User login
Looking for an alternative to ABPN maintenance of certification?
The current American Board of Medical Specialties (ABMS)/American Board of Psychiatry and Neurology (ABPN) requirements for maintenance of certification (MOC) do not assure that a practicing physician has maintained competency to practice neurology. The ABMS acknowledges this concept, and one ABMS member website included the following statement: “Many qualities are necessary to be a competent physician, and many of these qualities cannot be quantified or measured. Thus, certification is not a guarantee of the competence of the physician specialist.” In other words, board certification is meant to demonstrate competence, but the board does not guarantee competence. This concept nullifies the notion that the American College of Physicians (ACP) raised, that if you become involved in litigation, board certification will somehow protect you. The fact is that if you are negligent, no piece of paper hanging on your wall will protect you.
The costs to practicing neurologists both in terms of time and money to complete this process are considerable. In a recent study, the cost of physician compliance with MOC was found to range from $23,607 to $40,495 over a 10-year period depending on specialty. Yet, there is no published evidence that demonstrates these requirements serve to improve quality of practice.
Action and reaction
In an article published in the New England Journal of Medicine, Dr. Paul Teirstein, chief of cardiology at the Scripps Clinic, criticized many aspects of MOC. Shortly after publication, the American Board of Internal Medicine issued a “mea culpa” and suspended some of the Practice Assessment, Patient Voice, and Patient Safety requirements.
On Feb. 24, 2015, former American Academy of Neurology (AAN) President Timothy A. Pedley issued a statement on behalf of the AAN arguing that Part IV of MOC is an onerous requirement, and that this ABPN requirement has imposed a hardship on neurologists.
In July 2015, the ABPN announced that as of Jan. 1, 2016, the Feedback Module (patient or peer surveys) will become a highly recommended yet optional component of MOC. The Part IV Clinical Module component (chart review) will remain a requirement.”
A new pathway
Fortunately, there is a viable alternative to the ABMS/ABPN pathway to MOC. The National Board of Physicians and Surgeons (NBPAS.org), is offering recertification in ABMS medical specialties. The board of directors of the NBPAS comprises members representing many of the country’s top academic institutions and specialty organizations. All physician members of NBPAS are volunteers (there is a small paid administrative staff), in contradistinction to the ABMS boards, in which the members of these boards are paid six-figure salaries.
The NBPAS board recertification criteria
1. Previous certification by an ABMS member board.
2. Valid license to practice medicine.
3. At least 50 hours of CME accredited by the Accreditation Council for Continuing Medical Education within the past 24 months.
4. Active hospital privileges (for select specialties).
5. Clinical privileges in certified specialty have not been permanently revoked.
6. Cost: $169 for a 2-year certification.
The MOC requirement itself is incorporated in Medicare law and under the Patient Protection and Affordable Care Act, although there is ambiguity regarding whether MOC must be obtained via the ABMS specialty boards. When these laws were written, the ABMS was essentially “the only game in town” for physicians. The ABMS has been challenged in terms of being a monopoly organization for specialty certification and recertification. Presumably because of this, or perhaps as a preemptive defense, the ABMS has recently acknowledged publicly that it does have competition in the form of the NBPAS. To punctuate this point, one ABMS member website has included the following statement, “Possession of a Board certificate does not indicate total qualification for practice privileges, nor does it imply exclusion of other physicians not so certified.”
Due to pressure from NBPAS and others, the ABMS boards have had to reconsider their position on MOC. Beginning in 2016, the American Board of Anesthesiology decided to discontinue their 10-year recertification examination. Instead, their diplomates will be taking an online 30-question quiz per calendar quarter (120 questions per year). Although this is a positive change, making a 120-question, online, open-book exam for all diplomates recertifying must be significantly cheaper to produce and administer than a secured 10-year exam. That being said, the cost of this new MOC program is $210 per year instead of a lump sum $2,100 to take the closed book exam every 10 years. Clearly, the boards feel a reduction in cost of production to the boards should not translate to a reduction in cost to the diplomates, and that the boards should actually generate even greater revenues.
The ABPN has also responded positively by forming an MOC clinical advisory committee to evaluate how MOC impacts practice and “potentially” improves patient care. Their use of the word “potentially” is particularly encouraging, because it implicitly suggests that evidence needs to be found to support that claim.
The future of board certification
The ABMS boards acknowledge that NBPAS exists as a legitimate alternative board, but they do not feel threatened at all. They are very confident that physicians, like sheep to be herded, will continue to blindly pay to do unnecessary work in the name of board certification.
Unfortunately for the ABMS boards, over 3,000 physicians have become diplomates of NBPAS, which has become accepted as a viable alternative to ABMS by an increasing number of hospital credentialing departments. It is only through an expanding number of diplomates that NBAPS can increase its acceptance and rival the inflexible, self-centered monopoly that ABMS has become.
With more institutions accepting NBPAS certification, the influence and leverage of NBPAS will grow, and physicians will be relieved of the burden of complying with costly and time-consuming requirements that do not improve practice. There is no harm in being dual-boarded, and becoming a diplomate of NBPAS prior to the expiration of an ABPN/ABMS board certification is a low-risk decision that supports a prophysician grassroots movement. During this time of unprecedented physician unity, organizations like NBPAS appear well positioned to help return the practice of medicine to physicians rather than detached administrators.
Dr. Mathew is a member of the Harvard Medical School Faculty. He is director of continuing medical education at the Brigham & Women’s Hospital, John R. Graham Headache Center, and is a staff neurologist at Harvard Vanguard Medical Associates and the Cambridge Health Alliance. He also serves as the neurology representative on the volunteer advisory board of the National Board of Physicians and Surgeons.
The current American Board of Medical Specialties (ABMS)/American Board of Psychiatry and Neurology (ABPN) requirements for maintenance of certification (MOC) do not assure that a practicing physician has maintained competency to practice neurology. The ABMS acknowledges this concept, and one ABMS member website included the following statement: “Many qualities are necessary to be a competent physician, and many of these qualities cannot be quantified or measured. Thus, certification is not a guarantee of the competence of the physician specialist.” In other words, board certification is meant to demonstrate competence, but the board does not guarantee competence. This concept nullifies the notion that the American College of Physicians (ACP) raised, that if you become involved in litigation, board certification will somehow protect you. The fact is that if you are negligent, no piece of paper hanging on your wall will protect you.
The costs to practicing neurologists both in terms of time and money to complete this process are considerable. In a recent study, the cost of physician compliance with MOC was found to range from $23,607 to $40,495 over a 10-year period depending on specialty. Yet, there is no published evidence that demonstrates these requirements serve to improve quality of practice.
Action and reaction
In an article published in the New England Journal of Medicine, Dr. Paul Teirstein, chief of cardiology at the Scripps Clinic, criticized many aspects of MOC. Shortly after publication, the American Board of Internal Medicine issued a “mea culpa” and suspended some of the Practice Assessment, Patient Voice, and Patient Safety requirements.
On Feb. 24, 2015, former American Academy of Neurology (AAN) President Timothy A. Pedley issued a statement on behalf of the AAN arguing that Part IV of MOC is an onerous requirement, and that this ABPN requirement has imposed a hardship on neurologists.
In July 2015, the ABPN announced that as of Jan. 1, 2016, the Feedback Module (patient or peer surveys) will become a highly recommended yet optional component of MOC. The Part IV Clinical Module component (chart review) will remain a requirement.”
A new pathway
Fortunately, there is a viable alternative to the ABMS/ABPN pathway to MOC. The National Board of Physicians and Surgeons (NBPAS.org), is offering recertification in ABMS medical specialties. The board of directors of the NBPAS comprises members representing many of the country’s top academic institutions and specialty organizations. All physician members of NBPAS are volunteers (there is a small paid administrative staff), in contradistinction to the ABMS boards, in which the members of these boards are paid six-figure salaries.
The NBPAS board recertification criteria
1. Previous certification by an ABMS member board.
2. Valid license to practice medicine.
3. At least 50 hours of CME accredited by the Accreditation Council for Continuing Medical Education within the past 24 months.
4. Active hospital privileges (for select specialties).
5. Clinical privileges in certified specialty have not been permanently revoked.
6. Cost: $169 for a 2-year certification.
The MOC requirement itself is incorporated in Medicare law and under the Patient Protection and Affordable Care Act, although there is ambiguity regarding whether MOC must be obtained via the ABMS specialty boards. When these laws were written, the ABMS was essentially “the only game in town” for physicians. The ABMS has been challenged in terms of being a monopoly organization for specialty certification and recertification. Presumably because of this, or perhaps as a preemptive defense, the ABMS has recently acknowledged publicly that it does have competition in the form of the NBPAS. To punctuate this point, one ABMS member website has included the following statement, “Possession of a Board certificate does not indicate total qualification for practice privileges, nor does it imply exclusion of other physicians not so certified.”
Due to pressure from NBPAS and others, the ABMS boards have had to reconsider their position on MOC. Beginning in 2016, the American Board of Anesthesiology decided to discontinue their 10-year recertification examination. Instead, their diplomates will be taking an online 30-question quiz per calendar quarter (120 questions per year). Although this is a positive change, making a 120-question, online, open-book exam for all diplomates recertifying must be significantly cheaper to produce and administer than a secured 10-year exam. That being said, the cost of this new MOC program is $210 per year instead of a lump sum $2,100 to take the closed book exam every 10 years. Clearly, the boards feel a reduction in cost of production to the boards should not translate to a reduction in cost to the diplomates, and that the boards should actually generate even greater revenues.
The ABPN has also responded positively by forming an MOC clinical advisory committee to evaluate how MOC impacts practice and “potentially” improves patient care. Their use of the word “potentially” is particularly encouraging, because it implicitly suggests that evidence needs to be found to support that claim.
The future of board certification
The ABMS boards acknowledge that NBPAS exists as a legitimate alternative board, but they do not feel threatened at all. They are very confident that physicians, like sheep to be herded, will continue to blindly pay to do unnecessary work in the name of board certification.
Unfortunately for the ABMS boards, over 3,000 physicians have become diplomates of NBPAS, which has become accepted as a viable alternative to ABMS by an increasing number of hospital credentialing departments. It is only through an expanding number of diplomates that NBAPS can increase its acceptance and rival the inflexible, self-centered monopoly that ABMS has become.
With more institutions accepting NBPAS certification, the influence and leverage of NBPAS will grow, and physicians will be relieved of the burden of complying with costly and time-consuming requirements that do not improve practice. There is no harm in being dual-boarded, and becoming a diplomate of NBPAS prior to the expiration of an ABPN/ABMS board certification is a low-risk decision that supports a prophysician grassroots movement. During this time of unprecedented physician unity, organizations like NBPAS appear well positioned to help return the practice of medicine to physicians rather than detached administrators.
Dr. Mathew is a member of the Harvard Medical School Faculty. He is director of continuing medical education at the Brigham & Women’s Hospital, John R. Graham Headache Center, and is a staff neurologist at Harvard Vanguard Medical Associates and the Cambridge Health Alliance. He also serves as the neurology representative on the volunteer advisory board of the National Board of Physicians and Surgeons.
The current American Board of Medical Specialties (ABMS)/American Board of Psychiatry and Neurology (ABPN) requirements for maintenance of certification (MOC) do not assure that a practicing physician has maintained competency to practice neurology. The ABMS acknowledges this concept, and one ABMS member website included the following statement: “Many qualities are necessary to be a competent physician, and many of these qualities cannot be quantified or measured. Thus, certification is not a guarantee of the competence of the physician specialist.” In other words, board certification is meant to demonstrate competence, but the board does not guarantee competence. This concept nullifies the notion that the American College of Physicians (ACP) raised, that if you become involved in litigation, board certification will somehow protect you. The fact is that if you are negligent, no piece of paper hanging on your wall will protect you.
The costs to practicing neurologists both in terms of time and money to complete this process are considerable. In a recent study, the cost of physician compliance with MOC was found to range from $23,607 to $40,495 over a 10-year period depending on specialty. Yet, there is no published evidence that demonstrates these requirements serve to improve quality of practice.
Action and reaction
In an article published in the New England Journal of Medicine, Dr. Paul Teirstein, chief of cardiology at the Scripps Clinic, criticized many aspects of MOC. Shortly after publication, the American Board of Internal Medicine issued a “mea culpa” and suspended some of the Practice Assessment, Patient Voice, and Patient Safety requirements.
On Feb. 24, 2015, former American Academy of Neurology (AAN) President Timothy A. Pedley issued a statement on behalf of the AAN arguing that Part IV of MOC is an onerous requirement, and that this ABPN requirement has imposed a hardship on neurologists.
In July 2015, the ABPN announced that as of Jan. 1, 2016, the Feedback Module (patient or peer surveys) will become a highly recommended yet optional component of MOC. The Part IV Clinical Module component (chart review) will remain a requirement.”
A new pathway
Fortunately, there is a viable alternative to the ABMS/ABPN pathway to MOC. The National Board of Physicians and Surgeons (NBPAS.org), is offering recertification in ABMS medical specialties. The board of directors of the NBPAS comprises members representing many of the country’s top academic institutions and specialty organizations. All physician members of NBPAS are volunteers (there is a small paid administrative staff), in contradistinction to the ABMS boards, in which the members of these boards are paid six-figure salaries.
The NBPAS board recertification criteria
1. Previous certification by an ABMS member board.
2. Valid license to practice medicine.
3. At least 50 hours of CME accredited by the Accreditation Council for Continuing Medical Education within the past 24 months.
4. Active hospital privileges (for select specialties).
5. Clinical privileges in certified specialty have not been permanently revoked.
6. Cost: $169 for a 2-year certification.
The MOC requirement itself is incorporated in Medicare law and under the Patient Protection and Affordable Care Act, although there is ambiguity regarding whether MOC must be obtained via the ABMS specialty boards. When these laws were written, the ABMS was essentially “the only game in town” for physicians. The ABMS has been challenged in terms of being a monopoly organization for specialty certification and recertification. Presumably because of this, or perhaps as a preemptive defense, the ABMS has recently acknowledged publicly that it does have competition in the form of the NBPAS. To punctuate this point, one ABMS member website has included the following statement, “Possession of a Board certificate does not indicate total qualification for practice privileges, nor does it imply exclusion of other physicians not so certified.”
Due to pressure from NBPAS and others, the ABMS boards have had to reconsider their position on MOC. Beginning in 2016, the American Board of Anesthesiology decided to discontinue their 10-year recertification examination. Instead, their diplomates will be taking an online 30-question quiz per calendar quarter (120 questions per year). Although this is a positive change, making a 120-question, online, open-book exam for all diplomates recertifying must be significantly cheaper to produce and administer than a secured 10-year exam. That being said, the cost of this new MOC program is $210 per year instead of a lump sum $2,100 to take the closed book exam every 10 years. Clearly, the boards feel a reduction in cost of production to the boards should not translate to a reduction in cost to the diplomates, and that the boards should actually generate even greater revenues.
The ABPN has also responded positively by forming an MOC clinical advisory committee to evaluate how MOC impacts practice and “potentially” improves patient care. Their use of the word “potentially” is particularly encouraging, because it implicitly suggests that evidence needs to be found to support that claim.
The future of board certification
The ABMS boards acknowledge that NBPAS exists as a legitimate alternative board, but they do not feel threatened at all. They are very confident that physicians, like sheep to be herded, will continue to blindly pay to do unnecessary work in the name of board certification.
Unfortunately for the ABMS boards, over 3,000 physicians have become diplomates of NBPAS, which has become accepted as a viable alternative to ABMS by an increasing number of hospital credentialing departments. It is only through an expanding number of diplomates that NBAPS can increase its acceptance and rival the inflexible, self-centered monopoly that ABMS has become.
With more institutions accepting NBPAS certification, the influence and leverage of NBPAS will grow, and physicians will be relieved of the burden of complying with costly and time-consuming requirements that do not improve practice. There is no harm in being dual-boarded, and becoming a diplomate of NBPAS prior to the expiration of an ABPN/ABMS board certification is a low-risk decision that supports a prophysician grassroots movement. During this time of unprecedented physician unity, organizations like NBPAS appear well positioned to help return the practice of medicine to physicians rather than detached administrators.
Dr. Mathew is a member of the Harvard Medical School Faculty. He is director of continuing medical education at the Brigham & Women’s Hospital, John R. Graham Headache Center, and is a staff neurologist at Harvard Vanguard Medical Associates and the Cambridge Health Alliance. He also serves as the neurology representative on the volunteer advisory board of the National Board of Physicians and Surgeons.
Who among us has not asked a patient to keep track of a mole?
“Keep an eye on that one, and call me if it changes,” is as much a stock phrase for dermatologists as “Wear your sunscreen.” Yet, how do patients know if a mole changes? I’m quite sure many of my patients wouldn’t notice if I shaved my head and grew a beard, let alone notice if 1 of 30 moles on their back changed color.
Mole Mapper is an iPhone app developed by the department of dermatology at Oregon Health and Science University (OHSU) to solve this problem. The app provides a framework for patients to photo, measure, and track their moles. With clear instructions, an anatomical map, and sophisticated markers, it is a significant aid for motivated patients who want medical-grade photos suitable for tracking.
To standardize the photos, the app prompts you to include a nickel, dime, or quarter in photos with nevi of interest. The user then calibrates the app by pinching onscreen circles overlying the photo such that they correspond exactly to the circumference of the coin and to the mole. Using a coin as a standard, the app then calculates the precise size of the mole regardless of the size of the photo. For example, photos taken 2 feet and 4 feet away both give the same diameter because both photos are calibrated by the dime in each.
The app was developed by a cancer biologist, Dan Webster, Ph.D., to help his wife monitor her moles between dermatology appointments. Interestingly, it was largely developed by a single person, a sign that creating apps is nearly entering into a DIY era. This increases the possibility for useful health care tools to be developed while also increasing the already crushing crowd of apps, few of which are truly useful.
The app’s functionality would not have been possible without the inclusion of Apple’s ResearchKit and Sage Bionetworks’ Bridge Server. ResearchKit provided open-source tools to facilitate informed consent over the phone and the ability to conduct participant surveys, among other activities. Bridge Server enabled the app to encrypt and securely transfer participant data from the phone to firewalled storage. The combination of these two software frameworks is paving the way for an exciting future of integrated technology and biomedical research.
According to Dan Webster, “ResearchKit is a game-changer because it provides an open-source platform for elegant informed consent, measurement tools, and participant data protection. The ability for participants to have so few barriers to contribute to a research study is the truly transformative aspect of ResearchKit, and we have seen unprecedented numbers of research study enrollees as a result.”
But that’s not all. The app is more than just a consumer tool for tracking – ResearchKit allows OHSU researchers to gather data on nevi, track them over time, and learn characteristics associated with melanoma from user-generated outcomes. This could significantly increase our understanding of melanoma and perhaps spawn an artificially intelligent app that learns to diagnose melanoma without human assistance.
Because of the institutional review board’s requirements for their research, users must be 18 years old to participate in the study. The app gracefully walks users through the consent process and even has a knowledge check at the end to ensure that they understood the risks and benefits of participating. The consent process is so streamlined that it ought to be a model for us to consent any patient for any reason.
To be clear, the app does not make diagnoses. It only provides a framework for patients to photograph their moles and track them. It also politely prompts users to rephotograph moles every 30 days so changes can be recorded.
There are apps with similar names, so be sure you have Mole Mapper from Sage Bionetworks. I tried it out to offer my experience here. Taking photos was as simple as any photo on an iPhone. Like any selfie, however, there are azimuth limits to the human arm – you can’t get shots in remote bodily corners easily. Also, placing a coin on yourself is easier said than done, unless you want to use your bubble gum to hold it in place while you take the shot. (I asked for assistance from my wife instead.)
The photos I took were accurate when compared with the measured diameter in real life, but there are still user-dependent adjustments that could lead to large artifacts. Making the measurement circles even slightly smaller or larger around the coin or the mole can lead to more than a millimeter of margins of error. If detecting melanoma requires less than 1-mm error in mole changes, then this could limit its usefulness.
Whether or not it leads to an app that automatically diagnoses melanoma from patient mole selfies, Mole Mapper has value. Any tool that empowers patients to be actively involved in their care and to meticulously monitor their moles will surely help us in keeping them safe.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter. He has no conflicts relating to the topic of this column.
“Keep an eye on that one, and call me if it changes,” is as much a stock phrase for dermatologists as “Wear your sunscreen.” Yet, how do patients know if a mole changes? I’m quite sure many of my patients wouldn’t notice if I shaved my head and grew a beard, let alone notice if 1 of 30 moles on their back changed color.
Mole Mapper is an iPhone app developed by the department of dermatology at Oregon Health and Science University (OHSU) to solve this problem. The app provides a framework for patients to photo, measure, and track their moles. With clear instructions, an anatomical map, and sophisticated markers, it is a significant aid for motivated patients who want medical-grade photos suitable for tracking.
To standardize the photos, the app prompts you to include a nickel, dime, or quarter in photos with nevi of interest. The user then calibrates the app by pinching onscreen circles overlying the photo such that they correspond exactly to the circumference of the coin and to the mole. Using a coin as a standard, the app then calculates the precise size of the mole regardless of the size of the photo. For example, photos taken 2 feet and 4 feet away both give the same diameter because both photos are calibrated by the dime in each.
The app was developed by a cancer biologist, Dan Webster, Ph.D., to help his wife monitor her moles between dermatology appointments. Interestingly, it was largely developed by a single person, a sign that creating apps is nearly entering into a DIY era. This increases the possibility for useful health care tools to be developed while also increasing the already crushing crowd of apps, few of which are truly useful.
The app’s functionality would not have been possible without the inclusion of Apple’s ResearchKit and Sage Bionetworks’ Bridge Server. ResearchKit provided open-source tools to facilitate informed consent over the phone and the ability to conduct participant surveys, among other activities. Bridge Server enabled the app to encrypt and securely transfer participant data from the phone to firewalled storage. The combination of these two software frameworks is paving the way for an exciting future of integrated technology and biomedical research.
According to Dan Webster, “ResearchKit is a game-changer because it provides an open-source platform for elegant informed consent, measurement tools, and participant data protection. The ability for participants to have so few barriers to contribute to a research study is the truly transformative aspect of ResearchKit, and we have seen unprecedented numbers of research study enrollees as a result.”
But that’s not all. The app is more than just a consumer tool for tracking – ResearchKit allows OHSU researchers to gather data on nevi, track them over time, and learn characteristics associated with melanoma from user-generated outcomes. This could significantly increase our understanding of melanoma and perhaps spawn an artificially intelligent app that learns to diagnose melanoma without human assistance.
Because of the institutional review board’s requirements for their research, users must be 18 years old to participate in the study. The app gracefully walks users through the consent process and even has a knowledge check at the end to ensure that they understood the risks and benefits of participating. The consent process is so streamlined that it ought to be a model for us to consent any patient for any reason.
To be clear, the app does not make diagnoses. It only provides a framework for patients to photograph their moles and track them. It also politely prompts users to rephotograph moles every 30 days so changes can be recorded.
There are apps with similar names, so be sure you have Mole Mapper from Sage Bionetworks. I tried it out to offer my experience here. Taking photos was as simple as any photo on an iPhone. Like any selfie, however, there are azimuth limits to the human arm – you can’t get shots in remote bodily corners easily. Also, placing a coin on yourself is easier said than done, unless you want to use your bubble gum to hold it in place while you take the shot. (I asked for assistance from my wife instead.)
The photos I took were accurate when compared with the measured diameter in real life, but there are still user-dependent adjustments that could lead to large artifacts. Making the measurement circles even slightly smaller or larger around the coin or the mole can lead to more than a millimeter of margins of error. If detecting melanoma requires less than 1-mm error in mole changes, then this could limit its usefulness.
Whether or not it leads to an app that automatically diagnoses melanoma from patient mole selfies, Mole Mapper has value. Any tool that empowers patients to be actively involved in their care and to meticulously monitor their moles will surely help us in keeping them safe.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter. He has no conflicts relating to the topic of this column.
“Keep an eye on that one, and call me if it changes,” is as much a stock phrase for dermatologists as “Wear your sunscreen.” Yet, how do patients know if a mole changes? I’m quite sure many of my patients wouldn’t notice if I shaved my head and grew a beard, let alone notice if 1 of 30 moles on their back changed color.
Mole Mapper is an iPhone app developed by the department of dermatology at Oregon Health and Science University (OHSU) to solve this problem. The app provides a framework for patients to photo, measure, and track their moles. With clear instructions, an anatomical map, and sophisticated markers, it is a significant aid for motivated patients who want medical-grade photos suitable for tracking.
To standardize the photos, the app prompts you to include a nickel, dime, or quarter in photos with nevi of interest. The user then calibrates the app by pinching onscreen circles overlying the photo such that they correspond exactly to the circumference of the coin and to the mole. Using a coin as a standard, the app then calculates the precise size of the mole regardless of the size of the photo. For example, photos taken 2 feet and 4 feet away both give the same diameter because both photos are calibrated by the dime in each.
The app was developed by a cancer biologist, Dan Webster, Ph.D., to help his wife monitor her moles between dermatology appointments. Interestingly, it was largely developed by a single person, a sign that creating apps is nearly entering into a DIY era. This increases the possibility for useful health care tools to be developed while also increasing the already crushing crowd of apps, few of which are truly useful.
The app’s functionality would not have been possible without the inclusion of Apple’s ResearchKit and Sage Bionetworks’ Bridge Server. ResearchKit provided open-source tools to facilitate informed consent over the phone and the ability to conduct participant surveys, among other activities. Bridge Server enabled the app to encrypt and securely transfer participant data from the phone to firewalled storage. The combination of these two software frameworks is paving the way for an exciting future of integrated technology and biomedical research.
According to Dan Webster, “ResearchKit is a game-changer because it provides an open-source platform for elegant informed consent, measurement tools, and participant data protection. The ability for participants to have so few barriers to contribute to a research study is the truly transformative aspect of ResearchKit, and we have seen unprecedented numbers of research study enrollees as a result.”
But that’s not all. The app is more than just a consumer tool for tracking – ResearchKit allows OHSU researchers to gather data on nevi, track them over time, and learn characteristics associated with melanoma from user-generated outcomes. This could significantly increase our understanding of melanoma and perhaps spawn an artificially intelligent app that learns to diagnose melanoma without human assistance.
Because of the institutional review board’s requirements for their research, users must be 18 years old to participate in the study. The app gracefully walks users through the consent process and even has a knowledge check at the end to ensure that they understood the risks and benefits of participating. The consent process is so streamlined that it ought to be a model for us to consent any patient for any reason.
To be clear, the app does not make diagnoses. It only provides a framework for patients to photograph their moles and track them. It also politely prompts users to rephotograph moles every 30 days so changes can be recorded.
There are apps with similar names, so be sure you have Mole Mapper from Sage Bionetworks. I tried it out to offer my experience here. Taking photos was as simple as any photo on an iPhone. Like any selfie, however, there are azimuth limits to the human arm – you can’t get shots in remote bodily corners easily. Also, placing a coin on yourself is easier said than done, unless you want to use your bubble gum to hold it in place while you take the shot. (I asked for assistance from my wife instead.)
The photos I took were accurate when compared with the measured diameter in real life, but there are still user-dependent adjustments that could lead to large artifacts. Making the measurement circles even slightly smaller or larger around the coin or the mole can lead to more than a millimeter of margins of error. If detecting melanoma requires less than 1-mm error in mole changes, then this could limit its usefulness.
Whether or not it leads to an app that automatically diagnoses melanoma from patient mole selfies, Mole Mapper has value. Any tool that empowers patients to be actively involved in their care and to meticulously monitor their moles will surely help us in keeping them safe.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter. He has no conflicts relating to the topic of this column.
Elephant in the room of dermatology
I have become increasingly dismayed by reports of dermatologists who allow their nurse practitioners and physician assistants to practice independently.
That is, the employing dermatologists only see the patients, new or established, if they are asked to, and often are not even on the premises. In fact, they might be thousands of miles away.
A little background is in order. Physician assistants and nurse practitioners are formally trained in primary care, not in dermatology, although there are currently three 1-year programs to help them specialize in dermatology. When Congress authorized their independent payment in 1997, they envisioned primary care nurses traveling the hills, hollers, and inner cities improving health care. Unfortunately, this hasn’t happened, and instead they have moved into suburban America, and increasingly, are practicing specialty medicine.
It can be argued that decreased access to primary care, which was the reason midlevels were created, is more important than is access to dermatology. In particular, extenders have targeted office-based specialties such as dermatology, but also neurology and pain medicine. These specialties are office based, and credentialing by hospitals is not required to bill insurance plans. Also, these specialties have good-paying, seemingly simple, small procedures. They have accomplished this with the avid help of dermatologists, I might add. There will be an estimated 10,000 “dermatology” nurse practitioners and physician assistants next year.
Let me be clear: I am not opposed to a dermatology extender who works closely with a dermatologist and does intake histories and physicals, then staffs with the physician, assists with surgery, or sees routine follow-ups (think acne, psoriasis, atopy, suture removal, and warts) on an established protocol with the full knowledge of the patient.
This is not what we are seeing. We have nurse practitioners buying retiring dermatologists’ practices, physician assistants independently setting up remote clinics then hiring “supervising” dermatologists to visit once a week to sign and review charts, and independent “dermatology” clinics with a doctor thousands of miles away available, if really needed, by telephone or the Internet. (This is not really telemedicine, is it?) These extenders are listed as dermatologists on the Internet, or they hide behind the name of a dermatologist, and when you call their offices, and ask if you will see a “real” dermatologist, the answer is often “Oh, don’t worry, our nurse or PA specializes in dermatology.”
I think this is grossly unfair to patients, who, when they call the dermatology center listed on the Internet, can’t conceive that their dermatology appointment is not being made with a dermatologist, not even being made with a physician, but with a nurse practitioner or physician assistant! I also think it does a huge disservice to the specialty. The “collaborating” dermatologists enabling these extenders are renting out the good name of our specialty.
Patients seen by these extenders may also be subject to unnecessary biopsies. (If you don’t know what it is, you must biopsy it!) It also results in additional charges for pathology and additional medical misadventures.
In addition, I think it is unfair to the extender who is put in this situation. They may have worked in a dermatologist’s office for a few months or even years but are now being asked to pretend to be something they are not and being expected to perform at the level of a medical professional who has had many years of intense, focused training in dermatology. If they are not uncomfortable being thrust into this situation, then they are delusional.
I think it is unfair to the medical system who pays for the less informed opinion and unnecessary procedures. This is not a “good value” except to the rent-seeking dermatologists, who are the front men for this money-making deception.
This is an elephant in the room of dermatology, and I think we have to confront it. This trivializes our specialty and helps allow other specialties and regulatory agencies to ignore or exclude us from the networks and from the conversation. Unfortunately, many of our members and some of our leadership have been corrupted by the “easy money” or “easy time” afforded by this cheapening of the specialty.
Let me give you some examples. The rent seekers piously claim, “there is a shortage of dermatologists, and we are just trying to help save the world.” They also say “my nurses are special and great.”
The honest ones in private practice, however, say, “Man, I make $200,000 a year off my PA while I am off.” The honest academics say, “Listen, I work in a gulag, and I would never be able to travel if my nurses didn’t see my patients.” Time is money, and the academic who gets an extra 10 hours a week out of clinic is benefiting as much as the guy who makes $200,000 a year.
Of course, this situation is not sustainable and will become less viable because of a coming tsunami of malpractice claims, more focused insurer benchmarks revealing excessive test ordering and minor procedures, and patients getting wise. One obvious solution to this would be to reimburse extenders only for evaluation and management codes, which will take a change in law.
Meanwhile, I encourage all of you who feel the same nausea I do to ask candidates for your state and national dermatology organizations if they employ unsupervised extenders. Then check their website for the names of the extenders they employ. Then go to the Medicare data and look up their extenders and see if they bill independently for dermatologic procedures. I think you will be very disturbed, as I was and am.
I hope this stimulates a little self-examination among dermatologists.
Dr. Coldiron is a past-president of the American Academy of Dermatology. He is currently in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. Reach him at [email protected].
I have become increasingly dismayed by reports of dermatologists who allow their nurse practitioners and physician assistants to practice independently.
That is, the employing dermatologists only see the patients, new or established, if they are asked to, and often are not even on the premises. In fact, they might be thousands of miles away.
A little background is in order. Physician assistants and nurse practitioners are formally trained in primary care, not in dermatology, although there are currently three 1-year programs to help them specialize in dermatology. When Congress authorized their independent payment in 1997, they envisioned primary care nurses traveling the hills, hollers, and inner cities improving health care. Unfortunately, this hasn’t happened, and instead they have moved into suburban America, and increasingly, are practicing specialty medicine.
It can be argued that decreased access to primary care, which was the reason midlevels were created, is more important than is access to dermatology. In particular, extenders have targeted office-based specialties such as dermatology, but also neurology and pain medicine. These specialties are office based, and credentialing by hospitals is not required to bill insurance plans. Also, these specialties have good-paying, seemingly simple, small procedures. They have accomplished this with the avid help of dermatologists, I might add. There will be an estimated 10,000 “dermatology” nurse practitioners and physician assistants next year.
Let me be clear: I am not opposed to a dermatology extender who works closely with a dermatologist and does intake histories and physicals, then staffs with the physician, assists with surgery, or sees routine follow-ups (think acne, psoriasis, atopy, suture removal, and warts) on an established protocol with the full knowledge of the patient.
This is not what we are seeing. We have nurse practitioners buying retiring dermatologists’ practices, physician assistants independently setting up remote clinics then hiring “supervising” dermatologists to visit once a week to sign and review charts, and independent “dermatology” clinics with a doctor thousands of miles away available, if really needed, by telephone or the Internet. (This is not really telemedicine, is it?) These extenders are listed as dermatologists on the Internet, or they hide behind the name of a dermatologist, and when you call their offices, and ask if you will see a “real” dermatologist, the answer is often “Oh, don’t worry, our nurse or PA specializes in dermatology.”
I think this is grossly unfair to patients, who, when they call the dermatology center listed on the Internet, can’t conceive that their dermatology appointment is not being made with a dermatologist, not even being made with a physician, but with a nurse practitioner or physician assistant! I also think it does a huge disservice to the specialty. The “collaborating” dermatologists enabling these extenders are renting out the good name of our specialty.
Patients seen by these extenders may also be subject to unnecessary biopsies. (If you don’t know what it is, you must biopsy it!) It also results in additional charges for pathology and additional medical misadventures.
In addition, I think it is unfair to the extender who is put in this situation. They may have worked in a dermatologist’s office for a few months or even years but are now being asked to pretend to be something they are not and being expected to perform at the level of a medical professional who has had many years of intense, focused training in dermatology. If they are not uncomfortable being thrust into this situation, then they are delusional.
I think it is unfair to the medical system who pays for the less informed opinion and unnecessary procedures. This is not a “good value” except to the rent-seeking dermatologists, who are the front men for this money-making deception.
This is an elephant in the room of dermatology, and I think we have to confront it. This trivializes our specialty and helps allow other specialties and regulatory agencies to ignore or exclude us from the networks and from the conversation. Unfortunately, many of our members and some of our leadership have been corrupted by the “easy money” or “easy time” afforded by this cheapening of the specialty.
Let me give you some examples. The rent seekers piously claim, “there is a shortage of dermatologists, and we are just trying to help save the world.” They also say “my nurses are special and great.”
The honest ones in private practice, however, say, “Man, I make $200,000 a year off my PA while I am off.” The honest academics say, “Listen, I work in a gulag, and I would never be able to travel if my nurses didn’t see my patients.” Time is money, and the academic who gets an extra 10 hours a week out of clinic is benefiting as much as the guy who makes $200,000 a year.
Of course, this situation is not sustainable and will become less viable because of a coming tsunami of malpractice claims, more focused insurer benchmarks revealing excessive test ordering and minor procedures, and patients getting wise. One obvious solution to this would be to reimburse extenders only for evaluation and management codes, which will take a change in law.
Meanwhile, I encourage all of you who feel the same nausea I do to ask candidates for your state and national dermatology organizations if they employ unsupervised extenders. Then check their website for the names of the extenders they employ. Then go to the Medicare data and look up their extenders and see if they bill independently for dermatologic procedures. I think you will be very disturbed, as I was and am.
I hope this stimulates a little self-examination among dermatologists.
Dr. Coldiron is a past-president of the American Academy of Dermatology. He is currently in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. Reach him at [email protected].
I have become increasingly dismayed by reports of dermatologists who allow their nurse practitioners and physician assistants to practice independently.
That is, the employing dermatologists only see the patients, new or established, if they are asked to, and often are not even on the premises. In fact, they might be thousands of miles away.
A little background is in order. Physician assistants and nurse practitioners are formally trained in primary care, not in dermatology, although there are currently three 1-year programs to help them specialize in dermatology. When Congress authorized their independent payment in 1997, they envisioned primary care nurses traveling the hills, hollers, and inner cities improving health care. Unfortunately, this hasn’t happened, and instead they have moved into suburban America, and increasingly, are practicing specialty medicine.
It can be argued that decreased access to primary care, which was the reason midlevels were created, is more important than is access to dermatology. In particular, extenders have targeted office-based specialties such as dermatology, but also neurology and pain medicine. These specialties are office based, and credentialing by hospitals is not required to bill insurance plans. Also, these specialties have good-paying, seemingly simple, small procedures. They have accomplished this with the avid help of dermatologists, I might add. There will be an estimated 10,000 “dermatology” nurse practitioners and physician assistants next year.
Let me be clear: I am not opposed to a dermatology extender who works closely with a dermatologist and does intake histories and physicals, then staffs with the physician, assists with surgery, or sees routine follow-ups (think acne, psoriasis, atopy, suture removal, and warts) on an established protocol with the full knowledge of the patient.
This is not what we are seeing. We have nurse practitioners buying retiring dermatologists’ practices, physician assistants independently setting up remote clinics then hiring “supervising” dermatologists to visit once a week to sign and review charts, and independent “dermatology” clinics with a doctor thousands of miles away available, if really needed, by telephone or the Internet. (This is not really telemedicine, is it?) These extenders are listed as dermatologists on the Internet, or they hide behind the name of a dermatologist, and when you call their offices, and ask if you will see a “real” dermatologist, the answer is often “Oh, don’t worry, our nurse or PA specializes in dermatology.”
I think this is grossly unfair to patients, who, when they call the dermatology center listed on the Internet, can’t conceive that their dermatology appointment is not being made with a dermatologist, not even being made with a physician, but with a nurse practitioner or physician assistant! I also think it does a huge disservice to the specialty. The “collaborating” dermatologists enabling these extenders are renting out the good name of our specialty.
Patients seen by these extenders may also be subject to unnecessary biopsies. (If you don’t know what it is, you must biopsy it!) It also results in additional charges for pathology and additional medical misadventures.
In addition, I think it is unfair to the extender who is put in this situation. They may have worked in a dermatologist’s office for a few months or even years but are now being asked to pretend to be something they are not and being expected to perform at the level of a medical professional who has had many years of intense, focused training in dermatology. If they are not uncomfortable being thrust into this situation, then they are delusional.
I think it is unfair to the medical system who pays for the less informed opinion and unnecessary procedures. This is not a “good value” except to the rent-seeking dermatologists, who are the front men for this money-making deception.
This is an elephant in the room of dermatology, and I think we have to confront it. This trivializes our specialty and helps allow other specialties and regulatory agencies to ignore or exclude us from the networks and from the conversation. Unfortunately, many of our members and some of our leadership have been corrupted by the “easy money” or “easy time” afforded by this cheapening of the specialty.
Let me give you some examples. The rent seekers piously claim, “there is a shortage of dermatologists, and we are just trying to help save the world.” They also say “my nurses are special and great.”
The honest ones in private practice, however, say, “Man, I make $200,000 a year off my PA while I am off.” The honest academics say, “Listen, I work in a gulag, and I would never be able to travel if my nurses didn’t see my patients.” Time is money, and the academic who gets an extra 10 hours a week out of clinic is benefiting as much as the guy who makes $200,000 a year.
Of course, this situation is not sustainable and will become less viable because of a coming tsunami of malpractice claims, more focused insurer benchmarks revealing excessive test ordering and minor procedures, and patients getting wise. One obvious solution to this would be to reimburse extenders only for evaluation and management codes, which will take a change in law.
Meanwhile, I encourage all of you who feel the same nausea I do to ask candidates for your state and national dermatology organizations if they employ unsupervised extenders. Then check their website for the names of the extenders they employ. Then go to the Medicare data and look up their extenders and see if they bill independently for dermatologic procedures. I think you will be very disturbed, as I was and am.
I hope this stimulates a little self-examination among dermatologists.
Dr. Coldiron is a past-president of the American Academy of Dermatology. He is currently in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. Reach him at [email protected].
A bone to pick
I have had a long and circuitous relationship with the radius. When I was 9 years old, I slipped on the wet grass of our front yard in an attempt to make a highlight-reel baseball catch and landed awkwardly on my left arm. After I continued to complain for a day and a half, my mother took me to see our pediatrician, Dr. Blum. After feeling up and down my forearm and asking me to squeeze his fingers, he pronounced me well.
A week and a half later, when I was still favoring what is my dominant arm, we returned to Dr. Blum. Apparently still unimpressed with my physical exam, he begrudgingly ordered an x-ray. Hurrah! I had a fracture! But then he announced that we would treat it with a splint and an ace wrap. Come on! Everyone knows that if you break a bone you get a cast. From then on he was Dr. Bum to me.
For the next 2 weeks, I was forbidden to play sports, meanwhile losing serious credibility points with my peers who suspected that I was a wimp and had fabricated the whole story. And of course, does anyone go around asking their friends to sign his ace wrap ... really? It took me years of overcompensation to regain even a hint of preteen machismo.
During my last year of medical school, I leapt at the opportunity to take an elective in pediatric orthopedics. It was great! With coaching from the residents, I learned when to suspect a buckle fracture of the radius, identify it on x-ray, and best of all, how to apply a cast.
When I finally entered practice here in Brunswick, we were seriously short of specialists, including orthopedists. When it was discovered that I knew how to apply a forearm cast, the orthopedists encouraged me to treat my own patients with simple forearm fractures. They were more than busy enough with really exciting stuff.
As an artist at heart, the chance to mold in plaster and plastic was a special treat. I took great pride in my creations, and making a beautiful crafted cast was sometimes the high point of my day. No splints or wimpy ace wraps for my patients!
Parents loved the one-stop shopping. History, exam, x-ray, casting, and out the door in less than an hour. Because I was the only primary care physician in town who was casting fractures, I occasionally had to remind the emergency room physicians to send me my patients with buckle fractures instead of knee-jerking a referral to an orthopedist.
But then about 10 years ago, some party-pooping orthopedists from who-knows-where looked at a very large series of pediatric patients with buckle fractures of the radius and discovered that those patients treated with splints had at least as good results as those who had been casted. And ... the patients and parents preferred the splints. I had to admit that maybe Dr. Blum wasn’t such a bum after all. Sadly, I had to respond to the evidence by giving up my hobby except when a child’s temperament or past history of injury suggested that he or she might benefit from the extra protection a cast could afford.
A recent study from Toronto published in Pediatrics, “Primary Care Physician Follow-up of Distal Radius Buckle Fractures,” by Koelink et al., makes me wonder whether a splint and ace wrap may even be overtreatment (Pediatrics. 2016 Jan;137[1]:11-9. doi: 10.1542/peds.2015-2262). In this review of 200 pediatric patients with distal radius buckle fractures, the investigators found that regardless of whether the primary care physician discussed how long to use the splint or when to return to activity, more than two-thirds of the patients wore their splints less than 3 weeks. Despite what the authors considered suboptimal primary care physician guidance, 99% of the patients returned to usual activities within 4 weeks.
My mother and Dr. Blum were on the right track from the beginning. They just needed to ignore my complaints a few days longer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
I have had a long and circuitous relationship with the radius. When I was 9 years old, I slipped on the wet grass of our front yard in an attempt to make a highlight-reel baseball catch and landed awkwardly on my left arm. After I continued to complain for a day and a half, my mother took me to see our pediatrician, Dr. Blum. After feeling up and down my forearm and asking me to squeeze his fingers, he pronounced me well.
A week and a half later, when I was still favoring what is my dominant arm, we returned to Dr. Blum. Apparently still unimpressed with my physical exam, he begrudgingly ordered an x-ray. Hurrah! I had a fracture! But then he announced that we would treat it with a splint and an ace wrap. Come on! Everyone knows that if you break a bone you get a cast. From then on he was Dr. Bum to me.
For the next 2 weeks, I was forbidden to play sports, meanwhile losing serious credibility points with my peers who suspected that I was a wimp and had fabricated the whole story. And of course, does anyone go around asking their friends to sign his ace wrap ... really? It took me years of overcompensation to regain even a hint of preteen machismo.
During my last year of medical school, I leapt at the opportunity to take an elective in pediatric orthopedics. It was great! With coaching from the residents, I learned when to suspect a buckle fracture of the radius, identify it on x-ray, and best of all, how to apply a cast.
When I finally entered practice here in Brunswick, we were seriously short of specialists, including orthopedists. When it was discovered that I knew how to apply a forearm cast, the orthopedists encouraged me to treat my own patients with simple forearm fractures. They were more than busy enough with really exciting stuff.
As an artist at heart, the chance to mold in plaster and plastic was a special treat. I took great pride in my creations, and making a beautiful crafted cast was sometimes the high point of my day. No splints or wimpy ace wraps for my patients!
Parents loved the one-stop shopping. History, exam, x-ray, casting, and out the door in less than an hour. Because I was the only primary care physician in town who was casting fractures, I occasionally had to remind the emergency room physicians to send me my patients with buckle fractures instead of knee-jerking a referral to an orthopedist.
But then about 10 years ago, some party-pooping orthopedists from who-knows-where looked at a very large series of pediatric patients with buckle fractures of the radius and discovered that those patients treated with splints had at least as good results as those who had been casted. And ... the patients and parents preferred the splints. I had to admit that maybe Dr. Blum wasn’t such a bum after all. Sadly, I had to respond to the evidence by giving up my hobby except when a child’s temperament or past history of injury suggested that he or she might benefit from the extra protection a cast could afford.
A recent study from Toronto published in Pediatrics, “Primary Care Physician Follow-up of Distal Radius Buckle Fractures,” by Koelink et al., makes me wonder whether a splint and ace wrap may even be overtreatment (Pediatrics. 2016 Jan;137[1]:11-9. doi: 10.1542/peds.2015-2262). In this review of 200 pediatric patients with distal radius buckle fractures, the investigators found that regardless of whether the primary care physician discussed how long to use the splint or when to return to activity, more than two-thirds of the patients wore their splints less than 3 weeks. Despite what the authors considered suboptimal primary care physician guidance, 99% of the patients returned to usual activities within 4 weeks.
My mother and Dr. Blum were on the right track from the beginning. They just needed to ignore my complaints a few days longer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
I have had a long and circuitous relationship with the radius. When I was 9 years old, I slipped on the wet grass of our front yard in an attempt to make a highlight-reel baseball catch and landed awkwardly on my left arm. After I continued to complain for a day and a half, my mother took me to see our pediatrician, Dr. Blum. After feeling up and down my forearm and asking me to squeeze his fingers, he pronounced me well.
A week and a half later, when I was still favoring what is my dominant arm, we returned to Dr. Blum. Apparently still unimpressed with my physical exam, he begrudgingly ordered an x-ray. Hurrah! I had a fracture! But then he announced that we would treat it with a splint and an ace wrap. Come on! Everyone knows that if you break a bone you get a cast. From then on he was Dr. Bum to me.
For the next 2 weeks, I was forbidden to play sports, meanwhile losing serious credibility points with my peers who suspected that I was a wimp and had fabricated the whole story. And of course, does anyone go around asking their friends to sign his ace wrap ... really? It took me years of overcompensation to regain even a hint of preteen machismo.
During my last year of medical school, I leapt at the opportunity to take an elective in pediatric orthopedics. It was great! With coaching from the residents, I learned when to suspect a buckle fracture of the radius, identify it on x-ray, and best of all, how to apply a cast.
When I finally entered practice here in Brunswick, we were seriously short of specialists, including orthopedists. When it was discovered that I knew how to apply a forearm cast, the orthopedists encouraged me to treat my own patients with simple forearm fractures. They were more than busy enough with really exciting stuff.
As an artist at heart, the chance to mold in plaster and plastic was a special treat. I took great pride in my creations, and making a beautiful crafted cast was sometimes the high point of my day. No splints or wimpy ace wraps for my patients!
Parents loved the one-stop shopping. History, exam, x-ray, casting, and out the door in less than an hour. Because I was the only primary care physician in town who was casting fractures, I occasionally had to remind the emergency room physicians to send me my patients with buckle fractures instead of knee-jerking a referral to an orthopedist.
But then about 10 years ago, some party-pooping orthopedists from who-knows-where looked at a very large series of pediatric patients with buckle fractures of the radius and discovered that those patients treated with splints had at least as good results as those who had been casted. And ... the patients and parents preferred the splints. I had to admit that maybe Dr. Blum wasn’t such a bum after all. Sadly, I had to respond to the evidence by giving up my hobby except when a child’s temperament or past history of injury suggested that he or she might benefit from the extra protection a cast could afford.
A recent study from Toronto published in Pediatrics, “Primary Care Physician Follow-up of Distal Radius Buckle Fractures,” by Koelink et al., makes me wonder whether a splint and ace wrap may even be overtreatment (Pediatrics. 2016 Jan;137[1]:11-9. doi: 10.1542/peds.2015-2262). In this review of 200 pediatric patients with distal radius buckle fractures, the investigators found that regardless of whether the primary care physician discussed how long to use the splint or when to return to activity, more than two-thirds of the patients wore their splints less than 3 weeks. Despite what the authors considered suboptimal primary care physician guidance, 99% of the patients returned to usual activities within 4 weeks.
My mother and Dr. Blum were on the right track from the beginning. They just needed to ignore my complaints a few days longer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
What is a weekend?
In her role as the Dowager Countess on Public Broadcasting Service’s Downton Abbey, Maggie Smith has delivered many memorable one-liners, but none as revealing of her character’s social isolation as the clueless query, “What is a weekend?” How could anyone not appreciate the qualitative differences between the first 4 days of the week and the trio of Friday, Saturday, and Sunday?
A recent study by two Stanford University sociologists suggests that one doesn’t even need to have a job to place a higher value on the weekend (“You Don’t Need More Free Time,” by Cristobal Young, New York Times, Jan. 8, 2016). Using data from more than 500,000 respondents to a Gallup Daily Poll, the investigators found that a variety of indicators of well-being were lowest during the beginning of the workweek and then not surprisingly began to climb on Friday, reaching a peak on Saturday and Sunday. However, it turns out that the emotions of the unemployed respondents tracked exactly the same pattern as those of the people who had jobs.
In an effort to explain this unexpected finding, one of the investigators points out that time, particularly free time, is a “network good.” And in sociologist lingo, “Network goods are things that derive their value from being widely shared.” Although someone without a job may have an abundance of free time, the majority of the people with whom he or she could share that time are busy at work.
This study suggests that you may feel that you would be happier if you had more time off from work; part of the problem may be that there is a mismatch between your schedule and the schedules of the people and activities that you value most. You may have done this kind of self-assessment when you were looking for a job, but how successful were you in negotiating your schedule? Have you been able to renegotiate your schedule to match changes in your social situation? Spouse? Children?
How creative have you been in seeking out arrangements with coworkers who don’t share your time-off value profile? Although you might be tempted to say that based on this recent Stanford study, everyone places the same high value on weekend time off, is this really the case? There are a few people out there whose interests, personalities, and social situations make them value time off when you would just as soon work.
For example, I recently encountered a new word as I was scanning the classified advertisements in the back of this month’s Pediatrics. A hospital in California was looking for a “nocturnist.” An Internet search quickly confirmed my suspicion that a nocturnist is a physician, often a hospitalist, who prefers to work the night shift. Now, it may be just for the money, but if I were an avid birdwatcher, I can imagine wanting to maximize my time off when the sun was up.
Of course the trick is finding those coworkers whose lifestyles are as dissimilar from yours as possible ... and who are willing to trade work schedules. While I think that on many campuses, “diversity” has become an overused buzzword, diversity at your workplace might give you the best chance of finding a time-off arrangement that better matches your value profile.
Finally, if you are really unhappy, it may be time to swallow hard and entertain an arrangement in which you worked more and actually had less total free time, but the time you do have off is time you can share with the people you value and the activities you enjoy. It’s all about choosing the right set of compromises and learning to live with them. Good luck!
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
In her role as the Dowager Countess on Public Broadcasting Service’s Downton Abbey, Maggie Smith has delivered many memorable one-liners, but none as revealing of her character’s social isolation as the clueless query, “What is a weekend?” How could anyone not appreciate the qualitative differences between the first 4 days of the week and the trio of Friday, Saturday, and Sunday?
A recent study by two Stanford University sociologists suggests that one doesn’t even need to have a job to place a higher value on the weekend (“You Don’t Need More Free Time,” by Cristobal Young, New York Times, Jan. 8, 2016). Using data from more than 500,000 respondents to a Gallup Daily Poll, the investigators found that a variety of indicators of well-being were lowest during the beginning of the workweek and then not surprisingly began to climb on Friday, reaching a peak on Saturday and Sunday. However, it turns out that the emotions of the unemployed respondents tracked exactly the same pattern as those of the people who had jobs.
In an effort to explain this unexpected finding, one of the investigators points out that time, particularly free time, is a “network good.” And in sociologist lingo, “Network goods are things that derive their value from being widely shared.” Although someone without a job may have an abundance of free time, the majority of the people with whom he or she could share that time are busy at work.
This study suggests that you may feel that you would be happier if you had more time off from work; part of the problem may be that there is a mismatch between your schedule and the schedules of the people and activities that you value most. You may have done this kind of self-assessment when you were looking for a job, but how successful were you in negotiating your schedule? Have you been able to renegotiate your schedule to match changes in your social situation? Spouse? Children?
How creative have you been in seeking out arrangements with coworkers who don’t share your time-off value profile? Although you might be tempted to say that based on this recent Stanford study, everyone places the same high value on weekend time off, is this really the case? There are a few people out there whose interests, personalities, and social situations make them value time off when you would just as soon work.
For example, I recently encountered a new word as I was scanning the classified advertisements in the back of this month’s Pediatrics. A hospital in California was looking for a “nocturnist.” An Internet search quickly confirmed my suspicion that a nocturnist is a physician, often a hospitalist, who prefers to work the night shift. Now, it may be just for the money, but if I were an avid birdwatcher, I can imagine wanting to maximize my time off when the sun was up.
Of course the trick is finding those coworkers whose lifestyles are as dissimilar from yours as possible ... and who are willing to trade work schedules. While I think that on many campuses, “diversity” has become an overused buzzword, diversity at your workplace might give you the best chance of finding a time-off arrangement that better matches your value profile.
Finally, if you are really unhappy, it may be time to swallow hard and entertain an arrangement in which you worked more and actually had less total free time, but the time you do have off is time you can share with the people you value and the activities you enjoy. It’s all about choosing the right set of compromises and learning to live with them. Good luck!
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
In her role as the Dowager Countess on Public Broadcasting Service’s Downton Abbey, Maggie Smith has delivered many memorable one-liners, but none as revealing of her character’s social isolation as the clueless query, “What is a weekend?” How could anyone not appreciate the qualitative differences between the first 4 days of the week and the trio of Friday, Saturday, and Sunday?
A recent study by two Stanford University sociologists suggests that one doesn’t even need to have a job to place a higher value on the weekend (“You Don’t Need More Free Time,” by Cristobal Young, New York Times, Jan. 8, 2016). Using data from more than 500,000 respondents to a Gallup Daily Poll, the investigators found that a variety of indicators of well-being were lowest during the beginning of the workweek and then not surprisingly began to climb on Friday, reaching a peak on Saturday and Sunday. However, it turns out that the emotions of the unemployed respondents tracked exactly the same pattern as those of the people who had jobs.
In an effort to explain this unexpected finding, one of the investigators points out that time, particularly free time, is a “network good.” And in sociologist lingo, “Network goods are things that derive their value from being widely shared.” Although someone without a job may have an abundance of free time, the majority of the people with whom he or she could share that time are busy at work.
This study suggests that you may feel that you would be happier if you had more time off from work; part of the problem may be that there is a mismatch between your schedule and the schedules of the people and activities that you value most. You may have done this kind of self-assessment when you were looking for a job, but how successful were you in negotiating your schedule? Have you been able to renegotiate your schedule to match changes in your social situation? Spouse? Children?
How creative have you been in seeking out arrangements with coworkers who don’t share your time-off value profile? Although you might be tempted to say that based on this recent Stanford study, everyone places the same high value on weekend time off, is this really the case? There are a few people out there whose interests, personalities, and social situations make them value time off when you would just as soon work.
For example, I recently encountered a new word as I was scanning the classified advertisements in the back of this month’s Pediatrics. A hospital in California was looking for a “nocturnist.” An Internet search quickly confirmed my suspicion that a nocturnist is a physician, often a hospitalist, who prefers to work the night shift. Now, it may be just for the money, but if I were an avid birdwatcher, I can imagine wanting to maximize my time off when the sun was up.
Of course the trick is finding those coworkers whose lifestyles are as dissimilar from yours as possible ... and who are willing to trade work schedules. While I think that on many campuses, “diversity” has become an overused buzzword, diversity at your workplace might give you the best chance of finding a time-off arrangement that better matches your value profile.
Finally, if you are really unhappy, it may be time to swallow hard and entertain an arrangement in which you worked more and actually had less total free time, but the time you do have off is time you can share with the people you value and the activities you enjoy. It’s all about choosing the right set of compromises and learning to live with them. Good luck!
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
A Perfect Storm: Tumor biology and genomics
This is the second installment of a five-part monthly series that will discuss the pathologic, genomic, and clinical factors that contribute to the racial survival disparity in breast cancer. The series, which is adapted from an article that originally appeared in CA: A Cancer Journal for Clinicians1, a journal of the American Cancer Society, will also review exciting and innovative interventions to close this survival gap. This month’s column reviews tumor biology and genomics—the first element in the perfect storm.
Hormone receptor status and human epidermal growth factor receptor 2 (HER2)/neu
Breast cancer is not a single disease, and breast cancer subtype classifications are used in the clinical setting to determine prognosis and guide management. These different molecular subtypes are based on tumor markers, which include the presence or absence of three proteins: estrogen receptor (ER), progesterone receptor (PR), and HER2/neu. Hormone receptor status is a main factor in planning breast cancer treatment. Hormone receptor–positive breast tumors benefit from hormone therapies, such as selective ER modulators (for example, tamoxifen) and aromatase inhibitors (for example, anastrozole). Thus, these tumors have a more favorable disease-specific survival than do hormone receptor–negative tumors.2
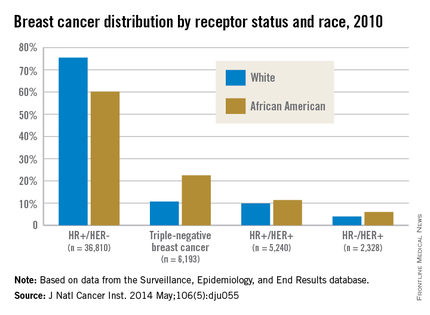
African American women are more likely to present with hormone receptor-negative tumors. In an analysis of the California Cancer Registry, which has collected patient ER and PR status since 1990, whites had a higher proportion of tumors that were ER positive or PR positive (or both) and HER2 negative (72% vs. 53%).3 DeSantis et al.4 reported similar results for this tumor type, with 76% of non-Hispanic whites having hormone receptor–positive, HER2-negative tumors vs. 62% of non-Hispanic blacks. Even with stratification by tumor stage, African Americans continue to have a significantly higher proportion of hormone receptor–negative tumors than do whites for localized and advanced disease.5
Although hormone receptor status varies significantly by race, HER2 status does not show the same divergence. HER2 overexpression is present in approximately 20% of invasive breast cancers. HER2-positive, hormone receptor–negative tumors demonstrate more-aggressive features and worse breast cancer–specific survival than do hormone receptor–positive and HER2-negative tumors,2 although survival has vastly improved with new HER2-targeted therapies such as trastuzumab and pertuzumab. Unlike hormone receptor status, there was no association between race and HER2-positive/ER-negative tumors in the Carolina Breast Cancer Study.2
Triple-negative breast cancer (TNBC)
TNBC is the subtype of breast cancer with the worst prognosis. TNBC gets its name because its tumor cells lack the markers for ER, PR, and HER2 overexpression. Thus, TNBC tumors are estrogen receptor negative (ER), progesterone receptor negative (PR), and HER2/neu negative (HER2). While other subtypes of breast cancer have benefited from drug development regarding hormonal therapies and HER2-targeted treatments, TNBC has not experienced the same pharmacologic breakthroughs.
As such, even after analyses control for the stage at diagnosis, women with this subtype have poorer survival than those with other breast cancers.6 African American women have a higher incidence of TNBC than white women.7 DeSantis et al.4 reported that 22% of breast cancers were triple negative in non-Hispanic black patients vs. only 11% in non-Hispanic white patients. The Carolina Breast Cancer Study found that 26% of African American women had TNBC, whereas 16% of non-African American women did.2 This subtype was most common among younger, premenopausal African American women (39% of diagnosed cancer subtypes). When TNBC patients were excluded from analysis in the Carolina Breast Cancer Study, breast cancer–specific survival remained significantly worse among premenopausal African American women, suggesting that although tumor biology in part explains the poor outcomes, the survival disparity story is more complex.
Germline mutations: BRCA1 and BRCA2 Mutations
In addition to tumor biology, cancer genomics has become increasingly important in determining cancer prognosis and guiding treatment. Approximately 5%-10% of breast cancer cases present in individuals with inherited mutations in autosomal dominant, highly penetrant breast cancer susceptibility genes.8 Accounting for 80%-90% of families containing multiple cases of breast and ovarian cancer, BRCA1 and BRCA2 germline mutations are the most common of the breast cancer susceptibility genes.9 These patients often are younger and have a higher-grade tumor that is hormone receptor negative, which also often matches the profile of the African American breast cancer patient.10
Despite similarities between BRCA1-associated breast cancers and breast cancer in African Americans, genetic abnormalities in African American breast cancer patients remain underresearched. Nanda et al.11 found that BRCA1 and BRCA2 mutations occur with appreciable frequency in high-risk families of African ancestry, with 28% testing positive for a deleterious mutation in one of these genes. This frequency was at a lower rate than that found in non-Hispanic, non-Jewish whites, who had a rate of 46%, because African Americans had a higher rate of polymorphisms or variants of unknown significance (44% vs. 12%). This large percentage of variants of unknown significance indicates that more analysis is needed to understand the clinical implications of these genetic variations. In another study from the Northern California site of the Breast Cancer Family Registry, the BRCA1 mutation prevalence was 16.7% in African American cases diagnosed under the age of 35 years vs. 7.2% in non-Hispanic, non-Ashkenazi Jewish whites in the same age category.12 High frequencies of mutations in BRCA1 and BRCA2 have also been reported in breast cancer patients of African ancestry from Nigeria and the Bahamas.13, 14
These results in African American patients highlight the need for further study of breast cancer genomics in minority populations. However, Armstrong et al.15 illuminated the existence of racial/ethnic disparities in patterns of referral to cancer risk clinics. In their study, African American women with a family history of breast or ovarian cancer were significantly less likely to undergo genetic counseling for BRCA1/2 testing than were white women with this family history. The results of this study were noteworthy for the magnitude of the disparity, with white women having almost five times greater odds of undergoing this clinically important evaluation. More than two decades after BRCA1 and BRCA2 genes were identified, larger studies are still needed in diverse populations to derive true estimates of the burden of mutations in both genes in underserved and understudied populations.
Although these differences in tumor biology and genomics tell part of the mortality disparity story, there is more to be told. In a study of African American and white patients in South Carolina, Adams et al.16 determined survival rates by ethnicity that were adjusted for disease stage and other prognostic characteristics. After they controlled for age, stage, ER, and HER2 expression as well as insurance status, African American women still had a twofold excess risk of death from breast cancer. Thus, in addition to differences in the innate characteristics of the breast tumors, racial differences in patterns of care for women with breast cancer must be considered in unraveling the observed disparity in mortality. The third installment of this series will discuss the second element of the perfect storm – patterns of care.
Other installments of this column can be found in the Related Content box.
1. Daly B, Olopade OI. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65(3):221-238.
2. Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492-502.
3. Kurian AW, Fish K, Shema SJ, Clarke CA. Lifetime risks of specific breast cancer subtypes among women in four racial/ethnic groups. Breast Cancer Res. 2010;12(6):R99.
4. DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2015 Oct 29. doi: 10.3322/caac.21320. [Epub ahead of print]
5. Setiawan VW, Monroe KR, Wilkens LR, Kolonel LN, Pike MC, Henderson BE. Breast cancer risk factors defined by estrogen and progesterone receptor status: the multiethnic cohort study. Am J Epidemiol. 2009;169(10):1251-9.
6. Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007;109(9):1721-8.
7. Ray M, Polite BN. Triple-negative breast cancers: a view from 10,000 feet. Cancer J. 2010;16(1):17-22.
8. Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318-24.
9. Easton DF, Bishop DT, Ford D, Crockford GP. Genetic linkage analysis in familial breast and ovarian cancer: results from 214 families. The Breast Cancer Linkage Consortium. Am J Hum Genet. 1993;52(4):678-701.
10. Polite BN, Olopade OI. Breast cancer and race: a rising tide does not lift all boats equally. Perspect Biol Med. 2005;48(1 Suppl):S166-75.
11. Nanda R, Schumm LP, Cummings S, et al. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294(15):1925-33.
12. John EM, Miron A, Gong G, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007;298(24):2869-76.
13. Fackenthal JD, Zhang J, Zhang B, et al. High prevalence of BRCA1 and BRCA2 mutations in unselected Nigerian breast cancer patients. Int J Cancer. 2012;131(5):1114-23.
14. Donenberg T, Lunn J, Curling D, et al. A high prevalence of BRCA1 mutations among breast cancer patients from the Bahamas. Breast Cancer Res Treat. 2011;125(2):591-6.
15. Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729-36.
16. Adams SA, Butler WM, Fulton J, et al. Racial disparities in breast cancer mortality in a multi-ethnic cohort in the Southeast. Cancer. 2012;118(10):2693-9.
Bobby Daly, MD, MBA, is the chief fellow in the section of hematology/oncology at the University of Chicago Medicine. His clinical focus is breast and thoracic oncology, and his research focus is health services. Specifically, Dr. Daly researches disparities in oncology care delivery, oncology health care utilization, aggressive end-of-life oncology care, and oncology payment models. He received his MD and MBA from Harvard Medical School and Harvard Business School, both in Boston, and a BA in Economics and History from Stanford (Calif.) University. He was the recipient of the Dean’s Award at Harvard Medical and Business Schools.
Olufunmilayo Olopade, MD, FACP, OON, is the Walter L. Palmer Distinguished Service Professor of Medicine and Human Genetics, and director, Center for Global Health at the University of Chicago. She is adopting emerging high throughput genomic and informatics strategies to identify genetic and nongenetic risk factors for breast cancer in order to implement precision health care in diverse populations. This innovative approach has the potential to improve the quality of care and reduce costs while saving more lives.
Disclosures: Dr. Olopade serves on the Medical Advisory Board for CancerIQ. Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. Frontline Medical Communications is a subsidiary of Quadrant Holdings Corporation.
Published in conjunction with Susan G. Komen®.
This is the second installment of a five-part monthly series that will discuss the pathologic, genomic, and clinical factors that contribute to the racial survival disparity in breast cancer. The series, which is adapted from an article that originally appeared in CA: A Cancer Journal for Clinicians1, a journal of the American Cancer Society, will also review exciting and innovative interventions to close this survival gap. This month’s column reviews tumor biology and genomics—the first element in the perfect storm.
Hormone receptor status and human epidermal growth factor receptor 2 (HER2)/neu
Breast cancer is not a single disease, and breast cancer subtype classifications are used in the clinical setting to determine prognosis and guide management. These different molecular subtypes are based on tumor markers, which include the presence or absence of three proteins: estrogen receptor (ER), progesterone receptor (PR), and HER2/neu. Hormone receptor status is a main factor in planning breast cancer treatment. Hormone receptor–positive breast tumors benefit from hormone therapies, such as selective ER modulators (for example, tamoxifen) and aromatase inhibitors (for example, anastrozole). Thus, these tumors have a more favorable disease-specific survival than do hormone receptor–negative tumors.2
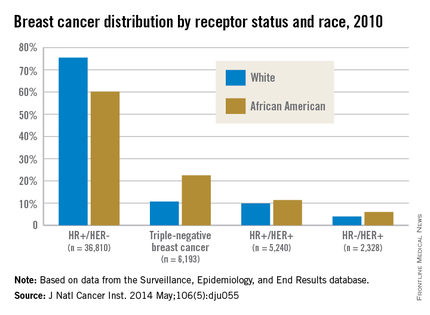
African American women are more likely to present with hormone receptor-negative tumors. In an analysis of the California Cancer Registry, which has collected patient ER and PR status since 1990, whites had a higher proportion of tumors that were ER positive or PR positive (or both) and HER2 negative (72% vs. 53%).3 DeSantis et al.4 reported similar results for this tumor type, with 76% of non-Hispanic whites having hormone receptor–positive, HER2-negative tumors vs. 62% of non-Hispanic blacks. Even with stratification by tumor stage, African Americans continue to have a significantly higher proportion of hormone receptor–negative tumors than do whites for localized and advanced disease.5
Although hormone receptor status varies significantly by race, HER2 status does not show the same divergence. HER2 overexpression is present in approximately 20% of invasive breast cancers. HER2-positive, hormone receptor–negative tumors demonstrate more-aggressive features and worse breast cancer–specific survival than do hormone receptor–positive and HER2-negative tumors,2 although survival has vastly improved with new HER2-targeted therapies such as trastuzumab and pertuzumab. Unlike hormone receptor status, there was no association between race and HER2-positive/ER-negative tumors in the Carolina Breast Cancer Study.2
Triple-negative breast cancer (TNBC)
TNBC is the subtype of breast cancer with the worst prognosis. TNBC gets its name because its tumor cells lack the markers for ER, PR, and HER2 overexpression. Thus, TNBC tumors are estrogen receptor negative (ER), progesterone receptor negative (PR), and HER2/neu negative (HER2). While other subtypes of breast cancer have benefited from drug development regarding hormonal therapies and HER2-targeted treatments, TNBC has not experienced the same pharmacologic breakthroughs.
As such, even after analyses control for the stage at diagnosis, women with this subtype have poorer survival than those with other breast cancers.6 African American women have a higher incidence of TNBC than white women.7 DeSantis et al.4 reported that 22% of breast cancers were triple negative in non-Hispanic black patients vs. only 11% in non-Hispanic white patients. The Carolina Breast Cancer Study found that 26% of African American women had TNBC, whereas 16% of non-African American women did.2 This subtype was most common among younger, premenopausal African American women (39% of diagnosed cancer subtypes). When TNBC patients were excluded from analysis in the Carolina Breast Cancer Study, breast cancer–specific survival remained significantly worse among premenopausal African American women, suggesting that although tumor biology in part explains the poor outcomes, the survival disparity story is more complex.
Germline mutations: BRCA1 and BRCA2 Mutations
In addition to tumor biology, cancer genomics has become increasingly important in determining cancer prognosis and guiding treatment. Approximately 5%-10% of breast cancer cases present in individuals with inherited mutations in autosomal dominant, highly penetrant breast cancer susceptibility genes.8 Accounting for 80%-90% of families containing multiple cases of breast and ovarian cancer, BRCA1 and BRCA2 germline mutations are the most common of the breast cancer susceptibility genes.9 These patients often are younger and have a higher-grade tumor that is hormone receptor negative, which also often matches the profile of the African American breast cancer patient.10
Despite similarities between BRCA1-associated breast cancers and breast cancer in African Americans, genetic abnormalities in African American breast cancer patients remain underresearched. Nanda et al.11 found that BRCA1 and BRCA2 mutations occur with appreciable frequency in high-risk families of African ancestry, with 28% testing positive for a deleterious mutation in one of these genes. This frequency was at a lower rate than that found in non-Hispanic, non-Jewish whites, who had a rate of 46%, because African Americans had a higher rate of polymorphisms or variants of unknown significance (44% vs. 12%). This large percentage of variants of unknown significance indicates that more analysis is needed to understand the clinical implications of these genetic variations. In another study from the Northern California site of the Breast Cancer Family Registry, the BRCA1 mutation prevalence was 16.7% in African American cases diagnosed under the age of 35 years vs. 7.2% in non-Hispanic, non-Ashkenazi Jewish whites in the same age category.12 High frequencies of mutations in BRCA1 and BRCA2 have also been reported in breast cancer patients of African ancestry from Nigeria and the Bahamas.13, 14
These results in African American patients highlight the need for further study of breast cancer genomics in minority populations. However, Armstrong et al.15 illuminated the existence of racial/ethnic disparities in patterns of referral to cancer risk clinics. In their study, African American women with a family history of breast or ovarian cancer were significantly less likely to undergo genetic counseling for BRCA1/2 testing than were white women with this family history. The results of this study were noteworthy for the magnitude of the disparity, with white women having almost five times greater odds of undergoing this clinically important evaluation. More than two decades after BRCA1 and BRCA2 genes were identified, larger studies are still needed in diverse populations to derive true estimates of the burden of mutations in both genes in underserved and understudied populations.
Although these differences in tumor biology and genomics tell part of the mortality disparity story, there is more to be told. In a study of African American and white patients in South Carolina, Adams et al.16 determined survival rates by ethnicity that were adjusted for disease stage and other prognostic characteristics. After they controlled for age, stage, ER, and HER2 expression as well as insurance status, African American women still had a twofold excess risk of death from breast cancer. Thus, in addition to differences in the innate characteristics of the breast tumors, racial differences in patterns of care for women with breast cancer must be considered in unraveling the observed disparity in mortality. The third installment of this series will discuss the second element of the perfect storm – patterns of care.
Other installments of this column can be found in the Related Content box.
1. Daly B, Olopade OI. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65(3):221-238.
2. Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492-502.
3. Kurian AW, Fish K, Shema SJ, Clarke CA. Lifetime risks of specific breast cancer subtypes among women in four racial/ethnic groups. Breast Cancer Res. 2010;12(6):R99.
4. DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2015 Oct 29. doi: 10.3322/caac.21320. [Epub ahead of print]
5. Setiawan VW, Monroe KR, Wilkens LR, Kolonel LN, Pike MC, Henderson BE. Breast cancer risk factors defined by estrogen and progesterone receptor status: the multiethnic cohort study. Am J Epidemiol. 2009;169(10):1251-9.
6. Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007;109(9):1721-8.
7. Ray M, Polite BN. Triple-negative breast cancers: a view from 10,000 feet. Cancer J. 2010;16(1):17-22.
8. Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318-24.
9. Easton DF, Bishop DT, Ford D, Crockford GP. Genetic linkage analysis in familial breast and ovarian cancer: results from 214 families. The Breast Cancer Linkage Consortium. Am J Hum Genet. 1993;52(4):678-701.
10. Polite BN, Olopade OI. Breast cancer and race: a rising tide does not lift all boats equally. Perspect Biol Med. 2005;48(1 Suppl):S166-75.
11. Nanda R, Schumm LP, Cummings S, et al. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294(15):1925-33.
12. John EM, Miron A, Gong G, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007;298(24):2869-76.
13. Fackenthal JD, Zhang J, Zhang B, et al. High prevalence of BRCA1 and BRCA2 mutations in unselected Nigerian breast cancer patients. Int J Cancer. 2012;131(5):1114-23.
14. Donenberg T, Lunn J, Curling D, et al. A high prevalence of BRCA1 mutations among breast cancer patients from the Bahamas. Breast Cancer Res Treat. 2011;125(2):591-6.
15. Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729-36.
16. Adams SA, Butler WM, Fulton J, et al. Racial disparities in breast cancer mortality in a multi-ethnic cohort in the Southeast. Cancer. 2012;118(10):2693-9.
Bobby Daly, MD, MBA, is the chief fellow in the section of hematology/oncology at the University of Chicago Medicine. His clinical focus is breast and thoracic oncology, and his research focus is health services. Specifically, Dr. Daly researches disparities in oncology care delivery, oncology health care utilization, aggressive end-of-life oncology care, and oncology payment models. He received his MD and MBA from Harvard Medical School and Harvard Business School, both in Boston, and a BA in Economics and History from Stanford (Calif.) University. He was the recipient of the Dean’s Award at Harvard Medical and Business Schools.
Olufunmilayo Olopade, MD, FACP, OON, is the Walter L. Palmer Distinguished Service Professor of Medicine and Human Genetics, and director, Center for Global Health at the University of Chicago. She is adopting emerging high throughput genomic and informatics strategies to identify genetic and nongenetic risk factors for breast cancer in order to implement precision health care in diverse populations. This innovative approach has the potential to improve the quality of care and reduce costs while saving more lives.
Disclosures: Dr. Olopade serves on the Medical Advisory Board for CancerIQ. Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. Frontline Medical Communications is a subsidiary of Quadrant Holdings Corporation.
Published in conjunction with Susan G. Komen®.
This is the second installment of a five-part monthly series that will discuss the pathologic, genomic, and clinical factors that contribute to the racial survival disparity in breast cancer. The series, which is adapted from an article that originally appeared in CA: A Cancer Journal for Clinicians1, a journal of the American Cancer Society, will also review exciting and innovative interventions to close this survival gap. This month’s column reviews tumor biology and genomics—the first element in the perfect storm.
Hormone receptor status and human epidermal growth factor receptor 2 (HER2)/neu
Breast cancer is not a single disease, and breast cancer subtype classifications are used in the clinical setting to determine prognosis and guide management. These different molecular subtypes are based on tumor markers, which include the presence or absence of three proteins: estrogen receptor (ER), progesterone receptor (PR), and HER2/neu. Hormone receptor status is a main factor in planning breast cancer treatment. Hormone receptor–positive breast tumors benefit from hormone therapies, such as selective ER modulators (for example, tamoxifen) and aromatase inhibitors (for example, anastrozole). Thus, these tumors have a more favorable disease-specific survival than do hormone receptor–negative tumors.2
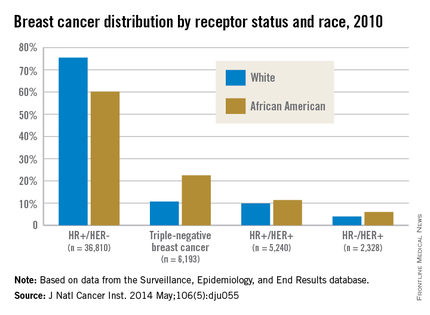
African American women are more likely to present with hormone receptor-negative tumors. In an analysis of the California Cancer Registry, which has collected patient ER and PR status since 1990, whites had a higher proportion of tumors that were ER positive or PR positive (or both) and HER2 negative (72% vs. 53%).3 DeSantis et al.4 reported similar results for this tumor type, with 76% of non-Hispanic whites having hormone receptor–positive, HER2-negative tumors vs. 62% of non-Hispanic blacks. Even with stratification by tumor stage, African Americans continue to have a significantly higher proportion of hormone receptor–negative tumors than do whites for localized and advanced disease.5
Although hormone receptor status varies significantly by race, HER2 status does not show the same divergence. HER2 overexpression is present in approximately 20% of invasive breast cancers. HER2-positive, hormone receptor–negative tumors demonstrate more-aggressive features and worse breast cancer–specific survival than do hormone receptor–positive and HER2-negative tumors,2 although survival has vastly improved with new HER2-targeted therapies such as trastuzumab and pertuzumab. Unlike hormone receptor status, there was no association between race and HER2-positive/ER-negative tumors in the Carolina Breast Cancer Study.2
Triple-negative breast cancer (TNBC)
TNBC is the subtype of breast cancer with the worst prognosis. TNBC gets its name because its tumor cells lack the markers for ER, PR, and HER2 overexpression. Thus, TNBC tumors are estrogen receptor negative (ER), progesterone receptor negative (PR), and HER2/neu negative (HER2). While other subtypes of breast cancer have benefited from drug development regarding hormonal therapies and HER2-targeted treatments, TNBC has not experienced the same pharmacologic breakthroughs.
As such, even after analyses control for the stage at diagnosis, women with this subtype have poorer survival than those with other breast cancers.6 African American women have a higher incidence of TNBC than white women.7 DeSantis et al.4 reported that 22% of breast cancers were triple negative in non-Hispanic black patients vs. only 11% in non-Hispanic white patients. The Carolina Breast Cancer Study found that 26% of African American women had TNBC, whereas 16% of non-African American women did.2 This subtype was most common among younger, premenopausal African American women (39% of diagnosed cancer subtypes). When TNBC patients were excluded from analysis in the Carolina Breast Cancer Study, breast cancer–specific survival remained significantly worse among premenopausal African American women, suggesting that although tumor biology in part explains the poor outcomes, the survival disparity story is more complex.
Germline mutations: BRCA1 and BRCA2 Mutations
In addition to tumor biology, cancer genomics has become increasingly important in determining cancer prognosis and guiding treatment. Approximately 5%-10% of breast cancer cases present in individuals with inherited mutations in autosomal dominant, highly penetrant breast cancer susceptibility genes.8 Accounting for 80%-90% of families containing multiple cases of breast and ovarian cancer, BRCA1 and BRCA2 germline mutations are the most common of the breast cancer susceptibility genes.9 These patients often are younger and have a higher-grade tumor that is hormone receptor negative, which also often matches the profile of the African American breast cancer patient.10
Despite similarities between BRCA1-associated breast cancers and breast cancer in African Americans, genetic abnormalities in African American breast cancer patients remain underresearched. Nanda et al.11 found that BRCA1 and BRCA2 mutations occur with appreciable frequency in high-risk families of African ancestry, with 28% testing positive for a deleterious mutation in one of these genes. This frequency was at a lower rate than that found in non-Hispanic, non-Jewish whites, who had a rate of 46%, because African Americans had a higher rate of polymorphisms or variants of unknown significance (44% vs. 12%). This large percentage of variants of unknown significance indicates that more analysis is needed to understand the clinical implications of these genetic variations. In another study from the Northern California site of the Breast Cancer Family Registry, the BRCA1 mutation prevalence was 16.7% in African American cases diagnosed under the age of 35 years vs. 7.2% in non-Hispanic, non-Ashkenazi Jewish whites in the same age category.12 High frequencies of mutations in BRCA1 and BRCA2 have also been reported in breast cancer patients of African ancestry from Nigeria and the Bahamas.13, 14
These results in African American patients highlight the need for further study of breast cancer genomics in minority populations. However, Armstrong et al.15 illuminated the existence of racial/ethnic disparities in patterns of referral to cancer risk clinics. In their study, African American women with a family history of breast or ovarian cancer were significantly less likely to undergo genetic counseling for BRCA1/2 testing than were white women with this family history. The results of this study were noteworthy for the magnitude of the disparity, with white women having almost five times greater odds of undergoing this clinically important evaluation. More than two decades after BRCA1 and BRCA2 genes were identified, larger studies are still needed in diverse populations to derive true estimates of the burden of mutations in both genes in underserved and understudied populations.
Although these differences in tumor biology and genomics tell part of the mortality disparity story, there is more to be told. In a study of African American and white patients in South Carolina, Adams et al.16 determined survival rates by ethnicity that were adjusted for disease stage and other prognostic characteristics. After they controlled for age, stage, ER, and HER2 expression as well as insurance status, African American women still had a twofold excess risk of death from breast cancer. Thus, in addition to differences in the innate characteristics of the breast tumors, racial differences in patterns of care for women with breast cancer must be considered in unraveling the observed disparity in mortality. The third installment of this series will discuss the second element of the perfect storm – patterns of care.
Other installments of this column can be found in the Related Content box.
1. Daly B, Olopade OI. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65(3):221-238.
2. Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492-502.
3. Kurian AW, Fish K, Shema SJ, Clarke CA. Lifetime risks of specific breast cancer subtypes among women in four racial/ethnic groups. Breast Cancer Res. 2010;12(6):R99.
4. DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2015 Oct 29. doi: 10.3322/caac.21320. [Epub ahead of print]
5. Setiawan VW, Monroe KR, Wilkens LR, Kolonel LN, Pike MC, Henderson BE. Breast cancer risk factors defined by estrogen and progesterone receptor status: the multiethnic cohort study. Am J Epidemiol. 2009;169(10):1251-9.
6. Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007;109(9):1721-8.
7. Ray M, Polite BN. Triple-negative breast cancers: a view from 10,000 feet. Cancer J. 2010;16(1):17-22.
8. Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318-24.
9. Easton DF, Bishop DT, Ford D, Crockford GP. Genetic linkage analysis in familial breast and ovarian cancer: results from 214 families. The Breast Cancer Linkage Consortium. Am J Hum Genet. 1993;52(4):678-701.
10. Polite BN, Olopade OI. Breast cancer and race: a rising tide does not lift all boats equally. Perspect Biol Med. 2005;48(1 Suppl):S166-75.
11. Nanda R, Schumm LP, Cummings S, et al. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294(15):1925-33.
12. John EM, Miron A, Gong G, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007;298(24):2869-76.
13. Fackenthal JD, Zhang J, Zhang B, et al. High prevalence of BRCA1 and BRCA2 mutations in unselected Nigerian breast cancer patients. Int J Cancer. 2012;131(5):1114-23.
14. Donenberg T, Lunn J, Curling D, et al. A high prevalence of BRCA1 mutations among breast cancer patients from the Bahamas. Breast Cancer Res Treat. 2011;125(2):591-6.
15. Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729-36.
16. Adams SA, Butler WM, Fulton J, et al. Racial disparities in breast cancer mortality in a multi-ethnic cohort in the Southeast. Cancer. 2012;118(10):2693-9.
Bobby Daly, MD, MBA, is the chief fellow in the section of hematology/oncology at the University of Chicago Medicine. His clinical focus is breast and thoracic oncology, and his research focus is health services. Specifically, Dr. Daly researches disparities in oncology care delivery, oncology health care utilization, aggressive end-of-life oncology care, and oncology payment models. He received his MD and MBA from Harvard Medical School and Harvard Business School, both in Boston, and a BA in Economics and History from Stanford (Calif.) University. He was the recipient of the Dean’s Award at Harvard Medical and Business Schools.
Olufunmilayo Olopade, MD, FACP, OON, is the Walter L. Palmer Distinguished Service Professor of Medicine and Human Genetics, and director, Center for Global Health at the University of Chicago. She is adopting emerging high throughput genomic and informatics strategies to identify genetic and nongenetic risk factors for breast cancer in order to implement precision health care in diverse populations. This innovative approach has the potential to improve the quality of care and reduce costs while saving more lives.
Disclosures: Dr. Olopade serves on the Medical Advisory Board for CancerIQ. Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. Frontline Medical Communications is a subsidiary of Quadrant Holdings Corporation.
Published in conjunction with Susan G. Komen®.
Terminalia chebula
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Reader reactions to modified American Cancer Society mammography guidelines
Why is ACOG so late?I am quite dismayed that the American College of Obstetricians and Gynecologists (ACOG), again, is the last kid on the block to accept data on a major recommendation like mammography. (ACOG was late to respond to cervical cancer screening changes.) There are growing data supporting the concept that we have over-done mammography and ignored the warnings that mammograms do not meet usual criteria for a good screening test, especially for those aged younger than 50 years. In the 70s and 80s, Dr. John Bailar of the National Cancer Institute warned of the dangers of radiation in “breast x-rays”.1,2 We must move forward and develop a more unified approach for this deadly disease.
James Kolter, MD
Paoli, Pennsylvania
References
- Bailar JC 3rd. Mammography: a time for caution. JAMA. 1977;237(10):997–998.
- Bailar JC 3rd. Mammography before age 50 years? JAMA. 1988;259(10):1548–1549.
Help me accept that we must let these women dieI have been a frontline gynecologist for about 40 years. When I was trained, the goal was to screen everyone. We sought to find diseases early enough to successfully treat and cure before they were too far advanced. In my years thus far I have seen it work: early breast cancers have been found on mammography and during clinical breast examinations. Many lives saved.
I have known most of my patients for 25 to 35 years. I am embarrassed to send an academic journal these experiential and anecdotal stories without numbers and percentages, but I treat individual people and not populations. I cannot get it into my brain that it is not worth saving these women.
Janet, a 37-year-old woman, had just lost her husband to a sudden heart attack, leaving her with 5- and 7-year-old daughters. At that time, baseline mammograms were ordered between ages 35 and 40 years. We were shocked when her mammography revealed breast cancer; she had no family history of breast cancer. Five years later it recurred, and 5 years after that, she was found to have something no one had known about earlier: the BRCA gene mutation. She has since had bilateral mastectomies and bilateral oophorectomies. Last week, at her annual check-up at age 62, she showed me pictures of her grandchildren.
I cannot help but feel that Janet would not be here today if we had not done that screening mammography years ago. But now I am asked to let someone like her go, so that the system does not have to pay for all the “normals.” There are many stories of lumps found during routine examination, of an aggressive cancer found on mammogram 1 year (not 2) after a perfectly normal mammogram.
Help me accept that we must let these people die, or identify their disease at a much more advanced state given these new guidelines. I cannot be the only bread-and-butter gynecologist who is having trouble agreeing with this new approach.
Are there not other ways to cut medical costs? Can we eliminate the “middlemen” in the system? Is there any way other than not screening to save women’s lives?
If a patient gets breast cancer before age 45 or within the 2-year interval between mammograms, would she sue their doctor for not recommending annual screening? We all know cases of women who have died of cervical cancer after having normal Papanicolaou (Pap) test results 2 years before. (Their survivors sued, and won). But if they had had a Pap after only 1 year, would their disease have been discovered and successfully treated?
Perhaps I reveal myself as politically incorrect or not “cost-effective” in this letter. But rest assured, many of my colleagues are retiring (as will I in time), so those trained in my era will disappear. The younger crop is thoroughly trained in this new way. I wonder what the pendulum will do, if after these guidelines sink in, advanced cancers that cannot be treated successfully reveal themselves.
Lois S. Goodman, MD
Weston, Massachusetts
Prevent rather than detectEarly detection is not prevention. Until medicine actually wants to work on prevention, the American Cancer Society guidelines are just more of the same old story, focusing on the symptoms rather than on the root causes. Using genomics and personalized, functional medicine in combination with breast thermography, many more breast cancers can potentially be prevented in the first place, with mammography (and ultrasonography) used as a diagnostic tool. This would be much more powerful than focusing only on early detection. ObGyns need to learn how to apply these new skills and help women get much more value from their preventive care. Until physicians reclaim their ability to think and evaluate critically with open, curious minds, they will continue to fail the very people they aim to serve—their patients.
Roberta Kline, MD
Santa Fe, New Mexico
Guidelines written by statisticians, not ObGynsI was happy to see Dr. Kopan’s article, as well as others about the new American Cancer Society (ACS) screening mammography guidelines. Initially, I was infuriated when I read the guidelines. Looking at the composition of the ACS committee, I can understand some of the conclusions: I believe there were 4 statisticians among the members.
Statisticians look at mammography statistics as numbers and significant figures. They do not consider that these numbers represent lives. In the guidelines it was stated that earlier and more frequent screening, as well as discontinuing screening after the age of 74, only saved the lives of 10 women out of 100,000. That would certainly be significant for the 10 women who are saved. What if one of them was a relative of one of the committee members?
Another silly recommendation was that women no longer have clinical breast examinations. The committee obviously does not realize how frequently cancers are found by clinical exam.
Norman D. Lindley, MD
Alamogordo, New Mexico
“MANUAL VACUUM ASPIRATION: A SAFE AND EFFECTIVE TREATMENT FOR EARLY MISCARRIAGE”PIYAPA PRADITPAN, MD, MPH, AND ANNE R. DAVIS, MD, MPH (NOVEMBER 2015)
Which antibiotic for prophylaxis at vacuum aspiration for miscarriage?Thank you to Drs. Praditpan and Davis for a great article. I think, however, there is more evidence for azithromycin 1 g PO (than doxycycline as the authors recommend) as prophylaxis for surgical abortion and no antibiotic prophylaxis for medi‑ cal abortion.
Tirun (Ty) Gopal, MD
San Francisco, California
Drs. Praditpan and Davis respond Thank you for your comment and for allowing us to provide clarification on the topic of antibiotic prophylaxis at the time of vacuum aspiration for miscarriage management. Few studies address the question of antibiotic prophylaxis at the time of surgical management of miscarriage, and a meta-analysis found insufficient data to yield a conclusion.1 Recommendations for infection prophylaxis in miscarriage management have been extrapolated from the abundance of data for induced abortion, since the surgical procedure is the same for both.
The 2011 Society of Family Planning (SFP) clinical guidelines on prevention of infection after induced abortion identified 14 randomized trials that examined the efficacy of antibiotic regimens administered preoperatively to prevent upper genital tract infection after first trimester surgical procedures.2 Five studies (involving a total of 5,380 patients) examined tetracyclines, while only 1 study (N = 378) examined macrolides. The trials comparing tetracycline prophylaxis with placebo showed significant risk reduction in upper genital tract infection in tetracycline users (up to 88%), with an overall postinfection rate similar to that reported in the United States (<1%). Regardless of antibiotic choice or duration, the risk of infection was lower in women who received any prophylactic antibiotics compared with women who received placebo.
Based on these data and doxycycline’s cost effectiveness and its minimal adverse effects, the SFP recommends doxycycline as the antibiotic of choice for prevention of infection after induced abortion. Antibiotics should be administered on the day of the procedure and, if clinicians prefer, for no more than 3 days afterwards. Azithromycin is a macrolide that can be used for presumptive treatment of chlamydia at the time of surgical abortion.3 No trials compare azithromycin to doxycycline for prevention of infection after vacuum aspiration.
References
- May W, Gulmezoglu AM, Ba-Thike K. Antibiotics for incomplete abortion. Cochrane Database Syst Rev. 2007;(4):CD001779.
- Achilles SL, Reeve MF; Society of Family Planning. Prevention of infection after induced abortion: release date October 2010: SFP Guideline 2010. Contraception. 2011;83(4):295–309.
- Royal College of Obstetricians and Gynaecologists. The care of women requesting induced abortion: Evidence-based clinical guideline number 7. https://www.rcog.org.uk/globalassets/documents/guidelines/abortion-guideline_web_1.pdf. Published November 2011. Accessed December 18, 2015.
Why is ACOG so late?I am quite dismayed that the American College of Obstetricians and Gynecologists (ACOG), again, is the last kid on the block to accept data on a major recommendation like mammography. (ACOG was late to respond to cervical cancer screening changes.) There are growing data supporting the concept that we have over-done mammography and ignored the warnings that mammograms do not meet usual criteria for a good screening test, especially for those aged younger than 50 years. In the 70s and 80s, Dr. John Bailar of the National Cancer Institute warned of the dangers of radiation in “breast x-rays”.1,2 We must move forward and develop a more unified approach for this deadly disease.
James Kolter, MD
Paoli, Pennsylvania
References
- Bailar JC 3rd. Mammography: a time for caution. JAMA. 1977;237(10):997–998.
- Bailar JC 3rd. Mammography before age 50 years? JAMA. 1988;259(10):1548–1549.
Help me accept that we must let these women dieI have been a frontline gynecologist for about 40 years. When I was trained, the goal was to screen everyone. We sought to find diseases early enough to successfully treat and cure before they were too far advanced. In my years thus far I have seen it work: early breast cancers have been found on mammography and during clinical breast examinations. Many lives saved.
I have known most of my patients for 25 to 35 years. I am embarrassed to send an academic journal these experiential and anecdotal stories without numbers and percentages, but I treat individual people and not populations. I cannot get it into my brain that it is not worth saving these women.
Janet, a 37-year-old woman, had just lost her husband to a sudden heart attack, leaving her with 5- and 7-year-old daughters. At that time, baseline mammograms were ordered between ages 35 and 40 years. We were shocked when her mammography revealed breast cancer; she had no family history of breast cancer. Five years later it recurred, and 5 years after that, she was found to have something no one had known about earlier: the BRCA gene mutation. She has since had bilateral mastectomies and bilateral oophorectomies. Last week, at her annual check-up at age 62, she showed me pictures of her grandchildren.
I cannot help but feel that Janet would not be here today if we had not done that screening mammography years ago. But now I am asked to let someone like her go, so that the system does not have to pay for all the “normals.” There are many stories of lumps found during routine examination, of an aggressive cancer found on mammogram 1 year (not 2) after a perfectly normal mammogram.
Help me accept that we must let these people die, or identify their disease at a much more advanced state given these new guidelines. I cannot be the only bread-and-butter gynecologist who is having trouble agreeing with this new approach.
Are there not other ways to cut medical costs? Can we eliminate the “middlemen” in the system? Is there any way other than not screening to save women’s lives?
If a patient gets breast cancer before age 45 or within the 2-year interval between mammograms, would she sue their doctor for not recommending annual screening? We all know cases of women who have died of cervical cancer after having normal Papanicolaou (Pap) test results 2 years before. (Their survivors sued, and won). But if they had had a Pap after only 1 year, would their disease have been discovered and successfully treated?
Perhaps I reveal myself as politically incorrect or not “cost-effective” in this letter. But rest assured, many of my colleagues are retiring (as will I in time), so those trained in my era will disappear. The younger crop is thoroughly trained in this new way. I wonder what the pendulum will do, if after these guidelines sink in, advanced cancers that cannot be treated successfully reveal themselves.
Lois S. Goodman, MD
Weston, Massachusetts
Prevent rather than detectEarly detection is not prevention. Until medicine actually wants to work on prevention, the American Cancer Society guidelines are just more of the same old story, focusing on the symptoms rather than on the root causes. Using genomics and personalized, functional medicine in combination with breast thermography, many more breast cancers can potentially be prevented in the first place, with mammography (and ultrasonography) used as a diagnostic tool. This would be much more powerful than focusing only on early detection. ObGyns need to learn how to apply these new skills and help women get much more value from their preventive care. Until physicians reclaim their ability to think and evaluate critically with open, curious minds, they will continue to fail the very people they aim to serve—their patients.
Roberta Kline, MD
Santa Fe, New Mexico
Guidelines written by statisticians, not ObGynsI was happy to see Dr. Kopan’s article, as well as others about the new American Cancer Society (ACS) screening mammography guidelines. Initially, I was infuriated when I read the guidelines. Looking at the composition of the ACS committee, I can understand some of the conclusions: I believe there were 4 statisticians among the members.
Statisticians look at mammography statistics as numbers and significant figures. They do not consider that these numbers represent lives. In the guidelines it was stated that earlier and more frequent screening, as well as discontinuing screening after the age of 74, only saved the lives of 10 women out of 100,000. That would certainly be significant for the 10 women who are saved. What if one of them was a relative of one of the committee members?
Another silly recommendation was that women no longer have clinical breast examinations. The committee obviously does not realize how frequently cancers are found by clinical exam.
Norman D. Lindley, MD
Alamogordo, New Mexico
“MANUAL VACUUM ASPIRATION: A SAFE AND EFFECTIVE TREATMENT FOR EARLY MISCARRIAGE”PIYAPA PRADITPAN, MD, MPH, AND ANNE R. DAVIS, MD, MPH (NOVEMBER 2015)
Which antibiotic for prophylaxis at vacuum aspiration for miscarriage?Thank you to Drs. Praditpan and Davis for a great article. I think, however, there is more evidence for azithromycin 1 g PO (than doxycycline as the authors recommend) as prophylaxis for surgical abortion and no antibiotic prophylaxis for medi‑ cal abortion.
Tirun (Ty) Gopal, MD
San Francisco, California
Drs. Praditpan and Davis respond Thank you for your comment and for allowing us to provide clarification on the topic of antibiotic prophylaxis at the time of vacuum aspiration for miscarriage management. Few studies address the question of antibiotic prophylaxis at the time of surgical management of miscarriage, and a meta-analysis found insufficient data to yield a conclusion.1 Recommendations for infection prophylaxis in miscarriage management have been extrapolated from the abundance of data for induced abortion, since the surgical procedure is the same for both.
The 2011 Society of Family Planning (SFP) clinical guidelines on prevention of infection after induced abortion identified 14 randomized trials that examined the efficacy of antibiotic regimens administered preoperatively to prevent upper genital tract infection after first trimester surgical procedures.2 Five studies (involving a total of 5,380 patients) examined tetracyclines, while only 1 study (N = 378) examined macrolides. The trials comparing tetracycline prophylaxis with placebo showed significant risk reduction in upper genital tract infection in tetracycline users (up to 88%), with an overall postinfection rate similar to that reported in the United States (<1%). Regardless of antibiotic choice or duration, the risk of infection was lower in women who received any prophylactic antibiotics compared with women who received placebo.
Based on these data and doxycycline’s cost effectiveness and its minimal adverse effects, the SFP recommends doxycycline as the antibiotic of choice for prevention of infection after induced abortion. Antibiotics should be administered on the day of the procedure and, if clinicians prefer, for no more than 3 days afterwards. Azithromycin is a macrolide that can be used for presumptive treatment of chlamydia at the time of surgical abortion.3 No trials compare azithromycin to doxycycline for prevention of infection after vacuum aspiration.
References
- May W, Gulmezoglu AM, Ba-Thike K. Antibiotics for incomplete abortion. Cochrane Database Syst Rev. 2007;(4):CD001779.
- Achilles SL, Reeve MF; Society of Family Planning. Prevention of infection after induced abortion: release date October 2010: SFP Guideline 2010. Contraception. 2011;83(4):295–309.
- Royal College of Obstetricians and Gynaecologists. The care of women requesting induced abortion: Evidence-based clinical guideline number 7. https://www.rcog.org.uk/globalassets/documents/guidelines/abortion-guideline_web_1.pdf. Published November 2011. Accessed December 18, 2015.
Why is ACOG so late?I am quite dismayed that the American College of Obstetricians and Gynecologists (ACOG), again, is the last kid on the block to accept data on a major recommendation like mammography. (ACOG was late to respond to cervical cancer screening changes.) There are growing data supporting the concept that we have over-done mammography and ignored the warnings that mammograms do not meet usual criteria for a good screening test, especially for those aged younger than 50 years. In the 70s and 80s, Dr. John Bailar of the National Cancer Institute warned of the dangers of radiation in “breast x-rays”.1,2 We must move forward and develop a more unified approach for this deadly disease.
James Kolter, MD
Paoli, Pennsylvania
References
- Bailar JC 3rd. Mammography: a time for caution. JAMA. 1977;237(10):997–998.
- Bailar JC 3rd. Mammography before age 50 years? JAMA. 1988;259(10):1548–1549.
Help me accept that we must let these women dieI have been a frontline gynecologist for about 40 years. When I was trained, the goal was to screen everyone. We sought to find diseases early enough to successfully treat and cure before they were too far advanced. In my years thus far I have seen it work: early breast cancers have been found on mammography and during clinical breast examinations. Many lives saved.
I have known most of my patients for 25 to 35 years. I am embarrassed to send an academic journal these experiential and anecdotal stories without numbers and percentages, but I treat individual people and not populations. I cannot get it into my brain that it is not worth saving these women.
Janet, a 37-year-old woman, had just lost her husband to a sudden heart attack, leaving her with 5- and 7-year-old daughters. At that time, baseline mammograms were ordered between ages 35 and 40 years. We were shocked when her mammography revealed breast cancer; she had no family history of breast cancer. Five years later it recurred, and 5 years after that, she was found to have something no one had known about earlier: the BRCA gene mutation. She has since had bilateral mastectomies and bilateral oophorectomies. Last week, at her annual check-up at age 62, she showed me pictures of her grandchildren.
I cannot help but feel that Janet would not be here today if we had not done that screening mammography years ago. But now I am asked to let someone like her go, so that the system does not have to pay for all the “normals.” There are many stories of lumps found during routine examination, of an aggressive cancer found on mammogram 1 year (not 2) after a perfectly normal mammogram.
Help me accept that we must let these people die, or identify their disease at a much more advanced state given these new guidelines. I cannot be the only bread-and-butter gynecologist who is having trouble agreeing with this new approach.
Are there not other ways to cut medical costs? Can we eliminate the “middlemen” in the system? Is there any way other than not screening to save women’s lives?
If a patient gets breast cancer before age 45 or within the 2-year interval between mammograms, would she sue their doctor for not recommending annual screening? We all know cases of women who have died of cervical cancer after having normal Papanicolaou (Pap) test results 2 years before. (Their survivors sued, and won). But if they had had a Pap after only 1 year, would their disease have been discovered and successfully treated?
Perhaps I reveal myself as politically incorrect or not “cost-effective” in this letter. But rest assured, many of my colleagues are retiring (as will I in time), so those trained in my era will disappear. The younger crop is thoroughly trained in this new way. I wonder what the pendulum will do, if after these guidelines sink in, advanced cancers that cannot be treated successfully reveal themselves.
Lois S. Goodman, MD
Weston, Massachusetts
Prevent rather than detectEarly detection is not prevention. Until medicine actually wants to work on prevention, the American Cancer Society guidelines are just more of the same old story, focusing on the symptoms rather than on the root causes. Using genomics and personalized, functional medicine in combination with breast thermography, many more breast cancers can potentially be prevented in the first place, with mammography (and ultrasonography) used as a diagnostic tool. This would be much more powerful than focusing only on early detection. ObGyns need to learn how to apply these new skills and help women get much more value from their preventive care. Until physicians reclaim their ability to think and evaluate critically with open, curious minds, they will continue to fail the very people they aim to serve—their patients.
Roberta Kline, MD
Santa Fe, New Mexico
Guidelines written by statisticians, not ObGynsI was happy to see Dr. Kopan’s article, as well as others about the new American Cancer Society (ACS) screening mammography guidelines. Initially, I was infuriated when I read the guidelines. Looking at the composition of the ACS committee, I can understand some of the conclusions: I believe there were 4 statisticians among the members.
Statisticians look at mammography statistics as numbers and significant figures. They do not consider that these numbers represent lives. In the guidelines it was stated that earlier and more frequent screening, as well as discontinuing screening after the age of 74, only saved the lives of 10 women out of 100,000. That would certainly be significant for the 10 women who are saved. What if one of them was a relative of one of the committee members?
Another silly recommendation was that women no longer have clinical breast examinations. The committee obviously does not realize how frequently cancers are found by clinical exam.
Norman D. Lindley, MD
Alamogordo, New Mexico
“MANUAL VACUUM ASPIRATION: A SAFE AND EFFECTIVE TREATMENT FOR EARLY MISCARRIAGE”PIYAPA PRADITPAN, MD, MPH, AND ANNE R. DAVIS, MD, MPH (NOVEMBER 2015)
Which antibiotic for prophylaxis at vacuum aspiration for miscarriage?Thank you to Drs. Praditpan and Davis for a great article. I think, however, there is more evidence for azithromycin 1 g PO (than doxycycline as the authors recommend) as prophylaxis for surgical abortion and no antibiotic prophylaxis for medi‑ cal abortion.
Tirun (Ty) Gopal, MD
San Francisco, California
Drs. Praditpan and Davis respond Thank you for your comment and for allowing us to provide clarification on the topic of antibiotic prophylaxis at the time of vacuum aspiration for miscarriage management. Few studies address the question of antibiotic prophylaxis at the time of surgical management of miscarriage, and a meta-analysis found insufficient data to yield a conclusion.1 Recommendations for infection prophylaxis in miscarriage management have been extrapolated from the abundance of data for induced abortion, since the surgical procedure is the same for both.
The 2011 Society of Family Planning (SFP) clinical guidelines on prevention of infection after induced abortion identified 14 randomized trials that examined the efficacy of antibiotic regimens administered preoperatively to prevent upper genital tract infection after first trimester surgical procedures.2 Five studies (involving a total of 5,380 patients) examined tetracyclines, while only 1 study (N = 378) examined macrolides. The trials comparing tetracycline prophylaxis with placebo showed significant risk reduction in upper genital tract infection in tetracycline users (up to 88%), with an overall postinfection rate similar to that reported in the United States (<1%). Regardless of antibiotic choice or duration, the risk of infection was lower in women who received any prophylactic antibiotics compared with women who received placebo.
Based on these data and doxycycline’s cost effectiveness and its minimal adverse effects, the SFP recommends doxycycline as the antibiotic of choice for prevention of infection after induced abortion. Antibiotics should be administered on the day of the procedure and, if clinicians prefer, for no more than 3 days afterwards. Azithromycin is a macrolide that can be used for presumptive treatment of chlamydia at the time of surgical abortion.3 No trials compare azithromycin to doxycycline for prevention of infection after vacuum aspiration.
References
- May W, Gulmezoglu AM, Ba-Thike K. Antibiotics for incomplete abortion. Cochrane Database Syst Rev. 2007;(4):CD001779.
- Achilles SL, Reeve MF; Society of Family Planning. Prevention of infection after induced abortion: release date October 2010: SFP Guideline 2010. Contraception. 2011;83(4):295–309.
- Royal College of Obstetricians and Gynaecologists. The care of women requesting induced abortion: Evidence-based clinical guideline number 7. https://www.rcog.org.uk/globalassets/documents/guidelines/abortion-guideline_web_1.pdf. Published November 2011. Accessed December 18, 2015.
Baby, back back back it up
As many young physicians might recognize, the title of today’s column is from a song by Prince Royce featuring Jennifer Lopez and Pitbull. This article, though, is about what we believe is likely an urgent matter for many of our readers – the issue of appropriately backing up information that resides on their personal computers. We were prompted to write about this after a colleague came to one of us in a panic after losing all of the information on her meticulously performed, but poorly conceived backup. For years she has been developing and storing her lectures on a flash drive, and every month she has been backing up her flash drive to her personal computer. She even set a reminder in her calendar to make sure that she perform those backups each and every month. Unfortunately, she lost her flash drive, and even more unfortunately discovered that what she thought were copies of files on her computer were actually only shortcuts to the files on her now-missing flash drive. All her files were gone.
We are going to organize our discussion in three parts: First, we want to convince you of the importance of making backups, essentially informational life insurance. Unlike life insurance, however, you have a pretty good chance of using your backups at some point over the next 10 years. Second, we are going to discuss locally based backups, and then lastly, we’ll cover cloud-based backups. This may seem like an incredibly dull topic to some, but we anticipate receiving emails of thanks over many years for the knowledge and actions that come out of today’s column.
Hard drive failure rates, derived from data published by companies that professionally manage large numbers of hard drives, is about 3%-5% in the first year. This remains at about 3% per year for the next 2-3 years, and then can go up to 10% or more per year as hard drives continue to age. That means that over a 4-year period, 15%-20% of hard drives are likely to fail.1,2 This fact underscores the importance of backing up your data, because there is a good chance that over time, loss of data will happen to you.
One strategy is to back up to an external drive. The drive can be either a flash drive if you have less than 128 GB to store, or a traditional external hard drive – a very affordable option for memory up to 4 TB (4,000 GB). There are many excellent external hard drives and flash drives from which to choose, but you also need to have backup software that will take the information from your personal computer and place it in an organized manner on your external drive. Many drives now come bundled with backup software. An example of such a drive is the Western Digital My Passport Elite. If the hard drive you have does not already have backup software, there are lots of good choices out there. Backup software solutions include Time Machine (built into all Mac Computers), and many software choices for PCs.3
While the speed of backup and recovery is fast – often just a few hours – there are two main issues that make external drives suboptimal as your main backup strategy. The first is that most people simply don’t remember to plug their external drive into their computer regularly; months and sometimes years can go by without backing up your files. The second issue, which is usually not considered, is that the hard drive usually sits on your desk next to your computer. Therefore, if there is a fire, a flood, an electrical surge, or even a simple spill on your desk, you may lose both your main files and your backup in one fell swoop. For this reason, if you choose to use an external drive as your backup method, you should back up to two different external drives and keep one drive in your office and one at home.
The best method of backup, and the one we recommend to everyone, eliminates the major disadvantages of local backups. This method is cloud-based backup. For cloud-based backup, you purchase a subscription with an annual fee, then you download software from the backup vendor to your computer. It usually takes about 15 minutes to set up the software by selecting the file folders that you would like to back up, then the software does the rest. The first backup can take a long time, typically a few days, as the speed of the backup is limited by the speed of your Internet connection. After that first time, though, backups don’t take long because they back up only the files that have changed since the previous backup.
The main advantages to cloud-based solutions is that once it has been set up, the software ensures that incremental backups occur automatically every time your computer is connected to the Internet. In addition, since the cloud backups are off-site, you are protected from an adverse occurrence taking out your backup drive and your computer when they are sitting next to each other on your desk. In addition, most cloud backup services also allow you to access your file from any computer or smartphone for access where and when you need the files.
So, let us end where we began, with lyrics from the music video, with which we agree, “Word of advice: Want a happy life … Back it up one more time.”
References
1. http://www.extremetech.com/computing/170748-how-long-do-hard-drives-actually-live-for
2. http://www.pcworld.com/article/131168/article.html
3. The Best Backup Software at http://www.pcmag.com/article2/0,2817,2278661,00.asp
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
As many young physicians might recognize, the title of today’s column is from a song by Prince Royce featuring Jennifer Lopez and Pitbull. This article, though, is about what we believe is likely an urgent matter for many of our readers – the issue of appropriately backing up information that resides on their personal computers. We were prompted to write about this after a colleague came to one of us in a panic after losing all of the information on her meticulously performed, but poorly conceived backup. For years she has been developing and storing her lectures on a flash drive, and every month she has been backing up her flash drive to her personal computer. She even set a reminder in her calendar to make sure that she perform those backups each and every month. Unfortunately, she lost her flash drive, and even more unfortunately discovered that what she thought were copies of files on her computer were actually only shortcuts to the files on her now-missing flash drive. All her files were gone.
We are going to organize our discussion in three parts: First, we want to convince you of the importance of making backups, essentially informational life insurance. Unlike life insurance, however, you have a pretty good chance of using your backups at some point over the next 10 years. Second, we are going to discuss locally based backups, and then lastly, we’ll cover cloud-based backups. This may seem like an incredibly dull topic to some, but we anticipate receiving emails of thanks over many years for the knowledge and actions that come out of today’s column.
Hard drive failure rates, derived from data published by companies that professionally manage large numbers of hard drives, is about 3%-5% in the first year. This remains at about 3% per year for the next 2-3 years, and then can go up to 10% or more per year as hard drives continue to age. That means that over a 4-year period, 15%-20% of hard drives are likely to fail.1,2 This fact underscores the importance of backing up your data, because there is a good chance that over time, loss of data will happen to you.
One strategy is to back up to an external drive. The drive can be either a flash drive if you have less than 128 GB to store, or a traditional external hard drive – a very affordable option for memory up to 4 TB (4,000 GB). There are many excellent external hard drives and flash drives from which to choose, but you also need to have backup software that will take the information from your personal computer and place it in an organized manner on your external drive. Many drives now come bundled with backup software. An example of such a drive is the Western Digital My Passport Elite. If the hard drive you have does not already have backup software, there are lots of good choices out there. Backup software solutions include Time Machine (built into all Mac Computers), and many software choices for PCs.3
While the speed of backup and recovery is fast – often just a few hours – there are two main issues that make external drives suboptimal as your main backup strategy. The first is that most people simply don’t remember to plug their external drive into their computer regularly; months and sometimes years can go by without backing up your files. The second issue, which is usually not considered, is that the hard drive usually sits on your desk next to your computer. Therefore, if there is a fire, a flood, an electrical surge, or even a simple spill on your desk, you may lose both your main files and your backup in one fell swoop. For this reason, if you choose to use an external drive as your backup method, you should back up to two different external drives and keep one drive in your office and one at home.
The best method of backup, and the one we recommend to everyone, eliminates the major disadvantages of local backups. This method is cloud-based backup. For cloud-based backup, you purchase a subscription with an annual fee, then you download software from the backup vendor to your computer. It usually takes about 15 minutes to set up the software by selecting the file folders that you would like to back up, then the software does the rest. The first backup can take a long time, typically a few days, as the speed of the backup is limited by the speed of your Internet connection. After that first time, though, backups don’t take long because they back up only the files that have changed since the previous backup.
The main advantages to cloud-based solutions is that once it has been set up, the software ensures that incremental backups occur automatically every time your computer is connected to the Internet. In addition, since the cloud backups are off-site, you are protected from an adverse occurrence taking out your backup drive and your computer when they are sitting next to each other on your desk. In addition, most cloud backup services also allow you to access your file from any computer or smartphone for access where and when you need the files.
So, let us end where we began, with lyrics from the music video, with which we agree, “Word of advice: Want a happy life … Back it up one more time.”
References
1. http://www.extremetech.com/computing/170748-how-long-do-hard-drives-actually-live-for
2. http://www.pcworld.com/article/131168/article.html
3. The Best Backup Software at http://www.pcmag.com/article2/0,2817,2278661,00.asp
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
As many young physicians might recognize, the title of today’s column is from a song by Prince Royce featuring Jennifer Lopez and Pitbull. This article, though, is about what we believe is likely an urgent matter for many of our readers – the issue of appropriately backing up information that resides on their personal computers. We were prompted to write about this after a colleague came to one of us in a panic after losing all of the information on her meticulously performed, but poorly conceived backup. For years she has been developing and storing her lectures on a flash drive, and every month she has been backing up her flash drive to her personal computer. She even set a reminder in her calendar to make sure that she perform those backups each and every month. Unfortunately, she lost her flash drive, and even more unfortunately discovered that what she thought were copies of files on her computer were actually only shortcuts to the files on her now-missing flash drive. All her files were gone.
We are going to organize our discussion in three parts: First, we want to convince you of the importance of making backups, essentially informational life insurance. Unlike life insurance, however, you have a pretty good chance of using your backups at some point over the next 10 years. Second, we are going to discuss locally based backups, and then lastly, we’ll cover cloud-based backups. This may seem like an incredibly dull topic to some, but we anticipate receiving emails of thanks over many years for the knowledge and actions that come out of today’s column.
Hard drive failure rates, derived from data published by companies that professionally manage large numbers of hard drives, is about 3%-5% in the first year. This remains at about 3% per year for the next 2-3 years, and then can go up to 10% or more per year as hard drives continue to age. That means that over a 4-year period, 15%-20% of hard drives are likely to fail.1,2 This fact underscores the importance of backing up your data, because there is a good chance that over time, loss of data will happen to you.
One strategy is to back up to an external drive. The drive can be either a flash drive if you have less than 128 GB to store, or a traditional external hard drive – a very affordable option for memory up to 4 TB (4,000 GB). There are many excellent external hard drives and flash drives from which to choose, but you also need to have backup software that will take the information from your personal computer and place it in an organized manner on your external drive. Many drives now come bundled with backup software. An example of such a drive is the Western Digital My Passport Elite. If the hard drive you have does not already have backup software, there are lots of good choices out there. Backup software solutions include Time Machine (built into all Mac Computers), and many software choices for PCs.3
While the speed of backup and recovery is fast – often just a few hours – there are two main issues that make external drives suboptimal as your main backup strategy. The first is that most people simply don’t remember to plug their external drive into their computer regularly; months and sometimes years can go by without backing up your files. The second issue, which is usually not considered, is that the hard drive usually sits on your desk next to your computer. Therefore, if there is a fire, a flood, an electrical surge, or even a simple spill on your desk, you may lose both your main files and your backup in one fell swoop. For this reason, if you choose to use an external drive as your backup method, you should back up to two different external drives and keep one drive in your office and one at home.
The best method of backup, and the one we recommend to everyone, eliminates the major disadvantages of local backups. This method is cloud-based backup. For cloud-based backup, you purchase a subscription with an annual fee, then you download software from the backup vendor to your computer. It usually takes about 15 minutes to set up the software by selecting the file folders that you would like to back up, then the software does the rest. The first backup can take a long time, typically a few days, as the speed of the backup is limited by the speed of your Internet connection. After that first time, though, backups don’t take long because they back up only the files that have changed since the previous backup.
The main advantages to cloud-based solutions is that once it has been set up, the software ensures that incremental backups occur automatically every time your computer is connected to the Internet. In addition, since the cloud backups are off-site, you are protected from an adverse occurrence taking out your backup drive and your computer when they are sitting next to each other on your desk. In addition, most cloud backup services also allow you to access your file from any computer or smartphone for access where and when you need the files.
So, let us end where we began, with lyrics from the music video, with which we agree, “Word of advice: Want a happy life … Back it up one more time.”
References
1. http://www.extremetech.com/computing/170748-how-long-do-hard-drives-actually-live-for
2. http://www.pcworld.com/article/131168/article.html
3. The Best Backup Software at http://www.pcmag.com/article2/0,2817,2278661,00.asp
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.