User login
Complex atypical hyperplasia: When is it appropriate to refer?
Complex atypical hyperplasia (CAH) of the endometrium is considered the precursor for endometrioid endometrial cancer, the most common gynecologic cancer in the United States. This disease is most frequently diagnosed by gynecologists who are evaluating symptoms of abnormal uterine bleeding in premenopausal women or in postmenopausal women who experience new bleeding. Medical therapies, typically progestin-based treatments, can be employed, particularly when fertility preservation is desired or among patients who are poor surgical candidates. However, the most definitive therapy remains surgery with total hysterectomy for two reasons: CAH is associated with a 28% risk for the development of invasive cancer, and occult invasive cancer frequently coexists with CAH.1,2 This raises a question for gynecologists: Given the risk for occult endometrial cancer, should patients be referred to a gynecologic oncologist for their surgery?
What is the risk for cancer?
What is the significance of occult malignancy with CAH?
If surgeons are aware of endometrial cancer preoperatively or intraoperatively, decisions can be made about staging, particularly the need for lymphadenectomy. The virtues of staging in endometrial cancer is a controversial and frequently debated topic. No survival (therapeutic) benefit from lymphadenectomy has been observed in prospective trials when the information from staging results is not used to guide adjuvant therapy.4 However, the administration of adjuvant chemotherapy is associated with improved survival for patients with lymph node metastases.5 Therefore, if there is a benefit to staging with lymphadenectomy, it is its ability to identify patients who most need this life-saving systemic therapy.
Not all patients with endometrial cancer are at equal risk for harboring lymph node metastases and the majority may not benefit from lymphadenectomy. Patients with tumors that are deeply invasive, moderate or high grade, larger than 2 cm, or that have lymphovascular space invasion are at higher risk for lymph node metastases. Women with low grade, minimally invasive tumors that are smaller than 2 cm have extremely low risk for metastases.6 These criteria are commonly employed to stratify women at lowest risk and minimize unnecessary lymphadenectomy procedures. It should be noted that all three of these low risk features must be present to convey that negligible risk profile. The finding of a grade 1 invasive tumor alone is not enough to exclude potential lymph node metastases, particularly in the case of large or deeply invasive cancers.
How can the diagnosis be made preoperatively or intraoperatively?
The gold standard for discriminating between CAH and endometrial cancer is definitive surgical pathology. However, if surgeons wait until these results are available, they have lost the opportunity to stage the patient without subjecting them to a second surgery. The preoperative discovery of cancer may be increased by performing diagnostic curettage rather than relying on office endometrial biopsy sampling.7 This is likely due to the increased volume of tissue removed with dilation and curettage, and a reduction in the risk for sampling error. The addition of hysteroscopy to curettage does not improve upon the detection of cancer. Preoperative MRI to evaluate for depth of myometrial invasion has been described in cases of known endometrial cancer; however, its role in discriminating between CAH and invasive cancer is not well studied.
Intraoperative frozen section is commonly employed to evaluate the hysterectomy specimen for cancer in order to triage patients to staging during that same surgery. However, the accuracy of frozen section with definitive pathology is only approximately 50%.8 This means that at least half of women with CAH will have a false negative frozen section result and will have lost the opportunity for staging at the same procedure. The inaccuracy of frozen section is often overlooked by surgeons who may feel that it is a very straightforward diagnostic procedure. In reality, the characterization of CAH and invasive cancer is technically challenging and relies on multiple sectioning and significant experience in gynecologic pathology.9
Should all patients with CAH be referred and staged?
An alternative to relying on the frozen section process and its inherent inaccuracies would be to routinely stage all women with CAH, knowing that approximately 40% of them have occult cancer, and more than a third of those will have high risk features for lymph node metastases. However, due to the risks associated with lymphadenectomy, particularly lymphedema, most gynecologic oncologists do not routinely stage patients with preoperative CAH with complete lymphadenectomy.
An alternative to the all (complete lymphadenectomy) or none (hysterectomy alone) approach is to perform sentinel lymph node (SLN) biopsy for patients with CAH. SLN biopsy involves removing scant, but high yield lymphatic tissue, and has been shown to be extremely sensitive in detecting metastatic disease.10 This approach is commonly employed by surgeons in the treatment of ductal carcinoma in situ of the breast which, like CAH, is a stage 0 cancer that can be associated with invasive carcinoma on final pathology. In the case of ductal carcinoma in situ, the risk for upstaging is actually substantially lower (25%) than what is observed in CAH.11 Therefore, it would seem even more compelling to apply this approach for endometrial pathologies. The ability to apply the SLN technique is lost after hysterectomy is performed, as there is no longer the target organ into which tracer can be injected; therefore, if SLN biopsy is to be offered to these patients, it needs to be performed using only the preoperative diagnosis of CAH. In this approach, there will be overtreatment of approximately two-thirds of patients, albeit with a less radical and morbid staging procedure.
Making the decision to refer
Ultimately, decisions to refer or not are guided by comprehensive discussions between patient and provider that outline the potential risks and benefits of various approaches. Patients frequently have strong relationships with confidence in their gynecologists who may have cared for them for many years, and may be motivated to have them perform their surgery. For others, the uncertainty and possibility of an unstaged cancer and the potential of a second surgery drives their decision to seek an oncology consultation. Clinicians should discuss the inherent uncertainties in the diagnosis of CAH and the potential for underlying cancer and lymph node metastases, and help patients determine the balance of their underlying competing concerns regarding the risk for inadequate surgery versus the risk of unnecessary surgical procedures.
Summary of recommendations
Invasive endometrial cancer will be identified in the hysterectomy specimens of approximately 40% of women with a preoperative diagnosis of complex endometrial hyperplasia. Preoperative dilation and curettage may reduce the potential for missed occult cancer. Frozen section is an option for determining which patients might benefit from staging but is associated with significant inaccuracies. Failure to diagnose malignancy pre- or intraoperatively handicaps postoperative decision making regarding the necessity of adjuvant chemotherapy, and prevents the ability to offer patients potentially less morbid staging techniques such as SLN biopsy. When gynecologists without oncology training perform these hysterectomies, they should discuss these scenarios to patients and consider referral to gynecologic oncology for patients who desire the potential for comprehensive staging if necessary.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina, Chapel Hill. She reports no relevant financial disclosures.
References
1. J Clin Oncol. 2010 Feb;28:788-92.
2. Cancer. 2006 Feb;106:812-9.
3. Int J Gynecol Cancer. 2005 Jan-Feb;15:127-31.
4. Lancet. 2009 Jan;373(9658):125-36.
5. J Clin Oncol. 2006 Jan;24:36-44.
6. Gynecol Oncol 2008 Apr;109:11-8.
7. Am J Obstet Gynecol. 2010 Oct;203(4):349. e1-6.
8. Am J Obstet Gynecol. 2007 May;196(5):e40-2.
9. Obstet Gynecol. 2012 Nov;120(5):1160-75.
10. Lancet Oncol. 2017 Mar;18(3):384-92.
11. Radiology. 2011 Jul;260:119-28.
Complex atypical hyperplasia (CAH) of the endometrium is considered the precursor for endometrioid endometrial cancer, the most common gynecologic cancer in the United States. This disease is most frequently diagnosed by gynecologists who are evaluating symptoms of abnormal uterine bleeding in premenopausal women or in postmenopausal women who experience new bleeding. Medical therapies, typically progestin-based treatments, can be employed, particularly when fertility preservation is desired or among patients who are poor surgical candidates. However, the most definitive therapy remains surgery with total hysterectomy for two reasons: CAH is associated with a 28% risk for the development of invasive cancer, and occult invasive cancer frequently coexists with CAH.1,2 This raises a question for gynecologists: Given the risk for occult endometrial cancer, should patients be referred to a gynecologic oncologist for their surgery?
What is the risk for cancer?
What is the significance of occult malignancy with CAH?
If surgeons are aware of endometrial cancer preoperatively or intraoperatively, decisions can be made about staging, particularly the need for lymphadenectomy. The virtues of staging in endometrial cancer is a controversial and frequently debated topic. No survival (therapeutic) benefit from lymphadenectomy has been observed in prospective trials when the information from staging results is not used to guide adjuvant therapy.4 However, the administration of adjuvant chemotherapy is associated with improved survival for patients with lymph node metastases.5 Therefore, if there is a benefit to staging with lymphadenectomy, it is its ability to identify patients who most need this life-saving systemic therapy.
Not all patients with endometrial cancer are at equal risk for harboring lymph node metastases and the majority may not benefit from lymphadenectomy. Patients with tumors that are deeply invasive, moderate or high grade, larger than 2 cm, or that have lymphovascular space invasion are at higher risk for lymph node metastases. Women with low grade, minimally invasive tumors that are smaller than 2 cm have extremely low risk for metastases.6 These criteria are commonly employed to stratify women at lowest risk and minimize unnecessary lymphadenectomy procedures. It should be noted that all three of these low risk features must be present to convey that negligible risk profile. The finding of a grade 1 invasive tumor alone is not enough to exclude potential lymph node metastases, particularly in the case of large or deeply invasive cancers.
How can the diagnosis be made preoperatively or intraoperatively?
The gold standard for discriminating between CAH and endometrial cancer is definitive surgical pathology. However, if surgeons wait until these results are available, they have lost the opportunity to stage the patient without subjecting them to a second surgery. The preoperative discovery of cancer may be increased by performing diagnostic curettage rather than relying on office endometrial biopsy sampling.7 This is likely due to the increased volume of tissue removed with dilation and curettage, and a reduction in the risk for sampling error. The addition of hysteroscopy to curettage does not improve upon the detection of cancer. Preoperative MRI to evaluate for depth of myometrial invasion has been described in cases of known endometrial cancer; however, its role in discriminating between CAH and invasive cancer is not well studied.
Intraoperative frozen section is commonly employed to evaluate the hysterectomy specimen for cancer in order to triage patients to staging during that same surgery. However, the accuracy of frozen section with definitive pathology is only approximately 50%.8 This means that at least half of women with CAH will have a false negative frozen section result and will have lost the opportunity for staging at the same procedure. The inaccuracy of frozen section is often overlooked by surgeons who may feel that it is a very straightforward diagnostic procedure. In reality, the characterization of CAH and invasive cancer is technically challenging and relies on multiple sectioning and significant experience in gynecologic pathology.9
Should all patients with CAH be referred and staged?
An alternative to relying on the frozen section process and its inherent inaccuracies would be to routinely stage all women with CAH, knowing that approximately 40% of them have occult cancer, and more than a third of those will have high risk features for lymph node metastases. However, due to the risks associated with lymphadenectomy, particularly lymphedema, most gynecologic oncologists do not routinely stage patients with preoperative CAH with complete lymphadenectomy.
An alternative to the all (complete lymphadenectomy) or none (hysterectomy alone) approach is to perform sentinel lymph node (SLN) biopsy for patients with CAH. SLN biopsy involves removing scant, but high yield lymphatic tissue, and has been shown to be extremely sensitive in detecting metastatic disease.10 This approach is commonly employed by surgeons in the treatment of ductal carcinoma in situ of the breast which, like CAH, is a stage 0 cancer that can be associated with invasive carcinoma on final pathology. In the case of ductal carcinoma in situ, the risk for upstaging is actually substantially lower (25%) than what is observed in CAH.11 Therefore, it would seem even more compelling to apply this approach for endometrial pathologies. The ability to apply the SLN technique is lost after hysterectomy is performed, as there is no longer the target organ into which tracer can be injected; therefore, if SLN biopsy is to be offered to these patients, it needs to be performed using only the preoperative diagnosis of CAH. In this approach, there will be overtreatment of approximately two-thirds of patients, albeit with a less radical and morbid staging procedure.
Making the decision to refer
Ultimately, decisions to refer or not are guided by comprehensive discussions between patient and provider that outline the potential risks and benefits of various approaches. Patients frequently have strong relationships with confidence in their gynecologists who may have cared for them for many years, and may be motivated to have them perform their surgery. For others, the uncertainty and possibility of an unstaged cancer and the potential of a second surgery drives their decision to seek an oncology consultation. Clinicians should discuss the inherent uncertainties in the diagnosis of CAH and the potential for underlying cancer and lymph node metastases, and help patients determine the balance of their underlying competing concerns regarding the risk for inadequate surgery versus the risk of unnecessary surgical procedures.
Summary of recommendations
Invasive endometrial cancer will be identified in the hysterectomy specimens of approximately 40% of women with a preoperative diagnosis of complex endometrial hyperplasia. Preoperative dilation and curettage may reduce the potential for missed occult cancer. Frozen section is an option for determining which patients might benefit from staging but is associated with significant inaccuracies. Failure to diagnose malignancy pre- or intraoperatively handicaps postoperative decision making regarding the necessity of adjuvant chemotherapy, and prevents the ability to offer patients potentially less morbid staging techniques such as SLN biopsy. When gynecologists without oncology training perform these hysterectomies, they should discuss these scenarios to patients and consider referral to gynecologic oncology for patients who desire the potential for comprehensive staging if necessary.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina, Chapel Hill. She reports no relevant financial disclosures.
References
1. J Clin Oncol. 2010 Feb;28:788-92.
2. Cancer. 2006 Feb;106:812-9.
3. Int J Gynecol Cancer. 2005 Jan-Feb;15:127-31.
4. Lancet. 2009 Jan;373(9658):125-36.
5. J Clin Oncol. 2006 Jan;24:36-44.
6. Gynecol Oncol 2008 Apr;109:11-8.
7. Am J Obstet Gynecol. 2010 Oct;203(4):349. e1-6.
8. Am J Obstet Gynecol. 2007 May;196(5):e40-2.
9. Obstet Gynecol. 2012 Nov;120(5):1160-75.
10. Lancet Oncol. 2017 Mar;18(3):384-92.
11. Radiology. 2011 Jul;260:119-28.
Complex atypical hyperplasia (CAH) of the endometrium is considered the precursor for endometrioid endometrial cancer, the most common gynecologic cancer in the United States. This disease is most frequently diagnosed by gynecologists who are evaluating symptoms of abnormal uterine bleeding in premenopausal women or in postmenopausal women who experience new bleeding. Medical therapies, typically progestin-based treatments, can be employed, particularly when fertility preservation is desired or among patients who are poor surgical candidates. However, the most definitive therapy remains surgery with total hysterectomy for two reasons: CAH is associated with a 28% risk for the development of invasive cancer, and occult invasive cancer frequently coexists with CAH.1,2 This raises a question for gynecologists: Given the risk for occult endometrial cancer, should patients be referred to a gynecologic oncologist for their surgery?
What is the risk for cancer?
What is the significance of occult malignancy with CAH?
If surgeons are aware of endometrial cancer preoperatively or intraoperatively, decisions can be made about staging, particularly the need for lymphadenectomy. The virtues of staging in endometrial cancer is a controversial and frequently debated topic. No survival (therapeutic) benefit from lymphadenectomy has been observed in prospective trials when the information from staging results is not used to guide adjuvant therapy.4 However, the administration of adjuvant chemotherapy is associated with improved survival for patients with lymph node metastases.5 Therefore, if there is a benefit to staging with lymphadenectomy, it is its ability to identify patients who most need this life-saving systemic therapy.
Not all patients with endometrial cancer are at equal risk for harboring lymph node metastases and the majority may not benefit from lymphadenectomy. Patients with tumors that are deeply invasive, moderate or high grade, larger than 2 cm, or that have lymphovascular space invasion are at higher risk for lymph node metastases. Women with low grade, minimally invasive tumors that are smaller than 2 cm have extremely low risk for metastases.6 These criteria are commonly employed to stratify women at lowest risk and minimize unnecessary lymphadenectomy procedures. It should be noted that all three of these low risk features must be present to convey that negligible risk profile. The finding of a grade 1 invasive tumor alone is not enough to exclude potential lymph node metastases, particularly in the case of large or deeply invasive cancers.
How can the diagnosis be made preoperatively or intraoperatively?
The gold standard for discriminating between CAH and endometrial cancer is definitive surgical pathology. However, if surgeons wait until these results are available, they have lost the opportunity to stage the patient without subjecting them to a second surgery. The preoperative discovery of cancer may be increased by performing diagnostic curettage rather than relying on office endometrial biopsy sampling.7 This is likely due to the increased volume of tissue removed with dilation and curettage, and a reduction in the risk for sampling error. The addition of hysteroscopy to curettage does not improve upon the detection of cancer. Preoperative MRI to evaluate for depth of myometrial invasion has been described in cases of known endometrial cancer; however, its role in discriminating between CAH and invasive cancer is not well studied.
Intraoperative frozen section is commonly employed to evaluate the hysterectomy specimen for cancer in order to triage patients to staging during that same surgery. However, the accuracy of frozen section with definitive pathology is only approximately 50%.8 This means that at least half of women with CAH will have a false negative frozen section result and will have lost the opportunity for staging at the same procedure. The inaccuracy of frozen section is often overlooked by surgeons who may feel that it is a very straightforward diagnostic procedure. In reality, the characterization of CAH and invasive cancer is technically challenging and relies on multiple sectioning and significant experience in gynecologic pathology.9
Should all patients with CAH be referred and staged?
An alternative to relying on the frozen section process and its inherent inaccuracies would be to routinely stage all women with CAH, knowing that approximately 40% of them have occult cancer, and more than a third of those will have high risk features for lymph node metastases. However, due to the risks associated with lymphadenectomy, particularly lymphedema, most gynecologic oncologists do not routinely stage patients with preoperative CAH with complete lymphadenectomy.
An alternative to the all (complete lymphadenectomy) or none (hysterectomy alone) approach is to perform sentinel lymph node (SLN) biopsy for patients with CAH. SLN biopsy involves removing scant, but high yield lymphatic tissue, and has been shown to be extremely sensitive in detecting metastatic disease.10 This approach is commonly employed by surgeons in the treatment of ductal carcinoma in situ of the breast which, like CAH, is a stage 0 cancer that can be associated with invasive carcinoma on final pathology. In the case of ductal carcinoma in situ, the risk for upstaging is actually substantially lower (25%) than what is observed in CAH.11 Therefore, it would seem even more compelling to apply this approach for endometrial pathologies. The ability to apply the SLN technique is lost after hysterectomy is performed, as there is no longer the target organ into which tracer can be injected; therefore, if SLN biopsy is to be offered to these patients, it needs to be performed using only the preoperative diagnosis of CAH. In this approach, there will be overtreatment of approximately two-thirds of patients, albeit with a less radical and morbid staging procedure.
Making the decision to refer
Ultimately, decisions to refer or not are guided by comprehensive discussions between patient and provider that outline the potential risks and benefits of various approaches. Patients frequently have strong relationships with confidence in their gynecologists who may have cared for them for many years, and may be motivated to have them perform their surgery. For others, the uncertainty and possibility of an unstaged cancer and the potential of a second surgery drives their decision to seek an oncology consultation. Clinicians should discuss the inherent uncertainties in the diagnosis of CAH and the potential for underlying cancer and lymph node metastases, and help patients determine the balance of their underlying competing concerns regarding the risk for inadequate surgery versus the risk of unnecessary surgical procedures.
Summary of recommendations
Invasive endometrial cancer will be identified in the hysterectomy specimens of approximately 40% of women with a preoperative diagnosis of complex endometrial hyperplasia. Preoperative dilation and curettage may reduce the potential for missed occult cancer. Frozen section is an option for determining which patients might benefit from staging but is associated with significant inaccuracies. Failure to diagnose malignancy pre- or intraoperatively handicaps postoperative decision making regarding the necessity of adjuvant chemotherapy, and prevents the ability to offer patients potentially less morbid staging techniques such as SLN biopsy. When gynecologists without oncology training perform these hysterectomies, they should discuss these scenarios to patients and consider referral to gynecologic oncology for patients who desire the potential for comprehensive staging if necessary.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina, Chapel Hill. She reports no relevant financial disclosures.
References
1. J Clin Oncol. 2010 Feb;28:788-92.
2. Cancer. 2006 Feb;106:812-9.
3. Int J Gynecol Cancer. 2005 Jan-Feb;15:127-31.
4. Lancet. 2009 Jan;373(9658):125-36.
5. J Clin Oncol. 2006 Jan;24:36-44.
6. Gynecol Oncol 2008 Apr;109:11-8.
7. Am J Obstet Gynecol. 2010 Oct;203(4):349. e1-6.
8. Am J Obstet Gynecol. 2007 May;196(5):e40-2.
9. Obstet Gynecol. 2012 Nov;120(5):1160-75.
10. Lancet Oncol. 2017 Mar;18(3):384-92.
11. Radiology. 2011 Jul;260:119-28.
Physician-assisted suicide – an update
Question: Choose the best answer regarding physician-assisted suicide in the United States:
A. It is now legal in most states.
B. Under California law, assisting or causing one to commit suicide, including physician-assisted suicide, still remains a felony.
C. Both the U.S. Supreme Court and the New York Court of Appeals have held there is no constitutional right to physician-assisted suicide.
D. The American Medical Association is neutral on the issue.
E. Pain relief is the overriding reason for patients who request physician-assisted suicide.
Answer: C. We reviewed this topic in one of our regular columns in 2013.1 At that time, efforts to legalize physician-assisted suicide (PAS) appeared to be gathering momentum across the country, with four jurisdictions having legalized the practice, beginning with Oregon in 1994. The other states were Washington, Vermont, and Montana, whose Supreme Court held that there was no public interest reason against the practice.2
Since that time, California, Colorado, and the District of Columbia have joined the group. Currently, PAS – but not euthanasia – is legally available in these jurisdictions and in Switzerland, but both can be legally practiced in Belgium, Canada, Colombia, Luxembourg, and the Netherlands.
All state statutes permitting PAS provide similar provisions and safeguards. Only competent individuals who are terminally ill, i.e., death expected within 6 months, can make a request for a lethal dose of medication to carry out the suicidal act. The request to the doctor is first made verbally, then in writing, and a second opinion must be obtained to confirm the patient’s intent, understanding, and free choice. There is also a waiting period.
Public support for euthanasia and PAS in the United States is said to have plateaued since the 1990s. But a significant number of Americans, 67%, still favor PAS, up from 56% a decade ago.3 However, not many patients resort to PAS – usually those with terminal cancers or neuromuscular conditions – and only a minority of physicians are participants.
For example, 61 physicians in Oregon wrote a total of 115 prescriptions in 2012; there were 77 known Death With Dignity Act deaths in Oregon that year.4 In Oregon and Washington State, less than 1% of licensed physicians write prescriptions for physician-assisted suicide each year. In contrast, about half or more of physicians in the Netherlands and Belgium reported ever having received a request, and 60% of Dutch physicians have granted such requests.
The California Department of Public Health reported that 111 terminally ill patients availed themselves of California’s End of Life Option Act in the 7 months after it became effective on June 9, 2016.
In a recent review on euthanasia and PAS for the period 1947-2016, Ezekiel Emanuel, MD, and colleagues noted that typical patients were older, white, and well educated, and pain was mostly not reported as the primary motivation.5 A large portion of patients receiving PAS in Oregon and Washington were enrolled in hospice or palliative care. Abuses have not been apparent.
In the vast majority of jurisdictions, assisting or causing one to commit suicide, including PAS, still remains a crime; for example, it is considered manslaughter under Hawaii state law §707-702.
In distinguishing between assisting suicide and withdrawing life-sustaining treatment, the U.S. Supreme Court’s landmark 1997 Vacco v. Quill decision emphasized issues of causation and intent.6 On causation, the court reasoned that when a patient refuses life-sustaining treatment, he dies from an underlying fatal disease; but if a patient ingests a lethal medication, he is killed by that medication. As to intent, a physician who honors a patient’s refusal of treatment purposefully intends only to respect his patient’s wishes and to cease doing futile or degrading things. On the other hand, a doctor who assists a suicide “must, necessarily and indubitably, intend primarily that the patient be made dead.”
In its companion case Washington v. Glucksberg, the Supreme Court held that the asserted “right” to assistance in committing suicide is not a fundamental liberty interest protected by the due process clause.7
State supreme courts in Florida, New Mexico, and elsewhere have likewise rebuffed claims of any constitutional right to PAS. The latest court to so rule is in New York, which has a long history of criminalizing assisted suicide.8 The New York Court of Appeals recently addressed claims brought by three terminally ill individuals, several medical providers, and a nonprofit entity seeking a declaration that New York’s “assisted suicide” statutes exclude physicians from prescribing a lethal dose of drugs to terminally ill, competent patients.
The court unequivocally rejected such claims and affirmed that a physician who assists a suicide by prescribing lethal doses of drugs is subject to criminal prosecution for second-degree manslaughter. It refused to regard PAS as being different from assisted suicide in general, and it rejected the constitutional claim to assisted suicide by a terminally ill person. The state appeals court reiterated the U.S. Supreme Court’s distinction between refusing life-sustaining treatment and assisted suicide, the former being “at least partially rooted in notions of bodily integrity, as the right to refuse treatment is a consequence of a person’s right to resist unwanted bodily invasions.” The New York Court of Appeals also noted that the state has a legitimate purpose and a rational basis for guarding against the risks of mistake and abuse.
These developments may signal a shift away from the legalization of PAS, as recently suggested in a Washington Post article.9 According to the end-of-life advocacy organization Compassion and Choices, none of the 27 states where such measures were introduced in 2017 passed them into law, including states such as Connecticut, Hawaii, and Rhode Island. In Central and Eastern Europe, support is decreasing, whereas the opposite is true in Western Europe.
U.S. federal lawmakers also appear to be pushing back. On July 13, 2017, the U.S. House Committee on Appropriations voted to block implementation of a “death with dignity” statute passed by the District of Columbia. Further, 11 House members – including 6 Democrats – have introduced a resolution asserting that PAS undermines a key safeguard that protects our nation’s most vulnerable citizens, including the elderly, people with disabilities, and people experiencing psychiatric diagnoses.10
The American Medical Association is steadfast in its opposition to PAS and euthanasia. In its latest Code of Ethics, the AMA reaffirmed its long-held position that “allowing physicians to engage in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks. … Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life.”11
References
1. “Physician-assisted suicide,” Internal Medicine News, Oct. 14, 2013.
2. Baxter v. State of Montana, 224 P. 3d 1211 (2010).
3. “Majority of Americans Remain Supportive of Euthanasia,” Gallup News, June 12, 2017.
4. Statistics available at public.health.oregon.gov under Oregon Death with Dignity Act.
5. JAMA. 2016 Jul 5;316(1):79-90.
6. Vacco v. Quill, 117 S. Ct. 2293 (1997).
7. Washington v. Glucksberg, 521 U.S. 702 (1997).
8. Myers v. Schneiderman, New York Court of Appeals, 2017.
9. “Legalizing assisted suicide has stalled at every level,” Washington Post, Oct. 24, 2017.
10. H. Con. Res. 80, 115th Congress (2017-2018).
11. AMA Code of Medical Ethics §5.7 (2017).
Question: Choose the best answer regarding physician-assisted suicide in the United States:
A. It is now legal in most states.
B. Under California law, assisting or causing one to commit suicide, including physician-assisted suicide, still remains a felony.
C. Both the U.S. Supreme Court and the New York Court of Appeals have held there is no constitutional right to physician-assisted suicide.
D. The American Medical Association is neutral on the issue.
E. Pain relief is the overriding reason for patients who request physician-assisted suicide.
Answer: C. We reviewed this topic in one of our regular columns in 2013.1 At that time, efforts to legalize physician-assisted suicide (PAS) appeared to be gathering momentum across the country, with four jurisdictions having legalized the practice, beginning with Oregon in 1994. The other states were Washington, Vermont, and Montana, whose Supreme Court held that there was no public interest reason against the practice.2
Since that time, California, Colorado, and the District of Columbia have joined the group. Currently, PAS – but not euthanasia – is legally available in these jurisdictions and in Switzerland, but both can be legally practiced in Belgium, Canada, Colombia, Luxembourg, and the Netherlands.
All state statutes permitting PAS provide similar provisions and safeguards. Only competent individuals who are terminally ill, i.e., death expected within 6 months, can make a request for a lethal dose of medication to carry out the suicidal act. The request to the doctor is first made verbally, then in writing, and a second opinion must be obtained to confirm the patient’s intent, understanding, and free choice. There is also a waiting period.
Public support for euthanasia and PAS in the United States is said to have plateaued since the 1990s. But a significant number of Americans, 67%, still favor PAS, up from 56% a decade ago.3 However, not many patients resort to PAS – usually those with terminal cancers or neuromuscular conditions – and only a minority of physicians are participants.
For example, 61 physicians in Oregon wrote a total of 115 prescriptions in 2012; there were 77 known Death With Dignity Act deaths in Oregon that year.4 In Oregon and Washington State, less than 1% of licensed physicians write prescriptions for physician-assisted suicide each year. In contrast, about half or more of physicians in the Netherlands and Belgium reported ever having received a request, and 60% of Dutch physicians have granted such requests.
The California Department of Public Health reported that 111 terminally ill patients availed themselves of California’s End of Life Option Act in the 7 months after it became effective on June 9, 2016.
In a recent review on euthanasia and PAS for the period 1947-2016, Ezekiel Emanuel, MD, and colleagues noted that typical patients were older, white, and well educated, and pain was mostly not reported as the primary motivation.5 A large portion of patients receiving PAS in Oregon and Washington were enrolled in hospice or palliative care. Abuses have not been apparent.
In the vast majority of jurisdictions, assisting or causing one to commit suicide, including PAS, still remains a crime; for example, it is considered manslaughter under Hawaii state law §707-702.
In distinguishing between assisting suicide and withdrawing life-sustaining treatment, the U.S. Supreme Court’s landmark 1997 Vacco v. Quill decision emphasized issues of causation and intent.6 On causation, the court reasoned that when a patient refuses life-sustaining treatment, he dies from an underlying fatal disease; but if a patient ingests a lethal medication, he is killed by that medication. As to intent, a physician who honors a patient’s refusal of treatment purposefully intends only to respect his patient’s wishes and to cease doing futile or degrading things. On the other hand, a doctor who assists a suicide “must, necessarily and indubitably, intend primarily that the patient be made dead.”
In its companion case Washington v. Glucksberg, the Supreme Court held that the asserted “right” to assistance in committing suicide is not a fundamental liberty interest protected by the due process clause.7
State supreme courts in Florida, New Mexico, and elsewhere have likewise rebuffed claims of any constitutional right to PAS. The latest court to so rule is in New York, which has a long history of criminalizing assisted suicide.8 The New York Court of Appeals recently addressed claims brought by three terminally ill individuals, several medical providers, and a nonprofit entity seeking a declaration that New York’s “assisted suicide” statutes exclude physicians from prescribing a lethal dose of drugs to terminally ill, competent patients.
The court unequivocally rejected such claims and affirmed that a physician who assists a suicide by prescribing lethal doses of drugs is subject to criminal prosecution for second-degree manslaughter. It refused to regard PAS as being different from assisted suicide in general, and it rejected the constitutional claim to assisted suicide by a terminally ill person. The state appeals court reiterated the U.S. Supreme Court’s distinction between refusing life-sustaining treatment and assisted suicide, the former being “at least partially rooted in notions of bodily integrity, as the right to refuse treatment is a consequence of a person’s right to resist unwanted bodily invasions.” The New York Court of Appeals also noted that the state has a legitimate purpose and a rational basis for guarding against the risks of mistake and abuse.
These developments may signal a shift away from the legalization of PAS, as recently suggested in a Washington Post article.9 According to the end-of-life advocacy organization Compassion and Choices, none of the 27 states where such measures were introduced in 2017 passed them into law, including states such as Connecticut, Hawaii, and Rhode Island. In Central and Eastern Europe, support is decreasing, whereas the opposite is true in Western Europe.
U.S. federal lawmakers also appear to be pushing back. On July 13, 2017, the U.S. House Committee on Appropriations voted to block implementation of a “death with dignity” statute passed by the District of Columbia. Further, 11 House members – including 6 Democrats – have introduced a resolution asserting that PAS undermines a key safeguard that protects our nation’s most vulnerable citizens, including the elderly, people with disabilities, and people experiencing psychiatric diagnoses.10
The American Medical Association is steadfast in its opposition to PAS and euthanasia. In its latest Code of Ethics, the AMA reaffirmed its long-held position that “allowing physicians to engage in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks. … Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life.”11
References
1. “Physician-assisted suicide,” Internal Medicine News, Oct. 14, 2013.
2. Baxter v. State of Montana, 224 P. 3d 1211 (2010).
3. “Majority of Americans Remain Supportive of Euthanasia,” Gallup News, June 12, 2017.
4. Statistics available at public.health.oregon.gov under Oregon Death with Dignity Act.
5. JAMA. 2016 Jul 5;316(1):79-90.
6. Vacco v. Quill, 117 S. Ct. 2293 (1997).
7. Washington v. Glucksberg, 521 U.S. 702 (1997).
8. Myers v. Schneiderman, New York Court of Appeals, 2017.
9. “Legalizing assisted suicide has stalled at every level,” Washington Post, Oct. 24, 2017.
10. H. Con. Res. 80, 115th Congress (2017-2018).
11. AMA Code of Medical Ethics §5.7 (2017).
Question: Choose the best answer regarding physician-assisted suicide in the United States:
A. It is now legal in most states.
B. Under California law, assisting or causing one to commit suicide, including physician-assisted suicide, still remains a felony.
C. Both the U.S. Supreme Court and the New York Court of Appeals have held there is no constitutional right to physician-assisted suicide.
D. The American Medical Association is neutral on the issue.
E. Pain relief is the overriding reason for patients who request physician-assisted suicide.
Answer: C. We reviewed this topic in one of our regular columns in 2013.1 At that time, efforts to legalize physician-assisted suicide (PAS) appeared to be gathering momentum across the country, with four jurisdictions having legalized the practice, beginning with Oregon in 1994. The other states were Washington, Vermont, and Montana, whose Supreme Court held that there was no public interest reason against the practice.2
Since that time, California, Colorado, and the District of Columbia have joined the group. Currently, PAS – but not euthanasia – is legally available in these jurisdictions and in Switzerland, but both can be legally practiced in Belgium, Canada, Colombia, Luxembourg, and the Netherlands.
All state statutes permitting PAS provide similar provisions and safeguards. Only competent individuals who are terminally ill, i.e., death expected within 6 months, can make a request for a lethal dose of medication to carry out the suicidal act. The request to the doctor is first made verbally, then in writing, and a second opinion must be obtained to confirm the patient’s intent, understanding, and free choice. There is also a waiting period.
Public support for euthanasia and PAS in the United States is said to have plateaued since the 1990s. But a significant number of Americans, 67%, still favor PAS, up from 56% a decade ago.3 However, not many patients resort to PAS – usually those with terminal cancers or neuromuscular conditions – and only a minority of physicians are participants.
For example, 61 physicians in Oregon wrote a total of 115 prescriptions in 2012; there were 77 known Death With Dignity Act deaths in Oregon that year.4 In Oregon and Washington State, less than 1% of licensed physicians write prescriptions for physician-assisted suicide each year. In contrast, about half or more of physicians in the Netherlands and Belgium reported ever having received a request, and 60% of Dutch physicians have granted such requests.
The California Department of Public Health reported that 111 terminally ill patients availed themselves of California’s End of Life Option Act in the 7 months after it became effective on June 9, 2016.
In a recent review on euthanasia and PAS for the period 1947-2016, Ezekiel Emanuel, MD, and colleagues noted that typical patients were older, white, and well educated, and pain was mostly not reported as the primary motivation.5 A large portion of patients receiving PAS in Oregon and Washington were enrolled in hospice or palliative care. Abuses have not been apparent.
In the vast majority of jurisdictions, assisting or causing one to commit suicide, including PAS, still remains a crime; for example, it is considered manslaughter under Hawaii state law §707-702.
In distinguishing between assisting suicide and withdrawing life-sustaining treatment, the U.S. Supreme Court’s landmark 1997 Vacco v. Quill decision emphasized issues of causation and intent.6 On causation, the court reasoned that when a patient refuses life-sustaining treatment, he dies from an underlying fatal disease; but if a patient ingests a lethal medication, he is killed by that medication. As to intent, a physician who honors a patient’s refusal of treatment purposefully intends only to respect his patient’s wishes and to cease doing futile or degrading things. On the other hand, a doctor who assists a suicide “must, necessarily and indubitably, intend primarily that the patient be made dead.”
In its companion case Washington v. Glucksberg, the Supreme Court held that the asserted “right” to assistance in committing suicide is not a fundamental liberty interest protected by the due process clause.7
State supreme courts in Florida, New Mexico, and elsewhere have likewise rebuffed claims of any constitutional right to PAS. The latest court to so rule is in New York, which has a long history of criminalizing assisted suicide.8 The New York Court of Appeals recently addressed claims brought by three terminally ill individuals, several medical providers, and a nonprofit entity seeking a declaration that New York’s “assisted suicide” statutes exclude physicians from prescribing a lethal dose of drugs to terminally ill, competent patients.
The court unequivocally rejected such claims and affirmed that a physician who assists a suicide by prescribing lethal doses of drugs is subject to criminal prosecution for second-degree manslaughter. It refused to regard PAS as being different from assisted suicide in general, and it rejected the constitutional claim to assisted suicide by a terminally ill person. The state appeals court reiterated the U.S. Supreme Court’s distinction between refusing life-sustaining treatment and assisted suicide, the former being “at least partially rooted in notions of bodily integrity, as the right to refuse treatment is a consequence of a person’s right to resist unwanted bodily invasions.” The New York Court of Appeals also noted that the state has a legitimate purpose and a rational basis for guarding against the risks of mistake and abuse.
These developments may signal a shift away from the legalization of PAS, as recently suggested in a Washington Post article.9 According to the end-of-life advocacy organization Compassion and Choices, none of the 27 states where such measures were introduced in 2017 passed them into law, including states such as Connecticut, Hawaii, and Rhode Island. In Central and Eastern Europe, support is decreasing, whereas the opposite is true in Western Europe.
U.S. federal lawmakers also appear to be pushing back. On July 13, 2017, the U.S. House Committee on Appropriations voted to block implementation of a “death with dignity” statute passed by the District of Columbia. Further, 11 House members – including 6 Democrats – have introduced a resolution asserting that PAS undermines a key safeguard that protects our nation’s most vulnerable citizens, including the elderly, people with disabilities, and people experiencing psychiatric diagnoses.10
The American Medical Association is steadfast in its opposition to PAS and euthanasia. In its latest Code of Ethics, the AMA reaffirmed its long-held position that “allowing physicians to engage in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks. … Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life.”11
References
1. “Physician-assisted suicide,” Internal Medicine News, Oct. 14, 2013.
2. Baxter v. State of Montana, 224 P. 3d 1211 (2010).
3. “Majority of Americans Remain Supportive of Euthanasia,” Gallup News, June 12, 2017.
4. Statistics available at public.health.oregon.gov under Oregon Death with Dignity Act.
5. JAMA. 2016 Jul 5;316(1):79-90.
6. Vacco v. Quill, 117 S. Ct. 2293 (1997).
7. Washington v. Glucksberg, 521 U.S. 702 (1997).
8. Myers v. Schneiderman, New York Court of Appeals, 2017.
9. “Legalizing assisted suicide has stalled at every level,” Washington Post, Oct. 24, 2017.
10. H. Con. Res. 80, 115th Congress (2017-2018).
11. AMA Code of Medical Ethics §5.7 (2017).
The (Friendly) Ghosts of Emergency Medicine Past, Present, and Yet to Come
Past…
Almost 40 years have elapsed since the American Board of Medical Specialties recognized emergency medicine (EM) as the 23rd medical specialty. Though the fundamental principles of patient care, medical education, and certification established by the American Board of Emergency Medicine (ABEM) have stood the test of time, the ED of today is a very different place than the “ER” of 1979. So too, today’s emergency physicians (EPs) are not only better trained and more capable of providing the highest quality of care in the ED, but are also increasingly doing so in venues outside of the traditional hospital-based ED.
Present...
In 1996, The New York Hospital – Cornell University Medical Center recruited me to be their first emergency physician-in-chief and EMS medical director, and to establish a first-rate academic ED and EM residency program. Starting with an “ER” staff of eight full-time and part-time non-EM-boarded attending physicians and a varying number of medical and surgical residents, over the next 20 years I expanded the complement of board-certified attending EPs to over 50, added attending-supervised nurse practitioners (NPs) and physician assistants (PAs), recruited a residency director, and helped him start a 4-year EM residency on both our Cornell and Columbia campuses. I also supported the initiation of 1-year ED nurse, PA, and NP residency programs. In corroboration with the chair of radiology, we added 24-hour dedicated sonography technologists to supplement the bedside emergency sonography that we had just been credentialed to perform, and established one of the very first divisions of emergency radiology, headed by EM board member and columnist, Keith Hentel, MD. Keith staffed his division with 24/7 attending radiologists to interpret all ED radiographic studies and provide imaging advice. More recently, I was able to arrange for dedicated 24/7 ED pharmacists, 24/7 ED social workers, and a patient safety/quality assurance division.
When I arrived at New York – Cornell, I supported the expansion of the ED patient services already in place, headed by an incredibly skilled and compassionate director, Constance Peterson, MA, who always insisted that her small office open directly off of the ED waiting room. Constance recruited and supervised a group of dedicated patient greeters and facilitators to ensure that no patient would get lost or fall through the “cracks” of our ever-expanding ED.
The plans for a new ED located at the front entrance to the hospital had literally been “carved in stone” by the time I arrived, but a decade later a magnificent gift from a donor gave me the opportunity to design a fourth patient-care area that expanded our ED to two full city blocks. I designed the new addition to serve the specific needs of a rapidly aging population and to provide a secure unit capable of managing patients with new or emerging infectious diseases and those with compromised immune systems. I also included in the new unit a large, state-of-the-art gynecologic (GYN) examination suite for conducting sexual assault exams and other GYN exams while providing the patient with a maximum level of comfort.
To coordinate activities throughout the ED and to provide a rapid expansion of staff when needed to manage surges in patient volume, I divided the ED into three acute areas and one urgent care area, each headed by an attending physician 24/7. One of the attendings was designated as the “administrative attending” or “AA.” Among other responsibilities, the AA was required to e-mail me and Associate Director Jeremy Sperling, MD, (now chair of EM at Einstein/Jacobi) a detailed note on patient volume, rate of new registrations, and any problems, at the end of every 8-hour shift—or more frequently when the need arose. Whenever patient volume was in danger of exceeding capacity, Jeremy immediately sent an urgent e-mail to all of our attending EPs, PAs, and NPs, offering double the hourly rate for 4 to 8 hours of patient care, while adhering to all relevant work-hour requirements. To cover the cost of these additional emergency clinical hours, I made a small portion of our fee-for-service revenues available. Two years ago, I initiated a physician scribe program to restore the physician-patient relationship during patient evaluations and treatments.
With the successful establishment of our EM residency program by Wallace Carter, MD, in 2003, I started 1- and 2-year fellowships in new disciplines for a 21st century ED—using a portion of our fee-for-service revenues designated for research and development to supplement the part-time attending base salaries of non-ACGME fellows. Beginning in 2005, I established the nation’s first geriatric EM fellowship, supported our newly established global EM program, recruited one of our attending EPs, Jay Lemery, MD, to start a wilderness medicine program in the Adirondack Mountains with Cornell (University) Outdoor Education, and appointed a director of EM/critical care. The ED expansion in 2009 enabled me to hire five attending EPs who were also board eligible/certified in medical toxicology, creating a “tox” group for bedside guidance and care in the ED and consultations throughout the hospital. The tox group also provided invaluable assistance to our secure psychiatric ED, headed by renowned emergency psychiatrists Lisa Sombrotto, MD, and Sharon Hird, MD. I also supported the activities of the pediatric EM fellowship, which had been established and nurtured by our extremely capable chief of pediatric EM, Shari Platt, MD. Most recently, I began to develop a new program in women’s health emergencies.
To expedite emergently needed care for an increasing number of oncology patients, I created a special “fast-track” to ensure that febrile cancer-treatment patients received needed antibiotics within an hour of arrival. I created a second fast-track to expedite the diagnosis and treatment (ie, transfer to the OR) of patients with surgical abdomens, and a third track to expedite the care of patients with community-acquired pneumonia.
And Yet to Come…
The programs and divisions described were developed over a 20-year period, always mindful of the standards and quality measures first promulgated by ABEM in 1979. New hospital-based ED initiatives will undoubtedly continue to be created in the future by EPs who are challenged to develop new and effective ways of caring for the ever-increasing numbers of patients in the face of continued hospital and ED closings.
At the same time, the increased numbers of patients seeking care in EDs, most recently created by the Affordable Care Act of 2010, is leading many EPs to apply the skills they learned as residents and their hospital-based ED experiences in new venues for emergency care. In recent years, there has been a virtual explosion in the number of urgent care centers, freestanding EDs, “convenient-care” centers, and even remote patient care in the form of “telehealth” or “telemedicine.” In 2014, when the National Hockey League mandated the presence of EPs at all games, I negotiated a contract that also enables our attending EPs to have senior residents accompany them and observe the practice of EM outside hospital walls. Prehospital and “interhospital” care also continues to expand with an increasing need for critical care and long-distance patient transfers to and from hospitals, and with a growing interest in community para-medicine programs.
In an October 2012 editorial (Emerg Med. 2012;44[10]:4), I wrote about French high-wire acrobat Philippe Petit who had rigged a cable between the two towers of the World Trade Center in August 1974, and then “aided only by a long, custom-made balancing pole, crossed, re-crossed, and danced on the wire without a safety net, for 45 minutes.” Most observers that day were certain he would fall to his death, and no one imagined that he would survive and outlast the 110-story towers he had anchored his cable to. So too, with EM: Hospital-based EDs will certainly remain an essential part of EM in the years to come, but EPs will also have increasing opportunities to practice their specialty in other important venues as well. The EP of the future will not be bound to a particular location to practice EM.
As I have this time of year for the past 11 years, I wish all of our readers, and all EPs everywhere, a joyous and safe holiday season and many happy and healthy new years to come.
Past…
Almost 40 years have elapsed since the American Board of Medical Specialties recognized emergency medicine (EM) as the 23rd medical specialty. Though the fundamental principles of patient care, medical education, and certification established by the American Board of Emergency Medicine (ABEM) have stood the test of time, the ED of today is a very different place than the “ER” of 1979. So too, today’s emergency physicians (EPs) are not only better trained and more capable of providing the highest quality of care in the ED, but are also increasingly doing so in venues outside of the traditional hospital-based ED.
Present...
In 1996, The New York Hospital – Cornell University Medical Center recruited me to be their first emergency physician-in-chief and EMS medical director, and to establish a first-rate academic ED and EM residency program. Starting with an “ER” staff of eight full-time and part-time non-EM-boarded attending physicians and a varying number of medical and surgical residents, over the next 20 years I expanded the complement of board-certified attending EPs to over 50, added attending-supervised nurse practitioners (NPs) and physician assistants (PAs), recruited a residency director, and helped him start a 4-year EM residency on both our Cornell and Columbia campuses. I also supported the initiation of 1-year ED nurse, PA, and NP residency programs. In corroboration with the chair of radiology, we added 24-hour dedicated sonography technologists to supplement the bedside emergency sonography that we had just been credentialed to perform, and established one of the very first divisions of emergency radiology, headed by EM board member and columnist, Keith Hentel, MD. Keith staffed his division with 24/7 attending radiologists to interpret all ED radiographic studies and provide imaging advice. More recently, I was able to arrange for dedicated 24/7 ED pharmacists, 24/7 ED social workers, and a patient safety/quality assurance division.
When I arrived at New York – Cornell, I supported the expansion of the ED patient services already in place, headed by an incredibly skilled and compassionate director, Constance Peterson, MA, who always insisted that her small office open directly off of the ED waiting room. Constance recruited and supervised a group of dedicated patient greeters and facilitators to ensure that no patient would get lost or fall through the “cracks” of our ever-expanding ED.
The plans for a new ED located at the front entrance to the hospital had literally been “carved in stone” by the time I arrived, but a decade later a magnificent gift from a donor gave me the opportunity to design a fourth patient-care area that expanded our ED to two full city blocks. I designed the new addition to serve the specific needs of a rapidly aging population and to provide a secure unit capable of managing patients with new or emerging infectious diseases and those with compromised immune systems. I also included in the new unit a large, state-of-the-art gynecologic (GYN) examination suite for conducting sexual assault exams and other GYN exams while providing the patient with a maximum level of comfort.
To coordinate activities throughout the ED and to provide a rapid expansion of staff when needed to manage surges in patient volume, I divided the ED into three acute areas and one urgent care area, each headed by an attending physician 24/7. One of the attendings was designated as the “administrative attending” or “AA.” Among other responsibilities, the AA was required to e-mail me and Associate Director Jeremy Sperling, MD, (now chair of EM at Einstein/Jacobi) a detailed note on patient volume, rate of new registrations, and any problems, at the end of every 8-hour shift—or more frequently when the need arose. Whenever patient volume was in danger of exceeding capacity, Jeremy immediately sent an urgent e-mail to all of our attending EPs, PAs, and NPs, offering double the hourly rate for 4 to 8 hours of patient care, while adhering to all relevant work-hour requirements. To cover the cost of these additional emergency clinical hours, I made a small portion of our fee-for-service revenues available. Two years ago, I initiated a physician scribe program to restore the physician-patient relationship during patient evaluations and treatments.
With the successful establishment of our EM residency program by Wallace Carter, MD, in 2003, I started 1- and 2-year fellowships in new disciplines for a 21st century ED—using a portion of our fee-for-service revenues designated for research and development to supplement the part-time attending base salaries of non-ACGME fellows. Beginning in 2005, I established the nation’s first geriatric EM fellowship, supported our newly established global EM program, recruited one of our attending EPs, Jay Lemery, MD, to start a wilderness medicine program in the Adirondack Mountains with Cornell (University) Outdoor Education, and appointed a director of EM/critical care. The ED expansion in 2009 enabled me to hire five attending EPs who were also board eligible/certified in medical toxicology, creating a “tox” group for bedside guidance and care in the ED and consultations throughout the hospital. The tox group also provided invaluable assistance to our secure psychiatric ED, headed by renowned emergency psychiatrists Lisa Sombrotto, MD, and Sharon Hird, MD. I also supported the activities of the pediatric EM fellowship, which had been established and nurtured by our extremely capable chief of pediatric EM, Shari Platt, MD. Most recently, I began to develop a new program in women’s health emergencies.
To expedite emergently needed care for an increasing number of oncology patients, I created a special “fast-track” to ensure that febrile cancer-treatment patients received needed antibiotics within an hour of arrival. I created a second fast-track to expedite the diagnosis and treatment (ie, transfer to the OR) of patients with surgical abdomens, and a third track to expedite the care of patients with community-acquired pneumonia.
And Yet to Come…
The programs and divisions described were developed over a 20-year period, always mindful of the standards and quality measures first promulgated by ABEM in 1979. New hospital-based ED initiatives will undoubtedly continue to be created in the future by EPs who are challenged to develop new and effective ways of caring for the ever-increasing numbers of patients in the face of continued hospital and ED closings.
At the same time, the increased numbers of patients seeking care in EDs, most recently created by the Affordable Care Act of 2010, is leading many EPs to apply the skills they learned as residents and their hospital-based ED experiences in new venues for emergency care. In recent years, there has been a virtual explosion in the number of urgent care centers, freestanding EDs, “convenient-care” centers, and even remote patient care in the form of “telehealth” or “telemedicine.” In 2014, when the National Hockey League mandated the presence of EPs at all games, I negotiated a contract that also enables our attending EPs to have senior residents accompany them and observe the practice of EM outside hospital walls. Prehospital and “interhospital” care also continues to expand with an increasing need for critical care and long-distance patient transfers to and from hospitals, and with a growing interest in community para-medicine programs.
In an October 2012 editorial (Emerg Med. 2012;44[10]:4), I wrote about French high-wire acrobat Philippe Petit who had rigged a cable between the two towers of the World Trade Center in August 1974, and then “aided only by a long, custom-made balancing pole, crossed, re-crossed, and danced on the wire without a safety net, for 45 minutes.” Most observers that day were certain he would fall to his death, and no one imagined that he would survive and outlast the 110-story towers he had anchored his cable to. So too, with EM: Hospital-based EDs will certainly remain an essential part of EM in the years to come, but EPs will also have increasing opportunities to practice their specialty in other important venues as well. The EP of the future will not be bound to a particular location to practice EM.
As I have this time of year for the past 11 years, I wish all of our readers, and all EPs everywhere, a joyous and safe holiday season and many happy and healthy new years to come.
Past…
Almost 40 years have elapsed since the American Board of Medical Specialties recognized emergency medicine (EM) as the 23rd medical specialty. Though the fundamental principles of patient care, medical education, and certification established by the American Board of Emergency Medicine (ABEM) have stood the test of time, the ED of today is a very different place than the “ER” of 1979. So too, today’s emergency physicians (EPs) are not only better trained and more capable of providing the highest quality of care in the ED, but are also increasingly doing so in venues outside of the traditional hospital-based ED.
Present...
In 1996, The New York Hospital – Cornell University Medical Center recruited me to be their first emergency physician-in-chief and EMS medical director, and to establish a first-rate academic ED and EM residency program. Starting with an “ER” staff of eight full-time and part-time non-EM-boarded attending physicians and a varying number of medical and surgical residents, over the next 20 years I expanded the complement of board-certified attending EPs to over 50, added attending-supervised nurse practitioners (NPs) and physician assistants (PAs), recruited a residency director, and helped him start a 4-year EM residency on both our Cornell and Columbia campuses. I also supported the initiation of 1-year ED nurse, PA, and NP residency programs. In corroboration with the chair of radiology, we added 24-hour dedicated sonography technologists to supplement the bedside emergency sonography that we had just been credentialed to perform, and established one of the very first divisions of emergency radiology, headed by EM board member and columnist, Keith Hentel, MD. Keith staffed his division with 24/7 attending radiologists to interpret all ED radiographic studies and provide imaging advice. More recently, I was able to arrange for dedicated 24/7 ED pharmacists, 24/7 ED social workers, and a patient safety/quality assurance division.
When I arrived at New York – Cornell, I supported the expansion of the ED patient services already in place, headed by an incredibly skilled and compassionate director, Constance Peterson, MA, who always insisted that her small office open directly off of the ED waiting room. Constance recruited and supervised a group of dedicated patient greeters and facilitators to ensure that no patient would get lost or fall through the “cracks” of our ever-expanding ED.
The plans for a new ED located at the front entrance to the hospital had literally been “carved in stone” by the time I arrived, but a decade later a magnificent gift from a donor gave me the opportunity to design a fourth patient-care area that expanded our ED to two full city blocks. I designed the new addition to serve the specific needs of a rapidly aging population and to provide a secure unit capable of managing patients with new or emerging infectious diseases and those with compromised immune systems. I also included in the new unit a large, state-of-the-art gynecologic (GYN) examination suite for conducting sexual assault exams and other GYN exams while providing the patient with a maximum level of comfort.
To coordinate activities throughout the ED and to provide a rapid expansion of staff when needed to manage surges in patient volume, I divided the ED into three acute areas and one urgent care area, each headed by an attending physician 24/7. One of the attendings was designated as the “administrative attending” or “AA.” Among other responsibilities, the AA was required to e-mail me and Associate Director Jeremy Sperling, MD, (now chair of EM at Einstein/Jacobi) a detailed note on patient volume, rate of new registrations, and any problems, at the end of every 8-hour shift—or more frequently when the need arose. Whenever patient volume was in danger of exceeding capacity, Jeremy immediately sent an urgent e-mail to all of our attending EPs, PAs, and NPs, offering double the hourly rate for 4 to 8 hours of patient care, while adhering to all relevant work-hour requirements. To cover the cost of these additional emergency clinical hours, I made a small portion of our fee-for-service revenues available. Two years ago, I initiated a physician scribe program to restore the physician-patient relationship during patient evaluations and treatments.
With the successful establishment of our EM residency program by Wallace Carter, MD, in 2003, I started 1- and 2-year fellowships in new disciplines for a 21st century ED—using a portion of our fee-for-service revenues designated for research and development to supplement the part-time attending base salaries of non-ACGME fellows. Beginning in 2005, I established the nation’s first geriatric EM fellowship, supported our newly established global EM program, recruited one of our attending EPs, Jay Lemery, MD, to start a wilderness medicine program in the Adirondack Mountains with Cornell (University) Outdoor Education, and appointed a director of EM/critical care. The ED expansion in 2009 enabled me to hire five attending EPs who were also board eligible/certified in medical toxicology, creating a “tox” group for bedside guidance and care in the ED and consultations throughout the hospital. The tox group also provided invaluable assistance to our secure psychiatric ED, headed by renowned emergency psychiatrists Lisa Sombrotto, MD, and Sharon Hird, MD. I also supported the activities of the pediatric EM fellowship, which had been established and nurtured by our extremely capable chief of pediatric EM, Shari Platt, MD. Most recently, I began to develop a new program in women’s health emergencies.
To expedite emergently needed care for an increasing number of oncology patients, I created a special “fast-track” to ensure that febrile cancer-treatment patients received needed antibiotics within an hour of arrival. I created a second fast-track to expedite the diagnosis and treatment (ie, transfer to the OR) of patients with surgical abdomens, and a third track to expedite the care of patients with community-acquired pneumonia.
And Yet to Come…
The programs and divisions described were developed over a 20-year period, always mindful of the standards and quality measures first promulgated by ABEM in 1979. New hospital-based ED initiatives will undoubtedly continue to be created in the future by EPs who are challenged to develop new and effective ways of caring for the ever-increasing numbers of patients in the face of continued hospital and ED closings.
At the same time, the increased numbers of patients seeking care in EDs, most recently created by the Affordable Care Act of 2010, is leading many EPs to apply the skills they learned as residents and their hospital-based ED experiences in new venues for emergency care. In recent years, there has been a virtual explosion in the number of urgent care centers, freestanding EDs, “convenient-care” centers, and even remote patient care in the form of “telehealth” or “telemedicine.” In 2014, when the National Hockey League mandated the presence of EPs at all games, I negotiated a contract that also enables our attending EPs to have senior residents accompany them and observe the practice of EM outside hospital walls. Prehospital and “interhospital” care also continues to expand with an increasing need for critical care and long-distance patient transfers to and from hospitals, and with a growing interest in community para-medicine programs.
In an October 2012 editorial (Emerg Med. 2012;44[10]:4), I wrote about French high-wire acrobat Philippe Petit who had rigged a cable between the two towers of the World Trade Center in August 1974, and then “aided only by a long, custom-made balancing pole, crossed, re-crossed, and danced on the wire without a safety net, for 45 minutes.” Most observers that day were certain he would fall to his death, and no one imagined that he would survive and outlast the 110-story towers he had anchored his cable to. So too, with EM: Hospital-based EDs will certainly remain an essential part of EM in the years to come, but EPs will also have increasing opportunities to practice their specialty in other important venues as well. The EP of the future will not be bound to a particular location to practice EM.
As I have this time of year for the past 11 years, I wish all of our readers, and all EPs everywhere, a joyous and safe holiday season and many happy and healthy new years to come.
Helping patients with addictions get, stay clean
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
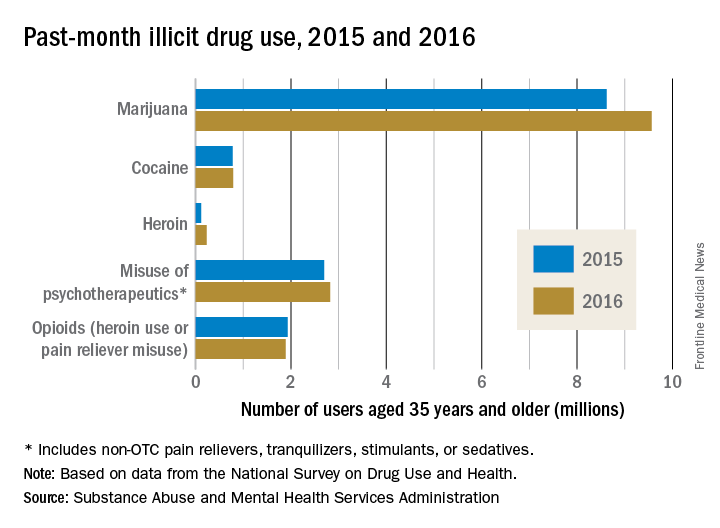
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
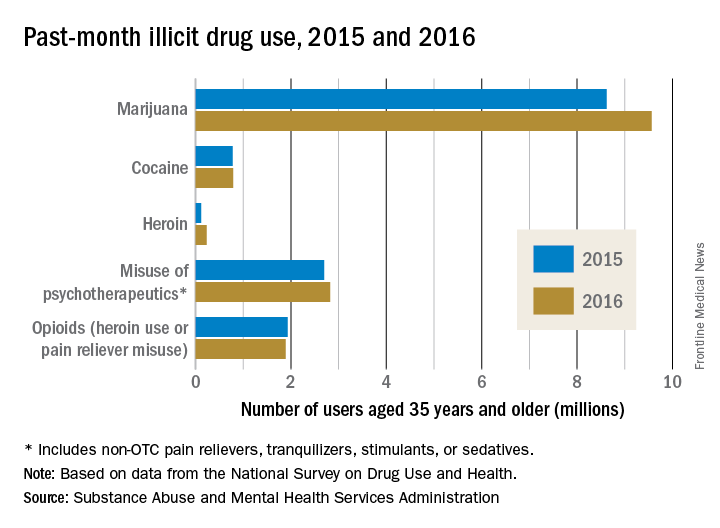
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Job Satisfaction
You know that good feeling you get when you think about what you do for a living? That’s job satisfaction. So, what contributes to that feeling? Why does it matter?
Job satisfaction among both NPs and PAs remains high since last year’s survey.
The major determinants of job satisfaction include autonomy, appropriate pay, having adequate time to interact with patients, collegial support, and opportunities for professional growth.1-3
Dissatisfaction—due, for example, to work-life imbalance, adverse working conditions, or threat of malpractice lawsuits—may motivate experienced clinicians to leave their jobs. Clearly, keeping NPs and PAs engaged and satisfied is key to creating and retaining effective health care teams, resulting in better patient care and lower health care costs.1,4
So, are you interested in discovering ways to increase your career satisfaction? Actively seeking a new position? Looking to hire or retain staff? Check out the PDF for information on pay, benefits, and reasons your peers leave their jobs—broken out by profession and by region.
You know that good feeling you get when you think about what you do for a living? That’s job satisfaction. So, what contributes to that feeling? Why does it matter?
Job satisfaction among both NPs and PAs remains high since last year’s survey.
The major determinants of job satisfaction include autonomy, appropriate pay, having adequate time to interact with patients, collegial support, and opportunities for professional growth.1-3
Dissatisfaction—due, for example, to work-life imbalance, adverse working conditions, or threat of malpractice lawsuits—may motivate experienced clinicians to leave their jobs. Clearly, keeping NPs and PAs engaged and satisfied is key to creating and retaining effective health care teams, resulting in better patient care and lower health care costs.1,4
So, are you interested in discovering ways to increase your career satisfaction? Actively seeking a new position? Looking to hire or retain staff? Check out the PDF for information on pay, benefits, and reasons your peers leave their jobs—broken out by profession and by region.
You know that good feeling you get when you think about what you do for a living? That’s job satisfaction. So, what contributes to that feeling? Why does it matter?
Job satisfaction among both NPs and PAs remains high since last year’s survey.
The major determinants of job satisfaction include autonomy, appropriate pay, having adequate time to interact with patients, collegial support, and opportunities for professional growth.1-3
Dissatisfaction—due, for example, to work-life imbalance, adverse working conditions, or threat of malpractice lawsuits—may motivate experienced clinicians to leave their jobs. Clearly, keeping NPs and PAs engaged and satisfied is key to creating and retaining effective health care teams, resulting in better patient care and lower health care costs.1,4
So, are you interested in discovering ways to increase your career satisfaction? Actively seeking a new position? Looking to hire or retain staff? Check out the PDF for information on pay, benefits, and reasons your peers leave their jobs—broken out by profession and by region.
RSS feeds are a versatile online tool
Recently I mentioned RSS news feeds as a useful, versatile online tool, but because it has been a while since I’ve discussed RSS feeds, an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you have become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular, but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an e-mail service to notify you of new content, but multiple e-mail subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS (which stands for “Rich Site Summary” or “Really Simple Syndication,” depending on whom you ask) is a file format, and websites use that format (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
Many readers are free, but those with the most advanced features usually charge a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive and more or less up-to-date list of available readers can be found in the Wikipedia article “Comparison of feed aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS,” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds, and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including e-mail newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. Next month, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Recently I mentioned RSS news feeds as a useful, versatile online tool, but because it has been a while since I’ve discussed RSS feeds, an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you have become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular, but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an e-mail service to notify you of new content, but multiple e-mail subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS (which stands for “Rich Site Summary” or “Really Simple Syndication,” depending on whom you ask) is a file format, and websites use that format (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
Many readers are free, but those with the most advanced features usually charge a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive and more or less up-to-date list of available readers can be found in the Wikipedia article “Comparison of feed aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS,” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds, and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including e-mail newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. Next month, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Recently I mentioned RSS news feeds as a useful, versatile online tool, but because it has been a while since I’ve discussed RSS feeds, an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you have become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular, but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an e-mail service to notify you of new content, but multiple e-mail subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS (which stands for “Rich Site Summary” or “Really Simple Syndication,” depending on whom you ask) is a file format, and websites use that format (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
Many readers are free, but those with the most advanced features usually charge a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive and more or less up-to-date list of available readers can be found in the Wikipedia article “Comparison of feed aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS,” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds, and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including e-mail newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. Next month, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
AHRQ Practice Toolbox: Health Literacy
This is the fifth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Members of primary care teams know that to be successful, they have to communicate effectively with patients and family members. Communication skills, however, are not emphasized in health professional schools. Furthermore, clear communication is important not only for clinicians, but for all members of primary care practices. In order to help patients be successful, practices also need to help patients navigate what is often a confusing health system with demands that frequently exceed patients’ abilities.
Health literacy universal precautions are aimed at the following three things:
- Simplifying communication with and confirming comprehension for all patients.
- Making the office environment and health care system easier to navigate.
- Supporting patients’ efforts to improve their health.
The AHRQ Health Literacy Universal Precautions Toolkit is designed for the busy adult or pediatric primary care practice. Each of its 21 tools is only 3-5 pages long, and a practice can jump in wherever it likes. The tools specify concrete action steps and link to other resources. A Quick Start Guide lets you watch a 6-minute video, then pick one of three tools to implement: Conduct Brown Bag Medicine Reviews, Communicate Clearly, or Use the Teach-Back Method. Practices that want to start the journey toward becoming a health literate organization can start with the first two tools: Form a Team and Create a Health Literate Improvement Plan, which includes a practice self-assessment. Practices can also choose focus their efforts on one of the four health literacy domains:
- Spoken Communication
- Written Communication
- Self-Management and Empowerment
- Supportive Systems
In addition to the Toolkit, AHRQ has created a companion guide with concrete advice based on the implementation experiences of diverse primary care practices. At least one person – such as a practice facilitator, quality improvement specialist, or health literacy team leader – should read it before you get started.
Adopting health literacy universal precautions can help you reach your practice’s goals, whether they are becoming a patient-centered medical home or preparing for value-based payment.
Links to health literacy resources:
AHRQ Health Literacy Universal Precautions Toolkit, 2nd edition: https://www.ahrq.gov/literacy
Guide to Implementing the Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices: https://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/impguide/index.html
Crosswalk between the tools included in the Toolkit and the PCMH certification standards (as of 2014) of the National Committee for Quality Assurance (NCQA), The Joint Commission, and the Utilization Review Accreditation Committee (URAC): https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/pcmh-crosswalk.pdf
Index of AHRQ Health Literacy Resources: https://www.ahrq.gov/professionals/clinicians-providers/resources/health-literacy.html
Diplomates of the American Board of Pediatrics and the American Board of Family Medicine can take health literacy modules (both knowledge self-assessment and performance improvement modules) for maintenance of certification.
Ms. Brach is Senior Health Care Researcher at AHRQ.
This is the fifth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Members of primary care teams know that to be successful, they have to communicate effectively with patients and family members. Communication skills, however, are not emphasized in health professional schools. Furthermore, clear communication is important not only for clinicians, but for all members of primary care practices. In order to help patients be successful, practices also need to help patients navigate what is often a confusing health system with demands that frequently exceed patients’ abilities.
Health literacy universal precautions are aimed at the following three things:
- Simplifying communication with and confirming comprehension for all patients.
- Making the office environment and health care system easier to navigate.
- Supporting patients’ efforts to improve their health.
The AHRQ Health Literacy Universal Precautions Toolkit is designed for the busy adult or pediatric primary care practice. Each of its 21 tools is only 3-5 pages long, and a practice can jump in wherever it likes. The tools specify concrete action steps and link to other resources. A Quick Start Guide lets you watch a 6-minute video, then pick one of three tools to implement: Conduct Brown Bag Medicine Reviews, Communicate Clearly, or Use the Teach-Back Method. Practices that want to start the journey toward becoming a health literate organization can start with the first two tools: Form a Team and Create a Health Literate Improvement Plan, which includes a practice self-assessment. Practices can also choose focus their efforts on one of the four health literacy domains:
- Spoken Communication
- Written Communication
- Self-Management and Empowerment
- Supportive Systems
In addition to the Toolkit, AHRQ has created a companion guide with concrete advice based on the implementation experiences of diverse primary care practices. At least one person – such as a practice facilitator, quality improvement specialist, or health literacy team leader – should read it before you get started.
Adopting health literacy universal precautions can help you reach your practice’s goals, whether they are becoming a patient-centered medical home or preparing for value-based payment.
Links to health literacy resources:
AHRQ Health Literacy Universal Precautions Toolkit, 2nd edition: https://www.ahrq.gov/literacy
Guide to Implementing the Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices: https://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/impguide/index.html
Crosswalk between the tools included in the Toolkit and the PCMH certification standards (as of 2014) of the National Committee for Quality Assurance (NCQA), The Joint Commission, and the Utilization Review Accreditation Committee (URAC): https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/pcmh-crosswalk.pdf
Index of AHRQ Health Literacy Resources: https://www.ahrq.gov/professionals/clinicians-providers/resources/health-literacy.html
Diplomates of the American Board of Pediatrics and the American Board of Family Medicine can take health literacy modules (both knowledge self-assessment and performance improvement modules) for maintenance of certification.
Ms. Brach is Senior Health Care Researcher at AHRQ.
This is the fifth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Members of primary care teams know that to be successful, they have to communicate effectively with patients and family members. Communication skills, however, are not emphasized in health professional schools. Furthermore, clear communication is important not only for clinicians, but for all members of primary care practices. In order to help patients be successful, practices also need to help patients navigate what is often a confusing health system with demands that frequently exceed patients’ abilities.
Health literacy universal precautions are aimed at the following three things:
- Simplifying communication with and confirming comprehension for all patients.
- Making the office environment and health care system easier to navigate.
- Supporting patients’ efforts to improve their health.
The AHRQ Health Literacy Universal Precautions Toolkit is designed for the busy adult or pediatric primary care practice. Each of its 21 tools is only 3-5 pages long, and a practice can jump in wherever it likes. The tools specify concrete action steps and link to other resources. A Quick Start Guide lets you watch a 6-minute video, then pick one of three tools to implement: Conduct Brown Bag Medicine Reviews, Communicate Clearly, or Use the Teach-Back Method. Practices that want to start the journey toward becoming a health literate organization can start with the first two tools: Form a Team and Create a Health Literate Improvement Plan, which includes a practice self-assessment. Practices can also choose focus their efforts on one of the four health literacy domains:
- Spoken Communication
- Written Communication
- Self-Management and Empowerment
- Supportive Systems
In addition to the Toolkit, AHRQ has created a companion guide with concrete advice based on the implementation experiences of diverse primary care practices. At least one person – such as a practice facilitator, quality improvement specialist, or health literacy team leader – should read it before you get started.
Adopting health literacy universal precautions can help you reach your practice’s goals, whether they are becoming a patient-centered medical home or preparing for value-based payment.
Links to health literacy resources:
AHRQ Health Literacy Universal Precautions Toolkit, 2nd edition: https://www.ahrq.gov/literacy
Guide to Implementing the Health Literacy Universal Precautions Toolkit: Practical Ideas for Primary Care Practices: https://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/impguide/index.html
Crosswalk between the tools included in the Toolkit and the PCMH certification standards (as of 2014) of the National Committee for Quality Assurance (NCQA), The Joint Commission, and the Utilization Review Accreditation Committee (URAC): https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/pcmh-crosswalk.pdf
Index of AHRQ Health Literacy Resources: https://www.ahrq.gov/professionals/clinicians-providers/resources/health-literacy.html
Diplomates of the American Board of Pediatrics and the American Board of Family Medicine can take health literacy modules (both knowledge self-assessment and performance improvement modules) for maintenance of certification.
Ms. Brach is Senior Health Care Researcher at AHRQ.
National Academy of Medicine should revisit issue of fetal alcohol exposure
More than 20 years ago the Institute of Medicine (recently renamed the National Academy of Medicine, or NAM) issued its landmark report on fetal alcohol syndrome. Since then, there has been an explosion of research on the issue of fetal alcohol exposure – and NAM needs to revisit the issue and release another report.
Unfortunately, too few physicians and not enough people in the larger society understand public health and that the health status of the unfortunate among us affects the health status of the most fortunate of us. In short, low-income people are the proverbial “canary in the coal mine.”
Accordingly, solving the health care problems of low-income people would solve the health care problems of the middle and upper class. Consider where the United States would be had we paid attention to the opioid epidemic in low-income communities instead of waiting until it spread into everyone’s “safe” communities. We would have tried and tested solutions to the problem as it currently exists.
Another reason NAM needs to revisit FASD – currently proposed to be called neurobehavioral disorders associated with prenatal alcohol exposure in the DSM-5 – are the new findings that link FASD to seizure disorders and other neurodevelopmental disorders of childhood, such as intellectual disability, attention-deficit/hyperactivity disorder, speech and language disorders, motor disorders, specific learning disorders, and autism. In fact, new research is emerging from Robert Freedman, MD, and his team at the University of Colorado Denver, to suggest that preventing choline deficiency in pregnancy (the mechanism producing neurodevelopmental defects in FASD) may not only prevent neurodevelopmental disorders of childhood but also schizophrenia. Further, it has become abundantly clear that choline deficiency (often generated by FASD), is responsible for affect dysregulation, which is a common thread in various forms of violence and suicide.
A recent report highlighted the findings that inmates incarcerated in Mexican prisons have high rates of intellectual disability, and we know that FASD is one of the leading causes of this problem, but we are not screening for it in our juvenile detention centers, jails, or prisons. Consequently, we need to look for the prevalence of FASD in special education as well as in foster care, because these services often feed our correctional institutions. There also is some recent animal evidence suggesting that sufficient prenatal choline during pregnancy may be protective against Alzheimer’s disease – soon to be an even greater public problem in the United States. Lastly, the neuroscience findings regarding FASD also are emerging.
Hence, there is substantial information growing in various, different but overlapping areas of our systems addressing the nation’s public health and well-being. One of the most respected sources of credible science in America is the National Academy Science. The NAM should convene a meeting of the experts to examine the current state of FASD knowledge. If there is sufficient new information, the NAM needs to develop a new report on FASD. It has been 21 years since the first FAS report from the Institute of Medicine and it needs to be revisited. But it appears that the correctional, child protective services, special education, and mental health fields are not aware of the breadth of available research and its importance to the nation’s public health. Determining how fetal alcohol exposure/choline deficiency affects children and adults in special education, foster care, juvenile and adult corrections systems – along with such other social issues as prematurity, disability, unemployment, homelessness, suicide, violence, and mental health – is critical to our nation’s future.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
More than 20 years ago the Institute of Medicine (recently renamed the National Academy of Medicine, or NAM) issued its landmark report on fetal alcohol syndrome. Since then, there has been an explosion of research on the issue of fetal alcohol exposure – and NAM needs to revisit the issue and release another report.
Unfortunately, too few physicians and not enough people in the larger society understand public health and that the health status of the unfortunate among us affects the health status of the most fortunate of us. In short, low-income people are the proverbial “canary in the coal mine.”
Accordingly, solving the health care problems of low-income people would solve the health care problems of the middle and upper class. Consider where the United States would be had we paid attention to the opioid epidemic in low-income communities instead of waiting until it spread into everyone’s “safe” communities. We would have tried and tested solutions to the problem as it currently exists.
Another reason NAM needs to revisit FASD – currently proposed to be called neurobehavioral disorders associated with prenatal alcohol exposure in the DSM-5 – are the new findings that link FASD to seizure disorders and other neurodevelopmental disorders of childhood, such as intellectual disability, attention-deficit/hyperactivity disorder, speech and language disorders, motor disorders, specific learning disorders, and autism. In fact, new research is emerging from Robert Freedman, MD, and his team at the University of Colorado Denver, to suggest that preventing choline deficiency in pregnancy (the mechanism producing neurodevelopmental defects in FASD) may not only prevent neurodevelopmental disorders of childhood but also schizophrenia. Further, it has become abundantly clear that choline deficiency (often generated by FASD), is responsible for affect dysregulation, which is a common thread in various forms of violence and suicide.
A recent report highlighted the findings that inmates incarcerated in Mexican prisons have high rates of intellectual disability, and we know that FASD is one of the leading causes of this problem, but we are not screening for it in our juvenile detention centers, jails, or prisons. Consequently, we need to look for the prevalence of FASD in special education as well as in foster care, because these services often feed our correctional institutions. There also is some recent animal evidence suggesting that sufficient prenatal choline during pregnancy may be protective against Alzheimer’s disease – soon to be an even greater public problem in the United States. Lastly, the neuroscience findings regarding FASD also are emerging.
Hence, there is substantial information growing in various, different but overlapping areas of our systems addressing the nation’s public health and well-being. One of the most respected sources of credible science in America is the National Academy Science. The NAM should convene a meeting of the experts to examine the current state of FASD knowledge. If there is sufficient new information, the NAM needs to develop a new report on FASD. It has been 21 years since the first FAS report from the Institute of Medicine and it needs to be revisited. But it appears that the correctional, child protective services, special education, and mental health fields are not aware of the breadth of available research and its importance to the nation’s public health. Determining how fetal alcohol exposure/choline deficiency affects children and adults in special education, foster care, juvenile and adult corrections systems – along with such other social issues as prematurity, disability, unemployment, homelessness, suicide, violence, and mental health – is critical to our nation’s future.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
More than 20 years ago the Institute of Medicine (recently renamed the National Academy of Medicine, or NAM) issued its landmark report on fetal alcohol syndrome. Since then, there has been an explosion of research on the issue of fetal alcohol exposure – and NAM needs to revisit the issue and release another report.
Unfortunately, too few physicians and not enough people in the larger society understand public health and that the health status of the unfortunate among us affects the health status of the most fortunate of us. In short, low-income people are the proverbial “canary in the coal mine.”
Accordingly, solving the health care problems of low-income people would solve the health care problems of the middle and upper class. Consider where the United States would be had we paid attention to the opioid epidemic in low-income communities instead of waiting until it spread into everyone’s “safe” communities. We would have tried and tested solutions to the problem as it currently exists.
Another reason NAM needs to revisit FASD – currently proposed to be called neurobehavioral disorders associated with prenatal alcohol exposure in the DSM-5 – are the new findings that link FASD to seizure disorders and other neurodevelopmental disorders of childhood, such as intellectual disability, attention-deficit/hyperactivity disorder, speech and language disorders, motor disorders, specific learning disorders, and autism. In fact, new research is emerging from Robert Freedman, MD, and his team at the University of Colorado Denver, to suggest that preventing choline deficiency in pregnancy (the mechanism producing neurodevelopmental defects in FASD) may not only prevent neurodevelopmental disorders of childhood but also schizophrenia. Further, it has become abundantly clear that choline deficiency (often generated by FASD), is responsible for affect dysregulation, which is a common thread in various forms of violence and suicide.
A recent report highlighted the findings that inmates incarcerated in Mexican prisons have high rates of intellectual disability, and we know that FASD is one of the leading causes of this problem, but we are not screening for it in our juvenile detention centers, jails, or prisons. Consequently, we need to look for the prevalence of FASD in special education as well as in foster care, because these services often feed our correctional institutions. There also is some recent animal evidence suggesting that sufficient prenatal choline during pregnancy may be protective against Alzheimer’s disease – soon to be an even greater public problem in the United States. Lastly, the neuroscience findings regarding FASD also are emerging.
Hence, there is substantial information growing in various, different but overlapping areas of our systems addressing the nation’s public health and well-being. One of the most respected sources of credible science in America is the National Academy Science. The NAM should convene a meeting of the experts to examine the current state of FASD knowledge. If there is sufficient new information, the NAM needs to develop a new report on FASD. It has been 21 years since the first FAS report from the Institute of Medicine and it needs to be revisited. But it appears that the correctional, child protective services, special education, and mental health fields are not aware of the breadth of available research and its importance to the nation’s public health. Determining how fetal alcohol exposure/choline deficiency affects children and adults in special education, foster care, juvenile and adult corrections systems – along with such other social issues as prematurity, disability, unemployment, homelessness, suicide, violence, and mental health – is critical to our nation’s future.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Urinary tract agents: A safety review in pregnancy
The reported frequency of use in pregnancy and during breastfeeding for most of these agents is very low or completely absent.
The five subclasses of urinary tract agents are analgesics, antispasmodics, urinary acidifiers, urinary alkalinizers, and urinary germicides. With the exception of the three urinary germicides, anti-infectives are not covered in this column.
Analgesics
The analgesic subclass includes pentosan and phenazopyridine. Pentosan (Elmiron), a heparinlike compound, is an oral drug that is indicated for the relief of bladder pain or discomfort associated with interstitial cystitis. Systemic absorption is low, at about 6%. Because of the high molecular weight (4,000-6,000), it does not appear to cross the placenta, at least in the first half of pregnancy. A 1975 reference described its use in five women with preeclampsia. Each patient received 100 mg intramuscularly every 8 hours for about 5 days in the last weeks of pregnancy. No maternal benefit from the therapy was observed. There was apparently no fetal harm, but the neonatal outcomes were not described.
There are substantial – more than 900 – human pregnancy exposures in the first trimester with phenazopyridine. The exposures were not related to an increased risk of embryo-fetal harm and so use of the drug in pregnancy can be classified as compatible. However, the low molecular weight (about 214 for the free base) suggests that the drug will cross to the embryo and fetus.
Antispasmodics
The eight antispasmodics are darifenacin (Enablex), fesoterodine (Toviaz), flavoxate, mirabegron (Myrbetriq), oxybutynin (Ditropan XL), solifenacin (Vesicare), tolterodine (Detrol LA), and trospium.
These agents are indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency. The molecular weights range between 342 and 508, suggesting that all will cross the human placenta. There are no human pregnancy data for six of these agents and very limited data for flavoxate and oxybutynin. There is no evidence of embryo-fetal harm from these two drugs, but only one case involved exposure in the first trimester.
In seven of these drugs, the animal data suggested low risk. There was no embryo harm from doses that were equal to or less than 10 times the human dose based on body surface area (BSA) or area under the concentration curve (AUC). Solifenacin did cause embryo toxicity in pregnant mice. There was no embryo toxicity in pregnant rats and rabbits, but the maximum doses used were very low. Overall, the available data suggest that exposure to an antispasmodic in pregnancy is low risk for embryo, fetal, and newborn harm.
Urinary acidifiers
Ammonium chloride is a urinary acidifier as well as a respiratory expectorant. There is a large amount of data related to when the drug was used as an expectorant. There was no evidence that this use was associated with large categories of major or minor malformations. However, there were possible associations with three individual defects: inguinal hernia, cataract, and any benign tumor. No reports describing its use as a urinary acidifier have been located. When large amounts are consumed near term, the drug may cause acidosis in the mother and fetus. The molecular weight (about 53) suggests that it will cross the placenta.
Urinary alkalinizers
Potassium citrate (Urocit-K) is indicated for the management of renal tubular acidosis with calcium stones, hypocitraturic calcium oxalate with nephrolithiasis of any etiology, and uric acid lithiasis with or without calcium stones. The molecular weight (about 307) suggests it will cross the placenta. Only one case of its use in pregnancy has been located. The newborn had an unspecified defect but no other information was provided. The animal data in four species suggest low risk.
Urinary germicides
There are three urinary germicides: methenamine, methylene blue, and nitrofurantoin. Methenamine is available as methenamine mandelate (molecular weight abut 292) and methenamine hippurate (molecular weight about 319). Both are metabolized to formaldehyde (molecular weight about 30), the active agent. The molecular weights suggest that all will cross the placenta. The use of methenamine during pregnancy has been reported in more than 750 pregnancies. There have been no embryo or fetal adverse effects attributed to the drug.
The human data involving oral methylene blue, a weak urinary germicide, is limited to 55 exposures. There were three infants with birth defects (type not specified). Several reports have described the use of intra-amniotic injections to assist in the diagnosis of suspected membrane rupture. This use has resulted in newborns with hemolytic anemia, hyperbilirubinemia with or without Heinz body formation, blue staining of the skin, and methemoglobinemia. Fetal deaths have also been described. Recommendations to avoid the intra-amniotic use of methylene blue were issued more than 10 years ago. Moreover, the use of oral methylene blue as a urinary germicide is no longer recommended.
The low molecular weight (about 238) of nitrofurantoin suggests that it will cross the placenta. It is commonly used in pregnancy for the treatment or prophylaxis of urinary tract infections. The large amount of human data indicates that the risk of drug-induced birth defects is low. Several cohort studies have found no increased risk for birth defects. However, some case-control studies have found increased risks for hypoplastic left heart syndrome and oral clefts. A 2015 review concluded that this difference was due to the increased sensitivity of case-control studies to detect adverse effects (J Obstet Gynaecol Can. 2015 Feb;37[2]:150-6).
Use of the drug close to term may cause hemolytic anemia in newborns who are glucose-6-phosphate dehydrogenase (G6PD) deficient. Although rare, this may also occur in newborns who are not G6PD deficient. The best course is to avoid use of the drug close to delivery. As for use of the drug in the first trimester, ACOG’s Committee on Obstetric Practice stated in Committee Opinion No. 717 that nitrofurantoin was still thought to be appropriate when no other suitable alternative antibiotics were available (Obstet Gynecol. 2017 Sept;130[3]:666-7).
Breastfeeding
Except for methenamine and nitrofurantoin, there are no data related to the use of the urinary tract drugs during breastfeeding. Peak levels of methenamine occur at 1 hour, but no reports of adverse effects on nursing infants have been located. Several reports have described the use of nitrofurantoin during breastfeeding. Minor diarrhea was noted in two infants. However, breastfeeding an infant with G6PD deficiency could lead to hemolytic anemia.
Phenazopyridine should be used with caution especially for an infant younger than 1 month or with G6PD deficiency because of the risk for methemoglobinemia, sulfhemoglobinemia, and hemolytic anemia.
Although there have been no reports of the use of mirabegron during lactation, the characteristics of the drug – low molecular weight (about 397), long elimination half life (50 hours), and moderate plasma protein binding (about 71%) – suggest that the drug will be excreted into milk, potentially in clinically significant amounts. There is also concern with use of tolterodine (molecular weight about 476) because both the primary drug and its equipotent metabolite may be excreted into milk.
Mr. Briggs is a clinical professor of pharmacy at the University of California, San Francisco, and an adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. He coauthored “Drugs in Pregnancy and Lactation” and coedited “Diseases, Complications, and Drug Therapy in Obstetrics.” He reported having no relevant financial disclosures.
The reported frequency of use in pregnancy and during breastfeeding for most of these agents is very low or completely absent.
The five subclasses of urinary tract agents are analgesics, antispasmodics, urinary acidifiers, urinary alkalinizers, and urinary germicides. With the exception of the three urinary germicides, anti-infectives are not covered in this column.
Analgesics
The analgesic subclass includes pentosan and phenazopyridine. Pentosan (Elmiron), a heparinlike compound, is an oral drug that is indicated for the relief of bladder pain or discomfort associated with interstitial cystitis. Systemic absorption is low, at about 6%. Because of the high molecular weight (4,000-6,000), it does not appear to cross the placenta, at least in the first half of pregnancy. A 1975 reference described its use in five women with preeclampsia. Each patient received 100 mg intramuscularly every 8 hours for about 5 days in the last weeks of pregnancy. No maternal benefit from the therapy was observed. There was apparently no fetal harm, but the neonatal outcomes were not described.
There are substantial – more than 900 – human pregnancy exposures in the first trimester with phenazopyridine. The exposures were not related to an increased risk of embryo-fetal harm and so use of the drug in pregnancy can be classified as compatible. However, the low molecular weight (about 214 for the free base) suggests that the drug will cross to the embryo and fetus.
Antispasmodics
The eight antispasmodics are darifenacin (Enablex), fesoterodine (Toviaz), flavoxate, mirabegron (Myrbetriq), oxybutynin (Ditropan XL), solifenacin (Vesicare), tolterodine (Detrol LA), and trospium.
These agents are indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency. The molecular weights range between 342 and 508, suggesting that all will cross the human placenta. There are no human pregnancy data for six of these agents and very limited data for flavoxate and oxybutynin. There is no evidence of embryo-fetal harm from these two drugs, but only one case involved exposure in the first trimester.
In seven of these drugs, the animal data suggested low risk. There was no embryo harm from doses that were equal to or less than 10 times the human dose based on body surface area (BSA) or area under the concentration curve (AUC). Solifenacin did cause embryo toxicity in pregnant mice. There was no embryo toxicity in pregnant rats and rabbits, but the maximum doses used were very low. Overall, the available data suggest that exposure to an antispasmodic in pregnancy is low risk for embryo, fetal, and newborn harm.
Urinary acidifiers
Ammonium chloride is a urinary acidifier as well as a respiratory expectorant. There is a large amount of data related to when the drug was used as an expectorant. There was no evidence that this use was associated with large categories of major or minor malformations. However, there were possible associations with three individual defects: inguinal hernia, cataract, and any benign tumor. No reports describing its use as a urinary acidifier have been located. When large amounts are consumed near term, the drug may cause acidosis in the mother and fetus. The molecular weight (about 53) suggests that it will cross the placenta.
Urinary alkalinizers
Potassium citrate (Urocit-K) is indicated for the management of renal tubular acidosis with calcium stones, hypocitraturic calcium oxalate with nephrolithiasis of any etiology, and uric acid lithiasis with or without calcium stones. The molecular weight (about 307) suggests it will cross the placenta. Only one case of its use in pregnancy has been located. The newborn had an unspecified defect but no other information was provided. The animal data in four species suggest low risk.
Urinary germicides
There are three urinary germicides: methenamine, methylene blue, and nitrofurantoin. Methenamine is available as methenamine mandelate (molecular weight abut 292) and methenamine hippurate (molecular weight about 319). Both are metabolized to formaldehyde (molecular weight about 30), the active agent. The molecular weights suggest that all will cross the placenta. The use of methenamine during pregnancy has been reported in more than 750 pregnancies. There have been no embryo or fetal adverse effects attributed to the drug.
The human data involving oral methylene blue, a weak urinary germicide, is limited to 55 exposures. There were three infants with birth defects (type not specified). Several reports have described the use of intra-amniotic injections to assist in the diagnosis of suspected membrane rupture. This use has resulted in newborns with hemolytic anemia, hyperbilirubinemia with or without Heinz body formation, blue staining of the skin, and methemoglobinemia. Fetal deaths have also been described. Recommendations to avoid the intra-amniotic use of methylene blue were issued more than 10 years ago. Moreover, the use of oral methylene blue as a urinary germicide is no longer recommended.
The low molecular weight (about 238) of nitrofurantoin suggests that it will cross the placenta. It is commonly used in pregnancy for the treatment or prophylaxis of urinary tract infections. The large amount of human data indicates that the risk of drug-induced birth defects is low. Several cohort studies have found no increased risk for birth defects. However, some case-control studies have found increased risks for hypoplastic left heart syndrome and oral clefts. A 2015 review concluded that this difference was due to the increased sensitivity of case-control studies to detect adverse effects (J Obstet Gynaecol Can. 2015 Feb;37[2]:150-6).
Use of the drug close to term may cause hemolytic anemia in newborns who are glucose-6-phosphate dehydrogenase (G6PD) deficient. Although rare, this may also occur in newborns who are not G6PD deficient. The best course is to avoid use of the drug close to delivery. As for use of the drug in the first trimester, ACOG’s Committee on Obstetric Practice stated in Committee Opinion No. 717 that nitrofurantoin was still thought to be appropriate when no other suitable alternative antibiotics were available (Obstet Gynecol. 2017 Sept;130[3]:666-7).
Breastfeeding
Except for methenamine and nitrofurantoin, there are no data related to the use of the urinary tract drugs during breastfeeding. Peak levels of methenamine occur at 1 hour, but no reports of adverse effects on nursing infants have been located. Several reports have described the use of nitrofurantoin during breastfeeding. Minor diarrhea was noted in two infants. However, breastfeeding an infant with G6PD deficiency could lead to hemolytic anemia.
Phenazopyridine should be used with caution especially for an infant younger than 1 month or with G6PD deficiency because of the risk for methemoglobinemia, sulfhemoglobinemia, and hemolytic anemia.
Although there have been no reports of the use of mirabegron during lactation, the characteristics of the drug – low molecular weight (about 397), long elimination half life (50 hours), and moderate plasma protein binding (about 71%) – suggest that the drug will be excreted into milk, potentially in clinically significant amounts. There is also concern with use of tolterodine (molecular weight about 476) because both the primary drug and its equipotent metabolite may be excreted into milk.
Mr. Briggs is a clinical professor of pharmacy at the University of California, San Francisco, and an adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. He coauthored “Drugs in Pregnancy and Lactation” and coedited “Diseases, Complications, and Drug Therapy in Obstetrics.” He reported having no relevant financial disclosures.
The reported frequency of use in pregnancy and during breastfeeding for most of these agents is very low or completely absent.
The five subclasses of urinary tract agents are analgesics, antispasmodics, urinary acidifiers, urinary alkalinizers, and urinary germicides. With the exception of the three urinary germicides, anti-infectives are not covered in this column.
Analgesics
The analgesic subclass includes pentosan and phenazopyridine. Pentosan (Elmiron), a heparinlike compound, is an oral drug that is indicated for the relief of bladder pain or discomfort associated with interstitial cystitis. Systemic absorption is low, at about 6%. Because of the high molecular weight (4,000-6,000), it does not appear to cross the placenta, at least in the first half of pregnancy. A 1975 reference described its use in five women with preeclampsia. Each patient received 100 mg intramuscularly every 8 hours for about 5 days in the last weeks of pregnancy. No maternal benefit from the therapy was observed. There was apparently no fetal harm, but the neonatal outcomes were not described.
There are substantial – more than 900 – human pregnancy exposures in the first trimester with phenazopyridine. The exposures were not related to an increased risk of embryo-fetal harm and so use of the drug in pregnancy can be classified as compatible. However, the low molecular weight (about 214 for the free base) suggests that the drug will cross to the embryo and fetus.
Antispasmodics
The eight antispasmodics are darifenacin (Enablex), fesoterodine (Toviaz), flavoxate, mirabegron (Myrbetriq), oxybutynin (Ditropan XL), solifenacin (Vesicare), tolterodine (Detrol LA), and trospium.
These agents are indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency. The molecular weights range between 342 and 508, suggesting that all will cross the human placenta. There are no human pregnancy data for six of these agents and very limited data for flavoxate and oxybutynin. There is no evidence of embryo-fetal harm from these two drugs, but only one case involved exposure in the first trimester.
In seven of these drugs, the animal data suggested low risk. There was no embryo harm from doses that were equal to or less than 10 times the human dose based on body surface area (BSA) or area under the concentration curve (AUC). Solifenacin did cause embryo toxicity in pregnant mice. There was no embryo toxicity in pregnant rats and rabbits, but the maximum doses used were very low. Overall, the available data suggest that exposure to an antispasmodic in pregnancy is low risk for embryo, fetal, and newborn harm.
Urinary acidifiers
Ammonium chloride is a urinary acidifier as well as a respiratory expectorant. There is a large amount of data related to when the drug was used as an expectorant. There was no evidence that this use was associated with large categories of major or minor malformations. However, there were possible associations with three individual defects: inguinal hernia, cataract, and any benign tumor. No reports describing its use as a urinary acidifier have been located. When large amounts are consumed near term, the drug may cause acidosis in the mother and fetus. The molecular weight (about 53) suggests that it will cross the placenta.
Urinary alkalinizers
Potassium citrate (Urocit-K) is indicated for the management of renal tubular acidosis with calcium stones, hypocitraturic calcium oxalate with nephrolithiasis of any etiology, and uric acid lithiasis with or without calcium stones. The molecular weight (about 307) suggests it will cross the placenta. Only one case of its use in pregnancy has been located. The newborn had an unspecified defect but no other information was provided. The animal data in four species suggest low risk.
Urinary germicides
There are three urinary germicides: methenamine, methylene blue, and nitrofurantoin. Methenamine is available as methenamine mandelate (molecular weight abut 292) and methenamine hippurate (molecular weight about 319). Both are metabolized to formaldehyde (molecular weight about 30), the active agent. The molecular weights suggest that all will cross the placenta. The use of methenamine during pregnancy has been reported in more than 750 pregnancies. There have been no embryo or fetal adverse effects attributed to the drug.
The human data involving oral methylene blue, a weak urinary germicide, is limited to 55 exposures. There were three infants with birth defects (type not specified). Several reports have described the use of intra-amniotic injections to assist in the diagnosis of suspected membrane rupture. This use has resulted in newborns with hemolytic anemia, hyperbilirubinemia with or without Heinz body formation, blue staining of the skin, and methemoglobinemia. Fetal deaths have also been described. Recommendations to avoid the intra-amniotic use of methylene blue were issued more than 10 years ago. Moreover, the use of oral methylene blue as a urinary germicide is no longer recommended.
The low molecular weight (about 238) of nitrofurantoin suggests that it will cross the placenta. It is commonly used in pregnancy for the treatment or prophylaxis of urinary tract infections. The large amount of human data indicates that the risk of drug-induced birth defects is low. Several cohort studies have found no increased risk for birth defects. However, some case-control studies have found increased risks for hypoplastic left heart syndrome and oral clefts. A 2015 review concluded that this difference was due to the increased sensitivity of case-control studies to detect adverse effects (J Obstet Gynaecol Can. 2015 Feb;37[2]:150-6).
Use of the drug close to term may cause hemolytic anemia in newborns who are glucose-6-phosphate dehydrogenase (G6PD) deficient. Although rare, this may also occur in newborns who are not G6PD deficient. The best course is to avoid use of the drug close to delivery. As for use of the drug in the first trimester, ACOG’s Committee on Obstetric Practice stated in Committee Opinion No. 717 that nitrofurantoin was still thought to be appropriate when no other suitable alternative antibiotics were available (Obstet Gynecol. 2017 Sept;130[3]:666-7).
Breastfeeding
Except for methenamine and nitrofurantoin, there are no data related to the use of the urinary tract drugs during breastfeeding. Peak levels of methenamine occur at 1 hour, but no reports of adverse effects on nursing infants have been located. Several reports have described the use of nitrofurantoin during breastfeeding. Minor diarrhea was noted in two infants. However, breastfeeding an infant with G6PD deficiency could lead to hemolytic anemia.
Phenazopyridine should be used with caution especially for an infant younger than 1 month or with G6PD deficiency because of the risk for methemoglobinemia, sulfhemoglobinemia, and hemolytic anemia.
Although there have been no reports of the use of mirabegron during lactation, the characteristics of the drug – low molecular weight (about 397), long elimination half life (50 hours), and moderate plasma protein binding (about 71%) – suggest that the drug will be excreted into milk, potentially in clinically significant amounts. There is also concern with use of tolterodine (molecular weight about 476) because both the primary drug and its equipotent metabolite may be excreted into milk.
Mr. Briggs is a clinical professor of pharmacy at the University of California, San Francisco, and an adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. He coauthored “Drugs in Pregnancy and Lactation” and coedited “Diseases, Complications, and Drug Therapy in Obstetrics.” He reported having no relevant financial disclosures.
¿No hablás español? Help Is Here
According to the 2015 US Census Bureau, more than 60 million individuals—about 19% of Americans—reported speaking a language other than English at home, and more than 25 million reported their English-speaking ability as less than “very well.” The top five non-English languages spoken at home were Spanish, French, Chinese, Tagalog, and Vietnamese, encompassing 72% of non-English speakers. 1,2
In the health care sector, translator services are essential for providing accurate and culturally competent care. Current options for translator services include face-to-face interpreters, phone-based translator services, and translator apps on mobile devices. In settings where face-to-face interpreters or phone-based translator services are not available, translator apps may be a reasonable alternative.
THREE TYPES OF TRANSLATOR APPS
Preset medical phrase translator apps require the user to search for or find a question or statement in order to facilitate a conversation. With these types of apps, a health care provider can choose fully conjugated sentences, which then can be played or read back to the patient in the chosen translated language. Within this group of apps, Canopy Speak and Universal Doctor Speaker are highly accessible, since both apps are available from the Apple iTunes and Google Play stores and both are free.
Medical dictionary apps require the user to search for a medical term in one language to receive a translation in another language. These apps are less practical, but they can help providers find and define specific terms in a given language.
General language translator apps require the user to enter a term, statement, or question in one language and then provide a translation in another language. Google Translate and Vocre Translate are examples.
Recommended apps
My colleagues, Dr. Amrin Khander and Dr. Sara Farag, and I identified and evaluated medical translator apps that are available from the Apple iTunes and Google Play stores, to aid clinicians in using such apps during clinical encounters with non-English speakers.3
The top recommended translator apps are listed in the table, evaluated with criteria from a shortened version of the APPLICATIONS scoring system: app comprehensiveness, price, platform, literature use, and important special features.4 We hope these tools will help you enhance communication with your patients who have limited English proficiency.
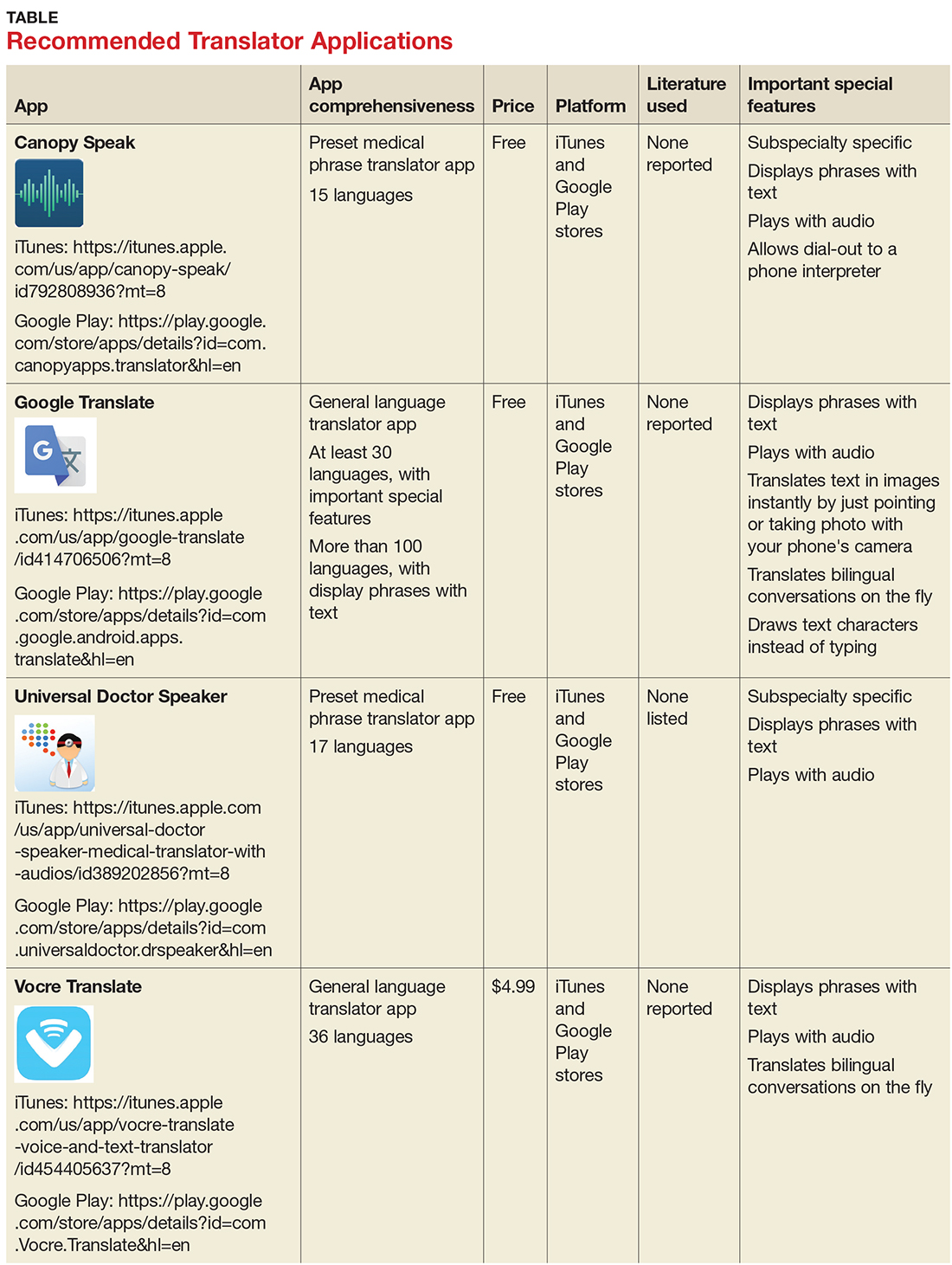
1. United States Census Bureau. Detailed language spoken at home and ability to speak English for the population 5 years and over: 2009–2013. www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Accessed November 1, 2017.
2. United States Census Bureau. U.S. and world population clock. www.census.gov/popclock/?intcmp=home_pop. Accessed November 1, 2017.
3. Khander A, Farag S, Chen KT. Identification and rating of medical translator mobile applications using the APPLICATIONS scoring system [abstract 321]. Obstet Gynecol. 2017;129(5 suppl):101S.
4. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125(6):1478-1483.
According to the 2015 US Census Bureau, more than 60 million individuals—about 19% of Americans—reported speaking a language other than English at home, and more than 25 million reported their English-speaking ability as less than “very well.” The top five non-English languages spoken at home were Spanish, French, Chinese, Tagalog, and Vietnamese, encompassing 72% of non-English speakers. 1,2
In the health care sector, translator services are essential for providing accurate and culturally competent care. Current options for translator services include face-to-face interpreters, phone-based translator services, and translator apps on mobile devices. In settings where face-to-face interpreters or phone-based translator services are not available, translator apps may be a reasonable alternative.
THREE TYPES OF TRANSLATOR APPS
Preset medical phrase translator apps require the user to search for or find a question or statement in order to facilitate a conversation. With these types of apps, a health care provider can choose fully conjugated sentences, which then can be played or read back to the patient in the chosen translated language. Within this group of apps, Canopy Speak and Universal Doctor Speaker are highly accessible, since both apps are available from the Apple iTunes and Google Play stores and both are free.
Medical dictionary apps require the user to search for a medical term in one language to receive a translation in another language. These apps are less practical, but they can help providers find and define specific terms in a given language.
General language translator apps require the user to enter a term, statement, or question in one language and then provide a translation in another language. Google Translate and Vocre Translate are examples.
Recommended apps
My colleagues, Dr. Amrin Khander and Dr. Sara Farag, and I identified and evaluated medical translator apps that are available from the Apple iTunes and Google Play stores, to aid clinicians in using such apps during clinical encounters with non-English speakers.3
The top recommended translator apps are listed in the table, evaluated with criteria from a shortened version of the APPLICATIONS scoring system: app comprehensiveness, price, platform, literature use, and important special features.4 We hope these tools will help you enhance communication with your patients who have limited English proficiency.
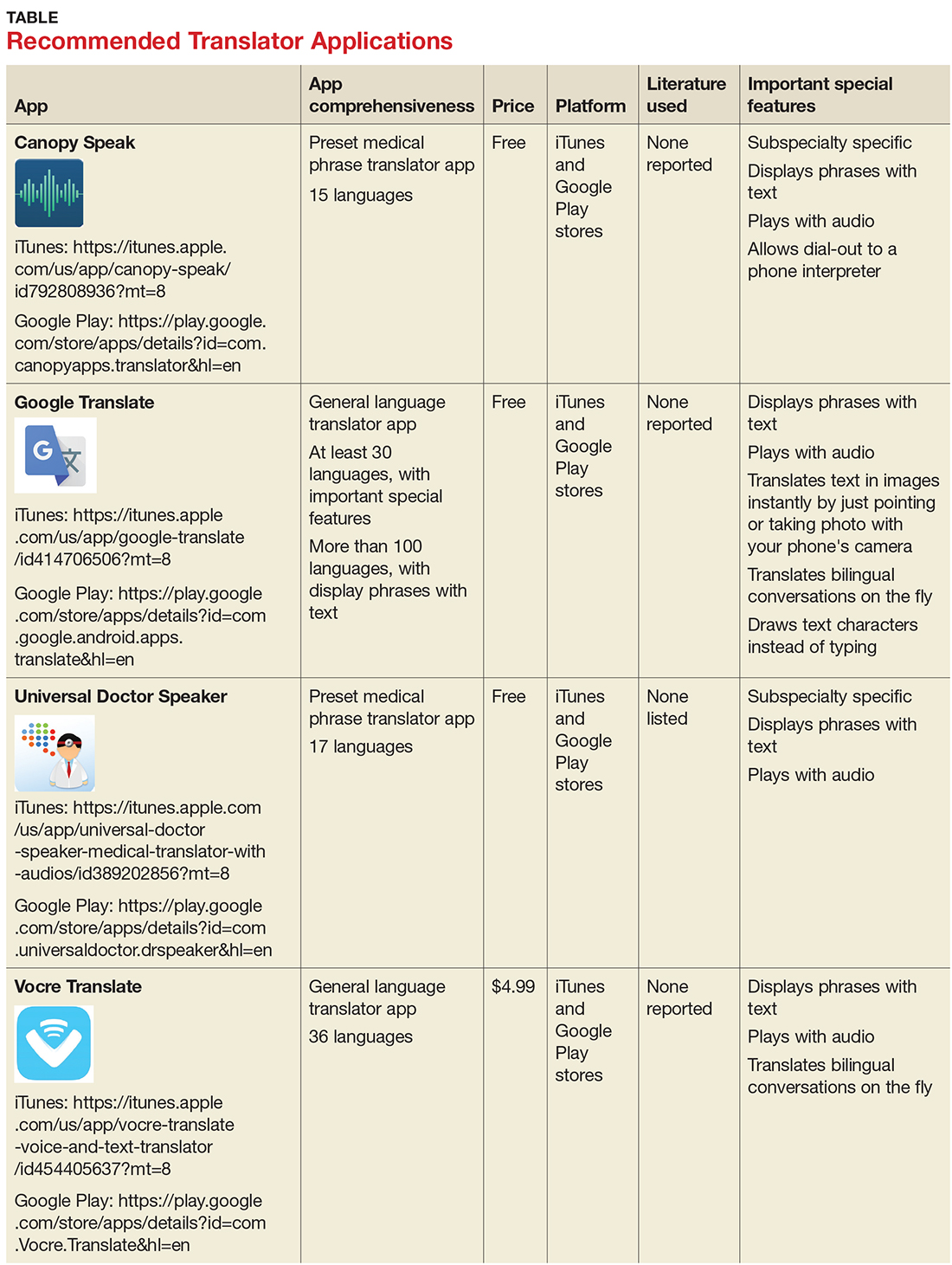
According to the 2015 US Census Bureau, more than 60 million individuals—about 19% of Americans—reported speaking a language other than English at home, and more than 25 million reported their English-speaking ability as less than “very well.” The top five non-English languages spoken at home were Spanish, French, Chinese, Tagalog, and Vietnamese, encompassing 72% of non-English speakers. 1,2
In the health care sector, translator services are essential for providing accurate and culturally competent care. Current options for translator services include face-to-face interpreters, phone-based translator services, and translator apps on mobile devices. In settings where face-to-face interpreters or phone-based translator services are not available, translator apps may be a reasonable alternative.
THREE TYPES OF TRANSLATOR APPS
Preset medical phrase translator apps require the user to search for or find a question or statement in order to facilitate a conversation. With these types of apps, a health care provider can choose fully conjugated sentences, which then can be played or read back to the patient in the chosen translated language. Within this group of apps, Canopy Speak and Universal Doctor Speaker are highly accessible, since both apps are available from the Apple iTunes and Google Play stores and both are free.
Medical dictionary apps require the user to search for a medical term in one language to receive a translation in another language. These apps are less practical, but they can help providers find and define specific terms in a given language.
General language translator apps require the user to enter a term, statement, or question in one language and then provide a translation in another language. Google Translate and Vocre Translate are examples.
Recommended apps
My colleagues, Dr. Amrin Khander and Dr. Sara Farag, and I identified and evaluated medical translator apps that are available from the Apple iTunes and Google Play stores, to aid clinicians in using such apps during clinical encounters with non-English speakers.3
The top recommended translator apps are listed in the table, evaluated with criteria from a shortened version of the APPLICATIONS scoring system: app comprehensiveness, price, platform, literature use, and important special features.4 We hope these tools will help you enhance communication with your patients who have limited English proficiency.
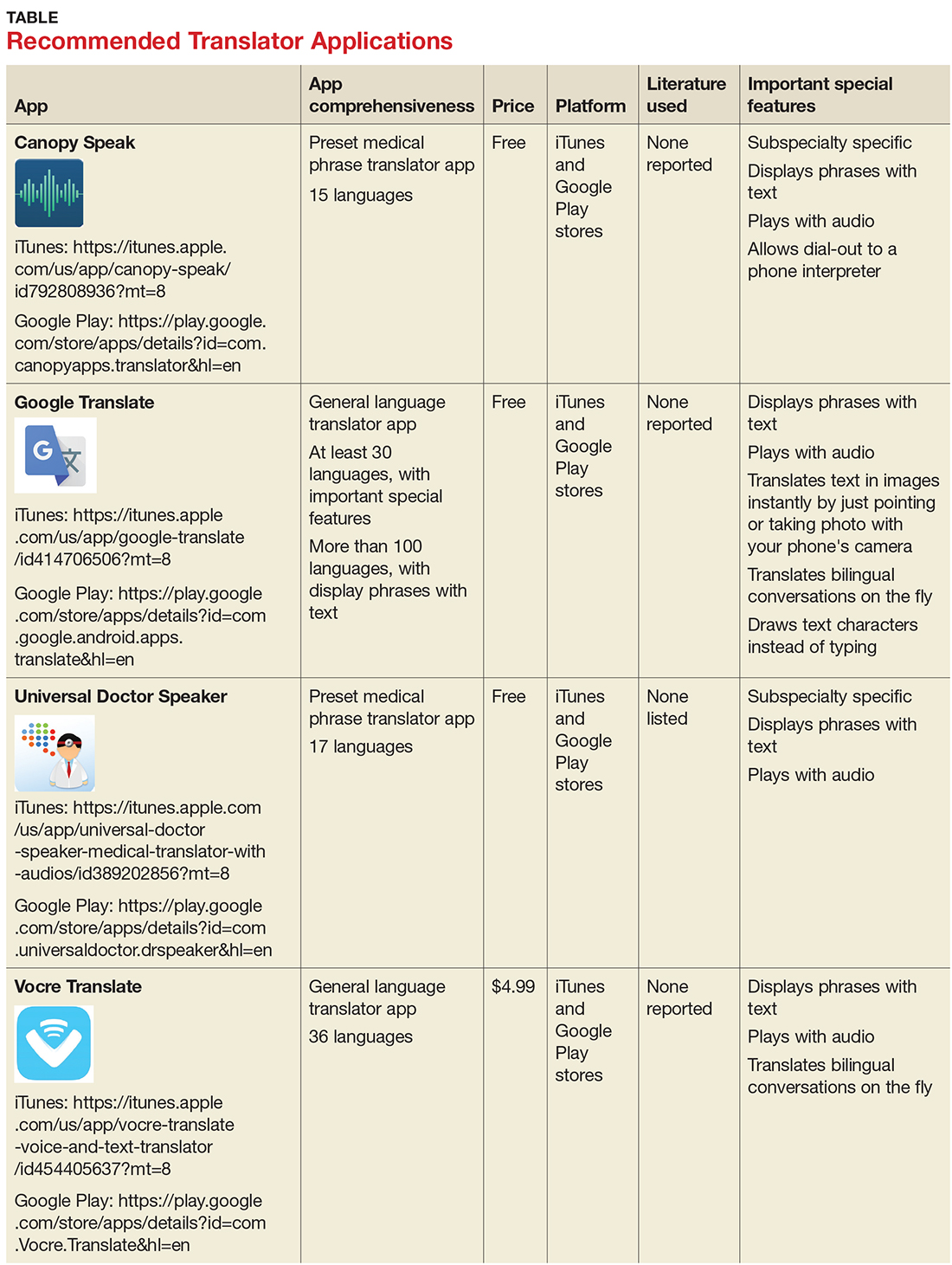
1. United States Census Bureau. Detailed language spoken at home and ability to speak English for the population 5 years and over: 2009–2013. www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Accessed November 1, 2017.
2. United States Census Bureau. U.S. and world population clock. www.census.gov/popclock/?intcmp=home_pop. Accessed November 1, 2017.
3. Khander A, Farag S, Chen KT. Identification and rating of medical translator mobile applications using the APPLICATIONS scoring system [abstract 321]. Obstet Gynecol. 2017;129(5 suppl):101S.
4. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125(6):1478-1483.
1. United States Census Bureau. Detailed language spoken at home and ability to speak English for the population 5 years and over: 2009–2013. www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Accessed November 1, 2017.
2. United States Census Bureau. U.S. and world population clock. www.census.gov/popclock/?intcmp=home_pop. Accessed November 1, 2017.
3. Khander A, Farag S, Chen KT. Identification and rating of medical translator mobile applications using the APPLICATIONS scoring system [abstract 321]. Obstet Gynecol. 2017;129(5 suppl):101S.
4. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125(6):1478-1483.