User login
Antibiotic prophylaxis for artificial joints
A 66-year-old woman 3 years status post hip replacement is seen for dental work. The dentist contacts the clinic for an antibiotic prescription. The patient has a penicillin allergy (rash). What do you recommend?
A. Clindamycin one dose before dental work.
B. Amoxicillin one dose before dental work.
C. Amoxicillin one dose before, one dose 4 hours after dental work.
D. Clindamycin one dose before dental work, one dose 4 hours after dental work.
E. No antibiotics.
Many patients with prosthetic joints will request antibiotics to take prior to dental procedures. Sometimes this request comes from the dental office.
When I ask patients why they feel they need antibiotics, they often reply that they were told by their orthopedic surgeons or their dentist that they would need to take antibiotics before dental procedures.
In an era when Clostridium difficile infection is a common and dangerous complication in the elderly, avoidance of unnecessary antibiotics is critical. In the United States, it is estimated that there are 240,000 patients infected with C. difficile annually, with 24,000 deaths at a cost of $6 billion.1
Is there compelling evidence to justify giving antibiotic prophylaxis for dental procedures to patients with prosthetic joints?
This information has called into question the wisdom of giving antibiotic prophylaxis for dental procedures when the same patients have transient bacteremias as a regular part of day-to-day life, and mouth organisms were infrequent causes of prosthetic joint infections.
The American Academy of Orthopaedic Surgeons (AAOS) and the American Dental Association (ADA) released an advisory statement 20 years ago on antibiotic prophylaxis for patients with dental replacements, which concluded: “Antibiotic prophylaxis is not indicated for dental patients with pins, plates, and screws, nor is it routinely indicated for most dental patients with total joint replacements.”4
In 2003, the AAOS and the ADA released updated guidelines that stated: “Presently, no scientific evidence supports the position that antibiotic prophylaxis to prevent hematogenous infections is required prior to dental treatment in patients with total joint prostheses. The risk/benefit and cost/effectiveness ratios fail to justify the administration of routine antibiotics.”5
Great confusion arose in 2009 when the AAOS published a position paper on its website that reversed this position.6 Interestingly, the statement was done by the AAOS alone, and not done in conjunction with the ADA.
In this position paper, the AAOS recommended that health care providers consider antibiotic prophylaxis prior to invasive procedures on all patients who had prosthetic joints, regardless of how long those joints have been in place. This major change in recommendations was not based on any new evidence that had been reviewed since the 2003 guidelines.
There are two studies that address outcome of patients with prosthetic joints who have and have not received prophylactic antibiotics.
Elie Berbari, MD, and colleagues reported on the results of a prospective case-control study comparing patients with prosthetic joints hospitalized with hip or knee infections with patients who had prosthetic joints hospitalized at the same time who did not have hip or knee infections.7
There was no increased risk of prosthetic hip or knee infection for patients undergoing a dental procedure who were not receiving antibiotic prophylaxis (odds ratio, 0.8; 95% confidence interval, 0.4-1.6), compared with the risk for patients not undergoing a dental procedure (OR, 0.6; 95% CI, 0.4-1.1). Antibiotic prophylaxis in patients undergoing high and low risk dental procedures did not decrease the risk of prosthetic joint infections.
In 2012, the AAOS and the ADA published updated guidelines with the following summary recommendation: “The practitioner might consider discontinuing the practice of routinely prescribing prophylactic antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures.”8 They referenced the Berbari study as the best available evidence.
Feng-Chen Kao, MD, and colleagues published a study this year with a design very similar to the Berbari study, with similar results.9 All Taiwanese residents who had received hip or knee replacements over a 12-year period were screened. Those who had received dental procedures were matched with individuals who had not had dental procedures. The dental procedure group was subdivided into a group that received antibiotics and one that didn’t.
There was no difference in infection rates between the group that had received dental procedures and the group that did not, and no difference in infection rates between those who received prophylactic antibiotics and those who didn’t.
I think this myth can be put to rest. There is no evidence to give patients with joint prostheses prophylactic antibiotics before dental procedures.
References
1. Steckelberg J.M., Osmon D.R. Prosthetic joint infections. In: Bisno A.L., Waldvogel F.A., eds. Infections associated with indwelling medical devices. Third ed., Washington, D.C.: American Society of Microbiology Press, 2000:173-209.
2. J Dent Res. 2004 Feb;83(2):170-4.
3. J Clin Periodontol. 2006 Feb;33(6):401-7.
4. J Am Dent Assoc. 1997 Jul;128(7):1004-8.
5. J Am Dent Assoc. 2003 Jul;134(7):895-9.
6. Spec Care Dentist. 2009 Nov-Dec;29(6):229-31.
7. Clin Infect Dis. 2010 Jan 1;50(1):8-16.
8. J Dent (Shiraz). 2013 Mar;14(1):49-52.
9. Infect Control Hosp Epidemiol. 2017 Feb;38(2):154-61.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 66-year-old woman 3 years status post hip replacement is seen for dental work. The dentist contacts the clinic for an antibiotic prescription. The patient has a penicillin allergy (rash). What do you recommend?
A. Clindamycin one dose before dental work.
B. Amoxicillin one dose before dental work.
C. Amoxicillin one dose before, one dose 4 hours after dental work.
D. Clindamycin one dose before dental work, one dose 4 hours after dental work.
E. No antibiotics.
Many patients with prosthetic joints will request antibiotics to take prior to dental procedures. Sometimes this request comes from the dental office.
When I ask patients why they feel they need antibiotics, they often reply that they were told by their orthopedic surgeons or their dentist that they would need to take antibiotics before dental procedures.
In an era when Clostridium difficile infection is a common and dangerous complication in the elderly, avoidance of unnecessary antibiotics is critical. In the United States, it is estimated that there are 240,000 patients infected with C. difficile annually, with 24,000 deaths at a cost of $6 billion.1
Is there compelling evidence to justify giving antibiotic prophylaxis for dental procedures to patients with prosthetic joints?
This information has called into question the wisdom of giving antibiotic prophylaxis for dental procedures when the same patients have transient bacteremias as a regular part of day-to-day life, and mouth organisms were infrequent causes of prosthetic joint infections.
The American Academy of Orthopaedic Surgeons (AAOS) and the American Dental Association (ADA) released an advisory statement 20 years ago on antibiotic prophylaxis for patients with dental replacements, which concluded: “Antibiotic prophylaxis is not indicated for dental patients with pins, plates, and screws, nor is it routinely indicated for most dental patients with total joint replacements.”4
In 2003, the AAOS and the ADA released updated guidelines that stated: “Presently, no scientific evidence supports the position that antibiotic prophylaxis to prevent hematogenous infections is required prior to dental treatment in patients with total joint prostheses. The risk/benefit and cost/effectiveness ratios fail to justify the administration of routine antibiotics.”5
Great confusion arose in 2009 when the AAOS published a position paper on its website that reversed this position.6 Interestingly, the statement was done by the AAOS alone, and not done in conjunction with the ADA.
In this position paper, the AAOS recommended that health care providers consider antibiotic prophylaxis prior to invasive procedures on all patients who had prosthetic joints, regardless of how long those joints have been in place. This major change in recommendations was not based on any new evidence that had been reviewed since the 2003 guidelines.
There are two studies that address outcome of patients with prosthetic joints who have and have not received prophylactic antibiotics.
Elie Berbari, MD, and colleagues reported on the results of a prospective case-control study comparing patients with prosthetic joints hospitalized with hip or knee infections with patients who had prosthetic joints hospitalized at the same time who did not have hip or knee infections.7
There was no increased risk of prosthetic hip or knee infection for patients undergoing a dental procedure who were not receiving antibiotic prophylaxis (odds ratio, 0.8; 95% confidence interval, 0.4-1.6), compared with the risk for patients not undergoing a dental procedure (OR, 0.6; 95% CI, 0.4-1.1). Antibiotic prophylaxis in patients undergoing high and low risk dental procedures did not decrease the risk of prosthetic joint infections.
In 2012, the AAOS and the ADA published updated guidelines with the following summary recommendation: “The practitioner might consider discontinuing the practice of routinely prescribing prophylactic antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures.”8 They referenced the Berbari study as the best available evidence.
Feng-Chen Kao, MD, and colleagues published a study this year with a design very similar to the Berbari study, with similar results.9 All Taiwanese residents who had received hip or knee replacements over a 12-year period were screened. Those who had received dental procedures were matched with individuals who had not had dental procedures. The dental procedure group was subdivided into a group that received antibiotics and one that didn’t.
There was no difference in infection rates between the group that had received dental procedures and the group that did not, and no difference in infection rates between those who received prophylactic antibiotics and those who didn’t.
I think this myth can be put to rest. There is no evidence to give patients with joint prostheses prophylactic antibiotics before dental procedures.
References
1. Steckelberg J.M., Osmon D.R. Prosthetic joint infections. In: Bisno A.L., Waldvogel F.A., eds. Infections associated with indwelling medical devices. Third ed., Washington, D.C.: American Society of Microbiology Press, 2000:173-209.
2. J Dent Res. 2004 Feb;83(2):170-4.
3. J Clin Periodontol. 2006 Feb;33(6):401-7.
4. J Am Dent Assoc. 1997 Jul;128(7):1004-8.
5. J Am Dent Assoc. 2003 Jul;134(7):895-9.
6. Spec Care Dentist. 2009 Nov-Dec;29(6):229-31.
7. Clin Infect Dis. 2010 Jan 1;50(1):8-16.
8. J Dent (Shiraz). 2013 Mar;14(1):49-52.
9. Infect Control Hosp Epidemiol. 2017 Feb;38(2):154-61.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 66-year-old woman 3 years status post hip replacement is seen for dental work. The dentist contacts the clinic for an antibiotic prescription. The patient has a penicillin allergy (rash). What do you recommend?
A. Clindamycin one dose before dental work.
B. Amoxicillin one dose before dental work.
C. Amoxicillin one dose before, one dose 4 hours after dental work.
D. Clindamycin one dose before dental work, one dose 4 hours after dental work.
E. No antibiotics.
Many patients with prosthetic joints will request antibiotics to take prior to dental procedures. Sometimes this request comes from the dental office.
When I ask patients why they feel they need antibiotics, they often reply that they were told by their orthopedic surgeons or their dentist that they would need to take antibiotics before dental procedures.
In an era when Clostridium difficile infection is a common and dangerous complication in the elderly, avoidance of unnecessary antibiotics is critical. In the United States, it is estimated that there are 240,000 patients infected with C. difficile annually, with 24,000 deaths at a cost of $6 billion.1
Is there compelling evidence to justify giving antibiotic prophylaxis for dental procedures to patients with prosthetic joints?
This information has called into question the wisdom of giving antibiotic prophylaxis for dental procedures when the same patients have transient bacteremias as a regular part of day-to-day life, and mouth organisms were infrequent causes of prosthetic joint infections.
The American Academy of Orthopaedic Surgeons (AAOS) and the American Dental Association (ADA) released an advisory statement 20 years ago on antibiotic prophylaxis for patients with dental replacements, which concluded: “Antibiotic prophylaxis is not indicated for dental patients with pins, plates, and screws, nor is it routinely indicated for most dental patients with total joint replacements.”4
In 2003, the AAOS and the ADA released updated guidelines that stated: “Presently, no scientific evidence supports the position that antibiotic prophylaxis to prevent hematogenous infections is required prior to dental treatment in patients with total joint prostheses. The risk/benefit and cost/effectiveness ratios fail to justify the administration of routine antibiotics.”5
Great confusion arose in 2009 when the AAOS published a position paper on its website that reversed this position.6 Interestingly, the statement was done by the AAOS alone, and not done in conjunction with the ADA.
In this position paper, the AAOS recommended that health care providers consider antibiotic prophylaxis prior to invasive procedures on all patients who had prosthetic joints, regardless of how long those joints have been in place. This major change in recommendations was not based on any new evidence that had been reviewed since the 2003 guidelines.
There are two studies that address outcome of patients with prosthetic joints who have and have not received prophylactic antibiotics.
Elie Berbari, MD, and colleagues reported on the results of a prospective case-control study comparing patients with prosthetic joints hospitalized with hip or knee infections with patients who had prosthetic joints hospitalized at the same time who did not have hip or knee infections.7
There was no increased risk of prosthetic hip or knee infection for patients undergoing a dental procedure who were not receiving antibiotic prophylaxis (odds ratio, 0.8; 95% confidence interval, 0.4-1.6), compared with the risk for patients not undergoing a dental procedure (OR, 0.6; 95% CI, 0.4-1.1). Antibiotic prophylaxis in patients undergoing high and low risk dental procedures did not decrease the risk of prosthetic joint infections.
In 2012, the AAOS and the ADA published updated guidelines with the following summary recommendation: “The practitioner might consider discontinuing the practice of routinely prescribing prophylactic antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures.”8 They referenced the Berbari study as the best available evidence.
Feng-Chen Kao, MD, and colleagues published a study this year with a design very similar to the Berbari study, with similar results.9 All Taiwanese residents who had received hip or knee replacements over a 12-year period were screened. Those who had received dental procedures were matched with individuals who had not had dental procedures. The dental procedure group was subdivided into a group that received antibiotics and one that didn’t.
There was no difference in infection rates between the group that had received dental procedures and the group that did not, and no difference in infection rates between those who received prophylactic antibiotics and those who didn’t.
I think this myth can be put to rest. There is no evidence to give patients with joint prostheses prophylactic antibiotics before dental procedures.
References
1. Steckelberg J.M., Osmon D.R. Prosthetic joint infections. In: Bisno A.L., Waldvogel F.A., eds. Infections associated with indwelling medical devices. Third ed., Washington, D.C.: American Society of Microbiology Press, 2000:173-209.
2. J Dent Res. 2004 Feb;83(2):170-4.
3. J Clin Periodontol. 2006 Feb;33(6):401-7.
4. J Am Dent Assoc. 1997 Jul;128(7):1004-8.
5. J Am Dent Assoc. 2003 Jul;134(7):895-9.
6. Spec Care Dentist. 2009 Nov-Dec;29(6):229-31.
7. Clin Infect Dis. 2010 Jan 1;50(1):8-16.
8. J Dent (Shiraz). 2013 Mar;14(1):49-52.
9. Infect Control Hosp Epidemiol. 2017 Feb;38(2):154-61.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Adverse childhood experiences
Adverse childhood experiences (ACEs) are the traumatic experiences in a person’s life occurring before the age of 18 years that the person remembers as an adult and that have consequences on a diverse set of outcomes. ACEs include physical abuse, sexual abuse, emotional abuse, mental illness of a household member, problematic drinking or alcoholism of a household member, illegal street or prescription drug use by a household member, divorce or separation of a parent, domestic violence toward a parent, and incarceration of a household member. Each of these experiences before the age of 18 years increases the likelihood of not only adulthood depression, suicide, and substance use disorders, but also a range of nonpsychiatric outcomes such as heart disease and chronic lung disease.
Case summary
Ellie is a 16-year-old girl with a past history of ADHD and oppositionality who arrives on her own in a walk-in clinic to be seen for a sports physical. Ellie has been generally healthy and was previously on a stable medical regimen of methylphenidate but has not been taking it for about 1 year. The oppositionality that she previously experienced in her early school-age years has slowly decreased. She generally does well in school and is in several clubs. In the course of the history, Ellie reveals that her mother’s depression has been worse lately to the point where her mother has resumed her drinking and illegal opiate use. You discuss safety with Ellie, and she reveals that, while she has never been threatened or injured, there has been domestic violence in the home that Ellie felt responsible to try to stop by calling the police. This led to the one and only time that Ellie was physically struck. Her father is now incarcerated, and Ellie feels guilty. After a discussion with Ellie, you report this situation to social services, who already has the case on file. Ellie’s mental status exam, including a thorough examination of symptoms of mood disorders, anxiety, substance use, and PTSD, is within normal limits.
Case discussion
Ellie has suffered a set of ACEs. Specifically, her mother has a mental illness, has a drinking problem, and uses illegal drugs; Ellie has witnessed domestic violence toward her mother, has a family member who is incarcerated, and has suffered from physical abuse. This ACEs score of 6 puts her at markedly increased risk for multiple psychiatric and nonpsychiatric medical outcomes. Individuals with scores of 4 or above on the simple ACEs questionnaire have demonstrated a 4- to 12-fold increased health risks for alcoholism, drug abuse, depression, and suicide attempts. Further, studies have shown a twofold to fourfold increase in smoking, poor self-rated health, increased numbers of sexual partners and sexually transmitted disease, and 1.4- to 1.6-fold increase in physical inactivity and severe obesity (Am J Prev Med. 1998 May;14[4]:245-58). In Ellie’s case, her history of ADHD and family history of substance use puts her at even further increased risk for later substance use disorders.
While there is no pharmacotherapy or psychotherapy specific to the treatment of having suffered adversity, it is critical for the clinician to note her increased risk. Ellie would be an individual for whom health promotion and prevention would be critical. It is excellent that she is exercising and participating in sports, which appear to be protective. Careful counseling and follow-up with regard to her increased risk for psychiatric and nonpsychiatric disorders is paramount.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
Adverse childhood experiences (ACEs) are the traumatic experiences in a person’s life occurring before the age of 18 years that the person remembers as an adult and that have consequences on a diverse set of outcomes. ACEs include physical abuse, sexual abuse, emotional abuse, mental illness of a household member, problematic drinking or alcoholism of a household member, illegal street or prescription drug use by a household member, divorce or separation of a parent, domestic violence toward a parent, and incarceration of a household member. Each of these experiences before the age of 18 years increases the likelihood of not only adulthood depression, suicide, and substance use disorders, but also a range of nonpsychiatric outcomes such as heart disease and chronic lung disease.
Case summary
Ellie is a 16-year-old girl with a past history of ADHD and oppositionality who arrives on her own in a walk-in clinic to be seen for a sports physical. Ellie has been generally healthy and was previously on a stable medical regimen of methylphenidate but has not been taking it for about 1 year. The oppositionality that she previously experienced in her early school-age years has slowly decreased. She generally does well in school and is in several clubs. In the course of the history, Ellie reveals that her mother’s depression has been worse lately to the point where her mother has resumed her drinking and illegal opiate use. You discuss safety with Ellie, and she reveals that, while she has never been threatened or injured, there has been domestic violence in the home that Ellie felt responsible to try to stop by calling the police. This led to the one and only time that Ellie was physically struck. Her father is now incarcerated, and Ellie feels guilty. After a discussion with Ellie, you report this situation to social services, who already has the case on file. Ellie’s mental status exam, including a thorough examination of symptoms of mood disorders, anxiety, substance use, and PTSD, is within normal limits.
Case discussion
Ellie has suffered a set of ACEs. Specifically, her mother has a mental illness, has a drinking problem, and uses illegal drugs; Ellie has witnessed domestic violence toward her mother, has a family member who is incarcerated, and has suffered from physical abuse. This ACEs score of 6 puts her at markedly increased risk for multiple psychiatric and nonpsychiatric medical outcomes. Individuals with scores of 4 or above on the simple ACEs questionnaire have demonstrated a 4- to 12-fold increased health risks for alcoholism, drug abuse, depression, and suicide attempts. Further, studies have shown a twofold to fourfold increase in smoking, poor self-rated health, increased numbers of sexual partners and sexually transmitted disease, and 1.4- to 1.6-fold increase in physical inactivity and severe obesity (Am J Prev Med. 1998 May;14[4]:245-58). In Ellie’s case, her history of ADHD and family history of substance use puts her at even further increased risk for later substance use disorders.
While there is no pharmacotherapy or psychotherapy specific to the treatment of having suffered adversity, it is critical for the clinician to note her increased risk. Ellie would be an individual for whom health promotion and prevention would be critical. It is excellent that she is exercising and participating in sports, which appear to be protective. Careful counseling and follow-up with regard to her increased risk for psychiatric and nonpsychiatric disorders is paramount.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
Adverse childhood experiences (ACEs) are the traumatic experiences in a person’s life occurring before the age of 18 years that the person remembers as an adult and that have consequences on a diverse set of outcomes. ACEs include physical abuse, sexual abuse, emotional abuse, mental illness of a household member, problematic drinking or alcoholism of a household member, illegal street or prescription drug use by a household member, divorce or separation of a parent, domestic violence toward a parent, and incarceration of a household member. Each of these experiences before the age of 18 years increases the likelihood of not only adulthood depression, suicide, and substance use disorders, but also a range of nonpsychiatric outcomes such as heart disease and chronic lung disease.
Case summary
Ellie is a 16-year-old girl with a past history of ADHD and oppositionality who arrives on her own in a walk-in clinic to be seen for a sports physical. Ellie has been generally healthy and was previously on a stable medical regimen of methylphenidate but has not been taking it for about 1 year. The oppositionality that she previously experienced in her early school-age years has slowly decreased. She generally does well in school and is in several clubs. In the course of the history, Ellie reveals that her mother’s depression has been worse lately to the point where her mother has resumed her drinking and illegal opiate use. You discuss safety with Ellie, and she reveals that, while she has never been threatened or injured, there has been domestic violence in the home that Ellie felt responsible to try to stop by calling the police. This led to the one and only time that Ellie was physically struck. Her father is now incarcerated, and Ellie feels guilty. After a discussion with Ellie, you report this situation to social services, who already has the case on file. Ellie’s mental status exam, including a thorough examination of symptoms of mood disorders, anxiety, substance use, and PTSD, is within normal limits.
Case discussion
Ellie has suffered a set of ACEs. Specifically, her mother has a mental illness, has a drinking problem, and uses illegal drugs; Ellie has witnessed domestic violence toward her mother, has a family member who is incarcerated, and has suffered from physical abuse. This ACEs score of 6 puts her at markedly increased risk for multiple psychiatric and nonpsychiatric medical outcomes. Individuals with scores of 4 or above on the simple ACEs questionnaire have demonstrated a 4- to 12-fold increased health risks for alcoholism, drug abuse, depression, and suicide attempts. Further, studies have shown a twofold to fourfold increase in smoking, poor self-rated health, increased numbers of sexual partners and sexually transmitted disease, and 1.4- to 1.6-fold increase in physical inactivity and severe obesity (Am J Prev Med. 1998 May;14[4]:245-58). In Ellie’s case, her history of ADHD and family history of substance use puts her at even further increased risk for later substance use disorders.
While there is no pharmacotherapy or psychotherapy specific to the treatment of having suffered adversity, it is critical for the clinician to note her increased risk. Ellie would be an individual for whom health promotion and prevention would be critical. It is excellent that she is exercising and participating in sports, which appear to be protective. Careful counseling and follow-up with regard to her increased risk for psychiatric and nonpsychiatric disorders is paramount.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
Mycobacterium tuberculosis: Overcoming one obstacle on the road to elimination
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
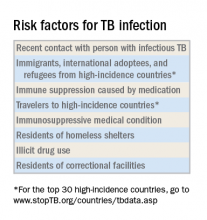
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Hot Threads in ACS Communities
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time
Cooperation must overcome polarization
Each profession has its own core set of knowledge, skills, and values. For physicians, the core set of knowledge is anatomy, pathophysiology, and pharmacology. Skills include taking a history, the physical exam, and surgical procedures. The core values traditionally have been compassion and altruism. For modern medical practice, I urge adding cooperation as a core value. Medical school and the apprenticeship of residency are designed to teach, role model, foster, develop, and groom these core competencies.
Getting into medical school is highly competitive. Medical training uses methods that are very different than those used to train elite Olympic and professional athletes. Some competitiveness persists in medical school, but in general the faculty emphasizes cooperation rather than competition. The metric is not whether one student or resident is better than another. Gold and silver medals are not awarded. It is about whether each physician-to-be has passed the milestones needed to practice medicine.
But American health care is threatened by the continued polarization of our government and our society. For years both Cleveland Clinic and Dana Farber have held annual fundraising events at Mar-a-Lago. In February 2017, because of that location’s association with President Trump, some people associated with the organizations advocated boycotting those important fund-raisers. These past few months, it seems every action and every purchase has become a political statement. One restaurant mentioned immigrants on its receipt. The action went viral and caused other people to advocate boycotting the restaurant or not tipping the wait staff (“The new political battleground: Your restaurant receipt,” The Washington Post, by Maura Judkis, Feb. 14, 2017).
Secondary boycotts are an ethical quandary. In labor disputes, organized unions can go on strike. In the 1970s, Japanese cars were not welcome in the employee parking lot of a Ford assembly plant. People do vote with their pocketbook. But in labor disputes, there are legal restrictions on secondary boycotts against other companies. People do need to get along with their neighbors and so do businesses. Politics is the art of encouraging cooperation on one project amongst people who disagree about the goals of many other proposed projects. The Preamble to the United States Constitution enumerates the benefits of cooperation.
In any large-scale human endeavor, conflicts arise that may limit cooperation. Accommodating conscientious objection is the safety valve that permits cooperation when dealing with contested government endeavors such as war, abortion, and physician-assisted suicide. It is meant as a last ditch effort to maintain cohesion of both societal and individual moral integrity. But if every proposed action is met with votes divided along party lines, conscientious objection loses its moral high ground.
Judge Neil Gorsuch, the nominee for the U.S. Supreme Court, has a record of supporting religious freedom in Yellowbear v. Lambert (10th Cir. 2014). He would likely support conscientious objection in relation to assisted dying by physicians, contrary to the arguments made recently by bioethicists Julian Savulescu and Udo Schuklenk. In related news, the liberty of physicians to address gun safety was affirmed when a Florida appeals court upheld the overturning of the state’s Privacy of Firearm Owners Act.
Summing up a tumultuous month of medical ethics, I leave you with the words of Voltaire: “Cherish those who seek the truth but beware of those who find it.”
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Each profession has its own core set of knowledge, skills, and values. For physicians, the core set of knowledge is anatomy, pathophysiology, and pharmacology. Skills include taking a history, the physical exam, and surgical procedures. The core values traditionally have been compassion and altruism. For modern medical practice, I urge adding cooperation as a core value. Medical school and the apprenticeship of residency are designed to teach, role model, foster, develop, and groom these core competencies.
Getting into medical school is highly competitive. Medical training uses methods that are very different than those used to train elite Olympic and professional athletes. Some competitiveness persists in medical school, but in general the faculty emphasizes cooperation rather than competition. The metric is not whether one student or resident is better than another. Gold and silver medals are not awarded. It is about whether each physician-to-be has passed the milestones needed to practice medicine.
But American health care is threatened by the continued polarization of our government and our society. For years both Cleveland Clinic and Dana Farber have held annual fundraising events at Mar-a-Lago. In February 2017, because of that location’s association with President Trump, some people associated with the organizations advocated boycotting those important fund-raisers. These past few months, it seems every action and every purchase has become a political statement. One restaurant mentioned immigrants on its receipt. The action went viral and caused other people to advocate boycotting the restaurant or not tipping the wait staff (“The new political battleground: Your restaurant receipt,” The Washington Post, by Maura Judkis, Feb. 14, 2017).
Secondary boycotts are an ethical quandary. In labor disputes, organized unions can go on strike. In the 1970s, Japanese cars were not welcome in the employee parking lot of a Ford assembly plant. People do vote with their pocketbook. But in labor disputes, there are legal restrictions on secondary boycotts against other companies. People do need to get along with their neighbors and so do businesses. Politics is the art of encouraging cooperation on one project amongst people who disagree about the goals of many other proposed projects. The Preamble to the United States Constitution enumerates the benefits of cooperation.
In any large-scale human endeavor, conflicts arise that may limit cooperation. Accommodating conscientious objection is the safety valve that permits cooperation when dealing with contested government endeavors such as war, abortion, and physician-assisted suicide. It is meant as a last ditch effort to maintain cohesion of both societal and individual moral integrity. But if every proposed action is met with votes divided along party lines, conscientious objection loses its moral high ground.
Judge Neil Gorsuch, the nominee for the U.S. Supreme Court, has a record of supporting religious freedom in Yellowbear v. Lambert (10th Cir. 2014). He would likely support conscientious objection in relation to assisted dying by physicians, contrary to the arguments made recently by bioethicists Julian Savulescu and Udo Schuklenk. In related news, the liberty of physicians to address gun safety was affirmed when a Florida appeals court upheld the overturning of the state’s Privacy of Firearm Owners Act.
Summing up a tumultuous month of medical ethics, I leave you with the words of Voltaire: “Cherish those who seek the truth but beware of those who find it.”
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Each profession has its own core set of knowledge, skills, and values. For physicians, the core set of knowledge is anatomy, pathophysiology, and pharmacology. Skills include taking a history, the physical exam, and surgical procedures. The core values traditionally have been compassion and altruism. For modern medical practice, I urge adding cooperation as a core value. Medical school and the apprenticeship of residency are designed to teach, role model, foster, develop, and groom these core competencies.
Getting into medical school is highly competitive. Medical training uses methods that are very different than those used to train elite Olympic and professional athletes. Some competitiveness persists in medical school, but in general the faculty emphasizes cooperation rather than competition. The metric is not whether one student or resident is better than another. Gold and silver medals are not awarded. It is about whether each physician-to-be has passed the milestones needed to practice medicine.
But American health care is threatened by the continued polarization of our government and our society. For years both Cleveland Clinic and Dana Farber have held annual fundraising events at Mar-a-Lago. In February 2017, because of that location’s association with President Trump, some people associated with the organizations advocated boycotting those important fund-raisers. These past few months, it seems every action and every purchase has become a political statement. One restaurant mentioned immigrants on its receipt. The action went viral and caused other people to advocate boycotting the restaurant or not tipping the wait staff (“The new political battleground: Your restaurant receipt,” The Washington Post, by Maura Judkis, Feb. 14, 2017).
Secondary boycotts are an ethical quandary. In labor disputes, organized unions can go on strike. In the 1970s, Japanese cars were not welcome in the employee parking lot of a Ford assembly plant. People do vote with their pocketbook. But in labor disputes, there are legal restrictions on secondary boycotts against other companies. People do need to get along with their neighbors and so do businesses. Politics is the art of encouraging cooperation on one project amongst people who disagree about the goals of many other proposed projects. The Preamble to the United States Constitution enumerates the benefits of cooperation.
In any large-scale human endeavor, conflicts arise that may limit cooperation. Accommodating conscientious objection is the safety valve that permits cooperation when dealing with contested government endeavors such as war, abortion, and physician-assisted suicide. It is meant as a last ditch effort to maintain cohesion of both societal and individual moral integrity. But if every proposed action is met with votes divided along party lines, conscientious objection loses its moral high ground.
Judge Neil Gorsuch, the nominee for the U.S. Supreme Court, has a record of supporting religious freedom in Yellowbear v. Lambert (10th Cir. 2014). He would likely support conscientious objection in relation to assisted dying by physicians, contrary to the arguments made recently by bioethicists Julian Savulescu and Udo Schuklenk. In related news, the liberty of physicians to address gun safety was affirmed when a Florida appeals court upheld the overturning of the state’s Privacy of Firearm Owners Act.
Summing up a tumultuous month of medical ethics, I leave you with the words of Voltaire: “Cherish those who seek the truth but beware of those who find it.”
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Medication for life
Some areas of psychiatry would benefit from more controversy. One of them is the prescription of antidepressants to young people dealing with romantic disappointments.
I have seen many young men and women given an antidepressant for the very painful, but ordinary, romantic break-ups characteristic of this phase of life, who then become habituated to the drug. They take the medication indefinitely, their brains accommodate neurophysiologically to the presence of the chemical, and they become unable to discontinue it without intolerable withdrawal symptoms that look like an underlying illness. A parallel phenomenon occurs not infrequently with the use of amphetamines (and other stimulants) for attention-deficit hyperactivity disorder that is at times mistakenly diagnosed in this age group.
Antidepressants for early romantic disappointments
Mr. A, now in his 30s, became sullen and withdrawn at age 16 after a girl refused his romantic approaches. His well-intentioned parents took him to a psychiatrist, who, after a brief evaluation, prescribed fluoxetine. Mr. A is now well adjusted and happily married but unable to get off fluoxetine. Even when it is carefully tapered, 2 or 3 months after it is discontinued, he becomes anxious and depressed. This is an iatrogenic problem. It is not related to goings-on in his mind or his life; rather it is the result of his brain’s accommodation to a medication, producing a serious withdrawal syndrome.
His original psychiatrist made only a descriptive diagnosis. He did not inquire about what was going on in Mr. A’s mind and thus could not make a dynamic diagnosis (that is, a diagnosis of a patient’s central emotional conflicts, ability to function in relation to other people, strengths, and weaknesses). Mr. A, like many adolescents, had a lot of anxiety and guilt about sexual and romantic involvement, and potential success. He defended against his anxiety and guilt by assuring himself life would never work out for him. When the girl he admired rebuffed him, he immediately concluded this would perpetually be his fate, so the girl’s refusal was particularly painful. Mr. A feels that had this dynamic been discussed with him at the time, he may well not have needed medication at all.
Ms. B, like Mr. A, was prescribed antidepressants for depressive reactions to early romantic disappointments. Likewise, she self-punitively convinced herself, despite easily attracting men’s attentions, that these disappointments meant a lifetime alone. Ms. B has a family history of depression (although neither of her brothers struggles with it), and she felt that she needed the medications to help negotiate difficult periods. But should she have been on them for extended periods of time? Therapeutic attention to her emotional conflicts helped her to form lasting relationships, marry, and have children. Unable to get off the medications, she had to deal with the risks of their use during pregnancy, which she then subjected to the same sort of guilty self-accusations as she previously had used to limit her romantic prospects.
Ms. C came to me on three medications – one for each of her significant romantic break-ups. She, too, was depressively self-diminishing, beginning therapy by letting me know all the things she could think of that might make me think less of her. Understanding some of the reasons for her self-deprecation helped her toward better romantic relationships but did not give her the courage to get off her medications. Pregnancy, however, led her to promptly and successfully discontinue an antidepressant and a mood stabilizer (she has never had any symptoms suggestive of manic depression). She remained on a low dose of a selective serotonin reuptake inhibitor, had an uneventful pregnancy, and then fell in love with a charming baby.
Principles for consideration
• Psychiatrists (and other mental health professionals and primary care physicians treating mental illness) should always make a dynamic, and not merely a descriptive, diagnosis. Even with a more clearly biologically driven problem, such as bipolar disorder, the patient’s personality and conflicts matter.
• Psychiatrists should be very judicious about prescribing medications in adolescence and young adulthood, especially for difficulties adapting to the typical events of those phases of life. Expert psychotherapy should be the first choice in these instances.
• Medication, when necessary, should be prescribed for as limited a time as possible. It is important for young people to advance their own development, not feel needlessly beholden to medications, not get iatrogenically dependent on them, and not feel that they have “diseases” they don’t have.
Amphetamines for misdiagnosed ADHD
When Ms. D’s family moved to a new house, she, her brother, and her sister, each attended a new school. Unlike her siblings, Ms. D, who was in high school, had a difficult adjustment. Her grades fell. She was taken to a psychiatrist who diagnosed ADHD and prescribed amphetamines. The psychiatrist paid little attention to her prior lack of difficulty in school or her struggles making new friends. Nor did the psychiatrist learn that Ms. D had to ward off the seductive advances of an older teacher (although Ms. D would likely not have been immediately forthcoming about this at the time).
When Ms. D came to me as a college student, for troubles with anger, anxiety, and some depression, she was religiously taking 70 mg of amphetamines daily. After I learned a bit about her and raised the question of whether she actually had ADHD, and whether it might make sense to consider tapering the amphetamines, she was appalled and looked like a toddler who was afraid I was about to steal her candy. Helping her to get off the unneeded medication was a multiyear process.
First, she had to recognize that it was prescribed to treat a problem she probably didn’t have, and second, that it was failing to help her with the problems she did have. As we attended to some of her actual emotional conflicts, she became willing to experiment with lower doses. She was able to see that her work was little changed as the dose was lowered, and that her difficulties with school had more to do with feelings toward classmates and teachers than with the presence or absence of amphetamines. After a protracted struggle, finally off the medication, she felt in charge of her life and no longer believed there was something inherently wrong with her mind or her brain.
Mr. E was the only son in a high-powered academic family. His older sisters were all intellectual standouts. Early in high school, he received his first B as a grade in a course. He was taken to a pediatrician, diagnosed with ADHD, and put on stimulants. Like Ms. D, he came to believe that he needed them. In college, he began to develop some magical aspects to his thinking, a potential side effect of the stimulants. It was very difficult to help him see either that he had a problem with his thinking or that it might be attributable to the medication.
Principles to consider
• If the ADHD wasn’t there in elementary school or before, it is unlikely that an adolescent or young adult has new-onset ADHD. A new or newly amplified conflict is occurring in the person’s mind and life A dynamic diagnosis, as always, is essential.
• When medication is prescribed for actual ADHD, as with anything else, the question of how long it will be taken must be asked. For life? Until other means of adaptation are accomplished? Until adequate outcome studies of long-term use of the medication are performed?
Helping patients to get off unneeded, or no longer needed, medications can be a difficult task. Their emotional attachments to the medications can be intense and varied. For some, the prescription is a sign of being loved and cared for. For others, it represents a certification of a deficit, appeases guilt about success, and/or attests to the need for special consideration. Insofar as the medication has been helpful, it may have come to be regarded as a dearly loved friend, or even a part of the self.
When medication has been helpful, there is also, of course, concern about the potential return of the difficulties for which it was prescribed. Few patients are told at the time of first prescription that there is potential risk of habituation and return of, or potential exaggeration of, symptoms with discontinuation. This type of discussion is more difficult to have in situations in which a prescription is urgently needed and the patient is reluctant, but is still not often done in those instances in which a prescription is more optional than essential. The picture is seldom simple.
These few comments only scratch the surface of the difficulties doctors and patients face in helping patients to discontinue their medications. Residency programs pay a lot of attention to helping trainees learn to prescribe medications; rarely do they sufficiently educate residents how to help patients discontinue them. The fact that so many residencies currently pay limited attention to interventions apart from medication contributes further to the difficulty.
Medications have saved the life of many a psychiatric patient. Some patients need medication for life. But some end up on medication for life, even in some instances when the medication may not have been needed in the first place. Although it is often a difficult task, we need to do a better job of distinguishing which patients are which.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
Some areas of psychiatry would benefit from more controversy. One of them is the prescription of antidepressants to young people dealing with romantic disappointments.
I have seen many young men and women given an antidepressant for the very painful, but ordinary, romantic break-ups characteristic of this phase of life, who then become habituated to the drug. They take the medication indefinitely, their brains accommodate neurophysiologically to the presence of the chemical, and they become unable to discontinue it without intolerable withdrawal symptoms that look like an underlying illness. A parallel phenomenon occurs not infrequently with the use of amphetamines (and other stimulants) for attention-deficit hyperactivity disorder that is at times mistakenly diagnosed in this age group.
Antidepressants for early romantic disappointments
Mr. A, now in his 30s, became sullen and withdrawn at age 16 after a girl refused his romantic approaches. His well-intentioned parents took him to a psychiatrist, who, after a brief evaluation, prescribed fluoxetine. Mr. A is now well adjusted and happily married but unable to get off fluoxetine. Even when it is carefully tapered, 2 or 3 months after it is discontinued, he becomes anxious and depressed. This is an iatrogenic problem. It is not related to goings-on in his mind or his life; rather it is the result of his brain’s accommodation to a medication, producing a serious withdrawal syndrome.
His original psychiatrist made only a descriptive diagnosis. He did not inquire about what was going on in Mr. A’s mind and thus could not make a dynamic diagnosis (that is, a diagnosis of a patient’s central emotional conflicts, ability to function in relation to other people, strengths, and weaknesses). Mr. A, like many adolescents, had a lot of anxiety and guilt about sexual and romantic involvement, and potential success. He defended against his anxiety and guilt by assuring himself life would never work out for him. When the girl he admired rebuffed him, he immediately concluded this would perpetually be his fate, so the girl’s refusal was particularly painful. Mr. A feels that had this dynamic been discussed with him at the time, he may well not have needed medication at all.
Ms. B, like Mr. A, was prescribed antidepressants for depressive reactions to early romantic disappointments. Likewise, she self-punitively convinced herself, despite easily attracting men’s attentions, that these disappointments meant a lifetime alone. Ms. B has a family history of depression (although neither of her brothers struggles with it), and she felt that she needed the medications to help negotiate difficult periods. But should she have been on them for extended periods of time? Therapeutic attention to her emotional conflicts helped her to form lasting relationships, marry, and have children. Unable to get off the medications, she had to deal with the risks of their use during pregnancy, which she then subjected to the same sort of guilty self-accusations as she previously had used to limit her romantic prospects.
Ms. C came to me on three medications – one for each of her significant romantic break-ups. She, too, was depressively self-diminishing, beginning therapy by letting me know all the things she could think of that might make me think less of her. Understanding some of the reasons for her self-deprecation helped her toward better romantic relationships but did not give her the courage to get off her medications. Pregnancy, however, led her to promptly and successfully discontinue an antidepressant and a mood stabilizer (she has never had any symptoms suggestive of manic depression). She remained on a low dose of a selective serotonin reuptake inhibitor, had an uneventful pregnancy, and then fell in love with a charming baby.
Principles for consideration
• Psychiatrists (and other mental health professionals and primary care physicians treating mental illness) should always make a dynamic, and not merely a descriptive, diagnosis. Even with a more clearly biologically driven problem, such as bipolar disorder, the patient’s personality and conflicts matter.
• Psychiatrists should be very judicious about prescribing medications in adolescence and young adulthood, especially for difficulties adapting to the typical events of those phases of life. Expert psychotherapy should be the first choice in these instances.
• Medication, when necessary, should be prescribed for as limited a time as possible. It is important for young people to advance their own development, not feel needlessly beholden to medications, not get iatrogenically dependent on them, and not feel that they have “diseases” they don’t have.
Amphetamines for misdiagnosed ADHD
When Ms. D’s family moved to a new house, she, her brother, and her sister, each attended a new school. Unlike her siblings, Ms. D, who was in high school, had a difficult adjustment. Her grades fell. She was taken to a psychiatrist who diagnosed ADHD and prescribed amphetamines. The psychiatrist paid little attention to her prior lack of difficulty in school or her struggles making new friends. Nor did the psychiatrist learn that Ms. D had to ward off the seductive advances of an older teacher (although Ms. D would likely not have been immediately forthcoming about this at the time).
When Ms. D came to me as a college student, for troubles with anger, anxiety, and some depression, she was religiously taking 70 mg of amphetamines daily. After I learned a bit about her and raised the question of whether she actually had ADHD, and whether it might make sense to consider tapering the amphetamines, she was appalled and looked like a toddler who was afraid I was about to steal her candy. Helping her to get off the unneeded medication was a multiyear process.
First, she had to recognize that it was prescribed to treat a problem she probably didn’t have, and second, that it was failing to help her with the problems she did have. As we attended to some of her actual emotional conflicts, she became willing to experiment with lower doses. She was able to see that her work was little changed as the dose was lowered, and that her difficulties with school had more to do with feelings toward classmates and teachers than with the presence or absence of amphetamines. After a protracted struggle, finally off the medication, she felt in charge of her life and no longer believed there was something inherently wrong with her mind or her brain.
Mr. E was the only son in a high-powered academic family. His older sisters were all intellectual standouts. Early in high school, he received his first B as a grade in a course. He was taken to a pediatrician, diagnosed with ADHD, and put on stimulants. Like Ms. D, he came to believe that he needed them. In college, he began to develop some magical aspects to his thinking, a potential side effect of the stimulants. It was very difficult to help him see either that he had a problem with his thinking or that it might be attributable to the medication.
Principles to consider
• If the ADHD wasn’t there in elementary school or before, it is unlikely that an adolescent or young adult has new-onset ADHD. A new or newly amplified conflict is occurring in the person’s mind and life A dynamic diagnosis, as always, is essential.
• When medication is prescribed for actual ADHD, as with anything else, the question of how long it will be taken must be asked. For life? Until other means of adaptation are accomplished? Until adequate outcome studies of long-term use of the medication are performed?
Helping patients to get off unneeded, or no longer needed, medications can be a difficult task. Their emotional attachments to the medications can be intense and varied. For some, the prescription is a sign of being loved and cared for. For others, it represents a certification of a deficit, appeases guilt about success, and/or attests to the need for special consideration. Insofar as the medication has been helpful, it may have come to be regarded as a dearly loved friend, or even a part of the self.
When medication has been helpful, there is also, of course, concern about the potential return of the difficulties for which it was prescribed. Few patients are told at the time of first prescription that there is potential risk of habituation and return of, or potential exaggeration of, symptoms with discontinuation. This type of discussion is more difficult to have in situations in which a prescription is urgently needed and the patient is reluctant, but is still not often done in those instances in which a prescription is more optional than essential. The picture is seldom simple.
These few comments only scratch the surface of the difficulties doctors and patients face in helping patients to discontinue their medications. Residency programs pay a lot of attention to helping trainees learn to prescribe medications; rarely do they sufficiently educate residents how to help patients discontinue them. The fact that so many residencies currently pay limited attention to interventions apart from medication contributes further to the difficulty.
Medications have saved the life of many a psychiatric patient. Some patients need medication for life. But some end up on medication for life, even in some instances when the medication may not have been needed in the first place. Although it is often a difficult task, we need to do a better job of distinguishing which patients are which.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
Some areas of psychiatry would benefit from more controversy. One of them is the prescription of antidepressants to young people dealing with romantic disappointments.
I have seen many young men and women given an antidepressant for the very painful, but ordinary, romantic break-ups characteristic of this phase of life, who then become habituated to the drug. They take the medication indefinitely, their brains accommodate neurophysiologically to the presence of the chemical, and they become unable to discontinue it without intolerable withdrawal symptoms that look like an underlying illness. A parallel phenomenon occurs not infrequently with the use of amphetamines (and other stimulants) for attention-deficit hyperactivity disorder that is at times mistakenly diagnosed in this age group.
Antidepressants for early romantic disappointments
Mr. A, now in his 30s, became sullen and withdrawn at age 16 after a girl refused his romantic approaches. His well-intentioned parents took him to a psychiatrist, who, after a brief evaluation, prescribed fluoxetine. Mr. A is now well adjusted and happily married but unable to get off fluoxetine. Even when it is carefully tapered, 2 or 3 months after it is discontinued, he becomes anxious and depressed. This is an iatrogenic problem. It is not related to goings-on in his mind or his life; rather it is the result of his brain’s accommodation to a medication, producing a serious withdrawal syndrome.
His original psychiatrist made only a descriptive diagnosis. He did not inquire about what was going on in Mr. A’s mind and thus could not make a dynamic diagnosis (that is, a diagnosis of a patient’s central emotional conflicts, ability to function in relation to other people, strengths, and weaknesses). Mr. A, like many adolescents, had a lot of anxiety and guilt about sexual and romantic involvement, and potential success. He defended against his anxiety and guilt by assuring himself life would never work out for him. When the girl he admired rebuffed him, he immediately concluded this would perpetually be his fate, so the girl’s refusal was particularly painful. Mr. A feels that had this dynamic been discussed with him at the time, he may well not have needed medication at all.
Ms. B, like Mr. A, was prescribed antidepressants for depressive reactions to early romantic disappointments. Likewise, she self-punitively convinced herself, despite easily attracting men’s attentions, that these disappointments meant a lifetime alone. Ms. B has a family history of depression (although neither of her brothers struggles with it), and she felt that she needed the medications to help negotiate difficult periods. But should she have been on them for extended periods of time? Therapeutic attention to her emotional conflicts helped her to form lasting relationships, marry, and have children. Unable to get off the medications, she had to deal with the risks of their use during pregnancy, which she then subjected to the same sort of guilty self-accusations as she previously had used to limit her romantic prospects.
Ms. C came to me on three medications – one for each of her significant romantic break-ups. She, too, was depressively self-diminishing, beginning therapy by letting me know all the things she could think of that might make me think less of her. Understanding some of the reasons for her self-deprecation helped her toward better romantic relationships but did not give her the courage to get off her medications. Pregnancy, however, led her to promptly and successfully discontinue an antidepressant and a mood stabilizer (she has never had any symptoms suggestive of manic depression). She remained on a low dose of a selective serotonin reuptake inhibitor, had an uneventful pregnancy, and then fell in love with a charming baby.
Principles for consideration
• Psychiatrists (and other mental health professionals and primary care physicians treating mental illness) should always make a dynamic, and not merely a descriptive, diagnosis. Even with a more clearly biologically driven problem, such as bipolar disorder, the patient’s personality and conflicts matter.
• Psychiatrists should be very judicious about prescribing medications in adolescence and young adulthood, especially for difficulties adapting to the typical events of those phases of life. Expert psychotherapy should be the first choice in these instances.
• Medication, when necessary, should be prescribed for as limited a time as possible. It is important for young people to advance their own development, not feel needlessly beholden to medications, not get iatrogenically dependent on them, and not feel that they have “diseases” they don’t have.
Amphetamines for misdiagnosed ADHD
When Ms. D’s family moved to a new house, she, her brother, and her sister, each attended a new school. Unlike her siblings, Ms. D, who was in high school, had a difficult adjustment. Her grades fell. She was taken to a psychiatrist who diagnosed ADHD and prescribed amphetamines. The psychiatrist paid little attention to her prior lack of difficulty in school or her struggles making new friends. Nor did the psychiatrist learn that Ms. D had to ward off the seductive advances of an older teacher (although Ms. D would likely not have been immediately forthcoming about this at the time).
When Ms. D came to me as a college student, for troubles with anger, anxiety, and some depression, she was religiously taking 70 mg of amphetamines daily. After I learned a bit about her and raised the question of whether she actually had ADHD, and whether it might make sense to consider tapering the amphetamines, she was appalled and looked like a toddler who was afraid I was about to steal her candy. Helping her to get off the unneeded medication was a multiyear process.
First, she had to recognize that it was prescribed to treat a problem she probably didn’t have, and second, that it was failing to help her with the problems she did have. As we attended to some of her actual emotional conflicts, she became willing to experiment with lower doses. She was able to see that her work was little changed as the dose was lowered, and that her difficulties with school had more to do with feelings toward classmates and teachers than with the presence or absence of amphetamines. After a protracted struggle, finally off the medication, she felt in charge of her life and no longer believed there was something inherently wrong with her mind or her brain.
Mr. E was the only son in a high-powered academic family. His older sisters were all intellectual standouts. Early in high school, he received his first B as a grade in a course. He was taken to a pediatrician, diagnosed with ADHD, and put on stimulants. Like Ms. D, he came to believe that he needed them. In college, he began to develop some magical aspects to his thinking, a potential side effect of the stimulants. It was very difficult to help him see either that he had a problem with his thinking or that it might be attributable to the medication.
Principles to consider
• If the ADHD wasn’t there in elementary school or before, it is unlikely that an adolescent or young adult has new-onset ADHD. A new or newly amplified conflict is occurring in the person’s mind and life A dynamic diagnosis, as always, is essential.
• When medication is prescribed for actual ADHD, as with anything else, the question of how long it will be taken must be asked. For life? Until other means of adaptation are accomplished? Until adequate outcome studies of long-term use of the medication are performed?
Helping patients to get off unneeded, or no longer needed, medications can be a difficult task. Their emotional attachments to the medications can be intense and varied. For some, the prescription is a sign of being loved and cared for. For others, it represents a certification of a deficit, appeases guilt about success, and/or attests to the need for special consideration. Insofar as the medication has been helpful, it may have come to be regarded as a dearly loved friend, or even a part of the self.
When medication has been helpful, there is also, of course, concern about the potential return of the difficulties for which it was prescribed. Few patients are told at the time of first prescription that there is potential risk of habituation and return of, or potential exaggeration of, symptoms with discontinuation. This type of discussion is more difficult to have in situations in which a prescription is urgently needed and the patient is reluctant, but is still not often done in those instances in which a prescription is more optional than essential. The picture is seldom simple.
These few comments only scratch the surface of the difficulties doctors and patients face in helping patients to discontinue their medications. Residency programs pay a lot of attention to helping trainees learn to prescribe medications; rarely do they sufficiently educate residents how to help patients discontinue them. The fact that so many residencies currently pay limited attention to interventions apart from medication contributes further to the difficulty.
Medications have saved the life of many a psychiatric patient. Some patients need medication for life. But some end up on medication for life, even in some instances when the medication may not have been needed in the first place. Although it is often a difficult task, we need to do a better job of distinguishing which patients are which.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
A Message from the President: The ACS: Dedicated to Doing What’s Right for the Patient
Do what’s right for the patient. That statement is the bedrock on which the American College of Surgeons (ACS) stands.
Throughout its nearly 104-year history, the ACS has promoted surgical education and quality improvement. The College’s dedication to education and quality can be traced to the guiding principles of its founder, Franklin H. Martin, MD, FACS. In Dr. Martin’s era, the early 20th century, medical education was in a deplorable state, as documented in the well-known Flexner report of 1910.
To help improve surgical education and training, Dr. Martin first established Surgery, Gynecology & Obstetrics (SG&O, now the Journal of the American College of Surgeons) as a practical journal for practicing surgeons, edited by active surgeons. He published an editorial in the journal inviting surgeons to “learn by watching” and encouraged “every physician in the U.S. and Canada who was interested in surgery to observe the clinics in one of the large medical centers.” Approximately 1,300 physicians responded to Dr. Martin’s charge, resulting in the first Clinical Congress of Surgeons of North America (CCSNA), November 7-9, 1910, in Chicago, IL. After the third CCSNA meeting in 1912, Dr. Martin concluded that further change was necessary, which eventually led to the formation of the ACS in November 1913.
Standards
The importance of establishing standards for hospitals and surgical training cannot be emphasized enough. These programs fundamentally changed surgical practice and training. If the College had ceased to exist after that achievement, it would have more than fulfilled the expectations of Dr. Martin and other ACS leaders. But this did not happen. Instead, the College continued to inspire quality and to maintain the highest standards for better outcomes through establishment of programs aimed at improving care for cancer and trauma patients.
Committees
The ACS Committee on Cancer published a Standardized Method for Reporting Cancer End Results in 1953. In 1965, other organizations partnered with the College to transform this committee into the Commission on Cancer (CoC), which today uses strict criteria and a rigorous on-site evaluation process to accredit more than 1,530 U.S. cancer centers. This accreditation process is used not only for initial verification of achievement of program standards, but also for periodic review for compliance to maintain accreditation.
Early in its history, the College also established a Committee on the Treatment of Fractures, which evolved into what we now know as the Committee on Trauma (COT). The COT’s guidelines for hospitals to attain or maintain verification as trauma centers—Resources for Optimal Care of the Injured Patient—was first issued in 1976 and now is in its sixth edition.
Another seminal event in trauma took place in 1976—an airplane crash involving James K. Styner, MD, FACS, and his family, in rural Nebraska. His wife died on impact, and his children were severely injured. Angered by the delays his family experienced in receiving appropriate care, Dr. Styner called for the development of adequate facilities and standardized approaches to care for severely injured patients. He combined forces with Paul E. “Skip” Collicott, MD, FACS, and other Nebraska surgeons, to develop the Advanced Trauma Life Support® program, which introduces physicians and other health care professionals around the world to best practices for initial evaluation and management of trauma patients.
ACS Regent Lenworth M. Jacobs, Jr., MD, MPH, FACS, has led more recent COT initiatives, including development of the Advanced Trauma Operative Management® course and the Hartford ConsensusTM. This panel—composed of trauma care professionals and government officials—developed the Stop the Bleed program—an initiative aimed at enhancing survival from mass casualty and active shooter events.
Another important committee that the College established to ensure surgeons are prepared to do what’s right for the patient is the Committee on Emerging Surgical Technology and Education (CESTE). Launched in 1992 with the late C. James Carrico, MD, FACS, as the inaugural Chair, CESTE was charged with developing processes to evaluate emerging surgical technology for safety and effectiveness, creating standardized education programs, and measuring outcomes. Two of the College’s most important education and quality programs sprang from CESTE—the Accredited Education Institutes, under the leadership of Ajit K. Sachdeva, MD, FACS, Director, ACS Division of Education, and the Division of Research and Optimal Patient Care, first led by R. Scott Jones, MD, FACS, and now under the purview of Clifford Y. Ko, MD, MS, FACS.
The future is in your hands
Unquestionably, the ACS and its leaders have a rich history of doing what’s right for the patient. The future, however, belongs to you. I want to encourage you to participate in all the activities of your College at the local, state, and national levels. Establish personal relationships with leaders. Be an advocate for our education and quality programs. I am confident that there are those among you who will become the leaders who will continue the evolution of the College and inspire quality, maintain the highest standards, and ensure better outcomes.
Dr. Townsend is the Robertson-Poth Distinguished Chair in General Surgery, department of surgery, University of Texas Medical Branch (UTMB), Galveston; professor of surgery, department of surgery, professor of physician assistant studies, School of Allied Health Sciences; and graduate faculty in the cell biology program, UTMB. He is the 97th President of the ACS.
Do what’s right for the patient. That statement is the bedrock on which the American College of Surgeons (ACS) stands.
Throughout its nearly 104-year history, the ACS has promoted surgical education and quality improvement. The College’s dedication to education and quality can be traced to the guiding principles of its founder, Franklin H. Martin, MD, FACS. In Dr. Martin’s era, the early 20th century, medical education was in a deplorable state, as documented in the well-known Flexner report of 1910.
To help improve surgical education and training, Dr. Martin first established Surgery, Gynecology & Obstetrics (SG&O, now the Journal of the American College of Surgeons) as a practical journal for practicing surgeons, edited by active surgeons. He published an editorial in the journal inviting surgeons to “learn by watching” and encouraged “every physician in the U.S. and Canada who was interested in surgery to observe the clinics in one of the large medical centers.” Approximately 1,300 physicians responded to Dr. Martin’s charge, resulting in the first Clinical Congress of Surgeons of North America (CCSNA), November 7-9, 1910, in Chicago, IL. After the third CCSNA meeting in 1912, Dr. Martin concluded that further change was necessary, which eventually led to the formation of the ACS in November 1913.
Standards
The importance of establishing standards for hospitals and surgical training cannot be emphasized enough. These programs fundamentally changed surgical practice and training. If the College had ceased to exist after that achievement, it would have more than fulfilled the expectations of Dr. Martin and other ACS leaders. But this did not happen. Instead, the College continued to inspire quality and to maintain the highest standards for better outcomes through establishment of programs aimed at improving care for cancer and trauma patients.
Committees
The ACS Committee on Cancer published a Standardized Method for Reporting Cancer End Results in 1953. In 1965, other organizations partnered with the College to transform this committee into the Commission on Cancer (CoC), which today uses strict criteria and a rigorous on-site evaluation process to accredit more than 1,530 U.S. cancer centers. This accreditation process is used not only for initial verification of achievement of program standards, but also for periodic review for compliance to maintain accreditation.
Early in its history, the College also established a Committee on the Treatment of Fractures, which evolved into what we now know as the Committee on Trauma (COT). The COT’s guidelines for hospitals to attain or maintain verification as trauma centers—Resources for Optimal Care of the Injured Patient—was first issued in 1976 and now is in its sixth edition.
Another seminal event in trauma took place in 1976—an airplane crash involving James K. Styner, MD, FACS, and his family, in rural Nebraska. His wife died on impact, and his children were severely injured. Angered by the delays his family experienced in receiving appropriate care, Dr. Styner called for the development of adequate facilities and standardized approaches to care for severely injured patients. He combined forces with Paul E. “Skip” Collicott, MD, FACS, and other Nebraska surgeons, to develop the Advanced Trauma Life Support® program, which introduces physicians and other health care professionals around the world to best practices for initial evaluation and management of trauma patients.
ACS Regent Lenworth M. Jacobs, Jr., MD, MPH, FACS, has led more recent COT initiatives, including development of the Advanced Trauma Operative Management® course and the Hartford ConsensusTM. This panel—composed of trauma care professionals and government officials—developed the Stop the Bleed program—an initiative aimed at enhancing survival from mass casualty and active shooter events.
Another important committee that the College established to ensure surgeons are prepared to do what’s right for the patient is the Committee on Emerging Surgical Technology and Education (CESTE). Launched in 1992 with the late C. James Carrico, MD, FACS, as the inaugural Chair, CESTE was charged with developing processes to evaluate emerging surgical technology for safety and effectiveness, creating standardized education programs, and measuring outcomes. Two of the College’s most important education and quality programs sprang from CESTE—the Accredited Education Institutes, under the leadership of Ajit K. Sachdeva, MD, FACS, Director, ACS Division of Education, and the Division of Research and Optimal Patient Care, first led by R. Scott Jones, MD, FACS, and now under the purview of Clifford Y. Ko, MD, MS, FACS.
The future is in your hands
Unquestionably, the ACS and its leaders have a rich history of doing what’s right for the patient. The future, however, belongs to you. I want to encourage you to participate in all the activities of your College at the local, state, and national levels. Establish personal relationships with leaders. Be an advocate for our education and quality programs. I am confident that there are those among you who will become the leaders who will continue the evolution of the College and inspire quality, maintain the highest standards, and ensure better outcomes.
Dr. Townsend is the Robertson-Poth Distinguished Chair in General Surgery, department of surgery, University of Texas Medical Branch (UTMB), Galveston; professor of surgery, department of surgery, professor of physician assistant studies, School of Allied Health Sciences; and graduate faculty in the cell biology program, UTMB. He is the 97th President of the ACS.
Do what’s right for the patient. That statement is the bedrock on which the American College of Surgeons (ACS) stands.
Throughout its nearly 104-year history, the ACS has promoted surgical education and quality improvement. The College’s dedication to education and quality can be traced to the guiding principles of its founder, Franklin H. Martin, MD, FACS. In Dr. Martin’s era, the early 20th century, medical education was in a deplorable state, as documented in the well-known Flexner report of 1910.
To help improve surgical education and training, Dr. Martin first established Surgery, Gynecology & Obstetrics (SG&O, now the Journal of the American College of Surgeons) as a practical journal for practicing surgeons, edited by active surgeons. He published an editorial in the journal inviting surgeons to “learn by watching” and encouraged “every physician in the U.S. and Canada who was interested in surgery to observe the clinics in one of the large medical centers.” Approximately 1,300 physicians responded to Dr. Martin’s charge, resulting in the first Clinical Congress of Surgeons of North America (CCSNA), November 7-9, 1910, in Chicago, IL. After the third CCSNA meeting in 1912, Dr. Martin concluded that further change was necessary, which eventually led to the formation of the ACS in November 1913.
Standards
The importance of establishing standards for hospitals and surgical training cannot be emphasized enough. These programs fundamentally changed surgical practice and training. If the College had ceased to exist after that achievement, it would have more than fulfilled the expectations of Dr. Martin and other ACS leaders. But this did not happen. Instead, the College continued to inspire quality and to maintain the highest standards for better outcomes through establishment of programs aimed at improving care for cancer and trauma patients.
Committees
The ACS Committee on Cancer published a Standardized Method for Reporting Cancer End Results in 1953. In 1965, other organizations partnered with the College to transform this committee into the Commission on Cancer (CoC), which today uses strict criteria and a rigorous on-site evaluation process to accredit more than 1,530 U.S. cancer centers. This accreditation process is used not only for initial verification of achievement of program standards, but also for periodic review for compliance to maintain accreditation.
Early in its history, the College also established a Committee on the Treatment of Fractures, which evolved into what we now know as the Committee on Trauma (COT). The COT’s guidelines for hospitals to attain or maintain verification as trauma centers—Resources for Optimal Care of the Injured Patient—was first issued in 1976 and now is in its sixth edition.
Another seminal event in trauma took place in 1976—an airplane crash involving James K. Styner, MD, FACS, and his family, in rural Nebraska. His wife died on impact, and his children were severely injured. Angered by the delays his family experienced in receiving appropriate care, Dr. Styner called for the development of adequate facilities and standardized approaches to care for severely injured patients. He combined forces with Paul E. “Skip” Collicott, MD, FACS, and other Nebraska surgeons, to develop the Advanced Trauma Life Support® program, which introduces physicians and other health care professionals around the world to best practices for initial evaluation and management of trauma patients.
ACS Regent Lenworth M. Jacobs, Jr., MD, MPH, FACS, has led more recent COT initiatives, including development of the Advanced Trauma Operative Management® course and the Hartford ConsensusTM. This panel—composed of trauma care professionals and government officials—developed the Stop the Bleed program—an initiative aimed at enhancing survival from mass casualty and active shooter events.
Another important committee that the College established to ensure surgeons are prepared to do what’s right for the patient is the Committee on Emerging Surgical Technology and Education (CESTE). Launched in 1992 with the late C. James Carrico, MD, FACS, as the inaugural Chair, CESTE was charged with developing processes to evaluate emerging surgical technology for safety and effectiveness, creating standardized education programs, and measuring outcomes. Two of the College’s most important education and quality programs sprang from CESTE—the Accredited Education Institutes, under the leadership of Ajit K. Sachdeva, MD, FACS, Director, ACS Division of Education, and the Division of Research and Optimal Patient Care, first led by R. Scott Jones, MD, FACS, and now under the purview of Clifford Y. Ko, MD, MS, FACS.
The future is in your hands
Unquestionably, the ACS and its leaders have a rich history of doing what’s right for the patient. The future, however, belongs to you. I want to encourage you to participate in all the activities of your College at the local, state, and national levels. Establish personal relationships with leaders. Be an advocate for our education and quality programs. I am confident that there are those among you who will become the leaders who will continue the evolution of the College and inspire quality, maintain the highest standards, and ensure better outcomes.
Dr. Townsend is the Robertson-Poth Distinguished Chair in General Surgery, department of surgery, University of Texas Medical Branch (UTMB), Galveston; professor of surgery, department of surgery, professor of physician assistant studies, School of Allied Health Sciences; and graduate faculty in the cell biology program, UTMB. He is the 97th President of the ACS.
Steroid use in adolescents
Anabolic androgenic steroid (AAS) use in athletes is not a new topic. In fact, many teens can relate a story involving a famous athlete and use of a performance-enhancing drug and the consequences associated with it. Although published data do not support a significant increase in use of performance-enhancing drugs among adolescents,1 more recent studies show that anabolic steroids are being found in nonprescription supplements, and their use among adolescents may be substantially underestimated.
Supplements are not regulated by the Food and Drug Administration, so many of these products are easily found on the Internet and sold in local stores.2,3 Some of these are marketed for increasing muscle mass, strength, and performance, which is appealing to the young athlete. Much of the marketing of these products minimize the side effects associated with their use and, therefore, most users are unaware of their harmful effects.
Approximately 5%-11% of teen athletes use AAS to improve physique and performance.3 Given its promotion for improved physique, many nonathletes also are turning to AAS for weight loss in both males and females. Side effects of steroid use are extrapolated from the data of therapeutic use, but most adolescents using steroids are not using under medical supervision. The dosing for building muscle mass uses a pyramid type dosing over a 6- to 12-week period and can be up to forty times the therapeutic dosing; therefore, the side effects can be greater than reported.4,5 Common side effects of AAS are hypogonadism, gynecomastia, decreased sperm count and infertility, acne, and aggressiveness. Liver tumors and psychosis have been reported, and increased depressed mood have been identified with discontinuation of use.4,6 Studies suggest that these side effects are reversible with discontinuation, but more studies are needed.4,6
Given that many of the side effects are not identifiable on physical exam, pediatricians must be proactive in questioning adolescents about their knowledge and use of AAS. Testing for steroid use is difficult and not very sensitive. Urine test for carbon isotopes 13/12 is the most common test, but if not done within hours of ingestion it will not be detected. T/E test (testosterone/epitestosterone glucuronide) is another test, but also limited by the timing of the test.6 Home screening also is available but the American Academy of Pediatrics 2014 guidelines warns against parents using these given the high false positive rate and risk of confrontation.7
Home and school screening may function more to deter athletes from using steroids to avoid consequences of being caught more than actually identifying use. If an athlete is suspected of using steroids, a test should be done. If negative, it should be repeated another time, as repeated testing is more likely to identify use. Studies have shown a correlation between steroid use and use of other illicit drugs so further screening should be done to identify if other drugs are being used.8
Widespread screening has not been shown to be cost effective and, therefore, should not be encouraged. Educating the patient on the risk of use and potential side effects along with healthy alternatives that improve performance and physique is much more effective.9 Being observant to signs and symptoms of AAS use helps to initiate conversation on the risk of using anabolic steroids.
References
1. Arch Pediatr Adolesc Med. 1997 Dec;151(12):1197-206.
2. Subst Use Misuse. 2012 Feb; 47(3):329-41.
3. Am J Clin Nutr. 2000 Feb;71(2):399-400.
4. J Sports Sci Med. 2006 Jun 1;5(2):182-93.
5. Br J Sports Med. 2006 Jul; 40(Suppl 1): i21-24.
6. J Athl Train. 1994 Mar; 29(1):60-4.
7. Pediatrics. 2014;133:e1798-1807.
8. Pediatrics. 1995 Jul;96(1 Pt 1):23-8.
9. Pediatrics. 1997 Jun;99(6):904-8.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
Anabolic androgenic steroid (AAS) use in athletes is not a new topic. In fact, many teens can relate a story involving a famous athlete and use of a performance-enhancing drug and the consequences associated with it. Although published data do not support a significant increase in use of performance-enhancing drugs among adolescents,1 more recent studies show that anabolic steroids are being found in nonprescription supplements, and their use among adolescents may be substantially underestimated.
Supplements are not regulated by the Food and Drug Administration, so many of these products are easily found on the Internet and sold in local stores.2,3 Some of these are marketed for increasing muscle mass, strength, and performance, which is appealing to the young athlete. Much of the marketing of these products minimize the side effects associated with their use and, therefore, most users are unaware of their harmful effects.
Approximately 5%-11% of teen athletes use AAS to improve physique and performance.3 Given its promotion for improved physique, many nonathletes also are turning to AAS for weight loss in both males and females. Side effects of steroid use are extrapolated from the data of therapeutic use, but most adolescents using steroids are not using under medical supervision. The dosing for building muscle mass uses a pyramid type dosing over a 6- to 12-week period and can be up to forty times the therapeutic dosing; therefore, the side effects can be greater than reported.4,5 Common side effects of AAS are hypogonadism, gynecomastia, decreased sperm count and infertility, acne, and aggressiveness. Liver tumors and psychosis have been reported, and increased depressed mood have been identified with discontinuation of use.4,6 Studies suggest that these side effects are reversible with discontinuation, but more studies are needed.4,6
Given that many of the side effects are not identifiable on physical exam, pediatricians must be proactive in questioning adolescents about their knowledge and use of AAS. Testing for steroid use is difficult and not very sensitive. Urine test for carbon isotopes 13/12 is the most common test, but if not done within hours of ingestion it will not be detected. T/E test (testosterone/epitestosterone glucuronide) is another test, but also limited by the timing of the test.6 Home screening also is available but the American Academy of Pediatrics 2014 guidelines warns against parents using these given the high false positive rate and risk of confrontation.7
Home and school screening may function more to deter athletes from using steroids to avoid consequences of being caught more than actually identifying use. If an athlete is suspected of using steroids, a test should be done. If negative, it should be repeated another time, as repeated testing is more likely to identify use. Studies have shown a correlation between steroid use and use of other illicit drugs so further screening should be done to identify if other drugs are being used.8
Widespread screening has not been shown to be cost effective and, therefore, should not be encouraged. Educating the patient on the risk of use and potential side effects along with healthy alternatives that improve performance and physique is much more effective.9 Being observant to signs and symptoms of AAS use helps to initiate conversation on the risk of using anabolic steroids.
References
1. Arch Pediatr Adolesc Med. 1997 Dec;151(12):1197-206.
2. Subst Use Misuse. 2012 Feb; 47(3):329-41.
3. Am J Clin Nutr. 2000 Feb;71(2):399-400.
4. J Sports Sci Med. 2006 Jun 1;5(2):182-93.
5. Br J Sports Med. 2006 Jul; 40(Suppl 1): i21-24.
6. J Athl Train. 1994 Mar; 29(1):60-4.
7. Pediatrics. 2014;133:e1798-1807.
8. Pediatrics. 1995 Jul;96(1 Pt 1):23-8.
9. Pediatrics. 1997 Jun;99(6):904-8.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
Anabolic androgenic steroid (AAS) use in athletes is not a new topic. In fact, many teens can relate a story involving a famous athlete and use of a performance-enhancing drug and the consequences associated with it. Although published data do not support a significant increase in use of performance-enhancing drugs among adolescents,1 more recent studies show that anabolic steroids are being found in nonprescription supplements, and their use among adolescents may be substantially underestimated.
Supplements are not regulated by the Food and Drug Administration, so many of these products are easily found on the Internet and sold in local stores.2,3 Some of these are marketed for increasing muscle mass, strength, and performance, which is appealing to the young athlete. Much of the marketing of these products minimize the side effects associated with their use and, therefore, most users are unaware of their harmful effects.
Approximately 5%-11% of teen athletes use AAS to improve physique and performance.3 Given its promotion for improved physique, many nonathletes also are turning to AAS for weight loss in both males and females. Side effects of steroid use are extrapolated from the data of therapeutic use, but most adolescents using steroids are not using under medical supervision. The dosing for building muscle mass uses a pyramid type dosing over a 6- to 12-week period and can be up to forty times the therapeutic dosing; therefore, the side effects can be greater than reported.4,5 Common side effects of AAS are hypogonadism, gynecomastia, decreased sperm count and infertility, acne, and aggressiveness. Liver tumors and psychosis have been reported, and increased depressed mood have been identified with discontinuation of use.4,6 Studies suggest that these side effects are reversible with discontinuation, but more studies are needed.4,6
Given that many of the side effects are not identifiable on physical exam, pediatricians must be proactive in questioning adolescents about their knowledge and use of AAS. Testing for steroid use is difficult and not very sensitive. Urine test for carbon isotopes 13/12 is the most common test, but if not done within hours of ingestion it will not be detected. T/E test (testosterone/epitestosterone glucuronide) is another test, but also limited by the timing of the test.6 Home screening also is available but the American Academy of Pediatrics 2014 guidelines warns against parents using these given the high false positive rate and risk of confrontation.7
Home and school screening may function more to deter athletes from using steroids to avoid consequences of being caught more than actually identifying use. If an athlete is suspected of using steroids, a test should be done. If negative, it should be repeated another time, as repeated testing is more likely to identify use. Studies have shown a correlation between steroid use and use of other illicit drugs so further screening should be done to identify if other drugs are being used.8
Widespread screening has not been shown to be cost effective and, therefore, should not be encouraged. Educating the patient on the risk of use and potential side effects along with healthy alternatives that improve performance and physique is much more effective.9 Being observant to signs and symptoms of AAS use helps to initiate conversation on the risk of using anabolic steroids.
References
1. Arch Pediatr Adolesc Med. 1997 Dec;151(12):1197-206.
2. Subst Use Misuse. 2012 Feb; 47(3):329-41.
3. Am J Clin Nutr. 2000 Feb;71(2):399-400.
4. J Sports Sci Med. 2006 Jun 1;5(2):182-93.
5. Br J Sports Med. 2006 Jul; 40(Suppl 1): i21-24.
6. J Athl Train. 1994 Mar; 29(1):60-4.
7. Pediatrics. 2014;133:e1798-1807.
8. Pediatrics. 1995 Jul;96(1 Pt 1):23-8.
9. Pediatrics. 1997 Jun;99(6):904-8.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
Eating disorders in transgender youth
The field of transgender health is growing. What began as a lone German physician in 1918 defying the norms of treating gender identity as a disease now has burgeoned into a field that includes 1,079 PubMed articles,two medical guidelines1,2, and a multitude of books. As we learn more about the complexity of gender and gender identity, we also are discovering potential problems that occur when providing care to our transgender patients. One is eating disorders.
A systematic review by Jones et al. showed only a handful of studies on eating disorders in transgender individuals, most of them restricted to case studies.3 In some situations, the issue of gender identity arises during treatment for an eating disorder, as the individual realizes that body dissatisfaction is due to the gender identity instead of a fear of gaining weight. In other cases, a transgender person in the process of transitioning to the affirmed gender develops an eating disorder.
There are two larger quantitative studies on eating disorders among transgender individuals. One study of 289,024 college students reveals that transgender students, compared to cisgender students, are almost five times as likely to report an eating disorder and two times as likely to use unhealthy compensatory methods (e.g., vomiting) for weight control.4 Another study of almost 2,500 teenagers shows that transgender individuals are almost three times as likely to restrict their eating, almost nine times as likely to take diet pills, and seven times as likely to take laxatives.5
The most commonly suggested reason for the possible elevated risk for eating disorders among transgender individuals is that many of them are trying to achieve the unrealistic standards of the ideal masculine or feminine body type. Another explanation is that eating disorders among transgender individuals are maladaptive coping mechanisms to stress from antitrans stigma and discrimination.4 However, these explanations are not mutually exclusive and could simultaneously drive disordered eating among transgender individuals.
To further appreciate the relationship between these two conditions, one must understand their similarities and differences. The Diagnostic Statistical Manual of Mental Disorders V characterizes eating disorders as “a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and ... significantly impairs physical health or psychosocial functioning.”6 Anorexia nervosa and bulimia nervosa are driven by fear of gaining weight or by a self-esteem unduly influenced by weight or appearance.6
Gender dysphoria, in comparison, is the distress caused by the incongruence between one’s gender identity and one’s anatomy, along with the desire to have the characteristics of one’s affirmed gender identity. This condition also could severely alter physical and psychosocial functioning,7 partly because of the distress from the incongruence, and partly because of the stress from antitrans stigma and discrimination, as an individual attempts to match the body with the gender identity8 (e.g., wearing clothing to match the gender identity).
The higher risk of developing an eating disorder among transgender individuals makes sense. Dissatisfaction with one’s body characterizes both conditions. The high standards on what is masculine or feminine affects everyone, especially transgender individuals who may feel that they’re “far behind” when they begin to transition to their affirmed gender. In addition, both involve identity. Those who have anorexia nervosa also incorporate this into their own identity.9 This is why treating an eating disorder can be very difficult.
Finally, individuals afflicted by an eating disorder or gender dysphoria engage in certain behaviors to achieve their desired appearance. However, this is where the similarities end. One major distinction between an eating disorder and gender dysphoria is the treatment approach. The goal in treating an eating disorder is to discourage the disordered behavior and encourage healthier eating habits and a more positive body image. Affirming the identity of someone with an eating disorder can be deadly, as it will encourage more disordered eating.10 In contrast, affirming the identity of someone with gender dysphoria through social transition, cross-sex hormones, and/or surgical reassignment is life-saving and therapeutic.11
There is little guidance on how to treat the these disorders simultaneously. What complicates treating both conditions at the same time is that when an eating disorder is accompanied by another mental health disorder (e.g., substance use), one condition over the other is prioritized.12 There is no guidance on whether the eating disorder or gender dysphoria should take priority over the other, or if it is possible to treat both conditions at the same time.
Strandjord et al. suggest a hierarchal approach, in which life-threatening issues (such as suicide or electrolyte disturbances) take priority.13 In addition, if the patient is malnourished, weight restoration should be the initial focus. A patient who is severely malnourished may not have the cognitive capacity nor the physiological ability to manage comorbidities such as anxiety or depression,12 much less have the capacity to process something as complex as gender and gender identity, nor understand the steps necessary for a successful transition to the affirmed gender. However, this does not mean providers should wait to successfully manage an eating disorder before addressing gender dysphoria. Studies have suggested that gender-affirming medical therapies (e.g., cross sex hormones) can be therapeutic for both gender dysphoria and eating disorder symptoms.14 Finally, because of the two ways a transgender patient with an eating disorder can present, I recommend screening for eating disorders in transgender individuals and inquiring about gender identity among those with an eating disorder. Doing so may save a life.
References
1. J Clin Endocrinol Metab. 2009 Sep;94(9):3132-54.
2. Adv Urol. 2012;2012:581712.
3. Int Rev Psychiatry. 2016;28(1):81-94.
4. J Adolesc Health. 2015 Aug;57(2):144-9.
5. J Adolesc Health. 2016. doi: 10.1016/j.jadohealth.2016.08.027.
6. Feeding and Eating Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
7. Gender Dysphoria. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
8. Psychol Bull. 2003 Sep;129(5):674-97.
9. Int J Law Psychiatry. 2003 Sep-Oct;26(5):533-48.
10. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
11. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
12. CNS drugs. 2006;20(8):655-63.
13. Int J Eat Disord. 2015 Nov;48(7):942-5.
14. Eat Disord. 2012;20(4):300-11.
The field of transgender health is growing. What began as a lone German physician in 1918 defying the norms of treating gender identity as a disease now has burgeoned into a field that includes 1,079 PubMed articles,two medical guidelines1,2, and a multitude of books. As we learn more about the complexity of gender and gender identity, we also are discovering potential problems that occur when providing care to our transgender patients. One is eating disorders.
A systematic review by Jones et al. showed only a handful of studies on eating disorders in transgender individuals, most of them restricted to case studies.3 In some situations, the issue of gender identity arises during treatment for an eating disorder, as the individual realizes that body dissatisfaction is due to the gender identity instead of a fear of gaining weight. In other cases, a transgender person in the process of transitioning to the affirmed gender develops an eating disorder.
There are two larger quantitative studies on eating disorders among transgender individuals. One study of 289,024 college students reveals that transgender students, compared to cisgender students, are almost five times as likely to report an eating disorder and two times as likely to use unhealthy compensatory methods (e.g., vomiting) for weight control.4 Another study of almost 2,500 teenagers shows that transgender individuals are almost three times as likely to restrict their eating, almost nine times as likely to take diet pills, and seven times as likely to take laxatives.5
The most commonly suggested reason for the possible elevated risk for eating disorders among transgender individuals is that many of them are trying to achieve the unrealistic standards of the ideal masculine or feminine body type. Another explanation is that eating disorders among transgender individuals are maladaptive coping mechanisms to stress from antitrans stigma and discrimination.4 However, these explanations are not mutually exclusive and could simultaneously drive disordered eating among transgender individuals.
To further appreciate the relationship between these two conditions, one must understand their similarities and differences. The Diagnostic Statistical Manual of Mental Disorders V characterizes eating disorders as “a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and ... significantly impairs physical health or psychosocial functioning.”6 Anorexia nervosa and bulimia nervosa are driven by fear of gaining weight or by a self-esteem unduly influenced by weight or appearance.6
Gender dysphoria, in comparison, is the distress caused by the incongruence between one’s gender identity and one’s anatomy, along with the desire to have the characteristics of one’s affirmed gender identity. This condition also could severely alter physical and psychosocial functioning,7 partly because of the distress from the incongruence, and partly because of the stress from antitrans stigma and discrimination, as an individual attempts to match the body with the gender identity8 (e.g., wearing clothing to match the gender identity).
The higher risk of developing an eating disorder among transgender individuals makes sense. Dissatisfaction with one’s body characterizes both conditions. The high standards on what is masculine or feminine affects everyone, especially transgender individuals who may feel that they’re “far behind” when they begin to transition to their affirmed gender. In addition, both involve identity. Those who have anorexia nervosa also incorporate this into their own identity.9 This is why treating an eating disorder can be very difficult.
Finally, individuals afflicted by an eating disorder or gender dysphoria engage in certain behaviors to achieve their desired appearance. However, this is where the similarities end. One major distinction between an eating disorder and gender dysphoria is the treatment approach. The goal in treating an eating disorder is to discourage the disordered behavior and encourage healthier eating habits and a more positive body image. Affirming the identity of someone with an eating disorder can be deadly, as it will encourage more disordered eating.10 In contrast, affirming the identity of someone with gender dysphoria through social transition, cross-sex hormones, and/or surgical reassignment is life-saving and therapeutic.11
There is little guidance on how to treat the these disorders simultaneously. What complicates treating both conditions at the same time is that when an eating disorder is accompanied by another mental health disorder (e.g., substance use), one condition over the other is prioritized.12 There is no guidance on whether the eating disorder or gender dysphoria should take priority over the other, or if it is possible to treat both conditions at the same time.
Strandjord et al. suggest a hierarchal approach, in which life-threatening issues (such as suicide or electrolyte disturbances) take priority.13 In addition, if the patient is malnourished, weight restoration should be the initial focus. A patient who is severely malnourished may not have the cognitive capacity nor the physiological ability to manage comorbidities such as anxiety or depression,12 much less have the capacity to process something as complex as gender and gender identity, nor understand the steps necessary for a successful transition to the affirmed gender. However, this does not mean providers should wait to successfully manage an eating disorder before addressing gender dysphoria. Studies have suggested that gender-affirming medical therapies (e.g., cross sex hormones) can be therapeutic for both gender dysphoria and eating disorder symptoms.14 Finally, because of the two ways a transgender patient with an eating disorder can present, I recommend screening for eating disorders in transgender individuals and inquiring about gender identity among those with an eating disorder. Doing so may save a life.
References
1. J Clin Endocrinol Metab. 2009 Sep;94(9):3132-54.
2. Adv Urol. 2012;2012:581712.
3. Int Rev Psychiatry. 2016;28(1):81-94.
4. J Adolesc Health. 2015 Aug;57(2):144-9.
5. J Adolesc Health. 2016. doi: 10.1016/j.jadohealth.2016.08.027.
6. Feeding and Eating Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
7. Gender Dysphoria. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
8. Psychol Bull. 2003 Sep;129(5):674-97.
9. Int J Law Psychiatry. 2003 Sep-Oct;26(5):533-48.
10. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
11. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
12. CNS drugs. 2006;20(8):655-63.
13. Int J Eat Disord. 2015 Nov;48(7):942-5.
14. Eat Disord. 2012;20(4):300-11.
The field of transgender health is growing. What began as a lone German physician in 1918 defying the norms of treating gender identity as a disease now has burgeoned into a field that includes 1,079 PubMed articles,two medical guidelines1,2, and a multitude of books. As we learn more about the complexity of gender and gender identity, we also are discovering potential problems that occur when providing care to our transgender patients. One is eating disorders.
A systematic review by Jones et al. showed only a handful of studies on eating disorders in transgender individuals, most of them restricted to case studies.3 In some situations, the issue of gender identity arises during treatment for an eating disorder, as the individual realizes that body dissatisfaction is due to the gender identity instead of a fear of gaining weight. In other cases, a transgender person in the process of transitioning to the affirmed gender develops an eating disorder.
There are two larger quantitative studies on eating disorders among transgender individuals. One study of 289,024 college students reveals that transgender students, compared to cisgender students, are almost five times as likely to report an eating disorder and two times as likely to use unhealthy compensatory methods (e.g., vomiting) for weight control.4 Another study of almost 2,500 teenagers shows that transgender individuals are almost three times as likely to restrict their eating, almost nine times as likely to take diet pills, and seven times as likely to take laxatives.5
The most commonly suggested reason for the possible elevated risk for eating disorders among transgender individuals is that many of them are trying to achieve the unrealistic standards of the ideal masculine or feminine body type. Another explanation is that eating disorders among transgender individuals are maladaptive coping mechanisms to stress from antitrans stigma and discrimination.4 However, these explanations are not mutually exclusive and could simultaneously drive disordered eating among transgender individuals.
To further appreciate the relationship between these two conditions, one must understand their similarities and differences. The Diagnostic Statistical Manual of Mental Disorders V characterizes eating disorders as “a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and ... significantly impairs physical health or psychosocial functioning.”6 Anorexia nervosa and bulimia nervosa are driven by fear of gaining weight or by a self-esteem unduly influenced by weight or appearance.6
Gender dysphoria, in comparison, is the distress caused by the incongruence between one’s gender identity and one’s anatomy, along with the desire to have the characteristics of one’s affirmed gender identity. This condition also could severely alter physical and psychosocial functioning,7 partly because of the distress from the incongruence, and partly because of the stress from antitrans stigma and discrimination, as an individual attempts to match the body with the gender identity8 (e.g., wearing clothing to match the gender identity).
The higher risk of developing an eating disorder among transgender individuals makes sense. Dissatisfaction with one’s body characterizes both conditions. The high standards on what is masculine or feminine affects everyone, especially transgender individuals who may feel that they’re “far behind” when they begin to transition to their affirmed gender. In addition, both involve identity. Those who have anorexia nervosa also incorporate this into their own identity.9 This is why treating an eating disorder can be very difficult.
Finally, individuals afflicted by an eating disorder or gender dysphoria engage in certain behaviors to achieve their desired appearance. However, this is where the similarities end. One major distinction between an eating disorder and gender dysphoria is the treatment approach. The goal in treating an eating disorder is to discourage the disordered behavior and encourage healthier eating habits and a more positive body image. Affirming the identity of someone with an eating disorder can be deadly, as it will encourage more disordered eating.10 In contrast, affirming the identity of someone with gender dysphoria through social transition, cross-sex hormones, and/or surgical reassignment is life-saving and therapeutic.11
There is little guidance on how to treat the these disorders simultaneously. What complicates treating both conditions at the same time is that when an eating disorder is accompanied by another mental health disorder (e.g., substance use), one condition over the other is prioritized.12 There is no guidance on whether the eating disorder or gender dysphoria should take priority over the other, or if it is possible to treat both conditions at the same time.
Strandjord et al. suggest a hierarchal approach, in which life-threatening issues (such as suicide or electrolyte disturbances) take priority.13 In addition, if the patient is malnourished, weight restoration should be the initial focus. A patient who is severely malnourished may not have the cognitive capacity nor the physiological ability to manage comorbidities such as anxiety or depression,12 much less have the capacity to process something as complex as gender and gender identity, nor understand the steps necessary for a successful transition to the affirmed gender. However, this does not mean providers should wait to successfully manage an eating disorder before addressing gender dysphoria. Studies have suggested that gender-affirming medical therapies (e.g., cross sex hormones) can be therapeutic for both gender dysphoria and eating disorder symptoms.14 Finally, because of the two ways a transgender patient with an eating disorder can present, I recommend screening for eating disorders in transgender individuals and inquiring about gender identity among those with an eating disorder. Doing so may save a life.
References
1. J Clin Endocrinol Metab. 2009 Sep;94(9):3132-54.
2. Adv Urol. 2012;2012:581712.
3. Int Rev Psychiatry. 2016;28(1):81-94.
4. J Adolesc Health. 2015 Aug;57(2):144-9.
5. J Adolesc Health. 2016. doi: 10.1016/j.jadohealth.2016.08.027.
6. Feeding and Eating Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
7. Gender Dysphoria. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
8. Psychol Bull. 2003 Sep;129(5):674-97.
9. Int J Law Psychiatry. 2003 Sep-Oct;26(5):533-48.
10. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
11. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
12. CNS drugs. 2006;20(8):655-63.
13. Int J Eat Disord. 2015 Nov;48(7):942-5.
14. Eat Disord. 2012;20(4):300-11.
Not enough time? Time to rethink
Raising children is a lot like drinking out of a fire hose. Feeding, cleaning, dressing, transporting, teaching, entertaining, protecting, comforting, and managing one child is demanding, but is increased exponentially by multiple children, a spouse, and a job.
In our dataset of more than 74,900 parents of 0- to 3-year-olds completing a routine previsit questionnaire about the “best” and “hardest” parts of parenting their child, the most frequent spontaneous comment for the hardest part was “time-life balance.” The goal of asking these questions is to broaden the agenda for the pediatric visit to address stresses that are highly relevant to the child’s life in the family, and their current well-being and future outcome. The hardest part also rather succinctly captures the stress I hear every day from parents coming to me not only for health supervision, but especially for child behavior problems.
Setting limits on work to free up more time is not possible for everyone. Many people are grateful to have a job at all or need multiple jobs to make ends meet. They may not be in a position to negotiate for fewer tasks, hours, or roles. But others more fortunate may have fallen into a habit of taking on extra duties, taking work home, or simply not examining where they might set limits to preserve time for themselves and their family.
Working parents may need to prepare themselves for the onslaught when they get home. If the returning parent retreats into TV, the computer, or the bedroom, it makes the children feel angry and rejected. The parent who has been managing the household for the preceding hour(s) feels resentful, unappreciated, and often exhausted. I sometimes suggest that the returning parent pause 15 minutes to take a walk before picking children up at day care or go to the gym before coming home to be ready to engage, accept, and be present for whatever happens when they open the door.
Eliciting the “hardest part” can insert a pause for some much-needed problem-solving. Pointing out to parents the value to their child of working on their own time-life balance often gives them needed permission to make changes.
Balancing time for some parents may include setting some privacy for “alone time.” Individual desire to be alone varies, but trouble getting it is universal, especially with young children who don’t even respect a closed bathroom door! Given a young child’s need for contact about every 3-5 minutes, parents need to revise their expectations, wait until after bedtime, get some help, learn to do “token” relaxation, or all of these.
Parents often feel guilty for not attending more to their child, but then feel irritable about getting behind on other chores. It can be useful to cite the fact that mothers at home full time typically spend only 20 minutes of exclusive playtime with their child. I regularly prescribe 15 minutes of “special time” daily to break this irritability cycle for both the parent and child. Getting a babysitter does not mean that the parent has to leave the house and the undone laundry. I often suggest to resource-strapped families that they pay an 8-year-old neighbor to play with their kids for an hour several times per week. While not expecting to leave the child alone with such a “sitter,” one could relax in the tub, read a magazine, or make an uninterrupted phone call to a friend with such help.
The same parents feeling the pinch of too little time often are lacking in social support, a major buffer of stress. Sometimes, the solutions overlap. For example, trading play dates with another family by taking all their kids on a regular basis and vice versa requires no money exchange. Several kids playing together are often easier to care for than one’s own with their usual sibling struggles or boredom. And sharing of this kind can build lasting friendships and social support for the adults. Another often forgotten source of adult rest coupled with social support is religious services that offer “Sunday School.” The service has built-in cues to meditation, the kids make new friends protected by accepting teachers, and the social hour builds social support for the parents.
But we can’t really insert more hours in the day, right? Actually, one of the most valuable suggestions may be for parents to keep a diary of their activities for a few days. The average American in 2015 clocked 147 minutes watching TV, 103 minutes in front of a computer, 151 minutes on smart phones, and 43 minutes with a tablet. These time wasters may not only not feel satisfying or even relaxing, but even prompt anxiety or envy, and certainly take away from sleep, exercise, and intimacy. The American Academy of Pediatrics recently provided a Media Calculator and Family Media Plan intended to help families consider these choices for their child’s media life within all the other required activities of a day (including sleep), but adults could benefit from the same approach to making decisions about how they budget their time.
By mapping out actual time spent, parents can then reevaluate and choose differently. A useful question we might ask frazzled parents is “What fills your tank?” to help them come up with a list of activities that (used to be) regenerative to put on the new schedule. Most people blurt out “go on a cruise” (not practical) when “token” activities can suffice and be immediately possible. Coach them to be creative! Instead of a cruise, take a walk around the block; instead of going to a spa, request a back rub at bedtime; instead of a movie, watch a YouTube clip. When allowing oneself to be fully present to such “tokens,” they can have immense value. The practice of mindfulness (for which many training apps are available) can heighten awareness of each moment and expand the sense of time. Meditation and yoga training both are proven to provide benefits for relaxation and well-being that can be fit into anyone’s day.
While this column is intended to help with pediatric practice, I’ll bet you thought I was talking about you! With the pace of current health care practice and emphasis on “productivity,” many pediatricians are struggling with balancing time for themselves and their families as well. All the ideas just discussed also apply to you, but maybe, just maybe, you have the resources to insist on limits on work you haven’t seized. Cherishing the years when you have children in your life is for you, too, not just your patients. Remember, “The days are long, but the years are short.”
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at [email protected].
Raising children is a lot like drinking out of a fire hose. Feeding, cleaning, dressing, transporting, teaching, entertaining, protecting, comforting, and managing one child is demanding, but is increased exponentially by multiple children, a spouse, and a job.
In our dataset of more than 74,900 parents of 0- to 3-year-olds completing a routine previsit questionnaire about the “best” and “hardest” parts of parenting their child, the most frequent spontaneous comment for the hardest part was “time-life balance.” The goal of asking these questions is to broaden the agenda for the pediatric visit to address stresses that are highly relevant to the child’s life in the family, and their current well-being and future outcome. The hardest part also rather succinctly captures the stress I hear every day from parents coming to me not only for health supervision, but especially for child behavior problems.
Setting limits on work to free up more time is not possible for everyone. Many people are grateful to have a job at all or need multiple jobs to make ends meet. They may not be in a position to negotiate for fewer tasks, hours, or roles. But others more fortunate may have fallen into a habit of taking on extra duties, taking work home, or simply not examining where they might set limits to preserve time for themselves and their family.
Working parents may need to prepare themselves for the onslaught when they get home. If the returning parent retreats into TV, the computer, or the bedroom, it makes the children feel angry and rejected. The parent who has been managing the household for the preceding hour(s) feels resentful, unappreciated, and often exhausted. I sometimes suggest that the returning parent pause 15 minutes to take a walk before picking children up at day care or go to the gym before coming home to be ready to engage, accept, and be present for whatever happens when they open the door.
Eliciting the “hardest part” can insert a pause for some much-needed problem-solving. Pointing out to parents the value to their child of working on their own time-life balance often gives them needed permission to make changes.
Balancing time for some parents may include setting some privacy for “alone time.” Individual desire to be alone varies, but trouble getting it is universal, especially with young children who don’t even respect a closed bathroom door! Given a young child’s need for contact about every 3-5 minutes, parents need to revise their expectations, wait until after bedtime, get some help, learn to do “token” relaxation, or all of these.
Parents often feel guilty for not attending more to their child, but then feel irritable about getting behind on other chores. It can be useful to cite the fact that mothers at home full time typically spend only 20 minutes of exclusive playtime with their child. I regularly prescribe 15 minutes of “special time” daily to break this irritability cycle for both the parent and child. Getting a babysitter does not mean that the parent has to leave the house and the undone laundry. I often suggest to resource-strapped families that they pay an 8-year-old neighbor to play with their kids for an hour several times per week. While not expecting to leave the child alone with such a “sitter,” one could relax in the tub, read a magazine, or make an uninterrupted phone call to a friend with such help.
The same parents feeling the pinch of too little time often are lacking in social support, a major buffer of stress. Sometimes, the solutions overlap. For example, trading play dates with another family by taking all their kids on a regular basis and vice versa requires no money exchange. Several kids playing together are often easier to care for than one’s own with their usual sibling struggles or boredom. And sharing of this kind can build lasting friendships and social support for the adults. Another often forgotten source of adult rest coupled with social support is religious services that offer “Sunday School.” The service has built-in cues to meditation, the kids make new friends protected by accepting teachers, and the social hour builds social support for the parents.
But we can’t really insert more hours in the day, right? Actually, one of the most valuable suggestions may be for parents to keep a diary of their activities for a few days. The average American in 2015 clocked 147 minutes watching TV, 103 minutes in front of a computer, 151 minutes on smart phones, and 43 minutes with a tablet. These time wasters may not only not feel satisfying or even relaxing, but even prompt anxiety or envy, and certainly take away from sleep, exercise, and intimacy. The American Academy of Pediatrics recently provided a Media Calculator and Family Media Plan intended to help families consider these choices for their child’s media life within all the other required activities of a day (including sleep), but adults could benefit from the same approach to making decisions about how they budget their time.
By mapping out actual time spent, parents can then reevaluate and choose differently. A useful question we might ask frazzled parents is “What fills your tank?” to help them come up with a list of activities that (used to be) regenerative to put on the new schedule. Most people blurt out “go on a cruise” (not practical) when “token” activities can suffice and be immediately possible. Coach them to be creative! Instead of a cruise, take a walk around the block; instead of going to a spa, request a back rub at bedtime; instead of a movie, watch a YouTube clip. When allowing oneself to be fully present to such “tokens,” they can have immense value. The practice of mindfulness (for which many training apps are available) can heighten awareness of each moment and expand the sense of time. Meditation and yoga training both are proven to provide benefits for relaxation and well-being that can be fit into anyone’s day.
While this column is intended to help with pediatric practice, I’ll bet you thought I was talking about you! With the pace of current health care practice and emphasis on “productivity,” many pediatricians are struggling with balancing time for themselves and their families as well. All the ideas just discussed also apply to you, but maybe, just maybe, you have the resources to insist on limits on work you haven’t seized. Cherishing the years when you have children in your life is for you, too, not just your patients. Remember, “The days are long, but the years are short.”
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at [email protected].
Raising children is a lot like drinking out of a fire hose. Feeding, cleaning, dressing, transporting, teaching, entertaining, protecting, comforting, and managing one child is demanding, but is increased exponentially by multiple children, a spouse, and a job.
In our dataset of more than 74,900 parents of 0- to 3-year-olds completing a routine previsit questionnaire about the “best” and “hardest” parts of parenting their child, the most frequent spontaneous comment for the hardest part was “time-life balance.” The goal of asking these questions is to broaden the agenda for the pediatric visit to address stresses that are highly relevant to the child’s life in the family, and their current well-being and future outcome. The hardest part also rather succinctly captures the stress I hear every day from parents coming to me not only for health supervision, but especially for child behavior problems.
Setting limits on work to free up more time is not possible for everyone. Many people are grateful to have a job at all or need multiple jobs to make ends meet. They may not be in a position to negotiate for fewer tasks, hours, or roles. But others more fortunate may have fallen into a habit of taking on extra duties, taking work home, or simply not examining where they might set limits to preserve time for themselves and their family.
Working parents may need to prepare themselves for the onslaught when they get home. If the returning parent retreats into TV, the computer, or the bedroom, it makes the children feel angry and rejected. The parent who has been managing the household for the preceding hour(s) feels resentful, unappreciated, and often exhausted. I sometimes suggest that the returning parent pause 15 minutes to take a walk before picking children up at day care or go to the gym before coming home to be ready to engage, accept, and be present for whatever happens when they open the door.
Eliciting the “hardest part” can insert a pause for some much-needed problem-solving. Pointing out to parents the value to their child of working on their own time-life balance often gives them needed permission to make changes.
Balancing time for some parents may include setting some privacy for “alone time.” Individual desire to be alone varies, but trouble getting it is universal, especially with young children who don’t even respect a closed bathroom door! Given a young child’s need for contact about every 3-5 minutes, parents need to revise their expectations, wait until after bedtime, get some help, learn to do “token” relaxation, or all of these.
Parents often feel guilty for not attending more to their child, but then feel irritable about getting behind on other chores. It can be useful to cite the fact that mothers at home full time typically spend only 20 minutes of exclusive playtime with their child. I regularly prescribe 15 minutes of “special time” daily to break this irritability cycle for both the parent and child. Getting a babysitter does not mean that the parent has to leave the house and the undone laundry. I often suggest to resource-strapped families that they pay an 8-year-old neighbor to play with their kids for an hour several times per week. While not expecting to leave the child alone with such a “sitter,” one could relax in the tub, read a magazine, or make an uninterrupted phone call to a friend with such help.
The same parents feeling the pinch of too little time often are lacking in social support, a major buffer of stress. Sometimes, the solutions overlap. For example, trading play dates with another family by taking all their kids on a regular basis and vice versa requires no money exchange. Several kids playing together are often easier to care for than one’s own with their usual sibling struggles or boredom. And sharing of this kind can build lasting friendships and social support for the adults. Another often forgotten source of adult rest coupled with social support is religious services that offer “Sunday School.” The service has built-in cues to meditation, the kids make new friends protected by accepting teachers, and the social hour builds social support for the parents.
But we can’t really insert more hours in the day, right? Actually, one of the most valuable suggestions may be for parents to keep a diary of their activities for a few days. The average American in 2015 clocked 147 minutes watching TV, 103 minutes in front of a computer, 151 minutes on smart phones, and 43 minutes with a tablet. These time wasters may not only not feel satisfying or even relaxing, but even prompt anxiety or envy, and certainly take away from sleep, exercise, and intimacy. The American Academy of Pediatrics recently provided a Media Calculator and Family Media Plan intended to help families consider these choices for their child’s media life within all the other required activities of a day (including sleep), but adults could benefit from the same approach to making decisions about how they budget their time.
By mapping out actual time spent, parents can then reevaluate and choose differently. A useful question we might ask frazzled parents is “What fills your tank?” to help them come up with a list of activities that (used to be) regenerative to put on the new schedule. Most people blurt out “go on a cruise” (not practical) when “token” activities can suffice and be immediately possible. Coach them to be creative! Instead of a cruise, take a walk around the block; instead of going to a spa, request a back rub at bedtime; instead of a movie, watch a YouTube clip. When allowing oneself to be fully present to such “tokens,” they can have immense value. The practice of mindfulness (for which many training apps are available) can heighten awareness of each moment and expand the sense of time. Meditation and yoga training both are proven to provide benefits for relaxation and well-being that can be fit into anyone’s day.
While this column is intended to help with pediatric practice, I’ll bet you thought I was talking about you! With the pace of current health care practice and emphasis on “productivity,” many pediatricians are struggling with balancing time for themselves and their families as well. All the ideas just discussed also apply to you, but maybe, just maybe, you have the resources to insist on limits on work you haven’t seized. Cherishing the years when you have children in your life is for you, too, not just your patients. Remember, “The days are long, but the years are short.”
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at [email protected].