User login
Can the U.S. keep COVID-19 variants in check? Here’s what it takes
The COVID-19 variants that have emerged in the United Kingdom, Brazil, South Africa and now Southern California are eliciting two notably distinct responses from U.S. public health officials.
First, broad concern. A variant that wreaked havoc in the United Kingdom, leading to a spike in cases and hospitalizations, is surfacing in a growing number of places in the United States. During the week of Jan. 24, another worrisome variant seen in Brazil surfaced in Minnesota. If these or other strains significantly change the way the virus transmits and attacks the body, as scientists fear they might, they could cause yet another prolonged surge in illness and death in the U.S., even as cases have begun to plateau and vaccines are rolling out.
On the other hand, variants aren’t novel or even uncommon in viral illnesses. The viruses that trigger common colds and flus regularly evolve. Even if a mutated strain of SARS-CoV-2, the virus that causes COVID-19, makes it more contagious or makes people sicker,
The problem is that the U.S. has struggled with every step of its public health response in its first year of battle against COVID-19. And that raises the question of whether the nation will devote the attention and resources needed to outflank the virus as it evolves.
Researchers are quick to stress that a coronavirus mutation in itself is no cause for alarm. In the course of making millions and billions of copies as part of the infection process, small changes to a virus’s genome happen all the time as a function of evolutionary biology.
“The word ‘variant’ and the word ‘mutation’ have these scary connotations, and they aren’t necessarily scary,” said Kelly Wroblewski, director of infectious disease programs for the Association of Public Health Laboratories.
When a mutation rings public health alarms, it’s typically because it has combined with other mutations and, collectively, changed how the virus behaves. At that point, it may be named a variant. A variant can make a virus spread faster, or more easily jump between species. It can make a virus more successful at making people sicker, or change how our immune systems respond.
SARS-CoV-2 has been mutating for as long as we’ve known about it; mutations were identified by scientists throughout 2020. Though relevant scientifically – mutations can actually be helpful, acting like a fingerprint that allows scientists to track a virus’s spread – the identified strains mostly carried little concern for public health.
Then came the end of the year, when several variants began drawing scrutiny. One of the most concerning, first detected in the United Kingdom, appears to make the virus more transmissible. Emerging evidence suggests it also could be deadlier, though scientists are still debating that.
We know more about the U.K. variant than others not because it’s necessarily worse, but because the British have one of the best virus surveillance programs in the world, said William Hanage, PhD, an epidemiologist and a professor at Harvard University.
By contrast, the U.S. has one of the weakest genomic surveillance programs of any rich country, Dr. Hanage said. “As it is, people like me cobble together partnerships with places and try and beg them” for samples, he said on a recent call with reporters.
Other variant strains were identified in South Africa and Brazil, and they share some mutations with the U.K. variant. That those changes evolved independently in several parts of the world suggests they might present an evolutionary advantage for the virus. Yet another strain was recently identified in Southern California and flagged due to its increasing presence in hard-hit cities like Los Angeles.
The Southern California strain was detected because a team of researchers at Cedars-Sinai, a hospital and research center in Los Angeles, has unfettered access to patient samples. They were able to see that the strain made up a growing share of cases at the hospital in recent weeks, as well as among the limited number of other samples haphazardly collected at a network of labs in the region.
Not only does the U.S. do less genomic sequencing than most wealthy countries, but it also does its surveillance by happenstance. That means it takes longer to detect new strains and draw conclusions about them. It’s not yet clear, for example, whether that Southern California strain was truly worthy of a press release.
Vast swaths of America’s privatized and decentralized system of health care aren’t set up to send samples to public health or academic labs. “I’m more concerned about the systems to detect variants than I am these particular variants,” said Mark Pandori, PhD, director of Nevada’s public health laboratory and associate professor at the University of Nevada-Reno School of Medicine.
Limited genomic surveillance of viruses is yet another side effect of a fragmented and underfunded public health system that’s struggled to test, track contacts and get COVID-19 under control throughout the pandemic, Ms. Wroblewski said.
The nation’s public health infrastructure, generally funded on a disease-by-disease basis, has decent systems set up to sequence flu, foodborne illnesses and tuberculosis, but there has been no national strategy on COVID-19. “To look for variants, it needs to be a national picture if it’s going to be done well,” Ms. Wroblewski said.
The Biden administration has outlined a strategy for a national response to COVID-19, which includes expanded surveillance for variants.
So far, vaccines for COVID-19 appear to protect against the known variants. Moderna has said its vaccine is effective against the U.K. and South African strains, though it yields fewer antibodies in the face of the latter. The company is working to develop a revised dose of the vaccine that could be added to the current two-shot regimen as a precaution.
But a lot of damage can be done in the time it will take to roll out the current vaccine, let alone an update.
Even with limited sampling, the U.K. variant has been detected in more than two dozen U.S. states, and the Centers for Disease Control and Prevention has warned it could be the predominant strain in the U.S. by March. When it took off in the United Kingdom at the end of last year, it caused a swell in cases, overwhelmed hospitals, and led to a holiday lockdown. Whether the U.S. faces the same fate could depend on which strains it is competing against, and how the public behaves in the weeks ahead.
Already risky interactions among people could, on average, get a little riskier. Many researchers are calling for better masks and better indoor ventilation. But any updates on recommendations likely would play at the margins. Even if variants spread more easily, the same recommendations public health experts have been espousing for months – masking, physical distancing, and limiting time indoors with others – will be the best way to ward them off, said Kirsten Bibbins-Domingo, MD, a physician and professor at the University of California, San Francisco.
“It’s very unsexy what the solutions are,” Dr. Bibbins-Domingo said. “But we need everyone to do them.”
That doesn’t make the task simple. Masking remains controversial in many states, and the public’s patience for maintaining physical distance has worn thin.
Adding to the concerns: Though case numbers stabilized in many parts of the U.S. in January, they have stabilized at rates many times what they were during previous periods in the pandemic or in other parts of the world. Having all that virus in so many bodies creates more opportunities for new mutations and new variants to emerge.
“If we keep letting this thing sneak around, it’s going to get around all the measures we take against it, and that’s the worst possible thing,” said Nevada’s Dr. Pandori.
Compared with less virulent strains, a more contagious variant likely will require that more people be vaccinated before a community can see the benefits of widespread immunity. It’s a bleak outlook for a nation already falling behind in the race to vaccinate enough people to bring the pandemic under control.
“When your best solution is to ask people to do the things that they don’t like to do anyway, that’s very scary,” said Dr. Bibbins-Domingo.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
The COVID-19 variants that have emerged in the United Kingdom, Brazil, South Africa and now Southern California are eliciting two notably distinct responses from U.S. public health officials.
First, broad concern. A variant that wreaked havoc in the United Kingdom, leading to a spike in cases and hospitalizations, is surfacing in a growing number of places in the United States. During the week of Jan. 24, another worrisome variant seen in Brazil surfaced in Minnesota. If these or other strains significantly change the way the virus transmits and attacks the body, as scientists fear they might, they could cause yet another prolonged surge in illness and death in the U.S., even as cases have begun to plateau and vaccines are rolling out.
On the other hand, variants aren’t novel or even uncommon in viral illnesses. The viruses that trigger common colds and flus regularly evolve. Even if a mutated strain of SARS-CoV-2, the virus that causes COVID-19, makes it more contagious or makes people sicker,
The problem is that the U.S. has struggled with every step of its public health response in its first year of battle against COVID-19. And that raises the question of whether the nation will devote the attention and resources needed to outflank the virus as it evolves.
Researchers are quick to stress that a coronavirus mutation in itself is no cause for alarm. In the course of making millions and billions of copies as part of the infection process, small changes to a virus’s genome happen all the time as a function of evolutionary biology.
“The word ‘variant’ and the word ‘mutation’ have these scary connotations, and they aren’t necessarily scary,” said Kelly Wroblewski, director of infectious disease programs for the Association of Public Health Laboratories.
When a mutation rings public health alarms, it’s typically because it has combined with other mutations and, collectively, changed how the virus behaves. At that point, it may be named a variant. A variant can make a virus spread faster, or more easily jump between species. It can make a virus more successful at making people sicker, or change how our immune systems respond.
SARS-CoV-2 has been mutating for as long as we’ve known about it; mutations were identified by scientists throughout 2020. Though relevant scientifically – mutations can actually be helpful, acting like a fingerprint that allows scientists to track a virus’s spread – the identified strains mostly carried little concern for public health.
Then came the end of the year, when several variants began drawing scrutiny. One of the most concerning, first detected in the United Kingdom, appears to make the virus more transmissible. Emerging evidence suggests it also could be deadlier, though scientists are still debating that.
We know more about the U.K. variant than others not because it’s necessarily worse, but because the British have one of the best virus surveillance programs in the world, said William Hanage, PhD, an epidemiologist and a professor at Harvard University.
By contrast, the U.S. has one of the weakest genomic surveillance programs of any rich country, Dr. Hanage said. “As it is, people like me cobble together partnerships with places and try and beg them” for samples, he said on a recent call with reporters.
Other variant strains were identified in South Africa and Brazil, and they share some mutations with the U.K. variant. That those changes evolved independently in several parts of the world suggests they might present an evolutionary advantage for the virus. Yet another strain was recently identified in Southern California and flagged due to its increasing presence in hard-hit cities like Los Angeles.
The Southern California strain was detected because a team of researchers at Cedars-Sinai, a hospital and research center in Los Angeles, has unfettered access to patient samples. They were able to see that the strain made up a growing share of cases at the hospital in recent weeks, as well as among the limited number of other samples haphazardly collected at a network of labs in the region.
Not only does the U.S. do less genomic sequencing than most wealthy countries, but it also does its surveillance by happenstance. That means it takes longer to detect new strains and draw conclusions about them. It’s not yet clear, for example, whether that Southern California strain was truly worthy of a press release.
Vast swaths of America’s privatized and decentralized system of health care aren’t set up to send samples to public health or academic labs. “I’m more concerned about the systems to detect variants than I am these particular variants,” said Mark Pandori, PhD, director of Nevada’s public health laboratory and associate professor at the University of Nevada-Reno School of Medicine.
Limited genomic surveillance of viruses is yet another side effect of a fragmented and underfunded public health system that’s struggled to test, track contacts and get COVID-19 under control throughout the pandemic, Ms. Wroblewski said.
The nation’s public health infrastructure, generally funded on a disease-by-disease basis, has decent systems set up to sequence flu, foodborne illnesses and tuberculosis, but there has been no national strategy on COVID-19. “To look for variants, it needs to be a national picture if it’s going to be done well,” Ms. Wroblewski said.
The Biden administration has outlined a strategy for a national response to COVID-19, which includes expanded surveillance for variants.
So far, vaccines for COVID-19 appear to protect against the known variants. Moderna has said its vaccine is effective against the U.K. and South African strains, though it yields fewer antibodies in the face of the latter. The company is working to develop a revised dose of the vaccine that could be added to the current two-shot regimen as a precaution.
But a lot of damage can be done in the time it will take to roll out the current vaccine, let alone an update.
Even with limited sampling, the U.K. variant has been detected in more than two dozen U.S. states, and the Centers for Disease Control and Prevention has warned it could be the predominant strain in the U.S. by March. When it took off in the United Kingdom at the end of last year, it caused a swell in cases, overwhelmed hospitals, and led to a holiday lockdown. Whether the U.S. faces the same fate could depend on which strains it is competing against, and how the public behaves in the weeks ahead.
Already risky interactions among people could, on average, get a little riskier. Many researchers are calling for better masks and better indoor ventilation. But any updates on recommendations likely would play at the margins. Even if variants spread more easily, the same recommendations public health experts have been espousing for months – masking, physical distancing, and limiting time indoors with others – will be the best way to ward them off, said Kirsten Bibbins-Domingo, MD, a physician and professor at the University of California, San Francisco.
“It’s very unsexy what the solutions are,” Dr. Bibbins-Domingo said. “But we need everyone to do them.”
That doesn’t make the task simple. Masking remains controversial in many states, and the public’s patience for maintaining physical distance has worn thin.
Adding to the concerns: Though case numbers stabilized in many parts of the U.S. in January, they have stabilized at rates many times what they were during previous periods in the pandemic or in other parts of the world. Having all that virus in so many bodies creates more opportunities for new mutations and new variants to emerge.
“If we keep letting this thing sneak around, it’s going to get around all the measures we take against it, and that’s the worst possible thing,” said Nevada’s Dr. Pandori.
Compared with less virulent strains, a more contagious variant likely will require that more people be vaccinated before a community can see the benefits of widespread immunity. It’s a bleak outlook for a nation already falling behind in the race to vaccinate enough people to bring the pandemic under control.
“When your best solution is to ask people to do the things that they don’t like to do anyway, that’s very scary,” said Dr. Bibbins-Domingo.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
The COVID-19 variants that have emerged in the United Kingdom, Brazil, South Africa and now Southern California are eliciting two notably distinct responses from U.S. public health officials.
First, broad concern. A variant that wreaked havoc in the United Kingdom, leading to a spike in cases and hospitalizations, is surfacing in a growing number of places in the United States. During the week of Jan. 24, another worrisome variant seen in Brazil surfaced in Minnesota. If these or other strains significantly change the way the virus transmits and attacks the body, as scientists fear they might, they could cause yet another prolonged surge in illness and death in the U.S., even as cases have begun to plateau and vaccines are rolling out.
On the other hand, variants aren’t novel or even uncommon in viral illnesses. The viruses that trigger common colds and flus regularly evolve. Even if a mutated strain of SARS-CoV-2, the virus that causes COVID-19, makes it more contagious or makes people sicker,
The problem is that the U.S. has struggled with every step of its public health response in its first year of battle against COVID-19. And that raises the question of whether the nation will devote the attention and resources needed to outflank the virus as it evolves.
Researchers are quick to stress that a coronavirus mutation in itself is no cause for alarm. In the course of making millions and billions of copies as part of the infection process, small changes to a virus’s genome happen all the time as a function of evolutionary biology.
“The word ‘variant’ and the word ‘mutation’ have these scary connotations, and they aren’t necessarily scary,” said Kelly Wroblewski, director of infectious disease programs for the Association of Public Health Laboratories.
When a mutation rings public health alarms, it’s typically because it has combined with other mutations and, collectively, changed how the virus behaves. At that point, it may be named a variant. A variant can make a virus spread faster, or more easily jump between species. It can make a virus more successful at making people sicker, or change how our immune systems respond.
SARS-CoV-2 has been mutating for as long as we’ve known about it; mutations were identified by scientists throughout 2020. Though relevant scientifically – mutations can actually be helpful, acting like a fingerprint that allows scientists to track a virus’s spread – the identified strains mostly carried little concern for public health.
Then came the end of the year, when several variants began drawing scrutiny. One of the most concerning, first detected in the United Kingdom, appears to make the virus more transmissible. Emerging evidence suggests it also could be deadlier, though scientists are still debating that.
We know more about the U.K. variant than others not because it’s necessarily worse, but because the British have one of the best virus surveillance programs in the world, said William Hanage, PhD, an epidemiologist and a professor at Harvard University.
By contrast, the U.S. has one of the weakest genomic surveillance programs of any rich country, Dr. Hanage said. “As it is, people like me cobble together partnerships with places and try and beg them” for samples, he said on a recent call with reporters.
Other variant strains were identified in South Africa and Brazil, and they share some mutations with the U.K. variant. That those changes evolved independently in several parts of the world suggests they might present an evolutionary advantage for the virus. Yet another strain was recently identified in Southern California and flagged due to its increasing presence in hard-hit cities like Los Angeles.
The Southern California strain was detected because a team of researchers at Cedars-Sinai, a hospital and research center in Los Angeles, has unfettered access to patient samples. They were able to see that the strain made up a growing share of cases at the hospital in recent weeks, as well as among the limited number of other samples haphazardly collected at a network of labs in the region.
Not only does the U.S. do less genomic sequencing than most wealthy countries, but it also does its surveillance by happenstance. That means it takes longer to detect new strains and draw conclusions about them. It’s not yet clear, for example, whether that Southern California strain was truly worthy of a press release.
Vast swaths of America’s privatized and decentralized system of health care aren’t set up to send samples to public health or academic labs. “I’m more concerned about the systems to detect variants than I am these particular variants,” said Mark Pandori, PhD, director of Nevada’s public health laboratory and associate professor at the University of Nevada-Reno School of Medicine.
Limited genomic surveillance of viruses is yet another side effect of a fragmented and underfunded public health system that’s struggled to test, track contacts and get COVID-19 under control throughout the pandemic, Ms. Wroblewski said.
The nation’s public health infrastructure, generally funded on a disease-by-disease basis, has decent systems set up to sequence flu, foodborne illnesses and tuberculosis, but there has been no national strategy on COVID-19. “To look for variants, it needs to be a national picture if it’s going to be done well,” Ms. Wroblewski said.
The Biden administration has outlined a strategy for a national response to COVID-19, which includes expanded surveillance for variants.
So far, vaccines for COVID-19 appear to protect against the known variants. Moderna has said its vaccine is effective against the U.K. and South African strains, though it yields fewer antibodies in the face of the latter. The company is working to develop a revised dose of the vaccine that could be added to the current two-shot regimen as a precaution.
But a lot of damage can be done in the time it will take to roll out the current vaccine, let alone an update.
Even with limited sampling, the U.K. variant has been detected in more than two dozen U.S. states, and the Centers for Disease Control and Prevention has warned it could be the predominant strain in the U.S. by March. When it took off in the United Kingdom at the end of last year, it caused a swell in cases, overwhelmed hospitals, and led to a holiday lockdown. Whether the U.S. faces the same fate could depend on which strains it is competing against, and how the public behaves in the weeks ahead.
Already risky interactions among people could, on average, get a little riskier. Many researchers are calling for better masks and better indoor ventilation. But any updates on recommendations likely would play at the margins. Even if variants spread more easily, the same recommendations public health experts have been espousing for months – masking, physical distancing, and limiting time indoors with others – will be the best way to ward them off, said Kirsten Bibbins-Domingo, MD, a physician and professor at the University of California, San Francisco.
“It’s very unsexy what the solutions are,” Dr. Bibbins-Domingo said. “But we need everyone to do them.”
That doesn’t make the task simple. Masking remains controversial in many states, and the public’s patience for maintaining physical distance has worn thin.
Adding to the concerns: Though case numbers stabilized in many parts of the U.S. in January, they have stabilized at rates many times what they were during previous periods in the pandemic or in other parts of the world. Having all that virus in so many bodies creates more opportunities for new mutations and new variants to emerge.
“If we keep letting this thing sneak around, it’s going to get around all the measures we take against it, and that’s the worst possible thing,” said Nevada’s Dr. Pandori.
Compared with less virulent strains, a more contagious variant likely will require that more people be vaccinated before a community can see the benefits of widespread immunity. It’s a bleak outlook for a nation already falling behind in the race to vaccinate enough people to bring the pandemic under control.
“When your best solution is to ask people to do the things that they don’t like to do anyway, that’s very scary,” said Dr. Bibbins-Domingo.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
Protecting patients with diabetes from impact of COVID-19
Experts discuss how to best protect people with diabetes from serious COVID-19 outcomes in a newly published article that summarizes in-depth discussions on the topic from a conference held online last year.
Lead author and Diabetes Technology Society founder and director David C. Klonoff, MD, said in an interview: “To my knowledge this is the largest article or learning that has been written anywhere ever about the co-occurrence of COVID-19 and diabetes and how COVID-19 affects diabetes ... There are a lot of different dimensions.”
The 37-page report covers all sessions from the Virtual International COVID-19 and Diabetes Summit, held Aug. 26-27, 2020, which had 800 attendees from six continents, on topics including pathophysiology and COVID-19 risk factors, the impact of social determinants of health on diabetes and COVID-19, and psychological aspects of the COVID-19 pandemic for people with diabetes.
The freely available report was published online Jan. 21 in the Journal of Diabetes Science and Technology by Jennifer Y. Zhang of the Diabetes Technology Society, Burlingame, Calif., and colleagues.
Other topics include medications and vaccines, outpatient diabetes management during the COVID-19 pandemic and the growth of telehealth, inpatient management of diabetes in patients with or without COVID-19, ethical considerations, children, pregnancy, economics of care for COVID-19, government policy, regulation of tests and treatments, patient surveillance/privacy, and research gaps and opportunities.
“A comprehensive report like this is so important because it covers such a wide range of topics that are all relevant when it comes to protecting patients with diabetes during a pandemic. Our report aims to bring together all these different aspects of policy during the pandemic, patient physiology, and patient psychology, so I hope it will be widely read and widely appreciated,” Ms. Zhang said in an interview.
Two important clinical trends arising as a result of the pandemic – the advent of telehealth in diabetes management and the use of continuous glucose monitoring (CGM) in hospital – are expected to continue even after COVID-19 abates, said Dr. Klonoff, medical director of the Diabetes Research Institute at Mills-Peninsula Medical Center, San Mateo, Calif.
Telehealth in diabetes here to stay, in U.S. at least
Dr. Klonoff noted that with diabetes telehealth, or “telediabetes” as it’s been dubbed, by using downloaded device data patients don’t have to travel, pay for parking, or take as much time off work. “There are advantages ... patients really like it,” he said.
And for health care providers, an advantage of remote visits is that the clinician can look at the patient while reviewing the patient’s data. “With telehealth for diabetes, the patient’s face and the software data are right next to each other on the same screen. Even as I’m typing I’m looking at the patient ... I consider that a huge advantage,” Dr. Klonoff said.
Rule changes early in the pandemic made the shift to telehealth in the United States possible, he said.
“Fortunately, Medicare and other payers are covering telehealth. It used to be there was no coverage, so that was a damper. Now that it’s covered I don’t think that’s going to go back. Everybody likes it,” he said.
CGM in hospitals helps detect hypoglycemia on wards
Regarding the increase of inpatient CGM (continuous glucose monitoring) prompted by the need to minimize patient exposure of nursing staff during the pandemic and the relaxing of Food and Drug Administration rules about its use, Dr. Klonoff said this phenomenon has led to two other positive developments.
“For FDA, it’s actually an opportunity to see some data collected. To do a clinical trial [prior to] March 2020 you had to go through a lot of processes to do a study. Once it becomes part of clinical care, then you can collect a lot of data,” he noted.
Moreover, Dr. Klonoff said there’s an important new area where hospital use of CGM is emerging: detection of hypoglycemia on wards.
“When a patient is in the ICU, if they become hypoglycemic or hyperglycemic it will likely be detected. But on the wards, they simply don’t get the same attention. Just about every doctor has had a case where somebody drifted into hypoglycemia that wasn’t recognized and maybe even died,” he explained.
If, however, “patients treated with insulin could all have CGMs that would be so useful. It would send out an alarm. A lot of times people don’t eat when you think they will. Suddenly the insulin dose is inappropriate and the nurse didn’t realize. Or, if IV nutrition stops and the insulin is given [it can be harmful].”
Another example, he said, is a common scenario when insulin is used in patients who are treated with steroids. “They need insulin, but then the steroid is decreased and the insulin dose isn’t decreased fast enough. All those situations can be helped with CGM.”
Overall, he concluded, COVID-19 has provided many lessons, which are “expanding our horizons.”
Ms. Zhang has reported no relevant financial relationships. Dr. Klonoff has reported being a consultant for Dexcom, EOFlow, Fractyl, Lifecare, Novo Nordisk, Roche Diagnostics, Samsung, and Thirdwayv.
A version of this article first appeared on Medscape.com.
Experts discuss how to best protect people with diabetes from serious COVID-19 outcomes in a newly published article that summarizes in-depth discussions on the topic from a conference held online last year.
Lead author and Diabetes Technology Society founder and director David C. Klonoff, MD, said in an interview: “To my knowledge this is the largest article or learning that has been written anywhere ever about the co-occurrence of COVID-19 and diabetes and how COVID-19 affects diabetes ... There are a lot of different dimensions.”
The 37-page report covers all sessions from the Virtual International COVID-19 and Diabetes Summit, held Aug. 26-27, 2020, which had 800 attendees from six continents, on topics including pathophysiology and COVID-19 risk factors, the impact of social determinants of health on diabetes and COVID-19, and psychological aspects of the COVID-19 pandemic for people with diabetes.
The freely available report was published online Jan. 21 in the Journal of Diabetes Science and Technology by Jennifer Y. Zhang of the Diabetes Technology Society, Burlingame, Calif., and colleagues.
Other topics include medications and vaccines, outpatient diabetes management during the COVID-19 pandemic and the growth of telehealth, inpatient management of diabetes in patients with or without COVID-19, ethical considerations, children, pregnancy, economics of care for COVID-19, government policy, regulation of tests and treatments, patient surveillance/privacy, and research gaps and opportunities.
“A comprehensive report like this is so important because it covers such a wide range of topics that are all relevant when it comes to protecting patients with diabetes during a pandemic. Our report aims to bring together all these different aspects of policy during the pandemic, patient physiology, and patient psychology, so I hope it will be widely read and widely appreciated,” Ms. Zhang said in an interview.
Two important clinical trends arising as a result of the pandemic – the advent of telehealth in diabetes management and the use of continuous glucose monitoring (CGM) in hospital – are expected to continue even after COVID-19 abates, said Dr. Klonoff, medical director of the Diabetes Research Institute at Mills-Peninsula Medical Center, San Mateo, Calif.
Telehealth in diabetes here to stay, in U.S. at least
Dr. Klonoff noted that with diabetes telehealth, or “telediabetes” as it’s been dubbed, by using downloaded device data patients don’t have to travel, pay for parking, or take as much time off work. “There are advantages ... patients really like it,” he said.
And for health care providers, an advantage of remote visits is that the clinician can look at the patient while reviewing the patient’s data. “With telehealth for diabetes, the patient’s face and the software data are right next to each other on the same screen. Even as I’m typing I’m looking at the patient ... I consider that a huge advantage,” Dr. Klonoff said.
Rule changes early in the pandemic made the shift to telehealth in the United States possible, he said.
“Fortunately, Medicare and other payers are covering telehealth. It used to be there was no coverage, so that was a damper. Now that it’s covered I don’t think that’s going to go back. Everybody likes it,” he said.
CGM in hospitals helps detect hypoglycemia on wards
Regarding the increase of inpatient CGM (continuous glucose monitoring) prompted by the need to minimize patient exposure of nursing staff during the pandemic and the relaxing of Food and Drug Administration rules about its use, Dr. Klonoff said this phenomenon has led to two other positive developments.
“For FDA, it’s actually an opportunity to see some data collected. To do a clinical trial [prior to] March 2020 you had to go through a lot of processes to do a study. Once it becomes part of clinical care, then you can collect a lot of data,” he noted.
Moreover, Dr. Klonoff said there’s an important new area where hospital use of CGM is emerging: detection of hypoglycemia on wards.
“When a patient is in the ICU, if they become hypoglycemic or hyperglycemic it will likely be detected. But on the wards, they simply don’t get the same attention. Just about every doctor has had a case where somebody drifted into hypoglycemia that wasn’t recognized and maybe even died,” he explained.
If, however, “patients treated with insulin could all have CGMs that would be so useful. It would send out an alarm. A lot of times people don’t eat when you think they will. Suddenly the insulin dose is inappropriate and the nurse didn’t realize. Or, if IV nutrition stops and the insulin is given [it can be harmful].”
Another example, he said, is a common scenario when insulin is used in patients who are treated with steroids. “They need insulin, but then the steroid is decreased and the insulin dose isn’t decreased fast enough. All those situations can be helped with CGM.”
Overall, he concluded, COVID-19 has provided many lessons, which are “expanding our horizons.”
Ms. Zhang has reported no relevant financial relationships. Dr. Klonoff has reported being a consultant for Dexcom, EOFlow, Fractyl, Lifecare, Novo Nordisk, Roche Diagnostics, Samsung, and Thirdwayv.
A version of this article first appeared on Medscape.com.
Experts discuss how to best protect people with diabetes from serious COVID-19 outcomes in a newly published article that summarizes in-depth discussions on the topic from a conference held online last year.
Lead author and Diabetes Technology Society founder and director David C. Klonoff, MD, said in an interview: “To my knowledge this is the largest article or learning that has been written anywhere ever about the co-occurrence of COVID-19 and diabetes and how COVID-19 affects diabetes ... There are a lot of different dimensions.”
The 37-page report covers all sessions from the Virtual International COVID-19 and Diabetes Summit, held Aug. 26-27, 2020, which had 800 attendees from six continents, on topics including pathophysiology and COVID-19 risk factors, the impact of social determinants of health on diabetes and COVID-19, and psychological aspects of the COVID-19 pandemic for people with diabetes.
The freely available report was published online Jan. 21 in the Journal of Diabetes Science and Technology by Jennifer Y. Zhang of the Diabetes Technology Society, Burlingame, Calif., and colleagues.
Other topics include medications and vaccines, outpatient diabetes management during the COVID-19 pandemic and the growth of telehealth, inpatient management of diabetes in patients with or without COVID-19, ethical considerations, children, pregnancy, economics of care for COVID-19, government policy, regulation of tests and treatments, patient surveillance/privacy, and research gaps and opportunities.
“A comprehensive report like this is so important because it covers such a wide range of topics that are all relevant when it comes to protecting patients with diabetes during a pandemic. Our report aims to bring together all these different aspects of policy during the pandemic, patient physiology, and patient psychology, so I hope it will be widely read and widely appreciated,” Ms. Zhang said in an interview.
Two important clinical trends arising as a result of the pandemic – the advent of telehealth in diabetes management and the use of continuous glucose monitoring (CGM) in hospital – are expected to continue even after COVID-19 abates, said Dr. Klonoff, medical director of the Diabetes Research Institute at Mills-Peninsula Medical Center, San Mateo, Calif.
Telehealth in diabetes here to stay, in U.S. at least
Dr. Klonoff noted that with diabetes telehealth, or “telediabetes” as it’s been dubbed, by using downloaded device data patients don’t have to travel, pay for parking, or take as much time off work. “There are advantages ... patients really like it,” he said.
And for health care providers, an advantage of remote visits is that the clinician can look at the patient while reviewing the patient’s data. “With telehealth for diabetes, the patient’s face and the software data are right next to each other on the same screen. Even as I’m typing I’m looking at the patient ... I consider that a huge advantage,” Dr. Klonoff said.
Rule changes early in the pandemic made the shift to telehealth in the United States possible, he said.
“Fortunately, Medicare and other payers are covering telehealth. It used to be there was no coverage, so that was a damper. Now that it’s covered I don’t think that’s going to go back. Everybody likes it,” he said.
CGM in hospitals helps detect hypoglycemia on wards
Regarding the increase of inpatient CGM (continuous glucose monitoring) prompted by the need to minimize patient exposure of nursing staff during the pandemic and the relaxing of Food and Drug Administration rules about its use, Dr. Klonoff said this phenomenon has led to two other positive developments.
“For FDA, it’s actually an opportunity to see some data collected. To do a clinical trial [prior to] March 2020 you had to go through a lot of processes to do a study. Once it becomes part of clinical care, then you can collect a lot of data,” he noted.
Moreover, Dr. Klonoff said there’s an important new area where hospital use of CGM is emerging: detection of hypoglycemia on wards.
“When a patient is in the ICU, if they become hypoglycemic or hyperglycemic it will likely be detected. But on the wards, they simply don’t get the same attention. Just about every doctor has had a case where somebody drifted into hypoglycemia that wasn’t recognized and maybe even died,” he explained.
If, however, “patients treated with insulin could all have CGMs that would be so useful. It would send out an alarm. A lot of times people don’t eat when you think they will. Suddenly the insulin dose is inappropriate and the nurse didn’t realize. Or, if IV nutrition stops and the insulin is given [it can be harmful].”
Another example, he said, is a common scenario when insulin is used in patients who are treated with steroids. “They need insulin, but then the steroid is decreased and the insulin dose isn’t decreased fast enough. All those situations can be helped with CGM.”
Overall, he concluded, COVID-19 has provided many lessons, which are “expanding our horizons.”
Ms. Zhang has reported no relevant financial relationships. Dr. Klonoff has reported being a consultant for Dexcom, EOFlow, Fractyl, Lifecare, Novo Nordisk, Roche Diagnostics, Samsung, and Thirdwayv.
A version of this article first appeared on Medscape.com.
Neprilysin, corin singled out for potential to guide heart failure therapy
Although not correlated with each other, increased levels of circulating according to prospective analysis involving 1,009 HF patients.
This implies that these enzymes might have value for individualizing care, including treatment of patients in heart failure with preserved ejection fraction (HFpEF), reported a team of investigators led by D.H. Frank Gommans, MD, PhD, department of cardiology, Radboud University Medical Center, Nijmegen, the Netherlands.
When followed for up to 7 years and after adjustment for differences in sex and age, the highest risk for the primary composite endpoint of cardiovascular (CV) death and heart failure hospitalization was observed in those with both high soluble neprilysin (sNEP) and high soluble corin (sCOR). The lowest risk was observed in the group with low levels of both enzymes.
The data suggest that monitoring these enzymes might provide “a step toward individualized CHF patient management,” Dr. Gommans reported in JACC Heart Failure, the adjusted hazard ratio for elevated sNEP and sCOR translated into a greater than 50% increase in the composite primary endpoint relative to low levels of both (HR, 1.56; P = .003). After a “comprehensive multivariable analysis,” the increased risk remained substantial and significant (HR, 1.41; P = .03).
In the natriuretic peptide pathway, which has long been recognized as a mediator of vasodilation, venous compliance, diuresis, and other processes dysregulated in heart failure, NEP and COR are “key mediators,” according to the investigators, who cited previously published studies. More attention has turned to these enzymes as potential biomarkers in the context of the PARADIGM trial, which associated an angiotensin-receptor neprilysin inhibitor (ARNI) with a survival benefit in CHF.
The observational study consisted of CHF patients attending a heart failure clinic and who were ARNI naive at inclusion. On the basis of circulating enzyme measurements undertaken from blood samples employing standard techniques, they were stratified into four groups. Those with low levels of both enzymes served as the reference. They were compared with those with low sNEP and high sCOR, those with high sNEP and low sCOR, and those with high levels of both enzymes.
Over the course of a median 4.5 years of follow-up, there were 511 deaths, of which 54% were from a CV cause. There were also 331 heart failure hospitalizations. In all, 449 patients reached the primary composite endpoint.
When compared with the group with low sNEP and low sCOR, an elevation in either enzyme was associated with a numerically but not significantly greater hazard ratio for the primary composite endpoint. The lack of correlation in the elevation of these two enzymes suggests each provides different prognostic information, although it appears that both must be considered together to predict outcomes.
Clinically, stratification of these enzymes might be most useful in HFpEF patients. Relative to the separation of event curves in the CHF patients with reduced ejection fraction (HFrEF), the divergence in the event curves for HFpEF were greater. In addition, event curves separated from the reference in HFpEF patients but not the HFrEF patients if either enzyme was elevated.
Asked if these data hold particular promise for monitoring and individualizing therapy in HFpEF patients, Dr. Gommans said yes. Although he cautioned that this was an observational study and that the differences between the HFpEF and HFrEF should be considered exploratory, he agreed that components of the natriuretic peptide pathway have particular potential to provide new prognostic information and individualize care in HFpEF, where therapeutic options remain limited.
Stratification of natriuretic peptide enzymes in this group might “present as an interesting alternative to ejection fraction” for prognosis and the consideration of treatment choices, he suggested.
Although further validation of the prognostic importance of sNEP and sCOR is needed, according to Dr. Gommans, he foresees the potential of therapeutic trials based on elevated levels of these enzymes. For example, he speculated that these levels might distinguish HFpEF patients who could benefit from a first-line ARNI.
In an accompanying editorial, significant doubts were expressed about simple measurements of sNEP and sCOR concentrations to predict clinical course or guide treatment decisions. The authors of the editorial agreed this is an important area of study but warned of its complexity.
“Concentrations of circulating neprilysin have been shown to correlate poorly with neprilysin activity. Thus the rate of natriuretic peptide degradation by neprilysin cannot be determined solely by measuring circulating levels,” cautioned Peder L. Myhre, MD, PhD, who is a cardiology fellow at Akershus University Hospital in Nordbyhagen, Norway, and postdoc researcher at the University of Oslo.
“Accordingly, concentrations of neprilysin and corin cannot alone be used to predict response to therapies interacting with these peptides,” he added. He agreed that neprilysin and corin might be appropriate biomarkers in CHF, but he thinks the focus must be on their enzymatic activity, not their circulating levels.
“Measuring the enzymatic activity may be a feasible strategy, but this remains to be seen,” he said.
Dr. Gommans reported a financial relationship with Novartis. Dr. Myhre reported financial relationships with Amgen, Novartis, and Novo Nordisk.
Although not correlated with each other, increased levels of circulating according to prospective analysis involving 1,009 HF patients.
This implies that these enzymes might have value for individualizing care, including treatment of patients in heart failure with preserved ejection fraction (HFpEF), reported a team of investigators led by D.H. Frank Gommans, MD, PhD, department of cardiology, Radboud University Medical Center, Nijmegen, the Netherlands.
When followed for up to 7 years and after adjustment for differences in sex and age, the highest risk for the primary composite endpoint of cardiovascular (CV) death and heart failure hospitalization was observed in those with both high soluble neprilysin (sNEP) and high soluble corin (sCOR). The lowest risk was observed in the group with low levels of both enzymes.
The data suggest that monitoring these enzymes might provide “a step toward individualized CHF patient management,” Dr. Gommans reported in JACC Heart Failure, the adjusted hazard ratio for elevated sNEP and sCOR translated into a greater than 50% increase in the composite primary endpoint relative to low levels of both (HR, 1.56; P = .003). After a “comprehensive multivariable analysis,” the increased risk remained substantial and significant (HR, 1.41; P = .03).
In the natriuretic peptide pathway, which has long been recognized as a mediator of vasodilation, venous compliance, diuresis, and other processes dysregulated in heart failure, NEP and COR are “key mediators,” according to the investigators, who cited previously published studies. More attention has turned to these enzymes as potential biomarkers in the context of the PARADIGM trial, which associated an angiotensin-receptor neprilysin inhibitor (ARNI) with a survival benefit in CHF.
The observational study consisted of CHF patients attending a heart failure clinic and who were ARNI naive at inclusion. On the basis of circulating enzyme measurements undertaken from blood samples employing standard techniques, they were stratified into four groups. Those with low levels of both enzymes served as the reference. They were compared with those with low sNEP and high sCOR, those with high sNEP and low sCOR, and those with high levels of both enzymes.
Over the course of a median 4.5 years of follow-up, there were 511 deaths, of which 54% were from a CV cause. There were also 331 heart failure hospitalizations. In all, 449 patients reached the primary composite endpoint.
When compared with the group with low sNEP and low sCOR, an elevation in either enzyme was associated with a numerically but not significantly greater hazard ratio for the primary composite endpoint. The lack of correlation in the elevation of these two enzymes suggests each provides different prognostic information, although it appears that both must be considered together to predict outcomes.
Clinically, stratification of these enzymes might be most useful in HFpEF patients. Relative to the separation of event curves in the CHF patients with reduced ejection fraction (HFrEF), the divergence in the event curves for HFpEF were greater. In addition, event curves separated from the reference in HFpEF patients but not the HFrEF patients if either enzyme was elevated.
Asked if these data hold particular promise for monitoring and individualizing therapy in HFpEF patients, Dr. Gommans said yes. Although he cautioned that this was an observational study and that the differences between the HFpEF and HFrEF should be considered exploratory, he agreed that components of the natriuretic peptide pathway have particular potential to provide new prognostic information and individualize care in HFpEF, where therapeutic options remain limited.
Stratification of natriuretic peptide enzymes in this group might “present as an interesting alternative to ejection fraction” for prognosis and the consideration of treatment choices, he suggested.
Although further validation of the prognostic importance of sNEP and sCOR is needed, according to Dr. Gommans, he foresees the potential of therapeutic trials based on elevated levels of these enzymes. For example, he speculated that these levels might distinguish HFpEF patients who could benefit from a first-line ARNI.
In an accompanying editorial, significant doubts were expressed about simple measurements of sNEP and sCOR concentrations to predict clinical course or guide treatment decisions. The authors of the editorial agreed this is an important area of study but warned of its complexity.
“Concentrations of circulating neprilysin have been shown to correlate poorly with neprilysin activity. Thus the rate of natriuretic peptide degradation by neprilysin cannot be determined solely by measuring circulating levels,” cautioned Peder L. Myhre, MD, PhD, who is a cardiology fellow at Akershus University Hospital in Nordbyhagen, Norway, and postdoc researcher at the University of Oslo.
“Accordingly, concentrations of neprilysin and corin cannot alone be used to predict response to therapies interacting with these peptides,” he added. He agreed that neprilysin and corin might be appropriate biomarkers in CHF, but he thinks the focus must be on their enzymatic activity, not their circulating levels.
“Measuring the enzymatic activity may be a feasible strategy, but this remains to be seen,” he said.
Dr. Gommans reported a financial relationship with Novartis. Dr. Myhre reported financial relationships with Amgen, Novartis, and Novo Nordisk.
Although not correlated with each other, increased levels of circulating according to prospective analysis involving 1,009 HF patients.
This implies that these enzymes might have value for individualizing care, including treatment of patients in heart failure with preserved ejection fraction (HFpEF), reported a team of investigators led by D.H. Frank Gommans, MD, PhD, department of cardiology, Radboud University Medical Center, Nijmegen, the Netherlands.
When followed for up to 7 years and after adjustment for differences in sex and age, the highest risk for the primary composite endpoint of cardiovascular (CV) death and heart failure hospitalization was observed in those with both high soluble neprilysin (sNEP) and high soluble corin (sCOR). The lowest risk was observed in the group with low levels of both enzymes.
The data suggest that monitoring these enzymes might provide “a step toward individualized CHF patient management,” Dr. Gommans reported in JACC Heart Failure, the adjusted hazard ratio for elevated sNEP and sCOR translated into a greater than 50% increase in the composite primary endpoint relative to low levels of both (HR, 1.56; P = .003). After a “comprehensive multivariable analysis,” the increased risk remained substantial and significant (HR, 1.41; P = .03).
In the natriuretic peptide pathway, which has long been recognized as a mediator of vasodilation, venous compliance, diuresis, and other processes dysregulated in heart failure, NEP and COR are “key mediators,” according to the investigators, who cited previously published studies. More attention has turned to these enzymes as potential biomarkers in the context of the PARADIGM trial, which associated an angiotensin-receptor neprilysin inhibitor (ARNI) with a survival benefit in CHF.
The observational study consisted of CHF patients attending a heart failure clinic and who were ARNI naive at inclusion. On the basis of circulating enzyme measurements undertaken from blood samples employing standard techniques, they were stratified into four groups. Those with low levels of both enzymes served as the reference. They were compared with those with low sNEP and high sCOR, those with high sNEP and low sCOR, and those with high levels of both enzymes.
Over the course of a median 4.5 years of follow-up, there were 511 deaths, of which 54% were from a CV cause. There were also 331 heart failure hospitalizations. In all, 449 patients reached the primary composite endpoint.
When compared with the group with low sNEP and low sCOR, an elevation in either enzyme was associated with a numerically but not significantly greater hazard ratio for the primary composite endpoint. The lack of correlation in the elevation of these two enzymes suggests each provides different prognostic information, although it appears that both must be considered together to predict outcomes.
Clinically, stratification of these enzymes might be most useful in HFpEF patients. Relative to the separation of event curves in the CHF patients with reduced ejection fraction (HFrEF), the divergence in the event curves for HFpEF were greater. In addition, event curves separated from the reference in HFpEF patients but not the HFrEF patients if either enzyme was elevated.
Asked if these data hold particular promise for monitoring and individualizing therapy in HFpEF patients, Dr. Gommans said yes. Although he cautioned that this was an observational study and that the differences between the HFpEF and HFrEF should be considered exploratory, he agreed that components of the natriuretic peptide pathway have particular potential to provide new prognostic information and individualize care in HFpEF, where therapeutic options remain limited.
Stratification of natriuretic peptide enzymes in this group might “present as an interesting alternative to ejection fraction” for prognosis and the consideration of treatment choices, he suggested.
Although further validation of the prognostic importance of sNEP and sCOR is needed, according to Dr. Gommans, he foresees the potential of therapeutic trials based on elevated levels of these enzymes. For example, he speculated that these levels might distinguish HFpEF patients who could benefit from a first-line ARNI.
In an accompanying editorial, significant doubts were expressed about simple measurements of sNEP and sCOR concentrations to predict clinical course or guide treatment decisions. The authors of the editorial agreed this is an important area of study but warned of its complexity.
“Concentrations of circulating neprilysin have been shown to correlate poorly with neprilysin activity. Thus the rate of natriuretic peptide degradation by neprilysin cannot be determined solely by measuring circulating levels,” cautioned Peder L. Myhre, MD, PhD, who is a cardiology fellow at Akershus University Hospital in Nordbyhagen, Norway, and postdoc researcher at the University of Oslo.
“Accordingly, concentrations of neprilysin and corin cannot alone be used to predict response to therapies interacting with these peptides,” he added. He agreed that neprilysin and corin might be appropriate biomarkers in CHF, but he thinks the focus must be on their enzymatic activity, not their circulating levels.
“Measuring the enzymatic activity may be a feasible strategy, but this remains to be seen,” he said.
Dr. Gommans reported a financial relationship with Novartis. Dr. Myhre reported financial relationships with Amgen, Novartis, and Novo Nordisk.
FROM JACC HEART FAILURE
Anticoagulation and antiplatelet therapy after GI bleed cut mortality, ischemic events
Background: Resumption of AC or AP therapy for patients following a GIB represents a common clinical challenge. Interruption of these medications following a GIB is associated with increased risk of macrovascular events, thrombosis, morbidity, and death. Prior studies have found inconsistent risk of rebleeding and death with resumption of these therapies following GIB. Little evidence exists for long-term outcomes and optimal timing of AC and AP resumption.
Study design: Retrospective observational cohort study.
Setting: Two general hospitals in Spain.
Synopsis: Overall 871 patients (mean age, 79 years) presenting with GIB on AC or AP therapy were followed for a median of 25 months. A total of 63% of patients experienced one of the following: thrombotic events, recurrent bleeding, or death during follow-up. Resumption of therapy was associated with a twofold risk of rebleeding, but lower rates of ischemic events (hazard ratio, 0.62; 95% confidence interval, 0.4-0.9) and death (HR, 0.60; 95% CI, 0.45-0.80). Early resumption (7 days or less) was associated with more rebleeding (30.6% vs. 23.1%; P = .04), fewer ischemic events (13.6% vs. 20.4%; P = .02%), and no difference in death. Bleeding was more frequent with AC agents, compared with AP agents.
Although resumption of AC or AP following a GIB increased bleeding risk, this may be outweighed by reductions in ischemic events and death if these agents are continued. For hospitalist clinicians, this remains a nuanced and patient-centered decision.
Interpretation is limited by variability in GIB location, agents used, and timing of resumption. Also, the study population included a limited number of elderly patients with multiple comorbidities and high overall death rate.
Bottom line: Resuming AC and AP medications following gastrointestinal bleeding doubled the rebleeding risk but lowered the risk of ischemic events and death, compared with the discontinuation of these medications.
Citation: Sostres C et al. Risk of rebleeding, vascular events and death after gastrointestinal bleeding in anticoagulant and/or antiplatelet users. Aliment Pharmcol Ther. 2019 Oct;50:919-29.
Dr. Berry is assistant professor of medicine, hospital medicine, at the Rocky Mountain Veterans Affairs Regional Medical Center, Aurora, Colo.
Background: Resumption of AC or AP therapy for patients following a GIB represents a common clinical challenge. Interruption of these medications following a GIB is associated with increased risk of macrovascular events, thrombosis, morbidity, and death. Prior studies have found inconsistent risk of rebleeding and death with resumption of these therapies following GIB. Little evidence exists for long-term outcomes and optimal timing of AC and AP resumption.
Study design: Retrospective observational cohort study.
Setting: Two general hospitals in Spain.
Synopsis: Overall 871 patients (mean age, 79 years) presenting with GIB on AC or AP therapy were followed for a median of 25 months. A total of 63% of patients experienced one of the following: thrombotic events, recurrent bleeding, or death during follow-up. Resumption of therapy was associated with a twofold risk of rebleeding, but lower rates of ischemic events (hazard ratio, 0.62; 95% confidence interval, 0.4-0.9) and death (HR, 0.60; 95% CI, 0.45-0.80). Early resumption (7 days or less) was associated with more rebleeding (30.6% vs. 23.1%; P = .04), fewer ischemic events (13.6% vs. 20.4%; P = .02%), and no difference in death. Bleeding was more frequent with AC agents, compared with AP agents.
Although resumption of AC or AP following a GIB increased bleeding risk, this may be outweighed by reductions in ischemic events and death if these agents are continued. For hospitalist clinicians, this remains a nuanced and patient-centered decision.
Interpretation is limited by variability in GIB location, agents used, and timing of resumption. Also, the study population included a limited number of elderly patients with multiple comorbidities and high overall death rate.
Bottom line: Resuming AC and AP medications following gastrointestinal bleeding doubled the rebleeding risk but lowered the risk of ischemic events and death, compared with the discontinuation of these medications.
Citation: Sostres C et al. Risk of rebleeding, vascular events and death after gastrointestinal bleeding in anticoagulant and/or antiplatelet users. Aliment Pharmcol Ther. 2019 Oct;50:919-29.
Dr. Berry is assistant professor of medicine, hospital medicine, at the Rocky Mountain Veterans Affairs Regional Medical Center, Aurora, Colo.
Background: Resumption of AC or AP therapy for patients following a GIB represents a common clinical challenge. Interruption of these medications following a GIB is associated with increased risk of macrovascular events, thrombosis, morbidity, and death. Prior studies have found inconsistent risk of rebleeding and death with resumption of these therapies following GIB. Little evidence exists for long-term outcomes and optimal timing of AC and AP resumption.
Study design: Retrospective observational cohort study.
Setting: Two general hospitals in Spain.
Synopsis: Overall 871 patients (mean age, 79 years) presenting with GIB on AC or AP therapy were followed for a median of 25 months. A total of 63% of patients experienced one of the following: thrombotic events, recurrent bleeding, or death during follow-up. Resumption of therapy was associated with a twofold risk of rebleeding, but lower rates of ischemic events (hazard ratio, 0.62; 95% confidence interval, 0.4-0.9) and death (HR, 0.60; 95% CI, 0.45-0.80). Early resumption (7 days or less) was associated with more rebleeding (30.6% vs. 23.1%; P = .04), fewer ischemic events (13.6% vs. 20.4%; P = .02%), and no difference in death. Bleeding was more frequent with AC agents, compared with AP agents.
Although resumption of AC or AP following a GIB increased bleeding risk, this may be outweighed by reductions in ischemic events and death if these agents are continued. For hospitalist clinicians, this remains a nuanced and patient-centered decision.
Interpretation is limited by variability in GIB location, agents used, and timing of resumption. Also, the study population included a limited number of elderly patients with multiple comorbidities and high overall death rate.
Bottom line: Resuming AC and AP medications following gastrointestinal bleeding doubled the rebleeding risk but lowered the risk of ischemic events and death, compared with the discontinuation of these medications.
Citation: Sostres C et al. Risk of rebleeding, vascular events and death after gastrointestinal bleeding in anticoagulant and/or antiplatelet users. Aliment Pharmcol Ther. 2019 Oct;50:919-29.
Dr. Berry is assistant professor of medicine, hospital medicine, at the Rocky Mountain Veterans Affairs Regional Medical Center, Aurora, Colo.
Myocarditis by CMR may be rare after COVID-19 in elite athletes
Two recent observational studies suggest that myocarditis, at least on cardiac magnetic resonance (CMR) imaging, might be far less common in elite-level athletes recovering from COVID-19 than suggested in influential earlier reports.
Both new studies documented a rate less than one-quarter as high as those previously reported from smaller cohorts, raising questions about the diagnostic yield of CMR in highly conditioned athletes with recent COVID-19 absent other evidence, such as from biomarker assays or electrocardiography (ECG).
That could have implications for some top-tier university athletics programs that mandate CMR imaging, biomarker assays, and other evaluations for myocarditis on all their players who test positive for SARS-CoV-2 before they can return to play.
The findings collectively point to CMR imaging features that might be a hallmark of an athlete’s heart, characterized by normal myocardial remodeling brought on by elite-level exercise training, which in athletes with recent COVID-19 could be misinterpreted as evidence of myocarditis. That may have thrown off prevalence estimates in the literature, the studies’ investigators speculated.
The two studies were retrospective takes on university athletes who underwent CMR imaging while recovering from COVID-19, who were either asymptomatic or with only mild to moderate symptoms and were generally without ECG or troponin evidence of myocarditis.
One of them showed a less than 2% incidence of myocarditis by CMR among 145 such cases, a low yield for imaging that is “raising doubt regarding its utility to evaluate athletes without a clinical presentation or abnormal ancillary tests to support the diagnosis of myocarditis,” argues a report published Jan. 14 in JAMA Cardiology, with lead author Jitka Starekova, MD, University of Wisconsin – Madison.
“Part of the problem is that occult myocarditis is, at least with other viruses, a risk factor for sudden death in competitive athletes. So you don’t want to let one slip through the cracks,” senior author Scott B. Reeder, MD, PhD, from the same institution, said in an interview.
Whether a policy of routine CMR imaging in elite athletes who test positive for the new coronavirus is better than more selective use driven by symptoms or other screening tests is unknown. But the more pressing issue, Dr. Reeder said, “is if they have a normal electrocardiogram and troponins, do they still need cardiac magnetic resonance imaging?”
The current study, he said, “certainly provides helpful evidence that maybe we don’t need as many.”
The other study, which featured two control groups, saw a similarly low incidence of myocarditis by CMR in athletes with recent COVID-19. One of the control groups included university athletes imaged prior to the advent of SARS-CoV-2 in the university’s region of the country. The other consisted of apparently healthy adult nonathletes.
Armed with two non-COVID-19 cohorts and two athlete cohorts, the researchers found comparable rates of myocarditis by CMR in both the COVID-19 athletes and the healthy athletes. And only 3% of the COVID-19 athletes had the tell-tale CMR signs, notes the report, published Dec. 17 in Circulation, with lead author Daniel E. Clark, MD, MPH, Vanderbilt University Medical Center, Nashville, Tenn.
Reassurance and concern
“The incidence is much lower than we feared, and so that’s reassuring,” Clark said in an interview. Still, the athletes with myocarditis by CMR “would have been completely missed by a protocol that did not include cardiac MR, and that’s concerning,” he said. “Both had active myocarditis.”
The study’s two non-COVID-19 control groups – elite athletes in one and nonathletes in the other – allowed them to tease out the potential contribution of athletic myocardial remodeling to CMR features that could be interpreted as scar tissue, which are characterized by late gadolinium enhancement (LGE).
As it turned out, focal regions of LGE located in the right ventricular (RV) septum on the scans were often seen in both athlete cohorts. “This kind of trivial nonischemic fibrosis in the mid RV septal insertion site was common among athletic control subjects. It was seen in 24% of them, which is almost identical to the percentage that we saw in the COVID-19 athletes, 22%,” Dr. Clark said.
The LGE finding, wrote Dr. Clark and coauthors, “may represent remodeling from athletic training, and should not be conflated with myocarditis.”
Of note, the other study saw a comparable incidence of the same or a very similar CMR feature in its athletes; 26% of the Wisconsin COVID-19 athlete cohort showed limited focal LGE in the inferior RV insertion site.
“And you get a little bit in the mid-septum, as well,” Dr. Reeder said. But the sign, in the absence of any corresponding T2 abnormalities, was not judged to represent myocarditis. “We interpreted all of these studies with this potential confounder in mind.”
Conceivably, Dr. Reeder proposed, the earlier studies may have “over-called” the prevalence of myocarditis in their cohorts. “I haven’t seen their images, but it’s possible there could be false-positives.”
It’s noteworthy that the Vanderbilt and Wisconsin reports saw closely similar incidences of the tell-tale CMR sign in all the athlete cohorts whether or not COVID-19 was involved, Aaron L. Baggish, MD, Massachusetts General Hospital, Boston, said in an interview.
“It looks very much like just an unrecognized part of athletic remodeling and isn’t in any way, shape, or form implicated as being a COVID-related issue,” said Dr. Baggish, who directs the cardiovascular performance program at his center and is unaffiliated with either study.
Still, that connection remains unproven given how little is yet known about the prevalence of clinically important myocarditis in milder cases of COVID-19, according to an accompanying editorial from Jonathan H. Kim, MD, MSc.
Although isolated LGE at the interventricular RV insertion site is “more commonly described among masters-level endurance athletes, the clinical significance and prevalence of this finding in youthful athletes is uncertain and should not be assumed to be a normal consequence of intense athletic training in young competitive athletes,” argued Dr. Kim, of Emory University, Atlanta.
There’s probably little about being a young competitive athlete that would render a person any more or less prone to COVID-19 cardiac involvement, Dr. Baggish said. Rather, “I think what we’re seeing, as the studies continue to come out, is that prevalence estimates are getting into the low single digits.”
The estimates are similar to those associated with influenza before the COVID-19 age; about 2% of patients showed cardiac involvement, Dr. Baggish said. “So the degree to which COVID is a special virus from this perspective, I think, is still a topic of some debate.”
The two current studies have limitations and neither is positioned to change practice, he said. “I would say that they are both kind of important, reassuring pieces of an unfinished jigsaw puzzle. But we still don’t know what the picture on the puzzle is.”
Routine CMR for positive cases
The University of Wisconsin group looked at all of the institution’s competitive athletes who underwent gadolinium-enhanced CMR imaging and other tests during recovery from COVID-19 from the beginning of the pandemic to the end of November 2020.
The imaging was performed on average about 2 weeks after a first positive SARS-CoV-2 assay result. About one-half and one-fourth of the cohort had experienced mild and moderate symptoms, respectively, and about 17% were asymptomatic; none had been hospitalized.
All CMR scans were reviewed by two experienced radiologists for, among other things, evidence of myocarditis according to modified Lake Louise criteria, the group wrote. Those criteria are based on CMR markers of fibrosis and other characteristics of scarring from myocarditis.
Such evidence was seen in only two members of the cohort, or 1.4%, one with elevated troponins but normal with respect to other biomarkers, and the other negative for all assays. Both were asymptomatic at the time of imaging, the report noted.
The Vanderbilt analysis from Dr. Clark and associates centered on 59 university athletes recently with COVID-19 who underwent CMR imaging along with other tests about 3 weeks after confirmation of SARS-CoV-2 infection. Symptoms had been mild in 78% of the group, and the remainder were asymptomatic.
They were compared with 60 retrospectively identified college athletes and elite-conditioned military personnel who had undergone CMR imaging prior to the advent of COVID-19, and to 27 apparently healthy nonathlete adults in whom CMR had been previously performed to define normal CMR imaging criteria at that center.
The only two post-COVID-19 athletes who met modified Lake Louise criteria for myocarditis showed no abnormalities on ECG or myocardial strain echocardiography, and had normal troponins, the group reported.
The COVID-19 athletes showed increased cardiac chamber volumes and myocardial mass “consistent with athletic remodeling,” compared with the healthy control subjects, the group wrote. But “most standard CMR parameters were similar” between the COVID-19 athletes and the control athletes, consistent with the 22% and 24% rates, respectively, for the finding of focal late LGE isolated to the inferoseptal RV insertion site.
At the end of the day, all published experiences on athletes with recent COVID-19 “are descriptive studies, without any hint of follow-up,” Dr. Baggish noted, so their clinical implications are unknown.
“We need time to sit and watch to see what happens to these individuals,” he said. “And if the answer is nothing, then that’s a very reassuring story. If the answer is that we start to see events, then that’s really important for us to take stock of.”
Dr. Starekova had no disclosures. Dr. Reeder reports that the University of Wisconsin receives research support from GE Healthcare and Bracco Diagnostics; and that he has ownership interests in Calimetrix, Reveal Pharmaceuticals, Cellectar Biosciences, Elucent Medical, and HeartVista; and has received grant support from Bayer Healthcare. Disclosures for the other coauthors are in the report. Dr. Clark and coauthors had no disclosures. Dr. Baggish reported no conflicts. Kim discloses receiving funding from the National Heart, Lung, and Blood Institute; compensation as team cardiologist for the Atlanta Falcons; and research stipends from the Atlanta Track Club.
A version of this article first appeared on Medscape.com.
Two recent observational studies suggest that myocarditis, at least on cardiac magnetic resonance (CMR) imaging, might be far less common in elite-level athletes recovering from COVID-19 than suggested in influential earlier reports.
Both new studies documented a rate less than one-quarter as high as those previously reported from smaller cohorts, raising questions about the diagnostic yield of CMR in highly conditioned athletes with recent COVID-19 absent other evidence, such as from biomarker assays or electrocardiography (ECG).
That could have implications for some top-tier university athletics programs that mandate CMR imaging, biomarker assays, and other evaluations for myocarditis on all their players who test positive for SARS-CoV-2 before they can return to play.
The findings collectively point to CMR imaging features that might be a hallmark of an athlete’s heart, characterized by normal myocardial remodeling brought on by elite-level exercise training, which in athletes with recent COVID-19 could be misinterpreted as evidence of myocarditis. That may have thrown off prevalence estimates in the literature, the studies’ investigators speculated.
The two studies were retrospective takes on university athletes who underwent CMR imaging while recovering from COVID-19, who were either asymptomatic or with only mild to moderate symptoms and were generally without ECG or troponin evidence of myocarditis.
One of them showed a less than 2% incidence of myocarditis by CMR among 145 such cases, a low yield for imaging that is “raising doubt regarding its utility to evaluate athletes without a clinical presentation or abnormal ancillary tests to support the diagnosis of myocarditis,” argues a report published Jan. 14 in JAMA Cardiology, with lead author Jitka Starekova, MD, University of Wisconsin – Madison.
“Part of the problem is that occult myocarditis is, at least with other viruses, a risk factor for sudden death in competitive athletes. So you don’t want to let one slip through the cracks,” senior author Scott B. Reeder, MD, PhD, from the same institution, said in an interview.
Whether a policy of routine CMR imaging in elite athletes who test positive for the new coronavirus is better than more selective use driven by symptoms or other screening tests is unknown. But the more pressing issue, Dr. Reeder said, “is if they have a normal electrocardiogram and troponins, do they still need cardiac magnetic resonance imaging?”
The current study, he said, “certainly provides helpful evidence that maybe we don’t need as many.”
The other study, which featured two control groups, saw a similarly low incidence of myocarditis by CMR in athletes with recent COVID-19. One of the control groups included university athletes imaged prior to the advent of SARS-CoV-2 in the university’s region of the country. The other consisted of apparently healthy adult nonathletes.
Armed with two non-COVID-19 cohorts and two athlete cohorts, the researchers found comparable rates of myocarditis by CMR in both the COVID-19 athletes and the healthy athletes. And only 3% of the COVID-19 athletes had the tell-tale CMR signs, notes the report, published Dec. 17 in Circulation, with lead author Daniel E. Clark, MD, MPH, Vanderbilt University Medical Center, Nashville, Tenn.
Reassurance and concern
“The incidence is much lower than we feared, and so that’s reassuring,” Clark said in an interview. Still, the athletes with myocarditis by CMR “would have been completely missed by a protocol that did not include cardiac MR, and that’s concerning,” he said. “Both had active myocarditis.”
The study’s two non-COVID-19 control groups – elite athletes in one and nonathletes in the other – allowed them to tease out the potential contribution of athletic myocardial remodeling to CMR features that could be interpreted as scar tissue, which are characterized by late gadolinium enhancement (LGE).
As it turned out, focal regions of LGE located in the right ventricular (RV) septum on the scans were often seen in both athlete cohorts. “This kind of trivial nonischemic fibrosis in the mid RV septal insertion site was common among athletic control subjects. It was seen in 24% of them, which is almost identical to the percentage that we saw in the COVID-19 athletes, 22%,” Dr. Clark said.
The LGE finding, wrote Dr. Clark and coauthors, “may represent remodeling from athletic training, and should not be conflated with myocarditis.”
Of note, the other study saw a comparable incidence of the same or a very similar CMR feature in its athletes; 26% of the Wisconsin COVID-19 athlete cohort showed limited focal LGE in the inferior RV insertion site.
“And you get a little bit in the mid-septum, as well,” Dr. Reeder said. But the sign, in the absence of any corresponding T2 abnormalities, was not judged to represent myocarditis. “We interpreted all of these studies with this potential confounder in mind.”
Conceivably, Dr. Reeder proposed, the earlier studies may have “over-called” the prevalence of myocarditis in their cohorts. “I haven’t seen their images, but it’s possible there could be false-positives.”
It’s noteworthy that the Vanderbilt and Wisconsin reports saw closely similar incidences of the tell-tale CMR sign in all the athlete cohorts whether or not COVID-19 was involved, Aaron L. Baggish, MD, Massachusetts General Hospital, Boston, said in an interview.
“It looks very much like just an unrecognized part of athletic remodeling and isn’t in any way, shape, or form implicated as being a COVID-related issue,” said Dr. Baggish, who directs the cardiovascular performance program at his center and is unaffiliated with either study.
Still, that connection remains unproven given how little is yet known about the prevalence of clinically important myocarditis in milder cases of COVID-19, according to an accompanying editorial from Jonathan H. Kim, MD, MSc.
Although isolated LGE at the interventricular RV insertion site is “more commonly described among masters-level endurance athletes, the clinical significance and prevalence of this finding in youthful athletes is uncertain and should not be assumed to be a normal consequence of intense athletic training in young competitive athletes,” argued Dr. Kim, of Emory University, Atlanta.
There’s probably little about being a young competitive athlete that would render a person any more or less prone to COVID-19 cardiac involvement, Dr. Baggish said. Rather, “I think what we’re seeing, as the studies continue to come out, is that prevalence estimates are getting into the low single digits.”
The estimates are similar to those associated with influenza before the COVID-19 age; about 2% of patients showed cardiac involvement, Dr. Baggish said. “So the degree to which COVID is a special virus from this perspective, I think, is still a topic of some debate.”
The two current studies have limitations and neither is positioned to change practice, he said. “I would say that they are both kind of important, reassuring pieces of an unfinished jigsaw puzzle. But we still don’t know what the picture on the puzzle is.”
Routine CMR for positive cases
The University of Wisconsin group looked at all of the institution’s competitive athletes who underwent gadolinium-enhanced CMR imaging and other tests during recovery from COVID-19 from the beginning of the pandemic to the end of November 2020.
The imaging was performed on average about 2 weeks after a first positive SARS-CoV-2 assay result. About one-half and one-fourth of the cohort had experienced mild and moderate symptoms, respectively, and about 17% were asymptomatic; none had been hospitalized.
All CMR scans were reviewed by two experienced radiologists for, among other things, evidence of myocarditis according to modified Lake Louise criteria, the group wrote. Those criteria are based on CMR markers of fibrosis and other characteristics of scarring from myocarditis.
Such evidence was seen in only two members of the cohort, or 1.4%, one with elevated troponins but normal with respect to other biomarkers, and the other negative for all assays. Both were asymptomatic at the time of imaging, the report noted.
The Vanderbilt analysis from Dr. Clark and associates centered on 59 university athletes recently with COVID-19 who underwent CMR imaging along with other tests about 3 weeks after confirmation of SARS-CoV-2 infection. Symptoms had been mild in 78% of the group, and the remainder were asymptomatic.
They were compared with 60 retrospectively identified college athletes and elite-conditioned military personnel who had undergone CMR imaging prior to the advent of COVID-19, and to 27 apparently healthy nonathlete adults in whom CMR had been previously performed to define normal CMR imaging criteria at that center.
The only two post-COVID-19 athletes who met modified Lake Louise criteria for myocarditis showed no abnormalities on ECG or myocardial strain echocardiography, and had normal troponins, the group reported.
The COVID-19 athletes showed increased cardiac chamber volumes and myocardial mass “consistent with athletic remodeling,” compared with the healthy control subjects, the group wrote. But “most standard CMR parameters were similar” between the COVID-19 athletes and the control athletes, consistent with the 22% and 24% rates, respectively, for the finding of focal late LGE isolated to the inferoseptal RV insertion site.
At the end of the day, all published experiences on athletes with recent COVID-19 “are descriptive studies, without any hint of follow-up,” Dr. Baggish noted, so their clinical implications are unknown.
“We need time to sit and watch to see what happens to these individuals,” he said. “And if the answer is nothing, then that’s a very reassuring story. If the answer is that we start to see events, then that’s really important for us to take stock of.”
Dr. Starekova had no disclosures. Dr. Reeder reports that the University of Wisconsin receives research support from GE Healthcare and Bracco Diagnostics; and that he has ownership interests in Calimetrix, Reveal Pharmaceuticals, Cellectar Biosciences, Elucent Medical, and HeartVista; and has received grant support from Bayer Healthcare. Disclosures for the other coauthors are in the report. Dr. Clark and coauthors had no disclosures. Dr. Baggish reported no conflicts. Kim discloses receiving funding from the National Heart, Lung, and Blood Institute; compensation as team cardiologist for the Atlanta Falcons; and research stipends from the Atlanta Track Club.
A version of this article first appeared on Medscape.com.
Two recent observational studies suggest that myocarditis, at least on cardiac magnetic resonance (CMR) imaging, might be far less common in elite-level athletes recovering from COVID-19 than suggested in influential earlier reports.
Both new studies documented a rate less than one-quarter as high as those previously reported from smaller cohorts, raising questions about the diagnostic yield of CMR in highly conditioned athletes with recent COVID-19 absent other evidence, such as from biomarker assays or electrocardiography (ECG).
That could have implications for some top-tier university athletics programs that mandate CMR imaging, biomarker assays, and other evaluations for myocarditis on all their players who test positive for SARS-CoV-2 before they can return to play.
The findings collectively point to CMR imaging features that might be a hallmark of an athlete’s heart, characterized by normal myocardial remodeling brought on by elite-level exercise training, which in athletes with recent COVID-19 could be misinterpreted as evidence of myocarditis. That may have thrown off prevalence estimates in the literature, the studies’ investigators speculated.
The two studies were retrospective takes on university athletes who underwent CMR imaging while recovering from COVID-19, who were either asymptomatic or with only mild to moderate symptoms and were generally without ECG or troponin evidence of myocarditis.
One of them showed a less than 2% incidence of myocarditis by CMR among 145 such cases, a low yield for imaging that is “raising doubt regarding its utility to evaluate athletes without a clinical presentation or abnormal ancillary tests to support the diagnosis of myocarditis,” argues a report published Jan. 14 in JAMA Cardiology, with lead author Jitka Starekova, MD, University of Wisconsin – Madison.
“Part of the problem is that occult myocarditis is, at least with other viruses, a risk factor for sudden death in competitive athletes. So you don’t want to let one slip through the cracks,” senior author Scott B. Reeder, MD, PhD, from the same institution, said in an interview.
Whether a policy of routine CMR imaging in elite athletes who test positive for the new coronavirus is better than more selective use driven by symptoms or other screening tests is unknown. But the more pressing issue, Dr. Reeder said, “is if they have a normal electrocardiogram and troponins, do they still need cardiac magnetic resonance imaging?”
The current study, he said, “certainly provides helpful evidence that maybe we don’t need as many.”
The other study, which featured two control groups, saw a similarly low incidence of myocarditis by CMR in athletes with recent COVID-19. One of the control groups included university athletes imaged prior to the advent of SARS-CoV-2 in the university’s region of the country. The other consisted of apparently healthy adult nonathletes.
Armed with two non-COVID-19 cohorts and two athlete cohorts, the researchers found comparable rates of myocarditis by CMR in both the COVID-19 athletes and the healthy athletes. And only 3% of the COVID-19 athletes had the tell-tale CMR signs, notes the report, published Dec. 17 in Circulation, with lead author Daniel E. Clark, MD, MPH, Vanderbilt University Medical Center, Nashville, Tenn.
Reassurance and concern
“The incidence is much lower than we feared, and so that’s reassuring,” Clark said in an interview. Still, the athletes with myocarditis by CMR “would have been completely missed by a protocol that did not include cardiac MR, and that’s concerning,” he said. “Both had active myocarditis.”
The study’s two non-COVID-19 control groups – elite athletes in one and nonathletes in the other – allowed them to tease out the potential contribution of athletic myocardial remodeling to CMR features that could be interpreted as scar tissue, which are characterized by late gadolinium enhancement (LGE).
As it turned out, focal regions of LGE located in the right ventricular (RV) septum on the scans were often seen in both athlete cohorts. “This kind of trivial nonischemic fibrosis in the mid RV septal insertion site was common among athletic control subjects. It was seen in 24% of them, which is almost identical to the percentage that we saw in the COVID-19 athletes, 22%,” Dr. Clark said.
The LGE finding, wrote Dr. Clark and coauthors, “may represent remodeling from athletic training, and should not be conflated with myocarditis.”
Of note, the other study saw a comparable incidence of the same or a very similar CMR feature in its athletes; 26% of the Wisconsin COVID-19 athlete cohort showed limited focal LGE in the inferior RV insertion site.
“And you get a little bit in the mid-septum, as well,” Dr. Reeder said. But the sign, in the absence of any corresponding T2 abnormalities, was not judged to represent myocarditis. “We interpreted all of these studies with this potential confounder in mind.”
Conceivably, Dr. Reeder proposed, the earlier studies may have “over-called” the prevalence of myocarditis in their cohorts. “I haven’t seen their images, but it’s possible there could be false-positives.”
It’s noteworthy that the Vanderbilt and Wisconsin reports saw closely similar incidences of the tell-tale CMR sign in all the athlete cohorts whether or not COVID-19 was involved, Aaron L. Baggish, MD, Massachusetts General Hospital, Boston, said in an interview.
“It looks very much like just an unrecognized part of athletic remodeling and isn’t in any way, shape, or form implicated as being a COVID-related issue,” said Dr. Baggish, who directs the cardiovascular performance program at his center and is unaffiliated with either study.
Still, that connection remains unproven given how little is yet known about the prevalence of clinically important myocarditis in milder cases of COVID-19, according to an accompanying editorial from Jonathan H. Kim, MD, MSc.
Although isolated LGE at the interventricular RV insertion site is “more commonly described among masters-level endurance athletes, the clinical significance and prevalence of this finding in youthful athletes is uncertain and should not be assumed to be a normal consequence of intense athletic training in young competitive athletes,” argued Dr. Kim, of Emory University, Atlanta.
There’s probably little about being a young competitive athlete that would render a person any more or less prone to COVID-19 cardiac involvement, Dr. Baggish said. Rather, “I think what we’re seeing, as the studies continue to come out, is that prevalence estimates are getting into the low single digits.”
The estimates are similar to those associated with influenza before the COVID-19 age; about 2% of patients showed cardiac involvement, Dr. Baggish said. “So the degree to which COVID is a special virus from this perspective, I think, is still a topic of some debate.”
The two current studies have limitations and neither is positioned to change practice, he said. “I would say that they are both kind of important, reassuring pieces of an unfinished jigsaw puzzle. But we still don’t know what the picture on the puzzle is.”
Routine CMR for positive cases
The University of Wisconsin group looked at all of the institution’s competitive athletes who underwent gadolinium-enhanced CMR imaging and other tests during recovery from COVID-19 from the beginning of the pandemic to the end of November 2020.
The imaging was performed on average about 2 weeks after a first positive SARS-CoV-2 assay result. About one-half and one-fourth of the cohort had experienced mild and moderate symptoms, respectively, and about 17% were asymptomatic; none had been hospitalized.
All CMR scans were reviewed by two experienced radiologists for, among other things, evidence of myocarditis according to modified Lake Louise criteria, the group wrote. Those criteria are based on CMR markers of fibrosis and other characteristics of scarring from myocarditis.
Such evidence was seen in only two members of the cohort, or 1.4%, one with elevated troponins but normal with respect to other biomarkers, and the other negative for all assays. Both were asymptomatic at the time of imaging, the report noted.
The Vanderbilt analysis from Dr. Clark and associates centered on 59 university athletes recently with COVID-19 who underwent CMR imaging along with other tests about 3 weeks after confirmation of SARS-CoV-2 infection. Symptoms had been mild in 78% of the group, and the remainder were asymptomatic.
They were compared with 60 retrospectively identified college athletes and elite-conditioned military personnel who had undergone CMR imaging prior to the advent of COVID-19, and to 27 apparently healthy nonathlete adults in whom CMR had been previously performed to define normal CMR imaging criteria at that center.
The only two post-COVID-19 athletes who met modified Lake Louise criteria for myocarditis showed no abnormalities on ECG or myocardial strain echocardiography, and had normal troponins, the group reported.
The COVID-19 athletes showed increased cardiac chamber volumes and myocardial mass “consistent with athletic remodeling,” compared with the healthy control subjects, the group wrote. But “most standard CMR parameters were similar” between the COVID-19 athletes and the control athletes, consistent with the 22% and 24% rates, respectively, for the finding of focal late LGE isolated to the inferoseptal RV insertion site.
At the end of the day, all published experiences on athletes with recent COVID-19 “are descriptive studies, without any hint of follow-up,” Dr. Baggish noted, so their clinical implications are unknown.
“We need time to sit and watch to see what happens to these individuals,” he said. “And if the answer is nothing, then that’s a very reassuring story. If the answer is that we start to see events, then that’s really important for us to take stock of.”
Dr. Starekova had no disclosures. Dr. Reeder reports that the University of Wisconsin receives research support from GE Healthcare and Bracco Diagnostics; and that he has ownership interests in Calimetrix, Reveal Pharmaceuticals, Cellectar Biosciences, Elucent Medical, and HeartVista; and has received grant support from Bayer Healthcare. Disclosures for the other coauthors are in the report. Dr. Clark and coauthors had no disclosures. Dr. Baggish reported no conflicts. Kim discloses receiving funding from the National Heart, Lung, and Blood Institute; compensation as team cardiologist for the Atlanta Falcons; and research stipends from the Atlanta Track Club.
A version of this article first appeared on Medscape.com.
COVID-19 Wellbeing
Resources for hospitalists
SHM is committed to supporting hospitalists and the health care team to safely deliver patient care while maintaining the health and wellbeing of the families and the community they serve. SHM has developed resources for hospitalists as well as compiled a listing of existing resources which you can find on our website. The resources include:
Hospital Medicine COVID-19 Check-in Guide for Self & Peers
This is the first resource produced by SHM’s Wellbeing Taskforce to address the issues of hospitalist burnout and mental health during COVID-19. It is designed to help hospitalists to break the culture of silence around wellbeing, burnout, and mental health during COVID-19 by encouraging open conversation around how they are handling and processing the pandemic. Download the guide at https://bit.ly/3nxikzl.
SHM’s Strategies for Hospitalist Wellbeing Initiatives during COVID-19
This resource was developed based on information shared during an April 2020 webinar on Provider Wellbeing. Included are examples of initiatives currently being implemented by various hospital medicine groups. You can find this resource at https://bit.ly/3seNBKQ.
Webinars
Hear experiences and examples of how hospitalists and hospital medicine grouups are managing their response to the clinical and practice implications of COVID-19. Webinars have included topics related to hospitalist wellbeing. For instance, a recent webinar featured Gail Gazelle, MD, MCC, a physician coach, author, and mentor focused on burnout and resilience. This was a virtual, confidential session created for hospitalists to have a space for honest reflection, support, and the exploration of strategies for navigating the stress and challenges of being on the front lines of the COVID-19 response and in caring for themselves and their families during a pandemic. See upcoming and recorded SHM webinars on the website: www.hospitalmedicine.org/clinical-topics/coronavirus-disease-2019-covid-19-resources-for-hospitalists/webinars.
Other resources not provided directly by SHM include:
Physician Support Line: volunteer psychiatrist-staffed helpline for free and confidential peer support to discuss immediate life stressors. Available 7 days a week, 8:00am-12:00am EST. Contact number: 888-409-0141
Talkspace: virtual therapy tool offering a free month of Unlimited Messaging Plus for health care providers by registering using their NPI. Download app in App Store or Google Play.
National Suicide Prevention Lifeline: free and confidential crisis hotline for anyone available 24/7 across the United States. Contact number: 800-273-8255.
Headspace Meditation App: app-based meditation tool. Premium version (Headspace Plus) available free for health care providers through 2020 by registering using their National Provider Identifier (NPI). Download app in App Store or Google Play.
Tide: A free app that uses natural sounds to help you sleep, relax, focus, and meditate. Tide also listens to your breathing to play an alarm during your lightest sleep phase, waking you up as gently as possible. Their premium service is available to all health care workers. Download app in App Store or Google Play.
Resources for hospitalists
Resources for hospitalists
SHM is committed to supporting hospitalists and the health care team to safely deliver patient care while maintaining the health and wellbeing of the families and the community they serve. SHM has developed resources for hospitalists as well as compiled a listing of existing resources which you can find on our website. The resources include:
Hospital Medicine COVID-19 Check-in Guide for Self & Peers
This is the first resource produced by SHM’s Wellbeing Taskforce to address the issues of hospitalist burnout and mental health during COVID-19. It is designed to help hospitalists to break the culture of silence around wellbeing, burnout, and mental health during COVID-19 by encouraging open conversation around how they are handling and processing the pandemic. Download the guide at https://bit.ly/3nxikzl.
SHM’s Strategies for Hospitalist Wellbeing Initiatives during COVID-19
This resource was developed based on information shared during an April 2020 webinar on Provider Wellbeing. Included are examples of initiatives currently being implemented by various hospital medicine groups. You can find this resource at https://bit.ly/3seNBKQ.
Webinars
Hear experiences and examples of how hospitalists and hospital medicine grouups are managing their response to the clinical and practice implications of COVID-19. Webinars have included topics related to hospitalist wellbeing. For instance, a recent webinar featured Gail Gazelle, MD, MCC, a physician coach, author, and mentor focused on burnout and resilience. This was a virtual, confidential session created for hospitalists to have a space for honest reflection, support, and the exploration of strategies for navigating the stress and challenges of being on the front lines of the COVID-19 response and in caring for themselves and their families during a pandemic. See upcoming and recorded SHM webinars on the website: www.hospitalmedicine.org/clinical-topics/coronavirus-disease-2019-covid-19-resources-for-hospitalists/webinars.
Other resources not provided directly by SHM include:
Physician Support Line: volunteer psychiatrist-staffed helpline for free and confidential peer support to discuss immediate life stressors. Available 7 days a week, 8:00am-12:00am EST. Contact number: 888-409-0141
Talkspace: virtual therapy tool offering a free month of Unlimited Messaging Plus for health care providers by registering using their NPI. Download app in App Store or Google Play.
National Suicide Prevention Lifeline: free and confidential crisis hotline for anyone available 24/7 across the United States. Contact number: 800-273-8255.
Headspace Meditation App: app-based meditation tool. Premium version (Headspace Plus) available free for health care providers through 2020 by registering using their National Provider Identifier (NPI). Download app in App Store or Google Play.
Tide: A free app that uses natural sounds to help you sleep, relax, focus, and meditate. Tide also listens to your breathing to play an alarm during your lightest sleep phase, waking you up as gently as possible. Their premium service is available to all health care workers. Download app in App Store or Google Play.
SHM is committed to supporting hospitalists and the health care team to safely deliver patient care while maintaining the health and wellbeing of the families and the community they serve. SHM has developed resources for hospitalists as well as compiled a listing of existing resources which you can find on our website. The resources include:
Hospital Medicine COVID-19 Check-in Guide for Self & Peers
This is the first resource produced by SHM’s Wellbeing Taskforce to address the issues of hospitalist burnout and mental health during COVID-19. It is designed to help hospitalists to break the culture of silence around wellbeing, burnout, and mental health during COVID-19 by encouraging open conversation around how they are handling and processing the pandemic. Download the guide at https://bit.ly/3nxikzl.
SHM’s Strategies for Hospitalist Wellbeing Initiatives during COVID-19
This resource was developed based on information shared during an April 2020 webinar on Provider Wellbeing. Included are examples of initiatives currently being implemented by various hospital medicine groups. You can find this resource at https://bit.ly/3seNBKQ.
Webinars
Hear experiences and examples of how hospitalists and hospital medicine grouups are managing their response to the clinical and practice implications of COVID-19. Webinars have included topics related to hospitalist wellbeing. For instance, a recent webinar featured Gail Gazelle, MD, MCC, a physician coach, author, and mentor focused on burnout and resilience. This was a virtual, confidential session created for hospitalists to have a space for honest reflection, support, and the exploration of strategies for navigating the stress and challenges of being on the front lines of the COVID-19 response and in caring for themselves and their families during a pandemic. See upcoming and recorded SHM webinars on the website: www.hospitalmedicine.org/clinical-topics/coronavirus-disease-2019-covid-19-resources-for-hospitalists/webinars.
Other resources not provided directly by SHM include:
Physician Support Line: volunteer psychiatrist-staffed helpline for free and confidential peer support to discuss immediate life stressors. Available 7 days a week, 8:00am-12:00am EST. Contact number: 888-409-0141
Talkspace: virtual therapy tool offering a free month of Unlimited Messaging Plus for health care providers by registering using their NPI. Download app in App Store or Google Play.
National Suicide Prevention Lifeline: free and confidential crisis hotline for anyone available 24/7 across the United States. Contact number: 800-273-8255.
Headspace Meditation App: app-based meditation tool. Premium version (Headspace Plus) available free for health care providers through 2020 by registering using their National Provider Identifier (NPI). Download app in App Store or Google Play.
Tide: A free app that uses natural sounds to help you sleep, relax, focus, and meditate. Tide also listens to your breathing to play an alarm during your lightest sleep phase, waking you up as gently as possible. Their premium service is available to all health care workers. Download app in App Store or Google Play.
Weekly COVID-19 cases in children dropped 22%
according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
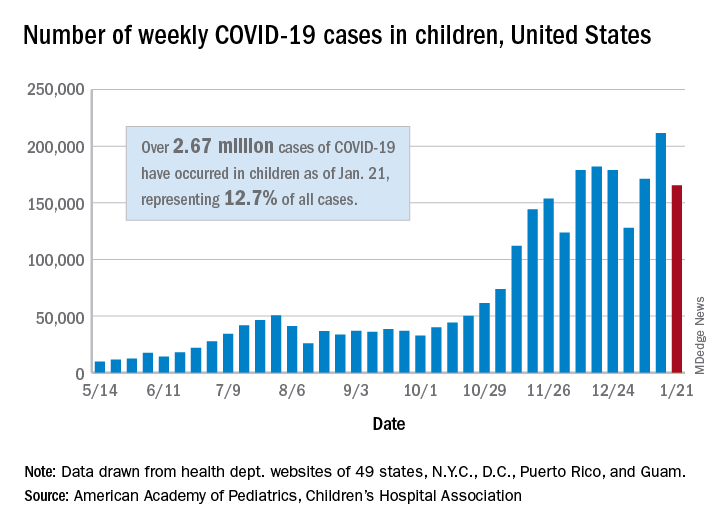
The 165,000 new cases reported during the week of Jan. 15-21 were down by almost 22% from the previous week’s 211,000, when the new-case count reached its highest point in the pandemic, the AAP and CHA said in their weekly COVID-19 report.
Cumulative cases in children now stand at just over 2.67 million, and children represent 12.7% of all COVID-19 cases reported by 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. For the week of Jan. 15-21, children made up 14.8% of all new cases, the highest proportion since late September, the AAP/CHA data show.
The cumulative rate of infection among children is up to 3,556 per 100,000 nationally, with states ranging from 943 per 100,000 in Hawaii to 8,195 in North Dakota. California has the most reported cases at 383,000, while Vermont has the fewest at 1,820, the two organizations reported.
There were 14 more deaths among children in the last week, bringing the total to 205 in the 43 states (plus New York City and Guam) reporting such data. Children represent just 0.06% of all coronavirus-related deaths, and only 0.01% of all cases in children have resulted in death, the AAP and CHA said. There are still 10 states where no children have died from COVID-19.
Although severe illness appears to be rare in children, the AAP and CHA noted, “there is an urgent need to collect more data on longer-term impacts of the pandemic on children, including ways the virus may harm the long-term physical health of infected children, as well as its emotional and mental health effects.”
according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
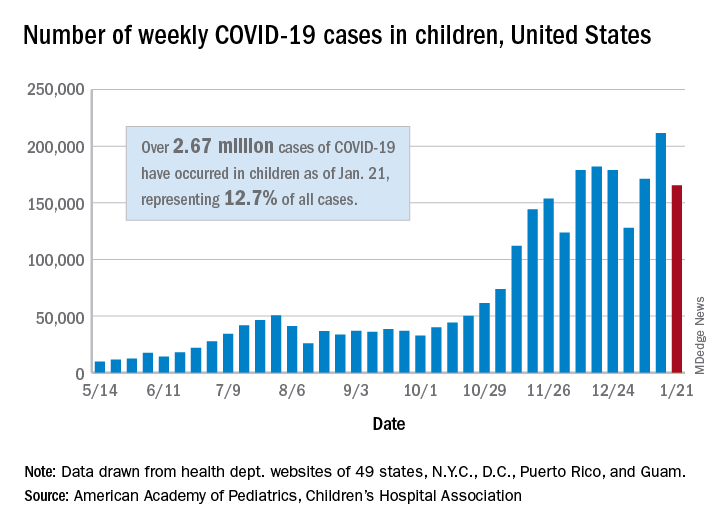
The 165,000 new cases reported during the week of Jan. 15-21 were down by almost 22% from the previous week’s 211,000, when the new-case count reached its highest point in the pandemic, the AAP and CHA said in their weekly COVID-19 report.
Cumulative cases in children now stand at just over 2.67 million, and children represent 12.7% of all COVID-19 cases reported by 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. For the week of Jan. 15-21, children made up 14.8% of all new cases, the highest proportion since late September, the AAP/CHA data show.
The cumulative rate of infection among children is up to 3,556 per 100,000 nationally, with states ranging from 943 per 100,000 in Hawaii to 8,195 in North Dakota. California has the most reported cases at 383,000, while Vermont has the fewest at 1,820, the two organizations reported.
There were 14 more deaths among children in the last week, bringing the total to 205 in the 43 states (plus New York City and Guam) reporting such data. Children represent just 0.06% of all coronavirus-related deaths, and only 0.01% of all cases in children have resulted in death, the AAP and CHA said. There are still 10 states where no children have died from COVID-19.
Although severe illness appears to be rare in children, the AAP and CHA noted, “there is an urgent need to collect more data on longer-term impacts of the pandemic on children, including ways the virus may harm the long-term physical health of infected children, as well as its emotional and mental health effects.”
according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
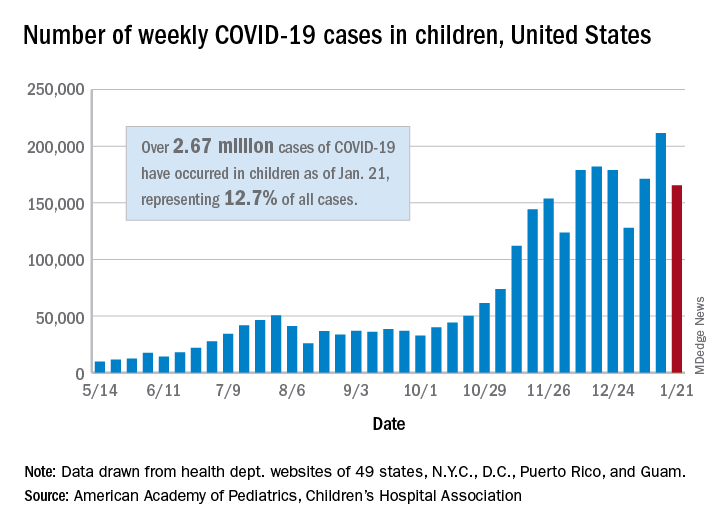
The 165,000 new cases reported during the week of Jan. 15-21 were down by almost 22% from the previous week’s 211,000, when the new-case count reached its highest point in the pandemic, the AAP and CHA said in their weekly COVID-19 report.
Cumulative cases in children now stand at just over 2.67 million, and children represent 12.7% of all COVID-19 cases reported by 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. For the week of Jan. 15-21, children made up 14.8% of all new cases, the highest proportion since late September, the AAP/CHA data show.
The cumulative rate of infection among children is up to 3,556 per 100,000 nationally, with states ranging from 943 per 100,000 in Hawaii to 8,195 in North Dakota. California has the most reported cases at 383,000, while Vermont has the fewest at 1,820, the two organizations reported.
There were 14 more deaths among children in the last week, bringing the total to 205 in the 43 states (plus New York City and Guam) reporting such data. Children represent just 0.06% of all coronavirus-related deaths, and only 0.01% of all cases in children have resulted in death, the AAP and CHA said. There are still 10 states where no children have died from COVID-19.
Although severe illness appears to be rare in children, the AAP and CHA noted, “there is an urgent need to collect more data on longer-term impacts of the pandemic on children, including ways the virus may harm the long-term physical health of infected children, as well as its emotional and mental health effects.”
Hospitalist movers and shakers: January 2021
Daniel Steinberg, MD, SFHM, recently was among 10 medical educators across the county to receive the Accreditation Council for Graduate Medical Education 2021 Parker J. Palmer Courage to Teach Award. Considered the most prestigious award given to graduate medical education program directors, it “recognizes program directors who have fostered innovation and improvement in their residency/fellowship program and served as exemplary role models for residents and fellows.”
Dr. Steinberg was program director for internal medicine residency at Mount Sinai Beth Israel, New York, for 11 years (2009-20) before becoming associate dean for quality and patient safety in graduate medical education in September. He is a professor of medicine and medical education at Icahn School of Medicine at Mount Sinai, New York.
Dr. Steinberg also is a leader within SHM, serving on the education, physicians-in-training, and annual conference committees. He is the course director for SHM Converge 2021.
Ann Sheehy, MD, SFHM, was honored in a virtual ceremony in December 2020 by the University of Wisconsin celebrating Physician Excellence Award winners. She was presented with the Physician Excellence Leadership Award.
Dr. Sheehy is division chief of the division of hospital medicine at the University of Wisconsin–Madison, and chair of the SHM Public Policy Committee.
Donald Schmidt, MD, has been named chief medical officer and vice president of medical affairs at Madonna Rehabilitation Hospitals in Omaha and Lincoln, Neb. He will replace Thomas Stalder, MD, who is retiring. Dr. Schmidt brings 20 years of experience to Madonna Rehabilitation Hospitals, including his most recent post as a hospitalist and medical director of the hospitalist program at Catholic Health Initiatives Health St. Elizabeth (Lincoln, Neb.).
Dr. Schmidt currently serves on the board of directors for OneHealth Nebraska, an independent physicians association.
Ezinne Nwude, MD, recently was presented with the SCP Health Excellence in Leadership Award during the organization’s Medical Leadership Conference. Dr. Nwude is chief of staff and hospitalist at the Medical Center of South Arkansas, El Dorado.
SCP Health coordinates staffing for more than 7,500 providers covering 30 states and is one of the nation’s largest clinical practice management companies. More than 420 medical leaders nationwide were eligible for the award. Dr. Nwude has focused on positive culture and health education since her start at MSCA in 2014. She has been chief of staff since October 2018.
RWJ Barnabas Health (West Orange, N.J.) recently named two new health system leaders from among its hospital medicine ranks, as Christopher Freer, MD, was tabbed as senior vice president for emergency and hospital medicine, and Maninder “Dolly” Abraham, MD, was picked as chief of hospital medicine. The moves were made as RWJBH takes over as the direct employer for Envision Physician Services in Nashville, Tenn.
Dr. Freer was elevated to his new role after spending the past 5 years as RWJBH’s system director for emergency services. He has nearly 3 decades of experience in hospital medicine.
Dr. Abraham comes to his new position after directing the hospitalist program at Saint Barnabas and serving as regional medical director with Envision.
Newman Regional Health (Emporia, Kan.) recently established a partnership with FreeState Healthcare (Wichita, Kan.). FreeState will be responsible for providing hospitalist services to adult inpatients and observation patients at Newman Regional Health during overnights.
Daniel Steinberg, MD, SFHM, recently was among 10 medical educators across the county to receive the Accreditation Council for Graduate Medical Education 2021 Parker J. Palmer Courage to Teach Award. Considered the most prestigious award given to graduate medical education program directors, it “recognizes program directors who have fostered innovation and improvement in their residency/fellowship program and served as exemplary role models for residents and fellows.”
Dr. Steinberg was program director for internal medicine residency at Mount Sinai Beth Israel, New York, for 11 years (2009-20) before becoming associate dean for quality and patient safety in graduate medical education in September. He is a professor of medicine and medical education at Icahn School of Medicine at Mount Sinai, New York.
Dr. Steinberg also is a leader within SHM, serving on the education, physicians-in-training, and annual conference committees. He is the course director for SHM Converge 2021.
Ann Sheehy, MD, SFHM, was honored in a virtual ceremony in December 2020 by the University of Wisconsin celebrating Physician Excellence Award winners. She was presented with the Physician Excellence Leadership Award.
Dr. Sheehy is division chief of the division of hospital medicine at the University of Wisconsin–Madison, and chair of the SHM Public Policy Committee.
Donald Schmidt, MD, has been named chief medical officer and vice president of medical affairs at Madonna Rehabilitation Hospitals in Omaha and Lincoln, Neb. He will replace Thomas Stalder, MD, who is retiring. Dr. Schmidt brings 20 years of experience to Madonna Rehabilitation Hospitals, including his most recent post as a hospitalist and medical director of the hospitalist program at Catholic Health Initiatives Health St. Elizabeth (Lincoln, Neb.).
Dr. Schmidt currently serves on the board of directors for OneHealth Nebraska, an independent physicians association.
Ezinne Nwude, MD, recently was presented with the SCP Health Excellence in Leadership Award during the organization’s Medical Leadership Conference. Dr. Nwude is chief of staff and hospitalist at the Medical Center of South Arkansas, El Dorado.
SCP Health coordinates staffing for more than 7,500 providers covering 30 states and is one of the nation’s largest clinical practice management companies. More than 420 medical leaders nationwide were eligible for the award. Dr. Nwude has focused on positive culture and health education since her start at MSCA in 2014. She has been chief of staff since October 2018.
RWJ Barnabas Health (West Orange, N.J.) recently named two new health system leaders from among its hospital medicine ranks, as Christopher Freer, MD, was tabbed as senior vice president for emergency and hospital medicine, and Maninder “Dolly” Abraham, MD, was picked as chief of hospital medicine. The moves were made as RWJBH takes over as the direct employer for Envision Physician Services in Nashville, Tenn.
Dr. Freer was elevated to his new role after spending the past 5 years as RWJBH’s system director for emergency services. He has nearly 3 decades of experience in hospital medicine.
Dr. Abraham comes to his new position after directing the hospitalist program at Saint Barnabas and serving as regional medical director with Envision.
Newman Regional Health (Emporia, Kan.) recently established a partnership with FreeState Healthcare (Wichita, Kan.). FreeState will be responsible for providing hospitalist services to adult inpatients and observation patients at Newman Regional Health during overnights.
Daniel Steinberg, MD, SFHM, recently was among 10 medical educators across the county to receive the Accreditation Council for Graduate Medical Education 2021 Parker J. Palmer Courage to Teach Award. Considered the most prestigious award given to graduate medical education program directors, it “recognizes program directors who have fostered innovation and improvement in their residency/fellowship program and served as exemplary role models for residents and fellows.”
Dr. Steinberg was program director for internal medicine residency at Mount Sinai Beth Israel, New York, for 11 years (2009-20) before becoming associate dean for quality and patient safety in graduate medical education in September. He is a professor of medicine and medical education at Icahn School of Medicine at Mount Sinai, New York.
Dr. Steinberg also is a leader within SHM, serving on the education, physicians-in-training, and annual conference committees. He is the course director for SHM Converge 2021.
Ann Sheehy, MD, SFHM, was honored in a virtual ceremony in December 2020 by the University of Wisconsin celebrating Physician Excellence Award winners. She was presented with the Physician Excellence Leadership Award.
Dr. Sheehy is division chief of the division of hospital medicine at the University of Wisconsin–Madison, and chair of the SHM Public Policy Committee.
Donald Schmidt, MD, has been named chief medical officer and vice president of medical affairs at Madonna Rehabilitation Hospitals in Omaha and Lincoln, Neb. He will replace Thomas Stalder, MD, who is retiring. Dr. Schmidt brings 20 years of experience to Madonna Rehabilitation Hospitals, including his most recent post as a hospitalist and medical director of the hospitalist program at Catholic Health Initiatives Health St. Elizabeth (Lincoln, Neb.).
Dr. Schmidt currently serves on the board of directors for OneHealth Nebraska, an independent physicians association.
Ezinne Nwude, MD, recently was presented with the SCP Health Excellence in Leadership Award during the organization’s Medical Leadership Conference. Dr. Nwude is chief of staff and hospitalist at the Medical Center of South Arkansas, El Dorado.
SCP Health coordinates staffing for more than 7,500 providers covering 30 states and is one of the nation’s largest clinical practice management companies. More than 420 medical leaders nationwide were eligible for the award. Dr. Nwude has focused on positive culture and health education since her start at MSCA in 2014. She has been chief of staff since October 2018.
RWJ Barnabas Health (West Orange, N.J.) recently named two new health system leaders from among its hospital medicine ranks, as Christopher Freer, MD, was tabbed as senior vice president for emergency and hospital medicine, and Maninder “Dolly” Abraham, MD, was picked as chief of hospital medicine. The moves were made as RWJBH takes over as the direct employer for Envision Physician Services in Nashville, Tenn.
Dr. Freer was elevated to his new role after spending the past 5 years as RWJBH’s system director for emergency services. He has nearly 3 decades of experience in hospital medicine.
Dr. Abraham comes to his new position after directing the hospitalist program at Saint Barnabas and serving as regional medical director with Envision.
Newman Regional Health (Emporia, Kan.) recently established a partnership with FreeState Healthcare (Wichita, Kan.). FreeState will be responsible for providing hospitalist services to adult inpatients and observation patients at Newman Regional Health during overnights.
Even patients with cancer in remission at risk for severe COVID-19
It’s been shown that hospitalized cancer patients and those undergoing active treatment are at high risk for severe COVID-19 complications. A new study shows that patients with cancer in remission are at higher risk, too.
For the study, investigators from the University of Pennsylvania, Philadelphia, analyzed 323 patients with SARS-CoV-2 infection in a research database with more than 4,800 patients. About 20% of database patients were Black, but they accounted for almost 65% of the infections, reflecting previous reports of increased risk for COVID among Black people.
A total of 67 of the infected patients had cancer, including 18 patients with active cancer and 49 patients whose cancer was in remission. After adjusting for demographics, smoking status, and comorbidities, a diagnosis of cancer more than doubled the odds of hospitalization and increased the odds of 30-day mortality nearly sixfold.
Worse outcomes were more strongly associated with active cancer, but patients whose cancer was in remission were also at higher risk than patients who did not have cancer.
It’s not only “patients hospitalized or on treatment ... all oncology patients need to take significant precautions during the pandemic to protect themselves,” senior investigator Kara Maxwell, MD, PhD, hematologist/oncologist and assistant professor at the University of Pennsylvania, said in a press release.
The study was published online on Jan. 21 in JNCI Cancer Spectrum.
The good news is that steps to prevent SARS-CoV-2 infection work, suggests a second report from the University of Pennsylvania. Among 124 cancer patients who underwent outpatient infusions from May to October 2020, not a single one experienced seroconversion over a median of 13 clinical visits. That second study was published on Jan. 16 in medRxiv and is pending peer review.
The zero seroconversion rate likely reflects “the success of transmission mitigation measures within health care facilities,” wrote investigators led by Lova Sun, MD, a hematology/oncology fellow at the University of Pennsylvania.
Like many institutions, the University of Pennsylvania Health System (Penn Medicine) is aggressive in protecting outpatients against the virus, the authors wrote. Among other steps, patients are queried about symptoms and contacts before their office visit, and their temperature is taken when they come in. Masks are worn, check-in is contactless, the number of visitors is limited, and patients who test positive are treated in a separate space.
In addition, patients in the study also reported that they wore masks and practiced social distancing in their daily lives.
Approached for comment, hematologist/oncologist Charles Shapiro, MD, a professor at the Icahn School of Medicine at Mount Sinai and director of translational breast cancer research at Mount Sinai Hospital, both in New York, said he wasn’t surprised that the prevention measures followed at Penn Medicine work. They are very similar to the measures followed at Mount Sinai oncology clinics, and “there’ve been very few COVID cases in our shop,” he added.
The bigger take-home message from both studies is that cancer patients, regardless of their age or if they are in remission, should be prioritized for vaccination against COVID-19, which is the best way to mitigate risk. “I strongly urge my patients to get it” if they can, he said.
The problem in New York is that immunizations are largely limited to people aged 65 years and older. Younger cancer patients are left out, and access has been spotty for all patients. “Vaccine is available one day, then not the next. It’s disheartening,” Dr. Shapiro said in an interview. “Hopefully, with the new administration, this will smooth out,” and the age limit will drop.
The study was supported by the National Institutes of Health, among other organizations. Dr. Lova, Dr. Maxwell, and Dr. Shapiro have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s been shown that hospitalized cancer patients and those undergoing active treatment are at high risk for severe COVID-19 complications. A new study shows that patients with cancer in remission are at higher risk, too.
For the study, investigators from the University of Pennsylvania, Philadelphia, analyzed 323 patients with SARS-CoV-2 infection in a research database with more than 4,800 patients. About 20% of database patients were Black, but they accounted for almost 65% of the infections, reflecting previous reports of increased risk for COVID among Black people.
A total of 67 of the infected patients had cancer, including 18 patients with active cancer and 49 patients whose cancer was in remission. After adjusting for demographics, smoking status, and comorbidities, a diagnosis of cancer more than doubled the odds of hospitalization and increased the odds of 30-day mortality nearly sixfold.
Worse outcomes were more strongly associated with active cancer, but patients whose cancer was in remission were also at higher risk than patients who did not have cancer.
It’s not only “patients hospitalized or on treatment ... all oncology patients need to take significant precautions during the pandemic to protect themselves,” senior investigator Kara Maxwell, MD, PhD, hematologist/oncologist and assistant professor at the University of Pennsylvania, said in a press release.
The study was published online on Jan. 21 in JNCI Cancer Spectrum.
The good news is that steps to prevent SARS-CoV-2 infection work, suggests a second report from the University of Pennsylvania. Among 124 cancer patients who underwent outpatient infusions from May to October 2020, not a single one experienced seroconversion over a median of 13 clinical visits. That second study was published on Jan. 16 in medRxiv and is pending peer review.
The zero seroconversion rate likely reflects “the success of transmission mitigation measures within health care facilities,” wrote investigators led by Lova Sun, MD, a hematology/oncology fellow at the University of Pennsylvania.
Like many institutions, the University of Pennsylvania Health System (Penn Medicine) is aggressive in protecting outpatients against the virus, the authors wrote. Among other steps, patients are queried about symptoms and contacts before their office visit, and their temperature is taken when they come in. Masks are worn, check-in is contactless, the number of visitors is limited, and patients who test positive are treated in a separate space.
In addition, patients in the study also reported that they wore masks and practiced social distancing in their daily lives.
Approached for comment, hematologist/oncologist Charles Shapiro, MD, a professor at the Icahn School of Medicine at Mount Sinai and director of translational breast cancer research at Mount Sinai Hospital, both in New York, said he wasn’t surprised that the prevention measures followed at Penn Medicine work. They are very similar to the measures followed at Mount Sinai oncology clinics, and “there’ve been very few COVID cases in our shop,” he added.
The bigger take-home message from both studies is that cancer patients, regardless of their age or if they are in remission, should be prioritized for vaccination against COVID-19, which is the best way to mitigate risk. “I strongly urge my patients to get it” if they can, he said.
The problem in New York is that immunizations are largely limited to people aged 65 years and older. Younger cancer patients are left out, and access has been spotty for all patients. “Vaccine is available one day, then not the next. It’s disheartening,” Dr. Shapiro said in an interview. “Hopefully, with the new administration, this will smooth out,” and the age limit will drop.
The study was supported by the National Institutes of Health, among other organizations. Dr. Lova, Dr. Maxwell, and Dr. Shapiro have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s been shown that hospitalized cancer patients and those undergoing active treatment are at high risk for severe COVID-19 complications. A new study shows that patients with cancer in remission are at higher risk, too.
For the study, investigators from the University of Pennsylvania, Philadelphia, analyzed 323 patients with SARS-CoV-2 infection in a research database with more than 4,800 patients. About 20% of database patients were Black, but they accounted for almost 65% of the infections, reflecting previous reports of increased risk for COVID among Black people.
A total of 67 of the infected patients had cancer, including 18 patients with active cancer and 49 patients whose cancer was in remission. After adjusting for demographics, smoking status, and comorbidities, a diagnosis of cancer more than doubled the odds of hospitalization and increased the odds of 30-day mortality nearly sixfold.
Worse outcomes were more strongly associated with active cancer, but patients whose cancer was in remission were also at higher risk than patients who did not have cancer.
It’s not only “patients hospitalized or on treatment ... all oncology patients need to take significant precautions during the pandemic to protect themselves,” senior investigator Kara Maxwell, MD, PhD, hematologist/oncologist and assistant professor at the University of Pennsylvania, said in a press release.
The study was published online on Jan. 21 in JNCI Cancer Spectrum.
The good news is that steps to prevent SARS-CoV-2 infection work, suggests a second report from the University of Pennsylvania. Among 124 cancer patients who underwent outpatient infusions from May to October 2020, not a single one experienced seroconversion over a median of 13 clinical visits. That second study was published on Jan. 16 in medRxiv and is pending peer review.
The zero seroconversion rate likely reflects “the success of transmission mitigation measures within health care facilities,” wrote investigators led by Lova Sun, MD, a hematology/oncology fellow at the University of Pennsylvania.
Like many institutions, the University of Pennsylvania Health System (Penn Medicine) is aggressive in protecting outpatients against the virus, the authors wrote. Among other steps, patients are queried about symptoms and contacts before their office visit, and their temperature is taken when they come in. Masks are worn, check-in is contactless, the number of visitors is limited, and patients who test positive are treated in a separate space.
In addition, patients in the study also reported that they wore masks and practiced social distancing in their daily lives.
Approached for comment, hematologist/oncologist Charles Shapiro, MD, a professor at the Icahn School of Medicine at Mount Sinai and director of translational breast cancer research at Mount Sinai Hospital, both in New York, said he wasn’t surprised that the prevention measures followed at Penn Medicine work. They are very similar to the measures followed at Mount Sinai oncology clinics, and “there’ve been very few COVID cases in our shop,” he added.
The bigger take-home message from both studies is that cancer patients, regardless of their age or if they are in remission, should be prioritized for vaccination against COVID-19, which is the best way to mitigate risk. “I strongly urge my patients to get it” if they can, he said.
The problem in New York is that immunizations are largely limited to people aged 65 years and older. Younger cancer patients are left out, and access has been spotty for all patients. “Vaccine is available one day, then not the next. It’s disheartening,” Dr. Shapiro said in an interview. “Hopefully, with the new administration, this will smooth out,” and the age limit will drop.
The study was supported by the National Institutes of Health, among other organizations. Dr. Lova, Dr. Maxwell, and Dr. Shapiro have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Full-dose anticoagulation reduces need for life support in COVID-19
Full-dose anticoagulation was superior to low, prophylactic doses in reducing the need for vital organ support such as ventilation in moderately ill patients hospitalized for COVID-19, according to a report released Jan. 22 by the National Institutes of Health (NIH).
“This is a major advance for patients hospitalized with COVID. Full dose of anticoagulation in these non-ICU patients improved outcomes and there’s a trend toward a reduction in mortality,” Judith Hochman, MD, director of the Cardiovascular Clinical Research Center at NYU Langone Medical Center, New York, said in an interview.
“We have treatments that are improving outcomes but not as many that reduce mortality, so we’re hopeful when the full dataset comes in that will be confirmed,” she said.
The observation of increased rates of blood clots and inflammation among COVID-19 patients, which can lead to complications such as lung failure, heart attack, and stroke, has given rise to various anticoagulant treatment protocols and a need for randomized data on routinely administering increased doses of anticoagulation to hospitalized patients.
Today’s top-line findings come from three linked clinical trials – REMAP-CAP, ACTIV-4, and ATTACC – examining the safety and efficacy of full-dose anticoagulation to treat moderately ill or critically ill adults hospitalized with COVID-19 compared with a lower dose typically used to prevent blood clots in hospitalized patients.
In December 2020, all three trials paused enrollment of the critically ill subgroup after results showed that full-dose anticoagulation started in the intensive care unit (ICU) was not beneficial and may have been harmful in some patients.
Moderately ill patients with COVID-19, defined as those who did not require ICU care or organ support, made up 80% of participants at enrollment in the three trials, Dr. Hochman said.
Among more than 1,000 moderately ill patients reviewed as of the data cut with the data safety monitoring board, full doses of low molecular weight or unfractionated heparin were superior to low prophylactic doses for the primary endpoint of need for ventilation or other organ supportive interventions at 21 days after randomization.
This met the predefined threshold for 99% probability of superiority and recruitment was stopped, Dr. Hochman reported. “Obviously safety figured into this decision. The risk/benefit ratio was very clear.”
The results do not pertain to patients with a previous indication for anticoagulation, who were excluded from the trials.
Data from an additional 1,000 patients will be reviewed and the data published sometime in the next 2-3 months, she said.
With large numbers of COVID-19 patients requiring hospitalization, the outcomes could help reduce the overload on intensive care units around the world, the NIH noted.
The results also highlight the critical role of timing in the course of COVID-19.
“We believe that full anticoagulation is effective early in the disease course,” Dr. Hochman said. “Based on the results so far from these three platform trials, those that were very, very sick at the time of enrollment really didn’t benefit and we needed to have caught them at an earlier stage.
“It’s possible that the people in the ICU are just different and the minute they get sick they need the ICU; so we haven’t clearly demonstrated this time course and when to intervene, but that’s the implication of the findings.”
The question of even earlier treatment is being examined in the partner ACTIV-4B trial, which is enrolling patients with COVID-19 illness not requiring hospitalization and randomizing them to the direct oral anticoagulant apixaban or aspirin or placebo.
“It’s a very important trial and we really want to get the message out that patients should volunteer for it,” said Dr. Hochman, principal investigator of the ACTIV-4 trial.
In the United States, the ACTIV-4 trial is being led by a collaborative effort involving a number of universities, including the University of Pittsburgh and New York University.
The REMAP-CAP, ACTIV-4, and ATTACC study platforms span five continents in more than 300 hospitals and are supported by multiple international funding organizations including the National Institutes of Health, Canadian Institutes of Health Research, the National Institute for Health Research (United Kingdom), the National Health and Medical Research Council (Australia), and the PREPARE and RECOVER consortia (European Union).
A version of this article first appeared on Medscape.com.
Full-dose anticoagulation was superior to low, prophylactic doses in reducing the need for vital organ support such as ventilation in moderately ill patients hospitalized for COVID-19, according to a report released Jan. 22 by the National Institutes of Health (NIH).
“This is a major advance for patients hospitalized with COVID. Full dose of anticoagulation in these non-ICU patients improved outcomes and there’s a trend toward a reduction in mortality,” Judith Hochman, MD, director of the Cardiovascular Clinical Research Center at NYU Langone Medical Center, New York, said in an interview.
“We have treatments that are improving outcomes but not as many that reduce mortality, so we’re hopeful when the full dataset comes in that will be confirmed,” she said.
The observation of increased rates of blood clots and inflammation among COVID-19 patients, which can lead to complications such as lung failure, heart attack, and stroke, has given rise to various anticoagulant treatment protocols and a need for randomized data on routinely administering increased doses of anticoagulation to hospitalized patients.
Today’s top-line findings come from three linked clinical trials – REMAP-CAP, ACTIV-4, and ATTACC – examining the safety and efficacy of full-dose anticoagulation to treat moderately ill or critically ill adults hospitalized with COVID-19 compared with a lower dose typically used to prevent blood clots in hospitalized patients.
In December 2020, all three trials paused enrollment of the critically ill subgroup after results showed that full-dose anticoagulation started in the intensive care unit (ICU) was not beneficial and may have been harmful in some patients.
Moderately ill patients with COVID-19, defined as those who did not require ICU care or organ support, made up 80% of participants at enrollment in the three trials, Dr. Hochman said.
Among more than 1,000 moderately ill patients reviewed as of the data cut with the data safety monitoring board, full doses of low molecular weight or unfractionated heparin were superior to low prophylactic doses for the primary endpoint of need for ventilation or other organ supportive interventions at 21 days after randomization.
This met the predefined threshold for 99% probability of superiority and recruitment was stopped, Dr. Hochman reported. “Obviously safety figured into this decision. The risk/benefit ratio was very clear.”
The results do not pertain to patients with a previous indication for anticoagulation, who were excluded from the trials.
Data from an additional 1,000 patients will be reviewed and the data published sometime in the next 2-3 months, she said.
With large numbers of COVID-19 patients requiring hospitalization, the outcomes could help reduce the overload on intensive care units around the world, the NIH noted.
The results also highlight the critical role of timing in the course of COVID-19.
“We believe that full anticoagulation is effective early in the disease course,” Dr. Hochman said. “Based on the results so far from these three platform trials, those that were very, very sick at the time of enrollment really didn’t benefit and we needed to have caught them at an earlier stage.
“It’s possible that the people in the ICU are just different and the minute they get sick they need the ICU; so we haven’t clearly demonstrated this time course and when to intervene, but that’s the implication of the findings.”
The question of even earlier treatment is being examined in the partner ACTIV-4B trial, which is enrolling patients with COVID-19 illness not requiring hospitalization and randomizing them to the direct oral anticoagulant apixaban or aspirin or placebo.
“It’s a very important trial and we really want to get the message out that patients should volunteer for it,” said Dr. Hochman, principal investigator of the ACTIV-4 trial.
In the United States, the ACTIV-4 trial is being led by a collaborative effort involving a number of universities, including the University of Pittsburgh and New York University.
The REMAP-CAP, ACTIV-4, and ATTACC study platforms span five continents in more than 300 hospitals and are supported by multiple international funding organizations including the National Institutes of Health, Canadian Institutes of Health Research, the National Institute for Health Research (United Kingdom), the National Health and Medical Research Council (Australia), and the PREPARE and RECOVER consortia (European Union).
A version of this article first appeared on Medscape.com.
Full-dose anticoagulation was superior to low, prophylactic doses in reducing the need for vital organ support such as ventilation in moderately ill patients hospitalized for COVID-19, according to a report released Jan. 22 by the National Institutes of Health (NIH).
“This is a major advance for patients hospitalized with COVID. Full dose of anticoagulation in these non-ICU patients improved outcomes and there’s a trend toward a reduction in mortality,” Judith Hochman, MD, director of the Cardiovascular Clinical Research Center at NYU Langone Medical Center, New York, said in an interview.
“We have treatments that are improving outcomes but not as many that reduce mortality, so we’re hopeful when the full dataset comes in that will be confirmed,” she said.
The observation of increased rates of blood clots and inflammation among COVID-19 patients, which can lead to complications such as lung failure, heart attack, and stroke, has given rise to various anticoagulant treatment protocols and a need for randomized data on routinely administering increased doses of anticoagulation to hospitalized patients.
Today’s top-line findings come from three linked clinical trials – REMAP-CAP, ACTIV-4, and ATTACC – examining the safety and efficacy of full-dose anticoagulation to treat moderately ill or critically ill adults hospitalized with COVID-19 compared with a lower dose typically used to prevent blood clots in hospitalized patients.
In December 2020, all three trials paused enrollment of the critically ill subgroup after results showed that full-dose anticoagulation started in the intensive care unit (ICU) was not beneficial and may have been harmful in some patients.
Moderately ill patients with COVID-19, defined as those who did not require ICU care or organ support, made up 80% of participants at enrollment in the three trials, Dr. Hochman said.
Among more than 1,000 moderately ill patients reviewed as of the data cut with the data safety monitoring board, full doses of low molecular weight or unfractionated heparin were superior to low prophylactic doses for the primary endpoint of need for ventilation or other organ supportive interventions at 21 days after randomization.
This met the predefined threshold for 99% probability of superiority and recruitment was stopped, Dr. Hochman reported. “Obviously safety figured into this decision. The risk/benefit ratio was very clear.”
The results do not pertain to patients with a previous indication for anticoagulation, who were excluded from the trials.
Data from an additional 1,000 patients will be reviewed and the data published sometime in the next 2-3 months, she said.
With large numbers of COVID-19 patients requiring hospitalization, the outcomes could help reduce the overload on intensive care units around the world, the NIH noted.
The results also highlight the critical role of timing in the course of COVID-19.
“We believe that full anticoagulation is effective early in the disease course,” Dr. Hochman said. “Based on the results so far from these three platform trials, those that were very, very sick at the time of enrollment really didn’t benefit and we needed to have caught them at an earlier stage.
“It’s possible that the people in the ICU are just different and the minute they get sick they need the ICU; so we haven’t clearly demonstrated this time course and when to intervene, but that’s the implication of the findings.”
The question of even earlier treatment is being examined in the partner ACTIV-4B trial, which is enrolling patients with COVID-19 illness not requiring hospitalization and randomizing them to the direct oral anticoagulant apixaban or aspirin or placebo.
“It’s a very important trial and we really want to get the message out that patients should volunteer for it,” said Dr. Hochman, principal investigator of the ACTIV-4 trial.
In the United States, the ACTIV-4 trial is being led by a collaborative effort involving a number of universities, including the University of Pittsburgh and New York University.
The REMAP-CAP, ACTIV-4, and ATTACC study platforms span five continents in more than 300 hospitals and are supported by multiple international funding organizations including the National Institutes of Health, Canadian Institutes of Health Research, the National Institute for Health Research (United Kingdom), the National Health and Medical Research Council (Australia), and the PREPARE and RECOVER consortia (European Union).
A version of this article first appeared on Medscape.com.