User login
Large scar after multiple procedures
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
2016 Obstetric code changes that could affect your reimbursement (very soon)
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
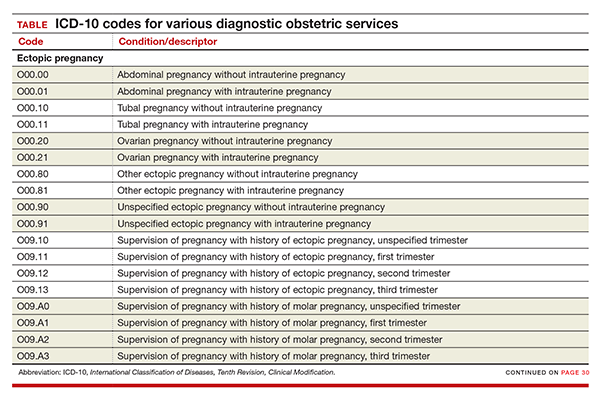
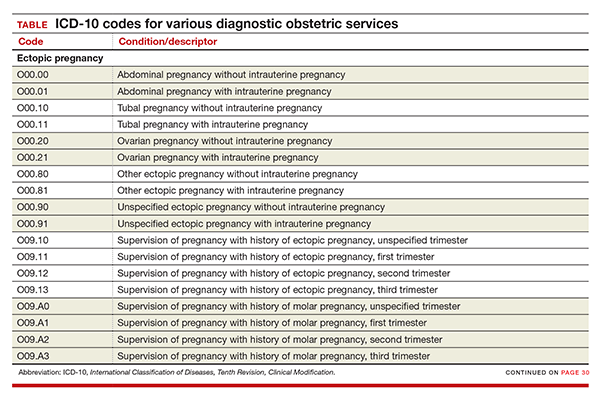
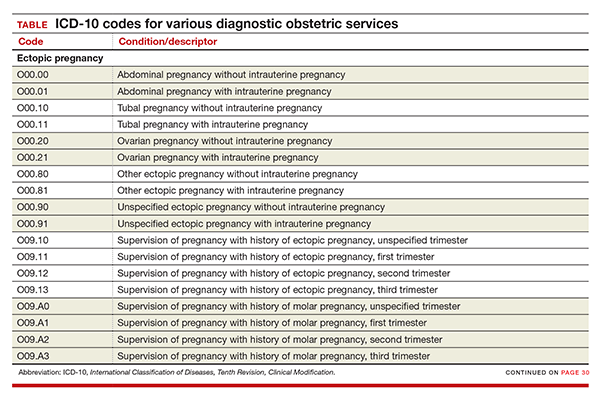
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
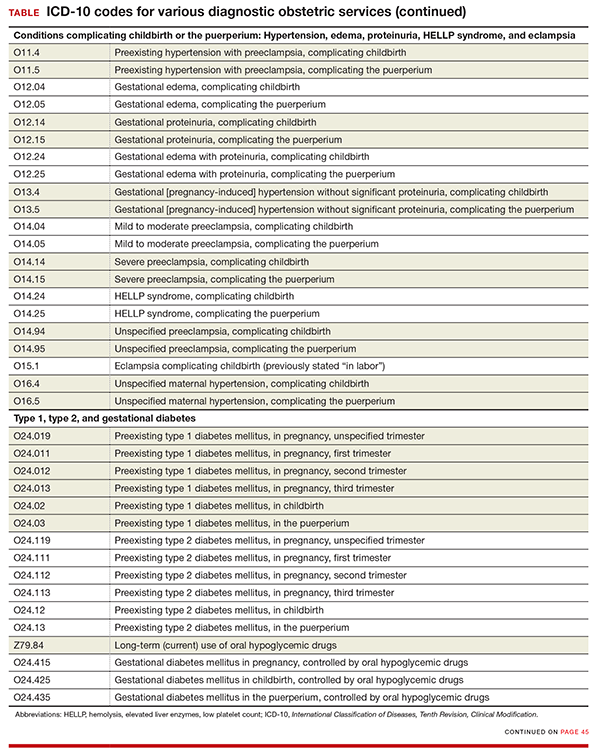
Codes added for complicating conditions of childbirth and the puerperium
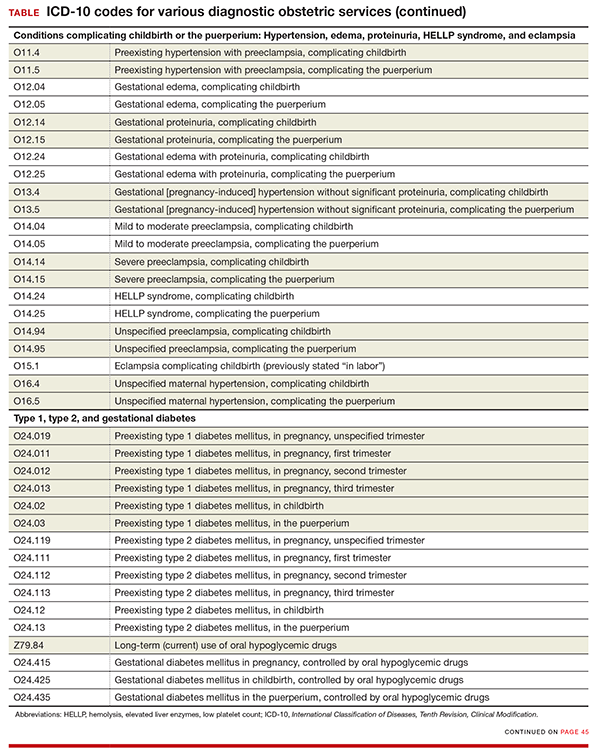
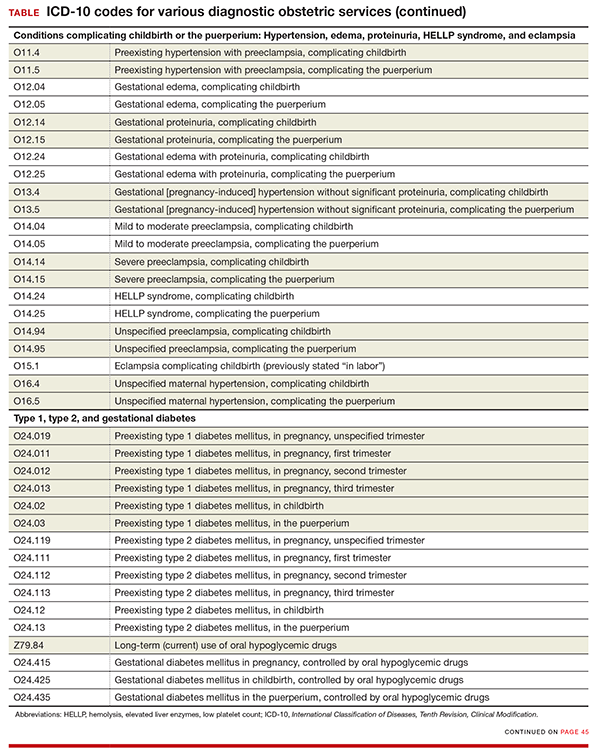
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
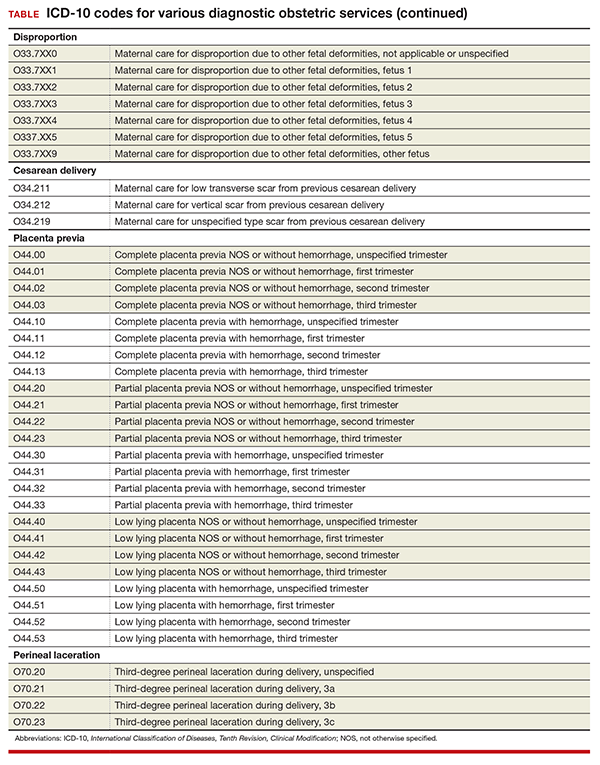
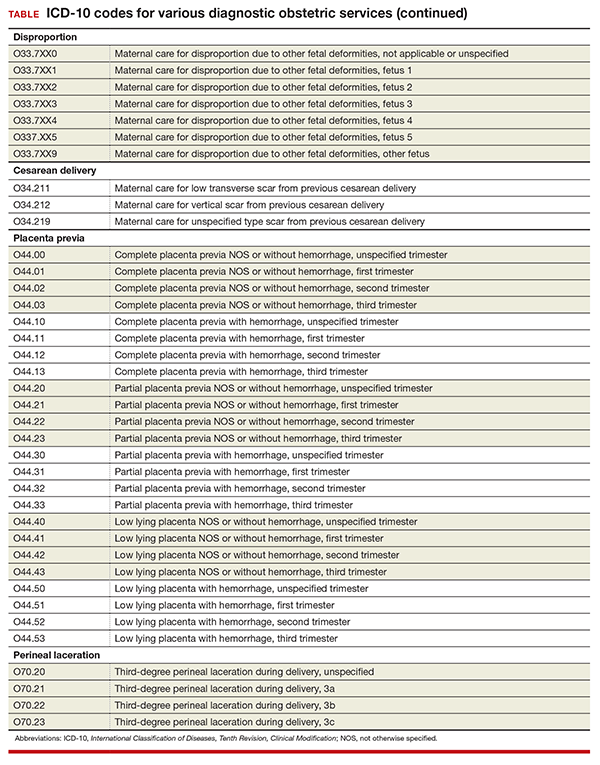
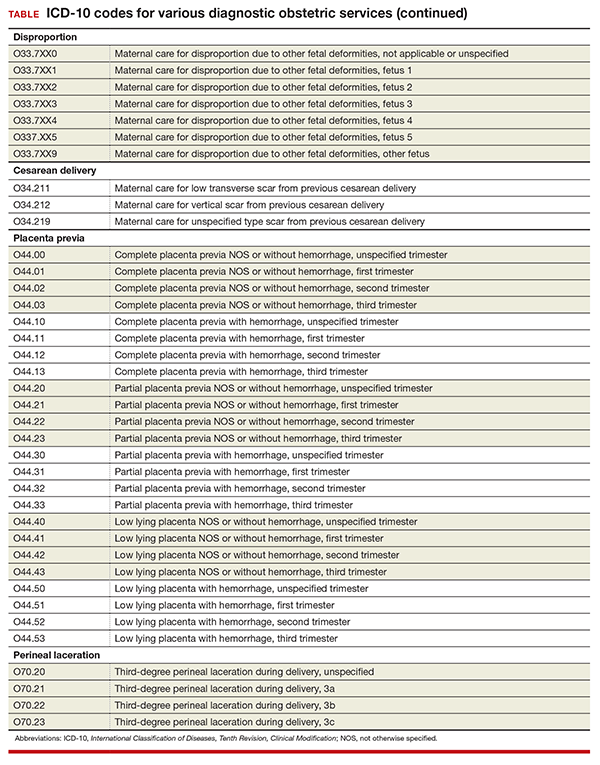
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
In this Article
- New and expanded codes
- Z code additions
- Table of codes
Resolving patients’ complaints
For most physicians, the resolution of patients’ complaints ranks second only to firing an employee on the Least Favorite Tasks List. With so many potential problems, and so many ways patients can react to them, it seems impossible to construct any sort of template for consistent, mutually satisfactory resolutions.
But it can be done, and it’s not as complex as it appears, once you realize that the vast majority of complaints have the same basic root: The patient’s expectations have not been met. Sometimes it’s your fault, sometimes the patient’s, and often a bit of both. Either way, the result is the same: You have an unhappy patient, and you must deal with it.
In most cases, this is not a job you should delegate. Unless the complaint is trivial or purely administrative, you should address it yourself. It’s what you would want if you were the complainant, and it’s often too important to trust to a subordinate.
I have distilled this unpleasant duty down to a simple three-part strategy:
• Discover which expectations went unmet, and why.
• Agree on a solution.
• Learn from the experience, to prevent similar future complaints.
At this point, you may be asking, “Why should I care? Is the personal expenditure of my time and effort necessary to resolve complaints really worth it?” Absolutely, because the old cliché is true: A satisfied patient will refer 5 new patients, but a dissatisfied one will chase away 20 or more. Besides, if the complaint is significant, and you won’t resolve it, the patient is likely to find someone who will; and chances are you won’t like the choice, or the venue – or the eventual resolution.
Of course, the easiest way to deal with complaints is to prevent as many as possible in the first place. Try to nip unrealistic expectations in the bud. Take the time to explain all treatments and procedures, and their most likely outcomes, in a clear and honest manner. And since even the most astute patients will not absorb everything you tell them, make liberal use of written handouts and other visual aids.
And, of course, document everything you have explained. Documentation is like garlic: There is no such thing as too much of it.
But despite your best efforts, there will always be complaints, and handling them is a skill set worth honing. The most important skill in that set is the one most people – especially physicians – do poorly: listening to the complaint. Before you can resolve a problem you have to know what it is, and this is precisely the wrong time to make assumptions or jump to conclusions.
So listen to the entire complaint without interrupting, defending, or justifying. Angry patients don’t care why the problem occurred, and they are not interested in your side of the story. This is not about you, so listen and understand.
As you listen, the unmet expectations will become clear. When the patient is finished, I like to summarize the complaint in that context: “So if I understand you correctly, you expected “X” to happen, but “Y” happened instead.” If I’m wrong, I modify my summary until the patient agrees that I understand the problem.
Once you know the problem, you can talk about a solution. The patient usually has one in mind – additional treatment, a referral elsewhere, a fee adjustment, or sometimes simply an apology. Consider it.
If the patient’s solution is reasonable, by all means, agree to it; if it is unreasonable, try to offer a reasonable alternative. The temptation here is to think more about protecting yourself than making the patient happy, but that often leads to bigger problems. Don’t be defensive. Again, this is not about you.
I am often asked if refunding a fee is a reasonable option. Some patients (and lawyers) will interpret a refund as a tacit admission of guilt, so I generally try to avoid them. However, canceling a small fee for an angry patient can be an expedient solution, and in my opinion looks exactly like what it is: an honest effort to rectify the situation. But in general, additional materials or services, at reduced or waived fees, are a better alternative than refunding money.
Once you have arrived at a mutually satisfactory solution, again, document everything; but consider reserving a “private” chart area for such documentation (unless it is a bona fide clinical issue), so that it won’t go out to referrers and other third parties with copies of your clinical notes. Also, consider having the patient sign off on the documentation, acknowledging that the complaint has been resolved.
Finally, always try to learn something from the experience. Ask yourself how you might prevent a repetition of the complaint, what you did that you can avoid doing next time, and how you might prevent unrealistic expectations in a similar future situation.
Above all, never take complaints personally – even when they are personal. It’s always worth reminding yourself that no matter how hard you try, you can never please everyone.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
For most physicians, the resolution of patients’ complaints ranks second only to firing an employee on the Least Favorite Tasks List. With so many potential problems, and so many ways patients can react to them, it seems impossible to construct any sort of template for consistent, mutually satisfactory resolutions.
But it can be done, and it’s not as complex as it appears, once you realize that the vast majority of complaints have the same basic root: The patient’s expectations have not been met. Sometimes it’s your fault, sometimes the patient’s, and often a bit of both. Either way, the result is the same: You have an unhappy patient, and you must deal with it.
In most cases, this is not a job you should delegate. Unless the complaint is trivial or purely administrative, you should address it yourself. It’s what you would want if you were the complainant, and it’s often too important to trust to a subordinate.
I have distilled this unpleasant duty down to a simple three-part strategy:
• Discover which expectations went unmet, and why.
• Agree on a solution.
• Learn from the experience, to prevent similar future complaints.
At this point, you may be asking, “Why should I care? Is the personal expenditure of my time and effort necessary to resolve complaints really worth it?” Absolutely, because the old cliché is true: A satisfied patient will refer 5 new patients, but a dissatisfied one will chase away 20 or more. Besides, if the complaint is significant, and you won’t resolve it, the patient is likely to find someone who will; and chances are you won’t like the choice, or the venue – or the eventual resolution.
Of course, the easiest way to deal with complaints is to prevent as many as possible in the first place. Try to nip unrealistic expectations in the bud. Take the time to explain all treatments and procedures, and their most likely outcomes, in a clear and honest manner. And since even the most astute patients will not absorb everything you tell them, make liberal use of written handouts and other visual aids.
And, of course, document everything you have explained. Documentation is like garlic: There is no such thing as too much of it.
But despite your best efforts, there will always be complaints, and handling them is a skill set worth honing. The most important skill in that set is the one most people – especially physicians – do poorly: listening to the complaint. Before you can resolve a problem you have to know what it is, and this is precisely the wrong time to make assumptions or jump to conclusions.
So listen to the entire complaint without interrupting, defending, or justifying. Angry patients don’t care why the problem occurred, and they are not interested in your side of the story. This is not about you, so listen and understand.
As you listen, the unmet expectations will become clear. When the patient is finished, I like to summarize the complaint in that context: “So if I understand you correctly, you expected “X” to happen, but “Y” happened instead.” If I’m wrong, I modify my summary until the patient agrees that I understand the problem.
Once you know the problem, you can talk about a solution. The patient usually has one in mind – additional treatment, a referral elsewhere, a fee adjustment, or sometimes simply an apology. Consider it.
If the patient’s solution is reasonable, by all means, agree to it; if it is unreasonable, try to offer a reasonable alternative. The temptation here is to think more about protecting yourself than making the patient happy, but that often leads to bigger problems. Don’t be defensive. Again, this is not about you.
I am often asked if refunding a fee is a reasonable option. Some patients (and lawyers) will interpret a refund as a tacit admission of guilt, so I generally try to avoid them. However, canceling a small fee for an angry patient can be an expedient solution, and in my opinion looks exactly like what it is: an honest effort to rectify the situation. But in general, additional materials or services, at reduced or waived fees, are a better alternative than refunding money.
Once you have arrived at a mutually satisfactory solution, again, document everything; but consider reserving a “private” chart area for such documentation (unless it is a bona fide clinical issue), so that it won’t go out to referrers and other third parties with copies of your clinical notes. Also, consider having the patient sign off on the documentation, acknowledging that the complaint has been resolved.
Finally, always try to learn something from the experience. Ask yourself how you might prevent a repetition of the complaint, what you did that you can avoid doing next time, and how you might prevent unrealistic expectations in a similar future situation.
Above all, never take complaints personally – even when they are personal. It’s always worth reminding yourself that no matter how hard you try, you can never please everyone.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
For most physicians, the resolution of patients’ complaints ranks second only to firing an employee on the Least Favorite Tasks List. With so many potential problems, and so many ways patients can react to them, it seems impossible to construct any sort of template for consistent, mutually satisfactory resolutions.
But it can be done, and it’s not as complex as it appears, once you realize that the vast majority of complaints have the same basic root: The patient’s expectations have not been met. Sometimes it’s your fault, sometimes the patient’s, and often a bit of both. Either way, the result is the same: You have an unhappy patient, and you must deal with it.
In most cases, this is not a job you should delegate. Unless the complaint is trivial or purely administrative, you should address it yourself. It’s what you would want if you were the complainant, and it’s often too important to trust to a subordinate.
I have distilled this unpleasant duty down to a simple three-part strategy:
• Discover which expectations went unmet, and why.
• Agree on a solution.
• Learn from the experience, to prevent similar future complaints.
At this point, you may be asking, “Why should I care? Is the personal expenditure of my time and effort necessary to resolve complaints really worth it?” Absolutely, because the old cliché is true: A satisfied patient will refer 5 new patients, but a dissatisfied one will chase away 20 or more. Besides, if the complaint is significant, and you won’t resolve it, the patient is likely to find someone who will; and chances are you won’t like the choice, or the venue – or the eventual resolution.
Of course, the easiest way to deal with complaints is to prevent as many as possible in the first place. Try to nip unrealistic expectations in the bud. Take the time to explain all treatments and procedures, and their most likely outcomes, in a clear and honest manner. And since even the most astute patients will not absorb everything you tell them, make liberal use of written handouts and other visual aids.
And, of course, document everything you have explained. Documentation is like garlic: There is no such thing as too much of it.
But despite your best efforts, there will always be complaints, and handling them is a skill set worth honing. The most important skill in that set is the one most people – especially physicians – do poorly: listening to the complaint. Before you can resolve a problem you have to know what it is, and this is precisely the wrong time to make assumptions or jump to conclusions.
So listen to the entire complaint without interrupting, defending, or justifying. Angry patients don’t care why the problem occurred, and they are not interested in your side of the story. This is not about you, so listen and understand.
As you listen, the unmet expectations will become clear. When the patient is finished, I like to summarize the complaint in that context: “So if I understand you correctly, you expected “X” to happen, but “Y” happened instead.” If I’m wrong, I modify my summary until the patient agrees that I understand the problem.
Once you know the problem, you can talk about a solution. The patient usually has one in mind – additional treatment, a referral elsewhere, a fee adjustment, or sometimes simply an apology. Consider it.
If the patient’s solution is reasonable, by all means, agree to it; if it is unreasonable, try to offer a reasonable alternative. The temptation here is to think more about protecting yourself than making the patient happy, but that often leads to bigger problems. Don’t be defensive. Again, this is not about you.
I am often asked if refunding a fee is a reasonable option. Some patients (and lawyers) will interpret a refund as a tacit admission of guilt, so I generally try to avoid them. However, canceling a small fee for an angry patient can be an expedient solution, and in my opinion looks exactly like what it is: an honest effort to rectify the situation. But in general, additional materials or services, at reduced or waived fees, are a better alternative than refunding money.
Once you have arrived at a mutually satisfactory solution, again, document everything; but consider reserving a “private” chart area for such documentation (unless it is a bona fide clinical issue), so that it won’t go out to referrers and other third parties with copies of your clinical notes. Also, consider having the patient sign off on the documentation, acknowledging that the complaint has been resolved.
Finally, always try to learn something from the experience. Ask yourself how you might prevent a repetition of the complaint, what you did that you can avoid doing next time, and how you might prevent unrealistic expectations in a similar future situation.
Above all, never take complaints personally – even when they are personal. It’s always worth reminding yourself that no matter how hard you try, you can never please everyone.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Team documentation—the good, the surprising
The clerical work involved in managing the electronic health record (EHR) is clearly not at the top of the skill set for physicians, yet many office-based clinicians find themselves bogged down in this work with no easy way out.
However, practices that are adopting team-based care—where each team member works at the top of his or her skill set—are finding a solution in the form of scribing or team documentation. This approach can ease that burden and perhaps even help to curb physician burnout in the process. But many questions still surround this approach, notably: What do we know about the quality of this documentation?
A recent study published by Misra-Hebert and colleagues reported on this issue.1 It provides some insight—and reason for optimism, especially because the study authors found that outpatient notes from trained staff stack up quite well when compared to those of physicians. Having worked myself with this approach to documentation, I can attest to its benefits, as well.
Team documented notes compare well
There are 2 different ways that physicians can get help with documentation. One involves the use of trained scribes, who come from a variety of backgrounds and are charged with writing down, or scribing, what the physician says. The other involves training staff, usually certified medical assistants (CMAs) or licensed practical nurses (LPNs), to take on a wide variety of additional duties including refill management, care gap closure, and most of the duties concerning the EHR—including documentation.
Misra-Hebert and colleagues studied the second approach in a retrospective chart review of ambulatory progress notes written before and after 8 practice sites transitioned to using medical assistants as scribes. Comparing notes relating to diabetes encounters and same-day appointments, the study authors found important evidence that using staff in this way does not adversely affect—and may even enhance—documentation previously done entirely by physicians. For diabetes encounters, scribed notes were rated higher in overall quality, as well as more up to date, thorough, useful, and comprehensible, than unscribed notes.1
Scribing versus team documentation: terminology can be important
A person who is serving in a medical scribe role is a "personal assistant to the physician; performing documentation in the [electronic health record], gathering information for the patient's visit, and partnering with the physician to deliver the pinnacle of efficient patient care," according to Scribe America, the largest US company that employs scribes, providing their services to hospitals, emergency departments, and outpatient care and urgent care facilities, etc.1
Scribes versus team-based care
Scribe America mainly employs medical students, offering students a way to become exposed to physicians, mentors, and medical care. In fact, they note on their website that "a background in medical scribing is quickly becoming the standard for premedical experience, and is suggested by medical school acceptance committees across the country."2
Bellin Health, and many practices transitioning to team-based care, do not use medical students as scribes but rather "train up" employed certified medical assistants and licensed practical nurses to perform what they call "team documentation." This is the model described by Misra-Hebert and colleagues.3 The advantage is that these licensed health care workers can perform many other aspects of patient care, such as agenda setting and basic health coaching, and can perform additional work in the electronic health record, such as order entry and pending refills.
References
- What is a medical scribe? ScribeAmerica website. http://www.scribeamerica.com/what_is_medical_scribe.html. Accessed June 20, 2016. .
- Why be a medical scribe? ScribeAmerica website. http://www.scribeamerica.com/why_be_a_medical_scribe.html. Accessed June 20, 2016.
- Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65(3):155−159.
In my experience
This change in the way we approach EHRs involves commitment, as I have seen first hand. There needs to be significant training to make this work and there needs to be more staff, since physicians require 2 of these valuable team members to function effectively. (At least that has been our experience.)
How has the physician’s role changed? Prior to team-based care, I would try to enter information into the EHR in the room while seeing the patient. After the visit, I would go to the computer at my station and use voice recognition software to add information. Now, the CMA/LPN does the initial documentation and other EHR work, while I am able to focus on the patient without the distraction of the computer. When I leave the room, the CMA/LPN stays with the patient, arranging necessary tests or consults, scheduling future labs and appointments, and reviewing the chart, all before seeing the next patient.
We are in the process of implementing team-based care throughout our 32-location health care system and have found that using CMAs and LPNs to assist with documentation is a “win” for everyone. And since the problems with burnout and all of the other reasons for making this transformation to team-based care applies to all office-based specialties, we plan to have our entire system adopt this model.
An ObGyn group was the first specialty group to pilot this model in our system. In fact, the American College of Obstetricians and Gynecologists’ interprofessional Task Force of Collaborative Practice published in March 2016 a strong recommendation that all practices across all specialties adopt team-based care.2 Among the aims of this care are that it should “respond to emerging demands and reduce undue burdens on health care providers.”
In order for this transformation to teambased care to be successful and sustainable at Bellin Health, we realized that we had to achieve 3 wins:
A win for the patient. Patients immediately notice that their physicians are now able to focus on them during the office visit, since the physicians no longer have to tend to the demands of the computer. In addition, since the CMAs/LPNs are with patients during the entire visit, the patients bond with them and feel the extra support from this relationship.
A win for the care team. Physician satisfaction has never been higher. Charts are usually closed at the end of each half-day. There is no need to take work home at night. CMAs/LPNs feel empowered and meaningfully involved in patient care. Their increase in satisfaction mirrors that of the physicians.
A win for the system. Not only are quality measures improving, but access improves since this team support increases efficiency. We are able to see more patients per day and are billing at a higher level of service, since there is more time to attend to more of the patient’s needs, thanks to the additional team support.
Team documentation can help bring the joy back
There is much talk about putting joy back into the practice of medicine. But the benchmark of any change needs to be whether it helps our patients. I believe that team documentation does. Happier, less burned-out physicians are able to better focus on patients during their visit. As one patient recently said to me at the end of a visit, “I feel like I’ve got my doctor back.” That is something that patients, and doctors alike, can feel good about.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65(3):155−159.
- Jennings J, Nielson P, Buck, ML, et al. Executive summary: Collaboration in Practice: Implementing Team-Based Care: Report of the American College of Obstetricians and Gynecologists’ Task Force on Collaborative Practice. Obstet Gynecol. 2016;127(3):612−627.
The clerical work involved in managing the electronic health record (EHR) is clearly not at the top of the skill set for physicians, yet many office-based clinicians find themselves bogged down in this work with no easy way out.
However, practices that are adopting team-based care—where each team member works at the top of his or her skill set—are finding a solution in the form of scribing or team documentation. This approach can ease that burden and perhaps even help to curb physician burnout in the process. But many questions still surround this approach, notably: What do we know about the quality of this documentation?
A recent study published by Misra-Hebert and colleagues reported on this issue.1 It provides some insight—and reason for optimism, especially because the study authors found that outpatient notes from trained staff stack up quite well when compared to those of physicians. Having worked myself with this approach to documentation, I can attest to its benefits, as well.
Team documented notes compare well
There are 2 different ways that physicians can get help with documentation. One involves the use of trained scribes, who come from a variety of backgrounds and are charged with writing down, or scribing, what the physician says. The other involves training staff, usually certified medical assistants (CMAs) or licensed practical nurses (LPNs), to take on a wide variety of additional duties including refill management, care gap closure, and most of the duties concerning the EHR—including documentation.
Misra-Hebert and colleagues studied the second approach in a retrospective chart review of ambulatory progress notes written before and after 8 practice sites transitioned to using medical assistants as scribes. Comparing notes relating to diabetes encounters and same-day appointments, the study authors found important evidence that using staff in this way does not adversely affect—and may even enhance—documentation previously done entirely by physicians. For diabetes encounters, scribed notes were rated higher in overall quality, as well as more up to date, thorough, useful, and comprehensible, than unscribed notes.1
Scribing versus team documentation: terminology can be important
A person who is serving in a medical scribe role is a "personal assistant to the physician; performing documentation in the [electronic health record], gathering information for the patient's visit, and partnering with the physician to deliver the pinnacle of efficient patient care," according to Scribe America, the largest US company that employs scribes, providing their services to hospitals, emergency departments, and outpatient care and urgent care facilities, etc.1
Scribes versus team-based care
Scribe America mainly employs medical students, offering students a way to become exposed to physicians, mentors, and medical care. In fact, they note on their website that "a background in medical scribing is quickly becoming the standard for premedical experience, and is suggested by medical school acceptance committees across the country."2
Bellin Health, and many practices transitioning to team-based care, do not use medical students as scribes but rather "train up" employed certified medical assistants and licensed practical nurses to perform what they call "team documentation." This is the model described by Misra-Hebert and colleagues.3 The advantage is that these licensed health care workers can perform many other aspects of patient care, such as agenda setting and basic health coaching, and can perform additional work in the electronic health record, such as order entry and pending refills.
References
- What is a medical scribe? ScribeAmerica website. http://www.scribeamerica.com/what_is_medical_scribe.html. Accessed June 20, 2016. .
- Why be a medical scribe? ScribeAmerica website. http://www.scribeamerica.com/why_be_a_medical_scribe.html. Accessed June 20, 2016.
- Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65(3):155−159.
In my experience
This change in the way we approach EHRs involves commitment, as I have seen first hand. There needs to be significant training to make this work and there needs to be more staff, since physicians require 2 of these valuable team members to function effectively. (At least that has been our experience.)
How has the physician’s role changed? Prior to team-based care, I would try to enter information into the EHR in the room while seeing the patient. After the visit, I would go to the computer at my station and use voice recognition software to add information. Now, the CMA/LPN does the initial documentation and other EHR work, while I am able to focus on the patient without the distraction of the computer. When I leave the room, the CMA/LPN stays with the patient, arranging necessary tests or consults, scheduling future labs and appointments, and reviewing the chart, all before seeing the next patient.
We are in the process of implementing team-based care throughout our 32-location health care system and have found that using CMAs and LPNs to assist with documentation is a “win” for everyone. And since the problems with burnout and all of the other reasons for making this transformation to team-based care applies to all office-based specialties, we plan to have our entire system adopt this model.
An ObGyn group was the first specialty group to pilot this model in our system. In fact, the American College of Obstetricians and Gynecologists’ interprofessional Task Force of Collaborative Practice published in March 2016 a strong recommendation that all practices across all specialties adopt team-based care.2 Among the aims of this care are that it should “respond to emerging demands and reduce undue burdens on health care providers.”
In order for this transformation to teambased care to be successful and sustainable at Bellin Health, we realized that we had to achieve 3 wins:
A win for the patient. Patients immediately notice that their physicians are now able to focus on them during the office visit, since the physicians no longer have to tend to the demands of the computer. In addition, since the CMAs/LPNs are with patients during the entire visit, the patients bond with them and feel the extra support from this relationship.
A win for the care team. Physician satisfaction has never been higher. Charts are usually closed at the end of each half-day. There is no need to take work home at night. CMAs/LPNs feel empowered and meaningfully involved in patient care. Their increase in satisfaction mirrors that of the physicians.
A win for the system. Not only are quality measures improving, but access improves since this team support increases efficiency. We are able to see more patients per day and are billing at a higher level of service, since there is more time to attend to more of the patient’s needs, thanks to the additional team support.
Team documentation can help bring the joy back
There is much talk about putting joy back into the practice of medicine. But the benchmark of any change needs to be whether it helps our patients. I believe that team documentation does. Happier, less burned-out physicians are able to better focus on patients during their visit. As one patient recently said to me at the end of a visit, “I feel like I’ve got my doctor back.” That is something that patients, and doctors alike, can feel good about.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The clerical work involved in managing the electronic health record (EHR) is clearly not at the top of the skill set for physicians, yet many office-based clinicians find themselves bogged down in this work with no easy way out.
However, practices that are adopting team-based care—where each team member works at the top of his or her skill set—are finding a solution in the form of scribing or team documentation. This approach can ease that burden and perhaps even help to curb physician burnout in the process. But many questions still surround this approach, notably: What do we know about the quality of this documentation?
A recent study published by Misra-Hebert and colleagues reported on this issue.1 It provides some insight—and reason for optimism, especially because the study authors found that outpatient notes from trained staff stack up quite well when compared to those of physicians. Having worked myself with this approach to documentation, I can attest to its benefits, as well.
Team documented notes compare well
There are 2 different ways that physicians can get help with documentation. One involves the use of trained scribes, who come from a variety of backgrounds and are charged with writing down, or scribing, what the physician says. The other involves training staff, usually certified medical assistants (CMAs) or licensed practical nurses (LPNs), to take on a wide variety of additional duties including refill management, care gap closure, and most of the duties concerning the EHR—including documentation.
Misra-Hebert and colleagues studied the second approach in a retrospective chart review of ambulatory progress notes written before and after 8 practice sites transitioned to using medical assistants as scribes. Comparing notes relating to diabetes encounters and same-day appointments, the study authors found important evidence that using staff in this way does not adversely affect—and may even enhance—documentation previously done entirely by physicians. For diabetes encounters, scribed notes were rated higher in overall quality, as well as more up to date, thorough, useful, and comprehensible, than unscribed notes.1
Scribing versus team documentation: terminology can be important
A person who is serving in a medical scribe role is a "personal assistant to the physician; performing documentation in the [electronic health record], gathering information for the patient's visit, and partnering with the physician to deliver the pinnacle of efficient patient care," according to Scribe America, the largest US company that employs scribes, providing their services to hospitals, emergency departments, and outpatient care and urgent care facilities, etc.1
Scribes versus team-based care
Scribe America mainly employs medical students, offering students a way to become exposed to physicians, mentors, and medical care. In fact, they note on their website that "a background in medical scribing is quickly becoming the standard for premedical experience, and is suggested by medical school acceptance committees across the country."2
Bellin Health, and many practices transitioning to team-based care, do not use medical students as scribes but rather "train up" employed certified medical assistants and licensed practical nurses to perform what they call "team documentation." This is the model described by Misra-Hebert and colleagues.3 The advantage is that these licensed health care workers can perform many other aspects of patient care, such as agenda setting and basic health coaching, and can perform additional work in the electronic health record, such as order entry and pending refills.
References
- What is a medical scribe? ScribeAmerica website. http://www.scribeamerica.com/what_is_medical_scribe.html. Accessed June 20, 2016. .
- Why be a medical scribe? ScribeAmerica website. http://www.scribeamerica.com/why_be_a_medical_scribe.html. Accessed June 20, 2016.
- Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65(3):155−159.
In my experience
This change in the way we approach EHRs involves commitment, as I have seen first hand. There needs to be significant training to make this work and there needs to be more staff, since physicians require 2 of these valuable team members to function effectively. (At least that has been our experience.)
How has the physician’s role changed? Prior to team-based care, I would try to enter information into the EHR in the room while seeing the patient. After the visit, I would go to the computer at my station and use voice recognition software to add information. Now, the CMA/LPN does the initial documentation and other EHR work, while I am able to focus on the patient without the distraction of the computer. When I leave the room, the CMA/LPN stays with the patient, arranging necessary tests or consults, scheduling future labs and appointments, and reviewing the chart, all before seeing the next patient.
We are in the process of implementing team-based care throughout our 32-location health care system and have found that using CMAs and LPNs to assist with documentation is a “win” for everyone. And since the problems with burnout and all of the other reasons for making this transformation to team-based care applies to all office-based specialties, we plan to have our entire system adopt this model.
An ObGyn group was the first specialty group to pilot this model in our system. In fact, the American College of Obstetricians and Gynecologists’ interprofessional Task Force of Collaborative Practice published in March 2016 a strong recommendation that all practices across all specialties adopt team-based care.2 Among the aims of this care are that it should “respond to emerging demands and reduce undue burdens on health care providers.”
In order for this transformation to teambased care to be successful and sustainable at Bellin Health, we realized that we had to achieve 3 wins:
A win for the patient. Patients immediately notice that their physicians are now able to focus on them during the office visit, since the physicians no longer have to tend to the demands of the computer. In addition, since the CMAs/LPNs are with patients during the entire visit, the patients bond with them and feel the extra support from this relationship.
A win for the care team. Physician satisfaction has never been higher. Charts are usually closed at the end of each half-day. There is no need to take work home at night. CMAs/LPNs feel empowered and meaningfully involved in patient care. Their increase in satisfaction mirrors that of the physicians.
A win for the system. Not only are quality measures improving, but access improves since this team support increases efficiency. We are able to see more patients per day and are billing at a higher level of service, since there is more time to attend to more of the patient’s needs, thanks to the additional team support.
Team documentation can help bring the joy back
There is much talk about putting joy back into the practice of medicine. But the benchmark of any change needs to be whether it helps our patients. I believe that team documentation does. Happier, less burned-out physicians are able to better focus on patients during their visit. As one patient recently said to me at the end of a visit, “I feel like I’ve got my doctor back.” That is something that patients, and doctors alike, can feel good about.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65(3):155−159.
- Jennings J, Nielson P, Buck, ML, et al. Executive summary: Collaboration in Practice: Implementing Team-Based Care: Report of the American College of Obstetricians and Gynecologists’ Task Force on Collaborative Practice. Obstet Gynecol. 2016;127(3):612−627.
- Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65(3):155−159.
- Jennings J, Nielson P, Buck, ML, et al. Executive summary: Collaboration in Practice: Implementing Team-Based Care: Report of the American College of Obstetricians and Gynecologists’ Task Force on Collaborative Practice. Obstet Gynecol. 2016;127(3):612−627.
In this Article
- Scribing vs team documentation
- How has the physician’s role changed?
Public speaking fundamentals. Preparation: Tips that lead to a solid, engaging presentation
Public speaking is one of the best ways to market and promote your skills as a physician. It is an ethical way of communicating and showcasing your areas of interest and expertise to professional or lay audiences. Most physicians and health care professionals take pride in their ability to communicate. After all, that is how we take a history, discuss our findings with patients, and educate individuals on restoring or maintaining their health. Public speaking, though, for the most part is a learned skill. Except for presentations to faculty at bedside or at grand rounds, we have received little training in public speaking.
Few of us are naturally comfortable in front of a live audience or a TV or video camera. But with a little practice and diligent preparation, we can become good or even excellent, confident public speakers. This article—the first in a series of 3—provides you with preparatory tips and techniques to enhance your public speaking skills.
First, know your audience
Whether you are presenting to a group of 20 or 200, you can do certain things in advance to ensure that your presentation achieves the desired response. Most important: Know your audience. Don’t assume the audience is like you. To connect with them, you need to understand why your topic is important to them. What do they expect to learn from the presentation? Each attendee will be asking, “What’s in it for me?”
To keep listeners interested and engaged, you also must know their level of knowledge about the topic. If you are speaking to a group of residents about pelvic organ prolapse, you would use different language and content than if you were speaking to practicing primary care doctors; and these elements would be different again if you were speaking to a group of practicing urogynecologists. It’s insulting to recite basic information to highly knowledgeable physicians, or to present sophisticated technical content and complicated slides to novice physicians or lay people.
When presenting in a foreign country, learn how the culture of the audience differs from yours. How do they dress? What style of humor do they favor? How do they typically communicate? What gestures are appropriate or inappropriate? Are there religious influences to consider?
Practical steps. Before the meeting or event, speak to the organizer or meeting planner and find out the audience’s level of knowledge on the topic. Ask about audience expectations as well as demographics (such as age and background). If you are speaking at an industry event, research the event’s website and familiarize yourself with the mission of the event and who are the typical attendees. If you are presenting to a corporation, learn as much as you can about it by visiting its website, reading news reports, and reviewing associated blogs.
In addition to knowing the needs of the audience, ask the meeting planner about the goals and objectives for the program to make certain you can deliver on the requests.
Know your talk stem to stern
Review your slide material thoroughly. Understand each slide in the presentation and be comfortable with its content.
Avoid reading from slides. Reciting content that viewers can read for themselves breeds boredom and makes them lose interest. Further, when you are looking at the slides, you are not making eye contact with the audience and risk losing their attention. Good speakers are so comfortable with their slides that they can discuss each one without having to look at it.
Rehearse. The best way to achieve the foregoing is to rehearse. Your audience will be able to tell if you took the slide deck directly from a CD and loaded it into a computer and are giving the talk for the first time. You’ll need to know how long the program is to last and how long you are to speak. We suggest you practice with a timer to be certain you do not exceed the allotted time. Rehearse your talk aloud several times with all the props and audiovisual equipment you plan to use. This practice will help to curb filler words such as “ah” and “um.” It is also helpful to practice slide transitions, pauses, and even your breathing.
Prepare for the unexpected, too. Dinner meetings, for instance, may not start on time due to office or hospital delays for attending physicians, possibly resulting in a need to shorten your presentation.
Ask about the meeting agenda. If a meal is to be served, will you be speaking beforehand? This is the least favorable time slot, as you are holding people hostage before they can eat. Our preference is to speak after the appetizer is served and the orders have been taken by the wait staff. This way, attendees are not starving and they have something to drink. You can assure the waiters they won’t be disturbing you, and you can ask them to avoid walking in front of the projector. Ideally, you should end your presentation before dessert arrives and use the remaining time to field questions.
We suggest that you prepare a handout to be distributed at the end of the program, not before. You want your audience focused on you and your slides as you are speaking. Tell the audience you will be providing a handout of your presentation, which will minimize note-taking during your talk.
Your speech opening
The first and last 30 seconds of any speech probably have the most impact.1 Give extra thought, time, and effort to your opening and closing remarks. Do not open with “Good evening, it is a pleasure to be here tonight.” That wastes precious seconds.
While opening a speech with a joke or funny story is the conventional wisdom, ask yourself1:
- Is my selection appropriate to the occasion and for this audience?
- Is it in good taste?
- Does it relate to me (my service) or to the event or the group? Does it support my topic or its key points?
A humorous story or inspirational vignette that relates to your topic or audience can grab the audience’s attention. If you feel that demands more presentation skill than you possess at the outset of your public-speaking career, give the audience what you know and what they most want to hear. You know the questions that you have heard most at cocktail receptions or professional society meetings. So, put the answers to those questions in your speech.
For example. A scientist working with a major corporation was preparing a speech for a lay audience. Since most of the audience did not know what scientists do, he offered the following analogy: “Being a scientist is like doing a jigsaw puzzle in a snowstorm at night...you don’t have all the pieces...and you don’t have the picture on the front of the box to work from.” You can say more with less.1
Your closing
The closing is an important aspect of your speech. Summarize the key elements to your presentation. If you are going to take questions, a good approach is to say, “Before my closing remarks, are there any questions?” Following the questions, finish with a takeaway message that ties into your theme.1
Prepare an autobiographical introduction
We suggest that you write your own introduction and e-mail it to the person who will be introducing you. Let them know it is a suggestion that they are welcome to modify. We have found that most emcees or meeting planners are delighted to have the introduction and will use it just as you have written it. Also bring hard copy with you; many emcees will have forgotten to download what you sent. The figure shows an example of the introduction that one of us (NHB) uses, and you are welcome to modify it for your own use.
Ask about and confirm audiovisual support
Ask the meeting planner ahead of time if they will be providing the computer, projector, and screen. And if, for instance, they will provide a projector but not a computer, make sure the computer you will bring is compatible with their projector. Also, you will probably not require a microphone for a small group, but if you are speaking in a loud restaurant, a portable microphone-speaker system may be helpful.
Arrive early at the program venue to make sure the computers, projector, screen placement, and seating arrangement are all in order. Nothing can sidetrack a speaker (even a seasoned one) like a problem with the computer or equipment setup—for example, your flash drive requiring a USB port cannot connect to the sponsor’s computer, or your program created on a Mac does not run on the sponsor’s PC.
Show time: Getting ready
Another benefit in arriving early, besides being able to check on the equipment, is the chance to greet the audience members as they enter. It is easier to speak to a group of friends than strangers. And if you can remember their names, you can call on them and ask their opinion or how they might manage a patient who has the condition you are discussing. You also could suggest to the meeting planner that name tags for attendees would be helpful.
Warming up. A public speaker, like an athlete, needs to warm up physically before the event. If the facility has an anteroom available, use it for the following exercises suggested by public speaking coach Patricia Fripp1:
- Stand on one leg and shake the other (remove high heels first). When you place your raised foot back on the floor, it will feel lighter than the other one. Repeat the exercise using the other leg. Imagine your energy going down through the floor and up out of your head. While this sounds quite comical, it is not. It is a practical technique used by actors.
- Shake your hands vigorously. Hold them above your head, bending your wrists and elbows, then return your arms to your sides. This will make your hand movements more natural.
- Warm up your facial muscles by chewing in a highly exaggerated way. Do shoulder and neck rolls. Imagine you are at eye level with a clock. As you look at 12 o’clock, pull as much of your face up to the 12 as you can; move your eyes to 3 and repeat, then down to 6, and finally over to 9.
Not only do these exercises warm you up but they also relax you. The exaggerated movements help your movements to flow more naturally.1
This is just the start
Thorough preparation is key to making a solid presentation. But other factors are important too. Your goal is for the audience to take action or to implement suggestions from your presentation. In part 2 of this series, we will share tips on elements of the presentation itself that will encourage audience engagement and message retention. We will discuss how to make your message “stick” and how to make a dynamic, effective presentation that holds your audience’s attention for your entire talk.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Fripp P. Add credibility to your business reputation through public speaking. Patricia Fripp website. http://www.fripp.com/add-credibility-to-your-business-reputation-through-public-speaking/. Accessed June 15, 2016.
Public speaking is one of the best ways to market and promote your skills as a physician. It is an ethical way of communicating and showcasing your areas of interest and expertise to professional or lay audiences. Most physicians and health care professionals take pride in their ability to communicate. After all, that is how we take a history, discuss our findings with patients, and educate individuals on restoring or maintaining their health. Public speaking, though, for the most part is a learned skill. Except for presentations to faculty at bedside or at grand rounds, we have received little training in public speaking.
Few of us are naturally comfortable in front of a live audience or a TV or video camera. But with a little practice and diligent preparation, we can become good or even excellent, confident public speakers. This article—the first in a series of 3—provides you with preparatory tips and techniques to enhance your public speaking skills.
First, know your audience
Whether you are presenting to a group of 20 or 200, you can do certain things in advance to ensure that your presentation achieves the desired response. Most important: Know your audience. Don’t assume the audience is like you. To connect with them, you need to understand why your topic is important to them. What do they expect to learn from the presentation? Each attendee will be asking, “What’s in it for me?”
To keep listeners interested and engaged, you also must know their level of knowledge about the topic. If you are speaking to a group of residents about pelvic organ prolapse, you would use different language and content than if you were speaking to practicing primary care doctors; and these elements would be different again if you were speaking to a group of practicing urogynecologists. It’s insulting to recite basic information to highly knowledgeable physicians, or to present sophisticated technical content and complicated slides to novice physicians or lay people.
When presenting in a foreign country, learn how the culture of the audience differs from yours. How do they dress? What style of humor do they favor? How do they typically communicate? What gestures are appropriate or inappropriate? Are there religious influences to consider?
Practical steps. Before the meeting or event, speak to the organizer or meeting planner and find out the audience’s level of knowledge on the topic. Ask about audience expectations as well as demographics (such as age and background). If you are speaking at an industry event, research the event’s website and familiarize yourself with the mission of the event and who are the typical attendees. If you are presenting to a corporation, learn as much as you can about it by visiting its website, reading news reports, and reviewing associated blogs.
In addition to knowing the needs of the audience, ask the meeting planner about the goals and objectives for the program to make certain you can deliver on the requests.
Know your talk stem to stern
Review your slide material thoroughly. Understand each slide in the presentation and be comfortable with its content.
Avoid reading from slides. Reciting content that viewers can read for themselves breeds boredom and makes them lose interest. Further, when you are looking at the slides, you are not making eye contact with the audience and risk losing their attention. Good speakers are so comfortable with their slides that they can discuss each one without having to look at it.
Rehearse. The best way to achieve the foregoing is to rehearse. Your audience will be able to tell if you took the slide deck directly from a CD and loaded it into a computer and are giving the talk for the first time. You’ll need to know how long the program is to last and how long you are to speak. We suggest you practice with a timer to be certain you do not exceed the allotted time. Rehearse your talk aloud several times with all the props and audiovisual equipment you plan to use. This practice will help to curb filler words such as “ah” and “um.” It is also helpful to practice slide transitions, pauses, and even your breathing.
Prepare for the unexpected, too. Dinner meetings, for instance, may not start on time due to office or hospital delays for attending physicians, possibly resulting in a need to shorten your presentation.
Ask about the meeting agenda. If a meal is to be served, will you be speaking beforehand? This is the least favorable time slot, as you are holding people hostage before they can eat. Our preference is to speak after the appetizer is served and the orders have been taken by the wait staff. This way, attendees are not starving and they have something to drink. You can assure the waiters they won’t be disturbing you, and you can ask them to avoid walking in front of the projector. Ideally, you should end your presentation before dessert arrives and use the remaining time to field questions.
We suggest that you prepare a handout to be distributed at the end of the program, not before. You want your audience focused on you and your slides as you are speaking. Tell the audience you will be providing a handout of your presentation, which will minimize note-taking during your talk.
Your speech opening
The first and last 30 seconds of any speech probably have the most impact.1 Give extra thought, time, and effort to your opening and closing remarks. Do not open with “Good evening, it is a pleasure to be here tonight.” That wastes precious seconds.
While opening a speech with a joke or funny story is the conventional wisdom, ask yourself1:
- Is my selection appropriate to the occasion and for this audience?
- Is it in good taste?
- Does it relate to me (my service) or to the event or the group? Does it support my topic or its key points?
A humorous story or inspirational vignette that relates to your topic or audience can grab the audience’s attention. If you feel that demands more presentation skill than you possess at the outset of your public-speaking career, give the audience what you know and what they most want to hear. You know the questions that you have heard most at cocktail receptions or professional society meetings. So, put the answers to those questions in your speech.
For example. A scientist working with a major corporation was preparing a speech for a lay audience. Since most of the audience did not know what scientists do, he offered the following analogy: “Being a scientist is like doing a jigsaw puzzle in a snowstorm at night...you don’t have all the pieces...and you don’t have the picture on the front of the box to work from.” You can say more with less.1
Your closing
The closing is an important aspect of your speech. Summarize the key elements to your presentation. If you are going to take questions, a good approach is to say, “Before my closing remarks, are there any questions?” Following the questions, finish with a takeaway message that ties into your theme.1
Prepare an autobiographical introduction
We suggest that you write your own introduction and e-mail it to the person who will be introducing you. Let them know it is a suggestion that they are welcome to modify. We have found that most emcees or meeting planners are delighted to have the introduction and will use it just as you have written it. Also bring hard copy with you; many emcees will have forgotten to download what you sent. The figure shows an example of the introduction that one of us (NHB) uses, and you are welcome to modify it for your own use.
Ask about and confirm audiovisual support
Ask the meeting planner ahead of time if they will be providing the computer, projector, and screen. And if, for instance, they will provide a projector but not a computer, make sure the computer you will bring is compatible with their projector. Also, you will probably not require a microphone for a small group, but if you are speaking in a loud restaurant, a portable microphone-speaker system may be helpful.
Arrive early at the program venue to make sure the computers, projector, screen placement, and seating arrangement are all in order. Nothing can sidetrack a speaker (even a seasoned one) like a problem with the computer or equipment setup—for example, your flash drive requiring a USB port cannot connect to the sponsor’s computer, or your program created on a Mac does not run on the sponsor’s PC.
Show time: Getting ready
Another benefit in arriving early, besides being able to check on the equipment, is the chance to greet the audience members as they enter. It is easier to speak to a group of friends than strangers. And if you can remember their names, you can call on them and ask their opinion or how they might manage a patient who has the condition you are discussing. You also could suggest to the meeting planner that name tags for attendees would be helpful.
Warming up. A public speaker, like an athlete, needs to warm up physically before the event. If the facility has an anteroom available, use it for the following exercises suggested by public speaking coach Patricia Fripp1:
- Stand on one leg and shake the other (remove high heels first). When you place your raised foot back on the floor, it will feel lighter than the other one. Repeat the exercise using the other leg. Imagine your energy going down through the floor and up out of your head. While this sounds quite comical, it is not. It is a practical technique used by actors.
- Shake your hands vigorously. Hold them above your head, bending your wrists and elbows, then return your arms to your sides. This will make your hand movements more natural.
- Warm up your facial muscles by chewing in a highly exaggerated way. Do shoulder and neck rolls. Imagine you are at eye level with a clock. As you look at 12 o’clock, pull as much of your face up to the 12 as you can; move your eyes to 3 and repeat, then down to 6, and finally over to 9.
Not only do these exercises warm you up but they also relax you. The exaggerated movements help your movements to flow more naturally.1
This is just the start
Thorough preparation is key to making a solid presentation. But other factors are important too. Your goal is for the audience to take action or to implement suggestions from your presentation. In part 2 of this series, we will share tips on elements of the presentation itself that will encourage audience engagement and message retention. We will discuss how to make your message “stick” and how to make a dynamic, effective presentation that holds your audience’s attention for your entire talk.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Public speaking is one of the best ways to market and promote your skills as a physician. It is an ethical way of communicating and showcasing your areas of interest and expertise to professional or lay audiences. Most physicians and health care professionals take pride in their ability to communicate. After all, that is how we take a history, discuss our findings with patients, and educate individuals on restoring or maintaining their health. Public speaking, though, for the most part is a learned skill. Except for presentations to faculty at bedside or at grand rounds, we have received little training in public speaking.
Few of us are naturally comfortable in front of a live audience or a TV or video camera. But with a little practice and diligent preparation, we can become good or even excellent, confident public speakers. This article—the first in a series of 3—provides you with preparatory tips and techniques to enhance your public speaking skills.
First, know your audience
Whether you are presenting to a group of 20 or 200, you can do certain things in advance to ensure that your presentation achieves the desired response. Most important: Know your audience. Don’t assume the audience is like you. To connect with them, you need to understand why your topic is important to them. What do they expect to learn from the presentation? Each attendee will be asking, “What’s in it for me?”
To keep listeners interested and engaged, you also must know their level of knowledge about the topic. If you are speaking to a group of residents about pelvic organ prolapse, you would use different language and content than if you were speaking to practicing primary care doctors; and these elements would be different again if you were speaking to a group of practicing urogynecologists. It’s insulting to recite basic information to highly knowledgeable physicians, or to present sophisticated technical content and complicated slides to novice physicians or lay people.
When presenting in a foreign country, learn how the culture of the audience differs from yours. How do they dress? What style of humor do they favor? How do they typically communicate? What gestures are appropriate or inappropriate? Are there religious influences to consider?
Practical steps. Before the meeting or event, speak to the organizer or meeting planner and find out the audience’s level of knowledge on the topic. Ask about audience expectations as well as demographics (such as age and background). If you are speaking at an industry event, research the event’s website and familiarize yourself with the mission of the event and who are the typical attendees. If you are presenting to a corporation, learn as much as you can about it by visiting its website, reading news reports, and reviewing associated blogs.
In addition to knowing the needs of the audience, ask the meeting planner about the goals and objectives for the program to make certain you can deliver on the requests.
Know your talk stem to stern
Review your slide material thoroughly. Understand each slide in the presentation and be comfortable with its content.
Avoid reading from slides. Reciting content that viewers can read for themselves breeds boredom and makes them lose interest. Further, when you are looking at the slides, you are not making eye contact with the audience and risk losing their attention. Good speakers are so comfortable with their slides that they can discuss each one without having to look at it.
Rehearse. The best way to achieve the foregoing is to rehearse. Your audience will be able to tell if you took the slide deck directly from a CD and loaded it into a computer and are giving the talk for the first time. You’ll need to know how long the program is to last and how long you are to speak. We suggest you practice with a timer to be certain you do not exceed the allotted time. Rehearse your talk aloud several times with all the props and audiovisual equipment you plan to use. This practice will help to curb filler words such as “ah” and “um.” It is also helpful to practice slide transitions, pauses, and even your breathing.
Prepare for the unexpected, too. Dinner meetings, for instance, may not start on time due to office or hospital delays for attending physicians, possibly resulting in a need to shorten your presentation.
Ask about the meeting agenda. If a meal is to be served, will you be speaking beforehand? This is the least favorable time slot, as you are holding people hostage before they can eat. Our preference is to speak after the appetizer is served and the orders have been taken by the wait staff. This way, attendees are not starving and they have something to drink. You can assure the waiters they won’t be disturbing you, and you can ask them to avoid walking in front of the projector. Ideally, you should end your presentation before dessert arrives and use the remaining time to field questions.
We suggest that you prepare a handout to be distributed at the end of the program, not before. You want your audience focused on you and your slides as you are speaking. Tell the audience you will be providing a handout of your presentation, which will minimize note-taking during your talk.
Your speech opening
The first and last 30 seconds of any speech probably have the most impact.1 Give extra thought, time, and effort to your opening and closing remarks. Do not open with “Good evening, it is a pleasure to be here tonight.” That wastes precious seconds.
While opening a speech with a joke or funny story is the conventional wisdom, ask yourself1:
- Is my selection appropriate to the occasion and for this audience?
- Is it in good taste?
- Does it relate to me (my service) or to the event or the group? Does it support my topic or its key points?
A humorous story or inspirational vignette that relates to your topic or audience can grab the audience’s attention. If you feel that demands more presentation skill than you possess at the outset of your public-speaking career, give the audience what you know and what they most want to hear. You know the questions that you have heard most at cocktail receptions or professional society meetings. So, put the answers to those questions in your speech.
For example. A scientist working with a major corporation was preparing a speech for a lay audience. Since most of the audience did not know what scientists do, he offered the following analogy: “Being a scientist is like doing a jigsaw puzzle in a snowstorm at night...you don’t have all the pieces...and you don’t have the picture on the front of the box to work from.” You can say more with less.1
Your closing
The closing is an important aspect of your speech. Summarize the key elements to your presentation. If you are going to take questions, a good approach is to say, “Before my closing remarks, are there any questions?” Following the questions, finish with a takeaway message that ties into your theme.1
Prepare an autobiographical introduction
We suggest that you write your own introduction and e-mail it to the person who will be introducing you. Let them know it is a suggestion that they are welcome to modify. We have found that most emcees or meeting planners are delighted to have the introduction and will use it just as you have written it. Also bring hard copy with you; many emcees will have forgotten to download what you sent. The figure shows an example of the introduction that one of us (NHB) uses, and you are welcome to modify it for your own use.
Ask about and confirm audiovisual support
Ask the meeting planner ahead of time if they will be providing the computer, projector, and screen. And if, for instance, they will provide a projector but not a computer, make sure the computer you will bring is compatible with their projector. Also, you will probably not require a microphone for a small group, but if you are speaking in a loud restaurant, a portable microphone-speaker system may be helpful.
Arrive early at the program venue to make sure the computers, projector, screen placement, and seating arrangement are all in order. Nothing can sidetrack a speaker (even a seasoned one) like a problem with the computer or equipment setup—for example, your flash drive requiring a USB port cannot connect to the sponsor’s computer, or your program created on a Mac does not run on the sponsor’s PC.
Show time: Getting ready
Another benefit in arriving early, besides being able to check on the equipment, is the chance to greet the audience members as they enter. It is easier to speak to a group of friends than strangers. And if you can remember their names, you can call on them and ask their opinion or how they might manage a patient who has the condition you are discussing. You also could suggest to the meeting planner that name tags for attendees would be helpful.
Warming up. A public speaker, like an athlete, needs to warm up physically before the event. If the facility has an anteroom available, use it for the following exercises suggested by public speaking coach Patricia Fripp1:
- Stand on one leg and shake the other (remove high heels first). When you place your raised foot back on the floor, it will feel lighter than the other one. Repeat the exercise using the other leg. Imagine your energy going down through the floor and up out of your head. While this sounds quite comical, it is not. It is a practical technique used by actors.
- Shake your hands vigorously. Hold them above your head, bending your wrists and elbows, then return your arms to your sides. This will make your hand movements more natural.
- Warm up your facial muscles by chewing in a highly exaggerated way. Do shoulder and neck rolls. Imagine you are at eye level with a clock. As you look at 12 o’clock, pull as much of your face up to the 12 as you can; move your eyes to 3 and repeat, then down to 6, and finally over to 9.
Not only do these exercises warm you up but they also relax you. The exaggerated movements help your movements to flow more naturally.1
This is just the start
Thorough preparation is key to making a solid presentation. But other factors are important too. Your goal is for the audience to take action or to implement suggestions from your presentation. In part 2 of this series, we will share tips on elements of the presentation itself that will encourage audience engagement and message retention. We will discuss how to make your message “stick” and how to make a dynamic, effective presentation that holds your audience’s attention for your entire talk.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Fripp P. Add credibility to your business reputation through public speaking. Patricia Fripp website. http://www.fripp.com/add-credibility-to-your-business-reputation-through-public-speaking/. Accessed June 15, 2016.
Reference
- Fripp P. Add credibility to your business reputation through public speaking. Patricia Fripp website. http://www.fripp.com/add-credibility-to-your-business-reputation-through-public-speaking/. Accessed June 15, 2016.
In this Article
- Preparing a presentation
- Your speech opening
- AV equipment and support
ObGyn salaries jumped in the last year
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The mean income for ObGyns rose by 10% in 2015 over 2014 ($277,000 compared with $249,000), according to a recent report from Medscape.1 This jump follows a gradual increase over the last few years ($243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1−3 The report included responses from 19,183 physicians across 26 specialties, 5% (nearly 1,000) of whom were ObGyns.1
The highest earners among all physician specialties were orthopedists ($443,000), cardiologists, and dermatologists. The lowest earners were pediatricians ($204,000), endocrinologists, and family physicians. The highest ObGyn earners lived in the Southwest ($307,000), the North Central region, and the West.1
Merritt Hawkins & Associates, a national physician search and consulting firm, recently evaluated the annual starting salaries and year-over-year increases of 3,342 of its physician and advanced practitioner recruiting assignments. They found that ObGyns had the second greatest increase in starting salaries among specialties, at 16%. They also found obstetrics and gynecology to be among the top 5 specialties most in demand.4
The gender picture
As in past years, male ObGyns reported higher earnings than their female counterparts: full-time male ObGyns earned $304,000 while full-time female ObGyns earned $256,000.1
According to a report published in the British Medical Journal in June 2016, there are drastic differences between the incomes of white and black male and female physicians in the United States.5 White male physicians had an adjusted median annual income of $253,042 (95% confidence interval [CI], $248,670−$257,413), compared with $188,230 ($170,844−$205,616) for black male physicians, $163,234 (95% CI, $159,912−$166,557) for white female physicians, and $152,784 (95% CI, $137,927−$167,641) for black female physicians.
How does employment status factor in? Of the self-employed, men earn $310,000 while women earn $285,000. Men who are employed report earning $293,000, with women reporting $244,000.5 (This includes full-time workers but does not control for the number of hours worked.) When Medscape evaluated full- versus part-time work (<40 hours per week), results indicated that, among primary care and most other specialties, more female physicians (25%) are part-timers than males (12%).6 However, among ObGyns, 13% of women report part-time employment versus 16% of men.1
Time with patients. Medscape reports that, among all physicians, 41% of men spent 17 minutes or more with their patients, compared with 49% of women. For office-based ObGyns, 31% of men and 39% of women spent 17 minutes or more with patients.1
Can disparity in leadership positions explain gender-related salary discrepancy?
In 2015, 48% of all medical students were female.7 In residency, the ratio of men to women is similar: For 2013−2014, the Association of American Medical Colleges (AAMC) reported that 46% of all residents were female.8 For ObGyn residency, however, the AMA’s FREIDA Online specialty training search (detailing 2014 general program information) indicates that, of the 5,018 active residents and fellows in ObGyn, 81.4% are female.9
Although the ObGyn field is becoming female-dominated, leadership within the specialty remains male dominated, points out Laura E. Baecher-Lind, MD, MPH, Director of the Division of General Obstetrics & Gynecology at Tufts Medical Center, Boston, Massachusetts. Dr. Baecher-Lind authored a study in 2012 in which she explored whether the proportions of ObGyn leadership positions held by women reflect the proportion of women who entered the field at the same time as current leaders.10 She found that very few academic department chair positions in ObGyn are held by women, although that number is gradually increasing.10 In addition, her study results indicated that women should hold 71 of the total of 194 ObGyn leadership positions. In actuality, 41 of the leadership positions were held by women (21.1%, P<.001) when based on the proportion of women entering residency programs. When considering only leaders who graduated during the years in which residency matching data were available, she found that women should hold 28 of 74 leadership positions, but they actually held 20 (27.0%, P = .05).10
Could the salary discrepancy disappear if more women held leadership positions? OBG <scaps>Management</scaps> posed this question to Dr. Baecher-Lind. “I suspect that the gender pay gap would persist,” she said. “Studies indicate that women hold implicit gender bias as strongly as men. This bias leads to devaluing women’s skills and accomplishments compared with men’s and is a strong contributor to the leadership and pay gaps in this country and in our specialty. We need to be mindful of this implicit bias and work against it with policies such as salary transparency and salary audits to encourage parity.”11
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients' gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting, May 14−17, in Washington, DC.1
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. "I was trying to decide if Obstetrics and Gynecology was the right field for me," he said. "I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results." After medical school Dr. Tobler pursued this current meta-analysis to address the conflict-ing results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association's medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health's database), Scopus (Elsevier's abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.1
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.1
"We were surprised by the numbers," comments Dr. Tobler. "The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin."
"We considered analyzing for age," he said, "but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers--the Middle East and Africa. But, in fact, results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference."1
References
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider. Accessed May 18, 2016.
What are ObGyns’ greatest practice concerns?
The Medicus Firm reported in its 2016 Physician Practice Preference and Relocation Survey that the top 3 major practice concerns for practicing physicians were compensation, work-life balance, and work-related burnout and stress.12 They found that physicians in general were slightly more satisfied with their 2015 income than their 2014 income, but less optimistic about the future. Only 29% projected that their 2016 income would increase over their 2015 earnings.
With ObGyn salaries on the up in 2015, less than half (46%) of ObGyns reported to Medscape that they feel fairly compensated; these physicians made $62,000 more than those who believed their pay was unfair.1 Fifty-four percent of employed male ObGyns and 64% of employed female ObGyns reported feeling fairly compensated, compared with 43% and 32%, respectively, who were self-employed.
ObGyns indicated in the 2016 Medscape report that the prime causes of stress were bureaucratic tasks and spending too many hours at work. More than half (52%) of ObGyns spend 30 to 45 hours per week seeing patients, and 40% spend more time than that.1 According to employment status, 56% of those who are self-employed and 58% of those who are employed spend 10 hours or more per week on administrative tasks.1
Lucia DiVenere, MA, Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists (ACOG) in Washington, DC, offers a brief look, with an in-depth focus to come in an upcoming issue, at the growing concern of burnout among physicians and how it can affect both ObGyns and their patients. She outlines ACOG’s efforts to help ObGyns maintain work-life balance in “ObGyn burnout: ACOG takes aim.”
ObGyn burnout: ACOG takes aim
Lucia DiVenere, MA
The good news: More women have access to coverage for health care than ever before--better insurance coverage for pregnancy, contraceptives, and well-woman care.
The bad news: America faces a shortage of ObGyns to provide that care, a shortage not likely to go away soon.
One of the imperatives of this dynamic is that we need to help every practicing ObGyn perform at his or her very best: your highest level of quality care, your best productivity, and your best ability to survive and thrive in an always changing and often challenging work environment.
This imperative is undermined when ObGyns are so stressed, overworked, overworried, and undersupported that you experience the very real effects of physician burnout.
Studies show that:
- ObGyns experience high rates of burnout
- rates of burnout are increasing over time
- women, the majority gender in obstetrics and gynecology, experience higher rates of burnout than their male counterparts.
Between 2011 and 2014, rates of physician burnout increased from 45.5% to 54.4%.1 Fifty-one percent of ObGyns reported experiencing burnout in 2015, with women reporting 55% compared to 46% for men.2
This insert is a quick look at this important issue, which can seriously erode an ObGyn's ability to provide high-quality care and continue enjoying practice. It can take a real toll on your personal health and well-being, too. In an upcoming issue of OBG Management, I will take a deeper dive, previewing the American College of Obstetricians and Gynecologists (ACOG) and American Medical Association resources to help you avoid burnout, plus highlighting ObGyns who provide insight and inspiration. I also will interview ACOG President Tom Gellhaus, MD, who is dedicating his presidency to providing you with opportunities to experience new and meaningful aspects of the ObGyn specialty. I will discuss ACOG's programs to help you combat burnout, as well as how you can:
- help underserved women around the globe through medical missions
- bring your leadership and passion for women's health to your state and national capitals
- explore your artistic side.
ObGyn burnout amounts to a public health challenge in women's health care. ACOG takes your well-being seriously, so that you can continue to ensure the well-being of women.
Lucia DiVenere, MA, is Officer, Government and Political Affairs, at the American Congress of Obstetricians and Gynecologists in Washington, DC.
Ms. DiVenere reports no financial relationships relevant to this article. .
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings. 2015;90(12):1600-1613.
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview. Published January 13, 2016. Accessed June 14, 2016.
Effects of the ACA on ObGyns
As of February 2016, 12.7 million Americans selected plans through the Health Insurance Marketplace of the Affordable Care Act (ACA).1 Physicians often have no choice in whether or not they participate in Health Insurance Exchanges; however, in 2016, 24% of ObGyns said they plan to participate in exchanges, 25% do not, and the rest are unsure.1
It is still unclear how the ACA affects physician income.1 When ObGyns who participated in Health Insurance Exchanges in 2015 were asked whether their income was affected, approximately 60% reported no change, 30% reported a decrease, and 9% said it increased.1
Medicus reported that physicians’ approval of the ACA has declined since last year. In their 2016 report, 71% of respondents gave the ACA a passing grade (A, B, C, or D), compared with 83% in 2015 and 77% in 2014. Fewer than 3% of 2016 respondents gave the ACA an “A.”12
Medscape reported that 36% of ObGyns have seen an increase in the number of patients due to the ACA.1 A 2015 report from the Kaiser Family Foundation and The Commonwealth Fund assessing the experiences and attitudes of primary care providers after the first year of ACA coverage found no association with lower- and higher-quality care whether or not patient load had increased.13 Among those in the Medscape report who said that quality of care had worsened, 21% had a greater patient load; 18% reported no increase in patient load. Seventy-eight percent of physicians whose patient load increased said that quality had stayed the same or improved; 82% of those who experienced no increase in patient load reported that quality had stayed the same or improved.1
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 8, 2016.
- Reale D, Yates J. ObGyn salaries continue gradual improvement. OBG Manag. 2015;27(7):34−37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed June 8, 2016.
- Merritt Hawkins. Survey: Starting salaries for physicians spiking. http://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/Merritt_Hawkins_Starting_Salaries_For_Physicians_Spiking.pdf. Published June 7, 2016. Accessed June 17, 2016.
- Ly DP, Seabury SA, Jena AB, Newhouse RL. Differences in incomes of physicians in the United States by race and sex: observational study [published online ahead of print June 7, 2016]. BMJ. 2016;353:i2923. http://dx.doi.org/10.1136/bmj.i2923. Accessed June 8, 2016.
- Peckham C. Medscape Physician Compensation Report 2016. Medscape website. http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=1. Published April 1, 2016. Accessed June 15, 2016.
- Kaiser Family Foundation. Distribution of medical school graduates by gender. http://kff.org/other/state-indicator/medical-school-graduates-by-gender/. Published 2016. Accessed June 22, 2016.
- Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The state of women in academic medicine, 2013-2014. Association of American Medical Colleges. 2014. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed June 17, 2016.
- American Medical Association. FREIDA Online specialty training search: Obstetrics and Gynecology, 2014. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&pageNumber=2&spcCd=220. Accessed June 17, 2016.
- Baecher-Lind L. Women in leadership positions within obstetrics and gynecology. Obstet Gynecol. 2012;120(6):1415−1418.
- Email correspondence with Laura E. Baecher-Lind, June 19, 2016.
- Medicus Firm. The Medicus Firm releases annual Physician Practice Preference Survey for 2016. http://www .themedicusfirm.com/the-medicus-firm-releases-annual-physician-practice-preference-survey-for-2016. Published May 4, 2016. Accessed June 10, 2016.
- Hamel L, Doty MM, Norton M, et al; Kaiser Family Foundation and The Commonwealth Fund. Experiences and attitudes of primary care providers under the first year of ACA coverage expansion. http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/primary-care-providers-first-year-aca. Published June 18, 2015. Accessed June 15, 2016.
In this Article
- ACOG takes aim at burnout
- Considering salary and leadership disparities
- ObGyns’ greatest practice concerns
Lesson in Improper Allocations, Unaccounted for NP/PA Contributions
I visited during a hot Florida summer in the mid 1990s and could readily see that the practice was great in most respects. The large multispecialty group had recruited talented hospitalists and had put in place effective operational practices. All seemed to be going well, but inappropriate overhead allocation was undermining the success of their efforts.
The multispecialty group employing the hospitalists used the same formula to allocate overhead to the hospitalists that was in place for other specialties. And compensation was essentially each doctor’s collections minus overhead, leaving the hospitalists with annual compensation much lower than they could reasonably expect. With the group deducting from hospitalist collections the same overhead expenses charged to other specialties, including a share of outpatient buildings, staff, and supplies, the hospitalists were paying a lot for services they weren’t using. This group corrected the errors but not until some talented doctors had resigned because of the compensation formula.
This was a common mistake made by multispecialty groups that employed hospitalists years ago. Today, nearly all such groups assess an appropriately smaller portion of overhead to hospitalists than office-based doctors.
Typical Hospitalist Overhead
It is still tricky to correctly assess and allocate hospitalist overhead. This meaningfully influences the apparent total cost of the program and hence the amount of support paid by the hospital or other entity. (This support is often referred to as a “subsidy,” though I don’t care for that term because of its negative connotation.)
For example, costs for billing and collections services, malpractice insurance, temporary staffing (locums), and an overhead allocation that pays for things like the salaries of medical group administrators and clerical staff may or may not be attributed to the hospitalist budget or “cost center.” This is one of several factors that make it awfully tricky to compare the total costs and/or hospital financial support between different hospitalist groups.
SHM’s State of Hospital Medicine report includes detailed instructions regarding which expenses the survey respondents should include as overhead costs, but I think it’s safe to assume that not all responses are fully compliant. I’m confident there is a meaningful amount of “noise” in these figures. Numbers like the median financial support per FTE hospitalist per year ($156,063 in the 2014 report) should only be used as a guideline and not a precise number that might apply in your setting. My reasoning is that the collections rate and compensation amount can vary tremendously from one practice to another and will typically have a far larger influence on the amount of financial support provided by the hospital than which expenses are or aren’t included as overhead. But I am confining this discussion to the latter.
APC Costs: One Factor Driving Increased Support
SHM has been surveying the financial support per physician FTE for about 15 years, and it has shown a steady increase. It was about $60,000 per FTE annually when first surveyed in the late 1990s; it has gone up every survey since. The best explanation for this seems to an increase in hospitalist compensation while production and revenue have remained relatively flat.
There likely are many other factors in play. One important one is physician assistant and nurse practitioner costs. The survey divides the total annual support provided to the whole hospitalist practice by the total number of physician FTEs. NPs and PAs are becoming more common in hospitalist groups; 65% of groups included them in 2014, up from 54% in 2012. Yet the cost of employing them, primarily salary and benefits, appears in the numerator but not the denominator of the support per physician FTE figure.
This means a group that adds NP/PA staffing, which typically requires an accompanying increase in hospital financial support, while maintaining the same number of physician FTEs will show an increase in hospital support per physician FTE. But this fails to capture that the practice’s work product (i.e., patients seen) has increased as a result of increasing its clinical staff.
This is a tricky issue to fix. SHM’s Practice Analysis Committee, which manages the survey, is aware of the issue and may make future adjustments to account for it. The best method might be to convert total staffing by physicians and NP/PAs into physician-equivalent FTEs (I described one method for doing this in my August 2009 column titled “Volume Variables”) or some other method that clearly accounts for both physician and NP/PA staffing levels. Other alternatives would be to divide the annual support by the number of billed encounters or some other measure of “work output” or to report percent of the total practice revenue that comes from hospital support versus professional fee collections and other sources.
Why Allocation of NP/PA Costs and FTEs Matter
Another way to think of this issue is that including NP/PA costs but not their work (FTEs) in the financial support per FTE figure overlooks the important work they can do for a hospitalist practice. And it can lead one to conclude hospitals’ costs per clinician FTE are rising faster than is actually the case.
This is only one of the tricky issues in accurately understanding hospitalist overhead and costs to the hospital they serve. TH

I visited during a hot Florida summer in the mid 1990s and could readily see that the practice was great in most respects. The large multispecialty group had recruited talented hospitalists and had put in place effective operational practices. All seemed to be going well, but inappropriate overhead allocation was undermining the success of their efforts.
The multispecialty group employing the hospitalists used the same formula to allocate overhead to the hospitalists that was in place for other specialties. And compensation was essentially each doctor’s collections minus overhead, leaving the hospitalists with annual compensation much lower than they could reasonably expect. With the group deducting from hospitalist collections the same overhead expenses charged to other specialties, including a share of outpatient buildings, staff, and supplies, the hospitalists were paying a lot for services they weren’t using. This group corrected the errors but not until some talented doctors had resigned because of the compensation formula.
This was a common mistake made by multispecialty groups that employed hospitalists years ago. Today, nearly all such groups assess an appropriately smaller portion of overhead to hospitalists than office-based doctors.
Typical Hospitalist Overhead
It is still tricky to correctly assess and allocate hospitalist overhead. This meaningfully influences the apparent total cost of the program and hence the amount of support paid by the hospital or other entity. (This support is often referred to as a “subsidy,” though I don’t care for that term because of its negative connotation.)
For example, costs for billing and collections services, malpractice insurance, temporary staffing (locums), and an overhead allocation that pays for things like the salaries of medical group administrators and clerical staff may or may not be attributed to the hospitalist budget or “cost center.” This is one of several factors that make it awfully tricky to compare the total costs and/or hospital financial support between different hospitalist groups.
SHM’s State of Hospital Medicine report includes detailed instructions regarding which expenses the survey respondents should include as overhead costs, but I think it’s safe to assume that not all responses are fully compliant. I’m confident there is a meaningful amount of “noise” in these figures. Numbers like the median financial support per FTE hospitalist per year ($156,063 in the 2014 report) should only be used as a guideline and not a precise number that might apply in your setting. My reasoning is that the collections rate and compensation amount can vary tremendously from one practice to another and will typically have a far larger influence on the amount of financial support provided by the hospital than which expenses are or aren’t included as overhead. But I am confining this discussion to the latter.
APC Costs: One Factor Driving Increased Support
SHM has been surveying the financial support per physician FTE for about 15 years, and it has shown a steady increase. It was about $60,000 per FTE annually when first surveyed in the late 1990s; it has gone up every survey since. The best explanation for this seems to an increase in hospitalist compensation while production and revenue have remained relatively flat.
There likely are many other factors in play. One important one is physician assistant and nurse practitioner costs. The survey divides the total annual support provided to the whole hospitalist practice by the total number of physician FTEs. NPs and PAs are becoming more common in hospitalist groups; 65% of groups included them in 2014, up from 54% in 2012. Yet the cost of employing them, primarily salary and benefits, appears in the numerator but not the denominator of the support per physician FTE figure.
This means a group that adds NP/PA staffing, which typically requires an accompanying increase in hospital financial support, while maintaining the same number of physician FTEs will show an increase in hospital support per physician FTE. But this fails to capture that the practice’s work product (i.e., patients seen) has increased as a result of increasing its clinical staff.
This is a tricky issue to fix. SHM’s Practice Analysis Committee, which manages the survey, is aware of the issue and may make future adjustments to account for it. The best method might be to convert total staffing by physicians and NP/PAs into physician-equivalent FTEs (I described one method for doing this in my August 2009 column titled “Volume Variables”) or some other method that clearly accounts for both physician and NP/PA staffing levels. Other alternatives would be to divide the annual support by the number of billed encounters or some other measure of “work output” or to report percent of the total practice revenue that comes from hospital support versus professional fee collections and other sources.
Why Allocation of NP/PA Costs and FTEs Matter
Another way to think of this issue is that including NP/PA costs but not their work (FTEs) in the financial support per FTE figure overlooks the important work they can do for a hospitalist practice. And it can lead one to conclude hospitals’ costs per clinician FTE are rising faster than is actually the case.
This is only one of the tricky issues in accurately understanding hospitalist overhead and costs to the hospital they serve. TH

I visited during a hot Florida summer in the mid 1990s and could readily see that the practice was great in most respects. The large multispecialty group had recruited talented hospitalists and had put in place effective operational practices. All seemed to be going well, but inappropriate overhead allocation was undermining the success of their efforts.
The multispecialty group employing the hospitalists used the same formula to allocate overhead to the hospitalists that was in place for other specialties. And compensation was essentially each doctor’s collections minus overhead, leaving the hospitalists with annual compensation much lower than they could reasonably expect. With the group deducting from hospitalist collections the same overhead expenses charged to other specialties, including a share of outpatient buildings, staff, and supplies, the hospitalists were paying a lot for services they weren’t using. This group corrected the errors but not until some talented doctors had resigned because of the compensation formula.
This was a common mistake made by multispecialty groups that employed hospitalists years ago. Today, nearly all such groups assess an appropriately smaller portion of overhead to hospitalists than office-based doctors.
Typical Hospitalist Overhead
It is still tricky to correctly assess and allocate hospitalist overhead. This meaningfully influences the apparent total cost of the program and hence the amount of support paid by the hospital or other entity. (This support is often referred to as a “subsidy,” though I don’t care for that term because of its negative connotation.)
For example, costs for billing and collections services, malpractice insurance, temporary staffing (locums), and an overhead allocation that pays for things like the salaries of medical group administrators and clerical staff may or may not be attributed to the hospitalist budget or “cost center.” This is one of several factors that make it awfully tricky to compare the total costs and/or hospital financial support between different hospitalist groups.
SHM’s State of Hospital Medicine report includes detailed instructions regarding which expenses the survey respondents should include as overhead costs, but I think it’s safe to assume that not all responses are fully compliant. I’m confident there is a meaningful amount of “noise” in these figures. Numbers like the median financial support per FTE hospitalist per year ($156,063 in the 2014 report) should only be used as a guideline and not a precise number that might apply in your setting. My reasoning is that the collections rate and compensation amount can vary tremendously from one practice to another and will typically have a far larger influence on the amount of financial support provided by the hospital than which expenses are or aren’t included as overhead. But I am confining this discussion to the latter.
APC Costs: One Factor Driving Increased Support
SHM has been surveying the financial support per physician FTE for about 15 years, and it has shown a steady increase. It was about $60,000 per FTE annually when first surveyed in the late 1990s; it has gone up every survey since. The best explanation for this seems to an increase in hospitalist compensation while production and revenue have remained relatively flat.
There likely are many other factors in play. One important one is physician assistant and nurse practitioner costs. The survey divides the total annual support provided to the whole hospitalist practice by the total number of physician FTEs. NPs and PAs are becoming more common in hospitalist groups; 65% of groups included them in 2014, up from 54% in 2012. Yet the cost of employing them, primarily salary and benefits, appears in the numerator but not the denominator of the support per physician FTE figure.
This means a group that adds NP/PA staffing, which typically requires an accompanying increase in hospital financial support, while maintaining the same number of physician FTEs will show an increase in hospital support per physician FTE. But this fails to capture that the practice’s work product (i.e., patients seen) has increased as a result of increasing its clinical staff.
This is a tricky issue to fix. SHM’s Practice Analysis Committee, which manages the survey, is aware of the issue and may make future adjustments to account for it. The best method might be to convert total staffing by physicians and NP/PAs into physician-equivalent FTEs (I described one method for doing this in my August 2009 column titled “Volume Variables”) or some other method that clearly accounts for both physician and NP/PA staffing levels. Other alternatives would be to divide the annual support by the number of billed encounters or some other measure of “work output” or to report percent of the total practice revenue that comes from hospital support versus professional fee collections and other sources.
Why Allocation of NP/PA Costs and FTEs Matter
Another way to think of this issue is that including NP/PA costs but not their work (FTEs) in the financial support per FTE figure overlooks the important work they can do for a hospitalist practice. And it can lead one to conclude hospitals’ costs per clinician FTE are rising faster than is actually the case.
This is only one of the tricky issues in accurately understanding hospitalist overhead and costs to the hospital they serve. TH

Setting up your own RSS feed
Last month, I discussed RSS news feeds as a useful tool for keeping abreast of frequently updated information, such as blog entries, news headlines, audio, and video, without having to visit a multitude of different Web pages each day.
This month, I’ll explain how to set up your own feed, which is useful if you want to increase the readership on your website, or publicize a podcast, or keep your patients abreast of your practice’s latest treatments and procedures. It will also alert you immediately if your name pops up in news or gossip sites.
There are several options, depending on your budget, and how involved you personally want to be in the process: Many Web hosting services will automatically create and update your feed for a monthly fee; so if you already have a professionally hosted website, check to see if your host offers that service. If not, Web services such as Feedity and Rapidfeeds allow you to manage multiple feeds, with automatic updates, so that you will not need to manually update your feed each time you update your website content. Feedity’s software can even generate an RSS file without your having to input each item. Other popular hosting options include Web Hosting Hub, Arvixe, and MyHosting, among many others. (As always, I have no financial interest in any service I mention here.)
Another option, used by many organizations that publish their own articles and news stories, is a content management system (CMS), an application designed to organize, store, and publish content, including tools for adding RSS feeds. Examples include Drupal and Plone – both free, open-source programs.
Alternatively, you can download a stand-alone RSS creation program, then create and update your feed manually. Again, there are many options to choose from. One popular example is RSS Builder, a free, open source RSS creation program that allows you to create RSS files, upload them to your website, and automatically manage them to some extent. Disadvantages of free systems include advertisements (sometimes removable for a monthly fee), scarce or nonexistent technical support, and in many cases, no option to create more than one feed. You may also have to manually add new headlines, links, and descriptive text yourself. Your “free” feed can become quite expensive if you or staffers are forced to spend an inordinate amount of time maintaining it. Paid programs such as FeedForAll allow easier creation and maintenance, and less time commitment.
Once you have chosen your service, create your first feed. The process will differ from program to program, but the general idea is the same for almost all of them. All feeds will need some basic data: A title (which should be the same as your website or podcast); the URL for your website, to help viewers link back to your home page; and a description – a sentence or two describing the general content on the feed.
Once you’ve entered this information, you can start populating the feed with content. Enter in the title of each article, blog post, podcast episode, etc., the URL that links directly to that content, and the publishing date. Each entry should have its own short but sweet description; this is what your readers will see before they choose to click your entry in their RSS readers. You can add author information and further comments if needed. Add a new entry for each piece of content that you want to broadcast.
Most RSS apps suggest that you assign each item in your feed a global unique identifier (GUID), which RSS readers use to determine if an item has been changed or updated. Each feed item should have its own GUID, particularly if multiple items are located at the same URL.
Once you’re done entering in all of your content to your feed, you need to export it to an XML file, which will allow visitors to subscribe to your feed. Then upload the XML file to your website, place it on your homepage, and click the Publish Feed button.
Once your feed is live, consider submitting it to some of the many RSS feed directories (also called aggregate sites) that collect articles from similar interests and can significantly increase your viewership. Search for medically oriented directories, and others that match the interests that your feed addresses, and submit each directory’s URL to your feed’s XML file.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Last month, I discussed RSS news feeds as a useful tool for keeping abreast of frequently updated information, such as blog entries, news headlines, audio, and video, without having to visit a multitude of different Web pages each day.
This month, I’ll explain how to set up your own feed, which is useful if you want to increase the readership on your website, or publicize a podcast, or keep your patients abreast of your practice’s latest treatments and procedures. It will also alert you immediately if your name pops up in news or gossip sites.
There are several options, depending on your budget, and how involved you personally want to be in the process: Many Web hosting services will automatically create and update your feed for a monthly fee; so if you already have a professionally hosted website, check to see if your host offers that service. If not, Web services such as Feedity and Rapidfeeds allow you to manage multiple feeds, with automatic updates, so that you will not need to manually update your feed each time you update your website content. Feedity’s software can even generate an RSS file without your having to input each item. Other popular hosting options include Web Hosting Hub, Arvixe, and MyHosting, among many others. (As always, I have no financial interest in any service I mention here.)
Another option, used by many organizations that publish their own articles and news stories, is a content management system (CMS), an application designed to organize, store, and publish content, including tools for adding RSS feeds. Examples include Drupal and Plone – both free, open-source programs.
Alternatively, you can download a stand-alone RSS creation program, then create and update your feed manually. Again, there are many options to choose from. One popular example is RSS Builder, a free, open source RSS creation program that allows you to create RSS files, upload them to your website, and automatically manage them to some extent. Disadvantages of free systems include advertisements (sometimes removable for a monthly fee), scarce or nonexistent technical support, and in many cases, no option to create more than one feed. You may also have to manually add new headlines, links, and descriptive text yourself. Your “free” feed can become quite expensive if you or staffers are forced to spend an inordinate amount of time maintaining it. Paid programs such as FeedForAll allow easier creation and maintenance, and less time commitment.
Once you have chosen your service, create your first feed. The process will differ from program to program, but the general idea is the same for almost all of them. All feeds will need some basic data: A title (which should be the same as your website or podcast); the URL for your website, to help viewers link back to your home page; and a description – a sentence or two describing the general content on the feed.
Once you’ve entered this information, you can start populating the feed with content. Enter in the title of each article, blog post, podcast episode, etc., the URL that links directly to that content, and the publishing date. Each entry should have its own short but sweet description; this is what your readers will see before they choose to click your entry in their RSS readers. You can add author information and further comments if needed. Add a new entry for each piece of content that you want to broadcast.
Most RSS apps suggest that you assign each item in your feed a global unique identifier (GUID), which RSS readers use to determine if an item has been changed or updated. Each feed item should have its own GUID, particularly if multiple items are located at the same URL.
Once you’re done entering in all of your content to your feed, you need to export it to an XML file, which will allow visitors to subscribe to your feed. Then upload the XML file to your website, place it on your homepage, and click the Publish Feed button.
Once your feed is live, consider submitting it to some of the many RSS feed directories (also called aggregate sites) that collect articles from similar interests and can significantly increase your viewership. Search for medically oriented directories, and others that match the interests that your feed addresses, and submit each directory’s URL to your feed’s XML file.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Last month, I discussed RSS news feeds as a useful tool for keeping abreast of frequently updated information, such as blog entries, news headlines, audio, and video, without having to visit a multitude of different Web pages each day.
This month, I’ll explain how to set up your own feed, which is useful if you want to increase the readership on your website, or publicize a podcast, or keep your patients abreast of your practice’s latest treatments and procedures. It will also alert you immediately if your name pops up in news or gossip sites.
There are several options, depending on your budget, and how involved you personally want to be in the process: Many Web hosting services will automatically create and update your feed for a monthly fee; so if you already have a professionally hosted website, check to see if your host offers that service. If not, Web services such as Feedity and Rapidfeeds allow you to manage multiple feeds, with automatic updates, so that you will not need to manually update your feed each time you update your website content. Feedity’s software can even generate an RSS file without your having to input each item. Other popular hosting options include Web Hosting Hub, Arvixe, and MyHosting, among many others. (As always, I have no financial interest in any service I mention here.)
Another option, used by many organizations that publish their own articles and news stories, is a content management system (CMS), an application designed to organize, store, and publish content, including tools for adding RSS feeds. Examples include Drupal and Plone – both free, open-source programs.
Alternatively, you can download a stand-alone RSS creation program, then create and update your feed manually. Again, there are many options to choose from. One popular example is RSS Builder, a free, open source RSS creation program that allows you to create RSS files, upload them to your website, and automatically manage them to some extent. Disadvantages of free systems include advertisements (sometimes removable for a monthly fee), scarce or nonexistent technical support, and in many cases, no option to create more than one feed. You may also have to manually add new headlines, links, and descriptive text yourself. Your “free” feed can become quite expensive if you or staffers are forced to spend an inordinate amount of time maintaining it. Paid programs such as FeedForAll allow easier creation and maintenance, and less time commitment.
Once you have chosen your service, create your first feed. The process will differ from program to program, but the general idea is the same for almost all of them. All feeds will need some basic data: A title (which should be the same as your website or podcast); the URL for your website, to help viewers link back to your home page; and a description – a sentence or two describing the general content on the feed.
Once you’ve entered this information, you can start populating the feed with content. Enter in the title of each article, blog post, podcast episode, etc., the URL that links directly to that content, and the publishing date. Each entry should have its own short but sweet description; this is what your readers will see before they choose to click your entry in their RSS readers. You can add author information and further comments if needed. Add a new entry for each piece of content that you want to broadcast.
Most RSS apps suggest that you assign each item in your feed a global unique identifier (GUID), which RSS readers use to determine if an item has been changed or updated. Each feed item should have its own GUID, particularly if multiple items are located at the same URL.
Once you’re done entering in all of your content to your feed, you need to export it to an XML file, which will allow visitors to subscribe to your feed. Then upload the XML file to your website, place it on your homepage, and click the Publish Feed button.
Once your feed is live, consider submitting it to some of the many RSS feed directories (also called aggregate sites) that collect articles from similar interests and can significantly increase your viewership. Search for medically oriented directories, and others that match the interests that your feed addresses, and submit each directory’s URL to your feed’s XML file.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Does U.S. Healthcare Need More Diverse Leadership?
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.
“My advancement speaks to hospital medicine and the fact that we are growing as a field,” she says. “Because of that, opportunities are presenting themselves.”
Dr. Kisuule’s ability to thrive in her position speaks to her professionalism but also to a number of other intentional factors: Dr. Howell’s continuing sponsorship to include her in leadership opportunities, an emergency call system for parents with sick children, and a women’s task force whose agenda calls for transparency in hiring and advancement.
Intentional Structure Change
Cardiologist Hannah A. Valantine, MD, recognizes the importance of addressing the lack of women and people from unrepresented groups in the Science, Technology, Engineering, and Mathematics (STEM) workforce. While at Stanford University School of Medicine, she developed and put into place a set of strategies to understand and mitigate the drivers of gender imbalance. Since then, Dr. Valantine was recruited to bring her expertise to the National Institutes of Health in Bethesda, Md., where she is the inaugural chief officer for scientific workforce diversity. In this role, she is committed “to promoting biomedical workforce diversity as an opportunity, not a problem.”
Dr. Valantine is pushing NIH to pursue a wide range of evidence-based programming to eliminate career-transition barriers that keep women and individuals from underrepresented groups from attaining spots in the top echelons of science and health leadership. She believes that applying scientific rigor to the issue of workforce diversity can lead to quantifiable, translatable, and repeatable methods for recruitment and retention of talent in the biomedical workforce (see “Building Blocks").
Before joining NIH, Dr. Valantine and her colleagues at Stanford surveyed gender composition and faculty satisfaction several years after initiating a multifaceted intervention to boost recruitment and development of women faculty.4 After making a visible commitment of resources to support faculty, with special attention to women, Stanford rose from below to above national benchmarks in the representation of women among faculty. Yet significant work remains to be done, Dr. Valantine says. Her work predicts that the estimated time to achieve 50% occupancy of full professorships by women nationally approaches 50 years—“far too long using current approaches.”
In a separate review article, Dr. Valantine and co-author Christy Sandborg, MD, described the Stanford University School of Medicine Academic Biomedical Career Customization (ABCC) model, which was adapted from Deloitte’s Mass Career Customization framework and allows for development of individual career plans that span a faculty member’s total career, not just a year or two at a time. Long-term planning can enable better alignment between the work culture and values of the workforce, which will improve the outlook for women faculty, Dr. Valantine says.
The issues of work-life balance may actually be generational, Dr. Valantine explains. Veteran hospitalist Janet Nagamine, MD, BSN, SFHM, of Santa Clara, Calif., agrees.
“Nowadays, men as well as women are looking for work-life balance,” she says.
In hospital medicine, Dr. Nagamine points out, the structural changes required to effect a work-life balance for hospital leaders are often difficult to achieve.
“As productivity surveys show, HM group leaders are putting in as many RVUs as the staff,” the former SHM board member says. “There is no dedicated time for administrative duties.”
Construct a Pipeline
Barriers to advancement often are particular to characteristics of diverse populations. For example, the AAMC’s report on the U.S. physician workforce documents that in African-American physicians 40 and younger, women outnumber their male counterparts. Therefore, in the association’s Diversity in Medical Education: Facts and Figures 2012 report, the executive summary points out the need to strengthen the medical education pipeline to increase the number of African-American males who enter the premed track.
Despite the fast-growing percentage of Latino and Hispanic populations in the United States, the shortage of Latino/Hispanic physicians increased from 1980 to 2010. Latinos/Hispanics are greatly underrepresented in the medical student, resident, and faculty populations, according to John Paul Sánchez, MD, MPH, assistant dean for diversity and inclusion in the Office for Diversity and Community Engagement at Rutgers, The State University of New Jersey. Likewise, Zeppenfeldt-Cestero believes that efforts must begin much earlier with Latino and other minority and underrepresented students.
“We have to make sure our students pursue the STEM disciplines and that they also later have the education and preparation to be competitive at the MBA or MPH levels,” he says.
Dr. Sánchez, an associate professor of emergency medicine and a diversity activist since his med school days, is the recipient of last year’s Association of Hispanic Healthcare Executives’ academic leader of the year award. Since September 2014, he has been involved with Building the Next Generation of Academic Physicians Inc., which collaborates with more than 40 medical schools across the country. The initiative offers conferences designed to develop diverse medical students’ and residents’ interest in pursuing academic medicine. Open to all medical students and residents, the conference curriculum is tailored for women, UREMs, and trainees who identify as lesbian, gay, bisexual, or transgender (LGBT), he says. Seven conferences were held in 2015, 10 are planned for this year, and seven for 2017.
Healthcare Leadership Gaps
Despite their omnipresence in healthcare, there is a dearth of women in chief executive and governance roles, as has been noted by both the American College of Healthcare Executives and the National Center for Healthcare Leadership. As with academic leadership positions, the leadership gap in the administrative sector does not seem to be due to a lack of women entering graduate programs in health administration. On the contrary, since the mid-1980s women have comprised 50% to 60% of graduate students.
“This is absolutely not a pipeline issue,” says Christy Harris Lemak, PhD, FACHE, professor and chair of the Department of Health Services Administration at the University of Alabama at Birmingham School of Health Professions and lead investigator of the National Center for Healthcare Leadership’s study of women in healthcare executive positions. Other factors come into play.
In the study, she and her co-authors queried female healthcare CEOs to ascertain the critical career inflection points that led to their success.6 Those who were strategic about their careers, sought out mentors, and voiced their intentions about pursuing leadership positions were more likely to be successful in those efforts. However, individual career efforts must be coupled with overall organizational commitment to fostering inclusion (see “Path to the Top: Strategic Advice for Women").
Hospitals and healthcare organizations must pursue the development of human capital (and the diversity of their leaders) in a systematic way. “We recommended [in the study] that organizations set expectations that leaders who mentor other potential leaders be rewarded in the same way as those who hit financial targets or readmission rate targets,” Dr. Lemak says.
Leadership matters, agrees Deborah J. Bowen, FACHE, CAE, president and CEO of Chicago-based American College of Healthcare Executives.
“I think we’re getting a little smarter. Organizational leaders and trustees have a better understanding that talent development is one of the most important jobs,” she says. “If you don’t have the right people in the right places making good decisions on behalf of the patients and the populations in the communities they’re serving, the rest falls apart.”
Nuances of Mentoring
Many conversations about encouraging diversity in healthcare leadership converge around the role of effective mentoring and sponsorship. A substantial body of research supports the impact of mentoring on retention, research productivity, career satisfaction, and career development for women. It’s important to ensure that the institutional culture is geared toward mentoring junior faculty, says Jessie Kimbrough Marshall, MD, MPH, assistant professor in the Division of General Medicine Hospitalist Program at the University of Michigan Health System in Ann Arbor (UMHS).
Several of our sources pointed out that leaders must learn how to be effective mentors. More attention is being given to enhancing leaders’ mentorship skills. One example is at the Institute for Diversity in Health Management, which conducts an intensive 12-month certificate in diversity management program for practitioners. León says the program fosters ongoing networking and support through the American Leadership Council on Diversity in Healthcare by building leadership competencies.
Dr. Valantine points out that mentoring is hardly a one-style-fits-all proposition but that it is a crucial element to creating and retaining diversity. She says it should be viewed “much more broadly than it is today, and it should focus beyond the trainer-trainee relationship.”
The process is a two-way street. Denege Ward, MD, hospitalist, assistant professor of internal medicine, and director of the medical short stay unit at UMHS, says minorities need to be ready to take a leap of faith.
“Underrepresented faculty and staff should take the risk of possible failure in challenging situations but learn from it and do better and not succumb to fear in face of challenges,” Dr. Ward says.
Although mentoring is one important component in building diversity in academic medicine, Dr. Sánchez asserts that role models, champions, and sponsors are equally important.
“In addition and separate from role models, there must be in place policies and procedures that promote a climate for diverse individuals to succeed,” he says. “What’s needed is an institutional vision and strategic plan that recognizes the importance of diversity. [It] has to become a core principle.”
Dr. Marshall echoes that refrain, noting the recruitment and retention of a diverse set of leaders will take time and intentionality. She is actively engaged in organizing annual meeting mentoring panels at the Society of General Internal Medicine.
“There are still quite a few barriers for women and minorities to advance into hospital leadership roles,” she says. “We still have a long way to go. However, I’m seeing more women and people of color get into these positions. The numbers are increasing, and that encourages me.” TH
Gretchen Henkel is a freelance writer in California.
References
- Institute for Diversity in Health Management. The state of health care diversity and disparities: a benchmarking study of U.S. hospitals. Available at: http://www.diversityconnection.org/diversityconnection/leadership-conferences/Benchmarking-Survey.jsp?fll=S11.
- Top issues confronting hospitals in 2015. American College of Healthcare Executives website. Available at: https://www.ache.org/pubs/research/ceoissues.cfm. Accessed March 5, 2016.
- Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2014. Available at: http://aamcdiversityfactsandfigures.org/.
- Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014;89(6):904-911.
- Valantine H, Sandborg CI. Changing the culture of academic medicine to eliminate the gender leadership gap: 50/50 by 2020. Acad Med. 2013;88(10):1411-1413.
- Sexton DW, Lemak CH, Wainio JA. Career inflection points of women who successfully achieved the hospital CEO position. J Healthc Manag. 2014;59(5):367-383.
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.
“My advancement speaks to hospital medicine and the fact that we are growing as a field,” she says. “Because of that, opportunities are presenting themselves.”
Dr. Kisuule’s ability to thrive in her position speaks to her professionalism but also to a number of other intentional factors: Dr. Howell’s continuing sponsorship to include her in leadership opportunities, an emergency call system for parents with sick children, and a women’s task force whose agenda calls for transparency in hiring and advancement.
Intentional Structure Change
Cardiologist Hannah A. Valantine, MD, recognizes the importance of addressing the lack of women and people from unrepresented groups in the Science, Technology, Engineering, and Mathematics (STEM) workforce. While at Stanford University School of Medicine, she developed and put into place a set of strategies to understand and mitigate the drivers of gender imbalance. Since then, Dr. Valantine was recruited to bring her expertise to the National Institutes of Health in Bethesda, Md., where she is the inaugural chief officer for scientific workforce diversity. In this role, she is committed “to promoting biomedical workforce diversity as an opportunity, not a problem.”
Dr. Valantine is pushing NIH to pursue a wide range of evidence-based programming to eliminate career-transition barriers that keep women and individuals from underrepresented groups from attaining spots in the top echelons of science and health leadership. She believes that applying scientific rigor to the issue of workforce diversity can lead to quantifiable, translatable, and repeatable methods for recruitment and retention of talent in the biomedical workforce (see “Building Blocks").
Before joining NIH, Dr. Valantine and her colleagues at Stanford surveyed gender composition and faculty satisfaction several years after initiating a multifaceted intervention to boost recruitment and development of women faculty.4 After making a visible commitment of resources to support faculty, with special attention to women, Stanford rose from below to above national benchmarks in the representation of women among faculty. Yet significant work remains to be done, Dr. Valantine says. Her work predicts that the estimated time to achieve 50% occupancy of full professorships by women nationally approaches 50 years—“far too long using current approaches.”
In a separate review article, Dr. Valantine and co-author Christy Sandborg, MD, described the Stanford University School of Medicine Academic Biomedical Career Customization (ABCC) model, which was adapted from Deloitte’s Mass Career Customization framework and allows for development of individual career plans that span a faculty member’s total career, not just a year or two at a time. Long-term planning can enable better alignment between the work culture and values of the workforce, which will improve the outlook for women faculty, Dr. Valantine says.
The issues of work-life balance may actually be generational, Dr. Valantine explains. Veteran hospitalist Janet Nagamine, MD, BSN, SFHM, of Santa Clara, Calif., agrees.
“Nowadays, men as well as women are looking for work-life balance,” she says.
In hospital medicine, Dr. Nagamine points out, the structural changes required to effect a work-life balance for hospital leaders are often difficult to achieve.
“As productivity surveys show, HM group leaders are putting in as many RVUs as the staff,” the former SHM board member says. “There is no dedicated time for administrative duties.”
Construct a Pipeline
Barriers to advancement often are particular to characteristics of diverse populations. For example, the AAMC’s report on the U.S. physician workforce documents that in African-American physicians 40 and younger, women outnumber their male counterparts. Therefore, in the association’s Diversity in Medical Education: Facts and Figures 2012 report, the executive summary points out the need to strengthen the medical education pipeline to increase the number of African-American males who enter the premed track.
Despite the fast-growing percentage of Latino and Hispanic populations in the United States, the shortage of Latino/Hispanic physicians increased from 1980 to 2010. Latinos/Hispanics are greatly underrepresented in the medical student, resident, and faculty populations, according to John Paul Sánchez, MD, MPH, assistant dean for diversity and inclusion in the Office for Diversity and Community Engagement at Rutgers, The State University of New Jersey. Likewise, Zeppenfeldt-Cestero believes that efforts must begin much earlier with Latino and other minority and underrepresented students.
“We have to make sure our students pursue the STEM disciplines and that they also later have the education and preparation to be competitive at the MBA or MPH levels,” he says.
Dr. Sánchez, an associate professor of emergency medicine and a diversity activist since his med school days, is the recipient of last year’s Association of Hispanic Healthcare Executives’ academic leader of the year award. Since September 2014, he has been involved with Building the Next Generation of Academic Physicians Inc., which collaborates with more than 40 medical schools across the country. The initiative offers conferences designed to develop diverse medical students’ and residents’ interest in pursuing academic medicine. Open to all medical students and residents, the conference curriculum is tailored for women, UREMs, and trainees who identify as lesbian, gay, bisexual, or transgender (LGBT), he says. Seven conferences were held in 2015, 10 are planned for this year, and seven for 2017.
Healthcare Leadership Gaps
Despite their omnipresence in healthcare, there is a dearth of women in chief executive and governance roles, as has been noted by both the American College of Healthcare Executives and the National Center for Healthcare Leadership. As with academic leadership positions, the leadership gap in the administrative sector does not seem to be due to a lack of women entering graduate programs in health administration. On the contrary, since the mid-1980s women have comprised 50% to 60% of graduate students.
“This is absolutely not a pipeline issue,” says Christy Harris Lemak, PhD, FACHE, professor and chair of the Department of Health Services Administration at the University of Alabama at Birmingham School of Health Professions and lead investigator of the National Center for Healthcare Leadership’s study of women in healthcare executive positions. Other factors come into play.
In the study, she and her co-authors queried female healthcare CEOs to ascertain the critical career inflection points that led to their success.6 Those who were strategic about their careers, sought out mentors, and voiced their intentions about pursuing leadership positions were more likely to be successful in those efforts. However, individual career efforts must be coupled with overall organizational commitment to fostering inclusion (see “Path to the Top: Strategic Advice for Women").
Hospitals and healthcare organizations must pursue the development of human capital (and the diversity of their leaders) in a systematic way. “We recommended [in the study] that organizations set expectations that leaders who mentor other potential leaders be rewarded in the same way as those who hit financial targets or readmission rate targets,” Dr. Lemak says.
Leadership matters, agrees Deborah J. Bowen, FACHE, CAE, president and CEO of Chicago-based American College of Healthcare Executives.
“I think we’re getting a little smarter. Organizational leaders and trustees have a better understanding that talent development is one of the most important jobs,” she says. “If you don’t have the right people in the right places making good decisions on behalf of the patients and the populations in the communities they’re serving, the rest falls apart.”
Nuances of Mentoring
Many conversations about encouraging diversity in healthcare leadership converge around the role of effective mentoring and sponsorship. A substantial body of research supports the impact of mentoring on retention, research productivity, career satisfaction, and career development for women. It’s important to ensure that the institutional culture is geared toward mentoring junior faculty, says Jessie Kimbrough Marshall, MD, MPH, assistant professor in the Division of General Medicine Hospitalist Program at the University of Michigan Health System in Ann Arbor (UMHS).
Several of our sources pointed out that leaders must learn how to be effective mentors. More attention is being given to enhancing leaders’ mentorship skills. One example is at the Institute for Diversity in Health Management, which conducts an intensive 12-month certificate in diversity management program for practitioners. León says the program fosters ongoing networking and support through the American Leadership Council on Diversity in Healthcare by building leadership competencies.
Dr. Valantine points out that mentoring is hardly a one-style-fits-all proposition but that it is a crucial element to creating and retaining diversity. She says it should be viewed “much more broadly than it is today, and it should focus beyond the trainer-trainee relationship.”
The process is a two-way street. Denege Ward, MD, hospitalist, assistant professor of internal medicine, and director of the medical short stay unit at UMHS, says minorities need to be ready to take a leap of faith.
“Underrepresented faculty and staff should take the risk of possible failure in challenging situations but learn from it and do better and not succumb to fear in face of challenges,” Dr. Ward says.
Although mentoring is one important component in building diversity in academic medicine, Dr. Sánchez asserts that role models, champions, and sponsors are equally important.
“In addition and separate from role models, there must be in place policies and procedures that promote a climate for diverse individuals to succeed,” he says. “What’s needed is an institutional vision and strategic plan that recognizes the importance of diversity. [It] has to become a core principle.”
Dr. Marshall echoes that refrain, noting the recruitment and retention of a diverse set of leaders will take time and intentionality. She is actively engaged in organizing annual meeting mentoring panels at the Society of General Internal Medicine.
“There are still quite a few barriers for women and minorities to advance into hospital leadership roles,” she says. “We still have a long way to go. However, I’m seeing more women and people of color get into these positions. The numbers are increasing, and that encourages me.” TH
Gretchen Henkel is a freelance writer in California.
References
- Institute for Diversity in Health Management. The state of health care diversity and disparities: a benchmarking study of U.S. hospitals. Available at: http://www.diversityconnection.org/diversityconnection/leadership-conferences/Benchmarking-Survey.jsp?fll=S11.
- Top issues confronting hospitals in 2015. American College of Healthcare Executives website. Available at: https://www.ache.org/pubs/research/ceoissues.cfm. Accessed March 5, 2016.
- Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2014. Available at: http://aamcdiversityfactsandfigures.org/.
- Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014;89(6):904-911.
- Valantine H, Sandborg CI. Changing the culture of academic medicine to eliminate the gender leadership gap: 50/50 by 2020. Acad Med. 2013;88(10):1411-1413.
- Sexton DW, Lemak CH, Wainio JA. Career inflection points of women who successfully achieved the hospital CEO position. J Healthc Manag. 2014;59(5):367-383.
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.
“My advancement speaks to hospital medicine and the fact that we are growing as a field,” she says. “Because of that, opportunities are presenting themselves.”
Dr. Kisuule’s ability to thrive in her position speaks to her professionalism but also to a number of other intentional factors: Dr. Howell’s continuing sponsorship to include her in leadership opportunities, an emergency call system for parents with sick children, and a women’s task force whose agenda calls for transparency in hiring and advancement.
Intentional Structure Change
Cardiologist Hannah A. Valantine, MD, recognizes the importance of addressing the lack of women and people from unrepresented groups in the Science, Technology, Engineering, and Mathematics (STEM) workforce. While at Stanford University School of Medicine, she developed and put into place a set of strategies to understand and mitigate the drivers of gender imbalance. Since then, Dr. Valantine was recruited to bring her expertise to the National Institutes of Health in Bethesda, Md., where she is the inaugural chief officer for scientific workforce diversity. In this role, she is committed “to promoting biomedical workforce diversity as an opportunity, not a problem.”
Dr. Valantine is pushing NIH to pursue a wide range of evidence-based programming to eliminate career-transition barriers that keep women and individuals from underrepresented groups from attaining spots in the top echelons of science and health leadership. She believes that applying scientific rigor to the issue of workforce diversity can lead to quantifiable, translatable, and repeatable methods for recruitment and retention of talent in the biomedical workforce (see “Building Blocks").
Before joining NIH, Dr. Valantine and her colleagues at Stanford surveyed gender composition and faculty satisfaction several years after initiating a multifaceted intervention to boost recruitment and development of women faculty.4 After making a visible commitment of resources to support faculty, with special attention to women, Stanford rose from below to above national benchmarks in the representation of women among faculty. Yet significant work remains to be done, Dr. Valantine says. Her work predicts that the estimated time to achieve 50% occupancy of full professorships by women nationally approaches 50 years—“far too long using current approaches.”
In a separate review article, Dr. Valantine and co-author Christy Sandborg, MD, described the Stanford University School of Medicine Academic Biomedical Career Customization (ABCC) model, which was adapted from Deloitte’s Mass Career Customization framework and allows for development of individual career plans that span a faculty member’s total career, not just a year or two at a time. Long-term planning can enable better alignment between the work culture and values of the workforce, which will improve the outlook for women faculty, Dr. Valantine says.
The issues of work-life balance may actually be generational, Dr. Valantine explains. Veteran hospitalist Janet Nagamine, MD, BSN, SFHM, of Santa Clara, Calif., agrees.
“Nowadays, men as well as women are looking for work-life balance,” she says.
In hospital medicine, Dr. Nagamine points out, the structural changes required to effect a work-life balance for hospital leaders are often difficult to achieve.
“As productivity surveys show, HM group leaders are putting in as many RVUs as the staff,” the former SHM board member says. “There is no dedicated time for administrative duties.”
Construct a Pipeline
Barriers to advancement often are particular to characteristics of diverse populations. For example, the AAMC’s report on the U.S. physician workforce documents that in African-American physicians 40 and younger, women outnumber their male counterparts. Therefore, in the association’s Diversity in Medical Education: Facts and Figures 2012 report, the executive summary points out the need to strengthen the medical education pipeline to increase the number of African-American males who enter the premed track.
Despite the fast-growing percentage of Latino and Hispanic populations in the United States, the shortage of Latino/Hispanic physicians increased from 1980 to 2010. Latinos/Hispanics are greatly underrepresented in the medical student, resident, and faculty populations, according to John Paul Sánchez, MD, MPH, assistant dean for diversity and inclusion in the Office for Diversity and Community Engagement at Rutgers, The State University of New Jersey. Likewise, Zeppenfeldt-Cestero believes that efforts must begin much earlier with Latino and other minority and underrepresented students.
“We have to make sure our students pursue the STEM disciplines and that they also later have the education and preparation to be competitive at the MBA or MPH levels,” he says.
Dr. Sánchez, an associate professor of emergency medicine and a diversity activist since his med school days, is the recipient of last year’s Association of Hispanic Healthcare Executives’ academic leader of the year award. Since September 2014, he has been involved with Building the Next Generation of Academic Physicians Inc., which collaborates with more than 40 medical schools across the country. The initiative offers conferences designed to develop diverse medical students’ and residents’ interest in pursuing academic medicine. Open to all medical students and residents, the conference curriculum is tailored for women, UREMs, and trainees who identify as lesbian, gay, bisexual, or transgender (LGBT), he says. Seven conferences were held in 2015, 10 are planned for this year, and seven for 2017.
Healthcare Leadership Gaps
Despite their omnipresence in healthcare, there is a dearth of women in chief executive and governance roles, as has been noted by both the American College of Healthcare Executives and the National Center for Healthcare Leadership. As with academic leadership positions, the leadership gap in the administrative sector does not seem to be due to a lack of women entering graduate programs in health administration. On the contrary, since the mid-1980s women have comprised 50% to 60% of graduate students.
“This is absolutely not a pipeline issue,” says Christy Harris Lemak, PhD, FACHE, professor and chair of the Department of Health Services Administration at the University of Alabama at Birmingham School of Health Professions and lead investigator of the National Center for Healthcare Leadership’s study of women in healthcare executive positions. Other factors come into play.
In the study, she and her co-authors queried female healthcare CEOs to ascertain the critical career inflection points that led to their success.6 Those who were strategic about their careers, sought out mentors, and voiced their intentions about pursuing leadership positions were more likely to be successful in those efforts. However, individual career efforts must be coupled with overall organizational commitment to fostering inclusion (see “Path to the Top: Strategic Advice for Women").
Hospitals and healthcare organizations must pursue the development of human capital (and the diversity of their leaders) in a systematic way. “We recommended [in the study] that organizations set expectations that leaders who mentor other potential leaders be rewarded in the same way as those who hit financial targets or readmission rate targets,” Dr. Lemak says.
Leadership matters, agrees Deborah J. Bowen, FACHE, CAE, president and CEO of Chicago-based American College of Healthcare Executives.
“I think we’re getting a little smarter. Organizational leaders and trustees have a better understanding that talent development is one of the most important jobs,” she says. “If you don’t have the right people in the right places making good decisions on behalf of the patients and the populations in the communities they’re serving, the rest falls apart.”
Nuances of Mentoring
Many conversations about encouraging diversity in healthcare leadership converge around the role of effective mentoring and sponsorship. A substantial body of research supports the impact of mentoring on retention, research productivity, career satisfaction, and career development for women. It’s important to ensure that the institutional culture is geared toward mentoring junior faculty, says Jessie Kimbrough Marshall, MD, MPH, assistant professor in the Division of General Medicine Hospitalist Program at the University of Michigan Health System in Ann Arbor (UMHS).
Several of our sources pointed out that leaders must learn how to be effective mentors. More attention is being given to enhancing leaders’ mentorship skills. One example is at the Institute for Diversity in Health Management, which conducts an intensive 12-month certificate in diversity management program for practitioners. León says the program fosters ongoing networking and support through the American Leadership Council on Diversity in Healthcare by building leadership competencies.
Dr. Valantine points out that mentoring is hardly a one-style-fits-all proposition but that it is a crucial element to creating and retaining diversity. She says it should be viewed “much more broadly than it is today, and it should focus beyond the trainer-trainee relationship.”
The process is a two-way street. Denege Ward, MD, hospitalist, assistant professor of internal medicine, and director of the medical short stay unit at UMHS, says minorities need to be ready to take a leap of faith.
“Underrepresented faculty and staff should take the risk of possible failure in challenging situations but learn from it and do better and not succumb to fear in face of challenges,” Dr. Ward says.
Although mentoring is one important component in building diversity in academic medicine, Dr. Sánchez asserts that role models, champions, and sponsors are equally important.
“In addition and separate from role models, there must be in place policies and procedures that promote a climate for diverse individuals to succeed,” he says. “What’s needed is an institutional vision and strategic plan that recognizes the importance of diversity. [It] has to become a core principle.”
Dr. Marshall echoes that refrain, noting the recruitment and retention of a diverse set of leaders will take time and intentionality. She is actively engaged in organizing annual meeting mentoring panels at the Society of General Internal Medicine.
“There are still quite a few barriers for women and minorities to advance into hospital leadership roles,” she says. “We still have a long way to go. However, I’m seeing more women and people of color get into these positions. The numbers are increasing, and that encourages me.” TH
Gretchen Henkel is a freelance writer in California.
References
- Institute for Diversity in Health Management. The state of health care diversity and disparities: a benchmarking study of U.S. hospitals. Available at: http://www.diversityconnection.org/diversityconnection/leadership-conferences/Benchmarking-Survey.jsp?fll=S11.
- Top issues confronting hospitals in 2015. American College of Healthcare Executives website. Available at: https://www.ache.org/pubs/research/ceoissues.cfm. Accessed March 5, 2016.
- Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2014. Available at: http://aamcdiversityfactsandfigures.org/.
- Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014;89(6):904-911.
- Valantine H, Sandborg CI. Changing the culture of academic medicine to eliminate the gender leadership gap: 50/50 by 2020. Acad Med. 2013;88(10):1411-1413.
- Sexton DW, Lemak CH, Wainio JA. Career inflection points of women who successfully achieved the hospital CEO position. J Healthc Manag. 2014;59(5):367-383.
Things Hospitalists Want Hospital Administrators to Know
I think it is really cool that this publication has a series of articles on “What Cardiologists [or infection disease specialists, nephrologists, etc.] Want Hospitalists to Know.” I’m always interested to see which clinical topics made the list and which I’m already reasonably familiar with versus know little about. I’ve added this series to my list of things that are always worth the time to read, along with the “What’s New” section in UpToDate, review articles in major journals, and the Cleveland Clinic Journal of Medicine.
Not long ago, I worked with a hospitalist group that had agreed to cardiologists’ request that new hospitalists round with a cardiologist for something like three days as part of their orientation. This seems like they’ve taken the idea of “What Cardiologists Want Hospitalists to Know” a lot further than I had ever considered. I’m sure it would have value on many levels, including positioning the new hospitalist to work more effectively with the cardiologists, but I’m not sure it’s worth the cost. And I’m really concerned it sends a signal that the relationship is one way—that is, the hospitalists need to understand what the cardiologists do and want from them and not the reverse. For many reasons, I think this should be a reciprocal relationship, and it seems reasonable that new cardiologists should orient by rounding with hospitalists.
Same goes for the “… Want Hospitalists to Know” series. I’d like to see articles enumerating what hospitalists want doctors in other fields to know either in this magazine or its counterpart in the other specialty. What follows is the first of these. It is my take on non-clinical topics hospitalists want hospital leaders to know, and I’ll leave it to others to write about clinical topics.
We Aren’t on ‘Vacation’ Every Other Week
If you always think of our days off as a vacation, as in, “Those hospitalists get 26 weeks of vacation a year,” you’re making a mistake. A significant portion of our weekdays off are just like your weekends; they’re days to take a breather.
And you’re likely forgetting how many weekends we work.
And maybe lots of nights also.
You probably work more hours annually, but having more days for a breather are one offset for our weekends and nights.
Insisting Hospitalists Work an Entire Shift (12 Hours) Doesn’t Make a Lot of Sense on Slow Days
Staying around after completing clinical work yields no value. Too often, the time is spent watching YouTube or similar activities. And it means the doctor will be much more frustrated, and more likely to lobby for overtime compensation, when needing to stay beyond the scheduled end of the shift on busy days.
Avoid measuring work effort in hours. And in many cases, it is best to avoid precise determinations of when a day shift ends. At most hospitals, you do need at least one daytime doctor to stay on duty until the next shift arrives, but it rarely makes sense to have all of the hospitalists stay.
Your hospitalists need to be professional enough not to dash out the door the minute they’ve put notes on every patient’s chart. Instead, rather than leaving at the first opportunity on slow days, they could do all of the discharge preparation (med rec, discharge summary, etc.) for patients likely ready for discharge the next day; this can help a lot to discharge patients early the next day. Or they could make “secondary” rounds focused on patient satisfaction, etc.
Obs Patients Usually Are No Less Complicated—or Labor-Intensive—to Care For
It’s best to think of observation as solely a payor classification and not a good indicator of risk, complexity, or work required. Unfortunately “observation” is often thought of as shorthand for simple, not sick, easy to manage, etc. While true for a small subset of observation patients, such as younger people with a single problem such as atypical chest pain, it isn’t true for older (Medicare) patients with multiple chronic illnesses, on multiple medications, and with complex social situations.
Shouldn’t We Measure Length of Stay for All Patients in Hours Rather Than Days?
Then we could better understand throughput issues such as whether afternoon discharges for inpatients are late discharges or really very early discharges that weren’t held until the next morning.
Even High-Performing Hospitalist Groups Are Likely to Have Patient Satisfaction Scores on the Lower End of Doctors at Your Hospital
Don’t decide that just because they have much lower scores than the orthopedists, cardiologists, obstetricians, and other specialties, it is the hospitalists who are falling furthest below their potential. It may be the cardiologists who have a long way to go to achieve great scores for their specialty.
This isn’t an excuse. Just about every hospitalist group can do better and should work to make it happen. And because in nearly every hospital more HCAHPS surveys are attributed to hospitalists than any other specialty by a wide margin, our scores have a huge impact on the overall hospital averages. But you should keep in mind that, for a variety of reasons, hospitalists everywhere have physician communication scores that are lower than many or most other specialties.
To my knowledge, there isn’t a data set that provides patient satisfaction scores by specialty. And scores seem to vary a lot by geographic region, e.g., they’re nearly always higher in the South than other parts of the country. So there isn’t a good way to control for all the variables and know you’re setting appropriate improvement goals for each specialty. But your hospitalists will appreciate it if you acknowledge it may be unreasonable to set the same goals across specialties.
We’d Love Your Help Getting Rid of Pagers
Secure text messaging between all caregivers seems to be the way to go, and we will look to the hospital to make an investment in technology to make it possible and train users to ensure that by making messaging easier the volume of messages (interruptions) doesn’t just skyrocket. We, the hospitalists at your hospital, are happy to help with all of this, from vendor selection to plans for implementation. Please ask! TH

I think it is really cool that this publication has a series of articles on “What Cardiologists [or infection disease specialists, nephrologists, etc.] Want Hospitalists to Know.” I’m always interested to see which clinical topics made the list and which I’m already reasonably familiar with versus know little about. I’ve added this series to my list of things that are always worth the time to read, along with the “What’s New” section in UpToDate, review articles in major journals, and the Cleveland Clinic Journal of Medicine.
Not long ago, I worked with a hospitalist group that had agreed to cardiologists’ request that new hospitalists round with a cardiologist for something like three days as part of their orientation. This seems like they’ve taken the idea of “What Cardiologists Want Hospitalists to Know” a lot further than I had ever considered. I’m sure it would have value on many levels, including positioning the new hospitalist to work more effectively with the cardiologists, but I’m not sure it’s worth the cost. And I’m really concerned it sends a signal that the relationship is one way—that is, the hospitalists need to understand what the cardiologists do and want from them and not the reverse. For many reasons, I think this should be a reciprocal relationship, and it seems reasonable that new cardiologists should orient by rounding with hospitalists.
Same goes for the “… Want Hospitalists to Know” series. I’d like to see articles enumerating what hospitalists want doctors in other fields to know either in this magazine or its counterpart in the other specialty. What follows is the first of these. It is my take on non-clinical topics hospitalists want hospital leaders to know, and I’ll leave it to others to write about clinical topics.
We Aren’t on ‘Vacation’ Every Other Week
If you always think of our days off as a vacation, as in, “Those hospitalists get 26 weeks of vacation a year,” you’re making a mistake. A significant portion of our weekdays off are just like your weekends; they’re days to take a breather.
And you’re likely forgetting how many weekends we work.
And maybe lots of nights also.
You probably work more hours annually, but having more days for a breather are one offset for our weekends and nights.
Insisting Hospitalists Work an Entire Shift (12 Hours) Doesn’t Make a Lot of Sense on Slow Days
Staying around after completing clinical work yields no value. Too often, the time is spent watching YouTube or similar activities. And it means the doctor will be much more frustrated, and more likely to lobby for overtime compensation, when needing to stay beyond the scheduled end of the shift on busy days.
Avoid measuring work effort in hours. And in many cases, it is best to avoid precise determinations of when a day shift ends. At most hospitals, you do need at least one daytime doctor to stay on duty until the next shift arrives, but it rarely makes sense to have all of the hospitalists stay.
Your hospitalists need to be professional enough not to dash out the door the minute they’ve put notes on every patient’s chart. Instead, rather than leaving at the first opportunity on slow days, they could do all of the discharge preparation (med rec, discharge summary, etc.) for patients likely ready for discharge the next day; this can help a lot to discharge patients early the next day. Or they could make “secondary” rounds focused on patient satisfaction, etc.
Obs Patients Usually Are No Less Complicated—or Labor-Intensive—to Care For
It’s best to think of observation as solely a payor classification and not a good indicator of risk, complexity, or work required. Unfortunately “observation” is often thought of as shorthand for simple, not sick, easy to manage, etc. While true for a small subset of observation patients, such as younger people with a single problem such as atypical chest pain, it isn’t true for older (Medicare) patients with multiple chronic illnesses, on multiple medications, and with complex social situations.
Shouldn’t We Measure Length of Stay for All Patients in Hours Rather Than Days?
Then we could better understand throughput issues such as whether afternoon discharges for inpatients are late discharges or really very early discharges that weren’t held until the next morning.
Even High-Performing Hospitalist Groups Are Likely to Have Patient Satisfaction Scores on the Lower End of Doctors at Your Hospital
Don’t decide that just because they have much lower scores than the orthopedists, cardiologists, obstetricians, and other specialties, it is the hospitalists who are falling furthest below their potential. It may be the cardiologists who have a long way to go to achieve great scores for their specialty.
This isn’t an excuse. Just about every hospitalist group can do better and should work to make it happen. And because in nearly every hospital more HCAHPS surveys are attributed to hospitalists than any other specialty by a wide margin, our scores have a huge impact on the overall hospital averages. But you should keep in mind that, for a variety of reasons, hospitalists everywhere have physician communication scores that are lower than many or most other specialties.
To my knowledge, there isn’t a data set that provides patient satisfaction scores by specialty. And scores seem to vary a lot by geographic region, e.g., they’re nearly always higher in the South than other parts of the country. So there isn’t a good way to control for all the variables and know you’re setting appropriate improvement goals for each specialty. But your hospitalists will appreciate it if you acknowledge it may be unreasonable to set the same goals across specialties.
We’d Love Your Help Getting Rid of Pagers
Secure text messaging between all caregivers seems to be the way to go, and we will look to the hospital to make an investment in technology to make it possible and train users to ensure that by making messaging easier the volume of messages (interruptions) doesn’t just skyrocket. We, the hospitalists at your hospital, are happy to help with all of this, from vendor selection to plans for implementation. Please ask! TH

I think it is really cool that this publication has a series of articles on “What Cardiologists [or infection disease specialists, nephrologists, etc.] Want Hospitalists to Know.” I’m always interested to see which clinical topics made the list and which I’m already reasonably familiar with versus know little about. I’ve added this series to my list of things that are always worth the time to read, along with the “What’s New” section in UpToDate, review articles in major journals, and the Cleveland Clinic Journal of Medicine.
Not long ago, I worked with a hospitalist group that had agreed to cardiologists’ request that new hospitalists round with a cardiologist for something like three days as part of their orientation. This seems like they’ve taken the idea of “What Cardiologists Want Hospitalists to Know” a lot further than I had ever considered. I’m sure it would have value on many levels, including positioning the new hospitalist to work more effectively with the cardiologists, but I’m not sure it’s worth the cost. And I’m really concerned it sends a signal that the relationship is one way—that is, the hospitalists need to understand what the cardiologists do and want from them and not the reverse. For many reasons, I think this should be a reciprocal relationship, and it seems reasonable that new cardiologists should orient by rounding with hospitalists.
Same goes for the “… Want Hospitalists to Know” series. I’d like to see articles enumerating what hospitalists want doctors in other fields to know either in this magazine or its counterpart in the other specialty. What follows is the first of these. It is my take on non-clinical topics hospitalists want hospital leaders to know, and I’ll leave it to others to write about clinical topics.
We Aren’t on ‘Vacation’ Every Other Week
If you always think of our days off as a vacation, as in, “Those hospitalists get 26 weeks of vacation a year,” you’re making a mistake. A significant portion of our weekdays off are just like your weekends; they’re days to take a breather.
And you’re likely forgetting how many weekends we work.
And maybe lots of nights also.
You probably work more hours annually, but having more days for a breather are one offset for our weekends and nights.
Insisting Hospitalists Work an Entire Shift (12 Hours) Doesn’t Make a Lot of Sense on Slow Days
Staying around after completing clinical work yields no value. Too often, the time is spent watching YouTube or similar activities. And it means the doctor will be much more frustrated, and more likely to lobby for overtime compensation, when needing to stay beyond the scheduled end of the shift on busy days.
Avoid measuring work effort in hours. And in many cases, it is best to avoid precise determinations of when a day shift ends. At most hospitals, you do need at least one daytime doctor to stay on duty until the next shift arrives, but it rarely makes sense to have all of the hospitalists stay.
Your hospitalists need to be professional enough not to dash out the door the minute they’ve put notes on every patient’s chart. Instead, rather than leaving at the first opportunity on slow days, they could do all of the discharge preparation (med rec, discharge summary, etc.) for patients likely ready for discharge the next day; this can help a lot to discharge patients early the next day. Or they could make “secondary” rounds focused on patient satisfaction, etc.
Obs Patients Usually Are No Less Complicated—or Labor-Intensive—to Care For
It’s best to think of observation as solely a payor classification and not a good indicator of risk, complexity, or work required. Unfortunately “observation” is often thought of as shorthand for simple, not sick, easy to manage, etc. While true for a small subset of observation patients, such as younger people with a single problem such as atypical chest pain, it isn’t true for older (Medicare) patients with multiple chronic illnesses, on multiple medications, and with complex social situations.
Shouldn’t We Measure Length of Stay for All Patients in Hours Rather Than Days?
Then we could better understand throughput issues such as whether afternoon discharges for inpatients are late discharges or really very early discharges that weren’t held until the next morning.
Even High-Performing Hospitalist Groups Are Likely to Have Patient Satisfaction Scores on the Lower End of Doctors at Your Hospital
Don’t decide that just because they have much lower scores than the orthopedists, cardiologists, obstetricians, and other specialties, it is the hospitalists who are falling furthest below their potential. It may be the cardiologists who have a long way to go to achieve great scores for their specialty.
This isn’t an excuse. Just about every hospitalist group can do better and should work to make it happen. And because in nearly every hospital more HCAHPS surveys are attributed to hospitalists than any other specialty by a wide margin, our scores have a huge impact on the overall hospital averages. But you should keep in mind that, for a variety of reasons, hospitalists everywhere have physician communication scores that are lower than many or most other specialties.
To my knowledge, there isn’t a data set that provides patient satisfaction scores by specialty. And scores seem to vary a lot by geographic region, e.g., they’re nearly always higher in the South than other parts of the country. So there isn’t a good way to control for all the variables and know you’re setting appropriate improvement goals for each specialty. But your hospitalists will appreciate it if you acknowledge it may be unreasonable to set the same goals across specialties.
We’d Love Your Help Getting Rid of Pagers
Secure text messaging between all caregivers seems to be the way to go, and we will look to the hospital to make an investment in technology to make it possible and train users to ensure that by making messaging easier the volume of messages (interruptions) doesn’t just skyrocket. We, the hospitalists at your hospital, are happy to help with all of this, from vendor selection to plans for implementation. Please ask! TH