User login
Heart failure drug a new treatment option for alcoholism?
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
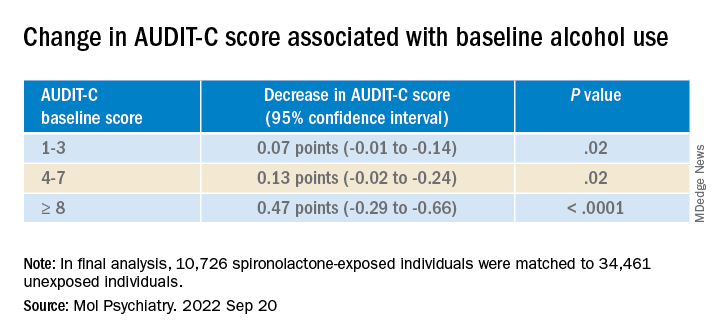
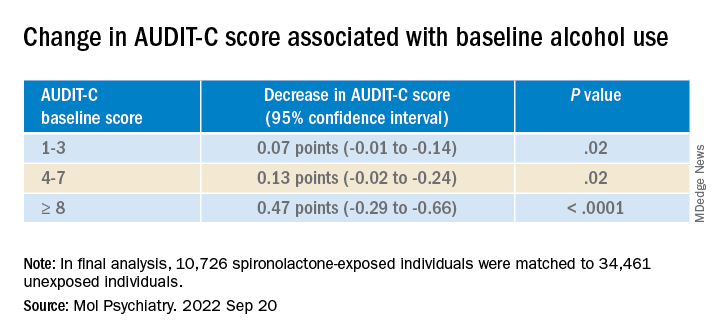
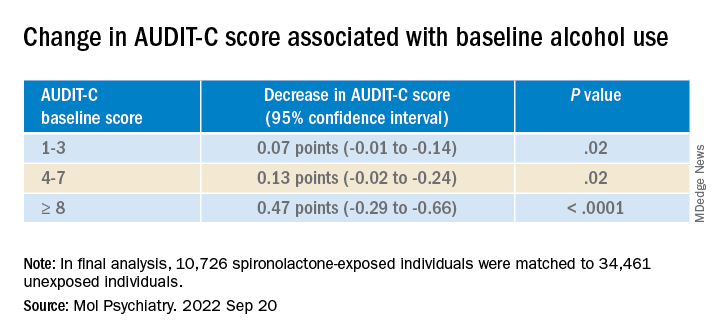
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.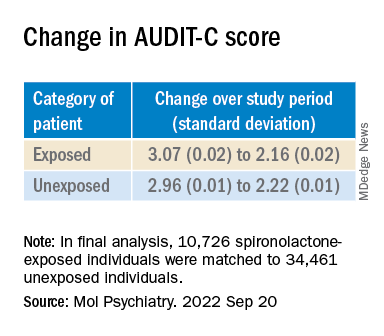
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.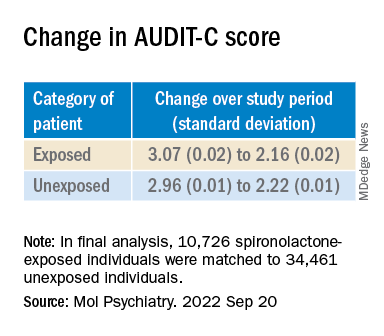
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.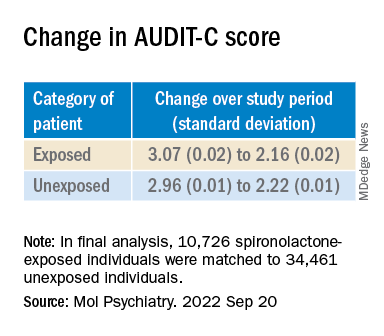
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MOLECULAR PSYCHIATRY
Minorities hit especially hard by overdose deaths during COVID
The results underscore the “urgency of expanding prevention, treatment, and harm reduction interventions tailored to specific populations, especially American Indian or Alaska Native and Black populations, given long-standing structural racism and inequities in accessing these services,” the researchers note.
The study was published online in JAMA Network Open.
‘Urgent need’ for education
From February 2020 to August 2021, drug overdose deaths in the United States rose 37%, and these deaths were largely due to synthetic opioids other than methadone – primarily fentanyl or analogs – and methamphetamine.
Yet, data are lacking regarding racial and ethnic disparities in overdose death rates.
To investigate, Beth Han, MD, PhD, with the National Institute on Drug Abuse, and colleagues analyzed federal drug overdose death data for individuals aged 15-34 and 35-64 from March 2018 to August 2021.
Among individuals aged 15-34, from March 2018 to August 2021, overdose death rates involving any drug, fentanyl, and methamphetamine with or without fentanyl, increased overall.
For the 6 months from March to August 2021, non-Hispanic Native American or Alaska Native men had the highest rates overall involving any drug, fentanyl, and methamphetamine without fentanyl, with rates of 42.0, 30.2, and 6.0 per 100,000, respectively.
The highest rates (per 100,000) of drug overdose deaths involving methamphetamine with fentanyl were for Native American or Alaska Native men (9.2) and women (8.0) and non-Hispanic White men (6.7).
Among people aged 35-64, from March to August 2021, overall drug overdose rates (per 100,000) were highest among non-Hispanic Black men (61.2) and Native American or Alaska Native men (60.0), and fentanyl-involved death rates were highest among Black men (43.3).
Rates involving methamphetamine with fentanyl were highest among Native American or Alaska Native men (12.6) and women (9.4) and White men (9.5).
Rates involving methamphetamine without fentanyl were highest among Native American or Alaska Native men (22.9).
The researchers note the findings highlight the “urgent need” for education on dangers of methamphetamine and fentanyl.
Expanding access to naloxone, fentanyl test strips, and treatments for substance use disorders to disproportionately affected populations is also critical to help curb disparities in drug overdose deaths, they add.
Limitations of the study are that overdose deaths may be underestimated because of the use of 2021 provisional data and that racial or ethnic identification may be misclassified, especially for Native American or Alaska Native people.
This study was sponsored by the National Institute on Drug Abuse of the National Institutes of Health and the Centers for Disease Control and Prevention. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
The results underscore the “urgency of expanding prevention, treatment, and harm reduction interventions tailored to specific populations, especially American Indian or Alaska Native and Black populations, given long-standing structural racism and inequities in accessing these services,” the researchers note.
The study was published online in JAMA Network Open.
‘Urgent need’ for education
From February 2020 to August 2021, drug overdose deaths in the United States rose 37%, and these deaths were largely due to synthetic opioids other than methadone – primarily fentanyl or analogs – and methamphetamine.
Yet, data are lacking regarding racial and ethnic disparities in overdose death rates.
To investigate, Beth Han, MD, PhD, with the National Institute on Drug Abuse, and colleagues analyzed federal drug overdose death data for individuals aged 15-34 and 35-64 from March 2018 to August 2021.
Among individuals aged 15-34, from March 2018 to August 2021, overdose death rates involving any drug, fentanyl, and methamphetamine with or without fentanyl, increased overall.
For the 6 months from March to August 2021, non-Hispanic Native American or Alaska Native men had the highest rates overall involving any drug, fentanyl, and methamphetamine without fentanyl, with rates of 42.0, 30.2, and 6.0 per 100,000, respectively.
The highest rates (per 100,000) of drug overdose deaths involving methamphetamine with fentanyl were for Native American or Alaska Native men (9.2) and women (8.0) and non-Hispanic White men (6.7).
Among people aged 35-64, from March to August 2021, overall drug overdose rates (per 100,000) were highest among non-Hispanic Black men (61.2) and Native American or Alaska Native men (60.0), and fentanyl-involved death rates were highest among Black men (43.3).
Rates involving methamphetamine with fentanyl were highest among Native American or Alaska Native men (12.6) and women (9.4) and White men (9.5).
Rates involving methamphetamine without fentanyl were highest among Native American or Alaska Native men (22.9).
The researchers note the findings highlight the “urgent need” for education on dangers of methamphetamine and fentanyl.
Expanding access to naloxone, fentanyl test strips, and treatments for substance use disorders to disproportionately affected populations is also critical to help curb disparities in drug overdose deaths, they add.
Limitations of the study are that overdose deaths may be underestimated because of the use of 2021 provisional data and that racial or ethnic identification may be misclassified, especially for Native American or Alaska Native people.
This study was sponsored by the National Institute on Drug Abuse of the National Institutes of Health and the Centers for Disease Control and Prevention. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
The results underscore the “urgency of expanding prevention, treatment, and harm reduction interventions tailored to specific populations, especially American Indian or Alaska Native and Black populations, given long-standing structural racism and inequities in accessing these services,” the researchers note.
The study was published online in JAMA Network Open.
‘Urgent need’ for education
From February 2020 to August 2021, drug overdose deaths in the United States rose 37%, and these deaths were largely due to synthetic opioids other than methadone – primarily fentanyl or analogs – and methamphetamine.
Yet, data are lacking regarding racial and ethnic disparities in overdose death rates.
To investigate, Beth Han, MD, PhD, with the National Institute on Drug Abuse, and colleagues analyzed federal drug overdose death data for individuals aged 15-34 and 35-64 from March 2018 to August 2021.
Among individuals aged 15-34, from March 2018 to August 2021, overdose death rates involving any drug, fentanyl, and methamphetamine with or without fentanyl, increased overall.
For the 6 months from March to August 2021, non-Hispanic Native American or Alaska Native men had the highest rates overall involving any drug, fentanyl, and methamphetamine without fentanyl, with rates of 42.0, 30.2, and 6.0 per 100,000, respectively.
The highest rates (per 100,000) of drug overdose deaths involving methamphetamine with fentanyl were for Native American or Alaska Native men (9.2) and women (8.0) and non-Hispanic White men (6.7).
Among people aged 35-64, from March to August 2021, overall drug overdose rates (per 100,000) were highest among non-Hispanic Black men (61.2) and Native American or Alaska Native men (60.0), and fentanyl-involved death rates were highest among Black men (43.3).
Rates involving methamphetamine with fentanyl were highest among Native American or Alaska Native men (12.6) and women (9.4) and White men (9.5).
Rates involving methamphetamine without fentanyl were highest among Native American or Alaska Native men (22.9).
The researchers note the findings highlight the “urgent need” for education on dangers of methamphetamine and fentanyl.
Expanding access to naloxone, fentanyl test strips, and treatments for substance use disorders to disproportionately affected populations is also critical to help curb disparities in drug overdose deaths, they add.
Limitations of the study are that overdose deaths may be underestimated because of the use of 2021 provisional data and that racial or ethnic identification may be misclassified, especially for Native American or Alaska Native people.
This study was sponsored by the National Institute on Drug Abuse of the National Institutes of Health and the Centers for Disease Control and Prevention. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Urgent need for research into psychedelic therapy for older adults
new research shows.
“Geriatric psychiatrists and others caring for older adults are interested in how much is known about psychedelic use in older adults,” study investigator C. Bree Johnston, MD, MPH, University of Arizona, Tucson, told this news organization.
“A major concern is how safe psychedelic-assisted therapy is for patients with heart disease, hypertension, neurological disorders, and multimorbidity,” Dr. Johnston said.
The study is published online in the American Journal of Geriatric Psychiatry.
‘Groundswell’ of research
The past few years have brought a “groundswell” of interest and promising research into the potential therapeutic benefit of psychedelic-assisted therapy for a variety of conditions affecting adults, the researchers noted.
They include psilocybin-assisted therapy for the distress associated with a terminal diagnosis, depression, and addiction, and MDMA-assisted therapy for PTSD.
However, in most studies, psychedelic therapy has been tested in relatively young healthy adults, raising the question of how generalizable the study results are for the patients that most geropsychiatrists will be treating, the investigators noted.
They reviewed “the most important” research studies on psilocybin- and MDMA-assisted therapies published over the past 2 decades that are likely to be relevant for geriatric psychiatrists and other professionals caring for older adults.
The researchers point out that psychedelics and related compounds have shown efficacy for the treatment of a number of conditions that are common among older adults, including mood disorders, distress associated with a serious medical illness, PTSD, substance use problems, and prolonged grief.
Psychedelics also have properties that may provide for cognitive impairment and dementia and promote personal growth among healthy older adults.
Research has shown that psychedelics can be safely administered to healthy adults in controlled conditions.
However, both psilocybin and MDMA can increase blood pressure and heart rate, which could be a concern if used in older adults with cardiovascular disease, the investigators noted.
“Healthy older adults are likely to face similar risks when undergoing psychedelic-assisted therapy as healthy younger adults,” said Dr. Johnston.
“In carefully selected adults, those risks appear to be minor when psychedelics are administered in controlled conditions under the guidance of a skilled therapist,” she added.
Given the potential of psychedelic compounds to benefit older adults, the authors call for more research to establish the safety and efficacy among older adults, particularly those with multiple comorbidities.
Pressing knowledge gaps
The exclusion of older adults from clinical trials of novel treatments is “one of contemporary psychiatry’s more pressing problems – one that extends beyond psychedelics,” Ipsit V. Vahia, MD, associate chief of the division of geriatric psychiatry, McLean Hospital, Belmont, Mass., who wasn’t involved in the review, told this news organization.
“Currently, there is little evidence that clinicians can lean on while considering the use of psychedelics in older adults,” Dr. Vahia said.
This paper highlights “the most pressing gaps in the evidence that bear addressing in order to develop more substantial best practices around the use of these drugs,” he added.
For example, little is known about appropriate dosing, pharmacokinetics, and pharmacodynamics of psychedelics in older adults, Dr. Vahia said.
“Their risks, particularly cardiovascular risks, are barely studied, and almost nothing is known about how these drugs may impact those in their 80s or older, or those with serious medical comorbidities who use multiple medications,” Dr. Vahia said. “The majority of the existing literature has excluded older adults, and the extremely limited evidence that does exist has been collected in relatively healthy, and relatively young (aged below 75) persons.”
Dr. Vahia noted that, before psychedelics as a class can be considered viable treatment options for a broader group of older adults, “more research is needed, particularly to establish safety.”
This research had no specific funding. Dr. Johnston and Dr. Vahia have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
new research shows.
“Geriatric psychiatrists and others caring for older adults are interested in how much is known about psychedelic use in older adults,” study investigator C. Bree Johnston, MD, MPH, University of Arizona, Tucson, told this news organization.
“A major concern is how safe psychedelic-assisted therapy is for patients with heart disease, hypertension, neurological disorders, and multimorbidity,” Dr. Johnston said.
The study is published online in the American Journal of Geriatric Psychiatry.
‘Groundswell’ of research
The past few years have brought a “groundswell” of interest and promising research into the potential therapeutic benefit of psychedelic-assisted therapy for a variety of conditions affecting adults, the researchers noted.
They include psilocybin-assisted therapy for the distress associated with a terminal diagnosis, depression, and addiction, and MDMA-assisted therapy for PTSD.
However, in most studies, psychedelic therapy has been tested in relatively young healthy adults, raising the question of how generalizable the study results are for the patients that most geropsychiatrists will be treating, the investigators noted.
They reviewed “the most important” research studies on psilocybin- and MDMA-assisted therapies published over the past 2 decades that are likely to be relevant for geriatric psychiatrists and other professionals caring for older adults.
The researchers point out that psychedelics and related compounds have shown efficacy for the treatment of a number of conditions that are common among older adults, including mood disorders, distress associated with a serious medical illness, PTSD, substance use problems, and prolonged grief.
Psychedelics also have properties that may provide for cognitive impairment and dementia and promote personal growth among healthy older adults.
Research has shown that psychedelics can be safely administered to healthy adults in controlled conditions.
However, both psilocybin and MDMA can increase blood pressure and heart rate, which could be a concern if used in older adults with cardiovascular disease, the investigators noted.
“Healthy older adults are likely to face similar risks when undergoing psychedelic-assisted therapy as healthy younger adults,” said Dr. Johnston.
“In carefully selected adults, those risks appear to be minor when psychedelics are administered in controlled conditions under the guidance of a skilled therapist,” she added.
Given the potential of psychedelic compounds to benefit older adults, the authors call for more research to establish the safety and efficacy among older adults, particularly those with multiple comorbidities.
Pressing knowledge gaps
The exclusion of older adults from clinical trials of novel treatments is “one of contemporary psychiatry’s more pressing problems – one that extends beyond psychedelics,” Ipsit V. Vahia, MD, associate chief of the division of geriatric psychiatry, McLean Hospital, Belmont, Mass., who wasn’t involved in the review, told this news organization.
“Currently, there is little evidence that clinicians can lean on while considering the use of psychedelics in older adults,” Dr. Vahia said.
This paper highlights “the most pressing gaps in the evidence that bear addressing in order to develop more substantial best practices around the use of these drugs,” he added.
For example, little is known about appropriate dosing, pharmacokinetics, and pharmacodynamics of psychedelics in older adults, Dr. Vahia said.
“Their risks, particularly cardiovascular risks, are barely studied, and almost nothing is known about how these drugs may impact those in their 80s or older, or those with serious medical comorbidities who use multiple medications,” Dr. Vahia said. “The majority of the existing literature has excluded older adults, and the extremely limited evidence that does exist has been collected in relatively healthy, and relatively young (aged below 75) persons.”
Dr. Vahia noted that, before psychedelics as a class can be considered viable treatment options for a broader group of older adults, “more research is needed, particularly to establish safety.”
This research had no specific funding. Dr. Johnston and Dr. Vahia have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
new research shows.
“Geriatric psychiatrists and others caring for older adults are interested in how much is known about psychedelic use in older adults,” study investigator C. Bree Johnston, MD, MPH, University of Arizona, Tucson, told this news organization.
“A major concern is how safe psychedelic-assisted therapy is for patients with heart disease, hypertension, neurological disorders, and multimorbidity,” Dr. Johnston said.
The study is published online in the American Journal of Geriatric Psychiatry.
‘Groundswell’ of research
The past few years have brought a “groundswell” of interest and promising research into the potential therapeutic benefit of psychedelic-assisted therapy for a variety of conditions affecting adults, the researchers noted.
They include psilocybin-assisted therapy for the distress associated with a terminal diagnosis, depression, and addiction, and MDMA-assisted therapy for PTSD.
However, in most studies, psychedelic therapy has been tested in relatively young healthy adults, raising the question of how generalizable the study results are for the patients that most geropsychiatrists will be treating, the investigators noted.
They reviewed “the most important” research studies on psilocybin- and MDMA-assisted therapies published over the past 2 decades that are likely to be relevant for geriatric psychiatrists and other professionals caring for older adults.
The researchers point out that psychedelics and related compounds have shown efficacy for the treatment of a number of conditions that are common among older adults, including mood disorders, distress associated with a serious medical illness, PTSD, substance use problems, and prolonged grief.
Psychedelics also have properties that may provide for cognitive impairment and dementia and promote personal growth among healthy older adults.
Research has shown that psychedelics can be safely administered to healthy adults in controlled conditions.
However, both psilocybin and MDMA can increase blood pressure and heart rate, which could be a concern if used in older adults with cardiovascular disease, the investigators noted.
“Healthy older adults are likely to face similar risks when undergoing psychedelic-assisted therapy as healthy younger adults,” said Dr. Johnston.
“In carefully selected adults, those risks appear to be minor when psychedelics are administered in controlled conditions under the guidance of a skilled therapist,” she added.
Given the potential of psychedelic compounds to benefit older adults, the authors call for more research to establish the safety and efficacy among older adults, particularly those with multiple comorbidities.
Pressing knowledge gaps
The exclusion of older adults from clinical trials of novel treatments is “one of contemporary psychiatry’s more pressing problems – one that extends beyond psychedelics,” Ipsit V. Vahia, MD, associate chief of the division of geriatric psychiatry, McLean Hospital, Belmont, Mass., who wasn’t involved in the review, told this news organization.
“Currently, there is little evidence that clinicians can lean on while considering the use of psychedelics in older adults,” Dr. Vahia said.
This paper highlights “the most pressing gaps in the evidence that bear addressing in order to develop more substantial best practices around the use of these drugs,” he added.
For example, little is known about appropriate dosing, pharmacokinetics, and pharmacodynamics of psychedelics in older adults, Dr. Vahia said.
“Their risks, particularly cardiovascular risks, are barely studied, and almost nothing is known about how these drugs may impact those in their 80s or older, or those with serious medical comorbidities who use multiple medications,” Dr. Vahia said. “The majority of the existing literature has excluded older adults, and the extremely limited evidence that does exist has been collected in relatively healthy, and relatively young (aged below 75) persons.”
Dr. Vahia noted that, before psychedelics as a class can be considered viable treatment options for a broader group of older adults, “more research is needed, particularly to establish safety.”
This research had no specific funding. Dr. Johnston and Dr. Vahia have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Clozapine may be best choice for cutting SUD risk in schizophrenia
results of a real-world study show.
“Our findings are in line with a recent meta-analysis showing superior efficacy of clozapine in schizophrenia and comorbid SUD and other studies pointing toward clozapine’s superiority over other antipsychotics in the treatment of individuals with schizophrenia and comorbid SUD,” the investigators, led by Jari Tiihonen MD, PhD, department of clinical neuroscience, Karolinska Institutet, Stockholm, write.
“The results on polypharmacy are in line with previous results from nationwide cohorts showing a favorable outcome, compared with oral monotherapies among persons with schizophrenia in general,” they add.
The study was published online Aug. 25 in The British Journal of Psychiatry.
Research gap
Research on the effectiveness of pharmacotherapies for schizophrenia and comorbid SUD is “very sparse, and more importantly, non-existent on the prevention of the development of SUDs in patients with schizophrenia,” the researchers note.
To investigate, they analyzed data on more than 45,000 patients with schizophrenia from Finnish and Swedish national registries, with follow-up lasting 22 years in Finland and 11 years in Sweden.
In patients with schizophrenia without SUD, treatment with clozapine was associated with lowest risk for an initial SUD in both Finland (adjusted hazard ratio, 0.20; 95% confidence interval, 0.16-0.24) and Sweden (aHR, 0.35; 95% CI, 0.24-0.50), compared with no use or use of other antipsychotics.
In Finland, aripiprazole was associated with the second lowest risk for an initial SUD (aHR, 0.36; 95% CI, 0.24-0.55) and antipsychotic polytherapy the third lowest risk (aHR, 0.47; 95% CI, 0.42-0.53).
In Sweden, antipsychotic polytherapy was associated with second lowest risk for an initial SUD (aHR, 0.54; 95% CI, 0.44-0.66) and olanzapine the third lowest risk (aHR, 0.67; 95% CI, 0.53-0.84).
In both countries, the risk for relapse as indicated by psychiatric hospital admission and SUD-related hospital admission were lowest for clozapine, antipsychotic polytherapy and long-acting injectables, the investigators report.
Interpret with caution
Reached for comment, Christoph U. Correll, MD, professor of psychiatry and molecular medicine, the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York, urged caution in interpreting the results.
“While the authors are experts in national database analyses and the study was conducted with state-of-the-art methodology, the onset of SUD analyses favoring clozapine are subject to survival bias and order effects,” Dr. Correll said.
“Since clozapine is generally used later in the illness and treatment course, after multiple other antipsychotics have been used, and since SUDs generally occur early in the illness course, most SUDs will already have arisen by the time that clozapine is considered and used,” Dr. Correll said.
“A similar potential bias exists for long-acting injectables (LAIs), as these have generally also been used late in the treatment algorithm,” he noted.
In terms of the significant reduction of SUD-related hospitalizations observed with clozapine, the “order effect” could also be relevant, Dr. Correll said, because over time, patients are less likely to be nonadherent and hospitalized and clozapine is systematically used later in life than other antipsychotics.
“Why antipsychotic polytherapy came out as the second-best treatment is much less clear. Clearly head-to-head randomized trials are needed to follow up on these interesting and intriguing naturalistic database study data,” said Dr. Correll.
This study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital. Dr. Tiihonen and three co-authors have participated in research projects funded by grants from Janssen-Cilag and Eli Lilly to their institution. Dr. Correll reports having been a consultant and/or advisor to or receiving honoraria from many companies. He has also provided expert testimony for Janssen and Otsuka; served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma, and Quantic.
A version of this article first appeared on Medscape.com.
results of a real-world study show.
“Our findings are in line with a recent meta-analysis showing superior efficacy of clozapine in schizophrenia and comorbid SUD and other studies pointing toward clozapine’s superiority over other antipsychotics in the treatment of individuals with schizophrenia and comorbid SUD,” the investigators, led by Jari Tiihonen MD, PhD, department of clinical neuroscience, Karolinska Institutet, Stockholm, write.
“The results on polypharmacy are in line with previous results from nationwide cohorts showing a favorable outcome, compared with oral monotherapies among persons with schizophrenia in general,” they add.
The study was published online Aug. 25 in The British Journal of Psychiatry.
Research gap
Research on the effectiveness of pharmacotherapies for schizophrenia and comorbid SUD is “very sparse, and more importantly, non-existent on the prevention of the development of SUDs in patients with schizophrenia,” the researchers note.
To investigate, they analyzed data on more than 45,000 patients with schizophrenia from Finnish and Swedish national registries, with follow-up lasting 22 years in Finland and 11 years in Sweden.
In patients with schizophrenia without SUD, treatment with clozapine was associated with lowest risk for an initial SUD in both Finland (adjusted hazard ratio, 0.20; 95% confidence interval, 0.16-0.24) and Sweden (aHR, 0.35; 95% CI, 0.24-0.50), compared with no use or use of other antipsychotics.
In Finland, aripiprazole was associated with the second lowest risk for an initial SUD (aHR, 0.36; 95% CI, 0.24-0.55) and antipsychotic polytherapy the third lowest risk (aHR, 0.47; 95% CI, 0.42-0.53).
In Sweden, antipsychotic polytherapy was associated with second lowest risk for an initial SUD (aHR, 0.54; 95% CI, 0.44-0.66) and olanzapine the third lowest risk (aHR, 0.67; 95% CI, 0.53-0.84).
In both countries, the risk for relapse as indicated by psychiatric hospital admission and SUD-related hospital admission were lowest for clozapine, antipsychotic polytherapy and long-acting injectables, the investigators report.
Interpret with caution
Reached for comment, Christoph U. Correll, MD, professor of psychiatry and molecular medicine, the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York, urged caution in interpreting the results.
“While the authors are experts in national database analyses and the study was conducted with state-of-the-art methodology, the onset of SUD analyses favoring clozapine are subject to survival bias and order effects,” Dr. Correll said.
“Since clozapine is generally used later in the illness and treatment course, after multiple other antipsychotics have been used, and since SUDs generally occur early in the illness course, most SUDs will already have arisen by the time that clozapine is considered and used,” Dr. Correll said.
“A similar potential bias exists for long-acting injectables (LAIs), as these have generally also been used late in the treatment algorithm,” he noted.
In terms of the significant reduction of SUD-related hospitalizations observed with clozapine, the “order effect” could also be relevant, Dr. Correll said, because over time, patients are less likely to be nonadherent and hospitalized and clozapine is systematically used later in life than other antipsychotics.
“Why antipsychotic polytherapy came out as the second-best treatment is much less clear. Clearly head-to-head randomized trials are needed to follow up on these interesting and intriguing naturalistic database study data,” said Dr. Correll.
This study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital. Dr. Tiihonen and three co-authors have participated in research projects funded by grants from Janssen-Cilag and Eli Lilly to their institution. Dr. Correll reports having been a consultant and/or advisor to or receiving honoraria from many companies. He has also provided expert testimony for Janssen and Otsuka; served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma, and Quantic.
A version of this article first appeared on Medscape.com.
results of a real-world study show.
“Our findings are in line with a recent meta-analysis showing superior efficacy of clozapine in schizophrenia and comorbid SUD and other studies pointing toward clozapine’s superiority over other antipsychotics in the treatment of individuals with schizophrenia and comorbid SUD,” the investigators, led by Jari Tiihonen MD, PhD, department of clinical neuroscience, Karolinska Institutet, Stockholm, write.
“The results on polypharmacy are in line with previous results from nationwide cohorts showing a favorable outcome, compared with oral monotherapies among persons with schizophrenia in general,” they add.
The study was published online Aug. 25 in The British Journal of Psychiatry.
Research gap
Research on the effectiveness of pharmacotherapies for schizophrenia and comorbid SUD is “very sparse, and more importantly, non-existent on the prevention of the development of SUDs in patients with schizophrenia,” the researchers note.
To investigate, they analyzed data on more than 45,000 patients with schizophrenia from Finnish and Swedish national registries, with follow-up lasting 22 years in Finland and 11 years in Sweden.
In patients with schizophrenia without SUD, treatment with clozapine was associated with lowest risk for an initial SUD in both Finland (adjusted hazard ratio, 0.20; 95% confidence interval, 0.16-0.24) and Sweden (aHR, 0.35; 95% CI, 0.24-0.50), compared with no use or use of other antipsychotics.
In Finland, aripiprazole was associated with the second lowest risk for an initial SUD (aHR, 0.36; 95% CI, 0.24-0.55) and antipsychotic polytherapy the third lowest risk (aHR, 0.47; 95% CI, 0.42-0.53).
In Sweden, antipsychotic polytherapy was associated with second lowest risk for an initial SUD (aHR, 0.54; 95% CI, 0.44-0.66) and olanzapine the third lowest risk (aHR, 0.67; 95% CI, 0.53-0.84).
In both countries, the risk for relapse as indicated by psychiatric hospital admission and SUD-related hospital admission were lowest for clozapine, antipsychotic polytherapy and long-acting injectables, the investigators report.
Interpret with caution
Reached for comment, Christoph U. Correll, MD, professor of psychiatry and molecular medicine, the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York, urged caution in interpreting the results.
“While the authors are experts in national database analyses and the study was conducted with state-of-the-art methodology, the onset of SUD analyses favoring clozapine are subject to survival bias and order effects,” Dr. Correll said.
“Since clozapine is generally used later in the illness and treatment course, after multiple other antipsychotics have been used, and since SUDs generally occur early in the illness course, most SUDs will already have arisen by the time that clozapine is considered and used,” Dr. Correll said.
“A similar potential bias exists for long-acting injectables (LAIs), as these have generally also been used late in the treatment algorithm,” he noted.
In terms of the significant reduction of SUD-related hospitalizations observed with clozapine, the “order effect” could also be relevant, Dr. Correll said, because over time, patients are less likely to be nonadherent and hospitalized and clozapine is systematically used later in life than other antipsychotics.
“Why antipsychotic polytherapy came out as the second-best treatment is much less clear. Clearly head-to-head randomized trials are needed to follow up on these interesting and intriguing naturalistic database study data,” said Dr. Correll.
This study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital. Dr. Tiihonen and three co-authors have participated in research projects funded by grants from Janssen-Cilag and Eli Lilly to their institution. Dr. Correll reports having been a consultant and/or advisor to or receiving honoraria from many companies. He has also provided expert testimony for Janssen and Otsuka; served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma, and Quantic.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF PSYCHIATRY
Largest-ever study into the effects of cannabis on the brain
The largest-ever independent study into the effects of cannabis on the brain is being carried out in the United Kingdom.
Even though cannabis is the most commonly used illegal drug in the United Kingdom and medicinal cannabis has been legal there since 2018 little is known about why some people react badly to it and others seem to benefit from it.
According to Home Office figures on drug use from 2019, 7.6% of adults aged 16-59 used cannabis in the previous year.
Medicinal cannabis in the United Kingdom can only be prescribed if no other licensed medicine could help the patient. At the moment, GPs can’t prescribe it, only specialist hospital doctors can. The National Health Service says it can only be used in three circumstances: in rare, severe epilepsy; to deal with chemotherapy side effects such as nausea; or to help with multiple sclerosis.
As part of the Cannabis&Me study, KCL needs to get 3,000 current cannabis users and 3,000 non–cannabis users to take part in an online survey, with a third of those survey respondents then taking part in a face-to-face assessment that includes virtual reality (VR) and psychological analysis. The study also aims to determine how the DNA of cannabis users and their endocannabinoid system impacts their experiences, both negative and positive, with the drug.
The study is spearheaded by Marta Di Forti, MD, PhD, and has been allocated over £2.5 million in funding by the Medical Research Council.
This news organization asked Dr. Di Forti about the study.
Question: How do you describe the study?
Answer: “It’s a really unique study. We are aiming to see what’s happening to people using cannabis in the privacy of their homes for medicinal, recreational reasons, or whatever other reason.
“The debate on cannabis has always been quite polarized. There have been people who experience adversities with cannabis use, especially psychosis, whose families may perhaps like cannabis to be abolished if possible. Then there are other people who are saying they get positive benefits from using cannabis.”
Q: So where does the study come in?
A: “The study wants to bring the two sides of the argument together and understand what’s really happening. The group I see as a clinician comes to severe harm when they use cannabis regularly. We want to find out who they are and whether we can identify them. While we need to make sure they never come to harm when using cannabis, we need to consider others who won’t come to harm from using cannabis and give them a chance to use it in a way that’s beneficial.”
Q: How does the study work?
A: “The first step of the study is to use an online questionnaire that can be filled in by anyone aged 18-45 who lives in the London area or can travel here if selected. The first set of questions are a general idea of their cannabis use: ‘Why do they use it?’ ‘What are its benefits?’ Then, general questions on what their life has been like up to that point: ‘Did they have any adversities in childhood?’ ‘How is their mood and anxiety levels?’ ‘Do they experience any paranoid responses in everyday life?’ It probably takes between 30 and 40 minutes to fill out the questionnaire.”
Q: Can you explain about paranoid responses?
A: “We go through the questionnaires looking at people’s paranoid response to everyday life, not in a clinical disorder term, just in terms of the differences in how we respond to certain circumstances. For example: ‘How do you feel if someone’s staring at you on the Tube?’ Some people are afraid, some feel uncomfortable, some people don’t notice, and others think a person is staring at them as they look good or another such positive feeling. So, we give people a paranoia score and will invite some at the top and some at the bottom of that score for a face-to-face assessment. We want to select those people who are using cannabis daily and they are getting either no paranoia or high paranoia.”
Q: What happens at the face-to-face assessments?
A: “We do two things which are very novel. We ask them to take part in a virtual reality experience. They are in a lovely shop and within this experience they come across challenges, which may or may not induce a benign paranoia response. We will ask them to donate a sample of blood before they go into the VR set. We will test for tetrahydrocannabinol (THC) and cannabidiol (CBD). We will also look at the metabolites of the two. People don’t take into account how differently individuals metabolize cannabis, which could be one of the reasons why some people can tolerate it and others can’t.”
Q: There’s also a genetic aspect of the study?
A: “From the same sample, we will extract DNA to look at the genetics across the genome and compare genetic variations between high and low paranoia in the context of cannabis use. Also, we will look at the epigenetics, as we have learned from neuroscience, and also cancer, that sometimes a substance we ingest has an effect on our health. It’s perhaps an interaction with the way our DNA is written but also with the changes to the way our DNA is read and translated into biology if exposed to that substance. We know that smoking tobacco does have an impact at an epigenetic level on the DNA. We do know that in people who stop smoking, these impacts on the epigenetics are partially reversed. This work hasn’t been done properly for cannabis.
“There have been four published studies that have looked at the effect of cannabis use on epigenetics but they have been quite inconclusive, and they haven’t looked at large numbers of current users taking into account how much they are using. Moreover, we do know that when THC and CBD get into our bodies, they interact with something that is already embedded in our biology which is the endocannabinoid system. Therefore, in the blood samples we also aim to measures the levels of the endocannabinoids we naturally produce.
“All of this data will then be analyzed to see if we can get close to understanding what makes some cannabis users susceptible to paranoia while others who are using cannabis get some benefits, even in the domain of mental health.”
Q: Who are you looking for to take part in your study?
A: “What we don’t want is to get only people who are the classic friends and family of academics to do the study. We want a representative sample of people out there who are using cannabis. My ideal candidate would be someone who hates me and usually sends me abusive emails saying I’m against cannabis, which is wrong. All I want to find out is who is susceptible to harm which will keep everybody else safe. We are not trying to demonize cannabis; it’s exactly the opposite. We would like people from all ethnic and socioeconomic backgrounds to join to give voice to everyone out there using cannabis, the reasons why, and the effects they experience.”
Q: Will this study perhaps give more information of when it’s appropriate to prescribe medicinal cannabis, as it’s still quite unusual for it to be prescribed in the United Kingdom isn’t it?
A: “Absolutely spot on. That’s exactly the point. We want to hear from people who are receiving medicinal cannabis as a prescription, as they are likely to take it on a daily basis and daily use is what epidemiological studies have linked to the highest risk of psychosis. There will be people taking THC everyday for pain, nausea, for Crohn’s disease, and more.
“Normally when you receive a prescription for a medication the physician in charge will tell you the potential side effects which will be monitored to make sure it’s safe, and you may have to swap to a different medication. Now this isn’t really happening with medicinal cannabis, which is one of the reasons clinicians are anxious about prescribing it, and they have been criticized for not prescribing it very much. There’s much less structure and guidance about ‘psychosis-related’ side effects monitoring. If we can really identify those people who are likely to develop psychosis or disabling paranoia when they use cannabis, physicians might be more prepared to prescribe more widely when indicated.
“You could even have a virtual reality scenario available as a screening tool when you get prescribed medicinal cannabis, to see if there are changes in your perception of the world, which is ultimately what psychosis is about. Could this be a way of implementing safe prescribing which will encourage physicians to use safe cannabis compounds and make some people less anxious about it?
“This study is not here to highlight the negativity of cannabis, on the contrary it’s to understand how it can be used recreationally, but even more important, medicinally in a safe way so people that are coming to no harm can continue to do so and people who are at risk can be kept safe, or at least monitored adequately.”
A version of this article first appeared on Medscape UK.
The largest-ever independent study into the effects of cannabis on the brain is being carried out in the United Kingdom.
Even though cannabis is the most commonly used illegal drug in the United Kingdom and medicinal cannabis has been legal there since 2018 little is known about why some people react badly to it and others seem to benefit from it.
According to Home Office figures on drug use from 2019, 7.6% of adults aged 16-59 used cannabis in the previous year.
Medicinal cannabis in the United Kingdom can only be prescribed if no other licensed medicine could help the patient. At the moment, GPs can’t prescribe it, only specialist hospital doctors can. The National Health Service says it can only be used in three circumstances: in rare, severe epilepsy; to deal with chemotherapy side effects such as nausea; or to help with multiple sclerosis.
As part of the Cannabis&Me study, KCL needs to get 3,000 current cannabis users and 3,000 non–cannabis users to take part in an online survey, with a third of those survey respondents then taking part in a face-to-face assessment that includes virtual reality (VR) and psychological analysis. The study also aims to determine how the DNA of cannabis users and their endocannabinoid system impacts their experiences, both negative and positive, with the drug.
The study is spearheaded by Marta Di Forti, MD, PhD, and has been allocated over £2.5 million in funding by the Medical Research Council.
This news organization asked Dr. Di Forti about the study.
Question: How do you describe the study?
Answer: “It’s a really unique study. We are aiming to see what’s happening to people using cannabis in the privacy of their homes for medicinal, recreational reasons, or whatever other reason.
“The debate on cannabis has always been quite polarized. There have been people who experience adversities with cannabis use, especially psychosis, whose families may perhaps like cannabis to be abolished if possible. Then there are other people who are saying they get positive benefits from using cannabis.”
Q: So where does the study come in?
A: “The study wants to bring the two sides of the argument together and understand what’s really happening. The group I see as a clinician comes to severe harm when they use cannabis regularly. We want to find out who they are and whether we can identify them. While we need to make sure they never come to harm when using cannabis, we need to consider others who won’t come to harm from using cannabis and give them a chance to use it in a way that’s beneficial.”
Q: How does the study work?
A: “The first step of the study is to use an online questionnaire that can be filled in by anyone aged 18-45 who lives in the London area or can travel here if selected. The first set of questions are a general idea of their cannabis use: ‘Why do they use it?’ ‘What are its benefits?’ Then, general questions on what their life has been like up to that point: ‘Did they have any adversities in childhood?’ ‘How is their mood and anxiety levels?’ ‘Do they experience any paranoid responses in everyday life?’ It probably takes between 30 and 40 minutes to fill out the questionnaire.”
Q: Can you explain about paranoid responses?
A: “We go through the questionnaires looking at people’s paranoid response to everyday life, not in a clinical disorder term, just in terms of the differences in how we respond to certain circumstances. For example: ‘How do you feel if someone’s staring at you on the Tube?’ Some people are afraid, some feel uncomfortable, some people don’t notice, and others think a person is staring at them as they look good or another such positive feeling. So, we give people a paranoia score and will invite some at the top and some at the bottom of that score for a face-to-face assessment. We want to select those people who are using cannabis daily and they are getting either no paranoia or high paranoia.”
Q: What happens at the face-to-face assessments?
A: “We do two things which are very novel. We ask them to take part in a virtual reality experience. They are in a lovely shop and within this experience they come across challenges, which may or may not induce a benign paranoia response. We will ask them to donate a sample of blood before they go into the VR set. We will test for tetrahydrocannabinol (THC) and cannabidiol (CBD). We will also look at the metabolites of the two. People don’t take into account how differently individuals metabolize cannabis, which could be one of the reasons why some people can tolerate it and others can’t.”
Q: There’s also a genetic aspect of the study?
A: “From the same sample, we will extract DNA to look at the genetics across the genome and compare genetic variations between high and low paranoia in the context of cannabis use. Also, we will look at the epigenetics, as we have learned from neuroscience, and also cancer, that sometimes a substance we ingest has an effect on our health. It’s perhaps an interaction with the way our DNA is written but also with the changes to the way our DNA is read and translated into biology if exposed to that substance. We know that smoking tobacco does have an impact at an epigenetic level on the DNA. We do know that in people who stop smoking, these impacts on the epigenetics are partially reversed. This work hasn’t been done properly for cannabis.
“There have been four published studies that have looked at the effect of cannabis use on epigenetics but they have been quite inconclusive, and they haven’t looked at large numbers of current users taking into account how much they are using. Moreover, we do know that when THC and CBD get into our bodies, they interact with something that is already embedded in our biology which is the endocannabinoid system. Therefore, in the blood samples we also aim to measures the levels of the endocannabinoids we naturally produce.
“All of this data will then be analyzed to see if we can get close to understanding what makes some cannabis users susceptible to paranoia while others who are using cannabis get some benefits, even in the domain of mental health.”
Q: Who are you looking for to take part in your study?
A: “What we don’t want is to get only people who are the classic friends and family of academics to do the study. We want a representative sample of people out there who are using cannabis. My ideal candidate would be someone who hates me and usually sends me abusive emails saying I’m against cannabis, which is wrong. All I want to find out is who is susceptible to harm which will keep everybody else safe. We are not trying to demonize cannabis; it’s exactly the opposite. We would like people from all ethnic and socioeconomic backgrounds to join to give voice to everyone out there using cannabis, the reasons why, and the effects they experience.”
Q: Will this study perhaps give more information of when it’s appropriate to prescribe medicinal cannabis, as it’s still quite unusual for it to be prescribed in the United Kingdom isn’t it?
A: “Absolutely spot on. That’s exactly the point. We want to hear from people who are receiving medicinal cannabis as a prescription, as they are likely to take it on a daily basis and daily use is what epidemiological studies have linked to the highest risk of psychosis. There will be people taking THC everyday for pain, nausea, for Crohn’s disease, and more.
“Normally when you receive a prescription for a medication the physician in charge will tell you the potential side effects which will be monitored to make sure it’s safe, and you may have to swap to a different medication. Now this isn’t really happening with medicinal cannabis, which is one of the reasons clinicians are anxious about prescribing it, and they have been criticized for not prescribing it very much. There’s much less structure and guidance about ‘psychosis-related’ side effects monitoring. If we can really identify those people who are likely to develop psychosis or disabling paranoia when they use cannabis, physicians might be more prepared to prescribe more widely when indicated.
“You could even have a virtual reality scenario available as a screening tool when you get prescribed medicinal cannabis, to see if there are changes in your perception of the world, which is ultimately what psychosis is about. Could this be a way of implementing safe prescribing which will encourage physicians to use safe cannabis compounds and make some people less anxious about it?
“This study is not here to highlight the negativity of cannabis, on the contrary it’s to understand how it can be used recreationally, but even more important, medicinally in a safe way so people that are coming to no harm can continue to do so and people who are at risk can be kept safe, or at least monitored adequately.”
A version of this article first appeared on Medscape UK.
The largest-ever independent study into the effects of cannabis on the brain is being carried out in the United Kingdom.
Even though cannabis is the most commonly used illegal drug in the United Kingdom and medicinal cannabis has been legal there since 2018 little is known about why some people react badly to it and others seem to benefit from it.
According to Home Office figures on drug use from 2019, 7.6% of adults aged 16-59 used cannabis in the previous year.
Medicinal cannabis in the United Kingdom can only be prescribed if no other licensed medicine could help the patient. At the moment, GPs can’t prescribe it, only specialist hospital doctors can. The National Health Service says it can only be used in three circumstances: in rare, severe epilepsy; to deal with chemotherapy side effects such as nausea; or to help with multiple sclerosis.
As part of the Cannabis&Me study, KCL needs to get 3,000 current cannabis users and 3,000 non–cannabis users to take part in an online survey, with a third of those survey respondents then taking part in a face-to-face assessment that includes virtual reality (VR) and psychological analysis. The study also aims to determine how the DNA of cannabis users and their endocannabinoid system impacts their experiences, both negative and positive, with the drug.
The study is spearheaded by Marta Di Forti, MD, PhD, and has been allocated over £2.5 million in funding by the Medical Research Council.
This news organization asked Dr. Di Forti about the study.
Question: How do you describe the study?
Answer: “It’s a really unique study. We are aiming to see what’s happening to people using cannabis in the privacy of their homes for medicinal, recreational reasons, or whatever other reason.
“The debate on cannabis has always been quite polarized. There have been people who experience adversities with cannabis use, especially psychosis, whose families may perhaps like cannabis to be abolished if possible. Then there are other people who are saying they get positive benefits from using cannabis.”
Q: So where does the study come in?
A: “The study wants to bring the two sides of the argument together and understand what’s really happening. The group I see as a clinician comes to severe harm when they use cannabis regularly. We want to find out who they are and whether we can identify them. While we need to make sure they never come to harm when using cannabis, we need to consider others who won’t come to harm from using cannabis and give them a chance to use it in a way that’s beneficial.”
Q: How does the study work?
A: “The first step of the study is to use an online questionnaire that can be filled in by anyone aged 18-45 who lives in the London area or can travel here if selected. The first set of questions are a general idea of their cannabis use: ‘Why do they use it?’ ‘What are its benefits?’ Then, general questions on what their life has been like up to that point: ‘Did they have any adversities in childhood?’ ‘How is their mood and anxiety levels?’ ‘Do they experience any paranoid responses in everyday life?’ It probably takes between 30 and 40 minutes to fill out the questionnaire.”
Q: Can you explain about paranoid responses?
A: “We go through the questionnaires looking at people’s paranoid response to everyday life, not in a clinical disorder term, just in terms of the differences in how we respond to certain circumstances. For example: ‘How do you feel if someone’s staring at you on the Tube?’ Some people are afraid, some feel uncomfortable, some people don’t notice, and others think a person is staring at them as they look good or another such positive feeling. So, we give people a paranoia score and will invite some at the top and some at the bottom of that score for a face-to-face assessment. We want to select those people who are using cannabis daily and they are getting either no paranoia or high paranoia.”
Q: What happens at the face-to-face assessments?
A: “We do two things which are very novel. We ask them to take part in a virtual reality experience. They are in a lovely shop and within this experience they come across challenges, which may or may not induce a benign paranoia response. We will ask them to donate a sample of blood before they go into the VR set. We will test for tetrahydrocannabinol (THC) and cannabidiol (CBD). We will also look at the metabolites of the two. People don’t take into account how differently individuals metabolize cannabis, which could be one of the reasons why some people can tolerate it and others can’t.”
Q: There’s also a genetic aspect of the study?
A: “From the same sample, we will extract DNA to look at the genetics across the genome and compare genetic variations between high and low paranoia in the context of cannabis use. Also, we will look at the epigenetics, as we have learned from neuroscience, and also cancer, that sometimes a substance we ingest has an effect on our health. It’s perhaps an interaction with the way our DNA is written but also with the changes to the way our DNA is read and translated into biology if exposed to that substance. We know that smoking tobacco does have an impact at an epigenetic level on the DNA. We do know that in people who stop smoking, these impacts on the epigenetics are partially reversed. This work hasn’t been done properly for cannabis.
“There have been four published studies that have looked at the effect of cannabis use on epigenetics but they have been quite inconclusive, and they haven’t looked at large numbers of current users taking into account how much they are using. Moreover, we do know that when THC and CBD get into our bodies, they interact with something that is already embedded in our biology which is the endocannabinoid system. Therefore, in the blood samples we also aim to measures the levels of the endocannabinoids we naturally produce.
“All of this data will then be analyzed to see if we can get close to understanding what makes some cannabis users susceptible to paranoia while others who are using cannabis get some benefits, even in the domain of mental health.”
Q: Who are you looking for to take part in your study?
A: “What we don’t want is to get only people who are the classic friends and family of academics to do the study. We want a representative sample of people out there who are using cannabis. My ideal candidate would be someone who hates me and usually sends me abusive emails saying I’m against cannabis, which is wrong. All I want to find out is who is susceptible to harm which will keep everybody else safe. We are not trying to demonize cannabis; it’s exactly the opposite. We would like people from all ethnic and socioeconomic backgrounds to join to give voice to everyone out there using cannabis, the reasons why, and the effects they experience.”
Q: Will this study perhaps give more information of when it’s appropriate to prescribe medicinal cannabis, as it’s still quite unusual for it to be prescribed in the United Kingdom isn’t it?
A: “Absolutely spot on. That’s exactly the point. We want to hear from people who are receiving medicinal cannabis as a prescription, as they are likely to take it on a daily basis and daily use is what epidemiological studies have linked to the highest risk of psychosis. There will be people taking THC everyday for pain, nausea, for Crohn’s disease, and more.
“Normally when you receive a prescription for a medication the physician in charge will tell you the potential side effects which will be monitored to make sure it’s safe, and you may have to swap to a different medication. Now this isn’t really happening with medicinal cannabis, which is one of the reasons clinicians are anxious about prescribing it, and they have been criticized for not prescribing it very much. There’s much less structure and guidance about ‘psychosis-related’ side effects monitoring. If we can really identify those people who are likely to develop psychosis or disabling paranoia when they use cannabis, physicians might be more prepared to prescribe more widely when indicated.
“You could even have a virtual reality scenario available as a screening tool when you get prescribed medicinal cannabis, to see if there are changes in your perception of the world, which is ultimately what psychosis is about. Could this be a way of implementing safe prescribing which will encourage physicians to use safe cannabis compounds and make some people less anxious about it?
“This study is not here to highlight the negativity of cannabis, on the contrary it’s to understand how it can be used recreationally, but even more important, medicinally in a safe way so people that are coming to no harm can continue to do so and people who are at risk can be kept safe, or at least monitored adequately.”
A version of this article first appeared on Medscape UK.
Psychiatrists’ views on psychoactive drugs clash with U.S. policy
“The consensus among experts, including psychiatrists, about specific drugs is not consistent or congruent with the schedule of these drugs” in the United States, lead author Adam Levin, MD, third-year psychiatry resident, Ohio State University, Columbus, and affiliate scholar at the Center for Psychedelic Drug Research and Education, Ohio State College of Social Work, told this news organization.
Dr. Levin stressed the importance of appropriate drug scheduling to improve access to treatments such as psilocybin (psychedelic mushrooms) and 4-methylenedioxy methamphetamine (MDMA), which are now being tested for psychiatric disorders.
“We are in the middle of a mental health crisis so having any new tools would be really important,” he said.
The survey findings were published online in the International Journal of Drug Policy.
Five drug schedules
The Controlled Substances Act of 1970 created five “schedules” that organized drugs from most to least dangerous (schedule I-V). However, Dr. Levin said that the schedules do not accurately reflect the harms or therapeutic benefits of the various drugs.
Some drugs in lower, less restrictive schedules have greater potential for harm than do those in higher schedules, he noted. For example, methamphetamine, which has been recalled in multiple formulations because of concerns about abuse and limited medical use, remains a schedule II drug.
In addition, several schedule I drugs, including psilocybin and MDMA that are deemed dangerous and of no medical value, have shown therapeutic potential and low rates of misuse, addiction, or physical harm, the investigators noted.
In fact, the Food and Drug Administration has granted breakthrough therapy status to psilocybin for treatment-resistant depression and major depressive disorder (MDD) and to MDMA for posttraumatic stress disorder. This has positioned these drugs for possible FDA approval within the next few years.
Access to schedule I drugs for research purposes is tightly controlled. “Once psilocybin was placed in schedule I, there was this massive drop-off in the research funding and amount of research; and we’re just now starting to understand the potential therapeutic value of this drug,” said Dr. Levin.
Even with a recent research resurgence, most studies are funded by charitable donations or for-profit companies because of continued hesitancy on the part of grant-making organizations, he added.
Apparent contradictions
Given the pending approval of several schedule I drugs and escalating abuse of drugs in lower schedules, there is a growing need to understand physician attitudes surrounding the apparent contradictions in the drug schedule, the investigators noted.
Their survey included a geographically diverse group of 181 mostly middle-aged psychiatrists (65.2% were men) with an average of 16.2 years of practice after residency.
Participants were randomly assigned to respond to a vignette depicting a clinical scenario where a patient wants one of four drugs to help treat severe depression: psilocybin, a schedule I drug; methamphetamine (Desoxyn), a schedule II drug; ketamine, a Schedule III drug; or alprazolam (Xanax), a schedule IV drug.
Each of these therapies has established antidepressant properties, but none are FDA approved for treatment of MDD. However, an intranasal formulation of the ketamine enantiomer Spravato (esketamine) was recently approved for treatment-resistant depression.
There were significant differences among the groups presented with different vignettes. Participants were more likely to warn against repeated use of and development of a new psychiatric problem with methamphetamine and alprazolam compared with psilocybin or ketamine.
Respondents were most concerned about increased suicide risk after the nonprescribed use of alprazolam compared with psilocybin and ketamine.
Compared with all other drugs, ketamine was more likely to be integrated into treatment plans.
Therapeutic value, abuse potential
Participants were asked to rate the safety, therapeutic value, and abuse potential of the four drugs as well as alcohol, a nonscheduled legal drug, if used properly or as directed.
Respondents viewed psilocybin and ketamine as similarly safe – and safer than methamphetamine and alprazolam. They considered ketamine as having the highest therapeutic potential, followed by psilocybin, and then alprazolam and methamphetamine. “Last was alcohol, which we expected because alcohol is not used therapeutically,” said Dr. Levin.
Survey completers viewed methamphetamine, alprazolam, and alcohol as having similarly high abuse potential, and ketamine as having mid-level abuse potential. Psilocybin was rated as having the lowest abuse potential, “which is exactly the opposite of what is implied by its schedule I status,” noted Dr. Levin.
The results provide evidence these drugs “are incorrectly scheduled,” he said.
“This suggests the schedule does not reflect current evidence, which I think is really important to understand because there are consequences to the drug schedule,” including criminal justice and research consequences, he added.
Dr. Levin pointed out that possession of drugs in more harmful schedules is linked to sometimes lengthy prison sentences.
The psychiatrists’ perceptions of the drugs “overlaps pretty significantly” with recent surveys of other mental health professionals, including psychologists and addiction experts, he noted.
The study was funded by the Drug Enforcement and Policy Center, Moritz College of Law, and The Ohio State University. Dr. Levin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“The consensus among experts, including psychiatrists, about specific drugs is not consistent or congruent with the schedule of these drugs” in the United States, lead author Adam Levin, MD, third-year psychiatry resident, Ohio State University, Columbus, and affiliate scholar at the Center for Psychedelic Drug Research and Education, Ohio State College of Social Work, told this news organization.
Dr. Levin stressed the importance of appropriate drug scheduling to improve access to treatments such as psilocybin (psychedelic mushrooms) and 4-methylenedioxy methamphetamine (MDMA), which are now being tested for psychiatric disorders.
“We are in the middle of a mental health crisis so having any new tools would be really important,” he said.
The survey findings were published online in the International Journal of Drug Policy.
Five drug schedules
The Controlled Substances Act of 1970 created five “schedules” that organized drugs from most to least dangerous (schedule I-V). However, Dr. Levin said that the schedules do not accurately reflect the harms or therapeutic benefits of the various drugs.
Some drugs in lower, less restrictive schedules have greater potential for harm than do those in higher schedules, he noted. For example, methamphetamine, which has been recalled in multiple formulations because of concerns about abuse and limited medical use, remains a schedule II drug.
In addition, several schedule I drugs, including psilocybin and MDMA that are deemed dangerous and of no medical value, have shown therapeutic potential and low rates of misuse, addiction, or physical harm, the investigators noted.
In fact, the Food and Drug Administration has granted breakthrough therapy status to psilocybin for treatment-resistant depression and major depressive disorder (MDD) and to MDMA for posttraumatic stress disorder. This has positioned these drugs for possible FDA approval within the next few years.
Access to schedule I drugs for research purposes is tightly controlled. “Once psilocybin was placed in schedule I, there was this massive drop-off in the research funding and amount of research; and we’re just now starting to understand the potential therapeutic value of this drug,” said Dr. Levin.
Even with a recent research resurgence, most studies are funded by charitable donations or for-profit companies because of continued hesitancy on the part of grant-making organizations, he added.
Apparent contradictions
Given the pending approval of several schedule I drugs and escalating abuse of drugs in lower schedules, there is a growing need to understand physician attitudes surrounding the apparent contradictions in the drug schedule, the investigators noted.
Their survey included a geographically diverse group of 181 mostly middle-aged psychiatrists (65.2% were men) with an average of 16.2 years of practice after residency.
Participants were randomly assigned to respond to a vignette depicting a clinical scenario where a patient wants one of four drugs to help treat severe depression: psilocybin, a schedule I drug; methamphetamine (Desoxyn), a schedule II drug; ketamine, a Schedule III drug; or alprazolam (Xanax), a schedule IV drug.
Each of these therapies has established antidepressant properties, but none are FDA approved for treatment of MDD. However, an intranasal formulation of the ketamine enantiomer Spravato (esketamine) was recently approved for treatment-resistant depression.
There were significant differences among the groups presented with different vignettes. Participants were more likely to warn against repeated use of and development of a new psychiatric problem with methamphetamine and alprazolam compared with psilocybin or ketamine.
Respondents were most concerned about increased suicide risk after the nonprescribed use of alprazolam compared with psilocybin and ketamine.
Compared with all other drugs, ketamine was more likely to be integrated into treatment plans.
Therapeutic value, abuse potential
Participants were asked to rate the safety, therapeutic value, and abuse potential of the four drugs as well as alcohol, a nonscheduled legal drug, if used properly or as directed.
Respondents viewed psilocybin and ketamine as similarly safe – and safer than methamphetamine and alprazolam. They considered ketamine as having the highest therapeutic potential, followed by psilocybin, and then alprazolam and methamphetamine. “Last was alcohol, which we expected because alcohol is not used therapeutically,” said Dr. Levin.
Survey completers viewed methamphetamine, alprazolam, and alcohol as having similarly high abuse potential, and ketamine as having mid-level abuse potential. Psilocybin was rated as having the lowest abuse potential, “which is exactly the opposite of what is implied by its schedule I status,” noted Dr. Levin.
The results provide evidence these drugs “are incorrectly scheduled,” he said.
“This suggests the schedule does not reflect current evidence, which I think is really important to understand because there are consequences to the drug schedule,” including criminal justice and research consequences, he added.
Dr. Levin pointed out that possession of drugs in more harmful schedules is linked to sometimes lengthy prison sentences.
The psychiatrists’ perceptions of the drugs “overlaps pretty significantly” with recent surveys of other mental health professionals, including psychologists and addiction experts, he noted.
The study was funded by the Drug Enforcement and Policy Center, Moritz College of Law, and The Ohio State University. Dr. Levin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“The consensus among experts, including psychiatrists, about specific drugs is not consistent or congruent with the schedule of these drugs” in the United States, lead author Adam Levin, MD, third-year psychiatry resident, Ohio State University, Columbus, and affiliate scholar at the Center for Psychedelic Drug Research and Education, Ohio State College of Social Work, told this news organization.
Dr. Levin stressed the importance of appropriate drug scheduling to improve access to treatments such as psilocybin (psychedelic mushrooms) and 4-methylenedioxy methamphetamine (MDMA), which are now being tested for psychiatric disorders.
“We are in the middle of a mental health crisis so having any new tools would be really important,” he said.
The survey findings were published online in the International Journal of Drug Policy.
Five drug schedules
The Controlled Substances Act of 1970 created five “schedules” that organized drugs from most to least dangerous (schedule I-V). However, Dr. Levin said that the schedules do not accurately reflect the harms or therapeutic benefits of the various drugs.
Some drugs in lower, less restrictive schedules have greater potential for harm than do those in higher schedules, he noted. For example, methamphetamine, which has been recalled in multiple formulations because of concerns about abuse and limited medical use, remains a schedule II drug.
In addition, several schedule I drugs, including psilocybin and MDMA that are deemed dangerous and of no medical value, have shown therapeutic potential and low rates of misuse, addiction, or physical harm, the investigators noted.
In fact, the Food and Drug Administration has granted breakthrough therapy status to psilocybin for treatment-resistant depression and major depressive disorder (MDD) and to MDMA for posttraumatic stress disorder. This has positioned these drugs for possible FDA approval within the next few years.
Access to schedule I drugs for research purposes is tightly controlled. “Once psilocybin was placed in schedule I, there was this massive drop-off in the research funding and amount of research; and we’re just now starting to understand the potential therapeutic value of this drug,” said Dr. Levin.
Even with a recent research resurgence, most studies are funded by charitable donations or for-profit companies because of continued hesitancy on the part of grant-making organizations, he added.
Apparent contradictions
Given the pending approval of several schedule I drugs and escalating abuse of drugs in lower schedules, there is a growing need to understand physician attitudes surrounding the apparent contradictions in the drug schedule, the investigators noted.
Their survey included a geographically diverse group of 181 mostly middle-aged psychiatrists (65.2% were men) with an average of 16.2 years of practice after residency.
Participants were randomly assigned to respond to a vignette depicting a clinical scenario where a patient wants one of four drugs to help treat severe depression: psilocybin, a schedule I drug; methamphetamine (Desoxyn), a schedule II drug; ketamine, a Schedule III drug; or alprazolam (Xanax), a schedule IV drug.
Each of these therapies has established antidepressant properties, but none are FDA approved for treatment of MDD. However, an intranasal formulation of the ketamine enantiomer Spravato (esketamine) was recently approved for treatment-resistant depression.
There were significant differences among the groups presented with different vignettes. Participants were more likely to warn against repeated use of and development of a new psychiatric problem with methamphetamine and alprazolam compared with psilocybin or ketamine.
Respondents were most concerned about increased suicide risk after the nonprescribed use of alprazolam compared with psilocybin and ketamine.
Compared with all other drugs, ketamine was more likely to be integrated into treatment plans.
Therapeutic value, abuse potential
Participants were asked to rate the safety, therapeutic value, and abuse potential of the four drugs as well as alcohol, a nonscheduled legal drug, if used properly or as directed.
Respondents viewed psilocybin and ketamine as similarly safe – and safer than methamphetamine and alprazolam. They considered ketamine as having the highest therapeutic potential, followed by psilocybin, and then alprazolam and methamphetamine. “Last was alcohol, which we expected because alcohol is not used therapeutically,” said Dr. Levin.
Survey completers viewed methamphetamine, alprazolam, and alcohol as having similarly high abuse potential, and ketamine as having mid-level abuse potential. Psilocybin was rated as having the lowest abuse potential, “which is exactly the opposite of what is implied by its schedule I status,” noted Dr. Levin.
The results provide evidence these drugs “are incorrectly scheduled,” he said.
“This suggests the schedule does not reflect current evidence, which I think is really important to understand because there are consequences to the drug schedule,” including criminal justice and research consequences, he added.
Dr. Levin pointed out that possession of drugs in more harmful schedules is linked to sometimes lengthy prison sentences.
The psychiatrists’ perceptions of the drugs “overlaps pretty significantly” with recent surveys of other mental health professionals, including psychologists and addiction experts, he noted.
The study was funded by the Drug Enforcement and Policy Center, Moritz College of Law, and The Ohio State University. Dr. Levin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF DRUG POLICY
How to identify and treat patients with substance use disorders
When Michael McGrath, MD, medical director of the Ohana Luxury Alcohol Rehab on the Big Island of Hawaii, trains primary care physicians, he tells them that talking with patients about substance use disorders is like having a stressful, weird conversation. But it’s a courageous one, because of the stigma associated with drug and alcohol disorders.
Dr. McGrath starts the conversation with patients by expressing that physicians now understand that addiction is a disease – one for which the patient isn’t responsible. He explains that there’s both a genetic and a nature/nurture component of the disorder and assures them that he won’t judge or abandon them but rather help them find treatment and make sure they get on the path to wellness.
It’s all too common to see patients with a substance use disorder in today’s primary care population. According to Medscape’s Physicians’ Views on Today’s Divisive Social Issues Report 2022,
According to the Recovery Research Institute, a leading nonprofit orgnaization from Massachusetts General Hospital dedicated to advancing addiction treatment and recovery, about 20 million people in the United States suffer from a substance use disorder. More than half (54%) need assistance with their recovery. The National Institute on Drug Abuse reports that substance abuse and addiction cost society more than $740 billion annually in workplace productivity, health care, and crime-related expenses.
Despite the challenges, physician experts provide advice on how to treat and help patients who have substance use disorders more effectively.
A courageous conversation
Often, the primary care physician or emergency physician is the first to be aware of a patient’s problem with a substance or a relapse. In many communities where shortages of specialized physicians and nonphysician treatment options for substance use disorders aren’t available, there’s usually limited time and resources to help patients with these disorders.
Patients often sense doctors are rushed and may not be interested in hearing about their drug or alcohol problems. Reddit threads are filled with stories like that of user “Cyralek,” who say that the two doctors they’ve seen since quitting drinking didn’t show much interest in the problem beyond ordering liver function tests.
In a nationwide study by researchers at Washington University School of Medicine, St. Louis, 80% of patients who met the diagnostic criteria for substance use disorder visited a doctor, hospital, or clinic for some reason over the past year. Only 1 in 10 were encouraged to cut back on drinking or receive any form of treatment or referral for substance misuse.
Emma Gordon, founder of a salvage yard in Los Angeles, says she used to abuse alcohol and that it affected every aspect of her life. Her brother tried to intervene, but nothing worked until she finally told a physician. “I admitted my problem and felt incredibly calm when she reacted as though it was all normal. I believe that was my first step to becoming a better me. I was thankful I had gone to see a doctor,” says Ms. Gordon.
Though physicians in primary care may not have more than a 15-minute appointment slot, seizing the opportunity to initiate a substance use disorder conversation when warranted is crucial, says Dr. McGrath. The CAGE-AID screening tool, which includes questions such as, “Have you ever felt you ought to cut down on your drinking or drug use?” is an excellent starter. Dr. McGrath also advises primary care clinicians to lower the threshold of concern to a single positive answer rather than several.
Doctors aren’t necessarily rewarded for the time it takes to develop a rapport with patients and to have a conversation that leads to asking, “How much are you drinking?”
“The system in primary care isn’t set up that way,” said Lucy McBride, MD, an internist in Washington, D.C.
Patients don’t often ask for help
In a perfect world, patients struggling with a substance use disorder would present with a request to discontinue using drugs or alcohol, as Ms. Gordon did. While that does happen sometimes, the onus is on the physician to screen for substance misuse.
“Remember, this is the disease that tells you that you don’t have a disease,” Dr. McGrath says. He also says that the use of screening instruments is a bare minimum. When patients are in the throes of a substance use disorder, the prefrontal cortex doesn’t work effectively. Dr. McGrath says there’s an alteration of consciousness so that the patient doesn’t realize the extent of the disease. “Often simply asking the patient is falling far short. It’s the biggest mistake I see,” he says.
Self-reporting from the patient may be unreliable. “That would be like a patient coming in and saying, ‘My blood sugar is 700, and I want you to give me some insulin,’ ” Dr. McGrath says. Instead, clinicians in the field need a more objective measurement.
Perhaps that means asking the patient to bring in a significant other at the next visit or digging deeper into the conversation about alcohol and drugs and their role in the patient’s life. And to really have an impact, Dr. McGrath said, the clinician should talk to the patient about referral for further evaluation.
“You have to get collateral history; that’s the goldmine for the clinician,” Dr. McGrath says. “It may take a few more minutes or mean talking to a family member, but it can make the difference between life and death.”
“I am thankful to my doctor who discussed this [substance use disorder] with me in detail,” says Ronald Williams, another Angeleno who braved the difficult discussion with his doctor. Mr. Williams says his doctor explained it in a good way and that if the doctor hadn’t guided him empathetically, the conversation might not have gone as well.
“We check patients’ cholesterol. We get them on the scale. But there is no blood test to discover how much they’re drinking, no PCR to test for social anxiety, no MRI that distinguishes between their recreational marijuana use and marijuana abuse,” said Dr. McBride.
Check the prescription drugs they’re taking
Another thing Dr. McGrath recommends is for primary care physicians to check the prescription drug monitoring program (PDMP) database in their state to help be alerted to a patient with a substance use disorder. The CDC’s PMPD guidelines recommend that the clinician check on a patient every 3 months or each time they write an opioid prescription. Assigning a staff member or a nurse to check the database can help uncover a history of doctor-shopping or use of controlled substances.
“There’s been a lot of times I’ve gone on self-report, and I’ve been bamboozled because I don’t have a truth-o-meter, and I can’t tell when a patient is telling the truth,” says Dr. McGrath.
He is also a huge proponent of point-of-service screening. Patients can urinate in a cup that has amino assay strips on the side, like an immediate COVID-19 test, or they can spit into a saliva cup. “It’s really beneficial for the patient and the clinician to know right then at the point of service if there is a substance present and what it is,” Dr. McGrath said.
It can be part of the larger conversation once a problem with substances has been uncovered. The clinician can say something like, “Let’s see where you are right now today as far as what you have in your system and where we should go from here.”
Other barriers physicians face
Many physicians may feel unprepared to meet the needs of patients with substance use disorders or prescribe medication that blunts cravings and reduces the urge to drink without the need for special training. Scientists at the National Institutes of Health found that only 1.6% of people with a substance use disorder were prescribed medication to help control it.
In the largest study on how primary care physicians address substance use disorders, fewer than 20% described themselves as very prepared to identify alcoholism or illegal drug use. Since most patients prefer to seek treatment from their primary care doctor, at least initially, not being prepared is a problem.
Although referral for specialty addiction treatment is recommended for patients with severe substance use disorders, primary care physicians with appropriate experience, training, and support can provide some of these services. “In an ideal world I wouldn’t have to refer patients out, since they’re much more likely to talk with their primary care provider about sensitive, intimate topics,” says Dr. McBride.
The issue of reimbursement
Billing for substance use disorder counseling or coordination of care is still challenging, and how to get compensated remains a conundrum for many physicians. Reimbursement may not adequately compensate providers for the additional time and staff needed, but some changes have been positive.
For instance, the American Society for Addiction Medicine reports that in 2022, Medicare expanded the physician fee schedule for opioid and SUD counseling to include reimbursement for telemedicine services.
Learning the billing CPT codes for various addiction treatments and counseling, or having a billing service that understands them, is crucial to reimbursement and keeping revenue running smoothly.
At the very least, developing relationships with treatment centers and specialists in the community can help physicians with referrals and with determining the level of care needed. Physicians can help facilitate that care with routine reassessment and frequent follow-ups, as well as by requesting reports from the treatment facility, continuing treatment of medical conditions, and reinforcing the importance of continued substance use disorder treatment.
Dr. McBride says that primary care physicians can and should make their office a safe, blame-free medical home for patients with substance use disorders. “Patients also need to understand they should bring their whole selves to the doctor – to talk about their sleep, what they consume, their depression, and not just about alcohol, but their relationship with it, and other substances,” she says.
“There needs to be time to talk about it.”
A version of this article first appeared on Medscape.com.
When Michael McGrath, MD, medical director of the Ohana Luxury Alcohol Rehab on the Big Island of Hawaii, trains primary care physicians, he tells them that talking with patients about substance use disorders is like having a stressful, weird conversation. But it’s a courageous one, because of the stigma associated with drug and alcohol disorders.
Dr. McGrath starts the conversation with patients by expressing that physicians now understand that addiction is a disease – one for which the patient isn’t responsible. He explains that there’s both a genetic and a nature/nurture component of the disorder and assures them that he won’t judge or abandon them but rather help them find treatment and make sure they get on the path to wellness.
It’s all too common to see patients with a substance use disorder in today’s primary care population. According to Medscape’s Physicians’ Views on Today’s Divisive Social Issues Report 2022,
According to the Recovery Research Institute, a leading nonprofit orgnaization from Massachusetts General Hospital dedicated to advancing addiction treatment and recovery, about 20 million people in the United States suffer from a substance use disorder. More than half (54%) need assistance with their recovery. The National Institute on Drug Abuse reports that substance abuse and addiction cost society more than $740 billion annually in workplace productivity, health care, and crime-related expenses.
Despite the challenges, physician experts provide advice on how to treat and help patients who have substance use disorders more effectively.
A courageous conversation
Often, the primary care physician or emergency physician is the first to be aware of a patient’s problem with a substance or a relapse. In many communities where shortages of specialized physicians and nonphysician treatment options for substance use disorders aren’t available, there’s usually limited time and resources to help patients with these disorders.
Patients often sense doctors are rushed and may not be interested in hearing about their drug or alcohol problems. Reddit threads are filled with stories like that of user “Cyralek,” who say that the two doctors they’ve seen since quitting drinking didn’t show much interest in the problem beyond ordering liver function tests.
In a nationwide study by researchers at Washington University School of Medicine, St. Louis, 80% of patients who met the diagnostic criteria for substance use disorder visited a doctor, hospital, or clinic for some reason over the past year. Only 1 in 10 were encouraged to cut back on drinking or receive any form of treatment or referral for substance misuse.
Emma Gordon, founder of a salvage yard in Los Angeles, says she used to abuse alcohol and that it affected every aspect of her life. Her brother tried to intervene, but nothing worked until she finally told a physician. “I admitted my problem and felt incredibly calm when she reacted as though it was all normal. I believe that was my first step to becoming a better me. I was thankful I had gone to see a doctor,” says Ms. Gordon.
Though physicians in primary care may not have more than a 15-minute appointment slot, seizing the opportunity to initiate a substance use disorder conversation when warranted is crucial, says Dr. McGrath. The CAGE-AID screening tool, which includes questions such as, “Have you ever felt you ought to cut down on your drinking or drug use?” is an excellent starter. Dr. McGrath also advises primary care clinicians to lower the threshold of concern to a single positive answer rather than several.
Doctors aren’t necessarily rewarded for the time it takes to develop a rapport with patients and to have a conversation that leads to asking, “How much are you drinking?”
“The system in primary care isn’t set up that way,” said Lucy McBride, MD, an internist in Washington, D.C.
Patients don’t often ask for help
In a perfect world, patients struggling with a substance use disorder would present with a request to discontinue using drugs or alcohol, as Ms. Gordon did. While that does happen sometimes, the onus is on the physician to screen for substance misuse.
“Remember, this is the disease that tells you that you don’t have a disease,” Dr. McGrath says. He also says that the use of screening instruments is a bare minimum. When patients are in the throes of a substance use disorder, the prefrontal cortex doesn’t work effectively. Dr. McGrath says there’s an alteration of consciousness so that the patient doesn’t realize the extent of the disease. “Often simply asking the patient is falling far short. It’s the biggest mistake I see,” he says.
Self-reporting from the patient may be unreliable. “That would be like a patient coming in and saying, ‘My blood sugar is 700, and I want you to give me some insulin,’ ” Dr. McGrath says. Instead, clinicians in the field need a more objective measurement.
Perhaps that means asking the patient to bring in a significant other at the next visit or digging deeper into the conversation about alcohol and drugs and their role in the patient’s life. And to really have an impact, Dr. McGrath said, the clinician should talk to the patient about referral for further evaluation.
“You have to get collateral history; that’s the goldmine for the clinician,” Dr. McGrath says. “It may take a few more minutes or mean talking to a family member, but it can make the difference between life and death.”
“I am thankful to my doctor who discussed this [substance use disorder] with me in detail,” says Ronald Williams, another Angeleno who braved the difficult discussion with his doctor. Mr. Williams says his doctor explained it in a good way and that if the doctor hadn’t guided him empathetically, the conversation might not have gone as well.
“We check patients’ cholesterol. We get them on the scale. But there is no blood test to discover how much they’re drinking, no PCR to test for social anxiety, no MRI that distinguishes between their recreational marijuana use and marijuana abuse,” said Dr. McBride.
Check the prescription drugs they’re taking
Another thing Dr. McGrath recommends is for primary care physicians to check the prescription drug monitoring program (PDMP) database in their state to help be alerted to a patient with a substance use disorder. The CDC’s PMPD guidelines recommend that the clinician check on a patient every 3 months or each time they write an opioid prescription. Assigning a staff member or a nurse to check the database can help uncover a history of doctor-shopping or use of controlled substances.
“There’s been a lot of times I’ve gone on self-report, and I’ve been bamboozled because I don’t have a truth-o-meter, and I can’t tell when a patient is telling the truth,” says Dr. McGrath.
He is also a huge proponent of point-of-service screening. Patients can urinate in a cup that has amino assay strips on the side, like an immediate COVID-19 test, or they can spit into a saliva cup. “It’s really beneficial for the patient and the clinician to know right then at the point of service if there is a substance present and what it is,” Dr. McGrath said.
It can be part of the larger conversation once a problem with substances has been uncovered. The clinician can say something like, “Let’s see where you are right now today as far as what you have in your system and where we should go from here.”
Other barriers physicians face
Many physicians may feel unprepared to meet the needs of patients with substance use disorders or prescribe medication that blunts cravings and reduces the urge to drink without the need for special training. Scientists at the National Institutes of Health found that only 1.6% of people with a substance use disorder were prescribed medication to help control it.
In the largest study on how primary care physicians address substance use disorders, fewer than 20% described themselves as very prepared to identify alcoholism or illegal drug use. Since most patients prefer to seek treatment from their primary care doctor, at least initially, not being prepared is a problem.
Although referral for specialty addiction treatment is recommended for patients with severe substance use disorders, primary care physicians with appropriate experience, training, and support can provide some of these services. “In an ideal world I wouldn’t have to refer patients out, since they’re much more likely to talk with their primary care provider about sensitive, intimate topics,” says Dr. McBride.
The issue of reimbursement
Billing for substance use disorder counseling or coordination of care is still challenging, and how to get compensated remains a conundrum for many physicians. Reimbursement may not adequately compensate providers for the additional time and staff needed, but some changes have been positive.
For instance, the American Society for Addiction Medicine reports that in 2022, Medicare expanded the physician fee schedule for opioid and SUD counseling to include reimbursement for telemedicine services.
Learning the billing CPT codes for various addiction treatments and counseling, or having a billing service that understands them, is crucial to reimbursement and keeping revenue running smoothly.
At the very least, developing relationships with treatment centers and specialists in the community can help physicians with referrals and with determining the level of care needed. Physicians can help facilitate that care with routine reassessment and frequent follow-ups, as well as by requesting reports from the treatment facility, continuing treatment of medical conditions, and reinforcing the importance of continued substance use disorder treatment.
Dr. McBride says that primary care physicians can and should make their office a safe, blame-free medical home for patients with substance use disorders. “Patients also need to understand they should bring their whole selves to the doctor – to talk about their sleep, what they consume, their depression, and not just about alcohol, but their relationship with it, and other substances,” she says.
“There needs to be time to talk about it.”
A version of this article first appeared on Medscape.com.
When Michael McGrath, MD, medical director of the Ohana Luxury Alcohol Rehab on the Big Island of Hawaii, trains primary care physicians, he tells them that talking with patients about substance use disorders is like having a stressful, weird conversation. But it’s a courageous one, because of the stigma associated with drug and alcohol disorders.
Dr. McGrath starts the conversation with patients by expressing that physicians now understand that addiction is a disease – one for which the patient isn’t responsible. He explains that there’s both a genetic and a nature/nurture component of the disorder and assures them that he won’t judge or abandon them but rather help them find treatment and make sure they get on the path to wellness.
It’s all too common to see patients with a substance use disorder in today’s primary care population. According to Medscape’s Physicians’ Views on Today’s Divisive Social Issues Report 2022,
According to the Recovery Research Institute, a leading nonprofit orgnaization from Massachusetts General Hospital dedicated to advancing addiction treatment and recovery, about 20 million people in the United States suffer from a substance use disorder. More than half (54%) need assistance with their recovery. The National Institute on Drug Abuse reports that substance abuse and addiction cost society more than $740 billion annually in workplace productivity, health care, and crime-related expenses.
Despite the challenges, physician experts provide advice on how to treat and help patients who have substance use disorders more effectively.
A courageous conversation
Often, the primary care physician or emergency physician is the first to be aware of a patient’s problem with a substance or a relapse. In many communities where shortages of specialized physicians and nonphysician treatment options for substance use disorders aren’t available, there’s usually limited time and resources to help patients with these disorders.
Patients often sense doctors are rushed and may not be interested in hearing about their drug or alcohol problems. Reddit threads are filled with stories like that of user “Cyralek,” who say that the two doctors they’ve seen since quitting drinking didn’t show much interest in the problem beyond ordering liver function tests.
In a nationwide study by researchers at Washington University School of Medicine, St. Louis, 80% of patients who met the diagnostic criteria for substance use disorder visited a doctor, hospital, or clinic for some reason over the past year. Only 1 in 10 were encouraged to cut back on drinking or receive any form of treatment or referral for substance misuse.
Emma Gordon, founder of a salvage yard in Los Angeles, says she used to abuse alcohol and that it affected every aspect of her life. Her brother tried to intervene, but nothing worked until she finally told a physician. “I admitted my problem and felt incredibly calm when she reacted as though it was all normal. I believe that was my first step to becoming a better me. I was thankful I had gone to see a doctor,” says Ms. Gordon.
Though physicians in primary care may not have more than a 15-minute appointment slot, seizing the opportunity to initiate a substance use disorder conversation when warranted is crucial, says Dr. McGrath. The CAGE-AID screening tool, which includes questions such as, “Have you ever felt you ought to cut down on your drinking or drug use?” is an excellent starter. Dr. McGrath also advises primary care clinicians to lower the threshold of concern to a single positive answer rather than several.
Doctors aren’t necessarily rewarded for the time it takes to develop a rapport with patients and to have a conversation that leads to asking, “How much are you drinking?”
“The system in primary care isn’t set up that way,” said Lucy McBride, MD, an internist in Washington, D.C.
Patients don’t often ask for help
In a perfect world, patients struggling with a substance use disorder would present with a request to discontinue using drugs or alcohol, as Ms. Gordon did. While that does happen sometimes, the onus is on the physician to screen for substance misuse.
“Remember, this is the disease that tells you that you don’t have a disease,” Dr. McGrath says. He also says that the use of screening instruments is a bare minimum. When patients are in the throes of a substance use disorder, the prefrontal cortex doesn’t work effectively. Dr. McGrath says there’s an alteration of consciousness so that the patient doesn’t realize the extent of the disease. “Often simply asking the patient is falling far short. It’s the biggest mistake I see,” he says.
Self-reporting from the patient may be unreliable. “That would be like a patient coming in and saying, ‘My blood sugar is 700, and I want you to give me some insulin,’ ” Dr. McGrath says. Instead, clinicians in the field need a more objective measurement.
Perhaps that means asking the patient to bring in a significant other at the next visit or digging deeper into the conversation about alcohol and drugs and their role in the patient’s life. And to really have an impact, Dr. McGrath said, the clinician should talk to the patient about referral for further evaluation.
“You have to get collateral history; that’s the goldmine for the clinician,” Dr. McGrath says. “It may take a few more minutes or mean talking to a family member, but it can make the difference between life and death.”
“I am thankful to my doctor who discussed this [substance use disorder] with me in detail,” says Ronald Williams, another Angeleno who braved the difficult discussion with his doctor. Mr. Williams says his doctor explained it in a good way and that if the doctor hadn’t guided him empathetically, the conversation might not have gone as well.
“We check patients’ cholesterol. We get them on the scale. But there is no blood test to discover how much they’re drinking, no PCR to test for social anxiety, no MRI that distinguishes between their recreational marijuana use and marijuana abuse,” said Dr. McBride.
Check the prescription drugs they’re taking
Another thing Dr. McGrath recommends is for primary care physicians to check the prescription drug monitoring program (PDMP) database in their state to help be alerted to a patient with a substance use disorder. The CDC’s PMPD guidelines recommend that the clinician check on a patient every 3 months or each time they write an opioid prescription. Assigning a staff member or a nurse to check the database can help uncover a history of doctor-shopping or use of controlled substances.
“There’s been a lot of times I’ve gone on self-report, and I’ve been bamboozled because I don’t have a truth-o-meter, and I can’t tell when a patient is telling the truth,” says Dr. McGrath.
He is also a huge proponent of point-of-service screening. Patients can urinate in a cup that has amino assay strips on the side, like an immediate COVID-19 test, or they can spit into a saliva cup. “It’s really beneficial for the patient and the clinician to know right then at the point of service if there is a substance present and what it is,” Dr. McGrath said.
It can be part of the larger conversation once a problem with substances has been uncovered. The clinician can say something like, “Let’s see where you are right now today as far as what you have in your system and where we should go from here.”
Other barriers physicians face
Many physicians may feel unprepared to meet the needs of patients with substance use disorders or prescribe medication that blunts cravings and reduces the urge to drink without the need for special training. Scientists at the National Institutes of Health found that only 1.6% of people with a substance use disorder were prescribed medication to help control it.
In the largest study on how primary care physicians address substance use disorders, fewer than 20% described themselves as very prepared to identify alcoholism or illegal drug use. Since most patients prefer to seek treatment from their primary care doctor, at least initially, not being prepared is a problem.
Although referral for specialty addiction treatment is recommended for patients with severe substance use disorders, primary care physicians with appropriate experience, training, and support can provide some of these services. “In an ideal world I wouldn’t have to refer patients out, since they’re much more likely to talk with their primary care provider about sensitive, intimate topics,” says Dr. McBride.
The issue of reimbursement
Billing for substance use disorder counseling or coordination of care is still challenging, and how to get compensated remains a conundrum for many physicians. Reimbursement may not adequately compensate providers for the additional time and staff needed, but some changes have been positive.
For instance, the American Society for Addiction Medicine reports that in 2022, Medicare expanded the physician fee schedule for opioid and SUD counseling to include reimbursement for telemedicine services.
Learning the billing CPT codes for various addiction treatments and counseling, or having a billing service that understands them, is crucial to reimbursement and keeping revenue running smoothly.
At the very least, developing relationships with treatment centers and specialists in the community can help physicians with referrals and with determining the level of care needed. Physicians can help facilitate that care with routine reassessment and frequent follow-ups, as well as by requesting reports from the treatment facility, continuing treatment of medical conditions, and reinforcing the importance of continued substance use disorder treatment.
Dr. McBride says that primary care physicians can and should make their office a safe, blame-free medical home for patients with substance use disorders. “Patients also need to understand they should bring their whole selves to the doctor – to talk about their sleep, what they consume, their depression, and not just about alcohol, but their relationship with it, and other substances,” she says.
“There needs to be time to talk about it.”
A version of this article first appeared on Medscape.com.
DOJ: Indiana nurses allowed controlled substances during opioid recovery
, according to a statement released Sept. 1.
In March, the U.S. Department of Justice (DOJ) announced the findings of its investigation, stating that the board “violated the ADA by prohibiting nurses who take medication to treat OUD from participating in the Indiana State Nursing Assistance Program [ISNAP].”
ISNAP rehabilitates and monitors nurses with substance use disorders, and the nursing board contracts with vendors to administer the program. Nurses seeking recovery must typically enroll in ISNAP and complete the 1-year program to maintain an active nursing license or have a license reinstated.
Following the investigation, the nursing board was instructed to implement corrective measures, such as revising policies and handbooks and training nursing board staff and vendors on ADA guidelines and nondiscriminatory practices.
The state’s professional organization for nurses said the remediation efforts will help nurses who are struggling with opioid addiction.
Katherine Feley, DNP, RN, chief executive officer of the Indiana State Nurses Association, told this news organization, “Allowing nurses who take medication to treat OUD to remain on their medication when participating in [ISNAP] will avoid making nurses choose between their health and their profession. This improvement will increase access to treatment resources, enabling more nurses to complete treatment and progress toward a safe return to work.”
The DOJ opened an investigation after receiving a complaint from a nurse in which she alleged that she was denied participation in ISNAP because of her use of prescription medication for OUD. In 2013, while participating in a methadone maintenance program, the nurse was told she had to taper off the medication because ISNAP utilizes an “abstinence-based” model. Because of these restrictions, she could not complete the program, and her nursing license was suspended in late 2014.
In 2016, her physician prescribed a new medication, buprenorphine, and the nurse attempted to enroll in ISNAP again. The program vendor instructed her to taper off the drug within 3 months of enrollment, something her physician believed “would come with a significant risk of relapse [and possibly] death.” The nurse was unable to qualify for reinstatement of her license.
As part of the settlement, the nursing board has agreed to pay a total of $70,000 in damages to the complainant and report compliance with new guidelines to the DOJ every 6 months.
The DOJ says ISNAP’s OUD abstinence policy does not conform with the state’s statute, which mandates that substance abuse rehabilitation services be provided for nurses.
“Indiana may not deny individuals lifesaving medications, including medications that treat [OUD], based on stereotypes and misinformation,” Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division said of the settlement. “Requiring nurses to stop taking prescribed medication as a condition of maintaining a nursing license violates the ADA and not only creates barriers to recovery but inappropriately limits employment opportunities based on disability.”
In April, the DOJ issued guidance for protecting the civil rights of people with OUD under the ADA to ensure that individuals seeking treatment or recovery can continue participating in society and the workplace.
“The opioid epidemic has greatly impacted professionals and families of all walks of life, and Indiana nurses have the right to seek medically approved treatment for [OUD] under federal law,” U.S. Attorney Zachary A. Myers, of the Southern District of Indiana, said of the settlement. “Following the Justice Department’s findings and the parties’ settlement agreement, Indiana must now enact policies to ensure that Hoosier nurses will not be forced to choose between their recovery and their livelihoods.”
Under the terms of the agreement, the nursing board must allow nurses who are taking OUD medication to participate in ISNAP when the medication is prescribed by a licensed practitioner as part of a medically necessary treatment plan and is incorporated into a recovery monitoring agreement.
A version of this article first appeared on Medscape.com.
, according to a statement released Sept. 1.
In March, the U.S. Department of Justice (DOJ) announced the findings of its investigation, stating that the board “violated the ADA by prohibiting nurses who take medication to treat OUD from participating in the Indiana State Nursing Assistance Program [ISNAP].”
ISNAP rehabilitates and monitors nurses with substance use disorders, and the nursing board contracts with vendors to administer the program. Nurses seeking recovery must typically enroll in ISNAP and complete the 1-year program to maintain an active nursing license or have a license reinstated.
Following the investigation, the nursing board was instructed to implement corrective measures, such as revising policies and handbooks and training nursing board staff and vendors on ADA guidelines and nondiscriminatory practices.
The state’s professional organization for nurses said the remediation efforts will help nurses who are struggling with opioid addiction.
Katherine Feley, DNP, RN, chief executive officer of the Indiana State Nurses Association, told this news organization, “Allowing nurses who take medication to treat OUD to remain on their medication when participating in [ISNAP] will avoid making nurses choose between their health and their profession. This improvement will increase access to treatment resources, enabling more nurses to complete treatment and progress toward a safe return to work.”
The DOJ opened an investigation after receiving a complaint from a nurse in which she alleged that she was denied participation in ISNAP because of her use of prescription medication for OUD. In 2013, while participating in a methadone maintenance program, the nurse was told she had to taper off the medication because ISNAP utilizes an “abstinence-based” model. Because of these restrictions, she could not complete the program, and her nursing license was suspended in late 2014.
In 2016, her physician prescribed a new medication, buprenorphine, and the nurse attempted to enroll in ISNAP again. The program vendor instructed her to taper off the drug within 3 months of enrollment, something her physician believed “would come with a significant risk of relapse [and possibly] death.” The nurse was unable to qualify for reinstatement of her license.
As part of the settlement, the nursing board has agreed to pay a total of $70,000 in damages to the complainant and report compliance with new guidelines to the DOJ every 6 months.
The DOJ says ISNAP’s OUD abstinence policy does not conform with the state’s statute, which mandates that substance abuse rehabilitation services be provided for nurses.
“Indiana may not deny individuals lifesaving medications, including medications that treat [OUD], based on stereotypes and misinformation,” Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division said of the settlement. “Requiring nurses to stop taking prescribed medication as a condition of maintaining a nursing license violates the ADA and not only creates barriers to recovery but inappropriately limits employment opportunities based on disability.”
In April, the DOJ issued guidance for protecting the civil rights of people with OUD under the ADA to ensure that individuals seeking treatment or recovery can continue participating in society and the workplace.
“The opioid epidemic has greatly impacted professionals and families of all walks of life, and Indiana nurses have the right to seek medically approved treatment for [OUD] under federal law,” U.S. Attorney Zachary A. Myers, of the Southern District of Indiana, said of the settlement. “Following the Justice Department’s findings and the parties’ settlement agreement, Indiana must now enact policies to ensure that Hoosier nurses will not be forced to choose between their recovery and their livelihoods.”
Under the terms of the agreement, the nursing board must allow nurses who are taking OUD medication to participate in ISNAP when the medication is prescribed by a licensed practitioner as part of a medically necessary treatment plan and is incorporated into a recovery monitoring agreement.
A version of this article first appeared on Medscape.com.
, according to a statement released Sept. 1.
In March, the U.S. Department of Justice (DOJ) announced the findings of its investigation, stating that the board “violated the ADA by prohibiting nurses who take medication to treat OUD from participating in the Indiana State Nursing Assistance Program [ISNAP].”
ISNAP rehabilitates and monitors nurses with substance use disorders, and the nursing board contracts with vendors to administer the program. Nurses seeking recovery must typically enroll in ISNAP and complete the 1-year program to maintain an active nursing license or have a license reinstated.
Following the investigation, the nursing board was instructed to implement corrective measures, such as revising policies and handbooks and training nursing board staff and vendors on ADA guidelines and nondiscriminatory practices.
The state’s professional organization for nurses said the remediation efforts will help nurses who are struggling with opioid addiction.
Katherine Feley, DNP, RN, chief executive officer of the Indiana State Nurses Association, told this news organization, “Allowing nurses who take medication to treat OUD to remain on their medication when participating in [ISNAP] will avoid making nurses choose between their health and their profession. This improvement will increase access to treatment resources, enabling more nurses to complete treatment and progress toward a safe return to work.”
The DOJ opened an investigation after receiving a complaint from a nurse in which she alleged that she was denied participation in ISNAP because of her use of prescription medication for OUD. In 2013, while participating in a methadone maintenance program, the nurse was told she had to taper off the medication because ISNAP utilizes an “abstinence-based” model. Because of these restrictions, she could not complete the program, and her nursing license was suspended in late 2014.
In 2016, her physician prescribed a new medication, buprenorphine, and the nurse attempted to enroll in ISNAP again. The program vendor instructed her to taper off the drug within 3 months of enrollment, something her physician believed “would come with a significant risk of relapse [and possibly] death.” The nurse was unable to qualify for reinstatement of her license.
As part of the settlement, the nursing board has agreed to pay a total of $70,000 in damages to the complainant and report compliance with new guidelines to the DOJ every 6 months.
The DOJ says ISNAP’s OUD abstinence policy does not conform with the state’s statute, which mandates that substance abuse rehabilitation services be provided for nurses.
“Indiana may not deny individuals lifesaving medications, including medications that treat [OUD], based on stereotypes and misinformation,” Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division said of the settlement. “Requiring nurses to stop taking prescribed medication as a condition of maintaining a nursing license violates the ADA and not only creates barriers to recovery but inappropriately limits employment opportunities based on disability.”
In April, the DOJ issued guidance for protecting the civil rights of people with OUD under the ADA to ensure that individuals seeking treatment or recovery can continue participating in society and the workplace.
“The opioid epidemic has greatly impacted professionals and families of all walks of life, and Indiana nurses have the right to seek medically approved treatment for [OUD] under federal law,” U.S. Attorney Zachary A. Myers, of the Southern District of Indiana, said of the settlement. “Following the Justice Department’s findings and the parties’ settlement agreement, Indiana must now enact policies to ensure that Hoosier nurses will not be forced to choose between their recovery and their livelihoods.”
Under the terms of the agreement, the nursing board must allow nurses who are taking OUD medication to participate in ISNAP when the medication is prescribed by a licensed practitioner as part of a medically necessary treatment plan and is incorporated into a recovery monitoring agreement.
A version of this article first appeared on Medscape.com.
Alcohol warning labels need updates to reflect harms: NEJM
The current labeling, which has not changed for 30 years, focuses on risks during pregnancy and with operating machinery and includes a vague statement that alcohol “may cause health problems.”
This is “so understated that it borders on being misleading,” the two researchers argued.
The science related to the use of alcohol has moved on, and there is now firm evidence of harm. Alcohol has been classified by the International Agency for Research on Cancer (IARC) as a group 1 carcinogen and has been linked to an increased risk of many types of cancer. Drinking alcohol has also been linked to a wide range of other diseases, from liver disease to pancreatitis to some types of heart disease, the authors noted.
Yet the general public is mostly unaware of the most serious health risks that are associated with alcohol consumption, they pointed out.
“We believe Americans deserve the opportunity to make well-informed decisions about their alcohol consumption,” said Anna H. Grummon, PhD, of the Harvard T. H. Chan School of Public Health, Boston, and Marissa G. Hall, PhD, of the University of North Carolina at Chapel Hill.
“Designing and adopting new alcohol warning labels should therefore be a research and policy priority,” they added.
The two researchers set out their arguments in a perspective article published in The New England Journal of Medicine.
“Alcohol consumption and its associated harms are reaching a crisis point in the United States,” they pointed out.
It now accounts for more than 140,000 deaths per year in the United States, according to the latest data from the Centers for Disease Control and Prevention. The COVID-19 pandemic has made the problem even worse – there was a 25% increase in alcohol-related deaths during 2020.
New, well-designed warning labels on alcohol is a common sense strategy for providing consumers with information and reducing the burden of alcohol-related harm, the authors suggested.
Warning Labels Prominently Displayed
Warning labels are most effective when they are prominently displayed, when they include pictures of some type, and when the messages alternate so as to avoid any one message from becoming “stale,” the authors noted. This approach has worked well with cigarette packs. This type of warning has increased smoking quit rates in comparison with smaller, side-of-pack, text-only warning labels.
There is some evidence that this type of labeling can be effective for alcohol. When large, pictorial warnings about cancer risk were temporarily added to the front of alcohol containers in some stores in Yukon, Canada, alcohol sales declined by 6%-10%, they pointed out.
However, pressure from the alcohol industry led to changes in the Yukon project, and while a general health warning remains, the label about increased cancer risk was removed.
The alcohol industry has tried to suppress efforts to educate the public, and this has created problems in conveying health information to consumers, the authors noted. The industry spends more than $1 billion each year to market its products in the United States.
The authors caution that without government intervention, the alcohol industry has little incentive to communicate the risks.
Some companies even link their products to health campaigns, such as selling pink ribbon–themed alcoholic drinks during October to promote their efforts to raise funds for breast cancer research, despite compelling evidence linking alcohol to an increased risk of breast cancer.
Petition at Congress calling for new labels
This is not the first call for a change in the warning labels on alcohol.
Last year, a number of medical groups petitioned Congress for a new cancer-specific warning label to be displayed on all alcoholic beverages.
The petition was signed by the American Society of Clinical Oncology (ASCO), the American Institute for Cancer Research (AICR), and Breast Cancer Prevention Partners, in collaboration with the American Public Health Association, the Consumer Federation of America, the Center for Science in the Public Interest, Alcohol Justice, and the U.S. Alcohol Policy Alliance.
They are advocating for a label that would say: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
That petition is still pending, Melissa Maitin-Shepard, MPP, policy expert at the AICR, said in an interview.
In addition, the AICR is “working to advocate for the addition of a cancer warning label to alcoholic beverages through multiple channels,” she said. “Given the strong evidence linking alcohol use with at least six types of cancer – and low awareness of the alcohol and cancer connection – there is a tremendous need to educate the public about alcohol and cancer risk.”
Noelle K. LoConte, MD, associate professor of medicine at the University of Wisconsin, Madison, who is the lead author of ASCO’s statement on alcohol and cancer risk, emphasized that there is no doubt that alcohol is a carcinogen, that it causes about 5% of cancers globally, and that its use has increased during the pandemic.
“Initiatives that raise awareness around this issue could help generate more public support for policies that limit alcohol access and thereby decrease the number of alcohol-associated cancers,” she said. “In ASCO’s statement on alcohol and cancer, we recommend several key strategies to reduce high-risk alcohol consumption, including limiting youth access to alcohol, giving municipalities more control over alcohol outlet density and points of sale, and increasing taxes on alcohol.”
However, she also had a small criticism of one point in the NEJM article. It shows a sample infographic that lists gastric cancer as being caused by alcohol. “But as of today, gastric cancer is not on the IARC list of alcohol-associated cancers,” she said. “I think this brings to mind one critical point, that these warning labels have to contain scientifically established facts.”
Dr. Grummon and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The current labeling, which has not changed for 30 years, focuses on risks during pregnancy and with operating machinery and includes a vague statement that alcohol “may cause health problems.”
This is “so understated that it borders on being misleading,” the two researchers argued.
The science related to the use of alcohol has moved on, and there is now firm evidence of harm. Alcohol has been classified by the International Agency for Research on Cancer (IARC) as a group 1 carcinogen and has been linked to an increased risk of many types of cancer. Drinking alcohol has also been linked to a wide range of other diseases, from liver disease to pancreatitis to some types of heart disease, the authors noted.
Yet the general public is mostly unaware of the most serious health risks that are associated with alcohol consumption, they pointed out.
“We believe Americans deserve the opportunity to make well-informed decisions about their alcohol consumption,” said Anna H. Grummon, PhD, of the Harvard T. H. Chan School of Public Health, Boston, and Marissa G. Hall, PhD, of the University of North Carolina at Chapel Hill.
“Designing and adopting new alcohol warning labels should therefore be a research and policy priority,” they added.
The two researchers set out their arguments in a perspective article published in The New England Journal of Medicine.
“Alcohol consumption and its associated harms are reaching a crisis point in the United States,” they pointed out.
It now accounts for more than 140,000 deaths per year in the United States, according to the latest data from the Centers for Disease Control and Prevention. The COVID-19 pandemic has made the problem even worse – there was a 25% increase in alcohol-related deaths during 2020.
New, well-designed warning labels on alcohol is a common sense strategy for providing consumers with information and reducing the burden of alcohol-related harm, the authors suggested.
Warning Labels Prominently Displayed
Warning labels are most effective when they are prominently displayed, when they include pictures of some type, and when the messages alternate so as to avoid any one message from becoming “stale,” the authors noted. This approach has worked well with cigarette packs. This type of warning has increased smoking quit rates in comparison with smaller, side-of-pack, text-only warning labels.
There is some evidence that this type of labeling can be effective for alcohol. When large, pictorial warnings about cancer risk were temporarily added to the front of alcohol containers in some stores in Yukon, Canada, alcohol sales declined by 6%-10%, they pointed out.
However, pressure from the alcohol industry led to changes in the Yukon project, and while a general health warning remains, the label about increased cancer risk was removed.
The alcohol industry has tried to suppress efforts to educate the public, and this has created problems in conveying health information to consumers, the authors noted. The industry spends more than $1 billion each year to market its products in the United States.
The authors caution that without government intervention, the alcohol industry has little incentive to communicate the risks.
Some companies even link their products to health campaigns, such as selling pink ribbon–themed alcoholic drinks during October to promote their efforts to raise funds for breast cancer research, despite compelling evidence linking alcohol to an increased risk of breast cancer.
Petition at Congress calling for new labels
This is not the first call for a change in the warning labels on alcohol.
Last year, a number of medical groups petitioned Congress for a new cancer-specific warning label to be displayed on all alcoholic beverages.
The petition was signed by the American Society of Clinical Oncology (ASCO), the American Institute for Cancer Research (AICR), and Breast Cancer Prevention Partners, in collaboration with the American Public Health Association, the Consumer Federation of America, the Center for Science in the Public Interest, Alcohol Justice, and the U.S. Alcohol Policy Alliance.
They are advocating for a label that would say: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
That petition is still pending, Melissa Maitin-Shepard, MPP, policy expert at the AICR, said in an interview.
In addition, the AICR is “working to advocate for the addition of a cancer warning label to alcoholic beverages through multiple channels,” she said. “Given the strong evidence linking alcohol use with at least six types of cancer – and low awareness of the alcohol and cancer connection – there is a tremendous need to educate the public about alcohol and cancer risk.”
Noelle K. LoConte, MD, associate professor of medicine at the University of Wisconsin, Madison, who is the lead author of ASCO’s statement on alcohol and cancer risk, emphasized that there is no doubt that alcohol is a carcinogen, that it causes about 5% of cancers globally, and that its use has increased during the pandemic.
“Initiatives that raise awareness around this issue could help generate more public support for policies that limit alcohol access and thereby decrease the number of alcohol-associated cancers,” she said. “In ASCO’s statement on alcohol and cancer, we recommend several key strategies to reduce high-risk alcohol consumption, including limiting youth access to alcohol, giving municipalities more control over alcohol outlet density and points of sale, and increasing taxes on alcohol.”
However, she also had a small criticism of one point in the NEJM article. It shows a sample infographic that lists gastric cancer as being caused by alcohol. “But as of today, gastric cancer is not on the IARC list of alcohol-associated cancers,” she said. “I think this brings to mind one critical point, that these warning labels have to contain scientifically established facts.”
Dr. Grummon and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The current labeling, which has not changed for 30 years, focuses on risks during pregnancy and with operating machinery and includes a vague statement that alcohol “may cause health problems.”
This is “so understated that it borders on being misleading,” the two researchers argued.
The science related to the use of alcohol has moved on, and there is now firm evidence of harm. Alcohol has been classified by the International Agency for Research on Cancer (IARC) as a group 1 carcinogen and has been linked to an increased risk of many types of cancer. Drinking alcohol has also been linked to a wide range of other diseases, from liver disease to pancreatitis to some types of heart disease, the authors noted.
Yet the general public is mostly unaware of the most serious health risks that are associated with alcohol consumption, they pointed out.
“We believe Americans deserve the opportunity to make well-informed decisions about their alcohol consumption,” said Anna H. Grummon, PhD, of the Harvard T. H. Chan School of Public Health, Boston, and Marissa G. Hall, PhD, of the University of North Carolina at Chapel Hill.
“Designing and adopting new alcohol warning labels should therefore be a research and policy priority,” they added.
The two researchers set out their arguments in a perspective article published in The New England Journal of Medicine.
“Alcohol consumption and its associated harms are reaching a crisis point in the United States,” they pointed out.
It now accounts for more than 140,000 deaths per year in the United States, according to the latest data from the Centers for Disease Control and Prevention. The COVID-19 pandemic has made the problem even worse – there was a 25% increase in alcohol-related deaths during 2020.
New, well-designed warning labels on alcohol is a common sense strategy for providing consumers with information and reducing the burden of alcohol-related harm, the authors suggested.
Warning Labels Prominently Displayed
Warning labels are most effective when they are prominently displayed, when they include pictures of some type, and when the messages alternate so as to avoid any one message from becoming “stale,” the authors noted. This approach has worked well with cigarette packs. This type of warning has increased smoking quit rates in comparison with smaller, side-of-pack, text-only warning labels.
There is some evidence that this type of labeling can be effective for alcohol. When large, pictorial warnings about cancer risk were temporarily added to the front of alcohol containers in some stores in Yukon, Canada, alcohol sales declined by 6%-10%, they pointed out.
However, pressure from the alcohol industry led to changes in the Yukon project, and while a general health warning remains, the label about increased cancer risk was removed.
The alcohol industry has tried to suppress efforts to educate the public, and this has created problems in conveying health information to consumers, the authors noted. The industry spends more than $1 billion each year to market its products in the United States.
The authors caution that without government intervention, the alcohol industry has little incentive to communicate the risks.
Some companies even link their products to health campaigns, such as selling pink ribbon–themed alcoholic drinks during October to promote their efforts to raise funds for breast cancer research, despite compelling evidence linking alcohol to an increased risk of breast cancer.
Petition at Congress calling for new labels
This is not the first call for a change in the warning labels on alcohol.
Last year, a number of medical groups petitioned Congress for a new cancer-specific warning label to be displayed on all alcoholic beverages.
The petition was signed by the American Society of Clinical Oncology (ASCO), the American Institute for Cancer Research (AICR), and Breast Cancer Prevention Partners, in collaboration with the American Public Health Association, the Consumer Federation of America, the Center for Science in the Public Interest, Alcohol Justice, and the U.S. Alcohol Policy Alliance.
They are advocating for a label that would say: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
That petition is still pending, Melissa Maitin-Shepard, MPP, policy expert at the AICR, said in an interview.
In addition, the AICR is “working to advocate for the addition of a cancer warning label to alcoholic beverages through multiple channels,” she said. “Given the strong evidence linking alcohol use with at least six types of cancer – and low awareness of the alcohol and cancer connection – there is a tremendous need to educate the public about alcohol and cancer risk.”
Noelle K. LoConte, MD, associate professor of medicine at the University of Wisconsin, Madison, who is the lead author of ASCO’s statement on alcohol and cancer risk, emphasized that there is no doubt that alcohol is a carcinogen, that it causes about 5% of cancers globally, and that its use has increased during the pandemic.
“Initiatives that raise awareness around this issue could help generate more public support for policies that limit alcohol access and thereby decrease the number of alcohol-associated cancers,” she said. “In ASCO’s statement on alcohol and cancer, we recommend several key strategies to reduce high-risk alcohol consumption, including limiting youth access to alcohol, giving municipalities more control over alcohol outlet density and points of sale, and increasing taxes on alcohol.”
However, she also had a small criticism of one point in the NEJM article. It shows a sample infographic that lists gastric cancer as being caused by alcohol. “But as of today, gastric cancer is not on the IARC list of alcohol-associated cancers,” she said. “I think this brings to mind one critical point, that these warning labels have to contain scientifically established facts.”
Dr. Grummon and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Laboratory monitoring for patients on buprenorphine: 10 questions
The opioid use disorder (OUD) epidemic is a major public health crisis in the United States.1 Naltrexone, methadone, and buprenorphine are first-line therapies for OUD and have high success rates.2 While studies have shown that naltrexone is effective, patients must achieve opioid detoxification and maintain 7 to 10 days of total abstinence to avoid a precipitated opioid withdrawal before it can be prescribed.3 Methadone does not require detoxification or a period of complete abstinence, but must be prescribed in special clinics and requires daily observed dosing for the first 90 days,4 though these requirements have been relaxed during the COVID-19 pandemic. In contrast, buprenorphine (with or without naloxone) can be used in office-based settings, which significantly improves the accessibility and availability of treatment for patients with OUD. Clinician knowledge and comfort prescribing buprenorphine are limiting factors to treatment.5 Increasing the number of clinicians proficient with buprenorphine management can improve access to effective treatment and recovery services, which is critical for patients with OUD.
Multiple resources are available for clinicians to learn how to prescribe buprenorphine, but clear guidance on laboratory testing for patients receiving buprenorphine is limited. To safely and effectively prescribe buprenorphine, clinicians need to understand its pharmacology (Box 16-9) and how laboratory testing influences treatment. In an effort to increase clinician knowledge of and proficiency with buprenorphine, this article answers 10 common questions about laboratory monitoring of patients receiving this medication.
Box 1
For patients with opioid use disorder, buprenorphine is indicated for opioid detoxification and maintenance. Oral formulations of buprenorphine (including tablets and buccal films) have long durations of action, and when dosed daily can prevent opioid withdrawal for at least 48 hours.6 The recommended formulation is a combination of buprenorphine and naloxone, because this formulation is associated with a lower risk of misuse and diversion compared to formulations containing only buprenorphine.7 However, buprenorphine alone can be effective in patients who experience adverse effects from or are unable to tolerate the combination buprenorphine/naloxone formulation.7 Despite the addition of naloxone, buprenorphine prescriptions may still be misused and diverted, so close monitoring is necessary.
Buprenorphine is metabolized by the cytochrome P450 system (CYP) (primarily CYP3A4) to its active metabolite, norbuprenorphine, both of which are primarily excreted in feces.8 However, small quantities of buprenorphine and norbuprenorphine are excreted in the urine,9 which makes urine specimen the best choice to monitor buprenorphine use for therapeutic purposes.
1. Why is laboratory monitoring important?
Proper laboratory monitoring discourages illicit substance use, encourages medication adherence, and influences treatment modifications. Patient self-reporting on medication compliance may be inaccurate or unreliable.10 Patients who relapse or use other illicit substances may also be reluctant to disclose their substance use.11
On the other hand, laboratory tests are objective markers of treatment outcome and adherence, and can verify a patient’s self-report.12 When used appropriately, laboratory monitoring can be therapeutic. It holds patients accountable, especially when used in conjunction with contingency management or other behavioral therapies.13 Laboratory monitoring is the most reliable method of determining if patients are abstaining from opioids and other illicit substances, or if the treatment plan requires revision.
2. Which tests should I order?
When initiating or maintaining a patient on buprenorphine, order a general urine drug screen (UDS), urine opioid screen (availability varies by institution), urine creatinine levels, urine buprenorphine/norbuprenorphine/naloxone/creatinine levels, urine alcohol metabolite levels, and a urine general toxicology test. It is also recommended to obtain a comprehensive metabolic panel (CMP) before starting buprenorphine,14,15 and to monitor CMP values at least once annually following treatment. Patients with a history of IV drug use or other high-risk factors should also be screened for hepatitis B, hepatitis C, and HIV.14,15
A general UDS can determine if opiates, amphetamines, cocaine, marijuana, or other common illicit substances are present to identify additional substance use. The proficiency of a general UDS may vary depending on the panels used at the respective institution. Some clinics use point-of-care UDS as part of their clinical management; these tests are inexpensive and provide immediate results.16 A basic UDS typically does not detect synthetic opioids due to the specificity of conventional immunoassays. As a result, specific tests for opioids such as oxycodone, hydrocodone, hydromorphone, oxymorphone, fentanyl, and methadone should also be considered, depending on their availability. Though buprenorphine treatment may trigger a positive opiate or other opioid screen,17 buprenorphine adherence should be confirmed using several urine tests, including creatinine, buprenorphine, norbuprenorphine, and naloxone urine levels.
In addition to screening for illicit substances and buprenorphine adherence, it is important to also screen for alcohol. Alcohol use disorder (AUD) is highly comorbid with OUD,18 and is associated with worse OUD treatment outcomes.19 Alcohol use may also affect liver function necessary for buprenorphine metabolism,8 so urine alcohol metabolites such as ethyl glucuronide and ethyl sulfate, serum transaminases, and gamma-glutamyl transferase should also be obtained.
Continue to: How frequently should patients be tested?
3. How frequently should patients be tested?
As part of the initial assessment, it is recommended to order CMP, UDS, and urine general toxicology.14 If indicated, specific laboratory tests such as specific opioid and alcohol metabolites screens can be ordered. After starting buprenorphine, the frequency of monitoring urine laboratory tests—including UDS, general drug toxicology, buprenorphine/norbuprenorphine/naloxone/creatinine, and alcohol and its metabolites—depends on a variety of factors, including a patient’s treatment response and stability as well as availability and cost of the tests. Ultimately, the frequency of laboratory monitoring should be determined on a patient-by-patient basis and clinicians should use their judgment.
The American Society of Addiction Medicine suggests testing more frequently earlier in the course of treatment (eg, weekly or biweekly), then spacing it out over time (eg, monthly or quarterly) as the patient’s recovery progresses.14,15 To conserve resources and reduce spending, some clinicians and guidelines recommend random monitoring as opposed to monitoring at every follow-up visit (eg, once out of every 3 to 5 visits, on average), which allows for longer intervals between testing while ensuring consistency with medication and abstinence from illicit substances.15,16 We suggest screening every 2 weeks for the first month, then spacing out to monthly and quarterly as patients demonstrate stability, with random screening as indicated. Monitoring of liver function should be done at least once annually.
4. How should urine buprenorphine and other results be interpreted?
There are several issues to consider when interpreting laboratory results. The clinician needs to know what to expect in the sample, and what approximate levels should be detected. To check treatment adherence, laboratory data should include stable urine buprenorphine and norbuprenorphine levels and negative urine screening for other illicit substances.14,15 While urine buprenorphine and norbuprenorphine levels have great interindividual variability due to genetic differences in hepatic metabolism, unusually high levels of buprenorphine (≥700 ng/mL) without norbuprenorphine suggests “urine spiking,” where patients put buprenorphine directly into their urine sample.20,21 Abnormally low or undetectable levels raise concern for medication nonadherence or diversion.
Though urine buprenorphine levels do not reliably correlate with dose, because there is typically not much intraindividual variability, patients should have relatively stable levels on each screen once a maintenance dose has been established.22 Furthermore, the buprenorphine-to-norbuprenorphine ratio (ie, “the metabolic ratio”) typically ranges from 1:2 to 1:4 across all individuals,20,21,23 regardless of dose or metabolic rate. Urine naloxone levels, which typically are included in commercial urine buprenorphine laboratory panels, also may aid in identifying tampered urine specimens when buprenorphine-to-norbuprenorphine ratios are abnormal or inconsistent with an individual’s prior ratio. Naloxone is typically (but not always) poorly absorbed and minimally detected in urine specimens.20 A high level of naloxone coupled with unusually high buprenorphine levels, particularly in the absence of norbuprenorphine in the urine, may indicate urine spiking.20,21,23
Urine creatinine is used to establish the reliability of the specimen. When urine creatinine concentration is <20 mg/dL, the concentration of most substances typically falls to subthreshold levels of detection.24 If a UDS is negative and the urine has a creatinine concentration <20 mg/dL, the patient should provide a new sample, because the urine was likely too diluted to detect any substances.
Continue to: The presence of alcohol...
The presence of alcohol metabolites can alert the clinician to recent alcohol use and possible AUD, which should be assessed and treated if indicated.
Liver enzymes should be normal or unchanged with short- and long-term buprenorphine use when taken as prescribed.25,26 However, acute liver injury may occur if patients inject buprenorphine intravenously, especially in those with underlying hepatitis C.25
5. What can cause a false negative result on UDS?
Laboratory monitoring may occasionally yield false negative drug screens. For urine buprenorphine levels, false negatives may occur in patients who are “rapid metabolizers,” infrequent or as-needed usage of the medication, patient mix-up, or laboratory error.27 For other substances, a false negative result may occur if the patient used the substance(s) outside the window of detection. The most common causes of false negative results, however, are overly diluted urine samples (eg, due to rapid water ingestion), or the use of an inappropriate test to measure a specific opioid or substance.27
Many laboratories use conventional immunoassays with morphine antibodies that react with various opioid substrates to determine the presence of a specific opioid. Some opioids—particularly synthetics such as oxycodone, hydrocodone, hydromorphone, oxymorphone, fentanyl, buprenorphine, and methadone—have poor cross-reactivity with the morphine antibody due to their distinct chemical structures, so standard immunoassays used to detect opioids may result in a false negative result.28 In such situations, a discussion with a clinical pathologist familiar with the laboratory detection method can help ensure proper testing. Additional tests for specific opioids should be ordered to more specifically target substances prone to false negative results.27
6. What can cause a false positive result on UDS?
The cross-reactivity of the morphine substrate may also result in a false positive result.28 Other over-the-counter (OTC) or prescription medications that have cross-reactivity with the morphine antibody include dextromethorphan, verapamil, quinine, fluoroquinolones, and rifampin, which can normally be found in urine 2 to 3 days after consumption.17,27 Poppy seeds have long been known to result in positive opiate screens on urine testing, particularly when laboratories use lower cutoff values (eg, 300 ng/mL), so advise patients to avoid consuming poppy seeds.29
Continue to: For other drugs of abuse...
For other drugs of abuse, false positives are typically caused by cross-reactivity with other prescription or OTC medications. Numerous substances cross-react with amphetamines and produce false positive results on amphetamine immunoassays, including amantadine, bupropion, ephedrine, labetalol, phentermine, pseudoephedrine, ranitidine, selegiline, and trazodone.27 Sertraline and efavirenz are known to produce false positive results on benzodiazepine UDS, and ibuprofen, naproxen, and efavirenz can produce false positive results for cannabinoids.27
7. How do I communicate the results to patients?
Effectively communicating test results to patients is just as important as the results themselves. A trusting, therapeutic alliance between patient and clinician is highly predictive of successful treatment,30 and how the clinician communicates affects the strength of this collaboration. A principle of addiction treatment is the use of neutral language when discussing laboratory results.31,32 To avoid unintentional shaming or moral judgment, use words such as “positive” or “negative” rather than stigmatizing terms such as “clean” or “dirty.”33
Additionally, make it clear that laboratory findings are not used to punish patients, but rather to improve treatment.34 Reassuring the patient that a positive screen will not result in withdrawal of care encourages a working relationship.14 All patients who receive buprenorphine treatment should be informed that collecting a UDS is the standard of care used to monitor their progress. You might want to compare using UDS in patients with OUD to monitoring HbA1c levels in patients with diabetes as an example to demonstrate how laboratory values inform treatment.35,36
Before reporting the results, a helpful strategy to maintain the therapeutic alliance in the face of a positive UDS is to ask the patient what they expect their UDS to show. When the patient has been reassured that treatment will not be withdrawn due to a positive result, they may be more likely to fully disclose substance use. This allows them the opportunity to self-disclose rather than be “called out” by the clinician.35
8. What happens when a patient tests positive for drugs of abuse?
If a patient tests positive for opioids or other drugs of abuse, convey this information to them, ideally by asking them what they expect to see on laboratory findings. Patients may have “slip ups” or relapses, or use certain prescription medications for medical reasons with the intention of establishing abstinence. It is essential to convey laboratory findings in a nonjudgmental tone while maintaining a supportive stance with clear boundaries.
Continue to: Though addiction specialists...
Though addiction specialists often advise complete abstinence from all substances, including alcohol, cannabis, and tobacco, the harm-reduction model emphasizes “meeting patients where they are” in terms of continued substance use.37 If a patient can reduce their substance use or abstain from some substances while continuing others, these accomplishments should be acknowledged.
For patients who continue to test positive for illicit substances (>3 instances) without a clear explanation, schedule an appointment to re-educate them about buprenorphine treatment and reassess the patient’s treatment goals. Consider changing the current treatment plan, such as by having more frequent follow-ups, increasing the dose of the buprenorphine for patients whose cravings are not sufficiently suppressed, switching to another medication such as methadone or naltrexone, or referring the patient to a higher level of care, such as intensive outpatient or residential treatment.
9. What should I do if the results indicate abnormal levels of buprenorphine, norbuprenorphine, and naloxone?
When urine buprenorphine, norbuprenorphine, or naloxone levels appear low or the results indicate a likely “spiking,” clarify whether the sample tampering is due to poor adherence or diversion. Similar to dealing with a positive result for substances of abuse, ask the patient what they expect to find in their urine, and discuss the results in a nonjudgmental manner. Patients who admit to difficulty following their medication regimen may require additional psychoeducation and motivational interviewing to identify and address barriers. Strategies to improve adherence include setting an alarm, involving the family, using a pillbox, or simplifying the regimen.38 A long-acting injectable form of buprenorphine is also available.
If you suspect diversion, refer to your clinic’s policy and use other clinical management skills, such as increasing the frequency of visits, random pill counts, and supervised medication administration in the clinic.39 If diversion occurs repetitively and the patient is not appropriate for or benefiting from buprenorphine treatment, it may make sense to terminate treatment and consider other treatment options (such as methadone or residential treatment).39
10. What should I do if a patient disagrees with laboratory findings?
It is common for patients to disagree with laboratory results. Maintaining an attitude of neutrality and allowing the patient to speak and provide explanations is necessary to ensure they feel heard. Explanations patients frequently provide include passive exposure (“I was around someone who was using it”) or accidental ingestion, when a patient reports taking a medication they were not aware was a substance of concern. In a calm and nonjudgmental manner, provide education on what leads to a positive drug screen, including the possibility of false positive findings.
Continue to: Because a screening test...
Because a screening test has high sensitivity and low specificity, false positives may occur.17,27 Therefore, when a result is in dispute, the use of a high-specificity confirmatory test is often needed (many laboratories have reflex confirmatory testing). However, in the case of diluted urine (urine creatinine concentrations <20 mg/dL), patients should be told the findings are physiologically implausible, and a new urine sample should be obtained.24
Goals of laboratory monitoring
Laboratory monitoring, including UDS and urine buprenorphine levels, is a mainstay of treatment for patients with OUD. The increased use of telehealth has affected how laboratory testing is conducted (Box 240,41). The goal of laboratory testing is to influence treatment and improve patient outcomes. Clinical data such as clinician assessment, patient self-reporting, and collateral information provide essential details for patient management. However, laboratory monitoring is often the most reliable and objective source by which to influence treatment.
Box 2
While delivering therapy via telehealth has been shown to decrease the stigma that surrounds treatment, reduce no-show rates, increase retention in care, improve treatment access for patients who have difficulty commuting, and allow for continuity of outpatient treatment during the COVID-19 pandemic, there are also challenges.40,41 Inducing patients on buprenorphine via telehealth, as well as managing complex treatment cases or repeated failed urine drug screen tests, can be especially challenging. However, treatment standards should be followed as much as possible, and laboratory monitoring as clinically indicated should still be used to improve treatment outcomes.
If needed, patients may be directed to community labs for urine screening and should have results sent to their clinicians prior to the telehealth visit. Complex treatment cases (eg, repeat positive opioid screens, or negative urine buprenorphine screens with comorbid psychiatric conditions) should be handled on an individual basis and in-person appointments may be needed. Video assessment is always preferable to telephone. For patients who are unable to use video and have difficulty maintaining negative drug screens, an in-person visit should be requested.
An increased understanding of recommended laboratory monitoring practices may improve your comfort with OUD treatment and motivate more clinicians to offer buprenorphine, a life-saving and disease-modifying treatment for OUD. Doing so would increase access to OUD treatment for patients to reduce the individual and public health risks associated with untreated OUD.
Bottom Line
Laboratory monitoring, particularly urine drug screens and urine buprenorphine levels, is the most reliable source of information in the treatment of patients with opioid use disorder (OUD). An increased understanding of monitoring practices may improve a clinician’s willingness to offer buprenorphine as an option for therapy and their ability to properly treat patients with OUD.
Related Resources
- Li X, Moore S, Olson C. Urine drug tests: how to make the most of them. Current Psychiatry. 2019;18(8):10-18,20.
- Moreno JL, Johnson JL, Peckham AM. Sublingual buprenorphine plus buprenorphine XR for opioid use disorder. Current Psychiatry. 2022;21(6):39-42,49. doi:10.12788/cp.0244
Drug Brand Names
Amantadine • Gocovri
Buprenorphine • Subutex, Sublocade
Bupropion • Wellbutrin, Zyban
Efavirenz • Sustiva
Fentanyl • Actiq
Hydrocodone • Hysingla
Hydromorphone • Dilaudid
Methadone • Methadose
Naloxone • Evzio
Naltrexone • Vivitrol
Oxycodone • Oxycontin
Oxymorphone • Opana
Phentermine • Ionamin
Quinine • Qualaquin
Ranitidine • Zantac
Rifampin • Rifadin
Selegiline • Eldepryl
Sertraline • Zoloft
Trazodone • Oleptro
Verapamil • Verelan
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. HHS Publication PEP19-5068, NSDUH Series H-54. May 2019. https://www.samhsa.gov/data/
2. Volkow ND, Frieden TR, Hyde PS, et al. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063-2066. doi:10.1056/NEJMp1402780
3. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391(10118):309-318. doi:10.1016/S0140-6736(17)32812-X
4. Sharma A, Kelly SM, Mitchell SG, et al. Update on barriers to pharmacotherapy for opioid use disorders. Curr Psychiatry Rep. 2017;19(6):35. doi:10.1007/s11920-017-0783-9
5. DeFlavio JR, Rolin SA, Nordstrom BR, et al. Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural Remote Health. 2015;15:3019. doi:10.22605/rrh3019
6. Kuhlman JJ Jr, Lalani S, Magluiolo J Jr, et al. Human pharmacokinetics of intravenous, sublingual, and buccal buprenorphine. J Anal Toxicol. 1996;20(6):369-378.
7. Fudala PJ, Bridge TP, Herbert S, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. N Engl J Med. 2003;349(10):949-958. doi:10.1056/NEJMoa022164
8. Brown SM, Holtzman M, Kim T, et al. Buprenorphine metabolites, buprenorphine-3-glucuronide and norbuprenorphine-3-glucuronide, are biologically active. Anesthesiology. 2011;115(6):1251-1260. doi:10.1097/ALN.0b013e318238fea0
9. Cone EJ, Gorodetzky CW, Yousefnejad D, et al. The metabolism and excretion of buprenorphine in humans. Drug Metab Dispos. 1984;12(5):577-581.
10. Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470-482. doi:10.1007/s13142-015-0315-2
11. Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction. 2000;95 Suppl 3:S347-S360. doi:10.1080/09652140020004278
12. Preston KL, Silverman K, Schuster CR, et al. Comparison of self-reported drug use with quantitative and qualitative urinalysis for assessment of drug use in treatment studies. NIDA Res Monogr. 1997;167:130-145.
13. Knezevic NN, Khan OM, Beiranvand A, et al. Repeated quantitative urine toxicology analysis may improve chronic pain patient compliance with opioid therapy. Pain Physician. 2017;20(2S):S135-S145. doi:10.36076/ppj.2017.s145
14. Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367.
15. The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med. 2020;14(2S Suppl 1):1-91. doi:10.1097/ADM.0000000000000633
16. McDonell MG, Graves MC, West II, et al. Utility of point-of-care urine drug tests in the treatment of primary care patients with drug use disorders. J Addict Med. 2016;10(3):196-201. doi:10.1097/ADM.0000000000000220
17. Algren DA, Christian MR. Buyer beware: pitfalls in toxicology laboratory testing. Mo Med. 2015;112(3):206-210.
18. Hartzler B, Donovan DM, Huang Z. Comparison of opiate-primary treatment seekers with and without alcohol use disorder. J Subst Abuse Treat. 2010;39(2):114-123. doi:10.1016/j.jsat.2010.05.008
19. Stapleton RD, Comiskey CM. Alcohol usage and associated treatment outcomes for opiate users entering treatment in Ireland. Drug Alcohol Depend. 2010;107(1):56-61. doi:10.1016/j.drugalcdep.2009.09.007
20. Warrington JS, Warrington GS, Francis-Fath S, et al. Urinary buprenorphine, norbuprenorphine and naloxone concentrations and ratios: review and potential clinical implications. J Addict Med. 2020;14(6):e344-e349. doi:10.1097/ADM.0000000000000676
21. Donroe JH, Holt SR, O’Connor PG, et al. Interpreting quantitative urine buprenorphine and norbuprenorphine levels in office-based clinical practice. Drug Alcohol Depend. 2017;180:46-51. doi:10.1016/j.drugalcdep.2017.07.040
22. Bai SA, Xiang Q, Finn A. Evaluation of the pharmacokinetics of single- and multiple-dose buprenorphine buccal film in healthy volunteers. Clin Ther. 2016;38(2):358-369. doi:10.1016/j.clinthera.2015.12.016
23. Suzuki J, Zinser J, Issa M, et al. Quantitative testing of buprenorphine and norbuprenorphine to identify urine sample spiking during office-based opioid treatment. Subst Abus. 2017;38(4):504-507. doi:10.1080/08897077.2017.1356796
24. Gowans EM, Fraser CG. Biological variation of serum and urine creatinine and creatinine clearance: ramifications for interpretation of results and patient care. Ann Clin Biochem. 1988;25( Pt 3):259-263. doi:10.1177/000456328802500312
25. Saxon AJ, Ling W, Hillhouse M, et al. Buprenorphine/naloxone and methadone effects on laboratory indices of liver health: a randomized trial. Drug Alcohol Depend. 2013;128(1-2):71-76. doi:10.1016/j.drugalcdep.2012.08.002
26. Fareed A, Eilender P, Ketchen B, et al. Factors affecting noncompliance with buprenorphine maintenance treatment. J Addict Med. 2014;8(5):345-350. doi:10.1097/ADM.0000000000000057
27. Moeller KE, Lee KC, Kissack JC. Urine drug screening: practical guide for clinicians. Mayo Clin Proc. 2008;83(1):66-76. doi:10.4065/83.1.66
28. Keary CJ, Wang Y, Moran JR, et al. Toxicologic testing for opiates: understanding false-positive and false-negative test results. Prim Care Companion CNS Disord. 2012;14(4).PCC.12f01371 doi:10.4088/PCC.12f01371
29. Zebelman AM, Troyer BL, Randall GL, et al. Detection of morphine and codeine following consumption of poppy seeds. J Anal Toxicol. 1987;11(3):131-132. doi:10.1093/jat/11.3.131
30. Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: a critical review of the literature. Addiction. 2005;100(3):304-316. doi:10.1111/j.1360-0443.2004.00935.x
31. Kelly JF, Saitz R, Wakeman S. Language, substance use disorders, and policy: the need to reach consensus on an “addiction-ary.” Alcohol Treat Q. 2016;34(1):116-123. doi:10.1080/07347324.2016.1113103
32. Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus. 2014;35(3):217-221. doi:10.1080/08897077.2014.930372
33. Kelly JF, Wakeman SE, Saitz R. Stop talking ‘dirty’: clinicians, language, and quality of care for the leading cause of preventable death in the United States. Am J Med. 2015;128(1):8-9. doi:10.1016/j.amjmed.2014.07.043
34. Jarvis M, Williams J, Hurford M, et al. Appropriate use of drug testing in clinical addiction medicine. J Addict Med. 2017;11(3):163-173. doi:10.1097/ADM.0000000000000323
35. Martin SA, Chiodo LM, Bosse JD, et al. The next stage of buprenorphine care for opioid use disorder. Ann Intern Med. 2018;169(9):628-635. doi:10.7326/M18-1652
36. Katz N, Fanciullo GJ. Role of urine toxicology testing in the management of chronic opioid therapy. Clin J Pain. 2002;18(4 Suppl):S76-S82.
37. Klein A. Harm reduction works: evidence and inclusion in drug policy and advocacy. Health Care Anal. 2020;28(4):404-414. doi:10.1007/s10728-020-00406-w
38. Patel MX, David AS. Medication adherence: predictive factors and enhancement strategies. Psychiatry. 2007;6(9):357-361. doi:10.1016/j.mppsy.2007.06.003
39. Lofwall MR, Walsh SL. A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world. J Addict Med. 2014;8(5):315-326. doi:10.1097/ADM.0000000000000045
40. Wang L, Weiss J, Ryan EB, et al. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021;124:108272. doi:10.1016/ j.jsat.2020.108272
41. Harris MTH, Lambert AM, Maschke AD, et al. “No home to take methadone to”: experiences with addiction services during the COVID-19 pandemic among survivors of opioid overdose in Boston. J Subst Abuse Treat. 2022;135:108655. doi:10.1016/j.jsat.2021.108655
The opioid use disorder (OUD) epidemic is a major public health crisis in the United States.1 Naltrexone, methadone, and buprenorphine are first-line therapies for OUD and have high success rates.2 While studies have shown that naltrexone is effective, patients must achieve opioid detoxification and maintain 7 to 10 days of total abstinence to avoid a precipitated opioid withdrawal before it can be prescribed.3 Methadone does not require detoxification or a period of complete abstinence, but must be prescribed in special clinics and requires daily observed dosing for the first 90 days,4 though these requirements have been relaxed during the COVID-19 pandemic. In contrast, buprenorphine (with or without naloxone) can be used in office-based settings, which significantly improves the accessibility and availability of treatment for patients with OUD. Clinician knowledge and comfort prescribing buprenorphine are limiting factors to treatment.5 Increasing the number of clinicians proficient with buprenorphine management can improve access to effective treatment and recovery services, which is critical for patients with OUD.
Multiple resources are available for clinicians to learn how to prescribe buprenorphine, but clear guidance on laboratory testing for patients receiving buprenorphine is limited. To safely and effectively prescribe buprenorphine, clinicians need to understand its pharmacology (Box 16-9) and how laboratory testing influences treatment. In an effort to increase clinician knowledge of and proficiency with buprenorphine, this article answers 10 common questions about laboratory monitoring of patients receiving this medication.
Box 1
For patients with opioid use disorder, buprenorphine is indicated for opioid detoxification and maintenance. Oral formulations of buprenorphine (including tablets and buccal films) have long durations of action, and when dosed daily can prevent opioid withdrawal for at least 48 hours.6 The recommended formulation is a combination of buprenorphine and naloxone, because this formulation is associated with a lower risk of misuse and diversion compared to formulations containing only buprenorphine.7 However, buprenorphine alone can be effective in patients who experience adverse effects from or are unable to tolerate the combination buprenorphine/naloxone formulation.7 Despite the addition of naloxone, buprenorphine prescriptions may still be misused and diverted, so close monitoring is necessary.
Buprenorphine is metabolized by the cytochrome P450 system (CYP) (primarily CYP3A4) to its active metabolite, norbuprenorphine, both of which are primarily excreted in feces.8 However, small quantities of buprenorphine and norbuprenorphine are excreted in the urine,9 which makes urine specimen the best choice to monitor buprenorphine use for therapeutic purposes.
1. Why is laboratory monitoring important?
Proper laboratory monitoring discourages illicit substance use, encourages medication adherence, and influences treatment modifications. Patient self-reporting on medication compliance may be inaccurate or unreliable.10 Patients who relapse or use other illicit substances may also be reluctant to disclose their substance use.11
On the other hand, laboratory tests are objective markers of treatment outcome and adherence, and can verify a patient’s self-report.12 When used appropriately, laboratory monitoring can be therapeutic. It holds patients accountable, especially when used in conjunction with contingency management or other behavioral therapies.13 Laboratory monitoring is the most reliable method of determining if patients are abstaining from opioids and other illicit substances, or if the treatment plan requires revision.
2. Which tests should I order?
When initiating or maintaining a patient on buprenorphine, order a general urine drug screen (UDS), urine opioid screen (availability varies by institution), urine creatinine levels, urine buprenorphine/norbuprenorphine/naloxone/creatinine levels, urine alcohol metabolite levels, and a urine general toxicology test. It is also recommended to obtain a comprehensive metabolic panel (CMP) before starting buprenorphine,14,15 and to monitor CMP values at least once annually following treatment. Patients with a history of IV drug use or other high-risk factors should also be screened for hepatitis B, hepatitis C, and HIV.14,15
A general UDS can determine if opiates, amphetamines, cocaine, marijuana, or other common illicit substances are present to identify additional substance use. The proficiency of a general UDS may vary depending on the panels used at the respective institution. Some clinics use point-of-care UDS as part of their clinical management; these tests are inexpensive and provide immediate results.16 A basic UDS typically does not detect synthetic opioids due to the specificity of conventional immunoassays. As a result, specific tests for opioids such as oxycodone, hydrocodone, hydromorphone, oxymorphone, fentanyl, and methadone should also be considered, depending on their availability. Though buprenorphine treatment may trigger a positive opiate or other opioid screen,17 buprenorphine adherence should be confirmed using several urine tests, including creatinine, buprenorphine, norbuprenorphine, and naloxone urine levels.
In addition to screening for illicit substances and buprenorphine adherence, it is important to also screen for alcohol. Alcohol use disorder (AUD) is highly comorbid with OUD,18 and is associated with worse OUD treatment outcomes.19 Alcohol use may also affect liver function necessary for buprenorphine metabolism,8 so urine alcohol metabolites such as ethyl glucuronide and ethyl sulfate, serum transaminases, and gamma-glutamyl transferase should also be obtained.
Continue to: How frequently should patients be tested?
3. How frequently should patients be tested?
As part of the initial assessment, it is recommended to order CMP, UDS, and urine general toxicology.14 If indicated, specific laboratory tests such as specific opioid and alcohol metabolites screens can be ordered. After starting buprenorphine, the frequency of monitoring urine laboratory tests—including UDS, general drug toxicology, buprenorphine/norbuprenorphine/naloxone/creatinine, and alcohol and its metabolites—depends on a variety of factors, including a patient’s treatment response and stability as well as availability and cost of the tests. Ultimately, the frequency of laboratory monitoring should be determined on a patient-by-patient basis and clinicians should use their judgment.
The American Society of Addiction Medicine suggests testing more frequently earlier in the course of treatment (eg, weekly or biweekly), then spacing it out over time (eg, monthly or quarterly) as the patient’s recovery progresses.14,15 To conserve resources and reduce spending, some clinicians and guidelines recommend random monitoring as opposed to monitoring at every follow-up visit (eg, once out of every 3 to 5 visits, on average), which allows for longer intervals between testing while ensuring consistency with medication and abstinence from illicit substances.15,16 We suggest screening every 2 weeks for the first month, then spacing out to monthly and quarterly as patients demonstrate stability, with random screening as indicated. Monitoring of liver function should be done at least once annually.
4. How should urine buprenorphine and other results be interpreted?
There are several issues to consider when interpreting laboratory results. The clinician needs to know what to expect in the sample, and what approximate levels should be detected. To check treatment adherence, laboratory data should include stable urine buprenorphine and norbuprenorphine levels and negative urine screening for other illicit substances.14,15 While urine buprenorphine and norbuprenorphine levels have great interindividual variability due to genetic differences in hepatic metabolism, unusually high levels of buprenorphine (≥700 ng/mL) without norbuprenorphine suggests “urine spiking,” where patients put buprenorphine directly into their urine sample.20,21 Abnormally low or undetectable levels raise concern for medication nonadherence or diversion.
Though urine buprenorphine levels do not reliably correlate with dose, because there is typically not much intraindividual variability, patients should have relatively stable levels on each screen once a maintenance dose has been established.22 Furthermore, the buprenorphine-to-norbuprenorphine ratio (ie, “the metabolic ratio”) typically ranges from 1:2 to 1:4 across all individuals,20,21,23 regardless of dose or metabolic rate. Urine naloxone levels, which typically are included in commercial urine buprenorphine laboratory panels, also may aid in identifying tampered urine specimens when buprenorphine-to-norbuprenorphine ratios are abnormal or inconsistent with an individual’s prior ratio. Naloxone is typically (but not always) poorly absorbed and minimally detected in urine specimens.20 A high level of naloxone coupled with unusually high buprenorphine levels, particularly in the absence of norbuprenorphine in the urine, may indicate urine spiking.20,21,23
Urine creatinine is used to establish the reliability of the specimen. When urine creatinine concentration is <20 mg/dL, the concentration of most substances typically falls to subthreshold levels of detection.24 If a UDS is negative and the urine has a creatinine concentration <20 mg/dL, the patient should provide a new sample, because the urine was likely too diluted to detect any substances.
Continue to: The presence of alcohol...
The presence of alcohol metabolites can alert the clinician to recent alcohol use and possible AUD, which should be assessed and treated if indicated.
Liver enzymes should be normal or unchanged with short- and long-term buprenorphine use when taken as prescribed.25,26 However, acute liver injury may occur if patients inject buprenorphine intravenously, especially in those with underlying hepatitis C.25
5. What can cause a false negative result on UDS?
Laboratory monitoring may occasionally yield false negative drug screens. For urine buprenorphine levels, false negatives may occur in patients who are “rapid metabolizers,” infrequent or as-needed usage of the medication, patient mix-up, or laboratory error.27 For other substances, a false negative result may occur if the patient used the substance(s) outside the window of detection. The most common causes of false negative results, however, are overly diluted urine samples (eg, due to rapid water ingestion), or the use of an inappropriate test to measure a specific opioid or substance.27
Many laboratories use conventional immunoassays with morphine antibodies that react with various opioid substrates to determine the presence of a specific opioid. Some opioids—particularly synthetics such as oxycodone, hydrocodone, hydromorphone, oxymorphone, fentanyl, buprenorphine, and methadone—have poor cross-reactivity with the morphine antibody due to their distinct chemical structures, so standard immunoassays used to detect opioids may result in a false negative result.28 In such situations, a discussion with a clinical pathologist familiar with the laboratory detection method can help ensure proper testing. Additional tests for specific opioids should be ordered to more specifically target substances prone to false negative results.27
6. What can cause a false positive result on UDS?
The cross-reactivity of the morphine substrate may also result in a false positive result.28 Other over-the-counter (OTC) or prescription medications that have cross-reactivity with the morphine antibody include dextromethorphan, verapamil, quinine, fluoroquinolones, and rifampin, which can normally be found in urine 2 to 3 days after consumption.17,27 Poppy seeds have long been known to result in positive opiate screens on urine testing, particularly when laboratories use lower cutoff values (eg, 300 ng/mL), so advise patients to avoid consuming poppy seeds.29
Continue to: For other drugs of abuse...
For other drugs of abuse, false positives are typically caused by cross-reactivity with other prescription or OTC medications. Numerous substances cross-react with amphetamines and produce false positive results on amphetamine immunoassays, including amantadine, bupropion, ephedrine, labetalol, phentermine, pseudoephedrine, ranitidine, selegiline, and trazodone.27 Sertraline and efavirenz are known to produce false positive results on benzodiazepine UDS, and ibuprofen, naproxen, and efavirenz can produce false positive results for cannabinoids.27
7. How do I communicate the results to patients?
Effectively communicating test results to patients is just as important as the results themselves. A trusting, therapeutic alliance between patient and clinician is highly predictive of successful treatment,30 and how the clinician communicates affects the strength of this collaboration. A principle of addiction treatment is the use of neutral language when discussing laboratory results.31,32 To avoid unintentional shaming or moral judgment, use words such as “positive” or “negative” rather than stigmatizing terms such as “clean” or “dirty.”33
Additionally, make it clear that laboratory findings are not used to punish patients, but rather to improve treatment.34 Reassuring the patient that a positive screen will not result in withdrawal of care encourages a working relationship.14 All patients who receive buprenorphine treatment should be informed that collecting a UDS is the standard of care used to monitor their progress. You might want to compare using UDS in patients with OUD to monitoring HbA1c levels in patients with diabetes as an example to demonstrate how laboratory values inform treatment.35,36
Before reporting the results, a helpful strategy to maintain the therapeutic alliance in the face of a positive UDS is to ask the patient what they expect their UDS to show. When the patient has been reassured that treatment will not be withdrawn due to a positive result, they may be more likely to fully disclose substance use. This allows them the opportunity to self-disclose rather than be “called out” by the clinician.35
8. What happens when a patient tests positive for drugs of abuse?
If a patient tests positive for opioids or other drugs of abuse, convey this information to them, ideally by asking them what they expect to see on laboratory findings. Patients may have “slip ups” or relapses, or use certain prescription medications for medical reasons with the intention of establishing abstinence. It is essential to convey laboratory findings in a nonjudgmental tone while maintaining a supportive stance with clear boundaries.
Continue to: Though addiction specialists...
Though addiction specialists often advise complete abstinence from all substances, including alcohol, cannabis, and tobacco, the harm-reduction model emphasizes “meeting patients where they are” in terms of continued substance use.37 If a patient can reduce their substance use or abstain from some substances while continuing others, these accomplishments should be acknowledged.
For patients who continue to test positive for illicit substances (>3 instances) without a clear explanation, schedule an appointment to re-educate them about buprenorphine treatment and reassess the patient’s treatment goals. Consider changing the current treatment plan, such as by having more frequent follow-ups, increasing the dose of the buprenorphine for patients whose cravings are not sufficiently suppressed, switching to another medication such as methadone or naltrexone, or referring the patient to a higher level of care, such as intensive outpatient or residential treatment.
9. What should I do if the results indicate abnormal levels of buprenorphine, norbuprenorphine, and naloxone?
When urine buprenorphine, norbuprenorphine, or naloxone levels appear low or the results indicate a likely “spiking,” clarify whether the sample tampering is due to poor adherence or diversion. Similar to dealing with a positive result for substances of abuse, ask the patient what they expect to find in their urine, and discuss the results in a nonjudgmental manner. Patients who admit to difficulty following their medication regimen may require additional psychoeducation and motivational interviewing to identify and address barriers. Strategies to improve adherence include setting an alarm, involving the family, using a pillbox, or simplifying the regimen.38 A long-acting injectable form of buprenorphine is also available.
If you suspect diversion, refer to your clinic’s policy and use other clinical management skills, such as increasing the frequency of visits, random pill counts, and supervised medication administration in the clinic.39 If diversion occurs repetitively and the patient is not appropriate for or benefiting from buprenorphine treatment, it may make sense to terminate treatment and consider other treatment options (such as methadone or residential treatment).39
10. What should I do if a patient disagrees with laboratory findings?
It is common for patients to disagree with laboratory results. Maintaining an attitude of neutrality and allowing the patient to speak and provide explanations is necessary to ensure they feel heard. Explanations patients frequently provide include passive exposure (“I was around someone who was using it”) or accidental ingestion, when a patient reports taking a medication they were not aware was a substance of concern. In a calm and nonjudgmental manner, provide education on what leads to a positive drug screen, including the possibility of false positive findings.
Continue to: Because a screening test...
Because a screening test has high sensitivity and low specificity, false positives may occur.17,27 Therefore, when a result is in dispute, the use of a high-specificity confirmatory test is often needed (many laboratories have reflex confirmatory testing). However, in the case of diluted urine (urine creatinine concentrations <20 mg/dL), patients should be told the findings are physiologically implausible, and a new urine sample should be obtained.24
Goals of laboratory monitoring
Laboratory monitoring, including UDS and urine buprenorphine levels, is a mainstay of treatment for patients with OUD. The increased use of telehealth has affected how laboratory testing is conducted (Box 240,41). The goal of laboratory testing is to influence treatment and improve patient outcomes. Clinical data such as clinician assessment, patient self-reporting, and collateral information provide essential details for patient management. However, laboratory monitoring is often the most reliable and objective source by which to influence treatment.
Box 2
While delivering therapy via telehealth has been shown to decrease the stigma that surrounds treatment, reduce no-show rates, increase retention in care, improve treatment access for patients who have difficulty commuting, and allow for continuity of outpatient treatment during the COVID-19 pandemic, there are also challenges.40,41 Inducing patients on buprenorphine via telehealth, as well as managing complex treatment cases or repeated failed urine drug screen tests, can be especially challenging. However, treatment standards should be followed as much as possible, and laboratory monitoring as clinically indicated should still be used to improve treatment outcomes.
If needed, patients may be directed to community labs for urine screening and should have results sent to their clinicians prior to the telehealth visit. Complex treatment cases (eg, repeat positive opioid screens, or negative urine buprenorphine screens with comorbid psychiatric conditions) should be handled on an individual basis and in-person appointments may be needed. Video assessment is always preferable to telephone. For patients who are unable to use video and have difficulty maintaining negative drug screens, an in-person visit should be requested.
An increased understanding of recommended laboratory monitoring practices may improve your comfort with OUD treatment and motivate more clinicians to offer buprenorphine, a life-saving and disease-modifying treatment for OUD. Doing so would increase access to OUD treatment for patients to reduce the individual and public health risks associated with untreated OUD.
Bottom Line
Laboratory monitoring, particularly urine drug screens and urine buprenorphine levels, is the most reliable source of information in the treatment of patients with opioid use disorder (OUD). An increased understanding of monitoring practices may improve a clinician’s willingness to offer buprenorphine as an option for therapy and their ability to properly treat patients with OUD.
Related Resources
- Li X, Moore S, Olson C. Urine drug tests: how to make the most of them. Current Psychiatry. 2019;18(8):10-18,20.
- Moreno JL, Johnson JL, Peckham AM. Sublingual buprenorphine plus buprenorphine XR for opioid use disorder. Current Psychiatry. 2022;21(6):39-42,49. doi:10.12788/cp.0244
Drug Brand Names
Amantadine • Gocovri
Buprenorphine • Subutex, Sublocade
Bupropion • Wellbutrin, Zyban
Efavirenz • Sustiva
Fentanyl • Actiq
Hydrocodone • Hysingla
Hydromorphone • Dilaudid
Methadone • Methadose
Naloxone • Evzio
Naltrexone • Vivitrol
Oxycodone • Oxycontin
Oxymorphone • Opana
Phentermine • Ionamin
Quinine • Qualaquin
Ranitidine • Zantac
Rifampin • Rifadin
Selegiline • Eldepryl
Sertraline • Zoloft
Trazodone • Oleptro
Verapamil • Verelan
The opioid use disorder (OUD) epidemic is a major public health crisis in the United States.1 Naltrexone, methadone, and buprenorphine are first-line therapies for OUD and have high success rates.2 While studies have shown that naltrexone is effective, patients must achieve opioid detoxification and maintain 7 to 10 days of total abstinence to avoid a precipitated opioid withdrawal before it can be prescribed.3 Methadone does not require detoxification or a period of complete abstinence, but must be prescribed in special clinics and requires daily observed dosing for the first 90 days,4 though these requirements have been relaxed during the COVID-19 pandemic. In contrast, buprenorphine (with or without naloxone) can be used in office-based settings, which significantly improves the accessibility and availability of treatment for patients with OUD. Clinician knowledge and comfort prescribing buprenorphine are limiting factors to treatment.5 Increasing the number of clinicians proficient with buprenorphine management can improve access to effective treatment and recovery services, which is critical for patients with OUD.
Multiple resources are available for clinicians to learn how to prescribe buprenorphine, but clear guidance on laboratory testing for patients receiving buprenorphine is limited. To safely and effectively prescribe buprenorphine, clinicians need to understand its pharmacology (Box 16-9) and how laboratory testing influences treatment. In an effort to increase clinician knowledge of and proficiency with buprenorphine, this article answers 10 common questions about laboratory monitoring of patients receiving this medication.
Box 1
For patients with opioid use disorder, buprenorphine is indicated for opioid detoxification and maintenance. Oral formulations of buprenorphine (including tablets and buccal films) have long durations of action, and when dosed daily can prevent opioid withdrawal for at least 48 hours.6 The recommended formulation is a combination of buprenorphine and naloxone, because this formulation is associated with a lower risk of misuse and diversion compared to formulations containing only buprenorphine.7 However, buprenorphine alone can be effective in patients who experience adverse effects from or are unable to tolerate the combination buprenorphine/naloxone formulation.7 Despite the addition of naloxone, buprenorphine prescriptions may still be misused and diverted, so close monitoring is necessary.
Buprenorphine is metabolized by the cytochrome P450 system (CYP) (primarily CYP3A4) to its active metabolite, norbuprenorphine, both of which are primarily excreted in feces.8 However, small quantities of buprenorphine and norbuprenorphine are excreted in the urine,9 which makes urine specimen the best choice to monitor buprenorphine use for therapeutic purposes.
1. Why is laboratory monitoring important?
Proper laboratory monitoring discourages illicit substance use, encourages medication adherence, and influences treatment modifications. Patient self-reporting on medication compliance may be inaccurate or unreliable.10 Patients who relapse or use other illicit substances may also be reluctant to disclose their substance use.11
On the other hand, laboratory tests are objective markers of treatment outcome and adherence, and can verify a patient’s self-report.12 When used appropriately, laboratory monitoring can be therapeutic. It holds patients accountable, especially when used in conjunction with contingency management or other behavioral therapies.13 Laboratory monitoring is the most reliable method of determining if patients are abstaining from opioids and other illicit substances, or if the treatment plan requires revision.
2. Which tests should I order?
When initiating or maintaining a patient on buprenorphine, order a general urine drug screen (UDS), urine opioid screen (availability varies by institution), urine creatinine levels, urine buprenorphine/norbuprenorphine/naloxone/creatinine levels, urine alcohol metabolite levels, and a urine general toxicology test. It is also recommended to obtain a comprehensive metabolic panel (CMP) before starting buprenorphine,14,15 and to monitor CMP values at least once annually following treatment. Patients with a history of IV drug use or other high-risk factors should also be screened for hepatitis B, hepatitis C, and HIV.14,15
A general UDS can determine if opiates, amphetamines, cocaine, marijuana, or other common illicit substances are present to identify additional substance use. The proficiency of a general UDS may vary depending on the panels used at the respective institution. Some clinics use point-of-care UDS as part of their clinical management; these tests are inexpensive and provide immediate results.16 A basic UDS typically does not detect synthetic opioids due to the specificity of conventional immunoassays. As a result, specific tests for opioids such as oxycodone, hydrocodone, hydromorphone, oxymorphone, fentanyl, and methadone should also be considered, depending on their availability. Though buprenorphine treatment may trigger a positive opiate or other opioid screen,17 buprenorphine adherence should be confirmed using several urine tests, including creatinine, buprenorphine, norbuprenorphine, and naloxone urine levels.
In addition to screening for illicit substances and buprenorphine adherence, it is important to also screen for alcohol. Alcohol use disorder (AUD) is highly comorbid with OUD,18 and is associated with worse OUD treatment outcomes.19 Alcohol use may also affect liver function necessary for buprenorphine metabolism,8 so urine alcohol metabolites such as ethyl glucuronide and ethyl sulfate, serum transaminases, and gamma-glutamyl transferase should also be obtained.
Continue to: How frequently should patients be tested?
3. How frequently should patients be tested?
As part of the initial assessment, it is recommended to order CMP, UDS, and urine general toxicology.14 If indicated, specific laboratory tests such as specific opioid and alcohol metabolites screens can be ordered. After starting buprenorphine, the frequency of monitoring urine laboratory tests—including UDS, general drug toxicology, buprenorphine/norbuprenorphine/naloxone/creatinine, and alcohol and its metabolites—depends on a variety of factors, including a patient’s treatment response and stability as well as availability and cost of the tests. Ultimately, the frequency of laboratory monitoring should be determined on a patient-by-patient basis and clinicians should use their judgment.
The American Society of Addiction Medicine suggests testing more frequently earlier in the course of treatment (eg, weekly or biweekly), then spacing it out over time (eg, monthly or quarterly) as the patient’s recovery progresses.14,15 To conserve resources and reduce spending, some clinicians and guidelines recommend random monitoring as opposed to monitoring at every follow-up visit (eg, once out of every 3 to 5 visits, on average), which allows for longer intervals between testing while ensuring consistency with medication and abstinence from illicit substances.15,16 We suggest screening every 2 weeks for the first month, then spacing out to monthly and quarterly as patients demonstrate stability, with random screening as indicated. Monitoring of liver function should be done at least once annually.
4. How should urine buprenorphine and other results be interpreted?
There are several issues to consider when interpreting laboratory results. The clinician needs to know what to expect in the sample, and what approximate levels should be detected. To check treatment adherence, laboratory data should include stable urine buprenorphine and norbuprenorphine levels and negative urine screening for other illicit substances.14,15 While urine buprenorphine and norbuprenorphine levels have great interindividual variability due to genetic differences in hepatic metabolism, unusually high levels of buprenorphine (≥700 ng/mL) without norbuprenorphine suggests “urine spiking,” where patients put buprenorphine directly into their urine sample.20,21 Abnormally low or undetectable levels raise concern for medication nonadherence or diversion.
Though urine buprenorphine levels do not reliably correlate with dose, because there is typically not much intraindividual variability, patients should have relatively stable levels on each screen once a maintenance dose has been established.22 Furthermore, the buprenorphine-to-norbuprenorphine ratio (ie, “the metabolic ratio”) typically ranges from 1:2 to 1:4 across all individuals,20,21,23 regardless of dose or metabolic rate. Urine naloxone levels, which typically are included in commercial urine buprenorphine laboratory panels, also may aid in identifying tampered urine specimens when buprenorphine-to-norbuprenorphine ratios are abnormal or inconsistent with an individual’s prior ratio. Naloxone is typically (but not always) poorly absorbed and minimally detected in urine specimens.20 A high level of naloxone coupled with unusually high buprenorphine levels, particularly in the absence of norbuprenorphine in the urine, may indicate urine spiking.20,21,23
Urine creatinine is used to establish the reliability of the specimen. When urine creatinine concentration is <20 mg/dL, the concentration of most substances typically falls to subthreshold levels of detection.24 If a UDS is negative and the urine has a creatinine concentration <20 mg/dL, the patient should provide a new sample, because the urine was likely too diluted to detect any substances.
Continue to: The presence of alcohol...
The presence of alcohol metabolites can alert the clinician to recent alcohol use and possible AUD, which should be assessed and treated if indicated.
Liver enzymes should be normal or unchanged with short- and long-term buprenorphine use when taken as prescribed.25,26 However, acute liver injury may occur if patients inject buprenorphine intravenously, especially in those with underlying hepatitis C.25
5. What can cause a false negative result on UDS?
Laboratory monitoring may occasionally yield false negative drug screens. For urine buprenorphine levels, false negatives may occur in patients who are “rapid metabolizers,” infrequent or as-needed usage of the medication, patient mix-up, or laboratory error.27 For other substances, a false negative result may occur if the patient used the substance(s) outside the window of detection. The most common causes of false negative results, however, are overly diluted urine samples (eg, due to rapid water ingestion), or the use of an inappropriate test to measure a specific opioid or substance.27
Many laboratories use conventional immunoassays with morphine antibodies that react with various opioid substrates to determine the presence of a specific opioid. Some opioids—particularly synthetics such as oxycodone, hydrocodone, hydromorphone, oxymorphone, fentanyl, buprenorphine, and methadone—have poor cross-reactivity with the morphine antibody due to their distinct chemical structures, so standard immunoassays used to detect opioids may result in a false negative result.28 In such situations, a discussion with a clinical pathologist familiar with the laboratory detection method can help ensure proper testing. Additional tests for specific opioids should be ordered to more specifically target substances prone to false negative results.27
6. What can cause a false positive result on UDS?
The cross-reactivity of the morphine substrate may also result in a false positive result.28 Other over-the-counter (OTC) or prescription medications that have cross-reactivity with the morphine antibody include dextromethorphan, verapamil, quinine, fluoroquinolones, and rifampin, which can normally be found in urine 2 to 3 days after consumption.17,27 Poppy seeds have long been known to result in positive opiate screens on urine testing, particularly when laboratories use lower cutoff values (eg, 300 ng/mL), so advise patients to avoid consuming poppy seeds.29
Continue to: For other drugs of abuse...
For other drugs of abuse, false positives are typically caused by cross-reactivity with other prescription or OTC medications. Numerous substances cross-react with amphetamines and produce false positive results on amphetamine immunoassays, including amantadine, bupropion, ephedrine, labetalol, phentermine, pseudoephedrine, ranitidine, selegiline, and trazodone.27 Sertraline and efavirenz are known to produce false positive results on benzodiazepine UDS, and ibuprofen, naproxen, and efavirenz can produce false positive results for cannabinoids.27
7. How do I communicate the results to patients?
Effectively communicating test results to patients is just as important as the results themselves. A trusting, therapeutic alliance between patient and clinician is highly predictive of successful treatment,30 and how the clinician communicates affects the strength of this collaboration. A principle of addiction treatment is the use of neutral language when discussing laboratory results.31,32 To avoid unintentional shaming or moral judgment, use words such as “positive” or “negative” rather than stigmatizing terms such as “clean” or “dirty.”33
Additionally, make it clear that laboratory findings are not used to punish patients, but rather to improve treatment.34 Reassuring the patient that a positive screen will not result in withdrawal of care encourages a working relationship.14 All patients who receive buprenorphine treatment should be informed that collecting a UDS is the standard of care used to monitor their progress. You might want to compare using UDS in patients with OUD to monitoring HbA1c levels in patients with diabetes as an example to demonstrate how laboratory values inform treatment.35,36
Before reporting the results, a helpful strategy to maintain the therapeutic alliance in the face of a positive UDS is to ask the patient what they expect their UDS to show. When the patient has been reassured that treatment will not be withdrawn due to a positive result, they may be more likely to fully disclose substance use. This allows them the opportunity to self-disclose rather than be “called out” by the clinician.35
8. What happens when a patient tests positive for drugs of abuse?
If a patient tests positive for opioids or other drugs of abuse, convey this information to them, ideally by asking them what they expect to see on laboratory findings. Patients may have “slip ups” or relapses, or use certain prescription medications for medical reasons with the intention of establishing abstinence. It is essential to convey laboratory findings in a nonjudgmental tone while maintaining a supportive stance with clear boundaries.
Continue to: Though addiction specialists...
Though addiction specialists often advise complete abstinence from all substances, including alcohol, cannabis, and tobacco, the harm-reduction model emphasizes “meeting patients where they are” in terms of continued substance use.37 If a patient can reduce their substance use or abstain from some substances while continuing others, these accomplishments should be acknowledged.
For patients who continue to test positive for illicit substances (>3 instances) without a clear explanation, schedule an appointment to re-educate them about buprenorphine treatment and reassess the patient’s treatment goals. Consider changing the current treatment plan, such as by having more frequent follow-ups, increasing the dose of the buprenorphine for patients whose cravings are not sufficiently suppressed, switching to another medication such as methadone or naltrexone, or referring the patient to a higher level of care, such as intensive outpatient or residential treatment.
9. What should I do if the results indicate abnormal levels of buprenorphine, norbuprenorphine, and naloxone?
When urine buprenorphine, norbuprenorphine, or naloxone levels appear low or the results indicate a likely “spiking,” clarify whether the sample tampering is due to poor adherence or diversion. Similar to dealing with a positive result for substances of abuse, ask the patient what they expect to find in their urine, and discuss the results in a nonjudgmental manner. Patients who admit to difficulty following their medication regimen may require additional psychoeducation and motivational interviewing to identify and address barriers. Strategies to improve adherence include setting an alarm, involving the family, using a pillbox, or simplifying the regimen.38 A long-acting injectable form of buprenorphine is also available.
If you suspect diversion, refer to your clinic’s policy and use other clinical management skills, such as increasing the frequency of visits, random pill counts, and supervised medication administration in the clinic.39 If diversion occurs repetitively and the patient is not appropriate for or benefiting from buprenorphine treatment, it may make sense to terminate treatment and consider other treatment options (such as methadone or residential treatment).39
10. What should I do if a patient disagrees with laboratory findings?
It is common for patients to disagree with laboratory results. Maintaining an attitude of neutrality and allowing the patient to speak and provide explanations is necessary to ensure they feel heard. Explanations patients frequently provide include passive exposure (“I was around someone who was using it”) or accidental ingestion, when a patient reports taking a medication they were not aware was a substance of concern. In a calm and nonjudgmental manner, provide education on what leads to a positive drug screen, including the possibility of false positive findings.
Continue to: Because a screening test...
Because a screening test has high sensitivity and low specificity, false positives may occur.17,27 Therefore, when a result is in dispute, the use of a high-specificity confirmatory test is often needed (many laboratories have reflex confirmatory testing). However, in the case of diluted urine (urine creatinine concentrations <20 mg/dL), patients should be told the findings are physiologically implausible, and a new urine sample should be obtained.24
Goals of laboratory monitoring
Laboratory monitoring, including UDS and urine buprenorphine levels, is a mainstay of treatment for patients with OUD. The increased use of telehealth has affected how laboratory testing is conducted (Box 240,41). The goal of laboratory testing is to influence treatment and improve patient outcomes. Clinical data such as clinician assessment, patient self-reporting, and collateral information provide essential details for patient management. However, laboratory monitoring is often the most reliable and objective source by which to influence treatment.
Box 2
While delivering therapy via telehealth has been shown to decrease the stigma that surrounds treatment, reduce no-show rates, increase retention in care, improve treatment access for patients who have difficulty commuting, and allow for continuity of outpatient treatment during the COVID-19 pandemic, there are also challenges.40,41 Inducing patients on buprenorphine via telehealth, as well as managing complex treatment cases or repeated failed urine drug screen tests, can be especially challenging. However, treatment standards should be followed as much as possible, and laboratory monitoring as clinically indicated should still be used to improve treatment outcomes.
If needed, patients may be directed to community labs for urine screening and should have results sent to their clinicians prior to the telehealth visit. Complex treatment cases (eg, repeat positive opioid screens, or negative urine buprenorphine screens with comorbid psychiatric conditions) should be handled on an individual basis and in-person appointments may be needed. Video assessment is always preferable to telephone. For patients who are unable to use video and have difficulty maintaining negative drug screens, an in-person visit should be requested.
An increased understanding of recommended laboratory monitoring practices may improve your comfort with OUD treatment and motivate more clinicians to offer buprenorphine, a life-saving and disease-modifying treatment for OUD. Doing so would increase access to OUD treatment for patients to reduce the individual and public health risks associated with untreated OUD.
Bottom Line
Laboratory monitoring, particularly urine drug screens and urine buprenorphine levels, is the most reliable source of information in the treatment of patients with opioid use disorder (OUD). An increased understanding of monitoring practices may improve a clinician’s willingness to offer buprenorphine as an option for therapy and their ability to properly treat patients with OUD.
Related Resources
- Li X, Moore S, Olson C. Urine drug tests: how to make the most of them. Current Psychiatry. 2019;18(8):10-18,20.
- Moreno JL, Johnson JL, Peckham AM. Sublingual buprenorphine plus buprenorphine XR for opioid use disorder. Current Psychiatry. 2022;21(6):39-42,49. doi:10.12788/cp.0244
Drug Brand Names
Amantadine • Gocovri
Buprenorphine • Subutex, Sublocade
Bupropion • Wellbutrin, Zyban
Efavirenz • Sustiva
Fentanyl • Actiq
Hydrocodone • Hysingla
Hydromorphone • Dilaudid
Methadone • Methadose
Naloxone • Evzio
Naltrexone • Vivitrol
Oxycodone • Oxycontin
Oxymorphone • Opana
Phentermine • Ionamin
Quinine • Qualaquin
Ranitidine • Zantac
Rifampin • Rifadin
Selegiline • Eldepryl
Sertraline • Zoloft
Trazodone • Oleptro
Verapamil • Verelan
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. HHS Publication PEP19-5068, NSDUH Series H-54. May 2019. https://www.samhsa.gov/data/
2. Volkow ND, Frieden TR, Hyde PS, et al. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063-2066. doi:10.1056/NEJMp1402780
3. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391(10118):309-318. doi:10.1016/S0140-6736(17)32812-X
4. Sharma A, Kelly SM, Mitchell SG, et al. Update on barriers to pharmacotherapy for opioid use disorders. Curr Psychiatry Rep. 2017;19(6):35. doi:10.1007/s11920-017-0783-9
5. DeFlavio JR, Rolin SA, Nordstrom BR, et al. Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural Remote Health. 2015;15:3019. doi:10.22605/rrh3019
6. Kuhlman JJ Jr, Lalani S, Magluiolo J Jr, et al. Human pharmacokinetics of intravenous, sublingual, and buccal buprenorphine. J Anal Toxicol. 1996;20(6):369-378.
7. Fudala PJ, Bridge TP, Herbert S, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. N Engl J Med. 2003;349(10):949-958. doi:10.1056/NEJMoa022164
8. Brown SM, Holtzman M, Kim T, et al. Buprenorphine metabolites, buprenorphine-3-glucuronide and norbuprenorphine-3-glucuronide, are biologically active. Anesthesiology. 2011;115(6):1251-1260. doi:10.1097/ALN.0b013e318238fea0
9. Cone EJ, Gorodetzky CW, Yousefnejad D, et al. The metabolism and excretion of buprenorphine in humans. Drug Metab Dispos. 1984;12(5):577-581.
10. Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470-482. doi:10.1007/s13142-015-0315-2
11. Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction. 2000;95 Suppl 3:S347-S360. doi:10.1080/09652140020004278
12. Preston KL, Silverman K, Schuster CR, et al. Comparison of self-reported drug use with quantitative and qualitative urinalysis for assessment of drug use in treatment studies. NIDA Res Monogr. 1997;167:130-145.
13. Knezevic NN, Khan OM, Beiranvand A, et al. Repeated quantitative urine toxicology analysis may improve chronic pain patient compliance with opioid therapy. Pain Physician. 2017;20(2S):S135-S145. doi:10.36076/ppj.2017.s145
14. Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367.
15. The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med. 2020;14(2S Suppl 1):1-91. doi:10.1097/ADM.0000000000000633
16. McDonell MG, Graves MC, West II, et al. Utility of point-of-care urine drug tests in the treatment of primary care patients with drug use disorders. J Addict Med. 2016;10(3):196-201. doi:10.1097/ADM.0000000000000220
17. Algren DA, Christian MR. Buyer beware: pitfalls in toxicology laboratory testing. Mo Med. 2015;112(3):206-210.
18. Hartzler B, Donovan DM, Huang Z. Comparison of opiate-primary treatment seekers with and without alcohol use disorder. J Subst Abuse Treat. 2010;39(2):114-123. doi:10.1016/j.jsat.2010.05.008
19. Stapleton RD, Comiskey CM. Alcohol usage and associated treatment outcomes for opiate users entering treatment in Ireland. Drug Alcohol Depend. 2010;107(1):56-61. doi:10.1016/j.drugalcdep.2009.09.007
20. Warrington JS, Warrington GS, Francis-Fath S, et al. Urinary buprenorphine, norbuprenorphine and naloxone concentrations and ratios: review and potential clinical implications. J Addict Med. 2020;14(6):e344-e349. doi:10.1097/ADM.0000000000000676
21. Donroe JH, Holt SR, O’Connor PG, et al. Interpreting quantitative urine buprenorphine and norbuprenorphine levels in office-based clinical practice. Drug Alcohol Depend. 2017;180:46-51. doi:10.1016/j.drugalcdep.2017.07.040
22. Bai SA, Xiang Q, Finn A. Evaluation of the pharmacokinetics of single- and multiple-dose buprenorphine buccal film in healthy volunteers. Clin Ther. 2016;38(2):358-369. doi:10.1016/j.clinthera.2015.12.016
23. Suzuki J, Zinser J, Issa M, et al. Quantitative testing of buprenorphine and norbuprenorphine to identify urine sample spiking during office-based opioid treatment. Subst Abus. 2017;38(4):504-507. doi:10.1080/08897077.2017.1356796
24. Gowans EM, Fraser CG. Biological variation of serum and urine creatinine and creatinine clearance: ramifications for interpretation of results and patient care. Ann Clin Biochem. 1988;25( Pt 3):259-263. doi:10.1177/000456328802500312
25. Saxon AJ, Ling W, Hillhouse M, et al. Buprenorphine/naloxone and methadone effects on laboratory indices of liver health: a randomized trial. Drug Alcohol Depend. 2013;128(1-2):71-76. doi:10.1016/j.drugalcdep.2012.08.002
26. Fareed A, Eilender P, Ketchen B, et al. Factors affecting noncompliance with buprenorphine maintenance treatment. J Addict Med. 2014;8(5):345-350. doi:10.1097/ADM.0000000000000057
27. Moeller KE, Lee KC, Kissack JC. Urine drug screening: practical guide for clinicians. Mayo Clin Proc. 2008;83(1):66-76. doi:10.4065/83.1.66
28. Keary CJ, Wang Y, Moran JR, et al. Toxicologic testing for opiates: understanding false-positive and false-negative test results. Prim Care Companion CNS Disord. 2012;14(4).PCC.12f01371 doi:10.4088/PCC.12f01371
29. Zebelman AM, Troyer BL, Randall GL, et al. Detection of morphine and codeine following consumption of poppy seeds. J Anal Toxicol. 1987;11(3):131-132. doi:10.1093/jat/11.3.131
30. Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: a critical review of the literature. Addiction. 2005;100(3):304-316. doi:10.1111/j.1360-0443.2004.00935.x
31. Kelly JF, Saitz R, Wakeman S. Language, substance use disorders, and policy: the need to reach consensus on an “addiction-ary.” Alcohol Treat Q. 2016;34(1):116-123. doi:10.1080/07347324.2016.1113103
32. Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus. 2014;35(3):217-221. doi:10.1080/08897077.2014.930372
33. Kelly JF, Wakeman SE, Saitz R. Stop talking ‘dirty’: clinicians, language, and quality of care for the leading cause of preventable death in the United States. Am J Med. 2015;128(1):8-9. doi:10.1016/j.amjmed.2014.07.043
34. Jarvis M, Williams J, Hurford M, et al. Appropriate use of drug testing in clinical addiction medicine. J Addict Med. 2017;11(3):163-173. doi:10.1097/ADM.0000000000000323
35. Martin SA, Chiodo LM, Bosse JD, et al. The next stage of buprenorphine care for opioid use disorder. Ann Intern Med. 2018;169(9):628-635. doi:10.7326/M18-1652
36. Katz N, Fanciullo GJ. Role of urine toxicology testing in the management of chronic opioid therapy. Clin J Pain. 2002;18(4 Suppl):S76-S82.
37. Klein A. Harm reduction works: evidence and inclusion in drug policy and advocacy. Health Care Anal. 2020;28(4):404-414. doi:10.1007/s10728-020-00406-w
38. Patel MX, David AS. Medication adherence: predictive factors and enhancement strategies. Psychiatry. 2007;6(9):357-361. doi:10.1016/j.mppsy.2007.06.003
39. Lofwall MR, Walsh SL. A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world. J Addict Med. 2014;8(5):315-326. doi:10.1097/ADM.0000000000000045
40. Wang L, Weiss J, Ryan EB, et al. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021;124:108272. doi:10.1016/ j.jsat.2020.108272
41. Harris MTH, Lambert AM, Maschke AD, et al. “No home to take methadone to”: experiences with addiction services during the COVID-19 pandemic among survivors of opioid overdose in Boston. J Subst Abuse Treat. 2022;135:108655. doi:10.1016/j.jsat.2021.108655
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. HHS Publication PEP19-5068, NSDUH Series H-54. May 2019. https://www.samhsa.gov/data/
2. Volkow ND, Frieden TR, Hyde PS, et al. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063-2066. doi:10.1056/NEJMp1402780
3. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391(10118):309-318. doi:10.1016/S0140-6736(17)32812-X
4. Sharma A, Kelly SM, Mitchell SG, et al. Update on barriers to pharmacotherapy for opioid use disorders. Curr Psychiatry Rep. 2017;19(6):35. doi:10.1007/s11920-017-0783-9
5. DeFlavio JR, Rolin SA, Nordstrom BR, et al. Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural Remote Health. 2015;15:3019. doi:10.22605/rrh3019
6. Kuhlman JJ Jr, Lalani S, Magluiolo J Jr, et al. Human pharmacokinetics of intravenous, sublingual, and buccal buprenorphine. J Anal Toxicol. 1996;20(6):369-378.
7. Fudala PJ, Bridge TP, Herbert S, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. N Engl J Med. 2003;349(10):949-958. doi:10.1056/NEJMoa022164
8. Brown SM, Holtzman M, Kim T, et al. Buprenorphine metabolites, buprenorphine-3-glucuronide and norbuprenorphine-3-glucuronide, are biologically active. Anesthesiology. 2011;115(6):1251-1260. doi:10.1097/ALN.0b013e318238fea0
9. Cone EJ, Gorodetzky CW, Yousefnejad D, et al. The metabolism and excretion of buprenorphine in humans. Drug Metab Dispos. 1984;12(5):577-581.
10. Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470-482. doi:10.1007/s13142-015-0315-2
11. Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction. 2000;95 Suppl 3:S347-S360. doi:10.1080/09652140020004278
12. Preston KL, Silverman K, Schuster CR, et al. Comparison of self-reported drug use with quantitative and qualitative urinalysis for assessment of drug use in treatment studies. NIDA Res Monogr. 1997;167:130-145.
13. Knezevic NN, Khan OM, Beiranvand A, et al. Repeated quantitative urine toxicology analysis may improve chronic pain patient compliance with opioid therapy. Pain Physician. 2017;20(2S):S135-S145. doi:10.36076/ppj.2017.s145
14. Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367.
15. The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med. 2020;14(2S Suppl 1):1-91. doi:10.1097/ADM.0000000000000633
16. McDonell MG, Graves MC, West II, et al. Utility of point-of-care urine drug tests in the treatment of primary care patients with drug use disorders. J Addict Med. 2016;10(3):196-201. doi:10.1097/ADM.0000000000000220
17. Algren DA, Christian MR. Buyer beware: pitfalls in toxicology laboratory testing. Mo Med. 2015;112(3):206-210.
18. Hartzler B, Donovan DM, Huang Z. Comparison of opiate-primary treatment seekers with and without alcohol use disorder. J Subst Abuse Treat. 2010;39(2):114-123. doi:10.1016/j.jsat.2010.05.008
19. Stapleton RD, Comiskey CM. Alcohol usage and associated treatment outcomes for opiate users entering treatment in Ireland. Drug Alcohol Depend. 2010;107(1):56-61. doi:10.1016/j.drugalcdep.2009.09.007
20. Warrington JS, Warrington GS, Francis-Fath S, et al. Urinary buprenorphine, norbuprenorphine and naloxone concentrations and ratios: review and potential clinical implications. J Addict Med. 2020;14(6):e344-e349. doi:10.1097/ADM.0000000000000676
21. Donroe JH, Holt SR, O’Connor PG, et al. Interpreting quantitative urine buprenorphine and norbuprenorphine levels in office-based clinical practice. Drug Alcohol Depend. 2017;180:46-51. doi:10.1016/j.drugalcdep.2017.07.040
22. Bai SA, Xiang Q, Finn A. Evaluation of the pharmacokinetics of single- and multiple-dose buprenorphine buccal film in healthy volunteers. Clin Ther. 2016;38(2):358-369. doi:10.1016/j.clinthera.2015.12.016
23. Suzuki J, Zinser J, Issa M, et al. Quantitative testing of buprenorphine and norbuprenorphine to identify urine sample spiking during office-based opioid treatment. Subst Abus. 2017;38(4):504-507. doi:10.1080/08897077.2017.1356796
24. Gowans EM, Fraser CG. Biological variation of serum and urine creatinine and creatinine clearance: ramifications for interpretation of results and patient care. Ann Clin Biochem. 1988;25( Pt 3):259-263. doi:10.1177/000456328802500312
25. Saxon AJ, Ling W, Hillhouse M, et al. Buprenorphine/naloxone and methadone effects on laboratory indices of liver health: a randomized trial. Drug Alcohol Depend. 2013;128(1-2):71-76. doi:10.1016/j.drugalcdep.2012.08.002
26. Fareed A, Eilender P, Ketchen B, et al. Factors affecting noncompliance with buprenorphine maintenance treatment. J Addict Med. 2014;8(5):345-350. doi:10.1097/ADM.0000000000000057
27. Moeller KE, Lee KC, Kissack JC. Urine drug screening: practical guide for clinicians. Mayo Clin Proc. 2008;83(1):66-76. doi:10.4065/83.1.66
28. Keary CJ, Wang Y, Moran JR, et al. Toxicologic testing for opiates: understanding false-positive and false-negative test results. Prim Care Companion CNS Disord. 2012;14(4).PCC.12f01371 doi:10.4088/PCC.12f01371
29. Zebelman AM, Troyer BL, Randall GL, et al. Detection of morphine and codeine following consumption of poppy seeds. J Anal Toxicol. 1987;11(3):131-132. doi:10.1093/jat/11.3.131
30. Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: a critical review of the literature. Addiction. 2005;100(3):304-316. doi:10.1111/j.1360-0443.2004.00935.x
31. Kelly JF, Saitz R, Wakeman S. Language, substance use disorders, and policy: the need to reach consensus on an “addiction-ary.” Alcohol Treat Q. 2016;34(1):116-123. doi:10.1080/07347324.2016.1113103
32. Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus. 2014;35(3):217-221. doi:10.1080/08897077.2014.930372
33. Kelly JF, Wakeman SE, Saitz R. Stop talking ‘dirty’: clinicians, language, and quality of care for the leading cause of preventable death in the United States. Am J Med. 2015;128(1):8-9. doi:10.1016/j.amjmed.2014.07.043
34. Jarvis M, Williams J, Hurford M, et al. Appropriate use of drug testing in clinical addiction medicine. J Addict Med. 2017;11(3):163-173. doi:10.1097/ADM.0000000000000323
35. Martin SA, Chiodo LM, Bosse JD, et al. The next stage of buprenorphine care for opioid use disorder. Ann Intern Med. 2018;169(9):628-635. doi:10.7326/M18-1652
36. Katz N, Fanciullo GJ. Role of urine toxicology testing in the management of chronic opioid therapy. Clin J Pain. 2002;18(4 Suppl):S76-S82.
37. Klein A. Harm reduction works: evidence and inclusion in drug policy and advocacy. Health Care Anal. 2020;28(4):404-414. doi:10.1007/s10728-020-00406-w
38. Patel MX, David AS. Medication adherence: predictive factors and enhancement strategies. Psychiatry. 2007;6(9):357-361. doi:10.1016/j.mppsy.2007.06.003
39. Lofwall MR, Walsh SL. A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world. J Addict Med. 2014;8(5):315-326. doi:10.1097/ADM.0000000000000045
40. Wang L, Weiss J, Ryan EB, et al. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021;124:108272. doi:10.1016/ j.jsat.2020.108272
41. Harris MTH, Lambert AM, Maschke AD, et al. “No home to take methadone to”: experiences with addiction services during the COVID-19 pandemic among survivors of opioid overdose in Boston. J Subst Abuse Treat. 2022;135:108655. doi:10.1016/j.jsat.2021.108655








