User login
Study shows imatinib response is durable and improves with time
SAN FRANCISCO—The longest duration study of imatinib treatment for patients with Ph+ CML shows 86% of patients are still alive 7 years after beginning therapy.
The International Randomized Interferon versus STI571 (IRIS) study revealed only 1 early chronic-phase patient progressed to a more advanced phase between years 6 and 7, Stephen O’Brien, MD, PhD, of Newcastle University in the UK, said at the 50th Annual Meeting of the American Society of Hematology.
IRIS is an open-label, phase 3 clinical trial enrolling 1106 newly diagnosed patients with chronic phase Ph+ CML in 177 centers across 16 countries. One group of 553 patients received imatinib 400 mg per day. Another group of 553 patients received a target dose of interferon (IFN) of 5 MIU/m2/day in combination with cytarabine at 20 mg/m2/day for 10 days each month.
Because of tolerability issues, lack of response, or loss of response, 65% of patients in the IFN/cytarabine arm crossed over to the imatinib arm. Only 3% of patients in the imatinib arm crossed over to the IFN/cytarabine arm.
A low rate of progression has been reported every year since this trial began in 2001. Seven percent of patients treated with imatinib progressed to advanced phases of CML after 7 years. Of the 456 patients (82%) who achieved a complete cytogenetic response, 17% lost their response and 3% progressed to advanced phases.
“After 1 year of treatment, there is a small risk of progression,” Dr O’Brien said. “If patients achieve and maintain a complete cytogenetic response after 3 years, they are fairly safe.”
Treatment with imatinib in the IRIS study was well tolerated, he said. No new serious adverse events occurred between the sixth and seventh year of treatment.
The results from the IRIS study also reveal that, by year 6, 85% to 90% of patients still taking imatinib achieved a major molecular response. This key milestone indicates a reduction in the abnormal protein responsible for the uncontrolled production of abnormal white blood cells and may be a sensitive predictor of long-term progression-free survival.
“There was a steady improvement in major molecular responses between 4 and 7 years of treatment,” said Timothy Hughes, MD, of the Institute of Medical and Veterinary Science in Adelaide, Australia. “By 7 years, the vast majority of patients who achieved a complete cytogenetic response also achieved a major molecular response.”
A major molecular response at any time point represents a “safe haven” for patients, Dr Hughes said. Both molecular and cytogenetic evaluations should be used to guide treatment decisions until a complete cytogenetic response is achieved, followed by measurements of molecular assessments.
“In this, the seventh year of the IRIS study, CML patients treated with imatinib continue to demonstrate impressive long-term survival,” Dr O’Brien said. “Imatinib 400 mg daily is confirmed as the standard of care for the initial therapy of chronic-phase CML.”
Imatinib, the first therapy to inhibit the activity of Bcr-Abl, revolutionized the treatment of Ph+ CML, Dr O’Brien said. Prior to imatinib, about 50% of patients with Ph+ CML progressed from the initial phase to more advanced stages after 3 to 5 years. Once patients reached the final blast crisis phase, survival was generally 3 to 6 months. ![]()
SAN FRANCISCO—The longest duration study of imatinib treatment for patients with Ph+ CML shows 86% of patients are still alive 7 years after beginning therapy.
The International Randomized Interferon versus STI571 (IRIS) study revealed only 1 early chronic-phase patient progressed to a more advanced phase between years 6 and 7, Stephen O’Brien, MD, PhD, of Newcastle University in the UK, said at the 50th Annual Meeting of the American Society of Hematology.
IRIS is an open-label, phase 3 clinical trial enrolling 1106 newly diagnosed patients with chronic phase Ph+ CML in 177 centers across 16 countries. One group of 553 patients received imatinib 400 mg per day. Another group of 553 patients received a target dose of interferon (IFN) of 5 MIU/m2/day in combination with cytarabine at 20 mg/m2/day for 10 days each month.
Because of tolerability issues, lack of response, or loss of response, 65% of patients in the IFN/cytarabine arm crossed over to the imatinib arm. Only 3% of patients in the imatinib arm crossed over to the IFN/cytarabine arm.
A low rate of progression has been reported every year since this trial began in 2001. Seven percent of patients treated with imatinib progressed to advanced phases of CML after 7 years. Of the 456 patients (82%) who achieved a complete cytogenetic response, 17% lost their response and 3% progressed to advanced phases.
“After 1 year of treatment, there is a small risk of progression,” Dr O’Brien said. “If patients achieve and maintain a complete cytogenetic response after 3 years, they are fairly safe.”
Treatment with imatinib in the IRIS study was well tolerated, he said. No new serious adverse events occurred between the sixth and seventh year of treatment.
The results from the IRIS study also reveal that, by year 6, 85% to 90% of patients still taking imatinib achieved a major molecular response. This key milestone indicates a reduction in the abnormal protein responsible for the uncontrolled production of abnormal white blood cells and may be a sensitive predictor of long-term progression-free survival.
“There was a steady improvement in major molecular responses between 4 and 7 years of treatment,” said Timothy Hughes, MD, of the Institute of Medical and Veterinary Science in Adelaide, Australia. “By 7 years, the vast majority of patients who achieved a complete cytogenetic response also achieved a major molecular response.”
A major molecular response at any time point represents a “safe haven” for patients, Dr Hughes said. Both molecular and cytogenetic evaluations should be used to guide treatment decisions until a complete cytogenetic response is achieved, followed by measurements of molecular assessments.
“In this, the seventh year of the IRIS study, CML patients treated with imatinib continue to demonstrate impressive long-term survival,” Dr O’Brien said. “Imatinib 400 mg daily is confirmed as the standard of care for the initial therapy of chronic-phase CML.”
Imatinib, the first therapy to inhibit the activity of Bcr-Abl, revolutionized the treatment of Ph+ CML, Dr O’Brien said. Prior to imatinib, about 50% of patients with Ph+ CML progressed from the initial phase to more advanced stages after 3 to 5 years. Once patients reached the final blast crisis phase, survival was generally 3 to 6 months. ![]()
SAN FRANCISCO—The longest duration study of imatinib treatment for patients with Ph+ CML shows 86% of patients are still alive 7 years after beginning therapy.
The International Randomized Interferon versus STI571 (IRIS) study revealed only 1 early chronic-phase patient progressed to a more advanced phase between years 6 and 7, Stephen O’Brien, MD, PhD, of Newcastle University in the UK, said at the 50th Annual Meeting of the American Society of Hematology.
IRIS is an open-label, phase 3 clinical trial enrolling 1106 newly diagnosed patients with chronic phase Ph+ CML in 177 centers across 16 countries. One group of 553 patients received imatinib 400 mg per day. Another group of 553 patients received a target dose of interferon (IFN) of 5 MIU/m2/day in combination with cytarabine at 20 mg/m2/day for 10 days each month.
Because of tolerability issues, lack of response, or loss of response, 65% of patients in the IFN/cytarabine arm crossed over to the imatinib arm. Only 3% of patients in the imatinib arm crossed over to the IFN/cytarabine arm.
A low rate of progression has been reported every year since this trial began in 2001. Seven percent of patients treated with imatinib progressed to advanced phases of CML after 7 years. Of the 456 patients (82%) who achieved a complete cytogenetic response, 17% lost their response and 3% progressed to advanced phases.
“After 1 year of treatment, there is a small risk of progression,” Dr O’Brien said. “If patients achieve and maintain a complete cytogenetic response after 3 years, they are fairly safe.”
Treatment with imatinib in the IRIS study was well tolerated, he said. No new serious adverse events occurred between the sixth and seventh year of treatment.
The results from the IRIS study also reveal that, by year 6, 85% to 90% of patients still taking imatinib achieved a major molecular response. This key milestone indicates a reduction in the abnormal protein responsible for the uncontrolled production of abnormal white blood cells and may be a sensitive predictor of long-term progression-free survival.
“There was a steady improvement in major molecular responses between 4 and 7 years of treatment,” said Timothy Hughes, MD, of the Institute of Medical and Veterinary Science in Adelaide, Australia. “By 7 years, the vast majority of patients who achieved a complete cytogenetic response also achieved a major molecular response.”
A major molecular response at any time point represents a “safe haven” for patients, Dr Hughes said. Both molecular and cytogenetic evaluations should be used to guide treatment decisions until a complete cytogenetic response is achieved, followed by measurements of molecular assessments.
“In this, the seventh year of the IRIS study, CML patients treated with imatinib continue to demonstrate impressive long-term survival,” Dr O’Brien said. “Imatinib 400 mg daily is confirmed as the standard of care for the initial therapy of chronic-phase CML.”
Imatinib, the first therapy to inhibit the activity of Bcr-Abl, revolutionized the treatment of Ph+ CML, Dr O’Brien said. Prior to imatinib, about 50% of patients with Ph+ CML progressed from the initial phase to more advanced stages after 3 to 5 years. Once patients reached the final blast crisis phase, survival was generally 3 to 6 months. ![]()
Dabigatran safe, effective in elderly surgery patients
San Francisco—Researchers confirmed the safety and efficacy of a lower dose of dabigatran etexilate in elderly hip and total knee replacement surgery patients.
Dabigatran is a new oral thrombin inhibitor recently approved in Europe for the prevention of VTE in patients undergoing this surgery. Ola E. Dahl, MD, of the Thrombosis Research Institute in London, reported the results of a post hoc pooled analysis of 2 pivotal trials comparing dabigatran with enoxaparin at the 50th Annual Meeting of the American Society of Hematology.
Dr Dahl and colleagues analyzed 883 patients older than 75 years who were enrolled in the RE-MODEL and RE-NOVATE trials. Researchers evaluated 220 mg and 150 mg once-daily doses of dabigatran compared to a 40 mg daily dose of enoxaparin.
The primary efficacy endpoint was total number of VTEs and all-cause mortality. Both doses of dabigatran reduced total VTEs compared to enoxaparin, though not significantly.
However, the higher dose of dabigatran produced a significant difference in the secondary endpoint, major VTEs and VTE-related mortality. Four of 216 patients (1.9%) receiving the 220 mg dose had a major VTE, compared with 13 of 218 patients receiving enoxaparin (P=0.045).
The safety endpoint was the difference in major bleeding events, including surgical site bleeding, which accounts for up to 90% of bleeding in these patients. Major bleeding events occurred in 3.7% of the patients receiving dabigatran at 220 mg and 1.4% receiving 150 mg, compared to 2.9% in the enoxaparin group. The study was not powered to show significance in the safety endpoint.
“If you look into the dabigatran regimens versus enoxaparin, you see that we have more efficacious 200 mg dosing with slightly increased bleeding,” Dr Dahl said. “The 150 mg dose has the same efficacy level, but with a little less bleeding. And that is exactly the profile we are looking for in the elderly.” ![]()
San Francisco—Researchers confirmed the safety and efficacy of a lower dose of dabigatran etexilate in elderly hip and total knee replacement surgery patients.
Dabigatran is a new oral thrombin inhibitor recently approved in Europe for the prevention of VTE in patients undergoing this surgery. Ola E. Dahl, MD, of the Thrombosis Research Institute in London, reported the results of a post hoc pooled analysis of 2 pivotal trials comparing dabigatran with enoxaparin at the 50th Annual Meeting of the American Society of Hematology.
Dr Dahl and colleagues analyzed 883 patients older than 75 years who were enrolled in the RE-MODEL and RE-NOVATE trials. Researchers evaluated 220 mg and 150 mg once-daily doses of dabigatran compared to a 40 mg daily dose of enoxaparin.
The primary efficacy endpoint was total number of VTEs and all-cause mortality. Both doses of dabigatran reduced total VTEs compared to enoxaparin, though not significantly.
However, the higher dose of dabigatran produced a significant difference in the secondary endpoint, major VTEs and VTE-related mortality. Four of 216 patients (1.9%) receiving the 220 mg dose had a major VTE, compared with 13 of 218 patients receiving enoxaparin (P=0.045).
The safety endpoint was the difference in major bleeding events, including surgical site bleeding, which accounts for up to 90% of bleeding in these patients. Major bleeding events occurred in 3.7% of the patients receiving dabigatran at 220 mg and 1.4% receiving 150 mg, compared to 2.9% in the enoxaparin group. The study was not powered to show significance in the safety endpoint.
“If you look into the dabigatran regimens versus enoxaparin, you see that we have more efficacious 200 mg dosing with slightly increased bleeding,” Dr Dahl said. “The 150 mg dose has the same efficacy level, but with a little less bleeding. And that is exactly the profile we are looking for in the elderly.” ![]()
San Francisco—Researchers confirmed the safety and efficacy of a lower dose of dabigatran etexilate in elderly hip and total knee replacement surgery patients.
Dabigatran is a new oral thrombin inhibitor recently approved in Europe for the prevention of VTE in patients undergoing this surgery. Ola E. Dahl, MD, of the Thrombosis Research Institute in London, reported the results of a post hoc pooled analysis of 2 pivotal trials comparing dabigatran with enoxaparin at the 50th Annual Meeting of the American Society of Hematology.
Dr Dahl and colleagues analyzed 883 patients older than 75 years who were enrolled in the RE-MODEL and RE-NOVATE trials. Researchers evaluated 220 mg and 150 mg once-daily doses of dabigatran compared to a 40 mg daily dose of enoxaparin.
The primary efficacy endpoint was total number of VTEs and all-cause mortality. Both doses of dabigatran reduced total VTEs compared to enoxaparin, though not significantly.
However, the higher dose of dabigatran produced a significant difference in the secondary endpoint, major VTEs and VTE-related mortality. Four of 216 patients (1.9%) receiving the 220 mg dose had a major VTE, compared with 13 of 218 patients receiving enoxaparin (P=0.045).
The safety endpoint was the difference in major bleeding events, including surgical site bleeding, which accounts for up to 90% of bleeding in these patients. Major bleeding events occurred in 3.7% of the patients receiving dabigatran at 220 mg and 1.4% receiving 150 mg, compared to 2.9% in the enoxaparin group. The study was not powered to show significance in the safety endpoint.
“If you look into the dabigatran regimens versus enoxaparin, you see that we have more efficacious 200 mg dosing with slightly increased bleeding,” Dr Dahl said. “The 150 mg dose has the same efficacy level, but with a little less bleeding. And that is exactly the profile we are looking for in the elderly.” ![]()
Fostamatinib for Lymphoma, Leukemia
Dr. Jonathan Friedberg discusses an experimental targeted oral agent, fostamatinib, that's being used to treat diffuse large B-cell lymphoma and chronic lymphocytic leukemia. Jane MacNeil of Elsevier Global Medical News (EGMN) reports from the annual meeting of the American Society of Hematology.
Dr. Jonathan Friedberg discusses an experimental targeted oral agent, fostamatinib, that's being used to treat diffuse large B-cell lymphoma and chronic lymphocytic leukemia. Jane MacNeil of Elsevier Global Medical News (EGMN) reports from the annual meeting of the American Society of Hematology.
Dr. Jonathan Friedberg discusses an experimental targeted oral agent, fostamatinib, that's being used to treat diffuse large B-cell lymphoma and chronic lymphocytic leukemia. Jane MacNeil of Elsevier Global Medical News (EGMN) reports from the annual meeting of the American Society of Hematology.
Eltrombopag in Chronic ITP
Dr. Gregory Cheng says patients with chronic idiopathic thrombocytopenia purpura are more likely to achieve target platelet counts when treated with oral eltrombopag. Jane MacNeil of Elsevier Global Medical News (EGMN) reports from the annual meeting of the American Society of Hematology.
Dr. Gregory Cheng says patients with chronic idiopathic thrombocytopenia purpura are more likely to achieve target platelet counts when treated with oral eltrombopag. Jane MacNeil of Elsevier Global Medical News (EGMN) reports from the annual meeting of the American Society of Hematology.
Dr. Gregory Cheng says patients with chronic idiopathic thrombocytopenia purpura are more likely to achieve target platelet counts when treated with oral eltrombopag. Jane MacNeil of Elsevier Global Medical News (EGMN) reports from the annual meeting of the American Society of Hematology.
IOM Recommends Resident Duty Hour Revisions
The Institute of Medicine (IOM) issued a report this month calling for limits to shifts worked by residents, a move that, if implemented, likely means more work for in-house hospitalists, according to one hospital medicine leader.
IOM recommends no change to the current maximum 80-hour workweek for residents, or to the maximum shift length of 30 hours. The report does, however, recommend residents only treat patients for up to 16 hours during their shift, down from the current recommendation of 24 hours. It also suggests residents take an uninterrupted five hours for a continuous sleep period between 10 p.m. and 8 a.m.
In 2003, the Accreditation Council for Graduate Medical Education restricted resident workweeks in order to protect patients and residents from unsafe conditions resulting from excessive fatigue. As mentioned in "While Residents Rest…" in The Hospitalist (August 2006), the resulting shift in workload stressed many hospitals relying on residents for coverage, and some believe it helped boost the need for hospitalists.
In teaching hospitals that follow the IOM recommendations, "I do think this work will go to hospitalists," says Sameer Badlani, MD, a hospitalist and instructor at the University of Chicago. "This is a good thing, in my opinion, as it will enhance the value a hospitalist program brings to an institution."
Dr. Badlani warns hospitals must be willing to help supplement additional costs to their hospitalist service.
The IOM report, "Resident Duty Hours: Enhancing Sleep, Supervision, and Safety," is available for purchase online, or you can download a report brief at www.iom.edu/CMS/3809/48553/60449.aspx.
The Institute of Medicine (IOM) issued a report this month calling for limits to shifts worked by residents, a move that, if implemented, likely means more work for in-house hospitalists, according to one hospital medicine leader.
IOM recommends no change to the current maximum 80-hour workweek for residents, or to the maximum shift length of 30 hours. The report does, however, recommend residents only treat patients for up to 16 hours during their shift, down from the current recommendation of 24 hours. It also suggests residents take an uninterrupted five hours for a continuous sleep period between 10 p.m. and 8 a.m.
In 2003, the Accreditation Council for Graduate Medical Education restricted resident workweeks in order to protect patients and residents from unsafe conditions resulting from excessive fatigue. As mentioned in "While Residents Rest…" in The Hospitalist (August 2006), the resulting shift in workload stressed many hospitals relying on residents for coverage, and some believe it helped boost the need for hospitalists.
In teaching hospitals that follow the IOM recommendations, "I do think this work will go to hospitalists," says Sameer Badlani, MD, a hospitalist and instructor at the University of Chicago. "This is a good thing, in my opinion, as it will enhance the value a hospitalist program brings to an institution."
Dr. Badlani warns hospitals must be willing to help supplement additional costs to their hospitalist service.
The IOM report, "Resident Duty Hours: Enhancing Sleep, Supervision, and Safety," is available for purchase online, or you can download a report brief at www.iom.edu/CMS/3809/48553/60449.aspx.
The Institute of Medicine (IOM) issued a report this month calling for limits to shifts worked by residents, a move that, if implemented, likely means more work for in-house hospitalists, according to one hospital medicine leader.
IOM recommends no change to the current maximum 80-hour workweek for residents, or to the maximum shift length of 30 hours. The report does, however, recommend residents only treat patients for up to 16 hours during their shift, down from the current recommendation of 24 hours. It also suggests residents take an uninterrupted five hours for a continuous sleep period between 10 p.m. and 8 a.m.
In 2003, the Accreditation Council for Graduate Medical Education restricted resident workweeks in order to protect patients and residents from unsafe conditions resulting from excessive fatigue. As mentioned in "While Residents Rest…" in The Hospitalist (August 2006), the resulting shift in workload stressed many hospitals relying on residents for coverage, and some believe it helped boost the need for hospitalists.
In teaching hospitals that follow the IOM recommendations, "I do think this work will go to hospitalists," says Sameer Badlani, MD, a hospitalist and instructor at the University of Chicago. "This is a good thing, in my opinion, as it will enhance the value a hospitalist program brings to an institution."
Dr. Badlani warns hospitals must be willing to help supplement additional costs to their hospitalist service.
The IOM report, "Resident Duty Hours: Enhancing Sleep, Supervision, and Safety," is available for purchase online, or you can download a report brief at www.iom.edu/CMS/3809/48553/60449.aspx.
Therapeutic Hypothermia in Cardiac Arrest
Mortality data estimates that there are about 400,000 to 460,000 sudden cardiac deaths (SCD) in the United States.1 In resuscitated cardiac arrest patients, morbidity and mortality remains high due to cerebral ischemic anoxia. Currently it is believed that following return of spontaneous circulation (ROSC) from successful resuscitation, secondary inflammatory responses characterized by the generation of chemical mediators and free radicals, as well as increased microvascular permeability, lead to further brain injury.2 Recently, 2 randomized controlled trials (RCT) showed that induced mild hypothermia (32C‐34C) in comatose patients after out‐of‐hospital cardiac arrest leads to improved neurologic outcomes and survival.3, 4 In 2002, the International Liaison Committee on Resuscitation (ILCOR) recommended induced mild hypothermia for the management of comatose patients with ROSC after cardiac arrest.5 Despite the recommendations by ILCOR and the supporting body of evidence proving the benefit of therapeutic hypothermia after cardiac arrest, this treatment remains underused.68
We present a case series of 8 cardiac arrest survivors treated using a hypothermia protocol at a community hospital.
TREATMENT PROTOCOL
Between June 2006 and December 2006, 8 patients presented to Unity Hospital, (a 200‐bed community teaching hospital with a 20‐bed intensive care unit [ICU]) in coma following cardiac arrest with ROSC after resuscitation. All the patients were managed using therapeutic hypothermia.
The hospital protocol, developed using the ILCOR guidelines, was used on all patients. The aim was to achieve a core temperature of 32C to 34C within 6 to 8 hours and maintain this for 24 hours from the start of cooling. The inclusion criteria were as follows: (1) coma within a 6‐hour postcardiac arrest window preceded by either ventricular fibrillation (VF), pulseless ventricular tachycardia, pulseless electrical activity, or asystole; (2) ability to maintain a blood pressure with or without pressors and/or fluid volume resuscitation after cardiopulmonary resuscitation; and (3) comatose at the time of cooling. The exclusion criteria were as follows: (1) coma from drug overdose, head trauma, stroke, or overt status epilepticus; (2) pregnancy; (3) temperature of 30C; (4) recent major surgery within 14 days; (5) systemic infections; (6) patients with known terminal illness; (7) Glasgow coma scale (GCS) of 10 and above; or (8) known bleeding diathesis or ongoing bleeding.
The Advanced Cardiac Life Support (ACLS) protocol was implemented in both in‐hospital and out‐of‐hospital cardiac arrests. The decision to initiate the protocol was made by the intensivist; however, in out‐of‐hospital cardiac arrest, the decision was taken in conjunction with the emergency room physician. A bladder temperature probe was used to monitor core body temperature. Cooling was achieved using iced saline gastric lavage and ice packs to the patient's neck, axillae, and groin while a cooling blanket (Mul‐T‐Blanket; Gaymar Industries, New York) was placed over and beneath the patient. In some cases, a Blanketrol cooling machine (Blanketrol II; CSZ Products, Inc., Cincinnati, OH) was used when available. All patients were maintained at a PaO2 above 90 mm Hg and PaCO2 around 35 mm Hg. Cisatacurium and midazolam were used to control shivering. Regular insulin intravenous drip was used to maintain tight blood glucose control (target blood glucose level of 140 mg/dL) when necessary. Target systolic and mean arterial blood pressures were 90 mm Hg and 80 mm Hg, respectively. Potassium was replaced to 3.4 mmol/L but not within 8 hours of commencing rewarming. Rewarming was started after 24 hours at a rate of not more than 1C in 4 hours. Clinical and laboratory parameters were continuously recorded and all patients were evaluated for complications, including electrolyte imbalance, cardiac arrhythmias, and seizures.
CASES
Table 1 summarizes all the cases. There were 4 men and 4 women. The mean age was 70 14 years (range, 44‐88 years). The main comorbidities were coronary artery disease (n = 6), hypertension (n = 5), diabetes mellitus (n = 5), and chronic or recurrent cardiac arrhythmia (n = 4). Cardiac arrest occurred out‐of‐hospital in 5 of 8 patients and was witnessed in 6 of the 8 cases. Ventricular fibrillation (VF) was the initial presenting rhythm in 5 of the 8 cases. The mean time from ROSC to initiation of cooling was 3 1.6 hours. The mean time from ROSC and attaining target temperature (34C) was 8.1 4.7 hours. The mean duration of cooling (initiation of cooling to onset of rewarming) was 23.8 0.6 hours. The mean duration at which target temperature was maintained (attainment of 32C‐34C to onset of rewarming) was 18.6 4.6 hours. The median time from onset of passive rewarming to attaining temperature of 36C was 7.25 hours. Two patients survived and were discharged to home (Patients B and C). Patient B had mild cognitive deficits on discharge.
| Patients | Age (Years) | Sex | Comorbidities | Location at the Time of Arrest | Witnessed Arrest? | Initial Rhythm | Time of Collapse to ROSC | Presenting GCS | Time from ROSC to Cooling Initiation (Hours) | Time from ROSC to Target Temperature of 34C (Hours) | Duration of Cooling (Cooling Initiation to Rewarming) (Hours) | Duration of Target Temperature Maintenance (Hours) | Onset of Passive Rewarming to Attainment of Temperature of >36C (Hours) | Complications by Day 5 | Outcome at Discharge |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
| A | 64 | M | DM, CAD, SSS, PTCA, PM, CHF, COPD | OOH | Yes | VF | 8 min | 3 | 1.7 | 1.7 | 16.9 | 24 | 6 | Pneumonia, hypokalemia, seizures | Death |
| B | 43 | F | Mitral valve prolapse | OOH | Yes | VF | 12 min | 5 | 6.3 | 5.3 | 12.0 | 24 | 7 | Hypokalemia | Good recovery |
| C | 64 | M | CAD, CABG | IH | No | VF | 7 min | 5 | 1.4 | 1.5 | 10.0 | 24 | 7.5 | Good recovery | |
| D | 76 | F | DM, HTN, CAD, PM | OOH | Yes | PEA | 36 min | 6 | 1.7 | 1.6 | 4.2 | 24 | 5 | Hypokalemia | Death |
| E | 88 | F | DM, HTN, CAD, AFIB, CHF, COPD | IH | Yes | Asystole | 6 min | 3 | 1.9 | 4.9 | 5.2 | 22.2 | 9.3 | Hypokalemia, elevated creatinine | Death |
| F | 70 | F | DM, HTN, CABG, PTCA, COPD | OOH | Yes | VF | 15 min | 5 | 1.4 | 2.1 | 5.6 | 18.3 | 3 | Seizures | Death |
| G | 71 | M | CAD, CABG, AICD | OOH | No | VF | >20 min | 3 | 4.7 | 4.6 | 6.7 | 22.5 | 12.3 | Hypokalemia, elevated creatinine, VT and VF | Death |
| H | 82 | M | HTN, CAD, AFIB, CHF | IH | Yes | Asystole | 19 min | 3 | 2.8 | 2.5 | 4.3 | 22.5 | 51 | Elevated creatinine | Death |
DISCUSSION
There is substantial clinical and public health concern over increasing incidence of sudden cardiac deaths despite decreasing overall mortality from coronary heart disease.6
Supportive management has been the norm for comatose patients following cardiac arrest until recently, when induced hypothermia was shown to have favorable outcomes in 2 landmark prospective RCTs.3, 4 Supportive management often led to prolonged unconsciousness due to severe anoxic brain injury, which eventually led to high morbidity and mortality rates.9, 10 The Hypothermia after Cardiac Arrest Study Group (HACA) study4 revealed that 6 patients would need to be treated with therapeutic hypothermia to prevent an adverse neurologic outcome, while 7 patients would need to be treated to prevent 1 death. Other authors have reported improved outcomes with induced hypothermia used in patients resuscitated following cardiac arrest.1114
Despite strong and encouraging evidence, therapeutic hypothermia has not been readily accepted into daily clinical critical care practice.68 In an Internet‐based survey of physicians by Abella et al.,6 87% of respondents (comprised of emergency medicine and critical care physicians, and cardiologists) had not used this treatment modality following cardiac arrest. Reasons given by most physicians included insufficient data to support the use of therapeutic hypothermia, technical difficulties including the immense amount of resources required, as well as inadequate training. Merchant et al.,7 using an Internet‐based survey also sought to ascertain the degree of therapeutic hypothermia use from physicians in the United States, the United Kingdom, Australia, and Finland. They found that 74% of respondents in the United States and 64% of respondents outside of the United States were yet to use induced therapeutic hypothermia. Factors predicting the use of therapeutic hypothermia by physicians were found to include practice in an academic hospital with more than 250 beds, critical care specialty training, and location of the hospital outside of the United States. Similarly, the major reasons given for nonutilization of therapeutic hypothermia in this study include lack of supportive data and technical difficulties. In yet another study by Laver et al.,8 73% of respondents (ICUs in the United Kingdom) revealed that therapeutic hypothermia after cardiac arrest had not been used in their service. They also gave the same reasons for nonusage as in the aforementioned studies.
In this case series we have presented our experience with therapeutic hypothermia in comatose patients following cardiac arrest. Evaluation of our cooling process compares favorably with the findings of the HACA study4: In our study, the mean time from ROSC to cooling initiation was 180 66 minutes compared to a median of 105 minutes (interquartile range, 61192 minutes) in the HACA study; mean time between ROSC and attaining target temperature was 8.1 4.7 hours in our study compared to a median of 8 hours in the HACA study; mean duration of cooling in our study was 23.8 0.6 hours compared to a median of 24 hours in the HACA study; target temperature was maintained for a mean duration of 18.6 4.6 hours in our study compared to a median of 24 hours in the HACA study; and last, median time from passive rewarming to attainment of temperature greater than 36C in our study was 7.25 hours compared to 8 hours in the HACA study.
There were few complications observed in this case series. These include hypokalemia, mildly elevated creatinine levels, and seizures. One patient developed pneumonia. Other potential complications of therapeutic hypothermia include cardiac arrhythmias, sepsis, hyperglycemia, coagulopathy, acid‐base disturbances, and electrolyte imbalance.15 The studies by Bernard et al.3 and the HACA;4 however, revealed no clinically significant unfavorable outcomes in the patients randomized to receive hypothermia treatment.
Our experience based on this case series leads us to conclude that therapeutic hypothermia is feasible in the community hospital setting. In our 200‐bed community teaching hospital, a multidisciplinary approach involving intensivists, emergency room physicians, internists, residents, and nursing staff lessens the technical difficulties associated with implementing a seemingly cumbersome yet inexpensive and effective treatment modality. Therapeutic hypothermia should be considered in appropriate patients in coma after resuscitation from cardiac arrest.
- Centers for Disease Control and Prevention.State specific mortality data from sudden cardiac death—United States, 1999.MMWR Morb Mortal Wkly Rep.2002;51(6):123– 126.
- .Bench to bedside: brain edema and cerebral resuscitation: the present and future.Acad Emerg Med.2002;9(9):933–946.
- ,,, et al.Treatment of comatose survivors of out of hospital cardiac arrest with induced hypothermia.N Engl J Med.2002;346(8):557–563.
- Hypothermia after Cardiac Arrest Study Group.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest.N Engl J Med.2002;346(8):549–556.
- Therapeutic hypothermia after cardiac arrest: an advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation.Circulation.2003;108:118–121.
- ,,, et al.Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey.Resuscitation.2005;64:181–186.
- ,,, et al.Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest.Crit Care Med.2006;34(7):1935–1940.
- ,,, et al.Therapeutic hypothermia after cardiac arrest: a survey of practice in intensive care units in the United Kingdom.Anaesthesia2006;61:873–877.
- .Hypothermia improves outcome from cardiac arrest.Crit Care Resusc.2005;7(4):325–327.
- ,,.Sudden cardiac death: epidemiology, transient risk, and intervention assessment.Ann Intern Med.1993;119(12):1187–1197.
- ,,, et al.Mild hypothermia induced by a helmet device: a clinical feasibility study.Resuscitation.2001;51:275–281.
- ,,, et al.Implementation of a standardized treatment protocol for post resuscitation care after out‐of‐hospital cardiac arrest.Resuscitation.2007;73(1):29–39.
- ,,,.Induced hypothermia following out‐of‐hospital cardiac arrest; initial experience in a community hospital.Clin Cardiol.2006;29(12):525–529.
- ,,,,.From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest.Crit Care Med.2006;34(7):1865–1873.
- ,.Induced hypothermia in critical care medicine: a review.Crit Care Med.2003;31(7):2041–2051.
Mortality data estimates that there are about 400,000 to 460,000 sudden cardiac deaths (SCD) in the United States.1 In resuscitated cardiac arrest patients, morbidity and mortality remains high due to cerebral ischemic anoxia. Currently it is believed that following return of spontaneous circulation (ROSC) from successful resuscitation, secondary inflammatory responses characterized by the generation of chemical mediators and free radicals, as well as increased microvascular permeability, lead to further brain injury.2 Recently, 2 randomized controlled trials (RCT) showed that induced mild hypothermia (32C‐34C) in comatose patients after out‐of‐hospital cardiac arrest leads to improved neurologic outcomes and survival.3, 4 In 2002, the International Liaison Committee on Resuscitation (ILCOR) recommended induced mild hypothermia for the management of comatose patients with ROSC after cardiac arrest.5 Despite the recommendations by ILCOR and the supporting body of evidence proving the benefit of therapeutic hypothermia after cardiac arrest, this treatment remains underused.68
We present a case series of 8 cardiac arrest survivors treated using a hypothermia protocol at a community hospital.
TREATMENT PROTOCOL
Between June 2006 and December 2006, 8 patients presented to Unity Hospital, (a 200‐bed community teaching hospital with a 20‐bed intensive care unit [ICU]) in coma following cardiac arrest with ROSC after resuscitation. All the patients were managed using therapeutic hypothermia.
The hospital protocol, developed using the ILCOR guidelines, was used on all patients. The aim was to achieve a core temperature of 32C to 34C within 6 to 8 hours and maintain this for 24 hours from the start of cooling. The inclusion criteria were as follows: (1) coma within a 6‐hour postcardiac arrest window preceded by either ventricular fibrillation (VF), pulseless ventricular tachycardia, pulseless electrical activity, or asystole; (2) ability to maintain a blood pressure with or without pressors and/or fluid volume resuscitation after cardiopulmonary resuscitation; and (3) comatose at the time of cooling. The exclusion criteria were as follows: (1) coma from drug overdose, head trauma, stroke, or overt status epilepticus; (2) pregnancy; (3) temperature of 30C; (4) recent major surgery within 14 days; (5) systemic infections; (6) patients with known terminal illness; (7) Glasgow coma scale (GCS) of 10 and above; or (8) known bleeding diathesis or ongoing bleeding.
The Advanced Cardiac Life Support (ACLS) protocol was implemented in both in‐hospital and out‐of‐hospital cardiac arrests. The decision to initiate the protocol was made by the intensivist; however, in out‐of‐hospital cardiac arrest, the decision was taken in conjunction with the emergency room physician. A bladder temperature probe was used to monitor core body temperature. Cooling was achieved using iced saline gastric lavage and ice packs to the patient's neck, axillae, and groin while a cooling blanket (Mul‐T‐Blanket; Gaymar Industries, New York) was placed over and beneath the patient. In some cases, a Blanketrol cooling machine (Blanketrol II; CSZ Products, Inc., Cincinnati, OH) was used when available. All patients were maintained at a PaO2 above 90 mm Hg and PaCO2 around 35 mm Hg. Cisatacurium and midazolam were used to control shivering. Regular insulin intravenous drip was used to maintain tight blood glucose control (target blood glucose level of 140 mg/dL) when necessary. Target systolic and mean arterial blood pressures were 90 mm Hg and 80 mm Hg, respectively. Potassium was replaced to 3.4 mmol/L but not within 8 hours of commencing rewarming. Rewarming was started after 24 hours at a rate of not more than 1C in 4 hours. Clinical and laboratory parameters were continuously recorded and all patients were evaluated for complications, including electrolyte imbalance, cardiac arrhythmias, and seizures.
CASES
Table 1 summarizes all the cases. There were 4 men and 4 women. The mean age was 70 14 years (range, 44‐88 years). The main comorbidities were coronary artery disease (n = 6), hypertension (n = 5), diabetes mellitus (n = 5), and chronic or recurrent cardiac arrhythmia (n = 4). Cardiac arrest occurred out‐of‐hospital in 5 of 8 patients and was witnessed in 6 of the 8 cases. Ventricular fibrillation (VF) was the initial presenting rhythm in 5 of the 8 cases. The mean time from ROSC to initiation of cooling was 3 1.6 hours. The mean time from ROSC and attaining target temperature (34C) was 8.1 4.7 hours. The mean duration of cooling (initiation of cooling to onset of rewarming) was 23.8 0.6 hours. The mean duration at which target temperature was maintained (attainment of 32C‐34C to onset of rewarming) was 18.6 4.6 hours. The median time from onset of passive rewarming to attaining temperature of 36C was 7.25 hours. Two patients survived and were discharged to home (Patients B and C). Patient B had mild cognitive deficits on discharge.
| Patients | Age (Years) | Sex | Comorbidities | Location at the Time of Arrest | Witnessed Arrest? | Initial Rhythm | Time of Collapse to ROSC | Presenting GCS | Time from ROSC to Cooling Initiation (Hours) | Time from ROSC to Target Temperature of 34C (Hours) | Duration of Cooling (Cooling Initiation to Rewarming) (Hours) | Duration of Target Temperature Maintenance (Hours) | Onset of Passive Rewarming to Attainment of Temperature of >36C (Hours) | Complications by Day 5 | Outcome at Discharge |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
| A | 64 | M | DM, CAD, SSS, PTCA, PM, CHF, COPD | OOH | Yes | VF | 8 min | 3 | 1.7 | 1.7 | 16.9 | 24 | 6 | Pneumonia, hypokalemia, seizures | Death |
| B | 43 | F | Mitral valve prolapse | OOH | Yes | VF | 12 min | 5 | 6.3 | 5.3 | 12.0 | 24 | 7 | Hypokalemia | Good recovery |
| C | 64 | M | CAD, CABG | IH | No | VF | 7 min | 5 | 1.4 | 1.5 | 10.0 | 24 | 7.5 | Good recovery | |
| D | 76 | F | DM, HTN, CAD, PM | OOH | Yes | PEA | 36 min | 6 | 1.7 | 1.6 | 4.2 | 24 | 5 | Hypokalemia | Death |
| E | 88 | F | DM, HTN, CAD, AFIB, CHF, COPD | IH | Yes | Asystole | 6 min | 3 | 1.9 | 4.9 | 5.2 | 22.2 | 9.3 | Hypokalemia, elevated creatinine | Death |
| F | 70 | F | DM, HTN, CABG, PTCA, COPD | OOH | Yes | VF | 15 min | 5 | 1.4 | 2.1 | 5.6 | 18.3 | 3 | Seizures | Death |
| G | 71 | M | CAD, CABG, AICD | OOH | No | VF | >20 min | 3 | 4.7 | 4.6 | 6.7 | 22.5 | 12.3 | Hypokalemia, elevated creatinine, VT and VF | Death |
| H | 82 | M | HTN, CAD, AFIB, CHF | IH | Yes | Asystole | 19 min | 3 | 2.8 | 2.5 | 4.3 | 22.5 | 51 | Elevated creatinine | Death |
DISCUSSION
There is substantial clinical and public health concern over increasing incidence of sudden cardiac deaths despite decreasing overall mortality from coronary heart disease.6
Supportive management has been the norm for comatose patients following cardiac arrest until recently, when induced hypothermia was shown to have favorable outcomes in 2 landmark prospective RCTs.3, 4 Supportive management often led to prolonged unconsciousness due to severe anoxic brain injury, which eventually led to high morbidity and mortality rates.9, 10 The Hypothermia after Cardiac Arrest Study Group (HACA) study4 revealed that 6 patients would need to be treated with therapeutic hypothermia to prevent an adverse neurologic outcome, while 7 patients would need to be treated to prevent 1 death. Other authors have reported improved outcomes with induced hypothermia used in patients resuscitated following cardiac arrest.1114
Despite strong and encouraging evidence, therapeutic hypothermia has not been readily accepted into daily clinical critical care practice.68 In an Internet‐based survey of physicians by Abella et al.,6 87% of respondents (comprised of emergency medicine and critical care physicians, and cardiologists) had not used this treatment modality following cardiac arrest. Reasons given by most physicians included insufficient data to support the use of therapeutic hypothermia, technical difficulties including the immense amount of resources required, as well as inadequate training. Merchant et al.,7 using an Internet‐based survey also sought to ascertain the degree of therapeutic hypothermia use from physicians in the United States, the United Kingdom, Australia, and Finland. They found that 74% of respondents in the United States and 64% of respondents outside of the United States were yet to use induced therapeutic hypothermia. Factors predicting the use of therapeutic hypothermia by physicians were found to include practice in an academic hospital with more than 250 beds, critical care specialty training, and location of the hospital outside of the United States. Similarly, the major reasons given for nonutilization of therapeutic hypothermia in this study include lack of supportive data and technical difficulties. In yet another study by Laver et al.,8 73% of respondents (ICUs in the United Kingdom) revealed that therapeutic hypothermia after cardiac arrest had not been used in their service. They also gave the same reasons for nonusage as in the aforementioned studies.
In this case series we have presented our experience with therapeutic hypothermia in comatose patients following cardiac arrest. Evaluation of our cooling process compares favorably with the findings of the HACA study4: In our study, the mean time from ROSC to cooling initiation was 180 66 minutes compared to a median of 105 minutes (interquartile range, 61192 minutes) in the HACA study; mean time between ROSC and attaining target temperature was 8.1 4.7 hours in our study compared to a median of 8 hours in the HACA study; mean duration of cooling in our study was 23.8 0.6 hours compared to a median of 24 hours in the HACA study; target temperature was maintained for a mean duration of 18.6 4.6 hours in our study compared to a median of 24 hours in the HACA study; and last, median time from passive rewarming to attainment of temperature greater than 36C in our study was 7.25 hours compared to 8 hours in the HACA study.
There were few complications observed in this case series. These include hypokalemia, mildly elevated creatinine levels, and seizures. One patient developed pneumonia. Other potential complications of therapeutic hypothermia include cardiac arrhythmias, sepsis, hyperglycemia, coagulopathy, acid‐base disturbances, and electrolyte imbalance.15 The studies by Bernard et al.3 and the HACA;4 however, revealed no clinically significant unfavorable outcomes in the patients randomized to receive hypothermia treatment.
Our experience based on this case series leads us to conclude that therapeutic hypothermia is feasible in the community hospital setting. In our 200‐bed community teaching hospital, a multidisciplinary approach involving intensivists, emergency room physicians, internists, residents, and nursing staff lessens the technical difficulties associated with implementing a seemingly cumbersome yet inexpensive and effective treatment modality. Therapeutic hypothermia should be considered in appropriate patients in coma after resuscitation from cardiac arrest.
Mortality data estimates that there are about 400,000 to 460,000 sudden cardiac deaths (SCD) in the United States.1 In resuscitated cardiac arrest patients, morbidity and mortality remains high due to cerebral ischemic anoxia. Currently it is believed that following return of spontaneous circulation (ROSC) from successful resuscitation, secondary inflammatory responses characterized by the generation of chemical mediators and free radicals, as well as increased microvascular permeability, lead to further brain injury.2 Recently, 2 randomized controlled trials (RCT) showed that induced mild hypothermia (32C‐34C) in comatose patients after out‐of‐hospital cardiac arrest leads to improved neurologic outcomes and survival.3, 4 In 2002, the International Liaison Committee on Resuscitation (ILCOR) recommended induced mild hypothermia for the management of comatose patients with ROSC after cardiac arrest.5 Despite the recommendations by ILCOR and the supporting body of evidence proving the benefit of therapeutic hypothermia after cardiac arrest, this treatment remains underused.68
We present a case series of 8 cardiac arrest survivors treated using a hypothermia protocol at a community hospital.
TREATMENT PROTOCOL
Between June 2006 and December 2006, 8 patients presented to Unity Hospital, (a 200‐bed community teaching hospital with a 20‐bed intensive care unit [ICU]) in coma following cardiac arrest with ROSC after resuscitation. All the patients were managed using therapeutic hypothermia.
The hospital protocol, developed using the ILCOR guidelines, was used on all patients. The aim was to achieve a core temperature of 32C to 34C within 6 to 8 hours and maintain this for 24 hours from the start of cooling. The inclusion criteria were as follows: (1) coma within a 6‐hour postcardiac arrest window preceded by either ventricular fibrillation (VF), pulseless ventricular tachycardia, pulseless electrical activity, or asystole; (2) ability to maintain a blood pressure with or without pressors and/or fluid volume resuscitation after cardiopulmonary resuscitation; and (3) comatose at the time of cooling. The exclusion criteria were as follows: (1) coma from drug overdose, head trauma, stroke, or overt status epilepticus; (2) pregnancy; (3) temperature of 30C; (4) recent major surgery within 14 days; (5) systemic infections; (6) patients with known terminal illness; (7) Glasgow coma scale (GCS) of 10 and above; or (8) known bleeding diathesis or ongoing bleeding.
The Advanced Cardiac Life Support (ACLS) protocol was implemented in both in‐hospital and out‐of‐hospital cardiac arrests. The decision to initiate the protocol was made by the intensivist; however, in out‐of‐hospital cardiac arrest, the decision was taken in conjunction with the emergency room physician. A bladder temperature probe was used to monitor core body temperature. Cooling was achieved using iced saline gastric lavage and ice packs to the patient's neck, axillae, and groin while a cooling blanket (Mul‐T‐Blanket; Gaymar Industries, New York) was placed over and beneath the patient. In some cases, a Blanketrol cooling machine (Blanketrol II; CSZ Products, Inc., Cincinnati, OH) was used when available. All patients were maintained at a PaO2 above 90 mm Hg and PaCO2 around 35 mm Hg. Cisatacurium and midazolam were used to control shivering. Regular insulin intravenous drip was used to maintain tight blood glucose control (target blood glucose level of 140 mg/dL) when necessary. Target systolic and mean arterial blood pressures were 90 mm Hg and 80 mm Hg, respectively. Potassium was replaced to 3.4 mmol/L but not within 8 hours of commencing rewarming. Rewarming was started after 24 hours at a rate of not more than 1C in 4 hours. Clinical and laboratory parameters were continuously recorded and all patients were evaluated for complications, including electrolyte imbalance, cardiac arrhythmias, and seizures.
CASES
Table 1 summarizes all the cases. There were 4 men and 4 women. The mean age was 70 14 years (range, 44‐88 years). The main comorbidities were coronary artery disease (n = 6), hypertension (n = 5), diabetes mellitus (n = 5), and chronic or recurrent cardiac arrhythmia (n = 4). Cardiac arrest occurred out‐of‐hospital in 5 of 8 patients and was witnessed in 6 of the 8 cases. Ventricular fibrillation (VF) was the initial presenting rhythm in 5 of the 8 cases. The mean time from ROSC to initiation of cooling was 3 1.6 hours. The mean time from ROSC and attaining target temperature (34C) was 8.1 4.7 hours. The mean duration of cooling (initiation of cooling to onset of rewarming) was 23.8 0.6 hours. The mean duration at which target temperature was maintained (attainment of 32C‐34C to onset of rewarming) was 18.6 4.6 hours. The median time from onset of passive rewarming to attaining temperature of 36C was 7.25 hours. Two patients survived and were discharged to home (Patients B and C). Patient B had mild cognitive deficits on discharge.
| Patients | Age (Years) | Sex | Comorbidities | Location at the Time of Arrest | Witnessed Arrest? | Initial Rhythm | Time of Collapse to ROSC | Presenting GCS | Time from ROSC to Cooling Initiation (Hours) | Time from ROSC to Target Temperature of 34C (Hours) | Duration of Cooling (Cooling Initiation to Rewarming) (Hours) | Duration of Target Temperature Maintenance (Hours) | Onset of Passive Rewarming to Attainment of Temperature of >36C (Hours) | Complications by Day 5 | Outcome at Discharge |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
| A | 64 | M | DM, CAD, SSS, PTCA, PM, CHF, COPD | OOH | Yes | VF | 8 min | 3 | 1.7 | 1.7 | 16.9 | 24 | 6 | Pneumonia, hypokalemia, seizures | Death |
| B | 43 | F | Mitral valve prolapse | OOH | Yes | VF | 12 min | 5 | 6.3 | 5.3 | 12.0 | 24 | 7 | Hypokalemia | Good recovery |
| C | 64 | M | CAD, CABG | IH | No | VF | 7 min | 5 | 1.4 | 1.5 | 10.0 | 24 | 7.5 | Good recovery | |
| D | 76 | F | DM, HTN, CAD, PM | OOH | Yes | PEA | 36 min | 6 | 1.7 | 1.6 | 4.2 | 24 | 5 | Hypokalemia | Death |
| E | 88 | F | DM, HTN, CAD, AFIB, CHF, COPD | IH | Yes | Asystole | 6 min | 3 | 1.9 | 4.9 | 5.2 | 22.2 | 9.3 | Hypokalemia, elevated creatinine | Death |
| F | 70 | F | DM, HTN, CABG, PTCA, COPD | OOH | Yes | VF | 15 min | 5 | 1.4 | 2.1 | 5.6 | 18.3 | 3 | Seizures | Death |
| G | 71 | M | CAD, CABG, AICD | OOH | No | VF | >20 min | 3 | 4.7 | 4.6 | 6.7 | 22.5 | 12.3 | Hypokalemia, elevated creatinine, VT and VF | Death |
| H | 82 | M | HTN, CAD, AFIB, CHF | IH | Yes | Asystole | 19 min | 3 | 2.8 | 2.5 | 4.3 | 22.5 | 51 | Elevated creatinine | Death |
DISCUSSION
There is substantial clinical and public health concern over increasing incidence of sudden cardiac deaths despite decreasing overall mortality from coronary heart disease.6
Supportive management has been the norm for comatose patients following cardiac arrest until recently, when induced hypothermia was shown to have favorable outcomes in 2 landmark prospective RCTs.3, 4 Supportive management often led to prolonged unconsciousness due to severe anoxic brain injury, which eventually led to high morbidity and mortality rates.9, 10 The Hypothermia after Cardiac Arrest Study Group (HACA) study4 revealed that 6 patients would need to be treated with therapeutic hypothermia to prevent an adverse neurologic outcome, while 7 patients would need to be treated to prevent 1 death. Other authors have reported improved outcomes with induced hypothermia used in patients resuscitated following cardiac arrest.1114
Despite strong and encouraging evidence, therapeutic hypothermia has not been readily accepted into daily clinical critical care practice.68 In an Internet‐based survey of physicians by Abella et al.,6 87% of respondents (comprised of emergency medicine and critical care physicians, and cardiologists) had not used this treatment modality following cardiac arrest. Reasons given by most physicians included insufficient data to support the use of therapeutic hypothermia, technical difficulties including the immense amount of resources required, as well as inadequate training. Merchant et al.,7 using an Internet‐based survey also sought to ascertain the degree of therapeutic hypothermia use from physicians in the United States, the United Kingdom, Australia, and Finland. They found that 74% of respondents in the United States and 64% of respondents outside of the United States were yet to use induced therapeutic hypothermia. Factors predicting the use of therapeutic hypothermia by physicians were found to include practice in an academic hospital with more than 250 beds, critical care specialty training, and location of the hospital outside of the United States. Similarly, the major reasons given for nonutilization of therapeutic hypothermia in this study include lack of supportive data and technical difficulties. In yet another study by Laver et al.,8 73% of respondents (ICUs in the United Kingdom) revealed that therapeutic hypothermia after cardiac arrest had not been used in their service. They also gave the same reasons for nonusage as in the aforementioned studies.
In this case series we have presented our experience with therapeutic hypothermia in comatose patients following cardiac arrest. Evaluation of our cooling process compares favorably with the findings of the HACA study4: In our study, the mean time from ROSC to cooling initiation was 180 66 minutes compared to a median of 105 minutes (interquartile range, 61192 minutes) in the HACA study; mean time between ROSC and attaining target temperature was 8.1 4.7 hours in our study compared to a median of 8 hours in the HACA study; mean duration of cooling in our study was 23.8 0.6 hours compared to a median of 24 hours in the HACA study; target temperature was maintained for a mean duration of 18.6 4.6 hours in our study compared to a median of 24 hours in the HACA study; and last, median time from passive rewarming to attainment of temperature greater than 36C in our study was 7.25 hours compared to 8 hours in the HACA study.
There were few complications observed in this case series. These include hypokalemia, mildly elevated creatinine levels, and seizures. One patient developed pneumonia. Other potential complications of therapeutic hypothermia include cardiac arrhythmias, sepsis, hyperglycemia, coagulopathy, acid‐base disturbances, and electrolyte imbalance.15 The studies by Bernard et al.3 and the HACA;4 however, revealed no clinically significant unfavorable outcomes in the patients randomized to receive hypothermia treatment.
Our experience based on this case series leads us to conclude that therapeutic hypothermia is feasible in the community hospital setting. In our 200‐bed community teaching hospital, a multidisciplinary approach involving intensivists, emergency room physicians, internists, residents, and nursing staff lessens the technical difficulties associated with implementing a seemingly cumbersome yet inexpensive and effective treatment modality. Therapeutic hypothermia should be considered in appropriate patients in coma after resuscitation from cardiac arrest.
- Centers for Disease Control and Prevention.State specific mortality data from sudden cardiac death—United States, 1999.MMWR Morb Mortal Wkly Rep.2002;51(6):123– 126.
- .Bench to bedside: brain edema and cerebral resuscitation: the present and future.Acad Emerg Med.2002;9(9):933–946.
- ,,, et al.Treatment of comatose survivors of out of hospital cardiac arrest with induced hypothermia.N Engl J Med.2002;346(8):557–563.
- Hypothermia after Cardiac Arrest Study Group.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest.N Engl J Med.2002;346(8):549–556.
- Therapeutic hypothermia after cardiac arrest: an advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation.Circulation.2003;108:118–121.
- ,,, et al.Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey.Resuscitation.2005;64:181–186.
- ,,, et al.Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest.Crit Care Med.2006;34(7):1935–1940.
- ,,, et al.Therapeutic hypothermia after cardiac arrest: a survey of practice in intensive care units in the United Kingdom.Anaesthesia2006;61:873–877.
- .Hypothermia improves outcome from cardiac arrest.Crit Care Resusc.2005;7(4):325–327.
- ,,.Sudden cardiac death: epidemiology, transient risk, and intervention assessment.Ann Intern Med.1993;119(12):1187–1197.
- ,,, et al.Mild hypothermia induced by a helmet device: a clinical feasibility study.Resuscitation.2001;51:275–281.
- ,,, et al.Implementation of a standardized treatment protocol for post resuscitation care after out‐of‐hospital cardiac arrest.Resuscitation.2007;73(1):29–39.
- ,,,.Induced hypothermia following out‐of‐hospital cardiac arrest; initial experience in a community hospital.Clin Cardiol.2006;29(12):525–529.
- ,,,,.From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest.Crit Care Med.2006;34(7):1865–1873.
- ,.Induced hypothermia in critical care medicine: a review.Crit Care Med.2003;31(7):2041–2051.
- Centers for Disease Control and Prevention.State specific mortality data from sudden cardiac death—United States, 1999.MMWR Morb Mortal Wkly Rep.2002;51(6):123– 126.
- .Bench to bedside: brain edema and cerebral resuscitation: the present and future.Acad Emerg Med.2002;9(9):933–946.
- ,,, et al.Treatment of comatose survivors of out of hospital cardiac arrest with induced hypothermia.N Engl J Med.2002;346(8):557–563.
- Hypothermia after Cardiac Arrest Study Group.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest.N Engl J Med.2002;346(8):549–556.
- Therapeutic hypothermia after cardiac arrest: an advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation.Circulation.2003;108:118–121.
- ,,, et al.Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey.Resuscitation.2005;64:181–186.
- ,,, et al.Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest.Crit Care Med.2006;34(7):1935–1940.
- ,,, et al.Therapeutic hypothermia after cardiac arrest: a survey of practice in intensive care units in the United Kingdom.Anaesthesia2006;61:873–877.
- .Hypothermia improves outcome from cardiac arrest.Crit Care Resusc.2005;7(4):325–327.
- ,,.Sudden cardiac death: epidemiology, transient risk, and intervention assessment.Ann Intern Med.1993;119(12):1187–1197.
- ,,, et al.Mild hypothermia induced by a helmet device: a clinical feasibility study.Resuscitation.2001;51:275–281.
- ,,, et al.Implementation of a standardized treatment protocol for post resuscitation care after out‐of‐hospital cardiac arrest.Resuscitation.2007;73(1):29–39.
- ,,,.Induced hypothermia following out‐of‐hospital cardiac arrest; initial experience in a community hospital.Clin Cardiol.2006;29(12):525–529.
- ,,,,.From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest.Crit Care Med.2006;34(7):1865–1873.
- ,.Induced hypothermia in critical care medicine: a review.Crit Care Med.2003;31(7):2041–2051.
Engaging Patients at Hospital Discharge
I first met G.M. (a pseudonym) a year ago during a hospitalization for a flare of his Crohn's disease. At the age of 26, he had accrued nearly 400 hospital days in more than 10 institutionsranging from academic to community medical centers from the East Coast to the West Coast. He had been admitted and discharged more than 25 times and endured several surgeries, intermittent struggles with chronic pain and depression, and mishaps due to poor discharge planning. He referred to discharge as the most chaotic time of hospitalization, a comment that prompted a memorable discussion.
He began by describing the emotions he felt when first told about being discharged, using words such as fear and helplessness. He repeatedly talked about the lack of planning and anticipation of discharge as well as the frustration of watching a system that required fixing. Speaking with tremendous emotion and insight, he also pointed out the discharge experiences that maintained his trust and faith in the system. The conversation then shifted to his mother, who pointed out that her experiences as the caretaker were quite different than her son's. She was equally passionate and genuine in trying to characterize the hospital discharge process.
The conversation was so moving that I asked G.M. and his mother to jot down their thoughts on discharge as well as participate in a multidisciplinary patient safety conference. The following are excerpts from our conversation, their letters, and the conference.
THE PATIENT'S VIEW
You never go into the hospital wanting to stay there, but you also worry tremendously about adjusting back to home life. In my case, I was often on heavy pain medications with a PCA (patient‐controlled analgesia), so the transition to orals always created a source of stress, particularly when the transition happened right at discharge. I've had a number of experiences when they told me I was going home, stopped the PCA, and then simply sent me on my way. Nothing is worse than being discharged from the hospital, spending the car ride home doubled over in pain, and then not being able to get pain meds from the pharmacy until the next day. On the other hand, I've had discharges that were better anticipated, so I could participate in the process. This made all the difference in the world. I don't think people realize that when you're on a PCA right up to discharge, you're not really in a state to receive counseling, education, or instructions about follow‐up plansI was just trying to get better.
Many times, I knew I was getting close to discharge, but I often didn't see anyone owning the process. Information would be fragmented or inconsistent, and while I may have been ready for discharge, I wasn't prepared for discharge. This was a combination of paperwork being incomplete or being left to arrange my own follow‐up appointments after getting home. When you're sick and depressed, you fall through the cracks of the system. You just don't have the resolve to make things happen.
Ultimately, a well orchestrated discharge prepared me to be independent on some level. I felt comfortable and ready for life outside the hospital. I didn't feel helpless because I was only responsible for getting wellnot for arranging my follow‐up appointments, ensuring the home care nurse was coming by, and confirming that my primary doctor knew what was going on. In these situations, there was always a discharge planner serving as a patient advocate of sorts. I also can't imagine what I would have done if I didn't have my mom with me all the time. She's my mom, my advocate, and my caretaker and I don't know how patients survive without someone like that.
HIS MOTHER'S VIEW
I wasn't the sick and helpless one but rather the one who was expected to make it all happen: keep tabs on the medications, understand the details of the discharge plan, and ultimately manage the execution of care postdischarge. In the majority of cases when we had a bad discharge experience, it was because the goals were confused. It became about the bed that was needed for the person still sitting in the emergency department. They may not have realized it, but we fully understood the tension, and we very much felt it during the spotty discharge communications. Safety for the patient being discharged seemed to fall off the radar.
The goals of the process must be clear. In good discharges, caregivers clearly outline the transition plan, transfer records to the outpatient physicians, and arrange referrals to specialists as needed. Perhaps equally important is addressing the patient's emotional state for discharge. This isn't about convincing us that he's safe to go home, but a simple acknowledgement of the difficult transitionparticularly after a long hospitalizationgoes a far way in providing reassurance and decreasing fear and anxiety. If the issue is always one about beds and cost, I would think someone would figure out that a good discharge prevents readmissions, which would have to be a cost‐effective investment.
DISCUSSION
The voice of the patient (or family member) is incredibly powerful. Rather than having a trainee present a case history to illustrate teaching points, it is sometimes more meaningful and instructive to let patients tell their own stories. We invited G.M. and his mother to discuss their discharge experiences at a multidisciplinary patient safety conference. There, representative members of the discharge team (eg, house staff, attending, bedside nurse, pharmacist, and discharge planner) responded to their comments and discussed their roles in the discharge process. Ultimately, the patient and his mother taught us the most about what we can do to improve a process fraught with complexity and the potential for errors: communicate and work better as a team.
G.M. and his mother listened to each of the experts discuss the tasks they must complete to ensure a smooth discharge. Each provider expressed how committed they were to safe discharges, yet all of them shared how easy it is for one to go awry. They knew their individual roles, but all relied on each other to make the process completehighlighting that communication failures frequently lead to poor discharge experiences for patients. Engaging patients in the process should not transfer ownership of discharge to them (ie, making them responsible to ensure we do our jobs), though our patient and his mother presented several examples of how they owned the process because it was clear no one else did.
Evaluating our hospital discharge systems must include identifying methods to improve communication with outpatient providers, ensuring medications are available to patients on discharge, and providing written instructions (including follow‐up appointments) to patients before they leave the hospital. G.M. and his mother remind us that the best systems still need to engage patients, make them an active part of the discharge process (rather than an outcome of it), and never underestimate what patients suffer through emotionally prior to discharge.
Providers often feel uneasy when having to explain to patients that they no longer require hospitalization and perhaps avoid emotional engagement in those discussions because of the fear that some patients may become upset about a planned discharge. Communicating with patients about discharge plans should be handled with the same compassion, patience, and skill as delivering bad news. Patients entrust their lives to our clinical decision making, and abandoning this trust just as they leave the hospital is an unintended message that our patient and his mother perceived during their poor discharge experiences.
In my practice, I frequently include trainees in bedside discussions with patients and families, both to illustrate how important these conversations are and to model skills I was taught during my training. I now use discussions about discharge as a specific bedside teaching moment as well, hoping to impress on trainees the overriding message shared by G.M. and his mother: do not forget to engage patients in a process that is designed for them rather than to them.
Many physicians remain dedicated to improving hospital systems, but perhaps we should all be including our patients more in quality improvement activities and hospital committee work, as they provide perspectives not easily captured by administrative data and run charts.
Acknowledgements
The author thanks G.M. and his mother for candidly sharing their thoughts and feelings about the discharge process. He also thanks Erin Hartman, MS, for her invaluable editorial assistance in preparing this manuscript. The patient safety conference described was part of the Triad for Optimal Patient Safety (TOPS), a project funded by the Gorden & Betty Moore Foundation.
I first met G.M. (a pseudonym) a year ago during a hospitalization for a flare of his Crohn's disease. At the age of 26, he had accrued nearly 400 hospital days in more than 10 institutionsranging from academic to community medical centers from the East Coast to the West Coast. He had been admitted and discharged more than 25 times and endured several surgeries, intermittent struggles with chronic pain and depression, and mishaps due to poor discharge planning. He referred to discharge as the most chaotic time of hospitalization, a comment that prompted a memorable discussion.
He began by describing the emotions he felt when first told about being discharged, using words such as fear and helplessness. He repeatedly talked about the lack of planning and anticipation of discharge as well as the frustration of watching a system that required fixing. Speaking with tremendous emotion and insight, he also pointed out the discharge experiences that maintained his trust and faith in the system. The conversation then shifted to his mother, who pointed out that her experiences as the caretaker were quite different than her son's. She was equally passionate and genuine in trying to characterize the hospital discharge process.
The conversation was so moving that I asked G.M. and his mother to jot down their thoughts on discharge as well as participate in a multidisciplinary patient safety conference. The following are excerpts from our conversation, their letters, and the conference.
THE PATIENT'S VIEW
You never go into the hospital wanting to stay there, but you also worry tremendously about adjusting back to home life. In my case, I was often on heavy pain medications with a PCA (patient‐controlled analgesia), so the transition to orals always created a source of stress, particularly when the transition happened right at discharge. I've had a number of experiences when they told me I was going home, stopped the PCA, and then simply sent me on my way. Nothing is worse than being discharged from the hospital, spending the car ride home doubled over in pain, and then not being able to get pain meds from the pharmacy until the next day. On the other hand, I've had discharges that were better anticipated, so I could participate in the process. This made all the difference in the world. I don't think people realize that when you're on a PCA right up to discharge, you're not really in a state to receive counseling, education, or instructions about follow‐up plansI was just trying to get better.
Many times, I knew I was getting close to discharge, but I often didn't see anyone owning the process. Information would be fragmented or inconsistent, and while I may have been ready for discharge, I wasn't prepared for discharge. This was a combination of paperwork being incomplete or being left to arrange my own follow‐up appointments after getting home. When you're sick and depressed, you fall through the cracks of the system. You just don't have the resolve to make things happen.
Ultimately, a well orchestrated discharge prepared me to be independent on some level. I felt comfortable and ready for life outside the hospital. I didn't feel helpless because I was only responsible for getting wellnot for arranging my follow‐up appointments, ensuring the home care nurse was coming by, and confirming that my primary doctor knew what was going on. In these situations, there was always a discharge planner serving as a patient advocate of sorts. I also can't imagine what I would have done if I didn't have my mom with me all the time. She's my mom, my advocate, and my caretaker and I don't know how patients survive without someone like that.
HIS MOTHER'S VIEW
I wasn't the sick and helpless one but rather the one who was expected to make it all happen: keep tabs on the medications, understand the details of the discharge plan, and ultimately manage the execution of care postdischarge. In the majority of cases when we had a bad discharge experience, it was because the goals were confused. It became about the bed that was needed for the person still sitting in the emergency department. They may not have realized it, but we fully understood the tension, and we very much felt it during the spotty discharge communications. Safety for the patient being discharged seemed to fall off the radar.
The goals of the process must be clear. In good discharges, caregivers clearly outline the transition plan, transfer records to the outpatient physicians, and arrange referrals to specialists as needed. Perhaps equally important is addressing the patient's emotional state for discharge. This isn't about convincing us that he's safe to go home, but a simple acknowledgement of the difficult transitionparticularly after a long hospitalizationgoes a far way in providing reassurance and decreasing fear and anxiety. If the issue is always one about beds and cost, I would think someone would figure out that a good discharge prevents readmissions, which would have to be a cost‐effective investment.
DISCUSSION
The voice of the patient (or family member) is incredibly powerful. Rather than having a trainee present a case history to illustrate teaching points, it is sometimes more meaningful and instructive to let patients tell their own stories. We invited G.M. and his mother to discuss their discharge experiences at a multidisciplinary patient safety conference. There, representative members of the discharge team (eg, house staff, attending, bedside nurse, pharmacist, and discharge planner) responded to their comments and discussed their roles in the discharge process. Ultimately, the patient and his mother taught us the most about what we can do to improve a process fraught with complexity and the potential for errors: communicate and work better as a team.
G.M. and his mother listened to each of the experts discuss the tasks they must complete to ensure a smooth discharge. Each provider expressed how committed they were to safe discharges, yet all of them shared how easy it is for one to go awry. They knew their individual roles, but all relied on each other to make the process completehighlighting that communication failures frequently lead to poor discharge experiences for patients. Engaging patients in the process should not transfer ownership of discharge to them (ie, making them responsible to ensure we do our jobs), though our patient and his mother presented several examples of how they owned the process because it was clear no one else did.
Evaluating our hospital discharge systems must include identifying methods to improve communication with outpatient providers, ensuring medications are available to patients on discharge, and providing written instructions (including follow‐up appointments) to patients before they leave the hospital. G.M. and his mother remind us that the best systems still need to engage patients, make them an active part of the discharge process (rather than an outcome of it), and never underestimate what patients suffer through emotionally prior to discharge.
Providers often feel uneasy when having to explain to patients that they no longer require hospitalization and perhaps avoid emotional engagement in those discussions because of the fear that some patients may become upset about a planned discharge. Communicating with patients about discharge plans should be handled with the same compassion, patience, and skill as delivering bad news. Patients entrust their lives to our clinical decision making, and abandoning this trust just as they leave the hospital is an unintended message that our patient and his mother perceived during their poor discharge experiences.
In my practice, I frequently include trainees in bedside discussions with patients and families, both to illustrate how important these conversations are and to model skills I was taught during my training. I now use discussions about discharge as a specific bedside teaching moment as well, hoping to impress on trainees the overriding message shared by G.M. and his mother: do not forget to engage patients in a process that is designed for them rather than to them.
Many physicians remain dedicated to improving hospital systems, but perhaps we should all be including our patients more in quality improvement activities and hospital committee work, as they provide perspectives not easily captured by administrative data and run charts.
Acknowledgements
The author thanks G.M. and his mother for candidly sharing their thoughts and feelings about the discharge process. He also thanks Erin Hartman, MS, for her invaluable editorial assistance in preparing this manuscript. The patient safety conference described was part of the Triad for Optimal Patient Safety (TOPS), a project funded by the Gorden & Betty Moore Foundation.
I first met G.M. (a pseudonym) a year ago during a hospitalization for a flare of his Crohn's disease. At the age of 26, he had accrued nearly 400 hospital days in more than 10 institutionsranging from academic to community medical centers from the East Coast to the West Coast. He had been admitted and discharged more than 25 times and endured several surgeries, intermittent struggles with chronic pain and depression, and mishaps due to poor discharge planning. He referred to discharge as the most chaotic time of hospitalization, a comment that prompted a memorable discussion.
He began by describing the emotions he felt when first told about being discharged, using words such as fear and helplessness. He repeatedly talked about the lack of planning and anticipation of discharge as well as the frustration of watching a system that required fixing. Speaking with tremendous emotion and insight, he also pointed out the discharge experiences that maintained his trust and faith in the system. The conversation then shifted to his mother, who pointed out that her experiences as the caretaker were quite different than her son's. She was equally passionate and genuine in trying to characterize the hospital discharge process.
The conversation was so moving that I asked G.M. and his mother to jot down their thoughts on discharge as well as participate in a multidisciplinary patient safety conference. The following are excerpts from our conversation, their letters, and the conference.
THE PATIENT'S VIEW
You never go into the hospital wanting to stay there, but you also worry tremendously about adjusting back to home life. In my case, I was often on heavy pain medications with a PCA (patient‐controlled analgesia), so the transition to orals always created a source of stress, particularly when the transition happened right at discharge. I've had a number of experiences when they told me I was going home, stopped the PCA, and then simply sent me on my way. Nothing is worse than being discharged from the hospital, spending the car ride home doubled over in pain, and then not being able to get pain meds from the pharmacy until the next day. On the other hand, I've had discharges that were better anticipated, so I could participate in the process. This made all the difference in the world. I don't think people realize that when you're on a PCA right up to discharge, you're not really in a state to receive counseling, education, or instructions about follow‐up plansI was just trying to get better.
Many times, I knew I was getting close to discharge, but I often didn't see anyone owning the process. Information would be fragmented or inconsistent, and while I may have been ready for discharge, I wasn't prepared for discharge. This was a combination of paperwork being incomplete or being left to arrange my own follow‐up appointments after getting home. When you're sick and depressed, you fall through the cracks of the system. You just don't have the resolve to make things happen.
Ultimately, a well orchestrated discharge prepared me to be independent on some level. I felt comfortable and ready for life outside the hospital. I didn't feel helpless because I was only responsible for getting wellnot for arranging my follow‐up appointments, ensuring the home care nurse was coming by, and confirming that my primary doctor knew what was going on. In these situations, there was always a discharge planner serving as a patient advocate of sorts. I also can't imagine what I would have done if I didn't have my mom with me all the time. She's my mom, my advocate, and my caretaker and I don't know how patients survive without someone like that.
HIS MOTHER'S VIEW
I wasn't the sick and helpless one but rather the one who was expected to make it all happen: keep tabs on the medications, understand the details of the discharge plan, and ultimately manage the execution of care postdischarge. In the majority of cases when we had a bad discharge experience, it was because the goals were confused. It became about the bed that was needed for the person still sitting in the emergency department. They may not have realized it, but we fully understood the tension, and we very much felt it during the spotty discharge communications. Safety for the patient being discharged seemed to fall off the radar.
The goals of the process must be clear. In good discharges, caregivers clearly outline the transition plan, transfer records to the outpatient physicians, and arrange referrals to specialists as needed. Perhaps equally important is addressing the patient's emotional state for discharge. This isn't about convincing us that he's safe to go home, but a simple acknowledgement of the difficult transitionparticularly after a long hospitalizationgoes a far way in providing reassurance and decreasing fear and anxiety. If the issue is always one about beds and cost, I would think someone would figure out that a good discharge prevents readmissions, which would have to be a cost‐effective investment.
DISCUSSION
The voice of the patient (or family member) is incredibly powerful. Rather than having a trainee present a case history to illustrate teaching points, it is sometimes more meaningful and instructive to let patients tell their own stories. We invited G.M. and his mother to discuss their discharge experiences at a multidisciplinary patient safety conference. There, representative members of the discharge team (eg, house staff, attending, bedside nurse, pharmacist, and discharge planner) responded to their comments and discussed their roles in the discharge process. Ultimately, the patient and his mother taught us the most about what we can do to improve a process fraught with complexity and the potential for errors: communicate and work better as a team.
G.M. and his mother listened to each of the experts discuss the tasks they must complete to ensure a smooth discharge. Each provider expressed how committed they were to safe discharges, yet all of them shared how easy it is for one to go awry. They knew their individual roles, but all relied on each other to make the process completehighlighting that communication failures frequently lead to poor discharge experiences for patients. Engaging patients in the process should not transfer ownership of discharge to them (ie, making them responsible to ensure we do our jobs), though our patient and his mother presented several examples of how they owned the process because it was clear no one else did.
Evaluating our hospital discharge systems must include identifying methods to improve communication with outpatient providers, ensuring medications are available to patients on discharge, and providing written instructions (including follow‐up appointments) to patients before they leave the hospital. G.M. and his mother remind us that the best systems still need to engage patients, make them an active part of the discharge process (rather than an outcome of it), and never underestimate what patients suffer through emotionally prior to discharge.
Providers often feel uneasy when having to explain to patients that they no longer require hospitalization and perhaps avoid emotional engagement in those discussions because of the fear that some patients may become upset about a planned discharge. Communicating with patients about discharge plans should be handled with the same compassion, patience, and skill as delivering bad news. Patients entrust their lives to our clinical decision making, and abandoning this trust just as they leave the hospital is an unintended message that our patient and his mother perceived during their poor discharge experiences.
In my practice, I frequently include trainees in bedside discussions with patients and families, both to illustrate how important these conversations are and to model skills I was taught during my training. I now use discussions about discharge as a specific bedside teaching moment as well, hoping to impress on trainees the overriding message shared by G.M. and his mother: do not forget to engage patients in a process that is designed for them rather than to them.
Many physicians remain dedicated to improving hospital systems, but perhaps we should all be including our patients more in quality improvement activities and hospital committee work, as they provide perspectives not easily captured by administrative data and run charts.
Acknowledgements
The author thanks G.M. and his mother for candidly sharing their thoughts and feelings about the discharge process. He also thanks Erin Hartman, MS, for her invaluable editorial assistance in preparing this manuscript. The patient safety conference described was part of the Triad for Optimal Patient Safety (TOPS), a project funded by the Gorden & Betty Moore Foundation.
Prepared for Discharge Scale
Patients are vulnerable to adverse events when they transition from the hospital to outpatient care.13 Approximately 19%‐23% of patients experience adverse events within 4 weeks after acute care hospitalization.3, 4 One cause of postdischarge adverse events is ineffective discharge planning1, 2, 5, 6 Efforts to study and improve the hospital discharge‐planning processes require appropriate and valid measurement instruments. These instruments must assess the discharge process from multiple perspectives. One of the important perspectives is the patient's.7, 8
The PREPARED Patient Questionnaire is a comprehensive quality improvement tool to assess hospital discharge‐planning processes and outcomes from the patient's perspective.9, 10 The PREPARED acronym describes the content of this tool used to investigate the following phenomena: 1) prescriptions, 2) ready to reenter community, 3) education, 4) placement, 5) assurance of safety, 6) realistic expectations, 7) empowerment, and 8) directed to appropriate services.9 The PREPARED questionnaire was developed for, modified for, and validated with patients at least 65 years old. When administered to elderly patients 1 week after hospital discharge, the PREPARED has face, content, and construct validity.9
We considered the PREPARED questionnaire when we designed a clinical trial to assess the value of a discharge intervention. We sought a survey questionnaire to assess the patients' perceptions after the discharge intervention. In 2004, we found noother validated questionnaires except the PREPARED. We also noted some limitations of the PREPARED. The validated population for the PREPARED was patients older than 65 years. In our clinical trial, we planned to enroll adults of all ages. Another limitation was the PREPARED response scoring system that assigned missing data values to patients who took no medicines, needed no services, or needed no equipment.10 We were concerned about the potential for unacceptably large numbers of patients with nonignorable missing data. We decided to address the above limitations with a validation study in our patient population and with a revised response scoring system.
In the present article, we describe item reduction and validation for the Brief PREPARED (B‐PREPARED) scale to measure patients' perceptions of their preparedness for hospital discharge. When we designed B‐PREPARED, we asked the following question: Does a subset of PREPARED items with a revised scoring system have internal consistency, construct validity, and predictive validity in a population of adult patients with broad age range? We also wanted a brief scale with acceptable, defined statistical properties for multiple users. One user class included clinicians who guide and assess discharge‐planning processes. Other users would be researchers like us who measure differences between treatment groups after discharge process interventions.
METHODS
The Peoria Institutional Review Board approved the protocol for human research. The patient sample for scale analysis was a prospective cohort. Follow‐up was 1 month after patient's discharge from a 730‐bed acute‐care teaching hospital in central Illinois. The patients were enrolled in an ongoing cluster randomized clinical trial with blinded outcome assessment. Willing patients or their proxies provided written consent for study participation. Enrollment occurred between December 2004 and July 2006.
Patient Inclusion Criteria
Trained research coordinators identified all consecutive adult inpatients who were discharged to the patient's home by internal medicine hospitalists. Patient inclusion in our cluster randomized trial required a probability of repeat admission (Pra) score of at least 0.40.11, 12 Hence, the patients in the scale analysis cohort had the same high probability for repeat admission. The research coordinators calculated the Pra within 2 days before discharge from the index hospitalization. The Pra score came from a logistic model of age, sex, prior hospitalizations, prior doctor visits, self‐rated health status, informal caregiver, and comorbid coronary heart disease and diabetes mellitus.11, 12
Patient Exclusion Criteria
We excluded patients if the discharge destination was a nursing home, another acute care hospital, or an inpatient rehabilitation unit. Patients were excluded if life expectancy was less than 6 months as estimated by the hospitalist. Because follow‐up occurred via interview, patients without telephones or English‐ or Spanish‐language skills were excluded. Patients with cognitive impairment could participate with consent from a legally authorized representative and with a proxy whospent a minimum of 3 hours daily with the patient and was willing to answer postdischarge interviews.
Baseline Assessment
During the index hospital admission, trained data abstractors recorded baseline patient data: age, sex, race, diabetes mellitus, heart failure, chronic obstructive pulmonary disease, and coronary heart disease. Patients or proxies provided the number of hospital admissions and doctor visits during the year before the index hospital admission. We recorded the availability of an informal caregiver in response to the question Is there a friend, relative, or neighbor who would take care of you for a few days if necessary? Patients rated their health status on the following scale: poor, fair, good, very good, or excellent.
Discharge and Postdischarge Procedures
At the end of the index hospitalization, hospitalists and ward nurses used standardized forms for discharge diagnoses, prescriptions, instructions, and appointments. Discharge‐planning nurses or social workers consulted with hospitalists and ward nurses and then coordinated service providers including home health nurses, physical therapists, home health aides, homemaker service providers, durable medical equipment vendors, home oxygen vendors, home infusion pharmacists, social workers, rehabilitation service providers, legal aide providers, and others. After discharge, trained research personnel conducted 2 telephone interviews with the patient or the patient's proxy. The first interview occurred 1 week after discharge. Interviewers read verbatim items from the PREPARED10 and the Satisfaction with Information about Medicines Scale (SIMS).13 During the second telephone interview 30 10 days after discharge, interviewers recorded if patients had experienced at least 1 emergency department visit during the month after discharge.
The purpose of the PREPARED items was to have a bank of items and responses that could be used to generate the B‐PREPARED scale. The PREPARED questionnaire was originally developed to provide feedback to hospital ward staff about the quality of discharge‐planning activities that occurred during hospitalization.9 Discriminant factor analysis on the original 16 process questions revealed 4 factors that explained 57% of the total variance in patient/caregiver responses. The PREPARED domains included information exchange on community services and equipment, management of medication, the process of preparing to cope after discharge, and having control over one's discharge circumstances.9 The purpose of the SIMS was as a construct to compare with the B‐PREPARED scale. The derivation and validity of the SIMS have been described extensively elsewhere.13 In summary, the SIMS items were derived from recommendations of the Association of the British Pharmaceutical Industry. The intent of the SIMS was to determine if a patient's medication information needs were met and to allow comparison between patients or groups. Respondents selected 1 of 5 options for each of the 17 items. The sum of scores for each of the SIMS items yielded a total score that ranged from 0 to 17. Patients with high total SIMS scores had high satisfaction with the amount of medication information they received. Validation samples included inpatients and outpatients with a variety of diseases and characteristics. SIMS demonstrated adequate internal consistency, test‐retest reliability, and criterion‐related validity.13
Item Selection and Scoring of the B‐PREPARED Instrument
We selected an initial pool of items from the PREPARED instrument.10 The goal was a parsimonious, comprehensive, and valid instrument for use in clinical and research environments. When we retained or deleted items, our decision process was conservative, conceptual, and statistical. We performed item reduction in the following steps defined a priori. First, we agreed on items consistent with domains in the prepared for discharge construct as defined by expert consensus.9 Second, we excluded items that assessed qualities of the discharge process that were imperceptible to the patient on the day of discharge. Third, we excluded items that elicited open‐ended responses unsuitable for quantitative scale development and analysis. Fourth, we assessed reliability as defined by the Cronbach's alpha statistic. We excluded items that substantially decreased Cronbach's alpha.
Measures of Construct Validity
We used 2 measures of construct validity in our assessment of B‐PREPARED. One construct was patient worry. During the interview 1 week after discharge, research personnel asked, Now that you have been out of the hospital for a while, has anything been worrying you about managing at home? Response options for the dichotomous worry item were no or yes. We anticipated worried patients would have lower B‐PREPARED scale values. The other construct, SIMS, evaluated patient preparedness related to medication information exchange. The hypothesis was a positive correlation between SIMS and B‐PREPARED scale values.
Measure of Predictive Validity
We asked if B‐PREPARED predicted and discriminated groups of patients who did or did not visit emergency departments after hospital discharge. Emergency department visits were relevant adverse outcomes because of their association with postdischarge adverse events due to inpatient treatment.4 Emergency department visits reflected new or worsening symptoms after discharge. In our scale analysis, the hypothesis was patients with at least 1 emergency department visit would have lower B‐PREPARED scale values.
Analysis
Analyses were performed with SPSS PC (Version 14.0.2, SPSS Inc, Chicago, IL). We reported descriptive statistics as means, standard deviations, and range for interval variables and percentages for nominal variables. To determine the internal consistency of the scale, we calculated Cronbach's alpha. We assessed the distribution of the B‐PREPARED scale with visual and statistical tests for skewness. While using the SPSS FACTOR program, we performed principal components extractions and then rotated components using the oblique promax technique. Component scores were saved using the regression score procedure. Component loadings above 0.30 were considered important. Statistical inference tests were the Mann‐Whitney U for median differences between 2 groups and the Spearman correlation for associations. We reported medians with 25th and 75th percentiles. Differences between 2 correlations were tested using Fischer z transformations. The accepted level of significance was P < 0.05.
RESULTS
Description of Cohort
We approached 5124 patients during the index hospital admission. After applying exclusion criteria, we obtained consent and enrolled 491 patients. The reasons for exclusion were low Pra score for 34.9% of ineligible patients, discharge to nursing home for 12.8%, declined consent for 10.8%, nonparticipating hospitalist service for 9.1%, discharged during screen for 8.5%, previously enrolled in study for 5.6%, and declined screening for 2.3%. Each of the other exclusion criteria accounted for less than 4% of the ineligible patients. After subtracting 6% of eligible patients (31 of 491) who died, withdrew, or were lost during the first month, there were 460 patients available for analysis. Table 1 describes the patients' characteristics. Most of the patients, 75.2% (346 of 460), were less than 65 years old, and the mean age was 53.9 15.5 years. Many patients had chronic diseases including diabetes mellitus, coronary heart disease, heart failure, and chronic obstructive pulmonary disease. Most patients, 81.5% (375 of 460), rated their health as poor or fair, and 53.5% (246/460) had 1 or more hospital admissions during the year before their index admission. Cohort patients had a high probability of repeat admission: mean Pra 0.49 0.07 (range 0.400.70).
| Characteristic | n (%) |
|---|---|
| Sex (male) | 193 (42.0%) |
| Age (years) | |
| 1930 | 35 (7.6%) |
| 3164 | 311 (67.6%) |
| 6598 | 114 (24.8%) |
| Race | |
| White | 275 (59.8%) |
| Black | 124 (27.0%) |
| Other | 61 (13.3%) |
| Self‐rated health status | |
| Poor | 139 (30.2%) |
| Fair | 236 (51.3%) |
| Good | 70 (15.2%) |
| Very good | 13 (2.8%) |
| Excellent | 2 (0.4%) |
| Diabetes mellitus | 259 (56.3%) |
| Chronic obstructive pulmonary disease | 79 (17.2%) |
| Coronary heart disease | 188 (40.9%) |
| Heart failure (n = 456) | 100 (21.7%) |
| Informal caregiver available (yes) | 459 (99.1%) |
| Hospital admissions during year prior to index admission | |
| 0 | 214 (46.5%) |
| 1 | 131 (28.5%) |
| 2 | 47 (10.2%) |
| 3 or 4 | 35 (7.6%) |
| 515 | 33 (7.2%) |
Item Reduction, Internal Consistency, and Score Distributions
Item reduction resulted in 12 items that fulfilled conceptual criteria. Table 2 shows the items and the distribution of responses. One of the 12 items, delays on the day you left the hospital (item 12, Table 2), was deleted because the item depressed the Cronbach's alpha. The B‐PREPARED with 11 items had acceptable internal consistency for the full cohort (Cronbach's alpha = 0.76).
| Item Text | Descriptor for Score 0 | Descriptor for Score 1 | Descriptor for Score 2 | |
|---|---|---|---|---|
| ||||
| 1 | While you were in the hospital, how much information did you receive about the medications that you were to take at home? | None (40, 8.7%) | Some, but not enough (95, 20.7%) | As much as I needed; or Not taking any medications (325, 70.7%) |
| 2 | While you were in the hospital, how much information did you receive about the side effects of the medications that you were to take at home? | None (198, 43.0%) | Some, but not enough (54, 11.7%) | As much as I needed; or Not taking any medications (208, 45.2%) |
| 3 | While you were in the hospital, were you given written instructions about your medications? If yes, did someone spend time explaining the written instructions? | No written instructions and no time spent (116, 25.2%) | Yes, received written instructions but no time spent (49, 10.7%) | Yes, received written instructions and yes, time spent; or, Not taking any medications (291, 63.3%) |
| 4 | While you were in the hospital, how much information did you receive on how you would manage your usual activities when you went home? | None (55, 12.0%) | Some, but not enough (90, 19.6%) | As much as I needed (315, 68.5%) |
| 5 | While you were in the hospital, how much information did you receive on community services you might use once you went home? | None (89, 19.3%) | Some, but not enough (40, 8.7%) | As much as I needed; or No services needed (331, 72.0%) |
| 6 | While you were in the hospital, how much information did you receive on equipment you might need once you went home? | None (49, 10.7%) | Some, but not enough (22, 4.8%) | As much as I needed; or No equipment needed (389, 84.6%) |
| 7 | Before you were discharged from the hospital, did anyone arrange community services for you to use at home? | No (42, 9.1%) | Yes; or No one needed to arrange because services were already in place or no services needed (418, 90.9%) | |
| 8 | Before you were discharged from the hospital, did anyone arrange equipment for you? | No (16, 3.5%) | Yes; or No one needed to because equipment already in place or no equipment needed (444, 96.5%) | |
| 9 | Before you were discharged from hospital, was there any other information you would have liked while you were in the hospital to prepare you for coping at home? | No (116, 25.2%) | Yes (344, 74.8%) | |
| 10 | After you were told you could leave the hospital, how confident did you feel about managing at home? | Not confident (25, 5.4%) | Unsure (103, 22.4%) | Confident (332, 72.2%) |
| 11 | Looking back to the time you left the hospital, overall, how prepared did you feel for returning home? | Unprepared (39, 8.5%) | Moderately prepared (132, 28.7%) | Very prepared (288, 62.6%) |
| 12 | After you were told you could leave the hospital, were there any delays on the day you left the hospital? | Yes (122, 26.5%) | No (338, 73.5%) | |
For an individual patient, the sum of the scores for each item yielded a B‐PREPARED scale value. In the 460‐patient cohort, B‐PREPARED scale values had a mean of 17.3 4.3 and a negatively skewed distribution. A high scale value reflected high perception of discharge preparedness. Each of the 11 items correlated significantly with the B‐PREPARED scale value (P < 0.001, 2‐tailed).
There were substantial ceiling effects with individual items but not in the B‐PREPARED total score. Five of the 9 items with 3 response options had a ceiling effect above 70%. Three items had a dichotomous response option (items 7, 8, and 9). In 2 of these 3 items, more than 90% of respondents selected the response indicating higher preparedness. The total B‐PREPARED did not have noteworthy floor or ceiling effects. In this sample's total B‐PREPARED scores, 0.2% of respondents had the lowest score of 3, and 20% had the highest score of 22.
Principal Component Analysis
In the component analysis, we evaluated the correlation matrix of the 11 items in the B‐PREPARED scale. A Kaiser‐Meyer‐Olkin statistic of 0.76 indicated sufficient sampling adequacy to extract components from the matrix. Principal components extracted 54.2% of the variance associated with the 11‐item B‐PREPARED scale. After inspection of scree plots, we determined that 3 components were extracted before the eigenvalue fell below 1. The pattern matrix for the promax rotation was inspected, and the factor loading of each item appears in Table 3. The item content identified the first component as self‐care information for medications and activities. The second component was equipment and services. The third component was confidence. All B‐PREPARED items loaded primarily on 1 of the 3 components (Table 3).
| Item text | Component | |||
|---|---|---|---|---|
| Self‐care Information for Medications and Activity | Equipment and Services | Confidence | ||
| 1 | While you were in the hospital, how much information did you receive about the medications that you were to take at home? | 0.749 | 0.032 | 0.019 |
| 2 | While you were in the hospital, how much information did you receive about the side effects of the medications that you were to take at home? | 0.778 | .008 | 0.003 |
| 3 | While you were in the hospital, were you given written instructions about your medications? If yes, did someone spend time explaining the written instructions? | 0.758 | 0.030 | 0.084 |
| 4 | While you were in the hospital, how much information did you receive on how you would manage your usual activities when you went home? | 0.581 | 0.101 | 0.195 |
| 5 | While you were in the hospital, how much information did you receive on community services you might use once you went home? | 0.158 | 0.639 | 0.124 |
| 6 | While you were in the hospital, how much information did you receive on equipment you might need once you went home? | 0.183 | 0.701 | ‐0.152 |
| 7 | Before you were discharged from the hospital, did anyone arrange community services for you to use at home? | 0.081 | 0.654 | 0.199 |
| 8 | Before you were discharged from the hospital, did anyone arrange equipment for you? | 0.138 | 0.655 | 0.095 |
| 9 | Before you were discharged from the hospital, was there any other information you would have liked while you were in the hospital to prepare you for coping at home? | 0.181 | 0.211 | 0.369 |
| 10 | After you were told you could leave the hospital, how confident did you feel about managing at home? | 0.036 | 0.058 | 0.876 |
| 11 | Looking back to the time you left the hospital, overall, how prepared did you feel for returning home? | 0.018 | 0.032 | 0.875 |
Construct Validity
We assessed 2 constructs: worry and satisfaction with medication information (SIMS). In the cohort, 25% of patients (115 of 460) reported worry about managing at home. Worried patients had significantly lower B‐PREPARED scale values (median [25%, 75%] = 14 [10, 16]) than patients who did not worry (median [25%, 75%] = 17 [14, 20], P < .001). We calculated SIMS and then correlated SIMS with B‐PREPARED and components. In the cohort, the mean SIMS was 12.1 4.7 (range 0‐17). Patients with greater satisfaction on the SIMS also had higher B‐PREPARED scale values (rho = 0.45, P < 0.001). There was a significant positive correlation between SIMS and the B‐PREPARED component called self‐care information for medications and activities (rho = 0.46, P < 0.001). The other 2 B‐PREPARED components, equipment/services and confidence, were positively correlated with SIMS at much lower levels (rho = 0.18 and rho = 0.24, respectively, both Fischer z transformations P < .001). The B‐PREPARED scale demonstrated validity with the constructs of worry and satisfaction with medication information.
Predictive Validity
We assessed the capacity of the B‐PREPARED to predict and discriminate groups of patients who did or did not visit emergency departments. Within 1 month of hospital discharge, 16.5% of the cohort (76 of 460 patients) had at least 1 visit to an emergency department. B‐PREPARED scale values were lower for those patients who visited emergency departments (median [25%, 75%] = 14 [12, 18]) than those who did not (median [25%, 75%] = 16 [13, 19], P = 0.011). The B‐PREPARED scale analysis supported the hypothesized relationship with emergency department visits.
Correlations between B‐PREPARED and Baseline Characteristics
We evaluated the correlations between a patient's B‐PREPARED scale value and baseline characteristics, shown in Table 1. There was a weak positive correlation with self‐rated health status (rho 0.17, P < .001). Patients who perceived better health status had higher B‐PREPARED scale values than those with poorer status. The other baseline characteristics in Table 1 were not associated with B‐PREPARED scale values.
DISCUSSION
The B‐PREPARED scale measures patients' perceptions of their preparedness for hospital discharge home. Scale items came from the PREPARED, a survey with validated psychometric properties in elderly patients. We assessed the B‐PREPARED in a cohort of young and elderly adult patients. We examined the B‐PREPARED instrument for internal consistency, construct validity, and predictive validity. In comparison with the domains identified in the full PREPARED instrument,9 the abbreviated B‐PREPARED scale identified similar domains. Some differences were anticipated because we limited items to those the respondents would be able to perceive before leaving the hospital.
The results of our study should be interpreted in the context of strengths and limitations. One of the strengths was the validity of the PREPARED, from which the B‐PREPARED was derived.7 The conceptually rigorous process used to develop the PREPARED questionnaire allowed us to draw from a bank of concise, well‐worded items.9 The B‐PREPARED extends validity to a population of adults of all ages with high risk for readmission. The other strength of the B‐PREPARED was the association with the clinically relevant constructs worry and satisfaction with medication information. The B‐PREPARED also discriminated between patients who did and those who did not return to emergency departments after discharge. Although the patient population for the B‐PREPARED validation was one of the strengths of this study, it is also a limitation. Our cohort lacked diversity with respect to readmission risk. The results of our study may not generalize to patients with low risk for repeated admission. Furthermore, all our patients were discharged home. The exclusion of other discharge destinations helped us to enroll a cohort with homogenous risk for readmission. However, our exclusion criteria did not allow us to validate the B‐PREPARED in patients discharged to nursing homes, inpatient rehabilitation units, or other acute care facilities.
Another limitation related to outpatient visits after discharge. We did not analyze outpatient sites other than emergency departments. For all of our study patients, the discharging hospitalist scheduled at least 1 outpatient visit with the primary care practitioner. For some patients, the hospitalist also scheduled postdischarge visits for diagnostic evaluations like cardiac stress tests, endoscopies, radiographs, or other laboratory tests. When these visits occurred, they represented successful execution of the discharge plan. Sometimes patients arrived for planned or unplanned outpatient visits with exacerbated symptoms or adverse events. These latter visits might represent failures of the discharge plan. Our data collection did not allow us to distinguish outpatient visits as successes or failures of the discharge plan. When we counted only emergency department visits, we may have underestimated the number of patients with adverse events who sought and received successful treatment in outpatient clinics. Future studies should consider ascertainment of planned and unplanned outpatient visits for exacerbated symptoms and adverse events.
After our study began enrollment, other investigators published the Readiness for Hospital Discharge Scale14 and Care Transitions Measure.15 The design and validation of these sampling instruments differed with each other and with the B‐PREPARED. The differences made the 3 scales complementary but not interchangeable. For example, investigators administered the 21‐item Readiness for Hospital Discharge Scale on the day of discharge to adult medical‐surgical patients, postpartum mothers, and parents of hospitalized children. In contrast, we administered the B‐PREPARED 1 week after discharge to adult internal medicine patients or their proxies. The Readiness for Hospital Discharge subscales were personal status, knowledge, coping ability, and expected support. These subscales were similar to the components of the B‐PREPARED. The Readiness for Hospital Discharge Scale demonstrated internal consistency and construct validity but did not predict patients who returned to emergency departments after hospital discharge.14 Future users of the Readiness for Hospital Discharge Scale or the B‐PREPARED should consider their patient populations and the date of administration when selecting 1 scale versus another. If brevity is important to a clinician or researcher, then the 11‐item B‐PREPARED scale may be considered.
The Care Transitions Measure also differed from the B‐PREPARED. The 15‐item Care Transitions Measure evaluated an adult population with a broad age range and with chronic obstructive pulmonary disease, heart failure, stroke, or hip fracture.15 The diseases represented in the population for the Care Transitions Measure were similar to those in the B‐PREPARED cohort, although the distribution of the diseases differed. When validating the Care Transitions Measure, investigators administered questionnaires 6 to 12 weeks after discharge. The Care Transitions Measure had 4 factors: critical understanding, preferences important, management preparation, and care plan. The factors of the Care Transitions Measure were comparable to the components of the B‐PREPARED, and both scales assessed medication self‐management. However, the Care Transitions Measure addressed patient preferences with specific items, whereas the B‐PREPARED used the scoring system to quantify patient preferences. Both the Care Transitions Measure and the B‐PREPARED demonstrated internal consistency and discriminated between patients who did and those who did not return to emergency departments after hospital discharge.15 When selecting a scale, future users should consider the B‐PREPARED only for assessments 1 week post discharge and should consider the Care Transitions Measure for later assessments.
There are applications of the B‐PREPARED scale in hospital quality improvement efforts. Hospitals have multiple motivations to pursue quality improvement projects related to discharge processes: satisfaction of patients, reduction in adverse events, relation with referring physicians, and accreditation by regulators.6, 16 When hospital‐based clinicians survey patients, they may wish to use a brief, reliable, and validated instrument like the B‐PREPARED questionnaire.
CONCLUSIONS
The B‐PREPARED provided a reliable and valid measure of patients' perceptions of their preparedness for hospital discharge home. Clinicians and researchers may find the B‐PREPARED useful to guide, assess, and compare discharge‐planning interventions.
Acknowledgements
The authors thank Dr. Karen Grimmer‐Somers, PhD, for permission to use the PREPARED instrument and for her thoughtful comments on the draft manuscript.
- ,,,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2004;(1):CD000313.
- ,,.Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home.Cochrane Database Syst Rev.2003;(4):CD003716.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- ,,,.Review of the literature on survey instruments used to collect data on hospital patients' perceptions of care.Health Serv Res.2005;40:1996–2017.
- ,.A patient‐centered model of care for hospital discharge.Clin Nurs Res.2004;13:117–136.
- ,.The development, validity and application of a new instrument to assess the quality of discharge planning activities from the community perspective.Int J Qual Health Care.2001;13:109–116.
- PREPARED Patient Questionnaire. Available at: http://www.unisa.edu.au/cahe/pubs/Patient%20scoring.pdf. Accessed June 14,2007.
- ,,.Predictive validity of a questionnaire that identifies older persons at risk for hospital admission.J Am Geriatr Soc.1995;43:374–377.
- ,,,.Predictive validity of the Pra instrument among older recipients of managed care.J Am Geriatr Soc.1997;45:614–617.
- ,,.The Satisfaction with Information about Medicines Scales (SIMS): a new measurement tool for audit and research.Qual Health Care.2001;10:135–140.
- ,.Psychometric properties of the Readiness for Hospital Discharge Scale.J Nurs Meas.2006;14:163–180.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43:246–255.
- 2007 Hospital/critical access hospital national patient safety goals. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals. Accessed June 14,2007.
Patients are vulnerable to adverse events when they transition from the hospital to outpatient care.13 Approximately 19%‐23% of patients experience adverse events within 4 weeks after acute care hospitalization.3, 4 One cause of postdischarge adverse events is ineffective discharge planning1, 2, 5, 6 Efforts to study and improve the hospital discharge‐planning processes require appropriate and valid measurement instruments. These instruments must assess the discharge process from multiple perspectives. One of the important perspectives is the patient's.7, 8
The PREPARED Patient Questionnaire is a comprehensive quality improvement tool to assess hospital discharge‐planning processes and outcomes from the patient's perspective.9, 10 The PREPARED acronym describes the content of this tool used to investigate the following phenomena: 1) prescriptions, 2) ready to reenter community, 3) education, 4) placement, 5) assurance of safety, 6) realistic expectations, 7) empowerment, and 8) directed to appropriate services.9 The PREPARED questionnaire was developed for, modified for, and validated with patients at least 65 years old. When administered to elderly patients 1 week after hospital discharge, the PREPARED has face, content, and construct validity.9
We considered the PREPARED questionnaire when we designed a clinical trial to assess the value of a discharge intervention. We sought a survey questionnaire to assess the patients' perceptions after the discharge intervention. In 2004, we found noother validated questionnaires except the PREPARED. We also noted some limitations of the PREPARED. The validated population for the PREPARED was patients older than 65 years. In our clinical trial, we planned to enroll adults of all ages. Another limitation was the PREPARED response scoring system that assigned missing data values to patients who took no medicines, needed no services, or needed no equipment.10 We were concerned about the potential for unacceptably large numbers of patients with nonignorable missing data. We decided to address the above limitations with a validation study in our patient population and with a revised response scoring system.
In the present article, we describe item reduction and validation for the Brief PREPARED (B‐PREPARED) scale to measure patients' perceptions of their preparedness for hospital discharge. When we designed B‐PREPARED, we asked the following question: Does a subset of PREPARED items with a revised scoring system have internal consistency, construct validity, and predictive validity in a population of adult patients with broad age range? We also wanted a brief scale with acceptable, defined statistical properties for multiple users. One user class included clinicians who guide and assess discharge‐planning processes. Other users would be researchers like us who measure differences between treatment groups after discharge process interventions.
METHODS
The Peoria Institutional Review Board approved the protocol for human research. The patient sample for scale analysis was a prospective cohort. Follow‐up was 1 month after patient's discharge from a 730‐bed acute‐care teaching hospital in central Illinois. The patients were enrolled in an ongoing cluster randomized clinical trial with blinded outcome assessment. Willing patients or their proxies provided written consent for study participation. Enrollment occurred between December 2004 and July 2006.
Patient Inclusion Criteria
Trained research coordinators identified all consecutive adult inpatients who were discharged to the patient's home by internal medicine hospitalists. Patient inclusion in our cluster randomized trial required a probability of repeat admission (Pra) score of at least 0.40.11, 12 Hence, the patients in the scale analysis cohort had the same high probability for repeat admission. The research coordinators calculated the Pra within 2 days before discharge from the index hospitalization. The Pra score came from a logistic model of age, sex, prior hospitalizations, prior doctor visits, self‐rated health status, informal caregiver, and comorbid coronary heart disease and diabetes mellitus.11, 12
Patient Exclusion Criteria
We excluded patients if the discharge destination was a nursing home, another acute care hospital, or an inpatient rehabilitation unit. Patients were excluded if life expectancy was less than 6 months as estimated by the hospitalist. Because follow‐up occurred via interview, patients without telephones or English‐ or Spanish‐language skills were excluded. Patients with cognitive impairment could participate with consent from a legally authorized representative and with a proxy whospent a minimum of 3 hours daily with the patient and was willing to answer postdischarge interviews.
Baseline Assessment
During the index hospital admission, trained data abstractors recorded baseline patient data: age, sex, race, diabetes mellitus, heart failure, chronic obstructive pulmonary disease, and coronary heart disease. Patients or proxies provided the number of hospital admissions and doctor visits during the year before the index hospital admission. We recorded the availability of an informal caregiver in response to the question Is there a friend, relative, or neighbor who would take care of you for a few days if necessary? Patients rated their health status on the following scale: poor, fair, good, very good, or excellent.
Discharge and Postdischarge Procedures
At the end of the index hospitalization, hospitalists and ward nurses used standardized forms for discharge diagnoses, prescriptions, instructions, and appointments. Discharge‐planning nurses or social workers consulted with hospitalists and ward nurses and then coordinated service providers including home health nurses, physical therapists, home health aides, homemaker service providers, durable medical equipment vendors, home oxygen vendors, home infusion pharmacists, social workers, rehabilitation service providers, legal aide providers, and others. After discharge, trained research personnel conducted 2 telephone interviews with the patient or the patient's proxy. The first interview occurred 1 week after discharge. Interviewers read verbatim items from the PREPARED10 and the Satisfaction with Information about Medicines Scale (SIMS).13 During the second telephone interview 30 10 days after discharge, interviewers recorded if patients had experienced at least 1 emergency department visit during the month after discharge.
The purpose of the PREPARED items was to have a bank of items and responses that could be used to generate the B‐PREPARED scale. The PREPARED questionnaire was originally developed to provide feedback to hospital ward staff about the quality of discharge‐planning activities that occurred during hospitalization.9 Discriminant factor analysis on the original 16 process questions revealed 4 factors that explained 57% of the total variance in patient/caregiver responses. The PREPARED domains included information exchange on community services and equipment, management of medication, the process of preparing to cope after discharge, and having control over one's discharge circumstances.9 The purpose of the SIMS was as a construct to compare with the B‐PREPARED scale. The derivation and validity of the SIMS have been described extensively elsewhere.13 In summary, the SIMS items were derived from recommendations of the Association of the British Pharmaceutical Industry. The intent of the SIMS was to determine if a patient's medication information needs were met and to allow comparison between patients or groups. Respondents selected 1 of 5 options for each of the 17 items. The sum of scores for each of the SIMS items yielded a total score that ranged from 0 to 17. Patients with high total SIMS scores had high satisfaction with the amount of medication information they received. Validation samples included inpatients and outpatients with a variety of diseases and characteristics. SIMS demonstrated adequate internal consistency, test‐retest reliability, and criterion‐related validity.13
Item Selection and Scoring of the B‐PREPARED Instrument
We selected an initial pool of items from the PREPARED instrument.10 The goal was a parsimonious, comprehensive, and valid instrument for use in clinical and research environments. When we retained or deleted items, our decision process was conservative, conceptual, and statistical. We performed item reduction in the following steps defined a priori. First, we agreed on items consistent with domains in the prepared for discharge construct as defined by expert consensus.9 Second, we excluded items that assessed qualities of the discharge process that were imperceptible to the patient on the day of discharge. Third, we excluded items that elicited open‐ended responses unsuitable for quantitative scale development and analysis. Fourth, we assessed reliability as defined by the Cronbach's alpha statistic. We excluded items that substantially decreased Cronbach's alpha.
Measures of Construct Validity
We used 2 measures of construct validity in our assessment of B‐PREPARED. One construct was patient worry. During the interview 1 week after discharge, research personnel asked, Now that you have been out of the hospital for a while, has anything been worrying you about managing at home? Response options for the dichotomous worry item were no or yes. We anticipated worried patients would have lower B‐PREPARED scale values. The other construct, SIMS, evaluated patient preparedness related to medication information exchange. The hypothesis was a positive correlation between SIMS and B‐PREPARED scale values.
Measure of Predictive Validity
We asked if B‐PREPARED predicted and discriminated groups of patients who did or did not visit emergency departments after hospital discharge. Emergency department visits were relevant adverse outcomes because of their association with postdischarge adverse events due to inpatient treatment.4 Emergency department visits reflected new or worsening symptoms after discharge. In our scale analysis, the hypothesis was patients with at least 1 emergency department visit would have lower B‐PREPARED scale values.
Analysis
Analyses were performed with SPSS PC (Version 14.0.2, SPSS Inc, Chicago, IL). We reported descriptive statistics as means, standard deviations, and range for interval variables and percentages for nominal variables. To determine the internal consistency of the scale, we calculated Cronbach's alpha. We assessed the distribution of the B‐PREPARED scale with visual and statistical tests for skewness. While using the SPSS FACTOR program, we performed principal components extractions and then rotated components using the oblique promax technique. Component scores were saved using the regression score procedure. Component loadings above 0.30 were considered important. Statistical inference tests were the Mann‐Whitney U for median differences between 2 groups and the Spearman correlation for associations. We reported medians with 25th and 75th percentiles. Differences between 2 correlations were tested using Fischer z transformations. The accepted level of significance was P < 0.05.
RESULTS
Description of Cohort
We approached 5124 patients during the index hospital admission. After applying exclusion criteria, we obtained consent and enrolled 491 patients. The reasons for exclusion were low Pra score for 34.9% of ineligible patients, discharge to nursing home for 12.8%, declined consent for 10.8%, nonparticipating hospitalist service for 9.1%, discharged during screen for 8.5%, previously enrolled in study for 5.6%, and declined screening for 2.3%. Each of the other exclusion criteria accounted for less than 4% of the ineligible patients. After subtracting 6% of eligible patients (31 of 491) who died, withdrew, or were lost during the first month, there were 460 patients available for analysis. Table 1 describes the patients' characteristics. Most of the patients, 75.2% (346 of 460), were less than 65 years old, and the mean age was 53.9 15.5 years. Many patients had chronic diseases including diabetes mellitus, coronary heart disease, heart failure, and chronic obstructive pulmonary disease. Most patients, 81.5% (375 of 460), rated their health as poor or fair, and 53.5% (246/460) had 1 or more hospital admissions during the year before their index admission. Cohort patients had a high probability of repeat admission: mean Pra 0.49 0.07 (range 0.400.70).
| Characteristic | n (%) |
|---|---|
| Sex (male) | 193 (42.0%) |
| Age (years) | |
| 1930 | 35 (7.6%) |
| 3164 | 311 (67.6%) |
| 6598 | 114 (24.8%) |
| Race | |
| White | 275 (59.8%) |
| Black | 124 (27.0%) |
| Other | 61 (13.3%) |
| Self‐rated health status | |
| Poor | 139 (30.2%) |
| Fair | 236 (51.3%) |
| Good | 70 (15.2%) |
| Very good | 13 (2.8%) |
| Excellent | 2 (0.4%) |
| Diabetes mellitus | 259 (56.3%) |
| Chronic obstructive pulmonary disease | 79 (17.2%) |
| Coronary heart disease | 188 (40.9%) |
| Heart failure (n = 456) | 100 (21.7%) |
| Informal caregiver available (yes) | 459 (99.1%) |
| Hospital admissions during year prior to index admission | |
| 0 | 214 (46.5%) |
| 1 | 131 (28.5%) |
| 2 | 47 (10.2%) |
| 3 or 4 | 35 (7.6%) |
| 515 | 33 (7.2%) |
Item Reduction, Internal Consistency, and Score Distributions
Item reduction resulted in 12 items that fulfilled conceptual criteria. Table 2 shows the items and the distribution of responses. One of the 12 items, delays on the day you left the hospital (item 12, Table 2), was deleted because the item depressed the Cronbach's alpha. The B‐PREPARED with 11 items had acceptable internal consistency for the full cohort (Cronbach's alpha = 0.76).
| Item Text | Descriptor for Score 0 | Descriptor for Score 1 | Descriptor for Score 2 | |
|---|---|---|---|---|
| ||||
| 1 | While you were in the hospital, how much information did you receive about the medications that you were to take at home? | None (40, 8.7%) | Some, but not enough (95, 20.7%) | As much as I needed; or Not taking any medications (325, 70.7%) |
| 2 | While you were in the hospital, how much information did you receive about the side effects of the medications that you were to take at home? | None (198, 43.0%) | Some, but not enough (54, 11.7%) | As much as I needed; or Not taking any medications (208, 45.2%) |
| 3 | While you were in the hospital, were you given written instructions about your medications? If yes, did someone spend time explaining the written instructions? | No written instructions and no time spent (116, 25.2%) | Yes, received written instructions but no time spent (49, 10.7%) | Yes, received written instructions and yes, time spent; or, Not taking any medications (291, 63.3%) |
| 4 | While you were in the hospital, how much information did you receive on how you would manage your usual activities when you went home? | None (55, 12.0%) | Some, but not enough (90, 19.6%) | As much as I needed (315, 68.5%) |
| 5 | While you were in the hospital, how much information did you receive on community services you might use once you went home? | None (89, 19.3%) | Some, but not enough (40, 8.7%) | As much as I needed; or No services needed (331, 72.0%) |
| 6 | While you were in the hospital, how much information did you receive on equipment you might need once you went home? | None (49, 10.7%) | Some, but not enough (22, 4.8%) | As much as I needed; or No equipment needed (389, 84.6%) |
| 7 | Before you were discharged from the hospital, did anyone arrange community services for you to use at home? | No (42, 9.1%) | Yes; or No one needed to arrange because services were already in place or no services needed (418, 90.9%) | |
| 8 | Before you were discharged from the hospital, did anyone arrange equipment for you? | No (16, 3.5%) | Yes; or No one needed to because equipment already in place or no equipment needed (444, 96.5%) | |
| 9 | Before you were discharged from hospital, was there any other information you would have liked while you were in the hospital to prepare you for coping at home? | No (116, 25.2%) | Yes (344, 74.8%) | |
| 10 | After you were told you could leave the hospital, how confident did you feel about managing at home? | Not confident (25, 5.4%) | Unsure (103, 22.4%) | Confident (332, 72.2%) |
| 11 | Looking back to the time you left the hospital, overall, how prepared did you feel for returning home? | Unprepared (39, 8.5%) | Moderately prepared (132, 28.7%) | Very prepared (288, 62.6%) |
| 12 | After you were told you could leave the hospital, were there any delays on the day you left the hospital? | Yes (122, 26.5%) | No (338, 73.5%) | |
For an individual patient, the sum of the scores for each item yielded a B‐PREPARED scale value. In the 460‐patient cohort, B‐PREPARED scale values had a mean of 17.3 4.3 and a negatively skewed distribution. A high scale value reflected high perception of discharge preparedness. Each of the 11 items correlated significantly with the B‐PREPARED scale value (P < 0.001, 2‐tailed).
There were substantial ceiling effects with individual items but not in the B‐PREPARED total score. Five of the 9 items with 3 response options had a ceiling effect above 70%. Three items had a dichotomous response option (items 7, 8, and 9). In 2 of these 3 items, more than 90% of respondents selected the response indicating higher preparedness. The total B‐PREPARED did not have noteworthy floor or ceiling effects. In this sample's total B‐PREPARED scores, 0.2% of respondents had the lowest score of 3, and 20% had the highest score of 22.
Principal Component Analysis
In the component analysis, we evaluated the correlation matrix of the 11 items in the B‐PREPARED scale. A Kaiser‐Meyer‐Olkin statistic of 0.76 indicated sufficient sampling adequacy to extract components from the matrix. Principal components extracted 54.2% of the variance associated with the 11‐item B‐PREPARED scale. After inspection of scree plots, we determined that 3 components were extracted before the eigenvalue fell below 1. The pattern matrix for the promax rotation was inspected, and the factor loading of each item appears in Table 3. The item content identified the first component as self‐care information for medications and activities. The second component was equipment and services. The third component was confidence. All B‐PREPARED items loaded primarily on 1 of the 3 components (Table 3).
| Item text | Component | |||
|---|---|---|---|---|
| Self‐care Information for Medications and Activity | Equipment and Services | Confidence | ||
| 1 | While you were in the hospital, how much information did you receive about the medications that you were to take at home? | 0.749 | 0.032 | 0.019 |
| 2 | While you were in the hospital, how much information did you receive about the side effects of the medications that you were to take at home? | 0.778 | .008 | 0.003 |
| 3 | While you were in the hospital, were you given written instructions about your medications? If yes, did someone spend time explaining the written instructions? | 0.758 | 0.030 | 0.084 |
| 4 | While you were in the hospital, how much information did you receive on how you would manage your usual activities when you went home? | 0.581 | 0.101 | 0.195 |
| 5 | While you were in the hospital, how much information did you receive on community services you might use once you went home? | 0.158 | 0.639 | 0.124 |
| 6 | While you were in the hospital, how much information did you receive on equipment you might need once you went home? | 0.183 | 0.701 | ‐0.152 |
| 7 | Before you were discharged from the hospital, did anyone arrange community services for you to use at home? | 0.081 | 0.654 | 0.199 |
| 8 | Before you were discharged from the hospital, did anyone arrange equipment for you? | 0.138 | 0.655 | 0.095 |
| 9 | Before you were discharged from the hospital, was there any other information you would have liked while you were in the hospital to prepare you for coping at home? | 0.181 | 0.211 | 0.369 |
| 10 | After you were told you could leave the hospital, how confident did you feel about managing at home? | 0.036 | 0.058 | 0.876 |
| 11 | Looking back to the time you left the hospital, overall, how prepared did you feel for returning home? | 0.018 | 0.032 | 0.875 |
Construct Validity
We assessed 2 constructs: worry and satisfaction with medication information (SIMS). In the cohort, 25% of patients (115 of 460) reported worry about managing at home. Worried patients had significantly lower B‐PREPARED scale values (median [25%, 75%] = 14 [10, 16]) than patients who did not worry (median [25%, 75%] = 17 [14, 20], P < .001). We calculated SIMS and then correlated SIMS with B‐PREPARED and components. In the cohort, the mean SIMS was 12.1 4.7 (range 0‐17). Patients with greater satisfaction on the SIMS also had higher B‐PREPARED scale values (rho = 0.45, P < 0.001). There was a significant positive correlation between SIMS and the B‐PREPARED component called self‐care information for medications and activities (rho = 0.46, P < 0.001). The other 2 B‐PREPARED components, equipment/services and confidence, were positively correlated with SIMS at much lower levels (rho = 0.18 and rho = 0.24, respectively, both Fischer z transformations P < .001). The B‐PREPARED scale demonstrated validity with the constructs of worry and satisfaction with medication information.
Predictive Validity
We assessed the capacity of the B‐PREPARED to predict and discriminate groups of patients who did or did not visit emergency departments. Within 1 month of hospital discharge, 16.5% of the cohort (76 of 460 patients) had at least 1 visit to an emergency department. B‐PREPARED scale values were lower for those patients who visited emergency departments (median [25%, 75%] = 14 [12, 18]) than those who did not (median [25%, 75%] = 16 [13, 19], P = 0.011). The B‐PREPARED scale analysis supported the hypothesized relationship with emergency department visits.
Correlations between B‐PREPARED and Baseline Characteristics
We evaluated the correlations between a patient's B‐PREPARED scale value and baseline characteristics, shown in Table 1. There was a weak positive correlation with self‐rated health status (rho 0.17, P < .001). Patients who perceived better health status had higher B‐PREPARED scale values than those with poorer status. The other baseline characteristics in Table 1 were not associated with B‐PREPARED scale values.
DISCUSSION
The B‐PREPARED scale measures patients' perceptions of their preparedness for hospital discharge home. Scale items came from the PREPARED, a survey with validated psychometric properties in elderly patients. We assessed the B‐PREPARED in a cohort of young and elderly adult patients. We examined the B‐PREPARED instrument for internal consistency, construct validity, and predictive validity. In comparison with the domains identified in the full PREPARED instrument,9 the abbreviated B‐PREPARED scale identified similar domains. Some differences were anticipated because we limited items to those the respondents would be able to perceive before leaving the hospital.
The results of our study should be interpreted in the context of strengths and limitations. One of the strengths was the validity of the PREPARED, from which the B‐PREPARED was derived.7 The conceptually rigorous process used to develop the PREPARED questionnaire allowed us to draw from a bank of concise, well‐worded items.9 The B‐PREPARED extends validity to a population of adults of all ages with high risk for readmission. The other strength of the B‐PREPARED was the association with the clinically relevant constructs worry and satisfaction with medication information. The B‐PREPARED also discriminated between patients who did and those who did not return to emergency departments after discharge. Although the patient population for the B‐PREPARED validation was one of the strengths of this study, it is also a limitation. Our cohort lacked diversity with respect to readmission risk. The results of our study may not generalize to patients with low risk for repeated admission. Furthermore, all our patients were discharged home. The exclusion of other discharge destinations helped us to enroll a cohort with homogenous risk for readmission. However, our exclusion criteria did not allow us to validate the B‐PREPARED in patients discharged to nursing homes, inpatient rehabilitation units, or other acute care facilities.
Another limitation related to outpatient visits after discharge. We did not analyze outpatient sites other than emergency departments. For all of our study patients, the discharging hospitalist scheduled at least 1 outpatient visit with the primary care practitioner. For some patients, the hospitalist also scheduled postdischarge visits for diagnostic evaluations like cardiac stress tests, endoscopies, radiographs, or other laboratory tests. When these visits occurred, they represented successful execution of the discharge plan. Sometimes patients arrived for planned or unplanned outpatient visits with exacerbated symptoms or adverse events. These latter visits might represent failures of the discharge plan. Our data collection did not allow us to distinguish outpatient visits as successes or failures of the discharge plan. When we counted only emergency department visits, we may have underestimated the number of patients with adverse events who sought and received successful treatment in outpatient clinics. Future studies should consider ascertainment of planned and unplanned outpatient visits for exacerbated symptoms and adverse events.
After our study began enrollment, other investigators published the Readiness for Hospital Discharge Scale14 and Care Transitions Measure.15 The design and validation of these sampling instruments differed with each other and with the B‐PREPARED. The differences made the 3 scales complementary but not interchangeable. For example, investigators administered the 21‐item Readiness for Hospital Discharge Scale on the day of discharge to adult medical‐surgical patients, postpartum mothers, and parents of hospitalized children. In contrast, we administered the B‐PREPARED 1 week after discharge to adult internal medicine patients or their proxies. The Readiness for Hospital Discharge subscales were personal status, knowledge, coping ability, and expected support. These subscales were similar to the components of the B‐PREPARED. The Readiness for Hospital Discharge Scale demonstrated internal consistency and construct validity but did not predict patients who returned to emergency departments after hospital discharge.14 Future users of the Readiness for Hospital Discharge Scale or the B‐PREPARED should consider their patient populations and the date of administration when selecting 1 scale versus another. If brevity is important to a clinician or researcher, then the 11‐item B‐PREPARED scale may be considered.
The Care Transitions Measure also differed from the B‐PREPARED. The 15‐item Care Transitions Measure evaluated an adult population with a broad age range and with chronic obstructive pulmonary disease, heart failure, stroke, or hip fracture.15 The diseases represented in the population for the Care Transitions Measure were similar to those in the B‐PREPARED cohort, although the distribution of the diseases differed. When validating the Care Transitions Measure, investigators administered questionnaires 6 to 12 weeks after discharge. The Care Transitions Measure had 4 factors: critical understanding, preferences important, management preparation, and care plan. The factors of the Care Transitions Measure were comparable to the components of the B‐PREPARED, and both scales assessed medication self‐management. However, the Care Transitions Measure addressed patient preferences with specific items, whereas the B‐PREPARED used the scoring system to quantify patient preferences. Both the Care Transitions Measure and the B‐PREPARED demonstrated internal consistency and discriminated between patients who did and those who did not return to emergency departments after hospital discharge.15 When selecting a scale, future users should consider the B‐PREPARED only for assessments 1 week post discharge and should consider the Care Transitions Measure for later assessments.
There are applications of the B‐PREPARED scale in hospital quality improvement efforts. Hospitals have multiple motivations to pursue quality improvement projects related to discharge processes: satisfaction of patients, reduction in adverse events, relation with referring physicians, and accreditation by regulators.6, 16 When hospital‐based clinicians survey patients, they may wish to use a brief, reliable, and validated instrument like the B‐PREPARED questionnaire.
CONCLUSIONS
The B‐PREPARED provided a reliable and valid measure of patients' perceptions of their preparedness for hospital discharge home. Clinicians and researchers may find the B‐PREPARED useful to guide, assess, and compare discharge‐planning interventions.
Acknowledgements
The authors thank Dr. Karen Grimmer‐Somers, PhD, for permission to use the PREPARED instrument and for her thoughtful comments on the draft manuscript.
Patients are vulnerable to adverse events when they transition from the hospital to outpatient care.13 Approximately 19%‐23% of patients experience adverse events within 4 weeks after acute care hospitalization.3, 4 One cause of postdischarge adverse events is ineffective discharge planning1, 2, 5, 6 Efforts to study and improve the hospital discharge‐planning processes require appropriate and valid measurement instruments. These instruments must assess the discharge process from multiple perspectives. One of the important perspectives is the patient's.7, 8
The PREPARED Patient Questionnaire is a comprehensive quality improvement tool to assess hospital discharge‐planning processes and outcomes from the patient's perspective.9, 10 The PREPARED acronym describes the content of this tool used to investigate the following phenomena: 1) prescriptions, 2) ready to reenter community, 3) education, 4) placement, 5) assurance of safety, 6) realistic expectations, 7) empowerment, and 8) directed to appropriate services.9 The PREPARED questionnaire was developed for, modified for, and validated with patients at least 65 years old. When administered to elderly patients 1 week after hospital discharge, the PREPARED has face, content, and construct validity.9
We considered the PREPARED questionnaire when we designed a clinical trial to assess the value of a discharge intervention. We sought a survey questionnaire to assess the patients' perceptions after the discharge intervention. In 2004, we found noother validated questionnaires except the PREPARED. We also noted some limitations of the PREPARED. The validated population for the PREPARED was patients older than 65 years. In our clinical trial, we planned to enroll adults of all ages. Another limitation was the PREPARED response scoring system that assigned missing data values to patients who took no medicines, needed no services, or needed no equipment.10 We were concerned about the potential for unacceptably large numbers of patients with nonignorable missing data. We decided to address the above limitations with a validation study in our patient population and with a revised response scoring system.
In the present article, we describe item reduction and validation for the Brief PREPARED (B‐PREPARED) scale to measure patients' perceptions of their preparedness for hospital discharge. When we designed B‐PREPARED, we asked the following question: Does a subset of PREPARED items with a revised scoring system have internal consistency, construct validity, and predictive validity in a population of adult patients with broad age range? We also wanted a brief scale with acceptable, defined statistical properties for multiple users. One user class included clinicians who guide and assess discharge‐planning processes. Other users would be researchers like us who measure differences between treatment groups after discharge process interventions.
METHODS
The Peoria Institutional Review Board approved the protocol for human research. The patient sample for scale analysis was a prospective cohort. Follow‐up was 1 month after patient's discharge from a 730‐bed acute‐care teaching hospital in central Illinois. The patients were enrolled in an ongoing cluster randomized clinical trial with blinded outcome assessment. Willing patients or their proxies provided written consent for study participation. Enrollment occurred between December 2004 and July 2006.
Patient Inclusion Criteria
Trained research coordinators identified all consecutive adult inpatients who were discharged to the patient's home by internal medicine hospitalists. Patient inclusion in our cluster randomized trial required a probability of repeat admission (Pra) score of at least 0.40.11, 12 Hence, the patients in the scale analysis cohort had the same high probability for repeat admission. The research coordinators calculated the Pra within 2 days before discharge from the index hospitalization. The Pra score came from a logistic model of age, sex, prior hospitalizations, prior doctor visits, self‐rated health status, informal caregiver, and comorbid coronary heart disease and diabetes mellitus.11, 12
Patient Exclusion Criteria
We excluded patients if the discharge destination was a nursing home, another acute care hospital, or an inpatient rehabilitation unit. Patients were excluded if life expectancy was less than 6 months as estimated by the hospitalist. Because follow‐up occurred via interview, patients without telephones or English‐ or Spanish‐language skills were excluded. Patients with cognitive impairment could participate with consent from a legally authorized representative and with a proxy whospent a minimum of 3 hours daily with the patient and was willing to answer postdischarge interviews.
Baseline Assessment
During the index hospital admission, trained data abstractors recorded baseline patient data: age, sex, race, diabetes mellitus, heart failure, chronic obstructive pulmonary disease, and coronary heart disease. Patients or proxies provided the number of hospital admissions and doctor visits during the year before the index hospital admission. We recorded the availability of an informal caregiver in response to the question Is there a friend, relative, or neighbor who would take care of you for a few days if necessary? Patients rated their health status on the following scale: poor, fair, good, very good, or excellent.
Discharge and Postdischarge Procedures
At the end of the index hospitalization, hospitalists and ward nurses used standardized forms for discharge diagnoses, prescriptions, instructions, and appointments. Discharge‐planning nurses or social workers consulted with hospitalists and ward nurses and then coordinated service providers including home health nurses, physical therapists, home health aides, homemaker service providers, durable medical equipment vendors, home oxygen vendors, home infusion pharmacists, social workers, rehabilitation service providers, legal aide providers, and others. After discharge, trained research personnel conducted 2 telephone interviews with the patient or the patient's proxy. The first interview occurred 1 week after discharge. Interviewers read verbatim items from the PREPARED10 and the Satisfaction with Information about Medicines Scale (SIMS).13 During the second telephone interview 30 10 days after discharge, interviewers recorded if patients had experienced at least 1 emergency department visit during the month after discharge.
The purpose of the PREPARED items was to have a bank of items and responses that could be used to generate the B‐PREPARED scale. The PREPARED questionnaire was originally developed to provide feedback to hospital ward staff about the quality of discharge‐planning activities that occurred during hospitalization.9 Discriminant factor analysis on the original 16 process questions revealed 4 factors that explained 57% of the total variance in patient/caregiver responses. The PREPARED domains included information exchange on community services and equipment, management of medication, the process of preparing to cope after discharge, and having control over one's discharge circumstances.9 The purpose of the SIMS was as a construct to compare with the B‐PREPARED scale. The derivation and validity of the SIMS have been described extensively elsewhere.13 In summary, the SIMS items were derived from recommendations of the Association of the British Pharmaceutical Industry. The intent of the SIMS was to determine if a patient's medication information needs were met and to allow comparison between patients or groups. Respondents selected 1 of 5 options for each of the 17 items. The sum of scores for each of the SIMS items yielded a total score that ranged from 0 to 17. Patients with high total SIMS scores had high satisfaction with the amount of medication information they received. Validation samples included inpatients and outpatients with a variety of diseases and characteristics. SIMS demonstrated adequate internal consistency, test‐retest reliability, and criterion‐related validity.13
Item Selection and Scoring of the B‐PREPARED Instrument
We selected an initial pool of items from the PREPARED instrument.10 The goal was a parsimonious, comprehensive, and valid instrument for use in clinical and research environments. When we retained or deleted items, our decision process was conservative, conceptual, and statistical. We performed item reduction in the following steps defined a priori. First, we agreed on items consistent with domains in the prepared for discharge construct as defined by expert consensus.9 Second, we excluded items that assessed qualities of the discharge process that were imperceptible to the patient on the day of discharge. Third, we excluded items that elicited open‐ended responses unsuitable for quantitative scale development and analysis. Fourth, we assessed reliability as defined by the Cronbach's alpha statistic. We excluded items that substantially decreased Cronbach's alpha.
Measures of Construct Validity
We used 2 measures of construct validity in our assessment of B‐PREPARED. One construct was patient worry. During the interview 1 week after discharge, research personnel asked, Now that you have been out of the hospital for a while, has anything been worrying you about managing at home? Response options for the dichotomous worry item were no or yes. We anticipated worried patients would have lower B‐PREPARED scale values. The other construct, SIMS, evaluated patient preparedness related to medication information exchange. The hypothesis was a positive correlation between SIMS and B‐PREPARED scale values.
Measure of Predictive Validity
We asked if B‐PREPARED predicted and discriminated groups of patients who did or did not visit emergency departments after hospital discharge. Emergency department visits were relevant adverse outcomes because of their association with postdischarge adverse events due to inpatient treatment.4 Emergency department visits reflected new or worsening symptoms after discharge. In our scale analysis, the hypothesis was patients with at least 1 emergency department visit would have lower B‐PREPARED scale values.
Analysis
Analyses were performed with SPSS PC (Version 14.0.2, SPSS Inc, Chicago, IL). We reported descriptive statistics as means, standard deviations, and range for interval variables and percentages for nominal variables. To determine the internal consistency of the scale, we calculated Cronbach's alpha. We assessed the distribution of the B‐PREPARED scale with visual and statistical tests for skewness. While using the SPSS FACTOR program, we performed principal components extractions and then rotated components using the oblique promax technique. Component scores were saved using the regression score procedure. Component loadings above 0.30 were considered important. Statistical inference tests were the Mann‐Whitney U for median differences between 2 groups and the Spearman correlation for associations. We reported medians with 25th and 75th percentiles. Differences between 2 correlations were tested using Fischer z transformations. The accepted level of significance was P < 0.05.
RESULTS
Description of Cohort
We approached 5124 patients during the index hospital admission. After applying exclusion criteria, we obtained consent and enrolled 491 patients. The reasons for exclusion were low Pra score for 34.9% of ineligible patients, discharge to nursing home for 12.8%, declined consent for 10.8%, nonparticipating hospitalist service for 9.1%, discharged during screen for 8.5%, previously enrolled in study for 5.6%, and declined screening for 2.3%. Each of the other exclusion criteria accounted for less than 4% of the ineligible patients. After subtracting 6% of eligible patients (31 of 491) who died, withdrew, or were lost during the first month, there were 460 patients available for analysis. Table 1 describes the patients' characteristics. Most of the patients, 75.2% (346 of 460), were less than 65 years old, and the mean age was 53.9 15.5 years. Many patients had chronic diseases including diabetes mellitus, coronary heart disease, heart failure, and chronic obstructive pulmonary disease. Most patients, 81.5% (375 of 460), rated their health as poor or fair, and 53.5% (246/460) had 1 or more hospital admissions during the year before their index admission. Cohort patients had a high probability of repeat admission: mean Pra 0.49 0.07 (range 0.400.70).
| Characteristic | n (%) |
|---|---|
| Sex (male) | 193 (42.0%) |
| Age (years) | |
| 1930 | 35 (7.6%) |
| 3164 | 311 (67.6%) |
| 6598 | 114 (24.8%) |
| Race | |
| White | 275 (59.8%) |
| Black | 124 (27.0%) |
| Other | 61 (13.3%) |
| Self‐rated health status | |
| Poor | 139 (30.2%) |
| Fair | 236 (51.3%) |
| Good | 70 (15.2%) |
| Very good | 13 (2.8%) |
| Excellent | 2 (0.4%) |
| Diabetes mellitus | 259 (56.3%) |
| Chronic obstructive pulmonary disease | 79 (17.2%) |
| Coronary heart disease | 188 (40.9%) |
| Heart failure (n = 456) | 100 (21.7%) |
| Informal caregiver available (yes) | 459 (99.1%) |
| Hospital admissions during year prior to index admission | |
| 0 | 214 (46.5%) |
| 1 | 131 (28.5%) |
| 2 | 47 (10.2%) |
| 3 or 4 | 35 (7.6%) |
| 515 | 33 (7.2%) |
Item Reduction, Internal Consistency, and Score Distributions
Item reduction resulted in 12 items that fulfilled conceptual criteria. Table 2 shows the items and the distribution of responses. One of the 12 items, delays on the day you left the hospital (item 12, Table 2), was deleted because the item depressed the Cronbach's alpha. The B‐PREPARED with 11 items had acceptable internal consistency for the full cohort (Cronbach's alpha = 0.76).
| Item Text | Descriptor for Score 0 | Descriptor for Score 1 | Descriptor for Score 2 | |
|---|---|---|---|---|
| ||||
| 1 | While you were in the hospital, how much information did you receive about the medications that you were to take at home? | None (40, 8.7%) | Some, but not enough (95, 20.7%) | As much as I needed; or Not taking any medications (325, 70.7%) |
| 2 | While you were in the hospital, how much information did you receive about the side effects of the medications that you were to take at home? | None (198, 43.0%) | Some, but not enough (54, 11.7%) | As much as I needed; or Not taking any medications (208, 45.2%) |
| 3 | While you were in the hospital, were you given written instructions about your medications? If yes, did someone spend time explaining the written instructions? | No written instructions and no time spent (116, 25.2%) | Yes, received written instructions but no time spent (49, 10.7%) | Yes, received written instructions and yes, time spent; or, Not taking any medications (291, 63.3%) |
| 4 | While you were in the hospital, how much information did you receive on how you would manage your usual activities when you went home? | None (55, 12.0%) | Some, but not enough (90, 19.6%) | As much as I needed (315, 68.5%) |
| 5 | While you were in the hospital, how much information did you receive on community services you might use once you went home? | None (89, 19.3%) | Some, but not enough (40, 8.7%) | As much as I needed; or No services needed (331, 72.0%) |
| 6 | While you were in the hospital, how much information did you receive on equipment you might need once you went home? | None (49, 10.7%) | Some, but not enough (22, 4.8%) | As much as I needed; or No equipment needed (389, 84.6%) |
| 7 | Before you were discharged from the hospital, did anyone arrange community services for you to use at home? | No (42, 9.1%) | Yes; or No one needed to arrange because services were already in place or no services needed (418, 90.9%) | |
| 8 | Before you were discharged from the hospital, did anyone arrange equipment for you? | No (16, 3.5%) | Yes; or No one needed to because equipment already in place or no equipment needed (444, 96.5%) | |
| 9 | Before you were discharged from hospital, was there any other information you would have liked while you were in the hospital to prepare you for coping at home? | No (116, 25.2%) | Yes (344, 74.8%) | |
| 10 | After you were told you could leave the hospital, how confident did you feel about managing at home? | Not confident (25, 5.4%) | Unsure (103, 22.4%) | Confident (332, 72.2%) |
| 11 | Looking back to the time you left the hospital, overall, how prepared did you feel for returning home? | Unprepared (39, 8.5%) | Moderately prepared (132, 28.7%) | Very prepared (288, 62.6%) |
| 12 | After you were told you could leave the hospital, were there any delays on the day you left the hospital? | Yes (122, 26.5%) | No (338, 73.5%) | |
For an individual patient, the sum of the scores for each item yielded a B‐PREPARED scale value. In the 460‐patient cohort, B‐PREPARED scale values had a mean of 17.3 4.3 and a negatively skewed distribution. A high scale value reflected high perception of discharge preparedness. Each of the 11 items correlated significantly with the B‐PREPARED scale value (P < 0.001, 2‐tailed).
There were substantial ceiling effects with individual items but not in the B‐PREPARED total score. Five of the 9 items with 3 response options had a ceiling effect above 70%. Three items had a dichotomous response option (items 7, 8, and 9). In 2 of these 3 items, more than 90% of respondents selected the response indicating higher preparedness. The total B‐PREPARED did not have noteworthy floor or ceiling effects. In this sample's total B‐PREPARED scores, 0.2% of respondents had the lowest score of 3, and 20% had the highest score of 22.
Principal Component Analysis
In the component analysis, we evaluated the correlation matrix of the 11 items in the B‐PREPARED scale. A Kaiser‐Meyer‐Olkin statistic of 0.76 indicated sufficient sampling adequacy to extract components from the matrix. Principal components extracted 54.2% of the variance associated with the 11‐item B‐PREPARED scale. After inspection of scree plots, we determined that 3 components were extracted before the eigenvalue fell below 1. The pattern matrix for the promax rotation was inspected, and the factor loading of each item appears in Table 3. The item content identified the first component as self‐care information for medications and activities. The second component was equipment and services. The third component was confidence. All B‐PREPARED items loaded primarily on 1 of the 3 components (Table 3).
| Item text | Component | |||
|---|---|---|---|---|
| Self‐care Information for Medications and Activity | Equipment and Services | Confidence | ||
| 1 | While you were in the hospital, how much information did you receive about the medications that you were to take at home? | 0.749 | 0.032 | 0.019 |
| 2 | While you were in the hospital, how much information did you receive about the side effects of the medications that you were to take at home? | 0.778 | .008 | 0.003 |
| 3 | While you were in the hospital, were you given written instructions about your medications? If yes, did someone spend time explaining the written instructions? | 0.758 | 0.030 | 0.084 |
| 4 | While you were in the hospital, how much information did you receive on how you would manage your usual activities when you went home? | 0.581 | 0.101 | 0.195 |
| 5 | While you were in the hospital, how much information did you receive on community services you might use once you went home? | 0.158 | 0.639 | 0.124 |
| 6 | While you were in the hospital, how much information did you receive on equipment you might need once you went home? | 0.183 | 0.701 | ‐0.152 |
| 7 | Before you were discharged from the hospital, did anyone arrange community services for you to use at home? | 0.081 | 0.654 | 0.199 |
| 8 | Before you were discharged from the hospital, did anyone arrange equipment for you? | 0.138 | 0.655 | 0.095 |
| 9 | Before you were discharged from the hospital, was there any other information you would have liked while you were in the hospital to prepare you for coping at home? | 0.181 | 0.211 | 0.369 |
| 10 | After you were told you could leave the hospital, how confident did you feel about managing at home? | 0.036 | 0.058 | 0.876 |
| 11 | Looking back to the time you left the hospital, overall, how prepared did you feel for returning home? | 0.018 | 0.032 | 0.875 |
Construct Validity
We assessed 2 constructs: worry and satisfaction with medication information (SIMS). In the cohort, 25% of patients (115 of 460) reported worry about managing at home. Worried patients had significantly lower B‐PREPARED scale values (median [25%, 75%] = 14 [10, 16]) than patients who did not worry (median [25%, 75%] = 17 [14, 20], P < .001). We calculated SIMS and then correlated SIMS with B‐PREPARED and components. In the cohort, the mean SIMS was 12.1 4.7 (range 0‐17). Patients with greater satisfaction on the SIMS also had higher B‐PREPARED scale values (rho = 0.45, P < 0.001). There was a significant positive correlation between SIMS and the B‐PREPARED component called self‐care information for medications and activities (rho = 0.46, P < 0.001). The other 2 B‐PREPARED components, equipment/services and confidence, were positively correlated with SIMS at much lower levels (rho = 0.18 and rho = 0.24, respectively, both Fischer z transformations P < .001). The B‐PREPARED scale demonstrated validity with the constructs of worry and satisfaction with medication information.
Predictive Validity
We assessed the capacity of the B‐PREPARED to predict and discriminate groups of patients who did or did not visit emergency departments. Within 1 month of hospital discharge, 16.5% of the cohort (76 of 460 patients) had at least 1 visit to an emergency department. B‐PREPARED scale values were lower for those patients who visited emergency departments (median [25%, 75%] = 14 [12, 18]) than those who did not (median [25%, 75%] = 16 [13, 19], P = 0.011). The B‐PREPARED scale analysis supported the hypothesized relationship with emergency department visits.
Correlations between B‐PREPARED and Baseline Characteristics
We evaluated the correlations between a patient's B‐PREPARED scale value and baseline characteristics, shown in Table 1. There was a weak positive correlation with self‐rated health status (rho 0.17, P < .001). Patients who perceived better health status had higher B‐PREPARED scale values than those with poorer status. The other baseline characteristics in Table 1 were not associated with B‐PREPARED scale values.
DISCUSSION
The B‐PREPARED scale measures patients' perceptions of their preparedness for hospital discharge home. Scale items came from the PREPARED, a survey with validated psychometric properties in elderly patients. We assessed the B‐PREPARED in a cohort of young and elderly adult patients. We examined the B‐PREPARED instrument for internal consistency, construct validity, and predictive validity. In comparison with the domains identified in the full PREPARED instrument,9 the abbreviated B‐PREPARED scale identified similar domains. Some differences were anticipated because we limited items to those the respondents would be able to perceive before leaving the hospital.
The results of our study should be interpreted in the context of strengths and limitations. One of the strengths was the validity of the PREPARED, from which the B‐PREPARED was derived.7 The conceptually rigorous process used to develop the PREPARED questionnaire allowed us to draw from a bank of concise, well‐worded items.9 The B‐PREPARED extends validity to a population of adults of all ages with high risk for readmission. The other strength of the B‐PREPARED was the association with the clinically relevant constructs worry and satisfaction with medication information. The B‐PREPARED also discriminated between patients who did and those who did not return to emergency departments after discharge. Although the patient population for the B‐PREPARED validation was one of the strengths of this study, it is also a limitation. Our cohort lacked diversity with respect to readmission risk. The results of our study may not generalize to patients with low risk for repeated admission. Furthermore, all our patients were discharged home. The exclusion of other discharge destinations helped us to enroll a cohort with homogenous risk for readmission. However, our exclusion criteria did not allow us to validate the B‐PREPARED in patients discharged to nursing homes, inpatient rehabilitation units, or other acute care facilities.
Another limitation related to outpatient visits after discharge. We did not analyze outpatient sites other than emergency departments. For all of our study patients, the discharging hospitalist scheduled at least 1 outpatient visit with the primary care practitioner. For some patients, the hospitalist also scheduled postdischarge visits for diagnostic evaluations like cardiac stress tests, endoscopies, radiographs, or other laboratory tests. When these visits occurred, they represented successful execution of the discharge plan. Sometimes patients arrived for planned or unplanned outpatient visits with exacerbated symptoms or adverse events. These latter visits might represent failures of the discharge plan. Our data collection did not allow us to distinguish outpatient visits as successes or failures of the discharge plan. When we counted only emergency department visits, we may have underestimated the number of patients with adverse events who sought and received successful treatment in outpatient clinics. Future studies should consider ascertainment of planned and unplanned outpatient visits for exacerbated symptoms and adverse events.
After our study began enrollment, other investigators published the Readiness for Hospital Discharge Scale14 and Care Transitions Measure.15 The design and validation of these sampling instruments differed with each other and with the B‐PREPARED. The differences made the 3 scales complementary but not interchangeable. For example, investigators administered the 21‐item Readiness for Hospital Discharge Scale on the day of discharge to adult medical‐surgical patients, postpartum mothers, and parents of hospitalized children. In contrast, we administered the B‐PREPARED 1 week after discharge to adult internal medicine patients or their proxies. The Readiness for Hospital Discharge subscales were personal status, knowledge, coping ability, and expected support. These subscales were similar to the components of the B‐PREPARED. The Readiness for Hospital Discharge Scale demonstrated internal consistency and construct validity but did not predict patients who returned to emergency departments after hospital discharge.14 Future users of the Readiness for Hospital Discharge Scale or the B‐PREPARED should consider their patient populations and the date of administration when selecting 1 scale versus another. If brevity is important to a clinician or researcher, then the 11‐item B‐PREPARED scale may be considered.
The Care Transitions Measure also differed from the B‐PREPARED. The 15‐item Care Transitions Measure evaluated an adult population with a broad age range and with chronic obstructive pulmonary disease, heart failure, stroke, or hip fracture.15 The diseases represented in the population for the Care Transitions Measure were similar to those in the B‐PREPARED cohort, although the distribution of the diseases differed. When validating the Care Transitions Measure, investigators administered questionnaires 6 to 12 weeks after discharge. The Care Transitions Measure had 4 factors: critical understanding, preferences important, management preparation, and care plan. The factors of the Care Transitions Measure were comparable to the components of the B‐PREPARED, and both scales assessed medication self‐management. However, the Care Transitions Measure addressed patient preferences with specific items, whereas the B‐PREPARED used the scoring system to quantify patient preferences. Both the Care Transitions Measure and the B‐PREPARED demonstrated internal consistency and discriminated between patients who did and those who did not return to emergency departments after hospital discharge.15 When selecting a scale, future users should consider the B‐PREPARED only for assessments 1 week post discharge and should consider the Care Transitions Measure for later assessments.
There are applications of the B‐PREPARED scale in hospital quality improvement efforts. Hospitals have multiple motivations to pursue quality improvement projects related to discharge processes: satisfaction of patients, reduction in adverse events, relation with referring physicians, and accreditation by regulators.6, 16 When hospital‐based clinicians survey patients, they may wish to use a brief, reliable, and validated instrument like the B‐PREPARED questionnaire.
CONCLUSIONS
The B‐PREPARED provided a reliable and valid measure of patients' perceptions of their preparedness for hospital discharge home. Clinicians and researchers may find the B‐PREPARED useful to guide, assess, and compare discharge‐planning interventions.
Acknowledgements
The authors thank Dr. Karen Grimmer‐Somers, PhD, for permission to use the PREPARED instrument and for her thoughtful comments on the draft manuscript.
- ,,,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2004;(1):CD000313.
- ,,.Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home.Cochrane Database Syst Rev.2003;(4):CD003716.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- ,,,.Review of the literature on survey instruments used to collect data on hospital patients' perceptions of care.Health Serv Res.2005;40:1996–2017.
- ,.A patient‐centered model of care for hospital discharge.Clin Nurs Res.2004;13:117–136.
- ,.The development, validity and application of a new instrument to assess the quality of discharge planning activities from the community perspective.Int J Qual Health Care.2001;13:109–116.
- PREPARED Patient Questionnaire. Available at: http://www.unisa.edu.au/cahe/pubs/Patient%20scoring.pdf. Accessed June 14,2007.
- ,,.Predictive validity of a questionnaire that identifies older persons at risk for hospital admission.J Am Geriatr Soc.1995;43:374–377.
- ,,,.Predictive validity of the Pra instrument among older recipients of managed care.J Am Geriatr Soc.1997;45:614–617.
- ,,.The Satisfaction with Information about Medicines Scales (SIMS): a new measurement tool for audit and research.Qual Health Care.2001;10:135–140.
- ,.Psychometric properties of the Readiness for Hospital Discharge Scale.J Nurs Meas.2006;14:163–180.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43:246–255.
- 2007 Hospital/critical access hospital national patient safety goals. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals. Accessed June 14,2007.
- ,,,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2004;(1):CD000313.
- ,,.Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home.Cochrane Database Syst Rev.2003;(4):CD003716.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- ,,,.Review of the literature on survey instruments used to collect data on hospital patients' perceptions of care.Health Serv Res.2005;40:1996–2017.
- ,.A patient‐centered model of care for hospital discharge.Clin Nurs Res.2004;13:117–136.
- ,.The development, validity and application of a new instrument to assess the quality of discharge planning activities from the community perspective.Int J Qual Health Care.2001;13:109–116.
- PREPARED Patient Questionnaire. Available at: http://www.unisa.edu.au/cahe/pubs/Patient%20scoring.pdf. Accessed June 14,2007.
- ,,.Predictive validity of a questionnaire that identifies older persons at risk for hospital admission.J Am Geriatr Soc.1995;43:374–377.
- ,,,.Predictive validity of the Pra instrument among older recipients of managed care.J Am Geriatr Soc.1997;45:614–617.
- ,,.The Satisfaction with Information about Medicines Scales (SIMS): a new measurement tool for audit and research.Qual Health Care.2001;10:135–140.
- ,.Psychometric properties of the Readiness for Hospital Discharge Scale.J Nurs Meas.2006;14:163–180.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43:246–255.
- 2007 Hospital/critical access hospital national patient safety goals. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals. Accessed June 14,2007.
Copyright © 2008 Society of Hospital Medicine
Soft‐tissue gangrene secondary to mixed cryoglobulinemia
A 61‐year‐old Hispanic male with chronic hepatitis C presented with a 4‐week history of a nonpruritic skin rash involving his lower extremities, hands, arms, and right ear. He also reported purple discoloration of his right foot, along with pain in the extremity that worsened with ambulation. Physical examination revealed diffuse purpura of both arms and legs (Figure 1). The right foot was cold to the touch and purple to black in color (Figure 2). There were multiple skin ulcers of various sizes covering the anterior aspect of his legs bilaterally. Pedal pulses were 2/4. Laboratory evaluation revealed positive cryoglobulins with low C4 and CH50 concentrations of 3 mg/dL (10‐40) and 2 units/mL (60‐144), respectively. Other immunological studies were negative. Lower extremity arterial Doppler studies were normal.


His clinical and laboratory findings were attributed to mixed cryoglobulinemia, and treatment, consisting of daily intravenous methylprednisolone, a single dose of intravenous cyclophosphamide, and plasmapheresis, was initiated. Despite these interventions, 5 days later, he developed severe burning pain in the right extremity with worsening discoloration and a line of demarcation at the level of his proximal midfoot. Eventually, right below the knee, amputation was performed, and histopathological examination showed soft‐tissue gangrene with avascular necrosis of the bone (Figure 3). The patient subsequently had an uneventful course. Plasmapheresis and oral prednisone were continued.
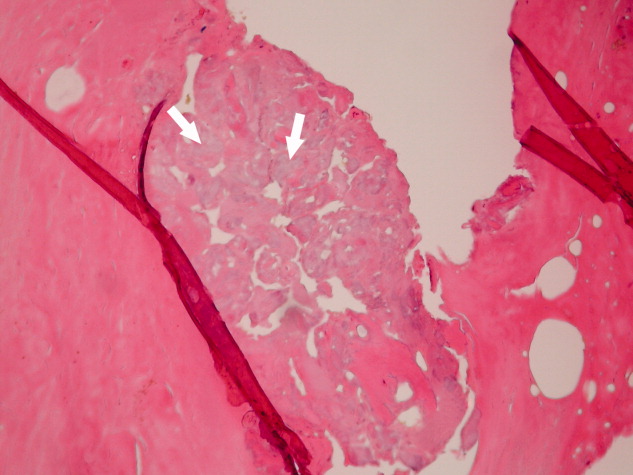
Cryoglobulinemia is a small‐ to medium‐vessel vasculitis due to cryoglobulin‐containing immune complexes. There are 3 types, with the classification based on an immunological analysis of the cryoglobulin composition. Hepatitis C virus infection is closely associated with type II mixed cryoglobulinemia. Cutaneous manifestations are the most common, consisting of palpable purpura, urticaria, postinflammatory hyperpigmentation, acrocyanosis, and skin ulcers. A serum cryoglobulin elevation is diagnostic and is usually accompanied by hypocomplementemia.
Treatment of the underlying disease is essential. However, aggressive therapy with plasmapheresis and immunosuppressive medications is warranted in severe cases involving limb‐ or organ‐threatening vasculitis.
A 61‐year‐old Hispanic male with chronic hepatitis C presented with a 4‐week history of a nonpruritic skin rash involving his lower extremities, hands, arms, and right ear. He also reported purple discoloration of his right foot, along with pain in the extremity that worsened with ambulation. Physical examination revealed diffuse purpura of both arms and legs (Figure 1). The right foot was cold to the touch and purple to black in color (Figure 2). There were multiple skin ulcers of various sizes covering the anterior aspect of his legs bilaterally. Pedal pulses were 2/4. Laboratory evaluation revealed positive cryoglobulins with low C4 and CH50 concentrations of 3 mg/dL (10‐40) and 2 units/mL (60‐144), respectively. Other immunological studies were negative. Lower extremity arterial Doppler studies were normal.


His clinical and laboratory findings were attributed to mixed cryoglobulinemia, and treatment, consisting of daily intravenous methylprednisolone, a single dose of intravenous cyclophosphamide, and plasmapheresis, was initiated. Despite these interventions, 5 days later, he developed severe burning pain in the right extremity with worsening discoloration and a line of demarcation at the level of his proximal midfoot. Eventually, right below the knee, amputation was performed, and histopathological examination showed soft‐tissue gangrene with avascular necrosis of the bone (Figure 3). The patient subsequently had an uneventful course. Plasmapheresis and oral prednisone were continued.
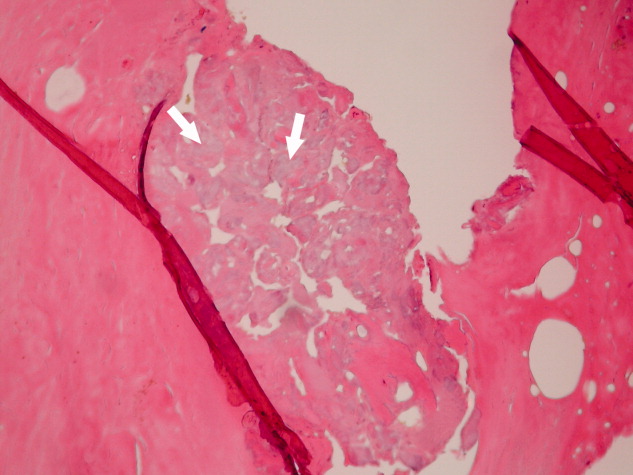
Cryoglobulinemia is a small‐ to medium‐vessel vasculitis due to cryoglobulin‐containing immune complexes. There are 3 types, with the classification based on an immunological analysis of the cryoglobulin composition. Hepatitis C virus infection is closely associated with type II mixed cryoglobulinemia. Cutaneous manifestations are the most common, consisting of palpable purpura, urticaria, postinflammatory hyperpigmentation, acrocyanosis, and skin ulcers. A serum cryoglobulin elevation is diagnostic and is usually accompanied by hypocomplementemia.
Treatment of the underlying disease is essential. However, aggressive therapy with plasmapheresis and immunosuppressive medications is warranted in severe cases involving limb‐ or organ‐threatening vasculitis.
A 61‐year‐old Hispanic male with chronic hepatitis C presented with a 4‐week history of a nonpruritic skin rash involving his lower extremities, hands, arms, and right ear. He also reported purple discoloration of his right foot, along with pain in the extremity that worsened with ambulation. Physical examination revealed diffuse purpura of both arms and legs (Figure 1). The right foot was cold to the touch and purple to black in color (Figure 2). There were multiple skin ulcers of various sizes covering the anterior aspect of his legs bilaterally. Pedal pulses were 2/4. Laboratory evaluation revealed positive cryoglobulins with low C4 and CH50 concentrations of 3 mg/dL (10‐40) and 2 units/mL (60‐144), respectively. Other immunological studies were negative. Lower extremity arterial Doppler studies were normal.


His clinical and laboratory findings were attributed to mixed cryoglobulinemia, and treatment, consisting of daily intravenous methylprednisolone, a single dose of intravenous cyclophosphamide, and plasmapheresis, was initiated. Despite these interventions, 5 days later, he developed severe burning pain in the right extremity with worsening discoloration and a line of demarcation at the level of his proximal midfoot. Eventually, right below the knee, amputation was performed, and histopathological examination showed soft‐tissue gangrene with avascular necrosis of the bone (Figure 3). The patient subsequently had an uneventful course. Plasmapheresis and oral prednisone were continued.
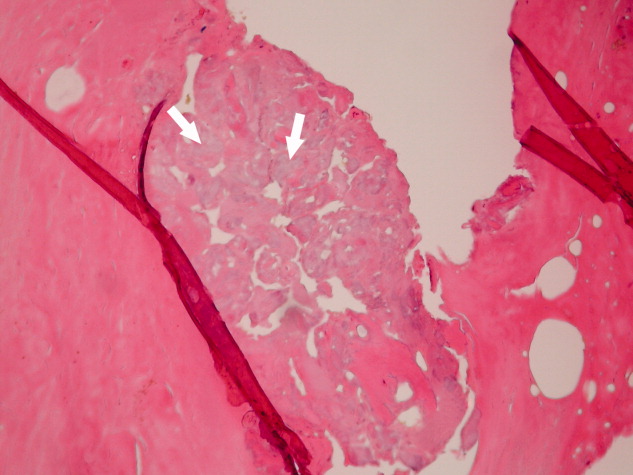
Cryoglobulinemia is a small‐ to medium‐vessel vasculitis due to cryoglobulin‐containing immune complexes. There are 3 types, with the classification based on an immunological analysis of the cryoglobulin composition. Hepatitis C virus infection is closely associated with type II mixed cryoglobulinemia. Cutaneous manifestations are the most common, consisting of palpable purpura, urticaria, postinflammatory hyperpigmentation, acrocyanosis, and skin ulcers. A serum cryoglobulin elevation is diagnostic and is usually accompanied by hypocomplementemia.
Treatment of the underlying disease is essential. However, aggressive therapy with plasmapheresis and immunosuppressive medications is warranted in severe cases involving limb‐ or organ‐threatening vasculitis.
SHM Medication Reconciliation Survey Results
The Joint Commission's (TJC) National Patient Safety Goal (NPSG) #8Accurately and completely reconcile medications across the continuum of carechallenges hospitals to design and implement new medication management processes. With medication errors contributing to patient morbidity and mortality,1 establishing a comprehensive process for reconciling a patient's medications during the hospitalization episode is an important quality improvement and patient safety goal.
However, the current state of inpatient medication management is highly fragmented. Standard documentation is lacking, as is integration of information between care settings.2 There are now reports describing implementation of various medication reconciliation processes for admissions,3 transfers,4 and discharges.5
Hospitalists are well‐positioned to contribute to the implementation of medication reconciliation. Indeed, because TJC does not explicitly specify what type of health care provider (eg, physician, nurse, etc.) should assume responsibility for this process, institutions have designed workflows to suit their own needs, while striving to comply with national standards.
Given the complexity and lack of standardization around this NPSG, a survey was distributed to attendees of a Society of Hospital Medicine (SHM) national meeting to determine the various processes implemented thus far, and to ascertain existing challenges to implementation. We report here on the results.
METHODS
A survey tool (Appendix) was designed to query demographic and institutional factors, involvement in the process, and barriers to implementation of medication reconciliation. Surveys were included in all attendees' registration materials, resulting in the distributions of approximately 800 surveys.
Responses were entered into an Excel spreadsheet. Simple descriptive statistics were used to determine proportions for providers, processes, and barriers to implementation. Where appropriate, variables were dichotomized, allowing for paired t‐test analysis. Statistical significance was defined as a P value less than .05. Subgroup analyses by hospital type, provider type, and process method were performed.
RESULTS
A total of 295 completed surveys were collected. The responses are tabulated in Table 1.
| |
| Primary practice setting | |
| Academic tertiary center | 23% |
| Community teaching hospital | 29% |
| Non‐academic hospital | 43% |
| Patient population | |
| Adults only | 90% |
| Pediatrics only | 5% |
| Adults and pediatrics | 5% |
| State of implementation | |
| Fully implemented | 48% |
| Partially implemented | 35% |
| Planning stages | 11% |
| Unaware of plans to implement | 2% |
| Unaware of med reconciliation | 4% |
| Hospitalist involvement | |
| Active role | 36% |
| Peripheral role | 24% |
| No role | 31% |
| Process format | |
| Paper | 47% |
| Computer | 11% |
| Both paper and computer | 31% |
| Don't know | 2% |
| Measuring compliance | |
| Yes | 42% |
| No | 14% |
| Don't know | 34% |
| Measuring outcomes | |
| Yes | 22% |
| No | 25% |
| Don't know | 41% |
| Impact of medication reconciliation | |
| No impact | 9% |
| Positive impact | 58% |
| Negative impact | 7% |
| Don't know | 14% |
Process
A paper process was used most often (47%), followed by a combined process (31%), and computers alone in just 11% of cases. Measurement of process compliance was reported in less than half (42%), with 34% unaware if their institutions were monitoring compliance. Outcome measurement was recorded as not performed (25%) or unknown (41%) in a majority of cases. Respondents reported a favorable view of the future impact of medication reconciliation, with 58% citing likely positive impacts on patient safety and patient care; fewer were unsure (14%) or anticipated no impact (9%) or negative impact (7%). Survey results regarding responsibility for individual process steps are detailed in Table 2. Notably, respondents often indicated that both physicians and nurses would share responsibility for a given step. Physicians were more often responsible for reconciling home medications, updating discharge medication lists, and communicating to outpatient providers. Nursing performed reconciliation in only 10% of cases. Results across all steps demonstrated very low participation rates by pharmacists, with pharmacist responsibility for reconciliation only 6% of the time.
| Process Step | Physician | Nurse | Physician and Nurse | Pharmacist | Other |
|---|---|---|---|---|---|
| |||||
| Obtaining home med list | 15% | 39% | 41% | 3% | 2% |
| Documenting home med list | 17% | 41% | 37% | 2% | 3% |
| Reconciling medications | 56% | 10% | 21% | 6% | 7% |
| Updating discharge med list | 64% | 6% | 17% | 3% | 10% |
| Providing instructions at discharge | 15% | 46% | 32% | 2% | 5% |
| Communicating changes at follow‐up | 84% | 6% | 4% | 6% | 1% |
Hospital Type
Results of subgroup analyses by hospital type are detailed in Table 3. Community teaching hospitals (CTHs) were significantly more likely (57%) than nonteaching hospitals (NTHs) (49%) or tertiary academic centers (TACs) (35%) to have achieved full implementation. NTHs were significantly less likely to have involved hospitalists in implementation. Use of computer‐based processes at TACs was more common (27%) than in CTHs (9%) or NTHs (7%). TACs were significantly more likely to have a physician obtain the medication list (33%, compared with 15% and 7% for CTHs and NTHs, respectively), whereas NTHs were more likely to use nurses (50%) than were CTHs (31%) or TACs (26%). Similar significant differences were found among hospital types with regard to obtaining the preadmission medication list. Physicians in TACs (25%) were more likely to be responsible for giving discharge medication instructions than in CTHs (10%) or NTHs (14%, not significant compared with TACs).
| Academic Centers [AC] | Community Teaching Hospitals [CT] | Non‐Teaching Hospitals [NT] | P values (2‐tailed) | |||
|---|---|---|---|---|---|---|
| AC vs. CT | AC vs. NT | CT vs. NT | ||||
| ||||||
| State of implementation | ||||||
| Fully implemented | 25/71 (35) | 48/84 (57) | 68/139 (49) | 0.007 | 0.06 | 0.25 |
| Partially implemented | 31/71 (44) | 25/84 (30) | 48/139 (35) | 0.07 | 0.21 | 0.44 |
| Planning stages | 9/71 (13) | 9/84 (11) | 14/139 (10) | 0.70 | 0.51 | 0.81 |
| Unaware of plans to implement | 2/71 (3) | 1/84 (1) | 3/139 (2) | 0.37 | 0.65 | 0.57 |
| Unaware of med reconciliation | 4/71 (5) | 1/84 (1) | 6/139 (4) | 0.14 | 0.74 | 0.19 |
| Hospitalist involvement | ||||||
| Active role | 28/59 (47) | 34/80 (43) | 43/127 (34) | 0.64 | 0.09 | 0.19 |
| Peripheral role | 12/59 (20) | 25/80 (31) | 34/127 (27) | 0.15 | 0.30 | 0.54 |
| No role | 19/59 (32) | 19/80 (24) | 50/127 (39) | 0.30 | 0.36 | 0.03 |
| Process format | ||||||
| Paper | 26/59 (44) | 47/81 (58) | 63/127 (50) | 0.10 | 0.45 | 0.26 |
| Computer | 16/59 (27) | 7/81 (9) | 9/127 (7) | 0.005 | 0.001 | 0.60 |
| Both paper and computer | 17/59 (29) | 25/81 (31) | 51/127 (40) | 0.80 | 0.15 | 0.19 |
| Don't know | 0/59 (0) | 2/81 (2) | 4/127 (3) | 0.28 | 0.18 | 0.66 |
| Process steps (selected questions) | ||||||
| Obtaining home med list | ||||||
| Physician | 19/58 (33) | 12/80 (15) | 9/125 (7) | 0.013 | 0.001 | 0.07 |
| Physician and Nurse | 19/58 (33) | 39/80 (49) | 49/125 (39) | 0.47 | 0.44 | 0.16 |
| Nurse | 15/58 (26) | 25/80 (31) | 62/125 (50) | 0.005 | 0.003 | 0.008 |
| Pharmacist | 5/58 (9) | 1/80 (1) | 2/125 (2) | 0.06 | 0.03 | 0.58 |
| Documenting home med list | ||||||
| Physician | 22/58 (38) | 11/80 (14) | 11/125 (9) | 0.001 | 0.001 | 0.26 |
| Physician and Nurse | 15/58 (26) | 37/80 (46) | 45/125 (36) | 0.02 | 0.18 | 0.16 |
| Nurse | 18/58 (31) | 26/80 (32) | 64/125 (51) | 0.90 | 0.012 | 0.008 |
| Pharmacist | 3/58 (5) | 2/80 (3) | 1/125 (1) | 0.55 | 0.09 | 0.29 |
| Reconciling medications | ||||||
| Physician | 33/58 (57) | 51/80 (64) | 63/125 (50) | 0.41 | 0.42 | 0.051 |
| Physician and Nurse | 8/58 (14) | 14/80 (18) | 32/125 (26) | 0.53 | 0.09 | 0.18 |
| Nurse | 6/58 (10) | 6/80 (8) | 15/125 (12) | 0.68 | 0.71 | 0.36 |
| Pharmacist | 8/58 (14) | 5/80 (6) | 3/125 (2) | 0.11 | 0.007 | 0.13 |
| Updating discharge med list | ||||||
| Physician | 42/58 (72) | 50/80 (63) | 76/125 (61) | 0.27 | 0.15 | 0.77 |
| Physician and Nurse | 7/58 (12) | 16/80 (20) | 23/125 (18) | 0.22 | 0.31 | 0.72 |
| Nurse | 2/58 (3) | 5/80 (6) | 10/125 (8) | 0.41 | 0.20 | 0.59 |
| Pharmacist | 3/58 (5) | 3/80 (4) | 3/125 (2) | 0.78 | 0.27 | 0.40 |
| Providing instructions at discharge | ||||||
| Physician | 14/57 (25) | 8/80 (10) | 17/125 (14) | 0.02 | 0.07 | 0.40 |
| Physician and Nurse | 14/57 (25) | 30/80 (38) | 39/125 (31) | 0.11 | 0.41 | 0.30 |
| Nurse | 25/57 (44) | 37/80 (46) | 60/125 (48) | 0.82 | 0.62 | 0.80 |
| Pharmacist | 4/57 (7) | 1/80 (1) | 0/125 (0) | 0.06 | 0.003 | 0.26 |
Barriers
Results regarding barriers to successful implementation are shown in Table 4. Patient lack of knowledge of medications (87%) and absence of a preadmission medication list from other sources (80%) were common. Both paper and computer medication reconciliation processes were associated with respondents citing cumbersome hospital systems as a barrier; this barrier was cited more often when the implemented process was paper‐only (Table 5). Respondents who stated the medication reconciliation process takes too long did so regardless of whether the implemented process was paper‐based or computer‐based. Despite these barriers, only 16% of respondents stated that medication reconciliation was not worth the effort of implementation. Barriers reported were similar across hospital type (Table 6) with 2 exceptions. Formulary differences were noted to be a barrier more often in CTHs (78%) compared with NTHs (60%) and TACs (64%, not significant compared with CTHs). Language barriers were problematic more often in TACs (48%) than in NTHs (28%) or CTHs (36%, not significant compared with TACs).
| Barrier to Implementation | Yes | No | Unsure |
|---|---|---|---|
| |||
| Patient not knowing meds | 87% | 2% | 0% |
| Process takes too long | 53% | 28% | 8% |
| Med list not available | 80% | 9% | 0% |
| Process not worth effort | 16% | 60% | 12% |
| Cumbersome hospital systems | 52% | 33% | 4% |
| Formulary differences | 59% | 24% | 5% |
| Language barriers | 31% | 53% | 4% |
| No access to outside records | 63% | 23% | 2% |
| Lack of job clarity in process | 38% | 48% | 3% |
| Availability of med list at discharge | 27% | 57% | 3% |
| Barriers (Selected Questions) | Paper Only [P] | Computer Only [C] | Paper and Computer [PC] | P values (2‐tailed) | ||
|---|---|---|---|---|---|---|
| P vs. C | P vs. PC | C vs. PC | ||||
| ||||||
| Process takes too long | ||||||
| Yes | 77/134 (57) | 19/31 (61) | 55/91 (60) | 0.69 | 0.65 | 0.92 |
| No | 43/134 (32) | 11/31 (35) | 28/91 (31) | 0.75 | 0.87 | 0.68 |
| Unsure | 14/134 (10) | 1/31 (3) | 8/91 (9) | 0.21 | 0.80 | 0.27 |
| Process not worth effort | ||||||
| Yes | 24/133 (18) | 3/31 (10) | 17/91 (19) | 0.28 | 0.85 | 0.25 |
| No | 93/133 (70) | 22/31 (71) | 62/91 (68) | 0.91 | 0.75 | 0.76 |
| Unsure | 16/133 (12) | 6/31 (19) | 12/91 (13) | 0.30 | 0.82 | 0.41 |
| Cumbersome hospital systems | ||||||
| Yes | 86/133 (65) | 16/31 (52) | 46/92 (50) | 0.18 | 0.03 | 0.85 |
| No | 42/133 (32) | 13/31 (42) | 42/92 (46) | 0.29 | 0.03 | 0.70 |
| Unsure | 5/133 (4) | 2/31 (6) | 4/92 (4) | 0.62 | 0.82 | 0.64 |
| Barrier to Implementation (Selected Questions) | Academic Centers [AC] | Community Teaching Hospitals [CT] | Non‐Teaching Hospitals [NT] | P values | ||
|---|---|---|---|---|---|---|
| AC vs. CT | AC vs. NT | CT vs. NT | ||||
| ||||||
| Process takes too long | ||||||
| Yes | 37/58 (64) | 49/78 (63) | 70/124 (56) | 0.90 | 0.31 | 0.37 |
| No | 15/58 (26) | 24/78 (31) | 42/124 (34) | 0.53 | 0.28 | 0.66 |
| Unsure | 6/58 (10) | 5/78 (6) | 12/124 (10) | 0.39 | 0.88 | 0.32 |
| Process not worth effort | ||||||
| Yes | 7/58 (12) | 16/78 (21) | 23/123 (19) | 0.17 | 0.24 | 0.73 |
| No | 42/58 (72) | 52/78 (67) | 84/123 (68) | 0.53 | 0.59 | 0.88 |
| Unsure | 9/58 (16) | 10/78 (12) | 16/123 (13) | 0.50 | 0.59 | 0.84 |
| Cumbersome hospital systems | ||||||
| Yes | 36/58 (62) | 46/79 (58) | 69/123 (56) | 0.64 | 0.45 | 0.78 |
| No | 19/58 (33) | 32/79 (41) | 46/123 (37) | 0.34 | 0.60 | 0.57 |
| Unsure | 3/58 (5) | 1/79 (1) | 8/123 (7) | 0.16 | 0.61 | 0.049 |
| Formulary differences | ||||||
| Yes | 37/58 (64) | 61/78 (78) | 74/123 (60) | 0.07 | 0.61 | 0.009 |
| No | 16/58 (28) | 14/78 (18) | 41/123 (33) | 0.17 | 0.50 | 0.02 |
| Unsure | 5/58 (8) | 2/78 (3) | 8/123 (7) | 0.19 | 0.81 | 0.22 |
| Language barriers | ||||||
| Yes | 28/58 (48) | 28/77 (36) | 34/123 (28) | 0.16 | 0.009 | 0.24 |
| No | 28/58 (48) | 46/77 (60) | 82/123 (67) | 0.17 | 0.016 | 0.32 |
| Unsure | 2/58 (3) | 3/77 (4) | 7/123 (5) | 0.76 | 0.54 | 0.74 |
| No access to outside records | ||||||
| Yes | 38/58 (66) | 60/79 (76) | 87/123 (71) | 0.20 | 0.50 | 0.44 |
| No | 18/58 (31) | 18/79 (23) | 33/123 (27) | 0.30 | 0.58 | 0.52 |
| Unsure | 2/58 (3) | 1/79 (1) | 3/123 (2) | 0.39 | 0.68 | 0.58 |
| Lack of job clarity in process | ||||||
| Yes | 26/58 (45) | 31/79 (39) | 49/121 (40) | 0.48 | 0.53 | 0.89 |
| No | 28/58 (48) | 46/79 (58) | 68/121 (56) | 0.25 | 0.32 | 0.78 |
| Unsure | 4/58 (7) | 2/79 (3) | 4/121 (3) | 0.28 | 0.22 | 0.75 |
| Availability of med list at discharge | ||||||
| Yes | 20/58 (34) | 24/79 (30) | 35/120 (29) | 0.62 | 0.50 | 0.88 |
| No | 36/58 (62) | 54/79 (68) | 78/120 (65) | 0.47 | 0.70 | 0.66 |
| Unsure | 0/58 (0) | 1/79 (1) | 7/120 (6) | 0.45 | 0.06 | 0.08 |
DISCUSSION
Managing medication information for inpatients is an extremely complex task. On admission, home medication lists are often inaccurate or absent,6 requiring extra time and effort to discover this information. By discharge, medication regimens have frequently been altered,7 making communication of changes to the next provider essential. One study described myriad provider, patient, and health system issues in maintaining accurate outpatient medication lists.8 These issues are further compounded by the multiple prescribers, necessary hand‐offs, and formulary differences in the inpatient setting.
Over half of the hospitalists in this survey reported hospitalist involvement in design and implementation of medication reconciliation. Given the familiarity with hospital systems and inpatient workflow, hospitalists are well‐positioned to contribute to successful implementation. Nonetheless, many were unaware of efforts to implement this NPSG.
Measurement of both process and outcome measures is important when determining value in quality improvement. Beyond process measures, outcome measures such as adverse drug events, readmission rates, mortality, patient satisfaction, and outpatient provider satisfaction may be appropriate in evaluating medication reconciliation strategies. Even measuring the accuracy of the process with respect to the admission orders written would be a valuable source of information for further improvement. Unfortunately, respondents indicated that evaluation was occurring infrequently. Potentially more problematic is the apparent lack of clarity regarding identification of healthcare provider responsibility for specific process steps. By far the least uniformity is in the acquisition and documentation of the preadmission medication list. There is variability in who is assigned to perform this task, but a substantial number of respondents indicated that their process involved a shared responsibility between physicians and nurses. It is unclear whether this phenomenon reflects the complexity of inpatient medication information management, or is simply an attempt to distribute the work among providers. Sharing the work between physicians and nurses may increase the overall likelihood for compliance and possibly improve the safety and accuracy of the process, especially if the physicians and nurses take the medication history in a redundant fashion and share their findings. Conversely, compliance may decrease if each provider merely expects the other to complete the process. Optimally, an interdisciplinary workflow for medication history taking would be in place, involving both physicians and nurses, with the availability of pharmacist consultation in complex cases. However, our survey data suggest this is infrequent; resident physicians appear to be the ones shouldering substantial responsibility for medication reconciliation in tertiary academic centers. Further research into the accuracy of medication reconciliation processes involving different strategies for medication information collection would be useful.
We documented several barriers to successful implementation of medication reconciliation. Physicians cited a lack of medication knowledge on the part of the patient and unavailable prior medication lists as substantial barriers to success. Many medication reconciliation processes are limited by issues of poor health literacy or inadequate patient knowledge about medications. This lack of medication knowledge is especially problematic for patients new to a healthcare system. It will be important to implement processes that not only reconcile medications accurately, but also make medication information available for future care episodes.
Time required to complete the process was also important. Certain elements of the medication reconciliation process are new work, and integrating the process into existing workflows is crucial. Given the significant time commitment required, the rare involvement of pharmacists at most institutions is striking. It appears that hospital pharmacists do not currently own any of the medication reconciliation process steps at most facilities, despite having formal training in medication history‐taking. In the 2006 ASHP national hospital pharmacy survey, one‐third of pharmacists stated that there were not enough pharmacy resources to meet medication reconciliation demands; only 19% of those surveyed stated pharmacists provided medication education at discharge to more than 25% of their patients.9
This report has several limitations. The survey used was not comprehensive, and only represents a convenience sample of hospitalists attending anational meeting. Nearly 300 physicians responded, representing both teaching and private hospital settings. We consider the response rate of 37% reasonable for a survey of this nature, and the variety of processes described is likely indicative of the overall status of medication reconciliation implementation. The over‐representation of certain institutions in our survey is possible, especially those with large or influential hospital medicine programs. Our survey did not ask respondents to name their home institutions. In addition, this design is open to a convenience sample bias, in that surveying only national meeting attendees (rather than the entire SHM membership) risks overinclusion of those hospitalists involved in leadership roles and quality improvement projects. Despite this, the variety of processes described is likely indicative of the overall status of medication reconciliation implementation in mid‐2006. It is possible that processes have become more uniform nationwide in the interim.
Our survey results reflect the complexity surrounding medication reconciliation. It appears that full implementation has not yet occurred everywhere, significant barriers remain, and outcome measurement is limited. Importantly, physicians, nurses, and pharmacists do not have standardized roles. Responsibility for medication reconciliation has predominantly been added to the existing duties of inpatient physicians and nurses, with limited involvement of pharmacists. Hospitalists are well‐positioned to lead the ongoing implementation of medication reconciliation processes and should take advantage of their systems knowledge to effectively partner with other physicians, nurses, and pharmacists to achieve success in medication reconciliation.
Acknowledgements
The authors thank Ken Epstein, MD, and Renee Meadows, MD, along with the entire SHM Medication Reconciliation Task Force for their helpful review and comments on the article.
Appendix
|
|
- Kohn LT,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999.
- .Medication reconciliation: transfer of medication information across settings – keeping it free from error.Am J Nurs.2005;105(3 Suppl):31–36.
- ,,, et al.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health‐Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- ,,,.Evaluation of a new integrated discharge prescription form.Ann Pharmacother.2001;35(7‐8):953–958.
- ,,, et al.Patient safety standardization as a mechanism to improve safety in health care.Jt Comm J Qual Saf.2004;30(1):5–14.
- ,,.What happens to long‐term medication when general practice patients are referred to hospital?Eur J Clin Pharmacol.1996;50(4):253–257.
- ,,, et al.An experiential interdisciplinary quality improvement education initiative.Am J Med Qual.2006;21(5):317–322.
- ,,.ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education‐2006.Am J Health‐Syst Pharm.2007;64(5):507–520.
The Joint Commission's (TJC) National Patient Safety Goal (NPSG) #8Accurately and completely reconcile medications across the continuum of carechallenges hospitals to design and implement new medication management processes. With medication errors contributing to patient morbidity and mortality,1 establishing a comprehensive process for reconciling a patient's medications during the hospitalization episode is an important quality improvement and patient safety goal.
However, the current state of inpatient medication management is highly fragmented. Standard documentation is lacking, as is integration of information between care settings.2 There are now reports describing implementation of various medication reconciliation processes for admissions,3 transfers,4 and discharges.5
Hospitalists are well‐positioned to contribute to the implementation of medication reconciliation. Indeed, because TJC does not explicitly specify what type of health care provider (eg, physician, nurse, etc.) should assume responsibility for this process, institutions have designed workflows to suit their own needs, while striving to comply with national standards.
Given the complexity and lack of standardization around this NPSG, a survey was distributed to attendees of a Society of Hospital Medicine (SHM) national meeting to determine the various processes implemented thus far, and to ascertain existing challenges to implementation. We report here on the results.
METHODS
A survey tool (Appendix) was designed to query demographic and institutional factors, involvement in the process, and barriers to implementation of medication reconciliation. Surveys were included in all attendees' registration materials, resulting in the distributions of approximately 800 surveys.
Responses were entered into an Excel spreadsheet. Simple descriptive statistics were used to determine proportions for providers, processes, and barriers to implementation. Where appropriate, variables were dichotomized, allowing for paired t‐test analysis. Statistical significance was defined as a P value less than .05. Subgroup analyses by hospital type, provider type, and process method were performed.
RESULTS
A total of 295 completed surveys were collected. The responses are tabulated in Table 1.
| |
| Primary practice setting | |
| Academic tertiary center | 23% |
| Community teaching hospital | 29% |
| Non‐academic hospital | 43% |
| Patient population | |
| Adults only | 90% |
| Pediatrics only | 5% |
| Adults and pediatrics | 5% |
| State of implementation | |
| Fully implemented | 48% |
| Partially implemented | 35% |
| Planning stages | 11% |
| Unaware of plans to implement | 2% |
| Unaware of med reconciliation | 4% |
| Hospitalist involvement | |
| Active role | 36% |
| Peripheral role | 24% |
| No role | 31% |
| Process format | |
| Paper | 47% |
| Computer | 11% |
| Both paper and computer | 31% |
| Don't know | 2% |
| Measuring compliance | |
| Yes | 42% |
| No | 14% |
| Don't know | 34% |
| Measuring outcomes | |
| Yes | 22% |
| No | 25% |
| Don't know | 41% |
| Impact of medication reconciliation | |
| No impact | 9% |
| Positive impact | 58% |
| Negative impact | 7% |
| Don't know | 14% |
Process
A paper process was used most often (47%), followed by a combined process (31%), and computers alone in just 11% of cases. Measurement of process compliance was reported in less than half (42%), with 34% unaware if their institutions were monitoring compliance. Outcome measurement was recorded as not performed (25%) or unknown (41%) in a majority of cases. Respondents reported a favorable view of the future impact of medication reconciliation, with 58% citing likely positive impacts on patient safety and patient care; fewer were unsure (14%) or anticipated no impact (9%) or negative impact (7%). Survey results regarding responsibility for individual process steps are detailed in Table 2. Notably, respondents often indicated that both physicians and nurses would share responsibility for a given step. Physicians were more often responsible for reconciling home medications, updating discharge medication lists, and communicating to outpatient providers. Nursing performed reconciliation in only 10% of cases. Results across all steps demonstrated very low participation rates by pharmacists, with pharmacist responsibility for reconciliation only 6% of the time.
| Process Step | Physician | Nurse | Physician and Nurse | Pharmacist | Other |
|---|---|---|---|---|---|
| |||||
| Obtaining home med list | 15% | 39% | 41% | 3% | 2% |
| Documenting home med list | 17% | 41% | 37% | 2% | 3% |
| Reconciling medications | 56% | 10% | 21% | 6% | 7% |
| Updating discharge med list | 64% | 6% | 17% | 3% | 10% |
| Providing instructions at discharge | 15% | 46% | 32% | 2% | 5% |
| Communicating changes at follow‐up | 84% | 6% | 4% | 6% | 1% |
Hospital Type
Results of subgroup analyses by hospital type are detailed in Table 3. Community teaching hospitals (CTHs) were significantly more likely (57%) than nonteaching hospitals (NTHs) (49%) or tertiary academic centers (TACs) (35%) to have achieved full implementation. NTHs were significantly less likely to have involved hospitalists in implementation. Use of computer‐based processes at TACs was more common (27%) than in CTHs (9%) or NTHs (7%). TACs were significantly more likely to have a physician obtain the medication list (33%, compared with 15% and 7% for CTHs and NTHs, respectively), whereas NTHs were more likely to use nurses (50%) than were CTHs (31%) or TACs (26%). Similar significant differences were found among hospital types with regard to obtaining the preadmission medication list. Physicians in TACs (25%) were more likely to be responsible for giving discharge medication instructions than in CTHs (10%) or NTHs (14%, not significant compared with TACs).
| Academic Centers [AC] | Community Teaching Hospitals [CT] | Non‐Teaching Hospitals [NT] | P values (2‐tailed) | |||
|---|---|---|---|---|---|---|
| AC vs. CT | AC vs. NT | CT vs. NT | ||||
| ||||||
| State of implementation | ||||||
| Fully implemented | 25/71 (35) | 48/84 (57) | 68/139 (49) | 0.007 | 0.06 | 0.25 |
| Partially implemented | 31/71 (44) | 25/84 (30) | 48/139 (35) | 0.07 | 0.21 | 0.44 |
| Planning stages | 9/71 (13) | 9/84 (11) | 14/139 (10) | 0.70 | 0.51 | 0.81 |
| Unaware of plans to implement | 2/71 (3) | 1/84 (1) | 3/139 (2) | 0.37 | 0.65 | 0.57 |
| Unaware of med reconciliation | 4/71 (5) | 1/84 (1) | 6/139 (4) | 0.14 | 0.74 | 0.19 |
| Hospitalist involvement | ||||||
| Active role | 28/59 (47) | 34/80 (43) | 43/127 (34) | 0.64 | 0.09 | 0.19 |
| Peripheral role | 12/59 (20) | 25/80 (31) | 34/127 (27) | 0.15 | 0.30 | 0.54 |
| No role | 19/59 (32) | 19/80 (24) | 50/127 (39) | 0.30 | 0.36 | 0.03 |
| Process format | ||||||
| Paper | 26/59 (44) | 47/81 (58) | 63/127 (50) | 0.10 | 0.45 | 0.26 |
| Computer | 16/59 (27) | 7/81 (9) | 9/127 (7) | 0.005 | 0.001 | 0.60 |
| Both paper and computer | 17/59 (29) | 25/81 (31) | 51/127 (40) | 0.80 | 0.15 | 0.19 |
| Don't know | 0/59 (0) | 2/81 (2) | 4/127 (3) | 0.28 | 0.18 | 0.66 |
| Process steps (selected questions) | ||||||
| Obtaining home med list | ||||||
| Physician | 19/58 (33) | 12/80 (15) | 9/125 (7) | 0.013 | 0.001 | 0.07 |
| Physician and Nurse | 19/58 (33) | 39/80 (49) | 49/125 (39) | 0.47 | 0.44 | 0.16 |
| Nurse | 15/58 (26) | 25/80 (31) | 62/125 (50) | 0.005 | 0.003 | 0.008 |
| Pharmacist | 5/58 (9) | 1/80 (1) | 2/125 (2) | 0.06 | 0.03 | 0.58 |
| Documenting home med list | ||||||
| Physician | 22/58 (38) | 11/80 (14) | 11/125 (9) | 0.001 | 0.001 | 0.26 |
| Physician and Nurse | 15/58 (26) | 37/80 (46) | 45/125 (36) | 0.02 | 0.18 | 0.16 |
| Nurse | 18/58 (31) | 26/80 (32) | 64/125 (51) | 0.90 | 0.012 | 0.008 |
| Pharmacist | 3/58 (5) | 2/80 (3) | 1/125 (1) | 0.55 | 0.09 | 0.29 |
| Reconciling medications | ||||||
| Physician | 33/58 (57) | 51/80 (64) | 63/125 (50) | 0.41 | 0.42 | 0.051 |
| Physician and Nurse | 8/58 (14) | 14/80 (18) | 32/125 (26) | 0.53 | 0.09 | 0.18 |
| Nurse | 6/58 (10) | 6/80 (8) | 15/125 (12) | 0.68 | 0.71 | 0.36 |
| Pharmacist | 8/58 (14) | 5/80 (6) | 3/125 (2) | 0.11 | 0.007 | 0.13 |
| Updating discharge med list | ||||||
| Physician | 42/58 (72) | 50/80 (63) | 76/125 (61) | 0.27 | 0.15 | 0.77 |
| Physician and Nurse | 7/58 (12) | 16/80 (20) | 23/125 (18) | 0.22 | 0.31 | 0.72 |
| Nurse | 2/58 (3) | 5/80 (6) | 10/125 (8) | 0.41 | 0.20 | 0.59 |
| Pharmacist | 3/58 (5) | 3/80 (4) | 3/125 (2) | 0.78 | 0.27 | 0.40 |
| Providing instructions at discharge | ||||||
| Physician | 14/57 (25) | 8/80 (10) | 17/125 (14) | 0.02 | 0.07 | 0.40 |
| Physician and Nurse | 14/57 (25) | 30/80 (38) | 39/125 (31) | 0.11 | 0.41 | 0.30 |
| Nurse | 25/57 (44) | 37/80 (46) | 60/125 (48) | 0.82 | 0.62 | 0.80 |
| Pharmacist | 4/57 (7) | 1/80 (1) | 0/125 (0) | 0.06 | 0.003 | 0.26 |
Barriers
Results regarding barriers to successful implementation are shown in Table 4. Patient lack of knowledge of medications (87%) and absence of a preadmission medication list from other sources (80%) were common. Both paper and computer medication reconciliation processes were associated with respondents citing cumbersome hospital systems as a barrier; this barrier was cited more often when the implemented process was paper‐only (Table 5). Respondents who stated the medication reconciliation process takes too long did so regardless of whether the implemented process was paper‐based or computer‐based. Despite these barriers, only 16% of respondents stated that medication reconciliation was not worth the effort of implementation. Barriers reported were similar across hospital type (Table 6) with 2 exceptions. Formulary differences were noted to be a barrier more often in CTHs (78%) compared with NTHs (60%) and TACs (64%, not significant compared with CTHs). Language barriers were problematic more often in TACs (48%) than in NTHs (28%) or CTHs (36%, not significant compared with TACs).
| Barrier to Implementation | Yes | No | Unsure |
|---|---|---|---|
| |||
| Patient not knowing meds | 87% | 2% | 0% |
| Process takes too long | 53% | 28% | 8% |
| Med list not available | 80% | 9% | 0% |
| Process not worth effort | 16% | 60% | 12% |
| Cumbersome hospital systems | 52% | 33% | 4% |
| Formulary differences | 59% | 24% | 5% |
| Language barriers | 31% | 53% | 4% |
| No access to outside records | 63% | 23% | 2% |
| Lack of job clarity in process | 38% | 48% | 3% |
| Availability of med list at discharge | 27% | 57% | 3% |
| Barriers (Selected Questions) | Paper Only [P] | Computer Only [C] | Paper and Computer [PC] | P values (2‐tailed) | ||
|---|---|---|---|---|---|---|
| P vs. C | P vs. PC | C vs. PC | ||||
| ||||||
| Process takes too long | ||||||
| Yes | 77/134 (57) | 19/31 (61) | 55/91 (60) | 0.69 | 0.65 | 0.92 |
| No | 43/134 (32) | 11/31 (35) | 28/91 (31) | 0.75 | 0.87 | 0.68 |
| Unsure | 14/134 (10) | 1/31 (3) | 8/91 (9) | 0.21 | 0.80 | 0.27 |
| Process not worth effort | ||||||
| Yes | 24/133 (18) | 3/31 (10) | 17/91 (19) | 0.28 | 0.85 | 0.25 |
| No | 93/133 (70) | 22/31 (71) | 62/91 (68) | 0.91 | 0.75 | 0.76 |
| Unsure | 16/133 (12) | 6/31 (19) | 12/91 (13) | 0.30 | 0.82 | 0.41 |
| Cumbersome hospital systems | ||||||
| Yes | 86/133 (65) | 16/31 (52) | 46/92 (50) | 0.18 | 0.03 | 0.85 |
| No | 42/133 (32) | 13/31 (42) | 42/92 (46) | 0.29 | 0.03 | 0.70 |
| Unsure | 5/133 (4) | 2/31 (6) | 4/92 (4) | 0.62 | 0.82 | 0.64 |
| Barrier to Implementation (Selected Questions) | Academic Centers [AC] | Community Teaching Hospitals [CT] | Non‐Teaching Hospitals [NT] | P values | ||
|---|---|---|---|---|---|---|
| AC vs. CT | AC vs. NT | CT vs. NT | ||||
| ||||||
| Process takes too long | ||||||
| Yes | 37/58 (64) | 49/78 (63) | 70/124 (56) | 0.90 | 0.31 | 0.37 |
| No | 15/58 (26) | 24/78 (31) | 42/124 (34) | 0.53 | 0.28 | 0.66 |
| Unsure | 6/58 (10) | 5/78 (6) | 12/124 (10) | 0.39 | 0.88 | 0.32 |
| Process not worth effort | ||||||
| Yes | 7/58 (12) | 16/78 (21) | 23/123 (19) | 0.17 | 0.24 | 0.73 |
| No | 42/58 (72) | 52/78 (67) | 84/123 (68) | 0.53 | 0.59 | 0.88 |
| Unsure | 9/58 (16) | 10/78 (12) | 16/123 (13) | 0.50 | 0.59 | 0.84 |
| Cumbersome hospital systems | ||||||
| Yes | 36/58 (62) | 46/79 (58) | 69/123 (56) | 0.64 | 0.45 | 0.78 |
| No | 19/58 (33) | 32/79 (41) | 46/123 (37) | 0.34 | 0.60 | 0.57 |
| Unsure | 3/58 (5) | 1/79 (1) | 8/123 (7) | 0.16 | 0.61 | 0.049 |
| Formulary differences | ||||||
| Yes | 37/58 (64) | 61/78 (78) | 74/123 (60) | 0.07 | 0.61 | 0.009 |
| No | 16/58 (28) | 14/78 (18) | 41/123 (33) | 0.17 | 0.50 | 0.02 |
| Unsure | 5/58 (8) | 2/78 (3) | 8/123 (7) | 0.19 | 0.81 | 0.22 |
| Language barriers | ||||||
| Yes | 28/58 (48) | 28/77 (36) | 34/123 (28) | 0.16 | 0.009 | 0.24 |
| No | 28/58 (48) | 46/77 (60) | 82/123 (67) | 0.17 | 0.016 | 0.32 |
| Unsure | 2/58 (3) | 3/77 (4) | 7/123 (5) | 0.76 | 0.54 | 0.74 |
| No access to outside records | ||||||
| Yes | 38/58 (66) | 60/79 (76) | 87/123 (71) | 0.20 | 0.50 | 0.44 |
| No | 18/58 (31) | 18/79 (23) | 33/123 (27) | 0.30 | 0.58 | 0.52 |
| Unsure | 2/58 (3) | 1/79 (1) | 3/123 (2) | 0.39 | 0.68 | 0.58 |
| Lack of job clarity in process | ||||||
| Yes | 26/58 (45) | 31/79 (39) | 49/121 (40) | 0.48 | 0.53 | 0.89 |
| No | 28/58 (48) | 46/79 (58) | 68/121 (56) | 0.25 | 0.32 | 0.78 |
| Unsure | 4/58 (7) | 2/79 (3) | 4/121 (3) | 0.28 | 0.22 | 0.75 |
| Availability of med list at discharge | ||||||
| Yes | 20/58 (34) | 24/79 (30) | 35/120 (29) | 0.62 | 0.50 | 0.88 |
| No | 36/58 (62) | 54/79 (68) | 78/120 (65) | 0.47 | 0.70 | 0.66 |
| Unsure | 0/58 (0) | 1/79 (1) | 7/120 (6) | 0.45 | 0.06 | 0.08 |
DISCUSSION
Managing medication information for inpatients is an extremely complex task. On admission, home medication lists are often inaccurate or absent,6 requiring extra time and effort to discover this information. By discharge, medication regimens have frequently been altered,7 making communication of changes to the next provider essential. One study described myriad provider, patient, and health system issues in maintaining accurate outpatient medication lists.8 These issues are further compounded by the multiple prescribers, necessary hand‐offs, and formulary differences in the inpatient setting.
Over half of the hospitalists in this survey reported hospitalist involvement in design and implementation of medication reconciliation. Given the familiarity with hospital systems and inpatient workflow, hospitalists are well‐positioned to contribute to successful implementation. Nonetheless, many were unaware of efforts to implement this NPSG.
Measurement of both process and outcome measures is important when determining value in quality improvement. Beyond process measures, outcome measures such as adverse drug events, readmission rates, mortality, patient satisfaction, and outpatient provider satisfaction may be appropriate in evaluating medication reconciliation strategies. Even measuring the accuracy of the process with respect to the admission orders written would be a valuable source of information for further improvement. Unfortunately, respondents indicated that evaluation was occurring infrequently. Potentially more problematic is the apparent lack of clarity regarding identification of healthcare provider responsibility for specific process steps. By far the least uniformity is in the acquisition and documentation of the preadmission medication list. There is variability in who is assigned to perform this task, but a substantial number of respondents indicated that their process involved a shared responsibility between physicians and nurses. It is unclear whether this phenomenon reflects the complexity of inpatient medication information management, or is simply an attempt to distribute the work among providers. Sharing the work between physicians and nurses may increase the overall likelihood for compliance and possibly improve the safety and accuracy of the process, especially if the physicians and nurses take the medication history in a redundant fashion and share their findings. Conversely, compliance may decrease if each provider merely expects the other to complete the process. Optimally, an interdisciplinary workflow for medication history taking would be in place, involving both physicians and nurses, with the availability of pharmacist consultation in complex cases. However, our survey data suggest this is infrequent; resident physicians appear to be the ones shouldering substantial responsibility for medication reconciliation in tertiary academic centers. Further research into the accuracy of medication reconciliation processes involving different strategies for medication information collection would be useful.
We documented several barriers to successful implementation of medication reconciliation. Physicians cited a lack of medication knowledge on the part of the patient and unavailable prior medication lists as substantial barriers to success. Many medication reconciliation processes are limited by issues of poor health literacy or inadequate patient knowledge about medications. This lack of medication knowledge is especially problematic for patients new to a healthcare system. It will be important to implement processes that not only reconcile medications accurately, but also make medication information available for future care episodes.
Time required to complete the process was also important. Certain elements of the medication reconciliation process are new work, and integrating the process into existing workflows is crucial. Given the significant time commitment required, the rare involvement of pharmacists at most institutions is striking. It appears that hospital pharmacists do not currently own any of the medication reconciliation process steps at most facilities, despite having formal training in medication history‐taking. In the 2006 ASHP national hospital pharmacy survey, one‐third of pharmacists stated that there were not enough pharmacy resources to meet medication reconciliation demands; only 19% of those surveyed stated pharmacists provided medication education at discharge to more than 25% of their patients.9
This report has several limitations. The survey used was not comprehensive, and only represents a convenience sample of hospitalists attending anational meeting. Nearly 300 physicians responded, representing both teaching and private hospital settings. We consider the response rate of 37% reasonable for a survey of this nature, and the variety of processes described is likely indicative of the overall status of medication reconciliation implementation. The over‐representation of certain institutions in our survey is possible, especially those with large or influential hospital medicine programs. Our survey did not ask respondents to name their home institutions. In addition, this design is open to a convenience sample bias, in that surveying only national meeting attendees (rather than the entire SHM membership) risks overinclusion of those hospitalists involved in leadership roles and quality improvement projects. Despite this, the variety of processes described is likely indicative of the overall status of medication reconciliation implementation in mid‐2006. It is possible that processes have become more uniform nationwide in the interim.
Our survey results reflect the complexity surrounding medication reconciliation. It appears that full implementation has not yet occurred everywhere, significant barriers remain, and outcome measurement is limited. Importantly, physicians, nurses, and pharmacists do not have standardized roles. Responsibility for medication reconciliation has predominantly been added to the existing duties of inpatient physicians and nurses, with limited involvement of pharmacists. Hospitalists are well‐positioned to lead the ongoing implementation of medication reconciliation processes and should take advantage of their systems knowledge to effectively partner with other physicians, nurses, and pharmacists to achieve success in medication reconciliation.
Acknowledgements
The authors thank Ken Epstein, MD, and Renee Meadows, MD, along with the entire SHM Medication Reconciliation Task Force for their helpful review and comments on the article.
Appendix
|
|
The Joint Commission's (TJC) National Patient Safety Goal (NPSG) #8Accurately and completely reconcile medications across the continuum of carechallenges hospitals to design and implement new medication management processes. With medication errors contributing to patient morbidity and mortality,1 establishing a comprehensive process for reconciling a patient's medications during the hospitalization episode is an important quality improvement and patient safety goal.
However, the current state of inpatient medication management is highly fragmented. Standard documentation is lacking, as is integration of information between care settings.2 There are now reports describing implementation of various medication reconciliation processes for admissions,3 transfers,4 and discharges.5
Hospitalists are well‐positioned to contribute to the implementation of medication reconciliation. Indeed, because TJC does not explicitly specify what type of health care provider (eg, physician, nurse, etc.) should assume responsibility for this process, institutions have designed workflows to suit their own needs, while striving to comply with national standards.
Given the complexity and lack of standardization around this NPSG, a survey was distributed to attendees of a Society of Hospital Medicine (SHM) national meeting to determine the various processes implemented thus far, and to ascertain existing challenges to implementation. We report here on the results.
METHODS
A survey tool (Appendix) was designed to query demographic and institutional factors, involvement in the process, and barriers to implementation of medication reconciliation. Surveys were included in all attendees' registration materials, resulting in the distributions of approximately 800 surveys.
Responses were entered into an Excel spreadsheet. Simple descriptive statistics were used to determine proportions for providers, processes, and barriers to implementation. Where appropriate, variables were dichotomized, allowing for paired t‐test analysis. Statistical significance was defined as a P value less than .05. Subgroup analyses by hospital type, provider type, and process method were performed.
RESULTS
A total of 295 completed surveys were collected. The responses are tabulated in Table 1.
| |
| Primary practice setting | |
| Academic tertiary center | 23% |
| Community teaching hospital | 29% |
| Non‐academic hospital | 43% |
| Patient population | |
| Adults only | 90% |
| Pediatrics only | 5% |
| Adults and pediatrics | 5% |
| State of implementation | |
| Fully implemented | 48% |
| Partially implemented | 35% |
| Planning stages | 11% |
| Unaware of plans to implement | 2% |
| Unaware of med reconciliation | 4% |
| Hospitalist involvement | |
| Active role | 36% |
| Peripheral role | 24% |
| No role | 31% |
| Process format | |
| Paper | 47% |
| Computer | 11% |
| Both paper and computer | 31% |
| Don't know | 2% |
| Measuring compliance | |
| Yes | 42% |
| No | 14% |
| Don't know | 34% |
| Measuring outcomes | |
| Yes | 22% |
| No | 25% |
| Don't know | 41% |
| Impact of medication reconciliation | |
| No impact | 9% |
| Positive impact | 58% |
| Negative impact | 7% |
| Don't know | 14% |
Process
A paper process was used most often (47%), followed by a combined process (31%), and computers alone in just 11% of cases. Measurement of process compliance was reported in less than half (42%), with 34% unaware if their institutions were monitoring compliance. Outcome measurement was recorded as not performed (25%) or unknown (41%) in a majority of cases. Respondents reported a favorable view of the future impact of medication reconciliation, with 58% citing likely positive impacts on patient safety and patient care; fewer were unsure (14%) or anticipated no impact (9%) or negative impact (7%). Survey results regarding responsibility for individual process steps are detailed in Table 2. Notably, respondents often indicated that both physicians and nurses would share responsibility for a given step. Physicians were more often responsible for reconciling home medications, updating discharge medication lists, and communicating to outpatient providers. Nursing performed reconciliation in only 10% of cases. Results across all steps demonstrated very low participation rates by pharmacists, with pharmacist responsibility for reconciliation only 6% of the time.
| Process Step | Physician | Nurse | Physician and Nurse | Pharmacist | Other |
|---|---|---|---|---|---|
| |||||
| Obtaining home med list | 15% | 39% | 41% | 3% | 2% |
| Documenting home med list | 17% | 41% | 37% | 2% | 3% |
| Reconciling medications | 56% | 10% | 21% | 6% | 7% |
| Updating discharge med list | 64% | 6% | 17% | 3% | 10% |
| Providing instructions at discharge | 15% | 46% | 32% | 2% | 5% |
| Communicating changes at follow‐up | 84% | 6% | 4% | 6% | 1% |
Hospital Type
Results of subgroup analyses by hospital type are detailed in Table 3. Community teaching hospitals (CTHs) were significantly more likely (57%) than nonteaching hospitals (NTHs) (49%) or tertiary academic centers (TACs) (35%) to have achieved full implementation. NTHs were significantly less likely to have involved hospitalists in implementation. Use of computer‐based processes at TACs was more common (27%) than in CTHs (9%) or NTHs (7%). TACs were significantly more likely to have a physician obtain the medication list (33%, compared with 15% and 7% for CTHs and NTHs, respectively), whereas NTHs were more likely to use nurses (50%) than were CTHs (31%) or TACs (26%). Similar significant differences were found among hospital types with regard to obtaining the preadmission medication list. Physicians in TACs (25%) were more likely to be responsible for giving discharge medication instructions than in CTHs (10%) or NTHs (14%, not significant compared with TACs).
| Academic Centers [AC] | Community Teaching Hospitals [CT] | Non‐Teaching Hospitals [NT] | P values (2‐tailed) | |||
|---|---|---|---|---|---|---|
| AC vs. CT | AC vs. NT | CT vs. NT | ||||
| ||||||
| State of implementation | ||||||
| Fully implemented | 25/71 (35) | 48/84 (57) | 68/139 (49) | 0.007 | 0.06 | 0.25 |
| Partially implemented | 31/71 (44) | 25/84 (30) | 48/139 (35) | 0.07 | 0.21 | 0.44 |
| Planning stages | 9/71 (13) | 9/84 (11) | 14/139 (10) | 0.70 | 0.51 | 0.81 |
| Unaware of plans to implement | 2/71 (3) | 1/84 (1) | 3/139 (2) | 0.37 | 0.65 | 0.57 |
| Unaware of med reconciliation | 4/71 (5) | 1/84 (1) | 6/139 (4) | 0.14 | 0.74 | 0.19 |
| Hospitalist involvement | ||||||
| Active role | 28/59 (47) | 34/80 (43) | 43/127 (34) | 0.64 | 0.09 | 0.19 |
| Peripheral role | 12/59 (20) | 25/80 (31) | 34/127 (27) | 0.15 | 0.30 | 0.54 |
| No role | 19/59 (32) | 19/80 (24) | 50/127 (39) | 0.30 | 0.36 | 0.03 |
| Process format | ||||||
| Paper | 26/59 (44) | 47/81 (58) | 63/127 (50) | 0.10 | 0.45 | 0.26 |
| Computer | 16/59 (27) | 7/81 (9) | 9/127 (7) | 0.005 | 0.001 | 0.60 |
| Both paper and computer | 17/59 (29) | 25/81 (31) | 51/127 (40) | 0.80 | 0.15 | 0.19 |
| Don't know | 0/59 (0) | 2/81 (2) | 4/127 (3) | 0.28 | 0.18 | 0.66 |
| Process steps (selected questions) | ||||||
| Obtaining home med list | ||||||
| Physician | 19/58 (33) | 12/80 (15) | 9/125 (7) | 0.013 | 0.001 | 0.07 |
| Physician and Nurse | 19/58 (33) | 39/80 (49) | 49/125 (39) | 0.47 | 0.44 | 0.16 |
| Nurse | 15/58 (26) | 25/80 (31) | 62/125 (50) | 0.005 | 0.003 | 0.008 |
| Pharmacist | 5/58 (9) | 1/80 (1) | 2/125 (2) | 0.06 | 0.03 | 0.58 |
| Documenting home med list | ||||||
| Physician | 22/58 (38) | 11/80 (14) | 11/125 (9) | 0.001 | 0.001 | 0.26 |
| Physician and Nurse | 15/58 (26) | 37/80 (46) | 45/125 (36) | 0.02 | 0.18 | 0.16 |
| Nurse | 18/58 (31) | 26/80 (32) | 64/125 (51) | 0.90 | 0.012 | 0.008 |
| Pharmacist | 3/58 (5) | 2/80 (3) | 1/125 (1) | 0.55 | 0.09 | 0.29 |
| Reconciling medications | ||||||
| Physician | 33/58 (57) | 51/80 (64) | 63/125 (50) | 0.41 | 0.42 | 0.051 |
| Physician and Nurse | 8/58 (14) | 14/80 (18) | 32/125 (26) | 0.53 | 0.09 | 0.18 |
| Nurse | 6/58 (10) | 6/80 (8) | 15/125 (12) | 0.68 | 0.71 | 0.36 |
| Pharmacist | 8/58 (14) | 5/80 (6) | 3/125 (2) | 0.11 | 0.007 | 0.13 |
| Updating discharge med list | ||||||
| Physician | 42/58 (72) | 50/80 (63) | 76/125 (61) | 0.27 | 0.15 | 0.77 |
| Physician and Nurse | 7/58 (12) | 16/80 (20) | 23/125 (18) | 0.22 | 0.31 | 0.72 |
| Nurse | 2/58 (3) | 5/80 (6) | 10/125 (8) | 0.41 | 0.20 | 0.59 |
| Pharmacist | 3/58 (5) | 3/80 (4) | 3/125 (2) | 0.78 | 0.27 | 0.40 |
| Providing instructions at discharge | ||||||
| Physician | 14/57 (25) | 8/80 (10) | 17/125 (14) | 0.02 | 0.07 | 0.40 |
| Physician and Nurse | 14/57 (25) | 30/80 (38) | 39/125 (31) | 0.11 | 0.41 | 0.30 |
| Nurse | 25/57 (44) | 37/80 (46) | 60/125 (48) | 0.82 | 0.62 | 0.80 |
| Pharmacist | 4/57 (7) | 1/80 (1) | 0/125 (0) | 0.06 | 0.003 | 0.26 |
Barriers
Results regarding barriers to successful implementation are shown in Table 4. Patient lack of knowledge of medications (87%) and absence of a preadmission medication list from other sources (80%) were common. Both paper and computer medication reconciliation processes were associated with respondents citing cumbersome hospital systems as a barrier; this barrier was cited more often when the implemented process was paper‐only (Table 5). Respondents who stated the medication reconciliation process takes too long did so regardless of whether the implemented process was paper‐based or computer‐based. Despite these barriers, only 16% of respondents stated that medication reconciliation was not worth the effort of implementation. Barriers reported were similar across hospital type (Table 6) with 2 exceptions. Formulary differences were noted to be a barrier more often in CTHs (78%) compared with NTHs (60%) and TACs (64%, not significant compared with CTHs). Language barriers were problematic more often in TACs (48%) than in NTHs (28%) or CTHs (36%, not significant compared with TACs).
| Barrier to Implementation | Yes | No | Unsure |
|---|---|---|---|
| |||
| Patient not knowing meds | 87% | 2% | 0% |
| Process takes too long | 53% | 28% | 8% |
| Med list not available | 80% | 9% | 0% |
| Process not worth effort | 16% | 60% | 12% |
| Cumbersome hospital systems | 52% | 33% | 4% |
| Formulary differences | 59% | 24% | 5% |
| Language barriers | 31% | 53% | 4% |
| No access to outside records | 63% | 23% | 2% |
| Lack of job clarity in process | 38% | 48% | 3% |
| Availability of med list at discharge | 27% | 57% | 3% |
| Barriers (Selected Questions) | Paper Only [P] | Computer Only [C] | Paper and Computer [PC] | P values (2‐tailed) | ||
|---|---|---|---|---|---|---|
| P vs. C | P vs. PC | C vs. PC | ||||
| ||||||
| Process takes too long | ||||||
| Yes | 77/134 (57) | 19/31 (61) | 55/91 (60) | 0.69 | 0.65 | 0.92 |
| No | 43/134 (32) | 11/31 (35) | 28/91 (31) | 0.75 | 0.87 | 0.68 |
| Unsure | 14/134 (10) | 1/31 (3) | 8/91 (9) | 0.21 | 0.80 | 0.27 |
| Process not worth effort | ||||||
| Yes | 24/133 (18) | 3/31 (10) | 17/91 (19) | 0.28 | 0.85 | 0.25 |
| No | 93/133 (70) | 22/31 (71) | 62/91 (68) | 0.91 | 0.75 | 0.76 |
| Unsure | 16/133 (12) | 6/31 (19) | 12/91 (13) | 0.30 | 0.82 | 0.41 |
| Cumbersome hospital systems | ||||||
| Yes | 86/133 (65) | 16/31 (52) | 46/92 (50) | 0.18 | 0.03 | 0.85 |
| No | 42/133 (32) | 13/31 (42) | 42/92 (46) | 0.29 | 0.03 | 0.70 |
| Unsure | 5/133 (4) | 2/31 (6) | 4/92 (4) | 0.62 | 0.82 | 0.64 |
| Barrier to Implementation (Selected Questions) | Academic Centers [AC] | Community Teaching Hospitals [CT] | Non‐Teaching Hospitals [NT] | P values | ||
|---|---|---|---|---|---|---|
| AC vs. CT | AC vs. NT | CT vs. NT | ||||
| ||||||
| Process takes too long | ||||||
| Yes | 37/58 (64) | 49/78 (63) | 70/124 (56) | 0.90 | 0.31 | 0.37 |
| No | 15/58 (26) | 24/78 (31) | 42/124 (34) | 0.53 | 0.28 | 0.66 |
| Unsure | 6/58 (10) | 5/78 (6) | 12/124 (10) | 0.39 | 0.88 | 0.32 |
| Process not worth effort | ||||||
| Yes | 7/58 (12) | 16/78 (21) | 23/123 (19) | 0.17 | 0.24 | 0.73 |
| No | 42/58 (72) | 52/78 (67) | 84/123 (68) | 0.53 | 0.59 | 0.88 |
| Unsure | 9/58 (16) | 10/78 (12) | 16/123 (13) | 0.50 | 0.59 | 0.84 |
| Cumbersome hospital systems | ||||||
| Yes | 36/58 (62) | 46/79 (58) | 69/123 (56) | 0.64 | 0.45 | 0.78 |
| No | 19/58 (33) | 32/79 (41) | 46/123 (37) | 0.34 | 0.60 | 0.57 |
| Unsure | 3/58 (5) | 1/79 (1) | 8/123 (7) | 0.16 | 0.61 | 0.049 |
| Formulary differences | ||||||
| Yes | 37/58 (64) | 61/78 (78) | 74/123 (60) | 0.07 | 0.61 | 0.009 |
| No | 16/58 (28) | 14/78 (18) | 41/123 (33) | 0.17 | 0.50 | 0.02 |
| Unsure | 5/58 (8) | 2/78 (3) | 8/123 (7) | 0.19 | 0.81 | 0.22 |
| Language barriers | ||||||
| Yes | 28/58 (48) | 28/77 (36) | 34/123 (28) | 0.16 | 0.009 | 0.24 |
| No | 28/58 (48) | 46/77 (60) | 82/123 (67) | 0.17 | 0.016 | 0.32 |
| Unsure | 2/58 (3) | 3/77 (4) | 7/123 (5) | 0.76 | 0.54 | 0.74 |
| No access to outside records | ||||||
| Yes | 38/58 (66) | 60/79 (76) | 87/123 (71) | 0.20 | 0.50 | 0.44 |
| No | 18/58 (31) | 18/79 (23) | 33/123 (27) | 0.30 | 0.58 | 0.52 |
| Unsure | 2/58 (3) | 1/79 (1) | 3/123 (2) | 0.39 | 0.68 | 0.58 |
| Lack of job clarity in process | ||||||
| Yes | 26/58 (45) | 31/79 (39) | 49/121 (40) | 0.48 | 0.53 | 0.89 |
| No | 28/58 (48) | 46/79 (58) | 68/121 (56) | 0.25 | 0.32 | 0.78 |
| Unsure | 4/58 (7) | 2/79 (3) | 4/121 (3) | 0.28 | 0.22 | 0.75 |
| Availability of med list at discharge | ||||||
| Yes | 20/58 (34) | 24/79 (30) | 35/120 (29) | 0.62 | 0.50 | 0.88 |
| No | 36/58 (62) | 54/79 (68) | 78/120 (65) | 0.47 | 0.70 | 0.66 |
| Unsure | 0/58 (0) | 1/79 (1) | 7/120 (6) | 0.45 | 0.06 | 0.08 |
DISCUSSION
Managing medication information for inpatients is an extremely complex task. On admission, home medication lists are often inaccurate or absent,6 requiring extra time and effort to discover this information. By discharge, medication regimens have frequently been altered,7 making communication of changes to the next provider essential. One study described myriad provider, patient, and health system issues in maintaining accurate outpatient medication lists.8 These issues are further compounded by the multiple prescribers, necessary hand‐offs, and formulary differences in the inpatient setting.
Over half of the hospitalists in this survey reported hospitalist involvement in design and implementation of medication reconciliation. Given the familiarity with hospital systems and inpatient workflow, hospitalists are well‐positioned to contribute to successful implementation. Nonetheless, many were unaware of efforts to implement this NPSG.
Measurement of both process and outcome measures is important when determining value in quality improvement. Beyond process measures, outcome measures such as adverse drug events, readmission rates, mortality, patient satisfaction, and outpatient provider satisfaction may be appropriate in evaluating medication reconciliation strategies. Even measuring the accuracy of the process with respect to the admission orders written would be a valuable source of information for further improvement. Unfortunately, respondents indicated that evaluation was occurring infrequently. Potentially more problematic is the apparent lack of clarity regarding identification of healthcare provider responsibility for specific process steps. By far the least uniformity is in the acquisition and documentation of the preadmission medication list. There is variability in who is assigned to perform this task, but a substantial number of respondents indicated that their process involved a shared responsibility between physicians and nurses. It is unclear whether this phenomenon reflects the complexity of inpatient medication information management, or is simply an attempt to distribute the work among providers. Sharing the work between physicians and nurses may increase the overall likelihood for compliance and possibly improve the safety and accuracy of the process, especially if the physicians and nurses take the medication history in a redundant fashion and share their findings. Conversely, compliance may decrease if each provider merely expects the other to complete the process. Optimally, an interdisciplinary workflow for medication history taking would be in place, involving both physicians and nurses, with the availability of pharmacist consultation in complex cases. However, our survey data suggest this is infrequent; resident physicians appear to be the ones shouldering substantial responsibility for medication reconciliation in tertiary academic centers. Further research into the accuracy of medication reconciliation processes involving different strategies for medication information collection would be useful.
We documented several barriers to successful implementation of medication reconciliation. Physicians cited a lack of medication knowledge on the part of the patient and unavailable prior medication lists as substantial barriers to success. Many medication reconciliation processes are limited by issues of poor health literacy or inadequate patient knowledge about medications. This lack of medication knowledge is especially problematic for patients new to a healthcare system. It will be important to implement processes that not only reconcile medications accurately, but also make medication information available for future care episodes.
Time required to complete the process was also important. Certain elements of the medication reconciliation process are new work, and integrating the process into existing workflows is crucial. Given the significant time commitment required, the rare involvement of pharmacists at most institutions is striking. It appears that hospital pharmacists do not currently own any of the medication reconciliation process steps at most facilities, despite having formal training in medication history‐taking. In the 2006 ASHP national hospital pharmacy survey, one‐third of pharmacists stated that there were not enough pharmacy resources to meet medication reconciliation demands; only 19% of those surveyed stated pharmacists provided medication education at discharge to more than 25% of their patients.9
This report has several limitations. The survey used was not comprehensive, and only represents a convenience sample of hospitalists attending anational meeting. Nearly 300 physicians responded, representing both teaching and private hospital settings. We consider the response rate of 37% reasonable for a survey of this nature, and the variety of processes described is likely indicative of the overall status of medication reconciliation implementation. The over‐representation of certain institutions in our survey is possible, especially those with large or influential hospital medicine programs. Our survey did not ask respondents to name their home institutions. In addition, this design is open to a convenience sample bias, in that surveying only national meeting attendees (rather than the entire SHM membership) risks overinclusion of those hospitalists involved in leadership roles and quality improvement projects. Despite this, the variety of processes described is likely indicative of the overall status of medication reconciliation implementation in mid‐2006. It is possible that processes have become more uniform nationwide in the interim.
Our survey results reflect the complexity surrounding medication reconciliation. It appears that full implementation has not yet occurred everywhere, significant barriers remain, and outcome measurement is limited. Importantly, physicians, nurses, and pharmacists do not have standardized roles. Responsibility for medication reconciliation has predominantly been added to the existing duties of inpatient physicians and nurses, with limited involvement of pharmacists. Hospitalists are well‐positioned to lead the ongoing implementation of medication reconciliation processes and should take advantage of their systems knowledge to effectively partner with other physicians, nurses, and pharmacists to achieve success in medication reconciliation.
Acknowledgements
The authors thank Ken Epstein, MD, and Renee Meadows, MD, along with the entire SHM Medication Reconciliation Task Force for their helpful review and comments on the article.
Appendix
|
|
- Kohn LT,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999.
- .Medication reconciliation: transfer of medication information across settings – keeping it free from error.Am J Nurs.2005;105(3 Suppl):31–36.
- ,,, et al.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health‐Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- ,,,.Evaluation of a new integrated discharge prescription form.Ann Pharmacother.2001;35(7‐8):953–958.
- ,,, et al.Patient safety standardization as a mechanism to improve safety in health care.Jt Comm J Qual Saf.2004;30(1):5–14.
- ,,.What happens to long‐term medication when general practice patients are referred to hospital?Eur J Clin Pharmacol.1996;50(4):253–257.
- ,,, et al.An experiential interdisciplinary quality improvement education initiative.Am J Med Qual.2006;21(5):317–322.
- ,,.ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education‐2006.Am J Health‐Syst Pharm.2007;64(5):507–520.
- Kohn LT,Corrigan JM,Donaldson MS, eds.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press;1999.
- .Medication reconciliation: transfer of medication information across settings – keeping it free from error.Am J Nurs.2005;105(3 Suppl):31–36.
- ,,, et al.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health‐Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- ,,,.Evaluation of a new integrated discharge prescription form.Ann Pharmacother.2001;35(7‐8):953–958.
- ,,, et al.Patient safety standardization as a mechanism to improve safety in health care.Jt Comm J Qual Saf.2004;30(1):5–14.
- ,,.What happens to long‐term medication when general practice patients are referred to hospital?Eur J Clin Pharmacol.1996;50(4):253–257.
- ,,, et al.An experiential interdisciplinary quality improvement education initiative.Am J Med Qual.2006;21(5):317–322.
- ,,.ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education‐2006.Am J Health‐Syst Pharm.2007;64(5):507–520.
