User login
Physician value thyself!
The Merriam-Webster dictionary defines value as “the regard that something is held to deserve; the importance, worth, or usefulness of something” and “relative worth, utility, or importance.” We usually assess our professional worth by how we are treated at work. In social valuing framework, we are given social status based on how others regard us for who we are, what we do, and what we are worth. This is described as “felt worth,” which encapsulates our feelings about how we are regarded by others, in contrast to self-esteem, which is more of an internally held belief.
Our power came from our relationship with our patients and our ability to communicate and influence our patients, peers and administrators. As owners of our practices and small businesses, our currency with hospitals and lawmakers was our ability to bring revenue to hospitals and patient concerns directly to legislators. Practicing in more than one hospital made us more valuable and hospitals battled with each other to provide us and our patients the latest tools and conveniences. In return, we gave our valuable time freely without compensation to hospitals as committee members, task force members, and sounding boards for the betterment of the community. If I were a conspiracy theorist, which I am not, and wanted to devalue physicians I would seek to weaken the physician-patient bond. The way to implement this would be for a single hospital employer to put us on a treadmill chasing work relative value units, give us hard-to-accomplish goals, and keep moving the goalpost. Like I said, I do not believe in conspiracies.
The tsunami of byzantine regulations, Stark laws, and complicated reimbursement formulas has sapped our energy to counter the devaluation. Some are glad to see physicians, particularly surgeons, get their comeuppance because we are perceived as having large egos. This may be true in some instances. Yet, it turns out that the top three job titles with the largest egos are: private household cooks, chief executives, and farm and ranch managers.1
Physicians are also reputed to be possessing dominant leadership styles and seen as bossy and disruptive. Hence, we are made to have frequent training in how to ameliorate our disruptive behavior tendencies. Again, this may be true in a few cases. However, while reports mention how many people witness such unacceptable behavior, there is no valid data about the incidence in practicing physicians. Research also does not support the view that physicians have dominant and aggressive personalities leading to such behavior.
One of the leading interpersonal skills model is Social Styles. We happen to teach this to our faculty at the Ohio State Medical Center’s Faculty Leadership Institute. Turns out that physicians and nurses are almost equally placed into the four quadrants of leadership styles: driving, expressive, amiable, and analytical. I found similar findings in our society members participating in a leadership session I moderated. Indeed, we rank very high on “versatility,” a measure that enables us to adapt our behaviors to fit with our patients and coworkers.
Reported burnout rates of 50% in physicians may or may not be accurate, but burnout is real and so is depression and so are physician suicides. I have witnessed six physician suicides in my career thus far. Teaching resilience, celebrating doctor’s day, and giving out a few awards are all interventions after the fact. Preventive measures like employers and hospitals prioritizing removing daily obstacles eliminating meaningless work, providing more resources to deal with EMRs, and making our lives easier at work, so we can get to our loved ones sooner would help.
Physicians have been largely excluded themselves from participating in the health care debate. We want to see empirical evidence before we sign on to every new proposed care model. Otherwise, we cling on to the status quo and therefore, decision makers tend to leave us out. More important, value-based payment models have not thus far led to reduction in the cost of health care. Despite poor engagement scores at major health systems, physicians are “managed” and sidelined, and mandates are “done to them, not with them.”
In my 40-year career, our devaluation has been a slow and painful process. It started with being called a “provider.” This devalues me. Call me by what I am and do. Physician. Doctor. That is what our patients call us. But, we have been pushed to acquiesce. So, why do physicians undervalue themselves and are unable to be confident of their value to employers and hospital executives?
Some have theorized that physicians have low self-esteem and that denial and rationalization are simply defense mechanisms. The low self-esteem is traced back to medical student days and considered “posttraumatic” disorder. In one study of 189 medical students, 50% reported a decrease in their self-esteem/confidence. The students blamed their residents and attendings for this reaction. Some degree of intimidation may continue into training and employment where it may be part of the culture. We need to change this cycle and treat our students, residents, and mentees with respect as future peers.
Another aspect is related to our own well-being. Most physicians value their patient’s health more than their own. That concept is drilled into us throughout our life. Our spouses complain that we care more about our patients than we do for our families. We often ignore warning signs of serious issues in our own health, always downplaying textbook symptoms of burnout, depression, and even MI. Being too busy is a badge of honor to indicate how successful and wanted we are. This also needs to change.
Sheryl Sandberg in her book “Lean in” discusses the “tiara syndrome,” mainly referring to women. I would suggest that this applies to a lot of physicians, both men and women. Physicians tend to keep their heads down, work hard, and expect someone to come compliment them and place a “tiara” over their head. We may be wary of being called “self-promoters.” Sometimes it is cultural baggage for immigrant physicians who are taught to not brag about their accomplishments. It may behoove us to judiciously make peers and leadership aware of our positive activities in and outside the health system.
Some see physicians not as “pillars of any community,” but as “technicians on an assembly line” or “pawns in a money-making game for hospital administrators.” This degree of pessimism among physicians in surveys is well known but there is good news.
In a 2016 survey based upon responses by 17,236 physicians, 63% were pessimistic or very pessimistic about the medical profession, down from 77% in 2012.2 In another poll, medical doctors were rated as having very high or high ratings of honesty and ethical standards by 65%, higher than all except nurses, military officers, and grade school teachers.3 When the health care debate was at its peak in 2009, a public poll on who they trusted to recommend the right thing for reforming the healthcare system placed physicians at the very top (73%)ahead of health care professors, researchers, hospitals, the President, and politicians. Gallup surveyed 7,000 physicians about engagement in four hierarchical levels: Confidence, Integrity, Pride and Passion. Physicians scored highly on the Pride items in the survey (feel proud to work and being treated with respect).4 In other words, if we are treated well, we feel proud to tell others where we work.
Finally, like many I may consider myself an expert in all sorts of things not relevant to practicing medicine. Yet, I respectfully suggest we stay away from political hot potatoes like nuclear disarmament, gun control, climate change, immigration, and other controversial issues because they distract us from our primary mission. I would hate to see us viewed like Hollywood.
References
1. www.chicagotribune.com/business/ct-payscale-ego-survey-0830-biz-20160829-story.html
2. www.medpagetoday.com/primarycare/generalprimarycare/60446
3. https://nurse.org/articles/gallup-ethical-standards-poll-nurses-rank-highest/
4.https://news.gallup.com/poll/120890/healthcare-americans-trust-physicians-politicians.aspx
Bhagwan Satiani, MD, MBA, is professor of clinical surgery in the division of vascular diseases and surgery at Ohio State University, Columbus. He blogs at www.savvy-medicine.com . Reach him on Twitter @savvycutter.
The Merriam-Webster dictionary defines value as “the regard that something is held to deserve; the importance, worth, or usefulness of something” and “relative worth, utility, or importance.” We usually assess our professional worth by how we are treated at work. In social valuing framework, we are given social status based on how others regard us for who we are, what we do, and what we are worth. This is described as “felt worth,” which encapsulates our feelings about how we are regarded by others, in contrast to self-esteem, which is more of an internally held belief.
Our power came from our relationship with our patients and our ability to communicate and influence our patients, peers and administrators. As owners of our practices and small businesses, our currency with hospitals and lawmakers was our ability to bring revenue to hospitals and patient concerns directly to legislators. Practicing in more than one hospital made us more valuable and hospitals battled with each other to provide us and our patients the latest tools and conveniences. In return, we gave our valuable time freely without compensation to hospitals as committee members, task force members, and sounding boards for the betterment of the community. If I were a conspiracy theorist, which I am not, and wanted to devalue physicians I would seek to weaken the physician-patient bond. The way to implement this would be for a single hospital employer to put us on a treadmill chasing work relative value units, give us hard-to-accomplish goals, and keep moving the goalpost. Like I said, I do not believe in conspiracies.
The tsunami of byzantine regulations, Stark laws, and complicated reimbursement formulas has sapped our energy to counter the devaluation. Some are glad to see physicians, particularly surgeons, get their comeuppance because we are perceived as having large egos. This may be true in some instances. Yet, it turns out that the top three job titles with the largest egos are: private household cooks, chief executives, and farm and ranch managers.1
Physicians are also reputed to be possessing dominant leadership styles and seen as bossy and disruptive. Hence, we are made to have frequent training in how to ameliorate our disruptive behavior tendencies. Again, this may be true in a few cases. However, while reports mention how many people witness such unacceptable behavior, there is no valid data about the incidence in practicing physicians. Research also does not support the view that physicians have dominant and aggressive personalities leading to such behavior.
One of the leading interpersonal skills model is Social Styles. We happen to teach this to our faculty at the Ohio State Medical Center’s Faculty Leadership Institute. Turns out that physicians and nurses are almost equally placed into the four quadrants of leadership styles: driving, expressive, amiable, and analytical. I found similar findings in our society members participating in a leadership session I moderated. Indeed, we rank very high on “versatility,” a measure that enables us to adapt our behaviors to fit with our patients and coworkers.
Reported burnout rates of 50% in physicians may or may not be accurate, but burnout is real and so is depression and so are physician suicides. I have witnessed six physician suicides in my career thus far. Teaching resilience, celebrating doctor’s day, and giving out a few awards are all interventions after the fact. Preventive measures like employers and hospitals prioritizing removing daily obstacles eliminating meaningless work, providing more resources to deal with EMRs, and making our lives easier at work, so we can get to our loved ones sooner would help.
Physicians have been largely excluded themselves from participating in the health care debate. We want to see empirical evidence before we sign on to every new proposed care model. Otherwise, we cling on to the status quo and therefore, decision makers tend to leave us out. More important, value-based payment models have not thus far led to reduction in the cost of health care. Despite poor engagement scores at major health systems, physicians are “managed” and sidelined, and mandates are “done to them, not with them.”
In my 40-year career, our devaluation has been a slow and painful process. It started with being called a “provider.” This devalues me. Call me by what I am and do. Physician. Doctor. That is what our patients call us. But, we have been pushed to acquiesce. So, why do physicians undervalue themselves and are unable to be confident of their value to employers and hospital executives?
Some have theorized that physicians have low self-esteem and that denial and rationalization are simply defense mechanisms. The low self-esteem is traced back to medical student days and considered “posttraumatic” disorder. In one study of 189 medical students, 50% reported a decrease in their self-esteem/confidence. The students blamed their residents and attendings for this reaction. Some degree of intimidation may continue into training and employment where it may be part of the culture. We need to change this cycle and treat our students, residents, and mentees with respect as future peers.
Another aspect is related to our own well-being. Most physicians value their patient’s health more than their own. That concept is drilled into us throughout our life. Our spouses complain that we care more about our patients than we do for our families. We often ignore warning signs of serious issues in our own health, always downplaying textbook symptoms of burnout, depression, and even MI. Being too busy is a badge of honor to indicate how successful and wanted we are. This also needs to change.
Sheryl Sandberg in her book “Lean in” discusses the “tiara syndrome,” mainly referring to women. I would suggest that this applies to a lot of physicians, both men and women. Physicians tend to keep their heads down, work hard, and expect someone to come compliment them and place a “tiara” over their head. We may be wary of being called “self-promoters.” Sometimes it is cultural baggage for immigrant physicians who are taught to not brag about their accomplishments. It may behoove us to judiciously make peers and leadership aware of our positive activities in and outside the health system.
Some see physicians not as “pillars of any community,” but as “technicians on an assembly line” or “pawns in a money-making game for hospital administrators.” This degree of pessimism among physicians in surveys is well known but there is good news.
In a 2016 survey based upon responses by 17,236 physicians, 63% were pessimistic or very pessimistic about the medical profession, down from 77% in 2012.2 In another poll, medical doctors were rated as having very high or high ratings of honesty and ethical standards by 65%, higher than all except nurses, military officers, and grade school teachers.3 When the health care debate was at its peak in 2009, a public poll on who they trusted to recommend the right thing for reforming the healthcare system placed physicians at the very top (73%)ahead of health care professors, researchers, hospitals, the President, and politicians. Gallup surveyed 7,000 physicians about engagement in four hierarchical levels: Confidence, Integrity, Pride and Passion. Physicians scored highly on the Pride items in the survey (feel proud to work and being treated with respect).4 In other words, if we are treated well, we feel proud to tell others where we work.
Finally, like many I may consider myself an expert in all sorts of things not relevant to practicing medicine. Yet, I respectfully suggest we stay away from political hot potatoes like nuclear disarmament, gun control, climate change, immigration, and other controversial issues because they distract us from our primary mission. I would hate to see us viewed like Hollywood.
References
1. www.chicagotribune.com/business/ct-payscale-ego-survey-0830-biz-20160829-story.html
2. www.medpagetoday.com/primarycare/generalprimarycare/60446
3. https://nurse.org/articles/gallup-ethical-standards-poll-nurses-rank-highest/
4.https://news.gallup.com/poll/120890/healthcare-americans-trust-physicians-politicians.aspx
Bhagwan Satiani, MD, MBA, is professor of clinical surgery in the division of vascular diseases and surgery at Ohio State University, Columbus. He blogs at www.savvy-medicine.com . Reach him on Twitter @savvycutter.
The Merriam-Webster dictionary defines value as “the regard that something is held to deserve; the importance, worth, or usefulness of something” and “relative worth, utility, or importance.” We usually assess our professional worth by how we are treated at work. In social valuing framework, we are given social status based on how others regard us for who we are, what we do, and what we are worth. This is described as “felt worth,” which encapsulates our feelings about how we are regarded by others, in contrast to self-esteem, which is more of an internally held belief.
Our power came from our relationship with our patients and our ability to communicate and influence our patients, peers and administrators. As owners of our practices and small businesses, our currency with hospitals and lawmakers was our ability to bring revenue to hospitals and patient concerns directly to legislators. Practicing in more than one hospital made us more valuable and hospitals battled with each other to provide us and our patients the latest tools and conveniences. In return, we gave our valuable time freely without compensation to hospitals as committee members, task force members, and sounding boards for the betterment of the community. If I were a conspiracy theorist, which I am not, and wanted to devalue physicians I would seek to weaken the physician-patient bond. The way to implement this would be for a single hospital employer to put us on a treadmill chasing work relative value units, give us hard-to-accomplish goals, and keep moving the goalpost. Like I said, I do not believe in conspiracies.
The tsunami of byzantine regulations, Stark laws, and complicated reimbursement formulas has sapped our energy to counter the devaluation. Some are glad to see physicians, particularly surgeons, get their comeuppance because we are perceived as having large egos. This may be true in some instances. Yet, it turns out that the top three job titles with the largest egos are: private household cooks, chief executives, and farm and ranch managers.1
Physicians are also reputed to be possessing dominant leadership styles and seen as bossy and disruptive. Hence, we are made to have frequent training in how to ameliorate our disruptive behavior tendencies. Again, this may be true in a few cases. However, while reports mention how many people witness such unacceptable behavior, there is no valid data about the incidence in practicing physicians. Research also does not support the view that physicians have dominant and aggressive personalities leading to such behavior.
One of the leading interpersonal skills model is Social Styles. We happen to teach this to our faculty at the Ohio State Medical Center’s Faculty Leadership Institute. Turns out that physicians and nurses are almost equally placed into the four quadrants of leadership styles: driving, expressive, amiable, and analytical. I found similar findings in our society members participating in a leadership session I moderated. Indeed, we rank very high on “versatility,” a measure that enables us to adapt our behaviors to fit with our patients and coworkers.
Reported burnout rates of 50% in physicians may or may not be accurate, but burnout is real and so is depression and so are physician suicides. I have witnessed six physician suicides in my career thus far. Teaching resilience, celebrating doctor’s day, and giving out a few awards are all interventions after the fact. Preventive measures like employers and hospitals prioritizing removing daily obstacles eliminating meaningless work, providing more resources to deal with EMRs, and making our lives easier at work, so we can get to our loved ones sooner would help.
Physicians have been largely excluded themselves from participating in the health care debate. We want to see empirical evidence before we sign on to every new proposed care model. Otherwise, we cling on to the status quo and therefore, decision makers tend to leave us out. More important, value-based payment models have not thus far led to reduction in the cost of health care. Despite poor engagement scores at major health systems, physicians are “managed” and sidelined, and mandates are “done to them, not with them.”
In my 40-year career, our devaluation has been a slow and painful process. It started with being called a “provider.” This devalues me. Call me by what I am and do. Physician. Doctor. That is what our patients call us. But, we have been pushed to acquiesce. So, why do physicians undervalue themselves and are unable to be confident of their value to employers and hospital executives?
Some have theorized that physicians have low self-esteem and that denial and rationalization are simply defense mechanisms. The low self-esteem is traced back to medical student days and considered “posttraumatic” disorder. In one study of 189 medical students, 50% reported a decrease in their self-esteem/confidence. The students blamed their residents and attendings for this reaction. Some degree of intimidation may continue into training and employment where it may be part of the culture. We need to change this cycle and treat our students, residents, and mentees with respect as future peers.
Another aspect is related to our own well-being. Most physicians value their patient’s health more than their own. That concept is drilled into us throughout our life. Our spouses complain that we care more about our patients than we do for our families. We often ignore warning signs of serious issues in our own health, always downplaying textbook symptoms of burnout, depression, and even MI. Being too busy is a badge of honor to indicate how successful and wanted we are. This also needs to change.
Sheryl Sandberg in her book “Lean in” discusses the “tiara syndrome,” mainly referring to women. I would suggest that this applies to a lot of physicians, both men and women. Physicians tend to keep their heads down, work hard, and expect someone to come compliment them and place a “tiara” over their head. We may be wary of being called “self-promoters.” Sometimes it is cultural baggage for immigrant physicians who are taught to not brag about their accomplishments. It may behoove us to judiciously make peers and leadership aware of our positive activities in and outside the health system.
Some see physicians not as “pillars of any community,” but as “technicians on an assembly line” or “pawns in a money-making game for hospital administrators.” This degree of pessimism among physicians in surveys is well known but there is good news.
In a 2016 survey based upon responses by 17,236 physicians, 63% were pessimistic or very pessimistic about the medical profession, down from 77% in 2012.2 In another poll, medical doctors were rated as having very high or high ratings of honesty and ethical standards by 65%, higher than all except nurses, military officers, and grade school teachers.3 When the health care debate was at its peak in 2009, a public poll on who they trusted to recommend the right thing for reforming the healthcare system placed physicians at the very top (73%)ahead of health care professors, researchers, hospitals, the President, and politicians. Gallup surveyed 7,000 physicians about engagement in four hierarchical levels: Confidence, Integrity, Pride and Passion. Physicians scored highly on the Pride items in the survey (feel proud to work and being treated with respect).4 In other words, if we are treated well, we feel proud to tell others where we work.
Finally, like many I may consider myself an expert in all sorts of things not relevant to practicing medicine. Yet, I respectfully suggest we stay away from political hot potatoes like nuclear disarmament, gun control, climate change, immigration, and other controversial issues because they distract us from our primary mission. I would hate to see us viewed like Hollywood.
References
1. www.chicagotribune.com/business/ct-payscale-ego-survey-0830-biz-20160829-story.html
2. www.medpagetoday.com/primarycare/generalprimarycare/60446
3. https://nurse.org/articles/gallup-ethical-standards-poll-nurses-rank-highest/
4.https://news.gallup.com/poll/120890/healthcare-americans-trust-physicians-politicians.aspx
Bhagwan Satiani, MD, MBA, is professor of clinical surgery in the division of vascular diseases and surgery at Ohio State University, Columbus. He blogs at www.savvy-medicine.com . Reach him on Twitter @savvycutter.
Continuous certification – Not just one more hoop to jump through
Maintenance of Certification (MOC) is an American Board of Medical Specialties (ABMS) requirement for their 24 member boards. The MOC process has received much criticism, especially in recent years. To date, a 5-hour exam at a secure testing center every 10 years covering comprehensive vascular surgery knowledge has been the routine. This requirement had the surgeon take off a day from work for the exam, in addition to the time it took to prepare. Burnout, at least in part, is related to the sheer volume of busywork not directly relevant to being a practicing surgeon.
The American Board of Surgery is sensitive to both the relevance of MOC and needs of the diplomate, and is striving to make appropriate changes. Diplomates were surveyed regarding MOC and the accompanying exam in both 2016 and 2017. Using this input, the development of the 10-year exam format was studied carefully by the board directors and executive staff, all of whom are active in the clinical practice of surgery, and a new process now known as Continuous Certification was introduced. The intent of the new Continuous Certification Assessment (to replace the every-10-year MOC exam) is to be an activity that is convenient, timely, and more reflective of the surgeon’s daily practice. The assessment is to be done every 2 years and is online, open book, and taken at a place of the examinee’s choosing, such as the home or in the office. Another key feature of the continuous certification process is that the total number of CME required is decreased and the self-assessment requirement is eliminated.
In November 2018, I took the first General Surgery Continuous Certification Assessment. There was approximately a 2-month window to register, and online registration was simple, taking only about 15 minutes to complete. All the references were listed on the ABS website and the vast majority were open access and directly linked to the article. For those articles that were not open access, there was a link to the PubMed abstract. I downloaded all of the articles (actually this part my assistant did) and requested five articles from the library. I did not review the articles in advance, but used them when going sequentially through the assessment questions. Depending on the article, I read it or looked up the specific aspect I was looking for. I worked on the test three different times – at the airport during a long layover, at home, and at my office. After answering each question, I received feedback on what was the correct answer and a one-paragraph explanation which I read completely. After completing all 40 questions, each question for which I had an incorrect answer (not more than one or two of course, Ha!) was shown again with the opportunity to answer the question. The total time took me was about 4.5 hours. All in all, it was a good experience, and I learned something.
The general surgery assessment is modular. Twenty questions (half) were core surgery topics, and the other twenty questions came from one of four specialty modules of the examinee’s choice – breast, abdomen, alimentary tract, or comprehensive general surgery. I took the core and the abdomen modules. The core topics were, for the most part, areas that a surgeon who does patient care would find relevant (for example, perioperative management of a patient on corticosteroids, postoperative delirium, and prophylaxis for venous thromboembolism).
A couple of other details should be mentioned about this new process. From the time of initiation of the assessment, there are 2 weeks allocated for completion. One needs 80% correct to pass. If the examinee receives less than 80% but higher than 40% on the first assessment attempt, he/she will have a second attempt to answer the questions that were incorrect on the first try. If a cumulative score of less than 80% is achieved after the second attempt, a grace year will be provided, which is an extension of certification for 1 year with the opportunity to take the next year’s assessment. If after the grace year (four attempts) the diplomate is unsuccessful, then a secure exam is required to regain certification.
Overall, there has been much positive feedback. Of the 2,164 diplomates taking the Continuous Certification Assessment, only 21 were unsuccessful. Therefore, the pass rate was over 99% for the inaugural year. The average examinee took just over 3 hours to complete the assessment.
In 2018, the 10-year recertification examination in vascular surgery with 10 years of credit was given for the last time. The Vascular Surgery Continuous Certification Assessment is in preparation now and will roll out in the fall of 2019. It will follow a format similar to general surgery with 40 questions on a number of topics in vascular surgery. However, the vascular surgery assessment will not be modular. This activity will incorporate general knowledge (for example, from consensus guidelines), as well as late breaking trials. So far, this process looks to be a better one, as well as more efficient and relevant for the busy surgeon.
Dr. Gahtan is professor and chief, division of vascular surgery and endovascular services, State University of New York Upstate Medical University, Syracuse.
Maintenance of Certification (MOC) is an American Board of Medical Specialties (ABMS) requirement for their 24 member boards. The MOC process has received much criticism, especially in recent years. To date, a 5-hour exam at a secure testing center every 10 years covering comprehensive vascular surgery knowledge has been the routine. This requirement had the surgeon take off a day from work for the exam, in addition to the time it took to prepare. Burnout, at least in part, is related to the sheer volume of busywork not directly relevant to being a practicing surgeon.
The American Board of Surgery is sensitive to both the relevance of MOC and needs of the diplomate, and is striving to make appropriate changes. Diplomates were surveyed regarding MOC and the accompanying exam in both 2016 and 2017. Using this input, the development of the 10-year exam format was studied carefully by the board directors and executive staff, all of whom are active in the clinical practice of surgery, and a new process now known as Continuous Certification was introduced. The intent of the new Continuous Certification Assessment (to replace the every-10-year MOC exam) is to be an activity that is convenient, timely, and more reflective of the surgeon’s daily practice. The assessment is to be done every 2 years and is online, open book, and taken at a place of the examinee’s choosing, such as the home or in the office. Another key feature of the continuous certification process is that the total number of CME required is decreased and the self-assessment requirement is eliminated.
In November 2018, I took the first General Surgery Continuous Certification Assessment. There was approximately a 2-month window to register, and online registration was simple, taking only about 15 minutes to complete. All the references were listed on the ABS website and the vast majority were open access and directly linked to the article. For those articles that were not open access, there was a link to the PubMed abstract. I downloaded all of the articles (actually this part my assistant did) and requested five articles from the library. I did not review the articles in advance, but used them when going sequentially through the assessment questions. Depending on the article, I read it or looked up the specific aspect I was looking for. I worked on the test three different times – at the airport during a long layover, at home, and at my office. After answering each question, I received feedback on what was the correct answer and a one-paragraph explanation which I read completely. After completing all 40 questions, each question for which I had an incorrect answer (not more than one or two of course, Ha!) was shown again with the opportunity to answer the question. The total time took me was about 4.5 hours. All in all, it was a good experience, and I learned something.
The general surgery assessment is modular. Twenty questions (half) were core surgery topics, and the other twenty questions came from one of four specialty modules of the examinee’s choice – breast, abdomen, alimentary tract, or comprehensive general surgery. I took the core and the abdomen modules. The core topics were, for the most part, areas that a surgeon who does patient care would find relevant (for example, perioperative management of a patient on corticosteroids, postoperative delirium, and prophylaxis for venous thromboembolism).
A couple of other details should be mentioned about this new process. From the time of initiation of the assessment, there are 2 weeks allocated for completion. One needs 80% correct to pass. If the examinee receives less than 80% but higher than 40% on the first assessment attempt, he/she will have a second attempt to answer the questions that were incorrect on the first try. If a cumulative score of less than 80% is achieved after the second attempt, a grace year will be provided, which is an extension of certification for 1 year with the opportunity to take the next year’s assessment. If after the grace year (four attempts) the diplomate is unsuccessful, then a secure exam is required to regain certification.
Overall, there has been much positive feedback. Of the 2,164 diplomates taking the Continuous Certification Assessment, only 21 were unsuccessful. Therefore, the pass rate was over 99% for the inaugural year. The average examinee took just over 3 hours to complete the assessment.
In 2018, the 10-year recertification examination in vascular surgery with 10 years of credit was given for the last time. The Vascular Surgery Continuous Certification Assessment is in preparation now and will roll out in the fall of 2019. It will follow a format similar to general surgery with 40 questions on a number of topics in vascular surgery. However, the vascular surgery assessment will not be modular. This activity will incorporate general knowledge (for example, from consensus guidelines), as well as late breaking trials. So far, this process looks to be a better one, as well as more efficient and relevant for the busy surgeon.
Dr. Gahtan is professor and chief, division of vascular surgery and endovascular services, State University of New York Upstate Medical University, Syracuse.
Maintenance of Certification (MOC) is an American Board of Medical Specialties (ABMS) requirement for their 24 member boards. The MOC process has received much criticism, especially in recent years. To date, a 5-hour exam at a secure testing center every 10 years covering comprehensive vascular surgery knowledge has been the routine. This requirement had the surgeon take off a day from work for the exam, in addition to the time it took to prepare. Burnout, at least in part, is related to the sheer volume of busywork not directly relevant to being a practicing surgeon.
The American Board of Surgery is sensitive to both the relevance of MOC and needs of the diplomate, and is striving to make appropriate changes. Diplomates were surveyed regarding MOC and the accompanying exam in both 2016 and 2017. Using this input, the development of the 10-year exam format was studied carefully by the board directors and executive staff, all of whom are active in the clinical practice of surgery, and a new process now known as Continuous Certification was introduced. The intent of the new Continuous Certification Assessment (to replace the every-10-year MOC exam) is to be an activity that is convenient, timely, and more reflective of the surgeon’s daily practice. The assessment is to be done every 2 years and is online, open book, and taken at a place of the examinee’s choosing, such as the home or in the office. Another key feature of the continuous certification process is that the total number of CME required is decreased and the self-assessment requirement is eliminated.
In November 2018, I took the first General Surgery Continuous Certification Assessment. There was approximately a 2-month window to register, and online registration was simple, taking only about 15 minutes to complete. All the references were listed on the ABS website and the vast majority were open access and directly linked to the article. For those articles that were not open access, there was a link to the PubMed abstract. I downloaded all of the articles (actually this part my assistant did) and requested five articles from the library. I did not review the articles in advance, but used them when going sequentially through the assessment questions. Depending on the article, I read it or looked up the specific aspect I was looking for. I worked on the test three different times – at the airport during a long layover, at home, and at my office. After answering each question, I received feedback on what was the correct answer and a one-paragraph explanation which I read completely. After completing all 40 questions, each question for which I had an incorrect answer (not more than one or two of course, Ha!) was shown again with the opportunity to answer the question. The total time took me was about 4.5 hours. All in all, it was a good experience, and I learned something.
The general surgery assessment is modular. Twenty questions (half) were core surgery topics, and the other twenty questions came from one of four specialty modules of the examinee’s choice – breast, abdomen, alimentary tract, or comprehensive general surgery. I took the core and the abdomen modules. The core topics were, for the most part, areas that a surgeon who does patient care would find relevant (for example, perioperative management of a patient on corticosteroids, postoperative delirium, and prophylaxis for venous thromboembolism).
A couple of other details should be mentioned about this new process. From the time of initiation of the assessment, there are 2 weeks allocated for completion. One needs 80% correct to pass. If the examinee receives less than 80% but higher than 40% on the first assessment attempt, he/she will have a second attempt to answer the questions that were incorrect on the first try. If a cumulative score of less than 80% is achieved after the second attempt, a grace year will be provided, which is an extension of certification for 1 year with the opportunity to take the next year’s assessment. If after the grace year (four attempts) the diplomate is unsuccessful, then a secure exam is required to regain certification.
Overall, there has been much positive feedback. Of the 2,164 diplomates taking the Continuous Certification Assessment, only 21 were unsuccessful. Therefore, the pass rate was over 99% for the inaugural year. The average examinee took just over 3 hours to complete the assessment.
In 2018, the 10-year recertification examination in vascular surgery with 10 years of credit was given for the last time. The Vascular Surgery Continuous Certification Assessment is in preparation now and will roll out in the fall of 2019. It will follow a format similar to general surgery with 40 questions on a number of topics in vascular surgery. However, the vascular surgery assessment will not be modular. This activity will incorporate general knowledge (for example, from consensus guidelines), as well as late breaking trials. So far, this process looks to be a better one, as well as more efficient and relevant for the busy surgeon.
Dr. Gahtan is professor and chief, division of vascular surgery and endovascular services, State University of New York Upstate Medical University, Syracuse.
My recommendations for the best books of 2018
There were .
“Enlightenment Now: The Case for Reason, Science, Humanism, and Progress,” by Steven Pinker, PhD (New York:Viking, 2018). Think life was better 50 years ago? 100? 500? Steven Pinker would say you’re wrong. Whether or not we feel it, empirically, life is better today than it ever has been. We are living longer, healthier lives, have better access to health care, have fewer war-related deaths and food shortages and higher levels of literacy and equal rights. However, Dr. Pinker acknowledges our shortcomings (e.g., providing a living wage) and potential societal pitfalls (e.g., increasing tribalism), although he could have addressed other crucial issues such as climate change more fully. If you’re looking for an optimistic, science-based outlook on humanity, look no further than this book.
“Aware: The Science and Practice of Presence – The Groundbreaking Meditation Practice,” by Daniel J. Siegel, MD (New York:TarcherPerigee, 2018). A clinical professor of psychiatry and director of the UCLA Mindful Awareness Research Center, Dr. Siegel, in his latest book, constructs a compelling argument for practicing presence that is supported by ample scientific evidence. His “Wheel of Awareness” is a tool to cultivate presence, self-awareness, and compassion. He deftly shows how developing “open awareness” and “kind intention” has not only psychological benefits, but also physical ones, such as improving immune function and increasing neural integration in the brain. As he writes, “The scientific findings are now in: Your mind can change the health of your body and slow aging.” That’s a message both we physicians and our patients could benefit from hearing more often.
“When: The Scientific Secrets of Perfect Timing,” by Daniel H. Pink (New York: Riverhead Books, 2018). In his latest book, Mr. Pink delves into timing, and the evolving science of timing, which draws from fields that include biology, psychology, neuroscience, and economics. Through extensive research (he analyzed over 700 studies) and fascinating real-life examples, the data are clear: We overwhelmingly perform optimally in the morning, suffer a mid-day slump, then rally once more in the evening (of course, there are productive night owls too). These peaks and dips affect both our moods and decision-making abilities, resulting in real-world impact (judges, for example, are more lenient in sentencing following a break). With practical takeaways you can immediately incorporate into your daily routine, you can start to feel more productive, energized, and happy, which is good news for both you and your patients.
“Natural Causes An Epidemic of Wellness, the Certainty of Dying, and Killing Ourselves to Live Longer,” by Barbara Ehrenreich, PhD (New York:Twelve, 2018). Infuriating, tender, disquieting, moving. Barbara Ehrenreich’s latest book is provocative. As a septuagenarian and cancer survivor who has forsworn most future medical measures, including Pap smears and cancer screenings (even though she has medical insurance), Dr. Ehrenreich castigates both the traditional medical and integrative holistic health establishments. Yes, she’s critical of us and nurses and fitness gurus and mindfulness coaches and Silicon Valley. Why should I read this you ask? Because it’s good to understand contrarian views, especially when they are thoughtfully articulated. Because there are many patients who share her beliefs, and understanding opposing perspectives might help us become better clinicians. Because she may cause you to be reflective. Do we order too many tests? Do we overprescribe meds? Are we setting up patients for false hopes of longevity? Is providing more care always the best option? This exercise is beneficial for all types of healers.
“Leadership in Turbulent Times,” by Doris Kearns Goodwin, PhD, (New York:Simon & Schuster, 2018). I’m a presidential biography junkie. As physicians in what some may rightly call a turbulent health care culture, we face challenges each day that require our best intentions, our best diagnostic skills, our best empathic efforts, our best selves. Dr. Goodwin, in her prototypical engaging and informative prose, shows us four American presidents, Abraham Lincoln, Theodore Roosevelt, Franklin D. Roosevelt, and Lyndon B. Johnson, who persevered through devastatingly turbulent times. While we don’t have to make decisions regarding warfare, we do have an unmistakable impact on the lives of thousands of patients, and this book provides insights that can help all of us become better informed, better prepared leaders for our patients, our coworkers, and our communities at large.
“You and I Eat the Same: On the Countless Ways Food and Cooking Connect Us to One Another,” edited by Chris Ying; foreword by René Redzepi (New York:Artisan, 2018). Open a newspaper or turn on the news, and it’s difficult not to feel as if we live in an alarmingly polarized society. We can find many issues that divide us, but as healers, I hope we also strive to find ways to connect us. In 19 engaging and thought-provoking essays, this book explores the various ways that food connects us as humans. Whether it’s an historical deep dive into our love of meat wrapped in flatbread (which we’ve been doing for over 1,000 years) or tackling philosophical questions like, “Is there such a thing as a ‘non-ethnic’ restaurant?” this book will inform, inspire, and delight, and provide delicious topics for a bite of small talk with your patients.
“The Great Alone,” by Kristin Hannah (New York:St. Martin’s Press, 2018). Lured by Alaska’s majestic splendor and remoteness, the Allbright family (former POW, Ernt; abused wife, Cora; and coming-of-age daughter, Leni) are happy with their new life. For a minute. What ensues, namely punishing 16-hour days of darkness punctuated by episodes of oppressive snowfall, paranoia, and domestic violence, is grueling: “Night swept in like nothing Leni had ever seen before, like the winged shadow of a creature too big and predatory to comprehend.” Yet, this book is also a story about the bonds of family, both those we are born into and those we choose, love, sacrifice, and resilience.
If you have any books you read over the last to year to add to this list, please write to me at [email protected].
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter.
There were .
“Enlightenment Now: The Case for Reason, Science, Humanism, and Progress,” by Steven Pinker, PhD (New York:Viking, 2018). Think life was better 50 years ago? 100? 500? Steven Pinker would say you’re wrong. Whether or not we feel it, empirically, life is better today than it ever has been. We are living longer, healthier lives, have better access to health care, have fewer war-related deaths and food shortages and higher levels of literacy and equal rights. However, Dr. Pinker acknowledges our shortcomings (e.g., providing a living wage) and potential societal pitfalls (e.g., increasing tribalism), although he could have addressed other crucial issues such as climate change more fully. If you’re looking for an optimistic, science-based outlook on humanity, look no further than this book.
“Aware: The Science and Practice of Presence – The Groundbreaking Meditation Practice,” by Daniel J. Siegel, MD (New York:TarcherPerigee, 2018). A clinical professor of psychiatry and director of the UCLA Mindful Awareness Research Center, Dr. Siegel, in his latest book, constructs a compelling argument for practicing presence that is supported by ample scientific evidence. His “Wheel of Awareness” is a tool to cultivate presence, self-awareness, and compassion. He deftly shows how developing “open awareness” and “kind intention” has not only psychological benefits, but also physical ones, such as improving immune function and increasing neural integration in the brain. As he writes, “The scientific findings are now in: Your mind can change the health of your body and slow aging.” That’s a message both we physicians and our patients could benefit from hearing more often.
“When: The Scientific Secrets of Perfect Timing,” by Daniel H. Pink (New York: Riverhead Books, 2018). In his latest book, Mr. Pink delves into timing, and the evolving science of timing, which draws from fields that include biology, psychology, neuroscience, and economics. Through extensive research (he analyzed over 700 studies) and fascinating real-life examples, the data are clear: We overwhelmingly perform optimally in the morning, suffer a mid-day slump, then rally once more in the evening (of course, there are productive night owls too). These peaks and dips affect both our moods and decision-making abilities, resulting in real-world impact (judges, for example, are more lenient in sentencing following a break). With practical takeaways you can immediately incorporate into your daily routine, you can start to feel more productive, energized, and happy, which is good news for both you and your patients.
“Natural Causes An Epidemic of Wellness, the Certainty of Dying, and Killing Ourselves to Live Longer,” by Barbara Ehrenreich, PhD (New York:Twelve, 2018). Infuriating, tender, disquieting, moving. Barbara Ehrenreich’s latest book is provocative. As a septuagenarian and cancer survivor who has forsworn most future medical measures, including Pap smears and cancer screenings (even though she has medical insurance), Dr. Ehrenreich castigates both the traditional medical and integrative holistic health establishments. Yes, she’s critical of us and nurses and fitness gurus and mindfulness coaches and Silicon Valley. Why should I read this you ask? Because it’s good to understand contrarian views, especially when they are thoughtfully articulated. Because there are many patients who share her beliefs, and understanding opposing perspectives might help us become better clinicians. Because she may cause you to be reflective. Do we order too many tests? Do we overprescribe meds? Are we setting up patients for false hopes of longevity? Is providing more care always the best option? This exercise is beneficial for all types of healers.
“Leadership in Turbulent Times,” by Doris Kearns Goodwin, PhD, (New York:Simon & Schuster, 2018). I’m a presidential biography junkie. As physicians in what some may rightly call a turbulent health care culture, we face challenges each day that require our best intentions, our best diagnostic skills, our best empathic efforts, our best selves. Dr. Goodwin, in her prototypical engaging and informative prose, shows us four American presidents, Abraham Lincoln, Theodore Roosevelt, Franklin D. Roosevelt, and Lyndon B. Johnson, who persevered through devastatingly turbulent times. While we don’t have to make decisions regarding warfare, we do have an unmistakable impact on the lives of thousands of patients, and this book provides insights that can help all of us become better informed, better prepared leaders for our patients, our coworkers, and our communities at large.
“You and I Eat the Same: On the Countless Ways Food and Cooking Connect Us to One Another,” edited by Chris Ying; foreword by René Redzepi (New York:Artisan, 2018). Open a newspaper or turn on the news, and it’s difficult not to feel as if we live in an alarmingly polarized society. We can find many issues that divide us, but as healers, I hope we also strive to find ways to connect us. In 19 engaging and thought-provoking essays, this book explores the various ways that food connects us as humans. Whether it’s an historical deep dive into our love of meat wrapped in flatbread (which we’ve been doing for over 1,000 years) or tackling philosophical questions like, “Is there such a thing as a ‘non-ethnic’ restaurant?” this book will inform, inspire, and delight, and provide delicious topics for a bite of small talk with your patients.
“The Great Alone,” by Kristin Hannah (New York:St. Martin’s Press, 2018). Lured by Alaska’s majestic splendor and remoteness, the Allbright family (former POW, Ernt; abused wife, Cora; and coming-of-age daughter, Leni) are happy with their new life. For a minute. What ensues, namely punishing 16-hour days of darkness punctuated by episodes of oppressive snowfall, paranoia, and domestic violence, is grueling: “Night swept in like nothing Leni had ever seen before, like the winged shadow of a creature too big and predatory to comprehend.” Yet, this book is also a story about the bonds of family, both those we are born into and those we choose, love, sacrifice, and resilience.
If you have any books you read over the last to year to add to this list, please write to me at [email protected].
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter.
There were .
“Enlightenment Now: The Case for Reason, Science, Humanism, and Progress,” by Steven Pinker, PhD (New York:Viking, 2018). Think life was better 50 years ago? 100? 500? Steven Pinker would say you’re wrong. Whether or not we feel it, empirically, life is better today than it ever has been. We are living longer, healthier lives, have better access to health care, have fewer war-related deaths and food shortages and higher levels of literacy and equal rights. However, Dr. Pinker acknowledges our shortcomings (e.g., providing a living wage) and potential societal pitfalls (e.g., increasing tribalism), although he could have addressed other crucial issues such as climate change more fully. If you’re looking for an optimistic, science-based outlook on humanity, look no further than this book.
“Aware: The Science and Practice of Presence – The Groundbreaking Meditation Practice,” by Daniel J. Siegel, MD (New York:TarcherPerigee, 2018). A clinical professor of psychiatry and director of the UCLA Mindful Awareness Research Center, Dr. Siegel, in his latest book, constructs a compelling argument for practicing presence that is supported by ample scientific evidence. His “Wheel of Awareness” is a tool to cultivate presence, self-awareness, and compassion. He deftly shows how developing “open awareness” and “kind intention” has not only psychological benefits, but also physical ones, such as improving immune function and increasing neural integration in the brain. As he writes, “The scientific findings are now in: Your mind can change the health of your body and slow aging.” That’s a message both we physicians and our patients could benefit from hearing more often.
“When: The Scientific Secrets of Perfect Timing,” by Daniel H. Pink (New York: Riverhead Books, 2018). In his latest book, Mr. Pink delves into timing, and the evolving science of timing, which draws from fields that include biology, psychology, neuroscience, and economics. Through extensive research (he analyzed over 700 studies) and fascinating real-life examples, the data are clear: We overwhelmingly perform optimally in the morning, suffer a mid-day slump, then rally once more in the evening (of course, there are productive night owls too). These peaks and dips affect both our moods and decision-making abilities, resulting in real-world impact (judges, for example, are more lenient in sentencing following a break). With practical takeaways you can immediately incorporate into your daily routine, you can start to feel more productive, energized, and happy, which is good news for both you and your patients.
“Natural Causes An Epidemic of Wellness, the Certainty of Dying, and Killing Ourselves to Live Longer,” by Barbara Ehrenreich, PhD (New York:Twelve, 2018). Infuriating, tender, disquieting, moving. Barbara Ehrenreich’s latest book is provocative. As a septuagenarian and cancer survivor who has forsworn most future medical measures, including Pap smears and cancer screenings (even though she has medical insurance), Dr. Ehrenreich castigates both the traditional medical and integrative holistic health establishments. Yes, she’s critical of us and nurses and fitness gurus and mindfulness coaches and Silicon Valley. Why should I read this you ask? Because it’s good to understand contrarian views, especially when they are thoughtfully articulated. Because there are many patients who share her beliefs, and understanding opposing perspectives might help us become better clinicians. Because she may cause you to be reflective. Do we order too many tests? Do we overprescribe meds? Are we setting up patients for false hopes of longevity? Is providing more care always the best option? This exercise is beneficial for all types of healers.
“Leadership in Turbulent Times,” by Doris Kearns Goodwin, PhD, (New York:Simon & Schuster, 2018). I’m a presidential biography junkie. As physicians in what some may rightly call a turbulent health care culture, we face challenges each day that require our best intentions, our best diagnostic skills, our best empathic efforts, our best selves. Dr. Goodwin, in her prototypical engaging and informative prose, shows us four American presidents, Abraham Lincoln, Theodore Roosevelt, Franklin D. Roosevelt, and Lyndon B. Johnson, who persevered through devastatingly turbulent times. While we don’t have to make decisions regarding warfare, we do have an unmistakable impact on the lives of thousands of patients, and this book provides insights that can help all of us become better informed, better prepared leaders for our patients, our coworkers, and our communities at large.
“You and I Eat the Same: On the Countless Ways Food and Cooking Connect Us to One Another,” edited by Chris Ying; foreword by René Redzepi (New York:Artisan, 2018). Open a newspaper or turn on the news, and it’s difficult not to feel as if we live in an alarmingly polarized society. We can find many issues that divide us, but as healers, I hope we also strive to find ways to connect us. In 19 engaging and thought-provoking essays, this book explores the various ways that food connects us as humans. Whether it’s an historical deep dive into our love of meat wrapped in flatbread (which we’ve been doing for over 1,000 years) or tackling philosophical questions like, “Is there such a thing as a ‘non-ethnic’ restaurant?” this book will inform, inspire, and delight, and provide delicious topics for a bite of small talk with your patients.
“The Great Alone,” by Kristin Hannah (New York:St. Martin’s Press, 2018). Lured by Alaska’s majestic splendor and remoteness, the Allbright family (former POW, Ernt; abused wife, Cora; and coming-of-age daughter, Leni) are happy with their new life. For a minute. What ensues, namely punishing 16-hour days of darkness punctuated by episodes of oppressive snowfall, paranoia, and domestic violence, is grueling: “Night swept in like nothing Leni had ever seen before, like the winged shadow of a creature too big and predatory to comprehend.” Yet, this book is also a story about the bonds of family, both those we are born into and those we choose, love, sacrifice, and resilience.
If you have any books you read over the last to year to add to this list, please write to me at [email protected].
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter.
TOO GOOD TO LAST?
When I first started in my training, I could not wait until the next issue of Emergency Medicine arrived in my mailbox (not yet inbox!). Emergency Medicine provided a service to our community and specialty at a time when no other publication was willing or able to do so. For no cost, no membership requirements, and no strings attached, we all received a monthly treasure trove of contemporary and practical information. The articles within were written by credible authors, in an approachable style, with professional illustrations that focused on key clinical issues that we saw in our everyday clinical practices.
As my career matured, I was asked to write and subsequently oversee a recurring feature on practical aspects of managing poisoning. Unclear if this was going to be well read, I agreed with trepidation. I quickly learned just how widely appreciated this journal was. People around the country wrote to let me know their thoughts on our thoughts (which meant they were reading it at least!). And people around the country offered to submit interesting toxicology cases for publication. For many of these authors, and many of my med tox trainees, this journal represented the first time they saw their name in print.
Clearly, to me at least, despite all the available blogs, podcasts, reddit and subreddit streams, and continuing medical education programs out there, people still loved getting this small but effective educational tool sent to them. And it is certainly sad to me, and likely many, that this wonderful benefactor of high-quality EM knowledge is losing its hard-fought battle against the modern reality of medical publishing.
I rest assured that there are other credible sources of education that we all can access. I know that our authors and readers will miss the journal dearly. But to paraphrase an unknown author: We should not be sad that it’s over, but glad that it happened.
Lewis S. Nelson, MD
Rutgers New Jersey Medical School
When I first started in my training, I could not wait until the next issue of Emergency Medicine arrived in my mailbox (not yet inbox!). Emergency Medicine provided a service to our community and specialty at a time when no other publication was willing or able to do so. For no cost, no membership requirements, and no strings attached, we all received a monthly treasure trove of contemporary and practical information. The articles within were written by credible authors, in an approachable style, with professional illustrations that focused on key clinical issues that we saw in our everyday clinical practices.
As my career matured, I was asked to write and subsequently oversee a recurring feature on practical aspects of managing poisoning. Unclear if this was going to be well read, I agreed with trepidation. I quickly learned just how widely appreciated this journal was. People around the country wrote to let me know their thoughts on our thoughts (which meant they were reading it at least!). And people around the country offered to submit interesting toxicology cases for publication. For many of these authors, and many of my med tox trainees, this journal represented the first time they saw their name in print.
Clearly, to me at least, despite all the available blogs, podcasts, reddit and subreddit streams, and continuing medical education programs out there, people still loved getting this small but effective educational tool sent to them. And it is certainly sad to me, and likely many, that this wonderful benefactor of high-quality EM knowledge is losing its hard-fought battle against the modern reality of medical publishing.
I rest assured that there are other credible sources of education that we all can access. I know that our authors and readers will miss the journal dearly. But to paraphrase an unknown author: We should not be sad that it’s over, but glad that it happened.
Lewis S. Nelson, MD
Rutgers New Jersey Medical School
When I first started in my training, I could not wait until the next issue of Emergency Medicine arrived in my mailbox (not yet inbox!). Emergency Medicine provided a service to our community and specialty at a time when no other publication was willing or able to do so. For no cost, no membership requirements, and no strings attached, we all received a monthly treasure trove of contemporary and practical information. The articles within were written by credible authors, in an approachable style, with professional illustrations that focused on key clinical issues that we saw in our everyday clinical practices.
As my career matured, I was asked to write and subsequently oversee a recurring feature on practical aspects of managing poisoning. Unclear if this was going to be well read, I agreed with trepidation. I quickly learned just how widely appreciated this journal was. People around the country wrote to let me know their thoughts on our thoughts (which meant they were reading it at least!). And people around the country offered to submit interesting toxicology cases for publication. For many of these authors, and many of my med tox trainees, this journal represented the first time they saw their name in print.
Clearly, to me at least, despite all the available blogs, podcasts, reddit and subreddit streams, and continuing medical education programs out there, people still loved getting this small but effective educational tool sent to them. And it is certainly sad to me, and likely many, that this wonderful benefactor of high-quality EM knowledge is losing its hard-fought battle against the modern reality of medical publishing.
I rest assured that there are other credible sources of education that we all can access. I know that our authors and readers will miss the journal dearly. But to paraphrase an unknown author: We should not be sad that it’s over, but glad that it happened.
Lewis S. Nelson, MD
Rutgers New Jersey Medical School
Guest editorial: Best of both worlds
Within 3 minutes of the car engine rumbling to a roar in the morning air, cruise control is set, freshly ground coffee is in hand and NPR is playing on WOSU 90.5. I settle in for the morning news on my 45-minute commute to the hospital. Sure, I could’ve found a hospital closer to shorten my commute, especially since I live in the 14th largest metropolitan city in the country.
If I’d wanted, I could be knocking out carotid endarterectomies at a level 1 trauma center, three blocks away from my front door. But no, that’s not what does it for me. What does? It’s having the opportunity to be my own boss and care for salt-of-the-earth folks in rural America.
You see, 5 years ago when I finished my vascular surgery fellowship at Good Samaritan Hospital in Cincinnati, I opened my own solo private practice in a rural community: population 30,000. Yep, that’s right, you heard it. I hung a shingle and went old school. And now as I reflect over the lessons learned during the first half-decade of my practice at Ohio Vein & Vascular Inc., I can tell you it has been a hell of a ride, and boy have we learned a lot.
The better half of the ‘we’ is my wife, Crystal, who doubles as my practice administrator, with her own solid foundation coming from a doctorate in physical therapy. We have successfully built a small company with four full-time employees, one contract registered vascular technologist, and two therapy dogs who serve more than 3,500 patients to date.
From the first day I opened my doors to this small-town rural community, I realized that it’s not what you know, but rather who you know. Well frankly, I didn’t know a soul!
Fortunately, my front office manager was born, raised, and still lives in Wilmington and knows everyone’s mother, brother, sister, niece, and grandchild in what felt like a 60-mile radius. She gave this young, slick city kid from Columbus instant street cred despite all the fancy credentials behind my name. I ditched the tie and fancy shoes and embraced my new ‘work’ home with open arms.
In a community such as Wilmington, Ohio, it’s the little things that count. I wear my own scrubs on days when I operate. Not only do they have my practice logo embroidered on the chest pocket, but they are also adorned with the brown leather symbol for Carhart, a clothing brand. In rural America, Carhart denim clothing – overall bibs, jackets, gloves, etc., are considered king. When my patients see that symbol, there is an instant point of mutual appreciation and it almost always results in some good laughs – who knew Carhart made scrubs?
As a result, I’ve been offered opportunities to ride combines, go drag racing, and go hunting for the infamous morel mushrooms. Just to be clear, I haven’t found a morel yet, so I guess I will stick to my day job as a surgeon.
Having a good laugh and connecting with my patients was something I was not accustomed to in my training. I was there to operate, and rarely participated in office days. At times this routine left me feeling unappreciated by my patients and their families. I was just a surgeon delivering bad news. I now find myself fortunate to have the opportunity to get to know my patients and participate in their health care, and I know they appreciate me for it.
A recent malpractice survey cited a finding that the more patients ‘like’ their physicians, the less likely they are to file malpractice lawsuits against them.1 Other reports have suggested that the relationship a physician has with a patient is a critical factor, more so than any single medical mistake, in determining whether or not a lawsuit is filed.2,3
While I feel appreciated and ‘liked’ by my patients, I’ve learned that I am not necessarily their favorite employee in the office. This honor is most often bestowed upon Claire and Whitney, aka “The Girls” – our two, miniature Labradoodles who serve in the capacity of therapy dogs and have perfected the ability to nap in nearly any situation. Try as I may to convince patients that what I am saying is important, they never lose focus on The Girls. They are the first thing patients ask about, I swear they receive more gifts than I do, and they always are on the receiving end of some good ‘pets’ as my patients leave the office. Despite any bad news they may have been told, very rarely do patients leave my office without smiles on their faces. It keeps me humble, as I think most of my patients aren’t really here to see me; after all I am just a fancy plumber.
Speaking of plumbing, I could’ve sworn that the ginormous two-volume Rutherford edition always gave me the impression that vascular disease is composed of 75% venous disease and 25% arterial disease. However, our fellowship training in the United States makes Rutherford seem like he had his numbers flipped – 99.8% was arterial with a splash of venous as an afterthought. Truth be told though, I see roughly 55% venous, 25% dialysis, and 20% arterial. I guess that wasn’t made up after all.
If my practice name, Ohio Vein & Vascular, didn’t give it away, I admit that I focus marketing efforts toward venous pathology. This has significantly improved my work-life balance. Let’s face it, not everything we do as a surgeon is fun and can certainly carry a large amount of stress. I devote an honest amount of time to developing what ‘type’ of practice I desire. I communicate regularly with my referring docs about the types of disease I focus on, write press releases to the local paper, and always have my elevator speech handy when speaking with fellow physicians and potential patients about what I do as a surgical subspecialist.
In such a small community, the more my vascular surgery practice grows, the more likely the podiatrist and his wife (also a podiatrist) across the hall will grow their practice. Same holds true of the cardiologist upstairs and the nephrologist down the hall. It’s not rocket science that the more I help their businesses thrive, the more likely they are to do the same for mine. We are all one large family working together with the common goal to stay independent, a rarity these days amongst the conglomerate of hospitals taking over.
Wait, did I mention that I have never run a business before? Well, let me tell the most important lesson I have learned ... some days it is really hard. I remember having to let go my first medical assistant after her 90-day review. All of my medical training never prepared me for a how hard that conversation was going to be, and she wasn’t even losing her leg. My wife, a trained physical therapist, jumped right in until we eventually got the gusto to hire another MA. Fortunately, we found a remarkable individual who is worth her weight in gold. The same holds true for our other employees and we aren’t about to let them leave so we pay them well, fund 80% of their health insurance premiums, established a 401K with matching funds, and profit share with each employee. We foster an environment that makes our employees want to work hard, although like my patients, sometimes I think they come to work just to see The Girls.
All in all, we treat our staff with respect and provide a significant monetary carrot to each of them at the holidays; this is unmatched in our area. Happy employees are instrumental to my work life and have a direct impact on the success of my practice. All boats rise with the rising tide, and we are sailing smoothly.
Despite all the challenges and hard work, nothing is better than being your own boss. Nothing. I don’t know a single physician whose desire was to trek through grueling medical school and years of residency and fellowship to ultimately become an employee of an overly glorified postgraduate degree holder in health care administration. I cannot recall having had a single conversation with any surgeon or physician who is 100% happy with his or her working situation who isn’t self-employed. Do I work now more than I ever thought I would? Absolutely. But the work I am doing isn’t simply waking up at all hours to operate or trudge through countless hours in a lab or clinic. No, the work I do is running a successful small business – and even better yet, it is great!
Here I am on a Saturday morning writing a guest editorial for publication in the official newspaper of the Society for Vascular Surgery and I am loving it. Life is short and I’m trying to enjoy every minute that I have on this planet by spending my time working in a manner that I find enjoyable.
Being the fancy plumber in rural America provides me that opportunity. I hope others realize that it is still possible to navigate health care’s oftentimes unknown waters as a solo private practitioner and be successful. That they too could be taking the bull by the horns and changing up their work-life balance for the betterment of themselves, the care they provide to patients, and their families.
And in the meantime, I’ll jump back in my car and head due north for a 45-minute decompressing drive, chat with family and friends, dictate the last case of the day, and continue to enjoy the best of both worlds living in the big city and working with the most genuine folks in rural America. You should try it.
Dr. Santin is a vascular surgeon in private practice at Ohio Vein & Vascular, Wilmington.
References
1. Medscape Malpractice Report 2015: Why Most Doctors Get Sued, by Carol Peckham, Dec. 9, 2015.
2. Decrease Your Risk of Being Successfully Sued, by Nancy Young, Crozer-Chester Medical Center.
3. To Be Sued Less, Doctors Should Consider Talking to Patients More, by Aaron E. Carroll, New York Times, June 1, 2015.
Within 3 minutes of the car engine rumbling to a roar in the morning air, cruise control is set, freshly ground coffee is in hand and NPR is playing on WOSU 90.5. I settle in for the morning news on my 45-minute commute to the hospital. Sure, I could’ve found a hospital closer to shorten my commute, especially since I live in the 14th largest metropolitan city in the country.
If I’d wanted, I could be knocking out carotid endarterectomies at a level 1 trauma center, three blocks away from my front door. But no, that’s not what does it for me. What does? It’s having the opportunity to be my own boss and care for salt-of-the-earth folks in rural America.
You see, 5 years ago when I finished my vascular surgery fellowship at Good Samaritan Hospital in Cincinnati, I opened my own solo private practice in a rural community: population 30,000. Yep, that’s right, you heard it. I hung a shingle and went old school. And now as I reflect over the lessons learned during the first half-decade of my practice at Ohio Vein & Vascular Inc., I can tell you it has been a hell of a ride, and boy have we learned a lot.
The better half of the ‘we’ is my wife, Crystal, who doubles as my practice administrator, with her own solid foundation coming from a doctorate in physical therapy. We have successfully built a small company with four full-time employees, one contract registered vascular technologist, and two therapy dogs who serve more than 3,500 patients to date.
From the first day I opened my doors to this small-town rural community, I realized that it’s not what you know, but rather who you know. Well frankly, I didn’t know a soul!
Fortunately, my front office manager was born, raised, and still lives in Wilmington and knows everyone’s mother, brother, sister, niece, and grandchild in what felt like a 60-mile radius. She gave this young, slick city kid from Columbus instant street cred despite all the fancy credentials behind my name. I ditched the tie and fancy shoes and embraced my new ‘work’ home with open arms.
In a community such as Wilmington, Ohio, it’s the little things that count. I wear my own scrubs on days when I operate. Not only do they have my practice logo embroidered on the chest pocket, but they are also adorned with the brown leather symbol for Carhart, a clothing brand. In rural America, Carhart denim clothing – overall bibs, jackets, gloves, etc., are considered king. When my patients see that symbol, there is an instant point of mutual appreciation and it almost always results in some good laughs – who knew Carhart made scrubs?
As a result, I’ve been offered opportunities to ride combines, go drag racing, and go hunting for the infamous morel mushrooms. Just to be clear, I haven’t found a morel yet, so I guess I will stick to my day job as a surgeon.
Having a good laugh and connecting with my patients was something I was not accustomed to in my training. I was there to operate, and rarely participated in office days. At times this routine left me feeling unappreciated by my patients and their families. I was just a surgeon delivering bad news. I now find myself fortunate to have the opportunity to get to know my patients and participate in their health care, and I know they appreciate me for it.
A recent malpractice survey cited a finding that the more patients ‘like’ their physicians, the less likely they are to file malpractice lawsuits against them.1 Other reports have suggested that the relationship a physician has with a patient is a critical factor, more so than any single medical mistake, in determining whether or not a lawsuit is filed.2,3
While I feel appreciated and ‘liked’ by my patients, I’ve learned that I am not necessarily their favorite employee in the office. This honor is most often bestowed upon Claire and Whitney, aka “The Girls” – our two, miniature Labradoodles who serve in the capacity of therapy dogs and have perfected the ability to nap in nearly any situation. Try as I may to convince patients that what I am saying is important, they never lose focus on The Girls. They are the first thing patients ask about, I swear they receive more gifts than I do, and they always are on the receiving end of some good ‘pets’ as my patients leave the office. Despite any bad news they may have been told, very rarely do patients leave my office without smiles on their faces. It keeps me humble, as I think most of my patients aren’t really here to see me; after all I am just a fancy plumber.
Speaking of plumbing, I could’ve sworn that the ginormous two-volume Rutherford edition always gave me the impression that vascular disease is composed of 75% venous disease and 25% arterial disease. However, our fellowship training in the United States makes Rutherford seem like he had his numbers flipped – 99.8% was arterial with a splash of venous as an afterthought. Truth be told though, I see roughly 55% venous, 25% dialysis, and 20% arterial. I guess that wasn’t made up after all.
If my practice name, Ohio Vein & Vascular, didn’t give it away, I admit that I focus marketing efforts toward venous pathology. This has significantly improved my work-life balance. Let’s face it, not everything we do as a surgeon is fun and can certainly carry a large amount of stress. I devote an honest amount of time to developing what ‘type’ of practice I desire. I communicate regularly with my referring docs about the types of disease I focus on, write press releases to the local paper, and always have my elevator speech handy when speaking with fellow physicians and potential patients about what I do as a surgical subspecialist.
In such a small community, the more my vascular surgery practice grows, the more likely the podiatrist and his wife (also a podiatrist) across the hall will grow their practice. Same holds true of the cardiologist upstairs and the nephrologist down the hall. It’s not rocket science that the more I help their businesses thrive, the more likely they are to do the same for mine. We are all one large family working together with the common goal to stay independent, a rarity these days amongst the conglomerate of hospitals taking over.
Wait, did I mention that I have never run a business before? Well, let me tell the most important lesson I have learned ... some days it is really hard. I remember having to let go my first medical assistant after her 90-day review. All of my medical training never prepared me for a how hard that conversation was going to be, and she wasn’t even losing her leg. My wife, a trained physical therapist, jumped right in until we eventually got the gusto to hire another MA. Fortunately, we found a remarkable individual who is worth her weight in gold. The same holds true for our other employees and we aren’t about to let them leave so we pay them well, fund 80% of their health insurance premiums, established a 401K with matching funds, and profit share with each employee. We foster an environment that makes our employees want to work hard, although like my patients, sometimes I think they come to work just to see The Girls.
All in all, we treat our staff with respect and provide a significant monetary carrot to each of them at the holidays; this is unmatched in our area. Happy employees are instrumental to my work life and have a direct impact on the success of my practice. All boats rise with the rising tide, and we are sailing smoothly.
Despite all the challenges and hard work, nothing is better than being your own boss. Nothing. I don’t know a single physician whose desire was to trek through grueling medical school and years of residency and fellowship to ultimately become an employee of an overly glorified postgraduate degree holder in health care administration. I cannot recall having had a single conversation with any surgeon or physician who is 100% happy with his or her working situation who isn’t self-employed. Do I work now more than I ever thought I would? Absolutely. But the work I am doing isn’t simply waking up at all hours to operate or trudge through countless hours in a lab or clinic. No, the work I do is running a successful small business – and even better yet, it is great!
Here I am on a Saturday morning writing a guest editorial for publication in the official newspaper of the Society for Vascular Surgery and I am loving it. Life is short and I’m trying to enjoy every minute that I have on this planet by spending my time working in a manner that I find enjoyable.
Being the fancy plumber in rural America provides me that opportunity. I hope others realize that it is still possible to navigate health care’s oftentimes unknown waters as a solo private practitioner and be successful. That they too could be taking the bull by the horns and changing up their work-life balance for the betterment of themselves, the care they provide to patients, and their families.
And in the meantime, I’ll jump back in my car and head due north for a 45-minute decompressing drive, chat with family and friends, dictate the last case of the day, and continue to enjoy the best of both worlds living in the big city and working with the most genuine folks in rural America. You should try it.
Dr. Santin is a vascular surgeon in private practice at Ohio Vein & Vascular, Wilmington.
References
1. Medscape Malpractice Report 2015: Why Most Doctors Get Sued, by Carol Peckham, Dec. 9, 2015.
2. Decrease Your Risk of Being Successfully Sued, by Nancy Young, Crozer-Chester Medical Center.
3. To Be Sued Less, Doctors Should Consider Talking to Patients More, by Aaron E. Carroll, New York Times, June 1, 2015.
Within 3 minutes of the car engine rumbling to a roar in the morning air, cruise control is set, freshly ground coffee is in hand and NPR is playing on WOSU 90.5. I settle in for the morning news on my 45-minute commute to the hospital. Sure, I could’ve found a hospital closer to shorten my commute, especially since I live in the 14th largest metropolitan city in the country.
If I’d wanted, I could be knocking out carotid endarterectomies at a level 1 trauma center, three blocks away from my front door. But no, that’s not what does it for me. What does? It’s having the opportunity to be my own boss and care for salt-of-the-earth folks in rural America.
You see, 5 years ago when I finished my vascular surgery fellowship at Good Samaritan Hospital in Cincinnati, I opened my own solo private practice in a rural community: population 30,000. Yep, that’s right, you heard it. I hung a shingle and went old school. And now as I reflect over the lessons learned during the first half-decade of my practice at Ohio Vein & Vascular Inc., I can tell you it has been a hell of a ride, and boy have we learned a lot.
The better half of the ‘we’ is my wife, Crystal, who doubles as my practice administrator, with her own solid foundation coming from a doctorate in physical therapy. We have successfully built a small company with four full-time employees, one contract registered vascular technologist, and two therapy dogs who serve more than 3,500 patients to date.
From the first day I opened my doors to this small-town rural community, I realized that it’s not what you know, but rather who you know. Well frankly, I didn’t know a soul!
Fortunately, my front office manager was born, raised, and still lives in Wilmington and knows everyone’s mother, brother, sister, niece, and grandchild in what felt like a 60-mile radius. She gave this young, slick city kid from Columbus instant street cred despite all the fancy credentials behind my name. I ditched the tie and fancy shoes and embraced my new ‘work’ home with open arms.
In a community such as Wilmington, Ohio, it’s the little things that count. I wear my own scrubs on days when I operate. Not only do they have my practice logo embroidered on the chest pocket, but they are also adorned with the brown leather symbol for Carhart, a clothing brand. In rural America, Carhart denim clothing – overall bibs, jackets, gloves, etc., are considered king. When my patients see that symbol, there is an instant point of mutual appreciation and it almost always results in some good laughs – who knew Carhart made scrubs?
As a result, I’ve been offered opportunities to ride combines, go drag racing, and go hunting for the infamous morel mushrooms. Just to be clear, I haven’t found a morel yet, so I guess I will stick to my day job as a surgeon.
Having a good laugh and connecting with my patients was something I was not accustomed to in my training. I was there to operate, and rarely participated in office days. At times this routine left me feeling unappreciated by my patients and their families. I was just a surgeon delivering bad news. I now find myself fortunate to have the opportunity to get to know my patients and participate in their health care, and I know they appreciate me for it.
A recent malpractice survey cited a finding that the more patients ‘like’ their physicians, the less likely they are to file malpractice lawsuits against them.1 Other reports have suggested that the relationship a physician has with a patient is a critical factor, more so than any single medical mistake, in determining whether or not a lawsuit is filed.2,3
While I feel appreciated and ‘liked’ by my patients, I’ve learned that I am not necessarily their favorite employee in the office. This honor is most often bestowed upon Claire and Whitney, aka “The Girls” – our two, miniature Labradoodles who serve in the capacity of therapy dogs and have perfected the ability to nap in nearly any situation. Try as I may to convince patients that what I am saying is important, they never lose focus on The Girls. They are the first thing patients ask about, I swear they receive more gifts than I do, and they always are on the receiving end of some good ‘pets’ as my patients leave the office. Despite any bad news they may have been told, very rarely do patients leave my office without smiles on their faces. It keeps me humble, as I think most of my patients aren’t really here to see me; after all I am just a fancy plumber.
Speaking of plumbing, I could’ve sworn that the ginormous two-volume Rutherford edition always gave me the impression that vascular disease is composed of 75% venous disease and 25% arterial disease. However, our fellowship training in the United States makes Rutherford seem like he had his numbers flipped – 99.8% was arterial with a splash of venous as an afterthought. Truth be told though, I see roughly 55% venous, 25% dialysis, and 20% arterial. I guess that wasn’t made up after all.
If my practice name, Ohio Vein & Vascular, didn’t give it away, I admit that I focus marketing efforts toward venous pathology. This has significantly improved my work-life balance. Let’s face it, not everything we do as a surgeon is fun and can certainly carry a large amount of stress. I devote an honest amount of time to developing what ‘type’ of practice I desire. I communicate regularly with my referring docs about the types of disease I focus on, write press releases to the local paper, and always have my elevator speech handy when speaking with fellow physicians and potential patients about what I do as a surgical subspecialist.
In such a small community, the more my vascular surgery practice grows, the more likely the podiatrist and his wife (also a podiatrist) across the hall will grow their practice. Same holds true of the cardiologist upstairs and the nephrologist down the hall. It’s not rocket science that the more I help their businesses thrive, the more likely they are to do the same for mine. We are all one large family working together with the common goal to stay independent, a rarity these days amongst the conglomerate of hospitals taking over.
Wait, did I mention that I have never run a business before? Well, let me tell the most important lesson I have learned ... some days it is really hard. I remember having to let go my first medical assistant after her 90-day review. All of my medical training never prepared me for a how hard that conversation was going to be, and she wasn’t even losing her leg. My wife, a trained physical therapist, jumped right in until we eventually got the gusto to hire another MA. Fortunately, we found a remarkable individual who is worth her weight in gold. The same holds true for our other employees and we aren’t about to let them leave so we pay them well, fund 80% of their health insurance premiums, established a 401K with matching funds, and profit share with each employee. We foster an environment that makes our employees want to work hard, although like my patients, sometimes I think they come to work just to see The Girls.
All in all, we treat our staff with respect and provide a significant monetary carrot to each of them at the holidays; this is unmatched in our area. Happy employees are instrumental to my work life and have a direct impact on the success of my practice. All boats rise with the rising tide, and we are sailing smoothly.
Despite all the challenges and hard work, nothing is better than being your own boss. Nothing. I don’t know a single physician whose desire was to trek through grueling medical school and years of residency and fellowship to ultimately become an employee of an overly glorified postgraduate degree holder in health care administration. I cannot recall having had a single conversation with any surgeon or physician who is 100% happy with his or her working situation who isn’t self-employed. Do I work now more than I ever thought I would? Absolutely. But the work I am doing isn’t simply waking up at all hours to operate or trudge through countless hours in a lab or clinic. No, the work I do is running a successful small business – and even better yet, it is great!
Here I am on a Saturday morning writing a guest editorial for publication in the official newspaper of the Society for Vascular Surgery and I am loving it. Life is short and I’m trying to enjoy every minute that I have on this planet by spending my time working in a manner that I find enjoyable.
Being the fancy plumber in rural America provides me that opportunity. I hope others realize that it is still possible to navigate health care’s oftentimes unknown waters as a solo private practitioner and be successful. That they too could be taking the bull by the horns and changing up their work-life balance for the betterment of themselves, the care they provide to patients, and their families.
And in the meantime, I’ll jump back in my car and head due north for a 45-minute decompressing drive, chat with family and friends, dictate the last case of the day, and continue to enjoy the best of both worlds living in the big city and working with the most genuine folks in rural America. You should try it.
Dr. Santin is a vascular surgeon in private practice at Ohio Vein & Vascular, Wilmington.
References
1. Medscape Malpractice Report 2015: Why Most Doctors Get Sued, by Carol Peckham, Dec. 9, 2015.
2. Decrease Your Risk of Being Successfully Sued, by Nancy Young, Crozer-Chester Medical Center.
3. To Be Sued Less, Doctors Should Consider Talking to Patients More, by Aaron E. Carroll, New York Times, June 1, 2015.
End of an Era
It is with a heavy heart I inform you that this issue—December 2018—of Emergency Medicine will be its last. Unfortunately, the print industry is facing enormous challenges financially, and the very difficult decision was made by Frontline Medical Communications, Inc, to stop publishing the journal, both in print and digital format. The fact that 2018 is the 50th anniversary of Emergency Medicine makes the decision even more poignant.
When the journal launched in 1968, it looked very different from the current version. In the early ears, it was a primary care journal focusing on an audience of general practitioners—predominantly family medicine and internal medicine physicians with an interest in emergency medicine. In many ways, its maturation as a journal mirrored that of Emergency Medicine as a recognized specialty within the house of medicine.
I started reading Emergency Medicine when I was an EM resident in the mid-1980s. Although I read other journals, I always enjoyed reading Emergency Medicine more—it was much less intimidating and easier to understand than its fellows. I also frequently learned something that I could immediately put to use in my practice. It was only as time passed that I found I was a member of a large group of practicing emergency physicians who felt exactly the same way. The comments I heard from colleagues had a consistent theme: practical, useful, helpful. I think this explains why it has been the most widely read journal in our specialty.
Like most things in life, success is due to the work of many. Emergency Medicine’s 50 years of excellence could not have been possible without the hard work and effort of the Editorial Board (both past and present), the authors and contributors, and our reviewers. A special thanks to the staff I have had the privilege to work with over the past many years: Harry Adkins, Martin Dicarlantonio, Maura Griffin, Mary Jo Dales, Jeff Bauer, Tracey Giannouris, and Kellie DeSantis. It has been my extreme fortune and honor to have worked with so many amazing physicians and staff. Please never forget the critically important role you played in a journal that was highly respected and valued by so many practicing emergency physicians. To our readers, I say thank you for your support, encouragement, and loyalty over the years.
Saying goodbye is difficult for me, so I will leave with the words of Drake: "I may regret the way we ended, but I will never regret what we had."
Francis L. Counselman, MD, CPE, FACEP
Editor-In-Chief
Emergency Medicine
It is with a heavy heart I inform you that this issue—December 2018—of Emergency Medicine will be its last. Unfortunately, the print industry is facing enormous challenges financially, and the very difficult decision was made by Frontline Medical Communications, Inc, to stop publishing the journal, both in print and digital format. The fact that 2018 is the 50th anniversary of Emergency Medicine makes the decision even more poignant.
When the journal launched in 1968, it looked very different from the current version. In the early ears, it was a primary care journal focusing on an audience of general practitioners—predominantly family medicine and internal medicine physicians with an interest in emergency medicine. In many ways, its maturation as a journal mirrored that of Emergency Medicine as a recognized specialty within the house of medicine.
I started reading Emergency Medicine when I was an EM resident in the mid-1980s. Although I read other journals, I always enjoyed reading Emergency Medicine more—it was much less intimidating and easier to understand than its fellows. I also frequently learned something that I could immediately put to use in my practice. It was only as time passed that I found I was a member of a large group of practicing emergency physicians who felt exactly the same way. The comments I heard from colleagues had a consistent theme: practical, useful, helpful. I think this explains why it has been the most widely read journal in our specialty.
Like most things in life, success is due to the work of many. Emergency Medicine’s 50 years of excellence could not have been possible without the hard work and effort of the Editorial Board (both past and present), the authors and contributors, and our reviewers. A special thanks to the staff I have had the privilege to work with over the past many years: Harry Adkins, Martin Dicarlantonio, Maura Griffin, Mary Jo Dales, Jeff Bauer, Tracey Giannouris, and Kellie DeSantis. It has been my extreme fortune and honor to have worked with so many amazing physicians and staff. Please never forget the critically important role you played in a journal that was highly respected and valued by so many practicing emergency physicians. To our readers, I say thank you for your support, encouragement, and loyalty over the years.
Saying goodbye is difficult for me, so I will leave with the words of Drake: "I may regret the way we ended, but I will never regret what we had."
Francis L. Counselman, MD, CPE, FACEP
Editor-In-Chief
Emergency Medicine
It is with a heavy heart I inform you that this issue—December 2018—of Emergency Medicine will be its last. Unfortunately, the print industry is facing enormous challenges financially, and the very difficult decision was made by Frontline Medical Communications, Inc, to stop publishing the journal, both in print and digital format. The fact that 2018 is the 50th anniversary of Emergency Medicine makes the decision even more poignant.
When the journal launched in 1968, it looked very different from the current version. In the early ears, it was a primary care journal focusing on an audience of general practitioners—predominantly family medicine and internal medicine physicians with an interest in emergency medicine. In many ways, its maturation as a journal mirrored that of Emergency Medicine as a recognized specialty within the house of medicine.
I started reading Emergency Medicine when I was an EM resident in the mid-1980s. Although I read other journals, I always enjoyed reading Emergency Medicine more—it was much less intimidating and easier to understand than its fellows. I also frequently learned something that I could immediately put to use in my practice. It was only as time passed that I found I was a member of a large group of practicing emergency physicians who felt exactly the same way. The comments I heard from colleagues had a consistent theme: practical, useful, helpful. I think this explains why it has been the most widely read journal in our specialty.
Like most things in life, success is due to the work of many. Emergency Medicine’s 50 years of excellence could not have been possible without the hard work and effort of the Editorial Board (both past and present), the authors and contributors, and our reviewers. A special thanks to the staff I have had the privilege to work with over the past many years: Harry Adkins, Martin Dicarlantonio, Maura Griffin, Mary Jo Dales, Jeff Bauer, Tracey Giannouris, and Kellie DeSantis. It has been my extreme fortune and honor to have worked with so many amazing physicians and staff. Please never forget the critically important role you played in a journal that was highly respected and valued by so many practicing emergency physicians. To our readers, I say thank you for your support, encouragement, and loyalty over the years.
Saying goodbye is difficult for me, so I will leave with the words of Drake: "I may regret the way we ended, but I will never regret what we had."
Francis L. Counselman, MD, CPE, FACEP
Editor-In-Chief
Emergency Medicine
Uptick in adult syphilis means congenital syphilis may be lurking
While many pediatric clinicians have not frequently managed newborns of mothers with reactive syphilis serology, increased adult syphilis may change that.1
Diagnosing/managing congenital syphilis is not always clear cut. A positive rapid plasma reagin (RPR) titer in a newborn may not indicate congenital infection but merely may reflect transplacental, passively acquired maternal IgG from the mother’s current or previous infection rather than antibodies produced by the newborn. Because currently no IgM assay for syphilis is recommended by the Centers for Disease Control and Prevention for newborn testing, we must deal with IgG test results.
Often initial management decisions are needed while the infant’s status is evolving. The questions to answer to make final decisions include the following2:
- Was the mother actively infected with Treponema pallidum during pregnancy?
- If so, was the mother appropriately treated and when?
- Does the infant have any clinical, laboratory, or radiographic evidence of syphilis?
- How do the mother’s and infant’s nontreponemal serologic titers (NTT) compare at delivery using the same test?
Note: All infants assessed for congenital syphilis need a full evaluation for HIV.
Managing the infant of a mother with positive tests3,4
All such neonates need an examination for evidence of congenital syphilis. The clinical signs of congenital syphilis in neonates include nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of extremity. Also, consider dark-field examination or polymerase chain reaction (PCR) of lesions (such as bullae) or secretions (nasal). If available, have the placenta examined histologically (silver stain) or by PCR (Clinical Laboratory Improvement Amendments–validated test). Skeletal radiographic surveys are more useful for stillborn than live born infants. (The complete algorithm can be found in Figure 3.10 of reference 4.)
Order a quantitative NTT, using the Venereal Disease Research Laboratory (VDRL) test or RPR test on neonatal serum. Umbilical cord blood is not appropriate because of potential maternal blood contamination, which could give a false-positive result, or Wharton’s jelly, which could give a false-negative result. Use of treponemal-specific tests that are used for maternal diagnosis – such as T. pallidum particle agglutination (TP-PA), T. pallidum enzyme-linked immunosorbent assay (TP-EIA), fluorescent treponemal antibody absorption (FTA-ABS) test, or T. pallidum chemiluminescence immunoassay (TP-CIA) – on neonatal serum is not recommended because of difficulties in interpretation.
Diagnostic results allow designation of an infant into one of four CDC categories: proven/highly probable syphilis; possible syphilis; syphilis less likely; and syphilis unlikely. Treatment recommendations are based on these categories.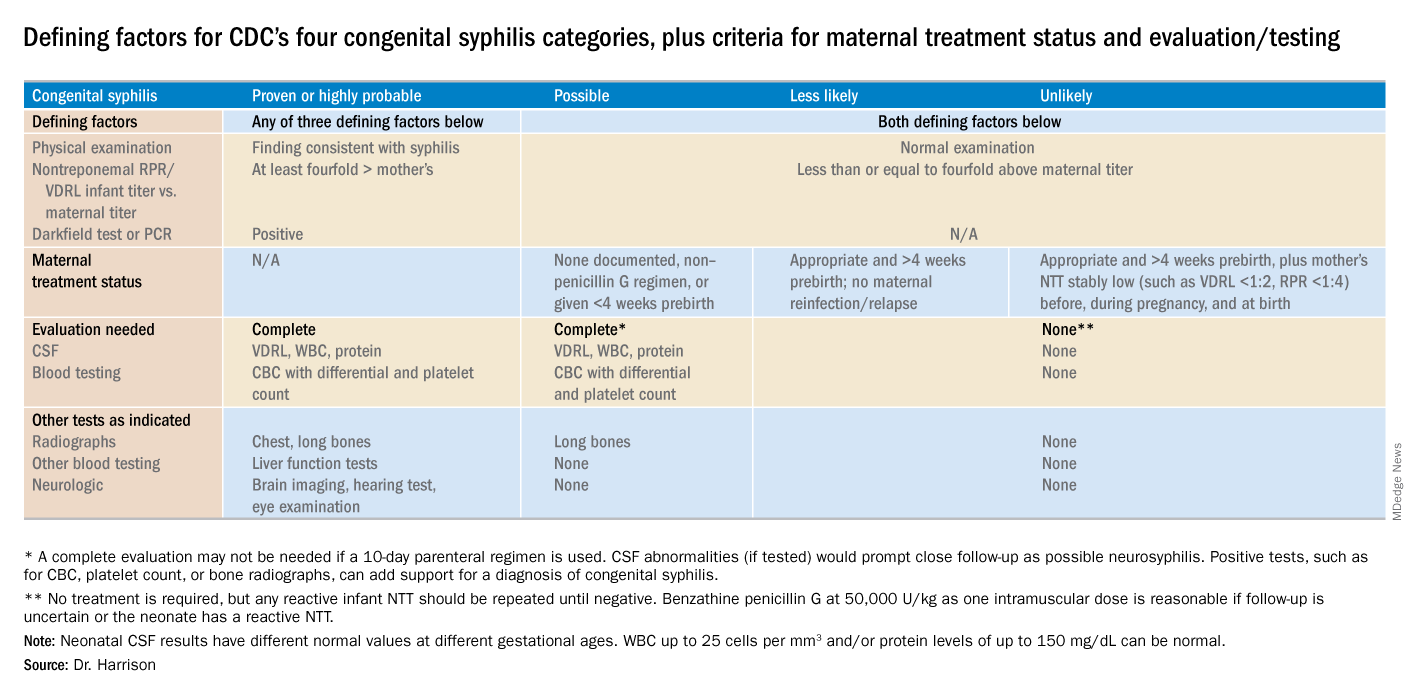
Proven or highly probable syphilis
There are two alternative recommended 10-day treatment regimens.
A. Aqueous crystalline penicillin G 100,000-150,000 U/kg per day by IV at 50,000 U/kg per dose, given every 12 hours through 7 days of age or every 8 hours if greater than 7 days old.
B. Procaine penicillin G at 50,000 U/kg per dose intramuscularly in one dose each day.
More than 1 day of missed therapy requires restarting a new 10-day course. Use of other antimicrobial agents (such as ampicillin) is not validated, so any empiric ampicillin initially given for possible sepsis does not count toward the 10-day penicillin regimen. If nonpenicillin drugs must be used, close serologic follow-up must occur to ensure adequacy of response to therapy.
Possible syphilis
There are three alternative regimens, the same two as in proven/highly probable syphilis (above) plus a single-dose option
A. Aqueous crystalline penicillin G, as described above.
B. Procaine penicillin G, as described above.
C. Benzathine penicillin G at 50,000 U/kg per dose intramuscularly in a single dose.
Note: To be eligible for regimen C, an infant must have a complete evaluation that is normal (cerebrospinal fluid [CSF] examination, long-bone radiographs, and complete blood count with platelet count) and follow-up must be assured. Exception: Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Less likely syphilis
One antibiotic regimen is available, but no treatment also may be an option.
A. Benzathine penicillin G as described above.
B. If mother’s NTT has decreased at least fourfold after appropriate early syphilis therapy or remained stably low, which indicates latent syphilis (VDRL less than 1:2; RPR less than 1:4), no treatment is an option but requires repeat serology every 2-3 months until infant is 6 months old.
Unlikely syphilis
No treatment is recommended unless follow-up is uncertain, in which case it is appropriate to give the infant benzathine penicillin G as described above.
Infant with positive NTT at birth
All neonates with reactive NTT need careful follow-up examinations and repeat NTT every 2-3 months until nonreactive. NTT in infants who are not treated because of less likely or unlikely syphilis status should drop by 3 months and be nonreactive by 6 months; this indicates NTT was passively transferred maternal IgG. If NTT remains reactive at 6 months, the infant is likely infected and needs treatment. Persistent NTT at 6-12 months in treated neonates should trigger repeat CSF examination and infectious diseases consultation about a possible repeat of the 10-day penicillin G regimen. If the mother was seroreactive, but the newborn’s NTT was negative at birth, testing of the infant’s NTT needs repeating at 3 months to exclude the possibility that the congenital syphilis was incubating when prior testing occurred at birth. Note: Treponemal-specific tests are not useful in assessing treatment because detectable maternal IgG treponemal antibody can persist at least 15 months.
Neonates with abnormal CSF at birth
Repeat cerebrospinal fluid evaluation every 6 months until results normalize. Persistently reactive CSF VDRL or abnormal CSF indexes not caused by another known cause requires retreatment for possible neurosyphilis, as well as consultation with an expert.
Summary
NTT are the essential test for newborns and some degree of laboratory or imaging work up often are needed. Consider consulting an expert in infectious diseases and/or perinatology if the gray areas do not readily become clear. Treatment of the correct patients with the right drug for the right duration remains the goal, as usual.
Dr. Harrison is a professor of pediatrics at University of Missouri-Kansas City and Director of Research Affairs in the pediatric infectious diseases division at Children’s Mercy Hospital – Kansas City. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. MMWR. 2015 Nov 13;64(44);1241-5.
2. “Congenital Syphilis,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
3. “Syphilis During Pregnancy,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
4. Syphilis – Section 3: Summaries of Infectious Diseases. Red Book Online. 2018.
While many pediatric clinicians have not frequently managed newborns of mothers with reactive syphilis serology, increased adult syphilis may change that.1
Diagnosing/managing congenital syphilis is not always clear cut. A positive rapid plasma reagin (RPR) titer in a newborn may not indicate congenital infection but merely may reflect transplacental, passively acquired maternal IgG from the mother’s current or previous infection rather than antibodies produced by the newborn. Because currently no IgM assay for syphilis is recommended by the Centers for Disease Control and Prevention for newborn testing, we must deal with IgG test results.
Often initial management decisions are needed while the infant’s status is evolving. The questions to answer to make final decisions include the following2:
- Was the mother actively infected with Treponema pallidum during pregnancy?
- If so, was the mother appropriately treated and when?
- Does the infant have any clinical, laboratory, or radiographic evidence of syphilis?
- How do the mother’s and infant’s nontreponemal serologic titers (NTT) compare at delivery using the same test?
Note: All infants assessed for congenital syphilis need a full evaluation for HIV.
Managing the infant of a mother with positive tests3,4
All such neonates need an examination for evidence of congenital syphilis. The clinical signs of congenital syphilis in neonates include nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of extremity. Also, consider dark-field examination or polymerase chain reaction (PCR) of lesions (such as bullae) or secretions (nasal). If available, have the placenta examined histologically (silver stain) or by PCR (Clinical Laboratory Improvement Amendments–validated test). Skeletal radiographic surveys are more useful for stillborn than live born infants. (The complete algorithm can be found in Figure 3.10 of reference 4.)
Order a quantitative NTT, using the Venereal Disease Research Laboratory (VDRL) test or RPR test on neonatal serum. Umbilical cord blood is not appropriate because of potential maternal blood contamination, which could give a false-positive result, or Wharton’s jelly, which could give a false-negative result. Use of treponemal-specific tests that are used for maternal diagnosis – such as T. pallidum particle agglutination (TP-PA), T. pallidum enzyme-linked immunosorbent assay (TP-EIA), fluorescent treponemal antibody absorption (FTA-ABS) test, or T. pallidum chemiluminescence immunoassay (TP-CIA) – on neonatal serum is not recommended because of difficulties in interpretation.
Diagnostic results allow designation of an infant into one of four CDC categories: proven/highly probable syphilis; possible syphilis; syphilis less likely; and syphilis unlikely. Treatment recommendations are based on these categories.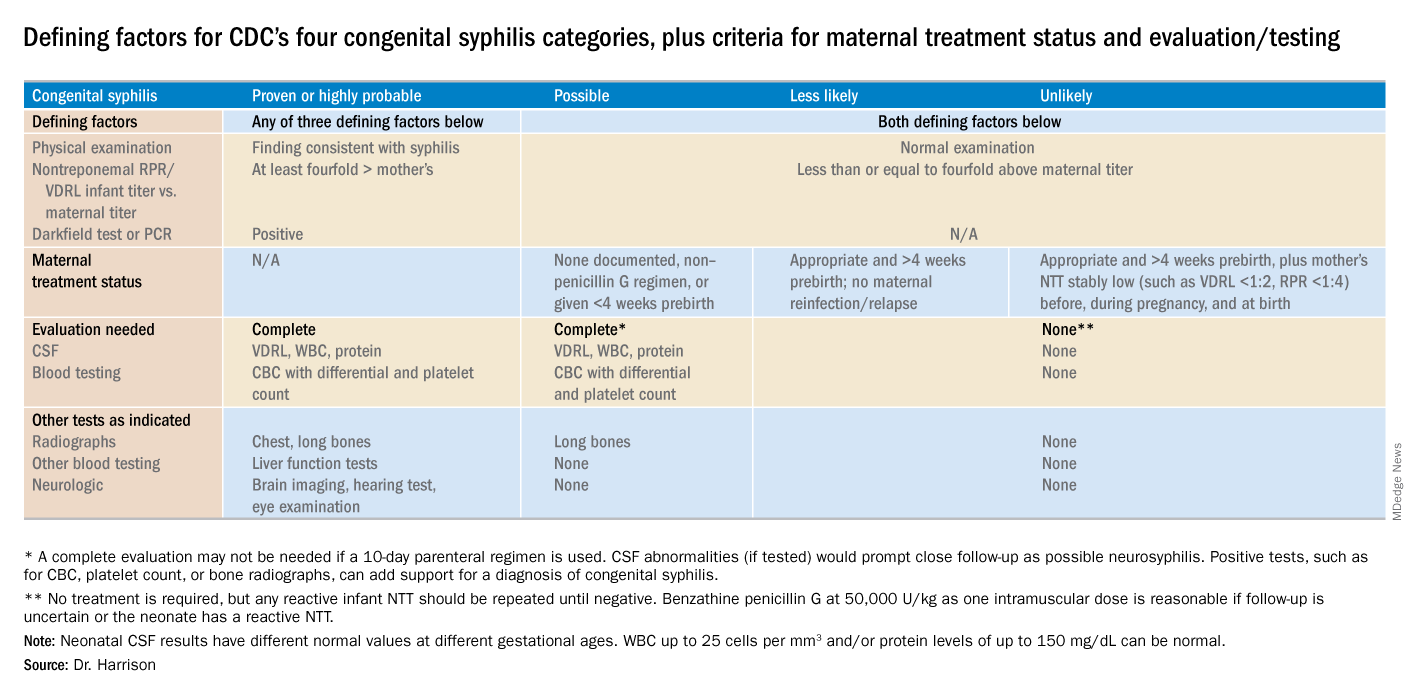
Proven or highly probable syphilis
There are two alternative recommended 10-day treatment regimens.
A. Aqueous crystalline penicillin G 100,000-150,000 U/kg per day by IV at 50,000 U/kg per dose, given every 12 hours through 7 days of age or every 8 hours if greater than 7 days old.
B. Procaine penicillin G at 50,000 U/kg per dose intramuscularly in one dose each day.
More than 1 day of missed therapy requires restarting a new 10-day course. Use of other antimicrobial agents (such as ampicillin) is not validated, so any empiric ampicillin initially given for possible sepsis does not count toward the 10-day penicillin regimen. If nonpenicillin drugs must be used, close serologic follow-up must occur to ensure adequacy of response to therapy.
Possible syphilis
There are three alternative regimens, the same two as in proven/highly probable syphilis (above) plus a single-dose option
A. Aqueous crystalline penicillin G, as described above.
B. Procaine penicillin G, as described above.
C. Benzathine penicillin G at 50,000 U/kg per dose intramuscularly in a single dose.
Note: To be eligible for regimen C, an infant must have a complete evaluation that is normal (cerebrospinal fluid [CSF] examination, long-bone radiographs, and complete blood count with platelet count) and follow-up must be assured. Exception: Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Less likely syphilis
One antibiotic regimen is available, but no treatment also may be an option.
A. Benzathine penicillin G as described above.
B. If mother’s NTT has decreased at least fourfold after appropriate early syphilis therapy or remained stably low, which indicates latent syphilis (VDRL less than 1:2; RPR less than 1:4), no treatment is an option but requires repeat serology every 2-3 months until infant is 6 months old.
Unlikely syphilis
No treatment is recommended unless follow-up is uncertain, in which case it is appropriate to give the infant benzathine penicillin G as described above.
Infant with positive NTT at birth
All neonates with reactive NTT need careful follow-up examinations and repeat NTT every 2-3 months until nonreactive. NTT in infants who are not treated because of less likely or unlikely syphilis status should drop by 3 months and be nonreactive by 6 months; this indicates NTT was passively transferred maternal IgG. If NTT remains reactive at 6 months, the infant is likely infected and needs treatment. Persistent NTT at 6-12 months in treated neonates should trigger repeat CSF examination and infectious diseases consultation about a possible repeat of the 10-day penicillin G regimen. If the mother was seroreactive, but the newborn’s NTT was negative at birth, testing of the infant’s NTT needs repeating at 3 months to exclude the possibility that the congenital syphilis was incubating when prior testing occurred at birth. Note: Treponemal-specific tests are not useful in assessing treatment because detectable maternal IgG treponemal antibody can persist at least 15 months.
Neonates with abnormal CSF at birth
Repeat cerebrospinal fluid evaluation every 6 months until results normalize. Persistently reactive CSF VDRL or abnormal CSF indexes not caused by another known cause requires retreatment for possible neurosyphilis, as well as consultation with an expert.
Summary
NTT are the essential test for newborns and some degree of laboratory or imaging work up often are needed. Consider consulting an expert in infectious diseases and/or perinatology if the gray areas do not readily become clear. Treatment of the correct patients with the right drug for the right duration remains the goal, as usual.
Dr. Harrison is a professor of pediatrics at University of Missouri-Kansas City and Director of Research Affairs in the pediatric infectious diseases division at Children’s Mercy Hospital – Kansas City. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. MMWR. 2015 Nov 13;64(44);1241-5.
2. “Congenital Syphilis,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
3. “Syphilis During Pregnancy,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
4. Syphilis – Section 3: Summaries of Infectious Diseases. Red Book Online. 2018.
While many pediatric clinicians have not frequently managed newborns of mothers with reactive syphilis serology, increased adult syphilis may change that.1
Diagnosing/managing congenital syphilis is not always clear cut. A positive rapid plasma reagin (RPR) titer in a newborn may not indicate congenital infection but merely may reflect transplacental, passively acquired maternal IgG from the mother’s current or previous infection rather than antibodies produced by the newborn. Because currently no IgM assay for syphilis is recommended by the Centers for Disease Control and Prevention for newborn testing, we must deal with IgG test results.
Often initial management decisions are needed while the infant’s status is evolving. The questions to answer to make final decisions include the following2:
- Was the mother actively infected with Treponema pallidum during pregnancy?
- If so, was the mother appropriately treated and when?
- Does the infant have any clinical, laboratory, or radiographic evidence of syphilis?
- How do the mother’s and infant’s nontreponemal serologic titers (NTT) compare at delivery using the same test?
Note: All infants assessed for congenital syphilis need a full evaluation for HIV.
Managing the infant of a mother with positive tests3,4
All such neonates need an examination for evidence of congenital syphilis. The clinical signs of congenital syphilis in neonates include nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of extremity. Also, consider dark-field examination or polymerase chain reaction (PCR) of lesions (such as bullae) or secretions (nasal). If available, have the placenta examined histologically (silver stain) or by PCR (Clinical Laboratory Improvement Amendments–validated test). Skeletal radiographic surveys are more useful for stillborn than live born infants. (The complete algorithm can be found in Figure 3.10 of reference 4.)
Order a quantitative NTT, using the Venereal Disease Research Laboratory (VDRL) test or RPR test on neonatal serum. Umbilical cord blood is not appropriate because of potential maternal blood contamination, which could give a false-positive result, or Wharton’s jelly, which could give a false-negative result. Use of treponemal-specific tests that are used for maternal diagnosis – such as T. pallidum particle agglutination (TP-PA), T. pallidum enzyme-linked immunosorbent assay (TP-EIA), fluorescent treponemal antibody absorption (FTA-ABS) test, or T. pallidum chemiluminescence immunoassay (TP-CIA) – on neonatal serum is not recommended because of difficulties in interpretation.
Diagnostic results allow designation of an infant into one of four CDC categories: proven/highly probable syphilis; possible syphilis; syphilis less likely; and syphilis unlikely. Treatment recommendations are based on these categories.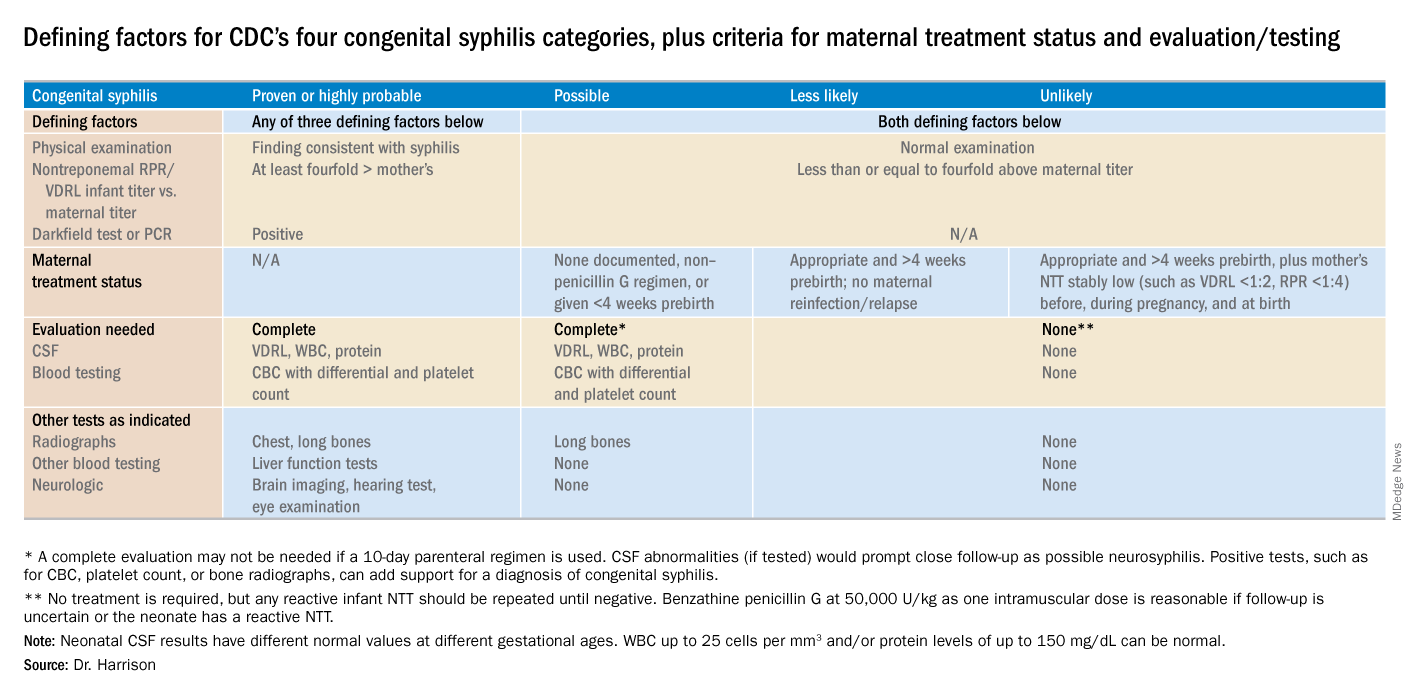
Proven or highly probable syphilis
There are two alternative recommended 10-day treatment regimens.
A. Aqueous crystalline penicillin G 100,000-150,000 U/kg per day by IV at 50,000 U/kg per dose, given every 12 hours through 7 days of age or every 8 hours if greater than 7 days old.
B. Procaine penicillin G at 50,000 U/kg per dose intramuscularly in one dose each day.
More than 1 day of missed therapy requires restarting a new 10-day course. Use of other antimicrobial agents (such as ampicillin) is not validated, so any empiric ampicillin initially given for possible sepsis does not count toward the 10-day penicillin regimen. If nonpenicillin drugs must be used, close serologic follow-up must occur to ensure adequacy of response to therapy.
Possible syphilis
There are three alternative regimens, the same two as in proven/highly probable syphilis (above) plus a single-dose option
A. Aqueous crystalline penicillin G, as described above.
B. Procaine penicillin G, as described above.
C. Benzathine penicillin G at 50,000 U/kg per dose intramuscularly in a single dose.
Note: To be eligible for regimen C, an infant must have a complete evaluation that is normal (cerebrospinal fluid [CSF] examination, long-bone radiographs, and complete blood count with platelet count) and follow-up must be assured. Exception: Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Less likely syphilis
One antibiotic regimen is available, but no treatment also may be an option.
A. Benzathine penicillin G as described above.
B. If mother’s NTT has decreased at least fourfold after appropriate early syphilis therapy or remained stably low, which indicates latent syphilis (VDRL less than 1:2; RPR less than 1:4), no treatment is an option but requires repeat serology every 2-3 months until infant is 6 months old.
Unlikely syphilis
No treatment is recommended unless follow-up is uncertain, in which case it is appropriate to give the infant benzathine penicillin G as described above.
Infant with positive NTT at birth
All neonates with reactive NTT need careful follow-up examinations and repeat NTT every 2-3 months until nonreactive. NTT in infants who are not treated because of less likely or unlikely syphilis status should drop by 3 months and be nonreactive by 6 months; this indicates NTT was passively transferred maternal IgG. If NTT remains reactive at 6 months, the infant is likely infected and needs treatment. Persistent NTT at 6-12 months in treated neonates should trigger repeat CSF examination and infectious diseases consultation about a possible repeat of the 10-day penicillin G regimen. If the mother was seroreactive, but the newborn’s NTT was negative at birth, testing of the infant’s NTT needs repeating at 3 months to exclude the possibility that the congenital syphilis was incubating when prior testing occurred at birth. Note: Treponemal-specific tests are not useful in assessing treatment because detectable maternal IgG treponemal antibody can persist at least 15 months.
Neonates with abnormal CSF at birth
Repeat cerebrospinal fluid evaluation every 6 months until results normalize. Persistently reactive CSF VDRL or abnormal CSF indexes not caused by another known cause requires retreatment for possible neurosyphilis, as well as consultation with an expert.
Summary
NTT are the essential test for newborns and some degree of laboratory or imaging work up often are needed. Consider consulting an expert in infectious diseases and/or perinatology if the gray areas do not readily become clear. Treatment of the correct patients with the right drug for the right duration remains the goal, as usual.
Dr. Harrison is a professor of pediatrics at University of Missouri-Kansas City and Director of Research Affairs in the pediatric infectious diseases division at Children’s Mercy Hospital – Kansas City. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. MMWR. 2015 Nov 13;64(44);1241-5.
2. “Congenital Syphilis,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
3. “Syphilis During Pregnancy,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
4. Syphilis – Section 3: Summaries of Infectious Diseases. Red Book Online. 2018.
We Asked, You Told Us
Dear Readers,
As 2018 draws to a close, Clinician Reviews is looking ahead to its 29th year of publication. In 1991, when our publication was founded, it was a unique idea to present information to both NPs and PAs together—a recognition of common educational needs and a unified focus on delivering the best possible patient care. For the past six years, as Editor, I have been privileged to ensure the fulfillment of CR’s editorial purpose—keeping NPs and PAs up to date on all aspects of clinical practice—while navigating changes both internal and external.
When CR started, personal computers existed but were not yet in widespread use (the office had one, to be shared). Manuscripts, peer reviews, even radiographs—all were submitted on paper, via the US Postal Service. How far the world has come in the ensuing decades. Now, we can stay connected to anyone, anywhere, via devices that fit in our pockets.
And so I’m excited to share with you one of the changes we’re making: In 2019, Clinician Reviews will be published 100% digitally! Why? Yes, printing and postage costs have increased to the point of unsustainability (and all that paper is not very environmentally friendly). But most importantly, online publication allows us to provide you with more of what you need for your practice—at any time of day or night, on any device you choose. And this gives us more scope to be creative in presenting information in engaging ways.
To ensure that we are moving in the right direction in making ClinicianReviews.com a more robust and useful resource, we surveyed NPs and PAs like you about our site, our competitors’ sites, and potential new offerings. Your answers were very enlightening, providing us guidance on
Building new functionality to make the site more user friendly
✓ Automatic notification when new content is posted
✓ Video player with a list of recently posted videos
Providing new content, including
✓ Clinical crossword puzzle
✓ Malpractice Chronicle by David Lang (both of which make their debut in this print issue)
Continue to: Offering you must-have content
Offering you must-have content
✓ Enhanced disease-specific content
✓ CE/CME with transcript tracking
✓ Peer-reviewed, evidence-based articles
✓ NP/PA- and MD-specific content
✓ Real-time news and conference reports
To ensure you stay informed about new offerings—and can continue to find the content you’ve enjoyed for years—we invite you to register on our website. You can do so by scanning the QR code below, and as a thank you, you’ll be able to download a free pocket guide, “PURLs in Primary Care.” And don’t forget to bookmark ClinicianReviews.com so that you can easily access our continually updated content.
We’re excited to take this step forward—and as always, we appreciate your support. We’re here to continue to serve the NP and PA professions, so please don’t hesitate to share your feedback and suggestions with us.
Best regards,
Karen J. Clemments
Dear Readers,
As 2018 draws to a close, Clinician Reviews is looking ahead to its 29th year of publication. In 1991, when our publication was founded, it was a unique idea to present information to both NPs and PAs together—a recognition of common educational needs and a unified focus on delivering the best possible patient care. For the past six years, as Editor, I have been privileged to ensure the fulfillment of CR’s editorial purpose—keeping NPs and PAs up to date on all aspects of clinical practice—while navigating changes both internal and external.
When CR started, personal computers existed but were not yet in widespread use (the office had one, to be shared). Manuscripts, peer reviews, even radiographs—all were submitted on paper, via the US Postal Service. How far the world has come in the ensuing decades. Now, we can stay connected to anyone, anywhere, via devices that fit in our pockets.
And so I’m excited to share with you one of the changes we’re making: In 2019, Clinician Reviews will be published 100% digitally! Why? Yes, printing and postage costs have increased to the point of unsustainability (and all that paper is not very environmentally friendly). But most importantly, online publication allows us to provide you with more of what you need for your practice—at any time of day or night, on any device you choose. And this gives us more scope to be creative in presenting information in engaging ways.
To ensure that we are moving in the right direction in making ClinicianReviews.com a more robust and useful resource, we surveyed NPs and PAs like you about our site, our competitors’ sites, and potential new offerings. Your answers were very enlightening, providing us guidance on
Building new functionality to make the site more user friendly
✓ Automatic notification when new content is posted
✓ Video player with a list of recently posted videos
Providing new content, including
✓ Clinical crossword puzzle
✓ Malpractice Chronicle by David Lang (both of which make their debut in this print issue)
Continue to: Offering you must-have content
Offering you must-have content
✓ Enhanced disease-specific content
✓ CE/CME with transcript tracking
✓ Peer-reviewed, evidence-based articles
✓ NP/PA- and MD-specific content
✓ Real-time news and conference reports
To ensure you stay informed about new offerings—and can continue to find the content you’ve enjoyed for years—we invite you to register on our website. You can do so by scanning the QR code below, and as a thank you, you’ll be able to download a free pocket guide, “PURLs in Primary Care.” And don’t forget to bookmark ClinicianReviews.com so that you can easily access our continually updated content.
We’re excited to take this step forward—and as always, we appreciate your support. We’re here to continue to serve the NP and PA professions, so please don’t hesitate to share your feedback and suggestions with us.
Best regards,
Karen J. Clemments
Dear Readers,
As 2018 draws to a close, Clinician Reviews is looking ahead to its 29th year of publication. In 1991, when our publication was founded, it was a unique idea to present information to both NPs and PAs together—a recognition of common educational needs and a unified focus on delivering the best possible patient care. For the past six years, as Editor, I have been privileged to ensure the fulfillment of CR’s editorial purpose—keeping NPs and PAs up to date on all aspects of clinical practice—while navigating changes both internal and external.
When CR started, personal computers existed but were not yet in widespread use (the office had one, to be shared). Manuscripts, peer reviews, even radiographs—all were submitted on paper, via the US Postal Service. How far the world has come in the ensuing decades. Now, we can stay connected to anyone, anywhere, via devices that fit in our pockets.
And so I’m excited to share with you one of the changes we’re making: In 2019, Clinician Reviews will be published 100% digitally! Why? Yes, printing and postage costs have increased to the point of unsustainability (and all that paper is not very environmentally friendly). But most importantly, online publication allows us to provide you with more of what you need for your practice—at any time of day or night, on any device you choose. And this gives us more scope to be creative in presenting information in engaging ways.
To ensure that we are moving in the right direction in making ClinicianReviews.com a more robust and useful resource, we surveyed NPs and PAs like you about our site, our competitors’ sites, and potential new offerings. Your answers were very enlightening, providing us guidance on
Building new functionality to make the site more user friendly
✓ Automatic notification when new content is posted
✓ Video player with a list of recently posted videos
Providing new content, including
✓ Clinical crossword puzzle
✓ Malpractice Chronicle by David Lang (both of which make their debut in this print issue)
Continue to: Offering you must-have content
Offering you must-have content
✓ Enhanced disease-specific content
✓ CE/CME with transcript tracking
✓ Peer-reviewed, evidence-based articles
✓ NP/PA- and MD-specific content
✓ Real-time news and conference reports
To ensure you stay informed about new offerings—and can continue to find the content you’ve enjoyed for years—we invite you to register on our website. You can do so by scanning the QR code below, and as a thank you, you’ll be able to download a free pocket guide, “PURLs in Primary Care.” And don’t forget to bookmark ClinicianReviews.com so that you can easily access our continually updated content.
We’re excited to take this step forward—and as always, we appreciate your support. We’re here to continue to serve the NP and PA professions, so please don’t hesitate to share your feedback and suggestions with us.
Best regards,
Karen J. Clemments
Letter to the Editor: Strengthening the relationships between transferring and accepting surgeons
“Nobody is happy when a patient needs to be transferred.” As the general surgery group who receives requests for transfer of patients to our tertiary care hospital, we understand and sympathize with many of the issues raised in Dr. Puls’ article (“Rural Surgery – A view from the front lines” ‘I need to transfer this patient,” ACS Surgery News, September 2018, p. 7).
There is no doubt that sometimes patients benefit from support only available at a tertiary care center. The need can be for subspeciality surgical expertise, but many times it is driven by other available hospital-level support (critical care, interventional radiology, etc.).
Transfers are time consuming for physicians on both ends – while referring physicians have the responsibility of reaching out, accepting physicians have the responsibility of timely response to a request, regardless of other demands on their time and attention. We agree wholeheartedly with Dr. Puls’s argument that the phone call process “should not be delegated to the hospitalist or anyone else.” The benefit of speaking directly to the surgeon who has personally evaluated the patient cannot be overemphasized. When referrals for surgical care are initiated by the hospitalist or emergency department physician caring for a patient, there is almost always a lack of clarity around the surgical history, reason for transfer, and ongoing needs of the patient. It is our practice to request to speak to the surgeon who has evaluated and cared for the patient so we can fully understand the clinical course. It is the rare, typically life-threatening, situation in which we transfer patients without this crucial conversation.
Another crucial conversation, one in which the receiving physicians have room for improvement, is that of closing the loop after transfer. Dr. Puls recommended that there be periodic communication between the referring physician and the accepting physician, as well as closing the loop at the time the patient is discharged. There is a lack of “best practice” and infrastructure to support this work in many institutions, including ours, in part complicated by the variable EHRs utilized by individual hospitals. We believe the burden of this communication is shared by both parties and critical to optimal patient outcomes. At our hospital, we are currently working on standardizing this process and hope it will continue to strengthen the relationships we are building with our community surgeons.
At the end of the day, referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients, by optimally matching patient needs with appropriate resources. or this reason, we disagree with Dr. Puls’ statement that “accepting physicians at larger hospitals should be treated like gold.” The work of “networking” should not be placed solely on the shoulders of rural surgeons. We believe it is best practice for the tertiary care hospital team to visit their community hospitals to better understand their resources, rather than the other way around. The Atrium Health National Surgical Quality Improvement Program Collaborative has been a valuable platform for making these connections for hospitals within our system and provides infrastructure for ongoing collaboration. Surgeons at tertiary care centers should also make themselves available for phone consultation for the complicated patient for whom a surgeon may simply need a second opinion. Not all “transfer calls” result in a transfer, and if both parties agree that the patient can continue to receive the same care at the local hospital that is often in his or her best interest.
Strengthening relationships with our community surgeons will allow surgeons at tertiary care centers to partner with them to optimally match patient needs to available resources. We truly appreciate our referring surgeons and thank them for the incredible work they do in serving our communities. Without their care on the front lines, we would not be able to provide the complex care and support to patients who need it most.
I very much appreciate the comments made by Drs. Reinke, Matthews, Paton, and Schiffern of the Carolinas Medical Center, Atrium Health, regarding my commentary on a rural surgeon’s take on transferring patients. They have provided the important perspective of the surgeon at a tertiary care center accepting a transferred patient. They also point out some of the important responsibilities that accepting surgeons have regarding the patient transfer process. If all tertiary facilities had the philosophy described by Drs. Reinke, Matthews, Paton, and Schiffern regarding patient transfers, many more patients would benefit
I agree that more easily arranged phone consultations between a rural surgeon and a tertiary surgeon regarding the need for a potential patient transfer would be helpful. Sometimes the simple reassurance from a tertiary care surgeon that the rural surgeon is doing the right thing, and the comfort the patient and his/her family derives from knowing that their surgeon has spoken with a surgeon at a tertiary care center, can be enough to prevent the need for an immediate transfer.
I also agree that “closing the loop” after a transfer is an important responsibility of both the transferring surgeon and the accepting surgeon. This is difficult partly because everyone is busy, but also because of factors such as the incompatibility of EHRs. Perhaps if part of the transfer process involved the transferring surgeon and accepting surgeon exchanging cell phone numbers and email addresses, then a quick phone call, text, or email every couple of days could help to “close the loop.
I accept their mild criticism of my statement that “accepting physicians at larger hospitals should be treated like gold” since they really are saying that there is a shared responsibility between tertiary care surgeons and rural surgeons to develop relationships that allow for the optimal care of transferred patients. I couldn’t agree more with their statement that “referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients.” When we do this, we are treating the patient like gold, which is our ultimate objective.
Mark Puls, MD, FACS, is a general surgeon in Alpena, Mich. He serves as vice chair of the ACS Advisory Council for Rural Surgery. octor’s Name and Bio
I very much appreciate the comments made by Drs. Reinke, Matthews, Paton, and Schiffern of the Carolinas Medical Center, Atrium Health, regarding my commentary on a rural surgeon’s take on transferring patients. They have provided the important perspective of the surgeon at a tertiary care center accepting a transferred patient. They also point out some of the important responsibilities that accepting surgeons have regarding the patient transfer process. If all tertiary facilities had the philosophy described by Drs. Reinke, Matthews, Paton, and Schiffern regarding patient transfers, many more patients would benefit
I agree that more easily arranged phone consultations between a rural surgeon and a tertiary surgeon regarding the need for a potential patient transfer would be helpful. Sometimes the simple reassurance from a tertiary care surgeon that the rural surgeon is doing the right thing, and the comfort the patient and his/her family derives from knowing that their surgeon has spoken with a surgeon at a tertiary care center, can be enough to prevent the need for an immediate transfer.
I also agree that “closing the loop” after a transfer is an important responsibility of both the transferring surgeon and the accepting surgeon. This is difficult partly because everyone is busy, but also because of factors such as the incompatibility of EHRs. Perhaps if part of the transfer process involved the transferring surgeon and accepting surgeon exchanging cell phone numbers and email addresses, then a quick phone call, text, or email every couple of days could help to “close the loop.
I accept their mild criticism of my statement that “accepting physicians at larger hospitals should be treated like gold” since they really are saying that there is a shared responsibility between tertiary care surgeons and rural surgeons to develop relationships that allow for the optimal care of transferred patients. I couldn’t agree more with their statement that “referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients.” When we do this, we are treating the patient like gold, which is our ultimate objective.
Mark Puls, MD, FACS, is a general surgeon in Alpena, Mich. He serves as vice chair of the ACS Advisory Council for Rural Surgery. octor’s Name and Bio
I very much appreciate the comments made by Drs. Reinke, Matthews, Paton, and Schiffern of the Carolinas Medical Center, Atrium Health, regarding my commentary on a rural surgeon’s take on transferring patients. They have provided the important perspective of the surgeon at a tertiary care center accepting a transferred patient. They also point out some of the important responsibilities that accepting surgeons have regarding the patient transfer process. If all tertiary facilities had the philosophy described by Drs. Reinke, Matthews, Paton, and Schiffern regarding patient transfers, many more patients would benefit
I agree that more easily arranged phone consultations between a rural surgeon and a tertiary surgeon regarding the need for a potential patient transfer would be helpful. Sometimes the simple reassurance from a tertiary care surgeon that the rural surgeon is doing the right thing, and the comfort the patient and his/her family derives from knowing that their surgeon has spoken with a surgeon at a tertiary care center, can be enough to prevent the need for an immediate transfer.
I also agree that “closing the loop” after a transfer is an important responsibility of both the transferring surgeon and the accepting surgeon. This is difficult partly because everyone is busy, but also because of factors such as the incompatibility of EHRs. Perhaps if part of the transfer process involved the transferring surgeon and accepting surgeon exchanging cell phone numbers and email addresses, then a quick phone call, text, or email every couple of days could help to “close the loop.
I accept their mild criticism of my statement that “accepting physicians at larger hospitals should be treated like gold” since they really are saying that there is a shared responsibility between tertiary care surgeons and rural surgeons to develop relationships that allow for the optimal care of transferred patients. I couldn’t agree more with their statement that “referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients.” When we do this, we are treating the patient like gold, which is our ultimate objective.
Mark Puls, MD, FACS, is a general surgeon in Alpena, Mich. He serves as vice chair of the ACS Advisory Council for Rural Surgery. octor’s Name and Bio
“Nobody is happy when a patient needs to be transferred.” As the general surgery group who receives requests for transfer of patients to our tertiary care hospital, we understand and sympathize with many of the issues raised in Dr. Puls’ article (“Rural Surgery – A view from the front lines” ‘I need to transfer this patient,” ACS Surgery News, September 2018, p. 7).
There is no doubt that sometimes patients benefit from support only available at a tertiary care center. The need can be for subspeciality surgical expertise, but many times it is driven by other available hospital-level support (critical care, interventional radiology, etc.).
Transfers are time consuming for physicians on both ends – while referring physicians have the responsibility of reaching out, accepting physicians have the responsibility of timely response to a request, regardless of other demands on their time and attention. We agree wholeheartedly with Dr. Puls’s argument that the phone call process “should not be delegated to the hospitalist or anyone else.” The benefit of speaking directly to the surgeon who has personally evaluated the patient cannot be overemphasized. When referrals for surgical care are initiated by the hospitalist or emergency department physician caring for a patient, there is almost always a lack of clarity around the surgical history, reason for transfer, and ongoing needs of the patient. It is our practice to request to speak to the surgeon who has evaluated and cared for the patient so we can fully understand the clinical course. It is the rare, typically life-threatening, situation in which we transfer patients without this crucial conversation.
Another crucial conversation, one in which the receiving physicians have room for improvement, is that of closing the loop after transfer. Dr. Puls recommended that there be periodic communication between the referring physician and the accepting physician, as well as closing the loop at the time the patient is discharged. There is a lack of “best practice” and infrastructure to support this work in many institutions, including ours, in part complicated by the variable EHRs utilized by individual hospitals. We believe the burden of this communication is shared by both parties and critical to optimal patient outcomes. At our hospital, we are currently working on standardizing this process and hope it will continue to strengthen the relationships we are building with our community surgeons.
At the end of the day, referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients, by optimally matching patient needs with appropriate resources. or this reason, we disagree with Dr. Puls’ statement that “accepting physicians at larger hospitals should be treated like gold.” The work of “networking” should not be placed solely on the shoulders of rural surgeons. We believe it is best practice for the tertiary care hospital team to visit their community hospitals to better understand their resources, rather than the other way around. The Atrium Health National Surgical Quality Improvement Program Collaborative has been a valuable platform for making these connections for hospitals within our system and provides infrastructure for ongoing collaboration. Surgeons at tertiary care centers should also make themselves available for phone consultation for the complicated patient for whom a surgeon may simply need a second opinion. Not all “transfer calls” result in a transfer, and if both parties agree that the patient can continue to receive the same care at the local hospital that is often in his or her best interest.
Strengthening relationships with our community surgeons will allow surgeons at tertiary care centers to partner with them to optimally match patient needs to available resources. We truly appreciate our referring surgeons and thank them for the incredible work they do in serving our communities. Without their care on the front lines, we would not be able to provide the complex care and support to patients who need it most.
“Nobody is happy when a patient needs to be transferred.” As the general surgery group who receives requests for transfer of patients to our tertiary care hospital, we understand and sympathize with many of the issues raised in Dr. Puls’ article (“Rural Surgery – A view from the front lines” ‘I need to transfer this patient,” ACS Surgery News, September 2018, p. 7).
There is no doubt that sometimes patients benefit from support only available at a tertiary care center. The need can be for subspeciality surgical expertise, but many times it is driven by other available hospital-level support (critical care, interventional radiology, etc.).
Transfers are time consuming for physicians on both ends – while referring physicians have the responsibility of reaching out, accepting physicians have the responsibility of timely response to a request, regardless of other demands on their time and attention. We agree wholeheartedly with Dr. Puls’s argument that the phone call process “should not be delegated to the hospitalist or anyone else.” The benefit of speaking directly to the surgeon who has personally evaluated the patient cannot be overemphasized. When referrals for surgical care are initiated by the hospitalist or emergency department physician caring for a patient, there is almost always a lack of clarity around the surgical history, reason for transfer, and ongoing needs of the patient. It is our practice to request to speak to the surgeon who has evaluated and cared for the patient so we can fully understand the clinical course. It is the rare, typically life-threatening, situation in which we transfer patients without this crucial conversation.
Another crucial conversation, one in which the receiving physicians have room for improvement, is that of closing the loop after transfer. Dr. Puls recommended that there be periodic communication between the referring physician and the accepting physician, as well as closing the loop at the time the patient is discharged. There is a lack of “best practice” and infrastructure to support this work in many institutions, including ours, in part complicated by the variable EHRs utilized by individual hospitals. We believe the burden of this communication is shared by both parties and critical to optimal patient outcomes. At our hospital, we are currently working on standardizing this process and hope it will continue to strengthen the relationships we are building with our community surgeons.
At the end of the day, referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients, by optimally matching patient needs with appropriate resources. or this reason, we disagree with Dr. Puls’ statement that “accepting physicians at larger hospitals should be treated like gold.” The work of “networking” should not be placed solely on the shoulders of rural surgeons. We believe it is best practice for the tertiary care hospital team to visit their community hospitals to better understand their resources, rather than the other way around. The Atrium Health National Surgical Quality Improvement Program Collaborative has been a valuable platform for making these connections for hospitals within our system and provides infrastructure for ongoing collaboration. Surgeons at tertiary care centers should also make themselves available for phone consultation for the complicated patient for whom a surgeon may simply need a second opinion. Not all “transfer calls” result in a transfer, and if both parties agree that the patient can continue to receive the same care at the local hospital that is often in his or her best interest.
Strengthening relationships with our community surgeons will allow surgeons at tertiary care centers to partner with them to optimally match patient needs to available resources. We truly appreciate our referring surgeons and thank them for the incredible work they do in serving our communities. Without their care on the front lines, we would not be able to provide the complex care and support to patients who need it most.
The power of the turkey sandwich
A relatively high proportion of pediatric visits to the emergency department are related to psychiatric symptoms, oftentimes with suicidal or violent ideation.1 Given that pediatric emergencies related to psychiatric symptoms are on the increase, clinicians frequently are called to assess children and adolescents with symptoms of aggression and violence. Management of these cases can be tricky.
Case presentation
Henry is a 6-year-old boy with mild developmental delays and possible anxiety who was brought to the emergency department because of concerns on the bus. For about a month, Henry, who is repeating his kindergarten year, had been struggling with getting on and off the bus and with other transitions at school. These struggles had been attributed to anxiety. He was started on sertraline and the dose was increased about 2 weeks later. Soon thereafter he complained of stomach upset with the sertraline, refused to take the medicine, and had a very hard day at school. He required one-on-one attention for unsafe behavior most of that day, and he missed most of his lunch and recess. His school support team was able to get him onto the bus at the end of the day, but he refused to get off of the bus at home. He became violent with the bus driver, kicking and biting him until the police were called. The police called EMS and he was brought into the emergency department after fighting to get on the transport stretcher. He was eventually brought into a secure exam room in the emergency department, but was unable to be fully assessed because he would only make animal noises when approached. His father already had been called, but was unable to calm him down. The emergency department physician was unable to approach Henry because he began swinging at him as soon as the physician entered the room. An emergent psychiatric consultation was called to determine what medication to give to Henry to calm him down and to assess him for possible psychosis.
Case discussion
It sounds like Henry was having a severe tantrum exacerbated by a number of factors. First of all, this is a child who struggles with transitions. That day had been loaded with transitions, eventually leading him to be in an unfamiliar environment with many unfamiliar faces. Even the familiar face of his father wasn’t enough to help because he was overly stimulated and scared. Next, he was probably hungry. We know for certain that he missed lunch, and several hours into his presentation there were no breaks to deal with his basic needs. The first approach to assessment of aggressive behavior in the emergency setting is to try to care for the basic needs of the individual to deescalate the situation. Finally, he had recently been started on sertraline, a selective serotonin reuptake inhibitor. He had been having some dyspepsia and/or nausea with the sertraline, leading to his having missed some doses. Some children and adolescents have a discontinuation syndrome, which can be more severe in younger children and with medications that have shorter half-lives.2 In Henry’s case, a missed dose or two can be enough to trigger this discontinuation response leading to more aggressive behavior.
Case follow-up
The child and adolescent psychiatrist called to the case received a history from the primary team. When he started to try to talk with the parent outside of the room, the child became upset. He was able to gather the information that Henry also had skipped breakfast. In an attempt to calm the patient down, the psychiatrist addressed Henry using a nonjudgmental, nonconfrontational, collaborative approach, incorporating play. Henry responded to this approach and allowed the psychiatrist to ask a few questions about basic needs, and admitted that he was hungry. He was offered a turkey sandwich, which was rapidly ingested. The tantrum slowly subsided. Within about 30 minutes (and with some more food), the child was able to sit on his parent’s lap and finish the interview. The decision was made to have him follow up with his primary care provider to change to an SSRI with a longer half-life, such as fluoxetine, as he did seem to be experiencing some discontinuation even after missing just a dose or two of sertraline.
When dealing with emergent, aggressive behavior, food isn’t always the best medicine, but sometimes it is. Environmental barriers to the child’s regaining control include hunger, thirst, a full bladder, constipation, or other pain. Attending to these issues first sometimes can help avoid sedating medications, which can prolong emergency visits and lead to unwelcome side effects.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. Pediatrics. 2011 May;127(5):e1356-66.
2. J Can Acad Child Adolesc Psychiatry. 2011 Feb;20(1):60-7.
A relatively high proportion of pediatric visits to the emergency department are related to psychiatric symptoms, oftentimes with suicidal or violent ideation.1 Given that pediatric emergencies related to psychiatric symptoms are on the increase, clinicians frequently are called to assess children and adolescents with symptoms of aggression and violence. Management of these cases can be tricky.
Case presentation
Henry is a 6-year-old boy with mild developmental delays and possible anxiety who was brought to the emergency department because of concerns on the bus. For about a month, Henry, who is repeating his kindergarten year, had been struggling with getting on and off the bus and with other transitions at school. These struggles had been attributed to anxiety. He was started on sertraline and the dose was increased about 2 weeks later. Soon thereafter he complained of stomach upset with the sertraline, refused to take the medicine, and had a very hard day at school. He required one-on-one attention for unsafe behavior most of that day, and he missed most of his lunch and recess. His school support team was able to get him onto the bus at the end of the day, but he refused to get off of the bus at home. He became violent with the bus driver, kicking and biting him until the police were called. The police called EMS and he was brought into the emergency department after fighting to get on the transport stretcher. He was eventually brought into a secure exam room in the emergency department, but was unable to be fully assessed because he would only make animal noises when approached. His father already had been called, but was unable to calm him down. The emergency department physician was unable to approach Henry because he began swinging at him as soon as the physician entered the room. An emergent psychiatric consultation was called to determine what medication to give to Henry to calm him down and to assess him for possible psychosis.
Case discussion
It sounds like Henry was having a severe tantrum exacerbated by a number of factors. First of all, this is a child who struggles with transitions. That day had been loaded with transitions, eventually leading him to be in an unfamiliar environment with many unfamiliar faces. Even the familiar face of his father wasn’t enough to help because he was overly stimulated and scared. Next, he was probably hungry. We know for certain that he missed lunch, and several hours into his presentation there were no breaks to deal with his basic needs. The first approach to assessment of aggressive behavior in the emergency setting is to try to care for the basic needs of the individual to deescalate the situation. Finally, he had recently been started on sertraline, a selective serotonin reuptake inhibitor. He had been having some dyspepsia and/or nausea with the sertraline, leading to his having missed some doses. Some children and adolescents have a discontinuation syndrome, which can be more severe in younger children and with medications that have shorter half-lives.2 In Henry’s case, a missed dose or two can be enough to trigger this discontinuation response leading to more aggressive behavior.
Case follow-up
The child and adolescent psychiatrist called to the case received a history from the primary team. When he started to try to talk with the parent outside of the room, the child became upset. He was able to gather the information that Henry also had skipped breakfast. In an attempt to calm the patient down, the psychiatrist addressed Henry using a nonjudgmental, nonconfrontational, collaborative approach, incorporating play. Henry responded to this approach and allowed the psychiatrist to ask a few questions about basic needs, and admitted that he was hungry. He was offered a turkey sandwich, which was rapidly ingested. The tantrum slowly subsided. Within about 30 minutes (and with some more food), the child was able to sit on his parent’s lap and finish the interview. The decision was made to have him follow up with his primary care provider to change to an SSRI with a longer half-life, such as fluoxetine, as he did seem to be experiencing some discontinuation even after missing just a dose or two of sertraline.
When dealing with emergent, aggressive behavior, food isn’t always the best medicine, but sometimes it is. Environmental barriers to the child’s regaining control include hunger, thirst, a full bladder, constipation, or other pain. Attending to these issues first sometimes can help avoid sedating medications, which can prolong emergency visits and lead to unwelcome side effects.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. Pediatrics. 2011 May;127(5):e1356-66.
2. J Can Acad Child Adolesc Psychiatry. 2011 Feb;20(1):60-7.
A relatively high proportion of pediatric visits to the emergency department are related to psychiatric symptoms, oftentimes with suicidal or violent ideation.1 Given that pediatric emergencies related to psychiatric symptoms are on the increase, clinicians frequently are called to assess children and adolescents with symptoms of aggression and violence. Management of these cases can be tricky.
Case presentation
Henry is a 6-year-old boy with mild developmental delays and possible anxiety who was brought to the emergency department because of concerns on the bus. For about a month, Henry, who is repeating his kindergarten year, had been struggling with getting on and off the bus and with other transitions at school. These struggles had been attributed to anxiety. He was started on sertraline and the dose was increased about 2 weeks later. Soon thereafter he complained of stomach upset with the sertraline, refused to take the medicine, and had a very hard day at school. He required one-on-one attention for unsafe behavior most of that day, and he missed most of his lunch and recess. His school support team was able to get him onto the bus at the end of the day, but he refused to get off of the bus at home. He became violent with the bus driver, kicking and biting him until the police were called. The police called EMS and he was brought into the emergency department after fighting to get on the transport stretcher. He was eventually brought into a secure exam room in the emergency department, but was unable to be fully assessed because he would only make animal noises when approached. His father already had been called, but was unable to calm him down. The emergency department physician was unable to approach Henry because he began swinging at him as soon as the physician entered the room. An emergent psychiatric consultation was called to determine what medication to give to Henry to calm him down and to assess him for possible psychosis.
Case discussion
It sounds like Henry was having a severe tantrum exacerbated by a number of factors. First of all, this is a child who struggles with transitions. That day had been loaded with transitions, eventually leading him to be in an unfamiliar environment with many unfamiliar faces. Even the familiar face of his father wasn’t enough to help because he was overly stimulated and scared. Next, he was probably hungry. We know for certain that he missed lunch, and several hours into his presentation there were no breaks to deal with his basic needs. The first approach to assessment of aggressive behavior in the emergency setting is to try to care for the basic needs of the individual to deescalate the situation. Finally, he had recently been started on sertraline, a selective serotonin reuptake inhibitor. He had been having some dyspepsia and/or nausea with the sertraline, leading to his having missed some doses. Some children and adolescents have a discontinuation syndrome, which can be more severe in younger children and with medications that have shorter half-lives.2 In Henry’s case, a missed dose or two can be enough to trigger this discontinuation response leading to more aggressive behavior.
Case follow-up
The child and adolescent psychiatrist called to the case received a history from the primary team. When he started to try to talk with the parent outside of the room, the child became upset. He was able to gather the information that Henry also had skipped breakfast. In an attempt to calm the patient down, the psychiatrist addressed Henry using a nonjudgmental, nonconfrontational, collaborative approach, incorporating play. Henry responded to this approach and allowed the psychiatrist to ask a few questions about basic needs, and admitted that he was hungry. He was offered a turkey sandwich, which was rapidly ingested. The tantrum slowly subsided. Within about 30 minutes (and with some more food), the child was able to sit on his parent’s lap and finish the interview. The decision was made to have him follow up with his primary care provider to change to an SSRI with a longer half-life, such as fluoxetine, as he did seem to be experiencing some discontinuation even after missing just a dose or two of sertraline.
When dealing with emergent, aggressive behavior, food isn’t always the best medicine, but sometimes it is. Environmental barriers to the child’s regaining control include hunger, thirst, a full bladder, constipation, or other pain. Attending to these issues first sometimes can help avoid sedating medications, which can prolong emergency visits and lead to unwelcome side effects.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. Pediatrics. 2011 May;127(5):e1356-66.
2. J Can Acad Child Adolesc Psychiatry. 2011 Feb;20(1):60-7.