User login
A Boxed Warning for Inadequate Psoriasis Treatment
The US Food and Drug Administration uses the term boxed warning to highlight potentially dangerous situations associated with prescription drugs. A boxed warning is used when “[T]here is an adverse reaction so serious in proportion to the potential benefit from the drug (e.g., a fatal, life-threatening or permanently disabling adverse reaction) that it is essential that it be considered in assessing the risks and benefits of using the drug.”1 However, drugs are not the only potential cause of severe adverse outcomes in patients with psoriasis. Untreated psoriasis also is a well-established cause of serious morbidity and mortality. What are the risks of inadequate psoriasis treatment?
Psoriasis is associated with an increased risk for cardiovascular disease.2-4 Patients with psoriasis also have a higher prevalence of classic cardiovascular risk factors including smoking, diabetes mellitus, hypertension, obesity, and hyperlipidemia.5,6 Psoriasis is a T-cell mediated disease process driven by IL-23 and TH17 helper cell–derived proinflammatory cytokines, sharing certain genetic aspects with metabolic syndrome.6 Cytokine actions on insulin signaling, lipid metabolism, and adipogenesis may underlie the increased prevalence of metabolic syndrome and cardiovascular risk factors in patients with psoriasis. In addition to treating the cutaneous manifestations of psoriasis, reducing inflammation in these patients reduces C-reactive protein and lipid peroxidation and increases high-density lipoprotein levels.6 Tumor necrosis factor α blockers decrease the risk for cardiovascular disease in patients with psoriasis.7,8 Lower than expected rates of cardiovascular disease also have been reported in a large cohort of psoriasis patients (ie, PSOLAR [Psoriasis Longitudinal Assessment and Registry] registry) being treated with either ustekinumab or tumor necrosis factor α blockers.9
Psoriatic arthritis is a chronic inflammatory disease in which active inflammation results in progressive joint destruction.10 Tumor necrosis factor α inhibitors suppress disease progression, preserve function, and delay destruction of the joints. Ustekinumab also helps control psoriatic arthritis and inhibits radiographic progression of joint disease.11
Importantly, untreated moderate to severe psoriasis is associated with several comorbidities that may lead to early death such as heart attacks and strokes.12 Furthermore, patients not taking biologic medications may have higher death rates than patients taking biologic medications.9 Psoriasis also is associated with tremendous suffering and negative psychosocial effects. The mental and physical impact of the disease is comparable to other major medical conditions (eg, cancer, arthritis, hypertension, heart disease, diabetes, depression).13 Patients also may experience physical discomfort from pain and itching.14 Children with psoriasis may experience bullying, which is associated with an increased number of depressive episodes, thereby increasing their risk for developing psychiatric conditions such as depression and anxiety as adults.15 The stigma associated with psoriasis may affect patients’ ability to build relationships. Patients with psoriasis experience higher divorce rates than patients with other chronic medical conditions, and direct involvement of genital regions may negatively impact patients’ sex lives. Patients have noted that the stigma of psoriasis also is associated with the inability to obtain employment.15 Almost one-third of patients with psoriasis who are either not working or are retired base their work status on their skin condition.16 Furthermore, psoriasis may contribute to economic burden for patients due to indirect costs associated with work absenteeism.17
Adequate treatment of psoriasis improves patients’ physical and psychological health as well as their ability to function in the workplace. However, despite the benefits of treatment, 30% of patients with severe psoriasis and 53% of patients with moderate psoriasis receive no treatment or only topical medications instead of systemic therapies.16 The potential adverse events of inadequate psoriasis treatment far outweigh any potential benefits of withholding treatment. Perhaps a boxed warning should be issued for inadequate treatment of psoriasis patients.
- US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. Guidance for industry: warning and precautions, contraindications, and boxed warning sections of labeling for human prescription drug and biological products—content and format. US Food and Drug Administration website. http://www.fda.gov/downloads/Drugs/.../Guidances/ucm075096.pdf. Published October 6, 2011. Accessed August 10, 2016.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Rose S, Sheth NH, Baker JF, et al. A comparison of vascular inflammation in psoriasis, rheumatoid arthritis, and healthy subjects by FDG-PET/CT: a pilot study. Am J Cardiovasc Dis. 2013;3:273-278.
- Shlyankevich J, Mehta NN, Krueger JG, et al. Accumulating evidence for the association and shared pathogenic mechanisms between psoriasis and cardiovascular-related comorbidities. Am J Med. 2014;127:1148-1153.
- Lee MK, Kim HS, Cho EB, et al. A study of awareness and screening behavior of cardiovascular risk factors in patients with psoriasis and dermatologists. Ann Dermatol. 2015;27:59-65.
- Voiculescu VM, Lupu M, Papagheorghe L, et al. Psoriasis and metabolic syndrome—scientific evidence and therapeutic implications. J Med Life. 2014;7:468-471.
- Wu JJ, Poon KY, Bebchuk JD. Association between the type and length of tumor necrosis factor inhibitor therapy and myocardial infarction risk in patients with psoriasis. J Drugs Dermatol. 2013;12:899-903.
- Famenini S, Sako EY, Wu JJ. Effect of treating psoriasis on cardiovascular comorbidities: focus on TNF inhibitors. Am J Clin Dermatol. 2014;15:45-50.
- Gottlieb AB, Kalb RE, Langley RG, et al. Safety observations in 12095 patients with psoriasis enrolled in an international registry (PSOLAR): experience with infliximab and other systemic and biologic therapies. J Drugs Dermatol. 2014;13:1441-1448.
- Chimenti MS, Graceffa D, Perricone R. Anti-TNFα discontinuation in rheumatoid and psoriatic arthritis: is it possible after disease remission [published online Apr 21, 2011]? Autoimmun Rev. 2011;10:636-640.
- Kavanaugh A, Ritchlin C, Rahman P, et al. Ustekinumab, an anti-IL-12/23 p40 monoclonal antibody, inhibits radiographic progression in patients with active psoriatic arthritis: results of an integrated analysis of radiographic data from the phase 3, multicentre, randomised, double-blind, placebo-controlled PSUMMIT-1 and PSUMMIT-2 trials. Ann Rheum Dis. 2014;73:1000-1006.
- Pietrzak A, Bartosinska J, Blaszczyk R, et al. Increased serum level of N-terminal Pro-B-type natriuretic peptide as a possible biomarker of cardiovascular risk in psoriatic patients. J Eur Acad Dermatol Venereol. 2015;29:1010-1014.
- Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3, pt 1):401-407.
- Pettey AA, Balkrishnan R, Rapp SR, et al. Patients with palmoplantar psoriasis have more physical disability and discomfort than patients with other forms of psoriasis: implications for clinical practice. J Am Acad Dermatol. 2003;49:271-275.
- Garshick MK, Kimball AB. Psoriasis and the life cycle of persistent life effects. Dermatol Clin. 2015;33:25-39.
- Feldman SR, Malakouti M, Koo JY. Social impact of the burden of psoriasis: effects on patients and practice. Dermatol Online J. August 17, 2014;20. pii:13030/qt48r4w8h2.
- Brezinski EA, Dhillon JS, Armstrong AW. Economic burden of psoriasis in the United States: a systematic review. JAMA Dermatol. 2015;151:651-658.
The US Food and Drug Administration uses the term boxed warning to highlight potentially dangerous situations associated with prescription drugs. A boxed warning is used when “[T]here is an adverse reaction so serious in proportion to the potential benefit from the drug (e.g., a fatal, life-threatening or permanently disabling adverse reaction) that it is essential that it be considered in assessing the risks and benefits of using the drug.”1 However, drugs are not the only potential cause of severe adverse outcomes in patients with psoriasis. Untreated psoriasis also is a well-established cause of serious morbidity and mortality. What are the risks of inadequate psoriasis treatment?
Psoriasis is associated with an increased risk for cardiovascular disease.2-4 Patients with psoriasis also have a higher prevalence of classic cardiovascular risk factors including smoking, diabetes mellitus, hypertension, obesity, and hyperlipidemia.5,6 Psoriasis is a T-cell mediated disease process driven by IL-23 and TH17 helper cell–derived proinflammatory cytokines, sharing certain genetic aspects with metabolic syndrome.6 Cytokine actions on insulin signaling, lipid metabolism, and adipogenesis may underlie the increased prevalence of metabolic syndrome and cardiovascular risk factors in patients with psoriasis. In addition to treating the cutaneous manifestations of psoriasis, reducing inflammation in these patients reduces C-reactive protein and lipid peroxidation and increases high-density lipoprotein levels.6 Tumor necrosis factor α blockers decrease the risk for cardiovascular disease in patients with psoriasis.7,8 Lower than expected rates of cardiovascular disease also have been reported in a large cohort of psoriasis patients (ie, PSOLAR [Psoriasis Longitudinal Assessment and Registry] registry) being treated with either ustekinumab or tumor necrosis factor α blockers.9
Psoriatic arthritis is a chronic inflammatory disease in which active inflammation results in progressive joint destruction.10 Tumor necrosis factor α inhibitors suppress disease progression, preserve function, and delay destruction of the joints. Ustekinumab also helps control psoriatic arthritis and inhibits radiographic progression of joint disease.11
Importantly, untreated moderate to severe psoriasis is associated with several comorbidities that may lead to early death such as heart attacks and strokes.12 Furthermore, patients not taking biologic medications may have higher death rates than patients taking biologic medications.9 Psoriasis also is associated with tremendous suffering and negative psychosocial effects. The mental and physical impact of the disease is comparable to other major medical conditions (eg, cancer, arthritis, hypertension, heart disease, diabetes, depression).13 Patients also may experience physical discomfort from pain and itching.14 Children with psoriasis may experience bullying, which is associated with an increased number of depressive episodes, thereby increasing their risk for developing psychiatric conditions such as depression and anxiety as adults.15 The stigma associated with psoriasis may affect patients’ ability to build relationships. Patients with psoriasis experience higher divorce rates than patients with other chronic medical conditions, and direct involvement of genital regions may negatively impact patients’ sex lives. Patients have noted that the stigma of psoriasis also is associated with the inability to obtain employment.15 Almost one-third of patients with psoriasis who are either not working or are retired base their work status on their skin condition.16 Furthermore, psoriasis may contribute to economic burden for patients due to indirect costs associated with work absenteeism.17
Adequate treatment of psoriasis improves patients’ physical and psychological health as well as their ability to function in the workplace. However, despite the benefits of treatment, 30% of patients with severe psoriasis and 53% of patients with moderate psoriasis receive no treatment or only topical medications instead of systemic therapies.16 The potential adverse events of inadequate psoriasis treatment far outweigh any potential benefits of withholding treatment. Perhaps a boxed warning should be issued for inadequate treatment of psoriasis patients.
The US Food and Drug Administration uses the term boxed warning to highlight potentially dangerous situations associated with prescription drugs. A boxed warning is used when “[T]here is an adverse reaction so serious in proportion to the potential benefit from the drug (e.g., a fatal, life-threatening or permanently disabling adverse reaction) that it is essential that it be considered in assessing the risks and benefits of using the drug.”1 However, drugs are not the only potential cause of severe adverse outcomes in patients with psoriasis. Untreated psoriasis also is a well-established cause of serious morbidity and mortality. What are the risks of inadequate psoriasis treatment?
Psoriasis is associated with an increased risk for cardiovascular disease.2-4 Patients with psoriasis also have a higher prevalence of classic cardiovascular risk factors including smoking, diabetes mellitus, hypertension, obesity, and hyperlipidemia.5,6 Psoriasis is a T-cell mediated disease process driven by IL-23 and TH17 helper cell–derived proinflammatory cytokines, sharing certain genetic aspects with metabolic syndrome.6 Cytokine actions on insulin signaling, lipid metabolism, and adipogenesis may underlie the increased prevalence of metabolic syndrome and cardiovascular risk factors in patients with psoriasis. In addition to treating the cutaneous manifestations of psoriasis, reducing inflammation in these patients reduces C-reactive protein and lipid peroxidation and increases high-density lipoprotein levels.6 Tumor necrosis factor α blockers decrease the risk for cardiovascular disease in patients with psoriasis.7,8 Lower than expected rates of cardiovascular disease also have been reported in a large cohort of psoriasis patients (ie, PSOLAR [Psoriasis Longitudinal Assessment and Registry] registry) being treated with either ustekinumab or tumor necrosis factor α blockers.9
Psoriatic arthritis is a chronic inflammatory disease in which active inflammation results in progressive joint destruction.10 Tumor necrosis factor α inhibitors suppress disease progression, preserve function, and delay destruction of the joints. Ustekinumab also helps control psoriatic arthritis and inhibits radiographic progression of joint disease.11
Importantly, untreated moderate to severe psoriasis is associated with several comorbidities that may lead to early death such as heart attacks and strokes.12 Furthermore, patients not taking biologic medications may have higher death rates than patients taking biologic medications.9 Psoriasis also is associated with tremendous suffering and negative psychosocial effects. The mental and physical impact of the disease is comparable to other major medical conditions (eg, cancer, arthritis, hypertension, heart disease, diabetes, depression).13 Patients also may experience physical discomfort from pain and itching.14 Children with psoriasis may experience bullying, which is associated with an increased number of depressive episodes, thereby increasing their risk for developing psychiatric conditions such as depression and anxiety as adults.15 The stigma associated with psoriasis may affect patients’ ability to build relationships. Patients with psoriasis experience higher divorce rates than patients with other chronic medical conditions, and direct involvement of genital regions may negatively impact patients’ sex lives. Patients have noted that the stigma of psoriasis also is associated with the inability to obtain employment.15 Almost one-third of patients with psoriasis who are either not working or are retired base their work status on their skin condition.16 Furthermore, psoriasis may contribute to economic burden for patients due to indirect costs associated with work absenteeism.17
Adequate treatment of psoriasis improves patients’ physical and psychological health as well as their ability to function in the workplace. However, despite the benefits of treatment, 30% of patients with severe psoriasis and 53% of patients with moderate psoriasis receive no treatment or only topical medications instead of systemic therapies.16 The potential adverse events of inadequate psoriasis treatment far outweigh any potential benefits of withholding treatment. Perhaps a boxed warning should be issued for inadequate treatment of psoriasis patients.
- US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. Guidance for industry: warning and precautions, contraindications, and boxed warning sections of labeling for human prescription drug and biological products—content and format. US Food and Drug Administration website. http://www.fda.gov/downloads/Drugs/.../Guidances/ucm075096.pdf. Published October 6, 2011. Accessed August 10, 2016.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Rose S, Sheth NH, Baker JF, et al. A comparison of vascular inflammation in psoriasis, rheumatoid arthritis, and healthy subjects by FDG-PET/CT: a pilot study. Am J Cardiovasc Dis. 2013;3:273-278.
- Shlyankevich J, Mehta NN, Krueger JG, et al. Accumulating evidence for the association and shared pathogenic mechanisms between psoriasis and cardiovascular-related comorbidities. Am J Med. 2014;127:1148-1153.
- Lee MK, Kim HS, Cho EB, et al. A study of awareness and screening behavior of cardiovascular risk factors in patients with psoriasis and dermatologists. Ann Dermatol. 2015;27:59-65.
- Voiculescu VM, Lupu M, Papagheorghe L, et al. Psoriasis and metabolic syndrome—scientific evidence and therapeutic implications. J Med Life. 2014;7:468-471.
- Wu JJ, Poon KY, Bebchuk JD. Association between the type and length of tumor necrosis factor inhibitor therapy and myocardial infarction risk in patients with psoriasis. J Drugs Dermatol. 2013;12:899-903.
- Famenini S, Sako EY, Wu JJ. Effect of treating psoriasis on cardiovascular comorbidities: focus on TNF inhibitors. Am J Clin Dermatol. 2014;15:45-50.
- Gottlieb AB, Kalb RE, Langley RG, et al. Safety observations in 12095 patients with psoriasis enrolled in an international registry (PSOLAR): experience with infliximab and other systemic and biologic therapies. J Drugs Dermatol. 2014;13:1441-1448.
- Chimenti MS, Graceffa D, Perricone R. Anti-TNFα discontinuation in rheumatoid and psoriatic arthritis: is it possible after disease remission [published online Apr 21, 2011]? Autoimmun Rev. 2011;10:636-640.
- Kavanaugh A, Ritchlin C, Rahman P, et al. Ustekinumab, an anti-IL-12/23 p40 monoclonal antibody, inhibits radiographic progression in patients with active psoriatic arthritis: results of an integrated analysis of radiographic data from the phase 3, multicentre, randomised, double-blind, placebo-controlled PSUMMIT-1 and PSUMMIT-2 trials. Ann Rheum Dis. 2014;73:1000-1006.
- Pietrzak A, Bartosinska J, Blaszczyk R, et al. Increased serum level of N-terminal Pro-B-type natriuretic peptide as a possible biomarker of cardiovascular risk in psoriatic patients. J Eur Acad Dermatol Venereol. 2015;29:1010-1014.
- Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3, pt 1):401-407.
- Pettey AA, Balkrishnan R, Rapp SR, et al. Patients with palmoplantar psoriasis have more physical disability and discomfort than patients with other forms of psoriasis: implications for clinical practice. J Am Acad Dermatol. 2003;49:271-275.
- Garshick MK, Kimball AB. Psoriasis and the life cycle of persistent life effects. Dermatol Clin. 2015;33:25-39.
- Feldman SR, Malakouti M, Koo JY. Social impact of the burden of psoriasis: effects on patients and practice. Dermatol Online J. August 17, 2014;20. pii:13030/qt48r4w8h2.
- Brezinski EA, Dhillon JS, Armstrong AW. Economic burden of psoriasis in the United States: a systematic review. JAMA Dermatol. 2015;151:651-658.
- US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. Guidance for industry: warning and precautions, contraindications, and boxed warning sections of labeling for human prescription drug and biological products—content and format. US Food and Drug Administration website. http://www.fda.gov/downloads/Drugs/.../Guidances/ucm075096.pdf. Published October 6, 2011. Accessed August 10, 2016.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Rose S, Sheth NH, Baker JF, et al. A comparison of vascular inflammation in psoriasis, rheumatoid arthritis, and healthy subjects by FDG-PET/CT: a pilot study. Am J Cardiovasc Dis. 2013;3:273-278.
- Shlyankevich J, Mehta NN, Krueger JG, et al. Accumulating evidence for the association and shared pathogenic mechanisms between psoriasis and cardiovascular-related comorbidities. Am J Med. 2014;127:1148-1153.
- Lee MK, Kim HS, Cho EB, et al. A study of awareness and screening behavior of cardiovascular risk factors in patients with psoriasis and dermatologists. Ann Dermatol. 2015;27:59-65.
- Voiculescu VM, Lupu M, Papagheorghe L, et al. Psoriasis and metabolic syndrome—scientific evidence and therapeutic implications. J Med Life. 2014;7:468-471.
- Wu JJ, Poon KY, Bebchuk JD. Association between the type and length of tumor necrosis factor inhibitor therapy and myocardial infarction risk in patients with psoriasis. J Drugs Dermatol. 2013;12:899-903.
- Famenini S, Sako EY, Wu JJ. Effect of treating psoriasis on cardiovascular comorbidities: focus on TNF inhibitors. Am J Clin Dermatol. 2014;15:45-50.
- Gottlieb AB, Kalb RE, Langley RG, et al. Safety observations in 12095 patients with psoriasis enrolled in an international registry (PSOLAR): experience with infliximab and other systemic and biologic therapies. J Drugs Dermatol. 2014;13:1441-1448.
- Chimenti MS, Graceffa D, Perricone R. Anti-TNFα discontinuation in rheumatoid and psoriatic arthritis: is it possible after disease remission [published online Apr 21, 2011]? Autoimmun Rev. 2011;10:636-640.
- Kavanaugh A, Ritchlin C, Rahman P, et al. Ustekinumab, an anti-IL-12/23 p40 monoclonal antibody, inhibits radiographic progression in patients with active psoriatic arthritis: results of an integrated analysis of radiographic data from the phase 3, multicentre, randomised, double-blind, placebo-controlled PSUMMIT-1 and PSUMMIT-2 trials. Ann Rheum Dis. 2014;73:1000-1006.
- Pietrzak A, Bartosinska J, Blaszczyk R, et al. Increased serum level of N-terminal Pro-B-type natriuretic peptide as a possible biomarker of cardiovascular risk in psoriatic patients. J Eur Acad Dermatol Venereol. 2015;29:1010-1014.
- Rapp SR, Feldman SR, Exum ML, et al. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3, pt 1):401-407.
- Pettey AA, Balkrishnan R, Rapp SR, et al. Patients with palmoplantar psoriasis have more physical disability and discomfort than patients with other forms of psoriasis: implications for clinical practice. J Am Acad Dermatol. 2003;49:271-275.
- Garshick MK, Kimball AB. Psoriasis and the life cycle of persistent life effects. Dermatol Clin. 2015;33:25-39.
- Feldman SR, Malakouti M, Koo JY. Social impact of the burden of psoriasis: effects on patients and practice. Dermatol Online J. August 17, 2014;20. pii:13030/qt48r4w8h2.
- Brezinski EA, Dhillon JS, Armstrong AW. Economic burden of psoriasis in the United States: a systematic review. JAMA Dermatol. 2015;151:651-658.
Back to Basics: The Role of the Team Physician
Editor’s Note: AJO Deputy Editor-in-Chief Robin West, MD, is the Head Team Physician for the Washington Redskins and the Washington Nationals. She has previously served as a team physician for 2 Super Bowl-winning Pittsburgh Steelers teams. I am pleased to “hand off” this issue to her.
—Bryan T. Hanypsiak, MD
The summer is over, football season has begun, and team physicians are busy trying to manage and treat the plethora of injuries that come with the game. Football is one of the most popular sports played by young athletes. Youth participation (ages 6-14 years) in tackle football was 2.169 million in 2015, according to a study conducted by the Physical Activity Council and presented by USA Football. There were 1.084 million boys (and 1500 girls) playing high school football in the 2014-2015 season, nearly twice the number of the next most popular sport, track and field, according to the National Federation of State High School Associations.Due to the sheer volume of athletes and high-impact nature of the game, football leads all other sports in the number of sustained injuries.
Team physicians have the leadership role in the organization, management, and provision of care of the athletes on the team. The roles and responsibilities of the team physician are ever-evolving. The team physician has to meet certain medical qualifications and education requirements, and understand the ethical and medicolegal issues.
The American Academy of Orthopaedic Surgeons and several other medical associations have put together a Team Physician Consensus Statement (available at http://bit.ly/2b8rOzS). All team physicians, coaches, and athletic trainers should read and understand this statement, as it delineates the qualifications, duties, and responsibilities of the team physician.
Our Football Issue focuses on the most common injuries that the team physician will encounter during the season. Our goal is to create a comprehensive guide for the team physician on the acute management of these injuries. As team physicians, we have to make quick return-to-play decisions that are often difficult, as we are dealing with extremely competitive athletes and coaches in the heat of the moment. Since we can’t control the high levels of adrenalin, loud stadium, or rapid speed of the game, we need to be prepared to perform a comprehensive evaluation and diagnosis under these circumstances. This return-to-play decision should be based solely on the severity of the injury and safety of the player. As a team physician, you are responsible for making the “final call” on when the player is safe to return to the game.
This issue includes a section on the most common medical issues (ophthalmology, dental, and dermatology), concussion, exertional heat stroke, knee injuries, and foot and ankle injuries. We also have a special list of the most common items to include in the athletic trainer’s medical bag when covering a high school or collegiate football game (see page 376). Our prominent contributing authors all have extensive experience covering high school, collegiate, and professional teams.
I hope that our Football Issue helps you to keep your athletes safe and injury-free, which is necessary to have a successful season. Remember, as the team physician, your primary focus is the well being of the players. The success of the team only comes when the players are healthy. A cohesive, well-organized medical team, led by the head athletic trainer and team physician, is a key component to the care of the athletes. It truly takes a village to provide top-notch medical care to a football team.
Am J Orthop. 2016;45(6):338. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Editor’s Note: AJO Deputy Editor-in-Chief Robin West, MD, is the Head Team Physician for the Washington Redskins and the Washington Nationals. She has previously served as a team physician for 2 Super Bowl-winning Pittsburgh Steelers teams. I am pleased to “hand off” this issue to her.
—Bryan T. Hanypsiak, MD
The summer is over, football season has begun, and team physicians are busy trying to manage and treat the plethora of injuries that come with the game. Football is one of the most popular sports played by young athletes. Youth participation (ages 6-14 years) in tackle football was 2.169 million in 2015, according to a study conducted by the Physical Activity Council and presented by USA Football. There were 1.084 million boys (and 1500 girls) playing high school football in the 2014-2015 season, nearly twice the number of the next most popular sport, track and field, according to the National Federation of State High School Associations.Due to the sheer volume of athletes and high-impact nature of the game, football leads all other sports in the number of sustained injuries.
Team physicians have the leadership role in the organization, management, and provision of care of the athletes on the team. The roles and responsibilities of the team physician are ever-evolving. The team physician has to meet certain medical qualifications and education requirements, and understand the ethical and medicolegal issues.
The American Academy of Orthopaedic Surgeons and several other medical associations have put together a Team Physician Consensus Statement (available at http://bit.ly/2b8rOzS). All team physicians, coaches, and athletic trainers should read and understand this statement, as it delineates the qualifications, duties, and responsibilities of the team physician.
Our Football Issue focuses on the most common injuries that the team physician will encounter during the season. Our goal is to create a comprehensive guide for the team physician on the acute management of these injuries. As team physicians, we have to make quick return-to-play decisions that are often difficult, as we are dealing with extremely competitive athletes and coaches in the heat of the moment. Since we can’t control the high levels of adrenalin, loud stadium, or rapid speed of the game, we need to be prepared to perform a comprehensive evaluation and diagnosis under these circumstances. This return-to-play decision should be based solely on the severity of the injury and safety of the player. As a team physician, you are responsible for making the “final call” on when the player is safe to return to the game.
This issue includes a section on the most common medical issues (ophthalmology, dental, and dermatology), concussion, exertional heat stroke, knee injuries, and foot and ankle injuries. We also have a special list of the most common items to include in the athletic trainer’s medical bag when covering a high school or collegiate football game (see page 376). Our prominent contributing authors all have extensive experience covering high school, collegiate, and professional teams.
I hope that our Football Issue helps you to keep your athletes safe and injury-free, which is necessary to have a successful season. Remember, as the team physician, your primary focus is the well being of the players. The success of the team only comes when the players are healthy. A cohesive, well-organized medical team, led by the head athletic trainer and team physician, is a key component to the care of the athletes. It truly takes a village to provide top-notch medical care to a football team.
Am J Orthop. 2016;45(6):338. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Editor’s Note: AJO Deputy Editor-in-Chief Robin West, MD, is the Head Team Physician for the Washington Redskins and the Washington Nationals. She has previously served as a team physician for 2 Super Bowl-winning Pittsburgh Steelers teams. I am pleased to “hand off” this issue to her.
—Bryan T. Hanypsiak, MD
The summer is over, football season has begun, and team physicians are busy trying to manage and treat the plethora of injuries that come with the game. Football is one of the most popular sports played by young athletes. Youth participation (ages 6-14 years) in tackle football was 2.169 million in 2015, according to a study conducted by the Physical Activity Council and presented by USA Football. There were 1.084 million boys (and 1500 girls) playing high school football in the 2014-2015 season, nearly twice the number of the next most popular sport, track and field, according to the National Federation of State High School Associations.Due to the sheer volume of athletes and high-impact nature of the game, football leads all other sports in the number of sustained injuries.
Team physicians have the leadership role in the organization, management, and provision of care of the athletes on the team. The roles and responsibilities of the team physician are ever-evolving. The team physician has to meet certain medical qualifications and education requirements, and understand the ethical and medicolegal issues.
The American Academy of Orthopaedic Surgeons and several other medical associations have put together a Team Physician Consensus Statement (available at http://bit.ly/2b8rOzS). All team physicians, coaches, and athletic trainers should read and understand this statement, as it delineates the qualifications, duties, and responsibilities of the team physician.
Our Football Issue focuses on the most common injuries that the team physician will encounter during the season. Our goal is to create a comprehensive guide for the team physician on the acute management of these injuries. As team physicians, we have to make quick return-to-play decisions that are often difficult, as we are dealing with extremely competitive athletes and coaches in the heat of the moment. Since we can’t control the high levels of adrenalin, loud stadium, or rapid speed of the game, we need to be prepared to perform a comprehensive evaluation and diagnosis under these circumstances. This return-to-play decision should be based solely on the severity of the injury and safety of the player. As a team physician, you are responsible for making the “final call” on when the player is safe to return to the game.
This issue includes a section on the most common medical issues (ophthalmology, dental, and dermatology), concussion, exertional heat stroke, knee injuries, and foot and ankle injuries. We also have a special list of the most common items to include in the athletic trainer’s medical bag when covering a high school or collegiate football game (see page 376). Our prominent contributing authors all have extensive experience covering high school, collegiate, and professional teams.
I hope that our Football Issue helps you to keep your athletes safe and injury-free, which is necessary to have a successful season. Remember, as the team physician, your primary focus is the well being of the players. The success of the team only comes when the players are healthy. A cohesive, well-organized medical team, led by the head athletic trainer and team physician, is a key component to the care of the athletes. It truly takes a village to provide top-notch medical care to a football team.
Am J Orthop. 2016;45(6):338. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Taking hysteroscopy to the office
Along with global endometrial ablation, diagnostic and minor operative hysteroscopy are excellent procedures to bring into your office environment. These operations are generally of short duration and provide little risk to the patient. Moreover, reimbursement exceeds that for the hospital setting. A constant revenue stream can be created after an initial moderate expenditure.
The key to a successful office procedure is patient comfort; this begins with minimizing pain and trauma. In our practice, we note decreased pain when performing vaginoscopy and hysteroscopy without the use of a speculum or tenaculum. This is well substantiated in literature by Professor Stefano Bettocchi, who immediately preceded me as president of the International Society for Gynecologic Endoscopy (ISGE).
In this issue of Master Class in Gynecologic Surgery, I have asked my partner, Aarathi Cholkeri-Singh, MD, to discuss vaginoscopy. Dr. Cholkeri-Singh is clinical assistant professor at the University of Illinois at Chicago, lecturer at Rosalind Franklin University of Medicine and Science, and associate director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.
She also serves as codirector of the AAGL/Society of Reproductive Surgeons fellowship in minimally invasive gynecologic surgery and director of gynecologic surgical education at Advocate Lutheran, and is chair for a postgraduate course on hysteroscopy at the upcoming AAGL 45th Annual Global Congress. Among her publications is a recent review in the Journal of Minimally Invasive Gynecology on hysteroscopy for infertile women (doi:10.1016/j.jmig.2014.12.163).
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/SRS fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. He reported having no financial disclosures relevant to this column. Email him at [email protected].
Along with global endometrial ablation, diagnostic and minor operative hysteroscopy are excellent procedures to bring into your office environment. These operations are generally of short duration and provide little risk to the patient. Moreover, reimbursement exceeds that for the hospital setting. A constant revenue stream can be created after an initial moderate expenditure.
The key to a successful office procedure is patient comfort; this begins with minimizing pain and trauma. In our practice, we note decreased pain when performing vaginoscopy and hysteroscopy without the use of a speculum or tenaculum. This is well substantiated in literature by Professor Stefano Bettocchi, who immediately preceded me as president of the International Society for Gynecologic Endoscopy (ISGE).
In this issue of Master Class in Gynecologic Surgery, I have asked my partner, Aarathi Cholkeri-Singh, MD, to discuss vaginoscopy. Dr. Cholkeri-Singh is clinical assistant professor at the University of Illinois at Chicago, lecturer at Rosalind Franklin University of Medicine and Science, and associate director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.
She also serves as codirector of the AAGL/Society of Reproductive Surgeons fellowship in minimally invasive gynecologic surgery and director of gynecologic surgical education at Advocate Lutheran, and is chair for a postgraduate course on hysteroscopy at the upcoming AAGL 45th Annual Global Congress. Among her publications is a recent review in the Journal of Minimally Invasive Gynecology on hysteroscopy for infertile women (doi:10.1016/j.jmig.2014.12.163).
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/SRS fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. He reported having no financial disclosures relevant to this column. Email him at [email protected].
Along with global endometrial ablation, diagnostic and minor operative hysteroscopy are excellent procedures to bring into your office environment. These operations are generally of short duration and provide little risk to the patient. Moreover, reimbursement exceeds that for the hospital setting. A constant revenue stream can be created after an initial moderate expenditure.
The key to a successful office procedure is patient comfort; this begins with minimizing pain and trauma. In our practice, we note decreased pain when performing vaginoscopy and hysteroscopy without the use of a speculum or tenaculum. This is well substantiated in literature by Professor Stefano Bettocchi, who immediately preceded me as president of the International Society for Gynecologic Endoscopy (ISGE).
In this issue of Master Class in Gynecologic Surgery, I have asked my partner, Aarathi Cholkeri-Singh, MD, to discuss vaginoscopy. Dr. Cholkeri-Singh is clinical assistant professor at the University of Illinois at Chicago, lecturer at Rosalind Franklin University of Medicine and Science, and associate director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.
She also serves as codirector of the AAGL/Society of Reproductive Surgeons fellowship in minimally invasive gynecologic surgery and director of gynecologic surgical education at Advocate Lutheran, and is chair for a postgraduate course on hysteroscopy at the upcoming AAGL 45th Annual Global Congress. Among her publications is a recent review in the Journal of Minimally Invasive Gynecology on hysteroscopy for infertile women (doi:10.1016/j.jmig.2014.12.163).
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/SRS fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. He reported having no financial disclosures relevant to this column. Email him at [email protected].
The benefits of integrating in-office hysteroscopy
The benefits of integrating hysteroscopy into office practice are compelling. Most importantly, patients appreciate the comfort and convenience of having hysteroscopic procedures done in a familiar setting. Patients can generally be in and out of the office in less than 30 minutes for a diagnostic procedure, and in less than 1-2 hours for an operative procedure.
Not only is an in-office approach patient centered and clinically valuable, but it is more efficient and economically favorable for the gynecologic surgeon. Physicians earn higher reimbursement for diagnostic hysteroscopies, as well as many therapeutic and operative hysteroscopies, when these procedures are done in the office rather than when they’re performed in a hospital or an outpatient center.
Transitioning to in-office hysteroscopy need not be daunting: The setup is relatively simple and does not require an operating suite, just a dedicated exam room. And the need for premedication and local anesthesia can be low, particularly when a vaginoscopic approach to hysteroscopy is employed. For most gynecologic surgeons, the necessary skills and comfort levels fall into place after only a few vaginoscopic procedures.
A vaginoscopic approach avoids the use of a vaginal speculum or cervical tenaculum, significantly decreasing discomfort or pain. Not using these instruments is the only difference between this and traditional hysteroscopy. It is a less invasive approach that is much more tolerable for patients. And for the surgeon, it can be easier and quicker and provides equally good visualization without any impairment in cervical passage.
Described in the literature as far back as the 1950s, vaginoscopy has its roots in the pediatric/adolescent population, where it was used for the removal of foreign bodies and evaluation of the vagina and external cervical os.
More recently, Stefano Bettocchi, MD, and Luigi Selvaggi, MD, in Italy were the first to describe a vaginoscopic approach to hysteroscopy for evaluating the endocervical canal and uterine cavity.
In a series of papers from 1997 to 2004, Dr. Bettocchi and Dr. Selvaggi documented their efforts to improve patient tolerance during diagnostic hysteroscopies. When they used both the speculum and tenaculum in 163 patients, with local anesthesia, 8% reported severe pain, 11% reported moderate pain, and 69% reported mild pain. Only 12% reported no discomfort. With speculum use only, and no anesthesia, in 308 patients, none reported severe pain, 2% reported moderate pain, 32% reported mild pain, and 66% reported no discomfort. When neither instrument was used (again, no anesthesia), patient discomfort was nearly eliminated: In 680 procedures, patients had a 96% no-discomfort rate (J Am Assoc Gynecol Laparosc. 1997 Feb;4[2]:255-8; Curr Opin Obstet Gynecol. 2003 Aug;15[4]:303-8; Obstet Gynecol Clin North Am. 2004 Sep;31[3]:641-54, xi).
Since then, research has affirmed the differences in patient tolerance and has shown that there is no significant difference between traditional and vaginoscopic hysteroscopy in the rate of procedure failure (0%-10%).
In my practice, in addition to vaginal or cervical examination and evaluation of the uterine cavity, I utilize a vaginoscopic approach to perform minor therapeutic and operative procedures such as biopsies, polypectomies, tubal occlusion using the Essure system, and removal of lost intrauterine devices. I can assess infertility, trauma, abnormal uterine bleeding, and mesh erosion, and provide pre- and postsurgical evaluations. In all of these cases, I use minimal premedication and only rarely need any local anesthetic and/or sedation.
Instrumentation and technique
There are a variety of hysteroscopes available on the market, from single-channel flexible diagnostic hysteroscopes that are 3 mm to 4 mm in diameter, to “see-and-treat” operative hysteroscopes that are rigid and have various diameters and camera lens angles.
A hysteroscope with a 5.5-mm outer diameter works well for a vaginoscopic approach that avoids cervical dilation. Accessory instrumentation includes semirigid 5 Fr 35-cm–long biopsy forceps, scissors, and alligator forceps.
In timing the procedure, our main goal is a thin uterine lining. This can be achieved by scheduling the procedure during the early proliferative phase of the menstrual cycle or by using a gonadotropin-releasing hormone agonist or a transdermal or transvaginal contraceptive medication.
By far the most important element of pain control and analgesia is the time spent with each patient to thoroughly discuss the experience of hysteroscopy and to set expectations about what she will hear, see, and feel. An unexpected experience can worsen anxiety, which in turn can worsen pain. If everything is as familiar and relaxed as possible, there will be little need for analgesia.
I tell patients in preprocedure counseling that the distention of the uterine walls usually causes some cramping, and that NSAIDs can minimize this cramping. In rare cases, when a patient is very worried about her pain tolerance, I will prescribe diazepam. However, many of my patients opt to do nothing other than take ibuprofen. On a case-by-case basis, you can determine with your patient what type and level of analgesia and preprocedure medication will be best.
Paracervical blocks are an option for some surgical patients, but I advise my patients to move forward without the block and assure them that it can be administered later if needed. Thus far, I’ve never proceeded with a paracervical block. There are other methods and sites for introducing local anesthesia, including intracervical, by injection or topical, or topical intracavitary techniques. Nevertheless, it is unclear from randomized controlled trials whether local anesthesia is effective. Trials of paracervical blocks similarly have had inconsistent outcomes.
I do commonly premedicate patients – mainly nulliparous patients and postmenopausal patients – with misoprostol, which softens the cervix and facilitates an easier entry of the hysteroscope into the cervix.
Published studies on misoprostol administration before hysteroscopy have had mixed results. A Cochrane review from 2015 concluded there is moderate-quality evidence in support of preoperative ripening with the agent, while another meta-analysis also published in 2015 concluded that data are poor and do not support its use. Recently, however, there appear to be more supportive studies demonstrating or suggesting that misoprostol is effective in reducing discomfort.
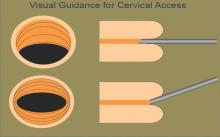
Patient discomfort is also minimized when there is little manipulation of the hysteroscope. Scopes that are angled (12, 25, or 30 degrees) allow optimal visualization with minimal movement; the scope can be brought to the midline of the uterine cavity and the light cord rotated to the 3:00 and 9:00 o’clock positions to enable visualization of the cornu. A 0-degree scope, on the other hand, must be manipulated quite a bit for the same degree of visualization, potentially increasing patient discomfort.
Prior to hysteroscopy, the cervix and vagina are cleaned with a small-diameter swab dipped in povidone-iodine or chlorhexidine gluconate in the case of allergies. One or two 1,000-cc bags of saline inserted into pressure bags are attached to Y-type tubing. (A diagnostic procedure rarely will require two bags.) I spread the labia initially while guiding the scope into the posterior fornix of the vagina. If the leakage of fluid causes inadequate distension of the vaginal walls, I will gently pinch the labia together with gauze.
I then gently pull back the scope and manipulate it posteriorly to visualize the external cervical os anteriorly. The hysteroscope may then be introduced through the cervical os, endocervical canal, and uterine cavity, with care taken so that the instrument does not rub against the cervix or the uterine tissue and cause trauma, pain, and bleeding. The uterus will progressively align with the cervix and vagina, thereby eliminating the need for a tenaculum to straighten the uterine axis.
Fluid monitoring is important, especially during operative hysteroscopy. In my practice, a nurse watches inflow and outflow amounts while I explain what I am doing and visualizing. Some patients like to be able to view the surgery, so I am always ready to tilt the screen accordingly.
The economics
How do you know if office hysteroscopy is right for you? Your own surgical skill and the skills of your staff, who must be trained to handle and sterilize equipment and to consistently assist you, are major factors, as is ensurance of a return on your investment.
One manufacturer contacted for this Master Class lists the price of a complete office tower (light source, camera, and monitor) at approximately $9,700 and the price of a rigid hysteroscope, sheath, and hand instruments at about $6,300. A complete setup for office hysteroscopy, including a standard operative (rigid) hysteroscope, should therefore cost between $15,000 and $17,000. Companies also offer leasing options for about $300-400/month.
Flexible hysteroscopes cost about $6,000 more, which prompts many gynecologic surgeons to focus their investment on a rigid scope that can be used for both diagnostic and therapeutic procedures. Disposables cost $10 or less, and $40-50 or less, for each diagnostic and operative hysteroscopy, respectively.
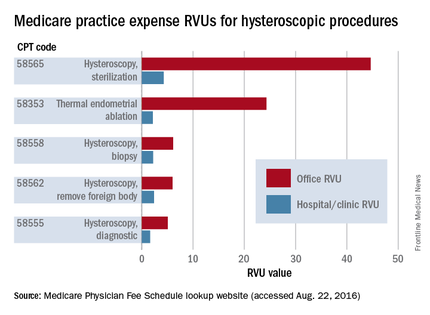
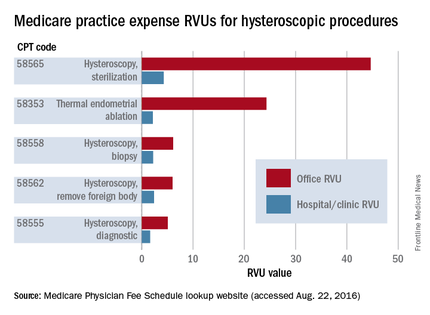
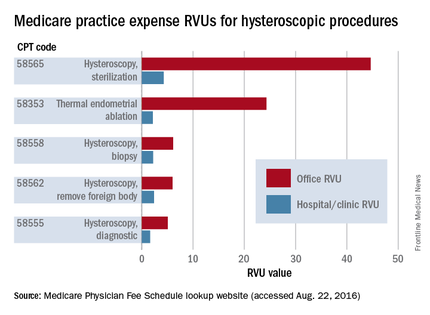
A look at the Medicare Relative Value Units (RVUs) – a key component of the Medicare reimbursement system and a standard for many payers in determining compensation – shows higher reimbursement for quite a few hysteroscopic codes when these procedures are performed in the office.
Total RVUs have three components:
1. Physician work, including time and the technical skill and intensity of effort it takes to perform a service or procedure.
2. Practice expenses, such as rent, equipment and supplies, and nonphysician salaries.
3. Malpractice insurance premiums.
Each component is multiplied by a factor that accounts for geographic cost variations, and each total RVU is multiplied by a dollar amount known as the conversion factor.
Practice expense (PE) RVUs for services provided in a “facility” (e.g., hospital or outpatient clinic) are often lower than office-based PE RVUs for the same services. Hysteroscopy is no exception. The PE RVU value for diagnostic hysteroscopy performed in the office, for instance, is approximately 5 units, compared with 1.64 units for diagnostic hysteroscopy performed in a facility.
Information on hysteroscopic procedures, and their associated RVUs, on geographic practice cost indices and on pricing, can be accessed using Medicare’s Physician Fee Schedule lookup tool (www.cms.gov/apps/physician-fee-schedule/overview.aspx).
This tool is useful for calculating returns on investment. According to national payment amounts listed in August, a diagnostic hysteroscopy performed in the office will earn an average of $315.08 vs. $192.27 for each case performed in the hospital. If you perform 12 such procedures a year, that’s about $3,781 in the office, compared with $2,307 in the hospital.
This difference alone might not be worth an investment of $15,000 or more, but if you anticipate performing additional procedures with higher margins and higher reimbursement, such as 12 thermal endometrial ablations a year in combination with diagnostic hysteroscopy (which, according to the Medicare national fee schedule averages would earn $15,962 in the office vs. $4,971 in the hospital), or 12 Essure tubal occlusions ($22,595 vs. $5,263), the investment will look more favorable.
And if your patients are largely privately insured, your return on investment will occur much more quickly. In metropolitan Chicago, Blue Cross Blue Shield is reimbursing in-office diagnostic hysteroscopy at approximately $568, hysteroscopic ablations at $3,844, and Essure tubal occlusions at $3,885.
In addition to reimbursement levels, it’s important to consider the efficiencies of in-office hysteroscopy. You can perform an annual exam while the assistant sets up the room and greets each patient, for instance, or see another established patient while the assistant discharges your patient and turns the room over. Our patients, in turn, benefit from increased accessibility, with less time spent away from work or family, as well as more familiarity and comfort and reduced out-of-pocket expenses.
Dr. Cholkeri-Singh is clinical assistant professor at the University of Illinois in Chicago and is director of gynecologic surgical education and associate director of minimally invasive gynecology at Advocate Lutheran General Hospital. She is in private practice with Dr. Charles Miller and Dr. Kristen Sasaki at the Advanced Gynecologic Surgical Institute in Chicago. She is a consultant for DySIS Medical, Hologic, and Bayer HealthCare.
The benefits of integrating hysteroscopy into office practice are compelling. Most importantly, patients appreciate the comfort and convenience of having hysteroscopic procedures done in a familiar setting. Patients can generally be in and out of the office in less than 30 minutes for a diagnostic procedure, and in less than 1-2 hours for an operative procedure.
Not only is an in-office approach patient centered and clinically valuable, but it is more efficient and economically favorable for the gynecologic surgeon. Physicians earn higher reimbursement for diagnostic hysteroscopies, as well as many therapeutic and operative hysteroscopies, when these procedures are done in the office rather than when they’re performed in a hospital or an outpatient center.
Transitioning to in-office hysteroscopy need not be daunting: The setup is relatively simple and does not require an operating suite, just a dedicated exam room. And the need for premedication and local anesthesia can be low, particularly when a vaginoscopic approach to hysteroscopy is employed. For most gynecologic surgeons, the necessary skills and comfort levels fall into place after only a few vaginoscopic procedures.
A vaginoscopic approach avoids the use of a vaginal speculum or cervical tenaculum, significantly decreasing discomfort or pain. Not using these instruments is the only difference between this and traditional hysteroscopy. It is a less invasive approach that is much more tolerable for patients. And for the surgeon, it can be easier and quicker and provides equally good visualization without any impairment in cervical passage.
Described in the literature as far back as the 1950s, vaginoscopy has its roots in the pediatric/adolescent population, where it was used for the removal of foreign bodies and evaluation of the vagina and external cervical os.
More recently, Stefano Bettocchi, MD, and Luigi Selvaggi, MD, in Italy were the first to describe a vaginoscopic approach to hysteroscopy for evaluating the endocervical canal and uterine cavity.
In a series of papers from 1997 to 2004, Dr. Bettocchi and Dr. Selvaggi documented their efforts to improve patient tolerance during diagnostic hysteroscopies. When they used both the speculum and tenaculum in 163 patients, with local anesthesia, 8% reported severe pain, 11% reported moderate pain, and 69% reported mild pain. Only 12% reported no discomfort. With speculum use only, and no anesthesia, in 308 patients, none reported severe pain, 2% reported moderate pain, 32% reported mild pain, and 66% reported no discomfort. When neither instrument was used (again, no anesthesia), patient discomfort was nearly eliminated: In 680 procedures, patients had a 96% no-discomfort rate (J Am Assoc Gynecol Laparosc. 1997 Feb;4[2]:255-8; Curr Opin Obstet Gynecol. 2003 Aug;15[4]:303-8; Obstet Gynecol Clin North Am. 2004 Sep;31[3]:641-54, xi).
Since then, research has affirmed the differences in patient tolerance and has shown that there is no significant difference between traditional and vaginoscopic hysteroscopy in the rate of procedure failure (0%-10%).
In my practice, in addition to vaginal or cervical examination and evaluation of the uterine cavity, I utilize a vaginoscopic approach to perform minor therapeutic and operative procedures such as biopsies, polypectomies, tubal occlusion using the Essure system, and removal of lost intrauterine devices. I can assess infertility, trauma, abnormal uterine bleeding, and mesh erosion, and provide pre- and postsurgical evaluations. In all of these cases, I use minimal premedication and only rarely need any local anesthetic and/or sedation.
Instrumentation and technique
There are a variety of hysteroscopes available on the market, from single-channel flexible diagnostic hysteroscopes that are 3 mm to 4 mm in diameter, to “see-and-treat” operative hysteroscopes that are rigid and have various diameters and camera lens angles.
A hysteroscope with a 5.5-mm outer diameter works well for a vaginoscopic approach that avoids cervical dilation. Accessory instrumentation includes semirigid 5 Fr 35-cm–long biopsy forceps, scissors, and alligator forceps.
In timing the procedure, our main goal is a thin uterine lining. This can be achieved by scheduling the procedure during the early proliferative phase of the menstrual cycle or by using a gonadotropin-releasing hormone agonist or a transdermal or transvaginal contraceptive medication.
By far the most important element of pain control and analgesia is the time spent with each patient to thoroughly discuss the experience of hysteroscopy and to set expectations about what she will hear, see, and feel. An unexpected experience can worsen anxiety, which in turn can worsen pain. If everything is as familiar and relaxed as possible, there will be little need for analgesia.
I tell patients in preprocedure counseling that the distention of the uterine walls usually causes some cramping, and that NSAIDs can minimize this cramping. In rare cases, when a patient is very worried about her pain tolerance, I will prescribe diazepam. However, many of my patients opt to do nothing other than take ibuprofen. On a case-by-case basis, you can determine with your patient what type and level of analgesia and preprocedure medication will be best.
Paracervical blocks are an option for some surgical patients, but I advise my patients to move forward without the block and assure them that it can be administered later if needed. Thus far, I’ve never proceeded with a paracervical block. There are other methods and sites for introducing local anesthesia, including intracervical, by injection or topical, or topical intracavitary techniques. Nevertheless, it is unclear from randomized controlled trials whether local anesthesia is effective. Trials of paracervical blocks similarly have had inconsistent outcomes.
I do commonly premedicate patients – mainly nulliparous patients and postmenopausal patients – with misoprostol, which softens the cervix and facilitates an easier entry of the hysteroscope into the cervix.
Published studies on misoprostol administration before hysteroscopy have had mixed results. A Cochrane review from 2015 concluded there is moderate-quality evidence in support of preoperative ripening with the agent, while another meta-analysis also published in 2015 concluded that data are poor and do not support its use. Recently, however, there appear to be more supportive studies demonstrating or suggesting that misoprostol is effective in reducing discomfort.
Patient discomfort is also minimized when there is little manipulation of the hysteroscope. Scopes that are angled (12, 25, or 30 degrees) allow optimal visualization with minimal movement; the scope can be brought to the midline of the uterine cavity and the light cord rotated to the 3:00 and 9:00 o’clock positions to enable visualization of the cornu. A 0-degree scope, on the other hand, must be manipulated quite a bit for the same degree of visualization, potentially increasing patient discomfort.
Prior to hysteroscopy, the cervix and vagina are cleaned with a small-diameter swab dipped in povidone-iodine or chlorhexidine gluconate in the case of allergies. One or two 1,000-cc bags of saline inserted into pressure bags are attached to Y-type tubing. (A diagnostic procedure rarely will require two bags.) I spread the labia initially while guiding the scope into the posterior fornix of the vagina. If the leakage of fluid causes inadequate distension of the vaginal walls, I will gently pinch the labia together with gauze.
I then gently pull back the scope and manipulate it posteriorly to visualize the external cervical os anteriorly. The hysteroscope may then be introduced through the cervical os, endocervical canal, and uterine cavity, with care taken so that the instrument does not rub against the cervix or the uterine tissue and cause trauma, pain, and bleeding. The uterus will progressively align with the cervix and vagina, thereby eliminating the need for a tenaculum to straighten the uterine axis.
Fluid monitoring is important, especially during operative hysteroscopy. In my practice, a nurse watches inflow and outflow amounts while I explain what I am doing and visualizing. Some patients like to be able to view the surgery, so I am always ready to tilt the screen accordingly.
The economics
How do you know if office hysteroscopy is right for you? Your own surgical skill and the skills of your staff, who must be trained to handle and sterilize equipment and to consistently assist you, are major factors, as is ensurance of a return on your investment.
One manufacturer contacted for this Master Class lists the price of a complete office tower (light source, camera, and monitor) at approximately $9,700 and the price of a rigid hysteroscope, sheath, and hand instruments at about $6,300. A complete setup for office hysteroscopy, including a standard operative (rigid) hysteroscope, should therefore cost between $15,000 and $17,000. Companies also offer leasing options for about $300-400/month.
Flexible hysteroscopes cost about $6,000 more, which prompts many gynecologic surgeons to focus their investment on a rigid scope that can be used for both diagnostic and therapeutic procedures. Disposables cost $10 or less, and $40-50 or less, for each diagnostic and operative hysteroscopy, respectively.
A look at the Medicare Relative Value Units (RVUs) – a key component of the Medicare reimbursement system and a standard for many payers in determining compensation – shows higher reimbursement for quite a few hysteroscopic codes when these procedures are performed in the office.
Total RVUs have three components:
1. Physician work, including time and the technical skill and intensity of effort it takes to perform a service or procedure.
2. Practice expenses, such as rent, equipment and supplies, and nonphysician salaries.
3. Malpractice insurance premiums.
Each component is multiplied by a factor that accounts for geographic cost variations, and each total RVU is multiplied by a dollar amount known as the conversion factor.
Practice expense (PE) RVUs for services provided in a “facility” (e.g., hospital or outpatient clinic) are often lower than office-based PE RVUs for the same services. Hysteroscopy is no exception. The PE RVU value for diagnostic hysteroscopy performed in the office, for instance, is approximately 5 units, compared with 1.64 units for diagnostic hysteroscopy performed in a facility.
Information on hysteroscopic procedures, and their associated RVUs, on geographic practice cost indices and on pricing, can be accessed using Medicare’s Physician Fee Schedule lookup tool (www.cms.gov/apps/physician-fee-schedule/overview.aspx).
This tool is useful for calculating returns on investment. According to national payment amounts listed in August, a diagnostic hysteroscopy performed in the office will earn an average of $315.08 vs. $192.27 for each case performed in the hospital. If you perform 12 such procedures a year, that’s about $3,781 in the office, compared with $2,307 in the hospital.
This difference alone might not be worth an investment of $15,000 or more, but if you anticipate performing additional procedures with higher margins and higher reimbursement, such as 12 thermal endometrial ablations a year in combination with diagnostic hysteroscopy (which, according to the Medicare national fee schedule averages would earn $15,962 in the office vs. $4,971 in the hospital), or 12 Essure tubal occlusions ($22,595 vs. $5,263), the investment will look more favorable.
And if your patients are largely privately insured, your return on investment will occur much more quickly. In metropolitan Chicago, Blue Cross Blue Shield is reimbursing in-office diagnostic hysteroscopy at approximately $568, hysteroscopic ablations at $3,844, and Essure tubal occlusions at $3,885.
In addition to reimbursement levels, it’s important to consider the efficiencies of in-office hysteroscopy. You can perform an annual exam while the assistant sets up the room and greets each patient, for instance, or see another established patient while the assistant discharges your patient and turns the room over. Our patients, in turn, benefit from increased accessibility, with less time spent away from work or family, as well as more familiarity and comfort and reduced out-of-pocket expenses.
Dr. Cholkeri-Singh is clinical assistant professor at the University of Illinois in Chicago and is director of gynecologic surgical education and associate director of minimally invasive gynecology at Advocate Lutheran General Hospital. She is in private practice with Dr. Charles Miller and Dr. Kristen Sasaki at the Advanced Gynecologic Surgical Institute in Chicago. She is a consultant for DySIS Medical, Hologic, and Bayer HealthCare.
The benefits of integrating hysteroscopy into office practice are compelling. Most importantly, patients appreciate the comfort and convenience of having hysteroscopic procedures done in a familiar setting. Patients can generally be in and out of the office in less than 30 minutes for a diagnostic procedure, and in less than 1-2 hours for an operative procedure.
Not only is an in-office approach patient centered and clinically valuable, but it is more efficient and economically favorable for the gynecologic surgeon. Physicians earn higher reimbursement for diagnostic hysteroscopies, as well as many therapeutic and operative hysteroscopies, when these procedures are done in the office rather than when they’re performed in a hospital or an outpatient center.
Transitioning to in-office hysteroscopy need not be daunting: The setup is relatively simple and does not require an operating suite, just a dedicated exam room. And the need for premedication and local anesthesia can be low, particularly when a vaginoscopic approach to hysteroscopy is employed. For most gynecologic surgeons, the necessary skills and comfort levels fall into place after only a few vaginoscopic procedures.
A vaginoscopic approach avoids the use of a vaginal speculum or cervical tenaculum, significantly decreasing discomfort or pain. Not using these instruments is the only difference between this and traditional hysteroscopy. It is a less invasive approach that is much more tolerable for patients. And for the surgeon, it can be easier and quicker and provides equally good visualization without any impairment in cervical passage.
Described in the literature as far back as the 1950s, vaginoscopy has its roots in the pediatric/adolescent population, where it was used for the removal of foreign bodies and evaluation of the vagina and external cervical os.
More recently, Stefano Bettocchi, MD, and Luigi Selvaggi, MD, in Italy were the first to describe a vaginoscopic approach to hysteroscopy for evaluating the endocervical canal and uterine cavity.
In a series of papers from 1997 to 2004, Dr. Bettocchi and Dr. Selvaggi documented their efforts to improve patient tolerance during diagnostic hysteroscopies. When they used both the speculum and tenaculum in 163 patients, with local anesthesia, 8% reported severe pain, 11% reported moderate pain, and 69% reported mild pain. Only 12% reported no discomfort. With speculum use only, and no anesthesia, in 308 patients, none reported severe pain, 2% reported moderate pain, 32% reported mild pain, and 66% reported no discomfort. When neither instrument was used (again, no anesthesia), patient discomfort was nearly eliminated: In 680 procedures, patients had a 96% no-discomfort rate (J Am Assoc Gynecol Laparosc. 1997 Feb;4[2]:255-8; Curr Opin Obstet Gynecol. 2003 Aug;15[4]:303-8; Obstet Gynecol Clin North Am. 2004 Sep;31[3]:641-54, xi).
Since then, research has affirmed the differences in patient tolerance and has shown that there is no significant difference between traditional and vaginoscopic hysteroscopy in the rate of procedure failure (0%-10%).
In my practice, in addition to vaginal or cervical examination and evaluation of the uterine cavity, I utilize a vaginoscopic approach to perform minor therapeutic and operative procedures such as biopsies, polypectomies, tubal occlusion using the Essure system, and removal of lost intrauterine devices. I can assess infertility, trauma, abnormal uterine bleeding, and mesh erosion, and provide pre- and postsurgical evaluations. In all of these cases, I use minimal premedication and only rarely need any local anesthetic and/or sedation.
Instrumentation and technique
There are a variety of hysteroscopes available on the market, from single-channel flexible diagnostic hysteroscopes that are 3 mm to 4 mm in diameter, to “see-and-treat” operative hysteroscopes that are rigid and have various diameters and camera lens angles.
A hysteroscope with a 5.5-mm outer diameter works well for a vaginoscopic approach that avoids cervical dilation. Accessory instrumentation includes semirigid 5 Fr 35-cm–long biopsy forceps, scissors, and alligator forceps.
In timing the procedure, our main goal is a thin uterine lining. This can be achieved by scheduling the procedure during the early proliferative phase of the menstrual cycle or by using a gonadotropin-releasing hormone agonist or a transdermal or transvaginal contraceptive medication.
By far the most important element of pain control and analgesia is the time spent with each patient to thoroughly discuss the experience of hysteroscopy and to set expectations about what she will hear, see, and feel. An unexpected experience can worsen anxiety, which in turn can worsen pain. If everything is as familiar and relaxed as possible, there will be little need for analgesia.
I tell patients in preprocedure counseling that the distention of the uterine walls usually causes some cramping, and that NSAIDs can minimize this cramping. In rare cases, when a patient is very worried about her pain tolerance, I will prescribe diazepam. However, many of my patients opt to do nothing other than take ibuprofen. On a case-by-case basis, you can determine with your patient what type and level of analgesia and preprocedure medication will be best.
Paracervical blocks are an option for some surgical patients, but I advise my patients to move forward without the block and assure them that it can be administered later if needed. Thus far, I’ve never proceeded with a paracervical block. There are other methods and sites for introducing local anesthesia, including intracervical, by injection or topical, or topical intracavitary techniques. Nevertheless, it is unclear from randomized controlled trials whether local anesthesia is effective. Trials of paracervical blocks similarly have had inconsistent outcomes.
I do commonly premedicate patients – mainly nulliparous patients and postmenopausal patients – with misoprostol, which softens the cervix and facilitates an easier entry of the hysteroscope into the cervix.
Published studies on misoprostol administration before hysteroscopy have had mixed results. A Cochrane review from 2015 concluded there is moderate-quality evidence in support of preoperative ripening with the agent, while another meta-analysis also published in 2015 concluded that data are poor and do not support its use. Recently, however, there appear to be more supportive studies demonstrating or suggesting that misoprostol is effective in reducing discomfort.
Patient discomfort is also minimized when there is little manipulation of the hysteroscope. Scopes that are angled (12, 25, or 30 degrees) allow optimal visualization with minimal movement; the scope can be brought to the midline of the uterine cavity and the light cord rotated to the 3:00 and 9:00 o’clock positions to enable visualization of the cornu. A 0-degree scope, on the other hand, must be manipulated quite a bit for the same degree of visualization, potentially increasing patient discomfort.
Prior to hysteroscopy, the cervix and vagina are cleaned with a small-diameter swab dipped in povidone-iodine or chlorhexidine gluconate in the case of allergies. One or two 1,000-cc bags of saline inserted into pressure bags are attached to Y-type tubing. (A diagnostic procedure rarely will require two bags.) I spread the labia initially while guiding the scope into the posterior fornix of the vagina. If the leakage of fluid causes inadequate distension of the vaginal walls, I will gently pinch the labia together with gauze.
I then gently pull back the scope and manipulate it posteriorly to visualize the external cervical os anteriorly. The hysteroscope may then be introduced through the cervical os, endocervical canal, and uterine cavity, with care taken so that the instrument does not rub against the cervix or the uterine tissue and cause trauma, pain, and bleeding. The uterus will progressively align with the cervix and vagina, thereby eliminating the need for a tenaculum to straighten the uterine axis.
Fluid monitoring is important, especially during operative hysteroscopy. In my practice, a nurse watches inflow and outflow amounts while I explain what I am doing and visualizing. Some patients like to be able to view the surgery, so I am always ready to tilt the screen accordingly.
The economics
How do you know if office hysteroscopy is right for you? Your own surgical skill and the skills of your staff, who must be trained to handle and sterilize equipment and to consistently assist you, are major factors, as is ensurance of a return on your investment.
One manufacturer contacted for this Master Class lists the price of a complete office tower (light source, camera, and monitor) at approximately $9,700 and the price of a rigid hysteroscope, sheath, and hand instruments at about $6,300. A complete setup for office hysteroscopy, including a standard operative (rigid) hysteroscope, should therefore cost between $15,000 and $17,000. Companies also offer leasing options for about $300-400/month.
Flexible hysteroscopes cost about $6,000 more, which prompts many gynecologic surgeons to focus their investment on a rigid scope that can be used for both diagnostic and therapeutic procedures. Disposables cost $10 or less, and $40-50 or less, for each diagnostic and operative hysteroscopy, respectively.
A look at the Medicare Relative Value Units (RVUs) – a key component of the Medicare reimbursement system and a standard for many payers in determining compensation – shows higher reimbursement for quite a few hysteroscopic codes when these procedures are performed in the office.
Total RVUs have three components:
1. Physician work, including time and the technical skill and intensity of effort it takes to perform a service or procedure.
2. Practice expenses, such as rent, equipment and supplies, and nonphysician salaries.
3. Malpractice insurance premiums.
Each component is multiplied by a factor that accounts for geographic cost variations, and each total RVU is multiplied by a dollar amount known as the conversion factor.
Practice expense (PE) RVUs for services provided in a “facility” (e.g., hospital or outpatient clinic) are often lower than office-based PE RVUs for the same services. Hysteroscopy is no exception. The PE RVU value for diagnostic hysteroscopy performed in the office, for instance, is approximately 5 units, compared with 1.64 units for diagnostic hysteroscopy performed in a facility.
Information on hysteroscopic procedures, and their associated RVUs, on geographic practice cost indices and on pricing, can be accessed using Medicare’s Physician Fee Schedule lookup tool (www.cms.gov/apps/physician-fee-schedule/overview.aspx).
This tool is useful for calculating returns on investment. According to national payment amounts listed in August, a diagnostic hysteroscopy performed in the office will earn an average of $315.08 vs. $192.27 for each case performed in the hospital. If you perform 12 such procedures a year, that’s about $3,781 in the office, compared with $2,307 in the hospital.
This difference alone might not be worth an investment of $15,000 or more, but if you anticipate performing additional procedures with higher margins and higher reimbursement, such as 12 thermal endometrial ablations a year in combination with diagnostic hysteroscopy (which, according to the Medicare national fee schedule averages would earn $15,962 in the office vs. $4,971 in the hospital), or 12 Essure tubal occlusions ($22,595 vs. $5,263), the investment will look more favorable.
And if your patients are largely privately insured, your return on investment will occur much more quickly. In metropolitan Chicago, Blue Cross Blue Shield is reimbursing in-office diagnostic hysteroscopy at approximately $568, hysteroscopic ablations at $3,844, and Essure tubal occlusions at $3,885.
In addition to reimbursement levels, it’s important to consider the efficiencies of in-office hysteroscopy. You can perform an annual exam while the assistant sets up the room and greets each patient, for instance, or see another established patient while the assistant discharges your patient and turns the room over. Our patients, in turn, benefit from increased accessibility, with less time spent away from work or family, as well as more familiarity and comfort and reduced out-of-pocket expenses.
Dr. Cholkeri-Singh is clinical assistant professor at the University of Illinois in Chicago and is director of gynecologic surgical education and associate director of minimally invasive gynecology at Advocate Lutheran General Hospital. She is in private practice with Dr. Charles Miller and Dr. Kristen Sasaki at the Advanced Gynecologic Surgical Institute in Chicago. She is a consultant for DySIS Medical, Hologic, and Bayer HealthCare.
PAs Should Focus on Patient Care, Not Unnecessary Testing
PAs are highly educated, trusted health care providers who lead patient-centered medical teams. Trained as experts in general medicine, we often pursue multiple specialties over the course of our careers—typically in three or four. PAs can decide to work in surgery, emergency care, orthopedics, oncology, pediatrics, dermatology, and many other areas. Moving among and between specialties is a hallmark of our profession. Unfortunately, a new proposal would alter how PAs are tested in order to maintain their certification—and, in 20 states, potentially jeopardize their license to practice.
The National Commission on Certification of PAs (NCCPA) has proposed significant changes to how PAs are recertified by requiring multiple exams, including a proctored, closed-book exam in a specialty area and two or three take-home exams during every 10-year recertification cycle. The proposal would in effect force PAs to choose a specialty and as a result undermine their ability to fill care gaps in hospitals, health systems, and communities.
The new requirements are cumbersome and unnecessary. PAs already undergo rigorous medical training and have initial licensing requirements that are similar to those of our physician, nurse practitioner, and pharmacist colleagues—none of whom are required to retest. PAs must graduate from an accredited program and take a test in general medicine in order to be licensed and certified in the first place. Throughout their careers, they have to complete extensive continuing medical education (CME). They also practice in clinical settings that continually inform and enhance their experience and base of knowledge.
Additional testing would take valuable time away from patients and could even discourage PAs from staying in a profession that is in high demand. More to the point, NCCPA has pursued its proposal even though studies have shown that recertification testing is not related to improvements in patient outcomes or safety.
AAPA recently received a message from longtime PA Peter Schuman, who is as passionate about patient care as he is leery of NCCPA’s recertification plan. “[NCCPA has] no significant, scientifically valid evidence to support their claims. I can honestly say that their testing requirements have not helped me care for patients better or become more knowledgeable in my field of practice/expertise one bit,” he wrote. “The PANRE is a waste of time and effort and is a source of great stress, taking time away from my patients, practice, and family. Enough is enough, NCCPA!”
The AAPA board has reached out to NCCPA and still hopes that it will engage in substantive discussions. Given the seriousness of our concerns, however, the AAPA Board voted recently to take steps toward the creation of an alternative certifying body for PAs. This vote came after careful deliberation and in response to the concerns of the thousands of professionals that AAPA represents. The decision was not made lightly and it reflects the priority of PAs to put patient care ahead of unnecessary testing.
AAPA is not alone in its opposition to recertification testing. A growing number of medical associations, including the American Medical Association (AMA), reject it as unnecessary and overly burdensome. AMA has rightly identified these exams as high-stakes tests because, it said, “failure to pass can result in a physician’s loss of privileges or employment.” Every PA would face similar consequences and, in 20 states, put their license at risk. At least 19 state medical associations have adopted similar resolutions in opposition to unnecessary retesting.
To be clear, AAPA does not oppose initial testing for certification and licensing and embraces the value of an exam in the licensing process. AAPA also strongly supports extensive CME and the benefits it provides.
We have not yet decided whether to establish a new certification organization. But we do know that there is no reason PAs should be singled out for additional testing when the extra requirement does not help patients and when other medical professionals are not required to do the same. Let PAs focus on patient care, not unwarranted test-taking.
PAs are highly educated, trusted health care providers who lead patient-centered medical teams. Trained as experts in general medicine, we often pursue multiple specialties over the course of our careers—typically in three or four. PAs can decide to work in surgery, emergency care, orthopedics, oncology, pediatrics, dermatology, and many other areas. Moving among and between specialties is a hallmark of our profession. Unfortunately, a new proposal would alter how PAs are tested in order to maintain their certification—and, in 20 states, potentially jeopardize their license to practice.
The National Commission on Certification of PAs (NCCPA) has proposed significant changes to how PAs are recertified by requiring multiple exams, including a proctored, closed-book exam in a specialty area and two or three take-home exams during every 10-year recertification cycle. The proposal would in effect force PAs to choose a specialty and as a result undermine their ability to fill care gaps in hospitals, health systems, and communities.
The new requirements are cumbersome and unnecessary. PAs already undergo rigorous medical training and have initial licensing requirements that are similar to those of our physician, nurse practitioner, and pharmacist colleagues—none of whom are required to retest. PAs must graduate from an accredited program and take a test in general medicine in order to be licensed and certified in the first place. Throughout their careers, they have to complete extensive continuing medical education (CME). They also practice in clinical settings that continually inform and enhance their experience and base of knowledge.
Additional testing would take valuable time away from patients and could even discourage PAs from staying in a profession that is in high demand. More to the point, NCCPA has pursued its proposal even though studies have shown that recertification testing is not related to improvements in patient outcomes or safety.
AAPA recently received a message from longtime PA Peter Schuman, who is as passionate about patient care as he is leery of NCCPA’s recertification plan. “[NCCPA has] no significant, scientifically valid evidence to support their claims. I can honestly say that their testing requirements have not helped me care for patients better or become more knowledgeable in my field of practice/expertise one bit,” he wrote. “The PANRE is a waste of time and effort and is a source of great stress, taking time away from my patients, practice, and family. Enough is enough, NCCPA!”
The AAPA board has reached out to NCCPA and still hopes that it will engage in substantive discussions. Given the seriousness of our concerns, however, the AAPA Board voted recently to take steps toward the creation of an alternative certifying body for PAs. This vote came after careful deliberation and in response to the concerns of the thousands of professionals that AAPA represents. The decision was not made lightly and it reflects the priority of PAs to put patient care ahead of unnecessary testing.
AAPA is not alone in its opposition to recertification testing. A growing number of medical associations, including the American Medical Association (AMA), reject it as unnecessary and overly burdensome. AMA has rightly identified these exams as high-stakes tests because, it said, “failure to pass can result in a physician’s loss of privileges or employment.” Every PA would face similar consequences and, in 20 states, put their license at risk. At least 19 state medical associations have adopted similar resolutions in opposition to unnecessary retesting.
To be clear, AAPA does not oppose initial testing for certification and licensing and embraces the value of an exam in the licensing process. AAPA also strongly supports extensive CME and the benefits it provides.
We have not yet decided whether to establish a new certification organization. But we do know that there is no reason PAs should be singled out for additional testing when the extra requirement does not help patients and when other medical professionals are not required to do the same. Let PAs focus on patient care, not unwarranted test-taking.
PAs are highly educated, trusted health care providers who lead patient-centered medical teams. Trained as experts in general medicine, we often pursue multiple specialties over the course of our careers—typically in three or four. PAs can decide to work in surgery, emergency care, orthopedics, oncology, pediatrics, dermatology, and many other areas. Moving among and between specialties is a hallmark of our profession. Unfortunately, a new proposal would alter how PAs are tested in order to maintain their certification—and, in 20 states, potentially jeopardize their license to practice.
The National Commission on Certification of PAs (NCCPA) has proposed significant changes to how PAs are recertified by requiring multiple exams, including a proctored, closed-book exam in a specialty area and two or three take-home exams during every 10-year recertification cycle. The proposal would in effect force PAs to choose a specialty and as a result undermine their ability to fill care gaps in hospitals, health systems, and communities.
The new requirements are cumbersome and unnecessary. PAs already undergo rigorous medical training and have initial licensing requirements that are similar to those of our physician, nurse practitioner, and pharmacist colleagues—none of whom are required to retest. PAs must graduate from an accredited program and take a test in general medicine in order to be licensed and certified in the first place. Throughout their careers, they have to complete extensive continuing medical education (CME). They also practice in clinical settings that continually inform and enhance their experience and base of knowledge.
Additional testing would take valuable time away from patients and could even discourage PAs from staying in a profession that is in high demand. More to the point, NCCPA has pursued its proposal even though studies have shown that recertification testing is not related to improvements in patient outcomes or safety.
AAPA recently received a message from longtime PA Peter Schuman, who is as passionate about patient care as he is leery of NCCPA’s recertification plan. “[NCCPA has] no significant, scientifically valid evidence to support their claims. I can honestly say that their testing requirements have not helped me care for patients better or become more knowledgeable in my field of practice/expertise one bit,” he wrote. “The PANRE is a waste of time and effort and is a source of great stress, taking time away from my patients, practice, and family. Enough is enough, NCCPA!”
The AAPA board has reached out to NCCPA and still hopes that it will engage in substantive discussions. Given the seriousness of our concerns, however, the AAPA Board voted recently to take steps toward the creation of an alternative certifying body for PAs. This vote came after careful deliberation and in response to the concerns of the thousands of professionals that AAPA represents. The decision was not made lightly and it reflects the priority of PAs to put patient care ahead of unnecessary testing.
AAPA is not alone in its opposition to recertification testing. A growing number of medical associations, including the American Medical Association (AMA), reject it as unnecessary and overly burdensome. AMA has rightly identified these exams as high-stakes tests because, it said, “failure to pass can result in a physician’s loss of privileges or employment.” Every PA would face similar consequences and, in 20 states, put their license at risk. At least 19 state medical associations have adopted similar resolutions in opposition to unnecessary retesting.
To be clear, AAPA does not oppose initial testing for certification and licensing and embraces the value of an exam in the licensing process. AAPA also strongly supports extensive CME and the benefits it provides.
We have not yet decided whether to establish a new certification organization. But we do know that there is no reason PAs should be singled out for additional testing when the extra requirement does not help patients and when other medical professionals are not required to do the same. Let PAs focus on patient care, not unwarranted test-taking.
‘Enough!’ We need to take back our profession; More unresolved questions about psychiatry
‘Enough!’ We need to take back our profession
Every day, I am grateful that I became a physician and a psychiatrist. Every minute that I spend with patients is an honor and a privilege. I have never forgotten that. But it is heartbreaking to see my precious profession being destroyed by bureaucrats.
An example: I am concerned about the effect that passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) will have on physicians. I read articles telling us how we should handle this new plan for reimbursement, but I also read that 86% of physicians are not in favor of MACRA. How did we get stuck with it?
Another example of why it has become virtually impossible to do our job: I spend a fair amount of time obtaining prior authorization for generic medications that are available at big-box stores for $10 or $15; often, these authorizations need approval by the medical director. I have been beaten down enough over the years to learn that I should no longer prescribe brand-name medications—only generic medications (which still require authorization!), even when my patient has been taking the medication for 10 or 15 years. The last time I sought authorization to prescribe a medication, the reviewer asked me why I had not tried 3 different generics over the past year. I had to remind her that I had an active prior authorization in place from the year before, and so why would I do what she was proposing?
Physicians are some of the most highly trained professionals. It takes 7 to 15 years to be able to be somewhat proficient at the job, then another 30 or 40 years of practice to become really good at it. But we’ve become technicians at the mercy of business executives: We go to our office and spend our time checking off boxes, trying to figure out proper coding and the proper diagnosis, so that we can get an appropriate amount of money for the service we’re providing. How has it come to this? Why can’t we take back our profession?
Another problem is that physicians are being paid for their performance and the outcomes they produce. But people are not refrigerators: We can do everything right and the patient still dies. I have a number of patients who have no insight into their psychiatric illness; no matter what I say, or do, or how much time I spend with them, they are nonadherent. How is this my fault?
Physicians are not given the opportunity to think for themselves, or to prescribe treatments that they see fit and document in ways that they were trained. Where is the American Medical Association, the Connecticut State Medical Society, the Hartford County Medical Association, and all the other associations that supposedly represent us? How have they allowed this to happen?
In the future, health care will be provided by physician assistants and nurse practitioners; physicians will provide background supervision, or perform surgery, but the patient will never meet them. I respect NPs and PAs, but they do not have the rigorous training that physicians have. But they’re less expensive—and isn’t that what it’s all about?
If we are not going to speak up, or if we are not going to elect officials to truly represent us and advocate for us, then we have nobody to blame but ourselves.
Carole Black Cohen, MD
Private psychiatric practice
Farmington, Connecticut
More unresolved questions about psychiatry
In Dr. Nasrallah’s August essay (From the Editor,
H. Steven Moffic, MD
Retired Tenured Professor of Psychiatry
Medical College of Wisconsin
Milwaukee, Wisconsin
Dr. Nasrallah responds
Dr. Moffic is spot-on about the escalating rate of burnout among physicians, including psychiatrists. The reason I did not include burnout in the list of questions is because I intended to pose questions related to external forces that interfere with patient care. Burnout is a vicious internal typhoon of emotional turmoil that might be related to multiple idiosyncratic personal variables and only partially to frustrations in clinical practice.
Burnout is, one might say, a subcortical event (generated in the amygdala?)—not a cortical process like the “why” questions that beg for answers. Admittedly, however, the cumulative burden of practice frustrations—especially the inability to erase the personal, social, financial, and vocational stigmata that plague our patients’ lives—can, eventually, take a toll on our morale and quality of life.
Fortunately, we psychiatrists generally are a resilient breed. We can manage personal stress using techniques that we employ in our practices. That might be why burnout is lower in psychiatry than it is in other medical specialties.
Henry A. Nasrallah, MD
Professor and Chair
Department of Psychiatry
Saint Louis University School of Medicine
St. Louis, Missouri
‘Enough!’ We need to take back our profession
Every day, I am grateful that I became a physician and a psychiatrist. Every minute that I spend with patients is an honor and a privilege. I have never forgotten that. But it is heartbreaking to see my precious profession being destroyed by bureaucrats.
An example: I am concerned about the effect that passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) will have on physicians. I read articles telling us how we should handle this new plan for reimbursement, but I also read that 86% of physicians are not in favor of MACRA. How did we get stuck with it?
Another example of why it has become virtually impossible to do our job: I spend a fair amount of time obtaining prior authorization for generic medications that are available at big-box stores for $10 or $15; often, these authorizations need approval by the medical director. I have been beaten down enough over the years to learn that I should no longer prescribe brand-name medications—only generic medications (which still require authorization!), even when my patient has been taking the medication for 10 or 15 years. The last time I sought authorization to prescribe a medication, the reviewer asked me why I had not tried 3 different generics over the past year. I had to remind her that I had an active prior authorization in place from the year before, and so why would I do what she was proposing?
Physicians are some of the most highly trained professionals. It takes 7 to 15 years to be able to be somewhat proficient at the job, then another 30 or 40 years of practice to become really good at it. But we’ve become technicians at the mercy of business executives: We go to our office and spend our time checking off boxes, trying to figure out proper coding and the proper diagnosis, so that we can get an appropriate amount of money for the service we’re providing. How has it come to this? Why can’t we take back our profession?
Another problem is that physicians are being paid for their performance and the outcomes they produce. But people are not refrigerators: We can do everything right and the patient still dies. I have a number of patients who have no insight into their psychiatric illness; no matter what I say, or do, or how much time I spend with them, they are nonadherent. How is this my fault?
Physicians are not given the opportunity to think for themselves, or to prescribe treatments that they see fit and document in ways that they were trained. Where is the American Medical Association, the Connecticut State Medical Society, the Hartford County Medical Association, and all the other associations that supposedly represent us? How have they allowed this to happen?
In the future, health care will be provided by physician assistants and nurse practitioners; physicians will provide background supervision, or perform surgery, but the patient will never meet them. I respect NPs and PAs, but they do not have the rigorous training that physicians have. But they’re less expensive—and isn’t that what it’s all about?
If we are not going to speak up, or if we are not going to elect officials to truly represent us and advocate for us, then we have nobody to blame but ourselves.
Carole Black Cohen, MD
Private psychiatric practice
Farmington, Connecticut
More unresolved questions about psychiatry
In Dr. Nasrallah’s August essay (From the Editor,
H. Steven Moffic, MD
Retired Tenured Professor of Psychiatry
Medical College of Wisconsin
Milwaukee, Wisconsin
Dr. Nasrallah responds
Dr. Moffic is spot-on about the escalating rate of burnout among physicians, including psychiatrists. The reason I did not include burnout in the list of questions is because I intended to pose questions related to external forces that interfere with patient care. Burnout is a vicious internal typhoon of emotional turmoil that might be related to multiple idiosyncratic personal variables and only partially to frustrations in clinical practice.
Burnout is, one might say, a subcortical event (generated in the amygdala?)—not a cortical process like the “why” questions that beg for answers. Admittedly, however, the cumulative burden of practice frustrations—especially the inability to erase the personal, social, financial, and vocational stigmata that plague our patients’ lives—can, eventually, take a toll on our morale and quality of life.
Fortunately, we psychiatrists generally are a resilient breed. We can manage personal stress using techniques that we employ in our practices. That might be why burnout is lower in psychiatry than it is in other medical specialties.
Henry A. Nasrallah, MD
Professor and Chair
Department of Psychiatry
Saint Louis University School of Medicine
St. Louis, Missouri
‘Enough!’ We need to take back our profession
Every day, I am grateful that I became a physician and a psychiatrist. Every minute that I spend with patients is an honor and a privilege. I have never forgotten that. But it is heartbreaking to see my precious profession being destroyed by bureaucrats.
An example: I am concerned about the effect that passage of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) will have on physicians. I read articles telling us how we should handle this new plan for reimbursement, but I also read that 86% of physicians are not in favor of MACRA. How did we get stuck with it?
Another example of why it has become virtually impossible to do our job: I spend a fair amount of time obtaining prior authorization for generic medications that are available at big-box stores for $10 or $15; often, these authorizations need approval by the medical director. I have been beaten down enough over the years to learn that I should no longer prescribe brand-name medications—only generic medications (which still require authorization!), even when my patient has been taking the medication for 10 or 15 years. The last time I sought authorization to prescribe a medication, the reviewer asked me why I had not tried 3 different generics over the past year. I had to remind her that I had an active prior authorization in place from the year before, and so why would I do what she was proposing?
Physicians are some of the most highly trained professionals. It takes 7 to 15 years to be able to be somewhat proficient at the job, then another 30 or 40 years of practice to become really good at it. But we’ve become technicians at the mercy of business executives: We go to our office and spend our time checking off boxes, trying to figure out proper coding and the proper diagnosis, so that we can get an appropriate amount of money for the service we’re providing. How has it come to this? Why can’t we take back our profession?
Another problem is that physicians are being paid for their performance and the outcomes they produce. But people are not refrigerators: We can do everything right and the patient still dies. I have a number of patients who have no insight into their psychiatric illness; no matter what I say, or do, or how much time I spend with them, they are nonadherent. How is this my fault?
Physicians are not given the opportunity to think for themselves, or to prescribe treatments that they see fit and document in ways that they were trained. Where is the American Medical Association, the Connecticut State Medical Society, the Hartford County Medical Association, and all the other associations that supposedly represent us? How have they allowed this to happen?
In the future, health care will be provided by physician assistants and nurse practitioners; physicians will provide background supervision, or perform surgery, but the patient will never meet them. I respect NPs and PAs, but they do not have the rigorous training that physicians have. But they’re less expensive—and isn’t that what it’s all about?
If we are not going to speak up, or if we are not going to elect officials to truly represent us and advocate for us, then we have nobody to blame but ourselves.
Carole Black Cohen, MD
Private psychiatric practice
Farmington, Connecticut
More unresolved questions about psychiatry
In Dr. Nasrallah’s August essay (From the Editor,
H. Steven Moffic, MD
Retired Tenured Professor of Psychiatry
Medical College of Wisconsin
Milwaukee, Wisconsin
Dr. Nasrallah responds
Dr. Moffic is spot-on about the escalating rate of burnout among physicians, including psychiatrists. The reason I did not include burnout in the list of questions is because I intended to pose questions related to external forces that interfere with patient care. Burnout is a vicious internal typhoon of emotional turmoil that might be related to multiple idiosyncratic personal variables and only partially to frustrations in clinical practice.
Burnout is, one might say, a subcortical event (generated in the amygdala?)—not a cortical process like the “why” questions that beg for answers. Admittedly, however, the cumulative burden of practice frustrations—especially the inability to erase the personal, social, financial, and vocational stigmata that plague our patients’ lives—can, eventually, take a toll on our morale and quality of life.
Fortunately, we psychiatrists generally are a resilient breed. We can manage personal stress using techniques that we employ in our practices. That might be why burnout is lower in psychiatry than it is in other medical specialties.
Henry A. Nasrallah, MD
Professor and Chair
Department of Psychiatry
Saint Louis University School of Medicine
St. Louis, Missouri
A Melting Pot of Mail
VAPING DANGERS: CLEARING THE AIR
The liquid base of an e-cigarette contains either vegetable glycerin (VG) or propylene glycol, or more commonly, a proprietary combination of both. Each of these ingredients has varying effects on the body.
However, the first paragraph of Randy D. Danielsen’s editorial alluded to what I consider a bigger concern regarding the future medical complications of vaping. The description of a “… huge puff of cherry-scented smoke …” indicates that vapes are not puffed on the way cigarettes are.
Cigarette smoking is similar to drinking through a straw—the smoke is first captured in the mouth, then cooled and inhaled. In contrast, vaping involves inhaling smoke directly into the lungs. This action, along with the thick VG base, produces a high volume of smoke. Vape shops even sponsor contests to see who can produce the largest cloud of smoke.
Therefore, my concern regarding vaping is not limited to the toxicity of the ingredients; it extends to how the toxicants are delivered to the poor, unsuspecting alveoli.
Gary Dula, FNP-C
Houston, TX
Continue for Millenials: Not All Sitting at the Kids' Table >>
MILLENIALS: NOT ALL SITTING AT THE KIDS' TABLES
I received my master’s degree in 2015 and am nearing completion of a year-long FNP fellowship program. I was an Army nurse for four years and a float nurse at various hospitals for five. I am a “millennial”—and, according to the published letters about precepting, am hated by older nurses because of it. Considering I have practiced with many hard-working people my age who would lay down their lives for this country, I find this unprecedented.
I work hard, but the school I attended for my FNP did not prepare me well; it was difficult to get people to teach and precept me during school. This led me to apply for my current fellowship.
Throughout my nine-year nursing career, I have precepted many nurses, including those with associate degrees. I will continue to mentor and precept as an APRN. I take issue with the portrayal of millennials as lazy and unable to work hard. Why? Because we will not work for free, would like to collaboratively learn, and need help to develop our skills?
One day, you will grow old and need someone to take care of you. Why on earth would you berate the people who will be doing just that? Complaining about this generation is not going to change the fact that they are here and present in the workforce. We need more providers, and chastising the younger generation is not going to solve that problem.
Stephanie Butler-Cleland, FNP-BC
Colorado Springs, CO
Continue for The Pros of Precepting >>
THE PROS OF PRECEPTING
I am an urgent care NP in urban communities on the West Coast of Florida. I had taken a break from precepting as a result of negative experiences, but I recently resumed to precept my first NP student in years.
Prior to accepting the student I precepted, I received requests from two other students. One asked if I could change my schedule to be closer to where she lived. The other clearly didn’t want to commit to the drive or the hours I was available, and asked if I would work more weekends to accommodate her schedule. Needless to say, I refused both students.
Instead, I precepted a smart 28-year-old student from my alma mater, one of the Florida state universities. She was attentive, prepared, and eager. I was very, very impressed with her. She had been a nurse for four years and was a second-semester student. It was a pleasure to have her; I like being questioned and challenged. It was fun to see her enjoying my job, and it reminded me of why I love what I do.
Anne Conklin, MS, ARNP-C
Bradenton, FL
Continue for A Scheming Industry >>
A SCHEMING INDUSTRY
Intelligent health care policy has been frustrated by the enormous amount of money brought to bear on Congress by the insurance and pharmaceutical industries. Each dollar paid to an insurance company is used to construct buildings, hire workers, create a sales staff, and ultimately pay their shareholders a profit.
Since the insurance industry obtained an antitrust exemption in the 1940s, they are essentially immune from prosecution for price collusion. Until recently, it was difficult to know how much of the money paid was returned in the form of medical benefits. In order to keep profits rising, they must enroll more people. Promising coverage while impeding medical workups and care, making great profits, and needing more and more enrollees fits the definition of a Ponzi scheme.
Several years ago in California, the state insurance commission (under threat of decertification) got an industry representative to admit that the maximum percentage of dollars used for services was 70%. In other words, for each dollar spent, a patient would be lucky to get 70 cents worth of services.
All of us who practice know how the companies do this: We request a needed diagnostic test or treatment and are denied. I have interrupted my schedule on many days to call for a “peer to peer” review—only once was I denied. This is a roadblock that many busy practitioners will not challenge. Since insurance companies market how great their coverage is, patients often get angry at the provider.
The repeated argument is that the market forces will lower medical costs. This fallacy is easily debunked by noting the ever-escalating costs and comparing health care costs as a percent of gross domestic product (GDP) in our country versus others. France, for example, expends 12% of GDP on health and ranks first in health care outcomes by world standards. In the US, we are approaching 20% of GDP.
Since insurance adds nothing to care and increases costs dramatically (every provider has to have billers for the various insurance companies, since each has its own requirements), a single-payer system is the only system that will lower costs. Those who benefit from the current system declare that we can’t have “socialized medicine.” To which I would respond, fine; we’ll continue to pay 30% to 50% more so that insurance companies can have their profits at our expense.
Nelson Herilhy, PA-C, MHS
Concord, CA
VAPING DANGERS: CLEARING THE AIR
The liquid base of an e-cigarette contains either vegetable glycerin (VG) or propylene glycol, or more commonly, a proprietary combination of both. Each of these ingredients has varying effects on the body.
However, the first paragraph of Randy D. Danielsen’s editorial alluded to what I consider a bigger concern regarding the future medical complications of vaping. The description of a “… huge puff of cherry-scented smoke …” indicates that vapes are not puffed on the way cigarettes are.
Cigarette smoking is similar to drinking through a straw—the smoke is first captured in the mouth, then cooled and inhaled. In contrast, vaping involves inhaling smoke directly into the lungs. This action, along with the thick VG base, produces a high volume of smoke. Vape shops even sponsor contests to see who can produce the largest cloud of smoke.
Therefore, my concern regarding vaping is not limited to the toxicity of the ingredients; it extends to how the toxicants are delivered to the poor, unsuspecting alveoli.
Gary Dula, FNP-C
Houston, TX
Continue for Millenials: Not All Sitting at the Kids' Table >>
MILLENIALS: NOT ALL SITTING AT THE KIDS' TABLES
I received my master’s degree in 2015 and am nearing completion of a year-long FNP fellowship program. I was an Army nurse for four years and a float nurse at various hospitals for five. I am a “millennial”—and, according to the published letters about precepting, am hated by older nurses because of it. Considering I have practiced with many hard-working people my age who would lay down their lives for this country, I find this unprecedented.
I work hard, but the school I attended for my FNP did not prepare me well; it was difficult to get people to teach and precept me during school. This led me to apply for my current fellowship.
Throughout my nine-year nursing career, I have precepted many nurses, including those with associate degrees. I will continue to mentor and precept as an APRN. I take issue with the portrayal of millennials as lazy and unable to work hard. Why? Because we will not work for free, would like to collaboratively learn, and need help to develop our skills?
One day, you will grow old and need someone to take care of you. Why on earth would you berate the people who will be doing just that? Complaining about this generation is not going to change the fact that they are here and present in the workforce. We need more providers, and chastising the younger generation is not going to solve that problem.
Stephanie Butler-Cleland, FNP-BC
Colorado Springs, CO
Continue for The Pros of Precepting >>
THE PROS OF PRECEPTING
I am an urgent care NP in urban communities on the West Coast of Florida. I had taken a break from precepting as a result of negative experiences, but I recently resumed to precept my first NP student in years.
Prior to accepting the student I precepted, I received requests from two other students. One asked if I could change my schedule to be closer to where she lived. The other clearly didn’t want to commit to the drive or the hours I was available, and asked if I would work more weekends to accommodate her schedule. Needless to say, I refused both students.
Instead, I precepted a smart 28-year-old student from my alma mater, one of the Florida state universities. She was attentive, prepared, and eager. I was very, very impressed with her. She had been a nurse for four years and was a second-semester student. It was a pleasure to have her; I like being questioned and challenged. It was fun to see her enjoying my job, and it reminded me of why I love what I do.
Anne Conklin, MS, ARNP-C
Bradenton, FL
Continue for A Scheming Industry >>
A SCHEMING INDUSTRY
Intelligent health care policy has been frustrated by the enormous amount of money brought to bear on Congress by the insurance and pharmaceutical industries. Each dollar paid to an insurance company is used to construct buildings, hire workers, create a sales staff, and ultimately pay their shareholders a profit.
Since the insurance industry obtained an antitrust exemption in the 1940s, they are essentially immune from prosecution for price collusion. Until recently, it was difficult to know how much of the money paid was returned in the form of medical benefits. In order to keep profits rising, they must enroll more people. Promising coverage while impeding medical workups and care, making great profits, and needing more and more enrollees fits the definition of a Ponzi scheme.
Several years ago in California, the state insurance commission (under threat of decertification) got an industry representative to admit that the maximum percentage of dollars used for services was 70%. In other words, for each dollar spent, a patient would be lucky to get 70 cents worth of services.
All of us who practice know how the companies do this: We request a needed diagnostic test or treatment and are denied. I have interrupted my schedule on many days to call for a “peer to peer” review—only once was I denied. This is a roadblock that many busy practitioners will not challenge. Since insurance companies market how great their coverage is, patients often get angry at the provider.
The repeated argument is that the market forces will lower medical costs. This fallacy is easily debunked by noting the ever-escalating costs and comparing health care costs as a percent of gross domestic product (GDP) in our country versus others. France, for example, expends 12% of GDP on health and ranks first in health care outcomes by world standards. In the US, we are approaching 20% of GDP.
Since insurance adds nothing to care and increases costs dramatically (every provider has to have billers for the various insurance companies, since each has its own requirements), a single-payer system is the only system that will lower costs. Those who benefit from the current system declare that we can’t have “socialized medicine.” To which I would respond, fine; we’ll continue to pay 30% to 50% more so that insurance companies can have their profits at our expense.
Nelson Herilhy, PA-C, MHS
Concord, CA
VAPING DANGERS: CLEARING THE AIR
The liquid base of an e-cigarette contains either vegetable glycerin (VG) or propylene glycol, or more commonly, a proprietary combination of both. Each of these ingredients has varying effects on the body.
However, the first paragraph of Randy D. Danielsen’s editorial alluded to what I consider a bigger concern regarding the future medical complications of vaping. The description of a “… huge puff of cherry-scented smoke …” indicates that vapes are not puffed on the way cigarettes are.
Cigarette smoking is similar to drinking through a straw—the smoke is first captured in the mouth, then cooled and inhaled. In contrast, vaping involves inhaling smoke directly into the lungs. This action, along with the thick VG base, produces a high volume of smoke. Vape shops even sponsor contests to see who can produce the largest cloud of smoke.
Therefore, my concern regarding vaping is not limited to the toxicity of the ingredients; it extends to how the toxicants are delivered to the poor, unsuspecting alveoli.
Gary Dula, FNP-C
Houston, TX
Continue for Millenials: Not All Sitting at the Kids' Table >>
MILLENIALS: NOT ALL SITTING AT THE KIDS' TABLES
I received my master’s degree in 2015 and am nearing completion of a year-long FNP fellowship program. I was an Army nurse for four years and a float nurse at various hospitals for five. I am a “millennial”—and, according to the published letters about precepting, am hated by older nurses because of it. Considering I have practiced with many hard-working people my age who would lay down their lives for this country, I find this unprecedented.
I work hard, but the school I attended for my FNP did not prepare me well; it was difficult to get people to teach and precept me during school. This led me to apply for my current fellowship.
Throughout my nine-year nursing career, I have precepted many nurses, including those with associate degrees. I will continue to mentor and precept as an APRN. I take issue with the portrayal of millennials as lazy and unable to work hard. Why? Because we will not work for free, would like to collaboratively learn, and need help to develop our skills?
One day, you will grow old and need someone to take care of you. Why on earth would you berate the people who will be doing just that? Complaining about this generation is not going to change the fact that they are here and present in the workforce. We need more providers, and chastising the younger generation is not going to solve that problem.
Stephanie Butler-Cleland, FNP-BC
Colorado Springs, CO
Continue for The Pros of Precepting >>
THE PROS OF PRECEPTING
I am an urgent care NP in urban communities on the West Coast of Florida. I had taken a break from precepting as a result of negative experiences, but I recently resumed to precept my first NP student in years.
Prior to accepting the student I precepted, I received requests from two other students. One asked if I could change my schedule to be closer to where she lived. The other clearly didn’t want to commit to the drive or the hours I was available, and asked if I would work more weekends to accommodate her schedule. Needless to say, I refused both students.
Instead, I precepted a smart 28-year-old student from my alma mater, one of the Florida state universities. She was attentive, prepared, and eager. I was very, very impressed with her. She had been a nurse for four years and was a second-semester student. It was a pleasure to have her; I like being questioned and challenged. It was fun to see her enjoying my job, and it reminded me of why I love what I do.
Anne Conklin, MS, ARNP-C
Bradenton, FL
Continue for A Scheming Industry >>
A SCHEMING INDUSTRY
Intelligent health care policy has been frustrated by the enormous amount of money brought to bear on Congress by the insurance and pharmaceutical industries. Each dollar paid to an insurance company is used to construct buildings, hire workers, create a sales staff, and ultimately pay their shareholders a profit.
Since the insurance industry obtained an antitrust exemption in the 1940s, they are essentially immune from prosecution for price collusion. Until recently, it was difficult to know how much of the money paid was returned in the form of medical benefits. In order to keep profits rising, they must enroll more people. Promising coverage while impeding medical workups and care, making great profits, and needing more and more enrollees fits the definition of a Ponzi scheme.
Several years ago in California, the state insurance commission (under threat of decertification) got an industry representative to admit that the maximum percentage of dollars used for services was 70%. In other words, for each dollar spent, a patient would be lucky to get 70 cents worth of services.
All of us who practice know how the companies do this: We request a needed diagnostic test or treatment and are denied. I have interrupted my schedule on many days to call for a “peer to peer” review—only once was I denied. This is a roadblock that many busy practitioners will not challenge. Since insurance companies market how great their coverage is, patients often get angry at the provider.
The repeated argument is that the market forces will lower medical costs. This fallacy is easily debunked by noting the ever-escalating costs and comparing health care costs as a percent of gross domestic product (GDP) in our country versus others. France, for example, expends 12% of GDP on health and ranks first in health care outcomes by world standards. In the US, we are approaching 20% of GDP.
Since insurance adds nothing to care and increases costs dramatically (every provider has to have billers for the various insurance companies, since each has its own requirements), a single-payer system is the only system that will lower costs. Those who benefit from the current system declare that we can’t have “socialized medicine.” To which I would respond, fine; we’ll continue to pay 30% to 50% more so that insurance companies can have their profits at our expense.
Nelson Herilhy, PA-C, MHS
Concord, CA
“Unprecedented” VA Proposal? We Don’t Think So
On May 25, 2016, the Department of Veterans Affairs (VA) published a proposed rule change in the Federal Register under the simple heading “Advanced Practice Registered Nurses.” From such modest beginnings stemmed a potential game-changer for advanced practice clinicians in this country: In summary, the VA proposed to “amend its medical regulations to permit full practice authority of all VA advanced practice registered nurses (APRNs) when they are acting within the scope of their VA employment.”1
The impetus for the VA’s proposal is that 505,000 veterans wait 30 days to access care within the VA system—and 300,000 wait between 31 and 60 days for health services.2 Granting plenary practice to VA APRNs would enable them to respond to this backlog of patients, since veterans would have direct access to APRNs who practice within the VA system, regardless of their state of licensure.
More than 4,800 NPs work within the VA; they provide clinical assessments, order appropriate tests and medications, and develop patient-centered care plans.2,3 Research has documented that outcomes for patients whose care is managed by NPs are equal to or better than outcomes for similar patients who are managed by physicians.4 As Major General Vincent Boles of the US Army (retired) stated, “Veterans rely on VA health care to take care of them, and the VA’s nurse practitioners are qualified to provide our veterans with the care they need and deserve.”4
Allowing veterans access to high-quality care is a 21st century solution that is “zero risk, zero cost, zero delay,” according to Dr. Cindy Cooke, President of the American Association of Nurse Practitioners (AANP).4 And it is not just the AANP that supports this rule change. Ninety-one percent of US households that are home to a veteran, and 88% of Americans overall, express support for the VA proposal. In a Mellman Group survey of more than 1,000 adults, strong support was noted across party lines (91% of Republicans; 90% of Democrats)—a rarity in our current political climate.4
Support for full practice authority for NPs at the VA has come from more than 60 organizations, including the Military Officers’ Association of America, the Air Force Sergeants Association, AARP (with 3.7 million veteran households in its membership), and 80 bipartisan members of Congress.5 At the AANP annual conference in San Antonio, Dr. Cooke was joined by leaders from the local American Legion and retired military officers who announced their support for this “change in practice.”3
However, among the more than 162,000 comments received by the VA during the public comment period, there were dissenting opinions. On July 13, 2016, Dr. Robert Wergin, Chair of the Board of the American Academy of Family Physicians (AAFP), sent a letter to Dr. David Shulkin, the Undersecretary of Health in the VA, stating that there were “significant concerns” about the rule change. His main point was that granting full practice authority to NPs would “alter the consistent standards of care for veterans over nonveterans in the states; further fragment the health care system; and dismantle physician-led team-based health care models.” He also stated that “the AAFP strongly opposes the unprecedented proposal to dismiss state practice authority regarding the authority of NPs.”6
Unprecedented? I don’t think so. I practiced as a family NP in the Navy for more than 20 years. I had my own patient panel, cared for active duty members and their families, and evaluated outcomes the same way my physician colleagues did. We practiced collaboratively and respectfully. We discussed patient plan issues, provided peer review on one another’s charts, and accepted new patients into our panels. It was a true collaborative practice.
Military nurses only need to be licensed in one state. The guidelines for NP practice were not based on the rules of the state in which we were licensed but were established by our professional practice association—just as the guidelines for physician practice were not based on the rules extant in their licensing state. I practiced successfully in many states and overseas, although I was licensed in a state that did not recognize plenary practice at the time.
The VA is attempting to respond to veterans’ need for access to care by adopting a model similar to what the military employs. It’s not a matter of superseding state regulations; it’s a matter of recognizing the education and training of health care professionals who can improve patient outcomes.
The opportunity to respond to the proposed amendment has now closed. Through its grassroots Veterans Deserve Care campaign, the AANP and its partners and supporters—clinicians, veterans, families, and others—submitted nearly 60,000 comments.2 Now we wait for the VA to review the abundance of feedback and issue their final decision.
I am hopeful that the VA will acknowledge the overwhelming evidence that our veterans deserve access to care led by highly qualified professionals. The old system isn’t working. Einstein said that the definition of insanity was to do the same thing over and over and expect a different outcome; maintaining a faulty system fits that description. NPs have a well-tested, evidence-based, high-quality education that encourages their ability to lead health care teams, perform collaboratively, and improve outcomes for those who have served our country.
Caring for active duty military and veterans is in the DNA of nurses. Florence Nightingale spent much of her post-Crimea life using evidence-based proposals and political influence to improve the health care of the soldiers and veterans of the British Empire. In Notes on Nursing, she spurred nurses to political action: “Let whoever [sic] is in charge keep this simple question in her [sic] head (not how can I always do this right thing myself, but) how can I provide for this right thing to be always done?”7 This advice should be taken to heart by all health care professionals: We can honor our veterans by advocating for and providing the health care access they need.
To share your thoughts, please contact us at [email protected]
1. Advanced practice registered nurses [2016-12338]. Fed Regist. May 25, 2016. https://federalregister.gov/a/2016-12338.
2. American Association of Nurse Practitioners. AANP and Air Force Sergeants Association urge VA to swiftly enact proposed rule. July 25, 2016. www.aanp.org/legislation-regu lation/federal-legislation/va-proposed-rule/173-press-room/2016-press-releases/ 1987-aanp-and-air-force-sergeants-associa tion-urge-va-to-swiftly-enact-proposed-rule. Accessed August 9, 2016.
3. American Association of Nurse Practitioners. AANP and veterans groups call for streamlined access to veteran’s health care. June 23, 2016. www.aanp.org/press-room/press-releases/173-press-room/2016-press-releases/1959-aanp-veteran-groups-call-for-streamlined-access-to-veterans-health-care. Accessed August 9, 2016.
4. American Association of Nurse Practitioners. National survey finds overwhelming support for VA rule granting veterans direct access to nurse practitioner care. July 20, 2016. www.aanp.org/press-room/press-releases/173-press-room/2016-press-releases/1986-national-survey-finds-overwhelming-support-for-va-rule-granting-veterans-direct-access-to-nurse-practition er-care. Accessed August 9, 2016.
5. American Association of Nurse Anesthetists. Nursing coalition and veterans groups join forces in unprecedented response to VA proposed rule to increase veterans’ access to care. June 28, 2016. www.aana.com/newsandjournal/News/Pages/062816-Nursing-Coalition-and-Veterans-Groups-Join-Forces-in-Unprecedented-Response-to-VA-Proposed-Rule.aspx. Accessed August 9, 2016.
6. Wergin RL. Letter to David Shulkin. July 13, 2016. www.aafp.org/dam/AAFP/docu ments/advocacy/workforce/scope/LT-VHA-APRN-071316.pdf. Accessed August 9, 2016 .
7. Nightingale F. Notes on Nursing: What It Is and What It Is Not. New York, NY: D. Appleton and Company; 1860.
On May 25, 2016, the Department of Veterans Affairs (VA) published a proposed rule change in the Federal Register under the simple heading “Advanced Practice Registered Nurses.” From such modest beginnings stemmed a potential game-changer for advanced practice clinicians in this country: In summary, the VA proposed to “amend its medical regulations to permit full practice authority of all VA advanced practice registered nurses (APRNs) when they are acting within the scope of their VA employment.”1
The impetus for the VA’s proposal is that 505,000 veterans wait 30 days to access care within the VA system—and 300,000 wait between 31 and 60 days for health services.2 Granting plenary practice to VA APRNs would enable them to respond to this backlog of patients, since veterans would have direct access to APRNs who practice within the VA system, regardless of their state of licensure.
More than 4,800 NPs work within the VA; they provide clinical assessments, order appropriate tests and medications, and develop patient-centered care plans.2,3 Research has documented that outcomes for patients whose care is managed by NPs are equal to or better than outcomes for similar patients who are managed by physicians.4 As Major General Vincent Boles of the US Army (retired) stated, “Veterans rely on VA health care to take care of them, and the VA’s nurse practitioners are qualified to provide our veterans with the care they need and deserve.”4
Allowing veterans access to high-quality care is a 21st century solution that is “zero risk, zero cost, zero delay,” according to Dr. Cindy Cooke, President of the American Association of Nurse Practitioners (AANP).4 And it is not just the AANP that supports this rule change. Ninety-one percent of US households that are home to a veteran, and 88% of Americans overall, express support for the VA proposal. In a Mellman Group survey of more than 1,000 adults, strong support was noted across party lines (91% of Republicans; 90% of Democrats)—a rarity in our current political climate.4
Support for full practice authority for NPs at the VA has come from more than 60 organizations, including the Military Officers’ Association of America, the Air Force Sergeants Association, AARP (with 3.7 million veteran households in its membership), and 80 bipartisan members of Congress.5 At the AANP annual conference in San Antonio, Dr. Cooke was joined by leaders from the local American Legion and retired military officers who announced their support for this “change in practice.”3
However, among the more than 162,000 comments received by the VA during the public comment period, there were dissenting opinions. On July 13, 2016, Dr. Robert Wergin, Chair of the Board of the American Academy of Family Physicians (AAFP), sent a letter to Dr. David Shulkin, the Undersecretary of Health in the VA, stating that there were “significant concerns” about the rule change. His main point was that granting full practice authority to NPs would “alter the consistent standards of care for veterans over nonveterans in the states; further fragment the health care system; and dismantle physician-led team-based health care models.” He also stated that “the AAFP strongly opposes the unprecedented proposal to dismiss state practice authority regarding the authority of NPs.”6
Unprecedented? I don’t think so. I practiced as a family NP in the Navy for more than 20 years. I had my own patient panel, cared for active duty members and their families, and evaluated outcomes the same way my physician colleagues did. We practiced collaboratively and respectfully. We discussed patient plan issues, provided peer review on one another’s charts, and accepted new patients into our panels. It was a true collaborative practice.
Military nurses only need to be licensed in one state. The guidelines for NP practice were not based on the rules of the state in which we were licensed but were established by our professional practice association—just as the guidelines for physician practice were not based on the rules extant in their licensing state. I practiced successfully in many states and overseas, although I was licensed in a state that did not recognize plenary practice at the time.
The VA is attempting to respond to veterans’ need for access to care by adopting a model similar to what the military employs. It’s not a matter of superseding state regulations; it’s a matter of recognizing the education and training of health care professionals who can improve patient outcomes.
The opportunity to respond to the proposed amendment has now closed. Through its grassroots Veterans Deserve Care campaign, the AANP and its partners and supporters—clinicians, veterans, families, and others—submitted nearly 60,000 comments.2 Now we wait for the VA to review the abundance of feedback and issue their final decision.
I am hopeful that the VA will acknowledge the overwhelming evidence that our veterans deserve access to care led by highly qualified professionals. The old system isn’t working. Einstein said that the definition of insanity was to do the same thing over and over and expect a different outcome; maintaining a faulty system fits that description. NPs have a well-tested, evidence-based, high-quality education that encourages their ability to lead health care teams, perform collaboratively, and improve outcomes for those who have served our country.
Caring for active duty military and veterans is in the DNA of nurses. Florence Nightingale spent much of her post-Crimea life using evidence-based proposals and political influence to improve the health care of the soldiers and veterans of the British Empire. In Notes on Nursing, she spurred nurses to political action: “Let whoever [sic] is in charge keep this simple question in her [sic] head (not how can I always do this right thing myself, but) how can I provide for this right thing to be always done?”7 This advice should be taken to heart by all health care professionals: We can honor our veterans by advocating for and providing the health care access they need.
To share your thoughts, please contact us at [email protected]
On May 25, 2016, the Department of Veterans Affairs (VA) published a proposed rule change in the Federal Register under the simple heading “Advanced Practice Registered Nurses.” From such modest beginnings stemmed a potential game-changer for advanced practice clinicians in this country: In summary, the VA proposed to “amend its medical regulations to permit full practice authority of all VA advanced practice registered nurses (APRNs) when they are acting within the scope of their VA employment.”1
The impetus for the VA’s proposal is that 505,000 veterans wait 30 days to access care within the VA system—and 300,000 wait between 31 and 60 days for health services.2 Granting plenary practice to VA APRNs would enable them to respond to this backlog of patients, since veterans would have direct access to APRNs who practice within the VA system, regardless of their state of licensure.
More than 4,800 NPs work within the VA; they provide clinical assessments, order appropriate tests and medications, and develop patient-centered care plans.2,3 Research has documented that outcomes for patients whose care is managed by NPs are equal to or better than outcomes for similar patients who are managed by physicians.4 As Major General Vincent Boles of the US Army (retired) stated, “Veterans rely on VA health care to take care of them, and the VA’s nurse practitioners are qualified to provide our veterans with the care they need and deserve.”4
Allowing veterans access to high-quality care is a 21st century solution that is “zero risk, zero cost, zero delay,” according to Dr. Cindy Cooke, President of the American Association of Nurse Practitioners (AANP).4 And it is not just the AANP that supports this rule change. Ninety-one percent of US households that are home to a veteran, and 88% of Americans overall, express support for the VA proposal. In a Mellman Group survey of more than 1,000 adults, strong support was noted across party lines (91% of Republicans; 90% of Democrats)—a rarity in our current political climate.4
Support for full practice authority for NPs at the VA has come from more than 60 organizations, including the Military Officers’ Association of America, the Air Force Sergeants Association, AARP (with 3.7 million veteran households in its membership), and 80 bipartisan members of Congress.5 At the AANP annual conference in San Antonio, Dr. Cooke was joined by leaders from the local American Legion and retired military officers who announced their support for this “change in practice.”3
However, among the more than 162,000 comments received by the VA during the public comment period, there were dissenting opinions. On July 13, 2016, Dr. Robert Wergin, Chair of the Board of the American Academy of Family Physicians (AAFP), sent a letter to Dr. David Shulkin, the Undersecretary of Health in the VA, stating that there were “significant concerns” about the rule change. His main point was that granting full practice authority to NPs would “alter the consistent standards of care for veterans over nonveterans in the states; further fragment the health care system; and dismantle physician-led team-based health care models.” He also stated that “the AAFP strongly opposes the unprecedented proposal to dismiss state practice authority regarding the authority of NPs.”6
Unprecedented? I don’t think so. I practiced as a family NP in the Navy for more than 20 years. I had my own patient panel, cared for active duty members and their families, and evaluated outcomes the same way my physician colleagues did. We practiced collaboratively and respectfully. We discussed patient plan issues, provided peer review on one another’s charts, and accepted new patients into our panels. It was a true collaborative practice.
Military nurses only need to be licensed in one state. The guidelines for NP practice were not based on the rules of the state in which we were licensed but were established by our professional practice association—just as the guidelines for physician practice were not based on the rules extant in their licensing state. I practiced successfully in many states and overseas, although I was licensed in a state that did not recognize plenary practice at the time.
The VA is attempting to respond to veterans’ need for access to care by adopting a model similar to what the military employs. It’s not a matter of superseding state regulations; it’s a matter of recognizing the education and training of health care professionals who can improve patient outcomes.
The opportunity to respond to the proposed amendment has now closed. Through its grassroots Veterans Deserve Care campaign, the AANP and its partners and supporters—clinicians, veterans, families, and others—submitted nearly 60,000 comments.2 Now we wait for the VA to review the abundance of feedback and issue their final decision.
I am hopeful that the VA will acknowledge the overwhelming evidence that our veterans deserve access to care led by highly qualified professionals. The old system isn’t working. Einstein said that the definition of insanity was to do the same thing over and over and expect a different outcome; maintaining a faulty system fits that description. NPs have a well-tested, evidence-based, high-quality education that encourages their ability to lead health care teams, perform collaboratively, and improve outcomes for those who have served our country.
Caring for active duty military and veterans is in the DNA of nurses. Florence Nightingale spent much of her post-Crimea life using evidence-based proposals and political influence to improve the health care of the soldiers and veterans of the British Empire. In Notes on Nursing, she spurred nurses to political action: “Let whoever [sic] is in charge keep this simple question in her [sic] head (not how can I always do this right thing myself, but) how can I provide for this right thing to be always done?”7 This advice should be taken to heart by all health care professionals: We can honor our veterans by advocating for and providing the health care access they need.
To share your thoughts, please contact us at [email protected]
1. Advanced practice registered nurses [2016-12338]. Fed Regist. May 25, 2016. https://federalregister.gov/a/2016-12338.
2. American Association of Nurse Practitioners. AANP and Air Force Sergeants Association urge VA to swiftly enact proposed rule. July 25, 2016. www.aanp.org/legislation-regu lation/federal-legislation/va-proposed-rule/173-press-room/2016-press-releases/ 1987-aanp-and-air-force-sergeants-associa tion-urge-va-to-swiftly-enact-proposed-rule. Accessed August 9, 2016.
3. American Association of Nurse Practitioners. AANP and veterans groups call for streamlined access to veteran’s health care. June 23, 2016. www.aanp.org/press-room/press-releases/173-press-room/2016-press-releases/1959-aanp-veteran-groups-call-for-streamlined-access-to-veterans-health-care. Accessed August 9, 2016.
4. American Association of Nurse Practitioners. National survey finds overwhelming support for VA rule granting veterans direct access to nurse practitioner care. July 20, 2016. www.aanp.org/press-room/press-releases/173-press-room/2016-press-releases/1986-national-survey-finds-overwhelming-support-for-va-rule-granting-veterans-direct-access-to-nurse-practition er-care. Accessed August 9, 2016.
5. American Association of Nurse Anesthetists. Nursing coalition and veterans groups join forces in unprecedented response to VA proposed rule to increase veterans’ access to care. June 28, 2016. www.aana.com/newsandjournal/News/Pages/062816-Nursing-Coalition-and-Veterans-Groups-Join-Forces-in-Unprecedented-Response-to-VA-Proposed-Rule.aspx. Accessed August 9, 2016.
6. Wergin RL. Letter to David Shulkin. July 13, 2016. www.aafp.org/dam/AAFP/docu ments/advocacy/workforce/scope/LT-VHA-APRN-071316.pdf. Accessed August 9, 2016 .
7. Nightingale F. Notes on Nursing: What It Is and What It Is Not. New York, NY: D. Appleton and Company; 1860.
1. Advanced practice registered nurses [2016-12338]. Fed Regist. May 25, 2016. https://federalregister.gov/a/2016-12338.
2. American Association of Nurse Practitioners. AANP and Air Force Sergeants Association urge VA to swiftly enact proposed rule. July 25, 2016. www.aanp.org/legislation-regu lation/federal-legislation/va-proposed-rule/173-press-room/2016-press-releases/ 1987-aanp-and-air-force-sergeants-associa tion-urge-va-to-swiftly-enact-proposed-rule. Accessed August 9, 2016.
3. American Association of Nurse Practitioners. AANP and veterans groups call for streamlined access to veteran’s health care. June 23, 2016. www.aanp.org/press-room/press-releases/173-press-room/2016-press-releases/1959-aanp-veteran-groups-call-for-streamlined-access-to-veterans-health-care. Accessed August 9, 2016.
4. American Association of Nurse Practitioners. National survey finds overwhelming support for VA rule granting veterans direct access to nurse practitioner care. July 20, 2016. www.aanp.org/press-room/press-releases/173-press-room/2016-press-releases/1986-national-survey-finds-overwhelming-support-for-va-rule-granting-veterans-direct-access-to-nurse-practition er-care. Accessed August 9, 2016.
5. American Association of Nurse Anesthetists. Nursing coalition and veterans groups join forces in unprecedented response to VA proposed rule to increase veterans’ access to care. June 28, 2016. www.aana.com/newsandjournal/News/Pages/062816-Nursing-Coalition-and-Veterans-Groups-Join-Forces-in-Unprecedented-Response-to-VA-Proposed-Rule.aspx. Accessed August 9, 2016.
6. Wergin RL. Letter to David Shulkin. July 13, 2016. www.aafp.org/dam/AAFP/docu ments/advocacy/workforce/scope/LT-VHA-APRN-071316.pdf. Accessed August 9, 2016 .
7. Nightingale F. Notes on Nursing: What It Is and What It Is Not. New York, NY: D. Appleton and Company; 1860.
Maybe it is all in your head

Origin of pain: Brain vs body. Recent research provides strong evidence that in some cases of intractable chronic pain, the origin of the pain signal is in the brain—rather than the body. In this issue of JFP, Davis and Vanderah discuss this type of pain as “a third kind” that needs to be treated in a manner that completely differs from that for peripherally generated pain. They refer to the traditional kinds of pain as either nociceptive (resulting from tissue damage or insult), or neuropathic (due to dysfunctional stimulation of peripheral nerves). The neurophysiology of the third kind of pain, which I will call “centrally generated pain,” is not fully understood, but neuroimaging and other sophisticated methods are identifying areas of the brain that become activated by psychological trauma, leading to significant painful suffering in the absence of tissue damage, or that is far out of proportion to physical insult.
The bad news for primary care physicians is that this third kind of pain is difficult, if not impossible, to treat with our traditional armamentarium of pain medications and physical modalities. In fact, these patients are often at risk for addiction, as doses of ineffective narcotics are escalated.
The good news is that clinical researchers have begun to identify ways to effectively treat centrally generated pain. For example, Schubiner et al used a novel psychological approach that involved helping patients "learn that their pain is influenced primarily by central nervous system psychological processes, and to enhance awareness and expression of emotions related to psychological trauma or conflict."1 Thirty percent of the 72 participants in the preliminary, uncontrolled trial experienced a 70% reduction in pain. Dr. Schubiner’s research is ongoing and supported by funding from the National Institutes of Health.
Proper diagnosis is paramount. Of course, proper diagnosis is paramount because an individual may suffer from more than one of the 3 kinds of pain and require different approaches for each. Thorough evaluation at a multidisciplinary pain clinic is a good place to start. Once the diagnoses are sorted out, it will then be possible to treat each component of pain appropriately.
Dr. Schubiner’s methods and other new and developing treatment approaches to chronic pain will help us better relieve patients’ suffering, reduce narcotic overuse, and relieve our own anxiety about caring for these challenging patients.
1. Burger AJ, Lumley MA, Carty JN, et al. The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: a preliminary, uncontrolled trial. J Psychosom Res. 2016;81:1-8.

Origin of pain: Brain vs body. Recent research provides strong evidence that in some cases of intractable chronic pain, the origin of the pain signal is in the brain—rather than the body. In this issue of JFP, Davis and Vanderah discuss this type of pain as “a third kind” that needs to be treated in a manner that completely differs from that for peripherally generated pain. They refer to the traditional kinds of pain as either nociceptive (resulting from tissue damage or insult), or neuropathic (due to dysfunctional stimulation of peripheral nerves). The neurophysiology of the third kind of pain, which I will call “centrally generated pain,” is not fully understood, but neuroimaging and other sophisticated methods are identifying areas of the brain that become activated by psychological trauma, leading to significant painful suffering in the absence of tissue damage, or that is far out of proportion to physical insult.
The bad news for primary care physicians is that this third kind of pain is difficult, if not impossible, to treat with our traditional armamentarium of pain medications and physical modalities. In fact, these patients are often at risk for addiction, as doses of ineffective narcotics are escalated.
The good news is that clinical researchers have begun to identify ways to effectively treat centrally generated pain. For example, Schubiner et al used a novel psychological approach that involved helping patients "learn that their pain is influenced primarily by central nervous system psychological processes, and to enhance awareness and expression of emotions related to psychological trauma or conflict."1 Thirty percent of the 72 participants in the preliminary, uncontrolled trial experienced a 70% reduction in pain. Dr. Schubiner’s research is ongoing and supported by funding from the National Institutes of Health.
Proper diagnosis is paramount. Of course, proper diagnosis is paramount because an individual may suffer from more than one of the 3 kinds of pain and require different approaches for each. Thorough evaluation at a multidisciplinary pain clinic is a good place to start. Once the diagnoses are sorted out, it will then be possible to treat each component of pain appropriately.
Dr. Schubiner’s methods and other new and developing treatment approaches to chronic pain will help us better relieve patients’ suffering, reduce narcotic overuse, and relieve our own anxiety about caring for these challenging patients.
1. Burger AJ, Lumley MA, Carty JN, et al. The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: a preliminary, uncontrolled trial. J Psychosom Res. 2016;81:1-8.

Origin of pain: Brain vs body. Recent research provides strong evidence that in some cases of intractable chronic pain, the origin of the pain signal is in the brain—rather than the body. In this issue of JFP, Davis and Vanderah discuss this type of pain as “a third kind” that needs to be treated in a manner that completely differs from that for peripherally generated pain. They refer to the traditional kinds of pain as either nociceptive (resulting from tissue damage or insult), or neuropathic (due to dysfunctional stimulation of peripheral nerves). The neurophysiology of the third kind of pain, which I will call “centrally generated pain,” is not fully understood, but neuroimaging and other sophisticated methods are identifying areas of the brain that become activated by psychological trauma, leading to significant painful suffering in the absence of tissue damage, or that is far out of proportion to physical insult.
The bad news for primary care physicians is that this third kind of pain is difficult, if not impossible, to treat with our traditional armamentarium of pain medications and physical modalities. In fact, these patients are often at risk for addiction, as doses of ineffective narcotics are escalated.
The good news is that clinical researchers have begun to identify ways to effectively treat centrally generated pain. For example, Schubiner et al used a novel psychological approach that involved helping patients "learn that their pain is influenced primarily by central nervous system psychological processes, and to enhance awareness and expression of emotions related to psychological trauma or conflict."1 Thirty percent of the 72 participants in the preliminary, uncontrolled trial experienced a 70% reduction in pain. Dr. Schubiner’s research is ongoing and supported by funding from the National Institutes of Health.
Proper diagnosis is paramount. Of course, proper diagnosis is paramount because an individual may suffer from more than one of the 3 kinds of pain and require different approaches for each. Thorough evaluation at a multidisciplinary pain clinic is a good place to start. Once the diagnoses are sorted out, it will then be possible to treat each component of pain appropriately.
Dr. Schubiner’s methods and other new and developing treatment approaches to chronic pain will help us better relieve patients’ suffering, reduce narcotic overuse, and relieve our own anxiety about caring for these challenging patients.
1. Burger AJ, Lumley MA, Carty JN, et al. The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: a preliminary, uncontrolled trial. J Psychosom Res. 2016;81:1-8.
The Translational Revolution in Atopic Dermatitis, and How It Also Translates to Other Inflammatory Skin Diseases
Atopic dermatitis (AD) is the most common inflammatory skin disease in both adults and children.1 Unfortunately, the current treatment armamentarium is largely confined to topical calcineurin inhibitors, topical and systemic steroids, phototherapy, cyclosporine (not approved by the US Food and Drug Administration for AD), and other oral immunosuppressants.2 The availability of partially helpful and highly toxic treatments creates a huge unmet need for more effective and safer treatments, particularly for patients with moderate to severe AD who often require systemic approaches.
Recent extensive translational (bench top to bedside and back) investigations in skin of AD patients has shown that skin phenotype is characterized by increased T-cell infiltration and related inflammatory cytokines as well as epidermal abnormalities (eg, hyperplasia, aberrant differentiation).3 Clinical improvement of AD has been demonstrated with broad T-cell targeted therapeutics, such as cyclosporine and narrowband UVB, coupled with decreases of T-cell infiltrates and inflammatory gene products as well as improvement of the pathologic epidermal phenotype.4,5
In the past, AD was conceptualized as a T helper cell TH2 (acute disease)/TH1 (chronic disease) bipolar cytokine disorder.6 Acute lesions are characterized by high TH2, TH22, and some TH17 signals, with intensification of these axes and TH1 augmentation orchestrating the chronic phenotype.7 The identification of the inflammatory pathways underlying AD has led to the development and testing of more than 10 broad or targeted therapeutics (Table).8 Phase 1 and phase 2 studies of dupilumab (targeting IL-4Rα) have shown not only tremendous AD improvement (~70%) but also tissue reversal of the immune and barrier abnormalities, including inflammatory cytokines and epidermal hyperplasia.9-11 As a result, other TH2 axis inhibitors (anti–IL-13/tralokinumab, anti–IL-31RA/CIM 331) are now in clinical trials. The identification of IL-22 in AD lesions has prompted trials with an anti–IL-22 (ILV 094) and an IL-12/IL-23p40 (ustekinumab) inhibitor.12 For psoriasis, ustekinumab showed 75% improvement in approximately 70% of patients,13 but for AD, despite clear clinical and molecular effects, differences compared to placebo were not statistically significant,12 probably due to underdosing of the drug in an excessively immune-activated disease14 as well as allowing topical steroids in patients, which may minimize the differences in treatment effect between drug and placebo.
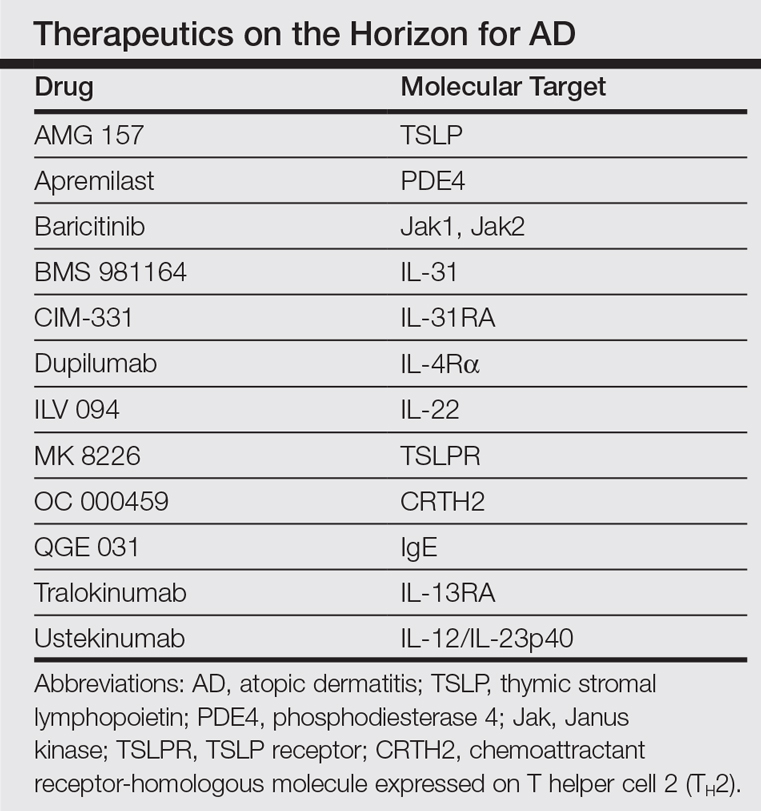
The developments seen in AD are now moving into other inflammatory skin diseases, particularly alopecia areata (AA), a T-cell–mediated disease that shares phenotypic similarities with AD and often is associated with it.15 There is a paucity of effective, remission-sustaining treatments of AA, particularly for patients with severe disease who rarely experience spontaneous hair regrowth and who have a limited response to topical interventions.16,17 Our clinical experience showed that successfully treating patients with concurrent AD and AA has led to hair regrowth. Inspired by these clinical observations and by results obtained in AD,9-12 studying AA skin showed an upregulation of not only the traditionally suspected culprit TH1 but also TH2 and TH9 axes, IL-23 cytokines, and phosphodiesterase 4.18 Subsequently, a pilot study of 3 patients with extensive AA treated with ustekinumab showed that all 3 patients not only experienced hair regrowth but also had a reduction in inflammatory markers in scalp lesions.19 Although these results are promising, AA is an immunologically complex disease and it is yet to be determined if therapeutically targeting 1 (eg, IL-4) rather than a wide array of cytokines can reverse disease phenotype. There are ongoing clinical trials directed at different pathogenic targets (eg, Jak inhibitors, IL-13 antagonist, IL-17 antagonist, phosphodiesterase 4 antagonist); some showed some efficacy in small studies.20,21
The finding of a commonly upregulated TH2 pathway in both AD and AA will pave the way for studies with TH2 antagonists in AA patients. Future targeted therapeutic studies will shed light on the pathogenic pathways of this devastating skin disease and answer the extensive unmet therapeutic need it presents.
- Czarnowicki T, Krueger JG, Guttman-Yassky E. Skin barrier and immune dysregulation in atopic dermatitis: an evolving story with important clinical implications. J Allergy Clin Immunol Pract. 2014;2:371-379; quiz 380-381.
- Roekevisch E, Spuls PI, Kuester D, et al. Efficacy and safety of systemic treatments for moderate-to-severe atopic dermatitis: a systematic review. J Allergy Clin Immunol. 2014;133:429-438.
- Guttman-Yassky E, Nograles KE, Krueger JG. Contrasting pathogenesis of atopic dermatitis and psoriasis—part
I: clinical and pathologic concepts. J Allergy Clin Immunol. 2011;127:1110-1118. - Khattri S, Shemer A, Rozenblit M, et al. Cyclosporine in patients with atopic dermatitis modulates activated inflammatory pathways and reverses epidermal pathology. J Allergy Clin Immunol. 2014;133:1626-1634.
- Tintle S, Shemer A, Suárez-Fariñas M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response [published online July 16, 2011]. J Allergy Clin Immunol. 2011;128:583-593.
- Eyerich K, Novak N. Immunology of atopic eczema: overcoming the Th1/Th2 paradigm. Allergy. 2013;68:974-982.
- Gittler JK, Shemer A, Suárez-Fariñas M, et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis [published online August 27, 2012]. J Allergy Clin Immunol. 2012;130:1344-1354.
- Noda S, Krueger JG, Guttman-Yassky E. The translational revolution and use of biologics in patients with inflammatory skin diseases. J Allergy Clin Immunol. 2015;135:324-336.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Hamilton JD, Suárez-Fariñas M, Dhingra N, et al. Dupilumab improves the molecular signature in skin of patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol. 2014;134:1293-1300.
- Hamilton J, Ren H, Weinstein SP, et al. Dupilumab improved all domains of Eczema Area and Severity Index (EASI) and 5-D pruritus scale in adults with atopic dermatitis in a phase 2 study. J Invest Dermatol. 2014;134:S104.
- Khattri S, Brunner PM, Garcet S, et al. Efficacy and safety of ustekinumab treatment in adults with moderate-to-severe atopic dermatitis [published online June 15, 2016]. Exp Dermatol. doi:10.1111/exd.13112.
- Griffiths CEM, Strober BE, van de Kerkhof P, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. N Engl J Med. 2010;362:118-128.
- Czarnowicki T, Malajian D, Shemer A, et al. Skin-homing and systemic T-cell subsets show higher activation in atopic dermatitis versus psoriasis. J Allergy Clin Immunol. 2015;136:208-211.
- Barahmani N, Schabath MB, Duvic M. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581-591.
- Price VH, Hordinsky MK, Olsen EA, et al. Subcutaneous efalizumab is not effective in the treatment of alopecia areata. J Am Acad Dermatol. 2008;58:395-402.
- Alkhalifah A, Alsantali A, Wang E, et al. Alopecia areata update part II. treatment. J Am Acad Dermatol. 2010;62:191-202.
- Suárez-Fariñas M, Ungar B, Noda S, et al. Alopecia areata profiling shows TH1, TH2, and IL-23 cytokine activation without parallel TH17/TH22 skewing. J Allergy Clin Immunol. 2015;136:1277-1287.
- Guttman-Yassky E, Ungar B, Noda S, et al. Extensive alopecia areata is reversed by IL-12/IL-23p40 cytokine antagonism. J Allergy Clin Immunol. 2016;137:301-304.
- Xing LZ, Dai ZP, Jabbari A, et al. Alopecia areata is driven by cytotoxic T lymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20:1043-1049.
- Castela E, Le Duff F, Butori C, et al. Effects of low-dose recombinant interleukin 2 to promote T-regulatory cells in alopecia areata. JAMA Dermatol. 2014;150:748-751.
Atopic dermatitis (AD) is the most common inflammatory skin disease in both adults and children.1 Unfortunately, the current treatment armamentarium is largely confined to topical calcineurin inhibitors, topical and systemic steroids, phototherapy, cyclosporine (not approved by the US Food and Drug Administration for AD), and other oral immunosuppressants.2 The availability of partially helpful and highly toxic treatments creates a huge unmet need for more effective and safer treatments, particularly for patients with moderate to severe AD who often require systemic approaches.
Recent extensive translational (bench top to bedside and back) investigations in skin of AD patients has shown that skin phenotype is characterized by increased T-cell infiltration and related inflammatory cytokines as well as epidermal abnormalities (eg, hyperplasia, aberrant differentiation).3 Clinical improvement of AD has been demonstrated with broad T-cell targeted therapeutics, such as cyclosporine and narrowband UVB, coupled with decreases of T-cell infiltrates and inflammatory gene products as well as improvement of the pathologic epidermal phenotype.4,5
In the past, AD was conceptualized as a T helper cell TH2 (acute disease)/TH1 (chronic disease) bipolar cytokine disorder.6 Acute lesions are characterized by high TH2, TH22, and some TH17 signals, with intensification of these axes and TH1 augmentation orchestrating the chronic phenotype.7 The identification of the inflammatory pathways underlying AD has led to the development and testing of more than 10 broad or targeted therapeutics (Table).8 Phase 1 and phase 2 studies of dupilumab (targeting IL-4Rα) have shown not only tremendous AD improvement (~70%) but also tissue reversal of the immune and barrier abnormalities, including inflammatory cytokines and epidermal hyperplasia.9-11 As a result, other TH2 axis inhibitors (anti–IL-13/tralokinumab, anti–IL-31RA/CIM 331) are now in clinical trials. The identification of IL-22 in AD lesions has prompted trials with an anti–IL-22 (ILV 094) and an IL-12/IL-23p40 (ustekinumab) inhibitor.12 For psoriasis, ustekinumab showed 75% improvement in approximately 70% of patients,13 but for AD, despite clear clinical and molecular effects, differences compared to placebo were not statistically significant,12 probably due to underdosing of the drug in an excessively immune-activated disease14 as well as allowing topical steroids in patients, which may minimize the differences in treatment effect between drug and placebo.
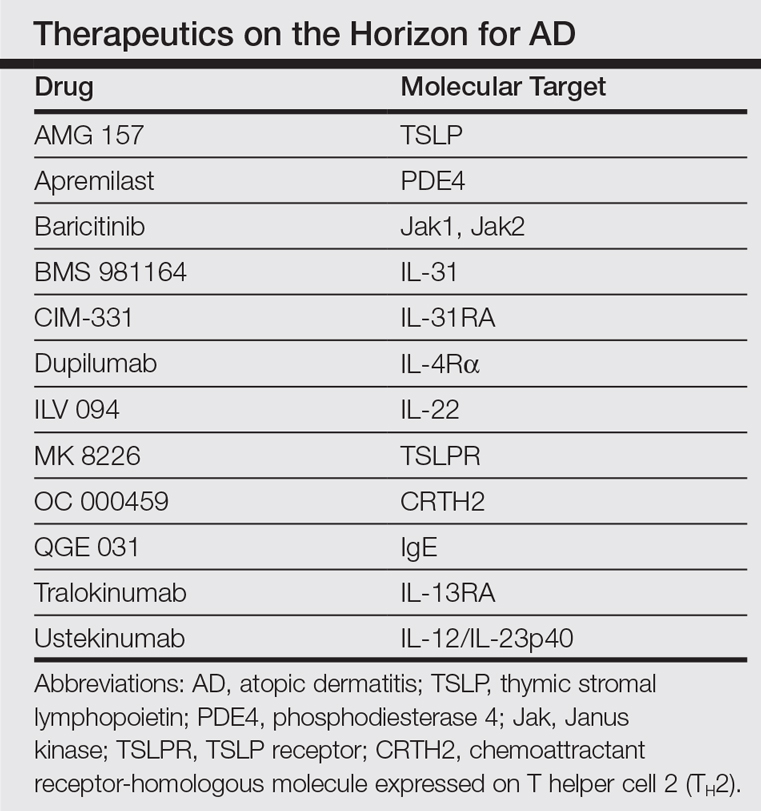
The developments seen in AD are now moving into other inflammatory skin diseases, particularly alopecia areata (AA), a T-cell–mediated disease that shares phenotypic similarities with AD and often is associated with it.15 There is a paucity of effective, remission-sustaining treatments of AA, particularly for patients with severe disease who rarely experience spontaneous hair regrowth and who have a limited response to topical interventions.16,17 Our clinical experience showed that successfully treating patients with concurrent AD and AA has led to hair regrowth. Inspired by these clinical observations and by results obtained in AD,9-12 studying AA skin showed an upregulation of not only the traditionally suspected culprit TH1 but also TH2 and TH9 axes, IL-23 cytokines, and phosphodiesterase 4.18 Subsequently, a pilot study of 3 patients with extensive AA treated with ustekinumab showed that all 3 patients not only experienced hair regrowth but also had a reduction in inflammatory markers in scalp lesions.19 Although these results are promising, AA is an immunologically complex disease and it is yet to be determined if therapeutically targeting 1 (eg, IL-4) rather than a wide array of cytokines can reverse disease phenotype. There are ongoing clinical trials directed at different pathogenic targets (eg, Jak inhibitors, IL-13 antagonist, IL-17 antagonist, phosphodiesterase 4 antagonist); some showed some efficacy in small studies.20,21
The finding of a commonly upregulated TH2 pathway in both AD and AA will pave the way for studies with TH2 antagonists in AA patients. Future targeted therapeutic studies will shed light on the pathogenic pathways of this devastating skin disease and answer the extensive unmet therapeutic need it presents.
Atopic dermatitis (AD) is the most common inflammatory skin disease in both adults and children.1 Unfortunately, the current treatment armamentarium is largely confined to topical calcineurin inhibitors, topical and systemic steroids, phototherapy, cyclosporine (not approved by the US Food and Drug Administration for AD), and other oral immunosuppressants.2 The availability of partially helpful and highly toxic treatments creates a huge unmet need for more effective and safer treatments, particularly for patients with moderate to severe AD who often require systemic approaches.
Recent extensive translational (bench top to bedside and back) investigations in skin of AD patients has shown that skin phenotype is characterized by increased T-cell infiltration and related inflammatory cytokines as well as epidermal abnormalities (eg, hyperplasia, aberrant differentiation).3 Clinical improvement of AD has been demonstrated with broad T-cell targeted therapeutics, such as cyclosporine and narrowband UVB, coupled with decreases of T-cell infiltrates and inflammatory gene products as well as improvement of the pathologic epidermal phenotype.4,5
In the past, AD was conceptualized as a T helper cell TH2 (acute disease)/TH1 (chronic disease) bipolar cytokine disorder.6 Acute lesions are characterized by high TH2, TH22, and some TH17 signals, with intensification of these axes and TH1 augmentation orchestrating the chronic phenotype.7 The identification of the inflammatory pathways underlying AD has led to the development and testing of more than 10 broad or targeted therapeutics (Table).8 Phase 1 and phase 2 studies of dupilumab (targeting IL-4Rα) have shown not only tremendous AD improvement (~70%) but also tissue reversal of the immune and barrier abnormalities, including inflammatory cytokines and epidermal hyperplasia.9-11 As a result, other TH2 axis inhibitors (anti–IL-13/tralokinumab, anti–IL-31RA/CIM 331) are now in clinical trials. The identification of IL-22 in AD lesions has prompted trials with an anti–IL-22 (ILV 094) and an IL-12/IL-23p40 (ustekinumab) inhibitor.12 For psoriasis, ustekinumab showed 75% improvement in approximately 70% of patients,13 but for AD, despite clear clinical and molecular effects, differences compared to placebo were not statistically significant,12 probably due to underdosing of the drug in an excessively immune-activated disease14 as well as allowing topical steroids in patients, which may minimize the differences in treatment effect between drug and placebo.
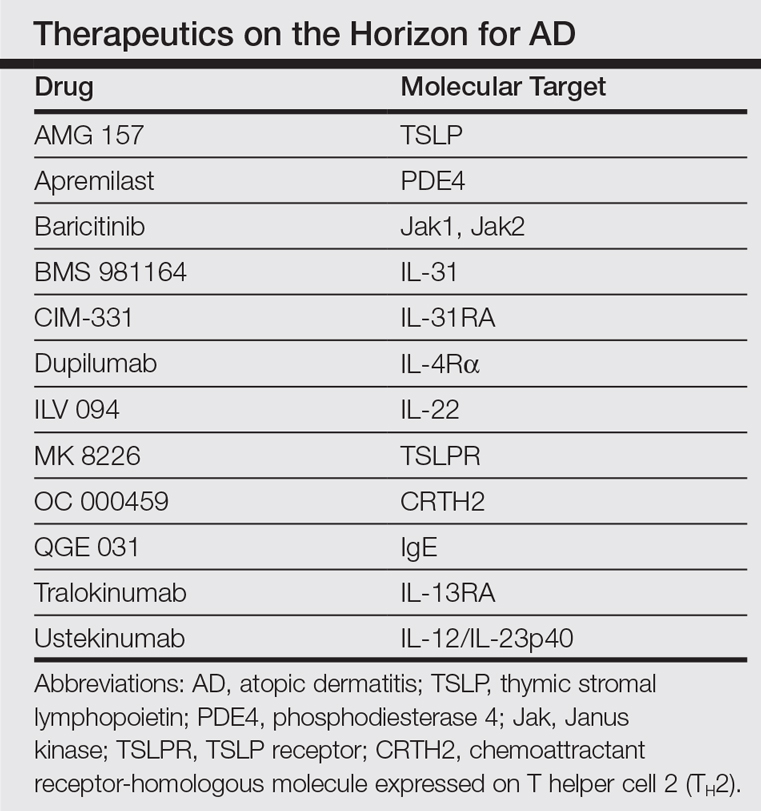
The developments seen in AD are now moving into other inflammatory skin diseases, particularly alopecia areata (AA), a T-cell–mediated disease that shares phenotypic similarities with AD and often is associated with it.15 There is a paucity of effective, remission-sustaining treatments of AA, particularly for patients with severe disease who rarely experience spontaneous hair regrowth and who have a limited response to topical interventions.16,17 Our clinical experience showed that successfully treating patients with concurrent AD and AA has led to hair regrowth. Inspired by these clinical observations and by results obtained in AD,9-12 studying AA skin showed an upregulation of not only the traditionally suspected culprit TH1 but also TH2 and TH9 axes, IL-23 cytokines, and phosphodiesterase 4.18 Subsequently, a pilot study of 3 patients with extensive AA treated with ustekinumab showed that all 3 patients not only experienced hair regrowth but also had a reduction in inflammatory markers in scalp lesions.19 Although these results are promising, AA is an immunologically complex disease and it is yet to be determined if therapeutically targeting 1 (eg, IL-4) rather than a wide array of cytokines can reverse disease phenotype. There are ongoing clinical trials directed at different pathogenic targets (eg, Jak inhibitors, IL-13 antagonist, IL-17 antagonist, phosphodiesterase 4 antagonist); some showed some efficacy in small studies.20,21
The finding of a commonly upregulated TH2 pathway in both AD and AA will pave the way for studies with TH2 antagonists in AA patients. Future targeted therapeutic studies will shed light on the pathogenic pathways of this devastating skin disease and answer the extensive unmet therapeutic need it presents.
- Czarnowicki T, Krueger JG, Guttman-Yassky E. Skin barrier and immune dysregulation in atopic dermatitis: an evolving story with important clinical implications. J Allergy Clin Immunol Pract. 2014;2:371-379; quiz 380-381.
- Roekevisch E, Spuls PI, Kuester D, et al. Efficacy and safety of systemic treatments for moderate-to-severe atopic dermatitis: a systematic review. J Allergy Clin Immunol. 2014;133:429-438.
- Guttman-Yassky E, Nograles KE, Krueger JG. Contrasting pathogenesis of atopic dermatitis and psoriasis—part
I: clinical and pathologic concepts. J Allergy Clin Immunol. 2011;127:1110-1118. - Khattri S, Shemer A, Rozenblit M, et al. Cyclosporine in patients with atopic dermatitis modulates activated inflammatory pathways and reverses epidermal pathology. J Allergy Clin Immunol. 2014;133:1626-1634.
- Tintle S, Shemer A, Suárez-Fariñas M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response [published online July 16, 2011]. J Allergy Clin Immunol. 2011;128:583-593.
- Eyerich K, Novak N. Immunology of atopic eczema: overcoming the Th1/Th2 paradigm. Allergy. 2013;68:974-982.
- Gittler JK, Shemer A, Suárez-Fariñas M, et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis [published online August 27, 2012]. J Allergy Clin Immunol. 2012;130:1344-1354.
- Noda S, Krueger JG, Guttman-Yassky E. The translational revolution and use of biologics in patients with inflammatory skin diseases. J Allergy Clin Immunol. 2015;135:324-336.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Hamilton JD, Suárez-Fariñas M, Dhingra N, et al. Dupilumab improves the molecular signature in skin of patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol. 2014;134:1293-1300.
- Hamilton J, Ren H, Weinstein SP, et al. Dupilumab improved all domains of Eczema Area and Severity Index (EASI) and 5-D pruritus scale in adults with atopic dermatitis in a phase 2 study. J Invest Dermatol. 2014;134:S104.
- Khattri S, Brunner PM, Garcet S, et al. Efficacy and safety of ustekinumab treatment in adults with moderate-to-severe atopic dermatitis [published online June 15, 2016]. Exp Dermatol. doi:10.1111/exd.13112.
- Griffiths CEM, Strober BE, van de Kerkhof P, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. N Engl J Med. 2010;362:118-128.
- Czarnowicki T, Malajian D, Shemer A, et al. Skin-homing and systemic T-cell subsets show higher activation in atopic dermatitis versus psoriasis. J Allergy Clin Immunol. 2015;136:208-211.
- Barahmani N, Schabath MB, Duvic M. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581-591.
- Price VH, Hordinsky MK, Olsen EA, et al. Subcutaneous efalizumab is not effective in the treatment of alopecia areata. J Am Acad Dermatol. 2008;58:395-402.
- Alkhalifah A, Alsantali A, Wang E, et al. Alopecia areata update part II. treatment. J Am Acad Dermatol. 2010;62:191-202.
- Suárez-Fariñas M, Ungar B, Noda S, et al. Alopecia areata profiling shows TH1, TH2, and IL-23 cytokine activation without parallel TH17/TH22 skewing. J Allergy Clin Immunol. 2015;136:1277-1287.
- Guttman-Yassky E, Ungar B, Noda S, et al. Extensive alopecia areata is reversed by IL-12/IL-23p40 cytokine antagonism. J Allergy Clin Immunol. 2016;137:301-304.
- Xing LZ, Dai ZP, Jabbari A, et al. Alopecia areata is driven by cytotoxic T lymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20:1043-1049.
- Castela E, Le Duff F, Butori C, et al. Effects of low-dose recombinant interleukin 2 to promote T-regulatory cells in alopecia areata. JAMA Dermatol. 2014;150:748-751.
- Czarnowicki T, Krueger JG, Guttman-Yassky E. Skin barrier and immune dysregulation in atopic dermatitis: an evolving story with important clinical implications. J Allergy Clin Immunol Pract. 2014;2:371-379; quiz 380-381.
- Roekevisch E, Spuls PI, Kuester D, et al. Efficacy and safety of systemic treatments for moderate-to-severe atopic dermatitis: a systematic review. J Allergy Clin Immunol. 2014;133:429-438.
- Guttman-Yassky E, Nograles KE, Krueger JG. Contrasting pathogenesis of atopic dermatitis and psoriasis—part
I: clinical and pathologic concepts. J Allergy Clin Immunol. 2011;127:1110-1118. - Khattri S, Shemer A, Rozenblit M, et al. Cyclosporine in patients with atopic dermatitis modulates activated inflammatory pathways and reverses epidermal pathology. J Allergy Clin Immunol. 2014;133:1626-1634.
- Tintle S, Shemer A, Suárez-Fariñas M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response [published online July 16, 2011]. J Allergy Clin Immunol. 2011;128:583-593.
- Eyerich K, Novak N. Immunology of atopic eczema: overcoming the Th1/Th2 paradigm. Allergy. 2013;68:974-982.
- Gittler JK, Shemer A, Suárez-Fariñas M, et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis [published online August 27, 2012]. J Allergy Clin Immunol. 2012;130:1344-1354.
- Noda S, Krueger JG, Guttman-Yassky E. The translational revolution and use of biologics in patients with inflammatory skin diseases. J Allergy Clin Immunol. 2015;135:324-336.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Hamilton JD, Suárez-Fariñas M, Dhingra N, et al. Dupilumab improves the molecular signature in skin of patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol. 2014;134:1293-1300.
- Hamilton J, Ren H, Weinstein SP, et al. Dupilumab improved all domains of Eczema Area and Severity Index (EASI) and 5-D pruritus scale in adults with atopic dermatitis in a phase 2 study. J Invest Dermatol. 2014;134:S104.
- Khattri S, Brunner PM, Garcet S, et al. Efficacy and safety of ustekinumab treatment in adults with moderate-to-severe atopic dermatitis [published online June 15, 2016]. Exp Dermatol. doi:10.1111/exd.13112.
- Griffiths CEM, Strober BE, van de Kerkhof P, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. N Engl J Med. 2010;362:118-128.
- Czarnowicki T, Malajian D, Shemer A, et al. Skin-homing and systemic T-cell subsets show higher activation in atopic dermatitis versus psoriasis. J Allergy Clin Immunol. 2015;136:208-211.
- Barahmani N, Schabath MB, Duvic M. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581-591.
- Price VH, Hordinsky MK, Olsen EA, et al. Subcutaneous efalizumab is not effective in the treatment of alopecia areata. J Am Acad Dermatol. 2008;58:395-402.
- Alkhalifah A, Alsantali A, Wang E, et al. Alopecia areata update part II. treatment. J Am Acad Dermatol. 2010;62:191-202.
- Suárez-Fariñas M, Ungar B, Noda S, et al. Alopecia areata profiling shows TH1, TH2, and IL-23 cytokine activation without parallel TH17/TH22 skewing. J Allergy Clin Immunol. 2015;136:1277-1287.
- Guttman-Yassky E, Ungar B, Noda S, et al. Extensive alopecia areata is reversed by IL-12/IL-23p40 cytokine antagonism. J Allergy Clin Immunol. 2016;137:301-304.
- Xing LZ, Dai ZP, Jabbari A, et al. Alopecia areata is driven by cytotoxic T lymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20:1043-1049.
- Castela E, Le Duff F, Butori C, et al. Effects of low-dose recombinant interleukin 2 to promote T-regulatory cells in alopecia areata. JAMA Dermatol. 2014;150:748-751.