User login
The month of new beginnings is here
This month’s Letter from the Editor is guest authored by Dr. Megan A. Adams, GI & Hepatology News Associate Editor
September is a month of new beginnings, as summer transitions to fall, kids go back to school, and we return to more consistent work routines, refreshed and reinvigorated after some well-deserved time off with family and friends. Among our cover stories this month is a study showing a novel application of deep learning to inform clinical care of patients with pancreatic cysts. We also feature several high-impact studies from AGA’s journals, including a large randomized controlled trial by Dr. Paul Moayyedi and colleagues, demonstrating that PPI therapy may be unnecessary in the majority of patients on oral anticoagulants, despite current guideline recommendations. This study has the potential to substantially change clinical practice, particularly in the context of the current discussion regarding PPI benefits and harms, and our transition to value-based care.
We also highlight a proof-of-concept study demonstrating a potential role for probiotics (specifically Bifidobacteria) in reducing the risk of NSAID-related gastrointestinal bleeding, and another study showing a possible role for clopidogrel in chemoprevention of colorectal cancer. Both articles are accompanied by expert commentaries highlighting their potential effect on clinical practice.
Our September issue also emphasizes the importance of professional advocacy by chronicling the participation of four AGA leaders (Dr. Carr, Dr. Kaufman, Dr. Ketwaroo, and Dr. Mathews) in the 2019 Alliance of Specialty Medicine Fly In, a multisociety effort to lobby legislators on key issues such as reducing prior authorization burdens and minimizing the strict constraints of step-therapy protocols. We also are pleased to acknowledge the future leaders of gastroenterology by recognizing the 17 exceptional fellows who demonstrated their passion for advancing GI clinical care by presenting their institutional quality improvement projects at a special session at DDW® 2019. We hope you find these stories to be thought provoking, inspiring, and directly relevant to your clinical practice – thank you for reading!
Megan A. Adams, MD, JD, MSc
Associate Editor
This month’s Letter from the Editor is guest authored by Dr. Megan A. Adams, GI & Hepatology News Associate Editor
September is a month of new beginnings, as summer transitions to fall, kids go back to school, and we return to more consistent work routines, refreshed and reinvigorated after some well-deserved time off with family and friends. Among our cover stories this month is a study showing a novel application of deep learning to inform clinical care of patients with pancreatic cysts. We also feature several high-impact studies from AGA’s journals, including a large randomized controlled trial by Dr. Paul Moayyedi and colleagues, demonstrating that PPI therapy may be unnecessary in the majority of patients on oral anticoagulants, despite current guideline recommendations. This study has the potential to substantially change clinical practice, particularly in the context of the current discussion regarding PPI benefits and harms, and our transition to value-based care.
We also highlight a proof-of-concept study demonstrating a potential role for probiotics (specifically Bifidobacteria) in reducing the risk of NSAID-related gastrointestinal bleeding, and another study showing a possible role for clopidogrel in chemoprevention of colorectal cancer. Both articles are accompanied by expert commentaries highlighting their potential effect on clinical practice.
Our September issue also emphasizes the importance of professional advocacy by chronicling the participation of four AGA leaders (Dr. Carr, Dr. Kaufman, Dr. Ketwaroo, and Dr. Mathews) in the 2019 Alliance of Specialty Medicine Fly In, a multisociety effort to lobby legislators on key issues such as reducing prior authorization burdens and minimizing the strict constraints of step-therapy protocols. We also are pleased to acknowledge the future leaders of gastroenterology by recognizing the 17 exceptional fellows who demonstrated their passion for advancing GI clinical care by presenting their institutional quality improvement projects at a special session at DDW® 2019. We hope you find these stories to be thought provoking, inspiring, and directly relevant to your clinical practice – thank you for reading!
Megan A. Adams, MD, JD, MSc
Associate Editor
This month’s Letter from the Editor is guest authored by Dr. Megan A. Adams, GI & Hepatology News Associate Editor
September is a month of new beginnings, as summer transitions to fall, kids go back to school, and we return to more consistent work routines, refreshed and reinvigorated after some well-deserved time off with family and friends. Among our cover stories this month is a study showing a novel application of deep learning to inform clinical care of patients with pancreatic cysts. We also feature several high-impact studies from AGA’s journals, including a large randomized controlled trial by Dr. Paul Moayyedi and colleagues, demonstrating that PPI therapy may be unnecessary in the majority of patients on oral anticoagulants, despite current guideline recommendations. This study has the potential to substantially change clinical practice, particularly in the context of the current discussion regarding PPI benefits and harms, and our transition to value-based care.
We also highlight a proof-of-concept study demonstrating a potential role for probiotics (specifically Bifidobacteria) in reducing the risk of NSAID-related gastrointestinal bleeding, and another study showing a possible role for clopidogrel in chemoprevention of colorectal cancer. Both articles are accompanied by expert commentaries highlighting their potential effect on clinical practice.
Our September issue also emphasizes the importance of professional advocacy by chronicling the participation of four AGA leaders (Dr. Carr, Dr. Kaufman, Dr. Ketwaroo, and Dr. Mathews) in the 2019 Alliance of Specialty Medicine Fly In, a multisociety effort to lobby legislators on key issues such as reducing prior authorization burdens and minimizing the strict constraints of step-therapy protocols. We also are pleased to acknowledge the future leaders of gastroenterology by recognizing the 17 exceptional fellows who demonstrated their passion for advancing GI clinical care by presenting their institutional quality improvement projects at a special session at DDW® 2019. We hope you find these stories to be thought provoking, inspiring, and directly relevant to your clinical practice – thank you for reading!
Megan A. Adams, MD, JD, MSc
Associate Editor
‘Miracle cures’ in psychiatry?
For a patient with a major mental illness, the road to wellness is long and uncertain. The medications commonly used to treat mood and thought disorders can take weeks to months to start providing benefits, and they carry significant risks for adverse effects, such as weight gain, sexual dysfunction, and movement disorders. Patients often have to take psychotropic medications for the rest of their lives. In addition to these downsides, there is no guarantee that these medications will provide complete or even partial relief.2,3
Recently, there has been growing excitement about new treatments that might be “miracle cures” for patients with mental illness, particularly for individuals with treatment-resistant depression (TRD). Two of these treatments—ketamine-related compounds, and hallucinogenic drugs—seem to promise therapeutic effects that are vastly different from those of other psychiatric medications: They appear to improve patients’ symptoms very quickly, and their effects may persist long after these drugs have been cleared from the body.
Intravenous ketamine is an older generic drug used in anesthesia; recently, it has been used off-label for TRD and other mental illnesses. On March 5, 2019, the FDA approved an intranasal formulation of esketamine—the S-enantiomer of ketamine—for TRD.4 Hallucinogens have also been tested in small studies and have seemingly significant effects in alleviating depression in patients with terminal illnesses5 and reducing smoking behavior in patients with tobacco use disorder.6,7
These miracle cures are becoming increasingly available to patients and continue to gain credibility among clinicians and researchers. How should we evaluate the usefulness of these new treatments? And how should we talk to our patients about them? To answer these questions, this article:
- explores our duty to our patients, ourselves, and our colleagues
- describes the dilemma
- discusses ways to evaluate claims made about these new miracle cures.
Duty: Protecting and helping our patients
The physician–patient relationship is a fiduciary relationship. According to both common law and medical ethics, a physician who enters into a treatment relationship with a patient creates a bond of special trust and confidence. Such a relationship requires a physician to act in good faith and in the patient’s best interests.8 As physicians, we have a duty to evaluate the safety and efficacy of new treatments that are available for our patients, whether or not they are FDA-approved.
We should also protect our patients from the adverse consequences of relatively untested drugs. For example, ketamine and hallucinogens both produce dissociative effects, and may carry high risks for patients who have a predisposition to psychosis.9 We should protect our patients from any false hopes that might lead them to abandon their current treatment regimens due to adverse effects and imperfect results. At the same time, we also have a duty to acknowledge our patients’ suffering and to recognize that they might be desperate for new treatment options. We should remain open-minded about new treatments, and acknowledge that they might work. Finally, we have a duty to be mindful of any financial benefits that we may derive from the development, marketing, and administration of these medications.
Dilemma: The need for new treatments
This is not the first time that novel treatments in mental health have seemed to hold incredible promise. In the late 1800s, Sigmund Freud began to regularly use a compound that led him to feel “the normal euphoria of a healthy person.” He wrote that this substance produced:
…exhilaration and lasting euphoria, which does not differ in any way from the normal euphoria of a healthy person. The feeling of excitement which accompanies stimulus by alcohol is completely lacking; the characteristic urge for immediate activity which alcohol produces is also absent. One senses an increase of self-control and feels more vigorous and more capable of work; on the other hand, if one works, one misses that heightening of the mental powers which alcohol, tea, or coffee induce. One is simply normal, and soon finds it difficult to believe that one is under the influence of any drug at all.1
Continue to: The compound Freud was describing...
The compound Freud was describing is cocaine, which we now know is an addictive and dangerous drug that can in fact worsen depression.10 Another treatment regarded as a miracle cure in its time involved placing patients with schizophrenia into an insulin-induced coma to treat their symptoms; this therapy was used from 1933 to 1960.11 We now recognize that this practice is unacceptably dangerous.
The past is filled with cautionary tales of the enthusiastic adoption of treatments for mental illness that later turned out to be ineffective, counterproductive, dangerous, or inhumane. Yet, the long, arduous journeys our patients go through continue to weigh heavily on us. We would love to offer our patients newer, more efficacious, and longer-lasting treatments with fewer adverse effects.
Discussion: How to best evaluate miracle cures
To help quickly assess a new treatment, the following 5 categories can help guide and organize our thought process.
1. Evidence
What type of evidence do we have that a new treatment is safe and effective? Psychiatric research may be even more susceptible to a placebo effect than other medical research, particularly for illnesses with subjective symptoms, such as depression.12 Double-blinded, placebo-controlled studies, such as the IV ketamine trial conducted by Singh et al,13 are the gold standard for separating a substance’s actual biologic effect from a placebo effect. Studies that do not include a control group should not be regarded as providing scientific evidence of efficacy.
2. Mechanism
If a new compound appears to have a beneficial effect on mental health, it is important to consider the potential mechanism underlying this effect to determine if it is biologically plausible. A compound that is claimed to be a panacea for every symptom of every mental illness should be heavily scrutinized. For example, based on available research, ketamine’s long-lasting effects seem to come from 2 mechanisms14,15:
- Activation of endogenous opioid receptors, which is also responsible for the euphoria induced by heroin and oxycodone.
- Blockade of N-methyl-
D -aspartate receptors. N-methyl-D -aspartate receptor activation is a key mechanism by which learning and memory function in the brain, and blocking these receptors may increase brain plasticity.
Continue to: Therefore, it seems plausible...
Therefore, it seems plausible that ketamine could produce both short- and long-term improvements in mood. Hallucinogenic drugs are thought to profoundly alter brain function through several mechanisms, including activating serotonin receptors, enhancing brain plasticity, and increasing brain connectivity.16
3. Reinforcement
Psychiatric medications that are acutely reinforcing have significant potential for abuse. Antidepressants and mood stabilizers are not acutely rewarding. They don’t make patients feel good right away. Medications such as stimulants and opioids do, and must be used with extreme care because of their abuse potential. The problem with acutely reinforcing medications is that in the long run, they can worsen depression by decreasing the brain’s ability to produce endogenous opioids.17
4.
A mental disorder is unlikely to have a single solution. Rather than regarding a new treatment as capable of rapidly alleviating every symptom of a patient’s illness, it should be viewed as a tool that can be helpful when used in combination with other treatments and lifestyle practices. In an interview with the web site STAT, Cristina Cusin, MD, co-director of the Intravenous Ketamine Clinic for Depression at Massachusetts General Hospital, said, “You don’t treat an advanced disease with just an infusion and a ‘see you next time.’ If [doctors] replace your knee but [you] don’t do physical therapy, you don’t walk again.”18 To sustain the benefits of a novel medication, patients with serious mental illnesses need to maintain strong social supports, see a mental health care provider regularly, and abstain from illicit drug and alcohol use.
5. Context matters
For a medication to obtain approval to treat a specific indication, the FDA usually require 2 trials that demonstrate efficacy. Off-label use of generic medications such as ketamine may have benefits, but it is unlikely that a generic drug would be put through a costly FDA-approval process.19
When learning about new medications, remember that patients might assume that these agents have undergone a thorough review process for safety and effectiveness. When our patients request such treatments—whether FDA-approved or off-label—it is our responsibility as physicians to educate them about the benefits, risks, effectiveness, and limitations of these treatments, as well as to evaluate the appropriateness of a treatment for a specific patient’s symptoms.
Continue to: Tempering excitement with caution
Tempering excitement with caution
Our patients are not the only ones desperate for a miracle cure. As psychiatrists, many of us are desperate, too. New compounds may ultimately change the way we treat mental illness. However, we have an obligation to temper our excitement with caution by remembering past mistakes, and systematically evaluating new miracle cures to determine if they are safe and effective.
1. Freud S. Cocaine papers. In: Freud S, Byck R. Sigmund Freud collection (Library of Congress). New York, NY: Stonehill; 1975;7.
2. Rush AJ. STAR*D: what have we learned? Am J Psychiatry. 2007;164(2):201-204.
3. Demjaha A, Lappin JM, Stahl D, et al. Antipsychotic treatment resistance in first-episode psychosis: prevalence, subtypes and predictors. Psychol Med. 2017;47(11):1981-1989.
4. Carey B. Fast-acting depression drug, newly approved, could help millions. The New York Times. https://www.nytimes.com/2019/03/05/health/depression-treatment-ketamine-fda.html. Published March 5, 2019. Accessed July 26, 2019.
5. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197.
6. Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43:55-60.
7. Garcia-Romeu A, Griffiths RR, Johnson MW. Psilocybin-occasioned mystical experiences in the treatment of tobacco addiction. Curr Drug Abuse Rev 2014;7(3):157-164.
8. Simon RI. Clinical psychiatry and the law. 2nd ed. Washington, DC: American Psychiatric Press; 1992.
9. Lahti AC, Weiler MA, Tamara Michaelidis BA, et al. Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology. 2001;25(4):455-467.
10. Perrine SA, Sheikh IS, Nwaneshiudu CA, et al. Withdrawal from chronic administration of cocaine decreases delta opioid receptor signaling and increases anxiety- and depression-like behaviors in the rat. Neuropharmacology. 2008;54(2):355-364.
11. Doroshow DB. Performing a cure for schizophrenia: insulin coma therapy on the wards. J Hist Med Allied Sci. 2007;62(2):213-243.
12. Khan A, Kolts RL, Rapaport MH, et al. Magnitude of placebo response and drug-placebo differences across psychiatric disorders. Psychol Med. 2005;35(5):743-749.
13. Singh JB, Fedgchin M, Daly EJ, et al. A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. Am J Psychiatry. 2016;173(8):816-826.
14. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
15. Duman RS, Aghajanian GK, Sanacora G, et al. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(2):238-249.
16. Carhart-Harris RL. How do psychedelics work? Curr Opin Psychiatry. 2019;32(1):16-21.
17. Martins SS, Fenton MC, Keyes KM, et al. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med. 2012;42(6):1261-1272.
18. Thielking M. Ketamine gives hope to patients with severe depression. But some clinics stray from the science and hype its benefits. STAT. https://www.statnews.com/2018/09/24/ketamine-clinics-severe-depression-treatment/. Published September 24, 2018. Accessed July 26, 2019.
19. Stafford RS. Regulating off-label drug use--rethinking the role of the FDA. N Engl J Med. 2008;358(14):1427-1429.
For a patient with a major mental illness, the road to wellness is long and uncertain. The medications commonly used to treat mood and thought disorders can take weeks to months to start providing benefits, and they carry significant risks for adverse effects, such as weight gain, sexual dysfunction, and movement disorders. Patients often have to take psychotropic medications for the rest of their lives. In addition to these downsides, there is no guarantee that these medications will provide complete or even partial relief.2,3
Recently, there has been growing excitement about new treatments that might be “miracle cures” for patients with mental illness, particularly for individuals with treatment-resistant depression (TRD). Two of these treatments—ketamine-related compounds, and hallucinogenic drugs—seem to promise therapeutic effects that are vastly different from those of other psychiatric medications: They appear to improve patients’ symptoms very quickly, and their effects may persist long after these drugs have been cleared from the body.
Intravenous ketamine is an older generic drug used in anesthesia; recently, it has been used off-label for TRD and other mental illnesses. On March 5, 2019, the FDA approved an intranasal formulation of esketamine—the S-enantiomer of ketamine—for TRD.4 Hallucinogens have also been tested in small studies and have seemingly significant effects in alleviating depression in patients with terminal illnesses5 and reducing smoking behavior in patients with tobacco use disorder.6,7
These miracle cures are becoming increasingly available to patients and continue to gain credibility among clinicians and researchers. How should we evaluate the usefulness of these new treatments? And how should we talk to our patients about them? To answer these questions, this article:
- explores our duty to our patients, ourselves, and our colleagues
- describes the dilemma
- discusses ways to evaluate claims made about these new miracle cures.
Duty: Protecting and helping our patients
The physician–patient relationship is a fiduciary relationship. According to both common law and medical ethics, a physician who enters into a treatment relationship with a patient creates a bond of special trust and confidence. Such a relationship requires a physician to act in good faith and in the patient’s best interests.8 As physicians, we have a duty to evaluate the safety and efficacy of new treatments that are available for our patients, whether or not they are FDA-approved.
We should also protect our patients from the adverse consequences of relatively untested drugs. For example, ketamine and hallucinogens both produce dissociative effects, and may carry high risks for patients who have a predisposition to psychosis.9 We should protect our patients from any false hopes that might lead them to abandon their current treatment regimens due to adverse effects and imperfect results. At the same time, we also have a duty to acknowledge our patients’ suffering and to recognize that they might be desperate for new treatment options. We should remain open-minded about new treatments, and acknowledge that they might work. Finally, we have a duty to be mindful of any financial benefits that we may derive from the development, marketing, and administration of these medications.
Dilemma: The need for new treatments
This is not the first time that novel treatments in mental health have seemed to hold incredible promise. In the late 1800s, Sigmund Freud began to regularly use a compound that led him to feel “the normal euphoria of a healthy person.” He wrote that this substance produced:
…exhilaration and lasting euphoria, which does not differ in any way from the normal euphoria of a healthy person. The feeling of excitement which accompanies stimulus by alcohol is completely lacking; the characteristic urge for immediate activity which alcohol produces is also absent. One senses an increase of self-control and feels more vigorous and more capable of work; on the other hand, if one works, one misses that heightening of the mental powers which alcohol, tea, or coffee induce. One is simply normal, and soon finds it difficult to believe that one is under the influence of any drug at all.1
Continue to: The compound Freud was describing...
The compound Freud was describing is cocaine, which we now know is an addictive and dangerous drug that can in fact worsen depression.10 Another treatment regarded as a miracle cure in its time involved placing patients with schizophrenia into an insulin-induced coma to treat their symptoms; this therapy was used from 1933 to 1960.11 We now recognize that this practice is unacceptably dangerous.
The past is filled with cautionary tales of the enthusiastic adoption of treatments for mental illness that later turned out to be ineffective, counterproductive, dangerous, or inhumane. Yet, the long, arduous journeys our patients go through continue to weigh heavily on us. We would love to offer our patients newer, more efficacious, and longer-lasting treatments with fewer adverse effects.
Discussion: How to best evaluate miracle cures
To help quickly assess a new treatment, the following 5 categories can help guide and organize our thought process.
1. Evidence
What type of evidence do we have that a new treatment is safe and effective? Psychiatric research may be even more susceptible to a placebo effect than other medical research, particularly for illnesses with subjective symptoms, such as depression.12 Double-blinded, placebo-controlled studies, such as the IV ketamine trial conducted by Singh et al,13 are the gold standard for separating a substance’s actual biologic effect from a placebo effect. Studies that do not include a control group should not be regarded as providing scientific evidence of efficacy.
2. Mechanism
If a new compound appears to have a beneficial effect on mental health, it is important to consider the potential mechanism underlying this effect to determine if it is biologically plausible. A compound that is claimed to be a panacea for every symptom of every mental illness should be heavily scrutinized. For example, based on available research, ketamine’s long-lasting effects seem to come from 2 mechanisms14,15:
- Activation of endogenous opioid receptors, which is also responsible for the euphoria induced by heroin and oxycodone.
- Blockade of N-methyl-
D -aspartate receptors. N-methyl-D -aspartate receptor activation is a key mechanism by which learning and memory function in the brain, and blocking these receptors may increase brain plasticity.
Continue to: Therefore, it seems plausible...
Therefore, it seems plausible that ketamine could produce both short- and long-term improvements in mood. Hallucinogenic drugs are thought to profoundly alter brain function through several mechanisms, including activating serotonin receptors, enhancing brain plasticity, and increasing brain connectivity.16
3. Reinforcement
Psychiatric medications that are acutely reinforcing have significant potential for abuse. Antidepressants and mood stabilizers are not acutely rewarding. They don’t make patients feel good right away. Medications such as stimulants and opioids do, and must be used with extreme care because of their abuse potential. The problem with acutely reinforcing medications is that in the long run, they can worsen depression by decreasing the brain’s ability to produce endogenous opioids.17
4.
A mental disorder is unlikely to have a single solution. Rather than regarding a new treatment as capable of rapidly alleviating every symptom of a patient’s illness, it should be viewed as a tool that can be helpful when used in combination with other treatments and lifestyle practices. In an interview with the web site STAT, Cristina Cusin, MD, co-director of the Intravenous Ketamine Clinic for Depression at Massachusetts General Hospital, said, “You don’t treat an advanced disease with just an infusion and a ‘see you next time.’ If [doctors] replace your knee but [you] don’t do physical therapy, you don’t walk again.”18 To sustain the benefits of a novel medication, patients with serious mental illnesses need to maintain strong social supports, see a mental health care provider regularly, and abstain from illicit drug and alcohol use.
5. Context matters
For a medication to obtain approval to treat a specific indication, the FDA usually require 2 trials that demonstrate efficacy. Off-label use of generic medications such as ketamine may have benefits, but it is unlikely that a generic drug would be put through a costly FDA-approval process.19
When learning about new medications, remember that patients might assume that these agents have undergone a thorough review process for safety and effectiveness. When our patients request such treatments—whether FDA-approved or off-label—it is our responsibility as physicians to educate them about the benefits, risks, effectiveness, and limitations of these treatments, as well as to evaluate the appropriateness of a treatment for a specific patient’s symptoms.
Continue to: Tempering excitement with caution
Tempering excitement with caution
Our patients are not the only ones desperate for a miracle cure. As psychiatrists, many of us are desperate, too. New compounds may ultimately change the way we treat mental illness. However, we have an obligation to temper our excitement with caution by remembering past mistakes, and systematically evaluating new miracle cures to determine if they are safe and effective.
For a patient with a major mental illness, the road to wellness is long and uncertain. The medications commonly used to treat mood and thought disorders can take weeks to months to start providing benefits, and they carry significant risks for adverse effects, such as weight gain, sexual dysfunction, and movement disorders. Patients often have to take psychotropic medications for the rest of their lives. In addition to these downsides, there is no guarantee that these medications will provide complete or even partial relief.2,3
Recently, there has been growing excitement about new treatments that might be “miracle cures” for patients with mental illness, particularly for individuals with treatment-resistant depression (TRD). Two of these treatments—ketamine-related compounds, and hallucinogenic drugs—seem to promise therapeutic effects that are vastly different from those of other psychiatric medications: They appear to improve patients’ symptoms very quickly, and their effects may persist long after these drugs have been cleared from the body.
Intravenous ketamine is an older generic drug used in anesthesia; recently, it has been used off-label for TRD and other mental illnesses. On March 5, 2019, the FDA approved an intranasal formulation of esketamine—the S-enantiomer of ketamine—for TRD.4 Hallucinogens have also been tested in small studies and have seemingly significant effects in alleviating depression in patients with terminal illnesses5 and reducing smoking behavior in patients with tobacco use disorder.6,7
These miracle cures are becoming increasingly available to patients and continue to gain credibility among clinicians and researchers. How should we evaluate the usefulness of these new treatments? And how should we talk to our patients about them? To answer these questions, this article:
- explores our duty to our patients, ourselves, and our colleagues
- describes the dilemma
- discusses ways to evaluate claims made about these new miracle cures.
Duty: Protecting and helping our patients
The physician–patient relationship is a fiduciary relationship. According to both common law and medical ethics, a physician who enters into a treatment relationship with a patient creates a bond of special trust and confidence. Such a relationship requires a physician to act in good faith and in the patient’s best interests.8 As physicians, we have a duty to evaluate the safety and efficacy of new treatments that are available for our patients, whether or not they are FDA-approved.
We should also protect our patients from the adverse consequences of relatively untested drugs. For example, ketamine and hallucinogens both produce dissociative effects, and may carry high risks for patients who have a predisposition to psychosis.9 We should protect our patients from any false hopes that might lead them to abandon their current treatment regimens due to adverse effects and imperfect results. At the same time, we also have a duty to acknowledge our patients’ suffering and to recognize that they might be desperate for new treatment options. We should remain open-minded about new treatments, and acknowledge that they might work. Finally, we have a duty to be mindful of any financial benefits that we may derive from the development, marketing, and administration of these medications.
Dilemma: The need for new treatments
This is not the first time that novel treatments in mental health have seemed to hold incredible promise. In the late 1800s, Sigmund Freud began to regularly use a compound that led him to feel “the normal euphoria of a healthy person.” He wrote that this substance produced:
…exhilaration and lasting euphoria, which does not differ in any way from the normal euphoria of a healthy person. The feeling of excitement which accompanies stimulus by alcohol is completely lacking; the characteristic urge for immediate activity which alcohol produces is also absent. One senses an increase of self-control and feels more vigorous and more capable of work; on the other hand, if one works, one misses that heightening of the mental powers which alcohol, tea, or coffee induce. One is simply normal, and soon finds it difficult to believe that one is under the influence of any drug at all.1
Continue to: The compound Freud was describing...
The compound Freud was describing is cocaine, which we now know is an addictive and dangerous drug that can in fact worsen depression.10 Another treatment regarded as a miracle cure in its time involved placing patients with schizophrenia into an insulin-induced coma to treat their symptoms; this therapy was used from 1933 to 1960.11 We now recognize that this practice is unacceptably dangerous.
The past is filled with cautionary tales of the enthusiastic adoption of treatments for mental illness that later turned out to be ineffective, counterproductive, dangerous, or inhumane. Yet, the long, arduous journeys our patients go through continue to weigh heavily on us. We would love to offer our patients newer, more efficacious, and longer-lasting treatments with fewer adverse effects.
Discussion: How to best evaluate miracle cures
To help quickly assess a new treatment, the following 5 categories can help guide and organize our thought process.
1. Evidence
What type of evidence do we have that a new treatment is safe and effective? Psychiatric research may be even more susceptible to a placebo effect than other medical research, particularly for illnesses with subjective symptoms, such as depression.12 Double-blinded, placebo-controlled studies, such as the IV ketamine trial conducted by Singh et al,13 are the gold standard for separating a substance’s actual biologic effect from a placebo effect. Studies that do not include a control group should not be regarded as providing scientific evidence of efficacy.
2. Mechanism
If a new compound appears to have a beneficial effect on mental health, it is important to consider the potential mechanism underlying this effect to determine if it is biologically plausible. A compound that is claimed to be a panacea for every symptom of every mental illness should be heavily scrutinized. For example, based on available research, ketamine’s long-lasting effects seem to come from 2 mechanisms14,15:
- Activation of endogenous opioid receptors, which is also responsible for the euphoria induced by heroin and oxycodone.
- Blockade of N-methyl-
D -aspartate receptors. N-methyl-D -aspartate receptor activation is a key mechanism by which learning and memory function in the brain, and blocking these receptors may increase brain plasticity.
Continue to: Therefore, it seems plausible...
Therefore, it seems plausible that ketamine could produce both short- and long-term improvements in mood. Hallucinogenic drugs are thought to profoundly alter brain function through several mechanisms, including activating serotonin receptors, enhancing brain plasticity, and increasing brain connectivity.16
3. Reinforcement
Psychiatric medications that are acutely reinforcing have significant potential for abuse. Antidepressants and mood stabilizers are not acutely rewarding. They don’t make patients feel good right away. Medications such as stimulants and opioids do, and must be used with extreme care because of their abuse potential. The problem with acutely reinforcing medications is that in the long run, they can worsen depression by decreasing the brain’s ability to produce endogenous opioids.17
4.
A mental disorder is unlikely to have a single solution. Rather than regarding a new treatment as capable of rapidly alleviating every symptom of a patient’s illness, it should be viewed as a tool that can be helpful when used in combination with other treatments and lifestyle practices. In an interview with the web site STAT, Cristina Cusin, MD, co-director of the Intravenous Ketamine Clinic for Depression at Massachusetts General Hospital, said, “You don’t treat an advanced disease with just an infusion and a ‘see you next time.’ If [doctors] replace your knee but [you] don’t do physical therapy, you don’t walk again.”18 To sustain the benefits of a novel medication, patients with serious mental illnesses need to maintain strong social supports, see a mental health care provider regularly, and abstain from illicit drug and alcohol use.
5. Context matters
For a medication to obtain approval to treat a specific indication, the FDA usually require 2 trials that demonstrate efficacy. Off-label use of generic medications such as ketamine may have benefits, but it is unlikely that a generic drug would be put through a costly FDA-approval process.19
When learning about new medications, remember that patients might assume that these agents have undergone a thorough review process for safety and effectiveness. When our patients request such treatments—whether FDA-approved or off-label—it is our responsibility as physicians to educate them about the benefits, risks, effectiveness, and limitations of these treatments, as well as to evaluate the appropriateness of a treatment for a specific patient’s symptoms.
Continue to: Tempering excitement with caution
Tempering excitement with caution
Our patients are not the only ones desperate for a miracle cure. As psychiatrists, many of us are desperate, too. New compounds may ultimately change the way we treat mental illness. However, we have an obligation to temper our excitement with caution by remembering past mistakes, and systematically evaluating new miracle cures to determine if they are safe and effective.
1. Freud S. Cocaine papers. In: Freud S, Byck R. Sigmund Freud collection (Library of Congress). New York, NY: Stonehill; 1975;7.
2. Rush AJ. STAR*D: what have we learned? Am J Psychiatry. 2007;164(2):201-204.
3. Demjaha A, Lappin JM, Stahl D, et al. Antipsychotic treatment resistance in first-episode psychosis: prevalence, subtypes and predictors. Psychol Med. 2017;47(11):1981-1989.
4. Carey B. Fast-acting depression drug, newly approved, could help millions. The New York Times. https://www.nytimes.com/2019/03/05/health/depression-treatment-ketamine-fda.html. Published March 5, 2019. Accessed July 26, 2019.
5. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197.
6. Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43:55-60.
7. Garcia-Romeu A, Griffiths RR, Johnson MW. Psilocybin-occasioned mystical experiences in the treatment of tobacco addiction. Curr Drug Abuse Rev 2014;7(3):157-164.
8. Simon RI. Clinical psychiatry and the law. 2nd ed. Washington, DC: American Psychiatric Press; 1992.
9. Lahti AC, Weiler MA, Tamara Michaelidis BA, et al. Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology. 2001;25(4):455-467.
10. Perrine SA, Sheikh IS, Nwaneshiudu CA, et al. Withdrawal from chronic administration of cocaine decreases delta opioid receptor signaling and increases anxiety- and depression-like behaviors in the rat. Neuropharmacology. 2008;54(2):355-364.
11. Doroshow DB. Performing a cure for schizophrenia: insulin coma therapy on the wards. J Hist Med Allied Sci. 2007;62(2):213-243.
12. Khan A, Kolts RL, Rapaport MH, et al. Magnitude of placebo response and drug-placebo differences across psychiatric disorders. Psychol Med. 2005;35(5):743-749.
13. Singh JB, Fedgchin M, Daly EJ, et al. A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. Am J Psychiatry. 2016;173(8):816-826.
14. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
15. Duman RS, Aghajanian GK, Sanacora G, et al. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(2):238-249.
16. Carhart-Harris RL. How do psychedelics work? Curr Opin Psychiatry. 2019;32(1):16-21.
17. Martins SS, Fenton MC, Keyes KM, et al. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med. 2012;42(6):1261-1272.
18. Thielking M. Ketamine gives hope to patients with severe depression. But some clinics stray from the science and hype its benefits. STAT. https://www.statnews.com/2018/09/24/ketamine-clinics-severe-depression-treatment/. Published September 24, 2018. Accessed July 26, 2019.
19. Stafford RS. Regulating off-label drug use--rethinking the role of the FDA. N Engl J Med. 2008;358(14):1427-1429.
1. Freud S. Cocaine papers. In: Freud S, Byck R. Sigmund Freud collection (Library of Congress). New York, NY: Stonehill; 1975;7.
2. Rush AJ. STAR*D: what have we learned? Am J Psychiatry. 2007;164(2):201-204.
3. Demjaha A, Lappin JM, Stahl D, et al. Antipsychotic treatment resistance in first-episode psychosis: prevalence, subtypes and predictors. Psychol Med. 2017;47(11):1981-1989.
4. Carey B. Fast-acting depression drug, newly approved, could help millions. The New York Times. https://www.nytimes.com/2019/03/05/health/depression-treatment-ketamine-fda.html. Published March 5, 2019. Accessed July 26, 2019.
5. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197.
6. Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43:55-60.
7. Garcia-Romeu A, Griffiths RR, Johnson MW. Psilocybin-occasioned mystical experiences in the treatment of tobacco addiction. Curr Drug Abuse Rev 2014;7(3):157-164.
8. Simon RI. Clinical psychiatry and the law. 2nd ed. Washington, DC: American Psychiatric Press; 1992.
9. Lahti AC, Weiler MA, Tamara Michaelidis BA, et al. Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology. 2001;25(4):455-467.
10. Perrine SA, Sheikh IS, Nwaneshiudu CA, et al. Withdrawal from chronic administration of cocaine decreases delta opioid receptor signaling and increases anxiety- and depression-like behaviors in the rat. Neuropharmacology. 2008;54(2):355-364.
11. Doroshow DB. Performing a cure for schizophrenia: insulin coma therapy on the wards. J Hist Med Allied Sci. 2007;62(2):213-243.
12. Khan A, Kolts RL, Rapaport MH, et al. Magnitude of placebo response and drug-placebo differences across psychiatric disorders. Psychol Med. 2005;35(5):743-749.
13. Singh JB, Fedgchin M, Daly EJ, et al. A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. Am J Psychiatry. 2016;173(8):816-826.
14. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
15. Duman RS, Aghajanian GK, Sanacora G, et al. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(2):238-249.
16. Carhart-Harris RL. How do psychedelics work? Curr Opin Psychiatry. 2019;32(1):16-21.
17. Martins SS, Fenton MC, Keyes KM, et al. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med. 2012;42(6):1261-1272.
18. Thielking M. Ketamine gives hope to patients with severe depression. But some clinics stray from the science and hype its benefits. STAT. https://www.statnews.com/2018/09/24/ketamine-clinics-severe-depression-treatment/. Published September 24, 2018. Accessed July 26, 2019.
19. Stafford RS. Regulating off-label drug use--rethinking the role of the FDA. N Engl J Med. 2008;358(14):1427-1429.
Transformative advances are unfolding in psychiatry
The future of psychiatry is bright, even scintillating. Disruptive changes are gradually unfolding and will proceed at a brisk pace. Psychiatric practice will be transformed into a clinical neuroscience that will heal the mind by repairing the brain. The ingredients of change are already in place, and the trend will accelerate.
Consider the following scientific, technical, and therapeutic advances that will continue to transform the psychiatric practice landscape.
Scientific advances
- Pluripotent cells. By dedifferentiating fibroblasts or skin cells and re-differentiating them into neurons and glia, the study of the structure and function of psychiatric patients’ brains can be conducted in a test tube. That will exponentially expand the knowledge of the neural circuitry that underpin psychiatric disorders and will lead to novel strategies for brain repair.1
- CRISPR. This revolutionary advance in excising and inserting genes will eventually lead to the prevention of a psychiatric disease by replacing risk genes or mutations.1
- Molecular genetics. The flurry of identifying risk genes, copy number variants (CNV), and de novo mutations using gene-wide association studies (GWAS) will facilitate gene therapy in psychiatric disorders.
- Neuroimmunology. The discovery of the role of neuroinflammation and oxidative stress (free radicals exceeding glutathione and other antioxidants) in neuropsychiatric disorders will ultimately lead to new insights into preventing the neurodegeneration associated with acute psychotic or mood disorders. Inhibiting the activation of microglia (the immune cells of the brain) is one example of innovative therapeutic targets in the future.2
- Recognizing the role of mitochondrial dysfunction as a pathogenic pathway to neuropsychiatric disorders such as depression, schizophrenia, bipolar disorder, and even the comorbid diabetes that is common among those psychiatric disorders will chart an entirely new approach to diagnosis and treatment.2
- The role of the microbiota and microbiome in psychiatric disorders has emerged as a fertile new frontier in psychiatry, both for etiology and as therapeutic targets.3
- The enteric brain in the gut, in close proximity with the microbiome, is now known to be a major source of neurotransmitters that modulate brain functions (dopamine, serotonin, and others). Consequently, it is implicated in psychopathology, rendering this “second brain” a target for therapeutic interventions in the future, in addition to the “cephalic brain.”4
- Biomarkers and endophenotypes. The rapid discoveries of biomarkers are setting the stage for the recognition of hundreds of biologic subtypes of complex neuropsychiatric syndromes such as schizophrenia, autism, depression, anxiety, and dementia. Biomarkers will steadily pave the road to precision psychiatry.5,6
Technical advances
- Artificial intelligence is beginning to revolutionize psychiatric practice by identifying psychopathology via voice patterns, facial features, motor activity, sleep patterns, and analysis of writing and language. It will significantly enhance the early detection and diagnosis of neuropsychiatric disorders.7
- Machine learning. As with other medical specialties, this radical and important new technology is likely to generate currently unrecognized information and decision options for psychiatric practitioners in the future.8
- Neuromodulation. The future is already here when it comes to employing neuromodulation as a therapeutic technique in psychiatry. The past was prologue with the discovery of electroconvulsive therapy (ECT) 30 years ago, evolving into vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS) over the past 2 decades. Their application will go beyond depression into several other psychiatric conditions. A flurry of other neuromodulation techniques are being developed, including cranial electrical stimulation (CES), deep brain stimulation (DBS), epidural cortical stimulation (ECS), focused ultrasound (FUS), low-field magnetic stimulation (LFMS), magnetic seizure therapy (MST), near infrared light therapy (NIR), and transcranial direct current stimulation (TDCS).9
Continue to: Therapeutic advances
Therapeutic advances
- Rapid-acting parenteral antidepressants are one of the most exciting paradigm shifts for the treatment of severe depression and suicidal urges. In controlled clinical trials, ketamine, scopolamine, and nitrous oxide were shown to reverse chronic depression that had failed to respond to multiple oral antidepressants in a matter of hours instead of weeks or months.10 This remarkable new frontier of psychiatric therapeutics has revolutionized our concept of the neurobiology of depression and its reversibility into rapid remission. The use of IV, intranasal, and inhalable delivery of pharmacotherapies is bound to become an integral component of the future of psychiatry.
- Telepsychiatry is an example of how the future has already arrived for psychiatric practice. Clinicians’ virtual access to patients living in remote areas for evaluation and treatment is certainly a totally new model of health care delivery when compared with traditional face-to-face psychiatry, where patients must travel to see a psychiatrist.
- New terminology for psychotropic agents is also an impending part of the future. The neuroscience-based nomenclature (NbN) will rename more than 100 psychotropic medications by their mechanisms of action rather than by their clinical indication.11 Not only will this new lexicon be more scientifically accurate, but it also will avoid pigeon-holing drugs such as selective serotonin reuptake inhibitor antidepressants, which also are used to treat obsessive-compulsive disorder (OCD), anxiety, bulimia nervosa, and pain, or second-generation “atypical” antipsychotics, which are indicated not only for schizophrenia but also for bipolar mania and bipolar depression, and have been reported to improve treatment-resistant major depression, treatment-resistant OCD, borderline personality disorder, posttraumatic stress disorder (PTSD), and delirium.12
- Early intervention during the prodromal phase of serious psychiatric disorders is already here and will advance rapidly in the future. This will spare patients the anguish and suffering of acute psychosis or mania, hospitalization, or disability. It will likely reduce the huge direct and indirect costs to society of serious psychiatric disorders.13
- Repurposing hallucinogens into therapeutic agents is one of the most interesting discoveries in psychiatry. As with ketamine, a dissociative hallucinogen that has been rebranded as a rapid antidepressant, other hallucinogens such as psilocybin, lysergic acid diethylamide (LSD), and 3,4-methylenedioxy-methamphetamine (MDMA) are being investigated as therapeutic agents for depression, anxiety, and PTSD. They will become part of our expanding future pharmacotherapeutic armamentarium.14
It is obvious that parts of the future of psychiatry are already in place today, but other trends will emerge and thrill us clinicians. These advances will gradually but certainly alter psychiatric practice for the better, as the neuroscience of the mind expands and guides psychiatrists to more objective diagnoses and precise treatment options. The pace of advances in psychiatry is one of the most rapid in medicine.
So hold on: This will be a fascinating journey of creative destruction of traditional psychiatry.15 But as Emily Dickinson wrote: “Truth must dazzle gradually, or every man be blind.”
1. Moslem M, Olive J, Falk A. Stem cell models of schizophrenia, what have we learned and what is the potential. Schizophrenia Res. 2019;210:3-12.
2. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2018;17(11):4-7.
3. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
4. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):19-20.
5. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2012;16(12):7-8,11.
6. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
7. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
8. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
9. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
10. Nasrallah HA. A brave new era of IV psychopharmacotherapy. Current Psychiatry. 2014;13(3):10-12.
11. Stahl SM. Neuroscience-based nomenclature: classifying psychotropics by mechanism of action rather than indication. Current Psychiatry. 2017;16(5):15-16.
12. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
13. Nasrallah HA. Psychiatry’s social impact: pervasive and multifaceted. Current Psychiatry. 2019;18(2):4,6-7.
14. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
15. Nasrallah HA. Is psychiatry ripe for creative destruction? Current Psychiatry. 2012;11(4):20-21.
The future of psychiatry is bright, even scintillating. Disruptive changes are gradually unfolding and will proceed at a brisk pace. Psychiatric practice will be transformed into a clinical neuroscience that will heal the mind by repairing the brain. The ingredients of change are already in place, and the trend will accelerate.
Consider the following scientific, technical, and therapeutic advances that will continue to transform the psychiatric practice landscape.
Scientific advances
- Pluripotent cells. By dedifferentiating fibroblasts or skin cells and re-differentiating them into neurons and glia, the study of the structure and function of psychiatric patients’ brains can be conducted in a test tube. That will exponentially expand the knowledge of the neural circuitry that underpin psychiatric disorders and will lead to novel strategies for brain repair.1
- CRISPR. This revolutionary advance in excising and inserting genes will eventually lead to the prevention of a psychiatric disease by replacing risk genes or mutations.1
- Molecular genetics. The flurry of identifying risk genes, copy number variants (CNV), and de novo mutations using gene-wide association studies (GWAS) will facilitate gene therapy in psychiatric disorders.
- Neuroimmunology. The discovery of the role of neuroinflammation and oxidative stress (free radicals exceeding glutathione and other antioxidants) in neuropsychiatric disorders will ultimately lead to new insights into preventing the neurodegeneration associated with acute psychotic or mood disorders. Inhibiting the activation of microglia (the immune cells of the brain) is one example of innovative therapeutic targets in the future.2
- Recognizing the role of mitochondrial dysfunction as a pathogenic pathway to neuropsychiatric disorders such as depression, schizophrenia, bipolar disorder, and even the comorbid diabetes that is common among those psychiatric disorders will chart an entirely new approach to diagnosis and treatment.2
- The role of the microbiota and microbiome in psychiatric disorders has emerged as a fertile new frontier in psychiatry, both for etiology and as therapeutic targets.3
- The enteric brain in the gut, in close proximity with the microbiome, is now known to be a major source of neurotransmitters that modulate brain functions (dopamine, serotonin, and others). Consequently, it is implicated in psychopathology, rendering this “second brain” a target for therapeutic interventions in the future, in addition to the “cephalic brain.”4
- Biomarkers and endophenotypes. The rapid discoveries of biomarkers are setting the stage for the recognition of hundreds of biologic subtypes of complex neuropsychiatric syndromes such as schizophrenia, autism, depression, anxiety, and dementia. Biomarkers will steadily pave the road to precision psychiatry.5,6
Technical advances
- Artificial intelligence is beginning to revolutionize psychiatric practice by identifying psychopathology via voice patterns, facial features, motor activity, sleep patterns, and analysis of writing and language. It will significantly enhance the early detection and diagnosis of neuropsychiatric disorders.7
- Machine learning. As with other medical specialties, this radical and important new technology is likely to generate currently unrecognized information and decision options for psychiatric practitioners in the future.8
- Neuromodulation. The future is already here when it comes to employing neuromodulation as a therapeutic technique in psychiatry. The past was prologue with the discovery of electroconvulsive therapy (ECT) 30 years ago, evolving into vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS) over the past 2 decades. Their application will go beyond depression into several other psychiatric conditions. A flurry of other neuromodulation techniques are being developed, including cranial electrical stimulation (CES), deep brain stimulation (DBS), epidural cortical stimulation (ECS), focused ultrasound (FUS), low-field magnetic stimulation (LFMS), magnetic seizure therapy (MST), near infrared light therapy (NIR), and transcranial direct current stimulation (TDCS).9
Continue to: Therapeutic advances
Therapeutic advances
- Rapid-acting parenteral antidepressants are one of the most exciting paradigm shifts for the treatment of severe depression and suicidal urges. In controlled clinical trials, ketamine, scopolamine, and nitrous oxide were shown to reverse chronic depression that had failed to respond to multiple oral antidepressants in a matter of hours instead of weeks or months.10 This remarkable new frontier of psychiatric therapeutics has revolutionized our concept of the neurobiology of depression and its reversibility into rapid remission. The use of IV, intranasal, and inhalable delivery of pharmacotherapies is bound to become an integral component of the future of psychiatry.
- Telepsychiatry is an example of how the future has already arrived for psychiatric practice. Clinicians’ virtual access to patients living in remote areas for evaluation and treatment is certainly a totally new model of health care delivery when compared with traditional face-to-face psychiatry, where patients must travel to see a psychiatrist.
- New terminology for psychotropic agents is also an impending part of the future. The neuroscience-based nomenclature (NbN) will rename more than 100 psychotropic medications by their mechanisms of action rather than by their clinical indication.11 Not only will this new lexicon be more scientifically accurate, but it also will avoid pigeon-holing drugs such as selective serotonin reuptake inhibitor antidepressants, which also are used to treat obsessive-compulsive disorder (OCD), anxiety, bulimia nervosa, and pain, or second-generation “atypical” antipsychotics, which are indicated not only for schizophrenia but also for bipolar mania and bipolar depression, and have been reported to improve treatment-resistant major depression, treatment-resistant OCD, borderline personality disorder, posttraumatic stress disorder (PTSD), and delirium.12
- Early intervention during the prodromal phase of serious psychiatric disorders is already here and will advance rapidly in the future. This will spare patients the anguish and suffering of acute psychosis or mania, hospitalization, or disability. It will likely reduce the huge direct and indirect costs to society of serious psychiatric disorders.13
- Repurposing hallucinogens into therapeutic agents is one of the most interesting discoveries in psychiatry. As with ketamine, a dissociative hallucinogen that has been rebranded as a rapid antidepressant, other hallucinogens such as psilocybin, lysergic acid diethylamide (LSD), and 3,4-methylenedioxy-methamphetamine (MDMA) are being investigated as therapeutic agents for depression, anxiety, and PTSD. They will become part of our expanding future pharmacotherapeutic armamentarium.14
It is obvious that parts of the future of psychiatry are already in place today, but other trends will emerge and thrill us clinicians. These advances will gradually but certainly alter psychiatric practice for the better, as the neuroscience of the mind expands and guides psychiatrists to more objective diagnoses and precise treatment options. The pace of advances in psychiatry is one of the most rapid in medicine.
So hold on: This will be a fascinating journey of creative destruction of traditional psychiatry.15 But as Emily Dickinson wrote: “Truth must dazzle gradually, or every man be blind.”
The future of psychiatry is bright, even scintillating. Disruptive changes are gradually unfolding and will proceed at a brisk pace. Psychiatric practice will be transformed into a clinical neuroscience that will heal the mind by repairing the brain. The ingredients of change are already in place, and the trend will accelerate.
Consider the following scientific, technical, and therapeutic advances that will continue to transform the psychiatric practice landscape.
Scientific advances
- Pluripotent cells. By dedifferentiating fibroblasts or skin cells and re-differentiating them into neurons and glia, the study of the structure and function of psychiatric patients’ brains can be conducted in a test tube. That will exponentially expand the knowledge of the neural circuitry that underpin psychiatric disorders and will lead to novel strategies for brain repair.1
- CRISPR. This revolutionary advance in excising and inserting genes will eventually lead to the prevention of a psychiatric disease by replacing risk genes or mutations.1
- Molecular genetics. The flurry of identifying risk genes, copy number variants (CNV), and de novo mutations using gene-wide association studies (GWAS) will facilitate gene therapy in psychiatric disorders.
- Neuroimmunology. The discovery of the role of neuroinflammation and oxidative stress (free radicals exceeding glutathione and other antioxidants) in neuropsychiatric disorders will ultimately lead to new insights into preventing the neurodegeneration associated with acute psychotic or mood disorders. Inhibiting the activation of microglia (the immune cells of the brain) is one example of innovative therapeutic targets in the future.2
- Recognizing the role of mitochondrial dysfunction as a pathogenic pathway to neuropsychiatric disorders such as depression, schizophrenia, bipolar disorder, and even the comorbid diabetes that is common among those psychiatric disorders will chart an entirely new approach to diagnosis and treatment.2
- The role of the microbiota and microbiome in psychiatric disorders has emerged as a fertile new frontier in psychiatry, both for etiology and as therapeutic targets.3
- The enteric brain in the gut, in close proximity with the microbiome, is now known to be a major source of neurotransmitters that modulate brain functions (dopamine, serotonin, and others). Consequently, it is implicated in psychopathology, rendering this “second brain” a target for therapeutic interventions in the future, in addition to the “cephalic brain.”4
- Biomarkers and endophenotypes. The rapid discoveries of biomarkers are setting the stage for the recognition of hundreds of biologic subtypes of complex neuropsychiatric syndromes such as schizophrenia, autism, depression, anxiety, and dementia. Biomarkers will steadily pave the road to precision psychiatry.5,6
Technical advances
- Artificial intelligence is beginning to revolutionize psychiatric practice by identifying psychopathology via voice patterns, facial features, motor activity, sleep patterns, and analysis of writing and language. It will significantly enhance the early detection and diagnosis of neuropsychiatric disorders.7
- Machine learning. As with other medical specialties, this radical and important new technology is likely to generate currently unrecognized information and decision options for psychiatric practitioners in the future.8
- Neuromodulation. The future is already here when it comes to employing neuromodulation as a therapeutic technique in psychiatry. The past was prologue with the discovery of electroconvulsive therapy (ECT) 30 years ago, evolving into vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS) over the past 2 decades. Their application will go beyond depression into several other psychiatric conditions. A flurry of other neuromodulation techniques are being developed, including cranial electrical stimulation (CES), deep brain stimulation (DBS), epidural cortical stimulation (ECS), focused ultrasound (FUS), low-field magnetic stimulation (LFMS), magnetic seizure therapy (MST), near infrared light therapy (NIR), and transcranial direct current stimulation (TDCS).9
Continue to: Therapeutic advances
Therapeutic advances
- Rapid-acting parenteral antidepressants are one of the most exciting paradigm shifts for the treatment of severe depression and suicidal urges. In controlled clinical trials, ketamine, scopolamine, and nitrous oxide were shown to reverse chronic depression that had failed to respond to multiple oral antidepressants in a matter of hours instead of weeks or months.10 This remarkable new frontier of psychiatric therapeutics has revolutionized our concept of the neurobiology of depression and its reversibility into rapid remission. The use of IV, intranasal, and inhalable delivery of pharmacotherapies is bound to become an integral component of the future of psychiatry.
- Telepsychiatry is an example of how the future has already arrived for psychiatric practice. Clinicians’ virtual access to patients living in remote areas for evaluation and treatment is certainly a totally new model of health care delivery when compared with traditional face-to-face psychiatry, where patients must travel to see a psychiatrist.
- New terminology for psychotropic agents is also an impending part of the future. The neuroscience-based nomenclature (NbN) will rename more than 100 psychotropic medications by their mechanisms of action rather than by their clinical indication.11 Not only will this new lexicon be more scientifically accurate, but it also will avoid pigeon-holing drugs such as selective serotonin reuptake inhibitor antidepressants, which also are used to treat obsessive-compulsive disorder (OCD), anxiety, bulimia nervosa, and pain, or second-generation “atypical” antipsychotics, which are indicated not only for schizophrenia but also for bipolar mania and bipolar depression, and have been reported to improve treatment-resistant major depression, treatment-resistant OCD, borderline personality disorder, posttraumatic stress disorder (PTSD), and delirium.12
- Early intervention during the prodromal phase of serious psychiatric disorders is already here and will advance rapidly in the future. This will spare patients the anguish and suffering of acute psychosis or mania, hospitalization, or disability. It will likely reduce the huge direct and indirect costs to society of serious psychiatric disorders.13
- Repurposing hallucinogens into therapeutic agents is one of the most interesting discoveries in psychiatry. As with ketamine, a dissociative hallucinogen that has been rebranded as a rapid antidepressant, other hallucinogens such as psilocybin, lysergic acid diethylamide (LSD), and 3,4-methylenedioxy-methamphetamine (MDMA) are being investigated as therapeutic agents for depression, anxiety, and PTSD. They will become part of our expanding future pharmacotherapeutic armamentarium.14
It is obvious that parts of the future of psychiatry are already in place today, but other trends will emerge and thrill us clinicians. These advances will gradually but certainly alter psychiatric practice for the better, as the neuroscience of the mind expands and guides psychiatrists to more objective diagnoses and precise treatment options. The pace of advances in psychiatry is one of the most rapid in medicine.
So hold on: This will be a fascinating journey of creative destruction of traditional psychiatry.15 But as Emily Dickinson wrote: “Truth must dazzle gradually, or every man be blind.”
1. Moslem M, Olive J, Falk A. Stem cell models of schizophrenia, what have we learned and what is the potential. Schizophrenia Res. 2019;210:3-12.
2. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2018;17(11):4-7.
3. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
4. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):19-20.
5. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2012;16(12):7-8,11.
6. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
7. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
8. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
9. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
10. Nasrallah HA. A brave new era of IV psychopharmacotherapy. Current Psychiatry. 2014;13(3):10-12.
11. Stahl SM. Neuroscience-based nomenclature: classifying psychotropics by mechanism of action rather than indication. Current Psychiatry. 2017;16(5):15-16.
12. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
13. Nasrallah HA. Psychiatry’s social impact: pervasive and multifaceted. Current Psychiatry. 2019;18(2):4,6-7.
14. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
15. Nasrallah HA. Is psychiatry ripe for creative destruction? Current Psychiatry. 2012;11(4):20-21.
1. Moslem M, Olive J, Falk A. Stem cell models of schizophrenia, what have we learned and what is the potential. Schizophrenia Res. 2019;210:3-12.
2. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2018;17(11):4-7.
3. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
4. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):19-20.
5. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2012;16(12):7-8,11.
6. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
7. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
8. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
9. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
10. Nasrallah HA. A brave new era of IV psychopharmacotherapy. Current Psychiatry. 2014;13(3):10-12.
11. Stahl SM. Neuroscience-based nomenclature: classifying psychotropics by mechanism of action rather than indication. Current Psychiatry. 2017;16(5):15-16.
12. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
13. Nasrallah HA. Psychiatry’s social impact: pervasive and multifaceted. Current Psychiatry. 2019;18(2):4,6-7.
14. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
15. Nasrallah HA. Is psychiatry ripe for creative destruction? Current Psychiatry. 2012;11(4):20-21.
Physician assistants in psychiatry: Helping to meet America’s mental health needs
“Canst thou not minister to a mind diseased, pluck from the memory a rooted sorrow, raze out the written troubles of the brain, and with some sweet oblivious antidote cleanse the stuffed bosom of that perilous stuff which weighs upon the heart?”
– William Shakespeare, Macbeth
For many years, the United States has been experiencing a shortage of psychiatrists. Currently, there are only 28,000 to 33,000 psychiatrists in active patient care practice in the United States.1,2 The lack of psychiatrists is pronounced in many areas of the country, including rural regions, some urban neighborhoods, and community health centers. In approximately half of US counties, there are no psychiatrists at all.3
While patients with mental illnesses often are treated in primary care settings, the need for qualified mental health clinicians remains acute. Two-thirds of primary care physicians report difficulty in referring patients for mental health care, due to the shortage of clinicians and long wait times for patients to be seen.4 In the Department of Veterans Affairs (VA), the shortage of qualified psychiatrists is even more acute, due to ongoing combat operations and an increased number of missions and manpower requirements to complete them, which also has increased veterans’ mental health needs during life after their service.5
The outlook for providing adequate numbers of psychiatrists in the future is even more concerning. Based on a population analysis, Satiani et al6 predicts an extreme shortage of psychiatrists for the next 30 years, with the availability of psychiatrists per population expected to reach an all-time low by 2024. Based on ratios from the Department of Health and Human Services, this would mean a shortage of 14,000 to 31,000 psychiatrists over the next 5 to 6 years alone. This is due primarily to the expected retirement of more than 25,000 psychiatrists age >55 during the next 5 years. With mental illness becoming the costliest medical condition in the United States, at $201 billion annually, the potential impact of this shortage is alarming.6
Addressing the shortage
Efforts aimed at increasing the number of psychiatrists, improving access to care, and improving efficiency of care have focused on expanding recruitment and training capacity in psychiatry residency programs, utilizing new models such as telepsychiatry and Assertive Community Treatment (ACT) teams, increasing the number of Certified Community Behavioral Health Clinics, and embedding psychiatrists in large primary care practices.7 Another avenue for addressing the psychiatrist shortage has been the training and hiring of more advanced practice clinicians, including physician assistants (PAs) and
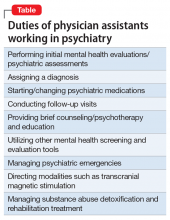
Physician assistants and NPs make up the largest group of non-physician mental health professionals who can prescribe medications. Physician assistant training is most closely aligned with the allopathic training model of physicians.9 Some typical duties of PAs working in a psychiatric setting are outlined in the Table.
How many PAs elect to specialize in psychiatry, compared with the percentage of physicians who choose psychiatry as a career? Data from the National Commission on Certification of Physician Assistants (NCCPA) revealed that in 2018 there were 1,470 PAs working in psychiatry, or approximately 1.5% of all PAs in practice.10 In comparison, approximately 5% of physicians complete residency training in psychiatry.2
Continue to: Although the need for more...
Although the need for more mental health professionals—especially those who can prescribe—is well documented, PA practice in psychiatry has been underrepresented, with PAs choosing to work in the field at a rate just over one-fourth that of physicians. While there is no clear explanation for the lack of PAs in psychiatry, PA programs’ training model has been to produce generalist clinicians who can work in numerous settings, particularly primary care. However, during the past several decades, PA practice choice has shifted largely from primary care to specialty care. In 1974, an estimated 68.8% of PAs worked in primary care settings (family medicine/general practice, general internal medicine, and general pediatrics), while the remainder worked in specialty areas.11 In contrast, by 2018, only 25.8% of PAs worked in primary care settings.10 Despite more PAs choosing to work in medical specialties, the number choosing psychiatry remains very low. With the great need for well-trained mental health prescribers, the opportunity for growth in this area of medicine and increased salary incentive should serve as an impetus for PAs to consider psychiatry. Like their physician counterparts, PAs working in specialty areas of medicine tend to be paid more, sometimes substantially more.12
Training requirements
What is the level of training and experience for PAs who choose to work in psychiatry? Physician assistant program applicants generally come from a pre-med background with a Bachelor’s degree in a hard science, and often have medical experience as a nurse, paramedic, emergency medical technician, or other health profession. Physician assistants are trained in the same medical model of care as physicians, although their training is structured over an average 27-month cycle, with 1 year devoted to didactic education and 1 year or more devoted to clinical training.13 They are qualified to “go to work” soon after graduating and passing the NCCPA Physician Assistant National Certifying Examination (PANCE), and may require a state license. Upon graduation, PAs have received approximately 1,000 hours of didactic and 2,000 hours of clinical training across the general spectrum of medicine.
Physician assistants who choose to specialize in psychiatry may complete a residency/fellowship in psychiatry of approximately 1 year, and/or obtain the Certificate of Added Qualification (CAQ) in psychiatry from the NCCPA. Most PAs who work in psychiatry have done so through “on-the-job” training, where their knowledge and skills have expanded through working with their supervising physician(s) and gaining experience from their clinical practice and self-study. For many years, there were only 1 or 2 PA residency/fellowship opportunities in psychiatry in the United States for PAs wanting to acquire additional formal didactic and clinical knowledge and skills in psychiatry. Fortunately, there has been a growing number of PA residencies/fellowships in psychiatry. These programs are typically 1 year in length and can provide a PA who wants to specialize in psychiatry with an additional 300 to >500 didactic and 1,500 to 2,000 clinical hours of training in the assessment, diagnosis, and treatment of the spectrum of psychiatric conditions. Currently, there are 10 to 12 programs in the United States that offer this training to PAs, producing approximately 18 to 20 residency-trained psychiatric PAs each year. Almost one-half of PAs who are residency-trained in psychiatry are being trained in VA facilities and affiliated institutions sponsored by the VA Office of Academic Affiliations. Along with the PA’s basic education, the additional knowledge and skills acquired in residency prepare the PA to be a highly capable psychiatric clinician, with a combined 1,500 didactic and 4,000 clinical hours of training in general medicine plus psychiatry. The addition of the CAQ demonstrates the PA’s commitment to additional learning in psychiatry, as the added work experience requirements, the additional postgraduate continuing medical education requirements in psychiatry, and the psychiatry board exam clearly show dedication to a higher level of knowledge and skill in the specialty.
Because PAs have been trained as generalists who are able to work in any setting or specialty, they have a broad range of knowledge in medicine and surgery. This can be especially helpful when working in a psychiatric practice, where they can provide an added medical focus to patient care when needed. As more PAs are choosing to work in a specialty area for much or all of their practice, they are able to gain significant knowledge and skills in that specialty.
Getting more PAs into psychiatry
So what does the future hold for PAs in psychiatry? The increased need and opportunity in mental health will likely draw a higher percentage of PAs to this specialty. Hopefully, an increase in the number of PA psychiatry residencies or advanced mental health training opportunities, and the continued goal of obtaining the CAQ in psychiatry, will serve to increase the number of psychiatric PAs.14
Continue to: The NCCPA has also recognized...
The NCCPA has also recognized the importance of increasing PA knowledge and integration in mental health care by establishing a PArtners in Mental Health Steering Committee, composed of leaders from the largest PA organizations, including the American Academy of Physician Assistants, the Accreditation Review Commission on Education for the Physician Assistant, the Physician Assistant Education Association, the Physician Assistant Foundation, and other PA and interprofessional members. The NCCPA’s PArtners in Mental Health Initiative: Stakeholders Report 2018 outlines an ongoing strategy to increase PA engagement in and awareness of mental health among the PA community and future providers via outreach to member organizations, state societies, PA programs, and those at the state and national level who legislate and reimburse PA services for mental health care.15 The Steering Committee’s recommendations include:
- enhancing PA educational approaches in mental health
- strengthening the PA practice environment to address mental health needs and foster integration
- promoting national campaigns to raise the profile of PAs addressing mental health across disciplines
- creating an organizational structure that incorporates current participants, offers backbone support to this movement, and plans for communication and financing.16
The role of PA educators
In the end, PA leaders and educators will play a substantial role in influencing future PAs to seek a career in psychiatry. Currently, psychiatry education varies among PA programs. Some offer robust didactic and clinical education and training, while other programs are limited in the number of hours of psychiatric didactic education, and may offer psychiatry clinical opportunities only in the context of a primary care setting, rather than in a dedicated psychiatric setting. Additionally, the mission of training PAs for generalist, primary care practice may limit many PAs from considering psychiatry because they do not necessarily view psychiatry as closely aligning with primary care generalist practice the way cardiology, pulmonology, gastroenterology, or other internal medicine specialties do.
In terms of PA postgraduate education, many PAs have completed residencies in surgical specialties or emergency medicine. Coincidentally, surgery and emergency medicine residencies are the most prolific of the postgraduate residency programs, adding a significant number of well-trained PAs to these specialties. The NCCPA also offers the CAQ for Cardiovascular and Thoracic Surgery, Orthopedic Surgery, and Emergency Medicine, which may attract PAs into these specialties, with or without completing a residency.
Because the NCCPA also offers the CAQ in Psychiatry, it would be reasonable and attractive for PAs who complete a psychiatry residency to obtain this certification. In fact, the PA psychiatry residency at our own institution trains our residents to be fully prepared and board-eligible to take the CAQ in Psychiatry upon completing residency. To date, every PA residency graduate who has completed our program and taken the CAQ in Psychiatry exam has passed and been awarded the CAQ in Psychiatry. They have proven themselves to the program and the NCCPA, and have impressed their employers with their clinical abilities and medical knowledge.
For psychiatrists, the addition of a well-trained or willing-to-be-trained PA to the practice can provide an economic advantage and strong team partnership that ensures optimal care for patients in this time of shortage of skilled mental health clinicians. The need is clear and will continue. Physician assistant educators must provide adequate didactic and clinical training in psychiatry to PA students, and support students interested in pursuing a career path in this specialty. Physician assistant organizations must meet the challenge of increasing the number of PAs in psychiatry, and encourage the establishment of additional post-graduate residency programs in psychiatry for PAs. Lastly, more PAs need to be made aware that psychiatry is an in-demand specialty that offers broad autonomy and rewarding clinical work.
Continue to: Bottom Line
Bottom Line
Physician assistants (PAs) who choose to specialize in psychiatry will find enormous opportunity, as the need for well-trained and knowledgeable mental health providers is acute. Those PAs who obtain additional training and/or certification in psychiatry will be highly valued and sought-after, with an abundance of job opportunities. Physician assistant programs should continue to improve didactic and clinical training for their students in psychiatry, and encourage increased numbers of PAs to consider psychiatry as a career path.
Related Resources
- National Commission on Certification of Physician Assistants. Psychiatry Certificate of Added Qualifications. https://www.nccpa.net/psychiatry.
- Association of Physician Assistants in Psychiatry. http://psychpa.com/.
1. Japen B. Psychiatrist shortage escalates as U.S. mental health needs grow. Forbes. https://www.forbes.com/sites/brucejapsen/2018/02/25/psychiatrist-shortage-escalates-as-u-s-mental-health-needs-grow/. Published February 25, 2018. Accessed February 1, 2019.
2. Association of American Medical Colleges. Active physicians in the largest specialties, 2017. Table 1.1. Number of active physicians in the largest specialties by major professional activity, 2017. www.aamc.org/data/workforce/reports/492556/1-1-chart.html. Published December 2017. Accessed February 1, 2019.
3. Weiner S. Addressing the escalating psychiatrist shortage. Association of American Medical Colleges AAMCNews. https://news.aamc.org/patient-care/article/addressing-escalating-psychiatrist-shortage/. Published February 13, 2018. Accessed February 1, 2019.
4. Cunningham P. Beyond parity: Primary care physicians’ perspectives on access to mental health care. Health Affairs. 2009;28(S1). https://www.healthaffairs.org/doi/full/10.1377/hlthaff.28.3.w490. Accessed February 1, 2019.
5. Psychiatrist shortage felt nationwide - and in VA system. The Gazette. https://www.thegazette.com/subject/news/government/psychiatrist-shortage-felt-nationwide-x2014-and-in-va-system-20170813. Published August 13, 2017. Accessed February 1, 2019.
6. Satiani A, Niedermier J, Satiani B, et al. Projected workforce of psychiatrists in the United States: a population analysis. Psychiatr Serv. 2018;69(6):710-713.
7. Levine D. What’s the answer to the shortage of mental health care providers? U.S. News & World Report. https://health.usnews.com/health-care/patient-advice/articles/2018-05-25/whats-the-answer-to-the-shortage-of-mental-health-care-providers. Published May 25, 2018. Accessed February 1, 2019.
8. Martsolf GR, Barnes H, Richards MR, et al. Employment of advanced practice clinicians in physician practices. JAMA Intern Med. 2018;178(7):988-990.
9. Hass V. Physician assistants and nurse practitioners are not interchangeable. JAAPA. 2016;29(4):9-12.
10. National Commission on Certification of Physician Assistants. 2018 Statistical profile of certified physician assistants by specialty. Annual report. https://prodcmsstoragesa.blob.core.windows.net/uploads/files/2018StatisticalProfileofCertifiedPAsbySpecialty1.pdf. Published July 2019. Accessed February 1, 2019.
11. Larson EH, Hart LG. Growth and change in the physician assistant workforce in the United States, 1967-2000. J Allied Health. 2007;36(3):121-130.
12. Perna G. NPs and PAs are joining docs in specialty care. Physicians Practice. http://www.physicianspractice.com/staff-salary-survey/nps-and-pas-are-joining-docs-specialty-care. Published May 9, 2016. Accessed February 1, 2019.
13. Pasquini S. Does PA program length matter? The Physician Assistant Life. www.thepalife.com/does-pa-program-length-matter/. Accessed February 1, 2019.
14. National Commission on Certification of Physician Assistants. PAs in specialty practice. An analysis of need, growth and future. http://prodcmsstoragesa.blob.core.windows.net/uploads/files/Whitepaper-PAsinSpecialtyPractice.pdf. Published October 2018. Accessed February 1, 2019.
15. National Commission on Certification of Physician Assistants. PArtners in Mental Health Initiative: Stakeholders Report 2018. http://www.nccpahealthfoundation.net/Portals/0/PDFs/PArtnersinMentalHealthInitiativeStakeholderReport2018.pdf. Published 2018. Accessed February 1, 2019.
16. National Commission on Certification of Physician Assistants. PArtners in Mental Health Summit: proceedings and Recommendations. Leesburg, Virginia – June 4-6, 2017. https://www.nccpahealthfoundation.net/Portals/0/PDFs/SummitProceedings.pdf. Published 2017. Accessed August 7, 2019.
“Canst thou not minister to a mind diseased, pluck from the memory a rooted sorrow, raze out the written troubles of the brain, and with some sweet oblivious antidote cleanse the stuffed bosom of that perilous stuff which weighs upon the heart?”
– William Shakespeare, Macbeth
For many years, the United States has been experiencing a shortage of psychiatrists. Currently, there are only 28,000 to 33,000 psychiatrists in active patient care practice in the United States.1,2 The lack of psychiatrists is pronounced in many areas of the country, including rural regions, some urban neighborhoods, and community health centers. In approximately half of US counties, there are no psychiatrists at all.3
While patients with mental illnesses often are treated in primary care settings, the need for qualified mental health clinicians remains acute. Two-thirds of primary care physicians report difficulty in referring patients for mental health care, due to the shortage of clinicians and long wait times for patients to be seen.4 In the Department of Veterans Affairs (VA), the shortage of qualified psychiatrists is even more acute, due to ongoing combat operations and an increased number of missions and manpower requirements to complete them, which also has increased veterans’ mental health needs during life after their service.5
The outlook for providing adequate numbers of psychiatrists in the future is even more concerning. Based on a population analysis, Satiani et al6 predicts an extreme shortage of psychiatrists for the next 30 years, with the availability of psychiatrists per population expected to reach an all-time low by 2024. Based on ratios from the Department of Health and Human Services, this would mean a shortage of 14,000 to 31,000 psychiatrists over the next 5 to 6 years alone. This is due primarily to the expected retirement of more than 25,000 psychiatrists age >55 during the next 5 years. With mental illness becoming the costliest medical condition in the United States, at $201 billion annually, the potential impact of this shortage is alarming.6
Addressing the shortage
Efforts aimed at increasing the number of psychiatrists, improving access to care, and improving efficiency of care have focused on expanding recruitment and training capacity in psychiatry residency programs, utilizing new models such as telepsychiatry and Assertive Community Treatment (ACT) teams, increasing the number of Certified Community Behavioral Health Clinics, and embedding psychiatrists in large primary care practices.7 Another avenue for addressing the psychiatrist shortage has been the training and hiring of more advanced practice clinicians, including physician assistants (PAs) and
Physician assistants and NPs make up the largest group of non-physician mental health professionals who can prescribe medications. Physician assistant training is most closely aligned with the allopathic training model of physicians.9 Some typical duties of PAs working in a psychiatric setting are outlined in the Table.
How many PAs elect to specialize in psychiatry, compared with the percentage of physicians who choose psychiatry as a career? Data from the National Commission on Certification of Physician Assistants (NCCPA) revealed that in 2018 there were 1,470 PAs working in psychiatry, or approximately 1.5% of all PAs in practice.10 In comparison, approximately 5% of physicians complete residency training in psychiatry.2
Continue to: Although the need for more...
Although the need for more mental health professionals—especially those who can prescribe—is well documented, PA practice in psychiatry has been underrepresented, with PAs choosing to work in the field at a rate just over one-fourth that of physicians. While there is no clear explanation for the lack of PAs in psychiatry, PA programs’ training model has been to produce generalist clinicians who can work in numerous settings, particularly primary care. However, during the past several decades, PA practice choice has shifted largely from primary care to specialty care. In 1974, an estimated 68.8% of PAs worked in primary care settings (family medicine/general practice, general internal medicine, and general pediatrics), while the remainder worked in specialty areas.11 In contrast, by 2018, only 25.8% of PAs worked in primary care settings.10 Despite more PAs choosing to work in medical specialties, the number choosing psychiatry remains very low. With the great need for well-trained mental health prescribers, the opportunity for growth in this area of medicine and increased salary incentive should serve as an impetus for PAs to consider psychiatry. Like their physician counterparts, PAs working in specialty areas of medicine tend to be paid more, sometimes substantially more.12
Training requirements
What is the level of training and experience for PAs who choose to work in psychiatry? Physician assistant program applicants generally come from a pre-med background with a Bachelor’s degree in a hard science, and often have medical experience as a nurse, paramedic, emergency medical technician, or other health profession. Physician assistants are trained in the same medical model of care as physicians, although their training is structured over an average 27-month cycle, with 1 year devoted to didactic education and 1 year or more devoted to clinical training.13 They are qualified to “go to work” soon after graduating and passing the NCCPA Physician Assistant National Certifying Examination (PANCE), and may require a state license. Upon graduation, PAs have received approximately 1,000 hours of didactic and 2,000 hours of clinical training across the general spectrum of medicine.
Physician assistants who choose to specialize in psychiatry may complete a residency/fellowship in psychiatry of approximately 1 year, and/or obtain the Certificate of Added Qualification (CAQ) in psychiatry from the NCCPA. Most PAs who work in psychiatry have done so through “on-the-job” training, where their knowledge and skills have expanded through working with their supervising physician(s) and gaining experience from their clinical practice and self-study. For many years, there were only 1 or 2 PA residency/fellowship opportunities in psychiatry in the United States for PAs wanting to acquire additional formal didactic and clinical knowledge and skills in psychiatry. Fortunately, there has been a growing number of PA residencies/fellowships in psychiatry. These programs are typically 1 year in length and can provide a PA who wants to specialize in psychiatry with an additional 300 to >500 didactic and 1,500 to 2,000 clinical hours of training in the assessment, diagnosis, and treatment of the spectrum of psychiatric conditions. Currently, there are 10 to 12 programs in the United States that offer this training to PAs, producing approximately 18 to 20 residency-trained psychiatric PAs each year. Almost one-half of PAs who are residency-trained in psychiatry are being trained in VA facilities and affiliated institutions sponsored by the VA Office of Academic Affiliations. Along with the PA’s basic education, the additional knowledge and skills acquired in residency prepare the PA to be a highly capable psychiatric clinician, with a combined 1,500 didactic and 4,000 clinical hours of training in general medicine plus psychiatry. The addition of the CAQ demonstrates the PA’s commitment to additional learning in psychiatry, as the added work experience requirements, the additional postgraduate continuing medical education requirements in psychiatry, and the psychiatry board exam clearly show dedication to a higher level of knowledge and skill in the specialty.
Because PAs have been trained as generalists who are able to work in any setting or specialty, they have a broad range of knowledge in medicine and surgery. This can be especially helpful when working in a psychiatric practice, where they can provide an added medical focus to patient care when needed. As more PAs are choosing to work in a specialty area for much or all of their practice, they are able to gain significant knowledge and skills in that specialty.
Getting more PAs into psychiatry
So what does the future hold for PAs in psychiatry? The increased need and opportunity in mental health will likely draw a higher percentage of PAs to this specialty. Hopefully, an increase in the number of PA psychiatry residencies or advanced mental health training opportunities, and the continued goal of obtaining the CAQ in psychiatry, will serve to increase the number of psychiatric PAs.14
Continue to: The NCCPA has also recognized...
The NCCPA has also recognized the importance of increasing PA knowledge and integration in mental health care by establishing a PArtners in Mental Health Steering Committee, composed of leaders from the largest PA organizations, including the American Academy of Physician Assistants, the Accreditation Review Commission on Education for the Physician Assistant, the Physician Assistant Education Association, the Physician Assistant Foundation, and other PA and interprofessional members. The NCCPA’s PArtners in Mental Health Initiative: Stakeholders Report 2018 outlines an ongoing strategy to increase PA engagement in and awareness of mental health among the PA community and future providers via outreach to member organizations, state societies, PA programs, and those at the state and national level who legislate and reimburse PA services for mental health care.15 The Steering Committee’s recommendations include:
- enhancing PA educational approaches in mental health
- strengthening the PA practice environment to address mental health needs and foster integration
- promoting national campaigns to raise the profile of PAs addressing mental health across disciplines
- creating an organizational structure that incorporates current participants, offers backbone support to this movement, and plans for communication and financing.16
The role of PA educators
In the end, PA leaders and educators will play a substantial role in influencing future PAs to seek a career in psychiatry. Currently, psychiatry education varies among PA programs. Some offer robust didactic and clinical education and training, while other programs are limited in the number of hours of psychiatric didactic education, and may offer psychiatry clinical opportunities only in the context of a primary care setting, rather than in a dedicated psychiatric setting. Additionally, the mission of training PAs for generalist, primary care practice may limit many PAs from considering psychiatry because they do not necessarily view psychiatry as closely aligning with primary care generalist practice the way cardiology, pulmonology, gastroenterology, or other internal medicine specialties do.
In terms of PA postgraduate education, many PAs have completed residencies in surgical specialties or emergency medicine. Coincidentally, surgery and emergency medicine residencies are the most prolific of the postgraduate residency programs, adding a significant number of well-trained PAs to these specialties. The NCCPA also offers the CAQ for Cardiovascular and Thoracic Surgery, Orthopedic Surgery, and Emergency Medicine, which may attract PAs into these specialties, with or without completing a residency.
Because the NCCPA also offers the CAQ in Psychiatry, it would be reasonable and attractive for PAs who complete a psychiatry residency to obtain this certification. In fact, the PA psychiatry residency at our own institution trains our residents to be fully prepared and board-eligible to take the CAQ in Psychiatry upon completing residency. To date, every PA residency graduate who has completed our program and taken the CAQ in Psychiatry exam has passed and been awarded the CAQ in Psychiatry. They have proven themselves to the program and the NCCPA, and have impressed their employers with their clinical abilities and medical knowledge.
For psychiatrists, the addition of a well-trained or willing-to-be-trained PA to the practice can provide an economic advantage and strong team partnership that ensures optimal care for patients in this time of shortage of skilled mental health clinicians. The need is clear and will continue. Physician assistant educators must provide adequate didactic and clinical training in psychiatry to PA students, and support students interested in pursuing a career path in this specialty. Physician assistant organizations must meet the challenge of increasing the number of PAs in psychiatry, and encourage the establishment of additional post-graduate residency programs in psychiatry for PAs. Lastly, more PAs need to be made aware that psychiatry is an in-demand specialty that offers broad autonomy and rewarding clinical work.
Continue to: Bottom Line
Bottom Line
Physician assistants (PAs) who choose to specialize in psychiatry will find enormous opportunity, as the need for well-trained and knowledgeable mental health providers is acute. Those PAs who obtain additional training and/or certification in psychiatry will be highly valued and sought-after, with an abundance of job opportunities. Physician assistant programs should continue to improve didactic and clinical training for their students in psychiatry, and encourage increased numbers of PAs to consider psychiatry as a career path.
Related Resources
- National Commission on Certification of Physician Assistants. Psychiatry Certificate of Added Qualifications. https://www.nccpa.net/psychiatry.
- Association of Physician Assistants in Psychiatry. http://psychpa.com/.
“Canst thou not minister to a mind diseased, pluck from the memory a rooted sorrow, raze out the written troubles of the brain, and with some sweet oblivious antidote cleanse the stuffed bosom of that perilous stuff which weighs upon the heart?”
– William Shakespeare, Macbeth
For many years, the United States has been experiencing a shortage of psychiatrists. Currently, there are only 28,000 to 33,000 psychiatrists in active patient care practice in the United States.1,2 The lack of psychiatrists is pronounced in many areas of the country, including rural regions, some urban neighborhoods, and community health centers. In approximately half of US counties, there are no psychiatrists at all.3
While patients with mental illnesses often are treated in primary care settings, the need for qualified mental health clinicians remains acute. Two-thirds of primary care physicians report difficulty in referring patients for mental health care, due to the shortage of clinicians and long wait times for patients to be seen.4 In the Department of Veterans Affairs (VA), the shortage of qualified psychiatrists is even more acute, due to ongoing combat operations and an increased number of missions and manpower requirements to complete them, which also has increased veterans’ mental health needs during life after their service.5
The outlook for providing adequate numbers of psychiatrists in the future is even more concerning. Based on a population analysis, Satiani et al6 predicts an extreme shortage of psychiatrists for the next 30 years, with the availability of psychiatrists per population expected to reach an all-time low by 2024. Based on ratios from the Department of Health and Human Services, this would mean a shortage of 14,000 to 31,000 psychiatrists over the next 5 to 6 years alone. This is due primarily to the expected retirement of more than 25,000 psychiatrists age >55 during the next 5 years. With mental illness becoming the costliest medical condition in the United States, at $201 billion annually, the potential impact of this shortage is alarming.6
Addressing the shortage
Efforts aimed at increasing the number of psychiatrists, improving access to care, and improving efficiency of care have focused on expanding recruitment and training capacity in psychiatry residency programs, utilizing new models such as telepsychiatry and Assertive Community Treatment (ACT) teams, increasing the number of Certified Community Behavioral Health Clinics, and embedding psychiatrists in large primary care practices.7 Another avenue for addressing the psychiatrist shortage has been the training and hiring of more advanced practice clinicians, including physician assistants (PAs) and
Physician assistants and NPs make up the largest group of non-physician mental health professionals who can prescribe medications. Physician assistant training is most closely aligned with the allopathic training model of physicians.9 Some typical duties of PAs working in a psychiatric setting are outlined in the Table.
How many PAs elect to specialize in psychiatry, compared with the percentage of physicians who choose psychiatry as a career? Data from the National Commission on Certification of Physician Assistants (NCCPA) revealed that in 2018 there were 1,470 PAs working in psychiatry, or approximately 1.5% of all PAs in practice.10 In comparison, approximately 5% of physicians complete residency training in psychiatry.2
Continue to: Although the need for more...
Although the need for more mental health professionals—especially those who can prescribe—is well documented, PA practice in psychiatry has been underrepresented, with PAs choosing to work in the field at a rate just over one-fourth that of physicians. While there is no clear explanation for the lack of PAs in psychiatry, PA programs’ training model has been to produce generalist clinicians who can work in numerous settings, particularly primary care. However, during the past several decades, PA practice choice has shifted largely from primary care to specialty care. In 1974, an estimated 68.8% of PAs worked in primary care settings (family medicine/general practice, general internal medicine, and general pediatrics), while the remainder worked in specialty areas.11 In contrast, by 2018, only 25.8% of PAs worked in primary care settings.10 Despite more PAs choosing to work in medical specialties, the number choosing psychiatry remains very low. With the great need for well-trained mental health prescribers, the opportunity for growth in this area of medicine and increased salary incentive should serve as an impetus for PAs to consider psychiatry. Like their physician counterparts, PAs working in specialty areas of medicine tend to be paid more, sometimes substantially more.12
Training requirements
What is the level of training and experience for PAs who choose to work in psychiatry? Physician assistant program applicants generally come from a pre-med background with a Bachelor’s degree in a hard science, and often have medical experience as a nurse, paramedic, emergency medical technician, or other health profession. Physician assistants are trained in the same medical model of care as physicians, although their training is structured over an average 27-month cycle, with 1 year devoted to didactic education and 1 year or more devoted to clinical training.13 They are qualified to “go to work” soon after graduating and passing the NCCPA Physician Assistant National Certifying Examination (PANCE), and may require a state license. Upon graduation, PAs have received approximately 1,000 hours of didactic and 2,000 hours of clinical training across the general spectrum of medicine.
Physician assistants who choose to specialize in psychiatry may complete a residency/fellowship in psychiatry of approximately 1 year, and/or obtain the Certificate of Added Qualification (CAQ) in psychiatry from the NCCPA. Most PAs who work in psychiatry have done so through “on-the-job” training, where their knowledge and skills have expanded through working with their supervising physician(s) and gaining experience from their clinical practice and self-study. For many years, there were only 1 or 2 PA residency/fellowship opportunities in psychiatry in the United States for PAs wanting to acquire additional formal didactic and clinical knowledge and skills in psychiatry. Fortunately, there has been a growing number of PA residencies/fellowships in psychiatry. These programs are typically 1 year in length and can provide a PA who wants to specialize in psychiatry with an additional 300 to >500 didactic and 1,500 to 2,000 clinical hours of training in the assessment, diagnosis, and treatment of the spectrum of psychiatric conditions. Currently, there are 10 to 12 programs in the United States that offer this training to PAs, producing approximately 18 to 20 residency-trained psychiatric PAs each year. Almost one-half of PAs who are residency-trained in psychiatry are being trained in VA facilities and affiliated institutions sponsored by the VA Office of Academic Affiliations. Along with the PA’s basic education, the additional knowledge and skills acquired in residency prepare the PA to be a highly capable psychiatric clinician, with a combined 1,500 didactic and 4,000 clinical hours of training in general medicine plus psychiatry. The addition of the CAQ demonstrates the PA’s commitment to additional learning in psychiatry, as the added work experience requirements, the additional postgraduate continuing medical education requirements in psychiatry, and the psychiatry board exam clearly show dedication to a higher level of knowledge and skill in the specialty.
Because PAs have been trained as generalists who are able to work in any setting or specialty, they have a broad range of knowledge in medicine and surgery. This can be especially helpful when working in a psychiatric practice, where they can provide an added medical focus to patient care when needed. As more PAs are choosing to work in a specialty area for much or all of their practice, they are able to gain significant knowledge and skills in that specialty.
Getting more PAs into psychiatry
So what does the future hold for PAs in psychiatry? The increased need and opportunity in mental health will likely draw a higher percentage of PAs to this specialty. Hopefully, an increase in the number of PA psychiatry residencies or advanced mental health training opportunities, and the continued goal of obtaining the CAQ in psychiatry, will serve to increase the number of psychiatric PAs.14
Continue to: The NCCPA has also recognized...
The NCCPA has also recognized the importance of increasing PA knowledge and integration in mental health care by establishing a PArtners in Mental Health Steering Committee, composed of leaders from the largest PA organizations, including the American Academy of Physician Assistants, the Accreditation Review Commission on Education for the Physician Assistant, the Physician Assistant Education Association, the Physician Assistant Foundation, and other PA and interprofessional members. The NCCPA’s PArtners in Mental Health Initiative: Stakeholders Report 2018 outlines an ongoing strategy to increase PA engagement in and awareness of mental health among the PA community and future providers via outreach to member organizations, state societies, PA programs, and those at the state and national level who legislate and reimburse PA services for mental health care.15 The Steering Committee’s recommendations include:
- enhancing PA educational approaches in mental health
- strengthening the PA practice environment to address mental health needs and foster integration
- promoting national campaigns to raise the profile of PAs addressing mental health across disciplines
- creating an organizational structure that incorporates current participants, offers backbone support to this movement, and plans for communication and financing.16
The role of PA educators
In the end, PA leaders and educators will play a substantial role in influencing future PAs to seek a career in psychiatry. Currently, psychiatry education varies among PA programs. Some offer robust didactic and clinical education and training, while other programs are limited in the number of hours of psychiatric didactic education, and may offer psychiatry clinical opportunities only in the context of a primary care setting, rather than in a dedicated psychiatric setting. Additionally, the mission of training PAs for generalist, primary care practice may limit many PAs from considering psychiatry because they do not necessarily view psychiatry as closely aligning with primary care generalist practice the way cardiology, pulmonology, gastroenterology, or other internal medicine specialties do.
In terms of PA postgraduate education, many PAs have completed residencies in surgical specialties or emergency medicine. Coincidentally, surgery and emergency medicine residencies are the most prolific of the postgraduate residency programs, adding a significant number of well-trained PAs to these specialties. The NCCPA also offers the CAQ for Cardiovascular and Thoracic Surgery, Orthopedic Surgery, and Emergency Medicine, which may attract PAs into these specialties, with or without completing a residency.
Because the NCCPA also offers the CAQ in Psychiatry, it would be reasonable and attractive for PAs who complete a psychiatry residency to obtain this certification. In fact, the PA psychiatry residency at our own institution trains our residents to be fully prepared and board-eligible to take the CAQ in Psychiatry upon completing residency. To date, every PA residency graduate who has completed our program and taken the CAQ in Psychiatry exam has passed and been awarded the CAQ in Psychiatry. They have proven themselves to the program and the NCCPA, and have impressed their employers with their clinical abilities and medical knowledge.
For psychiatrists, the addition of a well-trained or willing-to-be-trained PA to the practice can provide an economic advantage and strong team partnership that ensures optimal care for patients in this time of shortage of skilled mental health clinicians. The need is clear and will continue. Physician assistant educators must provide adequate didactic and clinical training in psychiatry to PA students, and support students interested in pursuing a career path in this specialty. Physician assistant organizations must meet the challenge of increasing the number of PAs in psychiatry, and encourage the establishment of additional post-graduate residency programs in psychiatry for PAs. Lastly, more PAs need to be made aware that psychiatry is an in-demand specialty that offers broad autonomy and rewarding clinical work.
Continue to: Bottom Line
Bottom Line
Physician assistants (PAs) who choose to specialize in psychiatry will find enormous opportunity, as the need for well-trained and knowledgeable mental health providers is acute. Those PAs who obtain additional training and/or certification in psychiatry will be highly valued and sought-after, with an abundance of job opportunities. Physician assistant programs should continue to improve didactic and clinical training for their students in psychiatry, and encourage increased numbers of PAs to consider psychiatry as a career path.
Related Resources
- National Commission on Certification of Physician Assistants. Psychiatry Certificate of Added Qualifications. https://www.nccpa.net/psychiatry.
- Association of Physician Assistants in Psychiatry. http://psychpa.com/.
1. Japen B. Psychiatrist shortage escalates as U.S. mental health needs grow. Forbes. https://www.forbes.com/sites/brucejapsen/2018/02/25/psychiatrist-shortage-escalates-as-u-s-mental-health-needs-grow/. Published February 25, 2018. Accessed February 1, 2019.
2. Association of American Medical Colleges. Active physicians in the largest specialties, 2017. Table 1.1. Number of active physicians in the largest specialties by major professional activity, 2017. www.aamc.org/data/workforce/reports/492556/1-1-chart.html. Published December 2017. Accessed February 1, 2019.
3. Weiner S. Addressing the escalating psychiatrist shortage. Association of American Medical Colleges AAMCNews. https://news.aamc.org/patient-care/article/addressing-escalating-psychiatrist-shortage/. Published February 13, 2018. Accessed February 1, 2019.
4. Cunningham P. Beyond parity: Primary care physicians’ perspectives on access to mental health care. Health Affairs. 2009;28(S1). https://www.healthaffairs.org/doi/full/10.1377/hlthaff.28.3.w490. Accessed February 1, 2019.
5. Psychiatrist shortage felt nationwide - and in VA system. The Gazette. https://www.thegazette.com/subject/news/government/psychiatrist-shortage-felt-nationwide-x2014-and-in-va-system-20170813. Published August 13, 2017. Accessed February 1, 2019.
6. Satiani A, Niedermier J, Satiani B, et al. Projected workforce of psychiatrists in the United States: a population analysis. Psychiatr Serv. 2018;69(6):710-713.
7. Levine D. What’s the answer to the shortage of mental health care providers? U.S. News & World Report. https://health.usnews.com/health-care/patient-advice/articles/2018-05-25/whats-the-answer-to-the-shortage-of-mental-health-care-providers. Published May 25, 2018. Accessed February 1, 2019.
8. Martsolf GR, Barnes H, Richards MR, et al. Employment of advanced practice clinicians in physician practices. JAMA Intern Med. 2018;178(7):988-990.
9. Hass V. Physician assistants and nurse practitioners are not interchangeable. JAAPA. 2016;29(4):9-12.
10. National Commission on Certification of Physician Assistants. 2018 Statistical profile of certified physician assistants by specialty. Annual report. https://prodcmsstoragesa.blob.core.windows.net/uploads/files/2018StatisticalProfileofCertifiedPAsbySpecialty1.pdf. Published July 2019. Accessed February 1, 2019.
11. Larson EH, Hart LG. Growth and change in the physician assistant workforce in the United States, 1967-2000. J Allied Health. 2007;36(3):121-130.
12. Perna G. NPs and PAs are joining docs in specialty care. Physicians Practice. http://www.physicianspractice.com/staff-salary-survey/nps-and-pas-are-joining-docs-specialty-care. Published May 9, 2016. Accessed February 1, 2019.
13. Pasquini S. Does PA program length matter? The Physician Assistant Life. www.thepalife.com/does-pa-program-length-matter/. Accessed February 1, 2019.
14. National Commission on Certification of Physician Assistants. PAs in specialty practice. An analysis of need, growth and future. http://prodcmsstoragesa.blob.core.windows.net/uploads/files/Whitepaper-PAsinSpecialtyPractice.pdf. Published October 2018. Accessed February 1, 2019.
15. National Commission on Certification of Physician Assistants. PArtners in Mental Health Initiative: Stakeholders Report 2018. http://www.nccpahealthfoundation.net/Portals/0/PDFs/PArtnersinMentalHealthInitiativeStakeholderReport2018.pdf. Published 2018. Accessed February 1, 2019.
16. National Commission on Certification of Physician Assistants. PArtners in Mental Health Summit: proceedings and Recommendations. Leesburg, Virginia – June 4-6, 2017. https://www.nccpahealthfoundation.net/Portals/0/PDFs/SummitProceedings.pdf. Published 2017. Accessed August 7, 2019.
1. Japen B. Psychiatrist shortage escalates as U.S. mental health needs grow. Forbes. https://www.forbes.com/sites/brucejapsen/2018/02/25/psychiatrist-shortage-escalates-as-u-s-mental-health-needs-grow/. Published February 25, 2018. Accessed February 1, 2019.
2. Association of American Medical Colleges. Active physicians in the largest specialties, 2017. Table 1.1. Number of active physicians in the largest specialties by major professional activity, 2017. www.aamc.org/data/workforce/reports/492556/1-1-chart.html. Published December 2017. Accessed February 1, 2019.
3. Weiner S. Addressing the escalating psychiatrist shortage. Association of American Medical Colleges AAMCNews. https://news.aamc.org/patient-care/article/addressing-escalating-psychiatrist-shortage/. Published February 13, 2018. Accessed February 1, 2019.
4. Cunningham P. Beyond parity: Primary care physicians’ perspectives on access to mental health care. Health Affairs. 2009;28(S1). https://www.healthaffairs.org/doi/full/10.1377/hlthaff.28.3.w490. Accessed February 1, 2019.
5. Psychiatrist shortage felt nationwide - and in VA system. The Gazette. https://www.thegazette.com/subject/news/government/psychiatrist-shortage-felt-nationwide-x2014-and-in-va-system-20170813. Published August 13, 2017. Accessed February 1, 2019.
6. Satiani A, Niedermier J, Satiani B, et al. Projected workforce of psychiatrists in the United States: a population analysis. Psychiatr Serv. 2018;69(6):710-713.
7. Levine D. What’s the answer to the shortage of mental health care providers? U.S. News & World Report. https://health.usnews.com/health-care/patient-advice/articles/2018-05-25/whats-the-answer-to-the-shortage-of-mental-health-care-providers. Published May 25, 2018. Accessed February 1, 2019.
8. Martsolf GR, Barnes H, Richards MR, et al. Employment of advanced practice clinicians in physician practices. JAMA Intern Med. 2018;178(7):988-990.
9. Hass V. Physician assistants and nurse practitioners are not interchangeable. JAAPA. 2016;29(4):9-12.
10. National Commission on Certification of Physician Assistants. 2018 Statistical profile of certified physician assistants by specialty. Annual report. https://prodcmsstoragesa.blob.core.windows.net/uploads/files/2018StatisticalProfileofCertifiedPAsbySpecialty1.pdf. Published July 2019. Accessed February 1, 2019.
11. Larson EH, Hart LG. Growth and change in the physician assistant workforce in the United States, 1967-2000. J Allied Health. 2007;36(3):121-130.
12. Perna G. NPs and PAs are joining docs in specialty care. Physicians Practice. http://www.physicianspractice.com/staff-salary-survey/nps-and-pas-are-joining-docs-specialty-care. Published May 9, 2016. Accessed February 1, 2019.
13. Pasquini S. Does PA program length matter? The Physician Assistant Life. www.thepalife.com/does-pa-program-length-matter/. Accessed February 1, 2019.
14. National Commission on Certification of Physician Assistants. PAs in specialty practice. An analysis of need, growth and future. http://prodcmsstoragesa.blob.core.windows.net/uploads/files/Whitepaper-PAsinSpecialtyPractice.pdf. Published October 2018. Accessed February 1, 2019.
15. National Commission on Certification of Physician Assistants. PArtners in Mental Health Initiative: Stakeholders Report 2018. http://www.nccpahealthfoundation.net/Portals/0/PDFs/PArtnersinMentalHealthInitiativeStakeholderReport2018.pdf. Published 2018. Accessed February 1, 2019.
16. National Commission on Certification of Physician Assistants. PArtners in Mental Health Summit: proceedings and Recommendations. Leesburg, Virginia – June 4-6, 2017. https://www.nccpahealthfoundation.net/Portals/0/PDFs/SummitProceedings.pdf. Published 2017. Accessed August 7, 2019.
Minimally invasive surgery for cervical cancer: Is surgeon volume a factor?
The role of minimally invasive surgery for early-stage cervical cancer has been the subject of heated debate since the presentation of the results of the Laparoscopic Approach to Cervical Cancer (LACC) Trial at the Society of Gynecologic Oncology Annual Meeting on Women’s Cancer in 2018. This was an international, randomized, phase 3 trial comparing minimally invasive radical hysterectomy (MH) to open radical hysterectomy (OH) in the treatment of early-stage cervical cancer. The trial was closed early by the study’s Data and Safety Monitoring Committee due to an imbalance of deaths between the groups, with a higher rate in the minimally invasive arm. The final results, which were largely unexpected by the medical community, showed that the disease-free survival (DFS) at 4.5 years was 86.0% in the MH arm and 96.5% in the OH arm, which was a larger difference than their noninferiority cutoff of -7.2 percentage points.1 Results of an epidemiologic study, which used data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Cancer Database, also were presented at this meeting, and they reinforced the findings of the LACC trial.2
The combined results have caused significant concern and confusion from the medical community regarding the clinical implication that minimally invasive surgery may be an unacceptable approach for radical hysterectomy in cervical cancer. Prior to this study, retrospective data supported similar outcomes between the two approaches.3 Additionally, robotic surgery has made radical hysterectomy an option for those with a higher body mass index, as an open radical hysterectomy can be technically challenging in larger patients and result in a higher rate of adverse outcomes.
LACC trial questioned by US surgeons
Many in the United States have questioned the design and conclusions of the LACC trial. This trial was conducted primarily outside of North America and utilized conventional laparoscopic surgery 85% of the time as opposed to robotic surgery. Additionally, the found difference in DFS between MH and OH may have been driven more by the superior performance of the OH group (compared with historical data) than the poorly performing MH group.4 Other criticisms have touched on the low number of overall survival events, the low bar for surgeon volume or skill assessment, and the inability to make conclusions regarding “low-risk” lesions (<2 cm, no lymphovascular space invasion, <1 cm depth of invasion).
Were requirements for surgical skill adequate? Regarding surgeon skill, the LACC trial required documentation of the perioperative outcomes from 10 laparoscopic or robotic radical hysterectomies, as well as 2 unedited videos of each surgeon participating in the study to verify their technique, which some have considered inadequate to sufficiently vet a surgeon’s ability. Additionally, 14 of the 33 centers enrolled in the study accrued 71% of the patients, and concerns about the surgeon volume of the remaining 19 centers have been raised. Finally, there has been discussion about whether the variance in surgical approach can even be adequately assessed in a trial of this nature, as surgical skill is not a binary variable that is easily amenable to randomization. Unlike other trials, which have clear exposure and control arms, no 2 surgeries are exactly alike, and surgical technique is highly variable between surgeons, institutions, and countries.
Continue to: New data evaluate for surgeon volume
New data evaluate for surgeon volume
In an effort to address the concerns regarding surgical approach and expertise, the recently published study by Cusimano and colleagues uses population-based data from Ontario for all women undergoing radical hysterectomy for cervical cancer over a 10-year period from 2006 through 2016.5 The primary outcome was all-cause death, but the study also sought to address whether surgeon volume has an impact on recurrence rates for patients undergoing MH versus OH. To measure this impact the authors stratified surgeon characteristics by technique-specific volume and cervical cancer volume, splitting these volumes at the 50% percentile for low- and high-volume surgeons. They defined technique-specific volume as the number of simple and radical hysterectomies performed in the prior year using the selected approach (MH or OH). Cervical cancer volume was calculated as the number of hysterectomies of any type for cervical cancer in the previous 2 years. The technique-specific volume variable was subsequently re-categorized into tertiles, examined as a continuous variable, and analyzed at the 50th percentile for each year of the study.
Death and recurrence rates better in the OH group. The final cohort included 958 women that were relatively evenly split between MH and OH procedures. Results from their analysis show no difference in terms of all-cause death, cervical cancer–specific death, or recurrence. However, all 3 of these parameters were significantly different in favor of the OH group in women with Stage IB disease, which comprised over half of the overall cohort. Importantly, neither technique-specific volume nor cervical cancer volume had an effect on death or recurrence in Stage IB patients in any of the investigators’ analyses.
Important limitations. There are several limitations to this study that have to be taken into account before drawing any conclusions. Pathologic data were obtained from the database and did not include some important details about the tumor specimens (including specifying subgroups of Stage IA and IB disease, tumor size, presence of lymphovascular space invasion, and depth of stromal invasion). All of these details have been shown to be important prognostic variables in early-stage cervical cancer. Additionally, the MH group included a predominantly laparoscopic approach with only 10% of cases performed robotically, which again brings into question the generalizability of the data.
However, despite some of these shortcomings, the study authors do make a compelling argument that surgeon volume alone does not seem to play a significant role in cancer outcomes after MH.
With surgical approaches hard to compare, turn to careful patient counseling
Definitive assessment of the impact of surgical skill and experience on cervical cancer outcomes is probably an impossible task, as even a perfectly designed trial cannot entirely account for the intricacies of a complex surgical procedure. Variations in tumor characteristics and patient anatomy that affect operative decision making are not likely to be reflected when a patient’s outcome is plugged into a database. As a result, some surgeons and departments have turned to reporting personal or institutional recurrence rates for MH, which they believe may b
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895-1904.
- Melamed A, Margul DJ, Chen L, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379:1905-1914.
- Wang Y, Deng L, Cao L, et al. The outcome of laparoscopy versus laparotomy for the management of early stage cervical cancer-meta analysis. J Minim Invasive Gynecol. 2015;22:S4-S5.
- Leitao MM Jr. The LACC Trial: has minimally invasive surgery for early-stage cervical cancer been dealt a knockout punch? Int J Gynecol Cancer. 2018;28:1248-1250.
- Cusimano MC, Baxter NN, Gien LT, et al. Impact of surgical approach on oncologic outcomes in women undergoing radical hysterectomy for cervical cancer. Am J Obstet Gynecol. July 6, 2019. doi:10.1016/j.ajog.2019.07.009.
The role of minimally invasive surgery for early-stage cervical cancer has been the subject of heated debate since the presentation of the results of the Laparoscopic Approach to Cervical Cancer (LACC) Trial at the Society of Gynecologic Oncology Annual Meeting on Women’s Cancer in 2018. This was an international, randomized, phase 3 trial comparing minimally invasive radical hysterectomy (MH) to open radical hysterectomy (OH) in the treatment of early-stage cervical cancer. The trial was closed early by the study’s Data and Safety Monitoring Committee due to an imbalance of deaths between the groups, with a higher rate in the minimally invasive arm. The final results, which were largely unexpected by the medical community, showed that the disease-free survival (DFS) at 4.5 years was 86.0% in the MH arm and 96.5% in the OH arm, which was a larger difference than their noninferiority cutoff of -7.2 percentage points.1 Results of an epidemiologic study, which used data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Cancer Database, also were presented at this meeting, and they reinforced the findings of the LACC trial.2
The combined results have caused significant concern and confusion from the medical community regarding the clinical implication that minimally invasive surgery may be an unacceptable approach for radical hysterectomy in cervical cancer. Prior to this study, retrospective data supported similar outcomes between the two approaches.3 Additionally, robotic surgery has made radical hysterectomy an option for those with a higher body mass index, as an open radical hysterectomy can be technically challenging in larger patients and result in a higher rate of adverse outcomes.
LACC trial questioned by US surgeons
Many in the United States have questioned the design and conclusions of the LACC trial. This trial was conducted primarily outside of North America and utilized conventional laparoscopic surgery 85% of the time as opposed to robotic surgery. Additionally, the found difference in DFS between MH and OH may have been driven more by the superior performance of the OH group (compared with historical data) than the poorly performing MH group.4 Other criticisms have touched on the low number of overall survival events, the low bar for surgeon volume or skill assessment, and the inability to make conclusions regarding “low-risk” lesions (<2 cm, no lymphovascular space invasion, <1 cm depth of invasion).
Were requirements for surgical skill adequate? Regarding surgeon skill, the LACC trial required documentation of the perioperative outcomes from 10 laparoscopic or robotic radical hysterectomies, as well as 2 unedited videos of each surgeon participating in the study to verify their technique, which some have considered inadequate to sufficiently vet a surgeon’s ability. Additionally, 14 of the 33 centers enrolled in the study accrued 71% of the patients, and concerns about the surgeon volume of the remaining 19 centers have been raised. Finally, there has been discussion about whether the variance in surgical approach can even be adequately assessed in a trial of this nature, as surgical skill is not a binary variable that is easily amenable to randomization. Unlike other trials, which have clear exposure and control arms, no 2 surgeries are exactly alike, and surgical technique is highly variable between surgeons, institutions, and countries.
Continue to: New data evaluate for surgeon volume
New data evaluate for surgeon volume
In an effort to address the concerns regarding surgical approach and expertise, the recently published study by Cusimano and colleagues uses population-based data from Ontario for all women undergoing radical hysterectomy for cervical cancer over a 10-year period from 2006 through 2016.5 The primary outcome was all-cause death, but the study also sought to address whether surgeon volume has an impact on recurrence rates for patients undergoing MH versus OH. To measure this impact the authors stratified surgeon characteristics by technique-specific volume and cervical cancer volume, splitting these volumes at the 50% percentile for low- and high-volume surgeons. They defined technique-specific volume as the number of simple and radical hysterectomies performed in the prior year using the selected approach (MH or OH). Cervical cancer volume was calculated as the number of hysterectomies of any type for cervical cancer in the previous 2 years. The technique-specific volume variable was subsequently re-categorized into tertiles, examined as a continuous variable, and analyzed at the 50th percentile for each year of the study.
Death and recurrence rates better in the OH group. The final cohort included 958 women that were relatively evenly split between MH and OH procedures. Results from their analysis show no difference in terms of all-cause death, cervical cancer–specific death, or recurrence. However, all 3 of these parameters were significantly different in favor of the OH group in women with Stage IB disease, which comprised over half of the overall cohort. Importantly, neither technique-specific volume nor cervical cancer volume had an effect on death or recurrence in Stage IB patients in any of the investigators’ analyses.
Important limitations. There are several limitations to this study that have to be taken into account before drawing any conclusions. Pathologic data were obtained from the database and did not include some important details about the tumor specimens (including specifying subgroups of Stage IA and IB disease, tumor size, presence of lymphovascular space invasion, and depth of stromal invasion). All of these details have been shown to be important prognostic variables in early-stage cervical cancer. Additionally, the MH group included a predominantly laparoscopic approach with only 10% of cases performed robotically, which again brings into question the generalizability of the data.
However, despite some of these shortcomings, the study authors do make a compelling argument that surgeon volume alone does not seem to play a significant role in cancer outcomes after MH.
With surgical approaches hard to compare, turn to careful patient counseling
Definitive assessment of the impact of surgical skill and experience on cervical cancer outcomes is probably an impossible task, as even a perfectly designed trial cannot entirely account for the intricacies of a complex surgical procedure. Variations in tumor characteristics and patient anatomy that affect operative decision making are not likely to be reflected when a patient’s outcome is plugged into a database. As a result, some surgeons and departments have turned to reporting personal or institutional recurrence rates for MH, which they believe may b
The role of minimally invasive surgery for early-stage cervical cancer has been the subject of heated debate since the presentation of the results of the Laparoscopic Approach to Cervical Cancer (LACC) Trial at the Society of Gynecologic Oncology Annual Meeting on Women’s Cancer in 2018. This was an international, randomized, phase 3 trial comparing minimally invasive radical hysterectomy (MH) to open radical hysterectomy (OH) in the treatment of early-stage cervical cancer. The trial was closed early by the study’s Data and Safety Monitoring Committee due to an imbalance of deaths between the groups, with a higher rate in the minimally invasive arm. The final results, which were largely unexpected by the medical community, showed that the disease-free survival (DFS) at 4.5 years was 86.0% in the MH arm and 96.5% in the OH arm, which was a larger difference than their noninferiority cutoff of -7.2 percentage points.1 Results of an epidemiologic study, which used data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Cancer Database, also were presented at this meeting, and they reinforced the findings of the LACC trial.2
The combined results have caused significant concern and confusion from the medical community regarding the clinical implication that minimally invasive surgery may be an unacceptable approach for radical hysterectomy in cervical cancer. Prior to this study, retrospective data supported similar outcomes between the two approaches.3 Additionally, robotic surgery has made radical hysterectomy an option for those with a higher body mass index, as an open radical hysterectomy can be technically challenging in larger patients and result in a higher rate of adverse outcomes.
LACC trial questioned by US surgeons
Many in the United States have questioned the design and conclusions of the LACC trial. This trial was conducted primarily outside of North America and utilized conventional laparoscopic surgery 85% of the time as opposed to robotic surgery. Additionally, the found difference in DFS between MH and OH may have been driven more by the superior performance of the OH group (compared with historical data) than the poorly performing MH group.4 Other criticisms have touched on the low number of overall survival events, the low bar for surgeon volume or skill assessment, and the inability to make conclusions regarding “low-risk” lesions (<2 cm, no lymphovascular space invasion, <1 cm depth of invasion).
Were requirements for surgical skill adequate? Regarding surgeon skill, the LACC trial required documentation of the perioperative outcomes from 10 laparoscopic or robotic radical hysterectomies, as well as 2 unedited videos of each surgeon participating in the study to verify their technique, which some have considered inadequate to sufficiently vet a surgeon’s ability. Additionally, 14 of the 33 centers enrolled in the study accrued 71% of the patients, and concerns about the surgeon volume of the remaining 19 centers have been raised. Finally, there has been discussion about whether the variance in surgical approach can even be adequately assessed in a trial of this nature, as surgical skill is not a binary variable that is easily amenable to randomization. Unlike other trials, which have clear exposure and control arms, no 2 surgeries are exactly alike, and surgical technique is highly variable between surgeons, institutions, and countries.
Continue to: New data evaluate for surgeon volume
New data evaluate for surgeon volume
In an effort to address the concerns regarding surgical approach and expertise, the recently published study by Cusimano and colleagues uses population-based data from Ontario for all women undergoing radical hysterectomy for cervical cancer over a 10-year period from 2006 through 2016.5 The primary outcome was all-cause death, but the study also sought to address whether surgeon volume has an impact on recurrence rates for patients undergoing MH versus OH. To measure this impact the authors stratified surgeon characteristics by technique-specific volume and cervical cancer volume, splitting these volumes at the 50% percentile for low- and high-volume surgeons. They defined technique-specific volume as the number of simple and radical hysterectomies performed in the prior year using the selected approach (MH or OH). Cervical cancer volume was calculated as the number of hysterectomies of any type for cervical cancer in the previous 2 years. The technique-specific volume variable was subsequently re-categorized into tertiles, examined as a continuous variable, and analyzed at the 50th percentile for each year of the study.
Death and recurrence rates better in the OH group. The final cohort included 958 women that were relatively evenly split between MH and OH procedures. Results from their analysis show no difference in terms of all-cause death, cervical cancer–specific death, or recurrence. However, all 3 of these parameters were significantly different in favor of the OH group in women with Stage IB disease, which comprised over half of the overall cohort. Importantly, neither technique-specific volume nor cervical cancer volume had an effect on death or recurrence in Stage IB patients in any of the investigators’ analyses.
Important limitations. There are several limitations to this study that have to be taken into account before drawing any conclusions. Pathologic data were obtained from the database and did not include some important details about the tumor specimens (including specifying subgroups of Stage IA and IB disease, tumor size, presence of lymphovascular space invasion, and depth of stromal invasion). All of these details have been shown to be important prognostic variables in early-stage cervical cancer. Additionally, the MH group included a predominantly laparoscopic approach with only 10% of cases performed robotically, which again brings into question the generalizability of the data.
However, despite some of these shortcomings, the study authors do make a compelling argument that surgeon volume alone does not seem to play a significant role in cancer outcomes after MH.
With surgical approaches hard to compare, turn to careful patient counseling
Definitive assessment of the impact of surgical skill and experience on cervical cancer outcomes is probably an impossible task, as even a perfectly designed trial cannot entirely account for the intricacies of a complex surgical procedure. Variations in tumor characteristics and patient anatomy that affect operative decision making are not likely to be reflected when a patient’s outcome is plugged into a database. As a result, some surgeons and departments have turned to reporting personal or institutional recurrence rates for MH, which they believe may b
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895-1904.
- Melamed A, Margul DJ, Chen L, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379:1905-1914.
- Wang Y, Deng L, Cao L, et al. The outcome of laparoscopy versus laparotomy for the management of early stage cervical cancer-meta analysis. J Minim Invasive Gynecol. 2015;22:S4-S5.
- Leitao MM Jr. The LACC Trial: has minimally invasive surgery for early-stage cervical cancer been dealt a knockout punch? Int J Gynecol Cancer. 2018;28:1248-1250.
- Cusimano MC, Baxter NN, Gien LT, et al. Impact of surgical approach on oncologic outcomes in women undergoing radical hysterectomy for cervical cancer. Am J Obstet Gynecol. July 6, 2019. doi:10.1016/j.ajog.2019.07.009.
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895-1904.
- Melamed A, Margul DJ, Chen L, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379:1905-1914.
- Wang Y, Deng L, Cao L, et al. The outcome of laparoscopy versus laparotomy for the management of early stage cervical cancer-meta analysis. J Minim Invasive Gynecol. 2015;22:S4-S5.
- Leitao MM Jr. The LACC Trial: has minimally invasive surgery for early-stage cervical cancer been dealt a knockout punch? Int J Gynecol Cancer. 2018;28:1248-1250.
- Cusimano MC, Baxter NN, Gien LT, et al. Impact of surgical approach on oncologic outcomes in women undergoing radical hysterectomy for cervical cancer. Am J Obstet Gynecol. July 6, 2019. doi:10.1016/j.ajog.2019.07.009.
Studies reinforce clinical experience and intuition
In this edition of “How I will treat my next patient,” I examine two recently published efforts to enlighten our sensitivity to the seriousness of immune-related adverse events (IrAEs) in patients on immune checkpoint inhibitors (ICIs) and the effect of delays in initiating systemic adjuvant therapy on the long-term outcomes of patients with resected pancreatic cancer.
IrAEs requiring hospitalization
Investigators led by Aanika Balaji of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore, reviewed a 6-month audit of inpatient oncology admissions of solid-tumor patients who had ever received ICIs and ascertained the prevalence of hospitalization for management of IrAEs (J Oncol Pract. 2019 Aug 6. doi: 10.1200/JOP.18.00703). To determine that an IrAE had occurred they required: consensus among two oncologists, clinical improvement with immune-directed therapy, exclusion of alternative diagnoses or pathologic confirmation of an IrAE, or chronic management of an IrAE for more than 6 months.
The bottom line: They found a cumulative incidence of a confirmed IrAEs among hospitalized ICI-treated solid tumor patients of 23%. As expected, the majority (65%) were grade 3-4 in severity. In total, 91% required multidisciplinary management, and 65% improved or resolved. But 87% of patients never received an ICI again.
Patients with preexisting autoimmune disease (25% of patients, although they included hypothyroidism in that group) were not more vulnerable to an IrAE with ICI therapy (odds ratio, 1.0; 95% confidence interval, 0.3-4.0). Not unsurprisingly, the median age was higher for ICI-treated patients who were admitted for IrAEs than for those not admitted (68 years vs. 59 years; OR, 5.4; 95% CI, 1.6-17.8), and more admitted patients had received combination ICIs than single agents (OR, 6.8; 95% CI, 2.0-23.2).
The median time from beginning ICIs to an IrAE-related hospitalization was 64 days, and the median number of ICI doses was one, with a wide range for both days and doses. The authors were quick to comment that this is a small, academic, single-institution survey over a brief period of time and that the generalizability of the results is uncertain.
What this means in practice
This publication changes very little for most practicing oncologists, but it does reinforce that ICI therapy can cause unpredictable, severe IrAEs. Clinical markers for selecting patients at highest risk are imperfect. As with chemotherapy, the patients we worry about the most – older individuals and patients treated with drug combinations – are, in fact, the ones we should be worrying about the most.
In view of the potential severity and impact of IrAEs, research efforts should place equal priority on identifying biomarkers of toxicity, such as tumor mutation burden, and biomarkers of efficacy (JAMA Oncol. 2019 Aug 22. doi: 10.1001/jamaoncol.2019.3221). The potential financial and societal effects, as well as lost opportunity costs in the form of alternative therapies and early referral to hospice, demand no less, particularly in an era of value-based health care reimbursement.
Timing of adjuvant treatment
Sung Jun Ma, MD, department of radiation medicine at Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., and colleagues analyzed data from the more than 7,500 stage I-II resected pancreatic cancer patients in the National Cancer Database, of whom more than 5,400 ultimately received adjuvant therapy (chemotherapy with or without radiation). The patients were treated during 2004-2015. Appropriately, the investigators focused on correlating survival duration with the interval between surgery and initiation of adjuvant therapy. Other endpoints would be hard to accurately measure and verify without detailed clinical information (JAMA Network Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9126).
They found that the best overall survival was associated with starting adjuvant treatment 28-59 days after surgery – not earlier (17% higher mortality) and not later (9% higher). Patients who did not start adjuvant treatment until more than 90 days post operatively still had an overall survival benefit (hazard ratio, 0.75; 95% confidence interval, 0.66-0.85; P less than .001), a more impressive hazard ratio than that seen for any particular interval between surgery and adjuvant treatment. Overall survival at 2 years was 47.2% versus 38% for the adjuvant therapy and surgery alone cohorts, respectively, with no overlap in the 95% confidence intervals.
As expected, longer delays to receive adjuvant treatment were associated with longer inpatient surgical stays, advanced age, black race, lower income, and a readmission for a postoperative complication within 30 days.
What this means in practice
This is another study that verifies that the patients we worry about most – older patients, those with a complicated recovery from surgery, and those with fewer supportive resources – are exactly the patients we should worry about most. It changes very little for most practicing oncologists. The analysis validates the importance of adjuvant therapy for patients who are able to receive it – whenever that is.
The data collection in this publication precedes recent improvements in adjuvant chemotherapy for resected pancreatic cancer, such as FOLFIRINOX or gemcitabine plus capecitabine. In an era of improved treatment, delays in initiating therapy may be less important since better treatment overcomes many prognostic variables that are significant for less effective therapy.
In my opinion, this large-data analysis is not really hypothesis-generating or practice-changing, but it does compel us to continue research efforts to improve surgical morbidity, identify better adjuvant and advanced disease regimens, and consider neoadjuvant treatment so that more than 72% of patients can receive all components of the multimodality treatment they need.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I examine two recently published efforts to enlighten our sensitivity to the seriousness of immune-related adverse events (IrAEs) in patients on immune checkpoint inhibitors (ICIs) and the effect of delays in initiating systemic adjuvant therapy on the long-term outcomes of patients with resected pancreatic cancer.
IrAEs requiring hospitalization
Investigators led by Aanika Balaji of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore, reviewed a 6-month audit of inpatient oncology admissions of solid-tumor patients who had ever received ICIs and ascertained the prevalence of hospitalization for management of IrAEs (J Oncol Pract. 2019 Aug 6. doi: 10.1200/JOP.18.00703). To determine that an IrAE had occurred they required: consensus among two oncologists, clinical improvement with immune-directed therapy, exclusion of alternative diagnoses or pathologic confirmation of an IrAE, or chronic management of an IrAE for more than 6 months.
The bottom line: They found a cumulative incidence of a confirmed IrAEs among hospitalized ICI-treated solid tumor patients of 23%. As expected, the majority (65%) were grade 3-4 in severity. In total, 91% required multidisciplinary management, and 65% improved or resolved. But 87% of patients never received an ICI again.
Patients with preexisting autoimmune disease (25% of patients, although they included hypothyroidism in that group) were not more vulnerable to an IrAE with ICI therapy (odds ratio, 1.0; 95% confidence interval, 0.3-4.0). Not unsurprisingly, the median age was higher for ICI-treated patients who were admitted for IrAEs than for those not admitted (68 years vs. 59 years; OR, 5.4; 95% CI, 1.6-17.8), and more admitted patients had received combination ICIs than single agents (OR, 6.8; 95% CI, 2.0-23.2).
The median time from beginning ICIs to an IrAE-related hospitalization was 64 days, and the median number of ICI doses was one, with a wide range for both days and doses. The authors were quick to comment that this is a small, academic, single-institution survey over a brief period of time and that the generalizability of the results is uncertain.
What this means in practice
This publication changes very little for most practicing oncologists, but it does reinforce that ICI therapy can cause unpredictable, severe IrAEs. Clinical markers for selecting patients at highest risk are imperfect. As with chemotherapy, the patients we worry about the most – older individuals and patients treated with drug combinations – are, in fact, the ones we should be worrying about the most.
In view of the potential severity and impact of IrAEs, research efforts should place equal priority on identifying biomarkers of toxicity, such as tumor mutation burden, and biomarkers of efficacy (JAMA Oncol. 2019 Aug 22. doi: 10.1001/jamaoncol.2019.3221). The potential financial and societal effects, as well as lost opportunity costs in the form of alternative therapies and early referral to hospice, demand no less, particularly in an era of value-based health care reimbursement.
Timing of adjuvant treatment
Sung Jun Ma, MD, department of radiation medicine at Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., and colleagues analyzed data from the more than 7,500 stage I-II resected pancreatic cancer patients in the National Cancer Database, of whom more than 5,400 ultimately received adjuvant therapy (chemotherapy with or without radiation). The patients were treated during 2004-2015. Appropriately, the investigators focused on correlating survival duration with the interval between surgery and initiation of adjuvant therapy. Other endpoints would be hard to accurately measure and verify without detailed clinical information (JAMA Network Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9126).
They found that the best overall survival was associated with starting adjuvant treatment 28-59 days after surgery – not earlier (17% higher mortality) and not later (9% higher). Patients who did not start adjuvant treatment until more than 90 days post operatively still had an overall survival benefit (hazard ratio, 0.75; 95% confidence interval, 0.66-0.85; P less than .001), a more impressive hazard ratio than that seen for any particular interval between surgery and adjuvant treatment. Overall survival at 2 years was 47.2% versus 38% for the adjuvant therapy and surgery alone cohorts, respectively, with no overlap in the 95% confidence intervals.
As expected, longer delays to receive adjuvant treatment were associated with longer inpatient surgical stays, advanced age, black race, lower income, and a readmission for a postoperative complication within 30 days.
What this means in practice
This is another study that verifies that the patients we worry about most – older patients, those with a complicated recovery from surgery, and those with fewer supportive resources – are exactly the patients we should worry about most. It changes very little for most practicing oncologists. The analysis validates the importance of adjuvant therapy for patients who are able to receive it – whenever that is.
The data collection in this publication precedes recent improvements in adjuvant chemotherapy for resected pancreatic cancer, such as FOLFIRINOX or gemcitabine plus capecitabine. In an era of improved treatment, delays in initiating therapy may be less important since better treatment overcomes many prognostic variables that are significant for less effective therapy.
In my opinion, this large-data analysis is not really hypothesis-generating or practice-changing, but it does compel us to continue research efforts to improve surgical morbidity, identify better adjuvant and advanced disease regimens, and consider neoadjuvant treatment so that more than 72% of patients can receive all components of the multimodality treatment they need.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I examine two recently published efforts to enlighten our sensitivity to the seriousness of immune-related adverse events (IrAEs) in patients on immune checkpoint inhibitors (ICIs) and the effect of delays in initiating systemic adjuvant therapy on the long-term outcomes of patients with resected pancreatic cancer.
IrAEs requiring hospitalization
Investigators led by Aanika Balaji of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore, reviewed a 6-month audit of inpatient oncology admissions of solid-tumor patients who had ever received ICIs and ascertained the prevalence of hospitalization for management of IrAEs (J Oncol Pract. 2019 Aug 6. doi: 10.1200/JOP.18.00703). To determine that an IrAE had occurred they required: consensus among two oncologists, clinical improvement with immune-directed therapy, exclusion of alternative diagnoses or pathologic confirmation of an IrAE, or chronic management of an IrAE for more than 6 months.
The bottom line: They found a cumulative incidence of a confirmed IrAEs among hospitalized ICI-treated solid tumor patients of 23%. As expected, the majority (65%) were grade 3-4 in severity. In total, 91% required multidisciplinary management, and 65% improved or resolved. But 87% of patients never received an ICI again.
Patients with preexisting autoimmune disease (25% of patients, although they included hypothyroidism in that group) were not more vulnerable to an IrAE with ICI therapy (odds ratio, 1.0; 95% confidence interval, 0.3-4.0). Not unsurprisingly, the median age was higher for ICI-treated patients who were admitted for IrAEs than for those not admitted (68 years vs. 59 years; OR, 5.4; 95% CI, 1.6-17.8), and more admitted patients had received combination ICIs than single agents (OR, 6.8; 95% CI, 2.0-23.2).
The median time from beginning ICIs to an IrAE-related hospitalization was 64 days, and the median number of ICI doses was one, with a wide range for both days and doses. The authors were quick to comment that this is a small, academic, single-institution survey over a brief period of time and that the generalizability of the results is uncertain.
What this means in practice
This publication changes very little for most practicing oncologists, but it does reinforce that ICI therapy can cause unpredictable, severe IrAEs. Clinical markers for selecting patients at highest risk are imperfect. As with chemotherapy, the patients we worry about the most – older individuals and patients treated with drug combinations – are, in fact, the ones we should be worrying about the most.
In view of the potential severity and impact of IrAEs, research efforts should place equal priority on identifying biomarkers of toxicity, such as tumor mutation burden, and biomarkers of efficacy (JAMA Oncol. 2019 Aug 22. doi: 10.1001/jamaoncol.2019.3221). The potential financial and societal effects, as well as lost opportunity costs in the form of alternative therapies and early referral to hospice, demand no less, particularly in an era of value-based health care reimbursement.
Timing of adjuvant treatment
Sung Jun Ma, MD, department of radiation medicine at Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., and colleagues analyzed data from the more than 7,500 stage I-II resected pancreatic cancer patients in the National Cancer Database, of whom more than 5,400 ultimately received adjuvant therapy (chemotherapy with or without radiation). The patients were treated during 2004-2015. Appropriately, the investigators focused on correlating survival duration with the interval between surgery and initiation of adjuvant therapy. Other endpoints would be hard to accurately measure and verify without detailed clinical information (JAMA Network Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9126).
They found that the best overall survival was associated with starting adjuvant treatment 28-59 days after surgery – not earlier (17% higher mortality) and not later (9% higher). Patients who did not start adjuvant treatment until more than 90 days post operatively still had an overall survival benefit (hazard ratio, 0.75; 95% confidence interval, 0.66-0.85; P less than .001), a more impressive hazard ratio than that seen for any particular interval between surgery and adjuvant treatment. Overall survival at 2 years was 47.2% versus 38% for the adjuvant therapy and surgery alone cohorts, respectively, with no overlap in the 95% confidence intervals.
As expected, longer delays to receive adjuvant treatment were associated with longer inpatient surgical stays, advanced age, black race, lower income, and a readmission for a postoperative complication within 30 days.
What this means in practice
This is another study that verifies that the patients we worry about most – older patients, those with a complicated recovery from surgery, and those with fewer supportive resources – are exactly the patients we should worry about most. It changes very little for most practicing oncologists. The analysis validates the importance of adjuvant therapy for patients who are able to receive it – whenever that is.
The data collection in this publication precedes recent improvements in adjuvant chemotherapy for resected pancreatic cancer, such as FOLFIRINOX or gemcitabine plus capecitabine. In an era of improved treatment, delays in initiating therapy may be less important since better treatment overcomes many prognostic variables that are significant for less effective therapy.
In my opinion, this large-data analysis is not really hypothesis-generating or practice-changing, but it does compel us to continue research efforts to improve surgical morbidity, identify better adjuvant and advanced disease regimens, and consider neoadjuvant treatment so that more than 72% of patients can receive all components of the multimodality treatment they need.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
Time or money?
The authors of a recent study published in the Annals of Internal Medicine estimate that physician burnout is costing this country’s health care system $4.6 billion annually, using a conservative base-case model (Ann Intern Med. 2019;170[11]:784-90). I guess we shouldn’t be surprised at the magnitude of the drain on our economy caused by unhappy physicians. We all know colleagues who are showing signs of burnout. And, you may be feeling yourself that the challenges of work are taking too great a toll on your physical and mental health? Would you be happier if you had more time?
A study reported in Harvard Business Review has looked at recent college graduates to determine if how they prioritize time and money can predict their future happiness (“Are New Graduates Happier Making More Money or Having More Time?” July 25, 2019). The researchers at the Harvard Business School surveyed 1,000 college students in the 2015 and 2016 classes of the University of British Columbia, Vancouver. The students were asked to match themselves with descriptions of fictitious individuals to determine whether in general they prioritized time or money. The researchers then assessed the students’ level of happiness by asking them, “How satisfied are you with life overall?”
At a 2-year follow-up, the researchers found that, even taking into account the students’ level of happiness at the beginning of the study, “those who prioritized time were happier.” The authors also found that time-oriented people don’t necessarily work less or even earn more money, prompting their conclusion there is “strong evidence that valuing time puts people on a trajectory toward job satisfaction and well-being.”
Do the results of this study of Canadian college students provide any answers for our epidemic of physician burnout? One could argue that, if we wanted to minimize burnout, medical schools should include an assessment of each applicant’s level of happiness and how she or he prioritizes time and money using methods similar those used in this study? The problem is that some students are so heavily committed to becoming physicians that they would game the system and provide answers that will project the image that they are happy and prioritize time over money, when in reality they are ticking time bombs of discontent.
The bigger problem with interpreting the results of this study is that the subjects were Canadians who have significantly less educational debt than the medical students in this country. And as the authors observe, “people with objective financial constraints ... are more likely to focus on having more money.” Until we solve the problem of the high cost of medical education the system will continue to select for physicians whose decisions are too heavily influenced by their educational debt.
Finally, it is important to consider that time-oriented individuals don’t always work less, rather they make decisions that make it more likely that they will pursue activities they find enjoyable. For example, accepting a higher-paying job that requires an additional 3 hours of commute each day lays the foundation for a life in which a large portion of one’s day is expended in an activity that few of us find enjoyable. Choosing a long commute is a personal decision. Spending nearly 2 hours each day tethered to an EHR system was not something most physicians anticipated when they were choosing a career.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
The authors of a recent study published in the Annals of Internal Medicine estimate that physician burnout is costing this country’s health care system $4.6 billion annually, using a conservative base-case model (Ann Intern Med. 2019;170[11]:784-90). I guess we shouldn’t be surprised at the magnitude of the drain on our economy caused by unhappy physicians. We all know colleagues who are showing signs of burnout. And, you may be feeling yourself that the challenges of work are taking too great a toll on your physical and mental health? Would you be happier if you had more time?
A study reported in Harvard Business Review has looked at recent college graduates to determine if how they prioritize time and money can predict their future happiness (“Are New Graduates Happier Making More Money or Having More Time?” July 25, 2019). The researchers at the Harvard Business School surveyed 1,000 college students in the 2015 and 2016 classes of the University of British Columbia, Vancouver. The students were asked to match themselves with descriptions of fictitious individuals to determine whether in general they prioritized time or money. The researchers then assessed the students’ level of happiness by asking them, “How satisfied are you with life overall?”
At a 2-year follow-up, the researchers found that, even taking into account the students’ level of happiness at the beginning of the study, “those who prioritized time were happier.” The authors also found that time-oriented people don’t necessarily work less or even earn more money, prompting their conclusion there is “strong evidence that valuing time puts people on a trajectory toward job satisfaction and well-being.”
Do the results of this study of Canadian college students provide any answers for our epidemic of physician burnout? One could argue that, if we wanted to minimize burnout, medical schools should include an assessment of each applicant’s level of happiness and how she or he prioritizes time and money using methods similar those used in this study? The problem is that some students are so heavily committed to becoming physicians that they would game the system and provide answers that will project the image that they are happy and prioritize time over money, when in reality they are ticking time bombs of discontent.
The bigger problem with interpreting the results of this study is that the subjects were Canadians who have significantly less educational debt than the medical students in this country. And as the authors observe, “people with objective financial constraints ... are more likely to focus on having more money.” Until we solve the problem of the high cost of medical education the system will continue to select for physicians whose decisions are too heavily influenced by their educational debt.
Finally, it is important to consider that time-oriented individuals don’t always work less, rather they make decisions that make it more likely that they will pursue activities they find enjoyable. For example, accepting a higher-paying job that requires an additional 3 hours of commute each day lays the foundation for a life in which a large portion of one’s day is expended in an activity that few of us find enjoyable. Choosing a long commute is a personal decision. Spending nearly 2 hours each day tethered to an EHR system was not something most physicians anticipated when they were choosing a career.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
The authors of a recent study published in the Annals of Internal Medicine estimate that physician burnout is costing this country’s health care system $4.6 billion annually, using a conservative base-case model (Ann Intern Med. 2019;170[11]:784-90). I guess we shouldn’t be surprised at the magnitude of the drain on our economy caused by unhappy physicians. We all know colleagues who are showing signs of burnout. And, you may be feeling yourself that the challenges of work are taking too great a toll on your physical and mental health? Would you be happier if you had more time?
A study reported in Harvard Business Review has looked at recent college graduates to determine if how they prioritize time and money can predict their future happiness (“Are New Graduates Happier Making More Money or Having More Time?” July 25, 2019). The researchers at the Harvard Business School surveyed 1,000 college students in the 2015 and 2016 classes of the University of British Columbia, Vancouver. The students were asked to match themselves with descriptions of fictitious individuals to determine whether in general they prioritized time or money. The researchers then assessed the students’ level of happiness by asking them, “How satisfied are you with life overall?”
At a 2-year follow-up, the researchers found that, even taking into account the students’ level of happiness at the beginning of the study, “those who prioritized time were happier.” The authors also found that time-oriented people don’t necessarily work less or even earn more money, prompting their conclusion there is “strong evidence that valuing time puts people on a trajectory toward job satisfaction and well-being.”
Do the results of this study of Canadian college students provide any answers for our epidemic of physician burnout? One could argue that, if we wanted to minimize burnout, medical schools should include an assessment of each applicant’s level of happiness and how she or he prioritizes time and money using methods similar those used in this study? The problem is that some students are so heavily committed to becoming physicians that they would game the system and provide answers that will project the image that they are happy and prioritize time over money, when in reality they are ticking time bombs of discontent.
The bigger problem with interpreting the results of this study is that the subjects were Canadians who have significantly less educational debt than the medical students in this country. And as the authors observe, “people with objective financial constraints ... are more likely to focus on having more money.” Until we solve the problem of the high cost of medical education the system will continue to select for physicians whose decisions are too heavily influenced by their educational debt.
Finally, it is important to consider that time-oriented individuals don’t always work less, rather they make decisions that make it more likely that they will pursue activities they find enjoyable. For example, accepting a higher-paying job that requires an additional 3 hours of commute each day lays the foundation for a life in which a large portion of one’s day is expended in an activity that few of us find enjoyable. Choosing a long commute is a personal decision. Spending nearly 2 hours each day tethered to an EHR system was not something most physicians anticipated when they were choosing a career.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Direct-to-patient telemedicine has benefits for providers, patients, and the practice
Innovations in care delivery, as previously introduced by Dr. Robert Gabbay, can enhance the patient and physician experience. Providing care via telemedicine can bring joy to work by introducing variety to practice. It also carries the satisfaction of easing access to care for the patient.
Broadly speaking, telemedicine can be seen as a tool for delivering care when a hands-on exam is not required. In direct-to-patient telemedicine, the patient can use a personal smartphone, tablet, or computer to connect with a provider in a real-time audio and/or video “visit” from home or work. The engagement can be scheduled or on demand. Although telemedicine is generally associated with the delivery of care to patients in remote or rural locations, it is increasingly being used in urban areas, especially with older patients and those for whom transport or time away from work might be difficult.
How the patient benefits
This built-in flexibility is appealing to patients – the easier access and convenience can translate into reduced time away from work or school and possibly a reduction in patient “no-shows.” Patients are more likely to enjoy the benefits of continuity of care with their own providers, rather than seeking independent, consumer-marketed services. In a nationwide survey of 4,345 respondents about attitudes toward telemedicine in primary care, 52% of respondents said they would like to see their own providers via telemedicine, 35% were willing to see a different provider from the same organization, and 15% said they would consider leaving their current provider to see one who offered telemedicine (BMC Health Services Research. 2017;17:784).
In addition, numerous studies have reported on the equivalent clinical outcomes and improved cost-of-care benefits in patients who receive diabetes care through telemedicine. Lui and colleagues looked at patients at the Denver VA Medical Center who were newly diagnosed with diabetes and they compared short-term glycemic control in patients who had telemedicine consultations with patients who had in-person visits. They found that the telemedicine consultations improved short-term glycemic control as effectively as the in-person visits, but with possible added financial benefits for both the patients and the health care system. (J Diabetes Sci Technol. 2016;10[5]:1079-86). Likewise, Fatehi and colleagues have reported that method of consultation – telemedicine or in-person consultation – did not affect concordance of advice between two endocrinologists (Diabetes Technol Ther. 2015;17[10]:717-25).
What telemedicine has to offer
When appropriate diagnostic labs have already been performed, newly diagnosed patients can be counseled on their diagnosis and started on therapy. For patients who have already been diagnosed, follow-up and monitoring of therapy adherence and glycemic control can be more convenient and done more routinely, compared with in-person visits, and thus yield better outcomes.
Use of cloud-based services to review data from glucometers, insulin pumps, and continuous glucose monitors allows the clinicians to access the same data they would in the office. Combining this data review with a video visit, rather than looking at the data in isolation, allows for increased patient engagement, shared decision making, and patient counseling.
Other diagnoses that readily fit at-home telemedicine care include gestational diabetes, as these patients need frequent follow-up, and doing some of their visits via telemedicine can reduce their burden of travel. Hypothyroidism follow-ups, with labs completed before the visit, can be very efficient via telemedicine. Internal surveys of direct-to-patient services at my institution demonstrated a high level of patient satisfaction, with 91% of patients indicating they were satisfied overall, and 81% saying that connection with the provider matched that of an in-person visit.
Gains for the provider, the care team, and the practice
Endocrinologists can derive benefit from telemedicine engagement with their patients, which could have positive implications for other members of the care team and for the practice as a whole. For the provider, being able to streamline clinical workflows and increase practice efficiency can help reduce personal and workplace-related stress and translate into greater personal satisfaction in one’s work and delivery of better-quality care.
At the practice level, the use of telemedicine presents opportunities for expanding the patient base and perhaps working more flexible hours to better accommodate the personal and professional time demands on providers and their staff. In addition, offering telemedicine as a medium of consultation could be a practice differentiator that could give you a competitive edge. That, along with smaller changes, such as enhancing or even reducing space utilization, could contribute to reduced overheads and a boost in revenue, which would have a positive impact on the practice’s bottom line.
Getting started
There is important groundwork to be done before a telemedicine program can get underway. First, bear in mind that there is considerable state-based variation in regulations and insurance coverage, so you need to be sure that you are in compliance with the requirements for your state. If direct-to-patient telemedicine is not widely reimbursed in your state, direct-payment models may be feasible. Providers who accept Medicare payments need to understand restrictions on self-payment for those patients. You may also be able to negotiate with payers to include reimbursement for telemedicine visits in your contracts. Negotiation with payers and direct-pay models may be possible.
Key guidelines. In addition to understanding your state’s regulations around telemedicine, there are specific aspects of practice about which you need to be clear, for example:
- You must be licensed in the state in which your patient is located at the time of their visit.
- Understand any restrictions on prescribing via telemedicine in your state.
- Be aware that Medicare has very specific guidelines and, at this time, does not recognize home as a place of service.
- You must be sure that you use HIPAA-compliant video software.
- If in any doubt, seek guidance from an attorney or your organization’s compliance office.
Infrastructure and outlay. Your infrastructure needs will depend on the specific services that you provide, but in general, you should include a communication platform and video conferencing equipment; sufficient bandwidth and a secure, reliable Internet connection; ready access to sound IT support; and comprehensive staff training at the outset, with subsequent refresher training sessions on a regular basis. Within the practice, you will need to think about adjustments to your existing workflow to accommodate the telemedicine services you plan to offer.
Resources. Two nonprofit groups that offer nonpartisan guidance in telemedicine are the Center for Connected Health Policy and the Regional Telehealth Resource Centers.
Dr. Griffith is assistant professor of medicine and medical director, Ambulatory Telehealth Services, Vanderbilt University Medical Center, in Nashville, Tenn. This article is part of a series based on presentations from the annual meeting of the Endocrine Society in March 2019. Dr. Griffith has no disclosures. Write to her at [email protected].
Innovations in care delivery, as previously introduced by Dr. Robert Gabbay, can enhance the patient and physician experience. Providing care via telemedicine can bring joy to work by introducing variety to practice. It also carries the satisfaction of easing access to care for the patient.
Broadly speaking, telemedicine can be seen as a tool for delivering care when a hands-on exam is not required. In direct-to-patient telemedicine, the patient can use a personal smartphone, tablet, or computer to connect with a provider in a real-time audio and/or video “visit” from home or work. The engagement can be scheduled or on demand. Although telemedicine is generally associated with the delivery of care to patients in remote or rural locations, it is increasingly being used in urban areas, especially with older patients and those for whom transport or time away from work might be difficult.
How the patient benefits
This built-in flexibility is appealing to patients – the easier access and convenience can translate into reduced time away from work or school and possibly a reduction in patient “no-shows.” Patients are more likely to enjoy the benefits of continuity of care with their own providers, rather than seeking independent, consumer-marketed services. In a nationwide survey of 4,345 respondents about attitudes toward telemedicine in primary care, 52% of respondents said they would like to see their own providers via telemedicine, 35% were willing to see a different provider from the same organization, and 15% said they would consider leaving their current provider to see one who offered telemedicine (BMC Health Services Research. 2017;17:784).
In addition, numerous studies have reported on the equivalent clinical outcomes and improved cost-of-care benefits in patients who receive diabetes care through telemedicine. Lui and colleagues looked at patients at the Denver VA Medical Center who were newly diagnosed with diabetes and they compared short-term glycemic control in patients who had telemedicine consultations with patients who had in-person visits. They found that the telemedicine consultations improved short-term glycemic control as effectively as the in-person visits, but with possible added financial benefits for both the patients and the health care system. (J Diabetes Sci Technol. 2016;10[5]:1079-86). Likewise, Fatehi and colleagues have reported that method of consultation – telemedicine or in-person consultation – did not affect concordance of advice between two endocrinologists (Diabetes Technol Ther. 2015;17[10]:717-25).
What telemedicine has to offer
When appropriate diagnostic labs have already been performed, newly diagnosed patients can be counseled on their diagnosis and started on therapy. For patients who have already been diagnosed, follow-up and monitoring of therapy adherence and glycemic control can be more convenient and done more routinely, compared with in-person visits, and thus yield better outcomes.
Use of cloud-based services to review data from glucometers, insulin pumps, and continuous glucose monitors allows the clinicians to access the same data they would in the office. Combining this data review with a video visit, rather than looking at the data in isolation, allows for increased patient engagement, shared decision making, and patient counseling.
Other diagnoses that readily fit at-home telemedicine care include gestational diabetes, as these patients need frequent follow-up, and doing some of their visits via telemedicine can reduce their burden of travel. Hypothyroidism follow-ups, with labs completed before the visit, can be very efficient via telemedicine. Internal surveys of direct-to-patient services at my institution demonstrated a high level of patient satisfaction, with 91% of patients indicating they were satisfied overall, and 81% saying that connection with the provider matched that of an in-person visit.
Gains for the provider, the care team, and the practice
Endocrinologists can derive benefit from telemedicine engagement with their patients, which could have positive implications for other members of the care team and for the practice as a whole. For the provider, being able to streamline clinical workflows and increase practice efficiency can help reduce personal and workplace-related stress and translate into greater personal satisfaction in one’s work and delivery of better-quality care.
At the practice level, the use of telemedicine presents opportunities for expanding the patient base and perhaps working more flexible hours to better accommodate the personal and professional time demands on providers and their staff. In addition, offering telemedicine as a medium of consultation could be a practice differentiator that could give you a competitive edge. That, along with smaller changes, such as enhancing or even reducing space utilization, could contribute to reduced overheads and a boost in revenue, which would have a positive impact on the practice’s bottom line.
Getting started
There is important groundwork to be done before a telemedicine program can get underway. First, bear in mind that there is considerable state-based variation in regulations and insurance coverage, so you need to be sure that you are in compliance with the requirements for your state. If direct-to-patient telemedicine is not widely reimbursed in your state, direct-payment models may be feasible. Providers who accept Medicare payments need to understand restrictions on self-payment for those patients. You may also be able to negotiate with payers to include reimbursement for telemedicine visits in your contracts. Negotiation with payers and direct-pay models may be possible.
Key guidelines. In addition to understanding your state’s regulations around telemedicine, there are specific aspects of practice about which you need to be clear, for example:
- You must be licensed in the state in which your patient is located at the time of their visit.
- Understand any restrictions on prescribing via telemedicine in your state.
- Be aware that Medicare has very specific guidelines and, at this time, does not recognize home as a place of service.
- You must be sure that you use HIPAA-compliant video software.
- If in any doubt, seek guidance from an attorney or your organization’s compliance office.
Infrastructure and outlay. Your infrastructure needs will depend on the specific services that you provide, but in general, you should include a communication platform and video conferencing equipment; sufficient bandwidth and a secure, reliable Internet connection; ready access to sound IT support; and comprehensive staff training at the outset, with subsequent refresher training sessions on a regular basis. Within the practice, you will need to think about adjustments to your existing workflow to accommodate the telemedicine services you plan to offer.
Resources. Two nonprofit groups that offer nonpartisan guidance in telemedicine are the Center for Connected Health Policy and the Regional Telehealth Resource Centers.
Dr. Griffith is assistant professor of medicine and medical director, Ambulatory Telehealth Services, Vanderbilt University Medical Center, in Nashville, Tenn. This article is part of a series based on presentations from the annual meeting of the Endocrine Society in March 2019. Dr. Griffith has no disclosures. Write to her at [email protected].
Innovations in care delivery, as previously introduced by Dr. Robert Gabbay, can enhance the patient and physician experience. Providing care via telemedicine can bring joy to work by introducing variety to practice. It also carries the satisfaction of easing access to care for the patient.
Broadly speaking, telemedicine can be seen as a tool for delivering care when a hands-on exam is not required. In direct-to-patient telemedicine, the patient can use a personal smartphone, tablet, or computer to connect with a provider in a real-time audio and/or video “visit” from home or work. The engagement can be scheduled or on demand. Although telemedicine is generally associated with the delivery of care to patients in remote or rural locations, it is increasingly being used in urban areas, especially with older patients and those for whom transport or time away from work might be difficult.
How the patient benefits
This built-in flexibility is appealing to patients – the easier access and convenience can translate into reduced time away from work or school and possibly a reduction in patient “no-shows.” Patients are more likely to enjoy the benefits of continuity of care with their own providers, rather than seeking independent, consumer-marketed services. In a nationwide survey of 4,345 respondents about attitudes toward telemedicine in primary care, 52% of respondents said they would like to see their own providers via telemedicine, 35% were willing to see a different provider from the same organization, and 15% said they would consider leaving their current provider to see one who offered telemedicine (BMC Health Services Research. 2017;17:784).
In addition, numerous studies have reported on the equivalent clinical outcomes and improved cost-of-care benefits in patients who receive diabetes care through telemedicine. Lui and colleagues looked at patients at the Denver VA Medical Center who were newly diagnosed with diabetes and they compared short-term glycemic control in patients who had telemedicine consultations with patients who had in-person visits. They found that the telemedicine consultations improved short-term glycemic control as effectively as the in-person visits, but with possible added financial benefits for both the patients and the health care system. (J Diabetes Sci Technol. 2016;10[5]:1079-86). Likewise, Fatehi and colleagues have reported that method of consultation – telemedicine or in-person consultation – did not affect concordance of advice between two endocrinologists (Diabetes Technol Ther. 2015;17[10]:717-25).
What telemedicine has to offer
When appropriate diagnostic labs have already been performed, newly diagnosed patients can be counseled on their diagnosis and started on therapy. For patients who have already been diagnosed, follow-up and monitoring of therapy adherence and glycemic control can be more convenient and done more routinely, compared with in-person visits, and thus yield better outcomes.
Use of cloud-based services to review data from glucometers, insulin pumps, and continuous glucose monitors allows the clinicians to access the same data they would in the office. Combining this data review with a video visit, rather than looking at the data in isolation, allows for increased patient engagement, shared decision making, and patient counseling.
Other diagnoses that readily fit at-home telemedicine care include gestational diabetes, as these patients need frequent follow-up, and doing some of their visits via telemedicine can reduce their burden of travel. Hypothyroidism follow-ups, with labs completed before the visit, can be very efficient via telemedicine. Internal surveys of direct-to-patient services at my institution demonstrated a high level of patient satisfaction, with 91% of patients indicating they were satisfied overall, and 81% saying that connection with the provider matched that of an in-person visit.
Gains for the provider, the care team, and the practice
Endocrinologists can derive benefit from telemedicine engagement with their patients, which could have positive implications for other members of the care team and for the practice as a whole. For the provider, being able to streamline clinical workflows and increase practice efficiency can help reduce personal and workplace-related stress and translate into greater personal satisfaction in one’s work and delivery of better-quality care.
At the practice level, the use of telemedicine presents opportunities for expanding the patient base and perhaps working more flexible hours to better accommodate the personal and professional time demands on providers and their staff. In addition, offering telemedicine as a medium of consultation could be a practice differentiator that could give you a competitive edge. That, along with smaller changes, such as enhancing or even reducing space utilization, could contribute to reduced overheads and a boost in revenue, which would have a positive impact on the practice’s bottom line.
Getting started
There is important groundwork to be done before a telemedicine program can get underway. First, bear in mind that there is considerable state-based variation in regulations and insurance coverage, so you need to be sure that you are in compliance with the requirements for your state. If direct-to-patient telemedicine is not widely reimbursed in your state, direct-payment models may be feasible. Providers who accept Medicare payments need to understand restrictions on self-payment for those patients. You may also be able to negotiate with payers to include reimbursement for telemedicine visits in your contracts. Negotiation with payers and direct-pay models may be possible.
Key guidelines. In addition to understanding your state’s regulations around telemedicine, there are specific aspects of practice about which you need to be clear, for example:
- You must be licensed in the state in which your patient is located at the time of their visit.
- Understand any restrictions on prescribing via telemedicine in your state.
- Be aware that Medicare has very specific guidelines and, at this time, does not recognize home as a place of service.
- You must be sure that you use HIPAA-compliant video software.
- If in any doubt, seek guidance from an attorney or your organization’s compliance office.
Infrastructure and outlay. Your infrastructure needs will depend on the specific services that you provide, but in general, you should include a communication platform and video conferencing equipment; sufficient bandwidth and a secure, reliable Internet connection; ready access to sound IT support; and comprehensive staff training at the outset, with subsequent refresher training sessions on a regular basis. Within the practice, you will need to think about adjustments to your existing workflow to accommodate the telemedicine services you plan to offer.
Resources. Two nonprofit groups that offer nonpartisan guidance in telemedicine are the Center for Connected Health Policy and the Regional Telehealth Resource Centers.
Dr. Griffith is assistant professor of medicine and medical director, Ambulatory Telehealth Services, Vanderbilt University Medical Center, in Nashville, Tenn. This article is part of a series based on presentations from the annual meeting of the Endocrine Society in March 2019. Dr. Griffith has no disclosures. Write to her at [email protected].
How innovation can bring more joy to your work
As the incidence of physician burnout increases, so does the overall cost to the health system, both in quality of care and financially, and findings from a recent study suggested that patients are becoming aware of burnout among providers and are concerned about its impact on the quality of the care that they are receiving.2
Burnout can be described as a form of extreme work-related stress manifesting as physical and/or emotional exhaustion that can generate a range of psychological ripple effects, such as depression, mood and anxiety disorders, a crippling sense of worthlessness, and a loss of sense of self. Anyone can be affected by burnout, but there seems to be a greater prevalence among women (50% vs 30% for men); younger doctors, especially residents; and providers of color.3,4
The fallout from burnout affects both our personal and professional lives. In our personal lives, it can translate into broken or strained relationships, alcohol and substance abuse, depression and mood or anxiety disorders, financial difficulties, and suicide (14% have reported thoughts of suicide; 1% have committed suicide). Juggling work and family can be overwhelming, and additional strains, such as caring for a parent or a sick family member, having a child, going through a divorce or a family bereavement, dealing with student debt, and pressure to achieve, can be cumulatively devastating for a hardworking provider.5
In the practice, we see burnout translate into an increase in the number of medical errors, diminished quality of care, lower patient satisfaction with care, decreased productivity and professional effort, dissatisfaction among staff, and an increase in physician turnover.6 Workplace-specific factors that can contribute to burnout include daily use of health information technology, especially the EHR; workplace inequities; pressures to keep abreast with changes in the specialty; and time management challenges and constraints that go along with the continual pressure to deliver better quality care, for less money, in less time.7
Our group wanted to devise innovative, practice-based strategies that would help our colleagues address the burnout crisis. We asked ourselves how – through new, innovative models of care – we could rediscover the joy in our work, and what the steppingstones of “meaningful work” would be. It seemed to us that working as a team and revisiting the care we deliver might be good starting points, and that, if we drilled down further, common themes to address burnout and find joy in work revolve around choice, camaraderie, equity, and cocreating solutions.
Evidence suggests that physicians who spend at least 20% of their professional effort focused on work they find most meaningful have a notably lower risk for burnout.8 Each 1% reduction below this threshold increases the risk of burnout, and there is a ceiling effect to the benefit at 20% – for example, spending 50% of your time in the most meaningful area is associated with similar rates of burnout as spending 20% on it.
So how do we to get to that meaningful threshold of 20%? You can begin with identifying your passion, making the business case, speaking to your boss, getting your colleagues’ buy-in, and even looking for grants and other funding if needed. We came up with five ways you might bring more joy to your work by adopting innovative models of diabetes care: the first – implementing a direct-to-patient telemedicine program – has been written by Michelle Griffith, MD, and is featured here. In coming articles, we will take a look at tackling the impediments of clinical inertia, coordinating care through use of a transfer summary, shifting to team-based care, how to use e-consultations to connect with primary care providers, and devising a business case for these and other innovations.
References
1. Kane L. National Physician Burnout, Depression & Suicide Report 2019. Medscape. Published online Jan 16, 2019.
2. American Society of Health-System Pharmacists. Press release. 2019 Jun 17.
3. Oakes K. Female family physicians come up short in burnout gender divide. Family Practice News. Published online November 27, 2017.
4. Dyrbye L. JAMA Network Open. 2019 Jul 26. doi: 10.1001/jamanetworkopen.2019.7457.
5. Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
6 . Panagioti M et al. JAMA Intern Med. 2018;178(10):1317-31.
7. Gardner R et al. J Am Med Inform Assoc. doi: 10.1093/jamia/ocy145.
8. Shanafelt T et al. Am J Med Qual. 2017;32(5):563-5.
Dr. Gabbay is chief medical officer at Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston. This is the introduction to a series of articles based on presentations from the annual meeting of the Endocrine Society in March 2019. Dr. Gabbay reports being an adviser to Lark, Onduo, and HealthReveal. Write to him at [email protected].
As the incidence of physician burnout increases, so does the overall cost to the health system, both in quality of care and financially, and findings from a recent study suggested that patients are becoming aware of burnout among providers and are concerned about its impact on the quality of the care that they are receiving.2
Burnout can be described as a form of extreme work-related stress manifesting as physical and/or emotional exhaustion that can generate a range of psychological ripple effects, such as depression, mood and anxiety disorders, a crippling sense of worthlessness, and a loss of sense of self. Anyone can be affected by burnout, but there seems to be a greater prevalence among women (50% vs 30% for men); younger doctors, especially residents; and providers of color.3,4
The fallout from burnout affects both our personal and professional lives. In our personal lives, it can translate into broken or strained relationships, alcohol and substance abuse, depression and mood or anxiety disorders, financial difficulties, and suicide (14% have reported thoughts of suicide; 1% have committed suicide). Juggling work and family can be overwhelming, and additional strains, such as caring for a parent or a sick family member, having a child, going through a divorce or a family bereavement, dealing with student debt, and pressure to achieve, can be cumulatively devastating for a hardworking provider.5
In the practice, we see burnout translate into an increase in the number of medical errors, diminished quality of care, lower patient satisfaction with care, decreased productivity and professional effort, dissatisfaction among staff, and an increase in physician turnover.6 Workplace-specific factors that can contribute to burnout include daily use of health information technology, especially the EHR; workplace inequities; pressures to keep abreast with changes in the specialty; and time management challenges and constraints that go along with the continual pressure to deliver better quality care, for less money, in less time.7
Our group wanted to devise innovative, practice-based strategies that would help our colleagues address the burnout crisis. We asked ourselves how – through new, innovative models of care – we could rediscover the joy in our work, and what the steppingstones of “meaningful work” would be. It seemed to us that working as a team and revisiting the care we deliver might be good starting points, and that, if we drilled down further, common themes to address burnout and find joy in work revolve around choice, camaraderie, equity, and cocreating solutions.
Evidence suggests that physicians who spend at least 20% of their professional effort focused on work they find most meaningful have a notably lower risk for burnout.8 Each 1% reduction below this threshold increases the risk of burnout, and there is a ceiling effect to the benefit at 20% – for example, spending 50% of your time in the most meaningful area is associated with similar rates of burnout as spending 20% on it.
So how do we to get to that meaningful threshold of 20%? You can begin with identifying your passion, making the business case, speaking to your boss, getting your colleagues’ buy-in, and even looking for grants and other funding if needed. We came up with five ways you might bring more joy to your work by adopting innovative models of diabetes care: the first – implementing a direct-to-patient telemedicine program – has been written by Michelle Griffith, MD, and is featured here. In coming articles, we will take a look at tackling the impediments of clinical inertia, coordinating care through use of a transfer summary, shifting to team-based care, how to use e-consultations to connect with primary care providers, and devising a business case for these and other innovations.
References
1. Kane L. National Physician Burnout, Depression & Suicide Report 2019. Medscape. Published online Jan 16, 2019.
2. American Society of Health-System Pharmacists. Press release. 2019 Jun 17.
3. Oakes K. Female family physicians come up short in burnout gender divide. Family Practice News. Published online November 27, 2017.
4. Dyrbye L. JAMA Network Open. 2019 Jul 26. doi: 10.1001/jamanetworkopen.2019.7457.
5. Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
6 . Panagioti M et al. JAMA Intern Med. 2018;178(10):1317-31.
7. Gardner R et al. J Am Med Inform Assoc. doi: 10.1093/jamia/ocy145.
8. Shanafelt T et al. Am J Med Qual. 2017;32(5):563-5.
Dr. Gabbay is chief medical officer at Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston. This is the introduction to a series of articles based on presentations from the annual meeting of the Endocrine Society in March 2019. Dr. Gabbay reports being an adviser to Lark, Onduo, and HealthReveal. Write to him at [email protected].
As the incidence of physician burnout increases, so does the overall cost to the health system, both in quality of care and financially, and findings from a recent study suggested that patients are becoming aware of burnout among providers and are concerned about its impact on the quality of the care that they are receiving.2
Burnout can be described as a form of extreme work-related stress manifesting as physical and/or emotional exhaustion that can generate a range of psychological ripple effects, such as depression, mood and anxiety disorders, a crippling sense of worthlessness, and a loss of sense of self. Anyone can be affected by burnout, but there seems to be a greater prevalence among women (50% vs 30% for men); younger doctors, especially residents; and providers of color.3,4
The fallout from burnout affects both our personal and professional lives. In our personal lives, it can translate into broken or strained relationships, alcohol and substance abuse, depression and mood or anxiety disorders, financial difficulties, and suicide (14% have reported thoughts of suicide; 1% have committed suicide). Juggling work and family can be overwhelming, and additional strains, such as caring for a parent or a sick family member, having a child, going through a divorce or a family bereavement, dealing with student debt, and pressure to achieve, can be cumulatively devastating for a hardworking provider.5
In the practice, we see burnout translate into an increase in the number of medical errors, diminished quality of care, lower patient satisfaction with care, decreased productivity and professional effort, dissatisfaction among staff, and an increase in physician turnover.6 Workplace-specific factors that can contribute to burnout include daily use of health information technology, especially the EHR; workplace inequities; pressures to keep abreast with changes in the specialty; and time management challenges and constraints that go along with the continual pressure to deliver better quality care, for less money, in less time.7
Our group wanted to devise innovative, practice-based strategies that would help our colleagues address the burnout crisis. We asked ourselves how – through new, innovative models of care – we could rediscover the joy in our work, and what the steppingstones of “meaningful work” would be. It seemed to us that working as a team and revisiting the care we deliver might be good starting points, and that, if we drilled down further, common themes to address burnout and find joy in work revolve around choice, camaraderie, equity, and cocreating solutions.
Evidence suggests that physicians who spend at least 20% of their professional effort focused on work they find most meaningful have a notably lower risk for burnout.8 Each 1% reduction below this threshold increases the risk of burnout, and there is a ceiling effect to the benefit at 20% – for example, spending 50% of your time in the most meaningful area is associated with similar rates of burnout as spending 20% on it.
So how do we to get to that meaningful threshold of 20%? You can begin with identifying your passion, making the business case, speaking to your boss, getting your colleagues’ buy-in, and even looking for grants and other funding if needed. We came up with five ways you might bring more joy to your work by adopting innovative models of diabetes care: the first – implementing a direct-to-patient telemedicine program – has been written by Michelle Griffith, MD, and is featured here. In coming articles, we will take a look at tackling the impediments of clinical inertia, coordinating care through use of a transfer summary, shifting to team-based care, how to use e-consultations to connect with primary care providers, and devising a business case for these and other innovations.
References
1. Kane L. National Physician Burnout, Depression & Suicide Report 2019. Medscape. Published online Jan 16, 2019.
2. American Society of Health-System Pharmacists. Press release. 2019 Jun 17.
3. Oakes K. Female family physicians come up short in burnout gender divide. Family Practice News. Published online November 27, 2017.
4. Dyrbye L. JAMA Network Open. 2019 Jul 26. doi: 10.1001/jamanetworkopen.2019.7457.
5. Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
6 . Panagioti M et al. JAMA Intern Med. 2018;178(10):1317-31.
7. Gardner R et al. J Am Med Inform Assoc. doi: 10.1093/jamia/ocy145.
8. Shanafelt T et al. Am J Med Qual. 2017;32(5):563-5.
Dr. Gabbay is chief medical officer at Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston. This is the introduction to a series of articles based on presentations from the annual meeting of the Endocrine Society in March 2019. Dr. Gabbay reports being an adviser to Lark, Onduo, and HealthReveal. Write to him at [email protected].