User login
A creative diversion
Do you have a creative diversion – a hobby for lack of a better word? One frequently hears of physicians who have creative skills not directly related to their professional careers. Furniture-building surgeons, fly-tying orthopedists, pediatrician poets, painting dermatologists ... I have even heard unsubstantiated claims that the traits that encourage individuals to become physicians make it more likely that they will have creative skills. Another one of those left brain/right brain things that probably doesn’t hold water.
If you do have a hobby or have the seed of a creative impulse you think could blossom into a hobby, I bet you wish that you could have an unlimited amount of time to invest in that activity. I am going to argue that this is another example of a situation in which you should be careful what you wish for.
When I was 9 or 10 years old, I bought a small carving of a sandpiper in a gift shop on Cape Cod. I still have it with its chipped bill and yellowed paper label on its driftwood base. That little bird triggered my interest in carving, and with gaps sometimes measured in decades I have been a self-taught bird carver. Some are attempts at realism with burned in feathers that takes weeks to complete. Others are free form painted whimsically, and are created in a few hours. They aren’t for sale, but to keep my inventory in check I distribute them as birthday and hostess gifts.
Ten years ago, after decades of visiting art galleries and grumbling to my wife, “I could do that,” I decided to try my hand at two-dimensional landscape painting. It was a fun challenge, and after a year or 2, I was ready to see what other people thought of my work. The first show that I entered stipulated that all of the entries be for sale. With no intention of parting with my work, I priced mine several orders of magnitude above what I thought they were worth.
One sold, and with that began a 7-year period during which pretty much anything I painted with a maritime theme sold for hundreds of dollars. It was a nice ego trip, but it took me down a dark path in which I began to choose my subjects and style based on what I knew would sell. Creating was no longer something I did for a change of pace. I was now retired, but painting had become my job. I felt burdened by the obligation to paint enough to cover the walls of the restaurant that graciously hung my work.
Luckily, the epiphany that I had sacrificed my creative diversion, which began with that little sandpiper, coincided with the restaurant’s decision to redecorate and the loss of much of my hanging space. I was now free to paint subjects I was interested in, and return to the comfort of carving when I felt the need to create.
If you already have a creative diversion, remember that a large part of its appeal is that it plays counterpoint to your job. Even if you are retired, a hobby provides a change of pace from which we can all benefit.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Do you have a creative diversion – a hobby for lack of a better word? One frequently hears of physicians who have creative skills not directly related to their professional careers. Furniture-building surgeons, fly-tying orthopedists, pediatrician poets, painting dermatologists ... I have even heard unsubstantiated claims that the traits that encourage individuals to become physicians make it more likely that they will have creative skills. Another one of those left brain/right brain things that probably doesn’t hold water.
If you do have a hobby or have the seed of a creative impulse you think could blossom into a hobby, I bet you wish that you could have an unlimited amount of time to invest in that activity. I am going to argue that this is another example of a situation in which you should be careful what you wish for.
When I was 9 or 10 years old, I bought a small carving of a sandpiper in a gift shop on Cape Cod. I still have it with its chipped bill and yellowed paper label on its driftwood base. That little bird triggered my interest in carving, and with gaps sometimes measured in decades I have been a self-taught bird carver. Some are attempts at realism with burned in feathers that takes weeks to complete. Others are free form painted whimsically, and are created in a few hours. They aren’t for sale, but to keep my inventory in check I distribute them as birthday and hostess gifts.
Ten years ago, after decades of visiting art galleries and grumbling to my wife, “I could do that,” I decided to try my hand at two-dimensional landscape painting. It was a fun challenge, and after a year or 2, I was ready to see what other people thought of my work. The first show that I entered stipulated that all of the entries be for sale. With no intention of parting with my work, I priced mine several orders of magnitude above what I thought they were worth.
One sold, and with that began a 7-year period during which pretty much anything I painted with a maritime theme sold for hundreds of dollars. It was a nice ego trip, but it took me down a dark path in which I began to choose my subjects and style based on what I knew would sell. Creating was no longer something I did for a change of pace. I was now retired, but painting had become my job. I felt burdened by the obligation to paint enough to cover the walls of the restaurant that graciously hung my work.
Luckily, the epiphany that I had sacrificed my creative diversion, which began with that little sandpiper, coincided with the restaurant’s decision to redecorate and the loss of much of my hanging space. I was now free to paint subjects I was interested in, and return to the comfort of carving when I felt the need to create.
If you already have a creative diversion, remember that a large part of its appeal is that it plays counterpoint to your job. Even if you are retired, a hobby provides a change of pace from which we can all benefit.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Do you have a creative diversion – a hobby for lack of a better word? One frequently hears of physicians who have creative skills not directly related to their professional careers. Furniture-building surgeons, fly-tying orthopedists, pediatrician poets, painting dermatologists ... I have even heard unsubstantiated claims that the traits that encourage individuals to become physicians make it more likely that they will have creative skills. Another one of those left brain/right brain things that probably doesn’t hold water.
If you do have a hobby or have the seed of a creative impulse you think could blossom into a hobby, I bet you wish that you could have an unlimited amount of time to invest in that activity. I am going to argue that this is another example of a situation in which you should be careful what you wish for.
When I was 9 or 10 years old, I bought a small carving of a sandpiper in a gift shop on Cape Cod. I still have it with its chipped bill and yellowed paper label on its driftwood base. That little bird triggered my interest in carving, and with gaps sometimes measured in decades I have been a self-taught bird carver. Some are attempts at realism with burned in feathers that takes weeks to complete. Others are free form painted whimsically, and are created in a few hours. They aren’t for sale, but to keep my inventory in check I distribute them as birthday and hostess gifts.
Ten years ago, after decades of visiting art galleries and grumbling to my wife, “I could do that,” I decided to try my hand at two-dimensional landscape painting. It was a fun challenge, and after a year or 2, I was ready to see what other people thought of my work. The first show that I entered stipulated that all of the entries be for sale. With no intention of parting with my work, I priced mine several orders of magnitude above what I thought they were worth.
One sold, and with that began a 7-year period during which pretty much anything I painted with a maritime theme sold for hundreds of dollars. It was a nice ego trip, but it took me down a dark path in which I began to choose my subjects and style based on what I knew would sell. Creating was no longer something I did for a change of pace. I was now retired, but painting had become my job. I felt burdened by the obligation to paint enough to cover the walls of the restaurant that graciously hung my work.
Luckily, the epiphany that I had sacrificed my creative diversion, which began with that little sandpiper, coincided with the restaurant’s decision to redecorate and the loss of much of my hanging space. I was now free to paint subjects I was interested in, and return to the comfort of carving when I felt the need to create.
If you already have a creative diversion, remember that a large part of its appeal is that it plays counterpoint to your job. Even if you are retired, a hobby provides a change of pace from which we can all benefit.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Evaluating fever in the first 90 days of life
Fever in the youngest of infants creates a challenge for the pediatric clinician. Fever is a common presentation for serious bacterial infection (SBI) although most fevers are due to viral infection. However, the clinical presentation does not necessarily differ, and the risk for a poor outcome in this age group is substantial.
In the early stages of my pediatric career, most febrile infants less than 90 days of age were evaluated for sepsis, admitted, and treated with antibiotics pending culture results. Group B streptococcal sepsis or Escherichia coli sepsis were common in the first month of life, and Haemophilus influenza type B or Streptococcus pneumoniae in the second and third months of life. The approach to fever in the first 90 days has changed following both the introduction of haemophilus and pneumococcal conjugate vaccines, the experience with risk stratification criteria for identifying infants at low risk for SBI, and the recognition of urinary tract infection (UTI) as a common source of infection in this age group as well as development of criteria for diagnosis.
A further nuance was subsequently added with the introduction of rapid diagnostics for viral infection. Byington et al. found that the majority of febrile infants less than 90 days of age had viral infection with enterovirus, respiratory syncytial virus (RSV), influenza or rotavirus.1 Using the Rochester risk stratification and the presence or absence of viral infection, she demonstrated that the risk of SBI was reduced in both high- and low-risk infants in the presence of viral infection; in low risk infants with viral infection, SBI was identified in 1.8%, compared with 3.1% in those without viral infection, and in high-risk infants. 5.5% has SBI when viral infection was found, compared to 16.7% in the absence of viral infection. She also proposed risk features to identify those infected with herpes simplex virus; age less than 42 days, vesicular rash, elevated alanine transaminase (ALT) and aspartate aminotransferase (AST), CSF pleocytosis, and seizure or twitching.
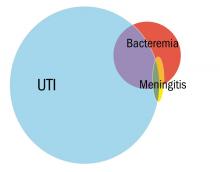
Greenhow et al. reported on the experience with “serious” bacterial infection in infants less than 90 days of age receiving care at Northern California Kaiser Permanente during the period 2005-2011.2 As pictured, the majority of children have UTI, and smaller numbers have bacteremia or meningitis. A small group of children with UTI have urosepsis as well; those with urosepsis can be differentiated from those with only UTI by age (less than 21 days), clinical exam (ill appearing), and elevated C reactive protein (greater than 20 mg/L) or elevated procalcitonin (greater than 0.5 ng/mL).3 Further evaluation of procalcitonin by other groups appears to validate its role in identifying children at low risk of SBI (procalcitonin less than 0.3 ng/mL).4
Currently, studies of febrile infants less than 90 days of age demonstrate that E. coli dominates in bacteremia, UTI, and meningitis, with Group B streptococcus as the next most frequent pathogen identified.2 Increasingly ampicillin resistance has been reported among E. coli isolates from both early- and late-onset disease as well as rare isolates that are resistant to third generation cephalosporins or gentamicin. Surveillance to identify changes in antimicrobial susceptibility will need to be ongoing to ensure that current approaches for initial therapy in high-risk infants aligns with current susceptibility patterns.
Dr. Pelton is chief of the section of pediatric infectious diseases and coordinator of the maternal-child HIV program at Boston Medical Center. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Pediatrics. 2004 Jun;113(6):1662-6.
2. Pediatr Infect Dis J. 2014 Jun;33(6):595-9.
3. Pediatr Infect Dis J. 2015 Jan;34(1):17-21.
4. JAMA Pediatr. 2016;170(1):17-18.
5. “AAP Proposes Update to Evaluating, Managing Febrile Infants Guideline,” The Hospitalist, 2016.
Fever in the youngest of infants creates a challenge for the pediatric clinician. Fever is a common presentation for serious bacterial infection (SBI) although most fevers are due to viral infection. However, the clinical presentation does not necessarily differ, and the risk for a poor outcome in this age group is substantial.
In the early stages of my pediatric career, most febrile infants less than 90 days of age were evaluated for sepsis, admitted, and treated with antibiotics pending culture results. Group B streptococcal sepsis or Escherichia coli sepsis were common in the first month of life, and Haemophilus influenza type B or Streptococcus pneumoniae in the second and third months of life. The approach to fever in the first 90 days has changed following both the introduction of haemophilus and pneumococcal conjugate vaccines, the experience with risk stratification criteria for identifying infants at low risk for SBI, and the recognition of urinary tract infection (UTI) as a common source of infection in this age group as well as development of criteria for diagnosis.
A further nuance was subsequently added with the introduction of rapid diagnostics for viral infection. Byington et al. found that the majority of febrile infants less than 90 days of age had viral infection with enterovirus, respiratory syncytial virus (RSV), influenza or rotavirus.1 Using the Rochester risk stratification and the presence or absence of viral infection, she demonstrated that the risk of SBI was reduced in both high- and low-risk infants in the presence of viral infection; in low risk infants with viral infection, SBI was identified in 1.8%, compared with 3.1% in those without viral infection, and in high-risk infants. 5.5% has SBI when viral infection was found, compared to 16.7% in the absence of viral infection. She also proposed risk features to identify those infected with herpes simplex virus; age less than 42 days, vesicular rash, elevated alanine transaminase (ALT) and aspartate aminotransferase (AST), CSF pleocytosis, and seizure or twitching.
Greenhow et al. reported on the experience with “serious” bacterial infection in infants less than 90 days of age receiving care at Northern California Kaiser Permanente during the period 2005-2011.2 As pictured, the majority of children have UTI, and smaller numbers have bacteremia or meningitis. A small group of children with UTI have urosepsis as well; those with urosepsis can be differentiated from those with only UTI by age (less than 21 days), clinical exam (ill appearing), and elevated C reactive protein (greater than 20 mg/L) or elevated procalcitonin (greater than 0.5 ng/mL).3 Further evaluation of procalcitonin by other groups appears to validate its role in identifying children at low risk of SBI (procalcitonin less than 0.3 ng/mL).4
Currently, studies of febrile infants less than 90 days of age demonstrate that E. coli dominates in bacteremia, UTI, and meningitis, with Group B streptococcus as the next most frequent pathogen identified.2 Increasingly ampicillin resistance has been reported among E. coli isolates from both early- and late-onset disease as well as rare isolates that are resistant to third generation cephalosporins or gentamicin. Surveillance to identify changes in antimicrobial susceptibility will need to be ongoing to ensure that current approaches for initial therapy in high-risk infants aligns with current susceptibility patterns.
Dr. Pelton is chief of the section of pediatric infectious diseases and coordinator of the maternal-child HIV program at Boston Medical Center. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Pediatrics. 2004 Jun;113(6):1662-6.
2. Pediatr Infect Dis J. 2014 Jun;33(6):595-9.
3. Pediatr Infect Dis J. 2015 Jan;34(1):17-21.
4. JAMA Pediatr. 2016;170(1):17-18.
5. “AAP Proposes Update to Evaluating, Managing Febrile Infants Guideline,” The Hospitalist, 2016.
Fever in the youngest of infants creates a challenge for the pediatric clinician. Fever is a common presentation for serious bacterial infection (SBI) although most fevers are due to viral infection. However, the clinical presentation does not necessarily differ, and the risk for a poor outcome in this age group is substantial.
In the early stages of my pediatric career, most febrile infants less than 90 days of age were evaluated for sepsis, admitted, and treated with antibiotics pending culture results. Group B streptococcal sepsis or Escherichia coli sepsis were common in the first month of life, and Haemophilus influenza type B or Streptococcus pneumoniae in the second and third months of life. The approach to fever in the first 90 days has changed following both the introduction of haemophilus and pneumococcal conjugate vaccines, the experience with risk stratification criteria for identifying infants at low risk for SBI, and the recognition of urinary tract infection (UTI) as a common source of infection in this age group as well as development of criteria for diagnosis.
A further nuance was subsequently added with the introduction of rapid diagnostics for viral infection. Byington et al. found that the majority of febrile infants less than 90 days of age had viral infection with enterovirus, respiratory syncytial virus (RSV), influenza or rotavirus.1 Using the Rochester risk stratification and the presence or absence of viral infection, she demonstrated that the risk of SBI was reduced in both high- and low-risk infants in the presence of viral infection; in low risk infants with viral infection, SBI was identified in 1.8%, compared with 3.1% in those without viral infection, and in high-risk infants. 5.5% has SBI when viral infection was found, compared to 16.7% in the absence of viral infection. She also proposed risk features to identify those infected with herpes simplex virus; age less than 42 days, vesicular rash, elevated alanine transaminase (ALT) and aspartate aminotransferase (AST), CSF pleocytosis, and seizure or twitching.
Greenhow et al. reported on the experience with “serious” bacterial infection in infants less than 90 days of age receiving care at Northern California Kaiser Permanente during the period 2005-2011.2 As pictured, the majority of children have UTI, and smaller numbers have bacteremia or meningitis. A small group of children with UTI have urosepsis as well; those with urosepsis can be differentiated from those with only UTI by age (less than 21 days), clinical exam (ill appearing), and elevated C reactive protein (greater than 20 mg/L) or elevated procalcitonin (greater than 0.5 ng/mL).3 Further evaluation of procalcitonin by other groups appears to validate its role in identifying children at low risk of SBI (procalcitonin less than 0.3 ng/mL).4
Currently, studies of febrile infants less than 90 days of age demonstrate that E. coli dominates in bacteremia, UTI, and meningitis, with Group B streptococcus as the next most frequent pathogen identified.2 Increasingly ampicillin resistance has been reported among E. coli isolates from both early- and late-onset disease as well as rare isolates that are resistant to third generation cephalosporins or gentamicin. Surveillance to identify changes in antimicrobial susceptibility will need to be ongoing to ensure that current approaches for initial therapy in high-risk infants aligns with current susceptibility patterns.
Dr. Pelton is chief of the section of pediatric infectious diseases and coordinator of the maternal-child HIV program at Boston Medical Center. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Pediatrics. 2004 Jun;113(6):1662-6.
2. Pediatr Infect Dis J. 2014 Jun;33(6):595-9.
3. Pediatr Infect Dis J. 2015 Jan;34(1):17-21.
4. JAMA Pediatr. 2016;170(1):17-18.
5. “AAP Proposes Update to Evaluating, Managing Febrile Infants Guideline,” The Hospitalist, 2016.
Complementary and Integrative Health Therapies for Opioid Overuse
The US has seen a rise in the number of prescriptions of opioids to treat chronic pain; however, the rise has been associated with increased rates of addiction and deaths related to opioid abuse and heroin use. Chronic pain is associated with the use of prescription opioids in veterans, which sometimes complicates the concurrent treatment of mental health disorders.1-3 Also, opioid use issues, including suicide, have affected veterans at higher numbers than it has in the nonveteran population.4,5
Unfortunately, the prevailing Western medical model with its focus on treating disease has not proven to be adequate in solving the problem. Hence, the Department of Veterans Affairs (VA) is in the process of a paradigm shift to a whole person model that prioritizes health and well-being, as defined by the individual, while proactively addressing risk factors before illness develops.
The new model includes an emphasis on complementary and integrative health (CIH) therapies to promote optimal health, healing, and well-being.6 Yoga, massage, acupuncture, meditation, and guided imagery are some examples of VA-approved CIH therapies favored by veterans and their health care providers (HCPs) to treat and/or divert the subject’s attention from physical pain or mental anguish.7,8
In response to opioid overuse, Congress passed the Comprehensive Addiction and Recovery Act of 2016 (CARA).9 Title IX of CARA mandates the VA to work with the Department of Defense (DoD) to limit the amount of time a patient is prescribed an opioid.
Replacing opioids with other ways to control chronic pain may be helpful in addressing the real distress experienced by persons with these diagnoses. Hence, the CARA suggests augmenting opioid therapy with other pain management therapies and modalities, including CIH. Instead of focusing on the treatment of a specific illness after it develops, CIH therapies aim to promote wellness in the whole person. However, good intentions are not enough. Due to existing institutional culture and prioritization of resources, the adoption of CIH therapies across the VA has been inconsistent.10
The CARA furnishes the VA with an opportunity to serve as a leader in the innovative use of CIH therapies. Previous research conducted by the VA has shown that veterans and their HCPs would like increased availability of CIH through the VA.7,10,11 Research also suggests CIH for specific conditions in veterans, such as posttraumatic stress disorder or postoperative pain.12,13 For its part, the VA has declared the provision of personalized, proactive, patient-driven health care for veterans as its top strategic priority.
To achieve the organizational transformation associated with providing this type of care, the VA established the Office of Patient Centered Care and Cultural Transformation (OPCC&CT), which created the Integrative Health Coordinating Center (IHCC).6 The main functions of the IHCC are to identify and remove barriers to providing CIH within VA and to serve as a resource for practice and education for veterans as well as HCPs.
Several VA facilities already have demonstrated what can be done with the support and encouragement of the OPCC&CT plus an enormous amount of dedicated effort from local HCPs and highly supportive service chiefs. Examples include the Perry Point VA Residential Wellness Center in Maryland and the Integrative Medicine and Wellness Center in the Central Arkansas VA Healthcare System in Little Rock. Perry Point has a focus on veterans with substance abuse diagnoses and uses multiple therapies, including acupuncture, yoga, guided meditation, osteopathic manipulation, music, and creative arts. The Little Rock center focuses on skills building, self-care, and accountability with modalities such as yoga, acupuncture, mindfulness, and chiropractic.
The CARA mandates the continuance and expansion of similar pilot projects that assess the feasibility and advisability of CIH programs to complement the provision of pain management and related health care services, including mental health care services to veterans. Thus, the VA Secretary was directed to select at least 15 geographically diverse locations for the pilot projects. The VA has committed to conducting 18 full-scale demonstration projects in 2018—1 project in each VISN (Veterans Integrated Service Network). Section 933 of the CARA, prioritizes medical centers where the “prescription rate of opioids conflicts with or is otherwise inconsistent with the standards of appropriate and safe care.”9
Several issues must be addressed to make the provision of CIH in the VA a success.14 They include but are not limited to the following:
- Clarification that CIH services for veterans are included in the Medical Benefits Package, which requires that care meets generally accepted standards of medical practice.
- Vetting of CIH therapies to determine which ones should be recommended for inclusion in the Medical Benefits Package. Factors to consider include clinical evidence, community standards, practice guidelines, licensing and credentialing requirements, potential for harm, and veteran demand.
- Changes to VA business processes to provide the infrastructure for CIH delivery.
- Competition with existing VA programs for resources.
- Education of HCPs and administrators about CIH through the development of CIH instruction manuals, curriculum, and faculty.
Although the VA faces the daunting task of reducing opioid use while continuing to treat chronic physical and mental pain, CIH therapies seem to offer a viable adjunctive therapy. It will be incumbent on the VA to explore through ongoing research all that CIH therapies may have to offer; veterans deserve no less. If the VA can demonstrate the effectiveness of CIH in treating the challenges faced by veterans, the results will serve as a useful example for treating chronic pain in the nonveteran population as well.
1. Lovejoy TI, Dobscha SK, Turk DC, Weimer MB, Morasco BJ. Correlates of prescription opioid therapy in veterans with chronic pain and history of substance use disorder. J Rehabil Res Dev. 2016;53(1):25-36.
2. Deyo RA, Smith DH, Johnson ES, et al. Opioids for back pain patients: primary care prescribing patterns and use of service. J Am Board Fam Med. 2011;24(6):717-727.
3. Hawkins EJ, Malte CA, Grossbard JR, Saxon AJ. Prevalence and trends of concurrent opioid analgesic and benzodiazepine use among Veterans Affairs patients with post-traumatic stress disorder, 2003-2011. Pain Med. 2015;16(10):1943-1954.
4. Jonas WB, Schoomaker EB. Pain and opioids in the military: we must do better. JAMA Intern Med. 2014;174(8):1402-1403.
5. Ilgen MA, Bohnert ASB, Ganoczy D, Bair MJ, McCarthy JF, Blow FC. Opioid dose and risk of suicide. Pain. 2016;157(5):1079-1084.
6. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12) (suppl 5):S5-S8.
7. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Perceptions of other integrative health therapies by veterans with pain who are receiving massage. J Rehabil Res Dev. 2016;53(1):117-126.
8. US Department of Veterans Affairs, Office of Patient Centered Care & Cultural Transformation. IHCC approved CIH. https://vaww.infoshare.va.gov/sites/OPCC/SitePages/IHCC-Approved-CIH.aspx . Published August 8, 2017. Accessed March 26, 2018. [Nonpublic document.]
9. 114th US Congress. Comprehensive Addiction and Recovery Act of 2016 . Public Law 114-198. July 22, 2016 130 STAT.695.
10. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Providers’ and administrators’ perceptions of complementary and integrative health practices across the Veterans Health Administration. J Altern Complement Med. 2017;23(1):26-34.
11. Davis MT, Mulvaney-Day N, Larson MJ, Hoover R, Mauch D. Complementary and alternative medicine among veterans and military personnel: a synthesis of population studies. Med Care. 2014;52(12)(suppl 5):S83-S90.
12. Bormann JE, Oman D, Walter KH, Johnson BD. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care. 2014;52(12)(suppl 5):S13-S18.
13. Mitchinson AR, Kim HM, Rosenberg JM, et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg. 2007;142(12):1158-1167.
14. US Department of Veterans Affairs, Veterans Health Administration. Complementary and integrative health – expanding research, education, delivery and integration of complementary and integrative health services into the health care services provided to veterans. https://vaww.infoshare.va.gov/sites/OPCC/SiteAssets/SitePages/IHCC-home/2017%20CIH%20Plan_CARA%20932.pdf . Published March 2017. Accessed March 23, 2018. [Nonpublic document.]
The US has seen a rise in the number of prescriptions of opioids to treat chronic pain; however, the rise has been associated with increased rates of addiction and deaths related to opioid abuse and heroin use. Chronic pain is associated with the use of prescription opioids in veterans, which sometimes complicates the concurrent treatment of mental health disorders.1-3 Also, opioid use issues, including suicide, have affected veterans at higher numbers than it has in the nonveteran population.4,5
Unfortunately, the prevailing Western medical model with its focus on treating disease has not proven to be adequate in solving the problem. Hence, the Department of Veterans Affairs (VA) is in the process of a paradigm shift to a whole person model that prioritizes health and well-being, as defined by the individual, while proactively addressing risk factors before illness develops.
The new model includes an emphasis on complementary and integrative health (CIH) therapies to promote optimal health, healing, and well-being.6 Yoga, massage, acupuncture, meditation, and guided imagery are some examples of VA-approved CIH therapies favored by veterans and their health care providers (HCPs) to treat and/or divert the subject’s attention from physical pain or mental anguish.7,8
In response to opioid overuse, Congress passed the Comprehensive Addiction and Recovery Act of 2016 (CARA).9 Title IX of CARA mandates the VA to work with the Department of Defense (DoD) to limit the amount of time a patient is prescribed an opioid.
Replacing opioids with other ways to control chronic pain may be helpful in addressing the real distress experienced by persons with these diagnoses. Hence, the CARA suggests augmenting opioid therapy with other pain management therapies and modalities, including CIH. Instead of focusing on the treatment of a specific illness after it develops, CIH therapies aim to promote wellness in the whole person. However, good intentions are not enough. Due to existing institutional culture and prioritization of resources, the adoption of CIH therapies across the VA has been inconsistent.10
The CARA furnishes the VA with an opportunity to serve as a leader in the innovative use of CIH therapies. Previous research conducted by the VA has shown that veterans and their HCPs would like increased availability of CIH through the VA.7,10,11 Research also suggests CIH for specific conditions in veterans, such as posttraumatic stress disorder or postoperative pain.12,13 For its part, the VA has declared the provision of personalized, proactive, patient-driven health care for veterans as its top strategic priority.
To achieve the organizational transformation associated with providing this type of care, the VA established the Office of Patient Centered Care and Cultural Transformation (OPCC&CT), which created the Integrative Health Coordinating Center (IHCC).6 The main functions of the IHCC are to identify and remove barriers to providing CIH within VA and to serve as a resource for practice and education for veterans as well as HCPs.
Several VA facilities already have demonstrated what can be done with the support and encouragement of the OPCC&CT plus an enormous amount of dedicated effort from local HCPs and highly supportive service chiefs. Examples include the Perry Point VA Residential Wellness Center in Maryland and the Integrative Medicine and Wellness Center in the Central Arkansas VA Healthcare System in Little Rock. Perry Point has a focus on veterans with substance abuse diagnoses and uses multiple therapies, including acupuncture, yoga, guided meditation, osteopathic manipulation, music, and creative arts. The Little Rock center focuses on skills building, self-care, and accountability with modalities such as yoga, acupuncture, mindfulness, and chiropractic.
The CARA mandates the continuance and expansion of similar pilot projects that assess the feasibility and advisability of CIH programs to complement the provision of pain management and related health care services, including mental health care services to veterans. Thus, the VA Secretary was directed to select at least 15 geographically diverse locations for the pilot projects. The VA has committed to conducting 18 full-scale demonstration projects in 2018—1 project in each VISN (Veterans Integrated Service Network). Section 933 of the CARA, prioritizes medical centers where the “prescription rate of opioids conflicts with or is otherwise inconsistent with the standards of appropriate and safe care.”9
Several issues must be addressed to make the provision of CIH in the VA a success.14 They include but are not limited to the following:
- Clarification that CIH services for veterans are included in the Medical Benefits Package, which requires that care meets generally accepted standards of medical practice.
- Vetting of CIH therapies to determine which ones should be recommended for inclusion in the Medical Benefits Package. Factors to consider include clinical evidence, community standards, practice guidelines, licensing and credentialing requirements, potential for harm, and veteran demand.
- Changes to VA business processes to provide the infrastructure for CIH delivery.
- Competition with existing VA programs for resources.
- Education of HCPs and administrators about CIH through the development of CIH instruction manuals, curriculum, and faculty.
Although the VA faces the daunting task of reducing opioid use while continuing to treat chronic physical and mental pain, CIH therapies seem to offer a viable adjunctive therapy. It will be incumbent on the VA to explore through ongoing research all that CIH therapies may have to offer; veterans deserve no less. If the VA can demonstrate the effectiveness of CIH in treating the challenges faced by veterans, the results will serve as a useful example for treating chronic pain in the nonveteran population as well.
The US has seen a rise in the number of prescriptions of opioids to treat chronic pain; however, the rise has been associated with increased rates of addiction and deaths related to opioid abuse and heroin use. Chronic pain is associated with the use of prescription opioids in veterans, which sometimes complicates the concurrent treatment of mental health disorders.1-3 Also, opioid use issues, including suicide, have affected veterans at higher numbers than it has in the nonveteran population.4,5
Unfortunately, the prevailing Western medical model with its focus on treating disease has not proven to be adequate in solving the problem. Hence, the Department of Veterans Affairs (VA) is in the process of a paradigm shift to a whole person model that prioritizes health and well-being, as defined by the individual, while proactively addressing risk factors before illness develops.
The new model includes an emphasis on complementary and integrative health (CIH) therapies to promote optimal health, healing, and well-being.6 Yoga, massage, acupuncture, meditation, and guided imagery are some examples of VA-approved CIH therapies favored by veterans and their health care providers (HCPs) to treat and/or divert the subject’s attention from physical pain or mental anguish.7,8
In response to opioid overuse, Congress passed the Comprehensive Addiction and Recovery Act of 2016 (CARA).9 Title IX of CARA mandates the VA to work with the Department of Defense (DoD) to limit the amount of time a patient is prescribed an opioid.
Replacing opioids with other ways to control chronic pain may be helpful in addressing the real distress experienced by persons with these diagnoses. Hence, the CARA suggests augmenting opioid therapy with other pain management therapies and modalities, including CIH. Instead of focusing on the treatment of a specific illness after it develops, CIH therapies aim to promote wellness in the whole person. However, good intentions are not enough. Due to existing institutional culture and prioritization of resources, the adoption of CIH therapies across the VA has been inconsistent.10
The CARA furnishes the VA with an opportunity to serve as a leader in the innovative use of CIH therapies. Previous research conducted by the VA has shown that veterans and their HCPs would like increased availability of CIH through the VA.7,10,11 Research also suggests CIH for specific conditions in veterans, such as posttraumatic stress disorder or postoperative pain.12,13 For its part, the VA has declared the provision of personalized, proactive, patient-driven health care for veterans as its top strategic priority.
To achieve the organizational transformation associated with providing this type of care, the VA established the Office of Patient Centered Care and Cultural Transformation (OPCC&CT), which created the Integrative Health Coordinating Center (IHCC).6 The main functions of the IHCC are to identify and remove barriers to providing CIH within VA and to serve as a resource for practice and education for veterans as well as HCPs.
Several VA facilities already have demonstrated what can be done with the support and encouragement of the OPCC&CT plus an enormous amount of dedicated effort from local HCPs and highly supportive service chiefs. Examples include the Perry Point VA Residential Wellness Center in Maryland and the Integrative Medicine and Wellness Center in the Central Arkansas VA Healthcare System in Little Rock. Perry Point has a focus on veterans with substance abuse diagnoses and uses multiple therapies, including acupuncture, yoga, guided meditation, osteopathic manipulation, music, and creative arts. The Little Rock center focuses on skills building, self-care, and accountability with modalities such as yoga, acupuncture, mindfulness, and chiropractic.
The CARA mandates the continuance and expansion of similar pilot projects that assess the feasibility and advisability of CIH programs to complement the provision of pain management and related health care services, including mental health care services to veterans. Thus, the VA Secretary was directed to select at least 15 geographically diverse locations for the pilot projects. The VA has committed to conducting 18 full-scale demonstration projects in 2018—1 project in each VISN (Veterans Integrated Service Network). Section 933 of the CARA, prioritizes medical centers where the “prescription rate of opioids conflicts with or is otherwise inconsistent with the standards of appropriate and safe care.”9
Several issues must be addressed to make the provision of CIH in the VA a success.14 They include but are not limited to the following:
- Clarification that CIH services for veterans are included in the Medical Benefits Package, which requires that care meets generally accepted standards of medical practice.
- Vetting of CIH therapies to determine which ones should be recommended for inclusion in the Medical Benefits Package. Factors to consider include clinical evidence, community standards, practice guidelines, licensing and credentialing requirements, potential for harm, and veteran demand.
- Changes to VA business processes to provide the infrastructure for CIH delivery.
- Competition with existing VA programs for resources.
- Education of HCPs and administrators about CIH through the development of CIH instruction manuals, curriculum, and faculty.
Although the VA faces the daunting task of reducing opioid use while continuing to treat chronic physical and mental pain, CIH therapies seem to offer a viable adjunctive therapy. It will be incumbent on the VA to explore through ongoing research all that CIH therapies may have to offer; veterans deserve no less. If the VA can demonstrate the effectiveness of CIH in treating the challenges faced by veterans, the results will serve as a useful example for treating chronic pain in the nonveteran population as well.
1. Lovejoy TI, Dobscha SK, Turk DC, Weimer MB, Morasco BJ. Correlates of prescription opioid therapy in veterans with chronic pain and history of substance use disorder. J Rehabil Res Dev. 2016;53(1):25-36.
2. Deyo RA, Smith DH, Johnson ES, et al. Opioids for back pain patients: primary care prescribing patterns and use of service. J Am Board Fam Med. 2011;24(6):717-727.
3. Hawkins EJ, Malte CA, Grossbard JR, Saxon AJ. Prevalence and trends of concurrent opioid analgesic and benzodiazepine use among Veterans Affairs patients with post-traumatic stress disorder, 2003-2011. Pain Med. 2015;16(10):1943-1954.
4. Jonas WB, Schoomaker EB. Pain and opioids in the military: we must do better. JAMA Intern Med. 2014;174(8):1402-1403.
5. Ilgen MA, Bohnert ASB, Ganoczy D, Bair MJ, McCarthy JF, Blow FC. Opioid dose and risk of suicide. Pain. 2016;157(5):1079-1084.
6. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12) (suppl 5):S5-S8.
7. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Perceptions of other integrative health therapies by veterans with pain who are receiving massage. J Rehabil Res Dev. 2016;53(1):117-126.
8. US Department of Veterans Affairs, Office of Patient Centered Care & Cultural Transformation. IHCC approved CIH. https://vaww.infoshare.va.gov/sites/OPCC/SitePages/IHCC-Approved-CIH.aspx . Published August 8, 2017. Accessed March 26, 2018. [Nonpublic document.]
9. 114th US Congress. Comprehensive Addiction and Recovery Act of 2016 . Public Law 114-198. July 22, 2016 130 STAT.695.
10. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Providers’ and administrators’ perceptions of complementary and integrative health practices across the Veterans Health Administration. J Altern Complement Med. 2017;23(1):26-34.
11. Davis MT, Mulvaney-Day N, Larson MJ, Hoover R, Mauch D. Complementary and alternative medicine among veterans and military personnel: a synthesis of population studies. Med Care. 2014;52(12)(suppl 5):S83-S90.
12. Bormann JE, Oman D, Walter KH, Johnson BD. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care. 2014;52(12)(suppl 5):S13-S18.
13. Mitchinson AR, Kim HM, Rosenberg JM, et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg. 2007;142(12):1158-1167.
14. US Department of Veterans Affairs, Veterans Health Administration. Complementary and integrative health – expanding research, education, delivery and integration of complementary and integrative health services into the health care services provided to veterans. https://vaww.infoshare.va.gov/sites/OPCC/SiteAssets/SitePages/IHCC-home/2017%20CIH%20Plan_CARA%20932.pdf . Published March 2017. Accessed March 23, 2018. [Nonpublic document.]
1. Lovejoy TI, Dobscha SK, Turk DC, Weimer MB, Morasco BJ. Correlates of prescription opioid therapy in veterans with chronic pain and history of substance use disorder. J Rehabil Res Dev. 2016;53(1):25-36.
2. Deyo RA, Smith DH, Johnson ES, et al. Opioids for back pain patients: primary care prescribing patterns and use of service. J Am Board Fam Med. 2011;24(6):717-727.
3. Hawkins EJ, Malte CA, Grossbard JR, Saxon AJ. Prevalence and trends of concurrent opioid analgesic and benzodiazepine use among Veterans Affairs patients with post-traumatic stress disorder, 2003-2011. Pain Med. 2015;16(10):1943-1954.
4. Jonas WB, Schoomaker EB. Pain and opioids in the military: we must do better. JAMA Intern Med. 2014;174(8):1402-1403.
5. Ilgen MA, Bohnert ASB, Ganoczy D, Bair MJ, McCarthy JF, Blow FC. Opioid dose and risk of suicide. Pain. 2016;157(5):1079-1084.
6. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12) (suppl 5):S5-S8.
7. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Perceptions of other integrative health therapies by veterans with pain who are receiving massage. J Rehabil Res Dev. 2016;53(1):117-126.
8. US Department of Veterans Affairs, Office of Patient Centered Care & Cultural Transformation. IHCC approved CIH. https://vaww.infoshare.va.gov/sites/OPCC/SitePages/IHCC-Approved-CIH.aspx . Published August 8, 2017. Accessed March 26, 2018. [Nonpublic document.]
9. 114th US Congress. Comprehensive Addiction and Recovery Act of 2016 . Public Law 114-198. July 22, 2016 130 STAT.695.
10. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Providers’ and administrators’ perceptions of complementary and integrative health practices across the Veterans Health Administration. J Altern Complement Med. 2017;23(1):26-34.
11. Davis MT, Mulvaney-Day N, Larson MJ, Hoover R, Mauch D. Complementary and alternative medicine among veterans and military personnel: a synthesis of population studies. Med Care. 2014;52(12)(suppl 5):S83-S90.
12. Bormann JE, Oman D, Walter KH, Johnson BD. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care. 2014;52(12)(suppl 5):S13-S18.
13. Mitchinson AR, Kim HM, Rosenberg JM, et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg. 2007;142(12):1158-1167.
14. US Department of Veterans Affairs, Veterans Health Administration. Complementary and integrative health – expanding research, education, delivery and integration of complementary and integrative health services into the health care services provided to veterans. https://vaww.infoshare.va.gov/sites/OPCC/SiteAssets/SitePages/IHCC-home/2017%20CIH%20Plan_CARA%20932.pdf . Published March 2017. Accessed March 23, 2018. [Nonpublic document.]
Cleaning Out Your Emotional Junk Drawer
It’s no secret that health care providers are at high risk for burnout. In my time as a provider, a patient, and a supportive companion to family members, I have witnessed too many of what I call “walking dead” providers—those who barely function in their jobs, leave the profession reluctantly, or count the days until retirement.
One key to avoiding burnout is self-care. I know, you’ve heard this before. But knowing something and acting on it are entirely different.
In my case, it was my employer who broke down my self-care barrier. Through the hospital I work for, I received repeated invitations to participate in free workshops. The first email read: “Healing loss workshops provided for interested staff.” The workshops were based on the Kübler-Ross model (otherwise known as the five stages of grief). First introduced by Swiss psychiatrist Elisabeth Kübler-Ross in 1969, the model postulates a series of emotional reactions to loss.
At the time, I thought grief and loss were only about someone dying. I didn’t know that it could encompass other forms of loss, such as relationships, jobs, physical mobility, major rejection, childhood dreams, or children. So, even though around this time I was in the middle of a divorce, ending a 20-year relationship, breaking up a family, and leaving a house I had lived in for two decades (talk about grief and loss!), I deleted several of these messages before I decided to consider the invitation.
Even when I did, my reason for filling out an application was based on the fact that the workshop, food, and lodgings were free—and I would receive continuing education credit! My mindset was focused on what I could gain tangibly rather than emotionally. I was surprised when I was accepted as a participant—and unaware of how much this experience would change both my personal and professional lives.
I arrived for the two-and-a-half-day seminar with no expectations. I knew that the workshop was touted as providing a safe, comfortable, and confidential environment in which facilitators and staff would provide education on and tools for healing. It was emphasized that this was not a form of medical therapy and that participants could choose to discontinue the workshop at any time. The goal was for participants to learn how to resolve inner issues they have built up and carried around with them.
It is difficult to explain in words the internal change that took place within me during my first workshop. The group participation helped me to recognize that everyone carries a mask. Behind that mask, every individual—strangers, colleagues, patients, even family—has his or her own story and journey. Witnessing others sharing their personal pain and grief in a confidential, nonjudgmental environment made me more compassionate.
Continue to: But I also learned more about myself ...
But I also learned more about myself than I expected to, including that I need to continually take care of myself. Otherwise, I will carry baggage with me wherever I am. And the contents of that baggage came as a surprise to me. Yes, I was dealing with loss in my immediate life—divorce, moving, etc—but I became aware that my earlier life experiences were impacting my current behaviors and relationships.
It was difficult for me to conceive that my loving parents, who had given me food and shelter, had neglected my emotional needs. I love my parents, but the resentments I uncovered during that first workshop startled me. I realized that, while they did not overtly teach me prejudice, their actions caused me to cultivate a general distrust of others. They would often say, “Don’t tell anyone.” I now understand that this cast others as untrustworthy and suspicious.
The memory that encapsulated this best for me was of one summer, when I returned home from traveling abroad and was unable to find my old toys (which were always in a large cardboard box in our garage). My parents didn’t have any explanation for where they had gone. I continued to search the garage for years, literally, not understanding how the toys had disappeared. It was only many years later, when the subject of the toys came up in a conversation with my mother, that she replied, nonchalantly, “Oh, your father threw them out.” It’s no wonder I had issues with trust!
I often hear people say, “I just want to forget about what happened to me,” “I don’t want to think about my past,” or “I buried all that old stuff.” But if I learned one thing from these workshops, it’s that life experiences do not stay buried. I carry the effects of my experiences around with me without being conscious of it. The workshop taught me how to acknowledge my grief and loss and work on becoming more emotionally available. I learned that it is OK to be angry about my parents’ behavior and to express my emotions about it, while still loving my parents very much. Acknowledging these suppressed emotions and the effects they had on my life has helped me to grow and move forward.
By the time the
Continue to: Some of the changes I've made ...
Some of the changes I’ve made as a result might seem subtle to an outsider, but they have made a huge difference to me internally—and that seems to reflect onto the people surrounding me.
The biggest complaints I hear from hospitalized patients are that “nobody tells me anything” or “they come in with one leg out the door.” So now I ask for permission to enter the patient’s room. I introduce myself, then ask if it’s OK to sit down with them. This seemingly small action makes such an impact. I began to notice that, in response, patients were thanking me for coming to see them, for listening, and for spending time with them.
The best example I have is a hospitalized patient who had undergone major surgery. She was upset about her care and getting frustrated with staff. I had seen her once before, and when she looked up and saw me at the door of her room, she said, “Oh, let her in! I know she’s really ‘here’ with me.” What a confirmation that this simple change of mindset on my part is helping to make a difference in the care I deliver to my patients!
I realize many of you might be as skeptical as I was when I read the first workshop invitation. You may be thinking, “This won’t help me.” I understand your doubts—I shared them. But that first workshop was so inspiring that I felt compelled to share my experience with others. I believe in the benefits so completely that I pursued training to become a voluntary facilitator. It is indescribable the results I witness in participants. I can only encourage you to give these types of workshops a chance. (If you are uncomfortable about doing a workshop with coworkers in attendance, or just want to do some traveling, workshops are available in many states and different countries.) A simple search for “internalization/externalization workshops” could change your life as much as it did mine!
It’s no secret that health care providers are at high risk for burnout. In my time as a provider, a patient, and a supportive companion to family members, I have witnessed too many of what I call “walking dead” providers—those who barely function in their jobs, leave the profession reluctantly, or count the days until retirement.
One key to avoiding burnout is self-care. I know, you’ve heard this before. But knowing something and acting on it are entirely different.
In my case, it was my employer who broke down my self-care barrier. Through the hospital I work for, I received repeated invitations to participate in free workshops. The first email read: “Healing loss workshops provided for interested staff.” The workshops were based on the Kübler-Ross model (otherwise known as the five stages of grief). First introduced by Swiss psychiatrist Elisabeth Kübler-Ross in 1969, the model postulates a series of emotional reactions to loss.
At the time, I thought grief and loss were only about someone dying. I didn’t know that it could encompass other forms of loss, such as relationships, jobs, physical mobility, major rejection, childhood dreams, or children. So, even though around this time I was in the middle of a divorce, ending a 20-year relationship, breaking up a family, and leaving a house I had lived in for two decades (talk about grief and loss!), I deleted several of these messages before I decided to consider the invitation.
Even when I did, my reason for filling out an application was based on the fact that the workshop, food, and lodgings were free—and I would receive continuing education credit! My mindset was focused on what I could gain tangibly rather than emotionally. I was surprised when I was accepted as a participant—and unaware of how much this experience would change both my personal and professional lives.
I arrived for the two-and-a-half-day seminar with no expectations. I knew that the workshop was touted as providing a safe, comfortable, and confidential environment in which facilitators and staff would provide education on and tools for healing. It was emphasized that this was not a form of medical therapy and that participants could choose to discontinue the workshop at any time. The goal was for participants to learn how to resolve inner issues they have built up and carried around with them.
It is difficult to explain in words the internal change that took place within me during my first workshop. The group participation helped me to recognize that everyone carries a mask. Behind that mask, every individual—strangers, colleagues, patients, even family—has his or her own story and journey. Witnessing others sharing their personal pain and grief in a confidential, nonjudgmental environment made me more compassionate.
Continue to: But I also learned more about myself ...
But I also learned more about myself than I expected to, including that I need to continually take care of myself. Otherwise, I will carry baggage with me wherever I am. And the contents of that baggage came as a surprise to me. Yes, I was dealing with loss in my immediate life—divorce, moving, etc—but I became aware that my earlier life experiences were impacting my current behaviors and relationships.
It was difficult for me to conceive that my loving parents, who had given me food and shelter, had neglected my emotional needs. I love my parents, but the resentments I uncovered during that first workshop startled me. I realized that, while they did not overtly teach me prejudice, their actions caused me to cultivate a general distrust of others. They would often say, “Don’t tell anyone.” I now understand that this cast others as untrustworthy and suspicious.
The memory that encapsulated this best for me was of one summer, when I returned home from traveling abroad and was unable to find my old toys (which were always in a large cardboard box in our garage). My parents didn’t have any explanation for where they had gone. I continued to search the garage for years, literally, not understanding how the toys had disappeared. It was only many years later, when the subject of the toys came up in a conversation with my mother, that she replied, nonchalantly, “Oh, your father threw them out.” It’s no wonder I had issues with trust!
I often hear people say, “I just want to forget about what happened to me,” “I don’t want to think about my past,” or “I buried all that old stuff.” But if I learned one thing from these workshops, it’s that life experiences do not stay buried. I carry the effects of my experiences around with me without being conscious of it. The workshop taught me how to acknowledge my grief and loss and work on becoming more emotionally available. I learned that it is OK to be angry about my parents’ behavior and to express my emotions about it, while still loving my parents very much. Acknowledging these suppressed emotions and the effects they had on my life has helped me to grow and move forward.
By the time the
Continue to: Some of the changes I've made ...
Some of the changes I’ve made as a result might seem subtle to an outsider, but they have made a huge difference to me internally—and that seems to reflect onto the people surrounding me.
The biggest complaints I hear from hospitalized patients are that “nobody tells me anything” or “they come in with one leg out the door.” So now I ask for permission to enter the patient’s room. I introduce myself, then ask if it’s OK to sit down with them. This seemingly small action makes such an impact. I began to notice that, in response, patients were thanking me for coming to see them, for listening, and for spending time with them.
The best example I have is a hospitalized patient who had undergone major surgery. She was upset about her care and getting frustrated with staff. I had seen her once before, and when she looked up and saw me at the door of her room, she said, “Oh, let her in! I know she’s really ‘here’ with me.” What a confirmation that this simple change of mindset on my part is helping to make a difference in the care I deliver to my patients!
I realize many of you might be as skeptical as I was when I read the first workshop invitation. You may be thinking, “This won’t help me.” I understand your doubts—I shared them. But that first workshop was so inspiring that I felt compelled to share my experience with others. I believe in the benefits so completely that I pursued training to become a voluntary facilitator. It is indescribable the results I witness in participants. I can only encourage you to give these types of workshops a chance. (If you are uncomfortable about doing a workshop with coworkers in attendance, or just want to do some traveling, workshops are available in many states and different countries.) A simple search for “internalization/externalization workshops” could change your life as much as it did mine!
It’s no secret that health care providers are at high risk for burnout. In my time as a provider, a patient, and a supportive companion to family members, I have witnessed too many of what I call “walking dead” providers—those who barely function in their jobs, leave the profession reluctantly, or count the days until retirement.
One key to avoiding burnout is self-care. I know, you’ve heard this before. But knowing something and acting on it are entirely different.
In my case, it was my employer who broke down my self-care barrier. Through the hospital I work for, I received repeated invitations to participate in free workshops. The first email read: “Healing loss workshops provided for interested staff.” The workshops were based on the Kübler-Ross model (otherwise known as the five stages of grief). First introduced by Swiss psychiatrist Elisabeth Kübler-Ross in 1969, the model postulates a series of emotional reactions to loss.
At the time, I thought grief and loss were only about someone dying. I didn’t know that it could encompass other forms of loss, such as relationships, jobs, physical mobility, major rejection, childhood dreams, or children. So, even though around this time I was in the middle of a divorce, ending a 20-year relationship, breaking up a family, and leaving a house I had lived in for two decades (talk about grief and loss!), I deleted several of these messages before I decided to consider the invitation.
Even when I did, my reason for filling out an application was based on the fact that the workshop, food, and lodgings were free—and I would receive continuing education credit! My mindset was focused on what I could gain tangibly rather than emotionally. I was surprised when I was accepted as a participant—and unaware of how much this experience would change both my personal and professional lives.
I arrived for the two-and-a-half-day seminar with no expectations. I knew that the workshop was touted as providing a safe, comfortable, and confidential environment in which facilitators and staff would provide education on and tools for healing. It was emphasized that this was not a form of medical therapy and that participants could choose to discontinue the workshop at any time. The goal was for participants to learn how to resolve inner issues they have built up and carried around with them.
It is difficult to explain in words the internal change that took place within me during my first workshop. The group participation helped me to recognize that everyone carries a mask. Behind that mask, every individual—strangers, colleagues, patients, even family—has his or her own story and journey. Witnessing others sharing their personal pain and grief in a confidential, nonjudgmental environment made me more compassionate.
Continue to: But I also learned more about myself ...
But I also learned more about myself than I expected to, including that I need to continually take care of myself. Otherwise, I will carry baggage with me wherever I am. And the contents of that baggage came as a surprise to me. Yes, I was dealing with loss in my immediate life—divorce, moving, etc—but I became aware that my earlier life experiences were impacting my current behaviors and relationships.
It was difficult for me to conceive that my loving parents, who had given me food and shelter, had neglected my emotional needs. I love my parents, but the resentments I uncovered during that first workshop startled me. I realized that, while they did not overtly teach me prejudice, their actions caused me to cultivate a general distrust of others. They would often say, “Don’t tell anyone.” I now understand that this cast others as untrustworthy and suspicious.
The memory that encapsulated this best for me was of one summer, when I returned home from traveling abroad and was unable to find my old toys (which were always in a large cardboard box in our garage). My parents didn’t have any explanation for where they had gone. I continued to search the garage for years, literally, not understanding how the toys had disappeared. It was only many years later, when the subject of the toys came up in a conversation with my mother, that she replied, nonchalantly, “Oh, your father threw them out.” It’s no wonder I had issues with trust!
I often hear people say, “I just want to forget about what happened to me,” “I don’t want to think about my past,” or “I buried all that old stuff.” But if I learned one thing from these workshops, it’s that life experiences do not stay buried. I carry the effects of my experiences around with me without being conscious of it. The workshop taught me how to acknowledge my grief and loss and work on becoming more emotionally available. I learned that it is OK to be angry about my parents’ behavior and to express my emotions about it, while still loving my parents very much. Acknowledging these suppressed emotions and the effects they had on my life has helped me to grow and move forward.
By the time the
Continue to: Some of the changes I've made ...
Some of the changes I’ve made as a result might seem subtle to an outsider, but they have made a huge difference to me internally—and that seems to reflect onto the people surrounding me.
The biggest complaints I hear from hospitalized patients are that “nobody tells me anything” or “they come in with one leg out the door.” So now I ask for permission to enter the patient’s room. I introduce myself, then ask if it’s OK to sit down with them. This seemingly small action makes such an impact. I began to notice that, in response, patients were thanking me for coming to see them, for listening, and for spending time with them.
The best example I have is a hospitalized patient who had undergone major surgery. She was upset about her care and getting frustrated with staff. I had seen her once before, and when she looked up and saw me at the door of her room, she said, “Oh, let her in! I know she’s really ‘here’ with me.” What a confirmation that this simple change of mindset on my part is helping to make a difference in the care I deliver to my patients!
I realize many of you might be as skeptical as I was when I read the first workshop invitation. You may be thinking, “This won’t help me.” I understand your doubts—I shared them. But that first workshop was so inspiring that I felt compelled to share my experience with others. I believe in the benefits so completely that I pursued training to become a voluntary facilitator. It is indescribable the results I witness in participants. I can only encourage you to give these types of workshops a chance. (If you are uncomfortable about doing a workshop with coworkers in attendance, or just want to do some traveling, workshops are available in many states and different countries.) A simple search for “internalization/externalization workshops” could change your life as much as it did mine!
How precision psychiatry helped my patient; Ketamine: The next ‘opioid crisis’?
How precision psychiatry helped my patient
I applaud Dr. Nasrallah’s editorial “The dawn of precision psychiatry” (From the Editor,
Ms. G, age 14, presented with periodic emotional “meltdowns,” which would occur in any setting, and I determined that they were precipitated by a high glycemic intake. By carefully controlling her glycemic intake and starting her on caprylic acid (a medium-chain triglyceride, which was used to maintain a ketotic state), 1 tablespoon 3 times daily, we were able to reduce the frequency of her episodes by 80% to 90%. Using data from commercially available DNA testing, I determined that she had single nucleotide polymorphisms (SNPs) in an alpha-ketoglutarate dehydrogenase gene, which is primarily located in the prefrontal cortex (PFC), and whose function is supported by thiamine and impaired by high glycemic intake.1 After adding oral thiamine hydrochloride, 100 mg twice a day, and correcting other abnormalities (eg, she was hypothyroid), her episodes are now rare. She is functioning well, has been getting high grades, and recently wrote a 40-page short story.
Once she improved, she was able to describe having a partial seizure, with a rising sensation, which often improves with ketosis. Clearly, disruption of her PFC energetics due to the SNPs described above contributed to the disinhibition of the temporal lobe structures. Furthermore, she has an APOE3/4 status, which puts her at risk for Alzheimer’s disease. Her mother was educated about the importance of good health habits, which is personalized and preventative medicine.
Robert Hedaya, MD, DLFAPA
Clinical Professor
MedStar Georgetown University Hospital
Washington, DC
Faculty
Institute for Functional Medicine
Gig Harbor, Washington, DC
Founder
National Center for Whole Psychiatry
Rockville, Maryland
Reference
1. Tretter L, Adam-Vizi V. Alpha-ketoglutarate dehydrogenase: a target and generator of oxidative stress. Philos Trans R Soc Lond B Biol Sci. 2005;360(1464):2335-2345.
Dr. Nasrallah responds
My thanks to Dr. Hedaya for his letter and for providing an excellent example of precision psychiatry. His brief case vignette brings it to life! I commend him for practicing on the cutting-edge of psychiatry’s scientific frontier.
Continue to: Ketamine: The next 'opioid crisis'?
Ketamine: The next ‘opioid crisis’?
The chief of the FDA, Scott Gottlieb, MD, recently discussed the
There are many similarities between the use of opioids to treat pain and the potential use of ketamine to treat suicidality. Physical and mental pain are subjective, qualitative, and difficult to quantify, which makes it difficult to develop accurate measurements of symptom severity. Chronic physical pain and suicidality are not illnesses, but symptoms of myriad types of pathologies with differing etiologies and treatment options.5 Due to the ambiguous and subjective experience of physical and mental pain, we tend to lump them together as 1 pathological category without understanding pathophysiologic differences. The most commonly reported types of pain include low back pain, migraine/headache, neck pain, and facial pain.6 However, each of these pain types would likely have a different pathophysiology and treatment. Likewise, suicide can be associated with various psychiatric conditions,7 and suicidality resulting from these conditions may require a different etiology and treatment.
We already know that both opioids and ketamine are addictive. For example, there is a report of a nurse stealing a hospital’s supply of ketamine and self-treating for depression, which led to an inpatient detox admission after she developed toxicity and addiction.8 Some ketamine research supports its safe use, but it may be biased due to conflicts of interest. For example, several authors of a recent study proclaiming the effectiveness of a single dose of ketamine in treating suicidal ideation
Warnings stating how both opioid and ketamine should be used were published years ago but have since been ignored. For example, a 1977 article advocated that opioids should only be used for a “short duration and limited to patients with acute diseases or inoperable or metastatic cancer who require long-term relief.”10 The rationale for this distinction was foretelling of the current opioid epidemic: “Continued and prolonged use of narcotics in patients with chronic benign pain is not recommended because of serious behavioral consequences, the development of tolerance, and addiction liability. Long-term use of analgesic drugs in chronic pain usually produces negative behavioral complications that are more difficult to manage than the pain it was desired to eliminate.”10 We knew better then.
The earliest report of ketamine dependency I could find was published in 1987, which predates its classification as a controlled substance.11 More recently, ketamine dependency has been associated with adverse effects that are similar to “not only cocaine and amphetamine but also with opiates, alcohol and cannabis, as well as the psychological attractions of its distinctive psychedelic properties.”12 We should consider ourselves warned.
Michael Shapiro, MD
Assistant Professor
Department of Psychiatry
University of Florida
Gainesville, Florida
References
1. Jayne O’Donnell. FDA chief supports opioid prescription limits, regrets agency’s prior inaction. USA TODAY. https://www.usatoday.com/story/news/politics/2017/10/23/fda-chief-supports-opioid-prescription-limits-regrets-agencys-prior-inaction/774007001. Published October 23, 2017. Accessed January 25, 2018.
2. Bill Whitaker. Ex-DEA agent: opioid crisis fueled by drug industry and Congress. CBS News. https://www.cbsnews.com/news/ex-dea-agent-opioid-crisis-fueled-by-drug-industry-and-congress. Published October 15, 2017. Accessed January 25, 2018.
3. Drug Enforcement Administration. Diversion of Control Division. Ketamine. https://www.deadiversion.usdoj.gov/drug_chem_info/ketamine.pdf. Published August 2013. Accessed January 25, 2018.
4. Bell RF. Ketamine for chronic noncancer pain: concerns regarding toxicity. Curr Opin Support Palliat Care. 2012;6(2):183-187.
5. Barzilay S, Apter A. Psychological models of suicide. Arch Suicide Res. 2014;18(4):295-312.
6. American Academy of Pain Medicine. AAPM facts and figures on pain. http://www.painmed.org/patientcenter/facts_on_pain.aspx.
7. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
8. Bonnet U. Long-term ketamine self-injections in major depressive disorder: focus on tolerance in ketamine’s antidepressant response and the development of ketamine addiction. J Psychoactive Drugs. 2015;47(4):276-85.
9. Wilkinson ST, Ballard ED, Bloch MH, et al. The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. Am J Psychiatry 2017. https://doi.org/10.1176/appi.ajp.2017.17040472
10. Halpern LM. Analgesic drugs in the management of pain. Arch Surg. 1977;112(7):861-869.
11. Kamaya H, Krishna PR. Anesthesiology. 1987;67(5):861-862.
12. Jansen KL, Darracot-Cankovic R. The nonmedical use of ketamine, part two: a review of problem use and dependence. J Psychoactive Drugs. 2001;33(2):151-158.
How precision psychiatry helped my patient
I applaud Dr. Nasrallah’s editorial “The dawn of precision psychiatry” (From the Editor,
Ms. G, age 14, presented with periodic emotional “meltdowns,” which would occur in any setting, and I determined that they were precipitated by a high glycemic intake. By carefully controlling her glycemic intake and starting her on caprylic acid (a medium-chain triglyceride, which was used to maintain a ketotic state), 1 tablespoon 3 times daily, we were able to reduce the frequency of her episodes by 80% to 90%. Using data from commercially available DNA testing, I determined that she had single nucleotide polymorphisms (SNPs) in an alpha-ketoglutarate dehydrogenase gene, which is primarily located in the prefrontal cortex (PFC), and whose function is supported by thiamine and impaired by high glycemic intake.1 After adding oral thiamine hydrochloride, 100 mg twice a day, and correcting other abnormalities (eg, she was hypothyroid), her episodes are now rare. She is functioning well, has been getting high grades, and recently wrote a 40-page short story.
Once she improved, she was able to describe having a partial seizure, with a rising sensation, which often improves with ketosis. Clearly, disruption of her PFC energetics due to the SNPs described above contributed to the disinhibition of the temporal lobe structures. Furthermore, she has an APOE3/4 status, which puts her at risk for Alzheimer’s disease. Her mother was educated about the importance of good health habits, which is personalized and preventative medicine.
Robert Hedaya, MD, DLFAPA
Clinical Professor
MedStar Georgetown University Hospital
Washington, DC
Faculty
Institute for Functional Medicine
Gig Harbor, Washington, DC
Founder
National Center for Whole Psychiatry
Rockville, Maryland
Reference
1. Tretter L, Adam-Vizi V. Alpha-ketoglutarate dehydrogenase: a target and generator of oxidative stress. Philos Trans R Soc Lond B Biol Sci. 2005;360(1464):2335-2345.
Dr. Nasrallah responds
My thanks to Dr. Hedaya for his letter and for providing an excellent example of precision psychiatry. His brief case vignette brings it to life! I commend him for practicing on the cutting-edge of psychiatry’s scientific frontier.
Continue to: Ketamine: The next 'opioid crisis'?
Ketamine: The next ‘opioid crisis’?
The chief of the FDA, Scott Gottlieb, MD, recently discussed the
There are many similarities between the use of opioids to treat pain and the potential use of ketamine to treat suicidality. Physical and mental pain are subjective, qualitative, and difficult to quantify, which makes it difficult to develop accurate measurements of symptom severity. Chronic physical pain and suicidality are not illnesses, but symptoms of myriad types of pathologies with differing etiologies and treatment options.5 Due to the ambiguous and subjective experience of physical and mental pain, we tend to lump them together as 1 pathological category without understanding pathophysiologic differences. The most commonly reported types of pain include low back pain, migraine/headache, neck pain, and facial pain.6 However, each of these pain types would likely have a different pathophysiology and treatment. Likewise, suicide can be associated with various psychiatric conditions,7 and suicidality resulting from these conditions may require a different etiology and treatment.
We already know that both opioids and ketamine are addictive. For example, there is a report of a nurse stealing a hospital’s supply of ketamine and self-treating for depression, which led to an inpatient detox admission after she developed toxicity and addiction.8 Some ketamine research supports its safe use, but it may be biased due to conflicts of interest. For example, several authors of a recent study proclaiming the effectiveness of a single dose of ketamine in treating suicidal ideation
Warnings stating how both opioid and ketamine should be used were published years ago but have since been ignored. For example, a 1977 article advocated that opioids should only be used for a “short duration and limited to patients with acute diseases or inoperable or metastatic cancer who require long-term relief.”10 The rationale for this distinction was foretelling of the current opioid epidemic: “Continued and prolonged use of narcotics in patients with chronic benign pain is not recommended because of serious behavioral consequences, the development of tolerance, and addiction liability. Long-term use of analgesic drugs in chronic pain usually produces negative behavioral complications that are more difficult to manage than the pain it was desired to eliminate.”10 We knew better then.
The earliest report of ketamine dependency I could find was published in 1987, which predates its classification as a controlled substance.11 More recently, ketamine dependency has been associated with adverse effects that are similar to “not only cocaine and amphetamine but also with opiates, alcohol and cannabis, as well as the psychological attractions of its distinctive psychedelic properties.”12 We should consider ourselves warned.
Michael Shapiro, MD
Assistant Professor
Department of Psychiatry
University of Florida
Gainesville, Florida
References
1. Jayne O’Donnell. FDA chief supports opioid prescription limits, regrets agency’s prior inaction. USA TODAY. https://www.usatoday.com/story/news/politics/2017/10/23/fda-chief-supports-opioid-prescription-limits-regrets-agencys-prior-inaction/774007001. Published October 23, 2017. Accessed January 25, 2018.
2. Bill Whitaker. Ex-DEA agent: opioid crisis fueled by drug industry and Congress. CBS News. https://www.cbsnews.com/news/ex-dea-agent-opioid-crisis-fueled-by-drug-industry-and-congress. Published October 15, 2017. Accessed January 25, 2018.
3. Drug Enforcement Administration. Diversion of Control Division. Ketamine. https://www.deadiversion.usdoj.gov/drug_chem_info/ketamine.pdf. Published August 2013. Accessed January 25, 2018.
4. Bell RF. Ketamine for chronic noncancer pain: concerns regarding toxicity. Curr Opin Support Palliat Care. 2012;6(2):183-187.
5. Barzilay S, Apter A. Psychological models of suicide. Arch Suicide Res. 2014;18(4):295-312.
6. American Academy of Pain Medicine. AAPM facts and figures on pain. http://www.painmed.org/patientcenter/facts_on_pain.aspx.
7. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
8. Bonnet U. Long-term ketamine self-injections in major depressive disorder: focus on tolerance in ketamine’s antidepressant response and the development of ketamine addiction. J Psychoactive Drugs. 2015;47(4):276-85.
9. Wilkinson ST, Ballard ED, Bloch MH, et al. The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. Am J Psychiatry 2017. https://doi.org/10.1176/appi.ajp.2017.17040472
10. Halpern LM. Analgesic drugs in the management of pain. Arch Surg. 1977;112(7):861-869.
11. Kamaya H, Krishna PR. Anesthesiology. 1987;67(5):861-862.
12. Jansen KL, Darracot-Cankovic R. The nonmedical use of ketamine, part two: a review of problem use and dependence. J Psychoactive Drugs. 2001;33(2):151-158.
How precision psychiatry helped my patient
I applaud Dr. Nasrallah’s editorial “The dawn of precision psychiatry” (From the Editor,
Ms. G, age 14, presented with periodic emotional “meltdowns,” which would occur in any setting, and I determined that they were precipitated by a high glycemic intake. By carefully controlling her glycemic intake and starting her on caprylic acid (a medium-chain triglyceride, which was used to maintain a ketotic state), 1 tablespoon 3 times daily, we were able to reduce the frequency of her episodes by 80% to 90%. Using data from commercially available DNA testing, I determined that she had single nucleotide polymorphisms (SNPs) in an alpha-ketoglutarate dehydrogenase gene, which is primarily located in the prefrontal cortex (PFC), and whose function is supported by thiamine and impaired by high glycemic intake.1 After adding oral thiamine hydrochloride, 100 mg twice a day, and correcting other abnormalities (eg, she was hypothyroid), her episodes are now rare. She is functioning well, has been getting high grades, and recently wrote a 40-page short story.
Once she improved, she was able to describe having a partial seizure, with a rising sensation, which often improves with ketosis. Clearly, disruption of her PFC energetics due to the SNPs described above contributed to the disinhibition of the temporal lobe structures. Furthermore, she has an APOE3/4 status, which puts her at risk for Alzheimer’s disease. Her mother was educated about the importance of good health habits, which is personalized and preventative medicine.
Robert Hedaya, MD, DLFAPA
Clinical Professor
MedStar Georgetown University Hospital
Washington, DC
Faculty
Institute for Functional Medicine
Gig Harbor, Washington, DC
Founder
National Center for Whole Psychiatry
Rockville, Maryland
Reference
1. Tretter L, Adam-Vizi V. Alpha-ketoglutarate dehydrogenase: a target and generator of oxidative stress. Philos Trans R Soc Lond B Biol Sci. 2005;360(1464):2335-2345.
Dr. Nasrallah responds
My thanks to Dr. Hedaya for his letter and for providing an excellent example of precision psychiatry. His brief case vignette brings it to life! I commend him for practicing on the cutting-edge of psychiatry’s scientific frontier.
Continue to: Ketamine: The next 'opioid crisis'?
Ketamine: The next ‘opioid crisis’?
The chief of the FDA, Scott Gottlieb, MD, recently discussed the
There are many similarities between the use of opioids to treat pain and the potential use of ketamine to treat suicidality. Physical and mental pain are subjective, qualitative, and difficult to quantify, which makes it difficult to develop accurate measurements of symptom severity. Chronic physical pain and suicidality are not illnesses, but symptoms of myriad types of pathologies with differing etiologies and treatment options.5 Due to the ambiguous and subjective experience of physical and mental pain, we tend to lump them together as 1 pathological category without understanding pathophysiologic differences. The most commonly reported types of pain include low back pain, migraine/headache, neck pain, and facial pain.6 However, each of these pain types would likely have a different pathophysiology and treatment. Likewise, suicide can be associated with various psychiatric conditions,7 and suicidality resulting from these conditions may require a different etiology and treatment.
We already know that both opioids and ketamine are addictive. For example, there is a report of a nurse stealing a hospital’s supply of ketamine and self-treating for depression, which led to an inpatient detox admission after she developed toxicity and addiction.8 Some ketamine research supports its safe use, but it may be biased due to conflicts of interest. For example, several authors of a recent study proclaiming the effectiveness of a single dose of ketamine in treating suicidal ideation
Warnings stating how both opioid and ketamine should be used were published years ago but have since been ignored. For example, a 1977 article advocated that opioids should only be used for a “short duration and limited to patients with acute diseases or inoperable or metastatic cancer who require long-term relief.”10 The rationale for this distinction was foretelling of the current opioid epidemic: “Continued and prolonged use of narcotics in patients with chronic benign pain is not recommended because of serious behavioral consequences, the development of tolerance, and addiction liability. Long-term use of analgesic drugs in chronic pain usually produces negative behavioral complications that are more difficult to manage than the pain it was desired to eliminate.”10 We knew better then.
The earliest report of ketamine dependency I could find was published in 1987, which predates its classification as a controlled substance.11 More recently, ketamine dependency has been associated with adverse effects that are similar to “not only cocaine and amphetamine but also with opiates, alcohol and cannabis, as well as the psychological attractions of its distinctive psychedelic properties.”12 We should consider ourselves warned.
Michael Shapiro, MD
Assistant Professor
Department of Psychiatry
University of Florida
Gainesville, Florida
References
1. Jayne O’Donnell. FDA chief supports opioid prescription limits, regrets agency’s prior inaction. USA TODAY. https://www.usatoday.com/story/news/politics/2017/10/23/fda-chief-supports-opioid-prescription-limits-regrets-agencys-prior-inaction/774007001. Published October 23, 2017. Accessed January 25, 2018.
2. Bill Whitaker. Ex-DEA agent: opioid crisis fueled by drug industry and Congress. CBS News. https://www.cbsnews.com/news/ex-dea-agent-opioid-crisis-fueled-by-drug-industry-and-congress. Published October 15, 2017. Accessed January 25, 2018.
3. Drug Enforcement Administration. Diversion of Control Division. Ketamine. https://www.deadiversion.usdoj.gov/drug_chem_info/ketamine.pdf. Published August 2013. Accessed January 25, 2018.
4. Bell RF. Ketamine for chronic noncancer pain: concerns regarding toxicity. Curr Opin Support Palliat Care. 2012;6(2):183-187.
5. Barzilay S, Apter A. Psychological models of suicide. Arch Suicide Res. 2014;18(4):295-312.
6. American Academy of Pain Medicine. AAPM facts and figures on pain. http://www.painmed.org/patientcenter/facts_on_pain.aspx.
7. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
8. Bonnet U. Long-term ketamine self-injections in major depressive disorder: focus on tolerance in ketamine’s antidepressant response and the development of ketamine addiction. J Psychoactive Drugs. 2015;47(4):276-85.
9. Wilkinson ST, Ballard ED, Bloch MH, et al. The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. Am J Psychiatry 2017. https://doi.org/10.1176/appi.ajp.2017.17040472
10. Halpern LM. Analgesic drugs in the management of pain. Arch Surg. 1977;112(7):861-869.
11. Kamaya H, Krishna PR. Anesthesiology. 1987;67(5):861-862.
12. Jansen KL, Darracot-Cankovic R. The nonmedical use of ketamine, part two: a review of problem use and dependence. J Psychoactive Drugs. 2001;33(2):151-158.
Do You Trust Your Employer?
Recently, I was talking with a colleague who works for a large hospital and health care system. While discussing his experiences over the past five years, he suddenly stopped and blurted out, “I don’t trust this organization. Nobody trusts this organization!”
Taken aback, I asked what made him say that.
First of all, he explained, there is a complete and pervasive lack of transparency as to both short- and long-term goals for the organization. Information is treated as proprietary thinking by nonclinical “corporate folks” and not released to the boots-on-the-ground clinician—which makes it difficult to work toward goals efficiently.
Furthermore, he related, there is consistent failure to provide accurate financial data or any plans to improve the organization’s financial position in the marketplace. This prevents providers from making a positive impact on cost containment. No one is invested. Provider compensation packages are neither universal nor simple. The financial folks devise complex formulas that do not account for the vagaries and complexities of health care. This health care organization views every patient as a Financial Information Number and makes no allowance for the fact that many have complex illnesses requiring significant time and attention.
Lastly, he described a systematic and insidious elimination of support staff at all levels—but particularly bedside nurses. The traditional “nursing safety net”—especially relevant in academic institutions—is in tatters, which threatens to undermine day-to-day success in patient care. Staffing of ancillary providers (those in physical, occupational, or speech-language therapy) has been cut back, which means patients wait longer to see these specialists and primary medical providers are frustrated by the lack of progress their patients make.
Stunned by his comments, I started thinking: How many of us recognize some or all of this description? How many trust the organization we work for? Realizing that a huge percentage of NPs, PAs, and physicians work for large entities, these are important questions.
Trust is central to human interaction on both personal and professional levels. Tschannen-Moran defines it as “one’s willingness to be vulnerable to another, based on the confidence that the other is benevolent, honest, open, reliable, and competent.”1
Continue to: A more focused definition of organizational trust
Organizational trust may require a broader and yet more focused definition—such as that of Cummings and Bromley, who stipulate that trust is a belief, held by an individual or groups of individuals, that another individual or group
- Makes a good faith effort to behave in accordance with any (explicit or implicit) commitments
- Is honest
- Does not take excessive advantage of another, even when the opportunity to do so exists.2
Thus, organizational (or collective) trust refers to the propensity of workgroups, administrators, and employees to trust others within the organization.
But does it really matter if we experience this kind of trust for our employer? Can’t we just show up and do our jobs? Frankly, no (at least, if we truly care about the work that we do).
Research has demonstrated that trust is a critical part of creating a shared vision; employees tend to help one another and work collaboratively when trust is present.3,4 Trust is also the foundation for flexibility and innovation.5 Employees are generally happier, more satisfied, and less stressed in high-trust organizations—and it has been shown that organizations benefit, too.6
By contrast, low-trust organizations usually create barriers to effective performance. In the absence of trust, people create rules and restrictions that mandate how others should act.4 Valuable time is then spent studying, enforcing, discussing, and rewriting rules. This yields low-flexibility results and leaves employees to simply follow and enforce policies. Another outcome is high transaction costs and less efficient work—meaning that processes become slower and more restricted by policies and paperwork.4 Low trust is also a barrier to change.7
Although we recognize organizational trust as an essential component of effective leadership, it remains an issue—one that can make or break an organization’s culture. Lack of trust, particularly between management and employees, creates a hostile work environment in which stress levels are high and productivity is reduced.
Continue to: Three dimensions of trust
There are three dimensions of trust, according to the Grunig Relationship Instrument:
Competence: The belief that an organization has the ability to do what it says it will do (this includes effectiveness and survivability in the marketplace).
Integrity: The belief that an organization is fair and just.
Dependability/reliability: The belief that an organization will do what it says it will do (ie, acts consistently and dependably).8
These concepts have been integrated into a “trust measurement questionnaire” that assists in the assessment of an organization’s trustworthiness. While this tool has been used in a variety of industries and has even been used to assess business-to-business relationships, some of the most relevant items for individual employees are outlined in the Table.8
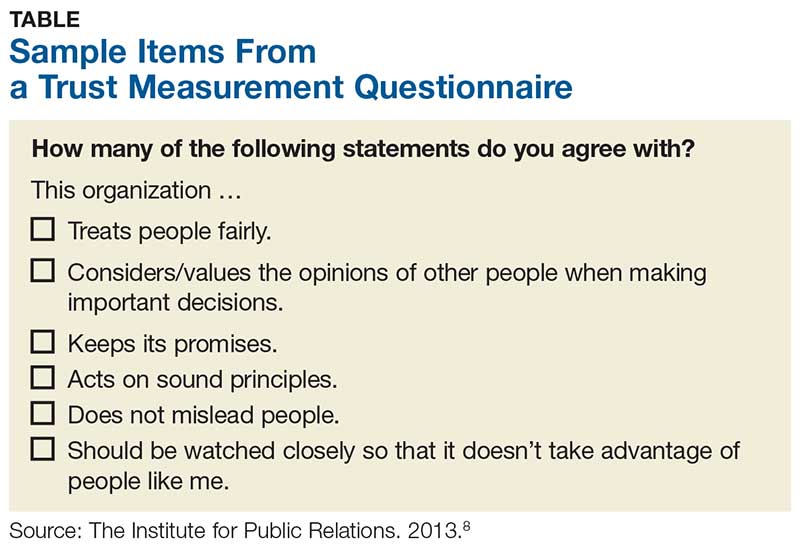
But measuring trust is only effective if it leads to action. Once you’ve realized you don’t trust your employer, what should you do about it? Unfortunately, the answer is often “push for change or leave!” Aside from voicing your concerns or requesting more information (or leaving), the onus is really on the leaders of the organization to improve communication (among other things).
Continue to: 7 ways leaders can improve trust within their organization
According to Gleeson, there are seven ways leaders can improve trust within their organization, which include
- Having the right people in the right job, since trust must be demonstrated from top to bottom and vice versa
- Being transparent
- Sharing information with all vested parties, from industry partners to customers to employees
- Providing resources to all parties in an equitable manner
- Offering feedback to employees at all levels, perhaps through regular “status update” meetings
- Facing challenges head-on, using teamwork to promote trust and positive attitudes
- Leading by example—the organization’s values and mission should be exemplified by everyone.9
If we want to be leaders, not only within our professions but within our workplaces, we must nurture the ideas of trust, transparency, and communication. I am very interested in hearing from you about organizations that you feel are trustworthy and what makes them so—and what experiences you’ve had that led you to avoid or leave employment situations (you need not “name names,” of course). You can reach me at [email protected].
1. Tschannen-Moran M. Trust Matters: Leadership for Successful Schools. San Francisco, CA: Jossey-Bass; 2004.
2. Cummings LL, Bromley P. The organizational trust inventory (OTI): development and validation. In: Kramer R, Tyler E, eds. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996:302, 330, 429.
3. Roueche JE, Baker GA, Rose RR, eds. Shared Vision: Transformational Leadership in American Community Colleges. Washington, DC: American Association of Community and Junior Colleges; 1989.
4. Henkin AB, Dee JR. The power of trust: teams and collective action in self-managed schools. J School Leadership. 2001;11(1):48-62.
5. Dervitsiotis KN. Building trust for excellence in performance and adaptation to change. Total Qual Manage Bus Excellence. 2006;17(7):795-810.
6. Costa AC, Roe RA, Taillieu T. Trust within teams: the relation with performance effectiveness. Eur J Work Org Psychol. 2001;10(3):225.
7. Kesler R, Perry C, Shay G. So they are resistant to change? Strategies for moving an immovable object. In: The Olympics of Leadership: Overcoming Obstacles, Balancing Skills, Taking Risks: Proceedings of the Annual International Conference of the National Community College Chair Academy (5th, Phoenix, Arizona, February 14-17, 1996). Mesa, AZ: National Community College Chair Academy; 1996.
8. The Institute for Public Relations Commission on PR Measurement and Evaluation, University of Florida. Guidelines for measuring trust in organizations. 2013. http://painepublishing.com/wp-content/uploads/2013/10/Grunig-relationship-instrument.pdf. Accessed March 13, 2018.
9. Gleeson B. 7 ways leaders can improve trust within their organizations. Published June 24, 2015. Inc.com. www.inc.com/brent-gleeson/7-ways-leaders-can-improve-trust-within-their-organizations.html. Accessed March 13, 2018.
Recently, I was talking with a colleague who works for a large hospital and health care system. While discussing his experiences over the past five years, he suddenly stopped and blurted out, “I don’t trust this organization. Nobody trusts this organization!”
Taken aback, I asked what made him say that.
First of all, he explained, there is a complete and pervasive lack of transparency as to both short- and long-term goals for the organization. Information is treated as proprietary thinking by nonclinical “corporate folks” and not released to the boots-on-the-ground clinician—which makes it difficult to work toward goals efficiently.
Furthermore, he related, there is consistent failure to provide accurate financial data or any plans to improve the organization’s financial position in the marketplace. This prevents providers from making a positive impact on cost containment. No one is invested. Provider compensation packages are neither universal nor simple. The financial folks devise complex formulas that do not account for the vagaries and complexities of health care. This health care organization views every patient as a Financial Information Number and makes no allowance for the fact that many have complex illnesses requiring significant time and attention.
Lastly, he described a systematic and insidious elimination of support staff at all levels—but particularly bedside nurses. The traditional “nursing safety net”—especially relevant in academic institutions—is in tatters, which threatens to undermine day-to-day success in patient care. Staffing of ancillary providers (those in physical, occupational, or speech-language therapy) has been cut back, which means patients wait longer to see these specialists and primary medical providers are frustrated by the lack of progress their patients make.
Stunned by his comments, I started thinking: How many of us recognize some or all of this description? How many trust the organization we work for? Realizing that a huge percentage of NPs, PAs, and physicians work for large entities, these are important questions.
Trust is central to human interaction on both personal and professional levels. Tschannen-Moran defines it as “one’s willingness to be vulnerable to another, based on the confidence that the other is benevolent, honest, open, reliable, and competent.”1
Continue to: A more focused definition of organizational trust
Organizational trust may require a broader and yet more focused definition—such as that of Cummings and Bromley, who stipulate that trust is a belief, held by an individual or groups of individuals, that another individual or group
- Makes a good faith effort to behave in accordance with any (explicit or implicit) commitments
- Is honest
- Does not take excessive advantage of another, even when the opportunity to do so exists.2
Thus, organizational (or collective) trust refers to the propensity of workgroups, administrators, and employees to trust others within the organization.
But does it really matter if we experience this kind of trust for our employer? Can’t we just show up and do our jobs? Frankly, no (at least, if we truly care about the work that we do).
Research has demonstrated that trust is a critical part of creating a shared vision; employees tend to help one another and work collaboratively when trust is present.3,4 Trust is also the foundation for flexibility and innovation.5 Employees are generally happier, more satisfied, and less stressed in high-trust organizations—and it has been shown that organizations benefit, too.6
By contrast, low-trust organizations usually create barriers to effective performance. In the absence of trust, people create rules and restrictions that mandate how others should act.4 Valuable time is then spent studying, enforcing, discussing, and rewriting rules. This yields low-flexibility results and leaves employees to simply follow and enforce policies. Another outcome is high transaction costs and less efficient work—meaning that processes become slower and more restricted by policies and paperwork.4 Low trust is also a barrier to change.7
Although we recognize organizational trust as an essential component of effective leadership, it remains an issue—one that can make or break an organization’s culture. Lack of trust, particularly between management and employees, creates a hostile work environment in which stress levels are high and productivity is reduced.
Continue to: Three dimensions of trust
There are three dimensions of trust, according to the Grunig Relationship Instrument:
Competence: The belief that an organization has the ability to do what it says it will do (this includes effectiveness and survivability in the marketplace).
Integrity: The belief that an organization is fair and just.
Dependability/reliability: The belief that an organization will do what it says it will do (ie, acts consistently and dependably).8
These concepts have been integrated into a “trust measurement questionnaire” that assists in the assessment of an organization’s trustworthiness. While this tool has been used in a variety of industries and has even been used to assess business-to-business relationships, some of the most relevant items for individual employees are outlined in the Table.8
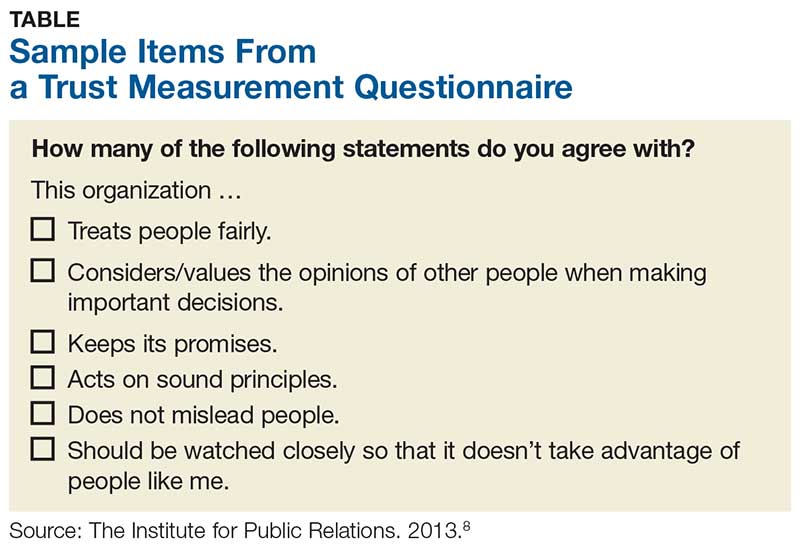
But measuring trust is only effective if it leads to action. Once you’ve realized you don’t trust your employer, what should you do about it? Unfortunately, the answer is often “push for change or leave!” Aside from voicing your concerns or requesting more information (or leaving), the onus is really on the leaders of the organization to improve communication (among other things).
Continue to: 7 ways leaders can improve trust within their organization
According to Gleeson, there are seven ways leaders can improve trust within their organization, which include
- Having the right people in the right job, since trust must be demonstrated from top to bottom and vice versa
- Being transparent
- Sharing information with all vested parties, from industry partners to customers to employees
- Providing resources to all parties in an equitable manner
- Offering feedback to employees at all levels, perhaps through regular “status update” meetings
- Facing challenges head-on, using teamwork to promote trust and positive attitudes
- Leading by example—the organization’s values and mission should be exemplified by everyone.9
If we want to be leaders, not only within our professions but within our workplaces, we must nurture the ideas of trust, transparency, and communication. I am very interested in hearing from you about organizations that you feel are trustworthy and what makes them so—and what experiences you’ve had that led you to avoid or leave employment situations (you need not “name names,” of course). You can reach me at [email protected].
Recently, I was talking with a colleague who works for a large hospital and health care system. While discussing his experiences over the past five years, he suddenly stopped and blurted out, “I don’t trust this organization. Nobody trusts this organization!”
Taken aback, I asked what made him say that.
First of all, he explained, there is a complete and pervasive lack of transparency as to both short- and long-term goals for the organization. Information is treated as proprietary thinking by nonclinical “corporate folks” and not released to the boots-on-the-ground clinician—which makes it difficult to work toward goals efficiently.
Furthermore, he related, there is consistent failure to provide accurate financial data or any plans to improve the organization’s financial position in the marketplace. This prevents providers from making a positive impact on cost containment. No one is invested. Provider compensation packages are neither universal nor simple. The financial folks devise complex formulas that do not account for the vagaries and complexities of health care. This health care organization views every patient as a Financial Information Number and makes no allowance for the fact that many have complex illnesses requiring significant time and attention.
Lastly, he described a systematic and insidious elimination of support staff at all levels—but particularly bedside nurses. The traditional “nursing safety net”—especially relevant in academic institutions—is in tatters, which threatens to undermine day-to-day success in patient care. Staffing of ancillary providers (those in physical, occupational, or speech-language therapy) has been cut back, which means patients wait longer to see these specialists and primary medical providers are frustrated by the lack of progress their patients make.
Stunned by his comments, I started thinking: How many of us recognize some or all of this description? How many trust the organization we work for? Realizing that a huge percentage of NPs, PAs, and physicians work for large entities, these are important questions.
Trust is central to human interaction on both personal and professional levels. Tschannen-Moran defines it as “one’s willingness to be vulnerable to another, based on the confidence that the other is benevolent, honest, open, reliable, and competent.”1
Continue to: A more focused definition of organizational trust
Organizational trust may require a broader and yet more focused definition—such as that of Cummings and Bromley, who stipulate that trust is a belief, held by an individual or groups of individuals, that another individual or group
- Makes a good faith effort to behave in accordance with any (explicit or implicit) commitments
- Is honest
- Does not take excessive advantage of another, even when the opportunity to do so exists.2
Thus, organizational (or collective) trust refers to the propensity of workgroups, administrators, and employees to trust others within the organization.
But does it really matter if we experience this kind of trust for our employer? Can’t we just show up and do our jobs? Frankly, no (at least, if we truly care about the work that we do).
Research has demonstrated that trust is a critical part of creating a shared vision; employees tend to help one another and work collaboratively when trust is present.3,4 Trust is also the foundation for flexibility and innovation.5 Employees are generally happier, more satisfied, and less stressed in high-trust organizations—and it has been shown that organizations benefit, too.6
By contrast, low-trust organizations usually create barriers to effective performance. In the absence of trust, people create rules and restrictions that mandate how others should act.4 Valuable time is then spent studying, enforcing, discussing, and rewriting rules. This yields low-flexibility results and leaves employees to simply follow and enforce policies. Another outcome is high transaction costs and less efficient work—meaning that processes become slower and more restricted by policies and paperwork.4 Low trust is also a barrier to change.7
Although we recognize organizational trust as an essential component of effective leadership, it remains an issue—one that can make or break an organization’s culture. Lack of trust, particularly between management and employees, creates a hostile work environment in which stress levels are high and productivity is reduced.
Continue to: Three dimensions of trust
There are three dimensions of trust, according to the Grunig Relationship Instrument:
Competence: The belief that an organization has the ability to do what it says it will do (this includes effectiveness and survivability in the marketplace).
Integrity: The belief that an organization is fair and just.
Dependability/reliability: The belief that an organization will do what it says it will do (ie, acts consistently and dependably).8
These concepts have been integrated into a “trust measurement questionnaire” that assists in the assessment of an organization’s trustworthiness. While this tool has been used in a variety of industries and has even been used to assess business-to-business relationships, some of the most relevant items for individual employees are outlined in the Table.8
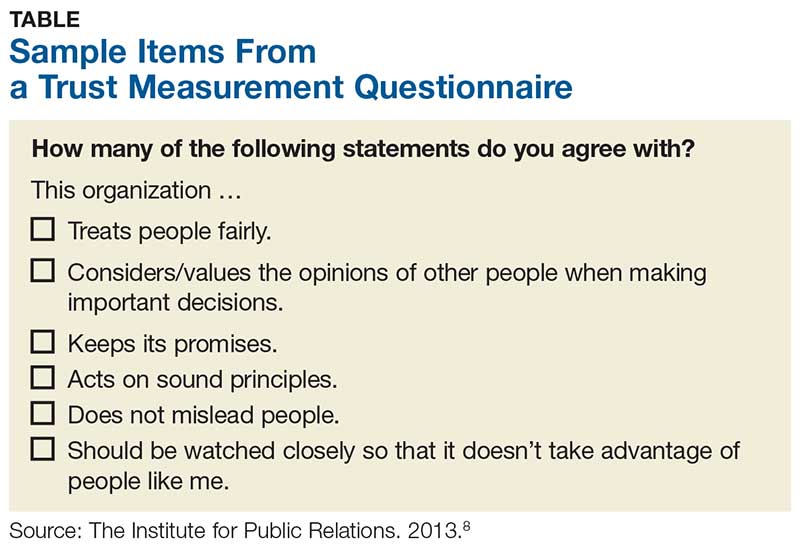
But measuring trust is only effective if it leads to action. Once you’ve realized you don’t trust your employer, what should you do about it? Unfortunately, the answer is often “push for change or leave!” Aside from voicing your concerns or requesting more information (or leaving), the onus is really on the leaders of the organization to improve communication (among other things).
Continue to: 7 ways leaders can improve trust within their organization
According to Gleeson, there are seven ways leaders can improve trust within their organization, which include
- Having the right people in the right job, since trust must be demonstrated from top to bottom and vice versa
- Being transparent
- Sharing information with all vested parties, from industry partners to customers to employees
- Providing resources to all parties in an equitable manner
- Offering feedback to employees at all levels, perhaps through regular “status update” meetings
- Facing challenges head-on, using teamwork to promote trust and positive attitudes
- Leading by example—the organization’s values and mission should be exemplified by everyone.9
If we want to be leaders, not only within our professions but within our workplaces, we must nurture the ideas of trust, transparency, and communication. I am very interested in hearing from you about organizations that you feel are trustworthy and what makes them so—and what experiences you’ve had that led you to avoid or leave employment situations (you need not “name names,” of course). You can reach me at [email protected].
1. Tschannen-Moran M. Trust Matters: Leadership for Successful Schools. San Francisco, CA: Jossey-Bass; 2004.
2. Cummings LL, Bromley P. The organizational trust inventory (OTI): development and validation. In: Kramer R, Tyler E, eds. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996:302, 330, 429.
3. Roueche JE, Baker GA, Rose RR, eds. Shared Vision: Transformational Leadership in American Community Colleges. Washington, DC: American Association of Community and Junior Colleges; 1989.
4. Henkin AB, Dee JR. The power of trust: teams and collective action in self-managed schools. J School Leadership. 2001;11(1):48-62.
5. Dervitsiotis KN. Building trust for excellence in performance and adaptation to change. Total Qual Manage Bus Excellence. 2006;17(7):795-810.
6. Costa AC, Roe RA, Taillieu T. Trust within teams: the relation with performance effectiveness. Eur J Work Org Psychol. 2001;10(3):225.
7. Kesler R, Perry C, Shay G. So they are resistant to change? Strategies for moving an immovable object. In: The Olympics of Leadership: Overcoming Obstacles, Balancing Skills, Taking Risks: Proceedings of the Annual International Conference of the National Community College Chair Academy (5th, Phoenix, Arizona, February 14-17, 1996). Mesa, AZ: National Community College Chair Academy; 1996.
8. The Institute for Public Relations Commission on PR Measurement and Evaluation, University of Florida. Guidelines for measuring trust in organizations. 2013. http://painepublishing.com/wp-content/uploads/2013/10/Grunig-relationship-instrument.pdf. Accessed March 13, 2018.
9. Gleeson B. 7 ways leaders can improve trust within their organizations. Published June 24, 2015. Inc.com. www.inc.com/brent-gleeson/7-ways-leaders-can-improve-trust-within-their-organizations.html. Accessed March 13, 2018.
1. Tschannen-Moran M. Trust Matters: Leadership for Successful Schools. San Francisco, CA: Jossey-Bass; 2004.
2. Cummings LL, Bromley P. The organizational trust inventory (OTI): development and validation. In: Kramer R, Tyler E, eds. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996:302, 330, 429.
3. Roueche JE, Baker GA, Rose RR, eds. Shared Vision: Transformational Leadership in American Community Colleges. Washington, DC: American Association of Community and Junior Colleges; 1989.
4. Henkin AB, Dee JR. The power of trust: teams and collective action in self-managed schools. J School Leadership. 2001;11(1):48-62.
5. Dervitsiotis KN. Building trust for excellence in performance and adaptation to change. Total Qual Manage Bus Excellence. 2006;17(7):795-810.
6. Costa AC, Roe RA, Taillieu T. Trust within teams: the relation with performance effectiveness. Eur J Work Org Psychol. 2001;10(3):225.
7. Kesler R, Perry C, Shay G. So they are resistant to change? Strategies for moving an immovable object. In: The Olympics of Leadership: Overcoming Obstacles, Balancing Skills, Taking Risks: Proceedings of the Annual International Conference of the National Community College Chair Academy (5th, Phoenix, Arizona, February 14-17, 1996). Mesa, AZ: National Community College Chair Academy; 1996.
8. The Institute for Public Relations Commission on PR Measurement and Evaluation, University of Florida. Guidelines for measuring trust in organizations. 2013. http://painepublishing.com/wp-content/uploads/2013/10/Grunig-relationship-instrument.pdf. Accessed March 13, 2018.
9. Gleeson B. 7 ways leaders can improve trust within their organizations. Published June 24, 2015. Inc.com. www.inc.com/brent-gleeson/7-ways-leaders-can-improve-trust-within-their-organizations.html. Accessed March 13, 2018.
We need to treat gun violence like an epidemic
In an interesting bit of timing, just one month before the tragic shooting at the Marjory Stoneman Douglas High School in Parkland, Florida, the AMA Journal of Ethics devoted its entire January issue to the role of physicians in preventing violence. Part of the discussion centered on the idea of treating gun violence as an infectious disease epidemic.1
Dr. Gary Slutkin, an infectious disease specialist and former Centers for Disease Control and Prevention epidemiologist, is a proponent of this approach. His research has demonstrated that epidemic disease control measures are effective in reducing violence and violence-related deaths.2-5
Just look at incidence. Violent deaths in the United States are at an epidemic proportion, just like deaths due to narcotic overdoses. In 2015, there were approximately 33,091 deaths due to narcotic overdoses and 36,252 deaths due to gun violence.6,7
Geographic and social factors. Like infectious disease epidemics, violence tends to cluster in certain geographic areas and social networks. The cause of violence is multifactorial, just like other infectious disease epidemics, such as tuberculosis. Poverty, poor education, and inadequate family structure act as modulating factors that increase the rate of violence in those exposed to it.
Enlisting the community. This contagious disease prevention approach uses community health workers to map areas of high transmission, reach out to those exposed, and intervene to reduce risk factors. For example, gang-related deaths are often due to retaliation. A thorough investigation of a patient who arrives in the emergency department (ED) with a gunshot wound can reveal the next likely perpetrators and victims. Then community violence prevention workers can go directly to these people and others in their social networks, such as parents and friends, to attempt to prevent the next shooting. This approach, dubbed “Cure Violence” (CureViolence.org), has resulted in up to a 70% decrease in violence in some areas of Chicago.2 Some neighborhoods of Baltimore and New York have seen similar reductions.3-5
What can family practitioners do? Dr. Slutkin believes his approach could be expanded from EDs to other health care settings, like primary care, where we can identify people at risk and refer them to community violence prevention resources. Imagine it—a day when violence goes the way of polio.
1. Slutkin G, Ransford C, Zvetina D. How the health sector can reduce violence by treating it as a contagion. AMA J Ethics. 2018;20:47-55.
2. Skogan WG, Hartnett SM, Bump N, et al. Evaluation of CeaseFire-Chicago. Evanston, IL: Northwestern University Institute for Policy Research; 2008. Available at: https://www.ncjrs.gov/pdffiles1/nij/grants/227181.pdf. Accessed September 11, 2017.
3. Webster DW, Whitehill JM, Vernick JS, et al. Evaluation of Baltimore’s Safe Streets program: effects on attitudes, participants’ experiences, and gun violence. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; January 11, 2012. Available at: http://baltimorehealth.org/wp-content/uploads/2016/06/2012_01_10_JHSPH_Safe_Streets_evaluation.pdf. Accessed September 11, 2017.
4. Delgado SA, Alsabahi L, Wolff K, et al. Demoralizing violence: the effects of Cure Violence in the South Bronx and East New York, Brooklyn. John Jay College of Criminal Justice Research and Evaluation Center. Available at: https://johnjayrec.nyc/2017/10/02/cvinsobronxeastny/. Published October 2, 2017. Accessed November 15, 2017.
5. Picard-Fritsche S, Cerniglia L. Testing a public approach to gun violence: an evaluation of Crown Heights Save Our Streets, a replication of the Cure Violence Model. Center for Court Innovation; 2013. Available at: https://www.courtinnovation.org/sites/default/files/documents/SOS_Evaluation.pdf. Accessed November 28, 2017.
6. Murphy SL, Xu J, Kochanek KD, et al. Deaths: Final Data for 2015. Natl Vital Stat Rep. 2017;66:1-75.
7. Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445-1452.
In an interesting bit of timing, just one month before the tragic shooting at the Marjory Stoneman Douglas High School in Parkland, Florida, the AMA Journal of Ethics devoted its entire January issue to the role of physicians in preventing violence. Part of the discussion centered on the idea of treating gun violence as an infectious disease epidemic.1
Dr. Gary Slutkin, an infectious disease specialist and former Centers for Disease Control and Prevention epidemiologist, is a proponent of this approach. His research has demonstrated that epidemic disease control measures are effective in reducing violence and violence-related deaths.2-5
Just look at incidence. Violent deaths in the United States are at an epidemic proportion, just like deaths due to narcotic overdoses. In 2015, there were approximately 33,091 deaths due to narcotic overdoses and 36,252 deaths due to gun violence.6,7
Geographic and social factors. Like infectious disease epidemics, violence tends to cluster in certain geographic areas and social networks. The cause of violence is multifactorial, just like other infectious disease epidemics, such as tuberculosis. Poverty, poor education, and inadequate family structure act as modulating factors that increase the rate of violence in those exposed to it.
Enlisting the community. This contagious disease prevention approach uses community health workers to map areas of high transmission, reach out to those exposed, and intervene to reduce risk factors. For example, gang-related deaths are often due to retaliation. A thorough investigation of a patient who arrives in the emergency department (ED) with a gunshot wound can reveal the next likely perpetrators and victims. Then community violence prevention workers can go directly to these people and others in their social networks, such as parents and friends, to attempt to prevent the next shooting. This approach, dubbed “Cure Violence” (CureViolence.org), has resulted in up to a 70% decrease in violence in some areas of Chicago.2 Some neighborhoods of Baltimore and New York have seen similar reductions.3-5
What can family practitioners do? Dr. Slutkin believes his approach could be expanded from EDs to other health care settings, like primary care, where we can identify people at risk and refer them to community violence prevention resources. Imagine it—a day when violence goes the way of polio.
In an interesting bit of timing, just one month before the tragic shooting at the Marjory Stoneman Douglas High School in Parkland, Florida, the AMA Journal of Ethics devoted its entire January issue to the role of physicians in preventing violence. Part of the discussion centered on the idea of treating gun violence as an infectious disease epidemic.1
Dr. Gary Slutkin, an infectious disease specialist and former Centers for Disease Control and Prevention epidemiologist, is a proponent of this approach. His research has demonstrated that epidemic disease control measures are effective in reducing violence and violence-related deaths.2-5
Just look at incidence. Violent deaths in the United States are at an epidemic proportion, just like deaths due to narcotic overdoses. In 2015, there were approximately 33,091 deaths due to narcotic overdoses and 36,252 deaths due to gun violence.6,7
Geographic and social factors. Like infectious disease epidemics, violence tends to cluster in certain geographic areas and social networks. The cause of violence is multifactorial, just like other infectious disease epidemics, such as tuberculosis. Poverty, poor education, and inadequate family structure act as modulating factors that increase the rate of violence in those exposed to it.
Enlisting the community. This contagious disease prevention approach uses community health workers to map areas of high transmission, reach out to those exposed, and intervene to reduce risk factors. For example, gang-related deaths are often due to retaliation. A thorough investigation of a patient who arrives in the emergency department (ED) with a gunshot wound can reveal the next likely perpetrators and victims. Then community violence prevention workers can go directly to these people and others in their social networks, such as parents and friends, to attempt to prevent the next shooting. This approach, dubbed “Cure Violence” (CureViolence.org), has resulted in up to a 70% decrease in violence in some areas of Chicago.2 Some neighborhoods of Baltimore and New York have seen similar reductions.3-5
What can family practitioners do? Dr. Slutkin believes his approach could be expanded from EDs to other health care settings, like primary care, where we can identify people at risk and refer them to community violence prevention resources. Imagine it—a day when violence goes the way of polio.
1. Slutkin G, Ransford C, Zvetina D. How the health sector can reduce violence by treating it as a contagion. AMA J Ethics. 2018;20:47-55.
2. Skogan WG, Hartnett SM, Bump N, et al. Evaluation of CeaseFire-Chicago. Evanston, IL: Northwestern University Institute for Policy Research; 2008. Available at: https://www.ncjrs.gov/pdffiles1/nij/grants/227181.pdf. Accessed September 11, 2017.
3. Webster DW, Whitehill JM, Vernick JS, et al. Evaluation of Baltimore’s Safe Streets program: effects on attitudes, participants’ experiences, and gun violence. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; January 11, 2012. Available at: http://baltimorehealth.org/wp-content/uploads/2016/06/2012_01_10_JHSPH_Safe_Streets_evaluation.pdf. Accessed September 11, 2017.
4. Delgado SA, Alsabahi L, Wolff K, et al. Demoralizing violence: the effects of Cure Violence in the South Bronx and East New York, Brooklyn. John Jay College of Criminal Justice Research and Evaluation Center. Available at: https://johnjayrec.nyc/2017/10/02/cvinsobronxeastny/. Published October 2, 2017. Accessed November 15, 2017.
5. Picard-Fritsche S, Cerniglia L. Testing a public approach to gun violence: an evaluation of Crown Heights Save Our Streets, a replication of the Cure Violence Model. Center for Court Innovation; 2013. Available at: https://www.courtinnovation.org/sites/default/files/documents/SOS_Evaluation.pdf. Accessed November 28, 2017.
6. Murphy SL, Xu J, Kochanek KD, et al. Deaths: Final Data for 2015. Natl Vital Stat Rep. 2017;66:1-75.
7. Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445-1452.
1. Slutkin G, Ransford C, Zvetina D. How the health sector can reduce violence by treating it as a contagion. AMA J Ethics. 2018;20:47-55.
2. Skogan WG, Hartnett SM, Bump N, et al. Evaluation of CeaseFire-Chicago. Evanston, IL: Northwestern University Institute for Policy Research; 2008. Available at: https://www.ncjrs.gov/pdffiles1/nij/grants/227181.pdf. Accessed September 11, 2017.
3. Webster DW, Whitehill JM, Vernick JS, et al. Evaluation of Baltimore’s Safe Streets program: effects on attitudes, participants’ experiences, and gun violence. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; January 11, 2012. Available at: http://baltimorehealth.org/wp-content/uploads/2016/06/2012_01_10_JHSPH_Safe_Streets_evaluation.pdf. Accessed September 11, 2017.
4. Delgado SA, Alsabahi L, Wolff K, et al. Demoralizing violence: the effects of Cure Violence in the South Bronx and East New York, Brooklyn. John Jay College of Criminal Justice Research and Evaluation Center. Available at: https://johnjayrec.nyc/2017/10/02/cvinsobronxeastny/. Published October 2, 2017. Accessed November 15, 2017.
5. Picard-Fritsche S, Cerniglia L. Testing a public approach to gun violence: an evaluation of Crown Heights Save Our Streets, a replication of the Cure Violence Model. Center for Court Innovation; 2013. Available at: https://www.courtinnovation.org/sites/default/files/documents/SOS_Evaluation.pdf. Accessed November 28, 2017.
6. Murphy SL, Xu J, Kochanek KD, et al. Deaths: Final Data for 2015. Natl Vital Stat Rep. 2017;66:1-75.
7. Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445-1452.
Hope, hepatology, and social determinants of health
Welcome to the April edition of GI & Hepatology News. April has always been a month where we have a sense of renewal and hope. For those of us living in northern climates, the distinct change in daylight and the melting of the snow (finally) both lifts us from the doldrums of winter darkness. In just over a month, we will gather in Washington for Digestive Disease Week® (DDW). I have seen a preview of AGA plenary sessions (basic science and clinical). They will be terrific. We will hear about advances in areas such as the microbiome, IBD-related inflammatory pathways, new insights into functional bowel disorders, and myriad new therapeutics (both medical and device) for us to share with our patients.
Substantial work is being done to better define an IBD severity index. These metrics are of critical importance for clinical researchers to use as we investigate the efficacy and effectiveness of new IBD drugs. You can also read about incorporating psychological care in the management of chronic diseases – a topic becoming more important as we expand our focus beyond just the biology of disease and into social determinants of health as we continue our transition to value-based reimbursement. Another topic included this month (and to which several DDW sessions are dedicated) is the devastating impact of opiates on our patients.
We have included a number of hepatology articles this month, such as the front-page story on NASH and its relationship with hepatocellular cancer. Pioglitazone benefits NASH patients with and without type 2 diabetes and biomarkers may predict liver transplant failures. There are selected articles about Barrett’s esophagus progression and risk stratification for colorectal cancer.
From Washington, we have received some good news. Please see the AGA commentary on the proposed budget. We were reminded last month about how Federal politics can impact U.S. medicine. With the (very late) reauthorization of the Children’s Health Insurance Plan (CHIP), we saw how political dysfunction can impact millions of American family’s lives. Changes in 340-B funding, continued transition from commercial to government payers, a tightening labor market, relentless increases in overhead expenses, all combine to reduce financial margins of both academic and nonacademic health systems. Economic pressures are leading to massive consolidations within the health care delivery system. Vertical integrations now have supplanted horizontal integrations as the industry trend. This situation that will impact many of our independent gastroenterology practices as demand-side management by large national corporations increases.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Welcome to the April edition of GI & Hepatology News. April has always been a month where we have a sense of renewal and hope. For those of us living in northern climates, the distinct change in daylight and the melting of the snow (finally) both lifts us from the doldrums of winter darkness. In just over a month, we will gather in Washington for Digestive Disease Week® (DDW). I have seen a preview of AGA plenary sessions (basic science and clinical). They will be terrific. We will hear about advances in areas such as the microbiome, IBD-related inflammatory pathways, new insights into functional bowel disorders, and myriad new therapeutics (both medical and device) for us to share with our patients.
Substantial work is being done to better define an IBD severity index. These metrics are of critical importance for clinical researchers to use as we investigate the efficacy and effectiveness of new IBD drugs. You can also read about incorporating psychological care in the management of chronic diseases – a topic becoming more important as we expand our focus beyond just the biology of disease and into social determinants of health as we continue our transition to value-based reimbursement. Another topic included this month (and to which several DDW sessions are dedicated) is the devastating impact of opiates on our patients.
We have included a number of hepatology articles this month, such as the front-page story on NASH and its relationship with hepatocellular cancer. Pioglitazone benefits NASH patients with and without type 2 diabetes and biomarkers may predict liver transplant failures. There are selected articles about Barrett’s esophagus progression and risk stratification for colorectal cancer.
From Washington, we have received some good news. Please see the AGA commentary on the proposed budget. We were reminded last month about how Federal politics can impact U.S. medicine. With the (very late) reauthorization of the Children’s Health Insurance Plan (CHIP), we saw how political dysfunction can impact millions of American family’s lives. Changes in 340-B funding, continued transition from commercial to government payers, a tightening labor market, relentless increases in overhead expenses, all combine to reduce financial margins of both academic and nonacademic health systems. Economic pressures are leading to massive consolidations within the health care delivery system. Vertical integrations now have supplanted horizontal integrations as the industry trend. This situation that will impact many of our independent gastroenterology practices as demand-side management by large national corporations increases.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Welcome to the April edition of GI & Hepatology News. April has always been a month where we have a sense of renewal and hope. For those of us living in northern climates, the distinct change in daylight and the melting of the snow (finally) both lifts us from the doldrums of winter darkness. In just over a month, we will gather in Washington for Digestive Disease Week® (DDW). I have seen a preview of AGA plenary sessions (basic science and clinical). They will be terrific. We will hear about advances in areas such as the microbiome, IBD-related inflammatory pathways, new insights into functional bowel disorders, and myriad new therapeutics (both medical and device) for us to share with our patients.
Substantial work is being done to better define an IBD severity index. These metrics are of critical importance for clinical researchers to use as we investigate the efficacy and effectiveness of new IBD drugs. You can also read about incorporating psychological care in the management of chronic diseases – a topic becoming more important as we expand our focus beyond just the biology of disease and into social determinants of health as we continue our transition to value-based reimbursement. Another topic included this month (and to which several DDW sessions are dedicated) is the devastating impact of opiates on our patients.
We have included a number of hepatology articles this month, such as the front-page story on NASH and its relationship with hepatocellular cancer. Pioglitazone benefits NASH patients with and without type 2 diabetes and biomarkers may predict liver transplant failures. There are selected articles about Barrett’s esophagus progression and risk stratification for colorectal cancer.
From Washington, we have received some good news. Please see the AGA commentary on the proposed budget. We were reminded last month about how Federal politics can impact U.S. medicine. With the (very late) reauthorization of the Children’s Health Insurance Plan (CHIP), we saw how political dysfunction can impact millions of American family’s lives. Changes in 340-B funding, continued transition from commercial to government payers, a tightening labor market, relentless increases in overhead expenses, all combine to reduce financial margins of both academic and nonacademic health systems. Economic pressures are leading to massive consolidations within the health care delivery system. Vertical integrations now have supplanted horizontal integrations as the industry trend. This situation that will impact many of our independent gastroenterology practices as demand-side management by large national corporations increases.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Arm teachers with mental health providers
The gun control bill passed recently in Florida is a promising step forward in helping to protect children from deadly violence in schools. While various attempts to minimize gun violence have been stalled in state legislatures, in some cases for decades, this bill, which includes funding to expand mental health services for students, highlights a simple, sustainable, and nonpolitical solution: mental health providers.
School-based health centers arm educators with the powerful combination of on-site medical, mental health, and community health services that could address and aid in preventing violence through education, screening, ongoing care, crisis management, and advocacy.
At Montefiore Health System in the Bronx, our school health program plays a crucial role in keeping kids safe and healthy, and sometimes even saving lives. This past fall a potential tragedy was averted when a student disclosed to one of our on-site mental health providers a plan to murder a classmate after school. The child was fully assessed, resulting in a brief hospitalization. The child is back in school, receiving on-site services and being carefully monitored.
Our dedicated staff works closely with teachers and school staff to identify children in need of services. Barriers to care are eliminated as services are provided directly in the school in collaboration with teachers and school administrators. Coordination with the school and family allows for comprehensive, high-quality treatment that cannot be provided in any other setting.
School-based health centers offer protection and support on many levels. Mental health professionals can train teachers and other school staff to recognize red flags in students. They can collaborate with educators to carry out regular school-wide screenings to identify students who need immediate follow-up. And primary care providers in the clinic also screen for troubling behaviors and refer students for treatment within the clinic.
We know mental health providers make a difference. But we also must acknowledge that accessing these services often is a challenge. Estimates suggest that only half of children aged 8-15 years who need mental services actually get them. This is why having school-based health centers and mental health providers located where children spend most of their day is so vital. Often, school-based mental health providers have a chance to reach kids who are the least likely to receive care in the community.
Mental health professionals and school based clinics are invaluable resources; they are on the front lines of recognizing and treating worrisome student behaviors. Funding and providing these services is essential.
Dr. Appel is director of the Montefiore School Health Program, which makes primary care, mental health, dental and vision services available to almost 40,000 K-12 students in 26 school-based health centers throughout the Bronx.
*This article was updated 3/29/2018.
The gun control bill passed recently in Florida is a promising step forward in helping to protect children from deadly violence in schools. While various attempts to minimize gun violence have been stalled in state legislatures, in some cases for decades, this bill, which includes funding to expand mental health services for students, highlights a simple, sustainable, and nonpolitical solution: mental health providers.
School-based health centers arm educators with the powerful combination of on-site medical, mental health, and community health services that could address and aid in preventing violence through education, screening, ongoing care, crisis management, and advocacy.
At Montefiore Health System in the Bronx, our school health program plays a crucial role in keeping kids safe and healthy, and sometimes even saving lives. This past fall a potential tragedy was averted when a student disclosed to one of our on-site mental health providers a plan to murder a classmate after school. The child was fully assessed, resulting in a brief hospitalization. The child is back in school, receiving on-site services and being carefully monitored.
Our dedicated staff works closely with teachers and school staff to identify children in need of services. Barriers to care are eliminated as services are provided directly in the school in collaboration with teachers and school administrators. Coordination with the school and family allows for comprehensive, high-quality treatment that cannot be provided in any other setting.
School-based health centers offer protection and support on many levels. Mental health professionals can train teachers and other school staff to recognize red flags in students. They can collaborate with educators to carry out regular school-wide screenings to identify students who need immediate follow-up. And primary care providers in the clinic also screen for troubling behaviors and refer students for treatment within the clinic.
We know mental health providers make a difference. But we also must acknowledge that accessing these services often is a challenge. Estimates suggest that only half of children aged 8-15 years who need mental services actually get them. This is why having school-based health centers and mental health providers located where children spend most of their day is so vital. Often, school-based mental health providers have a chance to reach kids who are the least likely to receive care in the community.
Mental health professionals and school based clinics are invaluable resources; they are on the front lines of recognizing and treating worrisome student behaviors. Funding and providing these services is essential.
Dr. Appel is director of the Montefiore School Health Program, which makes primary care, mental health, dental and vision services available to almost 40,000 K-12 students in 26 school-based health centers throughout the Bronx.
*This article was updated 3/29/2018.
The gun control bill passed recently in Florida is a promising step forward in helping to protect children from deadly violence in schools. While various attempts to minimize gun violence have been stalled in state legislatures, in some cases for decades, this bill, which includes funding to expand mental health services for students, highlights a simple, sustainable, and nonpolitical solution: mental health providers.
School-based health centers arm educators with the powerful combination of on-site medical, mental health, and community health services that could address and aid in preventing violence through education, screening, ongoing care, crisis management, and advocacy.
At Montefiore Health System in the Bronx, our school health program plays a crucial role in keeping kids safe and healthy, and sometimes even saving lives. This past fall a potential tragedy was averted when a student disclosed to one of our on-site mental health providers a plan to murder a classmate after school. The child was fully assessed, resulting in a brief hospitalization. The child is back in school, receiving on-site services and being carefully monitored.
Our dedicated staff works closely with teachers and school staff to identify children in need of services. Barriers to care are eliminated as services are provided directly in the school in collaboration with teachers and school administrators. Coordination with the school and family allows for comprehensive, high-quality treatment that cannot be provided in any other setting.
School-based health centers offer protection and support on many levels. Mental health professionals can train teachers and other school staff to recognize red flags in students. They can collaborate with educators to carry out regular school-wide screenings to identify students who need immediate follow-up. And primary care providers in the clinic also screen for troubling behaviors and refer students for treatment within the clinic.
We know mental health providers make a difference. But we also must acknowledge that accessing these services often is a challenge. Estimates suggest that only half of children aged 8-15 years who need mental services actually get them. This is why having school-based health centers and mental health providers located where children spend most of their day is so vital. Often, school-based mental health providers have a chance to reach kids who are the least likely to receive care in the community.
Mental health professionals and school based clinics are invaluable resources; they are on the front lines of recognizing and treating worrisome student behaviors. Funding and providing these services is essential.
Dr. Appel is director of the Montefiore School Health Program, which makes primary care, mental health, dental and vision services available to almost 40,000 K-12 students in 26 school-based health centers throughout the Bronx.
*This article was updated 3/29/2018.