User login
ERRATUM
In the October, 2017 audiocast, “Statins for primary prevention of CVD: To start or not to start?” Dr. Doug Campos-Outcalt drew an incorrect conclusion when he used himself as an example to demonstrate the application of recommendations from the American College of Cardiology/American Heart Association (ACC/AHA) and the US Preventive Services Task Force. He indicated that he would qualify for starting low- to moderate-dose statins under both sets of recommendations when, in fact, he would qualify only under the ACC/AHA recommendations. The audio file has been revised to reflect the proper conclusion.
In the October, 2017 audiocast, “Statins for primary prevention of CVD: To start or not to start?” Dr. Doug Campos-Outcalt drew an incorrect conclusion when he used himself as an example to demonstrate the application of recommendations from the American College of Cardiology/American Heart Association (ACC/AHA) and the US Preventive Services Task Force. He indicated that he would qualify for starting low- to moderate-dose statins under both sets of recommendations when, in fact, he would qualify only under the ACC/AHA recommendations. The audio file has been revised to reflect the proper conclusion.
In the October, 2017 audiocast, “Statins for primary prevention of CVD: To start or not to start?” Dr. Doug Campos-Outcalt drew an incorrect conclusion when he used himself as an example to demonstrate the application of recommendations from the American College of Cardiology/American Heart Association (ACC/AHA) and the US Preventive Services Task Force. He indicated that he would qualify for starting low- to moderate-dose statins under both sets of recommendations when, in fact, he would qualify only under the ACC/AHA recommendations. The audio file has been revised to reflect the proper conclusion.
Let’s get physical!
We see many patients in our office with acute or chronic musculoskeletal complaints. Most acute musculoskeletal injuries resolve with rest and a short course of a narcotic or over-the-counter pain medication.
But when pain lingers beyond a few weeks, patients get nervous and so do we. This is the critical time period during which patients may request more narcotic pain medication and/or develop chronic pain syndromes, which are enormously difficult to treat. What treatments can we suggest at this point that have good evidence of effectiveness?
Reassurance. The simplest effective intervention is reassurance—especially from a physician. Patients who are reassured are more likely to recover from low back pain.1 Patients often have unrealistic goals, expecting to be pain free in a couple of weeks, whereas the natural healing of soft tissue injuries takes 8 to 12 weeks (and sometimes longer) for more severe injuries.
Physical modalities. Nearly all of the other non-medicinal, effective interventions for subacute and chronic musculoskeletal pain are physical in nature. The article by Slattengren et al provides an evidence-based review of osteopathic manipulation techniques (OMT) for pain and other conditions, as well. The evidence for the effectiveness of OMT for low back pain is the strongest.
There is evidence for the effectiveness of other types of physical techniques for low back pain, too. A recent meta-analysis of spinal manipulation for acute low back pain concluded that it is moderately effective in reducing pain and increasing function.2 And although the evidence is not considered strong, the American College of Physicians included massage, tai chi, yoga, acupuncture, motor control exercises, and progressive relaxation in their recent recommendations for the treatment of acute, subacute, and chronic low back pain.3
My personal favorite treatment for chronic low back pain is walking. In a clever randomized trial, Irish researchers randomized patients with chronic low back pain to 3 groups: standard physical therapy, weekly exercise classes designed for people with low back pain, and a tailored, gradually increasing walking program.4 Participants in the last group were instructed to walk at least 4 days a week, starting with 10 minutes/day and working up to 30 minutes of brisk walking 5 days/week. The improvement in pain and disability after 2 months, although modest, was as good in the walking group as in the other 2 treatment groups.
So let’s try relying more on physical activity to help our patients manage their aches and pains. It may produce benefits for other health problems, too, and start many patients down a road to healthier living.
1. Traeger AC, Hübscher M, Henschke N, et al. Effect of primary care-based education on reassurance in patients with acute low back pain: systematic review and meta-analysis. JAMA Intern Med. 2015;175:733-743.
2. Paige NM, Miake-Lye IM, Booth MS, et al. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. JAMA. 2017;317:1451-1460.
3. Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Ann Intern Med. 2017;166:514-530.
4. Hurley DA, Tully MA, Lonsdale C, et al. Supervised walking in comparison with fitness training for chronic back pain in physiotherapy: results of the SWIFT single-blinded randomized controlled trial (ISRCTN17592092). Pain. 2015;156:131-147.
We see many patients in our office with acute or chronic musculoskeletal complaints. Most acute musculoskeletal injuries resolve with rest and a short course of a narcotic or over-the-counter pain medication.
But when pain lingers beyond a few weeks, patients get nervous and so do we. This is the critical time period during which patients may request more narcotic pain medication and/or develop chronic pain syndromes, which are enormously difficult to treat. What treatments can we suggest at this point that have good evidence of effectiveness?
Reassurance. The simplest effective intervention is reassurance—especially from a physician. Patients who are reassured are more likely to recover from low back pain.1 Patients often have unrealistic goals, expecting to be pain free in a couple of weeks, whereas the natural healing of soft tissue injuries takes 8 to 12 weeks (and sometimes longer) for more severe injuries.
Physical modalities. Nearly all of the other non-medicinal, effective interventions for subacute and chronic musculoskeletal pain are physical in nature. The article by Slattengren et al provides an evidence-based review of osteopathic manipulation techniques (OMT) for pain and other conditions, as well. The evidence for the effectiveness of OMT for low back pain is the strongest.
There is evidence for the effectiveness of other types of physical techniques for low back pain, too. A recent meta-analysis of spinal manipulation for acute low back pain concluded that it is moderately effective in reducing pain and increasing function.2 And although the evidence is not considered strong, the American College of Physicians included massage, tai chi, yoga, acupuncture, motor control exercises, and progressive relaxation in their recent recommendations for the treatment of acute, subacute, and chronic low back pain.3
My personal favorite treatment for chronic low back pain is walking. In a clever randomized trial, Irish researchers randomized patients with chronic low back pain to 3 groups: standard physical therapy, weekly exercise classes designed for people with low back pain, and a tailored, gradually increasing walking program.4 Participants in the last group were instructed to walk at least 4 days a week, starting with 10 minutes/day and working up to 30 minutes of brisk walking 5 days/week. The improvement in pain and disability after 2 months, although modest, was as good in the walking group as in the other 2 treatment groups.
So let’s try relying more on physical activity to help our patients manage their aches and pains. It may produce benefits for other health problems, too, and start many patients down a road to healthier living.
We see many patients in our office with acute or chronic musculoskeletal complaints. Most acute musculoskeletal injuries resolve with rest and a short course of a narcotic or over-the-counter pain medication.
But when pain lingers beyond a few weeks, patients get nervous and so do we. This is the critical time period during which patients may request more narcotic pain medication and/or develop chronic pain syndromes, which are enormously difficult to treat. What treatments can we suggest at this point that have good evidence of effectiveness?
Reassurance. The simplest effective intervention is reassurance—especially from a physician. Patients who are reassured are more likely to recover from low back pain.1 Patients often have unrealistic goals, expecting to be pain free in a couple of weeks, whereas the natural healing of soft tissue injuries takes 8 to 12 weeks (and sometimes longer) for more severe injuries.
Physical modalities. Nearly all of the other non-medicinal, effective interventions for subacute and chronic musculoskeletal pain are physical in nature. The article by Slattengren et al provides an evidence-based review of osteopathic manipulation techniques (OMT) for pain and other conditions, as well. The evidence for the effectiveness of OMT for low back pain is the strongest.
There is evidence for the effectiveness of other types of physical techniques for low back pain, too. A recent meta-analysis of spinal manipulation for acute low back pain concluded that it is moderately effective in reducing pain and increasing function.2 And although the evidence is not considered strong, the American College of Physicians included massage, tai chi, yoga, acupuncture, motor control exercises, and progressive relaxation in their recent recommendations for the treatment of acute, subacute, and chronic low back pain.3
My personal favorite treatment for chronic low back pain is walking. In a clever randomized trial, Irish researchers randomized patients with chronic low back pain to 3 groups: standard physical therapy, weekly exercise classes designed for people with low back pain, and a tailored, gradually increasing walking program.4 Participants in the last group were instructed to walk at least 4 days a week, starting with 10 minutes/day and working up to 30 minutes of brisk walking 5 days/week. The improvement in pain and disability after 2 months, although modest, was as good in the walking group as in the other 2 treatment groups.
So let’s try relying more on physical activity to help our patients manage their aches and pains. It may produce benefits for other health problems, too, and start many patients down a road to healthier living.
1. Traeger AC, Hübscher M, Henschke N, et al. Effect of primary care-based education on reassurance in patients with acute low back pain: systematic review and meta-analysis. JAMA Intern Med. 2015;175:733-743.
2. Paige NM, Miake-Lye IM, Booth MS, et al. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. JAMA. 2017;317:1451-1460.
3. Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Ann Intern Med. 2017;166:514-530.
4. Hurley DA, Tully MA, Lonsdale C, et al. Supervised walking in comparison with fitness training for chronic back pain in physiotherapy: results of the SWIFT single-blinded randomized controlled trial (ISRCTN17592092). Pain. 2015;156:131-147.
1. Traeger AC, Hübscher M, Henschke N, et al. Effect of primary care-based education on reassurance in patients with acute low back pain: systematic review and meta-analysis. JAMA Intern Med. 2015;175:733-743.
2. Paige NM, Miake-Lye IM, Booth MS, et al. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. JAMA. 2017;317:1451-1460.
3. Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Ann Intern Med. 2017;166:514-530.
4. Hurley DA, Tully MA, Lonsdale C, et al. Supervised walking in comparison with fitness training for chronic back pain in physiotherapy: results of the SWIFT single-blinded randomized controlled trial (ISRCTN17592092). Pain. 2015;156:131-147.
Letter from the Editor
This month we learned of the passing of Dr. Marv Sleisenger. There are few physicians who have had a greater impact on our field than Dr. Sleisenger. He was a consummate gentleman, enthusiastic teacher, great mentor, authored hundreds of research papers, and edited the most famous textbook of gastroenterology. Our thoughts and hearts are with his family and friends.
I would like to highlight our liver coverage. AASLD had their annual meeting in Washington in November. My colleague at University of Michigan (Anna Lok, MD) is the current president and helped spearhead a meeting that was packed with research and clinical information. We will be covering AASLD in greater depth in the months to come.
And while initial efforts to repeal the ACA have stalled, several key parts of the ACA continue to be modified or repealed either by Executive Orders or as part of the current tax reform efforts. We continue to view these efforts through the lens of our patients’ access to care.
John I. Allen, MD, MBA, AGAF
Editor in Chief
This month we learned of the passing of Dr. Marv Sleisenger. There are few physicians who have had a greater impact on our field than Dr. Sleisenger. He was a consummate gentleman, enthusiastic teacher, great mentor, authored hundreds of research papers, and edited the most famous textbook of gastroenterology. Our thoughts and hearts are with his family and friends.
I would like to highlight our liver coverage. AASLD had their annual meeting in Washington in November. My colleague at University of Michigan (Anna Lok, MD) is the current president and helped spearhead a meeting that was packed with research and clinical information. We will be covering AASLD in greater depth in the months to come.
And while initial efforts to repeal the ACA have stalled, several key parts of the ACA continue to be modified or repealed either by Executive Orders or as part of the current tax reform efforts. We continue to view these efforts through the lens of our patients’ access to care.
John I. Allen, MD, MBA, AGAF
Editor in Chief
This month we learned of the passing of Dr. Marv Sleisenger. There are few physicians who have had a greater impact on our field than Dr. Sleisenger. He was a consummate gentleman, enthusiastic teacher, great mentor, authored hundreds of research papers, and edited the most famous textbook of gastroenterology. Our thoughts and hearts are with his family and friends.
I would like to highlight our liver coverage. AASLD had their annual meeting in Washington in November. My colleague at University of Michigan (Anna Lok, MD) is the current president and helped spearhead a meeting that was packed with research and clinical information. We will be covering AASLD in greater depth in the months to come.
And while initial efforts to repeal the ACA have stalled, several key parts of the ACA continue to be modified or repealed either by Executive Orders or as part of the current tax reform efforts. We continue to view these efforts through the lens of our patients’ access to care.
John I. Allen, MD, MBA, AGAF
Editor in Chief
VA, Kaiser lauded for hypertension control
At a time when the Department of Veterans Affairs is criticized for the care it delivers, and when some also see it threatened by privatization, it was refreshing to hear the VA praised for the quality of its hypertension care, a model for success in a new era of reduced blood pressure treatment targets and revised hypertension guidelines that classify millions more Americans as having hypertension.
“In systems of care, like the VA and Kaiser Permanente Northern California, we are doing much better with hypertension control, reaching control rates greater than 90%,” Paul Whelton, MD, said in November during a talk at the American Heart Association scientific sessions in Anaheim, Calif. In a separate report at the same meeting, Dr. Whelton, a professor of public health at Tulane University in New Orleans, first presented the new hypertension diagnosis and management guidelines, produced by the American College of Cardiology/American Heart Association panel that he chaired (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.006).
He again stressed that the VA and Kaiser are doing “remarkably well” when it came to controlling hypertension in the vast majority of their patients.
That assessment seems especially appropriate for Kaiser Permanente Northern California, Oakland, Calif. Data from an audit of Kaiser’s hypertension registry showed that during 2000-2013 the percentage of patients with hypertension at their goal blood pressure rose from 44% in 2000 to 90% in 2013 (J Clin Hypertension. 2016 April;18[4]:260-1). The two Kaiser researchers who reported these findings attributed the rise in control rates to a hypertension treatment program that Kaiser Permanente Northern California put into practice starting in 2000.
Current success in the VA Health System is harder to pin down and put in the Kaiser ballpark. The most up-to-date audit I could find was a 2012 report from a team of VA researchers who reviewed control rates of more than half a million hypertensive veterans at 15 VA medical centers during 2000-2010. They found that, during that 11-year period, the percentage of hypertensive patients with their blood pressure controlled to their target level had risen from 46% in 2000 to 76% in 2010 (Circulation. 2012 May 22;125[20]:2462-68).
While this 76% rate of control in 2010 is short of the 90% rate in Kaiser in 2013, it’s still not shabby. To put the 76% control rate in perspective, consider data reported at the AHA meeting from TargetBP, a national program begun in late 2015 to aid all U.S. health care programs in improving their hypertension control rates: This data showed that, among 310 participating programs that filed 2016 control-rate data with TargetBP, the average control rate was 66%. Specifically, of those 310 reporting programs, 191 (62%) had control rates that exceeded 70%, with an average control rate among these more successful programs of 76%.
As-yet-unpublished data collected by the VA show that other centers in the system beyond those 15 included in the study discussed above have also recently reached a similar control level of about 75%, said Vasilios Papademetriou, MD, a professor of medicine at Georgetown University and the director of the Interventional Hypertension and Vascular Medicine Program at the VA Medical Center in Washington. Plus, certain VA centers are now up to an 85% control rate, he added in an interview. “Blood pressure control rates have been exceptionally good in the VA medical system,” he declared. Dr. Papademetriou attributed the rising control rates to a concerted hypertension program the VA instituted starting in the early 2000s.
“The VA has had some physicians who have championed this issue, and they have built computer-based systems to identify patients with uncontrolled hypertension, and then they plug these patients into their care algorithms,” commented Donald M. Lloyd-Jones, MD, a professor and chairman of preventive medicine at Northwestern University in Chicago. “Often, when there are champions, things change,” he noted.
William C. Cushman, MD, a hypertension specialist who is chief of preventive medicine for the VA Medical Center in Memphis and professor of preventive medicine at the University of Tennessee, also in Memphis, highlighted several steps the VA took that have helped fuel the program’s success in controlling blood pressure.
Dr. Cushman couldn’t resist adding that this successful approach to hypertension management is now threatened by potential changes to the VA system that could take some patients out of the existing program and move them to privatized medical care. “If that happens, patients will not get the same comprehensive care” that until now has produced such high rates of hypertension control, he warned.
[email protected]
On Twitter @mitchelzoler
At a time when the Department of Veterans Affairs is criticized for the care it delivers, and when some also see it threatened by privatization, it was refreshing to hear the VA praised for the quality of its hypertension care, a model for success in a new era of reduced blood pressure treatment targets and revised hypertension guidelines that classify millions more Americans as having hypertension.
“In systems of care, like the VA and Kaiser Permanente Northern California, we are doing much better with hypertension control, reaching control rates greater than 90%,” Paul Whelton, MD, said in November during a talk at the American Heart Association scientific sessions in Anaheim, Calif. In a separate report at the same meeting, Dr. Whelton, a professor of public health at Tulane University in New Orleans, first presented the new hypertension diagnosis and management guidelines, produced by the American College of Cardiology/American Heart Association panel that he chaired (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.006).
He again stressed that the VA and Kaiser are doing “remarkably well” when it came to controlling hypertension in the vast majority of their patients.
That assessment seems especially appropriate for Kaiser Permanente Northern California, Oakland, Calif. Data from an audit of Kaiser’s hypertension registry showed that during 2000-2013 the percentage of patients with hypertension at their goal blood pressure rose from 44% in 2000 to 90% in 2013 (J Clin Hypertension. 2016 April;18[4]:260-1). The two Kaiser researchers who reported these findings attributed the rise in control rates to a hypertension treatment program that Kaiser Permanente Northern California put into practice starting in 2000.
Current success in the VA Health System is harder to pin down and put in the Kaiser ballpark. The most up-to-date audit I could find was a 2012 report from a team of VA researchers who reviewed control rates of more than half a million hypertensive veterans at 15 VA medical centers during 2000-2010. They found that, during that 11-year period, the percentage of hypertensive patients with their blood pressure controlled to their target level had risen from 46% in 2000 to 76% in 2010 (Circulation. 2012 May 22;125[20]:2462-68).
While this 76% rate of control in 2010 is short of the 90% rate in Kaiser in 2013, it’s still not shabby. To put the 76% control rate in perspective, consider data reported at the AHA meeting from TargetBP, a national program begun in late 2015 to aid all U.S. health care programs in improving their hypertension control rates: This data showed that, among 310 participating programs that filed 2016 control-rate data with TargetBP, the average control rate was 66%. Specifically, of those 310 reporting programs, 191 (62%) had control rates that exceeded 70%, with an average control rate among these more successful programs of 76%.
As-yet-unpublished data collected by the VA show that other centers in the system beyond those 15 included in the study discussed above have also recently reached a similar control level of about 75%, said Vasilios Papademetriou, MD, a professor of medicine at Georgetown University and the director of the Interventional Hypertension and Vascular Medicine Program at the VA Medical Center in Washington. Plus, certain VA centers are now up to an 85% control rate, he added in an interview. “Blood pressure control rates have been exceptionally good in the VA medical system,” he declared. Dr. Papademetriou attributed the rising control rates to a concerted hypertension program the VA instituted starting in the early 2000s.
“The VA has had some physicians who have championed this issue, and they have built computer-based systems to identify patients with uncontrolled hypertension, and then they plug these patients into their care algorithms,” commented Donald M. Lloyd-Jones, MD, a professor and chairman of preventive medicine at Northwestern University in Chicago. “Often, when there are champions, things change,” he noted.
William C. Cushman, MD, a hypertension specialist who is chief of preventive medicine for the VA Medical Center in Memphis and professor of preventive medicine at the University of Tennessee, also in Memphis, highlighted several steps the VA took that have helped fuel the program’s success in controlling blood pressure.
Dr. Cushman couldn’t resist adding that this successful approach to hypertension management is now threatened by potential changes to the VA system that could take some patients out of the existing program and move them to privatized medical care. “If that happens, patients will not get the same comprehensive care” that until now has produced such high rates of hypertension control, he warned.
[email protected]
On Twitter @mitchelzoler
At a time when the Department of Veterans Affairs is criticized for the care it delivers, and when some also see it threatened by privatization, it was refreshing to hear the VA praised for the quality of its hypertension care, a model for success in a new era of reduced blood pressure treatment targets and revised hypertension guidelines that classify millions more Americans as having hypertension.
“In systems of care, like the VA and Kaiser Permanente Northern California, we are doing much better with hypertension control, reaching control rates greater than 90%,” Paul Whelton, MD, said in November during a talk at the American Heart Association scientific sessions in Anaheim, Calif. In a separate report at the same meeting, Dr. Whelton, a professor of public health at Tulane University in New Orleans, first presented the new hypertension diagnosis and management guidelines, produced by the American College of Cardiology/American Heart Association panel that he chaired (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.006).
He again stressed that the VA and Kaiser are doing “remarkably well” when it came to controlling hypertension in the vast majority of their patients.
That assessment seems especially appropriate for Kaiser Permanente Northern California, Oakland, Calif. Data from an audit of Kaiser’s hypertension registry showed that during 2000-2013 the percentage of patients with hypertension at their goal blood pressure rose from 44% in 2000 to 90% in 2013 (J Clin Hypertension. 2016 April;18[4]:260-1). The two Kaiser researchers who reported these findings attributed the rise in control rates to a hypertension treatment program that Kaiser Permanente Northern California put into practice starting in 2000.
Current success in the VA Health System is harder to pin down and put in the Kaiser ballpark. The most up-to-date audit I could find was a 2012 report from a team of VA researchers who reviewed control rates of more than half a million hypertensive veterans at 15 VA medical centers during 2000-2010. They found that, during that 11-year period, the percentage of hypertensive patients with their blood pressure controlled to their target level had risen from 46% in 2000 to 76% in 2010 (Circulation. 2012 May 22;125[20]:2462-68).
While this 76% rate of control in 2010 is short of the 90% rate in Kaiser in 2013, it’s still not shabby. To put the 76% control rate in perspective, consider data reported at the AHA meeting from TargetBP, a national program begun in late 2015 to aid all U.S. health care programs in improving their hypertension control rates: This data showed that, among 310 participating programs that filed 2016 control-rate data with TargetBP, the average control rate was 66%. Specifically, of those 310 reporting programs, 191 (62%) had control rates that exceeded 70%, with an average control rate among these more successful programs of 76%.
As-yet-unpublished data collected by the VA show that other centers in the system beyond those 15 included in the study discussed above have also recently reached a similar control level of about 75%, said Vasilios Papademetriou, MD, a professor of medicine at Georgetown University and the director of the Interventional Hypertension and Vascular Medicine Program at the VA Medical Center in Washington. Plus, certain VA centers are now up to an 85% control rate, he added in an interview. “Blood pressure control rates have been exceptionally good in the VA medical system,” he declared. Dr. Papademetriou attributed the rising control rates to a concerted hypertension program the VA instituted starting in the early 2000s.
“The VA has had some physicians who have championed this issue, and they have built computer-based systems to identify patients with uncontrolled hypertension, and then they plug these patients into their care algorithms,” commented Donald M. Lloyd-Jones, MD, a professor and chairman of preventive medicine at Northwestern University in Chicago. “Often, when there are champions, things change,” he noted.
William C. Cushman, MD, a hypertension specialist who is chief of preventive medicine for the VA Medical Center in Memphis and professor of preventive medicine at the University of Tennessee, also in Memphis, highlighted several steps the VA took that have helped fuel the program’s success in controlling blood pressure.
Dr. Cushman couldn’t resist adding that this successful approach to hypertension management is now threatened by potential changes to the VA system that could take some patients out of the existing program and move them to privatized medical care. “If that happens, patients will not get the same comprehensive care” that until now has produced such high rates of hypertension control, he warned.
[email protected]
On Twitter @mitchelzoler
Eating disorders over the holidays
For many, the holiday season is a time to celebrate, relax, and enjoy the company of family. Much of this celebrating centers on eating and food. Historically, eating disorders were associated with young, straight, cisgender, white females. Data collected over the past 15 years suggest that eating disorders can affect youth of all ethnicities and genders.
Below are some tips from the National Eating Disorder Association that may be helpful for youth struggling with an eating disorder over the holiday season:
• Eat regularly and in a consistent pattern. Avoid skipping meals or restricting intake in preparation for a holiday meal.
• Discuss any anticipated struggles around food or family with your parents, therapist, health care provider, dietitian, or other members of your support group. This can allow you to plan ahead for any challenges that may arise, and could prevent potential negative or harmful coping behaviors
• Consider choosing a loved one to be your “reality check” with food, to either help fix a plate for you or to give you sound feedback on the food portion sizes you make for yourself.
• Have a game plan before you go to a holiday event. Know who your support people are and how you’ll recognize when it may be time to make a quick exit and get connected with needed support.
• Avoid overextending yourself. A lower stress level can decrease the need to turn to eating-disordered behaviors or other unhelpful coping strategies.
• Work on being flexible in your thoughts. Learn to be flexible when setting guidelines for yourself and expectations of yourself and others. Strive to be flexible in what you can eat during the holidays. Take a holiday from self-imposed criticism, rigidity, and perfectionism.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at [email protected].
Resources
National Eating Disorders Association: www.nationaleatingdisorders.org
“Body image and eating disorders among lesbian, gay, bisexual, and transgender youth” (Pediatr Clin North Am. 2016 Dec;63[6]:1079-90.
References
1. Prev Chronic Dis. 2008 Oct;5(4):A114.
2. Arch Gen Psychiatry. 2011 Jul;68(7):714-23.
3. Pediatr Clin North Am. 2016 Dec;63(6):1079-90.
4. Curr Psychiatry Rep. 2012 Aug;14(4):391-7.
5. J Adolesc Health. 2015 Aug;57(2):144-9.
6. Am J Public Health. 2013 Feb;103(2):e16-22.
7. J Adolesc Health. 2009 Sep;45(3):238-45.
For many, the holiday season is a time to celebrate, relax, and enjoy the company of family. Much of this celebrating centers on eating and food. Historically, eating disorders were associated with young, straight, cisgender, white females. Data collected over the past 15 years suggest that eating disorders can affect youth of all ethnicities and genders.
Below are some tips from the National Eating Disorder Association that may be helpful for youth struggling with an eating disorder over the holiday season:
• Eat regularly and in a consistent pattern. Avoid skipping meals or restricting intake in preparation for a holiday meal.
• Discuss any anticipated struggles around food or family with your parents, therapist, health care provider, dietitian, or other members of your support group. This can allow you to plan ahead for any challenges that may arise, and could prevent potential negative or harmful coping behaviors
• Consider choosing a loved one to be your “reality check” with food, to either help fix a plate for you or to give you sound feedback on the food portion sizes you make for yourself.
• Have a game plan before you go to a holiday event. Know who your support people are and how you’ll recognize when it may be time to make a quick exit and get connected with needed support.
• Avoid overextending yourself. A lower stress level can decrease the need to turn to eating-disordered behaviors or other unhelpful coping strategies.
• Work on being flexible in your thoughts. Learn to be flexible when setting guidelines for yourself and expectations of yourself and others. Strive to be flexible in what you can eat during the holidays. Take a holiday from self-imposed criticism, rigidity, and perfectionism.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at [email protected].
Resources
National Eating Disorders Association: www.nationaleatingdisorders.org
“Body image and eating disorders among lesbian, gay, bisexual, and transgender youth” (Pediatr Clin North Am. 2016 Dec;63[6]:1079-90.
References
1. Prev Chronic Dis. 2008 Oct;5(4):A114.
2. Arch Gen Psychiatry. 2011 Jul;68(7):714-23.
3. Pediatr Clin North Am. 2016 Dec;63(6):1079-90.
4. Curr Psychiatry Rep. 2012 Aug;14(4):391-7.
5. J Adolesc Health. 2015 Aug;57(2):144-9.
6. Am J Public Health. 2013 Feb;103(2):e16-22.
7. J Adolesc Health. 2009 Sep;45(3):238-45.
For many, the holiday season is a time to celebrate, relax, and enjoy the company of family. Much of this celebrating centers on eating and food. Historically, eating disorders were associated with young, straight, cisgender, white females. Data collected over the past 15 years suggest that eating disorders can affect youth of all ethnicities and genders.
Below are some tips from the National Eating Disorder Association that may be helpful for youth struggling with an eating disorder over the holiday season:
• Eat regularly and in a consistent pattern. Avoid skipping meals or restricting intake in preparation for a holiday meal.
• Discuss any anticipated struggles around food or family with your parents, therapist, health care provider, dietitian, or other members of your support group. This can allow you to plan ahead for any challenges that may arise, and could prevent potential negative or harmful coping behaviors
• Consider choosing a loved one to be your “reality check” with food, to either help fix a plate for you or to give you sound feedback on the food portion sizes you make for yourself.
• Have a game plan before you go to a holiday event. Know who your support people are and how you’ll recognize when it may be time to make a quick exit and get connected with needed support.
• Avoid overextending yourself. A lower stress level can decrease the need to turn to eating-disordered behaviors or other unhelpful coping strategies.
• Work on being flexible in your thoughts. Learn to be flexible when setting guidelines for yourself and expectations of yourself and others. Strive to be flexible in what you can eat during the holidays. Take a holiday from self-imposed criticism, rigidity, and perfectionism.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at [email protected].
Resources
National Eating Disorders Association: www.nationaleatingdisorders.org
“Body image and eating disorders among lesbian, gay, bisexual, and transgender youth” (Pediatr Clin North Am. 2016 Dec;63[6]:1079-90.
References
1. Prev Chronic Dis. 2008 Oct;5(4):A114.
2. Arch Gen Psychiatry. 2011 Jul;68(7):714-23.
3. Pediatr Clin North Am. 2016 Dec;63(6):1079-90.
4. Curr Psychiatry Rep. 2012 Aug;14(4):391-7.
5. J Adolesc Health. 2015 Aug;57(2):144-9.
6. Am J Public Health. 2013 Feb;103(2):e16-22.
7. J Adolesc Health. 2009 Sep;45(3):238-45.
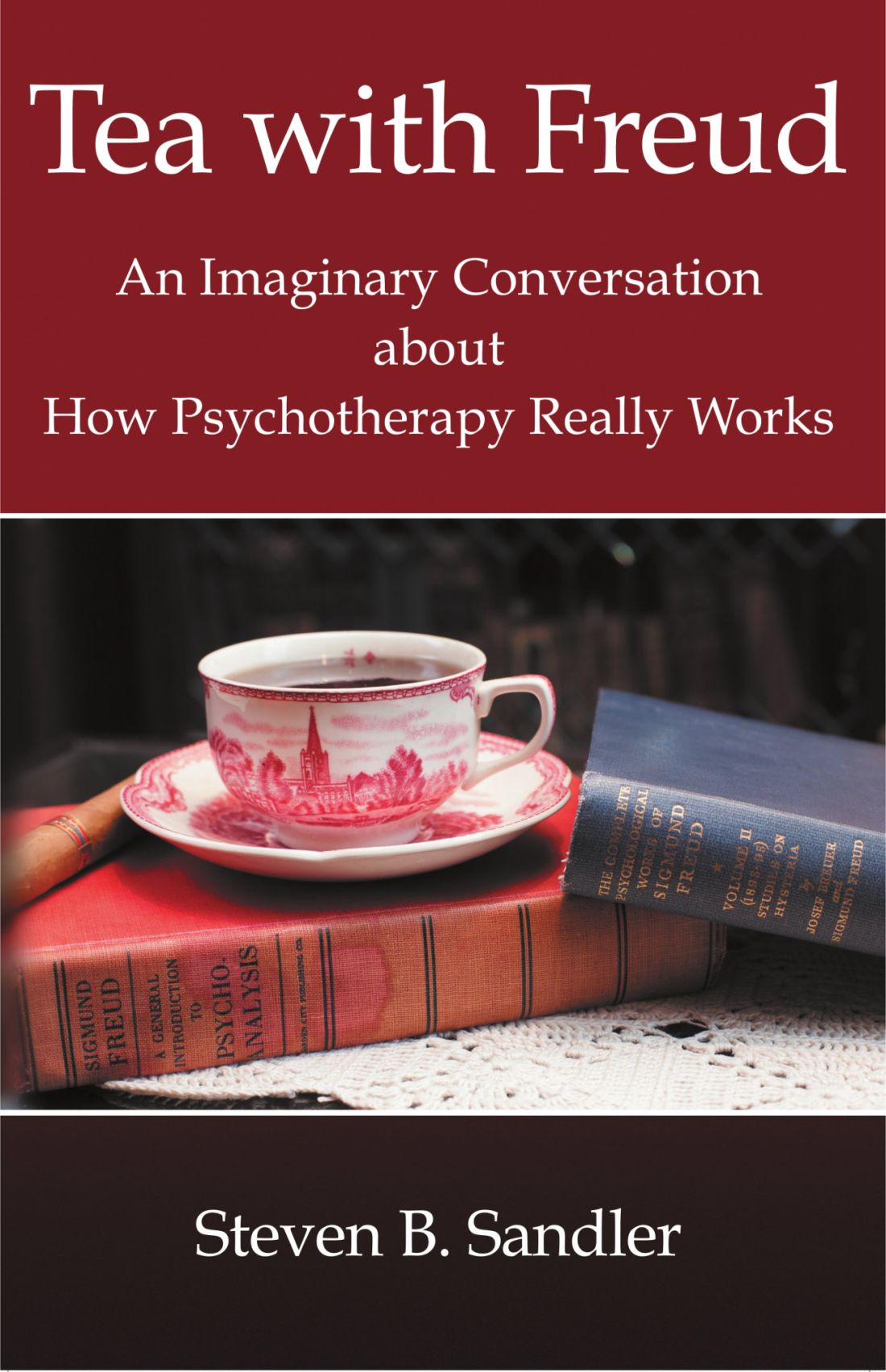
‘Tea with Freud’: Engaging, authentic, but nonanalytic
If I traveled back in time to meet with a 60-year-old Sigmund Freud, the first thing I would say to him is: “Stop smoking, and get out of Austria!”
That was my thought as I read “Tea with Freud: An Imaginary Conversation about How Psychotherapy Really Works” (Dog Ear Publishing, 2016), in which the author, psychiatrist Steven B. Sandler, MD, holds a series of imaginary meetings with Freud to discuss the evolution of psychoanalysis into Sandler’s preferred mode of short-term dynamic psychotherapy (STDP) and to present case material for Freud’s supervision.
The chapters in “Tea with Freud” alternate between the imagined meetings with Freud and Sandler’s clinical work, presented from what I assume are transcripts of videotaped sessions with some disguises and composites to protect patients’ privacy. These clinical vignettes bring the reader into the nitty-gritty of the treatment room, which may be highly instructive for a lay person – particularly one who has never been in therapy.
At the same time, the book has the potential to be quite misleading. This would not be the case if Sandler were simply trying to introduce the reader to STDP. Instead, he attempts to convince the reader, and apparently himself, that the therapy he practices is a modern rendition of psychoanalysis because it tries to access the patient’s unacceptable, unconscious feelings; encourages her to “remember with emotion” or “experience” her feelings; and leads to some sort of cathartic resolution and improvement in symptoms and outlook.
While, “Aha!” moments and cathartic abreaction were characteristic of very early analyses, modern psychoanalysis is about slow but permanent change in character structure. The unwritten message in the book is that Freud’s true heirs practice psychotherapy as Sandler does. He does not seem to consider the significance of the many psychoanalysts, myself included, practicing psychoanalysis today.
Sandler uses a (mercifully) attenuated Davanloo technique to provoke patients into dramatic enactments. He is highly directive, with statements like, “We don’t solve any particular problem if we jump around all over.” I wonder how he can possibly learn about his patients when he begins with a foregone conclusion about where they should be headed.
His treatments are very brief. During his first session with a patient named Carla, he deduces that she is suffering from unresolved anger related to childhood trauma and manifesting it in chronic anxiety with angry outbursts. He then proceeds to “cure” her in five sessions.
Sandler wonders why some of his patients relapse and decides it is because they have not explored their “positive memories” in treatment, as though memories were univalent.
And he talks way too much.
All of this is decidedly un-analytic, which, again, would not matter if he were only trying to demonstrate STDP in action. Nonanalytic psychotherapies are entitled to be nonanalytic. Sandler has Freud point out precisely these analytic errors, so he must be aware that he is making them. And, yet, he stubbornly maintains his position that his work is analytic. What a waste of time travel it would be to meet with Freud only to reinforce one’s own opinions.
“Tea with Freud” is a way for Sandler to promote STDP and his theories about “positive memories” using an established authority, Freud, to validate them. This makes the book disappointing, but fortunately, there is something more to it. I kept wondering why it was so important to the author to seek out Freud’s – that is, his father’s – approval for his work. The book never answers that question. But in his attempts to understand his motives, Sandler, who is very adept at describing his own thoughts and feelings, becomes a model for the awareness of internal states and the effects of unconscious processes. Perhaps this is the most important lesson in “Tea with Freud.”
Dr. Twersky-Kengmana is a psychiatrist and psychoanalyst in private practice in New York.
If I traveled back in time to meet with a 60-year-old Sigmund Freud, the first thing I would say to him is: “Stop smoking, and get out of Austria!”
That was my thought as I read “Tea with Freud: An Imaginary Conversation about How Psychotherapy Really Works” (Dog Ear Publishing, 2016), in which the author, psychiatrist Steven B. Sandler, MD, holds a series of imaginary meetings with Freud to discuss the evolution of psychoanalysis into Sandler’s preferred mode of short-term dynamic psychotherapy (STDP) and to present case material for Freud’s supervision.
The chapters in “Tea with Freud” alternate between the imagined meetings with Freud and Sandler’s clinical work, presented from what I assume are transcripts of videotaped sessions with some disguises and composites to protect patients’ privacy. These clinical vignettes bring the reader into the nitty-gritty of the treatment room, which may be highly instructive for a lay person – particularly one who has never been in therapy.
At the same time, the book has the potential to be quite misleading. This would not be the case if Sandler were simply trying to introduce the reader to STDP. Instead, he attempts to convince the reader, and apparently himself, that the therapy he practices is a modern rendition of psychoanalysis because it tries to access the patient’s unacceptable, unconscious feelings; encourages her to “remember with emotion” or “experience” her feelings; and leads to some sort of cathartic resolution and improvement in symptoms and outlook.
While, “Aha!” moments and cathartic abreaction were characteristic of very early analyses, modern psychoanalysis is about slow but permanent change in character structure. The unwritten message in the book is that Freud’s true heirs practice psychotherapy as Sandler does. He does not seem to consider the significance of the many psychoanalysts, myself included, practicing psychoanalysis today.
Sandler uses a (mercifully) attenuated Davanloo technique to provoke patients into dramatic enactments. He is highly directive, with statements like, “We don’t solve any particular problem if we jump around all over.” I wonder how he can possibly learn about his patients when he begins with a foregone conclusion about where they should be headed.
His treatments are very brief. During his first session with a patient named Carla, he deduces that she is suffering from unresolved anger related to childhood trauma and manifesting it in chronic anxiety with angry outbursts. He then proceeds to “cure” her in five sessions.
Sandler wonders why some of his patients relapse and decides it is because they have not explored their “positive memories” in treatment, as though memories were univalent.
And he talks way too much.
All of this is decidedly un-analytic, which, again, would not matter if he were only trying to demonstrate STDP in action. Nonanalytic psychotherapies are entitled to be nonanalytic. Sandler has Freud point out precisely these analytic errors, so he must be aware that he is making them. And, yet, he stubbornly maintains his position that his work is analytic. What a waste of time travel it would be to meet with Freud only to reinforce one’s own opinions.
“Tea with Freud” is a way for Sandler to promote STDP and his theories about “positive memories” using an established authority, Freud, to validate them. This makes the book disappointing, but fortunately, there is something more to it. I kept wondering why it was so important to the author to seek out Freud’s – that is, his father’s – approval for his work. The book never answers that question. But in his attempts to understand his motives, Sandler, who is very adept at describing his own thoughts and feelings, becomes a model for the awareness of internal states and the effects of unconscious processes. Perhaps this is the most important lesson in “Tea with Freud.”
Dr. Twersky-Kengmana is a psychiatrist and psychoanalyst in private practice in New York.
If I traveled back in time to meet with a 60-year-old Sigmund Freud, the first thing I would say to him is: “Stop smoking, and get out of Austria!”
That was my thought as I read “Tea with Freud: An Imaginary Conversation about How Psychotherapy Really Works” (Dog Ear Publishing, 2016), in which the author, psychiatrist Steven B. Sandler, MD, holds a series of imaginary meetings with Freud to discuss the evolution of psychoanalysis into Sandler’s preferred mode of short-term dynamic psychotherapy (STDP) and to present case material for Freud’s supervision.
The chapters in “Tea with Freud” alternate between the imagined meetings with Freud and Sandler’s clinical work, presented from what I assume are transcripts of videotaped sessions with some disguises and composites to protect patients’ privacy. These clinical vignettes bring the reader into the nitty-gritty of the treatment room, which may be highly instructive for a lay person – particularly one who has never been in therapy.
At the same time, the book has the potential to be quite misleading. This would not be the case if Sandler were simply trying to introduce the reader to STDP. Instead, he attempts to convince the reader, and apparently himself, that the therapy he practices is a modern rendition of psychoanalysis because it tries to access the patient’s unacceptable, unconscious feelings; encourages her to “remember with emotion” or “experience” her feelings; and leads to some sort of cathartic resolution and improvement in symptoms and outlook.
While, “Aha!” moments and cathartic abreaction were characteristic of very early analyses, modern psychoanalysis is about slow but permanent change in character structure. The unwritten message in the book is that Freud’s true heirs practice psychotherapy as Sandler does. He does not seem to consider the significance of the many psychoanalysts, myself included, practicing psychoanalysis today.
Sandler uses a (mercifully) attenuated Davanloo technique to provoke patients into dramatic enactments. He is highly directive, with statements like, “We don’t solve any particular problem if we jump around all over.” I wonder how he can possibly learn about his patients when he begins with a foregone conclusion about where they should be headed.
His treatments are very brief. During his first session with a patient named Carla, he deduces that she is suffering from unresolved anger related to childhood trauma and manifesting it in chronic anxiety with angry outbursts. He then proceeds to “cure” her in five sessions.
Sandler wonders why some of his patients relapse and decides it is because they have not explored their “positive memories” in treatment, as though memories were univalent.
And he talks way too much.
All of this is decidedly un-analytic, which, again, would not matter if he were only trying to demonstrate STDP in action. Nonanalytic psychotherapies are entitled to be nonanalytic. Sandler has Freud point out precisely these analytic errors, so he must be aware that he is making them. And, yet, he stubbornly maintains his position that his work is analytic. What a waste of time travel it would be to meet with Freud only to reinforce one’s own opinions.
“Tea with Freud” is a way for Sandler to promote STDP and his theories about “positive memories” using an established authority, Freud, to validate them. This makes the book disappointing, but fortunately, there is something more to it. I kept wondering why it was so important to the author to seek out Freud’s – that is, his father’s – approval for his work. The book never answers that question. But in his attempts to understand his motives, Sandler, who is very adept at describing his own thoughts and feelings, becomes a model for the awareness of internal states and the effects of unconscious processes. Perhaps this is the most important lesson in “Tea with Freud.”
Dr. Twersky-Kengmana is a psychiatrist and psychoanalyst in private practice in New York.
Luxury drug treatment centers: Close scrutiny advised
About 2.5 million people received mental and/or substance use disorder treatment last year, according to the Substance Abuse and Mental Health Services Administration.1 Of those, a small but significant percentage chose support from a luxury type facility. This article intends to provide clinicians with guidance in addressing medically supervised luxury detox and/or rehabilitation programs for drug and alcohol abuse.
We recommend that individuals entering substance abuse services pursue these treatments with “eyes wide open.” A vast amount of literature indicates a rise in programs designed to attract vulnerable clients seeking treatment.2 They offer an array of luxury services such as equine, massage, and yoga therapy, as well as holistic approaches. These services are all packaged in a five-star hotel–like environment in a desirable area (by the sea, mountains, etc.).
The question is whether a $50,000-per-month treatment center is better at keeping its clients in remission than a facility that charges a fraction of the price per month. We believe that success rates may be less a function of financial cost and more a function of evidenced-based treatment strategies that are specific to recovery.
We would like to advise individuals to look for the following elements when reviewing a potential treatment center:
• Accepted by major insurance companies such as Blue Cross/Blue Shield and United Healthcare, to name a few.
• No cookie-cutter approaches: Programs allowing for inter-individual flexibility regarding length of stay (not specifically 21, 30, or 45 days), as well as flexibility of services.
• Group therapy should have no more than 15 clients. Some individuals may not be appropriate for group therapy or may have a strong aversion to this modality.
• Licensed and/or certified staff (not peer coaching and/or paraprofessionals alone).
• Minimum of 20 hours per week, per client, of clinically supervised evidence-based methods, techniques, and/or practices including individual counseling, group therapies, and family involvement.
• If the length of stay is longer, fewer staff members may be more appropriate.
• Availability of higher level of professional staff, psychologists, psychiatrists, and other physicians to address all comorbid concerns.
• Adequate aftercare treatment.
After reviewing social media that rate treatment facilities, one common thread we noticed was the total absence of aftercare services.3 Aftercare services were something that clients may not think of at the initial intake.
References
1 Substance Abuse and Mental Health Services Administration (SAMHSA). “Behavioral Health Treatments and Services.”
2 The Verge, Sept. 6, 2017
3 Rehabs.com
4. The New York Times, Sept. 14, 2017
Dr. Lesser is executive director of RANE, Medical & Mental Health, in New York City. In his recent positions as medical director for New York City and State, he was instrumental in developing and implementing nationally recognized emergency and response programs. Dr. Brenner is chief of Behavioral Health Service Line for Catholic Health Services of Long Island, in New York. He is a clinical professor of psychiatry for the State University of New York, Brooklyn, and medical director and CEO of Neurobehavioral Research Inc. Dr. Ferber is a licensed psychologist in New York and California. He has been the director of Behavioral Health Central Intake at Catholic Health Services of Long Island for the last 2 years. Dr. Ferber specializes in addiction treatment. Ms. Howard is a psychologist in training with specialization in clinical psychology. She currently treats numerous dual-diagnosed patients with comorbidities on an acute psychiatric ward.
About 2.5 million people received mental and/or substance use disorder treatment last year, according to the Substance Abuse and Mental Health Services Administration.1 Of those, a small but significant percentage chose support from a luxury type facility. This article intends to provide clinicians with guidance in addressing medically supervised luxury detox and/or rehabilitation programs for drug and alcohol abuse.
We recommend that individuals entering substance abuse services pursue these treatments with “eyes wide open.” A vast amount of literature indicates a rise in programs designed to attract vulnerable clients seeking treatment.2 They offer an array of luxury services such as equine, massage, and yoga therapy, as well as holistic approaches. These services are all packaged in a five-star hotel–like environment in a desirable area (by the sea, mountains, etc.).
The question is whether a $50,000-per-month treatment center is better at keeping its clients in remission than a facility that charges a fraction of the price per month. We believe that success rates may be less a function of financial cost and more a function of evidenced-based treatment strategies that are specific to recovery.
We would like to advise individuals to look for the following elements when reviewing a potential treatment center:
• Accepted by major insurance companies such as Blue Cross/Blue Shield and United Healthcare, to name a few.
• No cookie-cutter approaches: Programs allowing for inter-individual flexibility regarding length of stay (not specifically 21, 30, or 45 days), as well as flexibility of services.
• Group therapy should have no more than 15 clients. Some individuals may not be appropriate for group therapy or may have a strong aversion to this modality.
• Licensed and/or certified staff (not peer coaching and/or paraprofessionals alone).
• Minimum of 20 hours per week, per client, of clinically supervised evidence-based methods, techniques, and/or practices including individual counseling, group therapies, and family involvement.
• If the length of stay is longer, fewer staff members may be more appropriate.
• Availability of higher level of professional staff, psychologists, psychiatrists, and other physicians to address all comorbid concerns.
• Adequate aftercare treatment.
After reviewing social media that rate treatment facilities, one common thread we noticed was the total absence of aftercare services.3 Aftercare services were something that clients may not think of at the initial intake.
References
1 Substance Abuse and Mental Health Services Administration (SAMHSA). “Behavioral Health Treatments and Services.”
2 The Verge, Sept. 6, 2017
3 Rehabs.com
4. The New York Times, Sept. 14, 2017
Dr. Lesser is executive director of RANE, Medical & Mental Health, in New York City. In his recent positions as medical director for New York City and State, he was instrumental in developing and implementing nationally recognized emergency and response programs. Dr. Brenner is chief of Behavioral Health Service Line for Catholic Health Services of Long Island, in New York. He is a clinical professor of psychiatry for the State University of New York, Brooklyn, and medical director and CEO of Neurobehavioral Research Inc. Dr. Ferber is a licensed psychologist in New York and California. He has been the director of Behavioral Health Central Intake at Catholic Health Services of Long Island for the last 2 years. Dr. Ferber specializes in addiction treatment. Ms. Howard is a psychologist in training with specialization in clinical psychology. She currently treats numerous dual-diagnosed patients with comorbidities on an acute psychiatric ward.
About 2.5 million people received mental and/or substance use disorder treatment last year, according to the Substance Abuse and Mental Health Services Administration.1 Of those, a small but significant percentage chose support from a luxury type facility. This article intends to provide clinicians with guidance in addressing medically supervised luxury detox and/or rehabilitation programs for drug and alcohol abuse.
We recommend that individuals entering substance abuse services pursue these treatments with “eyes wide open.” A vast amount of literature indicates a rise in programs designed to attract vulnerable clients seeking treatment.2 They offer an array of luxury services such as equine, massage, and yoga therapy, as well as holistic approaches. These services are all packaged in a five-star hotel–like environment in a desirable area (by the sea, mountains, etc.).
The question is whether a $50,000-per-month treatment center is better at keeping its clients in remission than a facility that charges a fraction of the price per month. We believe that success rates may be less a function of financial cost and more a function of evidenced-based treatment strategies that are specific to recovery.
We would like to advise individuals to look for the following elements when reviewing a potential treatment center:
• Accepted by major insurance companies such as Blue Cross/Blue Shield and United Healthcare, to name a few.
• No cookie-cutter approaches: Programs allowing for inter-individual flexibility regarding length of stay (not specifically 21, 30, or 45 days), as well as flexibility of services.
• Group therapy should have no more than 15 clients. Some individuals may not be appropriate for group therapy or may have a strong aversion to this modality.
• Licensed and/or certified staff (not peer coaching and/or paraprofessionals alone).
• Minimum of 20 hours per week, per client, of clinically supervised evidence-based methods, techniques, and/or practices including individual counseling, group therapies, and family involvement.
• If the length of stay is longer, fewer staff members may be more appropriate.
• Availability of higher level of professional staff, psychologists, psychiatrists, and other physicians to address all comorbid concerns.
• Adequate aftercare treatment.
After reviewing social media that rate treatment facilities, one common thread we noticed was the total absence of aftercare services.3 Aftercare services were something that clients may not think of at the initial intake.
References
1 Substance Abuse and Mental Health Services Administration (SAMHSA). “Behavioral Health Treatments and Services.”
2 The Verge, Sept. 6, 2017
3 Rehabs.com
4. The New York Times, Sept. 14, 2017
Dr. Lesser is executive director of RANE, Medical & Mental Health, in New York City. In his recent positions as medical director for New York City and State, he was instrumental in developing and implementing nationally recognized emergency and response programs. Dr. Brenner is chief of Behavioral Health Service Line for Catholic Health Services of Long Island, in New York. He is a clinical professor of psychiatry for the State University of New York, Brooklyn, and medical director and CEO of Neurobehavioral Research Inc. Dr. Ferber is a licensed psychologist in New York and California. He has been the director of Behavioral Health Central Intake at Catholic Health Services of Long Island for the last 2 years. Dr. Ferber specializes in addiction treatment. Ms. Howard is a psychologist in training with specialization in clinical psychology. She currently treats numerous dual-diagnosed patients with comorbidities on an acute psychiatric ward.
Confluent and reticulated papillomatosis
Confluent and reticulated papillomatosis of Gougerot and Carteaud, also known as Gougerot-Carteaud syndrome, is an uncommon skin disorder of young individuals characterized by hyperkeratotic or verrucous brown papules or plaques that coalesce centrally and by a reticulated pattern peripherally. It was first described by two French dermatologists, Gougerot and Carteaud, in 1927.1 Initially, the distinct entity of CARP was contested, with some dermatologists believing it to be a variant of acanthosis nigricans. However, CARP is now recognized as a distinct, though rare, dermatosis.
Histopathology reveals findings similar to those that may be found in acanthosis nigricans and epidermal nevi. Classic characteristics of CARP include hyperkeratosis, papillomatosis, increased basal melanin pigmentation, and mild acanthosis. Occasionally, there may be perivascular lymphocytic infiltrates in the superficial dermis.3,4
The etiology of CARP is unknown. CARP’s resolution in response to antibiotics and the isolation of two bacterial actinomycetes, Rhodococcus and Dietzia papillomatosis, from skin scrapings of CARP patients have led some to believe that its etiology is bacterial. However, no bacterial species have been consistently isolated from CARP patients. The prevailing theory of the past was that CARP was an abnormal host response to the fungus Malassezia furfur. Inconsistent detection of the fungus in skin scrapings, as well as persistence of the skin lesions after fungal clearance with antifungal therapy, has debunked this theory. An underlying disorder of keratinization resulting in hyperproliferation also has been suggested given reports of familial CARP and electron microscopy studies demonstrating focal-enhanced expression of keratin-16 in the stratum granulosom.5 Other theories include a cutaneous response to underlying endocrinopathies, ultraviolet light, and localized amyloidosis.1
Diagnosis and differential
CARP is poorly recognized by clinicians and frequently initially misdiagnosed due to its similar appearance to other disorders, most commonly tinea versicolor and acanthosis nigricans. Davis et al. proposed criteria for diagnosis of CARP requiring 1) presence of scaly, reticulated and papillomatous brown macules and patches; 2) distribution over the upper trunk and neck; 3) negative fungal staining of scales; 4) no improvement following antifungal treatment; and 5) improvement following minocycline.2
Tinea versicolor may appear similar to CARP, but unlike CARP, will respond to antifungal treatment and may demonstrate hyphae and yeast on KOH preparation. Acanthosis nigricans and CARP both may present with velvety, hyperpigmented plaques in individuals of obese habitus or with insulin resistance, but peripheral reticulation will be absent in acanthosis nigricans. However, acanthosis nigricans and CARP may coexist, and this coexistence is not uncommonly seen in individuals with obesity and/or insulin resistance. Darier’s disease may look similar to cases of CARP without pigmentary change, but it often will have accompanying nail changes. Macular or lichen amyloidosis may present with pruritic brown macules or papules, but skin biopsy will have positive amyloid staining. The use of 70% alcohol swabbing to diagnose terra firma-forme dermatosis, with lesions disappearing with swabbing, is classic and used to differentiate it from CARP. Other conditions to consider include seborrheic dermatitis, epidermal nevi, verruca plana, epidermodysplasia verruciformis, and acne vulgaris.1,2,4
Treatment
Minocycline is the first-line treatment for CARP: 80% of patients may have complete resolution with minocycline, while the remainder experience at least 50% clearance of skin lesions.2 However, recurrence after stopping minocycline treatment is not uncommon. The mechanism by which minocycline works is unknown. Second-line treatment for those who cannot tolerate minocycline are macrolide antibiotics.6 Other treatment options with reported success include oral isotretinoin and topical retinoids, including tretinoin gel and tazarotene cream.3,7 Appropriate strength topical corticosteroids may be used for pruritus.
Ms. Han is a medical student at the University of California, San Diego. Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego, as well as the vice chair of the department of dermatology and a professor of dermatology and pediatrics at UC San Diego. They report having no conflicts of interest or financial disclosures. Email them at [email protected].
References
1. Clin Cosmet Investig Dermatol. 2016 Aug 25;9:217-23.
2. Br J Dermatol. 2006 Feb;154(2):287-93.
3. Arch Dermatol. 2012 Apr;148(4):505-8.
4. J Am Acad Dermatol. 2003 Dec;49(6):1182-4.
5. Arch Dermatol. 2002 Feb;138(2):276-7.
6. J Am Acad Dermatol. 2001;44(4):652-5.
7. Am J Clin Dermatol. 2006;7(5):305-13.
Confluent and reticulated papillomatosis of Gougerot and Carteaud, also known as Gougerot-Carteaud syndrome, is an uncommon skin disorder of young individuals characterized by hyperkeratotic or verrucous brown papules or plaques that coalesce centrally and by a reticulated pattern peripherally. It was first described by two French dermatologists, Gougerot and Carteaud, in 1927.1 Initially, the distinct entity of CARP was contested, with some dermatologists believing it to be a variant of acanthosis nigricans. However, CARP is now recognized as a distinct, though rare, dermatosis.
Histopathology reveals findings similar to those that may be found in acanthosis nigricans and epidermal nevi. Classic characteristics of CARP include hyperkeratosis, papillomatosis, increased basal melanin pigmentation, and mild acanthosis. Occasionally, there may be perivascular lymphocytic infiltrates in the superficial dermis.3,4
The etiology of CARP is unknown. CARP’s resolution in response to antibiotics and the isolation of two bacterial actinomycetes, Rhodococcus and Dietzia papillomatosis, from skin scrapings of CARP patients have led some to believe that its etiology is bacterial. However, no bacterial species have been consistently isolated from CARP patients. The prevailing theory of the past was that CARP was an abnormal host response to the fungus Malassezia furfur. Inconsistent detection of the fungus in skin scrapings, as well as persistence of the skin lesions after fungal clearance with antifungal therapy, has debunked this theory. An underlying disorder of keratinization resulting in hyperproliferation also has been suggested given reports of familial CARP and electron microscopy studies demonstrating focal-enhanced expression of keratin-16 in the stratum granulosom.5 Other theories include a cutaneous response to underlying endocrinopathies, ultraviolet light, and localized amyloidosis.1
Diagnosis and differential
CARP is poorly recognized by clinicians and frequently initially misdiagnosed due to its similar appearance to other disorders, most commonly tinea versicolor and acanthosis nigricans. Davis et al. proposed criteria for diagnosis of CARP requiring 1) presence of scaly, reticulated and papillomatous brown macules and patches; 2) distribution over the upper trunk and neck; 3) negative fungal staining of scales; 4) no improvement following antifungal treatment; and 5) improvement following minocycline.2
Tinea versicolor may appear similar to CARP, but unlike CARP, will respond to antifungal treatment and may demonstrate hyphae and yeast on KOH preparation. Acanthosis nigricans and CARP both may present with velvety, hyperpigmented plaques in individuals of obese habitus or with insulin resistance, but peripheral reticulation will be absent in acanthosis nigricans. However, acanthosis nigricans and CARP may coexist, and this coexistence is not uncommonly seen in individuals with obesity and/or insulin resistance. Darier’s disease may look similar to cases of CARP without pigmentary change, but it often will have accompanying nail changes. Macular or lichen amyloidosis may present with pruritic brown macules or papules, but skin biopsy will have positive amyloid staining. The use of 70% alcohol swabbing to diagnose terra firma-forme dermatosis, with lesions disappearing with swabbing, is classic and used to differentiate it from CARP. Other conditions to consider include seborrheic dermatitis, epidermal nevi, verruca plana, epidermodysplasia verruciformis, and acne vulgaris.1,2,4
Treatment
Minocycline is the first-line treatment for CARP: 80% of patients may have complete resolution with minocycline, while the remainder experience at least 50% clearance of skin lesions.2 However, recurrence after stopping minocycline treatment is not uncommon. The mechanism by which minocycline works is unknown. Second-line treatment for those who cannot tolerate minocycline are macrolide antibiotics.6 Other treatment options with reported success include oral isotretinoin and topical retinoids, including tretinoin gel and tazarotene cream.3,7 Appropriate strength topical corticosteroids may be used for pruritus.
Ms. Han is a medical student at the University of California, San Diego. Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego, as well as the vice chair of the department of dermatology and a professor of dermatology and pediatrics at UC San Diego. They report having no conflicts of interest or financial disclosures. Email them at [email protected].
References
1. Clin Cosmet Investig Dermatol. 2016 Aug 25;9:217-23.
2. Br J Dermatol. 2006 Feb;154(2):287-93.
3. Arch Dermatol. 2012 Apr;148(4):505-8.
4. J Am Acad Dermatol. 2003 Dec;49(6):1182-4.
5. Arch Dermatol. 2002 Feb;138(2):276-7.
6. J Am Acad Dermatol. 2001;44(4):652-5.
7. Am J Clin Dermatol. 2006;7(5):305-13.
Confluent and reticulated papillomatosis of Gougerot and Carteaud, also known as Gougerot-Carteaud syndrome, is an uncommon skin disorder of young individuals characterized by hyperkeratotic or verrucous brown papules or plaques that coalesce centrally and by a reticulated pattern peripherally. It was first described by two French dermatologists, Gougerot and Carteaud, in 1927.1 Initially, the distinct entity of CARP was contested, with some dermatologists believing it to be a variant of acanthosis nigricans. However, CARP is now recognized as a distinct, though rare, dermatosis.
Histopathology reveals findings similar to those that may be found in acanthosis nigricans and epidermal nevi. Classic characteristics of CARP include hyperkeratosis, papillomatosis, increased basal melanin pigmentation, and mild acanthosis. Occasionally, there may be perivascular lymphocytic infiltrates in the superficial dermis.3,4
The etiology of CARP is unknown. CARP’s resolution in response to antibiotics and the isolation of two bacterial actinomycetes, Rhodococcus and Dietzia papillomatosis, from skin scrapings of CARP patients have led some to believe that its etiology is bacterial. However, no bacterial species have been consistently isolated from CARP patients. The prevailing theory of the past was that CARP was an abnormal host response to the fungus Malassezia furfur. Inconsistent detection of the fungus in skin scrapings, as well as persistence of the skin lesions after fungal clearance with antifungal therapy, has debunked this theory. An underlying disorder of keratinization resulting in hyperproliferation also has been suggested given reports of familial CARP and electron microscopy studies demonstrating focal-enhanced expression of keratin-16 in the stratum granulosom.5 Other theories include a cutaneous response to underlying endocrinopathies, ultraviolet light, and localized amyloidosis.1
Diagnosis and differential
CARP is poorly recognized by clinicians and frequently initially misdiagnosed due to its similar appearance to other disorders, most commonly tinea versicolor and acanthosis nigricans. Davis et al. proposed criteria for diagnosis of CARP requiring 1) presence of scaly, reticulated and papillomatous brown macules and patches; 2) distribution over the upper trunk and neck; 3) negative fungal staining of scales; 4) no improvement following antifungal treatment; and 5) improvement following minocycline.2
Tinea versicolor may appear similar to CARP, but unlike CARP, will respond to antifungal treatment and may demonstrate hyphae and yeast on KOH preparation. Acanthosis nigricans and CARP both may present with velvety, hyperpigmented plaques in individuals of obese habitus or with insulin resistance, but peripheral reticulation will be absent in acanthosis nigricans. However, acanthosis nigricans and CARP may coexist, and this coexistence is not uncommonly seen in individuals with obesity and/or insulin resistance. Darier’s disease may look similar to cases of CARP without pigmentary change, but it often will have accompanying nail changes. Macular or lichen amyloidosis may present with pruritic brown macules or papules, but skin biopsy will have positive amyloid staining. The use of 70% alcohol swabbing to diagnose terra firma-forme dermatosis, with lesions disappearing with swabbing, is classic and used to differentiate it from CARP. Other conditions to consider include seborrheic dermatitis, epidermal nevi, verruca plana, epidermodysplasia verruciformis, and acne vulgaris.1,2,4
Treatment
Minocycline is the first-line treatment for CARP: 80% of patients may have complete resolution with minocycline, while the remainder experience at least 50% clearance of skin lesions.2 However, recurrence after stopping minocycline treatment is not uncommon. The mechanism by which minocycline works is unknown. Second-line treatment for those who cannot tolerate minocycline are macrolide antibiotics.6 Other treatment options with reported success include oral isotretinoin and topical retinoids, including tretinoin gel and tazarotene cream.3,7 Appropriate strength topical corticosteroids may be used for pruritus.
Ms. Han is a medical student at the University of California, San Diego. Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego, as well as the vice chair of the department of dermatology and a professor of dermatology and pediatrics at UC San Diego. They report having no conflicts of interest or financial disclosures. Email them at [email protected].
References
1. Clin Cosmet Investig Dermatol. 2016 Aug 25;9:217-23.
2. Br J Dermatol. 2006 Feb;154(2):287-93.
3. Arch Dermatol. 2012 Apr;148(4):505-8.
4. J Am Acad Dermatol. 2003 Dec;49(6):1182-4.
5. Arch Dermatol. 2002 Feb;138(2):276-7.
6. J Am Acad Dermatol. 2001;44(4):652-5.
7. Am J Clin Dermatol. 2006;7(5):305-13.
A 17-year-old male presents to the dermatology clinic for brown lesions on his central chest and back that have been present for about a year. The brown areas gradually have become scaly over time. They are asymptomatic. His pediatrician had given him hydrocortisone ointment to apply to the lesions, but there was no improvement. Review of systems was otherwise negative.