User login
Merino wool clothing improves atopic dermatitis, studies find
Conventional wisdom holds that Joseph F. Fowler, Jr., MD, said at MedscapeLive’s annual Las Vegas Dermatology Seminar, held virtually.
“We’ve always though that wool is bad in atopics, right? Indeed, rough wool might be. But fine wool garments can actually improve atopic dermatitis, probably because wool is the most breathable fabric and has the best temperature regulation qualities of any fabric we can wear,” said Dr. Fowler, a dermatologist at the University of Louisville (Ky).
He was first author of a randomized, 12-week, crossover, assessor-blinded clinical trial which showed precisely that. And a second, similarly designed study, this one conducted in Australia, also concluded that fine merino wool assists in the management of AD.
The study by Dr. Fowler and coinvestigators included 50 children and adults with mild or moderate AD who either wore top-and-bottom base layer merino wool ensembles for 6 weeks and then switched to their regular nonwoolen clothing, or vice versa. The mean Eczema Area and Severity Index (EASI) score in those initially randomized to merino wool improved from a mean baseline of 4.5 to 1.7 at week 6, a significantly greater improvement than in the group wearing their regular clothing. Similarly, those who switched to merino wool after 6 weeks experienced a significant decrease in EASI scores from that point on to week 12, while those who switched from merino wool to their regular clothing did not.
Mean Dermatology Life Quality Index (DLQI) scores in patients who wore merino wool first improved from 6.9 at baseline to 3.4 at week 6. Those who wore their regular clothing first went from a mean baseline DLQI of 6.7 to 6.2 at week 6 – a nonsignificant change – but then improved to a week 12 mean DLQI of 3.7 while wearing wool. There was no improvement in DLQI scores while participants were wearing their regular clothing.
Static Investigator’s Global Assessment scores showed significantly greater improvement while patients wore merino wool garments than their regular clothing.
The Australian study included 39 patients with mild to moderate AD aged between 4 weeks and 3 years. This, too, was a 12-week, randomized, crossover, assessor-blinded clinical trial. Participating children wore merino wool for 6 weeks and cotton ensembles chosen by their parents for an equal time. The primary endpoint was change in the SCORing Atopic Dermatitis (SCORAD) index after each 6-week period. The mean 7.6-point greater SCORAD reduction at 6 weeks while wearing merino wool, compared with cotton, was “a pretty impressive reduction,” Dr. Fowler observed.
Reductions in the secondary endpoints of Atopic Dermatitis Severity Index and Infants’ Dermatitis Quality of Life Index while wearing merino wool followed suit. In contrast, switching from wool to cotton resulted in an increase in both scores. Also, use of topical corticosteroids was significantly reduced while patients wore merino wool.
Wool harvested from merino sheep is characterized by fine-diameter fibers. In Dr. Fowler’s study the mean fiber diameter was 17.5 mcm. This makes for a soft fabric with outstanding moisture absorbance capacity, a quality that’s beneficial in patients with AD, since their lesional skin loses the ability to regulate moisture, the dermatologist explained.
Both randomized trials were funded by Australian Wool Innovation and the Australian government.
MedscapeLive and this news organization are owned by the same parent company.
Conventional wisdom holds that Joseph F. Fowler, Jr., MD, said at MedscapeLive’s annual Las Vegas Dermatology Seminar, held virtually.
“We’ve always though that wool is bad in atopics, right? Indeed, rough wool might be. But fine wool garments can actually improve atopic dermatitis, probably because wool is the most breathable fabric and has the best temperature regulation qualities of any fabric we can wear,” said Dr. Fowler, a dermatologist at the University of Louisville (Ky).
He was first author of a randomized, 12-week, crossover, assessor-blinded clinical trial which showed precisely that. And a second, similarly designed study, this one conducted in Australia, also concluded that fine merino wool assists in the management of AD.
The study by Dr. Fowler and coinvestigators included 50 children and adults with mild or moderate AD who either wore top-and-bottom base layer merino wool ensembles for 6 weeks and then switched to their regular nonwoolen clothing, or vice versa. The mean Eczema Area and Severity Index (EASI) score in those initially randomized to merino wool improved from a mean baseline of 4.5 to 1.7 at week 6, a significantly greater improvement than in the group wearing their regular clothing. Similarly, those who switched to merino wool after 6 weeks experienced a significant decrease in EASI scores from that point on to week 12, while those who switched from merino wool to their regular clothing did not.
Mean Dermatology Life Quality Index (DLQI) scores in patients who wore merino wool first improved from 6.9 at baseline to 3.4 at week 6. Those who wore their regular clothing first went from a mean baseline DLQI of 6.7 to 6.2 at week 6 – a nonsignificant change – but then improved to a week 12 mean DLQI of 3.7 while wearing wool. There was no improvement in DLQI scores while participants were wearing their regular clothing.
Static Investigator’s Global Assessment scores showed significantly greater improvement while patients wore merino wool garments than their regular clothing.
The Australian study included 39 patients with mild to moderate AD aged between 4 weeks and 3 years. This, too, was a 12-week, randomized, crossover, assessor-blinded clinical trial. Participating children wore merino wool for 6 weeks and cotton ensembles chosen by their parents for an equal time. The primary endpoint was change in the SCORing Atopic Dermatitis (SCORAD) index after each 6-week period. The mean 7.6-point greater SCORAD reduction at 6 weeks while wearing merino wool, compared with cotton, was “a pretty impressive reduction,” Dr. Fowler observed.
Reductions in the secondary endpoints of Atopic Dermatitis Severity Index and Infants’ Dermatitis Quality of Life Index while wearing merino wool followed suit. In contrast, switching from wool to cotton resulted in an increase in both scores. Also, use of topical corticosteroids was significantly reduced while patients wore merino wool.
Wool harvested from merino sheep is characterized by fine-diameter fibers. In Dr. Fowler’s study the mean fiber diameter was 17.5 mcm. This makes for a soft fabric with outstanding moisture absorbance capacity, a quality that’s beneficial in patients with AD, since their lesional skin loses the ability to regulate moisture, the dermatologist explained.
Both randomized trials were funded by Australian Wool Innovation and the Australian government.
MedscapeLive and this news organization are owned by the same parent company.
Conventional wisdom holds that Joseph F. Fowler, Jr., MD, said at MedscapeLive’s annual Las Vegas Dermatology Seminar, held virtually.
“We’ve always though that wool is bad in atopics, right? Indeed, rough wool might be. But fine wool garments can actually improve atopic dermatitis, probably because wool is the most breathable fabric and has the best temperature regulation qualities of any fabric we can wear,” said Dr. Fowler, a dermatologist at the University of Louisville (Ky).
He was first author of a randomized, 12-week, crossover, assessor-blinded clinical trial which showed precisely that. And a second, similarly designed study, this one conducted in Australia, also concluded that fine merino wool assists in the management of AD.
The study by Dr. Fowler and coinvestigators included 50 children and adults with mild or moderate AD who either wore top-and-bottom base layer merino wool ensembles for 6 weeks and then switched to their regular nonwoolen clothing, or vice versa. The mean Eczema Area and Severity Index (EASI) score in those initially randomized to merino wool improved from a mean baseline of 4.5 to 1.7 at week 6, a significantly greater improvement than in the group wearing their regular clothing. Similarly, those who switched to merino wool after 6 weeks experienced a significant decrease in EASI scores from that point on to week 12, while those who switched from merino wool to their regular clothing did not.
Mean Dermatology Life Quality Index (DLQI) scores in patients who wore merino wool first improved from 6.9 at baseline to 3.4 at week 6. Those who wore their regular clothing first went from a mean baseline DLQI of 6.7 to 6.2 at week 6 – a nonsignificant change – but then improved to a week 12 mean DLQI of 3.7 while wearing wool. There was no improvement in DLQI scores while participants were wearing their regular clothing.
Static Investigator’s Global Assessment scores showed significantly greater improvement while patients wore merino wool garments than their regular clothing.
The Australian study included 39 patients with mild to moderate AD aged between 4 weeks and 3 years. This, too, was a 12-week, randomized, crossover, assessor-blinded clinical trial. Participating children wore merino wool for 6 weeks and cotton ensembles chosen by their parents for an equal time. The primary endpoint was change in the SCORing Atopic Dermatitis (SCORAD) index after each 6-week period. The mean 7.6-point greater SCORAD reduction at 6 weeks while wearing merino wool, compared with cotton, was “a pretty impressive reduction,” Dr. Fowler observed.
Reductions in the secondary endpoints of Atopic Dermatitis Severity Index and Infants’ Dermatitis Quality of Life Index while wearing merino wool followed suit. In contrast, switching from wool to cotton resulted in an increase in both scores. Also, use of topical corticosteroids was significantly reduced while patients wore merino wool.
Wool harvested from merino sheep is characterized by fine-diameter fibers. In Dr. Fowler’s study the mean fiber diameter was 17.5 mcm. This makes for a soft fabric with outstanding moisture absorbance capacity, a quality that’s beneficial in patients with AD, since their lesional skin loses the ability to regulate moisture, the dermatologist explained.
Both randomized trials were funded by Australian Wool Innovation and the Australian government.
MedscapeLive and this news organization are owned by the same parent company.
FROM MEDSCAPELIVE LAS VEGAS DERMATOLOGY SEMINAR
‘Uptake is only the first step’ for effective HIV PrEP protection
To Amanda Allmacher, DNP, RN, nurse practitioner at the Detroit Public Health STD Clinic, that means that same-day PrEP prescribing works and is acceptable. But there’s more work to do on the clinic and pharmacy side to make HIV protection a reality for most of her patients. Allmacher presented her data at the Association of Nurses in AIDS Care 2020 virtual annual meeting.
Dawn K. Smith, MD, epidemiologist and medical officer in the Division of HIV/AIDS Prevention at the Centers for Disease Control and Prevention’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said this adds to other data to show that we’re now entering the next phase of PrEP implementation.
“Our original focus was on uptake — informing folks what PrEP is, why they might benefit from its use, and then prescribing it if accepted,” Smith told Medscape Medical News via email. “Whether standard or same-day [PrEP prescribing], it is clear that uptake is only the first step.”
Nurses help navigate
Patients who attended the Detroit Public Health STD Clinic are more likely to be younger, have no insurance, and otherwise “have little to no contact with the healthcare system,” Allmacher said in her presentation. They also tend to come from communities that bear the greatest burden of HIV in the US — in other words, they are often the people most missed in PrEP rollouts thus far.
In response, the clinic implemented a same-day PrEP protocol, in which registered nurses trained in HIV risk assessment identify clients who might most benefit from PrEP. Criteria often include the presence of other STIs. Once the nurse explains what PrEP is and how it works, if the patient is interested, clients meet with a nurse practitioner right then to get the prescription for PrEP. The clinic also does labs to rule out current HIV infection, hepatitis B, metabolic issues, and other STI screening.
But it doesn’t stop there. The clinic used grant funding to offer PrEP navigation and financial counseling services, which help clients navigate the sometimes-thorny process of paying for PrEP. Payment comes either through Medicaid, which in Michigan charges $3 a month for a PrEP prescription, through patient assistance programs, or through private insurance. With clients under age 18 who are interested in PrEP, the clinic works to find a way to access PrEP without having to inform their parents. These same navigators schedule follow-up appointments, offer appointment reminders, and contact clients when they miss an appointment.
“Our navigators and financial counselors are a huge support for our same-day PrEP starts, helping with financial assistance, prior authorization, navigating different plans, and helping patients apply for Medicaid when appropriate,” she said.
The clinic also offers community outreach and incentives, which can include gift cards, bus passes, and pill containers, among other things.
This was a key lesson in setting up the program, Allmacher told Medscape Medical News.
“Starting PrEP at that initial visit allows for clinicians to meet patients where they are and administer care in a more equitable manner,” Allmacher said via email. “Use all available resources and funding sources. We have a versatile team working together to increase access for patients and promote HIV prevention and risk reduction.”
Script vs. follow-up
This approach is common, used in places like New York City and San Francisco. So once it was set up Allmacher sat back and waited to see how the program helped clients protect themselves from HIV.
Of the 451 clients eligible for PrEP in 2019, 336 were gay and bisexual men, 6 were transgender women, 61 were heterosexual, cisgender men, and 48 were cisgender women. One transgender man also screened as eligible. Allmacher did not break down data by race.
Uptake was high: 70% of all eligible clients did receive a prescription for PrEP, either generic tenofovir disoproxil fumarate/emtricitabine (Truvada) or tenofovir alafenamide/emtricitabine (Descovy). And uptake was high among people most at risk: 80% of gay and bisexual men who were eligible got a prescription, 60% of eligible cisgender women, 50% of the small number of transgender women, and 32.7% of heterosexual cisgender men did as well. The 1 transgender man also received a prescription.
This is a higher rate than found in a recent PrEP demonstration project, which found that despite gay and bisexual men, transgender adults, and Black people having the highest risk for HIV in the US, state health departments were more likely to refer heterosexual adults for PrEP.
That high uptake rate is encouraging, but follow-up? Not so much. After initial intake, clients are meant to return in a month to double-check their labs, ask about side effects, and start their 90-day supply of the medication. But just 40% showed up for their 30-day appointment, Allmacher said. And only one third of those showed up for the follow-up in 90 days.
By the end of 2019, just 73 of the original 451 clients screened were still taking PrEP.
“It was surprising to see just how significant the follow-up dropped off after that first visit, when the patient initially accepted the prescription,” Allmacher said.
And while it’s possible that some clients get their follow-up care from their primary care providers, “our clinic serves individuals regardless of insurance status and many do not identify having access to primary care for any type of service, PrEP or otherwise,” she said.
5 HIV acquisitions
In addition, the program review identified five clients who had been offered PrEP or had taken PrEP briefly who later acquired HIV. Those clients were offered same-day antiretroviral treatment, Allmacher said.
“So we’re finding people who are at high risk for HIV and we can prevent them, but we’re still not quite doing enough,” Allmacher said of those acquisitions. “Clearly we have a lot of work to do to focus on HIV prevention, and we are looking to create a more formal follow-up process” from the clinic’s side.
For instance, clinic staff call clients 1 week after their initial visit to share lab results. “This was identified as a missed opportunity for us to ask about their status, whether they filled their prescription, or if they need further assistance,” she said. “This is an area where our registered nurses are going to be taking on a greater role moving forward.”
Allmacher and team also discovered that, despite PrEP navigators arranging insurance coverage for clients on the day they receive their prescription, sometimes there were still barriers when the client showed up at the pharmacy to pick up their meds. The clinic does not have an in-house pharmacy and does not currently have the funding that would allow them to hand patients a bottle of the appropriate medication when they leave the clinic.
“Navigating the copays and the insurance coverage and using financial assistance through the drug manufacturer — even though we have the support in the clinic, it seems like there’s a disconnect between our clinic and getting to the pharmacy. Not every pharmacy is super familiar with navigating those,” she said. “So we have started to identify some area pharmacies near our clinic that are great at navigating these, and we really try to get our patients to go to places we know can give them assistance.”
A version of this story originally appeared on Medscape.com.
To Amanda Allmacher, DNP, RN, nurse practitioner at the Detroit Public Health STD Clinic, that means that same-day PrEP prescribing works and is acceptable. But there’s more work to do on the clinic and pharmacy side to make HIV protection a reality for most of her patients. Allmacher presented her data at the Association of Nurses in AIDS Care 2020 virtual annual meeting.
Dawn K. Smith, MD, epidemiologist and medical officer in the Division of HIV/AIDS Prevention at the Centers for Disease Control and Prevention’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said this adds to other data to show that we’re now entering the next phase of PrEP implementation.
“Our original focus was on uptake — informing folks what PrEP is, why they might benefit from its use, and then prescribing it if accepted,” Smith told Medscape Medical News via email. “Whether standard or same-day [PrEP prescribing], it is clear that uptake is only the first step.”
Nurses help navigate
Patients who attended the Detroit Public Health STD Clinic are more likely to be younger, have no insurance, and otherwise “have little to no contact with the healthcare system,” Allmacher said in her presentation. They also tend to come from communities that bear the greatest burden of HIV in the US — in other words, they are often the people most missed in PrEP rollouts thus far.
In response, the clinic implemented a same-day PrEP protocol, in which registered nurses trained in HIV risk assessment identify clients who might most benefit from PrEP. Criteria often include the presence of other STIs. Once the nurse explains what PrEP is and how it works, if the patient is interested, clients meet with a nurse practitioner right then to get the prescription for PrEP. The clinic also does labs to rule out current HIV infection, hepatitis B, metabolic issues, and other STI screening.
But it doesn’t stop there. The clinic used grant funding to offer PrEP navigation and financial counseling services, which help clients navigate the sometimes-thorny process of paying for PrEP. Payment comes either through Medicaid, which in Michigan charges $3 a month for a PrEP prescription, through patient assistance programs, or through private insurance. With clients under age 18 who are interested in PrEP, the clinic works to find a way to access PrEP without having to inform their parents. These same navigators schedule follow-up appointments, offer appointment reminders, and contact clients when they miss an appointment.
“Our navigators and financial counselors are a huge support for our same-day PrEP starts, helping with financial assistance, prior authorization, navigating different plans, and helping patients apply for Medicaid when appropriate,” she said.
The clinic also offers community outreach and incentives, which can include gift cards, bus passes, and pill containers, among other things.
This was a key lesson in setting up the program, Allmacher told Medscape Medical News.
“Starting PrEP at that initial visit allows for clinicians to meet patients where they are and administer care in a more equitable manner,” Allmacher said via email. “Use all available resources and funding sources. We have a versatile team working together to increase access for patients and promote HIV prevention and risk reduction.”
Script vs. follow-up
This approach is common, used in places like New York City and San Francisco. So once it was set up Allmacher sat back and waited to see how the program helped clients protect themselves from HIV.
Of the 451 clients eligible for PrEP in 2019, 336 were gay and bisexual men, 6 were transgender women, 61 were heterosexual, cisgender men, and 48 were cisgender women. One transgender man also screened as eligible. Allmacher did not break down data by race.
Uptake was high: 70% of all eligible clients did receive a prescription for PrEP, either generic tenofovir disoproxil fumarate/emtricitabine (Truvada) or tenofovir alafenamide/emtricitabine (Descovy). And uptake was high among people most at risk: 80% of gay and bisexual men who were eligible got a prescription, 60% of eligible cisgender women, 50% of the small number of transgender women, and 32.7% of heterosexual cisgender men did as well. The 1 transgender man also received a prescription.
This is a higher rate than found in a recent PrEP demonstration project, which found that despite gay and bisexual men, transgender adults, and Black people having the highest risk for HIV in the US, state health departments were more likely to refer heterosexual adults for PrEP.
That high uptake rate is encouraging, but follow-up? Not so much. After initial intake, clients are meant to return in a month to double-check their labs, ask about side effects, and start their 90-day supply of the medication. But just 40% showed up for their 30-day appointment, Allmacher said. And only one third of those showed up for the follow-up in 90 days.
By the end of 2019, just 73 of the original 451 clients screened were still taking PrEP.
“It was surprising to see just how significant the follow-up dropped off after that first visit, when the patient initially accepted the prescription,” Allmacher said.
And while it’s possible that some clients get their follow-up care from their primary care providers, “our clinic serves individuals regardless of insurance status and many do not identify having access to primary care for any type of service, PrEP or otherwise,” she said.
5 HIV acquisitions
In addition, the program review identified five clients who had been offered PrEP or had taken PrEP briefly who later acquired HIV. Those clients were offered same-day antiretroviral treatment, Allmacher said.
“So we’re finding people who are at high risk for HIV and we can prevent them, but we’re still not quite doing enough,” Allmacher said of those acquisitions. “Clearly we have a lot of work to do to focus on HIV prevention, and we are looking to create a more formal follow-up process” from the clinic’s side.
For instance, clinic staff call clients 1 week after their initial visit to share lab results. “This was identified as a missed opportunity for us to ask about their status, whether they filled their prescription, or if they need further assistance,” she said. “This is an area where our registered nurses are going to be taking on a greater role moving forward.”
Allmacher and team also discovered that, despite PrEP navigators arranging insurance coverage for clients on the day they receive their prescription, sometimes there were still barriers when the client showed up at the pharmacy to pick up their meds. The clinic does not have an in-house pharmacy and does not currently have the funding that would allow them to hand patients a bottle of the appropriate medication when they leave the clinic.
“Navigating the copays and the insurance coverage and using financial assistance through the drug manufacturer — even though we have the support in the clinic, it seems like there’s a disconnect between our clinic and getting to the pharmacy. Not every pharmacy is super familiar with navigating those,” she said. “So we have started to identify some area pharmacies near our clinic that are great at navigating these, and we really try to get our patients to go to places we know can give them assistance.”
A version of this story originally appeared on Medscape.com.
To Amanda Allmacher, DNP, RN, nurse practitioner at the Detroit Public Health STD Clinic, that means that same-day PrEP prescribing works and is acceptable. But there’s more work to do on the clinic and pharmacy side to make HIV protection a reality for most of her patients. Allmacher presented her data at the Association of Nurses in AIDS Care 2020 virtual annual meeting.
Dawn K. Smith, MD, epidemiologist and medical officer in the Division of HIV/AIDS Prevention at the Centers for Disease Control and Prevention’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said this adds to other data to show that we’re now entering the next phase of PrEP implementation.
“Our original focus was on uptake — informing folks what PrEP is, why they might benefit from its use, and then prescribing it if accepted,” Smith told Medscape Medical News via email. “Whether standard or same-day [PrEP prescribing], it is clear that uptake is only the first step.”
Nurses help navigate
Patients who attended the Detroit Public Health STD Clinic are more likely to be younger, have no insurance, and otherwise “have little to no contact with the healthcare system,” Allmacher said in her presentation. They also tend to come from communities that bear the greatest burden of HIV in the US — in other words, they are often the people most missed in PrEP rollouts thus far.
In response, the clinic implemented a same-day PrEP protocol, in which registered nurses trained in HIV risk assessment identify clients who might most benefit from PrEP. Criteria often include the presence of other STIs. Once the nurse explains what PrEP is and how it works, if the patient is interested, clients meet with a nurse practitioner right then to get the prescription for PrEP. The clinic also does labs to rule out current HIV infection, hepatitis B, metabolic issues, and other STI screening.
But it doesn’t stop there. The clinic used grant funding to offer PrEP navigation and financial counseling services, which help clients navigate the sometimes-thorny process of paying for PrEP. Payment comes either through Medicaid, which in Michigan charges $3 a month for a PrEP prescription, through patient assistance programs, or through private insurance. With clients under age 18 who are interested in PrEP, the clinic works to find a way to access PrEP without having to inform their parents. These same navigators schedule follow-up appointments, offer appointment reminders, and contact clients when they miss an appointment.
“Our navigators and financial counselors are a huge support for our same-day PrEP starts, helping with financial assistance, prior authorization, navigating different plans, and helping patients apply for Medicaid when appropriate,” she said.
The clinic also offers community outreach and incentives, which can include gift cards, bus passes, and pill containers, among other things.
This was a key lesson in setting up the program, Allmacher told Medscape Medical News.
“Starting PrEP at that initial visit allows for clinicians to meet patients where they are and administer care in a more equitable manner,” Allmacher said via email. “Use all available resources and funding sources. We have a versatile team working together to increase access for patients and promote HIV prevention and risk reduction.”
Script vs. follow-up
This approach is common, used in places like New York City and San Francisco. So once it was set up Allmacher sat back and waited to see how the program helped clients protect themselves from HIV.
Of the 451 clients eligible for PrEP in 2019, 336 were gay and bisexual men, 6 were transgender women, 61 were heterosexual, cisgender men, and 48 were cisgender women. One transgender man also screened as eligible. Allmacher did not break down data by race.
Uptake was high: 70% of all eligible clients did receive a prescription for PrEP, either generic tenofovir disoproxil fumarate/emtricitabine (Truvada) or tenofovir alafenamide/emtricitabine (Descovy). And uptake was high among people most at risk: 80% of gay and bisexual men who were eligible got a prescription, 60% of eligible cisgender women, 50% of the small number of transgender women, and 32.7% of heterosexual cisgender men did as well. The 1 transgender man also received a prescription.
This is a higher rate than found in a recent PrEP demonstration project, which found that despite gay and bisexual men, transgender adults, and Black people having the highest risk for HIV in the US, state health departments were more likely to refer heterosexual adults for PrEP.
That high uptake rate is encouraging, but follow-up? Not so much. After initial intake, clients are meant to return in a month to double-check their labs, ask about side effects, and start their 90-day supply of the medication. But just 40% showed up for their 30-day appointment, Allmacher said. And only one third of those showed up for the follow-up in 90 days.
By the end of 2019, just 73 of the original 451 clients screened were still taking PrEP.
“It was surprising to see just how significant the follow-up dropped off after that first visit, when the patient initially accepted the prescription,” Allmacher said.
And while it’s possible that some clients get their follow-up care from their primary care providers, “our clinic serves individuals regardless of insurance status and many do not identify having access to primary care for any type of service, PrEP or otherwise,” she said.
5 HIV acquisitions
In addition, the program review identified five clients who had been offered PrEP or had taken PrEP briefly who later acquired HIV. Those clients were offered same-day antiretroviral treatment, Allmacher said.
“So we’re finding people who are at high risk for HIV and we can prevent them, but we’re still not quite doing enough,” Allmacher said of those acquisitions. “Clearly we have a lot of work to do to focus on HIV prevention, and we are looking to create a more formal follow-up process” from the clinic’s side.
For instance, clinic staff call clients 1 week after their initial visit to share lab results. “This was identified as a missed opportunity for us to ask about their status, whether they filled their prescription, or if they need further assistance,” she said. “This is an area where our registered nurses are going to be taking on a greater role moving forward.”
Allmacher and team also discovered that, despite PrEP navigators arranging insurance coverage for clients on the day they receive their prescription, sometimes there were still barriers when the client showed up at the pharmacy to pick up their meds. The clinic does not have an in-house pharmacy and does not currently have the funding that would allow them to hand patients a bottle of the appropriate medication when they leave the clinic.
“Navigating the copays and the insurance coverage and using financial assistance through the drug manufacturer — even though we have the support in the clinic, it seems like there’s a disconnect between our clinic and getting to the pharmacy. Not every pharmacy is super familiar with navigating those,” she said. “So we have started to identify some area pharmacies near our clinic that are great at navigating these, and we really try to get our patients to go to places we know can give them assistance.”
A version of this story originally appeared on Medscape.com.
Experts disagree with USPSTF’s take on pediatric blood pressure screening
Current evidence is insufficient to assess the balance of benefits and harms of screening for high blood pressure in children and adolescents, the U.S. Preventive Services Task Force reported in JAMA.
However, two experts in this area suggested there is evidence if you know where to look, and pediatric BP testing is crucial now.
In this update to the 2013 statement, the USPSTF’s systematic review focused on evidence surrounding the benefits of screening, test accuracy, treatment effectiveness and harms, and links between hypertension and cardiovascular disease (CVD) markers in childhood and adulthood.
Limited information was available on the accuracy of screening tests. No studies were found that directly evaluated screening for pediatric high BP or reported effectiveness in delayed onset or risk reduction for cardiovascular outcomes related to hypertension. Additionally, no studies were found that addressed screening for secondary hypertension in asymptomatic pediatric patients. No studies were found that evaluated the treatment of primary childhood hypertension and BP reduction or other outcomes in adulthood. The panel also was unable to identify any studies that reported on harms of screening and treatment.
When the adult framework for cardiovascular risk reduction is extended in pediatric patients, there are methodological challenges that make it harder to determine how much of the potential burden can actually be prevented, the panel said. The clinical and epidemiologic significance of percentile thresholds that are used to determine their ties to adult CVD has limited supporting evidence. Inconsistent performance characteristics of current diagnostic methods, of which there are few, tend to yield unfavorable high false-positive rates. Such false positives are potentially harmful, because they lead to “unnecessary secondary evaluations or treatments.” Because pharmacologic management of pediatric hypertension is continued for a much longer period, it is the increased likelihood of adverse events that should be cause for concern.
Should the focus for screening be shifted to significant risk factors?
In an accompanying editorial, Joseph T. Flynn, MD, MS, of Seattle Children’s Hospital, said that the outcome of the latest statement is expected, “given how the key questions were framed and the analysis performed.” To begin, he suggested restating the question: “What is the best approach to assess whether childhood BP measurement is associated with adult CVD or whether treatment of high BP in childhood is associated with reducing the burden of adult CVD?” The answer is to tackle these questions with randomized clinical trials that compare screening to no screening and treatment to no treatment. But such studies are likely infeasible, partly because of the required length of follow-up of 5-6 decades.
Perhaps a better question would be: “Does BP measurement in childhood identify children and adolescents who already have markers of CVD or who are at risk of developing them as adults?” Were these youth to be identified, they would become candidates for approaches that seek to prevent disease progression. Reframing the question in this manner better positions physicians to focus on prevention and sidestep “the requirement that the only acceptable outcome is prevention of CVD events in adulthood,” he explained.
The next step would be to identify data already available to address the reframed question. Cross-sectional studies could be used to make the association between BP levels and cardiovascular risk markers already present. For example, several publications from the multicenter Study of High Blood Pressure in Pediatrics: Adult Hypertension Onset in Youth (SHIP-AHOY), which enrolled roughly 400 youth, provided data that reinforce prior single-center studies that essentially proved there are adverse consequences for youth with high BP, and they “set the stage for the institution of measures designed to reverse target-organ damage and reduce cardiovascular risk in youth,” said Dr. Flynn.
More specifically, results from SHIP-AHOY “have demonstrated that increased left ventricular mass can be demonstrated at BP levels currently classified as normotensive and that abnormal left ventricular function can be seen at similar BP levels,” Dr. Flynn noted. In addition, “they have established a substantial association between an abnormal metabolic phenotype and several forms of target-organ damage associated with high BP.”
One approach is to analyze longitudinal cohort studies
Because there is a paucity of prospective clinical trials, Dr. Flynn suggested that analyzing longitudinal cohort studies would be the most effective approach for evaluating the potential link between current BP levels and future CVD. Such studies already have “data that address an important point raised in the USPSTF statement, namely whether the pediatric percentile-based BP cut points, such as those in the 2017 AAP [American Academy of Pediatrics] guideline, are associated with adult hypertension and CVD,” noted Dr. Flynn. “In the International Childhood Cardiovascular Cohort Consortium study, the specific childhood BP levels that were associated with increased adult carotid intima-medial thickness were remarkably similar to the BP percentile cut points in the AAP guideline for children of similar ages.”
Analysis of data from the Bogalusa Heart Study found looking at children classified as having high BP by the 2017 AAP guideline had “increased relative risks of having hypertension, left ventricular hypertrophy, or metabolic syndrome as adults 36 years later.”
“The conclusions of the USPSTF statement underscore the need for additional research on childhood high BP and its association with adult CVD. The starting points for such research can be deduced from currently available cross-sectional and longitudinal data, which demonstrate the detrimental outcomes associated with high BP in youth. Using these data to reframe and answer the questions raised by the USPSTF should point the way toward effective prevention of adult CVD,” concluded Dr. Flynn.
In a separate interview, Kristen Sexson Tejtel, MD, PhD, MPH, medical director of the preventive cardiology clinic at Texas Children’s Hospital and Baylor College of Medicine, both in Houston, noted that in spite of USPSTF’s findings, there is actually an association between children with high blood pressure and intermediate outcomes in adults.
“Dr. Flynn suggests reframing the question. In fact, evidence exists that children with high blood pressure are at higher risk of left ventricular hypertrophy, increased arterial stiffness, and changes in retinal arteries,” noted Dr. Sexson Tejtel.
Evidence of pediatric heart damage has been documented in autopsies
“It is imperative that children have blood pressure evaluation,” she urged. “There is evidence that there are changes similar to those seen in adults with cardiovascular compromise. It has been shown that children dying of other causes [accidents] who have these problems also have more plaque on autopsy, indicating that those with high blood pressure are more likely to have markers of CVD already present in childhood.
“One of the keys of pediatric medicine is prevention and the counseling for prevention of adult diseases. The duration of study necessary to objectively determine whether treatment of hypertension in childhood reduces the risk of adult cardiac problems is extensive. If nothing is done now, we are putting more future generations in danger. We must provide appropriate counseling for children and their families regarding lifestyle improvements, to have a chance to improve cardiovascular risk factors in adults, including hypertension, hyperlipidemia and/or obesity,” urged Dr. Sexson Tejtel.
All members of the USPSTF received travel reimbursement and honoraria. Dr. Barry received grants and personal fees from Healthwise. The U.S. Congress mandates that the Agency for Healthcare Research and Quality support the operations of the USPSTF. Dr. Flynn reported receiving grants from the National Institutes of Health and royalties from UpToDate and Springer outside the submitted work. Dr. Sexson Tejtel said she had no relevant financial disclosures or conflicts of interest.
SOURCE: USPSTF. JAMA. 2020 Nov 10. doi: 10.1001/jama.2020.20122.
Current evidence is insufficient to assess the balance of benefits and harms of screening for high blood pressure in children and adolescents, the U.S. Preventive Services Task Force reported in JAMA.
However, two experts in this area suggested there is evidence if you know where to look, and pediatric BP testing is crucial now.
In this update to the 2013 statement, the USPSTF’s systematic review focused on evidence surrounding the benefits of screening, test accuracy, treatment effectiveness and harms, and links between hypertension and cardiovascular disease (CVD) markers in childhood and adulthood.
Limited information was available on the accuracy of screening tests. No studies were found that directly evaluated screening for pediatric high BP or reported effectiveness in delayed onset or risk reduction for cardiovascular outcomes related to hypertension. Additionally, no studies were found that addressed screening for secondary hypertension in asymptomatic pediatric patients. No studies were found that evaluated the treatment of primary childhood hypertension and BP reduction or other outcomes in adulthood. The panel also was unable to identify any studies that reported on harms of screening and treatment.
When the adult framework for cardiovascular risk reduction is extended in pediatric patients, there are methodological challenges that make it harder to determine how much of the potential burden can actually be prevented, the panel said. The clinical and epidemiologic significance of percentile thresholds that are used to determine their ties to adult CVD has limited supporting evidence. Inconsistent performance characteristics of current diagnostic methods, of which there are few, tend to yield unfavorable high false-positive rates. Such false positives are potentially harmful, because they lead to “unnecessary secondary evaluations or treatments.” Because pharmacologic management of pediatric hypertension is continued for a much longer period, it is the increased likelihood of adverse events that should be cause for concern.
Should the focus for screening be shifted to significant risk factors?
In an accompanying editorial, Joseph T. Flynn, MD, MS, of Seattle Children’s Hospital, said that the outcome of the latest statement is expected, “given how the key questions were framed and the analysis performed.” To begin, he suggested restating the question: “What is the best approach to assess whether childhood BP measurement is associated with adult CVD or whether treatment of high BP in childhood is associated with reducing the burden of adult CVD?” The answer is to tackle these questions with randomized clinical trials that compare screening to no screening and treatment to no treatment. But such studies are likely infeasible, partly because of the required length of follow-up of 5-6 decades.
Perhaps a better question would be: “Does BP measurement in childhood identify children and adolescents who already have markers of CVD or who are at risk of developing them as adults?” Were these youth to be identified, they would become candidates for approaches that seek to prevent disease progression. Reframing the question in this manner better positions physicians to focus on prevention and sidestep “the requirement that the only acceptable outcome is prevention of CVD events in adulthood,” he explained.
The next step would be to identify data already available to address the reframed question. Cross-sectional studies could be used to make the association between BP levels and cardiovascular risk markers already present. For example, several publications from the multicenter Study of High Blood Pressure in Pediatrics: Adult Hypertension Onset in Youth (SHIP-AHOY), which enrolled roughly 400 youth, provided data that reinforce prior single-center studies that essentially proved there are adverse consequences for youth with high BP, and they “set the stage for the institution of measures designed to reverse target-organ damage and reduce cardiovascular risk in youth,” said Dr. Flynn.
More specifically, results from SHIP-AHOY “have demonstrated that increased left ventricular mass can be demonstrated at BP levels currently classified as normotensive and that abnormal left ventricular function can be seen at similar BP levels,” Dr. Flynn noted. In addition, “they have established a substantial association between an abnormal metabolic phenotype and several forms of target-organ damage associated with high BP.”
One approach is to analyze longitudinal cohort studies
Because there is a paucity of prospective clinical trials, Dr. Flynn suggested that analyzing longitudinal cohort studies would be the most effective approach for evaluating the potential link between current BP levels and future CVD. Such studies already have “data that address an important point raised in the USPSTF statement, namely whether the pediatric percentile-based BP cut points, such as those in the 2017 AAP [American Academy of Pediatrics] guideline, are associated with adult hypertension and CVD,” noted Dr. Flynn. “In the International Childhood Cardiovascular Cohort Consortium study, the specific childhood BP levels that were associated with increased adult carotid intima-medial thickness were remarkably similar to the BP percentile cut points in the AAP guideline for children of similar ages.”
Analysis of data from the Bogalusa Heart Study found looking at children classified as having high BP by the 2017 AAP guideline had “increased relative risks of having hypertension, left ventricular hypertrophy, or metabolic syndrome as adults 36 years later.”
“The conclusions of the USPSTF statement underscore the need for additional research on childhood high BP and its association with adult CVD. The starting points for such research can be deduced from currently available cross-sectional and longitudinal data, which demonstrate the detrimental outcomes associated with high BP in youth. Using these data to reframe and answer the questions raised by the USPSTF should point the way toward effective prevention of adult CVD,” concluded Dr. Flynn.
In a separate interview, Kristen Sexson Tejtel, MD, PhD, MPH, medical director of the preventive cardiology clinic at Texas Children’s Hospital and Baylor College of Medicine, both in Houston, noted that in spite of USPSTF’s findings, there is actually an association between children with high blood pressure and intermediate outcomes in adults.
“Dr. Flynn suggests reframing the question. In fact, evidence exists that children with high blood pressure are at higher risk of left ventricular hypertrophy, increased arterial stiffness, and changes in retinal arteries,” noted Dr. Sexson Tejtel.
Evidence of pediatric heart damage has been documented in autopsies
“It is imperative that children have blood pressure evaluation,” she urged. “There is evidence that there are changes similar to those seen in adults with cardiovascular compromise. It has been shown that children dying of other causes [accidents] who have these problems also have more plaque on autopsy, indicating that those with high blood pressure are more likely to have markers of CVD already present in childhood.
“One of the keys of pediatric medicine is prevention and the counseling for prevention of adult diseases. The duration of study necessary to objectively determine whether treatment of hypertension in childhood reduces the risk of adult cardiac problems is extensive. If nothing is done now, we are putting more future generations in danger. We must provide appropriate counseling for children and their families regarding lifestyle improvements, to have a chance to improve cardiovascular risk factors in adults, including hypertension, hyperlipidemia and/or obesity,” urged Dr. Sexson Tejtel.
All members of the USPSTF received travel reimbursement and honoraria. Dr. Barry received grants and personal fees from Healthwise. The U.S. Congress mandates that the Agency for Healthcare Research and Quality support the operations of the USPSTF. Dr. Flynn reported receiving grants from the National Institutes of Health and royalties from UpToDate and Springer outside the submitted work. Dr. Sexson Tejtel said she had no relevant financial disclosures or conflicts of interest.
SOURCE: USPSTF. JAMA. 2020 Nov 10. doi: 10.1001/jama.2020.20122.
Current evidence is insufficient to assess the balance of benefits and harms of screening for high blood pressure in children and adolescents, the U.S. Preventive Services Task Force reported in JAMA.
However, two experts in this area suggested there is evidence if you know where to look, and pediatric BP testing is crucial now.
In this update to the 2013 statement, the USPSTF’s systematic review focused on evidence surrounding the benefits of screening, test accuracy, treatment effectiveness and harms, and links between hypertension and cardiovascular disease (CVD) markers in childhood and adulthood.
Limited information was available on the accuracy of screening tests. No studies were found that directly evaluated screening for pediatric high BP or reported effectiveness in delayed onset or risk reduction for cardiovascular outcomes related to hypertension. Additionally, no studies were found that addressed screening for secondary hypertension in asymptomatic pediatric patients. No studies were found that evaluated the treatment of primary childhood hypertension and BP reduction or other outcomes in adulthood. The panel also was unable to identify any studies that reported on harms of screening and treatment.
When the adult framework for cardiovascular risk reduction is extended in pediatric patients, there are methodological challenges that make it harder to determine how much of the potential burden can actually be prevented, the panel said. The clinical and epidemiologic significance of percentile thresholds that are used to determine their ties to adult CVD has limited supporting evidence. Inconsistent performance characteristics of current diagnostic methods, of which there are few, tend to yield unfavorable high false-positive rates. Such false positives are potentially harmful, because they lead to “unnecessary secondary evaluations or treatments.” Because pharmacologic management of pediatric hypertension is continued for a much longer period, it is the increased likelihood of adverse events that should be cause for concern.
Should the focus for screening be shifted to significant risk factors?
In an accompanying editorial, Joseph T. Flynn, MD, MS, of Seattle Children’s Hospital, said that the outcome of the latest statement is expected, “given how the key questions were framed and the analysis performed.” To begin, he suggested restating the question: “What is the best approach to assess whether childhood BP measurement is associated with adult CVD or whether treatment of high BP in childhood is associated with reducing the burden of adult CVD?” The answer is to tackle these questions with randomized clinical trials that compare screening to no screening and treatment to no treatment. But such studies are likely infeasible, partly because of the required length of follow-up of 5-6 decades.
Perhaps a better question would be: “Does BP measurement in childhood identify children and adolescents who already have markers of CVD or who are at risk of developing them as adults?” Were these youth to be identified, they would become candidates for approaches that seek to prevent disease progression. Reframing the question in this manner better positions physicians to focus on prevention and sidestep “the requirement that the only acceptable outcome is prevention of CVD events in adulthood,” he explained.
The next step would be to identify data already available to address the reframed question. Cross-sectional studies could be used to make the association between BP levels and cardiovascular risk markers already present. For example, several publications from the multicenter Study of High Blood Pressure in Pediatrics: Adult Hypertension Onset in Youth (SHIP-AHOY), which enrolled roughly 400 youth, provided data that reinforce prior single-center studies that essentially proved there are adverse consequences for youth with high BP, and they “set the stage for the institution of measures designed to reverse target-organ damage and reduce cardiovascular risk in youth,” said Dr. Flynn.
More specifically, results from SHIP-AHOY “have demonstrated that increased left ventricular mass can be demonstrated at BP levels currently classified as normotensive and that abnormal left ventricular function can be seen at similar BP levels,” Dr. Flynn noted. In addition, “they have established a substantial association between an abnormal metabolic phenotype and several forms of target-organ damage associated with high BP.”
One approach is to analyze longitudinal cohort studies
Because there is a paucity of prospective clinical trials, Dr. Flynn suggested that analyzing longitudinal cohort studies would be the most effective approach for evaluating the potential link between current BP levels and future CVD. Such studies already have “data that address an important point raised in the USPSTF statement, namely whether the pediatric percentile-based BP cut points, such as those in the 2017 AAP [American Academy of Pediatrics] guideline, are associated with adult hypertension and CVD,” noted Dr. Flynn. “In the International Childhood Cardiovascular Cohort Consortium study, the specific childhood BP levels that were associated with increased adult carotid intima-medial thickness were remarkably similar to the BP percentile cut points in the AAP guideline for children of similar ages.”
Analysis of data from the Bogalusa Heart Study found looking at children classified as having high BP by the 2017 AAP guideline had “increased relative risks of having hypertension, left ventricular hypertrophy, or metabolic syndrome as adults 36 years later.”
“The conclusions of the USPSTF statement underscore the need for additional research on childhood high BP and its association with adult CVD. The starting points for such research can be deduced from currently available cross-sectional and longitudinal data, which demonstrate the detrimental outcomes associated with high BP in youth. Using these data to reframe and answer the questions raised by the USPSTF should point the way toward effective prevention of adult CVD,” concluded Dr. Flynn.
In a separate interview, Kristen Sexson Tejtel, MD, PhD, MPH, medical director of the preventive cardiology clinic at Texas Children’s Hospital and Baylor College of Medicine, both in Houston, noted that in spite of USPSTF’s findings, there is actually an association between children with high blood pressure and intermediate outcomes in adults.
“Dr. Flynn suggests reframing the question. In fact, evidence exists that children with high blood pressure are at higher risk of left ventricular hypertrophy, increased arterial stiffness, and changes in retinal arteries,” noted Dr. Sexson Tejtel.
Evidence of pediatric heart damage has been documented in autopsies
“It is imperative that children have blood pressure evaluation,” she urged. “There is evidence that there are changes similar to those seen in adults with cardiovascular compromise. It has been shown that children dying of other causes [accidents] who have these problems also have more plaque on autopsy, indicating that those with high blood pressure are more likely to have markers of CVD already present in childhood.
“One of the keys of pediatric medicine is prevention and the counseling for prevention of adult diseases. The duration of study necessary to objectively determine whether treatment of hypertension in childhood reduces the risk of adult cardiac problems is extensive. If nothing is done now, we are putting more future generations in danger. We must provide appropriate counseling for children and their families regarding lifestyle improvements, to have a chance to improve cardiovascular risk factors in adults, including hypertension, hyperlipidemia and/or obesity,” urged Dr. Sexson Tejtel.
All members of the USPSTF received travel reimbursement and honoraria. Dr. Barry received grants and personal fees from Healthwise. The U.S. Congress mandates that the Agency for Healthcare Research and Quality support the operations of the USPSTF. Dr. Flynn reported receiving grants from the National Institutes of Health and royalties from UpToDate and Springer outside the submitted work. Dr. Sexson Tejtel said she had no relevant financial disclosures or conflicts of interest.
SOURCE: USPSTF. JAMA. 2020 Nov 10. doi: 10.1001/jama.2020.20122.
FROM JAMA
Should our patients really go home for the holidays?
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
United States adds nearly 74,000 more children with COVID-19
The new weekly high for COVID-19 cases in children announced last week has been surpassed already, as the United States experienced almost 74,000 new pediatric cases for the week ending Nov. 5, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The total number of COVID-19 cases in children is now 927,518 in 49 states, the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly report.
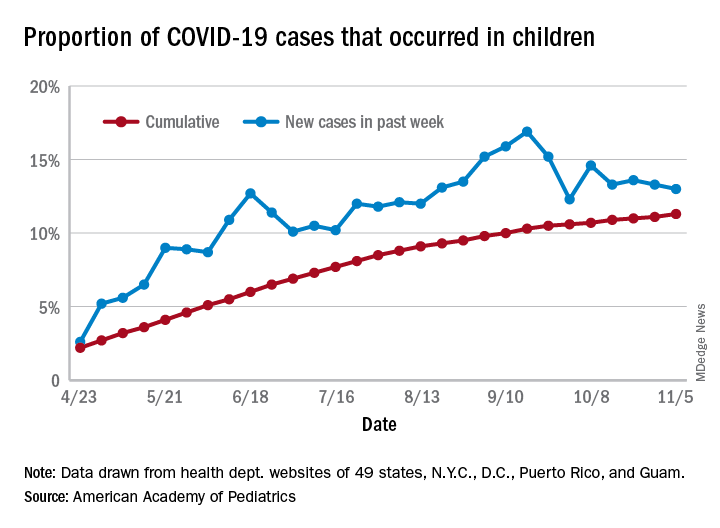
Cumulatively, children represent 11.3% of all COVID-19 cases in those jurisdictions, up from 11.1% a week ago. For just the past week, those 73,883 children represent 13.0% of the 567,672 new cases reported among all ages. That proportion peaked at 16.9% in mid-September, the AAP/CHA data show.
Dropping down to the state level, cumulative proportions as of Nov. 5 range from 5.2% in New Jersey to 23.3% in Wyoming, with 11 other states over 15%. California has had more cases, 100,856, than any other state, and Vermont the fewest at 329, the AAP and CHA said.
The national rate per 100,000 children is now 1,232, up from 1,134 the previous week and more than doubled since mid-August (582.2 per 100,000 on Aug. 20). North Dakota’s rate of 3,990 per 100,000 children is the highest of any state (South Dakota is next at 2,779), while Vermont is again the lowest at 245 per 100,000, based on data collected from state health department websites.
Two COVID-19–related deaths in children were reported during the week ending Nov. 5, bringing the total to 123 but leaving the overall proportion of deaths in children unchanged at 0.06% of all deaths. Texas has reported the most COVID-19 deaths in children with 29, while 15 states have recorded no deaths so far (mortality data in children reported by 42 states and New York City), the AAP and CHA said.
The new weekly high for COVID-19 cases in children announced last week has been surpassed already, as the United States experienced almost 74,000 new pediatric cases for the week ending Nov. 5, according to the American Academy of Pediatrics and the Children’s Hospital Association.
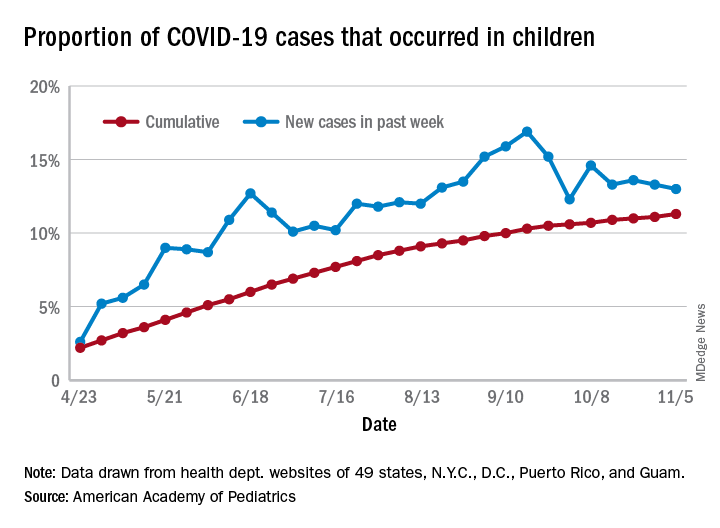
The total number of COVID-19 cases in children is now 927,518 in 49 states, the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly report.
Cumulatively, children represent 11.3% of all COVID-19 cases in those jurisdictions, up from 11.1% a week ago. For just the past week, those 73,883 children represent 13.0% of the 567,672 new cases reported among all ages. That proportion peaked at 16.9% in mid-September, the AAP/CHA data show.
Dropping down to the state level, cumulative proportions as of Nov. 5 range from 5.2% in New Jersey to 23.3% in Wyoming, with 11 other states over 15%. California has had more cases, 100,856, than any other state, and Vermont the fewest at 329, the AAP and CHA said.
The national rate per 100,000 children is now 1,232, up from 1,134 the previous week and more than doubled since mid-August (582.2 per 100,000 on Aug. 20). North Dakota’s rate of 3,990 per 100,000 children is the highest of any state (South Dakota is next at 2,779), while Vermont is again the lowest at 245 per 100,000, based on data collected from state health department websites.
Two COVID-19–related deaths in children were reported during the week ending Nov. 5, bringing the total to 123 but leaving the overall proportion of deaths in children unchanged at 0.06% of all deaths. Texas has reported the most COVID-19 deaths in children with 29, while 15 states have recorded no deaths so far (mortality data in children reported by 42 states and New York City), the AAP and CHA said.
The new weekly high for COVID-19 cases in children announced last week has been surpassed already, as the United States experienced almost 74,000 new pediatric cases for the week ending Nov. 5, according to the American Academy of Pediatrics and the Children’s Hospital Association.
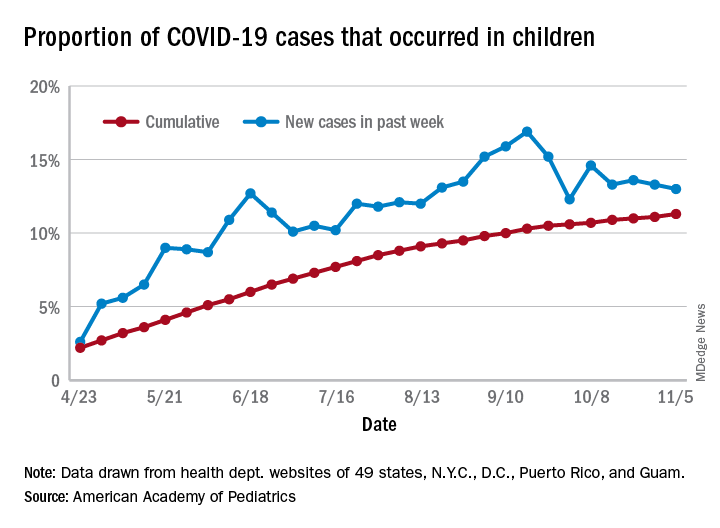
The total number of COVID-19 cases in children is now 927,518 in 49 states, the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly report.
Cumulatively, children represent 11.3% of all COVID-19 cases in those jurisdictions, up from 11.1% a week ago. For just the past week, those 73,883 children represent 13.0% of the 567,672 new cases reported among all ages. That proportion peaked at 16.9% in mid-September, the AAP/CHA data show.
Dropping down to the state level, cumulative proportions as of Nov. 5 range from 5.2% in New Jersey to 23.3% in Wyoming, with 11 other states over 15%. California has had more cases, 100,856, than any other state, and Vermont the fewest at 329, the AAP and CHA said.
The national rate per 100,000 children is now 1,232, up from 1,134 the previous week and more than doubled since mid-August (582.2 per 100,000 on Aug. 20). North Dakota’s rate of 3,990 per 100,000 children is the highest of any state (South Dakota is next at 2,779), while Vermont is again the lowest at 245 per 100,000, based on data collected from state health department websites.
Two COVID-19–related deaths in children were reported during the week ending Nov. 5, bringing the total to 123 but leaving the overall proportion of deaths in children unchanged at 0.06% of all deaths. Texas has reported the most COVID-19 deaths in children with 29, while 15 states have recorded no deaths so far (mortality data in children reported by 42 states and New York City), the AAP and CHA said.
Food insecurity called urgent issue you must address
and advocate on behalf of those experiencing or at risk of food insecurity, according to Kofi Essel, MD, MPH, a pediatrician at Children’s National Hospital in Washington.
More than one in four adults are dealing with food access hardships during the pandemic, Dr. Essel said at the virtual annual meeting of the American Academy of Pediatrics. Food insecurity is often interchangeable with hunger and refers to limited or uncertain availability of foods that are nutritious and safe.
“Food insecurity is as much about the threat of deprivation as it is about deprivation itself: A food-insecure life means a life lived in fear of hunger, and the psychological toll that takes,” according to a 2020 New York Times photo feature on food insecurity by Brenda Ann Kenneally that Dr. Essel quoted.
The lived experience of food insecure households includes food anxiety, a preoccupation with being able to get enough food that takes up cognitive bandwidth and prevents people from being able to focus on other important things. Another feature of food-insecure homes is a monotony of diet, which often involves an increase in caloric density and decrease in nutritional quality. As food insecurity grows more dire, adults’ food intake decreases, and then children’s intake decreases as adults seek out any way to get food, including “socially unacceptable” ways, which can include food pantries and bartering for food.
Food insecurity is associated with a wide range of negative outcomes even after accounting for other confounders, including decreased overall health, mental health, and educational outcomes. It’s also associated with an increase in developmental delays, hospitalizations, iron deficiency, asthma, and birth defects, among other problems. Somewhat paradoxically, it’s associated with both an increase and a decrease in obesity in the research.
Megan J. Gray, MD, MPH, assistant professor of pediatrics and population health at Dell Medical School at the The University of Texas at Austin, attended Dr. Essel’s session because food insecurity during COVID-19 now affects about half her patients, according to screening research she’s conducted.
“I wanted to learn more about the nuances of screening and using language and talking points that are helpful with families and with staff in building a culture of discussing food insecurity in our clinics,” Dr. Gray said in an interview. “What I’ve learned in my clinic is that if we don’t ask about it, families aren’t telling us – food insecurity is hiding in plain sight.”
She particularly appreciated Dr. Essel’s slides on the progression of food insecurity and how they acknowledged the mental health burden of food insecurity among parents.
“Right now during COVID-19, I see more patients I would call ‘socially complex’ rather than ‘medically complex,’ ” she said. “We all need to get a crash course in social work and Dr. Essel’s presentation is a great starting place.”
Screening for food insecurity
Beginning in 2015, an AAP policy statement charged pediatricians to “screen and intervene” with regard to food insecurity and their patients, Dr. Essel said. The statement also called for pediatricians to advocate for programs and policies that end childhood food insecurity.
The policy statement recommended a validated two-question screening tool called the Hunger Vital Sign:
1. “Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
2. “Within the past 12 months, the food that we bought just didn’t last and we didn’t have money to get more.”
But in screening, you need to be conscious of how dignity intersects with food insecurity concerns, Dr. Essel said.
“We need to create dignity for our families,” he said. “We need to create a safe environment for our families and use appropriate tools when necessary to be able to identify families that are struggling with food insecurity.”
That need is seen in research on food screening. The Hunger Vital Signs questions can be asked with a dichotomous variable, as a yes/no question, or on a Likert scale, though the latter is a more complex way to ask.
A 2017 study found, however, that asking with “yes/no” answers missed more than a quarter of at-risk families. In the AAP survey using “yes/no” answers, 31% of families screened positive for being at risk of food insecurity, compared with 46% when the same question was asked on a Likert scale. It seems the ability to answer with “sometimes” feels “safer” than answering “yes,” Dr. Essel said.
Another factor that potentially affects answers is how doctors ask. In a March 2020 study at a single primary care practice, 16% of families screened positive with yes/no responses to a food insecurity screen when the questions were written, compared with 10% of positive screens with verbal responses (P < .001).
Epidemiology of food insecurity
The most updated United States Department of Agriculture report on food insecurity released in September shows the United States finally reached prerecession levels in 2019, with 11% of families designated as “food insecure.” But 2019 data cannot show what has occurred since the pandemic.
Further, the numbers are higher in households with children: Fourteen percent, or one in seven households with children, are experiencing food insecurity. Racial and ethnic disparities in food insecurity have remained consistent over the past 2 decades, with about twice as many Black and Hispanic homes experiencing food insecurity as White homes.
More recent research using Census Household Pulse Surveys has found a tremendous increase in food insecurity for children in 2020. One in three Black children and one in four Hispanic children are food insecure, according to these surveys. The rates are one in six for Asian households and one in ten for White households.
“The disparity is consistent,” Dr. Essel said. “We see what COVID has done. We once may have described it as a great equalizer – everyone is touched in the same way – but the reality is, this is actually a great magnifier. It’s revealing to us and magnifying disparities that have existed for far too long and has really allowed us to see it in a new way.”
A big part of disparities in food insecurity is disparities in wealth, “the safety net or cushion for families when things go wrong,” Dr. Essel said. The median wealth of White Americans in 2016 was $171,000, compared to $20,700 among Latinx Americans and $17,600 among Black Americans, according to the Federal Reserve Board Survey of Consumer Finances.
Food insecurity interventions
Federal nutrition programs – such as Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and school meal programs – are key to addressing food insecurity, Dr. Essel said.
“They have a long track record of rescuing families out of poverty, of rescuing families from food security and improving overall health of families,” he said.
But emergency food relief programs are important as well. Four in 10 families currently coming into food pantries are new recipients, and these resources have seen a 60% increase in clients, he said.
“This is utterly unreasonable for them to be able to manage,” he said. “Food pantries are essential but inadequate to compensate for large numbers of families,” even while they also may be the only option for families unable or unwilling to access federal programs. For example, for every one meal that food banks can provide, SNAP can provide nine meals, Dr. Essel said. Further, during times of economic downtown, every SNAP $1 spent generates $1.50 to $2 in economic activity.
Currently, the Pandemic Electronic Benefit Transfer (P-EBT) program provides benefits to families for school breakfast and lunch and has been extended through December 2021. Another federal pandemic response was to increase SNAP to the maximum household benefit for families, about $646 for a family of four, although 40% of households were already receiving the maximum benefit.
Food insecurity advocacy
You can advocate for any one of multiple pillars when it comes to food insecurity, Dr. Essel said. “Food cannot solve food insecurity by itself,” he said. “We have to think about root causes – systemic causes – and think about unemployment, livable wage, systemic racism, oppression, an inequitable food system. All of these things are pillars that any of you can advocate for when recognizing a family that is struggling with food insecurity.”
He offered several suggestions for advocacy:
- Join your local AAP chapter and prioritize food insecurity.
- Join a local antihunger task force.
- Make your clinical environment as safe as possible for families to respond to questions about food insecurity.
- Know what’s happening in your community immigrant populations.
- Provide up-to-date information to families about eligibility for federal programs.
- Share stories through op-eds and letters to the editor, and by contacting congressional representatives and providing expert testimony to school boards and city councils.
- Educate others about food insecurity through the above channels and on social media.
Jessica Lazerov, MD, a general pediatrician at Children’s National Anacostia and assistant professor of pediatrics at George Washington University, Washington, said the session was fantastic.
“Dr. Essel went beyond the basics of food insecurity, delving into the root causes, potential solutions, and important considerations when screening for food insecurity in practice,” Dr. Lazerov said in an interview. “I enjoyed his focus on advocacy, as well as the fact that he spent a bit of time reviewing how the COVID pandemic has affected food insecurity. I truly felt empowered to take my advocacy efforts a step further as Dr. Essel laid out concrete, actionable next steps, as well as a review of the most relevant and current information about food insecurity.”
Dr. Essel, Dr. Lazerov, and Dr. Gray have no relevant financial disclosures.
and advocate on behalf of those experiencing or at risk of food insecurity, according to Kofi Essel, MD, MPH, a pediatrician at Children’s National Hospital in Washington.
More than one in four adults are dealing with food access hardships during the pandemic, Dr. Essel said at the virtual annual meeting of the American Academy of Pediatrics. Food insecurity is often interchangeable with hunger and refers to limited or uncertain availability of foods that are nutritious and safe.
“Food insecurity is as much about the threat of deprivation as it is about deprivation itself: A food-insecure life means a life lived in fear of hunger, and the psychological toll that takes,” according to a 2020 New York Times photo feature on food insecurity by Brenda Ann Kenneally that Dr. Essel quoted.
The lived experience of food insecure households includes food anxiety, a preoccupation with being able to get enough food that takes up cognitive bandwidth and prevents people from being able to focus on other important things. Another feature of food-insecure homes is a monotony of diet, which often involves an increase in caloric density and decrease in nutritional quality. As food insecurity grows more dire, adults’ food intake decreases, and then children’s intake decreases as adults seek out any way to get food, including “socially unacceptable” ways, which can include food pantries and bartering for food.
Food insecurity is associated with a wide range of negative outcomes even after accounting for other confounders, including decreased overall health, mental health, and educational outcomes. It’s also associated with an increase in developmental delays, hospitalizations, iron deficiency, asthma, and birth defects, among other problems. Somewhat paradoxically, it’s associated with both an increase and a decrease in obesity in the research.
Megan J. Gray, MD, MPH, assistant professor of pediatrics and population health at Dell Medical School at the The University of Texas at Austin, attended Dr. Essel’s session because food insecurity during COVID-19 now affects about half her patients, according to screening research she’s conducted.
“I wanted to learn more about the nuances of screening and using language and talking points that are helpful with families and with staff in building a culture of discussing food insecurity in our clinics,” Dr. Gray said in an interview. “What I’ve learned in my clinic is that if we don’t ask about it, families aren’t telling us – food insecurity is hiding in plain sight.”
She particularly appreciated Dr. Essel’s slides on the progression of food insecurity and how they acknowledged the mental health burden of food insecurity among parents.
“Right now during COVID-19, I see more patients I would call ‘socially complex’ rather than ‘medically complex,’ ” she said. “We all need to get a crash course in social work and Dr. Essel’s presentation is a great starting place.”
Screening for food insecurity
Beginning in 2015, an AAP policy statement charged pediatricians to “screen and intervene” with regard to food insecurity and their patients, Dr. Essel said. The statement also called for pediatricians to advocate for programs and policies that end childhood food insecurity.
The policy statement recommended a validated two-question screening tool called the Hunger Vital Sign:
1. “Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
2. “Within the past 12 months, the food that we bought just didn’t last and we didn’t have money to get more.”
But in screening, you need to be conscious of how dignity intersects with food insecurity concerns, Dr. Essel said.
“We need to create dignity for our families,” he said. “We need to create a safe environment for our families and use appropriate tools when necessary to be able to identify families that are struggling with food insecurity.”
That need is seen in research on food screening. The Hunger Vital Signs questions can be asked with a dichotomous variable, as a yes/no question, or on a Likert scale, though the latter is a more complex way to ask.
A 2017 study found, however, that asking with “yes/no” answers missed more than a quarter of at-risk families. In the AAP survey using “yes/no” answers, 31% of families screened positive for being at risk of food insecurity, compared with 46% when the same question was asked on a Likert scale. It seems the ability to answer with “sometimes” feels “safer” than answering “yes,” Dr. Essel said.
Another factor that potentially affects answers is how doctors ask. In a March 2020 study at a single primary care practice, 16% of families screened positive with yes/no responses to a food insecurity screen when the questions were written, compared with 10% of positive screens with verbal responses (P < .001).
Epidemiology of food insecurity
The most updated United States Department of Agriculture report on food insecurity released in September shows the United States finally reached prerecession levels in 2019, with 11% of families designated as “food insecure.” But 2019 data cannot show what has occurred since the pandemic.
Further, the numbers are higher in households with children: Fourteen percent, or one in seven households with children, are experiencing food insecurity. Racial and ethnic disparities in food insecurity have remained consistent over the past 2 decades, with about twice as many Black and Hispanic homes experiencing food insecurity as White homes.
More recent research using Census Household Pulse Surveys has found a tremendous increase in food insecurity for children in 2020. One in three Black children and one in four Hispanic children are food insecure, according to these surveys. The rates are one in six for Asian households and one in ten for White households.
“The disparity is consistent,” Dr. Essel said. “We see what COVID has done. We once may have described it as a great equalizer – everyone is touched in the same way – but the reality is, this is actually a great magnifier. It’s revealing to us and magnifying disparities that have existed for far too long and has really allowed us to see it in a new way.”
A big part of disparities in food insecurity is disparities in wealth, “the safety net or cushion for families when things go wrong,” Dr. Essel said. The median wealth of White Americans in 2016 was $171,000, compared to $20,700 among Latinx Americans and $17,600 among Black Americans, according to the Federal Reserve Board Survey of Consumer Finances.
Food insecurity interventions
Federal nutrition programs – such as Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and school meal programs – are key to addressing food insecurity, Dr. Essel said.
“They have a long track record of rescuing families out of poverty, of rescuing families from food security and improving overall health of families,” he said.
But emergency food relief programs are important as well. Four in 10 families currently coming into food pantries are new recipients, and these resources have seen a 60% increase in clients, he said.
“This is utterly unreasonable for them to be able to manage,” he said. “Food pantries are essential but inadequate to compensate for large numbers of families,” even while they also may be the only option for families unable or unwilling to access federal programs. For example, for every one meal that food banks can provide, SNAP can provide nine meals, Dr. Essel said. Further, during times of economic downtown, every SNAP $1 spent generates $1.50 to $2 in economic activity.
Currently, the Pandemic Electronic Benefit Transfer (P-EBT) program provides benefits to families for school breakfast and lunch and has been extended through December 2021. Another federal pandemic response was to increase SNAP to the maximum household benefit for families, about $646 for a family of four, although 40% of households were already receiving the maximum benefit.
Food insecurity advocacy
You can advocate for any one of multiple pillars when it comes to food insecurity, Dr. Essel said. “Food cannot solve food insecurity by itself,” he said. “We have to think about root causes – systemic causes – and think about unemployment, livable wage, systemic racism, oppression, an inequitable food system. All of these things are pillars that any of you can advocate for when recognizing a family that is struggling with food insecurity.”
He offered several suggestions for advocacy:
- Join your local AAP chapter and prioritize food insecurity.
- Join a local antihunger task force.
- Make your clinical environment as safe as possible for families to respond to questions about food insecurity.
- Know what’s happening in your community immigrant populations.
- Provide up-to-date information to families about eligibility for federal programs.
- Share stories through op-eds and letters to the editor, and by contacting congressional representatives and providing expert testimony to school boards and city councils.
- Educate others about food insecurity through the above channels and on social media.
Jessica Lazerov, MD, a general pediatrician at Children’s National Anacostia and assistant professor of pediatrics at George Washington University, Washington, said the session was fantastic.
“Dr. Essel went beyond the basics of food insecurity, delving into the root causes, potential solutions, and important considerations when screening for food insecurity in practice,” Dr. Lazerov said in an interview. “I enjoyed his focus on advocacy, as well as the fact that he spent a bit of time reviewing how the COVID pandemic has affected food insecurity. I truly felt empowered to take my advocacy efforts a step further as Dr. Essel laid out concrete, actionable next steps, as well as a review of the most relevant and current information about food insecurity.”
Dr. Essel, Dr. Lazerov, and Dr. Gray have no relevant financial disclosures.
and advocate on behalf of those experiencing or at risk of food insecurity, according to Kofi Essel, MD, MPH, a pediatrician at Children’s National Hospital in Washington.
More than one in four adults are dealing with food access hardships during the pandemic, Dr. Essel said at the virtual annual meeting of the American Academy of Pediatrics. Food insecurity is often interchangeable with hunger and refers to limited or uncertain availability of foods that are nutritious and safe.
“Food insecurity is as much about the threat of deprivation as it is about deprivation itself: A food-insecure life means a life lived in fear of hunger, and the psychological toll that takes,” according to a 2020 New York Times photo feature on food insecurity by Brenda Ann Kenneally that Dr. Essel quoted.
The lived experience of food insecure households includes food anxiety, a preoccupation with being able to get enough food that takes up cognitive bandwidth and prevents people from being able to focus on other important things. Another feature of food-insecure homes is a monotony of diet, which often involves an increase in caloric density and decrease in nutritional quality. As food insecurity grows more dire, adults’ food intake decreases, and then children’s intake decreases as adults seek out any way to get food, including “socially unacceptable” ways, which can include food pantries and bartering for food.
Food insecurity is associated with a wide range of negative outcomes even after accounting for other confounders, including decreased overall health, mental health, and educational outcomes. It’s also associated with an increase in developmental delays, hospitalizations, iron deficiency, asthma, and birth defects, among other problems. Somewhat paradoxically, it’s associated with both an increase and a decrease in obesity in the research.
Megan J. Gray, MD, MPH, assistant professor of pediatrics and population health at Dell Medical School at the The University of Texas at Austin, attended Dr. Essel’s session because food insecurity during COVID-19 now affects about half her patients, according to screening research she’s conducted.
“I wanted to learn more about the nuances of screening and using language and talking points that are helpful with families and with staff in building a culture of discussing food insecurity in our clinics,” Dr. Gray said in an interview. “What I’ve learned in my clinic is that if we don’t ask about it, families aren’t telling us – food insecurity is hiding in plain sight.”
She particularly appreciated Dr. Essel’s slides on the progression of food insecurity and how they acknowledged the mental health burden of food insecurity among parents.
“Right now during COVID-19, I see more patients I would call ‘socially complex’ rather than ‘medically complex,’ ” she said. “We all need to get a crash course in social work and Dr. Essel’s presentation is a great starting place.”
Screening for food insecurity
Beginning in 2015, an AAP policy statement charged pediatricians to “screen and intervene” with regard to food insecurity and their patients, Dr. Essel said. The statement also called for pediatricians to advocate for programs and policies that end childhood food insecurity.
The policy statement recommended a validated two-question screening tool called the Hunger Vital Sign:
1. “Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
2. “Within the past 12 months, the food that we bought just didn’t last and we didn’t have money to get more.”
But in screening, you need to be conscious of how dignity intersects with food insecurity concerns, Dr. Essel said.
“We need to create dignity for our families,” he said. “We need to create a safe environment for our families and use appropriate tools when necessary to be able to identify families that are struggling with food insecurity.”
That need is seen in research on food screening. The Hunger Vital Signs questions can be asked with a dichotomous variable, as a yes/no question, or on a Likert scale, though the latter is a more complex way to ask.
A 2017 study found, however, that asking with “yes/no” answers missed more than a quarter of at-risk families. In the AAP survey using “yes/no” answers, 31% of families screened positive for being at risk of food insecurity, compared with 46% when the same question was asked on a Likert scale. It seems the ability to answer with “sometimes” feels “safer” than answering “yes,” Dr. Essel said.
Another factor that potentially affects answers is how doctors ask. In a March 2020 study at a single primary care practice, 16% of families screened positive with yes/no responses to a food insecurity screen when the questions were written, compared with 10% of positive screens with verbal responses (P < .001).
Epidemiology of food insecurity
The most updated United States Department of Agriculture report on food insecurity released in September shows the United States finally reached prerecession levels in 2019, with 11% of families designated as “food insecure.” But 2019 data cannot show what has occurred since the pandemic.
Further, the numbers are higher in households with children: Fourteen percent, or one in seven households with children, are experiencing food insecurity. Racial and ethnic disparities in food insecurity have remained consistent over the past 2 decades, with about twice as many Black and Hispanic homes experiencing food insecurity as White homes.
More recent research using Census Household Pulse Surveys has found a tremendous increase in food insecurity for children in 2020. One in three Black children and one in four Hispanic children are food insecure, according to these surveys. The rates are one in six for Asian households and one in ten for White households.
“The disparity is consistent,” Dr. Essel said. “We see what COVID has done. We once may have described it as a great equalizer – everyone is touched in the same way – but the reality is, this is actually a great magnifier. It’s revealing to us and magnifying disparities that have existed for far too long and has really allowed us to see it in a new way.”
A big part of disparities in food insecurity is disparities in wealth, “the safety net or cushion for families when things go wrong,” Dr. Essel said. The median wealth of White Americans in 2016 was $171,000, compared to $20,700 among Latinx Americans and $17,600 among Black Americans, according to the Federal Reserve Board Survey of Consumer Finances.
Food insecurity interventions
Federal nutrition programs – such as Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and school meal programs – are key to addressing food insecurity, Dr. Essel said.
“They have a long track record of rescuing families out of poverty, of rescuing families from food security and improving overall health of families,” he said.
But emergency food relief programs are important as well. Four in 10 families currently coming into food pantries are new recipients, and these resources have seen a 60% increase in clients, he said.
“This is utterly unreasonable for them to be able to manage,” he said. “Food pantries are essential but inadequate to compensate for large numbers of families,” even while they also may be the only option for families unable or unwilling to access federal programs. For example, for every one meal that food banks can provide, SNAP can provide nine meals, Dr. Essel said. Further, during times of economic downtown, every SNAP $1 spent generates $1.50 to $2 in economic activity.
Currently, the Pandemic Electronic Benefit Transfer (P-EBT) program provides benefits to families for school breakfast and lunch and has been extended through December 2021. Another federal pandemic response was to increase SNAP to the maximum household benefit for families, about $646 for a family of four, although 40% of households were already receiving the maximum benefit.
Food insecurity advocacy
You can advocate for any one of multiple pillars when it comes to food insecurity, Dr. Essel said. “Food cannot solve food insecurity by itself,” he said. “We have to think about root causes – systemic causes – and think about unemployment, livable wage, systemic racism, oppression, an inequitable food system. All of these things are pillars that any of you can advocate for when recognizing a family that is struggling with food insecurity.”
He offered several suggestions for advocacy:
- Join your local AAP chapter and prioritize food insecurity.
- Join a local antihunger task force.
- Make your clinical environment as safe as possible for families to respond to questions about food insecurity.
- Know what’s happening in your community immigrant populations.
- Provide up-to-date information to families about eligibility for federal programs.
- Share stories through op-eds and letters to the editor, and by contacting congressional representatives and providing expert testimony to school boards and city councils.
- Educate others about food insecurity through the above channels and on social media.
Jessica Lazerov, MD, a general pediatrician at Children’s National Anacostia and assistant professor of pediatrics at George Washington University, Washington, said the session was fantastic.
“Dr. Essel went beyond the basics of food insecurity, delving into the root causes, potential solutions, and important considerations when screening for food insecurity in practice,” Dr. Lazerov said in an interview. “I enjoyed his focus on advocacy, as well as the fact that he spent a bit of time reviewing how the COVID pandemic has affected food insecurity. I truly felt empowered to take my advocacy efforts a step further as Dr. Essel laid out concrete, actionable next steps, as well as a review of the most relevant and current information about food insecurity.”
Dr. Essel, Dr. Lazerov, and Dr. Gray have no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 2020
Five pediatric heart health practices that may be unnecessary
the American Academy of Pediatrics explained in guidance released Nov. 2.
The AAP Section on Cardiology and Cardiac Surgery developed the recommendations as part of the Choosing Wisely campaign after reviewing evidence pertaining to practices common during pediatric visits, such as routinely ordering an electrocardiogram (ECG) as part of a sports exam.
The guidance lets physicians know what is not necessary or not indicated, with noted exceptions, Christopher S. Snyder, MD, chair of the section, said in an interview.
In all cases, family history is key, said Dr. Snyder, who is also chief of the division of pediatric cardiology at University Hospitals Cleveland Medical Center. That means taking the time necessary to ask about aunts, uncles, and all first-degree relatives, not just asking the single question of whether a patient has a family history of cardiac problems.
The following are the targeted practices and the AAP’s guidance on each.
ECG for sports participation
A screening ECG should not be ordered as part of a routine sports entry examination in otherwise healthy patients who have no symptoms and no personal or family history of cardiac disease, the committee says.
Some medical societies argue that all children who participate in sports should have an ECG, but, Dr. Snyder said, “Currently there are no data that support that, especially in the United States.”
ECGs often yield false positive findings, he noted: “About 10% of them will say the child is a little abnormal.”
That can be a particular problem in places with few or no pediatric cardiologists because kids can become sidelined from sports without access to experts who could clear them.
“In the U.S.,” he said, “we believe that the preparticipation physical exam and screening, which is routine for all high school athletes for sure and most athletes who compete in sports, is currently good enough.”
However, he warned, patients with a family history of heart disease need to see a pediatric cardiologist and “those patients need an ECG.”
The test is not perfect, though, he noted: “You could get your screening, go home, get a fever, COVID, something like that, and come back and have myocarditis and drop dead.”
ECG before ADHD therapy
Similarly, a screening ECG is not routinely needed before initiating therapy for ADHD in asymptomatic, otherwise healthy children who have no personal or family history of cardiac disease, according to the new guidance.
Dr. Snyder said that it has become routine for children to undergo an ECG before ADHD therapy, but evidence doesn’t support the practice, and with the rise in the number of ADHD diagnoses, the tests have increasingly become a burden.
Twenty years ago, the prevalence of ADHD was 3%-4%, Dr. Snyder said. It is now almost threefold higher.
The AAP committee points out that, when ECG abnormalities are identified, they rarely lead to a change in ADHD therapy. Additionally, the typical stimulants used to treat ADHD “have never shown any major effect on the heart,” Dr. Snyder said.
“Black box warnings have been put on these medications, but nothing has been found in the very routine stimulants in normal, routine doses to warrant an ECG,” he said.
Echocardiogram for syncope
The committee says routine use of echocardiograms for children with syncope is unnecessary unless a child has a concerning history or ECG abnormalities.
Most patient who have true syncope or are passing out or fainting are diagnosed through thorough family history, Dr. Snyder said.
“The vast majority of those need an ECG to rule out one other cause that can do this and a physical exam. If those things are normal, there really is no indication to do an echocardiogram,” he said.
“If the patient passes out while they’re running, they pass out doing strenuous exercise, or they pass out for 10-15 minutes as opposed to 20 seconds – those are the ones that need a thorough cardiac workup. But routine passing out, waking up in seconds, those do not.”
Echocardiogram for chest pain
Children with chest pain do not need an echocardiogram unless an ECG is abnormal or the patient has a concerning history, according to the new recommendations.
Too often, Dr. Snyder said, providers treat kids as they would adults.
“Often it comes down to what you learn in medical school,” Dr. Snyder said. “In medical school, we have 6 weeks of cardiology and we had 1 hour of pediatric cardiology.”
That younger patients will clog their arteries with fatty foods and high lipids “is really exceptionally rare,” Dr. Snyder said.
Chest pain “rarely, if ever” means heart attack in younger children, he added.
A thorough history and complete physical exam are critical, “without jumping immediately to an echocardiogram, which 99.9% of the time is going to be normal,” he said.
Troponins for chest pain
In addition, a typical workup for pediatric chest pain need not include evaluating troponins unless there is a concerning history or ECG abnormalities.
Snyder notes that kids with chest pain are often brought to emergency departments that are not pediatric specific, and thus clinicians turn to the standard treatment for adults with chest pain: ECG and troponin.
“The reason we in pediatric cardiology don’t love this is that troponins tend not to be specific just for heart in kids,” Dr. Snyder said. “If someone has anginal chest pain – shortness of breath, chest pain doing anything and everything, [chest pain that] occurs when they’re exercising, feels like an elephant standing on their chest – then we do encourage troponins on those patients.”
The guidance discourages ordering troponins without careful consideration of the patient’s age and condition, he said.
This list was developed by faculty in Pediatric Cardiology at University Hospitals in Cleveland. It was revised and approved by the AAP Section on Cardiology and Cardiac Surgery and the AAP Executive Committee.
A version of this article originally appeared on Medscape.com.
the American Academy of Pediatrics explained in guidance released Nov. 2.
The AAP Section on Cardiology and Cardiac Surgery developed the recommendations as part of the Choosing Wisely campaign after reviewing evidence pertaining to practices common during pediatric visits, such as routinely ordering an electrocardiogram (ECG) as part of a sports exam.
The guidance lets physicians know what is not necessary or not indicated, with noted exceptions, Christopher S. Snyder, MD, chair of the section, said in an interview.
In all cases, family history is key, said Dr. Snyder, who is also chief of the division of pediatric cardiology at University Hospitals Cleveland Medical Center. That means taking the time necessary to ask about aunts, uncles, and all first-degree relatives, not just asking the single question of whether a patient has a family history of cardiac problems.
The following are the targeted practices and the AAP’s guidance on each.
ECG for sports participation
A screening ECG should not be ordered as part of a routine sports entry examination in otherwise healthy patients who have no symptoms and no personal or family history of cardiac disease, the committee says.
Some medical societies argue that all children who participate in sports should have an ECG, but, Dr. Snyder said, “Currently there are no data that support that, especially in the United States.”
ECGs often yield false positive findings, he noted: “About 10% of them will say the child is a little abnormal.”
That can be a particular problem in places with few or no pediatric cardiologists because kids can become sidelined from sports without access to experts who could clear them.
“In the U.S.,” he said, “we believe that the preparticipation physical exam and screening, which is routine for all high school athletes for sure and most athletes who compete in sports, is currently good enough.”
However, he warned, patients with a family history of heart disease need to see a pediatric cardiologist and “those patients need an ECG.”
The test is not perfect, though, he noted: “You could get your screening, go home, get a fever, COVID, something like that, and come back and have myocarditis and drop dead.”
ECG before ADHD therapy
Similarly, a screening ECG is not routinely needed before initiating therapy for ADHD in asymptomatic, otherwise healthy children who have no personal or family history of cardiac disease, according to the new guidance.
Dr. Snyder said that it has become routine for children to undergo an ECG before ADHD therapy, but evidence doesn’t support the practice, and with the rise in the number of ADHD diagnoses, the tests have increasingly become a burden.
Twenty years ago, the prevalence of ADHD was 3%-4%, Dr. Snyder said. It is now almost threefold higher.
The AAP committee points out that, when ECG abnormalities are identified, they rarely lead to a change in ADHD therapy. Additionally, the typical stimulants used to treat ADHD “have never shown any major effect on the heart,” Dr. Snyder said.
“Black box warnings have been put on these medications, but nothing has been found in the very routine stimulants in normal, routine doses to warrant an ECG,” he said.
Echocardiogram for syncope
The committee says routine use of echocardiograms for children with syncope is unnecessary unless a child has a concerning history or ECG abnormalities.
Most patient who have true syncope or are passing out or fainting are diagnosed through thorough family history, Dr. Snyder said.
“The vast majority of those need an ECG to rule out one other cause that can do this and a physical exam. If those things are normal, there really is no indication to do an echocardiogram,” he said.
“If the patient passes out while they’re running, they pass out doing strenuous exercise, or they pass out for 10-15 minutes as opposed to 20 seconds – those are the ones that need a thorough cardiac workup. But routine passing out, waking up in seconds, those do not.”
Echocardiogram for chest pain
Children with chest pain do not need an echocardiogram unless an ECG is abnormal or the patient has a concerning history, according to the new recommendations.
Too often, Dr. Snyder said, providers treat kids as they would adults.
“Often it comes down to what you learn in medical school,” Dr. Snyder said. “In medical school, we have 6 weeks of cardiology and we had 1 hour of pediatric cardiology.”
That younger patients will clog their arteries with fatty foods and high lipids “is really exceptionally rare,” Dr. Snyder said.
Chest pain “rarely, if ever” means heart attack in younger children, he added.
A thorough history and complete physical exam are critical, “without jumping immediately to an echocardiogram, which 99.9% of the time is going to be normal,” he said.
Troponins for chest pain
In addition, a typical workup for pediatric chest pain need not include evaluating troponins unless there is a concerning history or ECG abnormalities.
Snyder notes that kids with chest pain are often brought to emergency departments that are not pediatric specific, and thus clinicians turn to the standard treatment for adults with chest pain: ECG and troponin.
“The reason we in pediatric cardiology don’t love this is that troponins tend not to be specific just for heart in kids,” Dr. Snyder said. “If someone has anginal chest pain – shortness of breath, chest pain doing anything and everything, [chest pain that] occurs when they’re exercising, feels like an elephant standing on their chest – then we do encourage troponins on those patients.”
The guidance discourages ordering troponins without careful consideration of the patient’s age and condition, he said.
This list was developed by faculty in Pediatric Cardiology at University Hospitals in Cleveland. It was revised and approved by the AAP Section on Cardiology and Cardiac Surgery and the AAP Executive Committee.
A version of this article originally appeared on Medscape.com.
the American Academy of Pediatrics explained in guidance released Nov. 2.
The AAP Section on Cardiology and Cardiac Surgery developed the recommendations as part of the Choosing Wisely campaign after reviewing evidence pertaining to practices common during pediatric visits, such as routinely ordering an electrocardiogram (ECG) as part of a sports exam.
The guidance lets physicians know what is not necessary or not indicated, with noted exceptions, Christopher S. Snyder, MD, chair of the section, said in an interview.
In all cases, family history is key, said Dr. Snyder, who is also chief of the division of pediatric cardiology at University Hospitals Cleveland Medical Center. That means taking the time necessary to ask about aunts, uncles, and all first-degree relatives, not just asking the single question of whether a patient has a family history of cardiac problems.
The following are the targeted practices and the AAP’s guidance on each.
ECG for sports participation
A screening ECG should not be ordered as part of a routine sports entry examination in otherwise healthy patients who have no symptoms and no personal or family history of cardiac disease, the committee says.
Some medical societies argue that all children who participate in sports should have an ECG, but, Dr. Snyder said, “Currently there are no data that support that, especially in the United States.”
ECGs often yield false positive findings, he noted: “About 10% of them will say the child is a little abnormal.”
That can be a particular problem in places with few or no pediatric cardiologists because kids can become sidelined from sports without access to experts who could clear them.
“In the U.S.,” he said, “we believe that the preparticipation physical exam and screening, which is routine for all high school athletes for sure and most athletes who compete in sports, is currently good enough.”
However, he warned, patients with a family history of heart disease need to see a pediatric cardiologist and “those patients need an ECG.”
The test is not perfect, though, he noted: “You could get your screening, go home, get a fever, COVID, something like that, and come back and have myocarditis and drop dead.”
ECG before ADHD therapy
Similarly, a screening ECG is not routinely needed before initiating therapy for ADHD in asymptomatic, otherwise healthy children who have no personal or family history of cardiac disease, according to the new guidance.
Dr. Snyder said that it has become routine for children to undergo an ECG before ADHD therapy, but evidence doesn’t support the practice, and with the rise in the number of ADHD diagnoses, the tests have increasingly become a burden.
Twenty years ago, the prevalence of ADHD was 3%-4%, Dr. Snyder said. It is now almost threefold higher.
The AAP committee points out that, when ECG abnormalities are identified, they rarely lead to a change in ADHD therapy. Additionally, the typical stimulants used to treat ADHD “have never shown any major effect on the heart,” Dr. Snyder said.
“Black box warnings have been put on these medications, but nothing has been found in the very routine stimulants in normal, routine doses to warrant an ECG,” he said.
Echocardiogram for syncope
The committee says routine use of echocardiograms for children with syncope is unnecessary unless a child has a concerning history or ECG abnormalities.
Most patient who have true syncope or are passing out or fainting are diagnosed through thorough family history, Dr. Snyder said.
“The vast majority of those need an ECG to rule out one other cause that can do this and a physical exam. If those things are normal, there really is no indication to do an echocardiogram,” he said.
“If the patient passes out while they’re running, they pass out doing strenuous exercise, or they pass out for 10-15 minutes as opposed to 20 seconds – those are the ones that need a thorough cardiac workup. But routine passing out, waking up in seconds, those do not.”
Echocardiogram for chest pain
Children with chest pain do not need an echocardiogram unless an ECG is abnormal or the patient has a concerning history, according to the new recommendations.
Too often, Dr. Snyder said, providers treat kids as they would adults.
“Often it comes down to what you learn in medical school,” Dr. Snyder said. “In medical school, we have 6 weeks of cardiology and we had 1 hour of pediatric cardiology.”
That younger patients will clog their arteries with fatty foods and high lipids “is really exceptionally rare,” Dr. Snyder said.
Chest pain “rarely, if ever” means heart attack in younger children, he added.
A thorough history and complete physical exam are critical, “without jumping immediately to an echocardiogram, which 99.9% of the time is going to be normal,” he said.
Troponins for chest pain
In addition, a typical workup for pediatric chest pain need not include evaluating troponins unless there is a concerning history or ECG abnormalities.
Snyder notes that kids with chest pain are often brought to emergency departments that are not pediatric specific, and thus clinicians turn to the standard treatment for adults with chest pain: ECG and troponin.
“The reason we in pediatric cardiology don’t love this is that troponins tend not to be specific just for heart in kids,” Dr. Snyder said. “If someone has anginal chest pain – shortness of breath, chest pain doing anything and everything, [chest pain that] occurs when they’re exercising, feels like an elephant standing on their chest – then we do encourage troponins on those patients.”
The guidance discourages ordering troponins without careful consideration of the patient’s age and condition, he said.
This list was developed by faculty in Pediatric Cardiology at University Hospitals in Cleveland. It was revised and approved by the AAP Section on Cardiology and Cardiac Surgery and the AAP Executive Committee.
A version of this article originally appeared on Medscape.com.
‘Disordered eating’ drops after teens undergo bariatric surgery
Kristina M. Decker, PhD, a postdoctoral fellow at Cincinnati Children’s Hospital Medical Center, presented these findings during the virtual ObesityWeek 2020.
Dr. Decker and associates examined rates of disordered eating in more than 200 adolescents (aged 13-18 years) who were severely obese, of whom 141 underwent bariatric surgery and the remainder did not.
At baseline (presurgery), the teens in both groups had rates of disordered eating ranging from 11% to 50%, with higher rates in those who went on to have bariatric surgery.
Six years later, rates of disordered eating were much lower in those who had bariatric surgery.
The data nevertheless “underscore that young adults with persistent severe obesity are at high risk for poor health and well-being,” Dr. Decker said in an interview.
“This means disordered eating behaviors should be closely monitored” in all such patients, both those who undergo surgery and those who don’t, she stressed.
Robust findings because of long follow-up and controls
The findings are not unexpected, based on adult bariatric literature, but are “novel because of the age of the patients,” senior author Margaret H. Zeller, PhD, Cincinnati Children’s Hospital Medical Center and professor at the University of Cincinnati, added.
In a comment comment, psychologist Kajsa Järvholm, PhD, of the Childhood Obesity Unit at Skåne University Hospital, Malmö̈, Sweden, who has published related work, said that this is “a needed study.”
Notably, it had “long-term follow-up and a control group,” and it “confirms that adolescents are in better control of their eating after surgery.”
However, an important additional takeaway for clinicians is that “disordered eating is associated with other mental health problems and self-worth. Clinicians treating obesity must address problems related to eating disorders to improve outcomes and well-being,” she stressed.
How does bariatric surgery impact overeating, binge eating, in teens?
“For teens with severe obesity, metabolic and bariatric surgery is the most effective treatment for improved cardiometabolic functioning, weight loss, and improved quality of life,” Dr. Decker stressed.
However, pre- and postsurgical disordered eating behaviors have been associated with a lower percentage change in body mass index (BMI), although this has not been well studied.
To investigate how disordered eating is affected by bariatric surgery in adolescents with severe obesity, researchers used data from Teen-LABS, which enrolled 242 participants aged 19 years and under who mainly underwent Roux-en-Y gastric bypass (67%) or sleeve gastrectomy (28%) from 2007 to 2012 at five adolescent bariatric surgery centers.
The current analysis examined data from 141 participants in Teen-LABS who underwent bariatric surgery at a mean age of 16.8 years. Mean BMI was 51.5, most were girls (80%), and they had diverse race/ethnicity (66% were White).
Researchers also identified a control group of 83 adolescents of a similar age and gender who had diverse race/ethnicity (54% White) and a mean BMI of 46.9.
At year 6, data were available for 123 young adults in the surgery group (who by then had a mean BMI of 39.7) and 63 young adults in the nonsurgery group (who had a mean BMI of 52.6).
At baseline and year 6, participants replied to questionnaires that identified three eating disorders: continuous eating (eating in an unplanned and repetitious way between meals and snacks), objective overeating (eating a “large” amount of food without loss of control), and objective binge eating (eating a “large” amount of food with loss of control).
At baseline, rates of continuous eating, overeating, and binge eating were higher in the surgical group (50%, 40%, and 30%, respectively) than the nonsurgical group (40%, 22%, and 11%, respectively).
Six years later, when participants were aged 19-24 years, rates of continuous eating, overeating, and binge eating had declined in the surgical group (to 17%, 5%, and 1%, respectively). In the nonsurgical group, only continuous eating and overeating declined (to 24% and 7%, respectively), and binge eating increased slightly (to 13%).
Disordered eating associated with low self-worth, anxiety, and depression
In young adulthood in both groups, disordered eating was associated with lower self-worth. In the surgical group, it was also associated with lower weight-related quality of life, and in the nonsurgical group, it was also associated with anxiety and/or depression.
“The current findings cannot tell us whether disordered eating is a direct result or caused by anxiety, depression, low self-worth, or poor quality of life,” Dr. Decker said.
“These findings do give us insight about what other areas of clinical concern might present together [in] young adults (e.g., disordered eating, low self-esteem).”
Bariatric surgery affects the amount of food people can eat at one time, she noted in reply to a question from the audience. If people eat too much at a time they can experience vomiting, dumping syndrome (where certain food is “dumped” into the small intestine without being digested, causing nausea and vomiting), and plugging (a sense of food becoming stuck).
The home environment and transition to adulthood might impact disordered eating in young adults, she said in reply to another question, but these issues were not examined in this study.
A version of this article originally appeared on Medscape.com.
Kristina M. Decker, PhD, a postdoctoral fellow at Cincinnati Children’s Hospital Medical Center, presented these findings during the virtual ObesityWeek 2020.
Dr. Decker and associates examined rates of disordered eating in more than 200 adolescents (aged 13-18 years) who were severely obese, of whom 141 underwent bariatric surgery and the remainder did not.
At baseline (presurgery), the teens in both groups had rates of disordered eating ranging from 11% to 50%, with higher rates in those who went on to have bariatric surgery.
Six years later, rates of disordered eating were much lower in those who had bariatric surgery.
The data nevertheless “underscore that young adults with persistent severe obesity are at high risk for poor health and well-being,” Dr. Decker said in an interview.
“This means disordered eating behaviors should be closely monitored” in all such patients, both those who undergo surgery and those who don’t, she stressed.
Robust findings because of long follow-up and controls
The findings are not unexpected, based on adult bariatric literature, but are “novel because of the age of the patients,” senior author Margaret H. Zeller, PhD, Cincinnati Children’s Hospital Medical Center and professor at the University of Cincinnati, added.
In a comment comment, psychologist Kajsa Järvholm, PhD, of the Childhood Obesity Unit at Skåne University Hospital, Malmö̈, Sweden, who has published related work, said that this is “a needed study.”
Notably, it had “long-term follow-up and a control group,” and it “confirms that adolescents are in better control of their eating after surgery.”
However, an important additional takeaway for clinicians is that “disordered eating is associated with other mental health problems and self-worth. Clinicians treating obesity must address problems related to eating disorders to improve outcomes and well-being,” she stressed.
How does bariatric surgery impact overeating, binge eating, in teens?
“For teens with severe obesity, metabolic and bariatric surgery is the most effective treatment for improved cardiometabolic functioning, weight loss, and improved quality of life,” Dr. Decker stressed.
However, pre- and postsurgical disordered eating behaviors have been associated with a lower percentage change in body mass index (BMI), although this has not been well studied.
To investigate how disordered eating is affected by bariatric surgery in adolescents with severe obesity, researchers used data from Teen-LABS, which enrolled 242 participants aged 19 years and under who mainly underwent Roux-en-Y gastric bypass (67%) or sleeve gastrectomy (28%) from 2007 to 2012 at five adolescent bariatric surgery centers.
The current analysis examined data from 141 participants in Teen-LABS who underwent bariatric surgery at a mean age of 16.8 years. Mean BMI was 51.5, most were girls (80%), and they had diverse race/ethnicity (66% were White).
Researchers also identified a control group of 83 adolescents of a similar age and gender who had diverse race/ethnicity (54% White) and a mean BMI of 46.9.
At year 6, data were available for 123 young adults in the surgery group (who by then had a mean BMI of 39.7) and 63 young adults in the nonsurgery group (who had a mean BMI of 52.6).
At baseline and year 6, participants replied to questionnaires that identified three eating disorders: continuous eating (eating in an unplanned and repetitious way between meals and snacks), objective overeating (eating a “large” amount of food without loss of control), and objective binge eating (eating a “large” amount of food with loss of control).
At baseline, rates of continuous eating, overeating, and binge eating were higher in the surgical group (50%, 40%, and 30%, respectively) than the nonsurgical group (40%, 22%, and 11%, respectively).
Six years later, when participants were aged 19-24 years, rates of continuous eating, overeating, and binge eating had declined in the surgical group (to 17%, 5%, and 1%, respectively). In the nonsurgical group, only continuous eating and overeating declined (to 24% and 7%, respectively), and binge eating increased slightly (to 13%).
Disordered eating associated with low self-worth, anxiety, and depression
In young adulthood in both groups, disordered eating was associated with lower self-worth. In the surgical group, it was also associated with lower weight-related quality of life, and in the nonsurgical group, it was also associated with anxiety and/or depression.
“The current findings cannot tell us whether disordered eating is a direct result or caused by anxiety, depression, low self-worth, or poor quality of life,” Dr. Decker said.
“These findings do give us insight about what other areas of clinical concern might present together [in] young adults (e.g., disordered eating, low self-esteem).”
Bariatric surgery affects the amount of food people can eat at one time, she noted in reply to a question from the audience. If people eat too much at a time they can experience vomiting, dumping syndrome (where certain food is “dumped” into the small intestine without being digested, causing nausea and vomiting), and plugging (a sense of food becoming stuck).
The home environment and transition to adulthood might impact disordered eating in young adults, she said in reply to another question, but these issues were not examined in this study.
A version of this article originally appeared on Medscape.com.
Kristina M. Decker, PhD, a postdoctoral fellow at Cincinnati Children’s Hospital Medical Center, presented these findings during the virtual ObesityWeek 2020.
Dr. Decker and associates examined rates of disordered eating in more than 200 adolescents (aged 13-18 years) who were severely obese, of whom 141 underwent bariatric surgery and the remainder did not.
At baseline (presurgery), the teens in both groups had rates of disordered eating ranging from 11% to 50%, with higher rates in those who went on to have bariatric surgery.
Six years later, rates of disordered eating were much lower in those who had bariatric surgery.
The data nevertheless “underscore that young adults with persistent severe obesity are at high risk for poor health and well-being,” Dr. Decker said in an interview.
“This means disordered eating behaviors should be closely monitored” in all such patients, both those who undergo surgery and those who don’t, she stressed.
Robust findings because of long follow-up and controls
The findings are not unexpected, based on adult bariatric literature, but are “novel because of the age of the patients,” senior author Margaret H. Zeller, PhD, Cincinnati Children’s Hospital Medical Center and professor at the University of Cincinnati, added.
In a comment comment, psychologist Kajsa Järvholm, PhD, of the Childhood Obesity Unit at Skåne University Hospital, Malmö̈, Sweden, who has published related work, said that this is “a needed study.”
Notably, it had “long-term follow-up and a control group,” and it “confirms that adolescents are in better control of their eating after surgery.”
However, an important additional takeaway for clinicians is that “disordered eating is associated with other mental health problems and self-worth. Clinicians treating obesity must address problems related to eating disorders to improve outcomes and well-being,” she stressed.
How does bariatric surgery impact overeating, binge eating, in teens?
“For teens with severe obesity, metabolic and bariatric surgery is the most effective treatment for improved cardiometabolic functioning, weight loss, and improved quality of life,” Dr. Decker stressed.
However, pre- and postsurgical disordered eating behaviors have been associated with a lower percentage change in body mass index (BMI), although this has not been well studied.
To investigate how disordered eating is affected by bariatric surgery in adolescents with severe obesity, researchers used data from Teen-LABS, which enrolled 242 participants aged 19 years and under who mainly underwent Roux-en-Y gastric bypass (67%) or sleeve gastrectomy (28%) from 2007 to 2012 at five adolescent bariatric surgery centers.
The current analysis examined data from 141 participants in Teen-LABS who underwent bariatric surgery at a mean age of 16.8 years. Mean BMI was 51.5, most were girls (80%), and they had diverse race/ethnicity (66% were White).
Researchers also identified a control group of 83 adolescents of a similar age and gender who had diverse race/ethnicity (54% White) and a mean BMI of 46.9.
At year 6, data were available for 123 young adults in the surgery group (who by then had a mean BMI of 39.7) and 63 young adults in the nonsurgery group (who had a mean BMI of 52.6).
At baseline and year 6, participants replied to questionnaires that identified three eating disorders: continuous eating (eating in an unplanned and repetitious way between meals and snacks), objective overeating (eating a “large” amount of food without loss of control), and objective binge eating (eating a “large” amount of food with loss of control).
At baseline, rates of continuous eating, overeating, and binge eating were higher in the surgical group (50%, 40%, and 30%, respectively) than the nonsurgical group (40%, 22%, and 11%, respectively).
Six years later, when participants were aged 19-24 years, rates of continuous eating, overeating, and binge eating had declined in the surgical group (to 17%, 5%, and 1%, respectively). In the nonsurgical group, only continuous eating and overeating declined (to 24% and 7%, respectively), and binge eating increased slightly (to 13%).
Disordered eating associated with low self-worth, anxiety, and depression
In young adulthood in both groups, disordered eating was associated with lower self-worth. In the surgical group, it was also associated with lower weight-related quality of life, and in the nonsurgical group, it was also associated with anxiety and/or depression.
“The current findings cannot tell us whether disordered eating is a direct result or caused by anxiety, depression, low self-worth, or poor quality of life,” Dr. Decker said.
“These findings do give us insight about what other areas of clinical concern might present together [in] young adults (e.g., disordered eating, low self-esteem).”
Bariatric surgery affects the amount of food people can eat at one time, she noted in reply to a question from the audience. If people eat too much at a time they can experience vomiting, dumping syndrome (where certain food is “dumped” into the small intestine without being digested, causing nausea and vomiting), and plugging (a sense of food becoming stuck).
The home environment and transition to adulthood might impact disordered eating in young adults, she said in reply to another question, but these issues were not examined in this study.
A version of this article originally appeared on Medscape.com.
Who’s at risk for depression on isotretinoin?
A Sanaa Butt, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
This was, however, the sole identifiable risk factor for treatment-limiting depressive symptoms in acne patients on isotretinoin in the study of 3,151 consecutive acne patients taking isotretinoin. There was no significant difference between those who did or did not develop depression on the oral retinoid in terms of age, gender, or daily dose of the drug at the time it was discontinued.
“Depressive symptoms occurred at any time from the date of initiation of isotretinoin up to 6 months into therapy, with no identifiable peak time period,” said Dr. Butt, a dermatologist with the U.K. National Health Service Tayside district at Ninewells Hospital, Dundee, Scotland. “Lower doses appear not to be protective,” she added.
The Tayside district has a catchment of roughly 450,000 people. The local population tends to stay put because Tayside is an economically disadvantaged and remote part of Scotland. There are very few private practice dermatologists in the area, so Dr. Butt and coinvestigators are confident their observational study of NHS patients captured the great majority of isotretinoin users in northern Scotland.
The investigators utilized software to analyze the contents of more than 8,000 digitized letters exchanged between NHS Tayside dermatologists and general practitioners during 2005-2018, zeroing in on 3,151 consecutive patients on isotretinoin for acne and 158 on the drug for other conditions, most often rosacea or folliculitis. They then drilled down further through the letters, electronically searching for key words such as suicide, depression, and anxiety. In this way, they ultimately identified 30 patients who discontinued the drug because they developed depressive symptoms. All 30 were on the drug for acne.
The annual incidence of treatment-limiting depressive mood changes was 0.96%, a figure that remained steady over the 13-year study period, even though prescribing of isotretinoin increased over time. This flat incidence rate effectively rules out the potential for confounding because of assessor bias, especially since many different NHS dermatologists were prescribing the drug, Dr. Butt said.
Half of acne patients prescribed isotretinoin were female and 50% were male. And 15 cases of treatment discontinuation caused by development of depressive symptoms occurred in females, 15 in males. A history of past depressive illness was present in 9.3% of females who started on isotretinoin and in 4.5% of the males. The relative risk of treatment-limiting depressive mood changes was increased 790% among females with a prior history of depressive illness and 440% in males with such a history.
Dr. Butt reported having no financial conflicts regarding her NHS-funded study.
A Sanaa Butt, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
This was, however, the sole identifiable risk factor for treatment-limiting depressive symptoms in acne patients on isotretinoin in the study of 3,151 consecutive acne patients taking isotretinoin. There was no significant difference between those who did or did not develop depression on the oral retinoid in terms of age, gender, or daily dose of the drug at the time it was discontinued.
“Depressive symptoms occurred at any time from the date of initiation of isotretinoin up to 6 months into therapy, with no identifiable peak time period,” said Dr. Butt, a dermatologist with the U.K. National Health Service Tayside district at Ninewells Hospital, Dundee, Scotland. “Lower doses appear not to be protective,” she added.
The Tayside district has a catchment of roughly 450,000 people. The local population tends to stay put because Tayside is an economically disadvantaged and remote part of Scotland. There are very few private practice dermatologists in the area, so Dr. Butt and coinvestigators are confident their observational study of NHS patients captured the great majority of isotretinoin users in northern Scotland.
The investigators utilized software to analyze the contents of more than 8,000 digitized letters exchanged between NHS Tayside dermatologists and general practitioners during 2005-2018, zeroing in on 3,151 consecutive patients on isotretinoin for acne and 158 on the drug for other conditions, most often rosacea or folliculitis. They then drilled down further through the letters, electronically searching for key words such as suicide, depression, and anxiety. In this way, they ultimately identified 30 patients who discontinued the drug because they developed depressive symptoms. All 30 were on the drug for acne.
The annual incidence of treatment-limiting depressive mood changes was 0.96%, a figure that remained steady over the 13-year study period, even though prescribing of isotretinoin increased over time. This flat incidence rate effectively rules out the potential for confounding because of assessor bias, especially since many different NHS dermatologists were prescribing the drug, Dr. Butt said.
Half of acne patients prescribed isotretinoin were female and 50% were male. And 15 cases of treatment discontinuation caused by development of depressive symptoms occurred in females, 15 in males. A history of past depressive illness was present in 9.3% of females who started on isotretinoin and in 4.5% of the males. The relative risk of treatment-limiting depressive mood changes was increased 790% among females with a prior history of depressive illness and 440% in males with such a history.
Dr. Butt reported having no financial conflicts regarding her NHS-funded study.
A Sanaa Butt, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
This was, however, the sole identifiable risk factor for treatment-limiting depressive symptoms in acne patients on isotretinoin in the study of 3,151 consecutive acne patients taking isotretinoin. There was no significant difference between those who did or did not develop depression on the oral retinoid in terms of age, gender, or daily dose of the drug at the time it was discontinued.
“Depressive symptoms occurred at any time from the date of initiation of isotretinoin up to 6 months into therapy, with no identifiable peak time period,” said Dr. Butt, a dermatologist with the U.K. National Health Service Tayside district at Ninewells Hospital, Dundee, Scotland. “Lower doses appear not to be protective,” she added.
The Tayside district has a catchment of roughly 450,000 people. The local population tends to stay put because Tayside is an economically disadvantaged and remote part of Scotland. There are very few private practice dermatologists in the area, so Dr. Butt and coinvestigators are confident their observational study of NHS patients captured the great majority of isotretinoin users in northern Scotland.
The investigators utilized software to analyze the contents of more than 8,000 digitized letters exchanged between NHS Tayside dermatologists and general practitioners during 2005-2018, zeroing in on 3,151 consecutive patients on isotretinoin for acne and 158 on the drug for other conditions, most often rosacea or folliculitis. They then drilled down further through the letters, electronically searching for key words such as suicide, depression, and anxiety. In this way, they ultimately identified 30 patients who discontinued the drug because they developed depressive symptoms. All 30 were on the drug for acne.
The annual incidence of treatment-limiting depressive mood changes was 0.96%, a figure that remained steady over the 13-year study period, even though prescribing of isotretinoin increased over time. This flat incidence rate effectively rules out the potential for confounding because of assessor bias, especially since many different NHS dermatologists were prescribing the drug, Dr. Butt said.
Half of acne patients prescribed isotretinoin were female and 50% were male. And 15 cases of treatment discontinuation caused by development of depressive symptoms occurred in females, 15 in males. A history of past depressive illness was present in 9.3% of females who started on isotretinoin and in 4.5% of the males. The relative risk of treatment-limiting depressive mood changes was increased 790% among females with a prior history of depressive illness and 440% in males with such a history.
Dr. Butt reported having no financial conflicts regarding her NHS-funded study.
FROM THE EADV CONGRESS
Information blocking: Adolescent confidentiality is collateral damage
On April 4, 2021, a rule implementing the federal regulations of the Information Blocking 21st Century Cures Act will be enacted. This Act furthers the seamless release of medical records to promote improved outcomes, access to medical information, and transparency of costs. Each state will need to be thoughtful balancing the action or inaction of allowing access to confidential or sensitive progress notes, as interference with access may be considered information blocking and subject to penalties and fines.
With adolescent confidential notes, protection rules may not apply under the information blocking regulations. These regulations will release progress notes, imaging narratives, procedure notes, and labs to parents via their EHR portals. The release of information is not limited, and both inpatient and outpatient records will be released. These regulations are written for adults with the assumption that all information is released to the individual receiving the care and shared with outside providers.
Unfortunately, the rules do not take into consideration adolescent confidential care. There are eight rules for the exception of releasing information, but it may be a stretch to place adolescent confidential progress notes under any of these eight exceptions. These exceptions are ambiguous and open to interpretation yet require specific documentation as to the limitation of access. Exceptions are prevention of harm; privacy conflicts; the security of the electronic health information; infeasibility, which includes challenges limiting the ability to comply; Health IT performance; content and manner; fees; and licensing.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
On April 4, 2021, a rule implementing the federal regulations of the Information Blocking 21st Century Cures Act will be enacted. This Act furthers the seamless release of medical records to promote improved outcomes, access to medical information, and transparency of costs. Each state will need to be thoughtful balancing the action or inaction of allowing access to confidential or sensitive progress notes, as interference with access may be considered information blocking and subject to penalties and fines.
With adolescent confidential notes, protection rules may not apply under the information blocking regulations. These regulations will release progress notes, imaging narratives, procedure notes, and labs to parents via their EHR portals. The release of information is not limited, and both inpatient and outpatient records will be released. These regulations are written for adults with the assumption that all information is released to the individual receiving the care and shared with outside providers.
Unfortunately, the rules do not take into consideration adolescent confidential care. There are eight rules for the exception of releasing information, but it may be a stretch to place adolescent confidential progress notes under any of these eight exceptions. These exceptions are ambiguous and open to interpretation yet require specific documentation as to the limitation of access. Exceptions are prevention of harm; privacy conflicts; the security of the electronic health information; infeasibility, which includes challenges limiting the ability to comply; Health IT performance; content and manner; fees; and licensing.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
On April 4, 2021, a rule implementing the federal regulations of the Information Blocking 21st Century Cures Act will be enacted. This Act furthers the seamless release of medical records to promote improved outcomes, access to medical information, and transparency of costs. Each state will need to be thoughtful balancing the action or inaction of allowing access to confidential or sensitive progress notes, as interference with access may be considered information blocking and subject to penalties and fines.
With adolescent confidential notes, protection rules may not apply under the information blocking regulations. These regulations will release progress notes, imaging narratives, procedure notes, and labs to parents via their EHR portals. The release of information is not limited, and both inpatient and outpatient records will be released. These regulations are written for adults with the assumption that all information is released to the individual receiving the care and shared with outside providers.
Unfortunately, the rules do not take into consideration adolescent confidential care. There are eight rules for the exception of releasing information, but it may be a stretch to place adolescent confidential progress notes under any of these eight exceptions. These exceptions are ambiguous and open to interpretation yet require specific documentation as to the limitation of access. Exceptions are prevention of harm; privacy conflicts; the security of the electronic health information; infeasibility, which includes challenges limiting the ability to comply; Health IT performance; content and manner; fees; and licensing.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].











