User login
Getting past bad drug outcomes
In my first year of fellowship, I met a delightful old man who had temporal arteritis. We naturally treated him with steroids, but he consequently suffered a vertebral fracture. He passed away soon after that from pneumonia that was probably aggravated by his inability to breathe deeply and cough appropriately.
An elderly patient with rheumatoid arthritis was diagnosed with lymphoma. For want of something to blame, his children blamed it on the methotrexate.
A woman with lupus nephritis got pregnant while on mycophenolate despite being on contraception. Her baby was born with malformed ears and eyes, and by all accounts will probably be deaf and blind.
We have been gifted with this mind-blowing ability to make our patients’ lives much better. That sense of accomplishment can be intoxicating. After all, how many of your polymyalgia rheumatica patients worship you because you made the diagnosis and made them 100% better by putting them on prednisone? Yet we forget that although bad things rarely happen, that does not mean that they won’t happen.
In a beautiful book called "Where’d You Go, Bernadette?" the husband of the title character says that the brain is a discounting mechanism: "Let’s say you get a crack in your windshield and you’re really upset. Oh no, my windshield, it’s ruined, I can hardly see out of it, this is a tragedy! But you don’t have enough money to fix it, so you drive with it. In a month, someone asks you what happened to your windshield, and you say, What do you mean? Because your brain has discounted it. ... It’s for survival. You need to be prepared for novel experiences because often they signal danger."
The book is about an artist who we are led to believe has completed her downward spiral, going from genius to wacko. In the above passage, the artist’s husband is explaining to their daughter why they loved their family home so much, despite its state of extreme disrepair. They loved the house so much that they couldn’t see that it was a safety hazard.
As a fresh graduate I insisted on weaning everyone off prednisone, terrified of the potential side effects. Five years later and with the benefit of the collected wisdom of hundreds of rheumatologists before me, I have accepted that some people need a low dose of steroid to keep their disease quiet. I have used this and other, more toxic drugs to such great effects – taking for granted their ability to make people better – that I forget sometimes that they can cause serious problems.
Bad outcomes can and do happen in spite of our best intentions. In my case, my default is to blame myself. In my more melodramatic moments, I wonder if I deserve to be a doctor. But when I am done feeling angry or sad, or, frankly, feeling sorry for myself, then I need that discounting mechanism to kick in, to remind myself that this is one bad outcome out of many good outcomes. There are things beyond my control, and I cannot let a bad outcome keep me from doing the good work that I am still able to do.
There is a scene from the TV series "The West Wing" where the president asks one of his staffers if he thought the president was being kept from doing a great job because his demons were "shouting down the better angels" in his brain. Thankfully, my brain’s discounting mechanism helps keep the demons at bay.
Dr. Chan practices rheumatology in Pawtucket, R.I.
In my first year of fellowship, I met a delightful old man who had temporal arteritis. We naturally treated him with steroids, but he consequently suffered a vertebral fracture. He passed away soon after that from pneumonia that was probably aggravated by his inability to breathe deeply and cough appropriately.
An elderly patient with rheumatoid arthritis was diagnosed with lymphoma. For want of something to blame, his children blamed it on the methotrexate.
A woman with lupus nephritis got pregnant while on mycophenolate despite being on contraception. Her baby was born with malformed ears and eyes, and by all accounts will probably be deaf and blind.
We have been gifted with this mind-blowing ability to make our patients’ lives much better. That sense of accomplishment can be intoxicating. After all, how many of your polymyalgia rheumatica patients worship you because you made the diagnosis and made them 100% better by putting them on prednisone? Yet we forget that although bad things rarely happen, that does not mean that they won’t happen.
In a beautiful book called "Where’d You Go, Bernadette?" the husband of the title character says that the brain is a discounting mechanism: "Let’s say you get a crack in your windshield and you’re really upset. Oh no, my windshield, it’s ruined, I can hardly see out of it, this is a tragedy! But you don’t have enough money to fix it, so you drive with it. In a month, someone asks you what happened to your windshield, and you say, What do you mean? Because your brain has discounted it. ... It’s for survival. You need to be prepared for novel experiences because often they signal danger."
The book is about an artist who we are led to believe has completed her downward spiral, going from genius to wacko. In the above passage, the artist’s husband is explaining to their daughter why they loved their family home so much, despite its state of extreme disrepair. They loved the house so much that they couldn’t see that it was a safety hazard.
As a fresh graduate I insisted on weaning everyone off prednisone, terrified of the potential side effects. Five years later and with the benefit of the collected wisdom of hundreds of rheumatologists before me, I have accepted that some people need a low dose of steroid to keep their disease quiet. I have used this and other, more toxic drugs to such great effects – taking for granted their ability to make people better – that I forget sometimes that they can cause serious problems.
Bad outcomes can and do happen in spite of our best intentions. In my case, my default is to blame myself. In my more melodramatic moments, I wonder if I deserve to be a doctor. But when I am done feeling angry or sad, or, frankly, feeling sorry for myself, then I need that discounting mechanism to kick in, to remind myself that this is one bad outcome out of many good outcomes. There are things beyond my control, and I cannot let a bad outcome keep me from doing the good work that I am still able to do.
There is a scene from the TV series "The West Wing" where the president asks one of his staffers if he thought the president was being kept from doing a great job because his demons were "shouting down the better angels" in his brain. Thankfully, my brain’s discounting mechanism helps keep the demons at bay.
Dr. Chan practices rheumatology in Pawtucket, R.I.
In my first year of fellowship, I met a delightful old man who had temporal arteritis. We naturally treated him with steroids, but he consequently suffered a vertebral fracture. He passed away soon after that from pneumonia that was probably aggravated by his inability to breathe deeply and cough appropriately.
An elderly patient with rheumatoid arthritis was diagnosed with lymphoma. For want of something to blame, his children blamed it on the methotrexate.
A woman with lupus nephritis got pregnant while on mycophenolate despite being on contraception. Her baby was born with malformed ears and eyes, and by all accounts will probably be deaf and blind.
We have been gifted with this mind-blowing ability to make our patients’ lives much better. That sense of accomplishment can be intoxicating. After all, how many of your polymyalgia rheumatica patients worship you because you made the diagnosis and made them 100% better by putting them on prednisone? Yet we forget that although bad things rarely happen, that does not mean that they won’t happen.
In a beautiful book called "Where’d You Go, Bernadette?" the husband of the title character says that the brain is a discounting mechanism: "Let’s say you get a crack in your windshield and you’re really upset. Oh no, my windshield, it’s ruined, I can hardly see out of it, this is a tragedy! But you don’t have enough money to fix it, so you drive with it. In a month, someone asks you what happened to your windshield, and you say, What do you mean? Because your brain has discounted it. ... It’s for survival. You need to be prepared for novel experiences because often they signal danger."
The book is about an artist who we are led to believe has completed her downward spiral, going from genius to wacko. In the above passage, the artist’s husband is explaining to their daughter why they loved their family home so much, despite its state of extreme disrepair. They loved the house so much that they couldn’t see that it was a safety hazard.
As a fresh graduate I insisted on weaning everyone off prednisone, terrified of the potential side effects. Five years later and with the benefit of the collected wisdom of hundreds of rheumatologists before me, I have accepted that some people need a low dose of steroid to keep their disease quiet. I have used this and other, more toxic drugs to such great effects – taking for granted their ability to make people better – that I forget sometimes that they can cause serious problems.
Bad outcomes can and do happen in spite of our best intentions. In my case, my default is to blame myself. In my more melodramatic moments, I wonder if I deserve to be a doctor. But when I am done feeling angry or sad, or, frankly, feeling sorry for myself, then I need that discounting mechanism to kick in, to remind myself that this is one bad outcome out of many good outcomes. There are things beyond my control, and I cannot let a bad outcome keep me from doing the good work that I am still able to do.
There is a scene from the TV series "The West Wing" where the president asks one of his staffers if he thought the president was being kept from doing a great job because his demons were "shouting down the better angels" in his brain. Thankfully, my brain’s discounting mechanism helps keep the demons at bay.
Dr. Chan practices rheumatology in Pawtucket, R.I.
Firing your patient
How often do you fire patients? I do it here and there, maybe a few times a year, but certainly not as often as patients fire me.
Contrary to popular belief, I don’t get some sort of perverse thrill out of it. I am maybe relieved, knowing that I’m (hopefully) done with a difficult relationship. But it’s a pain, always requiring a trip to the post office to send the registered letter. There’s also the fear that they’ll report me to the board for it, and I’ll have to defend my actions. And I certainly can’t guard against the one-sided Yelp reviews.
What tips you over the edge? I consider myself pretty tolerant. In long-standing patients, I’ll generally let the occasional no-show slide. For drug abusers, I’m actually willing to continue with many of them, but will let them know that I’m not going to give them controlled substances anymore. Most of them leave at that point anyway.
I have zero tolerance for malicious behavior. Abuse my staff, and you’re out of here. I’m more willing to put up with someone who’s nasty to me than one who treats my staff the same way.
What other things do I fire them for? Occasionally noncompliance, especially if it’s putting their own safety in danger. Only once have I fired someone for refusing to have tests done. That was after, literally, 5 years of him repeatedly showing up annually to ask me to order them for his symptoms, then never following through and showing up a year later to start over again. At some point, my patience for that type of thing runs out, and I consider myself fairly patient.
Like most doctors, I’ve had more patients fire me than I’ve fired patients. For most, you don’t realize they’re gone. They just never come back. Occasionally, you get a release from another doctor, but more often you don’t.
Rarely, someone sends a nasty letter telling me why they went elsewhere and what they think of my medical skills/fashion sense/office décor ... whatever. The first time I got one of those, it hurt. Nowadays, I just don’t care.
Part of growing up as a doctor is realizing you’ll never make everyone happy or be able to help them all. Trying to do so will only lessen your sanity, so it’s a message best learned early.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How often do you fire patients? I do it here and there, maybe a few times a year, but certainly not as often as patients fire me.
Contrary to popular belief, I don’t get some sort of perverse thrill out of it. I am maybe relieved, knowing that I’m (hopefully) done with a difficult relationship. But it’s a pain, always requiring a trip to the post office to send the registered letter. There’s also the fear that they’ll report me to the board for it, and I’ll have to defend my actions. And I certainly can’t guard against the one-sided Yelp reviews.
What tips you over the edge? I consider myself pretty tolerant. In long-standing patients, I’ll generally let the occasional no-show slide. For drug abusers, I’m actually willing to continue with many of them, but will let them know that I’m not going to give them controlled substances anymore. Most of them leave at that point anyway.
I have zero tolerance for malicious behavior. Abuse my staff, and you’re out of here. I’m more willing to put up with someone who’s nasty to me than one who treats my staff the same way.
What other things do I fire them for? Occasionally noncompliance, especially if it’s putting their own safety in danger. Only once have I fired someone for refusing to have tests done. That was after, literally, 5 years of him repeatedly showing up annually to ask me to order them for his symptoms, then never following through and showing up a year later to start over again. At some point, my patience for that type of thing runs out, and I consider myself fairly patient.
Like most doctors, I’ve had more patients fire me than I’ve fired patients. For most, you don’t realize they’re gone. They just never come back. Occasionally, you get a release from another doctor, but more often you don’t.
Rarely, someone sends a nasty letter telling me why they went elsewhere and what they think of my medical skills/fashion sense/office décor ... whatever. The first time I got one of those, it hurt. Nowadays, I just don’t care.
Part of growing up as a doctor is realizing you’ll never make everyone happy or be able to help them all. Trying to do so will only lessen your sanity, so it’s a message best learned early.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How often do you fire patients? I do it here and there, maybe a few times a year, but certainly not as often as patients fire me.
Contrary to popular belief, I don’t get some sort of perverse thrill out of it. I am maybe relieved, knowing that I’m (hopefully) done with a difficult relationship. But it’s a pain, always requiring a trip to the post office to send the registered letter. There’s also the fear that they’ll report me to the board for it, and I’ll have to defend my actions. And I certainly can’t guard against the one-sided Yelp reviews.
What tips you over the edge? I consider myself pretty tolerant. In long-standing patients, I’ll generally let the occasional no-show slide. For drug abusers, I’m actually willing to continue with many of them, but will let them know that I’m not going to give them controlled substances anymore. Most of them leave at that point anyway.
I have zero tolerance for malicious behavior. Abuse my staff, and you’re out of here. I’m more willing to put up with someone who’s nasty to me than one who treats my staff the same way.
What other things do I fire them for? Occasionally noncompliance, especially if it’s putting their own safety in danger. Only once have I fired someone for refusing to have tests done. That was after, literally, 5 years of him repeatedly showing up annually to ask me to order them for his symptoms, then never following through and showing up a year later to start over again. At some point, my patience for that type of thing runs out, and I consider myself fairly patient.
Like most doctors, I’ve had more patients fire me than I’ve fired patients. For most, you don’t realize they’re gone. They just never come back. Occasionally, you get a release from another doctor, but more often you don’t.
Rarely, someone sends a nasty letter telling me why they went elsewhere and what they think of my medical skills/fashion sense/office décor ... whatever. The first time I got one of those, it hurt. Nowadays, I just don’t care.
Part of growing up as a doctor is realizing you’ll never make everyone happy or be able to help them all. Trying to do so will only lessen your sanity, so it’s a message best learned early.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Polyunsaturated fatty acid supplementation
Supplementation with polyunsaturated fatty acids – or omega-3 fatty acids – during pregnancy is an important topic because of unproven claims that polyunsaturated fatty acids (PUFAs) improve fetal brain and eye development if taken during pregnancy, resulting in unnecessary expense for many women who buy these products. In Canada, there are prenatal vitamins available that contain omega-3 fatty acids with a statement that the product "helps support cognitive health and/or brain function" or that omega-3 fatty acids "support "healthy fetal brain and eye development." These are misleading, inappropriate statements, considering that there is no compelling evidence to support these claims.
Claims about the benefits of PUFA supplementation during pregnancy, which have circulated for about a decade, originate from studies that show that when PUFAs are restricted during pregnancy, fetal brain development can be adversely affected, particularly in animals. Other data include several human studies that have linked high cognitive scores to a high seafood content of the maternal diet. The highest levels of PUFAs are measured in the retina, which is part of the visual acuity claim.
My colleagues and I addressed the uncertainties about the benefits of PUFA supplementation in a systematic review of nine randomized controlled trials comparing visual and neurobehavioral outcomes in infants whose mothers received PUFA supplements during gestation with control women who received placebos. Three studies evaluated retinal development and six evaluated neurodevelopment; most ended the supplement at delivery, and evaluations were conducted during the first year, or up to age 2.5, 4, and 7 years in different studies.
Overall, there was no evidence of a beneficial effect of PUFA supplementation during pregnancy on neurodevelopment (IQ, language behaviors) or on visual acuity. As we concluded, there were "very limited, if any" benefits identified, and in the studies with statistically significant differences between the two groups, "the differences were small and of little potential clinical importance" (Obstet. Gynecol. Int. 2012 [doi:10.1155/2012/591531]).
A study published in May 2014 also found no beneficial effect of prenatal supplementation with 800 mg/day of omega-3 fatty acid docosahexaenoic acid (DHA) on neurodevelopmental outcomes in children followed to age 4 years, and the authors concluded that the data "do not support prenatal DHA supplementation to enhance early childhood development." The randomized placebo-controlled study evaluated about 650 children at age 4 years, whose mothers had received the supplement or 333 who received placebo. The mean cognitive scores were not different between the two groups, and the proportion of children with delayed or advanced scores also did not differ between the two groups, nor did other objective assessments of cognition, language, and executive functioning (JAMA 2014;311:1802-4).
Based on the lack of evidence to date, there is no reason to add PUFAs to prenatal vitamins or recommend that women take a PUFA supplement during pregnancy.
The bottom line for clinicians/health care providers is that although the available evidence today has found no detrimental effects of even high doses of omega-3 fatty acid supplementation (up to 3.7 g/day), with the present state of knowledge, there is no evidence that prenatal supplementation with PUFAs improves brain development or acuity of vision in children. Instead of supplementation with PUFA during pregnancy, women should consume a diet with adequate PUFAs, with food that includes eggs and fish, with caution about the mercury content of fish.
Dr. Koren is professor of pediatrics, pharmacology, pharmacy, medicine, and medical genetics at the University of Toronto. He heads the Research Leadership for Better Pharmacotherapy During Pregnancy and Lactation at the Hospital for Sick Children, Toronto, where he is director of the Motherisk Program. He also holds the Ivey Chair in Molecular Toxicology at the department of medicine, University of Western Ontario, London. He had no disclosures relevant to this topic. E-mail him at [email protected].
Supplementation with polyunsaturated fatty acids – or omega-3 fatty acids – during pregnancy is an important topic because of unproven claims that polyunsaturated fatty acids (PUFAs) improve fetal brain and eye development if taken during pregnancy, resulting in unnecessary expense for many women who buy these products. In Canada, there are prenatal vitamins available that contain omega-3 fatty acids with a statement that the product "helps support cognitive health and/or brain function" or that omega-3 fatty acids "support "healthy fetal brain and eye development." These are misleading, inappropriate statements, considering that there is no compelling evidence to support these claims.
Claims about the benefits of PUFA supplementation during pregnancy, which have circulated for about a decade, originate from studies that show that when PUFAs are restricted during pregnancy, fetal brain development can be adversely affected, particularly in animals. Other data include several human studies that have linked high cognitive scores to a high seafood content of the maternal diet. The highest levels of PUFAs are measured in the retina, which is part of the visual acuity claim.
My colleagues and I addressed the uncertainties about the benefits of PUFA supplementation in a systematic review of nine randomized controlled trials comparing visual and neurobehavioral outcomes in infants whose mothers received PUFA supplements during gestation with control women who received placebos. Three studies evaluated retinal development and six evaluated neurodevelopment; most ended the supplement at delivery, and evaluations were conducted during the first year, or up to age 2.5, 4, and 7 years in different studies.
Overall, there was no evidence of a beneficial effect of PUFA supplementation during pregnancy on neurodevelopment (IQ, language behaviors) or on visual acuity. As we concluded, there were "very limited, if any" benefits identified, and in the studies with statistically significant differences between the two groups, "the differences were small and of little potential clinical importance" (Obstet. Gynecol. Int. 2012 [doi:10.1155/2012/591531]).
A study published in May 2014 also found no beneficial effect of prenatal supplementation with 800 mg/day of omega-3 fatty acid docosahexaenoic acid (DHA) on neurodevelopmental outcomes in children followed to age 4 years, and the authors concluded that the data "do not support prenatal DHA supplementation to enhance early childhood development." The randomized placebo-controlled study evaluated about 650 children at age 4 years, whose mothers had received the supplement or 333 who received placebo. The mean cognitive scores were not different between the two groups, and the proportion of children with delayed or advanced scores also did not differ between the two groups, nor did other objective assessments of cognition, language, and executive functioning (JAMA 2014;311:1802-4).
Based on the lack of evidence to date, there is no reason to add PUFAs to prenatal vitamins or recommend that women take a PUFA supplement during pregnancy.
The bottom line for clinicians/health care providers is that although the available evidence today has found no detrimental effects of even high doses of omega-3 fatty acid supplementation (up to 3.7 g/day), with the present state of knowledge, there is no evidence that prenatal supplementation with PUFAs improves brain development or acuity of vision in children. Instead of supplementation with PUFA during pregnancy, women should consume a diet with adequate PUFAs, with food that includes eggs and fish, with caution about the mercury content of fish.
Dr. Koren is professor of pediatrics, pharmacology, pharmacy, medicine, and medical genetics at the University of Toronto. He heads the Research Leadership for Better Pharmacotherapy During Pregnancy and Lactation at the Hospital for Sick Children, Toronto, where he is director of the Motherisk Program. He also holds the Ivey Chair in Molecular Toxicology at the department of medicine, University of Western Ontario, London. He had no disclosures relevant to this topic. E-mail him at [email protected].
Supplementation with polyunsaturated fatty acids – or omega-3 fatty acids – during pregnancy is an important topic because of unproven claims that polyunsaturated fatty acids (PUFAs) improve fetal brain and eye development if taken during pregnancy, resulting in unnecessary expense for many women who buy these products. In Canada, there are prenatal vitamins available that contain omega-3 fatty acids with a statement that the product "helps support cognitive health and/or brain function" or that omega-3 fatty acids "support "healthy fetal brain and eye development." These are misleading, inappropriate statements, considering that there is no compelling evidence to support these claims.
Claims about the benefits of PUFA supplementation during pregnancy, which have circulated for about a decade, originate from studies that show that when PUFAs are restricted during pregnancy, fetal brain development can be adversely affected, particularly in animals. Other data include several human studies that have linked high cognitive scores to a high seafood content of the maternal diet. The highest levels of PUFAs are measured in the retina, which is part of the visual acuity claim.
My colleagues and I addressed the uncertainties about the benefits of PUFA supplementation in a systematic review of nine randomized controlled trials comparing visual and neurobehavioral outcomes in infants whose mothers received PUFA supplements during gestation with control women who received placebos. Three studies evaluated retinal development and six evaluated neurodevelopment; most ended the supplement at delivery, and evaluations were conducted during the first year, or up to age 2.5, 4, and 7 years in different studies.
Overall, there was no evidence of a beneficial effect of PUFA supplementation during pregnancy on neurodevelopment (IQ, language behaviors) or on visual acuity. As we concluded, there were "very limited, if any" benefits identified, and in the studies with statistically significant differences between the two groups, "the differences were small and of little potential clinical importance" (Obstet. Gynecol. Int. 2012 [doi:10.1155/2012/591531]).
A study published in May 2014 also found no beneficial effect of prenatal supplementation with 800 mg/day of omega-3 fatty acid docosahexaenoic acid (DHA) on neurodevelopmental outcomes in children followed to age 4 years, and the authors concluded that the data "do not support prenatal DHA supplementation to enhance early childhood development." The randomized placebo-controlled study evaluated about 650 children at age 4 years, whose mothers had received the supplement or 333 who received placebo. The mean cognitive scores were not different between the two groups, and the proportion of children with delayed or advanced scores also did not differ between the two groups, nor did other objective assessments of cognition, language, and executive functioning (JAMA 2014;311:1802-4).
Based on the lack of evidence to date, there is no reason to add PUFAs to prenatal vitamins or recommend that women take a PUFA supplement during pregnancy.
The bottom line for clinicians/health care providers is that although the available evidence today has found no detrimental effects of even high doses of omega-3 fatty acid supplementation (up to 3.7 g/day), with the present state of knowledge, there is no evidence that prenatal supplementation with PUFAs improves brain development or acuity of vision in children. Instead of supplementation with PUFA during pregnancy, women should consume a diet with adequate PUFAs, with food that includes eggs and fish, with caution about the mercury content of fish.
Dr. Koren is professor of pediatrics, pharmacology, pharmacy, medicine, and medical genetics at the University of Toronto. He heads the Research Leadership for Better Pharmacotherapy During Pregnancy and Lactation at the Hospital for Sick Children, Toronto, where he is director of the Motherisk Program. He also holds the Ivey Chair in Molecular Toxicology at the department of medicine, University of Western Ontario, London. He had no disclosures relevant to this topic. E-mail him at [email protected].
Hormone therapy for menopausal vasomotor symptoms
Estrogen therapy is highly effective in the treatment of hot flashes among postmenopausal women. For postmenopausal women with a uterus, estrogen treatment for hot flashes is almost always combined with a progestin to reduce the risk of endometrial polyps, hyperplasia, and cancer. For instance, in the Postmenopausal Estrogen/Progestin Interventions Trial, 62% of the women with a uterus treated with conjugated equine estrogen (CEE) 0.625 mg daily without a progestin developed endometrial hyperplasia.1
In the United States, the most commonly prescribed progestin for hormone therapy has been medroxyprogesterone acetate (MPA; Provera). However, data from the Women’s Health Initiative (WHI) trials indicate that MPA, when combined with CEE, may have adverse health effects among postmenopausal women.
Let’s examine the WHI data
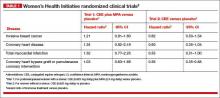
Among women 50 to 59 years of age with a uterus, the combination of CEE plus MPA was associated with a trend toward an increased risk of breast cancer, coronary heart disease, and myocardial infarction.2 In contrast, among women 50 to 59 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of invasive breast cancer, coronary heart disease, and myocardial infarction (TABLE 1).
Among women 50 to 79 years of age with a uterus, the combination of CEE plus MPA was associated with a significantly increased risk of breast cancer (hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.01–1.53; P = .04).2 In contrast, among women 50 to 79 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of breast cancer (HR, 0.79; 95% CI, 0.61–1.02, P = .07).2
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
When the analysis was limited to women consistently adherent to their CEE monotherapy, the estrogen treatment significantly decreased the risk of invasive breast cancer (HR, 0.67; 95% CI, 0.47–0.97; P = .03).3
The addition of MPA to CEE appears to reverse some of the health benefits of CEE monotherapy, although the biological mechanisms are unclear. This observation should prompt us to explore alternative and novel treatments of vasomotor symptoms that do not utilize MPA. Some options for MPA-free hormone therapy include:
- transdermal estradiol plus micronized progesterone
- CEE plus a levonorgestrel-releasing intrauterine system
- bazedoxifene plus CEE.
In addition, nonhormonal treatment of hot flashes is an option, with selective serotonin reuptake inhibitors (SSRIs).
Related article: Is one oral estrogen formulation safer than another for menopausal women? Andrew M. Kaunitz, MD (Examining the Evidence; January 2014)
MPA-free hormone therapy for hot flashes
Estrogen plus micronized progesterone
When using an estrogen plus progestin regimen to treat hot flashes, many experts favor a combination of low-dose transdermal estradiol and oral micronized progesterone (Prometrium). This combination is believed by some experts to result in a lower risk of venous thromboembolism, stroke, cardiovascular disease, and breast cancer than an estrogen-MPA combination.4–7
When prescribing transdermal estradiol plus oral micronized progesterone for a woman within 1 to 2 years of her last menses, a cyclic regimen can help reduce episodes of irregular, unscheduled uterine bleeding. I often use this cyclic regimen: transdermal estradiol 0.0375 mg plus cyclic oral micronized progesterone 200 mg prior to bedtime for calendar days 1 to 12.
When using transdermal estradiol plus oral micronized progesterone in a woman more than 2 years from her last menses, a continuous regimen is often prescribed. I often use this continuous regimen: transdermal estradiol 0.0375 mg plus continuous oral micronized progesterone 100 mg daily prior to bedtime.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Estrogen plus a levonorgestrel-releasing intrauterine systemThe levonorgestrel intrauterine system (LNG-IUS; 20 µg daily; Mirena) is frequently used in Europe to protect the endometrium against the adverse effects of estrogen therapy in postmenopausal women. In a meta-analysis of five clinical trials involving postmenopausal women, the LNG-IUS provided excellent protection against endometrial hyperplasia, compared with MPA.8
One caution about using the LNG-IUS system with estrogen in postmenopausal women is that an observational study of all women with breast cancer in Finland from 1995 through 2007 reported a significantly increased risk of breast cancer among postmenopausal women using an LNG-IUS compared with women who did not use hormones or used only estrogen because they had a hysterectomy (TABLE 2).9 This study was not a randomized clinical trial and patients at higher baseline risk for breast cancer, including women with a high body mass index, may have been preferentially treated with an LNG-IUS. More information is needed to better understand the relationship between the LNG-IUS and breast cancer in postmenopausal women.
Related article: What we’ve learned from 2 decades’ experience with the LNG-IUS. Q&A with Oskari Heikinheimo, MD, PhD (February 2011)
Progestin-free hormone treatment, bazedoxifene plus CEE
The main reason for adding a progestin to estrogen therapy for vasomotor symptoms in postmenopausal women with a uterus is to prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer. A major innovation in hormone therapy is the discovery that third-generation selective estrogen receptor modulators (SERMs), such as bazedoxifene (BZA), can prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer but do not interfere with the efficacy of estrogen in the treatment of vasomotor symptoms.
BZA is an estrogen agonist in bone and an estrogen antagonist in the endometrium.10–12 The combination of BZA (20 mg daily) plus CEE (0.45 mg daily) (Duavee) is approved for the treatment of moderate to severe vasomotor symptoms and prevention of osteoporosis.13–15 Over 24 months of therapy, various doses of BZA plus CEE reduced reported daily hot flashes by 52% to 86%.16 In the same study, placebo treatment was associated with a 17% reduction in hot flashes.16
The main adverse effect of BZA/CEE is an increased risk of deep venous thrombosis. Therefore, BZA/CEE is contraindicated in women with a known thrombophilia or a personal history of hormone-induced deep venous thrombosis. The effect of BZA/CEE on the risk of developing invasive breast cancer is not known; over 52 weeks of therapy it did not increase breast density on mammogram.17,18
BZA/CEE is a remarkable advance in hormone therapy. It is progestin-free, uses estrogen to treat vasomotor symptoms, and uses BZA to protect the endometrium against estrogen-induced hyperplasia.
Related article: New option for treating menopausal vasomotor symptoms receives FDA approval. (News for your Practice; October 2013)
Nonhormone treatment of vasomotor symptoms Paroxetine mesylateFor postmenopausal women with vasomotor symptoms who cannot take estrogen, SSRIs are modestly effective in reducing moderate to severe hot flashes. The US Food and Drug Administration recently approved paroxetine mesylate (Brisdelle) for the treatment of postmenopausal vasomotor symptoms. The approved dose is 7.5 mg daily taken at bedtime.
Data supporting the efficacy of paroxetine mesylate are available from two studies involving 1,184 menopausal women with vasomotor symptoms randomly assigned to receive paroxetine 7.5 mg daily or placebo for 12 weeks of treatment.19-22 In one of the two clinical trials, women treated with paroxetine mesylate 7.5 mg daily had 5.6 fewer moderate to severe hot flashes daily after 12 weeks of treatment compared with 3.9 fewer hot flashes with placebo (median treatment difference, 1.7; P<.001).21
Paroxetine can block the metabolism of tamoxifen to its highly potent metabolite, endoxifen. Consequently, paroxetine may reduce the effectiveness of tamoxifen treatment for breast cancer and should be used with caution in postmenopausal women with breast cancer being treated with tamoxifen.
Related article: Paroxetine mesylate 7.5 mg found to be a safe alternative to hormone therapy for menopausal women with hot flashes. (News for your Practice; June 2014)
Escitalopram
Gynecologists are familiar with the use of venlafaxine, desvenlafaxine, clonidine, citalopram, sertraline, and fluoxetine for the treatment of postmenopausal hot flashes. Recently, escitalopram (Lexapro) at doses of 10 to 20 mg daily has been shown to be more effective than placebo in the treatment of hot flashes and sleep disturbances in postmenopausal women.23,24 In one trial of escitalopram 10 to 20 mg daily versus placebo in 205 postmenopausal women averaging 9.8 hot flashes daily at baseline, escitalopram and placebo reduced mean daily hot flashes by 4.6 and 3.2, respectively (P<.001), after 8 weeks of treatment.
In a meta-analysis of SSRIs for the treatment of hot flashes, data from a mixed-treatment comparison analysis indicated that the rank order from most to least effective therapy for hot flashes was: escitalopram > paroxetine > sertraline > citalopram > fluoxetine.25 Venlafaxine and desvenlafaxine, two serotonin and norepinephrine reuptake inhibitors that are effective in the treatment of hot flashes, were not included in the mixed-treatment comparison.
Use of alternatives to MPA could mean fewer health risks for women on a wide scale
Substantial data indicate that MPA is not an optimal progestin to combine with estrogen for hormone therapy. Currently, many health insurance plans and Medicare use pharmacy management formularies that prioritize dispensing MPA for postmenopausal hormone therapy. Dispensing an alternative to MPA, such as micronized progesterone, often requires the patient to make a significant copayment.
Hopefully, health insurance companies, Medicare, and their affiliated pharmacy management administrators will soon stop their current policy of using financial incentives to favor dispensing MPA when hormone therapy is prescribed because alternatives to MPA appear to be associated with fewer health risks for postmenopausal women.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
1. The Writing Group for the PEPI Trial. Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. JAMA. 1996;275(5):370–375.
2. Manson JE, Chlebowski RT, Stefnick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310(13):1353–1368.
3. Stefanick ML, Anderson GL, Margolis KL, et al; WHI Investigators. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA. 2006;295(14):1647–1657.
4. Simon JA. What if the Women’s Health Initiative had used transdermal estradiol and oral progesterone instead? [published online head of print January 6, 2014]. Menopause. PMID: 24398406.
5. Manson JE. Current recommendations: What is the clinician to do? Fertil Steril. 2014;101(4):916–921.
6. Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: Results from the E3N cohort study [published correction appears in Breast Cancer Res Treat. 2008;107(2):307–308]. Breast Cancer Res Treat. 2008;107(1):103–111.
7. Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: A nested case-control study. BMJ. 2010;340:c2519.
8. Somboonpom W, Panna S, Temtanakitpaisan T, Kaewrudee S, Soontrapa S. Effects of the levonorgestrel-releasing intrauterine system plus estrogen therapy in perimenopausal and postmenopausal women: Systematic review and meta-analysis. Menopause. 2011;18(10):1060–1066.
9. Lyytinen HK, Dyba T, Ylikorkala O, Pukkala EI. A case-control study on hormone therapy as a risk factor for breast cancer in Finland: Intrauterine system carries a risk as well. Int J Cancer. 2010;126(2):483–489.
10. Komm BS, Mirkin S. An overview of current and emerging SERMs. J Steroid Biochem Mol Biol. 2014;143C:207–222.
11. Ethun KF, Wood CE, Cline JM, Register TC, Appt SE, Clarkson TB. Endometrial profile of bazedoxifene acetate alone and in combination with conjugated equine estrogens in a primate model. Menopause. 2013;20(7):777–784.
12. Pinkerton JV, Harvey JA, Lindsay R, et al; SMART-5 Investigators. Effects of bazedoxifene/conjugated estrogens on the endometrium and bone: A randomized trial. J Clin Endocrinol Metab. 2014;99(2):E189–E198.
13. Pinkerton JV, Pickar JH, Racketa J, Mirkin S. Bazedoxifene/conjugated estrogens for menopausal symptom treatment and osteoporosis prevention. Climacteric. 2012;15(5):411–418.
14. Pinkerton JV, Abraham L, Bushmakin AG, et al. Evaluation of the efficacy and safety of bazedoxifene/conjugated estrogens for secondary outcomes including vasomotor symptoms in postmenopausal women by years since menopause in the Selective estrogens, Menopause and Response to Therapy (SMART) trials. J Womens Health (Larchmt). 2014;23(1):18–28.
15. Pinkerton JV, Harvey JA, Pan K, et al. Breast effects of bazedoxifene-conjugated estrogens: A randomized controlled trial. Obstet Gynecol. 2013;121(5):959–968.
16. Lobo RA, Pinkerton JV, Gass ML, et al. Evaluation of bazedoxifene/conjugated estrogens for the treatment of menopausal symptoms and effects on metabolic parameters and overall safety profile. Fertil Steril. 2009;92(3):1025–1038.
17. Harvey JA, Holm MK, Ranganath R, Guse PA, Trott EA, Helzner E. The effects of bazedoxifene on mammographic breast density in postmenopausal women with osteoporosis. Menopause. 2009;16(6):1193–1196.
18. Harvey JA, Pinkerton JV, Baracat EC, Shi H, Chines AA, Mirkin S. Breast density changes in a randomized controlled trial evaluating bazedoxifene/conjugated estrogens. Menopause. 2013;20(2):138–145.
19. Simon JA, Portman DJ, Kaunitz AM, et al. Low-dose paroxetine 7.5 mg for menopausal vasomotor symptoms: Two randomized controlled trials. Menopause. 2013;20(10):1027–1035.
20. Simon JA, Portman DJ, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Safety profile of paroxetine 7.5 mg in women with moderate-to-severe vasomotor symptoms. Obstet Gynecol. 2014;123(suppl 1):132S–133S.
21. Orleans RJ, Li L, Kim MJ, et al. FDA approval of paroxetine for menopausal hot flashes. N Engl J Med. 2014;370(19):1777–1779.
22. Paroxetine (Brisdelle) for hot flashes. Med Lett Drugs Ther. 2013;55(1428):85–86.
23. Freeman EW, Guthrie KA, Caan B, et al. Efficacy of escitalopram for hot flashes in health menopausal women. A randomized controlled trial. JAMA. 2011;305(3):267–274.
24. Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: A randomized controlled trial. Menopause. 2012;19(8):848–855.
25. Shams T, Firwana B, Habib F, et al. SSRIs for hot flashes: A systematic review and meta-analysis of randomized trials. J Gen Intern Med. 2014;29(1):204–213.
Estrogen therapy is highly effective in the treatment of hot flashes among postmenopausal women. For postmenopausal women with a uterus, estrogen treatment for hot flashes is almost always combined with a progestin to reduce the risk of endometrial polyps, hyperplasia, and cancer. For instance, in the Postmenopausal Estrogen/Progestin Interventions Trial, 62% of the women with a uterus treated with conjugated equine estrogen (CEE) 0.625 mg daily without a progestin developed endometrial hyperplasia.1
In the United States, the most commonly prescribed progestin for hormone therapy has been medroxyprogesterone acetate (MPA; Provera). However, data from the Women’s Health Initiative (WHI) trials indicate that MPA, when combined with CEE, may have adverse health effects among postmenopausal women.
Let’s examine the WHI data
Among women 50 to 59 years of age with a uterus, the combination of CEE plus MPA was associated with a trend toward an increased risk of breast cancer, coronary heart disease, and myocardial infarction.2 In contrast, among women 50 to 59 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of invasive breast cancer, coronary heart disease, and myocardial infarction (TABLE 1).
Among women 50 to 79 years of age with a uterus, the combination of CEE plus MPA was associated with a significantly increased risk of breast cancer (hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.01–1.53; P = .04).2 In contrast, among women 50 to 79 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of breast cancer (HR, 0.79; 95% CI, 0.61–1.02, P = .07).2
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
When the analysis was limited to women consistently adherent to their CEE monotherapy, the estrogen treatment significantly decreased the risk of invasive breast cancer (HR, 0.67; 95% CI, 0.47–0.97; P = .03).3
The addition of MPA to CEE appears to reverse some of the health benefits of CEE monotherapy, although the biological mechanisms are unclear. This observation should prompt us to explore alternative and novel treatments of vasomotor symptoms that do not utilize MPA. Some options for MPA-free hormone therapy include:
- transdermal estradiol plus micronized progesterone
- CEE plus a levonorgestrel-releasing intrauterine system
- bazedoxifene plus CEE.
In addition, nonhormonal treatment of hot flashes is an option, with selective serotonin reuptake inhibitors (SSRIs).
Related article: Is one oral estrogen formulation safer than another for menopausal women? Andrew M. Kaunitz, MD (Examining the Evidence; January 2014)
MPA-free hormone therapy for hot flashes
Estrogen plus micronized progesterone
When using an estrogen plus progestin regimen to treat hot flashes, many experts favor a combination of low-dose transdermal estradiol and oral micronized progesterone (Prometrium). This combination is believed by some experts to result in a lower risk of venous thromboembolism, stroke, cardiovascular disease, and breast cancer than an estrogen-MPA combination.4–7
When prescribing transdermal estradiol plus oral micronized progesterone for a woman within 1 to 2 years of her last menses, a cyclic regimen can help reduce episodes of irregular, unscheduled uterine bleeding. I often use this cyclic regimen: transdermal estradiol 0.0375 mg plus cyclic oral micronized progesterone 200 mg prior to bedtime for calendar days 1 to 12.
When using transdermal estradiol plus oral micronized progesterone in a woman more than 2 years from her last menses, a continuous regimen is often prescribed. I often use this continuous regimen: transdermal estradiol 0.0375 mg plus continuous oral micronized progesterone 100 mg daily prior to bedtime.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Estrogen plus a levonorgestrel-releasing intrauterine systemThe levonorgestrel intrauterine system (LNG-IUS; 20 µg daily; Mirena) is frequently used in Europe to protect the endometrium against the adverse effects of estrogen therapy in postmenopausal women. In a meta-analysis of five clinical trials involving postmenopausal women, the LNG-IUS provided excellent protection against endometrial hyperplasia, compared with MPA.8
One caution about using the LNG-IUS system with estrogen in postmenopausal women is that an observational study of all women with breast cancer in Finland from 1995 through 2007 reported a significantly increased risk of breast cancer among postmenopausal women using an LNG-IUS compared with women who did not use hormones or used only estrogen because they had a hysterectomy (TABLE 2).9 This study was not a randomized clinical trial and patients at higher baseline risk for breast cancer, including women with a high body mass index, may have been preferentially treated with an LNG-IUS. More information is needed to better understand the relationship between the LNG-IUS and breast cancer in postmenopausal women.
Related article: What we’ve learned from 2 decades’ experience with the LNG-IUS. Q&A with Oskari Heikinheimo, MD, PhD (February 2011)
Progestin-free hormone treatment, bazedoxifene plus CEE
The main reason for adding a progestin to estrogen therapy for vasomotor symptoms in postmenopausal women with a uterus is to prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer. A major innovation in hormone therapy is the discovery that third-generation selective estrogen receptor modulators (SERMs), such as bazedoxifene (BZA), can prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer but do not interfere with the efficacy of estrogen in the treatment of vasomotor symptoms.
BZA is an estrogen agonist in bone and an estrogen antagonist in the endometrium.10–12 The combination of BZA (20 mg daily) plus CEE (0.45 mg daily) (Duavee) is approved for the treatment of moderate to severe vasomotor symptoms and prevention of osteoporosis.13–15 Over 24 months of therapy, various doses of BZA plus CEE reduced reported daily hot flashes by 52% to 86%.16 In the same study, placebo treatment was associated with a 17% reduction in hot flashes.16
The main adverse effect of BZA/CEE is an increased risk of deep venous thrombosis. Therefore, BZA/CEE is contraindicated in women with a known thrombophilia or a personal history of hormone-induced deep venous thrombosis. The effect of BZA/CEE on the risk of developing invasive breast cancer is not known; over 52 weeks of therapy it did not increase breast density on mammogram.17,18
BZA/CEE is a remarkable advance in hormone therapy. It is progestin-free, uses estrogen to treat vasomotor symptoms, and uses BZA to protect the endometrium against estrogen-induced hyperplasia.
Related article: New option for treating menopausal vasomotor symptoms receives FDA approval. (News for your Practice; October 2013)
Nonhormone treatment of vasomotor symptoms Paroxetine mesylateFor postmenopausal women with vasomotor symptoms who cannot take estrogen, SSRIs are modestly effective in reducing moderate to severe hot flashes. The US Food and Drug Administration recently approved paroxetine mesylate (Brisdelle) for the treatment of postmenopausal vasomotor symptoms. The approved dose is 7.5 mg daily taken at bedtime.
Data supporting the efficacy of paroxetine mesylate are available from two studies involving 1,184 menopausal women with vasomotor symptoms randomly assigned to receive paroxetine 7.5 mg daily or placebo for 12 weeks of treatment.19-22 In one of the two clinical trials, women treated with paroxetine mesylate 7.5 mg daily had 5.6 fewer moderate to severe hot flashes daily after 12 weeks of treatment compared with 3.9 fewer hot flashes with placebo (median treatment difference, 1.7; P<.001).21
Paroxetine can block the metabolism of tamoxifen to its highly potent metabolite, endoxifen. Consequently, paroxetine may reduce the effectiveness of tamoxifen treatment for breast cancer and should be used with caution in postmenopausal women with breast cancer being treated with tamoxifen.
Related article: Paroxetine mesylate 7.5 mg found to be a safe alternative to hormone therapy for menopausal women with hot flashes. (News for your Practice; June 2014)
Escitalopram
Gynecologists are familiar with the use of venlafaxine, desvenlafaxine, clonidine, citalopram, sertraline, and fluoxetine for the treatment of postmenopausal hot flashes. Recently, escitalopram (Lexapro) at doses of 10 to 20 mg daily has been shown to be more effective than placebo in the treatment of hot flashes and sleep disturbances in postmenopausal women.23,24 In one trial of escitalopram 10 to 20 mg daily versus placebo in 205 postmenopausal women averaging 9.8 hot flashes daily at baseline, escitalopram and placebo reduced mean daily hot flashes by 4.6 and 3.2, respectively (P<.001), after 8 weeks of treatment.
In a meta-analysis of SSRIs for the treatment of hot flashes, data from a mixed-treatment comparison analysis indicated that the rank order from most to least effective therapy for hot flashes was: escitalopram > paroxetine > sertraline > citalopram > fluoxetine.25 Venlafaxine and desvenlafaxine, two serotonin and norepinephrine reuptake inhibitors that are effective in the treatment of hot flashes, were not included in the mixed-treatment comparison.
Use of alternatives to MPA could mean fewer health risks for women on a wide scale
Substantial data indicate that MPA is not an optimal progestin to combine with estrogen for hormone therapy. Currently, many health insurance plans and Medicare use pharmacy management formularies that prioritize dispensing MPA for postmenopausal hormone therapy. Dispensing an alternative to MPA, such as micronized progesterone, often requires the patient to make a significant copayment.
Hopefully, health insurance companies, Medicare, and their affiliated pharmacy management administrators will soon stop their current policy of using financial incentives to favor dispensing MPA when hormone therapy is prescribed because alternatives to MPA appear to be associated with fewer health risks for postmenopausal women.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Estrogen therapy is highly effective in the treatment of hot flashes among postmenopausal women. For postmenopausal women with a uterus, estrogen treatment for hot flashes is almost always combined with a progestin to reduce the risk of endometrial polyps, hyperplasia, and cancer. For instance, in the Postmenopausal Estrogen/Progestin Interventions Trial, 62% of the women with a uterus treated with conjugated equine estrogen (CEE) 0.625 mg daily without a progestin developed endometrial hyperplasia.1
In the United States, the most commonly prescribed progestin for hormone therapy has been medroxyprogesterone acetate (MPA; Provera). However, data from the Women’s Health Initiative (WHI) trials indicate that MPA, when combined with CEE, may have adverse health effects among postmenopausal women.
Let’s examine the WHI data
Among women 50 to 59 years of age with a uterus, the combination of CEE plus MPA was associated with a trend toward an increased risk of breast cancer, coronary heart disease, and myocardial infarction.2 In contrast, among women 50 to 59 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of invasive breast cancer, coronary heart disease, and myocardial infarction (TABLE 1).
Among women 50 to 79 years of age with a uterus, the combination of CEE plus MPA was associated with a significantly increased risk of breast cancer (hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.01–1.53; P = .04).2 In contrast, among women 50 to 79 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of breast cancer (HR, 0.79; 95% CI, 0.61–1.02, P = .07).2
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
When the analysis was limited to women consistently adherent to their CEE monotherapy, the estrogen treatment significantly decreased the risk of invasive breast cancer (HR, 0.67; 95% CI, 0.47–0.97; P = .03).3
The addition of MPA to CEE appears to reverse some of the health benefits of CEE monotherapy, although the biological mechanisms are unclear. This observation should prompt us to explore alternative and novel treatments of vasomotor symptoms that do not utilize MPA. Some options for MPA-free hormone therapy include:
- transdermal estradiol plus micronized progesterone
- CEE plus a levonorgestrel-releasing intrauterine system
- bazedoxifene plus CEE.
In addition, nonhormonal treatment of hot flashes is an option, with selective serotonin reuptake inhibitors (SSRIs).
Related article: Is one oral estrogen formulation safer than another for menopausal women? Andrew M. Kaunitz, MD (Examining the Evidence; January 2014)
MPA-free hormone therapy for hot flashes
Estrogen plus micronized progesterone
When using an estrogen plus progestin regimen to treat hot flashes, many experts favor a combination of low-dose transdermal estradiol and oral micronized progesterone (Prometrium). This combination is believed by some experts to result in a lower risk of venous thromboembolism, stroke, cardiovascular disease, and breast cancer than an estrogen-MPA combination.4–7
When prescribing transdermal estradiol plus oral micronized progesterone for a woman within 1 to 2 years of her last menses, a cyclic regimen can help reduce episodes of irregular, unscheduled uterine bleeding. I often use this cyclic regimen: transdermal estradiol 0.0375 mg plus cyclic oral micronized progesterone 200 mg prior to bedtime for calendar days 1 to 12.
When using transdermal estradiol plus oral micronized progesterone in a woman more than 2 years from her last menses, a continuous regimen is often prescribed. I often use this continuous regimen: transdermal estradiol 0.0375 mg plus continuous oral micronized progesterone 100 mg daily prior to bedtime.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Estrogen plus a levonorgestrel-releasing intrauterine systemThe levonorgestrel intrauterine system (LNG-IUS; 20 µg daily; Mirena) is frequently used in Europe to protect the endometrium against the adverse effects of estrogen therapy in postmenopausal women. In a meta-analysis of five clinical trials involving postmenopausal women, the LNG-IUS provided excellent protection against endometrial hyperplasia, compared with MPA.8
One caution about using the LNG-IUS system with estrogen in postmenopausal women is that an observational study of all women with breast cancer in Finland from 1995 through 2007 reported a significantly increased risk of breast cancer among postmenopausal women using an LNG-IUS compared with women who did not use hormones or used only estrogen because they had a hysterectomy (TABLE 2).9 This study was not a randomized clinical trial and patients at higher baseline risk for breast cancer, including women with a high body mass index, may have been preferentially treated with an LNG-IUS. More information is needed to better understand the relationship between the LNG-IUS and breast cancer in postmenopausal women.
Related article: What we’ve learned from 2 decades’ experience with the LNG-IUS. Q&A with Oskari Heikinheimo, MD, PhD (February 2011)
Progestin-free hormone treatment, bazedoxifene plus CEE
The main reason for adding a progestin to estrogen therapy for vasomotor symptoms in postmenopausal women with a uterus is to prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer. A major innovation in hormone therapy is the discovery that third-generation selective estrogen receptor modulators (SERMs), such as bazedoxifene (BZA), can prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer but do not interfere with the efficacy of estrogen in the treatment of vasomotor symptoms.
BZA is an estrogen agonist in bone and an estrogen antagonist in the endometrium.10–12 The combination of BZA (20 mg daily) plus CEE (0.45 mg daily) (Duavee) is approved for the treatment of moderate to severe vasomotor symptoms and prevention of osteoporosis.13–15 Over 24 months of therapy, various doses of BZA plus CEE reduced reported daily hot flashes by 52% to 86%.16 In the same study, placebo treatment was associated with a 17% reduction in hot flashes.16
The main adverse effect of BZA/CEE is an increased risk of deep venous thrombosis. Therefore, BZA/CEE is contraindicated in women with a known thrombophilia or a personal history of hormone-induced deep venous thrombosis. The effect of BZA/CEE on the risk of developing invasive breast cancer is not known; over 52 weeks of therapy it did not increase breast density on mammogram.17,18
BZA/CEE is a remarkable advance in hormone therapy. It is progestin-free, uses estrogen to treat vasomotor symptoms, and uses BZA to protect the endometrium against estrogen-induced hyperplasia.
Related article: New option for treating menopausal vasomotor symptoms receives FDA approval. (News for your Practice; October 2013)
Nonhormone treatment of vasomotor symptoms Paroxetine mesylateFor postmenopausal women with vasomotor symptoms who cannot take estrogen, SSRIs are modestly effective in reducing moderate to severe hot flashes. The US Food and Drug Administration recently approved paroxetine mesylate (Brisdelle) for the treatment of postmenopausal vasomotor symptoms. The approved dose is 7.5 mg daily taken at bedtime.
Data supporting the efficacy of paroxetine mesylate are available from two studies involving 1,184 menopausal women with vasomotor symptoms randomly assigned to receive paroxetine 7.5 mg daily or placebo for 12 weeks of treatment.19-22 In one of the two clinical trials, women treated with paroxetine mesylate 7.5 mg daily had 5.6 fewer moderate to severe hot flashes daily after 12 weeks of treatment compared with 3.9 fewer hot flashes with placebo (median treatment difference, 1.7; P<.001).21
Paroxetine can block the metabolism of tamoxifen to its highly potent metabolite, endoxifen. Consequently, paroxetine may reduce the effectiveness of tamoxifen treatment for breast cancer and should be used with caution in postmenopausal women with breast cancer being treated with tamoxifen.
Related article: Paroxetine mesylate 7.5 mg found to be a safe alternative to hormone therapy for menopausal women with hot flashes. (News for your Practice; June 2014)
Escitalopram
Gynecologists are familiar with the use of venlafaxine, desvenlafaxine, clonidine, citalopram, sertraline, and fluoxetine for the treatment of postmenopausal hot flashes. Recently, escitalopram (Lexapro) at doses of 10 to 20 mg daily has been shown to be more effective than placebo in the treatment of hot flashes and sleep disturbances in postmenopausal women.23,24 In one trial of escitalopram 10 to 20 mg daily versus placebo in 205 postmenopausal women averaging 9.8 hot flashes daily at baseline, escitalopram and placebo reduced mean daily hot flashes by 4.6 and 3.2, respectively (P<.001), after 8 weeks of treatment.
In a meta-analysis of SSRIs for the treatment of hot flashes, data from a mixed-treatment comparison analysis indicated that the rank order from most to least effective therapy for hot flashes was: escitalopram > paroxetine > sertraline > citalopram > fluoxetine.25 Venlafaxine and desvenlafaxine, two serotonin and norepinephrine reuptake inhibitors that are effective in the treatment of hot flashes, were not included in the mixed-treatment comparison.
Use of alternatives to MPA could mean fewer health risks for women on a wide scale
Substantial data indicate that MPA is not an optimal progestin to combine with estrogen for hormone therapy. Currently, many health insurance plans and Medicare use pharmacy management formularies that prioritize dispensing MPA for postmenopausal hormone therapy. Dispensing an alternative to MPA, such as micronized progesterone, often requires the patient to make a significant copayment.
Hopefully, health insurance companies, Medicare, and their affiliated pharmacy management administrators will soon stop their current policy of using financial incentives to favor dispensing MPA when hormone therapy is prescribed because alternatives to MPA appear to be associated with fewer health risks for postmenopausal women.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
1. The Writing Group for the PEPI Trial. Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. JAMA. 1996;275(5):370–375.
2. Manson JE, Chlebowski RT, Stefnick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310(13):1353–1368.
3. Stefanick ML, Anderson GL, Margolis KL, et al; WHI Investigators. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA. 2006;295(14):1647–1657.
4. Simon JA. What if the Women’s Health Initiative had used transdermal estradiol and oral progesterone instead? [published online head of print January 6, 2014]. Menopause. PMID: 24398406.
5. Manson JE. Current recommendations: What is the clinician to do? Fertil Steril. 2014;101(4):916–921.
6. Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: Results from the E3N cohort study [published correction appears in Breast Cancer Res Treat. 2008;107(2):307–308]. Breast Cancer Res Treat. 2008;107(1):103–111.
7. Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: A nested case-control study. BMJ. 2010;340:c2519.
8. Somboonpom W, Panna S, Temtanakitpaisan T, Kaewrudee S, Soontrapa S. Effects of the levonorgestrel-releasing intrauterine system plus estrogen therapy in perimenopausal and postmenopausal women: Systematic review and meta-analysis. Menopause. 2011;18(10):1060–1066.
9. Lyytinen HK, Dyba T, Ylikorkala O, Pukkala EI. A case-control study on hormone therapy as a risk factor for breast cancer in Finland: Intrauterine system carries a risk as well. Int J Cancer. 2010;126(2):483–489.
10. Komm BS, Mirkin S. An overview of current and emerging SERMs. J Steroid Biochem Mol Biol. 2014;143C:207–222.
11. Ethun KF, Wood CE, Cline JM, Register TC, Appt SE, Clarkson TB. Endometrial profile of bazedoxifene acetate alone and in combination with conjugated equine estrogens in a primate model. Menopause. 2013;20(7):777–784.
12. Pinkerton JV, Harvey JA, Lindsay R, et al; SMART-5 Investigators. Effects of bazedoxifene/conjugated estrogens on the endometrium and bone: A randomized trial. J Clin Endocrinol Metab. 2014;99(2):E189–E198.
13. Pinkerton JV, Pickar JH, Racketa J, Mirkin S. Bazedoxifene/conjugated estrogens for menopausal symptom treatment and osteoporosis prevention. Climacteric. 2012;15(5):411–418.
14. Pinkerton JV, Abraham L, Bushmakin AG, et al. Evaluation of the efficacy and safety of bazedoxifene/conjugated estrogens for secondary outcomes including vasomotor symptoms in postmenopausal women by years since menopause in the Selective estrogens, Menopause and Response to Therapy (SMART) trials. J Womens Health (Larchmt). 2014;23(1):18–28.
15. Pinkerton JV, Harvey JA, Pan K, et al. Breast effects of bazedoxifene-conjugated estrogens: A randomized controlled trial. Obstet Gynecol. 2013;121(5):959–968.
16. Lobo RA, Pinkerton JV, Gass ML, et al. Evaluation of bazedoxifene/conjugated estrogens for the treatment of menopausal symptoms and effects on metabolic parameters and overall safety profile. Fertil Steril. 2009;92(3):1025–1038.
17. Harvey JA, Holm MK, Ranganath R, Guse PA, Trott EA, Helzner E. The effects of bazedoxifene on mammographic breast density in postmenopausal women with osteoporosis. Menopause. 2009;16(6):1193–1196.
18. Harvey JA, Pinkerton JV, Baracat EC, Shi H, Chines AA, Mirkin S. Breast density changes in a randomized controlled trial evaluating bazedoxifene/conjugated estrogens. Menopause. 2013;20(2):138–145.
19. Simon JA, Portman DJ, Kaunitz AM, et al. Low-dose paroxetine 7.5 mg for menopausal vasomotor symptoms: Two randomized controlled trials. Menopause. 2013;20(10):1027–1035.
20. Simon JA, Portman DJ, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Safety profile of paroxetine 7.5 mg in women with moderate-to-severe vasomotor symptoms. Obstet Gynecol. 2014;123(suppl 1):132S–133S.
21. Orleans RJ, Li L, Kim MJ, et al. FDA approval of paroxetine for menopausal hot flashes. N Engl J Med. 2014;370(19):1777–1779.
22. Paroxetine (Brisdelle) for hot flashes. Med Lett Drugs Ther. 2013;55(1428):85–86.
23. Freeman EW, Guthrie KA, Caan B, et al. Efficacy of escitalopram for hot flashes in health menopausal women. A randomized controlled trial. JAMA. 2011;305(3):267–274.
24. Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: A randomized controlled trial. Menopause. 2012;19(8):848–855.
25. Shams T, Firwana B, Habib F, et al. SSRIs for hot flashes: A systematic review and meta-analysis of randomized trials. J Gen Intern Med. 2014;29(1):204–213.
1. The Writing Group for the PEPI Trial. Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. JAMA. 1996;275(5):370–375.
2. Manson JE, Chlebowski RT, Stefnick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310(13):1353–1368.
3. Stefanick ML, Anderson GL, Margolis KL, et al; WHI Investigators. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA. 2006;295(14):1647–1657.
4. Simon JA. What if the Women’s Health Initiative had used transdermal estradiol and oral progesterone instead? [published online head of print January 6, 2014]. Menopause. PMID: 24398406.
5. Manson JE. Current recommendations: What is the clinician to do? Fertil Steril. 2014;101(4):916–921.
6. Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: Results from the E3N cohort study [published correction appears in Breast Cancer Res Treat. 2008;107(2):307–308]. Breast Cancer Res Treat. 2008;107(1):103–111.
7. Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: A nested case-control study. BMJ. 2010;340:c2519.
8. Somboonpom W, Panna S, Temtanakitpaisan T, Kaewrudee S, Soontrapa S. Effects of the levonorgestrel-releasing intrauterine system plus estrogen therapy in perimenopausal and postmenopausal women: Systematic review and meta-analysis. Menopause. 2011;18(10):1060–1066.
9. Lyytinen HK, Dyba T, Ylikorkala O, Pukkala EI. A case-control study on hormone therapy as a risk factor for breast cancer in Finland: Intrauterine system carries a risk as well. Int J Cancer. 2010;126(2):483–489.
10. Komm BS, Mirkin S. An overview of current and emerging SERMs. J Steroid Biochem Mol Biol. 2014;143C:207–222.
11. Ethun KF, Wood CE, Cline JM, Register TC, Appt SE, Clarkson TB. Endometrial profile of bazedoxifene acetate alone and in combination with conjugated equine estrogens in a primate model. Menopause. 2013;20(7):777–784.
12. Pinkerton JV, Harvey JA, Lindsay R, et al; SMART-5 Investigators. Effects of bazedoxifene/conjugated estrogens on the endometrium and bone: A randomized trial. J Clin Endocrinol Metab. 2014;99(2):E189–E198.
13. Pinkerton JV, Pickar JH, Racketa J, Mirkin S. Bazedoxifene/conjugated estrogens for menopausal symptom treatment and osteoporosis prevention. Climacteric. 2012;15(5):411–418.
14. Pinkerton JV, Abraham L, Bushmakin AG, et al. Evaluation of the efficacy and safety of bazedoxifene/conjugated estrogens for secondary outcomes including vasomotor symptoms in postmenopausal women by years since menopause in the Selective estrogens, Menopause and Response to Therapy (SMART) trials. J Womens Health (Larchmt). 2014;23(1):18–28.
15. Pinkerton JV, Harvey JA, Pan K, et al. Breast effects of bazedoxifene-conjugated estrogens: A randomized controlled trial. Obstet Gynecol. 2013;121(5):959–968.
16. Lobo RA, Pinkerton JV, Gass ML, et al. Evaluation of bazedoxifene/conjugated estrogens for the treatment of menopausal symptoms and effects on metabolic parameters and overall safety profile. Fertil Steril. 2009;92(3):1025–1038.
17. Harvey JA, Holm MK, Ranganath R, Guse PA, Trott EA, Helzner E. The effects of bazedoxifene on mammographic breast density in postmenopausal women with osteoporosis. Menopause. 2009;16(6):1193–1196.
18. Harvey JA, Pinkerton JV, Baracat EC, Shi H, Chines AA, Mirkin S. Breast density changes in a randomized controlled trial evaluating bazedoxifene/conjugated estrogens. Menopause. 2013;20(2):138–145.
19. Simon JA, Portman DJ, Kaunitz AM, et al. Low-dose paroxetine 7.5 mg for menopausal vasomotor symptoms: Two randomized controlled trials. Menopause. 2013;20(10):1027–1035.
20. Simon JA, Portman DJ, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Safety profile of paroxetine 7.5 mg in women with moderate-to-severe vasomotor symptoms. Obstet Gynecol. 2014;123(suppl 1):132S–133S.
21. Orleans RJ, Li L, Kim MJ, et al. FDA approval of paroxetine for menopausal hot flashes. N Engl J Med. 2014;370(19):1777–1779.
22. Paroxetine (Brisdelle) for hot flashes. Med Lett Drugs Ther. 2013;55(1428):85–86.
23. Freeman EW, Guthrie KA, Caan B, et al. Efficacy of escitalopram for hot flashes in health menopausal women. A randomized controlled trial. JAMA. 2011;305(3):267–274.
24. Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: A randomized controlled trial. Menopause. 2012;19(8):848–855.
25. Shams T, Firwana B, Habib F, et al. SSRIs for hot flashes: A systematic review and meta-analysis of randomized trials. J Gen Intern Med. 2014;29(1):204–213.
New Agents for the Treatment of Erythematotelangiectatic Rosacea
Rosacea is a common chronic disorder that predominantly manifests as facial erythema, telangiectasia, and flushing.1 Other primary clinical features include inflammatory lesions (eg, papules, pustules) and occasionally edema and rhinophyma. Ocular involvement also may occur. Rosacea patients routinely report sensitive skin with symptoms such as stinging, burning, and intolerance to topical agents (eg, medications, moisturizers, cosmetics).2,3
Rosacea affects facial appearance and can impair a patient’s emotional well-being. It may limit social and professional activities. Many patients and nonpatients alike presume the appearance of facial redness suggests alcohol overuse or emotional distress.4-6 A reduction in facial erythema as well as improvements in other clinical signs of rosacea have been shown to reduce patient self-consciousness and lead to increased socialization.7 Facial erythema is a major factor that adversely affects quality of life in rosacea patients.8
Although a number of options are available to successfully treat inflammatory lesions of rosacea, facial erythema has been the most difficult manifestation of the disease to medically treat.2,9 Chronic erythema and episodic flushing may be at least partially related to cutaneous vasomotor responses causing both transient and persistent dilation of facial blood vessels.10-12 The agents used for treating the inflammatory components of rosacea reduce erythema associated with papules and pustules but have little effect on the background erythema that is so noticeable. Oxymetazoline and brimonidine tartrate have been evaluated as potential rapid treatments of facial erythema. Daily application of oxymetazoline solution 0.05% has been shown to reduce facial erythema in rosacea patients.13
Brimonidine tartrate is a highly selective α2-adrenergic receptor agonist with potent vasoconstrictor activity.14 It has been used to treat open-angle glaucoma for more than 15 years with well-documented safety and efficacy.15 Phase 2 and 3 studies for once-daily application of brimonidine tartrate gel 0.5% have confirmed its efficacy and safety for the treatment of facial erythema in rosacea patients,9,12 and it was approved by the US Food and Drug Administration (brimonidine gel 0.33%) for persistent (nontransient) facial erythema of rosacea in late 2013. The effect was shown to occur in some patients as soon as 30 minutes following product application and usually persisted for approximately 9 to 12 hours. Erythema gradually returned as the effect waned, returning to baseline by 24 hours after application.12
Clinical efficacy of brimonidine gel was evaluated by a 2-grade improvement (primary end point) or 1-grade improvement (secondary end point) based on patient and clinician assessments using the patient self-assessment (PSA) and clinical erythema assessment (CEA), respectively, over the course of the 4-week studies. Patients also evaluated their satisfaction with the overall appearance of their facial skin.12 A 2-grade improvement on both PSA and CEA has been noted as a stringent criterion in evaluating the effectiveness of treatment of facial erythema.14 A 1-grade improvement on both PSA and CEA has been recognized as clinically relevant as a measure of effect that is noticeable to both patients and clinicians.12 Patients who achieved either a 1- or 2-grade improvement in both PSA and CEA were substantially more likely to report overall satisfaction with their appearance. A 2-grade improvement in both PSA and CEA scales was accompanied with 80% of patients rating their skin appearance as satisfactory or better. Conversely, few patients (ie, <10%) who did not achieve at least 1-grade composite success were satisfied with their appearance. Adverse effects were uncommon, with no evidence of tachyphylaxis and rare occurrence of rebound erythema.12
In summary, although there are a number of options available to reduce or eliminate inflammatory lesions of rosacea, effective medical treatment of the erythematous component of rosacea, which can be the most distressing aspect of the disease for patients, has been unsatisfactory. With the availability of topical brimonidine tartrate, dermatologists have a proven medication to improve facial redness in rosacea patients. Other options such as oxymetazoline may become available in the future.
- Crawford GH, Pelle MT, James WD. Rosacea: I. etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327-341.
- Wilkin J, Dahl M, Detmar M, et al. Standard grading system for rosacea: report of the National Rosacea Society expert committee on the classification and staging of rosacea. J Am Acad Dermatol. 2004;50:907-912.
- Odom R, Dahl M, Dover J, et al. Standard management options for rosacea, part I: overview and broad spectrum of care. Cutis. 2009;84:43-47.
- Baldwin HE. Systemic therapy for rosacea. Skin Therapy Lett. 2007;12:1-5.
- Drake L. Rosacea patients feel effects of their condition in social settings. Rosacea Review. Published Fall 2012. http://www.rosacea.org/rr/2012/fall/article_3.php. Accessed May 29, 2014.
- Aksoy B, Altaykan-Hapa A, Egemen D, et al. The impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalities. Br J Dermatol. 2010;163:719-725.
- Wolf JE Jr, Del Rosso JQ. The CLEAR trial: results of a large community-based study of metronidazole gel in rosacea. Cutis. 2007;79:73-80.
- Nicholson K, Abramova L, Chren MM, et al. A pilot quality-of-life instrument for acne rosacea. J Am Acad Dermatol. 2007;57:213-221.
- Fowler J, Jarratt M, Moore A, et al. Once-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicentre, randomized and vehicle-controlled studies. Br J Dermatol. 2012;166:633-641.
- Steinhoff M, Buddenkotte J, Aubert J, et al. Clinical, cellular and molecular aspects in the pathophysiology of rosacea. J Investig Dermatol Symp Proc. 2011;15:2-11.
- Wilkin JK. Rosacea: pathophysiology and treatment. Arch Dermatol. 1994;130:359-362.
- Fowler J, Jackson JM, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650-656.
- Del Rosso JQ. The central role, evaluation, and medical management of diffuse and persistent facial erythema of rosacea. J Clin Aesthet Dermatol. 2012;5:26-36.
- Rahman MQ, Ramaesh K, Montgomery DNI. Brimonidine for glaucoma. Expert Opin Drug Saf. 2010;9:483-491.
- Toris C, Camras C, Yablonski M. Acute versus chronic effects of brimonidine on aqueous humor dynamics in ocular hypertensive patients. Am J Ophthalmol. 1999;128:8-14.
Rosacea is a common chronic disorder that predominantly manifests as facial erythema, telangiectasia, and flushing.1 Other primary clinical features include inflammatory lesions (eg, papules, pustules) and occasionally edema and rhinophyma. Ocular involvement also may occur. Rosacea patients routinely report sensitive skin with symptoms such as stinging, burning, and intolerance to topical agents (eg, medications, moisturizers, cosmetics).2,3
Rosacea affects facial appearance and can impair a patient’s emotional well-being. It may limit social and professional activities. Many patients and nonpatients alike presume the appearance of facial redness suggests alcohol overuse or emotional distress.4-6 A reduction in facial erythema as well as improvements in other clinical signs of rosacea have been shown to reduce patient self-consciousness and lead to increased socialization.7 Facial erythema is a major factor that adversely affects quality of life in rosacea patients.8
Although a number of options are available to successfully treat inflammatory lesions of rosacea, facial erythema has been the most difficult manifestation of the disease to medically treat.2,9 Chronic erythema and episodic flushing may be at least partially related to cutaneous vasomotor responses causing both transient and persistent dilation of facial blood vessels.10-12 The agents used for treating the inflammatory components of rosacea reduce erythema associated with papules and pustules but have little effect on the background erythema that is so noticeable. Oxymetazoline and brimonidine tartrate have been evaluated as potential rapid treatments of facial erythema. Daily application of oxymetazoline solution 0.05% has been shown to reduce facial erythema in rosacea patients.13
Brimonidine tartrate is a highly selective α2-adrenergic receptor agonist with potent vasoconstrictor activity.14 It has been used to treat open-angle glaucoma for more than 15 years with well-documented safety and efficacy.15 Phase 2 and 3 studies for once-daily application of brimonidine tartrate gel 0.5% have confirmed its efficacy and safety for the treatment of facial erythema in rosacea patients,9,12 and it was approved by the US Food and Drug Administration (brimonidine gel 0.33%) for persistent (nontransient) facial erythema of rosacea in late 2013. The effect was shown to occur in some patients as soon as 30 minutes following product application and usually persisted for approximately 9 to 12 hours. Erythema gradually returned as the effect waned, returning to baseline by 24 hours after application.12
Clinical efficacy of brimonidine gel was evaluated by a 2-grade improvement (primary end point) or 1-grade improvement (secondary end point) based on patient and clinician assessments using the patient self-assessment (PSA) and clinical erythema assessment (CEA), respectively, over the course of the 4-week studies. Patients also evaluated their satisfaction with the overall appearance of their facial skin.12 A 2-grade improvement on both PSA and CEA has been noted as a stringent criterion in evaluating the effectiveness of treatment of facial erythema.14 A 1-grade improvement on both PSA and CEA has been recognized as clinically relevant as a measure of effect that is noticeable to both patients and clinicians.12 Patients who achieved either a 1- or 2-grade improvement in both PSA and CEA were substantially more likely to report overall satisfaction with their appearance. A 2-grade improvement in both PSA and CEA scales was accompanied with 80% of patients rating their skin appearance as satisfactory or better. Conversely, few patients (ie, <10%) who did not achieve at least 1-grade composite success were satisfied with their appearance. Adverse effects were uncommon, with no evidence of tachyphylaxis and rare occurrence of rebound erythema.12
In summary, although there are a number of options available to reduce or eliminate inflammatory lesions of rosacea, effective medical treatment of the erythematous component of rosacea, which can be the most distressing aspect of the disease for patients, has been unsatisfactory. With the availability of topical brimonidine tartrate, dermatologists have a proven medication to improve facial redness in rosacea patients. Other options such as oxymetazoline may become available in the future.
Rosacea is a common chronic disorder that predominantly manifests as facial erythema, telangiectasia, and flushing.1 Other primary clinical features include inflammatory lesions (eg, papules, pustules) and occasionally edema and rhinophyma. Ocular involvement also may occur. Rosacea patients routinely report sensitive skin with symptoms such as stinging, burning, and intolerance to topical agents (eg, medications, moisturizers, cosmetics).2,3
Rosacea affects facial appearance and can impair a patient’s emotional well-being. It may limit social and professional activities. Many patients and nonpatients alike presume the appearance of facial redness suggests alcohol overuse or emotional distress.4-6 A reduction in facial erythema as well as improvements in other clinical signs of rosacea have been shown to reduce patient self-consciousness and lead to increased socialization.7 Facial erythema is a major factor that adversely affects quality of life in rosacea patients.8
Although a number of options are available to successfully treat inflammatory lesions of rosacea, facial erythema has been the most difficult manifestation of the disease to medically treat.2,9 Chronic erythema and episodic flushing may be at least partially related to cutaneous vasomotor responses causing both transient and persistent dilation of facial blood vessels.10-12 The agents used for treating the inflammatory components of rosacea reduce erythema associated with papules and pustules but have little effect on the background erythema that is so noticeable. Oxymetazoline and brimonidine tartrate have been evaluated as potential rapid treatments of facial erythema. Daily application of oxymetazoline solution 0.05% has been shown to reduce facial erythema in rosacea patients.13
Brimonidine tartrate is a highly selective α2-adrenergic receptor agonist with potent vasoconstrictor activity.14 It has been used to treat open-angle glaucoma for more than 15 years with well-documented safety and efficacy.15 Phase 2 and 3 studies for once-daily application of brimonidine tartrate gel 0.5% have confirmed its efficacy and safety for the treatment of facial erythema in rosacea patients,9,12 and it was approved by the US Food and Drug Administration (brimonidine gel 0.33%) for persistent (nontransient) facial erythema of rosacea in late 2013. The effect was shown to occur in some patients as soon as 30 minutes following product application and usually persisted for approximately 9 to 12 hours. Erythema gradually returned as the effect waned, returning to baseline by 24 hours after application.12
Clinical efficacy of brimonidine gel was evaluated by a 2-grade improvement (primary end point) or 1-grade improvement (secondary end point) based on patient and clinician assessments using the patient self-assessment (PSA) and clinical erythema assessment (CEA), respectively, over the course of the 4-week studies. Patients also evaluated their satisfaction with the overall appearance of their facial skin.12 A 2-grade improvement on both PSA and CEA has been noted as a stringent criterion in evaluating the effectiveness of treatment of facial erythema.14 A 1-grade improvement on both PSA and CEA has been recognized as clinically relevant as a measure of effect that is noticeable to both patients and clinicians.12 Patients who achieved either a 1- or 2-grade improvement in both PSA and CEA were substantially more likely to report overall satisfaction with their appearance. A 2-grade improvement in both PSA and CEA scales was accompanied with 80% of patients rating their skin appearance as satisfactory or better. Conversely, few patients (ie, <10%) who did not achieve at least 1-grade composite success were satisfied with their appearance. Adverse effects were uncommon, with no evidence of tachyphylaxis and rare occurrence of rebound erythema.12
In summary, although there are a number of options available to reduce or eliminate inflammatory lesions of rosacea, effective medical treatment of the erythematous component of rosacea, which can be the most distressing aspect of the disease for patients, has been unsatisfactory. With the availability of topical brimonidine tartrate, dermatologists have a proven medication to improve facial redness in rosacea patients. Other options such as oxymetazoline may become available in the future.
- Crawford GH, Pelle MT, James WD. Rosacea: I. etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327-341.
- Wilkin J, Dahl M, Detmar M, et al. Standard grading system for rosacea: report of the National Rosacea Society expert committee on the classification and staging of rosacea. J Am Acad Dermatol. 2004;50:907-912.
- Odom R, Dahl M, Dover J, et al. Standard management options for rosacea, part I: overview and broad spectrum of care. Cutis. 2009;84:43-47.
- Baldwin HE. Systemic therapy for rosacea. Skin Therapy Lett. 2007;12:1-5.
- Drake L. Rosacea patients feel effects of their condition in social settings. Rosacea Review. Published Fall 2012. http://www.rosacea.org/rr/2012/fall/article_3.php. Accessed May 29, 2014.
- Aksoy B, Altaykan-Hapa A, Egemen D, et al. The impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalities. Br J Dermatol. 2010;163:719-725.
- Wolf JE Jr, Del Rosso JQ. The CLEAR trial: results of a large community-based study of metronidazole gel in rosacea. Cutis. 2007;79:73-80.
- Nicholson K, Abramova L, Chren MM, et al. A pilot quality-of-life instrument for acne rosacea. J Am Acad Dermatol. 2007;57:213-221.
- Fowler J, Jarratt M, Moore A, et al. Once-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicentre, randomized and vehicle-controlled studies. Br J Dermatol. 2012;166:633-641.
- Steinhoff M, Buddenkotte J, Aubert J, et al. Clinical, cellular and molecular aspects in the pathophysiology of rosacea. J Investig Dermatol Symp Proc. 2011;15:2-11.
- Wilkin JK. Rosacea: pathophysiology and treatment. Arch Dermatol. 1994;130:359-362.
- Fowler J, Jackson JM, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650-656.
- Del Rosso JQ. The central role, evaluation, and medical management of diffuse and persistent facial erythema of rosacea. J Clin Aesthet Dermatol. 2012;5:26-36.
- Rahman MQ, Ramaesh K, Montgomery DNI. Brimonidine for glaucoma. Expert Opin Drug Saf. 2010;9:483-491.
- Toris C, Camras C, Yablonski M. Acute versus chronic effects of brimonidine on aqueous humor dynamics in ocular hypertensive patients. Am J Ophthalmol. 1999;128:8-14.
- Crawford GH, Pelle MT, James WD. Rosacea: I. etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327-341.
- Wilkin J, Dahl M, Detmar M, et al. Standard grading system for rosacea: report of the National Rosacea Society expert committee on the classification and staging of rosacea. J Am Acad Dermatol. 2004;50:907-912.
- Odom R, Dahl M, Dover J, et al. Standard management options for rosacea, part I: overview and broad spectrum of care. Cutis. 2009;84:43-47.
- Baldwin HE. Systemic therapy for rosacea. Skin Therapy Lett. 2007;12:1-5.
- Drake L. Rosacea patients feel effects of their condition in social settings. Rosacea Review. Published Fall 2012. http://www.rosacea.org/rr/2012/fall/article_3.php. Accessed May 29, 2014.
- Aksoy B, Altaykan-Hapa A, Egemen D, et al. The impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalities. Br J Dermatol. 2010;163:719-725.
- Wolf JE Jr, Del Rosso JQ. The CLEAR trial: results of a large community-based study of metronidazole gel in rosacea. Cutis. 2007;79:73-80.
- Nicholson K, Abramova L, Chren MM, et al. A pilot quality-of-life instrument for acne rosacea. J Am Acad Dermatol. 2007;57:213-221.
- Fowler J, Jarratt M, Moore A, et al. Once-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicentre, randomized and vehicle-controlled studies. Br J Dermatol. 2012;166:633-641.
- Steinhoff M, Buddenkotte J, Aubert J, et al. Clinical, cellular and molecular aspects in the pathophysiology of rosacea. J Investig Dermatol Symp Proc. 2011;15:2-11.
- Wilkin JK. Rosacea: pathophysiology and treatment. Arch Dermatol. 1994;130:359-362.
- Fowler J, Jackson JM, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650-656.
- Del Rosso JQ. The central role, evaluation, and medical management of diffuse and persistent facial erythema of rosacea. J Clin Aesthet Dermatol. 2012;5:26-36.
- Rahman MQ, Ramaesh K, Montgomery DNI. Brimonidine for glaucoma. Expert Opin Drug Saf. 2010;9:483-491.
- Toris C, Camras C, Yablonski M. Acute versus chronic effects of brimonidine on aqueous humor dynamics in ocular hypertensive patients. Am J Ophthalmol. 1999;128:8-14.
Hospital employment or physician-led ACO?
Primary care physicians around the country are facing the largest decision of their lives: Do I stay independent and maybe form an accountable care organization with other independent physicians, or do I become an employee of a hospital or health system?
As accountable care is taking hold, new data may alter historic thinking on this "bet-the-practice" question.
Tired of being overworked, undersatisfied, and overwhelmed with growing regulatory requirements, many primary care physicians have sought the security and strength of hospital employment. They say the pressures to invest in technology, billing, coding, and continued reimbursement pressures are just too great.
Yet, the majority of these physicians miss their days of self-employed autonomy, are on average less productive, and worry that the clocks on their compensation guarantees are ticking down.
Most of the moves by your colleagues, and perhaps you, to hospital employment have been defensive. It was just no longer feasible to stay afloat in the current fee-for-service system. You cannot work any harder, faster, or cheaper. You can no longer spend satisfactory time with your patients.
On the other hand, some of you may have joined a hospital or health system to be proactive and gain a solid platform to prepare for the new value-based payment era.
You may have envisioned being integrated with a critical mass of like-minded physicians and facilities, aided by advanced population management tools and a strong balance sheet, and all linked together on the hospital’s health information technology platform. You read that primary care should be in a leadership position and financially incentivized in any accountable care organization – including a hospital’s. Independent physicians could theoretically form ACOs, too, but lack the up-front capital, know-how, and any spare intellectual bandwidth to do so.
So, from a strategic perspective, becoming employed with other physicians by a health system seemed the way to go.
The pace has quickened of health care’s movement away from fee for service or "pay for volume" to payment for better outcomes at lower overall costs, or "pay for value." The factors that applied to the decision to become employed in the fee-for-service era may be yielding to those in the accountable care era sooner than anticipated.
Independent physician-led ACOs appear to be adapting better than hospitals to this change. Although much better prepared fiscally, hospitals are conflicted, or at least hesitant, to make this switch, because much of the savings comes from avoidable admissions and readmissions. On the other hand, emerging data and experience are showing that physician-led ACOs can be very successful.
There are some very integrated and successful hospital-led ACOs or other value-delivery hospital/physician models. In fact, I believe that if the hospital is willing to right-size and truly commit to value, it can be the most successful model.
However, many physicians signed volume-only physician work relative value unit (wRVU) compensation formulas in their hospital employment agreements, with no incentive payments for value. They have not been involved as partners, much less leaders, in any ACO planning. Even though the fee-for-service days are waning and strains are showing for many hospitals that are not adapting, for many employed physicians, the pace of preparedness for the accountable care era has been disappointing.
New data show that while most of the early ACOs in the Medicare Shared Savings Program were hospital led, there are now more physician-led ACOs than any other. At the same time, early results of some modest primary care–only ACOs have been exciting. The rural primary care physician ACO previously reported on in this column, Rio Grande Valley Health Alliance in McAllen, Tex., is preliminarily looking at 90th-percentile quality results and more than $500,000 in (unofficial) savings per physician in their first year under the Medicare Shared Savings Program.
In fact, in a May 14, 2014, article in JAMA, its authors stated: "Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million in annual revenue" (JAMA 2014;311:1855-6). They noted that primary care receives only 5% of that spending, but can control much of the average of $5,000 in annual spending of their 2,000 or so patients. The independent physician-led Palm Beach ACO is cited as an example, with $22 million in savings their first year. The authors recommend physician-led ACOs as the best way to leverage that "CEO" power.
These new success lessons are being learned and need to be shared. Primary care physicians need to understand that the risk of change is now much less than the risk of maintaining the status quo. You need transparency regarding the realities of all your choices, including hospital employment and physician ACOs.
As readers of this column know, I heartily endorse the trend recognized in the JAMA article: "[A]n increasing number of primary care physicians see physician-led ACOs as a powerful opportunity to retain their autonomy and make a positive difference for their patient – as well as their practices’ bottom lines."
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Primary care physicians around the country are facing the largest decision of their lives: Do I stay independent and maybe form an accountable care organization with other independent physicians, or do I become an employee of a hospital or health system?
As accountable care is taking hold, new data may alter historic thinking on this "bet-the-practice" question.
Tired of being overworked, undersatisfied, and overwhelmed with growing regulatory requirements, many primary care physicians have sought the security and strength of hospital employment. They say the pressures to invest in technology, billing, coding, and continued reimbursement pressures are just too great.
Yet, the majority of these physicians miss their days of self-employed autonomy, are on average less productive, and worry that the clocks on their compensation guarantees are ticking down.
Most of the moves by your colleagues, and perhaps you, to hospital employment have been defensive. It was just no longer feasible to stay afloat in the current fee-for-service system. You cannot work any harder, faster, or cheaper. You can no longer spend satisfactory time with your patients.
On the other hand, some of you may have joined a hospital or health system to be proactive and gain a solid platform to prepare for the new value-based payment era.
You may have envisioned being integrated with a critical mass of like-minded physicians and facilities, aided by advanced population management tools and a strong balance sheet, and all linked together on the hospital’s health information technology platform. You read that primary care should be in a leadership position and financially incentivized in any accountable care organization – including a hospital’s. Independent physicians could theoretically form ACOs, too, but lack the up-front capital, know-how, and any spare intellectual bandwidth to do so.
So, from a strategic perspective, becoming employed with other physicians by a health system seemed the way to go.
The pace has quickened of health care’s movement away from fee for service or "pay for volume" to payment for better outcomes at lower overall costs, or "pay for value." The factors that applied to the decision to become employed in the fee-for-service era may be yielding to those in the accountable care era sooner than anticipated.
Independent physician-led ACOs appear to be adapting better than hospitals to this change. Although much better prepared fiscally, hospitals are conflicted, or at least hesitant, to make this switch, because much of the savings comes from avoidable admissions and readmissions. On the other hand, emerging data and experience are showing that physician-led ACOs can be very successful.
There are some very integrated and successful hospital-led ACOs or other value-delivery hospital/physician models. In fact, I believe that if the hospital is willing to right-size and truly commit to value, it can be the most successful model.
However, many physicians signed volume-only physician work relative value unit (wRVU) compensation formulas in their hospital employment agreements, with no incentive payments for value. They have not been involved as partners, much less leaders, in any ACO planning. Even though the fee-for-service days are waning and strains are showing for many hospitals that are not adapting, for many employed physicians, the pace of preparedness for the accountable care era has been disappointing.
New data show that while most of the early ACOs in the Medicare Shared Savings Program were hospital led, there are now more physician-led ACOs than any other. At the same time, early results of some modest primary care–only ACOs have been exciting. The rural primary care physician ACO previously reported on in this column, Rio Grande Valley Health Alliance in McAllen, Tex., is preliminarily looking at 90th-percentile quality results and more than $500,000 in (unofficial) savings per physician in their first year under the Medicare Shared Savings Program.
In fact, in a May 14, 2014, article in JAMA, its authors stated: "Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million in annual revenue" (JAMA 2014;311:1855-6). They noted that primary care receives only 5% of that spending, but can control much of the average of $5,000 in annual spending of their 2,000 or so patients. The independent physician-led Palm Beach ACO is cited as an example, with $22 million in savings their first year. The authors recommend physician-led ACOs as the best way to leverage that "CEO" power.
These new success lessons are being learned and need to be shared. Primary care physicians need to understand that the risk of change is now much less than the risk of maintaining the status quo. You need transparency regarding the realities of all your choices, including hospital employment and physician ACOs.
As readers of this column know, I heartily endorse the trend recognized in the JAMA article: "[A]n increasing number of primary care physicians see physician-led ACOs as a powerful opportunity to retain their autonomy and make a positive difference for their patient – as well as their practices’ bottom lines."
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Primary care physicians around the country are facing the largest decision of their lives: Do I stay independent and maybe form an accountable care organization with other independent physicians, or do I become an employee of a hospital or health system?
As accountable care is taking hold, new data may alter historic thinking on this "bet-the-practice" question.
Tired of being overworked, undersatisfied, and overwhelmed with growing regulatory requirements, many primary care physicians have sought the security and strength of hospital employment. They say the pressures to invest in technology, billing, coding, and continued reimbursement pressures are just too great.
Yet, the majority of these physicians miss their days of self-employed autonomy, are on average less productive, and worry that the clocks on their compensation guarantees are ticking down.
Most of the moves by your colleagues, and perhaps you, to hospital employment have been defensive. It was just no longer feasible to stay afloat in the current fee-for-service system. You cannot work any harder, faster, or cheaper. You can no longer spend satisfactory time with your patients.
On the other hand, some of you may have joined a hospital or health system to be proactive and gain a solid platform to prepare for the new value-based payment era.
You may have envisioned being integrated with a critical mass of like-minded physicians and facilities, aided by advanced population management tools and a strong balance sheet, and all linked together on the hospital’s health information technology platform. You read that primary care should be in a leadership position and financially incentivized in any accountable care organization – including a hospital’s. Independent physicians could theoretically form ACOs, too, but lack the up-front capital, know-how, and any spare intellectual bandwidth to do so.
So, from a strategic perspective, becoming employed with other physicians by a health system seemed the way to go.
The pace has quickened of health care’s movement away from fee for service or "pay for volume" to payment for better outcomes at lower overall costs, or "pay for value." The factors that applied to the decision to become employed in the fee-for-service era may be yielding to those in the accountable care era sooner than anticipated.
Independent physician-led ACOs appear to be adapting better than hospitals to this change. Although much better prepared fiscally, hospitals are conflicted, or at least hesitant, to make this switch, because much of the savings comes from avoidable admissions and readmissions. On the other hand, emerging data and experience are showing that physician-led ACOs can be very successful.
There are some very integrated and successful hospital-led ACOs or other value-delivery hospital/physician models. In fact, I believe that if the hospital is willing to right-size and truly commit to value, it can be the most successful model.
However, many physicians signed volume-only physician work relative value unit (wRVU) compensation formulas in their hospital employment agreements, with no incentive payments for value. They have not been involved as partners, much less leaders, in any ACO planning. Even though the fee-for-service days are waning and strains are showing for many hospitals that are not adapting, for many employed physicians, the pace of preparedness for the accountable care era has been disappointing.
New data show that while most of the early ACOs in the Medicare Shared Savings Program were hospital led, there are now more physician-led ACOs than any other. At the same time, early results of some modest primary care–only ACOs have been exciting. The rural primary care physician ACO previously reported on in this column, Rio Grande Valley Health Alliance in McAllen, Tex., is preliminarily looking at 90th-percentile quality results and more than $500,000 in (unofficial) savings per physician in their first year under the Medicare Shared Savings Program.
In fact, in a May 14, 2014, article in JAMA, its authors stated: "Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million in annual revenue" (JAMA 2014;311:1855-6). They noted that primary care receives only 5% of that spending, but can control much of the average of $5,000 in annual spending of their 2,000 or so patients. The independent physician-led Palm Beach ACO is cited as an example, with $22 million in savings their first year. The authors recommend physician-led ACOs as the best way to leverage that "CEO" power.
These new success lessons are being learned and need to be shared. Primary care physicians need to understand that the risk of change is now much less than the risk of maintaining the status quo. You need transparency regarding the realities of all your choices, including hospital employment and physician ACOs.
As readers of this column know, I heartily endorse the trend recognized in the JAMA article: "[A]n increasing number of primary care physicians see physician-led ACOs as a powerful opportunity to retain their autonomy and make a positive difference for their patient – as well as their practices’ bottom lines."
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Shifting our focus to HIV as a chronic disease
Last month in our practice we had a patient with a positive HIV enzyme-linked immunoassay (ELISA) test and a negative Western blot. The patient’s doctor was astute, elicited a history of a recent viral-like syndrome, and considered the possibility of recent HIV infection, which further testing confirmed as the correct diagnosis.
It has been fascinating to watch the discovery of HIV/acquired immunodeficiency syndrome (AIDS) and the evolution of diagnosis and treatment since the inception of the epidemic in 1981. In 1981, I was practicing in a small town in Michigan’s Upper Peninsula, and I did not see a patient with HIV infection in my office until 1990. In 2014, with an estimated prevalence of 1.1 million HIV cases in the United States,1 family physicians are likely to come into contact with several patients with HIV every year. Practicing on Chicago’s south side in 2008, I diagnosed 2 teenagers with HIV. It was a heartbreaking reality.
The discovery of highly active antiretroviral therapy (HAART) has transformed HIV/AIDS from an acute, infectious specialty disease to a chronic primary care disease. Although the annual incidence of HIV in the United States has dropped precipitously from its peak of 130,000 in the 1980s to about 50,000 in 2010,1 the prevalence continues to rise as more people with HIV infection are living for many years. People with HIV who receive proper care do have a shortened life span, but not by many years, and they are highly likely to show up in our offices for treatment of not only chronic illnesses that accompany HIV but also common diseases such as hypertension, diabetes, and coronary artery disease. More and more patients with HIV are being managed in primary care settings, with infectious disease specialists acting as consultants.
Universal screening for HIV is recommended and becoming the norm, and the stigma for testing appears to be decreasing. The burdensome informed consent process has been streamlined in many states, making screening seem routine to patients. Family physicians must do their part to help control the HIV epidemic by screening, properly diagnosing new cases of HIV, and providing chronic disease and preventive care. To that end, I encourage you to read “HIV screening: How we can do better,” by Editorial Board member Jeffrey T. Kirchner, DO, FAAFP, AAHIVS.
REFERENCE
1. Centers for Disease Control and Prevention (CDC). Today's HIV/AIDS epidemic. CDC Web site. Available at: http://www.cdc.gov/nchhstp/newsroom/docs/hivfactsheets/todaysepidemic-508.pdf. Accessed June 23, 2014.
Last month in our practice we had a patient with a positive HIV enzyme-linked immunoassay (ELISA) test and a negative Western blot. The patient’s doctor was astute, elicited a history of a recent viral-like syndrome, and considered the possibility of recent HIV infection, which further testing confirmed as the correct diagnosis.
It has been fascinating to watch the discovery of HIV/acquired immunodeficiency syndrome (AIDS) and the evolution of diagnosis and treatment since the inception of the epidemic in 1981. In 1981, I was practicing in a small town in Michigan’s Upper Peninsula, and I did not see a patient with HIV infection in my office until 1990. In 2014, with an estimated prevalence of 1.1 million HIV cases in the United States,1 family physicians are likely to come into contact with several patients with HIV every year. Practicing on Chicago’s south side in 2008, I diagnosed 2 teenagers with HIV. It was a heartbreaking reality.
The discovery of highly active antiretroviral therapy (HAART) has transformed HIV/AIDS from an acute, infectious specialty disease to a chronic primary care disease. Although the annual incidence of HIV in the United States has dropped precipitously from its peak of 130,000 in the 1980s to about 50,000 in 2010,1 the prevalence continues to rise as more people with HIV infection are living for many years. People with HIV who receive proper care do have a shortened life span, but not by many years, and they are highly likely to show up in our offices for treatment of not only chronic illnesses that accompany HIV but also common diseases such as hypertension, diabetes, and coronary artery disease. More and more patients with HIV are being managed in primary care settings, with infectious disease specialists acting as consultants.
Universal screening for HIV is recommended and becoming the norm, and the stigma for testing appears to be decreasing. The burdensome informed consent process has been streamlined in many states, making screening seem routine to patients. Family physicians must do their part to help control the HIV epidemic by screening, properly diagnosing new cases of HIV, and providing chronic disease and preventive care. To that end, I encourage you to read “HIV screening: How we can do better,” by Editorial Board member Jeffrey T. Kirchner, DO, FAAFP, AAHIVS.
Last month in our practice we had a patient with a positive HIV enzyme-linked immunoassay (ELISA) test and a negative Western blot. The patient’s doctor was astute, elicited a history of a recent viral-like syndrome, and considered the possibility of recent HIV infection, which further testing confirmed as the correct diagnosis.
It has been fascinating to watch the discovery of HIV/acquired immunodeficiency syndrome (AIDS) and the evolution of diagnosis and treatment since the inception of the epidemic in 1981. In 1981, I was practicing in a small town in Michigan’s Upper Peninsula, and I did not see a patient with HIV infection in my office until 1990. In 2014, with an estimated prevalence of 1.1 million HIV cases in the United States,1 family physicians are likely to come into contact with several patients with HIV every year. Practicing on Chicago’s south side in 2008, I diagnosed 2 teenagers with HIV. It was a heartbreaking reality.
The discovery of highly active antiretroviral therapy (HAART) has transformed HIV/AIDS from an acute, infectious specialty disease to a chronic primary care disease. Although the annual incidence of HIV in the United States has dropped precipitously from its peak of 130,000 in the 1980s to about 50,000 in 2010,1 the prevalence continues to rise as more people with HIV infection are living for many years. People with HIV who receive proper care do have a shortened life span, but not by many years, and they are highly likely to show up in our offices for treatment of not only chronic illnesses that accompany HIV but also common diseases such as hypertension, diabetes, and coronary artery disease. More and more patients with HIV are being managed in primary care settings, with infectious disease specialists acting as consultants.
Universal screening for HIV is recommended and becoming the norm, and the stigma for testing appears to be decreasing. The burdensome informed consent process has been streamlined in many states, making screening seem routine to patients. Family physicians must do their part to help control the HIV epidemic by screening, properly diagnosing new cases of HIV, and providing chronic disease and preventive care. To that end, I encourage you to read “HIV screening: How we can do better,” by Editorial Board member Jeffrey T. Kirchner, DO, FAAFP, AAHIVS.
REFERENCE
1. Centers for Disease Control and Prevention (CDC). Today's HIV/AIDS epidemic. CDC Web site. Available at: http://www.cdc.gov/nchhstp/newsroom/docs/hivfactsheets/todaysepidemic-508.pdf. Accessed June 23, 2014.
REFERENCE
1. Centers for Disease Control and Prevention (CDC). Today's HIV/AIDS epidemic. CDC Web site. Available at: http://www.cdc.gov/nchhstp/newsroom/docs/hivfactsheets/todaysepidemic-508.pdf. Accessed June 23, 2014.
Safety, Quality, Compassion...and Cost
Since the development of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles,1 we in the orthopedic trauma community have evaluated and reevaluated our work with a very critical eye.2-4 The desire to maximize our ability to restore functional mobility has not grown any less strong,5 but many of us are aware that we are reaching the limit of what a new implant or technical solution can do for our patients. Over the past 20 years, this realization has turned many in the orthopedic trauma community to debate the merits of particular solutions
to the same problem,6 to give appropriate weight to the patient’s subjective experience,7 and to feverishly debate the appropriate timing of fracture care.8 Dr. Vallier and her group in Cleveland have brought this conversation into the era of meaningful use in medicine with their article in this month’s issue of The American Journal of Orthopedics, “Cost Savings Associated With a Multidisciplinary Protocol That Expedites Definitive Fracture Care.”
This type of work is extremely difficult to accomplish in any system, and exceptionally so in the United States. In order to achieve even the simplest work in this domain, a number of obstacles must be overcome. First, we must reach consensus on the simplest data points to use in building a decision tree. Dr. Vallier’s group wisely chose straightforward endpoints of resuscitation readily and
rapidly available to any surgical team.9 Second, we must organize a hospital system (a system currently set up more to create turf battles than alliances) in a way that commits interdepartmental resources to an injured patient—one that inevitably appears without warning and often at the most inconvenient of times. Furthermore, we must agree to commit those resources within a relatively brief time frame (36 hours), requiring coordinated mobilization of various teams. Simply achieving these goals is a major accomplishment. Dr. Vallier’s real leadership in this area is her ability to argue the merits of this approach in terms that every administrator can understand.
Her team’s paper presents predicted savings to both patients and society when a uniform method is applied to determine when fracture care should be administered to the multiply injured patient. It is important to understand that “savings” in this context isn’t simply dollars not spent but includes preventable harm not inflicted. Complications can no longer be considered the cost of doing business, and not just because the Center for Medicare and Medicaid Services tells us so in the latest pay-for-performance dictum. We must expand our idea of primum non nocere to
include skillfully navigating the patient’s care in a way that predicts the most likely avoidance of trouble. This type of evaluation will require us to flexibly adapt our behavior in ways that may be personally inconvenient, seem redundant, or even appear to make little difference at all given our limited perspective at the sharp end of care.
It can be very difficult to understand why we should be trying to achieve better than 95% to 98% success rates when for an individual such success could easily be considered a measure of excellence. Moving health care into the realm of the High Reliability Organization, however, will require more than the work of expert individuals; it will require teams of people who know how to work together and who understand that expertise in their role both as an individual and as a team member is essential to an outcome even though they may be far removed from the
individual patient who experiences the successful outcome.
Finally, there can be little debate that safety, quality, and compassion are the pillars of effective health care.10-12 Though we can never have enough of these 3 elements, most of us now acknowledge the need to wrestle with the tension of dealing with the fourth pillar: cost in dollars spent on the systems level. Other systems (eg, the National Health Service in Great Britain, the Canadian Orthopaedic Trauma Society) have been leading the way for some time in developing integrated systems approaches for addressing both quality and cost. This is an extremely precarious but necessary marriage of goals, as we are now firmly in an era of shrinking resources even as we rightly demand higherquality, safer, and more compassionate care. Analyzing this type of work in the unique quilt that is the US health care system is extraordinarily difficult, as is evident in Dr. Vallier’s paper. I encourage you to read Dr. Vallier’s article, but more importantly, to ask yourself where you can take the baton she and others are handing us.
References
1. Muller ME, Allgower M, Willenegger H. Technique of Internal Fixation of
Fractures. Berlin, Germany: Springer-Verlag; 1965.
2. Schatzker J, Tile M. The Rationale of Operative Fracture Care. Berlin,
Germany: Springer-Verlag; 1987.
3. Letournel E, Judet R. Fractures of the Acetabulum. Berlin, Germany:
Springer-Verlag; 1981. 4. Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture
Surgery. Berlin, Germany: Springer-Verlag; 1989.
5. Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular
osteotomies in complex hip deformities. Clin Orthop. 2010;468(12):3168-3180.
6. Bhandari M, Devereaux PJ, Montori V, Cinà C, Tandan V, Guyatt GH;
Evidence-Based Surgery Working Group. Users’ guide to the surgical
literature: how to use a systematic literature review and meta-analysis.
Can J Surg. 2004;47(1):60-67.
7. Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague
S, de Vet HC. Outcome instruments: rationale for their use. J Bone Joint
Surg Am. 2009;91(suppl 3):41-49.
8. Pape HC, Rixen D, Morley J, et al; EPOFF Study Group. Impact of
method of initial stabilization for femoral shaft fractures in patients with
multiple injuries at risk for complications (borderline patients). Ann Surg.
2007;246(3):491-501.
9. Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic
surgery in multiple trauma patients: development of a protocol
for early appropriate care. J Orthop Trauma. 2013;27(10):543-551.
10. Jotterand F. The Hippocratic oath and contemporary medicine: dialectic
between past ideals and present reality? J Med Philos. 2005;30(1):107-128.
11. Seeskin K. Maimonides. In: Zalta EN, Nodelman U, Allen C, et al, eds.
Stanford Encyclopedia of Philosophy. http://plato.stanford.edu/archives
/spr2014/entries/maimonides/. Published January 24, 2006. Revised
June 12, 2013. Accessed April 27, 2014.
12. Osler W. Aequanimitas. In: Aequanimitas, With Other Addresses to Medical
Students, Nurses and Practitioners of Medicine. 2nd ed. Philadelphia,
PA: P. Blakiston’s Son & Co; 1925:chap 1. Celebrating the Contributions
of William Osler. http://www.medicalarchives.jhmi.edu/osler/aequessay.
htm. Published December 9, 1999. Accessed April 27, 2014.
Since the development of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles,1 we in the orthopedic trauma community have evaluated and reevaluated our work with a very critical eye.2-4 The desire to maximize our ability to restore functional mobility has not grown any less strong,5 but many of us are aware that we are reaching the limit of what a new implant or technical solution can do for our patients. Over the past 20 years, this realization has turned many in the orthopedic trauma community to debate the merits of particular solutions
to the same problem,6 to give appropriate weight to the patient’s subjective experience,7 and to feverishly debate the appropriate timing of fracture care.8 Dr. Vallier and her group in Cleveland have brought this conversation into the era of meaningful use in medicine with their article in this month’s issue of The American Journal of Orthopedics, “Cost Savings Associated With a Multidisciplinary Protocol That Expedites Definitive Fracture Care.”
This type of work is extremely difficult to accomplish in any system, and exceptionally so in the United States. In order to achieve even the simplest work in this domain, a number of obstacles must be overcome. First, we must reach consensus on the simplest data points to use in building a decision tree. Dr. Vallier’s group wisely chose straightforward endpoints of resuscitation readily and
rapidly available to any surgical team.9 Second, we must organize a hospital system (a system currently set up more to create turf battles than alliances) in a way that commits interdepartmental resources to an injured patient—one that inevitably appears without warning and often at the most inconvenient of times. Furthermore, we must agree to commit those resources within a relatively brief time frame (36 hours), requiring coordinated mobilization of various teams. Simply achieving these goals is a major accomplishment. Dr. Vallier’s real leadership in this area is her ability to argue the merits of this approach in terms that every administrator can understand.
Her team’s paper presents predicted savings to both patients and society when a uniform method is applied to determine when fracture care should be administered to the multiply injured patient. It is important to understand that “savings” in this context isn’t simply dollars not spent but includes preventable harm not inflicted. Complications can no longer be considered the cost of doing business, and not just because the Center for Medicare and Medicaid Services tells us so in the latest pay-for-performance dictum. We must expand our idea of primum non nocere to
include skillfully navigating the patient’s care in a way that predicts the most likely avoidance of trouble. This type of evaluation will require us to flexibly adapt our behavior in ways that may be personally inconvenient, seem redundant, or even appear to make little difference at all given our limited perspective at the sharp end of care.
It can be very difficult to understand why we should be trying to achieve better than 95% to 98% success rates when for an individual such success could easily be considered a measure of excellence. Moving health care into the realm of the High Reliability Organization, however, will require more than the work of expert individuals; it will require teams of people who know how to work together and who understand that expertise in their role both as an individual and as a team member is essential to an outcome even though they may be far removed from the
individual patient who experiences the successful outcome.
Finally, there can be little debate that safety, quality, and compassion are the pillars of effective health care.10-12 Though we can never have enough of these 3 elements, most of us now acknowledge the need to wrestle with the tension of dealing with the fourth pillar: cost in dollars spent on the systems level. Other systems (eg, the National Health Service in Great Britain, the Canadian Orthopaedic Trauma Society) have been leading the way for some time in developing integrated systems approaches for addressing both quality and cost. This is an extremely precarious but necessary marriage of goals, as we are now firmly in an era of shrinking resources even as we rightly demand higherquality, safer, and more compassionate care. Analyzing this type of work in the unique quilt that is the US health care system is extraordinarily difficult, as is evident in Dr. Vallier’s paper. I encourage you to read Dr. Vallier’s article, but more importantly, to ask yourself where you can take the baton she and others are handing us.
References
1. Muller ME, Allgower M, Willenegger H. Technique of Internal Fixation of
Fractures. Berlin, Germany: Springer-Verlag; 1965.
2. Schatzker J, Tile M. The Rationale of Operative Fracture Care. Berlin,
Germany: Springer-Verlag; 1987.
3. Letournel E, Judet R. Fractures of the Acetabulum. Berlin, Germany:
Springer-Verlag; 1981. 4. Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture
Surgery. Berlin, Germany: Springer-Verlag; 1989.
5. Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular
osteotomies in complex hip deformities. Clin Orthop. 2010;468(12):3168-3180.
6. Bhandari M, Devereaux PJ, Montori V, Cinà C, Tandan V, Guyatt GH;
Evidence-Based Surgery Working Group. Users’ guide to the surgical
literature: how to use a systematic literature review and meta-analysis.
Can J Surg. 2004;47(1):60-67.
7. Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague
S, de Vet HC. Outcome instruments: rationale for their use. J Bone Joint
Surg Am. 2009;91(suppl 3):41-49.
8. Pape HC, Rixen D, Morley J, et al; EPOFF Study Group. Impact of
method of initial stabilization for femoral shaft fractures in patients with
multiple injuries at risk for complications (borderline patients). Ann Surg.
2007;246(3):491-501.
9. Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic
surgery in multiple trauma patients: development of a protocol
for early appropriate care. J Orthop Trauma. 2013;27(10):543-551.
10. Jotterand F. The Hippocratic oath and contemporary medicine: dialectic
between past ideals and present reality? J Med Philos. 2005;30(1):107-128.
11. Seeskin K. Maimonides. In: Zalta EN, Nodelman U, Allen C, et al, eds.
Stanford Encyclopedia of Philosophy. http://plato.stanford.edu/archives
/spr2014/entries/maimonides/. Published January 24, 2006. Revised
June 12, 2013. Accessed April 27, 2014.
12. Osler W. Aequanimitas. In: Aequanimitas, With Other Addresses to Medical
Students, Nurses and Practitioners of Medicine. 2nd ed. Philadelphia,
PA: P. Blakiston’s Son & Co; 1925:chap 1. Celebrating the Contributions
of William Osler. http://www.medicalarchives.jhmi.edu/osler/aequessay.
htm. Published December 9, 1999. Accessed April 27, 2014.
Since the development of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles,1 we in the orthopedic trauma community have evaluated and reevaluated our work with a very critical eye.2-4 The desire to maximize our ability to restore functional mobility has not grown any less strong,5 but many of us are aware that we are reaching the limit of what a new implant or technical solution can do for our patients. Over the past 20 years, this realization has turned many in the orthopedic trauma community to debate the merits of particular solutions
to the same problem,6 to give appropriate weight to the patient’s subjective experience,7 and to feverishly debate the appropriate timing of fracture care.8 Dr. Vallier and her group in Cleveland have brought this conversation into the era of meaningful use in medicine with their article in this month’s issue of The American Journal of Orthopedics, “Cost Savings Associated With a Multidisciplinary Protocol That Expedites Definitive Fracture Care.”
This type of work is extremely difficult to accomplish in any system, and exceptionally so in the United States. In order to achieve even the simplest work in this domain, a number of obstacles must be overcome. First, we must reach consensus on the simplest data points to use in building a decision tree. Dr. Vallier’s group wisely chose straightforward endpoints of resuscitation readily and
rapidly available to any surgical team.9 Second, we must organize a hospital system (a system currently set up more to create turf battles than alliances) in a way that commits interdepartmental resources to an injured patient—one that inevitably appears without warning and often at the most inconvenient of times. Furthermore, we must agree to commit those resources within a relatively brief time frame (36 hours), requiring coordinated mobilization of various teams. Simply achieving these goals is a major accomplishment. Dr. Vallier’s real leadership in this area is her ability to argue the merits of this approach in terms that every administrator can understand.
Her team’s paper presents predicted savings to both patients and society when a uniform method is applied to determine when fracture care should be administered to the multiply injured patient. It is important to understand that “savings” in this context isn’t simply dollars not spent but includes preventable harm not inflicted. Complications can no longer be considered the cost of doing business, and not just because the Center for Medicare and Medicaid Services tells us so in the latest pay-for-performance dictum. We must expand our idea of primum non nocere to
include skillfully navigating the patient’s care in a way that predicts the most likely avoidance of trouble. This type of evaluation will require us to flexibly adapt our behavior in ways that may be personally inconvenient, seem redundant, or even appear to make little difference at all given our limited perspective at the sharp end of care.
It can be very difficult to understand why we should be trying to achieve better than 95% to 98% success rates when for an individual such success could easily be considered a measure of excellence. Moving health care into the realm of the High Reliability Organization, however, will require more than the work of expert individuals; it will require teams of people who know how to work together and who understand that expertise in their role both as an individual and as a team member is essential to an outcome even though they may be far removed from the
individual patient who experiences the successful outcome.
Finally, there can be little debate that safety, quality, and compassion are the pillars of effective health care.10-12 Though we can never have enough of these 3 elements, most of us now acknowledge the need to wrestle with the tension of dealing with the fourth pillar: cost in dollars spent on the systems level. Other systems (eg, the National Health Service in Great Britain, the Canadian Orthopaedic Trauma Society) have been leading the way for some time in developing integrated systems approaches for addressing both quality and cost. This is an extremely precarious but necessary marriage of goals, as we are now firmly in an era of shrinking resources even as we rightly demand higherquality, safer, and more compassionate care. Analyzing this type of work in the unique quilt that is the US health care system is extraordinarily difficult, as is evident in Dr. Vallier’s paper. I encourage you to read Dr. Vallier’s article, but more importantly, to ask yourself where you can take the baton she and others are handing us.
References
1. Muller ME, Allgower M, Willenegger H. Technique of Internal Fixation of
Fractures. Berlin, Germany: Springer-Verlag; 1965.
2. Schatzker J, Tile M. The Rationale of Operative Fracture Care. Berlin,
Germany: Springer-Verlag; 1987.
3. Letournel E, Judet R. Fractures of the Acetabulum. Berlin, Germany:
Springer-Verlag; 1981. 4. Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture
Surgery. Berlin, Germany: Springer-Verlag; 1989.
5. Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular
osteotomies in complex hip deformities. Clin Orthop. 2010;468(12):3168-3180.
6. Bhandari M, Devereaux PJ, Montori V, Cinà C, Tandan V, Guyatt GH;
Evidence-Based Surgery Working Group. Users’ guide to the surgical
literature: how to use a systematic literature review and meta-analysis.
Can J Surg. 2004;47(1):60-67.
7. Poolman RW, Swiontkowski MF, Fairbank JC, Schemitsch EH, Sprague
S, de Vet HC. Outcome instruments: rationale for their use. J Bone Joint
Surg Am. 2009;91(suppl 3):41-49.
8. Pape HC, Rixen D, Morley J, et al; EPOFF Study Group. Impact of
method of initial stabilization for femoral shaft fractures in patients with
multiple injuries at risk for complications (borderline patients). Ann Surg.
2007;246(3):491-501.
9. Vallier HA, Wang X, Moore TA, Wilber JH, Como JJ. Timing of orthopaedic
surgery in multiple trauma patients: development of a protocol
for early appropriate care. J Orthop Trauma. 2013;27(10):543-551.
10. Jotterand F. The Hippocratic oath and contemporary medicine: dialectic
between past ideals and present reality? J Med Philos. 2005;30(1):107-128.
11. Seeskin K. Maimonides. In: Zalta EN, Nodelman U, Allen C, et al, eds.
Stanford Encyclopedia of Philosophy. http://plato.stanford.edu/archives
/spr2014/entries/maimonides/. Published January 24, 2006. Revised
June 12, 2013. Accessed April 27, 2014.
12. Osler W. Aequanimitas. In: Aequanimitas, With Other Addresses to Medical
Students, Nurses and Practitioners of Medicine. 2nd ed. Philadelphia,
PA: P. Blakiston’s Son & Co; 1925:chap 1. Celebrating the Contributions
of William Osler. http://www.medicalarchives.jhmi.edu/osler/aequessay.
htm. Published December 9, 1999. Accessed April 27, 2014.
Editorial: A Night (and Week) to Remember!
Charlotte Yeh, MD, former chief of emergency medicine at Newton Wellesley Hospital and at Tufts Medical Center in Massachusetts before becoming Regional Administrator for CMS in Boston, is currently the chief medical officer for AARP Services. On a dark, rainy night in December 2011, Dr Yeh was struck by a car while crossing an intersection in Washington, DC.
After being placed on a backboard and C-collar, she was transported by ambulance to a Level I trauma center where, without identifying herself as an EP, she became another injured patient in a crowded ED.
The experiences Dr Yeh relates in the June 2014 issue of Health Affairs (http://content.healthaffairs.org/content/33/6/1094.full), which were also excerpted in the June 9, 2014 edition of the Washington Post (Go to washingtonpost.com and search for “Yeh.”), sound all too familiar, and none too comforting.
The triage nurse repeatedly asked Dr Yeh where in the car she was sitting despite her responses that she was not in a car but hit by a car—a “pedestrian struck” as they say in NYC. After triage, her pain was addressed, primary and secondary surveys were completed, and focused exams were conducted to enable safe removal of the C-collar and backboard. So far so good.
But over the next 2 days, Dr Yeh’s repeated complaints about knee and gluteal region pain went unaddressed, even as CT scans of the abdomen and pelvis, and X-rays of the chest were ordered and completed. When she returned to the ED from Radiology, Dr Yeh was “parked in a hallway” where she remained through the night after being informed by a new group of clinicians that she was going to be admitted, but “boarded” in the ED until an inpatient bed became available. After 15 hours, the day crew arrived and, recognizing that Dr Yeh was an EP, moved her from the hallway to a private ED room.
Later in the day, the trauma team informed Dr Yeh that with nothing broken, and no major injuries turning up since she arrived, she could go home—despite her excruciating pain and still unexamined knee and hip. After a physical therapy team realized that she could not stand up, the surgical resident told her “there’s no medical reason to admit you…but if you can’t walk, we’ll just have to.”
Upstairs in the first available bed (on the maternity ward!), she repeatedly requested a knee examination before an orthopedic consultant determined that Dr Yeh had a medial collateral ligament tear requiring splinting until an MRI could be obtained. Other lapses in care included a failure to identify early-on the sciatic and gluteal nerve contusions causing leg and hip numbness and tingling, and not noticing until the third hospital day that no admission history and physical exam had been performed by the admitting team. As soon as Dr Yeh was able to ambulate with assistance on day 4, she insisted on being transferred to a rehabilitation facility near her home.
Looking back at her experiences, Dr Yeh characterized the nature of her care as “uneven” and “marked by an over reliance on testing at the expense of [her] overall well-being.”
Uneven to be sure, also fragmented, episodic, sloppy, and, as she noted elsewhere, delivered with a callous attitude on the part of the trauma resident. But the picture that Dr Yeh draws is disturbing for another reason: a trauma patient in an overcrowded ED, with many different “providers” addressing specific issues, but no one coordinating all of these efforts, or looking for omissions, or caring for her as a patient. Where was the EP who should have been the captain of this ED ship ensuring the overall safety and well-being of his or her passengers? Isn’t that what an emergency physician is supposed to be doing?

Charlotte Yeh, MD, former chief of emergency medicine at Newton Wellesley Hospital and at Tufts Medical Center in Massachusetts before becoming Regional Administrator for CMS in Boston, is currently the chief medical officer for AARP Services. On a dark, rainy night in December 2011, Dr Yeh was struck by a car while crossing an intersection in Washington, DC.
After being placed on a backboard and C-collar, she was transported by ambulance to a Level I trauma center where, without identifying herself as an EP, she became another injured patient in a crowded ED.
The experiences Dr Yeh relates in the June 2014 issue of Health Affairs (http://content.healthaffairs.org/content/33/6/1094.full), which were also excerpted in the June 9, 2014 edition of the Washington Post (Go to washingtonpost.com and search for “Yeh.”), sound all too familiar, and none too comforting.
The triage nurse repeatedly asked Dr Yeh where in the car she was sitting despite her responses that she was not in a car but hit by a car—a “pedestrian struck” as they say in NYC. After triage, her pain was addressed, primary and secondary surveys were completed, and focused exams were conducted to enable safe removal of the C-collar and backboard. So far so good.
But over the next 2 days, Dr Yeh’s repeated complaints about knee and gluteal region pain went unaddressed, even as CT scans of the abdomen and pelvis, and X-rays of the chest were ordered and completed. When she returned to the ED from Radiology, Dr Yeh was “parked in a hallway” where she remained through the night after being informed by a new group of clinicians that she was going to be admitted, but “boarded” in the ED until an inpatient bed became available. After 15 hours, the day crew arrived and, recognizing that Dr Yeh was an EP, moved her from the hallway to a private ED room.
Later in the day, the trauma team informed Dr Yeh that with nothing broken, and no major injuries turning up since she arrived, she could go home—despite her excruciating pain and still unexamined knee and hip. After a physical therapy team realized that she could not stand up, the surgical resident told her “there’s no medical reason to admit you…but if you can’t walk, we’ll just have to.”
Upstairs in the first available bed (on the maternity ward!), she repeatedly requested a knee examination before an orthopedic consultant determined that Dr Yeh had a medial collateral ligament tear requiring splinting until an MRI could be obtained. Other lapses in care included a failure to identify early-on the sciatic and gluteal nerve contusions causing leg and hip numbness and tingling, and not noticing until the third hospital day that no admission history and physical exam had been performed by the admitting team. As soon as Dr Yeh was able to ambulate with assistance on day 4, she insisted on being transferred to a rehabilitation facility near her home.
Looking back at her experiences, Dr Yeh characterized the nature of her care as “uneven” and “marked by an over reliance on testing at the expense of [her] overall well-being.”
Uneven to be sure, also fragmented, episodic, sloppy, and, as she noted elsewhere, delivered with a callous attitude on the part of the trauma resident. But the picture that Dr Yeh draws is disturbing for another reason: a trauma patient in an overcrowded ED, with many different “providers” addressing specific issues, but no one coordinating all of these efforts, or looking for omissions, or caring for her as a patient. Where was the EP who should have been the captain of this ED ship ensuring the overall safety and well-being of his or her passengers? Isn’t that what an emergency physician is supposed to be doing?

Charlotte Yeh, MD, former chief of emergency medicine at Newton Wellesley Hospital and at Tufts Medical Center in Massachusetts before becoming Regional Administrator for CMS in Boston, is currently the chief medical officer for AARP Services. On a dark, rainy night in December 2011, Dr Yeh was struck by a car while crossing an intersection in Washington, DC.
After being placed on a backboard and C-collar, she was transported by ambulance to a Level I trauma center where, without identifying herself as an EP, she became another injured patient in a crowded ED.
The experiences Dr Yeh relates in the June 2014 issue of Health Affairs (http://content.healthaffairs.org/content/33/6/1094.full), which were also excerpted in the June 9, 2014 edition of the Washington Post (Go to washingtonpost.com and search for “Yeh.”), sound all too familiar, and none too comforting.
The triage nurse repeatedly asked Dr Yeh where in the car she was sitting despite her responses that she was not in a car but hit by a car—a “pedestrian struck” as they say in NYC. After triage, her pain was addressed, primary and secondary surveys were completed, and focused exams were conducted to enable safe removal of the C-collar and backboard. So far so good.
But over the next 2 days, Dr Yeh’s repeated complaints about knee and gluteal region pain went unaddressed, even as CT scans of the abdomen and pelvis, and X-rays of the chest were ordered and completed. When she returned to the ED from Radiology, Dr Yeh was “parked in a hallway” where she remained through the night after being informed by a new group of clinicians that she was going to be admitted, but “boarded” in the ED until an inpatient bed became available. After 15 hours, the day crew arrived and, recognizing that Dr Yeh was an EP, moved her from the hallway to a private ED room.
Later in the day, the trauma team informed Dr Yeh that with nothing broken, and no major injuries turning up since she arrived, she could go home—despite her excruciating pain and still unexamined knee and hip. After a physical therapy team realized that she could not stand up, the surgical resident told her “there’s no medical reason to admit you…but if you can’t walk, we’ll just have to.”
Upstairs in the first available bed (on the maternity ward!), she repeatedly requested a knee examination before an orthopedic consultant determined that Dr Yeh had a medial collateral ligament tear requiring splinting until an MRI could be obtained. Other lapses in care included a failure to identify early-on the sciatic and gluteal nerve contusions causing leg and hip numbness and tingling, and not noticing until the third hospital day that no admission history and physical exam had been performed by the admitting team. As soon as Dr Yeh was able to ambulate with assistance on day 4, she insisted on being transferred to a rehabilitation facility near her home.
Looking back at her experiences, Dr Yeh characterized the nature of her care as “uneven” and “marked by an over reliance on testing at the expense of [her] overall well-being.”
Uneven to be sure, also fragmented, episodic, sloppy, and, as she noted elsewhere, delivered with a callous attitude on the part of the trauma resident. But the picture that Dr Yeh draws is disturbing for another reason: a trauma patient in an overcrowded ED, with many different “providers” addressing specific issues, but no one coordinating all of these efforts, or looking for omissions, or caring for her as a patient. Where was the EP who should have been the captain of this ED ship ensuring the overall safety and well-being of his or her passengers? Isn’t that what an emergency physician is supposed to be doing?

Hard cases
"Hard cases," say the lawyers, "make bad law." That means something like, "Legislation works better when it’s drafted in response to average circumstances, not extreme ones."
This adage applies to our profession, too. You can learn more about how to practice and teach medicine from average cases than from rare and strange ones. Hard cases can make any of us look foolish.
Peter e-mailed me the other day. I’d seen him 6 months ago for an eczematous rash on his back. Something funny about it, though: The distribution didn’t work, and it wasn’t scaly. No response to triamcinolone. Biopsy: Nonspecific inflammation. CBC: Elevated white cells at 15,600, mostly lymphs. Hmmm.
I referred him to an academic center. They presented him at Grand Rounds, and set him up for patch testing. He avoided what they asked him to, with little success.
"The oncologist says I have lymphoma," Peter’s e-mail to the patch test clinic read, copying me. He apologetically canceled his allergy clinic follow-up. "I hope for a good prognosis, although diagnosis has been delayed for several months. I hope my example will be of value for future patients."
Peter puts his regrets gently. How valuable will his lesson be? His case teaches that strange presentations of uncommon conditions can make even good and conscientious doctors look lame.
We all congratulate ourselves on "good pick-ups," the diagnostic coups that hit the nail on the head. Fair enough, but we understandably look away when we got it right by dumb luck or got it wrong.
That subcutaneous fullness we thought was fine, but which the patient insisted be removed (and turned out to be dermatofibrosarcoma protuberans). That dark spot that looked like all the others, only the patient was nervous because he was sure it had changed (melanoma). The funny rash that ended up being measles in an unimmunized child, and when was the last time you saw measles?
Often, we never even find out about the hard cases we missed, because the people who had them got fed up with us and went elsewhere. Sometimes, they send an angry letter or – more common these days – write a bad review. "I went to another doctor who finally figured out my problem and prescribed the right treatment." Once in a while, a lawsuit.
Viewed through the "retrospectoscope," knowing how the story turned out, our initial fumblings look pretty clumsy, if not downright actionable. "Oh, come on," a critic might say, "Surely that lump was too irregular for you to pass it off as a fibroma." Or: "Why the surprise? Didn’t he tell you the mole changed?" "The kid was sick and had a funny rash, didn’t she?" says a third. "Don’t you read the papers about all the parents who won’t vaccinate their children for fear of autism?"
I’m not suggesting that these are bad questions or that we shouldn’t ask them, so we can learn what we can. What I am saying is that, even if we do, no matter how careful and thoughtful we are, we are never going to catch everything we are unprepared for – the rare, the atypical, the unexpected.
This spring, the media reported details of an outbreak that occurred 5 years ago at New Orleans Children’s Hospital of what turned out to be mucormycosis; it proved fatal for several children. Looking back, mistakes were made. Diagnostic biopsies were only done when parents demanded them. Soiled laundry was mishandled. All this at a well-respected tertiary care center staffed by clinicians no doubt as fine as specialists anywhere.
The resulting investigation will no doubt find clinical and administrative gaps and address them. Consciousness will be raised, systems streamlined, oversight tightened. This loophole will be closed. Then others will open, no doubt the way they usually do, when people are looking at something else.
I knew there was something fishy about Peter’s case, but I didn’t know what it was. The experienced and thoughtful academic physicians I sent him to didn’t figure it out, either. It is nice of Peter to be philosophical about this. I would not begrudge him a less considerate reaction.
As for us, we ought to be vigilant, thorough, and humble. Should we get full of ourselves, there’s a hard case out there just waiting to deflate us.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
"Hard cases," say the lawyers, "make bad law." That means something like, "Legislation works better when it’s drafted in response to average circumstances, not extreme ones."
This adage applies to our profession, too. You can learn more about how to practice and teach medicine from average cases than from rare and strange ones. Hard cases can make any of us look foolish.
Peter e-mailed me the other day. I’d seen him 6 months ago for an eczematous rash on his back. Something funny about it, though: The distribution didn’t work, and it wasn’t scaly. No response to triamcinolone. Biopsy: Nonspecific inflammation. CBC: Elevated white cells at 15,600, mostly lymphs. Hmmm.
I referred him to an academic center. They presented him at Grand Rounds, and set him up for patch testing. He avoided what they asked him to, with little success.
"The oncologist says I have lymphoma," Peter’s e-mail to the patch test clinic read, copying me. He apologetically canceled his allergy clinic follow-up. "I hope for a good prognosis, although diagnosis has been delayed for several months. I hope my example will be of value for future patients."
Peter puts his regrets gently. How valuable will his lesson be? His case teaches that strange presentations of uncommon conditions can make even good and conscientious doctors look lame.
We all congratulate ourselves on "good pick-ups," the diagnostic coups that hit the nail on the head. Fair enough, but we understandably look away when we got it right by dumb luck or got it wrong.
That subcutaneous fullness we thought was fine, but which the patient insisted be removed (and turned out to be dermatofibrosarcoma protuberans). That dark spot that looked like all the others, only the patient was nervous because he was sure it had changed (melanoma). The funny rash that ended up being measles in an unimmunized child, and when was the last time you saw measles?
Often, we never even find out about the hard cases we missed, because the people who had them got fed up with us and went elsewhere. Sometimes, they send an angry letter or – more common these days – write a bad review. "I went to another doctor who finally figured out my problem and prescribed the right treatment." Once in a while, a lawsuit.
Viewed through the "retrospectoscope," knowing how the story turned out, our initial fumblings look pretty clumsy, if not downright actionable. "Oh, come on," a critic might say, "Surely that lump was too irregular for you to pass it off as a fibroma." Or: "Why the surprise? Didn’t he tell you the mole changed?" "The kid was sick and had a funny rash, didn’t she?" says a third. "Don’t you read the papers about all the parents who won’t vaccinate their children for fear of autism?"
I’m not suggesting that these are bad questions or that we shouldn’t ask them, so we can learn what we can. What I am saying is that, even if we do, no matter how careful and thoughtful we are, we are never going to catch everything we are unprepared for – the rare, the atypical, the unexpected.
This spring, the media reported details of an outbreak that occurred 5 years ago at New Orleans Children’s Hospital of what turned out to be mucormycosis; it proved fatal for several children. Looking back, mistakes were made. Diagnostic biopsies were only done when parents demanded them. Soiled laundry was mishandled. All this at a well-respected tertiary care center staffed by clinicians no doubt as fine as specialists anywhere.
The resulting investigation will no doubt find clinical and administrative gaps and address them. Consciousness will be raised, systems streamlined, oversight tightened. This loophole will be closed. Then others will open, no doubt the way they usually do, when people are looking at something else.
I knew there was something fishy about Peter’s case, but I didn’t know what it was. The experienced and thoughtful academic physicians I sent him to didn’t figure it out, either. It is nice of Peter to be philosophical about this. I would not begrudge him a less considerate reaction.
As for us, we ought to be vigilant, thorough, and humble. Should we get full of ourselves, there’s a hard case out there just waiting to deflate us.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.
"Hard cases," say the lawyers, "make bad law." That means something like, "Legislation works better when it’s drafted in response to average circumstances, not extreme ones."
This adage applies to our profession, too. You can learn more about how to practice and teach medicine from average cases than from rare and strange ones. Hard cases can make any of us look foolish.
Peter e-mailed me the other day. I’d seen him 6 months ago for an eczematous rash on his back. Something funny about it, though: The distribution didn’t work, and it wasn’t scaly. No response to triamcinolone. Biopsy: Nonspecific inflammation. CBC: Elevated white cells at 15,600, mostly lymphs. Hmmm.
I referred him to an academic center. They presented him at Grand Rounds, and set him up for patch testing. He avoided what they asked him to, with little success.
"The oncologist says I have lymphoma," Peter’s e-mail to the patch test clinic read, copying me. He apologetically canceled his allergy clinic follow-up. "I hope for a good prognosis, although diagnosis has been delayed for several months. I hope my example will be of value for future patients."
Peter puts his regrets gently. How valuable will his lesson be? His case teaches that strange presentations of uncommon conditions can make even good and conscientious doctors look lame.
We all congratulate ourselves on "good pick-ups," the diagnostic coups that hit the nail on the head. Fair enough, but we understandably look away when we got it right by dumb luck or got it wrong.
That subcutaneous fullness we thought was fine, but which the patient insisted be removed (and turned out to be dermatofibrosarcoma protuberans). That dark spot that looked like all the others, only the patient was nervous because he was sure it had changed (melanoma). The funny rash that ended up being measles in an unimmunized child, and when was the last time you saw measles?
Often, we never even find out about the hard cases we missed, because the people who had them got fed up with us and went elsewhere. Sometimes, they send an angry letter or – more common these days – write a bad review. "I went to another doctor who finally figured out my problem and prescribed the right treatment." Once in a while, a lawsuit.
Viewed through the "retrospectoscope," knowing how the story turned out, our initial fumblings look pretty clumsy, if not downright actionable. "Oh, come on," a critic might say, "Surely that lump was too irregular for you to pass it off as a fibroma." Or: "Why the surprise? Didn’t he tell you the mole changed?" "The kid was sick and had a funny rash, didn’t she?" says a third. "Don’t you read the papers about all the parents who won’t vaccinate their children for fear of autism?"
I’m not suggesting that these are bad questions or that we shouldn’t ask them, so we can learn what we can. What I am saying is that, even if we do, no matter how careful and thoughtful we are, we are never going to catch everything we are unprepared for – the rare, the atypical, the unexpected.
This spring, the media reported details of an outbreak that occurred 5 years ago at New Orleans Children’s Hospital of what turned out to be mucormycosis; it proved fatal for several children. Looking back, mistakes were made. Diagnostic biopsies were only done when parents demanded them. Soiled laundry was mishandled. All this at a well-respected tertiary care center staffed by clinicians no doubt as fine as specialists anywhere.
The resulting investigation will no doubt find clinical and administrative gaps and address them. Consciousness will be raised, systems streamlined, oversight tightened. This loophole will be closed. Then others will open, no doubt the way they usually do, when people are looking at something else.
I knew there was something fishy about Peter’s case, but I didn’t know what it was. The experienced and thoughtful academic physicians I sent him to didn’t figure it out, either. It is nice of Peter to be philosophical about this. I would not begrudge him a less considerate reaction.
As for us, we ought to be vigilant, thorough, and humble. Should we get full of ourselves, there’s a hard case out there just waiting to deflate us.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Dr. Rockoff has contributed to the Under My Skin column in Skin & Allergy News since 1997.