User login
Studies help explain multidrug resistance in cancer

(right) and Sung Chang Lee
Photo courtesy of
The Scripps Research Institute
Scientists have discovered how the primary protein responsible for multidrug chemotherapy resistance changes shape and reacts to drugs.
They believe this information will aid the design of better molecules to inhibit or evade multidrug resistance.
The researchers noted that the proteins at work in multidrug resistance are ABC transporters. An important ABC transporter, P-glycoprotein (P-gp), catches harmful toxins in a “binding pocket” and expels them from cells.
The problem is that, in cancer patients, P-gp sometimes begins recognizing chemotherapy drugs and expelling them too. Over time, more and more cancer cells can develop multidrug resistance, eliminating all possible treatments.
“Virtually all cancer deaths can be attributed to the failure of chemotherapy,” said study author Qinghai Zhang, PhD, of The Scripps Research Institute in La Jolla, California.
He and his colleagues theorized that scientists might be able to design more effective cancer drugs if they had a better understanding of P-gp and how it binds to molecules.
A better look at transporters
For their first study, published in Structure, the researchers looked at P-gp and MsbA, a similar transporter protein found in bacteria, under an electron microscope. This helped them solve a major problem in transporter research.
Until recently, scientists could only compare images of crystal structures made from transporter proteins. These crystallography images showed single snapshots of the transporter but didn’t show how the shape of the transporters could change.
Using electron microscopy, however, a whole range of different conformations of the structures could be visualized, essentially capturing P-gp and MsbA in action.
The research was also aided by the development of new chemical tools. The team used a solution of lipids and peptides to mimic natural conditions in the cell membrane. They used a novel chemical called beta-sheet peptide to stabilize the protein and provide enough stability for a new perspective.
Together with electron microscopy, this technique enabled the researchers to capture a series of images showing how transporter proteins change shape in response to drug and nucleotide binding. They found that transporter proteins have an open binding pocket that constantly switches to face different sides of membranes.
“The transporter goes through many steps,” Dr Zhang said. “It’s like a machine.”
A closer look at binding
In a second study, published in Acta Crystallographica Section D, the scientists investigated the drug binding sites of P-gp using higher-resolution X-ray crystallography. And they discovered how P-gp interacts with ligands.
The researchers studied crystals of the transporter bound to 4 different ligands to see how the transporters reacted. They found that when certain ligands bind to P-gp, they trigger local conformational changes in the transporter.
Binding also increased the rate of ATP hydrolysis, which provides mechanical energy and may be the first step in the process by which the binding pocket closes.
The team also discovered that ligands could bind to different areas of the transporter, leaving nearby slots open for other molecules. This suggests it may be difficult to completely halt the drug expulsion process.
Dr Zhang said the next step for this research is to develop molecules to evade P-gp binding. ![]()

(right) and Sung Chang Lee
Photo courtesy of
The Scripps Research Institute
Scientists have discovered how the primary protein responsible for multidrug chemotherapy resistance changes shape and reacts to drugs.
They believe this information will aid the design of better molecules to inhibit or evade multidrug resistance.
The researchers noted that the proteins at work in multidrug resistance are ABC transporters. An important ABC transporter, P-glycoprotein (P-gp), catches harmful toxins in a “binding pocket” and expels them from cells.
The problem is that, in cancer patients, P-gp sometimes begins recognizing chemotherapy drugs and expelling them too. Over time, more and more cancer cells can develop multidrug resistance, eliminating all possible treatments.
“Virtually all cancer deaths can be attributed to the failure of chemotherapy,” said study author Qinghai Zhang, PhD, of The Scripps Research Institute in La Jolla, California.
He and his colleagues theorized that scientists might be able to design more effective cancer drugs if they had a better understanding of P-gp and how it binds to molecules.
A better look at transporters
For their first study, published in Structure, the researchers looked at P-gp and MsbA, a similar transporter protein found in bacteria, under an electron microscope. This helped them solve a major problem in transporter research.
Until recently, scientists could only compare images of crystal structures made from transporter proteins. These crystallography images showed single snapshots of the transporter but didn’t show how the shape of the transporters could change.
Using electron microscopy, however, a whole range of different conformations of the structures could be visualized, essentially capturing P-gp and MsbA in action.
The research was also aided by the development of new chemical tools. The team used a solution of lipids and peptides to mimic natural conditions in the cell membrane. They used a novel chemical called beta-sheet peptide to stabilize the protein and provide enough stability for a new perspective.
Together with electron microscopy, this technique enabled the researchers to capture a series of images showing how transporter proteins change shape in response to drug and nucleotide binding. They found that transporter proteins have an open binding pocket that constantly switches to face different sides of membranes.
“The transporter goes through many steps,” Dr Zhang said. “It’s like a machine.”
A closer look at binding
In a second study, published in Acta Crystallographica Section D, the scientists investigated the drug binding sites of P-gp using higher-resolution X-ray crystallography. And they discovered how P-gp interacts with ligands.
The researchers studied crystals of the transporter bound to 4 different ligands to see how the transporters reacted. They found that when certain ligands bind to P-gp, they trigger local conformational changes in the transporter.
Binding also increased the rate of ATP hydrolysis, which provides mechanical energy and may be the first step in the process by which the binding pocket closes.
The team also discovered that ligands could bind to different areas of the transporter, leaving nearby slots open for other molecules. This suggests it may be difficult to completely halt the drug expulsion process.
Dr Zhang said the next step for this research is to develop molecules to evade P-gp binding. ![]()

(right) and Sung Chang Lee
Photo courtesy of
The Scripps Research Institute
Scientists have discovered how the primary protein responsible for multidrug chemotherapy resistance changes shape and reacts to drugs.
They believe this information will aid the design of better molecules to inhibit or evade multidrug resistance.
The researchers noted that the proteins at work in multidrug resistance are ABC transporters. An important ABC transporter, P-glycoprotein (P-gp), catches harmful toxins in a “binding pocket” and expels them from cells.
The problem is that, in cancer patients, P-gp sometimes begins recognizing chemotherapy drugs and expelling them too. Over time, more and more cancer cells can develop multidrug resistance, eliminating all possible treatments.
“Virtually all cancer deaths can be attributed to the failure of chemotherapy,” said study author Qinghai Zhang, PhD, of The Scripps Research Institute in La Jolla, California.
He and his colleagues theorized that scientists might be able to design more effective cancer drugs if they had a better understanding of P-gp and how it binds to molecules.
A better look at transporters
For their first study, published in Structure, the researchers looked at P-gp and MsbA, a similar transporter protein found in bacteria, under an electron microscope. This helped them solve a major problem in transporter research.
Until recently, scientists could only compare images of crystal structures made from transporter proteins. These crystallography images showed single snapshots of the transporter but didn’t show how the shape of the transporters could change.
Using electron microscopy, however, a whole range of different conformations of the structures could be visualized, essentially capturing P-gp and MsbA in action.
The research was also aided by the development of new chemical tools. The team used a solution of lipids and peptides to mimic natural conditions in the cell membrane. They used a novel chemical called beta-sheet peptide to stabilize the protein and provide enough stability for a new perspective.
Together with electron microscopy, this technique enabled the researchers to capture a series of images showing how transporter proteins change shape in response to drug and nucleotide binding. They found that transporter proteins have an open binding pocket that constantly switches to face different sides of membranes.
“The transporter goes through many steps,” Dr Zhang said. “It’s like a machine.”
A closer look at binding
In a second study, published in Acta Crystallographica Section D, the scientists investigated the drug binding sites of P-gp using higher-resolution X-ray crystallography. And they discovered how P-gp interacts with ligands.
The researchers studied crystals of the transporter bound to 4 different ligands to see how the transporters reacted. They found that when certain ligands bind to P-gp, they trigger local conformational changes in the transporter.
Binding also increased the rate of ATP hydrolysis, which provides mechanical energy and may be the first step in the process by which the binding pocket closes.
The team also discovered that ligands could bind to different areas of the transporter, leaving nearby slots open for other molecules. This suggests it may be difficult to completely halt the drug expulsion process.
Dr Zhang said the next step for this research is to develop molecules to evade P-gp binding. ![]()
FDA’s new app provides info on drug shortages

a Nokia smart phone
Photo by Halvard Lundgaard
The US Food and Drug Administration (FDA) has launched the agency’s first mobile application (app) designed to speed public access to information on drug shortages.
The app provides details regarding current drug shortages, resolved shortages, and discontinued drug products.
It works just like the FDA’s drug shortages website. App users can search for a drug by its generic name or active ingredient, or they can browse by therapeutic category.
The app can also be used to report a suspected drug shortage or supply issue to the FDA.
The app is available for free download via iTunes (for Apple devices) and the Google Play store (for Android devices). It can be found by searching “FDA Drug Shortages.”
The FDA developed the app to improve access to information about drug shortages, as part of the agency’s efforts outlined in the Strategic Plan for Preventing and Mitigating Drug Shortages.
“The FDA understands that healthcare professionals and pharmacists need real-time information about drug shortages to make treatment decisions,” said Valerie Jensen, associate director of the Drug Shortage Staff in the FDA’s Center for Drug Evaluation and Research.
“The new mobile app is an innovative tool that will offer easier and faster access to important drug shortage information.” ![]()

a Nokia smart phone
Photo by Halvard Lundgaard
The US Food and Drug Administration (FDA) has launched the agency’s first mobile application (app) designed to speed public access to information on drug shortages.
The app provides details regarding current drug shortages, resolved shortages, and discontinued drug products.
It works just like the FDA’s drug shortages website. App users can search for a drug by its generic name or active ingredient, or they can browse by therapeutic category.
The app can also be used to report a suspected drug shortage or supply issue to the FDA.
The app is available for free download via iTunes (for Apple devices) and the Google Play store (for Android devices). It can be found by searching “FDA Drug Shortages.”
The FDA developed the app to improve access to information about drug shortages, as part of the agency’s efforts outlined in the Strategic Plan for Preventing and Mitigating Drug Shortages.
“The FDA understands that healthcare professionals and pharmacists need real-time information about drug shortages to make treatment decisions,” said Valerie Jensen, associate director of the Drug Shortage Staff in the FDA’s Center for Drug Evaluation and Research.
“The new mobile app is an innovative tool that will offer easier and faster access to important drug shortage information.” ![]()

a Nokia smart phone
Photo by Halvard Lundgaard
The US Food and Drug Administration (FDA) has launched the agency’s first mobile application (app) designed to speed public access to information on drug shortages.
The app provides details regarding current drug shortages, resolved shortages, and discontinued drug products.
It works just like the FDA’s drug shortages website. App users can search for a drug by its generic name or active ingredient, or they can browse by therapeutic category.
The app can also be used to report a suspected drug shortage or supply issue to the FDA.
The app is available for free download via iTunes (for Apple devices) and the Google Play store (for Android devices). It can be found by searching “FDA Drug Shortages.”
The FDA developed the app to improve access to information about drug shortages, as part of the agency’s efforts outlined in the Strategic Plan for Preventing and Mitigating Drug Shortages.
“The FDA understands that healthcare professionals and pharmacists need real-time information about drug shortages to make treatment decisions,” said Valerie Jensen, associate director of the Drug Shortage Staff in the FDA’s Center for Drug Evaluation and Research.
“The new mobile app is an innovative tool that will offer easier and faster access to important drug shortage information.” ![]()
Navigating Venous Access
Reliable venous access is fundamental for the safe and effective care of hospitalized patients. Venous access devices (VADs) are conduits for this purpose, providing delivery of intravenous medications, accurate measurement of central venous pressure, or administration of life‐saving blood products. Despite this important role, VADs are also often the source of hospital‐acquired complications. Although inpatient providers must balance the relative risks of VADs against their benefits, the evidence supporting such decisions is often limited. Advances in technology, scattered research, and growing availability of novel devices has only further fragmented provider knowledge in the field of vascular access.[1]
It is not surprising, then, that survey‐based studies of hospitalists reveal important knowledge gaps with regard to practices associated with VADs.[2] In this narrative review, we seek to bridge this gap by providing a concise and pragmatic overview of the fundamentals of venous access. We focus specifically on parameters that influence decisions regarding VAD placement in hospitalized patients, providing key takeaways for practicing hospitalists.
METHODS
To compile this review, we systematically searched Medline (via Ovid) for several keywords, including: peripheral intravenous catheters, ultrasound‐guided peripheral catheter, intraosseous, midline, peripherally inserted central catheter, central venous catheters, and vascular access device complications. We concentrated on full‐length articles in English only; no date restrictions were placed on the search. We reviewed guidelines and consensus statements (eg, from the Center for Disease Control [CDC] or Choosing Wisely criteria) as appropriate. Additional studies of interest were identified through content experts (M.P., C.M.R.) and bibliographies of included studies.
SCIENTIFIC PRINCIPLES UNDERPINNING VENOUS ACCESS
It is useful to begin by reviewing VAD‐related nomenclature and physiology. In the simplest sense, a VAD consists of a hub (providing access to various connectors), a hollow tube divided into 1 or many sections (lumens), and a tip that may terminate within a central or peripheral blood vessel. VADs are classified as central venous catheters (eg, centrally inserted central catheters [CICCs] or peripherally inserted central catheters [PICCs]) or peripheral intravenous catheters (eg, midlines or peripheral intravenous catheters) based on site of entry and location of the catheter tip. Therefore, VADs entering via proximal or distal veins of the arm are often referred to as peripheral lines, as their site of entry and tip both reside within peripheral veins. Conversely, the term central line is often used when VADs enter or terminate in a central vein (eg, subclavian vein insertion with the catheter tip in the lower superior vena cava).
Attention to a host of clinical and theoretical parameters is important when choosing a device for venous access. Some such parameters are summarized in Table 1.
| Parameter | Major Considerations |
|---|---|
| |
| Desired flow rate | Smaller diameter veins susceptible to damage with high flow rates. |
| Short, large‐bore catheters facilitate rapid infusion. | |
| Nature of infusion | pH, viscosity, and temperature may damage vessels. |
| Vesicants and irritants should always be administered into larger, central veins. | |
| Desired duration of vascular access, or dwell time | Vessel thrombosis or phlebitis increase over time with catheter in place. |
| Intermittent infusions increase complications in central catheters; often tunneled catheters are recommended. | |
| Urgency of placement | Access to large caliber vessels is often needed in emergencies. |
| Critically ill or hemodynamically unstable patients may require urgent access for invasive monitoring or rapid infusions. | |
| Patients with trauma often require large volumes of blood products and reliable access to central veins. | |
| Number of device lumens | VADs may have single or multiple lumens. |
| Multilumen allows for multiple functions (eg, infusion of multiple agents, measurement of central venous pressures, blood draws). | |
| Device gauge | In general, use of a smaller‐gauge catheter is preferred to prevent complications. |
| However, larger catheter diameter may be needed for specific clinical needs (eg, blood transfusion). | |
| Device coating | VADs may have antithrombotic or anti‐infective coatings. |
| These devices may be of value in patients at high risk of complications. | |
| Such devices, however, may be more costly than their counterparts. | |
| Self‐care compatibility | VADs that can be cared for by patients are ideal for outpatient care. |
| Conversely, VADs such as peripheral catheters, are highly prone to dislodgement and should be reserved for supervised settings only. | |
VENOUS ACCESS DEVICES
We will organize our discussion of VADs based on whether they terminate in peripheral or central vessels. These anatomical considerations are relevant as they determine physical characteristics, compatibility with particular infusates, dwell time, and risk of complications associated with each VAD discussed in Table 2.
| Complications | Major Considerations |
|---|---|
| |
| Infection | VADs breach the integrity of skin and permit skin pathogens to enter the blood stream (extraluminal infection). |
| Inadequate antisepsis of the VAD hub, including poor hand hygiene, failure to "scrub the hub," and multiple manipulations may also increase the risk of VAD‐related infection (endoluminal infection). | |
| Infections may be local (eg, exit‐site infections) or may spread hematogenously (eg, CLABSI). | |
| Type of VAD, duration of therapy, and host characteristics interact to influence infection risk. | |
| VADs with antiseptic coatings (eg, chlorhexidine) or antibiotic coatings (eg, minocycline) may reduce risk of infection in high‐risk patients. | |
| Antiseptic‐impregnated dressings may reduce risk of extraluminal infection. | |
| Venous thrombosis | VADs predispose to venous stasis and thrombosis. |
| Duration of VAD use, type and care of the VAD, and patient characteristics affect risk of thromboembolism. | |
| VAD tip position is a key determinant of venous thrombosis; central VADs that do not terminate at the cavo‐atrial junction should be repositioned to reduce the risk of thrombosis. | |
| Antithrombotic coated or eluting devices may reduce risk of thrombosis, though definitive data are lacking. | |
| Phlebitis | Inflammation caused by damage to tunica media.[18] |
| 3 types of phlebitis: | |
| Chemical: due to irritation of media from the infusate. | |
| Mechanical: VAD physically damages the vessel. | |
| Infective: bacteria invade vein and inflame vessel wall. | |
| Phlebitis may be limited by close attention to infusate compatibility with peripheral veins, appropriate dilution, and prompt removal of catheters that show signs of inflammation. | |
| Phlebitis may be prevented in PICCs by ensuring at least a 2:1 vein:catheter ratio. | |
| Extravasation | Extravasation (also called infiltration) is defined as leakage of infusate from intravascular to extravascular space. |
| Extravasation of vesicants/emrritants is particularly worrisome. | |
| May result in severe tissue injury, blistering, and tissue necrosis.[11] | |
| VADs should be checked frequently for adequate flushing and position prior to each infusion to minimize risk. | |
| Any VAD with redness, swelling, and tenderness at the entry site or problems with flushing should not be used without further examination and review of position. | |
Peripheral Venous Access
Short Peripheral Intravenous Catheter
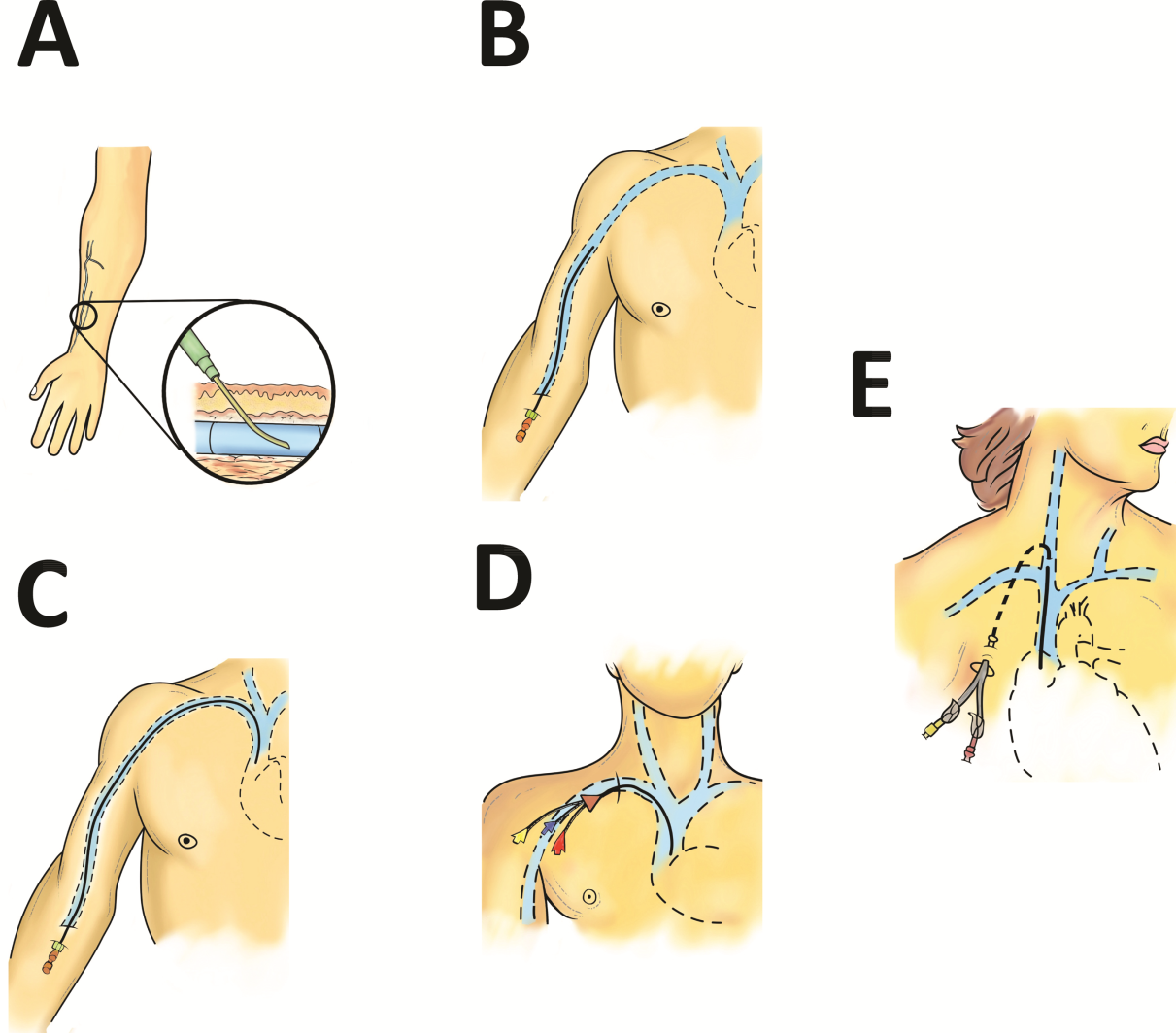
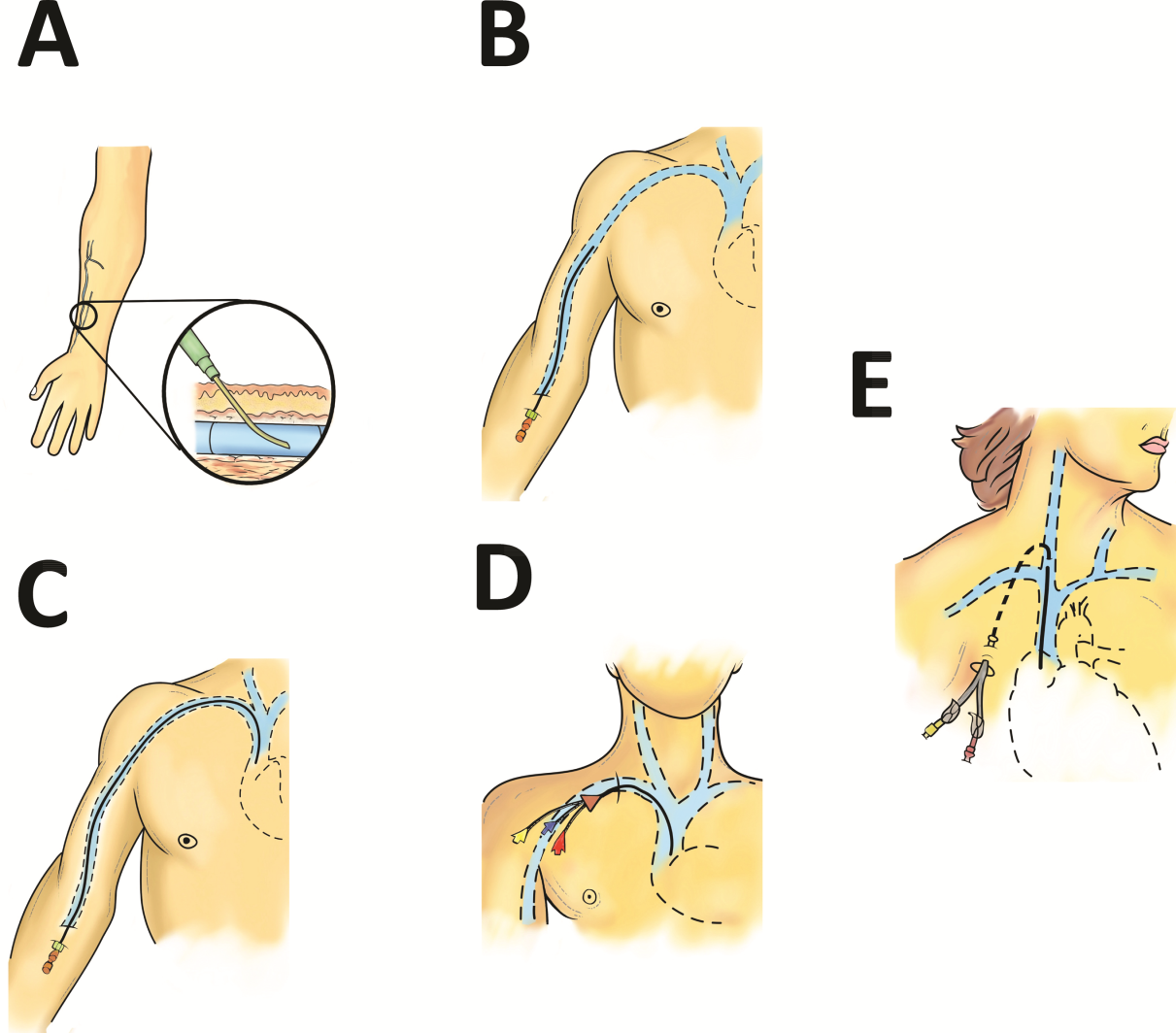
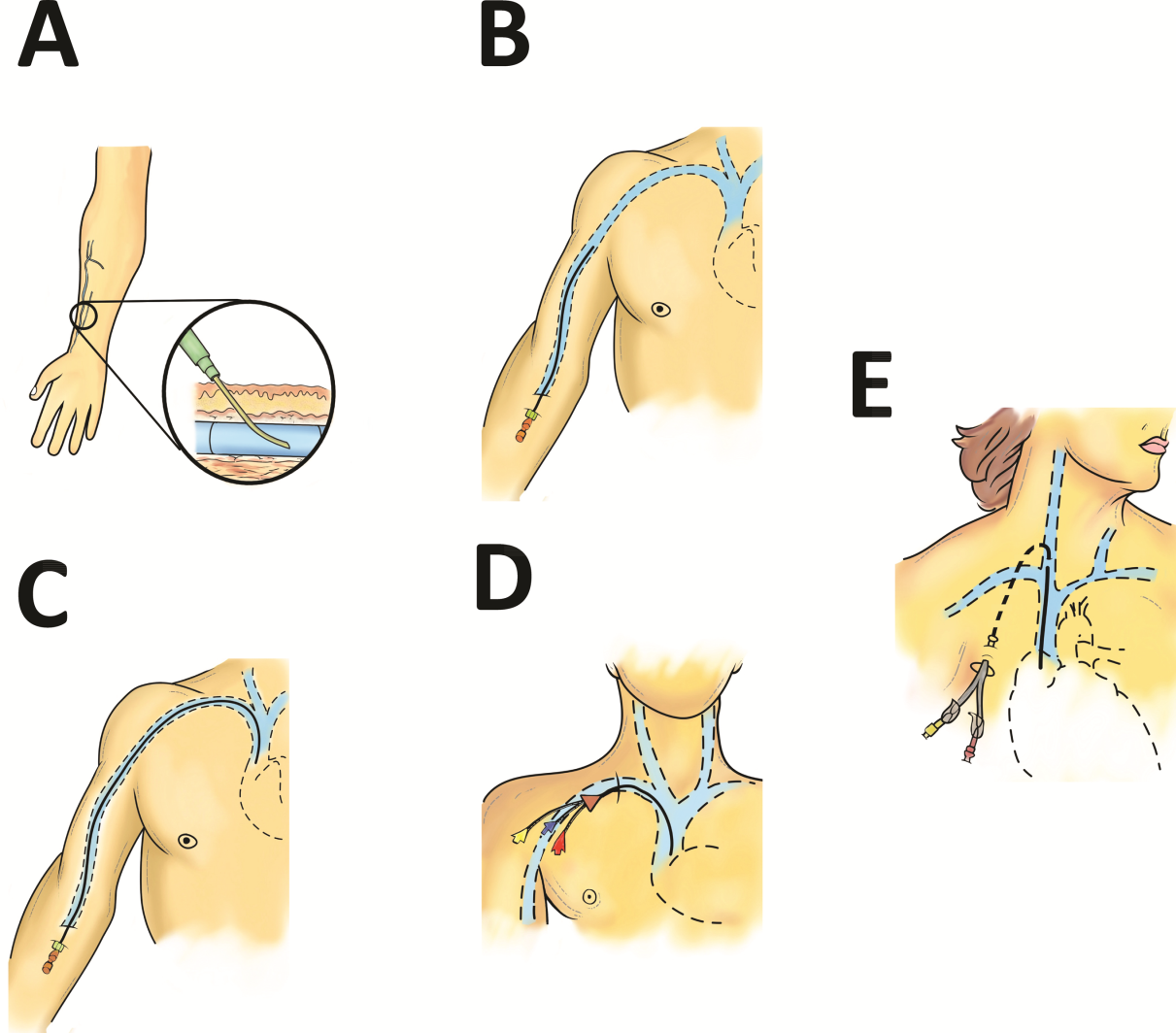
Approximately 200 million peripheral intravenous catheters (PIVs) are placed annually in the United States, making them the most common intravenous catheter.[3] PIVs are short devices, 3 to 6 cm in length, that enter and terminate in peripheral veins (Figure 1A). Placement is recommended in forearm veins rather than those of the hand, wrist, or upper arm, as forearm sites are less prone to occlusion, accidental removal, and phlebitis.[4] Additionally, placement in hand veins impedes activities of daily living (eg, hand washing) and is not preferred by patients.[5] PIV size ranges from 24 gauge (smallest) to 14 gauge (largest); larger catheters are often reserved for fluid resuscitation or blood transfusion as they accommodate greater flow and limit hemolysis. To decrease risk of phlebitis and thrombosis, the shortest catheter and smallest diameter should be used. However, unless adequately secured, smaller diameter catheters are also associated with greater rates of accidental removal.[4, 5]
By definition, PIVs are short‐term devices. The CDC currently recommends removal and replacement of these devices no more frequently than every 72 to 96 hours in adults. However, a recent randomized controlled trial found that replacing PIVs when clinically indicated (eg, device failure, phlebitis) rather than on a routine schedule added 30 hours to their lifespan without an increase in complications.[6] A systematic review by the Cochrane Collaboration echoes these findings.[3] These data have thus been incorporated into recommendations from the Infusion Nurses Society (INS) and the National Health Service in the United Kingdom.[5, 7] In hospitalized patients, this approach is relevant, as it preserves venous access sites, maximizes device dwell, and limits additional PIV insertions. In turn, these differences may reduce the need for invasive VADs such as PICCs. Furthermore, the projected 5‐year savings from implementation of clinically indicated PIV removal policies is US$300 million and 1 million health‐worker hours in the United States alone.[4]
PIVs offer many advantages. First, they are minimally invasive and require little training to insert. Second, they can be used for diverse indications in patients requiring short‐term (1 week) venous access. Third, PIVs do not require imaging to ensure correct placement; palpation of superficial veins is sufficient. Fourth, PIVs exhibit a risk of bloodstream infection that is about 40‐fold lower than more invasive, longer‐dwelling VADs[8] (0.06 bacteremia per 1000 catheter‐days).
Despite these advantages, PIVs also have important drawbacks. First, a quarter of all PIVs fail through occlusion or accidental dislodgement.[4] Infiltration, extravasation, and hematoma formation are important adverse events that may occur in such cases. Second, thrombophlebitis (pain and redness at the insertion site) is frequent, and may require device removal, especially in patients with catheters 20 guage.[9] Third, despite their relative safety, PIVs can cause localized or hematogenous infection. Septic thrombophlebitis (superficial thrombosis and bloodstream infection) and catheter‐related bloodstream infection, though rare, have been reported with PIVs and may lead to serious complications.[8, 10] In fact, some suggest that the overall burden of bloodstream infection risk posed by PIVs may be similar to that of CICCs given the substantially greater number of devices used and greater number of device days.[8]
PIVs and other peripheral VADs are not suitable for infusion of vesicants or irritants, which require larger, central veins for delivery. Vesicants (drugs that cause blistering on infusion) include chemotherapeutic agents (eg, dactinomycin, paclitaxel) and commonly used nonchemotherapeutical agents (eg, diazepam, piperacillin, vancomycin, esmolol, or total parenteral nutrition [TPN]).[11] Irritants (phlebitogenic drugs) cause short‐term inflammation and pain, and thus should not be peripherally infused for prolonged durations. Common irritants in the hospital setting include acyclovir, dobutamine, penicillin, and potassium chloride.
Of note, about one‐quarter of PIV insertions fail owing to difficult intravenous access.[12] Ultrasound‐guided peripheral intravenous (USGPIV) catheter placement is emerging as a technique to provide peripheral access for such patients to avoid placement of central venous access devices. Novel, longer devices (>8 cm) with built‐in guide wires have been developed to increase placement success of USGPIVs. These new designs provide easier access into deeper arm veins (brachial or basilic) not otherwise accessible by short PIVs. Although studies comparing the efficacy of USGPIV devices to other VADs are limited, a recent systematic review showed that time to successful cannulation was shorter, and fewer attempts were required to place USGPIVs compared to PIVs.[13] A recent study in France found that USGPIVs met the infusion needs of patients with difficult veins with minimal increase in complications.[14] Despite these encouraging data, future studies are needed to better evaluate this technology.
Midline Catheter
A midline is a VAD that is between 7.5 to 25 cm in length and is typically inserted into veins above the antecubital fossa. The catheter tip resides in a peripheral upper arm vein, often the basilic or cephalic vein, terminating just short of the subclavian vein (Figure 1B). Midline‐like devices were first developed in the 1950s and were initially used as an alternative to PIVs because they were thought to allow longer dwell times.[15] However, because they were originally constructed with a fairly rigid material, infiltration, mechanical phlebitis, and inflammation were common and tempered enthusiasm for their use.[15, 16] Newer midline devices obviate many of these problems and are inserted by ultrasound guidance and modified Seldinger technique.[17] Despite these advances, data regarding comparative efficacy are limited.
Midlines offer longer dwell times than standard PIVs owing to termination in the larger diameter basilic and brachial veins of the arm. Additionally, owing to their length, midlines are less prone to dislodgement. As they are inserted with greater antisepsis than PIVs and better secured to the skin, they are more durable than PIVs.[5, 9, 18] Current INS standards recommend use of midlines for 1 to 4 weeks.[5] Because they terminate in a peripheral vein, medications and infusions compatible with midlines are identical to those that are infused through a PIV. Thus, TPN, vesicants or irritants, or drugs that feature a pH 5 or pH >9, or >500 mOsm should not be infused through a midline.[15] New evidence suggests that diluted solutions of vancomycin (usually pH 5) may be safe to infuse for short durations (6 days) through a midline, and that concentration rather than pH may be more important in this regard.[19] Although it is possible that the use of midlines may extend to agents typically not deemed peripheral access compatible, limited evidence exists to support such a strategy at this time.
Midlines offer several advantages. First, because blood flow is greater in the more proximal veins of the arm, midlines can accommodate infusions at rates of 100 to 150 mL/min compared to 20 to 40 mL/min in smaller peripheral veins. Higher flow rates offer greater hemodilution (dilution of the infusion with blood), decreasing the likelihood of phlebitis and infiltration.[20] Second, midlines do not require x‐ray verification of tip placement; thus, their use is often favored in resource‐depleted settings such as skilled nursing facilities. Third, midlines offer longer dwell times than peripheral intravenous catheters and can thus serve as bridge devices for short‐term intravenous antibiotics or peripheral‐compatible infusions in an outpatient setting. Available evidence suggests that midlines are associated with low rates of bloodstream infection (0.30.8 per 1000 catheter‐days).[17] The most frequent complications include phlebitis (4.2%) and occlusion (3.3%).[20] Given these favorable statistics, midlines may offer a good alternative to PIVs in select patients who require peripheral infusions of intermediate duration.
Intraosseous Vascular Access
Intraosseous (IO) devices access the vascular system by piercing cortical bone. These devices provide access to the intramedullary cavity and venous plexi of long bones such as the tibia, femur, or humerus. Several insertion devices are now commercially available and have enhanced the ease and safety of IO placement. Using these newer devices, IO access may be obtained in 1 to 2 minutes with minimal training. By comparison, a central venous catheter often requires 10 to 15 minutes to insert with substantial training efforts for providers.[21, 22, 23]
IO devices thus offer several advantages. First, given the rapidity with which they can be inserted, they are often preferred in emergency settings (eg, trauma). Second, these devices are versatile and can accommodate both central and peripheral infusates.[24] Third, a recent meta‐analysis found that IOs have a low complication rate of 0.8%, with extravasation of infusate through the cortical entry site being the most common adverse event.[21] Of note, this study also reported zero local or distal infectious complications, a finding that may relate to the shorter dwell of these devices.[21] Some animal studies suggest that fat embolism from bone may occur at high rates with IO VADs.[25] However, death or significant morbidity from fat emboli in humans following IO access has not been described. Whether such emboli occur or are clinically significant in the context of IO devices remains unclear at this time.[21]
Central Venous Access Devices
Central venous access devices (CVADs) share in common tip termination in the cavo‐atrial junction, either in the lower portion of the superior vena cava or in the upper portion of the right atrium. CVADs can be safely used for irritant or vesicant medications as well as for blood withdrawal, blood exchange procedures (eg, dialysis), and hemodynamic monitoring. Traditionally, these devices are 15 to 25 cm in length and are directly inserted in the deep veins of the supra‐ or infraclavicular area, including the internal jugular, brachiocephalic, subclavian, or axillary veins. PICCs are unique CVADs in that they enter through peripheral veins but terminate in the proximity of the cavoatrial junction. Regarding nomenclature, CICC will be used to denote devices that enter directly into veins of the neck or chest, whereas PICC will be used for devices that are inserted peripherally but terminate centrally.
Peripherally Inserted Central Catheter
PICCs are inserted into peripheral veins of the upper arm (eg, brachial, basilica, or cephalic vein) and advanced such that the tip resides at the cavoatrial junction (Figure 1C). PICCs offer prolonged dwell times and are thus indicated when patients require venous access for weeks or months.[26] Additionally, they can accommodate a variety of infusates and are safer to insert than CICCs, given placement in peripheral veins of the arm rather than central veins of the chest/neck. Thus, insertion complications such as pneumothorax, hemothorax, or significant bleeding are rare with PICCs. In fact, a recent study reported that PICC insertion by hospitalists was associated with low rates of insertion or infectious complications.[27]
However, like CICCs, PICCs are associated with central lineassociated bloodstream infection (CLABSI), a serious complication known to prolong length of hospital stay, increase costs, and carry a 12% to 25% associated mortality.[28, 29] In the United States alone, over 250,000 CLASBI cases occur per year drawing considerable attention from the CDC and Joint Commission, who now mandate reporting and nonpayment for hospital‐acquired CLABSI.[30, 31, 32] A recent systematic review and meta‐analysis found that PICCs are associated with a substantial risk of CLABSI in hospitalized patients.[33] Importantly, no difference in CLABSI rates between PICCs and CICCs in hospitalized patients was evident in this meta‐analysis. Therefore, current guidelines specifically recommend against use of PICCs over CICCs as a strategy to reduce CLABSI.[34] Additionally, PICCs are associated with 2.5‐fold greater risk of deep vein thrombosis (DVT) compared to CICCs; thus, they should be used with caution in patients with cancer or those with underlying hypercoagulable states.
Of particular import to hospitalists is the fact that PICC placement is contraindicated in patients with stage IIIB or greater chronic kidney disease (CKD). In such patients, sequelae of PICC use, such as phlebitis or central vein stenosis, can be devastating in patients with CKD.[35] In a recent study, prior PICC placement was the strongest predictor of subsequent arteriovenous graft failure.[36] For this reason, Choosing Wisely recommendations call for avoidance of PICCs in such patients.[37]
Centrally Inserted Central Catheter
CICCs are CVADs placed by puncture and cannulation of the internal jugular, subclavian, brachiocephalic, or femoral veins (Figure 1D) and compose the vast majority of VADs placed in ICU settings.[38, 39] Central termination of CICCs allows for a variety of infusions, including irritants, vesicants, and vasopressors, as well as blood withdrawal and hemodynamic monitoring. CICCs are typically used for 7 to 14 days, but may remain for longer durations if they remain complication free and clinically necessary.[40] A key advantage of CICCs is that they can be placed in emergent settings to facilitate quick access for rapid infusion or hemodynamic monitoring. In particular, CICCs are inserted in the femoral vein and may be useful in emergency settings. However, owing to risk of infection and inability to monitor central pressures, these femoral devices should be replaced with a proper CICC or PICC when possible. Importantly, although CICCs are almost exclusively used in intensive or emergency care, PICCs may also be considered in such settings.[41, 42] CICCs usually have multiple lumens and often serve several simultaneous functions such as both infusions and hemodynamic monitoring.
Despite their benefits, CICCs have several disadvantages. First, insertion requires an experienced clinician and has historically been a task limited to physicians. However, this is changing rapidly (especially in Europe and Australia) where specially trained nurses are assuming responsibility for CICC placement.[43] Second, these devices are historically more likely to be associated with CLABSI, with estimates of infection rates varying between 2 and 5 infections per 1000 catheter‐days.[44] Third, CICCs pose a significant DVT risk, with rates around 22 DVTs per 1000 catheter‐days.[45] However, compared to PICCs, the DVT risk appears lower, and CICC use may be preferable in patients at high risk of DVT, such as critically ill or cancer populations.[46] An important note to prevent CICC insertion complications relates to use of ultrasound, a practice that has been associated with decreased accidental arterial puncture and hematoma formation. The role of ultrasound guidance with PICCs as well as implications for thrombotic and infectious events remains less characterized at this point.[47]
Tunneled Central Venous Access Devices
Tunneled devices (either CICCs or PICCs) are characterized by the fact that the insertion site on the skin and site of ultimate venipuncture are physically separated (Figure 1E). Tunneling limits bacterial entry from the extraluminal aspect of the CVAD to the bloodstream. For example, internal jugular veins are often ideal sites of puncture but inappropriate sites for catheter placement, as providing care to this area is challenging and may increase risk of infection.[34] Tunneling to the infraclavicular area provides a better option, as it provides an exit site that can be adequately cared for. Importantly, any CVAD (PICCs or CICCs) can be tunneled. Additionally, tunneled CICCs may be used in patients with chronic or impending renal failure where PICCs are contraindicated because entry into dialysis‐relevant vessels is to be avoided.[48] Such devices also allow regular blood sampling in patients who require frequent testing but have limited peripheral access, such as those with hematological malignancies. Additionally, tunneled catheters are more comfortable for patients and viewed as being more socially acceptable than nontunneled devices. However, the more invasive and permanent nature of these devices often requires deliberation prior to insertion.
Of note, tunneled devices and ports may be used as long‐term (>3 months to years) VADs. As our focus in this review is short‐term devices, we will not expand the discussion of these devices as they are almost always used for prolonged durations.[7]
OPERATIONALIZING THE DATA: AN ALGORITHMIC APPROACH TO VENOUS ACCESS
Hospitalists should consider approaching venous access using an algorithm based on a number of parameters. For example, a critically ill patient who requires vasopressor support and hemodynamic monitoring will need a CICC or a PICC. Given the potential greater risk of thromboses from PICCs, a CICC is preferable for critically ill patients provided an experienced inserter is available. Conversely, patients who require short‐term (710 days) venous access for infusion of nonirritant or nonvesicant therapy often only require a PIV. In patients with poor or difficult venous access, USGPIVs or midlines may be ideal and preferred over short PIVs. Finally, patients who require longer‐term or home‐based treatment may benefit from early placement of a midline or a PICC, depending again on the nature of the infusion, duration of treatment, and available venous access sites.
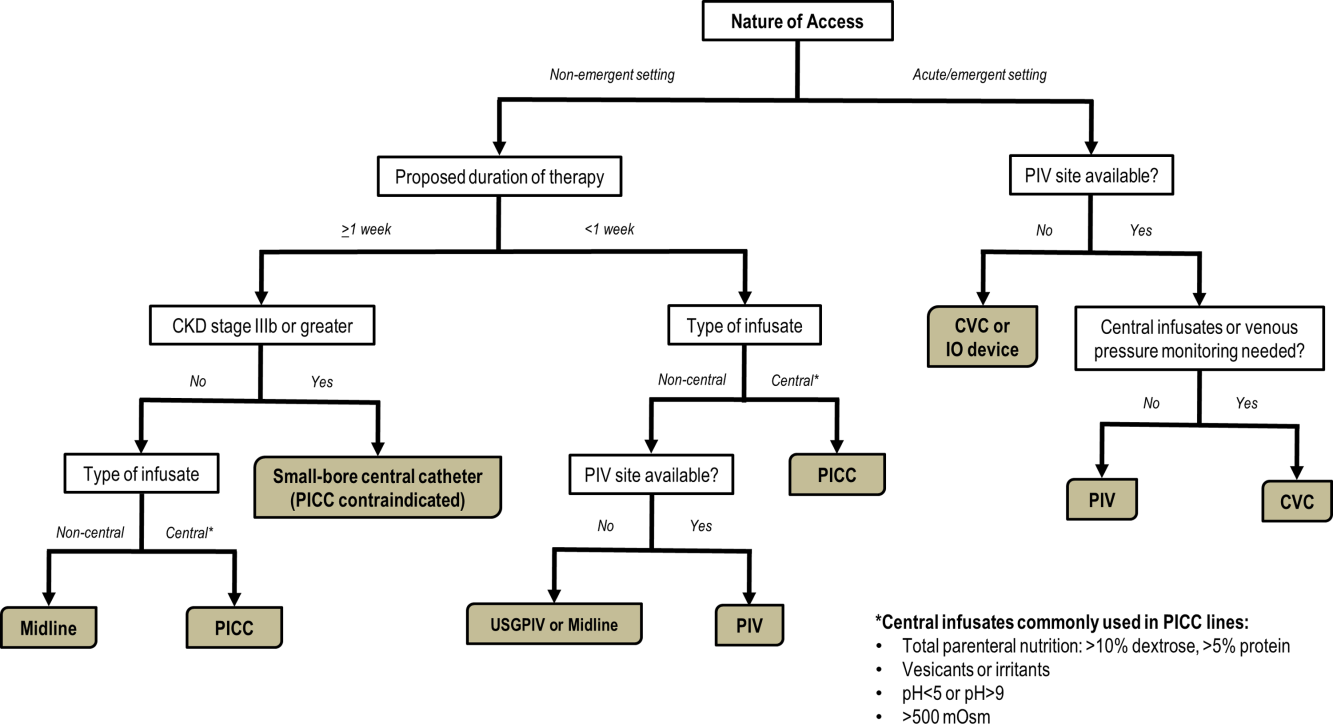
An algorithmic approach considering these parameters is suggested in Figure 2, and a brief overview of the devices and their considerations is shown in Table 3.
| Vascular Access Device | Central/Peripheral | Anatomical Location of Placement | Desired Duration of Placement | Common Uses | BSI Risk (Per 1,000 Catheter‐Days) | Thrombosis Risk | Important Considerations |
|---|---|---|---|---|---|---|---|
| |||||||
| Small peripheral IV | Peripheral | Peripheral veins, usually forearm | 710 days | Fluid resuscitation, most medications, blood products | 0.06[8] | Virtually no risk | Consider necessity of PIV daily and remove unnecessary devices |
| Midline | Peripheral | Inserted around antecubital fossa, reside within basilic or cephalic vein of the arm | 24 weeks | Long‐term medications excluding TPN, vesicants, corrosives | 0.30.8[17] | Insufficient data | Can be used as bridge devices for patients to complete short‐term antibiotics/emnfusions as an outpatient |
| Peripherally inserted central catheter | Central | Inserted into peripheral arm vein and advanced to larger veins (eg, internal jugular or subclavian) to the CAJ | >1 week, 3 months | Large variety of infusates, including TPN, vesicants, corrosives | 2.4[44] | 6.30% | Contraindicated in patients with CKD stage IIIb or higher |
| Centrally inserted central catheters | Central | Inserted above (internal jugular vein, brachiocephalic vein, subclavian vein), or below the clavicle (axillary vein) | >1 week, 3 months | Same infusate variety as PICC, measurement of central venous pressures, common in trauma/emergent settings | 2.3[44] | 1.30% | Given lower rates of DVT than PICC, preferred in ICU and hypercoagulable environments |
| Tunneled CICCs | Central | Placed percutaneously in any large vein in the arm, chest, neck or groin | >3 months to years | Central infusates, as in any CVAD; used for patients with CKD stage IIIb or greater when a PICC is indicated | Insufficient data | Insufficient data | May be superior when insertion site and puncture site are not congruent and may increase risk of infection |
CONCLUSIONS
With strides in technology and progress in medicine, hospitalists have access to an array of options for venous access. However, every VAD has limitations that can be easily overlooked in a perfunctory decision‐making process. The data presented in this review thus provide a first step to improving safety in this evolving science. Studies that further determine appropriateness of VADs in hospitalized settings are necessary. Only through such progressive scientific enquiry will complication‐free venous access be realized.
Disclosure
Nothing to report.
- , . The need for comparative data in vascular access: the rationale and design of the PICC registry. J Vasc Access. 2013; 18(4): 219–224.
- , , , et al. Hospitalist experiences, practice, opinions, and knowledge regarding peripherally inserted central catheters: a Michigan survey. J Hosp Med. 2013; 8(6): 309–314.
- , , , . Clinically‐indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2013; 4: CD007798.
- , , , et al. Cost‐effectiveness analysis of clinically indicated versus routine replacement of peripheral intravenous catheters. Appl Health Econ Health Policy. 2014; 12(1): 51–58.
- Infusion Nurses Society. Infusion Nursing Standards of Practice. Norwood, MA; Infusion Nurses Society; 2011.
- , , , et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012; 380(9847): 1066–1074.
- , , , et al. epic3: national evidence‐based guidelines for preventing healthcare‐associated infections in NHS hospitals in England. J Hosp Infect. 2014; 86(suppl 1): S1–S70.
- . Short peripheral intravenous catheters and infections. J Infus Nurs. 2012; 35(4): 230–240.
- , , , et al. Phlebitis risk varies by peripheral venous catheter site and increases after 96 hours: a large multi‐centre prospective study. J Adv Nurs. 2014; 70(11): 2539–2549.
- , . Intravenous catheter complications in the hand and forearm. J Trauma. 2004; 56(1): 123–127.
- , , , . Vesicant extravasation part I: Mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum. 2006; 33(6): 1134–1141.
- , . Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung. 2005; 34(5): 345–359.
- , , . Ultrasound‐guided peripheral venous access: a systematic review of randomized‐controlled trials. Eur J Emerg Med. 2014; 21(1): 18–23.
- , , , et al. Difficult peripheral venous access: clinical evaluation of a catheter inserted with the Seldinger method under ultrasound guidance. J Crit Care. 2014; 29(5): 823–827.
- . Choosing the right intravenous catheter. Home Healthc Nurse. 2007; 25(8): 523–531; quiz 532–523.
- Adverse reactions associated with midline catheters—United States, 1992–1995. MMWR Morb Mortal Wkly Rep. 1996; 45(5): 101–103.
- , , . The risk of midline catheterization in hospitalized patients. A prospective study. Ann Intern Med. 1995; 123(11): 841–844.
- . Midline catheters: indications, complications and maintenance. Nurs Stand. 2007; 22(11): 48–57; quiz 58.
- , . Safe administration of vancomycin through a novel midline catheter: a randomized, prospective clinical trial. J Vasc Access. 2014; 15(4): 251–256.
- . Midline catheters: the middle ground of intravenous therapy administration. J Infus Nurs. 2004; 27(5): 313–321.
- . Vascular access in resuscitation: is there a role for the intraosseous route? Anesthesiology. 2014; 120(4): 1015–1031.
- , , , et al. A new system for sternal intraosseous infusion in adults. Prehosp Emerg Care. 2000; 4(2): 173–177.
- , , , , , . Comparison of two intraosseous access devices in adult patients under resuscitation in the emergency department: a prospective, randomized study. Resuscitation. 2010; 81(8): 994–999.
- , , , , . Comparison study of intraosseous, central intravenous, and peripheral intravenous infusions of emergency drugs. Am J Dis Child. 1990; 144(1): 112–117.
- , , , , . The safety of intraosseous infusions: risks of fat and bone marrow emboli to the lungs. Ann Emerg Med. 1989; 18(10): 1062–1067.
- , , , , . ESPEN guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009; 28(4): 365–377.
- , . Peripherally inserted central catheter use in the hospitalized patient: is there a role for the hospitalist? J Hosp Med. 2009; 4(6): E1–E4.
- Vital signs: central line‐associated blood stream infections—United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep. 2011; 60(8): 243–248.
- , , , . Hospital costs of central line‐associated bloodstream infections and cost‐effectiveness of closed vs. open infusion containers. The case of Intensive Care Units in Italy. Cost Eff Resour Alloc. 2010; 8: 8.
- , , . The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006; 81(9): 1159–1171.
- The Joint Commission. Preventing Central Line‐Associated Bloodstream Infections: A Global Challenge, a Global Perspective. Oak Brook, IL: Joint Commission Resources; 2012.
- , , , et al. Guidelines for the prevention of intravascular catheter‐related infections. Am J Infect Control. 2011; 39(4 suppl 1): S1–S34.
- , , , , . The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta‐analysis. Infect Control Hosp Epidemiol. 2013; 34(9): 908–918.
- Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, American Hospital Association, Association for Professionals in Infection Control and Epidemiology, The Joint Commission. Compendium of Strategies to Prevent Healthcare‐Associated Infections in Acute Care Hospitals: 2014 Updates. Available at: http://www.shea‐online.org. Accessed August 1, 2014.
- , , , , . Guidelines for venous access in patients with chronic kidney disease. A Position Statement from the American Society of Diagnostic and Interventional Nephrology, Clinical Practice Committee and the Association for Vascular Access. Semin Dial. 2008; 21(2): 186–191.
- , , , et al. Association between prior peripherally inserted central catheters and lack of functioning arteriovenous fistulas: a case‐control study in hemodialysis patients. Am J Kidney Dis. 2012; 60(4): 601–608.
- , , , et al. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol. 2012; 7(10): 1664–1672.
- , , , et al. Do physicians know which of their patients have central venous catheters? A multi‐center observational study. Ann Intern Med. 2014; 161(8): 562–567.
- , , , et al. Hospital‐wide survey of the use of central venous catheters. J Hosp Infect. 2011; 77(4): 304–308.
- , , , , , . Peripherally inserted central catheter‐related deep vein thrombosis: contemporary patterns and predictors. J Thromb Haemost. 2014; 12(6): 847–854.
- , , , . An in vitro study comparing a peripherally inserted central catheter to a conventional central venous catheter: no difference in static and dynamic pressure transmission. BMC Anesthesiol. 2010; 10: 18.
- , , , et al. Clinical experience with power‐injectable PICCs in intensive care patients. Crit Care. 2012; 16(1): R21.
- , , , et al. Nurse‐led central venous catheter insertion‐procedural characteristics and outcomes of three intensive care based catheter placement services. Int J Nurs Stud. 2012; 49(2): 162–168.
- , , , et al. Peripherally inserted central venous catheters in the acute care setting: a safe alternative to high‐risk short‐term central venous catheters. Am J Infect Control. 2010; 38(2): 149–153.
- , , , et al. Which central venous catheters have the highest rate of catheter‐associated deep venous thrombosis: a prospective analysis of 2,128 catheter days in the surgical intensive care unit. J Trauma Acute Care Surg. 2013; 74(2): 454–460; discussion 461–452.
- , , , et al. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta‐analysis. Lancet. 2013; 382(9889): 311–325.
- , , , , . Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015; 1: CD011447.
- , , , et al. Tunneled jugular small‐bore central catheters as an alternative to peripherally inserted central catheters for intermediate‐term venous access in patients with hemodialysis and chronic renal insufficiency. Radiology. 1999; 213(1): 303–306.
Reliable venous access is fundamental for the safe and effective care of hospitalized patients. Venous access devices (VADs) are conduits for this purpose, providing delivery of intravenous medications, accurate measurement of central venous pressure, or administration of life‐saving blood products. Despite this important role, VADs are also often the source of hospital‐acquired complications. Although inpatient providers must balance the relative risks of VADs against their benefits, the evidence supporting such decisions is often limited. Advances in technology, scattered research, and growing availability of novel devices has only further fragmented provider knowledge in the field of vascular access.[1]
It is not surprising, then, that survey‐based studies of hospitalists reveal important knowledge gaps with regard to practices associated with VADs.[2] In this narrative review, we seek to bridge this gap by providing a concise and pragmatic overview of the fundamentals of venous access. We focus specifically on parameters that influence decisions regarding VAD placement in hospitalized patients, providing key takeaways for practicing hospitalists.
METHODS
To compile this review, we systematically searched Medline (via Ovid) for several keywords, including: peripheral intravenous catheters, ultrasound‐guided peripheral catheter, intraosseous, midline, peripherally inserted central catheter, central venous catheters, and vascular access device complications. We concentrated on full‐length articles in English only; no date restrictions were placed on the search. We reviewed guidelines and consensus statements (eg, from the Center for Disease Control [CDC] or Choosing Wisely criteria) as appropriate. Additional studies of interest were identified through content experts (M.P., C.M.R.) and bibliographies of included studies.
SCIENTIFIC PRINCIPLES UNDERPINNING VENOUS ACCESS
It is useful to begin by reviewing VAD‐related nomenclature and physiology. In the simplest sense, a VAD consists of a hub (providing access to various connectors), a hollow tube divided into 1 or many sections (lumens), and a tip that may terminate within a central or peripheral blood vessel. VADs are classified as central venous catheters (eg, centrally inserted central catheters [CICCs] or peripherally inserted central catheters [PICCs]) or peripheral intravenous catheters (eg, midlines or peripheral intravenous catheters) based on site of entry and location of the catheter tip. Therefore, VADs entering via proximal or distal veins of the arm are often referred to as peripheral lines, as their site of entry and tip both reside within peripheral veins. Conversely, the term central line is often used when VADs enter or terminate in a central vein (eg, subclavian vein insertion with the catheter tip in the lower superior vena cava).
Attention to a host of clinical and theoretical parameters is important when choosing a device for venous access. Some such parameters are summarized in Table 1.
| Parameter | Major Considerations |
|---|---|
| |
| Desired flow rate | Smaller diameter veins susceptible to damage with high flow rates. |
| Short, large‐bore catheters facilitate rapid infusion. | |
| Nature of infusion | pH, viscosity, and temperature may damage vessels. |
| Vesicants and irritants should always be administered into larger, central veins. | |
| Desired duration of vascular access, or dwell time | Vessel thrombosis or phlebitis increase over time with catheter in place. |
| Intermittent infusions increase complications in central catheters; often tunneled catheters are recommended. | |
| Urgency of placement | Access to large caliber vessels is often needed in emergencies. |
| Critically ill or hemodynamically unstable patients may require urgent access for invasive monitoring or rapid infusions. | |
| Patients with trauma often require large volumes of blood products and reliable access to central veins. | |
| Number of device lumens | VADs may have single or multiple lumens. |
| Multilumen allows for multiple functions (eg, infusion of multiple agents, measurement of central venous pressures, blood draws). | |
| Device gauge | In general, use of a smaller‐gauge catheter is preferred to prevent complications. |
| However, larger catheter diameter may be needed for specific clinical needs (eg, blood transfusion). | |
| Device coating | VADs may have antithrombotic or anti‐infective coatings. |
| These devices may be of value in patients at high risk of complications. | |
| Such devices, however, may be more costly than their counterparts. | |
| Self‐care compatibility | VADs that can be cared for by patients are ideal for outpatient care. |
| Conversely, VADs such as peripheral catheters, are highly prone to dislodgement and should be reserved for supervised settings only. | |
VENOUS ACCESS DEVICES
We will organize our discussion of VADs based on whether they terminate in peripheral or central vessels. These anatomical considerations are relevant as they determine physical characteristics, compatibility with particular infusates, dwell time, and risk of complications associated with each VAD discussed in Table 2.
| Complications | Major Considerations |
|---|---|
| |
| Infection | VADs breach the integrity of skin and permit skin pathogens to enter the blood stream (extraluminal infection). |
| Inadequate antisepsis of the VAD hub, including poor hand hygiene, failure to "scrub the hub," and multiple manipulations may also increase the risk of VAD‐related infection (endoluminal infection). | |
| Infections may be local (eg, exit‐site infections) or may spread hematogenously (eg, CLABSI). | |
| Type of VAD, duration of therapy, and host characteristics interact to influence infection risk. | |
| VADs with antiseptic coatings (eg, chlorhexidine) or antibiotic coatings (eg, minocycline) may reduce risk of infection in high‐risk patients. | |
| Antiseptic‐impregnated dressings may reduce risk of extraluminal infection. | |
| Venous thrombosis | VADs predispose to venous stasis and thrombosis. |
| Duration of VAD use, type and care of the VAD, and patient characteristics affect risk of thromboembolism. | |
| VAD tip position is a key determinant of venous thrombosis; central VADs that do not terminate at the cavo‐atrial junction should be repositioned to reduce the risk of thrombosis. | |
| Antithrombotic coated or eluting devices may reduce risk of thrombosis, though definitive data are lacking. | |
| Phlebitis | Inflammation caused by damage to tunica media.[18] |
| 3 types of phlebitis: | |
| Chemical: due to irritation of media from the infusate. | |
| Mechanical: VAD physically damages the vessel. | |
| Infective: bacteria invade vein and inflame vessel wall. | |
| Phlebitis may be limited by close attention to infusate compatibility with peripheral veins, appropriate dilution, and prompt removal of catheters that show signs of inflammation. | |
| Phlebitis may be prevented in PICCs by ensuring at least a 2:1 vein:catheter ratio. | |
| Extravasation | Extravasation (also called infiltration) is defined as leakage of infusate from intravascular to extravascular space. |
| Extravasation of vesicants/emrritants is particularly worrisome. | |
| May result in severe tissue injury, blistering, and tissue necrosis.[11] | |
| VADs should be checked frequently for adequate flushing and position prior to each infusion to minimize risk. | |
| Any VAD with redness, swelling, and tenderness at the entry site or problems with flushing should not be used without further examination and review of position. | |
Peripheral Venous Access
Short Peripheral Intravenous Catheter
Approximately 200 million peripheral intravenous catheters (PIVs) are placed annually in the United States, making them the most common intravenous catheter.[3] PIVs are short devices, 3 to 6 cm in length, that enter and terminate in peripheral veins (Figure 1A). Placement is recommended in forearm veins rather than those of the hand, wrist, or upper arm, as forearm sites are less prone to occlusion, accidental removal, and phlebitis.[4] Additionally, placement in hand veins impedes activities of daily living (eg, hand washing) and is not preferred by patients.[5] PIV size ranges from 24 gauge (smallest) to 14 gauge (largest); larger catheters are often reserved for fluid resuscitation or blood transfusion as they accommodate greater flow and limit hemolysis. To decrease risk of phlebitis and thrombosis, the shortest catheter and smallest diameter should be used. However, unless adequately secured, smaller diameter catheters are also associated with greater rates of accidental removal.[4, 5]
By definition, PIVs are short‐term devices. The CDC currently recommends removal and replacement of these devices no more frequently than every 72 to 96 hours in adults. However, a recent randomized controlled trial found that replacing PIVs when clinically indicated (eg, device failure, phlebitis) rather than on a routine schedule added 30 hours to their lifespan without an increase in complications.[6] A systematic review by the Cochrane Collaboration echoes these findings.[3] These data have thus been incorporated into recommendations from the Infusion Nurses Society (INS) and the National Health Service in the United Kingdom.[5, 7] In hospitalized patients, this approach is relevant, as it preserves venous access sites, maximizes device dwell, and limits additional PIV insertions. In turn, these differences may reduce the need for invasive VADs such as PICCs. Furthermore, the projected 5‐year savings from implementation of clinically indicated PIV removal policies is US$300 million and 1 million health‐worker hours in the United States alone.[4]
PIVs offer many advantages. First, they are minimally invasive and require little training to insert. Second, they can be used for diverse indications in patients requiring short‐term (1 week) venous access. Third, PIVs do not require imaging to ensure correct placement; palpation of superficial veins is sufficient. Fourth, PIVs exhibit a risk of bloodstream infection that is about 40‐fold lower than more invasive, longer‐dwelling VADs[8] (0.06 bacteremia per 1000 catheter‐days).
Despite these advantages, PIVs also have important drawbacks. First, a quarter of all PIVs fail through occlusion or accidental dislodgement.[4] Infiltration, extravasation, and hematoma formation are important adverse events that may occur in such cases. Second, thrombophlebitis (pain and redness at the insertion site) is frequent, and may require device removal, especially in patients with catheters 20 guage.[9] Third, despite their relative safety, PIVs can cause localized or hematogenous infection. Septic thrombophlebitis (superficial thrombosis and bloodstream infection) and catheter‐related bloodstream infection, though rare, have been reported with PIVs and may lead to serious complications.[8, 10] In fact, some suggest that the overall burden of bloodstream infection risk posed by PIVs may be similar to that of CICCs given the substantially greater number of devices used and greater number of device days.[8]
PIVs and other peripheral VADs are not suitable for infusion of vesicants or irritants, which require larger, central veins for delivery. Vesicants (drugs that cause blistering on infusion) include chemotherapeutic agents (eg, dactinomycin, paclitaxel) and commonly used nonchemotherapeutical agents (eg, diazepam, piperacillin, vancomycin, esmolol, or total parenteral nutrition [TPN]).[11] Irritants (phlebitogenic drugs) cause short‐term inflammation and pain, and thus should not be peripherally infused for prolonged durations. Common irritants in the hospital setting include acyclovir, dobutamine, penicillin, and potassium chloride.
Of note, about one‐quarter of PIV insertions fail owing to difficult intravenous access.[12] Ultrasound‐guided peripheral intravenous (USGPIV) catheter placement is emerging as a technique to provide peripheral access for such patients to avoid placement of central venous access devices. Novel, longer devices (>8 cm) with built‐in guide wires have been developed to increase placement success of USGPIVs. These new designs provide easier access into deeper arm veins (brachial or basilic) not otherwise accessible by short PIVs. Although studies comparing the efficacy of USGPIV devices to other VADs are limited, a recent systematic review showed that time to successful cannulation was shorter, and fewer attempts were required to place USGPIVs compared to PIVs.[13] A recent study in France found that USGPIVs met the infusion needs of patients with difficult veins with minimal increase in complications.[14] Despite these encouraging data, future studies are needed to better evaluate this technology.
Midline Catheter
A midline is a VAD that is between 7.5 to 25 cm in length and is typically inserted into veins above the antecubital fossa. The catheter tip resides in a peripheral upper arm vein, often the basilic or cephalic vein, terminating just short of the subclavian vein (Figure 1B). Midline‐like devices were first developed in the 1950s and were initially used as an alternative to PIVs because they were thought to allow longer dwell times.[15] However, because they were originally constructed with a fairly rigid material, infiltration, mechanical phlebitis, and inflammation were common and tempered enthusiasm for their use.[15, 16] Newer midline devices obviate many of these problems and are inserted by ultrasound guidance and modified Seldinger technique.[17] Despite these advances, data regarding comparative efficacy are limited.
Midlines offer longer dwell times than standard PIVs owing to termination in the larger diameter basilic and brachial veins of the arm. Additionally, owing to their length, midlines are less prone to dislodgement. As they are inserted with greater antisepsis than PIVs and better secured to the skin, they are more durable than PIVs.[5, 9, 18] Current INS standards recommend use of midlines for 1 to 4 weeks.[5] Because they terminate in a peripheral vein, medications and infusions compatible with midlines are identical to those that are infused through a PIV. Thus, TPN, vesicants or irritants, or drugs that feature a pH 5 or pH >9, or >500 mOsm should not be infused through a midline.[15] New evidence suggests that diluted solutions of vancomycin (usually pH 5) may be safe to infuse for short durations (6 days) through a midline, and that concentration rather than pH may be more important in this regard.[19] Although it is possible that the use of midlines may extend to agents typically not deemed peripheral access compatible, limited evidence exists to support such a strategy at this time.
Midlines offer several advantages. First, because blood flow is greater in the more proximal veins of the arm, midlines can accommodate infusions at rates of 100 to 150 mL/min compared to 20 to 40 mL/min in smaller peripheral veins. Higher flow rates offer greater hemodilution (dilution of the infusion with blood), decreasing the likelihood of phlebitis and infiltration.[20] Second, midlines do not require x‐ray verification of tip placement; thus, their use is often favored in resource‐depleted settings such as skilled nursing facilities. Third, midlines offer longer dwell times than peripheral intravenous catheters and can thus serve as bridge devices for short‐term intravenous antibiotics or peripheral‐compatible infusions in an outpatient setting. Available evidence suggests that midlines are associated with low rates of bloodstream infection (0.30.8 per 1000 catheter‐days).[17] The most frequent complications include phlebitis (4.2%) and occlusion (3.3%).[20] Given these favorable statistics, midlines may offer a good alternative to PIVs in select patients who require peripheral infusions of intermediate duration.
Intraosseous Vascular Access
Intraosseous (IO) devices access the vascular system by piercing cortical bone. These devices provide access to the intramedullary cavity and venous plexi of long bones such as the tibia, femur, or humerus. Several insertion devices are now commercially available and have enhanced the ease and safety of IO placement. Using these newer devices, IO access may be obtained in 1 to 2 minutes with minimal training. By comparison, a central venous catheter often requires 10 to 15 minutes to insert with substantial training efforts for providers.[21, 22, 23]
IO devices thus offer several advantages. First, given the rapidity with which they can be inserted, they are often preferred in emergency settings (eg, trauma). Second, these devices are versatile and can accommodate both central and peripheral infusates.[24] Third, a recent meta‐analysis found that IOs have a low complication rate of 0.8%, with extravasation of infusate through the cortical entry site being the most common adverse event.[21] Of note, this study also reported zero local or distal infectious complications, a finding that may relate to the shorter dwell of these devices.[21] Some animal studies suggest that fat embolism from bone may occur at high rates with IO VADs.[25] However, death or significant morbidity from fat emboli in humans following IO access has not been described. Whether such emboli occur or are clinically significant in the context of IO devices remains unclear at this time.[21]
Central Venous Access Devices
Central venous access devices (CVADs) share in common tip termination in the cavo‐atrial junction, either in the lower portion of the superior vena cava or in the upper portion of the right atrium. CVADs can be safely used for irritant or vesicant medications as well as for blood withdrawal, blood exchange procedures (eg, dialysis), and hemodynamic monitoring. Traditionally, these devices are 15 to 25 cm in length and are directly inserted in the deep veins of the supra‐ or infraclavicular area, including the internal jugular, brachiocephalic, subclavian, or axillary veins. PICCs are unique CVADs in that they enter through peripheral veins but terminate in the proximity of the cavoatrial junction. Regarding nomenclature, CICC will be used to denote devices that enter directly into veins of the neck or chest, whereas PICC will be used for devices that are inserted peripherally but terminate centrally.
Peripherally Inserted Central Catheter
PICCs are inserted into peripheral veins of the upper arm (eg, brachial, basilica, or cephalic vein) and advanced such that the tip resides at the cavoatrial junction (Figure 1C). PICCs offer prolonged dwell times and are thus indicated when patients require venous access for weeks or months.[26] Additionally, they can accommodate a variety of infusates and are safer to insert than CICCs, given placement in peripheral veins of the arm rather than central veins of the chest/neck. Thus, insertion complications such as pneumothorax, hemothorax, or significant bleeding are rare with PICCs. In fact, a recent study reported that PICC insertion by hospitalists was associated with low rates of insertion or infectious complications.[27]
However, like CICCs, PICCs are associated with central lineassociated bloodstream infection (CLABSI), a serious complication known to prolong length of hospital stay, increase costs, and carry a 12% to 25% associated mortality.[28, 29] In the United States alone, over 250,000 CLASBI cases occur per year drawing considerable attention from the CDC and Joint Commission, who now mandate reporting and nonpayment for hospital‐acquired CLABSI.[30, 31, 32] A recent systematic review and meta‐analysis found that PICCs are associated with a substantial risk of CLABSI in hospitalized patients.[33] Importantly, no difference in CLABSI rates between PICCs and CICCs in hospitalized patients was evident in this meta‐analysis. Therefore, current guidelines specifically recommend against use of PICCs over CICCs as a strategy to reduce CLABSI.[34] Additionally, PICCs are associated with 2.5‐fold greater risk of deep vein thrombosis (DVT) compared to CICCs; thus, they should be used with caution in patients with cancer or those with underlying hypercoagulable states.
Of particular import to hospitalists is the fact that PICC placement is contraindicated in patients with stage IIIB or greater chronic kidney disease (CKD). In such patients, sequelae of PICC use, such as phlebitis or central vein stenosis, can be devastating in patients with CKD.[35] In a recent study, prior PICC placement was the strongest predictor of subsequent arteriovenous graft failure.[36] For this reason, Choosing Wisely recommendations call for avoidance of PICCs in such patients.[37]
Centrally Inserted Central Catheter
CICCs are CVADs placed by puncture and cannulation of the internal jugular, subclavian, brachiocephalic, or femoral veins (Figure 1D) and compose the vast majority of VADs placed in ICU settings.[38, 39] Central termination of CICCs allows for a variety of infusions, including irritants, vesicants, and vasopressors, as well as blood withdrawal and hemodynamic monitoring. CICCs are typically used for 7 to 14 days, but may remain for longer durations if they remain complication free and clinically necessary.[40] A key advantage of CICCs is that they can be placed in emergent settings to facilitate quick access for rapid infusion or hemodynamic monitoring. In particular, CICCs are inserted in the femoral vein and may be useful in emergency settings. However, owing to risk of infection and inability to monitor central pressures, these femoral devices should be replaced with a proper CICC or PICC when possible. Importantly, although CICCs are almost exclusively used in intensive or emergency care, PICCs may also be considered in such settings.[41, 42] CICCs usually have multiple lumens and often serve several simultaneous functions such as both infusions and hemodynamic monitoring.
Despite their benefits, CICCs have several disadvantages. First, insertion requires an experienced clinician and has historically been a task limited to physicians. However, this is changing rapidly (especially in Europe and Australia) where specially trained nurses are assuming responsibility for CICC placement.[43] Second, these devices are historically more likely to be associated with CLABSI, with estimates of infection rates varying between 2 and 5 infections per 1000 catheter‐days.[44] Third, CICCs pose a significant DVT risk, with rates around 22 DVTs per 1000 catheter‐days.[45] However, compared to PICCs, the DVT risk appears lower, and CICC use may be preferable in patients at high risk of DVT, such as critically ill or cancer populations.[46] An important note to prevent CICC insertion complications relates to use of ultrasound, a practice that has been associated with decreased accidental arterial puncture and hematoma formation. The role of ultrasound guidance with PICCs as well as implications for thrombotic and infectious events remains less characterized at this point.[47]
Tunneled Central Venous Access Devices
Tunneled devices (either CICCs or PICCs) are characterized by the fact that the insertion site on the skin and site of ultimate venipuncture are physically separated (Figure 1E). Tunneling limits bacterial entry from the extraluminal aspect of the CVAD to the bloodstream. For example, internal jugular veins are often ideal sites of puncture but inappropriate sites for catheter placement, as providing care to this area is challenging and may increase risk of infection.[34] Tunneling to the infraclavicular area provides a better option, as it provides an exit site that can be adequately cared for. Importantly, any CVAD (PICCs or CICCs) can be tunneled. Additionally, tunneled CICCs may be used in patients with chronic or impending renal failure where PICCs are contraindicated because entry into dialysis‐relevant vessels is to be avoided.[48] Such devices also allow regular blood sampling in patients who require frequent testing but have limited peripheral access, such as those with hematological malignancies. Additionally, tunneled catheters are more comfortable for patients and viewed as being more socially acceptable than nontunneled devices. However, the more invasive and permanent nature of these devices often requires deliberation prior to insertion.
Of note, tunneled devices and ports may be used as long‐term (>3 months to years) VADs. As our focus in this review is short‐term devices, we will not expand the discussion of these devices as they are almost always used for prolonged durations.[7]
OPERATIONALIZING THE DATA: AN ALGORITHMIC APPROACH TO VENOUS ACCESS
Hospitalists should consider approaching venous access using an algorithm based on a number of parameters. For example, a critically ill patient who requires vasopressor support and hemodynamic monitoring will need a CICC or a PICC. Given the potential greater risk of thromboses from PICCs, a CICC is preferable for critically ill patients provided an experienced inserter is available. Conversely, patients who require short‐term (710 days) venous access for infusion of nonirritant or nonvesicant therapy often only require a PIV. In patients with poor or difficult venous access, USGPIVs or midlines may be ideal and preferred over short PIVs. Finally, patients who require longer‐term or home‐based treatment may benefit from early placement of a midline or a PICC, depending again on the nature of the infusion, duration of treatment, and available venous access sites.
An algorithmic approach considering these parameters is suggested in Figure 2, and a brief overview of the devices and their considerations is shown in Table 3.
| Vascular Access Device | Central/Peripheral | Anatomical Location of Placement | Desired Duration of Placement | Common Uses | BSI Risk (Per 1,000 Catheter‐Days) | Thrombosis Risk | Important Considerations |
|---|---|---|---|---|---|---|---|
| |||||||
| Small peripheral IV | Peripheral | Peripheral veins, usually forearm | 710 days | Fluid resuscitation, most medications, blood products | 0.06[8] | Virtually no risk | Consider necessity of PIV daily and remove unnecessary devices |
| Midline | Peripheral | Inserted around antecubital fossa, reside within basilic or cephalic vein of the arm | 24 weeks | Long‐term medications excluding TPN, vesicants, corrosives | 0.30.8[17] | Insufficient data | Can be used as bridge devices for patients to complete short‐term antibiotics/emnfusions as an outpatient |
| Peripherally inserted central catheter | Central | Inserted into peripheral arm vein and advanced to larger veins (eg, internal jugular or subclavian) to the CAJ | >1 week, 3 months | Large variety of infusates, including TPN, vesicants, corrosives | 2.4[44] | 6.30% | Contraindicated in patients with CKD stage IIIb or higher |
| Centrally inserted central catheters | Central | Inserted above (internal jugular vein, brachiocephalic vein, subclavian vein), or below the clavicle (axillary vein) | >1 week, 3 months | Same infusate variety as PICC, measurement of central venous pressures, common in trauma/emergent settings | 2.3[44] | 1.30% | Given lower rates of DVT than PICC, preferred in ICU and hypercoagulable environments |
| Tunneled CICCs | Central | Placed percutaneously in any large vein in the arm, chest, neck or groin | >3 months to years | Central infusates, as in any CVAD; used for patients with CKD stage IIIb or greater when a PICC is indicated | Insufficient data | Insufficient data | May be superior when insertion site and puncture site are not congruent and may increase risk of infection |
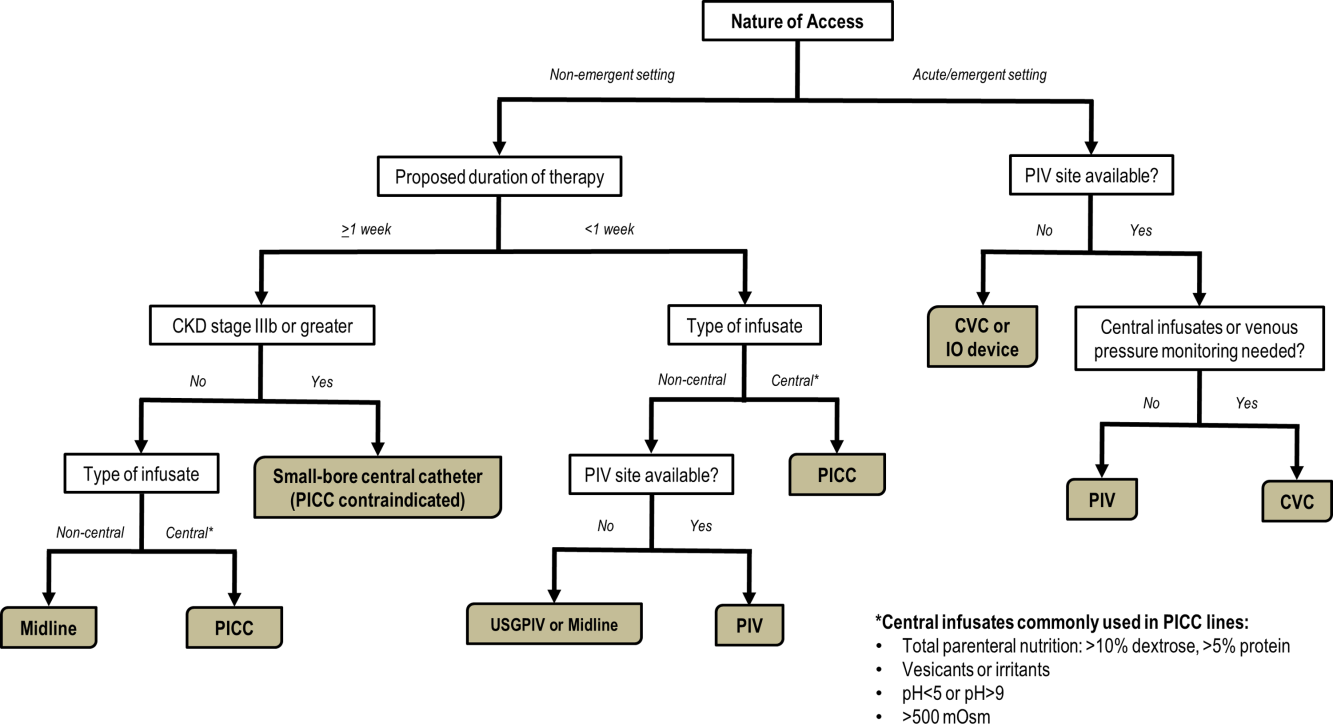
CONCLUSIONS
With strides in technology and progress in medicine, hospitalists have access to an array of options for venous access. However, every VAD has limitations that can be easily overlooked in a perfunctory decision‐making process. The data presented in this review thus provide a first step to improving safety in this evolving science. Studies that further determine appropriateness of VADs in hospitalized settings are necessary. Only through such progressive scientific enquiry will complication‐free venous access be realized.
Disclosure
Nothing to report.
Reliable venous access is fundamental for the safe and effective care of hospitalized patients. Venous access devices (VADs) are conduits for this purpose, providing delivery of intravenous medications, accurate measurement of central venous pressure, or administration of life‐saving blood products. Despite this important role, VADs are also often the source of hospital‐acquired complications. Although inpatient providers must balance the relative risks of VADs against their benefits, the evidence supporting such decisions is often limited. Advances in technology, scattered research, and growing availability of novel devices has only further fragmented provider knowledge in the field of vascular access.[1]
It is not surprising, then, that survey‐based studies of hospitalists reveal important knowledge gaps with regard to practices associated with VADs.[2] In this narrative review, we seek to bridge this gap by providing a concise and pragmatic overview of the fundamentals of venous access. We focus specifically on parameters that influence decisions regarding VAD placement in hospitalized patients, providing key takeaways for practicing hospitalists.
METHODS
To compile this review, we systematically searched Medline (via Ovid) for several keywords, including: peripheral intravenous catheters, ultrasound‐guided peripheral catheter, intraosseous, midline, peripherally inserted central catheter, central venous catheters, and vascular access device complications. We concentrated on full‐length articles in English only; no date restrictions were placed on the search. We reviewed guidelines and consensus statements (eg, from the Center for Disease Control [CDC] or Choosing Wisely criteria) as appropriate. Additional studies of interest were identified through content experts (M.P., C.M.R.) and bibliographies of included studies.
SCIENTIFIC PRINCIPLES UNDERPINNING VENOUS ACCESS
It is useful to begin by reviewing VAD‐related nomenclature and physiology. In the simplest sense, a VAD consists of a hub (providing access to various connectors), a hollow tube divided into 1 or many sections (lumens), and a tip that may terminate within a central or peripheral blood vessel. VADs are classified as central venous catheters (eg, centrally inserted central catheters [CICCs] or peripherally inserted central catheters [PICCs]) or peripheral intravenous catheters (eg, midlines or peripheral intravenous catheters) based on site of entry and location of the catheter tip. Therefore, VADs entering via proximal or distal veins of the arm are often referred to as peripheral lines, as their site of entry and tip both reside within peripheral veins. Conversely, the term central line is often used when VADs enter or terminate in a central vein (eg, subclavian vein insertion with the catheter tip in the lower superior vena cava).
Attention to a host of clinical and theoretical parameters is important when choosing a device for venous access. Some such parameters are summarized in Table 1.
| Parameter | Major Considerations |
|---|---|
| |
| Desired flow rate | Smaller diameter veins susceptible to damage with high flow rates. |
| Short, large‐bore catheters facilitate rapid infusion. | |
| Nature of infusion | pH, viscosity, and temperature may damage vessels. |
| Vesicants and irritants should always be administered into larger, central veins. | |
| Desired duration of vascular access, or dwell time | Vessel thrombosis or phlebitis increase over time with catheter in place. |
| Intermittent infusions increase complications in central catheters; often tunneled catheters are recommended. | |
| Urgency of placement | Access to large caliber vessels is often needed in emergencies. |
| Critically ill or hemodynamically unstable patients may require urgent access for invasive monitoring or rapid infusions. | |
| Patients with trauma often require large volumes of blood products and reliable access to central veins. | |
| Number of device lumens | VADs may have single or multiple lumens. |
| Multilumen allows for multiple functions (eg, infusion of multiple agents, measurement of central venous pressures, blood draws). | |
| Device gauge | In general, use of a smaller‐gauge catheter is preferred to prevent complications. |
| However, larger catheter diameter may be needed for specific clinical needs (eg, blood transfusion). | |
| Device coating | VADs may have antithrombotic or anti‐infective coatings. |
| These devices may be of value in patients at high risk of complications. | |
| Such devices, however, may be more costly than their counterparts. | |
| Self‐care compatibility | VADs that can be cared for by patients are ideal for outpatient care. |
| Conversely, VADs such as peripheral catheters, are highly prone to dislodgement and should be reserved for supervised settings only. | |
VENOUS ACCESS DEVICES
We will organize our discussion of VADs based on whether they terminate in peripheral or central vessels. These anatomical considerations are relevant as they determine physical characteristics, compatibility with particular infusates, dwell time, and risk of complications associated with each VAD discussed in Table 2.
| Complications | Major Considerations |
|---|---|
| |
| Infection | VADs breach the integrity of skin and permit skin pathogens to enter the blood stream (extraluminal infection). |
| Inadequate antisepsis of the VAD hub, including poor hand hygiene, failure to "scrub the hub," and multiple manipulations may also increase the risk of VAD‐related infection (endoluminal infection). | |
| Infections may be local (eg, exit‐site infections) or may spread hematogenously (eg, CLABSI). | |
| Type of VAD, duration of therapy, and host characteristics interact to influence infection risk. | |
| VADs with antiseptic coatings (eg, chlorhexidine) or antibiotic coatings (eg, minocycline) may reduce risk of infection in high‐risk patients. | |
| Antiseptic‐impregnated dressings may reduce risk of extraluminal infection. | |
| Venous thrombosis | VADs predispose to venous stasis and thrombosis. |
| Duration of VAD use, type and care of the VAD, and patient characteristics affect risk of thromboembolism. | |
| VAD tip position is a key determinant of venous thrombosis; central VADs that do not terminate at the cavo‐atrial junction should be repositioned to reduce the risk of thrombosis. | |
| Antithrombotic coated or eluting devices may reduce risk of thrombosis, though definitive data are lacking. | |
| Phlebitis | Inflammation caused by damage to tunica media.[18] |
| 3 types of phlebitis: | |
| Chemical: due to irritation of media from the infusate. | |
| Mechanical: VAD physically damages the vessel. | |
| Infective: bacteria invade vein and inflame vessel wall. | |
| Phlebitis may be limited by close attention to infusate compatibility with peripheral veins, appropriate dilution, and prompt removal of catheters that show signs of inflammation. | |
| Phlebitis may be prevented in PICCs by ensuring at least a 2:1 vein:catheter ratio. | |
| Extravasation | Extravasation (also called infiltration) is defined as leakage of infusate from intravascular to extravascular space. |
| Extravasation of vesicants/emrritants is particularly worrisome. | |
| May result in severe tissue injury, blistering, and tissue necrosis.[11] | |
| VADs should be checked frequently for adequate flushing and position prior to each infusion to minimize risk. | |
| Any VAD with redness, swelling, and tenderness at the entry site or problems with flushing should not be used without further examination and review of position. | |
Peripheral Venous Access
Short Peripheral Intravenous Catheter
Approximately 200 million peripheral intravenous catheters (PIVs) are placed annually in the United States, making them the most common intravenous catheter.[3] PIVs are short devices, 3 to 6 cm in length, that enter and terminate in peripheral veins (Figure 1A). Placement is recommended in forearm veins rather than those of the hand, wrist, or upper arm, as forearm sites are less prone to occlusion, accidental removal, and phlebitis.[4] Additionally, placement in hand veins impedes activities of daily living (eg, hand washing) and is not preferred by patients.[5] PIV size ranges from 24 gauge (smallest) to 14 gauge (largest); larger catheters are often reserved for fluid resuscitation or blood transfusion as they accommodate greater flow and limit hemolysis. To decrease risk of phlebitis and thrombosis, the shortest catheter and smallest diameter should be used. However, unless adequately secured, smaller diameter catheters are also associated with greater rates of accidental removal.[4, 5]
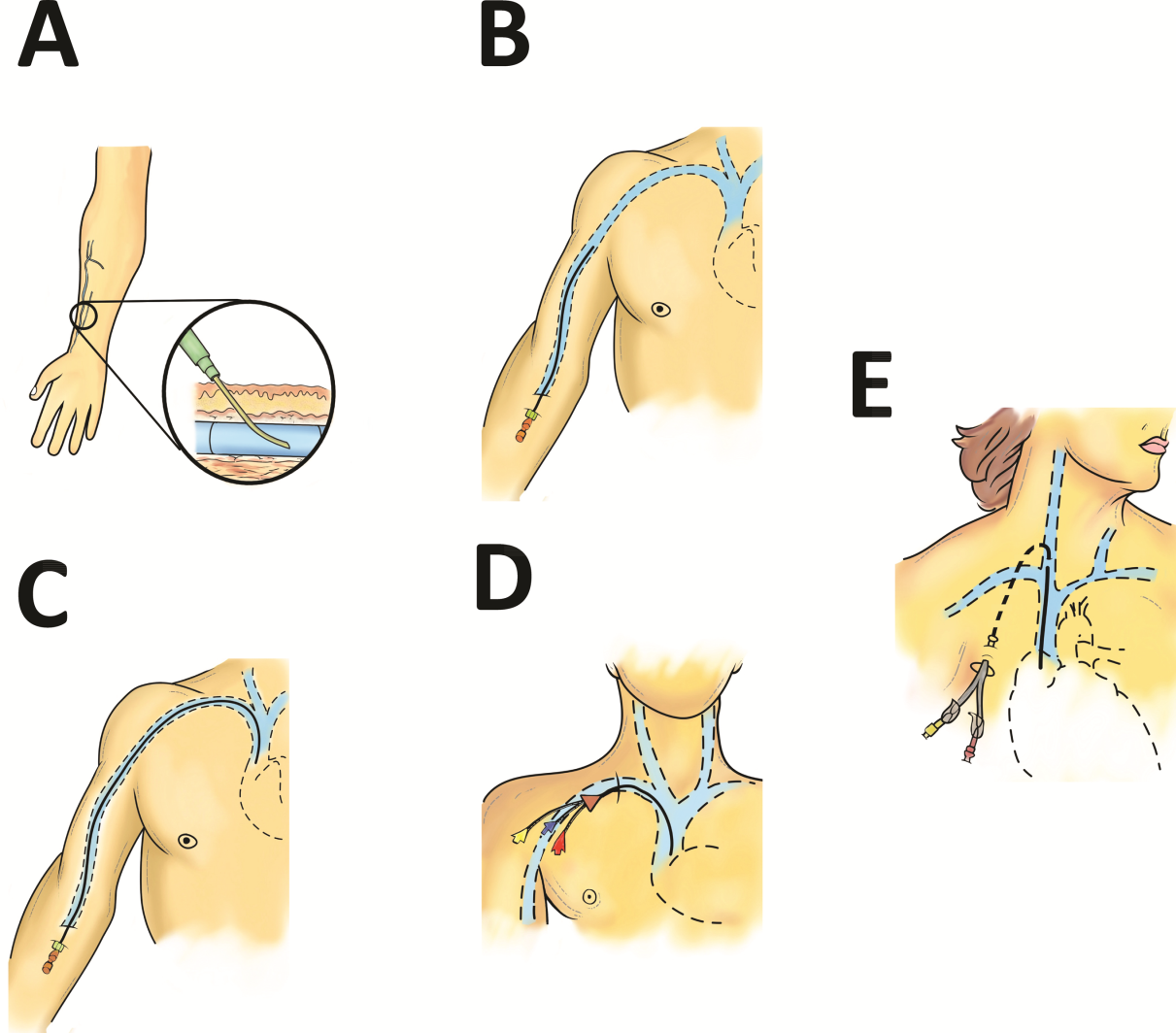
By definition, PIVs are short‐term devices. The CDC currently recommends removal and replacement of these devices no more frequently than every 72 to 96 hours in adults. However, a recent randomized controlled trial found that replacing PIVs when clinically indicated (eg, device failure, phlebitis) rather than on a routine schedule added 30 hours to their lifespan without an increase in complications.[6] A systematic review by the Cochrane Collaboration echoes these findings.[3] These data have thus been incorporated into recommendations from the Infusion Nurses Society (INS) and the National Health Service in the United Kingdom.[5, 7] In hospitalized patients, this approach is relevant, as it preserves venous access sites, maximizes device dwell, and limits additional PIV insertions. In turn, these differences may reduce the need for invasive VADs such as PICCs. Furthermore, the projected 5‐year savings from implementation of clinically indicated PIV removal policies is US$300 million and 1 million health‐worker hours in the United States alone.[4]
PIVs offer many advantages. First, they are minimally invasive and require little training to insert. Second, they can be used for diverse indications in patients requiring short‐term (1 week) venous access. Third, PIVs do not require imaging to ensure correct placement; palpation of superficial veins is sufficient. Fourth, PIVs exhibit a risk of bloodstream infection that is about 40‐fold lower than more invasive, longer‐dwelling VADs[8] (0.06 bacteremia per 1000 catheter‐days).
Despite these advantages, PIVs also have important drawbacks. First, a quarter of all PIVs fail through occlusion or accidental dislodgement.[4] Infiltration, extravasation, and hematoma formation are important adverse events that may occur in such cases. Second, thrombophlebitis (pain and redness at the insertion site) is frequent, and may require device removal, especially in patients with catheters 20 guage.[9] Third, despite their relative safety, PIVs can cause localized or hematogenous infection. Septic thrombophlebitis (superficial thrombosis and bloodstream infection) and catheter‐related bloodstream infection, though rare, have been reported with PIVs and may lead to serious complications.[8, 10] In fact, some suggest that the overall burden of bloodstream infection risk posed by PIVs may be similar to that of CICCs given the substantially greater number of devices used and greater number of device days.[8]
PIVs and other peripheral VADs are not suitable for infusion of vesicants or irritants, which require larger, central veins for delivery. Vesicants (drugs that cause blistering on infusion) include chemotherapeutic agents (eg, dactinomycin, paclitaxel) and commonly used nonchemotherapeutical agents (eg, diazepam, piperacillin, vancomycin, esmolol, or total parenteral nutrition [TPN]).[11] Irritants (phlebitogenic drugs) cause short‐term inflammation and pain, and thus should not be peripherally infused for prolonged durations. Common irritants in the hospital setting include acyclovir, dobutamine, penicillin, and potassium chloride.
Of note, about one‐quarter of PIV insertions fail owing to difficult intravenous access.[12] Ultrasound‐guided peripheral intravenous (USGPIV) catheter placement is emerging as a technique to provide peripheral access for such patients to avoid placement of central venous access devices. Novel, longer devices (>8 cm) with built‐in guide wires have been developed to increase placement success of USGPIVs. These new designs provide easier access into deeper arm veins (brachial or basilic) not otherwise accessible by short PIVs. Although studies comparing the efficacy of USGPIV devices to other VADs are limited, a recent systematic review showed that time to successful cannulation was shorter, and fewer attempts were required to place USGPIVs compared to PIVs.[13] A recent study in France found that USGPIVs met the infusion needs of patients with difficult veins with minimal increase in complications.[14] Despite these encouraging data, future studies are needed to better evaluate this technology.
Midline Catheter
A midline is a VAD that is between 7.5 to 25 cm in length and is typically inserted into veins above the antecubital fossa. The catheter tip resides in a peripheral upper arm vein, often the basilic or cephalic vein, terminating just short of the subclavian vein (Figure 1B). Midline‐like devices were first developed in the 1950s and were initially used as an alternative to PIVs because they were thought to allow longer dwell times.[15] However, because they were originally constructed with a fairly rigid material, infiltration, mechanical phlebitis, and inflammation were common and tempered enthusiasm for their use.[15, 16] Newer midline devices obviate many of these problems and are inserted by ultrasound guidance and modified Seldinger technique.[17] Despite these advances, data regarding comparative efficacy are limited.
Midlines offer longer dwell times than standard PIVs owing to termination in the larger diameter basilic and brachial veins of the arm. Additionally, owing to their length, midlines are less prone to dislodgement. As they are inserted with greater antisepsis than PIVs and better secured to the skin, they are more durable than PIVs.[5, 9, 18] Current INS standards recommend use of midlines for 1 to 4 weeks.[5] Because they terminate in a peripheral vein, medications and infusions compatible with midlines are identical to those that are infused through a PIV. Thus, TPN, vesicants or irritants, or drugs that feature a pH 5 or pH >9, or >500 mOsm should not be infused through a midline.[15] New evidence suggests that diluted solutions of vancomycin (usually pH 5) may be safe to infuse for short durations (6 days) through a midline, and that concentration rather than pH may be more important in this regard.[19] Although it is possible that the use of midlines may extend to agents typically not deemed peripheral access compatible, limited evidence exists to support such a strategy at this time.
Midlines offer several advantages. First, because blood flow is greater in the more proximal veins of the arm, midlines can accommodate infusions at rates of 100 to 150 mL/min compared to 20 to 40 mL/min in smaller peripheral veins. Higher flow rates offer greater hemodilution (dilution of the infusion with blood), decreasing the likelihood of phlebitis and infiltration.[20] Second, midlines do not require x‐ray verification of tip placement; thus, their use is often favored in resource‐depleted settings such as skilled nursing facilities. Third, midlines offer longer dwell times than peripheral intravenous catheters and can thus serve as bridge devices for short‐term intravenous antibiotics or peripheral‐compatible infusions in an outpatient setting. Available evidence suggests that midlines are associated with low rates of bloodstream infection (0.30.8 per 1000 catheter‐days).[17] The most frequent complications include phlebitis (4.2%) and occlusion (3.3%).[20] Given these favorable statistics, midlines may offer a good alternative to PIVs in select patients who require peripheral infusions of intermediate duration.
Intraosseous Vascular Access
Intraosseous (IO) devices access the vascular system by piercing cortical bone. These devices provide access to the intramedullary cavity and venous plexi of long bones such as the tibia, femur, or humerus. Several insertion devices are now commercially available and have enhanced the ease and safety of IO placement. Using these newer devices, IO access may be obtained in 1 to 2 minutes with minimal training. By comparison, a central venous catheter often requires 10 to 15 minutes to insert with substantial training efforts for providers.[21, 22, 23]
IO devices thus offer several advantages. First, given the rapidity with which they can be inserted, they are often preferred in emergency settings (eg, trauma). Second, these devices are versatile and can accommodate both central and peripheral infusates.[24] Third, a recent meta‐analysis found that IOs have a low complication rate of 0.8%, with extravasation of infusate through the cortical entry site being the most common adverse event.[21] Of note, this study also reported zero local or distal infectious complications, a finding that may relate to the shorter dwell of these devices.[21] Some animal studies suggest that fat embolism from bone may occur at high rates with IO VADs.[25] However, death or significant morbidity from fat emboli in humans following IO access has not been described. Whether such emboli occur or are clinically significant in the context of IO devices remains unclear at this time.[21]
Central Venous Access Devices
Central venous access devices (CVADs) share in common tip termination in the cavo‐atrial junction, either in the lower portion of the superior vena cava or in the upper portion of the right atrium. CVADs can be safely used for irritant or vesicant medications as well as for blood withdrawal, blood exchange procedures (eg, dialysis), and hemodynamic monitoring. Traditionally, these devices are 15 to 25 cm in length and are directly inserted in the deep veins of the supra‐ or infraclavicular area, including the internal jugular, brachiocephalic, subclavian, or axillary veins. PICCs are unique CVADs in that they enter through peripheral veins but terminate in the proximity of the cavoatrial junction. Regarding nomenclature, CICC will be used to denote devices that enter directly into veins of the neck or chest, whereas PICC will be used for devices that are inserted peripherally but terminate centrally.
Peripherally Inserted Central Catheter
PICCs are inserted into peripheral veins of the upper arm (eg, brachial, basilica, or cephalic vein) and advanced such that the tip resides at the cavoatrial junction (Figure 1C). PICCs offer prolonged dwell times and are thus indicated when patients require venous access for weeks or months.[26] Additionally, they can accommodate a variety of infusates and are safer to insert than CICCs, given placement in peripheral veins of the arm rather than central veins of the chest/neck. Thus, insertion complications such as pneumothorax, hemothorax, or significant bleeding are rare with PICCs. In fact, a recent study reported that PICC insertion by hospitalists was associated with low rates of insertion or infectious complications.[27]
However, like CICCs, PICCs are associated with central lineassociated bloodstream infection (CLABSI), a serious complication known to prolong length of hospital stay, increase costs, and carry a 12% to 25% associated mortality.[28, 29] In the United States alone, over 250,000 CLASBI cases occur per year drawing considerable attention from the CDC and Joint Commission, who now mandate reporting and nonpayment for hospital‐acquired CLABSI.[30, 31, 32] A recent systematic review and meta‐analysis found that PICCs are associated with a substantial risk of CLABSI in hospitalized patients.[33] Importantly, no difference in CLABSI rates between PICCs and CICCs in hospitalized patients was evident in this meta‐analysis. Therefore, current guidelines specifically recommend against use of PICCs over CICCs as a strategy to reduce CLABSI.[34] Additionally, PICCs are associated with 2.5‐fold greater risk of deep vein thrombosis (DVT) compared to CICCs; thus, they should be used with caution in patients with cancer or those with underlying hypercoagulable states.
Of particular import to hospitalists is the fact that PICC placement is contraindicated in patients with stage IIIB or greater chronic kidney disease (CKD). In such patients, sequelae of PICC use, such as phlebitis or central vein stenosis, can be devastating in patients with CKD.[35] In a recent study, prior PICC placement was the strongest predictor of subsequent arteriovenous graft failure.[36] For this reason, Choosing Wisely recommendations call for avoidance of PICCs in such patients.[37]
Centrally Inserted Central Catheter
CICCs are CVADs placed by puncture and cannulation of the internal jugular, subclavian, brachiocephalic, or femoral veins (Figure 1D) and compose the vast majority of VADs placed in ICU settings.[38, 39] Central termination of CICCs allows for a variety of infusions, including irritants, vesicants, and vasopressors, as well as blood withdrawal and hemodynamic monitoring. CICCs are typically used for 7 to 14 days, but may remain for longer durations if they remain complication free and clinically necessary.[40] A key advantage of CICCs is that they can be placed in emergent settings to facilitate quick access for rapid infusion or hemodynamic monitoring. In particular, CICCs are inserted in the femoral vein and may be useful in emergency settings. However, owing to risk of infection and inability to monitor central pressures, these femoral devices should be replaced with a proper CICC or PICC when possible. Importantly, although CICCs are almost exclusively used in intensive or emergency care, PICCs may also be considered in such settings.[41, 42] CICCs usually have multiple lumens and often serve several simultaneous functions such as both infusions and hemodynamic monitoring.
Despite their benefits, CICCs have several disadvantages. First, insertion requires an experienced clinician and has historically been a task limited to physicians. However, this is changing rapidly (especially in Europe and Australia) where specially trained nurses are assuming responsibility for CICC placement.[43] Second, these devices are historically more likely to be associated with CLABSI, with estimates of infection rates varying between 2 and 5 infections per 1000 catheter‐days.[44] Third, CICCs pose a significant DVT risk, with rates around 22 DVTs per 1000 catheter‐days.[45] However, compared to PICCs, the DVT risk appears lower, and CICC use may be preferable in patients at high risk of DVT, such as critically ill or cancer populations.[46] An important note to prevent CICC insertion complications relates to use of ultrasound, a practice that has been associated with decreased accidental arterial puncture and hematoma formation. The role of ultrasound guidance with PICCs as well as implications for thrombotic and infectious events remains less characterized at this point.[47]
Tunneled Central Venous Access Devices
Tunneled devices (either CICCs or PICCs) are characterized by the fact that the insertion site on the skin and site of ultimate venipuncture are physically separated (Figure 1E). Tunneling limits bacterial entry from the extraluminal aspect of the CVAD to the bloodstream. For example, internal jugular veins are often ideal sites of puncture but inappropriate sites for catheter placement, as providing care to this area is challenging and may increase risk of infection.[34] Tunneling to the infraclavicular area provides a better option, as it provides an exit site that can be adequately cared for. Importantly, any CVAD (PICCs or CICCs) can be tunneled. Additionally, tunneled CICCs may be used in patients with chronic or impending renal failure where PICCs are contraindicated because entry into dialysis‐relevant vessels is to be avoided.[48] Such devices also allow regular blood sampling in patients who require frequent testing but have limited peripheral access, such as those with hematological malignancies. Additionally, tunneled catheters are more comfortable for patients and viewed as being more socially acceptable than nontunneled devices. However, the more invasive and permanent nature of these devices often requires deliberation prior to insertion.
Of note, tunneled devices and ports may be used as long‐term (>3 months to years) VADs. As our focus in this review is short‐term devices, we will not expand the discussion of these devices as they are almost always used for prolonged durations.[7]
OPERATIONALIZING THE DATA: AN ALGORITHMIC APPROACH TO VENOUS ACCESS
Hospitalists should consider approaching venous access using an algorithm based on a number of parameters. For example, a critically ill patient who requires vasopressor support and hemodynamic monitoring will need a CICC or a PICC. Given the potential greater risk of thromboses from PICCs, a CICC is preferable for critically ill patients provided an experienced inserter is available. Conversely, patients who require short‐term (710 days) venous access for infusion of nonirritant or nonvesicant therapy often only require a PIV. In patients with poor or difficult venous access, USGPIVs or midlines may be ideal and preferred over short PIVs. Finally, patients who require longer‐term or home‐based treatment may benefit from early placement of a midline or a PICC, depending again on the nature of the infusion, duration of treatment, and available venous access sites.
An algorithmic approach considering these parameters is suggested in Figure 2, and a brief overview of the devices and their considerations is shown in Table 3.
| Vascular Access Device | Central/Peripheral | Anatomical Location of Placement | Desired Duration of Placement | Common Uses | BSI Risk (Per 1,000 Catheter‐Days) | Thrombosis Risk | Important Considerations |
|---|---|---|---|---|---|---|---|
| |||||||
| Small peripheral IV | Peripheral | Peripheral veins, usually forearm | 710 days | Fluid resuscitation, most medications, blood products | 0.06[8] | Virtually no risk | Consider necessity of PIV daily and remove unnecessary devices |
| Midline | Peripheral | Inserted around antecubital fossa, reside within basilic or cephalic vein of the arm | 24 weeks | Long‐term medications excluding TPN, vesicants, corrosives | 0.30.8[17] | Insufficient data | Can be used as bridge devices for patients to complete short‐term antibiotics/emnfusions as an outpatient |
| Peripherally inserted central catheter | Central | Inserted into peripheral arm vein and advanced to larger veins (eg, internal jugular or subclavian) to the CAJ | >1 week, 3 months | Large variety of infusates, including TPN, vesicants, corrosives | 2.4[44] | 6.30% | Contraindicated in patients with CKD stage IIIb or higher |
| Centrally inserted central catheters | Central | Inserted above (internal jugular vein, brachiocephalic vein, subclavian vein), or below the clavicle (axillary vein) | >1 week, 3 months | Same infusate variety as PICC, measurement of central venous pressures, common in trauma/emergent settings | 2.3[44] | 1.30% | Given lower rates of DVT than PICC, preferred in ICU and hypercoagulable environments |
| Tunneled CICCs | Central | Placed percutaneously in any large vein in the arm, chest, neck or groin | >3 months to years | Central infusates, as in any CVAD; used for patients with CKD stage IIIb or greater when a PICC is indicated | Insufficient data | Insufficient data | May be superior when insertion site and puncture site are not congruent and may increase risk of infection |
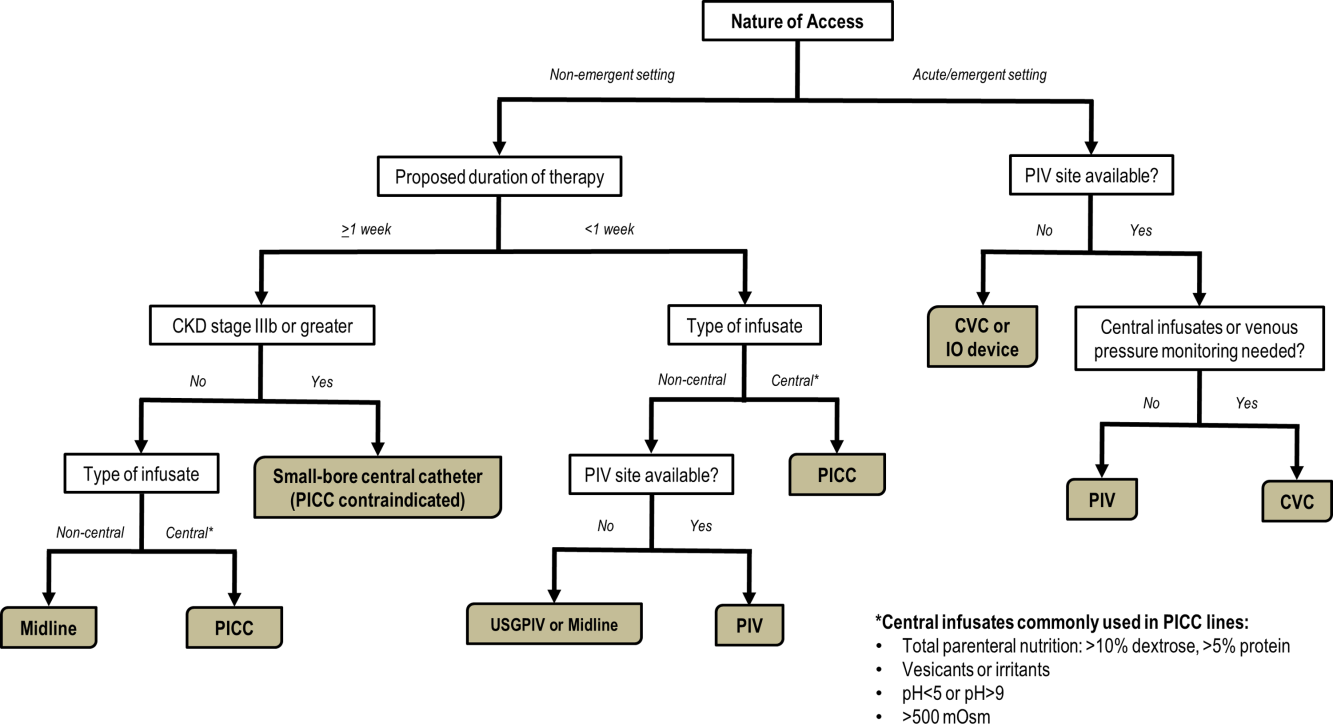
CONCLUSIONS
With strides in technology and progress in medicine, hospitalists have access to an array of options for venous access. However, every VAD has limitations that can be easily overlooked in a perfunctory decision‐making process. The data presented in this review thus provide a first step to improving safety in this evolving science. Studies that further determine appropriateness of VADs in hospitalized settings are necessary. Only through such progressive scientific enquiry will complication‐free venous access be realized.
Disclosure
Nothing to report.
- , . The need for comparative data in vascular access: the rationale and design of the PICC registry. J Vasc Access. 2013; 18(4): 219–224.
- , , , et al. Hospitalist experiences, practice, opinions, and knowledge regarding peripherally inserted central catheters: a Michigan survey. J Hosp Med. 2013; 8(6): 309–314.
- , , , . Clinically‐indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2013; 4: CD007798.
- , , , et al. Cost‐effectiveness analysis of clinically indicated versus routine replacement of peripheral intravenous catheters. Appl Health Econ Health Policy. 2014; 12(1): 51–58.
- Infusion Nurses Society. Infusion Nursing Standards of Practice. Norwood, MA; Infusion Nurses Society; 2011.
- , , , et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012; 380(9847): 1066–1074.
- , , , et al. epic3: national evidence‐based guidelines for preventing healthcare‐associated infections in NHS hospitals in England. J Hosp Infect. 2014; 86(suppl 1): S1–S70.
- . Short peripheral intravenous catheters and infections. J Infus Nurs. 2012; 35(4): 230–240.
- , , , et al. Phlebitis risk varies by peripheral venous catheter site and increases after 96 hours: a large multi‐centre prospective study. J Adv Nurs. 2014; 70(11): 2539–2549.
- , . Intravenous catheter complications in the hand and forearm. J Trauma. 2004; 56(1): 123–127.
- , , , . Vesicant extravasation part I: Mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum. 2006; 33(6): 1134–1141.
- , . Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung. 2005; 34(5): 345–359.
- , , . Ultrasound‐guided peripheral venous access: a systematic review of randomized‐controlled trials. Eur J Emerg Med. 2014; 21(1): 18–23.
- , , , et al. Difficult peripheral venous access: clinical evaluation of a catheter inserted with the Seldinger method under ultrasound guidance. J Crit Care. 2014; 29(5): 823–827.
- . Choosing the right intravenous catheter. Home Healthc Nurse. 2007; 25(8): 523–531; quiz 532–523.
- Adverse reactions associated with midline catheters—United States, 1992–1995. MMWR Morb Mortal Wkly Rep. 1996; 45(5): 101–103.
- , , . The risk of midline catheterization in hospitalized patients. A prospective study. Ann Intern Med. 1995; 123(11): 841–844.
- . Midline catheters: indications, complications and maintenance. Nurs Stand. 2007; 22(11): 48–57; quiz 58.
- , . Safe administration of vancomycin through a novel midline catheter: a randomized, prospective clinical trial. J Vasc Access. 2014; 15(4): 251–256.
- . Midline catheters: the middle ground of intravenous therapy administration. J Infus Nurs. 2004; 27(5): 313–321.
- . Vascular access in resuscitation: is there a role for the intraosseous route? Anesthesiology. 2014; 120(4): 1015–1031.
- , , , et al. A new system for sternal intraosseous infusion in adults. Prehosp Emerg Care. 2000; 4(2): 173–177.
- , , , , , . Comparison of two intraosseous access devices in adult patients under resuscitation in the emergency department: a prospective, randomized study. Resuscitation. 2010; 81(8): 994–999.
- , , , , . Comparison study of intraosseous, central intravenous, and peripheral intravenous infusions of emergency drugs. Am J Dis Child. 1990; 144(1): 112–117.
- , , , , . The safety of intraosseous infusions: risks of fat and bone marrow emboli to the lungs. Ann Emerg Med. 1989; 18(10): 1062–1067.
- , , , , . ESPEN guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009; 28(4): 365–377.
- , . Peripherally inserted central catheter use in the hospitalized patient: is there a role for the hospitalist? J Hosp Med. 2009; 4(6): E1–E4.
- Vital signs: central line‐associated blood stream infections—United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep. 2011; 60(8): 243–248.
- , , , . Hospital costs of central line‐associated bloodstream infections and cost‐effectiveness of closed vs. open infusion containers. The case of Intensive Care Units in Italy. Cost Eff Resour Alloc. 2010; 8: 8.
- , , . The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006; 81(9): 1159–1171.
- The Joint Commission. Preventing Central Line‐Associated Bloodstream Infections: A Global Challenge, a Global Perspective. Oak Brook, IL: Joint Commission Resources; 2012.
- , , , et al. Guidelines for the prevention of intravascular catheter‐related infections. Am J Infect Control. 2011; 39(4 suppl 1): S1–S34.
- , , , , . The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta‐analysis. Infect Control Hosp Epidemiol. 2013; 34(9): 908–918.
- Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, American Hospital Association, Association for Professionals in Infection Control and Epidemiology, The Joint Commission. Compendium of Strategies to Prevent Healthcare‐Associated Infections in Acute Care Hospitals: 2014 Updates. Available at: http://www.shea‐online.org. Accessed August 1, 2014.
- , , , , . Guidelines for venous access in patients with chronic kidney disease. A Position Statement from the American Society of Diagnostic and Interventional Nephrology, Clinical Practice Committee and the Association for Vascular Access. Semin Dial. 2008; 21(2): 186–191.
- , , , et al. Association between prior peripherally inserted central catheters and lack of functioning arteriovenous fistulas: a case‐control study in hemodialysis patients. Am J Kidney Dis. 2012; 60(4): 601–608.
- , , , et al. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol. 2012; 7(10): 1664–1672.
- , , , et al. Do physicians know which of their patients have central venous catheters? A multi‐center observational study. Ann Intern Med. 2014; 161(8): 562–567.
- , , , et al. Hospital‐wide survey of the use of central venous catheters. J Hosp Infect. 2011; 77(4): 304–308.
- , , , , , . Peripherally inserted central catheter‐related deep vein thrombosis: contemporary patterns and predictors. J Thromb Haemost. 2014; 12(6): 847–854.
- , , , . An in vitro study comparing a peripherally inserted central catheter to a conventional central venous catheter: no difference in static and dynamic pressure transmission. BMC Anesthesiol. 2010; 10: 18.
- , , , et al. Clinical experience with power‐injectable PICCs in intensive care patients. Crit Care. 2012; 16(1): R21.
- , , , et al. Nurse‐led central venous catheter insertion‐procedural characteristics and outcomes of three intensive care based catheter placement services. Int J Nurs Stud. 2012; 49(2): 162–168.
- , , , et al. Peripherally inserted central venous catheters in the acute care setting: a safe alternative to high‐risk short‐term central venous catheters. Am J Infect Control. 2010; 38(2): 149–153.
- , , , et al. Which central venous catheters have the highest rate of catheter‐associated deep venous thrombosis: a prospective analysis of 2,128 catheter days in the surgical intensive care unit. J Trauma Acute Care Surg. 2013; 74(2): 454–460; discussion 461–452.
- , , , et al. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta‐analysis. Lancet. 2013; 382(9889): 311–325.
- , , , , . Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015; 1: CD011447.
- , , , et al. Tunneled jugular small‐bore central catheters as an alternative to peripherally inserted central catheters for intermediate‐term venous access in patients with hemodialysis and chronic renal insufficiency. Radiology. 1999; 213(1): 303–306.
- , . The need for comparative data in vascular access: the rationale and design of the PICC registry. J Vasc Access. 2013; 18(4): 219–224.
- , , , et al. Hospitalist experiences, practice, opinions, and knowledge regarding peripherally inserted central catheters: a Michigan survey. J Hosp Med. 2013; 8(6): 309–314.
- , , , . Clinically‐indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2013; 4: CD007798.
- , , , et al. Cost‐effectiveness analysis of clinically indicated versus routine replacement of peripheral intravenous catheters. Appl Health Econ Health Policy. 2014; 12(1): 51–58.
- Infusion Nurses Society. Infusion Nursing Standards of Practice. Norwood, MA; Infusion Nurses Society; 2011.
- , , , et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012; 380(9847): 1066–1074.
- , , , et al. epic3: national evidence‐based guidelines for preventing healthcare‐associated infections in NHS hospitals in England. J Hosp Infect. 2014; 86(suppl 1): S1–S70.
- . Short peripheral intravenous catheters and infections. J Infus Nurs. 2012; 35(4): 230–240.
- , , , et al. Phlebitis risk varies by peripheral venous catheter site and increases after 96 hours: a large multi‐centre prospective study. J Adv Nurs. 2014; 70(11): 2539–2549.
- , . Intravenous catheter complications in the hand and forearm. J Trauma. 2004; 56(1): 123–127.
- , , , . Vesicant extravasation part I: Mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum. 2006; 33(6): 1134–1141.
- , . Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung. 2005; 34(5): 345–359.
- , , . Ultrasound‐guided peripheral venous access: a systematic review of randomized‐controlled trials. Eur J Emerg Med. 2014; 21(1): 18–23.
- , , , et al. Difficult peripheral venous access: clinical evaluation of a catheter inserted with the Seldinger method under ultrasound guidance. J Crit Care. 2014; 29(5): 823–827.
- . Choosing the right intravenous catheter. Home Healthc Nurse. 2007; 25(8): 523–531; quiz 532–523.
- Adverse reactions associated with midline catheters—United States, 1992–1995. MMWR Morb Mortal Wkly Rep. 1996; 45(5): 101–103.
- , , . The risk of midline catheterization in hospitalized patients. A prospective study. Ann Intern Med. 1995; 123(11): 841–844.
- . Midline catheters: indications, complications and maintenance. Nurs Stand. 2007; 22(11): 48–57; quiz 58.
- , . Safe administration of vancomycin through a novel midline catheter: a randomized, prospective clinical trial. J Vasc Access. 2014; 15(4): 251–256.
- . Midline catheters: the middle ground of intravenous therapy administration. J Infus Nurs. 2004; 27(5): 313–321.
- . Vascular access in resuscitation: is there a role for the intraosseous route? Anesthesiology. 2014; 120(4): 1015–1031.
- , , , et al. A new system for sternal intraosseous infusion in adults. Prehosp Emerg Care. 2000; 4(2): 173–177.
- , , , , , . Comparison of two intraosseous access devices in adult patients under resuscitation in the emergency department: a prospective, randomized study. Resuscitation. 2010; 81(8): 994–999.
- , , , , . Comparison study of intraosseous, central intravenous, and peripheral intravenous infusions of emergency drugs. Am J Dis Child. 1990; 144(1): 112–117.
- , , , , . The safety of intraosseous infusions: risks of fat and bone marrow emboli to the lungs. Ann Emerg Med. 1989; 18(10): 1062–1067.
- , , , , . ESPEN guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009; 28(4): 365–377.
- , . Peripherally inserted central catheter use in the hospitalized patient: is there a role for the hospitalist? J Hosp Med. 2009; 4(6): E1–E4.
- Vital signs: central line‐associated blood stream infections—United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep. 2011; 60(8): 243–248.
- , , , . Hospital costs of central line‐associated bloodstream infections and cost‐effectiveness of closed vs. open infusion containers. The case of Intensive Care Units in Italy. Cost Eff Resour Alloc. 2010; 8: 8.
- , , . The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006; 81(9): 1159–1171.
- The Joint Commission. Preventing Central Line‐Associated Bloodstream Infections: A Global Challenge, a Global Perspective. Oak Brook, IL: Joint Commission Resources; 2012.
- , , , et al. Guidelines for the prevention of intravascular catheter‐related infections. Am J Infect Control. 2011; 39(4 suppl 1): S1–S34.
- , , , , . The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta‐analysis. Infect Control Hosp Epidemiol. 2013; 34(9): 908–918.
- Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, American Hospital Association, Association for Professionals in Infection Control and Epidemiology, The Joint Commission. Compendium of Strategies to Prevent Healthcare‐Associated Infections in Acute Care Hospitals: 2014 Updates. Available at: http://www.shea‐online.org. Accessed August 1, 2014.
- , , , , . Guidelines for venous access in patients with chronic kidney disease. A Position Statement from the American Society of Diagnostic and Interventional Nephrology, Clinical Practice Committee and the Association for Vascular Access. Semin Dial. 2008; 21(2): 186–191.
- , , , et al. Association between prior peripherally inserted central catheters and lack of functioning arteriovenous fistulas: a case‐control study in hemodialysis patients. Am J Kidney Dis. 2012; 60(4): 601–608.
- , , , et al. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol. 2012; 7(10): 1664–1672.
- , , , et al. Do physicians know which of their patients have central venous catheters? A multi‐center observational study. Ann Intern Med. 2014; 161(8): 562–567.
- , , , et al. Hospital‐wide survey of the use of central venous catheters. J Hosp Infect. 2011; 77(4): 304–308.
- , , , , , . Peripherally inserted central catheter‐related deep vein thrombosis: contemporary patterns and predictors. J Thromb Haemost. 2014; 12(6): 847–854.
- , , , . An in vitro study comparing a peripherally inserted central catheter to a conventional central venous catheter: no difference in static and dynamic pressure transmission. BMC Anesthesiol. 2010; 10: 18.
- , , , et al. Clinical experience with power‐injectable PICCs in intensive care patients. Crit Care. 2012; 16(1): R21.
- , , , et al. Nurse‐led central venous catheter insertion‐procedural characteristics and outcomes of three intensive care based catheter placement services. Int J Nurs Stud. 2012; 49(2): 162–168.
- , , , et al. Peripherally inserted central venous catheters in the acute care setting: a safe alternative to high‐risk short‐term central venous catheters. Am J Infect Control. 2010; 38(2): 149–153.
- , , , et al. Which central venous catheters have the highest rate of catheter‐associated deep venous thrombosis: a prospective analysis of 2,128 catheter days in the surgical intensive care unit. J Trauma Acute Care Surg. 2013; 74(2): 454–460; discussion 461–452.
- , , , et al. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta‐analysis. Lancet. 2013; 382(9889): 311–325.
- , , , , . Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015; 1: CD011447.
- , , , et al. Tunneled jugular small‐bore central catheters as an alternative to peripherally inserted central catheters for intermediate‐term venous access in patients with hemodialysis and chronic renal insufficiency. Radiology. 1999; 213(1): 303–306.
Early Career Pediatric Hospitalists
Pediatric hospital medicine (PHM) has established itself as a well‐defined field of pediatrics dedicated to improving the care of hospitalized children.[1] In 2010, the PHM core competencies were established to identify a specific knowledge base and skill set needed to provide the highest quality care for hospitalized children.[2] With these competencies, many are re‐evaluating training needs, particularly given the rapid advancement of the field.[1, 3] Previous workforce evaluations estimated that less than half of hospitalists surveyed had any specific hospitalist training.[4] In 2004 and 2008, studies of the current roles and training needs of pediatric hospitalists revealed advanced training needs in administration, research, quality improvement (QI), and education.[5, 6] Currently, there are 27 US PHM fellowship programs, but the majority of hospitalists are entering the field without PHM‐specific training. There is little evidence regarding our current residency and fellowship training models' abilities to help participants achieve proficiency in the PHM core competencies.
The objectives of this study were to compare the perceived PHM core competency achievements of fellowship and non‐fellowship‐trained early career pediatric hospitalists and identify perceived knowledge gaps in our current training models.
METHODS
Study Design
An anonymous Web‐based survey was conducted in November 2013. The survey was electronically distributed to the American Academy of Pediatrics (AAP) Section on Hospital Medicine (SOHM) Listserv, current PHM fellows present at the annual PHM Fellows Conference, as well as PHM division directors and fellowship directors to distribute to eligible hospitalists. The AAP SOHM Listserv functions as a convenience sample, representing the single largest listing of pediatric hospitalists, currently with over 2100 subscribers (email communication with Nicole Alexander, AAP Manager of the Division of Hospital and Surgical Services). An email announcing the survey was distributed to the aforementioned parties with 1 reminder email sent to the SOHM Listserv encouraging participation.
Inclusion criteria were current practicing hospitalists who had graduated from a US Accreditation Council for Graduate Medical Education‐approved residency program within the last 5 years. Recruiting individuals within 5 years of residency graduation was chosen in an effort to capture the experience of our current training models. Practicing hospitalists included current PHM fellows, PHM fellowship graduates (both defined as fellowship‐trained), and non‐fellowship‐trained individuals.
Survey Development
The survey obtained demographic data including type of residency training, chief residency, postresidency training, advanced degrees, practice environment, and professional positions. Competency was self‐assessed using an interactive sliding scale where participants could indicate their perceived competency by placing the cursor along a continuum with the anchors novice, competent, and expert. Each anchor was defined as follows: novice is the inability to perform the skill or require supervision/assistance to complete the activity; competent is the ability to perform unsupervised execution of a task, not requiring substantial mastery or advanced ability; and expert is demonstrating initiative and adaptability to special problem situations and can lead others in performing the skill.[7] Cursor position along the sliding scale was converted by the survey tool to a value from 0 to 100 for data analysis. Within each group, a mean score below 50 was considered an area respondents perceived themselves less than competent. Select PHM core competencies were chosen in consultation with the authors of the PHM core competencies to provide a representative sample from each of the 4 domains (Table 1) as well as restrict the survey to a reasonable length. The survey was pilot tested in small groups and revised for content and readability based on the feedback received.
| Clinical Diagnosis | Core Skills | Specialized Clinical Skills | Healthcare Systems |
|---|---|---|---|
| |||
| Abdominal pain | Bladder catheterization | Child abuse* | Advocacy* |
| ALTE | ECG interpretation | Hospice and palliative care | Business practice* |
| Asthma | Feeding tubes | Leading healthcare team* | Communication |
| Bone and joint infection | Fluid/electrolytes | Newborn care* | Quality improvement* |
| Bronchiolitis | IV access/ phlebotomy* | Technology‐dependent children* | Cost‐effective care* |
| CNS infections | Lumbar puncture* | Transport of the critically ill | Education* |
| Diabetes | Noninvasive monitoring | Evidence‐based medicine* | |
| Failure to thrive | Nutrition* | Health information systems | |
| Fever unknown origin | Oxygen delivery and airway management | Legal, risk management | |
| Gastroenteritis | Pain management* | Patient safety* | |
| Kawasaki disease | PALS | Research* | |
| Neonatal fever | Procedural sedation* | Transitions of care* | |
| Neonatal jaundice | Radiographic interpretation | ||
| Pneumonia | |||
| Respiratory failure | |||
| Seizures | |||
| Shock | |||
| Sickle cell disease | |||
| Skin and soft tissue infection | |||
| Upper airway infections | |||
| UTI | |||
| Single summative question included in the survey. | |||
Data Collection
Study data were collected and managed using the Research Electronic Data Capture (REDcap) tool hosted at Children's National Health System. REDcap is a secure, Web‐based application designed to support data capture for research studies.[8]
Data Analysis
Analysis was performed using SPSS version 22 (IBM, Armonk, NY). Demographic data comparing fellowship‐trained and non‐fellowship‐trained individuals were analyzed by [2] testing for categorical variables. Mean competency values between non‐fellows and those who have completed or are in the process of completing fellowship were analyzed using multiprobit regression. Values were adjusted for years since residency graduation (regardless of whether the individual was a current fellow, a fellowship graduate, or non‐fellowship‐trained), type of residency, and chief residency. P values were calculated based on the estimate and standard error of the slope term within the probit model. The effect of fellowship was qualitatively analyzed by comparing the values between the groups at different years since residency graduation. Incomplete data were excluded only for responses missing.
Institutional review board approval was obtained from Children's National Medical Center in Washington, DC.
RESULTS
One hundred ninety‐seven pediatric hospitalists responded to the survey. All were included in the analysis. One hundred forty‐seven respondents were non‐fellowship‐trained and 50 were PHM fellowship graduates or current PHM fellows. Demographic characteristics are listed in Table 2. Current and former PHM fellows were on average 2.1 years from residency graduation, whereas non‐fellowship‐trained hospitalists were 2.6 years from residency graduation (P=0.05). A significantly higher proportion of fellowship‐trained hospitalists reported working at a university‐affiliated free‐standing children's hospital, whereas a higher proportion of non‐fellowship‐trained hospitalists reported working at a non‐university‐affiliated community hospital. The majority of practice domains included hospitalists worked were similar between the 2 groups. A significantly higher proportion of fellowship‐trained hospitalists reported working in research and QI/safety. Surgical comanagement and newborn nursery were domains a significantly higher proportion of non‐fellowship‐trained hospitalists reported working.
| Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value | |
|---|---|---|---|
| |||
| Average years experience (since residency graduation) | 2.1 | 2.6 | 0.05 |
| Type of residency | 0.82 | ||
| Pediatric | 48 (96%) | 140 (95%) | |
| Medicine‐pediatric | 2 (4%) | 7 (5%) | |
| Family medicine | 0 | 0 | |
| Chief residency | 17 (34%) | 37 (25%) | 0.23 |
| Advanced degree obtained | 0.12 | ||
| Master's Public Health | 2 (4%) | 8 (5.5%) | |
| Master's of Education | 0 | 1 (0.7%) | |
| Master's Clinical and Translational Research | 1 (2%) | 0 | |
| Master's Business Administration | 1 (2%) | 0 | |
| PhD | 0 | 1 (0.7%) | |
| Other | 3 (6%) | 8 (5.5%) | |
| Currently pursuing | 14 (28%) | 6 (4.1%) | |
| Practice environment | |||
| University‐affiliated free‐standing children's hospital | 40 (80%) | 68 (46.3%) | <0.001 |
| University‐affiliated pediatric ward | 7 (14%) | 37 (25.2%) | 0.1 |
| University‐affiliated community hospital | 2 (4%) | 25 (17%) | 0.02 |
| Non‐university affiliated community hospital | 2 (4%) | 35 (23.8%) | 0.002 |
| Practice domain | |||
| General pediatrics inpatient unit | 49/49 (100%) | 139/143 (97.2%) | 0.24 |
| Subspecialty wards | 19/46 (41.3%) | 47/130 (36.1%) | 0.54 |
| Surgical comanagement | 36/46 (78.3%) | 119/133 (89.5%) | 0.05 |
| NICU | 8/47 (17.0%) | 36/128 (28.1%) | 0.13 |
| PICU | 11/47 (17.0%) | 16/126 (12.0%) | 0.08 |
| Intermediate care unit | 17/47 (36.2%) | 36/128 (28.1%) | 0.09 |
| ED | 16/47 (34.0%) | 55/128 (43.0%) | 0.42 |
| Newborn nursery | 11/45 (24.4%) | 68/132 (51.5%) | 0.002 |
| Sedation | 20/48 (41.7%) | 48/133 (36.1%) | 0.49 |
| Medical education | 47/48 (97.9%) | 123/137 (89.8%) | 0.08 |
| Hospital committee work | 42/48 (87.5%) | 109/138 (79.0%) | 0.3 |
| Research | 44/49 (90.0%) | 72/137 (52.6%) | <0.001 |
| Quality improvement/safety | 44/48 (91.7%) | 103/134 (76.9%) | 0.003 |
| Advocacy | 23/47 (47.9%) | 49/128 (38.2%) | 0.19 |
The adjusted mean perceived competency scores for fellowship and non‐fellowship‐trained hospitalists are shown in Table 3. Reported competency scores for management of common acute inpatient medical conditions in an otherwise healthy child were similar between the 2 groups. Both fellowship and non‐fellowship‐trained hospitalists reported feeling less than competent (scores <50) in sedation, understanding basic components of PHM business practice, and defining a relative value unit. Fellowship‐trained hospitalists indicated perceived competency (scores >50) in the remainder of the competencies surveyed. Non‐fellowship‐trained hospitalists additionally had average scores <50 with statistically significant lower reported competency scores than fellowship‐trained hospitalists in IV access/phlebotomy, managing emergencies in technology‐dependent children, performing Plan‐Do‐Study‐Act (PDSA) cycles to achieve QI, performing root‐cause analysis (RCA), defining basic statistical terms, and identifying resources required to conduct research. Non‐fellowship‐trained hospitalists reported statistically significant higher mean competency scores in pain management, newborn care, and transitions in care. In each of these competencies, though, mean scores for both groups were in the competent range.
| Core Competency | Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value |
|---|---|---|---|
| |||
| Common diagnoses | 78.4 | 78.6 | 0.717 |
| Core skills | |||
| IV access/phlebotomy | 52.9 | 30.6 | 0.012 |
| Lumbar puncture | 76.2 | 77.0 | 0.245 |
| Sedation | 30.9 | 28.3 | 0.001 |
| Pain management | 70.7 | 72.6 | 0.014 |
| Nutrition | 68.0 | 66.1 | 0.026 |
| Specialized clinical skills | |||
| Leading a health care team | |||
| Team leadership | 74.9 | 72.0 | <0.001 |
| FCR | 75.3 | 72.6 | <0.001 |
| Technology‐dependent patient | |||
| General management | 71.4 | 65.9 | <0.001 |
| Emergencies | 53.2 | 49.4 | <0.001 |
| Newborn care | 56.6 | 61.6 | <0.001 |
| Child abuse | |||
| Diagnosing | 68.6 | 68.7 | 0.925 |
| Reporting | 68.9 | 68.5 | 0.630 |
| Healthcare systems | |||
| Transitions in care | 77.4 | 79.6 | 0.002 |
| Advocacy | 57.4 | 53.5 | <0.001 |
| Business practice | |||
| Basic components | 36.4 | 32.0 | <0.001 |
| Concept of RVU | 30.2 | 30.2 | 0.972 |
| Billing/coding | 61.4 | 63.9 | 0.004 |
| Quality Improvement | |||
| PDSA cycles | 63.7 | 42.8 | <0.001 |
| Best practice guidelines | 64.7 | 51.8 | <0.001 |
| Safety | |||
| Identify and address harm | 65.9 | 59.1 | <0.001 |
| Perform RCA | 56.7 | 36.0 | <0.001 |
| Cost‐effective care | 58.4 | 51.6 | <0.001 |
| Medical education | |||
| Needs assessment | 69.4 | 65.6 | <0.001 |
| Large group teaching | 67.6 | 60.6 | <0.001 |
| Small group teaching | 74.2 | 72.6 | 0.040 |
| Feedback | 73.8 | 68.9 | <0.001 |
| Evidence‐based medicine | |||
| Literature search | 75.9 | 69.0 | <0.001 |
| Literature appraisal | 63.4 | 57.2 | <0.001 |
| Apply study results | 70.2 | 64.8 | <0.001 |
| Research | |||
| Comparing study design | 62.6 | 54.1 | <0.001 |
| Basic statistics | 57.2 | 41.7 | <0.001 |
| Identifying resources | 56.0 | 36.1 | <0.001 |
The mean adjusted competency scores in areas with some of the largest differences between the 2 groups were plotted by time since residency graduation and depicted in Figure 1. This does not represent a single cohort of hospitalists over time, rather individual hospitalists at different post‐graduate years from their residency graduation. In performing PDSA cycles, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean score indicating competency (57.3), whereas only non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation reported a mean score approaching competency (49.1) (Figure 1A). For development of best practice guidelines, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean competency score (61.8), similar to non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation (60.8) (Figure 1B). Competency in performing RCA was reported by fellowship‐trained hospitalists 2 years postresidency (72.1), whereas non‐fellowship‐trained hospitalists up to 5 years post‐residency report a mean score below competency (Figure 1C). Regarding research competencies, fellowship‐trained hospitalists reported increased perceived competency at each year postresidency graduation, whereas non‐fellowship‐trained hospitalists reported lower mean competency scores with each year post‐residency (Figure 1D,E).
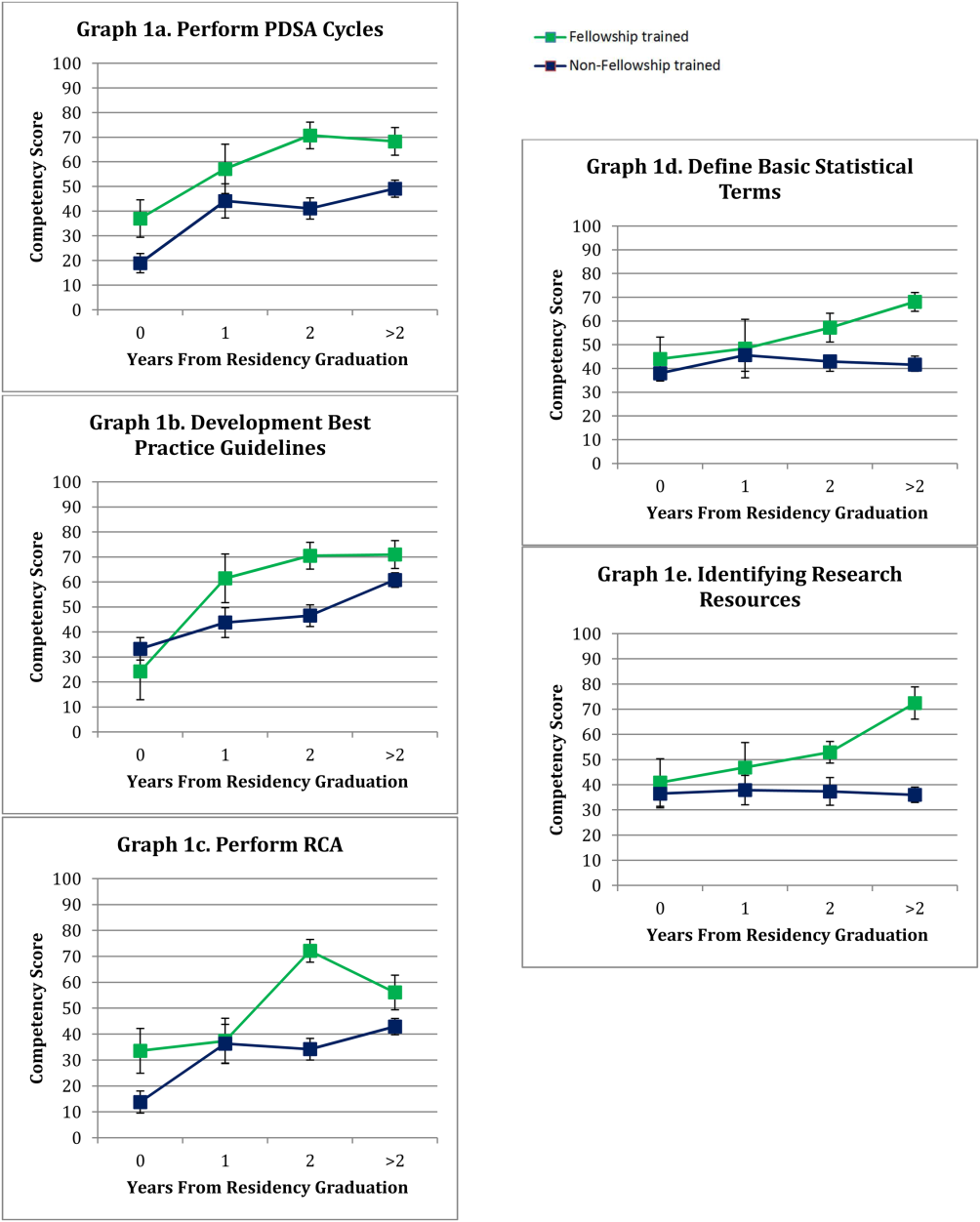
DISCUSSION
Our study results reveal significant differences in perceived competency between fellowship‐trained and non‐fellowship‐trained hospitalists, identifying several perceived knowledge gaps. Early career hospitalists, regardless of their training, perceive they have not achieved competency in sedation and aspects of PHM business practice. Early career hospitalists who did not pursue PHM fellowship training reported also feeling less than competent in intravenous access/phlebotomy, managing emergencies in technology‐dependent children, performing PDSA cycles to achieve QI, performing RCA, defining basic statistical terms, and identifying resources required to conduct research. Although both groups perceived themselves as competent in newborn care, pain management, and transitions in care, non‐fellowship‐trained hospitalists did report statistically significant higher competency scores compared to fellowship‐trained hospitalists in these skills.
Our findings support previous studies on the roles and training needs of pediatric hospitalists. In 2004, Ottolini et al. conducted a survey of pediatric hospitalists through Pediatric Research in Inpatient Settings, finding additional training needs in program/division management, practice guidelines, QI, safety, teaching, evidence‐based medicine (EBM), and research. The majority of hospitalists surveyed did not believe their pediatric residency training provided all of the skills necessary to practice as pediatric hospitalists.[5] Maniscalco et al. repeated the study in 2008 with similar findings.[6] In the field of adult internal medicine, Plauth et al. surveyed practicing hospitalists regarding the adequacy of their residency training, and found that systems issues (ie, QI, health economics, practice guidelines development) were reported as important to their current practice and not adequately emphasized in residency training.[9] Collectively, these findings highlight the need to critically evaluate our current training models' ability to prepare an individual for a career in hospital medicine. There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified,[1] but it is important to identify where the current knowledge gaps exist to optimize this process.
Not surprisingly, the majority of the hospitalists surveyed self‐reported competency in most of the clinical skills included. Residency training is heavily weighted toward acquisition of clinical skills, with a significant amount of time spent on inpatient clinical rotations.[10] The exception was sedation, which had some of the lowest mean perceived competency scores for all early career hospitalists surveyed. There is growing demand for safe and effective procedural sedation nationally, and pediatric hospitalists have been recognized as well poised to augment sedation services provided by anesthesiologists.[11, 12] This study demonstrates that current residency and PHM fellowship training may not adequately address this skill set to produce hospitalists prepared to take on this potential role.
Significant findings in the non‐clinical domains were the healthcare systems competencies. It is increasingly evident that a hospitalist's job description includes addressing communication, coordination of care, quality of care, and patient safety.[13] Yet, our findings indicate that non‐fellowship‐trained early career hospitalists do not feel competent in several of these aspects of hospital medicine practice. Our findings suggest that residency training alone may not provide adequate instruction for perceived competency, as no hospitalists with <1 year since residency graduation reported competency in PDSA cycles, best practice guidelines, and RCA. Interestingly, examining these competencies at different years following residency graduation, experience alone also does not ensure perceived competency early in one's career. Hospitalists are establishing themselves as a catalyst for change and the driving forces behind healthcare systems improvements within the hospital setting, often as our value added to an institution.[14, 15, 16, 17] Therefore, every pediatric hospitalist will need to acquire competency in these skills in a timely manner to effectively deliver high‐quality care to hospitalized children.
Finally, research was another area in which non‐fellowship‐trained hospitalists had low self‐perceived competency. When evaluating competency at different years postresidency graduation, non‐fellowship‐trained individuals appeared to lose a sense of competency each year, whereas fellowship‐trained hospitalists reported escalating competency with each year post‐residency. This finding may be due to the fellowship training itself, mentorship established in fellowship, or resources available in their chosen practice environment following fellowship. In 2011, Bekmezian et al. found that the majority of pediatric hospitalists wanted to conduct research but cited lack of dedicated time and mentorship as barriers to their productivity.[18] High‐quality studies including clinical, QI, and comparative effectiveness research are necessary to allow practicing hospitalists to make better decisions regarding patient care and to advance the field. This need transcends practice environment evidenced by the latest movement to transition away from the more traditional academic and non‐academic nomenclature. Even if one is not planning to conduct research, a basic foundation of research knowledge is required to critically appraise literature and apply EBM principles to clinical practice. This study suggests these skills are not being adequately obtained in residency for perceived competency or acquired with experience alone early in one's career.
There are several limitations of this study that should be considered. Most notably, the competency scores are based on self‐perceived assessments and therefore are not validated with objective measures of an individual's knowledge and skill, risking bias based on an individual's level of personal insight. We also did not quantify differences in training experience based on specific institutions, residency size, patient volume, and exposure to a hospitalist service, which could influence perceived competency and generalizability. Similarly, there is wide variation in current PHM fellowship curriculums, which is not accounted for in this study. Professional competency is challenging to define as well as measure.[19] Although this study is based on subjective measures, one can postulate that self‐perceived competency may impact an individual's approach to clinical practice, projects pursued, and career aspirations.
A second significant limitation was our inability to accurately determine a response rate. Other pediatric hospitalist surveys have faced similar limitations utilizing the AAP SOHM Listserv, because there is no centralized database of practicing hospitalists.[18, 20, 21] Attempts to collect workforce data from the American Board of Pediatrics (ABP) regarding estimates of the number of hospitalists within 5 years of their residency graduation revealed that they changed their data collection methods during our study period, therefore direct comparisons could not be made before and after 2012 (email communication with Cathy Koenig, Psychometric Data Analyst, ABP). Additionally, the AAP SOHM Listserv does not collect demographic data on subscribers, therefore we were unable to determine how many of the 2100 subscribers are within 5 years of their residency graduation. Nevertheless, it is the largest listserv of pediatric hospitalists and enabled us to attempt to collect data from the most representative population. PHM fellowship programs have also rapidly expanded, and only recently has there been a more centralized, comprehensive database of programs and fellows. With the available information, we could not accurately estimate a response rate. Despite the potential for response bias and small sample size, we feel the information collected is a valuable first look at important and timely data that can inform future studies.
Overall, this study provides important information regarding the perceived competency of early career pediatric hospitalists. Although different practice environments may afford different experiences and influence competency over time, we believe the majority of the PHM core competencies transcend practice environment and are ones all early career hospitalists should strive to achieve. To ensure the ongoing advancement of our field, we must guarantee that hospitalists are provided the resources and training to attain these competencies. This may include developing hospital medicine residency tracks, continuing medical education offerings, and/or PHM fellowships whose objectives are aligned with the established core competencies. Although this study was not designed to determine which of these options are optimal, the results can help identify the existing gaps to inform curriculum development in the future. As our field continues to evolve and advance, it will be important to continuously re‐evaluate our training programs' abilities to produce pediatric hospitalists with clinical, quality, scholarly, and leadership skills that meet our field's core competency standards.
CONCLUSIONS
Early career pediatric hospitalists report deficits in several of the PHM core competencies, which should be considered when designing PHM‐specific training in the future. PHM fellowship‐trained hospitalists report higher levels of self‐perceived competency in many core areas.
Disclosure: Nothing to report.
- , , , et al. Pediatric hospital medicine: a strategic planning roundtable to chart the future. J Hosp Med. 2012;7(4):329–334.
- , , , et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i–xv, 1–114.
- , . Pediatric hospital medicine and education: why we can't stand still. JAMA Pediatr. 2013;167(5):412–413.
- , , Research Advisory Committee of the American Board of Pediatrics. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179–186.
- , , , . PRIS Survey: pediatric hospitalist roles and training needs. Pediatr Res. 2004;55:360A.
- , , , , . Current roles and training needs of pediatric hospitalists: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. Paper presented at: Pediatric Academic Societies; 2008; Honolulu, HI.
- , , , . From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767.
- , , , , , . Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , , , . Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111(3):247–254.
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2012. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf. Accessed August 14, 2014.
- , . Pediatric sedation. Pediatr Clin North Am. 2014;61(4):703–717.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , , , et al. Guiding principles for pediatric hospital medicine programs. Pediatrics. 2013;132(4):782–786.
- , , , . Pediatric hospitalists: a systematic review of the literature. Pediatrics. 2006;117(5):1736–1744.
- , . Pediatric hospitalist systems versus traditional models of care: effect on quality and cost outcomes. J Hosp Med. 2012;7(4):350–357.
- . Pediatric hospital medicine: historical perspectives, inspired future. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):107–112.
- . Pediatric hospitalists working in community hospitals. Pediatr Clin North Am. 2014;61(4):681–691.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , . Defining and assessing professional competence. JAMA. 2002;287(2):226–235.
- , , . Transition of care: what Is the pediatric hospitalist's role? An exploratory survey of current attitudes. J Hosp Med. 2012;7(4):277–281.
- , , . Association between practice setting and pediatric hospitalist career satisfaction. Hosp Pediatr. 2013;3(3):285–291.
Pediatric hospital medicine (PHM) has established itself as a well‐defined field of pediatrics dedicated to improving the care of hospitalized children.[1] In 2010, the PHM core competencies were established to identify a specific knowledge base and skill set needed to provide the highest quality care for hospitalized children.[2] With these competencies, many are re‐evaluating training needs, particularly given the rapid advancement of the field.[1, 3] Previous workforce evaluations estimated that less than half of hospitalists surveyed had any specific hospitalist training.[4] In 2004 and 2008, studies of the current roles and training needs of pediatric hospitalists revealed advanced training needs in administration, research, quality improvement (QI), and education.[5, 6] Currently, there are 27 US PHM fellowship programs, but the majority of hospitalists are entering the field without PHM‐specific training. There is little evidence regarding our current residency and fellowship training models' abilities to help participants achieve proficiency in the PHM core competencies.
The objectives of this study were to compare the perceived PHM core competency achievements of fellowship and non‐fellowship‐trained early career pediatric hospitalists and identify perceived knowledge gaps in our current training models.
METHODS
Study Design
An anonymous Web‐based survey was conducted in November 2013. The survey was electronically distributed to the American Academy of Pediatrics (AAP) Section on Hospital Medicine (SOHM) Listserv, current PHM fellows present at the annual PHM Fellows Conference, as well as PHM division directors and fellowship directors to distribute to eligible hospitalists. The AAP SOHM Listserv functions as a convenience sample, representing the single largest listing of pediatric hospitalists, currently with over 2100 subscribers (email communication with Nicole Alexander, AAP Manager of the Division of Hospital and Surgical Services). An email announcing the survey was distributed to the aforementioned parties with 1 reminder email sent to the SOHM Listserv encouraging participation.
Inclusion criteria were current practicing hospitalists who had graduated from a US Accreditation Council for Graduate Medical Education‐approved residency program within the last 5 years. Recruiting individuals within 5 years of residency graduation was chosen in an effort to capture the experience of our current training models. Practicing hospitalists included current PHM fellows, PHM fellowship graduates (both defined as fellowship‐trained), and non‐fellowship‐trained individuals.
Survey Development
The survey obtained demographic data including type of residency training, chief residency, postresidency training, advanced degrees, practice environment, and professional positions. Competency was self‐assessed using an interactive sliding scale where participants could indicate their perceived competency by placing the cursor along a continuum with the anchors novice, competent, and expert. Each anchor was defined as follows: novice is the inability to perform the skill or require supervision/assistance to complete the activity; competent is the ability to perform unsupervised execution of a task, not requiring substantial mastery or advanced ability; and expert is demonstrating initiative and adaptability to special problem situations and can lead others in performing the skill.[7] Cursor position along the sliding scale was converted by the survey tool to a value from 0 to 100 for data analysis. Within each group, a mean score below 50 was considered an area respondents perceived themselves less than competent. Select PHM core competencies were chosen in consultation with the authors of the PHM core competencies to provide a representative sample from each of the 4 domains (Table 1) as well as restrict the survey to a reasonable length. The survey was pilot tested in small groups and revised for content and readability based on the feedback received.
| Clinical Diagnosis | Core Skills | Specialized Clinical Skills | Healthcare Systems |
|---|---|---|---|
| |||
| Abdominal pain | Bladder catheterization | Child abuse* | Advocacy* |
| ALTE | ECG interpretation | Hospice and palliative care | Business practice* |
| Asthma | Feeding tubes | Leading healthcare team* | Communication |
| Bone and joint infection | Fluid/electrolytes | Newborn care* | Quality improvement* |
| Bronchiolitis | IV access/ phlebotomy* | Technology‐dependent children* | Cost‐effective care* |
| CNS infections | Lumbar puncture* | Transport of the critically ill | Education* |
| Diabetes | Noninvasive monitoring | Evidence‐based medicine* | |
| Failure to thrive | Nutrition* | Health information systems | |
| Fever unknown origin | Oxygen delivery and airway management | Legal, risk management | |
| Gastroenteritis | Pain management* | Patient safety* | |
| Kawasaki disease | PALS | Research* | |
| Neonatal fever | Procedural sedation* | Transitions of care* | |
| Neonatal jaundice | Radiographic interpretation | ||
| Pneumonia | |||
| Respiratory failure | |||
| Seizures | |||
| Shock | |||
| Sickle cell disease | |||
| Skin and soft tissue infection | |||
| Upper airway infections | |||
| UTI | |||
| Single summative question included in the survey. | |||
Data Collection
Study data were collected and managed using the Research Electronic Data Capture (REDcap) tool hosted at Children's National Health System. REDcap is a secure, Web‐based application designed to support data capture for research studies.[8]
Data Analysis
Analysis was performed using SPSS version 22 (IBM, Armonk, NY). Demographic data comparing fellowship‐trained and non‐fellowship‐trained individuals were analyzed by [2] testing for categorical variables. Mean competency values between non‐fellows and those who have completed or are in the process of completing fellowship were analyzed using multiprobit regression. Values were adjusted for years since residency graduation (regardless of whether the individual was a current fellow, a fellowship graduate, or non‐fellowship‐trained), type of residency, and chief residency. P values were calculated based on the estimate and standard error of the slope term within the probit model. The effect of fellowship was qualitatively analyzed by comparing the values between the groups at different years since residency graduation. Incomplete data were excluded only for responses missing.
Institutional review board approval was obtained from Children's National Medical Center in Washington, DC.
RESULTS
One hundred ninety‐seven pediatric hospitalists responded to the survey. All were included in the analysis. One hundred forty‐seven respondents were non‐fellowship‐trained and 50 were PHM fellowship graduates or current PHM fellows. Demographic characteristics are listed in Table 2. Current and former PHM fellows were on average 2.1 years from residency graduation, whereas non‐fellowship‐trained hospitalists were 2.6 years from residency graduation (P=0.05). A significantly higher proportion of fellowship‐trained hospitalists reported working at a university‐affiliated free‐standing children's hospital, whereas a higher proportion of non‐fellowship‐trained hospitalists reported working at a non‐university‐affiliated community hospital. The majority of practice domains included hospitalists worked were similar between the 2 groups. A significantly higher proportion of fellowship‐trained hospitalists reported working in research and QI/safety. Surgical comanagement and newborn nursery were domains a significantly higher proportion of non‐fellowship‐trained hospitalists reported working.
| Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value | |
|---|---|---|---|
| |||
| Average years experience (since residency graduation) | 2.1 | 2.6 | 0.05 |
| Type of residency | 0.82 | ||
| Pediatric | 48 (96%) | 140 (95%) | |
| Medicine‐pediatric | 2 (4%) | 7 (5%) | |
| Family medicine | 0 | 0 | |
| Chief residency | 17 (34%) | 37 (25%) | 0.23 |
| Advanced degree obtained | 0.12 | ||
| Master's Public Health | 2 (4%) | 8 (5.5%) | |
| Master's of Education | 0 | 1 (0.7%) | |
| Master's Clinical and Translational Research | 1 (2%) | 0 | |
| Master's Business Administration | 1 (2%) | 0 | |
| PhD | 0 | 1 (0.7%) | |
| Other | 3 (6%) | 8 (5.5%) | |
| Currently pursuing | 14 (28%) | 6 (4.1%) | |
| Practice environment | |||
| University‐affiliated free‐standing children's hospital | 40 (80%) | 68 (46.3%) | <0.001 |
| University‐affiliated pediatric ward | 7 (14%) | 37 (25.2%) | 0.1 |
| University‐affiliated community hospital | 2 (4%) | 25 (17%) | 0.02 |
| Non‐university affiliated community hospital | 2 (4%) | 35 (23.8%) | 0.002 |
| Practice domain | |||
| General pediatrics inpatient unit | 49/49 (100%) | 139/143 (97.2%) | 0.24 |
| Subspecialty wards | 19/46 (41.3%) | 47/130 (36.1%) | 0.54 |
| Surgical comanagement | 36/46 (78.3%) | 119/133 (89.5%) | 0.05 |
| NICU | 8/47 (17.0%) | 36/128 (28.1%) | 0.13 |
| PICU | 11/47 (17.0%) | 16/126 (12.0%) | 0.08 |
| Intermediate care unit | 17/47 (36.2%) | 36/128 (28.1%) | 0.09 |
| ED | 16/47 (34.0%) | 55/128 (43.0%) | 0.42 |
| Newborn nursery | 11/45 (24.4%) | 68/132 (51.5%) | 0.002 |
| Sedation | 20/48 (41.7%) | 48/133 (36.1%) | 0.49 |
| Medical education | 47/48 (97.9%) | 123/137 (89.8%) | 0.08 |
| Hospital committee work | 42/48 (87.5%) | 109/138 (79.0%) | 0.3 |
| Research | 44/49 (90.0%) | 72/137 (52.6%) | <0.001 |
| Quality improvement/safety | 44/48 (91.7%) | 103/134 (76.9%) | 0.003 |
| Advocacy | 23/47 (47.9%) | 49/128 (38.2%) | 0.19 |
The adjusted mean perceived competency scores for fellowship and non‐fellowship‐trained hospitalists are shown in Table 3. Reported competency scores for management of common acute inpatient medical conditions in an otherwise healthy child were similar between the 2 groups. Both fellowship and non‐fellowship‐trained hospitalists reported feeling less than competent (scores <50) in sedation, understanding basic components of PHM business practice, and defining a relative value unit. Fellowship‐trained hospitalists indicated perceived competency (scores >50) in the remainder of the competencies surveyed. Non‐fellowship‐trained hospitalists additionally had average scores <50 with statistically significant lower reported competency scores than fellowship‐trained hospitalists in IV access/phlebotomy, managing emergencies in technology‐dependent children, performing Plan‐Do‐Study‐Act (PDSA) cycles to achieve QI, performing root‐cause analysis (RCA), defining basic statistical terms, and identifying resources required to conduct research. Non‐fellowship‐trained hospitalists reported statistically significant higher mean competency scores in pain management, newborn care, and transitions in care. In each of these competencies, though, mean scores for both groups were in the competent range.
| Core Competency | Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value |
|---|---|---|---|
| |||
| Common diagnoses | 78.4 | 78.6 | 0.717 |
| Core skills | |||
| IV access/phlebotomy | 52.9 | 30.6 | 0.012 |
| Lumbar puncture | 76.2 | 77.0 | 0.245 |
| Sedation | 30.9 | 28.3 | 0.001 |
| Pain management | 70.7 | 72.6 | 0.014 |
| Nutrition | 68.0 | 66.1 | 0.026 |
| Specialized clinical skills | |||
| Leading a health care team | |||
| Team leadership | 74.9 | 72.0 | <0.001 |
| FCR | 75.3 | 72.6 | <0.001 |
| Technology‐dependent patient | |||
| General management | 71.4 | 65.9 | <0.001 |
| Emergencies | 53.2 | 49.4 | <0.001 |
| Newborn care | 56.6 | 61.6 | <0.001 |
| Child abuse | |||
| Diagnosing | 68.6 | 68.7 | 0.925 |
| Reporting | 68.9 | 68.5 | 0.630 |
| Healthcare systems | |||
| Transitions in care | 77.4 | 79.6 | 0.002 |
| Advocacy | 57.4 | 53.5 | <0.001 |
| Business practice | |||
| Basic components | 36.4 | 32.0 | <0.001 |
| Concept of RVU | 30.2 | 30.2 | 0.972 |
| Billing/coding | 61.4 | 63.9 | 0.004 |
| Quality Improvement | |||
| PDSA cycles | 63.7 | 42.8 | <0.001 |
| Best practice guidelines | 64.7 | 51.8 | <0.001 |
| Safety | |||
| Identify and address harm | 65.9 | 59.1 | <0.001 |
| Perform RCA | 56.7 | 36.0 | <0.001 |
| Cost‐effective care | 58.4 | 51.6 | <0.001 |
| Medical education | |||
| Needs assessment | 69.4 | 65.6 | <0.001 |
| Large group teaching | 67.6 | 60.6 | <0.001 |
| Small group teaching | 74.2 | 72.6 | 0.040 |
| Feedback | 73.8 | 68.9 | <0.001 |
| Evidence‐based medicine | |||
| Literature search | 75.9 | 69.0 | <0.001 |
| Literature appraisal | 63.4 | 57.2 | <0.001 |
| Apply study results | 70.2 | 64.8 | <0.001 |
| Research | |||
| Comparing study design | 62.6 | 54.1 | <0.001 |
| Basic statistics | 57.2 | 41.7 | <0.001 |
| Identifying resources | 56.0 | 36.1 | <0.001 |
The mean adjusted competency scores in areas with some of the largest differences between the 2 groups were plotted by time since residency graduation and depicted in Figure 1. This does not represent a single cohort of hospitalists over time, rather individual hospitalists at different post‐graduate years from their residency graduation. In performing PDSA cycles, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean score indicating competency (57.3), whereas only non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation reported a mean score approaching competency (49.1) (Figure 1A). For development of best practice guidelines, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean competency score (61.8), similar to non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation (60.8) (Figure 1B). Competency in performing RCA was reported by fellowship‐trained hospitalists 2 years postresidency (72.1), whereas non‐fellowship‐trained hospitalists up to 5 years post‐residency report a mean score below competency (Figure 1C). Regarding research competencies, fellowship‐trained hospitalists reported increased perceived competency at each year postresidency graduation, whereas non‐fellowship‐trained hospitalists reported lower mean competency scores with each year post‐residency (Figure 1D,E).
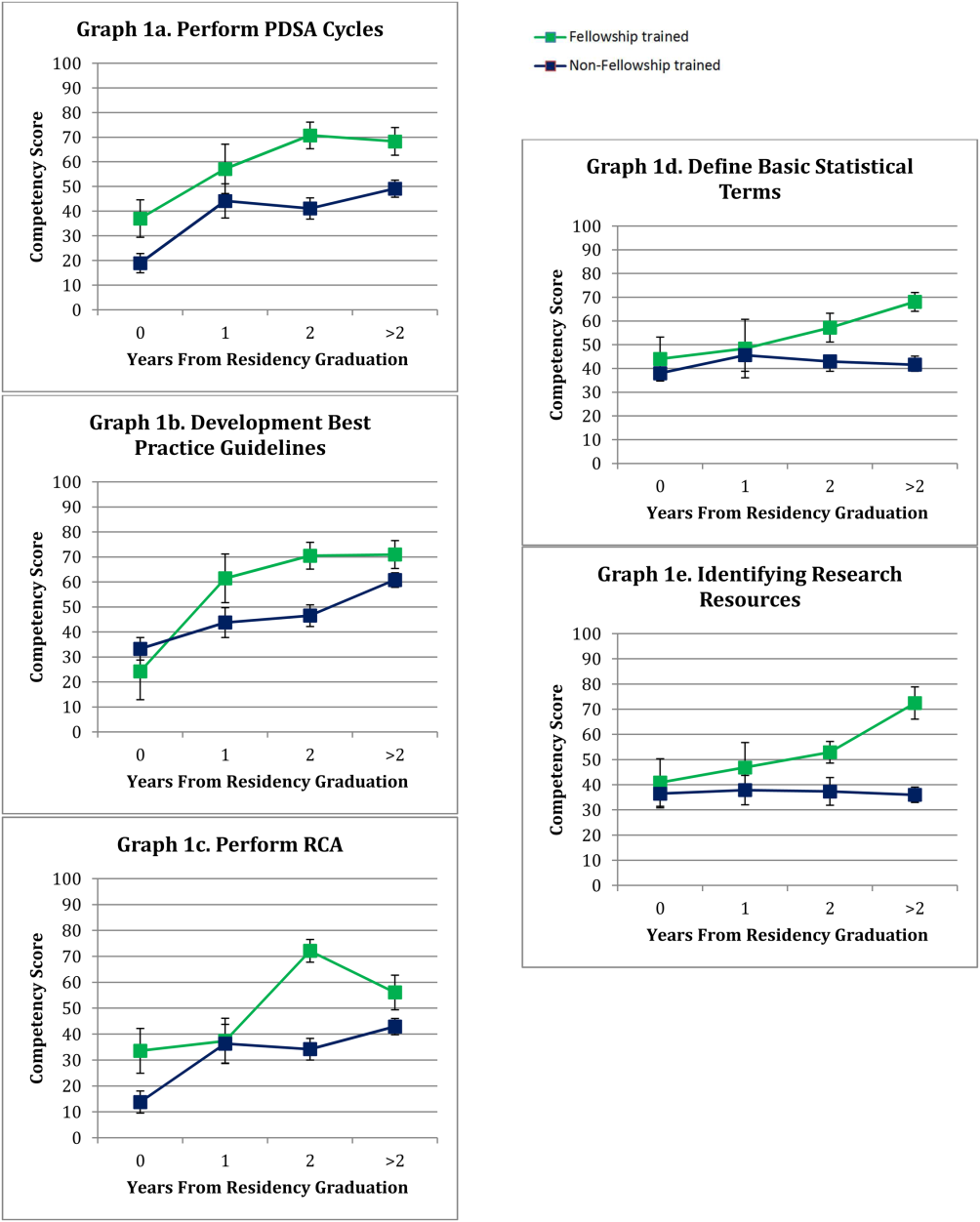
DISCUSSION
Our study results reveal significant differences in perceived competency between fellowship‐trained and non‐fellowship‐trained hospitalists, identifying several perceived knowledge gaps. Early career hospitalists, regardless of their training, perceive they have not achieved competency in sedation and aspects of PHM business practice. Early career hospitalists who did not pursue PHM fellowship training reported also feeling less than competent in intravenous access/phlebotomy, managing emergencies in technology‐dependent children, performing PDSA cycles to achieve QI, performing RCA, defining basic statistical terms, and identifying resources required to conduct research. Although both groups perceived themselves as competent in newborn care, pain management, and transitions in care, non‐fellowship‐trained hospitalists did report statistically significant higher competency scores compared to fellowship‐trained hospitalists in these skills.
Our findings support previous studies on the roles and training needs of pediatric hospitalists. In 2004, Ottolini et al. conducted a survey of pediatric hospitalists through Pediatric Research in Inpatient Settings, finding additional training needs in program/division management, practice guidelines, QI, safety, teaching, evidence‐based medicine (EBM), and research. The majority of hospitalists surveyed did not believe their pediatric residency training provided all of the skills necessary to practice as pediatric hospitalists.[5] Maniscalco et al. repeated the study in 2008 with similar findings.[6] In the field of adult internal medicine, Plauth et al. surveyed practicing hospitalists regarding the adequacy of their residency training, and found that systems issues (ie, QI, health economics, practice guidelines development) were reported as important to their current practice and not adequately emphasized in residency training.[9] Collectively, these findings highlight the need to critically evaluate our current training models' ability to prepare an individual for a career in hospital medicine. There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified,[1] but it is important to identify where the current knowledge gaps exist to optimize this process.
Not surprisingly, the majority of the hospitalists surveyed self‐reported competency in most of the clinical skills included. Residency training is heavily weighted toward acquisition of clinical skills, with a significant amount of time spent on inpatient clinical rotations.[10] The exception was sedation, which had some of the lowest mean perceived competency scores for all early career hospitalists surveyed. There is growing demand for safe and effective procedural sedation nationally, and pediatric hospitalists have been recognized as well poised to augment sedation services provided by anesthesiologists.[11, 12] This study demonstrates that current residency and PHM fellowship training may not adequately address this skill set to produce hospitalists prepared to take on this potential role.
Significant findings in the non‐clinical domains were the healthcare systems competencies. It is increasingly evident that a hospitalist's job description includes addressing communication, coordination of care, quality of care, and patient safety.[13] Yet, our findings indicate that non‐fellowship‐trained early career hospitalists do not feel competent in several of these aspects of hospital medicine practice. Our findings suggest that residency training alone may not provide adequate instruction for perceived competency, as no hospitalists with <1 year since residency graduation reported competency in PDSA cycles, best practice guidelines, and RCA. Interestingly, examining these competencies at different years following residency graduation, experience alone also does not ensure perceived competency early in one's career. Hospitalists are establishing themselves as a catalyst for change and the driving forces behind healthcare systems improvements within the hospital setting, often as our value added to an institution.[14, 15, 16, 17] Therefore, every pediatric hospitalist will need to acquire competency in these skills in a timely manner to effectively deliver high‐quality care to hospitalized children.
Finally, research was another area in which non‐fellowship‐trained hospitalists had low self‐perceived competency. When evaluating competency at different years postresidency graduation, non‐fellowship‐trained individuals appeared to lose a sense of competency each year, whereas fellowship‐trained hospitalists reported escalating competency with each year post‐residency. This finding may be due to the fellowship training itself, mentorship established in fellowship, or resources available in their chosen practice environment following fellowship. In 2011, Bekmezian et al. found that the majority of pediatric hospitalists wanted to conduct research but cited lack of dedicated time and mentorship as barriers to their productivity.[18] High‐quality studies including clinical, QI, and comparative effectiveness research are necessary to allow practicing hospitalists to make better decisions regarding patient care and to advance the field. This need transcends practice environment evidenced by the latest movement to transition away from the more traditional academic and non‐academic nomenclature. Even if one is not planning to conduct research, a basic foundation of research knowledge is required to critically appraise literature and apply EBM principles to clinical practice. This study suggests these skills are not being adequately obtained in residency for perceived competency or acquired with experience alone early in one's career.
There are several limitations of this study that should be considered. Most notably, the competency scores are based on self‐perceived assessments and therefore are not validated with objective measures of an individual's knowledge and skill, risking bias based on an individual's level of personal insight. We also did not quantify differences in training experience based on specific institutions, residency size, patient volume, and exposure to a hospitalist service, which could influence perceived competency and generalizability. Similarly, there is wide variation in current PHM fellowship curriculums, which is not accounted for in this study. Professional competency is challenging to define as well as measure.[19] Although this study is based on subjective measures, one can postulate that self‐perceived competency may impact an individual's approach to clinical practice, projects pursued, and career aspirations.
A second significant limitation was our inability to accurately determine a response rate. Other pediatric hospitalist surveys have faced similar limitations utilizing the AAP SOHM Listserv, because there is no centralized database of practicing hospitalists.[18, 20, 21] Attempts to collect workforce data from the American Board of Pediatrics (ABP) regarding estimates of the number of hospitalists within 5 years of their residency graduation revealed that they changed their data collection methods during our study period, therefore direct comparisons could not be made before and after 2012 (email communication with Cathy Koenig, Psychometric Data Analyst, ABP). Additionally, the AAP SOHM Listserv does not collect demographic data on subscribers, therefore we were unable to determine how many of the 2100 subscribers are within 5 years of their residency graduation. Nevertheless, it is the largest listserv of pediatric hospitalists and enabled us to attempt to collect data from the most representative population. PHM fellowship programs have also rapidly expanded, and only recently has there been a more centralized, comprehensive database of programs and fellows. With the available information, we could not accurately estimate a response rate. Despite the potential for response bias and small sample size, we feel the information collected is a valuable first look at important and timely data that can inform future studies.
Overall, this study provides important information regarding the perceived competency of early career pediatric hospitalists. Although different practice environments may afford different experiences and influence competency over time, we believe the majority of the PHM core competencies transcend practice environment and are ones all early career hospitalists should strive to achieve. To ensure the ongoing advancement of our field, we must guarantee that hospitalists are provided the resources and training to attain these competencies. This may include developing hospital medicine residency tracks, continuing medical education offerings, and/or PHM fellowships whose objectives are aligned with the established core competencies. Although this study was not designed to determine which of these options are optimal, the results can help identify the existing gaps to inform curriculum development in the future. As our field continues to evolve and advance, it will be important to continuously re‐evaluate our training programs' abilities to produce pediatric hospitalists with clinical, quality, scholarly, and leadership skills that meet our field's core competency standards.
CONCLUSIONS
Early career pediatric hospitalists report deficits in several of the PHM core competencies, which should be considered when designing PHM‐specific training in the future. PHM fellowship‐trained hospitalists report higher levels of self‐perceived competency in many core areas.
Disclosure: Nothing to report.
Pediatric hospital medicine (PHM) has established itself as a well‐defined field of pediatrics dedicated to improving the care of hospitalized children.[1] In 2010, the PHM core competencies were established to identify a specific knowledge base and skill set needed to provide the highest quality care for hospitalized children.[2] With these competencies, many are re‐evaluating training needs, particularly given the rapid advancement of the field.[1, 3] Previous workforce evaluations estimated that less than half of hospitalists surveyed had any specific hospitalist training.[4] In 2004 and 2008, studies of the current roles and training needs of pediatric hospitalists revealed advanced training needs in administration, research, quality improvement (QI), and education.[5, 6] Currently, there are 27 US PHM fellowship programs, but the majority of hospitalists are entering the field without PHM‐specific training. There is little evidence regarding our current residency and fellowship training models' abilities to help participants achieve proficiency in the PHM core competencies.
The objectives of this study were to compare the perceived PHM core competency achievements of fellowship and non‐fellowship‐trained early career pediatric hospitalists and identify perceived knowledge gaps in our current training models.
METHODS
Study Design
An anonymous Web‐based survey was conducted in November 2013. The survey was electronically distributed to the American Academy of Pediatrics (AAP) Section on Hospital Medicine (SOHM) Listserv, current PHM fellows present at the annual PHM Fellows Conference, as well as PHM division directors and fellowship directors to distribute to eligible hospitalists. The AAP SOHM Listserv functions as a convenience sample, representing the single largest listing of pediatric hospitalists, currently with over 2100 subscribers (email communication with Nicole Alexander, AAP Manager of the Division of Hospital and Surgical Services). An email announcing the survey was distributed to the aforementioned parties with 1 reminder email sent to the SOHM Listserv encouraging participation.
Inclusion criteria were current practicing hospitalists who had graduated from a US Accreditation Council for Graduate Medical Education‐approved residency program within the last 5 years. Recruiting individuals within 5 years of residency graduation was chosen in an effort to capture the experience of our current training models. Practicing hospitalists included current PHM fellows, PHM fellowship graduates (both defined as fellowship‐trained), and non‐fellowship‐trained individuals.
Survey Development
The survey obtained demographic data including type of residency training, chief residency, postresidency training, advanced degrees, practice environment, and professional positions. Competency was self‐assessed using an interactive sliding scale where participants could indicate their perceived competency by placing the cursor along a continuum with the anchors novice, competent, and expert. Each anchor was defined as follows: novice is the inability to perform the skill or require supervision/assistance to complete the activity; competent is the ability to perform unsupervised execution of a task, not requiring substantial mastery or advanced ability; and expert is demonstrating initiative and adaptability to special problem situations and can lead others in performing the skill.[7] Cursor position along the sliding scale was converted by the survey tool to a value from 0 to 100 for data analysis. Within each group, a mean score below 50 was considered an area respondents perceived themselves less than competent. Select PHM core competencies were chosen in consultation with the authors of the PHM core competencies to provide a representative sample from each of the 4 domains (Table 1) as well as restrict the survey to a reasonable length. The survey was pilot tested in small groups and revised for content and readability based on the feedback received.
| Clinical Diagnosis | Core Skills | Specialized Clinical Skills | Healthcare Systems |
|---|---|---|---|
| |||
| Abdominal pain | Bladder catheterization | Child abuse* | Advocacy* |
| ALTE | ECG interpretation | Hospice and palliative care | Business practice* |
| Asthma | Feeding tubes | Leading healthcare team* | Communication |
| Bone and joint infection | Fluid/electrolytes | Newborn care* | Quality improvement* |
| Bronchiolitis | IV access/ phlebotomy* | Technology‐dependent children* | Cost‐effective care* |
| CNS infections | Lumbar puncture* | Transport of the critically ill | Education* |
| Diabetes | Noninvasive monitoring | Evidence‐based medicine* | |
| Failure to thrive | Nutrition* | Health information systems | |
| Fever unknown origin | Oxygen delivery and airway management | Legal, risk management | |
| Gastroenteritis | Pain management* | Patient safety* | |
| Kawasaki disease | PALS | Research* | |
| Neonatal fever | Procedural sedation* | Transitions of care* | |
| Neonatal jaundice | Radiographic interpretation | ||
| Pneumonia | |||
| Respiratory failure | |||
| Seizures | |||
| Shock | |||
| Sickle cell disease | |||
| Skin and soft tissue infection | |||
| Upper airway infections | |||
| UTI | |||
| Single summative question included in the survey. | |||
Data Collection
Study data were collected and managed using the Research Electronic Data Capture (REDcap) tool hosted at Children's National Health System. REDcap is a secure, Web‐based application designed to support data capture for research studies.[8]
Data Analysis
Analysis was performed using SPSS version 22 (IBM, Armonk, NY). Demographic data comparing fellowship‐trained and non‐fellowship‐trained individuals were analyzed by [2] testing for categorical variables. Mean competency values between non‐fellows and those who have completed or are in the process of completing fellowship were analyzed using multiprobit regression. Values were adjusted for years since residency graduation (regardless of whether the individual was a current fellow, a fellowship graduate, or non‐fellowship‐trained), type of residency, and chief residency. P values were calculated based on the estimate and standard error of the slope term within the probit model. The effect of fellowship was qualitatively analyzed by comparing the values between the groups at different years since residency graduation. Incomplete data were excluded only for responses missing.
Institutional review board approval was obtained from Children's National Medical Center in Washington, DC.
RESULTS
One hundred ninety‐seven pediatric hospitalists responded to the survey. All were included in the analysis. One hundred forty‐seven respondents were non‐fellowship‐trained and 50 were PHM fellowship graduates or current PHM fellows. Demographic characteristics are listed in Table 2. Current and former PHM fellows were on average 2.1 years from residency graduation, whereas non‐fellowship‐trained hospitalists were 2.6 years from residency graduation (P=0.05). A significantly higher proportion of fellowship‐trained hospitalists reported working at a university‐affiliated free‐standing children's hospital, whereas a higher proportion of non‐fellowship‐trained hospitalists reported working at a non‐university‐affiliated community hospital. The majority of practice domains included hospitalists worked were similar between the 2 groups. A significantly higher proportion of fellowship‐trained hospitalists reported working in research and QI/safety. Surgical comanagement and newborn nursery were domains a significantly higher proportion of non‐fellowship‐trained hospitalists reported working.
| Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value | |
|---|---|---|---|
| |||
| Average years experience (since residency graduation) | 2.1 | 2.6 | 0.05 |
| Type of residency | 0.82 | ||
| Pediatric | 48 (96%) | 140 (95%) | |
| Medicine‐pediatric | 2 (4%) | 7 (5%) | |
| Family medicine | 0 | 0 | |
| Chief residency | 17 (34%) | 37 (25%) | 0.23 |
| Advanced degree obtained | 0.12 | ||
| Master's Public Health | 2 (4%) | 8 (5.5%) | |
| Master's of Education | 0 | 1 (0.7%) | |
| Master's Clinical and Translational Research | 1 (2%) | 0 | |
| Master's Business Administration | 1 (2%) | 0 | |
| PhD | 0 | 1 (0.7%) | |
| Other | 3 (6%) | 8 (5.5%) | |
| Currently pursuing | 14 (28%) | 6 (4.1%) | |
| Practice environment | |||
| University‐affiliated free‐standing children's hospital | 40 (80%) | 68 (46.3%) | <0.001 |
| University‐affiliated pediatric ward | 7 (14%) | 37 (25.2%) | 0.1 |
| University‐affiliated community hospital | 2 (4%) | 25 (17%) | 0.02 |
| Non‐university affiliated community hospital | 2 (4%) | 35 (23.8%) | 0.002 |
| Practice domain | |||
| General pediatrics inpatient unit | 49/49 (100%) | 139/143 (97.2%) | 0.24 |
| Subspecialty wards | 19/46 (41.3%) | 47/130 (36.1%) | 0.54 |
| Surgical comanagement | 36/46 (78.3%) | 119/133 (89.5%) | 0.05 |
| NICU | 8/47 (17.0%) | 36/128 (28.1%) | 0.13 |
| PICU | 11/47 (17.0%) | 16/126 (12.0%) | 0.08 |
| Intermediate care unit | 17/47 (36.2%) | 36/128 (28.1%) | 0.09 |
| ED | 16/47 (34.0%) | 55/128 (43.0%) | 0.42 |
| Newborn nursery | 11/45 (24.4%) | 68/132 (51.5%) | 0.002 |
| Sedation | 20/48 (41.7%) | 48/133 (36.1%) | 0.49 |
| Medical education | 47/48 (97.9%) | 123/137 (89.8%) | 0.08 |
| Hospital committee work | 42/48 (87.5%) | 109/138 (79.0%) | 0.3 |
| Research | 44/49 (90.0%) | 72/137 (52.6%) | <0.001 |
| Quality improvement/safety | 44/48 (91.7%) | 103/134 (76.9%) | 0.003 |
| Advocacy | 23/47 (47.9%) | 49/128 (38.2%) | 0.19 |
The adjusted mean perceived competency scores for fellowship and non‐fellowship‐trained hospitalists are shown in Table 3. Reported competency scores for management of common acute inpatient medical conditions in an otherwise healthy child were similar between the 2 groups. Both fellowship and non‐fellowship‐trained hospitalists reported feeling less than competent (scores <50) in sedation, understanding basic components of PHM business practice, and defining a relative value unit. Fellowship‐trained hospitalists indicated perceived competency (scores >50) in the remainder of the competencies surveyed. Non‐fellowship‐trained hospitalists additionally had average scores <50 with statistically significant lower reported competency scores than fellowship‐trained hospitalists in IV access/phlebotomy, managing emergencies in technology‐dependent children, performing Plan‐Do‐Study‐Act (PDSA) cycles to achieve QI, performing root‐cause analysis (RCA), defining basic statistical terms, and identifying resources required to conduct research. Non‐fellowship‐trained hospitalists reported statistically significant higher mean competency scores in pain management, newborn care, and transitions in care. In each of these competencies, though, mean scores for both groups were in the competent range.
| Core Competency | Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value |
|---|---|---|---|
| |||
| Common diagnoses | 78.4 | 78.6 | 0.717 |
| Core skills | |||
| IV access/phlebotomy | 52.9 | 30.6 | 0.012 |
| Lumbar puncture | 76.2 | 77.0 | 0.245 |
| Sedation | 30.9 | 28.3 | 0.001 |
| Pain management | 70.7 | 72.6 | 0.014 |
| Nutrition | 68.0 | 66.1 | 0.026 |
| Specialized clinical skills | |||
| Leading a health care team | |||
| Team leadership | 74.9 | 72.0 | <0.001 |
| FCR | 75.3 | 72.6 | <0.001 |
| Technology‐dependent patient | |||
| General management | 71.4 | 65.9 | <0.001 |
| Emergencies | 53.2 | 49.4 | <0.001 |
| Newborn care | 56.6 | 61.6 | <0.001 |
| Child abuse | |||
| Diagnosing | 68.6 | 68.7 | 0.925 |
| Reporting | 68.9 | 68.5 | 0.630 |
| Healthcare systems | |||
| Transitions in care | 77.4 | 79.6 | 0.002 |
| Advocacy | 57.4 | 53.5 | <0.001 |
| Business practice | |||
| Basic components | 36.4 | 32.0 | <0.001 |
| Concept of RVU | 30.2 | 30.2 | 0.972 |
| Billing/coding | 61.4 | 63.9 | 0.004 |
| Quality Improvement | |||
| PDSA cycles | 63.7 | 42.8 | <0.001 |
| Best practice guidelines | 64.7 | 51.8 | <0.001 |
| Safety | |||
| Identify and address harm | 65.9 | 59.1 | <0.001 |
| Perform RCA | 56.7 | 36.0 | <0.001 |
| Cost‐effective care | 58.4 | 51.6 | <0.001 |
| Medical education | |||
| Needs assessment | 69.4 | 65.6 | <0.001 |
| Large group teaching | 67.6 | 60.6 | <0.001 |
| Small group teaching | 74.2 | 72.6 | 0.040 |
| Feedback | 73.8 | 68.9 | <0.001 |
| Evidence‐based medicine | |||
| Literature search | 75.9 | 69.0 | <0.001 |
| Literature appraisal | 63.4 | 57.2 | <0.001 |
| Apply study results | 70.2 | 64.8 | <0.001 |
| Research | |||
| Comparing study design | 62.6 | 54.1 | <0.001 |
| Basic statistics | 57.2 | 41.7 | <0.001 |
| Identifying resources | 56.0 | 36.1 | <0.001 |
The mean adjusted competency scores in areas with some of the largest differences between the 2 groups were plotted by time since residency graduation and depicted in Figure 1. This does not represent a single cohort of hospitalists over time, rather individual hospitalists at different post‐graduate years from their residency graduation. In performing PDSA cycles, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean score indicating competency (57.3), whereas only non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation reported a mean score approaching competency (49.1) (Figure 1A). For development of best practice guidelines, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean competency score (61.8), similar to non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation (60.8) (Figure 1B). Competency in performing RCA was reported by fellowship‐trained hospitalists 2 years postresidency (72.1), whereas non‐fellowship‐trained hospitalists up to 5 years post‐residency report a mean score below competency (Figure 1C). Regarding research competencies, fellowship‐trained hospitalists reported increased perceived competency at each year postresidency graduation, whereas non‐fellowship‐trained hospitalists reported lower mean competency scores with each year post‐residency (Figure 1D,E).
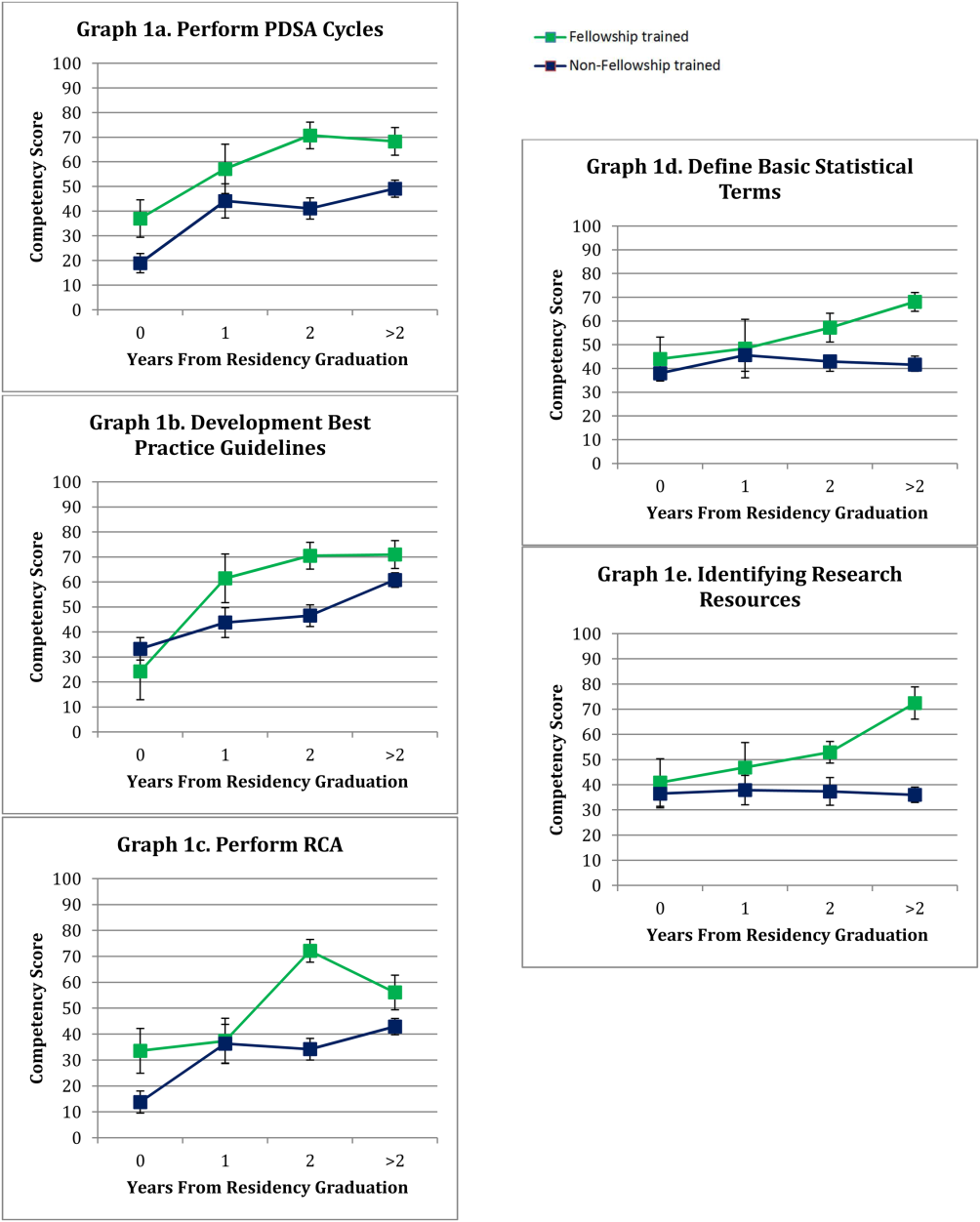
DISCUSSION
Our study results reveal significant differences in perceived competency between fellowship‐trained and non‐fellowship‐trained hospitalists, identifying several perceived knowledge gaps. Early career hospitalists, regardless of their training, perceive they have not achieved competency in sedation and aspects of PHM business practice. Early career hospitalists who did not pursue PHM fellowship training reported also feeling less than competent in intravenous access/phlebotomy, managing emergencies in technology‐dependent children, performing PDSA cycles to achieve QI, performing RCA, defining basic statistical terms, and identifying resources required to conduct research. Although both groups perceived themselves as competent in newborn care, pain management, and transitions in care, non‐fellowship‐trained hospitalists did report statistically significant higher competency scores compared to fellowship‐trained hospitalists in these skills.
Our findings support previous studies on the roles and training needs of pediatric hospitalists. In 2004, Ottolini et al. conducted a survey of pediatric hospitalists through Pediatric Research in Inpatient Settings, finding additional training needs in program/division management, practice guidelines, QI, safety, teaching, evidence‐based medicine (EBM), and research. The majority of hospitalists surveyed did not believe their pediatric residency training provided all of the skills necessary to practice as pediatric hospitalists.[5] Maniscalco et al. repeated the study in 2008 with similar findings.[6] In the field of adult internal medicine, Plauth et al. surveyed practicing hospitalists regarding the adequacy of their residency training, and found that systems issues (ie, QI, health economics, practice guidelines development) were reported as important to their current practice and not adequately emphasized in residency training.[9] Collectively, these findings highlight the need to critically evaluate our current training models' ability to prepare an individual for a career in hospital medicine. There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified,[1] but it is important to identify where the current knowledge gaps exist to optimize this process.
Not surprisingly, the majority of the hospitalists surveyed self‐reported competency in most of the clinical skills included. Residency training is heavily weighted toward acquisition of clinical skills, with a significant amount of time spent on inpatient clinical rotations.[10] The exception was sedation, which had some of the lowest mean perceived competency scores for all early career hospitalists surveyed. There is growing demand for safe and effective procedural sedation nationally, and pediatric hospitalists have been recognized as well poised to augment sedation services provided by anesthesiologists.[11, 12] This study demonstrates that current residency and PHM fellowship training may not adequately address this skill set to produce hospitalists prepared to take on this potential role.
Significant findings in the non‐clinical domains were the healthcare systems competencies. It is increasingly evident that a hospitalist's job description includes addressing communication, coordination of care, quality of care, and patient safety.[13] Yet, our findings indicate that non‐fellowship‐trained early career hospitalists do not feel competent in several of these aspects of hospital medicine practice. Our findings suggest that residency training alone may not provide adequate instruction for perceived competency, as no hospitalists with <1 year since residency graduation reported competency in PDSA cycles, best practice guidelines, and RCA. Interestingly, examining these competencies at different years following residency graduation, experience alone also does not ensure perceived competency early in one's career. Hospitalists are establishing themselves as a catalyst for change and the driving forces behind healthcare systems improvements within the hospital setting, often as our value added to an institution.[14, 15, 16, 17] Therefore, every pediatric hospitalist will need to acquire competency in these skills in a timely manner to effectively deliver high‐quality care to hospitalized children.
Finally, research was another area in which non‐fellowship‐trained hospitalists had low self‐perceived competency. When evaluating competency at different years postresidency graduation, non‐fellowship‐trained individuals appeared to lose a sense of competency each year, whereas fellowship‐trained hospitalists reported escalating competency with each year post‐residency. This finding may be due to the fellowship training itself, mentorship established in fellowship, or resources available in their chosen practice environment following fellowship. In 2011, Bekmezian et al. found that the majority of pediatric hospitalists wanted to conduct research but cited lack of dedicated time and mentorship as barriers to their productivity.[18] High‐quality studies including clinical, QI, and comparative effectiveness research are necessary to allow practicing hospitalists to make better decisions regarding patient care and to advance the field. This need transcends practice environment evidenced by the latest movement to transition away from the more traditional academic and non‐academic nomenclature. Even if one is not planning to conduct research, a basic foundation of research knowledge is required to critically appraise literature and apply EBM principles to clinical practice. This study suggests these skills are not being adequately obtained in residency for perceived competency or acquired with experience alone early in one's career.
There are several limitations of this study that should be considered. Most notably, the competency scores are based on self‐perceived assessments and therefore are not validated with objective measures of an individual's knowledge and skill, risking bias based on an individual's level of personal insight. We also did not quantify differences in training experience based on specific institutions, residency size, patient volume, and exposure to a hospitalist service, which could influence perceived competency and generalizability. Similarly, there is wide variation in current PHM fellowship curriculums, which is not accounted for in this study. Professional competency is challenging to define as well as measure.[19] Although this study is based on subjective measures, one can postulate that self‐perceived competency may impact an individual's approach to clinical practice, projects pursued, and career aspirations.
A second significant limitation was our inability to accurately determine a response rate. Other pediatric hospitalist surveys have faced similar limitations utilizing the AAP SOHM Listserv, because there is no centralized database of practicing hospitalists.[18, 20, 21] Attempts to collect workforce data from the American Board of Pediatrics (ABP) regarding estimates of the number of hospitalists within 5 years of their residency graduation revealed that they changed their data collection methods during our study period, therefore direct comparisons could not be made before and after 2012 (email communication with Cathy Koenig, Psychometric Data Analyst, ABP). Additionally, the AAP SOHM Listserv does not collect demographic data on subscribers, therefore we were unable to determine how many of the 2100 subscribers are within 5 years of their residency graduation. Nevertheless, it is the largest listserv of pediatric hospitalists and enabled us to attempt to collect data from the most representative population. PHM fellowship programs have also rapidly expanded, and only recently has there been a more centralized, comprehensive database of programs and fellows. With the available information, we could not accurately estimate a response rate. Despite the potential for response bias and small sample size, we feel the information collected is a valuable first look at important and timely data that can inform future studies.
Overall, this study provides important information regarding the perceived competency of early career pediatric hospitalists. Although different practice environments may afford different experiences and influence competency over time, we believe the majority of the PHM core competencies transcend practice environment and are ones all early career hospitalists should strive to achieve. To ensure the ongoing advancement of our field, we must guarantee that hospitalists are provided the resources and training to attain these competencies. This may include developing hospital medicine residency tracks, continuing medical education offerings, and/or PHM fellowships whose objectives are aligned with the established core competencies. Although this study was not designed to determine which of these options are optimal, the results can help identify the existing gaps to inform curriculum development in the future. As our field continues to evolve and advance, it will be important to continuously re‐evaluate our training programs' abilities to produce pediatric hospitalists with clinical, quality, scholarly, and leadership skills that meet our field's core competency standards.
CONCLUSIONS
Early career pediatric hospitalists report deficits in several of the PHM core competencies, which should be considered when designing PHM‐specific training in the future. PHM fellowship‐trained hospitalists report higher levels of self‐perceived competency in many core areas.
Disclosure: Nothing to report.
- , , , et al. Pediatric hospital medicine: a strategic planning roundtable to chart the future. J Hosp Med. 2012;7(4):329–334.
- , , , et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i–xv, 1–114.
- , . Pediatric hospital medicine and education: why we can't stand still. JAMA Pediatr. 2013;167(5):412–413.
- , , Research Advisory Committee of the American Board of Pediatrics. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179–186.
- , , , . PRIS Survey: pediatric hospitalist roles and training needs. Pediatr Res. 2004;55:360A.
- , , , , . Current roles and training needs of pediatric hospitalists: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. Paper presented at: Pediatric Academic Societies; 2008; Honolulu, HI.
- , , , . From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767.
- , , , , , . Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , , , . Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111(3):247–254.
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2012. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf. Accessed August 14, 2014.
- , . Pediatric sedation. Pediatr Clin North Am. 2014;61(4):703–717.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , , , et al. Guiding principles for pediatric hospital medicine programs. Pediatrics. 2013;132(4):782–786.
- , , , . Pediatric hospitalists: a systematic review of the literature. Pediatrics. 2006;117(5):1736–1744.
- , . Pediatric hospitalist systems versus traditional models of care: effect on quality and cost outcomes. J Hosp Med. 2012;7(4):350–357.
- . Pediatric hospital medicine: historical perspectives, inspired future. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):107–112.
- . Pediatric hospitalists working in community hospitals. Pediatr Clin North Am. 2014;61(4):681–691.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , . Defining and assessing professional competence. JAMA. 2002;287(2):226–235.
- , , . Transition of care: what Is the pediatric hospitalist's role? An exploratory survey of current attitudes. J Hosp Med. 2012;7(4):277–281.
- , , . Association between practice setting and pediatric hospitalist career satisfaction. Hosp Pediatr. 2013;3(3):285–291.
- , , , et al. Pediatric hospital medicine: a strategic planning roundtable to chart the future. J Hosp Med. 2012;7(4):329–334.
- , , , et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i–xv, 1–114.
- , . Pediatric hospital medicine and education: why we can't stand still. JAMA Pediatr. 2013;167(5):412–413.
- , , Research Advisory Committee of the American Board of Pediatrics. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179–186.
- , , , . PRIS Survey: pediatric hospitalist roles and training needs. Pediatr Res. 2004;55:360A.
- , , , , . Current roles and training needs of pediatric hospitalists: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. Paper presented at: Pediatric Academic Societies; 2008; Honolulu, HI.
- , , , . From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767.
- , , , , , . Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , , , . Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111(3):247–254.
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2012. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf. Accessed August 14, 2014.
- , . Pediatric sedation. Pediatr Clin North Am. 2014;61(4):703–717.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , , , et al. Guiding principles for pediatric hospital medicine programs. Pediatrics. 2013;132(4):782–786.
- , , , . Pediatric hospitalists: a systematic review of the literature. Pediatrics. 2006;117(5):1736–1744.
- , . Pediatric hospitalist systems versus traditional models of care: effect on quality and cost outcomes. J Hosp Med. 2012;7(4):350–357.
- . Pediatric hospital medicine: historical perspectives, inspired future. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):107–112.
- . Pediatric hospitalists working in community hospitals. Pediatr Clin North Am. 2014;61(4):681–691.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , . Defining and assessing professional competence. JAMA. 2002;287(2):226–235.
- , , . Transition of care: what Is the pediatric hospitalist's role? An exploratory survey of current attitudes. J Hosp Med. 2012;7(4):277–281.
- , , . Association between practice setting and pediatric hospitalist career satisfaction. Hosp Pediatr. 2013;3(3):285–291.
© 2015 Society of Hospital Medicine
PCP Communication at Discharge
Transitions of care from hospital to home are high‐risk times for patients.[1, 2] Increasing complexity of hospital admissions and shorter lengths of stay demand more effective coordination of care between hospitalists and outpatient clinicians.[3, 4, 5] Inaccurate, delayed, or incomplete clinical handoversthat is, transfer of information and professional responsibility and accountability[6]can lead to patient harm, and has been recognized as a key cause of preventable morbidity by the World Health Organization and The Joint Commission.[6, 7, 8] Conversely, when done effectively, transitions can result in improved patient health outcomes, reduced readmission rates, and higher patient and provider satisfaction.3
Previous studies note deficits in communication at discharge and primary care provider (PCP) dissatisfaction with discharge practices.[4, 9, 10, 11, 12, 13] In studies at academic medical centers, there were low rates of direct communication between inpatient and outpatient providers, mainly because of providers' belief that the discharge summary was adequate and the presence of significant barriers to direct communication.[14, 15] However, studies have shown that discharge summaries often omit critical information, and often are not available to PCPs in a timely manner.[10, 11, 12, 16] In response, the Society of Hospital Medicine developed a discharge checklist to aide in standardization of safe discharge practices.[1, 5] Discharge summary templates further attempt to improve documentation of patients' hospital courses. An electronic medical record (EMR) system shared by both inpatient and outpatient clinicians should impart several advantages: (1) automated alerts provide timely notification to PCPs regarding admission and discharge, (2) discharge summaries are available to the PCP as soon as they are written, and (3) all patient information pertaining to the hospitalization is available to the PCP.
Although it is plausible that shared EMRs should facilitate transitions of care by streamlining communication between hospitalists and PCPs, guidelines on format and content of PCP communication at discharge in the era of a shared EMR have yet to be defined. In this study, we sought to understand current discharge communication practices and PCP satisfaction within a shared EMR at our institution, and to identify key areas in which communication can be improved.
METHODS
Participants and Setting
We surveyed all resident and attending PCPs (n=124) working in the Division of General Internal Medicine (DGIM) Outpatient Practice at the University of California, San Francisco (UCSF). In June 2012, the outpatient and inpatient practices of UCSF transitioned from having separate medical record systems to a shared EMR (Epic Systems Corp., Verona, WI) where all informationboth inpatient and outpatientis accessible among healthcare professionals. The EMR provides automated notifications of admission and discharge to PCPs, allows for review of inpatient notes, labs, and studies, and immediate access to templated discharge summaries (see Supporting Information, Appendix 1, in the online version of this article). The EMR also enables secure communication between clinicians. At our institution, over 90% of discharge summaries are completed within 24 hours of discharge.[17]
Study Design and Analysis
We developed a survey about the discharge communication practices of inpatient medicine patients based on a previously described survey in the literature (see Supporting Information, Appendix 2, in the online version of this article).[9] The anonymous, 17‐question survey was electronically distributed to resident and attending PCPs at the DGIM practice. The survey was designed to determine: (1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, (2) perceived adequacy of automatic discharge notifications, and (3) perception of the types of patients and hospitalizations requiring additional high‐touch communication at discharge.
We analyzed results of our survey using descriptive statistics. Differences in resident and attending responses were analyzed by 2tests.
RESULTS
Seventy‐five of 124 (60%) clinicians (46% residents, 54% attendings) completed the survey. Thirty‐nine (52%) PCPs were satisfied or very satisfied with communication at patient discharge. Although most reported receiving automated discharge notifications (71%), only 39% felt that the notifications plus the discharge summaries were adequate communication for safe transition of care from hospital to community. Fifty‐one percent desired direct contact beyond a discharge summary. There were no differences in preferences on discharge communication between resident and attending PCPs (P>0.05).
Over three‐fourths of PCPs surveyed preferred that for patients with complex hospitalizations (multiple readmissions, multiple active comorbidities, goals of care changes, high‐risk medication changes, time‐sensitive follow‐up needs), an additional e‐mail or verbal communication was needed to augment the information in the discharge summary (Figure 1). Only 31% reported receiving such communication.
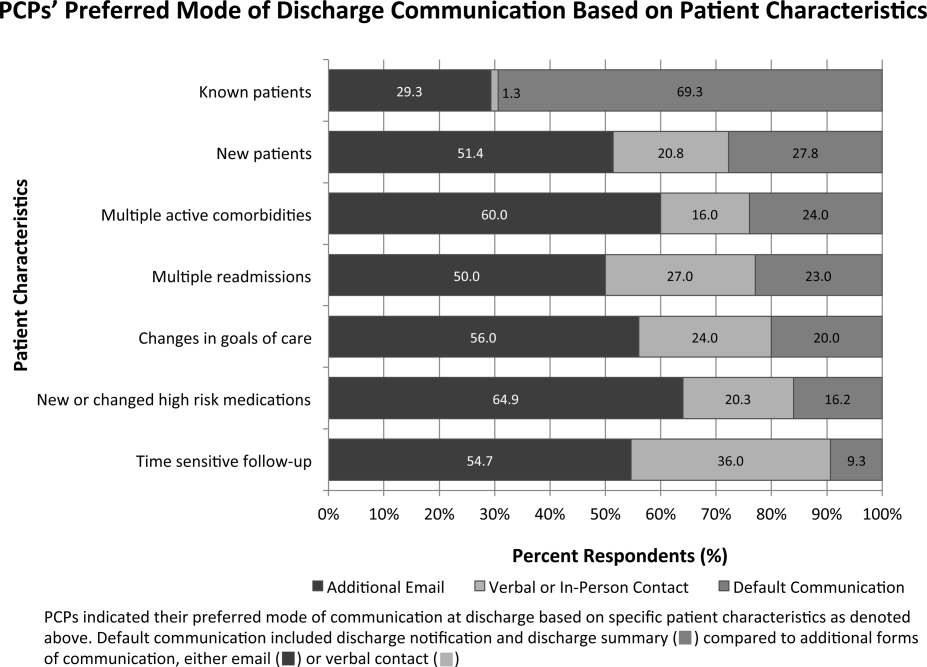
When asked about important items to communicate for safer transitions of care, PCPs reported finding the following elements most critical: (1) medication changes (93%), (2) follow‐up actions for the PCP (88%), and (3) active medical issues (84%) (Figure 2).
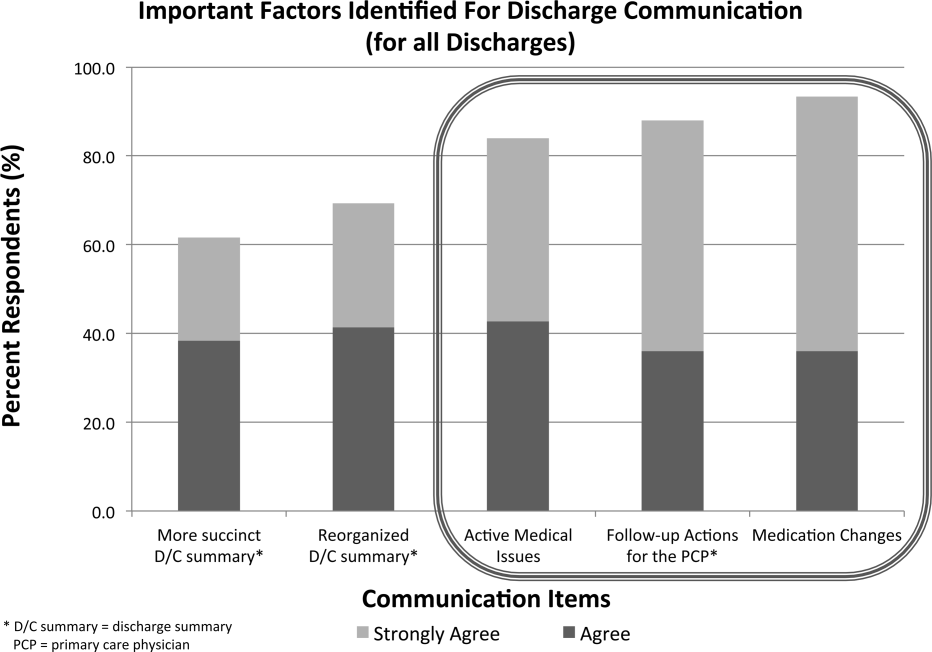
CONCLUSIONS
In the era of shared EMRs, real‐time access to medication lists, pending test results, and discharge summaries should facilitate care transitions at discharge.[18, 19] We conducted a study to determine PCP perceptions of discharge communication after implementation of a shared EMR. We found that although PCPs largely acknowledged timely receipt of automated discharge notifications and discharge summaries, the majority of PCPs felt that most discharges required additional communication to ensure safe transition of care.
Guidelines for discharge communication emphasize timely communication with the PCP, primarily through discharge summaries containing key safety elements.[1, 5, 10] At our institution, we have improved the timeliness and quality of discharge summaries according to guideline recommendations,[17] and conducted quality improvement projects to improve rates of direct communication with PCPs.[9] In addition, the shared EMR provides automated notifications to PCPs when their patients are discharged. Despite these interventions, our survey shows that PCP satisfaction with discharge communication is still inadequate. PCPs desired direct communication that highlights active medical issues, medication changes, and specific follow‐up actions. Although all of these topics are included in our discharge summary template (see Supporting Information, Appendix 1, in the online version of this article), it is possible that the templated discharge summaries lend themselves to longer documents and information overload, as prior studies have documented the desire for more succinct discharge summaries.[18] We also found that automated notifications of discharge were less reliable and useful for PCPs than anticipated. There were several reasons for this: (1) discharge summaries sometimes were sent to PCPs uncoupled from the discharge notification, (2) there were errors with the generation and delivery of automated messages at the rollout of the new system, and (3) PCPs received many other automated system messages, meaning that discharge notifications could be easily missed. These factors all likely contribute to PCPs' desire for high‐touch communication that highlights the most salient aspects of each patient's hospitalization. It is also possible that automated notifications and depersonalized discharge summaries create distance and a less‐collaborative feeling to patient care. PCPs want more direct communication, and desire to play a more active role in inpatient management, especially for complex hospitalizations.[18] This emphasis on direct communication resonates with previous studies conducted before shared EMRs existed.[9, 12, 19]
Our study had several limitations. First, because this is a single‐institution study at a tertiary care academic setting, the results may not be generalizable to all shared EMR settings, and may not reflect all the challenges of communication with the wider community of outpatient providers. One can postulate that inpatient and outpatient clinician relationships are stronger in an academic setting than in other more disparate environments, where direct communication may happen even less frequently. Of note, our low rates of direct communication are consistent with other single‐ and multi‐institution studies, suggesting that our findings are generalizable.[14, 15] Second, our survey is limited in its ability to distinguish those patients who require high‐touch communication and those who do not. Third, although we have used the survey to assess PCP satisfaction in previous studies, it is not a validated instrument, and therefore we cannot reliably say that increasing direct PCP communication would increase their satisfaction around discharge. Last, the PCP‐reported rates of discharge communication are subjective and may be influenced by recall bias. We did not have a systematic way to confirm the actual rates of communication at discharge, which could have occurred through EMR messages, e‐mails, phone calls, or pages.
Although a shared EMR allows for real‐time access to patient data, it does not eliminate PCPs' desire for direct 2‐way dialogue at discharge, especially for complex patients. Key information desired in such communication should include active medical issues, medication changes, and follow‐up needs, which is consistent with prior studies. Standardizing this direct communication process in an efficient way can be challenging. Further elucidation of PCP preferences around which patients necessitate higher‐level communication and preferred methods and timing of communication is needed, as well as determining the most efficient and effective method for hospitalists to provide such communication. Improving communication between hospitalists and PCPs requires not just the presence of a shared EMR, but additional, systematic efforts to engage both inpatient and outpatient clinicians in collaborative care.
Disclosure
Nothing to report.
- , , , et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449.
- , , , , The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–428.
- , , , , “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354−660.
- , , , , Improving measurement in clinical handover. Qual Saf Health Care. 2009;18:272–277.
- World Health Organization. Patient safety: action on patient safety: high 5s. 2007. Available at: http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html. Accessed January 28, 2015.
- The Joint Commission Center for Transforming Healthcare. Hand‐off communications. 2012. Available at: http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1. Accessed January 28, 2015.
- , , , et al. The effect of a resident‐led quality improvement project on improving communication between hospital‐based and outpatient physicians. Am J Med Qual. 2013;28(6):472–479.
- , , , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- , , , , , Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21:i97–i105.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA. 2013;173(8):624–629.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774.
- , , , et al. A Failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations [published online ahead of print October 15, 2014]. J Gen Intern Med. doi: 10.1007/s11606-014-3056-x.
- , , , et al. Pediatric hospitalists and primary care providers: a communication needs assessment. J Hosp Med. 2009;4(3):187–193.
Transitions of care from hospital to home are high‐risk times for patients.[1, 2] Increasing complexity of hospital admissions and shorter lengths of stay demand more effective coordination of care between hospitalists and outpatient clinicians.[3, 4, 5] Inaccurate, delayed, or incomplete clinical handoversthat is, transfer of information and professional responsibility and accountability[6]can lead to patient harm, and has been recognized as a key cause of preventable morbidity by the World Health Organization and The Joint Commission.[6, 7, 8] Conversely, when done effectively, transitions can result in improved patient health outcomes, reduced readmission rates, and higher patient and provider satisfaction.3
Previous studies note deficits in communication at discharge and primary care provider (PCP) dissatisfaction with discharge practices.[4, 9, 10, 11, 12, 13] In studies at academic medical centers, there were low rates of direct communication between inpatient and outpatient providers, mainly because of providers' belief that the discharge summary was adequate and the presence of significant barriers to direct communication.[14, 15] However, studies have shown that discharge summaries often omit critical information, and often are not available to PCPs in a timely manner.[10, 11, 12, 16] In response, the Society of Hospital Medicine developed a discharge checklist to aide in standardization of safe discharge practices.[1, 5] Discharge summary templates further attempt to improve documentation of patients' hospital courses. An electronic medical record (EMR) system shared by both inpatient and outpatient clinicians should impart several advantages: (1) automated alerts provide timely notification to PCPs regarding admission and discharge, (2) discharge summaries are available to the PCP as soon as they are written, and (3) all patient information pertaining to the hospitalization is available to the PCP.
Although it is plausible that shared EMRs should facilitate transitions of care by streamlining communication between hospitalists and PCPs, guidelines on format and content of PCP communication at discharge in the era of a shared EMR have yet to be defined. In this study, we sought to understand current discharge communication practices and PCP satisfaction within a shared EMR at our institution, and to identify key areas in which communication can be improved.
METHODS
Participants and Setting
We surveyed all resident and attending PCPs (n=124) working in the Division of General Internal Medicine (DGIM) Outpatient Practice at the University of California, San Francisco (UCSF). In June 2012, the outpatient and inpatient practices of UCSF transitioned from having separate medical record systems to a shared EMR (Epic Systems Corp., Verona, WI) where all informationboth inpatient and outpatientis accessible among healthcare professionals. The EMR provides automated notifications of admission and discharge to PCPs, allows for review of inpatient notes, labs, and studies, and immediate access to templated discharge summaries (see Supporting Information, Appendix 1, in the online version of this article). The EMR also enables secure communication between clinicians. At our institution, over 90% of discharge summaries are completed within 24 hours of discharge.[17]
Study Design and Analysis
We developed a survey about the discharge communication practices of inpatient medicine patients based on a previously described survey in the literature (see Supporting Information, Appendix 2, in the online version of this article).[9] The anonymous, 17‐question survey was electronically distributed to resident and attending PCPs at the DGIM practice. The survey was designed to determine: (1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, (2) perceived adequacy of automatic discharge notifications, and (3) perception of the types of patients and hospitalizations requiring additional high‐touch communication at discharge.
We analyzed results of our survey using descriptive statistics. Differences in resident and attending responses were analyzed by 2tests.
RESULTS
Seventy‐five of 124 (60%) clinicians (46% residents, 54% attendings) completed the survey. Thirty‐nine (52%) PCPs were satisfied or very satisfied with communication at patient discharge. Although most reported receiving automated discharge notifications (71%), only 39% felt that the notifications plus the discharge summaries were adequate communication for safe transition of care from hospital to community. Fifty‐one percent desired direct contact beyond a discharge summary. There were no differences in preferences on discharge communication between resident and attending PCPs (P>0.05).
Over three‐fourths of PCPs surveyed preferred that for patients with complex hospitalizations (multiple readmissions, multiple active comorbidities, goals of care changes, high‐risk medication changes, time‐sensitive follow‐up needs), an additional e‐mail or verbal communication was needed to augment the information in the discharge summary (Figure 1). Only 31% reported receiving such communication.
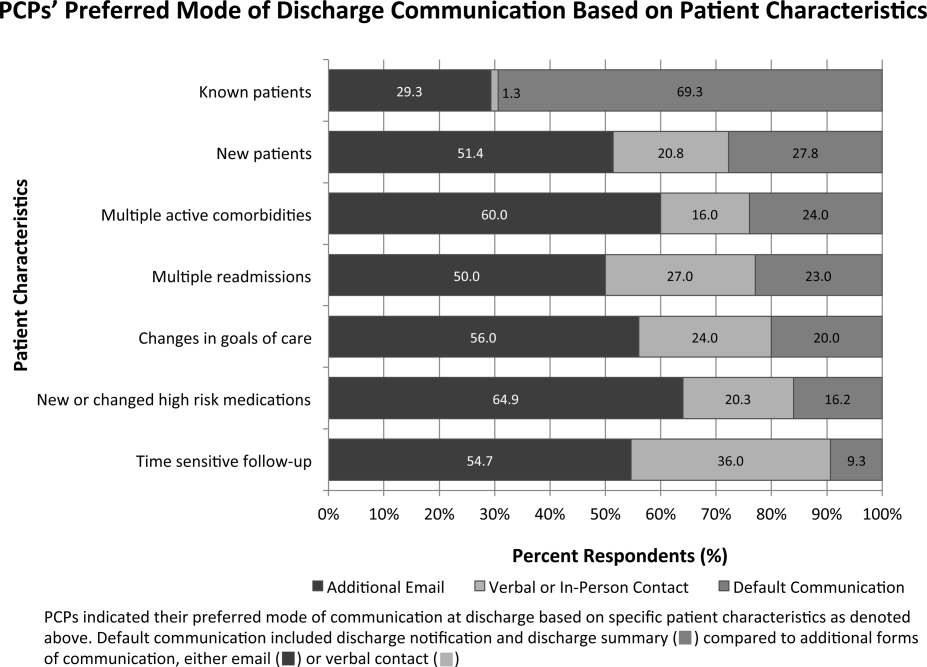
When asked about important items to communicate for safer transitions of care, PCPs reported finding the following elements most critical: (1) medication changes (93%), (2) follow‐up actions for the PCP (88%), and (3) active medical issues (84%) (Figure 2).
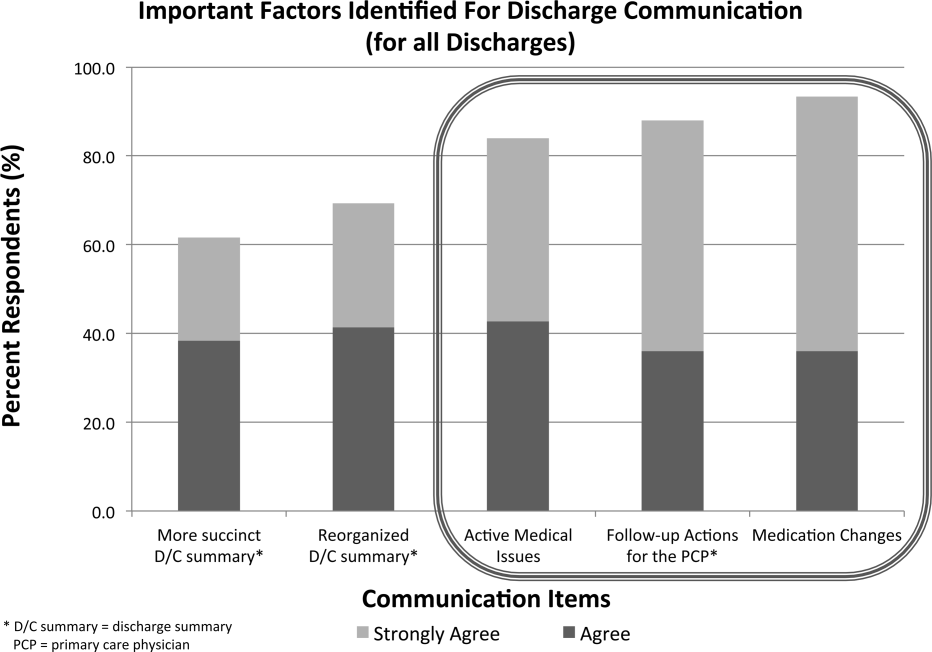
CONCLUSIONS
In the era of shared EMRs, real‐time access to medication lists, pending test results, and discharge summaries should facilitate care transitions at discharge.[18, 19] We conducted a study to determine PCP perceptions of discharge communication after implementation of a shared EMR. We found that although PCPs largely acknowledged timely receipt of automated discharge notifications and discharge summaries, the majority of PCPs felt that most discharges required additional communication to ensure safe transition of care.
Guidelines for discharge communication emphasize timely communication with the PCP, primarily through discharge summaries containing key safety elements.[1, 5, 10] At our institution, we have improved the timeliness and quality of discharge summaries according to guideline recommendations,[17] and conducted quality improvement projects to improve rates of direct communication with PCPs.[9] In addition, the shared EMR provides automated notifications to PCPs when their patients are discharged. Despite these interventions, our survey shows that PCP satisfaction with discharge communication is still inadequate. PCPs desired direct communication that highlights active medical issues, medication changes, and specific follow‐up actions. Although all of these topics are included in our discharge summary template (see Supporting Information, Appendix 1, in the online version of this article), it is possible that the templated discharge summaries lend themselves to longer documents and information overload, as prior studies have documented the desire for more succinct discharge summaries.[18] We also found that automated notifications of discharge were less reliable and useful for PCPs than anticipated. There were several reasons for this: (1) discharge summaries sometimes were sent to PCPs uncoupled from the discharge notification, (2) there were errors with the generation and delivery of automated messages at the rollout of the new system, and (3) PCPs received many other automated system messages, meaning that discharge notifications could be easily missed. These factors all likely contribute to PCPs' desire for high‐touch communication that highlights the most salient aspects of each patient's hospitalization. It is also possible that automated notifications and depersonalized discharge summaries create distance and a less‐collaborative feeling to patient care. PCPs want more direct communication, and desire to play a more active role in inpatient management, especially for complex hospitalizations.[18] This emphasis on direct communication resonates with previous studies conducted before shared EMRs existed.[9, 12, 19]
Our study had several limitations. First, because this is a single‐institution study at a tertiary care academic setting, the results may not be generalizable to all shared EMR settings, and may not reflect all the challenges of communication with the wider community of outpatient providers. One can postulate that inpatient and outpatient clinician relationships are stronger in an academic setting than in other more disparate environments, where direct communication may happen even less frequently. Of note, our low rates of direct communication are consistent with other single‐ and multi‐institution studies, suggesting that our findings are generalizable.[14, 15] Second, our survey is limited in its ability to distinguish those patients who require high‐touch communication and those who do not. Third, although we have used the survey to assess PCP satisfaction in previous studies, it is not a validated instrument, and therefore we cannot reliably say that increasing direct PCP communication would increase their satisfaction around discharge. Last, the PCP‐reported rates of discharge communication are subjective and may be influenced by recall bias. We did not have a systematic way to confirm the actual rates of communication at discharge, which could have occurred through EMR messages, e‐mails, phone calls, or pages.
Although a shared EMR allows for real‐time access to patient data, it does not eliminate PCPs' desire for direct 2‐way dialogue at discharge, especially for complex patients. Key information desired in such communication should include active medical issues, medication changes, and follow‐up needs, which is consistent with prior studies. Standardizing this direct communication process in an efficient way can be challenging. Further elucidation of PCP preferences around which patients necessitate higher‐level communication and preferred methods and timing of communication is needed, as well as determining the most efficient and effective method for hospitalists to provide such communication. Improving communication between hospitalists and PCPs requires not just the presence of a shared EMR, but additional, systematic efforts to engage both inpatient and outpatient clinicians in collaborative care.
Disclosure
Nothing to report.
Transitions of care from hospital to home are high‐risk times for patients.[1, 2] Increasing complexity of hospital admissions and shorter lengths of stay demand more effective coordination of care between hospitalists and outpatient clinicians.[3, 4, 5] Inaccurate, delayed, or incomplete clinical handoversthat is, transfer of information and professional responsibility and accountability[6]can lead to patient harm, and has been recognized as a key cause of preventable morbidity by the World Health Organization and The Joint Commission.[6, 7, 8] Conversely, when done effectively, transitions can result in improved patient health outcomes, reduced readmission rates, and higher patient and provider satisfaction.3
Previous studies note deficits in communication at discharge and primary care provider (PCP) dissatisfaction with discharge practices.[4, 9, 10, 11, 12, 13] In studies at academic medical centers, there were low rates of direct communication between inpatient and outpatient providers, mainly because of providers' belief that the discharge summary was adequate and the presence of significant barriers to direct communication.[14, 15] However, studies have shown that discharge summaries often omit critical information, and often are not available to PCPs in a timely manner.[10, 11, 12, 16] In response, the Society of Hospital Medicine developed a discharge checklist to aide in standardization of safe discharge practices.[1, 5] Discharge summary templates further attempt to improve documentation of patients' hospital courses. An electronic medical record (EMR) system shared by both inpatient and outpatient clinicians should impart several advantages: (1) automated alerts provide timely notification to PCPs regarding admission and discharge, (2) discharge summaries are available to the PCP as soon as they are written, and (3) all patient information pertaining to the hospitalization is available to the PCP.
Although it is plausible that shared EMRs should facilitate transitions of care by streamlining communication between hospitalists and PCPs, guidelines on format and content of PCP communication at discharge in the era of a shared EMR have yet to be defined. In this study, we sought to understand current discharge communication practices and PCP satisfaction within a shared EMR at our institution, and to identify key areas in which communication can be improved.
METHODS
Participants and Setting
We surveyed all resident and attending PCPs (n=124) working in the Division of General Internal Medicine (DGIM) Outpatient Practice at the University of California, San Francisco (UCSF). In June 2012, the outpatient and inpatient practices of UCSF transitioned from having separate medical record systems to a shared EMR (Epic Systems Corp., Verona, WI) where all informationboth inpatient and outpatientis accessible among healthcare professionals. The EMR provides automated notifications of admission and discharge to PCPs, allows for review of inpatient notes, labs, and studies, and immediate access to templated discharge summaries (see Supporting Information, Appendix 1, in the online version of this article). The EMR also enables secure communication between clinicians. At our institution, over 90% of discharge summaries are completed within 24 hours of discharge.[17]
Study Design and Analysis
We developed a survey about the discharge communication practices of inpatient medicine patients based on a previously described survey in the literature (see Supporting Information, Appendix 2, in the online version of this article).[9] The anonymous, 17‐question survey was electronically distributed to resident and attending PCPs at the DGIM practice. The survey was designed to determine: (1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, (2) perceived adequacy of automatic discharge notifications, and (3) perception of the types of patients and hospitalizations requiring additional high‐touch communication at discharge.
We analyzed results of our survey using descriptive statistics. Differences in resident and attending responses were analyzed by 2tests.
RESULTS
Seventy‐five of 124 (60%) clinicians (46% residents, 54% attendings) completed the survey. Thirty‐nine (52%) PCPs were satisfied or very satisfied with communication at patient discharge. Although most reported receiving automated discharge notifications (71%), only 39% felt that the notifications plus the discharge summaries were adequate communication for safe transition of care from hospital to community. Fifty‐one percent desired direct contact beyond a discharge summary. There were no differences in preferences on discharge communication between resident and attending PCPs (P>0.05).
Over three‐fourths of PCPs surveyed preferred that for patients with complex hospitalizations (multiple readmissions, multiple active comorbidities, goals of care changes, high‐risk medication changes, time‐sensitive follow‐up needs), an additional e‐mail or verbal communication was needed to augment the information in the discharge summary (Figure 1). Only 31% reported receiving such communication.
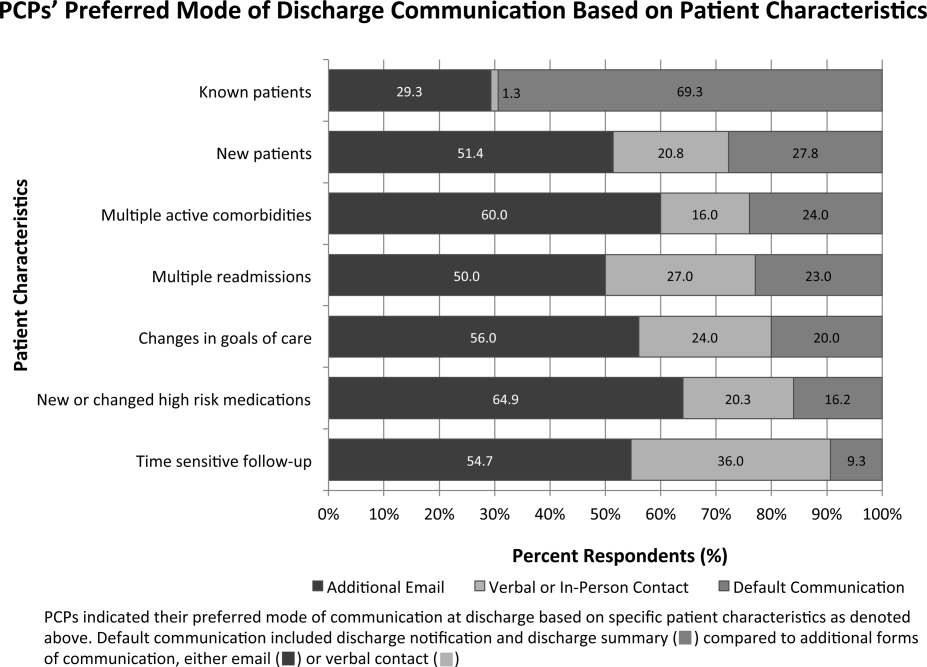
When asked about important items to communicate for safer transitions of care, PCPs reported finding the following elements most critical: (1) medication changes (93%), (2) follow‐up actions for the PCP (88%), and (3) active medical issues (84%) (Figure 2).
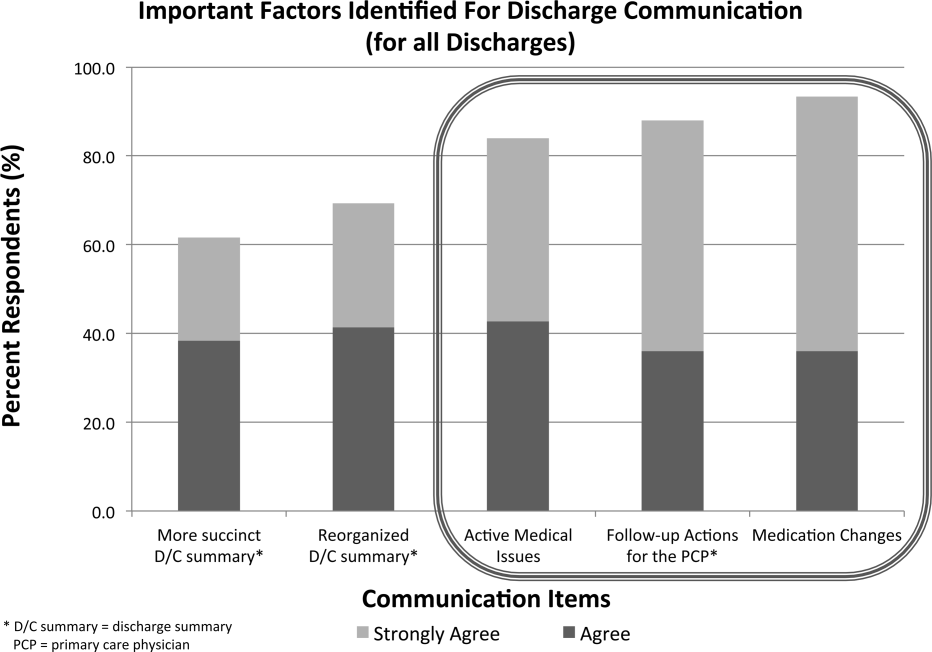
CONCLUSIONS
In the era of shared EMRs, real‐time access to medication lists, pending test results, and discharge summaries should facilitate care transitions at discharge.[18, 19] We conducted a study to determine PCP perceptions of discharge communication after implementation of a shared EMR. We found that although PCPs largely acknowledged timely receipt of automated discharge notifications and discharge summaries, the majority of PCPs felt that most discharges required additional communication to ensure safe transition of care.
Guidelines for discharge communication emphasize timely communication with the PCP, primarily through discharge summaries containing key safety elements.[1, 5, 10] At our institution, we have improved the timeliness and quality of discharge summaries according to guideline recommendations,[17] and conducted quality improvement projects to improve rates of direct communication with PCPs.[9] In addition, the shared EMR provides automated notifications to PCPs when their patients are discharged. Despite these interventions, our survey shows that PCP satisfaction with discharge communication is still inadequate. PCPs desired direct communication that highlights active medical issues, medication changes, and specific follow‐up actions. Although all of these topics are included in our discharge summary template (see Supporting Information, Appendix 1, in the online version of this article), it is possible that the templated discharge summaries lend themselves to longer documents and information overload, as prior studies have documented the desire for more succinct discharge summaries.[18] We also found that automated notifications of discharge were less reliable and useful for PCPs than anticipated. There were several reasons for this: (1) discharge summaries sometimes were sent to PCPs uncoupled from the discharge notification, (2) there were errors with the generation and delivery of automated messages at the rollout of the new system, and (3) PCPs received many other automated system messages, meaning that discharge notifications could be easily missed. These factors all likely contribute to PCPs' desire for high‐touch communication that highlights the most salient aspects of each patient's hospitalization. It is also possible that automated notifications and depersonalized discharge summaries create distance and a less‐collaborative feeling to patient care. PCPs want more direct communication, and desire to play a more active role in inpatient management, especially for complex hospitalizations.[18] This emphasis on direct communication resonates with previous studies conducted before shared EMRs existed.[9, 12, 19]
Our study had several limitations. First, because this is a single‐institution study at a tertiary care academic setting, the results may not be generalizable to all shared EMR settings, and may not reflect all the challenges of communication with the wider community of outpatient providers. One can postulate that inpatient and outpatient clinician relationships are stronger in an academic setting than in other more disparate environments, where direct communication may happen even less frequently. Of note, our low rates of direct communication are consistent with other single‐ and multi‐institution studies, suggesting that our findings are generalizable.[14, 15] Second, our survey is limited in its ability to distinguish those patients who require high‐touch communication and those who do not. Third, although we have used the survey to assess PCP satisfaction in previous studies, it is not a validated instrument, and therefore we cannot reliably say that increasing direct PCP communication would increase their satisfaction around discharge. Last, the PCP‐reported rates of discharge communication are subjective and may be influenced by recall bias. We did not have a systematic way to confirm the actual rates of communication at discharge, which could have occurred through EMR messages, e‐mails, phone calls, or pages.
Although a shared EMR allows for real‐time access to patient data, it does not eliminate PCPs' desire for direct 2‐way dialogue at discharge, especially for complex patients. Key information desired in such communication should include active medical issues, medication changes, and follow‐up needs, which is consistent with prior studies. Standardizing this direct communication process in an efficient way can be challenging. Further elucidation of PCP preferences around which patients necessitate higher‐level communication and preferred methods and timing of communication is needed, as well as determining the most efficient and effective method for hospitalists to provide such communication. Improving communication between hospitalists and PCPs requires not just the presence of a shared EMR, but additional, systematic efforts to engage both inpatient and outpatient clinicians in collaborative care.
Disclosure
Nothing to report.
- , , , et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449.
- , , , , The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–428.
- , , , , “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354−660.
- , , , , Improving measurement in clinical handover. Qual Saf Health Care. 2009;18:272–277.
- World Health Organization. Patient safety: action on patient safety: high 5s. 2007. Available at: http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html. Accessed January 28, 2015.
- The Joint Commission Center for Transforming Healthcare. Hand‐off communications. 2012. Available at: http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1. Accessed January 28, 2015.
- , , , et al. The effect of a resident‐led quality improvement project on improving communication between hospital‐based and outpatient physicians. Am J Med Qual. 2013;28(6):472–479.
- , , , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- , , , , , Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21:i97–i105.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA. 2013;173(8):624–629.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774.
- , , , et al. A Failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations [published online ahead of print October 15, 2014]. J Gen Intern Med. doi: 10.1007/s11606-014-3056-x.
- , , , et al. Pediatric hospitalists and primary care providers: a communication needs assessment. J Hosp Med. 2009;4(3):187–193.
- , , , et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449.
- , , , , The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–428.
- , , , , “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354−660.
- , , , , Improving measurement in clinical handover. Qual Saf Health Care. 2009;18:272–277.
- World Health Organization. Patient safety: action on patient safety: high 5s. 2007. Available at: http://www.who.int/patientsafety/implementation/solutions/high5s/en/index.html. Accessed January 28, 2015.
- The Joint Commission Center for Transforming Healthcare. Hand‐off communications. 2012. Available at: http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1. Accessed January 28, 2015.
- , , , et al. The effect of a resident‐led quality improvement project on improving communication between hospital‐based and outpatient physicians. Am J Med Qual. 2013;28(6):472–479.
- , , , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- , , , , , Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21:i97–i105.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA. 2013;173(8):624–629.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22(9):768–774.
- , , , et al. A Failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations [published online ahead of print October 15, 2014]. J Gen Intern Med. doi: 10.1007/s11606-014-3056-x.
- , , , et al. Pediatric hospitalists and primary care providers: a communication needs assessment. J Hosp Med. 2009;4(3):187–193.
Minimal residual disease could signify worse outcomes in acute myeloid leukemia treatment
Although peripheral count recovery and minimal residual disease level following induction therapy are linked, each is an independent prognostic factor for relapse and overall survival in patients with acute myeloid leukemia, investigators say in a report published online March 2 in Journal of Clinical Oncology. “Information about these post-treatment factors is likely more important than information about several traditional pretreatment prognostic factors and should play a major – and perhaps the dominant – role in planning postinduction therapy,” wrote Dr. Xueyan Chen and her associates.
The investigators retrospectively analyzed data from 245 adults with newly diagnosed, relapsed, or refractory acute myeloid leukemia (AML) who achieved either complete remission (CR), complete remission with incomplete platelet recovery (CRp), or complete remission with incomplete blood count recovery (CRi), after induction therapy. The 71% of patients who achieved CR had minimal residual disease (MRD) less frequently and had lower levels of MRD than the 19.6% of patients achieving CRp and 9.4% achieving CRi, suggesting that failure of blood count recovery may result from inadequate treatment of AML.
Read the entire article here: http://jco.ascopubs.org/content/early/2015/02/26/JCO.2014.58.3518
Although peripheral count recovery and minimal residual disease level following induction therapy are linked, each is an independent prognostic factor for relapse and overall survival in patients with acute myeloid leukemia, investigators say in a report published online March 2 in Journal of Clinical Oncology. “Information about these post-treatment factors is likely more important than information about several traditional pretreatment prognostic factors and should play a major – and perhaps the dominant – role in planning postinduction therapy,” wrote Dr. Xueyan Chen and her associates.
The investigators retrospectively analyzed data from 245 adults with newly diagnosed, relapsed, or refractory acute myeloid leukemia (AML) who achieved either complete remission (CR), complete remission with incomplete platelet recovery (CRp), or complete remission with incomplete blood count recovery (CRi), after induction therapy. The 71% of patients who achieved CR had minimal residual disease (MRD) less frequently and had lower levels of MRD than the 19.6% of patients achieving CRp and 9.4% achieving CRi, suggesting that failure of blood count recovery may result from inadequate treatment of AML.
Read the entire article here: http://jco.ascopubs.org/content/early/2015/02/26/JCO.2014.58.3518
Although peripheral count recovery and minimal residual disease level following induction therapy are linked, each is an independent prognostic factor for relapse and overall survival in patients with acute myeloid leukemia, investigators say in a report published online March 2 in Journal of Clinical Oncology. “Information about these post-treatment factors is likely more important than information about several traditional pretreatment prognostic factors and should play a major – and perhaps the dominant – role in planning postinduction therapy,” wrote Dr. Xueyan Chen and her associates.
The investigators retrospectively analyzed data from 245 adults with newly diagnosed, relapsed, or refractory acute myeloid leukemia (AML) who achieved either complete remission (CR), complete remission with incomplete platelet recovery (CRp), or complete remission with incomplete blood count recovery (CRi), after induction therapy. The 71% of patients who achieved CR had minimal residual disease (MRD) less frequently and had lower levels of MRD than the 19.6% of patients achieving CRp and 9.4% achieving CRi, suggesting that failure of blood count recovery may result from inadequate treatment of AML.
Read the entire article here: http://jco.ascopubs.org/content/early/2015/02/26/JCO.2014.58.3518
Studies of anesthesia’s effect on upper airway are limited
CORONADO, CALIF. – Studies of the most appropriate anesthetic agents for drug-induced sleep endoscopy are limited, but according to the best available evidence, local anesthetics appear to affect airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse, so they may not be ideal.
Those are key conclusions from a systematic review of literature on the effects of commonly used anesthetic agents and opioids on the upper airway presented at the Triological Society’s Combined Sections meeting. Drug-induced sleep endoscopy (DISE) “is a great tool to assess upper airway dynamics in order to determine optimal surgical therapy for obstructive sleep apnea,” said Dr. Zarmina Ehsan, a pediatric pulmonary medicine fellow at Cincinnati Children’s Hospital Medical Center. “There’s a lack of understanding regarding how upper airway dynamics are altered by anesthetic agents, compared with normal sleep. This is important because this hinders the development of universal guidelines and protocols for the use of DISE.”
Using PubMed, EMBASE, and other sources, she and her associates conducted a qualitative systematic review of studies related to common anesthetic agents and opioids in the medical literature through September 2014. To be eligible for inclusion, a study must have evaluated the agent’s effect on the upper airway, must have contained an abstract, and must have been published in English. Studies with fewer than seven subjects, no original data, review articles, and those involving animals were excluded. The researchers reviewed 180 abstracts and included 56 full text articles in the final analysis, for a total study population of 8,540 patients. At the meeting Dr. Ehsan summarized the following findings by agent:
• Lidocaine. This agent is safe for topical use, has a rapid onset of action, and an intermediate duration of efficacy. Lidocaine acts on muscles “which are potent dilators and tensors of the pharyngeal and laryngeal structures,” she said. Of 10 studies included in the analysis, 7 assessed the impact of lidocaine on upper airway obstruction. Of these, three showed increased airway obstruction while four showed no significant effects. There were two studies on sleep parameters with conflicting results: One showed an increase in mean apnea duration with lidocaine use while the other did not. From this the researchers concluded that lidocaine does affect upper airway dynamics.
• Propofol. This lipophilic intravenous agent has a quick onset of action and acts by global central nervous system depression. Of 12 studies included in the analysis, 4 examined dose-response characteristics and showed a dose-dependent decrease in airway cross-sectional area with increased dosing of propofol. “So increasing your dose makes airway obstruction more likely,” Dr. Ehsan said. “The levels of obstruction were greatest at the base of tongue, and the closure was primarily in the anterior-posterior direction.” Three studies found that propofol caused a decrease in genioglossus electromyogram activity, while the remaining five studies assessed heterogeneous outcomes. “Overall, the studies showed that propofol had a dose-dependent effect on the upper airway with increasing doses making airway obstruction more likely,” she said.
• Dexmedetomidine (DEX). This agent is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic effects. It’s typically given as a 10-minute loading dose followed by a continuous infusion, and is recommended when you want to preserve spontaneous respiration. Of the four DEX-related studies that were included in the analysis, all demonstrated a minimal effect on upper airway cross-sectional area. “One of the studies looked at sleep parameters and concluded that DEX does approximate non-REM sleep without causing respiratory depression,” Dr. Ehsan added. “So overall, DEX was less likely to result in upper airway obstruction, compared with propofol.”
• Midazolam. This agent is commonly used for procedural sedation, with an onset of action within 1-3 minutes and a duration of 15-60 minutes. Of the six studies involving midazolam, two evaluated sleep staging. One reported lack of REM sleep and increased duration of stage N3 sleep, while the other study found that all sleep stages were observed at a lower dosage. The remaining four studies had heterogeneous outcomes. This led the researchers to conclude that midazolam “may lead to upper airway obstruction,” Dr. Ehsan said. “It’s unclear if this is dose dependent.”
• Pentobarbital. Of the two studies involving this short-acting barbiturate, one showed no effect on pharyngeal critical pressure or respiratory muscle function, while the other found that pentobarbital can increase the upper airway cross-sectional area. “So the effect of pentobarbital is unclear,” she said.
• Ketamine. This N-methyl-D-aspartate receptor has a rapid onset and a minimal effect on the central respiratory drive. Of the three studies involving ketamine, one found a 10% incidence of transient laryngospasm, one found that the incidence of transient laryngospasm was higher when it was delivered intramuscularly vs. intravenously, and one found that ketamine was safe in infants undergoing upper airway endoscopy. The researchers concluded that overall, ketamine “could be useful during DISE.”
• Inhalation anesthetics. There were 11 studies of these agents. Of these, six found that inhalation anesthetics caused upper airway collapse while five had heterogeneous outcomes. “Overall, a majority of studies found that inhalation anesthetics exaggerate dynamic airway collapse,” Dr. Ehsan said.
• Opioids. Of the nine studies involving these agents, six found that opioids caused upper airway obstruction; two found that they caused depression of upper airway reflexes, and one found that they caused a decrease in respiratory compliance. “Overall, opioids increase upper airway obstruction,” she said.
Dr. Ehsan acknowledged certain limitations of the analysis, including the fact that there was little information on sleep state approximated by many of these agents, “which makes it difficult to determine the ideal anesthetic protocol. There was substantial heterogeneity in outcomes, and few prospective studies comparing the ability of anesthetics to approximate natural sleep.” She recommended that future efforts focus on comparative effectiveness studies between the agents, as well as evaluate the impact of combining anesthetic agents. “This is important, because most DISE protocols use a combination of agents,” she said.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons
Dr. Ehsan reported having no relevant financial conflicts.
On Twitter @dougbrunk
CORONADO, CALIF. – Studies of the most appropriate anesthetic agents for drug-induced sleep endoscopy are limited, but according to the best available evidence, local anesthetics appear to affect airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse, so they may not be ideal.
Those are key conclusions from a systematic review of literature on the effects of commonly used anesthetic agents and opioids on the upper airway presented at the Triological Society’s Combined Sections meeting. Drug-induced sleep endoscopy (DISE) “is a great tool to assess upper airway dynamics in order to determine optimal surgical therapy for obstructive sleep apnea,” said Dr. Zarmina Ehsan, a pediatric pulmonary medicine fellow at Cincinnati Children’s Hospital Medical Center. “There’s a lack of understanding regarding how upper airway dynamics are altered by anesthetic agents, compared with normal sleep. This is important because this hinders the development of universal guidelines and protocols for the use of DISE.”
Using PubMed, EMBASE, and other sources, she and her associates conducted a qualitative systematic review of studies related to common anesthetic agents and opioids in the medical literature through September 2014. To be eligible for inclusion, a study must have evaluated the agent’s effect on the upper airway, must have contained an abstract, and must have been published in English. Studies with fewer than seven subjects, no original data, review articles, and those involving animals were excluded. The researchers reviewed 180 abstracts and included 56 full text articles in the final analysis, for a total study population of 8,540 patients. At the meeting Dr. Ehsan summarized the following findings by agent:
• Lidocaine. This agent is safe for topical use, has a rapid onset of action, and an intermediate duration of efficacy. Lidocaine acts on muscles “which are potent dilators and tensors of the pharyngeal and laryngeal structures,” she said. Of 10 studies included in the analysis, 7 assessed the impact of lidocaine on upper airway obstruction. Of these, three showed increased airway obstruction while four showed no significant effects. There were two studies on sleep parameters with conflicting results: One showed an increase in mean apnea duration with lidocaine use while the other did not. From this the researchers concluded that lidocaine does affect upper airway dynamics.
• Propofol. This lipophilic intravenous agent has a quick onset of action and acts by global central nervous system depression. Of 12 studies included in the analysis, 4 examined dose-response characteristics and showed a dose-dependent decrease in airway cross-sectional area with increased dosing of propofol. “So increasing your dose makes airway obstruction more likely,” Dr. Ehsan said. “The levels of obstruction were greatest at the base of tongue, and the closure was primarily in the anterior-posterior direction.” Three studies found that propofol caused a decrease in genioglossus electromyogram activity, while the remaining five studies assessed heterogeneous outcomes. “Overall, the studies showed that propofol had a dose-dependent effect on the upper airway with increasing doses making airway obstruction more likely,” she said.
• Dexmedetomidine (DEX). This agent is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic effects. It’s typically given as a 10-minute loading dose followed by a continuous infusion, and is recommended when you want to preserve spontaneous respiration. Of the four DEX-related studies that were included in the analysis, all demonstrated a minimal effect on upper airway cross-sectional area. “One of the studies looked at sleep parameters and concluded that DEX does approximate non-REM sleep without causing respiratory depression,” Dr. Ehsan added. “So overall, DEX was less likely to result in upper airway obstruction, compared with propofol.”
• Midazolam. This agent is commonly used for procedural sedation, with an onset of action within 1-3 minutes and a duration of 15-60 minutes. Of the six studies involving midazolam, two evaluated sleep staging. One reported lack of REM sleep and increased duration of stage N3 sleep, while the other study found that all sleep stages were observed at a lower dosage. The remaining four studies had heterogeneous outcomes. This led the researchers to conclude that midazolam “may lead to upper airway obstruction,” Dr. Ehsan said. “It’s unclear if this is dose dependent.”
• Pentobarbital. Of the two studies involving this short-acting barbiturate, one showed no effect on pharyngeal critical pressure or respiratory muscle function, while the other found that pentobarbital can increase the upper airway cross-sectional area. “So the effect of pentobarbital is unclear,” she said.
• Ketamine. This N-methyl-D-aspartate receptor has a rapid onset and a minimal effect on the central respiratory drive. Of the three studies involving ketamine, one found a 10% incidence of transient laryngospasm, one found that the incidence of transient laryngospasm was higher when it was delivered intramuscularly vs. intravenously, and one found that ketamine was safe in infants undergoing upper airway endoscopy. The researchers concluded that overall, ketamine “could be useful during DISE.”
• Inhalation anesthetics. There were 11 studies of these agents. Of these, six found that inhalation anesthetics caused upper airway collapse while five had heterogeneous outcomes. “Overall, a majority of studies found that inhalation anesthetics exaggerate dynamic airway collapse,” Dr. Ehsan said.
• Opioids. Of the nine studies involving these agents, six found that opioids caused upper airway obstruction; two found that they caused depression of upper airway reflexes, and one found that they caused a decrease in respiratory compliance. “Overall, opioids increase upper airway obstruction,” she said.
Dr. Ehsan acknowledged certain limitations of the analysis, including the fact that there was little information on sleep state approximated by many of these agents, “which makes it difficult to determine the ideal anesthetic protocol. There was substantial heterogeneity in outcomes, and few prospective studies comparing the ability of anesthetics to approximate natural sleep.” She recommended that future efforts focus on comparative effectiveness studies between the agents, as well as evaluate the impact of combining anesthetic agents. “This is important, because most DISE protocols use a combination of agents,” she said.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons
Dr. Ehsan reported having no relevant financial conflicts.
On Twitter @dougbrunk
CORONADO, CALIF. – Studies of the most appropriate anesthetic agents for drug-induced sleep endoscopy are limited, but according to the best available evidence, local anesthetics appear to affect airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse, so they may not be ideal.
Those are key conclusions from a systematic review of literature on the effects of commonly used anesthetic agents and opioids on the upper airway presented at the Triological Society’s Combined Sections meeting. Drug-induced sleep endoscopy (DISE) “is a great tool to assess upper airway dynamics in order to determine optimal surgical therapy for obstructive sleep apnea,” said Dr. Zarmina Ehsan, a pediatric pulmonary medicine fellow at Cincinnati Children’s Hospital Medical Center. “There’s a lack of understanding regarding how upper airway dynamics are altered by anesthetic agents, compared with normal sleep. This is important because this hinders the development of universal guidelines and protocols for the use of DISE.”
Using PubMed, EMBASE, and other sources, she and her associates conducted a qualitative systematic review of studies related to common anesthetic agents and opioids in the medical literature through September 2014. To be eligible for inclusion, a study must have evaluated the agent’s effect on the upper airway, must have contained an abstract, and must have been published in English. Studies with fewer than seven subjects, no original data, review articles, and those involving animals were excluded. The researchers reviewed 180 abstracts and included 56 full text articles in the final analysis, for a total study population of 8,540 patients. At the meeting Dr. Ehsan summarized the following findings by agent:
• Lidocaine. This agent is safe for topical use, has a rapid onset of action, and an intermediate duration of efficacy. Lidocaine acts on muscles “which are potent dilators and tensors of the pharyngeal and laryngeal structures,” she said. Of 10 studies included in the analysis, 7 assessed the impact of lidocaine on upper airway obstruction. Of these, three showed increased airway obstruction while four showed no significant effects. There were two studies on sleep parameters with conflicting results: One showed an increase in mean apnea duration with lidocaine use while the other did not. From this the researchers concluded that lidocaine does affect upper airway dynamics.
• Propofol. This lipophilic intravenous agent has a quick onset of action and acts by global central nervous system depression. Of 12 studies included in the analysis, 4 examined dose-response characteristics and showed a dose-dependent decrease in airway cross-sectional area with increased dosing of propofol. “So increasing your dose makes airway obstruction more likely,” Dr. Ehsan said. “The levels of obstruction were greatest at the base of tongue, and the closure was primarily in the anterior-posterior direction.” Three studies found that propofol caused a decrease in genioglossus electromyogram activity, while the remaining five studies assessed heterogeneous outcomes. “Overall, the studies showed that propofol had a dose-dependent effect on the upper airway with increasing doses making airway obstruction more likely,” she said.
• Dexmedetomidine (DEX). This agent is an alpha-2 adrenergic agonist with sedative, anxiolytic, and analgesic effects. It’s typically given as a 10-minute loading dose followed by a continuous infusion, and is recommended when you want to preserve spontaneous respiration. Of the four DEX-related studies that were included in the analysis, all demonstrated a minimal effect on upper airway cross-sectional area. “One of the studies looked at sleep parameters and concluded that DEX does approximate non-REM sleep without causing respiratory depression,” Dr. Ehsan added. “So overall, DEX was less likely to result in upper airway obstruction, compared with propofol.”
• Midazolam. This agent is commonly used for procedural sedation, with an onset of action within 1-3 minutes and a duration of 15-60 minutes. Of the six studies involving midazolam, two evaluated sleep staging. One reported lack of REM sleep and increased duration of stage N3 sleep, while the other study found that all sleep stages were observed at a lower dosage. The remaining four studies had heterogeneous outcomes. This led the researchers to conclude that midazolam “may lead to upper airway obstruction,” Dr. Ehsan said. “It’s unclear if this is dose dependent.”
• Pentobarbital. Of the two studies involving this short-acting barbiturate, one showed no effect on pharyngeal critical pressure or respiratory muscle function, while the other found that pentobarbital can increase the upper airway cross-sectional area. “So the effect of pentobarbital is unclear,” she said.
• Ketamine. This N-methyl-D-aspartate receptor has a rapid onset and a minimal effect on the central respiratory drive. Of the three studies involving ketamine, one found a 10% incidence of transient laryngospasm, one found that the incidence of transient laryngospasm was higher when it was delivered intramuscularly vs. intravenously, and one found that ketamine was safe in infants undergoing upper airway endoscopy. The researchers concluded that overall, ketamine “could be useful during DISE.”
• Inhalation anesthetics. There were 11 studies of these agents. Of these, six found that inhalation anesthetics caused upper airway collapse while five had heterogeneous outcomes. “Overall, a majority of studies found that inhalation anesthetics exaggerate dynamic airway collapse,” Dr. Ehsan said.
• Opioids. Of the nine studies involving these agents, six found that opioids caused upper airway obstruction; two found that they caused depression of upper airway reflexes, and one found that they caused a decrease in respiratory compliance. “Overall, opioids increase upper airway obstruction,” she said.
Dr. Ehsan acknowledged certain limitations of the analysis, including the fact that there was little information on sleep state approximated by many of these agents, “which makes it difficult to determine the ideal anesthetic protocol. There was substantial heterogeneity in outcomes, and few prospective studies comparing the ability of anesthetics to approximate natural sleep.” She recommended that future efforts focus on comparative effectiveness studies between the agents, as well as evaluate the impact of combining anesthetic agents. “This is important, because most DISE protocols use a combination of agents,” she said.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons
Dr. Ehsan reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT THE COMBINED SECTIONS WINTER MEETING
Key clinical point: Choice of an appropriate anesthetic protocol for drug-induced sleep endoscopy must be based on a limited number of comparative studies.
Major finding: Local anesthetics appear to affect upper airway reflexes while inhalation anesthetics and opioids exaggerate dynamic airway collapse.
Data source: A qualitative systematic review of 56 studies related to common anesthetic agents and opioids published in the medical literature through September 2014.
Disclosures: Dr. Ehsan reported having no financial disclosures.
Smart diet remains potent cardiovascular medicine
SNOWMASS, COLO. – Cutting dietary fat intake remains a highly effective strategy for reducing coronary heart disease risk – but only so long as the replacement nutrients aren’t even bigger offenders, Dr. Robert A. Vogel said at the Annual Cardiovascular Conference at Snowmass.
In the face of decades of public health admonitions to reduce saturated fat intake, most Americans have increased their consumption of trans fats and simple carbohydrates, especially sugar. And therein lies a problem. Trans fats are far more harmful than saturated fats in terms of cardiovascular risk. And excessive sugar consumption is a major contributor to abdominal obesity, metabolic syndrome, hypertension, and endothelial dysfunction.
“In the United States, sugar is a bigger source of hypertension than is salt,” asserted Dr. Vogel, a cardiologist at the University of Colorado, Denver.
The editors of Time magazine ignited a public controversy last year with a cover story arrestingly titled, “Eat Butter – Scientists labelled fat the enemy. Why they were wrong.” The editors were picking up on a British meta-analysis of 32 observational studies that concluded there is no clear evidence to support the notion that saturated fats are harmful to cardiovascular health and that swapping them out for consumption of polyunsaturated fatty acids (PUFAs) is beneficial (Ann. Intern. Med. 2014;160:398-406).
Dr. Vogel said those investigators are in fact correct: Many of the observational studies – going all the way back to the pioneering work by Dr. Ancel Keys in the 1950s – are flawed. They don’t convincingly prove the case for PUFAs as a healthier alternative. But there is persuasive evidence from well-conducted, randomized, controlled trials that this is indeed so, he added.
Several of these studies were done in an earlier era when it was possible to slip around the challenges and limitations of dietary studies in free-living populations. These trials wouldn’t be possible today for ethical reasons involving lack of informed consent.
For example, in the Finnish Mental Hospital Study conducted during 1959-1971, the food served at two mental institutions was altered. Patients at one hospital got 6 years of a diet high in PUFAs, then were crossed over to a typical Finnish diet. At the other mental hospital, patients were fed a normal Finnish diet for 6 years, then crossed over to the high-PUFA diet for 6 years. During the experimental-diet years, the coronary heart disease event rate was reduced by nearly 60% (Int. J. Epidemiol. 1979;8:99-118).
Similarly, in a prospective randomized trial conducted at a Los Angeles Veterans Affairs institution for older, cognitively impaired men, a no-choice shift to a diet high in PUFAs with reduced saturated fats resulted in roughly a 30% reduction in CHD events compared to the usual institutional diet (Lancet 1968;2:1060-2). A similar magnitude of CHD event reduction was seen with a high-PUFA dietary intervention in the Oslo Diet-Heart Study, a prospective secondary prevention trial (Circulation 1970;42:935-42).
In the contemporary era, the standout randomized dietary intervention trial is the Lyon Diet Heart Study, a 46-month prospective secondary prevention trial in which a Mediterranean diet low in saturated fat and high in alpha-linoleic acid, a PUFA, reduced the combined endpoint of cardiac death and nonfatal MI by 70%, compared with the usual post-MI prudent diet recommended at that time. Yet total cholesterol levels in the two study arms did not differ (Circulation 1999;99:779-85).
To put these results into context, Dr. Vogel noted that the Cholesterol Treatment Trialists Collaboration headquartered at the University of Oxford (England) has shown that for every 40 mg/dL of LDL-lowering achieved with statin therapy, the result is roughly a 20% reduction in CHD. In contrast, the classic nonpharmacologic diet studies resulted in 30%-70% relative risk reductions.
“Heart disease is a dietary disease,” the cardiologist emphasized. “When you compare diet intervention to LDL lowering with statins, you see that diet is very, very effective. But you have to know the details of the diet. You can’t take something out and put just anything in. It doesn’t work like that.”
For example, an analysis of data from the National Health and Nutrition Examination Survey concluded that individuals who consumed 25% of their calories from added sugar – that’s the equivalent of three 12-oz cans of a sugary cola per day – had a 175% increased risk of cardiovascular mortality during a median 14.6 years of follow-up, compared with those who got less than 10% of their calories from added sugar (JAMA Intern. Med. 2014;174:516-24).
And as for the impact of the trans fat that’s liberally present in many processed foods, the Nurses Health Study showed that for every 5% increase in energy intake from saturated fat – that’s equivalent to one 8-oz steak per day – the relative risk for CHD rose by a relatively modest 17%, while for a 5% increase in energy intake from trans fat – the equivalent of 4 oz of butter – CHD risk shot up by 382% (N. Engl. J. Med. 1997;337:1491-9).
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center and receiving a research grant from Sanofi.
SNOWMASS, COLO. – Cutting dietary fat intake remains a highly effective strategy for reducing coronary heart disease risk – but only so long as the replacement nutrients aren’t even bigger offenders, Dr. Robert A. Vogel said at the Annual Cardiovascular Conference at Snowmass.
In the face of decades of public health admonitions to reduce saturated fat intake, most Americans have increased their consumption of trans fats and simple carbohydrates, especially sugar. And therein lies a problem. Trans fats are far more harmful than saturated fats in terms of cardiovascular risk. And excessive sugar consumption is a major contributor to abdominal obesity, metabolic syndrome, hypertension, and endothelial dysfunction.
“In the United States, sugar is a bigger source of hypertension than is salt,” asserted Dr. Vogel, a cardiologist at the University of Colorado, Denver.
The editors of Time magazine ignited a public controversy last year with a cover story arrestingly titled, “Eat Butter – Scientists labelled fat the enemy. Why they were wrong.” The editors were picking up on a British meta-analysis of 32 observational studies that concluded there is no clear evidence to support the notion that saturated fats are harmful to cardiovascular health and that swapping them out for consumption of polyunsaturated fatty acids (PUFAs) is beneficial (Ann. Intern. Med. 2014;160:398-406).
Dr. Vogel said those investigators are in fact correct: Many of the observational studies – going all the way back to the pioneering work by Dr. Ancel Keys in the 1950s – are flawed. They don’t convincingly prove the case for PUFAs as a healthier alternative. But there is persuasive evidence from well-conducted, randomized, controlled trials that this is indeed so, he added.
Several of these studies were done in an earlier era when it was possible to slip around the challenges and limitations of dietary studies in free-living populations. These trials wouldn’t be possible today for ethical reasons involving lack of informed consent.
For example, in the Finnish Mental Hospital Study conducted during 1959-1971, the food served at two mental institutions was altered. Patients at one hospital got 6 years of a diet high in PUFAs, then were crossed over to a typical Finnish diet. At the other mental hospital, patients were fed a normal Finnish diet for 6 years, then crossed over to the high-PUFA diet for 6 years. During the experimental-diet years, the coronary heart disease event rate was reduced by nearly 60% (Int. J. Epidemiol. 1979;8:99-118).
Similarly, in a prospective randomized trial conducted at a Los Angeles Veterans Affairs institution for older, cognitively impaired men, a no-choice shift to a diet high in PUFAs with reduced saturated fats resulted in roughly a 30% reduction in CHD events compared to the usual institutional diet (Lancet 1968;2:1060-2). A similar magnitude of CHD event reduction was seen with a high-PUFA dietary intervention in the Oslo Diet-Heart Study, a prospective secondary prevention trial (Circulation 1970;42:935-42).
In the contemporary era, the standout randomized dietary intervention trial is the Lyon Diet Heart Study, a 46-month prospective secondary prevention trial in which a Mediterranean diet low in saturated fat and high in alpha-linoleic acid, a PUFA, reduced the combined endpoint of cardiac death and nonfatal MI by 70%, compared with the usual post-MI prudent diet recommended at that time. Yet total cholesterol levels in the two study arms did not differ (Circulation 1999;99:779-85).
To put these results into context, Dr. Vogel noted that the Cholesterol Treatment Trialists Collaboration headquartered at the University of Oxford (England) has shown that for every 40 mg/dL of LDL-lowering achieved with statin therapy, the result is roughly a 20% reduction in CHD. In contrast, the classic nonpharmacologic diet studies resulted in 30%-70% relative risk reductions.
“Heart disease is a dietary disease,” the cardiologist emphasized. “When you compare diet intervention to LDL lowering with statins, you see that diet is very, very effective. But you have to know the details of the diet. You can’t take something out and put just anything in. It doesn’t work like that.”
For example, an analysis of data from the National Health and Nutrition Examination Survey concluded that individuals who consumed 25% of their calories from added sugar – that’s the equivalent of three 12-oz cans of a sugary cola per day – had a 175% increased risk of cardiovascular mortality during a median 14.6 years of follow-up, compared with those who got less than 10% of their calories from added sugar (JAMA Intern. Med. 2014;174:516-24).
And as for the impact of the trans fat that’s liberally present in many processed foods, the Nurses Health Study showed that for every 5% increase in energy intake from saturated fat – that’s equivalent to one 8-oz steak per day – the relative risk for CHD rose by a relatively modest 17%, while for a 5% increase in energy intake from trans fat – the equivalent of 4 oz of butter – CHD risk shot up by 382% (N. Engl. J. Med. 1997;337:1491-9).
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center and receiving a research grant from Sanofi.
SNOWMASS, COLO. – Cutting dietary fat intake remains a highly effective strategy for reducing coronary heart disease risk – but only so long as the replacement nutrients aren’t even bigger offenders, Dr. Robert A. Vogel said at the Annual Cardiovascular Conference at Snowmass.
In the face of decades of public health admonitions to reduce saturated fat intake, most Americans have increased their consumption of trans fats and simple carbohydrates, especially sugar. And therein lies a problem. Trans fats are far more harmful than saturated fats in terms of cardiovascular risk. And excessive sugar consumption is a major contributor to abdominal obesity, metabolic syndrome, hypertension, and endothelial dysfunction.
“In the United States, sugar is a bigger source of hypertension than is salt,” asserted Dr. Vogel, a cardiologist at the University of Colorado, Denver.
The editors of Time magazine ignited a public controversy last year with a cover story arrestingly titled, “Eat Butter – Scientists labelled fat the enemy. Why they were wrong.” The editors were picking up on a British meta-analysis of 32 observational studies that concluded there is no clear evidence to support the notion that saturated fats are harmful to cardiovascular health and that swapping them out for consumption of polyunsaturated fatty acids (PUFAs) is beneficial (Ann. Intern. Med. 2014;160:398-406).
Dr. Vogel said those investigators are in fact correct: Many of the observational studies – going all the way back to the pioneering work by Dr. Ancel Keys in the 1950s – are flawed. They don’t convincingly prove the case for PUFAs as a healthier alternative. But there is persuasive evidence from well-conducted, randomized, controlled trials that this is indeed so, he added.
Several of these studies were done in an earlier era when it was possible to slip around the challenges and limitations of dietary studies in free-living populations. These trials wouldn’t be possible today for ethical reasons involving lack of informed consent.
For example, in the Finnish Mental Hospital Study conducted during 1959-1971, the food served at two mental institutions was altered. Patients at one hospital got 6 years of a diet high in PUFAs, then were crossed over to a typical Finnish diet. At the other mental hospital, patients were fed a normal Finnish diet for 6 years, then crossed over to the high-PUFA diet for 6 years. During the experimental-diet years, the coronary heart disease event rate was reduced by nearly 60% (Int. J. Epidemiol. 1979;8:99-118).
Similarly, in a prospective randomized trial conducted at a Los Angeles Veterans Affairs institution for older, cognitively impaired men, a no-choice shift to a diet high in PUFAs with reduced saturated fats resulted in roughly a 30% reduction in CHD events compared to the usual institutional diet (Lancet 1968;2:1060-2). A similar magnitude of CHD event reduction was seen with a high-PUFA dietary intervention in the Oslo Diet-Heart Study, a prospective secondary prevention trial (Circulation 1970;42:935-42).
In the contemporary era, the standout randomized dietary intervention trial is the Lyon Diet Heart Study, a 46-month prospective secondary prevention trial in which a Mediterranean diet low in saturated fat and high in alpha-linoleic acid, a PUFA, reduced the combined endpoint of cardiac death and nonfatal MI by 70%, compared with the usual post-MI prudent diet recommended at that time. Yet total cholesterol levels in the two study arms did not differ (Circulation 1999;99:779-85).
To put these results into context, Dr. Vogel noted that the Cholesterol Treatment Trialists Collaboration headquartered at the University of Oxford (England) has shown that for every 40 mg/dL of LDL-lowering achieved with statin therapy, the result is roughly a 20% reduction in CHD. In contrast, the classic nonpharmacologic diet studies resulted in 30%-70% relative risk reductions.
“Heart disease is a dietary disease,” the cardiologist emphasized. “When you compare diet intervention to LDL lowering with statins, you see that diet is very, very effective. But you have to know the details of the diet. You can’t take something out and put just anything in. It doesn’t work like that.”
For example, an analysis of data from the National Health and Nutrition Examination Survey concluded that individuals who consumed 25% of their calories from added sugar – that’s the equivalent of three 12-oz cans of a sugary cola per day – had a 175% increased risk of cardiovascular mortality during a median 14.6 years of follow-up, compared with those who got less than 10% of their calories from added sugar (JAMA Intern. Med. 2014;174:516-24).
And as for the impact of the trans fat that’s liberally present in many processed foods, the Nurses Health Study showed that for every 5% increase in energy intake from saturated fat – that’s equivalent to one 8-oz steak per day – the relative risk for CHD rose by a relatively modest 17%, while for a 5% increase in energy intake from trans fat – the equivalent of 4 oz of butter – CHD risk shot up by 382% (N. Engl. J. Med. 1997;337:1491-9).
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center and receiving a research grant from Sanofi.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Experimental vaccine may have worked on Ebola-exposed physician
A U.S. physician exposed to Ebola virus received an investigational vaccine afterward and didn’t contract the disease, but the vaccine’s effectiveness remains unknown, according to report published online March 5 in JAMA.
The vaccine, VSV[Delta]G-ZEBOV, is based on a vesicular stomatitis virus with the glycoprotein gene replaced by a Zaire Ebola glycoprotein gene.
The physician received the vaccine slightly less than 2 days after Ebola exposure. After 12 hours, symptoms appeared that are associated with vesicular stomatitis virus. Those dissipated after 3-4 days, noted Dr. Lilin Lai of Emory University, Atlanta, and her colleagues.
No Ebola symptoms were detected, but the patient tested positive for Ebola virus glycoprotein-specific antibodies and T cells, which was an intended effect of the vaccine.
A single case report cannot provide a definitive answer to the effectiveness of VSV[Delta]G-ZEBOV, noted Thomas W. Geisbert, Ph.D. of the Galveston National Laboratory, University of Texas Medical Branch, in a related editorial. However, “this incident serves as an example of how important it is to have safe and effective countermeasures available in sufficient quantities that can be rapidly deployed for emergency use for both medical workers and affected populations.”
Find the full study and editorial in JAMA: (doi: 10.1001/jama.2015.1995) and (doi: 10.1001/jama.2015.2057).
A U.S. physician exposed to Ebola virus received an investigational vaccine afterward and didn’t contract the disease, but the vaccine’s effectiveness remains unknown, according to report published online March 5 in JAMA.
The vaccine, VSV[Delta]G-ZEBOV, is based on a vesicular stomatitis virus with the glycoprotein gene replaced by a Zaire Ebola glycoprotein gene.
The physician received the vaccine slightly less than 2 days after Ebola exposure. After 12 hours, symptoms appeared that are associated with vesicular stomatitis virus. Those dissipated after 3-4 days, noted Dr. Lilin Lai of Emory University, Atlanta, and her colleagues.
No Ebola symptoms were detected, but the patient tested positive for Ebola virus glycoprotein-specific antibodies and T cells, which was an intended effect of the vaccine.
A single case report cannot provide a definitive answer to the effectiveness of VSV[Delta]G-ZEBOV, noted Thomas W. Geisbert, Ph.D. of the Galveston National Laboratory, University of Texas Medical Branch, in a related editorial. However, “this incident serves as an example of how important it is to have safe and effective countermeasures available in sufficient quantities that can be rapidly deployed for emergency use for both medical workers and affected populations.”
Find the full study and editorial in JAMA: (doi: 10.1001/jama.2015.1995) and (doi: 10.1001/jama.2015.2057).
A U.S. physician exposed to Ebola virus received an investigational vaccine afterward and didn’t contract the disease, but the vaccine’s effectiveness remains unknown, according to report published online March 5 in JAMA.
The vaccine, VSV[Delta]G-ZEBOV, is based on a vesicular stomatitis virus with the glycoprotein gene replaced by a Zaire Ebola glycoprotein gene.
The physician received the vaccine slightly less than 2 days after Ebola exposure. After 12 hours, symptoms appeared that are associated with vesicular stomatitis virus. Those dissipated after 3-4 days, noted Dr. Lilin Lai of Emory University, Atlanta, and her colleagues.
No Ebola symptoms were detected, but the patient tested positive for Ebola virus glycoprotein-specific antibodies and T cells, which was an intended effect of the vaccine.
A single case report cannot provide a definitive answer to the effectiveness of VSV[Delta]G-ZEBOV, noted Thomas W. Geisbert, Ph.D. of the Galveston National Laboratory, University of Texas Medical Branch, in a related editorial. However, “this incident serves as an example of how important it is to have safe and effective countermeasures available in sufficient quantities that can be rapidly deployed for emergency use for both medical workers and affected populations.”
Find the full study and editorial in JAMA: (doi: 10.1001/jama.2015.1995) and (doi: 10.1001/jama.2015.2057).
Regimen prolongs PFS, increases AEs in MCL

Results of a phase 3 study suggest the VR-CAP regimen is more effective but less safe than R-CHOP in patients with newly diagnosed mantle cell lymphoma (MCL).
Patients who received VR-CAP (bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone) had superior progression-free survival (PFS) when compared to patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
But VR-CAP was also associated with more adverse events (AEs), particularly hematologic toxicities.
Tadeusz Robak, MD, of the Medical University of Lodz in Poland, and his colleagues reported results from this trial, known as LYM-3002, in NEJM. The study was funded by Janssen Research and Development and Millennium Pharmaceuticals.
LYM-3002 included 487 patients newly diagnosed with MCL who were not eligible for stem cell transplant.
Patients were randomized to receive six to eight 21-day cycles of R-CHOP intravenously on day 1 (with prednisone administered orally on days 1 to 5) or VR-CAP (similar to the R-CHOP regimen, but replacing vincristine with bortezomib at a dose of 1.3 mg per square meter of body-surface area on days 1, 4, 8, and 11).
The median follow-up was 40 months. The VR-CAP regimen significantly improved PFS, the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median PFS times of 24.7 months and 14.4 months, respectively (hazard ratio [HR]=0.63, P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median PFS times of 30.7 months and 16.1 months, respectively (HR=0.51, P<0.001).
Patients in the VR-CAP arm also fared better with regard to some secondary endpoints. The complete response rate was higher in the VR-CAP arm than the R-CHOP arm—53% and 42%, respectively (HR=1.29, P=0.007).
And patients in the VR-CAP arm had a longer median treatment-free interval—40.6 months and 20.5 months, respectively (HR=0.50, P<0.001).
However, there was no significant difference in overall survival between the treatment arms. The median overall survival was not reached in the VR-CAP arm and was 56.3 months in the R-CHOP arm (HR=0.80, P=0.17). The 4-year overall survival rate was 64% and 54%, respectively.
The investigators said VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious AEs were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Hematologic toxicity was more common in the VR-CAP arm than the R-CHOP arm. This included thrombocytopenia (72% vs 19%), neutropenia (88% vs 74%), anemia (51% vs 37%), leukopenia (50% vs 38%), lymphocytopenia (31% vs 13%), and febrile neutropenia (17% vs 14%).
Treatment discontinuation due to AEs occurred in 8% of patients in the VR-CAP arm and 6% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
It was based on these results that bortezomib was approved for use in patients with newly diagnosed MCL in the Europe Union and the US. ![]()

Results of a phase 3 study suggest the VR-CAP regimen is more effective but less safe than R-CHOP in patients with newly diagnosed mantle cell lymphoma (MCL).
Patients who received VR-CAP (bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone) had superior progression-free survival (PFS) when compared to patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
But VR-CAP was also associated with more adverse events (AEs), particularly hematologic toxicities.
Tadeusz Robak, MD, of the Medical University of Lodz in Poland, and his colleagues reported results from this trial, known as LYM-3002, in NEJM. The study was funded by Janssen Research and Development and Millennium Pharmaceuticals.
LYM-3002 included 487 patients newly diagnosed with MCL who were not eligible for stem cell transplant.
Patients were randomized to receive six to eight 21-day cycles of R-CHOP intravenously on day 1 (with prednisone administered orally on days 1 to 5) or VR-CAP (similar to the R-CHOP regimen, but replacing vincristine with bortezomib at a dose of 1.3 mg per square meter of body-surface area on days 1, 4, 8, and 11).
The median follow-up was 40 months. The VR-CAP regimen significantly improved PFS, the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median PFS times of 24.7 months and 14.4 months, respectively (hazard ratio [HR]=0.63, P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median PFS times of 30.7 months and 16.1 months, respectively (HR=0.51, P<0.001).
Patients in the VR-CAP arm also fared better with regard to some secondary endpoints. The complete response rate was higher in the VR-CAP arm than the R-CHOP arm—53% and 42%, respectively (HR=1.29, P=0.007).
And patients in the VR-CAP arm had a longer median treatment-free interval—40.6 months and 20.5 months, respectively (HR=0.50, P<0.001).
However, there was no significant difference in overall survival between the treatment arms. The median overall survival was not reached in the VR-CAP arm and was 56.3 months in the R-CHOP arm (HR=0.80, P=0.17). The 4-year overall survival rate was 64% and 54%, respectively.
The investigators said VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious AEs were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Hematologic toxicity was more common in the VR-CAP arm than the R-CHOP arm. This included thrombocytopenia (72% vs 19%), neutropenia (88% vs 74%), anemia (51% vs 37%), leukopenia (50% vs 38%), lymphocytopenia (31% vs 13%), and febrile neutropenia (17% vs 14%).
Treatment discontinuation due to AEs occurred in 8% of patients in the VR-CAP arm and 6% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
It was based on these results that bortezomib was approved for use in patients with newly diagnosed MCL in the Europe Union and the US. ![]()

Results of a phase 3 study suggest the VR-CAP regimen is more effective but less safe than R-CHOP in patients with newly diagnosed mantle cell lymphoma (MCL).
Patients who received VR-CAP (bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone) had superior progression-free survival (PFS) when compared to patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
But VR-CAP was also associated with more adverse events (AEs), particularly hematologic toxicities.
Tadeusz Robak, MD, of the Medical University of Lodz in Poland, and his colleagues reported results from this trial, known as LYM-3002, in NEJM. The study was funded by Janssen Research and Development and Millennium Pharmaceuticals.
LYM-3002 included 487 patients newly diagnosed with MCL who were not eligible for stem cell transplant.
Patients were randomized to receive six to eight 21-day cycles of R-CHOP intravenously on day 1 (with prednisone administered orally on days 1 to 5) or VR-CAP (similar to the R-CHOP regimen, but replacing vincristine with bortezomib at a dose of 1.3 mg per square meter of body-surface area on days 1, 4, 8, and 11).
The median follow-up was 40 months. The VR-CAP regimen significantly improved PFS, the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median PFS times of 24.7 months and 14.4 months, respectively (hazard ratio [HR]=0.63, P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median PFS times of 30.7 months and 16.1 months, respectively (HR=0.51, P<0.001).
Patients in the VR-CAP arm also fared better with regard to some secondary endpoints. The complete response rate was higher in the VR-CAP arm than the R-CHOP arm—53% and 42%, respectively (HR=1.29, P=0.007).
And patients in the VR-CAP arm had a longer median treatment-free interval—40.6 months and 20.5 months, respectively (HR=0.50, P<0.001).
However, there was no significant difference in overall survival between the treatment arms. The median overall survival was not reached in the VR-CAP arm and was 56.3 months in the R-CHOP arm (HR=0.80, P=0.17). The 4-year overall survival rate was 64% and 54%, respectively.
The investigators said VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious AEs were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Hematologic toxicity was more common in the VR-CAP arm than the R-CHOP arm. This included thrombocytopenia (72% vs 19%), neutropenia (88% vs 74%), anemia (51% vs 37%), leukopenia (50% vs 38%), lymphocytopenia (31% vs 13%), and febrile neutropenia (17% vs 14%).
Treatment discontinuation due to AEs occurred in 8% of patients in the VR-CAP arm and 6% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
It was based on these results that bortezomib was approved for use in patients with newly diagnosed MCL in the Europe Union and the US. ![]()