User login
Rethinking antimicrobial prophylaxis for UTI
The RIVUR [Randomized Intervention for Children With Vesicoureteral Reflux] trial investigators set out to reevaluate the role of antimicrobial prophylaxis for the prevention of recurrences in children with vesicoureteral reflux. As recent randomized trials have produced conflicting results, the goal of the RIVUR investigators was to determine whether antimicrobial prophylaxis could prevent febrile or symptomatic urinary tract infection and whether prevention would reduce the likelihood of subsequent renal scarring. The results, recently published in the New England Journal of Medicine (2014;370:2367-76), demonstrated that nearly 18% of children, 2 months to 6 years of age, have a febrile or symptomatic recurrence within the first year after the initial or presenting episode. The recurrence rate for febrile or symptomatic episodes was reduced by approximately 50% in the treatment group (trimethoprim-sulfamethoxazole) to nearly 8%.
In addition, the proportion of children considered treatment failures (defined as a combination of febrile or symptomatic UTIs or development of new renal scarring) occurred twice as often in the placebo group as in the treatment group. However, despite the reduction in febrile or symptomatic episodes in the treatment group, approximately 8% of children in both treatment and placebo groups developed new renal scarring, as defined by a decreased uptake of tracer or cortical thinning.
The study confirmed that children with higher grades of reflux (III or IV at baseline) were more likely to have febrile or symptomatic recurrences, that children with bladder and bowel dysfunction (based on a modified Dysfunctional Voiding Symptom Score) also were more likely to have febrile or symptomatic recurrences, and that recurrences in children on prophylaxis were more likely to be resistant to trimethoprim-sulfamethoxazole than were those in children on placebo.
Implications for prevention of UTI
The American Academy of Pediatrics guidelines for the management of UTI in children were updated in 2011 (Pediatrics 2011;128:595-610). The authors contacted the six researchers who had conducted the most recent randomized controlled trials and completed a formal meta-analysis that did not detect a statistically significant benefit of prophylaxis for stopping the recurrence of febrile UTI/pyelonephritis in infants without reflux or those with grades I, II, III, or IV. The 2011 recommendations reflected the findings of an AAP subcommittee that antimicrobial prophylaxis was not effective, as had been presumed in a 1999 report (Pediatrics 1999;103:843-52).
The AAP subcommittee on urinary tract infection of the Steering Committee on Quality Improvement and Management – authors of the 2011 revised guidelines – have recently reviewed the RIVUR study data (AAP News, July 1 2014) and concluded that antimicrobial prophylaxis did not alter the development of new renal scarring/damage, that the benefits of daily antimicrobial prophylaxis were modest, and that the increased likelihood of resistance to trimethoprim-sulfamethoxazole at recurrences was significant. The subcommittee reaffirmed the 2011 guidance concerning a "less aggressive" approach: Renal and bladder ultrasound are adequate for assessment of risk for renal scarring at first episodes, and watchful waiting without performing voiding cystourethrography (VCUG) or initiating prophylaxis is appropriate. VCUG is indicated after a first episode if renal and bladder ultrasonography reveals hydronephrosis, scarring, or other findings that would suggest either high-grade vesicoureteral reflux (VUR) or obstructive uropathy and in other atypical or complex clinical circumstances. As well, VCUG also should be performed if there is a recurrence of a febrile UTI (Pediatrics 2011;128:595-610).
The current subcommittee opined that prompt diagnosis and effective treatment of a febrile UTI recurrence may be of greater importance, regardless of whether VUR is present or the child is receiving antimicrobial prophylaxis.
My take
For me, the RIVUR data provide further insights into both the risk of any recurrence (approximately 18% by 12 months, approximately 25% by 24 months) and the risk for multiple recurrences (approximately 10%). The data identify those at highest risk for recurrences (patients with bladder and bowel dysfunction or higher grades of reflux) and provide evidence that trimethoprim-sulfamethoxazole prophylaxis is highly effective in such groups. No serious side effects were observed during the RIVUR trial; however, Stevens-Johnson syndrome is documented to occur rarely after administration of trimethoprim-sulfamethoxazole, and the potential for this life-threatening event should be part of the decision process. I believe the value of the new data is that they provide confidence that antimicrobial prophylaxis can be effective for the prevention of febrile/symptomatic UTI, and that in select children at great risk for recurrences and subsequent renal damage, antimicrobial prophylaxis can be part of our toolbox.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. He said that he had no relevant financial disclosures.
The RIVUR [Randomized Intervention for Children With Vesicoureteral Reflux] trial investigators set out to reevaluate the role of antimicrobial prophylaxis for the prevention of recurrences in children with vesicoureteral reflux. As recent randomized trials have produced conflicting results, the goal of the RIVUR investigators was to determine whether antimicrobial prophylaxis could prevent febrile or symptomatic urinary tract infection and whether prevention would reduce the likelihood of subsequent renal scarring. The results, recently published in the New England Journal of Medicine (2014;370:2367-76), demonstrated that nearly 18% of children, 2 months to 6 years of age, have a febrile or symptomatic recurrence within the first year after the initial or presenting episode. The recurrence rate for febrile or symptomatic episodes was reduced by approximately 50% in the treatment group (trimethoprim-sulfamethoxazole) to nearly 8%.
In addition, the proportion of children considered treatment failures (defined as a combination of febrile or symptomatic UTIs or development of new renal scarring) occurred twice as often in the placebo group as in the treatment group. However, despite the reduction in febrile or symptomatic episodes in the treatment group, approximately 8% of children in both treatment and placebo groups developed new renal scarring, as defined by a decreased uptake of tracer or cortical thinning.
The study confirmed that children with higher grades of reflux (III or IV at baseline) were more likely to have febrile or symptomatic recurrences, that children with bladder and bowel dysfunction (based on a modified Dysfunctional Voiding Symptom Score) also were more likely to have febrile or symptomatic recurrences, and that recurrences in children on prophylaxis were more likely to be resistant to trimethoprim-sulfamethoxazole than were those in children on placebo.
Implications for prevention of UTI
The American Academy of Pediatrics guidelines for the management of UTI in children were updated in 2011 (Pediatrics 2011;128:595-610). The authors contacted the six researchers who had conducted the most recent randomized controlled trials and completed a formal meta-analysis that did not detect a statistically significant benefit of prophylaxis for stopping the recurrence of febrile UTI/pyelonephritis in infants without reflux or those with grades I, II, III, or IV. The 2011 recommendations reflected the findings of an AAP subcommittee that antimicrobial prophylaxis was not effective, as had been presumed in a 1999 report (Pediatrics 1999;103:843-52).
The AAP subcommittee on urinary tract infection of the Steering Committee on Quality Improvement and Management – authors of the 2011 revised guidelines – have recently reviewed the RIVUR study data (AAP News, July 1 2014) and concluded that antimicrobial prophylaxis did not alter the development of new renal scarring/damage, that the benefits of daily antimicrobial prophylaxis were modest, and that the increased likelihood of resistance to trimethoprim-sulfamethoxazole at recurrences was significant. The subcommittee reaffirmed the 2011 guidance concerning a "less aggressive" approach: Renal and bladder ultrasound are adequate for assessment of risk for renal scarring at first episodes, and watchful waiting without performing voiding cystourethrography (VCUG) or initiating prophylaxis is appropriate. VCUG is indicated after a first episode if renal and bladder ultrasonography reveals hydronephrosis, scarring, or other findings that would suggest either high-grade vesicoureteral reflux (VUR) or obstructive uropathy and in other atypical or complex clinical circumstances. As well, VCUG also should be performed if there is a recurrence of a febrile UTI (Pediatrics 2011;128:595-610).
The current subcommittee opined that prompt diagnosis and effective treatment of a febrile UTI recurrence may be of greater importance, regardless of whether VUR is present or the child is receiving antimicrobial prophylaxis.
My take
For me, the RIVUR data provide further insights into both the risk of any recurrence (approximately 18% by 12 months, approximately 25% by 24 months) and the risk for multiple recurrences (approximately 10%). The data identify those at highest risk for recurrences (patients with bladder and bowel dysfunction or higher grades of reflux) and provide evidence that trimethoprim-sulfamethoxazole prophylaxis is highly effective in such groups. No serious side effects were observed during the RIVUR trial; however, Stevens-Johnson syndrome is documented to occur rarely after administration of trimethoprim-sulfamethoxazole, and the potential for this life-threatening event should be part of the decision process. I believe the value of the new data is that they provide confidence that antimicrobial prophylaxis can be effective for the prevention of febrile/symptomatic UTI, and that in select children at great risk for recurrences and subsequent renal damage, antimicrobial prophylaxis can be part of our toolbox.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. He said that he had no relevant financial disclosures.
The RIVUR [Randomized Intervention for Children With Vesicoureteral Reflux] trial investigators set out to reevaluate the role of antimicrobial prophylaxis for the prevention of recurrences in children with vesicoureteral reflux. As recent randomized trials have produced conflicting results, the goal of the RIVUR investigators was to determine whether antimicrobial prophylaxis could prevent febrile or symptomatic urinary tract infection and whether prevention would reduce the likelihood of subsequent renal scarring. The results, recently published in the New England Journal of Medicine (2014;370:2367-76), demonstrated that nearly 18% of children, 2 months to 6 years of age, have a febrile or symptomatic recurrence within the first year after the initial or presenting episode. The recurrence rate for febrile or symptomatic episodes was reduced by approximately 50% in the treatment group (trimethoprim-sulfamethoxazole) to nearly 8%.
In addition, the proportion of children considered treatment failures (defined as a combination of febrile or symptomatic UTIs or development of new renal scarring) occurred twice as often in the placebo group as in the treatment group. However, despite the reduction in febrile or symptomatic episodes in the treatment group, approximately 8% of children in both treatment and placebo groups developed new renal scarring, as defined by a decreased uptake of tracer or cortical thinning.
The study confirmed that children with higher grades of reflux (III or IV at baseline) were more likely to have febrile or symptomatic recurrences, that children with bladder and bowel dysfunction (based on a modified Dysfunctional Voiding Symptom Score) also were more likely to have febrile or symptomatic recurrences, and that recurrences in children on prophylaxis were more likely to be resistant to trimethoprim-sulfamethoxazole than were those in children on placebo.
Implications for prevention of UTI
The American Academy of Pediatrics guidelines for the management of UTI in children were updated in 2011 (Pediatrics 2011;128:595-610). The authors contacted the six researchers who had conducted the most recent randomized controlled trials and completed a formal meta-analysis that did not detect a statistically significant benefit of prophylaxis for stopping the recurrence of febrile UTI/pyelonephritis in infants without reflux or those with grades I, II, III, or IV. The 2011 recommendations reflected the findings of an AAP subcommittee that antimicrobial prophylaxis was not effective, as had been presumed in a 1999 report (Pediatrics 1999;103:843-52).
The AAP subcommittee on urinary tract infection of the Steering Committee on Quality Improvement and Management – authors of the 2011 revised guidelines – have recently reviewed the RIVUR study data (AAP News, July 1 2014) and concluded that antimicrobial prophylaxis did not alter the development of new renal scarring/damage, that the benefits of daily antimicrobial prophylaxis were modest, and that the increased likelihood of resistance to trimethoprim-sulfamethoxazole at recurrences was significant. The subcommittee reaffirmed the 2011 guidance concerning a "less aggressive" approach: Renal and bladder ultrasound are adequate for assessment of risk for renal scarring at first episodes, and watchful waiting without performing voiding cystourethrography (VCUG) or initiating prophylaxis is appropriate. VCUG is indicated after a first episode if renal and bladder ultrasonography reveals hydronephrosis, scarring, or other findings that would suggest either high-grade vesicoureteral reflux (VUR) or obstructive uropathy and in other atypical or complex clinical circumstances. As well, VCUG also should be performed if there is a recurrence of a febrile UTI (Pediatrics 2011;128:595-610).
The current subcommittee opined that prompt diagnosis and effective treatment of a febrile UTI recurrence may be of greater importance, regardless of whether VUR is present or the child is receiving antimicrobial prophylaxis.
My take
For me, the RIVUR data provide further insights into both the risk of any recurrence (approximately 18% by 12 months, approximately 25% by 24 months) and the risk for multiple recurrences (approximately 10%). The data identify those at highest risk for recurrences (patients with bladder and bowel dysfunction or higher grades of reflux) and provide evidence that trimethoprim-sulfamethoxazole prophylaxis is highly effective in such groups. No serious side effects were observed during the RIVUR trial; however, Stevens-Johnson syndrome is documented to occur rarely after administration of trimethoprim-sulfamethoxazole, and the potential for this life-threatening event should be part of the decision process. I believe the value of the new data is that they provide confidence that antimicrobial prophylaxis can be effective for the prevention of febrile/symptomatic UTI, and that in select children at great risk for recurrences and subsequent renal damage, antimicrobial prophylaxis can be part of our toolbox.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. He said that he had no relevant financial disclosures.
Scandals, focus, leadership, and honesty
The biggest news in ethics recently is the Veterans Affairs scandal, in which secret wait lists were allegedly kept to obscure the long delays for appointments. I seem to have a different perspective than the president, who said:
"How do we make sure that there is no slippage between somebody making a phone call and them getting an appointment scheduled. And let’s have a realistic time for how soon they’re going to get an appointment. Those are things that don’t require rocket science. It requires execution; it requires discipline; it requires focus."1
Execution, discipline, focus. I think the word the president was looking for was honesty.
Meanwhile, a VA whistleblower who told CNN about the problems at the Phoenix facility said Friday he was saddened by [Gen. Eric] Shinseki’s resignation under such circumstances.
"The VA administrators got way too focused on having good numbers, and they forgot the most important mandate, the reason we all work at the VA – to take care of veterans, to save their lives and give them good medical care," Dr. Sam Foote said.
"The next secretary’s biggest challenge will be to get that refocused and make sure the number one job is taking care of veterans – not worrying about their bureaucratic careers," Dr. Foote added.2
This analysis of being "too focused" echoes the analysis 4 months ago of a scandal involving cheating on proficiency tests at missile bases in Montana. In that situation, people were similarly focused on meeting numbers and lost track of the big picture.
"Leadership’s focus on perfection led commanders to micromanage their people," said [Lt. Gen. Stephen Wilson, the commander of the Air Force’s Global Strike Command,] pointing to pressure to get 100% scores on monthly proficiency exams when only 90% was necessary to pass. ... Leaders lost sight of the fact that execution in the field is more important than what happens in the classroom."3
"This is absolutely unacceptable behavior and it is completely contrary to our core values in the Air Force, and as everybody here knows, the No. 1 core value for us is integrity," Air Force Secretary Deborah Lee James told reporters.4
I’ll accept integrity as equivalent to honesty.
As in the VA scandal, the missile scandal initially seemed isolated, but on further investigation was determined to be widespread, with up to 20% of the 190-member force implicated at one point. Equally concerning to leadership was the fact that many more people were aware cheating was going on, but did not act on it. I’ve often seen the term teamwork used to justify that behavior or lack thereof.
Are the delays at the VA hospitals unique? Not in my experience. Just last month while making an appointment to see a sub-subspecialist, I was told they were scheduling 5 months out. I called back to my primary care physician, who made a call, and I was soon contacted with an appointment for about a week later. Did I get any preferential consideration as a professional courtesy because I’m a physician? I don’t know. Very possibly. Did I benefit from knowing the system and anticipating that if I called my doctor, an earlier appointment would be arranged? Absolutely. I’ve made those calls myself advocating for my own patients when I hear about a delay that seems too long. It is part of being a patient advocate.
This is a fairly (that may be a poor choice of adjective) common practice when access is limited, but it can become a significant source of injustice. I’m aware of one health care system with long delays in scheduling subspecialty appointments after hospitalizations, up to 4-5 months. However, they do a great job, when called by a member of their panel of frequently referring primary doctors, at fitting people in early. The impact is that patients who have a personal physician (which correlates with good insurance) routinely jump the queue and get seen promptly. Patients who don’t have an advocate, or who go to one of the low-income clinics, may not get care or get frustrated and look elsewhere. This arrangement allows the system to claim it sees Medicaid patients while actually seeing only a limited fraction. Despicably evil, but effective. Is there discriminatory intent? Unknown and hard to prove. Disparate impact? Absolutely. Public outrage? Nope. Public ignorance, apathy, and a good public relations department seem to avert scandal.
Focusing on the numbers, pay for performance, Press Ganey scores, getting the top box checkmark – do these take focus away from providing the best clinical therapies? One would hope professionalism would keep pediatricians focused on the noble pursuit of providing health care for children. But leadership and an occasional emphasis on honesty couldn’t hurt.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
References
1. http://www.whitehouse.gov/the-press-office/2014/05/30/statement-president
2. http://www.cnn.com/2014/05/30/politics/va-hospitals-shinseki/index.html
3. http://www.cnn.com/2014/03/27/us/air-force-cheating-investigation
4. http://www.cnn.com/2014/01/15/politics/air-force-nuclear-scandal
The biggest news in ethics recently is the Veterans Affairs scandal, in which secret wait lists were allegedly kept to obscure the long delays for appointments. I seem to have a different perspective than the president, who said:
"How do we make sure that there is no slippage between somebody making a phone call and them getting an appointment scheduled. And let’s have a realistic time for how soon they’re going to get an appointment. Those are things that don’t require rocket science. It requires execution; it requires discipline; it requires focus."1
Execution, discipline, focus. I think the word the president was looking for was honesty.
Meanwhile, a VA whistleblower who told CNN about the problems at the Phoenix facility said Friday he was saddened by [Gen. Eric] Shinseki’s resignation under such circumstances.
"The VA administrators got way too focused on having good numbers, and they forgot the most important mandate, the reason we all work at the VA – to take care of veterans, to save their lives and give them good medical care," Dr. Sam Foote said.
"The next secretary’s biggest challenge will be to get that refocused and make sure the number one job is taking care of veterans – not worrying about their bureaucratic careers," Dr. Foote added.2
This analysis of being "too focused" echoes the analysis 4 months ago of a scandal involving cheating on proficiency tests at missile bases in Montana. In that situation, people were similarly focused on meeting numbers and lost track of the big picture.
"Leadership’s focus on perfection led commanders to micromanage their people," said [Lt. Gen. Stephen Wilson, the commander of the Air Force’s Global Strike Command,] pointing to pressure to get 100% scores on monthly proficiency exams when only 90% was necessary to pass. ... Leaders lost sight of the fact that execution in the field is more important than what happens in the classroom."3
"This is absolutely unacceptable behavior and it is completely contrary to our core values in the Air Force, and as everybody here knows, the No. 1 core value for us is integrity," Air Force Secretary Deborah Lee James told reporters.4
I’ll accept integrity as equivalent to honesty.
As in the VA scandal, the missile scandal initially seemed isolated, but on further investigation was determined to be widespread, with up to 20% of the 190-member force implicated at one point. Equally concerning to leadership was the fact that many more people were aware cheating was going on, but did not act on it. I’ve often seen the term teamwork used to justify that behavior or lack thereof.
Are the delays at the VA hospitals unique? Not in my experience. Just last month while making an appointment to see a sub-subspecialist, I was told they were scheduling 5 months out. I called back to my primary care physician, who made a call, and I was soon contacted with an appointment for about a week later. Did I get any preferential consideration as a professional courtesy because I’m a physician? I don’t know. Very possibly. Did I benefit from knowing the system and anticipating that if I called my doctor, an earlier appointment would be arranged? Absolutely. I’ve made those calls myself advocating for my own patients when I hear about a delay that seems too long. It is part of being a patient advocate.
This is a fairly (that may be a poor choice of adjective) common practice when access is limited, but it can become a significant source of injustice. I’m aware of one health care system with long delays in scheduling subspecialty appointments after hospitalizations, up to 4-5 months. However, they do a great job, when called by a member of their panel of frequently referring primary doctors, at fitting people in early. The impact is that patients who have a personal physician (which correlates with good insurance) routinely jump the queue and get seen promptly. Patients who don’t have an advocate, or who go to one of the low-income clinics, may not get care or get frustrated and look elsewhere. This arrangement allows the system to claim it sees Medicaid patients while actually seeing only a limited fraction. Despicably evil, but effective. Is there discriminatory intent? Unknown and hard to prove. Disparate impact? Absolutely. Public outrage? Nope. Public ignorance, apathy, and a good public relations department seem to avert scandal.
Focusing on the numbers, pay for performance, Press Ganey scores, getting the top box checkmark – do these take focus away from providing the best clinical therapies? One would hope professionalism would keep pediatricians focused on the noble pursuit of providing health care for children. But leadership and an occasional emphasis on honesty couldn’t hurt.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
References
1. http://www.whitehouse.gov/the-press-office/2014/05/30/statement-president
2. http://www.cnn.com/2014/05/30/politics/va-hospitals-shinseki/index.html
3. http://www.cnn.com/2014/03/27/us/air-force-cheating-investigation
4. http://www.cnn.com/2014/01/15/politics/air-force-nuclear-scandal
The biggest news in ethics recently is the Veterans Affairs scandal, in which secret wait lists were allegedly kept to obscure the long delays for appointments. I seem to have a different perspective than the president, who said:
"How do we make sure that there is no slippage between somebody making a phone call and them getting an appointment scheduled. And let’s have a realistic time for how soon they’re going to get an appointment. Those are things that don’t require rocket science. It requires execution; it requires discipline; it requires focus."1
Execution, discipline, focus. I think the word the president was looking for was honesty.
Meanwhile, a VA whistleblower who told CNN about the problems at the Phoenix facility said Friday he was saddened by [Gen. Eric] Shinseki’s resignation under such circumstances.
"The VA administrators got way too focused on having good numbers, and they forgot the most important mandate, the reason we all work at the VA – to take care of veterans, to save their lives and give them good medical care," Dr. Sam Foote said.
"The next secretary’s biggest challenge will be to get that refocused and make sure the number one job is taking care of veterans – not worrying about their bureaucratic careers," Dr. Foote added.2
This analysis of being "too focused" echoes the analysis 4 months ago of a scandal involving cheating on proficiency tests at missile bases in Montana. In that situation, people were similarly focused on meeting numbers and lost track of the big picture.
"Leadership’s focus on perfection led commanders to micromanage their people," said [Lt. Gen. Stephen Wilson, the commander of the Air Force’s Global Strike Command,] pointing to pressure to get 100% scores on monthly proficiency exams when only 90% was necessary to pass. ... Leaders lost sight of the fact that execution in the field is more important than what happens in the classroom."3
"This is absolutely unacceptable behavior and it is completely contrary to our core values in the Air Force, and as everybody here knows, the No. 1 core value for us is integrity," Air Force Secretary Deborah Lee James told reporters.4
I’ll accept integrity as equivalent to honesty.
As in the VA scandal, the missile scandal initially seemed isolated, but on further investigation was determined to be widespread, with up to 20% of the 190-member force implicated at one point. Equally concerning to leadership was the fact that many more people were aware cheating was going on, but did not act on it. I’ve often seen the term teamwork used to justify that behavior or lack thereof.
Are the delays at the VA hospitals unique? Not in my experience. Just last month while making an appointment to see a sub-subspecialist, I was told they were scheduling 5 months out. I called back to my primary care physician, who made a call, and I was soon contacted with an appointment for about a week later. Did I get any preferential consideration as a professional courtesy because I’m a physician? I don’t know. Very possibly. Did I benefit from knowing the system and anticipating that if I called my doctor, an earlier appointment would be arranged? Absolutely. I’ve made those calls myself advocating for my own patients when I hear about a delay that seems too long. It is part of being a patient advocate.
This is a fairly (that may be a poor choice of adjective) common practice when access is limited, but it can become a significant source of injustice. I’m aware of one health care system with long delays in scheduling subspecialty appointments after hospitalizations, up to 4-5 months. However, they do a great job, when called by a member of their panel of frequently referring primary doctors, at fitting people in early. The impact is that patients who have a personal physician (which correlates with good insurance) routinely jump the queue and get seen promptly. Patients who don’t have an advocate, or who go to one of the low-income clinics, may not get care or get frustrated and look elsewhere. This arrangement allows the system to claim it sees Medicaid patients while actually seeing only a limited fraction. Despicably evil, but effective. Is there discriminatory intent? Unknown and hard to prove. Disparate impact? Absolutely. Public outrage? Nope. Public ignorance, apathy, and a good public relations department seem to avert scandal.
Focusing on the numbers, pay for performance, Press Ganey scores, getting the top box checkmark – do these take focus away from providing the best clinical therapies? One would hope professionalism would keep pediatricians focused on the noble pursuit of providing health care for children. But leadership and an occasional emphasis on honesty couldn’t hurt.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
References
1. http://www.whitehouse.gov/the-press-office/2014/05/30/statement-president
2. http://www.cnn.com/2014/05/30/politics/va-hospitals-shinseki/index.html
3. http://www.cnn.com/2014/03/27/us/air-force-cheating-investigation
4. http://www.cnn.com/2014/01/15/politics/air-force-nuclear-scandal
Retail me not!
In an era where everything around us has moved toward an "I need it now and I need it fast" attitude, the face of medicine also has changed. The days of patients wanting to wait to see their physician have faded, and now there is a demand for a quick fix so they can keep their already hectic lives moving.
Retail clinics also have thrown a curve ball to practicing physicians because now patients can get their fast medicine right along with their fast food, all at the corner strip mall.
The Internet also has changed how office visits run. Now physicians spend a lot of time explaining diagnoses that patients have found during their exhaustive research of their symptoms, or dispelling erroneous information that has been found on the Internet. This adds to time per patient, as well as distrust. Patients are now smarter, busier, and more likely to have chronic illnesses, so how does medicine keep up with the times?
As physicians, we must remember that our expertise as medical doctors is to rule in and rule out serious diseases. The "bread and butter" of any medical practice is likely easy to identify and treat, but where the expertise comes in is how to distinguish minor acute illness from life-threatening or potentially chronic illness. Many disease states are efficiently diagnosed only because the patient presents with further complaints that put the entire picture together. How is that achieved when patients fast-track through "minute clinics"?
Experience is also golden. If you have practiced long enough, you have had your share of surprises and know that "oh, it’s nothing" is the diagnosis only after all the "somethings " have been ruled out. For example, in adolescent medicine I commonly get the complaints of abdominal pain and anxiety. So when a patient presents with ongoing complaints of abdominal pain with no other clinical signs of disease, there is a temptation to assume it is just the anxiety. But experience teaches you that viral hepatitis, appendicitis, or urological disorders could be the underlying problem.
Another lesson that is taught by experience is how children express themselves. I recently saw an adolescent who had a minor trauma where he was struck in the chest with a basketball. He subsequently complained of chest pain, but kept saying, "I feel like I’m going to die." His mother was insistent that this was just his already diagnosed anxiety, and that he would settle down. But stating he "felt like he was going to die" was such an unusual complaint for a child that I was prompted to do an EKG, which revealed a viral myocarditis. Although this may have been identified in an express clinic, knowing the patient helped in expediting the diagnosis.
As physicians, we must educate and ensure that our patients feel they are getting the best care by sticking with someone who knows them. We have to accept that patients have options, so if we are going to keep their business, we have to work more efficiently, form relationships, and provide good care. Many practices have moved toward a concierge service, where a fee is charged for immediate appointments or telephone access. Utilization of a nurse practitioner can allow you to run your office more efficiently to manage the more acute illnesses, shorten the wait times, and maximize patient visits.
Retail clinics are here to stay. If we are going to keep private practices afloat, we have to make the visit worth the wait!
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
In an era where everything around us has moved toward an "I need it now and I need it fast" attitude, the face of medicine also has changed. The days of patients wanting to wait to see their physician have faded, and now there is a demand for a quick fix so they can keep their already hectic lives moving.
Retail clinics also have thrown a curve ball to practicing physicians because now patients can get their fast medicine right along with their fast food, all at the corner strip mall.
The Internet also has changed how office visits run. Now physicians spend a lot of time explaining diagnoses that patients have found during their exhaustive research of their symptoms, or dispelling erroneous information that has been found on the Internet. This adds to time per patient, as well as distrust. Patients are now smarter, busier, and more likely to have chronic illnesses, so how does medicine keep up with the times?
As physicians, we must remember that our expertise as medical doctors is to rule in and rule out serious diseases. The "bread and butter" of any medical practice is likely easy to identify and treat, but where the expertise comes in is how to distinguish minor acute illness from life-threatening or potentially chronic illness. Many disease states are efficiently diagnosed only because the patient presents with further complaints that put the entire picture together. How is that achieved when patients fast-track through "minute clinics"?
Experience is also golden. If you have practiced long enough, you have had your share of surprises and know that "oh, it’s nothing" is the diagnosis only after all the "somethings " have been ruled out. For example, in adolescent medicine I commonly get the complaints of abdominal pain and anxiety. So when a patient presents with ongoing complaints of abdominal pain with no other clinical signs of disease, there is a temptation to assume it is just the anxiety. But experience teaches you that viral hepatitis, appendicitis, or urological disorders could be the underlying problem.
Another lesson that is taught by experience is how children express themselves. I recently saw an adolescent who had a minor trauma where he was struck in the chest with a basketball. He subsequently complained of chest pain, but kept saying, "I feel like I’m going to die." His mother was insistent that this was just his already diagnosed anxiety, and that he would settle down. But stating he "felt like he was going to die" was such an unusual complaint for a child that I was prompted to do an EKG, which revealed a viral myocarditis. Although this may have been identified in an express clinic, knowing the patient helped in expediting the diagnosis.
As physicians, we must educate and ensure that our patients feel they are getting the best care by sticking with someone who knows them. We have to accept that patients have options, so if we are going to keep their business, we have to work more efficiently, form relationships, and provide good care. Many practices have moved toward a concierge service, where a fee is charged for immediate appointments or telephone access. Utilization of a nurse practitioner can allow you to run your office more efficiently to manage the more acute illnesses, shorten the wait times, and maximize patient visits.
Retail clinics are here to stay. If we are going to keep private practices afloat, we have to make the visit worth the wait!
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
In an era where everything around us has moved toward an "I need it now and I need it fast" attitude, the face of medicine also has changed. The days of patients wanting to wait to see their physician have faded, and now there is a demand for a quick fix so they can keep their already hectic lives moving.
Retail clinics also have thrown a curve ball to practicing physicians because now patients can get their fast medicine right along with their fast food, all at the corner strip mall.
The Internet also has changed how office visits run. Now physicians spend a lot of time explaining diagnoses that patients have found during their exhaustive research of their symptoms, or dispelling erroneous information that has been found on the Internet. This adds to time per patient, as well as distrust. Patients are now smarter, busier, and more likely to have chronic illnesses, so how does medicine keep up with the times?
As physicians, we must remember that our expertise as medical doctors is to rule in and rule out serious diseases. The "bread and butter" of any medical practice is likely easy to identify and treat, but where the expertise comes in is how to distinguish minor acute illness from life-threatening or potentially chronic illness. Many disease states are efficiently diagnosed only because the patient presents with further complaints that put the entire picture together. How is that achieved when patients fast-track through "minute clinics"?
Experience is also golden. If you have practiced long enough, you have had your share of surprises and know that "oh, it’s nothing" is the diagnosis only after all the "somethings " have been ruled out. For example, in adolescent medicine I commonly get the complaints of abdominal pain and anxiety. So when a patient presents with ongoing complaints of abdominal pain with no other clinical signs of disease, there is a temptation to assume it is just the anxiety. But experience teaches you that viral hepatitis, appendicitis, or urological disorders could be the underlying problem.
Another lesson that is taught by experience is how children express themselves. I recently saw an adolescent who had a minor trauma where he was struck in the chest with a basketball. He subsequently complained of chest pain, but kept saying, "I feel like I’m going to die." His mother was insistent that this was just his already diagnosed anxiety, and that he would settle down. But stating he "felt like he was going to die" was such an unusual complaint for a child that I was prompted to do an EKG, which revealed a viral myocarditis. Although this may have been identified in an express clinic, knowing the patient helped in expediting the diagnosis.
As physicians, we must educate and ensure that our patients feel they are getting the best care by sticking with someone who knows them. We have to accept that patients have options, so if we are going to keep their business, we have to work more efficiently, form relationships, and provide good care. Many practices have moved toward a concierge service, where a fee is charged for immediate appointments or telephone access. Utilization of a nurse practitioner can allow you to run your office more efficiently to manage the more acute illnesses, shorten the wait times, and maximize patient visits.
Retail clinics are here to stay. If we are going to keep private practices afloat, we have to make the visit worth the wait!
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
Position paper on sports-related concussion sets the right tone
The American Academy of Neurology’s position paper on the evaluation and management of sports-related concussion states a belief in the ethical obligation of the treating physician to make sure an athlete is ready to return to play following a concussion and that he or she is educated and protected from what could be a serious neurological injury.
As a practicing sports neurologist for the past 30 years, I agree with the stance that the AAN has taken, and I have found in my own practice that while the injured player and coaches are often anxious for the injured player to get back on the field, it is imperative for the player sit out until he or she has been given the okay by a qualified physician.
In my work with athletes from different sports and of all ages – as an adviser for Pop Warner football up through working on the NFL Players Association Mackey-White Traumatic Brain Injury Committee – the care of the patient has always been and will always be my greatest concern. Contact and collision sports, like football, hockey, and boxing, will never be completely safe, but that doesn’t lessen our responsibility as physicians to shield players from unnecessary injury and to ensure they are well enough to continue the sport.
If a player returns to the game before he is ready, he raises the likelihood of sustaining a second concussion, which is most likely to occur within 10 days of the initial concussion. He also increases his risk of "second-impact syndrome." While this is rare, its effects can be disastrous: traumatic injury and even death has occurred. A concussion is not just a "bump on the head," and everyone involved in a player’s care should take that seriously.
The AAN statement also supports the inclusion of concussion evaluation and training for neurology residency programs. Education on this particular issue is paramount in the fight to keep athletes safe. Making sure that all neurologists have the proper tools and are kept abreast of any changes to concussion management guidelines and testing will continue to ensure players’ safety.
Education for athletes, coaches, athletic trainers, parents, and the community in general also is critical. Once they know and understand the signs and symptoms – and the impact – of a concussion, the easier it will be for everyone to be on board with keeping an athlete out of play until she has been cleared by her doctor. It’s also important to have a better understanding of the scope of the problem and its impact. To that end, the AAN’s idea to create a mandatory national concussion registry is definitely a step in the right direction and could be an integral way to gain a better understanding of the issue at hand.
No matter whether a player has dedicated his life to the sport or if he is in his first Pop Warner season, it will always be tough to tell him that he has to sit out for one or more games. (And, for the younger set, that is often difficult for parents to hear.) But it is the ethical obligation of a physician to make sure a player has no visible signs or symptoms and is cognitively ready to return to play. That, combined with education and knowledge on the subject, as the AAN recommends, will help neurologists and other physicians throughout the country keep players safe and limit the number of concussions and their impact on today’s athletes.
Dr. Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He also serves as the assistant medical director there. He currently serves as the chief medical officer of the New York State Athletic Commission, as a team physician for USA Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
The American Academy of Neurology’s position paper on the evaluation and management of sports-related concussion states a belief in the ethical obligation of the treating physician to make sure an athlete is ready to return to play following a concussion and that he or she is educated and protected from what could be a serious neurological injury.
As a practicing sports neurologist for the past 30 years, I agree with the stance that the AAN has taken, and I have found in my own practice that while the injured player and coaches are often anxious for the injured player to get back on the field, it is imperative for the player sit out until he or she has been given the okay by a qualified physician.
In my work with athletes from different sports and of all ages – as an adviser for Pop Warner football up through working on the NFL Players Association Mackey-White Traumatic Brain Injury Committee – the care of the patient has always been and will always be my greatest concern. Contact and collision sports, like football, hockey, and boxing, will never be completely safe, but that doesn’t lessen our responsibility as physicians to shield players from unnecessary injury and to ensure they are well enough to continue the sport.
If a player returns to the game before he is ready, he raises the likelihood of sustaining a second concussion, which is most likely to occur within 10 days of the initial concussion. He also increases his risk of "second-impact syndrome." While this is rare, its effects can be disastrous: traumatic injury and even death has occurred. A concussion is not just a "bump on the head," and everyone involved in a player’s care should take that seriously.
The AAN statement also supports the inclusion of concussion evaluation and training for neurology residency programs. Education on this particular issue is paramount in the fight to keep athletes safe. Making sure that all neurologists have the proper tools and are kept abreast of any changes to concussion management guidelines and testing will continue to ensure players’ safety.
Education for athletes, coaches, athletic trainers, parents, and the community in general also is critical. Once they know and understand the signs and symptoms – and the impact – of a concussion, the easier it will be for everyone to be on board with keeping an athlete out of play until she has been cleared by her doctor. It’s also important to have a better understanding of the scope of the problem and its impact. To that end, the AAN’s idea to create a mandatory national concussion registry is definitely a step in the right direction and could be an integral way to gain a better understanding of the issue at hand.
No matter whether a player has dedicated his life to the sport or if he is in his first Pop Warner season, it will always be tough to tell him that he has to sit out for one or more games. (And, for the younger set, that is often difficult for parents to hear.) But it is the ethical obligation of a physician to make sure a player has no visible signs or symptoms and is cognitively ready to return to play. That, combined with education and knowledge on the subject, as the AAN recommends, will help neurologists and other physicians throughout the country keep players safe and limit the number of concussions and their impact on today’s athletes.
Dr. Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He also serves as the assistant medical director there. He currently serves as the chief medical officer of the New York State Athletic Commission, as a team physician for USA Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
The American Academy of Neurology’s position paper on the evaluation and management of sports-related concussion states a belief in the ethical obligation of the treating physician to make sure an athlete is ready to return to play following a concussion and that he or she is educated and protected from what could be a serious neurological injury.
As a practicing sports neurologist for the past 30 years, I agree with the stance that the AAN has taken, and I have found in my own practice that while the injured player and coaches are often anxious for the injured player to get back on the field, it is imperative for the player sit out until he or she has been given the okay by a qualified physician.
In my work with athletes from different sports and of all ages – as an adviser for Pop Warner football up through working on the NFL Players Association Mackey-White Traumatic Brain Injury Committee – the care of the patient has always been and will always be my greatest concern. Contact and collision sports, like football, hockey, and boxing, will never be completely safe, but that doesn’t lessen our responsibility as physicians to shield players from unnecessary injury and to ensure they are well enough to continue the sport.
If a player returns to the game before he is ready, he raises the likelihood of sustaining a second concussion, which is most likely to occur within 10 days of the initial concussion. He also increases his risk of "second-impact syndrome." While this is rare, its effects can be disastrous: traumatic injury and even death has occurred. A concussion is not just a "bump on the head," and everyone involved in a player’s care should take that seriously.
The AAN statement also supports the inclusion of concussion evaluation and training for neurology residency programs. Education on this particular issue is paramount in the fight to keep athletes safe. Making sure that all neurologists have the proper tools and are kept abreast of any changes to concussion management guidelines and testing will continue to ensure players’ safety.
Education for athletes, coaches, athletic trainers, parents, and the community in general also is critical. Once they know and understand the signs and symptoms – and the impact – of a concussion, the easier it will be for everyone to be on board with keeping an athlete out of play until she has been cleared by her doctor. It’s also important to have a better understanding of the scope of the problem and its impact. To that end, the AAN’s idea to create a mandatory national concussion registry is definitely a step in the right direction and could be an integral way to gain a better understanding of the issue at hand.
No matter whether a player has dedicated his life to the sport or if he is in his first Pop Warner season, it will always be tough to tell him that he has to sit out for one or more games. (And, for the younger set, that is often difficult for parents to hear.) But it is the ethical obligation of a physician to make sure a player has no visible signs or symptoms and is cognitively ready to return to play. That, combined with education and knowledge on the subject, as the AAN recommends, will help neurologists and other physicians throughout the country keep players safe and limit the number of concussions and their impact on today’s athletes.
Dr. Jordan is the director of the brain injury program and the memory evaluation treatment service at Burke Rehabilitation Hospital in White Plains, N.Y. He also serves as the assistant medical director there. He currently serves as the chief medical officer of the New York State Athletic Commission, as a team physician for USA Boxing, and as a member of the NFL Players Association Mackey-White Traumatic Brain Injury Committee and the NFL Neuro-Cognitive Disability Committee.
Helping breast cancer patients analyze risk
Dr. Sarah Hawley and her coinvestigators are to be applauded for generating insightful data regarding factors and concerns that motivate a woman to undergo contralateral prophylactic mastectomy in the setting of unilateral breast cancer (JAMA Surgery 2014 May 21 [doi:10.1001/jamasurg.2013.5689]).
Hawley et al. found that fear of recurrence was one of the strongest factors leading women to choose contralateral prophylactic mastectomy (CPM). This finding clearly demonstrates that we need to do a better job of explaining and defining the significance of (i) breast cancer local recurrence; (ii) breast cancer distant recurrence; and (iii) the development of a new/second primary breast cancer. Since cross-metastasis of a primary breast cancer to the contralateral breast is an extremely rare event, and since distant metastasis from the initial primary breast cancer tends to determine survival rates, CPM by definition will influence the incidence of only the third pattern. Furthermore, since the risk of experiencing a new contralateral malignancy is less than 1% per year for the general population of breast cancer patients, only a minority of these women will actually become bilateral breast cancer patients. Fear of recurrence is therefore a totally inappropriate reason for patients to pursue CPM, and the reasonableness of CPM to reduce the risk of a contralateral new primary breast cancer is debatable.
It can be reasonably stated that prophylactic surgery by definition is never a medically indicated necessity. Furthermore, despite the fact that a personal history of breast cancer is indeed a risk factor for developing a second primary cancer in the contralateral breast, numerous studies have demonstrated equivalent survival rates for women with unilateral breast cancer, compared with those diagnosed with bilateral/metachronous breast cancer (Cancer 2001;91:1845-53; Am. J. Clin. Oncol. 1997;20:541-5). Survival tends to be driven by the stage and effectiveness of treatment for the first cancer. By virtue of its earlier presentation, it is likely that the initially diagnosed cancer has established itself as the faster-growing malignancy with a lead time advantage in establishing distant organ micrometastatic disease; furthermore, patients with a unilateral breast cancer diagnosis are generally undergoing diligent surveillance and a contralateral malignancy is more often detected at an early stage.
Messages to our patients
It is essential for those of us who manage breast cancer to clearly emphasize several messages to our newly diagnosed breast cancer patients: First, although unilateral breast cancer increases the likelihood of developing a second primary tumor, it is certainly not inevitable, and in fact, the majority of patients are not destined to develop contralateral disease. Second, reducing the risk of being diagnosed with a contralateral breast cancer does not mitigate the mortality risk associated with the first cancer. And, finally, prophylactic mastectomy is the most aggressive and effective strategy for reducing the incidence of primary breast cancer (by approximately 90%), but it does not confer complete protection, as microscopic foci of breast tissue may be left behind in the mastectomy skin flaps, along the pectoralis, or in the axilla.
The messages above are critical: Our patients must understand that the priority is to address the known cancer. In this regard, appropriately selected patients should be encouraged to strongly consider breast-conserving surgery whenever feasible, as this low-morbidity treatment is equivalent to mastectomy from the perspective of overall survival. The question of CPM is most relevant for those patients that are ineligible for breast conservation or patients unwilling to undergo lumpectomy and breast radiation.
If a mastectomy for the cancerous breast is planned, we must then address the questions that routinely arise regarding bilateral surgery. In our efforts to clarify the reality of what CPM can and cannot achieve, we must also avoid being too dogmatic and paternalistic with our patients. There are clearly specific scenarios, as delineated in Dr. Hawley’s work, where the risk of a second primary breast cancer is likely to be considered excessive by most women, and where the decision to pursue CPM may be easier. Examples of such cases would be women known to harbor BRCA mutations or women with suspected hereditary susceptibility based on a strong family history of breast and/or ovarian cancer. The risk of a new contralateral breast cancer can be in the range of 4%-5% per year in cases of hereditary disease, compared with the general population of women with sporadic breast cancer, where the risk ranges from 0.25% to 1% per year.
Conveying an understanding of risk
Patients must understand that the risk to the contralateral breast is predominantly expressed in the future – the likelihood of having a clinically occult, incidentally detected cancer identified in the contralateral mastectomy specimen is only 6%, as demonstrated most recently by King et al. (Ann. Surg. 2011;254:2-7), and with ductal carcinoma in situ accounting for the high majority of these lesions.
Defining the threshold for the amount of risk that an individual woman finds to be acceptable, however, can be a very difficult and personal decision. Even after a patient comes to understand that CPM is unlikely to provide a survival advantage, she may continue to request bilateral surgery purely for the risk-reducing benefits, and out of a desire to minimize her chances of having to repeat the breast cancer diagnosis and treatment experience. In some cases this choice will be influenced by reconstruction factors. A woman may be motivated to pursue bilateral surgery if she has an adequate volume of abdominal tissue because of the fact that the autogenous TRAM (transverse rectus abdominis myocutaneous) flap can be harvested only once. In other cases the decision is influenced by body habitus, for example, a woman with large pendulous breasts who is not interested in breast reconstruction may decide that she is more comfortable with a symmetrically flat chest wall in order to avoid chest wall imbalance and the inconvenience of finding/wearing a prosthesis that matches the remaining breast.
As breast cancer surgeons we should openly discuss these issues with our patients and present viable alternatives when feasible, such as reduction mammoplasty for the large-breasted patient. Ultimately, however, the patient must decide the surgical approach that provides her with the optimal sense of treatment satisfaction, quality of life, and comfort.
Discussion strategies
In my own practice I have found two discussion strategies to be particularly useful in guiding patients through the decision about CPM.
The first approach is relevant for women who are lumpectomy candidates, but who express a "reflex" interest in bilateral mastectomy while they are still in the emotional fog of processing the new cancer diagnosis. For these women it is obviously important to stress the survival equivalence of mastectomy and breast-conserving surgery, and this is also a great opportunity to educate patients about the potential axillary surgery advantages of breast conservation. The American College of Surgeons Oncology Group Z11 trial (JAMA 2011;305:69-75) has provided strong evidence supporting the safety of avoiding an axillary lymph node dissection (ALND) in women with sentinel lymph node (SLN) metastatic disease if the primary breast cancer is managed by lumpectomy and breast radiation.
At this point in time, we do not have comparably strong data to justify avoiding the ALND in the setting of mastectomy patients with SLN metastatic disease. The mastectomy patient with SLN metastasis is usually committed to undergo the completion axillary lymph node dissection specifically so that definitive decisions can be made regarding the need for postmastectomy radiation, and many of these patients become ineligible for immediate reconstruction because of this possible radiation. I therefore accentuate the advantage of at least initiating treatment with lumpectomy and sentinel lymph node biopsy. The patient preserves all of her surgical options with the benefit of having more staging information. If she is found to have SLN metastatic disease then she is in a better position to avoid the ALND with lumpectomy and radiation, and the option of future mastectomy and immediate reconstruction would still be available to her in the future (after completing all of her cancer treatment and healing from her radiation); if the SLN is negative, she can either continue with the breast-conservation treatment plan or she can pursue mastectomy (with or without immediate breast reconstruction, since prophylactic mamillary radiation therapy is not likely to be indicated for node-negative disease).
The second approach is relevant to the patient requiring mastectomy but for whom delayed reconstruction is planned because of medical issues or anticipated postmastectomy radiation. I encourage these patients to at least consider deferring the decision for the CPM until they return for the delayed reconstruction of the cancerous mastectomy, because at that time they can undergo the prophylactic mastectomy with the cosmetic advantages of immediate reconstruction.
Cost considerations
From the public health and population-based breast cancer burden perspectives as well as for individual patients, there are additional issues to be factored into the CPM discussion. It is a basic reality that cost is relevant when it comes to sorting out the net benefit of particular medical interventions, especially those that are prophylactic. Interestingly, a cost analysis study by Zendejas et al. (J. Clin. Oncol. 2011;29:2993-3000) from the Mayo Clinic demonstrated that CPM is actually cost effective, compared with surveillance for patients diagnosed when they are younger than 70 years of age.
The Women’s Health and Cancer Rights Act was implemented in 1999, mandating insurance coverage for breast reconstruction after mastectomy performed for cancer. This legislation promoted more widespread acceptance (and reimbursement) for contralateral mastectomy/reconstruction, but patients should nonetheless be proactive about confirming that their individual policy will indeed cover the expenses of prophylactic surgery. Furthermore, we must continue to monitor outcomes in women who choose to undergo CPM, as advances in breast cancer therapies may influence the survival benefits of this surgical approach. Indeed, selected retrospective studies have recently demonstrated that patients undergoing CPM have an improved survival, compared with those focusing on unilateral breast cancer surgery (Ann. Surg. Oncol. 2010;17:2702-9; J. Natl. Cancer Inst. 2010;102:401-9; J. Clin. Oncol. 2005;23:4275-86; Am. J. Surg. 2000;180:439-45). These results suggest a survival advantage associated with avoidance of a contralateral breast cancer, in contrast to the historical data alluded to above, regarding survival equivalence for patients with unilateral compared to metachronous bilateral breast cancer. As adjuvant systemic therapies for breast cancer continue to improve in effectiveness and ability to completely eliminate distant organ micrometastases, it is likely that we will continue to increase the pool of women who are essentially "cured" of the first cancer. This in turn could potentially increase the longevity threat of a second/metachronous cancer though a renewed metastatic risk. Nonetheless, data on possible survival advantages of CPM have not yet matured to the point where it can be recommended as a medically "indicated" procedure.
Our breast cancer patients face an abundance of very legitimate fears related to the morbidity and mortality risks of the actual cancer as well as the adverse effects and toxicities of treatment for that cancer. Fortunately, we can assure them that for the majority of cases these treatments will be effective and their longevity will be protected. It is therefore understandable that the desire to avoid repeating this particular life experience may be strong. We have an obligation to explain the advantages and disadvantages, as well as the alternatives to CPM, with sensitivity and patience. We must also strive to make sure that our patients do not make premature decisions without understanding the consequences. Last, but certainly not least, we are ethically bound to offer only those treatments that we feel are medically reasonable and safe as well as oncologically sound. But we must also remember that the decision to pursue treatment and the choice between the options that we offer are ultimately rights that belong to the patient.
Dr. Newman in an ACS Fellow, professor of surgery, and director of the Breast Care Center and Multidisciplinary Breast Fellowship Program, University of Michigan Comprehensive Cancer Center, Ann Arbor.
Dr. Sarah Hawley and her coinvestigators are to be applauded for generating insightful data regarding factors and concerns that motivate a woman to undergo contralateral prophylactic mastectomy in the setting of unilateral breast cancer (JAMA Surgery 2014 May 21 [doi:10.1001/jamasurg.2013.5689]).
Hawley et al. found that fear of recurrence was one of the strongest factors leading women to choose contralateral prophylactic mastectomy (CPM). This finding clearly demonstrates that we need to do a better job of explaining and defining the significance of (i) breast cancer local recurrence; (ii) breast cancer distant recurrence; and (iii) the development of a new/second primary breast cancer. Since cross-metastasis of a primary breast cancer to the contralateral breast is an extremely rare event, and since distant metastasis from the initial primary breast cancer tends to determine survival rates, CPM by definition will influence the incidence of only the third pattern. Furthermore, since the risk of experiencing a new contralateral malignancy is less than 1% per year for the general population of breast cancer patients, only a minority of these women will actually become bilateral breast cancer patients. Fear of recurrence is therefore a totally inappropriate reason for patients to pursue CPM, and the reasonableness of CPM to reduce the risk of a contralateral new primary breast cancer is debatable.
It can be reasonably stated that prophylactic surgery by definition is never a medically indicated necessity. Furthermore, despite the fact that a personal history of breast cancer is indeed a risk factor for developing a second primary cancer in the contralateral breast, numerous studies have demonstrated equivalent survival rates for women with unilateral breast cancer, compared with those diagnosed with bilateral/metachronous breast cancer (Cancer 2001;91:1845-53; Am. J. Clin. Oncol. 1997;20:541-5). Survival tends to be driven by the stage and effectiveness of treatment for the first cancer. By virtue of its earlier presentation, it is likely that the initially diagnosed cancer has established itself as the faster-growing malignancy with a lead time advantage in establishing distant organ micrometastatic disease; furthermore, patients with a unilateral breast cancer diagnosis are generally undergoing diligent surveillance and a contralateral malignancy is more often detected at an early stage.
Messages to our patients
It is essential for those of us who manage breast cancer to clearly emphasize several messages to our newly diagnosed breast cancer patients: First, although unilateral breast cancer increases the likelihood of developing a second primary tumor, it is certainly not inevitable, and in fact, the majority of patients are not destined to develop contralateral disease. Second, reducing the risk of being diagnosed with a contralateral breast cancer does not mitigate the mortality risk associated with the first cancer. And, finally, prophylactic mastectomy is the most aggressive and effective strategy for reducing the incidence of primary breast cancer (by approximately 90%), but it does not confer complete protection, as microscopic foci of breast tissue may be left behind in the mastectomy skin flaps, along the pectoralis, or in the axilla.
The messages above are critical: Our patients must understand that the priority is to address the known cancer. In this regard, appropriately selected patients should be encouraged to strongly consider breast-conserving surgery whenever feasible, as this low-morbidity treatment is equivalent to mastectomy from the perspective of overall survival. The question of CPM is most relevant for those patients that are ineligible for breast conservation or patients unwilling to undergo lumpectomy and breast radiation.
If a mastectomy for the cancerous breast is planned, we must then address the questions that routinely arise regarding bilateral surgery. In our efforts to clarify the reality of what CPM can and cannot achieve, we must also avoid being too dogmatic and paternalistic with our patients. There are clearly specific scenarios, as delineated in Dr. Hawley’s work, where the risk of a second primary breast cancer is likely to be considered excessive by most women, and where the decision to pursue CPM may be easier. Examples of such cases would be women known to harbor BRCA mutations or women with suspected hereditary susceptibility based on a strong family history of breast and/or ovarian cancer. The risk of a new contralateral breast cancer can be in the range of 4%-5% per year in cases of hereditary disease, compared with the general population of women with sporadic breast cancer, where the risk ranges from 0.25% to 1% per year.
Conveying an understanding of risk
Patients must understand that the risk to the contralateral breast is predominantly expressed in the future – the likelihood of having a clinically occult, incidentally detected cancer identified in the contralateral mastectomy specimen is only 6%, as demonstrated most recently by King et al. (Ann. Surg. 2011;254:2-7), and with ductal carcinoma in situ accounting for the high majority of these lesions.
Defining the threshold for the amount of risk that an individual woman finds to be acceptable, however, can be a very difficult and personal decision. Even after a patient comes to understand that CPM is unlikely to provide a survival advantage, she may continue to request bilateral surgery purely for the risk-reducing benefits, and out of a desire to minimize her chances of having to repeat the breast cancer diagnosis and treatment experience. In some cases this choice will be influenced by reconstruction factors. A woman may be motivated to pursue bilateral surgery if she has an adequate volume of abdominal tissue because of the fact that the autogenous TRAM (transverse rectus abdominis myocutaneous) flap can be harvested only once. In other cases the decision is influenced by body habitus, for example, a woman with large pendulous breasts who is not interested in breast reconstruction may decide that she is more comfortable with a symmetrically flat chest wall in order to avoid chest wall imbalance and the inconvenience of finding/wearing a prosthesis that matches the remaining breast.
As breast cancer surgeons we should openly discuss these issues with our patients and present viable alternatives when feasible, such as reduction mammoplasty for the large-breasted patient. Ultimately, however, the patient must decide the surgical approach that provides her with the optimal sense of treatment satisfaction, quality of life, and comfort.
Discussion strategies
In my own practice I have found two discussion strategies to be particularly useful in guiding patients through the decision about CPM.
The first approach is relevant for women who are lumpectomy candidates, but who express a "reflex" interest in bilateral mastectomy while they are still in the emotional fog of processing the new cancer diagnosis. For these women it is obviously important to stress the survival equivalence of mastectomy and breast-conserving surgery, and this is also a great opportunity to educate patients about the potential axillary surgery advantages of breast conservation. The American College of Surgeons Oncology Group Z11 trial (JAMA 2011;305:69-75) has provided strong evidence supporting the safety of avoiding an axillary lymph node dissection (ALND) in women with sentinel lymph node (SLN) metastatic disease if the primary breast cancer is managed by lumpectomy and breast radiation.
At this point in time, we do not have comparably strong data to justify avoiding the ALND in the setting of mastectomy patients with SLN metastatic disease. The mastectomy patient with SLN metastasis is usually committed to undergo the completion axillary lymph node dissection specifically so that definitive decisions can be made regarding the need for postmastectomy radiation, and many of these patients become ineligible for immediate reconstruction because of this possible radiation. I therefore accentuate the advantage of at least initiating treatment with lumpectomy and sentinel lymph node biopsy. The patient preserves all of her surgical options with the benefit of having more staging information. If she is found to have SLN metastatic disease then she is in a better position to avoid the ALND with lumpectomy and radiation, and the option of future mastectomy and immediate reconstruction would still be available to her in the future (after completing all of her cancer treatment and healing from her radiation); if the SLN is negative, she can either continue with the breast-conservation treatment plan or she can pursue mastectomy (with or without immediate breast reconstruction, since prophylactic mamillary radiation therapy is not likely to be indicated for node-negative disease).
The second approach is relevant to the patient requiring mastectomy but for whom delayed reconstruction is planned because of medical issues or anticipated postmastectomy radiation. I encourage these patients to at least consider deferring the decision for the CPM until they return for the delayed reconstruction of the cancerous mastectomy, because at that time they can undergo the prophylactic mastectomy with the cosmetic advantages of immediate reconstruction.
Cost considerations
From the public health and population-based breast cancer burden perspectives as well as for individual patients, there are additional issues to be factored into the CPM discussion. It is a basic reality that cost is relevant when it comes to sorting out the net benefit of particular medical interventions, especially those that are prophylactic. Interestingly, a cost analysis study by Zendejas et al. (J. Clin. Oncol. 2011;29:2993-3000) from the Mayo Clinic demonstrated that CPM is actually cost effective, compared with surveillance for patients diagnosed when they are younger than 70 years of age.
The Women’s Health and Cancer Rights Act was implemented in 1999, mandating insurance coverage for breast reconstruction after mastectomy performed for cancer. This legislation promoted more widespread acceptance (and reimbursement) for contralateral mastectomy/reconstruction, but patients should nonetheless be proactive about confirming that their individual policy will indeed cover the expenses of prophylactic surgery. Furthermore, we must continue to monitor outcomes in women who choose to undergo CPM, as advances in breast cancer therapies may influence the survival benefits of this surgical approach. Indeed, selected retrospective studies have recently demonstrated that patients undergoing CPM have an improved survival, compared with those focusing on unilateral breast cancer surgery (Ann. Surg. Oncol. 2010;17:2702-9; J. Natl. Cancer Inst. 2010;102:401-9; J. Clin. Oncol. 2005;23:4275-86; Am. J. Surg. 2000;180:439-45). These results suggest a survival advantage associated with avoidance of a contralateral breast cancer, in contrast to the historical data alluded to above, regarding survival equivalence for patients with unilateral compared to metachronous bilateral breast cancer. As adjuvant systemic therapies for breast cancer continue to improve in effectiveness and ability to completely eliminate distant organ micrometastases, it is likely that we will continue to increase the pool of women who are essentially "cured" of the first cancer. This in turn could potentially increase the longevity threat of a second/metachronous cancer though a renewed metastatic risk. Nonetheless, data on possible survival advantages of CPM have not yet matured to the point where it can be recommended as a medically "indicated" procedure.
Our breast cancer patients face an abundance of very legitimate fears related to the morbidity and mortality risks of the actual cancer as well as the adverse effects and toxicities of treatment for that cancer. Fortunately, we can assure them that for the majority of cases these treatments will be effective and their longevity will be protected. It is therefore understandable that the desire to avoid repeating this particular life experience may be strong. We have an obligation to explain the advantages and disadvantages, as well as the alternatives to CPM, with sensitivity and patience. We must also strive to make sure that our patients do not make premature decisions without understanding the consequences. Last, but certainly not least, we are ethically bound to offer only those treatments that we feel are medically reasonable and safe as well as oncologically sound. But we must also remember that the decision to pursue treatment and the choice between the options that we offer are ultimately rights that belong to the patient.
Dr. Newman in an ACS Fellow, professor of surgery, and director of the Breast Care Center and Multidisciplinary Breast Fellowship Program, University of Michigan Comprehensive Cancer Center, Ann Arbor.
Dr. Sarah Hawley and her coinvestigators are to be applauded for generating insightful data regarding factors and concerns that motivate a woman to undergo contralateral prophylactic mastectomy in the setting of unilateral breast cancer (JAMA Surgery 2014 May 21 [doi:10.1001/jamasurg.2013.5689]).
Hawley et al. found that fear of recurrence was one of the strongest factors leading women to choose contralateral prophylactic mastectomy (CPM). This finding clearly demonstrates that we need to do a better job of explaining and defining the significance of (i) breast cancer local recurrence; (ii) breast cancer distant recurrence; and (iii) the development of a new/second primary breast cancer. Since cross-metastasis of a primary breast cancer to the contralateral breast is an extremely rare event, and since distant metastasis from the initial primary breast cancer tends to determine survival rates, CPM by definition will influence the incidence of only the third pattern. Furthermore, since the risk of experiencing a new contralateral malignancy is less than 1% per year for the general population of breast cancer patients, only a minority of these women will actually become bilateral breast cancer patients. Fear of recurrence is therefore a totally inappropriate reason for patients to pursue CPM, and the reasonableness of CPM to reduce the risk of a contralateral new primary breast cancer is debatable.
It can be reasonably stated that prophylactic surgery by definition is never a medically indicated necessity. Furthermore, despite the fact that a personal history of breast cancer is indeed a risk factor for developing a second primary cancer in the contralateral breast, numerous studies have demonstrated equivalent survival rates for women with unilateral breast cancer, compared with those diagnosed with bilateral/metachronous breast cancer (Cancer 2001;91:1845-53; Am. J. Clin. Oncol. 1997;20:541-5). Survival tends to be driven by the stage and effectiveness of treatment for the first cancer. By virtue of its earlier presentation, it is likely that the initially diagnosed cancer has established itself as the faster-growing malignancy with a lead time advantage in establishing distant organ micrometastatic disease; furthermore, patients with a unilateral breast cancer diagnosis are generally undergoing diligent surveillance and a contralateral malignancy is more often detected at an early stage.
Messages to our patients
It is essential for those of us who manage breast cancer to clearly emphasize several messages to our newly diagnosed breast cancer patients: First, although unilateral breast cancer increases the likelihood of developing a second primary tumor, it is certainly not inevitable, and in fact, the majority of patients are not destined to develop contralateral disease. Second, reducing the risk of being diagnosed with a contralateral breast cancer does not mitigate the mortality risk associated with the first cancer. And, finally, prophylactic mastectomy is the most aggressive and effective strategy for reducing the incidence of primary breast cancer (by approximately 90%), but it does not confer complete protection, as microscopic foci of breast tissue may be left behind in the mastectomy skin flaps, along the pectoralis, or in the axilla.
The messages above are critical: Our patients must understand that the priority is to address the known cancer. In this regard, appropriately selected patients should be encouraged to strongly consider breast-conserving surgery whenever feasible, as this low-morbidity treatment is equivalent to mastectomy from the perspective of overall survival. The question of CPM is most relevant for those patients that are ineligible for breast conservation or patients unwilling to undergo lumpectomy and breast radiation.
If a mastectomy for the cancerous breast is planned, we must then address the questions that routinely arise regarding bilateral surgery. In our efforts to clarify the reality of what CPM can and cannot achieve, we must also avoid being too dogmatic and paternalistic with our patients. There are clearly specific scenarios, as delineated in Dr. Hawley’s work, where the risk of a second primary breast cancer is likely to be considered excessive by most women, and where the decision to pursue CPM may be easier. Examples of such cases would be women known to harbor BRCA mutations or women with suspected hereditary susceptibility based on a strong family history of breast and/or ovarian cancer. The risk of a new contralateral breast cancer can be in the range of 4%-5% per year in cases of hereditary disease, compared with the general population of women with sporadic breast cancer, where the risk ranges from 0.25% to 1% per year.
Conveying an understanding of risk
Patients must understand that the risk to the contralateral breast is predominantly expressed in the future – the likelihood of having a clinically occult, incidentally detected cancer identified in the contralateral mastectomy specimen is only 6%, as demonstrated most recently by King et al. (Ann. Surg. 2011;254:2-7), and with ductal carcinoma in situ accounting for the high majority of these lesions.
Defining the threshold for the amount of risk that an individual woman finds to be acceptable, however, can be a very difficult and personal decision. Even after a patient comes to understand that CPM is unlikely to provide a survival advantage, she may continue to request bilateral surgery purely for the risk-reducing benefits, and out of a desire to minimize her chances of having to repeat the breast cancer diagnosis and treatment experience. In some cases this choice will be influenced by reconstruction factors. A woman may be motivated to pursue bilateral surgery if she has an adequate volume of abdominal tissue because of the fact that the autogenous TRAM (transverse rectus abdominis myocutaneous) flap can be harvested only once. In other cases the decision is influenced by body habitus, for example, a woman with large pendulous breasts who is not interested in breast reconstruction may decide that she is more comfortable with a symmetrically flat chest wall in order to avoid chest wall imbalance and the inconvenience of finding/wearing a prosthesis that matches the remaining breast.
As breast cancer surgeons we should openly discuss these issues with our patients and present viable alternatives when feasible, such as reduction mammoplasty for the large-breasted patient. Ultimately, however, the patient must decide the surgical approach that provides her with the optimal sense of treatment satisfaction, quality of life, and comfort.
Discussion strategies
In my own practice I have found two discussion strategies to be particularly useful in guiding patients through the decision about CPM.
The first approach is relevant for women who are lumpectomy candidates, but who express a "reflex" interest in bilateral mastectomy while they are still in the emotional fog of processing the new cancer diagnosis. For these women it is obviously important to stress the survival equivalence of mastectomy and breast-conserving surgery, and this is also a great opportunity to educate patients about the potential axillary surgery advantages of breast conservation. The American College of Surgeons Oncology Group Z11 trial (JAMA 2011;305:69-75) has provided strong evidence supporting the safety of avoiding an axillary lymph node dissection (ALND) in women with sentinel lymph node (SLN) metastatic disease if the primary breast cancer is managed by lumpectomy and breast radiation.
At this point in time, we do not have comparably strong data to justify avoiding the ALND in the setting of mastectomy patients with SLN metastatic disease. The mastectomy patient with SLN metastasis is usually committed to undergo the completion axillary lymph node dissection specifically so that definitive decisions can be made regarding the need for postmastectomy radiation, and many of these patients become ineligible for immediate reconstruction because of this possible radiation. I therefore accentuate the advantage of at least initiating treatment with lumpectomy and sentinel lymph node biopsy. The patient preserves all of her surgical options with the benefit of having more staging information. If she is found to have SLN metastatic disease then she is in a better position to avoid the ALND with lumpectomy and radiation, and the option of future mastectomy and immediate reconstruction would still be available to her in the future (after completing all of her cancer treatment and healing from her radiation); if the SLN is negative, she can either continue with the breast-conservation treatment plan or she can pursue mastectomy (with or without immediate breast reconstruction, since prophylactic mamillary radiation therapy is not likely to be indicated for node-negative disease).
The second approach is relevant to the patient requiring mastectomy but for whom delayed reconstruction is planned because of medical issues or anticipated postmastectomy radiation. I encourage these patients to at least consider deferring the decision for the CPM until they return for the delayed reconstruction of the cancerous mastectomy, because at that time they can undergo the prophylactic mastectomy with the cosmetic advantages of immediate reconstruction.
Cost considerations
From the public health and population-based breast cancer burden perspectives as well as for individual patients, there are additional issues to be factored into the CPM discussion. It is a basic reality that cost is relevant when it comes to sorting out the net benefit of particular medical interventions, especially those that are prophylactic. Interestingly, a cost analysis study by Zendejas et al. (J. Clin. Oncol. 2011;29:2993-3000) from the Mayo Clinic demonstrated that CPM is actually cost effective, compared with surveillance for patients diagnosed when they are younger than 70 years of age.
The Women’s Health and Cancer Rights Act was implemented in 1999, mandating insurance coverage for breast reconstruction after mastectomy performed for cancer. This legislation promoted more widespread acceptance (and reimbursement) for contralateral mastectomy/reconstruction, but patients should nonetheless be proactive about confirming that their individual policy will indeed cover the expenses of prophylactic surgery. Furthermore, we must continue to monitor outcomes in women who choose to undergo CPM, as advances in breast cancer therapies may influence the survival benefits of this surgical approach. Indeed, selected retrospective studies have recently demonstrated that patients undergoing CPM have an improved survival, compared with those focusing on unilateral breast cancer surgery (Ann. Surg. Oncol. 2010;17:2702-9; J. Natl. Cancer Inst. 2010;102:401-9; J. Clin. Oncol. 2005;23:4275-86; Am. J. Surg. 2000;180:439-45). These results suggest a survival advantage associated with avoidance of a contralateral breast cancer, in contrast to the historical data alluded to above, regarding survival equivalence for patients with unilateral compared to metachronous bilateral breast cancer. As adjuvant systemic therapies for breast cancer continue to improve in effectiveness and ability to completely eliminate distant organ micrometastases, it is likely that we will continue to increase the pool of women who are essentially "cured" of the first cancer. This in turn could potentially increase the longevity threat of a second/metachronous cancer though a renewed metastatic risk. Nonetheless, data on possible survival advantages of CPM have not yet matured to the point where it can be recommended as a medically "indicated" procedure.
Our breast cancer patients face an abundance of very legitimate fears related to the morbidity and mortality risks of the actual cancer as well as the adverse effects and toxicities of treatment for that cancer. Fortunately, we can assure them that for the majority of cases these treatments will be effective and their longevity will be protected. It is therefore understandable that the desire to avoid repeating this particular life experience may be strong. We have an obligation to explain the advantages and disadvantages, as well as the alternatives to CPM, with sensitivity and patience. We must also strive to make sure that our patients do not make premature decisions without understanding the consequences. Last, but certainly not least, we are ethically bound to offer only those treatments that we feel are medically reasonable and safe as well as oncologically sound. But we must also remember that the decision to pursue treatment and the choice between the options that we offer are ultimately rights that belong to the patient.
Dr. Newman in an ACS Fellow, professor of surgery, and director of the Breast Care Center and Multidisciplinary Breast Fellowship Program, University of Michigan Comprehensive Cancer Center, Ann Arbor.
Adaptability is the surgeon’s best friend
At my semiannual palliative medicine fellowship evaluation, I was asked, "What is your best strength?" and after a few seconds I said, "Adaptability."
Often, the most profound thoughts come spontaneously before habit interferes. As a practicing cardiothoracic surgeon for more than 16 years, my transition to palliative medicine and a hospice fellowship required the ability to reinvent myself, to embrace new ideas, to let go of old routines, and to accept new possibilities. In other words, to adapt to change.
During my surgical training I was most impressed with surgeons who could think calmly and rationally on the fly. As surgeons, we all understand the benefit of preparation and how contingency planning optimizes safety. But we also know from experience that no matter how well prepared you think you are, something can and almost invariably does happen that is unintentional, unanticipated, and unplanned that sabotages your preparation. So, too, is it with life.
I would never have predicted at the start of my career as a cardiothoracic and vascular surgeon that I would change, at midcareer, to palliative medicine. I am not going to explain all the events that pushed me to make a change, but suffice it to say I came to the proverbial fork in the road. I could have continued down the same path, frustrated and unhappy, but comfortable with my routines, or I could stop feeling sorry for myself, stop complaining, adapt to the changes, and go in a different direction. I chose the latter. I do miss the exhilaration and teamwork of surgery, but I have replaced it with the more profound collaboration of the palliative inter-disciplinary team that includes nurses, chaplains, social workers, therapists, and patients.
The most frequent question I am asked when people find out that I used to be a heart surgeon is why I changed careers. It’s really not as crazy as it seems. Fundamental to both surgery and palliative medicine are evidence-based options and patient-centered, informed decision making.
Historically, palliative care has had limited acceptance by the surgical community except at the end of life in an actively dying patient, but through the efforts of a few visionaries, palliative surgical care is now valued and deemed worthy of incorporation into general surgical residency training. During the past year I have been introduced to this interdisciplinary approach that improves the quality of life of patients and their families. Because this approach assesses and supports physical, psychological, social, and spiritual needs, it needs to occur with, not after, other appropriate medical treatments.
There is good empiric evidence that the earlier palliative medicine is involved in medical treatment, whether potentially curative or not, the quality of care improves: Caregiver, patient, and family satisfaction increases and resource utilization improves no matter what the delivery setting. These are very compelling data, and they validate the role of palliative medicine in a changing paradigm of health care delivery.
My vision for palliative medicine includes complete integration throughout the trajectory of all chronic illness, especially heart failure, cancer, and dementia, where coordination of care is critical and has been historically fragmented. Palliative medicine is increasing its role in acute care with improved symptom management and early consultation in the emergency department and ICU where better communication with the care team and advance care planning can help define goals of care and limit inappropriate and unwanted treatment.
The adaptability that is so crucial for patients and their families to adjust to progressive and critical illness is the same quality we need as practitioners to accommodate them. I challenge all my surgical colleagues to have the courage and wisdom to change, and to allow the integration of palliative medicine into your practice where and whenever possible.
Dr. Strzalka is a Fellow in Hospice and Palliative Medicine, Section of Palliative Medicine and Supportive Oncology, Taussig Cancer Institute, Cleveland Clinic.
At my semiannual palliative medicine fellowship evaluation, I was asked, "What is your best strength?" and after a few seconds I said, "Adaptability."
Often, the most profound thoughts come spontaneously before habit interferes. As a practicing cardiothoracic surgeon for more than 16 years, my transition to palliative medicine and a hospice fellowship required the ability to reinvent myself, to embrace new ideas, to let go of old routines, and to accept new possibilities. In other words, to adapt to change.
During my surgical training I was most impressed with surgeons who could think calmly and rationally on the fly. As surgeons, we all understand the benefit of preparation and how contingency planning optimizes safety. But we also know from experience that no matter how well prepared you think you are, something can and almost invariably does happen that is unintentional, unanticipated, and unplanned that sabotages your preparation. So, too, is it with life.
I would never have predicted at the start of my career as a cardiothoracic and vascular surgeon that I would change, at midcareer, to palliative medicine. I am not going to explain all the events that pushed me to make a change, but suffice it to say I came to the proverbial fork in the road. I could have continued down the same path, frustrated and unhappy, but comfortable with my routines, or I could stop feeling sorry for myself, stop complaining, adapt to the changes, and go in a different direction. I chose the latter. I do miss the exhilaration and teamwork of surgery, but I have replaced it with the more profound collaboration of the palliative inter-disciplinary team that includes nurses, chaplains, social workers, therapists, and patients.
The most frequent question I am asked when people find out that I used to be a heart surgeon is why I changed careers. It’s really not as crazy as it seems. Fundamental to both surgery and palliative medicine are evidence-based options and patient-centered, informed decision making.
Historically, palliative care has had limited acceptance by the surgical community except at the end of life in an actively dying patient, but through the efforts of a few visionaries, palliative surgical care is now valued and deemed worthy of incorporation into general surgical residency training. During the past year I have been introduced to this interdisciplinary approach that improves the quality of life of patients and their families. Because this approach assesses and supports physical, psychological, social, and spiritual needs, it needs to occur with, not after, other appropriate medical treatments.
There is good empiric evidence that the earlier palliative medicine is involved in medical treatment, whether potentially curative or not, the quality of care improves: Caregiver, patient, and family satisfaction increases and resource utilization improves no matter what the delivery setting. These are very compelling data, and they validate the role of palliative medicine in a changing paradigm of health care delivery.
My vision for palliative medicine includes complete integration throughout the trajectory of all chronic illness, especially heart failure, cancer, and dementia, where coordination of care is critical and has been historically fragmented. Palliative medicine is increasing its role in acute care with improved symptom management and early consultation in the emergency department and ICU where better communication with the care team and advance care planning can help define goals of care and limit inappropriate and unwanted treatment.
The adaptability that is so crucial for patients and their families to adjust to progressive and critical illness is the same quality we need as practitioners to accommodate them. I challenge all my surgical colleagues to have the courage and wisdom to change, and to allow the integration of palliative medicine into your practice where and whenever possible.
Dr. Strzalka is a Fellow in Hospice and Palliative Medicine, Section of Palliative Medicine and Supportive Oncology, Taussig Cancer Institute, Cleveland Clinic.
At my semiannual palliative medicine fellowship evaluation, I was asked, "What is your best strength?" and after a few seconds I said, "Adaptability."
Often, the most profound thoughts come spontaneously before habit interferes. As a practicing cardiothoracic surgeon for more than 16 years, my transition to palliative medicine and a hospice fellowship required the ability to reinvent myself, to embrace new ideas, to let go of old routines, and to accept new possibilities. In other words, to adapt to change.
During my surgical training I was most impressed with surgeons who could think calmly and rationally on the fly. As surgeons, we all understand the benefit of preparation and how contingency planning optimizes safety. But we also know from experience that no matter how well prepared you think you are, something can and almost invariably does happen that is unintentional, unanticipated, and unplanned that sabotages your preparation. So, too, is it with life.
I would never have predicted at the start of my career as a cardiothoracic and vascular surgeon that I would change, at midcareer, to palliative medicine. I am not going to explain all the events that pushed me to make a change, but suffice it to say I came to the proverbial fork in the road. I could have continued down the same path, frustrated and unhappy, but comfortable with my routines, or I could stop feeling sorry for myself, stop complaining, adapt to the changes, and go in a different direction. I chose the latter. I do miss the exhilaration and teamwork of surgery, but I have replaced it with the more profound collaboration of the palliative inter-disciplinary team that includes nurses, chaplains, social workers, therapists, and patients.
The most frequent question I am asked when people find out that I used to be a heart surgeon is why I changed careers. It’s really not as crazy as it seems. Fundamental to both surgery and palliative medicine are evidence-based options and patient-centered, informed decision making.
Historically, palliative care has had limited acceptance by the surgical community except at the end of life in an actively dying patient, but through the efforts of a few visionaries, palliative surgical care is now valued and deemed worthy of incorporation into general surgical residency training. During the past year I have been introduced to this interdisciplinary approach that improves the quality of life of patients and their families. Because this approach assesses and supports physical, psychological, social, and spiritual needs, it needs to occur with, not after, other appropriate medical treatments.
There is good empiric evidence that the earlier palliative medicine is involved in medical treatment, whether potentially curative or not, the quality of care improves: Caregiver, patient, and family satisfaction increases and resource utilization improves no matter what the delivery setting. These are very compelling data, and they validate the role of palliative medicine in a changing paradigm of health care delivery.
My vision for palliative medicine includes complete integration throughout the trajectory of all chronic illness, especially heart failure, cancer, and dementia, where coordination of care is critical and has been historically fragmented. Palliative medicine is increasing its role in acute care with improved symptom management and early consultation in the emergency department and ICU where better communication with the care team and advance care planning can help define goals of care and limit inappropriate and unwanted treatment.
The adaptability that is so crucial for patients and their families to adjust to progressive and critical illness is the same quality we need as practitioners to accommodate them. I challenge all my surgical colleagues to have the courage and wisdom to change, and to allow the integration of palliative medicine into your practice where and whenever possible.
Dr. Strzalka is a Fellow in Hospice and Palliative Medicine, Section of Palliative Medicine and Supportive Oncology, Taussig Cancer Institute, Cleveland Clinic.
Sleep
Questions about sleep – from newborns to teenagers – are among the most common in pediatric practice. A good night’s sleep is in everyone’s best interest for daily functioning and healthy development. Asking about sleep also provides a window into the family’s perspectives on discipline, parental cooperation, family stresses, and views on a child’s developing autonomy.
During their first year, infants may need as many as 18 hours of sleep daily, and the duration of sleep gradually declines thereafter to 8-10 hours nightly in adolescence. Sleep plays an essential role in consolidating memories, attention, and other cognitive functions; the immune system; and metabolism. Additionally, developing healthy sleep habits is one of the first and most profound ways that children learn to expect consistency from their parents, to soothe themselves, and to manage limits. As a child grows, her ability to plan, manage anxiety, and exercise discipline is cultivated through managing her sleep with increasing independence.
Preschoolers who are not getting adequate sleep may have behavioral problems, particularly in new settings (like school) or at transitional times (like bedtime). When a preschooler presents with hyperactivity, irritability, and tantrums, or failure to keep up with developmental expectations, asking about sleep patterns is a good early step. Although sleep disruption may be symptomatic of psychiatric disorders related to mood, anxiety, or attention, before you consider a disorder and treatment make sure that tensions at bedtime and poor sleeping habits are not a major factor.
How do you help tired, stressed parents encourage or enforce healthy sleep habits? Does the family have a routine after dinner that allows a child to settle down (such as taking a bath and then a quiet activity like reading a book with a parent)? Are the parents able to enforce this routine consistently, or does bedtime get dragged out for hours? And if so, why? In addition to ensuring that a child gets enough exercise during the day (but not in the hour before bed), parents will need to turn off the lights at a reasonably early hour so that a child may get adequate sleep before they will awaken with daylight.
Many parents will delay sleep until later as children push to stay awake and play. Sometimes, if both parents work and feel their only time with their children is after they return from work well into the evening, they may want more time with their children or feel guilty about having a strict, early bedtime routine. Reassure parents that even a short stretch of quality time with their children (reading to them, snuggling, asking about their day) is enough to nurture a profound connection.
"Screen time" merits special mention, especially in younger children. Letting children watch television or play on computers in order to "unwind" at the end of a long day is common, but in the time before bed, screen content can be very disruptive to restful sleep. Parents should assess if "screen time" is helping or hurting their child’s ability to fall asleep. Some families have found it helpful to have no screen time (any screen: television, computer, tablet, or cell phone) within 1 hour of lights going out: back-lit screens suppress endogenous melatonin release and can delay sleep. With school-age children, reading at bedtime is certainly preferable to an additional hour of computer time.
It is also worth asking where a child is sleeping. Do they have their own bed? Are they alone in their room? Is their room on the same level of the house as their parents’ room? Children who are anxious may sleep better if they share a room with a sibling or are close to their parents’ room. On the other hand, if they sleep with a sibling who is waking often during the night, they may have disrupted sleep.
It is worth finding out if a child is able to sleep through the night in their own bed. Many children have their own bed and room, but have a routine of sleeping in their parents’ bed. This usually results in inadequate sleep for both child and parents, and a child who does not learn how to appropriately soothe himself. Is it permissible for a child to climb into their parents’ bed in the middle of the night once in a while, if they have a bad dream, do not feel well, or have faced a stressful day? Yes. Is a child arguing to go to sleep in their parents’ bed, refusing to sleep in their own bed, with their parents "giving in"? Then it is a habit worth undoing.
School-age children who are not getting adequate sleep also may appear more irritable, forgetful, and inattentive, and they may have problems with academic, athletic, and social performance. These are years in which children start to have more independence and responsibility for their bedtime routines. They may have greater access to screens in the evening, and may be in charge of setting an alarm or turning their light out. These are also years in which children are more likely to experience anxiety, as they face and manage a host of new challenges. Anxiety can be very disruptive of restful sleep, and will in turn cause more problems about which these children get anxious. Alongside their greater responsibility, school-age children still need basic and consistently enforced ground rules about sleep in order to build independence. Clearly at this age, reading before bedtime is a good option.
Parents should help their school-age children to start their homework early, and to enjoy screen time, but not within an hour of bedtime, and to follow a consistent (and more independent) routine before bed. Do they have a consistent bedtime? Do they take a shower or bath each night? (A hot shower or bath naturally cues the body that it is time for sleep as the body’s core temperature rises and then drops.) Do they read before lights out? Is the house quiet at their bedtime? Parents should also find out if their children have worries that are making it difficult to go to sleep. Are they worried about a test or big game? Or about bigger issues of safety? Parents can help a child to discuss their worries and address those that are addressable; usually, this is enough to help children learn to master their worries. When a school-age child’s anxiety does not improve with open discussion, then it may be helpful to have a more formal evaluation for anxiety with a mental health clinician.
Adolescence is a time in which sleep patterns naturally shift, while the need for sleep remains robust. Teenagers become tired later and need to sleep in until later in the morning, just at the same time that school demands impinge on sleep with an earlier start to the day and more extensive homework at night. Older adolescents may go out with friends on weekends and shift their bedtime routine by 4 or more hours for two nights out of every seven, which is as profoundly disruptive to restful sleep as traveling across four time zones and back every week. These are years in which more independence can again lead to more screen use in the evening, whether for writing a paper on a computer or texting a friend late into the night.
An adolescent who is sleep deprived may have low energy, be forgetful and distractible, and see their academic and athletic performance suffer. They may appear more withdrawn or moody. This is an age in which serious mood problems, such as depression, are more likely to emerge, and are associated with sleep problems. But these problems will not improve with simple sleep hygiene interventions; thus, the teens who do not get better after these interventions may need a psychiatric evaluation.
The strategies that might help adolescents are not much different from those for younger children. It is important with adolescents, however, to explain why they should exercise regularly, have a consistent bedtime routine, and not bring their cell phone to bed. While parents should still be able to set and enforce ground rules, they also need to be equipping their adolescents to understand and manage their sleep independently, which they will need to do soon enough. Encouraging self-regulation between ages 13 and 17 is essential as college or independence approaches, and efforts at control are hard to enforce and send the wrong message.
Inconsistent, inadequate sleep often reflects what has been a frustrating struggle for parents. Asking questions about sleep gives parents the supportive message that sleep is challenging and important, and may empower them to approach it with renewed firmness and clarity. When you help parents to set routines and limits that support consistent, adequate sleep, their children will be on a path to healthy development.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
Questions about sleep – from newborns to teenagers – are among the most common in pediatric practice. A good night’s sleep is in everyone’s best interest for daily functioning and healthy development. Asking about sleep also provides a window into the family’s perspectives on discipline, parental cooperation, family stresses, and views on a child’s developing autonomy.
During their first year, infants may need as many as 18 hours of sleep daily, and the duration of sleep gradually declines thereafter to 8-10 hours nightly in adolescence. Sleep plays an essential role in consolidating memories, attention, and other cognitive functions; the immune system; and metabolism. Additionally, developing healthy sleep habits is one of the first and most profound ways that children learn to expect consistency from their parents, to soothe themselves, and to manage limits. As a child grows, her ability to plan, manage anxiety, and exercise discipline is cultivated through managing her sleep with increasing independence.
Preschoolers who are not getting adequate sleep may have behavioral problems, particularly in new settings (like school) or at transitional times (like bedtime). When a preschooler presents with hyperactivity, irritability, and tantrums, or failure to keep up with developmental expectations, asking about sleep patterns is a good early step. Although sleep disruption may be symptomatic of psychiatric disorders related to mood, anxiety, or attention, before you consider a disorder and treatment make sure that tensions at bedtime and poor sleeping habits are not a major factor.
How do you help tired, stressed parents encourage or enforce healthy sleep habits? Does the family have a routine after dinner that allows a child to settle down (such as taking a bath and then a quiet activity like reading a book with a parent)? Are the parents able to enforce this routine consistently, or does bedtime get dragged out for hours? And if so, why? In addition to ensuring that a child gets enough exercise during the day (but not in the hour before bed), parents will need to turn off the lights at a reasonably early hour so that a child may get adequate sleep before they will awaken with daylight.
Many parents will delay sleep until later as children push to stay awake and play. Sometimes, if both parents work and feel their only time with their children is after they return from work well into the evening, they may want more time with their children or feel guilty about having a strict, early bedtime routine. Reassure parents that even a short stretch of quality time with their children (reading to them, snuggling, asking about their day) is enough to nurture a profound connection.
"Screen time" merits special mention, especially in younger children. Letting children watch television or play on computers in order to "unwind" at the end of a long day is common, but in the time before bed, screen content can be very disruptive to restful sleep. Parents should assess if "screen time" is helping or hurting their child’s ability to fall asleep. Some families have found it helpful to have no screen time (any screen: television, computer, tablet, or cell phone) within 1 hour of lights going out: back-lit screens suppress endogenous melatonin release and can delay sleep. With school-age children, reading at bedtime is certainly preferable to an additional hour of computer time.
It is also worth asking where a child is sleeping. Do they have their own bed? Are they alone in their room? Is their room on the same level of the house as their parents’ room? Children who are anxious may sleep better if they share a room with a sibling or are close to their parents’ room. On the other hand, if they sleep with a sibling who is waking often during the night, they may have disrupted sleep.
It is worth finding out if a child is able to sleep through the night in their own bed. Many children have their own bed and room, but have a routine of sleeping in their parents’ bed. This usually results in inadequate sleep for both child and parents, and a child who does not learn how to appropriately soothe himself. Is it permissible for a child to climb into their parents’ bed in the middle of the night once in a while, if they have a bad dream, do not feel well, or have faced a stressful day? Yes. Is a child arguing to go to sleep in their parents’ bed, refusing to sleep in their own bed, with their parents "giving in"? Then it is a habit worth undoing.
School-age children who are not getting adequate sleep also may appear more irritable, forgetful, and inattentive, and they may have problems with academic, athletic, and social performance. These are years in which children start to have more independence and responsibility for their bedtime routines. They may have greater access to screens in the evening, and may be in charge of setting an alarm or turning their light out. These are also years in which children are more likely to experience anxiety, as they face and manage a host of new challenges. Anxiety can be very disruptive of restful sleep, and will in turn cause more problems about which these children get anxious. Alongside their greater responsibility, school-age children still need basic and consistently enforced ground rules about sleep in order to build independence. Clearly at this age, reading before bedtime is a good option.
Parents should help their school-age children to start their homework early, and to enjoy screen time, but not within an hour of bedtime, and to follow a consistent (and more independent) routine before bed. Do they have a consistent bedtime? Do they take a shower or bath each night? (A hot shower or bath naturally cues the body that it is time for sleep as the body’s core temperature rises and then drops.) Do they read before lights out? Is the house quiet at their bedtime? Parents should also find out if their children have worries that are making it difficult to go to sleep. Are they worried about a test or big game? Or about bigger issues of safety? Parents can help a child to discuss their worries and address those that are addressable; usually, this is enough to help children learn to master their worries. When a school-age child’s anxiety does not improve with open discussion, then it may be helpful to have a more formal evaluation for anxiety with a mental health clinician.
Adolescence is a time in which sleep patterns naturally shift, while the need for sleep remains robust. Teenagers become tired later and need to sleep in until later in the morning, just at the same time that school demands impinge on sleep with an earlier start to the day and more extensive homework at night. Older adolescents may go out with friends on weekends and shift their bedtime routine by 4 or more hours for two nights out of every seven, which is as profoundly disruptive to restful sleep as traveling across four time zones and back every week. These are years in which more independence can again lead to more screen use in the evening, whether for writing a paper on a computer or texting a friend late into the night.
An adolescent who is sleep deprived may have low energy, be forgetful and distractible, and see their academic and athletic performance suffer. They may appear more withdrawn or moody. This is an age in which serious mood problems, such as depression, are more likely to emerge, and are associated with sleep problems. But these problems will not improve with simple sleep hygiene interventions; thus, the teens who do not get better after these interventions may need a psychiatric evaluation.
The strategies that might help adolescents are not much different from those for younger children. It is important with adolescents, however, to explain why they should exercise regularly, have a consistent bedtime routine, and not bring their cell phone to bed. While parents should still be able to set and enforce ground rules, they also need to be equipping their adolescents to understand and manage their sleep independently, which they will need to do soon enough. Encouraging self-regulation between ages 13 and 17 is essential as college or independence approaches, and efforts at control are hard to enforce and send the wrong message.
Inconsistent, inadequate sleep often reflects what has been a frustrating struggle for parents. Asking questions about sleep gives parents the supportive message that sleep is challenging and important, and may empower them to approach it with renewed firmness and clarity. When you help parents to set routines and limits that support consistent, adequate sleep, their children will be on a path to healthy development.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
Questions about sleep – from newborns to teenagers – are among the most common in pediatric practice. A good night’s sleep is in everyone’s best interest for daily functioning and healthy development. Asking about sleep also provides a window into the family’s perspectives on discipline, parental cooperation, family stresses, and views on a child’s developing autonomy.
During their first year, infants may need as many as 18 hours of sleep daily, and the duration of sleep gradually declines thereafter to 8-10 hours nightly in adolescence. Sleep plays an essential role in consolidating memories, attention, and other cognitive functions; the immune system; and metabolism. Additionally, developing healthy sleep habits is one of the first and most profound ways that children learn to expect consistency from their parents, to soothe themselves, and to manage limits. As a child grows, her ability to plan, manage anxiety, and exercise discipline is cultivated through managing her sleep with increasing independence.
Preschoolers who are not getting adequate sleep may have behavioral problems, particularly in new settings (like school) or at transitional times (like bedtime). When a preschooler presents with hyperactivity, irritability, and tantrums, or failure to keep up with developmental expectations, asking about sleep patterns is a good early step. Although sleep disruption may be symptomatic of psychiatric disorders related to mood, anxiety, or attention, before you consider a disorder and treatment make sure that tensions at bedtime and poor sleeping habits are not a major factor.
How do you help tired, stressed parents encourage or enforce healthy sleep habits? Does the family have a routine after dinner that allows a child to settle down (such as taking a bath and then a quiet activity like reading a book with a parent)? Are the parents able to enforce this routine consistently, or does bedtime get dragged out for hours? And if so, why? In addition to ensuring that a child gets enough exercise during the day (but not in the hour before bed), parents will need to turn off the lights at a reasonably early hour so that a child may get adequate sleep before they will awaken with daylight.
Many parents will delay sleep until later as children push to stay awake and play. Sometimes, if both parents work and feel their only time with their children is after they return from work well into the evening, they may want more time with their children or feel guilty about having a strict, early bedtime routine. Reassure parents that even a short stretch of quality time with their children (reading to them, snuggling, asking about their day) is enough to nurture a profound connection.
"Screen time" merits special mention, especially in younger children. Letting children watch television or play on computers in order to "unwind" at the end of a long day is common, but in the time before bed, screen content can be very disruptive to restful sleep. Parents should assess if "screen time" is helping or hurting their child’s ability to fall asleep. Some families have found it helpful to have no screen time (any screen: television, computer, tablet, or cell phone) within 1 hour of lights going out: back-lit screens suppress endogenous melatonin release and can delay sleep. With school-age children, reading at bedtime is certainly preferable to an additional hour of computer time.
It is also worth asking where a child is sleeping. Do they have their own bed? Are they alone in their room? Is their room on the same level of the house as their parents’ room? Children who are anxious may sleep better if they share a room with a sibling or are close to their parents’ room. On the other hand, if they sleep with a sibling who is waking often during the night, they may have disrupted sleep.
It is worth finding out if a child is able to sleep through the night in their own bed. Many children have their own bed and room, but have a routine of sleeping in their parents’ bed. This usually results in inadequate sleep for both child and parents, and a child who does not learn how to appropriately soothe himself. Is it permissible for a child to climb into their parents’ bed in the middle of the night once in a while, if they have a bad dream, do not feel well, or have faced a stressful day? Yes. Is a child arguing to go to sleep in their parents’ bed, refusing to sleep in their own bed, with their parents "giving in"? Then it is a habit worth undoing.
School-age children who are not getting adequate sleep also may appear more irritable, forgetful, and inattentive, and they may have problems with academic, athletic, and social performance. These are years in which children start to have more independence and responsibility for their bedtime routines. They may have greater access to screens in the evening, and may be in charge of setting an alarm or turning their light out. These are also years in which children are more likely to experience anxiety, as they face and manage a host of new challenges. Anxiety can be very disruptive of restful sleep, and will in turn cause more problems about which these children get anxious. Alongside their greater responsibility, school-age children still need basic and consistently enforced ground rules about sleep in order to build independence. Clearly at this age, reading before bedtime is a good option.
Parents should help their school-age children to start their homework early, and to enjoy screen time, but not within an hour of bedtime, and to follow a consistent (and more independent) routine before bed. Do they have a consistent bedtime? Do they take a shower or bath each night? (A hot shower or bath naturally cues the body that it is time for sleep as the body’s core temperature rises and then drops.) Do they read before lights out? Is the house quiet at their bedtime? Parents should also find out if their children have worries that are making it difficult to go to sleep. Are they worried about a test or big game? Or about bigger issues of safety? Parents can help a child to discuss their worries and address those that are addressable; usually, this is enough to help children learn to master their worries. When a school-age child’s anxiety does not improve with open discussion, then it may be helpful to have a more formal evaluation for anxiety with a mental health clinician.
Adolescence is a time in which sleep patterns naturally shift, while the need for sleep remains robust. Teenagers become tired later and need to sleep in until later in the morning, just at the same time that school demands impinge on sleep with an earlier start to the day and more extensive homework at night. Older adolescents may go out with friends on weekends and shift their bedtime routine by 4 or more hours for two nights out of every seven, which is as profoundly disruptive to restful sleep as traveling across four time zones and back every week. These are years in which more independence can again lead to more screen use in the evening, whether for writing a paper on a computer or texting a friend late into the night.
An adolescent who is sleep deprived may have low energy, be forgetful and distractible, and see their academic and athletic performance suffer. They may appear more withdrawn or moody. This is an age in which serious mood problems, such as depression, are more likely to emerge, and are associated with sleep problems. But these problems will not improve with simple sleep hygiene interventions; thus, the teens who do not get better after these interventions may need a psychiatric evaluation.
The strategies that might help adolescents are not much different from those for younger children. It is important with adolescents, however, to explain why they should exercise regularly, have a consistent bedtime routine, and not bring their cell phone to bed. While parents should still be able to set and enforce ground rules, they also need to be equipping their adolescents to understand and manage their sleep independently, which they will need to do soon enough. Encouraging self-regulation between ages 13 and 17 is essential as college or independence approaches, and efforts at control are hard to enforce and send the wrong message.
Inconsistent, inadequate sleep often reflects what has been a frustrating struggle for parents. Asking questions about sleep gives parents the supportive message that sleep is challenging and important, and may empower them to approach it with renewed firmness and clarity. When you help parents to set routines and limits that support consistent, adequate sleep, their children will be on a path to healthy development.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
Shame
At 16, Eddie is tall and athletic. He’s been treating closed comedones on his forehead and chest off and on for a couple of years.
"I hope you can help him," his mother says. "There are days when he won’t go to school, he’s so embarrassed."
Really?
If you sat people down and asked them to list what people hate about their bodies, they wouldn’t come close to guessing what we dermatologists run into every day. Here are some cases I’ve seen lately. I’m sure you can easily come up with your own examples.
• A 50-year-old attorney with a wart on the dorsum of his right hand wanted me to take it off. "I sign a lot of documents," he said," and I’d prefer that clients remember me for my legal skills, not the wart on my hand."
• A 36-year-old waiter with a picker’s nodule over the proximal interphalangeal joint of his left fifth finger said I just had to get rid of it. "I’m a waiter," he said. "This is killing my tips."
• A 36-year-old woman gave up yoga a year ago, because she was sure the woman on the adjacent mat was disgusted by her plantar warts.
• A sprightly retiree, age 88(!), insisted on paying out of pocket to remove dermatosis papulosa nigra lesions from her face. Her explanation? "My children want me to stay at home, but I want to get out and be social!"
Self-consciousness doesn’t require lesions. For instance, I saw an 11-year-old last month with widespread atopic dermatitis, the kind that’s lifelong, miserably itchy, and hard to control. Yet she wasn’t even being treated. Why had she come now?
"What bothers you most about this?" I asked her.
"This brown patch on my neck," she said.
That’s right – not the itch, not the scratching, not the staying awake at night. What bothered her was the postinflammatory pigmentation on her neck that other kids would see and comment on.
She’s not alone. Another mother brought her 8-year-old daughter to see me. The girl’s eczema was being treated with nothing but moisturizer (which was "working, sort of").
"The reason we’re here," said Mom, "is that now she is starting to get self-conscious about the dark staining on her hand."
As doctors, we’re trained to think functionally so we can measure the ways disease impairs functionality: length of life, duration of fever, days out of work, oxygen saturation, percentage of involved body surface.
But you can’t measure shame. Nor can you predict what will produce it. Even after all these years, people surprise me all the time.
The secondary codes some insurers demand to cover wart treatment include pain, rapid growth, or bleeding. They do not include, "Clients are staring at my hand at real estate closings." Or, "This bump is reducing my tips." We could, of course, tell people not to mind being stared at, but they will not agree. They know how people look at them, and what parts of them they look at.
If any of us had a big welt over one eye, we might think twice before going to work, knowing that every patient and staff member are going to ask, "What bar were you in, and what does the other guy look like?" The teenager with the stain on her neck and the boy with the papules on his forehead and chest feel that way every morning.
Basically, nobody wants to stand out. If we do, we’d like it to be for some admirable quality. The truth is, we shouldn’t really take credit for being called handsome, smart, or healthy, but we do anyway. By the same token, it’s not our fault if we’re ill or different, but being singled out for either makes things worse – not functionally, just humanly.
Many years ago, a 15-year-old girl asked me to take off a mole from the top of her foot.
"The mole’s fine," I said. "Why do you want it off?"
"It’s embarrassing," she said.
"How?" I asked her. "Don’t you go to pools in the summer?"
"I stand with the one foot covering the spot on the other foot. Nobody has ever seen it."
Not everything people are embarrassed about can be removed with a cream or a hyfrecator. But shame is powerful, and we need to recognize it for what it is so we can address it if we can.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
At 16, Eddie is tall and athletic. He’s been treating closed comedones on his forehead and chest off and on for a couple of years.
"I hope you can help him," his mother says. "There are days when he won’t go to school, he’s so embarrassed."
Really?
If you sat people down and asked them to list what people hate about their bodies, they wouldn’t come close to guessing what we dermatologists run into every day. Here are some cases I’ve seen lately. I’m sure you can easily come up with your own examples.
• A 50-year-old attorney with a wart on the dorsum of his right hand wanted me to take it off. "I sign a lot of documents," he said," and I’d prefer that clients remember me for my legal skills, not the wart on my hand."
• A 36-year-old waiter with a picker’s nodule over the proximal interphalangeal joint of his left fifth finger said I just had to get rid of it. "I’m a waiter," he said. "This is killing my tips."
• A 36-year-old woman gave up yoga a year ago, because she was sure the woman on the adjacent mat was disgusted by her plantar warts.
• A sprightly retiree, age 88(!), insisted on paying out of pocket to remove dermatosis papulosa nigra lesions from her face. Her explanation? "My children want me to stay at home, but I want to get out and be social!"
Self-consciousness doesn’t require lesions. For instance, I saw an 11-year-old last month with widespread atopic dermatitis, the kind that’s lifelong, miserably itchy, and hard to control. Yet she wasn’t even being treated. Why had she come now?
"What bothers you most about this?" I asked her.
"This brown patch on my neck," she said.
That’s right – not the itch, not the scratching, not the staying awake at night. What bothered her was the postinflammatory pigmentation on her neck that other kids would see and comment on.
She’s not alone. Another mother brought her 8-year-old daughter to see me. The girl’s eczema was being treated with nothing but moisturizer (which was "working, sort of").
"The reason we’re here," said Mom, "is that now she is starting to get self-conscious about the dark staining on her hand."
As doctors, we’re trained to think functionally so we can measure the ways disease impairs functionality: length of life, duration of fever, days out of work, oxygen saturation, percentage of involved body surface.
But you can’t measure shame. Nor can you predict what will produce it. Even after all these years, people surprise me all the time.
The secondary codes some insurers demand to cover wart treatment include pain, rapid growth, or bleeding. They do not include, "Clients are staring at my hand at real estate closings." Or, "This bump is reducing my tips." We could, of course, tell people not to mind being stared at, but they will not agree. They know how people look at them, and what parts of them they look at.
If any of us had a big welt over one eye, we might think twice before going to work, knowing that every patient and staff member are going to ask, "What bar were you in, and what does the other guy look like?" The teenager with the stain on her neck and the boy with the papules on his forehead and chest feel that way every morning.
Basically, nobody wants to stand out. If we do, we’d like it to be for some admirable quality. The truth is, we shouldn’t really take credit for being called handsome, smart, or healthy, but we do anyway. By the same token, it’s not our fault if we’re ill or different, but being singled out for either makes things worse – not functionally, just humanly.
Many years ago, a 15-year-old girl asked me to take off a mole from the top of her foot.
"The mole’s fine," I said. "Why do you want it off?"
"It’s embarrassing," she said.
"How?" I asked her. "Don’t you go to pools in the summer?"
"I stand with the one foot covering the spot on the other foot. Nobody has ever seen it."
Not everything people are embarrassed about can be removed with a cream or a hyfrecator. But shame is powerful, and we need to recognize it for what it is so we can address it if we can.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
At 16, Eddie is tall and athletic. He’s been treating closed comedones on his forehead and chest off and on for a couple of years.
"I hope you can help him," his mother says. "There are days when he won’t go to school, he’s so embarrassed."
Really?
If you sat people down and asked them to list what people hate about their bodies, they wouldn’t come close to guessing what we dermatologists run into every day. Here are some cases I’ve seen lately. I’m sure you can easily come up with your own examples.
• A 50-year-old attorney with a wart on the dorsum of his right hand wanted me to take it off. "I sign a lot of documents," he said," and I’d prefer that clients remember me for my legal skills, not the wart on my hand."
• A 36-year-old waiter with a picker’s nodule over the proximal interphalangeal joint of his left fifth finger said I just had to get rid of it. "I’m a waiter," he said. "This is killing my tips."
• A 36-year-old woman gave up yoga a year ago, because she was sure the woman on the adjacent mat was disgusted by her plantar warts.
• A sprightly retiree, age 88(!), insisted on paying out of pocket to remove dermatosis papulosa nigra lesions from her face. Her explanation? "My children want me to stay at home, but I want to get out and be social!"
Self-consciousness doesn’t require lesions. For instance, I saw an 11-year-old last month with widespread atopic dermatitis, the kind that’s lifelong, miserably itchy, and hard to control. Yet she wasn’t even being treated. Why had she come now?
"What bothers you most about this?" I asked her.
"This brown patch on my neck," she said.
That’s right – not the itch, not the scratching, not the staying awake at night. What bothered her was the postinflammatory pigmentation on her neck that other kids would see and comment on.
She’s not alone. Another mother brought her 8-year-old daughter to see me. The girl’s eczema was being treated with nothing but moisturizer (which was "working, sort of").
"The reason we’re here," said Mom, "is that now she is starting to get self-conscious about the dark staining on her hand."
As doctors, we’re trained to think functionally so we can measure the ways disease impairs functionality: length of life, duration of fever, days out of work, oxygen saturation, percentage of involved body surface.
But you can’t measure shame. Nor can you predict what will produce it. Even after all these years, people surprise me all the time.
The secondary codes some insurers demand to cover wart treatment include pain, rapid growth, or bleeding. They do not include, "Clients are staring at my hand at real estate closings." Or, "This bump is reducing my tips." We could, of course, tell people not to mind being stared at, but they will not agree. They know how people look at them, and what parts of them they look at.
If any of us had a big welt over one eye, we might think twice before going to work, knowing that every patient and staff member are going to ask, "What bar were you in, and what does the other guy look like?" The teenager with the stain on her neck and the boy with the papules on his forehead and chest feel that way every morning.
Basically, nobody wants to stand out. If we do, we’d like it to be for some admirable quality. The truth is, we shouldn’t really take credit for being called handsome, smart, or healthy, but we do anyway. By the same token, it’s not our fault if we’re ill or different, but being singled out for either makes things worse – not functionally, just humanly.
Many years ago, a 15-year-old girl asked me to take off a mole from the top of her foot.
"The mole’s fine," I said. "Why do you want it off?"
"It’s embarrassing," she said.
"How?" I asked her. "Don’t you go to pools in the summer?"
"I stand with the one foot covering the spot on the other foot. Nobody has ever seen it."
Not everything people are embarrassed about can be removed with a cream or a hyfrecator. But shame is powerful, and we need to recognize it for what it is so we can address it if we can.
Dr. Rockoff practices dermatology in Brookline, Mass. He is on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
Diabesity – Fattening the U.S. health care budget
The world is not only getting older and warmer, but it’s getting heavier and more unfit each year. According to the World Health Organization’s most recent data, more than 1.4 billion adults were overweight in 2008, and 500 million of these adults were obese. In 2012, more than 40 million young children were overweight or obese. Diabetes, a disorder closely linked with obesity, affects about 347 million people worldwide – approximately ten times more people than those with HIV/AIDS. Although the number of AIDS-related deaths has steadily decreased over the last decade, even in developing countries, the number of diabetes-related deaths has steadily increased. The WHO projects that diabetes-related deaths will double by 2030, making it the seventh leading cause of death worldwide. In the United States, diabetes already is the seventh leading cause of death.
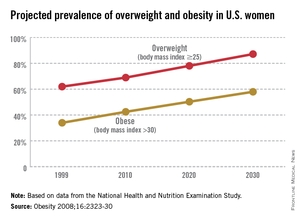
According to the Centers for Disease Control and Prevention, obesity-related diseases cost $147 billion annually, a number which dwarfs the health care costs associated with smoking ($96 billion). In addition to the link with type 2 diabetes, there are strong links between obesity and heart disease, kidney disease, depression, and hypertension. From 1987 to 2007, obesity was estimated to have caused more than a 20% increase in total health care spending.
The American Diabetes Association estimates that people diagnosed with diabetes have average yearly medical expenditures of over $13,000, which is over two times higher than the expenditures of a person without diagnosed diabetes. The 2012 estimated annual cost of care for diagnosed diabetes was $245 billion, which includes $176 billion in direct medical costs and $69 billion in reduced productivity (Diabetes Care 2013 [doi:10.2337/dc12-2625]). These figures, while staggering, do not include projected expenditures for people who have yet to receive a diabetes diagnosis.
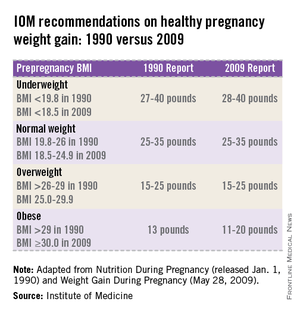
The federal government has chosen to take dramatic steps to help Americans lose weight. Since 2011, the Centers for Medicare & Medicaid Services has covered screening and intensive behavioral therapy for obesity by primary care physicians during office visits or outpatient hospital care. Additionally, the Affordable Care Act (ACA) now requires insurance companies to help overweight and obese patients try to lose weight and be healthier. The 2012 Institute of Medicine (IOM) report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation also has made major recommendations for health care practitioners, schools, and the food and beverage industry to take a more active part in improving our overall health.
Simple steps make a big impact on health
Despite the daunting – and perhaps somewhat disheartening – statistics on obesity and diabetes in the United States and around the world, research has shown that small steps to achieving a healthy weight and maintaining an active lifestyle can make a dramatic difference on the course of a person’s life. According to the Department of Agriculture, healthier diets could prevent about $71 billion in yearly health care costs, lost productivity, and premature deaths. This number is staggering, when you consider that the change could be as small as choosing a salad instead of fries for a side dish.
Medical research backs up the well-worn adage that "an apple a day keeps the doctor away." The Diabetes Prevention Program study, conducted in the early 2000s, found that lifestyle changes, such as getting more exercise and eating a balanced diet, had a major impact on whether a patient who is overweight with prediabetes developed type 2 diabetes (N. Engl. J. Med. 2002;346:393-403).
Lifestyle changes can also reduce the onset of diabetes in high-risk groups such as Asian Indians, where the incidence of diabetes is the highest in the world. The Indian Diabetes Prevention Programme showed that weight loss and healthy eating reduced the incidence of type 2 diabetes in this population at a rate similar to the use of metformin, one of the most common oral antidiabetic drugs (Diabetologia 2006;49:289-97).
The 16th U.S. Surgeon General, David Satcher, M.D., Ph.D., is famous for giving his "Prescription for Great Health" when he addresses colleges and universities, which includes not smoking, staying away from illicit drug use, and abstaining from unsafe sex. Importantly, the first two key points of his "prescription" are exercising at least five times a week for 30 minutes and eating at least five servings of fruits and vegetables daily. Again, very simple recommendations, but his advice has lasting and profound ramifications.
Do obstetrician/gynecologists have a role?
As ob.gyns., we always have played an incredibly critical role in maintaining the health and well-being of our patients. Now, more than ever, we have a significant opportunity to set our patients on a path to better eating, incorporating exercise into their daily routines and passing down these good habits to their children.
In the "old days," the ob.gyn. focused on a limited period in a patient’s life. Perhaps we only saw a patient for annual exams and then for a more intense time prior to and during pregnancy, and then for a checkup post partum where we may have examined our patients only for complications of the pregnancy and delivery and not much more. Although we may have included some counseling on maintaining a healthy pregnancy, many of us relied on a patient’s primary care physician to provide ongoing support.
Today, however, we must take a more active role in helping our patients establish and maintain a healthy lifestyle. Despite the increased insurance coverage under the ACA and the expansion of Medicaid, a woman’s ob.gyn. may be the only health care practitioner she will see on a routine basis. Many women do not visit a general practitioner for routine physical examinations, but women will see their ob.gyn. for regular exams. We can use these annual or biannual office visits to help women set goals to live a healthy life, approaching each patient as a whole person who needs comprehensive care throughout her reproductive life and beyond.
For patients who are overweight or obese, we may focus on helping them reduce their body mass index and blood pressure and encourage them to stay fit. We also should do everything we can to ensure that if a woman has had gestational diabetes, she’s doing what she can to reduce her risk of developing type 2 diabetes after pregnancy. For these patients, we should consider testing their blood glucose every 1-2 years during the annual checkup.
Healthy weight in pregnancy: to gain or to lose?
Whether or not an ob.gyn. practice implements a screening program and more intensive obesity and diabetes counseling, we all will face the same question: How much weight should my patient gain to have a healthy baby? Interestingly, in the first half of the 20th century, ob.gyns. were discouraged from recommending that their pregnant patients gain very much weight. Indeed, the 13th edition of "Williams Obstetrics" (New York: Appleton-Century-Crofts, 1966, p. 326) stated that obstetricians should limit their patients from gaining more than 25 pounds during gestation, and that the ideal weight gain was 15 pounds.
This guidance was called into question by a 1970 National Academy of Sciences report, "Maternal Nutrition and the Course of Pregnancy," which indicated a strong link between infant mortality and low maternal pregnancy weight. Further evidence suggested a need for new standards and, in 1990, the IOM issued recommendations on women’s nutrition during pregnancy (Nutrition During Pregnancy, Weight Gain and Nutrient Supplements. Washington, D.C.: National Academy Press, 1990). (See table.)
Americans consume 31% more calories today than they did 40 years ago. Because of this, a woman’s need to gain weight to improve the outcome of her pregnancy is significantly reduced. The calories that many people include in their diets often come from high-fat, sodium-loaded, processed foods. We also have become a more sedentary society, spending our days at a computer, browsing the internet, watching TV, and opting to drive rather than to walk. Taking these factors into account, revising the recommendations for weight gain seemed crucial. In 2009, the IOM revised its guidance on healthy weight gain in pregnancy, and these ranges are currently widely accepted by obstetricians today (iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx). (See table.)
With the obesity and diabetes epidemics on the rise, we may need to update the 2009 IOM guidelines again – and very soon. Isolated studies have indicated that, for women who are severely obese, moderate weight loss during pregnancy may improve pregnancy outcomes. These findings remain controversial, but the "heavy" burden of diabetes and obesity on the U.S. health care system in general, and the need to reduce obstetrical complications that accompany deliveries in patients who are overweight or obese and diabetic, means that we as a community may need to reexamine our practices and approaches much more closely.
"Food" for thought
We all know of patients who, once they become pregnant, begin justifying a greater intake of food as "eating for two." Many women may use their pregnancy as an excuse to overindulge in unhealthy foods or to forgo the gym and other regular exercise regimens. Recommending basic steps to change a patient’s lifestyle can make an incredible difference in improving maternal and fetal health outcomes.
Summary recommendations for healthy pregnancy
• A low-glycemic diet, combined with moderate exercise, can reduce or eliminate many of the negative consequences of obesity on pregnant women and their babies.
• Proper weight management during pregnancy can improve birth outcomes.
• Weight loss during pregnancy is not recommended, except, potentially, for morbidly obese women (BMI greater than 40).
• For women who are normal weight, overweight or obese, leading healthy lifestyles can greatly improve maternal and fetal health outcomes. These include physical exercise, balanced diet, and weight loss, in combination with medication in some cases.
• It is never too late to begin healthy habits!
If we microfocus only on a woman’s predelivery and postdelivery health, then we’re losing a big opportunity to improve her whole self and prevent future health complications during and outside of pregnancy. The good news for ob.gyns. is that this complex problem has a simple, well-documented, and proven solution.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
The world is not only getting older and warmer, but it’s getting heavier and more unfit each year. According to the World Health Organization’s most recent data, more than 1.4 billion adults were overweight in 2008, and 500 million of these adults were obese. In 2012, more than 40 million young children were overweight or obese. Diabetes, a disorder closely linked with obesity, affects about 347 million people worldwide – approximately ten times more people than those with HIV/AIDS. Although the number of AIDS-related deaths has steadily decreased over the last decade, even in developing countries, the number of diabetes-related deaths has steadily increased. The WHO projects that diabetes-related deaths will double by 2030, making it the seventh leading cause of death worldwide. In the United States, diabetes already is the seventh leading cause of death.
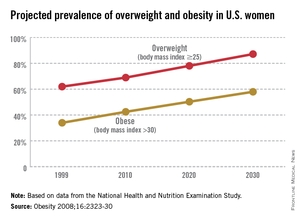
According to the Centers for Disease Control and Prevention, obesity-related diseases cost $147 billion annually, a number which dwarfs the health care costs associated with smoking ($96 billion). In addition to the link with type 2 diabetes, there are strong links between obesity and heart disease, kidney disease, depression, and hypertension. From 1987 to 2007, obesity was estimated to have caused more than a 20% increase in total health care spending.
The American Diabetes Association estimates that people diagnosed with diabetes have average yearly medical expenditures of over $13,000, which is over two times higher than the expenditures of a person without diagnosed diabetes. The 2012 estimated annual cost of care for diagnosed diabetes was $245 billion, which includes $176 billion in direct medical costs and $69 billion in reduced productivity (Diabetes Care 2013 [doi:10.2337/dc12-2625]). These figures, while staggering, do not include projected expenditures for people who have yet to receive a diabetes diagnosis.
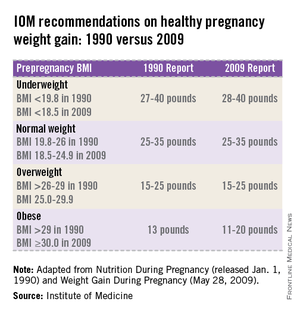
The federal government has chosen to take dramatic steps to help Americans lose weight. Since 2011, the Centers for Medicare & Medicaid Services has covered screening and intensive behavioral therapy for obesity by primary care physicians during office visits or outpatient hospital care. Additionally, the Affordable Care Act (ACA) now requires insurance companies to help overweight and obese patients try to lose weight and be healthier. The 2012 Institute of Medicine (IOM) report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation also has made major recommendations for health care practitioners, schools, and the food and beverage industry to take a more active part in improving our overall health.
Simple steps make a big impact on health
Despite the daunting – and perhaps somewhat disheartening – statistics on obesity and diabetes in the United States and around the world, research has shown that small steps to achieving a healthy weight and maintaining an active lifestyle can make a dramatic difference on the course of a person’s life. According to the Department of Agriculture, healthier diets could prevent about $71 billion in yearly health care costs, lost productivity, and premature deaths. This number is staggering, when you consider that the change could be as small as choosing a salad instead of fries for a side dish.
Medical research backs up the well-worn adage that "an apple a day keeps the doctor away." The Diabetes Prevention Program study, conducted in the early 2000s, found that lifestyle changes, such as getting more exercise and eating a balanced diet, had a major impact on whether a patient who is overweight with prediabetes developed type 2 diabetes (N. Engl. J. Med. 2002;346:393-403).
Lifestyle changes can also reduce the onset of diabetes in high-risk groups such as Asian Indians, where the incidence of diabetes is the highest in the world. The Indian Diabetes Prevention Programme showed that weight loss and healthy eating reduced the incidence of type 2 diabetes in this population at a rate similar to the use of metformin, one of the most common oral antidiabetic drugs (Diabetologia 2006;49:289-97).
The 16th U.S. Surgeon General, David Satcher, M.D., Ph.D., is famous for giving his "Prescription for Great Health" when he addresses colleges and universities, which includes not smoking, staying away from illicit drug use, and abstaining from unsafe sex. Importantly, the first two key points of his "prescription" are exercising at least five times a week for 30 minutes and eating at least five servings of fruits and vegetables daily. Again, very simple recommendations, but his advice has lasting and profound ramifications.
Do obstetrician/gynecologists have a role?
As ob.gyns., we always have played an incredibly critical role in maintaining the health and well-being of our patients. Now, more than ever, we have a significant opportunity to set our patients on a path to better eating, incorporating exercise into their daily routines and passing down these good habits to their children.
In the "old days," the ob.gyn. focused on a limited period in a patient’s life. Perhaps we only saw a patient for annual exams and then for a more intense time prior to and during pregnancy, and then for a checkup post partum where we may have examined our patients only for complications of the pregnancy and delivery and not much more. Although we may have included some counseling on maintaining a healthy pregnancy, many of us relied on a patient’s primary care physician to provide ongoing support.
Today, however, we must take a more active role in helping our patients establish and maintain a healthy lifestyle. Despite the increased insurance coverage under the ACA and the expansion of Medicaid, a woman’s ob.gyn. may be the only health care practitioner she will see on a routine basis. Many women do not visit a general practitioner for routine physical examinations, but women will see their ob.gyn. for regular exams. We can use these annual or biannual office visits to help women set goals to live a healthy life, approaching each patient as a whole person who needs comprehensive care throughout her reproductive life and beyond.
For patients who are overweight or obese, we may focus on helping them reduce their body mass index and blood pressure and encourage them to stay fit. We also should do everything we can to ensure that if a woman has had gestational diabetes, she’s doing what she can to reduce her risk of developing type 2 diabetes after pregnancy. For these patients, we should consider testing their blood glucose every 1-2 years during the annual checkup.
Healthy weight in pregnancy: to gain or to lose?
Whether or not an ob.gyn. practice implements a screening program and more intensive obesity and diabetes counseling, we all will face the same question: How much weight should my patient gain to have a healthy baby? Interestingly, in the first half of the 20th century, ob.gyns. were discouraged from recommending that their pregnant patients gain very much weight. Indeed, the 13th edition of "Williams Obstetrics" (New York: Appleton-Century-Crofts, 1966, p. 326) stated that obstetricians should limit their patients from gaining more than 25 pounds during gestation, and that the ideal weight gain was 15 pounds.
This guidance was called into question by a 1970 National Academy of Sciences report, "Maternal Nutrition and the Course of Pregnancy," which indicated a strong link between infant mortality and low maternal pregnancy weight. Further evidence suggested a need for new standards and, in 1990, the IOM issued recommendations on women’s nutrition during pregnancy (Nutrition During Pregnancy, Weight Gain and Nutrient Supplements. Washington, D.C.: National Academy Press, 1990). (See table.)
Americans consume 31% more calories today than they did 40 years ago. Because of this, a woman’s need to gain weight to improve the outcome of her pregnancy is significantly reduced. The calories that many people include in their diets often come from high-fat, sodium-loaded, processed foods. We also have become a more sedentary society, spending our days at a computer, browsing the internet, watching TV, and opting to drive rather than to walk. Taking these factors into account, revising the recommendations for weight gain seemed crucial. In 2009, the IOM revised its guidance on healthy weight gain in pregnancy, and these ranges are currently widely accepted by obstetricians today (iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx). (See table.)
With the obesity and diabetes epidemics on the rise, we may need to update the 2009 IOM guidelines again – and very soon. Isolated studies have indicated that, for women who are severely obese, moderate weight loss during pregnancy may improve pregnancy outcomes. These findings remain controversial, but the "heavy" burden of diabetes and obesity on the U.S. health care system in general, and the need to reduce obstetrical complications that accompany deliveries in patients who are overweight or obese and diabetic, means that we as a community may need to reexamine our practices and approaches much more closely.
"Food" for thought
We all know of patients who, once they become pregnant, begin justifying a greater intake of food as "eating for two." Many women may use their pregnancy as an excuse to overindulge in unhealthy foods or to forgo the gym and other regular exercise regimens. Recommending basic steps to change a patient’s lifestyle can make an incredible difference in improving maternal and fetal health outcomes.
Summary recommendations for healthy pregnancy
• A low-glycemic diet, combined with moderate exercise, can reduce or eliminate many of the negative consequences of obesity on pregnant women and their babies.
• Proper weight management during pregnancy can improve birth outcomes.
• Weight loss during pregnancy is not recommended, except, potentially, for morbidly obese women (BMI greater than 40).
• For women who are normal weight, overweight or obese, leading healthy lifestyles can greatly improve maternal and fetal health outcomes. These include physical exercise, balanced diet, and weight loss, in combination with medication in some cases.
• It is never too late to begin healthy habits!
If we microfocus only on a woman’s predelivery and postdelivery health, then we’re losing a big opportunity to improve her whole self and prevent future health complications during and outside of pregnancy. The good news for ob.gyns. is that this complex problem has a simple, well-documented, and proven solution.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
The world is not only getting older and warmer, but it’s getting heavier and more unfit each year. According to the World Health Organization’s most recent data, more than 1.4 billion adults were overweight in 2008, and 500 million of these adults were obese. In 2012, more than 40 million young children were overweight or obese. Diabetes, a disorder closely linked with obesity, affects about 347 million people worldwide – approximately ten times more people than those with HIV/AIDS. Although the number of AIDS-related deaths has steadily decreased over the last decade, even in developing countries, the number of diabetes-related deaths has steadily increased. The WHO projects that diabetes-related deaths will double by 2030, making it the seventh leading cause of death worldwide. In the United States, diabetes already is the seventh leading cause of death.
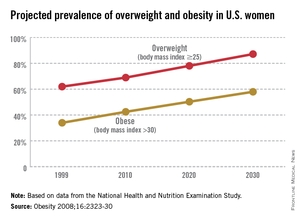
According to the Centers for Disease Control and Prevention, obesity-related diseases cost $147 billion annually, a number which dwarfs the health care costs associated with smoking ($96 billion). In addition to the link with type 2 diabetes, there are strong links between obesity and heart disease, kidney disease, depression, and hypertension. From 1987 to 2007, obesity was estimated to have caused more than a 20% increase in total health care spending.
The American Diabetes Association estimates that people diagnosed with diabetes have average yearly medical expenditures of over $13,000, which is over two times higher than the expenditures of a person without diagnosed diabetes. The 2012 estimated annual cost of care for diagnosed diabetes was $245 billion, which includes $176 billion in direct medical costs and $69 billion in reduced productivity (Diabetes Care 2013 [doi:10.2337/dc12-2625]). These figures, while staggering, do not include projected expenditures for people who have yet to receive a diabetes diagnosis.
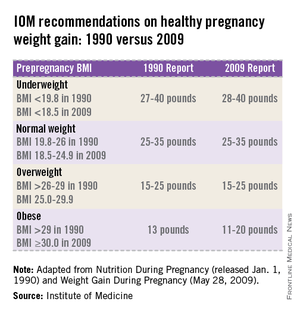
The federal government has chosen to take dramatic steps to help Americans lose weight. Since 2011, the Centers for Medicare & Medicaid Services has covered screening and intensive behavioral therapy for obesity by primary care physicians during office visits or outpatient hospital care. Additionally, the Affordable Care Act (ACA) now requires insurance companies to help overweight and obese patients try to lose weight and be healthier. The 2012 Institute of Medicine (IOM) report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation also has made major recommendations for health care practitioners, schools, and the food and beverage industry to take a more active part in improving our overall health.
Simple steps make a big impact on health
Despite the daunting – and perhaps somewhat disheartening – statistics on obesity and diabetes in the United States and around the world, research has shown that small steps to achieving a healthy weight and maintaining an active lifestyle can make a dramatic difference on the course of a person’s life. According to the Department of Agriculture, healthier diets could prevent about $71 billion in yearly health care costs, lost productivity, and premature deaths. This number is staggering, when you consider that the change could be as small as choosing a salad instead of fries for a side dish.
Medical research backs up the well-worn adage that "an apple a day keeps the doctor away." The Diabetes Prevention Program study, conducted in the early 2000s, found that lifestyle changes, such as getting more exercise and eating a balanced diet, had a major impact on whether a patient who is overweight with prediabetes developed type 2 diabetes (N. Engl. J. Med. 2002;346:393-403).
Lifestyle changes can also reduce the onset of diabetes in high-risk groups such as Asian Indians, where the incidence of diabetes is the highest in the world. The Indian Diabetes Prevention Programme showed that weight loss and healthy eating reduced the incidence of type 2 diabetes in this population at a rate similar to the use of metformin, one of the most common oral antidiabetic drugs (Diabetologia 2006;49:289-97).
The 16th U.S. Surgeon General, David Satcher, M.D., Ph.D., is famous for giving his "Prescription for Great Health" when he addresses colleges and universities, which includes not smoking, staying away from illicit drug use, and abstaining from unsafe sex. Importantly, the first two key points of his "prescription" are exercising at least five times a week for 30 minutes and eating at least five servings of fruits and vegetables daily. Again, very simple recommendations, but his advice has lasting and profound ramifications.
Do obstetrician/gynecologists have a role?
As ob.gyns., we always have played an incredibly critical role in maintaining the health and well-being of our patients. Now, more than ever, we have a significant opportunity to set our patients on a path to better eating, incorporating exercise into their daily routines and passing down these good habits to their children.
In the "old days," the ob.gyn. focused on a limited period in a patient’s life. Perhaps we only saw a patient for annual exams and then for a more intense time prior to and during pregnancy, and then for a checkup post partum where we may have examined our patients only for complications of the pregnancy and delivery and not much more. Although we may have included some counseling on maintaining a healthy pregnancy, many of us relied on a patient’s primary care physician to provide ongoing support.
Today, however, we must take a more active role in helping our patients establish and maintain a healthy lifestyle. Despite the increased insurance coverage under the ACA and the expansion of Medicaid, a woman’s ob.gyn. may be the only health care practitioner she will see on a routine basis. Many women do not visit a general practitioner for routine physical examinations, but women will see their ob.gyn. for regular exams. We can use these annual or biannual office visits to help women set goals to live a healthy life, approaching each patient as a whole person who needs comprehensive care throughout her reproductive life and beyond.
For patients who are overweight or obese, we may focus on helping them reduce their body mass index and blood pressure and encourage them to stay fit. We also should do everything we can to ensure that if a woman has had gestational diabetes, she’s doing what she can to reduce her risk of developing type 2 diabetes after pregnancy. For these patients, we should consider testing their blood glucose every 1-2 years during the annual checkup.
Healthy weight in pregnancy: to gain or to lose?
Whether or not an ob.gyn. practice implements a screening program and more intensive obesity and diabetes counseling, we all will face the same question: How much weight should my patient gain to have a healthy baby? Interestingly, in the first half of the 20th century, ob.gyns. were discouraged from recommending that their pregnant patients gain very much weight. Indeed, the 13th edition of "Williams Obstetrics" (New York: Appleton-Century-Crofts, 1966, p. 326) stated that obstetricians should limit their patients from gaining more than 25 pounds during gestation, and that the ideal weight gain was 15 pounds.
This guidance was called into question by a 1970 National Academy of Sciences report, "Maternal Nutrition and the Course of Pregnancy," which indicated a strong link between infant mortality and low maternal pregnancy weight. Further evidence suggested a need for new standards and, in 1990, the IOM issued recommendations on women’s nutrition during pregnancy (Nutrition During Pregnancy, Weight Gain and Nutrient Supplements. Washington, D.C.: National Academy Press, 1990). (See table.)
Americans consume 31% more calories today than they did 40 years ago. Because of this, a woman’s need to gain weight to improve the outcome of her pregnancy is significantly reduced. The calories that many people include in their diets often come from high-fat, sodium-loaded, processed foods. We also have become a more sedentary society, spending our days at a computer, browsing the internet, watching TV, and opting to drive rather than to walk. Taking these factors into account, revising the recommendations for weight gain seemed crucial. In 2009, the IOM revised its guidance on healthy weight gain in pregnancy, and these ranges are currently widely accepted by obstetricians today (iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx). (See table.)
With the obesity and diabetes epidemics on the rise, we may need to update the 2009 IOM guidelines again – and very soon. Isolated studies have indicated that, for women who are severely obese, moderate weight loss during pregnancy may improve pregnancy outcomes. These findings remain controversial, but the "heavy" burden of diabetes and obesity on the U.S. health care system in general, and the need to reduce obstetrical complications that accompany deliveries in patients who are overweight or obese and diabetic, means that we as a community may need to reexamine our practices and approaches much more closely.
"Food" for thought
We all know of patients who, once they become pregnant, begin justifying a greater intake of food as "eating for two." Many women may use their pregnancy as an excuse to overindulge in unhealthy foods or to forgo the gym and other regular exercise regimens. Recommending basic steps to change a patient’s lifestyle can make an incredible difference in improving maternal and fetal health outcomes.
Summary recommendations for healthy pregnancy
• A low-glycemic diet, combined with moderate exercise, can reduce or eliminate many of the negative consequences of obesity on pregnant women and their babies.
• Proper weight management during pregnancy can improve birth outcomes.
• Weight loss during pregnancy is not recommended, except, potentially, for morbidly obese women (BMI greater than 40).
• For women who are normal weight, overweight or obese, leading healthy lifestyles can greatly improve maternal and fetal health outcomes. These include physical exercise, balanced diet, and weight loss, in combination with medication in some cases.
• It is never too late to begin healthy habits!
If we microfocus only on a woman’s predelivery and postdelivery health, then we’re losing a big opportunity to improve her whole self and prevent future health complications during and outside of pregnancy. The good news for ob.gyns. is that this complex problem has a simple, well-documented, and proven solution.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Diabesity – Fattening the U.S. health care budget
The world is not only getting older and warmer, but it’s getting heavier and more unfit each year. According to the World Health Organization’s most recent data, more than 1.4 billion adults were overweight in 2008, and 500 million of these adults were obese. In 2012, more than 40 million young children were overweight or obese. Diabetes, a disorder closely linked with obesity, affects about 347 million people worldwide – approximately ten times more people than those with HIV/AIDS. Although the number of AIDS-related deaths has steadily decreased over the last decade, even in developing countries, the number of diabetes-related deaths has steadily increased. The WHO projects that diabetes-related deaths will double by 2030, making it the seventh leading cause of death worldwide. In the United States, diabetes already is the seventh leading cause of death.
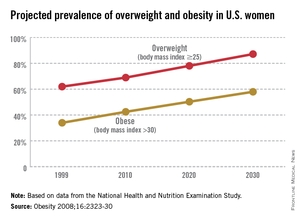
According to the Centers for Disease Control and Prevention, obesity-related diseases cost $147 billion annually, a number which dwarfs the health care costs associated with smoking ($96 billion). In addition to the link with type 2 diabetes, there are strong links between obesity and heart disease, kidney disease, depression, and hypertension. From 1987 to 2007, obesity was estimated to have caused more than a 20% increase in total health care spending.
The American Diabetes Association estimates that people diagnosed with diabetes have average yearly medical expenditures of over $13,000, which is over two times higher than the expenditures of a person without diagnosed diabetes. The 2012 estimated annual cost of care for diagnosed diabetes was $245 billion, which includes $176 billion in direct medical costs and $69 billion in reduced productivity (Diabetes Care 2013 [doi:10.2337/dc12-2625]). These figures, while staggering, do not include projected expenditures for people who have yet to receive a diabetes diagnosis.
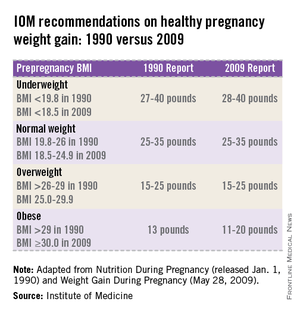
The federal government has chosen to take dramatic steps to help Americans lose weight. Since 2011, the Centers for Medicare & Medicaid Services has covered screening and intensive behavioral therapy for obesity by primary care physicians during office visits or outpatient hospital care. Additionally, the Affordable Care Act (ACA) now requires insurance companies to help overweight and obese patients try to lose weight and be healthier. The 2012 Institute of Medicine (IOM) report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation also has made major recommendations for health care practitioners, schools, and the food and beverage industry to take a more active part in improving our overall health.
Simple steps make a big impact on health
Despite the daunting – and perhaps somewhat disheartening – statistics on obesity and diabetes in the United States and around the world, research has shown that small steps to achieving a healthy weight and maintaining an active lifestyle can make a dramatic difference on the course of a person’s life. According to the Department of Agriculture, healthier diets could prevent about $71 billion in yearly health care costs, lost productivity, and premature deaths. This number is staggering, when you consider that the change could be as small as choosing a salad instead of fries for a side dish.
Medical research backs up the well-worn adage that "an apple a day keeps the doctor away." The Diabetes Prevention Program study, conducted in the early 2000s, found that lifestyle changes, such as getting more exercise and eating a balanced diet, had a major impact on whether a patient who is overweight with prediabetes developed type 2 diabetes (N. Engl. J. Med. 2002;346:393-403).
Lifestyle changes can also reduce the onset of diabetes in high-risk groups such as Asian Indians, where the incidence of diabetes is the highest in the world. The Indian Diabetes Prevention Programme showed that weight loss and healthy eating reduced the incidence of type 2 diabetes in this population at a rate similar to the use of metformin, one of the most common oral antidiabetic drugs (Diabetologia 2006;49:289-97).
The 16th U.S. Surgeon General, David Satcher, M.D., Ph.D., is famous for giving his "Prescription for Great Health" when he addresses colleges and universities, which includes not smoking, staying away from illicit drug use, and abstaining from unsafe sex. Importantly, the first two key points of his "prescription" are exercising at least five times a week for 30 minutes and eating at least five servings of fruits and vegetables daily. Again, very simple recommendations, but his advice has lasting and profound ramifications.
Do obstetrician/gynecologists have a role?
As ob.gyns., we always have played an incredibly critical role in maintaining the health and well-being of our patients. Now, more than ever, we have a significant opportunity to set our patients on a path to better eating, incorporating exercise into their daily routines and passing down these good habits to their children.
In the "old days," the ob.gyn. focused on a limited period in a patient’s life. Perhaps we only saw a patient for annual exams and then for a more intense time prior to and during pregnancy, and then for a checkup post partum where we may have examined our patients only for complications of the pregnancy and delivery and not much more. Although we may have included some counseling on maintaining a healthy pregnancy, many of us relied on a patient’s primary care physician to provide ongoing support.
Today, however, we must take a more active role in helping our patients establish and maintain a healthy lifestyle. Despite the increased insurance coverage under the ACA and the expansion of Medicaid, a woman’s ob.gyn. may be the only health care practitioner she will see on a routine basis. Many women do not visit a general practitioner for routine physical examinations, but women will see their ob.gyn. for regular exams. We can use these annual or biannual office visits to help women set goals to live a healthy life, approaching each patient as a whole person who needs comprehensive care throughout her reproductive life and beyond.
For patients who are overweight or obese, we may focus on helping them reduce their body mass index and blood pressure and encourage them to stay fit. We also should do everything we can to ensure that if a woman has had gestational diabetes, she’s doing what she can to reduce her risk of developing type 2 diabetes after pregnancy. For these patients, we should consider testing their blood glucose every 1-2 years during the annual checkup.
Healthy weight in pregnancy: to gain or to lose?
Whether or not an ob.gyn. practice implements a screening program and more intensive obesity and diabetes counseling, we all will face the same question: How much weight should my patient gain to have a healthy baby? Interestingly, in the first half of the 20th century, ob.gyns. were discouraged from recommending that their pregnant patients gain very much weight. Indeed, the 13th edition of "Williams Obstetrics" (New York: Appleton-Century-Crofts, 1966, p. 326) stated that obstetricians should limit their patients from gaining more than 25 pounds during gestation, and that the ideal weight gain was 15 pounds.
This guidance was called into question by a 1970 National Academy of Sciences report, "Maternal Nutrition and the Course of Pregnancy," which indicated a strong link between infant mortality and low maternal pregnancy weight. Further evidence suggested a need for new standards and, in 1990, the IOM issued recommendations on women’s nutrition during pregnancy (Nutrition During Pregnancy, Weight Gain and Nutrient Supplements. Washington, D.C.: National Academy Press, 1990). (See table.)
Americans consume 31% more calories today than they did 40 years ago. Because of this, a woman’s need to gain weight to improve the outcome of her pregnancy is significantly reduced. The calories that many people include in their diets often come from high-fat, sodium-loaded, processed foods. We also have become a more sedentary society, spending our days at a computer, browsing the internet, watching TV, and opting to drive rather than to walk. Taking these factors into account, revising the recommendations for weight gain seemed crucial. In 2009, the IOM revised its guidance on healthy weight gain in pregnancy, and these ranges are currently widely accepted by obstetricians today (iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx). (See table.)
With the obesity and diabetes epidemics on the rise, we may need to update the 2009 IOM guidelines again – and very soon. Isolated studies have indicated that, for women who are severely obese, moderate weight loss during pregnancy may improve pregnancy outcomes. These findings remain controversial, but the "heavy" burden of diabetes and obesity on the U.S. health care system in general, and the need to reduce obstetrical complications that accompany deliveries in patients who are overweight or obese and diabetic, means that we as a community may need to reexamine our practices and approaches much more closely.
"Food" for thought
We all know of patients who, once they become pregnant, begin justifying a greater intake of food as "eating for two." Many women may use their pregnancy as an excuse to overindulge in unhealthy foods or to forgo the gym and other regular exercise regimens. Recommending basic steps to change a patient’s lifestyle can make an incredible difference in improving maternal and fetal health outcomes.
Summary recommendations for healthy pregnancy
• A low-glycemic diet, combined with moderate exercise, can reduce or eliminate many of the negative consequences of obesity on pregnant women and their babies.
• Proper weight management during pregnancy can improve birth outcomes.
• Weight loss during pregnancy is not recommended, except, potentially, for morbidly obese women (BMI greater than 40).
• For women who are normal weight, overweight or obese, leading healthy lifestyles can greatly improve maternal and fetal health outcomes. These include physical exercise, balanced diet, and weight loss, in combination with medication in some cases.
• It is never too late to begin healthy habits!
If we microfocus only on a woman’s predelivery and postdelivery health, then we’re losing a big opportunity to improve her whole self and prevent future health complications during and outside of pregnancy. The good news for ob.gyns. is that this complex problem has a simple, well-documented, and proven solution.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
The world is not only getting older and warmer, but it’s getting heavier and more unfit each year. According to the World Health Organization’s most recent data, more than 1.4 billion adults were overweight in 2008, and 500 million of these adults were obese. In 2012, more than 40 million young children were overweight or obese. Diabetes, a disorder closely linked with obesity, affects about 347 million people worldwide – approximately ten times more people than those with HIV/AIDS. Although the number of AIDS-related deaths has steadily decreased over the last decade, even in developing countries, the number of diabetes-related deaths has steadily increased. The WHO projects that diabetes-related deaths will double by 2030, making it the seventh leading cause of death worldwide. In the United States, diabetes already is the seventh leading cause of death.
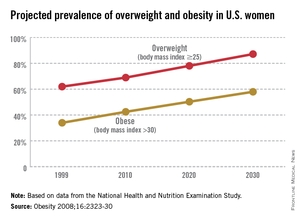
According to the Centers for Disease Control and Prevention, obesity-related diseases cost $147 billion annually, a number which dwarfs the health care costs associated with smoking ($96 billion). In addition to the link with type 2 diabetes, there are strong links between obesity and heart disease, kidney disease, depression, and hypertension. From 1987 to 2007, obesity was estimated to have caused more than a 20% increase in total health care spending.
The American Diabetes Association estimates that people diagnosed with diabetes have average yearly medical expenditures of over $13,000, which is over two times higher than the expenditures of a person without diagnosed diabetes. The 2012 estimated annual cost of care for diagnosed diabetes was $245 billion, which includes $176 billion in direct medical costs and $69 billion in reduced productivity (Diabetes Care 2013 [doi:10.2337/dc12-2625]). These figures, while staggering, do not include projected expenditures for people who have yet to receive a diabetes diagnosis.
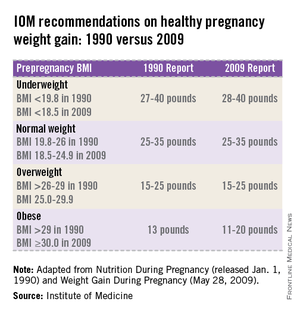
The federal government has chosen to take dramatic steps to help Americans lose weight. Since 2011, the Centers for Medicare & Medicaid Services has covered screening and intensive behavioral therapy for obesity by primary care physicians during office visits or outpatient hospital care. Additionally, the Affordable Care Act (ACA) now requires insurance companies to help overweight and obese patients try to lose weight and be healthier. The 2012 Institute of Medicine (IOM) report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation also has made major recommendations for health care practitioners, schools, and the food and beverage industry to take a more active part in improving our overall health.
Simple steps make a big impact on health
Despite the daunting – and perhaps somewhat disheartening – statistics on obesity and diabetes in the United States and around the world, research has shown that small steps to achieving a healthy weight and maintaining an active lifestyle can make a dramatic difference on the course of a person’s life. According to the Department of Agriculture, healthier diets could prevent about $71 billion in yearly health care costs, lost productivity, and premature deaths. This number is staggering, when you consider that the change could be as small as choosing a salad instead of fries for a side dish.
Medical research backs up the well-worn adage that "an apple a day keeps the doctor away." The Diabetes Prevention Program study, conducted in the early 2000s, found that lifestyle changes, such as getting more exercise and eating a balanced diet, had a major impact on whether a patient who is overweight with prediabetes developed type 2 diabetes (N. Engl. J. Med. 2002;346:393-403).
Lifestyle changes can also reduce the onset of diabetes in high-risk groups such as Asian Indians, where the incidence of diabetes is the highest in the world. The Indian Diabetes Prevention Programme showed that weight loss and healthy eating reduced the incidence of type 2 diabetes in this population at a rate similar to the use of metformin, one of the most common oral antidiabetic drugs (Diabetologia 2006;49:289-97).
The 16th U.S. Surgeon General, David Satcher, M.D., Ph.D., is famous for giving his "Prescription for Great Health" when he addresses colleges and universities, which includes not smoking, staying away from illicit drug use, and abstaining from unsafe sex. Importantly, the first two key points of his "prescription" are exercising at least five times a week for 30 minutes and eating at least five servings of fruits and vegetables daily. Again, very simple recommendations, but his advice has lasting and profound ramifications.
Do obstetrician/gynecologists have a role?
As ob.gyns., we always have played an incredibly critical role in maintaining the health and well-being of our patients. Now, more than ever, we have a significant opportunity to set our patients on a path to better eating, incorporating exercise into their daily routines and passing down these good habits to their children.
In the "old days," the ob.gyn. focused on a limited period in a patient’s life. Perhaps we only saw a patient for annual exams and then for a more intense time prior to and during pregnancy, and then for a checkup post partum where we may have examined our patients only for complications of the pregnancy and delivery and not much more. Although we may have included some counseling on maintaining a healthy pregnancy, many of us relied on a patient’s primary care physician to provide ongoing support.
Today, however, we must take a more active role in helping our patients establish and maintain a healthy lifestyle. Despite the increased insurance coverage under the ACA and the expansion of Medicaid, a woman’s ob.gyn. may be the only health care practitioner she will see on a routine basis. Many women do not visit a general practitioner for routine physical examinations, but women will see their ob.gyn. for regular exams. We can use these annual or biannual office visits to help women set goals to live a healthy life, approaching each patient as a whole person who needs comprehensive care throughout her reproductive life and beyond.
For patients who are overweight or obese, we may focus on helping them reduce their body mass index and blood pressure and encourage them to stay fit. We also should do everything we can to ensure that if a woman has had gestational diabetes, she’s doing what she can to reduce her risk of developing type 2 diabetes after pregnancy. For these patients, we should consider testing their blood glucose every 1-2 years during the annual checkup.
Healthy weight in pregnancy: to gain or to lose?
Whether or not an ob.gyn. practice implements a screening program and more intensive obesity and diabetes counseling, we all will face the same question: How much weight should my patient gain to have a healthy baby? Interestingly, in the first half of the 20th century, ob.gyns. were discouraged from recommending that their pregnant patients gain very much weight. Indeed, the 13th edition of "Williams Obstetrics" (New York: Appleton-Century-Crofts, 1966, p. 326) stated that obstetricians should limit their patients from gaining more than 25 pounds during gestation, and that the ideal weight gain was 15 pounds.
This guidance was called into question by a 1970 National Academy of Sciences report, "Maternal Nutrition and the Course of Pregnancy," which indicated a strong link between infant mortality and low maternal pregnancy weight. Further evidence suggested a need for new standards and, in 1990, the IOM issued recommendations on women’s nutrition during pregnancy (Nutrition During Pregnancy, Weight Gain and Nutrient Supplements. Washington, D.C.: National Academy Press, 1990). (See table.)
Americans consume 31% more calories today than they did 40 years ago. Because of this, a woman’s need to gain weight to improve the outcome of her pregnancy is significantly reduced. The calories that many people include in their diets often come from high-fat, sodium-loaded, processed foods. We also have become a more sedentary society, spending our days at a computer, browsing the internet, watching TV, and opting to drive rather than to walk. Taking these factors into account, revising the recommendations for weight gain seemed crucial. In 2009, the IOM revised its guidance on healthy weight gain in pregnancy, and these ranges are currently widely accepted by obstetricians today (iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx). (See table.)
With the obesity and diabetes epidemics on the rise, we may need to update the 2009 IOM guidelines again – and very soon. Isolated studies have indicated that, for women who are severely obese, moderate weight loss during pregnancy may improve pregnancy outcomes. These findings remain controversial, but the "heavy" burden of diabetes and obesity on the U.S. health care system in general, and the need to reduce obstetrical complications that accompany deliveries in patients who are overweight or obese and diabetic, means that we as a community may need to reexamine our practices and approaches much more closely.
"Food" for thought
We all know of patients who, once they become pregnant, begin justifying a greater intake of food as "eating for two." Many women may use their pregnancy as an excuse to overindulge in unhealthy foods or to forgo the gym and other regular exercise regimens. Recommending basic steps to change a patient’s lifestyle can make an incredible difference in improving maternal and fetal health outcomes.
Summary recommendations for healthy pregnancy
• A low-glycemic diet, combined with moderate exercise, can reduce or eliminate many of the negative consequences of obesity on pregnant women and their babies.
• Proper weight management during pregnancy can improve birth outcomes.
• Weight loss during pregnancy is not recommended, except, potentially, for morbidly obese women (BMI greater than 40).
• For women who are normal weight, overweight or obese, leading healthy lifestyles can greatly improve maternal and fetal health outcomes. These include physical exercise, balanced diet, and weight loss, in combination with medication in some cases.
• It is never too late to begin healthy habits!
If we microfocus only on a woman’s predelivery and postdelivery health, then we’re losing a big opportunity to improve her whole self and prevent future health complications during and outside of pregnancy. The good news for ob.gyns. is that this complex problem has a simple, well-documented, and proven solution.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
The world is not only getting older and warmer, but it’s getting heavier and more unfit each year. According to the World Health Organization’s most recent data, more than 1.4 billion adults were overweight in 2008, and 500 million of these adults were obese. In 2012, more than 40 million young children were overweight or obese. Diabetes, a disorder closely linked with obesity, affects about 347 million people worldwide – approximately ten times more people than those with HIV/AIDS. Although the number of AIDS-related deaths has steadily decreased over the last decade, even in developing countries, the number of diabetes-related deaths has steadily increased. The WHO projects that diabetes-related deaths will double by 2030, making it the seventh leading cause of death worldwide. In the United States, diabetes already is the seventh leading cause of death.
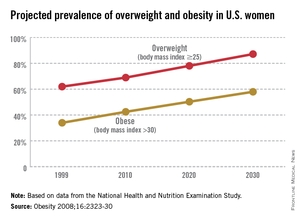
According to the Centers for Disease Control and Prevention, obesity-related diseases cost $147 billion annually, a number which dwarfs the health care costs associated with smoking ($96 billion). In addition to the link with type 2 diabetes, there are strong links between obesity and heart disease, kidney disease, depression, and hypertension. From 1987 to 2007, obesity was estimated to have caused more than a 20% increase in total health care spending.
The American Diabetes Association estimates that people diagnosed with diabetes have average yearly medical expenditures of over $13,000, which is over two times higher than the expenditures of a person without diagnosed diabetes. The 2012 estimated annual cost of care for diagnosed diabetes was $245 billion, which includes $176 billion in direct medical costs and $69 billion in reduced productivity (Diabetes Care 2013 [doi:10.2337/dc12-2625]). These figures, while staggering, do not include projected expenditures for people who have yet to receive a diabetes diagnosis.
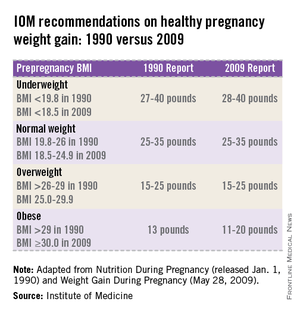
The federal government has chosen to take dramatic steps to help Americans lose weight. Since 2011, the Centers for Medicare & Medicaid Services has covered screening and intensive behavioral therapy for obesity by primary care physicians during office visits or outpatient hospital care. Additionally, the Affordable Care Act (ACA) now requires insurance companies to help overweight and obese patients try to lose weight and be healthier. The 2012 Institute of Medicine (IOM) report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation also has made major recommendations for health care practitioners, schools, and the food and beverage industry to take a more active part in improving our overall health.
Simple steps make a big impact on health
Despite the daunting – and perhaps somewhat disheartening – statistics on obesity and diabetes in the United States and around the world, research has shown that small steps to achieving a healthy weight and maintaining an active lifestyle can make a dramatic difference on the course of a person’s life. According to the Department of Agriculture, healthier diets could prevent about $71 billion in yearly health care costs, lost productivity, and premature deaths. This number is staggering, when you consider that the change could be as small as choosing a salad instead of fries for a side dish.
Medical research backs up the well-worn adage that "an apple a day keeps the doctor away." The Diabetes Prevention Program study, conducted in the early 2000s, found that lifestyle changes, such as getting more exercise and eating a balanced diet, had a major impact on whether a patient who is overweight with prediabetes developed type 2 diabetes (N. Engl. J. Med. 2002;346:393-403).
Lifestyle changes can also reduce the onset of diabetes in high-risk groups such as Asian Indians, where the incidence of diabetes is the highest in the world. The Indian Diabetes Prevention Programme showed that weight loss and healthy eating reduced the incidence of type 2 diabetes in this population at a rate similar to the use of metformin, one of the most common oral antidiabetic drugs (Diabetologia 2006;49:289-97).
The 16th U.S. Surgeon General, David Satcher, M.D., Ph.D., is famous for giving his "Prescription for Great Health" when he addresses colleges and universities, which includes not smoking, staying away from illicit drug use, and abstaining from unsafe sex. Importantly, the first two key points of his "prescription" are exercising at least five times a week for 30 minutes and eating at least five servings of fruits and vegetables daily. Again, very simple recommendations, but his advice has lasting and profound ramifications.
Do obstetrician/gynecologists have a role?
As ob.gyns., we always have played an incredibly critical role in maintaining the health and well-being of our patients. Now, more than ever, we have a significant opportunity to set our patients on a path to better eating, incorporating exercise into their daily routines and passing down these good habits to their children.
In the "old days," the ob.gyn. focused on a limited period in a patient’s life. Perhaps we only saw a patient for annual exams and then for a more intense time prior to and during pregnancy, and then for a checkup post partum where we may have examined our patients only for complications of the pregnancy and delivery and not much more. Although we may have included some counseling on maintaining a healthy pregnancy, many of us relied on a patient’s primary care physician to provide ongoing support.
Today, however, we must take a more active role in helping our patients establish and maintain a healthy lifestyle. Despite the increased insurance coverage under the ACA and the expansion of Medicaid, a woman’s ob.gyn. may be the only health care practitioner she will see on a routine basis. Many women do not visit a general practitioner for routine physical examinations, but women will see their ob.gyn. for regular exams. We can use these annual or biannual office visits to help women set goals to live a healthy life, approaching each patient as a whole person who needs comprehensive care throughout her reproductive life and beyond.
For patients who are overweight or obese, we may focus on helping them reduce their body mass index and blood pressure and encourage them to stay fit. We also should do everything we can to ensure that if a woman has had gestational diabetes, she’s doing what she can to reduce her risk of developing type 2 diabetes after pregnancy. For these patients, we should consider testing their blood glucose every 1-2 years during the annual checkup.
Healthy weight in pregnancy: to gain or to lose?
Whether or not an ob.gyn. practice implements a screening program and more intensive obesity and diabetes counseling, we all will face the same question: How much weight should my patient gain to have a healthy baby? Interestingly, in the first half of the 20th century, ob.gyns. were discouraged from recommending that their pregnant patients gain very much weight. Indeed, the 13th edition of "Williams Obstetrics" (New York: Appleton-Century-Crofts, 1966, p. 326) stated that obstetricians should limit their patients from gaining more than 25 pounds during gestation, and that the ideal weight gain was 15 pounds.
This guidance was called into question by a 1970 National Academy of Sciences report, "Maternal Nutrition and the Course of Pregnancy," which indicated a strong link between infant mortality and low maternal pregnancy weight. Further evidence suggested a need for new standards and, in 1990, the IOM issued recommendations on women’s nutrition during pregnancy (Nutrition During Pregnancy, Weight Gain and Nutrient Supplements. Washington, D.C.: National Academy Press, 1990). (See table.)
Americans consume 31% more calories today than they did 40 years ago. Because of this, a woman’s need to gain weight to improve the outcome of her pregnancy is significantly reduced. The calories that many people include in their diets often come from high-fat, sodium-loaded, processed foods. We also have become a more sedentary society, spending our days at a computer, browsing the internet, watching TV, and opting to drive rather than to walk. Taking these factors into account, revising the recommendations for weight gain seemed crucial. In 2009, the IOM revised its guidance on healthy weight gain in pregnancy, and these ranges are currently widely accepted by obstetricians today (iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx). (See table.)
With the obesity and diabetes epidemics on the rise, we may need to update the 2009 IOM guidelines again – and very soon. Isolated studies have indicated that, for women who are severely obese, moderate weight loss during pregnancy may improve pregnancy outcomes. These findings remain controversial, but the "heavy" burden of diabetes and obesity on the U.S. health care system in general, and the need to reduce obstetrical complications that accompany deliveries in patients who are overweight or obese and diabetic, means that we as a community may need to reexamine our practices and approaches much more closely.
"Food" for thought
We all know of patients who, once they become pregnant, begin justifying a greater intake of food as "eating for two." Many women may use their pregnancy as an excuse to overindulge in unhealthy foods or to forgo the gym and other regular exercise regimens. Recommending basic steps to change a patient’s lifestyle can make an incredible difference in improving maternal and fetal health outcomes.
Summary recommendations for healthy pregnancy
• A low-glycemic diet, combined with moderate exercise, can reduce or eliminate many of the negative consequences of obesity on pregnant women and their babies.
• Proper weight management during pregnancy can improve birth outcomes.
• Weight loss during pregnancy is not recommended, except, potentially, for morbidly obese women (BMI greater than 40).
• For women who are normal weight, overweight or obese, leading healthy lifestyles can greatly improve maternal and fetal health outcomes. These include physical exercise, balanced diet, and weight loss, in combination with medication in some cases.
• It is never too late to begin healthy habits!
If we microfocus only on a woman’s predelivery and postdelivery health, then we’re losing a big opportunity to improve her whole self and prevent future health complications during and outside of pregnancy. The good news for ob.gyns. is that this complex problem has a simple, well-documented, and proven solution.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].