User login
Obstetric hospitalists can screen for postpartum depression
Postpartum depression (PPD) is the most common complication of pregnancy, and onset can occur at any time from pregnancy until up to 1 year post partum.1,2 The immediate postpartum period is a time during which care is shared among multiple providers for both mother and child, and the transition from inpatient to outpatient postpartum care can impede communication between those caring for the patient in each setting. In 2018, the American College of Obstetricians and Gynecologists published a committee opinion emphasizing the importance of the “fourth trimester” and calling for health care providers to assist women in navigating the transition from pre- to postpartum care.3 An important consideration of perinatal care is mental health care for the mother, including screening and care for postpartum depression; however, the optimal role for the obstetric hospitalist in providing such services has been unclear.
Estimates of the prevalence of PPD in new mothers in the United States varied by state from 8% to 20% in 2012, with an overall average of 12%.2 Left untreated, PPD may result in significant negative outcomes for women, their children, and families. The depressive symptoms of PPD may persist for months or years afterward,4 with one study finding elevated depressive symptoms in women up to 11 years post partum.5 Suicide is also a leading cause of pregnancy-related mortality associated with depressive symptoms.6-9 In addition, maternal postpartum depression symptoms have been associated with impaired mother-infant bonding at 6 months of age10 and decreased cognitive and fine motor development of children at 18 months.11
Importance of screening
Evidence from the literature shows that, without proper screening, approximately 50% of cases of PPD go undiagnosed, and that increasing the number of women being screened by perinatal providers is an important first step to improving outcomes.12-18 Current recommendations for the timing and frequency of screening for PPD vary among the published guidelines. ACOG recommends screening at least once during the perinatal period for depression and anxiety using a standardized, validated tool; an update of the ACOG committee opinion in 2018 also states: “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.”19 The American Medical Association adopted new policies in 2017 promoting the implementation of a routine protocol for depression screening of perinatal women.20 The American Academy of Pediatrics recommends more frequent screening, with assessments at the 1-, 2-, 4-, and 6-month visits.21 Finally, the U.S. Preventive Services Task Force recommends screening for depression in the general population including pregnant and postpartum women.22
Multiple standardized, validated screening instruments are available for detecting possible symptoms of PPD, including the most widely used tools: the Edinburgh Postnatal Depression Scale (EPDS)19,23 and the Patient Health Questionnaire (PHQ-9).24 Two recent studies have shown that screening women for symptoms of PPD with a validated tool may reduce the duration or severity of depressive symptoms,25,26 further reinforcing the need to ensure that women experiencing symptoms of PPD are identified and treated early.
The inpatient hospitalization for labor, delivery, and birth of a child has not traditionally been viewed as an opportunity for PPD screening. While private practitioners and obstetric medical group practices typically have inquired about and documented the individual patient’s mental health history and risk factors for PPD, the obstetric hospitalist is most commonly meeting a patient in labor or in a postpartum encounter for the first time. As obstetric practices grow ever more consolidated, and as obstetric hospitalist care is implemented for a variety of reasons including, but not limited to, preventing burnout among private practitioners, serving as a safety net for all inpatient obstetric services, and increasing standardization in obstetric triage and obstetric emergency departments,
Barriers remain
Despite the need for early detection of PPD, screening practices remain inconsistent. A literature review of health care provider practices showed only one in four physicians reported using screening tools; obstetrician-gynecologists were most likely (36%) to use screening tools, followed by family practitioners (31%), with pediatricians the least likely (7%).27 This low rate is at least partially the result of perceived barriers to screening among health care providers, which contributes to underdiagnosis. A survey of more than 200 physicians who were members of ACOG showed that the top three barriers restricting screening practices were time constraints, inadequate training, and a lack of knowledge of the diagnostic criteria.28
Since 2017, Dignity Health has instituted routine screening of all inpatient postpartum patients at its 29 birth centers in Arizona, California, and Nevada. In this program, of which I am a physician participant, more than 30,000 women have been screened with the EPDS. In addition to providing screening, Dignity Health staff (physicians, certified nurse midwives, nurse practitioners, registered nurses, social workers, mental health therapists, lactation consultants, health educators, and others) have received in-person Perinatal Mental Health training. In this way, the entire care team coordinates inpatient screening and referral to outpatient care providers – thus bridging the gap in postpartum mental health care. For those patients who screen positive while an inpatient, a psychiatric telemedicine appointment is provided and, if necessary, short-course medications can be prescribed until the patient has outpatient follow-up and continuity of care. While we as obstetric hospitalists and community obstetrician-gynecologists recognize that inpatient postpartum screening may be limited in its sensitivity for capturing all women who will go on to develop PPD, there is definitely a benefit to having a discussion about PPD and maternal mental health early and often throughout the postpartum period. For many women suffering in silence, a 6-week postpartum outpatient visit is too late, especially given that approximately one-third of women are lost to postpartum follow-up.29,30
Addressing barriers
A growing number of states have enacted policies to address the challenge of peripartum behavioral health needs, and several states – Illinois, Massachusetts, New Jersey, and West Virginia – now mandate routine PPD screening by health care providers.31 However, few of these laws or policies contain specific guidance, such as the optimal timing for screening, instead leaving the details to providers.32 The proper identification and management of PPD cannot be achieved by state-level policy mandates alone, but must include clinician buy-in and participation.
Obstetricians play an essential role in the identification and treatment of PPD. Among nonpsychiatric specialists, obstetrician-gynecologists are the most likely providers to see and screen during the perinatal period.33 In addition, women prefer to receive help for PPD from either their obstetric practitioners or a mental-health specialists located at the obstetric clinic, and are more likely to receive mental-health services if they are provided at the same location as that of the obstetric provider.34,35 According to ACOG’s new guidance on the fourth trimester, obstetricians are encouraged to take responsibility for women’s care immediately after birth, and this care would include contact with all mothers within the first 3 weeks post partum, at follow-up visits as needed, and for a comprehensive postpartum visit at 12 weeks.3
Our specialty has and will continue to evolve, and obstetric hospitalists will play an ever more essential role in the care of women during their inpatient obstetric admission. Whether we are a patient’s primary inpatient obstetric provider or a practice extender for single or multigroup practice, we are in a unique role to screen, begin treatment for, and offer anticipatory guidance for maternal mental health and postpartum depression disorders. Obstetric hospitalists can be a bridge between inpatient and outpatient follow-up and catalysts for implementing universal inpatient PPD screening. Our role presents an opportunity to start the discussion early and often in the fourth trimester and to make a significant difference in addressing this critical unmet need in postnatal care.
Dr. van Dis is the medical director of the Ob Hospitalist Group in Burbank, Calif. She disclosed she received editorial assistance from Erik MacLaren, PhD, of Boston Strategic Partners Inc., with funding support from Sage Therapeutics Inc. E-mail [email protected].
References
1. Centers for Disease Control and Prevention. Postpartum Depression. 2017.
2. Morb Mortal Wkly Rep. 2017;66(6):153-8.
3. Obstet Gynecol. 2018;131(5):e140-e150.
4. Harv Rev Psychiatry. 2014;22(1):1-22.
5. JAMA Psychiatry. 2018;75(3):247-53.
6. J Womens Health (Larchmt). 2016;25(12):1219-24.
7. J Psychiatr Res. 2017;84:284-91.
8. Br J Psychiatry. 2003;183:279-81.
9. Obstet Gynecol Surv. 2005;60(3):183-90.
10. Arch Womens Ment Health. 2016;19(1):87-94.
11. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335-45.
12. J Reprod Med. 1999;44(4):351-8.
13. J Behav Health Serv Res. 2004;31(2):117-33.
14. J Clin Psychiatry. 2016;77(9):1189-200.
15. Am J Obstet Gynecol. 2000;182(5):1080-2.
16. J Fam Pract. 2001;50(2):117-22.
17. Obstet Gynecol. 1999;93(5 Pt 1):653-7.
18. J Womens Health (Larchmt). 2010;19(3):477-90.
19. Obstet Gynecol. 2018;132:e208-12.
20. “Physicians back programs to address maternal mortality, depression,” AMA, Nov. 15, 2017
21. Pediatrics. 2019 Jan 1;143(1):e20183260.
22. JAMA. 2016;315(4):380-7.
23. Br J Psychiatry. 1987;150:782-6.
24. Ann Fam Med. 2009;7(1):63-70.
25. Obstet Gynecol. 2016;127(5):917-25.
26. Pediatrics. 2017 Oct;140(4). pii: e20170110.
27. Womens Health Issues. 2015;25(6):703-10.
28. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
29. Matern Child Health J. 2016;20(Suppl 1):22-7.
30. National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC). 2018.
31. Psychiatr Serv. 2015;66(3):324-8.
32. Postpartum Support International. Legislation. 2018.
33. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, eds. Guidelines for Perinatal Care. 7th ed. (Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; Oct 2012.)
34. Birth. 2009;36(1):60-9.
35. Gen Hosp Psychiatry. 2009;31(2):155-62.
Postpartum depression (PPD) is the most common complication of pregnancy, and onset can occur at any time from pregnancy until up to 1 year post partum.1,2 The immediate postpartum period is a time during which care is shared among multiple providers for both mother and child, and the transition from inpatient to outpatient postpartum care can impede communication between those caring for the patient in each setting. In 2018, the American College of Obstetricians and Gynecologists published a committee opinion emphasizing the importance of the “fourth trimester” and calling for health care providers to assist women in navigating the transition from pre- to postpartum care.3 An important consideration of perinatal care is mental health care for the mother, including screening and care for postpartum depression; however, the optimal role for the obstetric hospitalist in providing such services has been unclear.
Estimates of the prevalence of PPD in new mothers in the United States varied by state from 8% to 20% in 2012, with an overall average of 12%.2 Left untreated, PPD may result in significant negative outcomes for women, their children, and families. The depressive symptoms of PPD may persist for months or years afterward,4 with one study finding elevated depressive symptoms in women up to 11 years post partum.5 Suicide is also a leading cause of pregnancy-related mortality associated with depressive symptoms.6-9 In addition, maternal postpartum depression symptoms have been associated with impaired mother-infant bonding at 6 months of age10 and decreased cognitive and fine motor development of children at 18 months.11
Importance of screening
Evidence from the literature shows that, without proper screening, approximately 50% of cases of PPD go undiagnosed, and that increasing the number of women being screened by perinatal providers is an important first step to improving outcomes.12-18 Current recommendations for the timing and frequency of screening for PPD vary among the published guidelines. ACOG recommends screening at least once during the perinatal period for depression and anxiety using a standardized, validated tool; an update of the ACOG committee opinion in 2018 also states: “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.”19 The American Medical Association adopted new policies in 2017 promoting the implementation of a routine protocol for depression screening of perinatal women.20 The American Academy of Pediatrics recommends more frequent screening, with assessments at the 1-, 2-, 4-, and 6-month visits.21 Finally, the U.S. Preventive Services Task Force recommends screening for depression in the general population including pregnant and postpartum women.22
Multiple standardized, validated screening instruments are available for detecting possible symptoms of PPD, including the most widely used tools: the Edinburgh Postnatal Depression Scale (EPDS)19,23 and the Patient Health Questionnaire (PHQ-9).24 Two recent studies have shown that screening women for symptoms of PPD with a validated tool may reduce the duration or severity of depressive symptoms,25,26 further reinforcing the need to ensure that women experiencing symptoms of PPD are identified and treated early.
The inpatient hospitalization for labor, delivery, and birth of a child has not traditionally been viewed as an opportunity for PPD screening. While private practitioners and obstetric medical group practices typically have inquired about and documented the individual patient’s mental health history and risk factors for PPD, the obstetric hospitalist is most commonly meeting a patient in labor or in a postpartum encounter for the first time. As obstetric practices grow ever more consolidated, and as obstetric hospitalist care is implemented for a variety of reasons including, but not limited to, preventing burnout among private practitioners, serving as a safety net for all inpatient obstetric services, and increasing standardization in obstetric triage and obstetric emergency departments,
Barriers remain
Despite the need for early detection of PPD, screening practices remain inconsistent. A literature review of health care provider practices showed only one in four physicians reported using screening tools; obstetrician-gynecologists were most likely (36%) to use screening tools, followed by family practitioners (31%), with pediatricians the least likely (7%).27 This low rate is at least partially the result of perceived barriers to screening among health care providers, which contributes to underdiagnosis. A survey of more than 200 physicians who were members of ACOG showed that the top three barriers restricting screening practices were time constraints, inadequate training, and a lack of knowledge of the diagnostic criteria.28
Since 2017, Dignity Health has instituted routine screening of all inpatient postpartum patients at its 29 birth centers in Arizona, California, and Nevada. In this program, of which I am a physician participant, more than 30,000 women have been screened with the EPDS. In addition to providing screening, Dignity Health staff (physicians, certified nurse midwives, nurse practitioners, registered nurses, social workers, mental health therapists, lactation consultants, health educators, and others) have received in-person Perinatal Mental Health training. In this way, the entire care team coordinates inpatient screening and referral to outpatient care providers – thus bridging the gap in postpartum mental health care. For those patients who screen positive while an inpatient, a psychiatric telemedicine appointment is provided and, if necessary, short-course medications can be prescribed until the patient has outpatient follow-up and continuity of care. While we as obstetric hospitalists and community obstetrician-gynecologists recognize that inpatient postpartum screening may be limited in its sensitivity for capturing all women who will go on to develop PPD, there is definitely a benefit to having a discussion about PPD and maternal mental health early and often throughout the postpartum period. For many women suffering in silence, a 6-week postpartum outpatient visit is too late, especially given that approximately one-third of women are lost to postpartum follow-up.29,30
Addressing barriers
A growing number of states have enacted policies to address the challenge of peripartum behavioral health needs, and several states – Illinois, Massachusetts, New Jersey, and West Virginia – now mandate routine PPD screening by health care providers.31 However, few of these laws or policies contain specific guidance, such as the optimal timing for screening, instead leaving the details to providers.32 The proper identification and management of PPD cannot be achieved by state-level policy mandates alone, but must include clinician buy-in and participation.
Obstetricians play an essential role in the identification and treatment of PPD. Among nonpsychiatric specialists, obstetrician-gynecologists are the most likely providers to see and screen during the perinatal period.33 In addition, women prefer to receive help for PPD from either their obstetric practitioners or a mental-health specialists located at the obstetric clinic, and are more likely to receive mental-health services if they are provided at the same location as that of the obstetric provider.34,35 According to ACOG’s new guidance on the fourth trimester, obstetricians are encouraged to take responsibility for women’s care immediately after birth, and this care would include contact with all mothers within the first 3 weeks post partum, at follow-up visits as needed, and for a comprehensive postpartum visit at 12 weeks.3
Our specialty has and will continue to evolve, and obstetric hospitalists will play an ever more essential role in the care of women during their inpatient obstetric admission. Whether we are a patient’s primary inpatient obstetric provider or a practice extender for single or multigroup practice, we are in a unique role to screen, begin treatment for, and offer anticipatory guidance for maternal mental health and postpartum depression disorders. Obstetric hospitalists can be a bridge between inpatient and outpatient follow-up and catalysts for implementing universal inpatient PPD screening. Our role presents an opportunity to start the discussion early and often in the fourth trimester and to make a significant difference in addressing this critical unmet need in postnatal care.
Dr. van Dis is the medical director of the Ob Hospitalist Group in Burbank, Calif. She disclosed she received editorial assistance from Erik MacLaren, PhD, of Boston Strategic Partners Inc., with funding support from Sage Therapeutics Inc. E-mail [email protected].
References
1. Centers for Disease Control and Prevention. Postpartum Depression. 2017.
2. Morb Mortal Wkly Rep. 2017;66(6):153-8.
3. Obstet Gynecol. 2018;131(5):e140-e150.
4. Harv Rev Psychiatry. 2014;22(1):1-22.
5. JAMA Psychiatry. 2018;75(3):247-53.
6. J Womens Health (Larchmt). 2016;25(12):1219-24.
7. J Psychiatr Res. 2017;84:284-91.
8. Br J Psychiatry. 2003;183:279-81.
9. Obstet Gynecol Surv. 2005;60(3):183-90.
10. Arch Womens Ment Health. 2016;19(1):87-94.
11. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335-45.
12. J Reprod Med. 1999;44(4):351-8.
13. J Behav Health Serv Res. 2004;31(2):117-33.
14. J Clin Psychiatry. 2016;77(9):1189-200.
15. Am J Obstet Gynecol. 2000;182(5):1080-2.
16. J Fam Pract. 2001;50(2):117-22.
17. Obstet Gynecol. 1999;93(5 Pt 1):653-7.
18. J Womens Health (Larchmt). 2010;19(3):477-90.
19. Obstet Gynecol. 2018;132:e208-12.
20. “Physicians back programs to address maternal mortality, depression,” AMA, Nov. 15, 2017
21. Pediatrics. 2019 Jan 1;143(1):e20183260.
22. JAMA. 2016;315(4):380-7.
23. Br J Psychiatry. 1987;150:782-6.
24. Ann Fam Med. 2009;7(1):63-70.
25. Obstet Gynecol. 2016;127(5):917-25.
26. Pediatrics. 2017 Oct;140(4). pii: e20170110.
27. Womens Health Issues. 2015;25(6):703-10.
28. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
29. Matern Child Health J. 2016;20(Suppl 1):22-7.
30. National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC). 2018.
31. Psychiatr Serv. 2015;66(3):324-8.
32. Postpartum Support International. Legislation. 2018.
33. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, eds. Guidelines for Perinatal Care. 7th ed. (Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; Oct 2012.)
34. Birth. 2009;36(1):60-9.
35. Gen Hosp Psychiatry. 2009;31(2):155-62.
Postpartum depression (PPD) is the most common complication of pregnancy, and onset can occur at any time from pregnancy until up to 1 year post partum.1,2 The immediate postpartum period is a time during which care is shared among multiple providers for both mother and child, and the transition from inpatient to outpatient postpartum care can impede communication between those caring for the patient in each setting. In 2018, the American College of Obstetricians and Gynecologists published a committee opinion emphasizing the importance of the “fourth trimester” and calling for health care providers to assist women in navigating the transition from pre- to postpartum care.3 An important consideration of perinatal care is mental health care for the mother, including screening and care for postpartum depression; however, the optimal role for the obstetric hospitalist in providing such services has been unclear.
Estimates of the prevalence of PPD in new mothers in the United States varied by state from 8% to 20% in 2012, with an overall average of 12%.2 Left untreated, PPD may result in significant negative outcomes for women, their children, and families. The depressive symptoms of PPD may persist for months or years afterward,4 with one study finding elevated depressive symptoms in women up to 11 years post partum.5 Suicide is also a leading cause of pregnancy-related mortality associated with depressive symptoms.6-9 In addition, maternal postpartum depression symptoms have been associated with impaired mother-infant bonding at 6 months of age10 and decreased cognitive and fine motor development of children at 18 months.11
Importance of screening
Evidence from the literature shows that, without proper screening, approximately 50% of cases of PPD go undiagnosed, and that increasing the number of women being screened by perinatal providers is an important first step to improving outcomes.12-18 Current recommendations for the timing and frequency of screening for PPD vary among the published guidelines. ACOG recommends screening at least once during the perinatal period for depression and anxiety using a standardized, validated tool; an update of the ACOG committee opinion in 2018 also states: “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.”19 The American Medical Association adopted new policies in 2017 promoting the implementation of a routine protocol for depression screening of perinatal women.20 The American Academy of Pediatrics recommends more frequent screening, with assessments at the 1-, 2-, 4-, and 6-month visits.21 Finally, the U.S. Preventive Services Task Force recommends screening for depression in the general population including pregnant and postpartum women.22
Multiple standardized, validated screening instruments are available for detecting possible symptoms of PPD, including the most widely used tools: the Edinburgh Postnatal Depression Scale (EPDS)19,23 and the Patient Health Questionnaire (PHQ-9).24 Two recent studies have shown that screening women for symptoms of PPD with a validated tool may reduce the duration or severity of depressive symptoms,25,26 further reinforcing the need to ensure that women experiencing symptoms of PPD are identified and treated early.
The inpatient hospitalization for labor, delivery, and birth of a child has not traditionally been viewed as an opportunity for PPD screening. While private practitioners and obstetric medical group practices typically have inquired about and documented the individual patient’s mental health history and risk factors for PPD, the obstetric hospitalist is most commonly meeting a patient in labor or in a postpartum encounter for the first time. As obstetric practices grow ever more consolidated, and as obstetric hospitalist care is implemented for a variety of reasons including, but not limited to, preventing burnout among private practitioners, serving as a safety net for all inpatient obstetric services, and increasing standardization in obstetric triage and obstetric emergency departments,
Barriers remain
Despite the need for early detection of PPD, screening practices remain inconsistent. A literature review of health care provider practices showed only one in four physicians reported using screening tools; obstetrician-gynecologists were most likely (36%) to use screening tools, followed by family practitioners (31%), with pediatricians the least likely (7%).27 This low rate is at least partially the result of perceived barriers to screening among health care providers, which contributes to underdiagnosis. A survey of more than 200 physicians who were members of ACOG showed that the top three barriers restricting screening practices were time constraints, inadequate training, and a lack of knowledge of the diagnostic criteria.28
Since 2017, Dignity Health has instituted routine screening of all inpatient postpartum patients at its 29 birth centers in Arizona, California, and Nevada. In this program, of which I am a physician participant, more than 30,000 women have been screened with the EPDS. In addition to providing screening, Dignity Health staff (physicians, certified nurse midwives, nurse practitioners, registered nurses, social workers, mental health therapists, lactation consultants, health educators, and others) have received in-person Perinatal Mental Health training. In this way, the entire care team coordinates inpatient screening and referral to outpatient care providers – thus bridging the gap in postpartum mental health care. For those patients who screen positive while an inpatient, a psychiatric telemedicine appointment is provided and, if necessary, short-course medications can be prescribed until the patient has outpatient follow-up and continuity of care. While we as obstetric hospitalists and community obstetrician-gynecologists recognize that inpatient postpartum screening may be limited in its sensitivity for capturing all women who will go on to develop PPD, there is definitely a benefit to having a discussion about PPD and maternal mental health early and often throughout the postpartum period. For many women suffering in silence, a 6-week postpartum outpatient visit is too late, especially given that approximately one-third of women are lost to postpartum follow-up.29,30
Addressing barriers
A growing number of states have enacted policies to address the challenge of peripartum behavioral health needs, and several states – Illinois, Massachusetts, New Jersey, and West Virginia – now mandate routine PPD screening by health care providers.31 However, few of these laws or policies contain specific guidance, such as the optimal timing for screening, instead leaving the details to providers.32 The proper identification and management of PPD cannot be achieved by state-level policy mandates alone, but must include clinician buy-in and participation.
Obstetricians play an essential role in the identification and treatment of PPD. Among nonpsychiatric specialists, obstetrician-gynecologists are the most likely providers to see and screen during the perinatal period.33 In addition, women prefer to receive help for PPD from either their obstetric practitioners or a mental-health specialists located at the obstetric clinic, and are more likely to receive mental-health services if they are provided at the same location as that of the obstetric provider.34,35 According to ACOG’s new guidance on the fourth trimester, obstetricians are encouraged to take responsibility for women’s care immediately after birth, and this care would include contact with all mothers within the first 3 weeks post partum, at follow-up visits as needed, and for a comprehensive postpartum visit at 12 weeks.3
Our specialty has and will continue to evolve, and obstetric hospitalists will play an ever more essential role in the care of women during their inpatient obstetric admission. Whether we are a patient’s primary inpatient obstetric provider or a practice extender for single or multigroup practice, we are in a unique role to screen, begin treatment for, and offer anticipatory guidance for maternal mental health and postpartum depression disorders. Obstetric hospitalists can be a bridge between inpatient and outpatient follow-up and catalysts for implementing universal inpatient PPD screening. Our role presents an opportunity to start the discussion early and often in the fourth trimester and to make a significant difference in addressing this critical unmet need in postnatal care.
Dr. van Dis is the medical director of the Ob Hospitalist Group in Burbank, Calif. She disclosed she received editorial assistance from Erik MacLaren, PhD, of Boston Strategic Partners Inc., with funding support from Sage Therapeutics Inc. E-mail [email protected].
References
1. Centers for Disease Control and Prevention. Postpartum Depression. 2017.
2. Morb Mortal Wkly Rep. 2017;66(6):153-8.
3. Obstet Gynecol. 2018;131(5):e140-e150.
4. Harv Rev Psychiatry. 2014;22(1):1-22.
5. JAMA Psychiatry. 2018;75(3):247-53.
6. J Womens Health (Larchmt). 2016;25(12):1219-24.
7. J Psychiatr Res. 2017;84:284-91.
8. Br J Psychiatry. 2003;183:279-81.
9. Obstet Gynecol Surv. 2005;60(3):183-90.
10. Arch Womens Ment Health. 2016;19(1):87-94.
11. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335-45.
12. J Reprod Med. 1999;44(4):351-8.
13. J Behav Health Serv Res. 2004;31(2):117-33.
14. J Clin Psychiatry. 2016;77(9):1189-200.
15. Am J Obstet Gynecol. 2000;182(5):1080-2.
16. J Fam Pract. 2001;50(2):117-22.
17. Obstet Gynecol. 1999;93(5 Pt 1):653-7.
18. J Womens Health (Larchmt). 2010;19(3):477-90.
19. Obstet Gynecol. 2018;132:e208-12.
20. “Physicians back programs to address maternal mortality, depression,” AMA, Nov. 15, 2017
21. Pediatrics. 2019 Jan 1;143(1):e20183260.
22. JAMA. 2016;315(4):380-7.
23. Br J Psychiatry. 1987;150:782-6.
24. Ann Fam Med. 2009;7(1):63-70.
25. Obstet Gynecol. 2016;127(5):917-25.
26. Pediatrics. 2017 Oct;140(4). pii: e20170110.
27. Womens Health Issues. 2015;25(6):703-10.
28. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
29. Matern Child Health J. 2016;20(Suppl 1):22-7.
30. National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC). 2018.
31. Psychiatr Serv. 2015;66(3):324-8.
32. Postpartum Support International. Legislation. 2018.
33. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, eds. Guidelines for Perinatal Care. 7th ed. (Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; Oct 2012.)
34. Birth. 2009;36(1):60-9.
35. Gen Hosp Psychiatry. 2009;31(2):155-62.
ADHD: When and how do we choose to start medications?
- A 9-year-old boy has poor impulse control, throws things in class, and cannot sit still. Teachers ask: Is this ADHD and should we start a medication?
- A 9-year-old girl is an inattentive daydreamer with poor class performance and trouble turning in homework. Her parents and teachers ask: Is this ADHD and should we start a medication?
- A 17-year-old boy who is a high achiever is taking the upcoming SATs and does poorly on timed tests because of poor focus and is now wondering: Do I have ADHD and would a medication help me perform better?
- A 17-year-old boy had poor grades for much of his early school years, but his parents always thought he was just a “lazy kid” although he insists he is trying his best. His parents now ask: Is this ADHD and has it been all along?
The above cases may sound familiar to you. They are an oversimplification of the patients who may come to you with two questions: Do I or someone I care about have ADHD and should they have medication for it? What may matter even more is how they are doing with that inattentiveness and how much it impacts their lives.
Sigmund Freud was known to think about goals for treatment as “liebe und arbeit” translated into “to love and to work.” As in, can someone live, love, and work or are their psychiatric symptoms impairing those functionalities? For a child, to live, work, and play (well with others) is most apt here. It is often more helpful to think in terms of childhood daily life when choosing to begin a medication or not. With inattention, a child can range from having a parent hoping for performance enhancement to having a severe impairment in their day-to-day functioning in a classroom. In the above case examples, each child or adolescent has varying impairments in performance – one is a high academic performer with very few issues outside of testing and another is a young child who can’t even sit still in a classroom to learn. Who should be prescribed a stimulant? Any or all of the above? It’s not as easy an answer as you may suspect, and there may not be one “right” answer either.
We know that stimulants can help a great deal of patients. They have the highest effect size for ADHD in that about 80% of children can benefit from stimulant treatment for ADHD. Specifically, “a high response rate of 70%-85% has been noted with methylphenidate and amphetamine formulations. The response rate is lower for atomoxetine [60%-65%] and guanfacine [30%-40%]” (Venkat B, Hechtman L. Considerations in selecting pharmacological treatments for attention deficit hyperactivity disorder. Clinical Pharmacist. 2016 Feb 11). In thinking about when to prescribe, we want to balance offering nonpharmacologic means to address symptoms of inattention (like mindfulness, exercise, and school supports such as individualized learning plans where applicable). We also do not want to withhold helpful treatments such as stimulants or other nonstimulant medications or trend toward overprescribing potentially habit-forming and imperfect medications.
It is important to make that distinction between impairment and the desire for medications to “enhance” life and optimize performance rather than treating symptoms of a disorder. It is most helpful to gain skills to navigate those challenges simultaneously to ultimately help our patients live, learn, love, and play to the best of their abilities.
Where to begin
When I was in training, I had difficulty teasing out the various ADHD stimulant formations. There were and are so many Ritalin preparations! Mostly there is a variation in shorter-acting to longer-acting effects. If the diagnosis is highly suspected and uncomplicated ADHD, I usually choose to start with Concerta 18 mg daily (a long-acting methylphenidate) for children aged over 6 years. Many times I don’t see the need to titrate that upwards much further toward the maximum clinically used dose of 54 mg daily (despite guidelines saying otherwise up to 72 mg daily, which I have found unnecessary usually and poorly tolerated). Concerta has an immediate effect (20%) and then slowly peaks until 12 p.m. (80%) and then is out of system by about 3 p.m. (for a total of 7 hours duration of action). There also are shorter-acting preparations (Ritalin, Methylin) which are “on/off” in 4 hours and use of these is more consistent with an antiquated way of prescribing, often up to twice daily and three times daily dosing schedules with the risk of the harder to tolerate “drop-off” effects with stimulants. And, if there is not an effect, I often reconsider the diagnosis and any co-occurring anxiety disorder, stressful life events, or depression or other illness with the knowledge that these medications so often are effective.
Anxiety + ADHD
If there is prominent anxiety, anxiety disorder, or tics, I often consider Strattera 10-20 mg daily up to around 40 mg. I tend to dose this lower than as written for tolerability and in a “dose low and go slow” approach with kids, which often results in better experiences with the medication. This medication also is recommended to be dosed by weight; this should be taken into account as well. Atomoxetine is a selective serotonin and norepinephrine reuptake inhibitor which is likely similar to Cymbalta (duloxetine). It may have a lower effect size of around less than 60% but this also is around the reported effect sizes for selective serotonin reuptake inhibitors (SSRIs) for depression. If a patient has both ADHD and an anxiety disorder, I often consider an SSRI alternatively first to manage attention issues associated with anxiety and then would add on a stimulant if attention issues persist once anxiety is better treated.
Second/third line ADHD treatments
As a second-line approach to long-acting Ritalin and if there is not a response to it, I would consider extended-release Adderall preparations such as Vyvanse, which is an amphetamine preparation supposedly less abusable than Adderall (one can’t snort it), but I also caution that it releases dopamine, peaks faster, and does not reduce to zero stimulant in 24 hours because of a variable half-life.
In this way, I always have imagined that these amphetamines may be more theoretically concerning than Ritalin/methylphenidate because they increase dopamine dumping into the synapse (which is a different and extra mechanism than just reuptake). For a third line, I may consider guanfacine depending on weight daily, which is an Food and Drug Administration–approved, nonstimulant alpha-2 agonist, which also acts longer than clonidine and may be better for hyperactivity symptoms. I may begin with doses as low as 0.25-0.5 mg in the evening for concerns with sedation or groggy aftereffects in the morning.
Throughout all treatment with medication, I emphasize the importance of assertively managing ADHD symptoms which may be in the form of “behavioral treatment,” like cognitive behavioral therapy, organizational coaching available at some educational centers, or even finding ways to train one’s focus with athletics or practices such as yoga and mindfulness. In addition to this combined approach to treatment, stimulants are not perfect medications. All stimulants have a “drop-off effect” and were made to work during a school day lasting from 8 a.m. to 3 p.m. Some patients and families complain about the drop-off effect and may want to “dose” around a medication more frequently, in the late afternoon and in the evening, which can lead to poor appetite at dinner and insomnia.
My answers to the cases above would be that all the patients could have ADHD, but they also may have anxiety or stress-related disorders, depression, worries about performance, or poor skills to manage inattention. They may not yet have received school supports, coaching, or found ways to manage these symptoms either. Because stimulants can improve and enhance performance but also have their own drawbacks and risks not covered here, it’s important to consider each case as a whole with thoughtfulness about a child’s unique ability to “live and work” in this world.
Dr. Pawlowski is an adult, adolescent, and child psychiatrist at the University of Vermont Medical Center and an assistant professor of psychiatry at UVM, both in Burlington. She reported no relevant financial disclosures. Email her at [email protected].
- A 9-year-old boy has poor impulse control, throws things in class, and cannot sit still. Teachers ask: Is this ADHD and should we start a medication?
- A 9-year-old girl is an inattentive daydreamer with poor class performance and trouble turning in homework. Her parents and teachers ask: Is this ADHD and should we start a medication?
- A 17-year-old boy who is a high achiever is taking the upcoming SATs and does poorly on timed tests because of poor focus and is now wondering: Do I have ADHD and would a medication help me perform better?
- A 17-year-old boy had poor grades for much of his early school years, but his parents always thought he was just a “lazy kid” although he insists he is trying his best. His parents now ask: Is this ADHD and has it been all along?
The above cases may sound familiar to you. They are an oversimplification of the patients who may come to you with two questions: Do I or someone I care about have ADHD and should they have medication for it? What may matter even more is how they are doing with that inattentiveness and how much it impacts their lives.
Sigmund Freud was known to think about goals for treatment as “liebe und arbeit” translated into “to love and to work.” As in, can someone live, love, and work or are their psychiatric symptoms impairing those functionalities? For a child, to live, work, and play (well with others) is most apt here. It is often more helpful to think in terms of childhood daily life when choosing to begin a medication or not. With inattention, a child can range from having a parent hoping for performance enhancement to having a severe impairment in their day-to-day functioning in a classroom. In the above case examples, each child or adolescent has varying impairments in performance – one is a high academic performer with very few issues outside of testing and another is a young child who can’t even sit still in a classroom to learn. Who should be prescribed a stimulant? Any or all of the above? It’s not as easy an answer as you may suspect, and there may not be one “right” answer either.
We know that stimulants can help a great deal of patients. They have the highest effect size for ADHD in that about 80% of children can benefit from stimulant treatment for ADHD. Specifically, “a high response rate of 70%-85% has been noted with methylphenidate and amphetamine formulations. The response rate is lower for atomoxetine [60%-65%] and guanfacine [30%-40%]” (Venkat B, Hechtman L. Considerations in selecting pharmacological treatments for attention deficit hyperactivity disorder. Clinical Pharmacist. 2016 Feb 11). In thinking about when to prescribe, we want to balance offering nonpharmacologic means to address symptoms of inattention (like mindfulness, exercise, and school supports such as individualized learning plans where applicable). We also do not want to withhold helpful treatments such as stimulants or other nonstimulant medications or trend toward overprescribing potentially habit-forming and imperfect medications.
It is important to make that distinction between impairment and the desire for medications to “enhance” life and optimize performance rather than treating symptoms of a disorder. It is most helpful to gain skills to navigate those challenges simultaneously to ultimately help our patients live, learn, love, and play to the best of their abilities.
Where to begin
When I was in training, I had difficulty teasing out the various ADHD stimulant formations. There were and are so many Ritalin preparations! Mostly there is a variation in shorter-acting to longer-acting effects. If the diagnosis is highly suspected and uncomplicated ADHD, I usually choose to start with Concerta 18 mg daily (a long-acting methylphenidate) for children aged over 6 years. Many times I don’t see the need to titrate that upwards much further toward the maximum clinically used dose of 54 mg daily (despite guidelines saying otherwise up to 72 mg daily, which I have found unnecessary usually and poorly tolerated). Concerta has an immediate effect (20%) and then slowly peaks until 12 p.m. (80%) and then is out of system by about 3 p.m. (for a total of 7 hours duration of action). There also are shorter-acting preparations (Ritalin, Methylin) which are “on/off” in 4 hours and use of these is more consistent with an antiquated way of prescribing, often up to twice daily and three times daily dosing schedules with the risk of the harder to tolerate “drop-off” effects with stimulants. And, if there is not an effect, I often reconsider the diagnosis and any co-occurring anxiety disorder, stressful life events, or depression or other illness with the knowledge that these medications so often are effective.
Anxiety + ADHD
If there is prominent anxiety, anxiety disorder, or tics, I often consider Strattera 10-20 mg daily up to around 40 mg. I tend to dose this lower than as written for tolerability and in a “dose low and go slow” approach with kids, which often results in better experiences with the medication. This medication also is recommended to be dosed by weight; this should be taken into account as well. Atomoxetine is a selective serotonin and norepinephrine reuptake inhibitor which is likely similar to Cymbalta (duloxetine). It may have a lower effect size of around less than 60% but this also is around the reported effect sizes for selective serotonin reuptake inhibitors (SSRIs) for depression. If a patient has both ADHD and an anxiety disorder, I often consider an SSRI alternatively first to manage attention issues associated with anxiety and then would add on a stimulant if attention issues persist once anxiety is better treated.
Second/third line ADHD treatments
As a second-line approach to long-acting Ritalin and if there is not a response to it, I would consider extended-release Adderall preparations such as Vyvanse, which is an amphetamine preparation supposedly less abusable than Adderall (one can’t snort it), but I also caution that it releases dopamine, peaks faster, and does not reduce to zero stimulant in 24 hours because of a variable half-life.
In this way, I always have imagined that these amphetamines may be more theoretically concerning than Ritalin/methylphenidate because they increase dopamine dumping into the synapse (which is a different and extra mechanism than just reuptake). For a third line, I may consider guanfacine depending on weight daily, which is an Food and Drug Administration–approved, nonstimulant alpha-2 agonist, which also acts longer than clonidine and may be better for hyperactivity symptoms. I may begin with doses as low as 0.25-0.5 mg in the evening for concerns with sedation or groggy aftereffects in the morning.
Throughout all treatment with medication, I emphasize the importance of assertively managing ADHD symptoms which may be in the form of “behavioral treatment,” like cognitive behavioral therapy, organizational coaching available at some educational centers, or even finding ways to train one’s focus with athletics or practices such as yoga and mindfulness. In addition to this combined approach to treatment, stimulants are not perfect medications. All stimulants have a “drop-off effect” and were made to work during a school day lasting from 8 a.m. to 3 p.m. Some patients and families complain about the drop-off effect and may want to “dose” around a medication more frequently, in the late afternoon and in the evening, which can lead to poor appetite at dinner and insomnia.
My answers to the cases above would be that all the patients could have ADHD, but they also may have anxiety or stress-related disorders, depression, worries about performance, or poor skills to manage inattention. They may not yet have received school supports, coaching, or found ways to manage these symptoms either. Because stimulants can improve and enhance performance but also have their own drawbacks and risks not covered here, it’s important to consider each case as a whole with thoughtfulness about a child’s unique ability to “live and work” in this world.
Dr. Pawlowski is an adult, adolescent, and child psychiatrist at the University of Vermont Medical Center and an assistant professor of psychiatry at UVM, both in Burlington. She reported no relevant financial disclosures. Email her at [email protected].
- A 9-year-old boy has poor impulse control, throws things in class, and cannot sit still. Teachers ask: Is this ADHD and should we start a medication?
- A 9-year-old girl is an inattentive daydreamer with poor class performance and trouble turning in homework. Her parents and teachers ask: Is this ADHD and should we start a medication?
- A 17-year-old boy who is a high achiever is taking the upcoming SATs and does poorly on timed tests because of poor focus and is now wondering: Do I have ADHD and would a medication help me perform better?
- A 17-year-old boy had poor grades for much of his early school years, but his parents always thought he was just a “lazy kid” although he insists he is trying his best. His parents now ask: Is this ADHD and has it been all along?
The above cases may sound familiar to you. They are an oversimplification of the patients who may come to you with two questions: Do I or someone I care about have ADHD and should they have medication for it? What may matter even more is how they are doing with that inattentiveness and how much it impacts their lives.
Sigmund Freud was known to think about goals for treatment as “liebe und arbeit” translated into “to love and to work.” As in, can someone live, love, and work or are their psychiatric symptoms impairing those functionalities? For a child, to live, work, and play (well with others) is most apt here. It is often more helpful to think in terms of childhood daily life when choosing to begin a medication or not. With inattention, a child can range from having a parent hoping for performance enhancement to having a severe impairment in their day-to-day functioning in a classroom. In the above case examples, each child or adolescent has varying impairments in performance – one is a high academic performer with very few issues outside of testing and another is a young child who can’t even sit still in a classroom to learn. Who should be prescribed a stimulant? Any or all of the above? It’s not as easy an answer as you may suspect, and there may not be one “right” answer either.
We know that stimulants can help a great deal of patients. They have the highest effect size for ADHD in that about 80% of children can benefit from stimulant treatment for ADHD. Specifically, “a high response rate of 70%-85% has been noted with methylphenidate and amphetamine formulations. The response rate is lower for atomoxetine [60%-65%] and guanfacine [30%-40%]” (Venkat B, Hechtman L. Considerations in selecting pharmacological treatments for attention deficit hyperactivity disorder. Clinical Pharmacist. 2016 Feb 11). In thinking about when to prescribe, we want to balance offering nonpharmacologic means to address symptoms of inattention (like mindfulness, exercise, and school supports such as individualized learning plans where applicable). We also do not want to withhold helpful treatments such as stimulants or other nonstimulant medications or trend toward overprescribing potentially habit-forming and imperfect medications.
It is important to make that distinction between impairment and the desire for medications to “enhance” life and optimize performance rather than treating symptoms of a disorder. It is most helpful to gain skills to navigate those challenges simultaneously to ultimately help our patients live, learn, love, and play to the best of their abilities.
Where to begin
When I was in training, I had difficulty teasing out the various ADHD stimulant formations. There were and are so many Ritalin preparations! Mostly there is a variation in shorter-acting to longer-acting effects. If the diagnosis is highly suspected and uncomplicated ADHD, I usually choose to start with Concerta 18 mg daily (a long-acting methylphenidate) for children aged over 6 years. Many times I don’t see the need to titrate that upwards much further toward the maximum clinically used dose of 54 mg daily (despite guidelines saying otherwise up to 72 mg daily, which I have found unnecessary usually and poorly tolerated). Concerta has an immediate effect (20%) and then slowly peaks until 12 p.m. (80%) and then is out of system by about 3 p.m. (for a total of 7 hours duration of action). There also are shorter-acting preparations (Ritalin, Methylin) which are “on/off” in 4 hours and use of these is more consistent with an antiquated way of prescribing, often up to twice daily and three times daily dosing schedules with the risk of the harder to tolerate “drop-off” effects with stimulants. And, if there is not an effect, I often reconsider the diagnosis and any co-occurring anxiety disorder, stressful life events, or depression or other illness with the knowledge that these medications so often are effective.
Anxiety + ADHD
If there is prominent anxiety, anxiety disorder, or tics, I often consider Strattera 10-20 mg daily up to around 40 mg. I tend to dose this lower than as written for tolerability and in a “dose low and go slow” approach with kids, which often results in better experiences with the medication. This medication also is recommended to be dosed by weight; this should be taken into account as well. Atomoxetine is a selective serotonin and norepinephrine reuptake inhibitor which is likely similar to Cymbalta (duloxetine). It may have a lower effect size of around less than 60% but this also is around the reported effect sizes for selective serotonin reuptake inhibitors (SSRIs) for depression. If a patient has both ADHD and an anxiety disorder, I often consider an SSRI alternatively first to manage attention issues associated with anxiety and then would add on a stimulant if attention issues persist once anxiety is better treated.
Second/third line ADHD treatments
As a second-line approach to long-acting Ritalin and if there is not a response to it, I would consider extended-release Adderall preparations such as Vyvanse, which is an amphetamine preparation supposedly less abusable than Adderall (one can’t snort it), but I also caution that it releases dopamine, peaks faster, and does not reduce to zero stimulant in 24 hours because of a variable half-life.
In this way, I always have imagined that these amphetamines may be more theoretically concerning than Ritalin/methylphenidate because they increase dopamine dumping into the synapse (which is a different and extra mechanism than just reuptake). For a third line, I may consider guanfacine depending on weight daily, which is an Food and Drug Administration–approved, nonstimulant alpha-2 agonist, which also acts longer than clonidine and may be better for hyperactivity symptoms. I may begin with doses as low as 0.25-0.5 mg in the evening for concerns with sedation or groggy aftereffects in the morning.
Throughout all treatment with medication, I emphasize the importance of assertively managing ADHD symptoms which may be in the form of “behavioral treatment,” like cognitive behavioral therapy, organizational coaching available at some educational centers, or even finding ways to train one’s focus with athletics or practices such as yoga and mindfulness. In addition to this combined approach to treatment, stimulants are not perfect medications. All stimulants have a “drop-off effect” and were made to work during a school day lasting from 8 a.m. to 3 p.m. Some patients and families complain about the drop-off effect and may want to “dose” around a medication more frequently, in the late afternoon and in the evening, which can lead to poor appetite at dinner and insomnia.
My answers to the cases above would be that all the patients could have ADHD, but they also may have anxiety or stress-related disorders, depression, worries about performance, or poor skills to manage inattention. They may not yet have received school supports, coaching, or found ways to manage these symptoms either. Because stimulants can improve and enhance performance but also have their own drawbacks and risks not covered here, it’s important to consider each case as a whole with thoughtfulness about a child’s unique ability to “live and work” in this world.
Dr. Pawlowski is an adult, adolescent, and child psychiatrist at the University of Vermont Medical Center and an assistant professor of psychiatry at UVM, both in Burlington. She reported no relevant financial disclosures. Email her at [email protected].
Clown-tox, tattooed immunity, and cingulum-bundle comedy
Quit clowning around
Would you like a balloon giraffe, elephant, or hypodermic needle? A recently published study examined how the use of “medical clowns” eased the anxiety and pain of children during botulinum toxin injections. These injections are used to treat spasticity in children, and researchers hypothesized that a clown might be an effective distraction.
As anyone who has been to a circus can surmise, the clowns did not perform better than the control distractions.
Researchers concluded that the clowns were appreciated by the parents but not particularly effective on the children. Maybe that’s because the parents weren’t the ones being stuck with needles while some crazy person in clown makeup attempted to distract them. Or maybe they were all just big fans of Stephen King’s “It.”
Inked immunity
Starting to feel a bit under the weather? Head to the local tattoo artist for the cure! Research from the University of Alabama at Birmingham found evidence that the immune systems of heavily tattooed people are stronger than those without, proving once and for all that tats = toughness. Hell's Angels were on to something all along.
While your immune system can actually grow temporarily weaker after one tattoo, multiple tattoos create a stronger immunological response. Researchers tested the immunoglobulin A levels in those getting a first tattoo and those with many tattoos. They found that the latter group had higher IgA levels.
Maybe that’s why Adam Levine showed off his ink at the Super Bowl halftime show – he was just signaling his strong immune system to the rest of us.
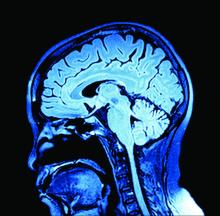
Brain surgery is a laughing matter
This certainly came as a surprise to us, but as it turns out, undergoing brain surgery while conscious and awake can be extremely stressful and panic inducing to the patient. We’re sure most people (including us) would prefer to be asleep for their surgery, but sometimes when dealing with the brain, the surgeon needs to be able to talk to the patient to accurately assess their faculties in case they damage something important.
So the question is: How do you keep brain surgery patients from panicking? Why, with the power of laughter, of course! Specifically, a group at Emory University, Atlanta, published a case study in the Journal of Clinical Investigation about their treatment of a patient with moderate anxiety. When the patient woke up from initial anesthesia, she began to panic. However, after electrical stimulation of the cingulum bundle, the patient immediately turned her frown upside down and began laughing and joking with the surgeons.
Sadly, while the team did not report on the quality of the jokes being told, we can only assume the phrase “this isn’t brain surgery” was thrown around multiple times.
A male brain is a terrible thing to waste
In the future, comedy may mean pressing a button to stimulate your cingulum bundle, but for now we still have jokes. One old joke goes like this: Some aliens land on earth and want to learn about humans, so they go into a store to buy some brains. “Why does the male brain cost twice as much as the female brain?” one asks the store owner, who replies, “It’s hardly been used.”
There may be another explanation: Womens’ brains appear to age more slowly than mens’, investigators at Washington University, St. Louis, said in the Proceedings of the National Academy of Sciences.
They performed PET scans on 121 women and 84 men aged 20-82 years to determine the fraction of sugar committed to aerobic glycolysis in various regions of the brain, and then a machine-learning algorithm used those data to calculate metabolic ages.
The womens’ brains were younger than the mens’ brains, with various calculations producing average differences of 2.7-5.3 years, they reported.
The male brain, it seems, is used for something, and after one LOTME staffer spent 5 minutes explaining total quarterback rating (QBR) to his wife, we think we’ve figured out what it is: sports trivia.
Quit clowning around
Would you like a balloon giraffe, elephant, or hypodermic needle? A recently published study examined how the use of “medical clowns” eased the anxiety and pain of children during botulinum toxin injections. These injections are used to treat spasticity in children, and researchers hypothesized that a clown might be an effective distraction.
As anyone who has been to a circus can surmise, the clowns did not perform better than the control distractions.
Researchers concluded that the clowns were appreciated by the parents but not particularly effective on the children. Maybe that’s because the parents weren’t the ones being stuck with needles while some crazy person in clown makeup attempted to distract them. Or maybe they were all just big fans of Stephen King’s “It.”
Inked immunity
Starting to feel a bit under the weather? Head to the local tattoo artist for the cure! Research from the University of Alabama at Birmingham found evidence that the immune systems of heavily tattooed people are stronger than those without, proving once and for all that tats = toughness. Hell's Angels were on to something all along.
While your immune system can actually grow temporarily weaker after one tattoo, multiple tattoos create a stronger immunological response. Researchers tested the immunoglobulin A levels in those getting a first tattoo and those with many tattoos. They found that the latter group had higher IgA levels.
Maybe that’s why Adam Levine showed off his ink at the Super Bowl halftime show – he was just signaling his strong immune system to the rest of us.
Brain surgery is a laughing matter
This certainly came as a surprise to us, but as it turns out, undergoing brain surgery while conscious and awake can be extremely stressful and panic inducing to the patient. We’re sure most people (including us) would prefer to be asleep for their surgery, but sometimes when dealing with the brain, the surgeon needs to be able to talk to the patient to accurately assess their faculties in case they damage something important.
So the question is: How do you keep brain surgery patients from panicking? Why, with the power of laughter, of course! Specifically, a group at Emory University, Atlanta, published a case study in the Journal of Clinical Investigation about their treatment of a patient with moderate anxiety. When the patient woke up from initial anesthesia, she began to panic. However, after electrical stimulation of the cingulum bundle, the patient immediately turned her frown upside down and began laughing and joking with the surgeons.
Sadly, while the team did not report on the quality of the jokes being told, we can only assume the phrase “this isn’t brain surgery” was thrown around multiple times.
A male brain is a terrible thing to waste
In the future, comedy may mean pressing a button to stimulate your cingulum bundle, but for now we still have jokes. One old joke goes like this: Some aliens land on earth and want to learn about humans, so they go into a store to buy some brains. “Why does the male brain cost twice as much as the female brain?” one asks the store owner, who replies, “It’s hardly been used.”
There may be another explanation: Womens’ brains appear to age more slowly than mens’, investigators at Washington University, St. Louis, said in the Proceedings of the National Academy of Sciences.
They performed PET scans on 121 women and 84 men aged 20-82 years to determine the fraction of sugar committed to aerobic glycolysis in various regions of the brain, and then a machine-learning algorithm used those data to calculate metabolic ages.
The womens’ brains were younger than the mens’ brains, with various calculations producing average differences of 2.7-5.3 years, they reported.
The male brain, it seems, is used for something, and after one LOTME staffer spent 5 minutes explaining total quarterback rating (QBR) to his wife, we think we’ve figured out what it is: sports trivia.
Quit clowning around
Would you like a balloon giraffe, elephant, or hypodermic needle? A recently published study examined how the use of “medical clowns” eased the anxiety and pain of children during botulinum toxin injections. These injections are used to treat spasticity in children, and researchers hypothesized that a clown might be an effective distraction.
As anyone who has been to a circus can surmise, the clowns did not perform better than the control distractions.
Researchers concluded that the clowns were appreciated by the parents but not particularly effective on the children. Maybe that’s because the parents weren’t the ones being stuck with needles while some crazy person in clown makeup attempted to distract them. Or maybe they were all just big fans of Stephen King’s “It.”
Inked immunity
Starting to feel a bit under the weather? Head to the local tattoo artist for the cure! Research from the University of Alabama at Birmingham found evidence that the immune systems of heavily tattooed people are stronger than those without, proving once and for all that tats = toughness. Hell's Angels were on to something all along.
While your immune system can actually grow temporarily weaker after one tattoo, multiple tattoos create a stronger immunological response. Researchers tested the immunoglobulin A levels in those getting a first tattoo and those with many tattoos. They found that the latter group had higher IgA levels.
Maybe that’s why Adam Levine showed off his ink at the Super Bowl halftime show – he was just signaling his strong immune system to the rest of us.
Brain surgery is a laughing matter
This certainly came as a surprise to us, but as it turns out, undergoing brain surgery while conscious and awake can be extremely stressful and panic inducing to the patient. We’re sure most people (including us) would prefer to be asleep for their surgery, but sometimes when dealing with the brain, the surgeon needs to be able to talk to the patient to accurately assess their faculties in case they damage something important.
So the question is: How do you keep brain surgery patients from panicking? Why, with the power of laughter, of course! Specifically, a group at Emory University, Atlanta, published a case study in the Journal of Clinical Investigation about their treatment of a patient with moderate anxiety. When the patient woke up from initial anesthesia, she began to panic. However, after electrical stimulation of the cingulum bundle, the patient immediately turned her frown upside down and began laughing and joking with the surgeons.
Sadly, while the team did not report on the quality of the jokes being told, we can only assume the phrase “this isn’t brain surgery” was thrown around multiple times.
A male brain is a terrible thing to waste
In the future, comedy may mean pressing a button to stimulate your cingulum bundle, but for now we still have jokes. One old joke goes like this: Some aliens land on earth and want to learn about humans, so they go into a store to buy some brains. “Why does the male brain cost twice as much as the female brain?” one asks the store owner, who replies, “It’s hardly been used.”
There may be another explanation: Womens’ brains appear to age more slowly than mens’, investigators at Washington University, St. Louis, said in the Proceedings of the National Academy of Sciences.
They performed PET scans on 121 women and 84 men aged 20-82 years to determine the fraction of sugar committed to aerobic glycolysis in various regions of the brain, and then a machine-learning algorithm used those data to calculate metabolic ages.
The womens’ brains were younger than the mens’ brains, with various calculations producing average differences of 2.7-5.3 years, they reported.
The male brain, it seems, is used for something, and after one LOTME staffer spent 5 minutes explaining total quarterback rating (QBR) to his wife, we think we’ve figured out what it is: sports trivia.
What’s New in Topical Treatments for Psoriasis
In an era when we have access to a dizzying array of biologics for psoriasis treatment, it is easy to forget that topical therapies are still the bread and butter of treatment. For the majority of patients living with psoriasis, topical treatment is the only therapy they receive; indeed, a recent study examining a large national payer database found that 86% of psoriasis patients were managed with topical medications only.1 Thus, it is extremely important to understand how to optimize topical treatments, recognize pitfalls in management, and utilize newer agents that can been added to our treatment armamentarium for psoriasis.
In general, steroids have been the mainstay of topical treatment of psoriasis. Their broad anti-inflammatory activity works well against both the visible signs and symptoms of psoriasis as well as the underlying inflammatory milieu of the disease; however, these treatments are not without their downsides. Hypothalamic-pituitary-adrenal (HPA) axis suppression, especially in higher-potency topical steroids, is a serious concern that limits their use. In one study comparing lotion and cream formulations of clobetasol propionate, HPA axis suppression was seen in 80% (8/10) of adults in the lotion group and 30% (3/10) in the cream group after 4 weeks of treatment.2 These findings are not new; a 1987 study found that patients using less than 50 g of topical clobetasol per week, which is considered a low dose, could still exhibit HPA axis suppression.3 Severe HPA axis suppression may occur; one study of various topical steroids found some degree of HPA axis suppression in 38% (19/50) of patients, with a direct correlation with topical steroid potency.4 Additionally, cutaneous side effects such as striae formation, atrophy, and the possibility of tachyphylaxis must be considered. Various treatment regimens have been developed to limit topical steroid use, including steroid-sparing medications (eg, calcipotriene) used in conjunction with topical steroids, systemic treatments (eg, phototherapy) added on, or higher-potency topical steroids rotated with lower-potency steroids. Implementing other agents, such as topical retinoids or keratolytics, into the treatment regimen also is an important consideration in the overall approach to topical psoriasis therapy.
Notably, a number of newly approved topical treatments for psoriasis have emerged, and more are in the pipeline. When evaluating these agents, important considerations include safety, length of treatment course, and efficacy. Several of these agents hold promise for patients with psoriasis.
An alcohol-free, fixed-combination aerosol foam formulation of calcipotriene 0.005% and betamethasone dipropionate 0.064% was approved by the US Food and Drug Administration for plaque psoriasis in 2015. This agent was shown to be more efficacious than the same combination of active ingredients in an ointment formulation as well as either agent alone, with psoriasis area and severity index 75 response achieved in more than 50% of patients at week 4 of treatment.5 Notably, this product offers once-daily application with positive patient satisfaction scores.6 The novelty of this foam is in its ability to supersaturate the active ingredients on the surface of the skin with improved penetration and drug delivery.
A novel spray formulation of betamethasone dipropionate 0.05% also has been developed and has been compared to augmented betamethasone dipropionate lotion. One benefit of this spray is that, based on the vasoconstriction test, the potency is similar to a mid-potency steroid while the efficacy is not significantly different from betamethasone dipropionate lotion, a class I steroid.7 Hypothalamic-pituitary-adrenal axis suppression was similar following a 4-week treatment course compared to a 2-week course of the lotion formulation.8
The newest agent, halobetasol propionate lotion 0.01%, was approved for treatment of psoriasis in October 2018. Compared to halobetasol 0.05% cream or ointment, halobetasol propionate lotion 0.01% has one-fifth the concentration of the active ingredient with the same degree of success in efficacy scores.9 This reduction in drug concentration is possible because the proprietary lotion base allows for better drug delivery of the active ingredient. Importantly, HPA axis suppression was assessed over an 8-week period of use and no suppression was noted.9 Generic class I steroids should only be used for 2 weeks, which is the standard treatment period used in comparator trials; however, many patients will still have active lesions on their body after 2 weeks of treatment, and if using generic clobetasol or betamethasone dipropionate, the choice becomes whether to keep applying the medication and risk HPA axis suppression and cutaneous side effects or switch to a less effective treatment. However, some of the newer agents are indicated for 4 to 8 weeks of treatment.
Utilizing other classes of agents such as retinoids and keratolytics in our treatment armamentarium for psoriasis often is helpful. It has long been known that tazarotene can be combined with topical steroids for increased efficacy and limitation of the irritating effects of the retinoid.10 Similarly, keratolytics play a role in allowing a topically applied medication to penetrate deep enough to affect the underlying inflammation of psoriasis. Medications that include salicylic acid or urea may help to remove ostraceous scales from thick psoriasis lesions that would otherwise prevent delivery of topical steroids to achieve clinically meaningful results. For scalp psoriasis, there are salicylic acid solutions as well as newer agents such as a dimethicone-based topical product.11
Nonsteroidal topical anti-inflammatories also have been used off label for psoriasis treatment. These agents are especially useful in patients who were not successfully treated with calcipotriene or need adjunctive therapy. Although not extremely effective against plaque psoriasis, topical tacrolimus in particular seems to have a place in the treatment of inverse psoriasis where it can be utilized without concern for long-term side effects.12 Crisaborole ointment, a topical medication approved for treatment of atopic dermatitis, was studied in phase 2 trials, but development has not progressed for a psoriasis indication.13 It is reasonable to consider this medication in the same way that tacrolimus has been used, however, considering that the mechanism of action—phosphodiesterase type 4 inhibition—has successfully been implemented in an oral medication to treat psoriasis, apremilast.
There are numerous topical medications in the pipeline that are being developed to treat psoriasis. Of them, the most relevant is a fixed-dose combination of halobetasol propionate 0.01% and tazarotene 0.045% in a proprietary lotion vehicle. A decision from the US Food and Drug Administration is expected in the first quarter of 2019. This medication capitalizes on the aforementioned synergistic effects of tazarotene and a superpotent topical steroid to achieve improved efficacy. Similar to halobetasol lotion 0.01%, this product was evaluated over an 8-week period, and no HPA axis suppression was observed. Efficacy was significantly improved versus both placebo and either halobetasol or tazarotene alone.14
Overall, it is promising that after a long period of relative stagnancy, we have numerous new agents available and upcoming for the topical treatment of psoriasis. For the vast majority of patients, topical medications still represent the mainstay of treatment, and it is important that we have access to better, safer medications in this category.
- Murage MJ, Kern DM, Chang L, et al. Treatment patterns among patients with psoriasis using a large national payer database in the United States: a retrospective study [published online October 25, 2018]. J Med Econ. doi:10.1080/13696998.2018.1540424.
- Clobex [package insert]. Fort Worth, TX: Galderma Laboratories, LP; 2005.
- Ohman EM, Rogers S, Meenan FO, et al. Adrenal suppression following low-dose topical clobetasol propionate. J R Soc Med. 1987;80:422-424.
- Kerner M, Ishay A, Ziv M, et al. Evaluation of the pituitary-adrenal axis function in patients on topical steroid therapy. J Am Acad Dermatol. 2011;65:215-216.
- Stein Gold L, Lebwohl M, Menter A, et al. Aerosol foam formulation of fixed combination calcipotriene plus betamethasone dipropionate is highly efficacious in patients with psoriasis vulgaris: pooled data from three randomized controlled studies. J Drugs Dermatol. 2016;15:951-957.
- Paul C, Bang B, Lebwohl M. Fixed combination calcipotriol plus betamethasone dipropionate aerosol foam in the treatment of psoriasis vulgaris: rationale for development and clinical profile. Expert Opin Pharmacother. 2017;18:115-121.
- Fowler JF Jr, Hebert AA, Sugarman J. DFD-01, a novel medium potency betamethasone dipropionate 0.05% emollient spray, demonstrates similar efficacy to augmented betamethasone dipropionate 0.05% lotion for the treatment of moderate plaque psoriasis. J Drugs Dermatol. 2016;15:154-162.
- Sidgiddi S, Pakunlu RI, Allenby K. Efficacy, safety, and potency of betamethasone dipropionate spray 0.05%: a treatment for adults with mildto-moderate plaque psoriasis. J Clin Aesthet Dermatol. 2018;11:14-22.
- Kerdel FA, Draelos ZD, Tyring SK, et al. A phase 2, multicenter, doubleblind, randomized, vehicle-controlled clinical study to compare the safety and efficacy of a halobetasol propionate 0.01% lotion and halobetasol propionate 0.05% cream in the treatment of plaque psoriasis [published online November 5, 2018]. J Dermatolog Treat. doi:10.1080/09 546634.2018.1523362.
- Lebwohl M, Poulin Y. Tazarotene in combination with topical corticosteroids. J Am Acad Dermatol. 1998;39(4 pt 2):S139-S143.
- Hengge UR, Roschmann K, Candler H. Single-center, noninterventional clinical trial to assess the safety, efficacy, and tolerability of a dimeticone-based medical device in facilitating the removal of scales after topical application in patients with psoriasis corporis or psoriasis capitis. Psoriasis (Auckl). 2017;7:41-49.
- Malecic N, Young H. Tacrolimus for the management of psoriasis: clinical utility and place in therapy. Psoriasis (Auckl). 2016;6:153-163.
- Nazarian R, Weinberg JM. AN-2728, a PDE4 inhibitor for the potential topical treatment of psoriasis and atopic dermatitis. Curr Opin Investig Drugs. 2009;10:1236-1242.
- Gold LS, Lebwohl MG, Sugarman JL, et al. Safety and efficacy of a fixed combination of halobetasol and tazarotene in the treatment of moderate-to-severe plaque psoriasis: results of 2 phase 3 randomized controlled trials. J Am Acad Dermatol. 2018;79:287-293.
In an era when we have access to a dizzying array of biologics for psoriasis treatment, it is easy to forget that topical therapies are still the bread and butter of treatment. For the majority of patients living with psoriasis, topical treatment is the only therapy they receive; indeed, a recent study examining a large national payer database found that 86% of psoriasis patients were managed with topical medications only.1 Thus, it is extremely important to understand how to optimize topical treatments, recognize pitfalls in management, and utilize newer agents that can been added to our treatment armamentarium for psoriasis.
In general, steroids have been the mainstay of topical treatment of psoriasis. Their broad anti-inflammatory activity works well against both the visible signs and symptoms of psoriasis as well as the underlying inflammatory milieu of the disease; however, these treatments are not without their downsides. Hypothalamic-pituitary-adrenal (HPA) axis suppression, especially in higher-potency topical steroids, is a serious concern that limits their use. In one study comparing lotion and cream formulations of clobetasol propionate, HPA axis suppression was seen in 80% (8/10) of adults in the lotion group and 30% (3/10) in the cream group after 4 weeks of treatment.2 These findings are not new; a 1987 study found that patients using less than 50 g of topical clobetasol per week, which is considered a low dose, could still exhibit HPA axis suppression.3 Severe HPA axis suppression may occur; one study of various topical steroids found some degree of HPA axis suppression in 38% (19/50) of patients, with a direct correlation with topical steroid potency.4 Additionally, cutaneous side effects such as striae formation, atrophy, and the possibility of tachyphylaxis must be considered. Various treatment regimens have been developed to limit topical steroid use, including steroid-sparing medications (eg, calcipotriene) used in conjunction with topical steroids, systemic treatments (eg, phototherapy) added on, or higher-potency topical steroids rotated with lower-potency steroids. Implementing other agents, such as topical retinoids or keratolytics, into the treatment regimen also is an important consideration in the overall approach to topical psoriasis therapy.
Notably, a number of newly approved topical treatments for psoriasis have emerged, and more are in the pipeline. When evaluating these agents, important considerations include safety, length of treatment course, and efficacy. Several of these agents hold promise for patients with psoriasis.
An alcohol-free, fixed-combination aerosol foam formulation of calcipotriene 0.005% and betamethasone dipropionate 0.064% was approved by the US Food and Drug Administration for plaque psoriasis in 2015. This agent was shown to be more efficacious than the same combination of active ingredients in an ointment formulation as well as either agent alone, with psoriasis area and severity index 75 response achieved in more than 50% of patients at week 4 of treatment.5 Notably, this product offers once-daily application with positive patient satisfaction scores.6 The novelty of this foam is in its ability to supersaturate the active ingredients on the surface of the skin with improved penetration and drug delivery.
A novel spray formulation of betamethasone dipropionate 0.05% also has been developed and has been compared to augmented betamethasone dipropionate lotion. One benefit of this spray is that, based on the vasoconstriction test, the potency is similar to a mid-potency steroid while the efficacy is not significantly different from betamethasone dipropionate lotion, a class I steroid.7 Hypothalamic-pituitary-adrenal axis suppression was similar following a 4-week treatment course compared to a 2-week course of the lotion formulation.8
The newest agent, halobetasol propionate lotion 0.01%, was approved for treatment of psoriasis in October 2018. Compared to halobetasol 0.05% cream or ointment, halobetasol propionate lotion 0.01% has one-fifth the concentration of the active ingredient with the same degree of success in efficacy scores.9 This reduction in drug concentration is possible because the proprietary lotion base allows for better drug delivery of the active ingredient. Importantly, HPA axis suppression was assessed over an 8-week period of use and no suppression was noted.9 Generic class I steroids should only be used for 2 weeks, which is the standard treatment period used in comparator trials; however, many patients will still have active lesions on their body after 2 weeks of treatment, and if using generic clobetasol or betamethasone dipropionate, the choice becomes whether to keep applying the medication and risk HPA axis suppression and cutaneous side effects or switch to a less effective treatment. However, some of the newer agents are indicated for 4 to 8 weeks of treatment.
Utilizing other classes of agents such as retinoids and keratolytics in our treatment armamentarium for psoriasis often is helpful. It has long been known that tazarotene can be combined with topical steroids for increased efficacy and limitation of the irritating effects of the retinoid.10 Similarly, keratolytics play a role in allowing a topically applied medication to penetrate deep enough to affect the underlying inflammation of psoriasis. Medications that include salicylic acid or urea may help to remove ostraceous scales from thick psoriasis lesions that would otherwise prevent delivery of topical steroids to achieve clinically meaningful results. For scalp psoriasis, there are salicylic acid solutions as well as newer agents such as a dimethicone-based topical product.11
Nonsteroidal topical anti-inflammatories also have been used off label for psoriasis treatment. These agents are especially useful in patients who were not successfully treated with calcipotriene or need adjunctive therapy. Although not extremely effective against plaque psoriasis, topical tacrolimus in particular seems to have a place in the treatment of inverse psoriasis where it can be utilized without concern for long-term side effects.12 Crisaborole ointment, a topical medication approved for treatment of atopic dermatitis, was studied in phase 2 trials, but development has not progressed for a psoriasis indication.13 It is reasonable to consider this medication in the same way that tacrolimus has been used, however, considering that the mechanism of action—phosphodiesterase type 4 inhibition—has successfully been implemented in an oral medication to treat psoriasis, apremilast.
There are numerous topical medications in the pipeline that are being developed to treat psoriasis. Of them, the most relevant is a fixed-dose combination of halobetasol propionate 0.01% and tazarotene 0.045% in a proprietary lotion vehicle. A decision from the US Food and Drug Administration is expected in the first quarter of 2019. This medication capitalizes on the aforementioned synergistic effects of tazarotene and a superpotent topical steroid to achieve improved efficacy. Similar to halobetasol lotion 0.01%, this product was evaluated over an 8-week period, and no HPA axis suppression was observed. Efficacy was significantly improved versus both placebo and either halobetasol or tazarotene alone.14
Overall, it is promising that after a long period of relative stagnancy, we have numerous new agents available and upcoming for the topical treatment of psoriasis. For the vast majority of patients, topical medications still represent the mainstay of treatment, and it is important that we have access to better, safer medications in this category.
In an era when we have access to a dizzying array of biologics for psoriasis treatment, it is easy to forget that topical therapies are still the bread and butter of treatment. For the majority of patients living with psoriasis, topical treatment is the only therapy they receive; indeed, a recent study examining a large national payer database found that 86% of psoriasis patients were managed with topical medications only.1 Thus, it is extremely important to understand how to optimize topical treatments, recognize pitfalls in management, and utilize newer agents that can been added to our treatment armamentarium for psoriasis.
In general, steroids have been the mainstay of topical treatment of psoriasis. Their broad anti-inflammatory activity works well against both the visible signs and symptoms of psoriasis as well as the underlying inflammatory milieu of the disease; however, these treatments are not without their downsides. Hypothalamic-pituitary-adrenal (HPA) axis suppression, especially in higher-potency topical steroids, is a serious concern that limits their use. In one study comparing lotion and cream formulations of clobetasol propionate, HPA axis suppression was seen in 80% (8/10) of adults in the lotion group and 30% (3/10) in the cream group after 4 weeks of treatment.2 These findings are not new; a 1987 study found that patients using less than 50 g of topical clobetasol per week, which is considered a low dose, could still exhibit HPA axis suppression.3 Severe HPA axis suppression may occur; one study of various topical steroids found some degree of HPA axis suppression in 38% (19/50) of patients, with a direct correlation with topical steroid potency.4 Additionally, cutaneous side effects such as striae formation, atrophy, and the possibility of tachyphylaxis must be considered. Various treatment regimens have been developed to limit topical steroid use, including steroid-sparing medications (eg, calcipotriene) used in conjunction with topical steroids, systemic treatments (eg, phototherapy) added on, or higher-potency topical steroids rotated with lower-potency steroids. Implementing other agents, such as topical retinoids or keratolytics, into the treatment regimen also is an important consideration in the overall approach to topical psoriasis therapy.
Notably, a number of newly approved topical treatments for psoriasis have emerged, and more are in the pipeline. When evaluating these agents, important considerations include safety, length of treatment course, and efficacy. Several of these agents hold promise for patients with psoriasis.
An alcohol-free, fixed-combination aerosol foam formulation of calcipotriene 0.005% and betamethasone dipropionate 0.064% was approved by the US Food and Drug Administration for plaque psoriasis in 2015. This agent was shown to be more efficacious than the same combination of active ingredients in an ointment formulation as well as either agent alone, with psoriasis area and severity index 75 response achieved in more than 50% of patients at week 4 of treatment.5 Notably, this product offers once-daily application with positive patient satisfaction scores.6 The novelty of this foam is in its ability to supersaturate the active ingredients on the surface of the skin with improved penetration and drug delivery.
A novel spray formulation of betamethasone dipropionate 0.05% also has been developed and has been compared to augmented betamethasone dipropionate lotion. One benefit of this spray is that, based on the vasoconstriction test, the potency is similar to a mid-potency steroid while the efficacy is not significantly different from betamethasone dipropionate lotion, a class I steroid.7 Hypothalamic-pituitary-adrenal axis suppression was similar following a 4-week treatment course compared to a 2-week course of the lotion formulation.8
The newest agent, halobetasol propionate lotion 0.01%, was approved for treatment of psoriasis in October 2018. Compared to halobetasol 0.05% cream or ointment, halobetasol propionate lotion 0.01% has one-fifth the concentration of the active ingredient with the same degree of success in efficacy scores.9 This reduction in drug concentration is possible because the proprietary lotion base allows for better drug delivery of the active ingredient. Importantly, HPA axis suppression was assessed over an 8-week period of use and no suppression was noted.9 Generic class I steroids should only be used for 2 weeks, which is the standard treatment period used in comparator trials; however, many patients will still have active lesions on their body after 2 weeks of treatment, and if using generic clobetasol or betamethasone dipropionate, the choice becomes whether to keep applying the medication and risk HPA axis suppression and cutaneous side effects or switch to a less effective treatment. However, some of the newer agents are indicated for 4 to 8 weeks of treatment.
Utilizing other classes of agents such as retinoids and keratolytics in our treatment armamentarium for psoriasis often is helpful. It has long been known that tazarotene can be combined with topical steroids for increased efficacy and limitation of the irritating effects of the retinoid.10 Similarly, keratolytics play a role in allowing a topically applied medication to penetrate deep enough to affect the underlying inflammation of psoriasis. Medications that include salicylic acid or urea may help to remove ostraceous scales from thick psoriasis lesions that would otherwise prevent delivery of topical steroids to achieve clinically meaningful results. For scalp psoriasis, there are salicylic acid solutions as well as newer agents such as a dimethicone-based topical product.11
Nonsteroidal topical anti-inflammatories also have been used off label for psoriasis treatment. These agents are especially useful in patients who were not successfully treated with calcipotriene or need adjunctive therapy. Although not extremely effective against plaque psoriasis, topical tacrolimus in particular seems to have a place in the treatment of inverse psoriasis where it can be utilized without concern for long-term side effects.12 Crisaborole ointment, a topical medication approved for treatment of atopic dermatitis, was studied in phase 2 trials, but development has not progressed for a psoriasis indication.13 It is reasonable to consider this medication in the same way that tacrolimus has been used, however, considering that the mechanism of action—phosphodiesterase type 4 inhibition—has successfully been implemented in an oral medication to treat psoriasis, apremilast.
There are numerous topical medications in the pipeline that are being developed to treat psoriasis. Of them, the most relevant is a fixed-dose combination of halobetasol propionate 0.01% and tazarotene 0.045% in a proprietary lotion vehicle. A decision from the US Food and Drug Administration is expected in the first quarter of 2019. This medication capitalizes on the aforementioned synergistic effects of tazarotene and a superpotent topical steroid to achieve improved efficacy. Similar to halobetasol lotion 0.01%, this product was evaluated over an 8-week period, and no HPA axis suppression was observed. Efficacy was significantly improved versus both placebo and either halobetasol or tazarotene alone.14
Overall, it is promising that after a long period of relative stagnancy, we have numerous new agents available and upcoming for the topical treatment of psoriasis. For the vast majority of patients, topical medications still represent the mainstay of treatment, and it is important that we have access to better, safer medications in this category.
- Murage MJ, Kern DM, Chang L, et al. Treatment patterns among patients with psoriasis using a large national payer database in the United States: a retrospective study [published online October 25, 2018]. J Med Econ. doi:10.1080/13696998.2018.1540424.
- Clobex [package insert]. Fort Worth, TX: Galderma Laboratories, LP; 2005.
- Ohman EM, Rogers S, Meenan FO, et al. Adrenal suppression following low-dose topical clobetasol propionate. J R Soc Med. 1987;80:422-424.
- Kerner M, Ishay A, Ziv M, et al. Evaluation of the pituitary-adrenal axis function in patients on topical steroid therapy. J Am Acad Dermatol. 2011;65:215-216.
- Stein Gold L, Lebwohl M, Menter A, et al. Aerosol foam formulation of fixed combination calcipotriene plus betamethasone dipropionate is highly efficacious in patients with psoriasis vulgaris: pooled data from three randomized controlled studies. J Drugs Dermatol. 2016;15:951-957.
- Paul C, Bang B, Lebwohl M. Fixed combination calcipotriol plus betamethasone dipropionate aerosol foam in the treatment of psoriasis vulgaris: rationale for development and clinical profile. Expert Opin Pharmacother. 2017;18:115-121.
- Fowler JF Jr, Hebert AA, Sugarman J. DFD-01, a novel medium potency betamethasone dipropionate 0.05% emollient spray, demonstrates similar efficacy to augmented betamethasone dipropionate 0.05% lotion for the treatment of moderate plaque psoriasis. J Drugs Dermatol. 2016;15:154-162.
- Sidgiddi S, Pakunlu RI, Allenby K. Efficacy, safety, and potency of betamethasone dipropionate spray 0.05%: a treatment for adults with mildto-moderate plaque psoriasis. J Clin Aesthet Dermatol. 2018;11:14-22.
- Kerdel FA, Draelos ZD, Tyring SK, et al. A phase 2, multicenter, doubleblind, randomized, vehicle-controlled clinical study to compare the safety and efficacy of a halobetasol propionate 0.01% lotion and halobetasol propionate 0.05% cream in the treatment of plaque psoriasis [published online November 5, 2018]. J Dermatolog Treat. doi:10.1080/09 546634.2018.1523362.
- Lebwohl M, Poulin Y. Tazarotene in combination with topical corticosteroids. J Am Acad Dermatol. 1998;39(4 pt 2):S139-S143.
- Hengge UR, Roschmann K, Candler H. Single-center, noninterventional clinical trial to assess the safety, efficacy, and tolerability of a dimeticone-based medical device in facilitating the removal of scales after topical application in patients with psoriasis corporis or psoriasis capitis. Psoriasis (Auckl). 2017;7:41-49.
- Malecic N, Young H. Tacrolimus for the management of psoriasis: clinical utility and place in therapy. Psoriasis (Auckl). 2016;6:153-163.
- Nazarian R, Weinberg JM. AN-2728, a PDE4 inhibitor for the potential topical treatment of psoriasis and atopic dermatitis. Curr Opin Investig Drugs. 2009;10:1236-1242.
- Gold LS, Lebwohl MG, Sugarman JL, et al. Safety and efficacy of a fixed combination of halobetasol and tazarotene in the treatment of moderate-to-severe plaque psoriasis: results of 2 phase 3 randomized controlled trials. J Am Acad Dermatol. 2018;79:287-293.
- Murage MJ, Kern DM, Chang L, et al. Treatment patterns among patients with psoriasis using a large national payer database in the United States: a retrospective study [published online October 25, 2018]. J Med Econ. doi:10.1080/13696998.2018.1540424.
- Clobex [package insert]. Fort Worth, TX: Galderma Laboratories, LP; 2005.
- Ohman EM, Rogers S, Meenan FO, et al. Adrenal suppression following low-dose topical clobetasol propionate. J R Soc Med. 1987;80:422-424.
- Kerner M, Ishay A, Ziv M, et al. Evaluation of the pituitary-adrenal axis function in patients on topical steroid therapy. J Am Acad Dermatol. 2011;65:215-216.
- Stein Gold L, Lebwohl M, Menter A, et al. Aerosol foam formulation of fixed combination calcipotriene plus betamethasone dipropionate is highly efficacious in patients with psoriasis vulgaris: pooled data from three randomized controlled studies. J Drugs Dermatol. 2016;15:951-957.
- Paul C, Bang B, Lebwohl M. Fixed combination calcipotriol plus betamethasone dipropionate aerosol foam in the treatment of psoriasis vulgaris: rationale for development and clinical profile. Expert Opin Pharmacother. 2017;18:115-121.
- Fowler JF Jr, Hebert AA, Sugarman J. DFD-01, a novel medium potency betamethasone dipropionate 0.05% emollient spray, demonstrates similar efficacy to augmented betamethasone dipropionate 0.05% lotion for the treatment of moderate plaque psoriasis. J Drugs Dermatol. 2016;15:154-162.
- Sidgiddi S, Pakunlu RI, Allenby K. Efficacy, safety, and potency of betamethasone dipropionate spray 0.05%: a treatment for adults with mildto-moderate plaque psoriasis. J Clin Aesthet Dermatol. 2018;11:14-22.
- Kerdel FA, Draelos ZD, Tyring SK, et al. A phase 2, multicenter, doubleblind, randomized, vehicle-controlled clinical study to compare the safety and efficacy of a halobetasol propionate 0.01% lotion and halobetasol propionate 0.05% cream in the treatment of plaque psoriasis [published online November 5, 2018]. J Dermatolog Treat. doi:10.1080/09 546634.2018.1523362.
- Lebwohl M, Poulin Y. Tazarotene in combination with topical corticosteroids. J Am Acad Dermatol. 1998;39(4 pt 2):S139-S143.
- Hengge UR, Roschmann K, Candler H. Single-center, noninterventional clinical trial to assess the safety, efficacy, and tolerability of a dimeticone-based medical device in facilitating the removal of scales after topical application in patients with psoriasis corporis or psoriasis capitis. Psoriasis (Auckl). 2017;7:41-49.
- Malecic N, Young H. Tacrolimus for the management of psoriasis: clinical utility and place in therapy. Psoriasis (Auckl). 2016;6:153-163.
- Nazarian R, Weinberg JM. AN-2728, a PDE4 inhibitor for the potential topical treatment of psoriasis and atopic dermatitis. Curr Opin Investig Drugs. 2009;10:1236-1242.
- Gold LS, Lebwohl MG, Sugarman JL, et al. Safety and efficacy of a fixed combination of halobetasol and tazarotene in the treatment of moderate-to-severe plaque psoriasis: results of 2 phase 3 randomized controlled trials. J Am Acad Dermatol. 2018;79:287-293.
One person’s snake oil is another’s improved bottom line
“I’d be a millionaire if I could get rid of my conscience.”
A friend of mine in obstetrics said that yesterday. We were talking about the various quackery products pushed over the Internet and in some stores. These things claim to heal anything from Parkinson’s disease to a broken heart, and are generally sold by someone without real medical training. Generally, they also include some comment about this being a cure that doctors are hiding from you.
Of course, all of this is untrue. If there were actually cure for some horrible neurologic disease, I’d be thrilled to prescribe it. I’m here to reduce suffering, not prolong it.
I get it. People want to believe there’s hope when there is none. Even if it’s just something like forgetting a broken relationship, they want to believe there’s a way to make it happen quickly and painlessly.
It would be nice if it worked that way, but it doesn’t. Worse, people in these unfortunate medical or emotional situations are often vulnerable to these sales pitches, and there’s no shortage of unscrupulous individuals willing to prey on them.
What bothers me most in these cases is when doctors, with training similar to mine, push these “remedies.” Often they’re sold in a case in the waiting room and recommended during the visit. I assume these physicians either have lost their conscience and don’t care, or over time have somehow convinced themselves that what they’re doing is right.
Having a doctor selling or endorsing such a product gives it a credibility that it usually won’t get from an average Internet huckster, even if it’s for the same thing.
I’m sure some doctors have convinced themselves that the product is harmless, and therefore falls under primum non nocere. But being harmless isn’t the same as being effective, which is what the patient wants.
Like my friend said, with the financial pressures modern physicians are under, it’s easy to look at things like this as a way to improve cash flow and the bottom line. But you can’t lose sight of the patients. They’re why we are here, and selling them a product that will do them no good isn’t right.
Hippocrates’ “Do no harm” is a key part of being a doctor, but Jiminy Cricket’s “always let your conscience be your guide” is part of being a good doctor. We should never forget that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I’d be a millionaire if I could get rid of my conscience.”
A friend of mine in obstetrics said that yesterday. We were talking about the various quackery products pushed over the Internet and in some stores. These things claim to heal anything from Parkinson’s disease to a broken heart, and are generally sold by someone without real medical training. Generally, they also include some comment about this being a cure that doctors are hiding from you.
Of course, all of this is untrue. If there were actually cure for some horrible neurologic disease, I’d be thrilled to prescribe it. I’m here to reduce suffering, not prolong it.
I get it. People want to believe there’s hope when there is none. Even if it’s just something like forgetting a broken relationship, they want to believe there’s a way to make it happen quickly and painlessly.
It would be nice if it worked that way, but it doesn’t. Worse, people in these unfortunate medical or emotional situations are often vulnerable to these sales pitches, and there’s no shortage of unscrupulous individuals willing to prey on them.
What bothers me most in these cases is when doctors, with training similar to mine, push these “remedies.” Often they’re sold in a case in the waiting room and recommended during the visit. I assume these physicians either have lost their conscience and don’t care, or over time have somehow convinced themselves that what they’re doing is right.
Having a doctor selling or endorsing such a product gives it a credibility that it usually won’t get from an average Internet huckster, even if it’s for the same thing.
I’m sure some doctors have convinced themselves that the product is harmless, and therefore falls under primum non nocere. But being harmless isn’t the same as being effective, which is what the patient wants.
Like my friend said, with the financial pressures modern physicians are under, it’s easy to look at things like this as a way to improve cash flow and the bottom line. But you can’t lose sight of the patients. They’re why we are here, and selling them a product that will do them no good isn’t right.
Hippocrates’ “Do no harm” is a key part of being a doctor, but Jiminy Cricket’s “always let your conscience be your guide” is part of being a good doctor. We should never forget that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I’d be a millionaire if I could get rid of my conscience.”
A friend of mine in obstetrics said that yesterday. We were talking about the various quackery products pushed over the Internet and in some stores. These things claim to heal anything from Parkinson’s disease to a broken heart, and are generally sold by someone without real medical training. Generally, they also include some comment about this being a cure that doctors are hiding from you.
Of course, all of this is untrue. If there were actually cure for some horrible neurologic disease, I’d be thrilled to prescribe it. I’m here to reduce suffering, not prolong it.
I get it. People want to believe there’s hope when there is none. Even if it’s just something like forgetting a broken relationship, they want to believe there’s a way to make it happen quickly and painlessly.
It would be nice if it worked that way, but it doesn’t. Worse, people in these unfortunate medical or emotional situations are often vulnerable to these sales pitches, and there’s no shortage of unscrupulous individuals willing to prey on them.
What bothers me most in these cases is when doctors, with training similar to mine, push these “remedies.” Often they’re sold in a case in the waiting room and recommended during the visit. I assume these physicians either have lost their conscience and don’t care, or over time have somehow convinced themselves that what they’re doing is right.
Having a doctor selling or endorsing such a product gives it a credibility that it usually won’t get from an average Internet huckster, even if it’s for the same thing.
I’m sure some doctors have convinced themselves that the product is harmless, and therefore falls under primum non nocere. But being harmless isn’t the same as being effective, which is what the patient wants.
Like my friend said, with the financial pressures modern physicians are under, it’s easy to look at things like this as a way to improve cash flow and the bottom line. But you can’t lose sight of the patients. They’re why we are here, and selling them a product that will do them no good isn’t right.
Hippocrates’ “Do no harm” is a key part of being a doctor, but Jiminy Cricket’s “always let your conscience be your guide” is part of being a good doctor. We should never forget that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Penicillin allergy
A 75-year-old man presents with fever, chills, and facial pain. He had an upper respiratory infection 3 weeks ago and has had persistent sinus drainage since. He has tried nasal irrigation and nasal steroids without improvement.
Over the past 5 days, he has had thicker postnasal drip, the development of facial pain, and today fevers as high as 102 degrees. He has a history of giant cell arteritis, for which he takes 30 mg of prednisone daily; coronary artery disease; and hypertension. He has a penicillin allergy (rash on chest, back, and arms 25 years ago). Exam reveals temperature of 101.5 and tenderness over left maxillary sinus.
What treatment do you recommend?
A. Amoxicillin/clavulanate.
B. Cefpodoxime.
C. Levofloxacin.
D. Trimethoprim/sulfamethoxazole.
I think cefpodoxime is probably the best of these choices to treat sinusitis in this patient. Choosing amoxicillin /clavulanate is an option only if you could give the patient a test dose in a controlled setting. I think giving this patient levofloxacin poses greater risk than a penicillin rechallenge. This patient is elderly and on prednisone, both of which increase his risk of tendon rupture if given a quinolone. Also, the Food and Drug Administration released a warning recently regarding increased risk of aortic disease in patients with cardiovascular risk factors who receive fluoroquinolones.1
Merin Kuruvilla, MD, and colleagues described oral amoxicillin challenge for patients with a history of low-risk penicillin allergy (described as benign rash, benign somatic symptoms, or unknown history with penicillin exposure more than 12 months prior).2 The study was done in a single allergy practice where 38 of 50 patients with penicillin allergy histories qualified for the study. Of the 38 eligible patients, 20 consented to oral rechallenge in clinic, and none of them developed immediate or delayed hypersensitivity reactions.
Melissa Iammatteo, MD, et al. studied 155 patients with a history of non–life-threatening penicillin reactions.3 Study participants received placebo followed by a two-step graded challenge to amoxicillin. No reaction occurred in 77% of patients, while 20% of patients had nonallergic reactions, which were equal between placebo and amoxicillin. Only 2.6 % had allergic reactions, all of which were classified as mild.
Reported penicillin allergy occurs in about 10% of community patients, but 90% of these patients can tolerate penicillins.4 Patients reporting a penicillin allergy have increased risk for drug resistance and prolonged hospital stays.5
The American Academy of Allergy, Asthma & Immunology recommended more widespread and routine performance of penicillin allergy testing in patients with a history of allergy to penicillin or other beta-lactam antibiotics.6 Patients who have penicillin allergy histories are more likely to receive drugs, such as clindamycin or a fluoroquinolone, that may carry much greater risks than a beta-lactam antibiotic. It also leads to more vancomycin use, which increases risk of vancomycin resistance.
Allergic reactions to cephalosporins are very infrequent in patients with a penicillin allergy. Eric Macy, MD, and colleagues studied all members of Kaiser Permanente Southern California health plan who had received cephalosporins over a 2-year period.7 More than 275,000 courses were given to patients with penicillin allergy, with only about 1% having an allergic reaction and only three cases of anaphylaxis.
Pearl: Most patients with a history of penicillin allergy will tolerate penicillins and cephalosporins. Penicillin allergy testing should be done to assess if they have a penicillin allergy, and in low-risk patients (patients who do not recall the allergy or had a maculopapular rash), consideration for oral rechallenge in a controlled setting may be an option. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Food and Drug Administration. “FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients,” 2018 Dec 20.
2. Ann Allergy Asthma Immunol. 2018 Nov;121(5):627-8.
3. J Allergy Clin Immunol Pract. 2019 Jan;7(1):236-43.
4. Immunol Allergy Clin North Am. 2017 Nov;37(4):643-62.
5. J Allergy Clin Immunol. 2014 Mar;133(3):790-6.
6. J Allergy Clin Immunol Pract. 2017 Mar - Apr;5(2):333-4.
7. J Allergy Clin Immunol. 2015 Mar;135(3):745-52.e5.
A 75-year-old man presents with fever, chills, and facial pain. He had an upper respiratory infection 3 weeks ago and has had persistent sinus drainage since. He has tried nasal irrigation and nasal steroids without improvement.
Over the past 5 days, he has had thicker postnasal drip, the development of facial pain, and today fevers as high as 102 degrees. He has a history of giant cell arteritis, for which he takes 30 mg of prednisone daily; coronary artery disease; and hypertension. He has a penicillin allergy (rash on chest, back, and arms 25 years ago). Exam reveals temperature of 101.5 and tenderness over left maxillary sinus.
What treatment do you recommend?
A. Amoxicillin/clavulanate.
B. Cefpodoxime.
C. Levofloxacin.
D. Trimethoprim/sulfamethoxazole.
I think cefpodoxime is probably the best of these choices to treat sinusitis in this patient. Choosing amoxicillin /clavulanate is an option only if you could give the patient a test dose in a controlled setting. I think giving this patient levofloxacin poses greater risk than a penicillin rechallenge. This patient is elderly and on prednisone, both of which increase his risk of tendon rupture if given a quinolone. Also, the Food and Drug Administration released a warning recently regarding increased risk of aortic disease in patients with cardiovascular risk factors who receive fluoroquinolones.1
Merin Kuruvilla, MD, and colleagues described oral amoxicillin challenge for patients with a history of low-risk penicillin allergy (described as benign rash, benign somatic symptoms, or unknown history with penicillin exposure more than 12 months prior).2 The study was done in a single allergy practice where 38 of 50 patients with penicillin allergy histories qualified for the study. Of the 38 eligible patients, 20 consented to oral rechallenge in clinic, and none of them developed immediate or delayed hypersensitivity reactions.
Melissa Iammatteo, MD, et al. studied 155 patients with a history of non–life-threatening penicillin reactions.3 Study participants received placebo followed by a two-step graded challenge to amoxicillin. No reaction occurred in 77% of patients, while 20% of patients had nonallergic reactions, which were equal between placebo and amoxicillin. Only 2.6 % had allergic reactions, all of which were classified as mild.
Reported penicillin allergy occurs in about 10% of community patients, but 90% of these patients can tolerate penicillins.4 Patients reporting a penicillin allergy have increased risk for drug resistance and prolonged hospital stays.5
The American Academy of Allergy, Asthma & Immunology recommended more widespread and routine performance of penicillin allergy testing in patients with a history of allergy to penicillin or other beta-lactam antibiotics.6 Patients who have penicillin allergy histories are more likely to receive drugs, such as clindamycin or a fluoroquinolone, that may carry much greater risks than a beta-lactam antibiotic. It also leads to more vancomycin use, which increases risk of vancomycin resistance.
Allergic reactions to cephalosporins are very infrequent in patients with a penicillin allergy. Eric Macy, MD, and colleagues studied all members of Kaiser Permanente Southern California health plan who had received cephalosporins over a 2-year period.7 More than 275,000 courses were given to patients with penicillin allergy, with only about 1% having an allergic reaction and only three cases of anaphylaxis.
Pearl: Most patients with a history of penicillin allergy will tolerate penicillins and cephalosporins. Penicillin allergy testing should be done to assess if they have a penicillin allergy, and in low-risk patients (patients who do not recall the allergy or had a maculopapular rash), consideration for oral rechallenge in a controlled setting may be an option. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Food and Drug Administration. “FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients,” 2018 Dec 20.
2. Ann Allergy Asthma Immunol. 2018 Nov;121(5):627-8.
3. J Allergy Clin Immunol Pract. 2019 Jan;7(1):236-43.
4. Immunol Allergy Clin North Am. 2017 Nov;37(4):643-62.
5. J Allergy Clin Immunol. 2014 Mar;133(3):790-6.
6. J Allergy Clin Immunol Pract. 2017 Mar - Apr;5(2):333-4.
7. J Allergy Clin Immunol. 2015 Mar;135(3):745-52.e5.
A 75-year-old man presents with fever, chills, and facial pain. He had an upper respiratory infection 3 weeks ago and has had persistent sinus drainage since. He has tried nasal irrigation and nasal steroids without improvement.
Over the past 5 days, he has had thicker postnasal drip, the development of facial pain, and today fevers as high as 102 degrees. He has a history of giant cell arteritis, for which he takes 30 mg of prednisone daily; coronary artery disease; and hypertension. He has a penicillin allergy (rash on chest, back, and arms 25 years ago). Exam reveals temperature of 101.5 and tenderness over left maxillary sinus.
What treatment do you recommend?
A. Amoxicillin/clavulanate.
B. Cefpodoxime.
C. Levofloxacin.
D. Trimethoprim/sulfamethoxazole.
I think cefpodoxime is probably the best of these choices to treat sinusitis in this patient. Choosing amoxicillin /clavulanate is an option only if you could give the patient a test dose in a controlled setting. I think giving this patient levofloxacin poses greater risk than a penicillin rechallenge. This patient is elderly and on prednisone, both of which increase his risk of tendon rupture if given a quinolone. Also, the Food and Drug Administration released a warning recently regarding increased risk of aortic disease in patients with cardiovascular risk factors who receive fluoroquinolones.1
Merin Kuruvilla, MD, and colleagues described oral amoxicillin challenge for patients with a history of low-risk penicillin allergy (described as benign rash, benign somatic symptoms, or unknown history with penicillin exposure more than 12 months prior).2 The study was done in a single allergy practice where 38 of 50 patients with penicillin allergy histories qualified for the study. Of the 38 eligible patients, 20 consented to oral rechallenge in clinic, and none of them developed immediate or delayed hypersensitivity reactions.
Melissa Iammatteo, MD, et al. studied 155 patients with a history of non–life-threatening penicillin reactions.3 Study participants received placebo followed by a two-step graded challenge to amoxicillin. No reaction occurred in 77% of patients, while 20% of patients had nonallergic reactions, which were equal between placebo and amoxicillin. Only 2.6 % had allergic reactions, all of which were classified as mild.
Reported penicillin allergy occurs in about 10% of community patients, but 90% of these patients can tolerate penicillins.4 Patients reporting a penicillin allergy have increased risk for drug resistance and prolonged hospital stays.5
The American Academy of Allergy, Asthma & Immunology recommended more widespread and routine performance of penicillin allergy testing in patients with a history of allergy to penicillin or other beta-lactam antibiotics.6 Patients who have penicillin allergy histories are more likely to receive drugs, such as clindamycin or a fluoroquinolone, that may carry much greater risks than a beta-lactam antibiotic. It also leads to more vancomycin use, which increases risk of vancomycin resistance.
Allergic reactions to cephalosporins are very infrequent in patients with a penicillin allergy. Eric Macy, MD, and colleagues studied all members of Kaiser Permanente Southern California health plan who had received cephalosporins over a 2-year period.7 More than 275,000 courses were given to patients with penicillin allergy, with only about 1% having an allergic reaction and only three cases of anaphylaxis.
Pearl: Most patients with a history of penicillin allergy will tolerate penicillins and cephalosporins. Penicillin allergy testing should be done to assess if they have a penicillin allergy, and in low-risk patients (patients who do not recall the allergy or had a maculopapular rash), consideration for oral rechallenge in a controlled setting may be an option. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Food and Drug Administration. “FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients,” 2018 Dec 20.
2. Ann Allergy Asthma Immunol. 2018 Nov;121(5):627-8.
3. J Allergy Clin Immunol Pract. 2019 Jan;7(1):236-43.
4. Immunol Allergy Clin North Am. 2017 Nov;37(4):643-62.
5. J Allergy Clin Immunol. 2014 Mar;133(3):790-6.
6. J Allergy Clin Immunol Pract. 2017 Mar - Apr;5(2):333-4.
7. J Allergy Clin Immunol. 2015 Mar;135(3):745-52.e5.
Tyranny by the numbers
“How come you retired?” I asked.
A few years my junior, Marty had taught in public school forever. “It was the MCAS,” he said. That’s the Massachusetts Comprehensive Assessment System, a standardized test meant to gauge student performance and teacher competence.
“They demanded that my students test at a fifth-grade level,” Marty said. “But they were all at a second-grade level.
“Plus, I had been teaching for thirty years, and some kid right out of college was telling me how to do my job. So I left.”
Of course, this tale will sound familiar to physicians. Pay for performance. Bean counters calling the shots. Dismissal of clinical experience as useless and self-serving.
A recent book lays it all out: Jerry Z. Muller’s The Tyranny of Metrics. This book is punchy, witty, and succinct – you can read it in a day. A historian of economics and culture, Muller shows the extent of what I had guessed at from chats with people in different fields. In all of these, if you don’t count it, it doesn’t count.
Metrics, it is assumed, are “hard” and “objective.” They must “replace judgment based on experience with standardized measurement.” Their promise is transparency, efficiency, accountability.
Muller began to study this when he became chair of his academic department. He thought his job was to nurture scholars and help students learn, only to find much of his time taken up with feeding often worthless data to remote administrators. He traces the metrical impulse, at root, to lack of trust. It’s not only doctors whom society doesn’t trust, but experts of all kinds.
Principal agents ... “employed in institutions are not to be trusted … their activity must be monitored and measured ... those measures need to be transparent to those without firsthand knowledge of the institutions ... and ... pecuniary rewards and punishments are the best way to motivate ‘agents.’ ”
What this analysis ignores, argues Muller, is that professionals respond not just to “extrinsic motivation[s]” (money) but to intrinsic ones: commitment to profession and clients, doing the right thing, making people happier and better, being recognized and honored by peers, doing interesting and stimulating work. When society denigrates and dismisses those considerations, professionals become demoralized. They leave, or they learn to game the system.
Muller gives many examples. Punish hospitals for readmissions within 30 days of discharge? Fine – readmit patients under “observation status” and call them outpatients. Dock hospitals for deaths within 30 days of leaving? Keep the respirator on for an extra day, and let the patient die on day 31. Risky case? Don’t operate. “Juking the stats” – arresting many small-fry drug pushers instead of focusing on the kingpins. Does U.S. News and World Report rank a college higher for classes with under 20 students? Schedule seminars with a maximum of 19. (My example, not Muller’s.) Teach to the MCAS (unless, like Marty, you decide that’s hopeless and just quit). Buff the numbers.
You know the drill. And if you need to learn it to succeed – or not be judged a failure – you’ll learn it.
Studies show that “pay for performance” often doesn’t work. Metric advocates ignore these and call for more studies. In Muller’s words, “Metric fixation, which aspires to imitate science, too often resembles faith.”
Muller argues with balance and nuance. He affirms that objective measurement has helped sweep away old dogmas no one had ever tested and culled markedly substandard teachers. But he shows that over the past 30 years just counting what you know how to count, counting things that cannot be counted, and privileging belief over disconfirming evidence has conferred on metrics “elements of a cult,” whose baleful effects doctors and others toiling in their professional vineyards know too well.
Faith in metrics will wane and its cult will pass away, though likely well after we have done so ourselves. At some point, so-called situated knowledge – what people who actually do something know – will again be valued.
In the meantime, please rate this column highly (give it a 6 on a scale of 1-5), and confirm that there are no barriers to your implementing its wisdom, which comes unsullied by any financial conflicts of interest.
And check out Muller’s book. You have nothing to lose but your chains.
Measurement without meaning is tyranny!
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
“How come you retired?” I asked.
A few years my junior, Marty had taught in public school forever. “It was the MCAS,” he said. That’s the Massachusetts Comprehensive Assessment System, a standardized test meant to gauge student performance and teacher competence.
“They demanded that my students test at a fifth-grade level,” Marty said. “But they were all at a second-grade level.
“Plus, I had been teaching for thirty years, and some kid right out of college was telling me how to do my job. So I left.”
Of course, this tale will sound familiar to physicians. Pay for performance. Bean counters calling the shots. Dismissal of clinical experience as useless and self-serving.
A recent book lays it all out: Jerry Z. Muller’s The Tyranny of Metrics. This book is punchy, witty, and succinct – you can read it in a day. A historian of economics and culture, Muller shows the extent of what I had guessed at from chats with people in different fields. In all of these, if you don’t count it, it doesn’t count.
Metrics, it is assumed, are “hard” and “objective.” They must “replace judgment based on experience with standardized measurement.” Their promise is transparency, efficiency, accountability.
Muller began to study this when he became chair of his academic department. He thought his job was to nurture scholars and help students learn, only to find much of his time taken up with feeding often worthless data to remote administrators. He traces the metrical impulse, at root, to lack of trust. It’s not only doctors whom society doesn’t trust, but experts of all kinds.
Principal agents ... “employed in institutions are not to be trusted … their activity must be monitored and measured ... those measures need to be transparent to those without firsthand knowledge of the institutions ... and ... pecuniary rewards and punishments are the best way to motivate ‘agents.’ ”
What this analysis ignores, argues Muller, is that professionals respond not just to “extrinsic motivation[s]” (money) but to intrinsic ones: commitment to profession and clients, doing the right thing, making people happier and better, being recognized and honored by peers, doing interesting and stimulating work. When society denigrates and dismisses those considerations, professionals become demoralized. They leave, or they learn to game the system.
Muller gives many examples. Punish hospitals for readmissions within 30 days of discharge? Fine – readmit patients under “observation status” and call them outpatients. Dock hospitals for deaths within 30 days of leaving? Keep the respirator on for an extra day, and let the patient die on day 31. Risky case? Don’t operate. “Juking the stats” – arresting many small-fry drug pushers instead of focusing on the kingpins. Does U.S. News and World Report rank a college higher for classes with under 20 students? Schedule seminars with a maximum of 19. (My example, not Muller’s.) Teach to the MCAS (unless, like Marty, you decide that’s hopeless and just quit). Buff the numbers.
You know the drill. And if you need to learn it to succeed – or not be judged a failure – you’ll learn it.
Studies show that “pay for performance” often doesn’t work. Metric advocates ignore these and call for more studies. In Muller’s words, “Metric fixation, which aspires to imitate science, too often resembles faith.”
Muller argues with balance and nuance. He affirms that objective measurement has helped sweep away old dogmas no one had ever tested and culled markedly substandard teachers. But he shows that over the past 30 years just counting what you know how to count, counting things that cannot be counted, and privileging belief over disconfirming evidence has conferred on metrics “elements of a cult,” whose baleful effects doctors and others toiling in their professional vineyards know too well.
Faith in metrics will wane and its cult will pass away, though likely well after we have done so ourselves. At some point, so-called situated knowledge – what people who actually do something know – will again be valued.
In the meantime, please rate this column highly (give it a 6 on a scale of 1-5), and confirm that there are no barriers to your implementing its wisdom, which comes unsullied by any financial conflicts of interest.
And check out Muller’s book. You have nothing to lose but your chains.
Measurement without meaning is tyranny!
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
“How come you retired?” I asked.
A few years my junior, Marty had taught in public school forever. “It was the MCAS,” he said. That’s the Massachusetts Comprehensive Assessment System, a standardized test meant to gauge student performance and teacher competence.
“They demanded that my students test at a fifth-grade level,” Marty said. “But they were all at a second-grade level.
“Plus, I had been teaching for thirty years, and some kid right out of college was telling me how to do my job. So I left.”
Of course, this tale will sound familiar to physicians. Pay for performance. Bean counters calling the shots. Dismissal of clinical experience as useless and self-serving.
A recent book lays it all out: Jerry Z. Muller’s The Tyranny of Metrics. This book is punchy, witty, and succinct – you can read it in a day. A historian of economics and culture, Muller shows the extent of what I had guessed at from chats with people in different fields. In all of these, if you don’t count it, it doesn’t count.
Metrics, it is assumed, are “hard” and “objective.” They must “replace judgment based on experience with standardized measurement.” Their promise is transparency, efficiency, accountability.
Muller began to study this when he became chair of his academic department. He thought his job was to nurture scholars and help students learn, only to find much of his time taken up with feeding often worthless data to remote administrators. He traces the metrical impulse, at root, to lack of trust. It’s not only doctors whom society doesn’t trust, but experts of all kinds.
Principal agents ... “employed in institutions are not to be trusted … their activity must be monitored and measured ... those measures need to be transparent to those without firsthand knowledge of the institutions ... and ... pecuniary rewards and punishments are the best way to motivate ‘agents.’ ”
What this analysis ignores, argues Muller, is that professionals respond not just to “extrinsic motivation[s]” (money) but to intrinsic ones: commitment to profession and clients, doing the right thing, making people happier and better, being recognized and honored by peers, doing interesting and stimulating work. When society denigrates and dismisses those considerations, professionals become demoralized. They leave, or they learn to game the system.
Muller gives many examples. Punish hospitals for readmissions within 30 days of discharge? Fine – readmit patients under “observation status” and call them outpatients. Dock hospitals for deaths within 30 days of leaving? Keep the respirator on for an extra day, and let the patient die on day 31. Risky case? Don’t operate. “Juking the stats” – arresting many small-fry drug pushers instead of focusing on the kingpins. Does U.S. News and World Report rank a college higher for classes with under 20 students? Schedule seminars with a maximum of 19. (My example, not Muller’s.) Teach to the MCAS (unless, like Marty, you decide that’s hopeless and just quit). Buff the numbers.
You know the drill. And if you need to learn it to succeed – or not be judged a failure – you’ll learn it.
Studies show that “pay for performance” often doesn’t work. Metric advocates ignore these and call for more studies. In Muller’s words, “Metric fixation, which aspires to imitate science, too often resembles faith.”
Muller argues with balance and nuance. He affirms that objective measurement has helped sweep away old dogmas no one had ever tested and culled markedly substandard teachers. But he shows that over the past 30 years just counting what you know how to count, counting things that cannot be counted, and privileging belief over disconfirming evidence has conferred on metrics “elements of a cult,” whose baleful effects doctors and others toiling in their professional vineyards know too well.
Faith in metrics will wane and its cult will pass away, though likely well after we have done so ourselves. At some point, so-called situated knowledge – what people who actually do something know – will again be valued.
In the meantime, please rate this column highly (give it a 6 on a scale of 1-5), and confirm that there are no barriers to your implementing its wisdom, which comes unsullied by any financial conflicts of interest.
And check out Muller’s book. You have nothing to lose but your chains.
Measurement without meaning is tyranny!
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
A shutdown, a lawsuit, and drug prices
As I write this editorial, regarding maintenance of certification. Being a doctor, these days, is neither easy nor relaxing.
The government shutdown is cheered by some, but it has real consequences for 800,000 government workers who are not getting paid, and our scientific community, where grant applications, hiring, data collection, and other critical roles of government are needed, is at a standstill. The class action suit against ABIM is the latest action of physicians telling the ABIM that enough is enough. Read more and form your opinion from our page one article. The ACA continues to be attacked in a variety of ways. To those who want to abolish it, please have a reasonable alternative in place so that real people with real diseases are not left in a desperate situation.
Drug prices continue to make news. The most recent example is the enormous increase in the cost of insulin. I read a lot about the inner workings of the pharmaceutical industry and cannot fathom how such prices are justified. Perhaps we physicians and our medical societies should consider raising our voices for our patients.
In this month’s issue there are several articles about polyp detection and the long-term protective effect of colonoscopy. We are doing really important and excellent work to reduce the burden of colon cancer.
As a heads up, Digestive Disease Week® (DDW) returns to San Diego this year. Housing choices are opening up and in San Diego fill rapidly; visit www.DDW.org/registration for more information. This year’s science is ground-breaking and will continue to advance our knowledge about IBD, the microbiome, and other important topics.
John I. Allen, MD, MBA, AGAF
Editor in Chief
As I write this editorial, regarding maintenance of certification. Being a doctor, these days, is neither easy nor relaxing.
The government shutdown is cheered by some, but it has real consequences for 800,000 government workers who are not getting paid, and our scientific community, where grant applications, hiring, data collection, and other critical roles of government are needed, is at a standstill. The class action suit against ABIM is the latest action of physicians telling the ABIM that enough is enough. Read more and form your opinion from our page one article. The ACA continues to be attacked in a variety of ways. To those who want to abolish it, please have a reasonable alternative in place so that real people with real diseases are not left in a desperate situation.
Drug prices continue to make news. The most recent example is the enormous increase in the cost of insulin. I read a lot about the inner workings of the pharmaceutical industry and cannot fathom how such prices are justified. Perhaps we physicians and our medical societies should consider raising our voices for our patients.
In this month’s issue there are several articles about polyp detection and the long-term protective effect of colonoscopy. We are doing really important and excellent work to reduce the burden of colon cancer.
As a heads up, Digestive Disease Week® (DDW) returns to San Diego this year. Housing choices are opening up and in San Diego fill rapidly; visit www.DDW.org/registration for more information. This year’s science is ground-breaking and will continue to advance our knowledge about IBD, the microbiome, and other important topics.
John I. Allen, MD, MBA, AGAF
Editor in Chief
As I write this editorial, regarding maintenance of certification. Being a doctor, these days, is neither easy nor relaxing.
The government shutdown is cheered by some, but it has real consequences for 800,000 government workers who are not getting paid, and our scientific community, where grant applications, hiring, data collection, and other critical roles of government are needed, is at a standstill. The class action suit against ABIM is the latest action of physicians telling the ABIM that enough is enough. Read more and form your opinion from our page one article. The ACA continues to be attacked in a variety of ways. To those who want to abolish it, please have a reasonable alternative in place so that real people with real diseases are not left in a desperate situation.
Drug prices continue to make news. The most recent example is the enormous increase in the cost of insulin. I read a lot about the inner workings of the pharmaceutical industry and cannot fathom how such prices are justified. Perhaps we physicians and our medical societies should consider raising our voices for our patients.
In this month’s issue there are several articles about polyp detection and the long-term protective effect of colonoscopy. We are doing really important and excellent work to reduce the burden of colon cancer.
As a heads up, Digestive Disease Week® (DDW) returns to San Diego this year. Housing choices are opening up and in San Diego fill rapidly; visit www.DDW.org/registration for more information. This year’s science is ground-breaking and will continue to advance our knowledge about IBD, the microbiome, and other important topics.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Understanding the terminology of gender identity
Use vocabulary to reduce barriers
TRANSforming Gynecology is a column about the ways in which ob.gyns. can become leaders in addressing the needs of the transgender/gender-nonconforming population. We hope to provide readers with some basic tools to help open the door to this marginalized population. We will lay the groundwork with an article on terminology and the importance of language before moving onto more focused discussions of topics that intersect with medical care of gender-nonconforming individuals. Transgender individuals experience among the worst health care outcomes of any demographic, and we hope that this column can be a starting point for providers to continue affirming the needs of marginalized populations in their everyday practice.

We live in a society in which most people’s gender identities are congruent with the sex they were assigned at birth based on physical characteristics. Transgender and gender-nonconforming people – often referred to as trans people, broadly – feel that their gender identity does not match their sex assigned at birth. This gender nonconformity, or the extent to which someone’s gender identity or expression differs from the cultural norm assigned to people with certain sexual organs, is in fact a matter of diversity, not pathology.
To truly provide sensitive care to trans patients, medical providers must first gain familiarity with the terminology used when discussing gender diversity. Gender identity, for starters, refers to an individual’s own personal and internal experience of themselves as a man, woman, some of both, or neither gender.1 It is only possible to learn a person’s gender identity through direct communication because gender identity is not always signaled by a certain gender expression. Gender expression is an external display usually through clothing, attitudes, or body language, that may or may not fit into socially recognized masculine or feminine categories.1 A separate aspect of the human experience is sexuality, such as gay, straight, bisexual, lesbian, etc. Sexuality should not be confused with sexual practices, which can sometimes deviate from a person’s sexuality. Gender identity is distinct from sexuality and sexual practices because people of any gender identity can hold any sexuality and engage in any sexual practices. Tied up in all of these categories is sex assigned at birth, which is a process by which health care providers categorize babies into two buckets based on the appearance of the external genitalia at the time of birth. It bears mentioning that the assignment of sex based on the appearance of external genitalia at the time of birth is a biologically inconsistent method that can lead to the exclusion of and nonconsensual mutilation of intersex people, who are individuals born with ambiguous genitalia and/or discrepancies between sex chromosome genotype and phenotype (stay tuned for more on people who are intersex in a future article).
A simplified way of remembering the distinctions between these concepts is that gender identity is who you go to bed as; gender expression is what you were wearing before you went to bed; sexuality is whom you tell others/yourself you go to bed with; sexual practice is whom you actually go to bed with; and sex assigned at birth is what you have between your legs when you are born (generally in a bed).
While cisgender persons feel that their experience of gender – their gender identity – agrees with the cultural norms surrounding their sex assigned at birth, transgender/gender-nonconforming (GNC) persons feel that their experience of gender is incongruent with their sex assigned at birth.1 Specifically, a transgender man is a person born with a vagina and therefore assigned female at birth who experiences himself as a man. A transgender woman is a person born with a penis and therefore assigned male at birth who experiences herself as a woman. A gender nonbinary person is someone with any sexual assignment at birth whose gender experience cannot be described using a binary that includes only male and female concepts, and a gender fluid person is someone whose internal experience of gender can oscillate.1 While these examples represent only a few of the many facets of gender diversity, the general terms trans and gender nonconforming (GNC) are widely accepted as inclusive, umbrella terms to describe all persons whose experience of gender is not congruent with their sex assigned at birth.
It is pivotal that medical providers understand that a person’s sex assigned at birth, gender identity, gender expression, sexuality, sexual practice, and romantic attraction can vary widely along a spectrum in each distinct category.2 For example, the current social norm dictates that someone born with a penis and assigned male at birth (AMAB) will feel that he is male, dress in a masculine fashion, and be both sexually and romantically attracted to someone born with a vagina who was assigned female at birth (AFAB), feels that she is female, dresses femininely, and likewise is sexually and romantically attracted to him. One possible alternative reality is a person who was born with a vagina that was therefore AFAB that experiences a masculine gender identity while engaging in a feminine gender expression in order to conform to social norms. In addition, they may be sexually attracted to people whom they perceive to be feminine while engaging in sexual activity with people who were AMAB. Informed medical care for trans persons starts with the basic understanding that an individual’s gender identity may not necessarily align with their gender expression, sex assigned at birth, sexual attraction, or romantic attraction.
As obstetrician-gynecologists, we are tasked by the American College of Obstetricians and Gynecologists to provide nondiscriminatory care to all patients, regardless of gender identity.3 We must be careful not to assume that all of our patients are cisgender women who use “she/hers/her” pronouns. By simply asking patients what names or pronouns they would like us to use before initiating care, we become more sensitive to variations in gender identity. Many providers may feel uncertain about how to initiate or respond to this line of questioning. One way that health care practices can begin to respectfully access information around gender identity is to create intake forms that include more than two options for gender or to alter their office visit note templates to include a section that prompts the provider to include a discussion surrounding gender identity. By offering these opportunities for inclusion, we become more welcoming of gender minorities like transgender men seeking cervical cancer screening.
There are a number of reasons that trans persons have limited access to the health care system, but the greatest barrier reported by transgender patients is the paucity of knowledgeable providers.4 to an already marginalized patient population. Familiarity with this terminology normalizes the idea of gender diversity and subsequently reduces the risk of providers making assumptions about patients that contributes to suboptimal care.
Dr. Joyner is an assistant professor at Emory University, Atlanta, and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Joey Bahng is a PGY-1 resident physician in Emory University’s gynecology & obstetrics residency program. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner and Dr. Bahng reported no financial disclosures.
1. Lancet. 2016 Jul 23;388(10042):390-400.
2. www.genderbread.org/resource/genderbread-person-v4-0.
3. Obstet Gynecol. 2011 Dec;118(6):1454-8.
4. Curr Opin Endocrinol Diabetes Obes. 2016 Apr 1;23(2):168-71.
Use vocabulary to reduce barriers
Use vocabulary to reduce barriers
TRANSforming Gynecology is a column about the ways in which ob.gyns. can become leaders in addressing the needs of the transgender/gender-nonconforming population. We hope to provide readers with some basic tools to help open the door to this marginalized population. We will lay the groundwork with an article on terminology and the importance of language before moving onto more focused discussions of topics that intersect with medical care of gender-nonconforming individuals. Transgender individuals experience among the worst health care outcomes of any demographic, and we hope that this column can be a starting point for providers to continue affirming the needs of marginalized populations in their everyday practice.

We live in a society in which most people’s gender identities are congruent with the sex they were assigned at birth based on physical characteristics. Transgender and gender-nonconforming people – often referred to as trans people, broadly – feel that their gender identity does not match their sex assigned at birth. This gender nonconformity, or the extent to which someone’s gender identity or expression differs from the cultural norm assigned to people with certain sexual organs, is in fact a matter of diversity, not pathology.
To truly provide sensitive care to trans patients, medical providers must first gain familiarity with the terminology used when discussing gender diversity. Gender identity, for starters, refers to an individual’s own personal and internal experience of themselves as a man, woman, some of both, or neither gender.1 It is only possible to learn a person’s gender identity through direct communication because gender identity is not always signaled by a certain gender expression. Gender expression is an external display usually through clothing, attitudes, or body language, that may or may not fit into socially recognized masculine or feminine categories.1 A separate aspect of the human experience is sexuality, such as gay, straight, bisexual, lesbian, etc. Sexuality should not be confused with sexual practices, which can sometimes deviate from a person’s sexuality. Gender identity is distinct from sexuality and sexual practices because people of any gender identity can hold any sexuality and engage in any sexual practices. Tied up in all of these categories is sex assigned at birth, which is a process by which health care providers categorize babies into two buckets based on the appearance of the external genitalia at the time of birth. It bears mentioning that the assignment of sex based on the appearance of external genitalia at the time of birth is a biologically inconsistent method that can lead to the exclusion of and nonconsensual mutilation of intersex people, who are individuals born with ambiguous genitalia and/or discrepancies between sex chromosome genotype and phenotype (stay tuned for more on people who are intersex in a future article).
A simplified way of remembering the distinctions between these concepts is that gender identity is who you go to bed as; gender expression is what you were wearing before you went to bed; sexuality is whom you tell others/yourself you go to bed with; sexual practice is whom you actually go to bed with; and sex assigned at birth is what you have between your legs when you are born (generally in a bed).
While cisgender persons feel that their experience of gender – their gender identity – agrees with the cultural norms surrounding their sex assigned at birth, transgender/gender-nonconforming (GNC) persons feel that their experience of gender is incongruent with their sex assigned at birth.1 Specifically, a transgender man is a person born with a vagina and therefore assigned female at birth who experiences himself as a man. A transgender woman is a person born with a penis and therefore assigned male at birth who experiences herself as a woman. A gender nonbinary person is someone with any sexual assignment at birth whose gender experience cannot be described using a binary that includes only male and female concepts, and a gender fluid person is someone whose internal experience of gender can oscillate.1 While these examples represent only a few of the many facets of gender diversity, the general terms trans and gender nonconforming (GNC) are widely accepted as inclusive, umbrella terms to describe all persons whose experience of gender is not congruent with their sex assigned at birth.
It is pivotal that medical providers understand that a person’s sex assigned at birth, gender identity, gender expression, sexuality, sexual practice, and romantic attraction can vary widely along a spectrum in each distinct category.2 For example, the current social norm dictates that someone born with a penis and assigned male at birth (AMAB) will feel that he is male, dress in a masculine fashion, and be both sexually and romantically attracted to someone born with a vagina who was assigned female at birth (AFAB), feels that she is female, dresses femininely, and likewise is sexually and romantically attracted to him. One possible alternative reality is a person who was born with a vagina that was therefore AFAB that experiences a masculine gender identity while engaging in a feminine gender expression in order to conform to social norms. In addition, they may be sexually attracted to people whom they perceive to be feminine while engaging in sexual activity with people who were AMAB. Informed medical care for trans persons starts with the basic understanding that an individual’s gender identity may not necessarily align with their gender expression, sex assigned at birth, sexual attraction, or romantic attraction.
As obstetrician-gynecologists, we are tasked by the American College of Obstetricians and Gynecologists to provide nondiscriminatory care to all patients, regardless of gender identity.3 We must be careful not to assume that all of our patients are cisgender women who use “she/hers/her” pronouns. By simply asking patients what names or pronouns they would like us to use before initiating care, we become more sensitive to variations in gender identity. Many providers may feel uncertain about how to initiate or respond to this line of questioning. One way that health care practices can begin to respectfully access information around gender identity is to create intake forms that include more than two options for gender or to alter their office visit note templates to include a section that prompts the provider to include a discussion surrounding gender identity. By offering these opportunities for inclusion, we become more welcoming of gender minorities like transgender men seeking cervical cancer screening.
There are a number of reasons that trans persons have limited access to the health care system, but the greatest barrier reported by transgender patients is the paucity of knowledgeable providers.4 to an already marginalized patient population. Familiarity with this terminology normalizes the idea of gender diversity and subsequently reduces the risk of providers making assumptions about patients that contributes to suboptimal care.
Dr. Joyner is an assistant professor at Emory University, Atlanta, and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Joey Bahng is a PGY-1 resident physician in Emory University’s gynecology & obstetrics residency program. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner and Dr. Bahng reported no financial disclosures.
1. Lancet. 2016 Jul 23;388(10042):390-400.
2. www.genderbread.org/resource/genderbread-person-v4-0.
3. Obstet Gynecol. 2011 Dec;118(6):1454-8.
4. Curr Opin Endocrinol Diabetes Obes. 2016 Apr 1;23(2):168-71.
TRANSforming Gynecology is a column about the ways in which ob.gyns. can become leaders in addressing the needs of the transgender/gender-nonconforming population. We hope to provide readers with some basic tools to help open the door to this marginalized population. We will lay the groundwork with an article on terminology and the importance of language before moving onto more focused discussions of topics that intersect with medical care of gender-nonconforming individuals. Transgender individuals experience among the worst health care outcomes of any demographic, and we hope that this column can be a starting point for providers to continue affirming the needs of marginalized populations in their everyday practice.

We live in a society in which most people’s gender identities are congruent with the sex they were assigned at birth based on physical characteristics. Transgender and gender-nonconforming people – often referred to as trans people, broadly – feel that their gender identity does not match their sex assigned at birth. This gender nonconformity, or the extent to which someone’s gender identity or expression differs from the cultural norm assigned to people with certain sexual organs, is in fact a matter of diversity, not pathology.
To truly provide sensitive care to trans patients, medical providers must first gain familiarity with the terminology used when discussing gender diversity. Gender identity, for starters, refers to an individual’s own personal and internal experience of themselves as a man, woman, some of both, or neither gender.1 It is only possible to learn a person’s gender identity through direct communication because gender identity is not always signaled by a certain gender expression. Gender expression is an external display usually through clothing, attitudes, or body language, that may or may not fit into socially recognized masculine or feminine categories.1 A separate aspect of the human experience is sexuality, such as gay, straight, bisexual, lesbian, etc. Sexuality should not be confused with sexual practices, which can sometimes deviate from a person’s sexuality. Gender identity is distinct from sexuality and sexual practices because people of any gender identity can hold any sexuality and engage in any sexual practices. Tied up in all of these categories is sex assigned at birth, which is a process by which health care providers categorize babies into two buckets based on the appearance of the external genitalia at the time of birth. It bears mentioning that the assignment of sex based on the appearance of external genitalia at the time of birth is a biologically inconsistent method that can lead to the exclusion of and nonconsensual mutilation of intersex people, who are individuals born with ambiguous genitalia and/or discrepancies between sex chromosome genotype and phenotype (stay tuned for more on people who are intersex in a future article).
A simplified way of remembering the distinctions between these concepts is that gender identity is who you go to bed as; gender expression is what you were wearing before you went to bed; sexuality is whom you tell others/yourself you go to bed with; sexual practice is whom you actually go to bed with; and sex assigned at birth is what you have between your legs when you are born (generally in a bed).
While cisgender persons feel that their experience of gender – their gender identity – agrees with the cultural norms surrounding their sex assigned at birth, transgender/gender-nonconforming (GNC) persons feel that their experience of gender is incongruent with their sex assigned at birth.1 Specifically, a transgender man is a person born with a vagina and therefore assigned female at birth who experiences himself as a man. A transgender woman is a person born with a penis and therefore assigned male at birth who experiences herself as a woman. A gender nonbinary person is someone with any sexual assignment at birth whose gender experience cannot be described using a binary that includes only male and female concepts, and a gender fluid person is someone whose internal experience of gender can oscillate.1 While these examples represent only a few of the many facets of gender diversity, the general terms trans and gender nonconforming (GNC) are widely accepted as inclusive, umbrella terms to describe all persons whose experience of gender is not congruent with their sex assigned at birth.
It is pivotal that medical providers understand that a person’s sex assigned at birth, gender identity, gender expression, sexuality, sexual practice, and romantic attraction can vary widely along a spectrum in each distinct category.2 For example, the current social norm dictates that someone born with a penis and assigned male at birth (AMAB) will feel that he is male, dress in a masculine fashion, and be both sexually and romantically attracted to someone born with a vagina who was assigned female at birth (AFAB), feels that she is female, dresses femininely, and likewise is sexually and romantically attracted to him. One possible alternative reality is a person who was born with a vagina that was therefore AFAB that experiences a masculine gender identity while engaging in a feminine gender expression in order to conform to social norms. In addition, they may be sexually attracted to people whom they perceive to be feminine while engaging in sexual activity with people who were AMAB. Informed medical care for trans persons starts with the basic understanding that an individual’s gender identity may not necessarily align with their gender expression, sex assigned at birth, sexual attraction, or romantic attraction.
As obstetrician-gynecologists, we are tasked by the American College of Obstetricians and Gynecologists to provide nondiscriminatory care to all patients, regardless of gender identity.3 We must be careful not to assume that all of our patients are cisgender women who use “she/hers/her” pronouns. By simply asking patients what names or pronouns they would like us to use before initiating care, we become more sensitive to variations in gender identity. Many providers may feel uncertain about how to initiate or respond to this line of questioning. One way that health care practices can begin to respectfully access information around gender identity is to create intake forms that include more than two options for gender or to alter their office visit note templates to include a section that prompts the provider to include a discussion surrounding gender identity. By offering these opportunities for inclusion, we become more welcoming of gender minorities like transgender men seeking cervical cancer screening.
There are a number of reasons that trans persons have limited access to the health care system, but the greatest barrier reported by transgender patients is the paucity of knowledgeable providers.4 to an already marginalized patient population. Familiarity with this terminology normalizes the idea of gender diversity and subsequently reduces the risk of providers making assumptions about patients that contributes to suboptimal care.
Dr. Joyner is an assistant professor at Emory University, Atlanta, and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Joey Bahng is a PGY-1 resident physician in Emory University’s gynecology & obstetrics residency program. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner and Dr. Bahng reported no financial disclosures.
1. Lancet. 2016 Jul 23;388(10042):390-400.
2. www.genderbread.org/resource/genderbread-person-v4-0.
3. Obstet Gynecol. 2011 Dec;118(6):1454-8.
4. Curr Opin Endocrinol Diabetes Obes. 2016 Apr 1;23(2):168-71.
Speaking in code
If you live in Spokane, Wash., 99213 and 99214 are important numbers. Interchanging the last two digits can send your mail into the Twilight Zone. Otherwise those five digit sequences have little significance to most Americans ... unless of course you are a physician. You have been told multiple times by practice administrators and business consultants that the failure to attach the proper sequence to your bill for services can threaten the sustainability of your practice’s bottom line or put you at risk for a costly fine.
Numerical codes for office visits were not handed down on stone tablets. There was a time when a physician simply charged for something he called an “office visit” and about half that for a “short” office visit that took less time and probably nothing for a “quick recheck.” He chose the fees based on what he felt was reasonable. I remember reading of one physician who pegged his charges at a dollar per penny of the cost of a regular postage stamp. For a variety of obvious and some unfortunate reasons, these loosely structured fee structures have disappeared.
Now a physician is asked to justify his or her charges by documenting what transpired during the office visit. The patient always has been the best witness, and at least has some sense of how much work the physician has had to do to arrive at diagnosis and suggest a treatment plan. Because the patient usually was paying the bill and had a personal stake in the value of the services provided, this system seemed to make sense.
However, now some large corporate entity or government agency probably is paying the bill and would like some idea of what it is being billed for. Justifying the service provided now falls on the physician. When the billing codes were first introduced and before the payers became more curious, it was easy. I simply applied 99213 to all my office visits and once or twice a day I would code out a visit that seemed more complex as a 99214. I wasn’t keeping track of how many minutes I spent in each visit, how many questions I asked, or how many body parts I examined. Except for patients with injured extremities, everyone was pretty much getting the same exam. My coding was based on my perception of value and effort. If it took more time than usual to remove a bit of cerumen or reassure an unusually concerned parent I chalked that up as my misfortune, not a reason to code the visit as a 99214. If I felt I needed more money, I assumed that my best option was to see more patients. Neither the patients nor the payers seemed to be complaining.
But obviously somewhere someone felt that there were too many providers gaming the system and there needed to be a better way to assign value to what a physician was doing in his or her examining room. I don’t have a workable alternative. However, I always have felt that if the folks who were paying the bills would come visit my office (unannounced if they wish) and spend a morning watching me see patients, they could more accurately assign a value to my work. I’m not sure how many of you would be comfortable with that degree of transparency. But for me it would be worth it if it freed me from the burden of coding to justify my effort.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If you live in Spokane, Wash., 99213 and 99214 are important numbers. Interchanging the last two digits can send your mail into the Twilight Zone. Otherwise those five digit sequences have little significance to most Americans ... unless of course you are a physician. You have been told multiple times by practice administrators and business consultants that the failure to attach the proper sequence to your bill for services can threaten the sustainability of your practice’s bottom line or put you at risk for a costly fine.
Numerical codes for office visits were not handed down on stone tablets. There was a time when a physician simply charged for something he called an “office visit” and about half that for a “short” office visit that took less time and probably nothing for a “quick recheck.” He chose the fees based on what he felt was reasonable. I remember reading of one physician who pegged his charges at a dollar per penny of the cost of a regular postage stamp. For a variety of obvious and some unfortunate reasons, these loosely structured fee structures have disappeared.
Now a physician is asked to justify his or her charges by documenting what transpired during the office visit. The patient always has been the best witness, and at least has some sense of how much work the physician has had to do to arrive at diagnosis and suggest a treatment plan. Because the patient usually was paying the bill and had a personal stake in the value of the services provided, this system seemed to make sense.
However, now some large corporate entity or government agency probably is paying the bill and would like some idea of what it is being billed for. Justifying the service provided now falls on the physician. When the billing codes were first introduced and before the payers became more curious, it was easy. I simply applied 99213 to all my office visits and once or twice a day I would code out a visit that seemed more complex as a 99214. I wasn’t keeping track of how many minutes I spent in each visit, how many questions I asked, or how many body parts I examined. Except for patients with injured extremities, everyone was pretty much getting the same exam. My coding was based on my perception of value and effort. If it took more time than usual to remove a bit of cerumen or reassure an unusually concerned parent I chalked that up as my misfortune, not a reason to code the visit as a 99214. If I felt I needed more money, I assumed that my best option was to see more patients. Neither the patients nor the payers seemed to be complaining.
But obviously somewhere someone felt that there were too many providers gaming the system and there needed to be a better way to assign value to what a physician was doing in his or her examining room. I don’t have a workable alternative. However, I always have felt that if the folks who were paying the bills would come visit my office (unannounced if they wish) and spend a morning watching me see patients, they could more accurately assign a value to my work. I’m not sure how many of you would be comfortable with that degree of transparency. But for me it would be worth it if it freed me from the burden of coding to justify my effort.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If you live in Spokane, Wash., 99213 and 99214 are important numbers. Interchanging the last two digits can send your mail into the Twilight Zone. Otherwise those five digit sequences have little significance to most Americans ... unless of course you are a physician. You have been told multiple times by practice administrators and business consultants that the failure to attach the proper sequence to your bill for services can threaten the sustainability of your practice’s bottom line or put you at risk for a costly fine.
Numerical codes for office visits were not handed down on stone tablets. There was a time when a physician simply charged for something he called an “office visit” and about half that for a “short” office visit that took less time and probably nothing for a “quick recheck.” He chose the fees based on what he felt was reasonable. I remember reading of one physician who pegged his charges at a dollar per penny of the cost of a regular postage stamp. For a variety of obvious and some unfortunate reasons, these loosely structured fee structures have disappeared.
Now a physician is asked to justify his or her charges by documenting what transpired during the office visit. The patient always has been the best witness, and at least has some sense of how much work the physician has had to do to arrive at diagnosis and suggest a treatment plan. Because the patient usually was paying the bill and had a personal stake in the value of the services provided, this system seemed to make sense.
However, now some large corporate entity or government agency probably is paying the bill and would like some idea of what it is being billed for. Justifying the service provided now falls on the physician. When the billing codes were first introduced and before the payers became more curious, it was easy. I simply applied 99213 to all my office visits and once or twice a day I would code out a visit that seemed more complex as a 99214. I wasn’t keeping track of how many minutes I spent in each visit, how many questions I asked, or how many body parts I examined. Except for patients with injured extremities, everyone was pretty much getting the same exam. My coding was based on my perception of value and effort. If it took more time than usual to remove a bit of cerumen or reassure an unusually concerned parent I chalked that up as my misfortune, not a reason to code the visit as a 99214. If I felt I needed more money, I assumed that my best option was to see more patients. Neither the patients nor the payers seemed to be complaining.
But obviously somewhere someone felt that there were too many providers gaming the system and there needed to be a better way to assign value to what a physician was doing in his or her examining room. I don’t have a workable alternative. However, I always have felt that if the folks who were paying the bills would come visit my office (unannounced if they wish) and spend a morning watching me see patients, they could more accurately assign a value to my work. I’m not sure how many of you would be comfortable with that degree of transparency. But for me it would be worth it if it freed me from the burden of coding to justify my effort.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].