User login
CAG Clinical Practice Guideline: Luminal Crohn’s disease
The Canadian Association of Gastroenterology has released a new clinical practice guideline for the treatment of luminal Crohn’s disease (CD) in adults.
“In the last decade, treatment paradigms have changed, recognizing that certain clinical parameters carry an increased risk of progressive and disabling disease,” wrote Remo Panaccione, MD, of the University of Calgary (Canada) and collaborators. Dr. Panaccione is the lead author of this practice guideline copublished in Clinical Gastroenterology and Hepatology and the Journal of the Canadian Association of Gastroenterology.
The expert consensus panel consisted of 20 voting members, including both academic and community gastroenterologists, in addition to a specialist nurse practitioner. Other nonvoting members included two GRADE experts, lay observers, and a patient representative.
The panel systematically reviewed the body of literature for studies related to the management of CD in adults. After applying the search criteria, the team found that the majority of evidence was extracted from systematic reviews and meta-analyses of randomized trials.
Quality of evidence and risk of bias was assessed using the GRADE (Grading of Recommendation Assessment, Development and Evaluation) methodology. The quality of evidence for each consensus statement was classified as either high, moderate, low, or very low, based on the methodology’s criteria.
The consensus statements were finalized at a face-to-face meeting in Toronto held in September 2016. Prior to completion, a web-based system was used to allow for anonymous voting on level of agreement for each consensus statement.
The new guideline provides evidence-based recommendations about optimal treatment approaches for patients with mild to severe active luminal CD in an ambulatory setting, with particular focus on six major drug classes, including corticosteroids, biologic therapies, immunosuppressants, 5-aminosalicylate, antibiotics, and other therapies.
The consensus group recommended against the use of 5-aminosalicylate or antibiotics as induction or maintenance treatment strategies. Alternatively, they suggested that corticosteroids, including budesonide, could be used as induction therapy, but not as maintenance therapy.
“Parenteral methotrexate was proposed for induction and maintenance therapy in patients with corticosteroid-dependent CD,” they wrote.
With respect to immunosuppressive therapy, thiopurine agents could be an appropriate option for maintenance therapy in certain low-risk patients, but were not recommended as induction therapy, according to the guideline.
In patients who fail with conventional induction therapies, Dr. Panaccione and colleagues recommended that biological treatments, including ustekinumab, vedolizumab, and anti–tumor necrosis factor agents, could be used. No consensus was reached on the concomitant use of immunosuppressants and biologics.
In recent years, an increasing amount of evidence has emphasized the importance of mucosal healing as a key goal of therapy. In particular, the use of some therapies can result in mucosal healing and symptomatic improvement in certain patients with luminal CD.
In addition, the authors explained that mucosal healing has been linked to better clinical outcomes over the short and long term. As a result, the recommendations in the guideline target complete remission, defined as both endoscopic and symptomatic remission.
“The outcome assessed in most randomized controlled trials (RCTs) has been either symptomatic remission or symptomatic response, with only more contemporary clinical trials including endoscopic outcomes,” the guideline authors wrote.
For this reason, the GRADE criteria–based quality of evidence for some of the consensus statements had to be lowered, they noted.
The panel acknowledged the importance of incorporating patient perspectives into treatment decision making; however, they reported that many gaps in clinical practice still remain.
“In many instances, factors that influence patient decisions relating to therapy choice and goals of therapy are not the same as those of the treating clinician,” they wrote. “[Current] surveys indicate a discrepancy between patient and physician treatment goals.”
In response, the guideline authors highlighted the importance of improved patient-physician collaboration and patient education.
The guideline was supported through grant funding provided by AbbVie, Janssen, Pfizer, and Takeda. The authors reported financial affiliations with AbbVie, Amgen, Baxter, Janssen, Shire, Takeda, and several others.
SOURCE: Panaccione R et al. Clin Gastroenterol Hepatol. 2019 Mar 7. doi: 10.1016/j.cgh.2019.02.043.
The Canadian Association of Gastroenterology has released a new clinical practice guideline for the treatment of luminal Crohn’s disease (CD) in adults.
“In the last decade, treatment paradigms have changed, recognizing that certain clinical parameters carry an increased risk of progressive and disabling disease,” wrote Remo Panaccione, MD, of the University of Calgary (Canada) and collaborators. Dr. Panaccione is the lead author of this practice guideline copublished in Clinical Gastroenterology and Hepatology and the Journal of the Canadian Association of Gastroenterology.
The expert consensus panel consisted of 20 voting members, including both academic and community gastroenterologists, in addition to a specialist nurse practitioner. Other nonvoting members included two GRADE experts, lay observers, and a patient representative.
The panel systematically reviewed the body of literature for studies related to the management of CD in adults. After applying the search criteria, the team found that the majority of evidence was extracted from systematic reviews and meta-analyses of randomized trials.
Quality of evidence and risk of bias was assessed using the GRADE (Grading of Recommendation Assessment, Development and Evaluation) methodology. The quality of evidence for each consensus statement was classified as either high, moderate, low, or very low, based on the methodology’s criteria.
The consensus statements were finalized at a face-to-face meeting in Toronto held in September 2016. Prior to completion, a web-based system was used to allow for anonymous voting on level of agreement for each consensus statement.
The new guideline provides evidence-based recommendations about optimal treatment approaches for patients with mild to severe active luminal CD in an ambulatory setting, with particular focus on six major drug classes, including corticosteroids, biologic therapies, immunosuppressants, 5-aminosalicylate, antibiotics, and other therapies.
The consensus group recommended against the use of 5-aminosalicylate or antibiotics as induction or maintenance treatment strategies. Alternatively, they suggested that corticosteroids, including budesonide, could be used as induction therapy, but not as maintenance therapy.
“Parenteral methotrexate was proposed for induction and maintenance therapy in patients with corticosteroid-dependent CD,” they wrote.
With respect to immunosuppressive therapy, thiopurine agents could be an appropriate option for maintenance therapy in certain low-risk patients, but were not recommended as induction therapy, according to the guideline.
In patients who fail with conventional induction therapies, Dr. Panaccione and colleagues recommended that biological treatments, including ustekinumab, vedolizumab, and anti–tumor necrosis factor agents, could be used. No consensus was reached on the concomitant use of immunosuppressants and biologics.
In recent years, an increasing amount of evidence has emphasized the importance of mucosal healing as a key goal of therapy. In particular, the use of some therapies can result in mucosal healing and symptomatic improvement in certain patients with luminal CD.
In addition, the authors explained that mucosal healing has been linked to better clinical outcomes over the short and long term. As a result, the recommendations in the guideline target complete remission, defined as both endoscopic and symptomatic remission.
“The outcome assessed in most randomized controlled trials (RCTs) has been either symptomatic remission or symptomatic response, with only more contemporary clinical trials including endoscopic outcomes,” the guideline authors wrote.
For this reason, the GRADE criteria–based quality of evidence for some of the consensus statements had to be lowered, they noted.
The panel acknowledged the importance of incorporating patient perspectives into treatment decision making; however, they reported that many gaps in clinical practice still remain.
“In many instances, factors that influence patient decisions relating to therapy choice and goals of therapy are not the same as those of the treating clinician,” they wrote. “[Current] surveys indicate a discrepancy between patient and physician treatment goals.”
In response, the guideline authors highlighted the importance of improved patient-physician collaboration and patient education.
The guideline was supported through grant funding provided by AbbVie, Janssen, Pfizer, and Takeda. The authors reported financial affiliations with AbbVie, Amgen, Baxter, Janssen, Shire, Takeda, and several others.
SOURCE: Panaccione R et al. Clin Gastroenterol Hepatol. 2019 Mar 7. doi: 10.1016/j.cgh.2019.02.043.
The Canadian Association of Gastroenterology has released a new clinical practice guideline for the treatment of luminal Crohn’s disease (CD) in adults.
“In the last decade, treatment paradigms have changed, recognizing that certain clinical parameters carry an increased risk of progressive and disabling disease,” wrote Remo Panaccione, MD, of the University of Calgary (Canada) and collaborators. Dr. Panaccione is the lead author of this practice guideline copublished in Clinical Gastroenterology and Hepatology and the Journal of the Canadian Association of Gastroenterology.
The expert consensus panel consisted of 20 voting members, including both academic and community gastroenterologists, in addition to a specialist nurse practitioner. Other nonvoting members included two GRADE experts, lay observers, and a patient representative.
The panel systematically reviewed the body of literature for studies related to the management of CD in adults. After applying the search criteria, the team found that the majority of evidence was extracted from systematic reviews and meta-analyses of randomized trials.
Quality of evidence and risk of bias was assessed using the GRADE (Grading of Recommendation Assessment, Development and Evaluation) methodology. The quality of evidence for each consensus statement was classified as either high, moderate, low, or very low, based on the methodology’s criteria.
The consensus statements were finalized at a face-to-face meeting in Toronto held in September 2016. Prior to completion, a web-based system was used to allow for anonymous voting on level of agreement for each consensus statement.
The new guideline provides evidence-based recommendations about optimal treatment approaches for patients with mild to severe active luminal CD in an ambulatory setting, with particular focus on six major drug classes, including corticosteroids, biologic therapies, immunosuppressants, 5-aminosalicylate, antibiotics, and other therapies.
The consensus group recommended against the use of 5-aminosalicylate or antibiotics as induction or maintenance treatment strategies. Alternatively, they suggested that corticosteroids, including budesonide, could be used as induction therapy, but not as maintenance therapy.
“Parenteral methotrexate was proposed for induction and maintenance therapy in patients with corticosteroid-dependent CD,” they wrote.
With respect to immunosuppressive therapy, thiopurine agents could be an appropriate option for maintenance therapy in certain low-risk patients, but were not recommended as induction therapy, according to the guideline.
In patients who fail with conventional induction therapies, Dr. Panaccione and colleagues recommended that biological treatments, including ustekinumab, vedolizumab, and anti–tumor necrosis factor agents, could be used. No consensus was reached on the concomitant use of immunosuppressants and biologics.
In recent years, an increasing amount of evidence has emphasized the importance of mucosal healing as a key goal of therapy. In particular, the use of some therapies can result in mucosal healing and symptomatic improvement in certain patients with luminal CD.
In addition, the authors explained that mucosal healing has been linked to better clinical outcomes over the short and long term. As a result, the recommendations in the guideline target complete remission, defined as both endoscopic and symptomatic remission.
“The outcome assessed in most randomized controlled trials (RCTs) has been either symptomatic remission or symptomatic response, with only more contemporary clinical trials including endoscopic outcomes,” the guideline authors wrote.
For this reason, the GRADE criteria–based quality of evidence for some of the consensus statements had to be lowered, they noted.
The panel acknowledged the importance of incorporating patient perspectives into treatment decision making; however, they reported that many gaps in clinical practice still remain.
“In many instances, factors that influence patient decisions relating to therapy choice and goals of therapy are not the same as those of the treating clinician,” they wrote. “[Current] surveys indicate a discrepancy between patient and physician treatment goals.”
In response, the guideline authors highlighted the importance of improved patient-physician collaboration and patient education.
The guideline was supported through grant funding provided by AbbVie, Janssen, Pfizer, and Takeda. The authors reported financial affiliations with AbbVie, Amgen, Baxter, Janssen, Shire, Takeda, and several others.
SOURCE: Panaccione R et al. Clin Gastroenterol Hepatol. 2019 Mar 7. doi: 10.1016/j.cgh.2019.02.043.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The Canadian Association of Gastroenterology has released a new clinical practice guideline for the treatment of mild to severe active luminal Crohn’s disease (CD).
Major finding: The new guideline includes 41 statements that focus on six major therapeutic classes.
Study details: The CAG Clinical Practice Guideline for Luminal CD.
Disclosures: The guideline was supported through grant funding provided by AbbVie, Janssen, Pfizer, and Takeda. The authors reported financial affiliations with AbbVie, Amgen, Baxter, Janssen, Shire, Takeda, and several others.
Source: Panaccione R et al. Clin Gastroenterol Hepatol. 2019 Mar 7. doi: 10.1016/j.cgh.2019.02.043.
Endocrine Society advises on diabetes care for older adults
according to a new guideline on diabetes care for older adults issued by the Endocrine Society.
“The prevalence of diabetes in the United States is projected to increase dramatically during the next 3 decades as the population ages, the numbers of higher-risk minority groups increase, and people with diabetes live longer because of decreasing rates of cardiovascular deaths,” wrote Derek LeRoith, MD, of Icahn School of Medicine at Mount Sinai, New York, and his writing committee colleagues. They said their goal was to provide health care providers with guidance for the management of type 1 or type 2 diabetes in older patients, with a focus on simplifying medication regimens and management strategies to avoid “unnecessary and/or harmful adverse effects.”
The guideline, published in the Journal of Clinical Endocrinology & Metabolism, is based mainly on evidence from controlled trials in two systematic reviews that specifically focused on adults aged 65 years and older. The guideline addresses six areas of consideration for this patient population:
- Role of the endocrinologist and diabetes care specialist.
- Screening for diabetes and prediabetes, and diabetes prevention.
- Assessment of older patients with diabetes.
- Treatment of hyperglycemia.
- Treating complications of diabetes.
- Special settings and populations.
Partnerships and screening
The guideline recommends that primary care providers partner with an endocrinologist or diabetes specialist in the care of patients aged 65 and older with newly diagnosed diabetes, and that the specialist take primary responsibility for diabetes care of patients with type 1 diabetes or those who need more complex intervention to achieve treatment goals.
Screening for diabetes in adults aged 65 years and older using fasting plasma glucose and/or hemoglobin A1c should occur every 2 years, but that schedule should be adjusted based on shared decision making with the patient, the committee said. Providers are advised to assess the patient’s overall health and personal values before settling on treatment goals and strategies. The writing group also recommends periodic cognitive screening and that medication regimens be simplified as much as possible.
Tackling hyperglycemia
For treatment of hyperglycemia, the guideline recommends outpatient strategies to minimize hypoglycemia and periodic or continuous glucose monitoring. The strategies include lifestyle modifications as a first-line intervention for ambulatory patients, as well as nutritional assessment. A high-protein diet is recommended for older patients with frailty, but no restrictions on diet are advised for patients who cannot meet glycemic targets with lifestyle modification and who are at risk for malnutrition.
Metformin is the first-choice recommendation for patients with diabetes aged 65 and older who need medical management in addition to lifestyle modification, but it is not recommended for individuals with impaired kidney function or gastrointestinal intolerance, according to the guideline. Oral and injectable drugs and/or insulin are recommended if metformin and lifestyle changes are insufficient to meet glycemic targets, the writers noted.
Managing complications
Hypertension is among the diabetes-related complications that need to be managed in older adults, and the guideline recommends a target blood pressure of 140/90 mm Hg, but other targets – based on patient-provider shared decision making – may be considered for patients in high-risk groups.
The guideline calls for management of hyperlipidemia with statin therapy and “use of an annual lipid profile to achieve the recommended levels for reducing absolute cardiovascular disease events and all-cause mortality.” The committee does not specify low-density lipoprotein cholesterol targets because of insufficient evidence, but recommends alternative treatments, including ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors, if statin therapy is not enough to help the patients meet goals. The writers also advocate fish oil and/or fenofibrate for patients with fasting triglycerides of more than 500 mg/dL.
To manage congestive heart failure in older patients with diabetes, the guideline recommends following standard clinical practice guidelines for the condition, and cautious use of oral hypoglycemic agents, including glinides, rosiglitazone, pioglitazone, and dipeptidyl peptidase–4 inhibitors. The writers noted that low-dose aspirin is recommended for patients with diabetes with a history of atherosclerotic cardiovascular disease.
The committee also recommends an annual comprehensive eye exam for patients with diabetes aged 65 years and older to identify retinal disease and suggests that actions, such as physical therapy and reduced use of sedatives, be taken to minimize the risk of falls in patients with neuropathy or problems with balance and gait.
Older patients with diabetes also should be screened annually for chronic kidney disease, and the dosage of diabetes medications should be adjusted to minimize side effects in patients with kidney problems.
Tailoring care to setting
Finally, the guideline addresses special settings and populations, including managing diabetes in hospitals or nursing homes, or in patients who are transitioning to homes or long-term care facilities. Recommendations in this category include simplifying medications for older adults with terminal illness or severe comorbidities, as well as setting glycemic targets as part of a hospital discharge plan.
“The most important aspect of successful transition is effective, detailed, and thorough bidirectional communication between the discharging and receiving teams of health care providers,” the writers emphasized.
The guideline is cosponsored by the European Society of Endocrinology, the Gerontological Society of America, and the Obesity Society. The chair of the committee had no relevant financial conflicts to disclose, and at least 50% of the committee members were free of relevant conflicts of interest.
SOURCE: LeRoith D et al. J Clin Endocrinol Metab. 2019;104:1520-74.
according to a new guideline on diabetes care for older adults issued by the Endocrine Society.
“The prevalence of diabetes in the United States is projected to increase dramatically during the next 3 decades as the population ages, the numbers of higher-risk minority groups increase, and people with diabetes live longer because of decreasing rates of cardiovascular deaths,” wrote Derek LeRoith, MD, of Icahn School of Medicine at Mount Sinai, New York, and his writing committee colleagues. They said their goal was to provide health care providers with guidance for the management of type 1 or type 2 diabetes in older patients, with a focus on simplifying medication regimens and management strategies to avoid “unnecessary and/or harmful adverse effects.”
The guideline, published in the Journal of Clinical Endocrinology & Metabolism, is based mainly on evidence from controlled trials in two systematic reviews that specifically focused on adults aged 65 years and older. The guideline addresses six areas of consideration for this patient population:
- Role of the endocrinologist and diabetes care specialist.
- Screening for diabetes and prediabetes, and diabetes prevention.
- Assessment of older patients with diabetes.
- Treatment of hyperglycemia.
- Treating complications of diabetes.
- Special settings and populations.
Partnerships and screening
The guideline recommends that primary care providers partner with an endocrinologist or diabetes specialist in the care of patients aged 65 and older with newly diagnosed diabetes, and that the specialist take primary responsibility for diabetes care of patients with type 1 diabetes or those who need more complex intervention to achieve treatment goals.
Screening for diabetes in adults aged 65 years and older using fasting plasma glucose and/or hemoglobin A1c should occur every 2 years, but that schedule should be adjusted based on shared decision making with the patient, the committee said. Providers are advised to assess the patient’s overall health and personal values before settling on treatment goals and strategies. The writing group also recommends periodic cognitive screening and that medication regimens be simplified as much as possible.
Tackling hyperglycemia
For treatment of hyperglycemia, the guideline recommends outpatient strategies to minimize hypoglycemia and periodic or continuous glucose monitoring. The strategies include lifestyle modifications as a first-line intervention for ambulatory patients, as well as nutritional assessment. A high-protein diet is recommended for older patients with frailty, but no restrictions on diet are advised for patients who cannot meet glycemic targets with lifestyle modification and who are at risk for malnutrition.
Metformin is the first-choice recommendation for patients with diabetes aged 65 and older who need medical management in addition to lifestyle modification, but it is not recommended for individuals with impaired kidney function or gastrointestinal intolerance, according to the guideline. Oral and injectable drugs and/or insulin are recommended if metformin and lifestyle changes are insufficient to meet glycemic targets, the writers noted.
Managing complications
Hypertension is among the diabetes-related complications that need to be managed in older adults, and the guideline recommends a target blood pressure of 140/90 mm Hg, but other targets – based on patient-provider shared decision making – may be considered for patients in high-risk groups.
The guideline calls for management of hyperlipidemia with statin therapy and “use of an annual lipid profile to achieve the recommended levels for reducing absolute cardiovascular disease events and all-cause mortality.” The committee does not specify low-density lipoprotein cholesterol targets because of insufficient evidence, but recommends alternative treatments, including ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors, if statin therapy is not enough to help the patients meet goals. The writers also advocate fish oil and/or fenofibrate for patients with fasting triglycerides of more than 500 mg/dL.
To manage congestive heart failure in older patients with diabetes, the guideline recommends following standard clinical practice guidelines for the condition, and cautious use of oral hypoglycemic agents, including glinides, rosiglitazone, pioglitazone, and dipeptidyl peptidase–4 inhibitors. The writers noted that low-dose aspirin is recommended for patients with diabetes with a history of atherosclerotic cardiovascular disease.
The committee also recommends an annual comprehensive eye exam for patients with diabetes aged 65 years and older to identify retinal disease and suggests that actions, such as physical therapy and reduced use of sedatives, be taken to minimize the risk of falls in patients with neuropathy or problems with balance and gait.
Older patients with diabetes also should be screened annually for chronic kidney disease, and the dosage of diabetes medications should be adjusted to minimize side effects in patients with kidney problems.
Tailoring care to setting
Finally, the guideline addresses special settings and populations, including managing diabetes in hospitals or nursing homes, or in patients who are transitioning to homes or long-term care facilities. Recommendations in this category include simplifying medications for older adults with terminal illness or severe comorbidities, as well as setting glycemic targets as part of a hospital discharge plan.
“The most important aspect of successful transition is effective, detailed, and thorough bidirectional communication between the discharging and receiving teams of health care providers,” the writers emphasized.
The guideline is cosponsored by the European Society of Endocrinology, the Gerontological Society of America, and the Obesity Society. The chair of the committee had no relevant financial conflicts to disclose, and at least 50% of the committee members were free of relevant conflicts of interest.
SOURCE: LeRoith D et al. J Clin Endocrinol Metab. 2019;104:1520-74.
according to a new guideline on diabetes care for older adults issued by the Endocrine Society.
“The prevalence of diabetes in the United States is projected to increase dramatically during the next 3 decades as the population ages, the numbers of higher-risk minority groups increase, and people with diabetes live longer because of decreasing rates of cardiovascular deaths,” wrote Derek LeRoith, MD, of Icahn School of Medicine at Mount Sinai, New York, and his writing committee colleagues. They said their goal was to provide health care providers with guidance for the management of type 1 or type 2 diabetes in older patients, with a focus on simplifying medication regimens and management strategies to avoid “unnecessary and/or harmful adverse effects.”
The guideline, published in the Journal of Clinical Endocrinology & Metabolism, is based mainly on evidence from controlled trials in two systematic reviews that specifically focused on adults aged 65 years and older. The guideline addresses six areas of consideration for this patient population:
- Role of the endocrinologist and diabetes care specialist.
- Screening for diabetes and prediabetes, and diabetes prevention.
- Assessment of older patients with diabetes.
- Treatment of hyperglycemia.
- Treating complications of diabetes.
- Special settings and populations.
Partnerships and screening
The guideline recommends that primary care providers partner with an endocrinologist or diabetes specialist in the care of patients aged 65 and older with newly diagnosed diabetes, and that the specialist take primary responsibility for diabetes care of patients with type 1 diabetes or those who need more complex intervention to achieve treatment goals.
Screening for diabetes in adults aged 65 years and older using fasting plasma glucose and/or hemoglobin A1c should occur every 2 years, but that schedule should be adjusted based on shared decision making with the patient, the committee said. Providers are advised to assess the patient’s overall health and personal values before settling on treatment goals and strategies. The writing group also recommends periodic cognitive screening and that medication regimens be simplified as much as possible.
Tackling hyperglycemia
For treatment of hyperglycemia, the guideline recommends outpatient strategies to minimize hypoglycemia and periodic or continuous glucose monitoring. The strategies include lifestyle modifications as a first-line intervention for ambulatory patients, as well as nutritional assessment. A high-protein diet is recommended for older patients with frailty, but no restrictions on diet are advised for patients who cannot meet glycemic targets with lifestyle modification and who are at risk for malnutrition.
Metformin is the first-choice recommendation for patients with diabetes aged 65 and older who need medical management in addition to lifestyle modification, but it is not recommended for individuals with impaired kidney function or gastrointestinal intolerance, according to the guideline. Oral and injectable drugs and/or insulin are recommended if metformin and lifestyle changes are insufficient to meet glycemic targets, the writers noted.
Managing complications
Hypertension is among the diabetes-related complications that need to be managed in older adults, and the guideline recommends a target blood pressure of 140/90 mm Hg, but other targets – based on patient-provider shared decision making – may be considered for patients in high-risk groups.
The guideline calls for management of hyperlipidemia with statin therapy and “use of an annual lipid profile to achieve the recommended levels for reducing absolute cardiovascular disease events and all-cause mortality.” The committee does not specify low-density lipoprotein cholesterol targets because of insufficient evidence, but recommends alternative treatments, including ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors, if statin therapy is not enough to help the patients meet goals. The writers also advocate fish oil and/or fenofibrate for patients with fasting triglycerides of more than 500 mg/dL.
To manage congestive heart failure in older patients with diabetes, the guideline recommends following standard clinical practice guidelines for the condition, and cautious use of oral hypoglycemic agents, including glinides, rosiglitazone, pioglitazone, and dipeptidyl peptidase–4 inhibitors. The writers noted that low-dose aspirin is recommended for patients with diabetes with a history of atherosclerotic cardiovascular disease.
The committee also recommends an annual comprehensive eye exam for patients with diabetes aged 65 years and older to identify retinal disease and suggests that actions, such as physical therapy and reduced use of sedatives, be taken to minimize the risk of falls in patients with neuropathy or problems with balance and gait.
Older patients with diabetes also should be screened annually for chronic kidney disease, and the dosage of diabetes medications should be adjusted to minimize side effects in patients with kidney problems.
Tailoring care to setting
Finally, the guideline addresses special settings and populations, including managing diabetes in hospitals or nursing homes, or in patients who are transitioning to homes or long-term care facilities. Recommendations in this category include simplifying medications for older adults with terminal illness or severe comorbidities, as well as setting glycemic targets as part of a hospital discharge plan.
“The most important aspect of successful transition is effective, detailed, and thorough bidirectional communication between the discharging and receiving teams of health care providers,” the writers emphasized.
The guideline is cosponsored by the European Society of Endocrinology, the Gerontological Society of America, and the Obesity Society. The chair of the committee had no relevant financial conflicts to disclose, and at least 50% of the committee members were free of relevant conflicts of interest.
SOURCE: LeRoith D et al. J Clin Endocrinol Metab. 2019;104:1520-74.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
AGA issues guideline for watery diarrhea
A new guideline from the American Gastroenterological Association (AGA) aims to help physicians diagnose the cause of chronic watery diarrhea, particularly to exclude diagnoses other than functional diarrhea or diarrhea-predominant irritable bowel syndrome (IBS). The guideline, published in Gastroenterology, does not apply to patients with concerning presentations like weight loss/anemia, diarrhea with signs of fat malabsorption, bloody diarrhea, cases with a family history of inflammatory bowel disease (IBD), colon cancer, or celiac disease or to those who have traveled to diarrheal disease–related regions.
To rule out IBD, physicians can use either fecal calprotectin (threshold value of 50 microg/g, sensitivity, 0.81; specificity, 0.87) or fecal lactoferrin (threshold, 4.0-7.25 mcg/g; pooled sensitivity for IBD, 0.79; specificity, 0.93). Neither erythrocyte sedimentation rate (ESR) nor C-reactive protein (CRP) should be used to diagnose IBD because tests have shown low pooled sensitivity and specificity. CRP might be useful in settings in which fecal lactoferrin or calprotectin tests are not available or covered by insurance.
Patients should be tested for giardia infection, using the antigen test or PCR, because this pathogen is common in the United States and easily treated.
Patients who have not recently traveled to or from high-risk areas should not be tested for ova and parasites because this is unlikely to identify a culprit. There are other guidelines for treating patients who have traveled to high-risk countries.
Celiac disease should be tested for using immunoglobulin-A tissue transglutaminase (IgA tTG) and a second test (IgG tTG and IgG or IgA deamidated gliadin peptide, or DGP) in case the patient has IgA deficiency that could lead to a false negative on the primary test. Thresholds of 7-15 AU/mL in IgA tTG typically provide sensitivity and specificity greater than 90%. A quantitative IgA level found to be normal confirms the IgA tTG test. In abnormal findings, either IgG tTG or a test for IgG DGP can be used. If no information on IgA levels is available, IgG tTG or IgG DGP can be combined with IgA tTG. Positive celiac disease tests should be confirmed by duodenal biopsy.
Bile acid diarrhea should be tested for in the United States by measuring total bile acids in a 48-hour stool collection to document increased fecal bile acids, or serum fibroblast growth factor 19, to identify defective feedback of bile acid synthesis. The Selenium HomotauroCholic Acid Test (SeHCAT) has moderate diagnostic efficiency, but it is not available in North America. A measurement of serum levels of 7alpha-hydroxy-4-cholesten-3-one (C4), which measures bile acid synthesis, is not yet available.
No recommendation was made for using available serologic tests for the diagnosis of IBS because existing evidence suggests they lack the diagnostic accuracy needed for routine use.
The guideline development was funded by AGA and had no outside funding.
SOURCE: Smalley W et al. Gastroenterology. 2019 Jul 11. doi: 10.1053/j.gastro.2019.07.004.
A new guideline from the American Gastroenterological Association (AGA) aims to help physicians diagnose the cause of chronic watery diarrhea, particularly to exclude diagnoses other than functional diarrhea or diarrhea-predominant irritable bowel syndrome (IBS). The guideline, published in Gastroenterology, does not apply to patients with concerning presentations like weight loss/anemia, diarrhea with signs of fat malabsorption, bloody diarrhea, cases with a family history of inflammatory bowel disease (IBD), colon cancer, or celiac disease or to those who have traveled to diarrheal disease–related regions.
To rule out IBD, physicians can use either fecal calprotectin (threshold value of 50 microg/g, sensitivity, 0.81; specificity, 0.87) or fecal lactoferrin (threshold, 4.0-7.25 mcg/g; pooled sensitivity for IBD, 0.79; specificity, 0.93). Neither erythrocyte sedimentation rate (ESR) nor C-reactive protein (CRP) should be used to diagnose IBD because tests have shown low pooled sensitivity and specificity. CRP might be useful in settings in which fecal lactoferrin or calprotectin tests are not available or covered by insurance.
Patients should be tested for giardia infection, using the antigen test or PCR, because this pathogen is common in the United States and easily treated.
Patients who have not recently traveled to or from high-risk areas should not be tested for ova and parasites because this is unlikely to identify a culprit. There are other guidelines for treating patients who have traveled to high-risk countries.
Celiac disease should be tested for using immunoglobulin-A tissue transglutaminase (IgA tTG) and a second test (IgG tTG and IgG or IgA deamidated gliadin peptide, or DGP) in case the patient has IgA deficiency that could lead to a false negative on the primary test. Thresholds of 7-15 AU/mL in IgA tTG typically provide sensitivity and specificity greater than 90%. A quantitative IgA level found to be normal confirms the IgA tTG test. In abnormal findings, either IgG tTG or a test for IgG DGP can be used. If no information on IgA levels is available, IgG tTG or IgG DGP can be combined with IgA tTG. Positive celiac disease tests should be confirmed by duodenal biopsy.
Bile acid diarrhea should be tested for in the United States by measuring total bile acids in a 48-hour stool collection to document increased fecal bile acids, or serum fibroblast growth factor 19, to identify defective feedback of bile acid synthesis. The Selenium HomotauroCholic Acid Test (SeHCAT) has moderate diagnostic efficiency, but it is not available in North America. A measurement of serum levels of 7alpha-hydroxy-4-cholesten-3-one (C4), which measures bile acid synthesis, is not yet available.
No recommendation was made for using available serologic tests for the diagnosis of IBS because existing evidence suggests they lack the diagnostic accuracy needed for routine use.
The guideline development was funded by AGA and had no outside funding.
SOURCE: Smalley W et al. Gastroenterology. 2019 Jul 11. doi: 10.1053/j.gastro.2019.07.004.
A new guideline from the American Gastroenterological Association (AGA) aims to help physicians diagnose the cause of chronic watery diarrhea, particularly to exclude diagnoses other than functional diarrhea or diarrhea-predominant irritable bowel syndrome (IBS). The guideline, published in Gastroenterology, does not apply to patients with concerning presentations like weight loss/anemia, diarrhea with signs of fat malabsorption, bloody diarrhea, cases with a family history of inflammatory bowel disease (IBD), colon cancer, or celiac disease or to those who have traveled to diarrheal disease–related regions.
To rule out IBD, physicians can use either fecal calprotectin (threshold value of 50 microg/g, sensitivity, 0.81; specificity, 0.87) or fecal lactoferrin (threshold, 4.0-7.25 mcg/g; pooled sensitivity for IBD, 0.79; specificity, 0.93). Neither erythrocyte sedimentation rate (ESR) nor C-reactive protein (CRP) should be used to diagnose IBD because tests have shown low pooled sensitivity and specificity. CRP might be useful in settings in which fecal lactoferrin or calprotectin tests are not available or covered by insurance.
Patients should be tested for giardia infection, using the antigen test or PCR, because this pathogen is common in the United States and easily treated.
Patients who have not recently traveled to or from high-risk areas should not be tested for ova and parasites because this is unlikely to identify a culprit. There are other guidelines for treating patients who have traveled to high-risk countries.
Celiac disease should be tested for using immunoglobulin-A tissue transglutaminase (IgA tTG) and a second test (IgG tTG and IgG or IgA deamidated gliadin peptide, or DGP) in case the patient has IgA deficiency that could lead to a false negative on the primary test. Thresholds of 7-15 AU/mL in IgA tTG typically provide sensitivity and specificity greater than 90%. A quantitative IgA level found to be normal confirms the IgA tTG test. In abnormal findings, either IgG tTG or a test for IgG DGP can be used. If no information on IgA levels is available, IgG tTG or IgG DGP can be combined with IgA tTG. Positive celiac disease tests should be confirmed by duodenal biopsy.
Bile acid diarrhea should be tested for in the United States by measuring total bile acids in a 48-hour stool collection to document increased fecal bile acids, or serum fibroblast growth factor 19, to identify defective feedback of bile acid synthesis. The Selenium HomotauroCholic Acid Test (SeHCAT) has moderate diagnostic efficiency, but it is not available in North America. A measurement of serum levels of 7alpha-hydroxy-4-cholesten-3-one (C4), which measures bile acid synthesis, is not yet available.
No recommendation was made for using available serologic tests for the diagnosis of IBS because existing evidence suggests they lack the diagnostic accuracy needed for routine use.
The guideline development was funded by AGA and had no outside funding.
SOURCE: Smalley W et al. Gastroenterology. 2019 Jul 11. doi: 10.1053/j.gastro.2019.07.004.
FROM GASTROENTEROLOGY
First adult APS recommendations released by European society
MADRID – Low-dose aspirin is recommended for the primary prevention of antiphospholipid syndrome (APS) in patients at high risk for developing the condition, according to new recommendations developed by the European League Against Rheumatism (EULAR).
Indeed, the NSAID should be given at a dose of between 75 mg and 100 mg per day, in patients with a “high risk” antiphospholipid (aPL) antibody profile, including asymptomatic aPL antibody carriers, patients with systemic lupus erythematosus (SLE) without APS, and in women who are not pregnant but who have a history of obstetric APS.
The recommendations aim to help guide practice and ultimately to improve the quality of care for patients and their outcomes following treatment, Maria G. Tektonidou, MD, PhD, said at the European Congress of Rheumatology.
The guidance is necessary as “clinical practice in APS remains highly variable,” said Dr. Tektonidou of the National and Kapodistrian University of Athens. This is perhaps because APS is a “rare disease and also because it’s a newly recognized disease – it’s only 35 years old – and knowledge about the clinical spectrum, classification, and management is continuously advancing.”
Dr. Tektonidou, who was the convener of the EULAR Task Force that wrote the recommendations, noted that they were now published in Annals of the Rheumatic Diseases and considered three main groups of patients: those with thrombotic APS, those with obstetric APS, and those with catastrophic APS (CAPS). There are three overarching principles, 12 recommendations, and 29 graded statements, she said.
The three overarching principles concerned risk stratification, general measures for managing patients who test positive for aPL antibodies, and patient education and counseling on various topics, such as treatment adherence, therapeutic drug monitoring, contraceptive use, and lifestyle interventions.
Dr. Tektonidou highlighted how risk stratification was important and that a high-risk aPL profile was defined as the presence of lupus anticoagulant (LA) on at least two occasions, measured 12 weeks apart according to International Society on Thrombosis and Haemostasis guidelines, or the presence of two or even three aPL antibodies, or persistently high aPL antibody titers. By contrast, a low-risk aPL profile was defined as the isolated presence of anticardiolipin (aCL) or anti–beta-2 glycoprotein I antibodies at low-medium titers, particularly if transiently positive.
“Risk stratification should include the determination of the high-risk aPL profile; a prior history of thrombotic or obstetric [APS]; the coexistence of other systemic autoimmune diseases, and the presence of traditional cardiovascular risk factors,” Dr. Tektonidou said.
Four of the recommendations focus on the secondary prevention of APS, giving guidance on anticoagulant treatment with definite APS, first provoked or unprovoked venous thrombosis, and how to manage recurrent venous thrombosis. There also is a recommendation for the management of patients with definite APS and a first arterial thrombosis, outlining the type and intensity of anticoagulant therapy that should be given. Another four of the recommendations focus on the management of obstetric APS, with a focus on how to manage the various types of complications seen in pregnant women. Then the final recommendation concerns CAPS, it’s prevention and first-line treatment, and how to manage refractory patients.
With regards to CAPS, Ricard Cervera, MD, PhD, of the Hospital Clinic of Barcelona, this is “terrible” but “thankfully rare” form of APS that was first described in the early 1990s.
Although fewer than 1% of the APS adult population have CAPS (Arthritis Rheum. 2002;46[4]:1019-27), it’s a condition in which several thrombotic events occur simultaneously, affecting multiple systems or organs and which can be life threatening if not treated quickly.
New treatment guidelines for catastrophic APS
During a separate clinical science session at the conference, Dr. Cervera discussed the development of treatment guidelines for CAPS, noting that this had been one of the focus points of the McMaster RARE-Bestpractices project group in 2016. The group selected CAPS for a pilot exercise in guideline development for a rare disease and published their recommendations in 2018 (J Thromb Haemost. 2018;16:1656-64). Ten recommendations were developed, most of which were conditional, Dr. Cervera said, due to the lack of, or very low certainty, of the evidence.
The new EULAR 2019 adult APS recommendations now include CAPS and recommendation number 12 is split into two parts. The first, part A, states that prompt treatment of infections is needed in all patients positive for aPL antibodies and that anticoagulation should have minimal interruption or be used at level to help prevent the development of CAPS.
The second, part B, states that the first-line treatment of CAPS should be a triple combination therapy of glucocorticoids, heparin, and plasma exchange, or intravenous immunoglobulins, rather than single-agent treatment. Plus, it says that any triggering factor should be treated accordingly.
“Finally,” Dr. Cervera said, “in patients with refractory CAPS, B-cell depletion with rituximab or complement inhibitors, for example eculizumab, may be considered.”
The adult APS recommendations project was funded by EULAR. Dr. Tektonidou and Dr. Cervera reported having no relevant conflicts of interest.
SOURCES: Tektonidou M. Ann Rheum Dis. Jun 2019;78(Suppl 2):59-60. Abstract SP0191, doi: 0.1136/annrheumdis-2019-eular.8601; and Cervera R et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):62. Abstract SP0201. doi: 10.1136/annrheumdis-2019-eular.8444.
MADRID – Low-dose aspirin is recommended for the primary prevention of antiphospholipid syndrome (APS) in patients at high risk for developing the condition, according to new recommendations developed by the European League Against Rheumatism (EULAR).
Indeed, the NSAID should be given at a dose of between 75 mg and 100 mg per day, in patients with a “high risk” antiphospholipid (aPL) antibody profile, including asymptomatic aPL antibody carriers, patients with systemic lupus erythematosus (SLE) without APS, and in women who are not pregnant but who have a history of obstetric APS.
The recommendations aim to help guide practice and ultimately to improve the quality of care for patients and their outcomes following treatment, Maria G. Tektonidou, MD, PhD, said at the European Congress of Rheumatology.
The guidance is necessary as “clinical practice in APS remains highly variable,” said Dr. Tektonidou of the National and Kapodistrian University of Athens. This is perhaps because APS is a “rare disease and also because it’s a newly recognized disease – it’s only 35 years old – and knowledge about the clinical spectrum, classification, and management is continuously advancing.”
Dr. Tektonidou, who was the convener of the EULAR Task Force that wrote the recommendations, noted that they were now published in Annals of the Rheumatic Diseases and considered three main groups of patients: those with thrombotic APS, those with obstetric APS, and those with catastrophic APS (CAPS). There are three overarching principles, 12 recommendations, and 29 graded statements, she said.
The three overarching principles concerned risk stratification, general measures for managing patients who test positive for aPL antibodies, and patient education and counseling on various topics, such as treatment adherence, therapeutic drug monitoring, contraceptive use, and lifestyle interventions.
Dr. Tektonidou highlighted how risk stratification was important and that a high-risk aPL profile was defined as the presence of lupus anticoagulant (LA) on at least two occasions, measured 12 weeks apart according to International Society on Thrombosis and Haemostasis guidelines, or the presence of two or even three aPL antibodies, or persistently high aPL antibody titers. By contrast, a low-risk aPL profile was defined as the isolated presence of anticardiolipin (aCL) or anti–beta-2 glycoprotein I antibodies at low-medium titers, particularly if transiently positive.
“Risk stratification should include the determination of the high-risk aPL profile; a prior history of thrombotic or obstetric [APS]; the coexistence of other systemic autoimmune diseases, and the presence of traditional cardiovascular risk factors,” Dr. Tektonidou said.
Four of the recommendations focus on the secondary prevention of APS, giving guidance on anticoagulant treatment with definite APS, first provoked or unprovoked venous thrombosis, and how to manage recurrent venous thrombosis. There also is a recommendation for the management of patients with definite APS and a first arterial thrombosis, outlining the type and intensity of anticoagulant therapy that should be given. Another four of the recommendations focus on the management of obstetric APS, with a focus on how to manage the various types of complications seen in pregnant women. Then the final recommendation concerns CAPS, it’s prevention and first-line treatment, and how to manage refractory patients.
With regards to CAPS, Ricard Cervera, MD, PhD, of the Hospital Clinic of Barcelona, this is “terrible” but “thankfully rare” form of APS that was first described in the early 1990s.
Although fewer than 1% of the APS adult population have CAPS (Arthritis Rheum. 2002;46[4]:1019-27), it’s a condition in which several thrombotic events occur simultaneously, affecting multiple systems or organs and which can be life threatening if not treated quickly.
New treatment guidelines for catastrophic APS
During a separate clinical science session at the conference, Dr. Cervera discussed the development of treatment guidelines for CAPS, noting that this had been one of the focus points of the McMaster RARE-Bestpractices project group in 2016. The group selected CAPS for a pilot exercise in guideline development for a rare disease and published their recommendations in 2018 (J Thromb Haemost. 2018;16:1656-64). Ten recommendations were developed, most of which were conditional, Dr. Cervera said, due to the lack of, or very low certainty, of the evidence.
The new EULAR 2019 adult APS recommendations now include CAPS and recommendation number 12 is split into two parts. The first, part A, states that prompt treatment of infections is needed in all patients positive for aPL antibodies and that anticoagulation should have minimal interruption or be used at level to help prevent the development of CAPS.
The second, part B, states that the first-line treatment of CAPS should be a triple combination therapy of glucocorticoids, heparin, and plasma exchange, or intravenous immunoglobulins, rather than single-agent treatment. Plus, it says that any triggering factor should be treated accordingly.
“Finally,” Dr. Cervera said, “in patients with refractory CAPS, B-cell depletion with rituximab or complement inhibitors, for example eculizumab, may be considered.”
The adult APS recommendations project was funded by EULAR. Dr. Tektonidou and Dr. Cervera reported having no relevant conflicts of interest.
SOURCES: Tektonidou M. Ann Rheum Dis. Jun 2019;78(Suppl 2):59-60. Abstract SP0191, doi: 0.1136/annrheumdis-2019-eular.8601; and Cervera R et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):62. Abstract SP0201. doi: 10.1136/annrheumdis-2019-eular.8444.
MADRID – Low-dose aspirin is recommended for the primary prevention of antiphospholipid syndrome (APS) in patients at high risk for developing the condition, according to new recommendations developed by the European League Against Rheumatism (EULAR).
Indeed, the NSAID should be given at a dose of between 75 mg and 100 mg per day, in patients with a “high risk” antiphospholipid (aPL) antibody profile, including asymptomatic aPL antibody carriers, patients with systemic lupus erythematosus (SLE) without APS, and in women who are not pregnant but who have a history of obstetric APS.
The recommendations aim to help guide practice and ultimately to improve the quality of care for patients and their outcomes following treatment, Maria G. Tektonidou, MD, PhD, said at the European Congress of Rheumatology.
The guidance is necessary as “clinical practice in APS remains highly variable,” said Dr. Tektonidou of the National and Kapodistrian University of Athens. This is perhaps because APS is a “rare disease and also because it’s a newly recognized disease – it’s only 35 years old – and knowledge about the clinical spectrum, classification, and management is continuously advancing.”
Dr. Tektonidou, who was the convener of the EULAR Task Force that wrote the recommendations, noted that they were now published in Annals of the Rheumatic Diseases and considered three main groups of patients: those with thrombotic APS, those with obstetric APS, and those with catastrophic APS (CAPS). There are three overarching principles, 12 recommendations, and 29 graded statements, she said.
The three overarching principles concerned risk stratification, general measures for managing patients who test positive for aPL antibodies, and patient education and counseling on various topics, such as treatment adherence, therapeutic drug monitoring, contraceptive use, and lifestyle interventions.
Dr. Tektonidou highlighted how risk stratification was important and that a high-risk aPL profile was defined as the presence of lupus anticoagulant (LA) on at least two occasions, measured 12 weeks apart according to International Society on Thrombosis and Haemostasis guidelines, or the presence of two or even three aPL antibodies, or persistently high aPL antibody titers. By contrast, a low-risk aPL profile was defined as the isolated presence of anticardiolipin (aCL) or anti–beta-2 glycoprotein I antibodies at low-medium titers, particularly if transiently positive.
“Risk stratification should include the determination of the high-risk aPL profile; a prior history of thrombotic or obstetric [APS]; the coexistence of other systemic autoimmune diseases, and the presence of traditional cardiovascular risk factors,” Dr. Tektonidou said.
Four of the recommendations focus on the secondary prevention of APS, giving guidance on anticoagulant treatment with definite APS, first provoked or unprovoked venous thrombosis, and how to manage recurrent venous thrombosis. There also is a recommendation for the management of patients with definite APS and a first arterial thrombosis, outlining the type and intensity of anticoagulant therapy that should be given. Another four of the recommendations focus on the management of obstetric APS, with a focus on how to manage the various types of complications seen in pregnant women. Then the final recommendation concerns CAPS, it’s prevention and first-line treatment, and how to manage refractory patients.
With regards to CAPS, Ricard Cervera, MD, PhD, of the Hospital Clinic of Barcelona, this is “terrible” but “thankfully rare” form of APS that was first described in the early 1990s.
Although fewer than 1% of the APS adult population have CAPS (Arthritis Rheum. 2002;46[4]:1019-27), it’s a condition in which several thrombotic events occur simultaneously, affecting multiple systems or organs and which can be life threatening if not treated quickly.
New treatment guidelines for catastrophic APS
During a separate clinical science session at the conference, Dr. Cervera discussed the development of treatment guidelines for CAPS, noting that this had been one of the focus points of the McMaster RARE-Bestpractices project group in 2016. The group selected CAPS for a pilot exercise in guideline development for a rare disease and published their recommendations in 2018 (J Thromb Haemost. 2018;16:1656-64). Ten recommendations were developed, most of which were conditional, Dr. Cervera said, due to the lack of, or very low certainty, of the evidence.
The new EULAR 2019 adult APS recommendations now include CAPS and recommendation number 12 is split into two parts. The first, part A, states that prompt treatment of infections is needed in all patients positive for aPL antibodies and that anticoagulation should have minimal interruption or be used at level to help prevent the development of CAPS.
The second, part B, states that the first-line treatment of CAPS should be a triple combination therapy of glucocorticoids, heparin, and plasma exchange, or intravenous immunoglobulins, rather than single-agent treatment. Plus, it says that any triggering factor should be treated accordingly.
“Finally,” Dr. Cervera said, “in patients with refractory CAPS, B-cell depletion with rituximab or complement inhibitors, for example eculizumab, may be considered.”
The adult APS recommendations project was funded by EULAR. Dr. Tektonidou and Dr. Cervera reported having no relevant conflicts of interest.
SOURCES: Tektonidou M. Ann Rheum Dis. Jun 2019;78(Suppl 2):59-60. Abstract SP0191, doi: 0.1136/annrheumdis-2019-eular.8601; and Cervera R et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):62. Abstract SP0201. doi: 10.1136/annrheumdis-2019-eular.8444.
REPORTING FROM THE EULAR 2019 Congress
Guidelines update donor selection criteria for HSCT
Newly updated guidelines can inform the selection of adult donors and cord blood units for allogeneic hematopoietic stem cell transplant.
The evidence-based guidelines suggest high-resolution human leukocyte antigen (HLA) matching and donor age are important when selecting adult donors, while HLA matching, cell dose, and banking practices should be considered when selecting cord blood units.
The guidelines were developed by the National Marrow Donor Program (NMDP) and Center for International Blood and Marrow Transplant Research (CIBMTR) and were recently published in Blood.
Adult donors
The guidelines recommend high-resolution HLA typing for adult donors and patients. This means typing for HLA-A, -B, -C, and -DRB1, at minimum. Typing at other loci – DPB1, DQB1, DRB3/4/5, DQA1, and DPA1 – is “optional but often helpful.”
An 8/8 HLA-matched donor is considered optimal. If only 7/8-matched donors are available, select a donor with a single allele mismatched at the patient’s homozygous locus if possible, and select an HLA-C*03:03 mismatch over an HLA-C*03:04 mismatch where applicable.
For both 8/8- and 7/8-matched donors, try to avoid mismatches at DQB1 and DRB3/4/5, and select DPB1 mismatches based on the DPB1 T-cell epitope algorithm. Mismatches of allotypes targeted by donor-specific HLA antibodies (DSA), including DQA1 and DPA1, should be avoided.
The guidelines recommend pursuing multiple donors because not all potential donors will be available. Younger donors should be prioritized over older donors. Other factors – such as sex or cytomegalovirus serostatus – should not affect donor selection.
Cord blood
For cord blood donations, testing attached segment identity is mandatory, red blood cell–replete units are not recommended, and both unit cryovolume and year of cryopreservation should be taken into consideration. The guidelines note that “some expert centers” favor red blood cell–depleted units with a postcryopreservation volume of about 25 ml/bag, and units banked more recently “may be linked to optimal banking practices.”
The guidelines recommend a minimum of eight high-resolution HLA typing for cord blood units and patients. A 4/6 match (HLA-A, -B, -DRB1) is acceptable, as is a 4/8 match (HLA-A, -B, -C, and -DRB1) or greater. In the case of a double-unit transplant, there is no need to match the units to each other.
“DSA must be considered on a case-by-case basis,” according to the guidelines. The patient’s diagnosis, prior immunosuppressive therapy, planned conditioning regimen, and DSA number/titer/specificity/complement fixation should be taken into consideration. DSA-targeted units should be avoided in patients with nonmalignant conditions and used with caution in patients with hematologic malignancies.
For single–cord blood units, the total nucleated cell dose should be at least 2.5 x 107/kg, and the number of CD34+ cells should be at least 1.5 x 105/kg. For double-unit transplants, the total nucleated cell dose should be at least 1.5 x 107/kg for each unit, and the number of CD34+ cells should be at least 1.0 x 105/kg for each unit.
The guidelines note that additional research is needed to inform how to balance cell dose against HLA match. However, cell dose should often take priority over HLA match for adults and larger pediatric patients, and HLA match can take priority in children, smaller adults, or patients with common HLA typing who have multiple units with a high cell dose.
The guidelines’ authors reported relationships with MolMed, NexImmune, AbbVie, Bellicum, Incyte, Medigene, Merck, Nektar, Novartis, Servier, Miltenyi, and the U.S. government/military.
SOURCE: Dehn J et al. Blood. 2019 Jul 10. doi: 10.1182/blood.2019001212.
Newly updated guidelines can inform the selection of adult donors and cord blood units for allogeneic hematopoietic stem cell transplant.
The evidence-based guidelines suggest high-resolution human leukocyte antigen (HLA) matching and donor age are important when selecting adult donors, while HLA matching, cell dose, and banking practices should be considered when selecting cord blood units.
The guidelines were developed by the National Marrow Donor Program (NMDP) and Center for International Blood and Marrow Transplant Research (CIBMTR) and were recently published in Blood.
Adult donors
The guidelines recommend high-resolution HLA typing for adult donors and patients. This means typing for HLA-A, -B, -C, and -DRB1, at minimum. Typing at other loci – DPB1, DQB1, DRB3/4/5, DQA1, and DPA1 – is “optional but often helpful.”
An 8/8 HLA-matched donor is considered optimal. If only 7/8-matched donors are available, select a donor with a single allele mismatched at the patient’s homozygous locus if possible, and select an HLA-C*03:03 mismatch over an HLA-C*03:04 mismatch where applicable.
For both 8/8- and 7/8-matched donors, try to avoid mismatches at DQB1 and DRB3/4/5, and select DPB1 mismatches based on the DPB1 T-cell epitope algorithm. Mismatches of allotypes targeted by donor-specific HLA antibodies (DSA), including DQA1 and DPA1, should be avoided.
The guidelines recommend pursuing multiple donors because not all potential donors will be available. Younger donors should be prioritized over older donors. Other factors – such as sex or cytomegalovirus serostatus – should not affect donor selection.
Cord blood
For cord blood donations, testing attached segment identity is mandatory, red blood cell–replete units are not recommended, and both unit cryovolume and year of cryopreservation should be taken into consideration. The guidelines note that “some expert centers” favor red blood cell–depleted units with a postcryopreservation volume of about 25 ml/bag, and units banked more recently “may be linked to optimal banking practices.”
The guidelines recommend a minimum of eight high-resolution HLA typing for cord blood units and patients. A 4/6 match (HLA-A, -B, -DRB1) is acceptable, as is a 4/8 match (HLA-A, -B, -C, and -DRB1) or greater. In the case of a double-unit transplant, there is no need to match the units to each other.
“DSA must be considered on a case-by-case basis,” according to the guidelines. The patient’s diagnosis, prior immunosuppressive therapy, planned conditioning regimen, and DSA number/titer/specificity/complement fixation should be taken into consideration. DSA-targeted units should be avoided in patients with nonmalignant conditions and used with caution in patients with hematologic malignancies.
For single–cord blood units, the total nucleated cell dose should be at least 2.5 x 107/kg, and the number of CD34+ cells should be at least 1.5 x 105/kg. For double-unit transplants, the total nucleated cell dose should be at least 1.5 x 107/kg for each unit, and the number of CD34+ cells should be at least 1.0 x 105/kg for each unit.
The guidelines note that additional research is needed to inform how to balance cell dose against HLA match. However, cell dose should often take priority over HLA match for adults and larger pediatric patients, and HLA match can take priority in children, smaller adults, or patients with common HLA typing who have multiple units with a high cell dose.
The guidelines’ authors reported relationships with MolMed, NexImmune, AbbVie, Bellicum, Incyte, Medigene, Merck, Nektar, Novartis, Servier, Miltenyi, and the U.S. government/military.
SOURCE: Dehn J et al. Blood. 2019 Jul 10. doi: 10.1182/blood.2019001212.
Newly updated guidelines can inform the selection of adult donors and cord blood units for allogeneic hematopoietic stem cell transplant.
The evidence-based guidelines suggest high-resolution human leukocyte antigen (HLA) matching and donor age are important when selecting adult donors, while HLA matching, cell dose, and banking practices should be considered when selecting cord blood units.
The guidelines were developed by the National Marrow Donor Program (NMDP) and Center for International Blood and Marrow Transplant Research (CIBMTR) and were recently published in Blood.
Adult donors
The guidelines recommend high-resolution HLA typing for adult donors and patients. This means typing for HLA-A, -B, -C, and -DRB1, at minimum. Typing at other loci – DPB1, DQB1, DRB3/4/5, DQA1, and DPA1 – is “optional but often helpful.”
An 8/8 HLA-matched donor is considered optimal. If only 7/8-matched donors are available, select a donor with a single allele mismatched at the patient’s homozygous locus if possible, and select an HLA-C*03:03 mismatch over an HLA-C*03:04 mismatch where applicable.
For both 8/8- and 7/8-matched donors, try to avoid mismatches at DQB1 and DRB3/4/5, and select DPB1 mismatches based on the DPB1 T-cell epitope algorithm. Mismatches of allotypes targeted by donor-specific HLA antibodies (DSA), including DQA1 and DPA1, should be avoided.
The guidelines recommend pursuing multiple donors because not all potential donors will be available. Younger donors should be prioritized over older donors. Other factors – such as sex or cytomegalovirus serostatus – should not affect donor selection.
Cord blood
For cord blood donations, testing attached segment identity is mandatory, red blood cell–replete units are not recommended, and both unit cryovolume and year of cryopreservation should be taken into consideration. The guidelines note that “some expert centers” favor red blood cell–depleted units with a postcryopreservation volume of about 25 ml/bag, and units banked more recently “may be linked to optimal banking practices.”
The guidelines recommend a minimum of eight high-resolution HLA typing for cord blood units and patients. A 4/6 match (HLA-A, -B, -DRB1) is acceptable, as is a 4/8 match (HLA-A, -B, -C, and -DRB1) or greater. In the case of a double-unit transplant, there is no need to match the units to each other.
“DSA must be considered on a case-by-case basis,” according to the guidelines. The patient’s diagnosis, prior immunosuppressive therapy, planned conditioning regimen, and DSA number/titer/specificity/complement fixation should be taken into consideration. DSA-targeted units should be avoided in patients with nonmalignant conditions and used with caution in patients with hematologic malignancies.
For single–cord blood units, the total nucleated cell dose should be at least 2.5 x 107/kg, and the number of CD34+ cells should be at least 1.5 x 105/kg. For double-unit transplants, the total nucleated cell dose should be at least 1.5 x 107/kg for each unit, and the number of CD34+ cells should be at least 1.0 x 105/kg for each unit.
The guidelines note that additional research is needed to inform how to balance cell dose against HLA match. However, cell dose should often take priority over HLA match for adults and larger pediatric patients, and HLA match can take priority in children, smaller adults, or patients with common HLA typing who have multiple units with a high cell dose.
The guidelines’ authors reported relationships with MolMed, NexImmune, AbbVie, Bellicum, Incyte, Medigene, Merck, Nektar, Novartis, Servier, Miltenyi, and the U.S. government/military.
SOURCE: Dehn J et al. Blood. 2019 Jul 10. doi: 10.1182/blood.2019001212.
FROM BLOOD
EULAR keeps csDMARDs as top PsA drugs
MADRID – The draft revision of the European League Against Rheumatism’s recommendations for managing psoriatic arthritis sticks with the group’s already-existing conviction that psoriatic arthritis treatment best starts with an NSAID, and if that fails follow with a conventional synthetic antirheumatic drug such as methotrexate, a position in stark contrast with the 2018 recommendation from the American College of Rheumatology to first treat with a tumor necrosis factor (TNF) inhibitor.
For patients with psoriatic arthritis (PsA) manifesting with polyarthritis, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) “should be first,” and should “start rapidly” if brief, initial treatment with an NSAID proves inadequate, Laure Gossec, MD, PhD, said while presenting a draft version of an update to the PsA management recommendations from EULAR at the European Congress of Rheumatology.
The EULAR recommendations-revision panel had about the same advice for managing PsA patients with oligoarthritis, monoarthritis, or peripheral arthritis. For oligo- and monoarthritis, “consider a csDMARD after failing NSAIDS, but also consider the patient’s prognostic factors,” like structural damage, and dactylitis. For PsA patients with peripheral arthritis, “it still makes sense to keep csDMARDs as the first line treatment,” said Dr. Gossec, professor of rheumatology at Pitie-Salpétriere Hospital and Sorbonne University, Paris. Once published, the revision will replace existing EULAR recommendations from 2015 (Ann Rheum Dis. 2016 Mar;75[3]:499-510).
The list of csDMARDs she cited included not just methotrexate, still the top csDMARD, but also sulfasalazine and leflunomide as alternatives, she noted, with methotrexate also the preferred csDMARD for patients with skin involvement. When a PsA patient fails at least one csDMARD, then switching to a biologic DMARD is recommended. For a patient with skin involvement, a drug that targets interleukin-17 or IL-12 and -23 is preferred. If skin involvement is not a major issue, then treatment with a TNF inhibitor is equally valid, she said.
The 2018 PsA management guideline from the American College of Rheumatology (ACR) proposed a strikingly different sequence, endorsing initial treatment with a TNF inhibitor first over all other options, including methotrexate and other “oral small molecules” (the ACR term for csDMARD), and also including NSAIDs (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
This schism between EULAR and the ACR could be seen as predictable, given the different constraints the two societies have set for themselves.
“EULAR recommendations take into account drug costs; the ACR guideline is supposed to be agnostic to costs,” explained Philip J. Mease, MD, a rheumatologist at Swedish Medical Center in Seattle and a member of the ACR panel that wrote the 2018 PsA guideline.
In fact it was a study Dr. Mease recently led and reported results from that provided the most recent and perhaps best assessment of a TNF inhibitor, compared with methotrexate, as initial treatment for PsA, with findings that suggest that, although the advice from the two societies may sharply differ, the viewpoints of both groups are evidence based.
The SEAM-PsA (Study of Etanercept and Methotrexate in Subjects with Psoriatic Arthritis) trial randomized 851 PsA patients receiving their first treatment to methotrexate only, the TNF inhibitor etanercept (Enbrel) only, or both drugs. The study’s two coprimary outcomes, the ACR 20 and minimal disease activity responses after 24 weeks, showed that etanercept monotherapy produced these responses in 61% and 36% of patients, respectively, while methotrexate monotherapy produced response rates of 51% and 23%, respectively. Both these differences between etanercept monotherapy and methotrexate monotherapy were statistically significant. Combining methotrexate with etanercept did not produce a significant improvement over etanercept alone.
Interpreting the meaning of this finding for clinical practice “depends on the lens you look through,” Dr. Mease said in an interview. “A lot of patients respond to methotrexate, which is good when treatment resources are challenged. But when there is no resource challenge, the data support going straight to a TNF inhibitor.”
Dr. Gossec confirmed the importance of the SEAM-PsA findings in the writing panel’s decision during discussion of the draft, replying to a question about consideration of the study’s findings. “We carefully looked at the SEAM-PsA trial results, which provide some of the only data we have on methotrexate” for PsA. “We felt that the results were in favor of methotrexate’s efficacy, and therefore did not go against our proposal to keep a graduated approach starting with a csDMARD.”
Patients who fail to receive adequate relief from a csDMARD could then try a biologic DMARD – a TNF inhibitor, IL-17 inhibitor, or IL-12/23 inhibitor, Dr. Gossec said. When skin involvement is minimal, any of these options are possible, she said. If skin involvement is significant, the panel recommended preferentially using an IL-17 or IL-12/23 inhibitor based on head-to-head trials in patients with psoriasis, she said.
When a biologic DMARD is not appropriate or fails, another option is to then try a targeted synthetic DMARD, such as a Janus kinase inhibitor. When none of these options are appropriate, or they all fail, another option for patients with mild oligo- or monoarthritis or in patients with limited skin involvement is apremilast (Otezla), a phosphodiesterase-4 inhibitor. The draft recommendations also advise clinicians to be sure to distinguish fibromyalgia pain from enthesitis involvement, and they introduce the possibility of, with “great caution,” tapering down DMARD treatment in PsA patients who show sustained remission.
Dr. Gossec and Dr. Mease have both been consultants to and received honoraria from several companies. SEAM-PsA was sponsored by Amgen, the company that markets Enbrel.
MADRID – The draft revision of the European League Against Rheumatism’s recommendations for managing psoriatic arthritis sticks with the group’s already-existing conviction that psoriatic arthritis treatment best starts with an NSAID, and if that fails follow with a conventional synthetic antirheumatic drug such as methotrexate, a position in stark contrast with the 2018 recommendation from the American College of Rheumatology to first treat with a tumor necrosis factor (TNF) inhibitor.
For patients with psoriatic arthritis (PsA) manifesting with polyarthritis, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) “should be first,” and should “start rapidly” if brief, initial treatment with an NSAID proves inadequate, Laure Gossec, MD, PhD, said while presenting a draft version of an update to the PsA management recommendations from EULAR at the European Congress of Rheumatology.
The EULAR recommendations-revision panel had about the same advice for managing PsA patients with oligoarthritis, monoarthritis, or peripheral arthritis. For oligo- and monoarthritis, “consider a csDMARD after failing NSAIDS, but also consider the patient’s prognostic factors,” like structural damage, and dactylitis. For PsA patients with peripheral arthritis, “it still makes sense to keep csDMARDs as the first line treatment,” said Dr. Gossec, professor of rheumatology at Pitie-Salpétriere Hospital and Sorbonne University, Paris. Once published, the revision will replace existing EULAR recommendations from 2015 (Ann Rheum Dis. 2016 Mar;75[3]:499-510).
The list of csDMARDs she cited included not just methotrexate, still the top csDMARD, but also sulfasalazine and leflunomide as alternatives, she noted, with methotrexate also the preferred csDMARD for patients with skin involvement. When a PsA patient fails at least one csDMARD, then switching to a biologic DMARD is recommended. For a patient with skin involvement, a drug that targets interleukin-17 or IL-12 and -23 is preferred. If skin involvement is not a major issue, then treatment with a TNF inhibitor is equally valid, she said.
The 2018 PsA management guideline from the American College of Rheumatology (ACR) proposed a strikingly different sequence, endorsing initial treatment with a TNF inhibitor first over all other options, including methotrexate and other “oral small molecules” (the ACR term for csDMARD), and also including NSAIDs (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
This schism between EULAR and the ACR could be seen as predictable, given the different constraints the two societies have set for themselves.
“EULAR recommendations take into account drug costs; the ACR guideline is supposed to be agnostic to costs,” explained Philip J. Mease, MD, a rheumatologist at Swedish Medical Center in Seattle and a member of the ACR panel that wrote the 2018 PsA guideline.
In fact it was a study Dr. Mease recently led and reported results from that provided the most recent and perhaps best assessment of a TNF inhibitor, compared with methotrexate, as initial treatment for PsA, with findings that suggest that, although the advice from the two societies may sharply differ, the viewpoints of both groups are evidence based.
The SEAM-PsA (Study of Etanercept and Methotrexate in Subjects with Psoriatic Arthritis) trial randomized 851 PsA patients receiving their first treatment to methotrexate only, the TNF inhibitor etanercept (Enbrel) only, or both drugs. The study’s two coprimary outcomes, the ACR 20 and minimal disease activity responses after 24 weeks, showed that etanercept monotherapy produced these responses in 61% and 36% of patients, respectively, while methotrexate monotherapy produced response rates of 51% and 23%, respectively. Both these differences between etanercept monotherapy and methotrexate monotherapy were statistically significant. Combining methotrexate with etanercept did not produce a significant improvement over etanercept alone.
Interpreting the meaning of this finding for clinical practice “depends on the lens you look through,” Dr. Mease said in an interview. “A lot of patients respond to methotrexate, which is good when treatment resources are challenged. But when there is no resource challenge, the data support going straight to a TNF inhibitor.”
Dr. Gossec confirmed the importance of the SEAM-PsA findings in the writing panel’s decision during discussion of the draft, replying to a question about consideration of the study’s findings. “We carefully looked at the SEAM-PsA trial results, which provide some of the only data we have on methotrexate” for PsA. “We felt that the results were in favor of methotrexate’s efficacy, and therefore did not go against our proposal to keep a graduated approach starting with a csDMARD.”
Patients who fail to receive adequate relief from a csDMARD could then try a biologic DMARD – a TNF inhibitor, IL-17 inhibitor, or IL-12/23 inhibitor, Dr. Gossec said. When skin involvement is minimal, any of these options are possible, she said. If skin involvement is significant, the panel recommended preferentially using an IL-17 or IL-12/23 inhibitor based on head-to-head trials in patients with psoriasis, she said.
When a biologic DMARD is not appropriate or fails, another option is to then try a targeted synthetic DMARD, such as a Janus kinase inhibitor. When none of these options are appropriate, or they all fail, another option for patients with mild oligo- or monoarthritis or in patients with limited skin involvement is apremilast (Otezla), a phosphodiesterase-4 inhibitor. The draft recommendations also advise clinicians to be sure to distinguish fibromyalgia pain from enthesitis involvement, and they introduce the possibility of, with “great caution,” tapering down DMARD treatment in PsA patients who show sustained remission.
Dr. Gossec and Dr. Mease have both been consultants to and received honoraria from several companies. SEAM-PsA was sponsored by Amgen, the company that markets Enbrel.
MADRID – The draft revision of the European League Against Rheumatism’s recommendations for managing psoriatic arthritis sticks with the group’s already-existing conviction that psoriatic arthritis treatment best starts with an NSAID, and if that fails follow with a conventional synthetic antirheumatic drug such as methotrexate, a position in stark contrast with the 2018 recommendation from the American College of Rheumatology to first treat with a tumor necrosis factor (TNF) inhibitor.
For patients with psoriatic arthritis (PsA) manifesting with polyarthritis, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) “should be first,” and should “start rapidly” if brief, initial treatment with an NSAID proves inadequate, Laure Gossec, MD, PhD, said while presenting a draft version of an update to the PsA management recommendations from EULAR at the European Congress of Rheumatology.
The EULAR recommendations-revision panel had about the same advice for managing PsA patients with oligoarthritis, monoarthritis, or peripheral arthritis. For oligo- and monoarthritis, “consider a csDMARD after failing NSAIDS, but also consider the patient’s prognostic factors,” like structural damage, and dactylitis. For PsA patients with peripheral arthritis, “it still makes sense to keep csDMARDs as the first line treatment,” said Dr. Gossec, professor of rheumatology at Pitie-Salpétriere Hospital and Sorbonne University, Paris. Once published, the revision will replace existing EULAR recommendations from 2015 (Ann Rheum Dis. 2016 Mar;75[3]:499-510).
The list of csDMARDs she cited included not just methotrexate, still the top csDMARD, but also sulfasalazine and leflunomide as alternatives, she noted, with methotrexate also the preferred csDMARD for patients with skin involvement. When a PsA patient fails at least one csDMARD, then switching to a biologic DMARD is recommended. For a patient with skin involvement, a drug that targets interleukin-17 or IL-12 and -23 is preferred. If skin involvement is not a major issue, then treatment with a TNF inhibitor is equally valid, she said.
The 2018 PsA management guideline from the American College of Rheumatology (ACR) proposed a strikingly different sequence, endorsing initial treatment with a TNF inhibitor first over all other options, including methotrexate and other “oral small molecules” (the ACR term for csDMARD), and also including NSAIDs (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
This schism between EULAR and the ACR could be seen as predictable, given the different constraints the two societies have set for themselves.
“EULAR recommendations take into account drug costs; the ACR guideline is supposed to be agnostic to costs,” explained Philip J. Mease, MD, a rheumatologist at Swedish Medical Center in Seattle and a member of the ACR panel that wrote the 2018 PsA guideline.
In fact it was a study Dr. Mease recently led and reported results from that provided the most recent and perhaps best assessment of a TNF inhibitor, compared with methotrexate, as initial treatment for PsA, with findings that suggest that, although the advice from the two societies may sharply differ, the viewpoints of both groups are evidence based.
The SEAM-PsA (Study of Etanercept and Methotrexate in Subjects with Psoriatic Arthritis) trial randomized 851 PsA patients receiving their first treatment to methotrexate only, the TNF inhibitor etanercept (Enbrel) only, or both drugs. The study’s two coprimary outcomes, the ACR 20 and minimal disease activity responses after 24 weeks, showed that etanercept monotherapy produced these responses in 61% and 36% of patients, respectively, while methotrexate monotherapy produced response rates of 51% and 23%, respectively. Both these differences between etanercept monotherapy and methotrexate monotherapy were statistically significant. Combining methotrexate with etanercept did not produce a significant improvement over etanercept alone.
Interpreting the meaning of this finding for clinical practice “depends on the lens you look through,” Dr. Mease said in an interview. “A lot of patients respond to methotrexate, which is good when treatment resources are challenged. But when there is no resource challenge, the data support going straight to a TNF inhibitor.”
Dr. Gossec confirmed the importance of the SEAM-PsA findings in the writing panel’s decision during discussion of the draft, replying to a question about consideration of the study’s findings. “We carefully looked at the SEAM-PsA trial results, which provide some of the only data we have on methotrexate” for PsA. “We felt that the results were in favor of methotrexate’s efficacy, and therefore did not go against our proposal to keep a graduated approach starting with a csDMARD.”
Patients who fail to receive adequate relief from a csDMARD could then try a biologic DMARD – a TNF inhibitor, IL-17 inhibitor, or IL-12/23 inhibitor, Dr. Gossec said. When skin involvement is minimal, any of these options are possible, she said. If skin involvement is significant, the panel recommended preferentially using an IL-17 or IL-12/23 inhibitor based on head-to-head trials in patients with psoriasis, she said.
When a biologic DMARD is not appropriate or fails, another option is to then try a targeted synthetic DMARD, such as a Janus kinase inhibitor. When none of these options are appropriate, or they all fail, another option for patients with mild oligo- or monoarthritis or in patients with limited skin involvement is apremilast (Otezla), a phosphodiesterase-4 inhibitor. The draft recommendations also advise clinicians to be sure to distinguish fibromyalgia pain from enthesitis involvement, and they introduce the possibility of, with “great caution,” tapering down DMARD treatment in PsA patients who show sustained remission.
Dr. Gossec and Dr. Mease have both been consultants to and received honoraria from several companies. SEAM-PsA was sponsored by Amgen, the company that markets Enbrel.
REPORTING FROM EULAR 2019 CONGRESS
Physical activity prevalence shows urban/rural divide
according to the Centers for Disease Control and Prevention.
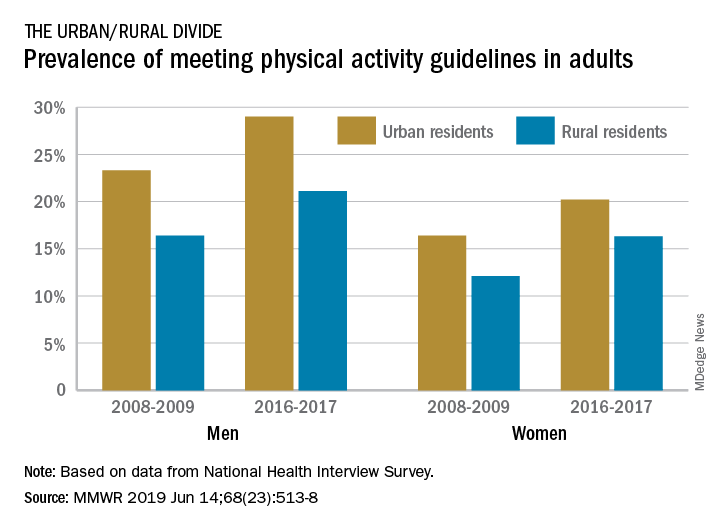
The prevalence of meeting the aerobic and muscle-strengthening recommendations in the 2008 Physical Activity Guidelines for Americans rose from 18.2% of adults in 2008 to 24.3% in 2017, but despite that increase, “insufficient participation in physical activity remains a public health concern,” Geoffrey P. Whitfield, PhD, and his associates said in the Morbidity and Mortality Weekly Report.
There was progress among both urban and rural residents, but those in rural areas were behind at the start of the study period in 2008 and remained behind in 2017. The prevalence of meeting the activity guideline started at 13.3% for rural residents and 19.4% for urbanites and rose to 19.6% and 25.3%, respectively, in 2017 – that’s an annual percentage point change of 0.5% for each population, the investigators reported. Rates among women were well below those of men in both populations.
Rural communities may lack the infrastructure, such as sidewalks, schoolyards, and parks, to support physical activities, or rural residents may get more exercise through occupational and domestic tasks, rather than through the leisure-time activities that are the focus of the National Health Interview Survey, which was the source of the study data, Dr. Whitfield and his associates suggested.
The 2008 federal guidelines recommend that adults get 150-300 minutes of moderate-intensity or 75-150 minutes of vigorous-intensity aerobic physical activity per week, along with muscle-strengthening activities of at least moderate intensity involving all major muscle groups on 2 or more days each week.
SOURCE: Whitfield GP et al. MMWR. 2019 Jun 14;68(23):514-8.
according to the Centers for Disease Control and Prevention.
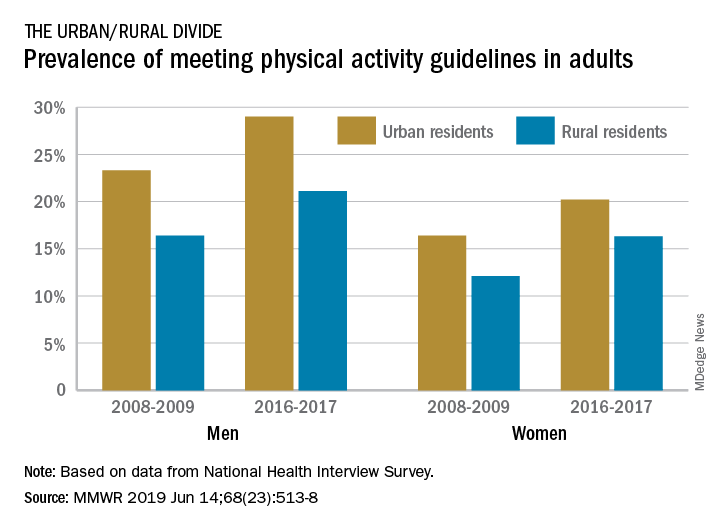
The prevalence of meeting the aerobic and muscle-strengthening recommendations in the 2008 Physical Activity Guidelines for Americans rose from 18.2% of adults in 2008 to 24.3% in 2017, but despite that increase, “insufficient participation in physical activity remains a public health concern,” Geoffrey P. Whitfield, PhD, and his associates said in the Morbidity and Mortality Weekly Report.
There was progress among both urban and rural residents, but those in rural areas were behind at the start of the study period in 2008 and remained behind in 2017. The prevalence of meeting the activity guideline started at 13.3% for rural residents and 19.4% for urbanites and rose to 19.6% and 25.3%, respectively, in 2017 – that’s an annual percentage point change of 0.5% for each population, the investigators reported. Rates among women were well below those of men in both populations.
Rural communities may lack the infrastructure, such as sidewalks, schoolyards, and parks, to support physical activities, or rural residents may get more exercise through occupational and domestic tasks, rather than through the leisure-time activities that are the focus of the National Health Interview Survey, which was the source of the study data, Dr. Whitfield and his associates suggested.
The 2008 federal guidelines recommend that adults get 150-300 minutes of moderate-intensity or 75-150 minutes of vigorous-intensity aerobic physical activity per week, along with muscle-strengthening activities of at least moderate intensity involving all major muscle groups on 2 or more days each week.
SOURCE: Whitfield GP et al. MMWR. 2019 Jun 14;68(23):514-8.
according to the Centers for Disease Control and Prevention.
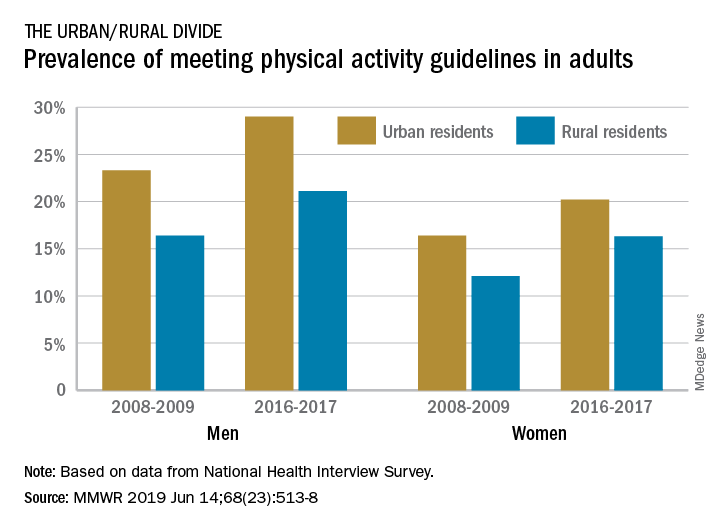
The prevalence of meeting the aerobic and muscle-strengthening recommendations in the 2008 Physical Activity Guidelines for Americans rose from 18.2% of adults in 2008 to 24.3% in 2017, but despite that increase, “insufficient participation in physical activity remains a public health concern,” Geoffrey P. Whitfield, PhD, and his associates said in the Morbidity and Mortality Weekly Report.
There was progress among both urban and rural residents, but those in rural areas were behind at the start of the study period in 2008 and remained behind in 2017. The prevalence of meeting the activity guideline started at 13.3% for rural residents and 19.4% for urbanites and rose to 19.6% and 25.3%, respectively, in 2017 – that’s an annual percentage point change of 0.5% for each population, the investigators reported. Rates among women were well below those of men in both populations.
Rural communities may lack the infrastructure, such as sidewalks, schoolyards, and parks, to support physical activities, or rural residents may get more exercise through occupational and domestic tasks, rather than through the leisure-time activities that are the focus of the National Health Interview Survey, which was the source of the study data, Dr. Whitfield and his associates suggested.
The 2008 federal guidelines recommend that adults get 150-300 minutes of moderate-intensity or 75-150 minutes of vigorous-intensity aerobic physical activity per week, along with muscle-strengthening activities of at least moderate intensity involving all major muscle groups on 2 or more days each week.
SOURCE: Whitfield GP et al. MMWR. 2019 Jun 14;68(23):514-8.
FROM MMWR
EULAR issues guidelines on managing rheumatic complications of cancer immunotherapies
MADRID – EULAR has issued recommendations to help rheumatologists address the increasingly common clinical issue of diagnosing and managing rheumatic-related adverse events associated with cancer immunotherapy.
“The rheumatic adverse events associated with immunotherapy represent a spectrum of new clinical entities, and they are challenging because they can be difficult to control while attempting to preserve the antitumor effects of oncological drugs,” Marie Kostine, MD, of the Centre Universitaire Hospitalier, Bordeaux, France, explained at the European Congress of Rheumatology.
The recommendations were drawn from the deliberations of an expert task force that identified the clinical issues to address and then developed a consensus about best practice recommendations. In addition to rheumatologists with expertise in this field, the task force included oncologists, allied health personnel, and two patient representatives.
The recommendations include four overarching principles and 10 recommendations.
“One of the overarching principles regards the importance of shared decision making between rheumatologists, oncologists, and patients,” Dr. Kostine said. Because of the expertise of rheumatologists in employing immunomodulatory therapies as they pertain to inflammation of the joints, the recommendations emphasize the value of their collaboration in clinical decisions.
The recommendations address patient referral, the assessment of preexisting rheumatic conditions, diagnosis, and therapeutic strategies.
“Rheumatologists should make themselves aware of the wide spectrum of potential clinical presentations of rheumatic adverse events following the initiation of immunotherapy,” Dr. Kostine said. While rheumatoid arthritis–like symptoms are common, the immune activation produced by checkpoint inhibitors and other immunotherapies can affect nearly every organ in the body, which includes diverse involvement of joint tissues.
In addition to joint pain, which has occurred in up to 40% of patients receiving a checkpoint inhibitor in some series, rheumatology-related events can include vasculitis, systemic sclerosis, and lupus. When associated with immunotherapy, these events sometimes develop in the absence of inflammatory markers or autoantibodies.
The new consensus guidelines emphasize that glucocorticoids can be “considered” to control rheumatic-related adverse events despite their immunosuppressive effect. However, because of their potential to attenuate the benefit of immune activation for treatment of the oncologic disease, such drugs, if used, “should be tapered to the lowest effective dose.”
The consensus recommendations were based on an extensive literature review, but Dr. Kostine acknowledged that prospective studies regarding the best practices for managing rheumatic-related adverse events of immunotherapies remain limited. She suggested that this knowledge gap was one reason for creating an expert task force.
“There has been an immunotherapy revolution, such that rheumatologists who have not yet seen these adverse events soon will,” said Dr. Kostine, noting that the number of approved immunotherapies and their clinical indications have been increasing rapidly.
The EULAR recommendations were created specifically for rheumatologists. In addition to guiding them toward best practice, the report from the task force provides background on the clinical issues raised by therapies that cause inflammatory side effects while stimulating immune function to treat malignancy.
MADRID – EULAR has issued recommendations to help rheumatologists address the increasingly common clinical issue of diagnosing and managing rheumatic-related adverse events associated with cancer immunotherapy.
“The rheumatic adverse events associated with immunotherapy represent a spectrum of new clinical entities, and they are challenging because they can be difficult to control while attempting to preserve the antitumor effects of oncological drugs,” Marie Kostine, MD, of the Centre Universitaire Hospitalier, Bordeaux, France, explained at the European Congress of Rheumatology.
The recommendations were drawn from the deliberations of an expert task force that identified the clinical issues to address and then developed a consensus about best practice recommendations. In addition to rheumatologists with expertise in this field, the task force included oncologists, allied health personnel, and two patient representatives.
The recommendations include four overarching principles and 10 recommendations.
“One of the overarching principles regards the importance of shared decision making between rheumatologists, oncologists, and patients,” Dr. Kostine said. Because of the expertise of rheumatologists in employing immunomodulatory therapies as they pertain to inflammation of the joints, the recommendations emphasize the value of their collaboration in clinical decisions.
The recommendations address patient referral, the assessment of preexisting rheumatic conditions, diagnosis, and therapeutic strategies.
“Rheumatologists should make themselves aware of the wide spectrum of potential clinical presentations of rheumatic adverse events following the initiation of immunotherapy,” Dr. Kostine said. While rheumatoid arthritis–like symptoms are common, the immune activation produced by checkpoint inhibitors and other immunotherapies can affect nearly every organ in the body, which includes diverse involvement of joint tissues.
In addition to joint pain, which has occurred in up to 40% of patients receiving a checkpoint inhibitor in some series, rheumatology-related events can include vasculitis, systemic sclerosis, and lupus. When associated with immunotherapy, these events sometimes develop in the absence of inflammatory markers or autoantibodies.
The new consensus guidelines emphasize that glucocorticoids can be “considered” to control rheumatic-related adverse events despite their immunosuppressive effect. However, because of their potential to attenuate the benefit of immune activation for treatment of the oncologic disease, such drugs, if used, “should be tapered to the lowest effective dose.”
The consensus recommendations were based on an extensive literature review, but Dr. Kostine acknowledged that prospective studies regarding the best practices for managing rheumatic-related adverse events of immunotherapies remain limited. She suggested that this knowledge gap was one reason for creating an expert task force.
“There has been an immunotherapy revolution, such that rheumatologists who have not yet seen these adverse events soon will,” said Dr. Kostine, noting that the number of approved immunotherapies and their clinical indications have been increasing rapidly.
The EULAR recommendations were created specifically for rheumatologists. In addition to guiding them toward best practice, the report from the task force provides background on the clinical issues raised by therapies that cause inflammatory side effects while stimulating immune function to treat malignancy.
MADRID – EULAR has issued recommendations to help rheumatologists address the increasingly common clinical issue of diagnosing and managing rheumatic-related adverse events associated with cancer immunotherapy.
“The rheumatic adverse events associated with immunotherapy represent a spectrum of new clinical entities, and they are challenging because they can be difficult to control while attempting to preserve the antitumor effects of oncological drugs,” Marie Kostine, MD, of the Centre Universitaire Hospitalier, Bordeaux, France, explained at the European Congress of Rheumatology.
The recommendations were drawn from the deliberations of an expert task force that identified the clinical issues to address and then developed a consensus about best practice recommendations. In addition to rheumatologists with expertise in this field, the task force included oncologists, allied health personnel, and two patient representatives.
The recommendations include four overarching principles and 10 recommendations.
“One of the overarching principles regards the importance of shared decision making between rheumatologists, oncologists, and patients,” Dr. Kostine said. Because of the expertise of rheumatologists in employing immunomodulatory therapies as they pertain to inflammation of the joints, the recommendations emphasize the value of their collaboration in clinical decisions.
The recommendations address patient referral, the assessment of preexisting rheumatic conditions, diagnosis, and therapeutic strategies.
“Rheumatologists should make themselves aware of the wide spectrum of potential clinical presentations of rheumatic adverse events following the initiation of immunotherapy,” Dr. Kostine said. While rheumatoid arthritis–like symptoms are common, the immune activation produced by checkpoint inhibitors and other immunotherapies can affect nearly every organ in the body, which includes diverse involvement of joint tissues.
In addition to joint pain, which has occurred in up to 40% of patients receiving a checkpoint inhibitor in some series, rheumatology-related events can include vasculitis, systemic sclerosis, and lupus. When associated with immunotherapy, these events sometimes develop in the absence of inflammatory markers or autoantibodies.
The new consensus guidelines emphasize that glucocorticoids can be “considered” to control rheumatic-related adverse events despite their immunosuppressive effect. However, because of their potential to attenuate the benefit of immune activation for treatment of the oncologic disease, such drugs, if used, “should be tapered to the lowest effective dose.”
The consensus recommendations were based on an extensive literature review, but Dr. Kostine acknowledged that prospective studies regarding the best practices for managing rheumatic-related adverse events of immunotherapies remain limited. She suggested that this knowledge gap was one reason for creating an expert task force.
“There has been an immunotherapy revolution, such that rheumatologists who have not yet seen these adverse events soon will,” said Dr. Kostine, noting that the number of approved immunotherapies and their clinical indications have been increasing rapidly.
The EULAR recommendations were created specifically for rheumatologists. In addition to guiding them toward best practice, the report from the task force provides background on the clinical issues raised by therapies that cause inflammatory side effects while stimulating immune function to treat malignancy.
REPORTING FROM EULAR 2019 CONGRESS
AGA introduces pathway to navigate IBD care
Inflammatory bowel disease (IBD) treatment remains a challenge in part because care is often fragmented among providers in different specialties, according to the American Gastroenterological Association. To address the need for provider coordination, the AGA has issued a new referral pathway for IBD care, published in Gastroenterology.
“The goal of this pathway is to offer guidance to primary care, emergency department, and gastroenterology providers, by helping identify patients at risk of or diagnosed with IBD and provide direction on initiating appropriate patient referrals,” wrote lead author Jami Kinnucan, MD, of the University of Michigan, Ann Arbor, and members of the AGA workgroup.
In particular, the pathway focuses on gaps in IBD care related to inflammatory issues, mental health, and nutrition. The work group included not only gastroenterologists, but also a primary care physician, mental/behavioral health specialist, registered dietitian/nutritionist, critical care specialist, nurse practitioner, physician group representative, and a patient advocacy representative.
The pathway identifies the top three areas where IBD patients usually present with symptoms: the emergency department, primary care office, and gastroenterology office.
The work group developed a list of key characteristics associated with increased morbidity, established IBD, or IBD-related complications that can be separated into high-risk, moderate-risk, and low-risk groups to help clinicians determine the timing of and need for referrals.
The pathway uses a sample patient presenting with GI symptoms such as bloody diarrhea; GI bleeding; anemia; fecal urgency; fever; abdominal pain; weight loss; and pain, swelling, or redness in the joints. Clinicians then apply the key characteristics to triage the patients into the risk groups.
High-risk characteristics include history of perianal or severe rectal disease, or deep ulcers in the GI mucosa; two or more emergency department visits for GI problems within the past 6 months, severe anemia, inadequate response to outpatient IBD therapy, history of IBD-related surgery, and malnourishment.
Moderate-risk characteristics include anemia without clinical symptoms, chronic corticosteroid use, and no emergency department or other GI medical visits within the past year.
Low-risk characteristics include chronic narcotic use, one or more comorbidities (such as heart failure, active hepatitis B, oncologic malignancy, lupus, GI infections, primary sclerosing cholangitis, viral hepatitis, and celiac disease), one or more relevant mental health conditions (such as depression, anxiety, or chronic pain), and nonadherence to IBD medical therapies.
“Referrals should be based on the highest level of risk present, in the event that a patient has characteristics that fall in more than one risk category,” the work group wrote.
To further guide clinicians in referring patients with possible or diagnosed IBD to gastroenterology specialists and to mental health and nutrition specialists, the work group developed an IBD Characteristics Assessment Checklist and a Referral Feedback form to accompany the pathway.
The checklist is designed for use by any health care professional to help identify whether a patient needs to be referred based on the key characteristics; the feedback form gives gastroenterologists a template to communicate with referring physicians about comanagement strategies for the patient.
The pathway also includes more details on how clinicians can tackle barriers to mental health and nutrition care for IBD patients.
“Until further evaluations are conducted, the work group encourages the immediate use of the pathway to begin addressing the needed improvements for IBD care coordination and communication between the different IBD providers,” the authors wrote.
Dr. Kinnucan disclosed serving as a consultant for AbbVie, Janssen, and Pfizer and serving on the Patient Education Committee of the Crohn’s and Colitis Foundation.
SOURCE: Kinnucan J et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.03.064.
Inflammatory bowel disease (IBD) treatment remains a challenge in part because care is often fragmented among providers in different specialties, according to the American Gastroenterological Association. To address the need for provider coordination, the AGA has issued a new referral pathway for IBD care, published in Gastroenterology.
“The goal of this pathway is to offer guidance to primary care, emergency department, and gastroenterology providers, by helping identify patients at risk of or diagnosed with IBD and provide direction on initiating appropriate patient referrals,” wrote lead author Jami Kinnucan, MD, of the University of Michigan, Ann Arbor, and members of the AGA workgroup.
In particular, the pathway focuses on gaps in IBD care related to inflammatory issues, mental health, and nutrition. The work group included not only gastroenterologists, but also a primary care physician, mental/behavioral health specialist, registered dietitian/nutritionist, critical care specialist, nurse practitioner, physician group representative, and a patient advocacy representative.
The pathway identifies the top three areas where IBD patients usually present with symptoms: the emergency department, primary care office, and gastroenterology office.
The work group developed a list of key characteristics associated with increased morbidity, established IBD, or IBD-related complications that can be separated into high-risk, moderate-risk, and low-risk groups to help clinicians determine the timing of and need for referrals.
The pathway uses a sample patient presenting with GI symptoms such as bloody diarrhea; GI bleeding; anemia; fecal urgency; fever; abdominal pain; weight loss; and pain, swelling, or redness in the joints. Clinicians then apply the key characteristics to triage the patients into the risk groups.
High-risk characteristics include history of perianal or severe rectal disease, or deep ulcers in the GI mucosa; two or more emergency department visits for GI problems within the past 6 months, severe anemia, inadequate response to outpatient IBD therapy, history of IBD-related surgery, and malnourishment.
Moderate-risk characteristics include anemia without clinical symptoms, chronic corticosteroid use, and no emergency department or other GI medical visits within the past year.
Low-risk characteristics include chronic narcotic use, one or more comorbidities (such as heart failure, active hepatitis B, oncologic malignancy, lupus, GI infections, primary sclerosing cholangitis, viral hepatitis, and celiac disease), one or more relevant mental health conditions (such as depression, anxiety, or chronic pain), and nonadherence to IBD medical therapies.
“Referrals should be based on the highest level of risk present, in the event that a patient has characteristics that fall in more than one risk category,” the work group wrote.
To further guide clinicians in referring patients with possible or diagnosed IBD to gastroenterology specialists and to mental health and nutrition specialists, the work group developed an IBD Characteristics Assessment Checklist and a Referral Feedback form to accompany the pathway.
The checklist is designed for use by any health care professional to help identify whether a patient needs to be referred based on the key characteristics; the feedback form gives gastroenterologists a template to communicate with referring physicians about comanagement strategies for the patient.
The pathway also includes more details on how clinicians can tackle barriers to mental health and nutrition care for IBD patients.
“Until further evaluations are conducted, the work group encourages the immediate use of the pathway to begin addressing the needed improvements for IBD care coordination and communication between the different IBD providers,” the authors wrote.
Dr. Kinnucan disclosed serving as a consultant for AbbVie, Janssen, and Pfizer and serving on the Patient Education Committee of the Crohn’s and Colitis Foundation.
SOURCE: Kinnucan J et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.03.064.
Inflammatory bowel disease (IBD) treatment remains a challenge in part because care is often fragmented among providers in different specialties, according to the American Gastroenterological Association. To address the need for provider coordination, the AGA has issued a new referral pathway for IBD care, published in Gastroenterology.
“The goal of this pathway is to offer guidance to primary care, emergency department, and gastroenterology providers, by helping identify patients at risk of or diagnosed with IBD and provide direction on initiating appropriate patient referrals,” wrote lead author Jami Kinnucan, MD, of the University of Michigan, Ann Arbor, and members of the AGA workgroup.
In particular, the pathway focuses on gaps in IBD care related to inflammatory issues, mental health, and nutrition. The work group included not only gastroenterologists, but also a primary care physician, mental/behavioral health specialist, registered dietitian/nutritionist, critical care specialist, nurse practitioner, physician group representative, and a patient advocacy representative.
The pathway identifies the top three areas where IBD patients usually present with symptoms: the emergency department, primary care office, and gastroenterology office.
The work group developed a list of key characteristics associated with increased morbidity, established IBD, or IBD-related complications that can be separated into high-risk, moderate-risk, and low-risk groups to help clinicians determine the timing of and need for referrals.
The pathway uses a sample patient presenting with GI symptoms such as bloody diarrhea; GI bleeding; anemia; fecal urgency; fever; abdominal pain; weight loss; and pain, swelling, or redness in the joints. Clinicians then apply the key characteristics to triage the patients into the risk groups.
High-risk characteristics include history of perianal or severe rectal disease, or deep ulcers in the GI mucosa; two or more emergency department visits for GI problems within the past 6 months, severe anemia, inadequate response to outpatient IBD therapy, history of IBD-related surgery, and malnourishment.
Moderate-risk characteristics include anemia without clinical symptoms, chronic corticosteroid use, and no emergency department or other GI medical visits within the past year.
Low-risk characteristics include chronic narcotic use, one or more comorbidities (such as heart failure, active hepatitis B, oncologic malignancy, lupus, GI infections, primary sclerosing cholangitis, viral hepatitis, and celiac disease), one or more relevant mental health conditions (such as depression, anxiety, or chronic pain), and nonadherence to IBD medical therapies.
“Referrals should be based on the highest level of risk present, in the event that a patient has characteristics that fall in more than one risk category,” the work group wrote.
To further guide clinicians in referring patients with possible or diagnosed IBD to gastroenterology specialists and to mental health and nutrition specialists, the work group developed an IBD Characteristics Assessment Checklist and a Referral Feedback form to accompany the pathway.
The checklist is designed for use by any health care professional to help identify whether a patient needs to be referred based on the key characteristics; the feedback form gives gastroenterologists a template to communicate with referring physicians about comanagement strategies for the patient.
The pathway also includes more details on how clinicians can tackle barriers to mental health and nutrition care for IBD patients.
“Until further evaluations are conducted, the work group encourages the immediate use of the pathway to begin addressing the needed improvements for IBD care coordination and communication between the different IBD providers,” the authors wrote.
Dr. Kinnucan disclosed serving as a consultant for AbbVie, Janssen, and Pfizer and serving on the Patient Education Committee of the Crohn’s and Colitis Foundation.
SOURCE: Kinnucan J et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.03.064.
FROM GASTROENTEROLOGY
Lipoprotein(a) levels can guide CV risk assessment and treatment
Lipoprotein(a) is an independent risk factor for atherosclerotic cardiovascular disease–related events, and plasma levels of Lp(a) could help refine risk assessment and influence treatment decisions, say the authors of a scientific statement from the National Lipid Association.
Don P. Wilson, MD, of Cook Children’s Medical Center, Fort Worth, Tex., and coauthors reviewed the evidence around testing of Lp(a) in clinical practice and its use in guiding treatment for both primary and secondary prevention. Their report is in the Journal of Clinical Lipidology.
Prospective, population-based studies point to a clear link between high Lp(a) levels and high risk of myocardial infarction, coronary heart disease, coronary artery stenosis, carotid stenosis, valvular aortic stenosis, ischemic stroke, cardiovascular mortality, and all-cause mortality, the authors wrote. This association was independent of the effect of other risk factors, including LDL cholesterol.
However, existing Lp(a) assays have not been globally standardized, and there is only incomplete evidence for age, sex, or ethnicity-specific cutoff points for high risk.
The authors suggested Lp(a) levels greater than 50 mg/dL (100 nmol/L) could be considered a risk factor that justifies the initiation of statin therapy. However ,they pointed out this level corresponded to the 80th population percentile in predominantly white populations, while in African American populations the equivalent cutoff was around 150 nmol/L.
On the issue of whom to test for Lp(a) serum levels, the authors said testing could reasonably be used to refine risk assessment for atherosclerotic cardiovascular disease in adults with first-degree relatives who experienced premature atherosclerotic cardiovascular disease, those with a personal history of the disease, or in those with severe hypercholesterolemia or suspected familial hypercholesterolemia.
However, statin therapy does not decrease Lp(a) levels, and there is also evidence that patients with high Lp(a) levels may not show as much LDL-C lowering in response to statin therapy.
“There is a lack of current evidence demonstrating that lowering Lp(a), independently of LDL-C, reduces ASCVD events in individuals with established ASCVD,” the authors wrote. “It appears that large absolute reductions in Lp(a) may be needed to demonstrate a significant clinical benefit.”
Despite this, the authors argued that in primary prevention, it was reasonable to use a Lp(a) level greater than 50 mg/dL (100 nmol/L) as a “risk-enhancing factor,” and in high-risk or very-high-risk patients with elevated LDL-C, it could prompt use of more intensive therapies.
Five authors disclosed honorarium or advisory board positions with the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Wilson D et al. J Clin Lipidol. 2019 May 17. doi: 10.1016/j.jacl.2019.04.010.
Lipoprotein(a) is an independent risk factor for atherosclerotic cardiovascular disease–related events, and plasma levels of Lp(a) could help refine risk assessment and influence treatment decisions, say the authors of a scientific statement from the National Lipid Association.
Don P. Wilson, MD, of Cook Children’s Medical Center, Fort Worth, Tex., and coauthors reviewed the evidence around testing of Lp(a) in clinical practice and its use in guiding treatment for both primary and secondary prevention. Their report is in the Journal of Clinical Lipidology.
Prospective, population-based studies point to a clear link between high Lp(a) levels and high risk of myocardial infarction, coronary heart disease, coronary artery stenosis, carotid stenosis, valvular aortic stenosis, ischemic stroke, cardiovascular mortality, and all-cause mortality, the authors wrote. This association was independent of the effect of other risk factors, including LDL cholesterol.
However, existing Lp(a) assays have not been globally standardized, and there is only incomplete evidence for age, sex, or ethnicity-specific cutoff points for high risk.
The authors suggested Lp(a) levels greater than 50 mg/dL (100 nmol/L) could be considered a risk factor that justifies the initiation of statin therapy. However ,they pointed out this level corresponded to the 80th population percentile in predominantly white populations, while in African American populations the equivalent cutoff was around 150 nmol/L.
On the issue of whom to test for Lp(a) serum levels, the authors said testing could reasonably be used to refine risk assessment for atherosclerotic cardiovascular disease in adults with first-degree relatives who experienced premature atherosclerotic cardiovascular disease, those with a personal history of the disease, or in those with severe hypercholesterolemia or suspected familial hypercholesterolemia.
However, statin therapy does not decrease Lp(a) levels, and there is also evidence that patients with high Lp(a) levels may not show as much LDL-C lowering in response to statin therapy.
“There is a lack of current evidence demonstrating that lowering Lp(a), independently of LDL-C, reduces ASCVD events in individuals with established ASCVD,” the authors wrote. “It appears that large absolute reductions in Lp(a) may be needed to demonstrate a significant clinical benefit.”
Despite this, the authors argued that in primary prevention, it was reasonable to use a Lp(a) level greater than 50 mg/dL (100 nmol/L) as a “risk-enhancing factor,” and in high-risk or very-high-risk patients with elevated LDL-C, it could prompt use of more intensive therapies.
Five authors disclosed honorarium or advisory board positions with the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Wilson D et al. J Clin Lipidol. 2019 May 17. doi: 10.1016/j.jacl.2019.04.010.
Lipoprotein(a) is an independent risk factor for atherosclerotic cardiovascular disease–related events, and plasma levels of Lp(a) could help refine risk assessment and influence treatment decisions, say the authors of a scientific statement from the National Lipid Association.
Don P. Wilson, MD, of Cook Children’s Medical Center, Fort Worth, Tex., and coauthors reviewed the evidence around testing of Lp(a) in clinical practice and its use in guiding treatment for both primary and secondary prevention. Their report is in the Journal of Clinical Lipidology.
Prospective, population-based studies point to a clear link between high Lp(a) levels and high risk of myocardial infarction, coronary heart disease, coronary artery stenosis, carotid stenosis, valvular aortic stenosis, ischemic stroke, cardiovascular mortality, and all-cause mortality, the authors wrote. This association was independent of the effect of other risk factors, including LDL cholesterol.
However, existing Lp(a) assays have not been globally standardized, and there is only incomplete evidence for age, sex, or ethnicity-specific cutoff points for high risk.
The authors suggested Lp(a) levels greater than 50 mg/dL (100 nmol/L) could be considered a risk factor that justifies the initiation of statin therapy. However ,they pointed out this level corresponded to the 80th population percentile in predominantly white populations, while in African American populations the equivalent cutoff was around 150 nmol/L.
On the issue of whom to test for Lp(a) serum levels, the authors said testing could reasonably be used to refine risk assessment for atherosclerotic cardiovascular disease in adults with first-degree relatives who experienced premature atherosclerotic cardiovascular disease, those with a personal history of the disease, or in those with severe hypercholesterolemia or suspected familial hypercholesterolemia.
However, statin therapy does not decrease Lp(a) levels, and there is also evidence that patients with high Lp(a) levels may not show as much LDL-C lowering in response to statin therapy.
“There is a lack of current evidence demonstrating that lowering Lp(a), independently of LDL-C, reduces ASCVD events in individuals with established ASCVD,” the authors wrote. “It appears that large absolute reductions in Lp(a) may be needed to demonstrate a significant clinical benefit.”
Despite this, the authors argued that in primary prevention, it was reasonable to use a Lp(a) level greater than 50 mg/dL (100 nmol/L) as a “risk-enhancing factor,” and in high-risk or very-high-risk patients with elevated LDL-C, it could prompt use of more intensive therapies.
Five authors disclosed honorarium or advisory board positions with the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Wilson D et al. J Clin Lipidol. 2019 May 17. doi: 10.1016/j.jacl.2019.04.010.
FROM THE JOURNAL OF CLINICAL LIPIDOLOGY







