User login
Reports of my departure are premature
Busy day at the office. Five different people asked when I plan to retire.
Dennis was first. I last saw him a year ago, as I’d been doing annually for 25 years. A few months later, he asked to have his records sent to his home. There was no obvious reason. Now he was back.
“I had an eventful year, medically,” he said. “You know, that biopsy you did on my nose was precancerous.”
I did know that. I had called him with the results. It was an actinic keratosis. I’d asked him to come back in a few months for me to recheck the area.
“I went to see another doctor,” he said. “He gave me a cream that made my skin turn red. I think it worked.”
It must have. After all, the keratosis had already been removed.
“But I didn’t like his office,” said Dennis, “so I decided to come back to you.”
Touching, I thought. “Nice to see you,” I said.
“I wanted a younger doctor,” said Dennis. “Someone who would be around for a while.”
“Well, I’m not planning to retire just yet.”
“Everyone retires eventually,” said Dennis.
“Yes,” I agreed. “I guess they do. See you next year.” Perhaps.
Well, that felt pretty good. Then I went in to see Phil.
“Good morning,” he said. “Are you thinking about retiring?”
“Not really,” I said.
“How old are you?” asked Phil.
“68,” I said.
Phil took a long look at me. “You look good,” he decided.
You don’t have to sound so surprised, I thought.
An hour later I saw Emma.
“I see you haven’t retired yet,” she said.
“No,” I replied. “It seems I haven’t. Would you like me to?”
“Oh, no!” said Emma. “I was just wondering. A lot of my doctors have been retiring.”
There it was. Fear of abandonment. Who will be there for me? I wanted to hold Emma’s hand and assure her that when the time came, someone would indeed be there for her when I wasn’t. But I didn’t. Like grown children, patients have to find out things like that for themselves.
A little later Mabel came by. Her rash was worrying her. “I saw a couple of doctors about it, but they didn’t seem to know what it was,” she said.
“It’s eczema,” I told her. “This is what I suggest you do.” I made some suggestions.
“I was here once before,” she said, “in the 80s. Then, when I couldn’t figure out what this rash I have was, I remembered your name. ‘No,’ I thought to myself. ‘He couldn’t possibly still be practicing.’ And then I found out that you were!”
Well, there you go.
This kind of thing can give you a complex. If so many people are surprised that you’re around, maybe you shouldn’t be. But the best was yet to come.
The last patient of the day was Jenna.
I introduced myself. “How did you get my name?” I asked. Nowadays, the most common answer I get goes something like, “I Googled you. I recognized your address and you got decent reviews.”
But Jenna answered, “My sister came here 10 years ago. She used to be a patient of Dr. Alvin Sherwin.”
“I took over Dr. Sherwin’s practice when he moved to Florida,” I told her. “That was in 1981, so it’s closer to 35 years ago, not 10.”
“My goodness,” she said. “That explains what my sister said.”
“What did your sister say?”
“Well, my mother found your name on a piece of paper. My mother likes to hold onto things.”
“I’ll say she does,” I said.
“My mother said, ‘Why don’t you call this guy Rockoff? He took care of your sister. He’s very good.’ So I looked you up and found your office.
“Anyway,” Jenna went on, “when I told my sister that I found you, she said, ‘Yes, I remember seeing him. You mean he’s still around? After all these years, I figured he was probably dead.’ ”
“Nope,” I said. “Not yet.”
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
Busy day at the office. Five different people asked when I plan to retire.
Dennis was first. I last saw him a year ago, as I’d been doing annually for 25 years. A few months later, he asked to have his records sent to his home. There was no obvious reason. Now he was back.
“I had an eventful year, medically,” he said. “You know, that biopsy you did on my nose was precancerous.”
I did know that. I had called him with the results. It was an actinic keratosis. I’d asked him to come back in a few months for me to recheck the area.
“I went to see another doctor,” he said. “He gave me a cream that made my skin turn red. I think it worked.”
It must have. After all, the keratosis had already been removed.
“But I didn’t like his office,” said Dennis, “so I decided to come back to you.”
Touching, I thought. “Nice to see you,” I said.
“I wanted a younger doctor,” said Dennis. “Someone who would be around for a while.”
“Well, I’m not planning to retire just yet.”
“Everyone retires eventually,” said Dennis.
“Yes,” I agreed. “I guess they do. See you next year.” Perhaps.
Well, that felt pretty good. Then I went in to see Phil.
“Good morning,” he said. “Are you thinking about retiring?”
“Not really,” I said.
“How old are you?” asked Phil.
“68,” I said.
Phil took a long look at me. “You look good,” he decided.
You don’t have to sound so surprised, I thought.
An hour later I saw Emma.
“I see you haven’t retired yet,” she said.
“No,” I replied. “It seems I haven’t. Would you like me to?”
“Oh, no!” said Emma. “I was just wondering. A lot of my doctors have been retiring.”
There it was. Fear of abandonment. Who will be there for me? I wanted to hold Emma’s hand and assure her that when the time came, someone would indeed be there for her when I wasn’t. But I didn’t. Like grown children, patients have to find out things like that for themselves.
A little later Mabel came by. Her rash was worrying her. “I saw a couple of doctors about it, but they didn’t seem to know what it was,” she said.
“It’s eczema,” I told her. “This is what I suggest you do.” I made some suggestions.
“I was here once before,” she said, “in the 80s. Then, when I couldn’t figure out what this rash I have was, I remembered your name. ‘No,’ I thought to myself. ‘He couldn’t possibly still be practicing.’ And then I found out that you were!”
Well, there you go.
This kind of thing can give you a complex. If so many people are surprised that you’re around, maybe you shouldn’t be. But the best was yet to come.
The last patient of the day was Jenna.
I introduced myself. “How did you get my name?” I asked. Nowadays, the most common answer I get goes something like, “I Googled you. I recognized your address and you got decent reviews.”
But Jenna answered, “My sister came here 10 years ago. She used to be a patient of Dr. Alvin Sherwin.”
“I took over Dr. Sherwin’s practice when he moved to Florida,” I told her. “That was in 1981, so it’s closer to 35 years ago, not 10.”
“My goodness,” she said. “That explains what my sister said.”
“What did your sister say?”
“Well, my mother found your name on a piece of paper. My mother likes to hold onto things.”
“I’ll say she does,” I said.
“My mother said, ‘Why don’t you call this guy Rockoff? He took care of your sister. He’s very good.’ So I looked you up and found your office.
“Anyway,” Jenna went on, “when I told my sister that I found you, she said, ‘Yes, I remember seeing him. You mean he’s still around? After all these years, I figured he was probably dead.’ ”
“Nope,” I said. “Not yet.”
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
Busy day at the office. Five different people asked when I plan to retire.
Dennis was first. I last saw him a year ago, as I’d been doing annually for 25 years. A few months later, he asked to have his records sent to his home. There was no obvious reason. Now he was back.
“I had an eventful year, medically,” he said. “You know, that biopsy you did on my nose was precancerous.”
I did know that. I had called him with the results. It was an actinic keratosis. I’d asked him to come back in a few months for me to recheck the area.
“I went to see another doctor,” he said. “He gave me a cream that made my skin turn red. I think it worked.”
It must have. After all, the keratosis had already been removed.
“But I didn’t like his office,” said Dennis, “so I decided to come back to you.”
Touching, I thought. “Nice to see you,” I said.
“I wanted a younger doctor,” said Dennis. “Someone who would be around for a while.”
“Well, I’m not planning to retire just yet.”
“Everyone retires eventually,” said Dennis.
“Yes,” I agreed. “I guess they do. See you next year.” Perhaps.
Well, that felt pretty good. Then I went in to see Phil.
“Good morning,” he said. “Are you thinking about retiring?”
“Not really,” I said.
“How old are you?” asked Phil.
“68,” I said.
Phil took a long look at me. “You look good,” he decided.
You don’t have to sound so surprised, I thought.
An hour later I saw Emma.
“I see you haven’t retired yet,” she said.
“No,” I replied. “It seems I haven’t. Would you like me to?”
“Oh, no!” said Emma. “I was just wondering. A lot of my doctors have been retiring.”
There it was. Fear of abandonment. Who will be there for me? I wanted to hold Emma’s hand and assure her that when the time came, someone would indeed be there for her when I wasn’t. But I didn’t. Like grown children, patients have to find out things like that for themselves.
A little later Mabel came by. Her rash was worrying her. “I saw a couple of doctors about it, but they didn’t seem to know what it was,” she said.
“It’s eczema,” I told her. “This is what I suggest you do.” I made some suggestions.
“I was here once before,” she said, “in the 80s. Then, when I couldn’t figure out what this rash I have was, I remembered your name. ‘No,’ I thought to myself. ‘He couldn’t possibly still be practicing.’ And then I found out that you were!”
Well, there you go.
This kind of thing can give you a complex. If so many people are surprised that you’re around, maybe you shouldn’t be. But the best was yet to come.
The last patient of the day was Jenna.
I introduced myself. “How did you get my name?” I asked. Nowadays, the most common answer I get goes something like, “I Googled you. I recognized your address and you got decent reviews.”
But Jenna answered, “My sister came here 10 years ago. She used to be a patient of Dr. Alvin Sherwin.”
“I took over Dr. Sherwin’s practice when he moved to Florida,” I told her. “That was in 1981, so it’s closer to 35 years ago, not 10.”
“My goodness,” she said. “That explains what my sister said.”
“What did your sister say?”
“Well, my mother found your name on a piece of paper. My mother likes to hold onto things.”
“I’ll say she does,” I said.
“My mother said, ‘Why don’t you call this guy Rockoff? He took care of your sister. He’s very good.’ So I looked you up and found your office.
“Anyway,” Jenna went on, “when I told my sister that I found you, she said, ‘Yes, I remember seeing him. You mean he’s still around? After all these years, I figured he was probably dead.’ ”
“Nope,” I said. “Not yet.”
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
New ACC/AHA/HRS Guideline for Management of SVT
NEW YORK - Catheter ablation is favored for the management of most forms of supraventricular tachycardia (SVT) in adults, according to revised guidelines from the American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS).
SVT affects 2.25 in 1000 individuals in the general population, with about 89,000 new cases of paroxysmal SVT (PSVT) per year. Women are twice as likely as men and individuals older than 65 are more than five times as likely as younger people to develop PSVT.
To provide a contemporary guideline for managing adults with all types of SVT except atrial fibrillation, ACC/AHA/HRS have now updated their 2003 guidelines.
Included are recommendations for managing sinus tachyarrhythmias, nonsinus focal atrial tachycardia and multifocal atrial tachycardia (MAT), atrioventricular nodal reentrant tachycardia (AVNRT), manifest and concealed accessory pathways, atrial flutter, and junctional tachycardia.
"Despite a 12-year gap in the update for these guidelines, there have been very few advances in antiarrhythmic drug therapy to offer patients with SVT," Dr. Gregory F. Michaud, director of the Center for Advanced Management of Atrial Fibrillation at Brigham and Women's Hospital in Boston, said by email.
"Catheter ablation has taken a stronger foothold in the chronic treatment of SVT and as such many physicians and patients are opting for invasive therapy earlier in the course of therapy," said Dr. Michaud, who wasn't involved in the guidelines.
The guidelines recommend vagal maneuvers, various drugs, and/or cardioversion as acute treatments, depending on the specific cause of SVT.
For most forms of symptomatic SVT, including those of unknown mechanism, the guidelines recommend electrophysiological (EP) studies and catheter ablation as definitive treatment for patients willing to undergo them, especially if medical therapy is ineffective.
Cardiac mapping is performed during EP studies to identify the site of origin of the arrhythmia or areas of critical conduction to allow targeting of ablation.
"One exception is inappropriate sinus tachycardia (IST) for which a more effective drug, ivabradine, is now available in the United States," Dr. Michaud said. "Catheter ablation is generally ineffective for IST patients."
Besides evaluation and treatment of possible reversible causes of IST, the guidelines recommend ivabradine, beta blockers, or their combination.
"SVT is generally not a life-threatening condition and treatment is based on eliminating symptoms and improving patient quality of life," Dr. Michaud explained. "However, physicians should be aware of three conditions associated with SVT that may be serious. First, sudden death is associated with the WPW (Wolff-Parkinson-White) syndrome and these patients, even if asymptomatic, should be referred to a cardiac electrophysiologist to consider management options."
He continued, "Second, SVT can cause cardiomyopathy and heart failure when incessant, even if the patient is asymptomatic. These patients should also be referred to a cardiac electrophysiologist to consider definitive therapy.
Third, patients with atrial flutter should be considered for oral anticoagulation to prevent stroke using the CHADS-Vasc risk scoring system, just as you would for patients with atrial fibrillation."
Dr. Michaud added, "Putting aside cost as an issue, there is significant regional variability in the accessibility of electrophysiologists or cardiologists with arrhythmia expertise. In my area, for instance, electrophysiologists are plentiful, and patients with SVT are often sent to us directly for further evaluation and treatment. Furthermore, training in arrhythmia management has become the purview of clinical cardiac electrophysiology, and many recently trained cardiologists are not as comfortable as their predecessors in managing patients with SVT."
The full report appears in the September 23 Journal of the American College of Cardiology online and was copublished in Circulation and Heart Rhythm.
Dr. Richard L. Page and Dr. Jose A. Joglar, chair and vice chair of the writing committee, did not respond to a request for comments.
NEW YORK - Catheter ablation is favored for the management of most forms of supraventricular tachycardia (SVT) in adults, according to revised guidelines from the American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS).
SVT affects 2.25 in 1000 individuals in the general population, with about 89,000 new cases of paroxysmal SVT (PSVT) per year. Women are twice as likely as men and individuals older than 65 are more than five times as likely as younger people to develop PSVT.
To provide a contemporary guideline for managing adults with all types of SVT except atrial fibrillation, ACC/AHA/HRS have now updated their 2003 guidelines.
Included are recommendations for managing sinus tachyarrhythmias, nonsinus focal atrial tachycardia and multifocal atrial tachycardia (MAT), atrioventricular nodal reentrant tachycardia (AVNRT), manifest and concealed accessory pathways, atrial flutter, and junctional tachycardia.
"Despite a 12-year gap in the update for these guidelines, there have been very few advances in antiarrhythmic drug therapy to offer patients with SVT," Dr. Gregory F. Michaud, director of the Center for Advanced Management of Atrial Fibrillation at Brigham and Women's Hospital in Boston, said by email.
"Catheter ablation has taken a stronger foothold in the chronic treatment of SVT and as such many physicians and patients are opting for invasive therapy earlier in the course of therapy," said Dr. Michaud, who wasn't involved in the guidelines.
The guidelines recommend vagal maneuvers, various drugs, and/or cardioversion as acute treatments, depending on the specific cause of SVT.
For most forms of symptomatic SVT, including those of unknown mechanism, the guidelines recommend electrophysiological (EP) studies and catheter ablation as definitive treatment for patients willing to undergo them, especially if medical therapy is ineffective.
Cardiac mapping is performed during EP studies to identify the site of origin of the arrhythmia or areas of critical conduction to allow targeting of ablation.
"One exception is inappropriate sinus tachycardia (IST) for which a more effective drug, ivabradine, is now available in the United States," Dr. Michaud said. "Catheter ablation is generally ineffective for IST patients."
Besides evaluation and treatment of possible reversible causes of IST, the guidelines recommend ivabradine, beta blockers, or their combination.
"SVT is generally not a life-threatening condition and treatment is based on eliminating symptoms and improving patient quality of life," Dr. Michaud explained. "However, physicians should be aware of three conditions associated with SVT that may be serious. First, sudden death is associated with the WPW (Wolff-Parkinson-White) syndrome and these patients, even if asymptomatic, should be referred to a cardiac electrophysiologist to consider management options."
He continued, "Second, SVT can cause cardiomyopathy and heart failure when incessant, even if the patient is asymptomatic. These patients should also be referred to a cardiac electrophysiologist to consider definitive therapy.
Third, patients with atrial flutter should be considered for oral anticoagulation to prevent stroke using the CHADS-Vasc risk scoring system, just as you would for patients with atrial fibrillation."
Dr. Michaud added, "Putting aside cost as an issue, there is significant regional variability in the accessibility of electrophysiologists or cardiologists with arrhythmia expertise. In my area, for instance, electrophysiologists are plentiful, and patients with SVT are often sent to us directly for further evaluation and treatment. Furthermore, training in arrhythmia management has become the purview of clinical cardiac electrophysiology, and many recently trained cardiologists are not as comfortable as their predecessors in managing patients with SVT."
The full report appears in the September 23 Journal of the American College of Cardiology online and was copublished in Circulation and Heart Rhythm.
Dr. Richard L. Page and Dr. Jose A. Joglar, chair and vice chair of the writing committee, did not respond to a request for comments.
NEW YORK - Catheter ablation is favored for the management of most forms of supraventricular tachycardia (SVT) in adults, according to revised guidelines from the American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS).
SVT affects 2.25 in 1000 individuals in the general population, with about 89,000 new cases of paroxysmal SVT (PSVT) per year. Women are twice as likely as men and individuals older than 65 are more than five times as likely as younger people to develop PSVT.
To provide a contemporary guideline for managing adults with all types of SVT except atrial fibrillation, ACC/AHA/HRS have now updated their 2003 guidelines.
Included are recommendations for managing sinus tachyarrhythmias, nonsinus focal atrial tachycardia and multifocal atrial tachycardia (MAT), atrioventricular nodal reentrant tachycardia (AVNRT), manifest and concealed accessory pathways, atrial flutter, and junctional tachycardia.
"Despite a 12-year gap in the update for these guidelines, there have been very few advances in antiarrhythmic drug therapy to offer patients with SVT," Dr. Gregory F. Michaud, director of the Center for Advanced Management of Atrial Fibrillation at Brigham and Women's Hospital in Boston, said by email.
"Catheter ablation has taken a stronger foothold in the chronic treatment of SVT and as such many physicians and patients are opting for invasive therapy earlier in the course of therapy," said Dr. Michaud, who wasn't involved in the guidelines.
The guidelines recommend vagal maneuvers, various drugs, and/or cardioversion as acute treatments, depending on the specific cause of SVT.
For most forms of symptomatic SVT, including those of unknown mechanism, the guidelines recommend electrophysiological (EP) studies and catheter ablation as definitive treatment for patients willing to undergo them, especially if medical therapy is ineffective.
Cardiac mapping is performed during EP studies to identify the site of origin of the arrhythmia or areas of critical conduction to allow targeting of ablation.
"One exception is inappropriate sinus tachycardia (IST) for which a more effective drug, ivabradine, is now available in the United States," Dr. Michaud said. "Catheter ablation is generally ineffective for IST patients."
Besides evaluation and treatment of possible reversible causes of IST, the guidelines recommend ivabradine, beta blockers, or their combination.
"SVT is generally not a life-threatening condition and treatment is based on eliminating symptoms and improving patient quality of life," Dr. Michaud explained. "However, physicians should be aware of three conditions associated with SVT that may be serious. First, sudden death is associated with the WPW (Wolff-Parkinson-White) syndrome and these patients, even if asymptomatic, should be referred to a cardiac electrophysiologist to consider management options."
He continued, "Second, SVT can cause cardiomyopathy and heart failure when incessant, even if the patient is asymptomatic. These patients should also be referred to a cardiac electrophysiologist to consider definitive therapy.
Third, patients with atrial flutter should be considered for oral anticoagulation to prevent stroke using the CHADS-Vasc risk scoring system, just as you would for patients with atrial fibrillation."
Dr. Michaud added, "Putting aside cost as an issue, there is significant regional variability in the accessibility of electrophysiologists or cardiologists with arrhythmia expertise. In my area, for instance, electrophysiologists are plentiful, and patients with SVT are often sent to us directly for further evaluation and treatment. Furthermore, training in arrhythmia management has become the purview of clinical cardiac electrophysiology, and many recently trained cardiologists are not as comfortable as their predecessors in managing patients with SVT."
The full report appears in the September 23 Journal of the American College of Cardiology online and was copublished in Circulation and Heart Rhythm.
Dr. Richard L. Page and Dr. Jose A. Joglar, chair and vice chair of the writing committee, did not respond to a request for comments.
The Power of Art in Medicine: The Patient Listening Project
[[{"attributes":{},"fields":{}}]]

Author
Lynn McKinley-Grant, MD
Associate Professor of Clinical Medicine/Dermatology
Georgetown University School of Medicine
Dr. McKinley-Grant discloses that she is a consultant for the Insight Institute and Novartis Pharmaceuticals Corporation.
Link
Click here to download this supplement.
12/15 XDP-1319483
[[{"attributes":{},"fields":{}}]]

Author
Lynn McKinley-Grant, MD
Associate Professor of Clinical Medicine/Dermatology
Georgetown University School of Medicine
Dr. McKinley-Grant discloses that she is a consultant for the Insight Institute and Novartis Pharmaceuticals Corporation.
Link
Click here to download this supplement.
12/15 XDP-1319483
[[{"attributes":{},"fields":{}}]]

Author
Lynn McKinley-Grant, MD
Associate Professor of Clinical Medicine/Dermatology
Georgetown University School of Medicine
Dr. McKinley-Grant discloses that she is a consultant for the Insight Institute and Novartis Pharmaceuticals Corporation.
Link
Click here to download this supplement.
12/15 XDP-1319483
New insight into infection-driven thrombosis
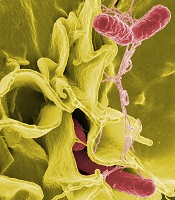
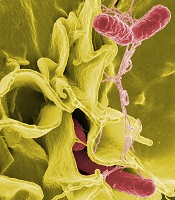
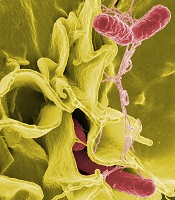
invading cultured human cells
Image courtesy of Rocky
Mountain Laboratories/NIAID
Preclinical research has shown how Salmonella infections that spread to the blood and organs can lead to life-threatening thrombosis.
Experiments in mice demonstrated that systemic infections prompt inflammation, which leads to thrombosis.
However, the sustained threat from thrombosis is independent of the continued presence of infection and instead parallels the regulation of inflammation within the host.
These findings, published in The Journal of Clinical Investigation, shed light on a poorly understood area of clinical medicine.
While some of the mechanisms that underpin the process of infection-driven thrombosis are known, particularly for Gram-positive organisms such as Staphylococci or Streptococci, they are not universally applicable.
Moreover, during sepsis, the causative pathogen is often never isolated or identified. The new study helps to explain why this is the case.
“For all of the advances we’ve made in this field, it is not always clear why people die from infection,” said study author Adam Cunningham, PhD, of the University of Birmingham in the UK.
“We think complications of thrombosis may be one reason. In Salmonella infections, severity is typically associated with the presence of bacteria in the blood, called bacteremia, even though the actual numbers of bacteria in the blood are very low. This suggested to us that the host response was crucial in determining the outcome.”
Dr Cunningham and his colleagues found that thrombi developed within the liver of murine models infected with Salmonella Typhimurium, and these thrombi persisted for many weeks.
The infection caused inflammation in the liver tissue, which then triggered thrombosis within vessels. This occurred via the ligation of C-type lectin-like receptor-2 (CLEC-2) on platelets by podoplanin, a molecule that is ordinarily absent in blood vessels but is expressed by macrophages responding to the infection.
The regulation and amplification of thrombosis was triggered by TLR4, a protein essential for the activation of the inflammatory cascade and the control of infection during its early stages.
Thrombosis remained at peak levels even when bacteria were absent from the blood and largely cleared from the infected organs.
“A little, controlled thrombosis is probably a good thing, as it helps to clear bacteria from the blood,” said study author Steve Watson, PhD, of the University of Birmingham.
“Therefore, any intervention would need to control, rather than deny, the host response. The problem only comes when it develops into a clot. Most of the current approaches to counter the development of these life-threatening thrombi do not account for the non-classical mechanism that we have shown to be at work.”
The researchers are now working to further understand how to manipulate and control this response, and how it can contribute to the complications of other infections and diseases. ![]()
invading cultured human cells
Image courtesy of Rocky
Mountain Laboratories/NIAID
Preclinical research has shown how Salmonella infections that spread to the blood and organs can lead to life-threatening thrombosis.
Experiments in mice demonstrated that systemic infections prompt inflammation, which leads to thrombosis.
However, the sustained threat from thrombosis is independent of the continued presence of infection and instead parallels the regulation of inflammation within the host.
These findings, published in The Journal of Clinical Investigation, shed light on a poorly understood area of clinical medicine.
While some of the mechanisms that underpin the process of infection-driven thrombosis are known, particularly for Gram-positive organisms such as Staphylococci or Streptococci, they are not universally applicable.
Moreover, during sepsis, the causative pathogen is often never isolated or identified. The new study helps to explain why this is the case.
“For all of the advances we’ve made in this field, it is not always clear why people die from infection,” said study author Adam Cunningham, PhD, of the University of Birmingham in the UK.
“We think complications of thrombosis may be one reason. In Salmonella infections, severity is typically associated with the presence of bacteria in the blood, called bacteremia, even though the actual numbers of bacteria in the blood are very low. This suggested to us that the host response was crucial in determining the outcome.”
Dr Cunningham and his colleagues found that thrombi developed within the liver of murine models infected with Salmonella Typhimurium, and these thrombi persisted for many weeks.
The infection caused inflammation in the liver tissue, which then triggered thrombosis within vessels. This occurred via the ligation of C-type lectin-like receptor-2 (CLEC-2) on platelets by podoplanin, a molecule that is ordinarily absent in blood vessels but is expressed by macrophages responding to the infection.
The regulation and amplification of thrombosis was triggered by TLR4, a protein essential for the activation of the inflammatory cascade and the control of infection during its early stages.
Thrombosis remained at peak levels even when bacteria were absent from the blood and largely cleared from the infected organs.
“A little, controlled thrombosis is probably a good thing, as it helps to clear bacteria from the blood,” said study author Steve Watson, PhD, of the University of Birmingham.
“Therefore, any intervention would need to control, rather than deny, the host response. The problem only comes when it develops into a clot. Most of the current approaches to counter the development of these life-threatening thrombi do not account for the non-classical mechanism that we have shown to be at work.”
The researchers are now working to further understand how to manipulate and control this response, and how it can contribute to the complications of other infections and diseases. ![]()
invading cultured human cells
Image courtesy of Rocky
Mountain Laboratories/NIAID
Preclinical research has shown how Salmonella infections that spread to the blood and organs can lead to life-threatening thrombosis.
Experiments in mice demonstrated that systemic infections prompt inflammation, which leads to thrombosis.
However, the sustained threat from thrombosis is independent of the continued presence of infection and instead parallels the regulation of inflammation within the host.
These findings, published in The Journal of Clinical Investigation, shed light on a poorly understood area of clinical medicine.
While some of the mechanisms that underpin the process of infection-driven thrombosis are known, particularly for Gram-positive organisms such as Staphylococci or Streptococci, they are not universally applicable.
Moreover, during sepsis, the causative pathogen is often never isolated or identified. The new study helps to explain why this is the case.
“For all of the advances we’ve made in this field, it is not always clear why people die from infection,” said study author Adam Cunningham, PhD, of the University of Birmingham in the UK.
“We think complications of thrombosis may be one reason. In Salmonella infections, severity is typically associated with the presence of bacteria in the blood, called bacteremia, even though the actual numbers of bacteria in the blood are very low. This suggested to us that the host response was crucial in determining the outcome.”
Dr Cunningham and his colleagues found that thrombi developed within the liver of murine models infected with Salmonella Typhimurium, and these thrombi persisted for many weeks.
The infection caused inflammation in the liver tissue, which then triggered thrombosis within vessels. This occurred via the ligation of C-type lectin-like receptor-2 (CLEC-2) on platelets by podoplanin, a molecule that is ordinarily absent in blood vessels but is expressed by macrophages responding to the infection.
The regulation and amplification of thrombosis was triggered by TLR4, a protein essential for the activation of the inflammatory cascade and the control of infection during its early stages.
Thrombosis remained at peak levels even when bacteria were absent from the blood and largely cleared from the infected organs.
“A little, controlled thrombosis is probably a good thing, as it helps to clear bacteria from the blood,” said study author Steve Watson, PhD, of the University of Birmingham.
“Therefore, any intervention would need to control, rather than deny, the host response. The problem only comes when it develops into a clot. Most of the current approaches to counter the development of these life-threatening thrombi do not account for the non-classical mechanism that we have shown to be at work.”
The researchers are now working to further understand how to manipulate and control this response, and how it can contribute to the complications of other infections and diseases. ![]()
FDA approves first monoclonal antibody for MM

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has granted accelerated approval for daratumumab (Darzalex).
The drug is now approved to treat patients with multiple myeloma (MM) who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are double-refractory to a proteasome inhibitor and an immunomodulatory agent.
Daratumumab is the first monoclonal antibody approved to treat MM.
The drug works by binding to CD38 on the surface of MM cells. It triggers the patient’s own immune system to attack MM cells, resulting in cell death through multiple mechanisms of action.
Daratumumab is being developed by Janssen Biotech. The drug was previously granted breakthrough designation, orphan designation, and priority review from the FDA.
Daratumumab was approved under the FDA’s accelerated approval program, which allows the agency to approve a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
As a condition of this accelerated approval, Janssen is required to conduct a multicenter, randomized trial establishing the superiority of daratumumab over standard therapy to verify and describe the clinical benefit of daratumumab. Janssen has several ongoing, multicenter, randomized trials with a primary endpoint of progression-free survival.
The recommended dose and schedule for daratumumab is 16 mg/kg once every week for 8 weeks, then once every 2 weeks for 16 weeks, then once every 4 weeks until disease progression.
The FDA said blood banks should be informed that patients are receiving daratumumab because the drug may interfere with tests such as antibody screening.
In addition, women who are pregnant should not use daratumumab, and women planning to become pregnant should use effective contraceptives during and for at least 3 months after stopping daratumumab.
Trial data
The FDA’s approval of daratumumab was based on results of 2 studies—the phase 2 MMY2002 (SIRIUS) study and the phase 1/2 GEN501 study.
The GEN501 study enrolled 102 patients with relapsed MM or relapsed MM that was refractory to 2 or more prior lines of therapy. The patients received daratumumab at a range of doses and on a number of different schedules.
The results suggested that daratumumab is most effective at a dose of 16 mg/kg. At this dose, the overall response rate was 36%.
Most adverse events in this study were grade 1 or 2, although serious events did occur.
The SIRIUS study enrolled 124 MM patients who had received 3 or more prior lines of therapy. They received daratumumab at different doses and on different schedules, but 106 of the patients received the drug at 16 mg/kg.
Twenty-nine percent of the 106 patients responded to treatment, and the median duration of response was 7 months. Thirty percent of patients experienced serious adverse events. ![]()

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has granted accelerated approval for daratumumab (Darzalex).
The drug is now approved to treat patients with multiple myeloma (MM) who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are double-refractory to a proteasome inhibitor and an immunomodulatory agent.
Daratumumab is the first monoclonal antibody approved to treat MM.
The drug works by binding to CD38 on the surface of MM cells. It triggers the patient’s own immune system to attack MM cells, resulting in cell death through multiple mechanisms of action.
Daratumumab is being developed by Janssen Biotech. The drug was previously granted breakthrough designation, orphan designation, and priority review from the FDA.
Daratumumab was approved under the FDA’s accelerated approval program, which allows the agency to approve a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
As a condition of this accelerated approval, Janssen is required to conduct a multicenter, randomized trial establishing the superiority of daratumumab over standard therapy to verify and describe the clinical benefit of daratumumab. Janssen has several ongoing, multicenter, randomized trials with a primary endpoint of progression-free survival.
The recommended dose and schedule for daratumumab is 16 mg/kg once every week for 8 weeks, then once every 2 weeks for 16 weeks, then once every 4 weeks until disease progression.
The FDA said blood banks should be informed that patients are receiving daratumumab because the drug may interfere with tests such as antibody screening.
In addition, women who are pregnant should not use daratumumab, and women planning to become pregnant should use effective contraceptives during and for at least 3 months after stopping daratumumab.
Trial data
The FDA’s approval of daratumumab was based on results of 2 studies—the phase 2 MMY2002 (SIRIUS) study and the phase 1/2 GEN501 study.
The GEN501 study enrolled 102 patients with relapsed MM or relapsed MM that was refractory to 2 or more prior lines of therapy. The patients received daratumumab at a range of doses and on a number of different schedules.
The results suggested that daratumumab is most effective at a dose of 16 mg/kg. At this dose, the overall response rate was 36%.
Most adverse events in this study were grade 1 or 2, although serious events did occur.
The SIRIUS study enrolled 124 MM patients who had received 3 or more prior lines of therapy. They received daratumumab at different doses and on different schedules, but 106 of the patients received the drug at 16 mg/kg.
Twenty-nine percent of the 106 patients responded to treatment, and the median duration of response was 7 months. Thirty percent of patients experienced serious adverse events. ![]()

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has granted accelerated approval for daratumumab (Darzalex).
The drug is now approved to treat patients with multiple myeloma (MM) who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are double-refractory to a proteasome inhibitor and an immunomodulatory agent.
Daratumumab is the first monoclonal antibody approved to treat MM.
The drug works by binding to CD38 on the surface of MM cells. It triggers the patient’s own immune system to attack MM cells, resulting in cell death through multiple mechanisms of action.
Daratumumab is being developed by Janssen Biotech. The drug was previously granted breakthrough designation, orphan designation, and priority review from the FDA.
Daratumumab was approved under the FDA’s accelerated approval program, which allows the agency to approve a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
As a condition of this accelerated approval, Janssen is required to conduct a multicenter, randomized trial establishing the superiority of daratumumab over standard therapy to verify and describe the clinical benefit of daratumumab. Janssen has several ongoing, multicenter, randomized trials with a primary endpoint of progression-free survival.
The recommended dose and schedule for daratumumab is 16 mg/kg once every week for 8 weeks, then once every 2 weeks for 16 weeks, then once every 4 weeks until disease progression.
The FDA said blood banks should be informed that patients are receiving daratumumab because the drug may interfere with tests such as antibody screening.
In addition, women who are pregnant should not use daratumumab, and women planning to become pregnant should use effective contraceptives during and for at least 3 months after stopping daratumumab.
Trial data
The FDA’s approval of daratumumab was based on results of 2 studies—the phase 2 MMY2002 (SIRIUS) study and the phase 1/2 GEN501 study.
The GEN501 study enrolled 102 patients with relapsed MM or relapsed MM that was refractory to 2 or more prior lines of therapy. The patients received daratumumab at a range of doses and on a number of different schedules.
The results suggested that daratumumab is most effective at a dose of 16 mg/kg. At this dose, the overall response rate was 36%.
Most adverse events in this study were grade 1 or 2, although serious events did occur.
The SIRIUS study enrolled 124 MM patients who had received 3 or more prior lines of therapy. They received daratumumab at different doses and on different schedules, but 106 of the patients received the drug at 16 mg/kg.
Twenty-nine percent of the 106 patients responded to treatment, and the median duration of response was 7 months. Thirty percent of patients experienced serious adverse events. ![]()
Strategy could slow spread of resistant malaria

Plasmodium falciparum
Image by Mae Melvin
A varied treatment approach could slow the spread of artemisinin-resistant malaria, according to research published in The Lancet Global Health.
Computer simulations suggested that giving a population multiple artemisinin-based combination therapies simultaneously, along with a non-artemisinin therapy, is the best way to combat malaria and reduce the spread of resistant disease.
Investigators found this approach worked best even when the non-artemisinin drug was only effective in treating malaria 85% of the time.
The team ran their computer simulations to determine if there was an optimal strategy that could stop the spread of drug-resistant Plasmodium falciparum parasites across populations while still effectively treating malaria in individual patients.
The simulations showed that simultaneously dosing a population with several artemisinin-combination therapies—for example, by prescribing artemisinin in combination with different partner drugs on different days of the week—was more effective than either cycling between different artemisinin combination therapies or sticking to one specific combination until that combination started failing.
The simulations also showed that if this simultaneous dosing included a combination without artemisinin, malaria parasites that were resistant to artemisinin were slower to emerge and slower to spread.
Including this potentially less effective treatment option didn’t necessarily mean that many more people would not recover from malaria.
In the worst-case scenario of the non-artemisinin treatment being only 75% as effective as artemisinin-based combination therapy, fewer than 7% of patients would still have post-treatment malaria parasites in their blood as a result of not receiving an artemisinin-based therapy.
“For this subgroup of patients, second-line treatment with an artemisinin combination therapy would be recommended,” said study author Maciej Boni, PhD, of the Hospital for Tropical Diseases in Ho Chi Minh City, Vietnam.
“The ethical implications of such a treatment policy will need to be weighed against the benefit of delaying and slowing down the spread of artemisinin resistance. But the nightmare we all want to avoid is the establishment of artemisinin resistance in Africa, where hundreds of millions of individuals rely on artemisinin-based therapies as their first-line antimalarial treatment.”
“By deploying different antimalarial therapies simultaneously—including non-artemisinin-based therapies—national malaria control programs in Africa should be able to slow down the spread of artemisinin-resistant parasites when they are imported into the continent.” ![]()

Plasmodium falciparum
Image by Mae Melvin
A varied treatment approach could slow the spread of artemisinin-resistant malaria, according to research published in The Lancet Global Health.
Computer simulations suggested that giving a population multiple artemisinin-based combination therapies simultaneously, along with a non-artemisinin therapy, is the best way to combat malaria and reduce the spread of resistant disease.
Investigators found this approach worked best even when the non-artemisinin drug was only effective in treating malaria 85% of the time.
The team ran their computer simulations to determine if there was an optimal strategy that could stop the spread of drug-resistant Plasmodium falciparum parasites across populations while still effectively treating malaria in individual patients.
The simulations showed that simultaneously dosing a population with several artemisinin-combination therapies—for example, by prescribing artemisinin in combination with different partner drugs on different days of the week—was more effective than either cycling between different artemisinin combination therapies or sticking to one specific combination until that combination started failing.
The simulations also showed that if this simultaneous dosing included a combination without artemisinin, malaria parasites that were resistant to artemisinin were slower to emerge and slower to spread.
Including this potentially less effective treatment option didn’t necessarily mean that many more people would not recover from malaria.
In the worst-case scenario of the non-artemisinin treatment being only 75% as effective as artemisinin-based combination therapy, fewer than 7% of patients would still have post-treatment malaria parasites in their blood as a result of not receiving an artemisinin-based therapy.
“For this subgroup of patients, second-line treatment with an artemisinin combination therapy would be recommended,” said study author Maciej Boni, PhD, of the Hospital for Tropical Diseases in Ho Chi Minh City, Vietnam.
“The ethical implications of such a treatment policy will need to be weighed against the benefit of delaying and slowing down the spread of artemisinin resistance. But the nightmare we all want to avoid is the establishment of artemisinin resistance in Africa, where hundreds of millions of individuals rely on artemisinin-based therapies as their first-line antimalarial treatment.”
“By deploying different antimalarial therapies simultaneously—including non-artemisinin-based therapies—national malaria control programs in Africa should be able to slow down the spread of artemisinin-resistant parasites when they are imported into the continent.” ![]()

Plasmodium falciparum
Image by Mae Melvin
A varied treatment approach could slow the spread of artemisinin-resistant malaria, according to research published in The Lancet Global Health.
Computer simulations suggested that giving a population multiple artemisinin-based combination therapies simultaneously, along with a non-artemisinin therapy, is the best way to combat malaria and reduce the spread of resistant disease.
Investigators found this approach worked best even when the non-artemisinin drug was only effective in treating malaria 85% of the time.
The team ran their computer simulations to determine if there was an optimal strategy that could stop the spread of drug-resistant Plasmodium falciparum parasites across populations while still effectively treating malaria in individual patients.
The simulations showed that simultaneously dosing a population with several artemisinin-combination therapies—for example, by prescribing artemisinin in combination with different partner drugs on different days of the week—was more effective than either cycling between different artemisinin combination therapies or sticking to one specific combination until that combination started failing.
The simulations also showed that if this simultaneous dosing included a combination without artemisinin, malaria parasites that were resistant to artemisinin were slower to emerge and slower to spread.
Including this potentially less effective treatment option didn’t necessarily mean that many more people would not recover from malaria.
In the worst-case scenario of the non-artemisinin treatment being only 75% as effective as artemisinin-based combination therapy, fewer than 7% of patients would still have post-treatment malaria parasites in their blood as a result of not receiving an artemisinin-based therapy.
“For this subgroup of patients, second-line treatment with an artemisinin combination therapy would be recommended,” said study author Maciej Boni, PhD, of the Hospital for Tropical Diseases in Ho Chi Minh City, Vietnam.
“The ethical implications of such a treatment policy will need to be weighed against the benefit of delaying and slowing down the spread of artemisinin resistance. But the nightmare we all want to avoid is the establishment of artemisinin resistance in Africa, where hundreds of millions of individuals rely on artemisinin-based therapies as their first-line antimalarial treatment.”
“By deploying different antimalarial therapies simultaneously—including non-artemisinin-based therapies—national malaria control programs in Africa should be able to slow down the spread of artemisinin-resistant parasites when they are imported into the continent.” ![]()
Role of inflammation and aging in leukemia

Image by Michael Zangani
Previous research has suggested the accumulation of cancer-causing mutations is to blame for the increased risk of cancer in the aging population.
But a study published in The Journal of Clinical Investigation tells another story.
Investigators found that, without age-associated inflammation, older mice developed leukemia no faster than young mice.
The study focused primarily on the “ecosystem” of B-cell progenitor pools.
The investigators wanted to determine what allows a population of healthy B-cell progenitors to be replaced over time with a population of cancerous B-cell progenitors.
“We chose to focus on the role of inflammation in the bone marrow—one of the hallmarks of age-associated tissue changes—where these B-cell progenitor pools live,” said study author Curtis Henry, PhD, of the University of Colorado Anschutz Medical Campus in Aurora, Colorado.
He and his colleagues found that inflammation hurts the growth and maintenance of B-progenitor cells, but that’s not all. Cancerous mutations tend to alter cells in ways that help them survive conditions of inflammation in the bone marrow.
“Suddenly, the healthy cells that were the fittest are no longer the most fit,” Dr Henry explained. “Because the tissue changed, cancer cells have a selective advantage.”
The investigators were able to observe this inflammation-driven natural selection in mouse models. The group worked with mice engineered to prevent inflammation and set out to determine how healthy and leukemia-initiated cells would fare in these conditions.
“Basically, without the effects of inflammation, B-cell progenitor pools stayed fit,” Dr Henry said.
And stopping inflammation reduced the ability of cells expressing the oncogene NRAS from taking over the bone marrow niche.
This study suggests that an increase in cancer risk with age may not be inevitable. Instead of simply being a matter of the passage of time, cancer development in aged populations may be partially dependent on inflammation-associated tissue changes.
“Despite the fact that cancer is largely a disease of old age, almost all cancer modeling in mice employs only young mice,” noted study author James DeGregori, PhD, of the University of Colorado Anschutz Medical Campus.
“This is based on the view that finding the genetic mutation that causes cancer should be enough to understand the disease.”
In these studies, the investigators tested both young and old mice. The older mice were more likely to develop leukemia, but only in the presence of age-associated inflammation. If age-associated inflammation was blocked, the older mice were no more likely than young mice to develop leukemia.
The work implies that stopping the effects of inflammation on tissue could stop cancers from forming. However, inflammation can be necessary in some circumstances. So the investigators said more work is needed to understand how to “tune” inflammation in the elderly to maximize its beneficial effects while minimizing negative effects.
“While it’s premature to suggest that people should take medicines to fight inflammation as they age, we believe our results warrant further study into this potential strategy to combat the age-associated increase in cancer risk,” Dr Henry concluded. ![]()

Image by Michael Zangani
Previous research has suggested the accumulation of cancer-causing mutations is to blame for the increased risk of cancer in the aging population.
But a study published in The Journal of Clinical Investigation tells another story.
Investigators found that, without age-associated inflammation, older mice developed leukemia no faster than young mice.
The study focused primarily on the “ecosystem” of B-cell progenitor pools.
The investigators wanted to determine what allows a population of healthy B-cell progenitors to be replaced over time with a population of cancerous B-cell progenitors.
“We chose to focus on the role of inflammation in the bone marrow—one of the hallmarks of age-associated tissue changes—where these B-cell progenitor pools live,” said study author Curtis Henry, PhD, of the University of Colorado Anschutz Medical Campus in Aurora, Colorado.
He and his colleagues found that inflammation hurts the growth and maintenance of B-progenitor cells, but that’s not all. Cancerous mutations tend to alter cells in ways that help them survive conditions of inflammation in the bone marrow.
“Suddenly, the healthy cells that were the fittest are no longer the most fit,” Dr Henry explained. “Because the tissue changed, cancer cells have a selective advantage.”
The investigators were able to observe this inflammation-driven natural selection in mouse models. The group worked with mice engineered to prevent inflammation and set out to determine how healthy and leukemia-initiated cells would fare in these conditions.
“Basically, without the effects of inflammation, B-cell progenitor pools stayed fit,” Dr Henry said.
And stopping inflammation reduced the ability of cells expressing the oncogene NRAS from taking over the bone marrow niche.
This study suggests that an increase in cancer risk with age may not be inevitable. Instead of simply being a matter of the passage of time, cancer development in aged populations may be partially dependent on inflammation-associated tissue changes.
“Despite the fact that cancer is largely a disease of old age, almost all cancer modeling in mice employs only young mice,” noted study author James DeGregori, PhD, of the University of Colorado Anschutz Medical Campus.
“This is based on the view that finding the genetic mutation that causes cancer should be enough to understand the disease.”
In these studies, the investigators tested both young and old mice. The older mice were more likely to develop leukemia, but only in the presence of age-associated inflammation. If age-associated inflammation was blocked, the older mice were no more likely than young mice to develop leukemia.
The work implies that stopping the effects of inflammation on tissue could stop cancers from forming. However, inflammation can be necessary in some circumstances. So the investigators said more work is needed to understand how to “tune” inflammation in the elderly to maximize its beneficial effects while minimizing negative effects.
“While it’s premature to suggest that people should take medicines to fight inflammation as they age, we believe our results warrant further study into this potential strategy to combat the age-associated increase in cancer risk,” Dr Henry concluded. ![]()

Image by Michael Zangani
Previous research has suggested the accumulation of cancer-causing mutations is to blame for the increased risk of cancer in the aging population.
But a study published in The Journal of Clinical Investigation tells another story.
Investigators found that, without age-associated inflammation, older mice developed leukemia no faster than young mice.
The study focused primarily on the “ecosystem” of B-cell progenitor pools.
The investigators wanted to determine what allows a population of healthy B-cell progenitors to be replaced over time with a population of cancerous B-cell progenitors.
“We chose to focus on the role of inflammation in the bone marrow—one of the hallmarks of age-associated tissue changes—where these B-cell progenitor pools live,” said study author Curtis Henry, PhD, of the University of Colorado Anschutz Medical Campus in Aurora, Colorado.
He and his colleagues found that inflammation hurts the growth and maintenance of B-progenitor cells, but that’s not all. Cancerous mutations tend to alter cells in ways that help them survive conditions of inflammation in the bone marrow.
“Suddenly, the healthy cells that were the fittest are no longer the most fit,” Dr Henry explained. “Because the tissue changed, cancer cells have a selective advantage.”
The investigators were able to observe this inflammation-driven natural selection in mouse models. The group worked with mice engineered to prevent inflammation and set out to determine how healthy and leukemia-initiated cells would fare in these conditions.
“Basically, without the effects of inflammation, B-cell progenitor pools stayed fit,” Dr Henry said.
And stopping inflammation reduced the ability of cells expressing the oncogene NRAS from taking over the bone marrow niche.
This study suggests that an increase in cancer risk with age may not be inevitable. Instead of simply being a matter of the passage of time, cancer development in aged populations may be partially dependent on inflammation-associated tissue changes.
“Despite the fact that cancer is largely a disease of old age, almost all cancer modeling in mice employs only young mice,” noted study author James DeGregori, PhD, of the University of Colorado Anschutz Medical Campus.
“This is based on the view that finding the genetic mutation that causes cancer should be enough to understand the disease.”
In these studies, the investigators tested both young and old mice. The older mice were more likely to develop leukemia, but only in the presence of age-associated inflammation. If age-associated inflammation was blocked, the older mice were no more likely than young mice to develop leukemia.
The work implies that stopping the effects of inflammation on tissue could stop cancers from forming. However, inflammation can be necessary in some circumstances. So the investigators said more work is needed to understand how to “tune” inflammation in the elderly to maximize its beneficial effects while minimizing negative effects.
“While it’s premature to suggest that people should take medicines to fight inflammation as they age, we believe our results warrant further study into this potential strategy to combat the age-associated increase in cancer risk,” Dr Henry concluded. ![]()
Product News: 11 2015
Carmex Winter Mint Lip Balm Click Stick
Carma Laboratories, Inc, introduces limited-edition Carmex Winter Mint Lip Balm Click Sticks. The new seasonal flavor, which comes in convenient click sticks that glide on lips easily, is available to consumers as part of specially marked 2-pack and 4-pack promotions. Both offers combine the Carmex Original Lip Balm Click Stick or Carmex Original Lip Balm Tube with a bonus Winter Mint seasonal stick and will be available at select retailers while supplies last. For more information, visit www.mycarmex.com.
Daytrana Patch
The US Food and Drug Administration (FDA) has added a new warning of chemical leukoderma to the drug label for the Daytrana patch (methylphenidate transdermal system)(Noven Therapeutics, LLC), which treats attention deficit hyperactivity disorder in children and adolescents. Chemical leukoderma is a condition that causes loss of skin color due to repeated exposure to specific chemical compounds. The areas of skin color loss described with the Daytrana patch ranged up to 8 inches in diameter. The FDA recommends that patients or their caregivers should watch for new areas of lighter skin, especially under the drug patch, and immediately report these changes to a health care professional. For more information, visit www.fda.gov/MedWatch.
Enstilar Foam
LEO Pharma Inc announces US Food and Drug Administration approval of Enstilar (calcipotriene and metamethasone dipropionate) Foam 0.005%/0.064% for topical treatment of plaque psoriasis in patients aged 18 years and older. Enstilar is an alcohol-free foam formulation in a pressurized spray can that allows application across large body areas of plaque psoriasis and should be applied to affected areas once daily for up to 4 weeks. The approval was based on pivotal clinical trial data at week 4 that also showed patients using Enstilar achieved efficacy as early as week 2. For more information, visit www.enstilar.com.
IMLYGIC
Amgen Inc announces that the US Food and Drug Administration has approved the Biologics License Application for IMLYGIC (talimogene laherparepvec), a genetically modified oncolytic viral therapy indicated for the local treatment of unresectable cutaneous, subcutaneous, and nodal lesions in patients with melanoma recurrent after initial surgery. IMLYGIC is the first oncolytic viral therapy approved based on therapeutic benefit demonstrated in a pivotal study, and variability of dosing from patient to patient is expected. IMLYGIC has not been shown to improve overall survival or have an effect on visceral metastases, and treatment is contraindicated in immunocompromised patients. For more information, visit www.imlygic.com.
Juvéderm Ultra XC
Allergan, Inc announces US Food and Drug Administration approval to market Juvéderm Ultra XC gel for injection into the lips and perioral area for lip augmentation in patients over the age of 21 years. Juvéderm Ultra XC is a smooth gel formulation made up of a modified form of hyaluronic acid, a naturally occurring sugar found in the human body whose role is to deliver nutrients and help the skin retain its natural moisture and softness. The gel formulation also contains a small amount of lidocaine, which improves the comfort of the injection. For more information, visit www.juvederm.com.
Opdivo + Yervoy Regimen
Bristol-Myers Squibb Company obtains US Food and Drug Administration approval for the Opdivo (nivolumab) + Yervoy (ipilimumab) regimen in BRAF V600 wild-type unresectable or metastatic melanoma. The approval, which is based on data from a pivotal study, marks the first approval of a regimen of 2 immuno-oncology agents in cancer. This indication is approved under accelerated approval based on tumor response rate and durability of response. Opdivo and Yervoy are immune checkpoint inhibitors that target separate, distinct, and complementary checkpoint pathways (PD-1 and CTLA-4). The mechanism of action involves dual immune checkpoint inhibition resulting in increased antitumor activity. For more information, visit www.bms.com.
If you would like your product included in Product News, please e-mail a press release to the Editorial Office at [email protected].
Carmex Winter Mint Lip Balm Click Stick
Carma Laboratories, Inc, introduces limited-edition Carmex Winter Mint Lip Balm Click Sticks. The new seasonal flavor, which comes in convenient click sticks that glide on lips easily, is available to consumers as part of specially marked 2-pack and 4-pack promotions. Both offers combine the Carmex Original Lip Balm Click Stick or Carmex Original Lip Balm Tube with a bonus Winter Mint seasonal stick and will be available at select retailers while supplies last. For more information, visit www.mycarmex.com.
Daytrana Patch
The US Food and Drug Administration (FDA) has added a new warning of chemical leukoderma to the drug label for the Daytrana patch (methylphenidate transdermal system)(Noven Therapeutics, LLC), which treats attention deficit hyperactivity disorder in children and adolescents. Chemical leukoderma is a condition that causes loss of skin color due to repeated exposure to specific chemical compounds. The areas of skin color loss described with the Daytrana patch ranged up to 8 inches in diameter. The FDA recommends that patients or their caregivers should watch for new areas of lighter skin, especially under the drug patch, and immediately report these changes to a health care professional. For more information, visit www.fda.gov/MedWatch.
Enstilar Foam
LEO Pharma Inc announces US Food and Drug Administration approval of Enstilar (calcipotriene and metamethasone dipropionate) Foam 0.005%/0.064% for topical treatment of plaque psoriasis in patients aged 18 years and older. Enstilar is an alcohol-free foam formulation in a pressurized spray can that allows application across large body areas of plaque psoriasis and should be applied to affected areas once daily for up to 4 weeks. The approval was based on pivotal clinical trial data at week 4 that also showed patients using Enstilar achieved efficacy as early as week 2. For more information, visit www.enstilar.com.
IMLYGIC
Amgen Inc announces that the US Food and Drug Administration has approved the Biologics License Application for IMLYGIC (talimogene laherparepvec), a genetically modified oncolytic viral therapy indicated for the local treatment of unresectable cutaneous, subcutaneous, and nodal lesions in patients with melanoma recurrent after initial surgery. IMLYGIC is the first oncolytic viral therapy approved based on therapeutic benefit demonstrated in a pivotal study, and variability of dosing from patient to patient is expected. IMLYGIC has not been shown to improve overall survival or have an effect on visceral metastases, and treatment is contraindicated in immunocompromised patients. For more information, visit www.imlygic.com.
Juvéderm Ultra XC
Allergan, Inc announces US Food and Drug Administration approval to market Juvéderm Ultra XC gel for injection into the lips and perioral area for lip augmentation in patients over the age of 21 years. Juvéderm Ultra XC is a smooth gel formulation made up of a modified form of hyaluronic acid, a naturally occurring sugar found in the human body whose role is to deliver nutrients and help the skin retain its natural moisture and softness. The gel formulation also contains a small amount of lidocaine, which improves the comfort of the injection. For more information, visit www.juvederm.com.
Opdivo + Yervoy Regimen
Bristol-Myers Squibb Company obtains US Food and Drug Administration approval for the Opdivo (nivolumab) + Yervoy (ipilimumab) regimen in BRAF V600 wild-type unresectable or metastatic melanoma. The approval, which is based on data from a pivotal study, marks the first approval of a regimen of 2 immuno-oncology agents in cancer. This indication is approved under accelerated approval based on tumor response rate and durability of response. Opdivo and Yervoy are immune checkpoint inhibitors that target separate, distinct, and complementary checkpoint pathways (PD-1 and CTLA-4). The mechanism of action involves dual immune checkpoint inhibition resulting in increased antitumor activity. For more information, visit www.bms.com.
If you would like your product included in Product News, please e-mail a press release to the Editorial Office at [email protected].
Carmex Winter Mint Lip Balm Click Stick
Carma Laboratories, Inc, introduces limited-edition Carmex Winter Mint Lip Balm Click Sticks. The new seasonal flavor, which comes in convenient click sticks that glide on lips easily, is available to consumers as part of specially marked 2-pack and 4-pack promotions. Both offers combine the Carmex Original Lip Balm Click Stick or Carmex Original Lip Balm Tube with a bonus Winter Mint seasonal stick and will be available at select retailers while supplies last. For more information, visit www.mycarmex.com.
Daytrana Patch
The US Food and Drug Administration (FDA) has added a new warning of chemical leukoderma to the drug label for the Daytrana patch (methylphenidate transdermal system)(Noven Therapeutics, LLC), which treats attention deficit hyperactivity disorder in children and adolescents. Chemical leukoderma is a condition that causes loss of skin color due to repeated exposure to specific chemical compounds. The areas of skin color loss described with the Daytrana patch ranged up to 8 inches in diameter. The FDA recommends that patients or their caregivers should watch for new areas of lighter skin, especially under the drug patch, and immediately report these changes to a health care professional. For more information, visit www.fda.gov/MedWatch.
Enstilar Foam
LEO Pharma Inc announces US Food and Drug Administration approval of Enstilar (calcipotriene and metamethasone dipropionate) Foam 0.005%/0.064% for topical treatment of plaque psoriasis in patients aged 18 years and older. Enstilar is an alcohol-free foam formulation in a pressurized spray can that allows application across large body areas of plaque psoriasis and should be applied to affected areas once daily for up to 4 weeks. The approval was based on pivotal clinical trial data at week 4 that also showed patients using Enstilar achieved efficacy as early as week 2. For more information, visit www.enstilar.com.
IMLYGIC
Amgen Inc announces that the US Food and Drug Administration has approved the Biologics License Application for IMLYGIC (talimogene laherparepvec), a genetically modified oncolytic viral therapy indicated for the local treatment of unresectable cutaneous, subcutaneous, and nodal lesions in patients with melanoma recurrent after initial surgery. IMLYGIC is the first oncolytic viral therapy approved based on therapeutic benefit demonstrated in a pivotal study, and variability of dosing from patient to patient is expected. IMLYGIC has not been shown to improve overall survival or have an effect on visceral metastases, and treatment is contraindicated in immunocompromised patients. For more information, visit www.imlygic.com.
Juvéderm Ultra XC
Allergan, Inc announces US Food and Drug Administration approval to market Juvéderm Ultra XC gel for injection into the lips and perioral area for lip augmentation in patients over the age of 21 years. Juvéderm Ultra XC is a smooth gel formulation made up of a modified form of hyaluronic acid, a naturally occurring sugar found in the human body whose role is to deliver nutrients and help the skin retain its natural moisture and softness. The gel formulation also contains a small amount of lidocaine, which improves the comfort of the injection. For more information, visit www.juvederm.com.
Opdivo + Yervoy Regimen
Bristol-Myers Squibb Company obtains US Food and Drug Administration approval for the Opdivo (nivolumab) + Yervoy (ipilimumab) regimen in BRAF V600 wild-type unresectable or metastatic melanoma. The approval, which is based on data from a pivotal study, marks the first approval of a regimen of 2 immuno-oncology agents in cancer. This indication is approved under accelerated approval based on tumor response rate and durability of response. Opdivo and Yervoy are immune checkpoint inhibitors that target separate, distinct, and complementary checkpoint pathways (PD-1 and CTLA-4). The mechanism of action involves dual immune checkpoint inhibition resulting in increased antitumor activity. For more information, visit www.bms.com.
If you would like your product included in Product News, please e-mail a press release to the Editorial Office at [email protected].
A modified olanzapine regimen for the prevention of chemotherapy-induced nausea and vomiting
Background At Kaiser Permanente Antioch and Walnut Creek Cancer Centers, a modified olanzapine regimen is used to prevent chemotherapy-induced nausea and vomiting (CINV) in patients who receive highly emetogenic chemotherapy (HEC).
Objective To determine if an olanzapine, ondansetron, dexamethasone (OOD) regimen is noninferior to a fosaprepitant, ondansetron, dexamethasone (FOD) regimen in preventing CINV in patients receiving HEC.
Methods This retrospective cohort study compared the rates of CINV in patients who were treated with HEC and received either the OOD or FOD regimen. Electronic medical records were assessed for documented reports of CINV. 148 patients were included in this study.
Results Complete response (CR), defined as no emesis after Cycle 1 of HEC, in patients receiving the OOD regimen was 95.7% in the acute phase, 94.3% in the delayed phase, and 92.9% overall. CR in patients receiving the FOD regimen was 98.7% in the acute phase, 89.7% in the delayed phase, and 89.7% overall. The percentage of patients who had no nausea on the OOD regimen was 87.1 in the acute phase, 75.5 in the delayed phase, and 71.4 overall, compared with 78.2 in the acute phase, 62.8 in the delayed phase, and 62.7 overall in patients on the FOD regimen.
Limitations This study was limited by its retrospective, nonrandomized design, and short follow-up period. This study did not assess adverse effects from the antiemetic regimens.
Conclusions A modified olanzapine regimen is noninferior to a standard fosaprepitant regimen in regard to CR in showing improved control of CINV. In addition, the use of the olanzapine regimen reduces patient exposure to corticosteroids and the risk of associated side effects, and it is significantly more cost effective, compared with the fosaprepitant regimen.
Click on the PDF icon at the top of this introduction to read the full article.
Background At Kaiser Permanente Antioch and Walnut Creek Cancer Centers, a modified olanzapine regimen is used to prevent chemotherapy-induced nausea and vomiting (CINV) in patients who receive highly emetogenic chemotherapy (HEC).
Objective To determine if an olanzapine, ondansetron, dexamethasone (OOD) regimen is noninferior to a fosaprepitant, ondansetron, dexamethasone (FOD) regimen in preventing CINV in patients receiving HEC.
Methods This retrospective cohort study compared the rates of CINV in patients who were treated with HEC and received either the OOD or FOD regimen. Electronic medical records were assessed for documented reports of CINV. 148 patients were included in this study.
Results Complete response (CR), defined as no emesis after Cycle 1 of HEC, in patients receiving the OOD regimen was 95.7% in the acute phase, 94.3% in the delayed phase, and 92.9% overall. CR in patients receiving the FOD regimen was 98.7% in the acute phase, 89.7% in the delayed phase, and 89.7% overall. The percentage of patients who had no nausea on the OOD regimen was 87.1 in the acute phase, 75.5 in the delayed phase, and 71.4 overall, compared with 78.2 in the acute phase, 62.8 in the delayed phase, and 62.7 overall in patients on the FOD regimen.
Limitations This study was limited by its retrospective, nonrandomized design, and short follow-up period. This study did not assess adverse effects from the antiemetic regimens.
Conclusions A modified olanzapine regimen is noninferior to a standard fosaprepitant regimen in regard to CR in showing improved control of CINV. In addition, the use of the olanzapine regimen reduces patient exposure to corticosteroids and the risk of associated side effects, and it is significantly more cost effective, compared with the fosaprepitant regimen.
Click on the PDF icon at the top of this introduction to read the full article.
Background At Kaiser Permanente Antioch and Walnut Creek Cancer Centers, a modified olanzapine regimen is used to prevent chemotherapy-induced nausea and vomiting (CINV) in patients who receive highly emetogenic chemotherapy (HEC).
Objective To determine if an olanzapine, ondansetron, dexamethasone (OOD) regimen is noninferior to a fosaprepitant, ondansetron, dexamethasone (FOD) regimen in preventing CINV in patients receiving HEC.
Methods This retrospective cohort study compared the rates of CINV in patients who were treated with HEC and received either the OOD or FOD regimen. Electronic medical records were assessed for documented reports of CINV. 148 patients were included in this study.
Results Complete response (CR), defined as no emesis after Cycle 1 of HEC, in patients receiving the OOD regimen was 95.7% in the acute phase, 94.3% in the delayed phase, and 92.9% overall. CR in patients receiving the FOD regimen was 98.7% in the acute phase, 89.7% in the delayed phase, and 89.7% overall. The percentage of patients who had no nausea on the OOD regimen was 87.1 in the acute phase, 75.5 in the delayed phase, and 71.4 overall, compared with 78.2 in the acute phase, 62.8 in the delayed phase, and 62.7 overall in patients on the FOD regimen.
Limitations This study was limited by its retrospective, nonrandomized design, and short follow-up period. This study did not assess adverse effects from the antiemetic regimens.
Conclusions A modified olanzapine regimen is noninferior to a standard fosaprepitant regimen in regard to CR in showing improved control of CINV. In addition, the use of the olanzapine regimen reduces patient exposure to corticosteroids and the risk of associated side effects, and it is significantly more cost effective, compared with the fosaprepitant regimen.
Click on the PDF icon at the top of this introduction to read the full article.
Balancing clinical and supportive care at every step of the disease continuum
It seems it was just yesterday that we did our first “mutation analysis” to help guide us in our treatment of patients with a drug that was more likely to work than not. Of course, I am referring to estrogen-receptor/progesterone receptor (ER/PR) blocking therapy, and “yesterday” actually goes all the way back to the 1970s! When tamoxifen was first given to unselected metastatic breast cancer patients, the response rate was low, but when the study population was “enriched” with breast cancer patients who were ER/ PR-positive, the response rates improved and the outcomes were more favorable. So began the era of tumor markers and enriching patient populations, and the process now referred to as mutation analysis, which is becoming more broadly applicable to other tumors as well.
Click on the PDF icon at the top of this introduction to read the full article.
It seems it was just yesterday that we did our first “mutation analysis” to help guide us in our treatment of patients with a drug that was more likely to work than not. Of course, I am referring to estrogen-receptor/progesterone receptor (ER/PR) blocking therapy, and “yesterday” actually goes all the way back to the 1970s! When tamoxifen was first given to unselected metastatic breast cancer patients, the response rate was low, but when the study population was “enriched” with breast cancer patients who were ER/ PR-positive, the response rates improved and the outcomes were more favorable. So began the era of tumor markers and enriching patient populations, and the process now referred to as mutation analysis, which is becoming more broadly applicable to other tumors as well.
Click on the PDF icon at the top of this introduction to read the full article.
It seems it was just yesterday that we did our first “mutation analysis” to help guide us in our treatment of patients with a drug that was more likely to work than not. Of course, I am referring to estrogen-receptor/progesterone receptor (ER/PR) blocking therapy, and “yesterday” actually goes all the way back to the 1970s! When tamoxifen was first given to unselected metastatic breast cancer patients, the response rate was low, but when the study population was “enriched” with breast cancer patients who were ER/ PR-positive, the response rates improved and the outcomes were more favorable. So began the era of tumor markers and enriching patient populations, and the process now referred to as mutation analysis, which is becoming more broadly applicable to other tumors as well.
Click on the PDF icon at the top of this introduction to read the full article.

