User login
Your patients are talking: Isn’t it time you take responsibility for your online reputation?
In a web-focused world, it should not take much convincing that monitoring your online reputation is time well spent. For some of us, it may be hard to believe that online reviews have evolved beyond restaurants and plumbers, but today your patients are flocking to the Internet to read and leave reviews about you, your staff, and your services. What can you do to protect your online reputation?
We first addressed this topic in December 2014 (“Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews”1). Have you implemented any of the tactics we offered then? We hope that you do take proactive steps to protect your online image.
What is a physician’s most precious asset?
You might answer this question with, “my patients” or “the training and education that I have obtained to practice my craft.” But the real answer is that your most precious asset is your reputation.
Physicians live and die by their reputations. We spend our entire medical careers polishing and protecting this status. The Internet dramatically has altered the way people gather information. It is sad but true that a single comment that only takes a few seconds and a single mouse-click to post can be seen by thousands and ruin that life-long effort.
How are physicians rated on the web?
Online physician reviews are positive 70% to 90% of the time.2 Most physicians have 5 or fewer reviews on any one site.3 Of the approximately 30 sites that monitor physicians and hospitals online, one of the most popular is AngiesList.com. This site requires registration and a fee; a member can review a physician every 6 months. On free websites such as Yelp.com and doctorsscorecard.com the reviewer can comment once. Other sites such as vitals.com or DrScore.com limit the reviews from 1 source, which prevents an angry patient from stuffing the ballot box.2
Pay attention
At a minimum, physicians should be monitoring their reputation by conducting periodic searches—“Googling” their name and practice name—to identify what information is already online. You may find that 3, 4, or even 10 reviews appear on various sites. If you are lucky, these reviews will be positive. Don’t be surprised, however, if 1 or 2 are not. Let’s face it: even the most accredited and experienced physician cannot possibly satisfy every patient who walks through the door.
Neil Baum, MD, and Ron Romano have offered tips on ways to manage online reputations in the past,1 and they urge Ob-Gyns to take an active role in this process in order to increase positive exposure to patients and maintain an active practice. Is active reputation management something that ObGyns are spending their valuable time on? To find out, OBG Management reached out to its Virtual Editorial Board. We found that many readers are paying attention to patient satisfaction. Some are soliciting online reviews and maintaining active upkeep on their online reputation. Here are a few responses we received from practicing ObGyns across the United States.
William E. McGrath Jr, MD, of Fernandina Beach, Florida, says that his office provides patients with a list of 5 popular review websites during their visits, and that approximately 1 in 10 will follow up with a review. Patient reviews are also prominently posted on his practice’s website. The large, private, single-specialty group to which his practice belongs requires patient satisfaction surveys for quality assurance review and insurance contract negotiations. “It is all about physician-patient communication,” he says.
Keith S. Merlin, MD, of Brockton, Massachusetts, says that he has checked online reviews to ensure their accuracy. His practice uses surveys, a suggestion box, and a mystery shopper to measure patient satisfaction, a worthwhile effort he says to understand where the practice is doing well and what needs to be done better.
Wesley Hambright, MD, of Jacksonville, North Carolina, reports that he has established a Google Alert to monitor for new content relating to his practice.
Patrick Pevoto, MD, MBA, of Austin, Texas, informs us that he has just started to think about ways to manage his online reputation. He has created a website and is writing a monthly blog, which he posts on his site. He acknowledges the importance of assessing patient satisfaction in his practice but is not applying large-scale measurement techniques yet. To keep his patients happy, he handles concerns that arise on a personal, case-by-case basis.
John Armstrong, MD, MS, of Napa, California, also reports that management of his online reputation is in the beginning stages. He uses focus groups and feels that listening to his patients when they do comment on their experience is important to his overall practice. Listening helps to “identify areas to improve and reaffirms when we are doing well,” he says. To keep his patients happy, he strives to “give extraordinary care and simply be nice to people.” When issues arise, making it right and being polite are important elements, he asserts.
Delos J. Clow, DO, MS, of Chillicothe, Missouri, does measure patient satisfaction, and feels this is very important to his practice in order to identify and correct any negative trends. He does not actively monitor his practice reputation online.
Robert del Rosario, MD, of Camp Hill, Pennsylvania, similarly does not actively manage an online reputation, but does focus on patient satisfaction. To enhance satisfaction, he tries to de-emphasize the electronic medical record to “make visits more personal and less interrogative.” Additionally, his practice objectively gauges aspects of care that might be able to be improved upon.
Reference
- Romano R, Baum NH. Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews. OBG Manag. 2014;26(12):23,24,26,28.
Tell your own story
As physicians, you may not have control over what others say about you, but you can take ownership of your online presence by establishing a website, blog, and social media platforms, ensuring your story is being properly communicated. Without an online presence, you are entirely at the mercy of directory and review sites.
Optimize your website
A site that successfully uses search engine optimization (SEO) will have the upper hand when patients hunt for a physician in your area because the information will be posted at the top of the search page, well above the reviews and listings left by patients and other third-party sources. This is a critical step for your online brand because it will be difficult for other sites to mask your credibility. This should motivate you to develop an online presence, regularly update information, and participate in Internet dialog with other sites.
Generate quality, natural reviews
If your site is in good standing in search results, the next step is to implement a patient reviews strategy to start acquiring positive online reviews. A third-party provider can work with you to launch a local search engine optimization strategy and a natural reviews management program tailored for your practice’s needs. For the most part, however, we do not recommend using an online reputation management company. It is far better and more economical to ask satisfied patients to provide reviews.
At first, you may be tempted to actively petition or solicit reviews through survey software, but this method is manipulative and can lead to reputation problems for your practice. Google actively tracks where reviews originate and uses advanced algorithms to determine the review’s integrity. A petitioned review is classified as less valid, and therefore Google will assume it was not written under the same pretense as a natural, unsolicited review.
Quality customer service and outstanding patient care are often what achieve the organic reviews you are striving for. To encourage a steady flow, administer a process that encourages your most satisfied, loyal patients to review your practice.
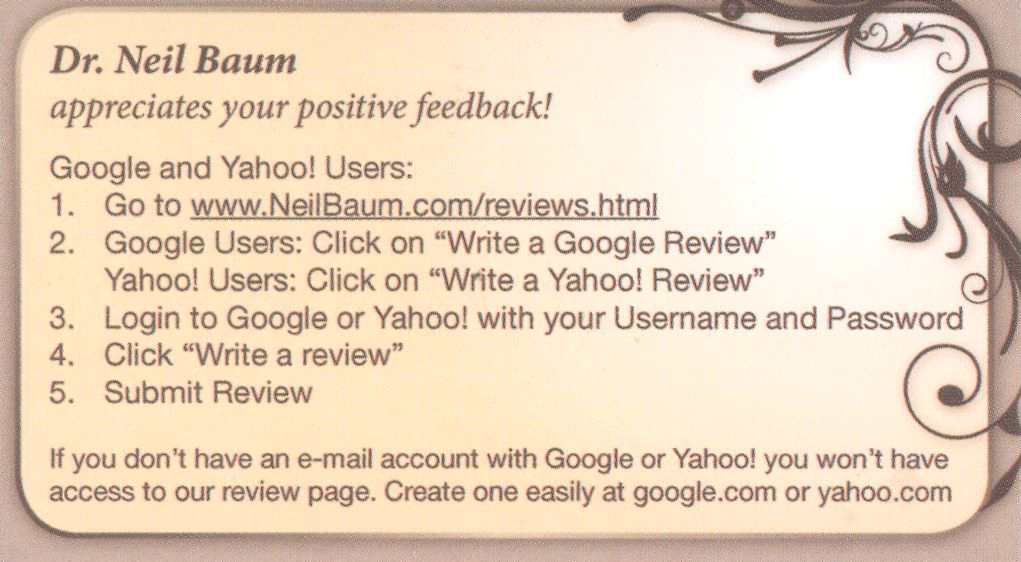
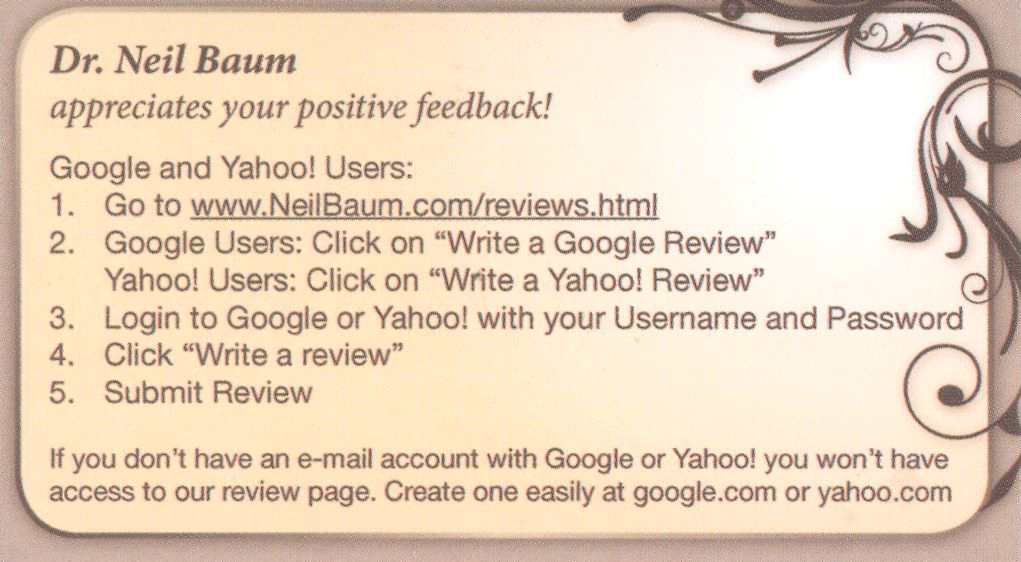
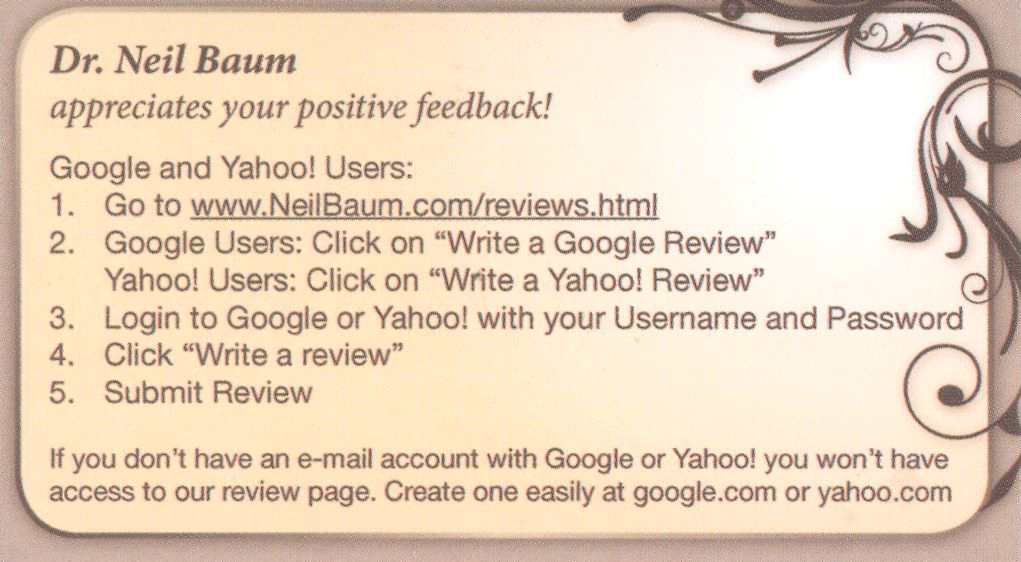
Keep the process simple. Capture positive compliments at the point of service. Before a patient leaves your office, hand her a card (FIGURE) with easy steps for posting an online review, or offer her a tablet that links directly to your website review section. If your patient is not computer savvy, ask her to complete a 4- to 5-question survey and give her a clipboard and a pen. Then have a staff member post it on your website.
In Dr. Baum’s practice, there is a poster in every exam room and in the reception area where patients can scan the quick response (QR) code and immediately submit a testimonial. Using this system, the practice is able to collect 3 to 5 positive reviews every day.
A patient pleased with your staff’s service will happily take 5 minutes to submit a review. Acquire 5 to 10 reviews monthly and within a year’s time you will have generated enough positive reviews to negate any damaging comments that inevitably will emerge from time to time.
CASE Patient criticizes physician in a review forum
A physician with a robust Internet presence will have his or her name and the practice appear at the top of search engine results pages (as is the case with Dr. Neil Baum when “urologist” plus “New Orleans” is typed into the Google search engine window). By far most of Dr. Baum’s reviews are positive. In one instance, however, a patient on a physician review website referred to Dr. Baum as “technologically advanced but more motivated to increase his income by performing too many diagnostic tests.”
If you find a negative comment in an online directory or review website, what should you do?
The Office for Civil Rights (OCR) within the US Department of Health and Human Services (HHS) is responsible for handling Health Insurance Portability and Accountability Act of 1996 (HIPAA)1 complaints. Deven McGraw, OCR’s deputy director of health information privacy, states that “just because patients have rated their health provider publicly doesn’t give their health provider permission to rate them in return.”2,3 In fact, some health care providers who responded to poor online reviews ran into trouble with privacy rules established by HIPAA.2,3
Mr. McGraw notes that, when responding to online reviews, health professionals should speak generally about the way they treat patients while complying with HIPAA regulations. He suggests, “If the complaint is about poor patient care … say, ‘I provide all of my patients with good patient care’ and ‘I’ve been reviewed in other contexts and have good reviews.’”2,3
According to Yelp’s senior director of litigation, Aaron Schur, most patient complaints center on practice-based concerns such as wait times, office staff, and billing, not about the medical service delivered. Although most physicians do not respond, says Mr. Schur, those who do, tend to ask patients to discuss the matter in private or to apologize.2,3
What are the consequences of a HIPAA violation?
OCR Director Jocelyn Samuels says that the office’s primary role is to help health providers follow HIPAA regulations.2,5 The OCR can resolve HIPPA violations privately and informally, impose fines of up to $50,000 per violation, or it can file criminal charges against violators.2,4
The majority of the office’s investigation and enforcement of HIPAA has been against large medical data breaches.2,5 Small privacy breaches by large health care providers (eg, CVS, Walmart, Lab Corp, Quest Diagnostics, and others) generally do not result in legal consequences; the providers are privately warned. According to ProPublica, even repeated HIPAA violations tend not to be fined.2,4
Small-scale infractions can be more damaging on a personal level to both patients and physicians. However, the OCR does not typically become involved in privacy breaches that include only a few individuals. Health care providers are rarely punished for small HIPPA breaches; instead, the OCR typically settles for pledges to fix any problems and issues reminders of HIPPA requirements.2,5
Although the OCR is often the only place patients can go to seek vindication, HIPAA does not support the right to sue for violation of personal privacy. People who seek a legal remedy must find another means, which is easier in some states than in others.2,5
Health care providers have tried myriad ways to attempt to combat negative reviews. Some have sued patients, attracting a flood of attention but achieving little legal success. Others have asked patients to remove their complaints.2,3
Best practices
Create and circulate a policy. Medical privacy breaches involving sensitive health details can occur when office or hospital staff share patient information due to personal hostility or lack of understanding of HIPPA policy.2,5 Have a practice policy for responding to online reviews by patients, and make sure the staff members who have access to the practice’s online accounts understand your policy and the possible repercussions of not following it. Teach and continue to remind your staff about HIPPA regulations and hold them to a high ethical level of privacy.
Solicit reviews on an ongoing basis. Jeffrey Segal, a review site critic, says that all reviews are valuable. Physicians should respond carefully to negative comments and encourage satisfied patients to post positive reviews. “’For doctors who get bent out of shape to get rid of negative reviews, it’s a denominator problem,’ he said. ‘If they only have three reviews and two are negative, the denominator is the problem. … If you can figure out a way to cultivate reviews from hundreds of patients rather than a few patients, the problem is solved.’”2,3
CASE Resolved
Dr. Baum never responded directly to the negative patient review, and others he has received. He balances the rare negative response with numerous and plentiful positive responses by making it a practice to encourage reviews from all of his patients.
References
- HIPAA for Professionals. US Department of Health & Human Services. http://www.hhs.gov/hipaa/for-professionals/index.html. Accessed October 11, 2016.
- Hall SD. Providers responding to Yelp reviews must be mindful of HIPAA. FierceHealthcare. http://www.fiercehealthcare.com/it/providers-responding-to-yelp-reviews-must-be-mindful-hipaa. Published May 31, 2016. Accessed October 7, 2016.
- Ornstein C. Stung by Yelp reviews, health providers spill patient secrets. ProPublica. https://www.propublica.org/article/stung-by-yelp-reviews-health -providers-spill-patient-secrets. Published May 27, 2016. Accessed October 11, 2016.
- Ornstein C, Waldman A. Few consequences for health privacy law’s repeat offenders. ProPublica. https://www.propublica.org/article/few-consequences-for-health-privacy-law-repeat-offenders. Published December 29, 2015. Accessed October 11, 2016.
- Ornstein C. Small-scale violations of medical privacy often cause the most harm. ProPublica. https://www.propublica.org/article/small-scale-violations-of-medical-privacy-often-cause-the-most-harm. Published December 10, 2015. Accessed October 11, 2016.
The bottom line
Patients are seeking and leaving reviews about you and your practice online and you need to actively manage your online reputation. Do not let one disgruntled patient ruin your reputation. Our advice: Do not wait for a negative review to begin your reputation management. Take an active role and generate positive reviews to drown out negative remarks made by an occasional patient. This is an inexpensive process that does work.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Romano R, Baum NH. Using the Internet in your practice. Part 4: Reputation management-how to gather kudos and combat negative online reviews. OBG Manag. 2014;26(12):23,24,26,28.
- Lagu T, Hannon NS, Rothberg MB, Lindenauer PK. Patients' evaluations of health care providers in the era of social networking: an analysis of physician rating websites. J Gen Intern Med. 2010;25(9):942-946.
- Gunter J. For better or maybe, worse, patients are judging your care online. OBG Manag. 2011;23(3):47-51.
In a web-focused world, it should not take much convincing that monitoring your online reputation is time well spent. For some of us, it may be hard to believe that online reviews have evolved beyond restaurants and plumbers, but today your patients are flocking to the Internet to read and leave reviews about you, your staff, and your services. What can you do to protect your online reputation?
We first addressed this topic in December 2014 (“Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews”1). Have you implemented any of the tactics we offered then? We hope that you do take proactive steps to protect your online image.
What is a physician’s most precious asset?
You might answer this question with, “my patients” or “the training and education that I have obtained to practice my craft.” But the real answer is that your most precious asset is your reputation.
Physicians live and die by their reputations. We spend our entire medical careers polishing and protecting this status. The Internet dramatically has altered the way people gather information. It is sad but true that a single comment that only takes a few seconds and a single mouse-click to post can be seen by thousands and ruin that life-long effort.
How are physicians rated on the web?
Online physician reviews are positive 70% to 90% of the time.2 Most physicians have 5 or fewer reviews on any one site.3 Of the approximately 30 sites that monitor physicians and hospitals online, one of the most popular is AngiesList.com. This site requires registration and a fee; a member can review a physician every 6 months. On free websites such as Yelp.com and doctorsscorecard.com the reviewer can comment once. Other sites such as vitals.com or DrScore.com limit the reviews from 1 source, which prevents an angry patient from stuffing the ballot box.2
Pay attention
At a minimum, physicians should be monitoring their reputation by conducting periodic searches—“Googling” their name and practice name—to identify what information is already online. You may find that 3, 4, or even 10 reviews appear on various sites. If you are lucky, these reviews will be positive. Don’t be surprised, however, if 1 or 2 are not. Let’s face it: even the most accredited and experienced physician cannot possibly satisfy every patient who walks through the door.
Neil Baum, MD, and Ron Romano have offered tips on ways to manage online reputations in the past,1 and they urge Ob-Gyns to take an active role in this process in order to increase positive exposure to patients and maintain an active practice. Is active reputation management something that ObGyns are spending their valuable time on? To find out, OBG Management reached out to its Virtual Editorial Board. We found that many readers are paying attention to patient satisfaction. Some are soliciting online reviews and maintaining active upkeep on their online reputation. Here are a few responses we received from practicing ObGyns across the United States.
William E. McGrath Jr, MD, of Fernandina Beach, Florida, says that his office provides patients with a list of 5 popular review websites during their visits, and that approximately 1 in 10 will follow up with a review. Patient reviews are also prominently posted on his practice’s website. The large, private, single-specialty group to which his practice belongs requires patient satisfaction surveys for quality assurance review and insurance contract negotiations. “It is all about physician-patient communication,” he says.
Keith S. Merlin, MD, of Brockton, Massachusetts, says that he has checked online reviews to ensure their accuracy. His practice uses surveys, a suggestion box, and a mystery shopper to measure patient satisfaction, a worthwhile effort he says to understand where the practice is doing well and what needs to be done better.
Wesley Hambright, MD, of Jacksonville, North Carolina, reports that he has established a Google Alert to monitor for new content relating to his practice.
Patrick Pevoto, MD, MBA, of Austin, Texas, informs us that he has just started to think about ways to manage his online reputation. He has created a website and is writing a monthly blog, which he posts on his site. He acknowledges the importance of assessing patient satisfaction in his practice but is not applying large-scale measurement techniques yet. To keep his patients happy, he handles concerns that arise on a personal, case-by-case basis.
John Armstrong, MD, MS, of Napa, California, also reports that management of his online reputation is in the beginning stages. He uses focus groups and feels that listening to his patients when they do comment on their experience is important to his overall practice. Listening helps to “identify areas to improve and reaffirms when we are doing well,” he says. To keep his patients happy, he strives to “give extraordinary care and simply be nice to people.” When issues arise, making it right and being polite are important elements, he asserts.
Delos J. Clow, DO, MS, of Chillicothe, Missouri, does measure patient satisfaction, and feels this is very important to his practice in order to identify and correct any negative trends. He does not actively monitor his practice reputation online.
Robert del Rosario, MD, of Camp Hill, Pennsylvania, similarly does not actively manage an online reputation, but does focus on patient satisfaction. To enhance satisfaction, he tries to de-emphasize the electronic medical record to “make visits more personal and less interrogative.” Additionally, his practice objectively gauges aspects of care that might be able to be improved upon.
Reference
- Romano R, Baum NH. Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews. OBG Manag. 2014;26(12):23,24,26,28.
Tell your own story
As physicians, you may not have control over what others say about you, but you can take ownership of your online presence by establishing a website, blog, and social media platforms, ensuring your story is being properly communicated. Without an online presence, you are entirely at the mercy of directory and review sites.
Optimize your website
A site that successfully uses search engine optimization (SEO) will have the upper hand when patients hunt for a physician in your area because the information will be posted at the top of the search page, well above the reviews and listings left by patients and other third-party sources. This is a critical step for your online brand because it will be difficult for other sites to mask your credibility. This should motivate you to develop an online presence, regularly update information, and participate in Internet dialog with other sites.
Generate quality, natural reviews
If your site is in good standing in search results, the next step is to implement a patient reviews strategy to start acquiring positive online reviews. A third-party provider can work with you to launch a local search engine optimization strategy and a natural reviews management program tailored for your practice’s needs. For the most part, however, we do not recommend using an online reputation management company. It is far better and more economical to ask satisfied patients to provide reviews.
At first, you may be tempted to actively petition or solicit reviews through survey software, but this method is manipulative and can lead to reputation problems for your practice. Google actively tracks where reviews originate and uses advanced algorithms to determine the review’s integrity. A petitioned review is classified as less valid, and therefore Google will assume it was not written under the same pretense as a natural, unsolicited review.
Quality customer service and outstanding patient care are often what achieve the organic reviews you are striving for. To encourage a steady flow, administer a process that encourages your most satisfied, loyal patients to review your practice.
Keep the process simple. Capture positive compliments at the point of service. Before a patient leaves your office, hand her a card (FIGURE) with easy steps for posting an online review, or offer her a tablet that links directly to your website review section. If your patient is not computer savvy, ask her to complete a 4- to 5-question survey and give her a clipboard and a pen. Then have a staff member post it on your website.
In Dr. Baum’s practice, there is a poster in every exam room and in the reception area where patients can scan the quick response (QR) code and immediately submit a testimonial. Using this system, the practice is able to collect 3 to 5 positive reviews every day.
A patient pleased with your staff’s service will happily take 5 minutes to submit a review. Acquire 5 to 10 reviews monthly and within a year’s time you will have generated enough positive reviews to negate any damaging comments that inevitably will emerge from time to time.
CASE Patient criticizes physician in a review forum
A physician with a robust Internet presence will have his or her name and the practice appear at the top of search engine results pages (as is the case with Dr. Neil Baum when “urologist” plus “New Orleans” is typed into the Google search engine window). By far most of Dr. Baum’s reviews are positive. In one instance, however, a patient on a physician review website referred to Dr. Baum as “technologically advanced but more motivated to increase his income by performing too many diagnostic tests.”
If you find a negative comment in an online directory or review website, what should you do?
The Office for Civil Rights (OCR) within the US Department of Health and Human Services (HHS) is responsible for handling Health Insurance Portability and Accountability Act of 1996 (HIPAA)1 complaints. Deven McGraw, OCR’s deputy director of health information privacy, states that “just because patients have rated their health provider publicly doesn’t give their health provider permission to rate them in return.”2,3 In fact, some health care providers who responded to poor online reviews ran into trouble with privacy rules established by HIPAA.2,3
Mr. McGraw notes that, when responding to online reviews, health professionals should speak generally about the way they treat patients while complying with HIPAA regulations. He suggests, “If the complaint is about poor patient care … say, ‘I provide all of my patients with good patient care’ and ‘I’ve been reviewed in other contexts and have good reviews.’”2,3
According to Yelp’s senior director of litigation, Aaron Schur, most patient complaints center on practice-based concerns such as wait times, office staff, and billing, not about the medical service delivered. Although most physicians do not respond, says Mr. Schur, those who do, tend to ask patients to discuss the matter in private or to apologize.2,3
What are the consequences of a HIPAA violation?
OCR Director Jocelyn Samuels says that the office’s primary role is to help health providers follow HIPAA regulations.2,5 The OCR can resolve HIPPA violations privately and informally, impose fines of up to $50,000 per violation, or it can file criminal charges against violators.2,4
The majority of the office’s investigation and enforcement of HIPAA has been against large medical data breaches.2,5 Small privacy breaches by large health care providers (eg, CVS, Walmart, Lab Corp, Quest Diagnostics, and others) generally do not result in legal consequences; the providers are privately warned. According to ProPublica, even repeated HIPAA violations tend not to be fined.2,4
Small-scale infractions can be more damaging on a personal level to both patients and physicians. However, the OCR does not typically become involved in privacy breaches that include only a few individuals. Health care providers are rarely punished for small HIPPA breaches; instead, the OCR typically settles for pledges to fix any problems and issues reminders of HIPPA requirements.2,5
Although the OCR is often the only place patients can go to seek vindication, HIPAA does not support the right to sue for violation of personal privacy. People who seek a legal remedy must find another means, which is easier in some states than in others.2,5
Health care providers have tried myriad ways to attempt to combat negative reviews. Some have sued patients, attracting a flood of attention but achieving little legal success. Others have asked patients to remove their complaints.2,3
Best practices
Create and circulate a policy. Medical privacy breaches involving sensitive health details can occur when office or hospital staff share patient information due to personal hostility or lack of understanding of HIPPA policy.2,5 Have a practice policy for responding to online reviews by patients, and make sure the staff members who have access to the practice’s online accounts understand your policy and the possible repercussions of not following it. Teach and continue to remind your staff about HIPPA regulations and hold them to a high ethical level of privacy.
Solicit reviews on an ongoing basis. Jeffrey Segal, a review site critic, says that all reviews are valuable. Physicians should respond carefully to negative comments and encourage satisfied patients to post positive reviews. “’For doctors who get bent out of shape to get rid of negative reviews, it’s a denominator problem,’ he said. ‘If they only have three reviews and two are negative, the denominator is the problem. … If you can figure out a way to cultivate reviews from hundreds of patients rather than a few patients, the problem is solved.’”2,3
CASE Resolved
Dr. Baum never responded directly to the negative patient review, and others he has received. He balances the rare negative response with numerous and plentiful positive responses by making it a practice to encourage reviews from all of his patients.
References
- HIPAA for Professionals. US Department of Health & Human Services. http://www.hhs.gov/hipaa/for-professionals/index.html. Accessed October 11, 2016.
- Hall SD. Providers responding to Yelp reviews must be mindful of HIPAA. FierceHealthcare. http://www.fiercehealthcare.com/it/providers-responding-to-yelp-reviews-must-be-mindful-hipaa. Published May 31, 2016. Accessed October 7, 2016.
- Ornstein C. Stung by Yelp reviews, health providers spill patient secrets. ProPublica. https://www.propublica.org/article/stung-by-yelp-reviews-health -providers-spill-patient-secrets. Published May 27, 2016. Accessed October 11, 2016.
- Ornstein C, Waldman A. Few consequences for health privacy law’s repeat offenders. ProPublica. https://www.propublica.org/article/few-consequences-for-health-privacy-law-repeat-offenders. Published December 29, 2015. Accessed October 11, 2016.
- Ornstein C. Small-scale violations of medical privacy often cause the most harm. ProPublica. https://www.propublica.org/article/small-scale-violations-of-medical-privacy-often-cause-the-most-harm. Published December 10, 2015. Accessed October 11, 2016.
The bottom line
Patients are seeking and leaving reviews about you and your practice online and you need to actively manage your online reputation. Do not let one disgruntled patient ruin your reputation. Our advice: Do not wait for a negative review to begin your reputation management. Take an active role and generate positive reviews to drown out negative remarks made by an occasional patient. This is an inexpensive process that does work.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In a web-focused world, it should not take much convincing that monitoring your online reputation is time well spent. For some of us, it may be hard to believe that online reviews have evolved beyond restaurants and plumbers, but today your patients are flocking to the Internet to read and leave reviews about you, your staff, and your services. What can you do to protect your online reputation?
We first addressed this topic in December 2014 (“Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews”1). Have you implemented any of the tactics we offered then? We hope that you do take proactive steps to protect your online image.
What is a physician’s most precious asset?
You might answer this question with, “my patients” or “the training and education that I have obtained to practice my craft.” But the real answer is that your most precious asset is your reputation.
Physicians live and die by their reputations. We spend our entire medical careers polishing and protecting this status. The Internet dramatically has altered the way people gather information. It is sad but true that a single comment that only takes a few seconds and a single mouse-click to post can be seen by thousands and ruin that life-long effort.
How are physicians rated on the web?
Online physician reviews are positive 70% to 90% of the time.2 Most physicians have 5 or fewer reviews on any one site.3 Of the approximately 30 sites that monitor physicians and hospitals online, one of the most popular is AngiesList.com. This site requires registration and a fee; a member can review a physician every 6 months. On free websites such as Yelp.com and doctorsscorecard.com the reviewer can comment once. Other sites such as vitals.com or DrScore.com limit the reviews from 1 source, which prevents an angry patient from stuffing the ballot box.2
Pay attention
At a minimum, physicians should be monitoring their reputation by conducting periodic searches—“Googling” their name and practice name—to identify what information is already online. You may find that 3, 4, or even 10 reviews appear on various sites. If you are lucky, these reviews will be positive. Don’t be surprised, however, if 1 or 2 are not. Let’s face it: even the most accredited and experienced physician cannot possibly satisfy every patient who walks through the door.
Neil Baum, MD, and Ron Romano have offered tips on ways to manage online reputations in the past,1 and they urge Ob-Gyns to take an active role in this process in order to increase positive exposure to patients and maintain an active practice. Is active reputation management something that ObGyns are spending their valuable time on? To find out, OBG Management reached out to its Virtual Editorial Board. We found that many readers are paying attention to patient satisfaction. Some are soliciting online reviews and maintaining active upkeep on their online reputation. Here are a few responses we received from practicing ObGyns across the United States.
William E. McGrath Jr, MD, of Fernandina Beach, Florida, says that his office provides patients with a list of 5 popular review websites during their visits, and that approximately 1 in 10 will follow up with a review. Patient reviews are also prominently posted on his practice’s website. The large, private, single-specialty group to which his practice belongs requires patient satisfaction surveys for quality assurance review and insurance contract negotiations. “It is all about physician-patient communication,” he says.
Keith S. Merlin, MD, of Brockton, Massachusetts, says that he has checked online reviews to ensure their accuracy. His practice uses surveys, a suggestion box, and a mystery shopper to measure patient satisfaction, a worthwhile effort he says to understand where the practice is doing well and what needs to be done better.
Wesley Hambright, MD, of Jacksonville, North Carolina, reports that he has established a Google Alert to monitor for new content relating to his practice.
Patrick Pevoto, MD, MBA, of Austin, Texas, informs us that he has just started to think about ways to manage his online reputation. He has created a website and is writing a monthly blog, which he posts on his site. He acknowledges the importance of assessing patient satisfaction in his practice but is not applying large-scale measurement techniques yet. To keep his patients happy, he handles concerns that arise on a personal, case-by-case basis.
John Armstrong, MD, MS, of Napa, California, also reports that management of his online reputation is in the beginning stages. He uses focus groups and feels that listening to his patients when they do comment on their experience is important to his overall practice. Listening helps to “identify areas to improve and reaffirms when we are doing well,” he says. To keep his patients happy, he strives to “give extraordinary care and simply be nice to people.” When issues arise, making it right and being polite are important elements, he asserts.
Delos J. Clow, DO, MS, of Chillicothe, Missouri, does measure patient satisfaction, and feels this is very important to his practice in order to identify and correct any negative trends. He does not actively monitor his practice reputation online.
Robert del Rosario, MD, of Camp Hill, Pennsylvania, similarly does not actively manage an online reputation, but does focus on patient satisfaction. To enhance satisfaction, he tries to de-emphasize the electronic medical record to “make visits more personal and less interrogative.” Additionally, his practice objectively gauges aspects of care that might be able to be improved upon.
Reference
- Romano R, Baum NH. Using the Internet in your practice. Part 4: Reputation management—how to gather kudos and combat negative online reviews. OBG Manag. 2014;26(12):23,24,26,28.
Tell your own story
As physicians, you may not have control over what others say about you, but you can take ownership of your online presence by establishing a website, blog, and social media platforms, ensuring your story is being properly communicated. Without an online presence, you are entirely at the mercy of directory and review sites.
Optimize your website
A site that successfully uses search engine optimization (SEO) will have the upper hand when patients hunt for a physician in your area because the information will be posted at the top of the search page, well above the reviews and listings left by patients and other third-party sources. This is a critical step for your online brand because it will be difficult for other sites to mask your credibility. This should motivate you to develop an online presence, regularly update information, and participate in Internet dialog with other sites.
Generate quality, natural reviews
If your site is in good standing in search results, the next step is to implement a patient reviews strategy to start acquiring positive online reviews. A third-party provider can work with you to launch a local search engine optimization strategy and a natural reviews management program tailored for your practice’s needs. For the most part, however, we do not recommend using an online reputation management company. It is far better and more economical to ask satisfied patients to provide reviews.
At first, you may be tempted to actively petition or solicit reviews through survey software, but this method is manipulative and can lead to reputation problems for your practice. Google actively tracks where reviews originate and uses advanced algorithms to determine the review’s integrity. A petitioned review is classified as less valid, and therefore Google will assume it was not written under the same pretense as a natural, unsolicited review.
Quality customer service and outstanding patient care are often what achieve the organic reviews you are striving for. To encourage a steady flow, administer a process that encourages your most satisfied, loyal patients to review your practice.
Keep the process simple. Capture positive compliments at the point of service. Before a patient leaves your office, hand her a card (FIGURE) with easy steps for posting an online review, or offer her a tablet that links directly to your website review section. If your patient is not computer savvy, ask her to complete a 4- to 5-question survey and give her a clipboard and a pen. Then have a staff member post it on your website.
In Dr. Baum’s practice, there is a poster in every exam room and in the reception area where patients can scan the quick response (QR) code and immediately submit a testimonial. Using this system, the practice is able to collect 3 to 5 positive reviews every day.
A patient pleased with your staff’s service will happily take 5 minutes to submit a review. Acquire 5 to 10 reviews monthly and within a year’s time you will have generated enough positive reviews to negate any damaging comments that inevitably will emerge from time to time.
CASE Patient criticizes physician in a review forum
A physician with a robust Internet presence will have his or her name and the practice appear at the top of search engine results pages (as is the case with Dr. Neil Baum when “urologist” plus “New Orleans” is typed into the Google search engine window). By far most of Dr. Baum’s reviews are positive. In one instance, however, a patient on a physician review website referred to Dr. Baum as “technologically advanced but more motivated to increase his income by performing too many diagnostic tests.”
If you find a negative comment in an online directory or review website, what should you do?
The Office for Civil Rights (OCR) within the US Department of Health and Human Services (HHS) is responsible for handling Health Insurance Portability and Accountability Act of 1996 (HIPAA)1 complaints. Deven McGraw, OCR’s deputy director of health information privacy, states that “just because patients have rated their health provider publicly doesn’t give their health provider permission to rate them in return.”2,3 In fact, some health care providers who responded to poor online reviews ran into trouble with privacy rules established by HIPAA.2,3
Mr. McGraw notes that, when responding to online reviews, health professionals should speak generally about the way they treat patients while complying with HIPAA regulations. He suggests, “If the complaint is about poor patient care … say, ‘I provide all of my patients with good patient care’ and ‘I’ve been reviewed in other contexts and have good reviews.’”2,3
According to Yelp’s senior director of litigation, Aaron Schur, most patient complaints center on practice-based concerns such as wait times, office staff, and billing, not about the medical service delivered. Although most physicians do not respond, says Mr. Schur, those who do, tend to ask patients to discuss the matter in private or to apologize.2,3
What are the consequences of a HIPAA violation?
OCR Director Jocelyn Samuels says that the office’s primary role is to help health providers follow HIPAA regulations.2,5 The OCR can resolve HIPPA violations privately and informally, impose fines of up to $50,000 per violation, or it can file criminal charges against violators.2,4
The majority of the office’s investigation and enforcement of HIPAA has been against large medical data breaches.2,5 Small privacy breaches by large health care providers (eg, CVS, Walmart, Lab Corp, Quest Diagnostics, and others) generally do not result in legal consequences; the providers are privately warned. According to ProPublica, even repeated HIPAA violations tend not to be fined.2,4
Small-scale infractions can be more damaging on a personal level to both patients and physicians. However, the OCR does not typically become involved in privacy breaches that include only a few individuals. Health care providers are rarely punished for small HIPPA breaches; instead, the OCR typically settles for pledges to fix any problems and issues reminders of HIPPA requirements.2,5
Although the OCR is often the only place patients can go to seek vindication, HIPAA does not support the right to sue for violation of personal privacy. People who seek a legal remedy must find another means, which is easier in some states than in others.2,5
Health care providers have tried myriad ways to attempt to combat negative reviews. Some have sued patients, attracting a flood of attention but achieving little legal success. Others have asked patients to remove their complaints.2,3
Best practices
Create and circulate a policy. Medical privacy breaches involving sensitive health details can occur when office or hospital staff share patient information due to personal hostility or lack of understanding of HIPPA policy.2,5 Have a practice policy for responding to online reviews by patients, and make sure the staff members who have access to the practice’s online accounts understand your policy and the possible repercussions of not following it. Teach and continue to remind your staff about HIPPA regulations and hold them to a high ethical level of privacy.
Solicit reviews on an ongoing basis. Jeffrey Segal, a review site critic, says that all reviews are valuable. Physicians should respond carefully to negative comments and encourage satisfied patients to post positive reviews. “’For doctors who get bent out of shape to get rid of negative reviews, it’s a denominator problem,’ he said. ‘If they only have three reviews and two are negative, the denominator is the problem. … If you can figure out a way to cultivate reviews from hundreds of patients rather than a few patients, the problem is solved.’”2,3
CASE Resolved
Dr. Baum never responded directly to the negative patient review, and others he has received. He balances the rare negative response with numerous and plentiful positive responses by making it a practice to encourage reviews from all of his patients.
References
- HIPAA for Professionals. US Department of Health & Human Services. http://www.hhs.gov/hipaa/for-professionals/index.html. Accessed October 11, 2016.
- Hall SD. Providers responding to Yelp reviews must be mindful of HIPAA. FierceHealthcare. http://www.fiercehealthcare.com/it/providers-responding-to-yelp-reviews-must-be-mindful-hipaa. Published May 31, 2016. Accessed October 7, 2016.
- Ornstein C. Stung by Yelp reviews, health providers spill patient secrets. ProPublica. https://www.propublica.org/article/stung-by-yelp-reviews-health -providers-spill-patient-secrets. Published May 27, 2016. Accessed October 11, 2016.
- Ornstein C, Waldman A. Few consequences for health privacy law’s repeat offenders. ProPublica. https://www.propublica.org/article/few-consequences-for-health-privacy-law-repeat-offenders. Published December 29, 2015. Accessed October 11, 2016.
- Ornstein C. Small-scale violations of medical privacy often cause the most harm. ProPublica. https://www.propublica.org/article/small-scale-violations-of-medical-privacy-often-cause-the-most-harm. Published December 10, 2015. Accessed October 11, 2016.
The bottom line
Patients are seeking and leaving reviews about you and your practice online and you need to actively manage your online reputation. Do not let one disgruntled patient ruin your reputation. Our advice: Do not wait for a negative review to begin your reputation management. Take an active role and generate positive reviews to drown out negative remarks made by an occasional patient. This is an inexpensive process that does work.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Romano R, Baum NH. Using the Internet in your practice. Part 4: Reputation management-how to gather kudos and combat negative online reviews. OBG Manag. 2014;26(12):23,24,26,28.
- Lagu T, Hannon NS, Rothberg MB, Lindenauer PK. Patients' evaluations of health care providers in the era of social networking: an analysis of physician rating websites. J Gen Intern Med. 2010;25(9):942-946.
- Gunter J. For better or maybe, worse, patients are judging your care online. OBG Manag. 2011;23(3):47-51.
- Romano R, Baum NH. Using the Internet in your practice. Part 4: Reputation management-how to gather kudos and combat negative online reviews. OBG Manag. 2014;26(12):23,24,26,28.
- Lagu T, Hannon NS, Rothberg MB, Lindenauer PK. Patients' evaluations of health care providers in the era of social networking: an analysis of physician rating websites. J Gen Intern Med. 2010;25(9):942-946.
- Gunter J. For better or maybe, worse, patients are judging your care online. OBG Manag. 2011;23(3):47-51.
In this Article
- How your peers manage online reputation
- Should you respond to a negative review?
- Generate quality, natural reviews
Public speaking fundamentals. Presentation follow-up: What to do after the last slide is shown
This third article in a series on public speaking describes steps you can take immediately following the program to strengthen the impact of your diligent preparation (“Preparation: Tips that lead to a solid, engaging presentation.” OBG Manag. 2016;28[7]:31–36) and honed presentation (“The program: Key elements in capturing and holding audience attention.” OBG Manag. 2016;28[9]:46–50). Don’t overlook these details.
Find ways to stay in touch
You have concluded your talk. The audience response was enthusiastic and the brief Q&A session productive. But it is not over yet. Postpone putting away your computer and disconnecting the audiovisual equipment. Instead, mingle with the attendees—as you also did, we hope, before the program began. There is always more you can learn about your listeners. And, importantly, a few of them would undoubtedly like to ask you one-on-one about a case related to the topic you covered or about another problem in your area of expertise.
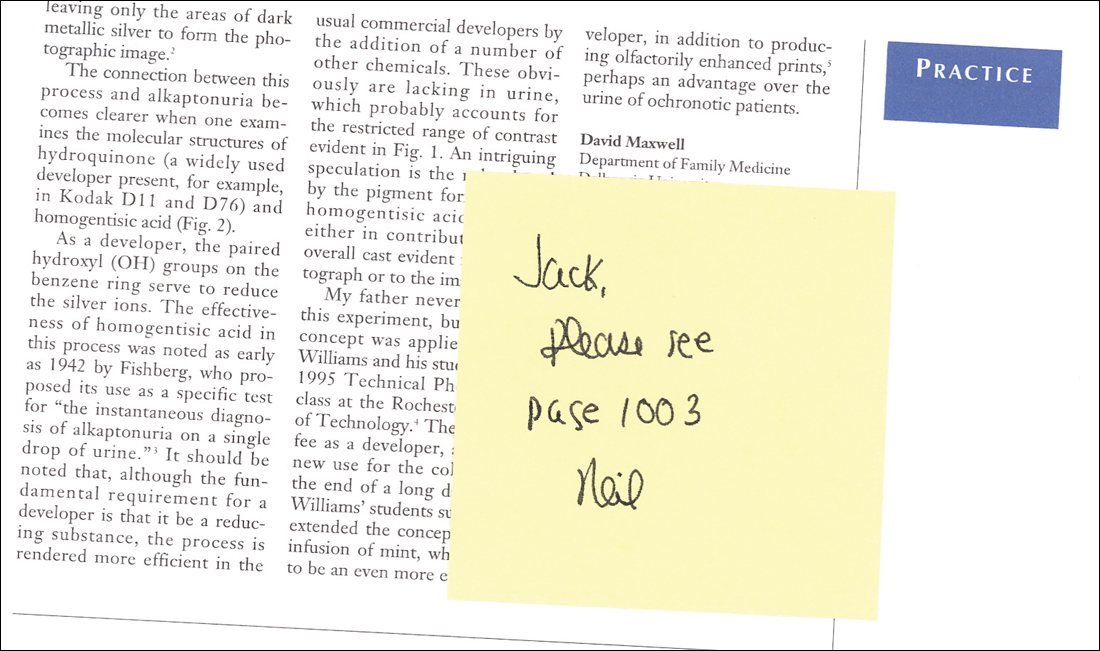
We suggest that, as part of your follow-up, you take the names of attendees you speak with. Make a note relevant to each one and plan to send a personal letter that perhaps includes an article you wrote or one published by a credible source. For example, if one of us (MK) gives a talk for a physician audience on a clinical topic, I will send the inquiring physician a note and an article on the topic, with the key sentences related to his or her question highlighted. A sticky note on the article’s front page directs the physician’s attention to the page containing the answer to his or her question (FIGURE). Using this simple technique can make you a value-added resource long after your presentation.
Alternatively, you could e-mail the article to a representative for the organization that you were speaking for. This makes you an asset to the representative, who will likely tell colleagues about your assistance, which could earn you a return speaking engagement.
Make sure, too, that you have an ample supply of business cards—the quickest and easiest way to give out your contact information.
You may also want to distribute a handout of your presentation. This could of course be a printout of your slide show presentation (assuming there are no copyright concerns). But we think it is better to distribute a single page with salient points you would like the audience to take away from your program. However you prepare your handout, be certain each page displays your name, address, phone numbers, and e-mail and website addresses.
Another suggestion: An unobtrusive way to obtain the names of those who attend your program is to collect their business cards in a container before the presentation and hold a drawing for a prize at the end of the program. We often give away a copy of one of our books, but any small gift would work.
Ask for feedback
If you are speaking on behalf of an organization or another sponsoring entity, it is helpful to ask the meeting planner what they thought of the program. Ask for constructive criticism and input on how you might improve the program. Also ask if you were able to get across your most important points.
Finally, send a note to the meeting planner or representative expressing your thanks for the invitation and offering to provide any additional information they might need or want.
Extend the reach of your message
If your talk would be appropriate for a broader audience, you could consider adapting it for publication. Be sure to understand the audience of the publication and review the selected journal’s guidance for authors.
If you do write an article, share it with your colleagues and perhaps your patients. You might also consider posting the article on your website. Yet another option would be to videotape your presentation, keeping it under 10 minutes, and upload it to the video-sharing website YouTube.
Bottom line. The payoff for your research and preparation need not end with the speaking engagement.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This third article in a series on public speaking describes steps you can take immediately following the program to strengthen the impact of your diligent preparation (“Preparation: Tips that lead to a solid, engaging presentation.” OBG Manag. 2016;28[7]:31–36) and honed presentation (“The program: Key elements in capturing and holding audience attention.” OBG Manag. 2016;28[9]:46–50). Don’t overlook these details.
Find ways to stay in touch
You have concluded your talk. The audience response was enthusiastic and the brief Q&A session productive. But it is not over yet. Postpone putting away your computer and disconnecting the audiovisual equipment. Instead, mingle with the attendees—as you also did, we hope, before the program began. There is always more you can learn about your listeners. And, importantly, a few of them would undoubtedly like to ask you one-on-one about a case related to the topic you covered or about another problem in your area of expertise.
We suggest that, as part of your follow-up, you take the names of attendees you speak with. Make a note relevant to each one and plan to send a personal letter that perhaps includes an article you wrote or one published by a credible source. For example, if one of us (MK) gives a talk for a physician audience on a clinical topic, I will send the inquiring physician a note and an article on the topic, with the key sentences related to his or her question highlighted. A sticky note on the article’s front page directs the physician’s attention to the page containing the answer to his or her question (FIGURE). Using this simple technique can make you a value-added resource long after your presentation.
Alternatively, you could e-mail the article to a representative for the organization that you were speaking for. This makes you an asset to the representative, who will likely tell colleagues about your assistance, which could earn you a return speaking engagement.
Make sure, too, that you have an ample supply of business cards—the quickest and easiest way to give out your contact information.
You may also want to distribute a handout of your presentation. This could of course be a printout of your slide show presentation (assuming there are no copyright concerns). But we think it is better to distribute a single page with salient points you would like the audience to take away from your program. However you prepare your handout, be certain each page displays your name, address, phone numbers, and e-mail and website addresses.
Another suggestion: An unobtrusive way to obtain the names of those who attend your program is to collect their business cards in a container before the presentation and hold a drawing for a prize at the end of the program. We often give away a copy of one of our books, but any small gift would work.
Ask for feedback
If you are speaking on behalf of an organization or another sponsoring entity, it is helpful to ask the meeting planner what they thought of the program. Ask for constructive criticism and input on how you might improve the program. Also ask if you were able to get across your most important points.
Finally, send a note to the meeting planner or representative expressing your thanks for the invitation and offering to provide any additional information they might need or want.
Extend the reach of your message
If your talk would be appropriate for a broader audience, you could consider adapting it for publication. Be sure to understand the audience of the publication and review the selected journal’s guidance for authors.
If you do write an article, share it with your colleagues and perhaps your patients. You might also consider posting the article on your website. Yet another option would be to videotape your presentation, keeping it under 10 minutes, and upload it to the video-sharing website YouTube.
Bottom line. The payoff for your research and preparation need not end with the speaking engagement.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
This third article in a series on public speaking describes steps you can take immediately following the program to strengthen the impact of your diligent preparation (“Preparation: Tips that lead to a solid, engaging presentation.” OBG Manag. 2016;28[7]:31–36) and honed presentation (“The program: Key elements in capturing and holding audience attention.” OBG Manag. 2016;28[9]:46–50). Don’t overlook these details.
Find ways to stay in touch
You have concluded your talk. The audience response was enthusiastic and the brief Q&A session productive. But it is not over yet. Postpone putting away your computer and disconnecting the audiovisual equipment. Instead, mingle with the attendees—as you also did, we hope, before the program began. There is always more you can learn about your listeners. And, importantly, a few of them would undoubtedly like to ask you one-on-one about a case related to the topic you covered or about another problem in your area of expertise.
We suggest that, as part of your follow-up, you take the names of attendees you speak with. Make a note relevant to each one and plan to send a personal letter that perhaps includes an article you wrote or one published by a credible source. For example, if one of us (MK) gives a talk for a physician audience on a clinical topic, I will send the inquiring physician a note and an article on the topic, with the key sentences related to his or her question highlighted. A sticky note on the article’s front page directs the physician’s attention to the page containing the answer to his or her question (FIGURE). Using this simple technique can make you a value-added resource long after your presentation.
Alternatively, you could e-mail the article to a representative for the organization that you were speaking for. This makes you an asset to the representative, who will likely tell colleagues about your assistance, which could earn you a return speaking engagement.
Make sure, too, that you have an ample supply of business cards—the quickest and easiest way to give out your contact information.
You may also want to distribute a handout of your presentation. This could of course be a printout of your slide show presentation (assuming there are no copyright concerns). But we think it is better to distribute a single page with salient points you would like the audience to take away from your program. However you prepare your handout, be certain each page displays your name, address, phone numbers, and e-mail and website addresses.
Another suggestion: An unobtrusive way to obtain the names of those who attend your program is to collect their business cards in a container before the presentation and hold a drawing for a prize at the end of the program. We often give away a copy of one of our books, but any small gift would work.
Ask for feedback
If you are speaking on behalf of an organization or another sponsoring entity, it is helpful to ask the meeting planner what they thought of the program. Ask for constructive criticism and input on how you might improve the program. Also ask if you were able to get across your most important points.
Finally, send a note to the meeting planner or representative expressing your thanks for the invitation and offering to provide any additional information they might need or want.
Extend the reach of your message
If your talk would be appropriate for a broader audience, you could consider adapting it for publication. Be sure to understand the audience of the publication and review the selected journal’s guidance for authors.
If you do write an article, share it with your colleagues and perhaps your patients. You might also consider posting the article on your website. Yet another option would be to videotape your presentation, keeping it under 10 minutes, and upload it to the video-sharing website YouTube.
Bottom line. The payoff for your research and preparation need not end with the speaking engagement.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CMS offering educational webinars on MACRA
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
MACRA
Given the copious amount of printed and blog space that has been devoted in recent months to MACRA – the Medicare Access and CHIP Reauthorization Act of 2015 – I felt no particular obligation to add to the din. Then I was startled to read a recent poll from Deloitte that found that half of all private-practice physicians had never heard of MACRA. Furthermore, only 21% of solo or small-group physicians, and 9% of those employed by hospitals or larger groups, were even somewhat familiar with its financial implications.
Since yet another significant percentage of your Medicare reimbursements will be at risk under this new bureaucracy, an introduction is in order.
When the new system is implemented in 2019, physicians must choose between two payment tracks: the Merit-Based Incentive System (MIPS) or one of the so-called Alternate Payment Models (APM).
The MIPS track will use the four reporting programs just mentioned to compile a composite score between 0 and 100 each year for every practitioner, based on four performance metrics: quality measures listed in Qualified Clinical Data Registries, such as Approved Quality Improvement; total resources used by each practitioner, as measured by VBM; “improvement activities” (MOC); and MU, in some new, as-yet-undefined form. You can earn a bonus of 4% of reimbursement in 2019, rising to 5% in 2020, 7% in 2021, and 9% in 2022 – or you can be penalized those amounts (“negative adjustments”) if your performance doesn’t measure up.
The Centers for Medicare & Medicaid Services initially estimated that most physicians in groups of 24 or fewer on the MIPS track would incur a penalty in 2019; but the final MACRA regulations, issued in mid-October, allow a more gradual implementation that should decrease the penalty burden for small practices, at least initially. For example, you can avoid a penalty – but not qualify for a bonus – in 2019 by reporting your performance in only one quality-of-care or practice-improvement category, or by reporting for only a portion of the year. A decrease in penalties, however, means a smaller pot for bonuses – and reprieves will be temporary.
The alternative, APM, is difficult to discuss at present as very few models have been presented, or even defined, to date. Only Accountable Care Organizations (ACOs) have been introduced in any quantity, and most have failed miserably in real-world settings. The Episode of Care model, which pays providers a fixed amount for all services rendered in a bundle (“episode”) of care, has been discussed at some length, but remains untested, and in the end, may turn out to be just another variant of capitation.
So, which to choose? Long term, I strongly suggest that everyone prepare for the APM track as soon as better, more efficient APMs become available, as it appears that there will be more financial security, with less risk of penalties; but you will probably need to start in the MIPS program, as most projections indicate that the great majority of practitioners, particularly those in smaller operations, will do.
While some may be prompted to join a larger organization or network to decrease their risk of MIPS penalties and gain quicker access to the APM track – which may well be one of CMS’ surreptitious goals in introducing MACRA in the first place – there are steps that those individuals and small groups who choose to remain independent can take now to maximize their chances of landing on the bonus side of the MIPS ledger.
First, make sure your practice data is accurate on the Medicare Provider Enrollment, Chain, and Ownership System (PECOS) – where CMS will gather data for the VBM and Physician Feedback Reports. Study the quality benchmarks, and review your Quality Resource and Use Report (QRUR), which gathers information about each practice’s quality and performance rates for the VBM. (Both PECOS and QRUR can be downloaded at CMS.gov.) And, of course, report successfully for PQRS, which will avoid an automatic penalty of 4% 2 years hence.
If the alphabet soup above has your head swimming, join the club – you’re far from alone; but don’t be discouraged. CMS has already indicated its willingness to make changes aimed at decreasing the administrative burden and, in its words, “making the transition to MACRA as simple and as flexible as possible.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected] .
Given the copious amount of printed and blog space that has been devoted in recent months to MACRA – the Medicare Access and CHIP Reauthorization Act of 2015 – I felt no particular obligation to add to the din. Then I was startled to read a recent poll from Deloitte that found that half of all private-practice physicians had never heard of MACRA. Furthermore, only 21% of solo or small-group physicians, and 9% of those employed by hospitals or larger groups, were even somewhat familiar with its financial implications.
Since yet another significant percentage of your Medicare reimbursements will be at risk under this new bureaucracy, an introduction is in order.
When the new system is implemented in 2019, physicians must choose between two payment tracks: the Merit-Based Incentive System (MIPS) or one of the so-called Alternate Payment Models (APM).
The MIPS track will use the four reporting programs just mentioned to compile a composite score between 0 and 100 each year for every practitioner, based on four performance metrics: quality measures listed in Qualified Clinical Data Registries, such as Approved Quality Improvement; total resources used by each practitioner, as measured by VBM; “improvement activities” (MOC); and MU, in some new, as-yet-undefined form. You can earn a bonus of 4% of reimbursement in 2019, rising to 5% in 2020, 7% in 2021, and 9% in 2022 – or you can be penalized those amounts (“negative adjustments”) if your performance doesn’t measure up.
The Centers for Medicare & Medicaid Services initially estimated that most physicians in groups of 24 or fewer on the MIPS track would incur a penalty in 2019; but the final MACRA regulations, issued in mid-October, allow a more gradual implementation that should decrease the penalty burden for small practices, at least initially. For example, you can avoid a penalty – but not qualify for a bonus – in 2019 by reporting your performance in only one quality-of-care or practice-improvement category, or by reporting for only a portion of the year. A decrease in penalties, however, means a smaller pot for bonuses – and reprieves will be temporary.
The alternative, APM, is difficult to discuss at present as very few models have been presented, or even defined, to date. Only Accountable Care Organizations (ACOs) have been introduced in any quantity, and most have failed miserably in real-world settings. The Episode of Care model, which pays providers a fixed amount for all services rendered in a bundle (“episode”) of care, has been discussed at some length, but remains untested, and in the end, may turn out to be just another variant of capitation.
So, which to choose? Long term, I strongly suggest that everyone prepare for the APM track as soon as better, more efficient APMs become available, as it appears that there will be more financial security, with less risk of penalties; but you will probably need to start in the MIPS program, as most projections indicate that the great majority of practitioners, particularly those in smaller operations, will do.
While some may be prompted to join a larger organization or network to decrease their risk of MIPS penalties and gain quicker access to the APM track – which may well be one of CMS’ surreptitious goals in introducing MACRA in the first place – there are steps that those individuals and small groups who choose to remain independent can take now to maximize their chances of landing on the bonus side of the MIPS ledger.
First, make sure your practice data is accurate on the Medicare Provider Enrollment, Chain, and Ownership System (PECOS) – where CMS will gather data for the VBM and Physician Feedback Reports. Study the quality benchmarks, and review your Quality Resource and Use Report (QRUR), which gathers information about each practice’s quality and performance rates for the VBM. (Both PECOS and QRUR can be downloaded at CMS.gov.) And, of course, report successfully for PQRS, which will avoid an automatic penalty of 4% 2 years hence.
If the alphabet soup above has your head swimming, join the club – you’re far from alone; but don’t be discouraged. CMS has already indicated its willingness to make changes aimed at decreasing the administrative burden and, in its words, “making the transition to MACRA as simple and as flexible as possible.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected] .
Given the copious amount of printed and blog space that has been devoted in recent months to MACRA – the Medicare Access and CHIP Reauthorization Act of 2015 – I felt no particular obligation to add to the din. Then I was startled to read a recent poll from Deloitte that found that half of all private-practice physicians had never heard of MACRA. Furthermore, only 21% of solo or small-group physicians, and 9% of those employed by hospitals or larger groups, were even somewhat familiar with its financial implications.
Since yet another significant percentage of your Medicare reimbursements will be at risk under this new bureaucracy, an introduction is in order.
When the new system is implemented in 2019, physicians must choose between two payment tracks: the Merit-Based Incentive System (MIPS) or one of the so-called Alternate Payment Models (APM).
The MIPS track will use the four reporting programs just mentioned to compile a composite score between 0 and 100 each year for every practitioner, based on four performance metrics: quality measures listed in Qualified Clinical Data Registries, such as Approved Quality Improvement; total resources used by each practitioner, as measured by VBM; “improvement activities” (MOC); and MU, in some new, as-yet-undefined form. You can earn a bonus of 4% of reimbursement in 2019, rising to 5% in 2020, 7% in 2021, and 9% in 2022 – or you can be penalized those amounts (“negative adjustments”) if your performance doesn’t measure up.
The Centers for Medicare & Medicaid Services initially estimated that most physicians in groups of 24 or fewer on the MIPS track would incur a penalty in 2019; but the final MACRA regulations, issued in mid-October, allow a more gradual implementation that should decrease the penalty burden for small practices, at least initially. For example, you can avoid a penalty – but not qualify for a bonus – in 2019 by reporting your performance in only one quality-of-care or practice-improvement category, or by reporting for only a portion of the year. A decrease in penalties, however, means a smaller pot for bonuses – and reprieves will be temporary.
The alternative, APM, is difficult to discuss at present as very few models have been presented, or even defined, to date. Only Accountable Care Organizations (ACOs) have been introduced in any quantity, and most have failed miserably in real-world settings. The Episode of Care model, which pays providers a fixed amount for all services rendered in a bundle (“episode”) of care, has been discussed at some length, but remains untested, and in the end, may turn out to be just another variant of capitation.
So, which to choose? Long term, I strongly suggest that everyone prepare for the APM track as soon as better, more efficient APMs become available, as it appears that there will be more financial security, with less risk of penalties; but you will probably need to start in the MIPS program, as most projections indicate that the great majority of practitioners, particularly those in smaller operations, will do.
While some may be prompted to join a larger organization or network to decrease their risk of MIPS penalties and gain quicker access to the APM track – which may well be one of CMS’ surreptitious goals in introducing MACRA in the first place – there are steps that those individuals and small groups who choose to remain independent can take now to maximize their chances of landing on the bonus side of the MIPS ledger.
First, make sure your practice data is accurate on the Medicare Provider Enrollment, Chain, and Ownership System (PECOS) – where CMS will gather data for the VBM and Physician Feedback Reports. Study the quality benchmarks, and review your Quality Resource and Use Report (QRUR), which gathers information about each practice’s quality and performance rates for the VBM. (Both PECOS and QRUR can be downloaded at CMS.gov.) And, of course, report successfully for PQRS, which will avoid an automatic penalty of 4% 2 years hence.
If the alphabet soup above has your head swimming, join the club – you’re far from alone; but don’t be discouraged. CMS has already indicated its willingness to make changes aimed at decreasing the administrative burden and, in its words, “making the transition to MACRA as simple and as flexible as possible.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected] .
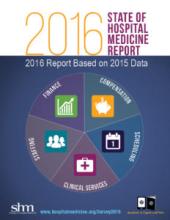
Observation Status Utilization by Hospitalist Groups Is Increasing
Editor's Note: Listen to Dr. Smith share more of his views on the State of Hospital Medicine report.
Hospitalist groups and their stakeholders must continually adapt to evolving reimbursement models and their attendant financial foci on quality. Even in the midst of care models that rely less heavily on volume of care as a marker for reimbursement, the use of criteria by insurers to separate hospital stays into inpatient or observation status remains widespread. Hospitalist groups vary in the reimbursement model environment they work in, and different reimbursement models can drive hospitalist group behavior in different ways.
SHM’s 2016 State of Hospital Medicine Report revisits the issue of observation status utilization raised in previous surveys.1 The 2012 survey’s methodology reports admissions classified as observation status based on CPT coding.2 The 2016 survey continues the 2014 survey methodology of using discharges classified as observation status based on CPT coding, along with same-day admission and discharge reported as a third hospitalization status category. In groups serving adults only, observation discharges accounted for 21.2% of all discharges, which represents an increase from 16.1% in the 2014 survey3 and a general return to the 2012-reported percentage of 20%. If same-day admissions and discharges, many of which are likely classified as observation status, are added, then observation status use in the 2016 survey may be as high as 24% of all admissions. This represents a considerable increase from the combined 19.6% rate in 2014.
Changes in non-academic status hospitalist groups largely account for this increase. Academic hospitalist groups reported an observation status utilization rate of 15.3% of admissions in 2012 and 19.4% in 2014, with a subsequent decrease to 17.5% reported in the 2016 survey. Inclusion of same-day admission and discharge with reported observation status use also reveals a decrease from 22.8% in 2014 to 20.8% in the new survey. In contrast, non-academic hospitalist groups now report a substantial change in observation status utilization, up to 21.4% in the 2016 survey from 15.6% in 2014 and similar to the 2012 level of 20.4%. When same-day admission and discharge codes are also included, the totals for non-academic hospitalist groups also evidence an increase, to 24.3% in the new survey from 19.2% in 2014.
I postulated in 2015 that the comparative increase in observation status utilization by academic groups as compared with non-academic groups in the 2014 survey may have been associated with greater proficiency in documentation and related billing inherent in a bedside clinical workforce entirely composed of physicians who have completed postgraduate training. Other phenomena may now potentially explain the increase in observation status use we see in the 2016 survey. These include adoption of the two-midnight rule by the Centers for Medicare & Medicaid Services, use of readmission rates in hospitalist group incentive structures, sharing of cost savings between hospitalist groups and healthcare organizations mutually engaged in third-party bundled payment arrangements, or risk-avoidant strategies executed by clinicians and institutional coders perhaps in excess of their institutions’ needs for risk avoidance. For many of these events, the 2016 State of Hospital Medicine Report provides further benchmark data, in a national and regional context, to inform understanding for hospitalist groups facing challenges associated with observation status utilization.
G. Randy Smith Jr., MD, MS, FRCP(Edin), SFHM, is an assistant professor in the Division of Hospital Medicine at Northwestern University Feinberg School of Medicine in Chicago.
References
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed September 11, 2016.
- 2012 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed September 11, 2016.
- 2014 State of Hospital Medicine Report. Society of Hospital Medicine website.
Accessed September 11, 2016.
Editor's Note: Listen to Dr. Smith share more of his views on the State of Hospital Medicine report.
Hospitalist groups and their stakeholders must continually adapt to evolving reimbursement models and their attendant financial foci on quality. Even in the midst of care models that rely less heavily on volume of care as a marker for reimbursement, the use of criteria by insurers to separate hospital stays into inpatient or observation status remains widespread. Hospitalist groups vary in the reimbursement model environment they work in, and different reimbursement models can drive hospitalist group behavior in different ways.
SHM’s 2016 State of Hospital Medicine Report revisits the issue of observation status utilization raised in previous surveys.1 The 2012 survey’s methodology reports admissions classified as observation status based on CPT coding.2 The 2016 survey continues the 2014 survey methodology of using discharges classified as observation status based on CPT coding, along with same-day admission and discharge reported as a third hospitalization status category. In groups serving adults only, observation discharges accounted for 21.2% of all discharges, which represents an increase from 16.1% in the 2014 survey3 and a general return to the 2012-reported percentage of 20%. If same-day admissions and discharges, many of which are likely classified as observation status, are added, then observation status use in the 2016 survey may be as high as 24% of all admissions. This represents a considerable increase from the combined 19.6% rate in 2014.
Changes in non-academic status hospitalist groups largely account for this increase. Academic hospitalist groups reported an observation status utilization rate of 15.3% of admissions in 2012 and 19.4% in 2014, with a subsequent decrease to 17.5% reported in the 2016 survey. Inclusion of same-day admission and discharge with reported observation status use also reveals a decrease from 22.8% in 2014 to 20.8% in the new survey. In contrast, non-academic hospitalist groups now report a substantial change in observation status utilization, up to 21.4% in the 2016 survey from 15.6% in 2014 and similar to the 2012 level of 20.4%. When same-day admission and discharge codes are also included, the totals for non-academic hospitalist groups also evidence an increase, to 24.3% in the new survey from 19.2% in 2014.
I postulated in 2015 that the comparative increase in observation status utilization by academic groups as compared with non-academic groups in the 2014 survey may have been associated with greater proficiency in documentation and related billing inherent in a bedside clinical workforce entirely composed of physicians who have completed postgraduate training. Other phenomena may now potentially explain the increase in observation status use we see in the 2016 survey. These include adoption of the two-midnight rule by the Centers for Medicare & Medicaid Services, use of readmission rates in hospitalist group incentive structures, sharing of cost savings between hospitalist groups and healthcare organizations mutually engaged in third-party bundled payment arrangements, or risk-avoidant strategies executed by clinicians and institutional coders perhaps in excess of their institutions’ needs for risk avoidance. For many of these events, the 2016 State of Hospital Medicine Report provides further benchmark data, in a national and regional context, to inform understanding for hospitalist groups facing challenges associated with observation status utilization.
G. Randy Smith Jr., MD, MS, FRCP(Edin), SFHM, is an assistant professor in the Division of Hospital Medicine at Northwestern University Feinberg School of Medicine in Chicago.
References
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed September 11, 2016.
- 2012 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed September 11, 2016.
- 2014 State of Hospital Medicine Report. Society of Hospital Medicine website.
Accessed September 11, 2016.
Editor's Note: Listen to Dr. Smith share more of his views on the State of Hospital Medicine report.
Hospitalist groups and their stakeholders must continually adapt to evolving reimbursement models and their attendant financial foci on quality. Even in the midst of care models that rely less heavily on volume of care as a marker for reimbursement, the use of criteria by insurers to separate hospital stays into inpatient or observation status remains widespread. Hospitalist groups vary in the reimbursement model environment they work in, and different reimbursement models can drive hospitalist group behavior in different ways.
SHM’s 2016 State of Hospital Medicine Report revisits the issue of observation status utilization raised in previous surveys.1 The 2012 survey’s methodology reports admissions classified as observation status based on CPT coding.2 The 2016 survey continues the 2014 survey methodology of using discharges classified as observation status based on CPT coding, along with same-day admission and discharge reported as a third hospitalization status category. In groups serving adults only, observation discharges accounted for 21.2% of all discharges, which represents an increase from 16.1% in the 2014 survey3 and a general return to the 2012-reported percentage of 20%. If same-day admissions and discharges, many of which are likely classified as observation status, are added, then observation status use in the 2016 survey may be as high as 24% of all admissions. This represents a considerable increase from the combined 19.6% rate in 2014.
Changes in non-academic status hospitalist groups largely account for this increase. Academic hospitalist groups reported an observation status utilization rate of 15.3% of admissions in 2012 and 19.4% in 2014, with a subsequent decrease to 17.5% reported in the 2016 survey. Inclusion of same-day admission and discharge with reported observation status use also reveals a decrease from 22.8% in 2014 to 20.8% in the new survey. In contrast, non-academic hospitalist groups now report a substantial change in observation status utilization, up to 21.4% in the 2016 survey from 15.6% in 2014 and similar to the 2012 level of 20.4%. When same-day admission and discharge codes are also included, the totals for non-academic hospitalist groups also evidence an increase, to 24.3% in the new survey from 19.2% in 2014.
I postulated in 2015 that the comparative increase in observation status utilization by academic groups as compared with non-academic groups in the 2014 survey may have been associated with greater proficiency in documentation and related billing inherent in a bedside clinical workforce entirely composed of physicians who have completed postgraduate training. Other phenomena may now potentially explain the increase in observation status use we see in the 2016 survey. These include adoption of the two-midnight rule by the Centers for Medicare & Medicaid Services, use of readmission rates in hospitalist group incentive structures, sharing of cost savings between hospitalist groups and healthcare organizations mutually engaged in third-party bundled payment arrangements, or risk-avoidant strategies executed by clinicians and institutional coders perhaps in excess of their institutions’ needs for risk avoidance. For many of these events, the 2016 State of Hospital Medicine Report provides further benchmark data, in a national and regional context, to inform understanding for hospitalist groups facing challenges associated with observation status utilization.
G. Randy Smith Jr., MD, MS, FRCP(Edin), SFHM, is an assistant professor in the Division of Hospital Medicine at Northwestern University Feinberg School of Medicine in Chicago.
References
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed September 11, 2016.
- 2012 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed September 11, 2016.
- 2014 State of Hospital Medicine Report. Society of Hospital Medicine website.
Accessed September 11, 2016.
Don’t forget about OSHA
Given the bewildering array of new bureaucracies that private practices have been forced to contend with in recent years, it’s easy to forget about the older ones – especially OSHA (Occupational Safety and Health Administration).
Now would be a good time – before the new year begins, and you’re forced to take on the MACRA meshugas, which I’ll discuss next month – to get out your OSHA logs, walk through your office, and confirm that you remain in compliance with all the applicable regulations. Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
I’m always amazed at how many offices lack an official OSHA poster, enumerating employee rights and explaining how to file complaints; it’s the first thing an OSHA inspector looks for. You can download one from OSHA’s website, or order it at no charge by calling 800-321-OSHA.
Next, check out your building’s exits. Everyone must be able to evacuate your office quickly in case of fire or other emergencies. At minimum, you (or the owner of the building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
Now, review your list of hazardous chemicals, which all employees have a right to know about. Keep in mind that OSHA’s list contains many substances – alcohol, disinfectants, even hydrogen peroxide – that you might not consider particularly dangerous but must nevertheless be on your written list of hazardous chemicals. For each of these, your employees must also have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific substance and for handling and containing it in a spill or other emergency.
How old is your written exposure control plan for blood-borne pathogens? It should document your use of such protective equipment as gloves, face and eye protection, and gowns, and your implementation of universal precautions – and it’s supposed to be updated annually, to reflect changes in technology. You need not adopt every new safety device as it comes on the market, but you should document which ones you are using, and why.
For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at your decision and what you plan to use instead.
You must provide all at-risk employees with hepatitis B vaccine, at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
Other components of the rule include proper containment of regulated medical waste, identification of regulated waste containers, sharps disposal boxes, and periodic employee training regarding all of those things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have such a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars.
How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you want to do that? Because in return for agreeing to have your office inspected, OSHA will agree not to cite you for any violations they find, as long as you fix them.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Given the bewildering array of new bureaucracies that private practices have been forced to contend with in recent years, it’s easy to forget about the older ones – especially OSHA (Occupational Safety and Health Administration).
Now would be a good time – before the new year begins, and you’re forced to take on the MACRA meshugas, which I’ll discuss next month – to get out your OSHA logs, walk through your office, and confirm that you remain in compliance with all the applicable regulations. Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
I’m always amazed at how many offices lack an official OSHA poster, enumerating employee rights and explaining how to file complaints; it’s the first thing an OSHA inspector looks for. You can download one from OSHA’s website, or order it at no charge by calling 800-321-OSHA.
Next, check out your building’s exits. Everyone must be able to evacuate your office quickly in case of fire or other emergencies. At minimum, you (or the owner of the building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
Now, review your list of hazardous chemicals, which all employees have a right to know about. Keep in mind that OSHA’s list contains many substances – alcohol, disinfectants, even hydrogen peroxide – that you might not consider particularly dangerous but must nevertheless be on your written list of hazardous chemicals. For each of these, your employees must also have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific substance and for handling and containing it in a spill or other emergency.
How old is your written exposure control plan for blood-borne pathogens? It should document your use of such protective equipment as gloves, face and eye protection, and gowns, and your implementation of universal precautions – and it’s supposed to be updated annually, to reflect changes in technology. You need not adopt every new safety device as it comes on the market, but you should document which ones you are using, and why.
For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at your decision and what you plan to use instead.
You must provide all at-risk employees with hepatitis B vaccine, at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
Other components of the rule include proper containment of regulated medical waste, identification of regulated waste containers, sharps disposal boxes, and periodic employee training regarding all of those things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have such a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars.
How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you want to do that? Because in return for agreeing to have your office inspected, OSHA will agree not to cite you for any violations they find, as long as you fix them.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Given the bewildering array of new bureaucracies that private practices have been forced to contend with in recent years, it’s easy to forget about the older ones – especially OSHA (Occupational Safety and Health Administration).
Now would be a good time – before the new year begins, and you’re forced to take on the MACRA meshugas, which I’ll discuss next month – to get out your OSHA logs, walk through your office, and confirm that you remain in compliance with all the applicable regulations. Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
I’m always amazed at how many offices lack an official OSHA poster, enumerating employee rights and explaining how to file complaints; it’s the first thing an OSHA inspector looks for. You can download one from OSHA’s website, or order it at no charge by calling 800-321-OSHA.
Next, check out your building’s exits. Everyone must be able to evacuate your office quickly in case of fire or other emergencies. At minimum, you (or the owner of the building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
Now, review your list of hazardous chemicals, which all employees have a right to know about. Keep in mind that OSHA’s list contains many substances – alcohol, disinfectants, even hydrogen peroxide – that you might not consider particularly dangerous but must nevertheless be on your written list of hazardous chemicals. For each of these, your employees must also have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific substance and for handling and containing it in a spill or other emergency.
How old is your written exposure control plan for blood-borne pathogens? It should document your use of such protective equipment as gloves, face and eye protection, and gowns, and your implementation of universal precautions – and it’s supposed to be updated annually, to reflect changes in technology. You need not adopt every new safety device as it comes on the market, but you should document which ones you are using, and why.
For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at your decision and what you plan to use instead.
You must provide all at-risk employees with hepatitis B vaccine, at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
Other components of the rule include proper containment of regulated medical waste, identification of regulated waste containers, sharps disposal boxes, and periodic employee training regarding all of those things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have such a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars.
How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you want to do that? Because in return for agreeing to have your office inspected, OSHA will agree not to cite you for any violations they find, as long as you fix them.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
The State of Hospital Medicine Is Strong
Editor's Note: Listen to Dr. Smith share more of his views on the State of Hospital Medicine report.
2016 is the “Year of the Hospitalist,” a sobriquet meant as a proud nod to the specialty’s maturation as a fixture in hospitals across the country. Hospital medicine is no longer the new kid on the block as it has assumed care for the vast majority of hospitalized patients nationwide.
One could understand then if the ever-rising salaries hospitalists have commanded for 20 years might have finally plateaued, particularly as tightening budgets have C-suite administrators looking to trim costs.
Think again.
“Growth suggests that there is still a huge demand,” says Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee. “The demand for hospitalists still exceeds the supply, and so recruiting hospitalists, particularly to nonurban areas, is really challenging and is requiring more money.”
The SoHM is a biennial partnership between SHM and MGMA that provides HM group leaders and rank-and-file hospitalists a litany of benchmarks for salaries, workloads, and everything that informs those two topics. Call it the specialty’s empirical roadmap.
“Often, compensation information relative to staffing information is proprietary, so hospitalists are in a position where they are dependent upon their hospital stakeholders to have access to this information, but they are also the same stakeholders with whom they negotiate their contracts,” says G. Randy Smith, MD, MS, FRCP(Edin), SFHM, an assistant professor in the Division of Hospital Medicine at Northwestern University Feinberg School of Medicine in Chicago and a member of SHM’s Practice Analysis Committee. “The State of Hospital Medicine report by SHM provides an opportunity for hospitalists to have an independent view of the compensation and workforce distribution factors that can impact negotiations with their hospital stakeholders. It’s a very powerful tool.”
Compensation Data
Rachel Lovins, MD, SFHM, CPE, voraciously reads every SoHM report because she uses its keynote compensation data to benchmark what she should pay her staff.
“I make a promise to my group,” says Dr. Lovins, chief of hospital medicine and vice chair of the Department of Medicine at Middlesex Hospital in Middletown, Conn. “I promise them that we will always be at or above what is standard for our areas. So for me, I have to look every time.”
Promises like that are getting more expensive to keep.
Hospitalists in the East region earn a median compensation of $245,977, up 3.1% from the $238,676 figure reported in 2014. But the East, where the bulk of the country’s population lives and where competition for hospitalists is typically lessened, is by far the lowest-paid region.
Hospitalists in the South continue to earn the most, with a median compensation of $301,833, up a whopping 16.9% from $258,020 from 2013. Hospitalists in the West earned a median of $275,658 (up 10.3% from $249,894), while Midwestern hospitalists saw a median compensation of $285,213 (up 8.9% from $261,868).
In addition to year-over-year growth, HM is also seeing outsized growth as compared with family medicine physicians, according to MGMA data. From 2011 to 2015, family medicine hospitalists saw an average compensation increase of 4.7%, bringing the average salary to $285,213. During the same period, family medicine physicians who are not hospitalists and don’t practice obstetrics saw an average annual compensation increase of only 3%, bringing the average salary to $230,456.
“The hospitalist can save the hospital considerable amounts of money because of their ability to better manage the patient and improve the quality of care at the same time,” says David Gans, MSHA, FACMPE, MGMA’s senior fellow of industry affairs. “Hospitals, they have recognized that, and therefore, there is considerable competition for recruiting and retaining hospitalists.”
To that end, 96.3% of HM groups (HMGs) received financial support in addition to their professional fee revenue. That’s up from 89% of HMGs that relied last year on their host hospitals. The median support is $157,535 per full-time employee (FTE), up just 1%. Correspondingly, SoHM reported 8.5% of HMGs received enough income from professional fee revenue to cover expenses, up from 6% two years ago.
Industry watchers predicted that, in two years, fee revenue would have to rise to offset hospitals’ inability to pay. The early returns seem to show that bearing out.
“We’re pretty close to that breaking point,” Flores says. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”
Productivity Stalls
While compensation continues to climb, productivity flattened out in this year’s report.
Median relative value units (RVUs) dipped slightly from the figure reported in 2014, to 4,252 from 4,297. But the tally is still ahead of 2012’s total of 4,159. Median collection-to-work RVUs also ticked down from 2014’s tally, to $50.29 from $51.50 in 2013.
Flores largely attributes the falling metrics of productivity to the evolution of HMGs that have standardized their scheduling to the point that most HMGs now offer vacation time.
“So the number of groups that are working 182 days is fewer, and we see a lot more groups that are working something like 168 days or 172 days,” she says. “And if a hospitalist works fewer shifts, even if they see the same number of patients per shift, they’re going to generate less productivity over the course of the year, so that’s part of it.”
Andrew White, MD, SFHM, director of the HM service at the University of Washington Medical Center in Seattle, says the report’s value is in avoiding a myopic approach to how HMGs operate. For example, RVUs are an important metric of productivity, but not all shifts should be expected to produce the same.
For example, it’d be valuable to use the report to see how hard your nocturnists are working compared with other sites, says Dr. White, also a member of the Practice Analysis Committee.
“The fundamental issue with working at night is that not everybody wants to do it, and so you have to recognize that it’s a pain to do and you have to either pay those people more, have them work less, or acknowledge that they’re going to be less productive,” he says. “We use the survey to assess all three of those things and then can work with our nocturnists to reach an agreement about a fair approach to their job structure that’s actually informed by national benchmarks. That process has helped us to pick, for example, how many nights per year they should work or what their salaries should look like compared to the day hospitalists.”
Dr. White says that because the report is comprehensive and includes broad participation, he’s able to use it as a benchmark to make hiring and service structure decisions.
“It also helps me to keep abreast of some trends that may be occurring in the broader workplace that we aren’t participating in but maybe should be or should be thinking about,” he says.
The report’s subsections are also critical for comparing one HMG to others, Dr. White says.
“Obviously, there is the aggregate data there to look at the average program,” he says. “But really as a hospitalist group leader, you want to know what are other programs like mine doing, and it allows you to drill down into that data.”
Survey Limitations
Any hospitalist worth their weight in scrubs knows that any medical study is only as good as its limitations. And while SoHM is a trove of valuable data information, Flores always cautions against taking data points as gospel.
“People should understand what the numbers are telling us, what goes into those numbers, and take them not with a grain of salt but take them for what they are,” she says.
For example, Flores says, look at productivity metrics per shift. Day shifts have traditionally driven that figure, and those shifts are typically busy. But night shifts have fewer patients and less productivity.
“So as more and more hospitals get 24-hour in-house coverage and have doctors working low-productivity night shifts, that [productivity] number might fall,” she says.
That sort of nuanced analysis of productivity can’t be found anywhere else, says Dr. Lovins.
These are “data that we don’t normally get from our administration,” she says, “information on things like staffing and patient loads, and how much more the director makes than the people that work for the director, and how much more nighttime people make than daytime people make. There is no other way for me to get that information, and it’s very important to make sure that our program is fair.”
Aside from fair, the data points are essential talking points as HMGs negotiate contracts and other arrangements with their administrators.
“It’s a reference point so that everybody feels like we’re using data from a national source that everyone can agree upon as fair,” says Dr. White.
In Dr. White’s case, he doesn’t have many local academic programs to benchmark against. And comparing to private, for-profit hospitals isn’t the proverbial apples-to-apples comparison. Having vetted regional and national figures for comparison is incredibly valuable, particularly since he doesn’t have to compile the data.
“If I had to go call all those group leaders and figure out what they were doing, it would be pretty exhausting,” he says.
Alternative Payment Models
Dr. Smith says that one area where the report will become even more valuable over the next few years is addressing alternative payment models (APMs). In particular, HM leaders say they’re excited about being drivers in one of the largest APMs: the Bundled Payments for Care Improvement (BCPI) initiative. In short, the program covers 48 defined episodes of care, including medical and surgical, that could begin three days prior to admission and stretch 30, 60, or 90 days post-discharge.
Dr. Smith thinks it’s still a bit too early to see from the report how APMs have affected compensation.
“We’re still relatively in the early days of bundled-payment models, so in that regard, the State of Hospital Medicine Report still represents very much a starting point with regard to where hospital medicine groups will find themselves as they start to encounter challenges,” he says.
Perhaps more important, Gans doesn’t expect that the maturation of APMs will result in decreased compensation for hospitalists.
“In a hospital environment where the hospital is being reimbursed a set amount for a complete hospital admission and follow-up care and potential readmissions, that is an episodic payment already,” he says. “Consequently, the incentive is there today to better manage the patient and to attain the care coordination and care management necessary for that patient to be discharged and not readmitted.”
In fact, the SHM/MGMA data tell him that the basic economic theory of supply and demand continues to drive hospitalist compensation even 20 years after the field was given its name. He says rising compensation, even as more practices look to hire nurse practitioners or physician assistants as less expensive alternatives, shows no sign of letting up.
“I think demand will continue to be there,” Gans adds. “There may be in the long run some lessening of demand for hospitalists, but I don’t see that for years.”
Richard Quinn is a freelance writer in New Jersey.
Editor's Note: Listen to Dr. Smith share more of his views on the State of Hospital Medicine report.
2016 is the “Year of the Hospitalist,” a sobriquet meant as a proud nod to the specialty’s maturation as a fixture in hospitals across the country. Hospital medicine is no longer the new kid on the block as it has assumed care for the vast majority of hospitalized patients nationwide.
One could understand then if the ever-rising salaries hospitalists have commanded for 20 years might have finally plateaued, particularly as tightening budgets have C-suite administrators looking to trim costs.
Think again.
“Growth suggests that there is still a huge demand,” says Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee. “The demand for hospitalists still exceeds the supply, and so recruiting hospitalists, particularly to nonurban areas, is really challenging and is requiring more money.”
The SoHM is a biennial partnership between SHM and MGMA that provides HM group leaders and rank-and-file hospitalists a litany of benchmarks for salaries, workloads, and everything that informs those two topics. Call it the specialty’s empirical roadmap.
“Often, compensation information relative to staffing information is proprietary, so hospitalists are in a position where they are dependent upon their hospital stakeholders to have access to this information, but they are also the same stakeholders with whom they negotiate their contracts,” says G. Randy Smith, MD, MS, FRCP(Edin), SFHM, an assistant professor in the Division of Hospital Medicine at Northwestern University Feinberg School of Medicine in Chicago and a member of SHM’s Practice Analysis Committee. “The State of Hospital Medicine report by SHM provides an opportunity for hospitalists to have an independent view of the compensation and workforce distribution factors that can impact negotiations with their hospital stakeholders. It’s a very powerful tool.”
Compensation Data
Rachel Lovins, MD, SFHM, CPE, voraciously reads every SoHM report because she uses its keynote compensation data to benchmark what she should pay her staff.
“I make a promise to my group,” says Dr. Lovins, chief of hospital medicine and vice chair of the Department of Medicine at Middlesex Hospital in Middletown, Conn. “I promise them that we will always be at or above what is standard for our areas. So for me, I have to look every time.”
Promises like that are getting more expensive to keep.
Hospitalists in the East region earn a median compensation of $245,977, up 3.1% from the $238,676 figure reported in 2014. But the East, where the bulk of the country’s population lives and where competition for hospitalists is typically lessened, is by far the lowest-paid region.
Hospitalists in the South continue to earn the most, with a median compensation of $301,833, up a whopping 16.9% from $258,020 from 2013. Hospitalists in the West earned a median of $275,658 (up 10.3% from $249,894), while Midwestern hospitalists saw a median compensation of $285,213 (up 8.9% from $261,868).
In addition to year-over-year growth, HM is also seeing outsized growth as compared with family medicine physicians, according to MGMA data. From 2011 to 2015, family medicine hospitalists saw an average compensation increase of 4.7%, bringing the average salary to $285,213. During the same period, family medicine physicians who are not hospitalists and don’t practice obstetrics saw an average annual compensation increase of only 3%, bringing the average salary to $230,456.
“The hospitalist can save the hospital considerable amounts of money because of their ability to better manage the patient and improve the quality of care at the same time,” says David Gans, MSHA, FACMPE, MGMA’s senior fellow of industry affairs. “Hospitals, they have recognized that, and therefore, there is considerable competition for recruiting and retaining hospitalists.”
To that end, 96.3% of HM groups (HMGs) received financial support in addition to their professional fee revenue. That’s up from 89% of HMGs that relied last year on their host hospitals. The median support is $157,535 per full-time employee (FTE), up just 1%. Correspondingly, SoHM reported 8.5% of HMGs received enough income from professional fee revenue to cover expenses, up from 6% two years ago.
Industry watchers predicted that, in two years, fee revenue would have to rise to offset hospitals’ inability to pay. The early returns seem to show that bearing out.
“We’re pretty close to that breaking point,” Flores says. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”
Productivity Stalls
While compensation continues to climb, productivity flattened out in this year’s report.
Median relative value units (RVUs) dipped slightly from the figure reported in 2014, to 4,252 from 4,297. But the tally is still ahead of 2012’s total of 4,159. Median collection-to-work RVUs also ticked down from 2014’s tally, to $50.29 from $51.50 in 2013.
Flores largely attributes the falling metrics of productivity to the evolution of HMGs that have standardized their scheduling to the point that most HMGs now offer vacation time.
“So the number of groups that are working 182 days is fewer, and we see a lot more groups that are working something like 168 days or 172 days,” she says. “And if a hospitalist works fewer shifts, even if they see the same number of patients per shift, they’re going to generate less productivity over the course of the year, so that’s part of it.”
Andrew White, MD, SFHM, director of the HM service at the University of Washington Medical Center in Seattle, says the report’s value is in avoiding a myopic approach to how HMGs operate. For example, RVUs are an important metric of productivity, but not all shifts should be expected to produce the same.
For example, it’d be valuable to use the report to see how hard your nocturnists are working compared with other sites, says Dr. White, also a member of the Practice Analysis Committee.
“The fundamental issue with working at night is that not everybody wants to do it, and so you have to recognize that it’s a pain to do and you have to either pay those people more, have them work less, or acknowledge that they’re going to be less productive,” he says. “We use the survey to assess all three of those things and then can work with our nocturnists to reach an agreement about a fair approach to their job structure that’s actually informed by national benchmarks. That process has helped us to pick, for example, how many nights per year they should work or what their salaries should look like compared to the day hospitalists.”
Dr. White says that because the report is comprehensive and includes broad participation, he’s able to use it as a benchmark to make hiring and service structure decisions.
“It also helps me to keep abreast of some trends that may be occurring in the broader workplace that we aren’t participating in but maybe should be or should be thinking about,” he says.
The report’s subsections are also critical for comparing one HMG to others, Dr. White says.
“Obviously, there is the aggregate data there to look at the average program,” he says. “But really as a hospitalist group leader, you want to know what are other programs like mine doing, and it allows you to drill down into that data.”
Survey Limitations
Any hospitalist worth their weight in scrubs knows that any medical study is only as good as its limitations. And while SoHM is a trove of valuable data information, Flores always cautions against taking data points as gospel.
“People should understand what the numbers are telling us, what goes into those numbers, and take them not with a grain of salt but take them for what they are,” she says.
For example, Flores says, look at productivity metrics per shift. Day shifts have traditionally driven that figure, and those shifts are typically busy. But night shifts have fewer patients and less productivity.
“So as more and more hospitals get 24-hour in-house coverage and have doctors working low-productivity night shifts, that [productivity] number might fall,” she says.
That sort of nuanced analysis of productivity can’t be found anywhere else, says Dr. Lovins.
These are “data that we don’t normally get from our administration,” she says, “information on things like staffing and patient loads, and how much more the director makes than the people that work for the director, and how much more nighttime people make than daytime people make. There is no other way for me to get that information, and it’s very important to make sure that our program is fair.”
Aside from fair, the data points are essential talking points as HMGs negotiate contracts and other arrangements with their administrators.
“It’s a reference point so that everybody feels like we’re using data from a national source that everyone can agree upon as fair,” says Dr. White.
In Dr. White’s case, he doesn’t have many local academic programs to benchmark against. And comparing to private, for-profit hospitals isn’t the proverbial apples-to-apples comparison. Having vetted regional and national figures for comparison is incredibly valuable, particularly since he doesn’t have to compile the data.
“If I had to go call all those group leaders and figure out what they were doing, it would be pretty exhausting,” he says.
Alternative Payment Models
Dr. Smith says that one area where the report will become even more valuable over the next few years is addressing alternative payment models (APMs). In particular, HM leaders say they’re excited about being drivers in one of the largest APMs: the Bundled Payments for Care Improvement (BCPI) initiative. In short, the program covers 48 defined episodes of care, including medical and surgical, that could begin three days prior to admission and stretch 30, 60, or 90 days post-discharge.
Dr. Smith thinks it’s still a bit too early to see from the report how APMs have affected compensation.
“We’re still relatively in the early days of bundled-payment models, so in that regard, the State of Hospital Medicine Report still represents very much a starting point with regard to where hospital medicine groups will find themselves as they start to encounter challenges,” he says.
Perhaps more important, Gans doesn’t expect that the maturation of APMs will result in decreased compensation for hospitalists.
“In a hospital environment where the hospital is being reimbursed a set amount for a complete hospital admission and follow-up care and potential readmissions, that is an episodic payment already,” he says. “Consequently, the incentive is there today to better manage the patient and to attain the care coordination and care management necessary for that patient to be discharged and not readmitted.”
In fact, the SHM/MGMA data tell him that the basic economic theory of supply and demand continues to drive hospitalist compensation even 20 years after the field was given its name. He says rising compensation, even as more practices look to hire nurse practitioners or physician assistants as less expensive alternatives, shows no sign of letting up.
“I think demand will continue to be there,” Gans adds. “There may be in the long run some lessening of demand for hospitalists, but I don’t see that for years.”
Richard Quinn is a freelance writer in New Jersey.
Editor's Note: Listen to Dr. Smith share more of his views on the State of Hospital Medicine report.
2016 is the “Year of the Hospitalist,” a sobriquet meant as a proud nod to the specialty’s maturation as a fixture in hospitals across the country. Hospital medicine is no longer the new kid on the block as it has assumed care for the vast majority of hospitalized patients nationwide.
One could understand then if the ever-rising salaries hospitalists have commanded for 20 years might have finally plateaued, particularly as tightening budgets have C-suite administrators looking to trim costs.
Think again.
“Growth suggests that there is still a huge demand,” says Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee. “The demand for hospitalists still exceeds the supply, and so recruiting hospitalists, particularly to nonurban areas, is really challenging and is requiring more money.”
The SoHM is a biennial partnership between SHM and MGMA that provides HM group leaders and rank-and-file hospitalists a litany of benchmarks for salaries, workloads, and everything that informs those two topics. Call it the specialty’s empirical roadmap.
“Often, compensation information relative to staffing information is proprietary, so hospitalists are in a position where they are dependent upon their hospital stakeholders to have access to this information, but they are also the same stakeholders with whom they negotiate their contracts,” says G. Randy Smith, MD, MS, FRCP(Edin), SFHM, an assistant professor in the Division of Hospital Medicine at Northwestern University Feinberg School of Medicine in Chicago and a member of SHM’s Practice Analysis Committee. “The State of Hospital Medicine report by SHM provides an opportunity for hospitalists to have an independent view of the compensation and workforce distribution factors that can impact negotiations with their hospital stakeholders. It’s a very powerful tool.”
Compensation Data
Rachel Lovins, MD, SFHM, CPE, voraciously reads every SoHM report because she uses its keynote compensation data to benchmark what she should pay her staff.
“I make a promise to my group,” says Dr. Lovins, chief of hospital medicine and vice chair of the Department of Medicine at Middlesex Hospital in Middletown, Conn. “I promise them that we will always be at or above what is standard for our areas. So for me, I have to look every time.”
Promises like that are getting more expensive to keep.
Hospitalists in the East region earn a median compensation of $245,977, up 3.1% from the $238,676 figure reported in 2014. But the East, where the bulk of the country’s population lives and where competition for hospitalists is typically lessened, is by far the lowest-paid region.
Hospitalists in the South continue to earn the most, with a median compensation of $301,833, up a whopping 16.9% from $258,020 from 2013. Hospitalists in the West earned a median of $275,658 (up 10.3% from $249,894), while Midwestern hospitalists saw a median compensation of $285,213 (up 8.9% from $261,868).
In addition to year-over-year growth, HM is also seeing outsized growth as compared with family medicine physicians, according to MGMA data. From 2011 to 2015, family medicine hospitalists saw an average compensation increase of 4.7%, bringing the average salary to $285,213. During the same period, family medicine physicians who are not hospitalists and don’t practice obstetrics saw an average annual compensation increase of only 3%, bringing the average salary to $230,456.
“The hospitalist can save the hospital considerable amounts of money because of their ability to better manage the patient and improve the quality of care at the same time,” says David Gans, MSHA, FACMPE, MGMA’s senior fellow of industry affairs. “Hospitals, they have recognized that, and therefore, there is considerable competition for recruiting and retaining hospitalists.”
To that end, 96.3% of HM groups (HMGs) received financial support in addition to their professional fee revenue. That’s up from 89% of HMGs that relied last year on their host hospitals. The median support is $157,535 per full-time employee (FTE), up just 1%. Correspondingly, SoHM reported 8.5% of HMGs received enough income from professional fee revenue to cover expenses, up from 6% two years ago.
Industry watchers predicted that, in two years, fee revenue would have to rise to offset hospitals’ inability to pay. The early returns seem to show that bearing out.
“We’re pretty close to that breaking point,” Flores says. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”
Productivity Stalls
While compensation continues to climb, productivity flattened out in this year’s report.
Median relative value units (RVUs) dipped slightly from the figure reported in 2014, to 4,252 from 4,297. But the tally is still ahead of 2012’s total of 4,159. Median collection-to-work RVUs also ticked down from 2014’s tally, to $50.29 from $51.50 in 2013.
Flores largely attributes the falling metrics of productivity to the evolution of HMGs that have standardized their scheduling to the point that most HMGs now offer vacation time.
“So the number of groups that are working 182 days is fewer, and we see a lot more groups that are working something like 168 days or 172 days,” she says. “And if a hospitalist works fewer shifts, even if they see the same number of patients per shift, they’re going to generate less productivity over the course of the year, so that’s part of it.”
Andrew White, MD, SFHM, director of the HM service at the University of Washington Medical Center in Seattle, says the report’s value is in avoiding a myopic approach to how HMGs operate. For example, RVUs are an important metric of productivity, but not all shifts should be expected to produce the same.
For example, it’d be valuable to use the report to see how hard your nocturnists are working compared with other sites, says Dr. White, also a member of the Practice Analysis Committee.
“The fundamental issue with working at night is that not everybody wants to do it, and so you have to recognize that it’s a pain to do and you have to either pay those people more, have them work less, or acknowledge that they’re going to be less productive,” he says. “We use the survey to assess all three of those things and then can work with our nocturnists to reach an agreement about a fair approach to their job structure that’s actually informed by national benchmarks. That process has helped us to pick, for example, how many nights per year they should work or what their salaries should look like compared to the day hospitalists.”
Dr. White says that because the report is comprehensive and includes broad participation, he’s able to use it as a benchmark to make hiring and service structure decisions.
“It also helps me to keep abreast of some trends that may be occurring in the broader workplace that we aren’t participating in but maybe should be or should be thinking about,” he says.
The report’s subsections are also critical for comparing one HMG to others, Dr. White says.
“Obviously, there is the aggregate data there to look at the average program,” he says. “But really as a hospitalist group leader, you want to know what are other programs like mine doing, and it allows you to drill down into that data.”
Survey Limitations
Any hospitalist worth their weight in scrubs knows that any medical study is only as good as its limitations. And while SoHM is a trove of valuable data information, Flores always cautions against taking data points as gospel.
“People should understand what the numbers are telling us, what goes into those numbers, and take them not with a grain of salt but take them for what they are,” she says.
For example, Flores says, look at productivity metrics per shift. Day shifts have traditionally driven that figure, and those shifts are typically busy. But night shifts have fewer patients and less productivity.
“So as more and more hospitals get 24-hour in-house coverage and have doctors working low-productivity night shifts, that [productivity] number might fall,” she says.
That sort of nuanced analysis of productivity can’t be found anywhere else, says Dr. Lovins.
These are “data that we don’t normally get from our administration,” she says, “information on things like staffing and patient loads, and how much more the director makes than the people that work for the director, and how much more nighttime people make than daytime people make. There is no other way for me to get that information, and it’s very important to make sure that our program is fair.”
Aside from fair, the data points are essential talking points as HMGs negotiate contracts and other arrangements with their administrators.
“It’s a reference point so that everybody feels like we’re using data from a national source that everyone can agree upon as fair,” says Dr. White.
In Dr. White’s case, he doesn’t have many local academic programs to benchmark against. And comparing to private, for-profit hospitals isn’t the proverbial apples-to-apples comparison. Having vetted regional and national figures for comparison is incredibly valuable, particularly since he doesn’t have to compile the data.
“If I had to go call all those group leaders and figure out what they were doing, it would be pretty exhausting,” he says.
Alternative Payment Models
Dr. Smith says that one area where the report will become even more valuable over the next few years is addressing alternative payment models (APMs). In particular, HM leaders say they’re excited about being drivers in one of the largest APMs: the Bundled Payments for Care Improvement (BCPI) initiative. In short, the program covers 48 defined episodes of care, including medical and surgical, that could begin three days prior to admission and stretch 30, 60, or 90 days post-discharge.
Dr. Smith thinks it’s still a bit too early to see from the report how APMs have affected compensation.
“We’re still relatively in the early days of bundled-payment models, so in that regard, the State of Hospital Medicine Report still represents very much a starting point with regard to where hospital medicine groups will find themselves as they start to encounter challenges,” he says.
Perhaps more important, Gans doesn’t expect that the maturation of APMs will result in decreased compensation for hospitalists.
“In a hospital environment where the hospital is being reimbursed a set amount for a complete hospital admission and follow-up care and potential readmissions, that is an episodic payment already,” he says. “Consequently, the incentive is there today to better manage the patient and to attain the care coordination and care management necessary for that patient to be discharged and not readmitted.”
In fact, the SHM/MGMA data tell him that the basic economic theory of supply and demand continues to drive hospitalist compensation even 20 years after the field was given its name. He says rising compensation, even as more practices look to hire nurse practitioners or physician assistants as less expensive alternatives, shows no sign of letting up.
“I think demand will continue to be there,” Gans adds. “There may be in the long run some lessening of demand for hospitalists, but I don’t see that for years.”
Richard Quinn is a freelance writer in New Jersey.
Setting Up Your New Physician for Success
Practices and hospitals invest significant time and money in recruiting a new physician. From phone interviews to site visits to contract negotiations, it’s a long and involved process.
Beyond setting up a new physician’s office and appointment schedule, completing human resources paperwork, and ordering business cards, what does your practice do to support new physicians to ensure they are successful? Although a new colleague may arrive with excellent clinical skills, even the most promising surgeon can fall short if not provided with the right expectations, training, and collegial support. Here’s how to fast track your new physician to professional heights.
Credentialing Is Key
At the crux of a new physician’s success is credentialing him or her with hospitals and insurance plans before the official start date to see patients.
“A state medical license is the first domino,” says orthopedic surgeon Michael R. Marks, MD, MBA, consultant and coding educator with KarenZupko & Associates, Inc. Marks has led or participated in physician recruitment in orthopedic and multispecialty groups. The firm has developed a comprehensive New Physician Onboarding Checklist, available at https://www.karenzupko.com/new-physician-onboarding-checklist/.
“Without a medical license,” Marks continues, “you can’t get the new physician hospital privileges and you can’t get him or her credentialed with plans. Without being credentialed, the physician can’t bill for patients treated.” Because commercial carriers won’t allow retrospective billing for services already rendered, “even a 3-month delay in credentialing could cost an orthopedic practice $60,000 to $180,000 in lost revenue.”
And if you think you can bill the new physician’s services under another partner’s name, you are incorrect. “The billing physician will have signed the note, but not have treated the patient,” warns Marks. “This is improper billing. Don’t do it.”
The remedy for ensuring that the new physician is credentialed is simple: get organized and plan ahead.
“When I first started participating in recruitment, I remember telling physicians, ‘I need you tomorrow!’” admits Amon T. Ferry, MD, a practicing orthopedist who leads recruitment efforts at IMS Orthopedics, a division of Integrated Medical Specialists in Phoenix, Arizona. “So they’d get hired before the practice was prepared and before credentialing was completed. Now, I set more realistic expectations,” he says, noting that in Arizona it takes 3 months to get a medical license, 6 months to contract with the hospital, and 9 months to get on insurance plans. And even after a plan has credentialed a new physician, “sometimes it still takes 4 to 6 weeks before the physician’s data is loaded into the plan’s computer systems.”
“The way to do credentialing right is to get all departments communicating,” Marks says. “If you keep everyone siloed, staff don’t understand that a lack of timeliness on their part impacts other areas of the practice.”
Ferry agrees, and says his group learned to organize its multiple departments after making mistakes and missing deadlines. “We now have an 8-page pre-employment application for new physicians,” he explains. “In addition to asking for contact information and everything we need to know in order to get the physician credentialed, we ask questions about malpractice suit history and whether there are issues with the medical board. We also ask about gaps in employment and details about where the physician has practiced in the past.” All of this is done to identify early whether credentialing will require more time and effort. Ferry says that the application has solved a number of processing problems the practice had in the past.
And whether credentialing is done within the practice or outsourced, Ferry says that it pays to be persistent. “Don’t sit back and assume it will get done. Even if you have outsourced credentialing to a company, someone must check with payers and hospitals weekly and provide the practice a status update.”
In one case, when getting a new physician contracted at a hospital was taking forever, Ferry directed the staff to call. “Turns out, they had been trying to reach us and had the wrong phone number,” he says. “When people are processing thousands of physician renewals, things get lost. You have to be proactive and be your own advocate. Don’t be afraid to be the squeaky wheel.”
Staff Relationships and Operational Wisdom
Marks points out that in many practices, the new physician is shown the examination rooms and his or her office, gets electronic health record (EHR) training, and that’s it. To be successful, Marks insists that the new physician must build relationships with personnel and understand operational basics. “In other business industries, successful leaders understand at least the basics of what everyone does. Part of how they do this is by getting to know the employees.”
Ideally, Marks advises that new physicians spend time with each staff member. “The best time to do this is in the first few weeks of employment,” he suggests. “Odds are, the new orthopedist doesn’t have 40 patients a day on the schedule. So schedule conversations within the first few weeks or month, and schedule observation time as well. When a patient complains about check-in, the physician will have an understanding of how things work up there if he or she knows the basic processes.” The new doctor should also spend time in the billing office getting to know the challenges faced by staff, and sit with the surgery coordinator to understand the process of getting cases booked and scheduled.
Plan for an initial and then periodic meetings with the practice administrator and other supervisors. Transparency about business operations, data, and strategy will help the new physician get up to speed faster.
“The executive director of our group was an absolutely invaluable information resource,” says Kathryn J. McCarthy, MD, an orthopedic spine surgeon with Arkansas Specialty Orthopaedics in Little Rock, Arkansas. McCarthy has been with the group for 3 years.
The practice’s executive director developed and presented a PowerPoint (Microsoft) explaining general business procedures, expectations for the coding and billing process, and pertinent compliance and risk issues. She had also developed an interactive model of the compensation formula and buy-in program, using Excel (Microsoft). McCarthy met with the executive director at 3 months, 6 months, and 9 months to review her patient and case volumes and how they were trending against the estimates made about her income, bonus, and buy-in status.
From the new physician’s perspective, McCarthy says having the new physician understand the complexities of certain business systems helps them understand things better. “If you sit in the business meetings long enough, you figure it out,” she says, “but it would have made some of the growing pains less painful if I understood what my overhead charge was going to, or more about the workflow of the clinic.” She adds that an overview of hospital relationships and any overlapping ownership interests will benefit new physicians as well.
“I think it’s useful to provide new physicians with a history of the practice and the vision of where things are going,” McCarthy says. “It’s important to outline the business vision, especially for subspecialties. If you explain to the new physician where you want to grow and when the practice plans on bringing on the next physician, it could really drive someone to grow their practice.”
Don’t Underestimate the Need for Coding Training
“When fellows come out of training, they are comfortable with clinical activity but uncomfortable with business administration,” Marks says. “And we know they don’t get training on coding and billing.”
Marks cites a recent conversation at an American Academy of Orthopaedic Surgeons (AAOS) coding workshop. “A surgeon new in practice told me, ‘I’ve been in practice for 4 months. I understand the clinical side but nobody educated me about coding and billing before this course.’” Practices must provide new physicians with coding and documentation training, and coach them to make sure they feel up to speed and comfortable. “The practice’s future revenue depends on it,” Marks says.
McCarthy agrees. “Having an administrative mentorship for coding is incredibly valuable. They don’t teach it in school.”
So from a practical standpoint, purchase AAOS’ Orthopaedic Code-X, a software tool that will help the new physician navigate and integrate Current Procedural Terminology (CPT), ICD-10 (International Classification of Diseases, Tenth Revision), and other coding data easily and accurately. Send him or her to one of the Academy’s regional coding and reimbursement workshops as well. “It will behoove the practice to send them even before they start seeing patients,” Marks says.
And don’t just stop there. High-performing groups conduct peer reviews of evaluation and management (E/M) and operative notes, blinding the codes billed and discussing which CPT and ICD-10 codes are appropriate for the visit or case. “It will take time for the new physician to completely integrate coding with their clinical care,” says Marks. “Peer review sessions, as well as having a partner review codes before they go to the billing office, can help speed learning.”
Collegial Coaching Counts
The week before her official start day, Mc-Carthy scrubbed in as a first assist with each of her new partners. “It was a great way to start ramping up,” she says. “I could see what kind of equipment was present in the hospitals, and got a touch point for hospital logistics. Plus, as a young surgeon it’s great to see how your skill sets match up with your new partners, and which best practices are being deployed by the group.”
This kind of “collegial coaching” is a vital part of the clinical and cultural integration to the practice. Beyond providing clinical support, it builds relationships and trust among the group, and fosters collaboration.
Arkansas Specialty Orthopaedics organized McCarthy’s clinic and operating room (OR) schedules so that a partner was always present. “There was also someone I could bounce ideas off of,” McCarthy explains. “Every day in the OR, there was a partner there at the same time. If I got into a sticky situation, one of my colleagues was willing to come in and scrub in the OR.”
McCarthy says that patients responded favorably when she told them her plan was developed in conjunction with her partners. “Patients find comfort in knowing that several people’s opinions were considered,” she says. “And as a young surgeon, knowing that you have backup, even if you don’t use it, when caring for high-risk and complex cases really means a lot,” she says.
And although her group didn’t offer a formal mentoring program, McCarthy found that an informal mentorship grew organically when a friendship developed with one of her new partners. “In the first 6 months, every single weekend we sat by the pool and rolled through a ton of cases,” she says. “That was fabulous and it alleviated so much stress for me.” And when it was time for McCarthy to move into board case selection, this colleague and another were instrumental in her board preparation because, “they knew my style and where I would need to focus.”
IMS Orthopedics’ approach is to provide the staff and systems that allow new physicians to step up and take responsibility. “If they want to scrub in with me, that’s great. If they’d like to visit additional facilities and get the lay of the land, we encourage it. But we don’t do a lot of handholding. We set them up for success and make sure people are in place to help them,” says Ferry.
A Marketing Plan Is a Must
“The vast majority of practices do very little when it comes to thinking about how to market and build the practice of their new physician,” Marks says. “Practice-building is more of a challenge for surgical specialists today than it was in the old days when new surgeons could easily meet internists as they were rounding at the hospital. Now, a new physician and the practice must come up with a game plan.”
That game plan starts with the easy things: order business cards, schedule a photo shoot, and update the practice’s Web site pages with the physician’s biography and an introductory video. But with social media, online reviews, and subspecialty competition, Marks says practices must think beyond the basics. Think through each element of marketing, from online to outreach to developing referral relationships.
“I tell practices to draft a written marketing plan,” he says. “Not only does it provide a roadmap for the new physician, but also indicates that the practice has put some thought into how he or she can build a practice. It can make the new physician feel less overwhelmed knowing that he or she doesn’t have to do the marketing alone.” Once you’ve developed a list of actions, Marks suggests creating a spreadsheet with deadlines, and ensuring each action is completed.
McCarthy was scheduled to visit family practice clinics, and joined by the administrator who “handed out cookies and cards while I talked,” she says. Arkansas Specialty Orthopaedics also hired an external marketing firm to develop promotional opportunities for her. For example, “I was scheduled to appear on news channels, where I discussed new and interesting procedures,” she says. “It got my name out into the community.”
If your practice is too small to hire an outside firm, Marks suggests reaching out to agencies such as nursing homes, fitness centers, or the YMCA, which frequently offers educational programs for members. “Contact the administrators or medical directors in these organizations. A few minutes on the phone or a short visit can go a long way to building these relationships and getting your new physician on the map.”
As the old saying goes, an ounce of prevention is worth a pound of cure. Scheduling time for orientation, training, staff integration, and collegial coaching will speed up a new physician’s integration into the practice, and increase his or her opportunity for success.
Practices and hospitals invest significant time and money in recruiting a new physician. From phone interviews to site visits to contract negotiations, it’s a long and involved process.
Beyond setting up a new physician’s office and appointment schedule, completing human resources paperwork, and ordering business cards, what does your practice do to support new physicians to ensure they are successful? Although a new colleague may arrive with excellent clinical skills, even the most promising surgeon can fall short if not provided with the right expectations, training, and collegial support. Here’s how to fast track your new physician to professional heights.
Credentialing Is Key
At the crux of a new physician’s success is credentialing him or her with hospitals and insurance plans before the official start date to see patients.
“A state medical license is the first domino,” says orthopedic surgeon Michael R. Marks, MD, MBA, consultant and coding educator with KarenZupko & Associates, Inc. Marks has led or participated in physician recruitment in orthopedic and multispecialty groups. The firm has developed a comprehensive New Physician Onboarding Checklist, available at https://www.karenzupko.com/new-physician-onboarding-checklist/.
“Without a medical license,” Marks continues, “you can’t get the new physician hospital privileges and you can’t get him or her credentialed with plans. Without being credentialed, the physician can’t bill for patients treated.” Because commercial carriers won’t allow retrospective billing for services already rendered, “even a 3-month delay in credentialing could cost an orthopedic practice $60,000 to $180,000 in lost revenue.”
And if you think you can bill the new physician’s services under another partner’s name, you are incorrect. “The billing physician will have signed the note, but not have treated the patient,” warns Marks. “This is improper billing. Don’t do it.”
The remedy for ensuring that the new physician is credentialed is simple: get organized and plan ahead.
“When I first started participating in recruitment, I remember telling physicians, ‘I need you tomorrow!’” admits Amon T. Ferry, MD, a practicing orthopedist who leads recruitment efforts at IMS Orthopedics, a division of Integrated Medical Specialists in Phoenix, Arizona. “So they’d get hired before the practice was prepared and before credentialing was completed. Now, I set more realistic expectations,” he says, noting that in Arizona it takes 3 months to get a medical license, 6 months to contract with the hospital, and 9 months to get on insurance plans. And even after a plan has credentialed a new physician, “sometimes it still takes 4 to 6 weeks before the physician’s data is loaded into the plan’s computer systems.”
“The way to do credentialing right is to get all departments communicating,” Marks says. “If you keep everyone siloed, staff don’t understand that a lack of timeliness on their part impacts other areas of the practice.”
Ferry agrees, and says his group learned to organize its multiple departments after making mistakes and missing deadlines. “We now have an 8-page pre-employment application for new physicians,” he explains. “In addition to asking for contact information and everything we need to know in order to get the physician credentialed, we ask questions about malpractice suit history and whether there are issues with the medical board. We also ask about gaps in employment and details about where the physician has practiced in the past.” All of this is done to identify early whether credentialing will require more time and effort. Ferry says that the application has solved a number of processing problems the practice had in the past.
And whether credentialing is done within the practice or outsourced, Ferry says that it pays to be persistent. “Don’t sit back and assume it will get done. Even if you have outsourced credentialing to a company, someone must check with payers and hospitals weekly and provide the practice a status update.”
In one case, when getting a new physician contracted at a hospital was taking forever, Ferry directed the staff to call. “Turns out, they had been trying to reach us and had the wrong phone number,” he says. “When people are processing thousands of physician renewals, things get lost. You have to be proactive and be your own advocate. Don’t be afraid to be the squeaky wheel.”
Staff Relationships and Operational Wisdom
Marks points out that in many practices, the new physician is shown the examination rooms and his or her office, gets electronic health record (EHR) training, and that’s it. To be successful, Marks insists that the new physician must build relationships with personnel and understand operational basics. “In other business industries, successful leaders understand at least the basics of what everyone does. Part of how they do this is by getting to know the employees.”
Ideally, Marks advises that new physicians spend time with each staff member. “The best time to do this is in the first few weeks of employment,” he suggests. “Odds are, the new orthopedist doesn’t have 40 patients a day on the schedule. So schedule conversations within the first few weeks or month, and schedule observation time as well. When a patient complains about check-in, the physician will have an understanding of how things work up there if he or she knows the basic processes.” The new doctor should also spend time in the billing office getting to know the challenges faced by staff, and sit with the surgery coordinator to understand the process of getting cases booked and scheduled.
Plan for an initial and then periodic meetings with the practice administrator and other supervisors. Transparency about business operations, data, and strategy will help the new physician get up to speed faster.
“The executive director of our group was an absolutely invaluable information resource,” says Kathryn J. McCarthy, MD, an orthopedic spine surgeon with Arkansas Specialty Orthopaedics in Little Rock, Arkansas. McCarthy has been with the group for 3 years.
The practice’s executive director developed and presented a PowerPoint (Microsoft) explaining general business procedures, expectations for the coding and billing process, and pertinent compliance and risk issues. She had also developed an interactive model of the compensation formula and buy-in program, using Excel (Microsoft). McCarthy met with the executive director at 3 months, 6 months, and 9 months to review her patient and case volumes and how they were trending against the estimates made about her income, bonus, and buy-in status.
From the new physician’s perspective, McCarthy says having the new physician understand the complexities of certain business systems helps them understand things better. “If you sit in the business meetings long enough, you figure it out,” she says, “but it would have made some of the growing pains less painful if I understood what my overhead charge was going to, or more about the workflow of the clinic.” She adds that an overview of hospital relationships and any overlapping ownership interests will benefit new physicians as well.
“I think it’s useful to provide new physicians with a history of the practice and the vision of where things are going,” McCarthy says. “It’s important to outline the business vision, especially for subspecialties. If you explain to the new physician where you want to grow and when the practice plans on bringing on the next physician, it could really drive someone to grow their practice.”
Don’t Underestimate the Need for Coding Training
“When fellows come out of training, they are comfortable with clinical activity but uncomfortable with business administration,” Marks says. “And we know they don’t get training on coding and billing.”
Marks cites a recent conversation at an American Academy of Orthopaedic Surgeons (AAOS) coding workshop. “A surgeon new in practice told me, ‘I’ve been in practice for 4 months. I understand the clinical side but nobody educated me about coding and billing before this course.’” Practices must provide new physicians with coding and documentation training, and coach them to make sure they feel up to speed and comfortable. “The practice’s future revenue depends on it,” Marks says.
McCarthy agrees. “Having an administrative mentorship for coding is incredibly valuable. They don’t teach it in school.”
So from a practical standpoint, purchase AAOS’ Orthopaedic Code-X, a software tool that will help the new physician navigate and integrate Current Procedural Terminology (CPT), ICD-10 (International Classification of Diseases, Tenth Revision), and other coding data easily and accurately. Send him or her to one of the Academy’s regional coding and reimbursement workshops as well. “It will behoove the practice to send them even before they start seeing patients,” Marks says.
And don’t just stop there. High-performing groups conduct peer reviews of evaluation and management (E/M) and operative notes, blinding the codes billed and discussing which CPT and ICD-10 codes are appropriate for the visit or case. “It will take time for the new physician to completely integrate coding with their clinical care,” says Marks. “Peer review sessions, as well as having a partner review codes before they go to the billing office, can help speed learning.”
Collegial Coaching Counts
The week before her official start day, Mc-Carthy scrubbed in as a first assist with each of her new partners. “It was a great way to start ramping up,” she says. “I could see what kind of equipment was present in the hospitals, and got a touch point for hospital logistics. Plus, as a young surgeon it’s great to see how your skill sets match up with your new partners, and which best practices are being deployed by the group.”
This kind of “collegial coaching” is a vital part of the clinical and cultural integration to the practice. Beyond providing clinical support, it builds relationships and trust among the group, and fosters collaboration.
Arkansas Specialty Orthopaedics organized McCarthy’s clinic and operating room (OR) schedules so that a partner was always present. “There was also someone I could bounce ideas off of,” McCarthy explains. “Every day in the OR, there was a partner there at the same time. If I got into a sticky situation, one of my colleagues was willing to come in and scrub in the OR.”
McCarthy says that patients responded favorably when she told them her plan was developed in conjunction with her partners. “Patients find comfort in knowing that several people’s opinions were considered,” she says. “And as a young surgeon, knowing that you have backup, even if you don’t use it, when caring for high-risk and complex cases really means a lot,” she says.
And although her group didn’t offer a formal mentoring program, McCarthy found that an informal mentorship grew organically when a friendship developed with one of her new partners. “In the first 6 months, every single weekend we sat by the pool and rolled through a ton of cases,” she says. “That was fabulous and it alleviated so much stress for me.” And when it was time for McCarthy to move into board case selection, this colleague and another were instrumental in her board preparation because, “they knew my style and where I would need to focus.”
IMS Orthopedics’ approach is to provide the staff and systems that allow new physicians to step up and take responsibility. “If they want to scrub in with me, that’s great. If they’d like to visit additional facilities and get the lay of the land, we encourage it. But we don’t do a lot of handholding. We set them up for success and make sure people are in place to help them,” says Ferry.
A Marketing Plan Is a Must
“The vast majority of practices do very little when it comes to thinking about how to market and build the practice of their new physician,” Marks says. “Practice-building is more of a challenge for surgical specialists today than it was in the old days when new surgeons could easily meet internists as they were rounding at the hospital. Now, a new physician and the practice must come up with a game plan.”
That game plan starts with the easy things: order business cards, schedule a photo shoot, and update the practice’s Web site pages with the physician’s biography and an introductory video. But with social media, online reviews, and subspecialty competition, Marks says practices must think beyond the basics. Think through each element of marketing, from online to outreach to developing referral relationships.
“I tell practices to draft a written marketing plan,” he says. “Not only does it provide a roadmap for the new physician, but also indicates that the practice has put some thought into how he or she can build a practice. It can make the new physician feel less overwhelmed knowing that he or she doesn’t have to do the marketing alone.” Once you’ve developed a list of actions, Marks suggests creating a spreadsheet with deadlines, and ensuring each action is completed.
McCarthy was scheduled to visit family practice clinics, and joined by the administrator who “handed out cookies and cards while I talked,” she says. Arkansas Specialty Orthopaedics also hired an external marketing firm to develop promotional opportunities for her. For example, “I was scheduled to appear on news channels, where I discussed new and interesting procedures,” she says. “It got my name out into the community.”
If your practice is too small to hire an outside firm, Marks suggests reaching out to agencies such as nursing homes, fitness centers, or the YMCA, which frequently offers educational programs for members. “Contact the administrators or medical directors in these organizations. A few minutes on the phone or a short visit can go a long way to building these relationships and getting your new physician on the map.”
As the old saying goes, an ounce of prevention is worth a pound of cure. Scheduling time for orientation, training, staff integration, and collegial coaching will speed up a new physician’s integration into the practice, and increase his or her opportunity for success.
Practices and hospitals invest significant time and money in recruiting a new physician. From phone interviews to site visits to contract negotiations, it’s a long and involved process.
Beyond setting up a new physician’s office and appointment schedule, completing human resources paperwork, and ordering business cards, what does your practice do to support new physicians to ensure they are successful? Although a new colleague may arrive with excellent clinical skills, even the most promising surgeon can fall short if not provided with the right expectations, training, and collegial support. Here’s how to fast track your new physician to professional heights.
Credentialing Is Key
At the crux of a new physician’s success is credentialing him or her with hospitals and insurance plans before the official start date to see patients.
“A state medical license is the first domino,” says orthopedic surgeon Michael R. Marks, MD, MBA, consultant and coding educator with KarenZupko & Associates, Inc. Marks has led or participated in physician recruitment in orthopedic and multispecialty groups. The firm has developed a comprehensive New Physician Onboarding Checklist, available at https://www.karenzupko.com/new-physician-onboarding-checklist/.
“Without a medical license,” Marks continues, “you can’t get the new physician hospital privileges and you can’t get him or her credentialed with plans. Without being credentialed, the physician can’t bill for patients treated.” Because commercial carriers won’t allow retrospective billing for services already rendered, “even a 3-month delay in credentialing could cost an orthopedic practice $60,000 to $180,000 in lost revenue.”
And if you think you can bill the new physician’s services under another partner’s name, you are incorrect. “The billing physician will have signed the note, but not have treated the patient,” warns Marks. “This is improper billing. Don’t do it.”
The remedy for ensuring that the new physician is credentialed is simple: get organized and plan ahead.
“When I first started participating in recruitment, I remember telling physicians, ‘I need you tomorrow!’” admits Amon T. Ferry, MD, a practicing orthopedist who leads recruitment efforts at IMS Orthopedics, a division of Integrated Medical Specialists in Phoenix, Arizona. “So they’d get hired before the practice was prepared and before credentialing was completed. Now, I set more realistic expectations,” he says, noting that in Arizona it takes 3 months to get a medical license, 6 months to contract with the hospital, and 9 months to get on insurance plans. And even after a plan has credentialed a new physician, “sometimes it still takes 4 to 6 weeks before the physician’s data is loaded into the plan’s computer systems.”
“The way to do credentialing right is to get all departments communicating,” Marks says. “If you keep everyone siloed, staff don’t understand that a lack of timeliness on their part impacts other areas of the practice.”
Ferry agrees, and says his group learned to organize its multiple departments after making mistakes and missing deadlines. “We now have an 8-page pre-employment application for new physicians,” he explains. “In addition to asking for contact information and everything we need to know in order to get the physician credentialed, we ask questions about malpractice suit history and whether there are issues with the medical board. We also ask about gaps in employment and details about where the physician has practiced in the past.” All of this is done to identify early whether credentialing will require more time and effort. Ferry says that the application has solved a number of processing problems the practice had in the past.
And whether credentialing is done within the practice or outsourced, Ferry says that it pays to be persistent. “Don’t sit back and assume it will get done. Even if you have outsourced credentialing to a company, someone must check with payers and hospitals weekly and provide the practice a status update.”
In one case, when getting a new physician contracted at a hospital was taking forever, Ferry directed the staff to call. “Turns out, they had been trying to reach us and had the wrong phone number,” he says. “When people are processing thousands of physician renewals, things get lost. You have to be proactive and be your own advocate. Don’t be afraid to be the squeaky wheel.”
Staff Relationships and Operational Wisdom
Marks points out that in many practices, the new physician is shown the examination rooms and his or her office, gets electronic health record (EHR) training, and that’s it. To be successful, Marks insists that the new physician must build relationships with personnel and understand operational basics. “In other business industries, successful leaders understand at least the basics of what everyone does. Part of how they do this is by getting to know the employees.”
Ideally, Marks advises that new physicians spend time with each staff member. “The best time to do this is in the first few weeks of employment,” he suggests. “Odds are, the new orthopedist doesn’t have 40 patients a day on the schedule. So schedule conversations within the first few weeks or month, and schedule observation time as well. When a patient complains about check-in, the physician will have an understanding of how things work up there if he or she knows the basic processes.” The new doctor should also spend time in the billing office getting to know the challenges faced by staff, and sit with the surgery coordinator to understand the process of getting cases booked and scheduled.
Plan for an initial and then periodic meetings with the practice administrator and other supervisors. Transparency about business operations, data, and strategy will help the new physician get up to speed faster.
“The executive director of our group was an absolutely invaluable information resource,” says Kathryn J. McCarthy, MD, an orthopedic spine surgeon with Arkansas Specialty Orthopaedics in Little Rock, Arkansas. McCarthy has been with the group for 3 years.
The practice’s executive director developed and presented a PowerPoint (Microsoft) explaining general business procedures, expectations for the coding and billing process, and pertinent compliance and risk issues. She had also developed an interactive model of the compensation formula and buy-in program, using Excel (Microsoft). McCarthy met with the executive director at 3 months, 6 months, and 9 months to review her patient and case volumes and how they were trending against the estimates made about her income, bonus, and buy-in status.
From the new physician’s perspective, McCarthy says having the new physician understand the complexities of certain business systems helps them understand things better. “If you sit in the business meetings long enough, you figure it out,” she says, “but it would have made some of the growing pains less painful if I understood what my overhead charge was going to, or more about the workflow of the clinic.” She adds that an overview of hospital relationships and any overlapping ownership interests will benefit new physicians as well.
“I think it’s useful to provide new physicians with a history of the practice and the vision of where things are going,” McCarthy says. “It’s important to outline the business vision, especially for subspecialties. If you explain to the new physician where you want to grow and when the practice plans on bringing on the next physician, it could really drive someone to grow their practice.”
Don’t Underestimate the Need for Coding Training
“When fellows come out of training, they are comfortable with clinical activity but uncomfortable with business administration,” Marks says. “And we know they don’t get training on coding and billing.”
Marks cites a recent conversation at an American Academy of Orthopaedic Surgeons (AAOS) coding workshop. “A surgeon new in practice told me, ‘I’ve been in practice for 4 months. I understand the clinical side but nobody educated me about coding and billing before this course.’” Practices must provide new physicians with coding and documentation training, and coach them to make sure they feel up to speed and comfortable. “The practice’s future revenue depends on it,” Marks says.
McCarthy agrees. “Having an administrative mentorship for coding is incredibly valuable. They don’t teach it in school.”
So from a practical standpoint, purchase AAOS’ Orthopaedic Code-X, a software tool that will help the new physician navigate and integrate Current Procedural Terminology (CPT), ICD-10 (International Classification of Diseases, Tenth Revision), and other coding data easily and accurately. Send him or her to one of the Academy’s regional coding and reimbursement workshops as well. “It will behoove the practice to send them even before they start seeing patients,” Marks says.
And don’t just stop there. High-performing groups conduct peer reviews of evaluation and management (E/M) and operative notes, blinding the codes billed and discussing which CPT and ICD-10 codes are appropriate for the visit or case. “It will take time for the new physician to completely integrate coding with their clinical care,” says Marks. “Peer review sessions, as well as having a partner review codes before they go to the billing office, can help speed learning.”
Collegial Coaching Counts
The week before her official start day, Mc-Carthy scrubbed in as a first assist with each of her new partners. “It was a great way to start ramping up,” she says. “I could see what kind of equipment was present in the hospitals, and got a touch point for hospital logistics. Plus, as a young surgeon it’s great to see how your skill sets match up with your new partners, and which best practices are being deployed by the group.”
This kind of “collegial coaching” is a vital part of the clinical and cultural integration to the practice. Beyond providing clinical support, it builds relationships and trust among the group, and fosters collaboration.
Arkansas Specialty Orthopaedics organized McCarthy’s clinic and operating room (OR) schedules so that a partner was always present. “There was also someone I could bounce ideas off of,” McCarthy explains. “Every day in the OR, there was a partner there at the same time. If I got into a sticky situation, one of my colleagues was willing to come in and scrub in the OR.”
McCarthy says that patients responded favorably when she told them her plan was developed in conjunction with her partners. “Patients find comfort in knowing that several people’s opinions were considered,” she says. “And as a young surgeon, knowing that you have backup, even if you don’t use it, when caring for high-risk and complex cases really means a lot,” she says.
And although her group didn’t offer a formal mentoring program, McCarthy found that an informal mentorship grew organically when a friendship developed with one of her new partners. “In the first 6 months, every single weekend we sat by the pool and rolled through a ton of cases,” she says. “That was fabulous and it alleviated so much stress for me.” And when it was time for McCarthy to move into board case selection, this colleague and another were instrumental in her board preparation because, “they knew my style and where I would need to focus.”
IMS Orthopedics’ approach is to provide the staff and systems that allow new physicians to step up and take responsibility. “If they want to scrub in with me, that’s great. If they’d like to visit additional facilities and get the lay of the land, we encourage it. But we don’t do a lot of handholding. We set them up for success and make sure people are in place to help them,” says Ferry.
A Marketing Plan Is a Must
“The vast majority of practices do very little when it comes to thinking about how to market and build the practice of their new physician,” Marks says. “Practice-building is more of a challenge for surgical specialists today than it was in the old days when new surgeons could easily meet internists as they were rounding at the hospital. Now, a new physician and the practice must come up with a game plan.”
That game plan starts with the easy things: order business cards, schedule a photo shoot, and update the practice’s Web site pages with the physician’s biography and an introductory video. But with social media, online reviews, and subspecialty competition, Marks says practices must think beyond the basics. Think through each element of marketing, from online to outreach to developing referral relationships.
“I tell practices to draft a written marketing plan,” he says. “Not only does it provide a roadmap for the new physician, but also indicates that the practice has put some thought into how he or she can build a practice. It can make the new physician feel less overwhelmed knowing that he or she doesn’t have to do the marketing alone.” Once you’ve developed a list of actions, Marks suggests creating a spreadsheet with deadlines, and ensuring each action is completed.
McCarthy was scheduled to visit family practice clinics, and joined by the administrator who “handed out cookies and cards while I talked,” she says. Arkansas Specialty Orthopaedics also hired an external marketing firm to develop promotional opportunities for her. For example, “I was scheduled to appear on news channels, where I discussed new and interesting procedures,” she says. “It got my name out into the community.”
If your practice is too small to hire an outside firm, Marks suggests reaching out to agencies such as nursing homes, fitness centers, or the YMCA, which frequently offers educational programs for members. “Contact the administrators or medical directors in these organizations. A few minutes on the phone or a short visit can go a long way to building these relationships and getting your new physician on the map.”
As the old saying goes, an ounce of prevention is worth a pound of cure. Scheduling time for orientation, training, staff integration, and collegial coaching will speed up a new physician’s integration into the practice, and increase his or her opportunity for success.
Public speaking fundamentals. The program: Key elements in capturing and holding audience attention
In the first part of this article series (“Preparation: Tips that lead to a solid, engaging presentation,” OBG Manag. 2016;28[7]:31–36.), we offered tips on preparing for a group presentation. In this article, part 2, we discuss the presentation itself and what you can do to capture and hold your audience’s attention.
How to connect with the audience
Let’s assume the meeting host has just introduced you to the audience using, as we suggested in the previous article, an autobiographical profile you provided. You now have the audience’s undivided attention. What you do and say in the next 30 to 60 seconds will set the stage for your program. Following the requisite “thank you” to the host and meeting sponsor, use this time to establish your expertise as a spokesperson on the chosen topic. Or, if the introductory remarks made your expertise plain, you may choose to connect with the audience on an informal, personal level. If you are from out of town, for instance, you could remark on an interesting aspect of the city or region you are visiting that you learned on the Internet before arriving.
Underscore the topic’s importance. On the other hand, you might want to begin with an insightful statistic germane to your talk. For example, a talk on breast cancer might begin with, “According to the American Cancer Society, there are nearly 250,000 new cases of breast cancer each year, and breast cancer accounts for more than 40,000 deaths per year. That means more women die from breast cancer than die in auto accidents each year. So this emphasizes the importance of appropriately screening women for breast cancer annually after age 40.”
An opening story about a patient can be powerful. Better yet, a personal experience reflecting your topic is a great way to connect with your audience members and get their attention. For example, one of us (NHB) gives talks on practice management and practice efficiency. I might talk about when I was called from an exam room 3 times to answer “emergency” phone calls from a patient who wanted only to request her medical records. To ensure that this embarrassment would never happen again, I put in place a system that I then describe for the audience.
Alternatively, an opening that addresses the audience’s unspoken question, “What’s in this for me?” is sure to grab their attention. For instance, a talk on office productivity might begin by promising to share a way to increase annual collections by $250,000 per physician through scheduling adjustments that can increase the number of examined patients by one per hour.
Steer clear of these openings. In general, avoid “I’m delighted to be here” and other clichés. One exception would be if you can make that cliché humorous. For example, if a speaker from the deep South is visiting the northern part of the country in summer, she might say, “Most speakers say they’re delighted to be here, and you may well question their sincerity. However, I’m from New Orleans where the temperature is approaching 105 degrees with 95% humidity. You know I’m really delighted to be here!”
Importantly, avoid starting with an apology. Do not mention problems with the audiovisual equipment or why you arrived late. The audience does not care, and you will immediately lose their attention. They want to be educated and entertained. There is no better way to do this than by offering a compelling and captivating opening that begins the moment after you are introduced.
Finally, avoid use of the “royal I,” as in “I am here to talk about XYZ.” It places you in a position superior to the audience, and that is a turnoff. Instead, you could say to the audience, “The reason you are here is to learn about XYZ.” This places the audience on an equal level with you, and they know there will be something in the presentation for them.
Housekeeping notes
The audience will appreciate knowing how long you plan to speak and whether you will take questions during or after the presentation. Based on our experience, if there are fewer than 20 attendees, we often encourage questions during the program instead of waiting until the end. This makes the program more conversational and usually generates more questions. With a dinner presentation, we prefer to speak while the audience is eating. We usually start after the waiters have taken the orders and the attendees have had their appetizers. We might say we will finish the program by the time they are ready for dessert. We also mention that we will distribute a handout after the presentation so they do not have to worry about following the handout, taking notes, and watching the speaker while trying to eat.
The main body of the program
As for structuring your talk, we suggest you follow this time-honored advice often attributed to Aristotle: Tell the audience what you are going to say, say it, and tell them what you said.
So we begin a presentation by stating the objectives of our program, usually limited to 3 and no more than 4. For example, a talk on hormone therapy (HT) for treating vasomotor symptoms of menopause might mention 1) the history of HT use, 2) which women are appropriate candidates for HT, and 3) how to monitor women who receive HT.
Enhance the talk’s relevance. We like to begin a clinical program with a case scenario wherein we describe how one of our patients had the specific problem and how we used a particular drug, treatment, or device to manage the case. We try to select a patient similar to ones who would be seen by members of the audience.
Simplify as much as possible. We then present the slides exactly as they have been provided by the pharmaceutical company. Most company slides contain too many words as well as diagrams that are too complex for the audience to grasp easily. We try to find one salient point on each slide and focus attention on that single word, phrase, or sentence. We can do this in a small audience by walking over to the screen and pointing it out, or we can use the laser pointer from a distance.
Change things up to keep the message fresh. Let’s be honest, most medical talks are dry and boring. Try to inject some energy and enthusiasm in the middle of the presentation. Every few minutes we tell a story or ask the audience a question. For example, during a program on practice management, one of us (NHB) will relate a story about an unhappy patient and then ask a physician in the audience how he or she might handle the disgruntled patient. This is a nice break from the main content of the presentation, re-engaging the audience in an interactive exchange.
Should you use humor?
Although many physicians attempt to use humor during a presentation, few are talented at stand-up comedy. However, used judiciously humor, like seasoning in fine cuisine, can do great things for a presentation. It can break the ice, drive home a point, and enhance your likeability. It can, though, also backfire. One of us (NHB) once gave a talk to a large audience of pharmaceutical representatives. As part of my wrap-up I displayed a slide from the cover of Economics that showed 2 camels in the mating position. My closing line was that reps need to “hump to it” and get involved with their physicians and be value-added in their product detailing. Afterward, the meeting planner told me that he would never hire me again. He said I had a great program, great material, and a good connection with the audience. But my closing was over the top. I learned my lesson. Never use material that has the potential to offend. If you want to use humor, the self-deprecatingkind is always safest.
Try using visual aids
Our observation is that few physician speakers use visual aids other than their slides. We have learned that audience attention will stay focused on you if you make use of visual aids. For example, if we are speaking to a lay audience about urinary incontinence, we might use a balloon to demonstrate the bladder and the urethra.
Studies have shown that there are more nerve endings from the eye to the brain than from the ear to the brain. Humans purportedly receive 25 times as much stimulus from visual cues than from auditory ones. To paraphrase an old proverb, “One seeing is better than 100 times hearing about”!
A few suggestions regarding the use of visual aids:
- Keep the visual aid out of sight until you are ready to use it. You do not want the audience staring at it when they should be focusing on you or your slide material. We usually keep our visual aids under the table that supports the computer and projector.
- Make certain the visual aid is large enough to be seen by everyone in the audience.
- Do not hand out the aid to the audience during your program. Doing so will divert their attention from you and your material.
- When you have finished using the aid, put it away.
Closing out the program
After we have covered the program’s 3 objectives, we let the audience know we are approaching the end of the presentation. For a dinner program, we try to time the ending just as plates are being cleared and before dessert is served. We then restate the 3 objectives as they might pertain to the attendees’ patients and practices. At this time, we take questions from the audience, even if some were asked during the presentation. We repeat each question when it is asked so that everyone can hear it. (This also gives us a few seconds to think about it and frame our answer.) If it appears that many questions will be asked, we assure everyone that we plan to finish on time and will remain after the program is over to answer additional questions.
Tips on fielding questions. When responding to a question, direct your attention initially to the person who asked it. After that, spend about 20% of the time focused on that person and 80% of the time on the rest of the audience. If you focus only on the questioner, it becomes a one-on-one conversation. You want to end your response with your eyes on the group and not on the questioner. Looking at the group will also act as a bridge to the next question. Although we used to reply to an inquiry with, “That’s a great question,” we now suggest avoiding this comment. Why? Because it is unlikely that you’ll keep using that line, and the next questioner who does not receive the same compliment might feel slighted.
Wrap up. When you announce, “I would like to conclude my program with…,” this is the magical time when you hold the complete attention of the audience. Often, the speaker’s last words are the ones the audience remembers the longest. So this is the time to offer your take-home message. For example, a talk on how to motivate your staff might conclude, “Remember, your staff members are the people that patients encounter first and the ones they see last as they leave the office. Every patient can have a positive experience with you and your practice if you ensure that your personnel are highly motivated. This happens in part by your effort to recognize their accomplishments.” Then hold up your hands and spread out your arms as you end with “Thank you.” The audience likely will applaud and, if your speech is truly exceptional, you might receive a gratifying standing ovation!
Be seated
Renowned for his speeches, Franklin Delano Roosevelt summarized the art of effective speaking when he said, “Be sincere. Be brief. Be seated.” When your time is up, turn the program back over to the meeting host and take a seat.
In the final article in this public speaking series, we will discuss the follow-up steps to take once the program is over, including the call to action or what you want the audience to do after you have left the podium or the speaking venue.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In the first part of this article series (“Preparation: Tips that lead to a solid, engaging presentation,” OBG Manag. 2016;28[7]:31–36.), we offered tips on preparing for a group presentation. In this article, part 2, we discuss the presentation itself and what you can do to capture and hold your audience’s attention.
How to connect with the audience
Let’s assume the meeting host has just introduced you to the audience using, as we suggested in the previous article, an autobiographical profile you provided. You now have the audience’s undivided attention. What you do and say in the next 30 to 60 seconds will set the stage for your program. Following the requisite “thank you” to the host and meeting sponsor, use this time to establish your expertise as a spokesperson on the chosen topic. Or, if the introductory remarks made your expertise plain, you may choose to connect with the audience on an informal, personal level. If you are from out of town, for instance, you could remark on an interesting aspect of the city or region you are visiting that you learned on the Internet before arriving.
Underscore the topic’s importance. On the other hand, you might want to begin with an insightful statistic germane to your talk. For example, a talk on breast cancer might begin with, “According to the American Cancer Society, there are nearly 250,000 new cases of breast cancer each year, and breast cancer accounts for more than 40,000 deaths per year. That means more women die from breast cancer than die in auto accidents each year. So this emphasizes the importance of appropriately screening women for breast cancer annually after age 40.”
An opening story about a patient can be powerful. Better yet, a personal experience reflecting your topic is a great way to connect with your audience members and get their attention. For example, one of us (NHB) gives talks on practice management and practice efficiency. I might talk about when I was called from an exam room 3 times to answer “emergency” phone calls from a patient who wanted only to request her medical records. To ensure that this embarrassment would never happen again, I put in place a system that I then describe for the audience.
Alternatively, an opening that addresses the audience’s unspoken question, “What’s in this for me?” is sure to grab their attention. For instance, a talk on office productivity might begin by promising to share a way to increase annual collections by $250,000 per physician through scheduling adjustments that can increase the number of examined patients by one per hour.
Steer clear of these openings. In general, avoid “I’m delighted to be here” and other clichés. One exception would be if you can make that cliché humorous. For example, if a speaker from the deep South is visiting the northern part of the country in summer, she might say, “Most speakers say they’re delighted to be here, and you may well question their sincerity. However, I’m from New Orleans where the temperature is approaching 105 degrees with 95% humidity. You know I’m really delighted to be here!”
Importantly, avoid starting with an apology. Do not mention problems with the audiovisual equipment or why you arrived late. The audience does not care, and you will immediately lose their attention. They want to be educated and entertained. There is no better way to do this than by offering a compelling and captivating opening that begins the moment after you are introduced.
Finally, avoid use of the “royal I,” as in “I am here to talk about XYZ.” It places you in a position superior to the audience, and that is a turnoff. Instead, you could say to the audience, “The reason you are here is to learn about XYZ.” This places the audience on an equal level with you, and they know there will be something in the presentation for them.
Housekeeping notes
The audience will appreciate knowing how long you plan to speak and whether you will take questions during or after the presentation. Based on our experience, if there are fewer than 20 attendees, we often encourage questions during the program instead of waiting until the end. This makes the program more conversational and usually generates more questions. With a dinner presentation, we prefer to speak while the audience is eating. We usually start after the waiters have taken the orders and the attendees have had their appetizers. We might say we will finish the program by the time they are ready for dessert. We also mention that we will distribute a handout after the presentation so they do not have to worry about following the handout, taking notes, and watching the speaker while trying to eat.
The main body of the program
As for structuring your talk, we suggest you follow this time-honored advice often attributed to Aristotle: Tell the audience what you are going to say, say it, and tell them what you said.
So we begin a presentation by stating the objectives of our program, usually limited to 3 and no more than 4. For example, a talk on hormone therapy (HT) for treating vasomotor symptoms of menopause might mention 1) the history of HT use, 2) which women are appropriate candidates for HT, and 3) how to monitor women who receive HT.
Enhance the talk’s relevance. We like to begin a clinical program with a case scenario wherein we describe how one of our patients had the specific problem and how we used a particular drug, treatment, or device to manage the case. We try to select a patient similar to ones who would be seen by members of the audience.
Simplify as much as possible. We then present the slides exactly as they have been provided by the pharmaceutical company. Most company slides contain too many words as well as diagrams that are too complex for the audience to grasp easily. We try to find one salient point on each slide and focus attention on that single word, phrase, or sentence. We can do this in a small audience by walking over to the screen and pointing it out, or we can use the laser pointer from a distance.
Change things up to keep the message fresh. Let’s be honest, most medical talks are dry and boring. Try to inject some energy and enthusiasm in the middle of the presentation. Every few minutes we tell a story or ask the audience a question. For example, during a program on practice management, one of us (NHB) will relate a story about an unhappy patient and then ask a physician in the audience how he or she might handle the disgruntled patient. This is a nice break from the main content of the presentation, re-engaging the audience in an interactive exchange.
Should you use humor?
Although many physicians attempt to use humor during a presentation, few are talented at stand-up comedy. However, used judiciously humor, like seasoning in fine cuisine, can do great things for a presentation. It can break the ice, drive home a point, and enhance your likeability. It can, though, also backfire. One of us (NHB) once gave a talk to a large audience of pharmaceutical representatives. As part of my wrap-up I displayed a slide from the cover of Economics that showed 2 camels in the mating position. My closing line was that reps need to “hump to it” and get involved with their physicians and be value-added in their product detailing. Afterward, the meeting planner told me that he would never hire me again. He said I had a great program, great material, and a good connection with the audience. But my closing was over the top. I learned my lesson. Never use material that has the potential to offend. If you want to use humor, the self-deprecatingkind is always safest.
Try using visual aids
Our observation is that few physician speakers use visual aids other than their slides. We have learned that audience attention will stay focused on you if you make use of visual aids. For example, if we are speaking to a lay audience about urinary incontinence, we might use a balloon to demonstrate the bladder and the urethra.
Studies have shown that there are more nerve endings from the eye to the brain than from the ear to the brain. Humans purportedly receive 25 times as much stimulus from visual cues than from auditory ones. To paraphrase an old proverb, “One seeing is better than 100 times hearing about”!
A few suggestions regarding the use of visual aids:
- Keep the visual aid out of sight until you are ready to use it. You do not want the audience staring at it when they should be focusing on you or your slide material. We usually keep our visual aids under the table that supports the computer and projector.
- Make certain the visual aid is large enough to be seen by everyone in the audience.
- Do not hand out the aid to the audience during your program. Doing so will divert their attention from you and your material.
- When you have finished using the aid, put it away.
Closing out the program
After we have covered the program’s 3 objectives, we let the audience know we are approaching the end of the presentation. For a dinner program, we try to time the ending just as plates are being cleared and before dessert is served. We then restate the 3 objectives as they might pertain to the attendees’ patients and practices. At this time, we take questions from the audience, even if some were asked during the presentation. We repeat each question when it is asked so that everyone can hear it. (This also gives us a few seconds to think about it and frame our answer.) If it appears that many questions will be asked, we assure everyone that we plan to finish on time and will remain after the program is over to answer additional questions.
Tips on fielding questions. When responding to a question, direct your attention initially to the person who asked it. After that, spend about 20% of the time focused on that person and 80% of the time on the rest of the audience. If you focus only on the questioner, it becomes a one-on-one conversation. You want to end your response with your eyes on the group and not on the questioner. Looking at the group will also act as a bridge to the next question. Although we used to reply to an inquiry with, “That’s a great question,” we now suggest avoiding this comment. Why? Because it is unlikely that you’ll keep using that line, and the next questioner who does not receive the same compliment might feel slighted.
Wrap up. When you announce, “I would like to conclude my program with…,” this is the magical time when you hold the complete attention of the audience. Often, the speaker’s last words are the ones the audience remembers the longest. So this is the time to offer your take-home message. For example, a talk on how to motivate your staff might conclude, “Remember, your staff members are the people that patients encounter first and the ones they see last as they leave the office. Every patient can have a positive experience with you and your practice if you ensure that your personnel are highly motivated. This happens in part by your effort to recognize their accomplishments.” Then hold up your hands and spread out your arms as you end with “Thank you.” The audience likely will applaud and, if your speech is truly exceptional, you might receive a gratifying standing ovation!
Be seated
Renowned for his speeches, Franklin Delano Roosevelt summarized the art of effective speaking when he said, “Be sincere. Be brief. Be seated.” When your time is up, turn the program back over to the meeting host and take a seat.
In the final article in this public speaking series, we will discuss the follow-up steps to take once the program is over, including the call to action or what you want the audience to do after you have left the podium or the speaking venue.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In the first part of this article series (“Preparation: Tips that lead to a solid, engaging presentation,” OBG Manag. 2016;28[7]:31–36.), we offered tips on preparing for a group presentation. In this article, part 2, we discuss the presentation itself and what you can do to capture and hold your audience’s attention.
How to connect with the audience
Let’s assume the meeting host has just introduced you to the audience using, as we suggested in the previous article, an autobiographical profile you provided. You now have the audience’s undivided attention. What you do and say in the next 30 to 60 seconds will set the stage for your program. Following the requisite “thank you” to the host and meeting sponsor, use this time to establish your expertise as a spokesperson on the chosen topic. Or, if the introductory remarks made your expertise plain, you may choose to connect with the audience on an informal, personal level. If you are from out of town, for instance, you could remark on an interesting aspect of the city or region you are visiting that you learned on the Internet before arriving.
Underscore the topic’s importance. On the other hand, you might want to begin with an insightful statistic germane to your talk. For example, a talk on breast cancer might begin with, “According to the American Cancer Society, there are nearly 250,000 new cases of breast cancer each year, and breast cancer accounts for more than 40,000 deaths per year. That means more women die from breast cancer than die in auto accidents each year. So this emphasizes the importance of appropriately screening women for breast cancer annually after age 40.”
An opening story about a patient can be powerful. Better yet, a personal experience reflecting your topic is a great way to connect with your audience members and get their attention. For example, one of us (NHB) gives talks on practice management and practice efficiency. I might talk about when I was called from an exam room 3 times to answer “emergency” phone calls from a patient who wanted only to request her medical records. To ensure that this embarrassment would never happen again, I put in place a system that I then describe for the audience.
Alternatively, an opening that addresses the audience’s unspoken question, “What’s in this for me?” is sure to grab their attention. For instance, a talk on office productivity might begin by promising to share a way to increase annual collections by $250,000 per physician through scheduling adjustments that can increase the number of examined patients by one per hour.
Steer clear of these openings. In general, avoid “I’m delighted to be here” and other clichés. One exception would be if you can make that cliché humorous. For example, if a speaker from the deep South is visiting the northern part of the country in summer, she might say, “Most speakers say they’re delighted to be here, and you may well question their sincerity. However, I’m from New Orleans where the temperature is approaching 105 degrees with 95% humidity. You know I’m really delighted to be here!”
Importantly, avoid starting with an apology. Do not mention problems with the audiovisual equipment or why you arrived late. The audience does not care, and you will immediately lose their attention. They want to be educated and entertained. There is no better way to do this than by offering a compelling and captivating opening that begins the moment after you are introduced.
Finally, avoid use of the “royal I,” as in “I am here to talk about XYZ.” It places you in a position superior to the audience, and that is a turnoff. Instead, you could say to the audience, “The reason you are here is to learn about XYZ.” This places the audience on an equal level with you, and they know there will be something in the presentation for them.
Housekeeping notes
The audience will appreciate knowing how long you plan to speak and whether you will take questions during or after the presentation. Based on our experience, if there are fewer than 20 attendees, we often encourage questions during the program instead of waiting until the end. This makes the program more conversational and usually generates more questions. With a dinner presentation, we prefer to speak while the audience is eating. We usually start after the waiters have taken the orders and the attendees have had their appetizers. We might say we will finish the program by the time they are ready for dessert. We also mention that we will distribute a handout after the presentation so they do not have to worry about following the handout, taking notes, and watching the speaker while trying to eat.
The main body of the program
As for structuring your talk, we suggest you follow this time-honored advice often attributed to Aristotle: Tell the audience what you are going to say, say it, and tell them what you said.
So we begin a presentation by stating the objectives of our program, usually limited to 3 and no more than 4. For example, a talk on hormone therapy (HT) for treating vasomotor symptoms of menopause might mention 1) the history of HT use, 2) which women are appropriate candidates for HT, and 3) how to monitor women who receive HT.
Enhance the talk’s relevance. We like to begin a clinical program with a case scenario wherein we describe how one of our patients had the specific problem and how we used a particular drug, treatment, or device to manage the case. We try to select a patient similar to ones who would be seen by members of the audience.
Simplify as much as possible. We then present the slides exactly as they have been provided by the pharmaceutical company. Most company slides contain too many words as well as diagrams that are too complex for the audience to grasp easily. We try to find one salient point on each slide and focus attention on that single word, phrase, or sentence. We can do this in a small audience by walking over to the screen and pointing it out, or we can use the laser pointer from a distance.
Change things up to keep the message fresh. Let’s be honest, most medical talks are dry and boring. Try to inject some energy and enthusiasm in the middle of the presentation. Every few minutes we tell a story or ask the audience a question. For example, during a program on practice management, one of us (NHB) will relate a story about an unhappy patient and then ask a physician in the audience how he or she might handle the disgruntled patient. This is a nice break from the main content of the presentation, re-engaging the audience in an interactive exchange.
Should you use humor?
Although many physicians attempt to use humor during a presentation, few are talented at stand-up comedy. However, used judiciously humor, like seasoning in fine cuisine, can do great things for a presentation. It can break the ice, drive home a point, and enhance your likeability. It can, though, also backfire. One of us (NHB) once gave a talk to a large audience of pharmaceutical representatives. As part of my wrap-up I displayed a slide from the cover of Economics that showed 2 camels in the mating position. My closing line was that reps need to “hump to it” and get involved with their physicians and be value-added in their product detailing. Afterward, the meeting planner told me that he would never hire me again. He said I had a great program, great material, and a good connection with the audience. But my closing was over the top. I learned my lesson. Never use material that has the potential to offend. If you want to use humor, the self-deprecatingkind is always safest.
Try using visual aids
Our observation is that few physician speakers use visual aids other than their slides. We have learned that audience attention will stay focused on you if you make use of visual aids. For example, if we are speaking to a lay audience about urinary incontinence, we might use a balloon to demonstrate the bladder and the urethra.
Studies have shown that there are more nerve endings from the eye to the brain than from the ear to the brain. Humans purportedly receive 25 times as much stimulus from visual cues than from auditory ones. To paraphrase an old proverb, “One seeing is better than 100 times hearing about”!
A few suggestions regarding the use of visual aids:
- Keep the visual aid out of sight until you are ready to use it. You do not want the audience staring at it when they should be focusing on you or your slide material. We usually keep our visual aids under the table that supports the computer and projector.
- Make certain the visual aid is large enough to be seen by everyone in the audience.
- Do not hand out the aid to the audience during your program. Doing so will divert their attention from you and your material.
- When you have finished using the aid, put it away.
Closing out the program
After we have covered the program’s 3 objectives, we let the audience know we are approaching the end of the presentation. For a dinner program, we try to time the ending just as plates are being cleared and before dessert is served. We then restate the 3 objectives as they might pertain to the attendees’ patients and practices. At this time, we take questions from the audience, even if some were asked during the presentation. We repeat each question when it is asked so that everyone can hear it. (This also gives us a few seconds to think about it and frame our answer.) If it appears that many questions will be asked, we assure everyone that we plan to finish on time and will remain after the program is over to answer additional questions.
Tips on fielding questions. When responding to a question, direct your attention initially to the person who asked it. After that, spend about 20% of the time focused on that person and 80% of the time on the rest of the audience. If you focus only on the questioner, it becomes a one-on-one conversation. You want to end your response with your eyes on the group and not on the questioner. Looking at the group will also act as a bridge to the next question. Although we used to reply to an inquiry with, “That’s a great question,” we now suggest avoiding this comment. Why? Because it is unlikely that you’ll keep using that line, and the next questioner who does not receive the same compliment might feel slighted.
Wrap up. When you announce, “I would like to conclude my program with…,” this is the magical time when you hold the complete attention of the audience. Often, the speaker’s last words are the ones the audience remembers the longest. So this is the time to offer your take-home message. For example, a talk on how to motivate your staff might conclude, “Remember, your staff members are the people that patients encounter first and the ones they see last as they leave the office. Every patient can have a positive experience with you and your practice if you ensure that your personnel are highly motivated. This happens in part by your effort to recognize their accomplishments.” Then hold up your hands and spread out your arms as you end with “Thank you.” The audience likely will applaud and, if your speech is truly exceptional, you might receive a gratifying standing ovation!
Be seated
Renowned for his speeches, Franklin Delano Roosevelt summarized the art of effective speaking when he said, “Be sincere. Be brief. Be seated.” When your time is up, turn the program back over to the meeting host and take a seat.
In the final article in this public speaking series, we will discuss the follow-up steps to take once the program is over, including the call to action or what you want the audience to do after you have left the podium or the speaking venue.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Don’t sell your practice short
I’ve written quite a lot over the past few years about the trend toward soloists and small groups selling their practices to hospitals, multispecialty groups, or larger practices. And I’ve made it fairly clear that I don’t think it’s a particularly good thing that the medical profession is going the way of the corner gas station and the mom-and-pop grocery store; it’s not good for physicians, patients, or private practice.
That said, if retirement looms with no individual buyers in sight, or your overhead is getting out of hand, selling to a larger entity is an option that you may need to consider. Too often, though, sellers are not receiving a fair return on the equity they have worked so hard to build over several decades, either because they have waited too long and must accept what is offered, or because they simply take the buyer’s word for their practice’s value. Don’t put yourself in either of those positions; and don’t entertain any offers until you obtain an objective appraisal from a neutral party.
Of course, a medical practice is trickier to value than is an ordinary business and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in 850 words; but three basic yardsticks are essential for determining the equity, or book value, of a practice:
• Tangible Assets: equipment, cash, accounts receivable, and other property owned by the practice.
• Liabilities: accounts payable, outstanding loans, and anything else owed to others.
• Intangible Assets: sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal, you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons why patients come back (if in fact they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place, and how well they pay, etc.), the extent and strength of the referral base, and the presence of supplemental income streams, such as clinical research.
It is also important to determine to what extent intangible assets are transferable. For example, unique skills with a laser, neurotoxins, or filler substances, or extraordinary personal charisma, may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again, there are many ways to estimate intangible asset value, and once again, you should ask which were used. Cash Flow Analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of Earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline Comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques that some consider a better estimate of intangible assets are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings (and thus its overall value) are.
Asset-based valuation is the most popular – but by no means the only – method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not its income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced and independent financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
I’ve written quite a lot over the past few years about the trend toward soloists and small groups selling their practices to hospitals, multispecialty groups, or larger practices. And I’ve made it fairly clear that I don’t think it’s a particularly good thing that the medical profession is going the way of the corner gas station and the mom-and-pop grocery store; it’s not good for physicians, patients, or private practice.
That said, if retirement looms with no individual buyers in sight, or your overhead is getting out of hand, selling to a larger entity is an option that you may need to consider. Too often, though, sellers are not receiving a fair return on the equity they have worked so hard to build over several decades, either because they have waited too long and must accept what is offered, or because they simply take the buyer’s word for their practice’s value. Don’t put yourself in either of those positions; and don’t entertain any offers until you obtain an objective appraisal from a neutral party.
Of course, a medical practice is trickier to value than is an ordinary business and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in 850 words; but three basic yardsticks are essential for determining the equity, or book value, of a practice:
• Tangible Assets: equipment, cash, accounts receivable, and other property owned by the practice.
• Liabilities: accounts payable, outstanding loans, and anything else owed to others.
• Intangible Assets: sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal, you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons why patients come back (if in fact they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place, and how well they pay, etc.), the extent and strength of the referral base, and the presence of supplemental income streams, such as clinical research.
It is also important to determine to what extent intangible assets are transferable. For example, unique skills with a laser, neurotoxins, or filler substances, or extraordinary personal charisma, may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again, there are many ways to estimate intangible asset value, and once again, you should ask which were used. Cash Flow Analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of Earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline Comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques that some consider a better estimate of intangible assets are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings (and thus its overall value) are.
Asset-based valuation is the most popular – but by no means the only – method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not its income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced and independent financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
I’ve written quite a lot over the past few years about the trend toward soloists and small groups selling their practices to hospitals, multispecialty groups, or larger practices. And I’ve made it fairly clear that I don’t think it’s a particularly good thing that the medical profession is going the way of the corner gas station and the mom-and-pop grocery store; it’s not good for physicians, patients, or private practice.
That said, if retirement looms with no individual buyers in sight, or your overhead is getting out of hand, selling to a larger entity is an option that you may need to consider. Too often, though, sellers are not receiving a fair return on the equity they have worked so hard to build over several decades, either because they have waited too long and must accept what is offered, or because they simply take the buyer’s word for their practice’s value. Don’t put yourself in either of those positions; and don’t entertain any offers until you obtain an objective appraisal from a neutral party.
Of course, a medical practice is trickier to value than is an ordinary business and usually requires the services of an experienced professional appraiser. Entire books have been written about the process, so I can’t hope to cover it completely in 850 words; but three basic yardsticks are essential for determining the equity, or book value, of a practice:
• Tangible Assets: equipment, cash, accounts receivable, and other property owned by the practice.
• Liabilities: accounts payable, outstanding loans, and anything else owed to others.
• Intangible Assets: sometimes called “good will” – the reputation of the physicians, the location and name recognition of the practice, the loyalty and volume of patients, and other, well, intangibles.
Valuing tangible assets is comparatively straightforward, but there are several ways to do it, and when reviewing a practice appraisal, you should ask which of them was used. Depreciated value is the book value of equipment and supplies as determined by their purchase price, less the amount their value has decreased since purchase. Remaining useful life value estimates how long the equipment can be expected to last. Market (or replacement) value is the amount it would cost on the open market to replace all equipment and supplies.
Intangible assets are more difficult to value. Many components are analyzed, including location, interior and exterior decor, accessibility to patients, age and functional status of equipment, systems in place to promote efficiency, reasons why patients come back (if in fact they do), and the overall reputation of the practice in the community. Other important factors include the “payer mix” (what percentage pays cash, how many third-party contracts are in place, and how well they pay, etc.), the extent and strength of the referral base, and the presence of supplemental income streams, such as clinical research.
It is also important to determine to what extent intangible assets are transferable. For example, unique skills with a laser, neurotoxins, or filler substances, or extraordinary personal charisma, may increase your practice’s value to you, but they are worthless to the next owner, and he or she will be unwilling to pay for them unless your services become part of the deal.
Once again, there are many ways to estimate intangible asset value, and once again, you should ask which were used. Cash Flow Analysis works on the assumption that cash flow is a measure of intangible value. Capitalization of Earnings puts a value, or capitalization, on the practice’s income streams using a variety of assumptions. Guideline Comparison uses various databases to compare your practice with other, similar ones that have changed hands in the past.
Two newer techniques that some consider a better estimate of intangible assets are the replacement method, which estimates the costs of starting the practice over again in the current market; and the excess earnings method, which measures how far above average your practice’s earnings (and thus its overall value) are.
Asset-based valuation is the most popular – but by no means the only – method available. Income-based valuation looks at the source and strength of a practice’s income stream as a creator of value, as well as whether or not its income stream under a different owner would mirror its present one. This in turn becomes the basis for an understanding of the fair market value of both tangible and intangible assets. Market valuation combines the asset-based and income-based approaches, along with an analysis of sales and mergers of comparable practices in the community, to determine the value of a practice in its local market.
Whatever methods are used, it is important that the appraisal be done by an experienced and independent financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation is supplied to support the conclusions reached. This is especially important if the appraisal will be relied upon in the sale or merger of the practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].