User login
Sacred cows
Within the academic pediatric community, there is little argument that the concepts “evidence based” and “early intervention” are gold standards against which we must measure our efforts.
It should be obvious to everyone that if we can intervene early in a child’s developmental trajectory, our chances of affecting his/her outcome are improved. And the earlier the better. If we aren’t supremely committed to prevention, then what sets pediatrics apart from the other specialties?
Likewise, if we aren’t willing to systematically measure our efforts at improving the health of our patients, we run the risk of simply spinning our wheels and even worse, squandering our patients’ time and their parents’ energies. However, a recent article in Pediatrics and a companion commentary suggest that we need to be more careful as we interpret the buzz that surrounds the terms “early intervention” and “evidence based.”
In their one-sentence conclusion of a paper reviewing 48 studies of early intervention in early childhood development, the authors observe, “Although several interventions resulted in improved child development outcomes age 0 to 3 years, comparison across studies and interventions is limited by the use of different outcome measures, time of evaluation, and variability of results” (“Primary Care Interventions for Early Childhood Development: A Systematic Review,” Peacock-Chambers et al. Pediatrics. 2017, Nov 14. doi: 10.1542/peds.2017-1661). Unless you are looking for another reason to slip further into an abyss of despair, I urge that you skip reading the details of the Peacock-Chambers paper and turn instead to Dr. Jack P. Shonkoff’s excellent commentary (“Rethinking the Definition of Evidence-Based Interventions to Promote Early Child Development,” Pediatrics. 2017, Dec. doi: 10.1542/peds.2017-3136).
Dr. Shonkoff observes that there is ample evidence to support the general concept of early intervention as it relates to childhood development. However, he acknowledges that the improvements observed generally have been small. And there has been little success in scaling these few successes to larger populations. It would seem that the sacred cow of early intervention remains standing, albeit on somewhat shaky legs.
Dr. Shonkoff points out that an obsession with statistical significance often has blinded some of us to the importance of the magnitude of (or the lack of) impact when interpreting studies of early intervention. As a result, we may have failed to realize how far research in early childhood development has fallen behind the other fields of biomedical research such as cancer, HIV, and AIDS. His plea is that we begin to leverage our successes in fields such as molecular biology, epigenetics, and neuroscience when designing future studies of early childhood development. He asserts that this kind of basic science – in concert with “on-the-ground experience” (that’s you and me) and “authentic parental engagement” – is more likely to result in greater scalable impact for our patients threatened by developmental delays.
It is refreshing and encouraging reading a critical consideration of the evidence-based sacred cow. Evidence can be viewed from a variety of perspectives. If we continue to filter all of our observations through a statistical significance filter, we run the risk of missing both the forest and the trees.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Within the academic pediatric community, there is little argument that the concepts “evidence based” and “early intervention” are gold standards against which we must measure our efforts.
It should be obvious to everyone that if we can intervene early in a child’s developmental trajectory, our chances of affecting his/her outcome are improved. And the earlier the better. If we aren’t supremely committed to prevention, then what sets pediatrics apart from the other specialties?
Likewise, if we aren’t willing to systematically measure our efforts at improving the health of our patients, we run the risk of simply spinning our wheels and even worse, squandering our patients’ time and their parents’ energies. However, a recent article in Pediatrics and a companion commentary suggest that we need to be more careful as we interpret the buzz that surrounds the terms “early intervention” and “evidence based.”
In their one-sentence conclusion of a paper reviewing 48 studies of early intervention in early childhood development, the authors observe, “Although several interventions resulted in improved child development outcomes age 0 to 3 years, comparison across studies and interventions is limited by the use of different outcome measures, time of evaluation, and variability of results” (“Primary Care Interventions for Early Childhood Development: A Systematic Review,” Peacock-Chambers et al. Pediatrics. 2017, Nov 14. doi: 10.1542/peds.2017-1661). Unless you are looking for another reason to slip further into an abyss of despair, I urge that you skip reading the details of the Peacock-Chambers paper and turn instead to Dr. Jack P. Shonkoff’s excellent commentary (“Rethinking the Definition of Evidence-Based Interventions to Promote Early Child Development,” Pediatrics. 2017, Dec. doi: 10.1542/peds.2017-3136).
Dr. Shonkoff observes that there is ample evidence to support the general concept of early intervention as it relates to childhood development. However, he acknowledges that the improvements observed generally have been small. And there has been little success in scaling these few successes to larger populations. It would seem that the sacred cow of early intervention remains standing, albeit on somewhat shaky legs.
Dr. Shonkoff points out that an obsession with statistical significance often has blinded some of us to the importance of the magnitude of (or the lack of) impact when interpreting studies of early intervention. As a result, we may have failed to realize how far research in early childhood development has fallen behind the other fields of biomedical research such as cancer, HIV, and AIDS. His plea is that we begin to leverage our successes in fields such as molecular biology, epigenetics, and neuroscience when designing future studies of early childhood development. He asserts that this kind of basic science – in concert with “on-the-ground experience” (that’s you and me) and “authentic parental engagement” – is more likely to result in greater scalable impact for our patients threatened by developmental delays.
It is refreshing and encouraging reading a critical consideration of the evidence-based sacred cow. Evidence can be viewed from a variety of perspectives. If we continue to filter all of our observations through a statistical significance filter, we run the risk of missing both the forest and the trees.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Within the academic pediatric community, there is little argument that the concepts “evidence based” and “early intervention” are gold standards against which we must measure our efforts.
It should be obvious to everyone that if we can intervene early in a child’s developmental trajectory, our chances of affecting his/her outcome are improved. And the earlier the better. If we aren’t supremely committed to prevention, then what sets pediatrics apart from the other specialties?
Likewise, if we aren’t willing to systematically measure our efforts at improving the health of our patients, we run the risk of simply spinning our wheels and even worse, squandering our patients’ time and their parents’ energies. However, a recent article in Pediatrics and a companion commentary suggest that we need to be more careful as we interpret the buzz that surrounds the terms “early intervention” and “evidence based.”
In their one-sentence conclusion of a paper reviewing 48 studies of early intervention in early childhood development, the authors observe, “Although several interventions resulted in improved child development outcomes age 0 to 3 years, comparison across studies and interventions is limited by the use of different outcome measures, time of evaluation, and variability of results” (“Primary Care Interventions for Early Childhood Development: A Systematic Review,” Peacock-Chambers et al. Pediatrics. 2017, Nov 14. doi: 10.1542/peds.2017-1661). Unless you are looking for another reason to slip further into an abyss of despair, I urge that you skip reading the details of the Peacock-Chambers paper and turn instead to Dr. Jack P. Shonkoff’s excellent commentary (“Rethinking the Definition of Evidence-Based Interventions to Promote Early Child Development,” Pediatrics. 2017, Dec. doi: 10.1542/peds.2017-3136).
Dr. Shonkoff observes that there is ample evidence to support the general concept of early intervention as it relates to childhood development. However, he acknowledges that the improvements observed generally have been small. And there has been little success in scaling these few successes to larger populations. It would seem that the sacred cow of early intervention remains standing, albeit on somewhat shaky legs.
Dr. Shonkoff points out that an obsession with statistical significance often has blinded some of us to the importance of the magnitude of (or the lack of) impact when interpreting studies of early intervention. As a result, we may have failed to realize how far research in early childhood development has fallen behind the other fields of biomedical research such as cancer, HIV, and AIDS. His plea is that we begin to leverage our successes in fields such as molecular biology, epigenetics, and neuroscience when designing future studies of early childhood development. He asserts that this kind of basic science – in concert with “on-the-ground experience” (that’s you and me) and “authentic parental engagement” – is more likely to result in greater scalable impact for our patients threatened by developmental delays.
It is refreshing and encouraging reading a critical consideration of the evidence-based sacred cow. Evidence can be viewed from a variety of perspectives. If we continue to filter all of our observations through a statistical significance filter, we run the risk of missing both the forest and the trees.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Stressed for Success
As I write this column, the holiday season has just begun, and its incumbent demands lie ahead. By the time this article reaches you, we will have outlasted the season and its associated stress. But it’s not just the holiday baking, gift-wrapping, and decorating that overwhelms us—we face enormous professional stress during this time of year, with its emphasis on home, family, good health, and harmony.
Stress is simply a part of human nature. And despite its bad rap, not all stress is problematic; it’s what motivates people to prepare or perform. Routine, “normal” stress that is temporary or short-lived can actually be beneficial. When placed in danger, the body prepares to either face the threat or flee to safety. During these times, your pulse quickens, you breathe faster, your muscles tense, your brain uses more oxygen and increases activity—all functions that aid in survival.1
But not every situation we encounter necessitates an increase in endorphin levels and blood pressure. Tell that to our stress levels, which are often persistently elevated! Chronic stress can cause the self-protective responses your body activates when threatened to suppress immune, digestive, sleep, and reproductive systems, leading them to cease normal functioning over time.1 This “bad” stress—or distress—can contribute to health problems such as hypertension, cardiovascular disease, obesity, and diabetes.
Stress can elicit a variety of responses: behavioral, psychologic/emotional, physical, cognitive, and social.2 For many, consumption (of tobacco, alcohol, drugs, sugar, fat, or caffeine) is a coping mechanism. While many people look to food for comfort and stress relief, research suggests it may have undesired effects. Eating a high-fat meal when under stress can slow your metabolism and result in significant weight gain.3 Stress can also influence whether people undereat or overeat and affect neurohormonal activity—which leads to increased production of cortisol, which leads to weight gain (particularly in women).4 Let’s be honest: Gaining weight seldom lowers someone’s stress level.
Everyone has different triggers that cause their stress levels to spike, but the workplace has been found to top the list. Within the “work” category, commonly reported stressors include
- Heavy workload or too much responsibility
- Long hours
- Poor management, unclear expectations, or having no say in decision-making.5
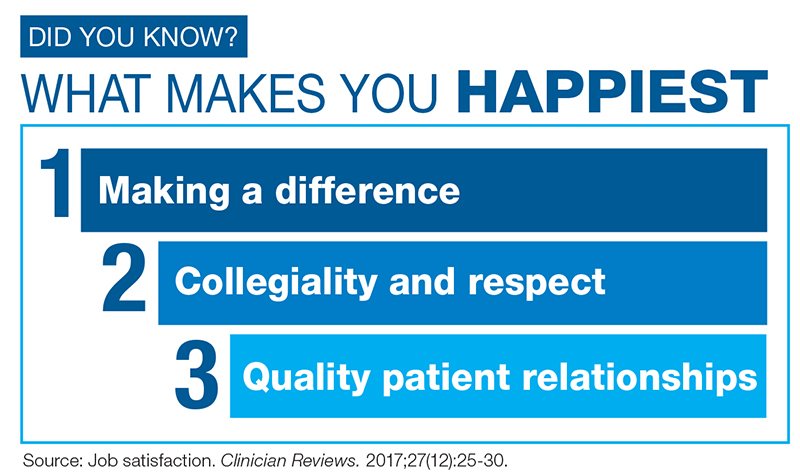
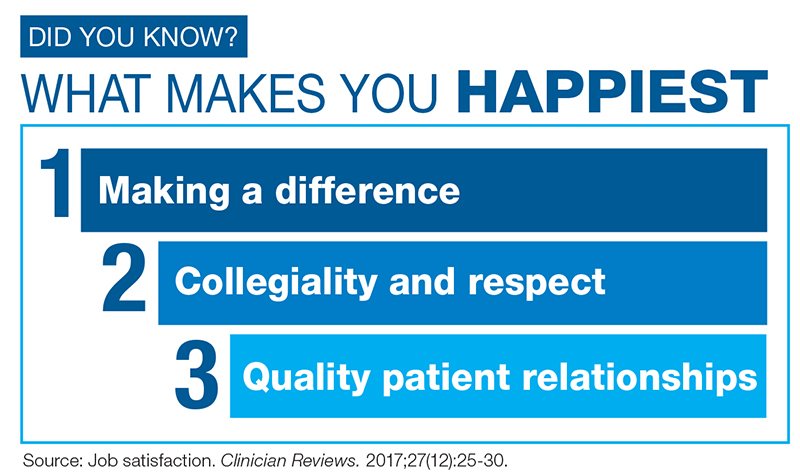
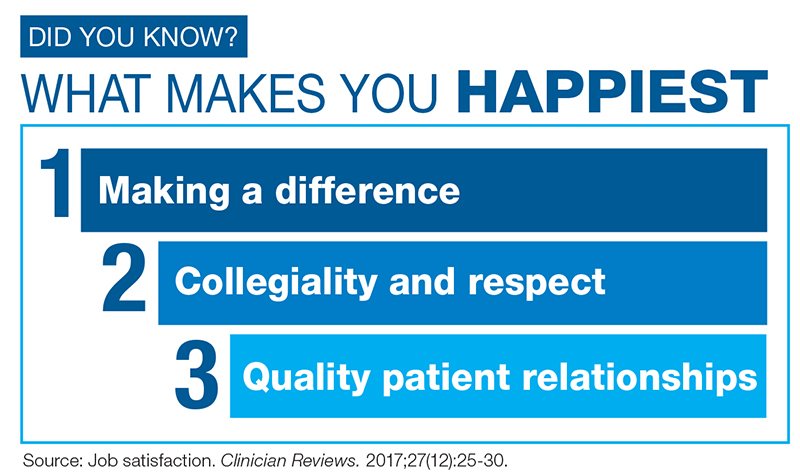
For health care providers, day-to-day stress is a chronic problem; responses to the Clinician Reviews annual job satisfaction survey have demonstrated that.6,7 Many of our readers report ongoing issues related to scheduling, work/life balance, compensation, and working conditions. That tension has a direct negative effect, not only on us, but on our families and our patients as well. A missed soccer game or a holiday on call are obvious stressors—but our inability to help patients achieve optimal health is a source of distress that we may not recognize the ramifications of. How often has a clinician felt caught in what feels like an unattainable quest?
Mitigating this workplace stress is the challenge. Changing jobs is another high-stress event, so up and quitting is probably not the answer. Identifying the problem is the first essential step.
If workload is the issue, focus on setting realistic goals for your day. Goal-setting provides purposeful direction and helps you feel in control. There will undeniably be days in which your plan must be completely abandoned. When this happens, don’t fret—reassess! Decide what must get done and what can wait. If possible, avoid scheduling patient appointments that will put you into overload. Learn to say “no” without feeling as though you are not a team player. And when you feel swamped, put a positive spin on the day by noting what you have accomplished, rather than what you have been unable to achieve.
If you find that your voice is but a whisper in the decision-making process, look for ways to become more involved. How can you provide direction on issues relating to organizational structure and clinical efficiency? Don’t suppress your feelings or concerns about the work environment. Pulling up a chair at the management table is crucial to improving the workplace and reducing stress for everyone (including the management!). Discuss key frustration points. Clear documentation of the issues that impede patient satisfaction (eg, long wait times) will aid in your dialogue.
Literature has identified common professional frustrations related to base pay rates, on-call pay, overtime pay, individual productivity compensation, and general incentive payments, which are further supported by our job satisfaction surveys.6-8 Knowing what’s included in the typical compensation packages in your region can reduce not only your own stress, but your employer’s as well. While this may seem a futile exercise, the investment in evaluating your own value, and the value your employer places on you, is well worth the return.
Previous experience dictates our ability to handle stress. If you have confidence in yourself, your contribution to your patients, and your ability to influence events and persevere through challenges, you are better equipped to handle the stress. If you can put the stressors in perspective by knowing the time frame of the stress, how long it will last, and what to expect, it will be easier to cope with the situation.
While trying to write this column, I was initially so stressed that I could barely compose a sentence! I knew that the stress of meeting my editorial deadline was “good” stress, though, so I kept taking short walks, and (as you can read) I got through it. Whether you turn to exercise or music or (as one friend does!) closet purging—managing your stress is key to maintaining good health.
[polldaddy:9906029]
1. National Institute of Mental Health. 5 things you should know about stress. www.nimh.nih.gov/health/publications/stress/index.shtml. Accessed December 4, 2017.
2. New York State Office of Mental Health. Common stress reactions: a self-assessment. www.omh.ny.gov/omhweb/disaster_resources/pandemic_influenza/doctors_nurses/Common_Stress_Reactions.html. Accessed December 7, 2017.
3. Smith M. Stress, high fat, and your metabolism [video]. WebMD. www.webmd.com/balance/stress-management/video/stress-high-fat-and-your-metabolism. Accessed December 7, 2017.
4. Slachta A. Stressed women more likely to develop obesity. Cardiovascular Business. November 15, 2017. www.cardiovascularbusiness.com/topics/lipid-metabolic/stressed-women-more-likely-develop-obesity-study-finds. Accessed December 7, 2017.
5. WebMD. Causes of stress. www.webmd.com/balance/guide/causes-of-stress#1. Accessed December 7, 2017.
6. Job satisfaction. Clinician Reviews. 2017;27(12):25-30.
7. Beyond salary: are you happy with your work? Clinician Reviews. 2016;26(12):23-26.
8. O’Hare S, Young AF. The advancing role of advanced practice clinicians: compensation, development, & leadership trends (2016). HealthLeaders Media. www.healthleadersmedia.com/whitepaper/advancing-role-advanced-practice-clinicians-compensation-development-leadership-trends. Accessed December 7, 2017.
As I write this column, the holiday season has just begun, and its incumbent demands lie ahead. By the time this article reaches you, we will have outlasted the season and its associated stress. But it’s not just the holiday baking, gift-wrapping, and decorating that overwhelms us—we face enormous professional stress during this time of year, with its emphasis on home, family, good health, and harmony.
Stress is simply a part of human nature. And despite its bad rap, not all stress is problematic; it’s what motivates people to prepare or perform. Routine, “normal” stress that is temporary or short-lived can actually be beneficial. When placed in danger, the body prepares to either face the threat or flee to safety. During these times, your pulse quickens, you breathe faster, your muscles tense, your brain uses more oxygen and increases activity—all functions that aid in survival.1
But not every situation we encounter necessitates an increase in endorphin levels and blood pressure. Tell that to our stress levels, which are often persistently elevated! Chronic stress can cause the self-protective responses your body activates when threatened to suppress immune, digestive, sleep, and reproductive systems, leading them to cease normal functioning over time.1 This “bad” stress—or distress—can contribute to health problems such as hypertension, cardiovascular disease, obesity, and diabetes.
Stress can elicit a variety of responses: behavioral, psychologic/emotional, physical, cognitive, and social.2 For many, consumption (of tobacco, alcohol, drugs, sugar, fat, or caffeine) is a coping mechanism. While many people look to food for comfort and stress relief, research suggests it may have undesired effects. Eating a high-fat meal when under stress can slow your metabolism and result in significant weight gain.3 Stress can also influence whether people undereat or overeat and affect neurohormonal activity—which leads to increased production of cortisol, which leads to weight gain (particularly in women).4 Let’s be honest: Gaining weight seldom lowers someone’s stress level.
Everyone has different triggers that cause their stress levels to spike, but the workplace has been found to top the list. Within the “work” category, commonly reported stressors include
- Heavy workload or too much responsibility
- Long hours
- Poor management, unclear expectations, or having no say in decision-making.5
For health care providers, day-to-day stress is a chronic problem; responses to the Clinician Reviews annual job satisfaction survey have demonstrated that.6,7 Many of our readers report ongoing issues related to scheduling, work/life balance, compensation, and working conditions. That tension has a direct negative effect, not only on us, but on our families and our patients as well. A missed soccer game or a holiday on call are obvious stressors—but our inability to help patients achieve optimal health is a source of distress that we may not recognize the ramifications of. How often has a clinician felt caught in what feels like an unattainable quest?
Mitigating this workplace stress is the challenge. Changing jobs is another high-stress event, so up and quitting is probably not the answer. Identifying the problem is the first essential step.
If workload is the issue, focus on setting realistic goals for your day. Goal-setting provides purposeful direction and helps you feel in control. There will undeniably be days in which your plan must be completely abandoned. When this happens, don’t fret—reassess! Decide what must get done and what can wait. If possible, avoid scheduling patient appointments that will put you into overload. Learn to say “no” without feeling as though you are not a team player. And when you feel swamped, put a positive spin on the day by noting what you have accomplished, rather than what you have been unable to achieve.
If you find that your voice is but a whisper in the decision-making process, look for ways to become more involved. How can you provide direction on issues relating to organizational structure and clinical efficiency? Don’t suppress your feelings or concerns about the work environment. Pulling up a chair at the management table is crucial to improving the workplace and reducing stress for everyone (including the management!). Discuss key frustration points. Clear documentation of the issues that impede patient satisfaction (eg, long wait times) will aid in your dialogue.
Literature has identified common professional frustrations related to base pay rates, on-call pay, overtime pay, individual productivity compensation, and general incentive payments, which are further supported by our job satisfaction surveys.6-8 Knowing what’s included in the typical compensation packages in your region can reduce not only your own stress, but your employer’s as well. While this may seem a futile exercise, the investment in evaluating your own value, and the value your employer places on you, is well worth the return.
Previous experience dictates our ability to handle stress. If you have confidence in yourself, your contribution to your patients, and your ability to influence events and persevere through challenges, you are better equipped to handle the stress. If you can put the stressors in perspective by knowing the time frame of the stress, how long it will last, and what to expect, it will be easier to cope with the situation.
While trying to write this column, I was initially so stressed that I could barely compose a sentence! I knew that the stress of meeting my editorial deadline was “good” stress, though, so I kept taking short walks, and (as you can read) I got through it. Whether you turn to exercise or music or (as one friend does!) closet purging—managing your stress is key to maintaining good health.
[polldaddy:9906029]
As I write this column, the holiday season has just begun, and its incumbent demands lie ahead. By the time this article reaches you, we will have outlasted the season and its associated stress. But it’s not just the holiday baking, gift-wrapping, and decorating that overwhelms us—we face enormous professional stress during this time of year, with its emphasis on home, family, good health, and harmony.
Stress is simply a part of human nature. And despite its bad rap, not all stress is problematic; it’s what motivates people to prepare or perform. Routine, “normal” stress that is temporary or short-lived can actually be beneficial. When placed in danger, the body prepares to either face the threat or flee to safety. During these times, your pulse quickens, you breathe faster, your muscles tense, your brain uses more oxygen and increases activity—all functions that aid in survival.1
But not every situation we encounter necessitates an increase in endorphin levels and blood pressure. Tell that to our stress levels, which are often persistently elevated! Chronic stress can cause the self-protective responses your body activates when threatened to suppress immune, digestive, sleep, and reproductive systems, leading them to cease normal functioning over time.1 This “bad” stress—or distress—can contribute to health problems such as hypertension, cardiovascular disease, obesity, and diabetes.
Stress can elicit a variety of responses: behavioral, psychologic/emotional, physical, cognitive, and social.2 For many, consumption (of tobacco, alcohol, drugs, sugar, fat, or caffeine) is a coping mechanism. While many people look to food for comfort and stress relief, research suggests it may have undesired effects. Eating a high-fat meal when under stress can slow your metabolism and result in significant weight gain.3 Stress can also influence whether people undereat or overeat and affect neurohormonal activity—which leads to increased production of cortisol, which leads to weight gain (particularly in women).4 Let’s be honest: Gaining weight seldom lowers someone’s stress level.
Everyone has different triggers that cause their stress levels to spike, but the workplace has been found to top the list. Within the “work” category, commonly reported stressors include
- Heavy workload or too much responsibility
- Long hours
- Poor management, unclear expectations, or having no say in decision-making.5
For health care providers, day-to-day stress is a chronic problem; responses to the Clinician Reviews annual job satisfaction survey have demonstrated that.6,7 Many of our readers report ongoing issues related to scheduling, work/life balance, compensation, and working conditions. That tension has a direct negative effect, not only on us, but on our families and our patients as well. A missed soccer game or a holiday on call are obvious stressors—but our inability to help patients achieve optimal health is a source of distress that we may not recognize the ramifications of. How often has a clinician felt caught in what feels like an unattainable quest?
Mitigating this workplace stress is the challenge. Changing jobs is another high-stress event, so up and quitting is probably not the answer. Identifying the problem is the first essential step.
If workload is the issue, focus on setting realistic goals for your day. Goal-setting provides purposeful direction and helps you feel in control. There will undeniably be days in which your plan must be completely abandoned. When this happens, don’t fret—reassess! Decide what must get done and what can wait. If possible, avoid scheduling patient appointments that will put you into overload. Learn to say “no” without feeling as though you are not a team player. And when you feel swamped, put a positive spin on the day by noting what you have accomplished, rather than what you have been unable to achieve.
If you find that your voice is but a whisper in the decision-making process, look for ways to become more involved. How can you provide direction on issues relating to organizational structure and clinical efficiency? Don’t suppress your feelings or concerns about the work environment. Pulling up a chair at the management table is crucial to improving the workplace and reducing stress for everyone (including the management!). Discuss key frustration points. Clear documentation of the issues that impede patient satisfaction (eg, long wait times) will aid in your dialogue.
Literature has identified common professional frustrations related to base pay rates, on-call pay, overtime pay, individual productivity compensation, and general incentive payments, which are further supported by our job satisfaction surveys.6-8 Knowing what’s included in the typical compensation packages in your region can reduce not only your own stress, but your employer’s as well. While this may seem a futile exercise, the investment in evaluating your own value, and the value your employer places on you, is well worth the return.
Previous experience dictates our ability to handle stress. If you have confidence in yourself, your contribution to your patients, and your ability to influence events and persevere through challenges, you are better equipped to handle the stress. If you can put the stressors in perspective by knowing the time frame of the stress, how long it will last, and what to expect, it will be easier to cope with the situation.
While trying to write this column, I was initially so stressed that I could barely compose a sentence! I knew that the stress of meeting my editorial deadline was “good” stress, though, so I kept taking short walks, and (as you can read) I got through it. Whether you turn to exercise or music or (as one friend does!) closet purging—managing your stress is key to maintaining good health.
[polldaddy:9906029]
1. National Institute of Mental Health. 5 things you should know about stress. www.nimh.nih.gov/health/publications/stress/index.shtml. Accessed December 4, 2017.
2. New York State Office of Mental Health. Common stress reactions: a self-assessment. www.omh.ny.gov/omhweb/disaster_resources/pandemic_influenza/doctors_nurses/Common_Stress_Reactions.html. Accessed December 7, 2017.
3. Smith M. Stress, high fat, and your metabolism [video]. WebMD. www.webmd.com/balance/stress-management/video/stress-high-fat-and-your-metabolism. Accessed December 7, 2017.
4. Slachta A. Stressed women more likely to develop obesity. Cardiovascular Business. November 15, 2017. www.cardiovascularbusiness.com/topics/lipid-metabolic/stressed-women-more-likely-develop-obesity-study-finds. Accessed December 7, 2017.
5. WebMD. Causes of stress. www.webmd.com/balance/guide/causes-of-stress#1. Accessed December 7, 2017.
6. Job satisfaction. Clinician Reviews. 2017;27(12):25-30.
7. Beyond salary: are you happy with your work? Clinician Reviews. 2016;26(12):23-26.
8. O’Hare S, Young AF. The advancing role of advanced practice clinicians: compensation, development, & leadership trends (2016). HealthLeaders Media. www.healthleadersmedia.com/whitepaper/advancing-role-advanced-practice-clinicians-compensation-development-leadership-trends. Accessed December 7, 2017.
1. National Institute of Mental Health. 5 things you should know about stress. www.nimh.nih.gov/health/publications/stress/index.shtml. Accessed December 4, 2017.
2. New York State Office of Mental Health. Common stress reactions: a self-assessment. www.omh.ny.gov/omhweb/disaster_resources/pandemic_influenza/doctors_nurses/Common_Stress_Reactions.html. Accessed December 7, 2017.
3. Smith M. Stress, high fat, and your metabolism [video]. WebMD. www.webmd.com/balance/stress-management/video/stress-high-fat-and-your-metabolism. Accessed December 7, 2017.
4. Slachta A. Stressed women more likely to develop obesity. Cardiovascular Business. November 15, 2017. www.cardiovascularbusiness.com/topics/lipid-metabolic/stressed-women-more-likely-develop-obesity-study-finds. Accessed December 7, 2017.
5. WebMD. Causes of stress. www.webmd.com/balance/guide/causes-of-stress#1. Accessed December 7, 2017.
6. Job satisfaction. Clinician Reviews. 2017;27(12):25-30.
7. Beyond salary: are you happy with your work? Clinician Reviews. 2016;26(12):23-26.
8. O’Hare S, Young AF. The advancing role of advanced practice clinicians: compensation, development, & leadership trends (2016). HealthLeaders Media. www.healthleadersmedia.com/whitepaper/advancing-role-advanced-practice-clinicians-compensation-development-leadership-trends. Accessed December 7, 2017.
See for yourself
About 800 million radiology exams were performed in this country in the past year, and they generated approximately 60 billion images, according to an article published in 2017 in the Wall Street Journal (“No need for radiologists to be negative on AI,” by Greg Ip, Nov. 24, 2017). How many of those millions of radiology studies did you order? And how many of the scores of images you requested did you see with your own two eyes? In fact, how many of the radiologists’ reports that were sent to you did you read in their entirety? How often did you just skip over the radiologist’s CYA disclaimers and simply read the final summary, “exam negative”?
I enjoy the challenge of interpreting x-ray images. In fact, I toyed with becoming a pediatric radiologist, but that career path would have meant settling in or near a large city, a compromise my wife and I were unwilling to make. I hoped to continue my habit of looking at all my patients’ x-rays, but because my practice was not in or near the hospital, I reluctantly had to bend my rules and admit I didn’t see every image I had ordered. But, I did read every report in its entirety. In one case, an offhand comment buried in the middle of the radiologist’s report referring to the “residual barium from a previous study” caught my eye, because I knew the patient hadn’t had a previous contrast study. Unfortunately, the neuroblastoma that the radiologist had missed initially, and I had seen the next day, never responded to treatment.
Toward the end of my career, digital imagery allowed me to view my patients’ x-rays without having to leave my desk, which got me closer to my goal of seeing all my patients’ studies. However, the advent of computerized axial tomography and magnetic resonance imaging meant that an increasing number of studies pushed my anatomic knowledge beyond its limits.
I suspect that many of you benefited from the if-you-order-it-look-at-it mantra during your training. How many of you have continued to follow the dictum? With the advent of digitized imagery, there is really little excuse for not taking a minute or 2 to pull up your patients’ images on your desktop. One could argue that looking inside your patient is part of a complete exam. Forcing yourself to take that extra step and look at the study may nudge you into thinking twice about whether you really needed the information the imaging study might add to the diagnostic process. Was your click to order the study just a reflex subliminally related to the fear of a lawsuit? Was it important enough to deserve a firsthand look?
At the very least, being able to say, “I’ve looked at your x-rays myself, and they look fine” may be more comforting to your patient than a third-hand relay of a “negative reading” performed by someone whom they have likely never met.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
About 800 million radiology exams were performed in this country in the past year, and they generated approximately 60 billion images, according to an article published in 2017 in the Wall Street Journal (“No need for radiologists to be negative on AI,” by Greg Ip, Nov. 24, 2017). How many of those millions of radiology studies did you order? And how many of the scores of images you requested did you see with your own two eyes? In fact, how many of the radiologists’ reports that were sent to you did you read in their entirety? How often did you just skip over the radiologist’s CYA disclaimers and simply read the final summary, “exam negative”?
I enjoy the challenge of interpreting x-ray images. In fact, I toyed with becoming a pediatric radiologist, but that career path would have meant settling in or near a large city, a compromise my wife and I were unwilling to make. I hoped to continue my habit of looking at all my patients’ x-rays, but because my practice was not in or near the hospital, I reluctantly had to bend my rules and admit I didn’t see every image I had ordered. But, I did read every report in its entirety. In one case, an offhand comment buried in the middle of the radiologist’s report referring to the “residual barium from a previous study” caught my eye, because I knew the patient hadn’t had a previous contrast study. Unfortunately, the neuroblastoma that the radiologist had missed initially, and I had seen the next day, never responded to treatment.
Toward the end of my career, digital imagery allowed me to view my patients’ x-rays without having to leave my desk, which got me closer to my goal of seeing all my patients’ studies. However, the advent of computerized axial tomography and magnetic resonance imaging meant that an increasing number of studies pushed my anatomic knowledge beyond its limits.
I suspect that many of you benefited from the if-you-order-it-look-at-it mantra during your training. How many of you have continued to follow the dictum? With the advent of digitized imagery, there is really little excuse for not taking a minute or 2 to pull up your patients’ images on your desktop. One could argue that looking inside your patient is part of a complete exam. Forcing yourself to take that extra step and look at the study may nudge you into thinking twice about whether you really needed the information the imaging study might add to the diagnostic process. Was your click to order the study just a reflex subliminally related to the fear of a lawsuit? Was it important enough to deserve a firsthand look?
At the very least, being able to say, “I’ve looked at your x-rays myself, and they look fine” may be more comforting to your patient than a third-hand relay of a “negative reading” performed by someone whom they have likely never met.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
About 800 million radiology exams were performed in this country in the past year, and they generated approximately 60 billion images, according to an article published in 2017 in the Wall Street Journal (“No need for radiologists to be negative on AI,” by Greg Ip, Nov. 24, 2017). How many of those millions of radiology studies did you order? And how many of the scores of images you requested did you see with your own two eyes? In fact, how many of the radiologists’ reports that were sent to you did you read in their entirety? How often did you just skip over the radiologist’s CYA disclaimers and simply read the final summary, “exam negative”?
I enjoy the challenge of interpreting x-ray images. In fact, I toyed with becoming a pediatric radiologist, but that career path would have meant settling in or near a large city, a compromise my wife and I were unwilling to make. I hoped to continue my habit of looking at all my patients’ x-rays, but because my practice was not in or near the hospital, I reluctantly had to bend my rules and admit I didn’t see every image I had ordered. But, I did read every report in its entirety. In one case, an offhand comment buried in the middle of the radiologist’s report referring to the “residual barium from a previous study” caught my eye, because I knew the patient hadn’t had a previous contrast study. Unfortunately, the neuroblastoma that the radiologist had missed initially, and I had seen the next day, never responded to treatment.
Toward the end of my career, digital imagery allowed me to view my patients’ x-rays without having to leave my desk, which got me closer to my goal of seeing all my patients’ studies. However, the advent of computerized axial tomography and magnetic resonance imaging meant that an increasing number of studies pushed my anatomic knowledge beyond its limits.
I suspect that many of you benefited from the if-you-order-it-look-at-it mantra during your training. How many of you have continued to follow the dictum? With the advent of digitized imagery, there is really little excuse for not taking a minute or 2 to pull up your patients’ images on your desktop. One could argue that looking inside your patient is part of a complete exam. Forcing yourself to take that extra step and look at the study may nudge you into thinking twice about whether you really needed the information the imaging study might add to the diagnostic process. Was your click to order the study just a reflex subliminally related to the fear of a lawsuit? Was it important enough to deserve a firsthand look?
At the very least, being able to say, “I’ve looked at your x-rays myself, and they look fine” may be more comforting to your patient than a third-hand relay of a “negative reading” performed by someone whom they have likely never met.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
ISSOP’s Budapest Declaration: A call to action for children on the move
In late October 2017, pediatricians from over 25 countries gathered at the annual meeting of the International Society of Social Pediatrics and Child Health in Budapest to develop strategies to address the health and well-being of children on the move. With the staggering global increase in the displacement of children – due to conflict, climate change, natural disasters, and economic deprivation – there is a critical need for action.
An international slate of experts, including pediatricians who are responding to the needs of these children, provided an evidence base for intervention and action. These discussions informed the development of a consensus statement, the Budapest Declaration, that establishes a framework for a global response to the exigencies confronting these children and families.
The Budapest Declaration is grounded in children’s rights as guaranteed in the United Nation’s Convention on the Rights of the Child (CRC). All countries in the world have signed onto the CRC, with a notable exception being the United States. But leading American pediatric groups, including the American Academy of Pediatrics, have endorsed the CRC, making it a basis of organizational advocacy. The CRC entitles all children to optimal survival and development (Article 6) and optimal health and health care (Article 24).
As prescribed by these accepted legal rights for children, children and youth on the move are entitled to the same services, including health care, as resident populations of children, regardless of their legal status. Countries can be held accountable to ensure they receive the full rights due them as articulated in the CRC. Furthermore, efforts to do so should be assessed in national periodic reports to the Committee on the Rights of the Child to ensure accountability.
The relevance of the Budapest Declaration to the United States cannot be overstated. National and regional public policy throughout our country, and in particular along our Southern border, is having a devastating effect on the physical and mental health of children and youth on the move – and will continue to do so throughout their life course.
The involvement of pediatricians and other child health providers is essential to the planning and implementation of clinical and public health programs for children on the move. Child health professionals, in conjunction with their professional organizations, must be engaged in all aspects of local, national, and global responses. Leadership and contributions by pediatricians and pediatric societies and academic institutions are integral to the success of key partners, such as UNICEF, the World Health Organization, the International Organization for Migration, and the UN High Commissioner for Refugees.
Systems of care should be provided that address the physical, mental, and social health care needs of these children without bias and prejudice. Pregnant mothers on the move also should receive services to ensure the delivery of healthy newborns. Every nation should develop approaches and commitments to advance equity in the health and well-being for these children and families.
For much of the world, working within the realm of children’s rights provides a strategy and moral and legal basis for our efforts. Pediatricians need to work with colleagues in a transdisciplinary approach to ensure all children live in nurturing, rights-respecting environments. Our ongoing efforts should include encouraging academic institutions to assist with professional education, research, and evaluation in this regard. We need evaluations that contribute to continuous quality improvement in our efforts and integrate the metrics of child rights, social justice, and health equity into our care of children on the move.
We call on other national and international public, private, and academic sector organizations to advance the health and well-being of children and youth on the move. These children and families are depending on us to do so.
For the complete text of the Budapest Declaration, see www.issop.org/2017/11/10/budapest-declaration-rights-health-well-children-youth-move/.
Dr. Rushton is medical director of the South Carolina Quality Through Innovation in Pediatrics (SCQTIP) network. Dr. Goldhagen is president-elect, International Society for Social Pediatrics and Child Health, and professor of pediatrics, University of Florida, Jacksonville. Email them at [email protected].
In late October 2017, pediatricians from over 25 countries gathered at the annual meeting of the International Society of Social Pediatrics and Child Health in Budapest to develop strategies to address the health and well-being of children on the move. With the staggering global increase in the displacement of children – due to conflict, climate change, natural disasters, and economic deprivation – there is a critical need for action.
An international slate of experts, including pediatricians who are responding to the needs of these children, provided an evidence base for intervention and action. These discussions informed the development of a consensus statement, the Budapest Declaration, that establishes a framework for a global response to the exigencies confronting these children and families.
The Budapest Declaration is grounded in children’s rights as guaranteed in the United Nation’s Convention on the Rights of the Child (CRC). All countries in the world have signed onto the CRC, with a notable exception being the United States. But leading American pediatric groups, including the American Academy of Pediatrics, have endorsed the CRC, making it a basis of organizational advocacy. The CRC entitles all children to optimal survival and development (Article 6) and optimal health and health care (Article 24).
As prescribed by these accepted legal rights for children, children and youth on the move are entitled to the same services, including health care, as resident populations of children, regardless of their legal status. Countries can be held accountable to ensure they receive the full rights due them as articulated in the CRC. Furthermore, efforts to do so should be assessed in national periodic reports to the Committee on the Rights of the Child to ensure accountability.
The relevance of the Budapest Declaration to the United States cannot be overstated. National and regional public policy throughout our country, and in particular along our Southern border, is having a devastating effect on the physical and mental health of children and youth on the move – and will continue to do so throughout their life course.
The involvement of pediatricians and other child health providers is essential to the planning and implementation of clinical and public health programs for children on the move. Child health professionals, in conjunction with their professional organizations, must be engaged in all aspects of local, national, and global responses. Leadership and contributions by pediatricians and pediatric societies and academic institutions are integral to the success of key partners, such as UNICEF, the World Health Organization, the International Organization for Migration, and the UN High Commissioner for Refugees.
Systems of care should be provided that address the physical, mental, and social health care needs of these children without bias and prejudice. Pregnant mothers on the move also should receive services to ensure the delivery of healthy newborns. Every nation should develop approaches and commitments to advance equity in the health and well-being for these children and families.
For much of the world, working within the realm of children’s rights provides a strategy and moral and legal basis for our efforts. Pediatricians need to work with colleagues in a transdisciplinary approach to ensure all children live in nurturing, rights-respecting environments. Our ongoing efforts should include encouraging academic institutions to assist with professional education, research, and evaluation in this regard. We need evaluations that contribute to continuous quality improvement in our efforts and integrate the metrics of child rights, social justice, and health equity into our care of children on the move.
We call on other national and international public, private, and academic sector organizations to advance the health and well-being of children and youth on the move. These children and families are depending on us to do so.
For the complete text of the Budapest Declaration, see www.issop.org/2017/11/10/budapest-declaration-rights-health-well-children-youth-move/.
Dr. Rushton is medical director of the South Carolina Quality Through Innovation in Pediatrics (SCQTIP) network. Dr. Goldhagen is president-elect, International Society for Social Pediatrics and Child Health, and professor of pediatrics, University of Florida, Jacksonville. Email them at [email protected].
In late October 2017, pediatricians from over 25 countries gathered at the annual meeting of the International Society of Social Pediatrics and Child Health in Budapest to develop strategies to address the health and well-being of children on the move. With the staggering global increase in the displacement of children – due to conflict, climate change, natural disasters, and economic deprivation – there is a critical need for action.
An international slate of experts, including pediatricians who are responding to the needs of these children, provided an evidence base for intervention and action. These discussions informed the development of a consensus statement, the Budapest Declaration, that establishes a framework for a global response to the exigencies confronting these children and families.
The Budapest Declaration is grounded in children’s rights as guaranteed in the United Nation’s Convention on the Rights of the Child (CRC). All countries in the world have signed onto the CRC, with a notable exception being the United States. But leading American pediatric groups, including the American Academy of Pediatrics, have endorsed the CRC, making it a basis of organizational advocacy. The CRC entitles all children to optimal survival and development (Article 6) and optimal health and health care (Article 24).
As prescribed by these accepted legal rights for children, children and youth on the move are entitled to the same services, including health care, as resident populations of children, regardless of their legal status. Countries can be held accountable to ensure they receive the full rights due them as articulated in the CRC. Furthermore, efforts to do so should be assessed in national periodic reports to the Committee on the Rights of the Child to ensure accountability.
The relevance of the Budapest Declaration to the United States cannot be overstated. National and regional public policy throughout our country, and in particular along our Southern border, is having a devastating effect on the physical and mental health of children and youth on the move – and will continue to do so throughout their life course.
The involvement of pediatricians and other child health providers is essential to the planning and implementation of clinical and public health programs for children on the move. Child health professionals, in conjunction with their professional organizations, must be engaged in all aspects of local, national, and global responses. Leadership and contributions by pediatricians and pediatric societies and academic institutions are integral to the success of key partners, such as UNICEF, the World Health Organization, the International Organization for Migration, and the UN High Commissioner for Refugees.
Systems of care should be provided that address the physical, mental, and social health care needs of these children without bias and prejudice. Pregnant mothers on the move also should receive services to ensure the delivery of healthy newborns. Every nation should develop approaches and commitments to advance equity in the health and well-being for these children and families.
For much of the world, working within the realm of children’s rights provides a strategy and moral and legal basis for our efforts. Pediatricians need to work with colleagues in a transdisciplinary approach to ensure all children live in nurturing, rights-respecting environments. Our ongoing efforts should include encouraging academic institutions to assist with professional education, research, and evaluation in this regard. We need evaluations that contribute to continuous quality improvement in our efforts and integrate the metrics of child rights, social justice, and health equity into our care of children on the move.
We call on other national and international public, private, and academic sector organizations to advance the health and well-being of children and youth on the move. These children and families are depending on us to do so.
For the complete text of the Budapest Declaration, see www.issop.org/2017/11/10/budapest-declaration-rights-health-well-children-youth-move/.
Dr. Rushton is medical director of the South Carolina Quality Through Innovation in Pediatrics (SCQTIP) network. Dr. Goldhagen is president-elect, International Society for Social Pediatrics and Child Health, and professor of pediatrics, University of Florida, Jacksonville. Email them at [email protected].
Don’t give up on influenza vaccine
I suspect most health care providers have heard the complaint, “The vaccine doesn’t work. One year I got the vaccine, and I still came down with the flu.”
Over the years, I’ve polished my responses to vaccine naysayers.
Influenza vaccine doesn’t protect you against every virus that can cause cold and flu symptoms. It only prevents influenza. It’s possible you had a different virus, such as adenovirus, coronavirus, parainfluenza virus, or respiratory syncytial virus.
Some years, the vaccine works better than others because there is a mismatch between the viruses chosen for the vaccine, and the viruses that end up circulating. Even when it doesn’t prevent flu, the vaccine can potentially reduce the severity of illness.
The discussion became a little more complicated in 2016 when the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices withdrew its support for the live attenuated influenza virus vaccine (LAIV4) because of concerns about effectiveness. During the 2015-2016 influenza season, LAIV4 demonstrated no statistically significant effectiveness in children 2-17 years of age against H1N1pdm09, the predominant influenza strain. Fortunately, inactivated injectable vaccine did offer protection. An estimated 41.8 million children aged 6 months to 17 years ultimately received this vaccine during the 2016-2017 influenza season.
Now with the 2017-2018 influenza season in full swing, some media reports are proclaiming the influenza vaccine is only 10% effective this year. This claim is based on an interim analysis of data from the most recent flu season in Australia and the effectiveness of the vaccine against the circulating H3N2 virus strain. News from the U.S. CDC is more encouraging. The H3N2 virus contained in this year’s vaccine is the same as that used last year, and so far, circulating H3N2 viruses in the United States are similar to the vaccine virus. Public health officials suggest that we can hope that the vaccine works as well as it did last year, when overall vaccine effectiveness against all circulating flu viruses was 39%, and effectiveness against the H3N2 virus specifically was 32%.
I’m upping my game when talking to parents about flu vaccine. I mention one study conducted between 2010 and 2012 in which influenza immunization reduced a child’s risk of being admitted to an intensive care unit with flu by 74% (J Infect Dis. 2014 Sep 1;210[5]:674-83). I emphasize that flu vaccine reduces the chance that a child will die from flu. According to a study published in 2017, influenza vaccine reduced the risk of death from flu by 65% in healthy children and 51% in children with high-risk medical conditions (Pediatrics. 2017 May. doi: 10.1542/peds.2016-4244).
When I’m talking to trainees, I no longer just focus on the match between circulating strains of flu and vaccine strains. I mention that viruses used to produce most seasonal flu vaccines are grown in eggs, a process that can result in minor antigenic changes in the hemagglutinin protein, especially in H3N2 viruses. These “egg-adapted changes” may result in a vaccine that stimulates a less effective immune response, even with a good match between circulating strains and vaccine strains. For example, Zost et al. found that the H3N2 virus that emerged during the 2014-2015 season possessed a new hemagglutinin-associated glycosylation site (Proc Natl Acad Sci U S A. 2017 Nov 21;114[47]:12578-83). Although this virus was represented in the 2016-2017 influenza vaccine, the egg-adapted version lost the glycosylation site, resulting in decreased vaccine immunogenicity and less protection against H3N2 viruses circulating in the community.
The real take-home message here is that we need better flu vaccines. In the short term, cell-based flu vaccines that use virus grown in animal cells are a potential alternative to egg-based vaccines. In the long term, we need a universal flu vaccine. The National Institute of Allergy and Infectious Diseases is prioritizing work on a vaccine that could provide long-lasting protection against multiple subtypes of the virus. According to a report on the National Institutes of Health website, such a vaccine could “eliminate the need to update and administer the seasonal flu vaccine each year and could provide protection against newly emerging flu strains,” including those with the potential to cause a pandemic. The NIH researchers acknowledge, however, that achieving this goal will require “a broad range of expertise and substantial resources.”
Until new vaccines are available, we need to do a better job of using available, albeit imperfect, flu vaccines. During the 2016-2017 season, only 59% of children 6 months to 17 years were immunized, and there were 110 influenza-associated deaths in children, according to the CDC. It’s likely that some of these were preventable.
The total magnitude of suffering associated with flu is more difficult to quantify, but anecdotes can be illuminating. A friend recently diagnosed with influenza shared her experience via Facebook. “Rough night. I’m seconds away from a meltdown. My body aches so bad that I can’t get comfortable on the couch or my bed. Can’t breathe, and I cough until I vomit. My head is about to burst along with my ears. Just took a hot bath hoping that would help. I don’t know what else to do. The flu really sucks.”
Indeed. Even a 1 in 10 chance of preventing the flu is better than no chance at all.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
I suspect most health care providers have heard the complaint, “The vaccine doesn’t work. One year I got the vaccine, and I still came down with the flu.”
Over the years, I’ve polished my responses to vaccine naysayers.
Influenza vaccine doesn’t protect you against every virus that can cause cold and flu symptoms. It only prevents influenza. It’s possible you had a different virus, such as adenovirus, coronavirus, parainfluenza virus, or respiratory syncytial virus.
Some years, the vaccine works better than others because there is a mismatch between the viruses chosen for the vaccine, and the viruses that end up circulating. Even when it doesn’t prevent flu, the vaccine can potentially reduce the severity of illness.
The discussion became a little more complicated in 2016 when the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices withdrew its support for the live attenuated influenza virus vaccine (LAIV4) because of concerns about effectiveness. During the 2015-2016 influenza season, LAIV4 demonstrated no statistically significant effectiveness in children 2-17 years of age against H1N1pdm09, the predominant influenza strain. Fortunately, inactivated injectable vaccine did offer protection. An estimated 41.8 million children aged 6 months to 17 years ultimately received this vaccine during the 2016-2017 influenza season.
Now with the 2017-2018 influenza season in full swing, some media reports are proclaiming the influenza vaccine is only 10% effective this year. This claim is based on an interim analysis of data from the most recent flu season in Australia and the effectiveness of the vaccine against the circulating H3N2 virus strain. News from the U.S. CDC is more encouraging. The H3N2 virus contained in this year’s vaccine is the same as that used last year, and so far, circulating H3N2 viruses in the United States are similar to the vaccine virus. Public health officials suggest that we can hope that the vaccine works as well as it did last year, when overall vaccine effectiveness against all circulating flu viruses was 39%, and effectiveness against the H3N2 virus specifically was 32%.
I’m upping my game when talking to parents about flu vaccine. I mention one study conducted between 2010 and 2012 in which influenza immunization reduced a child’s risk of being admitted to an intensive care unit with flu by 74% (J Infect Dis. 2014 Sep 1;210[5]:674-83). I emphasize that flu vaccine reduces the chance that a child will die from flu. According to a study published in 2017, influenza vaccine reduced the risk of death from flu by 65% in healthy children and 51% in children with high-risk medical conditions (Pediatrics. 2017 May. doi: 10.1542/peds.2016-4244).
When I’m talking to trainees, I no longer just focus on the match between circulating strains of flu and vaccine strains. I mention that viruses used to produce most seasonal flu vaccines are grown in eggs, a process that can result in minor antigenic changes in the hemagglutinin protein, especially in H3N2 viruses. These “egg-adapted changes” may result in a vaccine that stimulates a less effective immune response, even with a good match between circulating strains and vaccine strains. For example, Zost et al. found that the H3N2 virus that emerged during the 2014-2015 season possessed a new hemagglutinin-associated glycosylation site (Proc Natl Acad Sci U S A. 2017 Nov 21;114[47]:12578-83). Although this virus was represented in the 2016-2017 influenza vaccine, the egg-adapted version lost the glycosylation site, resulting in decreased vaccine immunogenicity and less protection against H3N2 viruses circulating in the community.
The real take-home message here is that we need better flu vaccines. In the short term, cell-based flu vaccines that use virus grown in animal cells are a potential alternative to egg-based vaccines. In the long term, we need a universal flu vaccine. The National Institute of Allergy and Infectious Diseases is prioritizing work on a vaccine that could provide long-lasting protection against multiple subtypes of the virus. According to a report on the National Institutes of Health website, such a vaccine could “eliminate the need to update and administer the seasonal flu vaccine each year and could provide protection against newly emerging flu strains,” including those with the potential to cause a pandemic. The NIH researchers acknowledge, however, that achieving this goal will require “a broad range of expertise and substantial resources.”
Until new vaccines are available, we need to do a better job of using available, albeit imperfect, flu vaccines. During the 2016-2017 season, only 59% of children 6 months to 17 years were immunized, and there were 110 influenza-associated deaths in children, according to the CDC. It’s likely that some of these were preventable.
The total magnitude of suffering associated with flu is more difficult to quantify, but anecdotes can be illuminating. A friend recently diagnosed with influenza shared her experience via Facebook. “Rough night. I’m seconds away from a meltdown. My body aches so bad that I can’t get comfortable on the couch or my bed. Can’t breathe, and I cough until I vomit. My head is about to burst along with my ears. Just took a hot bath hoping that would help. I don’t know what else to do. The flu really sucks.”
Indeed. Even a 1 in 10 chance of preventing the flu is better than no chance at all.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
I suspect most health care providers have heard the complaint, “The vaccine doesn’t work. One year I got the vaccine, and I still came down with the flu.”
Over the years, I’ve polished my responses to vaccine naysayers.
Influenza vaccine doesn’t protect you against every virus that can cause cold and flu symptoms. It only prevents influenza. It’s possible you had a different virus, such as adenovirus, coronavirus, parainfluenza virus, or respiratory syncytial virus.
Some years, the vaccine works better than others because there is a mismatch between the viruses chosen for the vaccine, and the viruses that end up circulating. Even when it doesn’t prevent flu, the vaccine can potentially reduce the severity of illness.
The discussion became a little more complicated in 2016 when the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices withdrew its support for the live attenuated influenza virus vaccine (LAIV4) because of concerns about effectiveness. During the 2015-2016 influenza season, LAIV4 demonstrated no statistically significant effectiveness in children 2-17 years of age against H1N1pdm09, the predominant influenza strain. Fortunately, inactivated injectable vaccine did offer protection. An estimated 41.8 million children aged 6 months to 17 years ultimately received this vaccine during the 2016-2017 influenza season.
Now with the 2017-2018 influenza season in full swing, some media reports are proclaiming the influenza vaccine is only 10% effective this year. This claim is based on an interim analysis of data from the most recent flu season in Australia and the effectiveness of the vaccine against the circulating H3N2 virus strain. News from the U.S. CDC is more encouraging. The H3N2 virus contained in this year’s vaccine is the same as that used last year, and so far, circulating H3N2 viruses in the United States are similar to the vaccine virus. Public health officials suggest that we can hope that the vaccine works as well as it did last year, when overall vaccine effectiveness against all circulating flu viruses was 39%, and effectiveness against the H3N2 virus specifically was 32%.
I’m upping my game when talking to parents about flu vaccine. I mention one study conducted between 2010 and 2012 in which influenza immunization reduced a child’s risk of being admitted to an intensive care unit with flu by 74% (J Infect Dis. 2014 Sep 1;210[5]:674-83). I emphasize that flu vaccine reduces the chance that a child will die from flu. According to a study published in 2017, influenza vaccine reduced the risk of death from flu by 65% in healthy children and 51% in children with high-risk medical conditions (Pediatrics. 2017 May. doi: 10.1542/peds.2016-4244).
When I’m talking to trainees, I no longer just focus on the match between circulating strains of flu and vaccine strains. I mention that viruses used to produce most seasonal flu vaccines are grown in eggs, a process that can result in minor antigenic changes in the hemagglutinin protein, especially in H3N2 viruses. These “egg-adapted changes” may result in a vaccine that stimulates a less effective immune response, even with a good match between circulating strains and vaccine strains. For example, Zost et al. found that the H3N2 virus that emerged during the 2014-2015 season possessed a new hemagglutinin-associated glycosylation site (Proc Natl Acad Sci U S A. 2017 Nov 21;114[47]:12578-83). Although this virus was represented in the 2016-2017 influenza vaccine, the egg-adapted version lost the glycosylation site, resulting in decreased vaccine immunogenicity and less protection against H3N2 viruses circulating in the community.
The real take-home message here is that we need better flu vaccines. In the short term, cell-based flu vaccines that use virus grown in animal cells are a potential alternative to egg-based vaccines. In the long term, we need a universal flu vaccine. The National Institute of Allergy and Infectious Diseases is prioritizing work on a vaccine that could provide long-lasting protection against multiple subtypes of the virus. According to a report on the National Institutes of Health website, such a vaccine could “eliminate the need to update and administer the seasonal flu vaccine each year and could provide protection against newly emerging flu strains,” including those with the potential to cause a pandemic. The NIH researchers acknowledge, however, that achieving this goal will require “a broad range of expertise and substantial resources.”
Until new vaccines are available, we need to do a better job of using available, albeit imperfect, flu vaccines. During the 2016-2017 season, only 59% of children 6 months to 17 years were immunized, and there were 110 influenza-associated deaths in children, according to the CDC. It’s likely that some of these were preventable.
The total magnitude of suffering associated with flu is more difficult to quantify, but anecdotes can be illuminating. A friend recently diagnosed with influenza shared her experience via Facebook. “Rough night. I’m seconds away from a meltdown. My body aches so bad that I can’t get comfortable on the couch or my bed. Can’t breathe, and I cough until I vomit. My head is about to burst along with my ears. Just took a hot bath hoping that would help. I don’t know what else to do. The flu really sucks.”
Indeed. Even a 1 in 10 chance of preventing the flu is better than no chance at all.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
Commentary—Study Heightens Awareness, But at What Cost?
The study conducted by Brookmeyer and colleagues is a logical and thoughtful attempt to size the potential impact of Alzheimer's disease now and in the future, updating old-technology estimates based on actual diagnoses with new technologically derived diagnoses of preclinical neurodegenerative states. They acknowledge that the uncertainty in the actual disease burden we will face is centered on the question of conversion rates, which vary between studies and are far less certain in the preclinical stages than the symptomatic ones.
Scientific interest aside, the main purpose of an article like this is to heighten awareness and concern by demonstrating that symptomatic Alzheimer's disease is the tip of a much larger iceberg and warrants more funding for research and clinical care. The worry that articles like this—or that the media attention they receive—create for me, however, is that they potentially contribute to a growing public panic at a time when we still lack truly meaningful therapy. As a doctor, I want to give my patients with MCI and dementia reason to believe they still have a meaningful life and that there is hope, rather than having them feel that I have just pronounced a death sentence.
The attention paid by the Alzheimer's Association is understandable, given its mission of increasing awareness and supporting more funding, but it omits to mention another important article showing that dementia rates are actually declining when data are adjusted for our aging population (observed vs expected).
We need to maintain public awareness without creating panic. There is no question that Alzheimer's disease is a major public health issue that warrants all the funding we can provide to researchers seeking a cure. How to balance that need with the need to give our population hope that all is not lost when they misplace their keys is the challenge this article raises.
—Richard J. Caselli, MD
Professor of Neurology
Mayo Clinic
Scottsdale, Arizona
The study conducted by Brookmeyer and colleagues is a logical and thoughtful attempt to size the potential impact of Alzheimer's disease now and in the future, updating old-technology estimates based on actual diagnoses with new technologically derived diagnoses of preclinical neurodegenerative states. They acknowledge that the uncertainty in the actual disease burden we will face is centered on the question of conversion rates, which vary between studies and are far less certain in the preclinical stages than the symptomatic ones.
Scientific interest aside, the main purpose of an article like this is to heighten awareness and concern by demonstrating that symptomatic Alzheimer's disease is the tip of a much larger iceberg and warrants more funding for research and clinical care. The worry that articles like this—or that the media attention they receive—create for me, however, is that they potentially contribute to a growing public panic at a time when we still lack truly meaningful therapy. As a doctor, I want to give my patients with MCI and dementia reason to believe they still have a meaningful life and that there is hope, rather than having them feel that I have just pronounced a death sentence.
The attention paid by the Alzheimer's Association is understandable, given its mission of increasing awareness and supporting more funding, but it omits to mention another important article showing that dementia rates are actually declining when data are adjusted for our aging population (observed vs expected).
We need to maintain public awareness without creating panic. There is no question that Alzheimer's disease is a major public health issue that warrants all the funding we can provide to researchers seeking a cure. How to balance that need with the need to give our population hope that all is not lost when they misplace their keys is the challenge this article raises.
—Richard J. Caselli, MD
Professor of Neurology
Mayo Clinic
Scottsdale, Arizona
The study conducted by Brookmeyer and colleagues is a logical and thoughtful attempt to size the potential impact of Alzheimer's disease now and in the future, updating old-technology estimates based on actual diagnoses with new technologically derived diagnoses of preclinical neurodegenerative states. They acknowledge that the uncertainty in the actual disease burden we will face is centered on the question of conversion rates, which vary between studies and are far less certain in the preclinical stages than the symptomatic ones.
Scientific interest aside, the main purpose of an article like this is to heighten awareness and concern by demonstrating that symptomatic Alzheimer's disease is the tip of a much larger iceberg and warrants more funding for research and clinical care. The worry that articles like this—or that the media attention they receive—create for me, however, is that they potentially contribute to a growing public panic at a time when we still lack truly meaningful therapy. As a doctor, I want to give my patients with MCI and dementia reason to believe they still have a meaningful life and that there is hope, rather than having them feel that I have just pronounced a death sentence.
The attention paid by the Alzheimer's Association is understandable, given its mission of increasing awareness and supporting more funding, but it omits to mention another important article showing that dementia rates are actually declining when data are adjusted for our aging population (observed vs expected).
We need to maintain public awareness without creating panic. There is no question that Alzheimer's disease is a major public health issue that warrants all the funding we can provide to researchers seeking a cure. How to balance that need with the need to give our population hope that all is not lost when they misplace their keys is the challenge this article raises.
—Richard J. Caselli, MD
Professor of Neurology
Mayo Clinic
Scottsdale, Arizona
Dementia: Past, Present, and Future
Jeffrey Cummings, MD, ScD
Director, Cleveland Clinic Lou Ruvo Center for Brain Health, Las Vegas
Disclosure: Jeffrey Cummings has provided consultation to Axovant, biOasis Technologies, Biogen, Boehinger-Ingelheim, Bracket, Dart, Eisai, Genentech, Grifols, Intracellular Therapies, Kyowa, Eli Lilly, Lundbeck, Medavante, Merck, Neurotrope, Novartis, Nutricia, Orion, Otsuka, Pfizer, Probiodrug, QR, Resverlogix, Servier, Suven, Takeda, Toyoma, and United Neuroscience companies.
As Neurology Reviews celebrates its 25th anniversary, we take this opportunity to look back and to look ahead in the area of dementia care and research. Most dementia research has focused on Alzheimer’s disease, although there have been important evolutions in the diagnosis, pathology, and potential interventions for frontotemporal dementia spectrum disorders, dementia with Lewy bodies, Parkinson’s disease dementia, and vascular dementia.
Alzheimer’s Disease
Twenty-five years ago—coinciding with the inauguration of Neurology Reviews—the first treatment for Alzheimer’s disease, the cholinesterase inhibitor tacrine, was approved by the FDA. Tacrine had many limitations, including a short half-life and a propensity to cause hepatotoxicity, but it represented an historical breakthrough in transforming an untreatable disease into a treatable one. The approval energized the field and gave hope to thousands of patients with Alzheimer’s disease dementia.
Tacrine was followed by other cholinesterase inhibitors and memantine in the next decade, with five drugs approved by the end of 2003. Unfortunately, no new agents have been approved for the treatment of Alzheimer’s disease since that fertile period.1 Tremendous efforts are now being devoted to developing disease-modifying treatments for Alzheimer’s disease and other dementias. There are promising preliminary observations for immunotherapies that remove amyloid-beta protein from the brain and stabilize cognitive decline.2 Progress in the development of disease-modifying treatments will transform the field, requiring much of the health care system and insurance companies, but offering an improved quality of life for millions of patients with Alzheimer’s disease.
Previous Advances
A major advance in understanding Alzheimer’s disease is the discovery that the disease begins with amyloid accumulation in mid-life, approximately 15 years before the onset of cognitive decline.3 The advent of amyloid imaging has allowed the visualization of fibrillar amyloid-comprising Alzheimer-type neuritic plaques in the brain of the living person. Scans become positive 15 years prior to the emergence of mild cognitive impairment (MCI) and progression to Alzheimer’s disease dementia. If one is destined to develop MCI at age 75, the scan would be positive by approximately age 60. CSF levels of amyloid beta decline simultaneously as the protein is trapped in the brain, thus resulting in positive amyloid imaging. More recently, findings from tau protein imaging have begun to remodel our understanding of the role of tau in Alzheimer’s disease. Tau imaging correlates with the emergence of symptoms in the MCI phase of Alzheimer’s disease.4 Tau correlates with cognitive decline; positive amyloid imaging does not.
Future Challenges
Looking to the future, it is likely that companion biomarkers such as amyloid and tau imaging will be approved for clinical use. They will enable neurologists to identify the patients whose brain changes match the mechanism of action of the intended treatment (eg, positive tau imaging for those to receive anti-tau therapy and positive amyloid imaging for individuals intended to receive anti-amyloid therapy).
Anticipated directions of therapy development include treatment of individuals before the onset of symptoms, phase-specific therapies that respond to the evolving state changes of Alzheimer’s disease, and combination therapies based on the observation that most patients with Alzheimer’s disease harbor multiple types of brain pathology.5 Alzheimer’s disease therapeutics will proceed in the direction of precision medicine with better matching of therapies to the features of the disorder for the individual patient.
The US health care system is unprepared for the advent of disease-modifying treatments for Alzheimer’s disease. Recognition of patients with mild changes, availability of amyloid imaging to support diagnosis and identify therapeutic targets, and the number of infusion centers to administer monoclonal antibodies are all insufficient to respon
Advances in the understanding of frontotemporal dementia have not yet led to a breakthrough therapy. Frontotemporal dementia has been shown to be pathologically heterogeneous, with about half of the patients having an underlying tauopathy, and about half having TDP-43 as the associated aggregated protein.6 A few cases have rarer forms of pathology. Major phenotypes of frontotemporal dementia include behavioral variant frontotemporal dementia, progressive nonfluent aphasia, and semantic dementia. Trials of new candidate therapies are progressing for frontotemporal dementia spectrum disorders, and new treatments are anticipated.
Progress in understanding dementia with Lewy bodies has led to the publication of diagnostic criteria.7 The phenotype of parkinsonism, fluctuating cognition, and visual hallucinations is supported by decreased dopamine uptake on dopamine transporter (DaT) scanning and the presence of REM sleep behavior disorder. Lewy bodies are found in the limbic and neocortex at autopsy; many cases have concomitant amyloid plaques similar to those of Alzheimer’s disease. Parkinson’s disease dementia has many of the same features and is distinguished from dementia with Lewy bodies only by the order of appearance of major symptoms—dementia first in dementia with Lewy bodies, parkinsonism first in Parkinson’s disease dementia. Rivastigmine is approved for the symptomatic treatment of cognitive deficits in Parkinson’s disease dementia, and trials of new therapies are being conducted in Parkinson’s disease dementia and dementia with Lewy bodies. Alpha-synuclein is present in both disorders and is the target of new disease-modifying treatments currently in clinical trials.
Improved understanding of the basic biology of neurodegenerative disease is critically important and must be accelerated. This knowledge will provide the foundation for improved diagnostics and therapeutics essential for responding to the needs of the burgeoning number of patients with these late-life brain disorders.
References
1. Cummings JL, Morstorf T, Zhong K. Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res Ther. 2014;6(4):37-43.
2. Sevigny J, Chiao P, Bussiere T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50-56.
3. Villemagne VL, Burnham S, Bourgeat P, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12(4):357-367.
4. Johnson KA, Schultz A, Betensky RA, et al. Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann Neurol. 2016;79(1):110-119.
5. James BD, Wilson RS, Boyle PA, et al. TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain. 2016;139(11):2983-2993.
6. Lashley T, Rohrer JD, Mead S, Revesz T. Review: an update on clinical, genetic and pathological aspects of frontotemporal lobar degenerations. Neuropathol Appl Neurobiol. 2015;41(7):858-881.
7. McKeith IG, Boeve BF, Dickson DW, et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88-100.
Jeffrey Cummings, MD, ScD
Director, Cleveland Clinic Lou Ruvo Center for Brain Health, Las Vegas
Disclosure: Jeffrey Cummings has provided consultation to Axovant, biOasis Technologies, Biogen, Boehinger-Ingelheim, Bracket, Dart, Eisai, Genentech, Grifols, Intracellular Therapies, Kyowa, Eli Lilly, Lundbeck, Medavante, Merck, Neurotrope, Novartis, Nutricia, Orion, Otsuka, Pfizer, Probiodrug, QR, Resverlogix, Servier, Suven, Takeda, Toyoma, and United Neuroscience companies.
As Neurology Reviews celebrates its 25th anniversary, we take this opportunity to look back and to look ahead in the area of dementia care and research. Most dementia research has focused on Alzheimer’s disease, although there have been important evolutions in the diagnosis, pathology, and potential interventions for frontotemporal dementia spectrum disorders, dementia with Lewy bodies, Parkinson’s disease dementia, and vascular dementia.
Alzheimer’s Disease
Twenty-five years ago—coinciding with the inauguration of Neurology Reviews—the first treatment for Alzheimer’s disease, the cholinesterase inhibitor tacrine, was approved by the FDA. Tacrine had many limitations, including a short half-life and a propensity to cause hepatotoxicity, but it represented an historical breakthrough in transforming an untreatable disease into a treatable one. The approval energized the field and gave hope to thousands of patients with Alzheimer’s disease dementia.
Tacrine was followed by other cholinesterase inhibitors and memantine in the next decade, with five drugs approved by the end of 2003. Unfortunately, no new agents have been approved for the treatment of Alzheimer’s disease since that fertile period.1 Tremendous efforts are now being devoted to developing disease-modifying treatments for Alzheimer’s disease and other dementias. There are promising preliminary observations for immunotherapies that remove amyloid-beta protein from the brain and stabilize cognitive decline.2 Progress in the development of disease-modifying treatments will transform the field, requiring much of the health care system and insurance companies, but offering an improved quality of life for millions of patients with Alzheimer’s disease.
Previous Advances
A major advance in understanding Alzheimer’s disease is the discovery that the disease begins with amyloid accumulation in mid-life, approximately 15 years before the onset of cognitive decline.3 The advent of amyloid imaging has allowed the visualization of fibrillar amyloid-comprising Alzheimer-type neuritic plaques in the brain of the living person. Scans become positive 15 years prior to the emergence of mild cognitive impairment (MCI) and progression to Alzheimer’s disease dementia. If one is destined to develop MCI at age 75, the scan would be positive by approximately age 60. CSF levels of amyloid beta decline simultaneously as the protein is trapped in the brain, thus resulting in positive amyloid imaging. More recently, findings from tau protein imaging have begun to remodel our understanding of the role of tau in Alzheimer’s disease. Tau imaging correlates with the emergence of symptoms in the MCI phase of Alzheimer’s disease.4 Tau correlates with cognitive decline; positive amyloid imaging does not.
Future Challenges
Looking to the future, it is likely that companion biomarkers such as amyloid and tau imaging will be approved for clinical use. They will enable neurologists to identify the patients whose brain changes match the mechanism of action of the intended treatment (eg, positive tau imaging for those to receive anti-tau therapy and positive amyloid imaging for individuals intended to receive anti-amyloid therapy).
Anticipated directions of therapy development include treatment of individuals before the onset of symptoms, phase-specific therapies that respond to the evolving state changes of Alzheimer’s disease, and combination therapies based on the observation that most patients with Alzheimer’s disease harbor multiple types of brain pathology.5 Alzheimer’s disease therapeutics will proceed in the direction of precision medicine with better matching of therapies to the features of the disorder for the individual patient.
The US health care system is unprepared for the advent of disease-modifying treatments for Alzheimer’s disease. Recognition of patients with mild changes, availability of amyloid imaging to support diagnosis and identify therapeutic targets, and the number of infusion centers to administer monoclonal antibodies are all insufficient to respon
Advances in the understanding of frontotemporal dementia have not yet led to a breakthrough therapy. Frontotemporal dementia has been shown to be pathologically heterogeneous, with about half of the patients having an underlying tauopathy, and about half having TDP-43 as the associated aggregated protein.6 A few cases have rarer forms of pathology. Major phenotypes of frontotemporal dementia include behavioral variant frontotemporal dementia, progressive nonfluent aphasia, and semantic dementia. Trials of new candidate therapies are progressing for frontotemporal dementia spectrum disorders, and new treatments are anticipated.
Progress in understanding dementia with Lewy bodies has led to the publication of diagnostic criteria.7 The phenotype of parkinsonism, fluctuating cognition, and visual hallucinations is supported by decreased dopamine uptake on dopamine transporter (DaT) scanning and the presence of REM sleep behavior disorder. Lewy bodies are found in the limbic and neocortex at autopsy; many cases have concomitant amyloid plaques similar to those of Alzheimer’s disease. Parkinson’s disease dementia has many of the same features and is distinguished from dementia with Lewy bodies only by the order of appearance of major symptoms—dementia first in dementia with Lewy bodies, parkinsonism first in Parkinson’s disease dementia. Rivastigmine is approved for the symptomatic treatment of cognitive deficits in Parkinson’s disease dementia, and trials of new therapies are being conducted in Parkinson’s disease dementia and dementia with Lewy bodies. Alpha-synuclein is present in both disorders and is the target of new disease-modifying treatments currently in clinical trials.
Improved understanding of the basic biology of neurodegenerative disease is critically important and must be accelerated. This knowledge will provide the foundation for improved diagnostics and therapeutics essential for responding to the needs of the burgeoning number of patients with these late-life brain disorders.
References
1. Cummings JL, Morstorf T, Zhong K. Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res Ther. 2014;6(4):37-43.
2. Sevigny J, Chiao P, Bussiere T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50-56.
3. Villemagne VL, Burnham S, Bourgeat P, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12(4):357-367.
4. Johnson KA, Schultz A, Betensky RA, et al. Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann Neurol. 2016;79(1):110-119.
5. James BD, Wilson RS, Boyle PA, et al. TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain. 2016;139(11):2983-2993.
6. Lashley T, Rohrer JD, Mead S, Revesz T. Review: an update on clinical, genetic and pathological aspects of frontotemporal lobar degenerations. Neuropathol Appl Neurobiol. 2015;41(7):858-881.
7. McKeith IG, Boeve BF, Dickson DW, et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88-100.
Jeffrey Cummings, MD, ScD
Director, Cleveland Clinic Lou Ruvo Center for Brain Health, Las Vegas
Disclosure: Jeffrey Cummings has provided consultation to Axovant, biOasis Technologies, Biogen, Boehinger-Ingelheim, Bracket, Dart, Eisai, Genentech, Grifols, Intracellular Therapies, Kyowa, Eli Lilly, Lundbeck, Medavante, Merck, Neurotrope, Novartis, Nutricia, Orion, Otsuka, Pfizer, Probiodrug, QR, Resverlogix, Servier, Suven, Takeda, Toyoma, and United Neuroscience companies.
As Neurology Reviews celebrates its 25th anniversary, we take this opportunity to look back and to look ahead in the area of dementia care and research. Most dementia research has focused on Alzheimer’s disease, although there have been important evolutions in the diagnosis, pathology, and potential interventions for frontotemporal dementia spectrum disorders, dementia with Lewy bodies, Parkinson’s disease dementia, and vascular dementia.
Alzheimer’s Disease
Twenty-five years ago—coinciding with the inauguration of Neurology Reviews—the first treatment for Alzheimer’s disease, the cholinesterase inhibitor tacrine, was approved by the FDA. Tacrine had many limitations, including a short half-life and a propensity to cause hepatotoxicity, but it represented an historical breakthrough in transforming an untreatable disease into a treatable one. The approval energized the field and gave hope to thousands of patients with Alzheimer’s disease dementia.
Tacrine was followed by other cholinesterase inhibitors and memantine in the next decade, with five drugs approved by the end of 2003. Unfortunately, no new agents have been approved for the treatment of Alzheimer’s disease since that fertile period.1 Tremendous efforts are now being devoted to developing disease-modifying treatments for Alzheimer’s disease and other dementias. There are promising preliminary observations for immunotherapies that remove amyloid-beta protein from the brain and stabilize cognitive decline.2 Progress in the development of disease-modifying treatments will transform the field, requiring much of the health care system and insurance companies, but offering an improved quality of life for millions of patients with Alzheimer’s disease.
Previous Advances
A major advance in understanding Alzheimer’s disease is the discovery that the disease begins with amyloid accumulation in mid-life, approximately 15 years before the onset of cognitive decline.3 The advent of amyloid imaging has allowed the visualization of fibrillar amyloid-comprising Alzheimer-type neuritic plaques in the brain of the living person. Scans become positive 15 years prior to the emergence of mild cognitive impairment (MCI) and progression to Alzheimer’s disease dementia. If one is destined to develop MCI at age 75, the scan would be positive by approximately age 60. CSF levels of amyloid beta decline simultaneously as the protein is trapped in the brain, thus resulting in positive amyloid imaging. More recently, findings from tau protein imaging have begun to remodel our understanding of the role of tau in Alzheimer’s disease. Tau imaging correlates with the emergence of symptoms in the MCI phase of Alzheimer’s disease.4 Tau correlates with cognitive decline; positive amyloid imaging does not.
Future Challenges
Looking to the future, it is likely that companion biomarkers such as amyloid and tau imaging will be approved for clinical use. They will enable neurologists to identify the patients whose brain changes match the mechanism of action of the intended treatment (eg, positive tau imaging for those to receive anti-tau therapy and positive amyloid imaging for individuals intended to receive anti-amyloid therapy).
Anticipated directions of therapy development include treatment of individuals before the onset of symptoms, phase-specific therapies that respond to the evolving state changes of Alzheimer’s disease, and combination therapies based on the observation that most patients with Alzheimer’s disease harbor multiple types of brain pathology.5 Alzheimer’s disease therapeutics will proceed in the direction of precision medicine with better matching of therapies to the features of the disorder for the individual patient.
The US health care system is unprepared for the advent of disease-modifying treatments for Alzheimer’s disease. Recognition of patients with mild changes, availability of amyloid imaging to support diagnosis and identify therapeutic targets, and the number of infusion centers to administer monoclonal antibodies are all insufficient to respon
Advances in the understanding of frontotemporal dementia have not yet led to a breakthrough therapy. Frontotemporal dementia has been shown to be pathologically heterogeneous, with about half of the patients having an underlying tauopathy, and about half having TDP-43 as the associated aggregated protein.6 A few cases have rarer forms of pathology. Major phenotypes of frontotemporal dementia include behavioral variant frontotemporal dementia, progressive nonfluent aphasia, and semantic dementia. Trials of new candidate therapies are progressing for frontotemporal dementia spectrum disorders, and new treatments are anticipated.
Progress in understanding dementia with Lewy bodies has led to the publication of diagnostic criteria.7 The phenotype of parkinsonism, fluctuating cognition, and visual hallucinations is supported by decreased dopamine uptake on dopamine transporter (DaT) scanning and the presence of REM sleep behavior disorder. Lewy bodies are found in the limbic and neocortex at autopsy; many cases have concomitant amyloid plaques similar to those of Alzheimer’s disease. Parkinson’s disease dementia has many of the same features and is distinguished from dementia with Lewy bodies only by the order of appearance of major symptoms—dementia first in dementia with Lewy bodies, parkinsonism first in Parkinson’s disease dementia. Rivastigmine is approved for the symptomatic treatment of cognitive deficits in Parkinson’s disease dementia, and trials of new therapies are being conducted in Parkinson’s disease dementia and dementia with Lewy bodies. Alpha-synuclein is present in both disorders and is the target of new disease-modifying treatments currently in clinical trials.
Improved understanding of the basic biology of neurodegenerative disease is critically important and must be accelerated. This knowledge will provide the foundation for improved diagnostics and therapeutics essential for responding to the needs of the burgeoning number of patients with these late-life brain disorders.
References
1. Cummings JL, Morstorf T, Zhong K. Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res Ther. 2014;6(4):37-43.
2. Sevigny J, Chiao P, Bussiere T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50-56.
3. Villemagne VL, Burnham S, Bourgeat P, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12(4):357-367.
4. Johnson KA, Schultz A, Betensky RA, et al. Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann Neurol. 2016;79(1):110-119.
5. James BD, Wilson RS, Boyle PA, et al. TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain. 2016;139(11):2983-2993.
6. Lashley T, Rohrer JD, Mead S, Revesz T. Review: an update on clinical, genetic and pathological aspects of frontotemporal lobar degenerations. Neuropathol Appl Neurobiol. 2015;41(7):858-881.
7. McKeith IG, Boeve BF, Dickson DW, et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88-100.
Snake in the grass
Most accomplished public speakers will tell you that critical to their success is the ability to understand and adapt to their audiences. It turns out that even chimpanzees accept and use this cornerstone of effective communication.
In a study published in Science Advances (2017 Nov 15;3[11]:e1701742), three scientists working in Uganda reported that chimpanzees who encounter a potential threat in the form of a realistic snake model will vocalize significantly fewer alert hoots if they hear other alert calls coming from the jungle in the vicinity. In other words, the chimp is saying to himself, “Why should I bother wasting my time and lung power hooting to warn my troop mates? Those guys already know about the snake.”
To select which anticipatory guidance topics to include and still be effective communicators, we have to know the families we are trying to help. Gaining this more nuanced picture of a family takes time and is fostered by continuity. Seeing a different provider at each visit doesn’t work very well here. What are this unique family’s concerns, regardless of what some committee thinks we should be asking?
How much can we rely on the media and groups such as the American Academy of Pediatrics and the Centers for Disease Control and Prevention to get out the messages that we have decided to skip over to address this family’s special concerns? Is the message about the benefits of breastfeeding so widely known that we will be wasting our limited office time repeating it? Is the same true for gun safety and seat belts? This is where research can help us decide where to target messages on a national level. But large population studies don’t always apply to our communities and the families we serve.
Where does our role as primary care physicians fit into the bigger picture of health education? The warning messages issued on a national level may have little relevance for our individual patients’ concerns. Is it our role to echo the message, or are we the ones who must do the fine-tuning?
And then there are the recent depressing and counterintuitive findings that for hot-button topics like immunization, education has little if any value. Those families with firmly held beliefs might acknowledge the rationale of our reasoning, but then quickly slide to another argument to tighten their grips on their original position.
Finally, we must be careful to avoid being labeled as the folks whose message is all about what parents should be afraid of. There are plenty of snakes out there in the jungle, but the chimpanzees have realized that when enough of the population is aware of the threat, then it is time to adjust their message. Certainly enough health problems exist on a national level to warrant continued messaging from the large groups in organized medicine. However, it is up to us out in the jungle to learn enough about our patients to know when we should echo those alerts and when it’s time to save our breath. We can’t hoot about every snake in the grass.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Most accomplished public speakers will tell you that critical to their success is the ability to understand and adapt to their audiences. It turns out that even chimpanzees accept and use this cornerstone of effective communication.
In a study published in Science Advances (2017 Nov 15;3[11]:e1701742), three scientists working in Uganda reported that chimpanzees who encounter a potential threat in the form of a realistic snake model will vocalize significantly fewer alert hoots if they hear other alert calls coming from the jungle in the vicinity. In other words, the chimp is saying to himself, “Why should I bother wasting my time and lung power hooting to warn my troop mates? Those guys already know about the snake.”
To select which anticipatory guidance topics to include and still be effective communicators, we have to know the families we are trying to help. Gaining this more nuanced picture of a family takes time and is fostered by continuity. Seeing a different provider at each visit doesn’t work very well here. What are this unique family’s concerns, regardless of what some committee thinks we should be asking?
How much can we rely on the media and groups such as the American Academy of Pediatrics and the Centers for Disease Control and Prevention to get out the messages that we have decided to skip over to address this family’s special concerns? Is the message about the benefits of breastfeeding so widely known that we will be wasting our limited office time repeating it? Is the same true for gun safety and seat belts? This is where research can help us decide where to target messages on a national level. But large population studies don’t always apply to our communities and the families we serve.
Where does our role as primary care physicians fit into the bigger picture of health education? The warning messages issued on a national level may have little relevance for our individual patients’ concerns. Is it our role to echo the message, or are we the ones who must do the fine-tuning?
And then there are the recent depressing and counterintuitive findings that for hot-button topics like immunization, education has little if any value. Those families with firmly held beliefs might acknowledge the rationale of our reasoning, but then quickly slide to another argument to tighten their grips on their original position.
Finally, we must be careful to avoid being labeled as the folks whose message is all about what parents should be afraid of. There are plenty of snakes out there in the jungle, but the chimpanzees have realized that when enough of the population is aware of the threat, then it is time to adjust their message. Certainly enough health problems exist on a national level to warrant continued messaging from the large groups in organized medicine. However, it is up to us out in the jungle to learn enough about our patients to know when we should echo those alerts and when it’s time to save our breath. We can’t hoot about every snake in the grass.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Most accomplished public speakers will tell you that critical to their success is the ability to understand and adapt to their audiences. It turns out that even chimpanzees accept and use this cornerstone of effective communication.
In a study published in Science Advances (2017 Nov 15;3[11]:e1701742), three scientists working in Uganda reported that chimpanzees who encounter a potential threat in the form of a realistic snake model will vocalize significantly fewer alert hoots if they hear other alert calls coming from the jungle in the vicinity. In other words, the chimp is saying to himself, “Why should I bother wasting my time and lung power hooting to warn my troop mates? Those guys already know about the snake.”
To select which anticipatory guidance topics to include and still be effective communicators, we have to know the families we are trying to help. Gaining this more nuanced picture of a family takes time and is fostered by continuity. Seeing a different provider at each visit doesn’t work very well here. What are this unique family’s concerns, regardless of what some committee thinks we should be asking?
How much can we rely on the media and groups such as the American Academy of Pediatrics and the Centers for Disease Control and Prevention to get out the messages that we have decided to skip over to address this family’s special concerns? Is the message about the benefits of breastfeeding so widely known that we will be wasting our limited office time repeating it? Is the same true for gun safety and seat belts? This is where research can help us decide where to target messages on a national level. But large population studies don’t always apply to our communities and the families we serve.
Where does our role as primary care physicians fit into the bigger picture of health education? The warning messages issued on a national level may have little relevance for our individual patients’ concerns. Is it our role to echo the message, or are we the ones who must do the fine-tuning?
And then there are the recent depressing and counterintuitive findings that for hot-button topics like immunization, education has little if any value. Those families with firmly held beliefs might acknowledge the rationale of our reasoning, but then quickly slide to another argument to tighten their grips on their original position.
Finally, we must be careful to avoid being labeled as the folks whose message is all about what parents should be afraid of. There are plenty of snakes out there in the jungle, but the chimpanzees have realized that when enough of the population is aware of the threat, then it is time to adjust their message. Certainly enough health problems exist on a national level to warrant continued messaging from the large groups in organized medicine. However, it is up to us out in the jungle to learn enough about our patients to know when we should echo those alerts and when it’s time to save our breath. We can’t hoot about every snake in the grass.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Withholding elective surgery in smokers, obese patients
No one will argue that obesity and tobacco aren’t serious public health issues, underlying many causes of morbidity and mortality. As a result, they’re driving factors behind a fair amount of health care spending.
In England, the county of Hertfordshire recently adopted a new approach to this: a ban on routine, nonurgent surgeries for both. Those with a body mass index of 30-40 kg/m2 must lose 10% of their weight over 9 months to qualify for a procedure, while those with a BMI above 40 must lose 15%. Smokers have to go 8 weeks without a cigarette and take breath tests to prove it.
The group that formulated the plan noted that resources to help these groups achieve such goals are (and will continue to be) freely available.
Not unexpectedly, the plan is controversial. Robert West, MD, a professor of health psychology and director of tobacco studies at the University College London, told CNN that “rationing treatment on the basis of unhealthy behaviors betrays an extraordinary naivety about what drives those behaviors.”
Of course, this debate is nothing new. In December 2014, I wrote about surgeons in the United States who were refusing to do elective hernia repairs on smokers because of their higher complication rates.
A lot of this is framed in terms of money, since that’s the driving factor. Obese patients and smokers do have higher rates of surgical complications in general, with longer recoveries and, hence, higher costs. This policy tries to put greater responsibility on patients to maintain their own health and well-being. After all, financial resources are a finite, shared commodity.
Like everything in modern health care, there’s no easy answer. Insurers and doctors try to balance better outcomes vs. greater good and cost savings.
Medicine is, and always will be, an ongoing experiment, where some things work, some don’t, and we learn from time and experience.
Unfortunately, patients and their doctors are often caught in the middle, trapped between market and political forces on one side and caring for those who need us on the other. That’s never good, or easy, for those directly involved with individual patients on the front lines of medical care.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
No one will argue that obesity and tobacco aren’t serious public health issues, underlying many causes of morbidity and mortality. As a result, they’re driving factors behind a fair amount of health care spending.
In England, the county of Hertfordshire recently adopted a new approach to this: a ban on routine, nonurgent surgeries for both. Those with a body mass index of 30-40 kg/m2 must lose 10% of their weight over 9 months to qualify for a procedure, while those with a BMI above 40 must lose 15%. Smokers have to go 8 weeks without a cigarette and take breath tests to prove it.
The group that formulated the plan noted that resources to help these groups achieve such goals are (and will continue to be) freely available.
Not unexpectedly, the plan is controversial. Robert West, MD, a professor of health psychology and director of tobacco studies at the University College London, told CNN that “rationing treatment on the basis of unhealthy behaviors betrays an extraordinary naivety about what drives those behaviors.”
Of course, this debate is nothing new. In December 2014, I wrote about surgeons in the United States who were refusing to do elective hernia repairs on smokers because of their higher complication rates.
A lot of this is framed in terms of money, since that’s the driving factor. Obese patients and smokers do have higher rates of surgical complications in general, with longer recoveries and, hence, higher costs. This policy tries to put greater responsibility on patients to maintain their own health and well-being. After all, financial resources are a finite, shared commodity.
Like everything in modern health care, there’s no easy answer. Insurers and doctors try to balance better outcomes vs. greater good and cost savings.
Medicine is, and always will be, an ongoing experiment, where some things work, some don’t, and we learn from time and experience.
Unfortunately, patients and their doctors are often caught in the middle, trapped between market and political forces on one side and caring for those who need us on the other. That’s never good, or easy, for those directly involved with individual patients on the front lines of medical care.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
No one will argue that obesity and tobacco aren’t serious public health issues, underlying many causes of morbidity and mortality. As a result, they’re driving factors behind a fair amount of health care spending.
In England, the county of Hertfordshire recently adopted a new approach to this: a ban on routine, nonurgent surgeries for both. Those with a body mass index of 30-40 kg/m2 must lose 10% of their weight over 9 months to qualify for a procedure, while those with a BMI above 40 must lose 15%. Smokers have to go 8 weeks without a cigarette and take breath tests to prove it.
The group that formulated the plan noted that resources to help these groups achieve such goals are (and will continue to be) freely available.
Not unexpectedly, the plan is controversial. Robert West, MD, a professor of health psychology and director of tobacco studies at the University College London, told CNN that “rationing treatment on the basis of unhealthy behaviors betrays an extraordinary naivety about what drives those behaviors.”
Of course, this debate is nothing new. In December 2014, I wrote about surgeons in the United States who were refusing to do elective hernia repairs on smokers because of their higher complication rates.
A lot of this is framed in terms of money, since that’s the driving factor. Obese patients and smokers do have higher rates of surgical complications in general, with longer recoveries and, hence, higher costs. This policy tries to put greater responsibility on patients to maintain their own health and well-being. After all, financial resources are a finite, shared commodity.
Like everything in modern health care, there’s no easy answer. Insurers and doctors try to balance better outcomes vs. greater good and cost savings.
Medicine is, and always will be, an ongoing experiment, where some things work, some don’t, and we learn from time and experience.
Unfortunately, patients and their doctors are often caught in the middle, trapped between market and political forces on one side and caring for those who need us on the other. That’s never good, or easy, for those directly involved with individual patients on the front lines of medical care.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Point/Counterpoint: Should FEVAR be used for a short neck?
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.
FEVAR is generally the best option
The advent of endovascular aortic aneurysm repair (EVAR) has steadily become the standard of care in the management of infrarenal abdominal aortic aneurysms (AAAs). In fact, it has now surpassed open surgical repair and is the predominant therapeutic modality in managing this disease entity. Clearly, there are specific anatomic and technical factors that may preclude the use of traditional EVAR – most notably, challenging proximal neck anatomy, be it insufficient length or severe angulation.
It is estimated that up to 30%-40% of patients are unsuitable candidates because of these concerns.1 Such patients are thus relegated to traditional open repair with the associated concerns for supravisceral clamping, including dramatic changes in hemodynamics and prolonged ICU and hospital stays.
Open surgical repair of pararenal, juxtarenal, and suprarenal AAAs is tried, tested, and durable. Knott and the group from Mayo Clinic reviewed their repair of 126 consecutive elective juxtarenal AAAs requiring suprarenal aortic clamping noting a 30-day mortality of .8%.2 More recent data from Kabbani and the Henry Ford group involved their 27-year clinical experience suggesting that open repair of complex proximal aortic aneurysms can be performed with clinical outcomes that are similar to those of open infrarenal repair.3 I respectfully accept this traditional – and historic – treatment modality.
However, we vascular surgeons are progressive and resilient in our quest to innovate and modernize – some of us even modified the traditional endografts on the back table. We charged forward despite the initial paucity of data on infrarenal EVAR compared to traditional open repair of aneurysms in the past. Now, a large percentage of infrarenal AAA repairs are performed via EVAR. In fact, our steadfast progression to advanced endovascular techniques has raised the concern that our graduating trainees are no longer proficient, competent, or even capable, in open complex aneurysm repair!
Tsilimparis and colleagues reported the first outcomes comparing open repair and FEVAR.4 They queried the NSQIP database comparing 1,091 patients undergoing open repair with 264 in the FEVAR group. There was an increased risk of morbidity in all combined endpoints including pulmonary and cardiovascular complications as well as length of stay in patients undergoing the open repair group. A larger comprehensive review pooled the results from 8 FEVAR and 12 open repair series. Analysis of the data found the groups to be identical. Open repair, however, was found to have an increased 30-day mortality when compared to FEVAR (relative risk 1.03, 2% increased absolute mortality).5
Gupta and colleagues reported the latest multi-institutional data noting that open repair was associated with higher risk than FEVAR for 30-day mortality, cardiac and pulmonary complications, renal failure requiring dialysis, return to the operating room, and in this age of cost-containment, length of stay (2 days vs. 7 days; P less than .0001).6
A further study by Donas and colleagues evaluated 90 consecutive patients with primary degenerative juxtarenal AAAs to different operative strategies based on morphologic and clinical characteristics – 29 FEVAR, 30 chEVAR, and 31 open repair.7 Early procedure-related and all-cause 30-day mortality was 0% in the endovascular group and 6.4% in the open group.
Although open repair for juxtarenal AAAs is the gold standard, short- and mid-term data on the outcomes for complex endovascular repair are excellent. Data on long-term durability, graft fixation/migration as well as the integrity of the graft and concerns for endoleaks and branch vessel patency, however, are limited. We do not have long-term data because we have not been doing these newer procedures for that long – but the data thus far show great promise.
We need to continue to challenge the status quo, particularly when the current data are satisfactory and the procedure feasible. With our continued appraisal of the data we publish as vascular surgeons, we can then identify if these innovations and techniques will withstand the test of time. After all, we are vascular surgeons (particularly those of us who have trained extensively in open repair) – and if open repair is necessary, then we will be ready.
But, if I can avoid a thoracoabdominal incision for a few percutaneous access sites, then sign me up!
Dr. Mouawad is chief of vascular and endovascular surgery, medical director of the vascular laboratory, and vice-chair of the department of surgery at McLaren Bay Region, Bay City, Mich. He is assistant professor of surgery at Michigan State University and Central Michigan University.
References
1. Perspect Vasc Surg Endovasc Ther. 2009;21:13-8.
2. J Vasc Surg. 2008;47:695-701.
3. J Vasc Surg. 2014;59:1488-94.
4. Ann Vasc Surg. 2013;27(3):267-73.
5. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
6. J Vasc Surg. 2017 Dec;66(6):1653-8.
7. J Vasc Surg. 2012 Aug;56(2):285-90.
FEVAR may not be the best choice
Over the past 3 decades, EVAR, with its very low periprocedural morbidity and mortality, and satisfactory long-term results, has become the primary treatment modality for the majority of infrarenal AAAs. The success of stent grafts for the repair of AAA relies heavily on satisfactory proximal and distal seal zones. Each commercially available standard EVAR graft has a manufacturer’s instructions for use requiring a proximal landing zone length of between 10 and 15 mm. Patients with less than this required length are considered to have “short necks.” Evaluation of this group of patients has demonstrated that this is not an uncommon finding and that EVAR performed outside the instructions for use has been associated with an increased risk of intraoperative failure, aneurysm expansion, and later complications.1-3
Current treatment options for patients with short necks include open surgical repair (OSR), FEVAR, and EVAR with the chimney graft technique (Ch-EVAR).
Thus, current knowledge acquired from case series, registries, and clinical experience must be used in deciding which therapeutic option to offer patients. Relevant factors influencing this decision include the availability and adaptability of the technique, early outcomes including technical success, morbidity and mortality, and late outcomes including survival, need for reintervention, and other late morbidity. Finally, in an era of value-based medical care, cost also must be considered.
Currently there is only one Food and Drug Administration–approved fenestrated graft. When used in properly selected patients, excellent periprocedural results have been reported approaching those of standard EVAR. However, there are limitations in both the availability and adaptability of FEVAR. These grafts are custom made for each patient, often requiring several weeks of lead time. Adaptability also has its limitations, including access vessels, severe neck angulation, calcification, mural thrombus, and branch vessel size, number, location, and associated arterial disease. Any of these factors may preclude the use of this technology. Open repair, on the other hand, is not limited by graft availability and allows for custom modification for each patient’s specific disease morphology. The essential limitation for open repair is the patient’s physiological ability to withstand the operation.
Several studies attempting to compare the early outcomes of FEVAR versus comparable patients undergoing OSR of similar aneurysms have reported significantly lower 30-day mortality and major morbidity rates for FEVAR.4,5 However, Rao et al., in a recent systematic review and meta-analysis that included data on 2,326 patients from 35 case series reporting on elective repair of juxtarenal aneurysms by either OSR or FEVAR, found perioperative mortality to not be significantly different (4.1% for both). Also, no significant difference was found between the two groups when evaluating postoperative renal insufficiency and need for permanent dialysis. However, OSR did have significantly higher major complication rates (25% vs. 15.7%).6 These findings suggest that both modalities can be performed successfully, but that long term outcomes need to be considered to determine if the increased initial morbidity of OSR is justified by differences in long term results between the two modalities.
Open surgical repair of juxtarenal AAA has been shown to be a durable repair.7 While early and even intermediate results of FEVAR appear to be satisfactory, long-term durability has yet to be determined.4,8 Along with continuing to exclude the aneurysm sac, as with standard EVAR, there is the additional concern regarding the outcome of the organs supplied by the fenestrated/stent-grafted branches with FEVAR. Longer-term follow-up in the same review by Rao et al. showed that significantly more FEVAR patients developed renal failure compared with OSR patients (19.7% vs. 7.7%). FEVAR patients also had a higher rate of reintervention.
And finally, long-term survival was significantly greater in OSR patients compared to FEVAR at 3 and 5 years (80% vs. 74% vs. 73% vs. 55%). These authors concluded that open repair remains the gold standard while FEVAR is a favorable option for high risk patients.6
These new and innovative stent graft devices come at considerable expense. While this aspect of FEVAR has not been extensively studied, Michel et al., in their report from the multicenter prospective Windows registry, attempted to evaluate the economic aspect of FEVAR. They compared a group of patients who underwent FEVAR to patients from a large national hospital discharge database who underwent OSR. No difference in 30-day mortality was noted between these two groups; however, there was a significantly greater cost with FEVAR. The authors concluded that FEVAR did not appear to be justified for patients fit for open surgery with juxtarenal AAA.9
For now, the roles of OSR and FEVAR would appear to be complementary. Current evidence suggests that OSR is the most appropriate intervention for good risk patients with an anticipated longer life expectancy. Patients with appropriate anatomy for FEVAR and who are at higher risk for open repair would benefit from FEVAR. As further experience and outcomes are accumulated, our ability to select the appropriate therapy for individual patients should improve.
Dr. Weaver is an assistant clinical professor for surgery at Wayne State School of Medicine, Detroit, and an attending in the division of vascular surgery, Henry Ford Hospital.
References
1. Ir J Med Sci. 2015;184(1):249-55.
2. Circulation. 2011;123(24):2848-55.
3. J Endovasc Therapy. 2001;8(5):457-64.
4. Eur J Vasc Endovasc Surg. 2009;38(1):35-41.
5. Ann Vasc Surg. 2013;27(3):267-73.
6. J Vasc Surg. 2015;61(1):242-55.
7. J Vasc Surg. 2012;56(1):2-7.
8. J Cardiovasc Surg. 2015;56(3):331-7.
9. Eur J Vasc Endovasc Surg. 2015;50(2):189-96.






















