User login
Breaking down blockchain: How this novel technology will unfetter health care
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
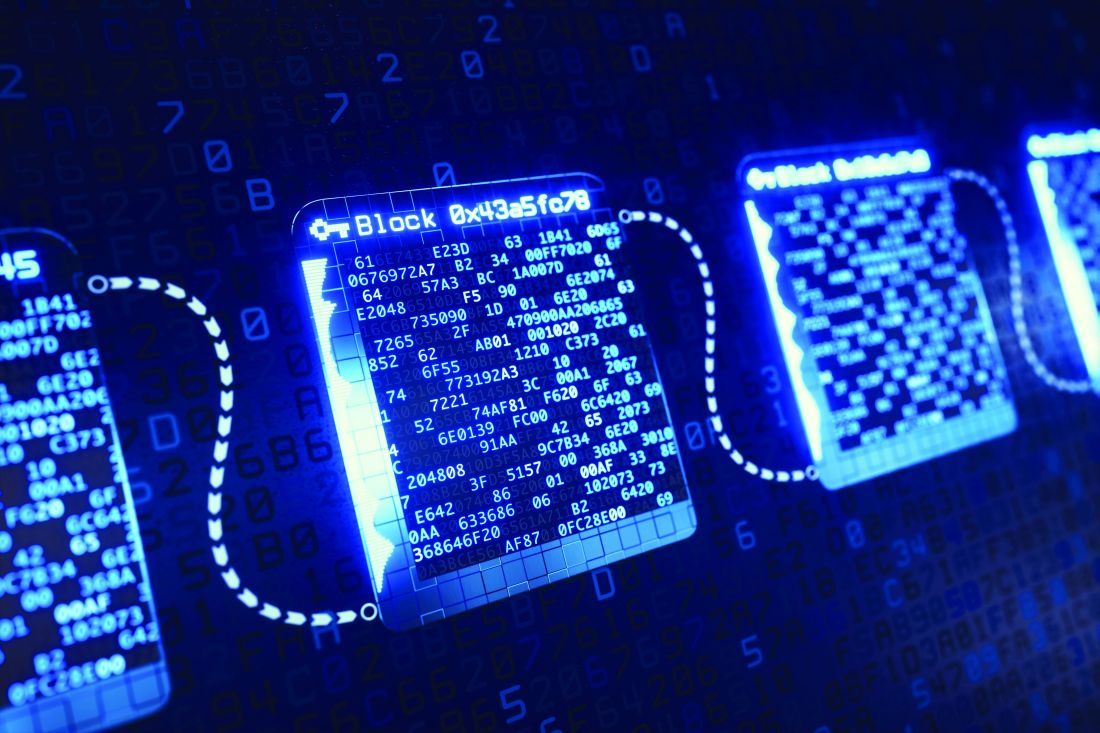
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
Keeping Your Brain in Shape
Every year, thousands of us vow to “get in shape” by eating right and exercising. (Whether we keep that resolution is another story.) But while we view physical exercise as a way to lose or maintain weight, reduce stress, or even hone athletic skills, we seldom think about exercising one of the most important muscles in our body: the brain.
“What?” you say. “The brain is not like other muscles.” No, it’s not … and yet, it isn’t as different as we used to think. Historically (maybe histologically?), it was believed that if nerve cells in the adult brain were damaged or had died, they, unlike other cells in t
But since the late 1990s, scientists have been debunking the negative myths about our brains as we age. They are not as static and unable to change as we have been led to fear! In fact, in 1998, American and Swedish scientists demonstrated that adult humans can generate new brain cells.1,2 Moreover, the brain does replicate neurons in the hippocampus, the area in our brains that is central to learning and memory. Neurons continue to grow and change beyond the first years of development and well into adulthood.
So learning (and teaching) movements to encourage the rebuilding of our neurons is key to keeping our minds sharp. In his work, Ratey found that “our physical movements can directly influence our ability to learn, think, and remember.”3 He also tells us that exercise enhances circulation to the brain, “priming it for improved function, including mental health as well as cognitive ability.”4
No, you can’t put your brain on a treadmill to get, and help keep, it “in shape.” But you can do something to maintain mental sharpness and delay decline in mental agility. And these exercises don’t require a health club membership or special equipment. They can be done anytime, anywhere … and no one knows you are doing them!
I’m talking about neurobics, a term coined to describe exercises that keep us mentally fit.5 The purpose of these activities is to work our brains in nonroutine or unexpected ways, using all of our senses to experience, or re-experience, a common activity.
Not sure what that means? Here are some examples:
Spend time in a new environment. Go to a different park or a new store. Travel, by the way, seems to slow age-related mental decline.
Continue to: Smell new odors in the morning
Smell new odors in the morning. Have new scents, like a bottle of mint extract, ready to smell first thing in the morning, to “wake up” your brain.
Take a shower with your eyes closed. Other senses become more active when you cannot see, and a shower engages several.
Try brushing your teeth with your nondominant hand. This may be difficult for some of us—and it definitely requires full attention the first time you try it!
Learn to read braille. This is a tough one, but learning to read with your fingers definitely involves one of your senses in a new context. Or, you could try learning American Sign Language, which also uses your fingers to communicate.
Respond to a situation differently. Catch yourself in a normal, unconscious response to a situation, and choose to respond in an alternate (and preferably better) way.
Continue to: Find a new route to work
Find a new route to work. It doesn’t have to be longer, just different. You may even find a faster way to work once you break your routine.
Act confidently. In a situation you are unsure about, choose to act confidently. You’ll notice that your mind gets very active once you adopt the assumption that you will know what to do.
Distinguish coins using only your sense of touch. This brain exercise can be used to kill time while waiting for an appointment. If you really want a challenge, see if you can distinguish paper currency denominations by touch.
Leave the lights off in the house. Get around your home by memory and feel. This certainly fully engages your attention—but be careful, of course!
If you give neurobics a try, let me know what you think! Or if you have other tips for staying mentally “fit,” please share them. I can be reached at [email protected]. And thank you to my friend Gail, who suggested this topic to me!
1. Kempermann G, Gage FH. New nerve cells for the adult brain. Scientific American. 1999;280(5):38-44.
2. Eriksson PS, Perfilieva E, Björk-Eriksson T, et al. Neurogenesis in the adult human hippocampus. Nature Medicine. 1998;4(11):1313-1317.
3. Ratey J. A User’s Guide to the Brain: Perception, Attention, and the Four Theaters of the Brain. New York, NY: Vintage Books; 2002.
4. Ratey J. SPARK: The Revolutionary New Science of Exercise and the Brain. New York, NY: Little, Brown and Company; 2008.
5. Katz LC, Rubin M. Keep Your Brain Alive: 83 Neurobic Exercises. New York, NY: Workman Publishing Company; 1999.
Every year, thousands of us vow to “get in shape” by eating right and exercising. (Whether we keep that resolution is another story.) But while we view physical exercise as a way to lose or maintain weight, reduce stress, or even hone athletic skills, we seldom think about exercising one of the most important muscles in our body: the brain.
“What?” you say. “The brain is not like other muscles.” No, it’s not … and yet, it isn’t as different as we used to think. Historically (maybe histologically?), it was believed that if nerve cells in the adult brain were damaged or had died, they, unlike other cells in t
But since the late 1990s, scientists have been debunking the negative myths about our brains as we age. They are not as static and unable to change as we have been led to fear! In fact, in 1998, American and Swedish scientists demonstrated that adult humans can generate new brain cells.1,2 Moreover, the brain does replicate neurons in the hippocampus, the area in our brains that is central to learning and memory. Neurons continue to grow and change beyond the first years of development and well into adulthood.
So learning (and teaching) movements to encourage the rebuilding of our neurons is key to keeping our minds sharp. In his work, Ratey found that “our physical movements can directly influence our ability to learn, think, and remember.”3 He also tells us that exercise enhances circulation to the brain, “priming it for improved function, including mental health as well as cognitive ability.”4
No, you can’t put your brain on a treadmill to get, and help keep, it “in shape.” But you can do something to maintain mental sharpness and delay decline in mental agility. And these exercises don’t require a health club membership or special equipment. They can be done anytime, anywhere … and no one knows you are doing them!
I’m talking about neurobics, a term coined to describe exercises that keep us mentally fit.5 The purpose of these activities is to work our brains in nonroutine or unexpected ways, using all of our senses to experience, or re-experience, a common activity.
Not sure what that means? Here are some examples:
Spend time in a new environment. Go to a different park or a new store. Travel, by the way, seems to slow age-related mental decline.
Continue to: Smell new odors in the morning
Smell new odors in the morning. Have new scents, like a bottle of mint extract, ready to smell first thing in the morning, to “wake up” your brain.
Take a shower with your eyes closed. Other senses become more active when you cannot see, and a shower engages several.
Try brushing your teeth with your nondominant hand. This may be difficult for some of us—and it definitely requires full attention the first time you try it!
Learn to read braille. This is a tough one, but learning to read with your fingers definitely involves one of your senses in a new context. Or, you could try learning American Sign Language, which also uses your fingers to communicate.
Respond to a situation differently. Catch yourself in a normal, unconscious response to a situation, and choose to respond in an alternate (and preferably better) way.
Continue to: Find a new route to work
Find a new route to work. It doesn’t have to be longer, just different. You may even find a faster way to work once you break your routine.
Act confidently. In a situation you are unsure about, choose to act confidently. You’ll notice that your mind gets very active once you adopt the assumption that you will know what to do.
Distinguish coins using only your sense of touch. This brain exercise can be used to kill time while waiting for an appointment. If you really want a challenge, see if you can distinguish paper currency denominations by touch.
Leave the lights off in the house. Get around your home by memory and feel. This certainly fully engages your attention—but be careful, of course!
If you give neurobics a try, let me know what you think! Or if you have other tips for staying mentally “fit,” please share them. I can be reached at [email protected]. And thank you to my friend Gail, who suggested this topic to me!
Every year, thousands of us vow to “get in shape” by eating right and exercising. (Whether we keep that resolution is another story.) But while we view physical exercise as a way to lose or maintain weight, reduce stress, or even hone athletic skills, we seldom think about exercising one of the most important muscles in our body: the brain.
“What?” you say. “The brain is not like other muscles.” No, it’s not … and yet, it isn’t as different as we used to think. Historically (maybe histologically?), it was believed that if nerve cells in the adult brain were damaged or had died, they, unlike other cells in t
But since the late 1990s, scientists have been debunking the negative myths about our brains as we age. They are not as static and unable to change as we have been led to fear! In fact, in 1998, American and Swedish scientists demonstrated that adult humans can generate new brain cells.1,2 Moreover, the brain does replicate neurons in the hippocampus, the area in our brains that is central to learning and memory. Neurons continue to grow and change beyond the first years of development and well into adulthood.
So learning (and teaching) movements to encourage the rebuilding of our neurons is key to keeping our minds sharp. In his work, Ratey found that “our physical movements can directly influence our ability to learn, think, and remember.”3 He also tells us that exercise enhances circulation to the brain, “priming it for improved function, including mental health as well as cognitive ability.”4
No, you can’t put your brain on a treadmill to get, and help keep, it “in shape.” But you can do something to maintain mental sharpness and delay decline in mental agility. And these exercises don’t require a health club membership or special equipment. They can be done anytime, anywhere … and no one knows you are doing them!
I’m talking about neurobics, a term coined to describe exercises that keep us mentally fit.5 The purpose of these activities is to work our brains in nonroutine or unexpected ways, using all of our senses to experience, or re-experience, a common activity.
Not sure what that means? Here are some examples:
Spend time in a new environment. Go to a different park or a new store. Travel, by the way, seems to slow age-related mental decline.
Continue to: Smell new odors in the morning
Smell new odors in the morning. Have new scents, like a bottle of mint extract, ready to smell first thing in the morning, to “wake up” your brain.
Take a shower with your eyes closed. Other senses become more active when you cannot see, and a shower engages several.
Try brushing your teeth with your nondominant hand. This may be difficult for some of us—and it definitely requires full attention the first time you try it!
Learn to read braille. This is a tough one, but learning to read with your fingers definitely involves one of your senses in a new context. Or, you could try learning American Sign Language, which also uses your fingers to communicate.
Respond to a situation differently. Catch yourself in a normal, unconscious response to a situation, and choose to respond in an alternate (and preferably better) way.
Continue to: Find a new route to work
Find a new route to work. It doesn’t have to be longer, just different. You may even find a faster way to work once you break your routine.
Act confidently. In a situation you are unsure about, choose to act confidently. You’ll notice that your mind gets very active once you adopt the assumption that you will know what to do.
Distinguish coins using only your sense of touch. This brain exercise can be used to kill time while waiting for an appointment. If you really want a challenge, see if you can distinguish paper currency denominations by touch.
Leave the lights off in the house. Get around your home by memory and feel. This certainly fully engages your attention—but be careful, of course!
If you give neurobics a try, let me know what you think! Or if you have other tips for staying mentally “fit,” please share them. I can be reached at [email protected]. And thank you to my friend Gail, who suggested this topic to me!
1. Kempermann G, Gage FH. New nerve cells for the adult brain. Scientific American. 1999;280(5):38-44.
2. Eriksson PS, Perfilieva E, Björk-Eriksson T, et al. Neurogenesis in the adult human hippocampus. Nature Medicine. 1998;4(11):1313-1317.
3. Ratey J. A User’s Guide to the Brain: Perception, Attention, and the Four Theaters of the Brain. New York, NY: Vintage Books; 2002.
4. Ratey J. SPARK: The Revolutionary New Science of Exercise and the Brain. New York, NY: Little, Brown and Company; 2008.
5. Katz LC, Rubin M. Keep Your Brain Alive: 83 Neurobic Exercises. New York, NY: Workman Publishing Company; 1999.
1. Kempermann G, Gage FH. New nerve cells for the adult brain. Scientific American. 1999;280(5):38-44.
2. Eriksson PS, Perfilieva E, Björk-Eriksson T, et al. Neurogenesis in the adult human hippocampus. Nature Medicine. 1998;4(11):1313-1317.
3. Ratey J. A User’s Guide to the Brain: Perception, Attention, and the Four Theaters of the Brain. New York, NY: Vintage Books; 2002.
4. Ratey J. SPARK: The Revolutionary New Science of Exercise and the Brain. New York, NY: Little, Brown and Company; 2008.
5. Katz LC, Rubin M. Keep Your Brain Alive: 83 Neurobic Exercises. New York, NY: Workman Publishing Company; 1999.
Preventing postpartum depression: Start with women at greatest risk
The last decade has brought appropriate attention to the high prevalence of postpartum mood and anxiety disorders, with postpartum depression (PPD) constituting the most common complication in modern obstetrics.
There have been very substantial efforts in more than 40 states in the United States to enhance screening for PPD and to increase support groups for women with postpartum depressive or anxiety symptoms. However, less focus has been paid to the outcomes of these screening initiatives.
A question that comes to mind is whether patients who are screened actually get referred for treatment, and if they do receive treatment, whether they recover and become well. One study referenced previously in this column noted that even in settings where women are screened for PPD, the vast majority of women are not referred, and of those who are referred, even fewer of those are treated or become well.1
It is noteworthy, then, that the U.S. Preventive Services Task Force has recommended screening for perinatal depression (just before and after birth) and issued draft recommendations regarding prevention of perinatal depression where it is suggested that patients at risk for perinatal depression be referred for appropriate “counseling interventions” – specifically, either cognitive-behavioral therapy (CBT) or interpersonal psychotherapy (IPT).2
The recommendation is a striking one because of the volume of patients who would be included. For example, the USPSTF recommends patients with histories of depression, depression during pregnancy, a history of child abuse, or even a family history of depression should receive preventive interventions with CBT or IPT. The recommendation is puzzling because of the data on risk for perinatal depression in those populations and the lack of available resources for patients who would be deemed “at risk.” Women with histories of depression are at a threefold increased risk for PPD (25%-30%). Depression during pregnancy is the strongest predictor of PPD and risk for PPD among these patients is as high as 75%.
So, there are a vast number of women who may be “at risk” for perinatal depression. But even with some data suggesting that IPT and CBT may be able to prevent perinatal depression, the suggestion that resources be made available to patients who are at risk is naive, because counseling interventions such as IPT or CBT, or even simply referrals to psychiatrists are not available even to patients who screen in for perinatal depression in real time during pregnancy and the postpartum period. I have previously written that the follow-up of women post partum who suffer from PPD is still far from meeting the needs who suffer from the disorder, and early detection and referrals to appropriate clinicians who are facile with both pharmacologic and nonpharmacologic interventions seem the most effective way to manage these patients and to see that they receive treatment.
The question then becomes: If the numbers or scale of the prevention initiative suggested in this draft recommendation from the USPSTF is an overreach, is there a group of patients for whom a preventive intervention could be pursued? The patients at highest risk for PPD include those with a history of PPD (50%), bipolar disorder (50%-60%), or postpartum psychosis (80%). And while there is not substantial literature for specifically using IPT, CBT, or other counseling interventions to mitigate risk for recurrence in women with histories of PPD, bipolar disorder, or postpartum psychosis, there are ways of identifying this population at risk and following them closely to mitigate the risk for recurrence.
To make this recommendation feasible, an infrastructure needs to be in place in both low resource settings and in all communities so that these patients can be referred and effectively treated. If we move to prevention, we ought to start with the populations that we already know are at greatest risk and that we can inquire about, and there are very easy-to-use screens that screen for bipolar disorder or that screen for past history of depression with which these women can be identified.
In committee opinion 757, the American College of Obstetricians and Gynecologists recommends women be screened at least once during the perinatal period for depression and anxiety symptoms and highlighted several validated tools, such as the Edinburgh Postnatal Depression Scale.3 We also need a better system of early detection and early intervention so that women at less-considerable risk for perinatal depression would have the opportunity for early identification, treatment, and referral, which we do not have at the current time.
An update of the ACOG committee opinion also states, “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.” This is recommended in addition to any screening for depression and anxiety during the pregnancy.
It is exciting that after decades of failing to attend to such a common complication of modern obstetrics, particularly now that we understand the adverse effects of PPD as it affects child development, family functioning, and risk for later childhood psychopathology. But in addition to recognizing the problem, we must come up with methods to carefully identify a navigable route for the women suffering from PPD to get their needs met. The route includes publicly identifying the illness, understanding which treatments are most effective and can be scaled for delivery to large numbers of women, and then, most critically, configuring social systems to absorb, effectively manage, and monitor the women we identify as needing treatment.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
References
1. J Clin Psychiatry. 2016 Sep;77[9]:1189-200.
2. Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. U.S. Preventive Services Task Force. Aug 2018.
The last decade has brought appropriate attention to the high prevalence of postpartum mood and anxiety disorders, with postpartum depression (PPD) constituting the most common complication in modern obstetrics.
There have been very substantial efforts in more than 40 states in the United States to enhance screening for PPD and to increase support groups for women with postpartum depressive or anxiety symptoms. However, less focus has been paid to the outcomes of these screening initiatives.
A question that comes to mind is whether patients who are screened actually get referred for treatment, and if they do receive treatment, whether they recover and become well. One study referenced previously in this column noted that even in settings where women are screened for PPD, the vast majority of women are not referred, and of those who are referred, even fewer of those are treated or become well.1
It is noteworthy, then, that the U.S. Preventive Services Task Force has recommended screening for perinatal depression (just before and after birth) and issued draft recommendations regarding prevention of perinatal depression where it is suggested that patients at risk for perinatal depression be referred for appropriate “counseling interventions” – specifically, either cognitive-behavioral therapy (CBT) or interpersonal psychotherapy (IPT).2
The recommendation is a striking one because of the volume of patients who would be included. For example, the USPSTF recommends patients with histories of depression, depression during pregnancy, a history of child abuse, or even a family history of depression should receive preventive interventions with CBT or IPT. The recommendation is puzzling because of the data on risk for perinatal depression in those populations and the lack of available resources for patients who would be deemed “at risk.” Women with histories of depression are at a threefold increased risk for PPD (25%-30%). Depression during pregnancy is the strongest predictor of PPD and risk for PPD among these patients is as high as 75%.
So, there are a vast number of women who may be “at risk” for perinatal depression. But even with some data suggesting that IPT and CBT may be able to prevent perinatal depression, the suggestion that resources be made available to patients who are at risk is naive, because counseling interventions such as IPT or CBT, or even simply referrals to psychiatrists are not available even to patients who screen in for perinatal depression in real time during pregnancy and the postpartum period. I have previously written that the follow-up of women post partum who suffer from PPD is still far from meeting the needs who suffer from the disorder, and early detection and referrals to appropriate clinicians who are facile with both pharmacologic and nonpharmacologic interventions seem the most effective way to manage these patients and to see that they receive treatment.
The question then becomes: If the numbers or scale of the prevention initiative suggested in this draft recommendation from the USPSTF is an overreach, is there a group of patients for whom a preventive intervention could be pursued? The patients at highest risk for PPD include those with a history of PPD (50%), bipolar disorder (50%-60%), or postpartum psychosis (80%). And while there is not substantial literature for specifically using IPT, CBT, or other counseling interventions to mitigate risk for recurrence in women with histories of PPD, bipolar disorder, or postpartum psychosis, there are ways of identifying this population at risk and following them closely to mitigate the risk for recurrence.
To make this recommendation feasible, an infrastructure needs to be in place in both low resource settings and in all communities so that these patients can be referred and effectively treated. If we move to prevention, we ought to start with the populations that we already know are at greatest risk and that we can inquire about, and there are very easy-to-use screens that screen for bipolar disorder or that screen for past history of depression with which these women can be identified.
In committee opinion 757, the American College of Obstetricians and Gynecologists recommends women be screened at least once during the perinatal period for depression and anxiety symptoms and highlighted several validated tools, such as the Edinburgh Postnatal Depression Scale.3 We also need a better system of early detection and early intervention so that women at less-considerable risk for perinatal depression would have the opportunity for early identification, treatment, and referral, which we do not have at the current time.
An update of the ACOG committee opinion also states, “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.” This is recommended in addition to any screening for depression and anxiety during the pregnancy.
It is exciting that after decades of failing to attend to such a common complication of modern obstetrics, particularly now that we understand the adverse effects of PPD as it affects child development, family functioning, and risk for later childhood psychopathology. But in addition to recognizing the problem, we must come up with methods to carefully identify a navigable route for the women suffering from PPD to get their needs met. The route includes publicly identifying the illness, understanding which treatments are most effective and can be scaled for delivery to large numbers of women, and then, most critically, configuring social systems to absorb, effectively manage, and monitor the women we identify as needing treatment.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
References
1. J Clin Psychiatry. 2016 Sep;77[9]:1189-200.
2. Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. U.S. Preventive Services Task Force. Aug 2018.
The last decade has brought appropriate attention to the high prevalence of postpartum mood and anxiety disorders, with postpartum depression (PPD) constituting the most common complication in modern obstetrics.
There have been very substantial efforts in more than 40 states in the United States to enhance screening for PPD and to increase support groups for women with postpartum depressive or anxiety symptoms. However, less focus has been paid to the outcomes of these screening initiatives.
A question that comes to mind is whether patients who are screened actually get referred for treatment, and if they do receive treatment, whether they recover and become well. One study referenced previously in this column noted that even in settings where women are screened for PPD, the vast majority of women are not referred, and of those who are referred, even fewer of those are treated or become well.1
It is noteworthy, then, that the U.S. Preventive Services Task Force has recommended screening for perinatal depression (just before and after birth) and issued draft recommendations regarding prevention of perinatal depression where it is suggested that patients at risk for perinatal depression be referred for appropriate “counseling interventions” – specifically, either cognitive-behavioral therapy (CBT) or interpersonal psychotherapy (IPT).2
The recommendation is a striking one because of the volume of patients who would be included. For example, the USPSTF recommends patients with histories of depression, depression during pregnancy, a history of child abuse, or even a family history of depression should receive preventive interventions with CBT or IPT. The recommendation is puzzling because of the data on risk for perinatal depression in those populations and the lack of available resources for patients who would be deemed “at risk.” Women with histories of depression are at a threefold increased risk for PPD (25%-30%). Depression during pregnancy is the strongest predictor of PPD and risk for PPD among these patients is as high as 75%.
So, there are a vast number of women who may be “at risk” for perinatal depression. But even with some data suggesting that IPT and CBT may be able to prevent perinatal depression, the suggestion that resources be made available to patients who are at risk is naive, because counseling interventions such as IPT or CBT, or even simply referrals to psychiatrists are not available even to patients who screen in for perinatal depression in real time during pregnancy and the postpartum period. I have previously written that the follow-up of women post partum who suffer from PPD is still far from meeting the needs who suffer from the disorder, and early detection and referrals to appropriate clinicians who are facile with both pharmacologic and nonpharmacologic interventions seem the most effective way to manage these patients and to see that they receive treatment.
The question then becomes: If the numbers or scale of the prevention initiative suggested in this draft recommendation from the USPSTF is an overreach, is there a group of patients for whom a preventive intervention could be pursued? The patients at highest risk for PPD include those with a history of PPD (50%), bipolar disorder (50%-60%), or postpartum psychosis (80%). And while there is not substantial literature for specifically using IPT, CBT, or other counseling interventions to mitigate risk for recurrence in women with histories of PPD, bipolar disorder, or postpartum psychosis, there are ways of identifying this population at risk and following them closely to mitigate the risk for recurrence.
To make this recommendation feasible, an infrastructure needs to be in place in both low resource settings and in all communities so that these patients can be referred and effectively treated. If we move to prevention, we ought to start with the populations that we already know are at greatest risk and that we can inquire about, and there are very easy-to-use screens that screen for bipolar disorder or that screen for past history of depression with which these women can be identified.
In committee opinion 757, the American College of Obstetricians and Gynecologists recommends women be screened at least once during the perinatal period for depression and anxiety symptoms and highlighted several validated tools, such as the Edinburgh Postnatal Depression Scale.3 We also need a better system of early detection and early intervention so that women at less-considerable risk for perinatal depression would have the opportunity for early identification, treatment, and referral, which we do not have at the current time.
An update of the ACOG committee opinion also states, “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.” This is recommended in addition to any screening for depression and anxiety during the pregnancy.
It is exciting that after decades of failing to attend to such a common complication of modern obstetrics, particularly now that we understand the adverse effects of PPD as it affects child development, family functioning, and risk for later childhood psychopathology. But in addition to recognizing the problem, we must come up with methods to carefully identify a navigable route for the women suffering from PPD to get their needs met. The route includes publicly identifying the illness, understanding which treatments are most effective and can be scaled for delivery to large numbers of women, and then, most critically, configuring social systems to absorb, effectively manage, and monitor the women we identify as needing treatment.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
References
1. J Clin Psychiatry. 2016 Sep;77[9]:1189-200.
2. Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. U.S. Preventive Services Task Force. Aug 2018.
Medical ethics and economics
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The fog may be lifting
One of the common symptoms described by postconcussion patients is that their heads feel a bit foggy. It may not be simply by chance that “foggy” is the best word to describe the atmosphere surrounding the entire field of concussion diagnosis and management.
Back in the Dark Ages, when the diagnosis of concussion was a simpler binary call, the issue of management seldom created much discussion. If the patient lost consciousness or was amnesic, he (it was less frequently she) could return to activity when his headache was gone and he could remember what he was supposed to do when the quarterback called for a “Red 34, Drive Right Smash” play. That may have even been during the second half of the game in which he was injured.
As it became more widely understood that the diagnosis of concussion didn’t require loss of consciousness and that repeated concussions could have serious sequelae, management became a bit fuzzier. No one had thought much about the recuperative process. Into this vacuum came a wide variety of researchers and providers. Not surprisingly, much of their advice was based on unproven assumptions, including the concept of “brain rest.”
It has taken time, but fortunately, folks with patience and wisdom have questioned these assumptions and begun collecting data. The result of these investigations and others has prompted the American Academy of Pediatrics to publish an updated set of guidelines on concussion management that includes the observation that extended school absence may slow the rehabilitation process (Pediatrics. 2018 Dec. doi: 10.1542/peds.2018-3074).
It is becoming clear that management of concussion can be rather complex and must be individualized to each patient. In my experience, the postconcussion period can unmask behavioral, cognitive, and emotional problems that were preexisting but had received little or no attention. For example, the trauma of the event may trigger anxiety about further injury or exacerbate depression that had been building for years. The student who “couldn’t do algebra” following a head injury may have had a lifelong learning disability that had gone unnoticed. The student athlete with prolonged postconcussion symptoms may indeed have another more serious problem. Hopefully, the new guidelines from the AAP will be a first step toward a more thoughtful and scientifically driven approach to concussion management.
It would be nice if that approach could filter down to the management of the more common but less dramatic pediatric injuries. There is hope. Choosing Wisely – a patient/parent–targeted initiative by the American Board of Internal Medicine Foundation in cooperation with the AAP – points out that, although half of the pediatric head injury patients seen in emergency departments received CT scan, only a third of those studies were indicated. Parents are encouraged to learn more about the risks of CT scans and question the physician when one is recommended.
But, doctors’ habits and old wives’ tales die slowly. I hope that you no longer recommend that parents keep their children awake after a head injury, or wake them every hour to check their pupils. Those counterproductive recommendations make about as much sense as staying out of the swimming pool for an hour after eating a chocolate chip cookie.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
One of the common symptoms described by postconcussion patients is that their heads feel a bit foggy. It may not be simply by chance that “foggy” is the best word to describe the atmosphere surrounding the entire field of concussion diagnosis and management.
Back in the Dark Ages, when the diagnosis of concussion was a simpler binary call, the issue of management seldom created much discussion. If the patient lost consciousness or was amnesic, he (it was less frequently she) could return to activity when his headache was gone and he could remember what he was supposed to do when the quarterback called for a “Red 34, Drive Right Smash” play. That may have even been during the second half of the game in which he was injured.
As it became more widely understood that the diagnosis of concussion didn’t require loss of consciousness and that repeated concussions could have serious sequelae, management became a bit fuzzier. No one had thought much about the recuperative process. Into this vacuum came a wide variety of researchers and providers. Not surprisingly, much of their advice was based on unproven assumptions, including the concept of “brain rest.”
It has taken time, but fortunately, folks with patience and wisdom have questioned these assumptions and begun collecting data. The result of these investigations and others has prompted the American Academy of Pediatrics to publish an updated set of guidelines on concussion management that includes the observation that extended school absence may slow the rehabilitation process (Pediatrics. 2018 Dec. doi: 10.1542/peds.2018-3074).
It is becoming clear that management of concussion can be rather complex and must be individualized to each patient. In my experience, the postconcussion period can unmask behavioral, cognitive, and emotional problems that were preexisting but had received little or no attention. For example, the trauma of the event may trigger anxiety about further injury or exacerbate depression that had been building for years. The student who “couldn’t do algebra” following a head injury may have had a lifelong learning disability that had gone unnoticed. The student athlete with prolonged postconcussion symptoms may indeed have another more serious problem. Hopefully, the new guidelines from the AAP will be a first step toward a more thoughtful and scientifically driven approach to concussion management.
It would be nice if that approach could filter down to the management of the more common but less dramatic pediatric injuries. There is hope. Choosing Wisely – a patient/parent–targeted initiative by the American Board of Internal Medicine Foundation in cooperation with the AAP – points out that, although half of the pediatric head injury patients seen in emergency departments received CT scan, only a third of those studies were indicated. Parents are encouraged to learn more about the risks of CT scans and question the physician when one is recommended.
But, doctors’ habits and old wives’ tales die slowly. I hope that you no longer recommend that parents keep their children awake after a head injury, or wake them every hour to check their pupils. Those counterproductive recommendations make about as much sense as staying out of the swimming pool for an hour after eating a chocolate chip cookie.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
One of the common symptoms described by postconcussion patients is that their heads feel a bit foggy. It may not be simply by chance that “foggy” is the best word to describe the atmosphere surrounding the entire field of concussion diagnosis and management.
Back in the Dark Ages, when the diagnosis of concussion was a simpler binary call, the issue of management seldom created much discussion. If the patient lost consciousness or was amnesic, he (it was less frequently she) could return to activity when his headache was gone and he could remember what he was supposed to do when the quarterback called for a “Red 34, Drive Right Smash” play. That may have even been during the second half of the game in which he was injured.
As it became more widely understood that the diagnosis of concussion didn’t require loss of consciousness and that repeated concussions could have serious sequelae, management became a bit fuzzier. No one had thought much about the recuperative process. Into this vacuum came a wide variety of researchers and providers. Not surprisingly, much of their advice was based on unproven assumptions, including the concept of “brain rest.”
It has taken time, but fortunately, folks with patience and wisdom have questioned these assumptions and begun collecting data. The result of these investigations and others has prompted the American Academy of Pediatrics to publish an updated set of guidelines on concussion management that includes the observation that extended school absence may slow the rehabilitation process (Pediatrics. 2018 Dec. doi: 10.1542/peds.2018-3074).
It is becoming clear that management of concussion can be rather complex and must be individualized to each patient. In my experience, the postconcussion period can unmask behavioral, cognitive, and emotional problems that were preexisting but had received little or no attention. For example, the trauma of the event may trigger anxiety about further injury or exacerbate depression that had been building for years. The student who “couldn’t do algebra” following a head injury may have had a lifelong learning disability that had gone unnoticed. The student athlete with prolonged postconcussion symptoms may indeed have another more serious problem. Hopefully, the new guidelines from the AAP will be a first step toward a more thoughtful and scientifically driven approach to concussion management.
It would be nice if that approach could filter down to the management of the more common but less dramatic pediatric injuries. There is hope. Choosing Wisely – a patient/parent–targeted initiative by the American Board of Internal Medicine Foundation in cooperation with the AAP – points out that, although half of the pediatric head injury patients seen in emergency departments received CT scan, only a third of those studies were indicated. Parents are encouraged to learn more about the risks of CT scans and question the physician when one is recommended.
But, doctors’ habits and old wives’ tales die slowly. I hope that you no longer recommend that parents keep their children awake after a head injury, or wake them every hour to check their pupils. Those counterproductive recommendations make about as much sense as staying out of the swimming pool for an hour after eating a chocolate chip cookie.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
The other side of activity
While the increasing prevalence of obesity has been obvious for nearly half a century, it is only in the last decade or two that the focus has broadened to include the associated decline in physical activity.
A recent paper attempts to sharpen that focus by examining the timeline of that decline (Pediatrics 2019 Jan. doi: 10.1542/peds.2018-0994.). Using a device incorporating five sensors, one of which was an accelerometer, the investigators collected data from 600 children from five European countries accumulating more than 1,200 observations. What they discovered was that their subjects’ physical activity declined by 75 minutes per day from ages 6 to 11 years of age while sedentary behavior increased more than 100 minutes over that same interval. This observation is concerning because previous attention has focused intervention on adolescents assuming that the erosion of physical activity was occurring primarily during the teen years.
Not surprisingly the authors suggest that more studies should be performed to aid in the design of more sharply targeted interventions. While more information may be helpful, their current findings and an abundance of anecdotal observations suggest that to be effective that intervention must begin well before children reach school age.
What should this intervention look like? Currently, the emphasis seems to have been on programs that encourage activity. The National Football League is promoting its NFL Play 60 initiative. The Afterschool Alliance has its Kids on the Move programs. Former First Lady Michelle Obama has been the spokesperson and driving force behind Let’s Move. And, the American Academy of Pediatrics has recently been encouraging both parents and pediatricians to appreciate The Power of Play to encourage children to get into more physical activity. All of these initiatives are well meaning, but I suspect their effectiveness is usually limited to the public awareness they generate.
We seem to have forgotten that there are two sides to the equation. The accelerometer study from Europe should remind us that our initiatives should also be addressing the problem of epidemic inactivity with equal vigor. Creating programs that focus on increasing activity can be expensive. There may be costs for equipment, spaces to be maintained, and staff to be paid. On the other hand, curbing sedentary behavior requires only an adult with the courage to say, “No.” “No, we will have the television for only an hour today.” “No, you can’t play your video game until after dinner.”
While addressing the disciplinary side of the activity-inactivity dichotomy may be relatively inexpensive, it does seem to have a cost on parents. It requires them to buy into the idea that, given even the most-limited supply of objects and infrastructure, most children can keep themselves entertained and active. There does seem to be a small subset of children who enter the world with a sedentary mindset, possibly inherited from their parents. This unfortunate minority will require some creative intervention to achieve a healthy level of activity.
However, most young children who have become accustomed to being amused by sedentary “activities” such as television and video games still retain their innate creativity and natural inclination to be physically active. Unfortunately, unmasking these health-sustaining attributes may require a long and unpleasant weaning period that many parents don’t seem to have the patience to endure. The longer the child has been allowed to engage in sedentary behaviors, the longer this adjustment period will be, yet another argument for early intervention.
Encouraging physical activity is something we should be doing every day in our offices, but it must go hand in hand with an equivalent emphasis on helping parents create a discipline framework that discourages sedentary behavior.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
While the increasing prevalence of obesity has been obvious for nearly half a century, it is only in the last decade or two that the focus has broadened to include the associated decline in physical activity.
A recent paper attempts to sharpen that focus by examining the timeline of that decline (Pediatrics 2019 Jan. doi: 10.1542/peds.2018-0994.). Using a device incorporating five sensors, one of which was an accelerometer, the investigators collected data from 600 children from five European countries accumulating more than 1,200 observations. What they discovered was that their subjects’ physical activity declined by 75 minutes per day from ages 6 to 11 years of age while sedentary behavior increased more than 100 minutes over that same interval. This observation is concerning because previous attention has focused intervention on adolescents assuming that the erosion of physical activity was occurring primarily during the teen years.
Not surprisingly the authors suggest that more studies should be performed to aid in the design of more sharply targeted interventions. While more information may be helpful, their current findings and an abundance of anecdotal observations suggest that to be effective that intervention must begin well before children reach school age.
What should this intervention look like? Currently, the emphasis seems to have been on programs that encourage activity. The National Football League is promoting its NFL Play 60 initiative. The Afterschool Alliance has its Kids on the Move programs. Former First Lady Michelle Obama has been the spokesperson and driving force behind Let’s Move. And, the American Academy of Pediatrics has recently been encouraging both parents and pediatricians to appreciate The Power of Play to encourage children to get into more physical activity. All of these initiatives are well meaning, but I suspect their effectiveness is usually limited to the public awareness they generate.
We seem to have forgotten that there are two sides to the equation. The accelerometer study from Europe should remind us that our initiatives should also be addressing the problem of epidemic inactivity with equal vigor. Creating programs that focus on increasing activity can be expensive. There may be costs for equipment, spaces to be maintained, and staff to be paid. On the other hand, curbing sedentary behavior requires only an adult with the courage to say, “No.” “No, we will have the television for only an hour today.” “No, you can’t play your video game until after dinner.”
While addressing the disciplinary side of the activity-inactivity dichotomy may be relatively inexpensive, it does seem to have a cost on parents. It requires them to buy into the idea that, given even the most-limited supply of objects and infrastructure, most children can keep themselves entertained and active. There does seem to be a small subset of children who enter the world with a sedentary mindset, possibly inherited from their parents. This unfortunate minority will require some creative intervention to achieve a healthy level of activity.
However, most young children who have become accustomed to being amused by sedentary “activities” such as television and video games still retain their innate creativity and natural inclination to be physically active. Unfortunately, unmasking these health-sustaining attributes may require a long and unpleasant weaning period that many parents don’t seem to have the patience to endure. The longer the child has been allowed to engage in sedentary behaviors, the longer this adjustment period will be, yet another argument for early intervention.
Encouraging physical activity is something we should be doing every day in our offices, but it must go hand in hand with an equivalent emphasis on helping parents create a discipline framework that discourages sedentary behavior.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
While the increasing prevalence of obesity has been obvious for nearly half a century, it is only in the last decade or two that the focus has broadened to include the associated decline in physical activity.
A recent paper attempts to sharpen that focus by examining the timeline of that decline (Pediatrics 2019 Jan. doi: 10.1542/peds.2018-0994.). Using a device incorporating five sensors, one of which was an accelerometer, the investigators collected data from 600 children from five European countries accumulating more than 1,200 observations. What they discovered was that their subjects’ physical activity declined by 75 minutes per day from ages 6 to 11 years of age while sedentary behavior increased more than 100 minutes over that same interval. This observation is concerning because previous attention has focused intervention on adolescents assuming that the erosion of physical activity was occurring primarily during the teen years.
Not surprisingly the authors suggest that more studies should be performed to aid in the design of more sharply targeted interventions. While more information may be helpful, their current findings and an abundance of anecdotal observations suggest that to be effective that intervention must begin well before children reach school age.
What should this intervention look like? Currently, the emphasis seems to have been on programs that encourage activity. The National Football League is promoting its NFL Play 60 initiative. The Afterschool Alliance has its Kids on the Move programs. Former First Lady Michelle Obama has been the spokesperson and driving force behind Let’s Move. And, the American Academy of Pediatrics has recently been encouraging both parents and pediatricians to appreciate The Power of Play to encourage children to get into more physical activity. All of these initiatives are well meaning, but I suspect their effectiveness is usually limited to the public awareness they generate.
We seem to have forgotten that there are two sides to the equation. The accelerometer study from Europe should remind us that our initiatives should also be addressing the problem of epidemic inactivity with equal vigor. Creating programs that focus on increasing activity can be expensive. There may be costs for equipment, spaces to be maintained, and staff to be paid. On the other hand, curbing sedentary behavior requires only an adult with the courage to say, “No.” “No, we will have the television for only an hour today.” “No, you can’t play your video game until after dinner.”
While addressing the disciplinary side of the activity-inactivity dichotomy may be relatively inexpensive, it does seem to have a cost on parents. It requires them to buy into the idea that, given even the most-limited supply of objects and infrastructure, most children can keep themselves entertained and active. There does seem to be a small subset of children who enter the world with a sedentary mindset, possibly inherited from their parents. This unfortunate minority will require some creative intervention to achieve a healthy level of activity.
However, most young children who have become accustomed to being amused by sedentary “activities” such as television and video games still retain their innate creativity and natural inclination to be physically active. Unfortunately, unmasking these health-sustaining attributes may require a long and unpleasant weaning period that many parents don’t seem to have the patience to endure. The longer the child has been allowed to engage in sedentary behaviors, the longer this adjustment period will be, yet another argument for early intervention.
Encouraging physical activity is something we should be doing every day in our offices, but it must go hand in hand with an equivalent emphasis on helping parents create a discipline framework that discourages sedentary behavior.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Timeout or not?
However, when it comes to timeout, child behavior specialists have failed to reach consensus. In a recent Washington Post article, Claire Gillespie quotes several experts who feel that timeout is ineffective at best and damaging and dangerous at its worst. (Timeouts are a dated and ineffective parenting strategy. So what’s a good alternative? Washington Post, Nov. 29, 2019.)
How do you feel about timeouts? Do you think they are effective? Do you think that brief periods of isolation in a home setting will increase a child’s anxiety? Will the threat of isolation create long-lasting psychological harm? Or do you believe that properly done timeout can be a safe consequence when a child misbehaves?
The disagreement seems to be another one of those issues of apples and oranges. Do I believe that solitary confinement in a prison or chained to a metal cot in the basement of mentally deranged and obsessive parent will leave psychological scars? Of course I do. But, do I believe that a few minutes alone in a child’s own room in a home in which her parents frequently express their affection will cause any harm? Not for a moment. It’s not so much where the child is. It’s where she isn’t. Of course, she doesn’t want to be isolated from the family and that sends a powerful but not harmful message. A big hug and a kiss at the end of the timeout wipes the slate clear.
Some critics believe that timeout should be condemned because it is a punishment. Here again, it’s a case of semantics. Punishments in my mind are inhumane, “a pound of flesh” or “an eye for an eye” response. A well-done timeout is a harmless consequence and one that particularly makes sense when the misbehavior has been or is creating an unpleasant atmosphere in the family.
Other critics will claim that timeouts aren’t an effective deterrent. Correct! They aren’t meant to be a deterrent. A detailed discussion, more likely a lecture, about the misbehavior before and even immediately after a timeout is a waste of time. If timeouts are a deterrent it is because of their safety. Parents will be more likely to use them as a consequence, and most importantly to follow up on their threats. A parent whose words can be believed is his or her own best deterrent.
Finally, many parents who have tried timeouts will claim that they don’t work. This is true if they were talking about deterrent value. Maybe the timeouts have been too long or too short. About 30-60 seconds after the child stops crying may be enough. However, if the parents mean that the child wouldn’t stay in timeout in his room, then they have not taken the difficult final step. If the parent doesn’t have the stamina to keep walking the child back into his room, then it is time to put a latch on the door. Whoops. ... I may have lost some of you who up to this point have been nodding agreement along with my rationale. I know, I know it smacks of prison. It may be used only once or twice, but it will remain as a tangible reminder that sometimes enough is enough. Frequent trips into the room to help the child self-calm make it clear he hasn’t been abandoned.
It’s hard to provide a fully nuanced argument for including timeout in the consequence arsenal in 500 words. I’m eager to hear how you feel on the subject. I can take the heat.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
However, when it comes to timeout, child behavior specialists have failed to reach consensus. In a recent Washington Post article, Claire Gillespie quotes several experts who feel that timeout is ineffective at best and damaging and dangerous at its worst. (Timeouts are a dated and ineffective parenting strategy. So what’s a good alternative? Washington Post, Nov. 29, 2019.)
How do you feel about timeouts? Do you think they are effective? Do you think that brief periods of isolation in a home setting will increase a child’s anxiety? Will the threat of isolation create long-lasting psychological harm? Or do you believe that properly done timeout can be a safe consequence when a child misbehaves?
The disagreement seems to be another one of those issues of apples and oranges. Do I believe that solitary confinement in a prison or chained to a metal cot in the basement of mentally deranged and obsessive parent will leave psychological scars? Of course I do. But, do I believe that a few minutes alone in a child’s own room in a home in which her parents frequently express their affection will cause any harm? Not for a moment. It’s not so much where the child is. It’s where she isn’t. Of course, she doesn’t want to be isolated from the family and that sends a powerful but not harmful message. A big hug and a kiss at the end of the timeout wipes the slate clear.
Some critics believe that timeout should be condemned because it is a punishment. Here again, it’s a case of semantics. Punishments in my mind are inhumane, “a pound of flesh” or “an eye for an eye” response. A well-done timeout is a harmless consequence and one that particularly makes sense when the misbehavior has been or is creating an unpleasant atmosphere in the family.
Other critics will claim that timeouts aren’t an effective deterrent. Correct! They aren’t meant to be a deterrent. A detailed discussion, more likely a lecture, about the misbehavior before and even immediately after a timeout is a waste of time. If timeouts are a deterrent it is because of their safety. Parents will be more likely to use them as a consequence, and most importantly to follow up on their threats. A parent whose words can be believed is his or her own best deterrent.
Finally, many parents who have tried timeouts will claim that they don’t work. This is true if they were talking about deterrent value. Maybe the timeouts have been too long or too short. About 30-60 seconds after the child stops crying may be enough. However, if the parents mean that the child wouldn’t stay in timeout in his room, then they have not taken the difficult final step. If the parent doesn’t have the stamina to keep walking the child back into his room, then it is time to put a latch on the door. Whoops. ... I may have lost some of you who up to this point have been nodding agreement along with my rationale. I know, I know it smacks of prison. It may be used only once or twice, but it will remain as a tangible reminder that sometimes enough is enough. Frequent trips into the room to help the child self-calm make it clear he hasn’t been abandoned.
It’s hard to provide a fully nuanced argument for including timeout in the consequence arsenal in 500 words. I’m eager to hear how you feel on the subject. I can take the heat.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
However, when it comes to timeout, child behavior specialists have failed to reach consensus. In a recent Washington Post article, Claire Gillespie quotes several experts who feel that timeout is ineffective at best and damaging and dangerous at its worst. (Timeouts are a dated and ineffective parenting strategy. So what’s a good alternative? Washington Post, Nov. 29, 2019.)
How do you feel about timeouts? Do you think they are effective? Do you think that brief periods of isolation in a home setting will increase a child’s anxiety? Will the threat of isolation create long-lasting psychological harm? Or do you believe that properly done timeout can be a safe consequence when a child misbehaves?
The disagreement seems to be another one of those issues of apples and oranges. Do I believe that solitary confinement in a prison or chained to a metal cot in the basement of mentally deranged and obsessive parent will leave psychological scars? Of course I do. But, do I believe that a few minutes alone in a child’s own room in a home in which her parents frequently express their affection will cause any harm? Not for a moment. It’s not so much where the child is. It’s where she isn’t. Of course, she doesn’t want to be isolated from the family and that sends a powerful but not harmful message. A big hug and a kiss at the end of the timeout wipes the slate clear.
Some critics believe that timeout should be condemned because it is a punishment. Here again, it’s a case of semantics. Punishments in my mind are inhumane, “a pound of flesh” or “an eye for an eye” response. A well-done timeout is a harmless consequence and one that particularly makes sense when the misbehavior has been or is creating an unpleasant atmosphere in the family.
Other critics will claim that timeouts aren’t an effective deterrent. Correct! They aren’t meant to be a deterrent. A detailed discussion, more likely a lecture, about the misbehavior before and even immediately after a timeout is a waste of time. If timeouts are a deterrent it is because of their safety. Parents will be more likely to use them as a consequence, and most importantly to follow up on their threats. A parent whose words can be believed is his or her own best deterrent.
Finally, many parents who have tried timeouts will claim that they don’t work. This is true if they were talking about deterrent value. Maybe the timeouts have been too long or too short. About 30-60 seconds after the child stops crying may be enough. However, if the parents mean that the child wouldn’t stay in timeout in his room, then they have not taken the difficult final step. If the parent doesn’t have the stamina to keep walking the child back into his room, then it is time to put a latch on the door. Whoops. ... I may have lost some of you who up to this point have been nodding agreement along with my rationale. I know, I know it smacks of prison. It may be used only once or twice, but it will remain as a tangible reminder that sometimes enough is enough. Frequent trips into the room to help the child self-calm make it clear he hasn’t been abandoned.
It’s hard to provide a fully nuanced argument for including timeout in the consequence arsenal in 500 words. I’m eager to hear how you feel on the subject. I can take the heat.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
When NOT to perform a Pap test
Pap tests have the reputation of being a simple, noninvasive, low-cost test to offer patients, and, therefore, it is understandable to believe there is no harm in offering it in all situations. However, if inappropriately applied in isolation, performing the Pap test may do more harm than good.
I recently saw a patient in consultation for cervical cancer. Her story was similar to one I’ve seen many times before. She was a 30-year-old non–English-speaking Hispanic woman who received regular care from the health department clinics.
In April of the prior year, she had noticed abnormal bleeding symptoms including intermenstrual and postcoital bleeding. She visited the health department and reported these symptoms to the provider who performed an examination. According to the provider’s notes, the cervix appeared “abnormal” and a Pap test was done. The result of this Pap test was high-grade dysplasia. The patient was promptly notified of the result and an appointment was arranged with the local ob.gyn. for a consultation, presumably for colposcopy and subsequent appropriate excisional procedure. Unfortunately, the patient did not attend that scheduled appointment. She later recounted to me that it was because she had not understood that it was important. She had a long history of abnormal Pap tests which, in the past, had only required repeat testing or minor interventions such as “freezing.”
Her bleeding symptoms became worse, and she developed abnormal discharge and pain. In November, she presented again for evaluation to the same provider. Now her cervix appeared very abnormal and was described as a “crater.” Again a Pap test was done. This time the Pap test showed “carcinoma,” and the patient was informed that she had cancer and was referred to gynecologic oncology. When I examined this unfortunate young woman, I discovered a 10 cm, stage IIB very locally advanced tumor. She is currently receiving primary chemotherapy/radiation with an approximately 60% probability of cure, and a high likelihood of lifelong sequelae of this toxic therapy.
This case highlights that, even when patients are engaged within our health care system, we can miss the opportunity to diagnose early-stage cancers if we are not utilizing screening versus diagnostic tests appropriately.
The purpose of a Pap test is as a screening test, which are designed to detect disease in asymptomatic individuals. The accuracy of these tests is determined in low-risk (asymptomatic) populations, which influences the pretest probability of disease. In asymptomatic patients with a normal screening test, it is safe to wait out the interval of time for the repeat screening test, because the combination of a low pretest probability and a high sensitivity of the test in finding disease means that there is a very low chance of missing disease.
Dysplasia rarely causes bleeding. However, invasive cervical cancer does. If a patient has a symptom such as abnormal bleeding, they no longer fit into the population with a low pretest probability for having cervical cancer. This same sensitivity of the Pap test in finding disease, combined with the now-higher pretest probability can raise the level of false-negative results to unacceptably high levels.
Patients with symptoms of cervical cancer should not receive screening tests exclusively; they should receive diagnostic tests. For example, Pap tests should not be used in isolation to diagnose pathology in patients with abnormal bleeding or discharge, just as screening mammograms should not be ordered in patients with symptomatic breast lumps, nipple discharge, retraction, etc. (these women should be referred for diagnostic mammography and ultrasound). It is not unusual for gynecologic oncologists to see patients with visible invasive cervical cancer who have only cervical intraepithelial neoplasia grade 3 on the preceding Pap test. There is a 34% positive predictive value that a cervical cancer will be found with a high-grade dysplastic Pap test.1 Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. It analyzes individual cells rather than a piece of tissue with intercellular relationships.
The take-home message for this column is that, if a provider sees an abnormal lesion on a cervix, they should biopsy the visible lesion to obtain a histologic diagnosis. Simply performing a Pap test alone may result in false reassurance and in underestimating the severity of disease.
Some providers will tell me that they have concerns about performing a biopsy on a grossly abnormal cervix for fear that the subsequent bleeding will be difficult to manage in the outpatient setting. This is understandable, although it is unlikely that an office equipped with the ability to perform colposcopy or excisional procedures would not have the necessary equipment to manage this. Prolonged pressure applied to the cervix with topical hemostatic agents or – in extreme cases – vaginal packing with gauze always has been effective for me in these circumstances.
The additional benefit of establishing histologic confirmation prior to referral is expediting care, including additional imaging and referrals to treating providers. If the diagnosis is inadequately established prior to their appointment with a gynecologic oncologist, it can add further delays before definitive surgical or nonsurgical management can be initiated, which is particularly problematic if the patient is experiencing severe bleeding. If the provider feels uncomfortable with proceeding with biopsy, they should inform the patient very clearly that they suspect that there is a cancer of the cervix, and it needs attention from a cancer specialist to confirm the diagnosis. This clear communication will minimize the likelihood that the patient may not show up for the subsequent appointments before her diagnosis is definitively established.
Another common scenario in which Pap tests are inappropriately applied is in the surveillance of endometrial cancer. In 2013, the Society of Gynecologic Oncology released its five “Choosing Wisely” recommendations. This included the recommendation to not perform Pap tests in the surveillance of endometrial cancer. This recommendation was based on a body of evidence that demonstrates screening for endometrial cancer recurrence with Pap smears does not detect vaginal mucosal recurrences any sooner than visualization of lesions on speculum examination.2,3 These Pap-positive recurrences almost always are visible on exam. Additionally, false positives are common in this population, particularly among women who have had radiation or have atrophic tissues.
Using Pap tests for the surveillance of cervical cancer is somewhat more complicated. Similarly, they do not detect cervical cancer recurrence any sooner than comprehensive examination does. However, this population may suffer from chronic human papillomavirus (HPV) infection, and there remains a role of the Pap test in screening for future, new HPV-related preinvasive vaginal disease. Therefore, Pap tests, and/or HPV testing can be offered to cervical cancer survivors in accordance with the American Society for Colposcopy and Cervical Pathology guidelines for noncervical cancer patients, with the caveat that, if radiation has been given, false positives are more likely.2
Pap tests clearly have an important role as a screening test in asymptomatic individuals. However, when the patient has a symptom that might be cervical cancer or a visibly suspicious lesion, she should receive a diagnostic test, and Pap tests are not designed for that purpose.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. Cytopathology. 2016 Jun;27(3):201-9.
2. Gynecol Oncol. 2017 Jul;146(1):3-10.
3. Gynecol Oncol. 2011 Nov;123(2):205-7.
Pap tests have the reputation of being a simple, noninvasive, low-cost test to offer patients, and, therefore, it is understandable to believe there is no harm in offering it in all situations. However, if inappropriately applied in isolation, performing the Pap test may do more harm than good.
I recently saw a patient in consultation for cervical cancer. Her story was similar to one I’ve seen many times before. She was a 30-year-old non–English-speaking Hispanic woman who received regular care from the health department clinics.
In April of the prior year, she had noticed abnormal bleeding symptoms including intermenstrual and postcoital bleeding. She visited the health department and reported these symptoms to the provider who performed an examination. According to the provider’s notes, the cervix appeared “abnormal” and a Pap test was done. The result of this Pap test was high-grade dysplasia. The patient was promptly notified of the result and an appointment was arranged with the local ob.gyn. for a consultation, presumably for colposcopy and subsequent appropriate excisional procedure. Unfortunately, the patient did not attend that scheduled appointment. She later recounted to me that it was because she had not understood that it was important. She had a long history of abnormal Pap tests which, in the past, had only required repeat testing or minor interventions such as “freezing.”
Her bleeding symptoms became worse, and she developed abnormal discharge and pain. In November, she presented again for evaluation to the same provider. Now her cervix appeared very abnormal and was described as a “crater.” Again a Pap test was done. This time the Pap test showed “carcinoma,” and the patient was informed that she had cancer and was referred to gynecologic oncology. When I examined this unfortunate young woman, I discovered a 10 cm, stage IIB very locally advanced tumor. She is currently receiving primary chemotherapy/radiation with an approximately 60% probability of cure, and a high likelihood of lifelong sequelae of this toxic therapy.
This case highlights that, even when patients are engaged within our health care system, we can miss the opportunity to diagnose early-stage cancers if we are not utilizing screening versus diagnostic tests appropriately.
The purpose of a Pap test is as a screening test, which are designed to detect disease in asymptomatic individuals. The accuracy of these tests is determined in low-risk (asymptomatic) populations, which influences the pretest probability of disease. In asymptomatic patients with a normal screening test, it is safe to wait out the interval of time for the repeat screening test, because the combination of a low pretest probability and a high sensitivity of the test in finding disease means that there is a very low chance of missing disease.
Dysplasia rarely causes bleeding. However, invasive cervical cancer does. If a patient has a symptom such as abnormal bleeding, they no longer fit into the population with a low pretest probability for having cervical cancer. This same sensitivity of the Pap test in finding disease, combined with the now-higher pretest probability can raise the level of false-negative results to unacceptably high levels.
Patients with symptoms of cervical cancer should not receive screening tests exclusively; they should receive diagnostic tests. For example, Pap tests should not be used in isolation to diagnose pathology in patients with abnormal bleeding or discharge, just as screening mammograms should not be ordered in patients with symptomatic breast lumps, nipple discharge, retraction, etc. (these women should be referred for diagnostic mammography and ultrasound). It is not unusual for gynecologic oncologists to see patients with visible invasive cervical cancer who have only cervical intraepithelial neoplasia grade 3 on the preceding Pap test. There is a 34% positive predictive value that a cervical cancer will be found with a high-grade dysplastic Pap test.1 Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. It analyzes individual cells rather than a piece of tissue with intercellular relationships.
The take-home message for this column is that, if a provider sees an abnormal lesion on a cervix, they should biopsy the visible lesion to obtain a histologic diagnosis. Simply performing a Pap test alone may result in false reassurance and in underestimating the severity of disease.
Some providers will tell me that they have concerns about performing a biopsy on a grossly abnormal cervix for fear that the subsequent bleeding will be difficult to manage in the outpatient setting. This is understandable, although it is unlikely that an office equipped with the ability to perform colposcopy or excisional procedures would not have the necessary equipment to manage this. Prolonged pressure applied to the cervix with topical hemostatic agents or – in extreme cases – vaginal packing with gauze always has been effective for me in these circumstances.
The additional benefit of establishing histologic confirmation prior to referral is expediting care, including additional imaging and referrals to treating providers. If the diagnosis is inadequately established prior to their appointment with a gynecologic oncologist, it can add further delays before definitive surgical or nonsurgical management can be initiated, which is particularly problematic if the patient is experiencing severe bleeding. If the provider feels uncomfortable with proceeding with biopsy, they should inform the patient very clearly that they suspect that there is a cancer of the cervix, and it needs attention from a cancer specialist to confirm the diagnosis. This clear communication will minimize the likelihood that the patient may not show up for the subsequent appointments before her diagnosis is definitively established.
Another common scenario in which Pap tests are inappropriately applied is in the surveillance of endometrial cancer. In 2013, the Society of Gynecologic Oncology released its five “Choosing Wisely” recommendations. This included the recommendation to not perform Pap tests in the surveillance of endometrial cancer. This recommendation was based on a body of evidence that demonstrates screening for endometrial cancer recurrence with Pap smears does not detect vaginal mucosal recurrences any sooner than visualization of lesions on speculum examination.2,3 These Pap-positive recurrences almost always are visible on exam. Additionally, false positives are common in this population, particularly among women who have had radiation or have atrophic tissues.
Using Pap tests for the surveillance of cervical cancer is somewhat more complicated. Similarly, they do not detect cervical cancer recurrence any sooner than comprehensive examination does. However, this population may suffer from chronic human papillomavirus (HPV) infection, and there remains a role of the Pap test in screening for future, new HPV-related preinvasive vaginal disease. Therefore, Pap tests, and/or HPV testing can be offered to cervical cancer survivors in accordance with the American Society for Colposcopy and Cervical Pathology guidelines for noncervical cancer patients, with the caveat that, if radiation has been given, false positives are more likely.2
Pap tests clearly have an important role as a screening test in asymptomatic individuals. However, when the patient has a symptom that might be cervical cancer or a visibly suspicious lesion, she should receive a diagnostic test, and Pap tests are not designed for that purpose.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. Cytopathology. 2016 Jun;27(3):201-9.
2. Gynecol Oncol. 2017 Jul;146(1):3-10.
3. Gynecol Oncol. 2011 Nov;123(2):205-7.
Pap tests have the reputation of being a simple, noninvasive, low-cost test to offer patients, and, therefore, it is understandable to believe there is no harm in offering it in all situations. However, if inappropriately applied in isolation, performing the Pap test may do more harm than good.
I recently saw a patient in consultation for cervical cancer. Her story was similar to one I’ve seen many times before. She was a 30-year-old non–English-speaking Hispanic woman who received regular care from the health department clinics.
In April of the prior year, she had noticed abnormal bleeding symptoms including intermenstrual and postcoital bleeding. She visited the health department and reported these symptoms to the provider who performed an examination. According to the provider’s notes, the cervix appeared “abnormal” and a Pap test was done. The result of this Pap test was high-grade dysplasia. The patient was promptly notified of the result and an appointment was arranged with the local ob.gyn. for a consultation, presumably for colposcopy and subsequent appropriate excisional procedure. Unfortunately, the patient did not attend that scheduled appointment. She later recounted to me that it was because she had not understood that it was important. She had a long history of abnormal Pap tests which, in the past, had only required repeat testing or minor interventions such as “freezing.”
Her bleeding symptoms became worse, and she developed abnormal discharge and pain. In November, she presented again for evaluation to the same provider. Now her cervix appeared very abnormal and was described as a “crater.” Again a Pap test was done. This time the Pap test showed “carcinoma,” and the patient was informed that she had cancer and was referred to gynecologic oncology. When I examined this unfortunate young woman, I discovered a 10 cm, stage IIB very locally advanced tumor. She is currently receiving primary chemotherapy/radiation with an approximately 60% probability of cure, and a high likelihood of lifelong sequelae of this toxic therapy.
This case highlights that, even when patients are engaged within our health care system, we can miss the opportunity to diagnose early-stage cancers if we are not utilizing screening versus diagnostic tests appropriately.
The purpose of a Pap test is as a screening test, which are designed to detect disease in asymptomatic individuals. The accuracy of these tests is determined in low-risk (asymptomatic) populations, which influences the pretest probability of disease. In asymptomatic patients with a normal screening test, it is safe to wait out the interval of time for the repeat screening test, because the combination of a low pretest probability and a high sensitivity of the test in finding disease means that there is a very low chance of missing disease.
Dysplasia rarely causes bleeding. However, invasive cervical cancer does. If a patient has a symptom such as abnormal bleeding, they no longer fit into the population with a low pretest probability for having cervical cancer. This same sensitivity of the Pap test in finding disease, combined with the now-higher pretest probability can raise the level of false-negative results to unacceptably high levels.
Patients with symptoms of cervical cancer should not receive screening tests exclusively; they should receive diagnostic tests. For example, Pap tests should not be used in isolation to diagnose pathology in patients with abnormal bleeding or discharge, just as screening mammograms should not be ordered in patients with symptomatic breast lumps, nipple discharge, retraction, etc. (these women should be referred for diagnostic mammography and ultrasound). It is not unusual for gynecologic oncologists to see patients with visible invasive cervical cancer who have only cervical intraepithelial neoplasia grade 3 on the preceding Pap test. There is a 34% positive predictive value that a cervical cancer will be found with a high-grade dysplastic Pap test.1 Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. It analyzes individual cells rather than a piece of tissue with intercellular relationships.
The take-home message for this column is that, if a provider sees an abnormal lesion on a cervix, they should biopsy the visible lesion to obtain a histologic diagnosis. Simply performing a Pap test alone may result in false reassurance and in underestimating the severity of disease.
Some providers will tell me that they have concerns about performing a biopsy on a grossly abnormal cervix for fear that the subsequent bleeding will be difficult to manage in the outpatient setting. This is understandable, although it is unlikely that an office equipped with the ability to perform colposcopy or excisional procedures would not have the necessary equipment to manage this. Prolonged pressure applied to the cervix with topical hemostatic agents or – in extreme cases – vaginal packing with gauze always has been effective for me in these circumstances.
The additional benefit of establishing histologic confirmation prior to referral is expediting care, including additional imaging and referrals to treating providers. If the diagnosis is inadequately established prior to their appointment with a gynecologic oncologist, it can add further delays before definitive surgical or nonsurgical management can be initiated, which is particularly problematic if the patient is experiencing severe bleeding. If the provider feels uncomfortable with proceeding with biopsy, they should inform the patient very clearly that they suspect that there is a cancer of the cervix, and it needs attention from a cancer specialist to confirm the diagnosis. This clear communication will minimize the likelihood that the patient may not show up for the subsequent appointments before her diagnosis is definitively established.
Another common scenario in which Pap tests are inappropriately applied is in the surveillance of endometrial cancer. In 2013, the Society of Gynecologic Oncology released its five “Choosing Wisely” recommendations. This included the recommendation to not perform Pap tests in the surveillance of endometrial cancer. This recommendation was based on a body of evidence that demonstrates screening for endometrial cancer recurrence with Pap smears does not detect vaginal mucosal recurrences any sooner than visualization of lesions on speculum examination.2,3 These Pap-positive recurrences almost always are visible on exam. Additionally, false positives are common in this population, particularly among women who have had radiation or have atrophic tissues.
Using Pap tests for the surveillance of cervical cancer is somewhat more complicated. Similarly, they do not detect cervical cancer recurrence any sooner than comprehensive examination does. However, this population may suffer from chronic human papillomavirus (HPV) infection, and there remains a role of the Pap test in screening for future, new HPV-related preinvasive vaginal disease. Therefore, Pap tests, and/or HPV testing can be offered to cervical cancer survivors in accordance with the American Society for Colposcopy and Cervical Pathology guidelines for noncervical cancer patients, with the caveat that, if radiation has been given, false positives are more likely.2
Pap tests clearly have an important role as a screening test in asymptomatic individuals. However, when the patient has a symptom that might be cervical cancer or a visibly suspicious lesion, she should receive a diagnostic test, and Pap tests are not designed for that purpose.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. Cytopathology. 2016 Jun;27(3):201-9.
2. Gynecol Oncol. 2017 Jul;146(1):3-10.
3. Gynecol Oncol. 2011 Nov;123(2):205-7.
We must counsel against heat-not-burn cigarettes
Tobacco companies are marketing a new version of cigarettes dubbed heat-not-burn (HNB) cigarettes.1,2 Offered as a “modified-risk tobacco product,” HNB cigarettes utilize a lithium battery-powered heating element and are available all over the world.1,2 Like conventional smokes, they contain tobacco, but deliver nicotine by heating leaves at 350° C rather than burning them at 600° C.1-3 Heating the tobacco produces an inhalable aerosol with tobacco flavor and nicotine, without smoke. These HNB cigarettes are also different from e-cigarettes that aerosolize a liquid.
Tobacco companies contend that HNB cigarettes are safer than smoking tobacco.1 Consumers inhale a heated tobacco aerosol that reportedly contains less nicotine and fewer toxicities; yet, HNB are not independently substantiated as being healthier, nor proven safe.1-5 Thermal decomposition, rather than combustion, may afford a less dangerous nicotine consumption; however, HNB aerosols deliver many of the same dangerous compounds as traditional cigarettes, including carbon monoxide, tar, and aromatic hydrocarbons.2-6 Despite possible harm reduction in the short-run, long-term safety remains unconfirmed.
Safety in passive environmental inhalations is not established.2 HNB cigarettes are contraindicated during pregnancy and/or lactation. Nicotine is provided in addictive quantities, enough to foster continued dependence. Exposure to HNB products can promote longer-term usage or lead to smoking traditional tobacco cigarettes. There is also an increased risk to non-smokers of exposure to HNB aerosols. Additionally, lithium batteries have been known to burn or explode. HNB devices may even lead to privacy concerns due micro-controller chips contained within that harvest information. These chips could inform manufacturers about device usage.7
Tobacco is a global health hazard and smoking is the number one preventable cause of disease.1,5,8 Global smoking prevalence is nearing 19%.9 There are concerns about dual use, rather than HNB cigarettes alone as a substitute for conventional smoking. The ultimate hope is to abstain from all tobacco and nicotine. Although HNB inhalations contain fewer toxic chemicals than by smoking, evidence regarding mitigation of tobacco-related diseases is inconclusive.10
Physicians have an obligation to minimize tobacco and nicotine-related hazards. Ongoing research and clinical exposure might better document the health impact of HNB cigarettes. Until the risks and benefits of HNB cigarettes are confirmed, health care professionals would be wise to counsel against their use.
Diksha Mohanty, MD; Steven Lippmann, MD
Louisville, Ky
1. Combustible cigarettes kill millions a year. Can Big Tobacco save them? The Economist Web site. https://www.economist.com/business/2017/12/19/combustible-cigarettes-kill-millions-a-year-can-big-tobacco-save-them. Accessed November 9, 2018.
2. Auer R, Concha-Lozano N, Jacot-Sadowski I, et al. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med. 2017;177:1050-1052.
3. Caputi TL. Industry watch: heat-not-burn tobacco products are about to reach their boiling point. Tob Control. 2016;26:609-610.
4. Jenssen BP, Walley SC, McGrath-Morrow SA. Heat-not-burn tobacco products: Tobacco industry claims no substitute for science. Pediatrics. 2018;141:e20172383.
5. Levy DT, Cummings KM, Villanti AC, et al. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction. 2017;112:8-17.
6. Bekki K, Inaba Y, Uchiyama S, et al. Comparison of chemicals in mainstream smoke in heat-not-burn tobacco and combustion cigarettes. J UOEH, 2017;39:201-207.
7. Lasseter T, Wilson D, Wilson T, et al. Philip Morris device knows a lot about your smoking habit. Reuters. https://www.reuters.com/investigates/special-report/tobacco-iqos-device. Accessed November 9, 2018.
8. Carter BD, Abnet CC, Feskanich D, et al. Smoking and mortality — beyond established causes. New Engl J Med. 2015;372:631-640.
9. World Health Organization. WHO global report on trends in tobacco smoking 2000-2025 - First edition. http://www.who.int/tobacco/publications/surveillance/reportontrendstobaccosmoking/en/index4.html. Accessed November 9, 2018.
10. U.S. Food & Drug Administration. CTPConnect—September 2017. https://www.fda.gov/TobaccoProducts/NewsEvents/ucm576895.htm. Updated June 14, 2018. Accessed Nov ember 9, 2018.
Tobacco companies are marketing a new version of cigarettes dubbed heat-not-burn (HNB) cigarettes.1,2 Offered as a “modified-risk tobacco product,” HNB cigarettes utilize a lithium battery-powered heating element and are available all over the world.1,2 Like conventional smokes, they contain tobacco, but deliver nicotine by heating leaves at 350° C rather than burning them at 600° C.1-3 Heating the tobacco produces an inhalable aerosol with tobacco flavor and nicotine, without smoke. These HNB cigarettes are also different from e-cigarettes that aerosolize a liquid.
Tobacco companies contend that HNB cigarettes are safer than smoking tobacco.1 Consumers inhale a heated tobacco aerosol that reportedly contains less nicotine and fewer toxicities; yet, HNB are not independently substantiated as being healthier, nor proven safe.1-5 Thermal decomposition, rather than combustion, may afford a less dangerous nicotine consumption; however, HNB aerosols deliver many of the same dangerous compounds as traditional cigarettes, including carbon monoxide, tar, and aromatic hydrocarbons.2-6 Despite possible harm reduction in the short-run, long-term safety remains unconfirmed.
Safety in passive environmental inhalations is not established.2 HNB cigarettes are contraindicated during pregnancy and/or lactation. Nicotine is provided in addictive quantities, enough to foster continued dependence. Exposure to HNB products can promote longer-term usage or lead to smoking traditional tobacco cigarettes. There is also an increased risk to non-smokers of exposure to HNB aerosols. Additionally, lithium batteries have been known to burn or explode. HNB devices may even lead to privacy concerns due micro-controller chips contained within that harvest information. These chips could inform manufacturers about device usage.7
Tobacco is a global health hazard and smoking is the number one preventable cause of disease.1,5,8 Global smoking prevalence is nearing 19%.9 There are concerns about dual use, rather than HNB cigarettes alone as a substitute for conventional smoking. The ultimate hope is to abstain from all tobacco and nicotine. Although HNB inhalations contain fewer toxic chemicals than by smoking, evidence regarding mitigation of tobacco-related diseases is inconclusive.10
Physicians have an obligation to minimize tobacco and nicotine-related hazards. Ongoing research and clinical exposure might better document the health impact of HNB cigarettes. Until the risks and benefits of HNB cigarettes are confirmed, health care professionals would be wise to counsel against their use.
Diksha Mohanty, MD; Steven Lippmann, MD
Louisville, Ky
Tobacco companies are marketing a new version of cigarettes dubbed heat-not-burn (HNB) cigarettes.1,2 Offered as a “modified-risk tobacco product,” HNB cigarettes utilize a lithium battery-powered heating element and are available all over the world.1,2 Like conventional smokes, they contain tobacco, but deliver nicotine by heating leaves at 350° C rather than burning them at 600° C.1-3 Heating the tobacco produces an inhalable aerosol with tobacco flavor and nicotine, without smoke. These HNB cigarettes are also different from e-cigarettes that aerosolize a liquid.
Tobacco companies contend that HNB cigarettes are safer than smoking tobacco.1 Consumers inhale a heated tobacco aerosol that reportedly contains less nicotine and fewer toxicities; yet, HNB are not independently substantiated as being healthier, nor proven safe.1-5 Thermal decomposition, rather than combustion, may afford a less dangerous nicotine consumption; however, HNB aerosols deliver many of the same dangerous compounds as traditional cigarettes, including carbon monoxide, tar, and aromatic hydrocarbons.2-6 Despite possible harm reduction in the short-run, long-term safety remains unconfirmed.
Safety in passive environmental inhalations is not established.2 HNB cigarettes are contraindicated during pregnancy and/or lactation. Nicotine is provided in addictive quantities, enough to foster continued dependence. Exposure to HNB products can promote longer-term usage or lead to smoking traditional tobacco cigarettes. There is also an increased risk to non-smokers of exposure to HNB aerosols. Additionally, lithium batteries have been known to burn or explode. HNB devices may even lead to privacy concerns due micro-controller chips contained within that harvest information. These chips could inform manufacturers about device usage.7
Tobacco is a global health hazard and smoking is the number one preventable cause of disease.1,5,8 Global smoking prevalence is nearing 19%.9 There are concerns about dual use, rather than HNB cigarettes alone as a substitute for conventional smoking. The ultimate hope is to abstain from all tobacco and nicotine. Although HNB inhalations contain fewer toxic chemicals than by smoking, evidence regarding mitigation of tobacco-related diseases is inconclusive.10
Physicians have an obligation to minimize tobacco and nicotine-related hazards. Ongoing research and clinical exposure might better document the health impact of HNB cigarettes. Until the risks and benefits of HNB cigarettes are confirmed, health care professionals would be wise to counsel against their use.
Diksha Mohanty, MD; Steven Lippmann, MD
Louisville, Ky
1. Combustible cigarettes kill millions a year. Can Big Tobacco save them? The Economist Web site. https://www.economist.com/business/2017/12/19/combustible-cigarettes-kill-millions-a-year-can-big-tobacco-save-them. Accessed November 9, 2018.
2. Auer R, Concha-Lozano N, Jacot-Sadowski I, et al. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med. 2017;177:1050-1052.
3. Caputi TL. Industry watch: heat-not-burn tobacco products are about to reach their boiling point. Tob Control. 2016;26:609-610.
4. Jenssen BP, Walley SC, McGrath-Morrow SA. Heat-not-burn tobacco products: Tobacco industry claims no substitute for science. Pediatrics. 2018;141:e20172383.
5. Levy DT, Cummings KM, Villanti AC, et al. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction. 2017;112:8-17.
6. Bekki K, Inaba Y, Uchiyama S, et al. Comparison of chemicals in mainstream smoke in heat-not-burn tobacco and combustion cigarettes. J UOEH, 2017;39:201-207.
7. Lasseter T, Wilson D, Wilson T, et al. Philip Morris device knows a lot about your smoking habit. Reuters. https://www.reuters.com/investigates/special-report/tobacco-iqos-device. Accessed November 9, 2018.
8. Carter BD, Abnet CC, Feskanich D, et al. Smoking and mortality — beyond established causes. New Engl J Med. 2015;372:631-640.
9. World Health Organization. WHO global report on trends in tobacco smoking 2000-2025 - First edition. http://www.who.int/tobacco/publications/surveillance/reportontrendstobaccosmoking/en/index4.html. Accessed November 9, 2018.
10. U.S. Food & Drug Administration. CTPConnect—September 2017. https://www.fda.gov/TobaccoProducts/NewsEvents/ucm576895.htm. Updated June 14, 2018. Accessed Nov ember 9, 2018.
1. Combustible cigarettes kill millions a year. Can Big Tobacco save them? The Economist Web site. https://www.economist.com/business/2017/12/19/combustible-cigarettes-kill-millions-a-year-can-big-tobacco-save-them. Accessed November 9, 2018.
2. Auer R, Concha-Lozano N, Jacot-Sadowski I, et al. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med. 2017;177:1050-1052.
3. Caputi TL. Industry watch: heat-not-burn tobacco products are about to reach their boiling point. Tob Control. 2016;26:609-610.
4. Jenssen BP, Walley SC, McGrath-Morrow SA. Heat-not-burn tobacco products: Tobacco industry claims no substitute for science. Pediatrics. 2018;141:e20172383.
5. Levy DT, Cummings KM, Villanti AC, et al. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction. 2017;112:8-17.
6. Bekki K, Inaba Y, Uchiyama S, et al. Comparison of chemicals in mainstream smoke in heat-not-burn tobacco and combustion cigarettes. J UOEH, 2017;39:201-207.
7. Lasseter T, Wilson D, Wilson T, et al. Philip Morris device knows a lot about your smoking habit. Reuters. https://www.reuters.com/investigates/special-report/tobacco-iqos-device. Accessed November 9, 2018.
8. Carter BD, Abnet CC, Feskanich D, et al. Smoking and mortality — beyond established causes. New Engl J Med. 2015;372:631-640.
9. World Health Organization. WHO global report on trends in tobacco smoking 2000-2025 - First edition. http://www.who.int/tobacco/publications/surveillance/reportontrendstobaccosmoking/en/index4.html. Accessed November 9, 2018.
10. U.S. Food & Drug Administration. CTPConnect—September 2017. https://www.fda.gov/TobaccoProducts/NewsEvents/ucm576895.htm. Updated June 14, 2018. Accessed Nov ember 9, 2018.
A skeptic’s view of bariatric surgery
Like JFP’s Editor-in-Chief, Dr. John Hickner, I have been skeptical about bariatric surgery (A [former] skeptic’s view of bariatric surgery. J Fam Pract. 2018;67:600), but I will recommend it for a select few patients who are unable or unwilling to undergo significant lifestyle changes. My experience in clinic has done nothing to change this skeptical view. I have many patients who opted for bariatric surgery, but did not change their lifestyle habits. These patients often regain weight and accumulate chronic diseases 2 to 7 years postop. In the end, if a patient does not change their lifestyle, bariatric surgery can push the consequences of obesity out 5 to 10 years, but at a very significant risk.
The most significant problem I see is that many primary care providers do not feel qualified to impart meaningful lifestyle recommendations to patients, which often leads to guidance that is inadequate and, in some cases, inaccurate. Furthermore, assuming patients have received evidence-based instructions, they often lack the support and means to apply these lifestyle changes. I would be very hesitant to recommend bariatric surgery before addressing all of these concerns.
An interesting study done by Lingvay et al1 showed that postsurgical starvation (600 kcal/d) without the bariatric surgery had better short-term outcomes than surgery with calorie restriction, which suggests that a period of starvation is better than surgery.
In general, the results of evidence-based lifestyle changes far surpass any medical or surgical treatment for obesity and its associated chronic diseases. The evidence for this is overwhelming. (See books by Drs. Joel Fuhrman, Michael Greger, Neal Barnard, Dean Ornish, and Garth Davis, as well as the hundreds of peer-reviewed studies cited in these books.) Yet most patients under-going bariatric surgery never receive proper instructions or attempt any meaningful lifestyle changes.
I think it is far more prudent to refer potential surgical candidates to someone who understands good nutrition and lifestyle changes, such as a doctor certified by the American College of Lifestyle Medicine (lifestylemedicine.org). Surgery, in my opinion, is a very poor and dangerous second choice.
John Reed, MD
Fishersville, Va
1. Lingvay I, GuthE, Eslam A, et al. Rapid improvement in diabetes after gastric bypass surgery: Is it the diet or surgery? Diabetes Care. 2013;36:2741-2747.
Like JFP’s Editor-in-Chief, Dr. John Hickner, I have been skeptical about bariatric surgery (A [former] skeptic’s view of bariatric surgery. J Fam Pract. 2018;67:600), but I will recommend it for a select few patients who are unable or unwilling to undergo significant lifestyle changes. My experience in clinic has done nothing to change this skeptical view. I have many patients who opted for bariatric surgery, but did not change their lifestyle habits. These patients often regain weight and accumulate chronic diseases 2 to 7 years postop. In the end, if a patient does not change their lifestyle, bariatric surgery can push the consequences of obesity out 5 to 10 years, but at a very significant risk.
The most significant problem I see is that many primary care providers do not feel qualified to impart meaningful lifestyle recommendations to patients, which often leads to guidance that is inadequate and, in some cases, inaccurate. Furthermore, assuming patients have received evidence-based instructions, they often lack the support and means to apply these lifestyle changes. I would be very hesitant to recommend bariatric surgery before addressing all of these concerns.
An interesting study done by Lingvay et al1 showed that postsurgical starvation (600 kcal/d) without the bariatric surgery had better short-term outcomes than surgery with calorie restriction, which suggests that a period of starvation is better than surgery.
In general, the results of evidence-based lifestyle changes far surpass any medical or surgical treatment for obesity and its associated chronic diseases. The evidence for this is overwhelming. (See books by Drs. Joel Fuhrman, Michael Greger, Neal Barnard, Dean Ornish, and Garth Davis, as well as the hundreds of peer-reviewed studies cited in these books.) Yet most patients under-going bariatric surgery never receive proper instructions or attempt any meaningful lifestyle changes.
I think it is far more prudent to refer potential surgical candidates to someone who understands good nutrition and lifestyle changes, such as a doctor certified by the American College of Lifestyle Medicine (lifestylemedicine.org). Surgery, in my opinion, is a very poor and dangerous second choice.
John Reed, MD
Fishersville, Va
Like JFP’s Editor-in-Chief, Dr. John Hickner, I have been skeptical about bariatric surgery (A [former] skeptic’s view of bariatric surgery. J Fam Pract. 2018;67:600), but I will recommend it for a select few patients who are unable or unwilling to undergo significant lifestyle changes. My experience in clinic has done nothing to change this skeptical view. I have many patients who opted for bariatric surgery, but did not change their lifestyle habits. These patients often regain weight and accumulate chronic diseases 2 to 7 years postop. In the end, if a patient does not change their lifestyle, bariatric surgery can push the consequences of obesity out 5 to 10 years, but at a very significant risk.
The most significant problem I see is that many primary care providers do not feel qualified to impart meaningful lifestyle recommendations to patients, which often leads to guidance that is inadequate and, in some cases, inaccurate. Furthermore, assuming patients have received evidence-based instructions, they often lack the support and means to apply these lifestyle changes. I would be very hesitant to recommend bariatric surgery before addressing all of these concerns.
An interesting study done by Lingvay et al1 showed that postsurgical starvation (600 kcal/d) without the bariatric surgery had better short-term outcomes than surgery with calorie restriction, which suggests that a period of starvation is better than surgery.
In general, the results of evidence-based lifestyle changes far surpass any medical or surgical treatment for obesity and its associated chronic diseases. The evidence for this is overwhelming. (See books by Drs. Joel Fuhrman, Michael Greger, Neal Barnard, Dean Ornish, and Garth Davis, as well as the hundreds of peer-reviewed studies cited in these books.) Yet most patients under-going bariatric surgery never receive proper instructions or attempt any meaningful lifestyle changes.
I think it is far more prudent to refer potential surgical candidates to someone who understands good nutrition and lifestyle changes, such as a doctor certified by the American College of Lifestyle Medicine (lifestylemedicine.org). Surgery, in my opinion, is a very poor and dangerous second choice.
John Reed, MD
Fishersville, Va
1. Lingvay I, GuthE, Eslam A, et al. Rapid improvement in diabetes after gastric bypass surgery: Is it the diet or surgery? Diabetes Care. 2013;36:2741-2747.
1. Lingvay I, GuthE, Eslam A, et al. Rapid improvement in diabetes after gastric bypass surgery: Is it the diet or surgery? Diabetes Care. 2013;36:2741-2747.