O’Sullivan criteria were established, essentially, based on their association with the development of diabetes after pregnancy. In addition to being a significant predictor of subsequent diabetes, a history of GDM also conferred a three- to fourfold increase in maternal mortality.
Fifty-some years later, these findings have been affirmed through additional research and are the crux of what drives the current recommendations for postpartum follow-up of women with a history of GDM.
Long-term maternal risks
Postpartum, the current recommendation from both the American Diabetes Association and the American College of Obstetricians and Gynecologists is that women with GDM be tested at 6-12 weeks after delivery to ensure that the diabetes has resolved.
This recommendation for initial postpartum testing carries with it a stipulation that’s different from subsequent postpartum testing. It says that postpartum testing at 6-12 weeks should be performed with either a fasting glucose test or a 2-hour OGTT. Since hemoglobin A1c may still be impacted by the rapid red blood cell turnover in pregnancy or blood loss at delivery, A1c testing lacks sensitivity for identifying diabetes during this window of time.
Initial postpartum testing also serves as a way to identify whether the diabetes during pregnancy was preexisting or purely secondary to the hormonal changes associated with the pregnancy.
If this first postpartum test shows diabetes, the patient most likely had preexisting diabetes, and therapy must be initiated immediately. In the case of a normal result, the patient remains at higher risk for the development of type 2 diabetes essentially for the rest of her life and should be tested at least every 3 years for the occurrence of the disease.
Much of the increased risk for different ethnic groups occurs within 5 years of the index pregnancy. This was shown in a systematic review led by Catherine Kim, MD; the review examined more than two dozen studies with follow-up of up to 28 years postpartum. The cumulative incidence of type 2 diabetes increased markedly in the first 5 years and then appeared to plateau after 10 years (Diabetes Care. 2002 Oct;25[10]:1862-8).
The best data on late-occurring diabetes following GDM comes from the multicenter National Institutes of Health–sponsored Diabetes Prevention Program (DPP) trial, which randomized more than 3,000 individuals with baseline impaired glucose tolerance – or prediabetes – to one of two interventions: metformin therapy or intensive lifestyle intervention, or to placebo.
Within this population, there were more than 1,700 women who had a previous live birth. Of these women, 350 reported a history of GDM at a mean of 12 years since the delivery of their first GDM pregnancy. The DPP gave us the opportunity, therefore, to look at a large group of women about 12 years away from their GDM pregnancy who had abnormal glucose levels but had not reached the level of type 2 diabetes, and compare them with women with similarly impaired glucose tolerance who did not have a history of GDM.
There were interesting similarities and differences. Women with a GDM history were on average 8 years younger than women without a GDM history, but they had comparable BMIs. In addition, within the placebo arm, we could observe the natural history of glucose intolerance in women with and without a history of GDM. Despite both groups entering the study with equivalent degrees of impaired glucose tolerance and similar BMI, women with a history of GDM had a 71% higher risk of developing diabetes during the 3-year intervention period than that of parous women without a history of GDM (J Clin Endocrinol Metab. 2008 Dec;93[12]:4774-9).
Clearly, there was something about the history of GDM that puts these women at greater risk for diabetes than women who had the same impaired glucose tolerance, but no GDM. The study demonstrated that GDM is an exceptionally strong predictor of the development of type 2 diabetes, even for those who manage to escape diabetes for the first 10 years.
Postpartum prevention
The DPP demonstrated, moreover, that intensive lifestyle therapy and metformin not only were both effective, but that they were equally effective, in delaying or preventing diabetes in women with impaired glucose tolerance and a history of GDM. Both reduced the risk by about 50% at 3 years. This was striking because in parous women without GDM, the reductions were 49% and 14%, respectively. Metformin thus appeared to be more effective in women with a history of GDM.
The effects of the interventions persisted over a 10-year follow up of the DPP population. In women with a history of GDM, the intensive lifestyle intervention and metformin reduced progression to diabetes by 35% and 40%, respectively, over 10 years (J Clin Endocrinol Metab. 2015 Apr;100[4]:1646-53).
Pregnancy presents a stress test for beta cell function, and gestational diabetes clearly is a harbinger of further deterioration in beta-cell function and metabolic abnormalities in the mother. Because of these risks and because early intervention makes a difference, surveillance is critically important. Most women see their ob.gyn. as their primary care physician in the 10 years following a pregnancy – the time when more than 50% of all cases of subsequent diabetes will occur – and many continue to see their ob.gyns. in the longer term, as their risk continues to linger.
Immediately after a pregnancy with GDM, ob.gyns. can counsel women not only about their risks of developing type 2 diabetes and the importance of screening, but also about the beneficial impact of lifestyle modification, caloric restriction and weight loss if necessary, and increased exercise. Mothers should also know that GDM is a family affair, and that lifestyle changes that are beneficial for the mother will be equally beneficial for the baby.
The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study taught us that there are continuous linear relationships between maternal glucose and adverse fetal outcomes like birth weight and percent body fat greater than the 90th percentile. Longitudinal studies of the Pima Indians showed us that offspring of women who had diabetes during pregnancy were more likely to be obese and more likely to develop diabetes than offspring of women who did not have diabetes during pregnancy. Even when GDM has been well treated and controlled, we should have heightened awareness to the potential risks in the fetus and the growing child and adolescent.
Patients who are found to have subsequent type 2 diabetes should know that aggressive therapy early on in the natural history of the disease reduces the risk of microvascular and macrovascular complications. And as the DPP has demonstrated, lifestyle interventions and metformin may also keep women who are found to have prediabetes outside of pregnancy from progressing on to diabetes.
Dr. Ratner is the chief scientific and medical officer for the American Diabetes Association. He reported having no financial disclosures relevant to this Master Class.
50 years of ob.gyn.: Has practice changed for the better?
As a practicing obstetrician-gynecologist for nearly 40 years, Leonard Brabson, MD, has watched his specialty transform in ways both large and small.
For starters, his regular work attire in 1977 – a shirt and tie – is now scrubs. The paper charts that once filled his office shelves have been replaced with electronic records. And the cumbersome machines that once took blurry, still pictures of a fetus have advanced by leaps and bounds and become a staple of prenatal care.
“Back then, we were expected to be generalists. If [a patient] had a cancer, you took care of it. If [she] had a fertility problem or problem with endocrinology, you took care of it. Of course, now if I have a female cancer, we refer them to the gyn-oncologist. But when you go back 40 years and beyond, we did mostly everything.”
The ob.gyns. of today are practicing in a vastly different environment than their predecessors, and while many of the differences have improved patient care and enhanced efficiency, physicians also note that some changes have harmed the doctor-patient relationship and created career dissatisfaction.
“Certainly, the advances of modern medicine have enabled the current physician to provide the patient a level of care unparalleled in history,” said Charles E. Miller, MD, a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.
More volume, less time
Most long-time physicians agree that higher patient volumes and increasing administrative burdens have diminished the time they are able to spend with patients.
Rising clinical documentation and coding are the top administrative tasks taking away from one-on-one patient care, said Kristen Zeligs, MD, chair of the American Congress of Obstetricians and Gynecologists’ Junior Fellow Congress Advisory Council and a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Md.
But there are other factors straining the doctor-patient relationship. Decades ago, first-time mothers often stayed with one doctor for a lifetime, Dr. Brabson recalled, having all of her babies delivered by a single ob.gyn. The same can’t be said for today, where insurance changes, job relocations, and a lack of connections often lead patients to switch physicians frequently.
“Now a lot of patients [move on] from one year to the next,” Dr. Brabson said. “There’s not that same loyalty.”
Doctors, too, traditionally stuck with patients over the long haul, he added. In the past, if an ob.gyn treated a patient during pregnancy, that same physician was present during the delivery, even if it meant leaving a vacation early or coming in on a night off.
“Now the younger docs, especially those that have families with small children, when it’s not their night on call and it’s 5 o’clock, they’re checking out,” Dr. Brabson said. “One of my partners right now, she started inducing someone yesterday. Well today’s her day off, so I’m going to do the delivery. That’s been a big change.”
Highs and lows of liability premiums
Another pressure on the specialty over the last couple of decades has been the high cost of liability insurance.
“2003 was really the peak of the liability crisis,” Dr. Montgomery said. “Hospitals were closing. Doctors were giving up practice. It’s a little better now than it was.”
While ob.gyns. still pay higher premiums than many other specialties, the legal climate has improved in recent years, said Paul Greve Jr., executive vice president and senior consultant for the Willis Healthcare Practice, and author of the 2016 Medical Liability Monitor, an annual report that surveys medical liability premiums.
“The best way to characterize the overall environment for medical professional liability is stable,” he said. “In the area of obstetrics, for the first time ever in recent years, we are seeing lower frequency and lower severity [of lawsuits].”
The lower number of filings are largely due to patient safety initiatives among ob.gyn. programs and tort reforms – many of which have been upheld by courts in the last decade, Mr. Greve said.
Of course, the rate of premiums greatly differs depending on location, with ob.gyns. in Eastern New York paying a high of $214,999 and ob.gyns. in Minnesota paying a low of $16,449 in 2016, according to the Medical Liability Monitor.
“The environment is specific to the region,” Mr. Greve said. “New York City is still very problematic. Chicago is still very problematic. There are some pockets around the country where there’s no damage caps, and it’s really tough to defend claims.”
Technology ups and downs
Another fairly new pressure on ob.gyns. is the integration of the electronic health record and the federal reporting requirements that go along with it.
“Most practicing ob.gyns. are really fed up with the computerization of medicine and the tasking and the charting,” Dr. Montgomery said. “For every hour you spend seeing patients, you spend 1 or 2 hours doing computer chart work and paperwork. Most doctors don’t go into medicine so they can type; they go into medicine to take care of patients.”
The Internet age also poses challenges when it comes to patients conducting their own “research,” said Megan Evans, MD, an ob.gyn. at Tufts Medical Center, Boston.
Protecting the security of patients’ medical records in the digital age is another worry, she said.
But for Dr. Evans, who completed her residency training in 2015, having dozens of digital tools at her disposal as she treats patients is definitely an upside to today’s practice environment.
“I can review a practice bulletin, look up the latest treatment regimens, and contact my colleagues with a quick question – all on my iPhone,” she said. “I also believe there is so much potential for electronic medical records and how they communicate with each other.”
Advancements in ultrasound, fetal monitoring, and other medical technologies have also allowed ob.gyns. to intervene earlier and save lives.
Dr. Brabson recalled the helplessness he and other physicians felt in the 1970s when it came to delivering extremely premature babies.
“We didn’t really feel like you could save a baby under 2 pounds,” he said. “When I was a medical student, if you had a baby under 2 pounds, very commonly what they would do is lay the baby up on the table and watch and see how vigorous it was going to be, and if it really did breathe and carry on for awhile, then you might take it to the nursery. The equipment that we have to save babies with today, compared to 40 years ago, that’s a dramatic change.”
A changing focus for the future
If current trends continue, Dr. Brabson’s early experience of being a generalist ob.gyn. won’t be the norm. Instead, more ob.gyns. will choose to subspecialize. Whether this change is positive or negative for the specialty depends on who you ask.
“You could argue the pros and cons for both sides,” Dr. Zeligs said. “For me, it takes away from what drew me to the specialty – the breadth that ob.gyn. offers, both as a primary care specialty and as a surgical subspecialty.”
However, choosing one focus may offer some doctors a way to capture that elusive professional and personal balance, she added.
Despite the changing landscape of clinical duties and business operations, some parts of ob.gyn. practice have remained intact, according to Dr. Brabson. “The most rewarding and enjoyable part of the job is developing a relationship of mutual trust and respect,” he said. “As a result of developing such a relationship, both the patient and the doctor come away with positive feelings. This has not changed.”
[email protected]
On Twitter @legal_med
As a practicing obstetrician-gynecologist for nearly 40 years, Leonard Brabson, MD, has watched his specialty transform in ways both large and small.
For starters, his regular work attire in 1977 – a shirt and tie – is now scrubs. The paper charts that once filled his office shelves have been replaced with electronic records. And the cumbersome machines that once took blurry, still pictures of a fetus have advanced by leaps and bounds and become a staple of prenatal care.
“Back then, we were expected to be generalists. If [a patient] had a cancer, you took care of it. If [she] had a fertility problem or problem with endocrinology, you took care of it. Of course, now if I have a female cancer, we refer them to the gyn-oncologist. But when you go back 40 years and beyond, we did mostly everything.”
The ob.gyns. of today are practicing in a vastly different environment than their predecessors, and while many of the differences have improved patient care and enhanced efficiency, physicians also note that some changes have harmed the doctor-patient relationship and created career dissatisfaction.
“Certainly, the advances of modern medicine have enabled the current physician to provide the patient a level of care unparalleled in history,” said Charles E. Miller, MD, a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.
More volume, less time
Most long-time physicians agree that higher patient volumes and increasing administrative burdens have diminished the time they are able to spend with patients.
Rising clinical documentation and coding are the top administrative tasks taking away from one-on-one patient care, said Kristen Zeligs, MD, chair of the American Congress of Obstetricians and Gynecologists’ Junior Fellow Congress Advisory Council and a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Md.
But there are other factors straining the doctor-patient relationship. Decades ago, first-time mothers often stayed with one doctor for a lifetime, Dr. Brabson recalled, having all of her babies delivered by a single ob.gyn. The same can’t be said for today, where insurance changes, job relocations, and a lack of connections often lead patients to switch physicians frequently.
“Now a lot of patients [move on] from one year to the next,” Dr. Brabson said. “There’s not that same loyalty.”
Doctors, too, traditionally stuck with patients over the long haul, he added. In the past, if an ob.gyn treated a patient during pregnancy, that same physician was present during the delivery, even if it meant leaving a vacation early or coming in on a night off.
“Now the younger docs, especially those that have families with small children, when it’s not their night on call and it’s 5 o’clock, they’re checking out,” Dr. Brabson said. “One of my partners right now, she started inducing someone yesterday. Well today’s her day off, so I’m going to do the delivery. That’s been a big change.”
Highs and lows of liability premiums
Another pressure on the specialty over the last couple of decades has been the high cost of liability insurance.
“2003 was really the peak of the liability crisis,” Dr. Montgomery said. “Hospitals were closing. Doctors were giving up practice. It’s a little better now than it was.”
While ob.gyns. still pay higher premiums than many other specialties, the legal climate has improved in recent years, said Paul Greve Jr., executive vice president and senior consultant for the Willis Healthcare Practice, and author of the 2016 Medical Liability Monitor, an annual report that surveys medical liability premiums.
“The best way to characterize the overall environment for medical professional liability is stable,” he said. “In the area of obstetrics, for the first time ever in recent years, we are seeing lower frequency and lower severity [of lawsuits].”
The lower number of filings are largely due to patient safety initiatives among ob.gyn. programs and tort reforms – many of which have been upheld by courts in the last decade, Mr. Greve said.
Of course, the rate of premiums greatly differs depending on location, with ob.gyns. in Eastern New York paying a high of $214,999 and ob.gyns. in Minnesota paying a low of $16,449 in 2016, according to the Medical Liability Monitor.
“The environment is specific to the region,” Mr. Greve said. “New York City is still very problematic. Chicago is still very problematic. There are some pockets around the country where there’s no damage caps, and it’s really tough to defend claims.”
Technology ups and downs
Another fairly new pressure on ob.gyns. is the integration of the electronic health record and the federal reporting requirements that go along with it.
“Most practicing ob.gyns. are really fed up with the computerization of medicine and the tasking and the charting,” Dr. Montgomery said. “For every hour you spend seeing patients, you spend 1 or 2 hours doing computer chart work and paperwork. Most doctors don’t go into medicine so they can type; they go into medicine to take care of patients.”
The Internet age also poses challenges when it comes to patients conducting their own “research,” said Megan Evans, MD, an ob.gyn. at Tufts Medical Center, Boston.
Protecting the security of patients’ medical records in the digital age is another worry, she said.
But for Dr. Evans, who completed her residency training in 2015, having dozens of digital tools at her disposal as she treats patients is definitely an upside to today’s practice environment.
“I can review a practice bulletin, look up the latest treatment regimens, and contact my colleagues with a quick question – all on my iPhone,” she said. “I also believe there is so much potential for electronic medical records and how they communicate with each other.”
Advancements in ultrasound, fetal monitoring, and other medical technologies have also allowed ob.gyns. to intervene earlier and save lives.
Dr. Brabson recalled the helplessness he and other physicians felt in the 1970s when it came to delivering extremely premature babies.
“We didn’t really feel like you could save a baby under 2 pounds,” he said. “When I was a medical student, if you had a baby under 2 pounds, very commonly what they would do is lay the baby up on the table and watch and see how vigorous it was going to be, and if it really did breathe and carry on for awhile, then you might take it to the nursery. The equipment that we have to save babies with today, compared to 40 years ago, that’s a dramatic change.”
A changing focus for the future
If current trends continue, Dr. Brabson’s early experience of being a generalist ob.gyn. won’t be the norm. Instead, more ob.gyns. will choose to subspecialize. Whether this change is positive or negative for the specialty depends on who you ask.
“You could argue the pros and cons for both sides,” Dr. Zeligs said. “For me, it takes away from what drew me to the specialty – the breadth that ob.gyn. offers, both as a primary care specialty and as a surgical subspecialty.”
However, choosing one focus may offer some doctors a way to capture that elusive professional and personal balance, she added.
Despite the changing landscape of clinical duties and business operations, some parts of ob.gyn. practice have remained intact, according to Dr. Brabson. “The most rewarding and enjoyable part of the job is developing a relationship of mutual trust and respect,” he said. “As a result of developing such a relationship, both the patient and the doctor come away with positive feelings. This has not changed.”
[email protected]
On Twitter @legal_med
As a practicing obstetrician-gynecologist for nearly 40 years, Leonard Brabson, MD, has watched his specialty transform in ways both large and small.
For starters, his regular work attire in 1977 – a shirt and tie – is now scrubs. The paper charts that once filled his office shelves have been replaced with electronic records. And the cumbersome machines that once took blurry, still pictures of a fetus have advanced by leaps and bounds and become a staple of prenatal care.
“Back then, we were expected to be generalists. If [a patient] had a cancer, you took care of it. If [she] had a fertility problem or problem with endocrinology, you took care of it. Of course, now if I have a female cancer, we refer them to the gyn-oncologist. But when you go back 40 years and beyond, we did mostly everything.”
The ob.gyns. of today are practicing in a vastly different environment than their predecessors, and while many of the differences have improved patient care and enhanced efficiency, physicians also note that some changes have harmed the doctor-patient relationship and created career dissatisfaction.
“Certainly, the advances of modern medicine have enabled the current physician to provide the patient a level of care unparalleled in history,” said Charles E. Miller, MD, a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.
More volume, less time
Most long-time physicians agree that higher patient volumes and increasing administrative burdens have diminished the time they are able to spend with patients.
Rising clinical documentation and coding are the top administrative tasks taking away from one-on-one patient care, said Kristen Zeligs, MD, chair of the American Congress of Obstetricians and Gynecologists’ Junior Fellow Congress Advisory Council and a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Md.
But there are other factors straining the doctor-patient relationship. Decades ago, first-time mothers often stayed with one doctor for a lifetime, Dr. Brabson recalled, having all of her babies delivered by a single ob.gyn. The same can’t be said for today, where insurance changes, job relocations, and a lack of connections often lead patients to switch physicians frequently.
“Now a lot of patients [move on] from one year to the next,” Dr. Brabson said. “There’s not that same loyalty.”
Doctors, too, traditionally stuck with patients over the long haul, he added. In the past, if an ob.gyn treated a patient during pregnancy, that same physician was present during the delivery, even if it meant leaving a vacation early or coming in on a night off.
“Now the younger docs, especially those that have families with small children, when it’s not their night on call and it’s 5 o’clock, they’re checking out,” Dr. Brabson said. “One of my partners right now, she started inducing someone yesterday. Well today’s her day off, so I’m going to do the delivery. That’s been a big change.”
Highs and lows of liability premiums
Another pressure on the specialty over the last couple of decades has been the high cost of liability insurance.
“2003 was really the peak of the liability crisis,” Dr. Montgomery said. “Hospitals were closing. Doctors were giving up practice. It’s a little better now than it was.”
While ob.gyns. still pay higher premiums than many other specialties, the legal climate has improved in recent years, said Paul Greve Jr., executive vice president and senior consultant for the Willis Healthcare Practice, and author of the 2016 Medical Liability Monitor, an annual report that surveys medical liability premiums.
“The best way to characterize the overall environment for medical professional liability is stable,” he said. “In the area of obstetrics, for the first time ever in recent years, we are seeing lower frequency and lower severity [of lawsuits].”
The lower number of filings are largely due to patient safety initiatives among ob.gyn. programs and tort reforms – many of which have been upheld by courts in the last decade, Mr. Greve said.
Of course, the rate of premiums greatly differs depending on location, with ob.gyns. in Eastern New York paying a high of $214,999 and ob.gyns. in Minnesota paying a low of $16,449 in 2016, according to the Medical Liability Monitor.
“The environment is specific to the region,” Mr. Greve said. “New York City is still very problematic. Chicago is still very problematic. There are some pockets around the country where there’s no damage caps, and it’s really tough to defend claims.”
Technology ups and downs
Another fairly new pressure on ob.gyns. is the integration of the electronic health record and the federal reporting requirements that go along with it.
“Most practicing ob.gyns. are really fed up with the computerization of medicine and the tasking and the charting,” Dr. Montgomery said. “For every hour you spend seeing patients, you spend 1 or 2 hours doing computer chart work and paperwork. Most doctors don’t go into medicine so they can type; they go into medicine to take care of patients.”
The Internet age also poses challenges when it comes to patients conducting their own “research,” said Megan Evans, MD, an ob.gyn. at Tufts Medical Center, Boston.
Protecting the security of patients’ medical records in the digital age is another worry, she said.
But for Dr. Evans, who completed her residency training in 2015, having dozens of digital tools at her disposal as she treats patients is definitely an upside to today’s practice environment.
“I can review a practice bulletin, look up the latest treatment regimens, and contact my colleagues with a quick question – all on my iPhone,” she said. “I also believe there is so much potential for electronic medical records and how they communicate with each other.”
Advancements in ultrasound, fetal monitoring, and other medical technologies have also allowed ob.gyns. to intervene earlier and save lives.
Dr. Brabson recalled the helplessness he and other physicians felt in the 1970s when it came to delivering extremely premature babies.
“We didn’t really feel like you could save a baby under 2 pounds,” he said. “When I was a medical student, if you had a baby under 2 pounds, very commonly what they would do is lay the baby up on the table and watch and see how vigorous it was going to be, and if it really did breathe and carry on for awhile, then you might take it to the nursery. The equipment that we have to save babies with today, compared to 40 years ago, that’s a dramatic change.”
A changing focus for the future
If current trends continue, Dr. Brabson’s early experience of being a generalist ob.gyn. won’t be the norm. Instead, more ob.gyns. will choose to subspecialize. Whether this change is positive or negative for the specialty depends on who you ask.
“You could argue the pros and cons for both sides,” Dr. Zeligs said. “For me, it takes away from what drew me to the specialty – the breadth that ob.gyn. offers, both as a primary care specialty and as a surgical subspecialty.”
However, choosing one focus may offer some doctors a way to capture that elusive professional and personal balance, she added.
Despite the changing landscape of clinical duties and business operations, some parts of ob.gyn. practice have remained intact, according to Dr. Brabson. “The most rewarding and enjoyable part of the job is developing a relationship of mutual trust and respect,” he said. “As a result of developing such a relationship, both the patient and the doctor come away with positive feelings. This has not changed.”
[email protected]
On Twitter @legal_med
Vitamin D supplementation recommended in all children, teens
SAN FRANCISCO – Vitamin D deficiency is common among children and adolescents, particularly those with chronic disease, Catherine Gordon, MD, said at the annual meeting of the American Academy of Pediatrics.
Yet the precise definition of vitamin D deficiency and the healthy threshold for vitamin D levels lack universally agreed-upon standards. Generally speaking, levels of at least 30 ng/mL (75 nmol/L) appear safe and reasonable for children with chronic disease, and additional research is confirming whether this range is appropriate for other pediatric groups as well. Although too much vitamin D can lead to hypercalcemia, vitamin D intoxication is very rare, said Dr. Gordon, director of the division of adolescents and transition medicine at the University of Cincinnati.
Severe vitamin D deficiency can lead to rickets, when bones have insufficient calcium and phosphorus levels, resulting in bone softening and weakening before growth plates close. If not treated with vitamin D and calcium supplementation, rickets becomes osteomalacia after the growth plates close.
Vitamin D deficiency rates vary by population
It’s difficult to pin down rates of vitamin D deficiency. One 2004 study of just over 300 children found nearly a quarter of them (24%) were deficient based on a threshold of levels below 15 ng/mL, and another 42% had insufficient levels, defined as 20 ng/mL or lower, but all were asymptomatic. Another 2008 study using different cut-offs found that 12% of healthy 8- to 24-month-olds were deficient, defined as levels below 20 ng/mL. Forty percent of the children had suboptimal levels below 30 ng/mL. Overall, a third of the children showed demineralization on their x-rays. While the season of the year and race/ethnicity did not emerge as predictors of vitamin D insufficiency, breastfeeding without supplementation and lack of milk consumption did.
Because the vitamin D content in human breast milk is low, breastfed infants typically develop low vitamin D levels unless they receive supplementation or plenty of exposure to sunlight. A maternal dose of 6,400 IU of vitamin D is needed for breastfed infants to reach normal vitamin D levels, Dr. Gordon said. Babies born to mothers with vitamin D deficiency have the highest risk of becoming deficient themselves, although formula-fed babies usually receive plenty through the vitamin D fortification in infant formula.
Among adolescents, obesity remains a common risk factor, and those with obesity require higher doses to correct deficiency or insufficiency. A study in the Journal of Pediatrics this year found that adult-sized teens need at least 5,000 IU of vitamin D3 a day for 8 weeks to correct deficiency. Similarly, a small 2012 study of 61 children and adolescents with inflammatory bowel disease found that supplementation of 2,000 IU of vitamin D3 daily or 50,000 IU of D2 weekly, for 6 weeks, more effectively corrected vitamin D deficiency than 2,000 IU daily of vitamin D2 without any changes to parathyroid hormone suppression.
How much to supplement
Much debate and uncertainty surround how much (if at all) healthy infants, children, and adolescents should be supplemented with vitamin D. The American Academy of Pediatrics recommends daily supplementation of 400 IU of vitamin D from birth through adolescence for all children and teens, although that’s far below the safe upper limit of vitamin D intake, Dr. Gordon said.
The health and sciences division (formerly the Institute of Medicine) of the National Academies of Sciences, Engineering, and Medicine, by contrast, recommends a daily intake of 400 IU of vitamin D for the first year of life and then 600 IU for age 1 through old age. The safe upper limits set by the health and sciences division include 1,000 IU for infants up to 6 months old, 1,500 IU for infants aged 6 months to 1 year, 2,500 IU for toddlers up to 3 years, 3,000 IU for children aged 4-8 years, and 4,000 IU for those 9 years and older.
Yet the Endocrine Society recommends a greater amount of supplementation for children at risk for vitamin D deficiency or low bone density mass: from 400 to 1,000 IU for children 1 year and younger, and 600-1,000 IU for all older children, adolescents, and adults. The Endocrine Society also cites a higher safe upper limit of 2,000 IU for infants up to 12 months and 4,000 IU for those aged 1 year and up.
Part of the discordance in these recommendations lies in what populations they are aimed at, Dr. Gordon explained. While the health and sciences division recommendations were written for healthy children and adolescents, the Endocrine Society is specifically addressing those in risk groups, such as transplant recipients, those with chronic conditions that can cause malabsorption, and those taking anticonvulsants or receiving other treatments that can threaten bone health. Among older children and adolescents, anorexia nervosa is also a risk factor for inadequate vitamin D levels.
Dr. Gordon recommended 600 IU of vitamin D daily for all healthy children and teens while noting that those in risk groups may require 1,000-2,000 IU to prevent vitamin D deficiency.
Additional concerns with inadequate vitamin D
Aside from bone mineral density and levels of 25(OH)D (25-hydroxy vitamin D) and parathyroid hormone, vitamin D insufficiency may be suspected based on several other biomarkers, including fractures or falls, intestinal calcium absorption, dental health, insulin sensitivity, beta-cell or immune functioning, respiratory disease such as wheezing or tuberculosis, and possibly hypertension.
Researchers have developed new interest in exploring whether factors during childhood and adolescence – critical years for bone acquisition – such as vitamin D levels might influence the risk for osteoporosis later in life, Dr. Gordon said.
Both males and females reach their peak bone mass and skeletal strength in their early to mid-20s and maintain these through about their mid-40s. While individuals have no control over intrinsic factors that help determine their bone mass, such as sex, family history, and ethnicity, other extrinsic factors are also bone mass determinants, including diet, body mass, a particular individual’s hormonal mix, illnesses and their treatments, physical activity level, and lifestyle choices.
Therefore, health providers should encourage patients to regularly exercise, maintain a healthy weight, eat healthfully, and take daily supplements, Dr. Gordon said. She only recommended testing 25(OH)D levels in those at risk for deficiency and/or low bone mass.
Dr. Gordon reported no relevant financial disclosures.
SAN FRANCISCO – Vitamin D deficiency is common among children and adolescents, particularly those with chronic disease, Catherine Gordon, MD, said at the annual meeting of the American Academy of Pediatrics.
Yet the precise definition of vitamin D deficiency and the healthy threshold for vitamin D levels lack universally agreed-upon standards. Generally speaking, levels of at least 30 ng/mL (75 nmol/L) appear safe and reasonable for children with chronic disease, and additional research is confirming whether this range is appropriate for other pediatric groups as well. Although too much vitamin D can lead to hypercalcemia, vitamin D intoxication is very rare, said Dr. Gordon, director of the division of adolescents and transition medicine at the University of Cincinnati.
Severe vitamin D deficiency can lead to rickets, when bones have insufficient calcium and phosphorus levels, resulting in bone softening and weakening before growth plates close. If not treated with vitamin D and calcium supplementation, rickets becomes osteomalacia after the growth plates close.
Vitamin D deficiency rates vary by population
It’s difficult to pin down rates of vitamin D deficiency. One 2004 study of just over 300 children found nearly a quarter of them (24%) were deficient based on a threshold of levels below 15 ng/mL, and another 42% had insufficient levels, defined as 20 ng/mL or lower, but all were asymptomatic. Another 2008 study using different cut-offs found that 12% of healthy 8- to 24-month-olds were deficient, defined as levels below 20 ng/mL. Forty percent of the children had suboptimal levels below 30 ng/mL. Overall, a third of the children showed demineralization on their x-rays. While the season of the year and race/ethnicity did not emerge as predictors of vitamin D insufficiency, breastfeeding without supplementation and lack of milk consumption did.
Because the vitamin D content in human breast milk is low, breastfed infants typically develop low vitamin D levels unless they receive supplementation or plenty of exposure to sunlight. A maternal dose of 6,400 IU of vitamin D is needed for breastfed infants to reach normal vitamin D levels, Dr. Gordon said. Babies born to mothers with vitamin D deficiency have the highest risk of becoming deficient themselves, although formula-fed babies usually receive plenty through the vitamin D fortification in infant formula.
Among adolescents, obesity remains a common risk factor, and those with obesity require higher doses to correct deficiency or insufficiency. A study in the Journal of Pediatrics this year found that adult-sized teens need at least 5,000 IU of vitamin D3 a day for 8 weeks to correct deficiency. Similarly, a small 2012 study of 61 children and adolescents with inflammatory bowel disease found that supplementation of 2,000 IU of vitamin D3 daily or 50,000 IU of D2 weekly, for 6 weeks, more effectively corrected vitamin D deficiency than 2,000 IU daily of vitamin D2 without any changes to parathyroid hormone suppression.
How much to supplement
Much debate and uncertainty surround how much (if at all) healthy infants, children, and adolescents should be supplemented with vitamin D. The American Academy of Pediatrics recommends daily supplementation of 400 IU of vitamin D from birth through adolescence for all children and teens, although that’s far below the safe upper limit of vitamin D intake, Dr. Gordon said.
The health and sciences division (formerly the Institute of Medicine) of the National Academies of Sciences, Engineering, and Medicine, by contrast, recommends a daily intake of 400 IU of vitamin D for the first year of life and then 600 IU for age 1 through old age. The safe upper limits set by the health and sciences division include 1,000 IU for infants up to 6 months old, 1,500 IU for infants aged 6 months to 1 year, 2,500 IU for toddlers up to 3 years, 3,000 IU for children aged 4-8 years, and 4,000 IU for those 9 years and older.
Yet the Endocrine Society recommends a greater amount of supplementation for children at risk for vitamin D deficiency or low bone density mass: from 400 to 1,000 IU for children 1 year and younger, and 600-1,000 IU for all older children, adolescents, and adults. The Endocrine Society also cites a higher safe upper limit of 2,000 IU for infants up to 12 months and 4,000 IU for those aged 1 year and up.
Part of the discordance in these recommendations lies in what populations they are aimed at, Dr. Gordon explained. While the health and sciences division recommendations were written for healthy children and adolescents, the Endocrine Society is specifically addressing those in risk groups, such as transplant recipients, those with chronic conditions that can cause malabsorption, and those taking anticonvulsants or receiving other treatments that can threaten bone health. Among older children and adolescents, anorexia nervosa is also a risk factor for inadequate vitamin D levels.
Dr. Gordon recommended 600 IU of vitamin D daily for all healthy children and teens while noting that those in risk groups may require 1,000-2,000 IU to prevent vitamin D deficiency.
Additional concerns with inadequate vitamin D
Aside from bone mineral density and levels of 25(OH)D (25-hydroxy vitamin D) and parathyroid hormone, vitamin D insufficiency may be suspected based on several other biomarkers, including fractures or falls, intestinal calcium absorption, dental health, insulin sensitivity, beta-cell or immune functioning, respiratory disease such as wheezing or tuberculosis, and possibly hypertension.
Researchers have developed new interest in exploring whether factors during childhood and adolescence – critical years for bone acquisition – such as vitamin D levels might influence the risk for osteoporosis later in life, Dr. Gordon said.
Both males and females reach their peak bone mass and skeletal strength in their early to mid-20s and maintain these through about their mid-40s. While individuals have no control over intrinsic factors that help determine their bone mass, such as sex, family history, and ethnicity, other extrinsic factors are also bone mass determinants, including diet, body mass, a particular individual’s hormonal mix, illnesses and their treatments, physical activity level, and lifestyle choices.
Therefore, health providers should encourage patients to regularly exercise, maintain a healthy weight, eat healthfully, and take daily supplements, Dr. Gordon said. She only recommended testing 25(OH)D levels in those at risk for deficiency and/or low bone mass.
Dr. Gordon reported no relevant financial disclosures.
SAN FRANCISCO – Vitamin D deficiency is common among children and adolescents, particularly those with chronic disease, Catherine Gordon, MD, said at the annual meeting of the American Academy of Pediatrics.
Yet the precise definition of vitamin D deficiency and the healthy threshold for vitamin D levels lack universally agreed-upon standards. Generally speaking, levels of at least 30 ng/mL (75 nmol/L) appear safe and reasonable for children with chronic disease, and additional research is confirming whether this range is appropriate for other pediatric groups as well. Although too much vitamin D can lead to hypercalcemia, vitamin D intoxication is very rare, said Dr. Gordon, director of the division of adolescents and transition medicine at the University of Cincinnati.
Severe vitamin D deficiency can lead to rickets, when bones have insufficient calcium and phosphorus levels, resulting in bone softening and weakening before growth plates close. If not treated with vitamin D and calcium supplementation, rickets becomes osteomalacia after the growth plates close.
Vitamin D deficiency rates vary by population
It’s difficult to pin down rates of vitamin D deficiency. One 2004 study of just over 300 children found nearly a quarter of them (24%) were deficient based on a threshold of levels below 15 ng/mL, and another 42% had insufficient levels, defined as 20 ng/mL or lower, but all were asymptomatic. Another 2008 study using different cut-offs found that 12% of healthy 8- to 24-month-olds were deficient, defined as levels below 20 ng/mL. Forty percent of the children had suboptimal levels below 30 ng/mL. Overall, a third of the children showed demineralization on their x-rays. While the season of the year and race/ethnicity did not emerge as predictors of vitamin D insufficiency, breastfeeding without supplementation and lack of milk consumption did.
Because the vitamin D content in human breast milk is low, breastfed infants typically develop low vitamin D levels unless they receive supplementation or plenty of exposure to sunlight. A maternal dose of 6,400 IU of vitamin D is needed for breastfed infants to reach normal vitamin D levels, Dr. Gordon said. Babies born to mothers with vitamin D deficiency have the highest risk of becoming deficient themselves, although formula-fed babies usually receive plenty through the vitamin D fortification in infant formula.
Among adolescents, obesity remains a common risk factor, and those with obesity require higher doses to correct deficiency or insufficiency. A study in the Journal of Pediatrics this year found that adult-sized teens need at least 5,000 IU of vitamin D3 a day for 8 weeks to correct deficiency. Similarly, a small 2012 study of 61 children and adolescents with inflammatory bowel disease found that supplementation of 2,000 IU of vitamin D3 daily or 50,000 IU of D2 weekly, for 6 weeks, more effectively corrected vitamin D deficiency than 2,000 IU daily of vitamin D2 without any changes to parathyroid hormone suppression.
How much to supplement
Much debate and uncertainty surround how much (if at all) healthy infants, children, and adolescents should be supplemented with vitamin D. The American Academy of Pediatrics recommends daily supplementation of 400 IU of vitamin D from birth through adolescence for all children and teens, although that’s far below the safe upper limit of vitamin D intake, Dr. Gordon said.
The health and sciences division (formerly the Institute of Medicine) of the National Academies of Sciences, Engineering, and Medicine, by contrast, recommends a daily intake of 400 IU of vitamin D for the first year of life and then 600 IU for age 1 through old age. The safe upper limits set by the health and sciences division include 1,000 IU for infants up to 6 months old, 1,500 IU for infants aged 6 months to 1 year, 2,500 IU for toddlers up to 3 years, 3,000 IU for children aged 4-8 years, and 4,000 IU for those 9 years and older.
Yet the Endocrine Society recommends a greater amount of supplementation for children at risk for vitamin D deficiency or low bone density mass: from 400 to 1,000 IU for children 1 year and younger, and 600-1,000 IU for all older children, adolescents, and adults. The Endocrine Society also cites a higher safe upper limit of 2,000 IU for infants up to 12 months and 4,000 IU for those aged 1 year and up.
Part of the discordance in these recommendations lies in what populations they are aimed at, Dr. Gordon explained. While the health and sciences division recommendations were written for healthy children and adolescents, the Endocrine Society is specifically addressing those in risk groups, such as transplant recipients, those with chronic conditions that can cause malabsorption, and those taking anticonvulsants or receiving other treatments that can threaten bone health. Among older children and adolescents, anorexia nervosa is also a risk factor for inadequate vitamin D levels.
Dr. Gordon recommended 600 IU of vitamin D daily for all healthy children and teens while noting that those in risk groups may require 1,000-2,000 IU to prevent vitamin D deficiency.
Additional concerns with inadequate vitamin D
Aside from bone mineral density and levels of 25(OH)D (25-hydroxy vitamin D) and parathyroid hormone, vitamin D insufficiency may be suspected based on several other biomarkers, including fractures or falls, intestinal calcium absorption, dental health, insulin sensitivity, beta-cell or immune functioning, respiratory disease such as wheezing or tuberculosis, and possibly hypertension.
Researchers have developed new interest in exploring whether factors during childhood and adolescence – critical years for bone acquisition – such as vitamin D levels might influence the risk for osteoporosis later in life, Dr. Gordon said.
Both males and females reach their peak bone mass and skeletal strength in their early to mid-20s and maintain these through about their mid-40s. While individuals have no control over intrinsic factors that help determine their bone mass, such as sex, family history, and ethnicity, other extrinsic factors are also bone mass determinants, including diet, body mass, a particular individual’s hormonal mix, illnesses and their treatments, physical activity level, and lifestyle choices.
Therefore, health providers should encourage patients to regularly exercise, maintain a healthy weight, eat healthfully, and take daily supplements, Dr. Gordon said. She only recommended testing 25(OH)D levels in those at risk for deficiency and/or low bone mass.
Dr. Gordon reported no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 16