User login
The EHR Report: Seeing through a glass, darkly
Recently, we were invited to take part in an case presentation focused on a young female patient. The reason for our specific invitation was because a key component in the patient’s case was centered on her electronic health record. This kind of story was not new to us – in fact, stories like these are becoming almost common everywhere. But this particular conference promised to be very special, because the patient herself was asked to take an active role and present the story from a unique perspective – her own.
Seated on stage in a hospital gown and accompanied by her I.V. pole, the patient related a 4-month history of symptoms. She had obviously told the story dozens of times – through seemingly endless encounters – to her primary physician, hospital residents, medical students, emergency physicians, and just about anyone else who would lend an ear. Listening to her share her story with a large audience while still a patient in the hospital was incredibly powerful; it was difficult not to become emotional with her as she welled up with tears. She told a complex, though very coherent tale that included her past medical and family histories, her employment, her hobbies, and her unusual signs and symptoms as they developed over an extended period of time. When the patient was done, her case was presented from another perspective: the way it was recorded in her electronic record. For a brief moment, those seated in the audience were confused. Then the theme of the conference became evident – these were completely different stories.
This was no case of mistaken identity or registration error. The chart presented at the conference did belong to the patient, but the story told by the chart was wrong. Reading through the chart, it would be easy to come away with the same sense as her care team; this must simply be a common illness that wasn’t responding to conventional treatment. Encounter after encounter, a new plan was devised to address the presumed diagnosis. But the patient’s telling of the history barely mentioned any symptoms related to that diagnosis. Her version focused more on how her life was affected, how she could no longer take care of her daughter, how she could no longer exercise (which she did avidly), and how she was sinking deeper into despair and losing hope. Woven through all of this were the historical details and seemingly obvious physical manifestations that might easily disclose the real cause of her symptoms. A few basic questions about her family history would also reveal multiple immediate family members who suffered from the same disease! But even if these questions had been asked, and even if the story had been heard, the image in the mirror – her chart – did not reflect an accurate understanding of the patient.
We often solicit comments from readers, and the response is alway encouraging. It is clear that our colleagues in the medical community feel a strong sense of obligation to their patients and care deeply for maintaining the sanctity of the physician-patient relationship. However, many feel the electronic health record has become a barrier to developing and nurturing that relationship, standing in the way understanding their stories. One poignant letter from a cardiologist in Florida, Eugene H. Eisman, MD, does a beautiful job in crystallizing this sentiment. Dr. Eisman writes:
“Many of my patients end up hospitalized where I do not have privileges. Almost every attending is attentive enough to send me a discharge summary. These, however, are EHR-generated. The patient may have been hospitalized for 3 days, yet the summary is seven pages long. It is filled with total nonsense, such as whether the patient had traveled to North Africa (even though he was hospitalized with a fractured hip while skiing in Colorado). The attending has managed to cut and paste reports of every chest film and CBC, and I have pages of normal studies. The final diagnosis and discharge medications are difficult to find in this morass of words. I cannot force myself to read this document, and it is thrown into his chart after a cursory glance. Yet, I can’t sleep at night. Is there buried in this seven-page document a discovery of malignancy, etc.?”
Dr. Eisman’s words are powerful because they reveal an oft-overlooked truth about modern medical records. The patient’s chart, once considered a sacred text containing the key inflection points in a patient’s story, has become merely a filing cabinet in which to stuff every piece of data about the patient, no matter how mundane or trivial. No thought need be put into preserving the important details, because now absolutely every detail can be included. We have become so overloaded with the unimportant, that we may lose the truly critical in this sea of information. It has become, therefore, imperative that physicians rediscover the patient in their story, and not rely solely on the poor reflection we may find in their chart.
Thousands of years ago, the apostle Paul wrote that “we see now as through a glass, darkly.” Borrowing from his original meaning, these ancient words have been quoted throughout literature to describe an “incomplete understanding,” often mixed with a state of despair. Today, we might think of the electronic record as the glass – or mirror – reflecting the patient’s story. Ironically, in spite of having more information than ever, the image we see may be incomplete, and possibly even wrong altogether. While the amount of available data may at first glance appear enlightening, the reflection in the glass may be rather dark indeed.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Neil Skolnik, MD, is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
Recently, we were invited to take part in an case presentation focused on a young female patient. The reason for our specific invitation was because a key component in the patient’s case was centered on her electronic health record. This kind of story was not new to us – in fact, stories like these are becoming almost common everywhere. But this particular conference promised to be very special, because the patient herself was asked to take an active role and present the story from a unique perspective – her own.
Seated on stage in a hospital gown and accompanied by her I.V. pole, the patient related a 4-month history of symptoms. She had obviously told the story dozens of times – through seemingly endless encounters – to her primary physician, hospital residents, medical students, emergency physicians, and just about anyone else who would lend an ear. Listening to her share her story with a large audience while still a patient in the hospital was incredibly powerful; it was difficult not to become emotional with her as she welled up with tears. She told a complex, though very coherent tale that included her past medical and family histories, her employment, her hobbies, and her unusual signs and symptoms as they developed over an extended period of time. When the patient was done, her case was presented from another perspective: the way it was recorded in her electronic record. For a brief moment, those seated in the audience were confused. Then the theme of the conference became evident – these were completely different stories.
This was no case of mistaken identity or registration error. The chart presented at the conference did belong to the patient, but the story told by the chart was wrong. Reading through the chart, it would be easy to come away with the same sense as her care team; this must simply be a common illness that wasn’t responding to conventional treatment. Encounter after encounter, a new plan was devised to address the presumed diagnosis. But the patient’s telling of the history barely mentioned any symptoms related to that diagnosis. Her version focused more on how her life was affected, how she could no longer take care of her daughter, how she could no longer exercise (which she did avidly), and how she was sinking deeper into despair and losing hope. Woven through all of this were the historical details and seemingly obvious physical manifestations that might easily disclose the real cause of her symptoms. A few basic questions about her family history would also reveal multiple immediate family members who suffered from the same disease! But even if these questions had been asked, and even if the story had been heard, the image in the mirror – her chart – did not reflect an accurate understanding of the patient.
We often solicit comments from readers, and the response is alway encouraging. It is clear that our colleagues in the medical community feel a strong sense of obligation to their patients and care deeply for maintaining the sanctity of the physician-patient relationship. However, many feel the electronic health record has become a barrier to developing and nurturing that relationship, standing in the way understanding their stories. One poignant letter from a cardiologist in Florida, Eugene H. Eisman, MD, does a beautiful job in crystallizing this sentiment. Dr. Eisman writes:
“Many of my patients end up hospitalized where I do not have privileges. Almost every attending is attentive enough to send me a discharge summary. These, however, are EHR-generated. The patient may have been hospitalized for 3 days, yet the summary is seven pages long. It is filled with total nonsense, such as whether the patient had traveled to North Africa (even though he was hospitalized with a fractured hip while skiing in Colorado). The attending has managed to cut and paste reports of every chest film and CBC, and I have pages of normal studies. The final diagnosis and discharge medications are difficult to find in this morass of words. I cannot force myself to read this document, and it is thrown into his chart after a cursory glance. Yet, I can’t sleep at night. Is there buried in this seven-page document a discovery of malignancy, etc.?”
Dr. Eisman’s words are powerful because they reveal an oft-overlooked truth about modern medical records. The patient’s chart, once considered a sacred text containing the key inflection points in a patient’s story, has become merely a filing cabinet in which to stuff every piece of data about the patient, no matter how mundane or trivial. No thought need be put into preserving the important details, because now absolutely every detail can be included. We have become so overloaded with the unimportant, that we may lose the truly critical in this sea of information. It has become, therefore, imperative that physicians rediscover the patient in their story, and not rely solely on the poor reflection we may find in their chart.
Thousands of years ago, the apostle Paul wrote that “we see now as through a glass, darkly.” Borrowing from his original meaning, these ancient words have been quoted throughout literature to describe an “incomplete understanding,” often mixed with a state of despair. Today, we might think of the electronic record as the glass – or mirror – reflecting the patient’s story. Ironically, in spite of having more information than ever, the image we see may be incomplete, and possibly even wrong altogether. While the amount of available data may at first glance appear enlightening, the reflection in the glass may be rather dark indeed.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Neil Skolnik, MD, is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
Recently, we were invited to take part in an case presentation focused on a young female patient. The reason for our specific invitation was because a key component in the patient’s case was centered on her electronic health record. This kind of story was not new to us – in fact, stories like these are becoming almost common everywhere. But this particular conference promised to be very special, because the patient herself was asked to take an active role and present the story from a unique perspective – her own.
Seated on stage in a hospital gown and accompanied by her I.V. pole, the patient related a 4-month history of symptoms. She had obviously told the story dozens of times – through seemingly endless encounters – to her primary physician, hospital residents, medical students, emergency physicians, and just about anyone else who would lend an ear. Listening to her share her story with a large audience while still a patient in the hospital was incredibly powerful; it was difficult not to become emotional with her as she welled up with tears. She told a complex, though very coherent tale that included her past medical and family histories, her employment, her hobbies, and her unusual signs and symptoms as they developed over an extended period of time. When the patient was done, her case was presented from another perspective: the way it was recorded in her electronic record. For a brief moment, those seated in the audience were confused. Then the theme of the conference became evident – these were completely different stories.
This was no case of mistaken identity or registration error. The chart presented at the conference did belong to the patient, but the story told by the chart was wrong. Reading through the chart, it would be easy to come away with the same sense as her care team; this must simply be a common illness that wasn’t responding to conventional treatment. Encounter after encounter, a new plan was devised to address the presumed diagnosis. But the patient’s telling of the history barely mentioned any symptoms related to that diagnosis. Her version focused more on how her life was affected, how she could no longer take care of her daughter, how she could no longer exercise (which she did avidly), and how she was sinking deeper into despair and losing hope. Woven through all of this were the historical details and seemingly obvious physical manifestations that might easily disclose the real cause of her symptoms. A few basic questions about her family history would also reveal multiple immediate family members who suffered from the same disease! But even if these questions had been asked, and even if the story had been heard, the image in the mirror – her chart – did not reflect an accurate understanding of the patient.
We often solicit comments from readers, and the response is alway encouraging. It is clear that our colleagues in the medical community feel a strong sense of obligation to their patients and care deeply for maintaining the sanctity of the physician-patient relationship. However, many feel the electronic health record has become a barrier to developing and nurturing that relationship, standing in the way understanding their stories. One poignant letter from a cardiologist in Florida, Eugene H. Eisman, MD, does a beautiful job in crystallizing this sentiment. Dr. Eisman writes:
“Many of my patients end up hospitalized where I do not have privileges. Almost every attending is attentive enough to send me a discharge summary. These, however, are EHR-generated. The patient may have been hospitalized for 3 days, yet the summary is seven pages long. It is filled with total nonsense, such as whether the patient had traveled to North Africa (even though he was hospitalized with a fractured hip while skiing in Colorado). The attending has managed to cut and paste reports of every chest film and CBC, and I have pages of normal studies. The final diagnosis and discharge medications are difficult to find in this morass of words. I cannot force myself to read this document, and it is thrown into his chart after a cursory glance. Yet, I can’t sleep at night. Is there buried in this seven-page document a discovery of malignancy, etc.?”
Dr. Eisman’s words are powerful because they reveal an oft-overlooked truth about modern medical records. The patient’s chart, once considered a sacred text containing the key inflection points in a patient’s story, has become merely a filing cabinet in which to stuff every piece of data about the patient, no matter how mundane or trivial. No thought need be put into preserving the important details, because now absolutely every detail can be included. We have become so overloaded with the unimportant, that we may lose the truly critical in this sea of information. It has become, therefore, imperative that physicians rediscover the patient in their story, and not rely solely on the poor reflection we may find in their chart.
Thousands of years ago, the apostle Paul wrote that “we see now as through a glass, darkly.” Borrowing from his original meaning, these ancient words have been quoted throughout literature to describe an “incomplete understanding,” often mixed with a state of despair. Today, we might think of the electronic record as the glass – or mirror – reflecting the patient’s story. Ironically, in spite of having more information than ever, the image we see may be incomplete, and possibly even wrong altogether. While the amount of available data may at first glance appear enlightening, the reflection in the glass may be rather dark indeed.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Neil Skolnik, MD, is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
Laboring in the Shadow of the Media: Care and Perceptions of Care in the VA
Just over 2 years ago, I finished a psychiatry residency at the Mayo Clinic, turned down an offer to stay on staff, and topped it off by taking a position at the VA. Not one of my brighter moments—or so one of my friends thought. “Are you off your rocker? Don’t you know that the VA is terrible? Why would you go work there?” he jabbed incredulously. I cringed, knowing that I had passed up an opportunity to stay in arguably the best hospital system in the nation, possibly the world, to work at what some (maybe even a lot) view as a corpulent and recalcitrant bastion of ineptitude bound by the dictates of a fickle Congress.
In the wake of the Phoenix wait-time scandal (and no, it’s not like Disneyland), the suicide by self-immolation of Charles Richard Ingram III outside a VA facility in New Jersey, the new data on veteran suicide showing progress but continued significant concern, and the ongoing VA privatization discussion, the prevailing discourse about the VA is largely negative.1,2 And in a high-voltage election cycle where public outrage can serve as an efficient tool to garner support, the VA risks getting pummeled.
Add to this the shocking research that shows nearly half of VA psychiatrists are considering leaving the VA within the next 2 years, and it’s clear that dissatisfaction within and outside the VA is high.3 This does not bode well for veterans at a time when suicide and mental health care needs are so critically important. But while the bureaucracy of the VA is often the focus of negative press, it also filters down and unfortunately has the potential to directly affect VA practitioners and veterans. When we lose sight of what the VA does well, we risk being caught up in a vortex of negativity and a profound sense of inadequacy and helplessness. More attention to what is already being done well can help us as a nation more realistically chart a path forward rather than being fueled by negative rhetoric and rage.
Despite the challenges, the VA is currently succeeding in a number of areas that deserve recognition:
Medical school and resident education and collaboration with VA. In 2014, > 41,000 medical residents and nearly 23,000 medical students had some or all of their training in a VA setting. More than 95% of allopathic medical schools and nearly 90% of osteopathic medical schools had affiliation agreements with the VA in 2014.4 Suffice it to say, if the educational endeavors of the VA were curtailed, there would be an unholy scramble to provide well-trained physicians for our nation. (This does not include the dentists, psychologists, pharmacists, social workers, nurses, and other health care professionals whose training involves the VA in some capacity.) In addition, the VA often provides loan repayment assistance, which is very important given that many young professionals carry substantial school debt after completing training.
Mental health and primary care integration. Medical care overall is changing, and there is an increasing shift away from volume-based, fee-for-service care to integrated, team-based models. The VA is one of several successful leaders at a time when most U.S. health care providers are being scrutinized for their use of health care dollars and overall national health outcomes.5 In addition to primary care integration, the VA uses home-based primary care and mental health intensive case management teams for vulnerable veterans, adding flexibility, continuity, and access for many.
Overall excellent mental health care. A recent study by Watkins and colleagues found that when comparing quality measures for medication evaluation and management for schizophrenia, bipolar disorder, posttraumatic stress disorder, depression, and substance use disorders, “In every case, VA performance was superior to that of the private sector by more than 30%.”6 This is not an aberration and not limited to mental health care. It is a consistent finding about which books have been written.7 However, the availability of evidence-based care may not be consistent across all VA facilities nationally, depending on demand and staffing.
Despite the rumors, VA has high customer satisfaction. According to the American Customer Satisfaction Index, the VA has consistently performed well in measures of customer satisfaction compared with those of the private sector health care providers.8 Let’s not ignore what veterans have actually said and continue to say about their care.
Once in, you’re in! I recently missed an initial appointment with a private sector pediatrician for one of my sons. I was tersely invited to find another doctor. This seemed scandalous since I have become accustomed in my role as a VA physician to reaching out, sometimes incessantly, to patients who do not come in for either a new or follow-up appointment. Yes, I call my patients; personally, directly, and often. In many clinics, patients receive reminder letters about upcoming appointments and then phone calls and sometimes letters when appointments are missed. My colleagues and I have jokingly referred to this practice as “benign stalking.”
Further, if a veteran is dissatisfied with care, there is a process to review and make adjustments if necessary, including transfer to a different doctor. Additionally, and sometimes alarmingly, veterans are not “fired” (and actually can’t be) for bad behavior (including direct threats to VA staff). Time, place, and manner of care can be tailored based on assessed risk, and VA police may be involved, but veterans continue to get care. I can assure you that if I made a threat to one of my doctors in private practice, I would very quickly be searching for a new doctor and answering some tough questions from law enforcement. Unlike many patients in private care, veterans have consistent access via phone (though admittedly not always user-friendly), walk-in appointments, after-hours availability in some locations, and secure messaging.
Electronic medical record and telehealth initiatives. The VA Computerized Patient Record System, has been around for some time and provides an excellent (although not perfect) system for documenting patient care. Each VA is linked to other VAs across the nation so patients don’t have to reinvent their story when they move and can actually get down to the business of being treated. Prior interventions, hospitalizations, medication trials, diagnostic impressions, imaging, lab work, etc, are all available at the touch of a button! And the VA’s telehealth initiative is all about access.
Veteran suicide prevention and opioid prescribing. Suicide is disproportionately high among veterans in the U.S. Recent data show that in 2014, an average of 20 veterans died by suicide per day.1 This accounted for 18% of all U.S. adult suicide deaths, even though veterans represent only 8.5% of the population. And while these recent statistics represent some improvement over prior research, prevention and care coordination remain major priorities in the VA. Veterans have access to same-day care (at least in Boise, Idaho) and a 24-hour crisis line that gives feedback to the patient’s local VA and can help coordinate follow-up care. The VA has specialized suicide prevention coordinators who attend to the needs of patients assessed to be at high risk for suicide and also disseminate training to providers in a variety of disciplines. All of this as the VA moves to ensure that suicide prevention remains a priority across disciplines and treatment sites.
Additionally, the VA is directly addressing the nationwide crisis of overprescription of opioids, beginning with education for both patients and staff and systemic encouragement of responsible prescribing via the national Opioid Safety Initiative and increased emphasis on providing at-risk veterans with naloxone kits.9
Research. VA research endeavors are wide ranging. The VA has been involved in pioneering clinical research in a substantial way since at least the 1920s and has contributed to important innovations in treatment, ranging from prosthetics to imaging, neuromodulation to medication intervention for a broad array of pathology.10
Drawing in professionals who want to work with veterans. The reason that many health care providers work at the VA is the veterans themselves. Veterans by and large represent a segment of our population who have demonstrated dedication, commitment to a shared goal, and the willingness to sacrifice their health or their lives for a greater good. The veteran identity and sacrifice has drawn many of us to want to serve them. My father’s and cousin’s service are truly inspirational on a personal level. I am not alone in this.
I recently had a veteran in my office who, once seated, pulled his chair closer to mine than I ordinarily prefer. He then gave me a penetrating stare, moved well within the comfort zone of even the closest of close-talkers, and began to scream about the wrongs he had heard about in the VA system. When he finished screaming (and once the other clinicians in the building realized that I wasn’t being physically attacked), he freely acknowledged that he had never actually experienced any of the VA shortcomings personally but, nonetheless, learned how reprehensible the VA is through the media. Our veterans deserve the best care that we as a nation can provide, and they also deserve to know the truth about the quality of VA care. But too often the negative media attention does not tell the whole story that directly impacts the well-being of our veterans.
I sit on the disruptive behavior committee at the Boise VAMC and see firsthand the stress that our veterans and staff are under. We review reports of veterans who disrupt the environment, sometimes by direct threats to shoot or in some way physically harm those taking care of them. Some of this is over pain medications or other specific health care issues. Some is due to frustration in trying to navigate an increasingly complex and nonintuitive system as the VA scrambles to implement congressional directives that sometimes clash with what is clinically appropriate and evidence-based. Some of the disruptive behavior, however, is fueled by the negative national discourse against the political establishment and its nearest representative—in this case, the VA. And again, this is often fueled, in my opinion, by incomplete media coverage.
The VA has problems. It would be delusional to argue otherwise. It is rightly open to public scrutiny as a tax-funded governmental agency, and lives are literally at stake as we grapple nationally with how best to deliver on Lincoln’s promise to “care for those who have borne the battle.”
As I reflect on my friend’s skepticism at my taking a VA position, I can answer that yes, the VA needs work. It has some major issues. But I no longer feel the need to cringe, because I now know firsthand the kind of care that is being delivered (at least to the veterans in Boise).
Wherever you stand on the quality of VA care, the movement to privatize, or the politicizing inevitable during an election year, to indiscriminately excoriate the VA is to risk marginalizing the superlative care that many currently receive by the thousands of physicians and other health care providers and administrators throughout the VA. Our veterans are a national treasure that deserve excellent care and real solutions to the problems that exist in the VA, not overwhelming negative rhetoric.
1. U.S. Department of Veterans Affairs, Office of Suicide Prevention. Suicide Among Veterans and Other Americans 2001-2014. http://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Published August 3, 2016. Accessed August 10, 2016.
2. Longman P, Gordon S. A conversation about the commission on care and the future of the VA. Washington Monthly. http://washingtonmonthly.com/2016/07/14/a-conversation-about-the-commission-on-care-and-the-future-of-the-va/. Published July 14, 2016. Accessed August 4, 2016.
3. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the Veterans Health Administration. Burnout Research. 2015;2(4):108-114.
4. U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and dental education program. http://www.va.gov/oaa/GME_default.asp. Updated December 9, 2015. Accessed August 4, 2016.
5. Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906.
6. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396.
7. Longman P. Best Care Anywhere: Why VA Health Care Would Work Better for Everyone. 3rd ed. San Francisco, CA: Berrett-Koehler; 2012.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. American customer satisfaction index 2013 customer satisfaction outpatient survey. http://www.va.gov/health/docs/VA2013OutpatientACSI.pdf. Published March 2014. Accessed August 10, 2016.
9. U.S. Department of Veterans Affairs. VHA pain management, Opioid Safety Initiative (OSI). http://www.va.gov/PAINMANAGEMENT/Opioid_Safety_Initiative_OSI.asp. Updated June 17, 2015. Accessed August 4, 2016.
10. U.S. Department of Veterans Affairs. Office of Research and Development. http://www.research.va.gov. Updated July 21, 2016. Accessed August 4, 2016.
Just over 2 years ago, I finished a psychiatry residency at the Mayo Clinic, turned down an offer to stay on staff, and topped it off by taking a position at the VA. Not one of my brighter moments—or so one of my friends thought. “Are you off your rocker? Don’t you know that the VA is terrible? Why would you go work there?” he jabbed incredulously. I cringed, knowing that I had passed up an opportunity to stay in arguably the best hospital system in the nation, possibly the world, to work at what some (maybe even a lot) view as a corpulent and recalcitrant bastion of ineptitude bound by the dictates of a fickle Congress.
In the wake of the Phoenix wait-time scandal (and no, it’s not like Disneyland), the suicide by self-immolation of Charles Richard Ingram III outside a VA facility in New Jersey, the new data on veteran suicide showing progress but continued significant concern, and the ongoing VA privatization discussion, the prevailing discourse about the VA is largely negative.1,2 And in a high-voltage election cycle where public outrage can serve as an efficient tool to garner support, the VA risks getting pummeled.
Add to this the shocking research that shows nearly half of VA psychiatrists are considering leaving the VA within the next 2 years, and it’s clear that dissatisfaction within and outside the VA is high.3 This does not bode well for veterans at a time when suicide and mental health care needs are so critically important. But while the bureaucracy of the VA is often the focus of negative press, it also filters down and unfortunately has the potential to directly affect VA practitioners and veterans. When we lose sight of what the VA does well, we risk being caught up in a vortex of negativity and a profound sense of inadequacy and helplessness. More attention to what is already being done well can help us as a nation more realistically chart a path forward rather than being fueled by negative rhetoric and rage.
Despite the challenges, the VA is currently succeeding in a number of areas that deserve recognition:
Medical school and resident education and collaboration with VA. In 2014, > 41,000 medical residents and nearly 23,000 medical students had some or all of their training in a VA setting. More than 95% of allopathic medical schools and nearly 90% of osteopathic medical schools had affiliation agreements with the VA in 2014.4 Suffice it to say, if the educational endeavors of the VA were curtailed, there would be an unholy scramble to provide well-trained physicians for our nation. (This does not include the dentists, psychologists, pharmacists, social workers, nurses, and other health care professionals whose training involves the VA in some capacity.) In addition, the VA often provides loan repayment assistance, which is very important given that many young professionals carry substantial school debt after completing training.
Mental health and primary care integration. Medical care overall is changing, and there is an increasing shift away from volume-based, fee-for-service care to integrated, team-based models. The VA is one of several successful leaders at a time when most U.S. health care providers are being scrutinized for their use of health care dollars and overall national health outcomes.5 In addition to primary care integration, the VA uses home-based primary care and mental health intensive case management teams for vulnerable veterans, adding flexibility, continuity, and access for many.
Overall excellent mental health care. A recent study by Watkins and colleagues found that when comparing quality measures for medication evaluation and management for schizophrenia, bipolar disorder, posttraumatic stress disorder, depression, and substance use disorders, “In every case, VA performance was superior to that of the private sector by more than 30%.”6 This is not an aberration and not limited to mental health care. It is a consistent finding about which books have been written.7 However, the availability of evidence-based care may not be consistent across all VA facilities nationally, depending on demand and staffing.
Despite the rumors, VA has high customer satisfaction. According to the American Customer Satisfaction Index, the VA has consistently performed well in measures of customer satisfaction compared with those of the private sector health care providers.8 Let’s not ignore what veterans have actually said and continue to say about their care.
Once in, you’re in! I recently missed an initial appointment with a private sector pediatrician for one of my sons. I was tersely invited to find another doctor. This seemed scandalous since I have become accustomed in my role as a VA physician to reaching out, sometimes incessantly, to patients who do not come in for either a new or follow-up appointment. Yes, I call my patients; personally, directly, and often. In many clinics, patients receive reminder letters about upcoming appointments and then phone calls and sometimes letters when appointments are missed. My colleagues and I have jokingly referred to this practice as “benign stalking.”
Further, if a veteran is dissatisfied with care, there is a process to review and make adjustments if necessary, including transfer to a different doctor. Additionally, and sometimes alarmingly, veterans are not “fired” (and actually can’t be) for bad behavior (including direct threats to VA staff). Time, place, and manner of care can be tailored based on assessed risk, and VA police may be involved, but veterans continue to get care. I can assure you that if I made a threat to one of my doctors in private practice, I would very quickly be searching for a new doctor and answering some tough questions from law enforcement. Unlike many patients in private care, veterans have consistent access via phone (though admittedly not always user-friendly), walk-in appointments, after-hours availability in some locations, and secure messaging.
Electronic medical record and telehealth initiatives. The VA Computerized Patient Record System, has been around for some time and provides an excellent (although not perfect) system for documenting patient care. Each VA is linked to other VAs across the nation so patients don’t have to reinvent their story when they move and can actually get down to the business of being treated. Prior interventions, hospitalizations, medication trials, diagnostic impressions, imaging, lab work, etc, are all available at the touch of a button! And the VA’s telehealth initiative is all about access.
Veteran suicide prevention and opioid prescribing. Suicide is disproportionately high among veterans in the U.S. Recent data show that in 2014, an average of 20 veterans died by suicide per day.1 This accounted for 18% of all U.S. adult suicide deaths, even though veterans represent only 8.5% of the population. And while these recent statistics represent some improvement over prior research, prevention and care coordination remain major priorities in the VA. Veterans have access to same-day care (at least in Boise, Idaho) and a 24-hour crisis line that gives feedback to the patient’s local VA and can help coordinate follow-up care. The VA has specialized suicide prevention coordinators who attend to the needs of patients assessed to be at high risk for suicide and also disseminate training to providers in a variety of disciplines. All of this as the VA moves to ensure that suicide prevention remains a priority across disciplines and treatment sites.
Additionally, the VA is directly addressing the nationwide crisis of overprescription of opioids, beginning with education for both patients and staff and systemic encouragement of responsible prescribing via the national Opioid Safety Initiative and increased emphasis on providing at-risk veterans with naloxone kits.9
Research. VA research endeavors are wide ranging. The VA has been involved in pioneering clinical research in a substantial way since at least the 1920s and has contributed to important innovations in treatment, ranging from prosthetics to imaging, neuromodulation to medication intervention for a broad array of pathology.10
Drawing in professionals who want to work with veterans. The reason that many health care providers work at the VA is the veterans themselves. Veterans by and large represent a segment of our population who have demonstrated dedication, commitment to a shared goal, and the willingness to sacrifice their health or their lives for a greater good. The veteran identity and sacrifice has drawn many of us to want to serve them. My father’s and cousin’s service are truly inspirational on a personal level. I am not alone in this.
I recently had a veteran in my office who, once seated, pulled his chair closer to mine than I ordinarily prefer. He then gave me a penetrating stare, moved well within the comfort zone of even the closest of close-talkers, and began to scream about the wrongs he had heard about in the VA system. When he finished screaming (and once the other clinicians in the building realized that I wasn’t being physically attacked), he freely acknowledged that he had never actually experienced any of the VA shortcomings personally but, nonetheless, learned how reprehensible the VA is through the media. Our veterans deserve the best care that we as a nation can provide, and they also deserve to know the truth about the quality of VA care. But too often the negative media attention does not tell the whole story that directly impacts the well-being of our veterans.
I sit on the disruptive behavior committee at the Boise VAMC and see firsthand the stress that our veterans and staff are under. We review reports of veterans who disrupt the environment, sometimes by direct threats to shoot or in some way physically harm those taking care of them. Some of this is over pain medications or other specific health care issues. Some is due to frustration in trying to navigate an increasingly complex and nonintuitive system as the VA scrambles to implement congressional directives that sometimes clash with what is clinically appropriate and evidence-based. Some of the disruptive behavior, however, is fueled by the negative national discourse against the political establishment and its nearest representative—in this case, the VA. And again, this is often fueled, in my opinion, by incomplete media coverage.
The VA has problems. It would be delusional to argue otherwise. It is rightly open to public scrutiny as a tax-funded governmental agency, and lives are literally at stake as we grapple nationally with how best to deliver on Lincoln’s promise to “care for those who have borne the battle.”
As I reflect on my friend’s skepticism at my taking a VA position, I can answer that yes, the VA needs work. It has some major issues. But I no longer feel the need to cringe, because I now know firsthand the kind of care that is being delivered (at least to the veterans in Boise).
Wherever you stand on the quality of VA care, the movement to privatize, or the politicizing inevitable during an election year, to indiscriminately excoriate the VA is to risk marginalizing the superlative care that many currently receive by the thousands of physicians and other health care providers and administrators throughout the VA. Our veterans are a national treasure that deserve excellent care and real solutions to the problems that exist in the VA, not overwhelming negative rhetoric.
Just over 2 years ago, I finished a psychiatry residency at the Mayo Clinic, turned down an offer to stay on staff, and topped it off by taking a position at the VA. Not one of my brighter moments—or so one of my friends thought. “Are you off your rocker? Don’t you know that the VA is terrible? Why would you go work there?” he jabbed incredulously. I cringed, knowing that I had passed up an opportunity to stay in arguably the best hospital system in the nation, possibly the world, to work at what some (maybe even a lot) view as a corpulent and recalcitrant bastion of ineptitude bound by the dictates of a fickle Congress.
In the wake of the Phoenix wait-time scandal (and no, it’s not like Disneyland), the suicide by self-immolation of Charles Richard Ingram III outside a VA facility in New Jersey, the new data on veteran suicide showing progress but continued significant concern, and the ongoing VA privatization discussion, the prevailing discourse about the VA is largely negative.1,2 And in a high-voltage election cycle where public outrage can serve as an efficient tool to garner support, the VA risks getting pummeled.
Add to this the shocking research that shows nearly half of VA psychiatrists are considering leaving the VA within the next 2 years, and it’s clear that dissatisfaction within and outside the VA is high.3 This does not bode well for veterans at a time when suicide and mental health care needs are so critically important. But while the bureaucracy of the VA is often the focus of negative press, it also filters down and unfortunately has the potential to directly affect VA practitioners and veterans. When we lose sight of what the VA does well, we risk being caught up in a vortex of negativity and a profound sense of inadequacy and helplessness. More attention to what is already being done well can help us as a nation more realistically chart a path forward rather than being fueled by negative rhetoric and rage.
Despite the challenges, the VA is currently succeeding in a number of areas that deserve recognition:
Medical school and resident education and collaboration with VA. In 2014, > 41,000 medical residents and nearly 23,000 medical students had some or all of their training in a VA setting. More than 95% of allopathic medical schools and nearly 90% of osteopathic medical schools had affiliation agreements with the VA in 2014.4 Suffice it to say, if the educational endeavors of the VA were curtailed, there would be an unholy scramble to provide well-trained physicians for our nation. (This does not include the dentists, psychologists, pharmacists, social workers, nurses, and other health care professionals whose training involves the VA in some capacity.) In addition, the VA often provides loan repayment assistance, which is very important given that many young professionals carry substantial school debt after completing training.
Mental health and primary care integration. Medical care overall is changing, and there is an increasing shift away from volume-based, fee-for-service care to integrated, team-based models. The VA is one of several successful leaders at a time when most U.S. health care providers are being scrutinized for their use of health care dollars and overall national health outcomes.5 In addition to primary care integration, the VA uses home-based primary care and mental health intensive case management teams for vulnerable veterans, adding flexibility, continuity, and access for many.
Overall excellent mental health care. A recent study by Watkins and colleagues found that when comparing quality measures for medication evaluation and management for schizophrenia, bipolar disorder, posttraumatic stress disorder, depression, and substance use disorders, “In every case, VA performance was superior to that of the private sector by more than 30%.”6 This is not an aberration and not limited to mental health care. It is a consistent finding about which books have been written.7 However, the availability of evidence-based care may not be consistent across all VA facilities nationally, depending on demand and staffing.
Despite the rumors, VA has high customer satisfaction. According to the American Customer Satisfaction Index, the VA has consistently performed well in measures of customer satisfaction compared with those of the private sector health care providers.8 Let’s not ignore what veterans have actually said and continue to say about their care.
Once in, you’re in! I recently missed an initial appointment with a private sector pediatrician for one of my sons. I was tersely invited to find another doctor. This seemed scandalous since I have become accustomed in my role as a VA physician to reaching out, sometimes incessantly, to patients who do not come in for either a new or follow-up appointment. Yes, I call my patients; personally, directly, and often. In many clinics, patients receive reminder letters about upcoming appointments and then phone calls and sometimes letters when appointments are missed. My colleagues and I have jokingly referred to this practice as “benign stalking.”
Further, if a veteran is dissatisfied with care, there is a process to review and make adjustments if necessary, including transfer to a different doctor. Additionally, and sometimes alarmingly, veterans are not “fired” (and actually can’t be) for bad behavior (including direct threats to VA staff). Time, place, and manner of care can be tailored based on assessed risk, and VA police may be involved, but veterans continue to get care. I can assure you that if I made a threat to one of my doctors in private practice, I would very quickly be searching for a new doctor and answering some tough questions from law enforcement. Unlike many patients in private care, veterans have consistent access via phone (though admittedly not always user-friendly), walk-in appointments, after-hours availability in some locations, and secure messaging.
Electronic medical record and telehealth initiatives. The VA Computerized Patient Record System, has been around for some time and provides an excellent (although not perfect) system for documenting patient care. Each VA is linked to other VAs across the nation so patients don’t have to reinvent their story when they move and can actually get down to the business of being treated. Prior interventions, hospitalizations, medication trials, diagnostic impressions, imaging, lab work, etc, are all available at the touch of a button! And the VA’s telehealth initiative is all about access.
Veteran suicide prevention and opioid prescribing. Suicide is disproportionately high among veterans in the U.S. Recent data show that in 2014, an average of 20 veterans died by suicide per day.1 This accounted for 18% of all U.S. adult suicide deaths, even though veterans represent only 8.5% of the population. And while these recent statistics represent some improvement over prior research, prevention and care coordination remain major priorities in the VA. Veterans have access to same-day care (at least in Boise, Idaho) and a 24-hour crisis line that gives feedback to the patient’s local VA and can help coordinate follow-up care. The VA has specialized suicide prevention coordinators who attend to the needs of patients assessed to be at high risk for suicide and also disseminate training to providers in a variety of disciplines. All of this as the VA moves to ensure that suicide prevention remains a priority across disciplines and treatment sites.
Additionally, the VA is directly addressing the nationwide crisis of overprescription of opioids, beginning with education for both patients and staff and systemic encouragement of responsible prescribing via the national Opioid Safety Initiative and increased emphasis on providing at-risk veterans with naloxone kits.9
Research. VA research endeavors are wide ranging. The VA has been involved in pioneering clinical research in a substantial way since at least the 1920s and has contributed to important innovations in treatment, ranging from prosthetics to imaging, neuromodulation to medication intervention for a broad array of pathology.10
Drawing in professionals who want to work with veterans. The reason that many health care providers work at the VA is the veterans themselves. Veterans by and large represent a segment of our population who have demonstrated dedication, commitment to a shared goal, and the willingness to sacrifice their health or their lives for a greater good. The veteran identity and sacrifice has drawn many of us to want to serve them. My father’s and cousin’s service are truly inspirational on a personal level. I am not alone in this.
I recently had a veteran in my office who, once seated, pulled his chair closer to mine than I ordinarily prefer. He then gave me a penetrating stare, moved well within the comfort zone of even the closest of close-talkers, and began to scream about the wrongs he had heard about in the VA system. When he finished screaming (and once the other clinicians in the building realized that I wasn’t being physically attacked), he freely acknowledged that he had never actually experienced any of the VA shortcomings personally but, nonetheless, learned how reprehensible the VA is through the media. Our veterans deserve the best care that we as a nation can provide, and they also deserve to know the truth about the quality of VA care. But too often the negative media attention does not tell the whole story that directly impacts the well-being of our veterans.
I sit on the disruptive behavior committee at the Boise VAMC and see firsthand the stress that our veterans and staff are under. We review reports of veterans who disrupt the environment, sometimes by direct threats to shoot or in some way physically harm those taking care of them. Some of this is over pain medications or other specific health care issues. Some is due to frustration in trying to navigate an increasingly complex and nonintuitive system as the VA scrambles to implement congressional directives that sometimes clash with what is clinically appropriate and evidence-based. Some of the disruptive behavior, however, is fueled by the negative national discourse against the political establishment and its nearest representative—in this case, the VA. And again, this is often fueled, in my opinion, by incomplete media coverage.
The VA has problems. It would be delusional to argue otherwise. It is rightly open to public scrutiny as a tax-funded governmental agency, and lives are literally at stake as we grapple nationally with how best to deliver on Lincoln’s promise to “care for those who have borne the battle.”
As I reflect on my friend’s skepticism at my taking a VA position, I can answer that yes, the VA needs work. It has some major issues. But I no longer feel the need to cringe, because I now know firsthand the kind of care that is being delivered (at least to the veterans in Boise).
Wherever you stand on the quality of VA care, the movement to privatize, or the politicizing inevitable during an election year, to indiscriminately excoriate the VA is to risk marginalizing the superlative care that many currently receive by the thousands of physicians and other health care providers and administrators throughout the VA. Our veterans are a national treasure that deserve excellent care and real solutions to the problems that exist in the VA, not overwhelming negative rhetoric.
1. U.S. Department of Veterans Affairs, Office of Suicide Prevention. Suicide Among Veterans and Other Americans 2001-2014. http://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Published August 3, 2016. Accessed August 10, 2016.
2. Longman P, Gordon S. A conversation about the commission on care and the future of the VA. Washington Monthly. http://washingtonmonthly.com/2016/07/14/a-conversation-about-the-commission-on-care-and-the-future-of-the-va/. Published July 14, 2016. Accessed August 4, 2016.
3. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the Veterans Health Administration. Burnout Research. 2015;2(4):108-114.
4. U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and dental education program. http://www.va.gov/oaa/GME_default.asp. Updated December 9, 2015. Accessed August 4, 2016.
5. Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906.
6. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396.
7. Longman P. Best Care Anywhere: Why VA Health Care Would Work Better for Everyone. 3rd ed. San Francisco, CA: Berrett-Koehler; 2012.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. American customer satisfaction index 2013 customer satisfaction outpatient survey. http://www.va.gov/health/docs/VA2013OutpatientACSI.pdf. Published March 2014. Accessed August 10, 2016.
9. U.S. Department of Veterans Affairs. VHA pain management, Opioid Safety Initiative (OSI). http://www.va.gov/PAINMANAGEMENT/Opioid_Safety_Initiative_OSI.asp. Updated June 17, 2015. Accessed August 4, 2016.
10. U.S. Department of Veterans Affairs. Office of Research and Development. http://www.research.va.gov. Updated July 21, 2016. Accessed August 4, 2016.
1. U.S. Department of Veterans Affairs, Office of Suicide Prevention. Suicide Among Veterans and Other Americans 2001-2014. http://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Published August 3, 2016. Accessed August 10, 2016.
2. Longman P, Gordon S. A conversation about the commission on care and the future of the VA. Washington Monthly. http://washingtonmonthly.com/2016/07/14/a-conversation-about-the-commission-on-care-and-the-future-of-the-va/. Published July 14, 2016. Accessed August 4, 2016.
3. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the Veterans Health Administration. Burnout Research. 2015;2(4):108-114.
4. U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and dental education program. http://www.va.gov/oaa/GME_default.asp. Updated December 9, 2015. Accessed August 4, 2016.
5. Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906.
6. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396.
7. Longman P. Best Care Anywhere: Why VA Health Care Would Work Better for Everyone. 3rd ed. San Francisco, CA: Berrett-Koehler; 2012.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. American customer satisfaction index 2013 customer satisfaction outpatient survey. http://www.va.gov/health/docs/VA2013OutpatientACSI.pdf. Published March 2014. Accessed August 10, 2016.
9. U.S. Department of Veterans Affairs. VHA pain management, Opioid Safety Initiative (OSI). http://www.va.gov/PAINMANAGEMENT/Opioid_Safety_Initiative_OSI.asp. Updated June 17, 2015. Accessed August 4, 2016.
10. U.S. Department of Veterans Affairs. Office of Research and Development. http://www.research.va.gov. Updated July 21, 2016. Accessed August 4, 2016.
What’s Hot in Our National Organizations: A Follow-Up
In “What’s Hot and What’s Not in Our National Organizations, An Emergency Medicine Panel, Parts 1 and 2” (Emergency Medicine, April 2016 and May 2016, respectively), we published highlights from a panel discussion that took place at the annual retreat of the Association of Academic Chairs in Emergency Medicine in Tempe, Arizona in February 2016. That discussion included seven EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Residency Directors in Emergency Medicine (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM). In this issue, we follow up with reports from the American College of Osteopathic Emergency Physicians (ACOEP) and the American Osteopathic Board of Emergency Medicine (AOBEM).
American College of Osteopathic Emergency Physicians
John C. Prestosh, DO, FACOEP-DPresident, ACOEP
Strategic Planning. The Board of Directors of ACOEP has recently adopted a revised mission statement and goals for the organization. The ACOEP “promotes patient-centric, holistic emergency care consistent with the osteopathic philosophy practiced by all emergency medicine professionals.” This statement is based on the belief that many non-osteopathic professionals practice aspects of holistic medicine, and will allow ACOEP to be a “home” for these practitioners. ACOEP’s goals are member engagement and value, advocacy and involvement, education and knowledge, improving awareness, and college strength and sustainability.
Workplace Issues. The ACOEP is aware of the issues emergency physicians (EPs) and professionals face every day. Therefore, we are including items for EPs on these issues in our educational programs. Upcoming events will include workshops on dealing with an active shooter scenario, ultrasound, and advanced airway management, which will be included in our Scientific Assembly in November.
The ACOEP is also a member of the White House Task Force addressing the opioid epidemic. Realizing there are times when opiates are necessary adjuncts to patient care, we also want to help educate physicians on the usage of alternative pain-relieving treatment plans when indicated.
Single Accreditation System and College Sustainability. Graduate medical education is undergoing an unprecedented change. The Single Accreditation System is currently being implemented with a target date of July 1, 2020 for all residency programs to fall under the jurisdiction of the Accreditation Council for Graduate Medical Education (ACGME) for accreditation. There is much anticipation regarding the changes that will occur.
We anticipate some American Osteopathic Association-accredited EM programs will become 3-year programs, thus precluding graduating residents from AOBEM certification. However, we expect a number of ACGME-accredited EM programs to establish “osteopathic-focused” tracks in which both DOs and MDs will learn osteopathic tenets and procedures to broaden their practice of EM. We anticipate this will allow residents to be certified by the AOBEM.
We believe the ACOEP can be a “home” for MD residents graduating from “osteopathic-focused” ACGME programs. Furthermore, the ACOEP is ready to amend its bylaws to offer active membership with full voting rights to MDs. We do not want to remain a closed organization, but are striving to have both DO and MD EPs belong to our College.
American Osteopathic Board of Emergency Medicine
Donald Phillips, DO, FACOEP-D, Executive Physician Director, AOBEM
Primary Certification News. The date for the 2017 Part I Examination (written examination) has been published. All candidates are advised that the examination has been moved from March to September beginning in 2017. Applications for Part I will be available on January 2, 2017. The deadline to submit the application is April 1, 2017. The examination will be administered at Prometric Testing Centers nationwide on September 12, 2017. Part II Examinations (oral examinations) are in March and November. Please refer to the AOBEM Web page at www.aobem.org for dates.
Subspecialty Certifications. AOBEM offers subspecialty certification opportunities to its diplomates in the following areas:
- Emergency medical services
- Hospice and palliative medicine
- Medical toxicology
- Sports medicine
- Undersea and hyperbaric medicine
- Internal medicine critical care
- Surgical critical care.
AOBEM and the American Osteopathic Board of Pediatrics are also engaged in the development of a pediatric EM subspecialty examination.
Osteopathic Continuous Certification (OCC). AOBEM continues to refine and evolve the OCC process. The Board has received approval to begin allowing group data for the Practice Performance Assessment portion of OCC. Diplomates may submit group data provided at least 30% of the charts reviewed are patients that the diplomate cared for personally. Diplomates may also submit unique projects that are not on the list of “preapproved” projects. It is recognized that many of our diplomates are involved in very advanced care systems. Many times, these systems have useful projects that will meet criteria for this component. If you wish to submit data for a unique project, they will be welcomed, but the Board asks that you contact us to have them approved before beginning the project.
Continuous Osteopathic Learning Assessments (COLAs) are a vital component. They demonstrate the diplomate is maintaining currency across the entire specialty of EM. We invite diplomates and candidates to submit journal articles they feel are significant to a topic for potential inclusion in the official list of COLA articles.
Candidates and diplomates are advised to keep apprised of important dates and announcements via the AOBEM Web page at www.aobem.org.
In “What’s Hot and What’s Not in Our National Organizations, An Emergency Medicine Panel, Parts 1 and 2” (Emergency Medicine, April 2016 and May 2016, respectively), we published highlights from a panel discussion that took place at the annual retreat of the Association of Academic Chairs in Emergency Medicine in Tempe, Arizona in February 2016. That discussion included seven EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Residency Directors in Emergency Medicine (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM). In this issue, we follow up with reports from the American College of Osteopathic Emergency Physicians (ACOEP) and the American Osteopathic Board of Emergency Medicine (AOBEM).
American College of Osteopathic Emergency Physicians
John C. Prestosh, DO, FACOEP-DPresident, ACOEP
Strategic Planning. The Board of Directors of ACOEP has recently adopted a revised mission statement and goals for the organization. The ACOEP “promotes patient-centric, holistic emergency care consistent with the osteopathic philosophy practiced by all emergency medicine professionals.” This statement is based on the belief that many non-osteopathic professionals practice aspects of holistic medicine, and will allow ACOEP to be a “home” for these practitioners. ACOEP’s goals are member engagement and value, advocacy and involvement, education and knowledge, improving awareness, and college strength and sustainability.
Workplace Issues. The ACOEP is aware of the issues emergency physicians (EPs) and professionals face every day. Therefore, we are including items for EPs on these issues in our educational programs. Upcoming events will include workshops on dealing with an active shooter scenario, ultrasound, and advanced airway management, which will be included in our Scientific Assembly in November.
The ACOEP is also a member of the White House Task Force addressing the opioid epidemic. Realizing there are times when opiates are necessary adjuncts to patient care, we also want to help educate physicians on the usage of alternative pain-relieving treatment plans when indicated.
Single Accreditation System and College Sustainability. Graduate medical education is undergoing an unprecedented change. The Single Accreditation System is currently being implemented with a target date of July 1, 2020 for all residency programs to fall under the jurisdiction of the Accreditation Council for Graduate Medical Education (ACGME) for accreditation. There is much anticipation regarding the changes that will occur.
We anticipate some American Osteopathic Association-accredited EM programs will become 3-year programs, thus precluding graduating residents from AOBEM certification. However, we expect a number of ACGME-accredited EM programs to establish “osteopathic-focused” tracks in which both DOs and MDs will learn osteopathic tenets and procedures to broaden their practice of EM. We anticipate this will allow residents to be certified by the AOBEM.
We believe the ACOEP can be a “home” for MD residents graduating from “osteopathic-focused” ACGME programs. Furthermore, the ACOEP is ready to amend its bylaws to offer active membership with full voting rights to MDs. We do not want to remain a closed organization, but are striving to have both DO and MD EPs belong to our College.
American Osteopathic Board of Emergency Medicine
Donald Phillips, DO, FACOEP-D, Executive Physician Director, AOBEM
Primary Certification News. The date for the 2017 Part I Examination (written examination) has been published. All candidates are advised that the examination has been moved from March to September beginning in 2017. Applications for Part I will be available on January 2, 2017. The deadline to submit the application is April 1, 2017. The examination will be administered at Prometric Testing Centers nationwide on September 12, 2017. Part II Examinations (oral examinations) are in March and November. Please refer to the AOBEM Web page at www.aobem.org for dates.
Subspecialty Certifications. AOBEM offers subspecialty certification opportunities to its diplomates in the following areas:
- Emergency medical services
- Hospice and palliative medicine
- Medical toxicology
- Sports medicine
- Undersea and hyperbaric medicine
- Internal medicine critical care
- Surgical critical care.
AOBEM and the American Osteopathic Board of Pediatrics are also engaged in the development of a pediatric EM subspecialty examination.
Osteopathic Continuous Certification (OCC). AOBEM continues to refine and evolve the OCC process. The Board has received approval to begin allowing group data for the Practice Performance Assessment portion of OCC. Diplomates may submit group data provided at least 30% of the charts reviewed are patients that the diplomate cared for personally. Diplomates may also submit unique projects that are not on the list of “preapproved” projects. It is recognized that many of our diplomates are involved in very advanced care systems. Many times, these systems have useful projects that will meet criteria for this component. If you wish to submit data for a unique project, they will be welcomed, but the Board asks that you contact us to have them approved before beginning the project.
Continuous Osteopathic Learning Assessments (COLAs) are a vital component. They demonstrate the diplomate is maintaining currency across the entire specialty of EM. We invite diplomates and candidates to submit journal articles they feel are significant to a topic for potential inclusion in the official list of COLA articles.
Candidates and diplomates are advised to keep apprised of important dates and announcements via the AOBEM Web page at www.aobem.org.
In “What’s Hot and What’s Not in Our National Organizations, An Emergency Medicine Panel, Parts 1 and 2” (Emergency Medicine, April 2016 and May 2016, respectively), we published highlights from a panel discussion that took place at the annual retreat of the Association of Academic Chairs in Emergency Medicine in Tempe, Arizona in February 2016. That discussion included seven EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Residency Directors in Emergency Medicine (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM). In this issue, we follow up with reports from the American College of Osteopathic Emergency Physicians (ACOEP) and the American Osteopathic Board of Emergency Medicine (AOBEM).
American College of Osteopathic Emergency Physicians
John C. Prestosh, DO, FACOEP-DPresident, ACOEP
Strategic Planning. The Board of Directors of ACOEP has recently adopted a revised mission statement and goals for the organization. The ACOEP “promotes patient-centric, holistic emergency care consistent with the osteopathic philosophy practiced by all emergency medicine professionals.” This statement is based on the belief that many non-osteopathic professionals practice aspects of holistic medicine, and will allow ACOEP to be a “home” for these practitioners. ACOEP’s goals are member engagement and value, advocacy and involvement, education and knowledge, improving awareness, and college strength and sustainability.
Workplace Issues. The ACOEP is aware of the issues emergency physicians (EPs) and professionals face every day. Therefore, we are including items for EPs on these issues in our educational programs. Upcoming events will include workshops on dealing with an active shooter scenario, ultrasound, and advanced airway management, which will be included in our Scientific Assembly in November.
The ACOEP is also a member of the White House Task Force addressing the opioid epidemic. Realizing there are times when opiates are necessary adjuncts to patient care, we also want to help educate physicians on the usage of alternative pain-relieving treatment plans when indicated.
Single Accreditation System and College Sustainability. Graduate medical education is undergoing an unprecedented change. The Single Accreditation System is currently being implemented with a target date of July 1, 2020 for all residency programs to fall under the jurisdiction of the Accreditation Council for Graduate Medical Education (ACGME) for accreditation. There is much anticipation regarding the changes that will occur.
We anticipate some American Osteopathic Association-accredited EM programs will become 3-year programs, thus precluding graduating residents from AOBEM certification. However, we expect a number of ACGME-accredited EM programs to establish “osteopathic-focused” tracks in which both DOs and MDs will learn osteopathic tenets and procedures to broaden their practice of EM. We anticipate this will allow residents to be certified by the AOBEM.
We believe the ACOEP can be a “home” for MD residents graduating from “osteopathic-focused” ACGME programs. Furthermore, the ACOEP is ready to amend its bylaws to offer active membership with full voting rights to MDs. We do not want to remain a closed organization, but are striving to have both DO and MD EPs belong to our College.
American Osteopathic Board of Emergency Medicine
Donald Phillips, DO, FACOEP-D, Executive Physician Director, AOBEM
Primary Certification News. The date for the 2017 Part I Examination (written examination) has been published. All candidates are advised that the examination has been moved from March to September beginning in 2017. Applications for Part I will be available on January 2, 2017. The deadline to submit the application is April 1, 2017. The examination will be administered at Prometric Testing Centers nationwide on September 12, 2017. Part II Examinations (oral examinations) are in March and November. Please refer to the AOBEM Web page at www.aobem.org for dates.
Subspecialty Certifications. AOBEM offers subspecialty certification opportunities to its diplomates in the following areas:
- Emergency medical services
- Hospice and palliative medicine
- Medical toxicology
- Sports medicine
- Undersea and hyperbaric medicine
- Internal medicine critical care
- Surgical critical care.
AOBEM and the American Osteopathic Board of Pediatrics are also engaged in the development of a pediatric EM subspecialty examination.
Osteopathic Continuous Certification (OCC). AOBEM continues to refine and evolve the OCC process. The Board has received approval to begin allowing group data for the Practice Performance Assessment portion of OCC. Diplomates may submit group data provided at least 30% of the charts reviewed are patients that the diplomate cared for personally. Diplomates may also submit unique projects that are not on the list of “preapproved” projects. It is recognized that many of our diplomates are involved in very advanced care systems. Many times, these systems have useful projects that will meet criteria for this component. If you wish to submit data for a unique project, they will be welcomed, but the Board asks that you contact us to have them approved before beginning the project.
Continuous Osteopathic Learning Assessments (COLAs) are a vital component. They demonstrate the diplomate is maintaining currency across the entire specialty of EM. We invite diplomates and candidates to submit journal articles they feel are significant to a topic for potential inclusion in the official list of COLA articles.
Candidates and diplomates are advised to keep apprised of important dates and announcements via the AOBEM Web page at www.aobem.org.
No more popping, swatting, slapping, and spanking
During a recent primary care rotation in northeast Philadelphia, I was privileged to witness a community experience on a daily basis. Each morning I took the elevated subway to the end of the line out of the city, and transferred to a bus to get to the office. The 24 bus at 8:30 a.m. has the same faces every day, making their way to work at various stops along the route. There was also a mother of a particularly cute set of twin boys. Every day she also got on the “El” and transferred to the bus with me, in order to get her boys to the day care she also went to as a child, where she told me she trusted her kids so much it was worth the daily trip.
On my last day of the rotation, enjoying the familiar scene again of people saying good morning to each other on the 24, everyone’s pleasant morning was suddenly interrupted. The twins were being particularly annoying to their mother that day, and she began disciplining them. The entire bus witnessed this: a mother “popping” her boys on the arms repeatedly while yelling loudly, “No hitting! You don’t hit each other and you don’t hit mommy!”
As a pediatrician, this was hard to watch. “Popping” is a common practice here in Philadelphia, and it involves a quick but loud slap that leaves no mark and I assume only stings a second or two, and thus is not too physically harmful. I chose not to speak up as they are not my patients, and it was not my place to be confrontational at that moment. But the thought that went through my head immediately was, “How can this caring and well-intentioned mother expect her sons to learn the lesson to not hit while she is doing exactly that?”
Get online and you’ll see plenty of bloggers arguing the topic of popping, swatting, slapping, and spanking. People say, “My generation was spanked and we turned out fine!” or “It toughens kids up and teaches them discipline.” But the main problem here is the mixed message. The old adage, “Do as I say and not as I do,” simply does not work in childhood. The young developing brain of a child can’t make that distinction, and learning by example from their most loved ones on this planet – their parents – is the single most influential factor in their education.
Just because something is common does not make it right. A few short decades ago seat belts were not commonly worn, and we all know of their benefits now. Currently in America, obesity is becoming the normal body shape for adults and children alike, and every physician is trying their best to combat it. Popping, swatting, slapping, and spanking, in this pediatric resident’s opinion, is far too common, and if explained to parents why the practice is counter-intuitive and ineffectual, I do hope it can be a thing of the past some day, too.
Dr. Beardmore is a pediatric resident at Albert Einstein Medical Center and St. Christopher’s Hospital for Children, Philadelphia. Email him at [email protected].
During a recent primary care rotation in northeast Philadelphia, I was privileged to witness a community experience on a daily basis. Each morning I took the elevated subway to the end of the line out of the city, and transferred to a bus to get to the office. The 24 bus at 8:30 a.m. has the same faces every day, making their way to work at various stops along the route. There was also a mother of a particularly cute set of twin boys. Every day she also got on the “El” and transferred to the bus with me, in order to get her boys to the day care she also went to as a child, where she told me she trusted her kids so much it was worth the daily trip.
On my last day of the rotation, enjoying the familiar scene again of people saying good morning to each other on the 24, everyone’s pleasant morning was suddenly interrupted. The twins were being particularly annoying to their mother that day, and she began disciplining them. The entire bus witnessed this: a mother “popping” her boys on the arms repeatedly while yelling loudly, “No hitting! You don’t hit each other and you don’t hit mommy!”
As a pediatrician, this was hard to watch. “Popping” is a common practice here in Philadelphia, and it involves a quick but loud slap that leaves no mark and I assume only stings a second or two, and thus is not too physically harmful. I chose not to speak up as they are not my patients, and it was not my place to be confrontational at that moment. But the thought that went through my head immediately was, “How can this caring and well-intentioned mother expect her sons to learn the lesson to not hit while she is doing exactly that?”
Get online and you’ll see plenty of bloggers arguing the topic of popping, swatting, slapping, and spanking. People say, “My generation was spanked and we turned out fine!” or “It toughens kids up and teaches them discipline.” But the main problem here is the mixed message. The old adage, “Do as I say and not as I do,” simply does not work in childhood. The young developing brain of a child can’t make that distinction, and learning by example from their most loved ones on this planet – their parents – is the single most influential factor in their education.
Just because something is common does not make it right. A few short decades ago seat belts were not commonly worn, and we all know of their benefits now. Currently in America, obesity is becoming the normal body shape for adults and children alike, and every physician is trying their best to combat it. Popping, swatting, slapping, and spanking, in this pediatric resident’s opinion, is far too common, and if explained to parents why the practice is counter-intuitive and ineffectual, I do hope it can be a thing of the past some day, too.
Dr. Beardmore is a pediatric resident at Albert Einstein Medical Center and St. Christopher’s Hospital for Children, Philadelphia. Email him at [email protected].
During a recent primary care rotation in northeast Philadelphia, I was privileged to witness a community experience on a daily basis. Each morning I took the elevated subway to the end of the line out of the city, and transferred to a bus to get to the office. The 24 bus at 8:30 a.m. has the same faces every day, making their way to work at various stops along the route. There was also a mother of a particularly cute set of twin boys. Every day she also got on the “El” and transferred to the bus with me, in order to get her boys to the day care she also went to as a child, where she told me she trusted her kids so much it was worth the daily trip.
On my last day of the rotation, enjoying the familiar scene again of people saying good morning to each other on the 24, everyone’s pleasant morning was suddenly interrupted. The twins were being particularly annoying to their mother that day, and she began disciplining them. The entire bus witnessed this: a mother “popping” her boys on the arms repeatedly while yelling loudly, “No hitting! You don’t hit each other and you don’t hit mommy!”
As a pediatrician, this was hard to watch. “Popping” is a common practice here in Philadelphia, and it involves a quick but loud slap that leaves no mark and I assume only stings a second or two, and thus is not too physically harmful. I chose not to speak up as they are not my patients, and it was not my place to be confrontational at that moment. But the thought that went through my head immediately was, “How can this caring and well-intentioned mother expect her sons to learn the lesson to not hit while she is doing exactly that?”
Get online and you’ll see plenty of bloggers arguing the topic of popping, swatting, slapping, and spanking. People say, “My generation was spanked and we turned out fine!” or “It toughens kids up and teaches them discipline.” But the main problem here is the mixed message. The old adage, “Do as I say and not as I do,” simply does not work in childhood. The young developing brain of a child can’t make that distinction, and learning by example from their most loved ones on this planet – their parents – is the single most influential factor in their education.
Just because something is common does not make it right. A few short decades ago seat belts were not commonly worn, and we all know of their benefits now. Currently in America, obesity is becoming the normal body shape for adults and children alike, and every physician is trying their best to combat it. Popping, swatting, slapping, and spanking, in this pediatric resident’s opinion, is far too common, and if explained to parents why the practice is counter-intuitive and ineffectual, I do hope it can be a thing of the past some day, too.
Dr. Beardmore is a pediatric resident at Albert Einstein Medical Center and St. Christopher’s Hospital for Children, Philadelphia. Email him at [email protected].
The ED Is a Safer Place…and Can Be Safer Still
Improving medication accuracy, transitions of care, health information technology, and other ED patient-safety strategies are offered in this month’s Emergency Medicine cover article, “Patient Safety in the Emergency Department,” by emergency physician (EP)/toxicologist Brenna M. Farmer, MD, a colleague for many years.
As Dr Farmer notes in her introduction, patient safety—in the ED and elsewhere—has received a great deal of attention since the publication of the two landmark Institute of Medicine (IOM) studies in 1999 and 2001 that documented an enormous number of medical errors and recommended improvements in medical care. More than a decade and a half after their publication, is there any evidence that these reports have led to a reduction in the number of serious adverse effects and deaths due to medical errors?
Although most EPs believe that ED safety measures have reduced the overall number of errors, there is a scarcity of published data demonstrating a direct cause-and-effect relationship in reducing the number of adverse events and deaths. A recent analysis of National Hospital Ambulatory Medical Care Survey data by EPs Kanzaria, Probst, and Hsia (Health Aff [Millwood]. 2016;35[7]:1303-1308) found that ED death rates dropped by nearly 50% between 1997 and 2011. Most of this reporting period includes the years following the IOM reports before the implementation of the Affordable Care Act measures. One might reasonably assume that the decrease in ED death rates since 1997 is at least partly due to the safety measures described by Dr Farmer. However, Kanzaria et al hypothesize that the reduction is probably due to palliative and prehospital care efforts which “shift the locus of deaths,” to recent advances in emergency critical care, and to public health successes in smoking cessation, motor vehicle safety, etc. Conspicuously absent from their list of possible measures responsible for the reduction in ED death rates are ED safety measures.
If Kanzaria et al are correct in attributing the reduction in ED deaths to measures taken by others to decrease the number of dying patients brought to EDs, then it may be reasonable to look for the benefit of eliminating serious ED errors to a decrease in death rates after patients leave the ED for inpatient services. Though inpatient death-rate data is available only since 2005, Kanzaria et al report no significant change in the inpatient death rate between 2005 and 2011. It is possible, however, that the improvements in ED critical care hypothesized by the authors to be partly responsible for reducing ED death rates enable sicker patients to survive longer and ultimately succumb to their serious illnesses as inpatients. If so, this could offset any evident reduction in inpatient mortality from the avoidance of serious errors in the ED.
In any case, Dr Farmer does present direct evidence that safety measures are effective in reducing morbidity, and probably mortality. For example, in one study cited, medication errors were 13.5 times less likely to occur when an ED pharmacist was present, and clearly, avoiding doubling the doses of potent cardiac medications or sedative hypnotics, avoiding dangerous drug interactions, and choosing the correct type, dose, and time of administration of antibiotics and all meds must be responsible for reducing morbidity and ultimately mortality. It is also worth recalling that with respect to patient safety, emergency medicine is undoubtedly the safest medical specialty ever created, pioneering from its inception 24/7 bedside attending presence and mandatory recertifications, years to decades before other specialties adopted these practices. Thanks to these efforts, EDs are much safer than they had been previously, and by implementing the measures described by Dr Farmer will be safer still.
Improving medication accuracy, transitions of care, health information technology, and other ED patient-safety strategies are offered in this month’s Emergency Medicine cover article, “Patient Safety in the Emergency Department,” by emergency physician (EP)/toxicologist Brenna M. Farmer, MD, a colleague for many years.
As Dr Farmer notes in her introduction, patient safety—in the ED and elsewhere—has received a great deal of attention since the publication of the two landmark Institute of Medicine (IOM) studies in 1999 and 2001 that documented an enormous number of medical errors and recommended improvements in medical care. More than a decade and a half after their publication, is there any evidence that these reports have led to a reduction in the number of serious adverse effects and deaths due to medical errors?
Although most EPs believe that ED safety measures have reduced the overall number of errors, there is a scarcity of published data demonstrating a direct cause-and-effect relationship in reducing the number of adverse events and deaths. A recent analysis of National Hospital Ambulatory Medical Care Survey data by EPs Kanzaria, Probst, and Hsia (Health Aff [Millwood]. 2016;35[7]:1303-1308) found that ED death rates dropped by nearly 50% between 1997 and 2011. Most of this reporting period includes the years following the IOM reports before the implementation of the Affordable Care Act measures. One might reasonably assume that the decrease in ED death rates since 1997 is at least partly due to the safety measures described by Dr Farmer. However, Kanzaria et al hypothesize that the reduction is probably due to palliative and prehospital care efforts which “shift the locus of deaths,” to recent advances in emergency critical care, and to public health successes in smoking cessation, motor vehicle safety, etc. Conspicuously absent from their list of possible measures responsible for the reduction in ED death rates are ED safety measures.
If Kanzaria et al are correct in attributing the reduction in ED deaths to measures taken by others to decrease the number of dying patients brought to EDs, then it may be reasonable to look for the benefit of eliminating serious ED errors to a decrease in death rates after patients leave the ED for inpatient services. Though inpatient death-rate data is available only since 2005, Kanzaria et al report no significant change in the inpatient death rate between 2005 and 2011. It is possible, however, that the improvements in ED critical care hypothesized by the authors to be partly responsible for reducing ED death rates enable sicker patients to survive longer and ultimately succumb to their serious illnesses as inpatients. If so, this could offset any evident reduction in inpatient mortality from the avoidance of serious errors in the ED.
In any case, Dr Farmer does present direct evidence that safety measures are effective in reducing morbidity, and probably mortality. For example, in one study cited, medication errors were 13.5 times less likely to occur when an ED pharmacist was present, and clearly, avoiding doubling the doses of potent cardiac medications or sedative hypnotics, avoiding dangerous drug interactions, and choosing the correct type, dose, and time of administration of antibiotics and all meds must be responsible for reducing morbidity and ultimately mortality. It is also worth recalling that with respect to patient safety, emergency medicine is undoubtedly the safest medical specialty ever created, pioneering from its inception 24/7 bedside attending presence and mandatory recertifications, years to decades before other specialties adopted these practices. Thanks to these efforts, EDs are much safer than they had been previously, and by implementing the measures described by Dr Farmer will be safer still.
Improving medication accuracy, transitions of care, health information technology, and other ED patient-safety strategies are offered in this month’s Emergency Medicine cover article, “Patient Safety in the Emergency Department,” by emergency physician (EP)/toxicologist Brenna M. Farmer, MD, a colleague for many years.
As Dr Farmer notes in her introduction, patient safety—in the ED and elsewhere—has received a great deal of attention since the publication of the two landmark Institute of Medicine (IOM) studies in 1999 and 2001 that documented an enormous number of medical errors and recommended improvements in medical care. More than a decade and a half after their publication, is there any evidence that these reports have led to a reduction in the number of serious adverse effects and deaths due to medical errors?
Although most EPs believe that ED safety measures have reduced the overall number of errors, there is a scarcity of published data demonstrating a direct cause-and-effect relationship in reducing the number of adverse events and deaths. A recent analysis of National Hospital Ambulatory Medical Care Survey data by EPs Kanzaria, Probst, and Hsia (Health Aff [Millwood]. 2016;35[7]:1303-1308) found that ED death rates dropped by nearly 50% between 1997 and 2011. Most of this reporting period includes the years following the IOM reports before the implementation of the Affordable Care Act measures. One might reasonably assume that the decrease in ED death rates since 1997 is at least partly due to the safety measures described by Dr Farmer. However, Kanzaria et al hypothesize that the reduction is probably due to palliative and prehospital care efforts which “shift the locus of deaths,” to recent advances in emergency critical care, and to public health successes in smoking cessation, motor vehicle safety, etc. Conspicuously absent from their list of possible measures responsible for the reduction in ED death rates are ED safety measures.
If Kanzaria et al are correct in attributing the reduction in ED deaths to measures taken by others to decrease the number of dying patients brought to EDs, then it may be reasonable to look for the benefit of eliminating serious ED errors to a decrease in death rates after patients leave the ED for inpatient services. Though inpatient death-rate data is available only since 2005, Kanzaria et al report no significant change in the inpatient death rate between 2005 and 2011. It is possible, however, that the improvements in ED critical care hypothesized by the authors to be partly responsible for reducing ED death rates enable sicker patients to survive longer and ultimately succumb to their serious illnesses as inpatients. If so, this could offset any evident reduction in inpatient mortality from the avoidance of serious errors in the ED.
In any case, Dr Farmer does present direct evidence that safety measures are effective in reducing morbidity, and probably mortality. For example, in one study cited, medication errors were 13.5 times less likely to occur when an ED pharmacist was present, and clearly, avoiding doubling the doses of potent cardiac medications or sedative hypnotics, avoiding dangerous drug interactions, and choosing the correct type, dose, and time of administration of antibiotics and all meds must be responsible for reducing morbidity and ultimately mortality. It is also worth recalling that with respect to patient safety, emergency medicine is undoubtedly the safest medical specialty ever created, pioneering from its inception 24/7 bedside attending presence and mandatory recertifications, years to decades before other specialties adopted these practices. Thanks to these efforts, EDs are much safer than they had been previously, and by implementing the measures described by Dr Farmer will be safer still.
The new NOACs are generally the best bet
New NOACs have largely replaced the need for vitamin K antagonists
The discovery of oral anticoagulants began in 1924, when Schofield linked the death of grazing cattle from internal hemorrhage to the consumption of spoiled sweet clover hay.1 It was not until 1941, however, while trying to understand this observation that Campbell and Link were able to identify the dicoumarol anticoagulant, which formed as a result of the spoiling process.2 Ultimately, after noting that vitamin K led to reversal of the dicoumarol effect, synthesis of the first class of oral anticoagulants, known as vitamin K antagonists (VKAs) began. Despite the numerous challenges associated with managing patients using this class of anticoagulants, VKAs have become the mainstay of oral anticoagulation therapy for the past 70 years. Over the past 5 years, however, new oral anticoagulants (NOACs) have emerged and are changing clinical practice. Mechanistically, these medications are targeted therapies and work as either direct thrombin inhibitors (dabigatran etexilate) or direct factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban). Given their favorable pharmacologic design, NOACs have the potential to replace VKAs as they not only have an encouraging safety profile, but also are therapeutically equivalent or even superior to VKAs when used in certain patient populations.
Pharmacologic design
The targeted drug design of NOACs provides many pharmacologic advantages. Compared with VKAs, NOACs have a notably more predictable pharmacologic profile and relatively wide therapeutic window, which allows for fixed dosing, a rapid onset and offset, and fewer drug interactions.3 These characteristics eliminate the need for the routine dose monitoring and serial dose adjustments frequently associated with VKAs. Additionally, NOACs less commonly require bridging therapy with parenteral unfractionated heparin or low molecular weight heparins (LMWH) while awaiting therapeutic drug levels, as these levels are reached sooner and more predictably than with VKAs.4 As with any medication, however, appropriate consideration should to be given to specific patient populations such as those who are older or have significant comorbidities which may influence drug effect and clearance.
Lastly, it should be mentioned that the pharmacologic benefits of NOACs are not only beneficial from a patient perspective, but also from a health care systems standpoint as their use may provide an opportunity to deliver more cost-effective care. Specifically, economic models using available clinical trial data for stroke prevention in nonvalvular atrial fibrillation have shown that NOACs (apixaban, dabigatran, and rivaroxaban) are cost-effective alternatives when compared with warfarin.5 Although the results from such economic analyses are limited by the modeling assumptions they rely upon, these findings suggest that, at least initially, cost should not be used as a prohibitive reason for adopting these new therapeutics.
Patient selection
The decision to institute oral anticoagulation therapy depends on each patient’s individualized bleeding risk to benefit of ischemia prevention ratio. A major determinant of this ratio is the clinical indication for which anticoagulation is begun. Numerous phase III clinical trials have been conducted comparing the use of NOACs versus VKAs or placebos for the management of nonvalvular atrial fibrillation (AF), venous thromboembolism (VTE), and as adjunctive therapy for patients with acute coronary syndrome.6 Meta-analyses of randomized trials have shown the most significant benefit to be in patients with nonvalvular atrial fibrillation where NOACs have significant reductions in stroke, intracranial hemorrhage, and all-cause mortality, compared with warfarin while displaying variable effects with regards to gastrointestinal bleeding.6,7
In patients with VTE, NOACs have been found to have similar efficacy, compared with VKAs, with regard to the prevention of VTE or VTE-related death, and have been noted to have a better safety profile.6 Lastly, when studied as an adjunctive agent to dual antiplatelet therapy in patients with acute coronary syndrome, it should be noted that NOACs have been associated with an increased bleeding risk without a significant decrease in thrombosis risk.6 Taken together, these data suggest that the primary indication for instituting NOAC therapy should be considered strongly when deciding upon the class of anticoagulant to use.
Overcoming challenges
Since the introduction of NOACs, there has been concern over the lack of specific antidotes to therapy, especially when administered in patients with impaired clearance, a high likelihood of need for an urgent or emergent procedure, or those presenting with life-threatening bleeding complications. Most recently, however, interim analysis from clinical trial data has shown complete reversal of the direct thrombin inhibitor dabigatran with the humanized monocolonal antibody idarucizumab within minutes of administration in greater than 88% of patients studied.8 Similarly, agents such as a PER977 are currently in phase II clinical trials as they have been shown to form noncovalent hydrogen bonds and charge-charge interactions with oral factor Xa inhibitors as well as oral thrombin inhibitors leading to their reversal.9 Given these promising findings, it likely will not be long until reversal agents for NOACs become clinically available. Until that time, it is encouraging that the bleeding profile of these drugs has been found to be favorable, compared with VKAs, and their short half-life allows for a relatively expeditious natural reversal of their anticoagulant effect as the drug is eliminated.
Conclusions
Unlike the serendipitous path leading to the discovery of the first class of oral anticoagulants (VKAs), NOACs have been specifically designed to provide targeted anticoagulation and to address the shortcomings of VKAs. To this end, NOACs are becoming increasingly important in the management of patients with specific clinical conditions such as nonvalvular atrial fibrillation and venous thromboembolism where they have been shown to provide a larger net clinical benefit relative to the available alternatives. Furthermore, with economic analyses providing evidence that NOACs are cost-effective for the health care system and clinical trial results suggesting progress in the development of antidotes for reversal, it is likely that with growing experience, these agents will replace VKAs as the mainstay for prophylactic and therapeutic oral anticoagulation in targeted patient populations.
Madhukar S. Patel, MD, and Elliot L. Chaikof, MD, are from the department of surgery, Beth Israel Deaconess Medical Center, Boston. They reported having no conflicts of interest.
References
1. J Am Vet Med Assoc 1924;64:553-575
3. Hematology Am Soc Hematol Educ Program 2013;2013:464-470
4. Eur Heart J 2013;34:2094-2106
6. Nat Rev Cardiol 2014;11:693-703
8. N Engl J Med 2015;373:511-520
9. N Engl J Med 2014;371:2141-2142
What the doctor didn’t order: unintended consequences and pitfalls of NOACs
Recently, several new oral anticoagulants (NOACs) have gained FDA approval to replace warfarin, capturing the attention of popular media. These include dabigatran, rivaroxaban, apixaban, and edoxaban. Dabigatran targets activated factor II (factor IIa), while rivaroxaban, apixaban, and edoxaban target activated factor X (factor Xa). Easy to take with a once or twice daily pill, with no cumbersome monitoring, they represent a seemingly ideal treatment for the chronically anticoagulated patient. All agents are currently FDA approved in the United States for treatment of acute VTE and AF.
Dabigatran and edoxaban
Similar to warfarin, dabigatran and edoxaban require the use of a LMWH or UFH “bridge” when therapy is beginning, while rivaroxaban and apixaban are instituted as monotherapy without such a bridge. Dabigatran etexilate (PradaxaR, Boehringer Ingelheim) has the longest half-life of all of the NOACs at 12-17 hours, and this half-life is prolonged with increasing age and decreasing renal function.1 It is the only new agent which can be at least partially reversed with dialysis.2 Edoxaban (SavaysaR, Daiichi Sankyo) carries a boxed warning stating that this agent is less effective in AF patients with a creatinine clearance greater than 95 mL/min, and that kidney function should be assessed prior to starting treatment: Such patients have a greater risk of stroke, compared with similar patients treated with warfarin. Edoxaban is the only agent specifically tested at a lower dose in patients at significantly increased risk of bleeding complications (low body weight and/or decreased creatinine clearance).3
Rivaroxaban and apixaban
Rivaroxaban (XareltoR, Bayer and Janssen), and apixaban (EliquisR, Bristol Myers-Squibb), unique amongst the NOACs, have been tested for extended therapy of acute deep vein thrombosis after treatment of 6-12 months. They were found to result in a significant decrease in recurrent VTE without an increase in major bleeding, compared with placebo.4,5 Rivaroxaban has once-daily dosing and apixaban has twice-daily dosing; both are immediate monotherapy, making them quite convenient for patients. Apixaban is the only agent among the NOACs to have a slight decrease in gastrointestinal bleeding, compared with warfarin.6
Consequences and pitfalls with NOACs
Problems with these new drugs, which may diminish our current level of enthusiasm for these agents to totally replace warfarin, include the inability to reliably follow their levels or reverse their anticoagulant effects, the lack of data available on bridging when other procedures need to be performed, their short half-lives, and the lack of data on their anti-inflammatory effects. With regard to monitoring of anticoagulation, the International Society of Thrombosis and Hemostasis (ISTH) has published the times when it might be useful to obtain levels. These times include:
• When a patient is bleeding.
• Before surgery or an invasive procedure when the patient has taken the drug in the previous 24 hours, or longer if creatinine clearance (CrCl) is less than 50 mL min.
• Identification of subtherapeutic or supratherapeutic levels in patients taking other drugs that are known to affect pharmacokinetics.
• Identification of subtherapeutic or supratherapeutic levels in patients at body weight extremes.
• Patients with deteriorating renal function.
• During perioperative management.
• During reversal of anticoagulation.
• When there is suspicion of overdose.
• Assessment of compliance in patients suffering thrombotic events while on treatment.7
Currently, there exists no commercially available reversal agent for any of the NOACs, and existing reversal agents for traditional anticoagulants are of limited, if any, use. Drugs under development include agents for the factor Xa inhibitors and for the thrombin inhibitor. Until the time that specific reversal agents exist, supportive care is the mainstay of therapy. In cases of trauma or severe or life-threatening bleeding, administration of concentrated clotting factors (prothrombin complex concentrate) or dialysis (dabigatran only) may be utilized. However, data from large clinical trials are lacking. A recent study of 90 patients receiving an antibody directed against dabigatran has revealed that the anticoagulant effects of dabigatran were reversed safely within minutes of administration; however drug levels were not consistently suppressed at 24 hours in 20% of the cohort.8
Currently there are no national guidelines or large scale studies to guide bridging NOACs for procedures.
The relatively short half-life for these agents makes it likely that traditional bridging as is practiced for warfarin is not necessary.9 However, this represents a double-edged sword; withholding anticoagulation for two doses (such as if a patient becomes ill or a clinician is overly cautious around the time of a procedure) may leave the patient unprotected.
The final question with the new agents is their anti-inflammatory effects. We know that heparin and LMWH have significant pleiotropic effects that are not necessarily related to their anticoagulant effects. These effects are important in order to decrease the inflammatory nature of the thrombus and its effect on the vein wall. We do not know if the new oral agents have similar effects, as this has never fully been tested. In view of the fact that two of the agents are being used as monotherapy agents without any heparin/LMWH bridge, the anti-inflammatory properties of these new agents should be defined to make sure that such a bridge is not necessary.
So, in summary, although these agents have much to offer, there are many questions that remain to be addressed and answered before they totally replace traditional approaches to anticoagulation, in the realm of VTE. It must not be overlooked that despite all the benefits, they also each carry a risk of bleeding as they all target portions of the coagulation mechanism. We caution that, as with any “gift horse,” physicians should perhaps examine the data more closely and proceed with caution.
Thomas Wakefield, MD, is the Stanley Professor of Vascular Surgery; head, section of vascular surgery; and director, Samuel and Jean Frankel Cardiovascular Center. Andrea Obi, MD, is a vascular surgery fellow and Dawn Coleman MD, is the program director, section of vascular surgery, all at the University of Michigan, Ann Arbor. They reported having no conflicts of interest.
References
1. N Engl J Med. 2009;361:2342-2352
2. J Vasc Surg: Venous and Lymphatic Disorders. 2013;1:418-426
3. N Engl J Med 2013;369:1406-1415
4. N Engl J Med 2010;363:2499-2510
5. N Engl J Med 2013;368:699-708
6. Arteriosclerosis, thrombosis, and vascular biology 2015;35:1056-1065
7. J Thrombosis and Haemostasis 2013;11:756-760
New NOACs have largely replaced the need for vitamin K antagonists
The discovery of oral anticoagulants began in 1924, when Schofield linked the death of grazing cattle from internal hemorrhage to the consumption of spoiled sweet clover hay.1 It was not until 1941, however, while trying to understand this observation that Campbell and Link were able to identify the dicoumarol anticoagulant, which formed as a result of the spoiling process.2 Ultimately, after noting that vitamin K led to reversal of the dicoumarol effect, synthesis of the first class of oral anticoagulants, known as vitamin K antagonists (VKAs) began. Despite the numerous challenges associated with managing patients using this class of anticoagulants, VKAs have become the mainstay of oral anticoagulation therapy for the past 70 years. Over the past 5 years, however, new oral anticoagulants (NOACs) have emerged and are changing clinical practice. Mechanistically, these medications are targeted therapies and work as either direct thrombin inhibitors (dabigatran etexilate) or direct factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban). Given their favorable pharmacologic design, NOACs have the potential to replace VKAs as they not only have an encouraging safety profile, but also are therapeutically equivalent or even superior to VKAs when used in certain patient populations.
Pharmacologic design
The targeted drug design of NOACs provides many pharmacologic advantages. Compared with VKAs, NOACs have a notably more predictable pharmacologic profile and relatively wide therapeutic window, which allows for fixed dosing, a rapid onset and offset, and fewer drug interactions.3 These characteristics eliminate the need for the routine dose monitoring and serial dose adjustments frequently associated with VKAs. Additionally, NOACs less commonly require bridging therapy with parenteral unfractionated heparin or low molecular weight heparins (LMWH) while awaiting therapeutic drug levels, as these levels are reached sooner and more predictably than with VKAs.4 As with any medication, however, appropriate consideration should to be given to specific patient populations such as those who are older or have significant comorbidities which may influence drug effect and clearance.
Lastly, it should be mentioned that the pharmacologic benefits of NOACs are not only beneficial from a patient perspective, but also from a health care systems standpoint as their use may provide an opportunity to deliver more cost-effective care. Specifically, economic models using available clinical trial data for stroke prevention in nonvalvular atrial fibrillation have shown that NOACs (apixaban, dabigatran, and rivaroxaban) are cost-effective alternatives when compared with warfarin.5 Although the results from such economic analyses are limited by the modeling assumptions they rely upon, these findings suggest that, at least initially, cost should not be used as a prohibitive reason for adopting these new therapeutics.
Patient selection
The decision to institute oral anticoagulation therapy depends on each patient’s individualized bleeding risk to benefit of ischemia prevention ratio. A major determinant of this ratio is the clinical indication for which anticoagulation is begun. Numerous phase III clinical trials have been conducted comparing the use of NOACs versus VKAs or placebos for the management of nonvalvular atrial fibrillation (AF), venous thromboembolism (VTE), and as adjunctive therapy for patients with acute coronary syndrome.6 Meta-analyses of randomized trials have shown the most significant benefit to be in patients with nonvalvular atrial fibrillation where NOACs have significant reductions in stroke, intracranial hemorrhage, and all-cause mortality, compared with warfarin while displaying variable effects with regards to gastrointestinal bleeding.6,7
In patients with VTE, NOACs have been found to have similar efficacy, compared with VKAs, with regard to the prevention of VTE or VTE-related death, and have been noted to have a better safety profile.6 Lastly, when studied as an adjunctive agent to dual antiplatelet therapy in patients with acute coronary syndrome, it should be noted that NOACs have been associated with an increased bleeding risk without a significant decrease in thrombosis risk.6 Taken together, these data suggest that the primary indication for instituting NOAC therapy should be considered strongly when deciding upon the class of anticoagulant to use.
Overcoming challenges
Since the introduction of NOACs, there has been concern over the lack of specific antidotes to therapy, especially when administered in patients with impaired clearance, a high likelihood of need for an urgent or emergent procedure, or those presenting with life-threatening bleeding complications. Most recently, however, interim analysis from clinical trial data has shown complete reversal of the direct thrombin inhibitor dabigatran with the humanized monocolonal antibody idarucizumab within minutes of administration in greater than 88% of patients studied.8 Similarly, agents such as a PER977 are currently in phase II clinical trials as they have been shown to form noncovalent hydrogen bonds and charge-charge interactions with oral factor Xa inhibitors as well as oral thrombin inhibitors leading to their reversal.9 Given these promising findings, it likely will not be long until reversal agents for NOACs become clinically available. Until that time, it is encouraging that the bleeding profile of these drugs has been found to be favorable, compared with VKAs, and their short half-life allows for a relatively expeditious natural reversal of their anticoagulant effect as the drug is eliminated.
Conclusions
Unlike the serendipitous path leading to the discovery of the first class of oral anticoagulants (VKAs), NOACs have been specifically designed to provide targeted anticoagulation and to address the shortcomings of VKAs. To this end, NOACs are becoming increasingly important in the management of patients with specific clinical conditions such as nonvalvular atrial fibrillation and venous thromboembolism where they have been shown to provide a larger net clinical benefit relative to the available alternatives. Furthermore, with economic analyses providing evidence that NOACs are cost-effective for the health care system and clinical trial results suggesting progress in the development of antidotes for reversal, it is likely that with growing experience, these agents will replace VKAs as the mainstay for prophylactic and therapeutic oral anticoagulation in targeted patient populations.
Madhukar S. Patel, MD, and Elliot L. Chaikof, MD, are from the department of surgery, Beth Israel Deaconess Medical Center, Boston. They reported having no conflicts of interest.
References
1. J Am Vet Med Assoc 1924;64:553-575
3. Hematology Am Soc Hematol Educ Program 2013;2013:464-470
4. Eur Heart J 2013;34:2094-2106
6. Nat Rev Cardiol 2014;11:693-703
8. N Engl J Med 2015;373:511-520
9. N Engl J Med 2014;371:2141-2142
What the doctor didn’t order: unintended consequences and pitfalls of NOACs
Recently, several new oral anticoagulants (NOACs) have gained FDA approval to replace warfarin, capturing the attention of popular media. These include dabigatran, rivaroxaban, apixaban, and edoxaban. Dabigatran targets activated factor II (factor IIa), while rivaroxaban, apixaban, and edoxaban target activated factor X (factor Xa). Easy to take with a once or twice daily pill, with no cumbersome monitoring, they represent a seemingly ideal treatment for the chronically anticoagulated patient. All agents are currently FDA approved in the United States for treatment of acute VTE and AF.
Dabigatran and edoxaban
Similar to warfarin, dabigatran and edoxaban require the use of a LMWH or UFH “bridge” when therapy is beginning, while rivaroxaban and apixaban are instituted as monotherapy without such a bridge. Dabigatran etexilate (PradaxaR, Boehringer Ingelheim) has the longest half-life of all of the NOACs at 12-17 hours, and this half-life is prolonged with increasing age and decreasing renal function.1 It is the only new agent which can be at least partially reversed with dialysis.2 Edoxaban (SavaysaR, Daiichi Sankyo) carries a boxed warning stating that this agent is less effective in AF patients with a creatinine clearance greater than 95 mL/min, and that kidney function should be assessed prior to starting treatment: Such patients have a greater risk of stroke, compared with similar patients treated with warfarin. Edoxaban is the only agent specifically tested at a lower dose in patients at significantly increased risk of bleeding complications (low body weight and/or decreased creatinine clearance).3
Rivaroxaban and apixaban
Rivaroxaban (XareltoR, Bayer and Janssen), and apixaban (EliquisR, Bristol Myers-Squibb), unique amongst the NOACs, have been tested for extended therapy of acute deep vein thrombosis after treatment of 6-12 months. They were found to result in a significant decrease in recurrent VTE without an increase in major bleeding, compared with placebo.4,5 Rivaroxaban has once-daily dosing and apixaban has twice-daily dosing; both are immediate monotherapy, making them quite convenient for patients. Apixaban is the only agent among the NOACs to have a slight decrease in gastrointestinal bleeding, compared with warfarin.6
Consequences and pitfalls with NOACs
Problems with these new drugs, which may diminish our current level of enthusiasm for these agents to totally replace warfarin, include the inability to reliably follow their levels or reverse their anticoagulant effects, the lack of data available on bridging when other procedures need to be performed, their short half-lives, and the lack of data on their anti-inflammatory effects. With regard to monitoring of anticoagulation, the International Society of Thrombosis and Hemostasis (ISTH) has published the times when it might be useful to obtain levels. These times include:
• When a patient is bleeding.
• Before surgery or an invasive procedure when the patient has taken the drug in the previous 24 hours, or longer if creatinine clearance (CrCl) is less than 50 mL min.
• Identification of subtherapeutic or supratherapeutic levels in patients taking other drugs that are known to affect pharmacokinetics.
• Identification of subtherapeutic or supratherapeutic levels in patients at body weight extremes.
• Patients with deteriorating renal function.
• During perioperative management.
• During reversal of anticoagulation.
• When there is suspicion of overdose.
• Assessment of compliance in patients suffering thrombotic events while on treatment.7
Currently, there exists no commercially available reversal agent for any of the NOACs, and existing reversal agents for traditional anticoagulants are of limited, if any, use. Drugs under development include agents for the factor Xa inhibitors and for the thrombin inhibitor. Until the time that specific reversal agents exist, supportive care is the mainstay of therapy. In cases of trauma or severe or life-threatening bleeding, administration of concentrated clotting factors (prothrombin complex concentrate) or dialysis (dabigatran only) may be utilized. However, data from large clinical trials are lacking. A recent study of 90 patients receiving an antibody directed against dabigatran has revealed that the anticoagulant effects of dabigatran were reversed safely within minutes of administration; however drug levels were not consistently suppressed at 24 hours in 20% of the cohort.8
Currently there are no national guidelines or large scale studies to guide bridging NOACs for procedures.
The relatively short half-life for these agents makes it likely that traditional bridging as is practiced for warfarin is not necessary.9 However, this represents a double-edged sword; withholding anticoagulation for two doses (such as if a patient becomes ill or a clinician is overly cautious around the time of a procedure) may leave the patient unprotected.
The final question with the new agents is their anti-inflammatory effects. We know that heparin and LMWH have significant pleiotropic effects that are not necessarily related to their anticoagulant effects. These effects are important in order to decrease the inflammatory nature of the thrombus and its effect on the vein wall. We do not know if the new oral agents have similar effects, as this has never fully been tested. In view of the fact that two of the agents are being used as monotherapy agents without any heparin/LMWH bridge, the anti-inflammatory properties of these new agents should be defined to make sure that such a bridge is not necessary.
So, in summary, although these agents have much to offer, there are many questions that remain to be addressed and answered before they totally replace traditional approaches to anticoagulation, in the realm of VTE. It must not be overlooked that despite all the benefits, they also each carry a risk of bleeding as they all target portions of the coagulation mechanism. We caution that, as with any “gift horse,” physicians should perhaps examine the data more closely and proceed with caution.
Thomas Wakefield, MD, is the Stanley Professor of Vascular Surgery; head, section of vascular surgery; and director, Samuel and Jean Frankel Cardiovascular Center. Andrea Obi, MD, is a vascular surgery fellow and Dawn Coleman MD, is the program director, section of vascular surgery, all at the University of Michigan, Ann Arbor. They reported having no conflicts of interest.
References
1. N Engl J Med. 2009;361:2342-2352
2. J Vasc Surg: Venous and Lymphatic Disorders. 2013;1:418-426
3. N Engl J Med 2013;369:1406-1415
4. N Engl J Med 2010;363:2499-2510
5. N Engl J Med 2013;368:699-708
6. Arteriosclerosis, thrombosis, and vascular biology 2015;35:1056-1065
7. J Thrombosis and Haemostasis 2013;11:756-760
New NOACs have largely replaced the need for vitamin K antagonists
The discovery of oral anticoagulants began in 1924, when Schofield linked the death of grazing cattle from internal hemorrhage to the consumption of spoiled sweet clover hay.1 It was not until 1941, however, while trying to understand this observation that Campbell and Link were able to identify the dicoumarol anticoagulant, which formed as a result of the spoiling process.2 Ultimately, after noting that vitamin K led to reversal of the dicoumarol effect, synthesis of the first class of oral anticoagulants, known as vitamin K antagonists (VKAs) began. Despite the numerous challenges associated with managing patients using this class of anticoagulants, VKAs have become the mainstay of oral anticoagulation therapy for the past 70 years. Over the past 5 years, however, new oral anticoagulants (NOACs) have emerged and are changing clinical practice. Mechanistically, these medications are targeted therapies and work as either direct thrombin inhibitors (dabigatran etexilate) or direct factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban). Given their favorable pharmacologic design, NOACs have the potential to replace VKAs as they not only have an encouraging safety profile, but also are therapeutically equivalent or even superior to VKAs when used in certain patient populations.
Pharmacologic design
The targeted drug design of NOACs provides many pharmacologic advantages. Compared with VKAs, NOACs have a notably more predictable pharmacologic profile and relatively wide therapeutic window, which allows for fixed dosing, a rapid onset and offset, and fewer drug interactions.3 These characteristics eliminate the need for the routine dose monitoring and serial dose adjustments frequently associated with VKAs. Additionally, NOACs less commonly require bridging therapy with parenteral unfractionated heparin or low molecular weight heparins (LMWH) while awaiting therapeutic drug levels, as these levels are reached sooner and more predictably than with VKAs.4 As with any medication, however, appropriate consideration should to be given to specific patient populations such as those who are older or have significant comorbidities which may influence drug effect and clearance.
Lastly, it should be mentioned that the pharmacologic benefits of NOACs are not only beneficial from a patient perspective, but also from a health care systems standpoint as their use may provide an opportunity to deliver more cost-effective care. Specifically, economic models using available clinical trial data for stroke prevention in nonvalvular atrial fibrillation have shown that NOACs (apixaban, dabigatran, and rivaroxaban) are cost-effective alternatives when compared with warfarin.5 Although the results from such economic analyses are limited by the modeling assumptions they rely upon, these findings suggest that, at least initially, cost should not be used as a prohibitive reason for adopting these new therapeutics.
Patient selection
The decision to institute oral anticoagulation therapy depends on each patient’s individualized bleeding risk to benefit of ischemia prevention ratio. A major determinant of this ratio is the clinical indication for which anticoagulation is begun. Numerous phase III clinical trials have been conducted comparing the use of NOACs versus VKAs or placebos for the management of nonvalvular atrial fibrillation (AF), venous thromboembolism (VTE), and as adjunctive therapy for patients with acute coronary syndrome.6 Meta-analyses of randomized trials have shown the most significant benefit to be in patients with nonvalvular atrial fibrillation where NOACs have significant reductions in stroke, intracranial hemorrhage, and all-cause mortality, compared with warfarin while displaying variable effects with regards to gastrointestinal bleeding.6,7
In patients with VTE, NOACs have been found to have similar efficacy, compared with VKAs, with regard to the prevention of VTE or VTE-related death, and have been noted to have a better safety profile.6 Lastly, when studied as an adjunctive agent to dual antiplatelet therapy in patients with acute coronary syndrome, it should be noted that NOACs have been associated with an increased bleeding risk without a significant decrease in thrombosis risk.6 Taken together, these data suggest that the primary indication for instituting NOAC therapy should be considered strongly when deciding upon the class of anticoagulant to use.
Overcoming challenges
Since the introduction of NOACs, there has been concern over the lack of specific antidotes to therapy, especially when administered in patients with impaired clearance, a high likelihood of need for an urgent or emergent procedure, or those presenting with life-threatening bleeding complications. Most recently, however, interim analysis from clinical trial data has shown complete reversal of the direct thrombin inhibitor dabigatran with the humanized monocolonal antibody idarucizumab within minutes of administration in greater than 88% of patients studied.8 Similarly, agents such as a PER977 are currently in phase II clinical trials as they have been shown to form noncovalent hydrogen bonds and charge-charge interactions with oral factor Xa inhibitors as well as oral thrombin inhibitors leading to their reversal.9 Given these promising findings, it likely will not be long until reversal agents for NOACs become clinically available. Until that time, it is encouraging that the bleeding profile of these drugs has been found to be favorable, compared with VKAs, and their short half-life allows for a relatively expeditious natural reversal of their anticoagulant effect as the drug is eliminated.
Conclusions
Unlike the serendipitous path leading to the discovery of the first class of oral anticoagulants (VKAs), NOACs have been specifically designed to provide targeted anticoagulation and to address the shortcomings of VKAs. To this end, NOACs are becoming increasingly important in the management of patients with specific clinical conditions such as nonvalvular atrial fibrillation and venous thromboembolism where they have been shown to provide a larger net clinical benefit relative to the available alternatives. Furthermore, with economic analyses providing evidence that NOACs are cost-effective for the health care system and clinical trial results suggesting progress in the development of antidotes for reversal, it is likely that with growing experience, these agents will replace VKAs as the mainstay for prophylactic and therapeutic oral anticoagulation in targeted patient populations.
Madhukar S. Patel, MD, and Elliot L. Chaikof, MD, are from the department of surgery, Beth Israel Deaconess Medical Center, Boston. They reported having no conflicts of interest.
References
1. J Am Vet Med Assoc 1924;64:553-575
3. Hematology Am Soc Hematol Educ Program 2013;2013:464-470
4. Eur Heart J 2013;34:2094-2106
6. Nat Rev Cardiol 2014;11:693-703
8. N Engl J Med 2015;373:511-520
9. N Engl J Med 2014;371:2141-2142
What the doctor didn’t order: unintended consequences and pitfalls of NOACs
Recently, several new oral anticoagulants (NOACs) have gained FDA approval to replace warfarin, capturing the attention of popular media. These include dabigatran, rivaroxaban, apixaban, and edoxaban. Dabigatran targets activated factor II (factor IIa), while rivaroxaban, apixaban, and edoxaban target activated factor X (factor Xa). Easy to take with a once or twice daily pill, with no cumbersome monitoring, they represent a seemingly ideal treatment for the chronically anticoagulated patient. All agents are currently FDA approved in the United States for treatment of acute VTE and AF.
Dabigatran and edoxaban
Similar to warfarin, dabigatran and edoxaban require the use of a LMWH or UFH “bridge” when therapy is beginning, while rivaroxaban and apixaban are instituted as monotherapy without such a bridge. Dabigatran etexilate (PradaxaR, Boehringer Ingelheim) has the longest half-life of all of the NOACs at 12-17 hours, and this half-life is prolonged with increasing age and decreasing renal function.1 It is the only new agent which can be at least partially reversed with dialysis.2 Edoxaban (SavaysaR, Daiichi Sankyo) carries a boxed warning stating that this agent is less effective in AF patients with a creatinine clearance greater than 95 mL/min, and that kidney function should be assessed prior to starting treatment: Such patients have a greater risk of stroke, compared with similar patients treated with warfarin. Edoxaban is the only agent specifically tested at a lower dose in patients at significantly increased risk of bleeding complications (low body weight and/or decreased creatinine clearance).3
Rivaroxaban and apixaban
Rivaroxaban (XareltoR, Bayer and Janssen), and apixaban (EliquisR, Bristol Myers-Squibb), unique amongst the NOACs, have been tested for extended therapy of acute deep vein thrombosis after treatment of 6-12 months. They were found to result in a significant decrease in recurrent VTE without an increase in major bleeding, compared with placebo.4,5 Rivaroxaban has once-daily dosing and apixaban has twice-daily dosing; both are immediate monotherapy, making them quite convenient for patients. Apixaban is the only agent among the NOACs to have a slight decrease in gastrointestinal bleeding, compared with warfarin.6
Consequences and pitfalls with NOACs
Problems with these new drugs, which may diminish our current level of enthusiasm for these agents to totally replace warfarin, include the inability to reliably follow their levels or reverse their anticoagulant effects, the lack of data available on bridging when other procedures need to be performed, their short half-lives, and the lack of data on their anti-inflammatory effects. With regard to monitoring of anticoagulation, the International Society of Thrombosis and Hemostasis (ISTH) has published the times when it might be useful to obtain levels. These times include:
• When a patient is bleeding.
• Before surgery or an invasive procedure when the patient has taken the drug in the previous 24 hours, or longer if creatinine clearance (CrCl) is less than 50 mL min.
• Identification of subtherapeutic or supratherapeutic levels in patients taking other drugs that are known to affect pharmacokinetics.
• Identification of subtherapeutic or supratherapeutic levels in patients at body weight extremes.
• Patients with deteriorating renal function.
• During perioperative management.
• During reversal of anticoagulation.
• When there is suspicion of overdose.
• Assessment of compliance in patients suffering thrombotic events while on treatment.7
Currently, there exists no commercially available reversal agent for any of the NOACs, and existing reversal agents for traditional anticoagulants are of limited, if any, use. Drugs under development include agents for the factor Xa inhibitors and for the thrombin inhibitor. Until the time that specific reversal agents exist, supportive care is the mainstay of therapy. In cases of trauma or severe or life-threatening bleeding, administration of concentrated clotting factors (prothrombin complex concentrate) or dialysis (dabigatran only) may be utilized. However, data from large clinical trials are lacking. A recent study of 90 patients receiving an antibody directed against dabigatran has revealed that the anticoagulant effects of dabigatran were reversed safely within minutes of administration; however drug levels were not consistently suppressed at 24 hours in 20% of the cohort.8
Currently there are no national guidelines or large scale studies to guide bridging NOACs for procedures.
The relatively short half-life for these agents makes it likely that traditional bridging as is practiced for warfarin is not necessary.9 However, this represents a double-edged sword; withholding anticoagulation for two doses (such as if a patient becomes ill or a clinician is overly cautious around the time of a procedure) may leave the patient unprotected.
The final question with the new agents is their anti-inflammatory effects. We know that heparin and LMWH have significant pleiotropic effects that are not necessarily related to their anticoagulant effects. These effects are important in order to decrease the inflammatory nature of the thrombus and its effect on the vein wall. We do not know if the new oral agents have similar effects, as this has never fully been tested. In view of the fact that two of the agents are being used as monotherapy agents without any heparin/LMWH bridge, the anti-inflammatory properties of these new agents should be defined to make sure that such a bridge is not necessary.
So, in summary, although these agents have much to offer, there are many questions that remain to be addressed and answered before they totally replace traditional approaches to anticoagulation, in the realm of VTE. It must not be overlooked that despite all the benefits, they also each carry a risk of bleeding as they all target portions of the coagulation mechanism. We caution that, as with any “gift horse,” physicians should perhaps examine the data more closely and proceed with caution.
Thomas Wakefield, MD, is the Stanley Professor of Vascular Surgery; head, section of vascular surgery; and director, Samuel and Jean Frankel Cardiovascular Center. Andrea Obi, MD, is a vascular surgery fellow and Dawn Coleman MD, is the program director, section of vascular surgery, all at the University of Michigan, Ann Arbor. They reported having no conflicts of interest.
References
1. N Engl J Med. 2009;361:2342-2352
2. J Vasc Surg: Venous and Lymphatic Disorders. 2013;1:418-426
3. N Engl J Med 2013;369:1406-1415
4. N Engl J Med 2010;363:2499-2510
5. N Engl J Med 2013;368:699-708
6. Arteriosclerosis, thrombosis, and vascular biology 2015;35:1056-1065
7. J Thrombosis and Haemostasis 2013;11:756-760
Commentary: INR instability in the NOAC era
Progress in the development of new oral anticoagulants (NOACs), as well as agents for their reversal, has lowered the threshold to use these therapeutics as first line agents for the management of nonvalvular atrial fibrillation and venous thromboembolism.1,2 Despite this increase in adoption, however, debate persists as to whether patients chronically maintained on vitamin K antagonists (VKAs), such as warfarin, should be switched to NOACs. The recently published research letter by Pokorney et al. assessed the stability of international normalized ratios (INRs) in patients on long-term warfarin therapy in order to address this question.3
Specifically, prospective registry data from 3,749 patients with at least three INR values in the first 6 months of therapy as well as six or more in the following year were included. Patients were deemed stable if 80% or more of their INRs were in a therapeutic range defined as an INR between 2 and 3.3 During the initiation period, only one in four patients taking warfarin had a stable INR.3 Furthermore, stability in the first 6 months was found to have limited ability to predict stability in the subsequent year (concordance index of 0.61). With regard to time in therapeutic range (TTR), only 32% of patients had a TTR of greater than 80% during the first 6 months with less than half (42%) of these patients able to maintain this in the following year.
Findings from Pokorney et al. add to the growing body of literature demonstrating the difficulty of achieving and maintaining a therapeutic INR while on warfarin therapy.4-7 Clinically, these findings are important, as deviations from TTR have been shown to be associated with increased risk of bleeding and thrombosis as well as increased health care costs.8-10 Mechanistically, patient factors such as differences in vitamin K consumption, comorbid conditions, drug-drug interactions, and medication compliance, as well as genetic differences that impact drug metabolism undoubtedly contribute to the variation of INR noted in patients on warfarin therapy.
Attempts to improve stability have included the administration of low-dose oral vitamin K. However, recent data from a multicenter randomized control trial suggests that while such therapy may help to decrease extreme variations in INR, it does not lead to an increased TTR.11 Furthermore, while significant work has been conducted in identifying specific gene variants, such as CYP2C9 and VKORC, which encode cytochrome P450 and vitamin K epoxide reductase enzymes, respectively, economic analyses suggest that testing for these gene variants would not be cost-effective.12 Additionally, clinical prediction tools, which incorporate important patient factors to help guide anticoagulation explain less than 10% of TTR variability.4
Nonetheless, some caution is warranted in the interpretation of the results reported by Pokorney and his colleagues. The proportion of registry patients treated with warfarin who had a low TTR was much lower than that previously reported by the pivotal U.S. trials of NOACs (55%-68%) and significantly lower than the results of a recent nationwide Swedish registry involving 40,449 patients.13
In the Swedish registry, the mean individual TTR was 70% with more than half the patients having a TTR of 70% or more, emphasizing the importance of health care system effects. Moreover, regardless of whether a patient is on warfarin or a NOAC, patients with a lower TTR have higher rates of diabetes, chronic obstructive pulmonary disease, heart failure, and renal failure, which may contribute to the need for additional therapies that may influence TTR.
For example, INR may be increased by ciprofloxacin or omeprazole when taken with warfarin, and CYP3A4 and P-glycoprotein (P-gp) inducers and inhibitors can result in an increased or decreased anticoagulation effect when used with NOACs. Recent reports have also highlighted variability in the safety of NOACs, particularly among patients with renal or liver insufficiency, African Americans, or patients with a prior history of GI bleeding.14-16 For these subgroups, determining NOAC activity to improve clinical safety of these agents is difficult.
PT or INR testing is largely insensitive or otherwise highly variable and the blood draw time relative to the most recent dose significantly influences the measured level of anti-Xa activity. Importantly, socioeconomic factors and family support systems also influence TTR, as important determinants of access to needed drugs or the ability to sustain related costs over time.
Taken together, prior INR stability on warfarin therapy does not ensure continued stability and, as a consequence, long-term warfarin therapy requires close monitoring in order to remain effective. To this end, further development of point-of-care coagulometers for self-testing and self-management, which have been found to be acceptable and preferred by patients, should be pursued.17 Similarly, attempts to decrease INR variability through research on optimizing computer assisted dosing programs remains warranted.18 NOACs offer an advantage over warfarin therapy in that they have a more predictable pharmacokinetic profile, which precludes the need for routine monitoring of anticoagulation parameters. However, many of the same factors, which influence TTR for warfarin do so for NOACs; NOACs have increased bleeding risk in comparison to warfarin for a number of demographic groups; and the high cost of NOACs may influence patient compliance.
Accordingly, until further data is available, consideration of the conversion of a patient on warfarin with a low TTR to a NOAC should be individualized.
Madhukar S. Patel, MD, is a general surgeon at the Department of Surgery, Massachusetts General Hospital, Boston, and Elliot L. Chaikof, MD, is Surgeon-in-Chief, Beth Israel Deaconess Medical Center, and Chairman, Roberta and Stephen R. Weiner Department of Surgery, Johnson and Johnson Professor of Surgery, Harvard Medical School. Dr. Chaikof is also an associate editor for Vascular Specialist. They have no relevant conflicts.
References
2. Nat Rev Cardiol. 2014;11:693-703.
5. J Thromb Haemost. 2010;8:2182-91.
6. Thromb Haemost. 2009;101:552-6.
7. Am J Cardiovasc Drugs. 2015;15:205-11.
8. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
10. J Med Econ. 2015;18:333-40.
11. Thromb Haemost. 2016;116:480-5.
12. Ann Intern Med. 2009;150:73-83.
13. JAMA Cardiol. 2016;1:172-80.
14. N Engl J Med. 2013;369:2093-104.
15. JAMA Intern Med. 2015;175:18-24.
16. J Am Coll Cardiol. 2014;63:891-900.
Progress in the development of new oral anticoagulants (NOACs), as well as agents for their reversal, has lowered the threshold to use these therapeutics as first line agents for the management of nonvalvular atrial fibrillation and venous thromboembolism.1,2 Despite this increase in adoption, however, debate persists as to whether patients chronically maintained on vitamin K antagonists (VKAs), such as warfarin, should be switched to NOACs. The recently published research letter by Pokorney et al. assessed the stability of international normalized ratios (INRs) in patients on long-term warfarin therapy in order to address this question.3
Specifically, prospective registry data from 3,749 patients with at least three INR values in the first 6 months of therapy as well as six or more in the following year were included. Patients were deemed stable if 80% or more of their INRs were in a therapeutic range defined as an INR between 2 and 3.3 During the initiation period, only one in four patients taking warfarin had a stable INR.3 Furthermore, stability in the first 6 months was found to have limited ability to predict stability in the subsequent year (concordance index of 0.61). With regard to time in therapeutic range (TTR), only 32% of patients had a TTR of greater than 80% during the first 6 months with less than half (42%) of these patients able to maintain this in the following year.
Findings from Pokorney et al. add to the growing body of literature demonstrating the difficulty of achieving and maintaining a therapeutic INR while on warfarin therapy.4-7 Clinically, these findings are important, as deviations from TTR have been shown to be associated with increased risk of bleeding and thrombosis as well as increased health care costs.8-10 Mechanistically, patient factors such as differences in vitamin K consumption, comorbid conditions, drug-drug interactions, and medication compliance, as well as genetic differences that impact drug metabolism undoubtedly contribute to the variation of INR noted in patients on warfarin therapy.
Attempts to improve stability have included the administration of low-dose oral vitamin K. However, recent data from a multicenter randomized control trial suggests that while such therapy may help to decrease extreme variations in INR, it does not lead to an increased TTR.11 Furthermore, while significant work has been conducted in identifying specific gene variants, such as CYP2C9 and VKORC, which encode cytochrome P450 and vitamin K epoxide reductase enzymes, respectively, economic analyses suggest that testing for these gene variants would not be cost-effective.12 Additionally, clinical prediction tools, which incorporate important patient factors to help guide anticoagulation explain less than 10% of TTR variability.4
Nonetheless, some caution is warranted in the interpretation of the results reported by Pokorney and his colleagues. The proportion of registry patients treated with warfarin who had a low TTR was much lower than that previously reported by the pivotal U.S. trials of NOACs (55%-68%) and significantly lower than the results of a recent nationwide Swedish registry involving 40,449 patients.13
In the Swedish registry, the mean individual TTR was 70% with more than half the patients having a TTR of 70% or more, emphasizing the importance of health care system effects. Moreover, regardless of whether a patient is on warfarin or a NOAC, patients with a lower TTR have higher rates of diabetes, chronic obstructive pulmonary disease, heart failure, and renal failure, which may contribute to the need for additional therapies that may influence TTR.
For example, INR may be increased by ciprofloxacin or omeprazole when taken with warfarin, and CYP3A4 and P-glycoprotein (P-gp) inducers and inhibitors can result in an increased or decreased anticoagulation effect when used with NOACs. Recent reports have also highlighted variability in the safety of NOACs, particularly among patients with renal or liver insufficiency, African Americans, or patients with a prior history of GI bleeding.14-16 For these subgroups, determining NOAC activity to improve clinical safety of these agents is difficult.
PT or INR testing is largely insensitive or otherwise highly variable and the blood draw time relative to the most recent dose significantly influences the measured level of anti-Xa activity. Importantly, socioeconomic factors and family support systems also influence TTR, as important determinants of access to needed drugs or the ability to sustain related costs over time.
Taken together, prior INR stability on warfarin therapy does not ensure continued stability and, as a consequence, long-term warfarin therapy requires close monitoring in order to remain effective. To this end, further development of point-of-care coagulometers for self-testing and self-management, which have been found to be acceptable and preferred by patients, should be pursued.17 Similarly, attempts to decrease INR variability through research on optimizing computer assisted dosing programs remains warranted.18 NOACs offer an advantage over warfarin therapy in that they have a more predictable pharmacokinetic profile, which precludes the need for routine monitoring of anticoagulation parameters. However, many of the same factors, which influence TTR for warfarin do so for NOACs; NOACs have increased bleeding risk in comparison to warfarin for a number of demographic groups; and the high cost of NOACs may influence patient compliance.
Accordingly, until further data is available, consideration of the conversion of a patient on warfarin with a low TTR to a NOAC should be individualized.
Madhukar S. Patel, MD, is a general surgeon at the Department of Surgery, Massachusetts General Hospital, Boston, and Elliot L. Chaikof, MD, is Surgeon-in-Chief, Beth Israel Deaconess Medical Center, and Chairman, Roberta and Stephen R. Weiner Department of Surgery, Johnson and Johnson Professor of Surgery, Harvard Medical School. Dr. Chaikof is also an associate editor for Vascular Specialist. They have no relevant conflicts.
References
2. Nat Rev Cardiol. 2014;11:693-703.
5. J Thromb Haemost. 2010;8:2182-91.
6. Thromb Haemost. 2009;101:552-6.
7. Am J Cardiovasc Drugs. 2015;15:205-11.
8. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
10. J Med Econ. 2015;18:333-40.
11. Thromb Haemost. 2016;116:480-5.
12. Ann Intern Med. 2009;150:73-83.
13. JAMA Cardiol. 2016;1:172-80.
14. N Engl J Med. 2013;369:2093-104.
15. JAMA Intern Med. 2015;175:18-24.
16. J Am Coll Cardiol. 2014;63:891-900.
Progress in the development of new oral anticoagulants (NOACs), as well as agents for their reversal, has lowered the threshold to use these therapeutics as first line agents for the management of nonvalvular atrial fibrillation and venous thromboembolism.1,2 Despite this increase in adoption, however, debate persists as to whether patients chronically maintained on vitamin K antagonists (VKAs), such as warfarin, should be switched to NOACs. The recently published research letter by Pokorney et al. assessed the stability of international normalized ratios (INRs) in patients on long-term warfarin therapy in order to address this question.3
Specifically, prospective registry data from 3,749 patients with at least three INR values in the first 6 months of therapy as well as six or more in the following year were included. Patients were deemed stable if 80% or more of their INRs were in a therapeutic range defined as an INR between 2 and 3.3 During the initiation period, only one in four patients taking warfarin had a stable INR.3 Furthermore, stability in the first 6 months was found to have limited ability to predict stability in the subsequent year (concordance index of 0.61). With regard to time in therapeutic range (TTR), only 32% of patients had a TTR of greater than 80% during the first 6 months with less than half (42%) of these patients able to maintain this in the following year.
Findings from Pokorney et al. add to the growing body of literature demonstrating the difficulty of achieving and maintaining a therapeutic INR while on warfarin therapy.4-7 Clinically, these findings are important, as deviations from TTR have been shown to be associated with increased risk of bleeding and thrombosis as well as increased health care costs.8-10 Mechanistically, patient factors such as differences in vitamin K consumption, comorbid conditions, drug-drug interactions, and medication compliance, as well as genetic differences that impact drug metabolism undoubtedly contribute to the variation of INR noted in patients on warfarin therapy.
Attempts to improve stability have included the administration of low-dose oral vitamin K. However, recent data from a multicenter randomized control trial suggests that while such therapy may help to decrease extreme variations in INR, it does not lead to an increased TTR.11 Furthermore, while significant work has been conducted in identifying specific gene variants, such as CYP2C9 and VKORC, which encode cytochrome P450 and vitamin K epoxide reductase enzymes, respectively, economic analyses suggest that testing for these gene variants would not be cost-effective.12 Additionally, clinical prediction tools, which incorporate important patient factors to help guide anticoagulation explain less than 10% of TTR variability.4
Nonetheless, some caution is warranted in the interpretation of the results reported by Pokorney and his colleagues. The proportion of registry patients treated with warfarin who had a low TTR was much lower than that previously reported by the pivotal U.S. trials of NOACs (55%-68%) and significantly lower than the results of a recent nationwide Swedish registry involving 40,449 patients.13
In the Swedish registry, the mean individual TTR was 70% with more than half the patients having a TTR of 70% or more, emphasizing the importance of health care system effects. Moreover, regardless of whether a patient is on warfarin or a NOAC, patients with a lower TTR have higher rates of diabetes, chronic obstructive pulmonary disease, heart failure, and renal failure, which may contribute to the need for additional therapies that may influence TTR.
For example, INR may be increased by ciprofloxacin or omeprazole when taken with warfarin, and CYP3A4 and P-glycoprotein (P-gp) inducers and inhibitors can result in an increased or decreased anticoagulation effect when used with NOACs. Recent reports have also highlighted variability in the safety of NOACs, particularly among patients with renal or liver insufficiency, African Americans, or patients with a prior history of GI bleeding.14-16 For these subgroups, determining NOAC activity to improve clinical safety of these agents is difficult.
PT or INR testing is largely insensitive or otherwise highly variable and the blood draw time relative to the most recent dose significantly influences the measured level of anti-Xa activity. Importantly, socioeconomic factors and family support systems also influence TTR, as important determinants of access to needed drugs or the ability to sustain related costs over time.
Taken together, prior INR stability on warfarin therapy does not ensure continued stability and, as a consequence, long-term warfarin therapy requires close monitoring in order to remain effective. To this end, further development of point-of-care coagulometers for self-testing and self-management, which have been found to be acceptable and preferred by patients, should be pursued.17 Similarly, attempts to decrease INR variability through research on optimizing computer assisted dosing programs remains warranted.18 NOACs offer an advantage over warfarin therapy in that they have a more predictable pharmacokinetic profile, which precludes the need for routine monitoring of anticoagulation parameters. However, many of the same factors, which influence TTR for warfarin do so for NOACs; NOACs have increased bleeding risk in comparison to warfarin for a number of demographic groups; and the high cost of NOACs may influence patient compliance.
Accordingly, until further data is available, consideration of the conversion of a patient on warfarin with a low TTR to a NOAC should be individualized.
Madhukar S. Patel, MD, is a general surgeon at the Department of Surgery, Massachusetts General Hospital, Boston, and Elliot L. Chaikof, MD, is Surgeon-in-Chief, Beth Israel Deaconess Medical Center, and Chairman, Roberta and Stephen R. Weiner Department of Surgery, Johnson and Johnson Professor of Surgery, Harvard Medical School. Dr. Chaikof is also an associate editor for Vascular Specialist. They have no relevant conflicts.
References
2. Nat Rev Cardiol. 2014;11:693-703.
5. J Thromb Haemost. 2010;8:2182-91.
6. Thromb Haemost. 2009;101:552-6.
7. Am J Cardiovasc Drugs. 2015;15:205-11.
8. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
10. J Med Econ. 2015;18:333-40.
11. Thromb Haemost. 2016;116:480-5.
12. Ann Intern Med. 2009;150:73-83.
13. JAMA Cardiol. 2016;1:172-80.
14. N Engl J Med. 2013;369:2093-104.
15. JAMA Intern Med. 2015;175:18-24.
16. J Am Coll Cardiol. 2014;63:891-900.
Size does matter
I grew up in a small town. I went to a small college. And I live and practiced in a small town in a sparsely populated state. Clearly, I’m partial to smallness. I have practiced in a two-man partnership, a solo practice, a small group, and finally in a large multicenter organization. The 10 years I practiced by myself were the most productive. It was also the most rewarding period of my life both professionally and financially.
The small group environment was a close second as a far as job satisfaction. What little I lost in autonomy was almost balanced by professional stimulation and camaraderie or working shoulder to shoulder with peers. However, all that was lost as our small group was engulfed by a larger entity. Our overhead inflated to a point that it was almost unsustainable. Meetings gobbled up productive office time. Even making little changes that might have allowed us to adapt to the changing clinical landscape seemed to take forever. That is, if they ever happened at all.
From my personal experience, health care delivery doesn’t benefit from the economics of scale that is claimed by other industries. Bigger is not better for health care delivery.
When the promoters of the Affordable Care Act promised that it would encourage cost saving and quality enhancing mergers of health delivery organizations, many other physicians and I had serious doubts about this claim. It turns that our concerns were well founded. The consolidations that were predicted and so eagerly anticipated by the architects of the ACA have occurred, but have not resulted in the promised cost savings or quality improvement.
The results have been so disappointing that Dr. Bob Kocher, special assistant to President Obama for health care and economic policy from 2009 to 2010, has felt the need to issue a mea culpa in the form of an op-ed piece in the Wall Street Journal (“How I Was Wrong About ObamaCare,” July 31, 2016). Although Dr. Kocher still believes organizing medicine into networks “that can share information, coordinate care for patients, and manage risk is critical for delivering higher-quality care, generating cost savings and improving the experience for patients,” he acknowledges, “having every provider in health care ‘owned’ by a single organization is more likely to be a barrier to better care.”
He cites recent evidence that “savings and quality improvement are generated much more often by independent primary care doctors than large hospital-centric health systems.” Small independent practices know their patients better. Unencumbered by the weight of multiple organizational layers, they can more nimbly adjust to change. And there will always be change.
Dr. Kocher also admits that he and his co-crafters of the ACA were mistaken in their belief that “it would take three to five years for physicians to use electronic health records effectively.” Unfortunately, he places the failure on what he views as delay tactics by organized medicine. Sadly, he shares this blind spot with too many other former and current government health care officials, most of whom who have never suffered under the burden of a user-unfriendly, free time–wasting, electronic medical record system.
While it is nice of Dr. Kocher to acknowledge his revelation about size, it comes too late. The bridges have already been burned. Most of the smaller independent practices he now realizes could have provided a solution to the accelerating cost of medical care are gone. In some cases, one of forces driving small practices to merge was the cost and complexity of converting to electronic medical records.
The mea culpa that we really need to hear now is the one admitting that the roll out of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009 and meaningful use requirements were poorly conceived and implemented. Electronic health record systems that are capable of seamlessly communicating with one another, and are inexpensive, intuitive, and user friendly might have allowed more small independent practices to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a small town. I went to a small college. And I live and practiced in a small town in a sparsely populated state. Clearly, I’m partial to smallness. I have practiced in a two-man partnership, a solo practice, a small group, and finally in a large multicenter organization. The 10 years I practiced by myself were the most productive. It was also the most rewarding period of my life both professionally and financially.
The small group environment was a close second as a far as job satisfaction. What little I lost in autonomy was almost balanced by professional stimulation and camaraderie or working shoulder to shoulder with peers. However, all that was lost as our small group was engulfed by a larger entity. Our overhead inflated to a point that it was almost unsustainable. Meetings gobbled up productive office time. Even making little changes that might have allowed us to adapt to the changing clinical landscape seemed to take forever. That is, if they ever happened at all.
From my personal experience, health care delivery doesn’t benefit from the economics of scale that is claimed by other industries. Bigger is not better for health care delivery.
When the promoters of the Affordable Care Act promised that it would encourage cost saving and quality enhancing mergers of health delivery organizations, many other physicians and I had serious doubts about this claim. It turns that our concerns were well founded. The consolidations that were predicted and so eagerly anticipated by the architects of the ACA have occurred, but have not resulted in the promised cost savings or quality improvement.
The results have been so disappointing that Dr. Bob Kocher, special assistant to President Obama for health care and economic policy from 2009 to 2010, has felt the need to issue a mea culpa in the form of an op-ed piece in the Wall Street Journal (“How I Was Wrong About ObamaCare,” July 31, 2016). Although Dr. Kocher still believes organizing medicine into networks “that can share information, coordinate care for patients, and manage risk is critical for delivering higher-quality care, generating cost savings and improving the experience for patients,” he acknowledges, “having every provider in health care ‘owned’ by a single organization is more likely to be a barrier to better care.”
He cites recent evidence that “savings and quality improvement are generated much more often by independent primary care doctors than large hospital-centric health systems.” Small independent practices know their patients better. Unencumbered by the weight of multiple organizational layers, they can more nimbly adjust to change. And there will always be change.
Dr. Kocher also admits that he and his co-crafters of the ACA were mistaken in their belief that “it would take three to five years for physicians to use electronic health records effectively.” Unfortunately, he places the failure on what he views as delay tactics by organized medicine. Sadly, he shares this blind spot with too many other former and current government health care officials, most of whom who have never suffered under the burden of a user-unfriendly, free time–wasting, electronic medical record system.
While it is nice of Dr. Kocher to acknowledge his revelation about size, it comes too late. The bridges have already been burned. Most of the smaller independent practices he now realizes could have provided a solution to the accelerating cost of medical care are gone. In some cases, one of forces driving small practices to merge was the cost and complexity of converting to electronic medical records.
The mea culpa that we really need to hear now is the one admitting that the roll out of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009 and meaningful use requirements were poorly conceived and implemented. Electronic health record systems that are capable of seamlessly communicating with one another, and are inexpensive, intuitive, and user friendly might have allowed more small independent practices to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a small town. I went to a small college. And I live and practiced in a small town in a sparsely populated state. Clearly, I’m partial to smallness. I have practiced in a two-man partnership, a solo practice, a small group, and finally in a large multicenter organization. The 10 years I practiced by myself were the most productive. It was also the most rewarding period of my life both professionally and financially.
The small group environment was a close second as a far as job satisfaction. What little I lost in autonomy was almost balanced by professional stimulation and camaraderie or working shoulder to shoulder with peers. However, all that was lost as our small group was engulfed by a larger entity. Our overhead inflated to a point that it was almost unsustainable. Meetings gobbled up productive office time. Even making little changes that might have allowed us to adapt to the changing clinical landscape seemed to take forever. That is, if they ever happened at all.
From my personal experience, health care delivery doesn’t benefit from the economics of scale that is claimed by other industries. Bigger is not better for health care delivery.
When the promoters of the Affordable Care Act promised that it would encourage cost saving and quality enhancing mergers of health delivery organizations, many other physicians and I had serious doubts about this claim. It turns that our concerns were well founded. The consolidations that were predicted and so eagerly anticipated by the architects of the ACA have occurred, but have not resulted in the promised cost savings or quality improvement.
The results have been so disappointing that Dr. Bob Kocher, special assistant to President Obama for health care and economic policy from 2009 to 2010, has felt the need to issue a mea culpa in the form of an op-ed piece in the Wall Street Journal (“How I Was Wrong About ObamaCare,” July 31, 2016). Although Dr. Kocher still believes organizing medicine into networks “that can share information, coordinate care for patients, and manage risk is critical for delivering higher-quality care, generating cost savings and improving the experience for patients,” he acknowledges, “having every provider in health care ‘owned’ by a single organization is more likely to be a barrier to better care.”
He cites recent evidence that “savings and quality improvement are generated much more often by independent primary care doctors than large hospital-centric health systems.” Small independent practices know their patients better. Unencumbered by the weight of multiple organizational layers, they can more nimbly adjust to change. And there will always be change.
Dr. Kocher also admits that he and his co-crafters of the ACA were mistaken in their belief that “it would take three to five years for physicians to use electronic health records effectively.” Unfortunately, he places the failure on what he views as delay tactics by organized medicine. Sadly, he shares this blind spot with too many other former and current government health care officials, most of whom who have never suffered under the burden of a user-unfriendly, free time–wasting, electronic medical record system.
While it is nice of Dr. Kocher to acknowledge his revelation about size, it comes too late. The bridges have already been burned. Most of the smaller independent practices he now realizes could have provided a solution to the accelerating cost of medical care are gone. In some cases, one of forces driving small practices to merge was the cost and complexity of converting to electronic medical records.
The mea culpa that we really need to hear now is the one admitting that the roll out of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009 and meaningful use requirements were poorly conceived and implemented. Electronic health record systems that are capable of seamlessly communicating with one another, and are inexpensive, intuitive, and user friendly might have allowed more small independent practices to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Help at a cost
Have you read the study with the weighty title of “Fully Capitated Payment Breakeven Rate for a Mid-Size Pediatric Practice?” (Pediatrics. 2016, July 29. doi: 10.1542/peds.2015-4367). You should! Of course, it’s easy for me to admonish you because my active practice days are behind me, and I have the time to read things with intimidating titles. But if you have had the time it takes to read the handwriting on the wall, you know that fee for service (FFS) is on the endangered list and is being replaced by a variety of other payment models, many of which are based on some form of capitation. Even just a cursory reading of this study from the Center of Healthcare Innovation and Policy Research at George Washington University should help you appreciate the complexities implicit in the transition from FFS to capitation and give you a sense of how it might affect the way you practice.
To amass the data they needed to run their computer models, the investigators had to make some assumptions. Here are just a few: The average pediatrician salary was pegged at $180,000, and she/he would be seeing 25 patients per day for 220 clinical days in the year. The practice she/he is working in has a staff to physician ratio of 3.2. Do you even know what your practice’s staff to physician ratio is? Is it ever discussed? How do their assumptions square with your reality?
The researchers also assumed that when practices transition to a capitated system many of them also adopt a primary care medical home (PCMH) model that often includes changes in staffing ratios almost always resulting in a higher staff to physician ratio. When the researchers fed their model even modest increases in staff to physician ratio from 3.2 to 4.0 or 4.4, the result was an increase in the break-even payment rate of between 12% and 23%. However, this study doesn’t answer whether related changes in panel size and patient outcome would make these increases sustainable.
It also doesn’t include the complexities that are inherent in the trend toward part-time employment. How good is your practice at optimizing physician to staff ratios when several physicians have chosen to work part-time? Are the physicians’ schedules arranged to minimize resource-wasting overlap in staffing? How efficient are you at utilizing support staff? For example, do you do your own measurements as part of your exam and give immunizations? How does this compare with your peers? Is your efficiency paying for some of their overhead?
If you are already using a PCMH model, how efficient have you been in using the additional support staff that it requires? Measuring the improvement in quality the change has created is difficult, but it should be fairly easy to determine the cost of the added staffing.
The investigators acknowledge that they have not included the cost of immunization in their models, and I don’t think that they expect to us take their numbers too seriously. But the first line in the authors’ conclusion is the reason that you should take the time to read this study. “Practices are more likely to succeed in capitated models if pediatricians understand how these models alter practice finances.”
You may have gone into pediatrics because of the noble causes that the specialty espouses. But it’s time to swallow hard and acknowledge that this is one of those situations in which it is all about the money. You need to keep informed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Have you read the study with the weighty title of “Fully Capitated Payment Breakeven Rate for a Mid-Size Pediatric Practice?” (Pediatrics. 2016, July 29. doi: 10.1542/peds.2015-4367). You should! Of course, it’s easy for me to admonish you because my active practice days are behind me, and I have the time to read things with intimidating titles. But if you have had the time it takes to read the handwriting on the wall, you know that fee for service (FFS) is on the endangered list and is being replaced by a variety of other payment models, many of which are based on some form of capitation. Even just a cursory reading of this study from the Center of Healthcare Innovation and Policy Research at George Washington University should help you appreciate the complexities implicit in the transition from FFS to capitation and give you a sense of how it might affect the way you practice.
To amass the data they needed to run their computer models, the investigators had to make some assumptions. Here are just a few: The average pediatrician salary was pegged at $180,000, and she/he would be seeing 25 patients per day for 220 clinical days in the year. The practice she/he is working in has a staff to physician ratio of 3.2. Do you even know what your practice’s staff to physician ratio is? Is it ever discussed? How do their assumptions square with your reality?
The researchers also assumed that when practices transition to a capitated system many of them also adopt a primary care medical home (PCMH) model that often includes changes in staffing ratios almost always resulting in a higher staff to physician ratio. When the researchers fed their model even modest increases in staff to physician ratio from 3.2 to 4.0 or 4.4, the result was an increase in the break-even payment rate of between 12% and 23%. However, this study doesn’t answer whether related changes in panel size and patient outcome would make these increases sustainable.
It also doesn’t include the complexities that are inherent in the trend toward part-time employment. How good is your practice at optimizing physician to staff ratios when several physicians have chosen to work part-time? Are the physicians’ schedules arranged to minimize resource-wasting overlap in staffing? How efficient are you at utilizing support staff? For example, do you do your own measurements as part of your exam and give immunizations? How does this compare with your peers? Is your efficiency paying for some of their overhead?
If you are already using a PCMH model, how efficient have you been in using the additional support staff that it requires? Measuring the improvement in quality the change has created is difficult, but it should be fairly easy to determine the cost of the added staffing.
The investigators acknowledge that they have not included the cost of immunization in their models, and I don’t think that they expect to us take their numbers too seriously. But the first line in the authors’ conclusion is the reason that you should take the time to read this study. “Practices are more likely to succeed in capitated models if pediatricians understand how these models alter practice finances.”
You may have gone into pediatrics because of the noble causes that the specialty espouses. But it’s time to swallow hard and acknowledge that this is one of those situations in which it is all about the money. You need to keep informed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Have you read the study with the weighty title of “Fully Capitated Payment Breakeven Rate for a Mid-Size Pediatric Practice?” (Pediatrics. 2016, July 29. doi: 10.1542/peds.2015-4367). You should! Of course, it’s easy for me to admonish you because my active practice days are behind me, and I have the time to read things with intimidating titles. But if you have had the time it takes to read the handwriting on the wall, you know that fee for service (FFS) is on the endangered list and is being replaced by a variety of other payment models, many of which are based on some form of capitation. Even just a cursory reading of this study from the Center of Healthcare Innovation and Policy Research at George Washington University should help you appreciate the complexities implicit in the transition from FFS to capitation and give you a sense of how it might affect the way you practice.
To amass the data they needed to run their computer models, the investigators had to make some assumptions. Here are just a few: The average pediatrician salary was pegged at $180,000, and she/he would be seeing 25 patients per day for 220 clinical days in the year. The practice she/he is working in has a staff to physician ratio of 3.2. Do you even know what your practice’s staff to physician ratio is? Is it ever discussed? How do their assumptions square with your reality?
The researchers also assumed that when practices transition to a capitated system many of them also adopt a primary care medical home (PCMH) model that often includes changes in staffing ratios almost always resulting in a higher staff to physician ratio. When the researchers fed their model even modest increases in staff to physician ratio from 3.2 to 4.0 or 4.4, the result was an increase in the break-even payment rate of between 12% and 23%. However, this study doesn’t answer whether related changes in panel size and patient outcome would make these increases sustainable.
It also doesn’t include the complexities that are inherent in the trend toward part-time employment. How good is your practice at optimizing physician to staff ratios when several physicians have chosen to work part-time? Are the physicians’ schedules arranged to minimize resource-wasting overlap in staffing? How efficient are you at utilizing support staff? For example, do you do your own measurements as part of your exam and give immunizations? How does this compare with your peers? Is your efficiency paying for some of their overhead?
If you are already using a PCMH model, how efficient have you been in using the additional support staff that it requires? Measuring the improvement in quality the change has created is difficult, but it should be fairly easy to determine the cost of the added staffing.
The investigators acknowledge that they have not included the cost of immunization in their models, and I don’t think that they expect to us take their numbers too seriously. But the first line in the authors’ conclusion is the reason that you should take the time to read this study. “Practices are more likely to succeed in capitated models if pediatricians understand how these models alter practice finances.”
You may have gone into pediatrics because of the noble causes that the specialty espouses. But it’s time to swallow hard and acknowledge that this is one of those situations in which it is all about the money. You need to keep informed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Commentary: Should board exams include a technical skill assessment? A European perspective
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
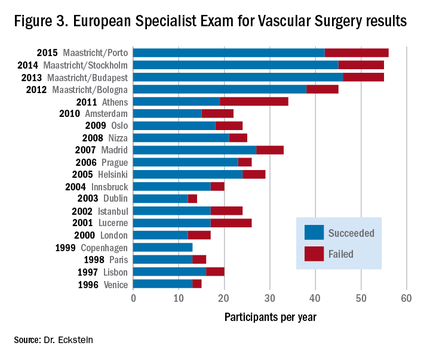
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8

|
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.

|
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.

|
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
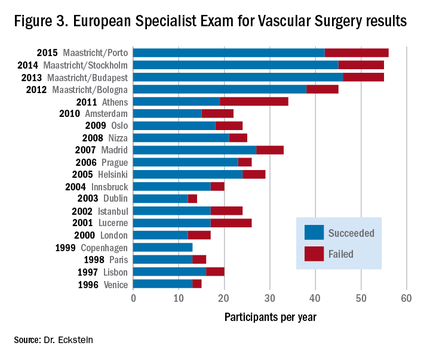
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
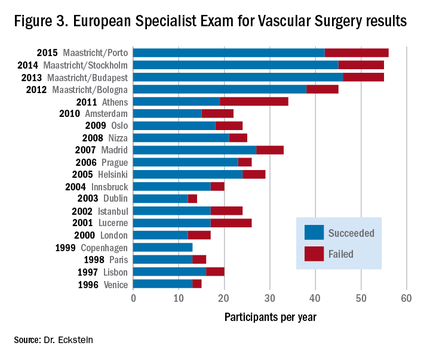
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8