User login
Heart failure med undertreatment because of older age common, flouts evidence
, suggests a large cohort study.
About 80% of patients aged 80 years or older were prescribed renin-angiotensin-system inhibitors (RASi) in a multivariate-adjusted analysis of more than 27,000 patients in the Swedish Heart Failure Registry (SwedeHF). In contrast, such drugs – which included angiotensin receptor-neprilysin inhibitors (ARNi), angiotensin receptor blockers, and ACE inhibitors – were prescribed to 95% of patients younger than 70 years.
Similarly, fewer of the oldest patients were offered meds from the two other drug classes core to HF management at the time: Beta blockers and mineralocorticoid receptor antagonists (MRA).
And among those in the 80-and-older age group who were prescribed RASi or beta blockers, their uptitration more often fell short of even half the target dosage, compared with the youngest patients in the analysis.
Physicians may hold back on full guideline-directed medical therapy in their very elderly patients with HFrEF for many reasons, including a perceived likelihood of drug intolerance due to frailty or multiple comorbidities, including renal dysfunction, Davide Stolfo, MD, Karolinska Institutet, Stockholm, and University of Trieste, Italy, told this news organization.
But the current analysis was adjusted for about 80 variables “that in our interpretation may be main reasons for not introducing drugs and using them in the older patients,” he said. They included care setting (that is, inpatient or outpatient), HF severity by several measures, a range of comorbidities, renal dysfunction, and history of serious illness such as cancer.
Even then, age emerged as a significant, independent predictor of medical therapy underuse in the oldest patients. Some physicians apparently see advanced age, by itself, as an “intrinsic reason” not to abide by HFrEF medical therapy recommendations, said Dr. Stolfo, who presented the analysis at HFA 2021, the annual meeting of the Heart Failure Association of the European Society of Cardiology (ESC-HFA), conducted both virtually and live in Florence, Italy.
Most major HF-drug trials have excluded or admitted few patients aged 80 years or older, but “the guidelines recommend treatment regardless of age, and in the trials there has been no influence from age on the effectiveness of drugs,” Dr. Stolfo observed.
Moreover, in a prior SwedeHF analysis with propensity matching, patients with HFrEF aged 80 or older showed steeper reductions in risk for death or HF hospitalization from treatment with RASi than those in younger age groups.
One of the few randomized trials to focus on the very elderly, called SENIORS, enrolled patients aged 70 years and older – the average age was 76 – and saw a significantly reduced risk of death or cardiovascular hospitalization for those assigned to the beta blocker nebivolol. The benefits in the trial, which was conducted 15 years ago, were independent of left ventricular function.
So in the oldest patients, “we could question the need to achieve full dose of an evidence-based drug, but we shouldn’t question the use of these drugs.”
The findings are consistent with a need to individualize medical therapy in senior patients with HFrEF, especially those of more advanced age, some of whom may be robust enough to be managed similarly to younger patients while others who may be less suitable for full guideline-directed medical therapy, Dr. Stolfo said.
Even for those who are more frail or have major comorbidities, drug therapy of HFrEF continues to be important for symptom control even if competing causes of death make it harder to prolong survival, Dr. Stolfo said.
“We should provide to all patients the best strategy they can tolerate,” he said. “If we cannot greatly impact on the long-term survival for these patients, treatment can be aimed to improve the quality of life and keep the patient out of the hospital.”
The analysis was supported by Boehringer Ingelheim. Dr. Stolfo disclosed personal fees from Novartis, Merck, GlaxoSmithKline, and Acceleron.
A version of this article first appeared on Medscape.com.
, suggests a large cohort study.
About 80% of patients aged 80 years or older were prescribed renin-angiotensin-system inhibitors (RASi) in a multivariate-adjusted analysis of more than 27,000 patients in the Swedish Heart Failure Registry (SwedeHF). In contrast, such drugs – which included angiotensin receptor-neprilysin inhibitors (ARNi), angiotensin receptor blockers, and ACE inhibitors – were prescribed to 95% of patients younger than 70 years.
Similarly, fewer of the oldest patients were offered meds from the two other drug classes core to HF management at the time: Beta blockers and mineralocorticoid receptor antagonists (MRA).
And among those in the 80-and-older age group who were prescribed RASi or beta blockers, their uptitration more often fell short of even half the target dosage, compared with the youngest patients in the analysis.
Physicians may hold back on full guideline-directed medical therapy in their very elderly patients with HFrEF for many reasons, including a perceived likelihood of drug intolerance due to frailty or multiple comorbidities, including renal dysfunction, Davide Stolfo, MD, Karolinska Institutet, Stockholm, and University of Trieste, Italy, told this news organization.
But the current analysis was adjusted for about 80 variables “that in our interpretation may be main reasons for not introducing drugs and using them in the older patients,” he said. They included care setting (that is, inpatient or outpatient), HF severity by several measures, a range of comorbidities, renal dysfunction, and history of serious illness such as cancer.
Even then, age emerged as a significant, independent predictor of medical therapy underuse in the oldest patients. Some physicians apparently see advanced age, by itself, as an “intrinsic reason” not to abide by HFrEF medical therapy recommendations, said Dr. Stolfo, who presented the analysis at HFA 2021, the annual meeting of the Heart Failure Association of the European Society of Cardiology (ESC-HFA), conducted both virtually and live in Florence, Italy.
Most major HF-drug trials have excluded or admitted few patients aged 80 years or older, but “the guidelines recommend treatment regardless of age, and in the trials there has been no influence from age on the effectiveness of drugs,” Dr. Stolfo observed.
Moreover, in a prior SwedeHF analysis with propensity matching, patients with HFrEF aged 80 or older showed steeper reductions in risk for death or HF hospitalization from treatment with RASi than those in younger age groups.
One of the few randomized trials to focus on the very elderly, called SENIORS, enrolled patients aged 70 years and older – the average age was 76 – and saw a significantly reduced risk of death or cardiovascular hospitalization for those assigned to the beta blocker nebivolol. The benefits in the trial, which was conducted 15 years ago, were independent of left ventricular function.
So in the oldest patients, “we could question the need to achieve full dose of an evidence-based drug, but we shouldn’t question the use of these drugs.”
The findings are consistent with a need to individualize medical therapy in senior patients with HFrEF, especially those of more advanced age, some of whom may be robust enough to be managed similarly to younger patients while others who may be less suitable for full guideline-directed medical therapy, Dr. Stolfo said.
Even for those who are more frail or have major comorbidities, drug therapy of HFrEF continues to be important for symptom control even if competing causes of death make it harder to prolong survival, Dr. Stolfo said.
“We should provide to all patients the best strategy they can tolerate,” he said. “If we cannot greatly impact on the long-term survival for these patients, treatment can be aimed to improve the quality of life and keep the patient out of the hospital.”
The analysis was supported by Boehringer Ingelheim. Dr. Stolfo disclosed personal fees from Novartis, Merck, GlaxoSmithKline, and Acceleron.
A version of this article first appeared on Medscape.com.
, suggests a large cohort study.
About 80% of patients aged 80 years or older were prescribed renin-angiotensin-system inhibitors (RASi) in a multivariate-adjusted analysis of more than 27,000 patients in the Swedish Heart Failure Registry (SwedeHF). In contrast, such drugs – which included angiotensin receptor-neprilysin inhibitors (ARNi), angiotensin receptor blockers, and ACE inhibitors – were prescribed to 95% of patients younger than 70 years.
Similarly, fewer of the oldest patients were offered meds from the two other drug classes core to HF management at the time: Beta blockers and mineralocorticoid receptor antagonists (MRA).
And among those in the 80-and-older age group who were prescribed RASi or beta blockers, their uptitration more often fell short of even half the target dosage, compared with the youngest patients in the analysis.
Physicians may hold back on full guideline-directed medical therapy in their very elderly patients with HFrEF for many reasons, including a perceived likelihood of drug intolerance due to frailty or multiple comorbidities, including renal dysfunction, Davide Stolfo, MD, Karolinska Institutet, Stockholm, and University of Trieste, Italy, told this news organization.
But the current analysis was adjusted for about 80 variables “that in our interpretation may be main reasons for not introducing drugs and using them in the older patients,” he said. They included care setting (that is, inpatient or outpatient), HF severity by several measures, a range of comorbidities, renal dysfunction, and history of serious illness such as cancer.
Even then, age emerged as a significant, independent predictor of medical therapy underuse in the oldest patients. Some physicians apparently see advanced age, by itself, as an “intrinsic reason” not to abide by HFrEF medical therapy recommendations, said Dr. Stolfo, who presented the analysis at HFA 2021, the annual meeting of the Heart Failure Association of the European Society of Cardiology (ESC-HFA), conducted both virtually and live in Florence, Italy.
Most major HF-drug trials have excluded or admitted few patients aged 80 years or older, but “the guidelines recommend treatment regardless of age, and in the trials there has been no influence from age on the effectiveness of drugs,” Dr. Stolfo observed.
Moreover, in a prior SwedeHF analysis with propensity matching, patients with HFrEF aged 80 or older showed steeper reductions in risk for death or HF hospitalization from treatment with RASi than those in younger age groups.
One of the few randomized trials to focus on the very elderly, called SENIORS, enrolled patients aged 70 years and older – the average age was 76 – and saw a significantly reduced risk of death or cardiovascular hospitalization for those assigned to the beta blocker nebivolol. The benefits in the trial, which was conducted 15 years ago, were independent of left ventricular function.
So in the oldest patients, “we could question the need to achieve full dose of an evidence-based drug, but we shouldn’t question the use of these drugs.”
The findings are consistent with a need to individualize medical therapy in senior patients with HFrEF, especially those of more advanced age, some of whom may be robust enough to be managed similarly to younger patients while others who may be less suitable for full guideline-directed medical therapy, Dr. Stolfo said.
Even for those who are more frail or have major comorbidities, drug therapy of HFrEF continues to be important for symptom control even if competing causes of death make it harder to prolong survival, Dr. Stolfo said.
“We should provide to all patients the best strategy they can tolerate,” he said. “If we cannot greatly impact on the long-term survival for these patients, treatment can be aimed to improve the quality of life and keep the patient out of the hospital.”
The analysis was supported by Boehringer Ingelheim. Dr. Stolfo disclosed personal fees from Novartis, Merck, GlaxoSmithKline, and Acceleron.
A version of this article first appeared on Medscape.com.
Huge trial casts doubt on bisphosphonates for breast cancer
say researchers reporting new results from a phase 3 trial with almost 3,000 women.
Current guidelines call for 3-5 years of bisphosphonate therapy on the theory that these drugs might reduce breast cancer recurrence as well as treatment-related bone problems.
However, the new results show no difference in disease-free survival, distant disease-free survival, and overall survival – regardless of menopausal status – between the 1,540 women who received intravenous zoledronate over a 5-year period and 1,447 women who received such therapy over a 2-year period.
What they did find was a substantially higher risk for adverse events with prolonged bisphosphonate treatment, including risks for grade 3/4 events, bone pain, bone fractures, arthralgia, and jaw necrosis, a rare but well- recognized possibility with bisphosphonates.
Lead investigator Thomas Friedl, PhD, a statistician at University Hospital Ulm (Germany), and colleagues concluded that the current duration of treatment can be reduced and that, short of good reason to use bisphosphonates longer, such as decreased bone density, “treatment with zoledronate for 5 years should not be considered in patients with early breast cancer.”
The study was published online on June 24 in JAMA Oncology.
An accompanying editorial went even further, stating not only that “shorter duration of treatment is sufficient” but also that the whole idea of bisphosphonates for breast cancer is in doubt.
With “the modest outcomes of bisphosphonates, compared with no bone-targeted therapy, in historical trials” and the low rates of recurrence with modern treatment – less than 10% in the trial – “what, if any, is the benefit from adjuvant bisphosphonates? It’s time to reevaluate the guidelines,” said the editorialists, led by Alexandra Desnoyers, MD, a breast cancer fellow at the University of Toronto.
“We suggest that zoledronate or other amino-bisphosphonates should not be given as standard adjuvant therapy for unselected women with breast cancer,” they wrote.
Risk for necrosis with 5 years of zoledronate
The women in the trial had primary invasive breast cancer and were at high risk for recurrence. They had either positive nodes or high-risk features, including age (median, 53 years). They were treated at 250 centers in Germany.
The first part of the trial was to see whether use of gemcitabine improved outcomes when added to docetaxel after standard fluorouracil, epirubicin, and cyclophosphamide adjuvant therapy following surgery. It did not, and the authors reported in 2020 that adjuvant gemcitabine should not be used in the treatment of high-risk early breast cancer.
The next phase of the trial involved zoledronate. Women were randomly assigned to receive zoledronate for 2 or 5 years after surgery and after undergoing chemotherapy. Dosing was 4 mg IV every 3 months for 2 years. The women in the 5-year group went on to receive 4 mg IV every 6 months for another 3 years.
At a mean of 5 years’ follow-up after the first zoledronate dose, there was no difference in any of the survival measures between the two dosage groups.
There was also no difference in rates of bone recurrence or in circulating tumor cells, which the bisphosphonates theory would have predicted. For instance, 10.5% of women in the 5-year group had one or more circulating tumor cells on follow-up versus 7.2% in the 2-year group.
Almost half of the women in the 5-year treatment group experienced adverse events with zoledronate – including 7.6% with grade 3/4 events – versus just over a quarter in the 2-year arm and only 5.1% with grade 3/4 events.
In the 5-year group, 8.3% of patients experienced bone pain and 5.1% experienced arthralgia versus 3.7% and 3.1%, respectively, in the 2-year arm.
Atypical fractures, such as femoral spiral fractures, are another concern with bisphosphonates. Although this trial did not report on fracture type, fractures were reported in 14 women in the 5-year group but in only 3 in the 2-year arm.
Jaw necrosis, another known adverse effect of bisphosphonates, was reported in 11 women in the 5-year group and in 5 in the 2-year group.
The study was funded by several pharmaceutical companies, including Novartis, the maker of zoledronate. The investigators have numerous industry ties. Dr. Friedl has received payments from Novartis.
A version of this article first appeared on Medscape.com.
say researchers reporting new results from a phase 3 trial with almost 3,000 women.
Current guidelines call for 3-5 years of bisphosphonate therapy on the theory that these drugs might reduce breast cancer recurrence as well as treatment-related bone problems.
However, the new results show no difference in disease-free survival, distant disease-free survival, and overall survival – regardless of menopausal status – between the 1,540 women who received intravenous zoledronate over a 5-year period and 1,447 women who received such therapy over a 2-year period.
What they did find was a substantially higher risk for adverse events with prolonged bisphosphonate treatment, including risks for grade 3/4 events, bone pain, bone fractures, arthralgia, and jaw necrosis, a rare but well- recognized possibility with bisphosphonates.
Lead investigator Thomas Friedl, PhD, a statistician at University Hospital Ulm (Germany), and colleagues concluded that the current duration of treatment can be reduced and that, short of good reason to use bisphosphonates longer, such as decreased bone density, “treatment with zoledronate for 5 years should not be considered in patients with early breast cancer.”
The study was published online on June 24 in JAMA Oncology.
An accompanying editorial went even further, stating not only that “shorter duration of treatment is sufficient” but also that the whole idea of bisphosphonates for breast cancer is in doubt.
With “the modest outcomes of bisphosphonates, compared with no bone-targeted therapy, in historical trials” and the low rates of recurrence with modern treatment – less than 10% in the trial – “what, if any, is the benefit from adjuvant bisphosphonates? It’s time to reevaluate the guidelines,” said the editorialists, led by Alexandra Desnoyers, MD, a breast cancer fellow at the University of Toronto.
“We suggest that zoledronate or other amino-bisphosphonates should not be given as standard adjuvant therapy for unselected women with breast cancer,” they wrote.
Risk for necrosis with 5 years of zoledronate
The women in the trial had primary invasive breast cancer and were at high risk for recurrence. They had either positive nodes or high-risk features, including age (median, 53 years). They were treated at 250 centers in Germany.
The first part of the trial was to see whether use of gemcitabine improved outcomes when added to docetaxel after standard fluorouracil, epirubicin, and cyclophosphamide adjuvant therapy following surgery. It did not, and the authors reported in 2020 that adjuvant gemcitabine should not be used in the treatment of high-risk early breast cancer.
The next phase of the trial involved zoledronate. Women were randomly assigned to receive zoledronate for 2 or 5 years after surgery and after undergoing chemotherapy. Dosing was 4 mg IV every 3 months for 2 years. The women in the 5-year group went on to receive 4 mg IV every 6 months for another 3 years.
At a mean of 5 years’ follow-up after the first zoledronate dose, there was no difference in any of the survival measures between the two dosage groups.
There was also no difference in rates of bone recurrence or in circulating tumor cells, which the bisphosphonates theory would have predicted. For instance, 10.5% of women in the 5-year group had one or more circulating tumor cells on follow-up versus 7.2% in the 2-year group.
Almost half of the women in the 5-year treatment group experienced adverse events with zoledronate – including 7.6% with grade 3/4 events – versus just over a quarter in the 2-year arm and only 5.1% with grade 3/4 events.
In the 5-year group, 8.3% of patients experienced bone pain and 5.1% experienced arthralgia versus 3.7% and 3.1%, respectively, in the 2-year arm.
Atypical fractures, such as femoral spiral fractures, are another concern with bisphosphonates. Although this trial did not report on fracture type, fractures were reported in 14 women in the 5-year group but in only 3 in the 2-year arm.
Jaw necrosis, another known adverse effect of bisphosphonates, was reported in 11 women in the 5-year group and in 5 in the 2-year group.
The study was funded by several pharmaceutical companies, including Novartis, the maker of zoledronate. The investigators have numerous industry ties. Dr. Friedl has received payments from Novartis.
A version of this article first appeared on Medscape.com.
say researchers reporting new results from a phase 3 trial with almost 3,000 women.
Current guidelines call for 3-5 years of bisphosphonate therapy on the theory that these drugs might reduce breast cancer recurrence as well as treatment-related bone problems.
However, the new results show no difference in disease-free survival, distant disease-free survival, and overall survival – regardless of menopausal status – between the 1,540 women who received intravenous zoledronate over a 5-year period and 1,447 women who received such therapy over a 2-year period.
What they did find was a substantially higher risk for adverse events with prolonged bisphosphonate treatment, including risks for grade 3/4 events, bone pain, bone fractures, arthralgia, and jaw necrosis, a rare but well- recognized possibility with bisphosphonates.
Lead investigator Thomas Friedl, PhD, a statistician at University Hospital Ulm (Germany), and colleagues concluded that the current duration of treatment can be reduced and that, short of good reason to use bisphosphonates longer, such as decreased bone density, “treatment with zoledronate for 5 years should not be considered in patients with early breast cancer.”
The study was published online on June 24 in JAMA Oncology.
An accompanying editorial went even further, stating not only that “shorter duration of treatment is sufficient” but also that the whole idea of bisphosphonates for breast cancer is in doubt.
With “the modest outcomes of bisphosphonates, compared with no bone-targeted therapy, in historical trials” and the low rates of recurrence with modern treatment – less than 10% in the trial – “what, if any, is the benefit from adjuvant bisphosphonates? It’s time to reevaluate the guidelines,” said the editorialists, led by Alexandra Desnoyers, MD, a breast cancer fellow at the University of Toronto.
“We suggest that zoledronate or other amino-bisphosphonates should not be given as standard adjuvant therapy for unselected women with breast cancer,” they wrote.
Risk for necrosis with 5 years of zoledronate
The women in the trial had primary invasive breast cancer and were at high risk for recurrence. They had either positive nodes or high-risk features, including age (median, 53 years). They were treated at 250 centers in Germany.
The first part of the trial was to see whether use of gemcitabine improved outcomes when added to docetaxel after standard fluorouracil, epirubicin, and cyclophosphamide adjuvant therapy following surgery. It did not, and the authors reported in 2020 that adjuvant gemcitabine should not be used in the treatment of high-risk early breast cancer.
The next phase of the trial involved zoledronate. Women were randomly assigned to receive zoledronate for 2 or 5 years after surgery and after undergoing chemotherapy. Dosing was 4 mg IV every 3 months for 2 years. The women in the 5-year group went on to receive 4 mg IV every 6 months for another 3 years.
At a mean of 5 years’ follow-up after the first zoledronate dose, there was no difference in any of the survival measures between the two dosage groups.
There was also no difference in rates of bone recurrence or in circulating tumor cells, which the bisphosphonates theory would have predicted. For instance, 10.5% of women in the 5-year group had one or more circulating tumor cells on follow-up versus 7.2% in the 2-year group.
Almost half of the women in the 5-year treatment group experienced adverse events with zoledronate – including 7.6% with grade 3/4 events – versus just over a quarter in the 2-year arm and only 5.1% with grade 3/4 events.
In the 5-year group, 8.3% of patients experienced bone pain and 5.1% experienced arthralgia versus 3.7% and 3.1%, respectively, in the 2-year arm.
Atypical fractures, such as femoral spiral fractures, are another concern with bisphosphonates. Although this trial did not report on fracture type, fractures were reported in 14 women in the 5-year group but in only 3 in the 2-year arm.
Jaw necrosis, another known adverse effect of bisphosphonates, was reported in 11 women in the 5-year group and in 5 in the 2-year group.
The study was funded by several pharmaceutical companies, including Novartis, the maker of zoledronate. The investigators have numerous industry ties. Dr. Friedl has received payments from Novartis.
A version of this article first appeared on Medscape.com.
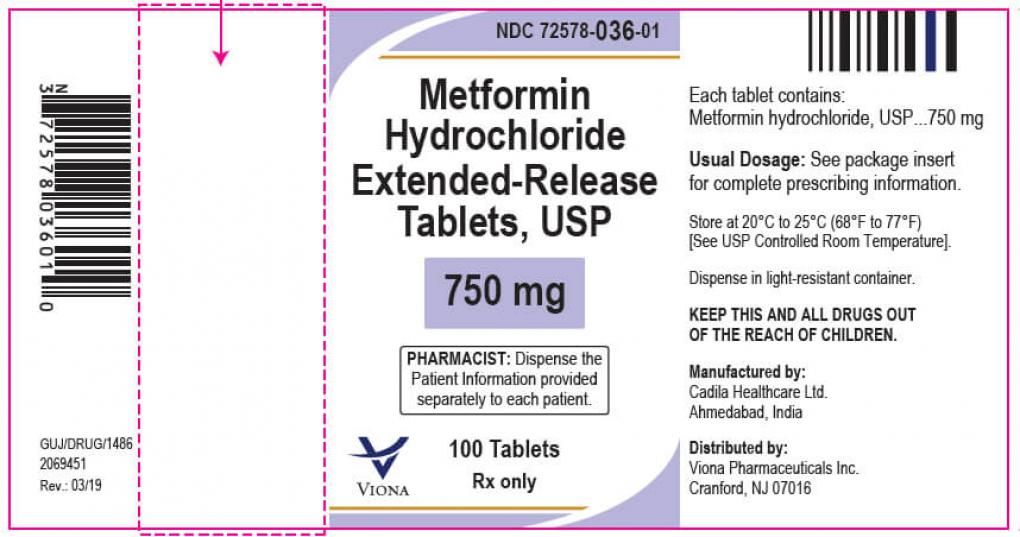
What’s best for diabetes after metformin? GRADE outdated at outset
Liraglutide and insulin glargine outperformed glimepiride and sitagliptin as single add-on agents to metformin for treating patients with type 2 diabetes in a multicenter U.S. trial that randomized just over 5,000 patients.
. Results were reported at the virtual American Diabetes Association (ADA) 81st Scientific Sessions.
The comparison included two oral medications – the sulfonylurea glimepiride and dipeptidyl peptidase-4 (DPP-4) inhibitor sitagliptin – and two injectable medications – insulin glargine and glucagon-like peptide 1 (GLP-1) receptor agonist liraglutide.
The primary endpoint was change in A1c level and overall glycemic control. Secondary endpoints include changes in weight, as well as cardiovascular, renal, gastrointestinal, and other complications.
For the primary endpoint – keeping A1c levels below 7% – liraglutide and the basal insulin glargine both did this best and were almost equivalent.
During the average 5-year follow-up, the rates of patients progressing to a confirmed A1c of 7% or higher were 67% among patients randomized to insulin glargine, 68% maintained on liraglutide, 72% taking the sulfonylurea glimepiride, and 77% taking sitagliptin, reported John M. Lachin, ScD, a biostatistician at George Washington University, Washington.
Too soon for take-aways, or are the data already obsolete?
“The ultimate goal of GRADE is to help clinicians select the therapies that will work best for individual patients, as diabetes care is not a one-size-fits all approach,” noted David M. Nathan, MD, chair of the study and director of the Diabetes Center at Massachusetts General Hospital, in an ADA press release.
Dr. Nathan, as well as several other members of the GRADE trial steering committee who presented results, repeatedly cautioned that the findings were preliminary because they represent 90% of outcomes, with the remaining 10% still to be adjudicated.
“We undertook this study to fill a gap in the guidelines,” said investigator Deborah J. Wexler, MD, clinical director of the Diabetes Center at Massachusetts General Hospital in Boston. “I would like to have all the results in ... before I comment on how the guidelines should change.”
“The metabolic data are solid, but the cardiovascular disease data are preliminary,” warned Dr. Nathan.
But that didn’t stop some from drawing their own conclusions, with Julio Rosenstock, MD, who comoderated the session but was not involved with the study, giving his own opinion.
“A pleasant surprise was the performance of basal insulin,” he said, calling the findings “a vindication” for basal insulin as a treatment for the types of patients with type 2 diabetes that enrolled in the study.
Steven E. Kahn, MB, ChB, another GRADE co-investigator agreed. “Based on the results, guidelines should say that you add insulin early on,” he observed.
A generic basal insulin and a generic sulfonylurea are both reasonable options, after metformin, for patients with limited resources, added Dr. Kahn, an endocrinologist and professor at the University of Washington, Seattle.
Dr. Rosenstock, director of the Dallas Diabetes Research Center, also saw the results as an indictment of agents in the DDP-4 inhibitor class, such as sitagliptin.
The DPP-4 inhibitors generate $9 billion a year, he said, wondering whether it “is justifiable to put them on the same level as other agents?”
Meanwhile the assigned discussant, David R. Matthews, DPhil, a professor of diabetes medicine at the University of Oxford, England – while congratulating the investigators on certain aspects of the study – said it ultimately fell short because it didn’t include an arm with an SGLT2 inhibitor.
“We should kick the authors for missing out on SGLT2 inhibitors,” Dr. Matthews said. “The omission means that the GRADE data are already obsolescent.”
In reply, Dr. Nathan admitted “we feel bad we did not include” an SGLT2 inhibitor, but he vigorously defended the dilemma faced by the trial’s organizers.
Oral SGLT2 inhibitors were not “well-established drugs” for type 2 diabetes when enrollment launched in 2013, and the researchers were wary of including what could turn out to be a problematic agent soon after controversy over the safety of agents in the thiazolidinedione drug class (such as rosiglitazone), he explained.
They also realized that adding a fifth drug to the study would necessitate doubling enrollment size, which would have undercut the funding plans already in place.
Dr. Matthews also derided GRADE as being underpowered to adequately address the impact of the tested agents on major adverse cardiovascular events (MACE) and hospitalizations for heart failure and too U.S.-centric to be generalizable elsewhere.
A study with lots of data
The roughly 5,000 patients enrolled in GRADE were an average age of 57 years old, 64% were men, 66% were White, and 20% were Black. They had had type 2 diabetes, on average, for 4.2 years. Mean body mass index at entry was about 34 kg/m2, average A1c was 7.5%, and average estimated glomerular filtration rate was 95 mL/min/1.73m2. The trial included a 6-12 week run-in period during which background metformin treatment was optimized and led to average A1c levels less than 7%.
Patients were then randomized to one of the four agents as add-on treatment.
Both liraglutide and insulin glargine performed well on many of the numerous metrics in the data-rich trial, largely funded by two branches of the National Institutes of Health, with commercial involvement limited to free supplies of the study drugs.
The secondary metabolic outcome, of disease progressing to a confirmed A1c of 7.5%, was reached by 39% of patients taking insulin glargine, significantly lower than the rate of 46% among patients taking liraglutide, and that rate, in turn, was significantly below the 50% rate among patients taking glimepiride and the 55% rate of those taking sitagliptin.
Mean doses of the second-line agents after 4 years of treatment were 38.3 units/day for glargine, 3.5 mg/day for glimepiride, 1.3 mg/day for subcutaneous liraglutide, and 82.9 mg/day for sitagliptin.
A trio of cardiovascular outcomes showed one significant benefit of liraglutide over the other three drugs for the endpoint of any cardiovascular event, which included not only major adverse cardiovascular events (MACE; cardiovascular death, myocardial infarction, or stroke), but also several other event types, including heart failure requiring hospitalization, unstable angina requiring hospitalization, revascularization or any arterial repairs, stent thrombosis, or transient ischemic attack.
For the endpoint of any cardiovascular event, the rate was 5.8% for patients taking liraglutide, significantly less than the rate of 7.6% of those taking insulin glargine, 8.0% for glimepiride, and 8.6% for sitagliptin, reported John B. Buse, MD, PhD, professor, chief of endocrinology, and director of the Diabetes Center at the University of North Carolina at Chapel Hill.
For each of the other two main cardiovascular endpoints – MACE and hospitalization for heart failure – liraglutide had a numeric advantage over the other three drugs but failed to reach significance.
Patients taking liraglutide also had a smaller but not significantly different point estimate for all-cause death, at 2.1%, compared with 3.1%-3.4% in the other three groups.
And, Dr. Nathan emphasized, the cardiovascular disease data are still considered preliminary.
Liraglutide scored a pair of additional outcome victories. Its use resulted in a significantly lower rate of patients who progressed during follow-up to either needing antihypertensive medications or having their blood pressure rise above 140/90 mm Hg compared with the other three drugs. (At baseline, average blood pressure for all patients was 128/77 mm Hg.)
And after 4 years, patients taking liraglutide lost an average of about 4 kg (8.8 lb) from their baseline weight (which averaged about 100 kg [220 lb]), roughly the same as patients taking sitagliptin but significantly better than with glimepiride or insulin glargine. Patients taking glargine gained a small amount of weight on average during their first couple of years of treatment, roughly 1 kg, but returned to around their baseline weight by the end of 4 years.
Four drugs performed equally well for some outcomes
Finally, the four drugs had similar results for some outcomes. This included their effects on renal function, distal sensory polyneuropathy, and low-density lipoprotein (LDL) cholesterol.
The four agents also had roughly similar safety profiles, with rates of serious adverse events all falling within the tight range of 33%-37%.
But the rate of severe hypoglycemic episodes that required assistance to treat showed significant separation, ranging from 2.3% for glimepiride, 1.4% for glargine, 0.9% for liraglutide, and 0.7% for sitagliptin. Gastrointestinal symptoms occurred in about 50% of patients in three of the treatment groups but were significantly higher in those taking liraglutide, affecting 60%.
GRADE received no commercial funding. Dr. Wexler has reported serving on data monitoring committees for Novo Nordisk. Dr. Buse has reported being a consultant for and holding stock in numerous companies. Dr. Rosenstock has reported being an advisor or consultant to Applied Therapeutics, Boehringer Ingelheim, Hanmi Pharmaceutical, Intarcia Therapeutics, Lilly, Novo Nordisk, Oramed, and Sanofi and has received research support from numerous companies. Dr. Kahn has reported being an advisor to or speaker on behalf of Bayer, Boehringer Ingelheim, Casma Therapeutics, Intarcia Therapeutics, Lilly, Merck, Novo Nordisk, Pfizer, and Third Rock Ventures. Dr. Matthews has reported receiving lecture and advisor fees from Merck, Novartis, Novo Nordisk, Sanofi Aventis, and Servier. Dr. Lachin and Dr. Nathan have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Liraglutide and insulin glargine outperformed glimepiride and sitagliptin as single add-on agents to metformin for treating patients with type 2 diabetes in a multicenter U.S. trial that randomized just over 5,000 patients.
. Results were reported at the virtual American Diabetes Association (ADA) 81st Scientific Sessions.
The comparison included two oral medications – the sulfonylurea glimepiride and dipeptidyl peptidase-4 (DPP-4) inhibitor sitagliptin – and two injectable medications – insulin glargine and glucagon-like peptide 1 (GLP-1) receptor agonist liraglutide.
The primary endpoint was change in A1c level and overall glycemic control. Secondary endpoints include changes in weight, as well as cardiovascular, renal, gastrointestinal, and other complications.
For the primary endpoint – keeping A1c levels below 7% – liraglutide and the basal insulin glargine both did this best and were almost equivalent.
During the average 5-year follow-up, the rates of patients progressing to a confirmed A1c of 7% or higher were 67% among patients randomized to insulin glargine, 68% maintained on liraglutide, 72% taking the sulfonylurea glimepiride, and 77% taking sitagliptin, reported John M. Lachin, ScD, a biostatistician at George Washington University, Washington.
Too soon for take-aways, or are the data already obsolete?
“The ultimate goal of GRADE is to help clinicians select the therapies that will work best for individual patients, as diabetes care is not a one-size-fits all approach,” noted David M. Nathan, MD, chair of the study and director of the Diabetes Center at Massachusetts General Hospital, in an ADA press release.
Dr. Nathan, as well as several other members of the GRADE trial steering committee who presented results, repeatedly cautioned that the findings were preliminary because they represent 90% of outcomes, with the remaining 10% still to be adjudicated.
“We undertook this study to fill a gap in the guidelines,” said investigator Deborah J. Wexler, MD, clinical director of the Diabetes Center at Massachusetts General Hospital in Boston. “I would like to have all the results in ... before I comment on how the guidelines should change.”
“The metabolic data are solid, but the cardiovascular disease data are preliminary,” warned Dr. Nathan.
But that didn’t stop some from drawing their own conclusions, with Julio Rosenstock, MD, who comoderated the session but was not involved with the study, giving his own opinion.
“A pleasant surprise was the performance of basal insulin,” he said, calling the findings “a vindication” for basal insulin as a treatment for the types of patients with type 2 diabetes that enrolled in the study.
Steven E. Kahn, MB, ChB, another GRADE co-investigator agreed. “Based on the results, guidelines should say that you add insulin early on,” he observed.
A generic basal insulin and a generic sulfonylurea are both reasonable options, after metformin, for patients with limited resources, added Dr. Kahn, an endocrinologist and professor at the University of Washington, Seattle.
Dr. Rosenstock, director of the Dallas Diabetes Research Center, also saw the results as an indictment of agents in the DDP-4 inhibitor class, such as sitagliptin.
The DPP-4 inhibitors generate $9 billion a year, he said, wondering whether it “is justifiable to put them on the same level as other agents?”
Meanwhile the assigned discussant, David R. Matthews, DPhil, a professor of diabetes medicine at the University of Oxford, England – while congratulating the investigators on certain aspects of the study – said it ultimately fell short because it didn’t include an arm with an SGLT2 inhibitor.
“We should kick the authors for missing out on SGLT2 inhibitors,” Dr. Matthews said. “The omission means that the GRADE data are already obsolescent.”
In reply, Dr. Nathan admitted “we feel bad we did not include” an SGLT2 inhibitor, but he vigorously defended the dilemma faced by the trial’s organizers.
Oral SGLT2 inhibitors were not “well-established drugs” for type 2 diabetes when enrollment launched in 2013, and the researchers were wary of including what could turn out to be a problematic agent soon after controversy over the safety of agents in the thiazolidinedione drug class (such as rosiglitazone), he explained.
They also realized that adding a fifth drug to the study would necessitate doubling enrollment size, which would have undercut the funding plans already in place.
Dr. Matthews also derided GRADE as being underpowered to adequately address the impact of the tested agents on major adverse cardiovascular events (MACE) and hospitalizations for heart failure and too U.S.-centric to be generalizable elsewhere.
A study with lots of data
The roughly 5,000 patients enrolled in GRADE were an average age of 57 years old, 64% were men, 66% were White, and 20% were Black. They had had type 2 diabetes, on average, for 4.2 years. Mean body mass index at entry was about 34 kg/m2, average A1c was 7.5%, and average estimated glomerular filtration rate was 95 mL/min/1.73m2. The trial included a 6-12 week run-in period during which background metformin treatment was optimized and led to average A1c levels less than 7%.
Patients were then randomized to one of the four agents as add-on treatment.
Both liraglutide and insulin glargine performed well on many of the numerous metrics in the data-rich trial, largely funded by two branches of the National Institutes of Health, with commercial involvement limited to free supplies of the study drugs.
The secondary metabolic outcome, of disease progressing to a confirmed A1c of 7.5%, was reached by 39% of patients taking insulin glargine, significantly lower than the rate of 46% among patients taking liraglutide, and that rate, in turn, was significantly below the 50% rate among patients taking glimepiride and the 55% rate of those taking sitagliptin.
Mean doses of the second-line agents after 4 years of treatment were 38.3 units/day for glargine, 3.5 mg/day for glimepiride, 1.3 mg/day for subcutaneous liraglutide, and 82.9 mg/day for sitagliptin.
A trio of cardiovascular outcomes showed one significant benefit of liraglutide over the other three drugs for the endpoint of any cardiovascular event, which included not only major adverse cardiovascular events (MACE; cardiovascular death, myocardial infarction, or stroke), but also several other event types, including heart failure requiring hospitalization, unstable angina requiring hospitalization, revascularization or any arterial repairs, stent thrombosis, or transient ischemic attack.
For the endpoint of any cardiovascular event, the rate was 5.8% for patients taking liraglutide, significantly less than the rate of 7.6% of those taking insulin glargine, 8.0% for glimepiride, and 8.6% for sitagliptin, reported John B. Buse, MD, PhD, professor, chief of endocrinology, and director of the Diabetes Center at the University of North Carolina at Chapel Hill.
For each of the other two main cardiovascular endpoints – MACE and hospitalization for heart failure – liraglutide had a numeric advantage over the other three drugs but failed to reach significance.
Patients taking liraglutide also had a smaller but not significantly different point estimate for all-cause death, at 2.1%, compared with 3.1%-3.4% in the other three groups.
And, Dr. Nathan emphasized, the cardiovascular disease data are still considered preliminary.
Liraglutide scored a pair of additional outcome victories. Its use resulted in a significantly lower rate of patients who progressed during follow-up to either needing antihypertensive medications or having their blood pressure rise above 140/90 mm Hg compared with the other three drugs. (At baseline, average blood pressure for all patients was 128/77 mm Hg.)
And after 4 years, patients taking liraglutide lost an average of about 4 kg (8.8 lb) from their baseline weight (which averaged about 100 kg [220 lb]), roughly the same as patients taking sitagliptin but significantly better than with glimepiride or insulin glargine. Patients taking glargine gained a small amount of weight on average during their first couple of years of treatment, roughly 1 kg, but returned to around their baseline weight by the end of 4 years.
Four drugs performed equally well for some outcomes
Finally, the four drugs had similar results for some outcomes. This included their effects on renal function, distal sensory polyneuropathy, and low-density lipoprotein (LDL) cholesterol.
The four agents also had roughly similar safety profiles, with rates of serious adverse events all falling within the tight range of 33%-37%.
But the rate of severe hypoglycemic episodes that required assistance to treat showed significant separation, ranging from 2.3% for glimepiride, 1.4% for glargine, 0.9% for liraglutide, and 0.7% for sitagliptin. Gastrointestinal symptoms occurred in about 50% of patients in three of the treatment groups but were significantly higher in those taking liraglutide, affecting 60%.
GRADE received no commercial funding. Dr. Wexler has reported serving on data monitoring committees for Novo Nordisk. Dr. Buse has reported being a consultant for and holding stock in numerous companies. Dr. Rosenstock has reported being an advisor or consultant to Applied Therapeutics, Boehringer Ingelheim, Hanmi Pharmaceutical, Intarcia Therapeutics, Lilly, Novo Nordisk, Oramed, and Sanofi and has received research support from numerous companies. Dr. Kahn has reported being an advisor to or speaker on behalf of Bayer, Boehringer Ingelheim, Casma Therapeutics, Intarcia Therapeutics, Lilly, Merck, Novo Nordisk, Pfizer, and Third Rock Ventures. Dr. Matthews has reported receiving lecture and advisor fees from Merck, Novartis, Novo Nordisk, Sanofi Aventis, and Servier. Dr. Lachin and Dr. Nathan have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Liraglutide and insulin glargine outperformed glimepiride and sitagliptin as single add-on agents to metformin for treating patients with type 2 diabetes in a multicenter U.S. trial that randomized just over 5,000 patients.
. Results were reported at the virtual American Diabetes Association (ADA) 81st Scientific Sessions.
The comparison included two oral medications – the sulfonylurea glimepiride and dipeptidyl peptidase-4 (DPP-4) inhibitor sitagliptin – and two injectable medications – insulin glargine and glucagon-like peptide 1 (GLP-1) receptor agonist liraglutide.
The primary endpoint was change in A1c level and overall glycemic control. Secondary endpoints include changes in weight, as well as cardiovascular, renal, gastrointestinal, and other complications.
For the primary endpoint – keeping A1c levels below 7% – liraglutide and the basal insulin glargine both did this best and were almost equivalent.
During the average 5-year follow-up, the rates of patients progressing to a confirmed A1c of 7% or higher were 67% among patients randomized to insulin glargine, 68% maintained on liraglutide, 72% taking the sulfonylurea glimepiride, and 77% taking sitagliptin, reported John M. Lachin, ScD, a biostatistician at George Washington University, Washington.
Too soon for take-aways, or are the data already obsolete?
“The ultimate goal of GRADE is to help clinicians select the therapies that will work best for individual patients, as diabetes care is not a one-size-fits all approach,” noted David M. Nathan, MD, chair of the study and director of the Diabetes Center at Massachusetts General Hospital, in an ADA press release.
Dr. Nathan, as well as several other members of the GRADE trial steering committee who presented results, repeatedly cautioned that the findings were preliminary because they represent 90% of outcomes, with the remaining 10% still to be adjudicated.
“We undertook this study to fill a gap in the guidelines,” said investigator Deborah J. Wexler, MD, clinical director of the Diabetes Center at Massachusetts General Hospital in Boston. “I would like to have all the results in ... before I comment on how the guidelines should change.”
“The metabolic data are solid, but the cardiovascular disease data are preliminary,” warned Dr. Nathan.
But that didn’t stop some from drawing their own conclusions, with Julio Rosenstock, MD, who comoderated the session but was not involved with the study, giving his own opinion.
“A pleasant surprise was the performance of basal insulin,” he said, calling the findings “a vindication” for basal insulin as a treatment for the types of patients with type 2 diabetes that enrolled in the study.
Steven E. Kahn, MB, ChB, another GRADE co-investigator agreed. “Based on the results, guidelines should say that you add insulin early on,” he observed.
A generic basal insulin and a generic sulfonylurea are both reasonable options, after metformin, for patients with limited resources, added Dr. Kahn, an endocrinologist and professor at the University of Washington, Seattle.
Dr. Rosenstock, director of the Dallas Diabetes Research Center, also saw the results as an indictment of agents in the DDP-4 inhibitor class, such as sitagliptin.
The DPP-4 inhibitors generate $9 billion a year, he said, wondering whether it “is justifiable to put them on the same level as other agents?”
Meanwhile the assigned discussant, David R. Matthews, DPhil, a professor of diabetes medicine at the University of Oxford, England – while congratulating the investigators on certain aspects of the study – said it ultimately fell short because it didn’t include an arm with an SGLT2 inhibitor.
“We should kick the authors for missing out on SGLT2 inhibitors,” Dr. Matthews said. “The omission means that the GRADE data are already obsolescent.”
In reply, Dr. Nathan admitted “we feel bad we did not include” an SGLT2 inhibitor, but he vigorously defended the dilemma faced by the trial’s organizers.
Oral SGLT2 inhibitors were not “well-established drugs” for type 2 diabetes when enrollment launched in 2013, and the researchers were wary of including what could turn out to be a problematic agent soon after controversy over the safety of agents in the thiazolidinedione drug class (such as rosiglitazone), he explained.
They also realized that adding a fifth drug to the study would necessitate doubling enrollment size, which would have undercut the funding plans already in place.
Dr. Matthews also derided GRADE as being underpowered to adequately address the impact of the tested agents on major adverse cardiovascular events (MACE) and hospitalizations for heart failure and too U.S.-centric to be generalizable elsewhere.
A study with lots of data
The roughly 5,000 patients enrolled in GRADE were an average age of 57 years old, 64% were men, 66% were White, and 20% were Black. They had had type 2 diabetes, on average, for 4.2 years. Mean body mass index at entry was about 34 kg/m2, average A1c was 7.5%, and average estimated glomerular filtration rate was 95 mL/min/1.73m2. The trial included a 6-12 week run-in period during which background metformin treatment was optimized and led to average A1c levels less than 7%.
Patients were then randomized to one of the four agents as add-on treatment.
Both liraglutide and insulin glargine performed well on many of the numerous metrics in the data-rich trial, largely funded by two branches of the National Institutes of Health, with commercial involvement limited to free supplies of the study drugs.
The secondary metabolic outcome, of disease progressing to a confirmed A1c of 7.5%, was reached by 39% of patients taking insulin glargine, significantly lower than the rate of 46% among patients taking liraglutide, and that rate, in turn, was significantly below the 50% rate among patients taking glimepiride and the 55% rate of those taking sitagliptin.
Mean doses of the second-line agents after 4 years of treatment were 38.3 units/day for glargine, 3.5 mg/day for glimepiride, 1.3 mg/day for subcutaneous liraglutide, and 82.9 mg/day for sitagliptin.
A trio of cardiovascular outcomes showed one significant benefit of liraglutide over the other three drugs for the endpoint of any cardiovascular event, which included not only major adverse cardiovascular events (MACE; cardiovascular death, myocardial infarction, or stroke), but also several other event types, including heart failure requiring hospitalization, unstable angina requiring hospitalization, revascularization or any arterial repairs, stent thrombosis, or transient ischemic attack.
For the endpoint of any cardiovascular event, the rate was 5.8% for patients taking liraglutide, significantly less than the rate of 7.6% of those taking insulin glargine, 8.0% for glimepiride, and 8.6% for sitagliptin, reported John B. Buse, MD, PhD, professor, chief of endocrinology, and director of the Diabetes Center at the University of North Carolina at Chapel Hill.
For each of the other two main cardiovascular endpoints – MACE and hospitalization for heart failure – liraglutide had a numeric advantage over the other three drugs but failed to reach significance.
Patients taking liraglutide also had a smaller but not significantly different point estimate for all-cause death, at 2.1%, compared with 3.1%-3.4% in the other three groups.
And, Dr. Nathan emphasized, the cardiovascular disease data are still considered preliminary.
Liraglutide scored a pair of additional outcome victories. Its use resulted in a significantly lower rate of patients who progressed during follow-up to either needing antihypertensive medications or having their blood pressure rise above 140/90 mm Hg compared with the other three drugs. (At baseline, average blood pressure for all patients was 128/77 mm Hg.)
And after 4 years, patients taking liraglutide lost an average of about 4 kg (8.8 lb) from their baseline weight (which averaged about 100 kg [220 lb]), roughly the same as patients taking sitagliptin but significantly better than with glimepiride or insulin glargine. Patients taking glargine gained a small amount of weight on average during their first couple of years of treatment, roughly 1 kg, but returned to around their baseline weight by the end of 4 years.
Four drugs performed equally well for some outcomes
Finally, the four drugs had similar results for some outcomes. This included their effects on renal function, distal sensory polyneuropathy, and low-density lipoprotein (LDL) cholesterol.
The four agents also had roughly similar safety profiles, with rates of serious adverse events all falling within the tight range of 33%-37%.
But the rate of severe hypoglycemic episodes that required assistance to treat showed significant separation, ranging from 2.3% for glimepiride, 1.4% for glargine, 0.9% for liraglutide, and 0.7% for sitagliptin. Gastrointestinal symptoms occurred in about 50% of patients in three of the treatment groups but were significantly higher in those taking liraglutide, affecting 60%.
GRADE received no commercial funding. Dr. Wexler has reported serving on data monitoring committees for Novo Nordisk. Dr. Buse has reported being a consultant for and holding stock in numerous companies. Dr. Rosenstock has reported being an advisor or consultant to Applied Therapeutics, Boehringer Ingelheim, Hanmi Pharmaceutical, Intarcia Therapeutics, Lilly, Novo Nordisk, Oramed, and Sanofi and has received research support from numerous companies. Dr. Kahn has reported being an advisor to or speaker on behalf of Bayer, Boehringer Ingelheim, Casma Therapeutics, Intarcia Therapeutics, Lilly, Merck, Novo Nordisk, Pfizer, and Third Rock Ventures. Dr. Matthews has reported receiving lecture and advisor fees from Merck, Novartis, Novo Nordisk, Sanofi Aventis, and Servier. Dr. Lachin and Dr. Nathan have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nocturnal hypoglycemia halved with insulin degludec vs. glargine
Patients with type 1 diabetes who used insulin degludec as their basal insulin had fewer than half the number of nocturnal hypoglycemia events, compared with patients who used insulin glargine U100, in a head-to-head crossover study with 51 patients who had a history of nighttime hypoglycemia episodes.
Patients with type 1 diabetes who are “struggling with nocturnal hypoglycemia would benefit from insulin degludec treatment,” said Julie M. Brøsen, MD, at the annual scientific sessions of the American Diabetes Association.
Accumulating evidence for less hypoglycemia with insulin degludec
Results from several studies comparing insulin degludec (Tresiba), a second-generation, longer-acting insulin with more stable steady-state performance, with the first-generation basal insulin analogue glargine (Lantus), have built the case that degludec produces fewer hypoglycemia events.
The landmark SWITCH 1 crossover study published in 2017 showed in about 500 patients with type 1 diabetes and a risk factor for hypoglycemia that treatment with insulin degludec led to significantly few total hypoglycemia episodes and significantly fewer nocturnal episodes, compared with insulin glargine.
Next came similar findings from ReFLeCT, a multicenter observational study that followed 556 unselected patients with type 1 diabetes in routine practice settings who switched to insulin degludec following treatment with a different basal insulin. The results again showed a significant drop-off in total, nonsevere, severe, and nocturnal hypoglycemia events.
Homing in on higher-risk patients
The current study, HypoDeg (Insulin Degludec and Symptomatic Nocturnal Hypoglycaemia), ran at 10 Danish centers and enrolled 149 adults with type 1 diabetes who had at least one episode of severe nocturnal hypoglycemia within the prior 2 years, focusing on patients most at risk for future nocturnal hypoglycemia events. In an unusual study design, researchers identified nocturnal hypoglycemic episodes with hourly venous blood samples drawn from a subcutaneous line.
They randomized the patients to basal insulin treatment with either insulin degludec or to insulin glargine U100, allowed their treatment to stabilize for 3 months, and then tallied nocturnal hypoglycemia events for 9 months. They then crossed patients to the alternative basal insulin and repeated the process.
Results from the full study have not yet appeared in published form but were in a pair of reports at the 2020 scientific sessions of the ADA.
One report included findings based on 136 episodes of severe hypoglycemia identified clinically and showed these events occurred 35% less often during treatment with insulin degludec, a significant difference. The overall finding was primarily driven by 48% fewer episodes of severe nocturnal hypoglycemia, but this difference was not significant.
The second report identified hypoglycemia events with continuous glucose monitoring in 74 of the study participants, which identified 193 episodes of nonsevere nocturnal hypoglycemia and found that treatment with insulin degludec cut the rate by 47%, primarily by reducing asymptomatic episodes.
Hourly blood draws track overnight hypoglycemia
The current study included 51 of the 149 HypoDeg patients who agreed to undergo overnight blood sampling and had this done at least once while treated with each of the two study insulins. (The study design called for two blood sampling nights for each willing patient during each of the two treatment periods.) The 51 patients had type 1 diabetes for an average of 28 years and an average age of 58 years. Two-thirds were men, their baseline A1c was 7.8%, and on average had 2.6 episodes of severe nocturnal hypoglycemia during the prior 2 years.
The researchers drew hourly blood specimens on a total of 196 nights from the 51 participating patients and identified 57 nights when blood glucose levels reached hypoglycemia thresholds in 33 patients. One-third of the events occurred when patients were on insulin degludec treatment, and two-thirds when they were on insulin glargine, reported Dr. Brøsen.
She presented three separate analyses of the data. One analysis focused on level 1 hypoglycemia events, when blood glucose dips to 70 mg/dL or less, which occurred 54% less often when patients were on insulin degludec. A second analysis looked at level 2 events, when blood glucose falls below 54 mg/dL, and treatment with insulin degludec cut this by 64% compared with insulin glargine. The third analysis focused on symptomatic events when blood glucose was 70 mg/dL or less, and treatment with insulin degludec linked with a 62% cut in this metric. All three between-group differences were significant.
Evidence supports already-changed practice
This new evidence “supports recommending” insulin degludec over insulin glargine, commented Bastiaan E. de Galan, MD, PhD, an endocrinologist and professor at Maastrict (the Netherlands) University Medical Center. The new results “extend those from previous trials in populations with type 1 diabetes that were unselected for the risk of hypoglycemia. In clinical practice, insulin degludec is already considered for patients who reported nocturnal hypoglycemia while on insulin glargine U100, but it’s great this study provides the scientific evidence,” said Dr. de Galan in an interview.
“The lower rate of nocturnal hypoglycemia with degludec, compared with glargine U100 is well established. Inpatient assessment of hypoglycemia with measurement of hourly plasma glucose allowed HypoDeg to provide stronger evidence than prior studies. The benefit of delgudec versus glargine U100 was significant and clinically meaningful, in hypo-prone patients who would benefit the most” by using insulin degludec, commented Gian Paolo Fadini, MD, an endocrinologist at the University of Padova (Italy), and a lead investigator on the ReFLeCT study.
But insulin degludec is not a completely silver bullet. Its prolonged duration of action and stability that may in part explain why it limits hypoglycemia events can also be a drawback: “It probably offers fewer options for flexibility. Any change in dose takes at least a day or 2 to settle, which may be unfavorable in certain circumstances,” noted Dr. de Galan.
“I wouldn’t recommend insulin degludec for all patients with type 1 diabetes. It’s an individual evaluation in each patient,” said Dr. Brøsen. “We will be looking into whether some patients are better off on insulin glargine.”
Cost makes a difference
Another, potentially more consequential flaw is insulin degludec’s relative expense.
“To date, use of degludec in routine practice has been limited by its cost, compared with older basal insulins,” observed Dr. Fadini in an interview. “In several countries, including the United States, degludec is substantially more expensive than glargine.”
The ADA’s Standards of Medical Care in Diabetes–2021 includes table 9.3 that lists the costs of various insulins and shows the median average wholesale price of insulin glargine U100 follow-on products as $190/vial, compared with a $407 price for a similar vial of insulin degludec.
Insulin degludec “is clearly superior from a hypoglycemia standpoint. Patients with type 1 diabetes like the reduction because hypoglycemia is scary, and dangerous. The main issue is cost, and the extent to which it may be covered by insurance,” commented Lisa Chow, MD, an endocrinologist at the University of Minnesota, Minneapolis. “We generally won’t prescribe degludec unless it is at a price affordable to the patient. We try to use patient assistance programs sponsored by the company [that markets insulin degludec: Novo Nordisk] to try to make it more affordable.”
Dr. Chow also highlighted that a new wrinkle has been introduction of a more concentrated formulation of insulin glargine, U300, which appears to cause less hypoglycemia than insulin glargine U100. Recent study results indicated that no significant difference exists in the incidence of hypoglycemia among patients treated with insulin glargine U300 and those treated with insulin degludec, such as findings from the BRIGHT trial, which included just over 900 patients, and in the CONCLUDE trial, which randomized more than 1,600 patients.
The HypoDeg study was sponsored by Novo Nordisk, the company that markets insulin degludec. Dr. Brøsen had no personal disclosures, but several of her coauthors were either Novo Nordisk employees or had financial relationships with the company. Dr. de Galan has received research funding from Novo Nordisk. Dr. Fadini has received lecture fees and research funding from Novo Nordisk, from Sanofi, the company that markets insulin glargine, and from several other companies. Dr. Chow has received research funding from Dexcom.
Patients with type 1 diabetes who used insulin degludec as their basal insulin had fewer than half the number of nocturnal hypoglycemia events, compared with patients who used insulin glargine U100, in a head-to-head crossover study with 51 patients who had a history of nighttime hypoglycemia episodes.
Patients with type 1 diabetes who are “struggling with nocturnal hypoglycemia would benefit from insulin degludec treatment,” said Julie M. Brøsen, MD, at the annual scientific sessions of the American Diabetes Association.
Accumulating evidence for less hypoglycemia with insulin degludec
Results from several studies comparing insulin degludec (Tresiba), a second-generation, longer-acting insulin with more stable steady-state performance, with the first-generation basal insulin analogue glargine (Lantus), have built the case that degludec produces fewer hypoglycemia events.
The landmark SWITCH 1 crossover study published in 2017 showed in about 500 patients with type 1 diabetes and a risk factor for hypoglycemia that treatment with insulin degludec led to significantly few total hypoglycemia episodes and significantly fewer nocturnal episodes, compared with insulin glargine.
Next came similar findings from ReFLeCT, a multicenter observational study that followed 556 unselected patients with type 1 diabetes in routine practice settings who switched to insulin degludec following treatment with a different basal insulin. The results again showed a significant drop-off in total, nonsevere, severe, and nocturnal hypoglycemia events.
Homing in on higher-risk patients
The current study, HypoDeg (Insulin Degludec and Symptomatic Nocturnal Hypoglycaemia), ran at 10 Danish centers and enrolled 149 adults with type 1 diabetes who had at least one episode of severe nocturnal hypoglycemia within the prior 2 years, focusing on patients most at risk for future nocturnal hypoglycemia events. In an unusual study design, researchers identified nocturnal hypoglycemic episodes with hourly venous blood samples drawn from a subcutaneous line.
They randomized the patients to basal insulin treatment with either insulin degludec or to insulin glargine U100, allowed their treatment to stabilize for 3 months, and then tallied nocturnal hypoglycemia events for 9 months. They then crossed patients to the alternative basal insulin and repeated the process.
Results from the full study have not yet appeared in published form but were in a pair of reports at the 2020 scientific sessions of the ADA.
One report included findings based on 136 episodes of severe hypoglycemia identified clinically and showed these events occurred 35% less often during treatment with insulin degludec, a significant difference. The overall finding was primarily driven by 48% fewer episodes of severe nocturnal hypoglycemia, but this difference was not significant.
The second report identified hypoglycemia events with continuous glucose monitoring in 74 of the study participants, which identified 193 episodes of nonsevere nocturnal hypoglycemia and found that treatment with insulin degludec cut the rate by 47%, primarily by reducing asymptomatic episodes.
Hourly blood draws track overnight hypoglycemia
The current study included 51 of the 149 HypoDeg patients who agreed to undergo overnight blood sampling and had this done at least once while treated with each of the two study insulins. (The study design called for two blood sampling nights for each willing patient during each of the two treatment periods.) The 51 patients had type 1 diabetes for an average of 28 years and an average age of 58 years. Two-thirds were men, their baseline A1c was 7.8%, and on average had 2.6 episodes of severe nocturnal hypoglycemia during the prior 2 years.
The researchers drew hourly blood specimens on a total of 196 nights from the 51 participating patients and identified 57 nights when blood glucose levels reached hypoglycemia thresholds in 33 patients. One-third of the events occurred when patients were on insulin degludec treatment, and two-thirds when they were on insulin glargine, reported Dr. Brøsen.
She presented three separate analyses of the data. One analysis focused on level 1 hypoglycemia events, when blood glucose dips to 70 mg/dL or less, which occurred 54% less often when patients were on insulin degludec. A second analysis looked at level 2 events, when blood glucose falls below 54 mg/dL, and treatment with insulin degludec cut this by 64% compared with insulin glargine. The third analysis focused on symptomatic events when blood glucose was 70 mg/dL or less, and treatment with insulin degludec linked with a 62% cut in this metric. All three between-group differences were significant.
Evidence supports already-changed practice
This new evidence “supports recommending” insulin degludec over insulin glargine, commented Bastiaan E. de Galan, MD, PhD, an endocrinologist and professor at Maastrict (the Netherlands) University Medical Center. The new results “extend those from previous trials in populations with type 1 diabetes that were unselected for the risk of hypoglycemia. In clinical practice, insulin degludec is already considered for patients who reported nocturnal hypoglycemia while on insulin glargine U100, but it’s great this study provides the scientific evidence,” said Dr. de Galan in an interview.
“The lower rate of nocturnal hypoglycemia with degludec, compared with glargine U100 is well established. Inpatient assessment of hypoglycemia with measurement of hourly plasma glucose allowed HypoDeg to provide stronger evidence than prior studies. The benefit of delgudec versus glargine U100 was significant and clinically meaningful, in hypo-prone patients who would benefit the most” by using insulin degludec, commented Gian Paolo Fadini, MD, an endocrinologist at the University of Padova (Italy), and a lead investigator on the ReFLeCT study.
But insulin degludec is not a completely silver bullet. Its prolonged duration of action and stability that may in part explain why it limits hypoglycemia events can also be a drawback: “It probably offers fewer options for flexibility. Any change in dose takes at least a day or 2 to settle, which may be unfavorable in certain circumstances,” noted Dr. de Galan.
“I wouldn’t recommend insulin degludec for all patients with type 1 diabetes. It’s an individual evaluation in each patient,” said Dr. Brøsen. “We will be looking into whether some patients are better off on insulin glargine.”
Cost makes a difference
Another, potentially more consequential flaw is insulin degludec’s relative expense.
“To date, use of degludec in routine practice has been limited by its cost, compared with older basal insulins,” observed Dr. Fadini in an interview. “In several countries, including the United States, degludec is substantially more expensive than glargine.”
The ADA’s Standards of Medical Care in Diabetes–2021 includes table 9.3 that lists the costs of various insulins and shows the median average wholesale price of insulin glargine U100 follow-on products as $190/vial, compared with a $407 price for a similar vial of insulin degludec.
Insulin degludec “is clearly superior from a hypoglycemia standpoint. Patients with type 1 diabetes like the reduction because hypoglycemia is scary, and dangerous. The main issue is cost, and the extent to which it may be covered by insurance,” commented Lisa Chow, MD, an endocrinologist at the University of Minnesota, Minneapolis. “We generally won’t prescribe degludec unless it is at a price affordable to the patient. We try to use patient assistance programs sponsored by the company [that markets insulin degludec: Novo Nordisk] to try to make it more affordable.”
Dr. Chow also highlighted that a new wrinkle has been introduction of a more concentrated formulation of insulin glargine, U300, which appears to cause less hypoglycemia than insulin glargine U100. Recent study results indicated that no significant difference exists in the incidence of hypoglycemia among patients treated with insulin glargine U300 and those treated with insulin degludec, such as findings from the BRIGHT trial, which included just over 900 patients, and in the CONCLUDE trial, which randomized more than 1,600 patients.
The HypoDeg study was sponsored by Novo Nordisk, the company that markets insulin degludec. Dr. Brøsen had no personal disclosures, but several of her coauthors were either Novo Nordisk employees or had financial relationships with the company. Dr. de Galan has received research funding from Novo Nordisk. Dr. Fadini has received lecture fees and research funding from Novo Nordisk, from Sanofi, the company that markets insulin glargine, and from several other companies. Dr. Chow has received research funding from Dexcom.
Patients with type 1 diabetes who used insulin degludec as their basal insulin had fewer than half the number of nocturnal hypoglycemia events, compared with patients who used insulin glargine U100, in a head-to-head crossover study with 51 patients who had a history of nighttime hypoglycemia episodes.
Patients with type 1 diabetes who are “struggling with nocturnal hypoglycemia would benefit from insulin degludec treatment,” said Julie M. Brøsen, MD, at the annual scientific sessions of the American Diabetes Association.
Accumulating evidence for less hypoglycemia with insulin degludec
Results from several studies comparing insulin degludec (Tresiba), a second-generation, longer-acting insulin with more stable steady-state performance, with the first-generation basal insulin analogue glargine (Lantus), have built the case that degludec produces fewer hypoglycemia events.
The landmark SWITCH 1 crossover study published in 2017 showed in about 500 patients with type 1 diabetes and a risk factor for hypoglycemia that treatment with insulin degludec led to significantly few total hypoglycemia episodes and significantly fewer nocturnal episodes, compared with insulin glargine.
Next came similar findings from ReFLeCT, a multicenter observational study that followed 556 unselected patients with type 1 diabetes in routine practice settings who switched to insulin degludec following treatment with a different basal insulin. The results again showed a significant drop-off in total, nonsevere, severe, and nocturnal hypoglycemia events.
Homing in on higher-risk patients
The current study, HypoDeg (Insulin Degludec and Symptomatic Nocturnal Hypoglycaemia), ran at 10 Danish centers and enrolled 149 adults with type 1 diabetes who had at least one episode of severe nocturnal hypoglycemia within the prior 2 years, focusing on patients most at risk for future nocturnal hypoglycemia events. In an unusual study design, researchers identified nocturnal hypoglycemic episodes with hourly venous blood samples drawn from a subcutaneous line.
They randomized the patients to basal insulin treatment with either insulin degludec or to insulin glargine U100, allowed their treatment to stabilize for 3 months, and then tallied nocturnal hypoglycemia events for 9 months. They then crossed patients to the alternative basal insulin and repeated the process.
Results from the full study have not yet appeared in published form but were in a pair of reports at the 2020 scientific sessions of the ADA.
One report included findings based on 136 episodes of severe hypoglycemia identified clinically and showed these events occurred 35% less often during treatment with insulin degludec, a significant difference. The overall finding was primarily driven by 48% fewer episodes of severe nocturnal hypoglycemia, but this difference was not significant.
The second report identified hypoglycemia events with continuous glucose monitoring in 74 of the study participants, which identified 193 episodes of nonsevere nocturnal hypoglycemia and found that treatment with insulin degludec cut the rate by 47%, primarily by reducing asymptomatic episodes.
Hourly blood draws track overnight hypoglycemia
The current study included 51 of the 149 HypoDeg patients who agreed to undergo overnight blood sampling and had this done at least once while treated with each of the two study insulins. (The study design called for two blood sampling nights for each willing patient during each of the two treatment periods.) The 51 patients had type 1 diabetes for an average of 28 years and an average age of 58 years. Two-thirds were men, their baseline A1c was 7.8%, and on average had 2.6 episodes of severe nocturnal hypoglycemia during the prior 2 years.
The researchers drew hourly blood specimens on a total of 196 nights from the 51 participating patients and identified 57 nights when blood glucose levels reached hypoglycemia thresholds in 33 patients. One-third of the events occurred when patients were on insulin degludec treatment, and two-thirds when they were on insulin glargine, reported Dr. Brøsen.
She presented three separate analyses of the data. One analysis focused on level 1 hypoglycemia events, when blood glucose dips to 70 mg/dL or less, which occurred 54% less often when patients were on insulin degludec. A second analysis looked at level 2 events, when blood glucose falls below 54 mg/dL, and treatment with insulin degludec cut this by 64% compared with insulin glargine. The third analysis focused on symptomatic events when blood glucose was 70 mg/dL or less, and treatment with insulin degludec linked with a 62% cut in this metric. All three between-group differences were significant.
Evidence supports already-changed practice
This new evidence “supports recommending” insulin degludec over insulin glargine, commented Bastiaan E. de Galan, MD, PhD, an endocrinologist and professor at Maastrict (the Netherlands) University Medical Center. The new results “extend those from previous trials in populations with type 1 diabetes that were unselected for the risk of hypoglycemia. In clinical practice, insulin degludec is already considered for patients who reported nocturnal hypoglycemia while on insulin glargine U100, but it’s great this study provides the scientific evidence,” said Dr. de Galan in an interview.
“The lower rate of nocturnal hypoglycemia with degludec, compared with glargine U100 is well established. Inpatient assessment of hypoglycemia with measurement of hourly plasma glucose allowed HypoDeg to provide stronger evidence than prior studies. The benefit of delgudec versus glargine U100 was significant and clinically meaningful, in hypo-prone patients who would benefit the most” by using insulin degludec, commented Gian Paolo Fadini, MD, an endocrinologist at the University of Padova (Italy), and a lead investigator on the ReFLeCT study.
But insulin degludec is not a completely silver bullet. Its prolonged duration of action and stability that may in part explain why it limits hypoglycemia events can also be a drawback: “It probably offers fewer options for flexibility. Any change in dose takes at least a day or 2 to settle, which may be unfavorable in certain circumstances,” noted Dr. de Galan.
“I wouldn’t recommend insulin degludec for all patients with type 1 diabetes. It’s an individual evaluation in each patient,” said Dr. Brøsen. “We will be looking into whether some patients are better off on insulin glargine.”
Cost makes a difference
Another, potentially more consequential flaw is insulin degludec’s relative expense.
“To date, use of degludec in routine practice has been limited by its cost, compared with older basal insulins,” observed Dr. Fadini in an interview. “In several countries, including the United States, degludec is substantially more expensive than glargine.”
The ADA’s Standards of Medical Care in Diabetes–2021 includes table 9.3 that lists the costs of various insulins and shows the median average wholesale price of insulin glargine U100 follow-on products as $190/vial, compared with a $407 price for a similar vial of insulin degludec.
Insulin degludec “is clearly superior from a hypoglycemia standpoint. Patients with type 1 diabetes like the reduction because hypoglycemia is scary, and dangerous. The main issue is cost, and the extent to which it may be covered by insurance,” commented Lisa Chow, MD, an endocrinologist at the University of Minnesota, Minneapolis. “We generally won’t prescribe degludec unless it is at a price affordable to the patient. We try to use patient assistance programs sponsored by the company [that markets insulin degludec: Novo Nordisk] to try to make it more affordable.”
Dr. Chow also highlighted that a new wrinkle has been introduction of a more concentrated formulation of insulin glargine, U300, which appears to cause less hypoglycemia than insulin glargine U100. Recent study results indicated that no significant difference exists in the incidence of hypoglycemia among patients treated with insulin glargine U300 and those treated with insulin degludec, such as findings from the BRIGHT trial, which included just over 900 patients, and in the CONCLUDE trial, which randomized more than 1,600 patients.
The HypoDeg study was sponsored by Novo Nordisk, the company that markets insulin degludec. Dr. Brøsen had no personal disclosures, but several of her coauthors were either Novo Nordisk employees or had financial relationships with the company. Dr. de Galan has received research funding from Novo Nordisk. Dr. Fadini has received lecture fees and research funding from Novo Nordisk, from Sanofi, the company that markets insulin glargine, and from several other companies. Dr. Chow has received research funding from Dexcom.
FROM ADA 2021
‘Stunning’ twincretin beats semaglutide for A1c, weight reduction in T2D
Tirzepatide, a novel “twincretin” agent, was superior to 1-mg semaglutide treatments for reducing both hemoglobin A1c levels and body weight in patients with type 2 diabetes in a pivotal, 40-week, head-to-head trial with nearly 1,900 randomized patients, one of four positive pivotal trial results reported for tirzepatide at the annual scientific sessions of the American Diabetes Association.
“Across all four studies we see a significant and clinically meaningful decrease in A1c, and robust weight loss. The results exceeded our expectations” for both these outcomes, said Laura Fernández Landó, MD, senior medical director for tirzepatide at Lilly, the company developing the agent, and a coauthor on the semaglutide comparison study as well as on other tirzepatide reports at the meeting.
“This opens up a new avenue for results in diabetes therapy,” Jens Juul Holst, MD, remarked in a press conference.
SURPASS-2 compared three different tirzepatide doses delivered once weekly by subcutaneous injection against a 1-mg weekly, subcutaneous dose of semaglutide (Ozempic) in 1,879 adults who had been diagnosed with type 2 diabetes for an average of almost 9 years. All patients were already on metformin treatment that had proved inadequate for controlling their hyperglycemia; enrolled patients had an average A1c of 8.28%. The trial’s primary endpoint was change from baseline in A1c levels after 40 weeks.
Significant differences at each dose level
Patients on each of the three tirzepatide doses – 5 mg, 10 mg, or 15 mg once weekly – showed dose-dependent reductions in A1c that, for each dose, were significantly better than the reduction achieved with semaglutide. The highest tirzepatide dose reduced A1c levels by an average of 0.45% more than what semaglutide achieved, reported first author Juan P. Frias, MD; Dr. Landó; and their coauthors.
One key secondary endpoint was weight reduction, and each of the three tirzepatide doses again produced significant incremental loss beyond what semaglutide produced. The 5-mg weekly dose of tirzepatide produced an average 1.9-kg additional weight loss, compared with semaglutide, while the 15-mg dose resulted in an average 5.5-kg loss beyond what semaglutide achieved and a total average weight loss of 11.2 kg from baseline.
The study’s additional key secondary endpoints, the percentages of patients reaching an A1c of less than 7%, and less than 5.7%, also showed significantly better numbers with tirzepatide. The highest tirzepatide dose pushed 86% of patients below the 7% mark, compared with 79% on semaglutide, and the top tirzepatide dose resulted in 46% of patients getting their A1c below 5.7%, compared with 19% of patients on semaglutide.
The findings are “stunning, I must stay, and those results included that up to half of the patients treated with high doses of tirzepatide may reach A1c levels of less than 5.7%, which is really, really unheard of,” said Dr. Holst, professor of endocrinology and metabolism at the University of Copenhagen. Along with the “weight losses at the same time of up to 12% in that patient group, we are seeing some completely unexpected and really shocking and wonderful new advances in the therapy,” added Dr. Holst.
The safety profile of tirzepatide was roughly similar to semaglutide’s and to that other agents in the glucagonlike peptide-1 receptor agonist (GLP-1 RA) class. Concurrently with the report at the meeting, the results also appeared in an article published online in the New England Journal of Medicine.
An ‘impressive’ weight loss effect
Weight loss on tirzepatide was “impressive,” commented Katherine R. Tuttle, MD, a nephrologist affiliated with the University of Washington and executive director for research at Providence Health Care in Spokane, Wash. Another striking feature of tirzepatide’s weight-loss effect was that it did not plateau during the 40 weeks of the study, Dr. Tuttle noted in an accompanying editorial that accompanied the published report, a finding that suggests the potential for additional weight loss from continued treatment .
“The weight loss is remarkable,” commented Rodolfo J. Galindo, MD, an endocrinologist at Emory University, Atlanta. While incremental reduction of A1c on the order of less than 0.5% is helpful, incremental weight loss of more than 10 lbs on tirzepatide, compared with semaglutide “will likely be a tie-breaker” for many clinicians and patients to favor tirzepatide over semaglutide or another GLP-1 RA agent, he said in an interview. Dr. Galindo also cited other important factors that he predicted will drive decisions on using tirzepatide or a GLP-1 RA once tirzepatide reaches the U.S. market: relative cost, access, and tolerability.
The important issue of dose
But the edge that tirzepatide showed over semaglutide for weight loss did not occur on a completely level playing field. The 1 mg/week dose of semaglutide used as the comparator in SURPASS-2 was the maximum dose available at the time the study began, but in June 2021 the Food and Drug Administration approved a 2.4 mg/week dose (Wegovy) labeled specifically for weight loss. Dr. Tuttle cited the limitation this introduces in her editorial.
“The dose issue is important,” she wrote. The doses of tirzepatide and semaglutide compared in SURPASS-2 “were not comparable in terms of weight outcomes” given that prior evidence showed that the 2.4 mg/week semaglutide dose is more appropriate for weight loss.
Dr. Tuttle also cited other factors to consider when assessing tirzepatide compared with agents in the GLP-1 RA class.
Several GLP-1 RA agents, including semaglutide, have proven efficacy for reducing rates of atherosclerotic cardiovascular events and albuminuria, and they also slow decline in kidney function and progression of diabetic kidney disease. No details on the renal effects of tirzepatide appeared in the SURPASS-2 report. A press release from Lilly in May 2021 briefly mentioned results from a meta-analysis of several clinical studies of tirzepatide that showed a nonsignificant effect from tirzepatide on the incidence of major cardiovascular adverse events (death from cardiovascular or undetermined causes, MI, stroke, and hospitalization for unstable angina) relative to comparator groups. Results from a dedicated cardiovascular outcomes trial in high-risk patients treated with tirzepatide, SURPASS-CVOT, are not expected until 2024.
A further limitation of SURPASS-2 was the demographics of the enrolled population, which had a low (0.4%) enrollment rate of Black patients, and a high proportion (70%) of Hispanic patients, Dr. Tuttle observed.
Low rates of hypoglycemia
Another notable finding from SURPASS-2 was the low incidence of clinically significant hypoglycemic events (blood glucose levels less than 54 mg/dL), which occurred in 0.2%-1.7% of patients on tirzepatide, depending on their dose, and in 0.4% of patients on semaglutide. Two patients in the tirzepatide cohort had severe hypoglycemia.
These numbers are reassuring, said Dr. Galindo, and reflect the safety of tirzepatide’s dual, incretin-like mechanisms of action that make it a “twincretin.” The molecule acts as both a GLP-1 RA, and as glucose-dependent insulinotropic polypeptide, an incretin that stimulates insulin release when blood sugar is high but also increases glucagon levels when blood sugar levels are normal or low. This dual action may help explain the apparent increased potency tirzepatide showed for both A1c reduction and weight loss, compared with semaglutide, which acts only as a GLP-1 RA.
Some experts have cited the uncertainty introduced by the open-label design of SURPASS-2, a decision necessitated by the distinctly different delivery devices used for tirzepatide and semaglutide, explained Dr. Landó. But she highlighted that double blinding applied to the three different tirzepatide dosages tested in the trial. Dr. Landó said that Lilly plans to seek FDA approval for all three tested tirzepatide doses to give clinicians and patients flexibility in applying the treatment.
SURPASS-2 used a prolonged dose-escalation protocol designed to minimize gastrointestinal adverse effects that started patients on a 2.5 mg weekly dose that then increased by 2.5 mg increments every 4 weeks until patients reached their assigned target dose. This meant that patients did not begin receiving the 15-mg/week dose until halfway through the trial.
Several more tirzepatide trials
Reports from two other pivotal trials for tirzepatide also appeared as posters at the meeting. SURPASS-5 compared tirzepatide with placebo in 475 patients inadequately controlled with titrated insulin glargine (Lantus). SURPASS-3 randomized 1,444 patients to tirzepatide or titrated insulin degludec (Tresiba). In both studies treatment with tirzepatide led to significantly better reductions in A1c and in weight loss than the comparator treatments. Results from a third pivotal trial, SURPASS-1 which compared tirzepatide against placebo in 478 treatment-naive patients, will come in a report scheduled for the second day of the meeting.
The results from all the recent tirzepatide trials show a consistent benefit across the continuum of patients with type 2 diabetes regardless of whether it’s recent onset or well-established disease, said Dr. Landó.
The SURPASS studies were sponsored by Lilly, the company developing tirzepatide, and the reports include several authors who are Lilly employees. Dr. Landó is a Lilly employee and stockholder. Dr. Tuttle has been a consultant to Lilly and to Novo Nordisk, the company that markets semaglutide, as well as to AstraZeneca, Bayer, Boehringer Ingelheim, Gilead, and Janssen. She has also received travel expenses from Kyokawa Hakko Kirin, and research funding from Bayer, Goldfinch Bio, and Lilly. Dr. Galindo has been a consultant to Lilly and to Novo Nordisk, as well as to Abbott Diabetes Care, Sanofi, Valeritas, and Weight Watchers, and his institution has received grant support on his behalf from Lilly, Novo Nordisk and Dexcom. Dr. Holst had no disclosures.
Tirzepatide, a novel “twincretin” agent, was superior to 1-mg semaglutide treatments for reducing both hemoglobin A1c levels and body weight in patients with type 2 diabetes in a pivotal, 40-week, head-to-head trial with nearly 1,900 randomized patients, one of four positive pivotal trial results reported for tirzepatide at the annual scientific sessions of the American Diabetes Association.
“Across all four studies we see a significant and clinically meaningful decrease in A1c, and robust weight loss. The results exceeded our expectations” for both these outcomes, said Laura Fernández Landó, MD, senior medical director for tirzepatide at Lilly, the company developing the agent, and a coauthor on the semaglutide comparison study as well as on other tirzepatide reports at the meeting.
“This opens up a new avenue for results in diabetes therapy,” Jens Juul Holst, MD, remarked in a press conference.
SURPASS-2 compared three different tirzepatide doses delivered once weekly by subcutaneous injection against a 1-mg weekly, subcutaneous dose of semaglutide (Ozempic) in 1,879 adults who had been diagnosed with type 2 diabetes for an average of almost 9 years. All patients were already on metformin treatment that had proved inadequate for controlling their hyperglycemia; enrolled patients had an average A1c of 8.28%. The trial’s primary endpoint was change from baseline in A1c levels after 40 weeks.
Significant differences at each dose level
Patients on each of the three tirzepatide doses – 5 mg, 10 mg, or 15 mg once weekly – showed dose-dependent reductions in A1c that, for each dose, were significantly better than the reduction achieved with semaglutide. The highest tirzepatide dose reduced A1c levels by an average of 0.45% more than what semaglutide achieved, reported first author Juan P. Frias, MD; Dr. Landó; and their coauthors.
One key secondary endpoint was weight reduction, and each of the three tirzepatide doses again produced significant incremental loss beyond what semaglutide produced. The 5-mg weekly dose of tirzepatide produced an average 1.9-kg additional weight loss, compared with semaglutide, while the 15-mg dose resulted in an average 5.5-kg loss beyond what semaglutide achieved and a total average weight loss of 11.2 kg from baseline.
The study’s additional key secondary endpoints, the percentages of patients reaching an A1c of less than 7%, and less than 5.7%, also showed significantly better numbers with tirzepatide. The highest tirzepatide dose pushed 86% of patients below the 7% mark, compared with 79% on semaglutide, and the top tirzepatide dose resulted in 46% of patients getting their A1c below 5.7%, compared with 19% of patients on semaglutide.
The findings are “stunning, I must stay, and those results included that up to half of the patients treated with high doses of tirzepatide may reach A1c levels of less than 5.7%, which is really, really unheard of,” said Dr. Holst, professor of endocrinology and metabolism at the University of Copenhagen. Along with the “weight losses at the same time of up to 12% in that patient group, we are seeing some completely unexpected and really shocking and wonderful new advances in the therapy,” added Dr. Holst.
The safety profile of tirzepatide was roughly similar to semaglutide’s and to that other agents in the glucagonlike peptide-1 receptor agonist (GLP-1 RA) class. Concurrently with the report at the meeting, the results also appeared in an article published online in the New England Journal of Medicine.
An ‘impressive’ weight loss effect
Weight loss on tirzepatide was “impressive,” commented Katherine R. Tuttle, MD, a nephrologist affiliated with the University of Washington and executive director for research at Providence Health Care in Spokane, Wash. Another striking feature of tirzepatide’s weight-loss effect was that it did not plateau during the 40 weeks of the study, Dr. Tuttle noted in an accompanying editorial that accompanied the published report, a finding that suggests the potential for additional weight loss from continued treatment .
“The weight loss is remarkable,” commented Rodolfo J. Galindo, MD, an endocrinologist at Emory University, Atlanta. While incremental reduction of A1c on the order of less than 0.5% is helpful, incremental weight loss of more than 10 lbs on tirzepatide, compared with semaglutide “will likely be a tie-breaker” for many clinicians and patients to favor tirzepatide over semaglutide or another GLP-1 RA agent, he said in an interview. Dr. Galindo also cited other important factors that he predicted will drive decisions on using tirzepatide or a GLP-1 RA once tirzepatide reaches the U.S. market: relative cost, access, and tolerability.
The important issue of dose
But the edge that tirzepatide showed over semaglutide for weight loss did not occur on a completely level playing field. The 1 mg/week dose of semaglutide used as the comparator in SURPASS-2 was the maximum dose available at the time the study began, but in June 2021 the Food and Drug Administration approved a 2.4 mg/week dose (Wegovy) labeled specifically for weight loss. Dr. Tuttle cited the limitation this introduces in her editorial.
“The dose issue is important,” she wrote. The doses of tirzepatide and semaglutide compared in SURPASS-2 “were not comparable in terms of weight outcomes” given that prior evidence showed that the 2.4 mg/week semaglutide dose is more appropriate for weight loss.
Dr. Tuttle also cited other factors to consider when assessing tirzepatide compared with agents in the GLP-1 RA class.
Several GLP-1 RA agents, including semaglutide, have proven efficacy for reducing rates of atherosclerotic cardiovascular events and albuminuria, and they also slow decline in kidney function and progression of diabetic kidney disease. No details on the renal effects of tirzepatide appeared in the SURPASS-2 report. A press release from Lilly in May 2021 briefly mentioned results from a meta-analysis of several clinical studies of tirzepatide that showed a nonsignificant effect from tirzepatide on the incidence of major cardiovascular adverse events (death from cardiovascular or undetermined causes, MI, stroke, and hospitalization for unstable angina) relative to comparator groups. Results from a dedicated cardiovascular outcomes trial in high-risk patients treated with tirzepatide, SURPASS-CVOT, are not expected until 2024.
A further limitation of SURPASS-2 was the demographics of the enrolled population, which had a low (0.4%) enrollment rate of Black patients, and a high proportion (70%) of Hispanic patients, Dr. Tuttle observed.
Low rates of hypoglycemia
Another notable finding from SURPASS-2 was the low incidence of clinically significant hypoglycemic events (blood glucose levels less than 54 mg/dL), which occurred in 0.2%-1.7% of patients on tirzepatide, depending on their dose, and in 0.4% of patients on semaglutide. Two patients in the tirzepatide cohort had severe hypoglycemia.
These numbers are reassuring, said Dr. Galindo, and reflect the safety of tirzepatide’s dual, incretin-like mechanisms of action that make it a “twincretin.” The molecule acts as both a GLP-1 RA, and as glucose-dependent insulinotropic polypeptide, an incretin that stimulates insulin release when blood sugar is high but also increases glucagon levels when blood sugar levels are normal or low. This dual action may help explain the apparent increased potency tirzepatide showed for both A1c reduction and weight loss, compared with semaglutide, which acts only as a GLP-1 RA.
Some experts have cited the uncertainty introduced by the open-label design of SURPASS-2, a decision necessitated by the distinctly different delivery devices used for tirzepatide and semaglutide, explained Dr. Landó. But she highlighted that double blinding applied to the three different tirzepatide dosages tested in the trial. Dr. Landó said that Lilly plans to seek FDA approval for all three tested tirzepatide doses to give clinicians and patients flexibility in applying the treatment.
SURPASS-2 used a prolonged dose-escalation protocol designed to minimize gastrointestinal adverse effects that started patients on a 2.5 mg weekly dose that then increased by 2.5 mg increments every 4 weeks until patients reached their assigned target dose. This meant that patients did not begin receiving the 15-mg/week dose until halfway through the trial.
Several more tirzepatide trials
Reports from two other pivotal trials for tirzepatide also appeared as posters at the meeting. SURPASS-5 compared tirzepatide with placebo in 475 patients inadequately controlled with titrated insulin glargine (Lantus). SURPASS-3 randomized 1,444 patients to tirzepatide or titrated insulin degludec (Tresiba). In both studies treatment with tirzepatide led to significantly better reductions in A1c and in weight loss than the comparator treatments. Results from a third pivotal trial, SURPASS-1 which compared tirzepatide against placebo in 478 treatment-naive patients, will come in a report scheduled for the second day of the meeting.
The results from all the recent tirzepatide trials show a consistent benefit across the continuum of patients with type 2 diabetes regardless of whether it’s recent onset or well-established disease, said Dr. Landó.
The SURPASS studies were sponsored by Lilly, the company developing tirzepatide, and the reports include several authors who are Lilly employees. Dr. Landó is a Lilly employee and stockholder. Dr. Tuttle has been a consultant to Lilly and to Novo Nordisk, the company that markets semaglutide, as well as to AstraZeneca, Bayer, Boehringer Ingelheim, Gilead, and Janssen. She has also received travel expenses from Kyokawa Hakko Kirin, and research funding from Bayer, Goldfinch Bio, and Lilly. Dr. Galindo has been a consultant to Lilly and to Novo Nordisk, as well as to Abbott Diabetes Care, Sanofi, Valeritas, and Weight Watchers, and his institution has received grant support on his behalf from Lilly, Novo Nordisk and Dexcom. Dr. Holst had no disclosures.
Tirzepatide, a novel “twincretin” agent, was superior to 1-mg semaglutide treatments for reducing both hemoglobin A1c levels and body weight in patients with type 2 diabetes in a pivotal, 40-week, head-to-head trial with nearly 1,900 randomized patients, one of four positive pivotal trial results reported for tirzepatide at the annual scientific sessions of the American Diabetes Association.
“Across all four studies we see a significant and clinically meaningful decrease in A1c, and robust weight loss. The results exceeded our expectations” for both these outcomes, said Laura Fernández Landó, MD, senior medical director for tirzepatide at Lilly, the company developing the agent, and a coauthor on the semaglutide comparison study as well as on other tirzepatide reports at the meeting.
“This opens up a new avenue for results in diabetes therapy,” Jens Juul Holst, MD, remarked in a press conference.
SURPASS-2 compared three different tirzepatide doses delivered once weekly by subcutaneous injection against a 1-mg weekly, subcutaneous dose of semaglutide (Ozempic) in 1,879 adults who had been diagnosed with type 2 diabetes for an average of almost 9 years. All patients were already on metformin treatment that had proved inadequate for controlling their hyperglycemia; enrolled patients had an average A1c of 8.28%. The trial’s primary endpoint was change from baseline in A1c levels after 40 weeks.
Significant differences at each dose level
Patients on each of the three tirzepatide doses – 5 mg, 10 mg, or 15 mg once weekly – showed dose-dependent reductions in A1c that, for each dose, were significantly better than the reduction achieved with semaglutide. The highest tirzepatide dose reduced A1c levels by an average of 0.45% more than what semaglutide achieved, reported first author Juan P. Frias, MD; Dr. Landó; and their coauthors.
One key secondary endpoint was weight reduction, and each of the three tirzepatide doses again produced significant incremental loss beyond what semaglutide produced. The 5-mg weekly dose of tirzepatide produced an average 1.9-kg additional weight loss, compared with semaglutide, while the 15-mg dose resulted in an average 5.5-kg loss beyond what semaglutide achieved and a total average weight loss of 11.2 kg from baseline.
The study’s additional key secondary endpoints, the percentages of patients reaching an A1c of less than 7%, and less than 5.7%, also showed significantly better numbers with tirzepatide. The highest tirzepatide dose pushed 86% of patients below the 7% mark, compared with 79% on semaglutide, and the top tirzepatide dose resulted in 46% of patients getting their A1c below 5.7%, compared with 19% of patients on semaglutide.
The findings are “stunning, I must stay, and those results included that up to half of the patients treated with high doses of tirzepatide may reach A1c levels of less than 5.7%, which is really, really unheard of,” said Dr. Holst, professor of endocrinology and metabolism at the University of Copenhagen. Along with the “weight losses at the same time of up to 12% in that patient group, we are seeing some completely unexpected and really shocking and wonderful new advances in the therapy,” added Dr. Holst.
The safety profile of tirzepatide was roughly similar to semaglutide’s and to that other agents in the glucagonlike peptide-1 receptor agonist (GLP-1 RA) class. Concurrently with the report at the meeting, the results also appeared in an article published online in the New England Journal of Medicine.
An ‘impressive’ weight loss effect
Weight loss on tirzepatide was “impressive,” commented Katherine R. Tuttle, MD, a nephrologist affiliated with the University of Washington and executive director for research at Providence Health Care in Spokane, Wash. Another striking feature of tirzepatide’s weight-loss effect was that it did not plateau during the 40 weeks of the study, Dr. Tuttle noted in an accompanying editorial that accompanied the published report, a finding that suggests the potential for additional weight loss from continued treatment .
“The weight loss is remarkable,” commented Rodolfo J. Galindo, MD, an endocrinologist at Emory University, Atlanta. While incremental reduction of A1c on the order of less than 0.5% is helpful, incremental weight loss of more than 10 lbs on tirzepatide, compared with semaglutide “will likely be a tie-breaker” for many clinicians and patients to favor tirzepatide over semaglutide or another GLP-1 RA agent, he said in an interview. Dr. Galindo also cited other important factors that he predicted will drive decisions on using tirzepatide or a GLP-1 RA once tirzepatide reaches the U.S. market: relative cost, access, and tolerability.
The important issue of dose
But the edge that tirzepatide showed over semaglutide for weight loss did not occur on a completely level playing field. The 1 mg/week dose of semaglutide used as the comparator in SURPASS-2 was the maximum dose available at the time the study began, but in June 2021 the Food and Drug Administration approved a 2.4 mg/week dose (Wegovy) labeled specifically for weight loss. Dr. Tuttle cited the limitation this introduces in her editorial.
“The dose issue is important,” she wrote. The doses of tirzepatide and semaglutide compared in SURPASS-2 “were not comparable in terms of weight outcomes” given that prior evidence showed that the 2.4 mg/week semaglutide dose is more appropriate for weight loss.
Dr. Tuttle also cited other factors to consider when assessing tirzepatide compared with agents in the GLP-1 RA class.
Several GLP-1 RA agents, including semaglutide, have proven efficacy for reducing rates of atherosclerotic cardiovascular events and albuminuria, and they also slow decline in kidney function and progression of diabetic kidney disease. No details on the renal effects of tirzepatide appeared in the SURPASS-2 report. A press release from Lilly in May 2021 briefly mentioned results from a meta-analysis of several clinical studies of tirzepatide that showed a nonsignificant effect from tirzepatide on the incidence of major cardiovascular adverse events (death from cardiovascular or undetermined causes, MI, stroke, and hospitalization for unstable angina) relative to comparator groups. Results from a dedicated cardiovascular outcomes trial in high-risk patients treated with tirzepatide, SURPASS-CVOT, are not expected until 2024.
A further limitation of SURPASS-2 was the demographics of the enrolled population, which had a low (0.4%) enrollment rate of Black patients, and a high proportion (70%) of Hispanic patients, Dr. Tuttle observed.
Low rates of hypoglycemia
Another notable finding from SURPASS-2 was the low incidence of clinically significant hypoglycemic events (blood glucose levels less than 54 mg/dL), which occurred in 0.2%-1.7% of patients on tirzepatide, depending on their dose, and in 0.4% of patients on semaglutide. Two patients in the tirzepatide cohort had severe hypoglycemia.
These numbers are reassuring, said Dr. Galindo, and reflect the safety of tirzepatide’s dual, incretin-like mechanisms of action that make it a “twincretin.” The molecule acts as both a GLP-1 RA, and as glucose-dependent insulinotropic polypeptide, an incretin that stimulates insulin release when blood sugar is high but also increases glucagon levels when blood sugar levels are normal or low. This dual action may help explain the apparent increased potency tirzepatide showed for both A1c reduction and weight loss, compared with semaglutide, which acts only as a GLP-1 RA.
Some experts have cited the uncertainty introduced by the open-label design of SURPASS-2, a decision necessitated by the distinctly different delivery devices used for tirzepatide and semaglutide, explained Dr. Landó. But she highlighted that double blinding applied to the three different tirzepatide dosages tested in the trial. Dr. Landó said that Lilly plans to seek FDA approval for all three tested tirzepatide doses to give clinicians and patients flexibility in applying the treatment.
SURPASS-2 used a prolonged dose-escalation protocol designed to minimize gastrointestinal adverse effects that started patients on a 2.5 mg weekly dose that then increased by 2.5 mg increments every 4 weeks until patients reached their assigned target dose. This meant that patients did not begin receiving the 15-mg/week dose until halfway through the trial.
Several more tirzepatide trials
Reports from two other pivotal trials for tirzepatide also appeared as posters at the meeting. SURPASS-5 compared tirzepatide with placebo in 475 patients inadequately controlled with titrated insulin glargine (Lantus). SURPASS-3 randomized 1,444 patients to tirzepatide or titrated insulin degludec (Tresiba). In both studies treatment with tirzepatide led to significantly better reductions in A1c and in weight loss than the comparator treatments. Results from a third pivotal trial, SURPASS-1 which compared tirzepatide against placebo in 478 treatment-naive patients, will come in a report scheduled for the second day of the meeting.
The results from all the recent tirzepatide trials show a consistent benefit across the continuum of patients with type 2 diabetes regardless of whether it’s recent onset or well-established disease, said Dr. Landó.
The SURPASS studies were sponsored by Lilly, the company developing tirzepatide, and the reports include several authors who are Lilly employees. Dr. Landó is a Lilly employee and stockholder. Dr. Tuttle has been a consultant to Lilly and to Novo Nordisk, the company that markets semaglutide, as well as to AstraZeneca, Bayer, Boehringer Ingelheim, Gilead, and Janssen. She has also received travel expenses from Kyokawa Hakko Kirin, and research funding from Bayer, Goldfinch Bio, and Lilly. Dr. Galindo has been a consultant to Lilly and to Novo Nordisk, as well as to Abbott Diabetes Care, Sanofi, Valeritas, and Weight Watchers, and his institution has received grant support on his behalf from Lilly, Novo Nordisk and Dexcom. Dr. Holst had no disclosures.
FROM ADA 2021
FDA approves OTC antihistamine nasal spray
, making it the first nasal antihistamine available over the counter in the United States.
The 0.15% strength of azelastine hydrochloride nasal spray is now approved for nonprescription treatment of seasonal and perennial allergic rhinitis in adults and children 6 years of age or older, the agency said. The 0.1% strength remains a prescription product that is indicated in younger children.
The “approval provides individuals an option for a safe and effective nasal antihistamine without requiring the assistance of a health care provider,” Theresa M. Michele, MD, director of the office of nonprescription drugs in the FDA’s Center for Drug Evaluation and Research, said in a prepared statement.
The FDA granted the nonprescription approval to Bayer Healthcare LLC, which said in a press release that the nasal spray would be available in national mass retail locations starting in the first quarter of 2022.
Oral antihistamines such as cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) have been on store shelves for years. Azelastine 0.15% will be the first and only over-the-counter antihistamine for indoor and outdoor allergy relief in a nasal formulation, Bayer said.
An over-the-counter nasal antihistamine could be a better option for some allergy sufferers when compared with what is already over the counter, said Tracy Prematta, MD, a private practice allergist in Havertown, Pa.
“In general, I like the nasal antihistamines,” Dr. Prematta said in an interview. “They work quickly, whereas the nasal steroids don’t, and I think a lot of people who go to the drugstore looking for allergy relief are actually looking for something quick-acting.”
However, the cost of the over-the-counter azelastine may play a big role in whether patients go with the prescription or nonprescription option, according to Dr. Prematta.
Bayer has not yet set the price for nonprescription azelastine, a company spokesperson told this news organization.
The change in azelastine approval status happened through a regulatory process called an Rx-to-OTC switch. According to the FDA, products switched to nonprescription status need to have data demonstrating that they are safe and effective as self-medication when used as directed.
The product manufacturer has to show that consumers know how to use the drug safely and effectively without a health care professional supervising them, the FDA said.
The FDA considers the change in status for azelastine a partial Rx-to-OTC switch, since the 0.15% strength is now over the counter and the 0.1% strength remains a prescription product.
The 0.1% strength is indicated for perennial allergies in children 6 months to 6 years old, and seasonal allergies for children 2-6 years old, according to the FDA.
Drowsiness is a side effect of azelastine, the FDA said. According to prescribing information, consumers using the nasal spray need to be careful when driving or operating machinery, and should avoid alcohol.
Using the product with alcohol, sedatives, or tranquilizers may increase drowsiness, the agency added.
Sedation is also common with the oral antihistamines people take to treat their allergies, said Dr. Prematta, who added that patients may also complain of dry mouth, nose, or throat.
Although some allergy sufferers dislike the taste of antihistamine nasal spray, they can try to overcome that issue by tilting the head forward, pointing the tip of the nozzle toward the outside of the nose, and sniffing gently, Dr. Prematta said.
“That really minimizes what gets in the back of your throat, so taste becomes less of a problem,” she explained.
Dr. Prematta has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, making it the first nasal antihistamine available over the counter in the United States.
The 0.15% strength of azelastine hydrochloride nasal spray is now approved for nonprescription treatment of seasonal and perennial allergic rhinitis in adults and children 6 years of age or older, the agency said. The 0.1% strength remains a prescription product that is indicated in younger children.
The “approval provides individuals an option for a safe and effective nasal antihistamine without requiring the assistance of a health care provider,” Theresa M. Michele, MD, director of the office of nonprescription drugs in the FDA’s Center for Drug Evaluation and Research, said in a prepared statement.
The FDA granted the nonprescription approval to Bayer Healthcare LLC, which said in a press release that the nasal spray would be available in national mass retail locations starting in the first quarter of 2022.
Oral antihistamines such as cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) have been on store shelves for years. Azelastine 0.15% will be the first and only over-the-counter antihistamine for indoor and outdoor allergy relief in a nasal formulation, Bayer said.
An over-the-counter nasal antihistamine could be a better option for some allergy sufferers when compared with what is already over the counter, said Tracy Prematta, MD, a private practice allergist in Havertown, Pa.
“In general, I like the nasal antihistamines,” Dr. Prematta said in an interview. “They work quickly, whereas the nasal steroids don’t, and I think a lot of people who go to the drugstore looking for allergy relief are actually looking for something quick-acting.”
However, the cost of the over-the-counter azelastine may play a big role in whether patients go with the prescription or nonprescription option, according to Dr. Prematta.
Bayer has not yet set the price for nonprescription azelastine, a company spokesperson told this news organization.
The change in azelastine approval status happened through a regulatory process called an Rx-to-OTC switch. According to the FDA, products switched to nonprescription status need to have data demonstrating that they are safe and effective as self-medication when used as directed.
The product manufacturer has to show that consumers know how to use the drug safely and effectively without a health care professional supervising them, the FDA said.
The FDA considers the change in status for azelastine a partial Rx-to-OTC switch, since the 0.15% strength is now over the counter and the 0.1% strength remains a prescription product.
The 0.1% strength is indicated for perennial allergies in children 6 months to 6 years old, and seasonal allergies for children 2-6 years old, according to the FDA.
Drowsiness is a side effect of azelastine, the FDA said. According to prescribing information, consumers using the nasal spray need to be careful when driving or operating machinery, and should avoid alcohol.
Using the product with alcohol, sedatives, or tranquilizers may increase drowsiness, the agency added.
Sedation is also common with the oral antihistamines people take to treat their allergies, said Dr. Prematta, who added that patients may also complain of dry mouth, nose, or throat.
Although some allergy sufferers dislike the taste of antihistamine nasal spray, they can try to overcome that issue by tilting the head forward, pointing the tip of the nozzle toward the outside of the nose, and sniffing gently, Dr. Prematta said.
“That really minimizes what gets in the back of your throat, so taste becomes less of a problem,” she explained.
Dr. Prematta has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, making it the first nasal antihistamine available over the counter in the United States.
The 0.15% strength of azelastine hydrochloride nasal spray is now approved for nonprescription treatment of seasonal and perennial allergic rhinitis in adults and children 6 years of age or older, the agency said. The 0.1% strength remains a prescription product that is indicated in younger children.
The “approval provides individuals an option for a safe and effective nasal antihistamine without requiring the assistance of a health care provider,” Theresa M. Michele, MD, director of the office of nonprescription drugs in the FDA’s Center for Drug Evaluation and Research, said in a prepared statement.
The FDA granted the nonprescription approval to Bayer Healthcare LLC, which said in a press release that the nasal spray would be available in national mass retail locations starting in the first quarter of 2022.
Oral antihistamines such as cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) have been on store shelves for years. Azelastine 0.15% will be the first and only over-the-counter antihistamine for indoor and outdoor allergy relief in a nasal formulation, Bayer said.
An over-the-counter nasal antihistamine could be a better option for some allergy sufferers when compared with what is already over the counter, said Tracy Prematta, MD, a private practice allergist in Havertown, Pa.
“In general, I like the nasal antihistamines,” Dr. Prematta said in an interview. “They work quickly, whereas the nasal steroids don’t, and I think a lot of people who go to the drugstore looking for allergy relief are actually looking for something quick-acting.”
However, the cost of the over-the-counter azelastine may play a big role in whether patients go with the prescription or nonprescription option, according to Dr. Prematta.
Bayer has not yet set the price for nonprescription azelastine, a company spokesperson told this news organization.
The change in azelastine approval status happened through a regulatory process called an Rx-to-OTC switch. According to the FDA, products switched to nonprescription status need to have data demonstrating that they are safe and effective as self-medication when used as directed.
The product manufacturer has to show that consumers know how to use the drug safely and effectively without a health care professional supervising them, the FDA said.
The FDA considers the change in status for azelastine a partial Rx-to-OTC switch, since the 0.15% strength is now over the counter and the 0.1% strength remains a prescription product.
The 0.1% strength is indicated for perennial allergies in children 6 months to 6 years old, and seasonal allergies for children 2-6 years old, according to the FDA.
Drowsiness is a side effect of azelastine, the FDA said. According to prescribing information, consumers using the nasal spray need to be careful when driving or operating machinery, and should avoid alcohol.
Using the product with alcohol, sedatives, or tranquilizers may increase drowsiness, the agency added.
Sedation is also common with the oral antihistamines people take to treat their allergies, said Dr. Prematta, who added that patients may also complain of dry mouth, nose, or throat.
Although some allergy sufferers dislike the taste of antihistamine nasal spray, they can try to overcome that issue by tilting the head forward, pointing the tip of the nozzle toward the outside of the nose, and sniffing gently, Dr. Prematta said.
“That really minimizes what gets in the back of your throat, so taste becomes less of a problem,” she explained.
Dr. Prematta has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Promising HER2+/HR– breast cancer survival with de-escalated therapy
It may not be always necessary to approach the treatment of HER2-positive, hormone receptor–negative (HER2+/HR–) early breast cancer with added chemotherapy, survival results of a prospective multicenter randomized trial suggest.
In the ADAPT-HER2+/HR– trial, comparing a de-escalated 12-week neoadjuvant regimen consisting of dual HER2 blockade with trastuzumab (Herceptin) and pertuzumab (Perjeta) with or without weekly paclitaxel, the three-drug regimen was associated with high pathologic complete response(pCR) rates and excellent 5-year survival, irrespective of whether patients received additional chemotherapy, reported Nadia Harbeck, MD, PhD, of the University of Munich.
“Chemotherapy-free regimens are promising in highly sensitive tumors with early response, but future investigation of such chemotherapy-free regimens need to be focused on selected patients, like those with HER2 3+ tumors, non–basal-like tumors, those showing early response to the de-escalated therapy, and those with predictive RNA signatures such as immune signatures,” she said in an oral abstract session during the American Society of Clinical Oncology annual meeting (Abstract 503).
Under the WGS umbrella
The ADAPT HER2+/HR– trial (NCT01779206) is one of several conducted by the West German Study Group (WGS) on therapy for intrinsic breast cancer types.
In this study, 134 patients with HER2-positive, estrogen and progesterone receptor–negative tumors with no metastatic disease and good performance status were assigned on a 5:2 basis to neoadjuvant therapy with trastuzumab at a loading dose of 8 mg/kg for the first cycle followed by 6 mg/kg for subsequent cycles every 3 weeks x 4, plus pertuzumab at a loading dose of 840 mg followed by 420 mg every 3 weeks x 4 (92 patients), or to trastuzumab and pertuzumab at the same dose and schedule plus paclitaxel 80 mg/m2 once weekly for 12 weeks.
Patients had surgery within 3 weeks of the end of study therapy unless they did not have a histologically confirmed pCR, in which case they went on to receive standard neoadjuvant therapy prior to surgery.
Adjuvant therapy was performed according to national guidelines, although patients with a pCR after 12 weeks of study therapy could be spared from adjuvant chemotherapy at the investigator’s discretion.
Patients underwent biopsy at 3 weeks for therapy for early response assessment, defined as either a Ki67 decrease of at least 30% from baseline, or low cellularity (less than 500 invasive tumor cells).
First survival results
The investigators previously reported the primary pCR endpoint from the trial, which showed a rate of 90% after 12 weeks in the three-drug arm, and a “substantial and clinically meaningful” pCR rate of 34% after the trastuzumab plus pertuzumab alone.
At ASCO 2021, Dr. Harbeck reported the first survival data from the trial.
After a median follow-up of 59.9 months, there were no statistically significant differences between trial arms in either overall survival, invasive disease-free survival (iDFS), or distant disease-free survival (dDFS).
The 5-year iDFS rate in the three-drug arm was 98%, compared with 87% for the dual HER2 blockade-only arm, a difference that was not statistically significant.
The 5-year dDFS rates were 98% and 92% respectively. There were only seven dDFS events during follow-up, Dr. Harbeck noted.
There were only six deaths during follow-up, with overall survival rates of 98% in the paclitaxel-containing arm, and 94% in the anti-HER2 antibodies–only arm, a difference of one overall survival event, Dr. Harbeck said.
pCR counts
However, patients who did not have pathologic complete responses at the end of first-line de-escalated therapy had worse outcomes, with a 5-year iDFS rate of 82%, compared with 98% for patients who had achieved a pCR. This translated into a hazard ratio for invasive disease in patients with pCRs of 0.14 (P = .011).
This difference occurred despite the study requirement that all patients who did not have pCR after 12 weeks of initial therapy would receive additional chemotherapy.
Looking at the tumor subtype among patients in the paclitaxel-free arm to see whether they could identify predictors of early response, the researchers found a pCR rate of 36.5% among 85 patients with nonbasal tumors, but 0% among 7 patients with basal tumors.
The investigators identified a population of patients whose tumors could be considered nonsensitive to dual HER2 blockade alone: Those with basal tumors, those tumors with low immunohistochemical HER2 expression, and those without an early response to therapy on biopsy 3 weeks into initial therapy. Among 31 of the 92 patients in the dual HER2 arm who met this description, 2 had pCRs, Dr. Harbeck noted.
The 5-year iDFS rate among patients in the dual blockade–only arm with nonsensitive tumors was 79%, compared with 93% for patients with treatment-responsive types, although there were only 13 invasive events total in this arm.
“If we look at the whole trial population, the negative prognostic impact of what we termed nonsensitive tumors was even significant regarding dDFS, with a hazard ratio of about 5,” she said.
‘A consistent theme’
Invited discussant Lisa A. Carey, MD, ScM, of the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, noted that the trial was underpowered for outcomes, but that results nonetheless suggest that patients with strongly HER2-driven tumors might get comparable benefits from less chemotherapy.
“This trial included only hormone receptor–negative, HER2-positive tumors, and these we know are likely to be HER2-enriched in terms of subtype, about three-quarters of them,”she said.
The previously reported pCR rate of 90% in the paclitaxel-containing arm, with 80% of patients requiring no further chemotherapy, resulted in the excellent 5-year iDFS and dDFS in this group, despite the relatively highly clinical stage, with about 60% of patients having clinical stage 2 or higher tumors, and more than 40% being node positive.
The idea that pCR itself can predict which patients could be spared from more intensive chemotherapy “is starting to look like a consistent theme,” she said.
Dr. Carey pointed out that in the KRISTINE trial comparing the combination of trastuzumab emtansine (T-DM1) and pertuzumab with standard chemotherapy in patients with HER2-positive stage I-III breast cancer, although the experimental combination was associated with lower pCR rates and worse event-free survival, rates of iDFS/dDFS were virtually identical for patients in both arms who achieved a pCR.
“So the question is can pCR mean that we can either eliminate additional therapy,” she said, noting that the question is currently being addressed prospectively in two clinical trials, COMPASS-pCR and DECRESCENDO.
ADAPT HER2+/HR- is sponsored by F. Hoffman-La Roche. Dr. Harbeck disclosed institutional research funding from Roche/Genentech, as well as honoraria and consulting/advising for multiple companies. Dr. Carey disclosed institutional research funding and other relationships with various companies.
It may not be always necessary to approach the treatment of HER2-positive, hormone receptor–negative (HER2+/HR–) early breast cancer with added chemotherapy, survival results of a prospective multicenter randomized trial suggest.
In the ADAPT-HER2+/HR– trial, comparing a de-escalated 12-week neoadjuvant regimen consisting of dual HER2 blockade with trastuzumab (Herceptin) and pertuzumab (Perjeta) with or without weekly paclitaxel, the three-drug regimen was associated with high pathologic complete response(pCR) rates and excellent 5-year survival, irrespective of whether patients received additional chemotherapy, reported Nadia Harbeck, MD, PhD, of the University of Munich.
“Chemotherapy-free regimens are promising in highly sensitive tumors with early response, but future investigation of such chemotherapy-free regimens need to be focused on selected patients, like those with HER2 3+ tumors, non–basal-like tumors, those showing early response to the de-escalated therapy, and those with predictive RNA signatures such as immune signatures,” she said in an oral abstract session during the American Society of Clinical Oncology annual meeting (Abstract 503).
Under the WGS umbrella
The ADAPT HER2+/HR– trial (NCT01779206) is one of several conducted by the West German Study Group (WGS) on therapy for intrinsic breast cancer types.
In this study, 134 patients with HER2-positive, estrogen and progesterone receptor–negative tumors with no metastatic disease and good performance status were assigned on a 5:2 basis to neoadjuvant therapy with trastuzumab at a loading dose of 8 mg/kg for the first cycle followed by 6 mg/kg for subsequent cycles every 3 weeks x 4, plus pertuzumab at a loading dose of 840 mg followed by 420 mg every 3 weeks x 4 (92 patients), or to trastuzumab and pertuzumab at the same dose and schedule plus paclitaxel 80 mg/m2 once weekly for 12 weeks.
Patients had surgery within 3 weeks of the end of study therapy unless they did not have a histologically confirmed pCR, in which case they went on to receive standard neoadjuvant therapy prior to surgery.
Adjuvant therapy was performed according to national guidelines, although patients with a pCR after 12 weeks of study therapy could be spared from adjuvant chemotherapy at the investigator’s discretion.
Patients underwent biopsy at 3 weeks for therapy for early response assessment, defined as either a Ki67 decrease of at least 30% from baseline, or low cellularity (less than 500 invasive tumor cells).
First survival results
The investigators previously reported the primary pCR endpoint from the trial, which showed a rate of 90% after 12 weeks in the three-drug arm, and a “substantial and clinically meaningful” pCR rate of 34% after the trastuzumab plus pertuzumab alone.
At ASCO 2021, Dr. Harbeck reported the first survival data from the trial.
After a median follow-up of 59.9 months, there were no statistically significant differences between trial arms in either overall survival, invasive disease-free survival (iDFS), or distant disease-free survival (dDFS).
The 5-year iDFS rate in the three-drug arm was 98%, compared with 87% for the dual HER2 blockade-only arm, a difference that was not statistically significant.
The 5-year dDFS rates were 98% and 92% respectively. There were only seven dDFS events during follow-up, Dr. Harbeck noted.
There were only six deaths during follow-up, with overall survival rates of 98% in the paclitaxel-containing arm, and 94% in the anti-HER2 antibodies–only arm, a difference of one overall survival event, Dr. Harbeck said.
pCR counts
However, patients who did not have pathologic complete responses at the end of first-line de-escalated therapy had worse outcomes, with a 5-year iDFS rate of 82%, compared with 98% for patients who had achieved a pCR. This translated into a hazard ratio for invasive disease in patients with pCRs of 0.14 (P = .011).
This difference occurred despite the study requirement that all patients who did not have pCR after 12 weeks of initial therapy would receive additional chemotherapy.
Looking at the tumor subtype among patients in the paclitaxel-free arm to see whether they could identify predictors of early response, the researchers found a pCR rate of 36.5% among 85 patients with nonbasal tumors, but 0% among 7 patients with basal tumors.
The investigators identified a population of patients whose tumors could be considered nonsensitive to dual HER2 blockade alone: Those with basal tumors, those tumors with low immunohistochemical HER2 expression, and those without an early response to therapy on biopsy 3 weeks into initial therapy. Among 31 of the 92 patients in the dual HER2 arm who met this description, 2 had pCRs, Dr. Harbeck noted.
The 5-year iDFS rate among patients in the dual blockade–only arm with nonsensitive tumors was 79%, compared with 93% for patients with treatment-responsive types, although there were only 13 invasive events total in this arm.
“If we look at the whole trial population, the negative prognostic impact of what we termed nonsensitive tumors was even significant regarding dDFS, with a hazard ratio of about 5,” she said.
‘A consistent theme’
Invited discussant Lisa A. Carey, MD, ScM, of the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, noted that the trial was underpowered for outcomes, but that results nonetheless suggest that patients with strongly HER2-driven tumors might get comparable benefits from less chemotherapy.
“This trial included only hormone receptor–negative, HER2-positive tumors, and these we know are likely to be HER2-enriched in terms of subtype, about three-quarters of them,”she said.
The previously reported pCR rate of 90% in the paclitaxel-containing arm, with 80% of patients requiring no further chemotherapy, resulted in the excellent 5-year iDFS and dDFS in this group, despite the relatively highly clinical stage, with about 60% of patients having clinical stage 2 or higher tumors, and more than 40% being node positive.
The idea that pCR itself can predict which patients could be spared from more intensive chemotherapy “is starting to look like a consistent theme,” she said.
Dr. Carey pointed out that in the KRISTINE trial comparing the combination of trastuzumab emtansine (T-DM1) and pertuzumab with standard chemotherapy in patients with HER2-positive stage I-III breast cancer, although the experimental combination was associated with lower pCR rates and worse event-free survival, rates of iDFS/dDFS were virtually identical for patients in both arms who achieved a pCR.
“So the question is can pCR mean that we can either eliminate additional therapy,” she said, noting that the question is currently being addressed prospectively in two clinical trials, COMPASS-pCR and DECRESCENDO.
ADAPT HER2+/HR- is sponsored by F. Hoffman-La Roche. Dr. Harbeck disclosed institutional research funding from Roche/Genentech, as well as honoraria and consulting/advising for multiple companies. Dr. Carey disclosed institutional research funding and other relationships with various companies.
It may not be always necessary to approach the treatment of HER2-positive, hormone receptor–negative (HER2+/HR–) early breast cancer with added chemotherapy, survival results of a prospective multicenter randomized trial suggest.
In the ADAPT-HER2+/HR– trial, comparing a de-escalated 12-week neoadjuvant regimen consisting of dual HER2 blockade with trastuzumab (Herceptin) and pertuzumab (Perjeta) with or without weekly paclitaxel, the three-drug regimen was associated with high pathologic complete response(pCR) rates and excellent 5-year survival, irrespective of whether patients received additional chemotherapy, reported Nadia Harbeck, MD, PhD, of the University of Munich.
“Chemotherapy-free regimens are promising in highly sensitive tumors with early response, but future investigation of such chemotherapy-free regimens need to be focused on selected patients, like those with HER2 3+ tumors, non–basal-like tumors, those showing early response to the de-escalated therapy, and those with predictive RNA signatures such as immune signatures,” she said in an oral abstract session during the American Society of Clinical Oncology annual meeting (Abstract 503).
Under the WGS umbrella
The ADAPT HER2+/HR– trial (NCT01779206) is one of several conducted by the West German Study Group (WGS) on therapy for intrinsic breast cancer types.
In this study, 134 patients with HER2-positive, estrogen and progesterone receptor–negative tumors with no metastatic disease and good performance status were assigned on a 5:2 basis to neoadjuvant therapy with trastuzumab at a loading dose of 8 mg/kg for the first cycle followed by 6 mg/kg for subsequent cycles every 3 weeks x 4, plus pertuzumab at a loading dose of 840 mg followed by 420 mg every 3 weeks x 4 (92 patients), or to trastuzumab and pertuzumab at the same dose and schedule plus paclitaxel 80 mg/m2 once weekly for 12 weeks.
Patients had surgery within 3 weeks of the end of study therapy unless they did not have a histologically confirmed pCR, in which case they went on to receive standard neoadjuvant therapy prior to surgery.
Adjuvant therapy was performed according to national guidelines, although patients with a pCR after 12 weeks of study therapy could be spared from adjuvant chemotherapy at the investigator’s discretion.
Patients underwent biopsy at 3 weeks for therapy for early response assessment, defined as either a Ki67 decrease of at least 30% from baseline, or low cellularity (less than 500 invasive tumor cells).
First survival results
The investigators previously reported the primary pCR endpoint from the trial, which showed a rate of 90% after 12 weeks in the three-drug arm, and a “substantial and clinically meaningful” pCR rate of 34% after the trastuzumab plus pertuzumab alone.
At ASCO 2021, Dr. Harbeck reported the first survival data from the trial.
After a median follow-up of 59.9 months, there were no statistically significant differences between trial arms in either overall survival, invasive disease-free survival (iDFS), or distant disease-free survival (dDFS).
The 5-year iDFS rate in the three-drug arm was 98%, compared with 87% for the dual HER2 blockade-only arm, a difference that was not statistically significant.
The 5-year dDFS rates were 98% and 92% respectively. There were only seven dDFS events during follow-up, Dr. Harbeck noted.
There were only six deaths during follow-up, with overall survival rates of 98% in the paclitaxel-containing arm, and 94% in the anti-HER2 antibodies–only arm, a difference of one overall survival event, Dr. Harbeck said.
pCR counts
However, patients who did not have pathologic complete responses at the end of first-line de-escalated therapy had worse outcomes, with a 5-year iDFS rate of 82%, compared with 98% for patients who had achieved a pCR. This translated into a hazard ratio for invasive disease in patients with pCRs of 0.14 (P = .011).
This difference occurred despite the study requirement that all patients who did not have pCR after 12 weeks of initial therapy would receive additional chemotherapy.
Looking at the tumor subtype among patients in the paclitaxel-free arm to see whether they could identify predictors of early response, the researchers found a pCR rate of 36.5% among 85 patients with nonbasal tumors, but 0% among 7 patients with basal tumors.
The investigators identified a population of patients whose tumors could be considered nonsensitive to dual HER2 blockade alone: Those with basal tumors, those tumors with low immunohistochemical HER2 expression, and those without an early response to therapy on biopsy 3 weeks into initial therapy. Among 31 of the 92 patients in the dual HER2 arm who met this description, 2 had pCRs, Dr. Harbeck noted.
The 5-year iDFS rate among patients in the dual blockade–only arm with nonsensitive tumors was 79%, compared with 93% for patients with treatment-responsive types, although there were only 13 invasive events total in this arm.
“If we look at the whole trial population, the negative prognostic impact of what we termed nonsensitive tumors was even significant regarding dDFS, with a hazard ratio of about 5,” she said.
‘A consistent theme’
Invited discussant Lisa A. Carey, MD, ScM, of the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill, noted that the trial was underpowered for outcomes, but that results nonetheless suggest that patients with strongly HER2-driven tumors might get comparable benefits from less chemotherapy.
“This trial included only hormone receptor–negative, HER2-positive tumors, and these we know are likely to be HER2-enriched in terms of subtype, about three-quarters of them,”she said.
The previously reported pCR rate of 90% in the paclitaxel-containing arm, with 80% of patients requiring no further chemotherapy, resulted in the excellent 5-year iDFS and dDFS in this group, despite the relatively highly clinical stage, with about 60% of patients having clinical stage 2 or higher tumors, and more than 40% being node positive.
The idea that pCR itself can predict which patients could be spared from more intensive chemotherapy “is starting to look like a consistent theme,” she said.
Dr. Carey pointed out that in the KRISTINE trial comparing the combination of trastuzumab emtansine (T-DM1) and pertuzumab with standard chemotherapy in patients with HER2-positive stage I-III breast cancer, although the experimental combination was associated with lower pCR rates and worse event-free survival, rates of iDFS/dDFS were virtually identical for patients in both arms who achieved a pCR.
“So the question is can pCR mean that we can either eliminate additional therapy,” she said, noting that the question is currently being addressed prospectively in two clinical trials, COMPASS-pCR and DECRESCENDO.
ADAPT HER2+/HR- is sponsored by F. Hoffman-La Roche. Dr. Harbeck disclosed institutional research funding from Roche/Genentech, as well as honoraria and consulting/advising for multiple companies. Dr. Carey disclosed institutional research funding and other relationships with various companies.
FROM ASCO 2021
FDA: More metformin extended-release tablets recalled
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
FROM THE FOOD AND DRUG ADMINISTRATION
Surgical outcomes favor addition of nivolumab to neoadjuvant chemo in resectable lung cancers
The addition of nivolumab to neoadjuvant chemotherapy did not impede the feasibility or timing of surgery in patients with resectable lung cancer, according to results from the phase 3 CheckMate 816 trial.
Adding nivolumab to chemotherapy was tolerable and did not increase the rate of surgical complications, investigator Jonathan Spicer, FRCPC, MD, PhD, of McGill University, Montreal, said in his presentation at the annual meeting of the American Society of Clinical Oncology.
His presentation comes about 2 months after the reporting of primary endpoint results of CheckMate 816 (NCT02998528). CheckMate 816 demonstrated that adding nivolumab to neoadjuvant chemotherapy significantly improved pathological complete response (pCR) in patients with resectable non–small cell lung cancer (NSCLC), according to results presented earlier at the American Association for Cancer Research annual meeting.
“The safety and surgical outcome data reported thus far from CheckMate 816, along with significant improvement in pathological complete response, support nivolumab in combination with chemotherapy as an attractive neoadjuvant option for patients with resectable NSCLC,” said Dr. Spicer (Abstract 8503).
Building on previous experience
The CheckMate 816 study builds on extensive experience in advanced NSCLC that has consistently shown better outcomes, including overall survival, with combinations of chemotherapy and immuno-oncology (IO) agents, compared to chemotherapy alone, said discussant Valerie W. Rusch, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Rusch called out “salient and interesting results” regarding surgical management in CheckMate 816, including a lower rate of surgery cancellations and shorter surgical duration in the chemotherapy-plus-IO arm, compared to the chemotherapy-alone arm.
Furthermore, fewer patients required a pneumonectomy and more patients had a complete resection in the chemotherapy-plus-IO arm, compared to chemotherapy alone, she noted.
“These excellent surgical results, along with the data previously presented at AACR regarding the primary endpoint, help to establish a new standard of neoadjuvant care,” Dr. Rusch said in her presentation.
Study details
CheckMate 816 included 358 patients with newly diagnosed, resectable, stage IB-IIIA NSCLC, Eastern Cooperative Oncology Group (ECOG) performance status of 0-1, and no known EGFR mutations or ALK alterations. Patients were randomized to receive nivolumab and platinum-doublet chemotherapy (nivolumab/chemotherapy) or chemotherapy alone every 3 weeks, with surgery to be performed within 6 weeks of the last dose of neoadjuvant treatment.
The median age of patients was 64 years in the nivolumab/chemotherapy arm and 65 years in the chemotherapy-alone arm. About one-third of patients had ECOG performance status of one, and about half had squamous tumor histology, Dr. Spicer said in his report. Almost two-thirds of patients had stage IIIA disease.
In the study results previously presented at the AACR meeting, both pCR and major pathologic response were significantly better following neoadjuvant chemotherapy and IO treatment, compared to chemotherapy alone.
In the intention-to-treat analysis, 24.0% of patients treated with nivolumab/chemotherapy achieved a pCR, compared to 2.2% in the chemotherapy arm, amounting to an approximate 12-fold increase in pCR, Dr. Spicer said. Similarly, the rate of major pathologic response in the intention-to-treat analysis was 36.9% and 8.9% for the nivolumab/chemotherapy and chemotherapy arms, respectively.
Surgical results
In his ASCO presentation, Dr. Spicer reported that definitive surgery was canceled in 16% of patients in the nivolumab/chemotherapy arm, and 21% of the chemotherapy arm. Reasons for surgery cancellation generally included patients declining surgery, unresectable disease, and poor lung function. “Cancellation of surgery due to neoadjuvant therapy toxicity was rare,” Dr. Spicer said in his presentation.
Among patients who did proceed to surgery, the median duration of the procedure was 184 minutes in the nivolumab/chemotherapy arm and 217 minutes in the chemotherapy arm. That half-hour difference in favor of the combination arm suggests that the complexity of surgery was not increased by the addition of nivolumab, Dr. Spicer said.
Median time to surgery was about 5 weeks in both arms, which was “well within accepted standards for a neoadjuvant therapeutic approach,” Dr. Spicer said. Most delays beyond 6 weeks were due to administrative issues, and occurred in similar proportions (21% of the nivolumab/chemotherapy arm and 18% of the chemotherapy arm).
The addition of nivolumab to chemotherapy improved pCR rates regardless of baseline stage of disease, according to Dr. Spicer. Furthermore, the depth of pathological regression in the primary tumor was “dramatically different” across stage groupings, he said. Median residual viable tumor percentage in stage IB/II patients was 28% for nivolumab/chemotherapy and 79% for chemotherapy, and in stage IIIA patients, it was 8% for nivolumab/chemotherapy and 70% for chemotherapy.
Overall, thoracotomy was the most frequent surgical approach in this international phase 3 trial, Dr. Spicer said. However, among patients with stage IIIA disease, minimally invasive approaches were used 30% of the time in the nivolumab/chemotherapy arm and 19% in the chemotherapy arm. Conversely, the rate of conversion from a minimally invasive to open approach in patients with stage IIIA disease was 11% for nivolumab/chemotherapy and 20% for chemotherapy alone.
Lobectomy was more frequent in the nivolumab/chemotherapy arm (77%) compared to the chemotherapy arm (61%), a difference that Dr. Spicer described as clinically important. He said the difference appears to be attributable to a lower rate of pneumonectomy in the nivolumab/chemotherapy arm (17%) than in the chemotherapy arm (25%).
Despite less extensive lung resection being required, the rate of R0 resection was numerically higher in the nivolumab/chemotherapy arm (83%) than in the chemotherapy arm (78%), said Dr. Spicer.
Length of hospital stay was “within expected ranges” from geographic regions represented in the trial, Dr. Spicer said. Median length of stay was 4.0 and 6.0 days, respectively, for nivolumab/chemotherapy and chemotherapy alone in North America, 9.5 and 13.0 days in Europe, and 11.0 and 13.0 days in Asia.
Likewise, 90-day surgical complications were well within expected ranges, according to the investigator, with anemia, pain, and wound complications being the most commonly reported. Rates were generally similar between study arms, other than a twofold higher rate of pain in the chemotherapy arm, possibly due to the lower rate of minimally invasive surgery or higher rate of conversion to an open procedure, compared to the nivolumab/chemotherapy arm, he said.
Awaiting survival
Rates of 30- and 90-day mortality are expected to be evaluated when survival endpoints are available, according to Dr. Spicer. Beyond pCR rate, event-free survival is also a primary endpoint of the study, while overall survival is a secondary endpoint.
The study was supported by Bristol Myers Squibb. Dr. Spicer reported disclosures related to AstraZeneca, Bristol Myers Squibb Foundation, Merck, and Roche. Dr. Rusch reported research funding with Genelux and Genentech, and travel expenses from Intuitive Surgical.
The addition of nivolumab to neoadjuvant chemotherapy did not impede the feasibility or timing of surgery in patients with resectable lung cancer, according to results from the phase 3 CheckMate 816 trial.
Adding nivolumab to chemotherapy was tolerable and did not increase the rate of surgical complications, investigator Jonathan Spicer, FRCPC, MD, PhD, of McGill University, Montreal, said in his presentation at the annual meeting of the American Society of Clinical Oncology.
His presentation comes about 2 months after the reporting of primary endpoint results of CheckMate 816 (NCT02998528). CheckMate 816 demonstrated that adding nivolumab to neoadjuvant chemotherapy significantly improved pathological complete response (pCR) in patients with resectable non–small cell lung cancer (NSCLC), according to results presented earlier at the American Association for Cancer Research annual meeting.
“The safety and surgical outcome data reported thus far from CheckMate 816, along with significant improvement in pathological complete response, support nivolumab in combination with chemotherapy as an attractive neoadjuvant option for patients with resectable NSCLC,” said Dr. Spicer (Abstract 8503).
Building on previous experience
The CheckMate 816 study builds on extensive experience in advanced NSCLC that has consistently shown better outcomes, including overall survival, with combinations of chemotherapy and immuno-oncology (IO) agents, compared to chemotherapy alone, said discussant Valerie W. Rusch, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Rusch called out “salient and interesting results” regarding surgical management in CheckMate 816, including a lower rate of surgery cancellations and shorter surgical duration in the chemotherapy-plus-IO arm, compared to the chemotherapy-alone arm.
Furthermore, fewer patients required a pneumonectomy and more patients had a complete resection in the chemotherapy-plus-IO arm, compared to chemotherapy alone, she noted.
“These excellent surgical results, along with the data previously presented at AACR regarding the primary endpoint, help to establish a new standard of neoadjuvant care,” Dr. Rusch said in her presentation.
Study details
CheckMate 816 included 358 patients with newly diagnosed, resectable, stage IB-IIIA NSCLC, Eastern Cooperative Oncology Group (ECOG) performance status of 0-1, and no known EGFR mutations or ALK alterations. Patients were randomized to receive nivolumab and platinum-doublet chemotherapy (nivolumab/chemotherapy) or chemotherapy alone every 3 weeks, with surgery to be performed within 6 weeks of the last dose of neoadjuvant treatment.
The median age of patients was 64 years in the nivolumab/chemotherapy arm and 65 years in the chemotherapy-alone arm. About one-third of patients had ECOG performance status of one, and about half had squamous tumor histology, Dr. Spicer said in his report. Almost two-thirds of patients had stage IIIA disease.
In the study results previously presented at the AACR meeting, both pCR and major pathologic response were significantly better following neoadjuvant chemotherapy and IO treatment, compared to chemotherapy alone.
In the intention-to-treat analysis, 24.0% of patients treated with nivolumab/chemotherapy achieved a pCR, compared to 2.2% in the chemotherapy arm, amounting to an approximate 12-fold increase in pCR, Dr. Spicer said. Similarly, the rate of major pathologic response in the intention-to-treat analysis was 36.9% and 8.9% for the nivolumab/chemotherapy and chemotherapy arms, respectively.
Surgical results
In his ASCO presentation, Dr. Spicer reported that definitive surgery was canceled in 16% of patients in the nivolumab/chemotherapy arm, and 21% of the chemotherapy arm. Reasons for surgery cancellation generally included patients declining surgery, unresectable disease, and poor lung function. “Cancellation of surgery due to neoadjuvant therapy toxicity was rare,” Dr. Spicer said in his presentation.
Among patients who did proceed to surgery, the median duration of the procedure was 184 minutes in the nivolumab/chemotherapy arm and 217 minutes in the chemotherapy arm. That half-hour difference in favor of the combination arm suggests that the complexity of surgery was not increased by the addition of nivolumab, Dr. Spicer said.
Median time to surgery was about 5 weeks in both arms, which was “well within accepted standards for a neoadjuvant therapeutic approach,” Dr. Spicer said. Most delays beyond 6 weeks were due to administrative issues, and occurred in similar proportions (21% of the nivolumab/chemotherapy arm and 18% of the chemotherapy arm).
The addition of nivolumab to chemotherapy improved pCR rates regardless of baseline stage of disease, according to Dr. Spicer. Furthermore, the depth of pathological regression in the primary tumor was “dramatically different” across stage groupings, he said. Median residual viable tumor percentage in stage IB/II patients was 28% for nivolumab/chemotherapy and 79% for chemotherapy, and in stage IIIA patients, it was 8% for nivolumab/chemotherapy and 70% for chemotherapy.
Overall, thoracotomy was the most frequent surgical approach in this international phase 3 trial, Dr. Spicer said. However, among patients with stage IIIA disease, minimally invasive approaches were used 30% of the time in the nivolumab/chemotherapy arm and 19% in the chemotherapy arm. Conversely, the rate of conversion from a minimally invasive to open approach in patients with stage IIIA disease was 11% for nivolumab/chemotherapy and 20% for chemotherapy alone.
Lobectomy was more frequent in the nivolumab/chemotherapy arm (77%) compared to the chemotherapy arm (61%), a difference that Dr. Spicer described as clinically important. He said the difference appears to be attributable to a lower rate of pneumonectomy in the nivolumab/chemotherapy arm (17%) than in the chemotherapy arm (25%).
Despite less extensive lung resection being required, the rate of R0 resection was numerically higher in the nivolumab/chemotherapy arm (83%) than in the chemotherapy arm (78%), said Dr. Spicer.
Length of hospital stay was “within expected ranges” from geographic regions represented in the trial, Dr. Spicer said. Median length of stay was 4.0 and 6.0 days, respectively, for nivolumab/chemotherapy and chemotherapy alone in North America, 9.5 and 13.0 days in Europe, and 11.0 and 13.0 days in Asia.
Likewise, 90-day surgical complications were well within expected ranges, according to the investigator, with anemia, pain, and wound complications being the most commonly reported. Rates were generally similar between study arms, other than a twofold higher rate of pain in the chemotherapy arm, possibly due to the lower rate of minimally invasive surgery or higher rate of conversion to an open procedure, compared to the nivolumab/chemotherapy arm, he said.
Awaiting survival
Rates of 30- and 90-day mortality are expected to be evaluated when survival endpoints are available, according to Dr. Spicer. Beyond pCR rate, event-free survival is also a primary endpoint of the study, while overall survival is a secondary endpoint.
The study was supported by Bristol Myers Squibb. Dr. Spicer reported disclosures related to AstraZeneca, Bristol Myers Squibb Foundation, Merck, and Roche. Dr. Rusch reported research funding with Genelux and Genentech, and travel expenses from Intuitive Surgical.
The addition of nivolumab to neoadjuvant chemotherapy did not impede the feasibility or timing of surgery in patients with resectable lung cancer, according to results from the phase 3 CheckMate 816 trial.
Adding nivolumab to chemotherapy was tolerable and did not increase the rate of surgical complications, investigator Jonathan Spicer, FRCPC, MD, PhD, of McGill University, Montreal, said in his presentation at the annual meeting of the American Society of Clinical Oncology.
His presentation comes about 2 months after the reporting of primary endpoint results of CheckMate 816 (NCT02998528). CheckMate 816 demonstrated that adding nivolumab to neoadjuvant chemotherapy significantly improved pathological complete response (pCR) in patients with resectable non–small cell lung cancer (NSCLC), according to results presented earlier at the American Association for Cancer Research annual meeting.
“The safety and surgical outcome data reported thus far from CheckMate 816, along with significant improvement in pathological complete response, support nivolumab in combination with chemotherapy as an attractive neoadjuvant option for patients with resectable NSCLC,” said Dr. Spicer (Abstract 8503).
Building on previous experience
The CheckMate 816 study builds on extensive experience in advanced NSCLC that has consistently shown better outcomes, including overall survival, with combinations of chemotherapy and immuno-oncology (IO) agents, compared to chemotherapy alone, said discussant Valerie W. Rusch, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Rusch called out “salient and interesting results” regarding surgical management in CheckMate 816, including a lower rate of surgery cancellations and shorter surgical duration in the chemotherapy-plus-IO arm, compared to the chemotherapy-alone arm.
Furthermore, fewer patients required a pneumonectomy and more patients had a complete resection in the chemotherapy-plus-IO arm, compared to chemotherapy alone, she noted.
“These excellent surgical results, along with the data previously presented at AACR regarding the primary endpoint, help to establish a new standard of neoadjuvant care,” Dr. Rusch said in her presentation.
Study details
CheckMate 816 included 358 patients with newly diagnosed, resectable, stage IB-IIIA NSCLC, Eastern Cooperative Oncology Group (ECOG) performance status of 0-1, and no known EGFR mutations or ALK alterations. Patients were randomized to receive nivolumab and platinum-doublet chemotherapy (nivolumab/chemotherapy) or chemotherapy alone every 3 weeks, with surgery to be performed within 6 weeks of the last dose of neoadjuvant treatment.
The median age of patients was 64 years in the nivolumab/chemotherapy arm and 65 years in the chemotherapy-alone arm. About one-third of patients had ECOG performance status of one, and about half had squamous tumor histology, Dr. Spicer said in his report. Almost two-thirds of patients had stage IIIA disease.
In the study results previously presented at the AACR meeting, both pCR and major pathologic response were significantly better following neoadjuvant chemotherapy and IO treatment, compared to chemotherapy alone.
In the intention-to-treat analysis, 24.0% of patients treated with nivolumab/chemotherapy achieved a pCR, compared to 2.2% in the chemotherapy arm, amounting to an approximate 12-fold increase in pCR, Dr. Spicer said. Similarly, the rate of major pathologic response in the intention-to-treat analysis was 36.9% and 8.9% for the nivolumab/chemotherapy and chemotherapy arms, respectively.
Surgical results
In his ASCO presentation, Dr. Spicer reported that definitive surgery was canceled in 16% of patients in the nivolumab/chemotherapy arm, and 21% of the chemotherapy arm. Reasons for surgery cancellation generally included patients declining surgery, unresectable disease, and poor lung function. “Cancellation of surgery due to neoadjuvant therapy toxicity was rare,” Dr. Spicer said in his presentation.
Among patients who did proceed to surgery, the median duration of the procedure was 184 minutes in the nivolumab/chemotherapy arm and 217 minutes in the chemotherapy arm. That half-hour difference in favor of the combination arm suggests that the complexity of surgery was not increased by the addition of nivolumab, Dr. Spicer said.
Median time to surgery was about 5 weeks in both arms, which was “well within accepted standards for a neoadjuvant therapeutic approach,” Dr. Spicer said. Most delays beyond 6 weeks were due to administrative issues, and occurred in similar proportions (21% of the nivolumab/chemotherapy arm and 18% of the chemotherapy arm).
The addition of nivolumab to chemotherapy improved pCR rates regardless of baseline stage of disease, according to Dr. Spicer. Furthermore, the depth of pathological regression in the primary tumor was “dramatically different” across stage groupings, he said. Median residual viable tumor percentage in stage IB/II patients was 28% for nivolumab/chemotherapy and 79% for chemotherapy, and in stage IIIA patients, it was 8% for nivolumab/chemotherapy and 70% for chemotherapy.
Overall, thoracotomy was the most frequent surgical approach in this international phase 3 trial, Dr. Spicer said. However, among patients with stage IIIA disease, minimally invasive approaches were used 30% of the time in the nivolumab/chemotherapy arm and 19% in the chemotherapy arm. Conversely, the rate of conversion from a minimally invasive to open approach in patients with stage IIIA disease was 11% for nivolumab/chemotherapy and 20% for chemotherapy alone.
Lobectomy was more frequent in the nivolumab/chemotherapy arm (77%) compared to the chemotherapy arm (61%), a difference that Dr. Spicer described as clinically important. He said the difference appears to be attributable to a lower rate of pneumonectomy in the nivolumab/chemotherapy arm (17%) than in the chemotherapy arm (25%).
Despite less extensive lung resection being required, the rate of R0 resection was numerically higher in the nivolumab/chemotherapy arm (83%) than in the chemotherapy arm (78%), said Dr. Spicer.
Length of hospital stay was “within expected ranges” from geographic regions represented in the trial, Dr. Spicer said. Median length of stay was 4.0 and 6.0 days, respectively, for nivolumab/chemotherapy and chemotherapy alone in North America, 9.5 and 13.0 days in Europe, and 11.0 and 13.0 days in Asia.
Likewise, 90-day surgical complications were well within expected ranges, according to the investigator, with anemia, pain, and wound complications being the most commonly reported. Rates were generally similar between study arms, other than a twofold higher rate of pain in the chemotherapy arm, possibly due to the lower rate of minimally invasive surgery or higher rate of conversion to an open procedure, compared to the nivolumab/chemotherapy arm, he said.
Awaiting survival
Rates of 30- and 90-day mortality are expected to be evaluated when survival endpoints are available, according to Dr. Spicer. Beyond pCR rate, event-free survival is also a primary endpoint of the study, while overall survival is a secondary endpoint.
The study was supported by Bristol Myers Squibb. Dr. Spicer reported disclosures related to AstraZeneca, Bristol Myers Squibb Foundation, Merck, and Roche. Dr. Rusch reported research funding with Genelux and Genentech, and travel expenses from Intuitive Surgical.
FROM ASCO 2021
Schizophrenia meds a key contributor to cognitive impairment
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.