User login
Randomized trial: When a vaginal approach is feasible, the robot offers no advantages for benign hysterectomy
When investigators compared the cost of vaginal hysterectomy with robot-assisted laparoscopic hysterectomy head to head, they found hospital costs of $4,579 and $7,059, respectively, with no other significant differences between the approaches. Accordingly, they concluded that vaginal hysterectomy should be the “first-choice” approach when it is feasible.
The randomized controlled trial by Lönnerfors and colleagues also compared “traditional” minimally invasive hysterectomy (vaginal or laparoscopic approach) with robot-assisted hysterectomy in 122 women undergoing hysterectomy for benign conditions. Women with a uterine size of 16 gestational weeks or smaller were randomly allocated to:
- traditional minimally invasive hysterectomy (n = 61) or
- robotic assisted hysterectomy (n = 61).
In the traditional group, vaginal hysterectomy was the first-choice approach when it was feasible; otherwise, laparoscopic hysterectomy was performed. Vaginal hysterectomy was possible in 41% of cases in this group.
When costs for vaginal and laparoscopic approaches were consolidated and compared with the cost of the robot-assisted approach, the differential was $993 for the robotic approach when the robot was considered a preexisting investment. The hospital cost increased by $1,607 for the robotic approach when investment costs and maintenance expenses were included.
When laparoscopic hysterectomy was compared directly with robot-assisted hysterectomy, costs were similar ($7,016 vs $7,059, respectively) when the robot was considered a preexisting investment, and the robotic approach was associated with less blood loss and fewer postoperative complications.
Investigators noted that: “per-protocol analysis indicates that laparoscopic and robotic-assisted hysterectomy can be performed at similar hospital cost because of higher robot capacity that entails excluding the cost of investment and maintenance, i.e., the basic cost of the robot. This cost differs among institutions, depending on the number of procedures performed; however, the difference becomes less pronounced when 300 to 400 procedures or more are performed annually and the cost for instruments and disposables accounts for most of the cost of the procedure.”
This randomized controlled trial was awarded the Robert B. Hunt Award at the 2015 AAGL Global Congress in Las Vegas as the best paper published over the past year in the Journal of Minimally Invasive Gynecology.
Reference
Lönnerfors C, Reynisson P, Persson J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J Minim Invasive Gynecol. 2015;22(1):78–86.
When investigators compared the cost of vaginal hysterectomy with robot-assisted laparoscopic hysterectomy head to head, they found hospital costs of $4,579 and $7,059, respectively, with no other significant differences between the approaches. Accordingly, they concluded that vaginal hysterectomy should be the “first-choice” approach when it is feasible.
The randomized controlled trial by Lönnerfors and colleagues also compared “traditional” minimally invasive hysterectomy (vaginal or laparoscopic approach) with robot-assisted hysterectomy in 122 women undergoing hysterectomy for benign conditions. Women with a uterine size of 16 gestational weeks or smaller were randomly allocated to:
- traditional minimally invasive hysterectomy (n = 61) or
- robotic assisted hysterectomy (n = 61).
In the traditional group, vaginal hysterectomy was the first-choice approach when it was feasible; otherwise, laparoscopic hysterectomy was performed. Vaginal hysterectomy was possible in 41% of cases in this group.
When costs for vaginal and laparoscopic approaches were consolidated and compared with the cost of the robot-assisted approach, the differential was $993 for the robotic approach when the robot was considered a preexisting investment. The hospital cost increased by $1,607 for the robotic approach when investment costs and maintenance expenses were included.
When laparoscopic hysterectomy was compared directly with robot-assisted hysterectomy, costs were similar ($7,016 vs $7,059, respectively) when the robot was considered a preexisting investment, and the robotic approach was associated with less blood loss and fewer postoperative complications.
Investigators noted that: “per-protocol analysis indicates that laparoscopic and robotic-assisted hysterectomy can be performed at similar hospital cost because of higher robot capacity that entails excluding the cost of investment and maintenance, i.e., the basic cost of the robot. This cost differs among institutions, depending on the number of procedures performed; however, the difference becomes less pronounced when 300 to 400 procedures or more are performed annually and the cost for instruments and disposables accounts for most of the cost of the procedure.”
This randomized controlled trial was awarded the Robert B. Hunt Award at the 2015 AAGL Global Congress in Las Vegas as the best paper published over the past year in the Journal of Minimally Invasive Gynecology.
When investigators compared the cost of vaginal hysterectomy with robot-assisted laparoscopic hysterectomy head to head, they found hospital costs of $4,579 and $7,059, respectively, with no other significant differences between the approaches. Accordingly, they concluded that vaginal hysterectomy should be the “first-choice” approach when it is feasible.
The randomized controlled trial by Lönnerfors and colleagues also compared “traditional” minimally invasive hysterectomy (vaginal or laparoscopic approach) with robot-assisted hysterectomy in 122 women undergoing hysterectomy for benign conditions. Women with a uterine size of 16 gestational weeks or smaller were randomly allocated to:
- traditional minimally invasive hysterectomy (n = 61) or
- robotic assisted hysterectomy (n = 61).
In the traditional group, vaginal hysterectomy was the first-choice approach when it was feasible; otherwise, laparoscopic hysterectomy was performed. Vaginal hysterectomy was possible in 41% of cases in this group.
When costs for vaginal and laparoscopic approaches were consolidated and compared with the cost of the robot-assisted approach, the differential was $993 for the robotic approach when the robot was considered a preexisting investment. The hospital cost increased by $1,607 for the robotic approach when investment costs and maintenance expenses were included.
When laparoscopic hysterectomy was compared directly with robot-assisted hysterectomy, costs were similar ($7,016 vs $7,059, respectively) when the robot was considered a preexisting investment, and the robotic approach was associated with less blood loss and fewer postoperative complications.
Investigators noted that: “per-protocol analysis indicates that laparoscopic and robotic-assisted hysterectomy can be performed at similar hospital cost because of higher robot capacity that entails excluding the cost of investment and maintenance, i.e., the basic cost of the robot. This cost differs among institutions, depending on the number of procedures performed; however, the difference becomes less pronounced when 300 to 400 procedures or more are performed annually and the cost for instruments and disposables accounts for most of the cost of the procedure.”
This randomized controlled trial was awarded the Robert B. Hunt Award at the 2015 AAGL Global Congress in Las Vegas as the best paper published over the past year in the Journal of Minimally Invasive Gynecology.
Reference
Lönnerfors C, Reynisson P, Persson J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J Minim Invasive Gynecol. 2015;22(1):78–86.
Reference
Lönnerfors C, Reynisson P, Persson J. A randomized trial comparing vaginal and laparoscopic hysterectomy vs robot-assisted hysterectomy. J Minim Invasive Gynecol. 2015;22(1):78–86.
When the surgeon is experienced, operative times are comparable for robot-assisted and standard laparoscopic hysterectomy
When investigators from the Penn State Milton S. Hershey Medical Center randomly allocated 144 women to robot-assisted or standard laparoscopic hysterectomy (n = 72 in each arm) and recorded complications for 12 weeks, they found no significant differences between groups in estimated blood loss.1 In addition, mean operative times (surgeon incision to surgeon stop, including docking in the robot-assisted group) were similar (73.9 min for robot-assisted surgery vs 74.9 min for standard laparoscopy), as were complication rates. In this trial, operative time was the primary outcome.
Pain was assessed at 2 postoperative hours and was found to be similar between groups.
Two intraoperative complications occurred in the robot-assisted group, compared with none for standard laparoscopy (P = .50). Six postoperative complications occurred in the robot-assisted group, compared with 9 in the standard laparoscopy group (P = 0.58).
Complications included: a need for reoperation/readmission (2 patients in each group; P = 1.00), infection (1 patient in each group; P = 1.00), hemorrhage/transfusion (4 in the standard laparoscopy group; P = 0.12), and vaginal cuff dehiscence (2 in the robot-assisted group vs 1 for standard laparoscopy; P = 1.00).
Investigators concluded that robot-assisted hysterectomy is “noninferior” to standard laparoscopy with regard to operative time when it is performed by experienced minimally invasive surgeons.
Gerald J. Harkins, MD, an author and primary surgeon of the trial, notes that it is the first randomized comparison involving surgeons with expertise in both robot-assisted and standard laparoscopic hysterectomy. As such, its findings represent Level I evidence. Dr. Harkins had completed more than 600 robot-assisted cases prior to initiation of the trial.
Cost was not analyzed in this study, the abstract of which won the Jay M. Cooper Award as the best paper on minimally invasive gynecology by a fellow and was presented on November 17 at the AAGL annual meeting in Las Vegas.
Reference
1. 1. Deimling TA, Eldridge JL, Riley KA, Kunselman AR, Harkins GJ. Standard versus robot-assisted laparoscopic hysterectomy: a prospective randomized trial [abstract]. Presented at the 2015 AAGL Global Congress in Las Vegas, Nevada, November 2015.
When investigators from the Penn State Milton S. Hershey Medical Center randomly allocated 144 women to robot-assisted or standard laparoscopic hysterectomy (n = 72 in each arm) and recorded complications for 12 weeks, they found no significant differences between groups in estimated blood loss.1 In addition, mean operative times (surgeon incision to surgeon stop, including docking in the robot-assisted group) were similar (73.9 min for robot-assisted surgery vs 74.9 min for standard laparoscopy), as were complication rates. In this trial, operative time was the primary outcome.
Pain was assessed at 2 postoperative hours and was found to be similar between groups.
Two intraoperative complications occurred in the robot-assisted group, compared with none for standard laparoscopy (P = .50). Six postoperative complications occurred in the robot-assisted group, compared with 9 in the standard laparoscopy group (P = 0.58).
Complications included: a need for reoperation/readmission (2 patients in each group; P = 1.00), infection (1 patient in each group; P = 1.00), hemorrhage/transfusion (4 in the standard laparoscopy group; P = 0.12), and vaginal cuff dehiscence (2 in the robot-assisted group vs 1 for standard laparoscopy; P = 1.00).
Investigators concluded that robot-assisted hysterectomy is “noninferior” to standard laparoscopy with regard to operative time when it is performed by experienced minimally invasive surgeons.
Gerald J. Harkins, MD, an author and primary surgeon of the trial, notes that it is the first randomized comparison involving surgeons with expertise in both robot-assisted and standard laparoscopic hysterectomy. As such, its findings represent Level I evidence. Dr. Harkins had completed more than 600 robot-assisted cases prior to initiation of the trial.
Cost was not analyzed in this study, the abstract of which won the Jay M. Cooper Award as the best paper on minimally invasive gynecology by a fellow and was presented on November 17 at the AAGL annual meeting in Las Vegas.
When investigators from the Penn State Milton S. Hershey Medical Center randomly allocated 144 women to robot-assisted or standard laparoscopic hysterectomy (n = 72 in each arm) and recorded complications for 12 weeks, they found no significant differences between groups in estimated blood loss.1 In addition, mean operative times (surgeon incision to surgeon stop, including docking in the robot-assisted group) were similar (73.9 min for robot-assisted surgery vs 74.9 min for standard laparoscopy), as were complication rates. In this trial, operative time was the primary outcome.
Pain was assessed at 2 postoperative hours and was found to be similar between groups.
Two intraoperative complications occurred in the robot-assisted group, compared with none for standard laparoscopy (P = .50). Six postoperative complications occurred in the robot-assisted group, compared with 9 in the standard laparoscopy group (P = 0.58).
Complications included: a need for reoperation/readmission (2 patients in each group; P = 1.00), infection (1 patient in each group; P = 1.00), hemorrhage/transfusion (4 in the standard laparoscopy group; P = 0.12), and vaginal cuff dehiscence (2 in the robot-assisted group vs 1 for standard laparoscopy; P = 1.00).
Investigators concluded that robot-assisted hysterectomy is “noninferior” to standard laparoscopy with regard to operative time when it is performed by experienced minimally invasive surgeons.
Gerald J. Harkins, MD, an author and primary surgeon of the trial, notes that it is the first randomized comparison involving surgeons with expertise in both robot-assisted and standard laparoscopic hysterectomy. As such, its findings represent Level I evidence. Dr. Harkins had completed more than 600 robot-assisted cases prior to initiation of the trial.
Cost was not analyzed in this study, the abstract of which won the Jay M. Cooper Award as the best paper on minimally invasive gynecology by a fellow and was presented on November 17 at the AAGL annual meeting in Las Vegas.
Reference
1. 1. Deimling TA, Eldridge JL, Riley KA, Kunselman AR, Harkins GJ. Standard versus robot-assisted laparoscopic hysterectomy: a prospective randomized trial [abstract]. Presented at the 2015 AAGL Global Congress in Las Vegas, Nevada, November 2015.
Reference
1. 1. Deimling TA, Eldridge JL, Riley KA, Kunselman AR, Harkins GJ. Standard versus robot-assisted laparoscopic hysterectomy: a prospective randomized trial [abstract]. Presented at the 2015 AAGL Global Congress in Las Vegas, Nevada, November 2015.
Design thinking
Design thinking isn’t only for products such as the Apple watch. It is a methodology used to improve customer experiences not only with products but also with services. Much in the same way that the SOAP note shaped our thinking about diagnosis and treatment, design thinking provides a scaffold to help us better understand the needs and wants of customers, or in our case, patients.
Design thinking uses specific tools and methodologies to understand experiences from others’ perspectives. From its roots in Silicon Valley, design thinking has grown steadily in its influence. Its first high priests were people such as Steve Jobs and David Kelly, who famously designed the computer mouse. The principles learned or applied to increasingly complicated products and services led to the growth of an entire industry in Palo Alto, Calif., with companies such as IDEO and gurus such as IDEO CEO and President Tim Brown of Stanford (Calif.) University has an entire graduate school program on design thinking called d.school while Coursera offers online courses on design thinking.
The principles are simple: The better you understand your customers and their needs, the better you can design your services. There are many toolkits that are available for you to try for free. Empathy Mapping is an easy one you could apply to your practice to enhance your patients’ experience.
The idea behind this technique is to immerse yourself in your patient’s world. Pick a time when your practice is closed. Then take a journey through your office as if you were a patient. It’s important that you keep the experience as close to reality as possible. Start before you even arrive at your office. What is the experience like driving to your office? Do patients have to fight traffic to get to you? Is parking easy to find? How far must they walk from their car to get to your office? What is your check-in process like? Are patients greeted by name? Are they first handed paperwork to complete? Or are they introduced and warmly welcomed to your practice first?
What’s the experience like in the waiting room? Take note of not only what your patients see but also what they hear, smell, touch, and say. What experience does your furniture give patients? What type of magazines are available to them? Do you have Wi-Fi? Is there a television? If so, is it showing simply an advertisement, or is it something that your patients would connect with? Is there music playing?
Using the same process, continue your journey through an entire patient visit. Make note of what the experience is like walking back to your exam rooms. What do your patients see and smell while sitting in an exam room waiting for you? Does it smell of isopropyl alcohol? Is it cold or hot? What’s it like to sit in your room wearing nothing but a patient gown? Are there instruments such as cryo guns that could be intimidating to patients? All of these factors can be modified and thus “designed” to optimize the experience for your patients. Continue this journey including a physical exam and discussion with the doctor and other providers and assistants.
This is a great exercise not only for you but more importantly for your staff. Ask your staff to take notes as they walk through the same empathy mapping journey. It will give them an entirely new and valuable perspective on what it’s like to be a patient in your office. Once you’ve completed your empathy mapping, sit with your team and brainstorm about opportunities to improve the experience for your patients. Ask yourselves what things surprised you. What things do you feel could have the largest impact on your patients’ experience in your office? In what ways can you modify the spaces in your office to optimize your patients’ experience?
Having done this exercise in my own clinic, I found it highly impactful. It gave me a deeper understanding of and appreciation for my patients and caused me to make several minor but important changes in my exam room and to my and my staff’s interactions with patients. I hope you have a similarly informative experience.
If you’re interested in learning more about design thinking, then check out the following books and articles:
• “Change by Design: How Design Thinking Transforms Organization and Inspires Innovation,” by Tim Brown (New York: Harper Business, 2009).
• “The Art of Innovation,” by Tom Kelley (New York: A Currency Book, Doubleday, Random House, 2001).
• Design Thinking Comes of Age, by Jon Kolko (Harv Bus Rev. Sep 2015;pp 66-71).
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Design thinking isn’t only for products such as the Apple watch. It is a methodology used to improve customer experiences not only with products but also with services. Much in the same way that the SOAP note shaped our thinking about diagnosis and treatment, design thinking provides a scaffold to help us better understand the needs and wants of customers, or in our case, patients.
Design thinking uses specific tools and methodologies to understand experiences from others’ perspectives. From its roots in Silicon Valley, design thinking has grown steadily in its influence. Its first high priests were people such as Steve Jobs and David Kelly, who famously designed the computer mouse. The principles learned or applied to increasingly complicated products and services led to the growth of an entire industry in Palo Alto, Calif., with companies such as IDEO and gurus such as IDEO CEO and President Tim Brown of Stanford (Calif.) University has an entire graduate school program on design thinking called d.school while Coursera offers online courses on design thinking.
The principles are simple: The better you understand your customers and their needs, the better you can design your services. There are many toolkits that are available for you to try for free. Empathy Mapping is an easy one you could apply to your practice to enhance your patients’ experience.
The idea behind this technique is to immerse yourself in your patient’s world. Pick a time when your practice is closed. Then take a journey through your office as if you were a patient. It’s important that you keep the experience as close to reality as possible. Start before you even arrive at your office. What is the experience like driving to your office? Do patients have to fight traffic to get to you? Is parking easy to find? How far must they walk from their car to get to your office? What is your check-in process like? Are patients greeted by name? Are they first handed paperwork to complete? Or are they introduced and warmly welcomed to your practice first?
What’s the experience like in the waiting room? Take note of not only what your patients see but also what they hear, smell, touch, and say. What experience does your furniture give patients? What type of magazines are available to them? Do you have Wi-Fi? Is there a television? If so, is it showing simply an advertisement, or is it something that your patients would connect with? Is there music playing?
Using the same process, continue your journey through an entire patient visit. Make note of what the experience is like walking back to your exam rooms. What do your patients see and smell while sitting in an exam room waiting for you? Does it smell of isopropyl alcohol? Is it cold or hot? What’s it like to sit in your room wearing nothing but a patient gown? Are there instruments such as cryo guns that could be intimidating to patients? All of these factors can be modified and thus “designed” to optimize the experience for your patients. Continue this journey including a physical exam and discussion with the doctor and other providers and assistants.
This is a great exercise not only for you but more importantly for your staff. Ask your staff to take notes as they walk through the same empathy mapping journey. It will give them an entirely new and valuable perspective on what it’s like to be a patient in your office. Once you’ve completed your empathy mapping, sit with your team and brainstorm about opportunities to improve the experience for your patients. Ask yourselves what things surprised you. What things do you feel could have the largest impact on your patients’ experience in your office? In what ways can you modify the spaces in your office to optimize your patients’ experience?
Having done this exercise in my own clinic, I found it highly impactful. It gave me a deeper understanding of and appreciation for my patients and caused me to make several minor but important changes in my exam room and to my and my staff’s interactions with patients. I hope you have a similarly informative experience.
If you’re interested in learning more about design thinking, then check out the following books and articles:
• “Change by Design: How Design Thinking Transforms Organization and Inspires Innovation,” by Tim Brown (New York: Harper Business, 2009).
• “The Art of Innovation,” by Tom Kelley (New York: A Currency Book, Doubleday, Random House, 2001).
• Design Thinking Comes of Age, by Jon Kolko (Harv Bus Rev. Sep 2015;pp 66-71).
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Design thinking isn’t only for products such as the Apple watch. It is a methodology used to improve customer experiences not only with products but also with services. Much in the same way that the SOAP note shaped our thinking about diagnosis and treatment, design thinking provides a scaffold to help us better understand the needs and wants of customers, or in our case, patients.
Design thinking uses specific tools and methodologies to understand experiences from others’ perspectives. From its roots in Silicon Valley, design thinking has grown steadily in its influence. Its first high priests were people such as Steve Jobs and David Kelly, who famously designed the computer mouse. The principles learned or applied to increasingly complicated products and services led to the growth of an entire industry in Palo Alto, Calif., with companies such as IDEO and gurus such as IDEO CEO and President Tim Brown of Stanford (Calif.) University has an entire graduate school program on design thinking called d.school while Coursera offers online courses on design thinking.
The principles are simple: The better you understand your customers and their needs, the better you can design your services. There are many toolkits that are available for you to try for free. Empathy Mapping is an easy one you could apply to your practice to enhance your patients’ experience.
The idea behind this technique is to immerse yourself in your patient’s world. Pick a time when your practice is closed. Then take a journey through your office as if you were a patient. It’s important that you keep the experience as close to reality as possible. Start before you even arrive at your office. What is the experience like driving to your office? Do patients have to fight traffic to get to you? Is parking easy to find? How far must they walk from their car to get to your office? What is your check-in process like? Are patients greeted by name? Are they first handed paperwork to complete? Or are they introduced and warmly welcomed to your practice first?
What’s the experience like in the waiting room? Take note of not only what your patients see but also what they hear, smell, touch, and say. What experience does your furniture give patients? What type of magazines are available to them? Do you have Wi-Fi? Is there a television? If so, is it showing simply an advertisement, or is it something that your patients would connect with? Is there music playing?
Using the same process, continue your journey through an entire patient visit. Make note of what the experience is like walking back to your exam rooms. What do your patients see and smell while sitting in an exam room waiting for you? Does it smell of isopropyl alcohol? Is it cold or hot? What’s it like to sit in your room wearing nothing but a patient gown? Are there instruments such as cryo guns that could be intimidating to patients? All of these factors can be modified and thus “designed” to optimize the experience for your patients. Continue this journey including a physical exam and discussion with the doctor and other providers and assistants.
This is a great exercise not only for you but more importantly for your staff. Ask your staff to take notes as they walk through the same empathy mapping journey. It will give them an entirely new and valuable perspective on what it’s like to be a patient in your office. Once you’ve completed your empathy mapping, sit with your team and brainstorm about opportunities to improve the experience for your patients. Ask yourselves what things surprised you. What things do you feel could have the largest impact on your patients’ experience in your office? In what ways can you modify the spaces in your office to optimize your patients’ experience?
Having done this exercise in my own clinic, I found it highly impactful. It gave me a deeper understanding of and appreciation for my patients and caused me to make several minor but important changes in my exam room and to my and my staff’s interactions with patients. I hope you have a similarly informative experience.
If you’re interested in learning more about design thinking, then check out the following books and articles:
• “Change by Design: How Design Thinking Transforms Organization and Inspires Innovation,” by Tim Brown (New York: Harper Business, 2009).
• “The Art of Innovation,” by Tom Kelley (New York: A Currency Book, Doubleday, Random House, 2001).
• Design Thinking Comes of Age, by Jon Kolko (Harv Bus Rev. Sep 2015;pp 66-71).
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
‘You’ve been served’: What to do if you receive a subpoena
Dear Dr. Mossman,
Psychiatrists should not reveal what their patients say except to avert a threat to health or safety or to report abuse. So, how can psychiatrists be subpoenaed to provide information for a trial? If I receive a subpoena, how can I comply without violating patient privacy? If I have to go to court, can I “plead the Fifth”?
Submitted by “Dr. S”
Physicians who are served with a subpoena feel upset for the reason Dr. S described: Complying with a subpoena seems to violate the obligation to protect patients’ privacy. But physicians can’t “plead the Fifth” under these circumstances, because the Fifth Amendment to the U.S. Constitution only bars forcing someone to give self-incriminating testimony.1
If you receive a subpoena for information gleaned during patient care, you should not ignore it. Failing to respond might place you in contempt of court and subject you to a fine or even jail time. Yet simply complying could have legal and professional implications, too.
Often, a psychiatrist who receives a subpoena should seek an attorney’s advice on how to best respond. But understanding what subpoenas are and how they work might let you feel less anxious as you go through the process of responding. With this goal in mind, this article covers:
• what a subpoena is and isn’t
• 2 types of privacy obligations
• legal options
• avoiding potential embarrassment (Box).2
What is a subpoena?
All citizens have a legal obligation to furnish courts with the information needed to decide legal issues.3 Statutes and legal rules dictate how such material comes to court.
Issuing a subpoena (from the Latin sub poena, “under penalty”) is one way of obtaining information needed for a legal proceeding. A subpoena ad testificandum directs the recipient to appear at a legal proceeding and provide testimony. A subpoena duces tecum (“you shall bring with you”) directs the recipient to produce specific records or to appear at a legal proceeding with the records.
Usually, subpoenas are issued by attorneys or court clerks, not by judges. As such, they are not court orders. If you receive a subpoena, you should make a timely response of some sort. But, ultimately, you might not have to release the information. Although physicians have to follow the same rules as other citizens, courts recognize that doctors also have professional obligations to their patients.
Confidentiality: Your reason to hesitate
Receiving a subpoena doesn’t change your obligation to protect your patient’s confidentiality. From the law’s standpoint, patient confidentiality is a function of the rules that govern use of information in legal proceedings.
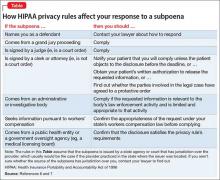
The Privacy Rule4 that arose from the Health Insurance Portability and Accountability Act (HIPAA) of 19965 provides guidance on acceptable responses to subpoenas by “covered entities,” which includes most physicians’ practices. HIPAA permits disclosure of the minimum amount of personal information needed to fulfill the demands of a subpoena. The Table6,7 explains HIPAA’s rules about specific responses to subpoenas, depending on their source.
Many states have patient privacy laws that are stricter than HIPAA rules. If you practice in one of those states, you have to follow the more stringent rule.8 For example, Ohio law does not let subpoenaed providers tender medical records for use in a grand jury proceeding without a release signed by the patient, although HIPAA would allow this (Table).6,7 Out of concern that “giving law enforcement unbridled access to medical records could discourage patients from seeking medical treatment,” Ohio protects patient records more than HIPAA does.9 New York State’s privilege rules also are stricter than HIPAA10 and contain specific provisions about releasing certain types of information (eg, HIV status11). State courts expect physicians to follow their laws about patient privacy and to consult attorneys to make sure that releasing information is done properly.12
Releasing information improperly could become grounds for legal action against you, even if you released the information in response to a subpoena. Legal action could take the form of a lawsuit for breach of confidentiality, a HIPAA-based complaint, a complaint to the state medical board, or all 3 of these.
Must you turn over information?
Before you testify or turn over documents, you need to verify that the legal and ethical requirements for the disclosure are met—as you would for any release of patient information. You can do this by obtaining your patient’s formal, written consent for the disclosure. Before you accept the patient’s agreement, however, you might—and in most cases should— consider discussing how the disclosure could affect the patient’s well-being or your treatment relationship.
If the patient will not agree to the disclosure, the patient or the patient’s attorney can seek to have the subpoena modified or quashed (declared void). One tactic for doing this is by asserting doctor–patient privilege, a legal doctrine codified in most state’s laws. The privilege recognizes that, because privacy is important in medical care, stopping clinical information from automatically coming in court serves an important social purpose.13
The doctor–patient privilege belongs to the litigant—here, your patient—not to you, so your patient has to raise the objection to releasing information.14 Also, the privilege is not absolute. If having the clinical information is necessary, the judge may issue a court order denying the patient’s motion to quash. Unless the judge later modifies or vacates the order, you risk being found in contempt of court if you still refuse to turn over documents demanded by the subpoena.
Fact witness or expert witness?
If the subpoena demands your testimony, the issuing party might want you to serve as a fact witness or expert witness. Persons with relevant personal knowledge to a legal proceeding can serve as fact witnesses, and testify about things they did or perceived.15 For example, a psychiatrist serving as a fact witness could recount having heard or seen a patient talking aloud as if arguing with someone when no real interlocutor was present.
A witness whom the court deems an “expert” by virtue of special knowledge, skill, experience, training, or education may offer opinions based on specific sets of facts. Courts hear such testimony when the expert’s specialized knowledge will help the jury understand the evidence or reach a verdict in a case.16 To return to the example above: a psychiatric expert witness might tell jurors that the patient’s “arguing” was evidence that she was hallucinating and suffered from schizophrenia.
If you receive a subpoena to testify about someone you have treated, you should notify the issuing party that you will provide fact testimony if required to do so. You cannot be compelled to serve as an expert witness, however. In many situations, attempting to provide objective expert testimony about one’s own patient could create unresolvable conflicts between the obligation to tell the truth and your obligation to serve your patient’s interests.17
If the subpoena requests deposition testimony about a patient, you probably will be able to schedule the deposition at a time that is convenient for you and the attorneys involved. Yet you should not agree to be deposed unless (a) you have received the patient’s authorization, (b) a court has ordered you to testify despite the patient’s objection, or (c) your attorney (whom you have consulted about the situation) has advised you that providing testimony is appropriate.
If you are called as a fact witness for a trial, the attorney or court that has subpoenaed you often will try to schedule things to minimize the time taken away from your other duties. Once in court, you can ask the judge (on the record) whether you must answer if you are asked questions about a patient who has not previously authorized you to release treatment information. A judge’s explicit command to respond absolves you of any further ethical obligation to withhold confidential information about the patient’s care.
Bottom Line
If you receive a subpoena for records or testimony, obtaining the patient’s written authorization should allow you to release the information without violating confidentiality obligations. If your patient won’t agree to the release, if turning over information might adversely affect the patient, or if you’re not sure what to do, seek advice from an attorney who knows about medical privacy rules. That way, you can be sure you are meeting all legal and professional standards that apply.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with any manufacturers of competing products.
1. Kastigar v United States, 406 US 441 (1972).
2. Barsky AE. Clinicians in court, second edition: A guide to subpoenas, depositions, testifying, and everything else you need to know. New York, NY: Guilford Press; 2012.
3. United States v Bryan, 339 US 323 (1950).
4. 45 CFR §164.50.
5. 45 CFR Parts 160 and 164.
6. 45 CFR §164.512.
7. Stanger K. HIPAA: responding to subpoenas, orders, and administrative demands. http://www.hhhealthlawblog.com/2013/10/hipaa-responding-to-subpoenas-orders-and-administrative-demands.html. Published October 9, 2013. Accessed September 22, 2015.
8. Zwerling AL, de Harder WA, Tarpey CM. To disclose or not to disclose, that is the question: issues to consider before responding to a subpoena. J Am Coll Radiol. 2012;9(4):279-281.
9. Turk v Oilier, 732 F Supp 2d 758 (ND Ohio 2010).
10. In re Antonia E, 16 Misc 3d 637 (Fam Ct Queens County 2007).
11. NY PBH Law §2785.
12. Crescenzo v Crane, 796 A2d 283 (NJ Super Ct App Div 2002).
13. In re Bruendl’s Will, 102 Wis 45, 78 NW 169 (1899).
14. In re Lifschutz, 2 Cal 3d 415, 85 Cal Rptr 829, 467 P2d 557 (1970).
15. Broun KS, Dix GE, Imwinkelried EJ, et al. McCormick on evidence. 7th ed. St. Paul, MN: West Group; 2013.
16. Fed Evid R 702.
17. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448-456.
Dear Dr. Mossman,
Psychiatrists should not reveal what their patients say except to avert a threat to health or safety or to report abuse. So, how can psychiatrists be subpoenaed to provide information for a trial? If I receive a subpoena, how can I comply without violating patient privacy? If I have to go to court, can I “plead the Fifth”?
Submitted by “Dr. S”
Physicians who are served with a subpoena feel upset for the reason Dr. S described: Complying with a subpoena seems to violate the obligation to protect patients’ privacy. But physicians can’t “plead the Fifth” under these circumstances, because the Fifth Amendment to the U.S. Constitution only bars forcing someone to give self-incriminating testimony.1
If you receive a subpoena for information gleaned during patient care, you should not ignore it. Failing to respond might place you in contempt of court and subject you to a fine or even jail time. Yet simply complying could have legal and professional implications, too.
Often, a psychiatrist who receives a subpoena should seek an attorney’s advice on how to best respond. But understanding what subpoenas are and how they work might let you feel less anxious as you go through the process of responding. With this goal in mind, this article covers:
• what a subpoena is and isn’t
• 2 types of privacy obligations
• legal options
• avoiding potential embarrassment (Box).2
What is a subpoena?
All citizens have a legal obligation to furnish courts with the information needed to decide legal issues.3 Statutes and legal rules dictate how such material comes to court.
Issuing a subpoena (from the Latin sub poena, “under penalty”) is one way of obtaining information needed for a legal proceeding. A subpoena ad testificandum directs the recipient to appear at a legal proceeding and provide testimony. A subpoena duces tecum (“you shall bring with you”) directs the recipient to produce specific records or to appear at a legal proceeding with the records.
Usually, subpoenas are issued by attorneys or court clerks, not by judges. As such, they are not court orders. If you receive a subpoena, you should make a timely response of some sort. But, ultimately, you might not have to release the information. Although physicians have to follow the same rules as other citizens, courts recognize that doctors also have professional obligations to their patients.
Confidentiality: Your reason to hesitate
Receiving a subpoena doesn’t change your obligation to protect your patient’s confidentiality. From the law’s standpoint, patient confidentiality is a function of the rules that govern use of information in legal proceedings.
The Privacy Rule4 that arose from the Health Insurance Portability and Accountability Act (HIPAA) of 19965 provides guidance on acceptable responses to subpoenas by “covered entities,” which includes most physicians’ practices. HIPAA permits disclosure of the minimum amount of personal information needed to fulfill the demands of a subpoena. The Table6,7 explains HIPAA’s rules about specific responses to subpoenas, depending on their source.
Many states have patient privacy laws that are stricter than HIPAA rules. If you practice in one of those states, you have to follow the more stringent rule.8 For example, Ohio law does not let subpoenaed providers tender medical records for use in a grand jury proceeding without a release signed by the patient, although HIPAA would allow this (Table).6,7 Out of concern that “giving law enforcement unbridled access to medical records could discourage patients from seeking medical treatment,” Ohio protects patient records more than HIPAA does.9 New York State’s privilege rules also are stricter than HIPAA10 and contain specific provisions about releasing certain types of information (eg, HIV status11). State courts expect physicians to follow their laws about patient privacy and to consult attorneys to make sure that releasing information is done properly.12
Releasing information improperly could become grounds for legal action against you, even if you released the information in response to a subpoena. Legal action could take the form of a lawsuit for breach of confidentiality, a HIPAA-based complaint, a complaint to the state medical board, or all 3 of these.
Must you turn over information?
Before you testify or turn over documents, you need to verify that the legal and ethical requirements for the disclosure are met—as you would for any release of patient information. You can do this by obtaining your patient’s formal, written consent for the disclosure. Before you accept the patient’s agreement, however, you might—and in most cases should— consider discussing how the disclosure could affect the patient’s well-being or your treatment relationship.
If the patient will not agree to the disclosure, the patient or the patient’s attorney can seek to have the subpoena modified or quashed (declared void). One tactic for doing this is by asserting doctor–patient privilege, a legal doctrine codified in most state’s laws. The privilege recognizes that, because privacy is important in medical care, stopping clinical information from automatically coming in court serves an important social purpose.13
The doctor–patient privilege belongs to the litigant—here, your patient—not to you, so your patient has to raise the objection to releasing information.14 Also, the privilege is not absolute. If having the clinical information is necessary, the judge may issue a court order denying the patient’s motion to quash. Unless the judge later modifies or vacates the order, you risk being found in contempt of court if you still refuse to turn over documents demanded by the subpoena.
Fact witness or expert witness?
If the subpoena demands your testimony, the issuing party might want you to serve as a fact witness or expert witness. Persons with relevant personal knowledge to a legal proceeding can serve as fact witnesses, and testify about things they did or perceived.15 For example, a psychiatrist serving as a fact witness could recount having heard or seen a patient talking aloud as if arguing with someone when no real interlocutor was present.
A witness whom the court deems an “expert” by virtue of special knowledge, skill, experience, training, or education may offer opinions based on specific sets of facts. Courts hear such testimony when the expert’s specialized knowledge will help the jury understand the evidence or reach a verdict in a case.16 To return to the example above: a psychiatric expert witness might tell jurors that the patient’s “arguing” was evidence that she was hallucinating and suffered from schizophrenia.
If you receive a subpoena to testify about someone you have treated, you should notify the issuing party that you will provide fact testimony if required to do so. You cannot be compelled to serve as an expert witness, however. In many situations, attempting to provide objective expert testimony about one’s own patient could create unresolvable conflicts between the obligation to tell the truth and your obligation to serve your patient’s interests.17
If the subpoena requests deposition testimony about a patient, you probably will be able to schedule the deposition at a time that is convenient for you and the attorneys involved. Yet you should not agree to be deposed unless (a) you have received the patient’s authorization, (b) a court has ordered you to testify despite the patient’s objection, or (c) your attorney (whom you have consulted about the situation) has advised you that providing testimony is appropriate.
If you are called as a fact witness for a trial, the attorney or court that has subpoenaed you often will try to schedule things to minimize the time taken away from your other duties. Once in court, you can ask the judge (on the record) whether you must answer if you are asked questions about a patient who has not previously authorized you to release treatment information. A judge’s explicit command to respond absolves you of any further ethical obligation to withhold confidential information about the patient’s care.
Bottom Line
If you receive a subpoena for records or testimony, obtaining the patient’s written authorization should allow you to release the information without violating confidentiality obligations. If your patient won’t agree to the release, if turning over information might adversely affect the patient, or if you’re not sure what to do, seek advice from an attorney who knows about medical privacy rules. That way, you can be sure you are meeting all legal and professional standards that apply.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with any manufacturers of competing products.
Dear Dr. Mossman,
Psychiatrists should not reveal what their patients say except to avert a threat to health or safety or to report abuse. So, how can psychiatrists be subpoenaed to provide information for a trial? If I receive a subpoena, how can I comply without violating patient privacy? If I have to go to court, can I “plead the Fifth”?
Submitted by “Dr. S”
Physicians who are served with a subpoena feel upset for the reason Dr. S described: Complying with a subpoena seems to violate the obligation to protect patients’ privacy. But physicians can’t “plead the Fifth” under these circumstances, because the Fifth Amendment to the U.S. Constitution only bars forcing someone to give self-incriminating testimony.1
If you receive a subpoena for information gleaned during patient care, you should not ignore it. Failing to respond might place you in contempt of court and subject you to a fine or even jail time. Yet simply complying could have legal and professional implications, too.
Often, a psychiatrist who receives a subpoena should seek an attorney’s advice on how to best respond. But understanding what subpoenas are and how they work might let you feel less anxious as you go through the process of responding. With this goal in mind, this article covers:
• what a subpoena is and isn’t
• 2 types of privacy obligations
• legal options
• avoiding potential embarrassment (Box).2
What is a subpoena?
All citizens have a legal obligation to furnish courts with the information needed to decide legal issues.3 Statutes and legal rules dictate how such material comes to court.
Issuing a subpoena (from the Latin sub poena, “under penalty”) is one way of obtaining information needed for a legal proceeding. A subpoena ad testificandum directs the recipient to appear at a legal proceeding and provide testimony. A subpoena duces tecum (“you shall bring with you”) directs the recipient to produce specific records or to appear at a legal proceeding with the records.
Usually, subpoenas are issued by attorneys or court clerks, not by judges. As such, they are not court orders. If you receive a subpoena, you should make a timely response of some sort. But, ultimately, you might not have to release the information. Although physicians have to follow the same rules as other citizens, courts recognize that doctors also have professional obligations to their patients.
Confidentiality: Your reason to hesitate
Receiving a subpoena doesn’t change your obligation to protect your patient’s confidentiality. From the law’s standpoint, patient confidentiality is a function of the rules that govern use of information in legal proceedings.
The Privacy Rule4 that arose from the Health Insurance Portability and Accountability Act (HIPAA) of 19965 provides guidance on acceptable responses to subpoenas by “covered entities,” which includes most physicians’ practices. HIPAA permits disclosure of the minimum amount of personal information needed to fulfill the demands of a subpoena. The Table6,7 explains HIPAA’s rules about specific responses to subpoenas, depending on their source.
Many states have patient privacy laws that are stricter than HIPAA rules. If you practice in one of those states, you have to follow the more stringent rule.8 For example, Ohio law does not let subpoenaed providers tender medical records for use in a grand jury proceeding without a release signed by the patient, although HIPAA would allow this (Table).6,7 Out of concern that “giving law enforcement unbridled access to medical records could discourage patients from seeking medical treatment,” Ohio protects patient records more than HIPAA does.9 New York State’s privilege rules also are stricter than HIPAA10 and contain specific provisions about releasing certain types of information (eg, HIV status11). State courts expect physicians to follow their laws about patient privacy and to consult attorneys to make sure that releasing information is done properly.12
Releasing information improperly could become grounds for legal action against you, even if you released the information in response to a subpoena. Legal action could take the form of a lawsuit for breach of confidentiality, a HIPAA-based complaint, a complaint to the state medical board, or all 3 of these.
Must you turn over information?
Before you testify or turn over documents, you need to verify that the legal and ethical requirements for the disclosure are met—as you would for any release of patient information. You can do this by obtaining your patient’s formal, written consent for the disclosure. Before you accept the patient’s agreement, however, you might—and in most cases should— consider discussing how the disclosure could affect the patient’s well-being or your treatment relationship.
If the patient will not agree to the disclosure, the patient or the patient’s attorney can seek to have the subpoena modified or quashed (declared void). One tactic for doing this is by asserting doctor–patient privilege, a legal doctrine codified in most state’s laws. The privilege recognizes that, because privacy is important in medical care, stopping clinical information from automatically coming in court serves an important social purpose.13
The doctor–patient privilege belongs to the litigant—here, your patient—not to you, so your patient has to raise the objection to releasing information.14 Also, the privilege is not absolute. If having the clinical information is necessary, the judge may issue a court order denying the patient’s motion to quash. Unless the judge later modifies or vacates the order, you risk being found in contempt of court if you still refuse to turn over documents demanded by the subpoena.
Fact witness or expert witness?
If the subpoena demands your testimony, the issuing party might want you to serve as a fact witness or expert witness. Persons with relevant personal knowledge to a legal proceeding can serve as fact witnesses, and testify about things they did or perceived.15 For example, a psychiatrist serving as a fact witness could recount having heard or seen a patient talking aloud as if arguing with someone when no real interlocutor was present.
A witness whom the court deems an “expert” by virtue of special knowledge, skill, experience, training, or education may offer opinions based on specific sets of facts. Courts hear such testimony when the expert’s specialized knowledge will help the jury understand the evidence or reach a verdict in a case.16 To return to the example above: a psychiatric expert witness might tell jurors that the patient’s “arguing” was evidence that she was hallucinating and suffered from schizophrenia.
If you receive a subpoena to testify about someone you have treated, you should notify the issuing party that you will provide fact testimony if required to do so. You cannot be compelled to serve as an expert witness, however. In many situations, attempting to provide objective expert testimony about one’s own patient could create unresolvable conflicts between the obligation to tell the truth and your obligation to serve your patient’s interests.17
If the subpoena requests deposition testimony about a patient, you probably will be able to schedule the deposition at a time that is convenient for you and the attorneys involved. Yet you should not agree to be deposed unless (a) you have received the patient’s authorization, (b) a court has ordered you to testify despite the patient’s objection, or (c) your attorney (whom you have consulted about the situation) has advised you that providing testimony is appropriate.
If you are called as a fact witness for a trial, the attorney or court that has subpoenaed you often will try to schedule things to minimize the time taken away from your other duties. Once in court, you can ask the judge (on the record) whether you must answer if you are asked questions about a patient who has not previously authorized you to release treatment information. A judge’s explicit command to respond absolves you of any further ethical obligation to withhold confidential information about the patient’s care.
Bottom Line
If you receive a subpoena for records or testimony, obtaining the patient’s written authorization should allow you to release the information without violating confidentiality obligations. If your patient won’t agree to the release, if turning over information might adversely affect the patient, or if you’re not sure what to do, seek advice from an attorney who knows about medical privacy rules. That way, you can be sure you are meeting all legal and professional standards that apply.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with any manufacturers of competing products.
1. Kastigar v United States, 406 US 441 (1972).
2. Barsky AE. Clinicians in court, second edition: A guide to subpoenas, depositions, testifying, and everything else you need to know. New York, NY: Guilford Press; 2012.
3. United States v Bryan, 339 US 323 (1950).
4. 45 CFR §164.50.
5. 45 CFR Parts 160 and 164.
6. 45 CFR §164.512.
7. Stanger K. HIPAA: responding to subpoenas, orders, and administrative demands. http://www.hhhealthlawblog.com/2013/10/hipaa-responding-to-subpoenas-orders-and-administrative-demands.html. Published October 9, 2013. Accessed September 22, 2015.
8. Zwerling AL, de Harder WA, Tarpey CM. To disclose or not to disclose, that is the question: issues to consider before responding to a subpoena. J Am Coll Radiol. 2012;9(4):279-281.
9. Turk v Oilier, 732 F Supp 2d 758 (ND Ohio 2010).
10. In re Antonia E, 16 Misc 3d 637 (Fam Ct Queens County 2007).
11. NY PBH Law §2785.
12. Crescenzo v Crane, 796 A2d 283 (NJ Super Ct App Div 2002).
13. In re Bruendl’s Will, 102 Wis 45, 78 NW 169 (1899).
14. In re Lifschutz, 2 Cal 3d 415, 85 Cal Rptr 829, 467 P2d 557 (1970).
15. Broun KS, Dix GE, Imwinkelried EJ, et al. McCormick on evidence. 7th ed. St. Paul, MN: West Group; 2013.
16. Fed Evid R 702.
17. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448-456.
1. Kastigar v United States, 406 US 441 (1972).
2. Barsky AE. Clinicians in court, second edition: A guide to subpoenas, depositions, testifying, and everything else you need to know. New York, NY: Guilford Press; 2012.
3. United States v Bryan, 339 US 323 (1950).
4. 45 CFR §164.50.
5. 45 CFR Parts 160 and 164.
6. 45 CFR §164.512.
7. Stanger K. HIPAA: responding to subpoenas, orders, and administrative demands. http://www.hhhealthlawblog.com/2013/10/hipaa-responding-to-subpoenas-orders-and-administrative-demands.html. Published October 9, 2013. Accessed September 22, 2015.
8. Zwerling AL, de Harder WA, Tarpey CM. To disclose or not to disclose, that is the question: issues to consider before responding to a subpoena. J Am Coll Radiol. 2012;9(4):279-281.
9. Turk v Oilier, 732 F Supp 2d 758 (ND Ohio 2010).
10. In re Antonia E, 16 Misc 3d 637 (Fam Ct Queens County 2007).
11. NY PBH Law §2785.
12. Crescenzo v Crane, 796 A2d 283 (NJ Super Ct App Div 2002).
13. In re Bruendl’s Will, 102 Wis 45, 78 NW 169 (1899).
14. In re Lifschutz, 2 Cal 3d 415, 85 Cal Rptr 829, 467 P2d 557 (1970).
15. Broun KS, Dix GE, Imwinkelried EJ, et al. McCormick on evidence. 7th ed. St. Paul, MN: West Group; 2013.
16. Fed Evid R 702.
17. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448-456.
FDA approves first naloxone nasal spray for opioid overdose
The Food and Drug Administration has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan by Adapt Pharma, a partner of Lightlake Therapeutics, the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr. Stephen Ostroff, FDA acting commissioner, said in a statement released with the Nov. 18 approval announcement. “We cannot stand by while Americans are dying. While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Dosage varies for each individual and should be determined by physicians.
Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training and can be performed by anyone.
Narcan’s approval comes less than 4 months after the FDA granted the medication a fast-track designation and priority review status, both of which are meant to expedite the review and approval processes for drugs that “demonstrate the potential to address an unmet medical need” and “offer a significant improvement in the safety or effectiveness of the treatment, prevention, or diagnosis of a serious condition,” according to the FDA’s approval statement.
Adverse events associated with opiate withdrawal have been noted in Narcan patients. Specifically, the FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
“Opioid overdose is responsible for the deaths of thousands of Americans in communities throughout the country, leaving a trail of devastation for friends and families,” Seamus Mulligan, Adapt Pharma’s chairman and CEO, said in a statement. “This new device makes naloxone readily available for emergency use by a friend, family member, or caregiver, as well as offering an alternative treatment option for first responders and health care providers.”
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the United States, cautioned Dr. Peter Friedmann, chief research officer at Baystate Health in Springfield, Mass.
“[Narcan] is just addressing overdose; we need more and better medications for treating addiction, we need more physicians and clinicians who are skilled in using these medications,” said Dr. Friedmann. “Given the ongoing crisis of deaths from opioid overuse, this expands the options that physicians, pharmacies, and community distribution programs can use to reduce these deaths.”
Dr. Friedmann also voiced his concern regarding the pricing of Narcan. Making the drug affordable is crucial to its success at successfully treating opioid overuse, he said.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Dr. Friedmann said that he hopes addiction medicine becomes a more attractive field for medical students and residents. It’s important for future physicians to know how to properly treat patients of addiction and administer drugs safely and effectively, he said.
“Addiction medicine is on the cusp of full recognition as a medical specialty, and we need people to go into that field to teach patients, medical students, and residents how to treat people with addiction,” Dr. Friedmann said. At the current rate, “we’re never going to have enough, so we need generalists to take this on.”
The Food and Drug Administration has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan by Adapt Pharma, a partner of Lightlake Therapeutics, the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr. Stephen Ostroff, FDA acting commissioner, said in a statement released with the Nov. 18 approval announcement. “We cannot stand by while Americans are dying. While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Dosage varies for each individual and should be determined by physicians.
Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training and can be performed by anyone.
Narcan’s approval comes less than 4 months after the FDA granted the medication a fast-track designation and priority review status, both of which are meant to expedite the review and approval processes for drugs that “demonstrate the potential to address an unmet medical need” and “offer a significant improvement in the safety or effectiveness of the treatment, prevention, or diagnosis of a serious condition,” according to the FDA’s approval statement.
Adverse events associated with opiate withdrawal have been noted in Narcan patients. Specifically, the FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
“Opioid overdose is responsible for the deaths of thousands of Americans in communities throughout the country, leaving a trail of devastation for friends and families,” Seamus Mulligan, Adapt Pharma’s chairman and CEO, said in a statement. “This new device makes naloxone readily available for emergency use by a friend, family member, or caregiver, as well as offering an alternative treatment option for first responders and health care providers.”
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the United States, cautioned Dr. Peter Friedmann, chief research officer at Baystate Health in Springfield, Mass.
“[Narcan] is just addressing overdose; we need more and better medications for treating addiction, we need more physicians and clinicians who are skilled in using these medications,” said Dr. Friedmann. “Given the ongoing crisis of deaths from opioid overuse, this expands the options that physicians, pharmacies, and community distribution programs can use to reduce these deaths.”
Dr. Friedmann also voiced his concern regarding the pricing of Narcan. Making the drug affordable is crucial to its success at successfully treating opioid overuse, he said.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Dr. Friedmann said that he hopes addiction medicine becomes a more attractive field for medical students and residents. It’s important for future physicians to know how to properly treat patients of addiction and administer drugs safely and effectively, he said.
“Addiction medicine is on the cusp of full recognition as a medical specialty, and we need people to go into that field to teach patients, medical students, and residents how to treat people with addiction,” Dr. Friedmann said. At the current rate, “we’re never going to have enough, so we need generalists to take this on.”
The Food and Drug Administration has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan by Adapt Pharma, a partner of Lightlake Therapeutics, the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr. Stephen Ostroff, FDA acting commissioner, said in a statement released with the Nov. 18 approval announcement. “We cannot stand by while Americans are dying. While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Dosage varies for each individual and should be determined by physicians.
Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training and can be performed by anyone.
Narcan’s approval comes less than 4 months after the FDA granted the medication a fast-track designation and priority review status, both of which are meant to expedite the review and approval processes for drugs that “demonstrate the potential to address an unmet medical need” and “offer a significant improvement in the safety or effectiveness of the treatment, prevention, or diagnosis of a serious condition,” according to the FDA’s approval statement.
Adverse events associated with opiate withdrawal have been noted in Narcan patients. Specifically, the FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
“Opioid overdose is responsible for the deaths of thousands of Americans in communities throughout the country, leaving a trail of devastation for friends and families,” Seamus Mulligan, Adapt Pharma’s chairman and CEO, said in a statement. “This new device makes naloxone readily available for emergency use by a friend, family member, or caregiver, as well as offering an alternative treatment option for first responders and health care providers.”
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the United States, cautioned Dr. Peter Friedmann, chief research officer at Baystate Health in Springfield, Mass.
“[Narcan] is just addressing overdose; we need more and better medications for treating addiction, we need more physicians and clinicians who are skilled in using these medications,” said Dr. Friedmann. “Given the ongoing crisis of deaths from opioid overuse, this expands the options that physicians, pharmacies, and community distribution programs can use to reduce these deaths.”
Dr. Friedmann also voiced his concern regarding the pricing of Narcan. Making the drug affordable is crucial to its success at successfully treating opioid overuse, he said.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Dr. Friedmann said that he hopes addiction medicine becomes a more attractive field for medical students and residents. It’s important for future physicians to know how to properly treat patients of addiction and administer drugs safely and effectively, he said.
“Addiction medicine is on the cusp of full recognition as a medical specialty, and we need people to go into that field to teach patients, medical students, and residents how to treat people with addiction,” Dr. Friedmann said. At the current rate, “we’re never going to have enough, so we need generalists to take this on.”
ACR: Criteria enable prompt diagnosis and treatment of CAPS
SAN FRANCISCO – Valid diagnostic criteria for cryopyrin-associated periodic syndromes are sorely needed, and a new model of CAPS diagnostic criteria enables rapid diagnosis of this rare, heterogeneous, inflammatory disease that can have devastating consequences if left undiagnosed and untreated.
“Our novel, unique approach integrated traditional methods of evidence synthesis with expert consensus, web-based decision tools, and innovative statistical methods. We hope this model can be of benefit in the diagnosis of other rare diseases,” said Dr. Jasmin B. Kümmerle-Deschner of the department of pediatrics at the University of Tübingen (Germany). She noted that the panel wanted to develop diagnostic criteria that could be used prior to genetic testing or in cases where no genetic mutation is identified.
Dr. Kümmerle-Deschner, who was on the multinational panel that developed the new diagnostic criteria, reviewed the process and presented the new criteria at the annual meeting of the American College of Rheumatology.
Cryopyrin-associated periodic syndromes (CAPS) comprise a rare, clinically heterogeneous group of devastating inflammatory diseases characterized by variable, severe system and organ inflammation resulting in permanent organ damage. The disease can manifest right after birth or later in life, and it can be associated with a mutation in the NLRP3 gene. Because the pathogenesis involves continually increased IL-1 secretion, early diagnosis and rapid initiation of IL-1 inhibition can control inflammation and prevent organ damage in children and adults with CAPS.
The lengthy process for developing the diagnostic criteria involved building an 18-member team of pediatric and adult subspecialists and experts in methods for rare disease. They generated 32 CAPS-typical items from a systematic literature review of 33 papers that described symptoms of CAPS and then reviewed the items in CAPS registries, weighting them via decision analysis software. Next, the panel refined these to 14 items plus the NLRP3 mutation. 1000Minds decision-making software ranked these 14 variables based on importance for the diagnosis of CAPS, with excellent correlation among experts.
Then a correspondence analysis determined variables consistently associated with the diagnosis of CAPS based on 284 cases and 873 controls; this process removed infrequently observed variables, such as “amyloidosis.” The remaining seven variables were found to be significantly associated with a diagnosis of CAPS (P less than .001 for all).
The final CAPS diagnosis model includes raised inflammatory markers (C-reactive protein/serum amyloid A) as a mandatory criterion, plus at least two of six different typical signs and symptoms of CAPS: urticaria-like rash, cold-stress triggered episodes, sensorineural hearing loss, musculoskeletal symptoms such as arthralgia, arthritis, and myalgia, chronic aseptic meningitis, and skeletal abnormalities such as epiphyseal overgrowth/frontal bossing. This model had a sensitivity of 81% and a specificity of 94%, performing well in all CAPS subtypes as well as in subgroups with or without evidence of germline NLRP3 mutations.
Dr. Kümmerle-Deschner opened her talk with a case description of an 81-year-old man who presented with a baffling disease. It turned out that his granddaughter was diagnosed with CAPS and 16 other family members were affected. She closed the talk by showing how this man could have been rapidly diagnosed by the new CAPS criteria. He presented with urticaria-like rash, arthralgia, arthritis, and cold-triggered episodes in the context of raised inflammatory markers.
“Early diagnosis enabling rapid treatment is possible,” she stated.
Dr. Kümmerle-Deschner disclosed financial ties with Novartis.
SAN FRANCISCO – Valid diagnostic criteria for cryopyrin-associated periodic syndromes are sorely needed, and a new model of CAPS diagnostic criteria enables rapid diagnosis of this rare, heterogeneous, inflammatory disease that can have devastating consequences if left undiagnosed and untreated.
“Our novel, unique approach integrated traditional methods of evidence synthesis with expert consensus, web-based decision tools, and innovative statistical methods. We hope this model can be of benefit in the diagnosis of other rare diseases,” said Dr. Jasmin B. Kümmerle-Deschner of the department of pediatrics at the University of Tübingen (Germany). She noted that the panel wanted to develop diagnostic criteria that could be used prior to genetic testing or in cases where no genetic mutation is identified.
Dr. Kümmerle-Deschner, who was on the multinational panel that developed the new diagnostic criteria, reviewed the process and presented the new criteria at the annual meeting of the American College of Rheumatology.
Cryopyrin-associated periodic syndromes (CAPS) comprise a rare, clinically heterogeneous group of devastating inflammatory diseases characterized by variable, severe system and organ inflammation resulting in permanent organ damage. The disease can manifest right after birth or later in life, and it can be associated with a mutation in the NLRP3 gene. Because the pathogenesis involves continually increased IL-1 secretion, early diagnosis and rapid initiation of IL-1 inhibition can control inflammation and prevent organ damage in children and adults with CAPS.
The lengthy process for developing the diagnostic criteria involved building an 18-member team of pediatric and adult subspecialists and experts in methods for rare disease. They generated 32 CAPS-typical items from a systematic literature review of 33 papers that described symptoms of CAPS and then reviewed the items in CAPS registries, weighting them via decision analysis software. Next, the panel refined these to 14 items plus the NLRP3 mutation. 1000Minds decision-making software ranked these 14 variables based on importance for the diagnosis of CAPS, with excellent correlation among experts.
Then a correspondence analysis determined variables consistently associated with the diagnosis of CAPS based on 284 cases and 873 controls; this process removed infrequently observed variables, such as “amyloidosis.” The remaining seven variables were found to be significantly associated with a diagnosis of CAPS (P less than .001 for all).
The final CAPS diagnosis model includes raised inflammatory markers (C-reactive protein/serum amyloid A) as a mandatory criterion, plus at least two of six different typical signs and symptoms of CAPS: urticaria-like rash, cold-stress triggered episodes, sensorineural hearing loss, musculoskeletal symptoms such as arthralgia, arthritis, and myalgia, chronic aseptic meningitis, and skeletal abnormalities such as epiphyseal overgrowth/frontal bossing. This model had a sensitivity of 81% and a specificity of 94%, performing well in all CAPS subtypes as well as in subgroups with or without evidence of germline NLRP3 mutations.
Dr. Kümmerle-Deschner opened her talk with a case description of an 81-year-old man who presented with a baffling disease. It turned out that his granddaughter was diagnosed with CAPS and 16 other family members were affected. She closed the talk by showing how this man could have been rapidly diagnosed by the new CAPS criteria. He presented with urticaria-like rash, arthralgia, arthritis, and cold-triggered episodes in the context of raised inflammatory markers.
“Early diagnosis enabling rapid treatment is possible,” she stated.
Dr. Kümmerle-Deschner disclosed financial ties with Novartis.
SAN FRANCISCO – Valid diagnostic criteria for cryopyrin-associated periodic syndromes are sorely needed, and a new model of CAPS diagnostic criteria enables rapid diagnosis of this rare, heterogeneous, inflammatory disease that can have devastating consequences if left undiagnosed and untreated.
“Our novel, unique approach integrated traditional methods of evidence synthesis with expert consensus, web-based decision tools, and innovative statistical methods. We hope this model can be of benefit in the diagnosis of other rare diseases,” said Dr. Jasmin B. Kümmerle-Deschner of the department of pediatrics at the University of Tübingen (Germany). She noted that the panel wanted to develop diagnostic criteria that could be used prior to genetic testing or in cases where no genetic mutation is identified.
Dr. Kümmerle-Deschner, who was on the multinational panel that developed the new diagnostic criteria, reviewed the process and presented the new criteria at the annual meeting of the American College of Rheumatology.
Cryopyrin-associated periodic syndromes (CAPS) comprise a rare, clinically heterogeneous group of devastating inflammatory diseases characterized by variable, severe system and organ inflammation resulting in permanent organ damage. The disease can manifest right after birth or later in life, and it can be associated with a mutation in the NLRP3 gene. Because the pathogenesis involves continually increased IL-1 secretion, early diagnosis and rapid initiation of IL-1 inhibition can control inflammation and prevent organ damage in children and adults with CAPS.
The lengthy process for developing the diagnostic criteria involved building an 18-member team of pediatric and adult subspecialists and experts in methods for rare disease. They generated 32 CAPS-typical items from a systematic literature review of 33 papers that described symptoms of CAPS and then reviewed the items in CAPS registries, weighting them via decision analysis software. Next, the panel refined these to 14 items plus the NLRP3 mutation. 1000Minds decision-making software ranked these 14 variables based on importance for the diagnosis of CAPS, with excellent correlation among experts.
Then a correspondence analysis determined variables consistently associated with the diagnosis of CAPS based on 284 cases and 873 controls; this process removed infrequently observed variables, such as “amyloidosis.” The remaining seven variables were found to be significantly associated with a diagnosis of CAPS (P less than .001 for all).
The final CAPS diagnosis model includes raised inflammatory markers (C-reactive protein/serum amyloid A) as a mandatory criterion, plus at least two of six different typical signs and symptoms of CAPS: urticaria-like rash, cold-stress triggered episodes, sensorineural hearing loss, musculoskeletal symptoms such as arthralgia, arthritis, and myalgia, chronic aseptic meningitis, and skeletal abnormalities such as epiphyseal overgrowth/frontal bossing. This model had a sensitivity of 81% and a specificity of 94%, performing well in all CAPS subtypes as well as in subgroups with or without evidence of germline NLRP3 mutations.
Dr. Kümmerle-Deschner opened her talk with a case description of an 81-year-old man who presented with a baffling disease. It turned out that his granddaughter was diagnosed with CAPS and 16 other family members were affected. She closed the talk by showing how this man could have been rapidly diagnosed by the new CAPS criteria. He presented with urticaria-like rash, arthralgia, arthritis, and cold-triggered episodes in the context of raised inflammatory markers.
“Early diagnosis enabling rapid treatment is possible,” she stated.
Dr. Kümmerle-Deschner disclosed financial ties with Novartis.
AT THE ACR ANNUAL MEETING
ICD-10 Under ACP Scrutiny
NEW YORK - While the new International Classification of Diseases, Tenth Revision, Clinical
Modification (ICD-10-CM) codes offer greater diagnostic precision, their implementation will require training of clinicians, coders, and other staff to minimize payment denials or delays from both public and private payers.
Brian Outland and colleagues from the American College of Physicians in Washington, D.C., outline some of the promises and challenges of ICD-10-CM implementation in a report online Sept. 22 in Annals of Internal Medicine.
Although completed and endorsed by the World Health Assembly in 1990, ICD-10-CM's implementation date has repeatedly been delayed, and was scheduled to take effect on Oct. 1.
The authors suggest that "the newer coding system will produce data that will indicate the clinical trajectory and other factors that will enable the data to be used in meaningful ways to better understand complications, design robust algorithms for clinical decision support, and track outcomes. Having these details built into the codes will decrease the need for health care providers to include supporting documentation with claims."
The new ICD-10-CM alphanumeric codes will contain as many as seven characters that specify categories, subcategories, laterality, severity and other features.
The use of codes that are not specific enough can result in payment denials or delays, so practices will need to keep current on payer reimbursement policies to ensure the reporting of ICD-10-CM codes that support reimbursement, the authors note.
The cost for the training of clinicians and staffs will depend on practice size, specialty, the method of training, current documentation quality, and technology readiness and availability.
Dr. Susan H. Fenton from UTHealth School of Biomedical Informatics in Houston, Texas, said by email, "One of the thoughts I cannot get away from is that the U.S. is trying to manage a 21st-century, rapidly evolving healthcare system with a 1970s technology. I can think of little else in healthcare that has remained as static since the 1970s."
"The diagnostic system added lots of codes, but the basic structure is the same," she said.
"Certainly, with more detail such as laterality, as well as first encounter, subsequent encounter, and sequelae, it will be much easier to track care for specific conditions across providers," Dr. Fenton said. "I think the issue of claims denials will have to play out over time."
Resources and tools from the Centers for Medicare & Medicaid Services (CMS) can be found online at www.roadto10.org.
The American College of Physicians also has helpful information available at www.acponline.org/ICD10.
Outland did not respond to a request for comment.
NEW YORK - While the new International Classification of Diseases, Tenth Revision, Clinical
Modification (ICD-10-CM) codes offer greater diagnostic precision, their implementation will require training of clinicians, coders, and other staff to minimize payment denials or delays from both public and private payers.
Brian Outland and colleagues from the American College of Physicians in Washington, D.C., outline some of the promises and challenges of ICD-10-CM implementation in a report online Sept. 22 in Annals of Internal Medicine.
Although completed and endorsed by the World Health Assembly in 1990, ICD-10-CM's implementation date has repeatedly been delayed, and was scheduled to take effect on Oct. 1.
The authors suggest that "the newer coding system will produce data that will indicate the clinical trajectory and other factors that will enable the data to be used in meaningful ways to better understand complications, design robust algorithms for clinical decision support, and track outcomes. Having these details built into the codes will decrease the need for health care providers to include supporting documentation with claims."
The new ICD-10-CM alphanumeric codes will contain as many as seven characters that specify categories, subcategories, laterality, severity and other features.
The use of codes that are not specific enough can result in payment denials or delays, so practices will need to keep current on payer reimbursement policies to ensure the reporting of ICD-10-CM codes that support reimbursement, the authors note.
The cost for the training of clinicians and staffs will depend on practice size, specialty, the method of training, current documentation quality, and technology readiness and availability.
Dr. Susan H. Fenton from UTHealth School of Biomedical Informatics in Houston, Texas, said by email, "One of the thoughts I cannot get away from is that the U.S. is trying to manage a 21st-century, rapidly evolving healthcare system with a 1970s technology. I can think of little else in healthcare that has remained as static since the 1970s."
"The diagnostic system added lots of codes, but the basic structure is the same," she said.
"Certainly, with more detail such as laterality, as well as first encounter, subsequent encounter, and sequelae, it will be much easier to track care for specific conditions across providers," Dr. Fenton said. "I think the issue of claims denials will have to play out over time."
Resources and tools from the Centers for Medicare & Medicaid Services (CMS) can be found online at www.roadto10.org.
The American College of Physicians also has helpful information available at www.acponline.org/ICD10.
Outland did not respond to a request for comment.
NEW YORK - While the new International Classification of Diseases, Tenth Revision, Clinical
Modification (ICD-10-CM) codes offer greater diagnostic precision, their implementation will require training of clinicians, coders, and other staff to minimize payment denials or delays from both public and private payers.
Brian Outland and colleagues from the American College of Physicians in Washington, D.C., outline some of the promises and challenges of ICD-10-CM implementation in a report online Sept. 22 in Annals of Internal Medicine.
Although completed and endorsed by the World Health Assembly in 1990, ICD-10-CM's implementation date has repeatedly been delayed, and was scheduled to take effect on Oct. 1.
The authors suggest that "the newer coding system will produce data that will indicate the clinical trajectory and other factors that will enable the data to be used in meaningful ways to better understand complications, design robust algorithms for clinical decision support, and track outcomes. Having these details built into the codes will decrease the need for health care providers to include supporting documentation with claims."
The new ICD-10-CM alphanumeric codes will contain as many as seven characters that specify categories, subcategories, laterality, severity and other features.
The use of codes that are not specific enough can result in payment denials or delays, so practices will need to keep current on payer reimbursement policies to ensure the reporting of ICD-10-CM codes that support reimbursement, the authors note.
The cost for the training of clinicians and staffs will depend on practice size, specialty, the method of training, current documentation quality, and technology readiness and availability.
Dr. Susan H. Fenton from UTHealth School of Biomedical Informatics in Houston, Texas, said by email, "One of the thoughts I cannot get away from is that the U.S. is trying to manage a 21st-century, rapidly evolving healthcare system with a 1970s technology. I can think of little else in healthcare that has remained as static since the 1970s."
"The diagnostic system added lots of codes, but the basic structure is the same," she said.
"Certainly, with more detail such as laterality, as well as first encounter, subsequent encounter, and sequelae, it will be much easier to track care for specific conditions across providers," Dr. Fenton said. "I think the issue of claims denials will have to play out over time."
Resources and tools from the Centers for Medicare & Medicaid Services (CMS) can be found online at www.roadto10.org.
The American College of Physicians also has helpful information available at www.acponline.org/ICD10.
Outland did not respond to a request for comment.
A surge in congenital syphilis reveals gaps in obstetric practice
The rate of congenital syphilis increased to 11.6 cases per 100,000 live births in 2014 in the United States—the highest rate documented since 2001, according to a new report from the Centers for Disease Control and Prevention (CDC).1 The increase in the rate of congenital syphilis reflects a rise in the rate of primary and secondary syphilis among US women, from 0.9 to 1.1 cases per 100,000 women, during the same period.1
The rate of congenital syphilis had declined between 2008 and 2012, from 10.5 cases to 8.4 cases per 100,000 live births.
Congenital syphilis occurs when an infected mother transmits the disease to her fetus during pregnancy. Among the adverse effects of congenital syphilis are deformities, stillbirth, and early infant death. “However, among mothers identified with syphilis who deliver past 20 weeks’ gestation, treatment with penicillin at least 30 days before delivery is 98% effective at preventing [congenital syphilis],” the CDC report notes.1
For the purposes of the CDC report, congenital syphilis includes “both infants and stillbirths with clinical evidence” of the disease, “as well as those infants and stillbirths born to mothers with untreated or inadequately treated syphilis, regardless of the infant’s manifestation of clinical disease.”1
CDC recommendations
The CDC notes that most of the increases in the rates of maternal and congenital syphilis likely stem from inadequate prenatal care.
“A large percentage of [congenital syphilis] cases continue to be attributable to a lack of prenatal care; even among those receiving some prenatal care, the detection and treatment of maternal syphilis is often not early enough….At particular risk are those who are uninsured or underinsured and those with substance use issues.”1
Among the recommendations of the CDC:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Screen women at elevated risk for syphilis, as well as those who live in “high-morbidity geographic areas” at the beginning of the third trimester and again at delivery.
- In cases where prenatal care has been lacking, screen the woman for syphilis using a rapid plasma reagin (RPR) card and treat the patient who tests positive at the time the pregnancy is confirmed.
- Do not discharge an infant from the hospital unless the syphilis serologic status of the mother has been tested at least once during pregnancy and, preferably, again at delivery (in high-risk cases).
- Test any woman who delivers a stillborn infant for syphilis.
Reference
1. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2008–2014. MMWR. 2015;64(44):1241–1245.
The rate of congenital syphilis increased to 11.6 cases per 100,000 live births in 2014 in the United States—the highest rate documented since 2001, according to a new report from the Centers for Disease Control and Prevention (CDC).1 The increase in the rate of congenital syphilis reflects a rise in the rate of primary and secondary syphilis among US women, from 0.9 to 1.1 cases per 100,000 women, during the same period.1
The rate of congenital syphilis had declined between 2008 and 2012, from 10.5 cases to 8.4 cases per 100,000 live births.
Congenital syphilis occurs when an infected mother transmits the disease to her fetus during pregnancy. Among the adverse effects of congenital syphilis are deformities, stillbirth, and early infant death. “However, among mothers identified with syphilis who deliver past 20 weeks’ gestation, treatment with penicillin at least 30 days before delivery is 98% effective at preventing [congenital syphilis],” the CDC report notes.1
For the purposes of the CDC report, congenital syphilis includes “both infants and stillbirths with clinical evidence” of the disease, “as well as those infants and stillbirths born to mothers with untreated or inadequately treated syphilis, regardless of the infant’s manifestation of clinical disease.”1
CDC recommendations
The CDC notes that most of the increases in the rates of maternal and congenital syphilis likely stem from inadequate prenatal care.
“A large percentage of [congenital syphilis] cases continue to be attributable to a lack of prenatal care; even among those receiving some prenatal care, the detection and treatment of maternal syphilis is often not early enough….At particular risk are those who are uninsured or underinsured and those with substance use issues.”1
Among the recommendations of the CDC:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Screen women at elevated risk for syphilis, as well as those who live in “high-morbidity geographic areas” at the beginning of the third trimester and again at delivery.
- In cases where prenatal care has been lacking, screen the woman for syphilis using a rapid plasma reagin (RPR) card and treat the patient who tests positive at the time the pregnancy is confirmed.
- Do not discharge an infant from the hospital unless the syphilis serologic status of the mother has been tested at least once during pregnancy and, preferably, again at delivery (in high-risk cases).
- Test any woman who delivers a stillborn infant for syphilis.
The rate of congenital syphilis increased to 11.6 cases per 100,000 live births in 2014 in the United States—the highest rate documented since 2001, according to a new report from the Centers for Disease Control and Prevention (CDC).1 The increase in the rate of congenital syphilis reflects a rise in the rate of primary and secondary syphilis among US women, from 0.9 to 1.1 cases per 100,000 women, during the same period.1
The rate of congenital syphilis had declined between 2008 and 2012, from 10.5 cases to 8.4 cases per 100,000 live births.
Congenital syphilis occurs when an infected mother transmits the disease to her fetus during pregnancy. Among the adverse effects of congenital syphilis are deformities, stillbirth, and early infant death. “However, among mothers identified with syphilis who deliver past 20 weeks’ gestation, treatment with penicillin at least 30 days before delivery is 98% effective at preventing [congenital syphilis],” the CDC report notes.1
For the purposes of the CDC report, congenital syphilis includes “both infants and stillbirths with clinical evidence” of the disease, “as well as those infants and stillbirths born to mothers with untreated or inadequately treated syphilis, regardless of the infant’s manifestation of clinical disease.”1
CDC recommendations
The CDC notes that most of the increases in the rates of maternal and congenital syphilis likely stem from inadequate prenatal care.
“A large percentage of [congenital syphilis] cases continue to be attributable to a lack of prenatal care; even among those receiving some prenatal care, the detection and treatment of maternal syphilis is often not early enough….At particular risk are those who are uninsured or underinsured and those with substance use issues.”1
Among the recommendations of the CDC:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Screen women at elevated risk for syphilis, as well as those who live in “high-morbidity geographic areas” at the beginning of the third trimester and again at delivery.
- In cases where prenatal care has been lacking, screen the woman for syphilis using a rapid plasma reagin (RPR) card and treat the patient who tests positive at the time the pregnancy is confirmed.
- Do not discharge an infant from the hospital unless the syphilis serologic status of the mother has been tested at least once during pregnancy and, preferably, again at delivery (in high-risk cases).
- Test any woman who delivers a stillborn infant for syphilis.
Reference
1. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2008–2014. MMWR. 2015;64(44):1241–1245.
Reference
1. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2008–2014. MMWR. 2015;64(44):1241–1245.
AK clearance rates maintained 1 year after thermally modulated PDT
Clearance rates for actinic keratoses (AKs) on the extremities were prolonged by adding thermal modulation to photodynamic therapy (PDT), a study has shown.
The single-site study of 17 adults with 10 or more AKs on their arms or legs evaluated thermally modulated PDT: 20% 5-aminolevulinic acid (ALA) applied to skin, occluded with plastic wrap and warmed with an electric heating pad to a median 41.2° C for one hour, then exposed to blue light. Treatment resulted in 90% clearance rates at 3 months and 12 months, reported Dr. Andrea Willey, a dermatologist in Sacramento, Calif., and her associates (Dermatol Surg. 2015 Nov;41[11]:1290-5).
They were inspired to conduct the study as a follow-on to a recently published pilot study of three patients, which found that clearance rates of AKs on the arm treated with thermally modulated 5-ALA blue light PDT persisted up to 14 months after treatment, when compared with the control arm, which was not heated.
In their study, there were 724 grade 1 and 2 AKs at baseline – a median of 15 per extremity; patients were followed up at 3, 6, 9, and 12 months. The total lesion count across the entire cohort was 70 at 3 months, 69 at 6 months, 64 at 9 months, and 72 at 1 year. No new AKs were seen in the treated areas during the 1-year follow-up.
There were 13 grade 3 hypertrophic AK lesions among all study participants. Although these lesions persisted, Dr. Willey and her coauthors noted that they did shrink initially after treatment.
Adverse events associated with the combination therapy were low, and included mild erythema and crusting up to 1 week post treatment, indicating the therapy was well tolerated, and patient satisfaction was high.
The results “suggest that mild skin warming may both improve efficacy and reduce variability of response to PDT in practice,” the authors wrote.
On Twitter @whitneymcknight
Clearance rates for actinic keratoses (AKs) on the extremities were prolonged by adding thermal modulation to photodynamic therapy (PDT), a study has shown.
The single-site study of 17 adults with 10 or more AKs on their arms or legs evaluated thermally modulated PDT: 20% 5-aminolevulinic acid (ALA) applied to skin, occluded with plastic wrap and warmed with an electric heating pad to a median 41.2° C for one hour, then exposed to blue light. Treatment resulted in 90% clearance rates at 3 months and 12 months, reported Dr. Andrea Willey, a dermatologist in Sacramento, Calif., and her associates (Dermatol Surg. 2015 Nov;41[11]:1290-5).
They were inspired to conduct the study as a follow-on to a recently published pilot study of three patients, which found that clearance rates of AKs on the arm treated with thermally modulated 5-ALA blue light PDT persisted up to 14 months after treatment, when compared with the control arm, which was not heated.
In their study, there were 724 grade 1 and 2 AKs at baseline – a median of 15 per extremity; patients were followed up at 3, 6, 9, and 12 months. The total lesion count across the entire cohort was 70 at 3 months, 69 at 6 months, 64 at 9 months, and 72 at 1 year. No new AKs were seen in the treated areas during the 1-year follow-up.
There were 13 grade 3 hypertrophic AK lesions among all study participants. Although these lesions persisted, Dr. Willey and her coauthors noted that they did shrink initially after treatment.
Adverse events associated with the combination therapy were low, and included mild erythema and crusting up to 1 week post treatment, indicating the therapy was well tolerated, and patient satisfaction was high.
The results “suggest that mild skin warming may both improve efficacy and reduce variability of response to PDT in practice,” the authors wrote.
On Twitter @whitneymcknight
Clearance rates for actinic keratoses (AKs) on the extremities were prolonged by adding thermal modulation to photodynamic therapy (PDT), a study has shown.
The single-site study of 17 adults with 10 or more AKs on their arms or legs evaluated thermally modulated PDT: 20% 5-aminolevulinic acid (ALA) applied to skin, occluded with plastic wrap and warmed with an electric heating pad to a median 41.2° C for one hour, then exposed to blue light. Treatment resulted in 90% clearance rates at 3 months and 12 months, reported Dr. Andrea Willey, a dermatologist in Sacramento, Calif., and her associates (Dermatol Surg. 2015 Nov;41[11]:1290-5).
They were inspired to conduct the study as a follow-on to a recently published pilot study of three patients, which found that clearance rates of AKs on the arm treated with thermally modulated 5-ALA blue light PDT persisted up to 14 months after treatment, when compared with the control arm, which was not heated.
In their study, there were 724 grade 1 and 2 AKs at baseline – a median of 15 per extremity; patients were followed up at 3, 6, 9, and 12 months. The total lesion count across the entire cohort was 70 at 3 months, 69 at 6 months, 64 at 9 months, and 72 at 1 year. No new AKs were seen in the treated areas during the 1-year follow-up.
There were 13 grade 3 hypertrophic AK lesions among all study participants. Although these lesions persisted, Dr. Willey and her coauthors noted that they did shrink initially after treatment.
Adverse events associated with the combination therapy were low, and included mild erythema and crusting up to 1 week post treatment, indicating the therapy was well tolerated, and patient satisfaction was high.
The results “suggest that mild skin warming may both improve efficacy and reduce variability of response to PDT in practice,” the authors wrote.
On Twitter @whitneymcknight
FROM DERMATOLOGIC SURGERY
Key clinical point: Mildly warming affected skin sites during photodynamic therapy can prolong the clearance rates for AKs on the extremities.
Major finding: AK clearance rates on the extremities remained at about 90% during the 1 year after treatment with thermally modulated PDT.
Data source: A single site, prospective 1-year study evaluating treatment with thermally modulated PDT for 17 adults with 10 or more AKs on their extremities.
Disclosures: Dr. Willey is a member of the scientific advisory board of DUSA Pharmaceuticals; she received a research grant, equipment loan, and study drug from the company. Her two coauthors had no relevant disclosures.
Myth of the Month: Does Colace work?
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].