User login
Edaravone: Costs versus benefits
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
Physician health programs: ‘Diagnosing for dollars’?
As medicine struggles with rising rates of physician burnout, dissatisfaction, depression, and suicide, one solution comes in the form of Physician Health Programs, or PHPs. These organizations were originally started by volunteer physicians, often doctors in recovery, and funded by medical societies, as a way of providing help while maintaining confidentiality. Now, they are run by independent corporations, by medical societies in some states, and sometimes by hospitals or health systems. The services they offer vary by PHP, and they may have relationships with state licensing boards. While they can provide a gateway to help for a troubled doctor, there has also been concern about the services that are being provided.
Louise Andrew, MD, JD, served as the liaison from the American College of Emergency Physicians (ACEP) to the the Federation of State Medical Boards from 2006 to 2014. In an online forum called Collective Wisdom, Andrew talked about the benefits of Physician Health Programs as entities that are helpful to stuggling doctors and urged her colleagues to use them as a safe alternative to suffering in silence.
More recently, Dr. Andrew has become concerned that PHPs may have taken on the role of what is more akin to “diagnosing for dollars.” In her May, 2016 column in Emergency Physician’s Monthly, Andrew noted, “A decade later, and my convictions have changed dramatically. Horror stories that colleagues related to me while I chaired ACEP’s Personal and Professional WellBeing Committee cannot all be isolated events. For example, physicians who self-referred to the PHP for management of stress and depression were reportedly railroaded into incredibly expensive and inconvenient out-of-state drug and alcohol treatment programs, even when there was no coexisting drug or alcohol problem.”
Dr. Andrew is not the only one voicing concerns about PHPs. In “Physician Health Programs: More harm than good?” (Medscape, Aug. 19, 2015), Pauline Anderson wrote about a several problems that have surfaced. In North Carolina, the state audited the PHPs after complaints that they were mandating physicians to lengthy and expensive inpatient programs. The complaints asserted that the physicians had no recourse and were not able to see their records. “The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat – the report determined that abuse could occur and potentially go undetected.
“It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.”
Finally, in a Florida Fox4News story, “Are FL doctors and nurses being sent to rehab unnecessarily? Accusations: Overdiagnosing; overcharging” (Nov. 16, 2017), reporters Katie Lagrone and Matthew Apthorp wrote about financial incentives for evaluators to refer doctors to inpatient substance abuse facilities.
The American Psychiatric Association has made it a priority to address physician burnout and mental health. Richard F. Summers, MD, APA Trustee-at-Large noted: “State PHPs are an essential resource for physicians, but there is a tremendous diversity in quality and approach. It is critical that these programs include attention to mental health problems as well as addiction, and that they support individual physicians’ treatment and journey toward well-being. They need to be accessible, private, and high quality, and they should be staffed by excellent psychiatrists and other mental health professionals.”
PHPs provide a much-needed and wanted service. But if the goal is to provide mental health and substance abuse services to physicians who are struggling – to prevent physicians from burning out, leaving medicine, and dying of suicide – then any whiff of corruption and any fear of professional repercussions become a reason not to use these services. If they are to be helpful, physicians must feel safe using them.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
As medicine struggles with rising rates of physician burnout, dissatisfaction, depression, and suicide, one solution comes in the form of Physician Health Programs, or PHPs. These organizations were originally started by volunteer physicians, often doctors in recovery, and funded by medical societies, as a way of providing help while maintaining confidentiality. Now, they are run by independent corporations, by medical societies in some states, and sometimes by hospitals or health systems. The services they offer vary by PHP, and they may have relationships with state licensing boards. While they can provide a gateway to help for a troubled doctor, there has also been concern about the services that are being provided.
Louise Andrew, MD, JD, served as the liaison from the American College of Emergency Physicians (ACEP) to the the Federation of State Medical Boards from 2006 to 2014. In an online forum called Collective Wisdom, Andrew talked about the benefits of Physician Health Programs as entities that are helpful to stuggling doctors and urged her colleagues to use them as a safe alternative to suffering in silence.
More recently, Dr. Andrew has become concerned that PHPs may have taken on the role of what is more akin to “diagnosing for dollars.” In her May, 2016 column in Emergency Physician’s Monthly, Andrew noted, “A decade later, and my convictions have changed dramatically. Horror stories that colleagues related to me while I chaired ACEP’s Personal and Professional WellBeing Committee cannot all be isolated events. For example, physicians who self-referred to the PHP for management of stress and depression were reportedly railroaded into incredibly expensive and inconvenient out-of-state drug and alcohol treatment programs, even when there was no coexisting drug or alcohol problem.”
Dr. Andrew is not the only one voicing concerns about PHPs. In “Physician Health Programs: More harm than good?” (Medscape, Aug. 19, 2015), Pauline Anderson wrote about a several problems that have surfaced. In North Carolina, the state audited the PHPs after complaints that they were mandating physicians to lengthy and expensive inpatient programs. The complaints asserted that the physicians had no recourse and were not able to see their records. “The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat – the report determined that abuse could occur and potentially go undetected.
“It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.”
Finally, in a Florida Fox4News story, “Are FL doctors and nurses being sent to rehab unnecessarily? Accusations: Overdiagnosing; overcharging” (Nov. 16, 2017), reporters Katie Lagrone and Matthew Apthorp wrote about financial incentives for evaluators to refer doctors to inpatient substance abuse facilities.
The American Psychiatric Association has made it a priority to address physician burnout and mental health. Richard F. Summers, MD, APA Trustee-at-Large noted: “State PHPs are an essential resource for physicians, but there is a tremendous diversity in quality and approach. It is critical that these programs include attention to mental health problems as well as addiction, and that they support individual physicians’ treatment and journey toward well-being. They need to be accessible, private, and high quality, and they should be staffed by excellent psychiatrists and other mental health professionals.”
PHPs provide a much-needed and wanted service. But if the goal is to provide mental health and substance abuse services to physicians who are struggling – to prevent physicians from burning out, leaving medicine, and dying of suicide – then any whiff of corruption and any fear of professional repercussions become a reason not to use these services. If they are to be helpful, physicians must feel safe using them.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
As medicine struggles with rising rates of physician burnout, dissatisfaction, depression, and suicide, one solution comes in the form of Physician Health Programs, or PHPs. These organizations were originally started by volunteer physicians, often doctors in recovery, and funded by medical societies, as a way of providing help while maintaining confidentiality. Now, they are run by independent corporations, by medical societies in some states, and sometimes by hospitals or health systems. The services they offer vary by PHP, and they may have relationships with state licensing boards. While they can provide a gateway to help for a troubled doctor, there has also been concern about the services that are being provided.
Louise Andrew, MD, JD, served as the liaison from the American College of Emergency Physicians (ACEP) to the the Federation of State Medical Boards from 2006 to 2014. In an online forum called Collective Wisdom, Andrew talked about the benefits of Physician Health Programs as entities that are helpful to stuggling doctors and urged her colleagues to use them as a safe alternative to suffering in silence.
More recently, Dr. Andrew has become concerned that PHPs may have taken on the role of what is more akin to “diagnosing for dollars.” In her May, 2016 column in Emergency Physician’s Monthly, Andrew noted, “A decade later, and my convictions have changed dramatically. Horror stories that colleagues related to me while I chaired ACEP’s Personal and Professional WellBeing Committee cannot all be isolated events. For example, physicians who self-referred to the PHP for management of stress and depression were reportedly railroaded into incredibly expensive and inconvenient out-of-state drug and alcohol treatment programs, even when there was no coexisting drug or alcohol problem.”
Dr. Andrew is not the only one voicing concerns about PHPs. In “Physician Health Programs: More harm than good?” (Medscape, Aug. 19, 2015), Pauline Anderson wrote about a several problems that have surfaced. In North Carolina, the state audited the PHPs after complaints that they were mandating physicians to lengthy and expensive inpatient programs. The complaints asserted that the physicians had no recourse and were not able to see their records. “The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat – the report determined that abuse could occur and potentially go undetected.
“It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.”
Finally, in a Florida Fox4News story, “Are FL doctors and nurses being sent to rehab unnecessarily? Accusations: Overdiagnosing; overcharging” (Nov. 16, 2017), reporters Katie Lagrone and Matthew Apthorp wrote about financial incentives for evaluators to refer doctors to inpatient substance abuse facilities.
The American Psychiatric Association has made it a priority to address physician burnout and mental health. Richard F. Summers, MD, APA Trustee-at-Large noted: “State PHPs are an essential resource for physicians, but there is a tremendous diversity in quality and approach. It is critical that these programs include attention to mental health problems as well as addiction, and that they support individual physicians’ treatment and journey toward well-being. They need to be accessible, private, and high quality, and they should be staffed by excellent psychiatrists and other mental health professionals.”
PHPs provide a much-needed and wanted service. But if the goal is to provide mental health and substance abuse services to physicians who are struggling – to prevent physicians from burning out, leaving medicine, and dying of suicide – then any whiff of corruption and any fear of professional repercussions become a reason not to use these services. If they are to be helpful, physicians must feel safe using them.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
Myth of the Month: MONA for acute treatment of chest pain?
A 66-year-old man presents with substernal chest pressure and dyspnea that has been present for 45 minutes. He has nausea. Vital signs: blood pressure, 110/60; pulse, 100; oxygen saturation, 92%. Neck: elevated jugular venous pressure. Chest: clear. Cardiac: normal S1 S2, no murmurs. ECG: ST elevation in 2, 3, and aVF leads.
Which of these treatments do you recommend?
A. Morphine, oxygen, nitroglycerin, and aspirin (ASA).
B. Oxygen, morphine, ASA.
C. ASA.
In this patient, I think the correct approach would be to just give aspirin. Nitroglycerin would be problematic, as it appears that this patient might be having a right ventricular infarct, and lowering right-sided filling pressures with nitroglycerin may lead to severe hypotension.
There is controversy over the safety of routine morphine use for patients with chest pain.
Trip J. Meine, MD, and colleagues found that use of morphine either alone or in combination with nitroglycerin for patients presenting with non–ST-elevation acute coronary syndrome (NSTE-ACS) was associated with higher mortality.1 Cian P. McCarthy, MD, and colleagues found the same results, with morphine use associated with larger infarct size, a longer hospital stay, and a trend toward increased mortality in invasively managed NSTE-ACS patients.2 Suzanne de Waha and colleagues found that morphine use in patients with ST-segment elevation MIs had larger infarct size and less reperfusion success, as measured by cardiac MRI.3
Not all recent studies show a detrimental effect of morphine. Etienne Puymirat et al. reviewed in-hospital complications (death, nonfatal re-MI, stroke, stent thrombosis, and bleeding) and 1-year survival according to prehospital morphine use in 2,438 ST-elevation MI (STEMI) patients from the French Registry of Acute ST-elevation and non–ST-elevation Myocardial Infarction (FAST-MI).4 They found no increase in in-hospital complications or 1-year mortality.
The practice of using supplemental oxygen to treat all patients with MI became standard nearly a century ago, after oxygen was found in 1900 to relieve angina, and led to clinical improvement in four MI patients in a 1930 case series.5,6
It was not studied in a controlled trial until 1976, when J.M. Rawles, MD, and colleagues randomized 157 patients with MI to 24 hours of oxygen at 8 L/min or to ambient air. They found no difference in mortality between the groups, but they did find a higher burden of MI in the intervention arm receiving supplemental oxygen, as measured by mean serum aspartate aminotransferase levels.7
The topic was not addressed again in a significant randomized trial until this century. Most notably, two recent studies again demonstrated no benefit of supplemental oxygen in normoxemic patients with MI.
In the AVOID trial in 2015, Dion Stub, MD, PhD, and colleagues randomized 441 patients with STEMI to oxygen at 8 L/min – from diagnosis in an ambulance until after cardiac catheterization – or to ambient air. They found no difference in death at 6 months, but did find an increased rate of in-hospital recurrent MIs, with 0.9% of the control group and 5.5% of the oxygen intervention arm suffering recurrence (P = .006).8 They also showed a larger area of myocardial infarct in the oxygen group, as measured by peak creatine kinase levels and cardiac MRI at 6 months.
Proposed mechanisms of increased myocardial injury from hyperoxia include increased coronary vascular resistance resulting in decreased myocardial perfusion, and increased reperfusion injury from formation of free radicals.9
Where does all this leave us in the treatment of suspected MI?
Morphine should only be used when the patient has pain, and is probably best reserved for severe pain, as the safety of its use is not clear. While hypoxemia is a common consequence of MI – and may correlate with worse outcomes – treatment with supplemental oxygen in the absence of hypoxemia is not supported by current evidence, and may carry risk of harm. Nitroglycerin should be avoided in patients with right ventricular infarcts, and in patients who present with hypotension.
Dr. Tubbesing is a senior resident in medicine at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Am Heart J. 2005 Jun;149(6):1043-9.
2. J Interv Cardiol. 2017 Nov 22. doi: 10.1111/joic.12464.
3. Clin Res Cardiol. 2015 Sep;104(9):727-34.
4. Eur Heart J. 2016 Apr 1;37(13):1063-71.
5. BMJ. 1900 Dec 1;2(2083):1568.
6. JAMA. 1930 May 3;94(18):1363-5.
7. Br Med J. 1976 May 8;1(6018):1121-3.
8. Circulation. 2015 Jun 16;131(24):2143-50.
9. Cochrane Database Syst Rev. 2016 Dec 19;12:CD007160.
10. N Engl J Med. 2017 Sep 28;377(13):1240-9.
A 66-year-old man presents with substernal chest pressure and dyspnea that has been present for 45 minutes. He has nausea. Vital signs: blood pressure, 110/60; pulse, 100; oxygen saturation, 92%. Neck: elevated jugular venous pressure. Chest: clear. Cardiac: normal S1 S2, no murmurs. ECG: ST elevation in 2, 3, and aVF leads.
Which of these treatments do you recommend?
A. Morphine, oxygen, nitroglycerin, and aspirin (ASA).
B. Oxygen, morphine, ASA.
C. ASA.
In this patient, I think the correct approach would be to just give aspirin. Nitroglycerin would be problematic, as it appears that this patient might be having a right ventricular infarct, and lowering right-sided filling pressures with nitroglycerin may lead to severe hypotension.
There is controversy over the safety of routine morphine use for patients with chest pain.
Trip J. Meine, MD, and colleagues found that use of morphine either alone or in combination with nitroglycerin for patients presenting with non–ST-elevation acute coronary syndrome (NSTE-ACS) was associated with higher mortality.1 Cian P. McCarthy, MD, and colleagues found the same results, with morphine use associated with larger infarct size, a longer hospital stay, and a trend toward increased mortality in invasively managed NSTE-ACS patients.2 Suzanne de Waha and colleagues found that morphine use in patients with ST-segment elevation MIs had larger infarct size and less reperfusion success, as measured by cardiac MRI.3
Not all recent studies show a detrimental effect of morphine. Etienne Puymirat et al. reviewed in-hospital complications (death, nonfatal re-MI, stroke, stent thrombosis, and bleeding) and 1-year survival according to prehospital morphine use in 2,438 ST-elevation MI (STEMI) patients from the French Registry of Acute ST-elevation and non–ST-elevation Myocardial Infarction (FAST-MI).4 They found no increase in in-hospital complications or 1-year mortality.
The practice of using supplemental oxygen to treat all patients with MI became standard nearly a century ago, after oxygen was found in 1900 to relieve angina, and led to clinical improvement in four MI patients in a 1930 case series.5,6
It was not studied in a controlled trial until 1976, when J.M. Rawles, MD, and colleagues randomized 157 patients with MI to 24 hours of oxygen at 8 L/min or to ambient air. They found no difference in mortality between the groups, but they did find a higher burden of MI in the intervention arm receiving supplemental oxygen, as measured by mean serum aspartate aminotransferase levels.7
The topic was not addressed again in a significant randomized trial until this century. Most notably, two recent studies again demonstrated no benefit of supplemental oxygen in normoxemic patients with MI.
In the AVOID trial in 2015, Dion Stub, MD, PhD, and colleagues randomized 441 patients with STEMI to oxygen at 8 L/min – from diagnosis in an ambulance until after cardiac catheterization – or to ambient air. They found no difference in death at 6 months, but did find an increased rate of in-hospital recurrent MIs, with 0.9% of the control group and 5.5% of the oxygen intervention arm suffering recurrence (P = .006).8 They also showed a larger area of myocardial infarct in the oxygen group, as measured by peak creatine kinase levels and cardiac MRI at 6 months.
Proposed mechanisms of increased myocardial injury from hyperoxia include increased coronary vascular resistance resulting in decreased myocardial perfusion, and increased reperfusion injury from formation of free radicals.9
Where does all this leave us in the treatment of suspected MI?
Morphine should only be used when the patient has pain, and is probably best reserved for severe pain, as the safety of its use is not clear. While hypoxemia is a common consequence of MI – and may correlate with worse outcomes – treatment with supplemental oxygen in the absence of hypoxemia is not supported by current evidence, and may carry risk of harm. Nitroglycerin should be avoided in patients with right ventricular infarcts, and in patients who present with hypotension.
Dr. Tubbesing is a senior resident in medicine at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Am Heart J. 2005 Jun;149(6):1043-9.
2. J Interv Cardiol. 2017 Nov 22. doi: 10.1111/joic.12464.
3. Clin Res Cardiol. 2015 Sep;104(9):727-34.
4. Eur Heart J. 2016 Apr 1;37(13):1063-71.
5. BMJ. 1900 Dec 1;2(2083):1568.
6. JAMA. 1930 May 3;94(18):1363-5.
7. Br Med J. 1976 May 8;1(6018):1121-3.
8. Circulation. 2015 Jun 16;131(24):2143-50.
9. Cochrane Database Syst Rev. 2016 Dec 19;12:CD007160.
10. N Engl J Med. 2017 Sep 28;377(13):1240-9.
A 66-year-old man presents with substernal chest pressure and dyspnea that has been present for 45 minutes. He has nausea. Vital signs: blood pressure, 110/60; pulse, 100; oxygen saturation, 92%. Neck: elevated jugular venous pressure. Chest: clear. Cardiac: normal S1 S2, no murmurs. ECG: ST elevation in 2, 3, and aVF leads.
Which of these treatments do you recommend?
A. Morphine, oxygen, nitroglycerin, and aspirin (ASA).
B. Oxygen, morphine, ASA.
C. ASA.
In this patient, I think the correct approach would be to just give aspirin. Nitroglycerin would be problematic, as it appears that this patient might be having a right ventricular infarct, and lowering right-sided filling pressures with nitroglycerin may lead to severe hypotension.
There is controversy over the safety of routine morphine use for patients with chest pain.
Trip J. Meine, MD, and colleagues found that use of morphine either alone or in combination with nitroglycerin for patients presenting with non–ST-elevation acute coronary syndrome (NSTE-ACS) was associated with higher mortality.1 Cian P. McCarthy, MD, and colleagues found the same results, with morphine use associated with larger infarct size, a longer hospital stay, and a trend toward increased mortality in invasively managed NSTE-ACS patients.2 Suzanne de Waha and colleagues found that morphine use in patients with ST-segment elevation MIs had larger infarct size and less reperfusion success, as measured by cardiac MRI.3
Not all recent studies show a detrimental effect of morphine. Etienne Puymirat et al. reviewed in-hospital complications (death, nonfatal re-MI, stroke, stent thrombosis, and bleeding) and 1-year survival according to prehospital morphine use in 2,438 ST-elevation MI (STEMI) patients from the French Registry of Acute ST-elevation and non–ST-elevation Myocardial Infarction (FAST-MI).4 They found no increase in in-hospital complications or 1-year mortality.
The practice of using supplemental oxygen to treat all patients with MI became standard nearly a century ago, after oxygen was found in 1900 to relieve angina, and led to clinical improvement in four MI patients in a 1930 case series.5,6
It was not studied in a controlled trial until 1976, when J.M. Rawles, MD, and colleagues randomized 157 patients with MI to 24 hours of oxygen at 8 L/min or to ambient air. They found no difference in mortality between the groups, but they did find a higher burden of MI in the intervention arm receiving supplemental oxygen, as measured by mean serum aspartate aminotransferase levels.7
The topic was not addressed again in a significant randomized trial until this century. Most notably, two recent studies again demonstrated no benefit of supplemental oxygen in normoxemic patients with MI.
In the AVOID trial in 2015, Dion Stub, MD, PhD, and colleagues randomized 441 patients with STEMI to oxygen at 8 L/min – from diagnosis in an ambulance until after cardiac catheterization – or to ambient air. They found no difference in death at 6 months, but did find an increased rate of in-hospital recurrent MIs, with 0.9% of the control group and 5.5% of the oxygen intervention arm suffering recurrence (P = .006).8 They also showed a larger area of myocardial infarct in the oxygen group, as measured by peak creatine kinase levels and cardiac MRI at 6 months.
Proposed mechanisms of increased myocardial injury from hyperoxia include increased coronary vascular resistance resulting in decreased myocardial perfusion, and increased reperfusion injury from formation of free radicals.9
Where does all this leave us in the treatment of suspected MI?
Morphine should only be used when the patient has pain, and is probably best reserved for severe pain, as the safety of its use is not clear. While hypoxemia is a common consequence of MI – and may correlate with worse outcomes – treatment with supplemental oxygen in the absence of hypoxemia is not supported by current evidence, and may carry risk of harm. Nitroglycerin should be avoided in patients with right ventricular infarcts, and in patients who present with hypotension.
Dr. Tubbesing is a senior resident in medicine at the University of Washington, Seattle. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Am Heart J. 2005 Jun;149(6):1043-9.
2. J Interv Cardiol. 2017 Nov 22. doi: 10.1111/joic.12464.
3. Clin Res Cardiol. 2015 Sep;104(9):727-34.
4. Eur Heart J. 2016 Apr 1;37(13):1063-71.
5. BMJ. 1900 Dec 1;2(2083):1568.
6. JAMA. 1930 May 3;94(18):1363-5.
7. Br Med J. 1976 May 8;1(6018):1121-3.
8. Circulation. 2015 Jun 16;131(24):2143-50.
9. Cochrane Database Syst Rev. 2016 Dec 19;12:CD007160.
10. N Engl J Med. 2017 Sep 28;377(13):1240-9.
Helping patients process sexual harassment
Years ago, after the revelation of sexual predations of male members of the U.S. Navy upon their female underlings, the Navy announced a “zero tolerance” policy. I, then the chair of the American Psychiatric Association Committee on Women, was invited to address a meeting of top Naval officers. They seemed dismayed when I told them that zero tolerance was just the beginning. Declarations that certain behaviors are unacceptable are facile, flimsy, and ultimately disingenuous substitutes for the infinitely more difficult task of monitoring and policing forbidden behaviors and protecting potential and actual victims.
The United States, I pointed out, has a zero tolerance policy on murder but still has to maintain a large force of police officers, detectives, judges, and prison guards to enforce that policy. The Navy had to have a similar approach to sexual assaults. Judging from the recent reports of female members of the military, that hasn’t happened.
Clarity in the law
Unwanted physical intrusion by one adult on another is against the law in the United States. Then why do we need laws specifically banning rape? In addition to the fact that rape, unlike any other assault, can result in conception, sexual assault is recognized as a particularly and uniquely evil and damaging invasion and degradation.
Although there are cultural differences about responsibility for rape, and whether marriage obviates a woman’s right to refuse sexual contact, there is little or no dispute about the need to recognize rape as a distinct, degrading, and particularly heinous attack. It is, therefore, no surprise that people who are raped feel soiled, shamed, and degraded. Those feelings are exacerbated by centuries of shifting responsibility for sexual assault, whether forced intercourse or other unwanted sexual behavior, from the perpetrator onto the victim.
The shifting of blame has been rejected in theory, but it very much persists in actuality. Who among us does not wonder how the victim was dressed or why (s)he was on that street, at that party, in that man’s room? Other forms of harassment echo the motivations of rape – to demonstrate the unanswerable power to degrade – and result in similar psychological responses.
The recent media revelations have lumped physical assault together with unwanted touching, sexual acts undergone as a result of psychological coercion, unwanted exposure to perpetrators’ genitalia and masturbation, and offensive sexual requests and comments. All of those acts are wrong, but they are not equivalent. An elderly man in a wheelchair grabbing an adult woman’s buttocks is not in the same category as an adult man sexually assaulting an underage girl.
What is the genesis of all this misbehavior? It’s not just about sex; it’s about sex and power. For many men, bragging about sexual conquests and making derogatory remarks about women’s physical appearance demonstrate machismo – define maleness.
It is not surprising that such comments are called “locker room talk”; sports are macho displays as well. Physically violating sexual boundaries is just the talk put into action. And macho works. Last November, more than 40% of female voters in the United States voted for the candidate who reportedly cheated on at least one of his three wives, bragged about unwanted sexual assault, and has been credibly accused of many other illegal and/or inappropriate behaviors.
Where does it end?
What is going to be the result of all this hullabaloo? The list of convincingly accused perpetrators grows by the day. Sexism and sexual misbehavior are endemic in every sphere of human endeavor, up to and including, of course, the clergy, who are meant to be models and protectors of virtue. The scope of recent revelations may be unusual, but revelations about one sector or another have happened every few years: the military, clergy, Wall Street, Silicon Valley, academia. What would happen if all the sexual misbehavior were to be revealed, and the perpetrators removed from their leadership and management positions? Would we have a film industry, a financial industry, a legislature? I saw a headline somewhere: “He’s always indispensable; you never are.” The argument, or myth, of indispensability is a powerful protection for powerful individuals. The powerful are too powerful to tolerate mass expulsions. Already, Congress has resorted to the time-honored and demonstrably useless response: training. Others among the accused report that they are undergoing treatment of sex addiction, a diagnosis our profession has wisely discarded, and for which there was no effective treatment.
Sex, while not addictive, does have a role in sexual misbehavior. Through the ages, women’s reproductive hormones have been a focus of social and medical attention, as the source of unpleasant behaviors, and, in fact, psychopathology: premenstrual dysphoric disorder, postpartum depression. Little or no attention has been paid to the problematic psychosocial effects of male reproductive hormones. In addition to the offensive behaviors currently in the headlines, there is the behavior of adolescent males. Isn’t reckless driving related to the pubertal influx of testosterone (Neurosci Biobehav Rev. 2006;30[3]:319-45)? This gender discrepancy deserves scientific and social attention.
What can psychiatrists do to help women (and men) who are affected by sexual misbehavior? This is a difficult problem. What would help most victims, of any injustice, most would be to confront those responsible, and see them removed from positions of power and otherwise punished. However, the recent reports of seemingly swift and severe responses are misleading. The responsible journalists who have reported these cases have, in most cases, devoted months to finding victimized women, persuading them to go public, and corroborating their accounts. The perpetrators, even when complaints have been made, have gone unpunished, and often been promoted, for years or even decades. Women who complain often are subject to employer retaliation.
So a treating psychiatrist is left with less-than-satisfactory recommendations and responses. The most important intervention is to identify and counter the patient’s inaccurate and damaging assumptions: that she was responsible, that she should and could have refused to tolerate the misbehavior, that she has been left tainted, impure. Some social groups and families will have reinforced the latter feeling. The remainder of the psychiatric intervention will be focused on the patient’s particular symptoms – of posttraumatic stress, anxiety, or depression – and the relationship between her symptoms, history, and psychodynamics. Group therapy or other support by women who have faced similar abuse may be helpful. I’m afraid that we will continue to have many such patients to treat.
Dr. Stotland, past president of the American Psychiatric Association, is professor of psychiatry, and obstetrics and gynecology, at Rush Medical College, Chicago. She has written numerous articles and books, including “Cutting Edge Medicine: What Psychiatrists Need to Know” (American Psychiatric Association Publishing, 2002).
Years ago, after the revelation of sexual predations of male members of the U.S. Navy upon their female underlings, the Navy announced a “zero tolerance” policy. I, then the chair of the American Psychiatric Association Committee on Women, was invited to address a meeting of top Naval officers. They seemed dismayed when I told them that zero tolerance was just the beginning. Declarations that certain behaviors are unacceptable are facile, flimsy, and ultimately disingenuous substitutes for the infinitely more difficult task of monitoring and policing forbidden behaviors and protecting potential and actual victims.
The United States, I pointed out, has a zero tolerance policy on murder but still has to maintain a large force of police officers, detectives, judges, and prison guards to enforce that policy. The Navy had to have a similar approach to sexual assaults. Judging from the recent reports of female members of the military, that hasn’t happened.
Clarity in the law
Unwanted physical intrusion by one adult on another is against the law in the United States. Then why do we need laws specifically banning rape? In addition to the fact that rape, unlike any other assault, can result in conception, sexual assault is recognized as a particularly and uniquely evil and damaging invasion and degradation.
Although there are cultural differences about responsibility for rape, and whether marriage obviates a woman’s right to refuse sexual contact, there is little or no dispute about the need to recognize rape as a distinct, degrading, and particularly heinous attack. It is, therefore, no surprise that people who are raped feel soiled, shamed, and degraded. Those feelings are exacerbated by centuries of shifting responsibility for sexual assault, whether forced intercourse or other unwanted sexual behavior, from the perpetrator onto the victim.
The shifting of blame has been rejected in theory, but it very much persists in actuality. Who among us does not wonder how the victim was dressed or why (s)he was on that street, at that party, in that man’s room? Other forms of harassment echo the motivations of rape – to demonstrate the unanswerable power to degrade – and result in similar psychological responses.
The recent media revelations have lumped physical assault together with unwanted touching, sexual acts undergone as a result of psychological coercion, unwanted exposure to perpetrators’ genitalia and masturbation, and offensive sexual requests and comments. All of those acts are wrong, but they are not equivalent. An elderly man in a wheelchair grabbing an adult woman’s buttocks is not in the same category as an adult man sexually assaulting an underage girl.
What is the genesis of all this misbehavior? It’s not just about sex; it’s about sex and power. For many men, bragging about sexual conquests and making derogatory remarks about women’s physical appearance demonstrate machismo – define maleness.
It is not surprising that such comments are called “locker room talk”; sports are macho displays as well. Physically violating sexual boundaries is just the talk put into action. And macho works. Last November, more than 40% of female voters in the United States voted for the candidate who reportedly cheated on at least one of his three wives, bragged about unwanted sexual assault, and has been credibly accused of many other illegal and/or inappropriate behaviors.
Where does it end?
What is going to be the result of all this hullabaloo? The list of convincingly accused perpetrators grows by the day. Sexism and sexual misbehavior are endemic in every sphere of human endeavor, up to and including, of course, the clergy, who are meant to be models and protectors of virtue. The scope of recent revelations may be unusual, but revelations about one sector or another have happened every few years: the military, clergy, Wall Street, Silicon Valley, academia. What would happen if all the sexual misbehavior were to be revealed, and the perpetrators removed from their leadership and management positions? Would we have a film industry, a financial industry, a legislature? I saw a headline somewhere: “He’s always indispensable; you never are.” The argument, or myth, of indispensability is a powerful protection for powerful individuals. The powerful are too powerful to tolerate mass expulsions. Already, Congress has resorted to the time-honored and demonstrably useless response: training. Others among the accused report that they are undergoing treatment of sex addiction, a diagnosis our profession has wisely discarded, and for which there was no effective treatment.
Sex, while not addictive, does have a role in sexual misbehavior. Through the ages, women’s reproductive hormones have been a focus of social and medical attention, as the source of unpleasant behaviors, and, in fact, psychopathology: premenstrual dysphoric disorder, postpartum depression. Little or no attention has been paid to the problematic psychosocial effects of male reproductive hormones. In addition to the offensive behaviors currently in the headlines, there is the behavior of adolescent males. Isn’t reckless driving related to the pubertal influx of testosterone (Neurosci Biobehav Rev. 2006;30[3]:319-45)? This gender discrepancy deserves scientific and social attention.
What can psychiatrists do to help women (and men) who are affected by sexual misbehavior? This is a difficult problem. What would help most victims, of any injustice, most would be to confront those responsible, and see them removed from positions of power and otherwise punished. However, the recent reports of seemingly swift and severe responses are misleading. The responsible journalists who have reported these cases have, in most cases, devoted months to finding victimized women, persuading them to go public, and corroborating their accounts. The perpetrators, even when complaints have been made, have gone unpunished, and often been promoted, for years or even decades. Women who complain often are subject to employer retaliation.
So a treating psychiatrist is left with less-than-satisfactory recommendations and responses. The most important intervention is to identify and counter the patient’s inaccurate and damaging assumptions: that she was responsible, that she should and could have refused to tolerate the misbehavior, that she has been left tainted, impure. Some social groups and families will have reinforced the latter feeling. The remainder of the psychiatric intervention will be focused on the patient’s particular symptoms – of posttraumatic stress, anxiety, or depression – and the relationship between her symptoms, history, and psychodynamics. Group therapy or other support by women who have faced similar abuse may be helpful. I’m afraid that we will continue to have many such patients to treat.
Dr. Stotland, past president of the American Psychiatric Association, is professor of psychiatry, and obstetrics and gynecology, at Rush Medical College, Chicago. She has written numerous articles and books, including “Cutting Edge Medicine: What Psychiatrists Need to Know” (American Psychiatric Association Publishing, 2002).
Years ago, after the revelation of sexual predations of male members of the U.S. Navy upon their female underlings, the Navy announced a “zero tolerance” policy. I, then the chair of the American Psychiatric Association Committee on Women, was invited to address a meeting of top Naval officers. They seemed dismayed when I told them that zero tolerance was just the beginning. Declarations that certain behaviors are unacceptable are facile, flimsy, and ultimately disingenuous substitutes for the infinitely more difficult task of monitoring and policing forbidden behaviors and protecting potential and actual victims.
The United States, I pointed out, has a zero tolerance policy on murder but still has to maintain a large force of police officers, detectives, judges, and prison guards to enforce that policy. The Navy had to have a similar approach to sexual assaults. Judging from the recent reports of female members of the military, that hasn’t happened.
Clarity in the law
Unwanted physical intrusion by one adult on another is against the law in the United States. Then why do we need laws specifically banning rape? In addition to the fact that rape, unlike any other assault, can result in conception, sexual assault is recognized as a particularly and uniquely evil and damaging invasion and degradation.
Although there are cultural differences about responsibility for rape, and whether marriage obviates a woman’s right to refuse sexual contact, there is little or no dispute about the need to recognize rape as a distinct, degrading, and particularly heinous attack. It is, therefore, no surprise that people who are raped feel soiled, shamed, and degraded. Those feelings are exacerbated by centuries of shifting responsibility for sexual assault, whether forced intercourse or other unwanted sexual behavior, from the perpetrator onto the victim.
The shifting of blame has been rejected in theory, but it very much persists in actuality. Who among us does not wonder how the victim was dressed or why (s)he was on that street, at that party, in that man’s room? Other forms of harassment echo the motivations of rape – to demonstrate the unanswerable power to degrade – and result in similar psychological responses.
The recent media revelations have lumped physical assault together with unwanted touching, sexual acts undergone as a result of psychological coercion, unwanted exposure to perpetrators’ genitalia and masturbation, and offensive sexual requests and comments. All of those acts are wrong, but they are not equivalent. An elderly man in a wheelchair grabbing an adult woman’s buttocks is not in the same category as an adult man sexually assaulting an underage girl.
What is the genesis of all this misbehavior? It’s not just about sex; it’s about sex and power. For many men, bragging about sexual conquests and making derogatory remarks about women’s physical appearance demonstrate machismo – define maleness.
It is not surprising that such comments are called “locker room talk”; sports are macho displays as well. Physically violating sexual boundaries is just the talk put into action. And macho works. Last November, more than 40% of female voters in the United States voted for the candidate who reportedly cheated on at least one of his three wives, bragged about unwanted sexual assault, and has been credibly accused of many other illegal and/or inappropriate behaviors.
Where does it end?
What is going to be the result of all this hullabaloo? The list of convincingly accused perpetrators grows by the day. Sexism and sexual misbehavior are endemic in every sphere of human endeavor, up to and including, of course, the clergy, who are meant to be models and protectors of virtue. The scope of recent revelations may be unusual, but revelations about one sector or another have happened every few years: the military, clergy, Wall Street, Silicon Valley, academia. What would happen if all the sexual misbehavior were to be revealed, and the perpetrators removed from their leadership and management positions? Would we have a film industry, a financial industry, a legislature? I saw a headline somewhere: “He’s always indispensable; you never are.” The argument, or myth, of indispensability is a powerful protection for powerful individuals. The powerful are too powerful to tolerate mass expulsions. Already, Congress has resorted to the time-honored and demonstrably useless response: training. Others among the accused report that they are undergoing treatment of sex addiction, a diagnosis our profession has wisely discarded, and for which there was no effective treatment.
Sex, while not addictive, does have a role in sexual misbehavior. Through the ages, women’s reproductive hormones have been a focus of social and medical attention, as the source of unpleasant behaviors, and, in fact, psychopathology: premenstrual dysphoric disorder, postpartum depression. Little or no attention has been paid to the problematic psychosocial effects of male reproductive hormones. In addition to the offensive behaviors currently in the headlines, there is the behavior of adolescent males. Isn’t reckless driving related to the pubertal influx of testosterone (Neurosci Biobehav Rev. 2006;30[3]:319-45)? This gender discrepancy deserves scientific and social attention.
What can psychiatrists do to help women (and men) who are affected by sexual misbehavior? This is a difficult problem. What would help most victims, of any injustice, most would be to confront those responsible, and see them removed from positions of power and otherwise punished. However, the recent reports of seemingly swift and severe responses are misleading. The responsible journalists who have reported these cases have, in most cases, devoted months to finding victimized women, persuading them to go public, and corroborating their accounts. The perpetrators, even when complaints have been made, have gone unpunished, and often been promoted, for years or even decades. Women who complain often are subject to employer retaliation.
So a treating psychiatrist is left with less-than-satisfactory recommendations and responses. The most important intervention is to identify and counter the patient’s inaccurate and damaging assumptions: that she was responsible, that she should and could have refused to tolerate the misbehavior, that she has been left tainted, impure. Some social groups and families will have reinforced the latter feeling. The remainder of the psychiatric intervention will be focused on the patient’s particular symptoms – of posttraumatic stress, anxiety, or depression – and the relationship between her symptoms, history, and psychodynamics. Group therapy or other support by women who have faced similar abuse may be helpful. I’m afraid that we will continue to have many such patients to treat.
Dr. Stotland, past president of the American Psychiatric Association, is professor of psychiatry, and obstetrics and gynecology, at Rush Medical College, Chicago. She has written numerous articles and books, including “Cutting Edge Medicine: What Psychiatrists Need to Know” (American Psychiatric Association Publishing, 2002).
The Right and Wrong of 2017
It is customary at the end of the year for editors of journals and magazines to publish “the best and the worst of the year” or top 10 lists of events or articles of the year, or even the “most important” discoveries or people of the year. Some publications survey their readers; others invite experts to opine on the selection. What is nearly always missing from these newsworthy roundups are the criteria for determining what meets the mark. But this is a crucial piece of missing information, and without it, many of these rankings have little worth.
Words like important, best, and worst are not factual claims but value judgments. For a value judgment to have validity, there must be a substantive basis for making the determination. Put less ponderously, readers need to understand what makes a person, action, or decision valuable or important.
Being a medical ethicist, I tend to think in terms of good and bad, right and wrong—hence, the title of this editorial. But even these essential terms of evaluation in our language must have a frame of reference or at least a description to have meaning when applied, especially if the terms are to be compared. For moral philosophy, the parent of medical ethics, these frames or bases for making judgments about the rightness or wrongness of conduct are often found in ethical theories.
Three of the most recognized and significant ethical theories are consequentialist, deontology, and virtue ethics. It is important to understand these theories to grasp how I decided on my list of the right and wrong of 2017. However due to space limitations, I will only provide a nutshell summary of these theories. Readers interested in cracking the nut wider may want to consult the references on ethical theory at the end of the essay.1
Consequentialist theories—utilitarianism being the most well known in health care—argue that what makes an action right or good is what brings about the most happiness for the most people. What is determinative of rightness is the outcome.
In direct opposition to consequentialism is deontology. The consequences do not matter at all to the deontologist, right and good have to do with intent, and the only truly right intent is acting for the sake of duty alone.
Virtue ethics finds the core of right and good in the character of the virtuous person. Right actions and good intent each spring from the root of an individual of moral excellence.2
Establishing these ethical theories as the criteria for judgment, I now turn to my choice for the right and the good, the “best” of federal practice in 2017. (Next month my editorial will focus on the bad or the “worst” of 2017 federal health care.) Upfront, I acknowledge these choices are subjective, but I justify them by using the theories set forth. We welcome readers to send us their selections.
The Best
While journalists and politicians have widely criticized the White House response (or lack thereof) to the destructive storms that occurred during this hurricane season, little attention has been paid to the response of the 3 federal health care agencies, which was quick, dedicated, and caring. And it is this response that makes it my best of 2017. The vulnerability of areas from Houston to Puerto Rico, some of which still lack the basic services of civilization, are struggling with loss of life and hope, powerless to protect what is left in the wake of the storms, only amplifies the desperate need for the human and material resources that the DoD, VA, and PHS have committed.
Testifying before the Senate Homeland Security and Governmental Affairs Committee, Robert G. Salesses, deputy assistant secretary of defense, chronicled the outpouring of DoD aid. “Military units cleared critical roadways, transported life-sustaining commodities, provided fuel distribution, conducted assessments of civilian hospitals, and provided medical support to include evacuating patients back to the continental United States.”3
The VA Disaster Emergency Medical Personnel system also went into high gear. In my facility and in many others, there were so many volunteers that facility leaders had to balance their clinical needs with the selfless desire to help the veterans and fellow federal practitioners who were in harm’s way.
According to Susan Wentzell, VISN 8 deputy communication manager and content manager:
“Despite the destruction caused by these monster storms, Veterans continued to receive vital health care and other support, thanks to the selfless efforts of thousands of dedicated VA employees who rallied together to provide around-the-clock care for patients sheltered-in-place in the eight large, hurricane-constructed VA hospitals and to get services back up and running in dozens of outpatient clinics impacted in the Southeast corridor of the U.S. and the Caribbean.”4
When Hurricane Maria ravaged Puerto Rico, medical personnel from the VA and the PHS Commissioned Corps staffed Federal Medical Stations in Manati and Bayamon, Puerto Rico, which provided cared for up to 250 people at a time. The officers of the Commissioned Corps also helped support the civilian health care infrastructure.
From a utilitarian perspective, the benefit of these relief efforts is obvious. They were literally life-saving and health preserving for the thousands who were injured in the wreckage of wind and rain, ill from the collapse of public services, as well as those psychologically traumatized. And had these men and women of the VA, PHS, and DoD not come to the aid of the victims of these unprecedented national disasters, the toll of human suffering and bereavement would have been far worse.
Deontologically, each of these government employees did their duty; many volunteered, and even those who were ordered to assist did so with a compassion and dedication that went far beyond doing a job. None of the historic drives of humankind to place themselves in harm’s way—power, money, or fame—motivated those who answered the call; only a duty to serve and an intention to help.
Each person who left the security of home and the comfort of friends and family displayed the highest qualities of virtue ethics: altruism, professionalism, empathy, and integrity among other virtues.
In preparing for this column, I read stories of health care practitioners and nonclinical staff who not only reached out, but also reached beyond any expectation, clearly demonstrating outstanding professionalism and humanism.
I end with just one of these inspirational accounts. As Hurricane Irma approached the Florida coast, veteran employee Tim Myers braved the coming storm to get to work. That is far harder and braver than it seems, because Myers, who is a pharmacy technician and delivers medications to inpatients at the James A. Haley VA, is a quadriplegic in a wheelchair. The humility of his laconic description of his supererogatory conduct is equally impressive. “I appreciate that, but it really wasn’t that big of a deal to me,” Myers said. “I mean, I had to get here.”5
1. Vaughn L. Bioethics Principles, Issues, and Cases. 3rd ed. New York, NY: Oxford University Press, 2017.
2. Kuhse H, Singer P, eds. A Companion to Bioethics. 2nd ed. Malden, MA: Wiley-Blackwell, 2012.
3. Garamone J. Officials detail DOD support during unprecedented hurricane season. https://www.defense.gov/News/Article/Article/1360033/officials-detail-dod-support-during-unprecedented-hurricane-season. Published November 1, 2017. Accessed November 18, 2017.
4. Wentzell S. Through hurricanes, VA continues efforts to care for Veterans. https://www.blogs.va.gov/VAntage/41864/through-hurricanes-va-continues-efforts-to-care-for-veterans/. Published October 3, 2017. Accessed November 19, 2017.
5. Drohan E. Dedication in the face of the storm. September 18, 2017. https://www.tampa.va.gov/TAMPA/features/Wheelchair_Through_Irma.asp. Published September 18, 2017. November 19, 2017.
It is customary at the end of the year for editors of journals and magazines to publish “the best and the worst of the year” or top 10 lists of events or articles of the year, or even the “most important” discoveries or people of the year. Some publications survey their readers; others invite experts to opine on the selection. What is nearly always missing from these newsworthy roundups are the criteria for determining what meets the mark. But this is a crucial piece of missing information, and without it, many of these rankings have little worth.
Words like important, best, and worst are not factual claims but value judgments. For a value judgment to have validity, there must be a substantive basis for making the determination. Put less ponderously, readers need to understand what makes a person, action, or decision valuable or important.
Being a medical ethicist, I tend to think in terms of good and bad, right and wrong—hence, the title of this editorial. But even these essential terms of evaluation in our language must have a frame of reference or at least a description to have meaning when applied, especially if the terms are to be compared. For moral philosophy, the parent of medical ethics, these frames or bases for making judgments about the rightness or wrongness of conduct are often found in ethical theories.
Three of the most recognized and significant ethical theories are consequentialist, deontology, and virtue ethics. It is important to understand these theories to grasp how I decided on my list of the right and wrong of 2017. However due to space limitations, I will only provide a nutshell summary of these theories. Readers interested in cracking the nut wider may want to consult the references on ethical theory at the end of the essay.1
Consequentialist theories—utilitarianism being the most well known in health care—argue that what makes an action right or good is what brings about the most happiness for the most people. What is determinative of rightness is the outcome.
In direct opposition to consequentialism is deontology. The consequences do not matter at all to the deontologist, right and good have to do with intent, and the only truly right intent is acting for the sake of duty alone.
Virtue ethics finds the core of right and good in the character of the virtuous person. Right actions and good intent each spring from the root of an individual of moral excellence.2
Establishing these ethical theories as the criteria for judgment, I now turn to my choice for the right and the good, the “best” of federal practice in 2017. (Next month my editorial will focus on the bad or the “worst” of 2017 federal health care.) Upfront, I acknowledge these choices are subjective, but I justify them by using the theories set forth. We welcome readers to send us their selections.
The Best
While journalists and politicians have widely criticized the White House response (or lack thereof) to the destructive storms that occurred during this hurricane season, little attention has been paid to the response of the 3 federal health care agencies, which was quick, dedicated, and caring. And it is this response that makes it my best of 2017. The vulnerability of areas from Houston to Puerto Rico, some of which still lack the basic services of civilization, are struggling with loss of life and hope, powerless to protect what is left in the wake of the storms, only amplifies the desperate need for the human and material resources that the DoD, VA, and PHS have committed.
Testifying before the Senate Homeland Security and Governmental Affairs Committee, Robert G. Salesses, deputy assistant secretary of defense, chronicled the outpouring of DoD aid. “Military units cleared critical roadways, transported life-sustaining commodities, provided fuel distribution, conducted assessments of civilian hospitals, and provided medical support to include evacuating patients back to the continental United States.”3
The VA Disaster Emergency Medical Personnel system also went into high gear. In my facility and in many others, there were so many volunteers that facility leaders had to balance their clinical needs with the selfless desire to help the veterans and fellow federal practitioners who were in harm’s way.
According to Susan Wentzell, VISN 8 deputy communication manager and content manager:
“Despite the destruction caused by these monster storms, Veterans continued to receive vital health care and other support, thanks to the selfless efforts of thousands of dedicated VA employees who rallied together to provide around-the-clock care for patients sheltered-in-place in the eight large, hurricane-constructed VA hospitals and to get services back up and running in dozens of outpatient clinics impacted in the Southeast corridor of the U.S. and the Caribbean.”4
When Hurricane Maria ravaged Puerto Rico, medical personnel from the VA and the PHS Commissioned Corps staffed Federal Medical Stations in Manati and Bayamon, Puerto Rico, which provided cared for up to 250 people at a time. The officers of the Commissioned Corps also helped support the civilian health care infrastructure.
From a utilitarian perspective, the benefit of these relief efforts is obvious. They were literally life-saving and health preserving for the thousands who were injured in the wreckage of wind and rain, ill from the collapse of public services, as well as those psychologically traumatized. And had these men and women of the VA, PHS, and DoD not come to the aid of the victims of these unprecedented national disasters, the toll of human suffering and bereavement would have been far worse.
Deontologically, each of these government employees did their duty; many volunteered, and even those who were ordered to assist did so with a compassion and dedication that went far beyond doing a job. None of the historic drives of humankind to place themselves in harm’s way—power, money, or fame—motivated those who answered the call; only a duty to serve and an intention to help.
Each person who left the security of home and the comfort of friends and family displayed the highest qualities of virtue ethics: altruism, professionalism, empathy, and integrity among other virtues.
In preparing for this column, I read stories of health care practitioners and nonclinical staff who not only reached out, but also reached beyond any expectation, clearly demonstrating outstanding professionalism and humanism.
I end with just one of these inspirational accounts. As Hurricane Irma approached the Florida coast, veteran employee Tim Myers braved the coming storm to get to work. That is far harder and braver than it seems, because Myers, who is a pharmacy technician and delivers medications to inpatients at the James A. Haley VA, is a quadriplegic in a wheelchair. The humility of his laconic description of his supererogatory conduct is equally impressive. “I appreciate that, but it really wasn’t that big of a deal to me,” Myers said. “I mean, I had to get here.”5
It is customary at the end of the year for editors of journals and magazines to publish “the best and the worst of the year” or top 10 lists of events or articles of the year, or even the “most important” discoveries or people of the year. Some publications survey their readers; others invite experts to opine on the selection. What is nearly always missing from these newsworthy roundups are the criteria for determining what meets the mark. But this is a crucial piece of missing information, and without it, many of these rankings have little worth.
Words like important, best, and worst are not factual claims but value judgments. For a value judgment to have validity, there must be a substantive basis for making the determination. Put less ponderously, readers need to understand what makes a person, action, or decision valuable or important.
Being a medical ethicist, I tend to think in terms of good and bad, right and wrong—hence, the title of this editorial. But even these essential terms of evaluation in our language must have a frame of reference or at least a description to have meaning when applied, especially if the terms are to be compared. For moral philosophy, the parent of medical ethics, these frames or bases for making judgments about the rightness or wrongness of conduct are often found in ethical theories.
Three of the most recognized and significant ethical theories are consequentialist, deontology, and virtue ethics. It is important to understand these theories to grasp how I decided on my list of the right and wrong of 2017. However due to space limitations, I will only provide a nutshell summary of these theories. Readers interested in cracking the nut wider may want to consult the references on ethical theory at the end of the essay.1
Consequentialist theories—utilitarianism being the most well known in health care—argue that what makes an action right or good is what brings about the most happiness for the most people. What is determinative of rightness is the outcome.
In direct opposition to consequentialism is deontology. The consequences do not matter at all to the deontologist, right and good have to do with intent, and the only truly right intent is acting for the sake of duty alone.
Virtue ethics finds the core of right and good in the character of the virtuous person. Right actions and good intent each spring from the root of an individual of moral excellence.2
Establishing these ethical theories as the criteria for judgment, I now turn to my choice for the right and the good, the “best” of federal practice in 2017. (Next month my editorial will focus on the bad or the “worst” of 2017 federal health care.) Upfront, I acknowledge these choices are subjective, but I justify them by using the theories set forth. We welcome readers to send us their selections.
The Best
While journalists and politicians have widely criticized the White House response (or lack thereof) to the destructive storms that occurred during this hurricane season, little attention has been paid to the response of the 3 federal health care agencies, which was quick, dedicated, and caring. And it is this response that makes it my best of 2017. The vulnerability of areas from Houston to Puerto Rico, some of which still lack the basic services of civilization, are struggling with loss of life and hope, powerless to protect what is left in the wake of the storms, only amplifies the desperate need for the human and material resources that the DoD, VA, and PHS have committed.
Testifying before the Senate Homeland Security and Governmental Affairs Committee, Robert G. Salesses, deputy assistant secretary of defense, chronicled the outpouring of DoD aid. “Military units cleared critical roadways, transported life-sustaining commodities, provided fuel distribution, conducted assessments of civilian hospitals, and provided medical support to include evacuating patients back to the continental United States.”3
The VA Disaster Emergency Medical Personnel system also went into high gear. In my facility and in many others, there were so many volunteers that facility leaders had to balance their clinical needs with the selfless desire to help the veterans and fellow federal practitioners who were in harm’s way.
According to Susan Wentzell, VISN 8 deputy communication manager and content manager:
“Despite the destruction caused by these monster storms, Veterans continued to receive vital health care and other support, thanks to the selfless efforts of thousands of dedicated VA employees who rallied together to provide around-the-clock care for patients sheltered-in-place in the eight large, hurricane-constructed VA hospitals and to get services back up and running in dozens of outpatient clinics impacted in the Southeast corridor of the U.S. and the Caribbean.”4
When Hurricane Maria ravaged Puerto Rico, medical personnel from the VA and the PHS Commissioned Corps staffed Federal Medical Stations in Manati and Bayamon, Puerto Rico, which provided cared for up to 250 people at a time. The officers of the Commissioned Corps also helped support the civilian health care infrastructure.
From a utilitarian perspective, the benefit of these relief efforts is obvious. They were literally life-saving and health preserving for the thousands who were injured in the wreckage of wind and rain, ill from the collapse of public services, as well as those psychologically traumatized. And had these men and women of the VA, PHS, and DoD not come to the aid of the victims of these unprecedented national disasters, the toll of human suffering and bereavement would have been far worse.
Deontologically, each of these government employees did their duty; many volunteered, and even those who were ordered to assist did so with a compassion and dedication that went far beyond doing a job. None of the historic drives of humankind to place themselves in harm’s way—power, money, or fame—motivated those who answered the call; only a duty to serve and an intention to help.
Each person who left the security of home and the comfort of friends and family displayed the highest qualities of virtue ethics: altruism, professionalism, empathy, and integrity among other virtues.
In preparing for this column, I read stories of health care practitioners and nonclinical staff who not only reached out, but also reached beyond any expectation, clearly demonstrating outstanding professionalism and humanism.
I end with just one of these inspirational accounts. As Hurricane Irma approached the Florida coast, veteran employee Tim Myers braved the coming storm to get to work. That is far harder and braver than it seems, because Myers, who is a pharmacy technician and delivers medications to inpatients at the James A. Haley VA, is a quadriplegic in a wheelchair. The humility of his laconic description of his supererogatory conduct is equally impressive. “I appreciate that, but it really wasn’t that big of a deal to me,” Myers said. “I mean, I had to get here.”5
1. Vaughn L. Bioethics Principles, Issues, and Cases. 3rd ed. New York, NY: Oxford University Press, 2017.
2. Kuhse H, Singer P, eds. A Companion to Bioethics. 2nd ed. Malden, MA: Wiley-Blackwell, 2012.
3. Garamone J. Officials detail DOD support during unprecedented hurricane season. https://www.defense.gov/News/Article/Article/1360033/officials-detail-dod-support-during-unprecedented-hurricane-season. Published November 1, 2017. Accessed November 18, 2017.
4. Wentzell S. Through hurricanes, VA continues efforts to care for Veterans. https://www.blogs.va.gov/VAntage/41864/through-hurricanes-va-continues-efforts-to-care-for-veterans/. Published October 3, 2017. Accessed November 19, 2017.
5. Drohan E. Dedication in the face of the storm. September 18, 2017. https://www.tampa.va.gov/TAMPA/features/Wheelchair_Through_Irma.asp. Published September 18, 2017. November 19, 2017.
1. Vaughn L. Bioethics Principles, Issues, and Cases. 3rd ed. New York, NY: Oxford University Press, 2017.
2. Kuhse H, Singer P, eds. A Companion to Bioethics. 2nd ed. Malden, MA: Wiley-Blackwell, 2012.
3. Garamone J. Officials detail DOD support during unprecedented hurricane season. https://www.defense.gov/News/Article/Article/1360033/officials-detail-dod-support-during-unprecedented-hurricane-season. Published November 1, 2017. Accessed November 18, 2017.
4. Wentzell S. Through hurricanes, VA continues efforts to care for Veterans. https://www.blogs.va.gov/VAntage/41864/through-hurricanes-va-continues-efforts-to-care-for-veterans/. Published October 3, 2017. Accessed November 19, 2017.
5. Drohan E. Dedication in the face of the storm. September 18, 2017. https://www.tampa.va.gov/TAMPA/features/Wheelchair_Through_Irma.asp. Published September 18, 2017. November 19, 2017.
Keeping Up With the … Clinicians?
This past week, I received “appointment reminder” text messages from two separate health care clinics requesting confirmation of my attendance—a practice that has become so commonplace, I didn’t think twice about it. But there was a time, not long ago, when this would’ve seemed like a scenario from the far-off future (like the flying cars on The Jetsons).
Times, they are a-changin’! Clinicians are becoming more electronically skilled and interested in connecting with patients in a more convenient, direct way. Accordingly, they are increasingly willing to embrace the world of social media—something health care institutions evaded for years and even discouraged employees from entering. Today, clinicians are starting to harness the potential of social media to increase health care awareness and improve access to care.
The popularity of social media has grown tremendously in recent years; 72% of US adults now use social media, up from 8% in 2005.1 Facebook—one of the most commonly used social networks, along with LinkedIn and Twitter—surpassed 1 billion users in the third quarter of 2012, making it the first to achieve this milestone.2
And that’s the beauty of social media: It’s a tool that’s all about speeding up and augmenting communication. Active users consider themselves part of a community and therefore tend to trust others within their social media “group.” As a result, patients—especially younger ones—are using social media to make health care decisions. They research and select their clinicians, hospitals, and even courses of treatment (for both themselves and their families) with input from this community.
Our patients are social media–savvy and expect us, as clinicians, to be equally skilled. Are we missing an opportunity by opting out of these networks? Or are we rightly avoiding a number of thorny legal and regulatory issues by staying “offline”?
Many clinicians believe that the dependability of social media can drive better quality of care. In fact, 60% of physicians are in favor of interacting with patients on social media for patient education, health monitoring, medication adherence, and promotion of behavioral change.4 And in a 2012 study, 56% of patients reported wanting clinicians to use “social media” (which included email) to set appointments, report diagnostic test results, send prescription notifications, provide health information, and answer questions.5
Social media provides a platform for the public, patients, and health care professionals to communicate about health issues and (possibly) improve health outcomes. It can be used for professional networking, education, organizational promotion, patient care, patient education, and public health programs.6 So, where’s the downside?
As use of social media increases, particularly in the health care industry, the risks for legal implications and noncompliance also rise. Numerous federal and state rules and regulations govern communication within the health care industry. One of the main challenges health care organizations face is the protection of the privacy of patient information (ie, HIPAA). To this end, organizations must exhibit that they are managing the activities of employees who have access to patient information (which includes social media use). Institutions planning to use social media also need to ensure that their electronic records are complete, secure, and tamper-proof for record retention and audit purposes. Noncompliance with health care regulations can not only damage the reputation of an institution, it can also impact the bottom line.
In addition, health care providers must consider legal issues related to patient privacy, litigation, and licensing before using social media. Federal and state privacy laws limit providers’ ability to interact with patients through social media, because anything that can be used to identify a patient
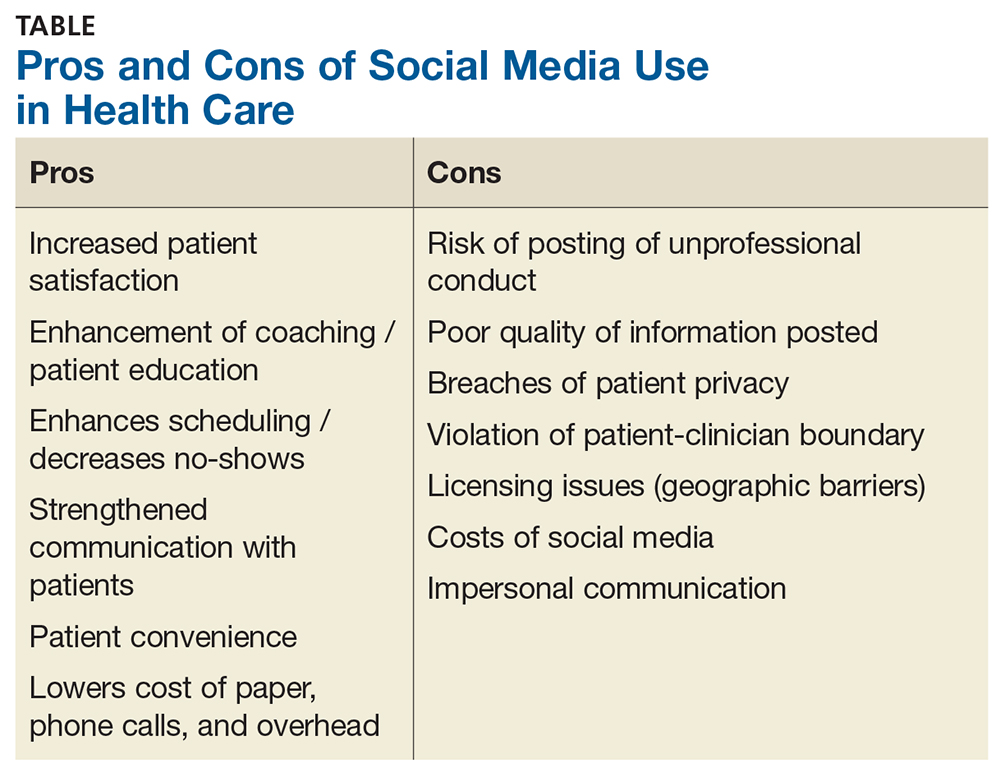
It’s no wonder some providers are leery of connecting with patients via social media. Many of them, however, have tested the waters by using social networks to connect with colleagues and peers, often sharing medical knowledge and opinions this way.
As social media has evolved, medically focused professional communities have been established. One example is SERMO, a popular, private, physician-only social network. SERMO (www.sermo.com/what-is-sermo/overview) is a virtual doctors’ lounge with more than 800,000 verified and credentialed physician members; it includes physicians from 150 countries, with plans for continued expansion. Another, the Medical Directors Forum (https://medicaldirectorsforum.com/site), is a verified, secure, closed-loop environment for peer-to-peer interaction between medical directors, which features discussion groups, calendar postings, and alerts. Finally, Doximity (www.doximity.com/review) is a social network for physicians, NPs, and PAs, which allows clinicians to call patients (with the physician’s office number displayed on caller ID), review pertinent medical articles, communicate with colleagues, and even fax and/or email documents. Additionally, the American Association of Nurse Practitioners (AANP), the American Academy of Physician Assistants (AAPA), and Clinician Reviews all have accounts on Facebook and Twitter, among other social media sites.

When it comes down to it, if used wisely, social media has the potential to promote individual and public health, as well as professional development and advancement. But carelessness can result in legal, ethical, and logistical issues, causing serious ramifications for the clinician—and possibly even the practice. So, which side of the social media debate are you on? Send your tips—or warnings—about integrating social media into your workplace to [email protected]
1. Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in healthcare: motives, barriers, and expectations. Patient Educ Couns. 2013;92(3):426-431.
2. Kaplan AM, Haenlein M. Users of the world unite! The challenges and opportunities of social media. Bus Horiz. 2010;53:59-68.
3. Statistica. Number of Facebook users worldwide as of 3rd quarter 2017 (in millions). www.statista.com/statistics/264810/number-of-monthly-active-facebook-users-worldwide/. Accessed November 16, 2017.
4. Househ M. The use of social media in healthcare: organizational, clinic, and patient perspectives. Stud Health Technol Inform. 2013;183:244-248.
5. Fisher J, Clayton M. Who gives a tweet: assessing patients’ interest in the use of social media for health care. Worldviews on Evid Based Nurs. 2012;9(2):100-108.
6. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
This past week, I received “appointment reminder” text messages from two separate health care clinics requesting confirmation of my attendance—a practice that has become so commonplace, I didn’t think twice about it. But there was a time, not long ago, when this would’ve seemed like a scenario from the far-off future (like the flying cars on The Jetsons).
Times, they are a-changin’! Clinicians are becoming more electronically skilled and interested in connecting with patients in a more convenient, direct way. Accordingly, they are increasingly willing to embrace the world of social media—something health care institutions evaded for years and even discouraged employees from entering. Today, clinicians are starting to harness the potential of social media to increase health care awareness and improve access to care.
The popularity of social media has grown tremendously in recent years; 72% of US adults now use social media, up from 8% in 2005.1 Facebook—one of the most commonly used social networks, along with LinkedIn and Twitter—surpassed 1 billion users in the third quarter of 2012, making it the first to achieve this milestone.2
And that’s the beauty of social media: It’s a tool that’s all about speeding up and augmenting communication. Active users consider themselves part of a community and therefore tend to trust others within their social media “group.” As a result, patients—especially younger ones—are using social media to make health care decisions. They research and select their clinicians, hospitals, and even courses of treatment (for both themselves and their families) with input from this community.
Our patients are social media–savvy and expect us, as clinicians, to be equally skilled. Are we missing an opportunity by opting out of these networks? Or are we rightly avoiding a number of thorny legal and regulatory issues by staying “offline”?
Many clinicians believe that the dependability of social media can drive better quality of care. In fact, 60% of physicians are in favor of interacting with patients on social media for patient education, health monitoring, medication adherence, and promotion of behavioral change.4 And in a 2012 study, 56% of patients reported wanting clinicians to use “social media” (which included email) to set appointments, report diagnostic test results, send prescription notifications, provide health information, and answer questions.5
Social media provides a platform for the public, patients, and health care professionals to communicate about health issues and (possibly) improve health outcomes. It can be used for professional networking, education, organizational promotion, patient care, patient education, and public health programs.6 So, where’s the downside?
As use of social media increases, particularly in the health care industry, the risks for legal implications and noncompliance also rise. Numerous federal and state rules and regulations govern communication within the health care industry. One of the main challenges health care organizations face is the protection of the privacy of patient information (ie, HIPAA). To this end, organizations must exhibit that they are managing the activities of employees who have access to patient information (which includes social media use). Institutions planning to use social media also need to ensure that their electronic records are complete, secure, and tamper-proof for record retention and audit purposes. Noncompliance with health care regulations can not only damage the reputation of an institution, it can also impact the bottom line.
In addition, health care providers must consider legal issues related to patient privacy, litigation, and licensing before using social media. Federal and state privacy laws limit providers’ ability to interact with patients through social media, because anything that can be used to identify a patient
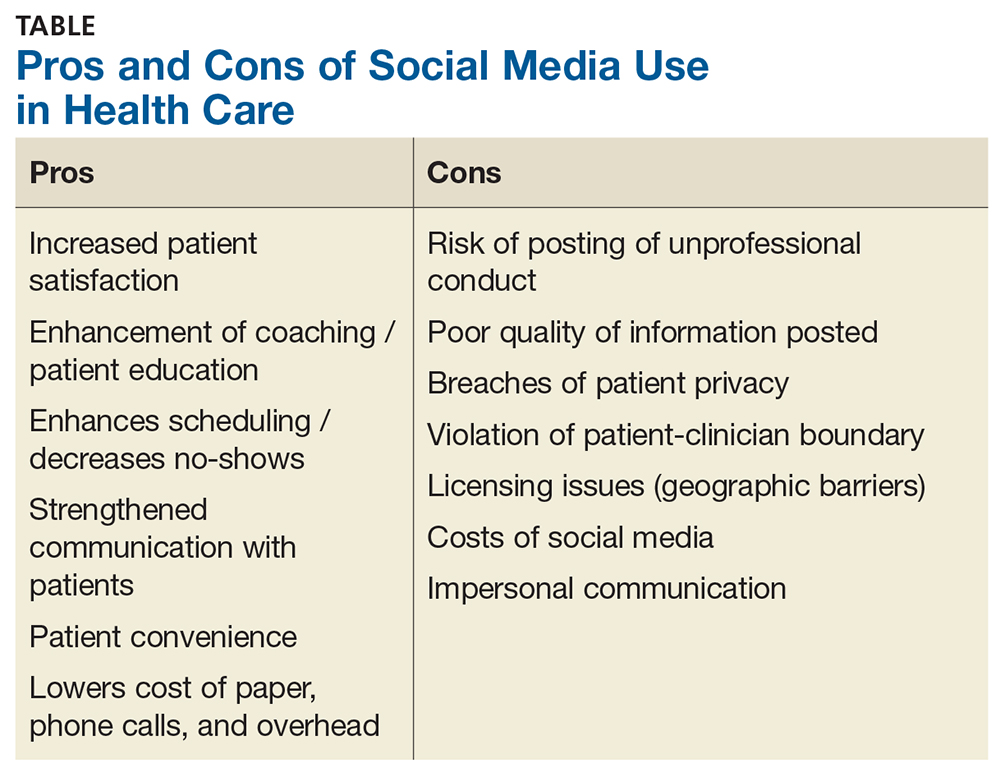
It’s no wonder some providers are leery of connecting with patients via social media. Many of them, however, have tested the waters by using social networks to connect with colleagues and peers, often sharing medical knowledge and opinions this way.
As social media has evolved, medically focused professional communities have been established. One example is SERMO, a popular, private, physician-only social network. SERMO (www.sermo.com/what-is-sermo/overview) is a virtual doctors’ lounge with more than 800,000 verified and credentialed physician members; it includes physicians from 150 countries, with plans for continued expansion. Another, the Medical Directors Forum (https://medicaldirectorsforum.com/site), is a verified, secure, closed-loop environment for peer-to-peer interaction between medical directors, which features discussion groups, calendar postings, and alerts. Finally, Doximity (www.doximity.com/review) is a social network for physicians, NPs, and PAs, which allows clinicians to call patients (with the physician’s office number displayed on caller ID), review pertinent medical articles, communicate with colleagues, and even fax and/or email documents. Additionally, the American Association of Nurse Practitioners (AANP), the American Academy of Physician Assistants (AAPA), and Clinician Reviews all have accounts on Facebook and Twitter, among other social media sites.

When it comes down to it, if used wisely, social media has the potential to promote individual and public health, as well as professional development and advancement. But carelessness can result in legal, ethical, and logistical issues, causing serious ramifications for the clinician—and possibly even the practice. So, which side of the social media debate are you on? Send your tips—or warnings—about integrating social media into your workplace to [email protected]
This past week, I received “appointment reminder” text messages from two separate health care clinics requesting confirmation of my attendance—a practice that has become so commonplace, I didn’t think twice about it. But there was a time, not long ago, when this would’ve seemed like a scenario from the far-off future (like the flying cars on The Jetsons).
Times, they are a-changin’! Clinicians are becoming more electronically skilled and interested in connecting with patients in a more convenient, direct way. Accordingly, they are increasingly willing to embrace the world of social media—something health care institutions evaded for years and even discouraged employees from entering. Today, clinicians are starting to harness the potential of social media to increase health care awareness and improve access to care.
The popularity of social media has grown tremendously in recent years; 72% of US adults now use social media, up from 8% in 2005.1 Facebook—one of the most commonly used social networks, along with LinkedIn and Twitter—surpassed 1 billion users in the third quarter of 2012, making it the first to achieve this milestone.2
And that’s the beauty of social media: It’s a tool that’s all about speeding up and augmenting communication. Active users consider themselves part of a community and therefore tend to trust others within their social media “group.” As a result, patients—especially younger ones—are using social media to make health care decisions. They research and select their clinicians, hospitals, and even courses of treatment (for both themselves and their families) with input from this community.
Our patients are social media–savvy and expect us, as clinicians, to be equally skilled. Are we missing an opportunity by opting out of these networks? Or are we rightly avoiding a number of thorny legal and regulatory issues by staying “offline”?
Many clinicians believe that the dependability of social media can drive better quality of care. In fact, 60% of physicians are in favor of interacting with patients on social media for patient education, health monitoring, medication adherence, and promotion of behavioral change.4 And in a 2012 study, 56% of patients reported wanting clinicians to use “social media” (which included email) to set appointments, report diagnostic test results, send prescription notifications, provide health information, and answer questions.5
Social media provides a platform for the public, patients, and health care professionals to communicate about health issues and (possibly) improve health outcomes. It can be used for professional networking, education, organizational promotion, patient care, patient education, and public health programs.6 So, where’s the downside?
As use of social media increases, particularly in the health care industry, the risks for legal implications and noncompliance also rise. Numerous federal and state rules and regulations govern communication within the health care industry. One of the main challenges health care organizations face is the protection of the privacy of patient information (ie, HIPAA). To this end, organizations must exhibit that they are managing the activities of employees who have access to patient information (which includes social media use). Institutions planning to use social media also need to ensure that their electronic records are complete, secure, and tamper-proof for record retention and audit purposes. Noncompliance with health care regulations can not only damage the reputation of an institution, it can also impact the bottom line.
In addition, health care providers must consider legal issues related to patient privacy, litigation, and licensing before using social media. Federal and state privacy laws limit providers’ ability to interact with patients through social media, because anything that can be used to identify a patient
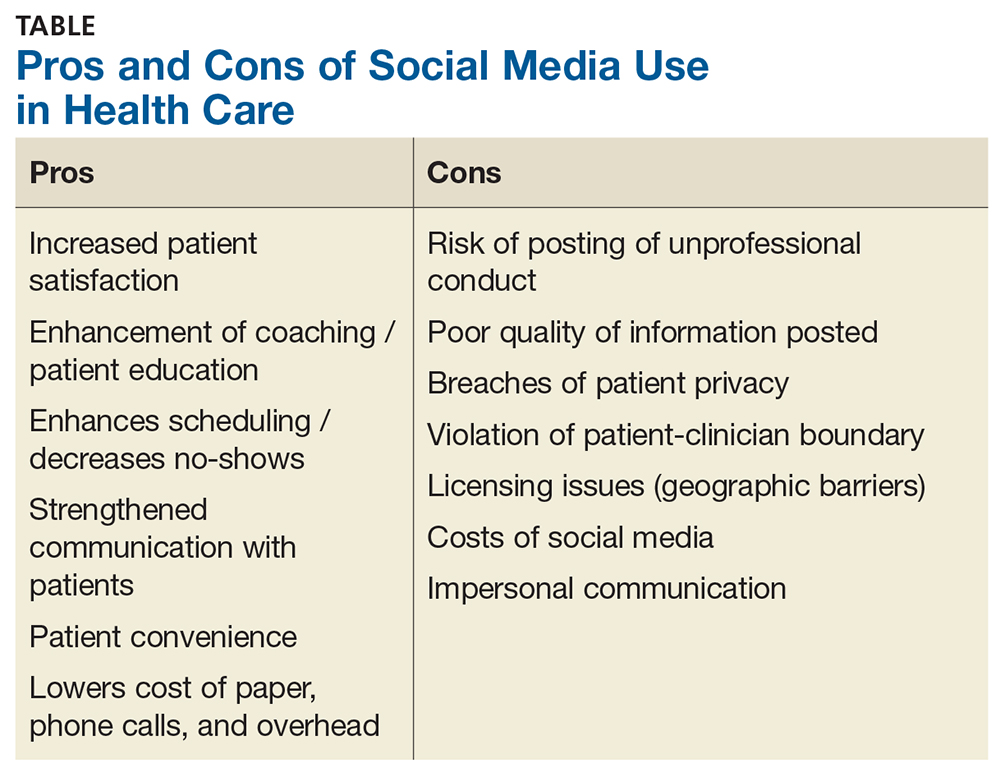
It’s no wonder some providers are leery of connecting with patients via social media. Many of them, however, have tested the waters by using social networks to connect with colleagues and peers, often sharing medical knowledge and opinions this way.
As social media has evolved, medically focused professional communities have been established. One example is SERMO, a popular, private, physician-only social network. SERMO (www.sermo.com/what-is-sermo/overview) is a virtual doctors’ lounge with more than 800,000 verified and credentialed physician members; it includes physicians from 150 countries, with plans for continued expansion. Another, the Medical Directors Forum (https://medicaldirectorsforum.com/site), is a verified, secure, closed-loop environment for peer-to-peer interaction between medical directors, which features discussion groups, calendar postings, and alerts. Finally, Doximity (www.doximity.com/review) is a social network for physicians, NPs, and PAs, which allows clinicians to call patients (with the physician’s office number displayed on caller ID), review pertinent medical articles, communicate with colleagues, and even fax and/or email documents. Additionally, the American Association of Nurse Practitioners (AANP), the American Academy of Physician Assistants (AAPA), and Clinician Reviews all have accounts on Facebook and Twitter, among other social media sites.

When it comes down to it, if used wisely, social media has the potential to promote individual and public health, as well as professional development and advancement. But carelessness can result in legal, ethical, and logistical issues, causing serious ramifications for the clinician—and possibly even the practice. So, which side of the social media debate are you on? Send your tips—or warnings—about integrating social media into your workplace to [email protected]
1. Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in healthcare: motives, barriers, and expectations. Patient Educ Couns. 2013;92(3):426-431.
2. Kaplan AM, Haenlein M. Users of the world unite! The challenges and opportunities of social media. Bus Horiz. 2010;53:59-68.
3. Statistica. Number of Facebook users worldwide as of 3rd quarter 2017 (in millions). www.statista.com/statistics/264810/number-of-monthly-active-facebook-users-worldwide/. Accessed November 16, 2017.
4. Househ M. The use of social media in healthcare: organizational, clinic, and patient perspectives. Stud Health Technol Inform. 2013;183:244-248.
5. Fisher J, Clayton M. Who gives a tweet: assessing patients’ interest in the use of social media for health care. Worldviews on Evid Based Nurs. 2012;9(2):100-108.
6. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
1. Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in healthcare: motives, barriers, and expectations. Patient Educ Couns. 2013;92(3):426-431.
2. Kaplan AM, Haenlein M. Users of the world unite! The challenges and opportunities of social media. Bus Horiz. 2010;53:59-68.
3. Statistica. Number of Facebook users worldwide as of 3rd quarter 2017 (in millions). www.statista.com/statistics/264810/number-of-monthly-active-facebook-users-worldwide/. Accessed November 16, 2017.
4. Househ M. The use of social media in healthcare: organizational, clinic, and patient perspectives. Stud Health Technol Inform. 2013;183:244-248.
5. Fisher J, Clayton M. Who gives a tweet: assessing patients’ interest in the use of social media for health care. Worldviews on Evid Based Nurs. 2012;9(2):100-108.
6. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
Which Is Junk: The Aspartame, or the Science?
A DIETARY DIAGNOSIS
I’m a hospital CEO and came across an NP colleague’s issue of Clinician Reviews; your September editorial on aspartame (2017;27[9]:6-7) caught my eye. While mine is another “n = 1” experience with the effects of aspartame, it was life-changing.
About 10 years ago, my former wife’s seizures suddenly increased in frequency after a fairly lengthy period without them. The problem was severe enough that she was faced with losing her ability to drive a car.
I had a good business relationship with the Massachusetts General Hospital and sought help from a prominent neurologist there. He asked us to keep a dietary journal before the appointment.
Though he ordered routine diagnostic tests, the journal told him all he needed to know: He told her to eliminate aspartame from her diet. It felt like a miracle when the seizures disappeared—no longer did I need to maintain bumpers on every sharp edge in the house!
Since this experience, I read every article that I can about this chemical additive and was interested to learn of your experiences.
Doug Jones
Ellsworth, ME
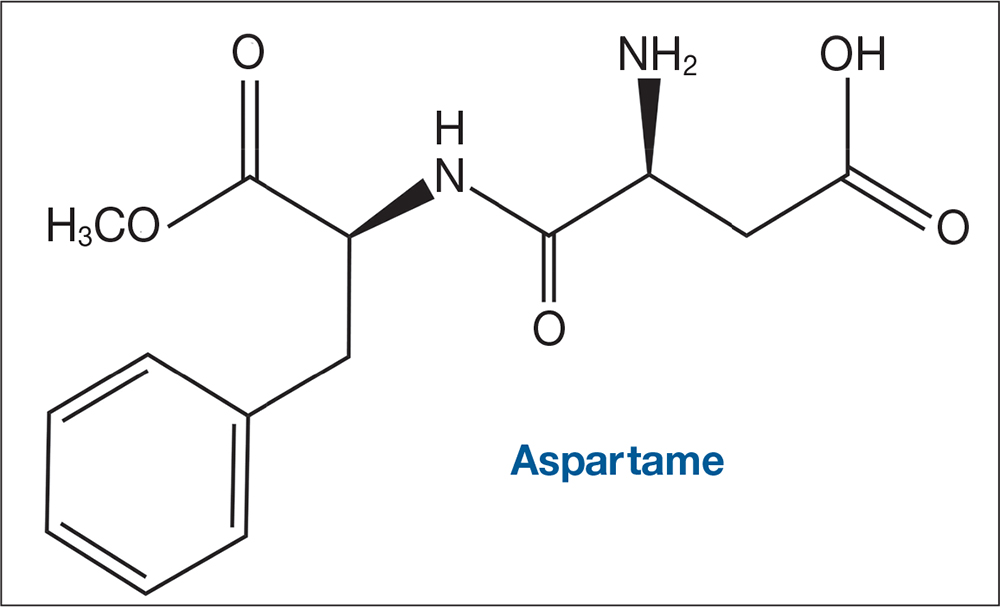
THE SCIENCE IS JUNK
I had to write because I can’t believe they allowed you to publish such a ridiculous article based on junk science. Anecdotal reports have no place in medicine. Aspartame is one of the most studied food items around. Many of these claims about the alleged danger of aspartame have been debunked by real scientists.
I am very disappointed.
Darlene Elliott, MSN, RN, CNP
Albuquerque, NM
STOP IGNORING THE BODY OF KNOWLEDGE
Thank you for addressing an issue that I believe to be of great importance. There is a huge body of knowledge that the medical community is ignoring regarding the correlation between diet and health in general, in particular the diabetes epidemic. As NPs, we are in a great position to lead.
I encourage you to read Jason Fung’s book, The Obesity Code. The entire book is eye popping, but chapter 15 (“The Diet Soda Delusion”) is particularly pertinent. He has the most thorough understanding of carbohydrate metabolism of all the authors I have read. However, Gary Taubes and Eric Westman have also published valuable resources; their books have changed my life, and I believe their knowledge could apply to many of our patients. If doctors will not embrace science, perhaps NPs will.
Martha DelGiudice, CNM
Smithtown, NY
MAYBE IT'S US …
Every time the “fasten seat belt” sign comes on, the ride gets very bumpy—so from now on, I’m going to ignore it. Aspartame “tricks our brain,” does it? What about agency? Or are we just passive leaves in the air blown about by gusts of aspartame?
Robert Pearlman, PA
Providence, RI
FAST TRACK FROM SWEET TO SOUR
Thank you for shedding light on the dangers of aspartame! My personal experience with it has not been good: One night, after drinking a large quantity of artificially sweetened powdered iced tea, I began to feel numb and experienced strange nerve sensations. I quickly learned that it is a migraine trigger for me. I now avoid aspartame and all other artificial sweeteners.
As a clinical dietitian (and NP), I’ve realized that fake food just doesn’t cut it for the body. Another issue in the dietary realm is that of folic acid. Yes, fortification has done wonders for preventing neural tube defects. But did you know that the folic acid put in our grains is a chemical that our bodies have to methylate to folinic acid, and that more than half of us do not do that well? This means excess synthetic folic acid is floating around in our bodies and brains, attributing to seizures, ADD, ADHD, migraines, miscarriages, etc.
I try to avoid eating foods with added folic acid. Talk about difficult! It means eating a lot of organic grains, whole grains, and natural vitamins with natural methylfolate to prevent anemia. Our bodies are designed to eat natural foods; the more processed something is, the more likely it is to be harmful to us.
Caroline Conneen, C-FNP, RD, IBCLC
Fredericksburg, VA
FAKE FOOD, NOT OUR FRIEND
My husband was habitually drinking flavored seltzer sweetened with aspartame when he became anxious, irritable, and developed insomnia. As soon as he stopped consuming it, the adverse effects dissipated. Since then, he has been astute about reading labels, and we do not support the use of any artificial sweeteners.
I believe aspartame should be taken off the market. The Internet is full of articles that report adverse effects from it. It seems more people are trying to avoid it. As an FNP and PMHNP, I educate my clients about aspartame and how it can exacerbate preexisting problems and contribute to insomnia, mood disorders, and panic/anxiety disorders.
I appreciate your scientific information about aspartame. We need to talk more about this chemical food additive; it is not our friend.
SUCRALOSE, ASPARTAME … ARE THE EFFECTS ONE AND THE SAME?
I have had negative thoughts concerning artificial sweeteners, including sucralose, which seems to be commonly used these days. I do not like the way I feel after ingesting these substances; it’s hard to describe—I just don’t feel right. I wonder if one answer lies in genomics and an individual’s inability to metabolize it? And to think of the byproducts you describe. Thank you for bringing this topic to light.
Anna Simon, CRNP
Allentown, PA
A DIETARY DIAGNOSIS
I’m a hospital CEO and came across an NP colleague’s issue of Clinician Reviews; your September editorial on aspartame (2017;27[9]:6-7) caught my eye. While mine is another “n = 1” experience with the effects of aspartame, it was life-changing.
About 10 years ago, my former wife’s seizures suddenly increased in frequency after a fairly lengthy period without them. The problem was severe enough that she was faced with losing her ability to drive a car.
I had a good business relationship with the Massachusetts General Hospital and sought help from a prominent neurologist there. He asked us to keep a dietary journal before the appointment.
Though he ordered routine diagnostic tests, the journal told him all he needed to know: He told her to eliminate aspartame from her diet. It felt like a miracle when the seizures disappeared—no longer did I need to maintain bumpers on every sharp edge in the house!
Since this experience, I read every article that I can about this chemical additive and was interested to learn of your experiences.
Doug Jones
Ellsworth, ME
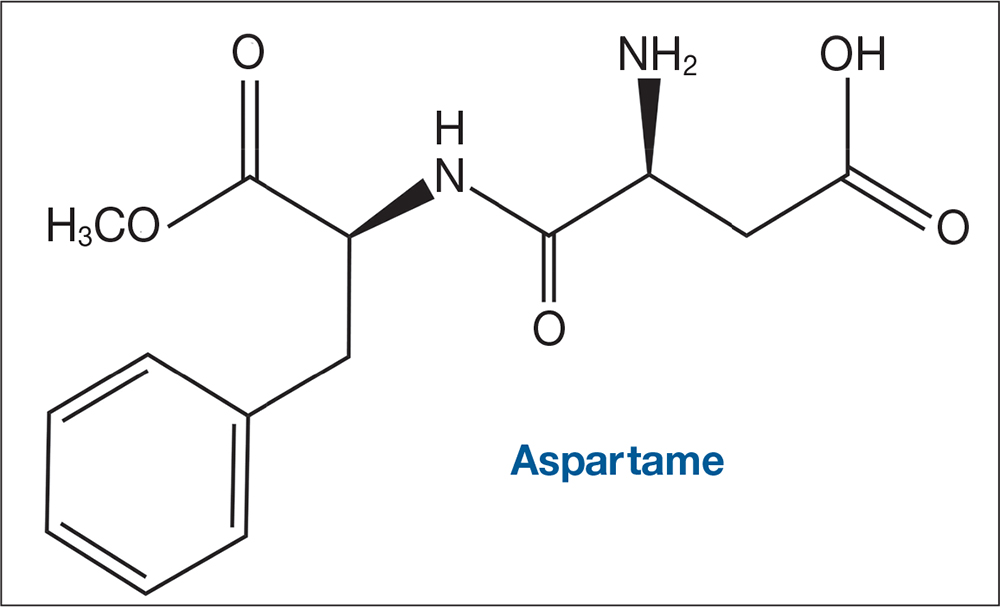
THE SCIENCE IS JUNK
I had to write because I can’t believe they allowed you to publish such a ridiculous article based on junk science. Anecdotal reports have no place in medicine. Aspartame is one of the most studied food items around. Many of these claims about the alleged danger of aspartame have been debunked by real scientists.
I am very disappointed.
Darlene Elliott, MSN, RN, CNP
Albuquerque, NM
STOP IGNORING THE BODY OF KNOWLEDGE
Thank you for addressing an issue that I believe to be of great importance. There is a huge body of knowledge that the medical community is ignoring regarding the correlation between diet and health in general, in particular the diabetes epidemic. As NPs, we are in a great position to lead.
I encourage you to read Jason Fung’s book, The Obesity Code. The entire book is eye popping, but chapter 15 (“The Diet Soda Delusion”) is particularly pertinent. He has the most thorough understanding of carbohydrate metabolism of all the authors I have read. However, Gary Taubes and Eric Westman have also published valuable resources; their books have changed my life, and I believe their knowledge could apply to many of our patients. If doctors will not embrace science, perhaps NPs will.
Martha DelGiudice, CNM
Smithtown, NY
MAYBE IT'S US …
Every time the “fasten seat belt” sign comes on, the ride gets very bumpy—so from now on, I’m going to ignore it. Aspartame “tricks our brain,” does it? What about agency? Or are we just passive leaves in the air blown about by gusts of aspartame?
Robert Pearlman, PA
Providence, RI
FAST TRACK FROM SWEET TO SOUR
Thank you for shedding light on the dangers of aspartame! My personal experience with it has not been good: One night, after drinking a large quantity of artificially sweetened powdered iced tea, I began to feel numb and experienced strange nerve sensations. I quickly learned that it is a migraine trigger for me. I now avoid aspartame and all other artificial sweeteners.
As a clinical dietitian (and NP), I’ve realized that fake food just doesn’t cut it for the body. Another issue in the dietary realm is that of folic acid. Yes, fortification has done wonders for preventing neural tube defects. But did you know that the folic acid put in our grains is a chemical that our bodies have to methylate to folinic acid, and that more than half of us do not do that well? This means excess synthetic folic acid is floating around in our bodies and brains, attributing to seizures, ADD, ADHD, migraines, miscarriages, etc.
I try to avoid eating foods with added folic acid. Talk about difficult! It means eating a lot of organic grains, whole grains, and natural vitamins with natural methylfolate to prevent anemia. Our bodies are designed to eat natural foods; the more processed something is, the more likely it is to be harmful to us.
Caroline Conneen, C-FNP, RD, IBCLC
Fredericksburg, VA
FAKE FOOD, NOT OUR FRIEND
My husband was habitually drinking flavored seltzer sweetened with aspartame when he became anxious, irritable, and developed insomnia. As soon as he stopped consuming it, the adverse effects dissipated. Since then, he has been astute about reading labels, and we do not support the use of any artificial sweeteners.
I believe aspartame should be taken off the market. The Internet is full of articles that report adverse effects from it. It seems more people are trying to avoid it. As an FNP and PMHNP, I educate my clients about aspartame and how it can exacerbate preexisting problems and contribute to insomnia, mood disorders, and panic/anxiety disorders.
I appreciate your scientific information about aspartame. We need to talk more about this chemical food additive; it is not our friend.
SUCRALOSE, ASPARTAME … ARE THE EFFECTS ONE AND THE SAME?
I have had negative thoughts concerning artificial sweeteners, including sucralose, which seems to be commonly used these days. I do not like the way I feel after ingesting these substances; it’s hard to describe—I just don’t feel right. I wonder if one answer lies in genomics and an individual’s inability to metabolize it? And to think of the byproducts you describe. Thank you for bringing this topic to light.
Anna Simon, CRNP
Allentown, PA
A DIETARY DIAGNOSIS
I’m a hospital CEO and came across an NP colleague’s issue of Clinician Reviews; your September editorial on aspartame (2017;27[9]:6-7) caught my eye. While mine is another “n = 1” experience with the effects of aspartame, it was life-changing.
About 10 years ago, my former wife’s seizures suddenly increased in frequency after a fairly lengthy period without them. The problem was severe enough that she was faced with losing her ability to drive a car.
I had a good business relationship with the Massachusetts General Hospital and sought help from a prominent neurologist there. He asked us to keep a dietary journal before the appointment.
Though he ordered routine diagnostic tests, the journal told him all he needed to know: He told her to eliminate aspartame from her diet. It felt like a miracle when the seizures disappeared—no longer did I need to maintain bumpers on every sharp edge in the house!
Since this experience, I read every article that I can about this chemical additive and was interested to learn of your experiences.
Doug Jones
Ellsworth, ME
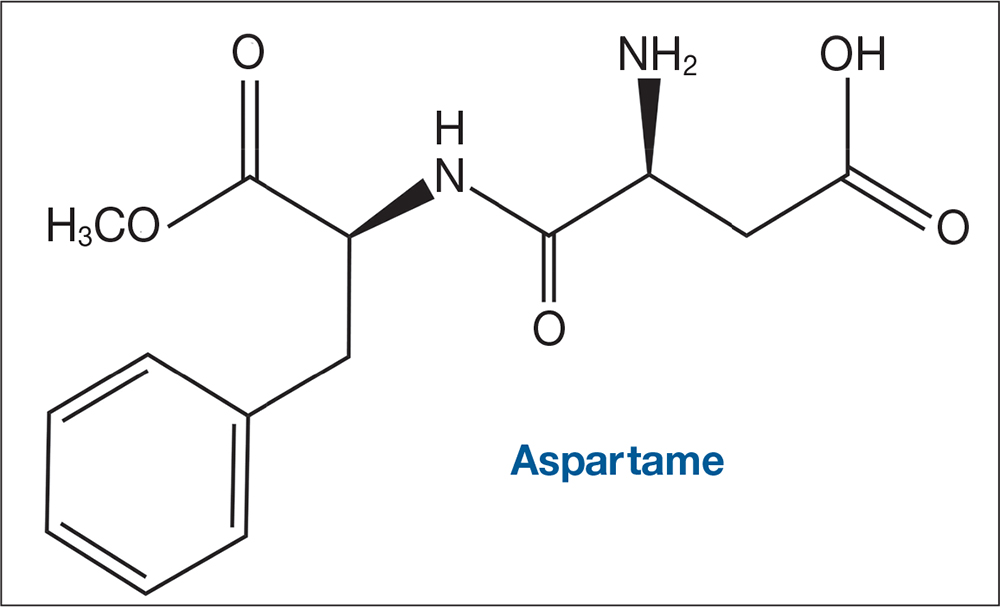
THE SCIENCE IS JUNK
I had to write because I can’t believe they allowed you to publish such a ridiculous article based on junk science. Anecdotal reports have no place in medicine. Aspartame is one of the most studied food items around. Many of these claims about the alleged danger of aspartame have been debunked by real scientists.
I am very disappointed.
Darlene Elliott, MSN, RN, CNP
Albuquerque, NM
STOP IGNORING THE BODY OF KNOWLEDGE
Thank you for addressing an issue that I believe to be of great importance. There is a huge body of knowledge that the medical community is ignoring regarding the correlation between diet and health in general, in particular the diabetes epidemic. As NPs, we are in a great position to lead.
I encourage you to read Jason Fung’s book, The Obesity Code. The entire book is eye popping, but chapter 15 (“The Diet Soda Delusion”) is particularly pertinent. He has the most thorough understanding of carbohydrate metabolism of all the authors I have read. However, Gary Taubes and Eric Westman have also published valuable resources; their books have changed my life, and I believe their knowledge could apply to many of our patients. If doctors will not embrace science, perhaps NPs will.
Martha DelGiudice, CNM
Smithtown, NY
MAYBE IT'S US …
Every time the “fasten seat belt” sign comes on, the ride gets very bumpy—so from now on, I’m going to ignore it. Aspartame “tricks our brain,” does it? What about agency? Or are we just passive leaves in the air blown about by gusts of aspartame?
Robert Pearlman, PA
Providence, RI
FAST TRACK FROM SWEET TO SOUR
Thank you for shedding light on the dangers of aspartame! My personal experience with it has not been good: One night, after drinking a large quantity of artificially sweetened powdered iced tea, I began to feel numb and experienced strange nerve sensations. I quickly learned that it is a migraine trigger for me. I now avoid aspartame and all other artificial sweeteners.
As a clinical dietitian (and NP), I’ve realized that fake food just doesn’t cut it for the body. Another issue in the dietary realm is that of folic acid. Yes, fortification has done wonders for preventing neural tube defects. But did you know that the folic acid put in our grains is a chemical that our bodies have to methylate to folinic acid, and that more than half of us do not do that well? This means excess synthetic folic acid is floating around in our bodies and brains, attributing to seizures, ADD, ADHD, migraines, miscarriages, etc.
I try to avoid eating foods with added folic acid. Talk about difficult! It means eating a lot of organic grains, whole grains, and natural vitamins with natural methylfolate to prevent anemia. Our bodies are designed to eat natural foods; the more processed something is, the more likely it is to be harmful to us.
Caroline Conneen, C-FNP, RD, IBCLC
Fredericksburg, VA
FAKE FOOD, NOT OUR FRIEND
My husband was habitually drinking flavored seltzer sweetened with aspartame when he became anxious, irritable, and developed insomnia. As soon as he stopped consuming it, the adverse effects dissipated. Since then, he has been astute about reading labels, and we do not support the use of any artificial sweeteners.
I believe aspartame should be taken off the market. The Internet is full of articles that report adverse effects from it. It seems more people are trying to avoid it. As an FNP and PMHNP, I educate my clients about aspartame and how it can exacerbate preexisting problems and contribute to insomnia, mood disorders, and panic/anxiety disorders.
I appreciate your scientific information about aspartame. We need to talk more about this chemical food additive; it is not our friend.
SUCRALOSE, ASPARTAME … ARE THE EFFECTS ONE AND THE SAME?
I have had negative thoughts concerning artificial sweeteners, including sucralose, which seems to be commonly used these days. I do not like the way I feel after ingesting these substances; it’s hard to describe—I just don’t feel right. I wonder if one answer lies in genomics and an individual’s inability to metabolize it? And to think of the byproducts you describe. Thank you for bringing this topic to light.
Anna Simon, CRNP
Allentown, PA
Diversity in the Dermatology Workforce: 2017 Status Update
Physician diversity benefits patient care: Patients are more satisfied during race-concordant visits, report their physicians as more engaged and responsive to their needs, and experience notably longer visits.1,2 Nonwhite physicians (ie, races and ethnicities that are underrepresented in medicine [URM] with respect to the general population) are more likely to care for underserved communities. Furthermore, increased diversity in the learning environment supports preparedness of all trainees to serve diverse patients.3 For these reasons, a more diverse physician workforce can contribute to better access to care in all communities, thus addressing health disparities.1,4
Increasing diversity in the dermatology workforce has been identified as an emerging priority.5 Dermatology is one of the least diverse specialties,5 and the representation of URM dermatologists is lower compared to other medical specialties and the general US population. The proportion of specialty leaders from underrepresented backgrounds may be even smaller. The lack of diversity in academic dermatology has negative consequences for patients and communities. Increasing the diversity of resident trainees is the only way to improve the diversity gap within the dermatology workforce.6
Recent commentary on this topic has highlighted several priorities for addressing the dermatology diversity gap,6-11 including the following: (1) making diversity an explicit goal in dermatology; (2) ensuring early exposure to dermatology in medical school; (3) supporting mentorship programs for minority medical students; (4) increasing medical student diversity; (5) encouraging that all dermatology program directors and leaders train in implicit bias; and (6) reviewing residency admission criteria to ensure they are objective and equitable, not biased against any applicants.
The process of reviewing residency selection criteria has begun. In 2017, Chen and Shinkai7 called for our specialty to rethink the selection process. The authors argued that emphasis on test scores, grades, and publications systematically disadvantages underrepresented minorities and students from lower socioeconomic statuses. The authors proposed several solutions: (1) make diversity an explicit goal of the selection process, (2) shift away from test scores for all applicants, (3) change the interview format, (4) prioritize other competencies such as observation skills, and (5) recruit and retain faculty who support URM trainees.7
Several dermatology leadership groups have taken action to promote programs that aim to improve diversity within dermatology. The Dermatology Diversity Champions initiative includes 6 US dermatology residency programs that are committed to increasing diversity and collaborate to evaluate pilot approaches. The American Academy of Dermatology President’s Conference on Diversity in Dermatology in Chicago, Illinois, in August 2017, as well as the focus on diversity in residency training programs at the Annual Meeting of the Association of Professors of Dermatology in Chicago, Illinois, in October 2017, are strong indicators that our specialty as a whole is aware and eager to embrace diversity as a priority. The American Academy of Dermatology President’s Conference, which was comprised of representatives from many leadership organizations and interest groups within dermatology, identified 3 action items: (1) increase the pipeline of URM students into medical school, (2) increase interest in dermatology among URM medical students, and (3) increase URM representation in residency training programs.
There are many strengths, weaknesses, opportunities, and threats/barriers (SWOT) to attaining this goal. Current strengths include strong support from dermatology leaders and activities that build on existing mentorship and diversity efforts by leaders within our specialty. SWOT analysis highlights several key opportunities of this mission, including connecting with the House of Medicine in shared efforts to improve diversity, as well as increased understanding of skin of color, health disparities, and implicit bias among physicians. Although faculty development will require time and financial investment, it will lead to tremendous benefits and opportunities for all dermatologists, including URM physicians. Other weaknesses and threats/barriers are outlined in the Figure.
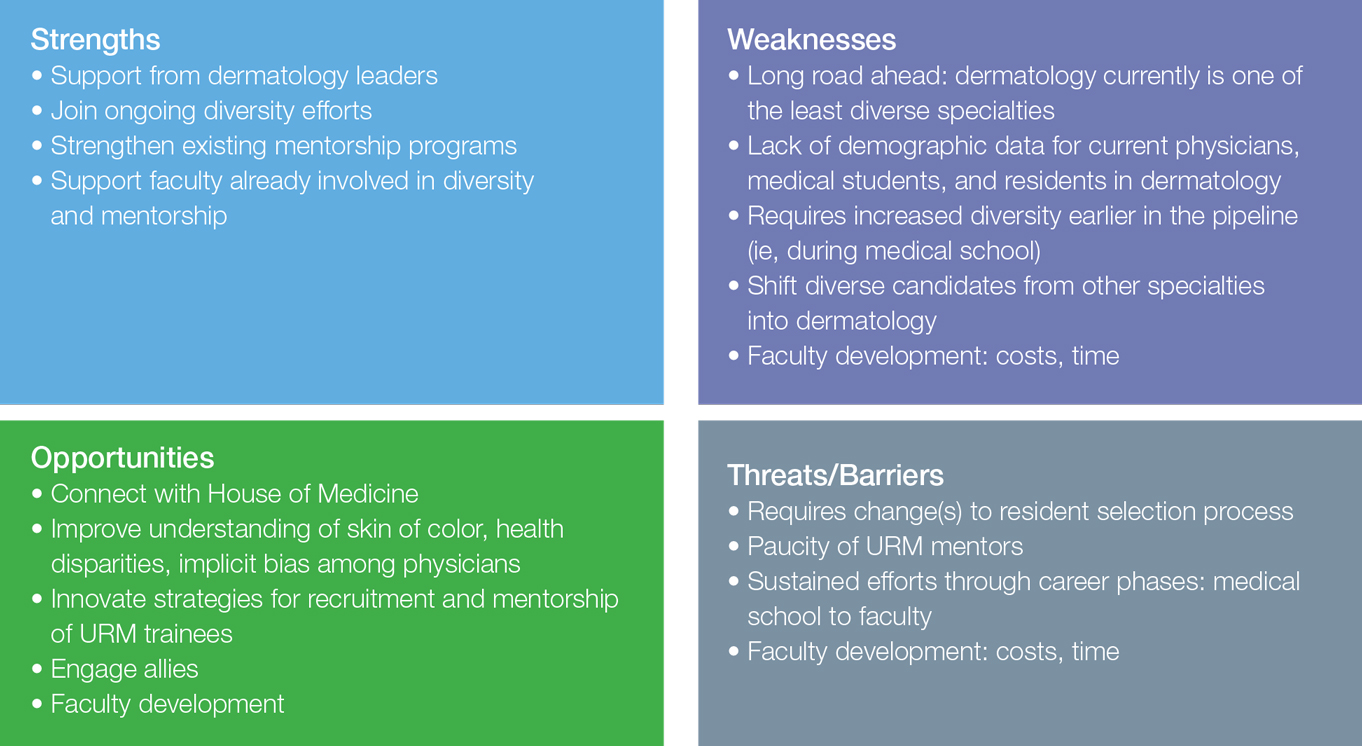
Final Thoughts
We are far from reaching our goal of a diverse dermatology workforce, and the road ahead is long. We have a start and we have momentum. We can move forward by spreading the word that all types of diversity are a priority for our specialty. Making a true difference will require commitment and sustained efforts. Dermatology can lead the way as all of American medicine strives to attain workforce diversity.
- Saha S. Taking diversity seriously: the merits of increasing minority representation in medicine. JAMA Intern Med. 2014;174:291-292.
- Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907-915.
- Saha S, Guiton G, Wimmers PF, et al. Student body racial and ethnic composition and diversity-related outcomes in US medical schools. JAMA. 2008;300:1135-1145.
- Marrast LM, Zallman L, Woolhandler S, et al. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289-291.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Lester J, Wintroub B, Linos E. Disparities in academic dermatology. JAMA Dermatol. 2016;152:878-879.
- Chen A, Shinkai K. Rethinking how we select dermatology applicants—turning the tide. JAMA Dermatol. 2017;153:259-260.
- Granstein RD, Cornelius L, Shinkai K. Diversity in dermatology—a call for action. JAMA Dermatol. 2017;153:499-500.
- McKesey J, Berger TG, Lim HW, et al. Cultural competence for the 21st century dermatologist practicing in the United States. J Am Acad Dermatol. 2017;77:1159-1169.
- Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18:S46-S49.
- Imadojemu S, James WD. Increasing African American representation in dermatology. JAMA Dermatol. 2016;152:15-16.
Physician diversity benefits patient care: Patients are more satisfied during race-concordant visits, report their physicians as more engaged and responsive to their needs, and experience notably longer visits.1,2 Nonwhite physicians (ie, races and ethnicities that are underrepresented in medicine [URM] with respect to the general population) are more likely to care for underserved communities. Furthermore, increased diversity in the learning environment supports preparedness of all trainees to serve diverse patients.3 For these reasons, a more diverse physician workforce can contribute to better access to care in all communities, thus addressing health disparities.1,4
Increasing diversity in the dermatology workforce has been identified as an emerging priority.5 Dermatology is one of the least diverse specialties,5 and the representation of URM dermatologists is lower compared to other medical specialties and the general US population. The proportion of specialty leaders from underrepresented backgrounds may be even smaller. The lack of diversity in academic dermatology has negative consequences for patients and communities. Increasing the diversity of resident trainees is the only way to improve the diversity gap within the dermatology workforce.6
Recent commentary on this topic has highlighted several priorities for addressing the dermatology diversity gap,6-11 including the following: (1) making diversity an explicit goal in dermatology; (2) ensuring early exposure to dermatology in medical school; (3) supporting mentorship programs for minority medical students; (4) increasing medical student diversity; (5) encouraging that all dermatology program directors and leaders train in implicit bias; and (6) reviewing residency admission criteria to ensure they are objective and equitable, not biased against any applicants.
The process of reviewing residency selection criteria has begun. In 2017, Chen and Shinkai7 called for our specialty to rethink the selection process. The authors argued that emphasis on test scores, grades, and publications systematically disadvantages underrepresented minorities and students from lower socioeconomic statuses. The authors proposed several solutions: (1) make diversity an explicit goal of the selection process, (2) shift away from test scores for all applicants, (3) change the interview format, (4) prioritize other competencies such as observation skills, and (5) recruit and retain faculty who support URM trainees.7
Several dermatology leadership groups have taken action to promote programs that aim to improve diversity within dermatology. The Dermatology Diversity Champions initiative includes 6 US dermatology residency programs that are committed to increasing diversity and collaborate to evaluate pilot approaches. The American Academy of Dermatology President’s Conference on Diversity in Dermatology in Chicago, Illinois, in August 2017, as well as the focus on diversity in residency training programs at the Annual Meeting of the Association of Professors of Dermatology in Chicago, Illinois, in October 2017, are strong indicators that our specialty as a whole is aware and eager to embrace diversity as a priority. The American Academy of Dermatology President’s Conference, which was comprised of representatives from many leadership organizations and interest groups within dermatology, identified 3 action items: (1) increase the pipeline of URM students into medical school, (2) increase interest in dermatology among URM medical students, and (3) increase URM representation in residency training programs.
There are many strengths, weaknesses, opportunities, and threats/barriers (SWOT) to attaining this goal. Current strengths include strong support from dermatology leaders and activities that build on existing mentorship and diversity efforts by leaders within our specialty. SWOT analysis highlights several key opportunities of this mission, including connecting with the House of Medicine in shared efforts to improve diversity, as well as increased understanding of skin of color, health disparities, and implicit bias among physicians. Although faculty development will require time and financial investment, it will lead to tremendous benefits and opportunities for all dermatologists, including URM physicians. Other weaknesses and threats/barriers are outlined in the Figure.
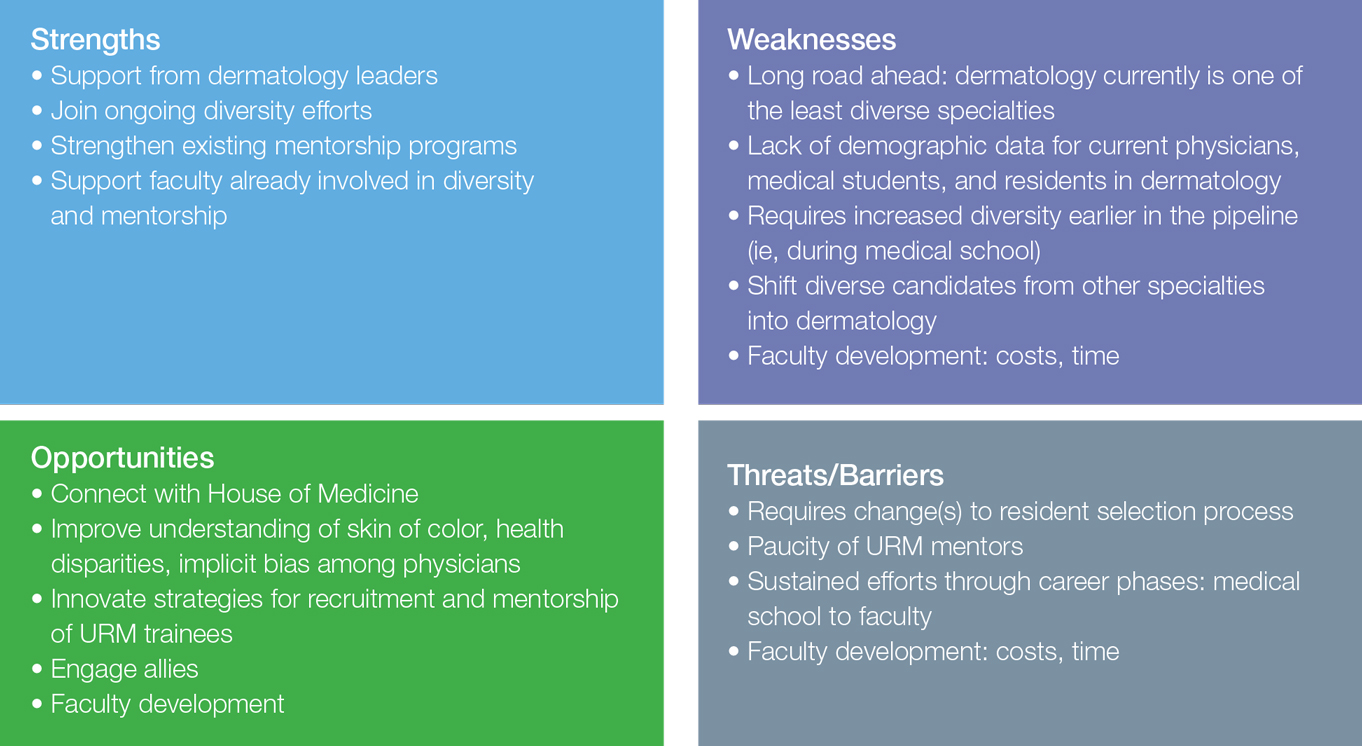
Final Thoughts
We are far from reaching our goal of a diverse dermatology workforce, and the road ahead is long. We have a start and we have momentum. We can move forward by spreading the word that all types of diversity are a priority for our specialty. Making a true difference will require commitment and sustained efforts. Dermatology can lead the way as all of American medicine strives to attain workforce diversity.
Physician diversity benefits patient care: Patients are more satisfied during race-concordant visits, report their physicians as more engaged and responsive to their needs, and experience notably longer visits.1,2 Nonwhite physicians (ie, races and ethnicities that are underrepresented in medicine [URM] with respect to the general population) are more likely to care for underserved communities. Furthermore, increased diversity in the learning environment supports preparedness of all trainees to serve diverse patients.3 For these reasons, a more diverse physician workforce can contribute to better access to care in all communities, thus addressing health disparities.1,4
Increasing diversity in the dermatology workforce has been identified as an emerging priority.5 Dermatology is one of the least diverse specialties,5 and the representation of URM dermatologists is lower compared to other medical specialties and the general US population. The proportion of specialty leaders from underrepresented backgrounds may be even smaller. The lack of diversity in academic dermatology has negative consequences for patients and communities. Increasing the diversity of resident trainees is the only way to improve the diversity gap within the dermatology workforce.6
Recent commentary on this topic has highlighted several priorities for addressing the dermatology diversity gap,6-11 including the following: (1) making diversity an explicit goal in dermatology; (2) ensuring early exposure to dermatology in medical school; (3) supporting mentorship programs for minority medical students; (4) increasing medical student diversity; (5) encouraging that all dermatology program directors and leaders train in implicit bias; and (6) reviewing residency admission criteria to ensure they are objective and equitable, not biased against any applicants.
The process of reviewing residency selection criteria has begun. In 2017, Chen and Shinkai7 called for our specialty to rethink the selection process. The authors argued that emphasis on test scores, grades, and publications systematically disadvantages underrepresented minorities and students from lower socioeconomic statuses. The authors proposed several solutions: (1) make diversity an explicit goal of the selection process, (2) shift away from test scores for all applicants, (3) change the interview format, (4) prioritize other competencies such as observation skills, and (5) recruit and retain faculty who support URM trainees.7
Several dermatology leadership groups have taken action to promote programs that aim to improve diversity within dermatology. The Dermatology Diversity Champions initiative includes 6 US dermatology residency programs that are committed to increasing diversity and collaborate to evaluate pilot approaches. The American Academy of Dermatology President’s Conference on Diversity in Dermatology in Chicago, Illinois, in August 2017, as well as the focus on diversity in residency training programs at the Annual Meeting of the Association of Professors of Dermatology in Chicago, Illinois, in October 2017, are strong indicators that our specialty as a whole is aware and eager to embrace diversity as a priority. The American Academy of Dermatology President’s Conference, which was comprised of representatives from many leadership organizations and interest groups within dermatology, identified 3 action items: (1) increase the pipeline of URM students into medical school, (2) increase interest in dermatology among URM medical students, and (3) increase URM representation in residency training programs.
There are many strengths, weaknesses, opportunities, and threats/barriers (SWOT) to attaining this goal. Current strengths include strong support from dermatology leaders and activities that build on existing mentorship and diversity efforts by leaders within our specialty. SWOT analysis highlights several key opportunities of this mission, including connecting with the House of Medicine in shared efforts to improve diversity, as well as increased understanding of skin of color, health disparities, and implicit bias among physicians. Although faculty development will require time and financial investment, it will lead to tremendous benefits and opportunities for all dermatologists, including URM physicians. Other weaknesses and threats/barriers are outlined in the Figure.
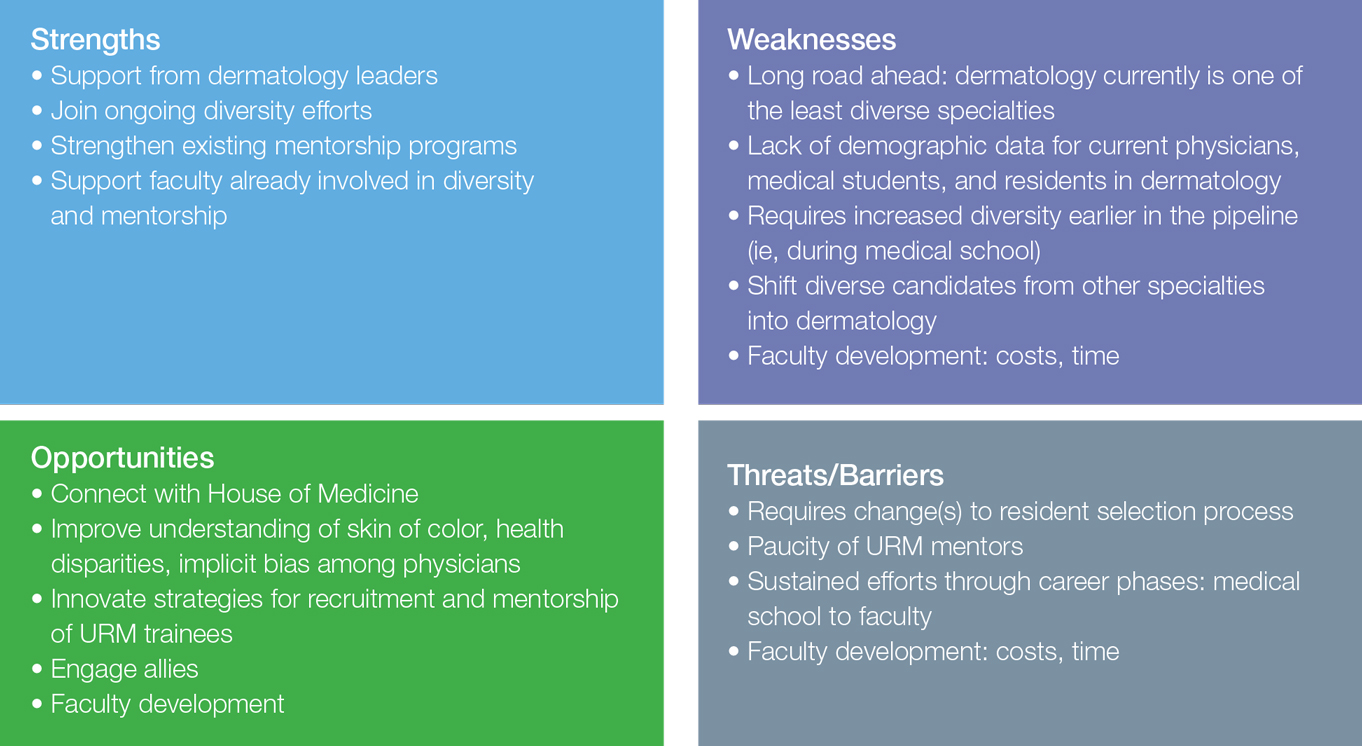
Final Thoughts
We are far from reaching our goal of a diverse dermatology workforce, and the road ahead is long. We have a start and we have momentum. We can move forward by spreading the word that all types of diversity are a priority for our specialty. Making a true difference will require commitment and sustained efforts. Dermatology can lead the way as all of American medicine strives to attain workforce diversity.
- Saha S. Taking diversity seriously: the merits of increasing minority representation in medicine. JAMA Intern Med. 2014;174:291-292.
- Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907-915.
- Saha S, Guiton G, Wimmers PF, et al. Student body racial and ethnic composition and diversity-related outcomes in US medical schools. JAMA. 2008;300:1135-1145.
- Marrast LM, Zallman L, Woolhandler S, et al. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289-291.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Lester J, Wintroub B, Linos E. Disparities in academic dermatology. JAMA Dermatol. 2016;152:878-879.
- Chen A, Shinkai K. Rethinking how we select dermatology applicants—turning the tide. JAMA Dermatol. 2017;153:259-260.
- Granstein RD, Cornelius L, Shinkai K. Diversity in dermatology—a call for action. JAMA Dermatol. 2017;153:499-500.
- McKesey J, Berger TG, Lim HW, et al. Cultural competence for the 21st century dermatologist practicing in the United States. J Am Acad Dermatol. 2017;77:1159-1169.
- Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18:S46-S49.
- Imadojemu S, James WD. Increasing African American representation in dermatology. JAMA Dermatol. 2016;152:15-16.
- Saha S. Taking diversity seriously: the merits of increasing minority representation in medicine. JAMA Intern Med. 2014;174:291-292.
- Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907-915.
- Saha S, Guiton G, Wimmers PF, et al. Student body racial and ethnic composition and diversity-related outcomes in US medical schools. JAMA. 2008;300:1135-1145.
- Marrast LM, Zallman L, Woolhandler S, et al. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289-291.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Lester J, Wintroub B, Linos E. Disparities in academic dermatology. JAMA Dermatol. 2016;152:878-879.
- Chen A, Shinkai K. Rethinking how we select dermatology applicants—turning the tide. JAMA Dermatol. 2017;153:259-260.
- Granstein RD, Cornelius L, Shinkai K. Diversity in dermatology—a call for action. JAMA Dermatol. 2017;153:499-500.
- McKesey J, Berger TG, Lim HW, et al. Cultural competence for the 21st century dermatologist practicing in the United States. J Am Acad Dermatol. 2017;77:1159-1169.
- Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18:S46-S49.
- Imadojemu S, James WD. Increasing African American representation in dermatology. JAMA Dermatol. 2016;152:15-16.
The Effects of Sunscreen on Marine Environments
Coastal travel accounts for 80% of all tourism worldwide, a number that continues to grow. The number of travelers to the Mediterranean Sea alone is expected to rise to 350 million individuals per year within the next 20 years.1 As the number of tourists visiting the world’s oceans increases, the rate of sunscreen unintentionally washed into these marine environments also rises. One study estimated that approximately one-quarter of the sunscreen applied to the skin is washed off over a 20-minute period spent in the water.2 Four of the most common sunscreen agents—benzophenone-3 (BP-3),
Benzophenone-3
4-Methylbenzylidene Camphor
Environmental concerns have also been raised about another common chemical UV filter: 4-MBC, or enzacamene. In laboratory studies, 4-MBC has been shown to cause oxidative stress to Tetrahymena thermophila, an aquatic protozoan, which results in inhibited growth. At higher concentrations, damage to the cellular membrane was seen as soon as 4 hours after exposure.6 In embryonic zebrafish, elevated 4-MBC levels were correlated to improper nerve and muscular development, resulting in developmental defects.7 Another study demonstrated that 4-MBC was toxic to Mytilus galloprovincialis, known as the Mediterranean mussel, and Paracentrotus lividus, a species of sea urchin.8 Although these studies utilized highly controlled laboratory settings, further studies are needed to examine the effects of 4-MBC on these species at environmentally relevant concentrations.
Physical Sunscreens
Physical sunscreens, as compared to the chemical filters referenced above, use either zinc or titanium to protect the skin from the sun’s rays. Nanoparticles, in particular, are preferred because they do not leave a white film on the skin.9 Both titanium dioxide and zinc oxide nanoparticles have been found to inhibit the growth and photosynthesis of marine phytoplankton, the most abundant primary producers on Earth.10,11 These metal contaminants can be transferred to organisms of higher trophic levels, including zooplankton,12 and filter-feeding organisms, including marine abalone13 and the Mediterranean mussel.14 These nanoparticles have been shown to cause oxidative stress to these organisms, making them less fit to withstand environmental stressors. It is difficult to show their true impact, however, as it is challenging to accurately detect and quantify nanoparticle concentrations in vivo.15
Final Thoughts
- Marine problems: tourism & coastal development. World Wide Fund for Nature website. http://wwf.panda.org/about_our_earth/blue_planet/problems/tourism/. Published 2017. Accessed November 14, 2017.
- Danovaro R, Bongiorni L, Corinaldesi C, et al. Sunscreens cause coral bleaching by promoting viral infections. Environ Health Perspect. 2008;116:441-447.
- Downs C, Kramarsky-Winter E, Segal R, et al. Toxicopathological effects of the sunscreen UV filter, oxybenzone (benzophenone-3), on coral planulae and cultured primary cells and its environmental contamination in Hawaii and the US Virgin Islands. Arch Environ Contam Toxicol. 2016;70:265-288.
- Sánchez Rodríguez A, Rodrigo Sanz M, Betancort Rodríguez JR. Occurrence of eight UV filters in beaches of Gran Canaria (Canary Islands)[published online March 17, 2015]. Chemosphere. 2015;131:85-90.
- Bratkovics S, Sapozhnikova Y. Determination of seven commonly used organic UV filters in fresh and saline waters by liquid chromatography-tandem mass spectrometry. Analytical Methods. 2011;3:2943-2950.
- Gao L, Yuan T, Zhou C, et al. Effects of four commonly used UV filters on the growth, cell viability and oxidative stress responses of the Tetrahymena thermophila. Chemosphere. 2013;93:2507-2513.
- Li VW, Tsui MP, Chen X, et al. Effects of 4-methylbenzylidene camphor (4-MBC) on neuronal and muscular development in zebrafish (Danio rerio) embryos [published online February 18, 2016]. Environ Sci Pollut Res Int. 2016;23:8275-8285.
- Paredes E, Perez S, Rodil R, et al. Ecotoxicological evaluation of four UV filters using marine organisms from different trophic levels Isochrysis galbana, Mytilus galloprovincialis, Paracentrotus lividus, and Siriella armata. Chemosphere. 2014;104:44-50.
- Osterwalder U, Sohn M, Herzog B. Global state of sunscreens. Photodermatol Photoimmunol Photomed. 2014;30:62-80.
- Miller RJ, Bennett S, Keller AA, et al. TiO2 nanoparticles are phototoxic to marine phytoplankton. PloS One. 2012;7:E30321.
- Spisni E. Toxicity Assessment of Industrial- and Sunscreen-derived ZnO Nanoparticles [master’s thesis]. Coral Gables, FL: University of Miami Libraries Scholarly Repository; 2016. http://scholarlyrepository.miami.edu/cgi/viewcontent.cgi?article=1625&context=oa_theses. Accessed November 10, 2017.
- Jarvis TA, Miller RJ, Lenihan HS, et al. Toxicity of ZnO nanoparticles to the copepod Acartia tonsa, exposed through a phytoplankton diet [published online April 15, 2013]. Environ Toxicol Chem. 2013;32:1264-1269.
- Zhu X, Zhou J, Cai Z. The toxicity and oxidative stress of TiO2 nanoparticles in marine abalone (Haliotis diversicolor supertexta). Mar Pollut Bull. 2011;63:334-338.
- Barmo C, Ciacci C, Canonico B, et al. In vivo effects of n-TiO2 on digestive gland and immune function of the marine bivalve Mytilus galloprovincialis. Aquatic Toxicol. 2013;132:9-18.
- Sánchez-Quiles D, Tovar-Sánchez A. Are sunscreens a new environmental risk associated with coastal tourism? Environ Int. 2015;83:158-170.
- Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
- Vesper I. Hawaii seeks to ban ‘reef-unfriendly’ sunscreen. Nature. February 3, 2017. https://www.nature.com/news/hawaii-seeks-to-ban-reef-unfriendly-sunscreen-1.21332. Accessed November 16, 2017.
Coastal travel accounts for 80% of all tourism worldwide, a number that continues to grow. The number of travelers to the Mediterranean Sea alone is expected to rise to 350 million individuals per year within the next 20 years.1 As the number of tourists visiting the world’s oceans increases, the rate of sunscreen unintentionally washed into these marine environments also rises. One study estimated that approximately one-quarter of the sunscreen applied to the skin is washed off over a 20-minute period spent in the water.2 Four of the most common sunscreen agents—benzophenone-3 (BP-3),
Benzophenone-3
4-Methylbenzylidene Camphor
Environmental concerns have also been raised about another common chemical UV filter: 4-MBC, or enzacamene. In laboratory studies, 4-MBC has been shown to cause oxidative stress to Tetrahymena thermophila, an aquatic protozoan, which results in inhibited growth. At higher concentrations, damage to the cellular membrane was seen as soon as 4 hours after exposure.6 In embryonic zebrafish, elevated 4-MBC levels were correlated to improper nerve and muscular development, resulting in developmental defects.7 Another study demonstrated that 4-MBC was toxic to Mytilus galloprovincialis, known as the Mediterranean mussel, and Paracentrotus lividus, a species of sea urchin.8 Although these studies utilized highly controlled laboratory settings, further studies are needed to examine the effects of 4-MBC on these species at environmentally relevant concentrations.
Physical Sunscreens
Physical sunscreens, as compared to the chemical filters referenced above, use either zinc or titanium to protect the skin from the sun’s rays. Nanoparticles, in particular, are preferred because they do not leave a white film on the skin.9 Both titanium dioxide and zinc oxide nanoparticles have been found to inhibit the growth and photosynthesis of marine phytoplankton, the most abundant primary producers on Earth.10,11 These metal contaminants can be transferred to organisms of higher trophic levels, including zooplankton,12 and filter-feeding organisms, including marine abalone13 and the Mediterranean mussel.14 These nanoparticles have been shown to cause oxidative stress to these organisms, making them less fit to withstand environmental stressors. It is difficult to show their true impact, however, as it is challenging to accurately detect and quantify nanoparticle concentrations in vivo.15
Final Thoughts
Coastal travel accounts for 80% of all tourism worldwide, a number that continues to grow. The number of travelers to the Mediterranean Sea alone is expected to rise to 350 million individuals per year within the next 20 years.1 As the number of tourists visiting the world’s oceans increases, the rate of sunscreen unintentionally washed into these marine environments also rises. One study estimated that approximately one-quarter of the sunscreen applied to the skin is washed off over a 20-minute period spent in the water.2 Four of the most common sunscreen agents—benzophenone-3 (BP-3),
Benzophenone-3
4-Methylbenzylidene Camphor
Environmental concerns have also been raised about another common chemical UV filter: 4-MBC, or enzacamene. In laboratory studies, 4-MBC has been shown to cause oxidative stress to Tetrahymena thermophila, an aquatic protozoan, which results in inhibited growth. At higher concentrations, damage to the cellular membrane was seen as soon as 4 hours after exposure.6 In embryonic zebrafish, elevated 4-MBC levels were correlated to improper nerve and muscular development, resulting in developmental defects.7 Another study demonstrated that 4-MBC was toxic to Mytilus galloprovincialis, known as the Mediterranean mussel, and Paracentrotus lividus, a species of sea urchin.8 Although these studies utilized highly controlled laboratory settings, further studies are needed to examine the effects of 4-MBC on these species at environmentally relevant concentrations.
Physical Sunscreens
Physical sunscreens, as compared to the chemical filters referenced above, use either zinc or titanium to protect the skin from the sun’s rays. Nanoparticles, in particular, are preferred because they do not leave a white film on the skin.9 Both titanium dioxide and zinc oxide nanoparticles have been found to inhibit the growth and photosynthesis of marine phytoplankton, the most abundant primary producers on Earth.10,11 These metal contaminants can be transferred to organisms of higher trophic levels, including zooplankton,12 and filter-feeding organisms, including marine abalone13 and the Mediterranean mussel.14 These nanoparticles have been shown to cause oxidative stress to these organisms, making them less fit to withstand environmental stressors. It is difficult to show their true impact, however, as it is challenging to accurately detect and quantify nanoparticle concentrations in vivo.15
Final Thoughts
- Marine problems: tourism & coastal development. World Wide Fund for Nature website. http://wwf.panda.org/about_our_earth/blue_planet/problems/tourism/. Published 2017. Accessed November 14, 2017.
- Danovaro R, Bongiorni L, Corinaldesi C, et al. Sunscreens cause coral bleaching by promoting viral infections. Environ Health Perspect. 2008;116:441-447.
- Downs C, Kramarsky-Winter E, Segal R, et al. Toxicopathological effects of the sunscreen UV filter, oxybenzone (benzophenone-3), on coral planulae and cultured primary cells and its environmental contamination in Hawaii and the US Virgin Islands. Arch Environ Contam Toxicol. 2016;70:265-288.
- Sánchez Rodríguez A, Rodrigo Sanz M, Betancort Rodríguez JR. Occurrence of eight UV filters in beaches of Gran Canaria (Canary Islands)[published online March 17, 2015]. Chemosphere. 2015;131:85-90.
- Bratkovics S, Sapozhnikova Y. Determination of seven commonly used organic UV filters in fresh and saline waters by liquid chromatography-tandem mass spectrometry. Analytical Methods. 2011;3:2943-2950.
- Gao L, Yuan T, Zhou C, et al. Effects of four commonly used UV filters on the growth, cell viability and oxidative stress responses of the Tetrahymena thermophila. Chemosphere. 2013;93:2507-2513.
- Li VW, Tsui MP, Chen X, et al. Effects of 4-methylbenzylidene camphor (4-MBC) on neuronal and muscular development in zebrafish (Danio rerio) embryos [published online February 18, 2016]. Environ Sci Pollut Res Int. 2016;23:8275-8285.
- Paredes E, Perez S, Rodil R, et al. Ecotoxicological evaluation of four UV filters using marine organisms from different trophic levels Isochrysis galbana, Mytilus galloprovincialis, Paracentrotus lividus, and Siriella armata. Chemosphere. 2014;104:44-50.
- Osterwalder U, Sohn M, Herzog B. Global state of sunscreens. Photodermatol Photoimmunol Photomed. 2014;30:62-80.
- Miller RJ, Bennett S, Keller AA, et al. TiO2 nanoparticles are phototoxic to marine phytoplankton. PloS One. 2012;7:E30321.
- Spisni E. Toxicity Assessment of Industrial- and Sunscreen-derived ZnO Nanoparticles [master’s thesis]. Coral Gables, FL: University of Miami Libraries Scholarly Repository; 2016. http://scholarlyrepository.miami.edu/cgi/viewcontent.cgi?article=1625&context=oa_theses. Accessed November 10, 2017.
- Jarvis TA, Miller RJ, Lenihan HS, et al. Toxicity of ZnO nanoparticles to the copepod Acartia tonsa, exposed through a phytoplankton diet [published online April 15, 2013]. Environ Toxicol Chem. 2013;32:1264-1269.
- Zhu X, Zhou J, Cai Z. The toxicity and oxidative stress of TiO2 nanoparticles in marine abalone (Haliotis diversicolor supertexta). Mar Pollut Bull. 2011;63:334-338.
- Barmo C, Ciacci C, Canonico B, et al. In vivo effects of n-TiO2 on digestive gland and immune function of the marine bivalve Mytilus galloprovincialis. Aquatic Toxicol. 2013;132:9-18.
- Sánchez-Quiles D, Tovar-Sánchez A. Are sunscreens a new environmental risk associated with coastal tourism? Environ Int. 2015;83:158-170.
- Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
- Vesper I. Hawaii seeks to ban ‘reef-unfriendly’ sunscreen. Nature. February 3, 2017. https://www.nature.com/news/hawaii-seeks-to-ban-reef-unfriendly-sunscreen-1.21332. Accessed November 16, 2017.
- Marine problems: tourism & coastal development. World Wide Fund for Nature website. http://wwf.panda.org/about_our_earth/blue_planet/problems/tourism/. Published 2017. Accessed November 14, 2017.
- Danovaro R, Bongiorni L, Corinaldesi C, et al. Sunscreens cause coral bleaching by promoting viral infections. Environ Health Perspect. 2008;116:441-447.
- Downs C, Kramarsky-Winter E, Segal R, et al. Toxicopathological effects of the sunscreen UV filter, oxybenzone (benzophenone-3), on coral planulae and cultured primary cells and its environmental contamination in Hawaii and the US Virgin Islands. Arch Environ Contam Toxicol. 2016;70:265-288.
- Sánchez Rodríguez A, Rodrigo Sanz M, Betancort Rodríguez JR. Occurrence of eight UV filters in beaches of Gran Canaria (Canary Islands)[published online March 17, 2015]. Chemosphere. 2015;131:85-90.
- Bratkovics S, Sapozhnikova Y. Determination of seven commonly used organic UV filters in fresh and saline waters by liquid chromatography-tandem mass spectrometry. Analytical Methods. 2011;3:2943-2950.
- Gao L, Yuan T, Zhou C, et al. Effects of four commonly used UV filters on the growth, cell viability and oxidative stress responses of the Tetrahymena thermophila. Chemosphere. 2013;93:2507-2513.
- Li VW, Tsui MP, Chen X, et al. Effects of 4-methylbenzylidene camphor (4-MBC) on neuronal and muscular development in zebrafish (Danio rerio) embryos [published online February 18, 2016]. Environ Sci Pollut Res Int. 2016;23:8275-8285.
- Paredes E, Perez S, Rodil R, et al. Ecotoxicological evaluation of four UV filters using marine organisms from different trophic levels Isochrysis galbana, Mytilus galloprovincialis, Paracentrotus lividus, and Siriella armata. Chemosphere. 2014;104:44-50.
- Osterwalder U, Sohn M, Herzog B. Global state of sunscreens. Photodermatol Photoimmunol Photomed. 2014;30:62-80.
- Miller RJ, Bennett S, Keller AA, et al. TiO2 nanoparticles are phototoxic to marine phytoplankton. PloS One. 2012;7:E30321.
- Spisni E. Toxicity Assessment of Industrial- and Sunscreen-derived ZnO Nanoparticles [master’s thesis]. Coral Gables, FL: University of Miami Libraries Scholarly Repository; 2016. http://scholarlyrepository.miami.edu/cgi/viewcontent.cgi?article=1625&context=oa_theses. Accessed November 10, 2017.
- Jarvis TA, Miller RJ, Lenihan HS, et al. Toxicity of ZnO nanoparticles to the copepod Acartia tonsa, exposed through a phytoplankton diet [published online April 15, 2013]. Environ Toxicol Chem. 2013;32:1264-1269.
- Zhu X, Zhou J, Cai Z. The toxicity and oxidative stress of TiO2 nanoparticles in marine abalone (Haliotis diversicolor supertexta). Mar Pollut Bull. 2011;63:334-338.
- Barmo C, Ciacci C, Canonico B, et al. In vivo effects of n-TiO2 on digestive gland and immune function of the marine bivalve Mytilus galloprovincialis. Aquatic Toxicol. 2013;132:9-18.
- Sánchez-Quiles D, Tovar-Sánchez A. Are sunscreens a new environmental risk associated with coastal tourism? Environ Int. 2015;83:158-170.
- Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
- Vesper I. Hawaii seeks to ban ‘reef-unfriendly’ sunscreen. Nature. February 3, 2017. https://www.nature.com/news/hawaii-seeks-to-ban-reef-unfriendly-sunscreen-1.21332. Accessed November 16, 2017.
Early inguinal hernia linked to schizophrenia
PARIS – One of the most unexpected and intriguing new developments in the field of schizophrenia has to be the discovery that the risk of the disease is significantly increased in men who were diagnosed with inguinal hernia before they were 13 years old.
“I think this is interesting because inguinal hernia in boys has to do with fibroblasts producing abnormal collagen structure,” according to Kristina Melkersson, MD, PhD, who presented her study findings at the annual congress of the European College of Neuropsychopharmacology.
She first detected a signal for a potential relationship in an earlier, small interview study in which she noticed that men with schizophrenia were more likely to have a history of inguinal hernia surgery than did men in the general population. This prompted her to try to confirm this preliminary observation in a large Swedish registry-based cohort study.
Among the nearly 1.3 million Swedes born during 1987-1999, there were 20,705 who were diagnosed with inguinal hernia before age 13 years. During a median 9.9 years of follow-up starting at age 13 years, 1,294 of these individuals were diagnosed with schizophrenia or schizoaffective disorder at a mean age of 21.4 years.
Among men, a history of inguinal hernia diagnosed before age 13 years was associated with a 56% increase in subsequent risk of schizophrenia or schizoaffective disorder, compared with men without such a history.
Women with a history of having inguinal hernia before age 13 years were at 16% increased risk; however, this modest increase in risk was not statistically significant, possibly because of small numbers. Inguinal hernia is 25 times more common in men than women.
Dr. Melkersson reported having no financial conflicts of interest regarding her study, which was supported by a grant from the Swedish Society of Medicine.
PARIS – One of the most unexpected and intriguing new developments in the field of schizophrenia has to be the discovery that the risk of the disease is significantly increased in men who were diagnosed with inguinal hernia before they were 13 years old.
“I think this is interesting because inguinal hernia in boys has to do with fibroblasts producing abnormal collagen structure,” according to Kristina Melkersson, MD, PhD, who presented her study findings at the annual congress of the European College of Neuropsychopharmacology.
She first detected a signal for a potential relationship in an earlier, small interview study in which she noticed that men with schizophrenia were more likely to have a history of inguinal hernia surgery than did men in the general population. This prompted her to try to confirm this preliminary observation in a large Swedish registry-based cohort study.
Among the nearly 1.3 million Swedes born during 1987-1999, there were 20,705 who were diagnosed with inguinal hernia before age 13 years. During a median 9.9 years of follow-up starting at age 13 years, 1,294 of these individuals were diagnosed with schizophrenia or schizoaffective disorder at a mean age of 21.4 years.
Among men, a history of inguinal hernia diagnosed before age 13 years was associated with a 56% increase in subsequent risk of schizophrenia or schizoaffective disorder, compared with men without such a history.
Women with a history of having inguinal hernia before age 13 years were at 16% increased risk; however, this modest increase in risk was not statistically significant, possibly because of small numbers. Inguinal hernia is 25 times more common in men than women.
Dr. Melkersson reported having no financial conflicts of interest regarding her study, which was supported by a grant from the Swedish Society of Medicine.
PARIS – One of the most unexpected and intriguing new developments in the field of schizophrenia has to be the discovery that the risk of the disease is significantly increased in men who were diagnosed with inguinal hernia before they were 13 years old.
“I think this is interesting because inguinal hernia in boys has to do with fibroblasts producing abnormal collagen structure,” according to Kristina Melkersson, MD, PhD, who presented her study findings at the annual congress of the European College of Neuropsychopharmacology.
She first detected a signal for a potential relationship in an earlier, small interview study in which she noticed that men with schizophrenia were more likely to have a history of inguinal hernia surgery than did men in the general population. This prompted her to try to confirm this preliminary observation in a large Swedish registry-based cohort study.
Among the nearly 1.3 million Swedes born during 1987-1999, there were 20,705 who were diagnosed with inguinal hernia before age 13 years. During a median 9.9 years of follow-up starting at age 13 years, 1,294 of these individuals were diagnosed with schizophrenia or schizoaffective disorder at a mean age of 21.4 years.
Among men, a history of inguinal hernia diagnosed before age 13 years was associated with a 56% increase in subsequent risk of schizophrenia or schizoaffective disorder, compared with men without such a history.
Women with a history of having inguinal hernia before age 13 years were at 16% increased risk; however, this modest increase in risk was not statistically significant, possibly because of small numbers. Inguinal hernia is 25 times more common in men than women.
Dr. Melkersson reported having no financial conflicts of interest regarding her study, which was supported by a grant from the Swedish Society of Medicine.
AT THE ECNP CONGRESS
Key clinical point:
Major finding: Swedish boys diagnosed with inguinal hernia before age 13 years were 56% more likely to be diagnosed with schizophrenia or schizoaffective disorder later in life.
Data source: This retrospective cohort study included nearly 1.3 million Swedes, 20,705 of whom were diagnosed with an inguinal hernia before age 13 years.
Disclosures: The study was supported by a grant from the Swedish Society of Medicine. The presenter reported having no financial conflicts.