User login
Stable, long-term opioid therapy safer than tapering?
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
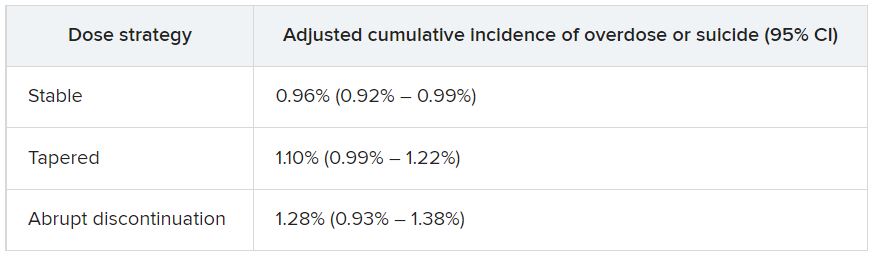
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
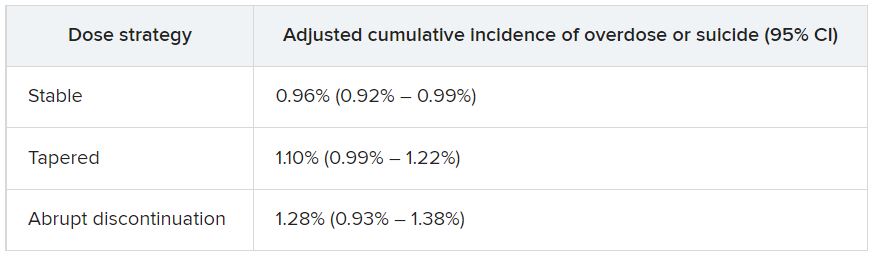
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
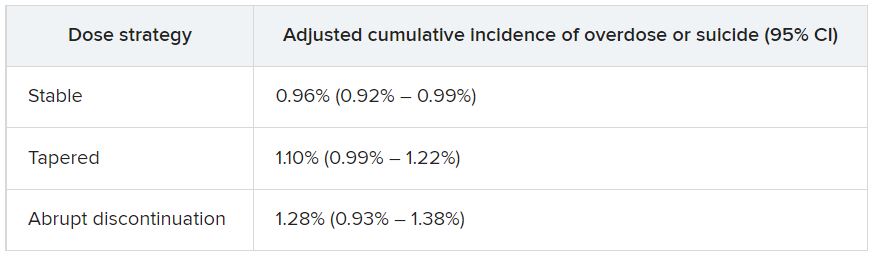
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
TikTok’s impact on adolescent mental health
For younger generations, TikTok is a go-to site for those who like short and catchy video clips. As a social media platform that allows concise video sharing, TikTok has over 1 billion monthly global users. Because of its platform size, a plethora of resources, and influence on media discourse, TikTok is the place for content creators to share visual media. Its cursory, condensed content delivery with videos capped at 1-minute focuses on high-yield information and rapid identification of fundamental points that are both engaging and entertaining.
Currently, on TikTok, 40 billion views are associated with the hashtag #mentalhealth. Content creators and regular users are employing this platform to share their own experiences, opinions, and strategies to overcome their struggles. While it is understandable for creators to share their personal stories that may be abusive, traumatic, or violent, they may not be prepared for their video to “go viral.”
Like any other social media platform, hateful speech such as racism, sexism, or xenophobia can accumulate on TikTok, which may cause more self-harm than self-help. Oversharing about personal strategies may lead to misconceived advice for TikTok viewers, while watching these TikTok videos can have negative mental health effects, even though there are no malicious intentions behind the creators who post these videos.
Hence, public health should pay more attention to the potential health-related implications this platform can create, as the quality of the information and the qualifications of the creators are mostly unrevealed. The concerns include undisclosed conflicts of interest, unchecked spread of misinformation, difficulty identifying source credibility, and excessive false information that viewers must filter through.1,2
Individual TikTok users may follow accounts and interpret these content creators as therapists and the content they see as therapy. They may also believe that a close relationship with the content creator exists when it does not. Specifically, these relationships may be defined as parasocial relationships, which are one-sided relationships where one person (the TikTok viewer) extends emotional energy, interest, and time, and the other party (the content creator) is completely unaware of the other’s existence.3 Additionally, Americans who are uninsured/underinsured may turn to this diluted version of therapy to compensate for the one-on-one or group therapy they need.
While TikTok may seem like a dangerous platform to browse through or post on, its growing influence cannot be underestimated. With 41% of TikTok users between the ages of 16 and 24, this is an ideal platform to disseminate public health information pertaining to this age group (for example, safe sex practices, substance abuse, and mental health issues).4 Because younger generations have incorporated social media into their daily lives, the medical community can harness TikTok’s potential to disseminate accurate information to potential patients for targeted medical education.
For example, Jake Goodman, MD, MBA, and Melissa Shepard, MD, each have more than a million TikTok followers and are notable psychiatrists who post a variety of content ranging from recognizing signs of depression to reducing stigma around mental health. Similarly, Justin Puder, PhD, is a licensed psychologist who advocates for ways to overcome mental health issues. By creating diverse content with appealing strategies, spreading accurate medical knowledge, and answering common medical questions for the public, these ‘mental health influencers’ educate potential patients to create patient-centered interactions.
While there are many pros and cons to social media platforms, it is undeniable that these platforms – such as TikTok – are here to stay. It is crucial for members of the medical community to recognize the outlets that younger generations use to express themselves and to exploit these media channels therapeutically.
Ms. Wong is a fourth-year medical student at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y. Dr. Chua is a psychiatrist with the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia, and assistant professor of clinical psychiatry at the University of Pennsylvania, also in Philadelphia.
References
1. Gottlieb M and Dyer S. Information and Disinformation: Social Media in the COVID-19 Crisis. Acad Emerg Med. 2020 Jul;27(7):640-1. doi: 10.1111/acem.14036.
2. De Veirman M et al. Front Psychol. 2019;10:2685. doi: 10.3389/fpsyg.2019.02685.
3. Bennett N-K et al. “Parasocial Relationships: The Nature of Celebrity Fascinations.” National Register of Health Service Psychologists. https://www.findapsychologist.org/parasocial-relationships-the-nature-of-celebrity-fascinations/.
4. Eghtesadi M and Florea A. Can J Public Health. 2020 Jun;111(3):389-91. doi: 10.17269/s41997-020-00343-0.
For younger generations, TikTok is a go-to site for those who like short and catchy video clips. As a social media platform that allows concise video sharing, TikTok has over 1 billion monthly global users. Because of its platform size, a plethora of resources, and influence on media discourse, TikTok is the place for content creators to share visual media. Its cursory, condensed content delivery with videos capped at 1-minute focuses on high-yield information and rapid identification of fundamental points that are both engaging and entertaining.
Currently, on TikTok, 40 billion views are associated with the hashtag #mentalhealth. Content creators and regular users are employing this platform to share their own experiences, opinions, and strategies to overcome their struggles. While it is understandable for creators to share their personal stories that may be abusive, traumatic, or violent, they may not be prepared for their video to “go viral.”
Like any other social media platform, hateful speech such as racism, sexism, or xenophobia can accumulate on TikTok, which may cause more self-harm than self-help. Oversharing about personal strategies may lead to misconceived advice for TikTok viewers, while watching these TikTok videos can have negative mental health effects, even though there are no malicious intentions behind the creators who post these videos.
Hence, public health should pay more attention to the potential health-related implications this platform can create, as the quality of the information and the qualifications of the creators are mostly unrevealed. The concerns include undisclosed conflicts of interest, unchecked spread of misinformation, difficulty identifying source credibility, and excessive false information that viewers must filter through.1,2
Individual TikTok users may follow accounts and interpret these content creators as therapists and the content they see as therapy. They may also believe that a close relationship with the content creator exists when it does not. Specifically, these relationships may be defined as parasocial relationships, which are one-sided relationships where one person (the TikTok viewer) extends emotional energy, interest, and time, and the other party (the content creator) is completely unaware of the other’s existence.3 Additionally, Americans who are uninsured/underinsured may turn to this diluted version of therapy to compensate for the one-on-one or group therapy they need.
While TikTok may seem like a dangerous platform to browse through or post on, its growing influence cannot be underestimated. With 41% of TikTok users between the ages of 16 and 24, this is an ideal platform to disseminate public health information pertaining to this age group (for example, safe sex practices, substance abuse, and mental health issues).4 Because younger generations have incorporated social media into their daily lives, the medical community can harness TikTok’s potential to disseminate accurate information to potential patients for targeted medical education.
For example, Jake Goodman, MD, MBA, and Melissa Shepard, MD, each have more than a million TikTok followers and are notable psychiatrists who post a variety of content ranging from recognizing signs of depression to reducing stigma around mental health. Similarly, Justin Puder, PhD, is a licensed psychologist who advocates for ways to overcome mental health issues. By creating diverse content with appealing strategies, spreading accurate medical knowledge, and answering common medical questions for the public, these ‘mental health influencers’ educate potential patients to create patient-centered interactions.
While there are many pros and cons to social media platforms, it is undeniable that these platforms – such as TikTok – are here to stay. It is crucial for members of the medical community to recognize the outlets that younger generations use to express themselves and to exploit these media channels therapeutically.
Ms. Wong is a fourth-year medical student at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y. Dr. Chua is a psychiatrist with the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia, and assistant professor of clinical psychiatry at the University of Pennsylvania, also in Philadelphia.
References
1. Gottlieb M and Dyer S. Information and Disinformation: Social Media in the COVID-19 Crisis. Acad Emerg Med. 2020 Jul;27(7):640-1. doi: 10.1111/acem.14036.
2. De Veirman M et al. Front Psychol. 2019;10:2685. doi: 10.3389/fpsyg.2019.02685.
3. Bennett N-K et al. “Parasocial Relationships: The Nature of Celebrity Fascinations.” National Register of Health Service Psychologists. https://www.findapsychologist.org/parasocial-relationships-the-nature-of-celebrity-fascinations/.
4. Eghtesadi M and Florea A. Can J Public Health. 2020 Jun;111(3):389-91. doi: 10.17269/s41997-020-00343-0.
For younger generations, TikTok is a go-to site for those who like short and catchy video clips. As a social media platform that allows concise video sharing, TikTok has over 1 billion monthly global users. Because of its platform size, a plethora of resources, and influence on media discourse, TikTok is the place for content creators to share visual media. Its cursory, condensed content delivery with videos capped at 1-minute focuses on high-yield information and rapid identification of fundamental points that are both engaging and entertaining.
Currently, on TikTok, 40 billion views are associated with the hashtag #mentalhealth. Content creators and regular users are employing this platform to share their own experiences, opinions, and strategies to overcome their struggles. While it is understandable for creators to share their personal stories that may be abusive, traumatic, or violent, they may not be prepared for their video to “go viral.”
Like any other social media platform, hateful speech such as racism, sexism, or xenophobia can accumulate on TikTok, which may cause more self-harm than self-help. Oversharing about personal strategies may lead to misconceived advice for TikTok viewers, while watching these TikTok videos can have negative mental health effects, even though there are no malicious intentions behind the creators who post these videos.
Hence, public health should pay more attention to the potential health-related implications this platform can create, as the quality of the information and the qualifications of the creators are mostly unrevealed. The concerns include undisclosed conflicts of interest, unchecked spread of misinformation, difficulty identifying source credibility, and excessive false information that viewers must filter through.1,2
Individual TikTok users may follow accounts and interpret these content creators as therapists and the content they see as therapy. They may also believe that a close relationship with the content creator exists when it does not. Specifically, these relationships may be defined as parasocial relationships, which are one-sided relationships where one person (the TikTok viewer) extends emotional energy, interest, and time, and the other party (the content creator) is completely unaware of the other’s existence.3 Additionally, Americans who are uninsured/underinsured may turn to this diluted version of therapy to compensate for the one-on-one or group therapy they need.
While TikTok may seem like a dangerous platform to browse through or post on, its growing influence cannot be underestimated. With 41% of TikTok users between the ages of 16 and 24, this is an ideal platform to disseminate public health information pertaining to this age group (for example, safe sex practices, substance abuse, and mental health issues).4 Because younger generations have incorporated social media into their daily lives, the medical community can harness TikTok’s potential to disseminate accurate information to potential patients for targeted medical education.
For example, Jake Goodman, MD, MBA, and Melissa Shepard, MD, each have more than a million TikTok followers and are notable psychiatrists who post a variety of content ranging from recognizing signs of depression to reducing stigma around mental health. Similarly, Justin Puder, PhD, is a licensed psychologist who advocates for ways to overcome mental health issues. By creating diverse content with appealing strategies, spreading accurate medical knowledge, and answering common medical questions for the public, these ‘mental health influencers’ educate potential patients to create patient-centered interactions.
While there are many pros and cons to social media platforms, it is undeniable that these platforms – such as TikTok – are here to stay. It is crucial for members of the medical community to recognize the outlets that younger generations use to express themselves and to exploit these media channels therapeutically.
Ms. Wong is a fourth-year medical student at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y. Dr. Chua is a psychiatrist with the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia, and assistant professor of clinical psychiatry at the University of Pennsylvania, also in Philadelphia.
References
1. Gottlieb M and Dyer S. Information and Disinformation: Social Media in the COVID-19 Crisis. Acad Emerg Med. 2020 Jul;27(7):640-1. doi: 10.1111/acem.14036.
2. De Veirman M et al. Front Psychol. 2019;10:2685. doi: 10.3389/fpsyg.2019.02685.
3. Bennett N-K et al. “Parasocial Relationships: The Nature of Celebrity Fascinations.” National Register of Health Service Psychologists. https://www.findapsychologist.org/parasocial-relationships-the-nature-of-celebrity-fascinations/.
4. Eghtesadi M and Florea A. Can J Public Health. 2020 Jun;111(3):389-91. doi: 10.17269/s41997-020-00343-0.
Psychedelic drug therapy a potential ‘breakthrough’ for alcohol dependence
Results from the first randomized, placebo-controlled trial of psilocybin for alcohol dependence showed that during the 8 months after first treatment dose, participants who received psilocybin had less than half as many heavy drinking days as their counterparts who received placebo.
In addition, 7 months after the last dose of medication, twice as many psilocybin-treated patients as placebo-treated patients were abstinent.
The effects observed with psilocybin were “considerably larger” than those of currently approved treatments for AUD, senior investigator Michael Bogenschutz, MD, psychiatrist and director of the NYU Langone Center for Psychedelic Medicine, New York, said during an Aug. 24 press briefing.
If the findings hold up in future trials, psilocybin will be a “real breakthrough” in the treatment of the condition, Dr. Bogenschutz said.
The findings were published online in JAMA Psychiatry.
83% reduction in drinking days
The study included 93 adults (mean age, 46 years) with alcohol dependence who consumed an average of seven drinks on the days they drank and had had at least four heavy drinking days during the month prior to treatment.
Of the participants, 48 were randomly assigned to receive two doses of psilocybin, and 45 were assigned to receive an antihistamine (diphenhydramine) placebo. Study medication was administered during 2 day-long sessions at week 4 and week 8.
The participants also received 12 psychotherapy sessions over a 12-week period. All were assessed at intervals from the beginning of the study until 32 weeks after the first medication session.
The primary outcome was percentage of days in which the patient drank heavily during the 32-week period following first medication dose. Heavy drinking was defined as having five or more drinks in a day for a man and four or more drinks in a day for a woman.
The percentage of heavy drinking days during the 32-week period was 9.7% for the psilocybin group and 23.6% for the placebo group, for a mean difference of 13.9% (P = .01).
“Compared to their baseline before the study, after receiving medication, the psilocybin group decreased their heavy drinking days by 83%, while the placebo group reduced their heavy drinking by 51%,” Dr. Bogenschutz reported.
During the last month of follow-up, which was 7 months after the final dose of study medication, 48% of the psilocybin group were entirely abstinent vs. 24% of the placebo group.
“It is remarkable that the effects of psilocybin treatment persisted for 7 months after people received the last dose of medication. This suggests that psilocybin is treating the underlying disorder of alcohol addiction rather than merely treating symptoms,” Dr. Bogenschutz noted.
Total alcohol consumption and problems related to alcohol use were also significantly less in the psilocybin group.
‘Encouraged and hopeful’
Adverse events related to psilocybin were mostly mild, self-limiting, and consistent with other recent trials that evaluated the drug’s effects in various conditions.
However, the current investigators note that they implemented measures to ensure safety, including careful medical and psychiatric screening, therapy, and monitoring that was provided by well-trained therapists, including a licensed psychiatrist. In addition, medications were available to treat acute psychiatric reactions.
A cited limitation of the study was that blinding was not maintained because the average intensity of experience with psilocybin was high, whereas it was low with diphenhydramine.
This difference undermined the masking of treatment such that more than 90% of participants and therapists correctly guessed the treatment assignment.
Another limitation was that objective measures to validate self-reported drinking outcomes were available for only 54% of study participants.
Despite these limitations, the study builds on earlier work by the NYU team that showed that two doses of psilocybin taken over a period of 8 weeks significantly reduced alcohol use and cravings in patients with AUD.
“We’re very encouraged by these findings and hopeful about where they could lead. Personally, it’s been very meaningful and rewarding for me to do this work and inspiring to witness the remarkable recoveries that some of our participants have experienced,” Dr. Bogenschutz told briefing attendees.
Urgent need
The authors of an accompanying editorial note that novel medications for alcohol dependence are “sorely needed. Recent renewed interest in the potential of hallucinogens for treating psychiatric disorders, including AUD, represents a potential move in that direction.”
Henry Kranzler, MD, and Emily Hartwell, PhD, both with the Center for Studies of Addiction, University of Pennsylvania, Philadelphia, write that the new findings “underscore the potential of developing psilocybin as an addition to the alcohol treatment pharmacopeia.”
They question, however, the feasibility of using hallucinogens in routine clinical practice because intensive psychotherapy, such as that provided in this study, requires a significant investment of time and labor.
“Such concomitant therapy, if necessary to realize the therapeutic benefits of psilocybin for treating AUD, could limit its uptake by clinicians,” Dr. Kranzler and Dr. Hartwell write.
The study was funded by the Heffter Research Institute and by individual donations from Carey and Claudia Turnbull, Dr. Efrem Nulman, Rodrigo Niño, and Cody Swift. Dr. Bogenschutz reports having received research funds from and serving as a consultant to Mind Medicine, the Multidisciplinary Association for Psychedelic Studies, B. More, AJNA Labs, Beckley Psytech, Journey Colab, and Bright Minds Biosciences. Dr. Kranzler and Dr. Hartwell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the first randomized, placebo-controlled trial of psilocybin for alcohol dependence showed that during the 8 months after first treatment dose, participants who received psilocybin had less than half as many heavy drinking days as their counterparts who received placebo.
In addition, 7 months after the last dose of medication, twice as many psilocybin-treated patients as placebo-treated patients were abstinent.
The effects observed with psilocybin were “considerably larger” than those of currently approved treatments for AUD, senior investigator Michael Bogenschutz, MD, psychiatrist and director of the NYU Langone Center for Psychedelic Medicine, New York, said during an Aug. 24 press briefing.
If the findings hold up in future trials, psilocybin will be a “real breakthrough” in the treatment of the condition, Dr. Bogenschutz said.
The findings were published online in JAMA Psychiatry.
83% reduction in drinking days
The study included 93 adults (mean age, 46 years) with alcohol dependence who consumed an average of seven drinks on the days they drank and had had at least four heavy drinking days during the month prior to treatment.
Of the participants, 48 were randomly assigned to receive two doses of psilocybin, and 45 were assigned to receive an antihistamine (diphenhydramine) placebo. Study medication was administered during 2 day-long sessions at week 4 and week 8.
The participants also received 12 psychotherapy sessions over a 12-week period. All were assessed at intervals from the beginning of the study until 32 weeks after the first medication session.
The primary outcome was percentage of days in which the patient drank heavily during the 32-week period following first medication dose. Heavy drinking was defined as having five or more drinks in a day for a man and four or more drinks in a day for a woman.
The percentage of heavy drinking days during the 32-week period was 9.7% for the psilocybin group and 23.6% for the placebo group, for a mean difference of 13.9% (P = .01).
“Compared to their baseline before the study, after receiving medication, the psilocybin group decreased their heavy drinking days by 83%, while the placebo group reduced their heavy drinking by 51%,” Dr. Bogenschutz reported.
During the last month of follow-up, which was 7 months after the final dose of study medication, 48% of the psilocybin group were entirely abstinent vs. 24% of the placebo group.
“It is remarkable that the effects of psilocybin treatment persisted for 7 months after people received the last dose of medication. This suggests that psilocybin is treating the underlying disorder of alcohol addiction rather than merely treating symptoms,” Dr. Bogenschutz noted.
Total alcohol consumption and problems related to alcohol use were also significantly less in the psilocybin group.
‘Encouraged and hopeful’
Adverse events related to psilocybin were mostly mild, self-limiting, and consistent with other recent trials that evaluated the drug’s effects in various conditions.
However, the current investigators note that they implemented measures to ensure safety, including careful medical and psychiatric screening, therapy, and monitoring that was provided by well-trained therapists, including a licensed psychiatrist. In addition, medications were available to treat acute psychiatric reactions.
A cited limitation of the study was that blinding was not maintained because the average intensity of experience with psilocybin was high, whereas it was low with diphenhydramine.
This difference undermined the masking of treatment such that more than 90% of participants and therapists correctly guessed the treatment assignment.
Another limitation was that objective measures to validate self-reported drinking outcomes were available for only 54% of study participants.
Despite these limitations, the study builds on earlier work by the NYU team that showed that two doses of psilocybin taken over a period of 8 weeks significantly reduced alcohol use and cravings in patients with AUD.
“We’re very encouraged by these findings and hopeful about where they could lead. Personally, it’s been very meaningful and rewarding for me to do this work and inspiring to witness the remarkable recoveries that some of our participants have experienced,” Dr. Bogenschutz told briefing attendees.
Urgent need
The authors of an accompanying editorial note that novel medications for alcohol dependence are “sorely needed. Recent renewed interest in the potential of hallucinogens for treating psychiatric disorders, including AUD, represents a potential move in that direction.”
Henry Kranzler, MD, and Emily Hartwell, PhD, both with the Center for Studies of Addiction, University of Pennsylvania, Philadelphia, write that the new findings “underscore the potential of developing psilocybin as an addition to the alcohol treatment pharmacopeia.”
They question, however, the feasibility of using hallucinogens in routine clinical practice because intensive psychotherapy, such as that provided in this study, requires a significant investment of time and labor.
“Such concomitant therapy, if necessary to realize the therapeutic benefits of psilocybin for treating AUD, could limit its uptake by clinicians,” Dr. Kranzler and Dr. Hartwell write.
The study was funded by the Heffter Research Institute and by individual donations from Carey and Claudia Turnbull, Dr. Efrem Nulman, Rodrigo Niño, and Cody Swift. Dr. Bogenschutz reports having received research funds from and serving as a consultant to Mind Medicine, the Multidisciplinary Association for Psychedelic Studies, B. More, AJNA Labs, Beckley Psytech, Journey Colab, and Bright Minds Biosciences. Dr. Kranzler and Dr. Hartwell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the first randomized, placebo-controlled trial of psilocybin for alcohol dependence showed that during the 8 months after first treatment dose, participants who received psilocybin had less than half as many heavy drinking days as their counterparts who received placebo.
In addition, 7 months after the last dose of medication, twice as many psilocybin-treated patients as placebo-treated patients were abstinent.
The effects observed with psilocybin were “considerably larger” than those of currently approved treatments for AUD, senior investigator Michael Bogenschutz, MD, psychiatrist and director of the NYU Langone Center for Psychedelic Medicine, New York, said during an Aug. 24 press briefing.
If the findings hold up in future trials, psilocybin will be a “real breakthrough” in the treatment of the condition, Dr. Bogenschutz said.
The findings were published online in JAMA Psychiatry.
83% reduction in drinking days
The study included 93 adults (mean age, 46 years) with alcohol dependence who consumed an average of seven drinks on the days they drank and had had at least four heavy drinking days during the month prior to treatment.
Of the participants, 48 were randomly assigned to receive two doses of psilocybin, and 45 were assigned to receive an antihistamine (diphenhydramine) placebo. Study medication was administered during 2 day-long sessions at week 4 and week 8.
The participants also received 12 psychotherapy sessions over a 12-week period. All were assessed at intervals from the beginning of the study until 32 weeks after the first medication session.
The primary outcome was percentage of days in which the patient drank heavily during the 32-week period following first medication dose. Heavy drinking was defined as having five or more drinks in a day for a man and four or more drinks in a day for a woman.
The percentage of heavy drinking days during the 32-week period was 9.7% for the psilocybin group and 23.6% for the placebo group, for a mean difference of 13.9% (P = .01).
“Compared to their baseline before the study, after receiving medication, the psilocybin group decreased their heavy drinking days by 83%, while the placebo group reduced their heavy drinking by 51%,” Dr. Bogenschutz reported.
During the last month of follow-up, which was 7 months after the final dose of study medication, 48% of the psilocybin group were entirely abstinent vs. 24% of the placebo group.
“It is remarkable that the effects of psilocybin treatment persisted for 7 months after people received the last dose of medication. This suggests that psilocybin is treating the underlying disorder of alcohol addiction rather than merely treating symptoms,” Dr. Bogenschutz noted.
Total alcohol consumption and problems related to alcohol use were also significantly less in the psilocybin group.
‘Encouraged and hopeful’
Adverse events related to psilocybin were mostly mild, self-limiting, and consistent with other recent trials that evaluated the drug’s effects in various conditions.
However, the current investigators note that they implemented measures to ensure safety, including careful medical and psychiatric screening, therapy, and monitoring that was provided by well-trained therapists, including a licensed psychiatrist. In addition, medications were available to treat acute psychiatric reactions.
A cited limitation of the study was that blinding was not maintained because the average intensity of experience with psilocybin was high, whereas it was low with diphenhydramine.
This difference undermined the masking of treatment such that more than 90% of participants and therapists correctly guessed the treatment assignment.
Another limitation was that objective measures to validate self-reported drinking outcomes were available for only 54% of study participants.
Despite these limitations, the study builds on earlier work by the NYU team that showed that two doses of psilocybin taken over a period of 8 weeks significantly reduced alcohol use and cravings in patients with AUD.
“We’re very encouraged by these findings and hopeful about where they could lead. Personally, it’s been very meaningful and rewarding for me to do this work and inspiring to witness the remarkable recoveries that some of our participants have experienced,” Dr. Bogenschutz told briefing attendees.
Urgent need
The authors of an accompanying editorial note that novel medications for alcohol dependence are “sorely needed. Recent renewed interest in the potential of hallucinogens for treating psychiatric disorders, including AUD, represents a potential move in that direction.”
Henry Kranzler, MD, and Emily Hartwell, PhD, both with the Center for Studies of Addiction, University of Pennsylvania, Philadelphia, write that the new findings “underscore the potential of developing psilocybin as an addition to the alcohol treatment pharmacopeia.”
They question, however, the feasibility of using hallucinogens in routine clinical practice because intensive psychotherapy, such as that provided in this study, requires a significant investment of time and labor.
“Such concomitant therapy, if necessary to realize the therapeutic benefits of psilocybin for treating AUD, could limit its uptake by clinicians,” Dr. Kranzler and Dr. Hartwell write.
The study was funded by the Heffter Research Institute and by individual donations from Carey and Claudia Turnbull, Dr. Efrem Nulman, Rodrigo Niño, and Cody Swift. Dr. Bogenschutz reports having received research funds from and serving as a consultant to Mind Medicine, the Multidisciplinary Association for Psychedelic Studies, B. More, AJNA Labs, Beckley Psytech, Journey Colab, and Bright Minds Biosciences. Dr. Kranzler and Dr. Hartwell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Reducing alcohol intake may reduce cancer risk
Alcohol is a major preventable risk factor for cancer. New data suggest that reducing alcohol intake reduces the risk of developing an alcohol-related cancer.
The findings, from a large population-based study conducted in Korea, underscore the importance of encouraging individuals to quit drinking or to reduce alcohol consumption to help reduce cancer risk, the authors noted.
The study was published online in JAMA Network Open.
It provides evidence “suggesting that cancer risk can be meaningfully altered by changing the amount of alcoholic beverages consumed,” wrote the authors of an accompanying editorial, Neal D. Freedman, PhD, and Christian C. Abnet, PhD, of the division of cancer epidemiology and genetics at the National Cancer Institute, Rockville, Md.
they wrote, adding that a “well examined dose-response association has been reported, with highest risks observed among people who drink 3 alcoholic beverages per day and higher.”
The new study shows that a “reduction in use was associated with lower risk, particularly among participants who started drinking at a heavy level,” they noted.
Previous studies have estimated that alcohol use accounts for nearly 4% of newly diagnosed cancers worldwide and nearly 5% of U.S. cancer cases overall.
But the figures are much higher for some specific cancers. That same U.S. study found that alcohol accounts for at least 45% of oral cavity/pharyngeal cancers and at least 25% of laryngeal cancers, as well as 12.1% of female breast cancers, 11.1% of colorectal cancers, 10.5% of liver cancers, and 7.7% of esophageal cancers, as previously reported by this news organization.
New findings on reducing intake
This latest study involved an analysis of data on 4.5 million individuals who were adult beneficiaries of the Korean National Health Insurance Service. The median age of the participants was 53.6 years, and they underwent a national health screening in 2009 and 2011.
During median follow-up of 6.4 years, the cancer incidence rate was 7.7 per 1,000 person-years.
Information on alcohol consumption was collected from self-administered questionnaires completed during the health screenings. Participants were categorized on the basis of alcohol consumption: none (0 g/d), mild ( less than 15 g/d), moderate (15-29.9 g/d), and heavy (30 or more g/d).
Compared with those who sustained their alcohol consumption level during the study period, those who increased their level were at higher risk of alcohol-related cancers and all cancers, the investigators found.
The increase in alcohol-related cancer incidence was dose dependent: Those who changed from nondrinking to mild, moderate, or heavy drinking were at increasingly higher risk for alcohol-related cancer, compared with those who remained nondrinkers (adjusted hazard ratios [aHRs], 1.03, 1.10, and 1.34, respectively).
Participants who were mild drinkers at baseline and who quit drinking were at lower risk of alcohol-related cancer, compared with those whose drinking level was sustained (aHR, 0.96). Those with moderate or heavy drinking levels who quit drinking were at higher overall cancer risk than were those who sustained their drinking levels. However, this difference was negated when quitting was sustained, the authors noted.
For heavy drinkers who reduced their drinking levels, cancer incidence was reduced, compared with those who sustained heavy drinking levels. This was true for those who changed from heavy to moderate drinking (aHR, 0.91 for alcohol-related cancers; 0.96 for alcohol-related cancers) and those who changed from heavy to mild drinking (aHR, 0.92 for alcohol-related cancers and all cancers).
“Alcohol cessation and reduction should be reinforced for the prevention of cancer,” concluded the authors.
Implications and future directions
The editorialists noted that the study is limited by several factors, such as a short interval between assessments and relatively short follow-up. There is also no information on participants’ alcohol consumption earlier in life or about other healthy lifestyle changes during the study period. In addition, there is no mention of a genetic variant affecting aldehyde dehydrogenase that leads to alcohol-induced flushing, which is common among East Asians.
Despite of these limitations, the study provides “important new findings about the potential role of changes in alcohol consumption in cancer risk,” Dr. Freedman and Dr. Abnet noted. Future studies should examine the association between alcohol intake and cancer risk in other populations and use longer intervals between assessments, they suggested.
“Such studies are needed to move the field forward and inform public health guidance on cancer prevention,” the editorialists concluded.
The authors of the study and the editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alcohol is a major preventable risk factor for cancer. New data suggest that reducing alcohol intake reduces the risk of developing an alcohol-related cancer.
The findings, from a large population-based study conducted in Korea, underscore the importance of encouraging individuals to quit drinking or to reduce alcohol consumption to help reduce cancer risk, the authors noted.
The study was published online in JAMA Network Open.
It provides evidence “suggesting that cancer risk can be meaningfully altered by changing the amount of alcoholic beverages consumed,” wrote the authors of an accompanying editorial, Neal D. Freedman, PhD, and Christian C. Abnet, PhD, of the division of cancer epidemiology and genetics at the National Cancer Institute, Rockville, Md.
they wrote, adding that a “well examined dose-response association has been reported, with highest risks observed among people who drink 3 alcoholic beverages per day and higher.”
The new study shows that a “reduction in use was associated with lower risk, particularly among participants who started drinking at a heavy level,” they noted.
Previous studies have estimated that alcohol use accounts for nearly 4% of newly diagnosed cancers worldwide and nearly 5% of U.S. cancer cases overall.
But the figures are much higher for some specific cancers. That same U.S. study found that alcohol accounts for at least 45% of oral cavity/pharyngeal cancers and at least 25% of laryngeal cancers, as well as 12.1% of female breast cancers, 11.1% of colorectal cancers, 10.5% of liver cancers, and 7.7% of esophageal cancers, as previously reported by this news organization.
New findings on reducing intake
This latest study involved an analysis of data on 4.5 million individuals who were adult beneficiaries of the Korean National Health Insurance Service. The median age of the participants was 53.6 years, and they underwent a national health screening in 2009 and 2011.
During median follow-up of 6.4 years, the cancer incidence rate was 7.7 per 1,000 person-years.
Information on alcohol consumption was collected from self-administered questionnaires completed during the health screenings. Participants were categorized on the basis of alcohol consumption: none (0 g/d), mild ( less than 15 g/d), moderate (15-29.9 g/d), and heavy (30 or more g/d).
Compared with those who sustained their alcohol consumption level during the study period, those who increased their level were at higher risk of alcohol-related cancers and all cancers, the investigators found.
The increase in alcohol-related cancer incidence was dose dependent: Those who changed from nondrinking to mild, moderate, or heavy drinking were at increasingly higher risk for alcohol-related cancer, compared with those who remained nondrinkers (adjusted hazard ratios [aHRs], 1.03, 1.10, and 1.34, respectively).
Participants who were mild drinkers at baseline and who quit drinking were at lower risk of alcohol-related cancer, compared with those whose drinking level was sustained (aHR, 0.96). Those with moderate or heavy drinking levels who quit drinking were at higher overall cancer risk than were those who sustained their drinking levels. However, this difference was negated when quitting was sustained, the authors noted.
For heavy drinkers who reduced their drinking levels, cancer incidence was reduced, compared with those who sustained heavy drinking levels. This was true for those who changed from heavy to moderate drinking (aHR, 0.91 for alcohol-related cancers; 0.96 for alcohol-related cancers) and those who changed from heavy to mild drinking (aHR, 0.92 for alcohol-related cancers and all cancers).
“Alcohol cessation and reduction should be reinforced for the prevention of cancer,” concluded the authors.
Implications and future directions
The editorialists noted that the study is limited by several factors, such as a short interval between assessments and relatively short follow-up. There is also no information on participants’ alcohol consumption earlier in life or about other healthy lifestyle changes during the study period. In addition, there is no mention of a genetic variant affecting aldehyde dehydrogenase that leads to alcohol-induced flushing, which is common among East Asians.
Despite of these limitations, the study provides “important new findings about the potential role of changes in alcohol consumption in cancer risk,” Dr. Freedman and Dr. Abnet noted. Future studies should examine the association between alcohol intake and cancer risk in other populations and use longer intervals between assessments, they suggested.
“Such studies are needed to move the field forward and inform public health guidance on cancer prevention,” the editorialists concluded.
The authors of the study and the editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alcohol is a major preventable risk factor for cancer. New data suggest that reducing alcohol intake reduces the risk of developing an alcohol-related cancer.
The findings, from a large population-based study conducted in Korea, underscore the importance of encouraging individuals to quit drinking or to reduce alcohol consumption to help reduce cancer risk, the authors noted.
The study was published online in JAMA Network Open.
It provides evidence “suggesting that cancer risk can be meaningfully altered by changing the amount of alcoholic beverages consumed,” wrote the authors of an accompanying editorial, Neal D. Freedman, PhD, and Christian C. Abnet, PhD, of the division of cancer epidemiology and genetics at the National Cancer Institute, Rockville, Md.
they wrote, adding that a “well examined dose-response association has been reported, with highest risks observed among people who drink 3 alcoholic beverages per day and higher.”
The new study shows that a “reduction in use was associated with lower risk, particularly among participants who started drinking at a heavy level,” they noted.
Previous studies have estimated that alcohol use accounts for nearly 4% of newly diagnosed cancers worldwide and nearly 5% of U.S. cancer cases overall.
But the figures are much higher for some specific cancers. That same U.S. study found that alcohol accounts for at least 45% of oral cavity/pharyngeal cancers and at least 25% of laryngeal cancers, as well as 12.1% of female breast cancers, 11.1% of colorectal cancers, 10.5% of liver cancers, and 7.7% of esophageal cancers, as previously reported by this news organization.
New findings on reducing intake
This latest study involved an analysis of data on 4.5 million individuals who were adult beneficiaries of the Korean National Health Insurance Service. The median age of the participants was 53.6 years, and they underwent a national health screening in 2009 and 2011.
During median follow-up of 6.4 years, the cancer incidence rate was 7.7 per 1,000 person-years.
Information on alcohol consumption was collected from self-administered questionnaires completed during the health screenings. Participants were categorized on the basis of alcohol consumption: none (0 g/d), mild ( less than 15 g/d), moderate (15-29.9 g/d), and heavy (30 or more g/d).
Compared with those who sustained their alcohol consumption level during the study period, those who increased their level were at higher risk of alcohol-related cancers and all cancers, the investigators found.
The increase in alcohol-related cancer incidence was dose dependent: Those who changed from nondrinking to mild, moderate, or heavy drinking were at increasingly higher risk for alcohol-related cancer, compared with those who remained nondrinkers (adjusted hazard ratios [aHRs], 1.03, 1.10, and 1.34, respectively).
Participants who were mild drinkers at baseline and who quit drinking were at lower risk of alcohol-related cancer, compared with those whose drinking level was sustained (aHR, 0.96). Those with moderate or heavy drinking levels who quit drinking were at higher overall cancer risk than were those who sustained their drinking levels. However, this difference was negated when quitting was sustained, the authors noted.
For heavy drinkers who reduced their drinking levels, cancer incidence was reduced, compared with those who sustained heavy drinking levels. This was true for those who changed from heavy to moderate drinking (aHR, 0.91 for alcohol-related cancers; 0.96 for alcohol-related cancers) and those who changed from heavy to mild drinking (aHR, 0.92 for alcohol-related cancers and all cancers).
“Alcohol cessation and reduction should be reinforced for the prevention of cancer,” concluded the authors.
Implications and future directions
The editorialists noted that the study is limited by several factors, such as a short interval between assessments and relatively short follow-up. There is also no information on participants’ alcohol consumption earlier in life or about other healthy lifestyle changes during the study period. In addition, there is no mention of a genetic variant affecting aldehyde dehydrogenase that leads to alcohol-induced flushing, which is common among East Asians.
Despite of these limitations, the study provides “important new findings about the potential role of changes in alcohol consumption in cancer risk,” Dr. Freedman and Dr. Abnet noted. Future studies should examine the association between alcohol intake and cancer risk in other populations and use longer intervals between assessments, they suggested.
“Such studies are needed to move the field forward and inform public health guidance on cancer prevention,” the editorialists concluded.
The authors of the study and the editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Brief Psychiatric Rating Scale succeeds as transdiagnostic measure
“Current DSM and ICD diagnoses do not depict psychopathology accurately, therefore their validity in research and utility in clinical practice is questioned,” wrote Andreas B. Hofmann, PhD, of the University of Zürich and colleagues.
The BPRS was developed to assess changes in psychopathology across a range of severe psychiatric disorders, but its potential to assess symptoms in nonpsychotic disorders has not been explored, the researchers said.
In a study published in Psychiatry Research, the investigators analyzed data from 600 adult psychiatric inpatients divided equally into six diagnostic categories: alcohol use disorder, major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and personality disorders. The mean age of the patients was 41.5 years and 45.5% were women. The demographic characteristics were similar across most groups, although patients with a personality disorder were significantly more likely than other patients to be younger and female.
Patients were assessed using the BPRS based on their main diagnosis. The mini-ICF-APP, another validated measure for assessing psychiatric disorders, served as a comparator, and both were compared to the Clinical Global Impression Scale (CGI).
Overall, the BPRS and mini-ICF-APP showed moderate correlation and good agreement, the researchers said. The Pearson correlation coefficient for the BPRS and mini-ICF-APP scales was 0.53 and the concordance correlation coefficient was 0.52. The mean sum scores for the BPRS, the mini-ICF-APP, and the CGI were 45.4 (standard deviation, 14.4), 19.93 (SD, 8.21), and 5.55 (SD, 0.84), respectively, which indicated “markedly ill” to “severely ill” patients, the researchers said.
The researchers were able to detect three clusters of symptoms corresponding to externalizing, internalizing, and thought disturbance domains using the BPRS, and four clusters using the mini-ICF-APP.
The symptoms using BPRS and the functionality domains using the mini-ICF-APP “showed a close interplay,” the researchers noted.
“The symptoms and functional domains we found to be central within the network structure are among the first targets of any psychiatric or psychotherapeutic intervention, namely the building of a common language and understanding as well as the establishment of confidence in relationships and a trustworthy therapeutic alliance,” they wrote in their discussion.
The study findings were limited by several factors including the collection of data from routine practice rather than clinical trials, the focus on only the main diagnosis without comorbidities, and the inclusion only of patients requiring hospitalization, the researchers noted.
However, the results were strengthened by the large sample size, and demonstrate the validity of the BPRS as a measurement tool across a range of psychiatric diagnoses, they said.
“Since the BPRS is a widely known and readily available psychometric scale, our results support its use as a transdiagnostic measurement instrument of psychopathology,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
“Current DSM and ICD diagnoses do not depict psychopathology accurately, therefore their validity in research and utility in clinical practice is questioned,” wrote Andreas B. Hofmann, PhD, of the University of Zürich and colleagues.
The BPRS was developed to assess changes in psychopathology across a range of severe psychiatric disorders, but its potential to assess symptoms in nonpsychotic disorders has not been explored, the researchers said.
In a study published in Psychiatry Research, the investigators analyzed data from 600 adult psychiatric inpatients divided equally into six diagnostic categories: alcohol use disorder, major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and personality disorders. The mean age of the patients was 41.5 years and 45.5% were women. The demographic characteristics were similar across most groups, although patients with a personality disorder were significantly more likely than other patients to be younger and female.
Patients were assessed using the BPRS based on their main diagnosis. The mini-ICF-APP, another validated measure for assessing psychiatric disorders, served as a comparator, and both were compared to the Clinical Global Impression Scale (CGI).
Overall, the BPRS and mini-ICF-APP showed moderate correlation and good agreement, the researchers said. The Pearson correlation coefficient for the BPRS and mini-ICF-APP scales was 0.53 and the concordance correlation coefficient was 0.52. The mean sum scores for the BPRS, the mini-ICF-APP, and the CGI were 45.4 (standard deviation, 14.4), 19.93 (SD, 8.21), and 5.55 (SD, 0.84), respectively, which indicated “markedly ill” to “severely ill” patients, the researchers said.
The researchers were able to detect three clusters of symptoms corresponding to externalizing, internalizing, and thought disturbance domains using the BPRS, and four clusters using the mini-ICF-APP.
The symptoms using BPRS and the functionality domains using the mini-ICF-APP “showed a close interplay,” the researchers noted.
“The symptoms and functional domains we found to be central within the network structure are among the first targets of any psychiatric or psychotherapeutic intervention, namely the building of a common language and understanding as well as the establishment of confidence in relationships and a trustworthy therapeutic alliance,” they wrote in their discussion.
The study findings were limited by several factors including the collection of data from routine practice rather than clinical trials, the focus on only the main diagnosis without comorbidities, and the inclusion only of patients requiring hospitalization, the researchers noted.
However, the results were strengthened by the large sample size, and demonstrate the validity of the BPRS as a measurement tool across a range of psychiatric diagnoses, they said.
“Since the BPRS is a widely known and readily available psychometric scale, our results support its use as a transdiagnostic measurement instrument of psychopathology,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
“Current DSM and ICD diagnoses do not depict psychopathology accurately, therefore their validity in research and utility in clinical practice is questioned,” wrote Andreas B. Hofmann, PhD, of the University of Zürich and colleagues.
The BPRS was developed to assess changes in psychopathology across a range of severe psychiatric disorders, but its potential to assess symptoms in nonpsychotic disorders has not been explored, the researchers said.
In a study published in Psychiatry Research, the investigators analyzed data from 600 adult psychiatric inpatients divided equally into six diagnostic categories: alcohol use disorder, major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and personality disorders. The mean age of the patients was 41.5 years and 45.5% were women. The demographic characteristics were similar across most groups, although patients with a personality disorder were significantly more likely than other patients to be younger and female.
Patients were assessed using the BPRS based on their main diagnosis. The mini-ICF-APP, another validated measure for assessing psychiatric disorders, served as a comparator, and both were compared to the Clinical Global Impression Scale (CGI).
Overall, the BPRS and mini-ICF-APP showed moderate correlation and good agreement, the researchers said. The Pearson correlation coefficient for the BPRS and mini-ICF-APP scales was 0.53 and the concordance correlation coefficient was 0.52. The mean sum scores for the BPRS, the mini-ICF-APP, and the CGI were 45.4 (standard deviation, 14.4), 19.93 (SD, 8.21), and 5.55 (SD, 0.84), respectively, which indicated “markedly ill” to “severely ill” patients, the researchers said.
The researchers were able to detect three clusters of symptoms corresponding to externalizing, internalizing, and thought disturbance domains using the BPRS, and four clusters using the mini-ICF-APP.
The symptoms using BPRS and the functionality domains using the mini-ICF-APP “showed a close interplay,” the researchers noted.
“The symptoms and functional domains we found to be central within the network structure are among the first targets of any psychiatric or psychotherapeutic intervention, namely the building of a common language and understanding as well as the establishment of confidence in relationships and a trustworthy therapeutic alliance,” they wrote in their discussion.
The study findings were limited by several factors including the collection of data from routine practice rather than clinical trials, the focus on only the main diagnosis without comorbidities, and the inclusion only of patients requiring hospitalization, the researchers noted.
However, the results were strengthened by the large sample size, and demonstrate the validity of the BPRS as a measurement tool across a range of psychiatric diagnoses, they said.
“Since the BPRS is a widely known and readily available psychometric scale, our results support its use as a transdiagnostic measurement instrument of psychopathology,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM PSYCHIATRY RESEARCH
Patients who engage in risky ‘chemsex’ benefit from appropriate treatment
Chemsex combines sex, drugs, and smartphones, and physicians know very little about it. Dedicated consultations were instituted in the fall of 2019 at the Infectious Diseases Department at the Saint-Louis Hospital in Paris. It’s estimated that 1,000 persons who were patients there practice chemsex.
Alexandre Aslan, MD, is one of the department’s physicians; he is also a sexologist and psychotherapist-psychoanalyst. At the ALBATROS International Congress of Addiction, which took place in the French capital in June, he presented the results of a study of patients who engage in chemsex and who regularly attend those consultations. Through this research, light is being shed on the phenomenon.
This news organization invited Dr. Aslan to discuss the issues connected with this practice.
Question: What exactly is chemsex, also known as party ‘n’ play (PnP)?
Dr. Aslan: Hearing the word “chemsex,” one would automatically think that it is what it sounds like it is: having sex while on drugs. That’s not really what it is. According to the definition that’s been published in the scientific literature, chemsex is a practice seen among men who have sex with men, where they take some very specific substances during sexual activity to sustain, enhance, or intensify the sexual experience, but also to “manage” issues related to intimacy, performance, and concerns about sexually transmitted infections (STIs). The substances are most commonly a cocktail of three drugs: GHB [gamma-hydroxybutyrate], cathinones, and crystal meth. In chemsex, smartphones play a central role as well, through the use of social networking and dating applications – those location-based apps that allow users to instantly find partners.
Question: In what ways does meeting through apps influence the sexual relationship and the use of substances?
Dr. Aslan: Because the plan to meet up for sex is being made through these kinds of apps, the promise to have sex is often implied – and this is before the individuals even meet up in real life. Let me explain. It’s not an encounter or a person that’s going to trigger sexual desire. Instead, it’s something within – the sexual “urge” inside of the individual – that’s going to drive them toward sexual activity. Now, finding yourself promising to have sex with someone – someone you don’t know, haven’t spoken to, and haven’t actually met – in an environment where it’s possible that you’ll meet several people and where the moments in which the sexual acts take place are predominantly characterized by pornography-related performance scripts: This can push you to take substances so you can “let go” and get to the point where you’re able to adapt to the requirements of the situation. Seeking to perform well and to not be overly inhibited, these individuals have found that this drug cocktail proves to be quite explosive, imparting a very strong capacity for experiencing excitement and even bringing about new sexual practices.
Question: Can you speak a bit about drug-enhanced sex?
Dr. Aslan: We sexologists consider it to be a very particular type of sex. People who engage in it feel that the sex is very intense, with unbelievable experiences, and that they have a deeper connection with their partner. In fact, it’s a type of sex where taking these substances does away with the very principles of sexual physiology – in other words, desire followed by excitement, plateau, orgasm, and resolution. Little by little, one’s sexual partner is no longer going to exist in the sex session, and the benefit is a succession of partners whose sole purpose is to keep the fire of excitement burning, an excitement that’s also reinforced by the substances taken. It’s “sex” under the influence rather than a sexual encounter linked to desire.
Question: What impact does it have on health?
Dr. Aslan: This practice brings with it numerous complications, such as STIs, but also physical injuries, as these sessions can last for 24 to more than 48 hours. There are also psychological complications, because these drugs can bring about depression, paranoia, self-harm, and even episodes of decompensation. And then, it should be noted that later on, the spotlight gets pulled away from the sex – the pretext from the very beginning – and shifts toward the taking of drugs: The individuals will no longer be able to separate the sexual encounter from the taking of drugs. Then, in a few years, there’s no longer the sexual encounter, only the taking of drugs. In the United States, between 2021 and 2022, there was a decrease in the number of deaths caused by heroin and prescription opioids. On the other hand, since 2020, the overdoses that have exploded in number are those related to fentanyl, nonprescription opioids, and stimulants – cocaine and methamphetamine, which can come back into the practices particularly through the seemingly “playful” arena of sex.
Question: How is it that things have gone from being a practice that’s under control to full-on drug addiction?
Dr. Aslan: You still have people who manage to keep things under control. But the kinds of drugs that are taken are highly addictive and compel the individual to take even more. It’s one big circle: The exciting sexual relationship itself, to which you add substances that cause even more dopamine to be released, and a smartphone screen with excitatory pornographic images on it all the time. In all the patients we see, we notice a trajectory that looks like the trajectory of every drug. When they’re at the beginning – in other words, the first year – after a first experience that they consider to be explosive, they may not return to the scene right away, and then they do return to it. They realize that it’s perhaps not as marvelous as the first time, but they’re going to give it another try. During this novelty phase, a strategy is pursued whereby they adapt and make adjustments in an attempt to feel again what they felt the first time. At the end of a year or two, they become disillusioned and they refocus on all activities having to do with drug use. Our hospital department conducted a survey where we asked detailed questions to over 100 individuals. It showed that people noticed the negative consequences that chemsex had on their work (60%), on their private lives and sex lives (55%), and on their relationships with friends and family (63%). This means that people are well aware of the negative effects that this practice has in very important areas of their lives. But even if they notice all of that, even if they resolve to have a certain number of sexual relations without drugs involved, these substances are so powerful in releasing a rush of dopamine that that very fact can sweep away any capacity the individual may have had to make a decision and stick to it, and they’re going to feel practically “compelled” to use. This is what’s called a craving.
Question: How do you identify patients who engage in chemsex among the patients in your infectious diseases department?
Dr. Aslan: As a rule, all patients admitted to our department are asked a series of questions. Do you use drugs to engage in sexual relations? Which drug do you prefer? How do you take it? Do you have a good time? Do you find that it’s good for you? Are you okay with how much you’re using? We also ask patients to tell us when they last had drug-free sex. It’s a very important question, because if we can identify someone who has had 10 or so partners a month but hasn’t had drug-free sex for over a month, we’ll try to steer the conversation to where they’ll come to think that it might not be such a bad idea to talk about it.
Question: Should a physician be asking younger patients whether they’re engaging in chemsex?
Dr. Aslan: Yes, but the physician has to be very careful. We often have a tendency to believe that we’re capable of speaking with our patients about relevant matters related to sex. We see ourselves as that kind of person, not to mention we’re open-minded. Now, as in all fields of medicine, we have to educate ourselves about how best to approach patients – in this case, about their sexual health. Because sometimes, despite our best intentions, we can do harm. The idea that we have of our own sexual behavior does not necessarily help provide counsel regarding another person’s sexual behavior, particularly when there are differences between the two. If you’re interested in the issue, you need to be trained on all the answers that could come up. There are training courses online. There’s a module on sexual health and chemsex at a site designed to give private practice physicians guidance about PrEP. It’s at least a place to start. This way, physicians will know what questions they can ask and when they should reach out to a specialist, such as a sexologist with training in these specific issues.
Question: What is the treatment based on?
Dr. Aslan: The traditional approach taken by addiction medicine physicians may not be comprehensive enough. Likewise, a sexologist’s approach alone can only go so far. It’s impossible to get by thinking that a single discipline can hold the solution, all the answers. So, it’s a multidisciplinary sexual health treatment. There should be a psychiatrist or addiction medicine physician who knows the drugs and is capable of navigating through this landscape of psychiatric comorbidities (such as psychoses and ADHD).
There also has to be a sexologist for the treatment of any sexual dysfunctions there may be. At Saint-Louis Hospital, 60% of patients who engage in chemsex said that engaging in the practice was related to a sexual problem that they noted – but never went to see a doctor about – before the first time they used. Be that as it may, it’s still the case that if these patients had been able to see a sexologist – who would have treated the problem – the drug may perhaps not have taken hold.
There also has to be a practitioner who can focus on risk reduction. In other words, someone capable of helping the patient get to the desired level of use where the craving, the need for instant gratification, can be kept in check.
In practice, one can sometimes, in addition to all of that, turn to medical treatments to manage the craving or medical comorbidities, an approach based on sexology to provide care for the sexual dysfunction or even to help the person learn how to evoke sexual or erotic fantasies without drugs, and an approach based on addiction medicine or psychotherapy, as some of our patients experienced sexual abuse in childhood. In the end, chemsex is just the outer layer – a problem that only seems to pertain to sex but that, in reality, covers up a wide range of issues. And not only sexual issues or issues that are related to drugs like chemsex is.
Question: What are the outcomes of this multidisciplinary treatment?
Dr. Aslan: Before we finish, I must point out and just state that the patients, when they’re cared for and when they’re provided with the appropriate treatment, change their practices. Some of our patients, even those with more advanced cases in terms of frequency, how often they’re injecting drugs – every 30 minutes over the course of 24 or 48 hours, with complications such as thrombosis, sepsis, and abscesses – they’ve completely stopped after several months of treatment. They now lead lives that, as they’ve told us, work better for them. So, those of us in the health care industry, we have to get organized and set things up in a way that will allow us to focus our efforts on treating these patients.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape French edition.
Chemsex combines sex, drugs, and smartphones, and physicians know very little about it. Dedicated consultations were instituted in the fall of 2019 at the Infectious Diseases Department at the Saint-Louis Hospital in Paris. It’s estimated that 1,000 persons who were patients there practice chemsex.
Alexandre Aslan, MD, is one of the department’s physicians; he is also a sexologist and psychotherapist-psychoanalyst. At the ALBATROS International Congress of Addiction, which took place in the French capital in June, he presented the results of a study of patients who engage in chemsex and who regularly attend those consultations. Through this research, light is being shed on the phenomenon.
This news organization invited Dr. Aslan to discuss the issues connected with this practice.
Question: What exactly is chemsex, also known as party ‘n’ play (PnP)?
Dr. Aslan: Hearing the word “chemsex,” one would automatically think that it is what it sounds like it is: having sex while on drugs. That’s not really what it is. According to the definition that’s been published in the scientific literature, chemsex is a practice seen among men who have sex with men, where they take some very specific substances during sexual activity to sustain, enhance, or intensify the sexual experience, but also to “manage” issues related to intimacy, performance, and concerns about sexually transmitted infections (STIs). The substances are most commonly a cocktail of three drugs: GHB [gamma-hydroxybutyrate], cathinones, and crystal meth. In chemsex, smartphones play a central role as well, through the use of social networking and dating applications – those location-based apps that allow users to instantly find partners.
Question: In what ways does meeting through apps influence the sexual relationship and the use of substances?
Dr. Aslan: Because the plan to meet up for sex is being made through these kinds of apps, the promise to have sex is often implied – and this is before the individuals even meet up in real life. Let me explain. It’s not an encounter or a person that’s going to trigger sexual desire. Instead, it’s something within – the sexual “urge” inside of the individual – that’s going to drive them toward sexual activity. Now, finding yourself promising to have sex with someone – someone you don’t know, haven’t spoken to, and haven’t actually met – in an environment where it’s possible that you’ll meet several people and where the moments in which the sexual acts take place are predominantly characterized by pornography-related performance scripts: This can push you to take substances so you can “let go” and get to the point where you’re able to adapt to the requirements of the situation. Seeking to perform well and to not be overly inhibited, these individuals have found that this drug cocktail proves to be quite explosive, imparting a very strong capacity for experiencing excitement and even bringing about new sexual practices.
Question: Can you speak a bit about drug-enhanced sex?
Dr. Aslan: We sexologists consider it to be a very particular type of sex. People who engage in it feel that the sex is very intense, with unbelievable experiences, and that they have a deeper connection with their partner. In fact, it’s a type of sex where taking these substances does away with the very principles of sexual physiology – in other words, desire followed by excitement, plateau, orgasm, and resolution. Little by little, one’s sexual partner is no longer going to exist in the sex session, and the benefit is a succession of partners whose sole purpose is to keep the fire of excitement burning, an excitement that’s also reinforced by the substances taken. It’s “sex” under the influence rather than a sexual encounter linked to desire.
Question: What impact does it have on health?
Dr. Aslan: This practice brings with it numerous complications, such as STIs, but also physical injuries, as these sessions can last for 24 to more than 48 hours. There are also psychological complications, because these drugs can bring about depression, paranoia, self-harm, and even episodes of decompensation. And then, it should be noted that later on, the spotlight gets pulled away from the sex – the pretext from the very beginning – and shifts toward the taking of drugs: The individuals will no longer be able to separate the sexual encounter from the taking of drugs. Then, in a few years, there’s no longer the sexual encounter, only the taking of drugs. In the United States, between 2021 and 2022, there was a decrease in the number of deaths caused by heroin and prescription opioids. On the other hand, since 2020, the overdoses that have exploded in number are those related to fentanyl, nonprescription opioids, and stimulants – cocaine and methamphetamine, which can come back into the practices particularly through the seemingly “playful” arena of sex.
Question: How is it that things have gone from being a practice that’s under control to full-on drug addiction?
Dr. Aslan: You still have people who manage to keep things under control. But the kinds of drugs that are taken are highly addictive and compel the individual to take even more. It’s one big circle: The exciting sexual relationship itself, to which you add substances that cause even more dopamine to be released, and a smartphone screen with excitatory pornographic images on it all the time. In all the patients we see, we notice a trajectory that looks like the trajectory of every drug. When they’re at the beginning – in other words, the first year – after a first experience that they consider to be explosive, they may not return to the scene right away, and then they do return to it. They realize that it’s perhaps not as marvelous as the first time, but they’re going to give it another try. During this novelty phase, a strategy is pursued whereby they adapt and make adjustments in an attempt to feel again what they felt the first time. At the end of a year or two, they become disillusioned and they refocus on all activities having to do with drug use. Our hospital department conducted a survey where we asked detailed questions to over 100 individuals. It showed that people noticed the negative consequences that chemsex had on their work (60%), on their private lives and sex lives (55%), and on their relationships with friends and family (63%). This means that people are well aware of the negative effects that this practice has in very important areas of their lives. But even if they notice all of that, even if they resolve to have a certain number of sexual relations without drugs involved, these substances are so powerful in releasing a rush of dopamine that that very fact can sweep away any capacity the individual may have had to make a decision and stick to it, and they’re going to feel practically “compelled” to use. This is what’s called a craving.
Question: How do you identify patients who engage in chemsex among the patients in your infectious diseases department?
Dr. Aslan: As a rule, all patients admitted to our department are asked a series of questions. Do you use drugs to engage in sexual relations? Which drug do you prefer? How do you take it? Do you have a good time? Do you find that it’s good for you? Are you okay with how much you’re using? We also ask patients to tell us when they last had drug-free sex. It’s a very important question, because if we can identify someone who has had 10 or so partners a month but hasn’t had drug-free sex for over a month, we’ll try to steer the conversation to where they’ll come to think that it might not be such a bad idea to talk about it.
Question: Should a physician be asking younger patients whether they’re engaging in chemsex?
Dr. Aslan: Yes, but the physician has to be very careful. We often have a tendency to believe that we’re capable of speaking with our patients about relevant matters related to sex. We see ourselves as that kind of person, not to mention we’re open-minded. Now, as in all fields of medicine, we have to educate ourselves about how best to approach patients – in this case, about their sexual health. Because sometimes, despite our best intentions, we can do harm. The idea that we have of our own sexual behavior does not necessarily help provide counsel regarding another person’s sexual behavior, particularly when there are differences between the two. If you’re interested in the issue, you need to be trained on all the answers that could come up. There are training courses online. There’s a module on sexual health and chemsex at a site designed to give private practice physicians guidance about PrEP. It’s at least a place to start. This way, physicians will know what questions they can ask and when they should reach out to a specialist, such as a sexologist with training in these specific issues.
Question: What is the treatment based on?
Dr. Aslan: The traditional approach taken by addiction medicine physicians may not be comprehensive enough. Likewise, a sexologist’s approach alone can only go so far. It’s impossible to get by thinking that a single discipline can hold the solution, all the answers. So, it’s a multidisciplinary sexual health treatment. There should be a psychiatrist or addiction medicine physician who knows the drugs and is capable of navigating through this landscape of psychiatric comorbidities (such as psychoses and ADHD).
There also has to be a sexologist for the treatment of any sexual dysfunctions there may be. At Saint-Louis Hospital, 60% of patients who engage in chemsex said that engaging in the practice was related to a sexual problem that they noted – but never went to see a doctor about – before the first time they used. Be that as it may, it’s still the case that if these patients had been able to see a sexologist – who would have treated the problem – the drug may perhaps not have taken hold.
There also has to be a practitioner who can focus on risk reduction. In other words, someone capable of helping the patient get to the desired level of use where the craving, the need for instant gratification, can be kept in check.
In practice, one can sometimes, in addition to all of that, turn to medical treatments to manage the craving or medical comorbidities, an approach based on sexology to provide care for the sexual dysfunction or even to help the person learn how to evoke sexual or erotic fantasies without drugs, and an approach based on addiction medicine or psychotherapy, as some of our patients experienced sexual abuse in childhood. In the end, chemsex is just the outer layer – a problem that only seems to pertain to sex but that, in reality, covers up a wide range of issues. And not only sexual issues or issues that are related to drugs like chemsex is.
Question: What are the outcomes of this multidisciplinary treatment?
Dr. Aslan: Before we finish, I must point out and just state that the patients, when they’re cared for and when they’re provided with the appropriate treatment, change their practices. Some of our patients, even those with more advanced cases in terms of frequency, how often they’re injecting drugs – every 30 minutes over the course of 24 or 48 hours, with complications such as thrombosis, sepsis, and abscesses – they’ve completely stopped after several months of treatment. They now lead lives that, as they’ve told us, work better for them. So, those of us in the health care industry, we have to get organized and set things up in a way that will allow us to focus our efforts on treating these patients.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape French edition.
Chemsex combines sex, drugs, and smartphones, and physicians know very little about it. Dedicated consultations were instituted in the fall of 2019 at the Infectious Diseases Department at the Saint-Louis Hospital in Paris. It’s estimated that 1,000 persons who were patients there practice chemsex.
Alexandre Aslan, MD, is one of the department’s physicians; he is also a sexologist and psychotherapist-psychoanalyst. At the ALBATROS International Congress of Addiction, which took place in the French capital in June, he presented the results of a study of patients who engage in chemsex and who regularly attend those consultations. Through this research, light is being shed on the phenomenon.
This news organization invited Dr. Aslan to discuss the issues connected with this practice.
Question: What exactly is chemsex, also known as party ‘n’ play (PnP)?
Dr. Aslan: Hearing the word “chemsex,” one would automatically think that it is what it sounds like it is: having sex while on drugs. That’s not really what it is. According to the definition that’s been published in the scientific literature, chemsex is a practice seen among men who have sex with men, where they take some very specific substances during sexual activity to sustain, enhance, or intensify the sexual experience, but also to “manage” issues related to intimacy, performance, and concerns about sexually transmitted infections (STIs). The substances are most commonly a cocktail of three drugs: GHB [gamma-hydroxybutyrate], cathinones, and crystal meth. In chemsex, smartphones play a central role as well, through the use of social networking and dating applications – those location-based apps that allow users to instantly find partners.
Question: In what ways does meeting through apps influence the sexual relationship and the use of substances?
Dr. Aslan: Because the plan to meet up for sex is being made through these kinds of apps, the promise to have sex is often implied – and this is before the individuals even meet up in real life. Let me explain. It’s not an encounter or a person that’s going to trigger sexual desire. Instead, it’s something within – the sexual “urge” inside of the individual – that’s going to drive them toward sexual activity. Now, finding yourself promising to have sex with someone – someone you don’t know, haven’t spoken to, and haven’t actually met – in an environment where it’s possible that you’ll meet several people and where the moments in which the sexual acts take place are predominantly characterized by pornography-related performance scripts: This can push you to take substances so you can “let go” and get to the point where you’re able to adapt to the requirements of the situation. Seeking to perform well and to not be overly inhibited, these individuals have found that this drug cocktail proves to be quite explosive, imparting a very strong capacity for experiencing excitement and even bringing about new sexual practices.
Question: Can you speak a bit about drug-enhanced sex?
Dr. Aslan: We sexologists consider it to be a very particular type of sex. People who engage in it feel that the sex is very intense, with unbelievable experiences, and that they have a deeper connection with their partner. In fact, it’s a type of sex where taking these substances does away with the very principles of sexual physiology – in other words, desire followed by excitement, plateau, orgasm, and resolution. Little by little, one’s sexual partner is no longer going to exist in the sex session, and the benefit is a succession of partners whose sole purpose is to keep the fire of excitement burning, an excitement that’s also reinforced by the substances taken. It’s “sex” under the influence rather than a sexual encounter linked to desire.
Question: What impact does it have on health?
Dr. Aslan: This practice brings with it numerous complications, such as STIs, but also physical injuries, as these sessions can last for 24 to more than 48 hours. There are also psychological complications, because these drugs can bring about depression, paranoia, self-harm, and even episodes of decompensation. And then, it should be noted that later on, the spotlight gets pulled away from the sex – the pretext from the very beginning – and shifts toward the taking of drugs: The individuals will no longer be able to separate the sexual encounter from the taking of drugs. Then, in a few years, there’s no longer the sexual encounter, only the taking of drugs. In the United States, between 2021 and 2022, there was a decrease in the number of deaths caused by heroin and prescription opioids. On the other hand, since 2020, the overdoses that have exploded in number are those related to fentanyl, nonprescription opioids, and stimulants – cocaine and methamphetamine, which can come back into the practices particularly through the seemingly “playful” arena of sex.
Question: How is it that things have gone from being a practice that’s under control to full-on drug addiction?
Dr. Aslan: You still have people who manage to keep things under control. But the kinds of drugs that are taken are highly addictive and compel the individual to take even more. It’s one big circle: The exciting sexual relationship itself, to which you add substances that cause even more dopamine to be released, and a smartphone screen with excitatory pornographic images on it all the time. In all the patients we see, we notice a trajectory that looks like the trajectory of every drug. When they’re at the beginning – in other words, the first year – after a first experience that they consider to be explosive, they may not return to the scene right away, and then they do return to it. They realize that it’s perhaps not as marvelous as the first time, but they’re going to give it another try. During this novelty phase, a strategy is pursued whereby they adapt and make adjustments in an attempt to feel again what they felt the first time. At the end of a year or two, they become disillusioned and they refocus on all activities having to do with drug use. Our hospital department conducted a survey where we asked detailed questions to over 100 individuals. It showed that people noticed the negative consequences that chemsex had on their work (60%), on their private lives and sex lives (55%), and on their relationships with friends and family (63%). This means that people are well aware of the negative effects that this practice has in very important areas of their lives. But even if they notice all of that, even if they resolve to have a certain number of sexual relations without drugs involved, these substances are so powerful in releasing a rush of dopamine that that very fact can sweep away any capacity the individual may have had to make a decision and stick to it, and they’re going to feel practically “compelled” to use. This is what’s called a craving.
Question: How do you identify patients who engage in chemsex among the patients in your infectious diseases department?
Dr. Aslan: As a rule, all patients admitted to our department are asked a series of questions. Do you use drugs to engage in sexual relations? Which drug do you prefer? How do you take it? Do you have a good time? Do you find that it’s good for you? Are you okay with how much you’re using? We also ask patients to tell us when they last had drug-free sex. It’s a very important question, because if we can identify someone who has had 10 or so partners a month but hasn’t had drug-free sex for over a month, we’ll try to steer the conversation to where they’ll come to think that it might not be such a bad idea to talk about it.
Question: Should a physician be asking younger patients whether they’re engaging in chemsex?
Dr. Aslan: Yes, but the physician has to be very careful. We often have a tendency to believe that we’re capable of speaking with our patients about relevant matters related to sex. We see ourselves as that kind of person, not to mention we’re open-minded. Now, as in all fields of medicine, we have to educate ourselves about how best to approach patients – in this case, about their sexual health. Because sometimes, despite our best intentions, we can do harm. The idea that we have of our own sexual behavior does not necessarily help provide counsel regarding another person’s sexual behavior, particularly when there are differences between the two. If you’re interested in the issue, you need to be trained on all the answers that could come up. There are training courses online. There’s a module on sexual health and chemsex at a site designed to give private practice physicians guidance about PrEP. It’s at least a place to start. This way, physicians will know what questions they can ask and when they should reach out to a specialist, such as a sexologist with training in these specific issues.
Question: What is the treatment based on?
Dr. Aslan: The traditional approach taken by addiction medicine physicians may not be comprehensive enough. Likewise, a sexologist’s approach alone can only go so far. It’s impossible to get by thinking that a single discipline can hold the solution, all the answers. So, it’s a multidisciplinary sexual health treatment. There should be a psychiatrist or addiction medicine physician who knows the drugs and is capable of navigating through this landscape of psychiatric comorbidities (such as psychoses and ADHD).
There also has to be a sexologist for the treatment of any sexual dysfunctions there may be. At Saint-Louis Hospital, 60% of patients who engage in chemsex said that engaging in the practice was related to a sexual problem that they noted – but never went to see a doctor about – before the first time they used. Be that as it may, it’s still the case that if these patients had been able to see a sexologist – who would have treated the problem – the drug may perhaps not have taken hold.
There also has to be a practitioner who can focus on risk reduction. In other words, someone capable of helping the patient get to the desired level of use where the craving, the need for instant gratification, can be kept in check.
In practice, one can sometimes, in addition to all of that, turn to medical treatments to manage the craving or medical comorbidities, an approach based on sexology to provide care for the sexual dysfunction or even to help the person learn how to evoke sexual or erotic fantasies without drugs, and an approach based on addiction medicine or psychotherapy, as some of our patients experienced sexual abuse in childhood. In the end, chemsex is just the outer layer – a problem that only seems to pertain to sex but that, in reality, covers up a wide range of issues. And not only sexual issues or issues that are related to drugs like chemsex is.
Question: What are the outcomes of this multidisciplinary treatment?
Dr. Aslan: Before we finish, I must point out and just state that the patients, when they’re cared for and when they’re provided with the appropriate treatment, change their practices. Some of our patients, even those with more advanced cases in terms of frequency, how often they’re injecting drugs – every 30 minutes over the course of 24 or 48 hours, with complications such as thrombosis, sepsis, and abscesses – they’ve completely stopped after several months of treatment. They now lead lives that, as they’ve told us, work better for them. So, those of us in the health care industry, we have to get organized and set things up in a way that will allow us to focus our efforts on treating these patients.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape French edition.
‘Shocking’ and persistent gap in treatment for opioid addiction
The vast majority of Americans with opioid use disorder (OUD) do not receive potentially lifesaving medications.
Drugs such as methadone, buprenorphine, and extended-release naltrexone have been shown to reduce opioid overdoses by more than 50%. Yet a new analysis shows that only about 1 in 10 people living with OUD receive these medications.
“Even though it’s not especially surprising, it’s still disturbing and shocking in a way that we have just made such little progress on this huge issue,” study investigator Noa Krawczyk, PhD, with the Center for Opioid Epidemiology and Policy, department of population health, NYU Langone, told this news organization.
The study was published online in the International Journal of Drug Policy.
Increased urgency
Despite efforts to increase capacity for OUD treatment in the United States, how receipt of treatment compares to need for treatment remains unclear.
Dr. Krawczyk and colleagues examined the gap between new estimates of OUD prevalence and treatment at the national and state levels from 2010 through 2019.
“,” the investigators write.
Adjusted estimates suggest that past-year OUD affected roughly 7.63 million individuals in the United States (2,773 per 100,000), yet only about 1.02 million received medication (365 per 100,000), they note.
Overall, there was a 106% increase in receipt of medications for OUD across the United States from 2010 to 2019 and a 5% increase from 2018 to 2019.
Yet, as of 2019, 87% of people with OUD were not receiving medication.
“While the number of people getting treatment doubled over the last decade, it’s nowhere near the amount of people who are still struggling with an opioid use disorder, and the urgency of the problem has become much worse because of the worsening fentanyl crisis and the lethality of the drug supply,” said Dr. Krawczyk.
The study also showed wide variation in past-year OUD prevalence and treatment across the United States.
Past-year OUD rates were highest in Washington, D.C., and lowest in Minnesota. Receipt of treatment was lowest in South Dakota and highest in Vermont.
However, in all 50 states and Washington, D.C., past-year OUD prevalence was greater than rates of medication use. As of 2019, the largest treatment gaps were in Iowa, North Dakota, and Washington, D.C. The smallest treatment gaps were in Connecticut, Maryland, and Rhode Island.
Long road ahead
“Even in states with the smallest treatment gaps, at least 50% of people who could benefit from medications for opioid use disorder are still not receiving them,” senior author Magdalena Cerdá, DrPH, director of the Center for Opioid Epidemiology and Policy in the department of population health at NYU Langone Health, said in a statement.
“We have a long way to go in reducing stigma surrounding treatment and in devising the types of policies and programs we need to ensure these medications reach the people who need them the most,” Dr. Cerdá added.
Access to OUD treatment is an ongoing problem in the United States.
“A lot of areas don’t have specialty treatment programs that provide methadone, or they might not have addiction-trained providers who are willing to prescribe buprenorphine or have a waiver to prescribe buprenorphine, so a lot places are really struggling with where people can get treatment,” said Dr. Krawczyk.
Recent data show that 46% of counties lack an OUD medication provider, and 32% have no specialty programs to treat substance use disorders.
Dr. Krawczyk and colleagues note that COVID-19–related policy changes and recently proposed legislation to allow more flexible and convenient access to OUD treatment may be a first step toward expanding access to this lifesaving treatment.
But improving initial access to medication for OUD is “only the first step – our research and health systems have a long way to go in addressing the needs of people with OUD to support retention in treatment and services to effectively reduce overdose and improve long-term health and well-being,” the researchers write.
The study was supported by the NYU Center for Epidemiology and Policy. Dr. Krawczyk has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The vast majority of Americans with opioid use disorder (OUD) do not receive potentially lifesaving medications.
Drugs such as methadone, buprenorphine, and extended-release naltrexone have been shown to reduce opioid overdoses by more than 50%. Yet a new analysis shows that only about 1 in 10 people living with OUD receive these medications.
“Even though it’s not especially surprising, it’s still disturbing and shocking in a way that we have just made such little progress on this huge issue,” study investigator Noa Krawczyk, PhD, with the Center for Opioid Epidemiology and Policy, department of population health, NYU Langone, told this news organization.
The study was published online in the International Journal of Drug Policy.
Increased urgency
Despite efforts to increase capacity for OUD treatment in the United States, how receipt of treatment compares to need for treatment remains unclear.
Dr. Krawczyk and colleagues examined the gap between new estimates of OUD prevalence and treatment at the national and state levels from 2010 through 2019.
“,” the investigators write.
Adjusted estimates suggest that past-year OUD affected roughly 7.63 million individuals in the United States (2,773 per 100,000), yet only about 1.02 million received medication (365 per 100,000), they note.
Overall, there was a 106% increase in receipt of medications for OUD across the United States from 2010 to 2019 and a 5% increase from 2018 to 2019.
Yet, as of 2019, 87% of people with OUD were not receiving medication.
“While the number of people getting treatment doubled over the last decade, it’s nowhere near the amount of people who are still struggling with an opioid use disorder, and the urgency of the problem has become much worse because of the worsening fentanyl crisis and the lethality of the drug supply,” said Dr. Krawczyk.
The study also showed wide variation in past-year OUD prevalence and treatment across the United States.
Past-year OUD rates were highest in Washington, D.C., and lowest in Minnesota. Receipt of treatment was lowest in South Dakota and highest in Vermont.
However, in all 50 states and Washington, D.C., past-year OUD prevalence was greater than rates of medication use. As of 2019, the largest treatment gaps were in Iowa, North Dakota, and Washington, D.C. The smallest treatment gaps were in Connecticut, Maryland, and Rhode Island.
Long road ahead
“Even in states with the smallest treatment gaps, at least 50% of people who could benefit from medications for opioid use disorder are still not receiving them,” senior author Magdalena Cerdá, DrPH, director of the Center for Opioid Epidemiology and Policy in the department of population health at NYU Langone Health, said in a statement.
“We have a long way to go in reducing stigma surrounding treatment and in devising the types of policies and programs we need to ensure these medications reach the people who need them the most,” Dr. Cerdá added.
Access to OUD treatment is an ongoing problem in the United States.
“A lot of areas don’t have specialty treatment programs that provide methadone, or they might not have addiction-trained providers who are willing to prescribe buprenorphine or have a waiver to prescribe buprenorphine, so a lot places are really struggling with where people can get treatment,” said Dr. Krawczyk.
Recent data show that 46% of counties lack an OUD medication provider, and 32% have no specialty programs to treat substance use disorders.
Dr. Krawczyk and colleagues note that COVID-19–related policy changes and recently proposed legislation to allow more flexible and convenient access to OUD treatment may be a first step toward expanding access to this lifesaving treatment.
But improving initial access to medication for OUD is “only the first step – our research and health systems have a long way to go in addressing the needs of people with OUD to support retention in treatment and services to effectively reduce overdose and improve long-term health and well-being,” the researchers write.
The study was supported by the NYU Center for Epidemiology and Policy. Dr. Krawczyk has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The vast majority of Americans with opioid use disorder (OUD) do not receive potentially lifesaving medications.
Drugs such as methadone, buprenorphine, and extended-release naltrexone have been shown to reduce opioid overdoses by more than 50%. Yet a new analysis shows that only about 1 in 10 people living with OUD receive these medications.
“Even though it’s not especially surprising, it’s still disturbing and shocking in a way that we have just made such little progress on this huge issue,” study investigator Noa Krawczyk, PhD, with the Center for Opioid Epidemiology and Policy, department of population health, NYU Langone, told this news organization.
The study was published online in the International Journal of Drug Policy.
Increased urgency
Despite efforts to increase capacity for OUD treatment in the United States, how receipt of treatment compares to need for treatment remains unclear.
Dr. Krawczyk and colleagues examined the gap between new estimates of OUD prevalence and treatment at the national and state levels from 2010 through 2019.
“,” the investigators write.
Adjusted estimates suggest that past-year OUD affected roughly 7.63 million individuals in the United States (2,773 per 100,000), yet only about 1.02 million received medication (365 per 100,000), they note.
Overall, there was a 106% increase in receipt of medications for OUD across the United States from 2010 to 2019 and a 5% increase from 2018 to 2019.
Yet, as of 2019, 87% of people with OUD were not receiving medication.
“While the number of people getting treatment doubled over the last decade, it’s nowhere near the amount of people who are still struggling with an opioid use disorder, and the urgency of the problem has become much worse because of the worsening fentanyl crisis and the lethality of the drug supply,” said Dr. Krawczyk.
The study also showed wide variation in past-year OUD prevalence and treatment across the United States.
Past-year OUD rates were highest in Washington, D.C., and lowest in Minnesota. Receipt of treatment was lowest in South Dakota and highest in Vermont.
However, in all 50 states and Washington, D.C., past-year OUD prevalence was greater than rates of medication use. As of 2019, the largest treatment gaps were in Iowa, North Dakota, and Washington, D.C. The smallest treatment gaps were in Connecticut, Maryland, and Rhode Island.
Long road ahead
“Even in states with the smallest treatment gaps, at least 50% of people who could benefit from medications for opioid use disorder are still not receiving them,” senior author Magdalena Cerdá, DrPH, director of the Center for Opioid Epidemiology and Policy in the department of population health at NYU Langone Health, said in a statement.
“We have a long way to go in reducing stigma surrounding treatment and in devising the types of policies and programs we need to ensure these medications reach the people who need them the most,” Dr. Cerdá added.
Access to OUD treatment is an ongoing problem in the United States.
“A lot of areas don’t have specialty treatment programs that provide methadone, or they might not have addiction-trained providers who are willing to prescribe buprenorphine or have a waiver to prescribe buprenorphine, so a lot places are really struggling with where people can get treatment,” said Dr. Krawczyk.
Recent data show that 46% of counties lack an OUD medication provider, and 32% have no specialty programs to treat substance use disorders.
Dr. Krawczyk and colleagues note that COVID-19–related policy changes and recently proposed legislation to allow more flexible and convenient access to OUD treatment may be a first step toward expanding access to this lifesaving treatment.
But improving initial access to medication for OUD is “only the first step – our research and health systems have a long way to go in addressing the needs of people with OUD to support retention in treatment and services to effectively reduce overdose and improve long-term health and well-being,” the researchers write.
The study was supported by the NYU Center for Epidemiology and Policy. Dr. Krawczyk has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF DRUG POLICY
HCV reinfection uncommon among people who inject drugs
The findings, which are based on prospective data from 13 countries, including the United States, and were published in Annals of Internal Medicine (2022 Aug 8. doi: 10.7326/M21-4119), should encourage physicians to treat HCV in people with a history of injection drug use, said lead author Jason Grebely, PhD. They should also pressure payers to lift reimbursement restrictions on the same population.
“Direct-acting antiviral medications for HCV infection are safe and effective among people receiving OAT and people with recent injecting-drug use,” the investigators wrote. “Concerns remain, however, that HCV reinfection may reduce the benefits of cure among people who inject drugs and compromise HCV elimination efforts.”
They explored these concerns through a 3-year extension of the phase 3 CO-STAR trial that evaluated elbasvir and grazoprevir in people consistently taking OAT. Participants in the CO-STAR trial, which had a 96% sustained virologic response rate among those who completed therapy, could elect to participate in the present study, offering a prospective look at long-term reinfection.
Out of 296 participants in the CO-STAR trial, 286 were evaluable for reinfection and 199 enrolled in the present extension. The majority were White (79.4%) and male (75.9%), with most taking methadone (79%), followed by buprenorphine (20%). At 6 months, 40 out of 191 respondents (21%) reported injection-drug use in the previous month. At the 3-year mark, 26 out of 142 respondents (18%) disclosed injection-drug use in the previous month.
For all participants in the CO-STAR trial, the overall rate of reinfection at 3 years was 1.7 per 100 person-years (95% confidence interval, 0.8-3.0), which is lower than the rate reported in systematic reviews (3.8 per 100 person-years), according to the investigators.
In the extension analysis, the 3-year reinfection rate was lower still, at 1.2 per 100 person-years. The rate was slightly higher among people who reported injection-drug use in the previous month (1.9 per 100 person-years), and slightly lower among those who did not report injection-drug use in the prior month (0.5 per 100 person-years). More pronounced differences in reinfection were observed among participants who shared needles (6.4 per 100 person-years), versus those who didn’t share needles (1.5 per 100 person years).
Low reinfection rate may help facilitate removal of reimbursement restrictions
“Most of the reinfections in this study occurred within 24 weeks of completing treatment, suggesting that this is a key period for optimizing treatment of opioid use disorder and for providing access to needle and syringe programs that have documented benefits in preventing HCV transmission,” the investigators wrote.
This is one of the largest observational studies of its kind to date, bolstered by “excellent study retention” and a “well-characterized cohort,” with findings that should prompt real-world action, said Dr. Grebely, who is head of the hepatitis C and drug use group in the viral hepatitis clinical research program at the Kirby Institute, University of New South Wales, Sydney.
“Given that reinfection has often been cited ... by some providers as a reason for not offering treatment to people receiving OAT, the low reinfection rate in this study will be incredibly important for guiding practice and ensuring therapy is not withheld from this group,” Dr. Grebely said in an interview. “In terms of policy implications, these data may also help to facilitate the removal of reimbursement restrictions based on recent drug/alcohol use criteria that are in place among many payers in the United States.”
More research needed to determine optimal intervention strategies
Carl Latkin, PhD, professor and vice chair of the department of health, behavior, and society at Johns Hopkins University, Baltimore, called the present publication a “great article and well-done study with long-term follow-up.”
Dr. Latkin, who investigates biobehavioral interventions for disadvantaged communities, said the reported rate of reinfection is “very low among a group of current and former injectors.”
Affirming Dr. Grebely’s call for supportive practices by physicians and payers, Dr. Latkin said: “The study highlights the importance of improving access to medication for opioid use disorder. This level of treatment adherence in this group is much higher than for many other medications. Given these data, it would be difficult for payers to have a rational reason for blanket restrictions for HCV treatment among people who use drugs.”
Dr. Latkin explained that “it isn’t simply injection drug use per se” that drives HCV reinfection; instead, he cited social factors, such as lack of housing, as well as withdrawal symptoms, especially among those without access to medications for opioid use disorder (MOUD).
Dr. Latkin and Grebely also agreed that more research is needed to determine optimal intervention strategies.
Dr. Grebely called for one to enhance HCV testing and linkage to care, a topic he covered in a recent review article (Lancet Gastroenterol Hepatol. 2022 May;7[5]:426-45.).
Dr. Latkin said that, while it’s clear that “syringe services programs, accessible HCV treatment, and MOUD are needed,” it is unclear how much coverage is necessary for a given population.
Findings support critical nature of needle and syringe exchange programs
Sarah M. Kattakuzhy, MD, an associate professor in the division of clinical care & research at the Institute of Human Virology, University of Maryland, Baltimore, agreed that the findings “support the critical nature of needle and syringe exchange programs.”
“As most cities in the United States fall well below the high coverage needle and syringe program threshold required to maximally prevent disease transmission, the study serves as a push toward an evidence-based harm reduction policy,” she said.
Dr. Kattakuzhy he added that the study “supports the need to longitudinally engage individuals after HCV treatment to monitor reinfection risk behaviors and test for reinfection,” she continued.
When it came to translating all the data to populations in the United States, she offered a more guarded view.
“Critically, the study population included only individuals who were engaged with OAT and adherent for 3 or more months, selecting to a population of individuals with high adherence and engagement in care,” Dr. Kattakuzhy said in an interview. “As such, the study findings are not applicable to other cross sections of the drug-using community, including individuals not engaged in OAT, and cohorts with higher rates of ongoing injection drug use. Furthermore, there are known genetic impacts on spontaneous clearance, and emerging data on the immunology of reinfection.
“Studies with a focus on less engaged, higher-risk, and minority populations with active drug use are required to answer the remaining questions in HCV reinfection,” she said.
The study was supported by Merck, the Australian Government Department of Health, and the Australian National Health and Medical Research Council. Dr. Grebely disclosed receiving funding from Cepheid, the manufacturer of the Xpert HCV assay. The other investigators disclosed additional relationships with Gilead, AbbVie, Cepheid, and others. Dr. Latkin and Dr. Kattakuzhy disclosed no relevant conflicts of interest.
The findings, which are based on prospective data from 13 countries, including the United States, and were published in Annals of Internal Medicine (2022 Aug 8. doi: 10.7326/M21-4119), should encourage physicians to treat HCV in people with a history of injection drug use, said lead author Jason Grebely, PhD. They should also pressure payers to lift reimbursement restrictions on the same population.
“Direct-acting antiviral medications for HCV infection are safe and effective among people receiving OAT and people with recent injecting-drug use,” the investigators wrote. “Concerns remain, however, that HCV reinfection may reduce the benefits of cure among people who inject drugs and compromise HCV elimination efforts.”
They explored these concerns through a 3-year extension of the phase 3 CO-STAR trial that evaluated elbasvir and grazoprevir in people consistently taking OAT. Participants in the CO-STAR trial, which had a 96% sustained virologic response rate among those who completed therapy, could elect to participate in the present study, offering a prospective look at long-term reinfection.
Out of 296 participants in the CO-STAR trial, 286 were evaluable for reinfection and 199 enrolled in the present extension. The majority were White (79.4%) and male (75.9%), with most taking methadone (79%), followed by buprenorphine (20%). At 6 months, 40 out of 191 respondents (21%) reported injection-drug use in the previous month. At the 3-year mark, 26 out of 142 respondents (18%) disclosed injection-drug use in the previous month.
For all participants in the CO-STAR trial, the overall rate of reinfection at 3 years was 1.7 per 100 person-years (95% confidence interval, 0.8-3.0), which is lower than the rate reported in systematic reviews (3.8 per 100 person-years), according to the investigators.
In the extension analysis, the 3-year reinfection rate was lower still, at 1.2 per 100 person-years. The rate was slightly higher among people who reported injection-drug use in the previous month (1.9 per 100 person-years), and slightly lower among those who did not report injection-drug use in the prior month (0.5 per 100 person-years). More pronounced differences in reinfection were observed among participants who shared needles (6.4 per 100 person-years), versus those who didn’t share needles (1.5 per 100 person years).
Low reinfection rate may help facilitate removal of reimbursement restrictions
“Most of the reinfections in this study occurred within 24 weeks of completing treatment, suggesting that this is a key period for optimizing treatment of opioid use disorder and for providing access to needle and syringe programs that have documented benefits in preventing HCV transmission,” the investigators wrote.
This is one of the largest observational studies of its kind to date, bolstered by “excellent study retention” and a “well-characterized cohort,” with findings that should prompt real-world action, said Dr. Grebely, who is head of the hepatitis C and drug use group in the viral hepatitis clinical research program at the Kirby Institute, University of New South Wales, Sydney.
“Given that reinfection has often been cited ... by some providers as a reason for not offering treatment to people receiving OAT, the low reinfection rate in this study will be incredibly important for guiding practice and ensuring therapy is not withheld from this group,” Dr. Grebely said in an interview. “In terms of policy implications, these data may also help to facilitate the removal of reimbursement restrictions based on recent drug/alcohol use criteria that are in place among many payers in the United States.”
More research needed to determine optimal intervention strategies
Carl Latkin, PhD, professor and vice chair of the department of health, behavior, and society at Johns Hopkins University, Baltimore, called the present publication a “great article and well-done study with long-term follow-up.”
Dr. Latkin, who investigates biobehavioral interventions for disadvantaged communities, said the reported rate of reinfection is “very low among a group of current and former injectors.”
Affirming Dr. Grebely’s call for supportive practices by physicians and payers, Dr. Latkin said: “The study highlights the importance of improving access to medication for opioid use disorder. This level of treatment adherence in this group is much higher than for many other medications. Given these data, it would be difficult for payers to have a rational reason for blanket restrictions for HCV treatment among people who use drugs.”
Dr. Latkin explained that “it isn’t simply injection drug use per se” that drives HCV reinfection; instead, he cited social factors, such as lack of housing, as well as withdrawal symptoms, especially among those without access to medications for opioid use disorder (MOUD).
Dr. Latkin and Grebely also agreed that more research is needed to determine optimal intervention strategies.
Dr. Grebely called for one to enhance HCV testing and linkage to care, a topic he covered in a recent review article (Lancet Gastroenterol Hepatol. 2022 May;7[5]:426-45.).
Dr. Latkin said that, while it’s clear that “syringe services programs, accessible HCV treatment, and MOUD are needed,” it is unclear how much coverage is necessary for a given population.
Findings support critical nature of needle and syringe exchange programs
Sarah M. Kattakuzhy, MD, an associate professor in the division of clinical care & research at the Institute of Human Virology, University of Maryland, Baltimore, agreed that the findings “support the critical nature of needle and syringe exchange programs.”
“As most cities in the United States fall well below the high coverage needle and syringe program threshold required to maximally prevent disease transmission, the study serves as a push toward an evidence-based harm reduction policy,” she said.
Dr. Kattakuzhy he added that the study “supports the need to longitudinally engage individuals after HCV treatment to monitor reinfection risk behaviors and test for reinfection,” she continued.
When it came to translating all the data to populations in the United States, she offered a more guarded view.
“Critically, the study population included only individuals who were engaged with OAT and adherent for 3 or more months, selecting to a population of individuals with high adherence and engagement in care,” Dr. Kattakuzhy said in an interview. “As such, the study findings are not applicable to other cross sections of the drug-using community, including individuals not engaged in OAT, and cohorts with higher rates of ongoing injection drug use. Furthermore, there are known genetic impacts on spontaneous clearance, and emerging data on the immunology of reinfection.
“Studies with a focus on less engaged, higher-risk, and minority populations with active drug use are required to answer the remaining questions in HCV reinfection,” she said.
The study was supported by Merck, the Australian Government Department of Health, and the Australian National Health and Medical Research Council. Dr. Grebely disclosed receiving funding from Cepheid, the manufacturer of the Xpert HCV assay. The other investigators disclosed additional relationships with Gilead, AbbVie, Cepheid, and others. Dr. Latkin and Dr. Kattakuzhy disclosed no relevant conflicts of interest.
The findings, which are based on prospective data from 13 countries, including the United States, and were published in Annals of Internal Medicine (2022 Aug 8. doi: 10.7326/M21-4119), should encourage physicians to treat HCV in people with a history of injection drug use, said lead author Jason Grebely, PhD. They should also pressure payers to lift reimbursement restrictions on the same population.
“Direct-acting antiviral medications for HCV infection are safe and effective among people receiving OAT and people with recent injecting-drug use,” the investigators wrote. “Concerns remain, however, that HCV reinfection may reduce the benefits of cure among people who inject drugs and compromise HCV elimination efforts.”
They explored these concerns through a 3-year extension of the phase 3 CO-STAR trial that evaluated elbasvir and grazoprevir in people consistently taking OAT. Participants in the CO-STAR trial, which had a 96% sustained virologic response rate among those who completed therapy, could elect to participate in the present study, offering a prospective look at long-term reinfection.
Out of 296 participants in the CO-STAR trial, 286 were evaluable for reinfection and 199 enrolled in the present extension. The majority were White (79.4%) and male (75.9%), with most taking methadone (79%), followed by buprenorphine (20%). At 6 months, 40 out of 191 respondents (21%) reported injection-drug use in the previous month. At the 3-year mark, 26 out of 142 respondents (18%) disclosed injection-drug use in the previous month.
For all participants in the CO-STAR trial, the overall rate of reinfection at 3 years was 1.7 per 100 person-years (95% confidence interval, 0.8-3.0), which is lower than the rate reported in systematic reviews (3.8 per 100 person-years), according to the investigators.
In the extension analysis, the 3-year reinfection rate was lower still, at 1.2 per 100 person-years. The rate was slightly higher among people who reported injection-drug use in the previous month (1.9 per 100 person-years), and slightly lower among those who did not report injection-drug use in the prior month (0.5 per 100 person-years). More pronounced differences in reinfection were observed among participants who shared needles (6.4 per 100 person-years), versus those who didn’t share needles (1.5 per 100 person years).
Low reinfection rate may help facilitate removal of reimbursement restrictions
“Most of the reinfections in this study occurred within 24 weeks of completing treatment, suggesting that this is a key period for optimizing treatment of opioid use disorder and for providing access to needle and syringe programs that have documented benefits in preventing HCV transmission,” the investigators wrote.
This is one of the largest observational studies of its kind to date, bolstered by “excellent study retention” and a “well-characterized cohort,” with findings that should prompt real-world action, said Dr. Grebely, who is head of the hepatitis C and drug use group in the viral hepatitis clinical research program at the Kirby Institute, University of New South Wales, Sydney.
“Given that reinfection has often been cited ... by some providers as a reason for not offering treatment to people receiving OAT, the low reinfection rate in this study will be incredibly important for guiding practice and ensuring therapy is not withheld from this group,” Dr. Grebely said in an interview. “In terms of policy implications, these data may also help to facilitate the removal of reimbursement restrictions based on recent drug/alcohol use criteria that are in place among many payers in the United States.”
More research needed to determine optimal intervention strategies
Carl Latkin, PhD, professor and vice chair of the department of health, behavior, and society at Johns Hopkins University, Baltimore, called the present publication a “great article and well-done study with long-term follow-up.”
Dr. Latkin, who investigates biobehavioral interventions for disadvantaged communities, said the reported rate of reinfection is “very low among a group of current and former injectors.”
Affirming Dr. Grebely’s call for supportive practices by physicians and payers, Dr. Latkin said: “The study highlights the importance of improving access to medication for opioid use disorder. This level of treatment adherence in this group is much higher than for many other medications. Given these data, it would be difficult for payers to have a rational reason for blanket restrictions for HCV treatment among people who use drugs.”
Dr. Latkin explained that “it isn’t simply injection drug use per se” that drives HCV reinfection; instead, he cited social factors, such as lack of housing, as well as withdrawal symptoms, especially among those without access to medications for opioid use disorder (MOUD).
Dr. Latkin and Grebely also agreed that more research is needed to determine optimal intervention strategies.
Dr. Grebely called for one to enhance HCV testing and linkage to care, a topic he covered in a recent review article (Lancet Gastroenterol Hepatol. 2022 May;7[5]:426-45.).
Dr. Latkin said that, while it’s clear that “syringe services programs, accessible HCV treatment, and MOUD are needed,” it is unclear how much coverage is necessary for a given population.
Findings support critical nature of needle and syringe exchange programs
Sarah M. Kattakuzhy, MD, an associate professor in the division of clinical care & research at the Institute of Human Virology, University of Maryland, Baltimore, agreed that the findings “support the critical nature of needle and syringe exchange programs.”
“As most cities in the United States fall well below the high coverage needle and syringe program threshold required to maximally prevent disease transmission, the study serves as a push toward an evidence-based harm reduction policy,” she said.
Dr. Kattakuzhy he added that the study “supports the need to longitudinally engage individuals after HCV treatment to monitor reinfection risk behaviors and test for reinfection,” she continued.
When it came to translating all the data to populations in the United States, she offered a more guarded view.
“Critically, the study population included only individuals who were engaged with OAT and adherent for 3 or more months, selecting to a population of individuals with high adherence and engagement in care,” Dr. Kattakuzhy said in an interview. “As such, the study findings are not applicable to other cross sections of the drug-using community, including individuals not engaged in OAT, and cohorts with higher rates of ongoing injection drug use. Furthermore, there are known genetic impacts on spontaneous clearance, and emerging data on the immunology of reinfection.
“Studies with a focus on less engaged, higher-risk, and minority populations with active drug use are required to answer the remaining questions in HCV reinfection,” she said.
The study was supported by Merck, the Australian Government Department of Health, and the Australian National Health and Medical Research Council. Dr. Grebely disclosed receiving funding from Cepheid, the manufacturer of the Xpert HCV assay. The other investigators disclosed additional relationships with Gilead, AbbVie, Cepheid, and others. Dr. Latkin and Dr. Kattakuzhy disclosed no relevant conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
‘Go Ask Alice’: A fake view of teen mental health
If you grew up in the 1970s and 1980s, chances are high you’re familiar with “Go Ask Alice.”
What was then said to be the real diary of a 15-year-old promising teen turned drug addict was released in 1971 as a cautionary tale and has since sold over 5 million copies. The diary was harrowing against the backdrop of the war on drugs and soon became both acclaimed and banned from classrooms across the country.
Schools citied “inappropriate” language that “borders on pornography” as grounds to prohibit teenagers from reading Alice’s story. But as much as the book’s vivid writing offended readers, it drew millions in with its profanity and graphic descriptions of sex, drugs, and mental health struggles.
At the time, The New York Times reviewed the book as “a strong, painfully honest, nakedly candid and true story ... a document of horrifying reality,” but the popular diary was later found to be a ploy – a fake story written by a 54-year-old Mormon youth counselor named Beatrice Sparks.
Now, Ms. Sparks, who died in 2012, has been further exposed in radio personality Rick Emerson’s new book, “Unmask Alice: LSD, Satanic Panic, and the Imposter Behind the World’s Most Notorious Diaries.” Mr. Emerson published the exposé in July, years after he had the idea to investigate Ms. Sparks’s work in 2015. The book details Ms. Sparks’s background, her journey in creating Alice, and her quest to be recognized for the teen diary she had published as “Anonymous.”
“After 30 years of trying, Beatrice Sparks had changed the world. And nobody knew it,” Mr. Emerson told the New York Post.In his work, Mr. Emerson also dives into the profound impact of the diary at a time when not as much research existed on teen mental health.
When the teenager whose diary inspired Ms. Sparks’s writing “died in March 1971, the very first true study of adolescent psychology had just barely come out,” Mr. Emerson said to Rolling Stone. “Mental health, especially for young people, was still very much on training wheels.”
According to Mr. Emerson, a lack of insight into mental health issues allowed Ms. Sparks’s description to go relatively unchallenged and for the book’s influence to spread despite its misinformation.
“It’s indisputable that large sections of ‘Go Ask Alice’ are just embellished and/or false,” he told the Post.
Then versus now
This landscape is in stark contrast to today, where thousands of studies on the topic have been done, compared with the mere dozens in the 1970s.
Anxiety and depression in minors have increased over time, a trend worsened by the COVID-19 pandemic, according to the CDC. Studies have shown that reported drug use in teens has decreased over time, proving significant during the pandemic, according to the National Institutes of Health.
While Alice from “Go Ask Alice” has not existed in either, comparing the two periods can offer insight into teen struggles in the 1970s versus today and sheds light on how literature – fiction or even faked nonfiction – can transform a nation.
A version of this article first appeared on WebMD.com.
If you grew up in the 1970s and 1980s, chances are high you’re familiar with “Go Ask Alice.”
What was then said to be the real diary of a 15-year-old promising teen turned drug addict was released in 1971 as a cautionary tale and has since sold over 5 million copies. The diary was harrowing against the backdrop of the war on drugs and soon became both acclaimed and banned from classrooms across the country.
Schools citied “inappropriate” language that “borders on pornography” as grounds to prohibit teenagers from reading Alice’s story. But as much as the book’s vivid writing offended readers, it drew millions in with its profanity and graphic descriptions of sex, drugs, and mental health struggles.
At the time, The New York Times reviewed the book as “a strong, painfully honest, nakedly candid and true story ... a document of horrifying reality,” but the popular diary was later found to be a ploy – a fake story written by a 54-year-old Mormon youth counselor named Beatrice Sparks.
Now, Ms. Sparks, who died in 2012, has been further exposed in radio personality Rick Emerson’s new book, “Unmask Alice: LSD, Satanic Panic, and the Imposter Behind the World’s Most Notorious Diaries.” Mr. Emerson published the exposé in July, years after he had the idea to investigate Ms. Sparks’s work in 2015. The book details Ms. Sparks’s background, her journey in creating Alice, and her quest to be recognized for the teen diary she had published as “Anonymous.”
“After 30 years of trying, Beatrice Sparks had changed the world. And nobody knew it,” Mr. Emerson told the New York Post.In his work, Mr. Emerson also dives into the profound impact of the diary at a time when not as much research existed on teen mental health.
When the teenager whose diary inspired Ms. Sparks’s writing “died in March 1971, the very first true study of adolescent psychology had just barely come out,” Mr. Emerson said to Rolling Stone. “Mental health, especially for young people, was still very much on training wheels.”
According to Mr. Emerson, a lack of insight into mental health issues allowed Ms. Sparks’s description to go relatively unchallenged and for the book’s influence to spread despite its misinformation.
“It’s indisputable that large sections of ‘Go Ask Alice’ are just embellished and/or false,” he told the Post.
Then versus now
This landscape is in stark contrast to today, where thousands of studies on the topic have been done, compared with the mere dozens in the 1970s.
Anxiety and depression in minors have increased over time, a trend worsened by the COVID-19 pandemic, according to the CDC. Studies have shown that reported drug use in teens has decreased over time, proving significant during the pandemic, according to the National Institutes of Health.
While Alice from “Go Ask Alice” has not existed in either, comparing the two periods can offer insight into teen struggles in the 1970s versus today and sheds light on how literature – fiction or even faked nonfiction – can transform a nation.
A version of this article first appeared on WebMD.com.
If you grew up in the 1970s and 1980s, chances are high you’re familiar with “Go Ask Alice.”
What was then said to be the real diary of a 15-year-old promising teen turned drug addict was released in 1971 as a cautionary tale and has since sold over 5 million copies. The diary was harrowing against the backdrop of the war on drugs and soon became both acclaimed and banned from classrooms across the country.
Schools citied “inappropriate” language that “borders on pornography” as grounds to prohibit teenagers from reading Alice’s story. But as much as the book’s vivid writing offended readers, it drew millions in with its profanity and graphic descriptions of sex, drugs, and mental health struggles.
At the time, The New York Times reviewed the book as “a strong, painfully honest, nakedly candid and true story ... a document of horrifying reality,” but the popular diary was later found to be a ploy – a fake story written by a 54-year-old Mormon youth counselor named Beatrice Sparks.
Now, Ms. Sparks, who died in 2012, has been further exposed in radio personality Rick Emerson’s new book, “Unmask Alice: LSD, Satanic Panic, and the Imposter Behind the World’s Most Notorious Diaries.” Mr. Emerson published the exposé in July, years after he had the idea to investigate Ms. Sparks’s work in 2015. The book details Ms. Sparks’s background, her journey in creating Alice, and her quest to be recognized for the teen diary she had published as “Anonymous.”
“After 30 years of trying, Beatrice Sparks had changed the world. And nobody knew it,” Mr. Emerson told the New York Post.In his work, Mr. Emerson also dives into the profound impact of the diary at a time when not as much research existed on teen mental health.
When the teenager whose diary inspired Ms. Sparks’s writing “died in March 1971, the very first true study of adolescent psychology had just barely come out,” Mr. Emerson said to Rolling Stone. “Mental health, especially for young people, was still very much on training wheels.”
According to Mr. Emerson, a lack of insight into mental health issues allowed Ms. Sparks’s description to go relatively unchallenged and for the book’s influence to spread despite its misinformation.
“It’s indisputable that large sections of ‘Go Ask Alice’ are just embellished and/or false,” he told the Post.
Then versus now
This landscape is in stark contrast to today, where thousands of studies on the topic have been done, compared with the mere dozens in the 1970s.
Anxiety and depression in minors have increased over time, a trend worsened by the COVID-19 pandemic, according to the CDC. Studies have shown that reported drug use in teens has decreased over time, proving significant during the pandemic, according to the National Institutes of Health.
While Alice from “Go Ask Alice” has not existed in either, comparing the two periods can offer insight into teen struggles in the 1970s versus today and sheds light on how literature – fiction or even faked nonfiction – can transform a nation.
A version of this article first appeared on WebMD.com.
University to train ‘trip facilitators’ for psychedelic therapy
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.













