User login
Product granted orphan designation for GVHD

Credit: PLOS ONE
The European Medicines Agency (EMA) has granted orphan drug status to ApoCell for the prevention of graft-vs-host disease (GVHD).
ApoCell consists of matched-donor, mononuclear-enriched, early apoptotic cells. It has been shown to immunomodulate macrophages and dendritic cells, both of which are involved in GVHD pathogenesis.
ApoCell showed early promise in a phase 1/2a study, and a phase 2b/3 trial of the product is set to begin this year.
ApoCell, which is under development by Enlivex Therapeutics, received orphan drug designation in the US in 2013.
In the European Union (EU), orphan designation is granted to products intended for the treatment, prevention, or diagnosis of a life-threatening or chronically debilitating disease with a prevalence of no more than 5 in 10,000, with no satisfactory method of diagnosis, prevention, or treatment authorized by the EMA.
Orphan designation in the EU comes with a number of benefits, including protocol assistance and 10-year market exclusivity following regulatory approval.
Phase 1/2a trial of ApoCell
For this study, researchers tested an infusion of ApoCell, in addition to cyclosporine and methotrexate, as prophylaxis for acute GVHD.
The trial enrolled 13 leukemia patients who had a median age of 37 (range, 20-59). All of the patients received an HLA-matched, myeloablative, allogeneic hematopoietic stem cell transplant (HSCT) from a related donor.
All patients engrafted. The median time to neutrophil recovery was 13 days after HSCT (range, 11 to 19), and the median time to platelet recovery was 15 days (range, 11 to 59).
At 100 days post-HSCT, the cumulative incidence of acute grade 2-4 GVHD was 23.1%, and the incidence of acute grade 3-4 GVHD was 15.4%. None of the patients developed acute GVHD beyond day 100.
Among patients who received the 2 higher doses of ApoCell (n=6), the rate of acute grade 2-4 GVHD was 0%.
Ten patients experienced serious adverse events, but 7 were considered unrelated to ApoCell, and 3 were likely unrelated to the treatment.
The nonrelapse mortality rate was 7.7% at both 100 and 180 days after HSCT. The overall survival rate was 92% at 100 days and 85% at 180 days.
The researchers said these results suggest a single infusion of ApoCell is safe and may effectively prevent acute GVHD. ![]()

Credit: PLOS ONE
The European Medicines Agency (EMA) has granted orphan drug status to ApoCell for the prevention of graft-vs-host disease (GVHD).
ApoCell consists of matched-donor, mononuclear-enriched, early apoptotic cells. It has been shown to immunomodulate macrophages and dendritic cells, both of which are involved in GVHD pathogenesis.
ApoCell showed early promise in a phase 1/2a study, and a phase 2b/3 trial of the product is set to begin this year.
ApoCell, which is under development by Enlivex Therapeutics, received orphan drug designation in the US in 2013.
In the European Union (EU), orphan designation is granted to products intended for the treatment, prevention, or diagnosis of a life-threatening or chronically debilitating disease with a prevalence of no more than 5 in 10,000, with no satisfactory method of diagnosis, prevention, or treatment authorized by the EMA.
Orphan designation in the EU comes with a number of benefits, including protocol assistance and 10-year market exclusivity following regulatory approval.
Phase 1/2a trial of ApoCell
For this study, researchers tested an infusion of ApoCell, in addition to cyclosporine and methotrexate, as prophylaxis for acute GVHD.
The trial enrolled 13 leukemia patients who had a median age of 37 (range, 20-59). All of the patients received an HLA-matched, myeloablative, allogeneic hematopoietic stem cell transplant (HSCT) from a related donor.
All patients engrafted. The median time to neutrophil recovery was 13 days after HSCT (range, 11 to 19), and the median time to platelet recovery was 15 days (range, 11 to 59).
At 100 days post-HSCT, the cumulative incidence of acute grade 2-4 GVHD was 23.1%, and the incidence of acute grade 3-4 GVHD was 15.4%. None of the patients developed acute GVHD beyond day 100.
Among patients who received the 2 higher doses of ApoCell (n=6), the rate of acute grade 2-4 GVHD was 0%.
Ten patients experienced serious adverse events, but 7 were considered unrelated to ApoCell, and 3 were likely unrelated to the treatment.
The nonrelapse mortality rate was 7.7% at both 100 and 180 days after HSCT. The overall survival rate was 92% at 100 days and 85% at 180 days.
The researchers said these results suggest a single infusion of ApoCell is safe and may effectively prevent acute GVHD. ![]()

Credit: PLOS ONE
The European Medicines Agency (EMA) has granted orphan drug status to ApoCell for the prevention of graft-vs-host disease (GVHD).
ApoCell consists of matched-donor, mononuclear-enriched, early apoptotic cells. It has been shown to immunomodulate macrophages and dendritic cells, both of which are involved in GVHD pathogenesis.
ApoCell showed early promise in a phase 1/2a study, and a phase 2b/3 trial of the product is set to begin this year.
ApoCell, which is under development by Enlivex Therapeutics, received orphan drug designation in the US in 2013.
In the European Union (EU), orphan designation is granted to products intended for the treatment, prevention, or diagnosis of a life-threatening or chronically debilitating disease with a prevalence of no more than 5 in 10,000, with no satisfactory method of diagnosis, prevention, or treatment authorized by the EMA.
Orphan designation in the EU comes with a number of benefits, including protocol assistance and 10-year market exclusivity following regulatory approval.
Phase 1/2a trial of ApoCell
For this study, researchers tested an infusion of ApoCell, in addition to cyclosporine and methotrexate, as prophylaxis for acute GVHD.
The trial enrolled 13 leukemia patients who had a median age of 37 (range, 20-59). All of the patients received an HLA-matched, myeloablative, allogeneic hematopoietic stem cell transplant (HSCT) from a related donor.
All patients engrafted. The median time to neutrophil recovery was 13 days after HSCT (range, 11 to 19), and the median time to platelet recovery was 15 days (range, 11 to 59).
At 100 days post-HSCT, the cumulative incidence of acute grade 2-4 GVHD was 23.1%, and the incidence of acute grade 3-4 GVHD was 15.4%. None of the patients developed acute GVHD beyond day 100.
Among patients who received the 2 higher doses of ApoCell (n=6), the rate of acute grade 2-4 GVHD was 0%.
Ten patients experienced serious adverse events, but 7 were considered unrelated to ApoCell, and 3 were likely unrelated to the treatment.
The nonrelapse mortality rate was 7.7% at both 100 and 180 days after HSCT. The overall survival rate was 92% at 100 days and 85% at 180 days.
The researchers said these results suggest a single infusion of ApoCell is safe and may effectively prevent acute GVHD. ![]()
NICE recommends rivaroxaban for ACS

Credit: NHS
In its final draft guidance, the UK’s National Institute for Health and Care Excellence (NICE) is recommending rivaroxaban (Xarelto) as an option for preventing adverse outcomes in patients with acute coronary syndromes (ACS).
The agency said it supports use of the factor Xa inhibitor in combination with aspirin and clopidogrel or aspirin alone to prevent atherothrombotic events in ACS patients with elevated cardiac biomarkers.
This includes patients who have had ST-segment-elevation myocardial infarctions (STEMIs) or non-ST-segment myocardial infarctions (NSTEMIs) but not unstable angina. In unstable angina, damage to the heart is not severe enough to result in the release of biomarkers into the blood, so this condition is not included in the guidance.
“Because rivaroxaban is associated with a higher risk of causing bleeding than clopidogrel in combination with aspirin or aspirin alone, the draft guidance recommends that, before starting treatment, doctors should carry out a careful assessment of a person’s bleeding risk,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“The decision to start treatment should be made after an informed discussion between the doctor and patient about the benefits and risks of rivaroxaban. Also, because there is limited experience of treatment with rivaroxaban up to 24 months, the draft guidance recommends careful consideration should be given to whether treatment is continued beyond 12 months.”
The final draft guidance is now with consultees, who have the opportunity to appeal against it. Once NICE issues its final guidance on a technology, it replaces local recommendations.
Cost and clinical effectiveness
An appraisal committee advising NICE concluded that rivaroxaban given at 2.5 mg twice daily in combination with aspirin plus clopidogrel or with aspirin alone was more effective than aspirin plus clopidogrel or aspirin alone for preventing further cardiovascular deaths and myocardial infarction in patients with ACS and raised cardiac biomarkers.
The committee also found rivaroxaban to be cost-effective. According to Bayer Healthcare (the company co-developing rivaroxaban with Janssen Research & Development, LLC), the base-case incremental cost-effectiveness ratio (ICER) was £6203 per quality-adjusted life-year (QALY) gained. The evidence review group’s preferred base-case estimate was £5622 per QALY gained.
The committee said there is uncertainty about the validity of these results, which were based on the ATLAS-ACS 2-TIMI 51 trial, because of the risk of bias resulting from missing trial data and informative censoring.
However, the committee considered that the ICERs presented were all within the range that could be considered cost-effective, and adjusting for the various types of bias that might have occurred was unlikely to increase the ICER to the extent that it would become unacceptable.
The list price of rivaroxaban is £58.88 per 2.5 mg, 56-capsule pack (excluding value-added tax). The license dose is 2.5 mg twice daily, which equates to a price of £2.10 per day.
Assuming a treatment duration of 12 months, total acquisition costs are £766.50. Costs may vary in different settings because of negotiated procurement discounts. ![]()

Credit: NHS
In its final draft guidance, the UK’s National Institute for Health and Care Excellence (NICE) is recommending rivaroxaban (Xarelto) as an option for preventing adverse outcomes in patients with acute coronary syndromes (ACS).
The agency said it supports use of the factor Xa inhibitor in combination with aspirin and clopidogrel or aspirin alone to prevent atherothrombotic events in ACS patients with elevated cardiac biomarkers.
This includes patients who have had ST-segment-elevation myocardial infarctions (STEMIs) or non-ST-segment myocardial infarctions (NSTEMIs) but not unstable angina. In unstable angina, damage to the heart is not severe enough to result in the release of biomarkers into the blood, so this condition is not included in the guidance.
“Because rivaroxaban is associated with a higher risk of causing bleeding than clopidogrel in combination with aspirin or aspirin alone, the draft guidance recommends that, before starting treatment, doctors should carry out a careful assessment of a person’s bleeding risk,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“The decision to start treatment should be made after an informed discussion between the doctor and patient about the benefits and risks of rivaroxaban. Also, because there is limited experience of treatment with rivaroxaban up to 24 months, the draft guidance recommends careful consideration should be given to whether treatment is continued beyond 12 months.”
The final draft guidance is now with consultees, who have the opportunity to appeal against it. Once NICE issues its final guidance on a technology, it replaces local recommendations.
Cost and clinical effectiveness
An appraisal committee advising NICE concluded that rivaroxaban given at 2.5 mg twice daily in combination with aspirin plus clopidogrel or with aspirin alone was more effective than aspirin plus clopidogrel or aspirin alone for preventing further cardiovascular deaths and myocardial infarction in patients with ACS and raised cardiac biomarkers.
The committee also found rivaroxaban to be cost-effective. According to Bayer Healthcare (the company co-developing rivaroxaban with Janssen Research & Development, LLC), the base-case incremental cost-effectiveness ratio (ICER) was £6203 per quality-adjusted life-year (QALY) gained. The evidence review group’s preferred base-case estimate was £5622 per QALY gained.
The committee said there is uncertainty about the validity of these results, which were based on the ATLAS-ACS 2-TIMI 51 trial, because of the risk of bias resulting from missing trial data and informative censoring.
However, the committee considered that the ICERs presented were all within the range that could be considered cost-effective, and adjusting for the various types of bias that might have occurred was unlikely to increase the ICER to the extent that it would become unacceptable.
The list price of rivaroxaban is £58.88 per 2.5 mg, 56-capsule pack (excluding value-added tax). The license dose is 2.5 mg twice daily, which equates to a price of £2.10 per day.
Assuming a treatment duration of 12 months, total acquisition costs are £766.50. Costs may vary in different settings because of negotiated procurement discounts. ![]()

Credit: NHS
In its final draft guidance, the UK’s National Institute for Health and Care Excellence (NICE) is recommending rivaroxaban (Xarelto) as an option for preventing adverse outcomes in patients with acute coronary syndromes (ACS).
The agency said it supports use of the factor Xa inhibitor in combination with aspirin and clopidogrel or aspirin alone to prevent atherothrombotic events in ACS patients with elevated cardiac biomarkers.
This includes patients who have had ST-segment-elevation myocardial infarctions (STEMIs) or non-ST-segment myocardial infarctions (NSTEMIs) but not unstable angina. In unstable angina, damage to the heart is not severe enough to result in the release of biomarkers into the blood, so this condition is not included in the guidance.
“Because rivaroxaban is associated with a higher risk of causing bleeding than clopidogrel in combination with aspirin or aspirin alone, the draft guidance recommends that, before starting treatment, doctors should carry out a careful assessment of a person’s bleeding risk,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“The decision to start treatment should be made after an informed discussion between the doctor and patient about the benefits and risks of rivaroxaban. Also, because there is limited experience of treatment with rivaroxaban up to 24 months, the draft guidance recommends careful consideration should be given to whether treatment is continued beyond 12 months.”
The final draft guidance is now with consultees, who have the opportunity to appeal against it. Once NICE issues its final guidance on a technology, it replaces local recommendations.
Cost and clinical effectiveness
An appraisal committee advising NICE concluded that rivaroxaban given at 2.5 mg twice daily in combination with aspirin plus clopidogrel or with aspirin alone was more effective than aspirin plus clopidogrel or aspirin alone for preventing further cardiovascular deaths and myocardial infarction in patients with ACS and raised cardiac biomarkers.
The committee also found rivaroxaban to be cost-effective. According to Bayer Healthcare (the company co-developing rivaroxaban with Janssen Research & Development, LLC), the base-case incremental cost-effectiveness ratio (ICER) was £6203 per quality-adjusted life-year (QALY) gained. The evidence review group’s preferred base-case estimate was £5622 per QALY gained.
The committee said there is uncertainty about the validity of these results, which were based on the ATLAS-ACS 2-TIMI 51 trial, because of the risk of bias resulting from missing trial data and informative censoring.
However, the committee considered that the ICERs presented were all within the range that could be considered cost-effective, and adjusting for the various types of bias that might have occurred was unlikely to increase the ICER to the extent that it would become unacceptable.
The list price of rivaroxaban is £58.88 per 2.5 mg, 56-capsule pack (excluding value-added tax). The license dose is 2.5 mg twice daily, which equates to a price of £2.10 per day.
Assuming a treatment duration of 12 months, total acquisition costs are £766.50. Costs may vary in different settings because of negotiated procurement discounts. ![]()
Pituitary Incidentaloma
Brian, 46, is referred to endocrinology for evaluation of a pituitary “mass.” The mass was an incidental finding of head and neck CT performed three months ago, when Brian went to an emergency department following a motor vehicle accident. He has fully recovered from the accident and feels well. He describes himself as a “completely healthy” person who has no chronic medical conditions and takes neither prescription nor OTC medications.
Brian denies significant headache, visual disturbance, change in appetite, unexplained weight change, skin rash (wide purple striae) or color changes (hyperpigmentation), polyuria or polydipsia, dizziness, syncopal episodes, low libido, erectile dysfunction, joint pain, and changes in ring or shoe size. He does not wear a hat or cap and is unaware of head size changes. He has not experienced changes in his facial features or trouble with chewing.
He is a happily married engineer with two healthy children and reports that he feels well except for this “brain tumor” finding that has been a shock to him and his family. There is no family history of pituitary adenoma or multiple endocrine neoplasia syndrome.
His vital signs, all within normal ranges, include a blood pressure of 103/65 mm Hg. His height is 6 ft and his weight, 180 lb. His BMI is 24.4.
HOW COMMON IS PITUITARY INCIDENTALOMA?
A pituitary incidentaloma is a lesion in the pituitary gland that was not previously suspected and was found through an imaging study ordered for other reasons. Pituitary incidentaloma is surprisingly common, with an average prevalence of 10.6% (as estimated from combined autopsy data), although it has been found in up to 20% of patients undergoing CT and 38% undergoing MRI.1,2 Most are microadenomas (< 1 cm in size).1
Continue for recommendations from the Endocrine Society >>
SHOULD AN ASYMPTOMATIC PATIENT BE EVALUATED FURTHER?
Endocrine Society guidelines2 recommend that all patients with pituitary incidentaloma, with or without symptoms, should undergo a complete history and physical examination and laboratory evaluation to exclude hypersecretion and hyposecretion of pituitary hormones.
The “classic” presentation of pituitary hormone hypersecretion—in the form of prolactinoma, adrenocorticotropic hormone (ACTH) excess (Cushing disease), growth hormone (GH) excess (gigantism/acromegaly), and TSH excess (secondary hyperthyroidism)—may be readily detectable on history and physical examination. Subtle cases, so-called subclinical disease, however, may exhibit little or no signs and symptoms initially but can be detrimental to the patient’s health if left untreated. For example, the estimated time from onset to diagnosis of acromegaly is approximately seven to 10 years—a delay that can significantly impact the patient’s morbidity and mortality.3
Prolactinoma can be more clinically apparent in premenopausal females due to irregular menstrual cycles (oligomenorrhea/amenorrhea). However, galactorrhea, or “milky” nipple discharge, occurs in only about 50% of women with prolactinoma and is extremely rare in men. Furthermore, the clinical presentation of prolactinoma in men is vague and related to hypogonadism, resulting from increased prolactin levels. Since men are essentially asymptomatic, these tumors can grow extensively (macroadenoma) and cause “mass effect,” such as headaches and visual impairment.
Therefore, without laboratory testing, abnormal pituitary function may go unrecognized.
WHAT LABS SHOULD I ORDER FOR THIS PATIENT?
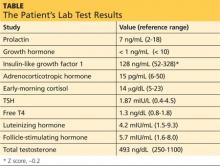
Guidelines suggest an initial screening panel of prolactin, GH, insulin-like growth factor 1 (IGF-1), ACTH, early-morning cortisol, TSH, free T4, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone.2
Note the use of “suggest” rather than “recommend.” Even among guideline task force members, there were differences in opinion as to whether certain tests (eg, TSH, LH, and FSH) should be included in initial screening. Those tests can be ordered at the clinician’s discretion, according to the level of suspicion, or can be added later if necessary.
Brian’s sample for laboratory testing is drawn at 7:50 am. Results can be found in the table (previous page).
Next page: Caveats and concerns >>
ARE THERE ANY CAVEATS TO THE INTERPRETATION OF LAB VALUES?
It is important to note that in postmenopausal women who are not taking hormone replacement therapy, LH and FSH will be elevated and estradiol may provide an additional clue in the detection of abnormal function. Conversely, low LH and FSH in postmenopausal women should raise a flag for hypopituitarism.
Another caveat is that GH secretion is pulsatile and serum levels are undetectable between pulses. Therefore, low/undetectable GH does not necessarily suggest deficiency. The GH measurement would only be helpful if it is significantly elevated (suggestive of hypersecretion—gigantism/acromegaly). Otherwise, GH has little value as a screening test.
Instead, IGF-1, which is secreted from the liver in response to GH secretion, has a longer half-life and serves as a better screening tool. IGF-1 has age- and sex-adjusted reference ranges, which are often reported by the lab or given as a Z score.
WHAT IS THE PREFERRED IMAGING STUDY FOR THE PITUITARY GLAND?
The best choice is MRI of the pituitary gland (not the whole brain) with gadolinium. If the incidentaloma was initially diagnosed by a CT, additional testing with MRI should be performed, unless contraindicated.2
Brian is referred for MRI with gadolinium. The radiologist’s report describes a 5 x 4 x 4–mm pituitary microadenoma without sellar extension or involvement of the optic chiasm.
AT WHAT POINT SHOULD OPTIC CHIASM BE A CONCERN?
Since the pituitary gland is located directly beneath the optic chiasm, any compressive effect of growth against the optic nerve(s) can cause visual impairment. This includes bitemporal hemianopsia (loss of peripheral vision) or ophthalmoplegia (abnormal movement of the ocular muscle). Since clinical signs and symptoms can be subtle or absent, all patients with evidence of a pituitary lesion abutting or compressing the optic chiasm should have a formal visual field exam.2
Continue for surgical intervention >>
WHO REQUIRES SURGICAL INTERVENTION?
Patients with mass effect (headache, increased intracranial pressure, compromised optic chiasm) and those with hyperfunctioning nonprolactin adenomas, some (but not all) macroprolactinomas, or pituitary apoplexy should be referred for surgery.2 Almost all cases involve macroadenomas rather than microadenomas.
The preferred treatment for GH-secreting tumors and ACTH-secreting tumors is surgery. However, prolactinoma can be well controlled with pharmacologic agents (dopamine agonists) in most cases. For prolactinomas refractory to these medications, surgical resection is recommended. (Detailed treatment approaches are available elsewhere; those for hyperprolactinoma can be found on the Clinician Reviews website: http://bit.ly/1HOb9Jf.)
Pituitary apoplexy, a life-threatening emergency that requires prompt surgical decompression, is an infarction of the gland due to abrupt cessation of the blood supply, caused by either pituitary artery hemorrhage or sudden hypovolemia. Increased blood supply is needed due to the extra tissue and volume of the pituitary mass; this may stress the pituitary arteries, which are not equipped for this increased flow, causing them to rupture. Hemorrhage anywhere else in the body can lead to hypovolemia and decrease the blood supply to the pituitary gland. A classic example would be postpartum hemorrhage causing pituitary infarct, called Sheehan syndrome.
Due to increased estrogen levels, the pituitary gland doubles in size during pregnancy.4 A preexisting mass may further develop and compress the optic chiasm. Therefore, women of childbearing age should be engaged in discussion of the potential risks and benefits of decompression surgery before actively pursuing pregnancy—especially if the lesion is close to the optic chiasm.
Surgery can also be considered for patients with significant growth in adenoma size during monitoring, loss of endocrinologic function due to mass effect on other pituitary cells, or unremitting headache.2
Next: How should patients be monitored?
HOW SHOULD PATIENTS BE MONITORED?
Those who do not meet criteria for surgery can be closely monitored with periodic testing. Imaging can be repeated six months after the first scan for macroadenoma and in one year for microadenoma. If there is no change in the size of the mass, imaging can be done yearly for macroadenoma and for microadenoma, every one to two years for three years and then gradually less often thereafter.2
Unless the lesion is abutting the optic chiasm (seen via imaging) or the patient reports symptoms, visual field testing does not need to be repeated.
Lab testing should be repeated six months after initial testing for macroadenoma and yearly thereafter. No further testing is suggested for nonsecretory microadenoma, unless clinically indicated.2
If there are any changes in status—noted clinically or via imaging—more frequent testing is suggested.
Brian is reassured that pituitary adenoma is not an uncommon finding and that his adenoma is relatively small in size and nonsecretory. Repeat pituitary MRI in one year is recommended.
CONCLUSION
Most pituitary incidentalomas have no consequences to a patient’s health. However, patients often become highly anxious about the “brain tumor” they were told they have. Appropriate patient education and thorough evaluation can reassure patients and alleviate their concerns.
REFERENCES
1. Molitch ME. Nonfunctioning pituitary tumors and pituitary incidentalomas. Endocrinol Metab Clin North Am. 2008;37(1):151-171.
2. Freda PU, Beckers AM, Katznelson L, et al. Pituitary incidentaloma: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96(4):894-904.
3. Katznelson L, Atkinson JL, Cook DM, et al. American Association of Clinical Endocrinologists Medical Guidelines For Clinical Practice For The Diagnosis And Treatment Of Acromegaly–2011 Update. Endocr Pract. 2011;17(suppl 4).
4. Jameson JL. Harrison’s Endocrinology. 2nd ed. China: McGraw-Hill; 2010:16-49.
Brian, 46, is referred to endocrinology for evaluation of a pituitary “mass.” The mass was an incidental finding of head and neck CT performed three months ago, when Brian went to an emergency department following a motor vehicle accident. He has fully recovered from the accident and feels well. He describes himself as a “completely healthy” person who has no chronic medical conditions and takes neither prescription nor OTC medications.
Brian denies significant headache, visual disturbance, change in appetite, unexplained weight change, skin rash (wide purple striae) or color changes (hyperpigmentation), polyuria or polydipsia, dizziness, syncopal episodes, low libido, erectile dysfunction, joint pain, and changes in ring or shoe size. He does not wear a hat or cap and is unaware of head size changes. He has not experienced changes in his facial features or trouble with chewing.
He is a happily married engineer with two healthy children and reports that he feels well except for this “brain tumor” finding that has been a shock to him and his family. There is no family history of pituitary adenoma or multiple endocrine neoplasia syndrome.
His vital signs, all within normal ranges, include a blood pressure of 103/65 mm Hg. His height is 6 ft and his weight, 180 lb. His BMI is 24.4.
HOW COMMON IS PITUITARY INCIDENTALOMA?
A pituitary incidentaloma is a lesion in the pituitary gland that was not previously suspected and was found through an imaging study ordered for other reasons. Pituitary incidentaloma is surprisingly common, with an average prevalence of 10.6% (as estimated from combined autopsy data), although it has been found in up to 20% of patients undergoing CT and 38% undergoing MRI.1,2 Most are microadenomas (< 1 cm in size).1
Continue for recommendations from the Endocrine Society >>
SHOULD AN ASYMPTOMATIC PATIENT BE EVALUATED FURTHER?
Endocrine Society guidelines2 recommend that all patients with pituitary incidentaloma, with or without symptoms, should undergo a complete history and physical examination and laboratory evaluation to exclude hypersecretion and hyposecretion of pituitary hormones.
The “classic” presentation of pituitary hormone hypersecretion—in the form of prolactinoma, adrenocorticotropic hormone (ACTH) excess (Cushing disease), growth hormone (GH) excess (gigantism/acromegaly), and TSH excess (secondary hyperthyroidism)—may be readily detectable on history and physical examination. Subtle cases, so-called subclinical disease, however, may exhibit little or no signs and symptoms initially but can be detrimental to the patient’s health if left untreated. For example, the estimated time from onset to diagnosis of acromegaly is approximately seven to 10 years—a delay that can significantly impact the patient’s morbidity and mortality.3
Prolactinoma can be more clinically apparent in premenopausal females due to irregular menstrual cycles (oligomenorrhea/amenorrhea). However, galactorrhea, or “milky” nipple discharge, occurs in only about 50% of women with prolactinoma and is extremely rare in men. Furthermore, the clinical presentation of prolactinoma in men is vague and related to hypogonadism, resulting from increased prolactin levels. Since men are essentially asymptomatic, these tumors can grow extensively (macroadenoma) and cause “mass effect,” such as headaches and visual impairment.
Therefore, without laboratory testing, abnormal pituitary function may go unrecognized.
WHAT LABS SHOULD I ORDER FOR THIS PATIENT?
Guidelines suggest an initial screening panel of prolactin, GH, insulin-like growth factor 1 (IGF-1), ACTH, early-morning cortisol, TSH, free T4, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone.2
Note the use of “suggest” rather than “recommend.” Even among guideline task force members, there were differences in opinion as to whether certain tests (eg, TSH, LH, and FSH) should be included in initial screening. Those tests can be ordered at the clinician’s discretion, according to the level of suspicion, or can be added later if necessary.
Brian’s sample for laboratory testing is drawn at 7:50 am. Results can be found in the table (previous page).
Next page: Caveats and concerns >>
ARE THERE ANY CAVEATS TO THE INTERPRETATION OF LAB VALUES?
It is important to note that in postmenopausal women who are not taking hormone replacement therapy, LH and FSH will be elevated and estradiol may provide an additional clue in the detection of abnormal function. Conversely, low LH and FSH in postmenopausal women should raise a flag for hypopituitarism.
Another caveat is that GH secretion is pulsatile and serum levels are undetectable between pulses. Therefore, low/undetectable GH does not necessarily suggest deficiency. The GH measurement would only be helpful if it is significantly elevated (suggestive of hypersecretion—gigantism/acromegaly). Otherwise, GH has little value as a screening test.
Instead, IGF-1, which is secreted from the liver in response to GH secretion, has a longer half-life and serves as a better screening tool. IGF-1 has age- and sex-adjusted reference ranges, which are often reported by the lab or given as a Z score.
WHAT IS THE PREFERRED IMAGING STUDY FOR THE PITUITARY GLAND?
The best choice is MRI of the pituitary gland (not the whole brain) with gadolinium. If the incidentaloma was initially diagnosed by a CT, additional testing with MRI should be performed, unless contraindicated.2
Brian is referred for MRI with gadolinium. The radiologist’s report describes a 5 x 4 x 4–mm pituitary microadenoma without sellar extension or involvement of the optic chiasm.
AT WHAT POINT SHOULD OPTIC CHIASM BE A CONCERN?
Since the pituitary gland is located directly beneath the optic chiasm, any compressive effect of growth against the optic nerve(s) can cause visual impairment. This includes bitemporal hemianopsia (loss of peripheral vision) or ophthalmoplegia (abnormal movement of the ocular muscle). Since clinical signs and symptoms can be subtle or absent, all patients with evidence of a pituitary lesion abutting or compressing the optic chiasm should have a formal visual field exam.2
Continue for surgical intervention >>
WHO REQUIRES SURGICAL INTERVENTION?
Patients with mass effect (headache, increased intracranial pressure, compromised optic chiasm) and those with hyperfunctioning nonprolactin adenomas, some (but not all) macroprolactinomas, or pituitary apoplexy should be referred for surgery.2 Almost all cases involve macroadenomas rather than microadenomas.
The preferred treatment for GH-secreting tumors and ACTH-secreting tumors is surgery. However, prolactinoma can be well controlled with pharmacologic agents (dopamine agonists) in most cases. For prolactinomas refractory to these medications, surgical resection is recommended. (Detailed treatment approaches are available elsewhere; those for hyperprolactinoma can be found on the Clinician Reviews website: http://bit.ly/1HOb9Jf.)
Pituitary apoplexy, a life-threatening emergency that requires prompt surgical decompression, is an infarction of the gland due to abrupt cessation of the blood supply, caused by either pituitary artery hemorrhage or sudden hypovolemia. Increased blood supply is needed due to the extra tissue and volume of the pituitary mass; this may stress the pituitary arteries, which are not equipped for this increased flow, causing them to rupture. Hemorrhage anywhere else in the body can lead to hypovolemia and decrease the blood supply to the pituitary gland. A classic example would be postpartum hemorrhage causing pituitary infarct, called Sheehan syndrome.
Due to increased estrogen levels, the pituitary gland doubles in size during pregnancy.4 A preexisting mass may further develop and compress the optic chiasm. Therefore, women of childbearing age should be engaged in discussion of the potential risks and benefits of decompression surgery before actively pursuing pregnancy—especially if the lesion is close to the optic chiasm.
Surgery can also be considered for patients with significant growth in adenoma size during monitoring, loss of endocrinologic function due to mass effect on other pituitary cells, or unremitting headache.2
Next: How should patients be monitored?
HOW SHOULD PATIENTS BE MONITORED?
Those who do not meet criteria for surgery can be closely monitored with periodic testing. Imaging can be repeated six months after the first scan for macroadenoma and in one year for microadenoma. If there is no change in the size of the mass, imaging can be done yearly for macroadenoma and for microadenoma, every one to two years for three years and then gradually less often thereafter.2
Unless the lesion is abutting the optic chiasm (seen via imaging) or the patient reports symptoms, visual field testing does not need to be repeated.
Lab testing should be repeated six months after initial testing for macroadenoma and yearly thereafter. No further testing is suggested for nonsecretory microadenoma, unless clinically indicated.2
If there are any changes in status—noted clinically or via imaging—more frequent testing is suggested.
Brian is reassured that pituitary adenoma is not an uncommon finding and that his adenoma is relatively small in size and nonsecretory. Repeat pituitary MRI in one year is recommended.
CONCLUSION
Most pituitary incidentalomas have no consequences to a patient’s health. However, patients often become highly anxious about the “brain tumor” they were told they have. Appropriate patient education and thorough evaluation can reassure patients and alleviate their concerns.
REFERENCES
1. Molitch ME. Nonfunctioning pituitary tumors and pituitary incidentalomas. Endocrinol Metab Clin North Am. 2008;37(1):151-171.
2. Freda PU, Beckers AM, Katznelson L, et al. Pituitary incidentaloma: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96(4):894-904.
3. Katznelson L, Atkinson JL, Cook DM, et al. American Association of Clinical Endocrinologists Medical Guidelines For Clinical Practice For The Diagnosis And Treatment Of Acromegaly–2011 Update. Endocr Pract. 2011;17(suppl 4).
4. Jameson JL. Harrison’s Endocrinology. 2nd ed. China: McGraw-Hill; 2010:16-49.
Brian, 46, is referred to endocrinology for evaluation of a pituitary “mass.” The mass was an incidental finding of head and neck CT performed three months ago, when Brian went to an emergency department following a motor vehicle accident. He has fully recovered from the accident and feels well. He describes himself as a “completely healthy” person who has no chronic medical conditions and takes neither prescription nor OTC medications.
Brian denies significant headache, visual disturbance, change in appetite, unexplained weight change, skin rash (wide purple striae) or color changes (hyperpigmentation), polyuria or polydipsia, dizziness, syncopal episodes, low libido, erectile dysfunction, joint pain, and changes in ring or shoe size. He does not wear a hat or cap and is unaware of head size changes. He has not experienced changes in his facial features or trouble with chewing.
He is a happily married engineer with two healthy children and reports that he feels well except for this “brain tumor” finding that has been a shock to him and his family. There is no family history of pituitary adenoma or multiple endocrine neoplasia syndrome.
His vital signs, all within normal ranges, include a blood pressure of 103/65 mm Hg. His height is 6 ft and his weight, 180 lb. His BMI is 24.4.
HOW COMMON IS PITUITARY INCIDENTALOMA?
A pituitary incidentaloma is a lesion in the pituitary gland that was not previously suspected and was found through an imaging study ordered for other reasons. Pituitary incidentaloma is surprisingly common, with an average prevalence of 10.6% (as estimated from combined autopsy data), although it has been found in up to 20% of patients undergoing CT and 38% undergoing MRI.1,2 Most are microadenomas (< 1 cm in size).1
Continue for recommendations from the Endocrine Society >>
SHOULD AN ASYMPTOMATIC PATIENT BE EVALUATED FURTHER?
Endocrine Society guidelines2 recommend that all patients with pituitary incidentaloma, with or without symptoms, should undergo a complete history and physical examination and laboratory evaluation to exclude hypersecretion and hyposecretion of pituitary hormones.
The “classic” presentation of pituitary hormone hypersecretion—in the form of prolactinoma, adrenocorticotropic hormone (ACTH) excess (Cushing disease), growth hormone (GH) excess (gigantism/acromegaly), and TSH excess (secondary hyperthyroidism)—may be readily detectable on history and physical examination. Subtle cases, so-called subclinical disease, however, may exhibit little or no signs and symptoms initially but can be detrimental to the patient’s health if left untreated. For example, the estimated time from onset to diagnosis of acromegaly is approximately seven to 10 years—a delay that can significantly impact the patient’s morbidity and mortality.3
Prolactinoma can be more clinically apparent in premenopausal females due to irregular menstrual cycles (oligomenorrhea/amenorrhea). However, galactorrhea, or “milky” nipple discharge, occurs in only about 50% of women with prolactinoma and is extremely rare in men. Furthermore, the clinical presentation of prolactinoma in men is vague and related to hypogonadism, resulting from increased prolactin levels. Since men are essentially asymptomatic, these tumors can grow extensively (macroadenoma) and cause “mass effect,” such as headaches and visual impairment.
Therefore, without laboratory testing, abnormal pituitary function may go unrecognized.
WHAT LABS SHOULD I ORDER FOR THIS PATIENT?
Guidelines suggest an initial screening panel of prolactin, GH, insulin-like growth factor 1 (IGF-1), ACTH, early-morning cortisol, TSH, free T4, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone.2
Note the use of “suggest” rather than “recommend.” Even among guideline task force members, there were differences in opinion as to whether certain tests (eg, TSH, LH, and FSH) should be included in initial screening. Those tests can be ordered at the clinician’s discretion, according to the level of suspicion, or can be added later if necessary.
Brian’s sample for laboratory testing is drawn at 7:50 am. Results can be found in the table (previous page).
Next page: Caveats and concerns >>
ARE THERE ANY CAVEATS TO THE INTERPRETATION OF LAB VALUES?
It is important to note that in postmenopausal women who are not taking hormone replacement therapy, LH and FSH will be elevated and estradiol may provide an additional clue in the detection of abnormal function. Conversely, low LH and FSH in postmenopausal women should raise a flag for hypopituitarism.
Another caveat is that GH secretion is pulsatile and serum levels are undetectable between pulses. Therefore, low/undetectable GH does not necessarily suggest deficiency. The GH measurement would only be helpful if it is significantly elevated (suggestive of hypersecretion—gigantism/acromegaly). Otherwise, GH has little value as a screening test.
Instead, IGF-1, which is secreted from the liver in response to GH secretion, has a longer half-life and serves as a better screening tool. IGF-1 has age- and sex-adjusted reference ranges, which are often reported by the lab or given as a Z score.
WHAT IS THE PREFERRED IMAGING STUDY FOR THE PITUITARY GLAND?
The best choice is MRI of the pituitary gland (not the whole brain) with gadolinium. If the incidentaloma was initially diagnosed by a CT, additional testing with MRI should be performed, unless contraindicated.2
Brian is referred for MRI with gadolinium. The radiologist’s report describes a 5 x 4 x 4–mm pituitary microadenoma without sellar extension or involvement of the optic chiasm.
AT WHAT POINT SHOULD OPTIC CHIASM BE A CONCERN?
Since the pituitary gland is located directly beneath the optic chiasm, any compressive effect of growth against the optic nerve(s) can cause visual impairment. This includes bitemporal hemianopsia (loss of peripheral vision) or ophthalmoplegia (abnormal movement of the ocular muscle). Since clinical signs and symptoms can be subtle or absent, all patients with evidence of a pituitary lesion abutting or compressing the optic chiasm should have a formal visual field exam.2
Continue for surgical intervention >>
WHO REQUIRES SURGICAL INTERVENTION?
Patients with mass effect (headache, increased intracranial pressure, compromised optic chiasm) and those with hyperfunctioning nonprolactin adenomas, some (but not all) macroprolactinomas, or pituitary apoplexy should be referred for surgery.2 Almost all cases involve macroadenomas rather than microadenomas.
The preferred treatment for GH-secreting tumors and ACTH-secreting tumors is surgery. However, prolactinoma can be well controlled with pharmacologic agents (dopamine agonists) in most cases. For prolactinomas refractory to these medications, surgical resection is recommended. (Detailed treatment approaches are available elsewhere; those for hyperprolactinoma can be found on the Clinician Reviews website: http://bit.ly/1HOb9Jf.)
Pituitary apoplexy, a life-threatening emergency that requires prompt surgical decompression, is an infarction of the gland due to abrupt cessation of the blood supply, caused by either pituitary artery hemorrhage or sudden hypovolemia. Increased blood supply is needed due to the extra tissue and volume of the pituitary mass; this may stress the pituitary arteries, which are not equipped for this increased flow, causing them to rupture. Hemorrhage anywhere else in the body can lead to hypovolemia and decrease the blood supply to the pituitary gland. A classic example would be postpartum hemorrhage causing pituitary infarct, called Sheehan syndrome.
Due to increased estrogen levels, the pituitary gland doubles in size during pregnancy.4 A preexisting mass may further develop and compress the optic chiasm. Therefore, women of childbearing age should be engaged in discussion of the potential risks and benefits of decompression surgery before actively pursuing pregnancy—especially if the lesion is close to the optic chiasm.
Surgery can also be considered for patients with significant growth in adenoma size during monitoring, loss of endocrinologic function due to mass effect on other pituitary cells, or unremitting headache.2
Next: How should patients be monitored?
HOW SHOULD PATIENTS BE MONITORED?
Those who do not meet criteria for surgery can be closely monitored with periodic testing. Imaging can be repeated six months after the first scan for macroadenoma and in one year for microadenoma. If there is no change in the size of the mass, imaging can be done yearly for macroadenoma and for microadenoma, every one to two years for three years and then gradually less often thereafter.2
Unless the lesion is abutting the optic chiasm (seen via imaging) or the patient reports symptoms, visual field testing does not need to be repeated.
Lab testing should be repeated six months after initial testing for macroadenoma and yearly thereafter. No further testing is suggested for nonsecretory microadenoma, unless clinically indicated.2
If there are any changes in status—noted clinically or via imaging—more frequent testing is suggested.
Brian is reassured that pituitary adenoma is not an uncommon finding and that his adenoma is relatively small in size and nonsecretory. Repeat pituitary MRI in one year is recommended.
CONCLUSION
Most pituitary incidentalomas have no consequences to a patient’s health. However, patients often become highly anxious about the “brain tumor” they were told they have. Appropriate patient education and thorough evaluation can reassure patients and alleviate their concerns.
REFERENCES
1. Molitch ME. Nonfunctioning pituitary tumors and pituitary incidentalomas. Endocrinol Metab Clin North Am. 2008;37(1):151-171.
2. Freda PU, Beckers AM, Katznelson L, et al. Pituitary incidentaloma: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96(4):894-904.
3. Katznelson L, Atkinson JL, Cook DM, et al. American Association of Clinical Endocrinologists Medical Guidelines For Clinical Practice For The Diagnosis And Treatment Of Acromegaly–2011 Update. Endocr Pract. 2011;17(suppl 4).
4. Jameson JL. Harrison’s Endocrinology. 2nd ed. China: McGraw-Hill; 2010:16-49.
Teledermoscopy referrals surpass paper for managing skin cancer patients
Smartphone teledermoscopy referrals were faster and allowed for more efficient management of patients with skin cancer, compared with paper referrals, according to Dr. Alexander Börve of the University of Gothenburg, Sweden, and his associates.
The waiting time was significantly shorter using teledermoscopy for patients with various melanomas and carcinomas when surgical treatment was necessary. “Triage decisions were also more reliable with teledermoscopy, and over 40% of the teledermoscopy patients could potentially have avoided face-to-face visits,” the researchers noted (Acta. Derm. Venereol. 2015;95:186-90).
Less than 1% of teledermoscopy referrals were excluded because of poor image quality, they said.
Read the full article at Acta Dermato-Venereologica (doi:10.2340/00015555-1906).
Smartphone teledermoscopy referrals were faster and allowed for more efficient management of patients with skin cancer, compared with paper referrals, according to Dr. Alexander Börve of the University of Gothenburg, Sweden, and his associates.
The waiting time was significantly shorter using teledermoscopy for patients with various melanomas and carcinomas when surgical treatment was necessary. “Triage decisions were also more reliable with teledermoscopy, and over 40% of the teledermoscopy patients could potentially have avoided face-to-face visits,” the researchers noted (Acta. Derm. Venereol. 2015;95:186-90).
Less than 1% of teledermoscopy referrals were excluded because of poor image quality, they said.
Read the full article at Acta Dermato-Venereologica (doi:10.2340/00015555-1906).
Smartphone teledermoscopy referrals were faster and allowed for more efficient management of patients with skin cancer, compared with paper referrals, according to Dr. Alexander Börve of the University of Gothenburg, Sweden, and his associates.
The waiting time was significantly shorter using teledermoscopy for patients with various melanomas and carcinomas when surgical treatment was necessary. “Triage decisions were also more reliable with teledermoscopy, and over 40% of the teledermoscopy patients could potentially have avoided face-to-face visits,” the researchers noted (Acta. Derm. Venereol. 2015;95:186-90).
Less than 1% of teledermoscopy referrals were excluded because of poor image quality, they said.
Read the full article at Acta Dermato-Venereologica (doi:10.2340/00015555-1906).
Residents reluctant to recommend DNR to patients
BOSTON – Medical residents in the United States appear to understand that cardiopulmonary resuscitation or intubation is highly unlikely to benefit patients with advanced cancers at the end of life, but the majority of residents surveyed said that they do not discuss code-status options or potentially beneficial palliative care with their dying patients.
“This was primarily due to residents’ perceptions of patient autonomy: Residents wanted patients to make their own decisions, without any influence from the doctor, which misses the concept of informed decision making. These incomplete discussions can cause at minimum improper documentation of patients’ wishes, and at most psychological harm, damage to the physician-patient relationship, and the potential for unwanted attempts at resuscitation,” said Dr. David J. Einstein, a resident at Beth Israel Deaconess Medical Center and Tufts Medical Center, both in Boston.
Despite their reluctance to have the discussion, however, the majority of residents said they preferred to discuss code status with patients themselves rather than hand it off to the attending physician, primarily out of a sense that it is their responsibility as physicians.
Yet these physicians in training did not seem to feel that they were also responsible for providing guidance to patients, Dr. Einstein said at the Palliative Care in Oncology Symposium.
“We felt that this represented an unmet need in training and practice. Residents and attendings should be providing guidance on all medical interventions, including CPR, and if they aren’t sure what to recommend, then they themselves should be seeking guidance from other experts, before asking a patient to falsely choose between an intervention and death,” he said.
The first discussion of code status – do not resuscitate (DNR) or do not intubate (DNI) – may occur in the hospital, and is often left to a resident physician. Ideally, the physician and patient should discuss the patient’s prognosis, goals for care, evaluation of CPR as a means of meeting those goals, and a recommendation.
But many residents lack training in the end-of-life discussion, which can have a significant impact on the quality of the patients’ remaining weeks or months of life.
Nationwide survey
Dr. Einstein and his colleagues conducted a nationwide survey to measure the likelihood that residents would discuss prognostic information and offer recommendations to patients with limited life expectancy. They also sought to determine why residents might be reluctant to provide discussion, and to evaluate their satisfaction with code-status discussions that both they and their attending physicians have conducted.
The survey presented respondents with a hypothetical case of a patient with stage IV adenocarcinoma of the lung metastatic to the brain. The patient, who has disease progression despite receiving first- and second-line therapy, presents to the emergency department with dyspnea and is slightly hypoxemic, but is not in distress. The patient has not previously established a code-status preference.
The investigators contacted 387 residency program directors by mail, 19 of whom agreed to participate and responded. They sent surveys to a total of 1,627 residents, 358 of which were completed and included.
The investigators found that slightly less than half of the respondents said they would share information with the patient about his/her prognosis and the relative benefit of CPR, and more than two-thirds said they would be unlikely to offer a specific recommendation.
“So even in the situation with a clearly declining patient, residents were as likely as not to provide the information needed to make an informed decision, and were far less likely to provide guidance on this decision,” Dr. Einstein said.
Asked the reason for their decisions, 69% of the residents who would not offer a recommendation said that the patient should make his/her own decision without any influence, and 26.5% said that the attending would not want them to offer a recommendation. Nonetheless, only 1.3% of this group said they believed that CPR would offer the patient a reasonable chance of resuscitation.
The majority of respondents who would offer a recommendation (93.5%) said they would recommend DNR and DNI.
Code-status talk a ‘responsibility’
When they were asked whether they would prefer the attending to discuss code status, nearly 70% of respondents disagreed.
Of those residents who said they preferred to retain the code-status discussion, 93.4% said they thought it was part of their responsibility as a physician, and 65.8% said they thought they had sufficient training and knowledge to do it. A minority in this group (2.5%) said that they would be likely to disagree with the attending’s estimate of prognosis, and 4.9% said they thought the attending would not share his/her estimate honestly.
When the authors asked about the residents’ general satisfaction with discussion of code status, “we learned two things: One, the residents are significantly more satisfied with their own discussions than their attendings’ discussions; and two, there is a substantial minority that is dissatisfied with all discussions, and a small number who are actually very satisfied,” Dr. Einstein said.
In a linear regression analysis testing for hypothesized correlations, the investigators found that more-senior residents were more likely to share prognostic information and make recommendations (P = .002). Residents who expressed an interest in hematology/oncology or palliative care specialization were also more likely to offer prognostic information, but not to make a recommendation about code status.
More-senior year of training correlated negatively with satisfaction with both the resident’s own and the attending’s discussion of code status.
“We found substantial dissatisfaction with code-status discussions in general, and we hypothesize that this is due to an internal conflict. When a resident knows that an intervention may be more harmful than beneficial, but thinks that the patient should make their own decision alone, then one may experience substantial frustration, and this would increase as training goes on and one becomes more sure of the outcomes of interventions like CPR,” Dr. Einstein said.
Generation gap
Evoking a potential generation gap between old-school doctors and the up-and-coming young physicians who by statute work fewer hours than their mentors had to, “I’m struck that [residents] don’t trust the attendings. When I was a resident, you didn’t do anything without asking the attending,” said Dr. Michael H. Levy, an invited discussant who is vice chair of medical oncology and director of the pain and palliative care program at Fox Chase Cancer Center, Philadelphia.
“I’m glad that the residents want to do it, but they have the same arrogance/ignorance that they don’t know how, so if we want them to do it, we have to train them,” he said. The symposium was cosponsored by AAHPM, ASCO, ASTRO, and MASCC. The study was supported in part by the Conquer Cancer Foundation. Dr. Einstein and Dr. Levy reported having no relevant disclosures.
Can you imagine a health care system where your treating physician cannot offer their patients information on code-status and end of life decisions? Seems somewhat preposterous, but in a national survey in the United States, more than two-thirds of medical residents said they would not offer end-of-life code-status prognostic information and recommendations to their patients with limited life expectancy. Granted that medical residents thought that invasive interventions in an individual with limited life expectancy were not warranted; they wanted patients to make these decisions on their own without influence from health care professionals. Although patient autonomy is one of the pillars in medical ethics, decisions made without undue influence should be made with the most accurate information at hand.

|
| Dr. Laura Drudi |
In vascular surgery, specialists are performing moderate- to high-risk interventions on an exponentially growing elderly population plagued with a significant cardiovascular disease burden. It is therefore essential that physicians, where appropriate, discuss end-of-life and code status with their patients. In my experience, surgical residents are inexperienced when it comes to having these dialogues with patients largely because there are no teaching opportunities to learn these communication skills. Further, there are few opportunities to learn by observing these sensitive discussions that are often performed out of earshot. Currently, there is an unmet need in training programs when it comes to providing appropriate guidance to residents who may need to have these difficult discussions.
It is our responsibility as medical professionals to provide the best medical as well as end of life care. Residents who are appropriately trained to participate in code- status discussions and end-of-life decisions will enable our patients to make well-advised and truly autonomous decisions about their ultimate care.
Dr. Laura Drudi is the resident medical editor for Vascular Specialist.
Can you imagine a health care system where your treating physician cannot offer their patients information on code-status and end of life decisions? Seems somewhat preposterous, but in a national survey in the United States, more than two-thirds of medical residents said they would not offer end-of-life code-status prognostic information and recommendations to their patients with limited life expectancy. Granted that medical residents thought that invasive interventions in an individual with limited life expectancy were not warranted; they wanted patients to make these decisions on their own without influence from health care professionals. Although patient autonomy is one of the pillars in medical ethics, decisions made without undue influence should be made with the most accurate information at hand.

|
| Dr. Laura Drudi |
In vascular surgery, specialists are performing moderate- to high-risk interventions on an exponentially growing elderly population plagued with a significant cardiovascular disease burden. It is therefore essential that physicians, where appropriate, discuss end-of-life and code status with their patients. In my experience, surgical residents are inexperienced when it comes to having these dialogues with patients largely because there are no teaching opportunities to learn these communication skills. Further, there are few opportunities to learn by observing these sensitive discussions that are often performed out of earshot. Currently, there is an unmet need in training programs when it comes to providing appropriate guidance to residents who may need to have these difficult discussions.
It is our responsibility as medical professionals to provide the best medical as well as end of life care. Residents who are appropriately trained to participate in code- status discussions and end-of-life decisions will enable our patients to make well-advised and truly autonomous decisions about their ultimate care.
Dr. Laura Drudi is the resident medical editor for Vascular Specialist.
Can you imagine a health care system where your treating physician cannot offer their patients information on code-status and end of life decisions? Seems somewhat preposterous, but in a national survey in the United States, more than two-thirds of medical residents said they would not offer end-of-life code-status prognostic information and recommendations to their patients with limited life expectancy. Granted that medical residents thought that invasive interventions in an individual with limited life expectancy were not warranted; they wanted patients to make these decisions on their own without influence from health care professionals. Although patient autonomy is one of the pillars in medical ethics, decisions made without undue influence should be made with the most accurate information at hand.

|
| Dr. Laura Drudi |
In vascular surgery, specialists are performing moderate- to high-risk interventions on an exponentially growing elderly population plagued with a significant cardiovascular disease burden. It is therefore essential that physicians, where appropriate, discuss end-of-life and code status with their patients. In my experience, surgical residents are inexperienced when it comes to having these dialogues with patients largely because there are no teaching opportunities to learn these communication skills. Further, there are few opportunities to learn by observing these sensitive discussions that are often performed out of earshot. Currently, there is an unmet need in training programs when it comes to providing appropriate guidance to residents who may need to have these difficult discussions.
It is our responsibility as medical professionals to provide the best medical as well as end of life care. Residents who are appropriately trained to participate in code- status discussions and end-of-life decisions will enable our patients to make well-advised and truly autonomous decisions about their ultimate care.
Dr. Laura Drudi is the resident medical editor for Vascular Specialist.
BOSTON – Medical residents in the United States appear to understand that cardiopulmonary resuscitation or intubation is highly unlikely to benefit patients with advanced cancers at the end of life, but the majority of residents surveyed said that they do not discuss code-status options or potentially beneficial palliative care with their dying patients.
“This was primarily due to residents’ perceptions of patient autonomy: Residents wanted patients to make their own decisions, without any influence from the doctor, which misses the concept of informed decision making. These incomplete discussions can cause at minimum improper documentation of patients’ wishes, and at most psychological harm, damage to the physician-patient relationship, and the potential for unwanted attempts at resuscitation,” said Dr. David J. Einstein, a resident at Beth Israel Deaconess Medical Center and Tufts Medical Center, both in Boston.
Despite their reluctance to have the discussion, however, the majority of residents said they preferred to discuss code status with patients themselves rather than hand it off to the attending physician, primarily out of a sense that it is their responsibility as physicians.
Yet these physicians in training did not seem to feel that they were also responsible for providing guidance to patients, Dr. Einstein said at the Palliative Care in Oncology Symposium.
“We felt that this represented an unmet need in training and practice. Residents and attendings should be providing guidance on all medical interventions, including CPR, and if they aren’t sure what to recommend, then they themselves should be seeking guidance from other experts, before asking a patient to falsely choose between an intervention and death,” he said.
The first discussion of code status – do not resuscitate (DNR) or do not intubate (DNI) – may occur in the hospital, and is often left to a resident physician. Ideally, the physician and patient should discuss the patient’s prognosis, goals for care, evaluation of CPR as a means of meeting those goals, and a recommendation.
But many residents lack training in the end-of-life discussion, which can have a significant impact on the quality of the patients’ remaining weeks or months of life.
Nationwide survey
Dr. Einstein and his colleagues conducted a nationwide survey to measure the likelihood that residents would discuss prognostic information and offer recommendations to patients with limited life expectancy. They also sought to determine why residents might be reluctant to provide discussion, and to evaluate their satisfaction with code-status discussions that both they and their attending physicians have conducted.
The survey presented respondents with a hypothetical case of a patient with stage IV adenocarcinoma of the lung metastatic to the brain. The patient, who has disease progression despite receiving first- and second-line therapy, presents to the emergency department with dyspnea and is slightly hypoxemic, but is not in distress. The patient has not previously established a code-status preference.
The investigators contacted 387 residency program directors by mail, 19 of whom agreed to participate and responded. They sent surveys to a total of 1,627 residents, 358 of which were completed and included.
The investigators found that slightly less than half of the respondents said they would share information with the patient about his/her prognosis and the relative benefit of CPR, and more than two-thirds said they would be unlikely to offer a specific recommendation.
“So even in the situation with a clearly declining patient, residents were as likely as not to provide the information needed to make an informed decision, and were far less likely to provide guidance on this decision,” Dr. Einstein said.
Asked the reason for their decisions, 69% of the residents who would not offer a recommendation said that the patient should make his/her own decision without any influence, and 26.5% said that the attending would not want them to offer a recommendation. Nonetheless, only 1.3% of this group said they believed that CPR would offer the patient a reasonable chance of resuscitation.
The majority of respondents who would offer a recommendation (93.5%) said they would recommend DNR and DNI.
Code-status talk a ‘responsibility’
When they were asked whether they would prefer the attending to discuss code status, nearly 70% of respondents disagreed.
Of those residents who said they preferred to retain the code-status discussion, 93.4% said they thought it was part of their responsibility as a physician, and 65.8% said they thought they had sufficient training and knowledge to do it. A minority in this group (2.5%) said that they would be likely to disagree with the attending’s estimate of prognosis, and 4.9% said they thought the attending would not share his/her estimate honestly.
When the authors asked about the residents’ general satisfaction with discussion of code status, “we learned two things: One, the residents are significantly more satisfied with their own discussions than their attendings’ discussions; and two, there is a substantial minority that is dissatisfied with all discussions, and a small number who are actually very satisfied,” Dr. Einstein said.
In a linear regression analysis testing for hypothesized correlations, the investigators found that more-senior residents were more likely to share prognostic information and make recommendations (P = .002). Residents who expressed an interest in hematology/oncology or palliative care specialization were also more likely to offer prognostic information, but not to make a recommendation about code status.
More-senior year of training correlated negatively with satisfaction with both the resident’s own and the attending’s discussion of code status.
“We found substantial dissatisfaction with code-status discussions in general, and we hypothesize that this is due to an internal conflict. When a resident knows that an intervention may be more harmful than beneficial, but thinks that the patient should make their own decision alone, then one may experience substantial frustration, and this would increase as training goes on and one becomes more sure of the outcomes of interventions like CPR,” Dr. Einstein said.
Generation gap
Evoking a potential generation gap between old-school doctors and the up-and-coming young physicians who by statute work fewer hours than their mentors had to, “I’m struck that [residents] don’t trust the attendings. When I was a resident, you didn’t do anything without asking the attending,” said Dr. Michael H. Levy, an invited discussant who is vice chair of medical oncology and director of the pain and palliative care program at Fox Chase Cancer Center, Philadelphia.
“I’m glad that the residents want to do it, but they have the same arrogance/ignorance that they don’t know how, so if we want them to do it, we have to train them,” he said. The symposium was cosponsored by AAHPM, ASCO, ASTRO, and MASCC. The study was supported in part by the Conquer Cancer Foundation. Dr. Einstein and Dr. Levy reported having no relevant disclosures.
BOSTON – Medical residents in the United States appear to understand that cardiopulmonary resuscitation or intubation is highly unlikely to benefit patients with advanced cancers at the end of life, but the majority of residents surveyed said that they do not discuss code-status options or potentially beneficial palliative care with their dying patients.
“This was primarily due to residents’ perceptions of patient autonomy: Residents wanted patients to make their own decisions, without any influence from the doctor, which misses the concept of informed decision making. These incomplete discussions can cause at minimum improper documentation of patients’ wishes, and at most psychological harm, damage to the physician-patient relationship, and the potential for unwanted attempts at resuscitation,” said Dr. David J. Einstein, a resident at Beth Israel Deaconess Medical Center and Tufts Medical Center, both in Boston.
Despite their reluctance to have the discussion, however, the majority of residents said they preferred to discuss code status with patients themselves rather than hand it off to the attending physician, primarily out of a sense that it is their responsibility as physicians.
Yet these physicians in training did not seem to feel that they were also responsible for providing guidance to patients, Dr. Einstein said at the Palliative Care in Oncology Symposium.
“We felt that this represented an unmet need in training and practice. Residents and attendings should be providing guidance on all medical interventions, including CPR, and if they aren’t sure what to recommend, then they themselves should be seeking guidance from other experts, before asking a patient to falsely choose between an intervention and death,” he said.
The first discussion of code status – do not resuscitate (DNR) or do not intubate (DNI) – may occur in the hospital, and is often left to a resident physician. Ideally, the physician and patient should discuss the patient’s prognosis, goals for care, evaluation of CPR as a means of meeting those goals, and a recommendation.
But many residents lack training in the end-of-life discussion, which can have a significant impact on the quality of the patients’ remaining weeks or months of life.
Nationwide survey
Dr. Einstein and his colleagues conducted a nationwide survey to measure the likelihood that residents would discuss prognostic information and offer recommendations to patients with limited life expectancy. They also sought to determine why residents might be reluctant to provide discussion, and to evaluate their satisfaction with code-status discussions that both they and their attending physicians have conducted.
The survey presented respondents with a hypothetical case of a patient with stage IV adenocarcinoma of the lung metastatic to the brain. The patient, who has disease progression despite receiving first- and second-line therapy, presents to the emergency department with dyspnea and is slightly hypoxemic, but is not in distress. The patient has not previously established a code-status preference.
The investigators contacted 387 residency program directors by mail, 19 of whom agreed to participate and responded. They sent surveys to a total of 1,627 residents, 358 of which were completed and included.
The investigators found that slightly less than half of the respondents said they would share information with the patient about his/her prognosis and the relative benefit of CPR, and more than two-thirds said they would be unlikely to offer a specific recommendation.
“So even in the situation with a clearly declining patient, residents were as likely as not to provide the information needed to make an informed decision, and were far less likely to provide guidance on this decision,” Dr. Einstein said.
Asked the reason for their decisions, 69% of the residents who would not offer a recommendation said that the patient should make his/her own decision without any influence, and 26.5% said that the attending would not want them to offer a recommendation. Nonetheless, only 1.3% of this group said they believed that CPR would offer the patient a reasonable chance of resuscitation.
The majority of respondents who would offer a recommendation (93.5%) said they would recommend DNR and DNI.
Code-status talk a ‘responsibility’
When they were asked whether they would prefer the attending to discuss code status, nearly 70% of respondents disagreed.
Of those residents who said they preferred to retain the code-status discussion, 93.4% said they thought it was part of their responsibility as a physician, and 65.8% said they thought they had sufficient training and knowledge to do it. A minority in this group (2.5%) said that they would be likely to disagree with the attending’s estimate of prognosis, and 4.9% said they thought the attending would not share his/her estimate honestly.
When the authors asked about the residents’ general satisfaction with discussion of code status, “we learned two things: One, the residents are significantly more satisfied with their own discussions than their attendings’ discussions; and two, there is a substantial minority that is dissatisfied with all discussions, and a small number who are actually very satisfied,” Dr. Einstein said.
In a linear regression analysis testing for hypothesized correlations, the investigators found that more-senior residents were more likely to share prognostic information and make recommendations (P = .002). Residents who expressed an interest in hematology/oncology or palliative care specialization were also more likely to offer prognostic information, but not to make a recommendation about code status.
More-senior year of training correlated negatively with satisfaction with both the resident’s own and the attending’s discussion of code status.
“We found substantial dissatisfaction with code-status discussions in general, and we hypothesize that this is due to an internal conflict. When a resident knows that an intervention may be more harmful than beneficial, but thinks that the patient should make their own decision alone, then one may experience substantial frustration, and this would increase as training goes on and one becomes more sure of the outcomes of interventions like CPR,” Dr. Einstein said.
Generation gap
Evoking a potential generation gap between old-school doctors and the up-and-coming young physicians who by statute work fewer hours than their mentors had to, “I’m struck that [residents] don’t trust the attendings. When I was a resident, you didn’t do anything without asking the attending,” said Dr. Michael H. Levy, an invited discussant who is vice chair of medical oncology and director of the pain and palliative care program at Fox Chase Cancer Center, Philadelphia.
“I’m glad that the residents want to do it, but they have the same arrogance/ignorance that they don’t know how, so if we want them to do it, we have to train them,” he said. The symposium was cosponsored by AAHPM, ASCO, ASTRO, and MASCC. The study was supported in part by the Conquer Cancer Foundation. Dr. Einstein and Dr. Levy reported having no relevant disclosures.
Ibuprofen superior to morphine following pediatric tonsillectomy
Ibuprofen appears to be an effective and safer pain reliever than morphine in children undergoing tonsillectomies, according to a recent study.
Although the two medications, administered with acetaminophen, treated pain about equally, morphine showed a greater risk for oxygen desaturation the night after surgery.
“Given the unpredictable posttonsillectomy respiratory response to opioids (codeine, morphine, and hydrocodone) and the analgesic effectiveness of ibuprofen, perhaps the time has come to question the postoperative use of all opioids in this population,” wrote Lauren Kelly, Ph.D., of Western University in London, Ontario, and her associates. The study was published online Jan. 26 (Pediatrics 2014 Jan. 26 [doi: 10.1542/peds.2014-1906].
The researchers randomized 91 children aged 1-10 years to acetaminophen (10-15 mg/kg per dose every 4 hours) with either an age appropriate dose of 0.2-0.5 mg/kg oral morphine every 4 hours or 10 mg/kg of oral ibuprofen every 6 hours after the children underwent a tonsillectomy with or without an adenoidectomy to treat sleep disordered breathing. The study ran from September 2012 to January 2014.
Parents put pulse oximeters on their children the nights before and after surgery to monitor oxygen saturation and apnea events.
The first evening after the surgery, 68% of children receiving ibuprofen showed improvement in oxygen desaturations, compared with 14% of children receiving morphine. The children receiving ibuprofen experienced an average 1.79 fewer desaturation events per hour, compared to an average 11.17 more desaturation events per hour in the morphine group.
No differences in average postsurgical oxygen saturation, pain relieving effectiveness, tonsillar bleeding or drug adverse events were identified.
“The results of this study support effective posttonsillectomy analgesia in children by using ibuprofen in combination with acetaminophen,” Dr. Kelly and her team wrote.
Ibuprofen appears to be an effective and safer pain reliever than morphine in children undergoing tonsillectomies, according to a recent study.
Although the two medications, administered with acetaminophen, treated pain about equally, morphine showed a greater risk for oxygen desaturation the night after surgery.
“Given the unpredictable posttonsillectomy respiratory response to opioids (codeine, morphine, and hydrocodone) and the analgesic effectiveness of ibuprofen, perhaps the time has come to question the postoperative use of all opioids in this population,” wrote Lauren Kelly, Ph.D., of Western University in London, Ontario, and her associates. The study was published online Jan. 26 (Pediatrics 2014 Jan. 26 [doi: 10.1542/peds.2014-1906].
The researchers randomized 91 children aged 1-10 years to acetaminophen (10-15 mg/kg per dose every 4 hours) with either an age appropriate dose of 0.2-0.5 mg/kg oral morphine every 4 hours or 10 mg/kg of oral ibuprofen every 6 hours after the children underwent a tonsillectomy with or without an adenoidectomy to treat sleep disordered breathing. The study ran from September 2012 to January 2014.
Parents put pulse oximeters on their children the nights before and after surgery to monitor oxygen saturation and apnea events.
The first evening after the surgery, 68% of children receiving ibuprofen showed improvement in oxygen desaturations, compared with 14% of children receiving morphine. The children receiving ibuprofen experienced an average 1.79 fewer desaturation events per hour, compared to an average 11.17 more desaturation events per hour in the morphine group.
No differences in average postsurgical oxygen saturation, pain relieving effectiveness, tonsillar bleeding or drug adverse events were identified.
“The results of this study support effective posttonsillectomy analgesia in children by using ibuprofen in combination with acetaminophen,” Dr. Kelly and her team wrote.
Ibuprofen appears to be an effective and safer pain reliever than morphine in children undergoing tonsillectomies, according to a recent study.
Although the two medications, administered with acetaminophen, treated pain about equally, morphine showed a greater risk for oxygen desaturation the night after surgery.
“Given the unpredictable posttonsillectomy respiratory response to opioids (codeine, morphine, and hydrocodone) and the analgesic effectiveness of ibuprofen, perhaps the time has come to question the postoperative use of all opioids in this population,” wrote Lauren Kelly, Ph.D., of Western University in London, Ontario, and her associates. The study was published online Jan. 26 (Pediatrics 2014 Jan. 26 [doi: 10.1542/peds.2014-1906].
The researchers randomized 91 children aged 1-10 years to acetaminophen (10-15 mg/kg per dose every 4 hours) with either an age appropriate dose of 0.2-0.5 mg/kg oral morphine every 4 hours or 10 mg/kg of oral ibuprofen every 6 hours after the children underwent a tonsillectomy with or without an adenoidectomy to treat sleep disordered breathing. The study ran from September 2012 to January 2014.
Parents put pulse oximeters on their children the nights before and after surgery to monitor oxygen saturation and apnea events.
The first evening after the surgery, 68% of children receiving ibuprofen showed improvement in oxygen desaturations, compared with 14% of children receiving morphine. The children receiving ibuprofen experienced an average 1.79 fewer desaturation events per hour, compared to an average 11.17 more desaturation events per hour in the morphine group.
No differences in average postsurgical oxygen saturation, pain relieving effectiveness, tonsillar bleeding or drug adverse events were identified.
“The results of this study support effective posttonsillectomy analgesia in children by using ibuprofen in combination with acetaminophen,” Dr. Kelly and her team wrote.
FROM PEDIATRICS
Key clinical point: Ibuprofen safely and effectively replaces morphine for children’s pain relief following tonsillectomy.
Major finding: Among children receiving ibuprofen, 68% improved the first night post surgery, compared with 14% of children receiving morphine.
Data source: A prospective randomized clinical trial of 91 children, aged 1-10 years, assigned to receive 10-15 mg/kg acetaminophen with either 0.2-0.5 mg/kg oral morphine or 10 mg/kg of oral ibuprofen following a tonsillectomy with or without adenoidectomy.
Disclosures: The Canadian Institutes for Health Research Drug Safety and Effectiveness Network funded the study. The authors reported no relevant financial disclosures.
Deaths in young leukemia patients on decline in UK

Credit: Bill Branson
Cancer deaths in children, adolescents, and young adults in the UK have fallen by 58% in the past 40 years, according to new figures from Cancer Research UK.*
Among cancer patients age 24 and under, the number of deaths each year dropped from about 1300 in the mid-1970s (1975-1977) to around 550 in more recent years (2010-2012).
And patients with leukemia have seen the steepest decline in mortality.
This is key because, according to Cancer Research UK, leukemia is the most commonly diagnosed cancer in children aged 14 and under and the sixth most commonly diagnosed cancer among 15- to 24-year-olds.
“These figures are testament to the real progress we’re making in treating children and young people with cancer,” said Pam Kearns, PhD, director of the Cancer Research UK Clinical Trials Unit in Birmingham.
“But hundreds of young people are dying from cancer each year in the UK, which means there’s still much more we need to do.”
Around 1600 children and 2200 adolescents and young adults are diagnosed with cancer every year in the UK.
And cancer remains the biggest killer of children and young people in the UK. It is the most common cause of death in children and young women aged 15 to 24 and the fourth most common cause of death in young men aged 15 to 24.
Still, the latest figures from Cancer Research UK show progress.
The mortality rate for all cancer patients ages 0 to 24 fell from 63.7 per million in 1975-1977 to 36.7 per million in 2001-2003 and then to 27.9 per million in 2010-2012. So the mortality rate has fallen 56% since 1975 and 24% in the last decade.
The average number of cancer deaths among children age 0 to 24 fell from 1325 in 1975-1977 to 681 in 2001-2003 and then to 550 in 2010-2012. That translates to a 58% decrease in deaths from 1975 and a 19% decrease in the last decade.
For leukemia patients ages 0 to 24, the mortality rate fell from 9.6 per million in 2001-2003 to 5.6 per million in 2010-2012, which translates to a 42% decrease. The annual average number of deaths dropped from 179 in 2001-2003 to 110 in 2010-2012, which translates to a 39% decrease.
“Cancer causes more deaths among children and young people than any other disease in the UK, so it’s hugely encouraging to see that death toll now falling steadily,” said Harpal Kumar, DSc, Cancer Research UK’s chief executive.
“But as the largest funder of research into children’s cancers in the UK, we will keep going until no young lives are lost to cancer.”
To that end, Cancer Research UK has launched “Cancer Research UK Kids & Teens,” an ongoing campaign to fund more research to find better treatments for young cancer patients.
“Money raised by ‘Cancer Research UK Kids & Teens’ will be restricted to research into cancers affecting children, teenagers, and young adults, enabling us to better understand these cancers and find better and kinder treatments and cures,” Dr Kumar said. “In the next 5 to 10 years, Cancer Research UK hopes to double the amount it spends on these cancers.” ![]()
*Some of the information in this article is not available on the Cancer Research UK website (and was sent to HematologyTimes upon request), but similar data and additional details are available on the organization’s Cancer Stats page.

Credit: Bill Branson
Cancer deaths in children, adolescents, and young adults in the UK have fallen by 58% in the past 40 years, according to new figures from Cancer Research UK.*
Among cancer patients age 24 and under, the number of deaths each year dropped from about 1300 in the mid-1970s (1975-1977) to around 550 in more recent years (2010-2012).
And patients with leukemia have seen the steepest decline in mortality.
This is key because, according to Cancer Research UK, leukemia is the most commonly diagnosed cancer in children aged 14 and under and the sixth most commonly diagnosed cancer among 15- to 24-year-olds.
“These figures are testament to the real progress we’re making in treating children and young people with cancer,” said Pam Kearns, PhD, director of the Cancer Research UK Clinical Trials Unit in Birmingham.
“But hundreds of young people are dying from cancer each year in the UK, which means there’s still much more we need to do.”
Around 1600 children and 2200 adolescents and young adults are diagnosed with cancer every year in the UK.
And cancer remains the biggest killer of children and young people in the UK. It is the most common cause of death in children and young women aged 15 to 24 and the fourth most common cause of death in young men aged 15 to 24.
Still, the latest figures from Cancer Research UK show progress.
The mortality rate for all cancer patients ages 0 to 24 fell from 63.7 per million in 1975-1977 to 36.7 per million in 2001-2003 and then to 27.9 per million in 2010-2012. So the mortality rate has fallen 56% since 1975 and 24% in the last decade.
The average number of cancer deaths among children age 0 to 24 fell from 1325 in 1975-1977 to 681 in 2001-2003 and then to 550 in 2010-2012. That translates to a 58% decrease in deaths from 1975 and a 19% decrease in the last decade.
For leukemia patients ages 0 to 24, the mortality rate fell from 9.6 per million in 2001-2003 to 5.6 per million in 2010-2012, which translates to a 42% decrease. The annual average number of deaths dropped from 179 in 2001-2003 to 110 in 2010-2012, which translates to a 39% decrease.
“Cancer causes more deaths among children and young people than any other disease in the UK, so it’s hugely encouraging to see that death toll now falling steadily,” said Harpal Kumar, DSc, Cancer Research UK’s chief executive.
“But as the largest funder of research into children’s cancers in the UK, we will keep going until no young lives are lost to cancer.”
To that end, Cancer Research UK has launched “Cancer Research UK Kids & Teens,” an ongoing campaign to fund more research to find better treatments for young cancer patients.
“Money raised by ‘Cancer Research UK Kids & Teens’ will be restricted to research into cancers affecting children, teenagers, and young adults, enabling us to better understand these cancers and find better and kinder treatments and cures,” Dr Kumar said. “In the next 5 to 10 years, Cancer Research UK hopes to double the amount it spends on these cancers.” ![]()
*Some of the information in this article is not available on the Cancer Research UK website (and was sent to HematologyTimes upon request), but similar data and additional details are available on the organization’s Cancer Stats page.

Credit: Bill Branson
Cancer deaths in children, adolescents, and young adults in the UK have fallen by 58% in the past 40 years, according to new figures from Cancer Research UK.*
Among cancer patients age 24 and under, the number of deaths each year dropped from about 1300 in the mid-1970s (1975-1977) to around 550 in more recent years (2010-2012).
And patients with leukemia have seen the steepest decline in mortality.
This is key because, according to Cancer Research UK, leukemia is the most commonly diagnosed cancer in children aged 14 and under and the sixth most commonly diagnosed cancer among 15- to 24-year-olds.
“These figures are testament to the real progress we’re making in treating children and young people with cancer,” said Pam Kearns, PhD, director of the Cancer Research UK Clinical Trials Unit in Birmingham.
“But hundreds of young people are dying from cancer each year in the UK, which means there’s still much more we need to do.”
Around 1600 children and 2200 adolescents and young adults are diagnosed with cancer every year in the UK.
And cancer remains the biggest killer of children and young people in the UK. It is the most common cause of death in children and young women aged 15 to 24 and the fourth most common cause of death in young men aged 15 to 24.
Still, the latest figures from Cancer Research UK show progress.
The mortality rate for all cancer patients ages 0 to 24 fell from 63.7 per million in 1975-1977 to 36.7 per million in 2001-2003 and then to 27.9 per million in 2010-2012. So the mortality rate has fallen 56% since 1975 and 24% in the last decade.
The average number of cancer deaths among children age 0 to 24 fell from 1325 in 1975-1977 to 681 in 2001-2003 and then to 550 in 2010-2012. That translates to a 58% decrease in deaths from 1975 and a 19% decrease in the last decade.
For leukemia patients ages 0 to 24, the mortality rate fell from 9.6 per million in 2001-2003 to 5.6 per million in 2010-2012, which translates to a 42% decrease. The annual average number of deaths dropped from 179 in 2001-2003 to 110 in 2010-2012, which translates to a 39% decrease.
“Cancer causes more deaths among children and young people than any other disease in the UK, so it’s hugely encouraging to see that death toll now falling steadily,” said Harpal Kumar, DSc, Cancer Research UK’s chief executive.
“But as the largest funder of research into children’s cancers in the UK, we will keep going until no young lives are lost to cancer.”
To that end, Cancer Research UK has launched “Cancer Research UK Kids & Teens,” an ongoing campaign to fund more research to find better treatments for young cancer patients.
“Money raised by ‘Cancer Research UK Kids & Teens’ will be restricted to research into cancers affecting children, teenagers, and young adults, enabling us to better understand these cancers and find better and kinder treatments and cures,” Dr Kumar said. “In the next 5 to 10 years, Cancer Research UK hopes to double the amount it spends on these cancers.” ![]()
*Some of the information in this article is not available on the Cancer Research UK website (and was sent to HematologyTimes upon request), but similar data and additional details are available on the organization’s Cancer Stats page.
EMA wants to suspend drugs due to data manipulation

Credit: Steven Harbour
The European Medicines Agency (EMA) has recommended suspending a number of drugs that were approved in the European Union (EU) based on clinical studies conducted at GVK Biosciences in Hyderabad, India.
An inspection of the site suggested GVK Bio employees may have manipulated data from trials that took place there.
So the EMA compiled a list of drugs—which includes clopidogrel, dexamethasone, and tacrolimus, among others—that should be suspended.
However, the EMA said there is no evidence of harm or lack of effectiveness linked to the conduct of studies by GVK Bio, and patients should continue taking their medicines as prescribed.
The EMA’s opinion has been forwarded to the European Commission (EC), which will adopt a legally binding decision.
It was at the request of the EC that the EMA’s Committee for Medicinal Products for Human Use (CHMP) reviewed the drugs set to be suspended.
An inspection by the French medicines agency, Agence nationale de sécurité du médicament et des produits de santé (ANSM), in May 2014 uncovered “non-compliance with good clinical practice” at the GVK Bio site in Hyderabad.
The ANSM inspector analyzed 9 studies conducted there from 2008 to 2013 and found evidence suggesting that data from electrocardiograms (ECGs) had been manipulated. It appeared that GVK Bio employees were taking multiple ECGs of one volunteer and presenting them as ECGs of other volunteers.
The EMA said the systematic nature of these data manipulations, the extended period of time during which they took place, and the number of staff members involved casts doubt on the integrity of the way trials were performed at the Hyderabad facility and on the reliability of data generated there.
With this in mind, the CHMP looked at more than 1000 pharmaceutical forms and strengths of medicines studied at the site. For more than 300 of the medications, there was sufficient data from other sources to support the drugs’ authorization, so these will remain on the market in the EU.
For drugs that lack data from other studies, the CHMP recommended suspension unless they are of critical importance for patients because alternatives will not be able to meet patients’ needs.
Whether a medicine is critical for patients will be determined by the national authorities of EU member states, depending on the situation in their country. For drugs that are considered critical, companies developing those drugs will be given 12 months to submit additional data.
The CHMP’s recommendation will be sent to the EC for a legally binding decision that will apply to all EU member states whether or not they have taken interim measures to suspend medicines.
GVK Bio responds
GVK Bio said an internal audit conducted following the ANSM inspection suggested that standard operating procedures were followed for the 9 trials analyzed. The organization also sought the opinion of 4 independent cardiologists, who said it was difficult to determine if the ECGs belong to the same volunteer or more than one person.
GVK Bio presented this information to the ANSM, but the agency concluded that the studies did not meet good clinical practice guidelines and should be rejected.
Following subsequent meetings and analyses, the EMA came to a similar conclusion—that the overall findings cast doubt on the results of trials conducted at the Hyderabad facility from 2008 to 2014.
GVK Bio said it respects the EMA’s decision, but their recommended suspension of drugs is “unprecedented and highly disproportional” for a few reasons.
First, the ANSM said the ECGs in question were not essential to demonstrate the bioequivalence of the drugs tested, and the agency’s recommendation to reject the 9 studies was a “precautionary” measure.
The ANSM also said the observations made during the inspection should not be extrapolated to other trial-related activities at the Hyderabad site or GVK Bio’s other site in Ahmedabad.
And finally, the EMA itself said there is no evidence proving that the drugs in question are ineffective or pose a risk to human health. ![]()

Credit: Steven Harbour
The European Medicines Agency (EMA) has recommended suspending a number of drugs that were approved in the European Union (EU) based on clinical studies conducted at GVK Biosciences in Hyderabad, India.
An inspection of the site suggested GVK Bio employees may have manipulated data from trials that took place there.
So the EMA compiled a list of drugs—which includes clopidogrel, dexamethasone, and tacrolimus, among others—that should be suspended.
However, the EMA said there is no evidence of harm or lack of effectiveness linked to the conduct of studies by GVK Bio, and patients should continue taking their medicines as prescribed.
The EMA’s opinion has been forwarded to the European Commission (EC), which will adopt a legally binding decision.
It was at the request of the EC that the EMA’s Committee for Medicinal Products for Human Use (CHMP) reviewed the drugs set to be suspended.
An inspection by the French medicines agency, Agence nationale de sécurité du médicament et des produits de santé (ANSM), in May 2014 uncovered “non-compliance with good clinical practice” at the GVK Bio site in Hyderabad.
The ANSM inspector analyzed 9 studies conducted there from 2008 to 2013 and found evidence suggesting that data from electrocardiograms (ECGs) had been manipulated. It appeared that GVK Bio employees were taking multiple ECGs of one volunteer and presenting them as ECGs of other volunteers.
The EMA said the systematic nature of these data manipulations, the extended period of time during which they took place, and the number of staff members involved casts doubt on the integrity of the way trials were performed at the Hyderabad facility and on the reliability of data generated there.
With this in mind, the CHMP looked at more than 1000 pharmaceutical forms and strengths of medicines studied at the site. For more than 300 of the medications, there was sufficient data from other sources to support the drugs’ authorization, so these will remain on the market in the EU.
For drugs that lack data from other studies, the CHMP recommended suspension unless they are of critical importance for patients because alternatives will not be able to meet patients’ needs.
Whether a medicine is critical for patients will be determined by the national authorities of EU member states, depending on the situation in their country. For drugs that are considered critical, companies developing those drugs will be given 12 months to submit additional data.
The CHMP’s recommendation will be sent to the EC for a legally binding decision that will apply to all EU member states whether or not they have taken interim measures to suspend medicines.
GVK Bio responds
GVK Bio said an internal audit conducted following the ANSM inspection suggested that standard operating procedures were followed for the 9 trials analyzed. The organization also sought the opinion of 4 independent cardiologists, who said it was difficult to determine if the ECGs belong to the same volunteer or more than one person.
GVK Bio presented this information to the ANSM, but the agency concluded that the studies did not meet good clinical practice guidelines and should be rejected.
Following subsequent meetings and analyses, the EMA came to a similar conclusion—that the overall findings cast doubt on the results of trials conducted at the Hyderabad facility from 2008 to 2014.
GVK Bio said it respects the EMA’s decision, but their recommended suspension of drugs is “unprecedented and highly disproportional” for a few reasons.
First, the ANSM said the ECGs in question were not essential to demonstrate the bioequivalence of the drugs tested, and the agency’s recommendation to reject the 9 studies was a “precautionary” measure.
The ANSM also said the observations made during the inspection should not be extrapolated to other trial-related activities at the Hyderabad site or GVK Bio’s other site in Ahmedabad.
And finally, the EMA itself said there is no evidence proving that the drugs in question are ineffective or pose a risk to human health. ![]()

Credit: Steven Harbour
The European Medicines Agency (EMA) has recommended suspending a number of drugs that were approved in the European Union (EU) based on clinical studies conducted at GVK Biosciences in Hyderabad, India.
An inspection of the site suggested GVK Bio employees may have manipulated data from trials that took place there.
So the EMA compiled a list of drugs—which includes clopidogrel, dexamethasone, and tacrolimus, among others—that should be suspended.
However, the EMA said there is no evidence of harm or lack of effectiveness linked to the conduct of studies by GVK Bio, and patients should continue taking their medicines as prescribed.
The EMA’s opinion has been forwarded to the European Commission (EC), which will adopt a legally binding decision.
It was at the request of the EC that the EMA’s Committee for Medicinal Products for Human Use (CHMP) reviewed the drugs set to be suspended.
An inspection by the French medicines agency, Agence nationale de sécurité du médicament et des produits de santé (ANSM), in May 2014 uncovered “non-compliance with good clinical practice” at the GVK Bio site in Hyderabad.
The ANSM inspector analyzed 9 studies conducted there from 2008 to 2013 and found evidence suggesting that data from electrocardiograms (ECGs) had been manipulated. It appeared that GVK Bio employees were taking multiple ECGs of one volunteer and presenting them as ECGs of other volunteers.
The EMA said the systematic nature of these data manipulations, the extended period of time during which they took place, and the number of staff members involved casts doubt on the integrity of the way trials were performed at the Hyderabad facility and on the reliability of data generated there.
With this in mind, the CHMP looked at more than 1000 pharmaceutical forms and strengths of medicines studied at the site. For more than 300 of the medications, there was sufficient data from other sources to support the drugs’ authorization, so these will remain on the market in the EU.
For drugs that lack data from other studies, the CHMP recommended suspension unless they are of critical importance for patients because alternatives will not be able to meet patients’ needs.
Whether a medicine is critical for patients will be determined by the national authorities of EU member states, depending on the situation in their country. For drugs that are considered critical, companies developing those drugs will be given 12 months to submit additional data.
The CHMP’s recommendation will be sent to the EC for a legally binding decision that will apply to all EU member states whether or not they have taken interim measures to suspend medicines.
GVK Bio responds
GVK Bio said an internal audit conducted following the ANSM inspection suggested that standard operating procedures were followed for the 9 trials analyzed. The organization also sought the opinion of 4 independent cardiologists, who said it was difficult to determine if the ECGs belong to the same volunteer or more than one person.
GVK Bio presented this information to the ANSM, but the agency concluded that the studies did not meet good clinical practice guidelines and should be rejected.
Following subsequent meetings and analyses, the EMA came to a similar conclusion—that the overall findings cast doubt on the results of trials conducted at the Hyderabad facility from 2008 to 2014.
GVK Bio said it respects the EMA’s decision, but their recommended suspension of drugs is “unprecedented and highly disproportional” for a few reasons.
First, the ANSM said the ECGs in question were not essential to demonstrate the bioequivalence of the drugs tested, and the agency’s recommendation to reject the 9 studies was a “precautionary” measure.
The ANSM also said the observations made during the inspection should not be extrapolated to other trial-related activities at the Hyderabad site or GVK Bio’s other site in Ahmedabad.
And finally, the EMA itself said there is no evidence proving that the drugs in question are ineffective or pose a risk to human health. ![]()
Analysis examines glossectomy as solo treatment for sleep apnea
CORONADO, CALIF. – Results from a new meta-analysis suggest that glossectomy significantly improves sleep outcomes when performed as part of a multi-level surgery for adults with obstructive sleep apnea.
However, “there is insufficient evidence to analyze the role of glossectomy as a stand-alone procedure for the treatment of sleep apnea,” lead study author Dr. Alexander W. Murphey said in an interview in advance of The Triological Society’s Combined Sections meeting, where the work was presented. “The lack of available data for glossectomy as a single treatment was disappointing, and points to the need for further studies in this population.”
Glossectomy for OSA was first reported in 1991 as a salvage surgery after uvulopalatopharyngoplasty, said Dr. Murphey, who is completing a clinical research fellowship in the department of otolaryngology-head and neck surgery at Medical University of South Carolina, Charleston, under the mentoring of Dr. Marion B. Gillespie and Dr. Shaun A. Nguyen. Since that time, “many modifications have been made regarding technique and instrumentation with recent focus on minimally invasive techniques aimed at maximizing tissue reduction while limiting the inherent morbidity associated with glossectomy,” he said. “The aim of our study was to review and analyze all of the available literature on partial glossectomy for OSA in one study. Overall, there is a significant lack of research into glossectomy, and what literature is available include small, case-series that analyze glossectomy as part of complex, multi-level surgeries. This study represents the first large scale meta-analysis on the role of glossectomy, and attempts to determine the role of glossectomy both as part of multi-level surgery, and as a single, stand-alone sleep apnea treatment.”
Dr. Murphey used the PubMed-NCBI literature database to identify studies with 10 or more patients and reported preoperative and postoperative apnea-hypopnea index (AHI) scores. The primary endpoint was change in AHI while secondary endpoints included predefined surgical success rates, and changes in additional reported sleep outcomes such as Epworth Sleep Scores (ESS), Lowest Oxygen Saturation (LSAT), and snoring visual analog scale (VAS). The researchers reported results from 15 articles with 442 patients treated with three glossectomy techniques (midline glossectomy, lingualplasty, and submucosal minimally invasive lingual excision (SMILE). In pooled analyses that compared baseline vs. post-surgery, investigators observed significant reductions in AHI (from 48 to 20); ESS (from 12 to 5), and VAS (from 9 to 3; all with a P of less than .0001). In addition, they observed a significant increase in LSAT (from 77% to 84%; P less than .0001), according to the findings, presented at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
Surgical success, which was defined as an AHI less than 20 and a greater than 50% reduction in AHI, was achieved in 56% of cases, while complications occurred in 18% of patients. Only 24 patients (5%) were treated with glossectomy as sole therapy for OSA. Among these 24 patients, significant reductions occurred in AHI (from 42 to 25; P=.0345) and ESS (from 12 to 7; P less than .0001).
Dr. Murphey acknowledged certain limitations of the analysis, including “a lack of quality research involving glossectomy, with the majority of available published data drawn from small, case-series without control arms,” he said. “Additionally, studies varied in surgical approach, inclusion criteria, and accompanying procedures in multi-level treatment. This makes it extremely difficult to truly compare treatments.”
The researchers reported having no relevant financial conflicts.
On Twitter @dougbrunk
CORONADO, CALIF. – Results from a new meta-analysis suggest that glossectomy significantly improves sleep outcomes when performed as part of a multi-level surgery for adults with obstructive sleep apnea.
However, “there is insufficient evidence to analyze the role of glossectomy as a stand-alone procedure for the treatment of sleep apnea,” lead study author Dr. Alexander W. Murphey said in an interview in advance of The Triological Society’s Combined Sections meeting, where the work was presented. “The lack of available data for glossectomy as a single treatment was disappointing, and points to the need for further studies in this population.”
Glossectomy for OSA was first reported in 1991 as a salvage surgery after uvulopalatopharyngoplasty, said Dr. Murphey, who is completing a clinical research fellowship in the department of otolaryngology-head and neck surgery at Medical University of South Carolina, Charleston, under the mentoring of Dr. Marion B. Gillespie and Dr. Shaun A. Nguyen. Since that time, “many modifications have been made regarding technique and instrumentation with recent focus on minimally invasive techniques aimed at maximizing tissue reduction while limiting the inherent morbidity associated with glossectomy,” he said. “The aim of our study was to review and analyze all of the available literature on partial glossectomy for OSA in one study. Overall, there is a significant lack of research into glossectomy, and what literature is available include small, case-series that analyze glossectomy as part of complex, multi-level surgeries. This study represents the first large scale meta-analysis on the role of glossectomy, and attempts to determine the role of glossectomy both as part of multi-level surgery, and as a single, stand-alone sleep apnea treatment.”
Dr. Murphey used the PubMed-NCBI literature database to identify studies with 10 or more patients and reported preoperative and postoperative apnea-hypopnea index (AHI) scores. The primary endpoint was change in AHI while secondary endpoints included predefined surgical success rates, and changes in additional reported sleep outcomes such as Epworth Sleep Scores (ESS), Lowest Oxygen Saturation (LSAT), and snoring visual analog scale (VAS). The researchers reported results from 15 articles with 442 patients treated with three glossectomy techniques (midline glossectomy, lingualplasty, and submucosal minimally invasive lingual excision (SMILE). In pooled analyses that compared baseline vs. post-surgery, investigators observed significant reductions in AHI (from 48 to 20); ESS (from 12 to 5), and VAS (from 9 to 3; all with a P of less than .0001). In addition, they observed a significant increase in LSAT (from 77% to 84%; P less than .0001), according to the findings, presented at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
Surgical success, which was defined as an AHI less than 20 and a greater than 50% reduction in AHI, was achieved in 56% of cases, while complications occurred in 18% of patients. Only 24 patients (5%) were treated with glossectomy as sole therapy for OSA. Among these 24 patients, significant reductions occurred in AHI (from 42 to 25; P=.0345) and ESS (from 12 to 7; P less than .0001).
Dr. Murphey acknowledged certain limitations of the analysis, including “a lack of quality research involving glossectomy, with the majority of available published data drawn from small, case-series without control arms,” he said. “Additionally, studies varied in surgical approach, inclusion criteria, and accompanying procedures in multi-level treatment. This makes it extremely difficult to truly compare treatments.”
The researchers reported having no relevant financial conflicts.
On Twitter @dougbrunk
CORONADO, CALIF. – Results from a new meta-analysis suggest that glossectomy significantly improves sleep outcomes when performed as part of a multi-level surgery for adults with obstructive sleep apnea.
However, “there is insufficient evidence to analyze the role of glossectomy as a stand-alone procedure for the treatment of sleep apnea,” lead study author Dr. Alexander W. Murphey said in an interview in advance of The Triological Society’s Combined Sections meeting, where the work was presented. “The lack of available data for glossectomy as a single treatment was disappointing, and points to the need for further studies in this population.”
Glossectomy for OSA was first reported in 1991 as a salvage surgery after uvulopalatopharyngoplasty, said Dr. Murphey, who is completing a clinical research fellowship in the department of otolaryngology-head and neck surgery at Medical University of South Carolina, Charleston, under the mentoring of Dr. Marion B. Gillespie and Dr. Shaun A. Nguyen. Since that time, “many modifications have been made regarding technique and instrumentation with recent focus on minimally invasive techniques aimed at maximizing tissue reduction while limiting the inherent morbidity associated with glossectomy,” he said. “The aim of our study was to review and analyze all of the available literature on partial glossectomy for OSA in one study. Overall, there is a significant lack of research into glossectomy, and what literature is available include small, case-series that analyze glossectomy as part of complex, multi-level surgeries. This study represents the first large scale meta-analysis on the role of glossectomy, and attempts to determine the role of glossectomy both as part of multi-level surgery, and as a single, stand-alone sleep apnea treatment.”
Dr. Murphey used the PubMed-NCBI literature database to identify studies with 10 or more patients and reported preoperative and postoperative apnea-hypopnea index (AHI) scores. The primary endpoint was change in AHI while secondary endpoints included predefined surgical success rates, and changes in additional reported sleep outcomes such as Epworth Sleep Scores (ESS), Lowest Oxygen Saturation (LSAT), and snoring visual analog scale (VAS). The researchers reported results from 15 articles with 442 patients treated with three glossectomy techniques (midline glossectomy, lingualplasty, and submucosal minimally invasive lingual excision (SMILE). In pooled analyses that compared baseline vs. post-surgery, investigators observed significant reductions in AHI (from 48 to 20); ESS (from 12 to 5), and VAS (from 9 to 3; all with a P of less than .0001). In addition, they observed a significant increase in LSAT (from 77% to 84%; P less than .0001), according to the findings, presented at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
Surgical success, which was defined as an AHI less than 20 and a greater than 50% reduction in AHI, was achieved in 56% of cases, while complications occurred in 18% of patients. Only 24 patients (5%) were treated with glossectomy as sole therapy for OSA. Among these 24 patients, significant reductions occurred in AHI (from 42 to 25; P=.0345) and ESS (from 12 to 7; P less than .0001).
Dr. Murphey acknowledged certain limitations of the analysis, including “a lack of quality research involving glossectomy, with the majority of available published data drawn from small, case-series without control arms,” he said. “Additionally, studies varied in surgical approach, inclusion criteria, and accompanying procedures in multi-level treatment. This makes it extremely difficult to truly compare treatments.”
The researchers reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT THE COMBINED SECTIONS WINTER MEETING
Key clinical point: Among adults with obstructive sleep apnea, glossectomy significantly improved sleep outcomes when performed as part of a multi-level surgery, though evidence is sparse.
Major finding: There are no available data on the role of glossectomy as a stand-alone procedure for the treatment of OSA.
Data source: A meta-analysis of 15 articles concerning 442 patients treated with three glossectomy techniques (midline glossectomy, lingualplasty, and submucosal minimally invasive lingual excision.
Disclosures: The researchers reported having no financial disclosures.
Some things vascular surgeons should know that they don’t learn in training
All vascular surgeons want to be good doctors and to take the best possible care of their patients. They, therefore, train diligently and strive to keep up with new developments by reading vascular journals and attending cutting edge vascular meetings. They seek to optimize their judgment, communicate well and honestly with patients, perform their procedures with care, and follow their patients closely.
However, doing all these things does not ensure ascendancy in the profession. There are other factors which go into being a successful vascular surgeon. Many of these are not taught in medical school or residency training, and failure to recognize their importance can derail an otherwise prominent career. It is, therefore, important to highlight some of these factors which can be pitfalls to even the best trained and most committed vascular surgeon.
Vascular surgeons exist in a professionally competitive environment. We compete for patients with several other specialists including interventional cardiologists, interventional radiologists, and some general and cardiac surgeons as well as other lesser competitors.
All are hungry for patients and all consider themselves expert in all or some of the things we do. We also face competition from other vascular surgeons, few of whom feel busy enough to turn away patients. Therefore, it is important that vascular surgeons consider the competitive landscape when they are choosing a location or institution in which to practice. Is there an empty niche for the particular skills one brings to the area or the institution, and will other physicians in the area recognize those skills? Even then they must compete effectively not only by providing superior care but also by engaging in appropriate public relations and marketing of their assets.
Recognizing the importance of professional relationships with nonphysicians and other physicians outside our specialty and cultivating these relationships are other keys to success. The need for good relationships with referring physicians is obvious. Not so obvious is the need to have good relationships with hospital administrators who control essential resources, with other specialists like anesthesiologists and intensivists who can optimize the care our patients receive, with industry representatives, and even with other vascular surgeons. To make these relationships work to our advantage it is crucial to make them mutually beneficial. People are much more inclined to be helpful if what they are doing also helps them. Mutual self-interest can even improve interactions with competitors.
It is also important to avoid making enemies. This is particularly hard to do in the competitive environment in which we work. It is even harder to do in the present health care setting in which others who we do not control are unreasonable or incompetent. This is particularly true with those in positions of administrative authority like hospital executives or operating room supervisors. Making enemies of these individuals can be disastrous since they often control resources that determine our destiny. Keeping such individuals supportive or at least neutral, despite their possible serious flaws, is worth the sometimes painful effort required.
One must also be aware that nothing elicits hostility like success. If a young vascular surgeon/specialist has introduced a new technique or is particularly charming and hard-working and therefore has a booming practice, rest assured that his or her competitors – or even non-competitors – will be covertly or overtly hostile and take every opportunity to damage or bring down the successful individual. It does not matter that the hostility is unjustified and based on jealousy. It can still be unfairly damaging. All should realize that jealousy and greed are among the most powerful motivators of human behavior.
In view of all these considerations, it is apparent that all vascular surgeons, especially talented and successful ones, will at various times in their careers face battles. All cannot be fought. So one has to decide which ones should be avoided and which ones to engage in. Battles to fight should be picked carefully because they will consume energy and leave scars, no matter the outcome.
Most battles are best avoided unless victory is certain. Multiple simultaneous battles should be avoided. Battles in which one faces numerous opponents at the same time should also be shunned. Ideally in unavoidable conflicts, one should have as many allies as possible, although the loyalty of allies cannot always be counted on. Self-interest will determine the loyalty of presumed allies.
Never underestimate enemies, or overestimate allies. If the outcome of a battle is uncertain or to be determined by a board or other group, know how that group will vote before taking on the fight. Always remember the role of jealousy and greed in determining human behavior in battle. Defeated opponents do not forget and are forever dangerous.
Time is a vascular surgeon’s most important asset. Anything that one can do to enlist others to protect or expand this time is helpful. To this end, loyal nurses, physician’s assistants, or nonprofessional associates are invaluable. Their loyalty, which must be reciprocated, can be earned by recognizing their contributions and rewarding them intellectually and financially. This mutual loyalty is essential to success in practice and in the inevitable conflicts that will occur.
All these concepts and many others are not covered in medical school or residency training. Yet all are important in a vascular surgery career, whether it be in a practice or academic setting. Human nature is a constant and its elements may often work against one’s success. Being aware of some of these often noxious and little discussed elements will hopefully enable vascular surgeons to cope with them better and ultimately survive in what can be a difficult environment.
Dr. Veith is professor of surgery at New York University Medical Center and the Cleveland Clinic and an associate medical editor for Vascular Specialist.
The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or publisher.
All vascular surgeons want to be good doctors and to take the best possible care of their patients. They, therefore, train diligently and strive to keep up with new developments by reading vascular journals and attending cutting edge vascular meetings. They seek to optimize their judgment, communicate well and honestly with patients, perform their procedures with care, and follow their patients closely.
However, doing all these things does not ensure ascendancy in the profession. There are other factors which go into being a successful vascular surgeon. Many of these are not taught in medical school or residency training, and failure to recognize their importance can derail an otherwise prominent career. It is, therefore, important to highlight some of these factors which can be pitfalls to even the best trained and most committed vascular surgeon.
Vascular surgeons exist in a professionally competitive environment. We compete for patients with several other specialists including interventional cardiologists, interventional radiologists, and some general and cardiac surgeons as well as other lesser competitors.
All are hungry for patients and all consider themselves expert in all or some of the things we do. We also face competition from other vascular surgeons, few of whom feel busy enough to turn away patients. Therefore, it is important that vascular surgeons consider the competitive landscape when they are choosing a location or institution in which to practice. Is there an empty niche for the particular skills one brings to the area or the institution, and will other physicians in the area recognize those skills? Even then they must compete effectively not only by providing superior care but also by engaging in appropriate public relations and marketing of their assets.
Recognizing the importance of professional relationships with nonphysicians and other physicians outside our specialty and cultivating these relationships are other keys to success. The need for good relationships with referring physicians is obvious. Not so obvious is the need to have good relationships with hospital administrators who control essential resources, with other specialists like anesthesiologists and intensivists who can optimize the care our patients receive, with industry representatives, and even with other vascular surgeons. To make these relationships work to our advantage it is crucial to make them mutually beneficial. People are much more inclined to be helpful if what they are doing also helps them. Mutual self-interest can even improve interactions with competitors.
It is also important to avoid making enemies. This is particularly hard to do in the competitive environment in which we work. It is even harder to do in the present health care setting in which others who we do not control are unreasonable or incompetent. This is particularly true with those in positions of administrative authority like hospital executives or operating room supervisors. Making enemies of these individuals can be disastrous since they often control resources that determine our destiny. Keeping such individuals supportive or at least neutral, despite their possible serious flaws, is worth the sometimes painful effort required.
One must also be aware that nothing elicits hostility like success. If a young vascular surgeon/specialist has introduced a new technique or is particularly charming and hard-working and therefore has a booming practice, rest assured that his or her competitors – or even non-competitors – will be covertly or overtly hostile and take every opportunity to damage or bring down the successful individual. It does not matter that the hostility is unjustified and based on jealousy. It can still be unfairly damaging. All should realize that jealousy and greed are among the most powerful motivators of human behavior.
In view of all these considerations, it is apparent that all vascular surgeons, especially talented and successful ones, will at various times in their careers face battles. All cannot be fought. So one has to decide which ones should be avoided and which ones to engage in. Battles to fight should be picked carefully because they will consume energy and leave scars, no matter the outcome.
Most battles are best avoided unless victory is certain. Multiple simultaneous battles should be avoided. Battles in which one faces numerous opponents at the same time should also be shunned. Ideally in unavoidable conflicts, one should have as many allies as possible, although the loyalty of allies cannot always be counted on. Self-interest will determine the loyalty of presumed allies.
Never underestimate enemies, or overestimate allies. If the outcome of a battle is uncertain or to be determined by a board or other group, know how that group will vote before taking on the fight. Always remember the role of jealousy and greed in determining human behavior in battle. Defeated opponents do not forget and are forever dangerous.
Time is a vascular surgeon’s most important asset. Anything that one can do to enlist others to protect or expand this time is helpful. To this end, loyal nurses, physician’s assistants, or nonprofessional associates are invaluable. Their loyalty, which must be reciprocated, can be earned by recognizing their contributions and rewarding them intellectually and financially. This mutual loyalty is essential to success in practice and in the inevitable conflicts that will occur.
All these concepts and many others are not covered in medical school or residency training. Yet all are important in a vascular surgery career, whether it be in a practice or academic setting. Human nature is a constant and its elements may often work against one’s success. Being aware of some of these often noxious and little discussed elements will hopefully enable vascular surgeons to cope with them better and ultimately survive in what can be a difficult environment.
Dr. Veith is professor of surgery at New York University Medical Center and the Cleveland Clinic and an associate medical editor for Vascular Specialist.
The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or publisher.
All vascular surgeons want to be good doctors and to take the best possible care of their patients. They, therefore, train diligently and strive to keep up with new developments by reading vascular journals and attending cutting edge vascular meetings. They seek to optimize their judgment, communicate well and honestly with patients, perform their procedures with care, and follow their patients closely.
However, doing all these things does not ensure ascendancy in the profession. There are other factors which go into being a successful vascular surgeon. Many of these are not taught in medical school or residency training, and failure to recognize their importance can derail an otherwise prominent career. It is, therefore, important to highlight some of these factors which can be pitfalls to even the best trained and most committed vascular surgeon.
Vascular surgeons exist in a professionally competitive environment. We compete for patients with several other specialists including interventional cardiologists, interventional radiologists, and some general and cardiac surgeons as well as other lesser competitors.
All are hungry for patients and all consider themselves expert in all or some of the things we do. We also face competition from other vascular surgeons, few of whom feel busy enough to turn away patients. Therefore, it is important that vascular surgeons consider the competitive landscape when they are choosing a location or institution in which to practice. Is there an empty niche for the particular skills one brings to the area or the institution, and will other physicians in the area recognize those skills? Even then they must compete effectively not only by providing superior care but also by engaging in appropriate public relations and marketing of their assets.
Recognizing the importance of professional relationships with nonphysicians and other physicians outside our specialty and cultivating these relationships are other keys to success. The need for good relationships with referring physicians is obvious. Not so obvious is the need to have good relationships with hospital administrators who control essential resources, with other specialists like anesthesiologists and intensivists who can optimize the care our patients receive, with industry representatives, and even with other vascular surgeons. To make these relationships work to our advantage it is crucial to make them mutually beneficial. People are much more inclined to be helpful if what they are doing also helps them. Mutual self-interest can even improve interactions with competitors.
It is also important to avoid making enemies. This is particularly hard to do in the competitive environment in which we work. It is even harder to do in the present health care setting in which others who we do not control are unreasonable or incompetent. This is particularly true with those in positions of administrative authority like hospital executives or operating room supervisors. Making enemies of these individuals can be disastrous since they often control resources that determine our destiny. Keeping such individuals supportive or at least neutral, despite their possible serious flaws, is worth the sometimes painful effort required.
One must also be aware that nothing elicits hostility like success. If a young vascular surgeon/specialist has introduced a new technique or is particularly charming and hard-working and therefore has a booming practice, rest assured that his or her competitors – or even non-competitors – will be covertly or overtly hostile and take every opportunity to damage or bring down the successful individual. It does not matter that the hostility is unjustified and based on jealousy. It can still be unfairly damaging. All should realize that jealousy and greed are among the most powerful motivators of human behavior.
In view of all these considerations, it is apparent that all vascular surgeons, especially talented and successful ones, will at various times in their careers face battles. All cannot be fought. So one has to decide which ones should be avoided and which ones to engage in. Battles to fight should be picked carefully because they will consume energy and leave scars, no matter the outcome.
Most battles are best avoided unless victory is certain. Multiple simultaneous battles should be avoided. Battles in which one faces numerous opponents at the same time should also be shunned. Ideally in unavoidable conflicts, one should have as many allies as possible, although the loyalty of allies cannot always be counted on. Self-interest will determine the loyalty of presumed allies.
Never underestimate enemies, or overestimate allies. If the outcome of a battle is uncertain or to be determined by a board or other group, know how that group will vote before taking on the fight. Always remember the role of jealousy and greed in determining human behavior in battle. Defeated opponents do not forget and are forever dangerous.
Time is a vascular surgeon’s most important asset. Anything that one can do to enlist others to protect or expand this time is helpful. To this end, loyal nurses, physician’s assistants, or nonprofessional associates are invaluable. Their loyalty, which must be reciprocated, can be earned by recognizing their contributions and rewarding them intellectually and financially. This mutual loyalty is essential to success in practice and in the inevitable conflicts that will occur.
All these concepts and many others are not covered in medical school or residency training. Yet all are important in a vascular surgery career, whether it be in a practice or academic setting. Human nature is a constant and its elements may often work against one’s success. Being aware of some of these often noxious and little discussed elements will hopefully enable vascular surgeons to cope with them better and ultimately survive in what can be a difficult environment.
Dr. Veith is professor of surgery at New York University Medical Center and the Cleveland Clinic and an associate medical editor for Vascular Specialist.
The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or publisher.