User login
Polychlorinated Biphenyls Are Associated With Risk of Parkinson’s Disease
PORTLAND, OR—Higher serum levels of polychlorinated biphenyls (PCBs) are associated with increased risk of Parkinson’s disease in two independent study populations, according to research presented at the Fourth World Parkinson Congress.
PCBs are persistent environmental pollutants that are detectable in most people despite a worldwide ban on their production that has been in place for more than 20 years. PCBs cause selective dopaminergic toxicity in animal models, but have been minimally studied in Parkinson’s disease, the researchers said.
The investigators recently reported a significantly increased risk of Parkinson’s disease associated with higher levels of serum PCBs in a case–control study of Alaska Native people. In the present study, they investigated this association in a demographically dissimilar study population.
They identified people with Parkinson’s disease within the Agricultural Health Study, a cohort of pesticide applicators and their spouses in Iowa and North Carolina. They also randomly selected controls matched for age, sex, and state. They confirmed Parkinson’s disease diagnoses by in-person neurologist evaluation and consensus review. PCB congeners 118, 138, 153, and 180 were measured as ng/g lipid in serum using gas chromatography-mass spectroscopy. To assess dose-response, the researchers constructed quartiles for each congener and for the sum of congeners. The used logistic regression, adjusting for age, gender, and state, to calculate odds ratios.
Ninety-seven people with Parkinson’s disease and 113 controls were included in the study. About 25% of the participants were women. Mean age was 69. Parkinson’s disease was associated with higher levels of PCBs. A significant dose-response was seen across quartiles. Participants in the second, third, and fourth quartiles of total PCB levels had a 1.7-, 2.4-, and 2.7-fold greater risk of Parkinson’s disease, respectively, compared with participants in the lowest quartile of total PCB levels. Odds ratios were similar in the Agricultural Heath Study and the Alaska study. In both studies, PCB levels correlated positively with age but not with disease duration, which argues against reverse causation, the researchers said.
—Jake Remaly
PORTLAND, OR—Higher serum levels of polychlorinated biphenyls (PCBs) are associated with increased risk of Parkinson’s disease in two independent study populations, according to research presented at the Fourth World Parkinson Congress.
PCBs are persistent environmental pollutants that are detectable in most people despite a worldwide ban on their production that has been in place for more than 20 years. PCBs cause selective dopaminergic toxicity in animal models, but have been minimally studied in Parkinson’s disease, the researchers said.
The investigators recently reported a significantly increased risk of Parkinson’s disease associated with higher levels of serum PCBs in a case–control study of Alaska Native people. In the present study, they investigated this association in a demographically dissimilar study population.
They identified people with Parkinson’s disease within the Agricultural Health Study, a cohort of pesticide applicators and their spouses in Iowa and North Carolina. They also randomly selected controls matched for age, sex, and state. They confirmed Parkinson’s disease diagnoses by in-person neurologist evaluation and consensus review. PCB congeners 118, 138, 153, and 180 were measured as ng/g lipid in serum using gas chromatography-mass spectroscopy. To assess dose-response, the researchers constructed quartiles for each congener and for the sum of congeners. The used logistic regression, adjusting for age, gender, and state, to calculate odds ratios.
Ninety-seven people with Parkinson’s disease and 113 controls were included in the study. About 25% of the participants were women. Mean age was 69. Parkinson’s disease was associated with higher levels of PCBs. A significant dose-response was seen across quartiles. Participants in the second, third, and fourth quartiles of total PCB levels had a 1.7-, 2.4-, and 2.7-fold greater risk of Parkinson’s disease, respectively, compared with participants in the lowest quartile of total PCB levels. Odds ratios were similar in the Agricultural Heath Study and the Alaska study. In both studies, PCB levels correlated positively with age but not with disease duration, which argues against reverse causation, the researchers said.
—Jake Remaly
PORTLAND, OR—Higher serum levels of polychlorinated biphenyls (PCBs) are associated with increased risk of Parkinson’s disease in two independent study populations, according to research presented at the Fourth World Parkinson Congress.
PCBs are persistent environmental pollutants that are detectable in most people despite a worldwide ban on their production that has been in place for more than 20 years. PCBs cause selective dopaminergic toxicity in animal models, but have been minimally studied in Parkinson’s disease, the researchers said.
The investigators recently reported a significantly increased risk of Parkinson’s disease associated with higher levels of serum PCBs in a case–control study of Alaska Native people. In the present study, they investigated this association in a demographically dissimilar study population.
They identified people with Parkinson’s disease within the Agricultural Health Study, a cohort of pesticide applicators and their spouses in Iowa and North Carolina. They also randomly selected controls matched for age, sex, and state. They confirmed Parkinson’s disease diagnoses by in-person neurologist evaluation and consensus review. PCB congeners 118, 138, 153, and 180 were measured as ng/g lipid in serum using gas chromatography-mass spectroscopy. To assess dose-response, the researchers constructed quartiles for each congener and for the sum of congeners. The used logistic regression, adjusting for age, gender, and state, to calculate odds ratios.
Ninety-seven people with Parkinson’s disease and 113 controls were included in the study. About 25% of the participants were women. Mean age was 69. Parkinson’s disease was associated with higher levels of PCBs. A significant dose-response was seen across quartiles. Participants in the second, third, and fourth quartiles of total PCB levels had a 1.7-, 2.4-, and 2.7-fold greater risk of Parkinson’s disease, respectively, compared with participants in the lowest quartile of total PCB levels. Odds ratios were similar in the Agricultural Heath Study and the Alaska study. In both studies, PCB levels correlated positively with age but not with disease duration, which argues against reverse causation, the researchers said.
—Jake Remaly
Does Transdermal Nicotine Benefit Patients With Parkinson’s Disease?
PORTLAND, OR—High doses of transdermal nicotine failed to improve off motor symptoms in patients with Parkinson’s disease, according to trial results presented at the Fourth World Parkinson Congress. Nicotine may have provided benefit on secondary outcome measures, researchers said.
Gabriel Villafane, MD, a neurologist at Henri Mondor University Hospital in Créteil, France, and colleagues conducted the Nicopark2 Study, a single-blind, controlled, randomized trial to evaluate the effect of high doses of transdermal nicotine (approximately 90 mg per day) on motor symptoms in Parkinson’s disease.
Cigarette smoking is associated with a dose-dependent reduction in risk of Parkinson’s disease. Nicotine’s effect on motor symptoms in Parkinson’s disease is controversial. Seven of eight open-label studies suggested that nicotine improves motor symptoms, but four placebo-controlled studies were negative.
The investigators enrolled 40 patients with Parkinson’s disease in the study. Eligible patients were nonsmokers age 35 to 70 with a Hoehn and Yahr off stage of four or less and a Hoehn and Yahr on stage of three or less. Patients had received levodopa treatment for at least three years. Exclusion criteria included neurosurgery, psychiatric disease, and symptomatic orthostatic hypotension.
The primary outcome was mean difference between groups in change of Unified Parkinson’s Disease Rating Scale off motor score from baseline to week 39 on blinded video rating.
Twenty patients were randomized to receive transdermal nicotine, and 20 patients were randomized to a control group. The change in motor score between groups was not statistically significant. Change in quality of life assessed by the Parkinson’s Disease Questionnaire was not statistically significant. At 39 weeks, a reduction in levodopa doses, a reduction in dyskinesias, and an improvement in activities of daily living were observed in the nicotine group, the researchers said.
Adverse events occurred in more patients the nicotine group than in the control group. They included worsening of parkinsonism (30% vs 5%), cutaneous reactions (35% vs 5%), gastrointestinal complaints (65% vs 15%), hypotension (25% vs 5%), insomnia (25% vs 5%), and nervousness and anxiety (20% vs 0%). Ten patients in the nicotine group had a serious adverse event, compared with three patients in the control group.
—Jake Remaly
Suggested Reading
Quik M, Bordia T, Zhang D, Perez XA. Nicotine and nicotinic receptor drugs: potential for Parkinson's disease and drug-induced movement disorders. Int Rev Neurobiol. 2015;124:247-271.
PORTLAND, OR—High doses of transdermal nicotine failed to improve off motor symptoms in patients with Parkinson’s disease, according to trial results presented at the Fourth World Parkinson Congress. Nicotine may have provided benefit on secondary outcome measures, researchers said.
Gabriel Villafane, MD, a neurologist at Henri Mondor University Hospital in Créteil, France, and colleagues conducted the Nicopark2 Study, a single-blind, controlled, randomized trial to evaluate the effect of high doses of transdermal nicotine (approximately 90 mg per day) on motor symptoms in Parkinson’s disease.
Cigarette smoking is associated with a dose-dependent reduction in risk of Parkinson’s disease. Nicotine’s effect on motor symptoms in Parkinson’s disease is controversial. Seven of eight open-label studies suggested that nicotine improves motor symptoms, but four placebo-controlled studies were negative.
The investigators enrolled 40 patients with Parkinson’s disease in the study. Eligible patients were nonsmokers age 35 to 70 with a Hoehn and Yahr off stage of four or less and a Hoehn and Yahr on stage of three or less. Patients had received levodopa treatment for at least three years. Exclusion criteria included neurosurgery, psychiatric disease, and symptomatic orthostatic hypotension.
The primary outcome was mean difference between groups in change of Unified Parkinson’s Disease Rating Scale off motor score from baseline to week 39 on blinded video rating.
Twenty patients were randomized to receive transdermal nicotine, and 20 patients were randomized to a control group. The change in motor score between groups was not statistically significant. Change in quality of life assessed by the Parkinson’s Disease Questionnaire was not statistically significant. At 39 weeks, a reduction in levodopa doses, a reduction in dyskinesias, and an improvement in activities of daily living were observed in the nicotine group, the researchers said.
Adverse events occurred in more patients the nicotine group than in the control group. They included worsening of parkinsonism (30% vs 5%), cutaneous reactions (35% vs 5%), gastrointestinal complaints (65% vs 15%), hypotension (25% vs 5%), insomnia (25% vs 5%), and nervousness and anxiety (20% vs 0%). Ten patients in the nicotine group had a serious adverse event, compared with three patients in the control group.
—Jake Remaly
PORTLAND, OR—High doses of transdermal nicotine failed to improve off motor symptoms in patients with Parkinson’s disease, according to trial results presented at the Fourth World Parkinson Congress. Nicotine may have provided benefit on secondary outcome measures, researchers said.
Gabriel Villafane, MD, a neurologist at Henri Mondor University Hospital in Créteil, France, and colleagues conducted the Nicopark2 Study, a single-blind, controlled, randomized trial to evaluate the effect of high doses of transdermal nicotine (approximately 90 mg per day) on motor symptoms in Parkinson’s disease.
Cigarette smoking is associated with a dose-dependent reduction in risk of Parkinson’s disease. Nicotine’s effect on motor symptoms in Parkinson’s disease is controversial. Seven of eight open-label studies suggested that nicotine improves motor symptoms, but four placebo-controlled studies were negative.
The investigators enrolled 40 patients with Parkinson’s disease in the study. Eligible patients were nonsmokers age 35 to 70 with a Hoehn and Yahr off stage of four or less and a Hoehn and Yahr on stage of three or less. Patients had received levodopa treatment for at least three years. Exclusion criteria included neurosurgery, psychiatric disease, and symptomatic orthostatic hypotension.
The primary outcome was mean difference between groups in change of Unified Parkinson’s Disease Rating Scale off motor score from baseline to week 39 on blinded video rating.
Twenty patients were randomized to receive transdermal nicotine, and 20 patients were randomized to a control group. The change in motor score between groups was not statistically significant. Change in quality of life assessed by the Parkinson’s Disease Questionnaire was not statistically significant. At 39 weeks, a reduction in levodopa doses, a reduction in dyskinesias, and an improvement in activities of daily living were observed in the nicotine group, the researchers said.
Adverse events occurred in more patients the nicotine group than in the control group. They included worsening of parkinsonism (30% vs 5%), cutaneous reactions (35% vs 5%), gastrointestinal complaints (65% vs 15%), hypotension (25% vs 5%), insomnia (25% vs 5%), and nervousness and anxiety (20% vs 0%). Ten patients in the nicotine group had a serious adverse event, compared with three patients in the control group.
—Jake Remaly
Suggested Reading
Quik M, Bordia T, Zhang D, Perez XA. Nicotine and nicotinic receptor drugs: potential for Parkinson's disease and drug-induced movement disorders. Int Rev Neurobiol. 2015;124:247-271.
Suggested Reading
Quik M, Bordia T, Zhang D, Perez XA. Nicotine and nicotinic receptor drugs: potential for Parkinson's disease and drug-induced movement disorders. Int Rev Neurobiol. 2015;124:247-271.
Patient-reported outcomes tied to long-term outcomes in bariatric surgery
Clinical outcomes of surgery and patient-reported outcomes of function, disability, and health status are two different measures of surgical success.
A large study of patients who had bariatric surgery showed that patient-reported outcomes were correlated with long-term weight loss but not with short-term complication rates. In addition, obesity-specific patient-reported quality of life scores were associated with a reduction in medications required for the treatment of obesity-related conditions.
“Clinical outcomes, such as perioperative morbidity and mortality, are commonly used to benchmark hospital performance,” reported Jennifer F. Waljee, MD, and her associates at the University of Michigan, Ann Arbor (Ann Surg. 2016. doi: 10.1097/SLA.0000000000001852).
“However, for many surgical procedures, such as bariatric surgery ... complications may be rare, and may not entirely reflect treatment effectiveness. Alternatively, patient-reported measures of function, disability, and health status may offer a unique and more reliable assessment of provider quality and performance,” she explained. Yet despite growing interest in using patient-reported measures, many important questions regarding their accuracy, applicability, and clinical utility remain. The purpose of this study was, therefore, to evaluate how patient-reported quality of life measures compared to short-term and long-term clinical outcomes in patients who underwent bariatric surgery.
The majority of the study’s 11,420 participants were female (79.8%), were white (84.1%), and underwent Roux-en-Y laparoscopic gastric bypass (56.8%). For each study participant, both short-term and long-term clinical outcome measures were obtained from medical board review. Short-term clinical outcomes were defined as the rate of perioperative complications within 30 days of bariatric surgery. Percent excess weight loss at 1 year post surgery was used as a long-term clinical outcome.
In addition, two patient-reported outcomes were collected: an overall health-related quality of life score called the Health and Activities Limitations Index (HALex) and an obesity-specific quality of life score, the Bariatric Quality of Life (BQL) index, which measures well-being, social and physical functioning, and obesity-related symptoms.
Multivariate and linear regression models demonstrated that short-term complication rates were not correlated to the overall patient-reported quality of life score (P = .32) or to the obesity-specific BQL score (P = .74).
However, the long-term measure of excess weight loss at 1 year post surgery was significantly associated with both overall and obesity-specific patient-reported measures of health-related quality of life (P less than .002 and P less than .001 respectively).
Moreover, scores indicating improved quality of life were associated with greater weight loss.
Finally, comorbidity resolution, estimated by the reduction in the use of medications taken to treat conditions related to obesity, was significantly associated with the obesity-specific measure, BQL, but not the overall quality of life measure, HALex.
“In conclusion, [patient-reported outcomes] are distinct from clinical outcomes,” investigators wrote. Patient-reported outcomes “provide an opportunity for improved population-based cost-effectiveness analyses using outcomes germane to procedures performed for symptomatology and improving QOL,” they added.
The Agency for Healthcare Research and Quality supported the research. The investigators reported having no disclosures.
On Twitter @jessnicolecraig
Clinical outcomes of surgery and patient-reported outcomes of function, disability, and health status are two different measures of surgical success.
A large study of patients who had bariatric surgery showed that patient-reported outcomes were correlated with long-term weight loss but not with short-term complication rates. In addition, obesity-specific patient-reported quality of life scores were associated with a reduction in medications required for the treatment of obesity-related conditions.
“Clinical outcomes, such as perioperative morbidity and mortality, are commonly used to benchmark hospital performance,” reported Jennifer F. Waljee, MD, and her associates at the University of Michigan, Ann Arbor (Ann Surg. 2016. doi: 10.1097/SLA.0000000000001852).
“However, for many surgical procedures, such as bariatric surgery ... complications may be rare, and may not entirely reflect treatment effectiveness. Alternatively, patient-reported measures of function, disability, and health status may offer a unique and more reliable assessment of provider quality and performance,” she explained. Yet despite growing interest in using patient-reported measures, many important questions regarding their accuracy, applicability, and clinical utility remain. The purpose of this study was, therefore, to evaluate how patient-reported quality of life measures compared to short-term and long-term clinical outcomes in patients who underwent bariatric surgery.
The majority of the study’s 11,420 participants were female (79.8%), were white (84.1%), and underwent Roux-en-Y laparoscopic gastric bypass (56.8%). For each study participant, both short-term and long-term clinical outcome measures were obtained from medical board review. Short-term clinical outcomes were defined as the rate of perioperative complications within 30 days of bariatric surgery. Percent excess weight loss at 1 year post surgery was used as a long-term clinical outcome.
In addition, two patient-reported outcomes were collected: an overall health-related quality of life score called the Health and Activities Limitations Index (HALex) and an obesity-specific quality of life score, the Bariatric Quality of Life (BQL) index, which measures well-being, social and physical functioning, and obesity-related symptoms.
Multivariate and linear regression models demonstrated that short-term complication rates were not correlated to the overall patient-reported quality of life score (P = .32) or to the obesity-specific BQL score (P = .74).
However, the long-term measure of excess weight loss at 1 year post surgery was significantly associated with both overall and obesity-specific patient-reported measures of health-related quality of life (P less than .002 and P less than .001 respectively).
Moreover, scores indicating improved quality of life were associated with greater weight loss.
Finally, comorbidity resolution, estimated by the reduction in the use of medications taken to treat conditions related to obesity, was significantly associated with the obesity-specific measure, BQL, but not the overall quality of life measure, HALex.
“In conclusion, [patient-reported outcomes] are distinct from clinical outcomes,” investigators wrote. Patient-reported outcomes “provide an opportunity for improved population-based cost-effectiveness analyses using outcomes germane to procedures performed for symptomatology and improving QOL,” they added.
The Agency for Healthcare Research and Quality supported the research. The investigators reported having no disclosures.
On Twitter @jessnicolecraig
Clinical outcomes of surgery and patient-reported outcomes of function, disability, and health status are two different measures of surgical success.
A large study of patients who had bariatric surgery showed that patient-reported outcomes were correlated with long-term weight loss but not with short-term complication rates. In addition, obesity-specific patient-reported quality of life scores were associated with a reduction in medications required for the treatment of obesity-related conditions.
“Clinical outcomes, such as perioperative morbidity and mortality, are commonly used to benchmark hospital performance,” reported Jennifer F. Waljee, MD, and her associates at the University of Michigan, Ann Arbor (Ann Surg. 2016. doi: 10.1097/SLA.0000000000001852).
“However, for many surgical procedures, such as bariatric surgery ... complications may be rare, and may not entirely reflect treatment effectiveness. Alternatively, patient-reported measures of function, disability, and health status may offer a unique and more reliable assessment of provider quality and performance,” she explained. Yet despite growing interest in using patient-reported measures, many important questions regarding their accuracy, applicability, and clinical utility remain. The purpose of this study was, therefore, to evaluate how patient-reported quality of life measures compared to short-term and long-term clinical outcomes in patients who underwent bariatric surgery.
The majority of the study’s 11,420 participants were female (79.8%), were white (84.1%), and underwent Roux-en-Y laparoscopic gastric bypass (56.8%). For each study participant, both short-term and long-term clinical outcome measures were obtained from medical board review. Short-term clinical outcomes were defined as the rate of perioperative complications within 30 days of bariatric surgery. Percent excess weight loss at 1 year post surgery was used as a long-term clinical outcome.
In addition, two patient-reported outcomes were collected: an overall health-related quality of life score called the Health and Activities Limitations Index (HALex) and an obesity-specific quality of life score, the Bariatric Quality of Life (BQL) index, which measures well-being, social and physical functioning, and obesity-related symptoms.
Multivariate and linear regression models demonstrated that short-term complication rates were not correlated to the overall patient-reported quality of life score (P = .32) or to the obesity-specific BQL score (P = .74).
However, the long-term measure of excess weight loss at 1 year post surgery was significantly associated with both overall and obesity-specific patient-reported measures of health-related quality of life (P less than .002 and P less than .001 respectively).
Moreover, scores indicating improved quality of life were associated with greater weight loss.
Finally, comorbidity resolution, estimated by the reduction in the use of medications taken to treat conditions related to obesity, was significantly associated with the obesity-specific measure, BQL, but not the overall quality of life measure, HALex.
“In conclusion, [patient-reported outcomes] are distinct from clinical outcomes,” investigators wrote. Patient-reported outcomes “provide an opportunity for improved population-based cost-effectiveness analyses using outcomes germane to procedures performed for symptomatology and improving QOL,” they added.
The Agency for Healthcare Research and Quality supported the research. The investigators reported having no disclosures.
On Twitter @jessnicolecraig
FROM ANNALS OF SURGERY
Key clinical point: Patient-reported quality of life measures were associated with long-term but not short-term clinical outcomes.
Major finding: Overall and obesity-specific patient-reported quality of life scores were associated with long-term excess weight loss (P less than .002 and P less than .001 respectively).
Data source: A retrospective study of 11,420 patients who underwent bariatric surgery.
Disclosures: The Agency for Healthcare Research and Quality supported the study. The investigators reported having no disclosures.
Two novel DNA Zika virus vaccines set for human trials
The search is on for clinical trial participants to help verify whether two genetically based vaccines that lowered Zika virus viremia in infected primates will be effective in humans.
Although much is still unknown about the pathogenesis, immunity, and transmission of the flavivirus, its devastating effects mean developing a vaccine is imperative, wrote Kimberly A. Dowd, PhD, a virologist at the National Institute of Allergy and Infectious Diseases, and her colleagues in a paper published online in Science.
According to Dr. Dowd and her coauthors, the quickest path to a Zika vaccine is to start with what is already known about flaviviruses and to avoid unnecessary bureaucracy.
“Advantages of DNA vaccines include the ability to rapidly test multiple candidate antigen designs, rapidly produce GMP material, and established safety profile in humans, and a relatively straightforward regulatory pathway into clinical evaluation,” Dr. Dowd and her colleagues wrote. The study details the results of two Zika vaccine candidates tested in primates. The clinical trial will now test these vaccines’ efficacy in humans (Science. 2016 Sept 22. doi: 10.1126/science.aai3197).
Starting with insights gained from DNA-based testing for a West Nile virus vaccine that showed vaccine-elicited neutralizing antibodies are associated with protection from flavivirus-mediated disease, and data showing that a single vaccine antigen will protect against all strains of Zika virus, Dr. Dowd and her coinvestigators developed two DNA-based vaccines that successfully bound to Zika subviral particles in infected mice. Then they tested the vaccines in rhesus macaques.
Six animals were injected with either 1 mg of VRC5283 at 0 and 4 weeks. Another six were injected with 4 mg of either VRC5283 or VRC5288 at 0 or 4 weeks. Another six were injected with a single 1-mg dose of VRC5288 at week 0. After the initial DNA dose, all animals were found to have detectable binding and neutralizing antibody activity, peaking at week 3. Compared with controls given the CMV-immediate early-promoter–containing vector VRC8400, all study animals had a significantly higher neutralizing antibody response (P = .022). The group given the single dose of VRC5288 had significantly lower neutralizing antibody titers, compared with macaques given two doses of either vaccine (P = .022).
Across the groups given two doses of either vaccine, there were no significant differences between titer levels, suggesting that both vaccine candidates elicit substantial Zika virus–specific neutralizing antibodies in primates. More to the point was that 8 weeks after immunization, when all animals in the study were challenged subcutaneously with the virus, viremia levels in the 18 total macaques given two doses of either amount and of either vaccine were undetectable in all but 1. Compared with controls, that had peak viral loads on day 3 or 4, the six animals given one dose of 1 mg VRC5288 were viremic on day 3, but at a significantly reduced rate (P = .041).
Taking into account one animal in the VRC5288 two-dose 4-mg group that had viral load blips above background on days 3 and 7, as well as the lowest titer levels of all the test animals, the investigators determined that 70% protection from Zika virus viremia would be possible if certain titer levels could be achieved.
Whether waning or incomplete immunity could lead to enhanced flavivirus disease is a concern when developing correct vaccination dosage, the investigators said. However, despite some breakthrough infection in the group given the single 1 mg dose of VRC5288, the animals’ illness remained subclinical, there were no signs of replication, and their viremia levels were lower than in unvaccinated controls.
Now, all eyes are on how the vaccines compare with one another while researchers try to establish an adequate serologic correlate of sterilizing immunity in humans. According to Dr. Dowd and her colleagues, the phase I trial is being designed in parallel with other trials looking into a purified, protein-based whole-inactivated Zika virus vaccine, as well as other antigens, delivery methods, and combination vaccines.
The multipronged approach improves the likelihood that enough immunogenicity data can be gathered and translated into a successful intervention for the women of child-bearing age most affected by the Zika virus, and the general population at large, Dr. Dowd and her colleagues concluded.
The research was supported by intramural funding from the National Institute of Allergy and Infectious Diseases; start-up funding from the department of diagnostic medicine and pathobiology, College of Veterinary Medicine, Kansas State University; and federal funds from the Frederick National Laboratory for Cancer Research, NIH. One of the coauthors also reported funding from Leidos Biomedical Research.
On Twitter @whitneymcknight
The search is on for clinical trial participants to help verify whether two genetically based vaccines that lowered Zika virus viremia in infected primates will be effective in humans.
Although much is still unknown about the pathogenesis, immunity, and transmission of the flavivirus, its devastating effects mean developing a vaccine is imperative, wrote Kimberly A. Dowd, PhD, a virologist at the National Institute of Allergy and Infectious Diseases, and her colleagues in a paper published online in Science.
According to Dr. Dowd and her coauthors, the quickest path to a Zika vaccine is to start with what is already known about flaviviruses and to avoid unnecessary bureaucracy.
“Advantages of DNA vaccines include the ability to rapidly test multiple candidate antigen designs, rapidly produce GMP material, and established safety profile in humans, and a relatively straightforward regulatory pathway into clinical evaluation,” Dr. Dowd and her colleagues wrote. The study details the results of two Zika vaccine candidates tested in primates. The clinical trial will now test these vaccines’ efficacy in humans (Science. 2016 Sept 22. doi: 10.1126/science.aai3197).
Starting with insights gained from DNA-based testing for a West Nile virus vaccine that showed vaccine-elicited neutralizing antibodies are associated with protection from flavivirus-mediated disease, and data showing that a single vaccine antigen will protect against all strains of Zika virus, Dr. Dowd and her coinvestigators developed two DNA-based vaccines that successfully bound to Zika subviral particles in infected mice. Then they tested the vaccines in rhesus macaques.
Six animals were injected with either 1 mg of VRC5283 at 0 and 4 weeks. Another six were injected with 4 mg of either VRC5283 or VRC5288 at 0 or 4 weeks. Another six were injected with a single 1-mg dose of VRC5288 at week 0. After the initial DNA dose, all animals were found to have detectable binding and neutralizing antibody activity, peaking at week 3. Compared with controls given the CMV-immediate early-promoter–containing vector VRC8400, all study animals had a significantly higher neutralizing antibody response (P = .022). The group given the single dose of VRC5288 had significantly lower neutralizing antibody titers, compared with macaques given two doses of either vaccine (P = .022).
Across the groups given two doses of either vaccine, there were no significant differences between titer levels, suggesting that both vaccine candidates elicit substantial Zika virus–specific neutralizing antibodies in primates. More to the point was that 8 weeks after immunization, when all animals in the study were challenged subcutaneously with the virus, viremia levels in the 18 total macaques given two doses of either amount and of either vaccine were undetectable in all but 1. Compared with controls, that had peak viral loads on day 3 or 4, the six animals given one dose of 1 mg VRC5288 were viremic on day 3, but at a significantly reduced rate (P = .041).
Taking into account one animal in the VRC5288 two-dose 4-mg group that had viral load blips above background on days 3 and 7, as well as the lowest titer levels of all the test animals, the investigators determined that 70% protection from Zika virus viremia would be possible if certain titer levels could be achieved.
Whether waning or incomplete immunity could lead to enhanced flavivirus disease is a concern when developing correct vaccination dosage, the investigators said. However, despite some breakthrough infection in the group given the single 1 mg dose of VRC5288, the animals’ illness remained subclinical, there were no signs of replication, and their viremia levels were lower than in unvaccinated controls.
Now, all eyes are on how the vaccines compare with one another while researchers try to establish an adequate serologic correlate of sterilizing immunity in humans. According to Dr. Dowd and her colleagues, the phase I trial is being designed in parallel with other trials looking into a purified, protein-based whole-inactivated Zika virus vaccine, as well as other antigens, delivery methods, and combination vaccines.
The multipronged approach improves the likelihood that enough immunogenicity data can be gathered and translated into a successful intervention for the women of child-bearing age most affected by the Zika virus, and the general population at large, Dr. Dowd and her colleagues concluded.
The research was supported by intramural funding from the National Institute of Allergy and Infectious Diseases; start-up funding from the department of diagnostic medicine and pathobiology, College of Veterinary Medicine, Kansas State University; and federal funds from the Frederick National Laboratory for Cancer Research, NIH. One of the coauthors also reported funding from Leidos Biomedical Research.
On Twitter @whitneymcknight
The search is on for clinical trial participants to help verify whether two genetically based vaccines that lowered Zika virus viremia in infected primates will be effective in humans.
Although much is still unknown about the pathogenesis, immunity, and transmission of the flavivirus, its devastating effects mean developing a vaccine is imperative, wrote Kimberly A. Dowd, PhD, a virologist at the National Institute of Allergy and Infectious Diseases, and her colleagues in a paper published online in Science.
According to Dr. Dowd and her coauthors, the quickest path to a Zika vaccine is to start with what is already known about flaviviruses and to avoid unnecessary bureaucracy.
“Advantages of DNA vaccines include the ability to rapidly test multiple candidate antigen designs, rapidly produce GMP material, and established safety profile in humans, and a relatively straightforward regulatory pathway into clinical evaluation,” Dr. Dowd and her colleagues wrote. The study details the results of two Zika vaccine candidates tested in primates. The clinical trial will now test these vaccines’ efficacy in humans (Science. 2016 Sept 22. doi: 10.1126/science.aai3197).
Starting with insights gained from DNA-based testing for a West Nile virus vaccine that showed vaccine-elicited neutralizing antibodies are associated with protection from flavivirus-mediated disease, and data showing that a single vaccine antigen will protect against all strains of Zika virus, Dr. Dowd and her coinvestigators developed two DNA-based vaccines that successfully bound to Zika subviral particles in infected mice. Then they tested the vaccines in rhesus macaques.
Six animals were injected with either 1 mg of VRC5283 at 0 and 4 weeks. Another six were injected with 4 mg of either VRC5283 or VRC5288 at 0 or 4 weeks. Another six were injected with a single 1-mg dose of VRC5288 at week 0. After the initial DNA dose, all animals were found to have detectable binding and neutralizing antibody activity, peaking at week 3. Compared with controls given the CMV-immediate early-promoter–containing vector VRC8400, all study animals had a significantly higher neutralizing antibody response (P = .022). The group given the single dose of VRC5288 had significantly lower neutralizing antibody titers, compared with macaques given two doses of either vaccine (P = .022).
Across the groups given two doses of either vaccine, there were no significant differences between titer levels, suggesting that both vaccine candidates elicit substantial Zika virus–specific neutralizing antibodies in primates. More to the point was that 8 weeks after immunization, when all animals in the study were challenged subcutaneously with the virus, viremia levels in the 18 total macaques given two doses of either amount and of either vaccine were undetectable in all but 1. Compared with controls, that had peak viral loads on day 3 or 4, the six animals given one dose of 1 mg VRC5288 were viremic on day 3, but at a significantly reduced rate (P = .041).
Taking into account one animal in the VRC5288 two-dose 4-mg group that had viral load blips above background on days 3 and 7, as well as the lowest titer levels of all the test animals, the investigators determined that 70% protection from Zika virus viremia would be possible if certain titer levels could be achieved.
Whether waning or incomplete immunity could lead to enhanced flavivirus disease is a concern when developing correct vaccination dosage, the investigators said. However, despite some breakthrough infection in the group given the single 1 mg dose of VRC5288, the animals’ illness remained subclinical, there were no signs of replication, and their viremia levels were lower than in unvaccinated controls.
Now, all eyes are on how the vaccines compare with one another while researchers try to establish an adequate serologic correlate of sterilizing immunity in humans. According to Dr. Dowd and her colleagues, the phase I trial is being designed in parallel with other trials looking into a purified, protein-based whole-inactivated Zika virus vaccine, as well as other antigens, delivery methods, and combination vaccines.
The multipronged approach improves the likelihood that enough immunogenicity data can be gathered and translated into a successful intervention for the women of child-bearing age most affected by the Zika virus, and the general population at large, Dr. Dowd and her colleagues concluded.
The research was supported by intramural funding from the National Institute of Allergy and Infectious Diseases; start-up funding from the department of diagnostic medicine and pathobiology, College of Veterinary Medicine, Kansas State University; and federal funds from the Frederick National Laboratory for Cancer Research, NIH. One of the coauthors also reported funding from Leidos Biomedical Research.
On Twitter @whitneymcknight
FROM SCIENCE
Key clinical point: A DNA vaccination could be a successful approach to protect against Zika virus infection.
Major finding: Two DNA vaccines with efficacy against the Zika virus in primates are set to begin testing in humans.
Data source: Animal trials of two DNA-based Zika virus vaccines in infected mice and rhesus macaques.
Disclosures: The research was supported by intramural funding from the National Institute of Allergy and Infectious Diseases; start-up funding from the department of diagnostic medicine and pathobiology, College of Veterinary Medicine, Kansas State University; and federal funds from the Frederick National Laboratory for Cancer Research, NIH. One of the coauthors also reported funding from Leidos Biomedical Research.
Inflammation, depression, slow gait define high-risk phenotype in seniors
SAN FRANCISCO – Patients with unchecked inflammation, depression, and slow gait make up a “depressed frail phenotype at grave risk of death,” Patrick J. Brown, PhD, said at the 2016 congress of the International Psychogeriatric Association..
“There are multiple pathways into this phenotypic cycle. Depression and slow gait share a bidirectional relationship, and inflammation may indirectly lead to depression because of its impact on mobility,” said Dr. Brown, a clinical psychologist in the department of psychiatry at Columbia University, New York. Clinicians should consider aggressive interventions for older patients with depression and frailty, recognizing that exercise and dietary changes may be “much more relevant” than switching or augmenting antidepressants and other psychotropic medications, which can be especially risky for seniors, he said.
Models of psychiatric illness, particularly depression, come from studies of younger adults “and have failed us in geriatric medicine,” Dr. Brown emphasized. About 3%-7% of adults above age 65 years meet criteria for major depressive disorder, and another 15% have “significant but subthreshold” depressive symptoms, but less than half of depressed seniors have responded to antidepressants in controlled trials. High rates of treatment failure in late-life depression suggest that it has diverse etiologies that have to be identified and targeted to improve outcomes, Dr. Brown said. Frailty, characterized by slowed gait, weak grip, and decreased physical activity and energy, resembles and often co-occurs with late-life depression, giving rise to the concept of a “depressed-frail” phenotype at potentially greater risk of imminent death, he added.
To test that idea, Dr. Brown and his associates analyzed 10-year longitudinal data for 3,075 white and African American adults aged 68-80 years who were free from significant disabilities or functional limitations at baseline. These participants were from the Dynamics of Health, Aging, and Body Composition study, which annually measured body composition, gait, grip strength, comorbidities, and other clinical data. Using a method called latent class analysis, the researchers examined trajectories of depression (defined as a score of at least 10 on the Center for Epidemiologic Studies Depression Scale, slow gait (walking speed less than 1.02 meters per second), and inflammation (serum interleukin-6 [IL-6] levels above 3.24 pg/mL) over time. They also used multivariable regression to understand how each of those features correlated with mortality.
The latent class analysis showed that 22% of participants had either rising or consistently high probabilities of inflammation, slow gait, and depression. Slow gait was associated with inflammation (r = 0.40; P less than .001) and depression (r = 0.49; P less than .001). Inflammation was independently associated with mortality (P less than .001), while slow gait was linked to mortality only in participants with depression that worsened over time (P less than .01). Among the 247 patients with a high level of inflammation and slow gait with increasing or a consistently high level of depression, the 10-year mortality was 85%, the highest of any group of patients in the study, Dr. Brown said.
The study also confirmed the overlap between depression and frailty. Depression and inflammation each independently predicted slow gait, with odds ratios of 1.37 (95% confidence interval, 1.17-1.60) and 1.22 (1.05-1.41), respectively. Slow gait also was a significant predictor of depression (OR, 1.27; 1.08-1.50), even after the investigators accounted for age, sex, body mass index, comorbidities, use of anti-inflammatories, and scores on the Modified Mini-Mental State Examination.
These and other recent findings highlight frailty as a physical manifestation of greater biologic aging, Dr. Brown said. Accordingly, researchers are studying whether combatting age-related deterioration can improve outcomes in late-life depression. Specific protocols under study include anaerobic exercise to reverse mitochondrial dysfunction, anti-inflammatories targeting acute phase proteins (C-reactive protein) and cytokines (IL-6 and tumor necrosis factor–alpha), and treatments that augment dopaminergic neurotransmission, he said.
The National Institutes of Health provided funding. Dr. Brown had no relevant financial disclosures.
SAN FRANCISCO – Patients with unchecked inflammation, depression, and slow gait make up a “depressed frail phenotype at grave risk of death,” Patrick J. Brown, PhD, said at the 2016 congress of the International Psychogeriatric Association..
“There are multiple pathways into this phenotypic cycle. Depression and slow gait share a bidirectional relationship, and inflammation may indirectly lead to depression because of its impact on mobility,” said Dr. Brown, a clinical psychologist in the department of psychiatry at Columbia University, New York. Clinicians should consider aggressive interventions for older patients with depression and frailty, recognizing that exercise and dietary changes may be “much more relevant” than switching or augmenting antidepressants and other psychotropic medications, which can be especially risky for seniors, he said.
Models of psychiatric illness, particularly depression, come from studies of younger adults “and have failed us in geriatric medicine,” Dr. Brown emphasized. About 3%-7% of adults above age 65 years meet criteria for major depressive disorder, and another 15% have “significant but subthreshold” depressive symptoms, but less than half of depressed seniors have responded to antidepressants in controlled trials. High rates of treatment failure in late-life depression suggest that it has diverse etiologies that have to be identified and targeted to improve outcomes, Dr. Brown said. Frailty, characterized by slowed gait, weak grip, and decreased physical activity and energy, resembles and often co-occurs with late-life depression, giving rise to the concept of a “depressed-frail” phenotype at potentially greater risk of imminent death, he added.
To test that idea, Dr. Brown and his associates analyzed 10-year longitudinal data for 3,075 white and African American adults aged 68-80 years who were free from significant disabilities or functional limitations at baseline. These participants were from the Dynamics of Health, Aging, and Body Composition study, which annually measured body composition, gait, grip strength, comorbidities, and other clinical data. Using a method called latent class analysis, the researchers examined trajectories of depression (defined as a score of at least 10 on the Center for Epidemiologic Studies Depression Scale, slow gait (walking speed less than 1.02 meters per second), and inflammation (serum interleukin-6 [IL-6] levels above 3.24 pg/mL) over time. They also used multivariable regression to understand how each of those features correlated with mortality.
The latent class analysis showed that 22% of participants had either rising or consistently high probabilities of inflammation, slow gait, and depression. Slow gait was associated with inflammation (r = 0.40; P less than .001) and depression (r = 0.49; P less than .001). Inflammation was independently associated with mortality (P less than .001), while slow gait was linked to mortality only in participants with depression that worsened over time (P less than .01). Among the 247 patients with a high level of inflammation and slow gait with increasing or a consistently high level of depression, the 10-year mortality was 85%, the highest of any group of patients in the study, Dr. Brown said.
The study also confirmed the overlap between depression and frailty. Depression and inflammation each independently predicted slow gait, with odds ratios of 1.37 (95% confidence interval, 1.17-1.60) and 1.22 (1.05-1.41), respectively. Slow gait also was a significant predictor of depression (OR, 1.27; 1.08-1.50), even after the investigators accounted for age, sex, body mass index, comorbidities, use of anti-inflammatories, and scores on the Modified Mini-Mental State Examination.
These and other recent findings highlight frailty as a physical manifestation of greater biologic aging, Dr. Brown said. Accordingly, researchers are studying whether combatting age-related deterioration can improve outcomes in late-life depression. Specific protocols under study include anaerobic exercise to reverse mitochondrial dysfunction, anti-inflammatories targeting acute phase proteins (C-reactive protein) and cytokines (IL-6 and tumor necrosis factor–alpha), and treatments that augment dopaminergic neurotransmission, he said.
The National Institutes of Health provided funding. Dr. Brown had no relevant financial disclosures.
SAN FRANCISCO – Patients with unchecked inflammation, depression, and slow gait make up a “depressed frail phenotype at grave risk of death,” Patrick J. Brown, PhD, said at the 2016 congress of the International Psychogeriatric Association..
“There are multiple pathways into this phenotypic cycle. Depression and slow gait share a bidirectional relationship, and inflammation may indirectly lead to depression because of its impact on mobility,” said Dr. Brown, a clinical psychologist in the department of psychiatry at Columbia University, New York. Clinicians should consider aggressive interventions for older patients with depression and frailty, recognizing that exercise and dietary changes may be “much more relevant” than switching or augmenting antidepressants and other psychotropic medications, which can be especially risky for seniors, he said.
Models of psychiatric illness, particularly depression, come from studies of younger adults “and have failed us in geriatric medicine,” Dr. Brown emphasized. About 3%-7% of adults above age 65 years meet criteria for major depressive disorder, and another 15% have “significant but subthreshold” depressive symptoms, but less than half of depressed seniors have responded to antidepressants in controlled trials. High rates of treatment failure in late-life depression suggest that it has diverse etiologies that have to be identified and targeted to improve outcomes, Dr. Brown said. Frailty, characterized by slowed gait, weak grip, and decreased physical activity and energy, resembles and often co-occurs with late-life depression, giving rise to the concept of a “depressed-frail” phenotype at potentially greater risk of imminent death, he added.
To test that idea, Dr. Brown and his associates analyzed 10-year longitudinal data for 3,075 white and African American adults aged 68-80 years who were free from significant disabilities or functional limitations at baseline. These participants were from the Dynamics of Health, Aging, and Body Composition study, which annually measured body composition, gait, grip strength, comorbidities, and other clinical data. Using a method called latent class analysis, the researchers examined trajectories of depression (defined as a score of at least 10 on the Center for Epidemiologic Studies Depression Scale, slow gait (walking speed less than 1.02 meters per second), and inflammation (serum interleukin-6 [IL-6] levels above 3.24 pg/mL) over time. They also used multivariable regression to understand how each of those features correlated with mortality.
The latent class analysis showed that 22% of participants had either rising or consistently high probabilities of inflammation, slow gait, and depression. Slow gait was associated with inflammation (r = 0.40; P less than .001) and depression (r = 0.49; P less than .001). Inflammation was independently associated with mortality (P less than .001), while slow gait was linked to mortality only in participants with depression that worsened over time (P less than .01). Among the 247 patients with a high level of inflammation and slow gait with increasing or a consistently high level of depression, the 10-year mortality was 85%, the highest of any group of patients in the study, Dr. Brown said.
The study also confirmed the overlap between depression and frailty. Depression and inflammation each independently predicted slow gait, with odds ratios of 1.37 (95% confidence interval, 1.17-1.60) and 1.22 (1.05-1.41), respectively. Slow gait also was a significant predictor of depression (OR, 1.27; 1.08-1.50), even after the investigators accounted for age, sex, body mass index, comorbidities, use of anti-inflammatories, and scores on the Modified Mini-Mental State Examination.
These and other recent findings highlight frailty as a physical manifestation of greater biologic aging, Dr. Brown said. Accordingly, researchers are studying whether combatting age-related deterioration can improve outcomes in late-life depression. Specific protocols under study include anaerobic exercise to reverse mitochondrial dysfunction, anti-inflammatories targeting acute phase proteins (C-reactive protein) and cytokines (IL-6 and tumor necrosis factor–alpha), and treatments that augment dopaminergic neurotransmission, he said.
The National Institutes of Health provided funding. Dr. Brown had no relevant financial disclosures.
AT IPA 2016
Key clinical point: Older adults with unchecked inflammation, depression, and slow gait are at high risk of death.
Major finding: The 10-year mortality was 85% among participants with increasing or consistently high levels of depression, and consistently high levels of inflammation and a slow gait.
Data source: A longitudinal analysis of 3,075 adults aged 68-80 years who were functioning well at initial evaluation.
Disclosures: The National Institutes of Health provided funding. Dr. Brown had no relevant financial disclosures.
GAD tied to twice the risk of cancer mortality in men
VIENNA – Generalized anxiety disorder in men over age 40 was independently associated with a greater than twofold increased risk of death due to cancer during 15 years of follow-up, compared with men without the psychiatric disorder, in a large longitudinal population-based study, Olivia Remes reported at the annual congress of the European College of Neuropsychopharmacology.
In contrast, women with generalized anxiety disorder (GAD) were at no increased risk for cancer mortality, according to Ms. Remes, a PhD candidate in the department of public health and primary care at the University of Cambridge, England.
“I think an important message of this study is that anxiety is not just a personality trait,” she said in an interview. “In some cases, it may be more than worries and stress; it can represent a possible marker for future ill physical health that general practitioners and psychiatrists ought to be aware of.”
This creates a dilemma, because individuals with GAD typically are high users of health care resources. They frequently present in physicians’ offices and emergency departments with a wide range of physical complaints, including stomach pain, breathing difficulty, fatigue, nausea, or peripheral numbness.
Ms. Remes presented an analysis of 7,139 men and 8,799 women over age 40 at enrollment in the European Prospective Investigation of Cancer–Norfolk Study from the period of 1996-2000. At entry, the patients underwent a physical examination and completed numerous health-related questionnaires. Among these was the Health and Life Experiences Questionnaire (HLEQ), the responses to which enabled investigators to identify 1.8% of the men and 2.4% of women as meeting DSM-IV diagnostic criteria for GAD.
During 15 years of follow-up, 796 men and 648 women died of cancer. In multivariate analysis, men with GAD were at a 2.14-fold increased risk of death due to cancer. This analysis was extensively adjusted for potential confounders, including age, marital status, education level, socioeconomic status, major chronic physical illnesses, smoking, alcohol intake, major depressive disorder, body mass index, physical activity level, and the use of antidepressants or antihypnotic agents.
This was the first large, long-term study to examine the relationship between GAD and cancer mortality. Prior studies yielded conflicting results but were limited by small sample size and/or short follow-up, Ms. Remes said.
Even with more than 1,400 cancer deaths in the study, the sample size is too small to say whether GAD in men is preferentially associated with death due to any specific type of cancer.
Severe chronic anxiety has been linked to increased systemic inflammation, an observation that points to a possible mechanism by which GAD might increase affected individuals’ risk of fatal cancer as well as cardiovascular disease, chronic lung disease, and other conditions where inflammation figures prominently. But that doesn’t explain the gender difference in cancer mortality risk, the source of which remains speculative. It’s not the result of men being more likely to be smokers or to abuse alcohol, since those carcinogenic lifestyle factors were controlled for in the multivariate analysis, she observed.
One hypothetical possibility is that men with GAD who develop a malignancy might be more likely to delay seeking medical attention for it than might men without the anxiety disorder. Ms. Remes and her coinvestigators plan to explore this possibility in a roundabout way by analyzing the Norfolk study database looking for differences between men with and without GAD in the time from cancer diagnosis to death.
To eliminate the possibility that GAD in men might be triggered by an occult and ultimately fatal cancer, the investigators reanalyzed the Norfolk study data after excluding deaths that occurred during the first 5 years of follow-up. The results remained unchanged, according to Ms. Remes.
She reported having no financial conflicts regarding this study, which was sponsored by the U.K. Medical Research Council and Cancer Research UK.
VIENNA – Generalized anxiety disorder in men over age 40 was independently associated with a greater than twofold increased risk of death due to cancer during 15 years of follow-up, compared with men without the psychiatric disorder, in a large longitudinal population-based study, Olivia Remes reported at the annual congress of the European College of Neuropsychopharmacology.
In contrast, women with generalized anxiety disorder (GAD) were at no increased risk for cancer mortality, according to Ms. Remes, a PhD candidate in the department of public health and primary care at the University of Cambridge, England.
“I think an important message of this study is that anxiety is not just a personality trait,” she said in an interview. “In some cases, it may be more than worries and stress; it can represent a possible marker for future ill physical health that general practitioners and psychiatrists ought to be aware of.”
This creates a dilemma, because individuals with GAD typically are high users of health care resources. They frequently present in physicians’ offices and emergency departments with a wide range of physical complaints, including stomach pain, breathing difficulty, fatigue, nausea, or peripheral numbness.
Ms. Remes presented an analysis of 7,139 men and 8,799 women over age 40 at enrollment in the European Prospective Investigation of Cancer–Norfolk Study from the period of 1996-2000. At entry, the patients underwent a physical examination and completed numerous health-related questionnaires. Among these was the Health and Life Experiences Questionnaire (HLEQ), the responses to which enabled investigators to identify 1.8% of the men and 2.4% of women as meeting DSM-IV diagnostic criteria for GAD.
During 15 years of follow-up, 796 men and 648 women died of cancer. In multivariate analysis, men with GAD were at a 2.14-fold increased risk of death due to cancer. This analysis was extensively adjusted for potential confounders, including age, marital status, education level, socioeconomic status, major chronic physical illnesses, smoking, alcohol intake, major depressive disorder, body mass index, physical activity level, and the use of antidepressants or antihypnotic agents.
This was the first large, long-term study to examine the relationship between GAD and cancer mortality. Prior studies yielded conflicting results but were limited by small sample size and/or short follow-up, Ms. Remes said.
Even with more than 1,400 cancer deaths in the study, the sample size is too small to say whether GAD in men is preferentially associated with death due to any specific type of cancer.
Severe chronic anxiety has been linked to increased systemic inflammation, an observation that points to a possible mechanism by which GAD might increase affected individuals’ risk of fatal cancer as well as cardiovascular disease, chronic lung disease, and other conditions where inflammation figures prominently. But that doesn’t explain the gender difference in cancer mortality risk, the source of which remains speculative. It’s not the result of men being more likely to be smokers or to abuse alcohol, since those carcinogenic lifestyle factors were controlled for in the multivariate analysis, she observed.
One hypothetical possibility is that men with GAD who develop a malignancy might be more likely to delay seeking medical attention for it than might men without the anxiety disorder. Ms. Remes and her coinvestigators plan to explore this possibility in a roundabout way by analyzing the Norfolk study database looking for differences between men with and without GAD in the time from cancer diagnosis to death.
To eliminate the possibility that GAD in men might be triggered by an occult and ultimately fatal cancer, the investigators reanalyzed the Norfolk study data after excluding deaths that occurred during the first 5 years of follow-up. The results remained unchanged, according to Ms. Remes.
She reported having no financial conflicts regarding this study, which was sponsored by the U.K. Medical Research Council and Cancer Research UK.
VIENNA – Generalized anxiety disorder in men over age 40 was independently associated with a greater than twofold increased risk of death due to cancer during 15 years of follow-up, compared with men without the psychiatric disorder, in a large longitudinal population-based study, Olivia Remes reported at the annual congress of the European College of Neuropsychopharmacology.
In contrast, women with generalized anxiety disorder (GAD) were at no increased risk for cancer mortality, according to Ms. Remes, a PhD candidate in the department of public health and primary care at the University of Cambridge, England.
“I think an important message of this study is that anxiety is not just a personality trait,” she said in an interview. “In some cases, it may be more than worries and stress; it can represent a possible marker for future ill physical health that general practitioners and psychiatrists ought to be aware of.”
This creates a dilemma, because individuals with GAD typically are high users of health care resources. They frequently present in physicians’ offices and emergency departments with a wide range of physical complaints, including stomach pain, breathing difficulty, fatigue, nausea, or peripheral numbness.
Ms. Remes presented an analysis of 7,139 men and 8,799 women over age 40 at enrollment in the European Prospective Investigation of Cancer–Norfolk Study from the period of 1996-2000. At entry, the patients underwent a physical examination and completed numerous health-related questionnaires. Among these was the Health and Life Experiences Questionnaire (HLEQ), the responses to which enabled investigators to identify 1.8% of the men and 2.4% of women as meeting DSM-IV diagnostic criteria for GAD.
During 15 years of follow-up, 796 men and 648 women died of cancer. In multivariate analysis, men with GAD were at a 2.14-fold increased risk of death due to cancer. This analysis was extensively adjusted for potential confounders, including age, marital status, education level, socioeconomic status, major chronic physical illnesses, smoking, alcohol intake, major depressive disorder, body mass index, physical activity level, and the use of antidepressants or antihypnotic agents.
This was the first large, long-term study to examine the relationship between GAD and cancer mortality. Prior studies yielded conflicting results but were limited by small sample size and/or short follow-up, Ms. Remes said.
Even with more than 1,400 cancer deaths in the study, the sample size is too small to say whether GAD in men is preferentially associated with death due to any specific type of cancer.
Severe chronic anxiety has been linked to increased systemic inflammation, an observation that points to a possible mechanism by which GAD might increase affected individuals’ risk of fatal cancer as well as cardiovascular disease, chronic lung disease, and other conditions where inflammation figures prominently. But that doesn’t explain the gender difference in cancer mortality risk, the source of which remains speculative. It’s not the result of men being more likely to be smokers or to abuse alcohol, since those carcinogenic lifestyle factors were controlled for in the multivariate analysis, she observed.
One hypothetical possibility is that men with GAD who develop a malignancy might be more likely to delay seeking medical attention for it than might men without the anxiety disorder. Ms. Remes and her coinvestigators plan to explore this possibility in a roundabout way by analyzing the Norfolk study database looking for differences between men with and without GAD in the time from cancer diagnosis to death.
To eliminate the possibility that GAD in men might be triggered by an occult and ultimately fatal cancer, the investigators reanalyzed the Norfolk study data after excluding deaths that occurred during the first 5 years of follow-up. The results remained unchanged, according to Ms. Remes.
She reported having no financial conflicts regarding this study, which was sponsored by the U.K. Medical Research Council and Cancer Research UK.
AT THE ECNP CONGRESS
Key clinical point: Men with generalized anxiety disorder are more than twice as likely to die from cancer, compared with men without the disorder.
Major finding: Men over age 40 with generalized anxiety disorder were 2.14 times more likely to die of cancer within 15 years than were those without the disorder.
Data source: A longitudinal, population-based study of nearly 16,000 Norfolk, England–area adults aged 40 or older who were followed for 15 years.
Disclosures: The U.K. Medical Research Council and Cancer Research UK sponsored the study. The presenter reported having no financial conflicts of interest.
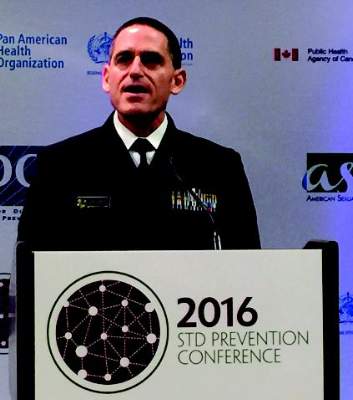
Gonorrhea cluster shows increased antibiotic resistance
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
AT THE 2016 STD PREVENTION CONFERENCE
Back pain: Let’s get it straight!
Back pain is a common complaint among adolescents. But there are several misconceptions about back pain that lead to excessive referrals and unnecessary imaging.
One of the most common of these misconceptions is that back pain in adolescents is caused by their carrying a heavy backpack. When this was researched, carrying a heavy backpack had a weak association with back pain,1,2 but because so many relate the two, the American Academy of Pediatrics came out with recommendations limiting the weight to 20% of the child’s body weight.3
Another misconception regarding back pain in children is that the cause is likely serious and needs a prompt work-up. A study followed 560 children who were diagnosed with low back pain and idiopathic scoliosis. In only 9% of cases was an underlying pathologic condition found: 29 patients had spondylolysis or spondylolisthesis, 9 had Scheuermann’s kyphosis, 5 had a syrinx, 2 had a herniated disk, 1 had hydromyelia, 1 had a tethered cord, and 1 had an intraspinal tumor.4
As with all diagnoses, a detailed history is very important. Is the pain acute or chronic? Does the pain radiate? Is there nighttime pain? Where exactly is the pain? Commonly, with acute onset there is an association of new activity or trauma. A good social history is also important because complaints of back pain are high on the list with psychosomatic issues as well.
The physical exam should include inspection of the back with the patient standing, bent forward, and in a hyperextended position. Identifying curvatures of the spine and pinpointing what increases the pain are helpful in getting the correct diagnosis. Middle back pain associated with an excessively rounded back, or kyphosis of the thoracic spine, is known as Scheuermann’s kyphosis. This is due to the vertebrae becoming wedged.5
Body habitus also is important to note. Adolescents with large breasts may complain of upper back pain especially, if they are not wearing a supportive bra. Weak abdominal muscles can also give rise to back pain, most commonly in the lower back. Tight hamstrings can cause posterior rotation of the pelvis, which can result in lumbosacral pain.
More worrisome causes of back pain are spondylosis or stress fractures; these are usually caused by a sports trauma such as gymnastics or diving, but also can be caused by a rapid growth spurt.1 Pain is usually mild initially. Spondylolisthesis is the forward movement of one vertebra on another. This causes pain in the lumbosacral area, with radiation into the lower extremities and weakness.4
Infection and tumor are rare causes of low back pain. Both can cause nighttime pain. Infection in the intervertebral disk space, or diskitis, is more common in younger children. Pain can be described in the back or the abdominal area.1 Limping or refusal to walk are also noted.
Tumors, although rare, are what parents worry the most about. Osteoid osteoma is the most common form, and should be considered whenever a scoliosis is of new onset or advances quickly.6
A work-up for acute low back pain associated with minor trauma and no radiation or limitation to movement can be done conservatively. If the physical exam reveals muscle imbalances or tightness and abdominal weakness, referral to physical therapy is warranted.
If low back pain is associated with abnormal findings, then an x-ray should be done. Anteroposterior and lateral views are usually sufficient. Oblique views should be added if there is suspicion of a stress fracture.
Referral to an orthopedist is warranted if there are any bowel or bladder changes, significant weakness, and/or sensory changes. A bone scan, CT scan and MRI are more definitive tests. The bone scan is not very sensitive (61%) but has a high specificity (80%). CT scans show soft tissue, but no marrow elements are seen, so it is not as helpful with a herniated disk.7
In this ever-changing medical arena, taking a detailed history and doing a good exam will not only save a lot of time but also decrease the number of unnecessary referrals, which is the name of the game!
References
1. J Pediatr Orthop. 2006 May-Jun;26(3):358-63.
2. Pediatrics. 2003 Apr;111(4 Pt 1):822-8.
3. American Academy of Pediatrics. Backpack safety.
4. J Bone Joint Surg Am. 1997 Mar;79(3):364-8.
6. J Paediatr Child Health. 2000 Jun;36(3):208-12.
7. Skeletal Radiol. 2005 Feb;34(2):63-73.
Dr. Pearce is a pediatrician in Frankfort, Ill.
Back pain is a common complaint among adolescents. But there are several misconceptions about back pain that lead to excessive referrals and unnecessary imaging.
One of the most common of these misconceptions is that back pain in adolescents is caused by their carrying a heavy backpack. When this was researched, carrying a heavy backpack had a weak association with back pain,1,2 but because so many relate the two, the American Academy of Pediatrics came out with recommendations limiting the weight to 20% of the child’s body weight.3
Another misconception regarding back pain in children is that the cause is likely serious and needs a prompt work-up. A study followed 560 children who were diagnosed with low back pain and idiopathic scoliosis. In only 9% of cases was an underlying pathologic condition found: 29 patients had spondylolysis or spondylolisthesis, 9 had Scheuermann’s kyphosis, 5 had a syrinx, 2 had a herniated disk, 1 had hydromyelia, 1 had a tethered cord, and 1 had an intraspinal tumor.4
As with all diagnoses, a detailed history is very important. Is the pain acute or chronic? Does the pain radiate? Is there nighttime pain? Where exactly is the pain? Commonly, with acute onset there is an association of new activity or trauma. A good social history is also important because complaints of back pain are high on the list with psychosomatic issues as well.
The physical exam should include inspection of the back with the patient standing, bent forward, and in a hyperextended position. Identifying curvatures of the spine and pinpointing what increases the pain are helpful in getting the correct diagnosis. Middle back pain associated with an excessively rounded back, or kyphosis of the thoracic spine, is known as Scheuermann’s kyphosis. This is due to the vertebrae becoming wedged.5
Body habitus also is important to note. Adolescents with large breasts may complain of upper back pain especially, if they are not wearing a supportive bra. Weak abdominal muscles can also give rise to back pain, most commonly in the lower back. Tight hamstrings can cause posterior rotation of the pelvis, which can result in lumbosacral pain.
More worrisome causes of back pain are spondylosis or stress fractures; these are usually caused by a sports trauma such as gymnastics or diving, but also can be caused by a rapid growth spurt.1 Pain is usually mild initially. Spondylolisthesis is the forward movement of one vertebra on another. This causes pain in the lumbosacral area, with radiation into the lower extremities and weakness.4
Infection and tumor are rare causes of low back pain. Both can cause nighttime pain. Infection in the intervertebral disk space, or diskitis, is more common in younger children. Pain can be described in the back or the abdominal area.1 Limping or refusal to walk are also noted.
Tumors, although rare, are what parents worry the most about. Osteoid osteoma is the most common form, and should be considered whenever a scoliosis is of new onset or advances quickly.6
A work-up for acute low back pain associated with minor trauma and no radiation or limitation to movement can be done conservatively. If the physical exam reveals muscle imbalances or tightness and abdominal weakness, referral to physical therapy is warranted.
If low back pain is associated with abnormal findings, then an x-ray should be done. Anteroposterior and lateral views are usually sufficient. Oblique views should be added if there is suspicion of a stress fracture.
Referral to an orthopedist is warranted if there are any bowel or bladder changes, significant weakness, and/or sensory changes. A bone scan, CT scan and MRI are more definitive tests. The bone scan is not very sensitive (61%) but has a high specificity (80%). CT scans show soft tissue, but no marrow elements are seen, so it is not as helpful with a herniated disk.7
In this ever-changing medical arena, taking a detailed history and doing a good exam will not only save a lot of time but also decrease the number of unnecessary referrals, which is the name of the game!
References
1. J Pediatr Orthop. 2006 May-Jun;26(3):358-63.
2. Pediatrics. 2003 Apr;111(4 Pt 1):822-8.
3. American Academy of Pediatrics. Backpack safety.
4. J Bone Joint Surg Am. 1997 Mar;79(3):364-8.
6. J Paediatr Child Health. 2000 Jun;36(3):208-12.
7. Skeletal Radiol. 2005 Feb;34(2):63-73.
Dr. Pearce is a pediatrician in Frankfort, Ill.
Back pain is a common complaint among adolescents. But there are several misconceptions about back pain that lead to excessive referrals and unnecessary imaging.
One of the most common of these misconceptions is that back pain in adolescents is caused by their carrying a heavy backpack. When this was researched, carrying a heavy backpack had a weak association with back pain,1,2 but because so many relate the two, the American Academy of Pediatrics came out with recommendations limiting the weight to 20% of the child’s body weight.3
Another misconception regarding back pain in children is that the cause is likely serious and needs a prompt work-up. A study followed 560 children who were diagnosed with low back pain and idiopathic scoliosis. In only 9% of cases was an underlying pathologic condition found: 29 patients had spondylolysis or spondylolisthesis, 9 had Scheuermann’s kyphosis, 5 had a syrinx, 2 had a herniated disk, 1 had hydromyelia, 1 had a tethered cord, and 1 had an intraspinal tumor.4
As with all diagnoses, a detailed history is very important. Is the pain acute or chronic? Does the pain radiate? Is there nighttime pain? Where exactly is the pain? Commonly, with acute onset there is an association of new activity or trauma. A good social history is also important because complaints of back pain are high on the list with psychosomatic issues as well.
The physical exam should include inspection of the back with the patient standing, bent forward, and in a hyperextended position. Identifying curvatures of the spine and pinpointing what increases the pain are helpful in getting the correct diagnosis. Middle back pain associated with an excessively rounded back, or kyphosis of the thoracic spine, is known as Scheuermann’s kyphosis. This is due to the vertebrae becoming wedged.5
Body habitus also is important to note. Adolescents with large breasts may complain of upper back pain especially, if they are not wearing a supportive bra. Weak abdominal muscles can also give rise to back pain, most commonly in the lower back. Tight hamstrings can cause posterior rotation of the pelvis, which can result in lumbosacral pain.
More worrisome causes of back pain are spondylosis or stress fractures; these are usually caused by a sports trauma such as gymnastics or diving, but also can be caused by a rapid growth spurt.1 Pain is usually mild initially. Spondylolisthesis is the forward movement of one vertebra on another. This causes pain in the lumbosacral area, with radiation into the lower extremities and weakness.4
Infection and tumor are rare causes of low back pain. Both can cause nighttime pain. Infection in the intervertebral disk space, or diskitis, is more common in younger children. Pain can be described in the back or the abdominal area.1 Limping or refusal to walk are also noted.
Tumors, although rare, are what parents worry the most about. Osteoid osteoma is the most common form, and should be considered whenever a scoliosis is of new onset or advances quickly.6
A work-up for acute low back pain associated with minor trauma and no radiation or limitation to movement can be done conservatively. If the physical exam reveals muscle imbalances or tightness and abdominal weakness, referral to physical therapy is warranted.
If low back pain is associated with abnormal findings, then an x-ray should be done. Anteroposterior and lateral views are usually sufficient. Oblique views should be added if there is suspicion of a stress fracture.
Referral to an orthopedist is warranted if there are any bowel or bladder changes, significant weakness, and/or sensory changes. A bone scan, CT scan and MRI are more definitive tests. The bone scan is not very sensitive (61%) but has a high specificity (80%). CT scans show soft tissue, but no marrow elements are seen, so it is not as helpful with a herniated disk.7
In this ever-changing medical arena, taking a detailed history and doing a good exam will not only save a lot of time but also decrease the number of unnecessary referrals, which is the name of the game!
References
1. J Pediatr Orthop. 2006 May-Jun;26(3):358-63.
2. Pediatrics. 2003 Apr;111(4 Pt 1):822-8.
3. American Academy of Pediatrics. Backpack safety.
4. J Bone Joint Surg Am. 1997 Mar;79(3):364-8.
6. J Paediatr Child Health. 2000 Jun;36(3):208-12.
7. Skeletal Radiol. 2005 Feb;34(2):63-73.
Dr. Pearce is a pediatrician in Frankfort, Ill.
CMS: Bundled payment initiative shows savings
The majority of clinical episode groups participating in the Bundled Payments for Care Improvement initiative are generating Medicare savings, according to a CMS analysis.
The study showed that orthopedic surgery under Model 2 generated savings of $864 per episode, while improving postdischarge outcomes. Cardiovascular surgery episodes under Model 2 did not show any savings, but quality of care was preserved, according to the analysis. In total, 11 out of the 15 clinical episode groups analyzed showed potential savings to Medicare.
“While there is more work to be done, CMS continues to move forward to achieving the administration’s goal to have 50% of traditional Medicare payments tied to alternative payment models by 2018,” Patrick Conway, MD, CMS acting principal deputy administrator and chief medical officer wrote in a blog post. “Bundled payments continue to be an integral part of transforming our health care system by creating innovative care delivery models that support hospitals, doctors, and other providers in their efforts to deliver better care for patients while spending taxpayer dollars more wisely.”
The Bundled Payments for Care Improvement (BPCI) initiative was designed to test whether linking payments for all providers involved in an episode of care reduces Medicare costs, while maintaining or improving quality of care. To participate, BPCI awardees – which include hospitals, physician groups, post-acute care (PAC) providers, and other entities – enter into agreements with the CMS that hold them accountable for total Medicare episode payments. Such agreements specify choices among four payment models, 48 clinical episodes, three episode lengths, and waiver options.
From October 2013 through September 2014, the first full year of the initiative, 94 awardees, including hospitals, physician groups, and post–acute care providers, entered into agreements with the CMS to be held accountable for total Medicare episode payments. Under the initiative, nearly 60,000 episodes of care were initiated, according to the CMS. BPCI-participating providers tended to be larger, operate in more affluent urban areas, and have higher episode costs than providers who did not participate.
An analysis of Model 2 showed that:
• Average standardized Medicare payments for hospitalization and 90 days post discharge were estimated to have declined by $864 per orthopedic surgery episode at BPCI-participating hospitals, compared with nonparticipating hospitals.
• For cardiovascular surgery, there was no statistically significant difference in Medicare payments for the index hospitalization and the 90-day post discharge period between the BPCI and comparison episodes.
• For cardiovascular surgery, there were no statistically significant changes in hospital readmissions within the 30 or 90 days post discharge, or any of the assessment-based quality measures between the BPCI and comparison populations.
For most clinical episode groups in Model 3, there were no statistically significant differences between BPCI and comparison episodes from the baseline to the intervention period in total Medicare standardized allowed payments during the qualifying inpatient stay and 90-day postdischarge period or in quality measures, the analysis found.
Over the next year, the CMS plans to have significantly more data available on the initiative, enabling the agency to better estimate effects on costs and quality, according to Dr. Conway. Future evaluation reports are expected to have greater ability to detect changes in payment and quality because of larger sample sizes and the recent growth in participation in the initiative.
On Twitter @legal_med
The majority of clinical episode groups participating in the Bundled Payments for Care Improvement initiative are generating Medicare savings, according to a CMS analysis.
The study showed that orthopedic surgery under Model 2 generated savings of $864 per episode, while improving postdischarge outcomes. Cardiovascular surgery episodes under Model 2 did not show any savings, but quality of care was preserved, according to the analysis. In total, 11 out of the 15 clinical episode groups analyzed showed potential savings to Medicare.
“While there is more work to be done, CMS continues to move forward to achieving the administration’s goal to have 50% of traditional Medicare payments tied to alternative payment models by 2018,” Patrick Conway, MD, CMS acting principal deputy administrator and chief medical officer wrote in a blog post. “Bundled payments continue to be an integral part of transforming our health care system by creating innovative care delivery models that support hospitals, doctors, and other providers in their efforts to deliver better care for patients while spending taxpayer dollars more wisely.”
The Bundled Payments for Care Improvement (BPCI) initiative was designed to test whether linking payments for all providers involved in an episode of care reduces Medicare costs, while maintaining or improving quality of care. To participate, BPCI awardees – which include hospitals, physician groups, post-acute care (PAC) providers, and other entities – enter into agreements with the CMS that hold them accountable for total Medicare episode payments. Such agreements specify choices among four payment models, 48 clinical episodes, three episode lengths, and waiver options.
From October 2013 through September 2014, the first full year of the initiative, 94 awardees, including hospitals, physician groups, and post–acute care providers, entered into agreements with the CMS to be held accountable for total Medicare episode payments. Under the initiative, nearly 60,000 episodes of care were initiated, according to the CMS. BPCI-participating providers tended to be larger, operate in more affluent urban areas, and have higher episode costs than providers who did not participate.
An analysis of Model 2 showed that:
• Average standardized Medicare payments for hospitalization and 90 days post discharge were estimated to have declined by $864 per orthopedic surgery episode at BPCI-participating hospitals, compared with nonparticipating hospitals.
• For cardiovascular surgery, there was no statistically significant difference in Medicare payments for the index hospitalization and the 90-day post discharge period between the BPCI and comparison episodes.
• For cardiovascular surgery, there were no statistically significant changes in hospital readmissions within the 30 or 90 days post discharge, or any of the assessment-based quality measures between the BPCI and comparison populations.
For most clinical episode groups in Model 3, there were no statistically significant differences between BPCI and comparison episodes from the baseline to the intervention period in total Medicare standardized allowed payments during the qualifying inpatient stay and 90-day postdischarge period or in quality measures, the analysis found.
Over the next year, the CMS plans to have significantly more data available on the initiative, enabling the agency to better estimate effects on costs and quality, according to Dr. Conway. Future evaluation reports are expected to have greater ability to detect changes in payment and quality because of larger sample sizes and the recent growth in participation in the initiative.
On Twitter @legal_med
The majority of clinical episode groups participating in the Bundled Payments for Care Improvement initiative are generating Medicare savings, according to a CMS analysis.
The study showed that orthopedic surgery under Model 2 generated savings of $864 per episode, while improving postdischarge outcomes. Cardiovascular surgery episodes under Model 2 did not show any savings, but quality of care was preserved, according to the analysis. In total, 11 out of the 15 clinical episode groups analyzed showed potential savings to Medicare.
“While there is more work to be done, CMS continues to move forward to achieving the administration’s goal to have 50% of traditional Medicare payments tied to alternative payment models by 2018,” Patrick Conway, MD, CMS acting principal deputy administrator and chief medical officer wrote in a blog post. “Bundled payments continue to be an integral part of transforming our health care system by creating innovative care delivery models that support hospitals, doctors, and other providers in their efforts to deliver better care for patients while spending taxpayer dollars more wisely.”
The Bundled Payments for Care Improvement (BPCI) initiative was designed to test whether linking payments for all providers involved in an episode of care reduces Medicare costs, while maintaining or improving quality of care. To participate, BPCI awardees – which include hospitals, physician groups, post-acute care (PAC) providers, and other entities – enter into agreements with the CMS that hold them accountable for total Medicare episode payments. Such agreements specify choices among four payment models, 48 clinical episodes, three episode lengths, and waiver options.
From October 2013 through September 2014, the first full year of the initiative, 94 awardees, including hospitals, physician groups, and post–acute care providers, entered into agreements with the CMS to be held accountable for total Medicare episode payments. Under the initiative, nearly 60,000 episodes of care were initiated, according to the CMS. BPCI-participating providers tended to be larger, operate in more affluent urban areas, and have higher episode costs than providers who did not participate.
An analysis of Model 2 showed that:
• Average standardized Medicare payments for hospitalization and 90 days post discharge were estimated to have declined by $864 per orthopedic surgery episode at BPCI-participating hospitals, compared with nonparticipating hospitals.
• For cardiovascular surgery, there was no statistically significant difference in Medicare payments for the index hospitalization and the 90-day post discharge period between the BPCI and comparison episodes.
• For cardiovascular surgery, there were no statistically significant changes in hospital readmissions within the 30 or 90 days post discharge, or any of the assessment-based quality measures between the BPCI and comparison populations.
For most clinical episode groups in Model 3, there were no statistically significant differences between BPCI and comparison episodes from the baseline to the intervention period in total Medicare standardized allowed payments during the qualifying inpatient stay and 90-day postdischarge period or in quality measures, the analysis found.
Over the next year, the CMS plans to have significantly more data available on the initiative, enabling the agency to better estimate effects on costs and quality, according to Dr. Conway. Future evaluation reports are expected to have greater ability to detect changes in payment and quality because of larger sample sizes and the recent growth in participation in the initiative.
On Twitter @legal_med
DEA licenses: Is it time for a graduated approach?
I sometimes think about giving up my DEA certificate. I can’t be the only one.
It’s not strictly about the money. $731 every 3 years is small change, compared with my rent, staff salaries, and malpractice insurance, although the savings would be nice.
Part of it is the desire to unfetter myself from prescribing controlled substances. I wouldn’t have to worry about drug seekers hitting me up, or dealing with the paperwork and pharmacy calls, or doing background checks on the state monitoring site.
But, realistically, I can’t do that. Even though I try to limit my narcotic scripts, the DEA number covers many other things, such as Lyrica, Vimpat, and Klonopin for epilepsy patients; Provigil for MS fatigue; and Valium to help someone get through an MRI scan.
There are, of course, the occasional narcotics. I don’t have many patients on chronic narcotics any more, but I’m sure all of us have a few migraine patients who keep an emergency supply of some narcotic (say, 5-10 pills) on hand to be used in lieu of an ER trip. They may only get it filled once a year, which doesn’t seem unreasonable.
I think it would be unfair to make patients, many of whom I’ve seen for many years, have to find a new neurologist over such things.
But what if there were a graduated DEA license? Say, one that limited me to schedules III-V or even just level IV and V substances? That would probably make life easier. The latter would still allow tramadol and Stadol-NS for breakthrough migraines, while adding level III would still allow Tylenol with codeine No. 3. Either way, it would take oxycodone, hydrocodone, morphine, amphetamines, and other drugs of greater abuse potential out of my hands. A few less things to worry about.
There are pros and cons of this. From one view, it would limit the number of docs prescribing higher level substances, making them easier to track and control. On the other hand, patients who need them, many of whom are legitimately in pain, would be forced to change to a dwindling number of narcotic prescribers. Many of these doctors would likely start to work on a cash-only basis knowing the demand they’d be in. Who knows where that would lead? Like so many things in medicine, there are always going to be unintended consequences.
For the time being I have no plans to drop my DEA license, but it would be nice to have options besides all or nothing.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I sometimes think about giving up my DEA certificate. I can’t be the only one.
It’s not strictly about the money. $731 every 3 years is small change, compared with my rent, staff salaries, and malpractice insurance, although the savings would be nice.
Part of it is the desire to unfetter myself from prescribing controlled substances. I wouldn’t have to worry about drug seekers hitting me up, or dealing with the paperwork and pharmacy calls, or doing background checks on the state monitoring site.
But, realistically, I can’t do that. Even though I try to limit my narcotic scripts, the DEA number covers many other things, such as Lyrica, Vimpat, and Klonopin for epilepsy patients; Provigil for MS fatigue; and Valium to help someone get through an MRI scan.
There are, of course, the occasional narcotics. I don’t have many patients on chronic narcotics any more, but I’m sure all of us have a few migraine patients who keep an emergency supply of some narcotic (say, 5-10 pills) on hand to be used in lieu of an ER trip. They may only get it filled once a year, which doesn’t seem unreasonable.
I think it would be unfair to make patients, many of whom I’ve seen for many years, have to find a new neurologist over such things.
But what if there were a graduated DEA license? Say, one that limited me to schedules III-V or even just level IV and V substances? That would probably make life easier. The latter would still allow tramadol and Stadol-NS for breakthrough migraines, while adding level III would still allow Tylenol with codeine No. 3. Either way, it would take oxycodone, hydrocodone, morphine, amphetamines, and other drugs of greater abuse potential out of my hands. A few less things to worry about.
There are pros and cons of this. From one view, it would limit the number of docs prescribing higher level substances, making them easier to track and control. On the other hand, patients who need them, many of whom are legitimately in pain, would be forced to change to a dwindling number of narcotic prescribers. Many of these doctors would likely start to work on a cash-only basis knowing the demand they’d be in. Who knows where that would lead? Like so many things in medicine, there are always going to be unintended consequences.
For the time being I have no plans to drop my DEA license, but it would be nice to have options besides all or nothing.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I sometimes think about giving up my DEA certificate. I can’t be the only one.
It’s not strictly about the money. $731 every 3 years is small change, compared with my rent, staff salaries, and malpractice insurance, although the savings would be nice.
Part of it is the desire to unfetter myself from prescribing controlled substances. I wouldn’t have to worry about drug seekers hitting me up, or dealing with the paperwork and pharmacy calls, or doing background checks on the state monitoring site.
But, realistically, I can’t do that. Even though I try to limit my narcotic scripts, the DEA number covers many other things, such as Lyrica, Vimpat, and Klonopin for epilepsy patients; Provigil for MS fatigue; and Valium to help someone get through an MRI scan.
There are, of course, the occasional narcotics. I don’t have many patients on chronic narcotics any more, but I’m sure all of us have a few migraine patients who keep an emergency supply of some narcotic (say, 5-10 pills) on hand to be used in lieu of an ER trip. They may only get it filled once a year, which doesn’t seem unreasonable.
I think it would be unfair to make patients, many of whom I’ve seen for many years, have to find a new neurologist over such things.
But what if there were a graduated DEA license? Say, one that limited me to schedules III-V or even just level IV and V substances? That would probably make life easier. The latter would still allow tramadol and Stadol-NS for breakthrough migraines, while adding level III would still allow Tylenol with codeine No. 3. Either way, it would take oxycodone, hydrocodone, morphine, amphetamines, and other drugs of greater abuse potential out of my hands. A few less things to worry about.
There are pros and cons of this. From one view, it would limit the number of docs prescribing higher level substances, making them easier to track and control. On the other hand, patients who need them, many of whom are legitimately in pain, would be forced to change to a dwindling number of narcotic prescribers. Many of these doctors would likely start to work on a cash-only basis knowing the demand they’d be in. Who knows where that would lead? Like so many things in medicine, there are always going to be unintended consequences.
For the time being I have no plans to drop my DEA license, but it would be nice to have options besides all or nothing.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.