User login
Two more and counting: Suicide in medical trainees
Like everyone in the arc of social media impact, I was shocked and terribly saddened by the recent suicides of two New York women in medicine – a final-year medical student on May 1 and a second-year resident on May 5. As a specialist in physician health, a former training director, a long-standing member of our institution’s medical student admissions committee, and the ombudsman for our medical students, I am finding these tragedies harder and harder to reconcile. Something isn’t working. But before I get to that, what follows is a bulleted list of some events of the past couple of weeks that may give a context for my statements and have informed my two recommendations.
- May 3, 2018: I give an invited GI grand rounds on stress, burnout, depression, and suicide in physicians. The residents are quiet and say nothing. Faculty members seem only concerned about preventing and eradicating burnout – and not that interested in anything more severe.
- May 5: A psychiatry resident from Melbourne arrives to spend 10 days with me to do an elective in physician health. As in the United States, there is a significant suicide death rate in medical students and residents Down Under. In the afternoon, I present a paper at the annual meeting of the American Academy of Psychodynamic Psychiatry and Psychoanalysis on the use of psychotherapy in treatment-resistant suicidal depression in physicians. There is increasing hope that this essential modality of care will return to the contemporary psychiatrist’s toolbox.
- May 6: At the annual meeting of the American Psychiatric Association in New York, I’m the discussant for powerful heartfelt papers of five psychiatrists (mostly early career psychiatrists and one resident) that talked about living with a psychiatric illness. The audience is huge, and we hear narratives about internal stigma, self-disclosure, external stigma, shunning, bullying, acceptance, rejection, alienation, connection, and love by peers and family. The authenticity and valor of the speakers create an atmosphere of safety, which enables psychiatrists in attendance from all over the world to share their personal stories – some at the microphone, some privately.
- May 7: Again at the APA, I chair and facilitate a workshop on physician suicide. We hear from four speakers, all women, who have lost a loved one to suicide – a husband, a father, a brother, a son – all doctors. Two of the speakers are psychiatrists. The stories are gripping, detailed, and tender. Yes, the atmosphere is very sad, but there is not a pall. We learn how these doctors lived, not just how they died. They all loved medicine; they were creative; they cared deeply; they suffered silently; and with shame, they lost hope. Again, a big audience of psychiatrists, many of whom share their own stories, that they, too, had lost a physician son, wife, or mother to suicide. Some of their deceased family members fell through the cracks and did not receive the life-saving care they deserved; some, fearing assaults to their medical license, hospital privileges, or insurance, refused to see anyone. They died untreated.
- May 8: Still at the APA, a psychiatrist colleague and I collaborate on a clinical case conference. Each of us describes losing a physician patient to suicide. We walk the attendees through the clinical details of assessment, treatment, and the aftermath of their deaths. We talk openly and frankly about our feelings, grief, outreach to colleagues and the family, and our own personal journeys of learning, growth, and healing. The clinician audience members give constructive feedback, and some share their own stories of losing patients to suicide. Like the day before, some psychiatrists are grieving the loss of a physician son or sibling to suicide. As mental health professionals, they suffer from an additional layer of failure and guilt that a loved one died “under their watch.”
- May 8: I rush across the Javits Center to catch the discussant for a concurrent symposium on physician burnout and depression. She foregoes any prepared remarks to share her previous 48 hours with the audience. She is the training director of the program that lost the second-year resident on May 5. She did not learn of the death until 24 hours later. We are all on the edge of our seats as we listen to this grieving, courageous woman, a seasoned psychiatrist and educator, who has been blindsided by this tragedy. She has not slept. She called all of her residents and broke the news personally as best she could. Aided by “After A Suicide: A Toolkit for Residency/Fellowship Programs” (American Foundation for Suicide Prevention), she and her colleagues instituted a plan of action and worked with administration and faculty. Her strength and commitment to the well-being of her trainees is palpable and magnanimous. When the session ends, many of us stand in line to give her a hug. It is a stark reminder of how many lives are affected when someone you know or care about takes his/her own life – and how, in the house of medicine, medical students and residents really are part of an institutional family.
- May 10: I facilitate a meeting of our 12 second-year residents, many of whom knew of or had met the resident who died. Almost everyone speaks, shares their feelings, poses questions, and calls for answers and change. There is disbelief, sadness, confusion, some guilt, and lots of anger. Also a feeling of disillusionment or paradox about the field of psychiatry: “Of all branches of medicine, shouldn’t residents who are struggling with psychiatric issues feel safe, protected, cared for in psychiatry?” There is also a feeling of lip service being paid to personal treatment, as in quoted statements: “By all means, get treatment for your issues, but don’t let it encroach on your duty hours” or “It’s good you’re getting help, but do you still have to go weekly?”
In the immediate aftermath of suicide, feelings run high, as they should. But rather than wait it out – and fearing a return to “business as usual” – let me make only two suggestions:
2. In psychiatry, we need to redouble our efforts in fighting the stigma attached to psychiatric illness in trainees. It is unconscionable that medical students and residents are dying of treatable disorders (I’ve never heard of a doctor dying of cancer who didn’t go to an oncologist at least once), yet too many are not availing themselves of services we provide – even when they’re free of charge or covered by insurance. And are we certain that, when they knock on our doors, we are providing them with state-of-the-art care? Is it possible that unrecognized internal stigma and shame deep within us might make us hesitant to help our trainees in their hour of need? Or cut corners? Or not get a second opinion? Very few psychiatrists on faculty of our medical schools divulge their personal experiences of depression, posttraumatic stress disorders, substance use disorders, and more (with the exception of being in therapy during residency, which is normative and isn’t stigmatized). Coming out is leveling, humane, and respectful – and it shrinks the power differential in the teaching dyad. It might even save a life.
Dr. Myers is a professor of clinical psychiatry at State University of New York, Brooklyn, and the author of “Why Physicians Die by Suicide: Lessons Learned From Their Families and Others Who Cared.”
Like everyone in the arc of social media impact, I was shocked and terribly saddened by the recent suicides of two New York women in medicine – a final-year medical student on May 1 and a second-year resident on May 5. As a specialist in physician health, a former training director, a long-standing member of our institution’s medical student admissions committee, and the ombudsman for our medical students, I am finding these tragedies harder and harder to reconcile. Something isn’t working. But before I get to that, what follows is a bulleted list of some events of the past couple of weeks that may give a context for my statements and have informed my two recommendations.
- May 3, 2018: I give an invited GI grand rounds on stress, burnout, depression, and suicide in physicians. The residents are quiet and say nothing. Faculty members seem only concerned about preventing and eradicating burnout – and not that interested in anything more severe.
- May 5: A psychiatry resident from Melbourne arrives to spend 10 days with me to do an elective in physician health. As in the United States, there is a significant suicide death rate in medical students and residents Down Under. In the afternoon, I present a paper at the annual meeting of the American Academy of Psychodynamic Psychiatry and Psychoanalysis on the use of psychotherapy in treatment-resistant suicidal depression in physicians. There is increasing hope that this essential modality of care will return to the contemporary psychiatrist’s toolbox.
- May 6: At the annual meeting of the American Psychiatric Association in New York, I’m the discussant for powerful heartfelt papers of five psychiatrists (mostly early career psychiatrists and one resident) that talked about living with a psychiatric illness. The audience is huge, and we hear narratives about internal stigma, self-disclosure, external stigma, shunning, bullying, acceptance, rejection, alienation, connection, and love by peers and family. The authenticity and valor of the speakers create an atmosphere of safety, which enables psychiatrists in attendance from all over the world to share their personal stories – some at the microphone, some privately.
- May 7: Again at the APA, I chair and facilitate a workshop on physician suicide. We hear from four speakers, all women, who have lost a loved one to suicide – a husband, a father, a brother, a son – all doctors. Two of the speakers are psychiatrists. The stories are gripping, detailed, and tender. Yes, the atmosphere is very sad, but there is not a pall. We learn how these doctors lived, not just how they died. They all loved medicine; they were creative; they cared deeply; they suffered silently; and with shame, they lost hope. Again, a big audience of psychiatrists, many of whom share their own stories, that they, too, had lost a physician son, wife, or mother to suicide. Some of their deceased family members fell through the cracks and did not receive the life-saving care they deserved; some, fearing assaults to their medical license, hospital privileges, or insurance, refused to see anyone. They died untreated.
- May 8: Still at the APA, a psychiatrist colleague and I collaborate on a clinical case conference. Each of us describes losing a physician patient to suicide. We walk the attendees through the clinical details of assessment, treatment, and the aftermath of their deaths. We talk openly and frankly about our feelings, grief, outreach to colleagues and the family, and our own personal journeys of learning, growth, and healing. The clinician audience members give constructive feedback, and some share their own stories of losing patients to suicide. Like the day before, some psychiatrists are grieving the loss of a physician son or sibling to suicide. As mental health professionals, they suffer from an additional layer of failure and guilt that a loved one died “under their watch.”
- May 8: I rush across the Javits Center to catch the discussant for a concurrent symposium on physician burnout and depression. She foregoes any prepared remarks to share her previous 48 hours with the audience. She is the training director of the program that lost the second-year resident on May 5. She did not learn of the death until 24 hours later. We are all on the edge of our seats as we listen to this grieving, courageous woman, a seasoned psychiatrist and educator, who has been blindsided by this tragedy. She has not slept. She called all of her residents and broke the news personally as best she could. Aided by “After A Suicide: A Toolkit for Residency/Fellowship Programs” (American Foundation for Suicide Prevention), she and her colleagues instituted a plan of action and worked with administration and faculty. Her strength and commitment to the well-being of her trainees is palpable and magnanimous. When the session ends, many of us stand in line to give her a hug. It is a stark reminder of how many lives are affected when someone you know or care about takes his/her own life – and how, in the house of medicine, medical students and residents really are part of an institutional family.
- May 10: I facilitate a meeting of our 12 second-year residents, many of whom knew of or had met the resident who died. Almost everyone speaks, shares their feelings, poses questions, and calls for answers and change. There is disbelief, sadness, confusion, some guilt, and lots of anger. Also a feeling of disillusionment or paradox about the field of psychiatry: “Of all branches of medicine, shouldn’t residents who are struggling with psychiatric issues feel safe, protected, cared for in psychiatry?” There is also a feeling of lip service being paid to personal treatment, as in quoted statements: “By all means, get treatment for your issues, but don’t let it encroach on your duty hours” or “It’s good you’re getting help, but do you still have to go weekly?”
In the immediate aftermath of suicide, feelings run high, as they should. But rather than wait it out – and fearing a return to “business as usual” – let me make only two suggestions:
2. In psychiatry, we need to redouble our efforts in fighting the stigma attached to psychiatric illness in trainees. It is unconscionable that medical students and residents are dying of treatable disorders (I’ve never heard of a doctor dying of cancer who didn’t go to an oncologist at least once), yet too many are not availing themselves of services we provide – even when they’re free of charge or covered by insurance. And are we certain that, when they knock on our doors, we are providing them with state-of-the-art care? Is it possible that unrecognized internal stigma and shame deep within us might make us hesitant to help our trainees in their hour of need? Or cut corners? Or not get a second opinion? Very few psychiatrists on faculty of our medical schools divulge their personal experiences of depression, posttraumatic stress disorders, substance use disorders, and more (with the exception of being in therapy during residency, which is normative and isn’t stigmatized). Coming out is leveling, humane, and respectful – and it shrinks the power differential in the teaching dyad. It might even save a life.
Dr. Myers is a professor of clinical psychiatry at State University of New York, Brooklyn, and the author of “Why Physicians Die by Suicide: Lessons Learned From Their Families and Others Who Cared.”
Like everyone in the arc of social media impact, I was shocked and terribly saddened by the recent suicides of two New York women in medicine – a final-year medical student on May 1 and a second-year resident on May 5. As a specialist in physician health, a former training director, a long-standing member of our institution’s medical student admissions committee, and the ombudsman for our medical students, I am finding these tragedies harder and harder to reconcile. Something isn’t working. But before I get to that, what follows is a bulleted list of some events of the past couple of weeks that may give a context for my statements and have informed my two recommendations.
- May 3, 2018: I give an invited GI grand rounds on stress, burnout, depression, and suicide in physicians. The residents are quiet and say nothing. Faculty members seem only concerned about preventing and eradicating burnout – and not that interested in anything more severe.
- May 5: A psychiatry resident from Melbourne arrives to spend 10 days with me to do an elective in physician health. As in the United States, there is a significant suicide death rate in medical students and residents Down Under. In the afternoon, I present a paper at the annual meeting of the American Academy of Psychodynamic Psychiatry and Psychoanalysis on the use of psychotherapy in treatment-resistant suicidal depression in physicians. There is increasing hope that this essential modality of care will return to the contemporary psychiatrist’s toolbox.
- May 6: At the annual meeting of the American Psychiatric Association in New York, I’m the discussant for powerful heartfelt papers of five psychiatrists (mostly early career psychiatrists and one resident) that talked about living with a psychiatric illness. The audience is huge, and we hear narratives about internal stigma, self-disclosure, external stigma, shunning, bullying, acceptance, rejection, alienation, connection, and love by peers and family. The authenticity and valor of the speakers create an atmosphere of safety, which enables psychiatrists in attendance from all over the world to share their personal stories – some at the microphone, some privately.
- May 7: Again at the APA, I chair and facilitate a workshop on physician suicide. We hear from four speakers, all women, who have lost a loved one to suicide – a husband, a father, a brother, a son – all doctors. Two of the speakers are psychiatrists. The stories are gripping, detailed, and tender. Yes, the atmosphere is very sad, but there is not a pall. We learn how these doctors lived, not just how they died. They all loved medicine; they were creative; they cared deeply; they suffered silently; and with shame, they lost hope. Again, a big audience of psychiatrists, many of whom share their own stories, that they, too, had lost a physician son, wife, or mother to suicide. Some of their deceased family members fell through the cracks and did not receive the life-saving care they deserved; some, fearing assaults to their medical license, hospital privileges, or insurance, refused to see anyone. They died untreated.
- May 8: Still at the APA, a psychiatrist colleague and I collaborate on a clinical case conference. Each of us describes losing a physician patient to suicide. We walk the attendees through the clinical details of assessment, treatment, and the aftermath of their deaths. We talk openly and frankly about our feelings, grief, outreach to colleagues and the family, and our own personal journeys of learning, growth, and healing. The clinician audience members give constructive feedback, and some share their own stories of losing patients to suicide. Like the day before, some psychiatrists are grieving the loss of a physician son or sibling to suicide. As mental health professionals, they suffer from an additional layer of failure and guilt that a loved one died “under their watch.”
- May 8: I rush across the Javits Center to catch the discussant for a concurrent symposium on physician burnout and depression. She foregoes any prepared remarks to share her previous 48 hours with the audience. She is the training director of the program that lost the second-year resident on May 5. She did not learn of the death until 24 hours later. We are all on the edge of our seats as we listen to this grieving, courageous woman, a seasoned psychiatrist and educator, who has been blindsided by this tragedy. She has not slept. She called all of her residents and broke the news personally as best she could. Aided by “After A Suicide: A Toolkit for Residency/Fellowship Programs” (American Foundation for Suicide Prevention), she and her colleagues instituted a plan of action and worked with administration and faculty. Her strength and commitment to the well-being of her trainees is palpable and magnanimous. When the session ends, many of us stand in line to give her a hug. It is a stark reminder of how many lives are affected when someone you know or care about takes his/her own life – and how, in the house of medicine, medical students and residents really are part of an institutional family.
- May 10: I facilitate a meeting of our 12 second-year residents, many of whom knew of or had met the resident who died. Almost everyone speaks, shares their feelings, poses questions, and calls for answers and change. There is disbelief, sadness, confusion, some guilt, and lots of anger. Also a feeling of disillusionment or paradox about the field of psychiatry: “Of all branches of medicine, shouldn’t residents who are struggling with psychiatric issues feel safe, protected, cared for in psychiatry?” There is also a feeling of lip service being paid to personal treatment, as in quoted statements: “By all means, get treatment for your issues, but don’t let it encroach on your duty hours” or “It’s good you’re getting help, but do you still have to go weekly?”
In the immediate aftermath of suicide, feelings run high, as they should. But rather than wait it out – and fearing a return to “business as usual” – let me make only two suggestions:
2. In psychiatry, we need to redouble our efforts in fighting the stigma attached to psychiatric illness in trainees. It is unconscionable that medical students and residents are dying of treatable disorders (I’ve never heard of a doctor dying of cancer who didn’t go to an oncologist at least once), yet too many are not availing themselves of services we provide – even when they’re free of charge or covered by insurance. And are we certain that, when they knock on our doors, we are providing them with state-of-the-art care? Is it possible that unrecognized internal stigma and shame deep within us might make us hesitant to help our trainees in their hour of need? Or cut corners? Or not get a second opinion? Very few psychiatrists on faculty of our medical schools divulge their personal experiences of depression, posttraumatic stress disorders, substance use disorders, and more (with the exception of being in therapy during residency, which is normative and isn’t stigmatized). Coming out is leveling, humane, and respectful – and it shrinks the power differential in the teaching dyad. It might even save a life.
Dr. Myers is a professor of clinical psychiatry at State University of New York, Brooklyn, and the author of “Why Physicians Die by Suicide: Lessons Learned From Their Families and Others Who Cared.”
How to harness value-based care codes
Many of you reading this column joined Medicare accountable care organizations (ACOs) sometime between 2011 and 2016. As the power of prevention, wellness, and the medical home model are starting to be realized and appreciated, those benefits may be swamped by two new Centers for Medicare and Medicaid Services value-based revenue streams that did not exist when many of you first joined your ACO.
The Medicare Access and CHIP Reauthorization Act (MACRA) was passed in 2015 and is just now being implemented. Value-based, fee-for-service payments started out rather modestly a few years ago as chronic care management codes, but they have exploded to include more than 20 codes, counting the new ones coming online in 2018. Let’s call them collectively value-based care codes, or VCCs.
Many practices are trying to understand and perform the basic requirements to avoid penalties under MACRA’s Merit-based Incentive Payment System (MIPS) program. Some primary care practices, however, see the upside potential and bonuses stacking up to 30% or more.
Did you know that even if you are in, let’s say, a basic Medicare Shared Savings Program ACO – the MSSP Track 1, with no exposure to risk – you get special treatment on reporting under MACRA as a MIPS Advanced Practice Model (APM)?
But more importantly, MACRA is a team game. Getting into an MSSP Track 1 is justified just to get practice for the care coordination you’ll need. Few physicians know that they are judged under MACRA MIPS for the total costs of their patients, not just their own costs. A primary care physician receives only up to 8% of the $10 million your patients consume on average. The best way to counter that is through an ACO.
Further, we are aware of ACOs that have chosen risk-taking Medicare models such as NextGen, even though they predict small losses. Those losses are because of the automatic 5% fee-for-service payment bump to its physicians for risk taking if they are in a MACRA Advanced Alternative Payment Model (AAPM).
There’s a wide range of primary care physicians who are seizing opportunities offered by VCCs.
A family physician friend of mine who practices in a rural area generated more than 50% of his revenue from value-based care coding last year. And he has personally generated more than $350,000 in additional annual revenue, not counting the revenue from additional medically necessary procedures revealed by this more proactive wellness assessment activity and early diagnoses.
On the other hand, because busy physicians have a hard time wading through all these regulations and implementing the required staff and technology changes, it is reported that only about 8% of physicians are employing even the chronic care management codes. And when they do, they only achieve an 18% eligible patient penetration. My friend has broken the code, so to speak; he has protocolized and templated the process, has happy patients, has an ongoing 93% penetration rate, and actually has more free time.
While you are busy saving lives, I have had the luxury of looking from a high level at these tectonic, value-based payment shifts. To me, it’s a no-brainer for a primary care physician to leverage their ACO to maximize all three revenue streams. Look at MACRA MIPS, MIPS-APM, and AAPM measures anew, and see how well they play into integrated care.
As quarterback of health care through the patient-centered medical home, you are in great position to drive substantial bonuses. Similarly, when one looks at VCCs, the ACO can: help you navigate through the paperwork, perform much of the required reporting, and select the highest value-adding initiatives to monitor and drive higher quality and shared savings for the ACO.
As readers know, we firmly believe that, to have sustained incentivization, every ACO needs to have a merit-based, shared savings distribution formula. Accordingly, your compensation should rise under MACRA, VCCs, and the ACO.
This shift to value care is hard. But your colleagues who have made these changes are enjoying practice as never before. Their professional and financial rewards have climbed. But, most important, their patients love it.
Mr. Bobbitt is head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He is president of Value Health Partners, a health care strategic consulting company. He has years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Many of you reading this column joined Medicare accountable care organizations (ACOs) sometime between 2011 and 2016. As the power of prevention, wellness, and the medical home model are starting to be realized and appreciated, those benefits may be swamped by two new Centers for Medicare and Medicaid Services value-based revenue streams that did not exist when many of you first joined your ACO.
The Medicare Access and CHIP Reauthorization Act (MACRA) was passed in 2015 and is just now being implemented. Value-based, fee-for-service payments started out rather modestly a few years ago as chronic care management codes, but they have exploded to include more than 20 codes, counting the new ones coming online in 2018. Let’s call them collectively value-based care codes, or VCCs.
Many practices are trying to understand and perform the basic requirements to avoid penalties under MACRA’s Merit-based Incentive Payment System (MIPS) program. Some primary care practices, however, see the upside potential and bonuses stacking up to 30% or more.
Did you know that even if you are in, let’s say, a basic Medicare Shared Savings Program ACO – the MSSP Track 1, with no exposure to risk – you get special treatment on reporting under MACRA as a MIPS Advanced Practice Model (APM)?
But more importantly, MACRA is a team game. Getting into an MSSP Track 1 is justified just to get practice for the care coordination you’ll need. Few physicians know that they are judged under MACRA MIPS for the total costs of their patients, not just their own costs. A primary care physician receives only up to 8% of the $10 million your patients consume on average. The best way to counter that is through an ACO.
Further, we are aware of ACOs that have chosen risk-taking Medicare models such as NextGen, even though they predict small losses. Those losses are because of the automatic 5% fee-for-service payment bump to its physicians for risk taking if they are in a MACRA Advanced Alternative Payment Model (AAPM).
There’s a wide range of primary care physicians who are seizing opportunities offered by VCCs.
A family physician friend of mine who practices in a rural area generated more than 50% of his revenue from value-based care coding last year. And he has personally generated more than $350,000 in additional annual revenue, not counting the revenue from additional medically necessary procedures revealed by this more proactive wellness assessment activity and early diagnoses.
On the other hand, because busy physicians have a hard time wading through all these regulations and implementing the required staff and technology changes, it is reported that only about 8% of physicians are employing even the chronic care management codes. And when they do, they only achieve an 18% eligible patient penetration. My friend has broken the code, so to speak; he has protocolized and templated the process, has happy patients, has an ongoing 93% penetration rate, and actually has more free time.
While you are busy saving lives, I have had the luxury of looking from a high level at these tectonic, value-based payment shifts. To me, it’s a no-brainer for a primary care physician to leverage their ACO to maximize all three revenue streams. Look at MACRA MIPS, MIPS-APM, and AAPM measures anew, and see how well they play into integrated care.
As quarterback of health care through the patient-centered medical home, you are in great position to drive substantial bonuses. Similarly, when one looks at VCCs, the ACO can: help you navigate through the paperwork, perform much of the required reporting, and select the highest value-adding initiatives to monitor and drive higher quality and shared savings for the ACO.
As readers know, we firmly believe that, to have sustained incentivization, every ACO needs to have a merit-based, shared savings distribution formula. Accordingly, your compensation should rise under MACRA, VCCs, and the ACO.
This shift to value care is hard. But your colleagues who have made these changes are enjoying practice as never before. Their professional and financial rewards have climbed. But, most important, their patients love it.
Mr. Bobbitt is head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He is president of Value Health Partners, a health care strategic consulting company. He has years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Many of you reading this column joined Medicare accountable care organizations (ACOs) sometime between 2011 and 2016. As the power of prevention, wellness, and the medical home model are starting to be realized and appreciated, those benefits may be swamped by two new Centers for Medicare and Medicaid Services value-based revenue streams that did not exist when many of you first joined your ACO.
The Medicare Access and CHIP Reauthorization Act (MACRA) was passed in 2015 and is just now being implemented. Value-based, fee-for-service payments started out rather modestly a few years ago as chronic care management codes, but they have exploded to include more than 20 codes, counting the new ones coming online in 2018. Let’s call them collectively value-based care codes, or VCCs.
Many practices are trying to understand and perform the basic requirements to avoid penalties under MACRA’s Merit-based Incentive Payment System (MIPS) program. Some primary care practices, however, see the upside potential and bonuses stacking up to 30% or more.
Did you know that even if you are in, let’s say, a basic Medicare Shared Savings Program ACO – the MSSP Track 1, with no exposure to risk – you get special treatment on reporting under MACRA as a MIPS Advanced Practice Model (APM)?
But more importantly, MACRA is a team game. Getting into an MSSP Track 1 is justified just to get practice for the care coordination you’ll need. Few physicians know that they are judged under MACRA MIPS for the total costs of their patients, not just their own costs. A primary care physician receives only up to 8% of the $10 million your patients consume on average. The best way to counter that is through an ACO.
Further, we are aware of ACOs that have chosen risk-taking Medicare models such as NextGen, even though they predict small losses. Those losses are because of the automatic 5% fee-for-service payment bump to its physicians for risk taking if they are in a MACRA Advanced Alternative Payment Model (AAPM).
There’s a wide range of primary care physicians who are seizing opportunities offered by VCCs.
A family physician friend of mine who practices in a rural area generated more than 50% of his revenue from value-based care coding last year. And he has personally generated more than $350,000 in additional annual revenue, not counting the revenue from additional medically necessary procedures revealed by this more proactive wellness assessment activity and early diagnoses.
On the other hand, because busy physicians have a hard time wading through all these regulations and implementing the required staff and technology changes, it is reported that only about 8% of physicians are employing even the chronic care management codes. And when they do, they only achieve an 18% eligible patient penetration. My friend has broken the code, so to speak; he has protocolized and templated the process, has happy patients, has an ongoing 93% penetration rate, and actually has more free time.
While you are busy saving lives, I have had the luxury of looking from a high level at these tectonic, value-based payment shifts. To me, it’s a no-brainer for a primary care physician to leverage their ACO to maximize all three revenue streams. Look at MACRA MIPS, MIPS-APM, and AAPM measures anew, and see how well they play into integrated care.
As quarterback of health care through the patient-centered medical home, you are in great position to drive substantial bonuses. Similarly, when one looks at VCCs, the ACO can: help you navigate through the paperwork, perform much of the required reporting, and select the highest value-adding initiatives to monitor and drive higher quality and shared savings for the ACO.
As readers know, we firmly believe that, to have sustained incentivization, every ACO needs to have a merit-based, shared savings distribution formula. Accordingly, your compensation should rise under MACRA, VCCs, and the ACO.
This shift to value care is hard. But your colleagues who have made these changes are enjoying practice as never before. Their professional and financial rewards have climbed. But, most important, their patients love it.
Mr. Bobbitt is head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He is president of Value Health Partners, a health care strategic consulting company. He has years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Diet
I’m about to embark on a controversial topic. Perhaps it’s safer to avoid, but I can’t put it off any longer. We need to talk about diet.
Discussing diet, like politics, religion, or salary, is best done just with oneself. Yet, I’m compelled to share what I’ve learned. First, I’m agnostic. I don’t believe you need to be vegan or paleo to be saved. I eat plant-based foods. I also eat things that eat plants. I’m sure you’d find a fine film of gluten in my kitchen. What I’ve learned is that for me, it doesn’t matter.
Specifically, I have little or nothing to eat from when I wake until dinner. As a busy dermatologist, that may seem draconian, but in fact it is easier than you might think. Patients are a constant all day, while hunger is fleeting. Got a craving at 10:15 a.m.? Easy. Walk in to see the next patient. Then repeat. Most days, this continues until 6:30 p.m. or so, when it’s time to head home. It’s not that hard, particularly when you don’t have anything in your office to eat except Dentyne Ice gum and green tea.
Now, this doesn’t always work. Why? Meetings. How do I manage fasting on those days? I don’t. If I know I have a lunch meeting scheduled, then I eat a healthy breakfast before I leave home, such as a protein smoothie or a bowl of hot oats with a dollop of Greek yogurt, sunflower seeds, walnuts, and berries. By eating a wholesome, well-balanced meal of fiber, carbs, lean protein, and good fats, I’m not starving before the meeting and am less likely to overeat. (That’s because I have also learned I’m not one of those enviable people who can simply say “no” to a crispy fish taco and guacamole if I’m hungry. I’m gonna eat it.) So, I avoid fasting and the inevitable frustration of breaking a fast on those days.
On days when I fast, I monitor how I feel. Fortunately, I have rarely felt hypoglycemic; except for that one Tuesday a couple of months ago. I had completed a long, hard early morning workout, and by mid-morning my hands were shaking and I felt nauseous. I quickly downed two RX bars and felt fine within minutes. Better for me, better for my patients.
Right now, intermittent fasting is working for me. Here’s my weekly plan:
I don’t fast on Fridays or weekends or when I travel. I eat out rarely. On weekends, my wife and I shop at the local farmers’ and fish markets to prepare ourselves for a week of healthy eating. And on Sundays, we continue our treasured family tradition of Sunday supper, which is basted with nostalgia and drizzled liberally with comfort. Often it requires long preparation, which is part of the appeal, and short attention is paid to its nutritional value. That’s not the point of Sunday dinner. A delicious dunk of fresh Italian bread in grassy-green olive oil or fresh pasta doused with homemade tomato basil sauce is the best possible meal I can have to prepare for a long, hard week ahead.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I’m about to embark on a controversial topic. Perhaps it’s safer to avoid, but I can’t put it off any longer. We need to talk about diet.
Discussing diet, like politics, religion, or salary, is best done just with oneself. Yet, I’m compelled to share what I’ve learned. First, I’m agnostic. I don’t believe you need to be vegan or paleo to be saved. I eat plant-based foods. I also eat things that eat plants. I’m sure you’d find a fine film of gluten in my kitchen. What I’ve learned is that for me, it doesn’t matter.
Specifically, I have little or nothing to eat from when I wake until dinner. As a busy dermatologist, that may seem draconian, but in fact it is easier than you might think. Patients are a constant all day, while hunger is fleeting. Got a craving at 10:15 a.m.? Easy. Walk in to see the next patient. Then repeat. Most days, this continues until 6:30 p.m. or so, when it’s time to head home. It’s not that hard, particularly when you don’t have anything in your office to eat except Dentyne Ice gum and green tea.
Now, this doesn’t always work. Why? Meetings. How do I manage fasting on those days? I don’t. If I know I have a lunch meeting scheduled, then I eat a healthy breakfast before I leave home, such as a protein smoothie or a bowl of hot oats with a dollop of Greek yogurt, sunflower seeds, walnuts, and berries. By eating a wholesome, well-balanced meal of fiber, carbs, lean protein, and good fats, I’m not starving before the meeting and am less likely to overeat. (That’s because I have also learned I’m not one of those enviable people who can simply say “no” to a crispy fish taco and guacamole if I’m hungry. I’m gonna eat it.) So, I avoid fasting and the inevitable frustration of breaking a fast on those days.
On days when I fast, I monitor how I feel. Fortunately, I have rarely felt hypoglycemic; except for that one Tuesday a couple of months ago. I had completed a long, hard early morning workout, and by mid-morning my hands were shaking and I felt nauseous. I quickly downed two RX bars and felt fine within minutes. Better for me, better for my patients.
Right now, intermittent fasting is working for me. Here’s my weekly plan:
I don’t fast on Fridays or weekends or when I travel. I eat out rarely. On weekends, my wife and I shop at the local farmers’ and fish markets to prepare ourselves for a week of healthy eating. And on Sundays, we continue our treasured family tradition of Sunday supper, which is basted with nostalgia and drizzled liberally with comfort. Often it requires long preparation, which is part of the appeal, and short attention is paid to its nutritional value. That’s not the point of Sunday dinner. A delicious dunk of fresh Italian bread in grassy-green olive oil or fresh pasta doused with homemade tomato basil sauce is the best possible meal I can have to prepare for a long, hard week ahead.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I’m about to embark on a controversial topic. Perhaps it’s safer to avoid, but I can’t put it off any longer. We need to talk about diet.
Discussing diet, like politics, religion, or salary, is best done just with oneself. Yet, I’m compelled to share what I’ve learned. First, I’m agnostic. I don’t believe you need to be vegan or paleo to be saved. I eat plant-based foods. I also eat things that eat plants. I’m sure you’d find a fine film of gluten in my kitchen. What I’ve learned is that for me, it doesn’t matter.
Specifically, I have little or nothing to eat from when I wake until dinner. As a busy dermatologist, that may seem draconian, but in fact it is easier than you might think. Patients are a constant all day, while hunger is fleeting. Got a craving at 10:15 a.m.? Easy. Walk in to see the next patient. Then repeat. Most days, this continues until 6:30 p.m. or so, when it’s time to head home. It’s not that hard, particularly when you don’t have anything in your office to eat except Dentyne Ice gum and green tea.
Now, this doesn’t always work. Why? Meetings. How do I manage fasting on those days? I don’t. If I know I have a lunch meeting scheduled, then I eat a healthy breakfast before I leave home, such as a protein smoothie or a bowl of hot oats with a dollop of Greek yogurt, sunflower seeds, walnuts, and berries. By eating a wholesome, well-balanced meal of fiber, carbs, lean protein, and good fats, I’m not starving before the meeting and am less likely to overeat. (That’s because I have also learned I’m not one of those enviable people who can simply say “no” to a crispy fish taco and guacamole if I’m hungry. I’m gonna eat it.) So, I avoid fasting and the inevitable frustration of breaking a fast on those days.
On days when I fast, I monitor how I feel. Fortunately, I have rarely felt hypoglycemic; except for that one Tuesday a couple of months ago. I had completed a long, hard early morning workout, and by mid-morning my hands were shaking and I felt nauseous. I quickly downed two RX bars and felt fine within minutes. Better for me, better for my patients.
Right now, intermittent fasting is working for me. Here’s my weekly plan:
I don’t fast on Fridays or weekends or when I travel. I eat out rarely. On weekends, my wife and I shop at the local farmers’ and fish markets to prepare ourselves for a week of healthy eating. And on Sundays, we continue our treasured family tradition of Sunday supper, which is basted with nostalgia and drizzled liberally with comfort. Often it requires long preparation, which is part of the appeal, and short attention is paid to its nutritional value. That’s not the point of Sunday dinner. A delicious dunk of fresh Italian bread in grassy-green olive oil or fresh pasta doused with homemade tomato basil sauce is the best possible meal I can have to prepare for a long, hard week ahead.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Patients who record office visits
Question: During an office visit, the patient used a smartphone to record his conversation with the doctor. Which of the following statements is best?
A. This is an intrusion into a private and confidential physician-patient encounter and violates laws against eavesdropping and wiretapping.
B. Recordings are rarely made in the doctor’s office.
C. Both parties must consent before the patient or doctor can legally make such a recording.
D. Surreptitious recording by one party is always illegal.
E. All are incorrect.
Answer: E.
Scholars from Dartmouth recently published their viewpoint on this topic in the Aug. 7, 2017, issue of JAMA.1 Many individuals believe that taping or recording a private conversation is per se illegal.
This is a misconception. Although it is a serious felony to violate wiretapping laws, in fact every jurisdiction permits the taping or recording of doctor-patient conversations where there is all-party consent. A majority of states actually allow the recording even if one party has not given his/her consent. This one-party consent rule is the law in 39 states, including Hawaii and New York. On the other hand, 11 states, such as California, Florida, Massachusetts, and Washington, deem such recordings illegal. A listing of the law in the various states can be found in the JAMA article, in which the authors call for “clear policies that facilitate the positive use of digital recordings.”
In a 2011 case against the Cleveland Clinic, a patient died of a cardiac arrest from hyperkalemia 3 days after elective knee surgery.2 The patient’s children had made a covert recording of a meeting with the chief medical officer when discussing the incident. The hospital attempted to bar the use of the recording, claiming that the information was nondiscoverable under the “peer review” privilege.
Both the trial court and the court of appeals disagreed, being unconvinced that such discussions fell within peer review protection. That the recording was made surreptitiously was not raised as an issue, as Ohio is a one-party consent state, i.e., the law permits a patient to legally tape his/her conversations without obtaining prior approval from the doctor.3
There are clear advantages to having a permanent record of a doctor’s professional opinion. The patient can review the information after the visit for a better understanding or for recall purposes, even sharing the information with family members, caregivers, or others, especially where there is a lack of clarity on instructions.4 In the area of informed consent, this is particularly useful for a reminder of medication side effects and potential complications of proposed surgery.
However, many doctors believe that recordings may be disruptive or prove inhibitory to free and open discussions, and they are concerned about their potential use should litigation arises.
Risk managers and malpractice carriers are divided in their views. For example, it has been stated that, “at the Barrow Neurological Institute, in Phoenix, Arizona, where patients are routinely offered video recordings of their visits, clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and $1 million extra liability coverage” (P.J. Barr, unpublished data, 2017, as cited in reference 1). Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the majority of jurisdictions, recordings are legal if consented to by one of the parties. This means that recordings by the patient with/without consent from or with/without knowledge of the doctor are fully legitimate. It also means that the recordings will be admissible into evidence in a courtroom, unless the information is privileged (protected from discovery) or is otherwise irrelevant or unreliable.
On the other hand, in states requiring all-party consent, such recordings are illegal absent across-the-board consent, and they will be inadmissible into evidence. This cardinal difference in state law raises vital implications for both plaintiff and defendant in litigation, because the recordings may contain incriminating or exculpatory information.
Recordings of conversations in the doctor’s office are by no means rare. A survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and 11% were aware of someone else doing the same.5 The concerned physician could proactively prohibit all office recordings by posting a “no recording” sign in the waiting room in the name of confidentiality and privacy. And should a physician discover that a patient is covertly recording, risk managers have suggested terminating the visit with a warning that a repeat attempt will result in discharge.
Like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., is likely to increase the prevalence of recordings. A practical approach for practicing physicians is to familiarize themselves with the law in the individual state in which they practice and to improve their communication skills irrespective of whether or not there is a recording.
They may wish to consider the view attributed to Richard Boothman, JD, chief risk officer at the University of Michigan Health System: “Recording should cause any caregiver to mind their professionalism and be disciplined in their remarks to their patients. … I believe it can be a very powerful tool to cement the patient/physician relationship and the patient’s understanding of the clinical messages and information. Physicians are significantly benefited by an informed patient.”6
References
1. JAMA. 2017 Aug 8;318(6):513-4.
2. Smith v. Cleveland Clinic, 197 Ohio App.3d 524, 2011.
3. Ohio Revised Code 2933.52.
4. JAMA. 2015 Apr 28;313(16):1615-6.
5. BMJ Open. 2015 Aug 11;5(8):e008566.
6. “Your office is being recorded.” Medscape, April 3, 2018.
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
Question: During an office visit, the patient used a smartphone to record his conversation with the doctor. Which of the following statements is best?
A. This is an intrusion into a private and confidential physician-patient encounter and violates laws against eavesdropping and wiretapping.
B. Recordings are rarely made in the doctor’s office.
C. Both parties must consent before the patient or doctor can legally make such a recording.
D. Surreptitious recording by one party is always illegal.
E. All are incorrect.
Answer: E.
Scholars from Dartmouth recently published their viewpoint on this topic in the Aug. 7, 2017, issue of JAMA.1 Many individuals believe that taping or recording a private conversation is per se illegal.
This is a misconception. Although it is a serious felony to violate wiretapping laws, in fact every jurisdiction permits the taping or recording of doctor-patient conversations where there is all-party consent. A majority of states actually allow the recording even if one party has not given his/her consent. This one-party consent rule is the law in 39 states, including Hawaii and New York. On the other hand, 11 states, such as California, Florida, Massachusetts, and Washington, deem such recordings illegal. A listing of the law in the various states can be found in the JAMA article, in which the authors call for “clear policies that facilitate the positive use of digital recordings.”
In a 2011 case against the Cleveland Clinic, a patient died of a cardiac arrest from hyperkalemia 3 days after elective knee surgery.2 The patient’s children had made a covert recording of a meeting with the chief medical officer when discussing the incident. The hospital attempted to bar the use of the recording, claiming that the information was nondiscoverable under the “peer review” privilege.
Both the trial court and the court of appeals disagreed, being unconvinced that such discussions fell within peer review protection. That the recording was made surreptitiously was not raised as an issue, as Ohio is a one-party consent state, i.e., the law permits a patient to legally tape his/her conversations without obtaining prior approval from the doctor.3
There are clear advantages to having a permanent record of a doctor’s professional opinion. The patient can review the information after the visit for a better understanding or for recall purposes, even sharing the information with family members, caregivers, or others, especially where there is a lack of clarity on instructions.4 In the area of informed consent, this is particularly useful for a reminder of medication side effects and potential complications of proposed surgery.
However, many doctors believe that recordings may be disruptive or prove inhibitory to free and open discussions, and they are concerned about their potential use should litigation arises.
Risk managers and malpractice carriers are divided in their views. For example, it has been stated that, “at the Barrow Neurological Institute, in Phoenix, Arizona, where patients are routinely offered video recordings of their visits, clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and $1 million extra liability coverage” (P.J. Barr, unpublished data, 2017, as cited in reference 1). Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the majority of jurisdictions, recordings are legal if consented to by one of the parties. This means that recordings by the patient with/without consent from or with/without knowledge of the doctor are fully legitimate. It also means that the recordings will be admissible into evidence in a courtroom, unless the information is privileged (protected from discovery) or is otherwise irrelevant or unreliable.
On the other hand, in states requiring all-party consent, such recordings are illegal absent across-the-board consent, and they will be inadmissible into evidence. This cardinal difference in state law raises vital implications for both plaintiff and defendant in litigation, because the recordings may contain incriminating or exculpatory information.
Recordings of conversations in the doctor’s office are by no means rare. A survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and 11% were aware of someone else doing the same.5 The concerned physician could proactively prohibit all office recordings by posting a “no recording” sign in the waiting room in the name of confidentiality and privacy. And should a physician discover that a patient is covertly recording, risk managers have suggested terminating the visit with a warning that a repeat attempt will result in discharge.
Like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., is likely to increase the prevalence of recordings. A practical approach for practicing physicians is to familiarize themselves with the law in the individual state in which they practice and to improve their communication skills irrespective of whether or not there is a recording.
They may wish to consider the view attributed to Richard Boothman, JD, chief risk officer at the University of Michigan Health System: “Recording should cause any caregiver to mind their professionalism and be disciplined in their remarks to their patients. … I believe it can be a very powerful tool to cement the patient/physician relationship and the patient’s understanding of the clinical messages and information. Physicians are significantly benefited by an informed patient.”6
References
1. JAMA. 2017 Aug 8;318(6):513-4.
2. Smith v. Cleveland Clinic, 197 Ohio App.3d 524, 2011.
3. Ohio Revised Code 2933.52.
4. JAMA. 2015 Apr 28;313(16):1615-6.
5. BMJ Open. 2015 Aug 11;5(8):e008566.
6. “Your office is being recorded.” Medscape, April 3, 2018.
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
Question: During an office visit, the patient used a smartphone to record his conversation with the doctor. Which of the following statements is best?
A. This is an intrusion into a private and confidential physician-patient encounter and violates laws against eavesdropping and wiretapping.
B. Recordings are rarely made in the doctor’s office.
C. Both parties must consent before the patient or doctor can legally make such a recording.
D. Surreptitious recording by one party is always illegal.
E. All are incorrect.
Answer: E.
Scholars from Dartmouth recently published their viewpoint on this topic in the Aug. 7, 2017, issue of JAMA.1 Many individuals believe that taping or recording a private conversation is per se illegal.
This is a misconception. Although it is a serious felony to violate wiretapping laws, in fact every jurisdiction permits the taping or recording of doctor-patient conversations where there is all-party consent. A majority of states actually allow the recording even if one party has not given his/her consent. This one-party consent rule is the law in 39 states, including Hawaii and New York. On the other hand, 11 states, such as California, Florida, Massachusetts, and Washington, deem such recordings illegal. A listing of the law in the various states can be found in the JAMA article, in which the authors call for “clear policies that facilitate the positive use of digital recordings.”
In a 2011 case against the Cleveland Clinic, a patient died of a cardiac arrest from hyperkalemia 3 days after elective knee surgery.2 The patient’s children had made a covert recording of a meeting with the chief medical officer when discussing the incident. The hospital attempted to bar the use of the recording, claiming that the information was nondiscoverable under the “peer review” privilege.
Both the trial court and the court of appeals disagreed, being unconvinced that such discussions fell within peer review protection. That the recording was made surreptitiously was not raised as an issue, as Ohio is a one-party consent state, i.e., the law permits a patient to legally tape his/her conversations without obtaining prior approval from the doctor.3
There are clear advantages to having a permanent record of a doctor’s professional opinion. The patient can review the information after the visit for a better understanding or for recall purposes, even sharing the information with family members, caregivers, or others, especially where there is a lack of clarity on instructions.4 In the area of informed consent, this is particularly useful for a reminder of medication side effects and potential complications of proposed surgery.
However, many doctors believe that recordings may be disruptive or prove inhibitory to free and open discussions, and they are concerned about their potential use should litigation arises.
Risk managers and malpractice carriers are divided in their views. For example, it has been stated that, “at the Barrow Neurological Institute, in Phoenix, Arizona, where patients are routinely offered video recordings of their visits, clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and $1 million extra liability coverage” (P.J. Barr, unpublished data, 2017, as cited in reference 1). Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the majority of jurisdictions, recordings are legal if consented to by one of the parties. This means that recordings by the patient with/without consent from or with/without knowledge of the doctor are fully legitimate. It also means that the recordings will be admissible into evidence in a courtroom, unless the information is privileged (protected from discovery) or is otherwise irrelevant or unreliable.
On the other hand, in states requiring all-party consent, such recordings are illegal absent across-the-board consent, and they will be inadmissible into evidence. This cardinal difference in state law raises vital implications for both plaintiff and defendant in litigation, because the recordings may contain incriminating or exculpatory information.
Recordings of conversations in the doctor’s office are by no means rare. A survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and 11% were aware of someone else doing the same.5 The concerned physician could proactively prohibit all office recordings by posting a “no recording” sign in the waiting room in the name of confidentiality and privacy. And should a physician discover that a patient is covertly recording, risk managers have suggested terminating the visit with a warning that a repeat attempt will result in discharge.
Like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., is likely to increase the prevalence of recordings. A practical approach for practicing physicians is to familiarize themselves with the law in the individual state in which they practice and to improve their communication skills irrespective of whether or not there is a recording.
They may wish to consider the view attributed to Richard Boothman, JD, chief risk officer at the University of Michigan Health System: “Recording should cause any caregiver to mind their professionalism and be disciplined in their remarks to their patients. … I believe it can be a very powerful tool to cement the patient/physician relationship and the patient’s understanding of the clinical messages and information. Physicians are significantly benefited by an informed patient.”6
References
1. JAMA. 2017 Aug 8;318(6):513-4.
2. Smith v. Cleveland Clinic, 197 Ohio App.3d 524, 2011.
3. Ohio Revised Code 2933.52.
4. JAMA. 2015 Apr 28;313(16):1615-6.
5. BMJ Open. 2015 Aug 11;5(8):e008566.
6. “Your office is being recorded.” Medscape, April 3, 2018.
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
Words do matter – especially in psychiatry
As psychiatrists, we must be more precise with our language. When we speak, we must not use psychiatric diagnoses to describe common, everyday problems in life.
For example, at the recent American Psychiatric Association meeting in New York City, I frequently heard my colleagues talking about being “traumatized” over a microinsult or a microaggression. Although these individuals suggested that they were so fragile and vulnerable that stressful events caused them to develop posttraumatic stress disorder (PTSD), I seriously doubted it. Moreover, with further dialogue, it became clear that they were stressed or distressed over the stressful event – not traumatized in the purest sense of the term.
Traumatic stress, on the other hand, is an event that is so painful and disruptive that it runs the risk of breaking the mind’s ability to process or make peace with the event because it is so overwhelming that it disrupts or destroys normal psychic life. Such an event has the potential of causing PTSD, which is a chronic anxiety disorder that needs to be addressed clinically. This precision may seem nitpicky; however, the research on traumatic stress is clear. If you expose 100 people to a genuine traumatic experience, about 10% of the males and 20% of the females will develop PTSD, thus, something must be protecting people from developing PTSD from exposure to trauma. The research also is lucid that catastrophizing increases the risk of developing PTSD from exposure to a trauma by about 33%, and not having a sense of self-efficacy increases the risk by an additional 33%. Accordingly, , as this is catastrophizing and minimizes the belief in self-efficacy.
Similarly, we must be careful how we use the word “depression.” My understanding is depression is a clinical phenomenon that can be disabling. Unfortunately, I often hear patients and others talking about how they are depressed over various events in life that to me are a part of living, for example, being out of a job and not being able to make a way in life. Of course, if you are out actively looking for a job, that is probably not a clinical depression that would respond to antidepressant medication, but which would respond to finding a job. If a person were depressed from not having a job and unable to summon the energy to look for a job for 2 weeks or longer, I possibly would consider them clinically depressed. It seems laypeople are always using the word “depression” interchangeably for “unhappy,” “sad,” “grief,” or even “demoralization,” and although they all have common threads and are interlinked to one another, they are also very different.
Finally, the use of the word “bipolar” seems to be creeping into common usage, as I frequently hear patients who have poor affect regulation, for example, bad tempers, referring to themselves as being “bipolar.” However, after more dialogue, it becomes clear that they are describing a loss of self-control that lasts for maybe for 30 minutes or an hour. What is more distressing are the number of psychiatrists who are willing to take the patients’ word for it that they are “bipolar” and willing to prescribe mood stabilizers for such patients.
We must do better. We must not mislead the public into thinking that the ordinary problems of living are psychiatric disorders.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Surgical-Medical/Psychiatric Inpatient Unit; clinical professor emeritus, department of psychiatry, University of Illinois at Chicago; and former director of the Institute for Juvenile Research (the birthplace of child psychiatry), all in Chicago. He also serves as chair of psychiatry at Windsor University, St. Kitts.
As psychiatrists, we must be more precise with our language. When we speak, we must not use psychiatric diagnoses to describe common, everyday problems in life.
For example, at the recent American Psychiatric Association meeting in New York City, I frequently heard my colleagues talking about being “traumatized” over a microinsult or a microaggression. Although these individuals suggested that they were so fragile and vulnerable that stressful events caused them to develop posttraumatic stress disorder (PTSD), I seriously doubted it. Moreover, with further dialogue, it became clear that they were stressed or distressed over the stressful event – not traumatized in the purest sense of the term.
Traumatic stress, on the other hand, is an event that is so painful and disruptive that it runs the risk of breaking the mind’s ability to process or make peace with the event because it is so overwhelming that it disrupts or destroys normal psychic life. Such an event has the potential of causing PTSD, which is a chronic anxiety disorder that needs to be addressed clinically. This precision may seem nitpicky; however, the research on traumatic stress is clear. If you expose 100 people to a genuine traumatic experience, about 10% of the males and 20% of the females will develop PTSD, thus, something must be protecting people from developing PTSD from exposure to trauma. The research also is lucid that catastrophizing increases the risk of developing PTSD from exposure to a trauma by about 33%, and not having a sense of self-efficacy increases the risk by an additional 33%. Accordingly, , as this is catastrophizing and minimizes the belief in self-efficacy.
Similarly, we must be careful how we use the word “depression.” My understanding is depression is a clinical phenomenon that can be disabling. Unfortunately, I often hear patients and others talking about how they are depressed over various events in life that to me are a part of living, for example, being out of a job and not being able to make a way in life. Of course, if you are out actively looking for a job, that is probably not a clinical depression that would respond to antidepressant medication, but which would respond to finding a job. If a person were depressed from not having a job and unable to summon the energy to look for a job for 2 weeks or longer, I possibly would consider them clinically depressed. It seems laypeople are always using the word “depression” interchangeably for “unhappy,” “sad,” “grief,” or even “demoralization,” and although they all have common threads and are interlinked to one another, they are also very different.
Finally, the use of the word “bipolar” seems to be creeping into common usage, as I frequently hear patients who have poor affect regulation, for example, bad tempers, referring to themselves as being “bipolar.” However, after more dialogue, it becomes clear that they are describing a loss of self-control that lasts for maybe for 30 minutes or an hour. What is more distressing are the number of psychiatrists who are willing to take the patients’ word for it that they are “bipolar” and willing to prescribe mood stabilizers for such patients.
We must do better. We must not mislead the public into thinking that the ordinary problems of living are psychiatric disorders.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Surgical-Medical/Psychiatric Inpatient Unit; clinical professor emeritus, department of psychiatry, University of Illinois at Chicago; and former director of the Institute for Juvenile Research (the birthplace of child psychiatry), all in Chicago. He also serves as chair of psychiatry at Windsor University, St. Kitts.
As psychiatrists, we must be more precise with our language. When we speak, we must not use psychiatric diagnoses to describe common, everyday problems in life.
For example, at the recent American Psychiatric Association meeting in New York City, I frequently heard my colleagues talking about being “traumatized” over a microinsult or a microaggression. Although these individuals suggested that they were so fragile and vulnerable that stressful events caused them to develop posttraumatic stress disorder (PTSD), I seriously doubted it. Moreover, with further dialogue, it became clear that they were stressed or distressed over the stressful event – not traumatized in the purest sense of the term.
Traumatic stress, on the other hand, is an event that is so painful and disruptive that it runs the risk of breaking the mind’s ability to process or make peace with the event because it is so overwhelming that it disrupts or destroys normal psychic life. Such an event has the potential of causing PTSD, which is a chronic anxiety disorder that needs to be addressed clinically. This precision may seem nitpicky; however, the research on traumatic stress is clear. If you expose 100 people to a genuine traumatic experience, about 10% of the males and 20% of the females will develop PTSD, thus, something must be protecting people from developing PTSD from exposure to trauma. The research also is lucid that catastrophizing increases the risk of developing PTSD from exposure to a trauma by about 33%, and not having a sense of self-efficacy increases the risk by an additional 33%. Accordingly, , as this is catastrophizing and minimizes the belief in self-efficacy.
Similarly, we must be careful how we use the word “depression.” My understanding is depression is a clinical phenomenon that can be disabling. Unfortunately, I often hear patients and others talking about how they are depressed over various events in life that to me are a part of living, for example, being out of a job and not being able to make a way in life. Of course, if you are out actively looking for a job, that is probably not a clinical depression that would respond to antidepressant medication, but which would respond to finding a job. If a person were depressed from not having a job and unable to summon the energy to look for a job for 2 weeks or longer, I possibly would consider them clinically depressed. It seems laypeople are always using the word “depression” interchangeably for “unhappy,” “sad,” “grief,” or even “demoralization,” and although they all have common threads and are interlinked to one another, they are also very different.
Finally, the use of the word “bipolar” seems to be creeping into common usage, as I frequently hear patients who have poor affect regulation, for example, bad tempers, referring to themselves as being “bipolar.” However, after more dialogue, it becomes clear that they are describing a loss of self-control that lasts for maybe for 30 minutes or an hour. What is more distressing are the number of psychiatrists who are willing to take the patients’ word for it that they are “bipolar” and willing to prescribe mood stabilizers for such patients.
We must do better. We must not mislead the public into thinking that the ordinary problems of living are psychiatric disorders.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Surgical-Medical/Psychiatric Inpatient Unit; clinical professor emeritus, department of psychiatry, University of Illinois at Chicago; and former director of the Institute for Juvenile Research (the birthplace of child psychiatry), all in Chicago. He also serves as chair of psychiatry at Windsor University, St. Kitts.
Make the Diagnosis - May 2018
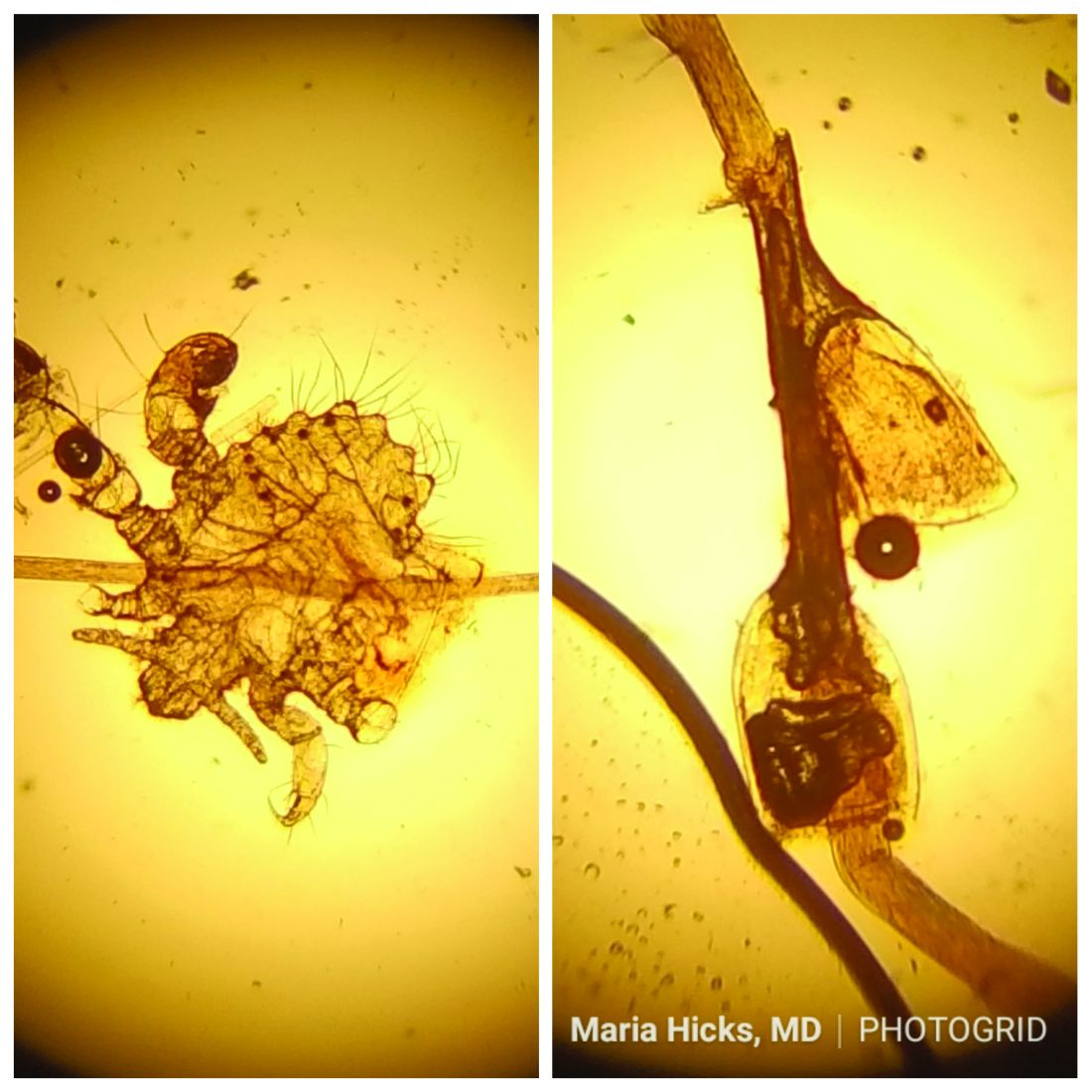
and through close skin contact, as well as contaminated clothes and bedding. Adult lice can live up to 36 hours away from its host. Pubic areas most commonly are affected, although other hair-bearing parts of the body often are affected, including eyelashes.
Pruritus can be severe. Secondary bacterial infections may occur as maculae ceruleae, or blue-colored macules, on the skin. The lice are visible to the naked eye and are approximately 1 mm in length. They have a crablike appearance, six legs, and a wide body. Nits may be present on the hair shaft. Unlike hair casts, which can be moved up and down along the hair shaft, nits firmly adhere to the hair. Diagnosis should prompt a workup for other sexually transmitted diseases, including HIV.
Treatment for patients and their sexual partners include permethrin topically; and laundering of clothing and bedding. Lice on the eyelashes can be treated with 8 days of twice-daily applications of petrolatum. Ivermectin can be used when topical therapy fails, although this is an off-label treatment (not approved by the Food and Drug Administration).
Pediculosis corporis – body lice or clothing lice – is also known as “vagabond’s disease” and is caused by Pediculus humanus var corporis. Body lice lay their eggs in clothing seams and can live in clothing for up to 1 month without feeding on human blood. Often homeless individuals and those living in overcrowded areas can be affected. The louse and nits also are visible to the naked eye. They have a longer, narrower body than Phthirus pubis and are more similar in appearance to head lice. They rarely are found on the skin.
Body lice may carry disease such as epidemic typhus, relapsing fever, and trench fever or endocarditis. Permethrin is the most widely used treatment to kill both lice and ova. Other treatments include Malathion, Lindane, and Crotamiton. Clothing and bedding should be laundered.
Scabies is a mite infestation caused by Sarcoptes scabiei. Unlike lice, scabies often affects the hands and feet. Characteristic linear burrows may be seen in the finger web spaces. The circle of Hebra describes the areas commonly infected by mites: axillae, antecubital fossa, wrists, hands, and the groin. Pruritus may be severe and worse at night. Patients may be afflicted with both lice and scabies at the same time. Mites are not visible to the naked eye but can be seen microscopically. Topical permethrin cream is used most often for treatment. All household contacts should be treated at the same time. As in louse infestations, clothing and bedding should be laundered. Ivermectin can be used for crusted scabies, although this is an off-label treatment.
This case and photo were submitted by Maria Hicks, MD, Advanced Dermatology and Cosmetic Surgery, Tampa, and Dr. Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
and through close skin contact, as well as contaminated clothes and bedding. Adult lice can live up to 36 hours away from its host. Pubic areas most commonly are affected, although other hair-bearing parts of the body often are affected, including eyelashes.
Pruritus can be severe. Secondary bacterial infections may occur as maculae ceruleae, or blue-colored macules, on the skin. The lice are visible to the naked eye and are approximately 1 mm in length. They have a crablike appearance, six legs, and a wide body. Nits may be present on the hair shaft. Unlike hair casts, which can be moved up and down along the hair shaft, nits firmly adhere to the hair. Diagnosis should prompt a workup for other sexually transmitted diseases, including HIV.
Treatment for patients and their sexual partners include permethrin topically; and laundering of clothing and bedding. Lice on the eyelashes can be treated with 8 days of twice-daily applications of petrolatum. Ivermectin can be used when topical therapy fails, although this is an off-label treatment (not approved by the Food and Drug Administration).
Pediculosis corporis – body lice or clothing lice – is also known as “vagabond’s disease” and is caused by Pediculus humanus var corporis. Body lice lay their eggs in clothing seams and can live in clothing for up to 1 month without feeding on human blood. Often homeless individuals and those living in overcrowded areas can be affected. The louse and nits also are visible to the naked eye. They have a longer, narrower body than Phthirus pubis and are more similar in appearance to head lice. They rarely are found on the skin.
Body lice may carry disease such as epidemic typhus, relapsing fever, and trench fever or endocarditis. Permethrin is the most widely used treatment to kill both lice and ova. Other treatments include Malathion, Lindane, and Crotamiton. Clothing and bedding should be laundered.
Scabies is a mite infestation caused by Sarcoptes scabiei. Unlike lice, scabies often affects the hands and feet. Characteristic linear burrows may be seen in the finger web spaces. The circle of Hebra describes the areas commonly infected by mites: axillae, antecubital fossa, wrists, hands, and the groin. Pruritus may be severe and worse at night. Patients may be afflicted with both lice and scabies at the same time. Mites are not visible to the naked eye but can be seen microscopically. Topical permethrin cream is used most often for treatment. All household contacts should be treated at the same time. As in louse infestations, clothing and bedding should be laundered. Ivermectin can be used for crusted scabies, although this is an off-label treatment.
This case and photo were submitted by Maria Hicks, MD, Advanced Dermatology and Cosmetic Surgery, Tampa, and Dr. Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
and through close skin contact, as well as contaminated clothes and bedding. Adult lice can live up to 36 hours away from its host. Pubic areas most commonly are affected, although other hair-bearing parts of the body often are affected, including eyelashes.
Pruritus can be severe. Secondary bacterial infections may occur as maculae ceruleae, or blue-colored macules, on the skin. The lice are visible to the naked eye and are approximately 1 mm in length. They have a crablike appearance, six legs, and a wide body. Nits may be present on the hair shaft. Unlike hair casts, which can be moved up and down along the hair shaft, nits firmly adhere to the hair. Diagnosis should prompt a workup for other sexually transmitted diseases, including HIV.
Treatment for patients and their sexual partners include permethrin topically; and laundering of clothing and bedding. Lice on the eyelashes can be treated with 8 days of twice-daily applications of petrolatum. Ivermectin can be used when topical therapy fails, although this is an off-label treatment (not approved by the Food and Drug Administration).
Pediculosis corporis – body lice or clothing lice – is also known as “vagabond’s disease” and is caused by Pediculus humanus var corporis. Body lice lay their eggs in clothing seams and can live in clothing for up to 1 month without feeding on human blood. Often homeless individuals and those living in overcrowded areas can be affected. The louse and nits also are visible to the naked eye. They have a longer, narrower body than Phthirus pubis and are more similar in appearance to head lice. They rarely are found on the skin.
Body lice may carry disease such as epidemic typhus, relapsing fever, and trench fever or endocarditis. Permethrin is the most widely used treatment to kill both lice and ova. Other treatments include Malathion, Lindane, and Crotamiton. Clothing and bedding should be laundered.
Scabies is a mite infestation caused by Sarcoptes scabiei. Unlike lice, scabies often affects the hands and feet. Characteristic linear burrows may be seen in the finger web spaces. The circle of Hebra describes the areas commonly infected by mites: axillae, antecubital fossa, wrists, hands, and the groin. Pruritus may be severe and worse at night. Patients may be afflicted with both lice and scabies at the same time. Mites are not visible to the naked eye but can be seen microscopically. Topical permethrin cream is used most often for treatment. All household contacts should be treated at the same time. As in louse infestations, clothing and bedding should be laundered. Ivermectin can be used for crusted scabies, although this is an off-label treatment.
This case and photo were submitted by Maria Hicks, MD, Advanced Dermatology and Cosmetic Surgery, Tampa, and Dr. Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
A 40-year-old HIV-positive male presented with a 1-month history of severely pruritic papules on his chest. The patient reported that he "removes bugs" from his skin. Microscopic examination of a hair clipping was performed.
Make the Diagnosis:
New Medicare cards
By now, you are probably aware that . The new, completely random number-letter combinations – dubbed Medicare Beneficiary Identifiers (MBI) – replace the old Social Security number–based Health Insurance Claim Numbers (HICN). The idea is to make citizens’ private information less vulnerable to identity thieves and other nefarious parties.
The switch began on April 1, and is expected to take about a year as the CMS processes about half a dozen states at a time. As I write this (at the beginning of May), the CMS is mailing out the first group of new cards to patients in Pennsylvania, Virginia, West Virginia, Maryland, Delaware, and the District of Columbia. But regardless of where you practice, you can expect to start seeing MBIs in your office soon – if you haven’t already – because people enrolling in Medicare for the first time are also receiving the new cards, no matter where they live.
Unlike the abrupt switch in 2015 from ICD-9 coding to ICD-10, this changeover has a transition period: Both HICNs and MBIs can be used on all billing and Medicare transactions from now until the end of 2019; after that, only claims with MBIs will be accepted. The last day of 2019 may sound like a long way off, but the time to get up to speed on everything MBI is now. That way, you can begin processing MBIs as soon as you start receiving them, and you will have time to solve any processing glitches well before the deadline.
First, you’ll need to make sure that your electronic health records and claims processing software will accept the new format, and that your electronic clearinghouse, if you use one, is geared up to accept and transmit the data on the new cards. Not all of them are. Some have been seduced by the year-and-a-half buffer – during which time HICNs can still be used – into dragging their feet on the MBI issue. Now is the time to find out if a vendor’s software is hard-wired to accept a maximum of 10 digits (MBIs have 11), not when your claims start bouncing.
Second, you will need to educate your front desk staff, so they will be able to recognize the new cards at a glance. Unfortunately, it looks a lot like the current card, though it is slightly smaller. It has the traditional red and blue colors with black printing, but there is no birthday or gender designation – again, in the interest of protecting patients’ identities. Knowing the difference will become particularly important after your state has been processed, when all of your Medicare patients should have the new card. Those who don’t will need to be identified and urged to get one before the December 2019 deadline.
Finally, once your staff and vendors are up to speed, you can begin educating your patients. Inevitably, some will not receive a new card, especially if they have moved and have not notified the CMS of the change; and some who are not expecting a new card will believe it is a duplicate, and throw it away. The CMS will be airing public service announcements and mailing education pieces to Medicare recipients, but a substantial portion of the education burden will fall on doctors and hospitals.
Have your front office staff remind patients to be sure their addresses are updated online with Medicare (www.Medicare.gov) or the Social Security Administration (www.ssa.gov). Encourage them to take advantage of the free resources available at www.cms.gov. These include both downloadable options and printed materials that illustrate what the new card will look like, explain how to update a mailing address with the Social Security Administration, and remind seniors to keep an eye out for their cards in the mail.
For the many Medicare-age patients who are not particularly computer savvy, the CMS has free resources for physicians as well. You will need to open an account at the agency’s Product Ordering website (productordering.cms.hhs.gov), which in turn needs to be approved by an administrator. The posters and other free literature can be displayed in your waiting room, exam rooms, and other “patient flow” areas. There is also a 1-minute video, downloadable from YouTube (https://youtu.be/DusRmgzQnLY), which can be looped in your waiting area.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
By now, you are probably aware that . The new, completely random number-letter combinations – dubbed Medicare Beneficiary Identifiers (MBI) – replace the old Social Security number–based Health Insurance Claim Numbers (HICN). The idea is to make citizens’ private information less vulnerable to identity thieves and other nefarious parties.
The switch began on April 1, and is expected to take about a year as the CMS processes about half a dozen states at a time. As I write this (at the beginning of May), the CMS is mailing out the first group of new cards to patients in Pennsylvania, Virginia, West Virginia, Maryland, Delaware, and the District of Columbia. But regardless of where you practice, you can expect to start seeing MBIs in your office soon – if you haven’t already – because people enrolling in Medicare for the first time are also receiving the new cards, no matter where they live.
Unlike the abrupt switch in 2015 from ICD-9 coding to ICD-10, this changeover has a transition period: Both HICNs and MBIs can be used on all billing and Medicare transactions from now until the end of 2019; after that, only claims with MBIs will be accepted. The last day of 2019 may sound like a long way off, but the time to get up to speed on everything MBI is now. That way, you can begin processing MBIs as soon as you start receiving them, and you will have time to solve any processing glitches well before the deadline.
First, you’ll need to make sure that your electronic health records and claims processing software will accept the new format, and that your electronic clearinghouse, if you use one, is geared up to accept and transmit the data on the new cards. Not all of them are. Some have been seduced by the year-and-a-half buffer – during which time HICNs can still be used – into dragging their feet on the MBI issue. Now is the time to find out if a vendor’s software is hard-wired to accept a maximum of 10 digits (MBIs have 11), not when your claims start bouncing.
Second, you will need to educate your front desk staff, so they will be able to recognize the new cards at a glance. Unfortunately, it looks a lot like the current card, though it is slightly smaller. It has the traditional red and blue colors with black printing, but there is no birthday or gender designation – again, in the interest of protecting patients’ identities. Knowing the difference will become particularly important after your state has been processed, when all of your Medicare patients should have the new card. Those who don’t will need to be identified and urged to get one before the December 2019 deadline.
Finally, once your staff and vendors are up to speed, you can begin educating your patients. Inevitably, some will not receive a new card, especially if they have moved and have not notified the CMS of the change; and some who are not expecting a new card will believe it is a duplicate, and throw it away. The CMS will be airing public service announcements and mailing education pieces to Medicare recipients, but a substantial portion of the education burden will fall on doctors and hospitals.
Have your front office staff remind patients to be sure their addresses are updated online with Medicare (www.Medicare.gov) or the Social Security Administration (www.ssa.gov). Encourage them to take advantage of the free resources available at www.cms.gov. These include both downloadable options and printed materials that illustrate what the new card will look like, explain how to update a mailing address with the Social Security Administration, and remind seniors to keep an eye out for their cards in the mail.
For the many Medicare-age patients who are not particularly computer savvy, the CMS has free resources for physicians as well. You will need to open an account at the agency’s Product Ordering website (productordering.cms.hhs.gov), which in turn needs to be approved by an administrator. The posters and other free literature can be displayed in your waiting room, exam rooms, and other “patient flow” areas. There is also a 1-minute video, downloadable from YouTube (https://youtu.be/DusRmgzQnLY), which can be looped in your waiting area.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
By now, you are probably aware that . The new, completely random number-letter combinations – dubbed Medicare Beneficiary Identifiers (MBI) – replace the old Social Security number–based Health Insurance Claim Numbers (HICN). The idea is to make citizens’ private information less vulnerable to identity thieves and other nefarious parties.
The switch began on April 1, and is expected to take about a year as the CMS processes about half a dozen states at a time. As I write this (at the beginning of May), the CMS is mailing out the first group of new cards to patients in Pennsylvania, Virginia, West Virginia, Maryland, Delaware, and the District of Columbia. But regardless of where you practice, you can expect to start seeing MBIs in your office soon – if you haven’t already – because people enrolling in Medicare for the first time are also receiving the new cards, no matter where they live.
Unlike the abrupt switch in 2015 from ICD-9 coding to ICD-10, this changeover has a transition period: Both HICNs and MBIs can be used on all billing and Medicare transactions from now until the end of 2019; after that, only claims with MBIs will be accepted. The last day of 2019 may sound like a long way off, but the time to get up to speed on everything MBI is now. That way, you can begin processing MBIs as soon as you start receiving them, and you will have time to solve any processing glitches well before the deadline.
First, you’ll need to make sure that your electronic health records and claims processing software will accept the new format, and that your electronic clearinghouse, if you use one, is geared up to accept and transmit the data on the new cards. Not all of them are. Some have been seduced by the year-and-a-half buffer – during which time HICNs can still be used – into dragging their feet on the MBI issue. Now is the time to find out if a vendor’s software is hard-wired to accept a maximum of 10 digits (MBIs have 11), not when your claims start bouncing.
Second, you will need to educate your front desk staff, so they will be able to recognize the new cards at a glance. Unfortunately, it looks a lot like the current card, though it is slightly smaller. It has the traditional red and blue colors with black printing, but there is no birthday or gender designation – again, in the interest of protecting patients’ identities. Knowing the difference will become particularly important after your state has been processed, when all of your Medicare patients should have the new card. Those who don’t will need to be identified and urged to get one before the December 2019 deadline.
Finally, once your staff and vendors are up to speed, you can begin educating your patients. Inevitably, some will not receive a new card, especially if they have moved and have not notified the CMS of the change; and some who are not expecting a new card will believe it is a duplicate, and throw it away. The CMS will be airing public service announcements and mailing education pieces to Medicare recipients, but a substantial portion of the education burden will fall on doctors and hospitals.
Have your front office staff remind patients to be sure their addresses are updated online with Medicare (www.Medicare.gov) or the Social Security Administration (www.ssa.gov). Encourage them to take advantage of the free resources available at www.cms.gov. These include both downloadable options and printed materials that illustrate what the new card will look like, explain how to update a mailing address with the Social Security Administration, and remind seniors to keep an eye out for their cards in the mail.
For the many Medicare-age patients who are not particularly computer savvy, the CMS has free resources for physicians as well. You will need to open an account at the agency’s Product Ordering website (productordering.cms.hhs.gov), which in turn needs to be approved by an administrator. The posters and other free literature can be displayed in your waiting room, exam rooms, and other “patient flow” areas. There is also a 1-minute video, downloadable from YouTube (https://youtu.be/DusRmgzQnLY), which can be looped in your waiting area.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Universal depression screening for adolescents not without controversy
When 14-year-old Ryan saw his pediatrician for his annual physical this past August, he was asked a few quick questions about whether he was having any problems, if he was feeling depressed or anxious, and if there was anything he wanted to discuss. Ryan said no to each question, then the doctor examined him, reminded him to get a flu shot, and signed off on the forms he needed to play team sports in high school. The doctor assured Ryan’s mother that he was healthy, and the visit was over. Next August, Ryan’s exam will likely include a more detailed look at his mental health.
In February 2018, the American Academy of Pediatrics updated its guidelines on screening for depression in adolescents in primary care settings. The guidelines address the problem of undiagnosed and untreated psychiatric illness in children over the age of 10 years, the shortage of available mental health professionals, and techniques primary care physicians might use to address psychiatric needs in adolescents. The AAP guidelines include a new recommendation for universal screening with an assessment tool: “Adolescent patients ages 12 years and older should be screened annually for depression [MDD or depressive disorders] with a formal self-report screening tool either on paper or electronically.”
Dr. Liu noted that some of his patients drive 4-5 hours each way to see him in Omaha, then spend the night before making the return trip. “There is a dire shortage of pediatric mental health services in every state. This shifts the responsibility for care to pediatricians, teachers, and parents who often lack the resources to keep kids safe and well. It’s an unconscionable gap in care.”
Dr. Doran’s practice has not yet implemented the use of a written screening tool for all adolescents. He anticipates doing this soon because of the new guidelines, but he was not enthusiastic about the prospect. “ We are already loaded down with administrative tasks and screening requirements.” Of note, in Dr. Doran’s 35 years in clinical practice, no child under his care has died of suicide.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
When 14-year-old Ryan saw his pediatrician for his annual physical this past August, he was asked a few quick questions about whether he was having any problems, if he was feeling depressed or anxious, and if there was anything he wanted to discuss. Ryan said no to each question, then the doctor examined him, reminded him to get a flu shot, and signed off on the forms he needed to play team sports in high school. The doctor assured Ryan’s mother that he was healthy, and the visit was over. Next August, Ryan’s exam will likely include a more detailed look at his mental health.
In February 2018, the American Academy of Pediatrics updated its guidelines on screening for depression in adolescents in primary care settings. The guidelines address the problem of undiagnosed and untreated psychiatric illness in children over the age of 10 years, the shortage of available mental health professionals, and techniques primary care physicians might use to address psychiatric needs in adolescents. The AAP guidelines include a new recommendation for universal screening with an assessment tool: “Adolescent patients ages 12 years and older should be screened annually for depression [MDD or depressive disorders] with a formal self-report screening tool either on paper or electronically.”
Dr. Liu noted that some of his patients drive 4-5 hours each way to see him in Omaha, then spend the night before making the return trip. “There is a dire shortage of pediatric mental health services in every state. This shifts the responsibility for care to pediatricians, teachers, and parents who often lack the resources to keep kids safe and well. It’s an unconscionable gap in care.”
Dr. Doran’s practice has not yet implemented the use of a written screening tool for all adolescents. He anticipates doing this soon because of the new guidelines, but he was not enthusiastic about the prospect. “ We are already loaded down with administrative tasks and screening requirements.” Of note, in Dr. Doran’s 35 years in clinical practice, no child under his care has died of suicide.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
When 14-year-old Ryan saw his pediatrician for his annual physical this past August, he was asked a few quick questions about whether he was having any problems, if he was feeling depressed or anxious, and if there was anything he wanted to discuss. Ryan said no to each question, then the doctor examined him, reminded him to get a flu shot, and signed off on the forms he needed to play team sports in high school. The doctor assured Ryan’s mother that he was healthy, and the visit was over. Next August, Ryan’s exam will likely include a more detailed look at his mental health.
In February 2018, the American Academy of Pediatrics updated its guidelines on screening for depression in adolescents in primary care settings. The guidelines address the problem of undiagnosed and untreated psychiatric illness in children over the age of 10 years, the shortage of available mental health professionals, and techniques primary care physicians might use to address psychiatric needs in adolescents. The AAP guidelines include a new recommendation for universal screening with an assessment tool: “Adolescent patients ages 12 years and older should be screened annually for depression [MDD or depressive disorders] with a formal self-report screening tool either on paper or electronically.”
Dr. Liu noted that some of his patients drive 4-5 hours each way to see him in Omaha, then spend the night before making the return trip. “There is a dire shortage of pediatric mental health services in every state. This shifts the responsibility for care to pediatricians, teachers, and parents who often lack the resources to keep kids safe and well. It’s an unconscionable gap in care.”
Dr. Doran’s practice has not yet implemented the use of a written screening tool for all adolescents. He anticipates doing this soon because of the new guidelines, but he was not enthusiastic about the prospect. “ We are already loaded down with administrative tasks and screening requirements.” Of note, in Dr. Doran’s 35 years in clinical practice, no child under his care has died of suicide.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
Thirteen Years and Still Growing: An AVAHO History (FULL)
The Association of VA Hematology/Oncology (AVAHO) is now 13 years old, and we have much to celebrate! Like an adolescent, the organization has grown significantly over the past 13 years, and there is still a lot to learn and plenty of opportunities to grow. To understand where we are going, it is helpful to reflect on our past before looking ahead to a bright future.
It is true that in the 1980s the VHA hosted an annual cancer symposium. This forum was focused on veterans with cancer and provided a unique opportunity for VA health care professionals (HCPs) to meet. Lack of funding, strict rules, concerns over conflicts of interest eventually meant that the symposia could not continue. There was a dire need to fill the void, and VA HCPs were nostalgic.
Because of the VA’s population of patients and structure, VA HCPs face unique challengesand opportunities. The founders of AVAHO saw the benefits and positive influences that providing a platform for education, networking, and research opportunities would bring to VA care. The seed for AVAHO was planted in the summer of 2005 by a group of passionate hematology and oncology professionals working at the VHA, including Abdul-Rahman Jazieh, MD, MPH, who was professor of medicine in the division of hematology/medical oncology at the University of Cincinnati in Ohio. This group sought to implement a forum for interaction among VA hematology/oncology professionals across the nation with the simple goal of providing the best care possible to our nation’s veterans facing cancer. Dr. Jazieh, developed a partnership that joined VA HCPs; the pharmaceutical industry (including Celgene’s Jackie Rychel), which provided financial support; and workforce Strategies (Tammy Pritchard); which provided logistic and legal support. Sue Lentz was employed as administrator.
The first official AVAHO inaugural meeting was held in Cincinnati, Ohio, on September 17, 2005, and the first executive committee consisted of Dr. Jazieh (president); Malek Safa, MD (vice president); Rami Komrokji, MD (secretary); and Zeina Nahleh, MD (treasurer).
A Maturing Organization
The society has grown over the past 13 years from fewer than 100 to a robust 630-member organization that provides a high-quality conference annually, including continuing medical education (CME) and non-CME sessions. Attendance at the annual conferences grew from 35 members in 2005 to nearly 400 in 2016. The first conference program lasted about 6 hours and included a business meeting and education and breakout sessions. Since 2005, the AVAHO meeting has expanded to 2 days to include CME and non-CME concurrent education sessions, special interest group breakout discussions, scientific posters, an exhibitor showcase, and networking opportunities. In addition, pharmaceutical company-sponsored satellite symposia have become very attractive to our members in the past 2 years and help support the organization’s goals. Now it has become difficult to fit the growing agenda into 2 days.
From its inception, AVAHO has been interdisciplinary so that professionals from across the cancer care team could connect, share their expertise and experience, and develop new strategies for cancer care delivery and research. From Nashville to Portland, Atlanta to Omaha, Washington, DC, to Dallas, the annual conference location varies to facilitate attendance from all areas of the country.
The society also has been at the vanguard of promoting cutting-edge science, precision medicine, and fostering innovation in cancer care as can be seen in the pages that follow. In addition, AVAHO is committed to providing essential CME for all hematology and oncology professionals and opportunities for HCPs to network and collaborate.
Beginning in 2012, AVAHO forged a strategic relationship with Federal Practitioner, and that relationship has grown to include the publication of AVAHO abstracts and a series of special issues focused on hematology and oncology—including this one.
A Unique Organization
AVAHO is unique. We are a 501(c)(3) nonprofit organization that is volunteer-led and managed with the support of a single paid staff member. This is the only professional association where all disciplines of hematology oncology professionals meet with only one focus—care of veterans with cancer.
The AVAHO mission is to provide leadership in delivering quality comprehensive care to veterans with cancer; education for members to improve the quality of cancer care for veterans; a mechanism for networking among members to gain knowledge and best practices from the experiences of colleagues; and a venue to explore and facilitate new multidisciplinary research. One priority has been to continually increase the benefits of being an AVAHO member. Members have access to a variety of resources to keep current with trends in cancer care as well as to low-cost continuing education credits that are essential for licensure across disciplines.
The education AVAHO provides is focused on the unique nature of providing “the best care, anywhere” inside the VHA system. In addition, AVAHO continues to help minimize the costs associated with travel to the conference site, cost of stay, some of the associated meals provided in part by AVAHO. As members, HCPs also have the opportunity to raise issues and concerns and share successes and almost-successes, and support career development of professional peers.
Last year, AVAHO announced its first scholarship, a $10,000 research scholarship to a young investigator. Anyone who completed education and/or training within the past 10 years and has a minimum 5/8ths appointment at a VA facility can apply for these funds.
The teen years are not always easy but offer great promise. Over the past 13 years, AVAHO has grown significantly as an organization and continues to offer more opportunities for education, research, and networking, all with the hope of improving the quality of care for veterans with cancer and increasing support for their caregivers.
Click here to read the digital edition.
The Association of VA Hematology/Oncology (AVAHO) is now 13 years old, and we have much to celebrate! Like an adolescent, the organization has grown significantly over the past 13 years, and there is still a lot to learn and plenty of opportunities to grow. To understand where we are going, it is helpful to reflect on our past before looking ahead to a bright future.
It is true that in the 1980s the VHA hosted an annual cancer symposium. This forum was focused on veterans with cancer and provided a unique opportunity for VA health care professionals (HCPs) to meet. Lack of funding, strict rules, concerns over conflicts of interest eventually meant that the symposia could not continue. There was a dire need to fill the void, and VA HCPs were nostalgic.
Because of the VA’s population of patients and structure, VA HCPs face unique challengesand opportunities. The founders of AVAHO saw the benefits and positive influences that providing a platform for education, networking, and research opportunities would bring to VA care. The seed for AVAHO was planted in the summer of 2005 by a group of passionate hematology and oncology professionals working at the VHA, including Abdul-Rahman Jazieh, MD, MPH, who was professor of medicine in the division of hematology/medical oncology at the University of Cincinnati in Ohio. This group sought to implement a forum for interaction among VA hematology/oncology professionals across the nation with the simple goal of providing the best care possible to our nation’s veterans facing cancer. Dr. Jazieh, developed a partnership that joined VA HCPs; the pharmaceutical industry (including Celgene’s Jackie Rychel), which provided financial support; and workforce Strategies (Tammy Pritchard); which provided logistic and legal support. Sue Lentz was employed as administrator.
The first official AVAHO inaugural meeting was held in Cincinnati, Ohio, on September 17, 2005, and the first executive committee consisted of Dr. Jazieh (president); Malek Safa, MD (vice president); Rami Komrokji, MD (secretary); and Zeina Nahleh, MD (treasurer).
A Maturing Organization
The society has grown over the past 13 years from fewer than 100 to a robust 630-member organization that provides a high-quality conference annually, including continuing medical education (CME) and non-CME sessions. Attendance at the annual conferences grew from 35 members in 2005 to nearly 400 in 2016. The first conference program lasted about 6 hours and included a business meeting and education and breakout sessions. Since 2005, the AVAHO meeting has expanded to 2 days to include CME and non-CME concurrent education sessions, special interest group breakout discussions, scientific posters, an exhibitor showcase, and networking opportunities. In addition, pharmaceutical company-sponsored satellite symposia have become very attractive to our members in the past 2 years and help support the organization’s goals. Now it has become difficult to fit the growing agenda into 2 days.
From its inception, AVAHO has been interdisciplinary so that professionals from across the cancer care team could connect, share their expertise and experience, and develop new strategies for cancer care delivery and research. From Nashville to Portland, Atlanta to Omaha, Washington, DC, to Dallas, the annual conference location varies to facilitate attendance from all areas of the country.
The society also has been at the vanguard of promoting cutting-edge science, precision medicine, and fostering innovation in cancer care as can be seen in the pages that follow. In addition, AVAHO is committed to providing essential CME for all hematology and oncology professionals and opportunities for HCPs to network and collaborate.
Beginning in 2012, AVAHO forged a strategic relationship with Federal Practitioner, and that relationship has grown to include the publication of AVAHO abstracts and a series of special issues focused on hematology and oncology—including this one.
A Unique Organization
AVAHO is unique. We are a 501(c)(3) nonprofit organization that is volunteer-led and managed with the support of a single paid staff member. This is the only professional association where all disciplines of hematology oncology professionals meet with only one focus—care of veterans with cancer.
The AVAHO mission is to provide leadership in delivering quality comprehensive care to veterans with cancer; education for members to improve the quality of cancer care for veterans; a mechanism for networking among members to gain knowledge and best practices from the experiences of colleagues; and a venue to explore and facilitate new multidisciplinary research. One priority has been to continually increase the benefits of being an AVAHO member. Members have access to a variety of resources to keep current with trends in cancer care as well as to low-cost continuing education credits that are essential for licensure across disciplines.
The education AVAHO provides is focused on the unique nature of providing “the best care, anywhere” inside the VHA system. In addition, AVAHO continues to help minimize the costs associated with travel to the conference site, cost of stay, some of the associated meals provided in part by AVAHO. As members, HCPs also have the opportunity to raise issues and concerns and share successes and almost-successes, and support career development of professional peers.
Last year, AVAHO announced its first scholarship, a $10,000 research scholarship to a young investigator. Anyone who completed education and/or training within the past 10 years and has a minimum 5/8ths appointment at a VA facility can apply for these funds.
The teen years are not always easy but offer great promise. Over the past 13 years, AVAHO has grown significantly as an organization and continues to offer more opportunities for education, research, and networking, all with the hope of improving the quality of care for veterans with cancer and increasing support for their caregivers.
Click here to read the digital edition.
The Association of VA Hematology/Oncology (AVAHO) is now 13 years old, and we have much to celebrate! Like an adolescent, the organization has grown significantly over the past 13 years, and there is still a lot to learn and plenty of opportunities to grow. To understand where we are going, it is helpful to reflect on our past before looking ahead to a bright future.
It is true that in the 1980s the VHA hosted an annual cancer symposium. This forum was focused on veterans with cancer and provided a unique opportunity for VA health care professionals (HCPs) to meet. Lack of funding, strict rules, concerns over conflicts of interest eventually meant that the symposia could not continue. There was a dire need to fill the void, and VA HCPs were nostalgic.
Because of the VA’s population of patients and structure, VA HCPs face unique challengesand opportunities. The founders of AVAHO saw the benefits and positive influences that providing a platform for education, networking, and research opportunities would bring to VA care. The seed for AVAHO was planted in the summer of 2005 by a group of passionate hematology and oncology professionals working at the VHA, including Abdul-Rahman Jazieh, MD, MPH, who was professor of medicine in the division of hematology/medical oncology at the University of Cincinnati in Ohio. This group sought to implement a forum for interaction among VA hematology/oncology professionals across the nation with the simple goal of providing the best care possible to our nation’s veterans facing cancer. Dr. Jazieh, developed a partnership that joined VA HCPs; the pharmaceutical industry (including Celgene’s Jackie Rychel), which provided financial support; and workforce Strategies (Tammy Pritchard); which provided logistic and legal support. Sue Lentz was employed as administrator.
The first official AVAHO inaugural meeting was held in Cincinnati, Ohio, on September 17, 2005, and the first executive committee consisted of Dr. Jazieh (president); Malek Safa, MD (vice president); Rami Komrokji, MD (secretary); and Zeina Nahleh, MD (treasurer).
A Maturing Organization
The society has grown over the past 13 years from fewer than 100 to a robust 630-member organization that provides a high-quality conference annually, including continuing medical education (CME) and non-CME sessions. Attendance at the annual conferences grew from 35 members in 2005 to nearly 400 in 2016. The first conference program lasted about 6 hours and included a business meeting and education and breakout sessions. Since 2005, the AVAHO meeting has expanded to 2 days to include CME and non-CME concurrent education sessions, special interest group breakout discussions, scientific posters, an exhibitor showcase, and networking opportunities. In addition, pharmaceutical company-sponsored satellite symposia have become very attractive to our members in the past 2 years and help support the organization’s goals. Now it has become difficult to fit the growing agenda into 2 days.
From its inception, AVAHO has been interdisciplinary so that professionals from across the cancer care team could connect, share their expertise and experience, and develop new strategies for cancer care delivery and research. From Nashville to Portland, Atlanta to Omaha, Washington, DC, to Dallas, the annual conference location varies to facilitate attendance from all areas of the country.
The society also has been at the vanguard of promoting cutting-edge science, precision medicine, and fostering innovation in cancer care as can be seen in the pages that follow. In addition, AVAHO is committed to providing essential CME for all hematology and oncology professionals and opportunities for HCPs to network and collaborate.
Beginning in 2012, AVAHO forged a strategic relationship with Federal Practitioner, and that relationship has grown to include the publication of AVAHO abstracts and a series of special issues focused on hematology and oncology—including this one.
A Unique Organization
AVAHO is unique. We are a 501(c)(3) nonprofit organization that is volunteer-led and managed with the support of a single paid staff member. This is the only professional association where all disciplines of hematology oncology professionals meet with only one focus—care of veterans with cancer.
The AVAHO mission is to provide leadership in delivering quality comprehensive care to veterans with cancer; education for members to improve the quality of cancer care for veterans; a mechanism for networking among members to gain knowledge and best practices from the experiences of colleagues; and a venue to explore and facilitate new multidisciplinary research. One priority has been to continually increase the benefits of being an AVAHO member. Members have access to a variety of resources to keep current with trends in cancer care as well as to low-cost continuing education credits that are essential for licensure across disciplines.
The education AVAHO provides is focused on the unique nature of providing “the best care, anywhere” inside the VHA system. In addition, AVAHO continues to help minimize the costs associated with travel to the conference site, cost of stay, some of the associated meals provided in part by AVAHO. As members, HCPs also have the opportunity to raise issues and concerns and share successes and almost-successes, and support career development of professional peers.
Last year, AVAHO announced its first scholarship, a $10,000 research scholarship to a young investigator. Anyone who completed education and/or training within the past 10 years and has a minimum 5/8ths appointment at a VA facility can apply for these funds.
The teen years are not always easy but offer great promise. Over the past 13 years, AVAHO has grown significantly as an organization and continues to offer more opportunities for education, research, and networking, all with the hope of improving the quality of care for veterans with cancer and increasing support for their caregivers.
Click here to read the digital edition.
Homelessness: A need for better care
In 1946, Psychiatrist Viktor Frankl postulated in “Man’s Search for Meaning” that the expected reaction to being placed in a concentration camp was dehumanization, apathy, and despair. The placement of a person in such a desolate environment, anticipating death, and seeing the affliction of horror, was believed to lead to hopelessness and mental illness. Facing such circumstances, Dr. Frankl advised finding a purpose as a means to stay mentally and physically alive.
As contemporary psychiatrists, we see ourselves confronted with a different kind of challenge. Modern society has left more than a half-million of our fellow Americans on the streets, homeless, and with little connection to the rest of society. Despite their isolation, their paths merge with ours in an array of settings, namely mental health services in emergency departments, community clinics, and local correctional institutions. Nearly all psychiatrists have worked with a homeless patient at some point in their careers. The connection between mental illness and homelessness may be apparent to some, but we remain perplexed and propose more questions than answers.
What is the expected reaction to homelessness?
How might a homeless person describe his fears? “I don’t want to go to the emergency room, doc; these are all the belongings I have, and I have nowhere safe to store them. I have to carry a knife for protection despite the fact that it is illegal. I used to have a circle of support, but my ‘friends’ stole from me, and now I don’t trust anyone. I don’t like to be around a lot of people; I’ve seen some people do really horrible things on the streets that I can’t unsee. Sometimes, I think the cops enjoy arresting me; I wonder if it helps their quotas.” Are those concerns a sign of an anxiety disorder or even paranoia? Or is it how most people would respond if they were placed in similar situations?
How might a homeless person describe her mood? “I have no home. I have not seen my family in a decade. I am so disconnected from society that I do not know who the president is, or what is the date. Nobody has shaken my hand in years.” Yet, we expect that person to possibly narrow and codify her suffering with an adjective on a Likert scale, or even a visual analog scale of mood with a happy or a frowny face. We assume that their mood can even be narrowed to an emoji or a label, despite their complex circumstances.
When asked about social history, we often hear responses such as, “I have no income. I tried to get a job, but it was too hard to maintain my hygiene and transportation, so I quit. I applied for disability once, and I was denied. I want to work, but when you’ve been on the streets this long it’s hard. I mean … look at me. I applied for affordable housing twice, but I didn’t get it because I’ve been evicted in the last 5 years. The only time I had stable housing for an extended period of time in the last 10 years was when I went to jail for trespassing. I want to live, but I can’t go on like this. I think people would be better off without me if I was gone. Heck, maybe they wouldn’t even notice.” Would we permit a patient like this to be heard in a safe and nonconfrontational environment? Do they meet criteria for grave disability and/or danger to self? Or are they doing the best they can to get their needs met in a broken system?
Our clinical experience has taught us that the homeless population suffers from many of the same symptoms as those of patients with mental illness, independent of a diagnosis. Careful examination of their lives can often explain these expected reactions better than contextualizing them through pathological or diagnostic lenses.
Should homelessness alone be a criterion for mental health treatment?
Despite the enormous challenges facing the homeless population, many are seen in our clinics hopeful and endorsing a fair mood. Many are polite and answer questions in an attempt to diminish the burden they feel they impose on others, including the medical system. Many display strong resiliency and find ways to cope, relate, and find meaning despite their challenging circumstances. Yet, many also come to us suffering and seeking assistance.
We routinely see the distress and hopelessness in our patients suffering from homelessness. We think that psychiatry is capable of softening those daily traumas using supportive therapy. We think that psychiatry is capable of positively challenging the despondency by activating meaning and purpose, as suggested by Dr. Frankl. While those are not typical interventions in modern psychiatry, they are established and validated. By considering homelessness in and of itself a criterion for mental health treatment, we can begin to address those challenges, and engage in alternative, longer lasting treatment considerations.
How to proceed?
Though the answer for caring for the homeless may not be in psychopharmacology, we think that psychiatry could enhance the care of the homeless by pursuit of two main goals.
The first is to advocate for access to mental health services for all homeless persons who desire it, even those who do not meet criteria for a DSM disorder. This charade we are forced to play with insurance companies and community organizations requiring the presence of a “disorder” to justify supportive therapy and/or occasional use of a crisis house bed does not appear warranted. While we understand that resources are limited, we do not think that homeless persons who are in need of care, but do not meet criteria for a DSM disorder, are any less worthy.
The second goal is to advocate for housing first initiatives that incorporate comprehensive supportive services into their facilities. While we acknowledge the problems that can arise by forcing programs to accept clients, we do not see how mental health treatment can be done adequately without an opportunity for housing. Psychiatry must acknowledge that this social determinant of health takes priority over medication adherence, drug use, the ability to fill out forms, and even symptomatology. Sometimes, medications aren’t even necessary – we’ve worked with homeless patients who present initially with insomnia, depression, and anxiety, and as soon as they get stable housing, these symptoms resolve. In these situations, social interventions are more sensical than medication management. The social nature of homelessness should not propel psychiatry to focus its efforts on the biological side of its specialty; it should be seen as an opportunity for us to develop skills in advocacy and lead, or at least support, interventions that target the social determinants of health.
Under our current medical model, as psychiatrists, we understand that our role is to diagnose, and then treat the diagnosed disorder. Homelessness brings a unique challenge; it is a factor, not based on biology, that can cause severe psychiatric symptomatology with or without the presence of a DSM disorder. We worry that current constructs of mental health narrow our reach and inhibit our potential benefit to society. We hope to encourage psychiatry in embracing public health interventions such as housing first and remembering the value of psychological interventions when working with this vulnerable population.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre mentors residents on projects, including the reduction in the use of solitary confinement of patients with mental illness and examination of the mentally ill offender. Dr. Badre can be reached at Badremd.com. Dr. Janowsky is a combined resident in family medicine and psychiatry at the University of California, San Diego. She spends most of her clinical time at St. Vincent de Paul Family Health Center, a clinic that primarily serves the homeless. Her interests include disease prevention, wellness promotion, and behavioral interventions for chronic disease management. Outside of work, you can find her recharging her batteries via yoga, musical meditation, hiking, beach journaling, and spending time with loved ones.
In 1946, Psychiatrist Viktor Frankl postulated in “Man’s Search for Meaning” that the expected reaction to being placed in a concentration camp was dehumanization, apathy, and despair. The placement of a person in such a desolate environment, anticipating death, and seeing the affliction of horror, was believed to lead to hopelessness and mental illness. Facing such circumstances, Dr. Frankl advised finding a purpose as a means to stay mentally and physically alive.
As contemporary psychiatrists, we see ourselves confronted with a different kind of challenge. Modern society has left more than a half-million of our fellow Americans on the streets, homeless, and with little connection to the rest of society. Despite their isolation, their paths merge with ours in an array of settings, namely mental health services in emergency departments, community clinics, and local correctional institutions. Nearly all psychiatrists have worked with a homeless patient at some point in their careers. The connection between mental illness and homelessness may be apparent to some, but we remain perplexed and propose more questions than answers.
What is the expected reaction to homelessness?
How might a homeless person describe his fears? “I don’t want to go to the emergency room, doc; these are all the belongings I have, and I have nowhere safe to store them. I have to carry a knife for protection despite the fact that it is illegal. I used to have a circle of support, but my ‘friends’ stole from me, and now I don’t trust anyone. I don’t like to be around a lot of people; I’ve seen some people do really horrible things on the streets that I can’t unsee. Sometimes, I think the cops enjoy arresting me; I wonder if it helps their quotas.” Are those concerns a sign of an anxiety disorder or even paranoia? Or is it how most people would respond if they were placed in similar situations?
How might a homeless person describe her mood? “I have no home. I have not seen my family in a decade. I am so disconnected from society that I do not know who the president is, or what is the date. Nobody has shaken my hand in years.” Yet, we expect that person to possibly narrow and codify her suffering with an adjective on a Likert scale, or even a visual analog scale of mood with a happy or a frowny face. We assume that their mood can even be narrowed to an emoji or a label, despite their complex circumstances.
When asked about social history, we often hear responses such as, “I have no income. I tried to get a job, but it was too hard to maintain my hygiene and transportation, so I quit. I applied for disability once, and I was denied. I want to work, but when you’ve been on the streets this long it’s hard. I mean … look at me. I applied for affordable housing twice, but I didn’t get it because I’ve been evicted in the last 5 years. The only time I had stable housing for an extended period of time in the last 10 years was when I went to jail for trespassing. I want to live, but I can’t go on like this. I think people would be better off without me if I was gone. Heck, maybe they wouldn’t even notice.” Would we permit a patient like this to be heard in a safe and nonconfrontational environment? Do they meet criteria for grave disability and/or danger to self? Or are they doing the best they can to get their needs met in a broken system?
Our clinical experience has taught us that the homeless population suffers from many of the same symptoms as those of patients with mental illness, independent of a diagnosis. Careful examination of their lives can often explain these expected reactions better than contextualizing them through pathological or diagnostic lenses.
Should homelessness alone be a criterion for mental health treatment?
Despite the enormous challenges facing the homeless population, many are seen in our clinics hopeful and endorsing a fair mood. Many are polite and answer questions in an attempt to diminish the burden they feel they impose on others, including the medical system. Many display strong resiliency and find ways to cope, relate, and find meaning despite their challenging circumstances. Yet, many also come to us suffering and seeking assistance.
We routinely see the distress and hopelessness in our patients suffering from homelessness. We think that psychiatry is capable of softening those daily traumas using supportive therapy. We think that psychiatry is capable of positively challenging the despondency by activating meaning and purpose, as suggested by Dr. Frankl. While those are not typical interventions in modern psychiatry, they are established and validated. By considering homelessness in and of itself a criterion for mental health treatment, we can begin to address those challenges, and engage in alternative, longer lasting treatment considerations.
How to proceed?
Though the answer for caring for the homeless may not be in psychopharmacology, we think that psychiatry could enhance the care of the homeless by pursuit of two main goals.
The first is to advocate for access to mental health services for all homeless persons who desire it, even those who do not meet criteria for a DSM disorder. This charade we are forced to play with insurance companies and community organizations requiring the presence of a “disorder” to justify supportive therapy and/or occasional use of a crisis house bed does not appear warranted. While we understand that resources are limited, we do not think that homeless persons who are in need of care, but do not meet criteria for a DSM disorder, are any less worthy.
The second goal is to advocate for housing first initiatives that incorporate comprehensive supportive services into their facilities. While we acknowledge the problems that can arise by forcing programs to accept clients, we do not see how mental health treatment can be done adequately without an opportunity for housing. Psychiatry must acknowledge that this social determinant of health takes priority over medication adherence, drug use, the ability to fill out forms, and even symptomatology. Sometimes, medications aren’t even necessary – we’ve worked with homeless patients who present initially with insomnia, depression, and anxiety, and as soon as they get stable housing, these symptoms resolve. In these situations, social interventions are more sensical than medication management. The social nature of homelessness should not propel psychiatry to focus its efforts on the biological side of its specialty; it should be seen as an opportunity for us to develop skills in advocacy and lead, or at least support, interventions that target the social determinants of health.
Under our current medical model, as psychiatrists, we understand that our role is to diagnose, and then treat the diagnosed disorder. Homelessness brings a unique challenge; it is a factor, not based on biology, that can cause severe psychiatric symptomatology with or without the presence of a DSM disorder. We worry that current constructs of mental health narrow our reach and inhibit our potential benefit to society. We hope to encourage psychiatry in embracing public health interventions such as housing first and remembering the value of psychological interventions when working with this vulnerable population.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre mentors residents on projects, including the reduction in the use of solitary confinement of patients with mental illness and examination of the mentally ill offender. Dr. Badre can be reached at Badremd.com. Dr. Janowsky is a combined resident in family medicine and psychiatry at the University of California, San Diego. She spends most of her clinical time at St. Vincent de Paul Family Health Center, a clinic that primarily serves the homeless. Her interests include disease prevention, wellness promotion, and behavioral interventions for chronic disease management. Outside of work, you can find her recharging her batteries via yoga, musical meditation, hiking, beach journaling, and spending time with loved ones.
In 1946, Psychiatrist Viktor Frankl postulated in “Man’s Search for Meaning” that the expected reaction to being placed in a concentration camp was dehumanization, apathy, and despair. The placement of a person in such a desolate environment, anticipating death, and seeing the affliction of horror, was believed to lead to hopelessness and mental illness. Facing such circumstances, Dr. Frankl advised finding a purpose as a means to stay mentally and physically alive.
As contemporary psychiatrists, we see ourselves confronted with a different kind of challenge. Modern society has left more than a half-million of our fellow Americans on the streets, homeless, and with little connection to the rest of society. Despite their isolation, their paths merge with ours in an array of settings, namely mental health services in emergency departments, community clinics, and local correctional institutions. Nearly all psychiatrists have worked with a homeless patient at some point in their careers. The connection between mental illness and homelessness may be apparent to some, but we remain perplexed and propose more questions than answers.
What is the expected reaction to homelessness?
How might a homeless person describe his fears? “I don’t want to go to the emergency room, doc; these are all the belongings I have, and I have nowhere safe to store them. I have to carry a knife for protection despite the fact that it is illegal. I used to have a circle of support, but my ‘friends’ stole from me, and now I don’t trust anyone. I don’t like to be around a lot of people; I’ve seen some people do really horrible things on the streets that I can’t unsee. Sometimes, I think the cops enjoy arresting me; I wonder if it helps their quotas.” Are those concerns a sign of an anxiety disorder or even paranoia? Or is it how most people would respond if they were placed in similar situations?
How might a homeless person describe her mood? “I have no home. I have not seen my family in a decade. I am so disconnected from society that I do not know who the president is, or what is the date. Nobody has shaken my hand in years.” Yet, we expect that person to possibly narrow and codify her suffering with an adjective on a Likert scale, or even a visual analog scale of mood with a happy or a frowny face. We assume that their mood can even be narrowed to an emoji or a label, despite their complex circumstances.
When asked about social history, we often hear responses such as, “I have no income. I tried to get a job, but it was too hard to maintain my hygiene and transportation, so I quit. I applied for disability once, and I was denied. I want to work, but when you’ve been on the streets this long it’s hard. I mean … look at me. I applied for affordable housing twice, but I didn’t get it because I’ve been evicted in the last 5 years. The only time I had stable housing for an extended period of time in the last 10 years was when I went to jail for trespassing. I want to live, but I can’t go on like this. I think people would be better off without me if I was gone. Heck, maybe they wouldn’t even notice.” Would we permit a patient like this to be heard in a safe and nonconfrontational environment? Do they meet criteria for grave disability and/or danger to self? Or are they doing the best they can to get their needs met in a broken system?
Our clinical experience has taught us that the homeless population suffers from many of the same symptoms as those of patients with mental illness, independent of a diagnosis. Careful examination of their lives can often explain these expected reactions better than contextualizing them through pathological or diagnostic lenses.
Should homelessness alone be a criterion for mental health treatment?
Despite the enormous challenges facing the homeless population, many are seen in our clinics hopeful and endorsing a fair mood. Many are polite and answer questions in an attempt to diminish the burden they feel they impose on others, including the medical system. Many display strong resiliency and find ways to cope, relate, and find meaning despite their challenging circumstances. Yet, many also come to us suffering and seeking assistance.
We routinely see the distress and hopelessness in our patients suffering from homelessness. We think that psychiatry is capable of softening those daily traumas using supportive therapy. We think that psychiatry is capable of positively challenging the despondency by activating meaning and purpose, as suggested by Dr. Frankl. While those are not typical interventions in modern psychiatry, they are established and validated. By considering homelessness in and of itself a criterion for mental health treatment, we can begin to address those challenges, and engage in alternative, longer lasting treatment considerations.
How to proceed?
Though the answer for caring for the homeless may not be in psychopharmacology, we think that psychiatry could enhance the care of the homeless by pursuit of two main goals.
The first is to advocate for access to mental health services for all homeless persons who desire it, even those who do not meet criteria for a DSM disorder. This charade we are forced to play with insurance companies and community organizations requiring the presence of a “disorder” to justify supportive therapy and/or occasional use of a crisis house bed does not appear warranted. While we understand that resources are limited, we do not think that homeless persons who are in need of care, but do not meet criteria for a DSM disorder, are any less worthy.
The second goal is to advocate for housing first initiatives that incorporate comprehensive supportive services into their facilities. While we acknowledge the problems that can arise by forcing programs to accept clients, we do not see how mental health treatment can be done adequately without an opportunity for housing. Psychiatry must acknowledge that this social determinant of health takes priority over medication adherence, drug use, the ability to fill out forms, and even symptomatology. Sometimes, medications aren’t even necessary – we’ve worked with homeless patients who present initially with insomnia, depression, and anxiety, and as soon as they get stable housing, these symptoms resolve. In these situations, social interventions are more sensical than medication management. The social nature of homelessness should not propel psychiatry to focus its efforts on the biological side of its specialty; it should be seen as an opportunity for us to develop skills in advocacy and lead, or at least support, interventions that target the social determinants of health.
Under our current medical model, as psychiatrists, we understand that our role is to diagnose, and then treat the diagnosed disorder. Homelessness brings a unique challenge; it is a factor, not based on biology, that can cause severe psychiatric symptomatology with or without the presence of a DSM disorder. We worry that current constructs of mental health narrow our reach and inhibit our potential benefit to society. We hope to encourage psychiatry in embracing public health interventions such as housing first and remembering the value of psychological interventions when working with this vulnerable population.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre mentors residents on projects, including the reduction in the use of solitary confinement of patients with mental illness and examination of the mentally ill offender. Dr. Badre can be reached at Badremd.com. Dr. Janowsky is a combined resident in family medicine and psychiatry at the University of California, San Diego. She spends most of her clinical time at St. Vincent de Paul Family Health Center, a clinic that primarily serves the homeless. Her interests include disease prevention, wellness promotion, and behavioral interventions for chronic disease management. Outside of work, you can find her recharging her batteries via yoga, musical meditation, hiking, beach journaling, and spending time with loved ones.