User login
Atopic Dermatitis Treatments Moving Forward: Report From the AAD Meeting
Although psoriasis was once at the forefront of therapeutic advancements in dermatology, atopic dermatitis (AD) is now taking center stage with several new treatments in the pipeline. Dr. Emma Guttman-Yassky provides an overview of the future of AD treatment, which includes new topical and systemic agents that currently are moving forward in advanced clinical trials or are close to registration. She also discusses strategies for improving disease management in AD patients, noting that prevention and education of both patients and their caregivers are key to effective treatment.
Although psoriasis was once at the forefront of therapeutic advancements in dermatology, atopic dermatitis (AD) is now taking center stage with several new treatments in the pipeline. Dr. Emma Guttman-Yassky provides an overview of the future of AD treatment, which includes new topical and systemic agents that currently are moving forward in advanced clinical trials or are close to registration. She also discusses strategies for improving disease management in AD patients, noting that prevention and education of both patients and their caregivers are key to effective treatment.
Although psoriasis was once at the forefront of therapeutic advancements in dermatology, atopic dermatitis (AD) is now taking center stage with several new treatments in the pipeline. Dr. Emma Guttman-Yassky provides an overview of the future of AD treatment, which includes new topical and systemic agents that currently are moving forward in advanced clinical trials or are close to registration. She also discusses strategies for improving disease management in AD patients, noting that prevention and education of both patients and their caregivers are key to effective treatment.
Tool May Help Predict Persistent Postconcussion Symptoms
A clinical risk score may help identify which children and adolescents with recent head injury are at risk for persistent postconcussion symptoms, according to an investigation published March 8 in JAMA.
Approximately one-third of pediatric patients with concussion have ongoing somatic, cognitive, psychological, or behavioral symptoms at 28 days. At present, neurologists have no tools to help predict which patients will be affected in this way. The 5P (Preventing Postconcussive Problems in Pediatrics) study was performed to develop and validate a clinical risk score for this purpose, said Roger Zemek, MD, a scientist at Children’s Hospital of Eastern Ontario Research Institute in Ottawa, Canada, and his associates.
This prospective cohort study involved patients between ages 5 and 17 (median age, 12) who presented to one of nine Canadian pediatric emergency departments within 48 hours of sustaining a concussion.
In the derivation cohort, 510 of 1,701 participants (30%) met the criteria for persistent postconcussion symptoms. The investigators assessed 47 possible predictive variables for their usefulness in predicting persistent postconcussion symptoms in this cohort. The variables were collected from demographic data, patient history, injury characteristics, physical examination, results on the Acute Concussion Evaluation Inventory and the Postconcussion Symptom Inventory, and patient and parent responses to weekly follow-up surveys during the month after the injury.
The investigators devised a clinical risk score using the following nine predictors that they found to be most accurate: age, gender, presence or absence of prior concussion, migraine history, presence or absence of current headache, sensitivity to noise, fatigue, slow responses to questions, and an abnormal tandem stance. They then selected three cutoff points to stratify the risk of persistent postconcussion symptoms: 0–3 points indicated low risk, 4–8 points indicated intermediate risk, and 9 or more points indicated high risk. Treating physicians also were asked to predict the likelihood of persistent postconcussion symptoms.
In the validation cohort, 291 of 883 participants (33%) met the criteria for persistent postconcussion symptoms. For low-risk patients, the sensitivity of the clinical risk score was 94%, the specificity was 18%, the negative predictive value was 85%, and the positive predictive value was 36%. For high-risk patients, the sensitivity of the clinical risk score was 20%, the specificity was 94%, the negative predictive value was 70%, and the positive predictive value was 60%.
In both sets of patients, the clinical risk score was significantly better than physician judgment in predicting persistent postconcussion symptoms. The clinical risk score has modest accuracy, however, at distinguishing between who will and who will not have persistent symptoms. This tool could be refined further, perhaps, by adding information regarding biomarkers, genetic susceptibility, or advanced neuroimaging, said Dr. Zemek and his associates.
—Mary Ann Moon
Suggested Reading
Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014-1025.
A clinical risk score may help identify which children and adolescents with recent head injury are at risk for persistent postconcussion symptoms, according to an investigation published March 8 in JAMA.
Approximately one-third of pediatric patients with concussion have ongoing somatic, cognitive, psychological, or behavioral symptoms at 28 days. At present, neurologists have no tools to help predict which patients will be affected in this way. The 5P (Preventing Postconcussive Problems in Pediatrics) study was performed to develop and validate a clinical risk score for this purpose, said Roger Zemek, MD, a scientist at Children’s Hospital of Eastern Ontario Research Institute in Ottawa, Canada, and his associates.
This prospective cohort study involved patients between ages 5 and 17 (median age, 12) who presented to one of nine Canadian pediatric emergency departments within 48 hours of sustaining a concussion.
In the derivation cohort, 510 of 1,701 participants (30%) met the criteria for persistent postconcussion symptoms. The investigators assessed 47 possible predictive variables for their usefulness in predicting persistent postconcussion symptoms in this cohort. The variables were collected from demographic data, patient history, injury characteristics, physical examination, results on the Acute Concussion Evaluation Inventory and the Postconcussion Symptom Inventory, and patient and parent responses to weekly follow-up surveys during the month after the injury.
The investigators devised a clinical risk score using the following nine predictors that they found to be most accurate: age, gender, presence or absence of prior concussion, migraine history, presence or absence of current headache, sensitivity to noise, fatigue, slow responses to questions, and an abnormal tandem stance. They then selected three cutoff points to stratify the risk of persistent postconcussion symptoms: 0–3 points indicated low risk, 4–8 points indicated intermediate risk, and 9 or more points indicated high risk. Treating physicians also were asked to predict the likelihood of persistent postconcussion symptoms.
In the validation cohort, 291 of 883 participants (33%) met the criteria for persistent postconcussion symptoms. For low-risk patients, the sensitivity of the clinical risk score was 94%, the specificity was 18%, the negative predictive value was 85%, and the positive predictive value was 36%. For high-risk patients, the sensitivity of the clinical risk score was 20%, the specificity was 94%, the negative predictive value was 70%, and the positive predictive value was 60%.
In both sets of patients, the clinical risk score was significantly better than physician judgment in predicting persistent postconcussion symptoms. The clinical risk score has modest accuracy, however, at distinguishing between who will and who will not have persistent symptoms. This tool could be refined further, perhaps, by adding information regarding biomarkers, genetic susceptibility, or advanced neuroimaging, said Dr. Zemek and his associates.
—Mary Ann Moon
A clinical risk score may help identify which children and adolescents with recent head injury are at risk for persistent postconcussion symptoms, according to an investigation published March 8 in JAMA.
Approximately one-third of pediatric patients with concussion have ongoing somatic, cognitive, psychological, or behavioral symptoms at 28 days. At present, neurologists have no tools to help predict which patients will be affected in this way. The 5P (Preventing Postconcussive Problems in Pediatrics) study was performed to develop and validate a clinical risk score for this purpose, said Roger Zemek, MD, a scientist at Children’s Hospital of Eastern Ontario Research Institute in Ottawa, Canada, and his associates.
This prospective cohort study involved patients between ages 5 and 17 (median age, 12) who presented to one of nine Canadian pediatric emergency departments within 48 hours of sustaining a concussion.
In the derivation cohort, 510 of 1,701 participants (30%) met the criteria for persistent postconcussion symptoms. The investigators assessed 47 possible predictive variables for their usefulness in predicting persistent postconcussion symptoms in this cohort. The variables were collected from demographic data, patient history, injury characteristics, physical examination, results on the Acute Concussion Evaluation Inventory and the Postconcussion Symptom Inventory, and patient and parent responses to weekly follow-up surveys during the month after the injury.
The investigators devised a clinical risk score using the following nine predictors that they found to be most accurate: age, gender, presence or absence of prior concussion, migraine history, presence or absence of current headache, sensitivity to noise, fatigue, slow responses to questions, and an abnormal tandem stance. They then selected three cutoff points to stratify the risk of persistent postconcussion symptoms: 0–3 points indicated low risk, 4–8 points indicated intermediate risk, and 9 or more points indicated high risk. Treating physicians also were asked to predict the likelihood of persistent postconcussion symptoms.
In the validation cohort, 291 of 883 participants (33%) met the criteria for persistent postconcussion symptoms. For low-risk patients, the sensitivity of the clinical risk score was 94%, the specificity was 18%, the negative predictive value was 85%, and the positive predictive value was 36%. For high-risk patients, the sensitivity of the clinical risk score was 20%, the specificity was 94%, the negative predictive value was 70%, and the positive predictive value was 60%.
In both sets of patients, the clinical risk score was significantly better than physician judgment in predicting persistent postconcussion symptoms. The clinical risk score has modest accuracy, however, at distinguishing between who will and who will not have persistent symptoms. This tool could be refined further, perhaps, by adding information regarding biomarkers, genetic susceptibility, or advanced neuroimaging, said Dr. Zemek and his associates.
—Mary Ann Moon
Suggested Reading
Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014-1025.
Suggested Reading
Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014-1025.
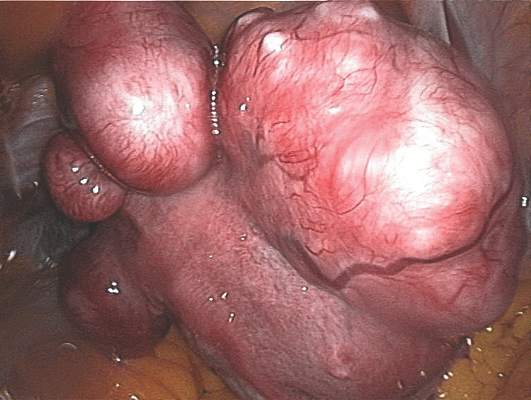
Bone sarcomas are not just for kids
The treatment of bone sarcomas in adults is guided as much by experience as it is by medical evidence, say sarcoma experts who should know.
“[L]arge prospective clinical trials in adults with bone sarcomas are lacking. Although translation of findings in pediatric studies to adults is possible, it is not clear if findings from pediatric studies truly apply to adults,” Dr. Michael J. Wagner and his colleagues from the University of Texas MD Anderson Cancer Center in Houston said.
In a review article in the Journal of Oncology Practice, the investigators outline how they have melded lessons learned from pediatric clinical trials with clinical experience treating adults with bone sarcomas.
Adult osteosarcomas
Although the peak incidence of osteosarcoma occurs in adolescents and young adults, some studies of various chemotherapy regimens have included middle-aged adults and even some patients in their 90s, although many have excluded patients older than 30, the authors noted.
In adults, and in children and adolescents and young adults, chemotherapy and definitive surgical resection are the mainstays of treatment, with the exception of osteosarcomas of the jaw, which are generally treated with resection alone. For the past three decades, adults with high-grade osteosarcomas have been treated with chemotherapy containing doxorubicin, cisplatin, high-dose methotrexate, and ifosfamide.
“However, important differences to consider in the treatment of older patients include, but are not limited to, the increased incidence of histologic variants of osteosarcoma (including secondary osteosarcomas) and medical comorbidities that may limit tolerance of older adults to dose-intense chemotherapy,” wrote Dr. Wagner and his colleagues (J Oncol Pract. 2016 Mar. doi: 10.1200/JOP.2015.009944).
High-grade localized osteosarcoma is treated with neoadjuvant chemotherapy, followed by limb-sparing surgery and adjuvant chemotherapy.
A poor response to neoadjuvant chemotherapy, defined as tumor necrosis of less than 90% at resection, is a marker for poor prognosis.
The authors previously reported that for patients with a poor response following a regimen of doxorubicin intravenous infusion at 90 mg/m2 over 96 hours plus cisplatin infused intra-arterially at 120-160 mg/m2 over 2 to 24 hours, the addition of high-dose methotrexate and ifosfamide resulted in significant improvement in continuous relapse-free survival.
At MD Anderson, adults with osteosarcoma receive preoperative chemotherapy with doxorubicin and cisplatin for three to four cycles and then undergo surgical resection. Those who have a good response go on to receive adjuvant chemotherapy with doxorubicin 75 mg/m2 and ifosfamide 10g/m2 for four cycles. Patients who have a poor response to neoadjuvant chemotherapy receive alternating courses of ifosfamide 14 g/m2, high-dose methotrexate 10 to 12 g/m2, and doxorubicin 75 mg/m2 and ifosfamide 10 g/m2 for up to 12 cycles or until intolerable adverse events.
Patients with metastatic relapsed/refractory osteosarcoma have 5-year overall survival rates ranging from 15% to 20%, the authors noted, adding that chemotherapy has “limited efficacy” in this setting.
Targeted agents, including the tyrosine kinase inhibitor sorafenib (Nexavar) and the mammalian target of rapamycin (mTOR) inhibitor everolimus (Afinitor) have been evaluated in phase II trials.
Ewing sarcoma
Evidence from clinical trials of chemotherapy regimens in Ewing sarcoma show that patients 18 and older tend to have less favorable outcomes than younger patients when treated with dose-dense regimens, the authors noted.
Their practice is to treat adults with Ewing sarcoma with upfront vincristine 2 mg on day 1, doxorubicin 75 to 90 mg/m2 in a continuous 72-hour infusion, and ifosfamide 2.5 g/m2 given over 3 hours daily for four doses, followed by surgery, and adjuvant chemotherapy with an ifosfamide-based regimen.
Giant cell tumors of bone
These rare osteolytic tumors are treated with surgery as the primary therapy if they are resectable. Patients with metastases (which paradoxically, are usually histologically benign) as well as those who have tumors in areas where surgery may cause unacceptable morbidities may be treated with serial embolization, denosumab (Xgeva), interferon, or pegylated interferon.
Chondrosarcoma
The so-called “conventional” sub-type of chondrosarcomas are not generally responsive to cytotoxic chemotherapy and best managed with surgery alone, the authors say. However, patients with mesenchymal chondrosarcoma are treated similarly to patients with Ewing sarcoma, and those with the dedifferentiated subtype are treated with an osteosarcoma regimens.
The authors noted that point mutations in IDH1 and IDH2 have recently been discovered in chondrosarcomas, making them potential targets for an experimental IDH-1 inhibitor.
Dr. Wagner and coauthor Dr. J. Andrew Livingston reported no relevant disclosures. Coauthors Dr. Shreyaskumar R. Patel and Dr. Robert S. Benjamin reported consulting, advisory roles, research funding, or ownership interests in various pharmaceutical companies.
The treatment of bone sarcomas in adults is guided as much by experience as it is by medical evidence, say sarcoma experts who should know.
“[L]arge prospective clinical trials in adults with bone sarcomas are lacking. Although translation of findings in pediatric studies to adults is possible, it is not clear if findings from pediatric studies truly apply to adults,” Dr. Michael J. Wagner and his colleagues from the University of Texas MD Anderson Cancer Center in Houston said.
In a review article in the Journal of Oncology Practice, the investigators outline how they have melded lessons learned from pediatric clinical trials with clinical experience treating adults with bone sarcomas.
Adult osteosarcomas
Although the peak incidence of osteosarcoma occurs in adolescents and young adults, some studies of various chemotherapy regimens have included middle-aged adults and even some patients in their 90s, although many have excluded patients older than 30, the authors noted.
In adults, and in children and adolescents and young adults, chemotherapy and definitive surgical resection are the mainstays of treatment, with the exception of osteosarcomas of the jaw, which are generally treated with resection alone. For the past three decades, adults with high-grade osteosarcomas have been treated with chemotherapy containing doxorubicin, cisplatin, high-dose methotrexate, and ifosfamide.
“However, important differences to consider in the treatment of older patients include, but are not limited to, the increased incidence of histologic variants of osteosarcoma (including secondary osteosarcomas) and medical comorbidities that may limit tolerance of older adults to dose-intense chemotherapy,” wrote Dr. Wagner and his colleagues (J Oncol Pract. 2016 Mar. doi: 10.1200/JOP.2015.009944).
High-grade localized osteosarcoma is treated with neoadjuvant chemotherapy, followed by limb-sparing surgery and adjuvant chemotherapy.
A poor response to neoadjuvant chemotherapy, defined as tumor necrosis of less than 90% at resection, is a marker for poor prognosis.
The authors previously reported that for patients with a poor response following a regimen of doxorubicin intravenous infusion at 90 mg/m2 over 96 hours plus cisplatin infused intra-arterially at 120-160 mg/m2 over 2 to 24 hours, the addition of high-dose methotrexate and ifosfamide resulted in significant improvement in continuous relapse-free survival.
At MD Anderson, adults with osteosarcoma receive preoperative chemotherapy with doxorubicin and cisplatin for three to four cycles and then undergo surgical resection. Those who have a good response go on to receive adjuvant chemotherapy with doxorubicin 75 mg/m2 and ifosfamide 10g/m2 for four cycles. Patients who have a poor response to neoadjuvant chemotherapy receive alternating courses of ifosfamide 14 g/m2, high-dose methotrexate 10 to 12 g/m2, and doxorubicin 75 mg/m2 and ifosfamide 10 g/m2 for up to 12 cycles or until intolerable adverse events.
Patients with metastatic relapsed/refractory osteosarcoma have 5-year overall survival rates ranging from 15% to 20%, the authors noted, adding that chemotherapy has “limited efficacy” in this setting.
Targeted agents, including the tyrosine kinase inhibitor sorafenib (Nexavar) and the mammalian target of rapamycin (mTOR) inhibitor everolimus (Afinitor) have been evaluated in phase II trials.
Ewing sarcoma
Evidence from clinical trials of chemotherapy regimens in Ewing sarcoma show that patients 18 and older tend to have less favorable outcomes than younger patients when treated with dose-dense regimens, the authors noted.
Their practice is to treat adults with Ewing sarcoma with upfront vincristine 2 mg on day 1, doxorubicin 75 to 90 mg/m2 in a continuous 72-hour infusion, and ifosfamide 2.5 g/m2 given over 3 hours daily for four doses, followed by surgery, and adjuvant chemotherapy with an ifosfamide-based regimen.
Giant cell tumors of bone
These rare osteolytic tumors are treated with surgery as the primary therapy if they are resectable. Patients with metastases (which paradoxically, are usually histologically benign) as well as those who have tumors in areas where surgery may cause unacceptable morbidities may be treated with serial embolization, denosumab (Xgeva), interferon, or pegylated interferon.
Chondrosarcoma
The so-called “conventional” sub-type of chondrosarcomas are not generally responsive to cytotoxic chemotherapy and best managed with surgery alone, the authors say. However, patients with mesenchymal chondrosarcoma are treated similarly to patients with Ewing sarcoma, and those with the dedifferentiated subtype are treated with an osteosarcoma regimens.
The authors noted that point mutations in IDH1 and IDH2 have recently been discovered in chondrosarcomas, making them potential targets for an experimental IDH-1 inhibitor.
Dr. Wagner and coauthor Dr. J. Andrew Livingston reported no relevant disclosures. Coauthors Dr. Shreyaskumar R. Patel and Dr. Robert S. Benjamin reported consulting, advisory roles, research funding, or ownership interests in various pharmaceutical companies.
The treatment of bone sarcomas in adults is guided as much by experience as it is by medical evidence, say sarcoma experts who should know.
“[L]arge prospective clinical trials in adults with bone sarcomas are lacking. Although translation of findings in pediatric studies to adults is possible, it is not clear if findings from pediatric studies truly apply to adults,” Dr. Michael J. Wagner and his colleagues from the University of Texas MD Anderson Cancer Center in Houston said.
In a review article in the Journal of Oncology Practice, the investigators outline how they have melded lessons learned from pediatric clinical trials with clinical experience treating adults with bone sarcomas.
Adult osteosarcomas
Although the peak incidence of osteosarcoma occurs in adolescents and young adults, some studies of various chemotherapy regimens have included middle-aged adults and even some patients in their 90s, although many have excluded patients older than 30, the authors noted.
In adults, and in children and adolescents and young adults, chemotherapy and definitive surgical resection are the mainstays of treatment, with the exception of osteosarcomas of the jaw, which are generally treated with resection alone. For the past three decades, adults with high-grade osteosarcomas have been treated with chemotherapy containing doxorubicin, cisplatin, high-dose methotrexate, and ifosfamide.
“However, important differences to consider in the treatment of older patients include, but are not limited to, the increased incidence of histologic variants of osteosarcoma (including secondary osteosarcomas) and medical comorbidities that may limit tolerance of older adults to dose-intense chemotherapy,” wrote Dr. Wagner and his colleagues (J Oncol Pract. 2016 Mar. doi: 10.1200/JOP.2015.009944).
High-grade localized osteosarcoma is treated with neoadjuvant chemotherapy, followed by limb-sparing surgery and adjuvant chemotherapy.
A poor response to neoadjuvant chemotherapy, defined as tumor necrosis of less than 90% at resection, is a marker for poor prognosis.
The authors previously reported that for patients with a poor response following a regimen of doxorubicin intravenous infusion at 90 mg/m2 over 96 hours plus cisplatin infused intra-arterially at 120-160 mg/m2 over 2 to 24 hours, the addition of high-dose methotrexate and ifosfamide resulted in significant improvement in continuous relapse-free survival.
At MD Anderson, adults with osteosarcoma receive preoperative chemotherapy with doxorubicin and cisplatin for three to four cycles and then undergo surgical resection. Those who have a good response go on to receive adjuvant chemotherapy with doxorubicin 75 mg/m2 and ifosfamide 10g/m2 for four cycles. Patients who have a poor response to neoadjuvant chemotherapy receive alternating courses of ifosfamide 14 g/m2, high-dose methotrexate 10 to 12 g/m2, and doxorubicin 75 mg/m2 and ifosfamide 10 g/m2 for up to 12 cycles or until intolerable adverse events.
Patients with metastatic relapsed/refractory osteosarcoma have 5-year overall survival rates ranging from 15% to 20%, the authors noted, adding that chemotherapy has “limited efficacy” in this setting.
Targeted agents, including the tyrosine kinase inhibitor sorafenib (Nexavar) and the mammalian target of rapamycin (mTOR) inhibitor everolimus (Afinitor) have been evaluated in phase II trials.
Ewing sarcoma
Evidence from clinical trials of chemotherapy regimens in Ewing sarcoma show that patients 18 and older tend to have less favorable outcomes than younger patients when treated with dose-dense regimens, the authors noted.
Their practice is to treat adults with Ewing sarcoma with upfront vincristine 2 mg on day 1, doxorubicin 75 to 90 mg/m2 in a continuous 72-hour infusion, and ifosfamide 2.5 g/m2 given over 3 hours daily for four doses, followed by surgery, and adjuvant chemotherapy with an ifosfamide-based regimen.
Giant cell tumors of bone
These rare osteolytic tumors are treated with surgery as the primary therapy if they are resectable. Patients with metastases (which paradoxically, are usually histologically benign) as well as those who have tumors in areas where surgery may cause unacceptable morbidities may be treated with serial embolization, denosumab (Xgeva), interferon, or pegylated interferon.
Chondrosarcoma
The so-called “conventional” sub-type of chondrosarcomas are not generally responsive to cytotoxic chemotherapy and best managed with surgery alone, the authors say. However, patients with mesenchymal chondrosarcoma are treated similarly to patients with Ewing sarcoma, and those with the dedifferentiated subtype are treated with an osteosarcoma regimens.
The authors noted that point mutations in IDH1 and IDH2 have recently been discovered in chondrosarcomas, making them potential targets for an experimental IDH-1 inhibitor.
Dr. Wagner and coauthor Dr. J. Andrew Livingston reported no relevant disclosures. Coauthors Dr. Shreyaskumar R. Patel and Dr. Robert S. Benjamin reported consulting, advisory roles, research funding, or ownership interests in various pharmaceutical companies.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
Key clinical point: Sarcomas of bone have their peak incidence in children and adolescents, but are also seen in adults.
Major finding: Findings from clinical trials in pediatric bone sarcomas may not be applicable to treatment of adults with the same malignancies.
Data source: Review of the medical literature and of clinical experience at the authors’ center.
Disclosures: Dr. Wagner and coauthor Dr. J. Andrew Livingston reported no relevant disclosures. Coauthors Dr. Shreyaskumar R. Patel and Dr. Robert S. Benjamin reported consulting, advisory roles, research funding, or ownership interests in various pharmaceutical companies.
High Coffee Consumption May Decrease Risk for MS
High coffee consumption decreases the odds of developing multiple sclerosis (MS), according to two case–control studies published online ahead of print March 3 in the Journal of Neurology, Neurosurgery & Psychiatry. Anna K. Hedström, MD, PhD, a postdoctoral researcher at the Karolinska Institute, Stockholm, and her associates conducted the studies.
The investigators analyzed coffee consumption among 1,620 adults with MS and 2,788 healthy controls in the Swedish Epidemiological Investigation of Multiple Sclerosis (EIMS). They also examined coffee consumption in 1,159 adults with MS and 1,172 healthy controls in the Kaiser Permanente Medical Care Plan, Northern California Region (KPNC).
In EIMS, the adjusted odds ratio (OR) for developing MS was 0.70 among participants who drank more than six cups of coffee (ie, greater than 900 mL) daily at the index year, which was defined as the year of the initial appearance of symptoms indicative of MS. The corresponding ORs for those who reported high coffee consumption at five or 10 years before the study were 0.72 and 0.71, respectively, but these results were not statistically significant.
In KPNC, those who consumed four or more cups of coffee (ie, more than 948 mL) daily were significantly less likely to develop MS than were those who never drank coffee (OR, 0.69). In addition, people who drank four or more cups of coffee daily at least five years prior to the index year had significantly reduced odds of MS (OR, 0.64).
A meta-analysis of the combined results of the two studies indicated a significant 29% reduction in the likelihood of developing MS among the people with the greatest coffee consumption (ie, greater than 900 mL daily in EIMS and greater than 948 mL in KPNC). The investigators adjusted all the analyses for many demographic and environmental risk factors for MS, including age, gender, residential area, ancestry, smoking habits, exposure to passive smoking, sun exposure habits, and BMI at age 20.
No evidence indicated any associations between increased amounts of tea or soda intake and MS.
“Further studies are required to establish if it is in fact caffeine, or if there is another molecule in coffee underlying the findings, to longitudinally assess the association between consumption of coffee and disease activity in MS, and to evaluate the mechanisms by which coffee may be acting, which could thus lead to new therapeutic targets,” the researchers concluded.
—Lori Laubach
Suggested Reading
Hedström AK, Mowry EM, Gianfrancesco MA, et al. High consumption of coffee is associated with decreased multiple sclerosis risk; results from two independent studies. J Neurol Neurosurg Psychiatry. 2016 March 3 [Epub ahead of print].
High coffee consumption decreases the odds of developing multiple sclerosis (MS), according to two case–control studies published online ahead of print March 3 in the Journal of Neurology, Neurosurgery & Psychiatry. Anna K. Hedström, MD, PhD, a postdoctoral researcher at the Karolinska Institute, Stockholm, and her associates conducted the studies.
The investigators analyzed coffee consumption among 1,620 adults with MS and 2,788 healthy controls in the Swedish Epidemiological Investigation of Multiple Sclerosis (EIMS). They also examined coffee consumption in 1,159 adults with MS and 1,172 healthy controls in the Kaiser Permanente Medical Care Plan, Northern California Region (KPNC).
In EIMS, the adjusted odds ratio (OR) for developing MS was 0.70 among participants who drank more than six cups of coffee (ie, greater than 900 mL) daily at the index year, which was defined as the year of the initial appearance of symptoms indicative of MS. The corresponding ORs for those who reported high coffee consumption at five or 10 years before the study were 0.72 and 0.71, respectively, but these results were not statistically significant.
In KPNC, those who consumed four or more cups of coffee (ie, more than 948 mL) daily were significantly less likely to develop MS than were those who never drank coffee (OR, 0.69). In addition, people who drank four or more cups of coffee daily at least five years prior to the index year had significantly reduced odds of MS (OR, 0.64).
A meta-analysis of the combined results of the two studies indicated a significant 29% reduction in the likelihood of developing MS among the people with the greatest coffee consumption (ie, greater than 900 mL daily in EIMS and greater than 948 mL in KPNC). The investigators adjusted all the analyses for many demographic and environmental risk factors for MS, including age, gender, residential area, ancestry, smoking habits, exposure to passive smoking, sun exposure habits, and BMI at age 20.
No evidence indicated any associations between increased amounts of tea or soda intake and MS.
“Further studies are required to establish if it is in fact caffeine, or if there is another molecule in coffee underlying the findings, to longitudinally assess the association between consumption of coffee and disease activity in MS, and to evaluate the mechanisms by which coffee may be acting, which could thus lead to new therapeutic targets,” the researchers concluded.
—Lori Laubach
High coffee consumption decreases the odds of developing multiple sclerosis (MS), according to two case–control studies published online ahead of print March 3 in the Journal of Neurology, Neurosurgery & Psychiatry. Anna K. Hedström, MD, PhD, a postdoctoral researcher at the Karolinska Institute, Stockholm, and her associates conducted the studies.
The investigators analyzed coffee consumption among 1,620 adults with MS and 2,788 healthy controls in the Swedish Epidemiological Investigation of Multiple Sclerosis (EIMS). They also examined coffee consumption in 1,159 adults with MS and 1,172 healthy controls in the Kaiser Permanente Medical Care Plan, Northern California Region (KPNC).
In EIMS, the adjusted odds ratio (OR) for developing MS was 0.70 among participants who drank more than six cups of coffee (ie, greater than 900 mL) daily at the index year, which was defined as the year of the initial appearance of symptoms indicative of MS. The corresponding ORs for those who reported high coffee consumption at five or 10 years before the study were 0.72 and 0.71, respectively, but these results were not statistically significant.
In KPNC, those who consumed four or more cups of coffee (ie, more than 948 mL) daily were significantly less likely to develop MS than were those who never drank coffee (OR, 0.69). In addition, people who drank four or more cups of coffee daily at least five years prior to the index year had significantly reduced odds of MS (OR, 0.64).
A meta-analysis of the combined results of the two studies indicated a significant 29% reduction in the likelihood of developing MS among the people with the greatest coffee consumption (ie, greater than 900 mL daily in EIMS and greater than 948 mL in KPNC). The investigators adjusted all the analyses for many demographic and environmental risk factors for MS, including age, gender, residential area, ancestry, smoking habits, exposure to passive smoking, sun exposure habits, and BMI at age 20.
No evidence indicated any associations between increased amounts of tea or soda intake and MS.
“Further studies are required to establish if it is in fact caffeine, or if there is another molecule in coffee underlying the findings, to longitudinally assess the association between consumption of coffee and disease activity in MS, and to evaluate the mechanisms by which coffee may be acting, which could thus lead to new therapeutic targets,” the researchers concluded.
—Lori Laubach
Suggested Reading
Hedström AK, Mowry EM, Gianfrancesco MA, et al. High consumption of coffee is associated with decreased multiple sclerosis risk; results from two independent studies. J Neurol Neurosurg Psychiatry. 2016 March 3 [Epub ahead of print].
Suggested Reading
Hedström AK, Mowry EM, Gianfrancesco MA, et al. High consumption of coffee is associated with decreased multiple sclerosis risk; results from two independent studies. J Neurol Neurosurg Psychiatry. 2016 March 3 [Epub ahead of print].
Home infusion policies called out in ACR position statement
Proper administration of intravenous biologics should take place under the close supervision of a physician in a physician’s office, infusion center, or hospital rather than in a patient’s home in order to address potential infusion reactions that can range from mild to life threatening, according to a position statement issued by the American College of Rheumatology’s Committee on Rheumatologic Care.
The “Patient Safety and Site of Service for Infusible Biologics” statement, issued in late February, comes in opposition to “policies that require home infusion” that appear to seek potential cost savings with home infusions rather than meet the standard of care with on-site physician supervision.
“One observation made by some but not all payers is that infusible biologics are about twice as expensive when infused in a hospital-based infusion center as compared to other locations, such as a clinic-based infusion center or the patient’s home. Thus, some payers are rolling out policies designed to shift patients from hospital-based infusion centers to less expensive sites. The ACR is opposed to policies that would force patients, solely for the purpose of cost containment, to receive infusible biologics in an improperly supervised setting. The purpose of the position statement is to outline that stance,” Dr. Douglas W. White, chair of the ACR’s Committee on Rheumatologic Care, said in an interview.
He noted that he’s “been in on conversations with two payers who are implementing policies to move patients away from hospital-based infusions, but we are aware that others are in various stages of implementing such policies, too. It’s not so much an issue of critical mass for us, rather we’re just trying to keep ahead of the trends, and we think this will be a big trend.”
The potential for adverse reactions is not uncommon during intravenous administration of biologics, the committee wrote, noting, for example, that 10% of patients given infliximab have acute infusion reactions. On-site physicians such as rheumatologists who have experience with the “tremendous heterogeneity of patients with autoimmune disease and the diversity of conditions treated with biologics” can determine the severity of infusion reactions and decide whether or not it is safe to continue a particular biologic agent, in addition to providing reassurance to patients during acute and potentially severe reactions, according to the ACR statement.
Infusion reactions can range in severity from a mild rash to life-threatening anaphylaxis that can involve multiple organ systems leading to respiratory and cardiovascular collapse and requiring immediate treatment with medications such as epinephrine or intravenous glucocorticoids.
The position statement recognizes unusual situations in which home infusion is necessary for a patient to receive treatment because of transportation problems to a medical facility or comorbid conditions in which the risk of no treatment may outweigh the risk of home infusion. In these circumstances, the ACR “encourages providers in such unusual and difficult situations to make the best medical decision based on the individual needs of the patient. Routine home infusion of biologics is considered an unnecessary and dangerous risk to patients and violates our current clinical standards of practice.”
Requirements for using home infusion also threaten “to reduce access to” intravenous biologics, the ACR contends, because “specially trained physicians are less likely to prescribe treatments that are not properly administered in the safest clinical setting [and] patient fear of biologic therapy may lead to noncompliance and inadequate control of disease.”
The ACR noted that home administration of subcutaneous biologics is medically appropriate and the injection site reactions that can occur with their use are often easily managed.
Proper administration of intravenous biologics should take place under the close supervision of a physician in a physician’s office, infusion center, or hospital rather than in a patient’s home in order to address potential infusion reactions that can range from mild to life threatening, according to a position statement issued by the American College of Rheumatology’s Committee on Rheumatologic Care.
The “Patient Safety and Site of Service for Infusible Biologics” statement, issued in late February, comes in opposition to “policies that require home infusion” that appear to seek potential cost savings with home infusions rather than meet the standard of care with on-site physician supervision.
“One observation made by some but not all payers is that infusible biologics are about twice as expensive when infused in a hospital-based infusion center as compared to other locations, such as a clinic-based infusion center or the patient’s home. Thus, some payers are rolling out policies designed to shift patients from hospital-based infusion centers to less expensive sites. The ACR is opposed to policies that would force patients, solely for the purpose of cost containment, to receive infusible biologics in an improperly supervised setting. The purpose of the position statement is to outline that stance,” Dr. Douglas W. White, chair of the ACR’s Committee on Rheumatologic Care, said in an interview.
He noted that he’s “been in on conversations with two payers who are implementing policies to move patients away from hospital-based infusions, but we are aware that others are in various stages of implementing such policies, too. It’s not so much an issue of critical mass for us, rather we’re just trying to keep ahead of the trends, and we think this will be a big trend.”
The potential for adverse reactions is not uncommon during intravenous administration of biologics, the committee wrote, noting, for example, that 10% of patients given infliximab have acute infusion reactions. On-site physicians such as rheumatologists who have experience with the “tremendous heterogeneity of patients with autoimmune disease and the diversity of conditions treated with biologics” can determine the severity of infusion reactions and decide whether or not it is safe to continue a particular biologic agent, in addition to providing reassurance to patients during acute and potentially severe reactions, according to the ACR statement.
Infusion reactions can range in severity from a mild rash to life-threatening anaphylaxis that can involve multiple organ systems leading to respiratory and cardiovascular collapse and requiring immediate treatment with medications such as epinephrine or intravenous glucocorticoids.
The position statement recognizes unusual situations in which home infusion is necessary for a patient to receive treatment because of transportation problems to a medical facility or comorbid conditions in which the risk of no treatment may outweigh the risk of home infusion. In these circumstances, the ACR “encourages providers in such unusual and difficult situations to make the best medical decision based on the individual needs of the patient. Routine home infusion of biologics is considered an unnecessary and dangerous risk to patients and violates our current clinical standards of practice.”
Requirements for using home infusion also threaten “to reduce access to” intravenous biologics, the ACR contends, because “specially trained physicians are less likely to prescribe treatments that are not properly administered in the safest clinical setting [and] patient fear of biologic therapy may lead to noncompliance and inadequate control of disease.”
The ACR noted that home administration of subcutaneous biologics is medically appropriate and the injection site reactions that can occur with their use are often easily managed.
Proper administration of intravenous biologics should take place under the close supervision of a physician in a physician’s office, infusion center, or hospital rather than in a patient’s home in order to address potential infusion reactions that can range from mild to life threatening, according to a position statement issued by the American College of Rheumatology’s Committee on Rheumatologic Care.
The “Patient Safety and Site of Service for Infusible Biologics” statement, issued in late February, comes in opposition to “policies that require home infusion” that appear to seek potential cost savings with home infusions rather than meet the standard of care with on-site physician supervision.
“One observation made by some but not all payers is that infusible biologics are about twice as expensive when infused in a hospital-based infusion center as compared to other locations, such as a clinic-based infusion center or the patient’s home. Thus, some payers are rolling out policies designed to shift patients from hospital-based infusion centers to less expensive sites. The ACR is opposed to policies that would force patients, solely for the purpose of cost containment, to receive infusible biologics in an improperly supervised setting. The purpose of the position statement is to outline that stance,” Dr. Douglas W. White, chair of the ACR’s Committee on Rheumatologic Care, said in an interview.
He noted that he’s “been in on conversations with two payers who are implementing policies to move patients away from hospital-based infusions, but we are aware that others are in various stages of implementing such policies, too. It’s not so much an issue of critical mass for us, rather we’re just trying to keep ahead of the trends, and we think this will be a big trend.”
The potential for adverse reactions is not uncommon during intravenous administration of biologics, the committee wrote, noting, for example, that 10% of patients given infliximab have acute infusion reactions. On-site physicians such as rheumatologists who have experience with the “tremendous heterogeneity of patients with autoimmune disease and the diversity of conditions treated with biologics” can determine the severity of infusion reactions and decide whether or not it is safe to continue a particular biologic agent, in addition to providing reassurance to patients during acute and potentially severe reactions, according to the ACR statement.
Infusion reactions can range in severity from a mild rash to life-threatening anaphylaxis that can involve multiple organ systems leading to respiratory and cardiovascular collapse and requiring immediate treatment with medications such as epinephrine or intravenous glucocorticoids.
The position statement recognizes unusual situations in which home infusion is necessary for a patient to receive treatment because of transportation problems to a medical facility or comorbid conditions in which the risk of no treatment may outweigh the risk of home infusion. In these circumstances, the ACR “encourages providers in such unusual and difficult situations to make the best medical decision based on the individual needs of the patient. Routine home infusion of biologics is considered an unnecessary and dangerous risk to patients and violates our current clinical standards of practice.”
Requirements for using home infusion also threaten “to reduce access to” intravenous biologics, the ACR contends, because “specially trained physicians are less likely to prescribe treatments that are not properly administered in the safest clinical setting [and] patient fear of biologic therapy may lead to noncompliance and inadequate control of disease.”
The ACR noted that home administration of subcutaneous biologics is medically appropriate and the injection site reactions that can occur with their use are often easily managed.
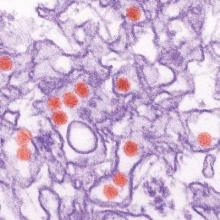
Zika virus: More questions than answers?
With spring break in full swing and summer vacations right around the corner, pediatricians are increasingly fielding questions from families about Zika virus.
“There are a lot of resources available online, but they’re constantly being updated, and it’s difficult to stay current,” a friend and fellow pediatrician confided. “It seems like there’s new information every day, but still as many questions as answers.”
A quick PubMed search validated her concern: More than 200 articles have been published about Zika virus since the beginning of the year. The Centers for Disease Control and Prevention and the World Health Organization post new information to their Zika websites regularly, if not daily, and the WHO has released a Zika app for clinicians. Understanding that the busy pediatrician may not always have time to peruse these authoritative references during the course of a day in the office, I’ve compiled some common questions and answers.
“Is Zika really as serious as the media portrays it?” asked the mother of two children as she contemplated Caribbean vacation plans. In truth, most healthy people infected with Zika virus never develop symptoms. Illness, when it occurs, is most often mild and includes low-grade fever, headache, arthralgia, myalgia, nonpurulent conjunctivitis, and a maculopapular rash. Unlike dengue, another Flavivirus carried by Aedes mosquitoes, Zika does not cause hemorrhagic fever, and death appears to be rare.
An understanding of Zika infection and neurologic complications is a work in progress. A 20-fold increase in the incidence of Guillain-Barré (GBS) cases was noted in French Polynesia during a 2013-2014 outbreak of Zika virus.
In a case-control study involving 42 patients hospitalized with GBS, 98% had anti–Zika virus IgM or IgG, and all had neutralizing antibodies against Zika virus, compared with 56% of 98 control patients (P less than .0001 ) (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
To date, 10 countries or territories have reported GBS cases with confirmed Zika virus infection. According to the World Health Organization, “Zika virus is highly likely to be a cause of the elevated incidence of GBS in countries and territories in the Western Pacific and Americas,” but further research is needed. Zika has recently been associated with other neurologic disorders, including myelitis, and the full spectrum of disease is likely not yet known.
Most Zika virus infections are transmitted from the bite of an Aedes mosquito. What we know about Zika transmission among humans continues to evolve. Viremia can persist for 14 or more days after the onset of symptoms, during which time blood is a potential source of infection. Two possible cases of transfusion-related viral transmission are under investigation in Brazil, and during the French Polynesia outbreak, 3% of samples from asymptomatic blood donors contained detectable Zika RNA. The U.S. Food and Drug Administration has recommended that individuals who have lived in or traveled to an area with active Zika virus transmission defer blood donation for 4 weeks after departure from the area .
Zika virus also has been detected in the urine and saliva of infected individuals, but these fluids have not been linked to transmission. Sexual transmission from infected men to their partners is well documented, but the period of risk remains undefined. The virus can persist in the semen long after viremia clears, and in one individual, Zika virus was detected in the semen 62 days after symptom onset.
Maternal-fetal transmission can occur as early as the first trimester and as late as at the time of delivery. Zika virus has been recovered from both amniotic fluid and placentas. The consequences of maternal-fetal transmission are less certain. Coincident with an epidemic of Zika in Brazil, that country has observed a marked increase in the incidence of microcephaly. Between Oct. 22, 2015, and March 12, 2016, 6,480 cases of microcephaly and/or central nervous system malformation were reported in Brazil, contrasting sharply with the average of 163 cases reported annually from 2001 to 2014. Zika virus has been linked to 863 cases of microcephaly investigated thus far. Proving causality takes time, but the World Health Organization says the link between microcephaly and Zika infection is “strongly suspected.”
Because of the association between Zika virus and birth defects, including abnormal brain development, eye abnormalities, and hearing deficits, the CDC currently recommends that pregnant women not travel to areas with Zika transmission, while men who have lived in or traveled to an area with Zika and who have a pregnant partner should either use condoms or not have sex for the duration of the pregnancy.
The good news for nonpregnant women who contract Zika infection is that the infection is not thought to pose any risk to future pregnancies. Currently, there is no evidence that a fetus conceived after maternal viremia has resolved would be at risk for infection. Still, many unanswered questions remain about Zika infection during pregnancy. For example, it’s currently unknown how often infection is transmitted from an infected mother to her fetus, or if infection is more severe at a particular point in gestation.
Although Zika virus has been isolated from breast milk, no infections have been linked to breastfeeding, and mothers are encouraged to continue to nurse, even in areas with widespread transmission. Infection with Zika at the time of birth or later in childhood has not been linked to microcephaly. Beyond that, the long-term health outcomes of infants and children with Zika virus infection are unknown.
“How far north do you think the virus will spread?” one mom asked me. “Do I need to be worried?”
For public health officials, that’s the sixty-four thousand dollar question. To date, there have been no cases acquired as a result of a mosquito bite in the United States, but the edge of the outbreak continues to creep north. Local transmission of the virus was reported in Cuba on March 14.
As of March 16, 2016, 258 travel-associated Zika virus cases have been diagnosed in the United States, including 18 in pregnant women. Six of these were sexually transmitted. Theoretically, “onward transmission” from one of these cases could occur if the right kind of mosquito bites an infected person during the period of active viremia and then bites someone else, transferring a tiny amount of the virus-contaminated blood.
According to CDC experts, “Texas, Florida, and Hawaii are likely to be the U.S. states with the highest risk of experiencing local transmission of Zika virus by mosquitoes.” Although this estimate is based on prior experience with similar viruses, the principal vector of Zika, Aedes aegypti, has been identified as far west as California and in a number of states across the South, including my home state of Kentucky. Aedes albopictus mosquitoes also have been proven competent vectors for Zika virus transmission and are more widely distributed throughout the continental United States.
In a thoughtful review published in JAMA Pediatrics, “What Pediatricians and Other Clinicians Should Know About Zika Virus,” Dr. Mark W. Kline and Dr. Gordon E. Schutze noted that up to two-thirds of the U.S. population live in an area where Aedes mosquitoes are present at least part of the year (JAMA Pediatr. 2016 Feb 18. doi: 10.1001/jamapediatrics.2016.0429). Fortunately, transmission of dengue and chikungunya, two other viruses carried by the same insect, is still very uncommon. Public health experts are urging individuals with Zika virus infection to avoid mosquito bites during the first week of illness, to protect others.
We should start now counseling our patients and families to avoid mosquito bites at home and abroad. Besides Zika virus, mosquitoes transmit several pathogens in the United States each year, including West Nile virus, LaCrosse encephalitis virus, St. Louis encephalitis virus, and dengue.
Any collections of standing water should be eliminated, as these can be mosquito breeding grounds. These include flower pots, buckets, barrels, and discarded tires. The water in bird baths and pet dishes should be changed at least weekly, and children’s wading pools should be drained and stored on their side after use.
To the extent practical, exposed skin should be covered with long-sleeved shirts, long pants, and socks when individuals are in areas with mosquito activity. To enhance protection, clothing can be treated with permethrin, or pretreated clothing can be worn. An FDA-registered insect repellent should be applied to exposed skin, especially during hours of highest mosquito activity. Zika-carrying mosquitoes bite during the day, or dawn to dusk. Effective repellents include DEET, picaridin, IR3535, and oil of lemon eucalyptus, although families should read labels carefully as instructions for use vary, as does the recommended time period of reapplication. Combination sunscreen/insect repellent products are not recommended as repellent usually does not need to be reapplied as often as sunscreen. Parents also should be reminded not to use oil of lemon eucalyptus–containing products on children under 3 years of age.
“We’re going to get a lot more questions as the weather turns warmer,” said a colleague of mine. “I’m just waiting for the first call about a child who develops fever and a rash after a mosquito bite. Parents will wonder if it could be Zika.”
It is going to be an interesting summer. Stay tuned.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Kosair Children’s Hospital, also in Louisville. She had no relevant financial disclosures.
With spring break in full swing and summer vacations right around the corner, pediatricians are increasingly fielding questions from families about Zika virus.
“There are a lot of resources available online, but they’re constantly being updated, and it’s difficult to stay current,” a friend and fellow pediatrician confided. “It seems like there’s new information every day, but still as many questions as answers.”
A quick PubMed search validated her concern: More than 200 articles have been published about Zika virus since the beginning of the year. The Centers for Disease Control and Prevention and the World Health Organization post new information to their Zika websites regularly, if not daily, and the WHO has released a Zika app for clinicians. Understanding that the busy pediatrician may not always have time to peruse these authoritative references during the course of a day in the office, I’ve compiled some common questions and answers.
“Is Zika really as serious as the media portrays it?” asked the mother of two children as she contemplated Caribbean vacation plans. In truth, most healthy people infected with Zika virus never develop symptoms. Illness, when it occurs, is most often mild and includes low-grade fever, headache, arthralgia, myalgia, nonpurulent conjunctivitis, and a maculopapular rash. Unlike dengue, another Flavivirus carried by Aedes mosquitoes, Zika does not cause hemorrhagic fever, and death appears to be rare.
An understanding of Zika infection and neurologic complications is a work in progress. A 20-fold increase in the incidence of Guillain-Barré (GBS) cases was noted in French Polynesia during a 2013-2014 outbreak of Zika virus.
In a case-control study involving 42 patients hospitalized with GBS, 98% had anti–Zika virus IgM or IgG, and all had neutralizing antibodies against Zika virus, compared with 56% of 98 control patients (P less than .0001 ) (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
To date, 10 countries or territories have reported GBS cases with confirmed Zika virus infection. According to the World Health Organization, “Zika virus is highly likely to be a cause of the elevated incidence of GBS in countries and territories in the Western Pacific and Americas,” but further research is needed. Zika has recently been associated with other neurologic disorders, including myelitis, and the full spectrum of disease is likely not yet known.
Most Zika virus infections are transmitted from the bite of an Aedes mosquito. What we know about Zika transmission among humans continues to evolve. Viremia can persist for 14 or more days after the onset of symptoms, during which time blood is a potential source of infection. Two possible cases of transfusion-related viral transmission are under investigation in Brazil, and during the French Polynesia outbreak, 3% of samples from asymptomatic blood donors contained detectable Zika RNA. The U.S. Food and Drug Administration has recommended that individuals who have lived in or traveled to an area with active Zika virus transmission defer blood donation for 4 weeks after departure from the area .
Zika virus also has been detected in the urine and saliva of infected individuals, but these fluids have not been linked to transmission. Sexual transmission from infected men to their partners is well documented, but the period of risk remains undefined. The virus can persist in the semen long after viremia clears, and in one individual, Zika virus was detected in the semen 62 days after symptom onset.
Maternal-fetal transmission can occur as early as the first trimester and as late as at the time of delivery. Zika virus has been recovered from both amniotic fluid and placentas. The consequences of maternal-fetal transmission are less certain. Coincident with an epidemic of Zika in Brazil, that country has observed a marked increase in the incidence of microcephaly. Between Oct. 22, 2015, and March 12, 2016, 6,480 cases of microcephaly and/or central nervous system malformation were reported in Brazil, contrasting sharply with the average of 163 cases reported annually from 2001 to 2014. Zika virus has been linked to 863 cases of microcephaly investigated thus far. Proving causality takes time, but the World Health Organization says the link between microcephaly and Zika infection is “strongly suspected.”
Because of the association between Zika virus and birth defects, including abnormal brain development, eye abnormalities, and hearing deficits, the CDC currently recommends that pregnant women not travel to areas with Zika transmission, while men who have lived in or traveled to an area with Zika and who have a pregnant partner should either use condoms or not have sex for the duration of the pregnancy.
The good news for nonpregnant women who contract Zika infection is that the infection is not thought to pose any risk to future pregnancies. Currently, there is no evidence that a fetus conceived after maternal viremia has resolved would be at risk for infection. Still, many unanswered questions remain about Zika infection during pregnancy. For example, it’s currently unknown how often infection is transmitted from an infected mother to her fetus, or if infection is more severe at a particular point in gestation.
Although Zika virus has been isolated from breast milk, no infections have been linked to breastfeeding, and mothers are encouraged to continue to nurse, even in areas with widespread transmission. Infection with Zika at the time of birth or later in childhood has not been linked to microcephaly. Beyond that, the long-term health outcomes of infants and children with Zika virus infection are unknown.
“How far north do you think the virus will spread?” one mom asked me. “Do I need to be worried?”
For public health officials, that’s the sixty-four thousand dollar question. To date, there have been no cases acquired as a result of a mosquito bite in the United States, but the edge of the outbreak continues to creep north. Local transmission of the virus was reported in Cuba on March 14.
As of March 16, 2016, 258 travel-associated Zika virus cases have been diagnosed in the United States, including 18 in pregnant women. Six of these were sexually transmitted. Theoretically, “onward transmission” from one of these cases could occur if the right kind of mosquito bites an infected person during the period of active viremia and then bites someone else, transferring a tiny amount of the virus-contaminated blood.
According to CDC experts, “Texas, Florida, and Hawaii are likely to be the U.S. states with the highest risk of experiencing local transmission of Zika virus by mosquitoes.” Although this estimate is based on prior experience with similar viruses, the principal vector of Zika, Aedes aegypti, has been identified as far west as California and in a number of states across the South, including my home state of Kentucky. Aedes albopictus mosquitoes also have been proven competent vectors for Zika virus transmission and are more widely distributed throughout the continental United States.
In a thoughtful review published in JAMA Pediatrics, “What Pediatricians and Other Clinicians Should Know About Zika Virus,” Dr. Mark W. Kline and Dr. Gordon E. Schutze noted that up to two-thirds of the U.S. population live in an area where Aedes mosquitoes are present at least part of the year (JAMA Pediatr. 2016 Feb 18. doi: 10.1001/jamapediatrics.2016.0429). Fortunately, transmission of dengue and chikungunya, two other viruses carried by the same insect, is still very uncommon. Public health experts are urging individuals with Zika virus infection to avoid mosquito bites during the first week of illness, to protect others.
We should start now counseling our patients and families to avoid mosquito bites at home and abroad. Besides Zika virus, mosquitoes transmit several pathogens in the United States each year, including West Nile virus, LaCrosse encephalitis virus, St. Louis encephalitis virus, and dengue.
Any collections of standing water should be eliminated, as these can be mosquito breeding grounds. These include flower pots, buckets, barrels, and discarded tires. The water in bird baths and pet dishes should be changed at least weekly, and children’s wading pools should be drained and stored on their side after use.
To the extent practical, exposed skin should be covered with long-sleeved shirts, long pants, and socks when individuals are in areas with mosquito activity. To enhance protection, clothing can be treated with permethrin, or pretreated clothing can be worn. An FDA-registered insect repellent should be applied to exposed skin, especially during hours of highest mosquito activity. Zika-carrying mosquitoes bite during the day, or dawn to dusk. Effective repellents include DEET, picaridin, IR3535, and oil of lemon eucalyptus, although families should read labels carefully as instructions for use vary, as does the recommended time period of reapplication. Combination sunscreen/insect repellent products are not recommended as repellent usually does not need to be reapplied as often as sunscreen. Parents also should be reminded not to use oil of lemon eucalyptus–containing products on children under 3 years of age.
“We’re going to get a lot more questions as the weather turns warmer,” said a colleague of mine. “I’m just waiting for the first call about a child who develops fever and a rash after a mosquito bite. Parents will wonder if it could be Zika.”
It is going to be an interesting summer. Stay tuned.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Kosair Children’s Hospital, also in Louisville. She had no relevant financial disclosures.
With spring break in full swing and summer vacations right around the corner, pediatricians are increasingly fielding questions from families about Zika virus.
“There are a lot of resources available online, but they’re constantly being updated, and it’s difficult to stay current,” a friend and fellow pediatrician confided. “It seems like there’s new information every day, but still as many questions as answers.”
A quick PubMed search validated her concern: More than 200 articles have been published about Zika virus since the beginning of the year. The Centers for Disease Control and Prevention and the World Health Organization post new information to their Zika websites regularly, if not daily, and the WHO has released a Zika app for clinicians. Understanding that the busy pediatrician may not always have time to peruse these authoritative references during the course of a day in the office, I’ve compiled some common questions and answers.
“Is Zika really as serious as the media portrays it?” asked the mother of two children as she contemplated Caribbean vacation plans. In truth, most healthy people infected with Zika virus never develop symptoms. Illness, when it occurs, is most often mild and includes low-grade fever, headache, arthralgia, myalgia, nonpurulent conjunctivitis, and a maculopapular rash. Unlike dengue, another Flavivirus carried by Aedes mosquitoes, Zika does not cause hemorrhagic fever, and death appears to be rare.
An understanding of Zika infection and neurologic complications is a work in progress. A 20-fold increase in the incidence of Guillain-Barré (GBS) cases was noted in French Polynesia during a 2013-2014 outbreak of Zika virus.
In a case-control study involving 42 patients hospitalized with GBS, 98% had anti–Zika virus IgM or IgG, and all had neutralizing antibodies against Zika virus, compared with 56% of 98 control patients (P less than .0001 ) (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
To date, 10 countries or territories have reported GBS cases with confirmed Zika virus infection. According to the World Health Organization, “Zika virus is highly likely to be a cause of the elevated incidence of GBS in countries and territories in the Western Pacific and Americas,” but further research is needed. Zika has recently been associated with other neurologic disorders, including myelitis, and the full spectrum of disease is likely not yet known.
Most Zika virus infections are transmitted from the bite of an Aedes mosquito. What we know about Zika transmission among humans continues to evolve. Viremia can persist for 14 or more days after the onset of symptoms, during which time blood is a potential source of infection. Two possible cases of transfusion-related viral transmission are under investigation in Brazil, and during the French Polynesia outbreak, 3% of samples from asymptomatic blood donors contained detectable Zika RNA. The U.S. Food and Drug Administration has recommended that individuals who have lived in or traveled to an area with active Zika virus transmission defer blood donation for 4 weeks after departure from the area .
Zika virus also has been detected in the urine and saliva of infected individuals, but these fluids have not been linked to transmission. Sexual transmission from infected men to their partners is well documented, but the period of risk remains undefined. The virus can persist in the semen long after viremia clears, and in one individual, Zika virus was detected in the semen 62 days after symptom onset.
Maternal-fetal transmission can occur as early as the first trimester and as late as at the time of delivery. Zika virus has been recovered from both amniotic fluid and placentas. The consequences of maternal-fetal transmission are less certain. Coincident with an epidemic of Zika in Brazil, that country has observed a marked increase in the incidence of microcephaly. Between Oct. 22, 2015, and March 12, 2016, 6,480 cases of microcephaly and/or central nervous system malformation were reported in Brazil, contrasting sharply with the average of 163 cases reported annually from 2001 to 2014. Zika virus has been linked to 863 cases of microcephaly investigated thus far. Proving causality takes time, but the World Health Organization says the link between microcephaly and Zika infection is “strongly suspected.”
Because of the association between Zika virus and birth defects, including abnormal brain development, eye abnormalities, and hearing deficits, the CDC currently recommends that pregnant women not travel to areas with Zika transmission, while men who have lived in or traveled to an area with Zika and who have a pregnant partner should either use condoms or not have sex for the duration of the pregnancy.
The good news for nonpregnant women who contract Zika infection is that the infection is not thought to pose any risk to future pregnancies. Currently, there is no evidence that a fetus conceived after maternal viremia has resolved would be at risk for infection. Still, many unanswered questions remain about Zika infection during pregnancy. For example, it’s currently unknown how often infection is transmitted from an infected mother to her fetus, or if infection is more severe at a particular point in gestation.
Although Zika virus has been isolated from breast milk, no infections have been linked to breastfeeding, and mothers are encouraged to continue to nurse, even in areas with widespread transmission. Infection with Zika at the time of birth or later in childhood has not been linked to microcephaly. Beyond that, the long-term health outcomes of infants and children with Zika virus infection are unknown.
“How far north do you think the virus will spread?” one mom asked me. “Do I need to be worried?”
For public health officials, that’s the sixty-four thousand dollar question. To date, there have been no cases acquired as a result of a mosquito bite in the United States, but the edge of the outbreak continues to creep north. Local transmission of the virus was reported in Cuba on March 14.
As of March 16, 2016, 258 travel-associated Zika virus cases have been diagnosed in the United States, including 18 in pregnant women. Six of these were sexually transmitted. Theoretically, “onward transmission” from one of these cases could occur if the right kind of mosquito bites an infected person during the period of active viremia and then bites someone else, transferring a tiny amount of the virus-contaminated blood.
According to CDC experts, “Texas, Florida, and Hawaii are likely to be the U.S. states with the highest risk of experiencing local transmission of Zika virus by mosquitoes.” Although this estimate is based on prior experience with similar viruses, the principal vector of Zika, Aedes aegypti, has been identified as far west as California and in a number of states across the South, including my home state of Kentucky. Aedes albopictus mosquitoes also have been proven competent vectors for Zika virus transmission and are more widely distributed throughout the continental United States.
In a thoughtful review published in JAMA Pediatrics, “What Pediatricians and Other Clinicians Should Know About Zika Virus,” Dr. Mark W. Kline and Dr. Gordon E. Schutze noted that up to two-thirds of the U.S. population live in an area where Aedes mosquitoes are present at least part of the year (JAMA Pediatr. 2016 Feb 18. doi: 10.1001/jamapediatrics.2016.0429). Fortunately, transmission of dengue and chikungunya, two other viruses carried by the same insect, is still very uncommon. Public health experts are urging individuals with Zika virus infection to avoid mosquito bites during the first week of illness, to protect others.
We should start now counseling our patients and families to avoid mosquito bites at home and abroad. Besides Zika virus, mosquitoes transmit several pathogens in the United States each year, including West Nile virus, LaCrosse encephalitis virus, St. Louis encephalitis virus, and dengue.
Any collections of standing water should be eliminated, as these can be mosquito breeding grounds. These include flower pots, buckets, barrels, and discarded tires. The water in bird baths and pet dishes should be changed at least weekly, and children’s wading pools should be drained and stored on their side after use.
To the extent practical, exposed skin should be covered with long-sleeved shirts, long pants, and socks when individuals are in areas with mosquito activity. To enhance protection, clothing can be treated with permethrin, or pretreated clothing can be worn. An FDA-registered insect repellent should be applied to exposed skin, especially during hours of highest mosquito activity. Zika-carrying mosquitoes bite during the day, or dawn to dusk. Effective repellents include DEET, picaridin, IR3535, and oil of lemon eucalyptus, although families should read labels carefully as instructions for use vary, as does the recommended time period of reapplication. Combination sunscreen/insect repellent products are not recommended as repellent usually does not need to be reapplied as often as sunscreen. Parents also should be reminded not to use oil of lemon eucalyptus–containing products on children under 3 years of age.
“We’re going to get a lot more questions as the weather turns warmer,” said a colleague of mine. “I’m just waiting for the first call about a child who develops fever and a rash after a mosquito bite. Parents will wonder if it could be Zika.”
It is going to be an interesting summer. Stay tuned.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Kosair Children’s Hospital, also in Louisville. She had no relevant financial disclosures.
Finding the right path for pain control
There has been a lot of publicity surrounding the increasing use of prescription painkillers and subsequent increase in deaths. In 2014, there were close to 19,000 deaths related to opioid painkiller overdose. State and federal governments have reacted with various initiatives, from changing the scheduling of Vicodin, to initiating prescription drug–monitoring programs, to limiting the number of pills dispensed. There are loud voices on either side of this debate, to be sure, but perhaps none so aggravating as the aggravated patient.
I did not start my practice with any prescribing “policy,” as I thought such policies were arbitrary. I am a physician, after all, so why wouldn’t I prescribe a narcotic if necessary? I also trained at a time when pain was considered “the fifth vital sign,” and we were taught to treat it aggressively.
But after a while you learn that trust in patients can be misplaced. You never forget the first nice lady whose urine drug screen comes back negative when you expected it to show the narcotic that you were prescribing her. You never forget the person who calls on a weekend claiming to be a patient of the practice and turns out not to be. And when your colleague gets her DEA number stolen and her signature forged, you finally learn that humanity is imperfect. What’s more, in your transition from young naive doctor to elder statesman, you learn that the push to treat pain so aggressively was achieved, in large part, by lobbying from the pharmaceutical industry.
Some patients of course can have a legitimate need for narcotics and truly derive benefit from them. In such patients, it is our practice to have the patient sign a pain “contract.” Such contracts are nonbinding, but give the narcotic prescription the gravitas that it deserves, underscoring the sacrosanct nature not just of the prescription but also of the physician-patient relationship. They specify the strength of the prescription, the number of pills dispensed, the pharmacy at which the prescription is to be filled, and the physician’s prerogative to do random drug screens.
The more vexing problem for rheumatologists involves patients with central sensitization and chronic pain. These patients seem predisposed to requiring escalating doses of narcotics, and they often have risk factors for developing narcotic abuse disorders. In addition, there is no evidence that chronic narcotic use provides any long-term benefit. But it is a rare chronic pain patient who is willing to accept that narcotics are not the answer to his or her problems.
One way to manage this is for the patients to not be given narcotics in the first place. That probably requires lobbying of a different kind: educating primary care providers and emergency department physicians on how to recognize chronic pain or central sensitization syndromes and disseminating the literature showing that narcotics have no long-term benefit in such cases.
Dr. Chan practices rheumatology in Pawtucket, R.I.
There has been a lot of publicity surrounding the increasing use of prescription painkillers and subsequent increase in deaths. In 2014, there were close to 19,000 deaths related to opioid painkiller overdose. State and federal governments have reacted with various initiatives, from changing the scheduling of Vicodin, to initiating prescription drug–monitoring programs, to limiting the number of pills dispensed. There are loud voices on either side of this debate, to be sure, but perhaps none so aggravating as the aggravated patient.
I did not start my practice with any prescribing “policy,” as I thought such policies were arbitrary. I am a physician, after all, so why wouldn’t I prescribe a narcotic if necessary? I also trained at a time when pain was considered “the fifth vital sign,” and we were taught to treat it aggressively.
But after a while you learn that trust in patients can be misplaced. You never forget the first nice lady whose urine drug screen comes back negative when you expected it to show the narcotic that you were prescribing her. You never forget the person who calls on a weekend claiming to be a patient of the practice and turns out not to be. And when your colleague gets her DEA number stolen and her signature forged, you finally learn that humanity is imperfect. What’s more, in your transition from young naive doctor to elder statesman, you learn that the push to treat pain so aggressively was achieved, in large part, by lobbying from the pharmaceutical industry.
Some patients of course can have a legitimate need for narcotics and truly derive benefit from them. In such patients, it is our practice to have the patient sign a pain “contract.” Such contracts are nonbinding, but give the narcotic prescription the gravitas that it deserves, underscoring the sacrosanct nature not just of the prescription but also of the physician-patient relationship. They specify the strength of the prescription, the number of pills dispensed, the pharmacy at which the prescription is to be filled, and the physician’s prerogative to do random drug screens.
The more vexing problem for rheumatologists involves patients with central sensitization and chronic pain. These patients seem predisposed to requiring escalating doses of narcotics, and they often have risk factors for developing narcotic abuse disorders. In addition, there is no evidence that chronic narcotic use provides any long-term benefit. But it is a rare chronic pain patient who is willing to accept that narcotics are not the answer to his or her problems.
One way to manage this is for the patients to not be given narcotics in the first place. That probably requires lobbying of a different kind: educating primary care providers and emergency department physicians on how to recognize chronic pain or central sensitization syndromes and disseminating the literature showing that narcotics have no long-term benefit in such cases.
Dr. Chan practices rheumatology in Pawtucket, R.I.
There has been a lot of publicity surrounding the increasing use of prescription painkillers and subsequent increase in deaths. In 2014, there were close to 19,000 deaths related to opioid painkiller overdose. State and federal governments have reacted with various initiatives, from changing the scheduling of Vicodin, to initiating prescription drug–monitoring programs, to limiting the number of pills dispensed. There are loud voices on either side of this debate, to be sure, but perhaps none so aggravating as the aggravated patient.
I did not start my practice with any prescribing “policy,” as I thought such policies were arbitrary. I am a physician, after all, so why wouldn’t I prescribe a narcotic if necessary? I also trained at a time when pain was considered “the fifth vital sign,” and we were taught to treat it aggressively.
But after a while you learn that trust in patients can be misplaced. You never forget the first nice lady whose urine drug screen comes back negative when you expected it to show the narcotic that you were prescribing her. You never forget the person who calls on a weekend claiming to be a patient of the practice and turns out not to be. And when your colleague gets her DEA number stolen and her signature forged, you finally learn that humanity is imperfect. What’s more, in your transition from young naive doctor to elder statesman, you learn that the push to treat pain so aggressively was achieved, in large part, by lobbying from the pharmaceutical industry.
Some patients of course can have a legitimate need for narcotics and truly derive benefit from them. In such patients, it is our practice to have the patient sign a pain “contract.” Such contracts are nonbinding, but give the narcotic prescription the gravitas that it deserves, underscoring the sacrosanct nature not just of the prescription but also of the physician-patient relationship. They specify the strength of the prescription, the number of pills dispensed, the pharmacy at which the prescription is to be filled, and the physician’s prerogative to do random drug screens.
The more vexing problem for rheumatologists involves patients with central sensitization and chronic pain. These patients seem predisposed to requiring escalating doses of narcotics, and they often have risk factors for developing narcotic abuse disorders. In addition, there is no evidence that chronic narcotic use provides any long-term benefit. But it is a rare chronic pain patient who is willing to accept that narcotics are not the answer to his or her problems.
One way to manage this is for the patients to not be given narcotics in the first place. That probably requires lobbying of a different kind: educating primary care providers and emergency department physicians on how to recognize chronic pain or central sensitization syndromes and disseminating the literature showing that narcotics have no long-term benefit in such cases.
Dr. Chan practices rheumatology in Pawtucket, R.I.
Fibroids, endometriosis linked to chemical exposures cost Europe $1.5 billion a year
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Key clinical point: Between 20% and 39% of uterine fibroids and endometriosis cases in Europe are linked to two chemical exposures, and the associated costs exceed $1.5 billion annually.
Major finding: DDE-attributable fibroids and phthalate-attributable endometriosis cases were about 56,700 and 145,000, respectively, in 2010, with total combined economic and health care costs of about $1.5 billion.
Data source: Cohort biomarker data were used to assess European women’s exposures, and disease burden estimated from national health care databases.
Disclosures: The Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation sponsored the study, whose authors disclosed no conflicts.
Intranasal Ketorolac Treats Migraine Effectively
Intranasal ketorolac is superior to placebo and noninferior to intranasal sumatriptan for the acute abortive treatment of moderate to severe migraine, according to data published in the February issue of Headache. Intranasal ketorolac may be appropriate for patients whose nausea makes the use of oral medications difficult, and the formulation also offers an effective alternative for patients who cannot or do not want to use a triptan nasal spray, according to the authors.
Research suggests that parenteral ketorolac may be as effective as or more effective than certain triptans and other acute abortive therapies. No previous study, however, had directly compared intranasal ketorolac with any migraine-specific therapy.
Aruna S. Rao, MD, Instructor of Neurology at Johns Hopkins University School of Medicine in Baltimore, and colleagues conducted a prospective, double-blind, double-dummy trial at an outpatient headache center in Baltimore from March 2013 to December 2014. Eligible patients were age 18 or older, had a history of episodic migraine for at least one year, and had two to 10 migraine attacks per month.
Participants were randomized in groups of equal size to one of six sequences of ketorolac nasal spray (31.5 mg), sumatriptan nasal spray (20 mg), and placebo. Each participant treated three moderate to severe migraine attacks and received a different treatment for each attack. During the 48 hours following the use of each treatment, patients used a four-point scale to assess headache severity, migraine-associated symptoms, and disability.
The study’s primary outcome was two-hour headache relief. Secondary outcomes included two-hour pain freedom, two-hour absence of migraine-associated symptoms, absence of allodynia, disability, and 24- and 48-hour sustained pain relief and sustained pain freedom.
In all, 72 participants were randomized, 54 used at least one dose of study medication, and 49 treated three attacks. A total of 152 attacks were analyzed. Patients’ mean age was 36. Approximately 80% of patients were Caucasian, and 98% were female.
About 73% of patients treated with ketorolac had two-hour pain relief, compared with 69% of patients treated with sumatriptan and 39% of controls. Ketorolac and sumatriptan thus were superior to placebo. In addition, 43% of patients treated with ketorolac had two-hour pain freedom, compared with 37% of patients treated with sumatriptan and 18% of controls. Ketorolac and sumatriptan were superior to placebo for time to pain relief, two-hour freedom from photophobia, and two-to-24-hour sustained pain relief. Only ketorolac was superior to placebo for two-hour freedom from nausea and phonophobia, two-to-24-hour sustained pain freedom, two-to-48-hour sustained pain relief, and two-to-48-hour sustained pain freedom.
The researchers found no statistically significant difference in two-hour freedom from allodynia in participants treated with ketorolac or sumatriptan, compared with placebo. In the first two hours after study treatment, participants who used ketorolac were 61% less likely, and participants who used sumatriptan were 53% less likely, to use rescue medication, compared with placebo. The most common adverse events reported for ketorolac and sumatriptan were nasal burning and an unusual taste. Both were mild to moderate for the majority of patients.
—Erik Greb
Suggested Reading
Rao AS, Gelaye B, Kurth T, et al. A randomized trial of ketorolac vs sumatripan vs placebo nasal spray (KSPN) for acute migraine. Headache. 2016;56(2):331-340.
Intranasal ketorolac is superior to placebo and noninferior to intranasal sumatriptan for the acute abortive treatment of moderate to severe migraine, according to data published in the February issue of Headache. Intranasal ketorolac may be appropriate for patients whose nausea makes the use of oral medications difficult, and the formulation also offers an effective alternative for patients who cannot or do not want to use a triptan nasal spray, according to the authors.
Research suggests that parenteral ketorolac may be as effective as or more effective than certain triptans and other acute abortive therapies. No previous study, however, had directly compared intranasal ketorolac with any migraine-specific therapy.
Aruna S. Rao, MD, Instructor of Neurology at Johns Hopkins University School of Medicine in Baltimore, and colleagues conducted a prospective, double-blind, double-dummy trial at an outpatient headache center in Baltimore from March 2013 to December 2014. Eligible patients were age 18 or older, had a history of episodic migraine for at least one year, and had two to 10 migraine attacks per month.
Participants were randomized in groups of equal size to one of six sequences of ketorolac nasal spray (31.5 mg), sumatriptan nasal spray (20 mg), and placebo. Each participant treated three moderate to severe migraine attacks and received a different treatment for each attack. During the 48 hours following the use of each treatment, patients used a four-point scale to assess headache severity, migraine-associated symptoms, and disability.
The study’s primary outcome was two-hour headache relief. Secondary outcomes included two-hour pain freedom, two-hour absence of migraine-associated symptoms, absence of allodynia, disability, and 24- and 48-hour sustained pain relief and sustained pain freedom.
In all, 72 participants were randomized, 54 used at least one dose of study medication, and 49 treated three attacks. A total of 152 attacks were analyzed. Patients’ mean age was 36. Approximately 80% of patients were Caucasian, and 98% were female.
About 73% of patients treated with ketorolac had two-hour pain relief, compared with 69% of patients treated with sumatriptan and 39% of controls. Ketorolac and sumatriptan thus were superior to placebo. In addition, 43% of patients treated with ketorolac had two-hour pain freedom, compared with 37% of patients treated with sumatriptan and 18% of controls. Ketorolac and sumatriptan were superior to placebo for time to pain relief, two-hour freedom from photophobia, and two-to-24-hour sustained pain relief. Only ketorolac was superior to placebo for two-hour freedom from nausea and phonophobia, two-to-24-hour sustained pain freedom, two-to-48-hour sustained pain relief, and two-to-48-hour sustained pain freedom.
The researchers found no statistically significant difference in two-hour freedom from allodynia in participants treated with ketorolac or sumatriptan, compared with placebo. In the first two hours after study treatment, participants who used ketorolac were 61% less likely, and participants who used sumatriptan were 53% less likely, to use rescue medication, compared with placebo. The most common adverse events reported for ketorolac and sumatriptan were nasal burning and an unusual taste. Both were mild to moderate for the majority of patients.
—Erik Greb
Intranasal ketorolac is superior to placebo and noninferior to intranasal sumatriptan for the acute abortive treatment of moderate to severe migraine, according to data published in the February issue of Headache. Intranasal ketorolac may be appropriate for patients whose nausea makes the use of oral medications difficult, and the formulation also offers an effective alternative for patients who cannot or do not want to use a triptan nasal spray, according to the authors.
Research suggests that parenteral ketorolac may be as effective as or more effective than certain triptans and other acute abortive therapies. No previous study, however, had directly compared intranasal ketorolac with any migraine-specific therapy.
Aruna S. Rao, MD, Instructor of Neurology at Johns Hopkins University School of Medicine in Baltimore, and colleagues conducted a prospective, double-blind, double-dummy trial at an outpatient headache center in Baltimore from March 2013 to December 2014. Eligible patients were age 18 or older, had a history of episodic migraine for at least one year, and had two to 10 migraine attacks per month.
Participants were randomized in groups of equal size to one of six sequences of ketorolac nasal spray (31.5 mg), sumatriptan nasal spray (20 mg), and placebo. Each participant treated three moderate to severe migraine attacks and received a different treatment for each attack. During the 48 hours following the use of each treatment, patients used a four-point scale to assess headache severity, migraine-associated symptoms, and disability.
The study’s primary outcome was two-hour headache relief. Secondary outcomes included two-hour pain freedom, two-hour absence of migraine-associated symptoms, absence of allodynia, disability, and 24- and 48-hour sustained pain relief and sustained pain freedom.
In all, 72 participants were randomized, 54 used at least one dose of study medication, and 49 treated three attacks. A total of 152 attacks were analyzed. Patients’ mean age was 36. Approximately 80% of patients were Caucasian, and 98% were female.
About 73% of patients treated with ketorolac had two-hour pain relief, compared with 69% of patients treated with sumatriptan and 39% of controls. Ketorolac and sumatriptan thus were superior to placebo. In addition, 43% of patients treated with ketorolac had two-hour pain freedom, compared with 37% of patients treated with sumatriptan and 18% of controls. Ketorolac and sumatriptan were superior to placebo for time to pain relief, two-hour freedom from photophobia, and two-to-24-hour sustained pain relief. Only ketorolac was superior to placebo for two-hour freedom from nausea and phonophobia, two-to-24-hour sustained pain freedom, two-to-48-hour sustained pain relief, and two-to-48-hour sustained pain freedom.
The researchers found no statistically significant difference in two-hour freedom from allodynia in participants treated with ketorolac or sumatriptan, compared with placebo. In the first two hours after study treatment, participants who used ketorolac were 61% less likely, and participants who used sumatriptan were 53% less likely, to use rescue medication, compared with placebo. The most common adverse events reported for ketorolac and sumatriptan were nasal burning and an unusual taste. Both were mild to moderate for the majority of patients.
—Erik Greb
Suggested Reading
Rao AS, Gelaye B, Kurth T, et al. A randomized trial of ketorolac vs sumatripan vs placebo nasal spray (KSPN) for acute migraine. Headache. 2016;56(2):331-340.
Suggested Reading
Rao AS, Gelaye B, Kurth T, et al. A randomized trial of ketorolac vs sumatripan vs placebo nasal spray (KSPN) for acute migraine. Headache. 2016;56(2):331-340.
Drugs for Progressive MS Could Target Multiple Disease Mechanisms
NEW ORLEANS—The lack of a therapy that slows or stops disease progression represents the greatest unmet need among patients with progressive multiple sclerosis (MS), according to a lecture presented at the ACTRIMS 2016 Forum. Future therapeutics for progressive MS will need to address mechanisms such as microglial and macrophage-driven neurodegeneration, mitochondrial dysfunction, and oxidative stress, said Claudia F. Lucchinetti, MD, Professor of Neurology at Mayo Clinic in Rochester, Minnesota.
Research efforts should aim to develop drugs that treat smoldering plaques and meningeal inflammation, she added. Furthermore, patients need a therapy that protects axons and promotes remyelination. “Finally, our therapies are going to need to consider targeting both inflammation and neurodegeneration early and concurrently,” said Dr. Lucchinetti.
White Matter Plaques Indicate Disease Duration
MS progression generally affects the white matter, the axons, the cortex, the meninges, and the deep gray matter. As white matter undergoes demyelination, it may develop any of four types of plaques, including active, inactive, smoldering, and remyelinated shadow plaques. In 2015, Dr. Lucchinetti and colleagues studied autopsy results for 120 patients with MS who had 2,476 white-matter plaques. They found that most plaques in early MS were active, while inactive plaques predominated in chronic MS. Smoldering plaques were rare in early MS, but reached peak levels at 18 to 20 years’ disease duration, which is when many patients convert to secondary progressive MS. The frequency of shadow plaques was similar throughout the disease duration.
In addition, the investigators found that active plaques predominated among patients with ongoing relapses, indicating that the plaques may be “the substrate of the relapse itself,” said Dr. Lucchinetti. Active plaques were less frequent in secondary progressive MS without attacks and in primary progressive MS. Shadow plaques occurred in all clinical forms of the disease, but smoldering plaques occurred only in progressive MS.
Axonal Injury May Promote Progression
Axonal injury in MS mostly occurs in small axons. The main causes of axonal loss are repeated demyelination, lack of trophic support for myelin in oligodendrocytes, Wallerian degeneration, and acute and chronic mitochondrial dysfunction, which may result from enhanced production of reactive oxygen species in macrophages and active microglia.
Mitochondria are especially susceptible to oxidative damage, and microarray gene studies have found mitochondrial dysfunction in MS. Oxidized lipids are common within active plaques and promote calcium accumulation in the axon and, hence, axonal degeneration. In cells such as oligodendrocytes, injury to the mitochondria activates apoptosis-inducible factor, which can be transferred into the nucleus. MS also causes chronic energy failure in axons, which leak current when they have been demyelinated. In a compensatory response, sodium channels increase within the axon, and mitochondria are recruited, but this response eventually fails. Demyelinated axons subsequently undergo neurodegeneration and irreversible injury, potentially leading to disease progression.
Cortical Lesions Predict Disability
“Cortical lesion load is the strongest predictor of MS disability,” said Dr. Lucchinetti. Cortical lesion load correlates with cognitive dysfunction and is present early in the disease. Approximately 40% of patients with clinically isolated syndrome have cortical lesions, which include leukocortical, intracortical, and subpial plaques.
Dr. Lucchinetti and colleagues demonstrated in one investigation that early MS lesions in the cortex are inflammatory, unlike lesions found in chronic MS. Furthermore, they found myelinated macrophages in early cortical plaques. A finding of large numbers of CD68 and CD8 cells near neurons suggests that early neurodegeneration occurs against a background of inflammation, said Dr. Lucchinetti.
Demyelination in the cortex is extensive in chronic MS. It occurs in multiple gyri and mainly affects areas involved in cognition. Research indicates that areas of cortical demyelination often are topographically related to areas in which one finds follicular light structures. “This topographical association of meningeal inflammation and cortical demyelination is striking, and it also seems to be associated with microglial activation in the underlying cortex and neuritic damage, again pointing to the fact that there is a potential soluble myelinotoxic factor mediating this aspect of MS pathology,” said Dr. Lucchinetti.
Meningeal Inflammation and Aggressive Disease
Although meningeal infiltrates may not be true follicles, meningeal inflammation is associated with greater inflammation and a shorter, more aggressive disease course. Data suggest that patients have more aggressive disease and die sooner when they have more meningeal inflammation.
In 2015, Absinta et al found that 3-T postcontrast T2-weighted FLAIR MRI may identify areas of fixed leptomeningeal inflammation. Histopathology indicated that the inflammation included perivascular lymphocytic and mononuclear infiltration in association with nearby subpial cortical demyelination. “When they looked further within these areas, they found prominent, meningeal diffuse inflammation positive for CD45 and CD68 cells,” said Dr. Lucchinetti.
The results indicate that neurologists may now have a marker to track this aspect of MS pathology, she continued. Diffuse and focal meningeal inflammation is present within days to weeks of initial presentation. This inflammation increases the likelihood of cortical demyelination and may contribute to disease progression. In a cohort of patients with early MS, meningeal inflammation was associated with subpial demyelination, similar to the association in chronic MS.
Mainero et al found that sparse areas of abnormality within the upper 25% of the brain tissue correspond with focal myelin loss or iron loss. Deeper areas of the cortex have more extensive involvement (ie, prolonged T2), and these changes are strongly associated with Expanded Disability Status Scale score. This process begins early and is not associated with white matter lesion burden, thus “highlighting the importance of this pathology to some elements of disease progression,” said Dr. Lucchinetti.
Deep Gray Matter Damage
Damage to deep gray matter in MS is focused in the caudate and the hypothalamus. As the disease progresses, it may involve the deep gray matter more extensively. Atrophy of the third ventricle is one potential way to measure the degree to which MS affects the thalamus. This atrophy seems to be associated with cognitive decline, motor deficits, and fatigue. It correlates with cortical demyelination, but not white matter demyelination.
Current approved therapies “are really targeting what we can see, [such as] inflammation and white matter plaques, but there’s much more going on,” concluded Dr. Lucchinetti.
—Erik Greb
Suggested Reading
Absinta M, Vuolo L, Rao A, et al. Gadolinium-based MRI characterization of leptomeningeal inflammation in multiple sclerosis. Neurology. 2015;85(1):18-28.
Frischer JM, Weigand SD, Guo Y, et al. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78(5):710-721.
Mainero C, Louapre C, Govindarajan ST, et al. A gradient in cortical pathology in multiple sclerosis by in vivo quantitative 7 T imaging. Brain. 2015;138(Pr 4):932-945.
Popescu BF, Lucchinetti CF. Meningeal and cortical grey matter pathology in multiple sclerosis. BMC Neurol. 2012;12:11.
NEW ORLEANS—The lack of a therapy that slows or stops disease progression represents the greatest unmet need among patients with progressive multiple sclerosis (MS), according to a lecture presented at the ACTRIMS 2016 Forum. Future therapeutics for progressive MS will need to address mechanisms such as microglial and macrophage-driven neurodegeneration, mitochondrial dysfunction, and oxidative stress, said Claudia F. Lucchinetti, MD, Professor of Neurology at Mayo Clinic in Rochester, Minnesota.
Research efforts should aim to develop drugs that treat smoldering plaques and meningeal inflammation, she added. Furthermore, patients need a therapy that protects axons and promotes remyelination. “Finally, our therapies are going to need to consider targeting both inflammation and neurodegeneration early and concurrently,” said Dr. Lucchinetti.
White Matter Plaques Indicate Disease Duration
MS progression generally affects the white matter, the axons, the cortex, the meninges, and the deep gray matter. As white matter undergoes demyelination, it may develop any of four types of plaques, including active, inactive, smoldering, and remyelinated shadow plaques. In 2015, Dr. Lucchinetti and colleagues studied autopsy results for 120 patients with MS who had 2,476 white-matter plaques. They found that most plaques in early MS were active, while inactive plaques predominated in chronic MS. Smoldering plaques were rare in early MS, but reached peak levels at 18 to 20 years’ disease duration, which is when many patients convert to secondary progressive MS. The frequency of shadow plaques was similar throughout the disease duration.
In addition, the investigators found that active plaques predominated among patients with ongoing relapses, indicating that the plaques may be “the substrate of the relapse itself,” said Dr. Lucchinetti. Active plaques were less frequent in secondary progressive MS without attacks and in primary progressive MS. Shadow plaques occurred in all clinical forms of the disease, but smoldering plaques occurred only in progressive MS.
Axonal Injury May Promote Progression
Axonal injury in MS mostly occurs in small axons. The main causes of axonal loss are repeated demyelination, lack of trophic support for myelin in oligodendrocytes, Wallerian degeneration, and acute and chronic mitochondrial dysfunction, which may result from enhanced production of reactive oxygen species in macrophages and active microglia.
Mitochondria are especially susceptible to oxidative damage, and microarray gene studies have found mitochondrial dysfunction in MS. Oxidized lipids are common within active plaques and promote calcium accumulation in the axon and, hence, axonal degeneration. In cells such as oligodendrocytes, injury to the mitochondria activates apoptosis-inducible factor, which can be transferred into the nucleus. MS also causes chronic energy failure in axons, which leak current when they have been demyelinated. In a compensatory response, sodium channels increase within the axon, and mitochondria are recruited, but this response eventually fails. Demyelinated axons subsequently undergo neurodegeneration and irreversible injury, potentially leading to disease progression.
Cortical Lesions Predict Disability
“Cortical lesion load is the strongest predictor of MS disability,” said Dr. Lucchinetti. Cortical lesion load correlates with cognitive dysfunction and is present early in the disease. Approximately 40% of patients with clinically isolated syndrome have cortical lesions, which include leukocortical, intracortical, and subpial plaques.
Dr. Lucchinetti and colleagues demonstrated in one investigation that early MS lesions in the cortex are inflammatory, unlike lesions found in chronic MS. Furthermore, they found myelinated macrophages in early cortical plaques. A finding of large numbers of CD68 and CD8 cells near neurons suggests that early neurodegeneration occurs against a background of inflammation, said Dr. Lucchinetti.
Demyelination in the cortex is extensive in chronic MS. It occurs in multiple gyri and mainly affects areas involved in cognition. Research indicates that areas of cortical demyelination often are topographically related to areas in which one finds follicular light structures. “This topographical association of meningeal inflammation and cortical demyelination is striking, and it also seems to be associated with microglial activation in the underlying cortex and neuritic damage, again pointing to the fact that there is a potential soluble myelinotoxic factor mediating this aspect of MS pathology,” said Dr. Lucchinetti.
Meningeal Inflammation and Aggressive Disease
Although meningeal infiltrates may not be true follicles, meningeal inflammation is associated with greater inflammation and a shorter, more aggressive disease course. Data suggest that patients have more aggressive disease and die sooner when they have more meningeal inflammation.
In 2015, Absinta et al found that 3-T postcontrast T2-weighted FLAIR MRI may identify areas of fixed leptomeningeal inflammation. Histopathology indicated that the inflammation included perivascular lymphocytic and mononuclear infiltration in association with nearby subpial cortical demyelination. “When they looked further within these areas, they found prominent, meningeal diffuse inflammation positive for CD45 and CD68 cells,” said Dr. Lucchinetti.
The results indicate that neurologists may now have a marker to track this aspect of MS pathology, she continued. Diffuse and focal meningeal inflammation is present within days to weeks of initial presentation. This inflammation increases the likelihood of cortical demyelination and may contribute to disease progression. In a cohort of patients with early MS, meningeal inflammation was associated with subpial demyelination, similar to the association in chronic MS.
Mainero et al found that sparse areas of abnormality within the upper 25% of the brain tissue correspond with focal myelin loss or iron loss. Deeper areas of the cortex have more extensive involvement (ie, prolonged T2), and these changes are strongly associated with Expanded Disability Status Scale score. This process begins early and is not associated with white matter lesion burden, thus “highlighting the importance of this pathology to some elements of disease progression,” said Dr. Lucchinetti.
Deep Gray Matter Damage
Damage to deep gray matter in MS is focused in the caudate and the hypothalamus. As the disease progresses, it may involve the deep gray matter more extensively. Atrophy of the third ventricle is one potential way to measure the degree to which MS affects the thalamus. This atrophy seems to be associated with cognitive decline, motor deficits, and fatigue. It correlates with cortical demyelination, but not white matter demyelination.
Current approved therapies “are really targeting what we can see, [such as] inflammation and white matter plaques, but there’s much more going on,” concluded Dr. Lucchinetti.
—Erik Greb
NEW ORLEANS—The lack of a therapy that slows or stops disease progression represents the greatest unmet need among patients with progressive multiple sclerosis (MS), according to a lecture presented at the ACTRIMS 2016 Forum. Future therapeutics for progressive MS will need to address mechanisms such as microglial and macrophage-driven neurodegeneration, mitochondrial dysfunction, and oxidative stress, said Claudia F. Lucchinetti, MD, Professor of Neurology at Mayo Clinic in Rochester, Minnesota.
Research efforts should aim to develop drugs that treat smoldering plaques and meningeal inflammation, she added. Furthermore, patients need a therapy that protects axons and promotes remyelination. “Finally, our therapies are going to need to consider targeting both inflammation and neurodegeneration early and concurrently,” said Dr. Lucchinetti.
White Matter Plaques Indicate Disease Duration
MS progression generally affects the white matter, the axons, the cortex, the meninges, and the deep gray matter. As white matter undergoes demyelination, it may develop any of four types of plaques, including active, inactive, smoldering, and remyelinated shadow plaques. In 2015, Dr. Lucchinetti and colleagues studied autopsy results for 120 patients with MS who had 2,476 white-matter plaques. They found that most plaques in early MS were active, while inactive plaques predominated in chronic MS. Smoldering plaques were rare in early MS, but reached peak levels at 18 to 20 years’ disease duration, which is when many patients convert to secondary progressive MS. The frequency of shadow plaques was similar throughout the disease duration.
In addition, the investigators found that active plaques predominated among patients with ongoing relapses, indicating that the plaques may be “the substrate of the relapse itself,” said Dr. Lucchinetti. Active plaques were less frequent in secondary progressive MS without attacks and in primary progressive MS. Shadow plaques occurred in all clinical forms of the disease, but smoldering plaques occurred only in progressive MS.
Axonal Injury May Promote Progression
Axonal injury in MS mostly occurs in small axons. The main causes of axonal loss are repeated demyelination, lack of trophic support for myelin in oligodendrocytes, Wallerian degeneration, and acute and chronic mitochondrial dysfunction, which may result from enhanced production of reactive oxygen species in macrophages and active microglia.
Mitochondria are especially susceptible to oxidative damage, and microarray gene studies have found mitochondrial dysfunction in MS. Oxidized lipids are common within active plaques and promote calcium accumulation in the axon and, hence, axonal degeneration. In cells such as oligodendrocytes, injury to the mitochondria activates apoptosis-inducible factor, which can be transferred into the nucleus. MS also causes chronic energy failure in axons, which leak current when they have been demyelinated. In a compensatory response, sodium channels increase within the axon, and mitochondria are recruited, but this response eventually fails. Demyelinated axons subsequently undergo neurodegeneration and irreversible injury, potentially leading to disease progression.
Cortical Lesions Predict Disability
“Cortical lesion load is the strongest predictor of MS disability,” said Dr. Lucchinetti. Cortical lesion load correlates with cognitive dysfunction and is present early in the disease. Approximately 40% of patients with clinically isolated syndrome have cortical lesions, which include leukocortical, intracortical, and subpial plaques.
Dr. Lucchinetti and colleagues demonstrated in one investigation that early MS lesions in the cortex are inflammatory, unlike lesions found in chronic MS. Furthermore, they found myelinated macrophages in early cortical plaques. A finding of large numbers of CD68 and CD8 cells near neurons suggests that early neurodegeneration occurs against a background of inflammation, said Dr. Lucchinetti.
Demyelination in the cortex is extensive in chronic MS. It occurs in multiple gyri and mainly affects areas involved in cognition. Research indicates that areas of cortical demyelination often are topographically related to areas in which one finds follicular light structures. “This topographical association of meningeal inflammation and cortical demyelination is striking, and it also seems to be associated with microglial activation in the underlying cortex and neuritic damage, again pointing to the fact that there is a potential soluble myelinotoxic factor mediating this aspect of MS pathology,” said Dr. Lucchinetti.
Meningeal Inflammation and Aggressive Disease
Although meningeal infiltrates may not be true follicles, meningeal inflammation is associated with greater inflammation and a shorter, more aggressive disease course. Data suggest that patients have more aggressive disease and die sooner when they have more meningeal inflammation.
In 2015, Absinta et al found that 3-T postcontrast T2-weighted FLAIR MRI may identify areas of fixed leptomeningeal inflammation. Histopathology indicated that the inflammation included perivascular lymphocytic and mononuclear infiltration in association with nearby subpial cortical demyelination. “When they looked further within these areas, they found prominent, meningeal diffuse inflammation positive for CD45 and CD68 cells,” said Dr. Lucchinetti.
The results indicate that neurologists may now have a marker to track this aspect of MS pathology, she continued. Diffuse and focal meningeal inflammation is present within days to weeks of initial presentation. This inflammation increases the likelihood of cortical demyelination and may contribute to disease progression. In a cohort of patients with early MS, meningeal inflammation was associated with subpial demyelination, similar to the association in chronic MS.
Mainero et al found that sparse areas of abnormality within the upper 25% of the brain tissue correspond with focal myelin loss or iron loss. Deeper areas of the cortex have more extensive involvement (ie, prolonged T2), and these changes are strongly associated with Expanded Disability Status Scale score. This process begins early and is not associated with white matter lesion burden, thus “highlighting the importance of this pathology to some elements of disease progression,” said Dr. Lucchinetti.
Deep Gray Matter Damage
Damage to deep gray matter in MS is focused in the caudate and the hypothalamus. As the disease progresses, it may involve the deep gray matter more extensively. Atrophy of the third ventricle is one potential way to measure the degree to which MS affects the thalamus. This atrophy seems to be associated with cognitive decline, motor deficits, and fatigue. It correlates with cortical demyelination, but not white matter demyelination.
Current approved therapies “are really targeting what we can see, [such as] inflammation and white matter plaques, but there’s much more going on,” concluded Dr. Lucchinetti.
—Erik Greb
Suggested Reading
Absinta M, Vuolo L, Rao A, et al. Gadolinium-based MRI characterization of leptomeningeal inflammation in multiple sclerosis. Neurology. 2015;85(1):18-28.
Frischer JM, Weigand SD, Guo Y, et al. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78(5):710-721.
Mainero C, Louapre C, Govindarajan ST, et al. A gradient in cortical pathology in multiple sclerosis by in vivo quantitative 7 T imaging. Brain. 2015;138(Pr 4):932-945.
Popescu BF, Lucchinetti CF. Meningeal and cortical grey matter pathology in multiple sclerosis. BMC Neurol. 2012;12:11.
Suggested Reading
Absinta M, Vuolo L, Rao A, et al. Gadolinium-based MRI characterization of leptomeningeal inflammation in multiple sclerosis. Neurology. 2015;85(1):18-28.
Frischer JM, Weigand SD, Guo Y, et al. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78(5):710-721.
Mainero C, Louapre C, Govindarajan ST, et al. A gradient in cortical pathology in multiple sclerosis by in vivo quantitative 7 T imaging. Brain. 2015;138(Pr 4):932-945.
Popescu BF, Lucchinetti CF. Meningeal and cortical grey matter pathology in multiple sclerosis. BMC Neurol. 2012;12:11.