User login
Slowing, not stopping, Alzheimer’s a better goal for clinical trials?
and may be a more realistic goal for clinical AD drug trials, a new report suggests.
The report is a yearlong undertaking by an expert work group convened by the Alzheimer’s Association and was prompted, in part, by the fallout from the U.S. Food and Drug Administration’s controversial decision to grant aducanumab (Aduhelm) accelerated approval, which came over the objection of an advisory panel that found the drug was ineffective.
The report’s authors call for a “reframing” of how researchers define “clinically meaningful” in randomized controlled trials (RCTs), noting that it’s time to adjust expectations of outcomes from relatively short clinical trials.
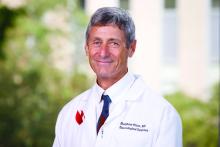
“Without lowering the bar, are we expecting too much from a clinical trial by expecting that unless the disease is halted in its tracks and there’s no progression, we failed at treatment?” the report’s lead author and group leader Ronald C. Petersen, MD, PhD, lead author, chair of the work group, and professor of neurology at the Mayo Clinic, Rochester, Minn., told this news organization.
Interpretations of clinical meaningfulness are used in the drug approval process and in decisions about whether an insurer will cover the cost of treatment, the authors note.
While the report doesn’t provide a consensus definition of clinically meaningful benefit, it does offer a starting point for a conversation about how the phrase should be defined in the context of RCTs for disease-modifying therapies (DMTs) in AD, Dr. Petersen said.
“What we tried to do was to put it into some kind of perspective and at least have people reflect on this: If you’re going to design the perfect drug trial in Alzheimer’s disease, what would it be? We wanted to get people to think about it without digging in their heels for or against,” he added.
The report was published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
A proactive measure
The expert group began its work in January 2022, less than a year after the FDA approved aducanumab. Since the panel began its work, the FDA has approved a second AD drug, lecanemab (Leqembi), and denied accelerated approval of a third medication, donanemab.
“At the time we started this group, we had one approved treatment, and we just knew that there were others on the way, and we needed to be prepared to have this conversation and be more proactive than reactive,” Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association and co-author of the report, said in an interview.
The work group suggests that simply slowing disease progression might be a desired goal for drug trials, especially early on, before cognition and memory are affected.
They also note that a benefit identified during an 18-month clinical trial may ultimately lead to even more meaningful changes over coming years, well beyond the trial’s end.
In addition, the report authors call for the development of better research tools to more accurately assess meaningful change. The Clinical Dementia Rating (CDR) scale is currently the key instrument used as a primary outcome measure in RCTs. However, the report’s authors note that it may not be adequate to measure meaningful change in early-stage disease.
“Developing better tools certainly should be on the radar screen for all of us, because I think we can do better,” Dr. Petersen said. “The CDR, as good as it is and as long as it’s been used in the field, is a pretty blunt instrument, and it’s the result of subjective ratings.”
‘Quality of mind’
Jason Karlawish, MD, professor of medicine, medical ethics, health policy, and neurology at the University of Pennsylvania, Philadelphia, said measuring the actual impact of a drug on a patient’s disease and quality of life has been a hot topic in the AD field for some time, but settling on a definition of “clinically meaningful” that everyone agrees upon will be a challenge.
“I think the idea of ‘clinically meaningful’ is truly a socially constructed idea,” said Dr. Karlawish, co-director of Penn’s Memory Center, who did not work on the report.
“You can come up with objective measures of cognition, but a measure to call something ‘clinically meaningful’ ultimately requires some sort of negotiated social order among clinicians and patients and others who have immediate interest in the health and well-being of the patient.”
Dr. Karlawish added that he’s interested in the conversations the report might prompt and the challenges it could highlight, especially when it comes to how meaningful clinical benefit can be measured, regardless of how it’s defined.
“Hidden in this conversation about clinically meaningful treatments in Alzheimer’s disease is, frankly, not quality of life, but quality of mind,” said Dr. Karlawish. “No measure captures acceptably the very thing that everyone actually cares a lot about and why we view this disease as so dreadful, which is damage to our mind.”
More evidence needed
The development of such tools will take time. What does that mean for drugs already in the pipeline? Members of the work group argue that those trials must move forward at the same time new tools are being created.
“We need to continue to refine, develop better instruments, [and] develop tools that are going to assess the disease in its more subtle features early on, even in the so-called ‘pre-symptomatic’ stage of the disease,” said lead author Dr. Petersen. “We shouldn’t wait for the development of that before intervening if we have a drug that seems to work.”
However, not everyone who agrees with the premise of the report agrees with this position, including Joel S. Perlmutter, MD, professor of neurology, Washington University School of Medicine, St. Louis, who also commented on the report.
As reported by this news organization, Dr. Perlmutter was one of three physicians who resigned from the FDA advisory panel that voted against approving aducanumab after the agency moved forward anyway.
“We have to be careful not to recommend DMTs that we hope will help without strong evidence, especially when potential side effects are not trivial,” Dr. Perlmutter said. “We have to have evidence before making these recommendations so we don’t end up harming people more than helping them.”
The report received no specific funding. Dr. Petersen received consulting fees from Roche, Nestle, Merck, Biogen, Eisai, and Genentech. Full disclosures are included in the original article. Dr. Perlmutter and Dr. Karlawish report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
and may be a more realistic goal for clinical AD drug trials, a new report suggests.
The report is a yearlong undertaking by an expert work group convened by the Alzheimer’s Association and was prompted, in part, by the fallout from the U.S. Food and Drug Administration’s controversial decision to grant aducanumab (Aduhelm) accelerated approval, which came over the objection of an advisory panel that found the drug was ineffective.
The report’s authors call for a “reframing” of how researchers define “clinically meaningful” in randomized controlled trials (RCTs), noting that it’s time to adjust expectations of outcomes from relatively short clinical trials.
“Without lowering the bar, are we expecting too much from a clinical trial by expecting that unless the disease is halted in its tracks and there’s no progression, we failed at treatment?” the report’s lead author and group leader Ronald C. Petersen, MD, PhD, lead author, chair of the work group, and professor of neurology at the Mayo Clinic, Rochester, Minn., told this news organization.
Interpretations of clinical meaningfulness are used in the drug approval process and in decisions about whether an insurer will cover the cost of treatment, the authors note.
While the report doesn’t provide a consensus definition of clinically meaningful benefit, it does offer a starting point for a conversation about how the phrase should be defined in the context of RCTs for disease-modifying therapies (DMTs) in AD, Dr. Petersen said.
“What we tried to do was to put it into some kind of perspective and at least have people reflect on this: If you’re going to design the perfect drug trial in Alzheimer’s disease, what would it be? We wanted to get people to think about it without digging in their heels for or against,” he added.
The report was published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
A proactive measure
The expert group began its work in January 2022, less than a year after the FDA approved aducanumab. Since the panel began its work, the FDA has approved a second AD drug, lecanemab (Leqembi), and denied accelerated approval of a third medication, donanemab.
“At the time we started this group, we had one approved treatment, and we just knew that there were others on the way, and we needed to be prepared to have this conversation and be more proactive than reactive,” Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association and co-author of the report, said in an interview.
The work group suggests that simply slowing disease progression might be a desired goal for drug trials, especially early on, before cognition and memory are affected.
They also note that a benefit identified during an 18-month clinical trial may ultimately lead to even more meaningful changes over coming years, well beyond the trial’s end.
In addition, the report authors call for the development of better research tools to more accurately assess meaningful change. The Clinical Dementia Rating (CDR) scale is currently the key instrument used as a primary outcome measure in RCTs. However, the report’s authors note that it may not be adequate to measure meaningful change in early-stage disease.
“Developing better tools certainly should be on the radar screen for all of us, because I think we can do better,” Dr. Petersen said. “The CDR, as good as it is and as long as it’s been used in the field, is a pretty blunt instrument, and it’s the result of subjective ratings.”
‘Quality of mind’
Jason Karlawish, MD, professor of medicine, medical ethics, health policy, and neurology at the University of Pennsylvania, Philadelphia, said measuring the actual impact of a drug on a patient’s disease and quality of life has been a hot topic in the AD field for some time, but settling on a definition of “clinically meaningful” that everyone agrees upon will be a challenge.
“I think the idea of ‘clinically meaningful’ is truly a socially constructed idea,” said Dr. Karlawish, co-director of Penn’s Memory Center, who did not work on the report.
“You can come up with objective measures of cognition, but a measure to call something ‘clinically meaningful’ ultimately requires some sort of negotiated social order among clinicians and patients and others who have immediate interest in the health and well-being of the patient.”
Dr. Karlawish added that he’s interested in the conversations the report might prompt and the challenges it could highlight, especially when it comes to how meaningful clinical benefit can be measured, regardless of how it’s defined.
“Hidden in this conversation about clinically meaningful treatments in Alzheimer’s disease is, frankly, not quality of life, but quality of mind,” said Dr. Karlawish. “No measure captures acceptably the very thing that everyone actually cares a lot about and why we view this disease as so dreadful, which is damage to our mind.”
More evidence needed
The development of such tools will take time. What does that mean for drugs already in the pipeline? Members of the work group argue that those trials must move forward at the same time new tools are being created.
“We need to continue to refine, develop better instruments, [and] develop tools that are going to assess the disease in its more subtle features early on, even in the so-called ‘pre-symptomatic’ stage of the disease,” said lead author Dr. Petersen. “We shouldn’t wait for the development of that before intervening if we have a drug that seems to work.”
However, not everyone who agrees with the premise of the report agrees with this position, including Joel S. Perlmutter, MD, professor of neurology, Washington University School of Medicine, St. Louis, who also commented on the report.
As reported by this news organization, Dr. Perlmutter was one of three physicians who resigned from the FDA advisory panel that voted against approving aducanumab after the agency moved forward anyway.
“We have to be careful not to recommend DMTs that we hope will help without strong evidence, especially when potential side effects are not trivial,” Dr. Perlmutter said. “We have to have evidence before making these recommendations so we don’t end up harming people more than helping them.”
The report received no specific funding. Dr. Petersen received consulting fees from Roche, Nestle, Merck, Biogen, Eisai, and Genentech. Full disclosures are included in the original article. Dr. Perlmutter and Dr. Karlawish report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
and may be a more realistic goal for clinical AD drug trials, a new report suggests.
The report is a yearlong undertaking by an expert work group convened by the Alzheimer’s Association and was prompted, in part, by the fallout from the U.S. Food and Drug Administration’s controversial decision to grant aducanumab (Aduhelm) accelerated approval, which came over the objection of an advisory panel that found the drug was ineffective.
The report’s authors call for a “reframing” of how researchers define “clinically meaningful” in randomized controlled trials (RCTs), noting that it’s time to adjust expectations of outcomes from relatively short clinical trials.
“Without lowering the bar, are we expecting too much from a clinical trial by expecting that unless the disease is halted in its tracks and there’s no progression, we failed at treatment?” the report’s lead author and group leader Ronald C. Petersen, MD, PhD, lead author, chair of the work group, and professor of neurology at the Mayo Clinic, Rochester, Minn., told this news organization.
Interpretations of clinical meaningfulness are used in the drug approval process and in decisions about whether an insurer will cover the cost of treatment, the authors note.
While the report doesn’t provide a consensus definition of clinically meaningful benefit, it does offer a starting point for a conversation about how the phrase should be defined in the context of RCTs for disease-modifying therapies (DMTs) in AD, Dr. Petersen said.
“What we tried to do was to put it into some kind of perspective and at least have people reflect on this: If you’re going to design the perfect drug trial in Alzheimer’s disease, what would it be? We wanted to get people to think about it without digging in their heels for or against,” he added.
The report was published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
A proactive measure
The expert group began its work in January 2022, less than a year after the FDA approved aducanumab. Since the panel began its work, the FDA has approved a second AD drug, lecanemab (Leqembi), and denied accelerated approval of a third medication, donanemab.
“At the time we started this group, we had one approved treatment, and we just knew that there were others on the way, and we needed to be prepared to have this conversation and be more proactive than reactive,” Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association and co-author of the report, said in an interview.
The work group suggests that simply slowing disease progression might be a desired goal for drug trials, especially early on, before cognition and memory are affected.
They also note that a benefit identified during an 18-month clinical trial may ultimately lead to even more meaningful changes over coming years, well beyond the trial’s end.
In addition, the report authors call for the development of better research tools to more accurately assess meaningful change. The Clinical Dementia Rating (CDR) scale is currently the key instrument used as a primary outcome measure in RCTs. However, the report’s authors note that it may not be adequate to measure meaningful change in early-stage disease.
“Developing better tools certainly should be on the radar screen for all of us, because I think we can do better,” Dr. Petersen said. “The CDR, as good as it is and as long as it’s been used in the field, is a pretty blunt instrument, and it’s the result of subjective ratings.”
‘Quality of mind’
Jason Karlawish, MD, professor of medicine, medical ethics, health policy, and neurology at the University of Pennsylvania, Philadelphia, said measuring the actual impact of a drug on a patient’s disease and quality of life has been a hot topic in the AD field for some time, but settling on a definition of “clinically meaningful” that everyone agrees upon will be a challenge.
“I think the idea of ‘clinically meaningful’ is truly a socially constructed idea,” said Dr. Karlawish, co-director of Penn’s Memory Center, who did not work on the report.
“You can come up with objective measures of cognition, but a measure to call something ‘clinically meaningful’ ultimately requires some sort of negotiated social order among clinicians and patients and others who have immediate interest in the health and well-being of the patient.”
Dr. Karlawish added that he’s interested in the conversations the report might prompt and the challenges it could highlight, especially when it comes to how meaningful clinical benefit can be measured, regardless of how it’s defined.
“Hidden in this conversation about clinically meaningful treatments in Alzheimer’s disease is, frankly, not quality of life, but quality of mind,” said Dr. Karlawish. “No measure captures acceptably the very thing that everyone actually cares a lot about and why we view this disease as so dreadful, which is damage to our mind.”
More evidence needed
The development of such tools will take time. What does that mean for drugs already in the pipeline? Members of the work group argue that those trials must move forward at the same time new tools are being created.
“We need to continue to refine, develop better instruments, [and] develop tools that are going to assess the disease in its more subtle features early on, even in the so-called ‘pre-symptomatic’ stage of the disease,” said lead author Dr. Petersen. “We shouldn’t wait for the development of that before intervening if we have a drug that seems to work.”
However, not everyone who agrees with the premise of the report agrees with this position, including Joel S. Perlmutter, MD, professor of neurology, Washington University School of Medicine, St. Louis, who also commented on the report.
As reported by this news organization, Dr. Perlmutter was one of three physicians who resigned from the FDA advisory panel that voted against approving aducanumab after the agency moved forward anyway.
“We have to be careful not to recommend DMTs that we hope will help without strong evidence, especially when potential side effects are not trivial,” Dr. Perlmutter said. “We have to have evidence before making these recommendations so we don’t end up harming people more than helping them.”
The report received no specific funding. Dr. Petersen received consulting fees from Roche, Nestle, Merck, Biogen, Eisai, and Genentech. Full disclosures are included in the original article. Dr. Perlmutter and Dr. Karlawish report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ALZHEIMER’S AND DEMENTIA
What’s new in brain health?
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
Drug combo promising in vascular cognitive impairment: LACI-2 trial results
and is seen as a new therapeutic approach for patients with cerebral small-vessel disease. The drugs – isosorbide mononitrate and cilostazol – stabilize endothelial function, which is a new therapeutic target for patients with small-vessel disease stroke.
The phase 2 LACI-2 study, evaluating these drugs individually and in combination in patients with lacunar stroke, showed promising trends toward reductions in recurrent stroke, cognitive impairment, and dependency, some of which became significant when the drugs were given together. There was also some suggestion of positive impacts on mood and quality of life.
“Isosorbide mononitrate was associated with a reduction in recurrent stroke, a tendency toward a reduction in dependency and a reduction in cognitive impairment, and cilostazol also seemed to reduce dependency,” study investigator Joanna M. Wardlaw, MD, professor of applied neuroimaging at Edinburgh University, reported.
“When used together, they seemed to have more benefits than either drug on its own. So this is good preliminary evidence that the drugs are working together in a positive way,” she said. But she cautioned that these potential benefits will need to be confirmed in a larger phase 3 trial.
The LACI-2 study was presented at the International Stroke Conference by Dr. Wardlaw and coinvestigator Philip Bath, DSc, professor of medicine at the University of Nottingham (England).
They both highlighted the effect seen on cognitive impairment at the conference presented by the American Stroke Association, a division of the American Heart Association.
“We saw a significant reduction in the number of patients with cognitive impairment with the two drugs together in this phase 2 study,” Dr. Wardlaw said. “This is very encouraging since no study has previously found any medications that positively affect cognitive impairment in small-vessel disease strokes. We cautiously hope that these medications may have wider implications for other types of small-vessel disease as well.”
Dr. Bath added: “The results on cognitive impairment are particularly important. Many patients rate cognitive impairment as one of the most dreaded outcomes of a stroke even if they also have quite significant physical disability. People simply don’t want to lose their memory and thinking ability.”
“The results of LACI-2 also raise interesting questions about whether these drugs would be beneficial for other types of small-vessel disease which do not present as stroke, but maybe may manifest as headaches or memory impairment,” he noted.
‘Very intriguing results’
Outside experts were enthusiastic about these preliminary results. In an ISC highlights presentation, program chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, N.J., said: “It is refreshing to finally see some positive signals in studies in small-vessel stroke. This is an area where we haven’t had answers for a long time.”
He described the reduction in cognitive impairment seen in the study as “very intriguing and very important.”
“I think we have underestimated the burden that cognitive impairment has in stroke, and the burden in general in society of vascular cognitive impairment. This is a very promising approach that definitely deserves to be investigated more thoroughly in a larger trial.”
Commenting on the study findings, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University Irving Medical Center, New York, said this study “provides evidence that points us in at least two important directions.”
“First, it suggests that endothelial dysfunction, or problems with the lining of the blood vessels, may be an important contributor to small-vessel disease and the cognitive decline that often accompanies it. This is a new mechanism of action and different from blood clotting, blood pressure, and other conventional targets of treatment,” Dr. Elkind said.
“Second, and more generally, it suggests that stroke trials, particularly in the subtype of small-vessel disease, can and should explore not only the incidence of recurrent acute events but also the steady decline that occurs after stroke. Poststroke cognitive decline is a relatively new area of stroke research.”
Dr. Wardlaw noted that lacunar stroke is a common type of ischemic stroke, but it has been rather neglected in terms of research. It is assumed to be caused by atherosclerosis of the small vessel but there is now mounting evidence suggesting that it is a result of problems in the endothelium of the small vessels.
“We looked for potential available drugs that targeted endothelial dysfunction. Both the drugs we tested are already widely used – isosorbide mononitrate for the treatment of coronary artery disease and angina, and cilostazol, mainly in Asia, for stroke prevention,” she said.
LACI-2 was primarily a feasibility study looking at whether it was possible to recruit enough patients who had had a lacunar stroke and would take the drugs, individually or in combination, for up to a year. Outcomes were investigated on an exploratory basis. The study enrolled 363 patients who had experienced lacunar stroke from 26 stroke centers throughout the United Kingdom. They were randomly assigned to one of four treatment groups for 1 year:
- 40-60 mg/day of oral isosorbide mononitrate alone.
- 200 mg/day of oral cilostazol alone.
- Both medications.
- Neither medication.
Patients completed phone surveys at 6 and 12 months to assess health status, including recurrent stroke, myocardial infarction, cognitive tests, symptoms, quality of life surveys, and they also had brain imaging at 12 months.
Results showed 98% of patients were still taking their study medication at 1 year, and the drugs appeared to be safe on top of usual care with few deaths or hemorrhages in the study.
The composite outcome including recurrent stroke, MI, cognitive impairment, dependency (modified Rankin score > 2) and death was reduced by 20% in the isosorbide mononitrate–alone group (adjusted hazard ratio, 0.80; 95% confidence interval, 0.59-1.09).
The composite endpoint was reduced by 23% in the cilostazol group (aHR, 0.77; 95% CI, 0.57-1.05) and by 42% in the combination group (aHR, 0.58, 95% CI, 0.36-0.92) compared with those taking neither drug.
Isosorbide mononitrate alone showed trends toward a reduction in recurrent stroke, cognitive impairment, and dependency, whereas cilostazol alone reduced dependency with a trend toward a reduction in cognitive impairment. When used together, the drugs showed large reductions in cognitive impairment (aHR, 0.44; 95% CI, 0.19-0.99) and dependency (aHR ,0.14; 95% CI, 0.03-0.59).
During the highlights session, Dr. Jovin commented: “It is obvious that the investigators have put a lot of thought into the design of this trial. Presumably because of the composite score they were able to increase the power. We are used to trials which require thousands of patients, but here we are able to see significant results, although exploratory, with just a few hundred patients.”
Dr. Bath stressed that this was only a phase 2 study. “We now need to see if we can confirm these results in a larger phase 3 study.” That study, LACI-3, is planned to start later this year. He also suggested that it would be interesting to investigate whether these drugs would work in other types of ischemic stroke such as those caused by large-artery disease or cardioembolic strokes, as well as other forms of small-vessel disease such as patients with vascular cognitive impairment.
“There are many areas to investigate in future. It might be that in a few years’ time these drugs may be standard of care across many different forms of small-vessel disease,” he said.
Dr. Wardlaw noted that lacunar strokes are generally quite mild strokes, which could be one of the reasons why they have not been the target of much research to date. But Dr. Bath added: “While they may be labeled as a mild stroke on the NIHSS scale, patients can still be quite badly affected. About half of patients with a lacunar stroke develop cognitive impairment and eventually dementia – that is certainly not mild.”
The study was funded primarily by the British Heart Foundation, with support from the UK Alzheimer’s Society, the UK Dementia Research Institute, the Stroke Association, the Fondation Leducq, NHS Research Scotland, and the UK National Institutes of Health Research Clinical Research Networks. Dr. Bath is an adviser to CoMind, DiaMedica, Phagenesis, and Roche. Dr. Wardlaw reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and is seen as a new therapeutic approach for patients with cerebral small-vessel disease. The drugs – isosorbide mononitrate and cilostazol – stabilize endothelial function, which is a new therapeutic target for patients with small-vessel disease stroke.
The phase 2 LACI-2 study, evaluating these drugs individually and in combination in patients with lacunar stroke, showed promising trends toward reductions in recurrent stroke, cognitive impairment, and dependency, some of which became significant when the drugs were given together. There was also some suggestion of positive impacts on mood and quality of life.
“Isosorbide mononitrate was associated with a reduction in recurrent stroke, a tendency toward a reduction in dependency and a reduction in cognitive impairment, and cilostazol also seemed to reduce dependency,” study investigator Joanna M. Wardlaw, MD, professor of applied neuroimaging at Edinburgh University, reported.
“When used together, they seemed to have more benefits than either drug on its own. So this is good preliminary evidence that the drugs are working together in a positive way,” she said. But she cautioned that these potential benefits will need to be confirmed in a larger phase 3 trial.
The LACI-2 study was presented at the International Stroke Conference by Dr. Wardlaw and coinvestigator Philip Bath, DSc, professor of medicine at the University of Nottingham (England).
They both highlighted the effect seen on cognitive impairment at the conference presented by the American Stroke Association, a division of the American Heart Association.
“We saw a significant reduction in the number of patients with cognitive impairment with the two drugs together in this phase 2 study,” Dr. Wardlaw said. “This is very encouraging since no study has previously found any medications that positively affect cognitive impairment in small-vessel disease strokes. We cautiously hope that these medications may have wider implications for other types of small-vessel disease as well.”
Dr. Bath added: “The results on cognitive impairment are particularly important. Many patients rate cognitive impairment as one of the most dreaded outcomes of a stroke even if they also have quite significant physical disability. People simply don’t want to lose their memory and thinking ability.”
“The results of LACI-2 also raise interesting questions about whether these drugs would be beneficial for other types of small-vessel disease which do not present as stroke, but maybe may manifest as headaches or memory impairment,” he noted.
‘Very intriguing results’
Outside experts were enthusiastic about these preliminary results. In an ISC highlights presentation, program chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, N.J., said: “It is refreshing to finally see some positive signals in studies in small-vessel stroke. This is an area where we haven’t had answers for a long time.”
He described the reduction in cognitive impairment seen in the study as “very intriguing and very important.”
“I think we have underestimated the burden that cognitive impairment has in stroke, and the burden in general in society of vascular cognitive impairment. This is a very promising approach that definitely deserves to be investigated more thoroughly in a larger trial.”
Commenting on the study findings, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University Irving Medical Center, New York, said this study “provides evidence that points us in at least two important directions.”
“First, it suggests that endothelial dysfunction, or problems with the lining of the blood vessels, may be an important contributor to small-vessel disease and the cognitive decline that often accompanies it. This is a new mechanism of action and different from blood clotting, blood pressure, and other conventional targets of treatment,” Dr. Elkind said.
“Second, and more generally, it suggests that stroke trials, particularly in the subtype of small-vessel disease, can and should explore not only the incidence of recurrent acute events but also the steady decline that occurs after stroke. Poststroke cognitive decline is a relatively new area of stroke research.”
Dr. Wardlaw noted that lacunar stroke is a common type of ischemic stroke, but it has been rather neglected in terms of research. It is assumed to be caused by atherosclerosis of the small vessel but there is now mounting evidence suggesting that it is a result of problems in the endothelium of the small vessels.
“We looked for potential available drugs that targeted endothelial dysfunction. Both the drugs we tested are already widely used – isosorbide mononitrate for the treatment of coronary artery disease and angina, and cilostazol, mainly in Asia, for stroke prevention,” she said.
LACI-2 was primarily a feasibility study looking at whether it was possible to recruit enough patients who had had a lacunar stroke and would take the drugs, individually or in combination, for up to a year. Outcomes were investigated on an exploratory basis. The study enrolled 363 patients who had experienced lacunar stroke from 26 stroke centers throughout the United Kingdom. They were randomly assigned to one of four treatment groups for 1 year:
- 40-60 mg/day of oral isosorbide mononitrate alone.
- 200 mg/day of oral cilostazol alone.
- Both medications.
- Neither medication.
Patients completed phone surveys at 6 and 12 months to assess health status, including recurrent stroke, myocardial infarction, cognitive tests, symptoms, quality of life surveys, and they also had brain imaging at 12 months.
Results showed 98% of patients were still taking their study medication at 1 year, and the drugs appeared to be safe on top of usual care with few deaths or hemorrhages in the study.
The composite outcome including recurrent stroke, MI, cognitive impairment, dependency (modified Rankin score > 2) and death was reduced by 20% in the isosorbide mononitrate–alone group (adjusted hazard ratio, 0.80; 95% confidence interval, 0.59-1.09).
The composite endpoint was reduced by 23% in the cilostazol group (aHR, 0.77; 95% CI, 0.57-1.05) and by 42% in the combination group (aHR, 0.58, 95% CI, 0.36-0.92) compared with those taking neither drug.
Isosorbide mononitrate alone showed trends toward a reduction in recurrent stroke, cognitive impairment, and dependency, whereas cilostazol alone reduced dependency with a trend toward a reduction in cognitive impairment. When used together, the drugs showed large reductions in cognitive impairment (aHR, 0.44; 95% CI, 0.19-0.99) and dependency (aHR ,0.14; 95% CI, 0.03-0.59).
During the highlights session, Dr. Jovin commented: “It is obvious that the investigators have put a lot of thought into the design of this trial. Presumably because of the composite score they were able to increase the power. We are used to trials which require thousands of patients, but here we are able to see significant results, although exploratory, with just a few hundred patients.”
Dr. Bath stressed that this was only a phase 2 study. “We now need to see if we can confirm these results in a larger phase 3 study.” That study, LACI-3, is planned to start later this year. He also suggested that it would be interesting to investigate whether these drugs would work in other types of ischemic stroke such as those caused by large-artery disease or cardioembolic strokes, as well as other forms of small-vessel disease such as patients with vascular cognitive impairment.
“There are many areas to investigate in future. It might be that in a few years’ time these drugs may be standard of care across many different forms of small-vessel disease,” he said.
Dr. Wardlaw noted that lacunar strokes are generally quite mild strokes, which could be one of the reasons why they have not been the target of much research to date. But Dr. Bath added: “While they may be labeled as a mild stroke on the NIHSS scale, patients can still be quite badly affected. About half of patients with a lacunar stroke develop cognitive impairment and eventually dementia – that is certainly not mild.”
The study was funded primarily by the British Heart Foundation, with support from the UK Alzheimer’s Society, the UK Dementia Research Institute, the Stroke Association, the Fondation Leducq, NHS Research Scotland, and the UK National Institutes of Health Research Clinical Research Networks. Dr. Bath is an adviser to CoMind, DiaMedica, Phagenesis, and Roche. Dr. Wardlaw reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and is seen as a new therapeutic approach for patients with cerebral small-vessel disease. The drugs – isosorbide mononitrate and cilostazol – stabilize endothelial function, which is a new therapeutic target for patients with small-vessel disease stroke.
The phase 2 LACI-2 study, evaluating these drugs individually and in combination in patients with lacunar stroke, showed promising trends toward reductions in recurrent stroke, cognitive impairment, and dependency, some of which became significant when the drugs were given together. There was also some suggestion of positive impacts on mood and quality of life.
“Isosorbide mononitrate was associated with a reduction in recurrent stroke, a tendency toward a reduction in dependency and a reduction in cognitive impairment, and cilostazol also seemed to reduce dependency,” study investigator Joanna M. Wardlaw, MD, professor of applied neuroimaging at Edinburgh University, reported.
“When used together, they seemed to have more benefits than either drug on its own. So this is good preliminary evidence that the drugs are working together in a positive way,” she said. But she cautioned that these potential benefits will need to be confirmed in a larger phase 3 trial.
The LACI-2 study was presented at the International Stroke Conference by Dr. Wardlaw and coinvestigator Philip Bath, DSc, professor of medicine at the University of Nottingham (England).
They both highlighted the effect seen on cognitive impairment at the conference presented by the American Stroke Association, a division of the American Heart Association.
“We saw a significant reduction in the number of patients with cognitive impairment with the two drugs together in this phase 2 study,” Dr. Wardlaw said. “This is very encouraging since no study has previously found any medications that positively affect cognitive impairment in small-vessel disease strokes. We cautiously hope that these medications may have wider implications for other types of small-vessel disease as well.”
Dr. Bath added: “The results on cognitive impairment are particularly important. Many patients rate cognitive impairment as one of the most dreaded outcomes of a stroke even if they also have quite significant physical disability. People simply don’t want to lose their memory and thinking ability.”
“The results of LACI-2 also raise interesting questions about whether these drugs would be beneficial for other types of small-vessel disease which do not present as stroke, but maybe may manifest as headaches or memory impairment,” he noted.
‘Very intriguing results’
Outside experts were enthusiastic about these preliminary results. In an ISC highlights presentation, program chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, N.J., said: “It is refreshing to finally see some positive signals in studies in small-vessel stroke. This is an area where we haven’t had answers for a long time.”
He described the reduction in cognitive impairment seen in the study as “very intriguing and very important.”
“I think we have underestimated the burden that cognitive impairment has in stroke, and the burden in general in society of vascular cognitive impairment. This is a very promising approach that definitely deserves to be investigated more thoroughly in a larger trial.”
Commenting on the study findings, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University Irving Medical Center, New York, said this study “provides evidence that points us in at least two important directions.”
“First, it suggests that endothelial dysfunction, or problems with the lining of the blood vessels, may be an important contributor to small-vessel disease and the cognitive decline that often accompanies it. This is a new mechanism of action and different from blood clotting, blood pressure, and other conventional targets of treatment,” Dr. Elkind said.
“Second, and more generally, it suggests that stroke trials, particularly in the subtype of small-vessel disease, can and should explore not only the incidence of recurrent acute events but also the steady decline that occurs after stroke. Poststroke cognitive decline is a relatively new area of stroke research.”
Dr. Wardlaw noted that lacunar stroke is a common type of ischemic stroke, but it has been rather neglected in terms of research. It is assumed to be caused by atherosclerosis of the small vessel but there is now mounting evidence suggesting that it is a result of problems in the endothelium of the small vessels.
“We looked for potential available drugs that targeted endothelial dysfunction. Both the drugs we tested are already widely used – isosorbide mononitrate for the treatment of coronary artery disease and angina, and cilostazol, mainly in Asia, for stroke prevention,” she said.
LACI-2 was primarily a feasibility study looking at whether it was possible to recruit enough patients who had had a lacunar stroke and would take the drugs, individually or in combination, for up to a year. Outcomes were investigated on an exploratory basis. The study enrolled 363 patients who had experienced lacunar stroke from 26 stroke centers throughout the United Kingdom. They were randomly assigned to one of four treatment groups for 1 year:
- 40-60 mg/day of oral isosorbide mononitrate alone.
- 200 mg/day of oral cilostazol alone.
- Both medications.
- Neither medication.
Patients completed phone surveys at 6 and 12 months to assess health status, including recurrent stroke, myocardial infarction, cognitive tests, symptoms, quality of life surveys, and they also had brain imaging at 12 months.
Results showed 98% of patients were still taking their study medication at 1 year, and the drugs appeared to be safe on top of usual care with few deaths or hemorrhages in the study.
The composite outcome including recurrent stroke, MI, cognitive impairment, dependency (modified Rankin score > 2) and death was reduced by 20% in the isosorbide mononitrate–alone group (adjusted hazard ratio, 0.80; 95% confidence interval, 0.59-1.09).
The composite endpoint was reduced by 23% in the cilostazol group (aHR, 0.77; 95% CI, 0.57-1.05) and by 42% in the combination group (aHR, 0.58, 95% CI, 0.36-0.92) compared with those taking neither drug.
Isosorbide mononitrate alone showed trends toward a reduction in recurrent stroke, cognitive impairment, and dependency, whereas cilostazol alone reduced dependency with a trend toward a reduction in cognitive impairment. When used together, the drugs showed large reductions in cognitive impairment (aHR, 0.44; 95% CI, 0.19-0.99) and dependency (aHR ,0.14; 95% CI, 0.03-0.59).
During the highlights session, Dr. Jovin commented: “It is obvious that the investigators have put a lot of thought into the design of this trial. Presumably because of the composite score they were able to increase the power. We are used to trials which require thousands of patients, but here we are able to see significant results, although exploratory, with just a few hundred patients.”
Dr. Bath stressed that this was only a phase 2 study. “We now need to see if we can confirm these results in a larger phase 3 study.” That study, LACI-3, is planned to start later this year. He also suggested that it would be interesting to investigate whether these drugs would work in other types of ischemic stroke such as those caused by large-artery disease or cardioembolic strokes, as well as other forms of small-vessel disease such as patients with vascular cognitive impairment.
“There are many areas to investigate in future. It might be that in a few years’ time these drugs may be standard of care across many different forms of small-vessel disease,” he said.
Dr. Wardlaw noted that lacunar strokes are generally quite mild strokes, which could be one of the reasons why they have not been the target of much research to date. But Dr. Bath added: “While they may be labeled as a mild stroke on the NIHSS scale, patients can still be quite badly affected. About half of patients with a lacunar stroke develop cognitive impairment and eventually dementia – that is certainly not mild.”
The study was funded primarily by the British Heart Foundation, with support from the UK Alzheimer’s Society, the UK Dementia Research Institute, the Stroke Association, the Fondation Leducq, NHS Research Scotland, and the UK National Institutes of Health Research Clinical Research Networks. Dr. Bath is an adviser to CoMind, DiaMedica, Phagenesis, and Roche. Dr. Wardlaw reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ISC 2023
Medicare ‘offers’ cancer patient a choice: Less life or more debt
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
Be aware of hepatic encephalopathy, dementia overlap in older patients with cirrhosis
, according to a new study involving U.S. veterans.
The overlap between dementia and HE was also independent of alcohol use, brain injury, age, and other metabolic risk factors.
“The aging of patients with cirrhosis leads us to encounter several individuals who may be prone to both of these diseases,” senior author Jasmohan Bajaj, MD, a professor of gastroenterology, hepatology, and nutrition at Virginia Commonwealth University Medical Center and GI section of the Central Virginia Veterans Healthcare System in Richmond, said in an interview.
“Given the epidemic of metabolic syndrome and alcohol, consider excluding cirrhosis in your patient [for] whom the presumptive diagnosis is dementia, since they could have concomitant HE,” he said.
“On the flip side, in those with HE who have predominant long-term memory issues and persistent cognitive changes, consider consulting a neuropsychiatrist or neurologist to ensure there is a resolution of the underlying disease process,” Dr. Bajaj added.
The study was published online in The American Journal of Gastroenterology.
Analyzing associations
HE is a common decompensating event in patients with cirrhosis. Because of the aging population of patients with cirrhosis, however, it’s important to differentiate HE from nonhepatic etiologies of cognitive impairment, such as dementia, the authors note.
Using data from the VA Corporate Data Warehouse, Dr. Bajaj and colleagues identified veterans with cirrhosis who received VA care between October 2019 and September 2021 and compared baseline characteristics between the cohorts based on the presence or absence of dementia. The research team then evaluated factors associated with having a diagnosis of dementia, adjusting for demographics, comorbid illnesses, cirrhosis etiology, and cirrhosis complications.
Investigators identified 71,522 veterans with diagnostic codes for cirrhosis who were engaged in VA care in 2019. They were mostly men (96.2%) and had a median age of 66. The most common etiologies of cirrhosis were alcohol and hepatitis C, followed by nonalcoholic steatohepatitis (NASH). The group also included veterans with predominantly compensated cirrhosis and a median MELD-Na score of 9. The MELD-Na score gauges the severity of chronic liver disease using values such as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium to predict survival.
Among those with cirrhosis, 5,647 (7.9%) also had dementia diagnosis codes. This rate is higher than the prevalence of dementia in the general population and equivalent to the rate of dementia in veterans without cirrhosis who are older than 65, the authors note.
In general, veterans with dementia tended to be older, to be White, to live in an urban area, and to have higher MELD-Na scores, and they were more frequently diagnosed with alcohol-related cirrhosis, alcohol and tobacco use disorder, diabetes, chronic kidney disease, chronic heart failure, brain trauma, and cerebrovascular disease.
In a multivariable analysis, the presence of any decompensating event was significantly associated with dementia. In subsequent analyses of individual decompensating events, however, the strongest association was with HE, while ascites or variceal bleeding did not add to the risk.
When HE was defined as patients who filled prescriptions for lactulose or rifaximin, the frequency of patients with HE decreased from 13.7% to 10.9%. In an analysis with HE as the decompensating event, the association between HE and dementia remained significant compared to when HE was defined by diagnostic codes alone.
“We were surprised by the high proportion of patients with dementia who also had cirrhosis, and given the genuine difficulty that clinicians have with defining HE vs. dementia, we were not very surprised at that overlap,” Dr. Bajaj said.
“We were also surprised at the specificity of this overlap only with HE and not with other decompensating events, which was also independent of head injury, alcohol use, and PTSD,” he added.
Additional research needed
Future research should look at the characteristics of HE, including the number of episodes or breakthrough episodes, and should focus on objective biomarkers to differentiate dementia and HE, the study authors write.
“The distinction and study of potential overlapping features among HE and dementia is important because HE is often treatable with medications and reverses after liver transplant, while this does not occur with dementia,” they add.
Dr. Bajaj and colleagues call for a greater awareness of disease processes and complications in older patients with cirrhosis, particularly since diagnostic imprecision can lead to patient and family confusion, distrust, and ineffective treatment.
The study will help physicians better understand the important overlap between dementia and HE, said Eric Orman, MD, an associate professor of medicine at Indiana University, Indianapolis.
Dr. Orman, who wasn’t involved with this study, has researched recent trends in the characteristics and outcomes of patients with newly diagnosed cirrhosis and has found that the proportion of older adults has increased, as well as those with alcoholic cirrhosis and NASH, which has implications for future patient care.
“It is important to recognize that both dementia and HE can occur either separately or concurrently in individuals with cirrhosis,” Dr. Orman told this news organization. “When seeing patients with cognitive impairment, having a high index of suspicion for both conditions is critical to ensure appropriate diagnosis and treatment.”
The study’s findings “represent the tip of the iceberg,” Neal Parikh, MD, an assistant professor of neurology and neuroscience at Weill Cornell Medicine in New York, said in an interview. “There is a tremendous amount left to be discovered regarding the role of the liver in brain health.”
Dr. Parikh, who wasn’t associated with this study, has researched the impact of chronic liver conditions on cognitive impairment and dementia. He is working on a project that addresses HE in detail.
“There is growing recognition of a so-called ‘liver-brain axis,’ with several researchers, including my group, showing that a range of chronic liver conditions may detrimentally impact cognitive function and increase the risk of dementia,” he said. “Studying the specific contributions of cirrhosis is critical for understanding the role of hepatic encephalopathy in age-related cognitive decline.”
The study received no financial support. The authors reported no potential competing interests.
A version of this article first appeared on Medscape.com.
, according to a new study involving U.S. veterans.
The overlap between dementia and HE was also independent of alcohol use, brain injury, age, and other metabolic risk factors.
“The aging of patients with cirrhosis leads us to encounter several individuals who may be prone to both of these diseases,” senior author Jasmohan Bajaj, MD, a professor of gastroenterology, hepatology, and nutrition at Virginia Commonwealth University Medical Center and GI section of the Central Virginia Veterans Healthcare System in Richmond, said in an interview.
“Given the epidemic of metabolic syndrome and alcohol, consider excluding cirrhosis in your patient [for] whom the presumptive diagnosis is dementia, since they could have concomitant HE,” he said.
“On the flip side, in those with HE who have predominant long-term memory issues and persistent cognitive changes, consider consulting a neuropsychiatrist or neurologist to ensure there is a resolution of the underlying disease process,” Dr. Bajaj added.
The study was published online in The American Journal of Gastroenterology.
Analyzing associations
HE is a common decompensating event in patients with cirrhosis. Because of the aging population of patients with cirrhosis, however, it’s important to differentiate HE from nonhepatic etiologies of cognitive impairment, such as dementia, the authors note.
Using data from the VA Corporate Data Warehouse, Dr. Bajaj and colleagues identified veterans with cirrhosis who received VA care between October 2019 and September 2021 and compared baseline characteristics between the cohorts based on the presence or absence of dementia. The research team then evaluated factors associated with having a diagnosis of dementia, adjusting for demographics, comorbid illnesses, cirrhosis etiology, and cirrhosis complications.
Investigators identified 71,522 veterans with diagnostic codes for cirrhosis who were engaged in VA care in 2019. They were mostly men (96.2%) and had a median age of 66. The most common etiologies of cirrhosis were alcohol and hepatitis C, followed by nonalcoholic steatohepatitis (NASH). The group also included veterans with predominantly compensated cirrhosis and a median MELD-Na score of 9. The MELD-Na score gauges the severity of chronic liver disease using values such as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium to predict survival.
Among those with cirrhosis, 5,647 (7.9%) also had dementia diagnosis codes. This rate is higher than the prevalence of dementia in the general population and equivalent to the rate of dementia in veterans without cirrhosis who are older than 65, the authors note.
In general, veterans with dementia tended to be older, to be White, to live in an urban area, and to have higher MELD-Na scores, and they were more frequently diagnosed with alcohol-related cirrhosis, alcohol and tobacco use disorder, diabetes, chronic kidney disease, chronic heart failure, brain trauma, and cerebrovascular disease.
In a multivariable analysis, the presence of any decompensating event was significantly associated with dementia. In subsequent analyses of individual decompensating events, however, the strongest association was with HE, while ascites or variceal bleeding did not add to the risk.
When HE was defined as patients who filled prescriptions for lactulose or rifaximin, the frequency of patients with HE decreased from 13.7% to 10.9%. In an analysis with HE as the decompensating event, the association between HE and dementia remained significant compared to when HE was defined by diagnostic codes alone.
“We were surprised by the high proportion of patients with dementia who also had cirrhosis, and given the genuine difficulty that clinicians have with defining HE vs. dementia, we were not very surprised at that overlap,” Dr. Bajaj said.
“We were also surprised at the specificity of this overlap only with HE and not with other decompensating events, which was also independent of head injury, alcohol use, and PTSD,” he added.
Additional research needed
Future research should look at the characteristics of HE, including the number of episodes or breakthrough episodes, and should focus on objective biomarkers to differentiate dementia and HE, the study authors write.
“The distinction and study of potential overlapping features among HE and dementia is important because HE is often treatable with medications and reverses after liver transplant, while this does not occur with dementia,” they add.
Dr. Bajaj and colleagues call for a greater awareness of disease processes and complications in older patients with cirrhosis, particularly since diagnostic imprecision can lead to patient and family confusion, distrust, and ineffective treatment.
The study will help physicians better understand the important overlap between dementia and HE, said Eric Orman, MD, an associate professor of medicine at Indiana University, Indianapolis.
Dr. Orman, who wasn’t involved with this study, has researched recent trends in the characteristics and outcomes of patients with newly diagnosed cirrhosis and has found that the proportion of older adults has increased, as well as those with alcoholic cirrhosis and NASH, which has implications for future patient care.
“It is important to recognize that both dementia and HE can occur either separately or concurrently in individuals with cirrhosis,” Dr. Orman told this news organization. “When seeing patients with cognitive impairment, having a high index of suspicion for both conditions is critical to ensure appropriate diagnosis and treatment.”
The study’s findings “represent the tip of the iceberg,” Neal Parikh, MD, an assistant professor of neurology and neuroscience at Weill Cornell Medicine in New York, said in an interview. “There is a tremendous amount left to be discovered regarding the role of the liver in brain health.”
Dr. Parikh, who wasn’t associated with this study, has researched the impact of chronic liver conditions on cognitive impairment and dementia. He is working on a project that addresses HE in detail.
“There is growing recognition of a so-called ‘liver-brain axis,’ with several researchers, including my group, showing that a range of chronic liver conditions may detrimentally impact cognitive function and increase the risk of dementia,” he said. “Studying the specific contributions of cirrhosis is critical for understanding the role of hepatic encephalopathy in age-related cognitive decline.”
The study received no financial support. The authors reported no potential competing interests.
A version of this article first appeared on Medscape.com.
, according to a new study involving U.S. veterans.
The overlap between dementia and HE was also independent of alcohol use, brain injury, age, and other metabolic risk factors.
“The aging of patients with cirrhosis leads us to encounter several individuals who may be prone to both of these diseases,” senior author Jasmohan Bajaj, MD, a professor of gastroenterology, hepatology, and nutrition at Virginia Commonwealth University Medical Center and GI section of the Central Virginia Veterans Healthcare System in Richmond, said in an interview.
“Given the epidemic of metabolic syndrome and alcohol, consider excluding cirrhosis in your patient [for] whom the presumptive diagnosis is dementia, since they could have concomitant HE,” he said.
“On the flip side, in those with HE who have predominant long-term memory issues and persistent cognitive changes, consider consulting a neuropsychiatrist or neurologist to ensure there is a resolution of the underlying disease process,” Dr. Bajaj added.
The study was published online in The American Journal of Gastroenterology.
Analyzing associations
HE is a common decompensating event in patients with cirrhosis. Because of the aging population of patients with cirrhosis, however, it’s important to differentiate HE from nonhepatic etiologies of cognitive impairment, such as dementia, the authors note.
Using data from the VA Corporate Data Warehouse, Dr. Bajaj and colleagues identified veterans with cirrhosis who received VA care between October 2019 and September 2021 and compared baseline characteristics between the cohorts based on the presence or absence of dementia. The research team then evaluated factors associated with having a diagnosis of dementia, adjusting for demographics, comorbid illnesses, cirrhosis etiology, and cirrhosis complications.
Investigators identified 71,522 veterans with diagnostic codes for cirrhosis who were engaged in VA care in 2019. They were mostly men (96.2%) and had a median age of 66. The most common etiologies of cirrhosis were alcohol and hepatitis C, followed by nonalcoholic steatohepatitis (NASH). The group also included veterans with predominantly compensated cirrhosis and a median MELD-Na score of 9. The MELD-Na score gauges the severity of chronic liver disease using values such as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium to predict survival.
Among those with cirrhosis, 5,647 (7.9%) also had dementia diagnosis codes. This rate is higher than the prevalence of dementia in the general population and equivalent to the rate of dementia in veterans without cirrhosis who are older than 65, the authors note.
In general, veterans with dementia tended to be older, to be White, to live in an urban area, and to have higher MELD-Na scores, and they were more frequently diagnosed with alcohol-related cirrhosis, alcohol and tobacco use disorder, diabetes, chronic kidney disease, chronic heart failure, brain trauma, and cerebrovascular disease.
In a multivariable analysis, the presence of any decompensating event was significantly associated with dementia. In subsequent analyses of individual decompensating events, however, the strongest association was with HE, while ascites or variceal bleeding did not add to the risk.
When HE was defined as patients who filled prescriptions for lactulose or rifaximin, the frequency of patients with HE decreased from 13.7% to 10.9%. In an analysis with HE as the decompensating event, the association between HE and dementia remained significant compared to when HE was defined by diagnostic codes alone.
“We were surprised by the high proportion of patients with dementia who also had cirrhosis, and given the genuine difficulty that clinicians have with defining HE vs. dementia, we were not very surprised at that overlap,” Dr. Bajaj said.
“We were also surprised at the specificity of this overlap only with HE and not with other decompensating events, which was also independent of head injury, alcohol use, and PTSD,” he added.
Additional research needed
Future research should look at the characteristics of HE, including the number of episodes or breakthrough episodes, and should focus on objective biomarkers to differentiate dementia and HE, the study authors write.
“The distinction and study of potential overlapping features among HE and dementia is important because HE is often treatable with medications and reverses after liver transplant, while this does not occur with dementia,” they add.
Dr. Bajaj and colleagues call for a greater awareness of disease processes and complications in older patients with cirrhosis, particularly since diagnostic imprecision can lead to patient and family confusion, distrust, and ineffective treatment.
The study will help physicians better understand the important overlap between dementia and HE, said Eric Orman, MD, an associate professor of medicine at Indiana University, Indianapolis.
Dr. Orman, who wasn’t involved with this study, has researched recent trends in the characteristics and outcomes of patients with newly diagnosed cirrhosis and has found that the proportion of older adults has increased, as well as those with alcoholic cirrhosis and NASH, which has implications for future patient care.
“It is important to recognize that both dementia and HE can occur either separately or concurrently in individuals with cirrhosis,” Dr. Orman told this news organization. “When seeing patients with cognitive impairment, having a high index of suspicion for both conditions is critical to ensure appropriate diagnosis and treatment.”
The study’s findings “represent the tip of the iceberg,” Neal Parikh, MD, an assistant professor of neurology and neuroscience at Weill Cornell Medicine in New York, said in an interview. “There is a tremendous amount left to be discovered regarding the role of the liver in brain health.”
Dr. Parikh, who wasn’t associated with this study, has researched the impact of chronic liver conditions on cognitive impairment and dementia. He is working on a project that addresses HE in detail.
“There is growing recognition of a so-called ‘liver-brain axis,’ with several researchers, including my group, showing that a range of chronic liver conditions may detrimentally impact cognitive function and increase the risk of dementia,” he said. “Studying the specific contributions of cirrhosis is critical for understanding the role of hepatic encephalopathy in age-related cognitive decline.”
The study received no financial support. The authors reported no potential competing interests.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
How a concussion led a former football player/WWE star to a pioneering neuroscience career
On Oct. 5, 2022, at 10:24 a.m., Chris Nowinski, PhD, cofounder of the Boston-based Concussion Legacy Foundation (CLF), was in his home office when the email came through.
“I pounded my desk, shouted YES! and went to find my wife so I could pick her up and give her a big hug,” he recalled. “It was the culmination of 15 years of research and hard work.”
Robert Cantu, MD, who has been studying head trauma for 50+ years and has published more than 500 papers about it, compares the announcement to the 1964 Surgeon General’s report that linked cigarette smoking with lung cancer and heart disease. With the NIH and the Centers of Disease Control and Prevention (CDC) now in agreement about the risks of participating in impact sports and activities, he said, “We’ve reached a tipping point that should finally prompt deniers such as the NHL, NCAA, FIFA, World Rugby, the International Olympic Committee, and other [sports organizations] to remove all unnecessary head trauma from their sports.”
“A lot of the credit for this must go to Chris,” added Dr. Cantu, medical director and director of clinical research at the Cantu Concussion Center at Emerson Hospital in Concord, Mass. “Clinicians like myself can reach only so many people by writing papers and giving speeches at medical conferences. For this to happen, the message needed to get out to parents, athletes, and society in general. And Chris was the vehicle for doing that.”
Dr. Nowinski didn’t set out to be the messenger. He played football at Harvard in the late 1990s, making second-team All-Ivy as a defensive tackle his senior year. In 2000, he enrolled in Killer Kowalski’s Wrestling Institute and eventually joined Vince McMahon’s World Wrestling Entertainment (WWE).
There he played the role of 295-pound villain “Chris Harvard,” an intellectual snob who dressed in crimson tights and insulted the crowd’s IQ. “Roses are red. Violets are blue. The reason I’m talking so slowly is because no one in [insert name of town he was appearing in] has passed grade 2!”
“I’d often apply my education during a match,” he wrote in his book, “Head Games: Football’s Concussion Crisis.“ In a match in Bridgeport, Conn., I assaulted [my opponent] with a human skeleton, ripped off the skull, got down on bended knee, and began reciting Hamlet. Those were good times.”
Those good times ended abruptly, however, during a match with Bubba Ray Dudley at the Hartford Civic Center in Connecticut in 2003. Even though pro wrestling matches are rehearsed, and the blows aren’t real, accidents happen. Mr. Dudley mistakenly kicked Dr. Nowinski in the jaw with enough force to put him on his back and make the whole ring shake.
“Holy shit, kid! You okay?” asked the referee. Before a foggy Dr. Nowinski could reply, 300-pound Mr. Dudley crashed down on him, hooked his leg, and the ref began counting, “One! Two! …” Dr. Nowinski instinctively kicked out but had forgotten the rest of the script. He managed to finish the match and stagger backstage.
His coherence and awareness gradually returned, but a “throbbing headache” persisted. A locker room doctor said he might have a concussion and recommended he wait to see how he felt before wrestling in Albany, N.Y., the next evening.
The following day the headache had subsided, but he still felt “a little strange.” Nonetheless, he told the doctor he was fine and strutted out to again battle Bubba Ray, this time in a match where he eventually got thrown through a ringside table and suffered the Dudley Death Drop. Afterward, “I crawled backstage and laid down. The headache was much, much worse.”
An event and a process
Dr. Nowinski continued to insist he was “fine” and wrestled a few more matches in the following days before finally acknowledging something was wrong. He’d had his bell rung numerous times in football, but this was different. Even more worrisome, none of the doctors he consulted could give him any definitive answers. He finally found his way to Emerson Hospital, where Dr. Cantu was the chief of neurosurgery.
“I remember that day vividly,” said Dr. Cantu. “Chris was this big, strapping, handsome guy – a hell of an athlete whose star was rising. He didn’t realize that he’d suffered a series of concussions and that trying to push through them was the worst thing he could be doing.”
Concussions and their effects were misunderstood by many athletes, coaches, and even physicians back then. It was assumed that the quarter inch of bone surrounding the adult brain provided adequate protection from common sports impacts and that any aftereffects were temporary. A common treatment was smelling salts and a pat on the back as the athlete returned to action.
However, the brain floats inside the skull in a bath of cerebral fluid. Any significant impact causes it to slosh violently from side to side, damaging tissue, synapses, and cells resulting in inflammation that can manifest as confusion and brain fog.
“A concussion is actually not defined by a physical injury,” explained Dr. Nowinski, “but by a loss of brain function that is induced by trauma. Concussion is not just an event, but also a process.” It’s almost as if the person has suffered a small seizure.
Fortunately, most concussion symptoms resolve within 2 weeks, but in some cases, especially if there’s been additional head trauma, they can persist, causing anxiety, depression, anger, and/or sleep disorders. Known as postconcussion syndrome (PCS), this is what Dr. Nowinski was unknowingly suffering from when he consulted Dr. Cantu.
In fact, one night it an Indianapolis hotel, weeks after his initial concussion, he awoke to find himself on the floor and the room in shambles. His girlfriend was yelling his name and shaking him. She told him he’d been having a nightmare and had suddenly started screaming and tearing up the room. “I didn’t remember any of it,” he said.
Dr. Cantu eventually advised Dr. Nowinski against ever returning to the ring or any activity with the risk for head injury. Research shows that sustaining a single significant concussion increases the risk of subsequent more-severe brain injuries.
“My diagnosis could have sent Chris off the deep end because he could no longer do what he wanted to do with this life,” said Dr. Cantu. “But instead, he used it as a tool to find meaning for his life.”
Dr. Nowinski decided to use his experience as a teaching opportunity, not just for other athletes but also for sports organizations and the medical community.
His book, which focused on the NFL’s “tobacco-industry-like refusal to acknowledge the depths of the problem,” was published in 2006. A year later, Dr. Nowinski partnered with Dr. Cantu to found the Sports Legacy Institute, which eventually became the Concussion Legacy Foundation (CLF).
Cold calling for brain donations
Robert Stern, PhD, is another highly respected authority in the study of neurodegenerative disease. In 2007, he was directing the clinical core of Boston University’s Alzheimer’s Disease Center. After giving a lecture to a group of financial planners and elder-law attorneys one morning, he got a request for a private meeting from a fellow named Chris Nowinski.
“I’d never heard of him, but I agreed,” recalled Dr. Stern, a professor of neurology, neurosurgery, anatomy, and neurobiology at Boston University. “A few days later, this larger-than-life guy walked into our conference room at the BU School of Medicine, exuding a great deal of passion, intellect, and determination. He told me his story and then started talking about the long-term consequences of concussions in sports.”
Dr. Stern had seen patients with dementia pugilistica, the old-school term for CTE. These were mostly boxers with cognitive and behavioral impairment. “But I had not heard about football players,” he said. “I hadn’t put the two together. And as I was listening to Chris, I realized if what he was saying was true then it was not only a potentially huge public health issue, but it was also a potentially huge scientific issue in the field of neurodegenerative disease.”
Dr. Nowinski introduced Dr. Stern to Dr. Cantu, and together with Ann McKee, MD, professor of neurology and pathology at BU, they cofounded the Center for the Study of Traumatic Encephalopathy (CSTE) in 2008. It was the first center of its kind devoted to the study of CTE in the world.
One of Dr. Nowinski’s first jobs at the CSTE was soliciting and procuring brain donations. Since CTE is generally a progressive condition that can take decades to manifest, autopsy was the only way to detect it.
The brains of two former Pittsburgh Steelers, Mike Webster and Terry Long, had been examined after their untimely deaths. After immunostaining, investigators found both former NFL players had “protein misfolds” characteristic of CTE.
This finding drew a lot of public and scientific attention, given that Mr. Long died by suicide and Mr. Webster was homeless when he died of a heart attack. But more scientific evidence was needed to prove a causal link between the head trauma and CTE.
Dr. Nowinski scoured obituaries looking for potential brains to study. When he found one, he would cold call the family and try to convince them to donate it to science. The first brain he secured for the center belonged to John Grimsley, a former NFL linebacker who in 2008 died at age 45 of an accidental gunshot wound. Often, Dr. Nowinski would even be the courier, traveling to pick up the brain after it had been harvested.
Over the next 10 years, Dr. Nowinski and his research team secured 500 brain donations. The research that resulted was staggering. In the beginning only 45 cases of CTE had been identified in the world, but in the first 111 NFL players who were autopsied, 110 had the disorder.
Of the first 53 college football players autopsied, 48 had CTE. Although Dr. Nowinski’s initial focus was football, evidence of CTE was soon detected among athletes in boxing, hockey, soccer, and rugby, as well as in combat veterans. However, the National Football League and other governing sports bodies initially denied any connection between sport-related head trauma and CTE.
Cumulative damage
In 2017, after 7 years of study, Dr. Nowinski earned a PhD in neurology. As the scientific evidence continued to accumulate, two shifts occurred that Dr. Stern said represent Dr. Nowinski’s greatest contributions. First, concussion is now widely recognized as an acute brain injury with symptoms that need to be immediately diagnosed and addressed.
“This is a completely different story from where things were just 10 years ago,” said Dr. Stern, “and Chris played a central role, if not the central role, in raising awareness about that.”
All 50 states and the District of Columbia now have laws regarding sports-related concussion. And there are brain banks in Australia, Canada, New Zealand, Brazil, and the United Kingdom studying CTE. More than 2,500 athletes in a variety of sports, including NASCAR’s Dale Earnhardt Jr. and NFL hall of famer Nick Buoniconti, have publicly pledged to donate their brains to science after their deaths.
Second, said Dr. Stern, we now know that although concussions can contribute to CTE, they are not the sole cause. It’s repetitive subconcussive trauma, without symptoms of concussion, that do the most damage.
“These happen during every practice and in every game,” said Dr. Stern. In fact, it’s estimated that pro football players suffer thousands of subconcussive incidents over the course of their careers. So, a player doesn’t have to see stars or lose consciousness to suffer brain damage; small impacts can accumulate over time.
Understanding this point is crucial for making youth sports safer. “Chris has played a critical role in raising awareness here, too,” said Dr. Stern. “Allowing our kids to get hit in the head over and over can put them at greater risk for later problems, plus it just doesn’t make common sense.”
“The biggest misconception surrounding head trauma in sports,” said Dr. Nowinski, “is the belief among players, coaches, and even the medical and scientific communities that if you get hit in the head and don’t have any symptoms then you’re okay and there hasn’t been any damage. That couldn’t be further from the truth. We now know that people are suffering serious brain injuries due to the accumulated effect of subconcussive impacts, and we need to get the word out about that.”
A major initiative from the Concussion Legacy Foundation called “Stop Hitting Kids in the Head” has the goal of convincing every sport to eliminate repetitive head impacts in players under age 14 – the time when the skull and brain are still developing and most vulnerable – by 2026. In fact, Dr. Nowinski wrote that “there could be a lot of kids who are misdiagnosed and medicated for various behavioral or emotional problems that may actually be head injury–related.”
Starting in 2009, the NFL adopted a series of rule changes designed to better protect its players against repeated head trauma. Among them is a ban on spearing or leading with the helmet, penalties for hitting defenseless players, and more stringent return-to-play guidelines, including concussion protocols.
The NFL has also put more emphasis on flag football options for youngsters and, for the first time, showcased this alternative in the 2023 Pro Bowl. But Dr. Nowinski is pressuring the league to go further. “While acknowledging that the game causes CTE, the NFL still underwrites recruiting 5-year-olds to play tackle football,” he said. “In my opinion, that’s unethical, and it needs to be addressed.”
WWE one of the most responsive organizations
Dr. Nowinski said WWE has been one of the most responsive sports organizations for protecting athletes. A doctor is now ringside at every match as is an observer who knows the script, thereby allowing for instant medical intervention if something goes wrong. “Since everyone is trying to look like they have a concussion all the time, it takes a deep understanding of the business to recognize a real one,” he said.
But this hasn’t been the case with other sports. “I am eternally disappointed in the response of the professional sports industry to the knowledge of CTE and long-term concussion symptoms,” said Dr. Nowinski.
“For example, FIFA [international soccer’s governing body] still doesn’t allow doctors to evaluate [potentially concussed] players on the sidelines and put them back in the game with a free substitution [if they’re deemed okay]. Not giving players proper medical care for a brain injury is unethical,” he said. BU’s Center for the Study of Traumatic Encephalopathy diagnosed the first CTE case in soccer in 2012, and in 2015 Dr. Nowinski successfully lobbied U.S. Soccer to ban heading the ball before age 11.
“Unfortunately, many governing bodies have circled the wagons in denying their sport causes CTE,” he continued. “FIFA, World Rugby, the NHL, even the NCAA and International Olympic Committee refuse to acknowledge it and, therefore, aren’t taking any steps to prevent it. They see it as a threat to their business model. Hopefully, now that the NIH and CDC are aligned about the risks of head impact in sports, this will begin to change.”
Meanwhile, research is continuing. Scientists are getting closer to being able to diagnose CTE in living humans, with ongoing studies using PET scans, blood markers, and spinal fluid markers. In 2019, researchers identified tau proteins specific to CTE that they believe are distinct from those of Alzheimer’s and other neurodegenerative diseases. Next step would be developing a drug to slow the development of CTE once detected.
Nonetheless, athletes at all levels in impact sports still don’t fully appreciate the risks of repeated head trauma and especially subconcussive blows. “I talk to former NFL and college players every week,” said Dr. Stern. “Some tell me, ‘I love the sport, it gave me so much, and I would do it again, but I’m not letting my grandchildren play.’ But others say, ‘As long as they know the risks, they can make their own decision.’ “
Dr. Nowinski has a daughter who is 4 and a son who’s 2. Both play soccer but, thanks to dad, heading isn’t allowed in their age groups. If they continue playing sports, Dr. Nowinski said he’ll make sure they understand the risks and how to protect themselves. This is a conversation all parents should have with their kids at every level to make sure they play safe, he added.
Those in the medical community can also volunteer their time to explain head trauma to athletes, coaches, and school administrators to be sure they understand its seriousness and are doing everything to protect players.
As you watch this year’s Super Bowl, Dr. Nowinski and his team would like you to keep something in mind. Those young men on the field for your entertainment are receiving mild brain trauma repeatedly throughout the game.
Even if it’s not a huge hit that gets replayed and makes everyone gasp, even if no one gets ushered into the little sideline tent for a concussion screening, even if no one loses consciousness, brain damage is still occurring. Watch the heads of the players during every play and think about what’s going on inside their skulls regardless of how big and strong those helmets look.
A version of this article first appeared on Medscape.com.
On Oct. 5, 2022, at 10:24 a.m., Chris Nowinski, PhD, cofounder of the Boston-based Concussion Legacy Foundation (CLF), was in his home office when the email came through.
“I pounded my desk, shouted YES! and went to find my wife so I could pick her up and give her a big hug,” he recalled. “It was the culmination of 15 years of research and hard work.”
Robert Cantu, MD, who has been studying head trauma for 50+ years and has published more than 500 papers about it, compares the announcement to the 1964 Surgeon General’s report that linked cigarette smoking with lung cancer and heart disease. With the NIH and the Centers of Disease Control and Prevention (CDC) now in agreement about the risks of participating in impact sports and activities, he said, “We’ve reached a tipping point that should finally prompt deniers such as the NHL, NCAA, FIFA, World Rugby, the International Olympic Committee, and other [sports organizations] to remove all unnecessary head trauma from their sports.”
“A lot of the credit for this must go to Chris,” added Dr. Cantu, medical director and director of clinical research at the Cantu Concussion Center at Emerson Hospital in Concord, Mass. “Clinicians like myself can reach only so many people by writing papers and giving speeches at medical conferences. For this to happen, the message needed to get out to parents, athletes, and society in general. And Chris was the vehicle for doing that.”
Dr. Nowinski didn’t set out to be the messenger. He played football at Harvard in the late 1990s, making second-team All-Ivy as a defensive tackle his senior year. In 2000, he enrolled in Killer Kowalski’s Wrestling Institute and eventually joined Vince McMahon’s World Wrestling Entertainment (WWE).
There he played the role of 295-pound villain “Chris Harvard,” an intellectual snob who dressed in crimson tights and insulted the crowd’s IQ. “Roses are red. Violets are blue. The reason I’m talking so slowly is because no one in [insert name of town he was appearing in] has passed grade 2!”
“I’d often apply my education during a match,” he wrote in his book, “Head Games: Football’s Concussion Crisis.“ In a match in Bridgeport, Conn., I assaulted [my opponent] with a human skeleton, ripped off the skull, got down on bended knee, and began reciting Hamlet. Those were good times.”
Those good times ended abruptly, however, during a match with Bubba Ray Dudley at the Hartford Civic Center in Connecticut in 2003. Even though pro wrestling matches are rehearsed, and the blows aren’t real, accidents happen. Mr. Dudley mistakenly kicked Dr. Nowinski in the jaw with enough force to put him on his back and make the whole ring shake.
“Holy shit, kid! You okay?” asked the referee. Before a foggy Dr. Nowinski could reply, 300-pound Mr. Dudley crashed down on him, hooked his leg, and the ref began counting, “One! Two! …” Dr. Nowinski instinctively kicked out but had forgotten the rest of the script. He managed to finish the match and stagger backstage.
His coherence and awareness gradually returned, but a “throbbing headache” persisted. A locker room doctor said he might have a concussion and recommended he wait to see how he felt before wrestling in Albany, N.Y., the next evening.
The following day the headache had subsided, but he still felt “a little strange.” Nonetheless, he told the doctor he was fine and strutted out to again battle Bubba Ray, this time in a match where he eventually got thrown through a ringside table and suffered the Dudley Death Drop. Afterward, “I crawled backstage and laid down. The headache was much, much worse.”
An event and a process
Dr. Nowinski continued to insist he was “fine” and wrestled a few more matches in the following days before finally acknowledging something was wrong. He’d had his bell rung numerous times in football, but this was different. Even more worrisome, none of the doctors he consulted could give him any definitive answers. He finally found his way to Emerson Hospital, where Dr. Cantu was the chief of neurosurgery.
“I remember that day vividly,” said Dr. Cantu. “Chris was this big, strapping, handsome guy – a hell of an athlete whose star was rising. He didn’t realize that he’d suffered a series of concussions and that trying to push through them was the worst thing he could be doing.”
Concussions and their effects were misunderstood by many athletes, coaches, and even physicians back then. It was assumed that the quarter inch of bone surrounding the adult brain provided adequate protection from common sports impacts and that any aftereffects were temporary. A common treatment was smelling salts and a pat on the back as the athlete returned to action.
However, the brain floats inside the skull in a bath of cerebral fluid. Any significant impact causes it to slosh violently from side to side, damaging tissue, synapses, and cells resulting in inflammation that can manifest as confusion and brain fog.
“A concussion is actually not defined by a physical injury,” explained Dr. Nowinski, “but by a loss of brain function that is induced by trauma. Concussion is not just an event, but also a process.” It’s almost as if the person has suffered a small seizure.
Fortunately, most concussion symptoms resolve within 2 weeks, but in some cases, especially if there’s been additional head trauma, they can persist, causing anxiety, depression, anger, and/or sleep disorders. Known as postconcussion syndrome (PCS), this is what Dr. Nowinski was unknowingly suffering from when he consulted Dr. Cantu.
In fact, one night it an Indianapolis hotel, weeks after his initial concussion, he awoke to find himself on the floor and the room in shambles. His girlfriend was yelling his name and shaking him. She told him he’d been having a nightmare and had suddenly started screaming and tearing up the room. “I didn’t remember any of it,” he said.
Dr. Cantu eventually advised Dr. Nowinski against ever returning to the ring or any activity with the risk for head injury. Research shows that sustaining a single significant concussion increases the risk of subsequent more-severe brain injuries.
“My diagnosis could have sent Chris off the deep end because he could no longer do what he wanted to do with this life,” said Dr. Cantu. “But instead, he used it as a tool to find meaning for his life.”
Dr. Nowinski decided to use his experience as a teaching opportunity, not just for other athletes but also for sports organizations and the medical community.
His book, which focused on the NFL’s “tobacco-industry-like refusal to acknowledge the depths of the problem,” was published in 2006. A year later, Dr. Nowinski partnered with Dr. Cantu to found the Sports Legacy Institute, which eventually became the Concussion Legacy Foundation (CLF).
Cold calling for brain donations
Robert Stern, PhD, is another highly respected authority in the study of neurodegenerative disease. In 2007, he was directing the clinical core of Boston University’s Alzheimer’s Disease Center. After giving a lecture to a group of financial planners and elder-law attorneys one morning, he got a request for a private meeting from a fellow named Chris Nowinski.
“I’d never heard of him, but I agreed,” recalled Dr. Stern, a professor of neurology, neurosurgery, anatomy, and neurobiology at Boston University. “A few days later, this larger-than-life guy walked into our conference room at the BU School of Medicine, exuding a great deal of passion, intellect, and determination. He told me his story and then started talking about the long-term consequences of concussions in sports.”
Dr. Stern had seen patients with dementia pugilistica, the old-school term for CTE. These were mostly boxers with cognitive and behavioral impairment. “But I had not heard about football players,” he said. “I hadn’t put the two together. And as I was listening to Chris, I realized if what he was saying was true then it was not only a potentially huge public health issue, but it was also a potentially huge scientific issue in the field of neurodegenerative disease.”
Dr. Nowinski introduced Dr. Stern to Dr. Cantu, and together with Ann McKee, MD, professor of neurology and pathology at BU, they cofounded the Center for the Study of Traumatic Encephalopathy (CSTE) in 2008. It was the first center of its kind devoted to the study of CTE in the world.
One of Dr. Nowinski’s first jobs at the CSTE was soliciting and procuring brain donations. Since CTE is generally a progressive condition that can take decades to manifest, autopsy was the only way to detect it.
The brains of two former Pittsburgh Steelers, Mike Webster and Terry Long, had been examined after their untimely deaths. After immunostaining, investigators found both former NFL players had “protein misfolds” characteristic of CTE.
This finding drew a lot of public and scientific attention, given that Mr. Long died by suicide and Mr. Webster was homeless when he died of a heart attack. But more scientific evidence was needed to prove a causal link between the head trauma and CTE.
Dr. Nowinski scoured obituaries looking for potential brains to study. When he found one, he would cold call the family and try to convince them to donate it to science. The first brain he secured for the center belonged to John Grimsley, a former NFL linebacker who in 2008 died at age 45 of an accidental gunshot wound. Often, Dr. Nowinski would even be the courier, traveling to pick up the brain after it had been harvested.
Over the next 10 years, Dr. Nowinski and his research team secured 500 brain donations. The research that resulted was staggering. In the beginning only 45 cases of CTE had been identified in the world, but in the first 111 NFL players who were autopsied, 110 had the disorder.
Of the first 53 college football players autopsied, 48 had CTE. Although Dr. Nowinski’s initial focus was football, evidence of CTE was soon detected among athletes in boxing, hockey, soccer, and rugby, as well as in combat veterans. However, the National Football League and other governing sports bodies initially denied any connection between sport-related head trauma and CTE.
Cumulative damage
In 2017, after 7 years of study, Dr. Nowinski earned a PhD in neurology. As the scientific evidence continued to accumulate, two shifts occurred that Dr. Stern said represent Dr. Nowinski’s greatest contributions. First, concussion is now widely recognized as an acute brain injury with symptoms that need to be immediately diagnosed and addressed.
“This is a completely different story from where things were just 10 years ago,” said Dr. Stern, “and Chris played a central role, if not the central role, in raising awareness about that.”
All 50 states and the District of Columbia now have laws regarding sports-related concussion. And there are brain banks in Australia, Canada, New Zealand, Brazil, and the United Kingdom studying CTE. More than 2,500 athletes in a variety of sports, including NASCAR’s Dale Earnhardt Jr. and NFL hall of famer Nick Buoniconti, have publicly pledged to donate their brains to science after their deaths.
Second, said Dr. Stern, we now know that although concussions can contribute to CTE, they are not the sole cause. It’s repetitive subconcussive trauma, without symptoms of concussion, that do the most damage.
“These happen during every practice and in every game,” said Dr. Stern. In fact, it’s estimated that pro football players suffer thousands of subconcussive incidents over the course of their careers. So, a player doesn’t have to see stars or lose consciousness to suffer brain damage; small impacts can accumulate over time.
Understanding this point is crucial for making youth sports safer. “Chris has played a critical role in raising awareness here, too,” said Dr. Stern. “Allowing our kids to get hit in the head over and over can put them at greater risk for later problems, plus it just doesn’t make common sense.”
“The biggest misconception surrounding head trauma in sports,” said Dr. Nowinski, “is the belief among players, coaches, and even the medical and scientific communities that if you get hit in the head and don’t have any symptoms then you’re okay and there hasn’t been any damage. That couldn’t be further from the truth. We now know that people are suffering serious brain injuries due to the accumulated effect of subconcussive impacts, and we need to get the word out about that.”
A major initiative from the Concussion Legacy Foundation called “Stop Hitting Kids in the Head” has the goal of convincing every sport to eliminate repetitive head impacts in players under age 14 – the time when the skull and brain are still developing and most vulnerable – by 2026. In fact, Dr. Nowinski wrote that “there could be a lot of kids who are misdiagnosed and medicated for various behavioral or emotional problems that may actually be head injury–related.”
Starting in 2009, the NFL adopted a series of rule changes designed to better protect its players against repeated head trauma. Among them is a ban on spearing or leading with the helmet, penalties for hitting defenseless players, and more stringent return-to-play guidelines, including concussion protocols.
The NFL has also put more emphasis on flag football options for youngsters and, for the first time, showcased this alternative in the 2023 Pro Bowl. But Dr. Nowinski is pressuring the league to go further. “While acknowledging that the game causes CTE, the NFL still underwrites recruiting 5-year-olds to play tackle football,” he said. “In my opinion, that’s unethical, and it needs to be addressed.”
WWE one of the most responsive organizations
Dr. Nowinski said WWE has been one of the most responsive sports organizations for protecting athletes. A doctor is now ringside at every match as is an observer who knows the script, thereby allowing for instant medical intervention if something goes wrong. “Since everyone is trying to look like they have a concussion all the time, it takes a deep understanding of the business to recognize a real one,” he said.
But this hasn’t been the case with other sports. “I am eternally disappointed in the response of the professional sports industry to the knowledge of CTE and long-term concussion symptoms,” said Dr. Nowinski.
“For example, FIFA [international soccer’s governing body] still doesn’t allow doctors to evaluate [potentially concussed] players on the sidelines and put them back in the game with a free substitution [if they’re deemed okay]. Not giving players proper medical care for a brain injury is unethical,” he said. BU’s Center for the Study of Traumatic Encephalopathy diagnosed the first CTE case in soccer in 2012, and in 2015 Dr. Nowinski successfully lobbied U.S. Soccer to ban heading the ball before age 11.
“Unfortunately, many governing bodies have circled the wagons in denying their sport causes CTE,” he continued. “FIFA, World Rugby, the NHL, even the NCAA and International Olympic Committee refuse to acknowledge it and, therefore, aren’t taking any steps to prevent it. They see it as a threat to their business model. Hopefully, now that the NIH and CDC are aligned about the risks of head impact in sports, this will begin to change.”
Meanwhile, research is continuing. Scientists are getting closer to being able to diagnose CTE in living humans, with ongoing studies using PET scans, blood markers, and spinal fluid markers. In 2019, researchers identified tau proteins specific to CTE that they believe are distinct from those of Alzheimer’s and other neurodegenerative diseases. Next step would be developing a drug to slow the development of CTE once detected.
Nonetheless, athletes at all levels in impact sports still don’t fully appreciate the risks of repeated head trauma and especially subconcussive blows. “I talk to former NFL and college players every week,” said Dr. Stern. “Some tell me, ‘I love the sport, it gave me so much, and I would do it again, but I’m not letting my grandchildren play.’ But others say, ‘As long as they know the risks, they can make their own decision.’ “
Dr. Nowinski has a daughter who is 4 and a son who’s 2. Both play soccer but, thanks to dad, heading isn’t allowed in their age groups. If they continue playing sports, Dr. Nowinski said he’ll make sure they understand the risks and how to protect themselves. This is a conversation all parents should have with their kids at every level to make sure they play safe, he added.
Those in the medical community can also volunteer their time to explain head trauma to athletes, coaches, and school administrators to be sure they understand its seriousness and are doing everything to protect players.
As you watch this year’s Super Bowl, Dr. Nowinski and his team would like you to keep something in mind. Those young men on the field for your entertainment are receiving mild brain trauma repeatedly throughout the game.
Even if it’s not a huge hit that gets replayed and makes everyone gasp, even if no one gets ushered into the little sideline tent for a concussion screening, even if no one loses consciousness, brain damage is still occurring. Watch the heads of the players during every play and think about what’s going on inside their skulls regardless of how big and strong those helmets look.
A version of this article first appeared on Medscape.com.
On Oct. 5, 2022, at 10:24 a.m., Chris Nowinski, PhD, cofounder of the Boston-based Concussion Legacy Foundation (CLF), was in his home office when the email came through.
“I pounded my desk, shouted YES! and went to find my wife so I could pick her up and give her a big hug,” he recalled. “It was the culmination of 15 years of research and hard work.”
Robert Cantu, MD, who has been studying head trauma for 50+ years and has published more than 500 papers about it, compares the announcement to the 1964 Surgeon General’s report that linked cigarette smoking with lung cancer and heart disease. With the NIH and the Centers of Disease Control and Prevention (CDC) now in agreement about the risks of participating in impact sports and activities, he said, “We’ve reached a tipping point that should finally prompt deniers such as the NHL, NCAA, FIFA, World Rugby, the International Olympic Committee, and other [sports organizations] to remove all unnecessary head trauma from their sports.”
“A lot of the credit for this must go to Chris,” added Dr. Cantu, medical director and director of clinical research at the Cantu Concussion Center at Emerson Hospital in Concord, Mass. “Clinicians like myself can reach only so many people by writing papers and giving speeches at medical conferences. For this to happen, the message needed to get out to parents, athletes, and society in general. And Chris was the vehicle for doing that.”
Dr. Nowinski didn’t set out to be the messenger. He played football at Harvard in the late 1990s, making second-team All-Ivy as a defensive tackle his senior year. In 2000, he enrolled in Killer Kowalski’s Wrestling Institute and eventually joined Vince McMahon’s World Wrestling Entertainment (WWE).
There he played the role of 295-pound villain “Chris Harvard,” an intellectual snob who dressed in crimson tights and insulted the crowd’s IQ. “Roses are red. Violets are blue. The reason I’m talking so slowly is because no one in [insert name of town he was appearing in] has passed grade 2!”
“I’d often apply my education during a match,” he wrote in his book, “Head Games: Football’s Concussion Crisis.“ In a match in Bridgeport, Conn., I assaulted [my opponent] with a human skeleton, ripped off the skull, got down on bended knee, and began reciting Hamlet. Those were good times.”
Those good times ended abruptly, however, during a match with Bubba Ray Dudley at the Hartford Civic Center in Connecticut in 2003. Even though pro wrestling matches are rehearsed, and the blows aren’t real, accidents happen. Mr. Dudley mistakenly kicked Dr. Nowinski in the jaw with enough force to put him on his back and make the whole ring shake.
“Holy shit, kid! You okay?” asked the referee. Before a foggy Dr. Nowinski could reply, 300-pound Mr. Dudley crashed down on him, hooked his leg, and the ref began counting, “One! Two! …” Dr. Nowinski instinctively kicked out but had forgotten the rest of the script. He managed to finish the match and stagger backstage.
His coherence and awareness gradually returned, but a “throbbing headache” persisted. A locker room doctor said he might have a concussion and recommended he wait to see how he felt before wrestling in Albany, N.Y., the next evening.
The following day the headache had subsided, but he still felt “a little strange.” Nonetheless, he told the doctor he was fine and strutted out to again battle Bubba Ray, this time in a match where he eventually got thrown through a ringside table and suffered the Dudley Death Drop. Afterward, “I crawled backstage and laid down. The headache was much, much worse.”
An event and a process
Dr. Nowinski continued to insist he was “fine” and wrestled a few more matches in the following days before finally acknowledging something was wrong. He’d had his bell rung numerous times in football, but this was different. Even more worrisome, none of the doctors he consulted could give him any definitive answers. He finally found his way to Emerson Hospital, where Dr. Cantu was the chief of neurosurgery.
“I remember that day vividly,” said Dr. Cantu. “Chris was this big, strapping, handsome guy – a hell of an athlete whose star was rising. He didn’t realize that he’d suffered a series of concussions and that trying to push through them was the worst thing he could be doing.”
Concussions and their effects were misunderstood by many athletes, coaches, and even physicians back then. It was assumed that the quarter inch of bone surrounding the adult brain provided adequate protection from common sports impacts and that any aftereffects were temporary. A common treatment was smelling salts and a pat on the back as the athlete returned to action.
However, the brain floats inside the skull in a bath of cerebral fluid. Any significant impact causes it to slosh violently from side to side, damaging tissue, synapses, and cells resulting in inflammation that can manifest as confusion and brain fog.
“A concussion is actually not defined by a physical injury,” explained Dr. Nowinski, “but by a loss of brain function that is induced by trauma. Concussion is not just an event, but also a process.” It’s almost as if the person has suffered a small seizure.
Fortunately, most concussion symptoms resolve within 2 weeks, but in some cases, especially if there’s been additional head trauma, they can persist, causing anxiety, depression, anger, and/or sleep disorders. Known as postconcussion syndrome (PCS), this is what Dr. Nowinski was unknowingly suffering from when he consulted Dr. Cantu.
In fact, one night it an Indianapolis hotel, weeks after his initial concussion, he awoke to find himself on the floor and the room in shambles. His girlfriend was yelling his name and shaking him. She told him he’d been having a nightmare and had suddenly started screaming and tearing up the room. “I didn’t remember any of it,” he said.
Dr. Cantu eventually advised Dr. Nowinski against ever returning to the ring or any activity with the risk for head injury. Research shows that sustaining a single significant concussion increases the risk of subsequent more-severe brain injuries.
“My diagnosis could have sent Chris off the deep end because he could no longer do what he wanted to do with this life,” said Dr. Cantu. “But instead, he used it as a tool to find meaning for his life.”
Dr. Nowinski decided to use his experience as a teaching opportunity, not just for other athletes but also for sports organizations and the medical community.
His book, which focused on the NFL’s “tobacco-industry-like refusal to acknowledge the depths of the problem,” was published in 2006. A year later, Dr. Nowinski partnered with Dr. Cantu to found the Sports Legacy Institute, which eventually became the Concussion Legacy Foundation (CLF).
Cold calling for brain donations
Robert Stern, PhD, is another highly respected authority in the study of neurodegenerative disease. In 2007, he was directing the clinical core of Boston University’s Alzheimer’s Disease Center. After giving a lecture to a group of financial planners and elder-law attorneys one morning, he got a request for a private meeting from a fellow named Chris Nowinski.
“I’d never heard of him, but I agreed,” recalled Dr. Stern, a professor of neurology, neurosurgery, anatomy, and neurobiology at Boston University. “A few days later, this larger-than-life guy walked into our conference room at the BU School of Medicine, exuding a great deal of passion, intellect, and determination. He told me his story and then started talking about the long-term consequences of concussions in sports.”
Dr. Stern had seen patients with dementia pugilistica, the old-school term for CTE. These were mostly boxers with cognitive and behavioral impairment. “But I had not heard about football players,” he said. “I hadn’t put the two together. And as I was listening to Chris, I realized if what he was saying was true then it was not only a potentially huge public health issue, but it was also a potentially huge scientific issue in the field of neurodegenerative disease.”
Dr. Nowinski introduced Dr. Stern to Dr. Cantu, and together with Ann McKee, MD, professor of neurology and pathology at BU, they cofounded the Center for the Study of Traumatic Encephalopathy (CSTE) in 2008. It was the first center of its kind devoted to the study of CTE in the world.
One of Dr. Nowinski’s first jobs at the CSTE was soliciting and procuring brain donations. Since CTE is generally a progressive condition that can take decades to manifest, autopsy was the only way to detect it.
The brains of two former Pittsburgh Steelers, Mike Webster and Terry Long, had been examined after their untimely deaths. After immunostaining, investigators found both former NFL players had “protein misfolds” characteristic of CTE.
This finding drew a lot of public and scientific attention, given that Mr. Long died by suicide and Mr. Webster was homeless when he died of a heart attack. But more scientific evidence was needed to prove a causal link between the head trauma and CTE.
Dr. Nowinski scoured obituaries looking for potential brains to study. When he found one, he would cold call the family and try to convince them to donate it to science. The first brain he secured for the center belonged to John Grimsley, a former NFL linebacker who in 2008 died at age 45 of an accidental gunshot wound. Often, Dr. Nowinski would even be the courier, traveling to pick up the brain after it had been harvested.
Over the next 10 years, Dr. Nowinski and his research team secured 500 brain donations. The research that resulted was staggering. In the beginning only 45 cases of CTE had been identified in the world, but in the first 111 NFL players who were autopsied, 110 had the disorder.
Of the first 53 college football players autopsied, 48 had CTE. Although Dr. Nowinski’s initial focus was football, evidence of CTE was soon detected among athletes in boxing, hockey, soccer, and rugby, as well as in combat veterans. However, the National Football League and other governing sports bodies initially denied any connection between sport-related head trauma and CTE.
Cumulative damage
In 2017, after 7 years of study, Dr. Nowinski earned a PhD in neurology. As the scientific evidence continued to accumulate, two shifts occurred that Dr. Stern said represent Dr. Nowinski’s greatest contributions. First, concussion is now widely recognized as an acute brain injury with symptoms that need to be immediately diagnosed and addressed.
“This is a completely different story from where things were just 10 years ago,” said Dr. Stern, “and Chris played a central role, if not the central role, in raising awareness about that.”
All 50 states and the District of Columbia now have laws regarding sports-related concussion. And there are brain banks in Australia, Canada, New Zealand, Brazil, and the United Kingdom studying CTE. More than 2,500 athletes in a variety of sports, including NASCAR’s Dale Earnhardt Jr. and NFL hall of famer Nick Buoniconti, have publicly pledged to donate their brains to science after their deaths.
Second, said Dr. Stern, we now know that although concussions can contribute to CTE, they are not the sole cause. It’s repetitive subconcussive trauma, without symptoms of concussion, that do the most damage.
“These happen during every practice and in every game,” said Dr. Stern. In fact, it’s estimated that pro football players suffer thousands of subconcussive incidents over the course of their careers. So, a player doesn’t have to see stars or lose consciousness to suffer brain damage; small impacts can accumulate over time.
Understanding this point is crucial for making youth sports safer. “Chris has played a critical role in raising awareness here, too,” said Dr. Stern. “Allowing our kids to get hit in the head over and over can put them at greater risk for later problems, plus it just doesn’t make common sense.”
“The biggest misconception surrounding head trauma in sports,” said Dr. Nowinski, “is the belief among players, coaches, and even the medical and scientific communities that if you get hit in the head and don’t have any symptoms then you’re okay and there hasn’t been any damage. That couldn’t be further from the truth. We now know that people are suffering serious brain injuries due to the accumulated effect of subconcussive impacts, and we need to get the word out about that.”
A major initiative from the Concussion Legacy Foundation called “Stop Hitting Kids in the Head” has the goal of convincing every sport to eliminate repetitive head impacts in players under age 14 – the time when the skull and brain are still developing and most vulnerable – by 2026. In fact, Dr. Nowinski wrote that “there could be a lot of kids who are misdiagnosed and medicated for various behavioral or emotional problems that may actually be head injury–related.”
Starting in 2009, the NFL adopted a series of rule changes designed to better protect its players against repeated head trauma. Among them is a ban on spearing or leading with the helmet, penalties for hitting defenseless players, and more stringent return-to-play guidelines, including concussion protocols.
The NFL has also put more emphasis on flag football options for youngsters and, for the first time, showcased this alternative in the 2023 Pro Bowl. But Dr. Nowinski is pressuring the league to go further. “While acknowledging that the game causes CTE, the NFL still underwrites recruiting 5-year-olds to play tackle football,” he said. “In my opinion, that’s unethical, and it needs to be addressed.”
WWE one of the most responsive organizations
Dr. Nowinski said WWE has been one of the most responsive sports organizations for protecting athletes. A doctor is now ringside at every match as is an observer who knows the script, thereby allowing for instant medical intervention if something goes wrong. “Since everyone is trying to look like they have a concussion all the time, it takes a deep understanding of the business to recognize a real one,” he said.
But this hasn’t been the case with other sports. “I am eternally disappointed in the response of the professional sports industry to the knowledge of CTE and long-term concussion symptoms,” said Dr. Nowinski.
“For example, FIFA [international soccer’s governing body] still doesn’t allow doctors to evaluate [potentially concussed] players on the sidelines and put them back in the game with a free substitution [if they’re deemed okay]. Not giving players proper medical care for a brain injury is unethical,” he said. BU’s Center for the Study of Traumatic Encephalopathy diagnosed the first CTE case in soccer in 2012, and in 2015 Dr. Nowinski successfully lobbied U.S. Soccer to ban heading the ball before age 11.
“Unfortunately, many governing bodies have circled the wagons in denying their sport causes CTE,” he continued. “FIFA, World Rugby, the NHL, even the NCAA and International Olympic Committee refuse to acknowledge it and, therefore, aren’t taking any steps to prevent it. They see it as a threat to their business model. Hopefully, now that the NIH and CDC are aligned about the risks of head impact in sports, this will begin to change.”
Meanwhile, research is continuing. Scientists are getting closer to being able to diagnose CTE in living humans, with ongoing studies using PET scans, blood markers, and spinal fluid markers. In 2019, researchers identified tau proteins specific to CTE that they believe are distinct from those of Alzheimer’s and other neurodegenerative diseases. Next step would be developing a drug to slow the development of CTE once detected.
Nonetheless, athletes at all levels in impact sports still don’t fully appreciate the risks of repeated head trauma and especially subconcussive blows. “I talk to former NFL and college players every week,” said Dr. Stern. “Some tell me, ‘I love the sport, it gave me so much, and I would do it again, but I’m not letting my grandchildren play.’ But others say, ‘As long as they know the risks, they can make their own decision.’ “
Dr. Nowinski has a daughter who is 4 and a son who’s 2. Both play soccer but, thanks to dad, heading isn’t allowed in their age groups. If they continue playing sports, Dr. Nowinski said he’ll make sure they understand the risks and how to protect themselves. This is a conversation all parents should have with their kids at every level to make sure they play safe, he added.
Those in the medical community can also volunteer their time to explain head trauma to athletes, coaches, and school administrators to be sure they understand its seriousness and are doing everything to protect players.
As you watch this year’s Super Bowl, Dr. Nowinski and his team would like you to keep something in mind. Those young men on the field for your entertainment are receiving mild brain trauma repeatedly throughout the game.
Even if it’s not a huge hit that gets replayed and makes everyone gasp, even if no one gets ushered into the little sideline tent for a concussion screening, even if no one loses consciousness, brain damage is still occurring. Watch the heads of the players during every play and think about what’s going on inside their skulls regardless of how big and strong those helmets look.
A version of this article first appeared on Medscape.com.
Unexpected link between light drinking and dementia risk
new research suggests.
Investigators assessed dementia risk using changes in alcohol consumption over a 2-year period in nearly 4 million people in South Korea. After about 7 years, dementia was 21% less likely in mild drinkers and 17% less likely in moderate drinkers. Heavy drinking was linked to an 8% increased risk.
Other studies of the relationship between alcohol and dementia have yielded mixed results, and this study does little to clear those murky waters. Nor do the results mean that drinking is recommended, the investigators note.
But the study does offer new information on how risk changes over time as people change their drinking habits, lead investigator Keun Hye Jeon, MD, assistant professor of family medicine at Cha Gumi Medical Center at Cha University, Gumi, South Korea, told this news organization.
“Although numerous studies have shown a relationship between alcohol consumption and dementia, there is a paucity of understanding as to how the incidence of dementia changes with changes in drinking habits,” Dr. Jeon said.
“By measuring alcohol consumption at two time points, we were able to study the relationship between reducing, ceasing, maintaining, and increasing alcohol consumption and incident dementia,” he added.
The findings were published online in JAMA Network Open.
Tracking drinking habits
Researchers analyzed data from nearly 4 million individuals aged 40 years and older in the Korean National Health Insurance Service who completed questionnaires and underwent physical exams in 2009 and 2011.
Study participants completed questionnaires on their drinking habits and were assigned to one of five groups according to change in alcohol consumption during the study period. These groups consisted of sustained nondrinkers; those who stopped drinking (quitters); those who reduced their consumption of alcohol but did not stop drinking (reducers); those who maintained the same level of consumption (sustainers); and those who increased their level of consumption (increasers).
A standard drink in the United States contains 14 g of alcohol. For this study, mild drinking was defined as less than 15 g/day, or one drink; moderate consumption as 15-29.9 g/day, or one to two drinks; and heavy drinking as 30 g/day or more, or three or more drinks.
At baseline, 54.8% of participants were nondrinkers, 26.7% were mild drinkers, 11.0% were moderate drinkers, and 7.5% were heavy drinkers.
From 2009 to 2011, 24.2% of mild drinkers, 8.4% of moderate drinkers, and 7.6% of heavy drinkers became quitters. In the same period, 13.9% of nondrinkers, 16.1% of mild drinkers, and 17.4% of moderate drinkers increased their drinking level.
After a mean follow-up of 6.3 years, 2.5% of participants were diagnosed with dementia, 2.0% with Alzheimer’s disease, and 0.3% with vascular dementia.
Unexpected finding
Compared with consistently not drinking, mild and moderate alcohol consumption was associated with a 21% (adjust hazard ratio, 0.79; 95% confidence interval, 0.77-0.81) and 17% (aHR, 0.83; 95% CI, 0.79-0.88) decreased risk for dementia, respectively.
Heavy drinking was linked to an 8% increased risk (aHR, 1.08; 95% CI, 1.03-1.12).
Similar associations were found between alcohol consumption and risk for Alzheimer’s disease and vascular dementia.
Reducing drinking habits from heavy to moderate led to a reduction in risk for dementia and Alzheimer’s, and increasing drinking levels led to an increase in risk for both conditions.
But when the researchers analyzed dementia risk for nondrinkers who began drinking at mild levels during the study period, they found something unexpected – the risk in this group decreased by 7% for dementia (aHR, 0.93; 95% CI, 0.90-0.96) and by 8% for Alzheimer’s (aHR, 0.92; 95% CI, 0.89-0.95), compared with sustained mild drinkers.
“Our study showed that initiation of mild alcohol consumption leads to a reduced risk of all-cause dementia and Alzheimer’s disease, which has never been reported in previous studies,” Dr. Jeon said.
However, Dr. Jeon was quick to point out that this doesn’t mean that people who don’t drink should start.
Previous studies have shown that heavy alcohol use can triple an individual’s dementia risk, while other studies have shown that no amount of alcohol consumption is good for the brain.
“None of the existing health guidelines recommend starting alcohol drinking,” Dr. Jeon said. “Our findings regarding an initiation of mild alcohol consumption cannot be directly translated into clinical recommendations,” but the findings do warrant additional study, he added.
Risks persist
Commenting on the findings, Percy Griffin, PhD, director of scientific engagement for the Alzheimer’s Association in Chicago, agrees.
“While this study is interesting, and this topic deserves further study, no one should drink alcohol as a method of reducing risk of Alzheimer’s disease or other dementia based on this study,” said Dr. Griffin, who was not part of the study.
The exact tipping point in alcohol consumption that can lead to problems with cognition or increased dementia risk is unknown, Dr. Griffin said. Nor do researchers understand why mild drinking may have a protective effect.
“We do know, however, that excessive alcohol consumption has negative effects on heart health and general health, which can lead to problems with brain function,” he said. “Clinicians should have discussions with their patients around their alcohol consumption patterns and the risks associated with drinking in excess, including potential damage to their cognition.”
Funding for the study was not disclosed. Dr. Jeon and Dr. Griffin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators assessed dementia risk using changes in alcohol consumption over a 2-year period in nearly 4 million people in South Korea. After about 7 years, dementia was 21% less likely in mild drinkers and 17% less likely in moderate drinkers. Heavy drinking was linked to an 8% increased risk.
Other studies of the relationship between alcohol and dementia have yielded mixed results, and this study does little to clear those murky waters. Nor do the results mean that drinking is recommended, the investigators note.
But the study does offer new information on how risk changes over time as people change their drinking habits, lead investigator Keun Hye Jeon, MD, assistant professor of family medicine at Cha Gumi Medical Center at Cha University, Gumi, South Korea, told this news organization.
“Although numerous studies have shown a relationship between alcohol consumption and dementia, there is a paucity of understanding as to how the incidence of dementia changes with changes in drinking habits,” Dr. Jeon said.
“By measuring alcohol consumption at two time points, we were able to study the relationship between reducing, ceasing, maintaining, and increasing alcohol consumption and incident dementia,” he added.
The findings were published online in JAMA Network Open.
Tracking drinking habits
Researchers analyzed data from nearly 4 million individuals aged 40 years and older in the Korean National Health Insurance Service who completed questionnaires and underwent physical exams in 2009 and 2011.
Study participants completed questionnaires on their drinking habits and were assigned to one of five groups according to change in alcohol consumption during the study period. These groups consisted of sustained nondrinkers; those who stopped drinking (quitters); those who reduced their consumption of alcohol but did not stop drinking (reducers); those who maintained the same level of consumption (sustainers); and those who increased their level of consumption (increasers).
A standard drink in the United States contains 14 g of alcohol. For this study, mild drinking was defined as less than 15 g/day, or one drink; moderate consumption as 15-29.9 g/day, or one to two drinks; and heavy drinking as 30 g/day or more, or three or more drinks.
At baseline, 54.8% of participants were nondrinkers, 26.7% were mild drinkers, 11.0% were moderate drinkers, and 7.5% were heavy drinkers.
From 2009 to 2011, 24.2% of mild drinkers, 8.4% of moderate drinkers, and 7.6% of heavy drinkers became quitters. In the same period, 13.9% of nondrinkers, 16.1% of mild drinkers, and 17.4% of moderate drinkers increased their drinking level.
After a mean follow-up of 6.3 years, 2.5% of participants were diagnosed with dementia, 2.0% with Alzheimer’s disease, and 0.3% with vascular dementia.
Unexpected finding
Compared with consistently not drinking, mild and moderate alcohol consumption was associated with a 21% (adjust hazard ratio, 0.79; 95% confidence interval, 0.77-0.81) and 17% (aHR, 0.83; 95% CI, 0.79-0.88) decreased risk for dementia, respectively.
Heavy drinking was linked to an 8% increased risk (aHR, 1.08; 95% CI, 1.03-1.12).
Similar associations were found between alcohol consumption and risk for Alzheimer’s disease and vascular dementia.
Reducing drinking habits from heavy to moderate led to a reduction in risk for dementia and Alzheimer’s, and increasing drinking levels led to an increase in risk for both conditions.
But when the researchers analyzed dementia risk for nondrinkers who began drinking at mild levels during the study period, they found something unexpected – the risk in this group decreased by 7% for dementia (aHR, 0.93; 95% CI, 0.90-0.96) and by 8% for Alzheimer’s (aHR, 0.92; 95% CI, 0.89-0.95), compared with sustained mild drinkers.
“Our study showed that initiation of mild alcohol consumption leads to a reduced risk of all-cause dementia and Alzheimer’s disease, which has never been reported in previous studies,” Dr. Jeon said.
However, Dr. Jeon was quick to point out that this doesn’t mean that people who don’t drink should start.
Previous studies have shown that heavy alcohol use can triple an individual’s dementia risk, while other studies have shown that no amount of alcohol consumption is good for the brain.
“None of the existing health guidelines recommend starting alcohol drinking,” Dr. Jeon said. “Our findings regarding an initiation of mild alcohol consumption cannot be directly translated into clinical recommendations,” but the findings do warrant additional study, he added.
Risks persist
Commenting on the findings, Percy Griffin, PhD, director of scientific engagement for the Alzheimer’s Association in Chicago, agrees.
“While this study is interesting, and this topic deserves further study, no one should drink alcohol as a method of reducing risk of Alzheimer’s disease or other dementia based on this study,” said Dr. Griffin, who was not part of the study.
The exact tipping point in alcohol consumption that can lead to problems with cognition or increased dementia risk is unknown, Dr. Griffin said. Nor do researchers understand why mild drinking may have a protective effect.
“We do know, however, that excessive alcohol consumption has negative effects on heart health and general health, which can lead to problems with brain function,” he said. “Clinicians should have discussions with their patients around their alcohol consumption patterns and the risks associated with drinking in excess, including potential damage to their cognition.”
Funding for the study was not disclosed. Dr. Jeon and Dr. Griffin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators assessed dementia risk using changes in alcohol consumption over a 2-year period in nearly 4 million people in South Korea. After about 7 years, dementia was 21% less likely in mild drinkers and 17% less likely in moderate drinkers. Heavy drinking was linked to an 8% increased risk.
Other studies of the relationship between alcohol and dementia have yielded mixed results, and this study does little to clear those murky waters. Nor do the results mean that drinking is recommended, the investigators note.
But the study does offer new information on how risk changes over time as people change their drinking habits, lead investigator Keun Hye Jeon, MD, assistant professor of family medicine at Cha Gumi Medical Center at Cha University, Gumi, South Korea, told this news organization.
“Although numerous studies have shown a relationship between alcohol consumption and dementia, there is a paucity of understanding as to how the incidence of dementia changes with changes in drinking habits,” Dr. Jeon said.
“By measuring alcohol consumption at two time points, we were able to study the relationship between reducing, ceasing, maintaining, and increasing alcohol consumption and incident dementia,” he added.
The findings were published online in JAMA Network Open.
Tracking drinking habits
Researchers analyzed data from nearly 4 million individuals aged 40 years and older in the Korean National Health Insurance Service who completed questionnaires and underwent physical exams in 2009 and 2011.
Study participants completed questionnaires on their drinking habits and were assigned to one of five groups according to change in alcohol consumption during the study period. These groups consisted of sustained nondrinkers; those who stopped drinking (quitters); those who reduced their consumption of alcohol but did not stop drinking (reducers); those who maintained the same level of consumption (sustainers); and those who increased their level of consumption (increasers).
A standard drink in the United States contains 14 g of alcohol. For this study, mild drinking was defined as less than 15 g/day, or one drink; moderate consumption as 15-29.9 g/day, or one to two drinks; and heavy drinking as 30 g/day or more, or three or more drinks.
At baseline, 54.8% of participants were nondrinkers, 26.7% were mild drinkers, 11.0% were moderate drinkers, and 7.5% were heavy drinkers.
From 2009 to 2011, 24.2% of mild drinkers, 8.4% of moderate drinkers, and 7.6% of heavy drinkers became quitters. In the same period, 13.9% of nondrinkers, 16.1% of mild drinkers, and 17.4% of moderate drinkers increased their drinking level.
After a mean follow-up of 6.3 years, 2.5% of participants were diagnosed with dementia, 2.0% with Alzheimer’s disease, and 0.3% with vascular dementia.
Unexpected finding
Compared with consistently not drinking, mild and moderate alcohol consumption was associated with a 21% (adjust hazard ratio, 0.79; 95% confidence interval, 0.77-0.81) and 17% (aHR, 0.83; 95% CI, 0.79-0.88) decreased risk for dementia, respectively.
Heavy drinking was linked to an 8% increased risk (aHR, 1.08; 95% CI, 1.03-1.12).
Similar associations were found between alcohol consumption and risk for Alzheimer’s disease and vascular dementia.
Reducing drinking habits from heavy to moderate led to a reduction in risk for dementia and Alzheimer’s, and increasing drinking levels led to an increase in risk for both conditions.
But when the researchers analyzed dementia risk for nondrinkers who began drinking at mild levels during the study period, they found something unexpected – the risk in this group decreased by 7% for dementia (aHR, 0.93; 95% CI, 0.90-0.96) and by 8% for Alzheimer’s (aHR, 0.92; 95% CI, 0.89-0.95), compared with sustained mild drinkers.
“Our study showed that initiation of mild alcohol consumption leads to a reduced risk of all-cause dementia and Alzheimer’s disease, which has never been reported in previous studies,” Dr. Jeon said.
However, Dr. Jeon was quick to point out that this doesn’t mean that people who don’t drink should start.
Previous studies have shown that heavy alcohol use can triple an individual’s dementia risk, while other studies have shown that no amount of alcohol consumption is good for the brain.
“None of the existing health guidelines recommend starting alcohol drinking,” Dr. Jeon said. “Our findings regarding an initiation of mild alcohol consumption cannot be directly translated into clinical recommendations,” but the findings do warrant additional study, he added.
Risks persist
Commenting on the findings, Percy Griffin, PhD, director of scientific engagement for the Alzheimer’s Association in Chicago, agrees.
“While this study is interesting, and this topic deserves further study, no one should drink alcohol as a method of reducing risk of Alzheimer’s disease or other dementia based on this study,” said Dr. Griffin, who was not part of the study.
The exact tipping point in alcohol consumption that can lead to problems with cognition or increased dementia risk is unknown, Dr. Griffin said. Nor do researchers understand why mild drinking may have a protective effect.
“We do know, however, that excessive alcohol consumption has negative effects on heart health and general health, which can lead to problems with brain function,” he said. “Clinicians should have discussions with their patients around their alcohol consumption patterns and the risks associated with drinking in excess, including potential damage to their cognition.”
Funding for the study was not disclosed. Dr. Jeon and Dr. Griffin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
We don’t lose our keys (or other things) as much as we think
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
FROM CURRENT BIOLOGY
Long-term depression may hasten brain aging in midlife
Previous research suggests a possible link between depression and increased risk of dementia in older adults, but the association between depression and brain health in early adulthood and midlife has not been well studied, wrote Christina S. Dintica, PhD, of the University of California, San Francisco, and colleagues.
In a study published in the Journal of Affective Disorders, the researchers identified 649 individuals aged 23-36 at baseline who were part of the Coronary Artery Risk Development in Young Adults (CARDIA) study. All participants underwent brain MRI and cognitive testing. Depressive symptoms were assessed six times over a 25-year period using the Center for Epidemiological Studies Depression scale (CES–D), and the scores were analyzed as time-weighted averages (TWA). Elevated depressive symptoms were defined as CES-D scores of 16 or higher. Brain age was assessed via high-dimensional neuroimaging. Approximately half of the participants were female, and half were Black.
Overall, each 5-point increment in TWA depression symptoms over 25 years was associated with a 1-year increase in brain age, and individuals with elevated TWA depression averaged a 3-year increase in brain age compared with those with lower levels of depression after controlling for factors including chronological age, sex, education, race, MRI scanning site, and intracranial volume, they said. The association was attenuated in a model controlling for antidepressant use, and further attenuated after adjusting for smoking, alcohol consumption, income, body mass index, diabetes, and physical exercise.
The researchers also investigated the impact of the age period of elevated depressive symptoms on brain age. Compared with low depressive symptoms, elevated TWA CES-D at ages 30-39 years, 40-49 years, and 50-59 years was associated with increased brain ages of 2.43, 3.19, and 1.82.
In addition, elevated depressive symptoms were associated with a threefold increase in the odds of poor cognitive function at midlife (odds ratio, 3.30), although these odds were reduced after adjusting for use of antidepressants (OR, 1.47).
The mechanisms of action for the link between depression and accelerated brain aging remains uncertain, the researchers wrote in their discussion. “Studies over the last 20 years have demonstrated that increased inflammation and hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis are two of the most consistent biological findings in major depression, which have been linked to premature aging,” they noted. “Alternative explanations for the link between depression and adverse brain health could be underlying factors that explain both outcomes rather independently, such as low socioeconomic status, childhood maltreatment, or shared genetic effects,” they added.
Adjustment for antidepressant use had little effect overall on the association between depressive symptom severity and brain age, they said.
The current study findings were limited by the single assessment of brain age, which prevented evaluation of the temporality of the association between brain aging and depression, the researchers noted.
However, the results were strengthened by the large and diverse cohort, long-term follow-up, and use of high-dimensional neuroimaging, they said. Longitudinal studies are needed to explore mechanisms of action and the potential benefits of antidepressants, they added.
In the meantime, monitoring and treating depressive symptoms in young adults may help promote brain health in midlife and older age, they concluded.
The CARDIA study was supported by the National Heart, Lung, and Blood Institute, the National Institute on Aging, and the Alzheimer’s Association. The researchers had no financial conflicts to disclose.
Previous research suggests a possible link between depression and increased risk of dementia in older adults, but the association between depression and brain health in early adulthood and midlife has not been well studied, wrote Christina S. Dintica, PhD, of the University of California, San Francisco, and colleagues.
In a study published in the Journal of Affective Disorders, the researchers identified 649 individuals aged 23-36 at baseline who were part of the Coronary Artery Risk Development in Young Adults (CARDIA) study. All participants underwent brain MRI and cognitive testing. Depressive symptoms were assessed six times over a 25-year period using the Center for Epidemiological Studies Depression scale (CES–D), and the scores were analyzed as time-weighted averages (TWA). Elevated depressive symptoms were defined as CES-D scores of 16 or higher. Brain age was assessed via high-dimensional neuroimaging. Approximately half of the participants were female, and half were Black.
Overall, each 5-point increment in TWA depression symptoms over 25 years was associated with a 1-year increase in brain age, and individuals with elevated TWA depression averaged a 3-year increase in brain age compared with those with lower levels of depression after controlling for factors including chronological age, sex, education, race, MRI scanning site, and intracranial volume, they said. The association was attenuated in a model controlling for antidepressant use, and further attenuated after adjusting for smoking, alcohol consumption, income, body mass index, diabetes, and physical exercise.
The researchers also investigated the impact of the age period of elevated depressive symptoms on brain age. Compared with low depressive symptoms, elevated TWA CES-D at ages 30-39 years, 40-49 years, and 50-59 years was associated with increased brain ages of 2.43, 3.19, and 1.82.
In addition, elevated depressive symptoms were associated with a threefold increase in the odds of poor cognitive function at midlife (odds ratio, 3.30), although these odds were reduced after adjusting for use of antidepressants (OR, 1.47).
The mechanisms of action for the link between depression and accelerated brain aging remains uncertain, the researchers wrote in their discussion. “Studies over the last 20 years have demonstrated that increased inflammation and hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis are two of the most consistent biological findings in major depression, which have been linked to premature aging,” they noted. “Alternative explanations for the link between depression and adverse brain health could be underlying factors that explain both outcomes rather independently, such as low socioeconomic status, childhood maltreatment, or shared genetic effects,” they added.
Adjustment for antidepressant use had little effect overall on the association between depressive symptom severity and brain age, they said.
The current study findings were limited by the single assessment of brain age, which prevented evaluation of the temporality of the association between brain aging and depression, the researchers noted.
However, the results were strengthened by the large and diverse cohort, long-term follow-up, and use of high-dimensional neuroimaging, they said. Longitudinal studies are needed to explore mechanisms of action and the potential benefits of antidepressants, they added.
In the meantime, monitoring and treating depressive symptoms in young adults may help promote brain health in midlife and older age, they concluded.
The CARDIA study was supported by the National Heart, Lung, and Blood Institute, the National Institute on Aging, and the Alzheimer’s Association. The researchers had no financial conflicts to disclose.
Previous research suggests a possible link between depression and increased risk of dementia in older adults, but the association between depression and brain health in early adulthood and midlife has not been well studied, wrote Christina S. Dintica, PhD, of the University of California, San Francisco, and colleagues.
In a study published in the Journal of Affective Disorders, the researchers identified 649 individuals aged 23-36 at baseline who were part of the Coronary Artery Risk Development in Young Adults (CARDIA) study. All participants underwent brain MRI and cognitive testing. Depressive symptoms were assessed six times over a 25-year period using the Center for Epidemiological Studies Depression scale (CES–D), and the scores were analyzed as time-weighted averages (TWA). Elevated depressive symptoms were defined as CES-D scores of 16 or higher. Brain age was assessed via high-dimensional neuroimaging. Approximately half of the participants were female, and half were Black.
Overall, each 5-point increment in TWA depression symptoms over 25 years was associated with a 1-year increase in brain age, and individuals with elevated TWA depression averaged a 3-year increase in brain age compared with those with lower levels of depression after controlling for factors including chronological age, sex, education, race, MRI scanning site, and intracranial volume, they said. The association was attenuated in a model controlling for antidepressant use, and further attenuated after adjusting for smoking, alcohol consumption, income, body mass index, diabetes, and physical exercise.
The researchers also investigated the impact of the age period of elevated depressive symptoms on brain age. Compared with low depressive symptoms, elevated TWA CES-D at ages 30-39 years, 40-49 years, and 50-59 years was associated with increased brain ages of 2.43, 3.19, and 1.82.
In addition, elevated depressive symptoms were associated with a threefold increase in the odds of poor cognitive function at midlife (odds ratio, 3.30), although these odds were reduced after adjusting for use of antidepressants (OR, 1.47).
The mechanisms of action for the link between depression and accelerated brain aging remains uncertain, the researchers wrote in their discussion. “Studies over the last 20 years have demonstrated that increased inflammation and hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis are two of the most consistent biological findings in major depression, which have been linked to premature aging,” they noted. “Alternative explanations for the link between depression and adverse brain health could be underlying factors that explain both outcomes rather independently, such as low socioeconomic status, childhood maltreatment, or shared genetic effects,” they added.
Adjustment for antidepressant use had little effect overall on the association between depressive symptom severity and brain age, they said.
The current study findings were limited by the single assessment of brain age, which prevented evaluation of the temporality of the association between brain aging and depression, the researchers noted.
However, the results were strengthened by the large and diverse cohort, long-term follow-up, and use of high-dimensional neuroimaging, they said. Longitudinal studies are needed to explore mechanisms of action and the potential benefits of antidepressants, they added.
In the meantime, monitoring and treating depressive symptoms in young adults may help promote brain health in midlife and older age, they concluded.
The CARDIA study was supported by the National Heart, Lung, and Blood Institute, the National Institute on Aging, and the Alzheimer’s Association. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Cognitive testing for older drivers: Is there a benefit?
, according to results from a large population-based study using data from Japan.
But the same study, published in the Journal of the American Geriatrics Society, also reported a concurrent increase in pedestrian and cycling injuries, possibly because more older former drivers were getting around by alternative means. That finding echoed a 2012 study from Denmark, which also looked at the effects of an age-based cognitive screening policy for older drivers, and saw more fatal road injuries among older people who were not driving.
While some governments, including those of Denmark, Taiwan, and Japan, have implemented age-based cognitive screening for older drivers, there has been little evidence to date that such policies improve road safety. Guidelines issued in 2010 by the American Academy of Neurology discourage age-based screening, advising instead that people diagnosed with cognitive disorders be carefully evaluated for driving fitness and recommending one widely used scale, the Clinical Dementia Rating, as useful in identifying potentially unsafe drivers.
Japan’s national screening policy: Did it work?
The new study, led by Haruhiko Inada, MD, PhD, an epidemiologist at Johns Hopkins University in Baltimore, used national crash data from Japan, where since 2017 all drivers 75 and older not only must take cognitive tests measuring temporal orientation and memory at license renewal, but are also referred for medical evaluation if they fail them. People receiving a subsequent dementia diagnosis can have their licenses suspended or revoked.
Dr. Inada and his colleagues looked at national data from nearly 603,000 police-reported vehicle collisions and nearly 197,000 pedestrian or cyclist road injuries between March 2012 and December 2019, all involving people aged 70 and older. To assess the screening policy’s impact, the researchers calculated estimated monthly collision or injury incidence rates per 100,000 person-years. This way, they could “control for secular trends that were unaffected by the policy, such as the decreasing incidence of motor vehicle collisions year by year,” the researchers explained.
After the screening was implemented, cumulative estimated collisions among drivers 75 or older decreased by 3,670 (95% confidence interval, 5,125-2,104), while reported pedestrian or cyclist injuries increased by an estimated 959 (95% CI, 24-1,834). Dr. Inada and colleagues found that crashes declined among men but not women, noting also that more older men than women are licensed to drive in Japan. Pedestrian and cyclist injuries were highest among men aged 80-84, and women aged 80 and older.
“Cognitively screening older drivers at license renewal and promoting voluntary surrender of licenses may prevent motor vehicle collisions,” Dr. Inada and his colleagues concluded. “However, they are associated with an increase in road injuries for older pedestrians and cyclists. Future studies should examine the effectiveness of mitigation measures, such as alternative, safe transportation, and accommodations for pedestrians and cyclists.”
No definitive answers
Two investigators who have studied cognitive screening related to road safety were contacted for commentary on the study findings.
Anu Siren, PhD, professor of gerontology at Tampere (Finland) University, who in 2012 reported higher injuries after implementation of older-driver cognitive screening in Denmark, commented that the new study, while benefiting from a much larger data set than earlier studies, still “fails to show that decrease in collisions is because ‘unfit’ drivers were removed from the road. But it does confirm previous findings about how strict screening policies make people shift from cars to unprotected modes of transportation,” which are riskier.
In studies measuring driving safety, the usual definition of risk is incidents per exposure, Dr. Siren noted. In Dr. Inada and colleagues’ study, “the incident measure, or numerator, is the number of collisions. The exposure measure or denominator is population. Because the study uses population and not driver licenses (or distance traveled) as an exposure measure, the observed decrease in collisions does not say much about how the collision risk develops after the implementation of screening.”
Older driver screening “is likely to cause some older persons to cease from driving and probably continue to travel as unprotected road users,” Dr. Siren continued. “Similar to what we found [in 2012], the injury rates for pedestrians and cyclists went up after the introduction of screening, which suggests that screening indirectly causes increasing number of injuries among older unprotected road users.”
Matthew Rizzo, MD, professor and chair of the department of neurological sciences at the University of Nebraska Medical Center and codirector of the Nebraska Neuroscience Alliance in Omaha, Neb., and the lead author of the 2010 AAN guidelines on cognitive impairment and driving risk, cautioned against ageism in designing policies meant to protect motorists.
“We find some erratic/weak effects of age here and there, but the big effects we consistently find are from cognitive and visual decline – which is somewhat correlated with age, but with huge variance,” Dr. Rizzo said. “It is hard to say what an optimal age threshold for risk would be, and if 75 is it.”
U.S. crash data from the last decade points to drivers 80 and older as significantly more accident-prone than those in their 70s, or even late 70s, Dr. Rizzo noted. Moreover, “willingness to get on the road, number of miles driven, type of road (urban, rural, highway, commercial, residential), type of vehicle driven, traffic, and environment (day, night, weather), et cetera, are all factors to consider in driving risk and restriction,” he said.
Dr. Rizzo added that the 2010 AAN guidelines might need to be revisited in light of newer vehicle safety systems and automation.
Dr. Inada and colleagues’ study was funded by Japanese government grants, and Dr. Inada and his coauthors reported no financial conflicts of interest. Dr. Siren and Dr. Rizzo reported no financial conflicts of interest.
, according to results from a large population-based study using data from Japan.
But the same study, published in the Journal of the American Geriatrics Society, also reported a concurrent increase in pedestrian and cycling injuries, possibly because more older former drivers were getting around by alternative means. That finding echoed a 2012 study from Denmark, which also looked at the effects of an age-based cognitive screening policy for older drivers, and saw more fatal road injuries among older people who were not driving.
While some governments, including those of Denmark, Taiwan, and Japan, have implemented age-based cognitive screening for older drivers, there has been little evidence to date that such policies improve road safety. Guidelines issued in 2010 by the American Academy of Neurology discourage age-based screening, advising instead that people diagnosed with cognitive disorders be carefully evaluated for driving fitness and recommending one widely used scale, the Clinical Dementia Rating, as useful in identifying potentially unsafe drivers.
Japan’s national screening policy: Did it work?
The new study, led by Haruhiko Inada, MD, PhD, an epidemiologist at Johns Hopkins University in Baltimore, used national crash data from Japan, where since 2017 all drivers 75 and older not only must take cognitive tests measuring temporal orientation and memory at license renewal, but are also referred for medical evaluation if they fail them. People receiving a subsequent dementia diagnosis can have their licenses suspended or revoked.
Dr. Inada and his colleagues looked at national data from nearly 603,000 police-reported vehicle collisions and nearly 197,000 pedestrian or cyclist road injuries between March 2012 and December 2019, all involving people aged 70 and older. To assess the screening policy’s impact, the researchers calculated estimated monthly collision or injury incidence rates per 100,000 person-years. This way, they could “control for secular trends that were unaffected by the policy, such as the decreasing incidence of motor vehicle collisions year by year,” the researchers explained.
After the screening was implemented, cumulative estimated collisions among drivers 75 or older decreased by 3,670 (95% confidence interval, 5,125-2,104), while reported pedestrian or cyclist injuries increased by an estimated 959 (95% CI, 24-1,834). Dr. Inada and colleagues found that crashes declined among men but not women, noting also that more older men than women are licensed to drive in Japan. Pedestrian and cyclist injuries were highest among men aged 80-84, and women aged 80 and older.
“Cognitively screening older drivers at license renewal and promoting voluntary surrender of licenses may prevent motor vehicle collisions,” Dr. Inada and his colleagues concluded. “However, they are associated with an increase in road injuries for older pedestrians and cyclists. Future studies should examine the effectiveness of mitigation measures, such as alternative, safe transportation, and accommodations for pedestrians and cyclists.”
No definitive answers
Two investigators who have studied cognitive screening related to road safety were contacted for commentary on the study findings.
Anu Siren, PhD, professor of gerontology at Tampere (Finland) University, who in 2012 reported higher injuries after implementation of older-driver cognitive screening in Denmark, commented that the new study, while benefiting from a much larger data set than earlier studies, still “fails to show that decrease in collisions is because ‘unfit’ drivers were removed from the road. But it does confirm previous findings about how strict screening policies make people shift from cars to unprotected modes of transportation,” which are riskier.
In studies measuring driving safety, the usual definition of risk is incidents per exposure, Dr. Siren noted. In Dr. Inada and colleagues’ study, “the incident measure, or numerator, is the number of collisions. The exposure measure or denominator is population. Because the study uses population and not driver licenses (or distance traveled) as an exposure measure, the observed decrease in collisions does not say much about how the collision risk develops after the implementation of screening.”
Older driver screening “is likely to cause some older persons to cease from driving and probably continue to travel as unprotected road users,” Dr. Siren continued. “Similar to what we found [in 2012], the injury rates for pedestrians and cyclists went up after the introduction of screening, which suggests that screening indirectly causes increasing number of injuries among older unprotected road users.”
Matthew Rizzo, MD, professor and chair of the department of neurological sciences at the University of Nebraska Medical Center and codirector of the Nebraska Neuroscience Alliance in Omaha, Neb., and the lead author of the 2010 AAN guidelines on cognitive impairment and driving risk, cautioned against ageism in designing policies meant to protect motorists.
“We find some erratic/weak effects of age here and there, but the big effects we consistently find are from cognitive and visual decline – which is somewhat correlated with age, but with huge variance,” Dr. Rizzo said. “It is hard to say what an optimal age threshold for risk would be, and if 75 is it.”
U.S. crash data from the last decade points to drivers 80 and older as significantly more accident-prone than those in their 70s, or even late 70s, Dr. Rizzo noted. Moreover, “willingness to get on the road, number of miles driven, type of road (urban, rural, highway, commercial, residential), type of vehicle driven, traffic, and environment (day, night, weather), et cetera, are all factors to consider in driving risk and restriction,” he said.
Dr. Rizzo added that the 2010 AAN guidelines might need to be revisited in light of newer vehicle safety systems and automation.
Dr. Inada and colleagues’ study was funded by Japanese government grants, and Dr. Inada and his coauthors reported no financial conflicts of interest. Dr. Siren and Dr. Rizzo reported no financial conflicts of interest.
, according to results from a large population-based study using data from Japan.
But the same study, published in the Journal of the American Geriatrics Society, also reported a concurrent increase in pedestrian and cycling injuries, possibly because more older former drivers were getting around by alternative means. That finding echoed a 2012 study from Denmark, which also looked at the effects of an age-based cognitive screening policy for older drivers, and saw more fatal road injuries among older people who were not driving.
While some governments, including those of Denmark, Taiwan, and Japan, have implemented age-based cognitive screening for older drivers, there has been little evidence to date that such policies improve road safety. Guidelines issued in 2010 by the American Academy of Neurology discourage age-based screening, advising instead that people diagnosed with cognitive disorders be carefully evaluated for driving fitness and recommending one widely used scale, the Clinical Dementia Rating, as useful in identifying potentially unsafe drivers.
Japan’s national screening policy: Did it work?
The new study, led by Haruhiko Inada, MD, PhD, an epidemiologist at Johns Hopkins University in Baltimore, used national crash data from Japan, where since 2017 all drivers 75 and older not only must take cognitive tests measuring temporal orientation and memory at license renewal, but are also referred for medical evaluation if they fail them. People receiving a subsequent dementia diagnosis can have their licenses suspended or revoked.
Dr. Inada and his colleagues looked at national data from nearly 603,000 police-reported vehicle collisions and nearly 197,000 pedestrian or cyclist road injuries between March 2012 and December 2019, all involving people aged 70 and older. To assess the screening policy’s impact, the researchers calculated estimated monthly collision or injury incidence rates per 100,000 person-years. This way, they could “control for secular trends that were unaffected by the policy, such as the decreasing incidence of motor vehicle collisions year by year,” the researchers explained.
After the screening was implemented, cumulative estimated collisions among drivers 75 or older decreased by 3,670 (95% confidence interval, 5,125-2,104), while reported pedestrian or cyclist injuries increased by an estimated 959 (95% CI, 24-1,834). Dr. Inada and colleagues found that crashes declined among men but not women, noting also that more older men than women are licensed to drive in Japan. Pedestrian and cyclist injuries were highest among men aged 80-84, and women aged 80 and older.
“Cognitively screening older drivers at license renewal and promoting voluntary surrender of licenses may prevent motor vehicle collisions,” Dr. Inada and his colleagues concluded. “However, they are associated with an increase in road injuries for older pedestrians and cyclists. Future studies should examine the effectiveness of mitigation measures, such as alternative, safe transportation, and accommodations for pedestrians and cyclists.”
No definitive answers
Two investigators who have studied cognitive screening related to road safety were contacted for commentary on the study findings.
Anu Siren, PhD, professor of gerontology at Tampere (Finland) University, who in 2012 reported higher injuries after implementation of older-driver cognitive screening in Denmark, commented that the new study, while benefiting from a much larger data set than earlier studies, still “fails to show that decrease in collisions is because ‘unfit’ drivers were removed from the road. But it does confirm previous findings about how strict screening policies make people shift from cars to unprotected modes of transportation,” which are riskier.
In studies measuring driving safety, the usual definition of risk is incidents per exposure, Dr. Siren noted. In Dr. Inada and colleagues’ study, “the incident measure, or numerator, is the number of collisions. The exposure measure or denominator is population. Because the study uses population and not driver licenses (or distance traveled) as an exposure measure, the observed decrease in collisions does not say much about how the collision risk develops after the implementation of screening.”
Older driver screening “is likely to cause some older persons to cease from driving and probably continue to travel as unprotected road users,” Dr. Siren continued. “Similar to what we found [in 2012], the injury rates for pedestrians and cyclists went up after the introduction of screening, which suggests that screening indirectly causes increasing number of injuries among older unprotected road users.”
Matthew Rizzo, MD, professor and chair of the department of neurological sciences at the University of Nebraska Medical Center and codirector of the Nebraska Neuroscience Alliance in Omaha, Neb., and the lead author of the 2010 AAN guidelines on cognitive impairment and driving risk, cautioned against ageism in designing policies meant to protect motorists.
“We find some erratic/weak effects of age here and there, but the big effects we consistently find are from cognitive and visual decline – which is somewhat correlated with age, but with huge variance,” Dr. Rizzo said. “It is hard to say what an optimal age threshold for risk would be, and if 75 is it.”
U.S. crash data from the last decade points to drivers 80 and older as significantly more accident-prone than those in their 70s, or even late 70s, Dr. Rizzo noted. Moreover, “willingness to get on the road, number of miles driven, type of road (urban, rural, highway, commercial, residential), type of vehicle driven, traffic, and environment (day, night, weather), et cetera, are all factors to consider in driving risk and restriction,” he said.
Dr. Rizzo added that the 2010 AAN guidelines might need to be revisited in light of newer vehicle safety systems and automation.
Dr. Inada and colleagues’ study was funded by Japanese government grants, and Dr. Inada and his coauthors reported no financial conflicts of interest. Dr. Siren and Dr. Rizzo reported no financial conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN GERIATRICS SOCIETY