User login
Universal anxiety screening recommendation is a good start
A very good thing happened this summer for patients with anxiety and the psychiatrists, psychologists, and other mental health professionals who provide treatment for them. The U.S. Preventive Services Task Force recommended anxiety screening for all adults younger than 65.
On the surface, this is a great recommendation for recognition and caring for those who deal with and suffer from an anxiety disorder or multiple anxiety disorders. Although the USPSTF recommendations are independent of the U.S. government and are not an official position of the Department of Health & Human Services, they are a wonderful start at recognizing the importance of mental health care.
After all, anxiety disorders are the most commonly experienced and diagnosed mental disorders, according to the DSM-5.
They range mainly from generalized anxiety disorder (GAD), to panic attacks and panic disorder, separation anxiety, specific type phobias (bridges, tunnels, insects, snakes, and the list goes on), to other phobias, including agoraphobia, social phobia, and of course, anxiety caused by medical conditions. GAD alone occurs in, at least, more than 3% of the population.
Those of us who have been treating anxiety disorders for decades recognize them as an issue affecting both mental and physical well-being, not only because of the emotional causes but the physical distress and illnesses that anxiety may precipitate or worsen.
For example, blood pressure– and heart-related issues, GI disorders, and musculoskeletal issues are just a few examples of how our bodies and organ systems are affected by anxiety. Just the momentary physical symptoms of tachycardia or the “runs” before an exam are fine examples of how anxiety may affect patients physically, and an ongoing, consistent anxiety is potentially more harmful.
In fact, a first panic attack or episode of generalized anxiety may be so serious that an emergency department or physician visit is necessary to rule out a heart attack, asthma, or breathing issues – even a hormone or thyroid emergency, or a cardiac arrhythmia. Panic attacks alone create a high number of ED visits.
Treatments mainly include medication management and a variety of psychotherapy techniques. Currently, the most preferred, first-choice medications are the SSRI antidepressants, which are Food and Drug Administration approved for anxiety as well. These include Zoloft (sertraline), Prozac/Sarafem (fluoxetine), Celexa (citalopram), and Lexapro (escitalopram).
For many years, benzodiazepines (that is, tranquillizers) such as Valium (diazepam), Ativan (lorazepam), and Klonopin/Rivotril (clonazepam) to name a few, were the mainstay of anxiety treatment, but they have proven addictive and may affect cognition and memory. As the current opioid epidemic has shown, when combined with opioids, benzodiazepines are a potentially lethal combination and when used, they need to be for shorter-term care and monitored very judiciously.
It should be noted that after ongoing long-term use of an SSRI for anxiety or depression, it should not be stopped abruptly, as a variety of physical symptoms (for example, flu-like symptoms) may occur.
Benefits of nonmedicinal therapies
There are a variety of talk therapies, from dynamic psychotherapies to cognitive-behavioral therapies (CBT), plus relaxation techniques and guided imagery that have all had a good amount of success in treating generalized anxiety, panic disorder, as well as various types of phobias.
When medications are stopped, the anxiety symptoms may well return. But when using nonmedicinal therapies, clinicians have discovered that when patients develop a new perspective on the anxiety problem or have a new technique to treat anxiety, it may well be long lasting.
For me, using CBT, relaxation techniques, hypnosis, and guided imagery has been very successful in treating anxiety disorders with long-lasting results. Once a person learns to relax, whether it’s from deep breathing exercises, hypnosis (which is not sleep), mindfulness, or meditation, a strategy of guided imagery can be taught, which allows a person to practice as well as control their anxiety as a lifetime process. For example, I like imagining a large movie screen to desensitize and project anxieties.
In many instances, a combination of a medication and a talk therapy approach works best, but there are an equal number of instances in which just medication or just talk therapy is needed. Once again, knowledge, clinical judgment, and the art of care are required to make these assessments.
In other words, recognizing and treating anxiety requires highly specialized training, which is why I thought the USPSTF recommendations raise a few critical questions.
Questions and concerns
One issue, of course, is the exclusion of those patients over age 65 because of a lack of “data.” Why such an exclusion? Does this mean that data are lacking for this age group?
The concept of using solely evidenced-based data in psychiatry is itself an interesting concept because our profession, like many other medical specialties, requires practitioners to use a combination of art and science. And much can be said either way about the clarity of accuracy in the diversity of issues that arise when treating emotional disorders.
When looking at the over-65 population, has anyone thought of clinical knowledge, judgment, experience, observation, and, of course, common sense?
Just consider the worry (a cardinal feature of anxiety) that besets people over 65 when it comes to issues such as retirement, financial security, “empty nesting,” physical health issues, decreased socialization that resulted from the COVID-19 pandemic, and the perpetual loss of relatives and friends.
In addition, as we age, anxiety can come simply from the loss of identity as active lifestyles decrease and the reality of nearing life’s end becomes more of a reality. It would seem that this population would benefit enormously from anxiety screening and possible treatment.
Another major concern is that the screening and potential treatment of patients is aimed at primary care physicians. Putting the sole responsibility of providing mental health care on these overworked PCPs defies common sense unless we’re okay with 1- to 2-minute assessments of mental health issues and no doubt, a pharmacology-only approach.
If this follows the same route as well-intentioned PCPs treating depression, where 5-minute medication management is far too common, the only proper diagnostic course – the in-depth interview necessary to make a proper diagnosis – is often missing.
For example, in depression alone, it takes psychiatric experience and time to differentiate a major depressive disorder from a bipolar depression and to provide the appropriate medication and treatment plan with careful follow-up. In my experience, this usually does not happen in the exceedingly overworked, time-driven day of a PCP.
Anxiety disorders and depression can prove debilitating, and if a PCP wants the responsibility of treatment, a mandated mental health program should be followed – just as here in New York, prescribers are mandated to take a pain control, opioid, and infection control CME course to keep our licenses up to date.
Short of mandating a mental health program for PCPs, it should be part of training and CME courses that Psychiatry is a super specialty, much like orthopedics and ophthalmology, and primary care physicians should never hesitate to make referrals to the specialist.
The big picture for me, and I hope for us all, is that the USPSTF has started things rolling by making it clear that PCPs and other health care clinicians need to screen for anxiety as a disabling disorder that is quite treatable.
This approach will help to advance the destigmatization of mental health disorders. But as result, with more patients diagnosed, there will be a need for more psychiatrists – and psychologists with PhDs or PsyDs – to fill the gaps in mental health care.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
A very good thing happened this summer for patients with anxiety and the psychiatrists, psychologists, and other mental health professionals who provide treatment for them. The U.S. Preventive Services Task Force recommended anxiety screening for all adults younger than 65.
On the surface, this is a great recommendation for recognition and caring for those who deal with and suffer from an anxiety disorder or multiple anxiety disorders. Although the USPSTF recommendations are independent of the U.S. government and are not an official position of the Department of Health & Human Services, they are a wonderful start at recognizing the importance of mental health care.
After all, anxiety disorders are the most commonly experienced and diagnosed mental disorders, according to the DSM-5.
They range mainly from generalized anxiety disorder (GAD), to panic attacks and panic disorder, separation anxiety, specific type phobias (bridges, tunnels, insects, snakes, and the list goes on), to other phobias, including agoraphobia, social phobia, and of course, anxiety caused by medical conditions. GAD alone occurs in, at least, more than 3% of the population.
Those of us who have been treating anxiety disorders for decades recognize them as an issue affecting both mental and physical well-being, not only because of the emotional causes but the physical distress and illnesses that anxiety may precipitate or worsen.
For example, blood pressure– and heart-related issues, GI disorders, and musculoskeletal issues are just a few examples of how our bodies and organ systems are affected by anxiety. Just the momentary physical symptoms of tachycardia or the “runs” before an exam are fine examples of how anxiety may affect patients physically, and an ongoing, consistent anxiety is potentially more harmful.
In fact, a first panic attack or episode of generalized anxiety may be so serious that an emergency department or physician visit is necessary to rule out a heart attack, asthma, or breathing issues – even a hormone or thyroid emergency, or a cardiac arrhythmia. Panic attacks alone create a high number of ED visits.
Treatments mainly include medication management and a variety of psychotherapy techniques. Currently, the most preferred, first-choice medications are the SSRI antidepressants, which are Food and Drug Administration approved for anxiety as well. These include Zoloft (sertraline), Prozac/Sarafem (fluoxetine), Celexa (citalopram), and Lexapro (escitalopram).
For many years, benzodiazepines (that is, tranquillizers) such as Valium (diazepam), Ativan (lorazepam), and Klonopin/Rivotril (clonazepam) to name a few, were the mainstay of anxiety treatment, but they have proven addictive and may affect cognition and memory. As the current opioid epidemic has shown, when combined with opioids, benzodiazepines are a potentially lethal combination and when used, they need to be for shorter-term care and monitored very judiciously.
It should be noted that after ongoing long-term use of an SSRI for anxiety or depression, it should not be stopped abruptly, as a variety of physical symptoms (for example, flu-like symptoms) may occur.
Benefits of nonmedicinal therapies
There are a variety of talk therapies, from dynamic psychotherapies to cognitive-behavioral therapies (CBT), plus relaxation techniques and guided imagery that have all had a good amount of success in treating generalized anxiety, panic disorder, as well as various types of phobias.
When medications are stopped, the anxiety symptoms may well return. But when using nonmedicinal therapies, clinicians have discovered that when patients develop a new perspective on the anxiety problem or have a new technique to treat anxiety, it may well be long lasting.
For me, using CBT, relaxation techniques, hypnosis, and guided imagery has been very successful in treating anxiety disorders with long-lasting results. Once a person learns to relax, whether it’s from deep breathing exercises, hypnosis (which is not sleep), mindfulness, or meditation, a strategy of guided imagery can be taught, which allows a person to practice as well as control their anxiety as a lifetime process. For example, I like imagining a large movie screen to desensitize and project anxieties.
In many instances, a combination of a medication and a talk therapy approach works best, but there are an equal number of instances in which just medication or just talk therapy is needed. Once again, knowledge, clinical judgment, and the art of care are required to make these assessments.
In other words, recognizing and treating anxiety requires highly specialized training, which is why I thought the USPSTF recommendations raise a few critical questions.
Questions and concerns
One issue, of course, is the exclusion of those patients over age 65 because of a lack of “data.” Why such an exclusion? Does this mean that data are lacking for this age group?
The concept of using solely evidenced-based data in psychiatry is itself an interesting concept because our profession, like many other medical specialties, requires practitioners to use a combination of art and science. And much can be said either way about the clarity of accuracy in the diversity of issues that arise when treating emotional disorders.
When looking at the over-65 population, has anyone thought of clinical knowledge, judgment, experience, observation, and, of course, common sense?
Just consider the worry (a cardinal feature of anxiety) that besets people over 65 when it comes to issues such as retirement, financial security, “empty nesting,” physical health issues, decreased socialization that resulted from the COVID-19 pandemic, and the perpetual loss of relatives and friends.
In addition, as we age, anxiety can come simply from the loss of identity as active lifestyles decrease and the reality of nearing life’s end becomes more of a reality. It would seem that this population would benefit enormously from anxiety screening and possible treatment.
Another major concern is that the screening and potential treatment of patients is aimed at primary care physicians. Putting the sole responsibility of providing mental health care on these overworked PCPs defies common sense unless we’re okay with 1- to 2-minute assessments of mental health issues and no doubt, a pharmacology-only approach.
If this follows the same route as well-intentioned PCPs treating depression, where 5-minute medication management is far too common, the only proper diagnostic course – the in-depth interview necessary to make a proper diagnosis – is often missing.
For example, in depression alone, it takes psychiatric experience and time to differentiate a major depressive disorder from a bipolar depression and to provide the appropriate medication and treatment plan with careful follow-up. In my experience, this usually does not happen in the exceedingly overworked, time-driven day of a PCP.
Anxiety disorders and depression can prove debilitating, and if a PCP wants the responsibility of treatment, a mandated mental health program should be followed – just as here in New York, prescribers are mandated to take a pain control, opioid, and infection control CME course to keep our licenses up to date.
Short of mandating a mental health program for PCPs, it should be part of training and CME courses that Psychiatry is a super specialty, much like orthopedics and ophthalmology, and primary care physicians should never hesitate to make referrals to the specialist.
The big picture for me, and I hope for us all, is that the USPSTF has started things rolling by making it clear that PCPs and other health care clinicians need to screen for anxiety as a disabling disorder that is quite treatable.
This approach will help to advance the destigmatization of mental health disorders. But as result, with more patients diagnosed, there will be a need for more psychiatrists – and psychologists with PhDs or PsyDs – to fill the gaps in mental health care.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
A very good thing happened this summer for patients with anxiety and the psychiatrists, psychologists, and other mental health professionals who provide treatment for them. The U.S. Preventive Services Task Force recommended anxiety screening for all adults younger than 65.
On the surface, this is a great recommendation for recognition and caring for those who deal with and suffer from an anxiety disorder or multiple anxiety disorders. Although the USPSTF recommendations are independent of the U.S. government and are not an official position of the Department of Health & Human Services, they are a wonderful start at recognizing the importance of mental health care.
After all, anxiety disorders are the most commonly experienced and diagnosed mental disorders, according to the DSM-5.
They range mainly from generalized anxiety disorder (GAD), to panic attacks and panic disorder, separation anxiety, specific type phobias (bridges, tunnels, insects, snakes, and the list goes on), to other phobias, including agoraphobia, social phobia, and of course, anxiety caused by medical conditions. GAD alone occurs in, at least, more than 3% of the population.
Those of us who have been treating anxiety disorders for decades recognize them as an issue affecting both mental and physical well-being, not only because of the emotional causes but the physical distress and illnesses that anxiety may precipitate or worsen.
For example, blood pressure– and heart-related issues, GI disorders, and musculoskeletal issues are just a few examples of how our bodies and organ systems are affected by anxiety. Just the momentary physical symptoms of tachycardia or the “runs” before an exam are fine examples of how anxiety may affect patients physically, and an ongoing, consistent anxiety is potentially more harmful.
In fact, a first panic attack or episode of generalized anxiety may be so serious that an emergency department or physician visit is necessary to rule out a heart attack, asthma, or breathing issues – even a hormone or thyroid emergency, or a cardiac arrhythmia. Panic attacks alone create a high number of ED visits.
Treatments mainly include medication management and a variety of psychotherapy techniques. Currently, the most preferred, first-choice medications are the SSRI antidepressants, which are Food and Drug Administration approved for anxiety as well. These include Zoloft (sertraline), Prozac/Sarafem (fluoxetine), Celexa (citalopram), and Lexapro (escitalopram).
For many years, benzodiazepines (that is, tranquillizers) such as Valium (diazepam), Ativan (lorazepam), and Klonopin/Rivotril (clonazepam) to name a few, were the mainstay of anxiety treatment, but they have proven addictive and may affect cognition and memory. As the current opioid epidemic has shown, when combined with opioids, benzodiazepines are a potentially lethal combination and when used, they need to be for shorter-term care and monitored very judiciously.
It should be noted that after ongoing long-term use of an SSRI for anxiety or depression, it should not be stopped abruptly, as a variety of physical symptoms (for example, flu-like symptoms) may occur.
Benefits of nonmedicinal therapies
There are a variety of talk therapies, from dynamic psychotherapies to cognitive-behavioral therapies (CBT), plus relaxation techniques and guided imagery that have all had a good amount of success in treating generalized anxiety, panic disorder, as well as various types of phobias.
When medications are stopped, the anxiety symptoms may well return. But when using nonmedicinal therapies, clinicians have discovered that when patients develop a new perspective on the anxiety problem or have a new technique to treat anxiety, it may well be long lasting.
For me, using CBT, relaxation techniques, hypnosis, and guided imagery has been very successful in treating anxiety disorders with long-lasting results. Once a person learns to relax, whether it’s from deep breathing exercises, hypnosis (which is not sleep), mindfulness, or meditation, a strategy of guided imagery can be taught, which allows a person to practice as well as control their anxiety as a lifetime process. For example, I like imagining a large movie screen to desensitize and project anxieties.
In many instances, a combination of a medication and a talk therapy approach works best, but there are an equal number of instances in which just medication or just talk therapy is needed. Once again, knowledge, clinical judgment, and the art of care are required to make these assessments.
In other words, recognizing and treating anxiety requires highly specialized training, which is why I thought the USPSTF recommendations raise a few critical questions.
Questions and concerns
One issue, of course, is the exclusion of those patients over age 65 because of a lack of “data.” Why such an exclusion? Does this mean that data are lacking for this age group?
The concept of using solely evidenced-based data in psychiatry is itself an interesting concept because our profession, like many other medical specialties, requires practitioners to use a combination of art and science. And much can be said either way about the clarity of accuracy in the diversity of issues that arise when treating emotional disorders.
When looking at the over-65 population, has anyone thought of clinical knowledge, judgment, experience, observation, and, of course, common sense?
Just consider the worry (a cardinal feature of anxiety) that besets people over 65 when it comes to issues such as retirement, financial security, “empty nesting,” physical health issues, decreased socialization that resulted from the COVID-19 pandemic, and the perpetual loss of relatives and friends.
In addition, as we age, anxiety can come simply from the loss of identity as active lifestyles decrease and the reality of nearing life’s end becomes more of a reality. It would seem that this population would benefit enormously from anxiety screening and possible treatment.
Another major concern is that the screening and potential treatment of patients is aimed at primary care physicians. Putting the sole responsibility of providing mental health care on these overworked PCPs defies common sense unless we’re okay with 1- to 2-minute assessments of mental health issues and no doubt, a pharmacology-only approach.
If this follows the same route as well-intentioned PCPs treating depression, where 5-minute medication management is far too common, the only proper diagnostic course – the in-depth interview necessary to make a proper diagnosis – is often missing.
For example, in depression alone, it takes psychiatric experience and time to differentiate a major depressive disorder from a bipolar depression and to provide the appropriate medication and treatment plan with careful follow-up. In my experience, this usually does not happen in the exceedingly overworked, time-driven day of a PCP.
Anxiety disorders and depression can prove debilitating, and if a PCP wants the responsibility of treatment, a mandated mental health program should be followed – just as here in New York, prescribers are mandated to take a pain control, opioid, and infection control CME course to keep our licenses up to date.
Short of mandating a mental health program for PCPs, it should be part of training and CME courses that Psychiatry is a super specialty, much like orthopedics and ophthalmology, and primary care physicians should never hesitate to make referrals to the specialist.
The big picture for me, and I hope for us all, is that the USPSTF has started things rolling by making it clear that PCPs and other health care clinicians need to screen for anxiety as a disabling disorder that is quite treatable.
This approach will help to advance the destigmatization of mental health disorders. But as result, with more patients diagnosed, there will be a need for more psychiatrists – and psychologists with PhDs or PsyDs – to fill the gaps in mental health care.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Barbie has an anxiety disorder
And it’s a great time to be a therapist
The Barbie movie is generating a lot of feelings, ranging from praise to vitriol. However one feels about the movie, let’s all pause and reflect for a moment on the fact that the number-one grossing film of 2023 is about our childhood doll trying to treat her anxiety disorder.
“Life imitates art more than art imitates life.” So said Oscar Wilde in 1889.
When my adult daughter, a childhood Barbie enthusiast, asked me to see the film, we put on pink and went. Twice. Little did I know that it would stir up so many thoughts and feelings. The one I want to share is how blessed I feel at this moment in time to be a mental health care provider! No longer is mental health something to be whispered about at the water cooler; instead, even Barbie is suffering. And with all the controversy in the press about the movie, no one seems at all surprised by this storyline.
I was raised by two child psychiatrists and have been practicing as an adult psychiatrist since 1991. The start of the pandemic was the most difficult time of my career, as almost every patient was struggling simultaneously, as was I. Three long years later, we are gradually emerging from our shared trauma. How ironic, now with the opportunity to go back to work, I have elected to maintain the majority of my practice online from home. It seems that most patients and providers prefer this mode of treatment, with a full 90 percent of practitioners saying they are using a hybrid model.
As mental health professionals, we know that anywhere from 3% to 49% of those experiencing trauma will develop posttraumatic stress disorder (PTSD), and we have been trained to treat them.
But what happens when an entire global population is exposed simultaneously to trauma? Historians and social scientists refer to such events by many different names, such as: Singularity, Black Swan Event, and Tipping Point. These events are incredibly rare, and afterwards everything is different. These global traumas always lead to massive change.
I think we are at that tipping point. This is the singularity. This is our Black Swan Event. Within a 3-year span, we have experienced the following:
- A global traumatic event (COVID-19).
- A sudden and seemingly permanent shift from office to remote video meetings mostly from home.
- Upending of traditional fundamentals of the stock market as the game literally stopped in January 2021.
- Rapid and widespread availability of Artificial Intelligence.
- The first generation to be fully raised on the Internet and social media (Gen Z) is now entering the workforce.
- Ongoing war in Ukraine.
That’s already an overwhelming list, and I could go on, but let’s get back to Barbie’s anxiety disorder.
The awareness about and acceptance of mental health issues has never been higher. The access to treatment never greater. There are now more online therapy options than ever. Treatment options have dramatically expanded in recent years, from Transcranial Magnetic Stimulation (TMS) to ketamine centers and psychedelics, as well as more mainstream options such as dialectical behavior therapy (DBT), cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), and so many more.
What is particularly unique about this moment is the direct access to care. Self-help books abound with many making it to the New York Times bestseller list. YouTube is loaded with fantastic content on overcoming many mental health issues, although one should be careful with selecting reliable sources. Apps like HeadSpace and Calm are being downloaded by millions of people around the globe. Investors provided a record-breaking $1.5 billion to mental health startups in 2020 alone.
For most practitioners, our phones have been ringing off the hook since 2020. Applications to psychology, psychiatric residency, social work, and counseling degree programs are on the rise, with workforce shortages expected to continue for decades. Psychological expertise has been embraced by businesses especially for DEI (diversity, equity, and inclusion). Mental health experts are the most asked-for experts through media request services. Elite athletes are talking openly about bringing us on their teams.
In this unique moment, when everything seems set to transform into something else, it is time for mental health professionals to exert some agency and influence over where mental health will go from here. I think the next frontier for mental health specialists is to figure out how to speak collectively and help guide society.
Neil Howe, in his sweeping book “The Fourth Turning is Here,” says we have another 10 years in this “Millennial Crisis” phase. He calls this our “winter,” and it remains to be seen how we will emerge from our current challenges. I think we can make a difference.
If the Barbie movie is indeed a canary in the coal mine, I see positive trends ahead as we move past some of the societal and structural issues facing us, and work together to create a more open and egalitarian society. We must find creative solutions that will solve truly massive problems threatening our well-being and perhaps even our existence.
I am so grateful to be able to continue to practice and share my thoughts with you here from my home office, and I hope you can take a break and see this movie, which is not only entertaining but also thought- and emotion-provoking.
Dr. Ritvo has almost 30 years’ experience in psychiatry and is currently practicing telemedicine. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She has no conflicts of interest.
And it’s a great time to be a therapist
And it’s a great time to be a therapist
The Barbie movie is generating a lot of feelings, ranging from praise to vitriol. However one feels about the movie, let’s all pause and reflect for a moment on the fact that the number-one grossing film of 2023 is about our childhood doll trying to treat her anxiety disorder.
“Life imitates art more than art imitates life.” So said Oscar Wilde in 1889.
When my adult daughter, a childhood Barbie enthusiast, asked me to see the film, we put on pink and went. Twice. Little did I know that it would stir up so many thoughts and feelings. The one I want to share is how blessed I feel at this moment in time to be a mental health care provider! No longer is mental health something to be whispered about at the water cooler; instead, even Barbie is suffering. And with all the controversy in the press about the movie, no one seems at all surprised by this storyline.
I was raised by two child psychiatrists and have been practicing as an adult psychiatrist since 1991. The start of the pandemic was the most difficult time of my career, as almost every patient was struggling simultaneously, as was I. Three long years later, we are gradually emerging from our shared trauma. How ironic, now with the opportunity to go back to work, I have elected to maintain the majority of my practice online from home. It seems that most patients and providers prefer this mode of treatment, with a full 90 percent of practitioners saying they are using a hybrid model.
As mental health professionals, we know that anywhere from 3% to 49% of those experiencing trauma will develop posttraumatic stress disorder (PTSD), and we have been trained to treat them.
But what happens when an entire global population is exposed simultaneously to trauma? Historians and social scientists refer to such events by many different names, such as: Singularity, Black Swan Event, and Tipping Point. These events are incredibly rare, and afterwards everything is different. These global traumas always lead to massive change.
I think we are at that tipping point. This is the singularity. This is our Black Swan Event. Within a 3-year span, we have experienced the following:
- A global traumatic event (COVID-19).
- A sudden and seemingly permanent shift from office to remote video meetings mostly from home.
- Upending of traditional fundamentals of the stock market as the game literally stopped in January 2021.
- Rapid and widespread availability of Artificial Intelligence.
- The first generation to be fully raised on the Internet and social media (Gen Z) is now entering the workforce.
- Ongoing war in Ukraine.
That’s already an overwhelming list, and I could go on, but let’s get back to Barbie’s anxiety disorder.
The awareness about and acceptance of mental health issues has never been higher. The access to treatment never greater. There are now more online therapy options than ever. Treatment options have dramatically expanded in recent years, from Transcranial Magnetic Stimulation (TMS) to ketamine centers and psychedelics, as well as more mainstream options such as dialectical behavior therapy (DBT), cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), and so many more.
What is particularly unique about this moment is the direct access to care. Self-help books abound with many making it to the New York Times bestseller list. YouTube is loaded with fantastic content on overcoming many mental health issues, although one should be careful with selecting reliable sources. Apps like HeadSpace and Calm are being downloaded by millions of people around the globe. Investors provided a record-breaking $1.5 billion to mental health startups in 2020 alone.
For most practitioners, our phones have been ringing off the hook since 2020. Applications to psychology, psychiatric residency, social work, and counseling degree programs are on the rise, with workforce shortages expected to continue for decades. Psychological expertise has been embraced by businesses especially for DEI (diversity, equity, and inclusion). Mental health experts are the most asked-for experts through media request services. Elite athletes are talking openly about bringing us on their teams.
In this unique moment, when everything seems set to transform into something else, it is time for mental health professionals to exert some agency and influence over where mental health will go from here. I think the next frontier for mental health specialists is to figure out how to speak collectively and help guide society.
Neil Howe, in his sweeping book “The Fourth Turning is Here,” says we have another 10 years in this “Millennial Crisis” phase. He calls this our “winter,” and it remains to be seen how we will emerge from our current challenges. I think we can make a difference.
If the Barbie movie is indeed a canary in the coal mine, I see positive trends ahead as we move past some of the societal and structural issues facing us, and work together to create a more open and egalitarian society. We must find creative solutions that will solve truly massive problems threatening our well-being and perhaps even our existence.
I am so grateful to be able to continue to practice and share my thoughts with you here from my home office, and I hope you can take a break and see this movie, which is not only entertaining but also thought- and emotion-provoking.
Dr. Ritvo has almost 30 years’ experience in psychiatry and is currently practicing telemedicine. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She has no conflicts of interest.
The Barbie movie is generating a lot of feelings, ranging from praise to vitriol. However one feels about the movie, let’s all pause and reflect for a moment on the fact that the number-one grossing film of 2023 is about our childhood doll trying to treat her anxiety disorder.
“Life imitates art more than art imitates life.” So said Oscar Wilde in 1889.
When my adult daughter, a childhood Barbie enthusiast, asked me to see the film, we put on pink and went. Twice. Little did I know that it would stir up so many thoughts and feelings. The one I want to share is how blessed I feel at this moment in time to be a mental health care provider! No longer is mental health something to be whispered about at the water cooler; instead, even Barbie is suffering. And with all the controversy in the press about the movie, no one seems at all surprised by this storyline.
I was raised by two child psychiatrists and have been practicing as an adult psychiatrist since 1991. The start of the pandemic was the most difficult time of my career, as almost every patient was struggling simultaneously, as was I. Three long years later, we are gradually emerging from our shared trauma. How ironic, now with the opportunity to go back to work, I have elected to maintain the majority of my practice online from home. It seems that most patients and providers prefer this mode of treatment, with a full 90 percent of practitioners saying they are using a hybrid model.
As mental health professionals, we know that anywhere from 3% to 49% of those experiencing trauma will develop posttraumatic stress disorder (PTSD), and we have been trained to treat them.
But what happens when an entire global population is exposed simultaneously to trauma? Historians and social scientists refer to such events by many different names, such as: Singularity, Black Swan Event, and Tipping Point. These events are incredibly rare, and afterwards everything is different. These global traumas always lead to massive change.
I think we are at that tipping point. This is the singularity. This is our Black Swan Event. Within a 3-year span, we have experienced the following:
- A global traumatic event (COVID-19).
- A sudden and seemingly permanent shift from office to remote video meetings mostly from home.
- Upending of traditional fundamentals of the stock market as the game literally stopped in January 2021.
- Rapid and widespread availability of Artificial Intelligence.
- The first generation to be fully raised on the Internet and social media (Gen Z) is now entering the workforce.
- Ongoing war in Ukraine.
That’s already an overwhelming list, and I could go on, but let’s get back to Barbie’s anxiety disorder.
The awareness about and acceptance of mental health issues has never been higher. The access to treatment never greater. There are now more online therapy options than ever. Treatment options have dramatically expanded in recent years, from Transcranial Magnetic Stimulation (TMS) to ketamine centers and psychedelics, as well as more mainstream options such as dialectical behavior therapy (DBT), cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), and so many more.
What is particularly unique about this moment is the direct access to care. Self-help books abound with many making it to the New York Times bestseller list. YouTube is loaded with fantastic content on overcoming many mental health issues, although one should be careful with selecting reliable sources. Apps like HeadSpace and Calm are being downloaded by millions of people around the globe. Investors provided a record-breaking $1.5 billion to mental health startups in 2020 alone.
For most practitioners, our phones have been ringing off the hook since 2020. Applications to psychology, psychiatric residency, social work, and counseling degree programs are on the rise, with workforce shortages expected to continue for decades. Psychological expertise has been embraced by businesses especially for DEI (diversity, equity, and inclusion). Mental health experts are the most asked-for experts through media request services. Elite athletes are talking openly about bringing us on their teams.
In this unique moment, when everything seems set to transform into something else, it is time for mental health professionals to exert some agency and influence over where mental health will go from here. I think the next frontier for mental health specialists is to figure out how to speak collectively and help guide society.
Neil Howe, in his sweeping book “The Fourth Turning is Here,” says we have another 10 years in this “Millennial Crisis” phase. He calls this our “winter,” and it remains to be seen how we will emerge from our current challenges. I think we can make a difference.
If the Barbie movie is indeed a canary in the coal mine, I see positive trends ahead as we move past some of the societal and structural issues facing us, and work together to create a more open and egalitarian society. We must find creative solutions that will solve truly massive problems threatening our well-being and perhaps even our existence.
I am so grateful to be able to continue to practice and share my thoughts with you here from my home office, and I hope you can take a break and see this movie, which is not only entertaining but also thought- and emotion-provoking.
Dr. Ritvo has almost 30 years’ experience in psychiatry and is currently practicing telemedicine. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She has no conflicts of interest.
Climate change and mental illness: What psychiatrists can do
“ Hope is engagement with the act of mapping our destinies.” 1
—Valerie Braithwaite
Why should psychiatrists care about climate change and try to mitigate its effects? First, we are tasked by society with managing the psychological and neuropsychiatric sequelae from disasters, which include climate change. The American Psychiatric Association’s position statement on climate change includes it as a legitimate focus for our specialty.2 Second, as physicians, we are morally obligated to do no harm. Since the health care sector contributes significantly to climate change (8.5% of national carbon emissions stem from health care) and causes demonstrable health impacts,3 managing these impacts and decarbonizing the health care industry is morally imperative.4 And third, psychiatric clinicians have transferrable skills that can address fears of climate change, challenge climate change denialism,5 motivate people to adopt more pro-environmental behaviors, and help communities not only endure the emotional impact of climate change but become more psychologically resilient.6
Most psychiatrists, however, did not receive formal training on climate change and the related field of disaster preparedness. For example, Harvard Medical School did not include a course on climate change in their medical student curriculum until 2023.7 In this article, we provide a basic framework of climate change and its impact on mental health, with particular focus on patients with serious mental illness (SMI). We offer concrete steps clinicians can take to prevent or mitigate harm from climate change for their patients, prepare for disasters at the level of individual patient encounters, and strengthen their clinics and communities. We also encourage clinicians to take active leadership roles in their professional organizations to be part of climate solutions, building on the trust patients continue to have in their physicians.8 Even if clinicians do not view climate change concerns under their conceived clinical care mandate, having a working knowledge about it is important because patients, paraprofessional staff, or medical trainees are likely to bring it up.9
Climate change and mental health
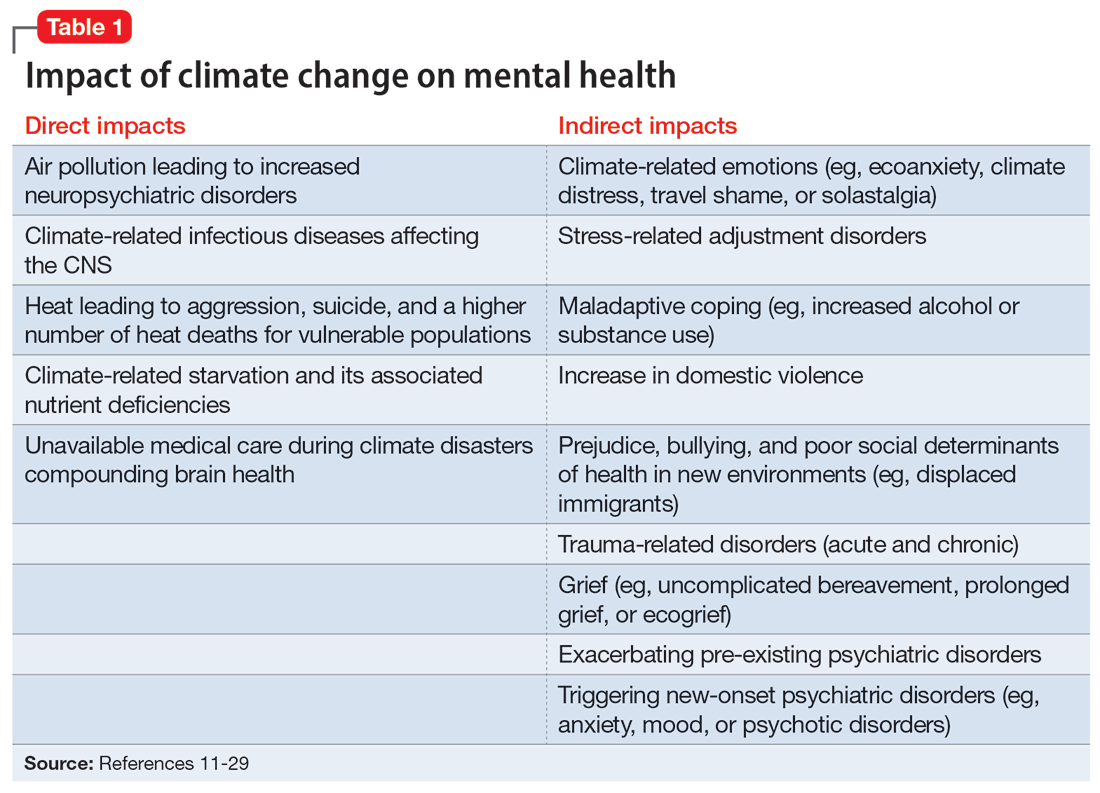
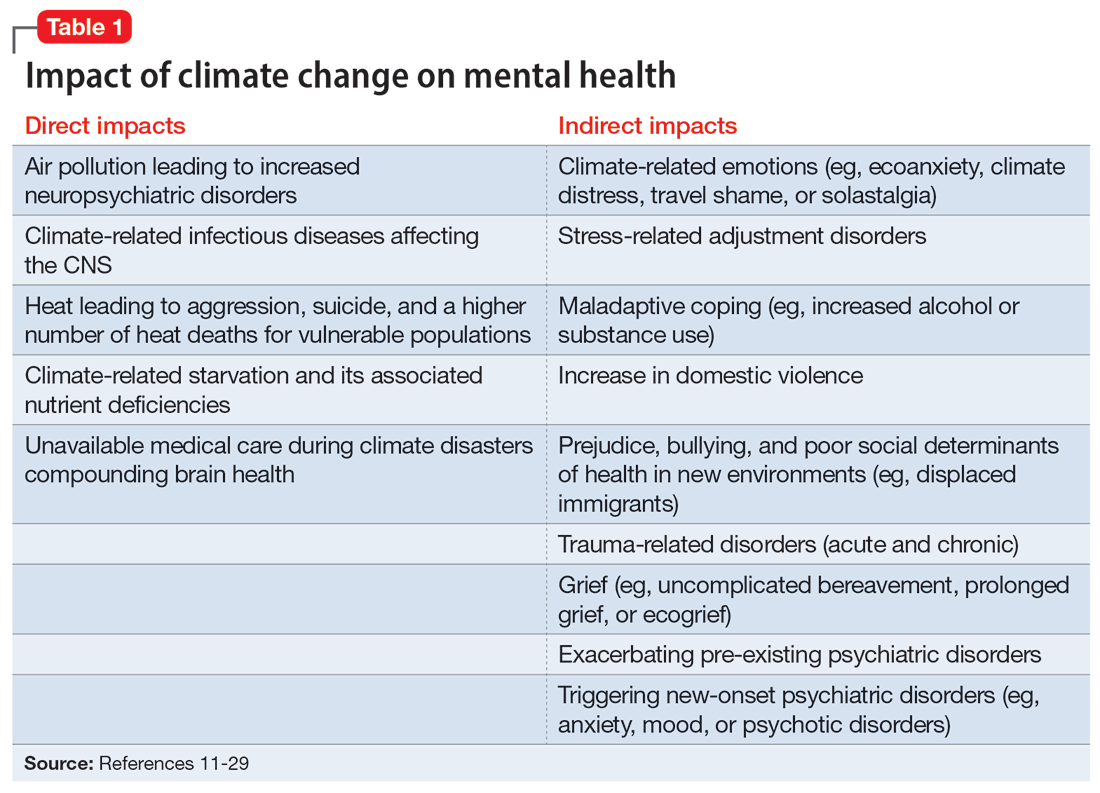
Climate change is harmful to human health, including mental health.10 It can impact mental health directly via its impact on brain function and neuropsychiatric sequelae, and indirectly via climate-related disasters leading to acute or chronic stress, losses, and displacement with psychiatric and psychological sequelae (Table 111-29).
Direct impact
The effects of air pollution, heat, infections, and starvation are examples of how climate change directly impacts mental health. Air pollution and brain health are a concern for psychiatry, given the well-described effects of air deterioration on the developing brain.11 In animal models, airborne pollutants lead to widespread neuroinflammation and cell loss via a multitude of mechanisms.12 This is consistent with worse cognitive and behavioral functions across a wide range of cognitive domains seen in children exposed to pollution compared to those who grew up in environments with healthy air.13 Even low-level exposure to air pollution increases the risk for later onset of depression, suicide, and anxiety.14 Hippocampal atrophy observed in patients with first-episode psychosis may also be partially attributable to air pollution.15 An association between heat and suicide (and to a lesser extent, aggression) has also been reported.16
Worse physical health (eg, strokes) due to excessive heat can further compound mental health via elevated rates of depression. Data from the United States and Mexico show that for each degree Celsius increase in ambient temperature, suicide rates may increase by approximately 1%.17 A meta-analysis by Frangione et al18 similarly concluded that each degree Celsius increase results in an overall risk ratio of 1.016 (95% CI, 1.012 to 1.019) for deaths by suicide and suicide attempts. Additionally, global warming is shifting the endemic areas for many infectious agents, particularly vector-borne diseases,19 to regions in which they had hitherto been unknown, increasing the risk for future outbreaks and even pandemics.20 These infectious illnesses often carry neuropsychiatric morbidity, with seizures, encephalopathy with incomplete recovery, and psychiatric syndromes occurring in many cases. Crop failure can lead to starvation during pregnancy and childhood, which has wide-ranging consequences for brain development and later physical and psychological health in adults.21,22 Mothers affected by starvation also experience negative impacts on childbearing and childrearing.23
Indirect impact
Climate change’s indirect impact on mental health can stem from the stress of living through a disaster such as an extreme weather event; from losses, including the death of friends and family members; and from becoming temporarily displaced.24 Some climate change–driven disasters can be viewed as slow-moving, such as drought and the rising of sea levels, where displacement becomes permanent. Managing mass migration from internally or externally displaced people who must abandon their communities because of climate change will have significant repercussions for all societies.25 The term “climate refugee” is not (yet) included in the United Nations’ official definition of refugees; it defines refugees as individuals who have fled their countries because of war, violence, or persecution.26 These and other bureaucratic issues can come up when clinicians are trying to help migrants with immigration-related paperwork.
Continue to: As the inevitability of climate change...
As the inevitability of climate change sinks in, its long-term ramifications have introduced a new lexicon of psychological suffering related to the crisis.27 Common terms for such distress include ecoanxiety (fear of what is happening and will happen with climate change), ecogrief (sadness about the destruction of species and natural habitats), solastalgia28 (the nostalgia an individual feels for emotionally treasured landscapes that have changed), and terrafuria or ecorage (the reaction to betrayal and inaction by governments and leaders).29 Climate-related emotions can lead to pessimism about the future and a nihilistic outlook on an individual’s ability to effect change and have agency over their life’s outcomes.
The categories of direct and indirect impacts are not mutually exclusive. A child may be starving due to weather-related crop failure as the family is forced to move to another country, then have to contend with prejudice and bullying as an immigrant, and later become anxiously preoccupied with climate change and its ability to cause further distress.
Effect on individuals with serious mental illness
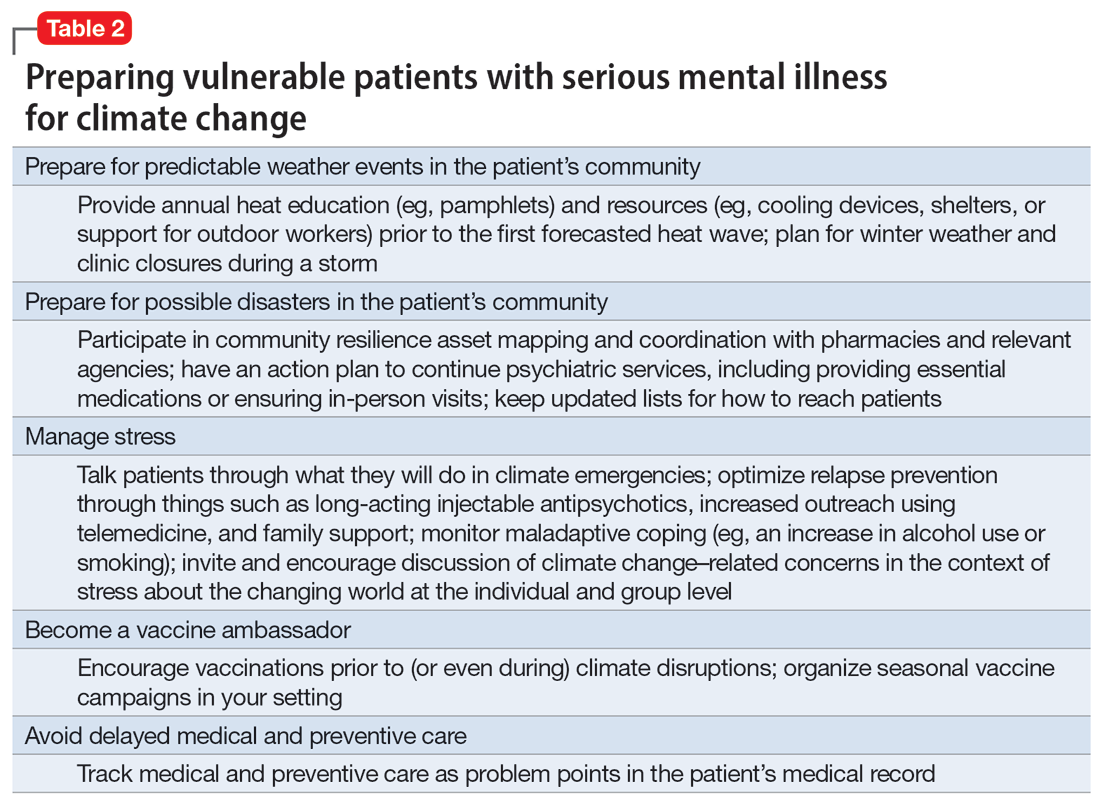
Patients with SMI are particularly vulnerable to the impact of climate change. They are less resilient to climate change–related events, such as heat waves or temporary displacement from flooding, both at the personal level due to illness factors (eg, negative symptoms or cognitive impairment) and at the community level due to social factors (eg, weaker social support or poverty).
Recognizing the increased vulnerability to heat waves and preparing for them is particularly important for patients with SMI because they are at an increased risk for heat-related illnesses.30 For example, patients may not appreciate the danger from heat and live in conditions that put them at risk (ie, not having air conditioning in their home or living alone). Their illness alone impairs heat regulation31; patients with depression and anxiety also dissipate heat less effectively.32,33 Additionally, many psychiatric medications, particularly antipsychotics, impair key mechanisms of heat dissipation.34,35 Antipsychotics render organisms more poikilothermic (susceptible to environmental temperature, like cold-blooded animals) and can be anticholinergic, which impedes sweating. A recent analysis of heat-related deaths during a period of extreme and prolonged heat in British Columbia in 2021 affirmed these concerns, reporting that patients with schizophrenia had the highest odds of death during this heat-related event.36
COVID-19 has shown that flexible models of care are needed to prevent disengagement from medical and psychiatric care37 and assure continued treatment with essential medications such as clozapine38 and long-acting injectable antipsychotics39 during periods of social change, as with climate change. While telehealth was critical during the COVID-19 pandemic40 and is here to stay, it alone may be insufficient given the digital divide (patients with SMI may be less likely to have access to or be proficient in the use of digital technologies). The pandemic has shown the importance of public health efforts, including benefits from targeted outreach, with regards to vaccinations for this patient group.41,42 Table 2 summarizes things clinicians should consider when preparing patients with SMI for the effects of climate change.
Continue to: The psychiatrist's role
The psychiatrist’s role
There are many ways a psychiatrist can professionally get involved in addressing climate change. Table 343-53 outlines the 3 Ps of climate action (taking actions to mitigate the effects of climate change): personal, patient (and clinic), and political (advocacy).
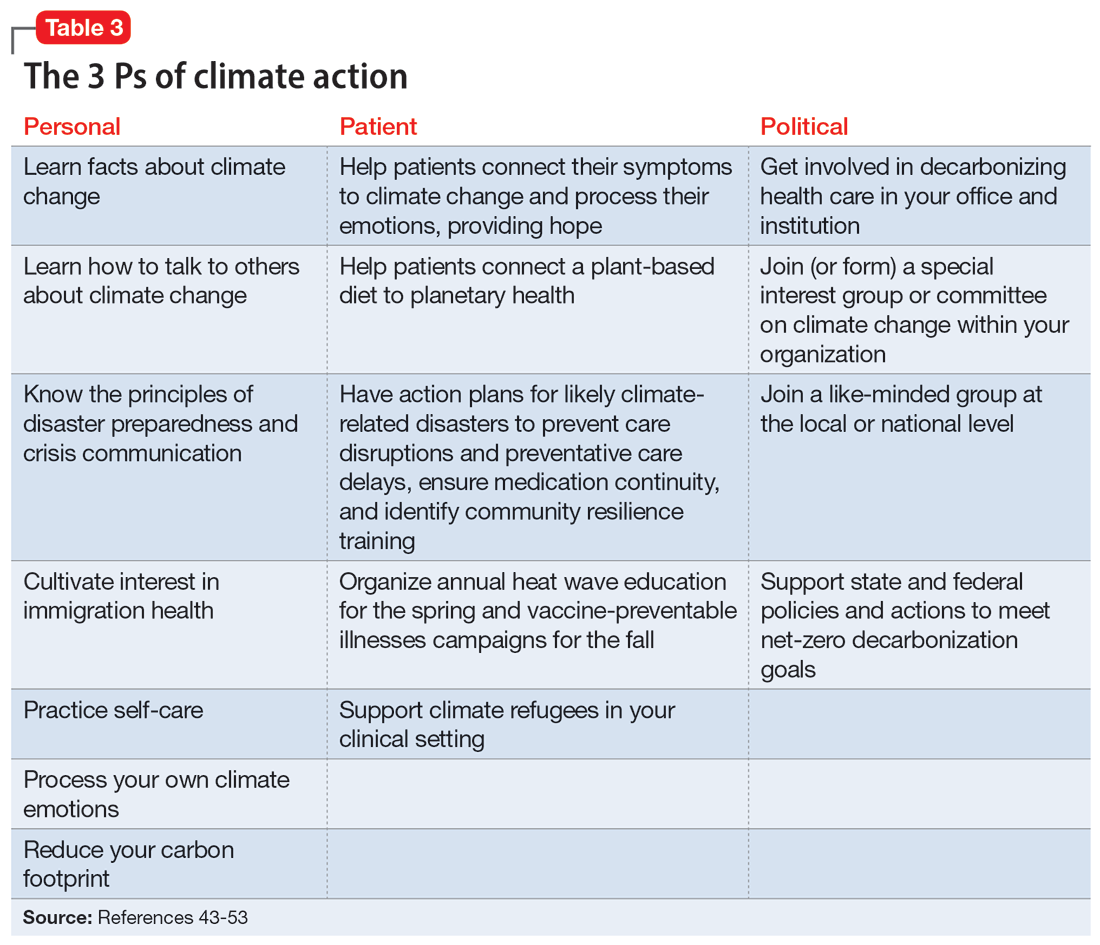
Personal
Even if clinicians believe climate change is important for their clinical work, they may still feel overwhelmed and unsure what to do in the context of competing responsibilities. A necessary first step is overcoming paralysis from the enormity of the problem, including the need to shift away from an expanding consumption model to environmental sustainability in a short period of time.
A good starting point is to get educated on the facts of climate change and how to discuss it in an office setting as well as in your personal life. A basic principle of climate change communication is that constructive hope (progress achieved despite everything) coupled with constructive doubt (the reality of the threat) can mobilize people towards action, whereas false hope or fatalistic doubt impedes action.43 The importance of optimal public health messaging cannot be overstated; well-meaning campaigns to change behavior can fail if they emphasize the wrong message. For example, in a study examining COVID-19 messaging in >80 countries, Dorison et al44 found that negatively framed messages mostly increased anxiety but had no benefit with regard to shifting people toward desired behaviors.
In addition, clinicians can learn how to confront climate disavowal and difficult emotions in themselves and even plan to shift to carbon neutrality, such as purchasing carbon offsets or green sources of energy and transportation. They may not be familiar with principles of disaster preparedness or crisis communication.46 Acquiring those professional skills may suggest next steps for action. Being familiar with the challenges and resources for immigrants, including individuals displaced due to climate change, may be necessary.47 Finally, to reduce the risk of burnout, it is important to practice self-care, including strategies to reduce feelings of being overwhelmed.
Patient
In clinical encounters, clinicians can be proactive in helping patients understand their climate-related anxieties around an uncertain future, including identifying barriers to climate action.48
Continue to: Clinics must prepare for disasters...
Clinics must prepare for disasters in their communities to prevent disruption of psychiatric care by having an action plan, including the provision of medications. Such action plans should be prioritized for the most likely scenarios in an individual’s setting (eg, heat waves, wildfires, hurricanes, or flooding).
It is important to educate clinic staff and include them in planning for emergencies, because an all-hands approach and buy-in from all team members is critical. Clinicians should review how patients would continue to receive services, particularly medications, in the event of a disaster. In some cases, providing a 90-day medication supply will suffice, while in others (eg, patients receiving long-acting antipsychotics or clozapine) more preparation is necessary. Some events are predictable and can be organized annually, such as clinicians becoming vaccine ambassadors and organizing vaccine campaigns every fall50; winter-related disaster preparation every fall; and heat wave education every spring (leaflets for patients, staff, and family members; review of safety of medications during heat waves). Plan for, monitor, and coordinate medical care and services for climate refugees and other populations that may otherwise delay medical care and impede illness prevention. Finally, support climate refugees, including connecting them to services or providing trauma-informed care.
Political
Some clinicians may feel compelled to become politically active to advocate for changes within the health care system. Two initiatives related to decarbonizing the health care sector are My Green Doctor51 and Health Care Without Harm,52 which offer help in shifting your office, clinic, or hospital towards carbon neutrality.
Climate change unevenly affects people and will continue to exacerbate inequalities in society, including individuals with mental illness.53 To work toward climate justice on behalf of their patients, clinicians could join (or form) climate committees of special interest groups in their professional organizations or setting. Joining like-minded groups working on climate change at the local or national level prevents an omission of a psychiatric voice and counteracts burnout. It is important to stay focused on the root causes of the problem during activism: doing something to reduce fossil fuel use is ultimately most important.54 The concrete goal of reaching the Paris 1.5-degree Celsius climate goal is a critical benchmark against which any other action can be measured.54
Planning for the future
Over the course of history, societies have always faced difficult periods in which they needed to rebuild after natural disasters or self-inflicted catastrophes such as terrorist attacks or wars. Since the advent of the nuclear age, people have lived under the existential threat of nuclear war. The Anthropocene is a proposed geological term that reflects the enormous and possibly disastrous impact human activity has had on our planet.55 While not yet formally adopted, this term has heuristic value, directing attention and reflection to our role and its now undisputed consequences. In the future, historians will debate if the scale of our current climate crisis has been different. It is, however, not controversial that humanity will be faced with the effects of climate change for the foreseeable future.10 Already, even “normal” weather events are fueled by energy in overcharged and altered weather systems due to global warming, leading to weather events ranging from droughts to floods and storms that are more severe, more frequent, and have longer-lasting effects on communities.56
Continue to: As physicians, we are tasked...
As physicians, we are tasked by society to create and maintain a health care system that addresses the needs of our patients and the communities in which they live. Increasingly, we are forced to contend with an addition to the traditional 5 phases of acute disaster management (prevention, mitigation, preparedness, response, and recovery) to manage prolonged or even parallel disasters, where a series of disasters occurs before the community has recovered and healed. We must grapple with a sense of an “extended period of insecurity and instability” (permacrisis) and must better prepare for and prevent the polycrisis (many simultaneous crises) or the metacrisis of our “age of turmoil”57 in which we must limit global warming, mitigate its damage, and increase community resilience to adapt.
Leading by personal example and providing hope may be what some patients need, as the reality of climate change contributes to the general uneasiness about the future and doomsday scenarios to which many fall victim. At the level of professional societies, many are calling for leadership, including from mental health organizations, to bolster the “social climate,” to help us strengthen our emotional resilience and social bonds to better withstand climate change together.58 It is becoming harder to justify standing on the sidelines,59 and it may be better for both our world and a clinician’s own sanity to be engaged in professional and private hopeful action1 to address climate change. Without ecological or planetary health, there can be no mental health.
Bottom Line
Clinicians can prepare their patients for climate-related disruptions and manage the impact climate change has on their mental health. Addressing climate change at clinical and political levels is consistent with the leadership roles and professional ethics clinicians face in daily practice.
Related Resources
- Lim C, MacLaurin S, Freudenreich O. Preparing patients with serious mental illness for extreme HEAT. Current Psychiatry. 2022;21(9):27-28. doi:10.12788/cp.0287
- My Green Doctor. https://mygreendoctor.org/
- The Climate Resilience for Frontline Clinics Toolkit from Americares. https://www.americares.org/what-we-do/community-health/climate-resilient-health-clinics
- Climate Psychiatry Alliance. https://www.climatepsychiatry.org/
Drug Brand Names
Clozapine • Clozaril
1. Kretz L. Hope in environmental philosophy. J Agricult Environ Ethics. 2013;26:925-944. doi:10.1007/s10806-012-9425-8
2. Ursano RJ, Morganstein JC, Cooper R. Position statement on mental health and climate change. American Psychiatric Association. March 2023. Accessed August 6, 2023. https://www.psychiatry.org/getattachment/0ce71f37-61a6-44d0-8fcd-c752b7e935fd/Position-Mental-Health-Climate-Change.pdf
3. Eckelman MJ, Huang K, Lagasse R, et al. Health care pollution and public health damage in the United States: an update. Health Aff (Millwood). 2020;39:2071-2079.
4. Dzau VJ, Levine R, Barrett G, et al. Decarbonizing the U.S. health sector - a call to action. N Engl J Med. 2021;385(23):2117-2119. doi:10.1056/NEJMp2115675
5. Haase E, Augustinavicius JH, K. Climate change and psychiatry. In: Tasman A, Riba MB, Alarcón RD, et al, eds. Tasman’s Psychiatry. 5th ed. Springer; 2023.
6. Belkin G. Mental health and the global race to resilience. Psychiatr Times. 2023;40(3):26.
7. Hu SR, Yang JQ. Harvard Medical School will integrate climate change into M.D. curriculum. The Harvard Crimson. February 3, 2023. Accessed August 6, 2023. https://www.thecrimson.com/article/2023/2/3/hms-climate-curriculum/#:~:text=The%20new%20climate%20change%20curriculum,in%20arriving%20at%20climate%20solutions
8. Funk C, Gramlich J. Amid coronavirus threat, Americans generally have a high level of trust in medical doctors. Pew Research Center. March 13, 2020. Accessed August 6, 2023. https://www.pewresearch.org/fact-tank/2020/03/13/amid-coronavirus-threat-americans-generally-have-a-high-level-of-trust-in-medical-doctors/
9. Coverdale J, Balon R, Beresin EV, et al. Climate change: a call to action for the psychiatric profession. Acad Psychiatry. 2018;42(3):317-323. doi:10.1007/s40596-018-0885-7
10. Intergovernmental Panel on Climate Change. AR6 synthesis report: climate change 2023. Accessed August 6, 2023. https://www.ipcc.ch/report/sixth-assessment-report-cycle/
11. Perera FP. Multiple threats to child health from fossil fuel combustion: impacts of air pollution and climate change. Environ Health Perspect. 2017;125(2):141-148. doi:10.1289/EHP299
12. Hahad O, Lelieveldz J, Birklein F, et al. Ambient air pollution increases the risk of cerebrovascular and neuropsychiatric disorders through induction of inflammation and oxidative stress. Int J Mol Sci. 2020;21(12):4306. doi:10.3390/ijms21124306
13. Brockmeyer S, D’Angiulli A. How air pollution alters brain development: the role of neuroinflammation. Translational Neurosci. 2016;7(1):24-30. doi:10.1515/tnsci-2016-0005
14. Yang T, Wang J, Huang J, et al. Long-term exposure to multiple ambient air pollutants and association with incident depression and anxiety. JAMA Psychiatry. 2023;80:305-313. doi:10.1001/jamapsychiatry.2022.4812
15. Worthington MA, Petkova E, Freudenreich O, et al. Air pollution and hippocampal atrophy in first episode schizophrenia. Schizophr Res. 2020;218:63-69. doi:10.1016/j.schres.2020.03.001
16. Dumont C, Haase E, Dolber T, et al. Climate change and risk of completed suicide. J Nerv Ment Dis. 2020;208(7):559-565. doi:10.1097/NMD.0000000000001162
17. Burke M, Gonzales F, Bayis P, et al. Higher temperatures increase suicide rates in the United States and Mexico. Nat Climate Change. 2018;8:723-729. doi:10.1038/s41558-018-0222-x
18. Frangione B, Villamizar LAR, Lang JJ, et al. Short-term changes in meteorological conditions and suicide: a systematic review and meta-analysis. Environ Res. 2022;207:112230. doi:10.1016/j.envres.2021.112230
19. Rocklov J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol. 2020;21(5):479-483. doi:10.1038/s41590-020-0648-y
20. Carlson CJ, Albery GF, Merow C, et al. Climate change increases cross-species viral transmission risk. Nature. 2022;607(7919):555-562. doi:10.1038/s41586-022-04788-w
21. Roseboom TJ, Painter RC, van Abeelen AFM, et al. Hungry in the womb: what are the consequences? Lessons from the Dutch famine. Maturitas. 2011;70(2):141-145. doi:10.1016/j.maturitas.2011.06.017
22. Liu Y, Diao L, Xu L. The impact of childhood experience of starvations on the health of older adults: evidence from China. Int J Health Plann Manage. 2021;36(2):515-531. doi:10.1002/hpm.3099
23. Rothschild J, Haase E. The mental health of women and climate change: direct neuropsychiatric impacts and associated psychological concerns. Int J Gynaecol Obstet. 2023;160(2):405-413. doi:10.1002/ijgo.14479
24. Cianconi P, Betro S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Frontiers Psychiatry. 2020;11:74. doi:10.3389/fpsyt.2020.00074
25. World Economic Forum. Climate refugees – the world’s forgotten victims. June 18, 2021. Accessed August 6, 2023. https://www.weforum.org/agenda/2021/06/climate-refugees-the-world-s-forgotten-victims
26. Climate Refugees. Accessed August 6, 2023. https://www.climate-refugees.org/why
27. Pihkala P. Anxiety and the ecological crisis: an analysis of eco-anxiety and climate anxiety. Sustainability. 2020;12(19):7836. doi:10.3390/su12197836
28. Galway LP, Beery T, Jones-Casey K, et al. Mapping the solastalgia literature: a scoping review study. Int J Environ Res Public Health. 2019;16(15):2662. doi:10.3390/ijerph16152662
29. Albrecht GA. Earth Emotions. New Words for a New World. Cornell University Press; 2019.
30. Sorensen C, Hess J. Treatment and prevention of heat-related illness. N Engl J Med. 2022;387(15):1404-1413. doi:10.1056/NEJMcp2210623
31. Chong TWH, Castle DJ. Layer upon layer: thermoregulation in schizophrenia. Schizophr Res. 2004;69(2-3):149-157. doi:10.1016/s0920-9964(03)00222-6
32. von Salis S, Ehlert U, Fischer S. Altered experienced thermoregulation in depression--no evidence for an effect of early life stress. Front Psychiatry. 2021;12:620656. doi:10.3389/fpsyt.2021.620656
33. Sarchiapone M, Gramaglia C, Iosue M, et al. The association between electrodermal activity (EDA), depression and suicidal behaviour: a systematic review and narrative synthesis. BMC Psychiatry. 2018;18(1):22. doi:10.1186/s12888-017-1551-4
34. Martin-Latry K, Goumy MP, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalisation. Eur Psychiatry. 2007;22(6):335-338. doi:10.1016/j.eurpsy.2007.03.007
35. Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. Lancet. 2021;398(10301):698-708. doi:10.1016/S0140-6736(21)01208-3
36. Lee MJ, McLean KE, Kuo M, et al. Chronic diseases associated with mortality in British Columbia, Canada during the 2021 Western North America extreme heat event. Geohealth. 2023;7(3):e2022GH000729. doi:10.1029/2022GH000729
37. Busch AB, Huskamp HA, Raja P, et al. Disruptions in care for Medicare beneficiaries with severe mental illness during the COVID-19 pandemic. JAMA Netw Open. 2022;5(1):e2145677. doi:10.1001/jamanetworkopen.2021.45677
38. Siskind D, Honer WG, Clark S, et al. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45(3):222-223. doi:10.1503/jpn.200061
39. MacLaurin SA, Mulligan C, Van Alphen MU, et al. Optimal long-acting injectable antipsychotic management during COVID-19. J Clin Psychiatry. 2021;82(1): 20l13730. doi:10.4088/JCP.20l13730
40. Bartels SJ, Baggett TP, Freudenreich O, et al. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness. Psychiatr Serv. 2020;71(10):1078-1081. doi:10.1176/appi.ps.202000244
41. Van Alphen MU, Lim C, Freudenreich O. Mobile vaccine clinics for patients with serious mental illness and health care workers in outpatient mental health clinics. Psychiatr Serv. February 8, 2023. doi:10.1176/appi.ps.20220460
42. Lim C, Van Alphen MU, Maclaurin S, et al. Increasing COVID-19 vaccination rates among patients with serious mental illness: a pilot intervention study. Psychiatr Serv. 2022;73(11):1274-1277. doi:10.1176/appi.ps.202100702
43. Marlon JR, Bloodhart B, Ballew MT, et al. How hope and doubt affect climate change mobilization. Front Commun. May 21, 2019. doi:10.3389/fcomm.2019.00020
44. Dorison CA, Lerner JS, Heller BH, et al. In COVID-19 health messaging, loss framing increases anxiety with little-to-no concomitant benefits: experimental evidence from 84 countries. Affective Sci. 2022;3(3):577-602. doi:10.1007/s42761-022-00128-3
45. Maibach E. Increasing public awareness and facilitating behavior change: two guiding heuristics. George Mason University, Center for Climate Change Communication. September 2015. Accessed August 6, 2023. https://www.climatechangecommunication.org/wp-content/uploads/2018/06/Maibach-Two-hueristics-September-2015-revised.pdf
46. Koh KA, Raviola G, Stoddard FJ Jr. Psychiatry and crisis communication during COVID-19: a view from the trenches. Psychiatr Serv. 2021;72(5):615. doi:10.1176/appi.ps.202000912
47. Velez G, Adam B, Shadid O, et al. The clock is ticking: are we prepared for mass climate migration? Psychiatr News. March 24, 2023. Accessed August 6, 2023. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2023.04.4.3
48. Ingle HE, Mikulewicz M. Mental health and climate change: tackling invisible injustice. Lancet Planet Health. 2020;4:e128-e130. doi:10.1016/S2542-5196(20)30081-4
49. Shah UA, Merlo G. Personal and planetary health--the connection with dietary choices. JAMA. 2023;329(21):1823-1824. doi:10.1001/jama.2023.6118
50. Lim C, Van Alphen MU, Freudenreich O. Becoming vaccine ambassadors: a new role for psychiatrists. Current Psychiatry. 2021;20(8):10-11,17-21,26-28,38. doi:10.12788/cp.0155
51. My Green Doctor. Accessed August 6, 2023. https://mygreendoctor.org/
52. Healthcare Without Harm. Accessed August 6, 2023. https://noharm.org/
53. Levy BS, Patz JA. Climate change, human rights, and social justice. Ann Glob Health. 2015;81:310-322.
54. Intergovernmental Panel on Climate Change. Global warming of 1.5° C 2018. Accessed August 6, 2023. https://www.ipcc.ch/sr15/
55. Steffen W, Crutzen J, McNeill JR. The Anthropocene: are humans now overwhelming the great forces of nature? Ambio. 2007;36(8):614-621. doi:10.1579/0044-7447(2007)36[614:taahno]2.0.co;2
56. American Meteorological Society. Explaining extreme events from a climate perspective. Accessed August 6, 2023. https://www.ametsoc.org/ams/index.cfm/publications/bulletin-of-the-american-meteorological-society-bams/explaining-extreme-events-from-a-climate-perspective/
57. Nierenberg AA. Coping in the age of turmoil. Psychiatr Ann. 2022;52(7):263. July 1, 2022. doi:10.3928/23258160-20220701-01
58. Belkin G. Leadership for the social climate. N Engl J Med. 2020;382(21):1975-1977. doi:10.1056/NEJMp2001507
59. Skinner JR. Doctors and climate change: first do no harm. J Paediatr Child Health. 2021;57(11):1754-1758. doi:10.1111/jpc.15658
“ Hope is engagement with the act of mapping our destinies.” 1
—Valerie Braithwaite
Why should psychiatrists care about climate change and try to mitigate its effects? First, we are tasked by society with managing the psychological and neuropsychiatric sequelae from disasters, which include climate change. The American Psychiatric Association’s position statement on climate change includes it as a legitimate focus for our specialty.2 Second, as physicians, we are morally obligated to do no harm. Since the health care sector contributes significantly to climate change (8.5% of national carbon emissions stem from health care) and causes demonstrable health impacts,3 managing these impacts and decarbonizing the health care industry is morally imperative.4 And third, psychiatric clinicians have transferrable skills that can address fears of climate change, challenge climate change denialism,5 motivate people to adopt more pro-environmental behaviors, and help communities not only endure the emotional impact of climate change but become more psychologically resilient.6
Most psychiatrists, however, did not receive formal training on climate change and the related field of disaster preparedness. For example, Harvard Medical School did not include a course on climate change in their medical student curriculum until 2023.7 In this article, we provide a basic framework of climate change and its impact on mental health, with particular focus on patients with serious mental illness (SMI). We offer concrete steps clinicians can take to prevent or mitigate harm from climate change for their patients, prepare for disasters at the level of individual patient encounters, and strengthen their clinics and communities. We also encourage clinicians to take active leadership roles in their professional organizations to be part of climate solutions, building on the trust patients continue to have in their physicians.8 Even if clinicians do not view climate change concerns under their conceived clinical care mandate, having a working knowledge about it is important because patients, paraprofessional staff, or medical trainees are likely to bring it up.9
Climate change and mental health
Climate change is harmful to human health, including mental health.10 It can impact mental health directly via its impact on brain function and neuropsychiatric sequelae, and indirectly via climate-related disasters leading to acute or chronic stress, losses, and displacement with psychiatric and psychological sequelae (Table 111-29).
Direct impact
The effects of air pollution, heat, infections, and starvation are examples of how climate change directly impacts mental health. Air pollution and brain health are a concern for psychiatry, given the well-described effects of air deterioration on the developing brain.11 In animal models, airborne pollutants lead to widespread neuroinflammation and cell loss via a multitude of mechanisms.12 This is consistent with worse cognitive and behavioral functions across a wide range of cognitive domains seen in children exposed to pollution compared to those who grew up in environments with healthy air.13 Even low-level exposure to air pollution increases the risk for later onset of depression, suicide, and anxiety.14 Hippocampal atrophy observed in patients with first-episode psychosis may also be partially attributable to air pollution.15 An association between heat and suicide (and to a lesser extent, aggression) has also been reported.16
Worse physical health (eg, strokes) due to excessive heat can further compound mental health via elevated rates of depression. Data from the United States and Mexico show that for each degree Celsius increase in ambient temperature, suicide rates may increase by approximately 1%.17 A meta-analysis by Frangione et al18 similarly concluded that each degree Celsius increase results in an overall risk ratio of 1.016 (95% CI, 1.012 to 1.019) for deaths by suicide and suicide attempts. Additionally, global warming is shifting the endemic areas for many infectious agents, particularly vector-borne diseases,19 to regions in which they had hitherto been unknown, increasing the risk for future outbreaks and even pandemics.20 These infectious illnesses often carry neuropsychiatric morbidity, with seizures, encephalopathy with incomplete recovery, and psychiatric syndromes occurring in many cases. Crop failure can lead to starvation during pregnancy and childhood, which has wide-ranging consequences for brain development and later physical and psychological health in adults.21,22 Mothers affected by starvation also experience negative impacts on childbearing and childrearing.23
Indirect impact
Climate change’s indirect impact on mental health can stem from the stress of living through a disaster such as an extreme weather event; from losses, including the death of friends and family members; and from becoming temporarily displaced.24 Some climate change–driven disasters can be viewed as slow-moving, such as drought and the rising of sea levels, where displacement becomes permanent. Managing mass migration from internally or externally displaced people who must abandon their communities because of climate change will have significant repercussions for all societies.25 The term “climate refugee” is not (yet) included in the United Nations’ official definition of refugees; it defines refugees as individuals who have fled their countries because of war, violence, or persecution.26 These and other bureaucratic issues can come up when clinicians are trying to help migrants with immigration-related paperwork.
Continue to: As the inevitability of climate change...
As the inevitability of climate change sinks in, its long-term ramifications have introduced a new lexicon of psychological suffering related to the crisis.27 Common terms for such distress include ecoanxiety (fear of what is happening and will happen with climate change), ecogrief (sadness about the destruction of species and natural habitats), solastalgia28 (the nostalgia an individual feels for emotionally treasured landscapes that have changed), and terrafuria or ecorage (the reaction to betrayal and inaction by governments and leaders).29 Climate-related emotions can lead to pessimism about the future and a nihilistic outlook on an individual’s ability to effect change and have agency over their life’s outcomes.
The categories of direct and indirect impacts are not mutually exclusive. A child may be starving due to weather-related crop failure as the family is forced to move to another country, then have to contend with prejudice and bullying as an immigrant, and later become anxiously preoccupied with climate change and its ability to cause further distress.
Effect on individuals with serious mental illness
Patients with SMI are particularly vulnerable to the impact of climate change. They are less resilient to climate change–related events, such as heat waves or temporary displacement from flooding, both at the personal level due to illness factors (eg, negative symptoms or cognitive impairment) and at the community level due to social factors (eg, weaker social support or poverty).
Recognizing the increased vulnerability to heat waves and preparing for them is particularly important for patients with SMI because they are at an increased risk for heat-related illnesses.30 For example, patients may not appreciate the danger from heat and live in conditions that put them at risk (ie, not having air conditioning in their home or living alone). Their illness alone impairs heat regulation31; patients with depression and anxiety also dissipate heat less effectively.32,33 Additionally, many psychiatric medications, particularly antipsychotics, impair key mechanisms of heat dissipation.34,35 Antipsychotics render organisms more poikilothermic (susceptible to environmental temperature, like cold-blooded animals) and can be anticholinergic, which impedes sweating. A recent analysis of heat-related deaths during a period of extreme and prolonged heat in British Columbia in 2021 affirmed these concerns, reporting that patients with schizophrenia had the highest odds of death during this heat-related event.36
COVID-19 has shown that flexible models of care are needed to prevent disengagement from medical and psychiatric care37 and assure continued treatment with essential medications such as clozapine38 and long-acting injectable antipsychotics39 during periods of social change, as with climate change. While telehealth was critical during the COVID-19 pandemic40 and is here to stay, it alone may be insufficient given the digital divide (patients with SMI may be less likely to have access to or be proficient in the use of digital technologies). The pandemic has shown the importance of public health efforts, including benefits from targeted outreach, with regards to vaccinations for this patient group.41,42 Table 2 summarizes things clinicians should consider when preparing patients with SMI for the effects of climate change.
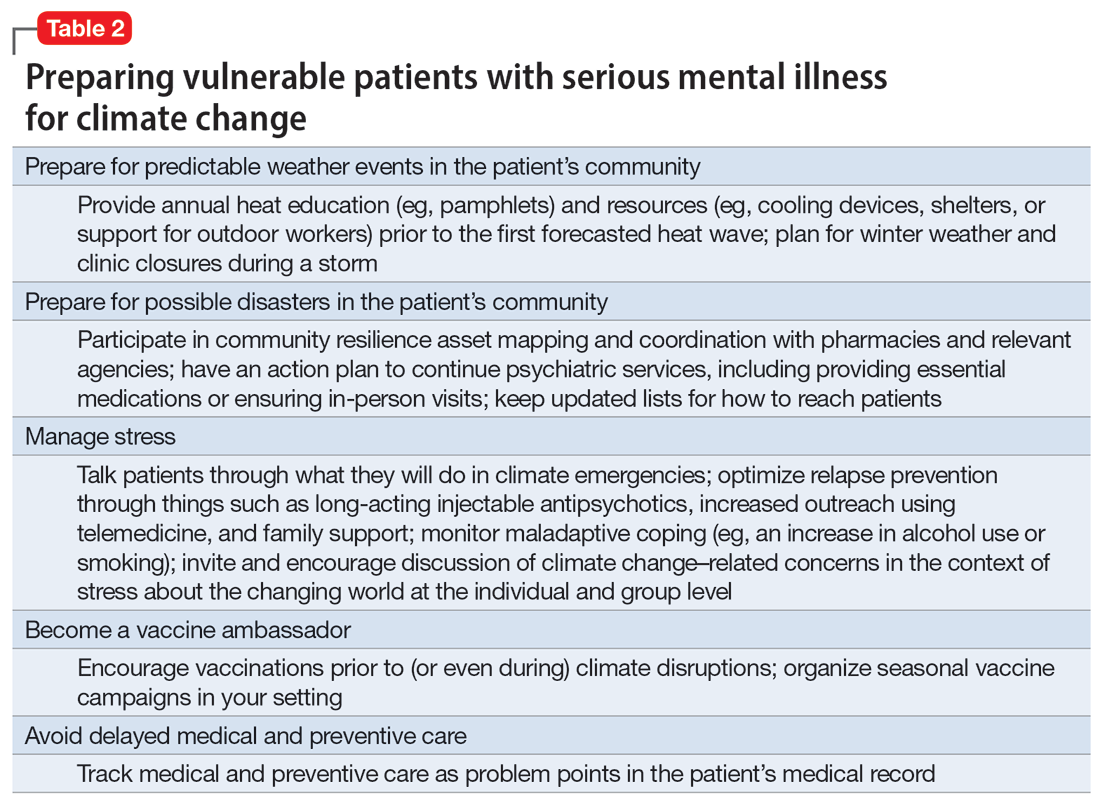
Continue to: The psychiatrist's role
The psychiatrist’s role
There are many ways a psychiatrist can professionally get involved in addressing climate change. Table 343-53 outlines the 3 Ps of climate action (taking actions to mitigate the effects of climate change): personal, patient (and clinic), and political (advocacy).
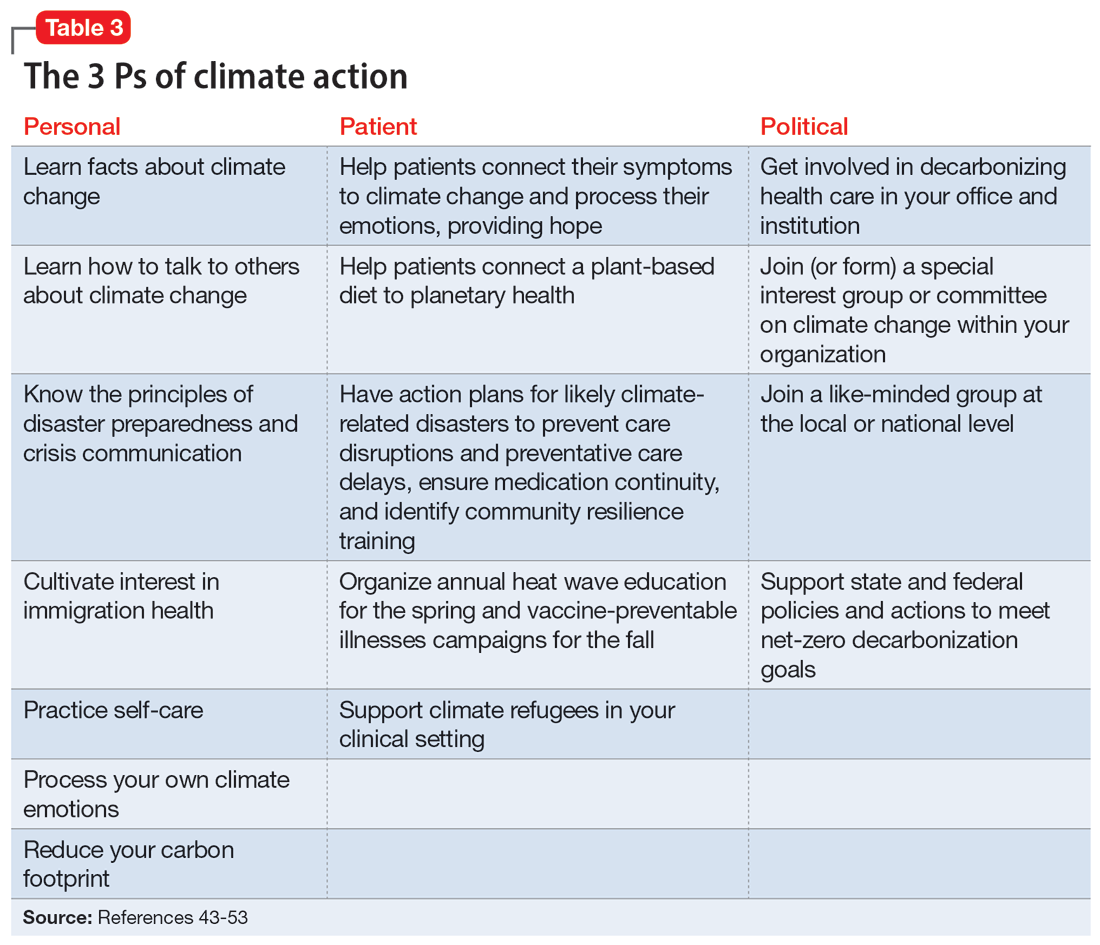
Personal
Even if clinicians believe climate change is important for their clinical work, they may still feel overwhelmed and unsure what to do in the context of competing responsibilities. A necessary first step is overcoming paralysis from the enormity of the problem, including the need to shift away from an expanding consumption model to environmental sustainability in a short period of time.
A good starting point is to get educated on the facts of climate change and how to discuss it in an office setting as well as in your personal life. A basic principle of climate change communication is that constructive hope (progress achieved despite everything) coupled with constructive doubt (the reality of the threat) can mobilize people towards action, whereas false hope or fatalistic doubt impedes action.43 The importance of optimal public health messaging cannot be overstated; well-meaning campaigns to change behavior can fail if they emphasize the wrong message. For example, in a study examining COVID-19 messaging in >80 countries, Dorison et al44 found that negatively framed messages mostly increased anxiety but had no benefit with regard to shifting people toward desired behaviors.
In addition, clinicians can learn how to confront climate disavowal and difficult emotions in themselves and even plan to shift to carbon neutrality, such as purchasing carbon offsets or green sources of energy and transportation. They may not be familiar with principles of disaster preparedness or crisis communication.46 Acquiring those professional skills may suggest next steps for action. Being familiar with the challenges and resources for immigrants, including individuals displaced due to climate change, may be necessary.47 Finally, to reduce the risk of burnout, it is important to practice self-care, including strategies to reduce feelings of being overwhelmed.
Patient
In clinical encounters, clinicians can be proactive in helping patients understand their climate-related anxieties around an uncertain future, including identifying barriers to climate action.48
Continue to: Clinics must prepare for disasters...
Clinics must prepare for disasters in their communities to prevent disruption of psychiatric care by having an action plan, including the provision of medications. Such action plans should be prioritized for the most likely scenarios in an individual’s setting (eg, heat waves, wildfires, hurricanes, or flooding).
It is important to educate clinic staff and include them in planning for emergencies, because an all-hands approach and buy-in from all team members is critical. Clinicians should review how patients would continue to receive services, particularly medications, in the event of a disaster. In some cases, providing a 90-day medication supply will suffice, while in others (eg, patients receiving long-acting antipsychotics or clozapine) more preparation is necessary. Some events are predictable and can be organized annually, such as clinicians becoming vaccine ambassadors and organizing vaccine campaigns every fall50; winter-related disaster preparation every fall; and heat wave education every spring (leaflets for patients, staff, and family members; review of safety of medications during heat waves). Plan for, monitor, and coordinate medical care and services for climate refugees and other populations that may otherwise delay medical care and impede illness prevention. Finally, support climate refugees, including connecting them to services or providing trauma-informed care.
Political
Some clinicians may feel compelled to become politically active to advocate for changes within the health care system. Two initiatives related to decarbonizing the health care sector are My Green Doctor51 and Health Care Without Harm,52 which offer help in shifting your office, clinic, or hospital towards carbon neutrality.
Climate change unevenly affects people and will continue to exacerbate inequalities in society, including individuals with mental illness.53 To work toward climate justice on behalf of their patients, clinicians could join (or form) climate committees of special interest groups in their professional organizations or setting. Joining like-minded groups working on climate change at the local or national level prevents an omission of a psychiatric voice and counteracts burnout. It is important to stay focused on the root causes of the problem during activism: doing something to reduce fossil fuel use is ultimately most important.54 The concrete goal of reaching the Paris 1.5-degree Celsius climate goal is a critical benchmark against which any other action can be measured.54
Planning for the future
Over the course of history, societies have always faced difficult periods in which they needed to rebuild after natural disasters or self-inflicted catastrophes such as terrorist attacks or wars. Since the advent of the nuclear age, people have lived under the existential threat of nuclear war. The Anthropocene is a proposed geological term that reflects the enormous and possibly disastrous impact human activity has had on our planet.55 While not yet formally adopted, this term has heuristic value, directing attention and reflection to our role and its now undisputed consequences. In the future, historians will debate if the scale of our current climate crisis has been different. It is, however, not controversial that humanity will be faced with the effects of climate change for the foreseeable future.10 Already, even “normal” weather events are fueled by energy in overcharged and altered weather systems due to global warming, leading to weather events ranging from droughts to floods and storms that are more severe, more frequent, and have longer-lasting effects on communities.56
Continue to: As physicians, we are tasked...
As physicians, we are tasked by society to create and maintain a health care system that addresses the needs of our patients and the communities in which they live. Increasingly, we are forced to contend with an addition to the traditional 5 phases of acute disaster management (prevention, mitigation, preparedness, response, and recovery) to manage prolonged or even parallel disasters, where a series of disasters occurs before the community has recovered and healed. We must grapple with a sense of an “extended period of insecurity and instability” (permacrisis) and must better prepare for and prevent the polycrisis (many simultaneous crises) or the metacrisis of our “age of turmoil”57 in which we must limit global warming, mitigate its damage, and increase community resilience to adapt.
Leading by personal example and providing hope may be what some patients need, as the reality of climate change contributes to the general uneasiness about the future and doomsday scenarios to which many fall victim. At the level of professional societies, many are calling for leadership, including from mental health organizations, to bolster the “social climate,” to help us strengthen our emotional resilience and social bonds to better withstand climate change together.58 It is becoming harder to justify standing on the sidelines,59 and it may be better for both our world and a clinician’s own sanity to be engaged in professional and private hopeful action1 to address climate change. Without ecological or planetary health, there can be no mental health.
Bottom Line
Clinicians can prepare their patients for climate-related disruptions and manage the impact climate change has on their mental health. Addressing climate change at clinical and political levels is consistent with the leadership roles and professional ethics clinicians face in daily practice.
Related Resources
- Lim C, MacLaurin S, Freudenreich O. Preparing patients with serious mental illness for extreme HEAT. Current Psychiatry. 2022;21(9):27-28. doi:10.12788/cp.0287
- My Green Doctor. https://mygreendoctor.org/
- The Climate Resilience for Frontline Clinics Toolkit from Americares. https://www.americares.org/what-we-do/community-health/climate-resilient-health-clinics
- Climate Psychiatry Alliance. https://www.climatepsychiatry.org/
Drug Brand Names
Clozapine • Clozaril
“ Hope is engagement with the act of mapping our destinies.” 1
—Valerie Braithwaite
Why should psychiatrists care about climate change and try to mitigate its effects? First, we are tasked by society with managing the psychological and neuropsychiatric sequelae from disasters, which include climate change. The American Psychiatric Association’s position statement on climate change includes it as a legitimate focus for our specialty.2 Second, as physicians, we are morally obligated to do no harm. Since the health care sector contributes significantly to climate change (8.5% of national carbon emissions stem from health care) and causes demonstrable health impacts,3 managing these impacts and decarbonizing the health care industry is morally imperative.4 And third, psychiatric clinicians have transferrable skills that can address fears of climate change, challenge climate change denialism,5 motivate people to adopt more pro-environmental behaviors, and help communities not only endure the emotional impact of climate change but become more psychologically resilient.6
Most psychiatrists, however, did not receive formal training on climate change and the related field of disaster preparedness. For example, Harvard Medical School did not include a course on climate change in their medical student curriculum until 2023.7 In this article, we provide a basic framework of climate change and its impact on mental health, with particular focus on patients with serious mental illness (SMI). We offer concrete steps clinicians can take to prevent or mitigate harm from climate change for their patients, prepare for disasters at the level of individual patient encounters, and strengthen their clinics and communities. We also encourage clinicians to take active leadership roles in their professional organizations to be part of climate solutions, building on the trust patients continue to have in their physicians.8 Even if clinicians do not view climate change concerns under their conceived clinical care mandate, having a working knowledge about it is important because patients, paraprofessional staff, or medical trainees are likely to bring it up.9
Climate change and mental health
Climate change is harmful to human health, including mental health.10 It can impact mental health directly via its impact on brain function and neuropsychiatric sequelae, and indirectly via climate-related disasters leading to acute or chronic stress, losses, and displacement with psychiatric and psychological sequelae (Table 111-29).
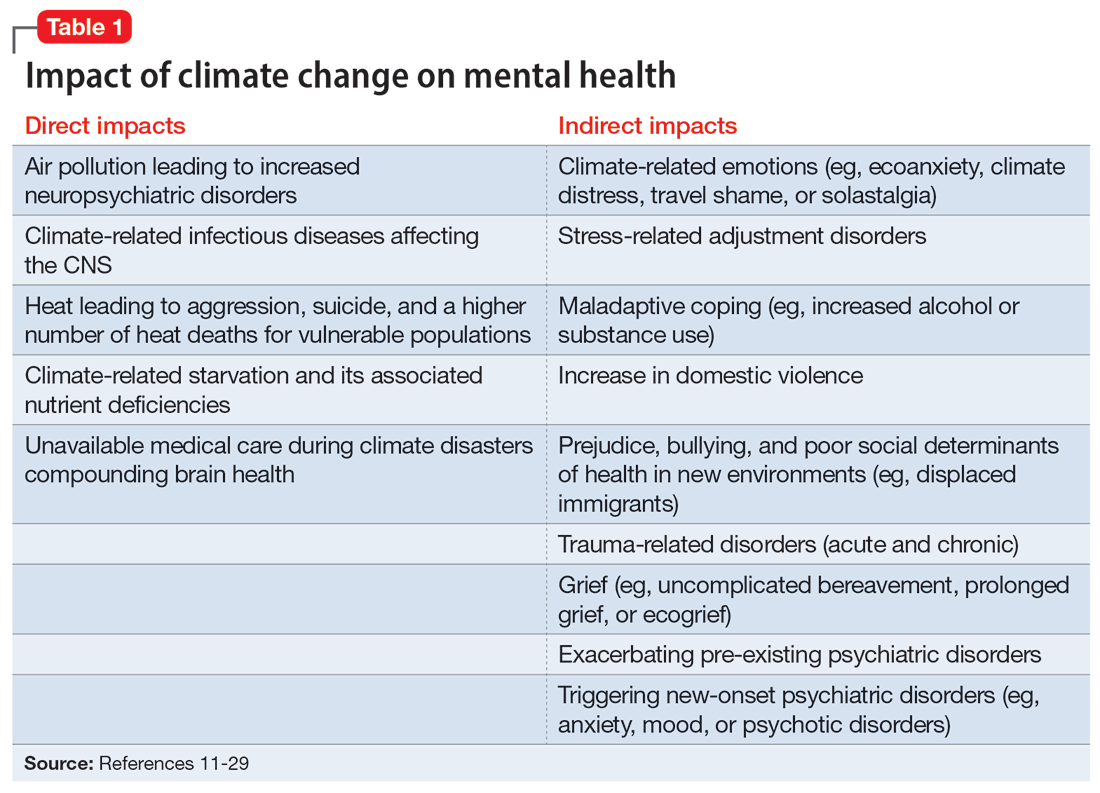
Direct impact
The effects of air pollution, heat, infections, and starvation are examples of how climate change directly impacts mental health. Air pollution and brain health are a concern for psychiatry, given the well-described effects of air deterioration on the developing brain.11 In animal models, airborne pollutants lead to widespread neuroinflammation and cell loss via a multitude of mechanisms.12 This is consistent with worse cognitive and behavioral functions across a wide range of cognitive domains seen in children exposed to pollution compared to those who grew up in environments with healthy air.13 Even low-level exposure to air pollution increases the risk for later onset of depression, suicide, and anxiety.14 Hippocampal atrophy observed in patients with first-episode psychosis may also be partially attributable to air pollution.15 An association between heat and suicide (and to a lesser extent, aggression) has also been reported.16
Worse physical health (eg, strokes) due to excessive heat can further compound mental health via elevated rates of depression. Data from the United States and Mexico show that for each degree Celsius increase in ambient temperature, suicide rates may increase by approximately 1%.17 A meta-analysis by Frangione et al18 similarly concluded that each degree Celsius increase results in an overall risk ratio of 1.016 (95% CI, 1.012 to 1.019) for deaths by suicide and suicide attempts. Additionally, global warming is shifting the endemic areas for many infectious agents, particularly vector-borne diseases,19 to regions in which they had hitherto been unknown, increasing the risk for future outbreaks and even pandemics.20 These infectious illnesses often carry neuropsychiatric morbidity, with seizures, encephalopathy with incomplete recovery, and psychiatric syndromes occurring in many cases. Crop failure can lead to starvation during pregnancy and childhood, which has wide-ranging consequences for brain development and later physical and psychological health in adults.21,22 Mothers affected by starvation also experience negative impacts on childbearing and childrearing.23
Indirect impact
Climate change’s indirect impact on mental health can stem from the stress of living through a disaster such as an extreme weather event; from losses, including the death of friends and family members; and from becoming temporarily displaced.24 Some climate change–driven disasters can be viewed as slow-moving, such as drought and the rising of sea levels, where displacement becomes permanent. Managing mass migration from internally or externally displaced people who must abandon their communities because of climate change will have significant repercussions for all societies.25 The term “climate refugee” is not (yet) included in the United Nations’ official definition of refugees; it defines refugees as individuals who have fled their countries because of war, violence, or persecution.26 These and other bureaucratic issues can come up when clinicians are trying to help migrants with immigration-related paperwork.
Continue to: As the inevitability of climate change...
As the inevitability of climate change sinks in, its long-term ramifications have introduced a new lexicon of psychological suffering related to the crisis.27 Common terms for such distress include ecoanxiety (fear of what is happening and will happen with climate change), ecogrief (sadness about the destruction of species and natural habitats), solastalgia28 (the nostalgia an individual feels for emotionally treasured landscapes that have changed), and terrafuria or ecorage (the reaction to betrayal and inaction by governments and leaders).29 Climate-related emotions can lead to pessimism about the future and a nihilistic outlook on an individual’s ability to effect change and have agency over their life’s outcomes.
The categories of direct and indirect impacts are not mutually exclusive. A child may be starving due to weather-related crop failure as the family is forced to move to another country, then have to contend with prejudice and bullying as an immigrant, and later become anxiously preoccupied with climate change and its ability to cause further distress.
Effect on individuals with serious mental illness
Patients with SMI are particularly vulnerable to the impact of climate change. They are less resilient to climate change–related events, such as heat waves or temporary displacement from flooding, both at the personal level due to illness factors (eg, negative symptoms or cognitive impairment) and at the community level due to social factors (eg, weaker social support or poverty).
Recognizing the increased vulnerability to heat waves and preparing for them is particularly important for patients with SMI because they are at an increased risk for heat-related illnesses.30 For example, patients may not appreciate the danger from heat and live in conditions that put them at risk (ie, not having air conditioning in their home or living alone). Their illness alone impairs heat regulation31; patients with depression and anxiety also dissipate heat less effectively.32,33 Additionally, many psychiatric medications, particularly antipsychotics, impair key mechanisms of heat dissipation.34,35 Antipsychotics render organisms more poikilothermic (susceptible to environmental temperature, like cold-blooded animals) and can be anticholinergic, which impedes sweating. A recent analysis of heat-related deaths during a period of extreme and prolonged heat in British Columbia in 2021 affirmed these concerns, reporting that patients with schizophrenia had the highest odds of death during this heat-related event.36
COVID-19 has shown that flexible models of care are needed to prevent disengagement from medical and psychiatric care37 and assure continued treatment with essential medications such as clozapine38 and long-acting injectable antipsychotics39 during periods of social change, as with climate change. While telehealth was critical during the COVID-19 pandemic40 and is here to stay, it alone may be insufficient given the digital divide (patients with SMI may be less likely to have access to or be proficient in the use of digital technologies). The pandemic has shown the importance of public health efforts, including benefits from targeted outreach, with regards to vaccinations for this patient group.41,42 Table 2 summarizes things clinicians should consider when preparing patients with SMI for the effects of climate change.
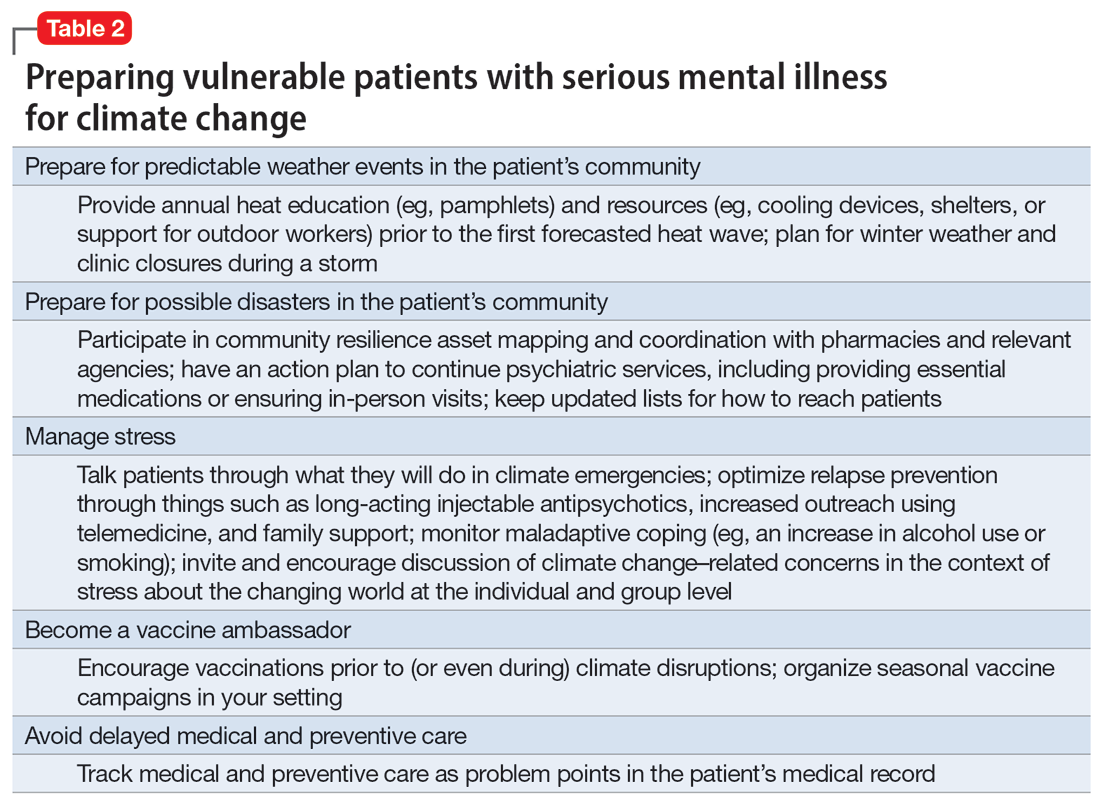
Continue to: The psychiatrist's role
The psychiatrist’s role
There are many ways a psychiatrist can professionally get involved in addressing climate change. Table 343-53 outlines the 3 Ps of climate action (taking actions to mitigate the effects of climate change): personal, patient (and clinic), and political (advocacy).
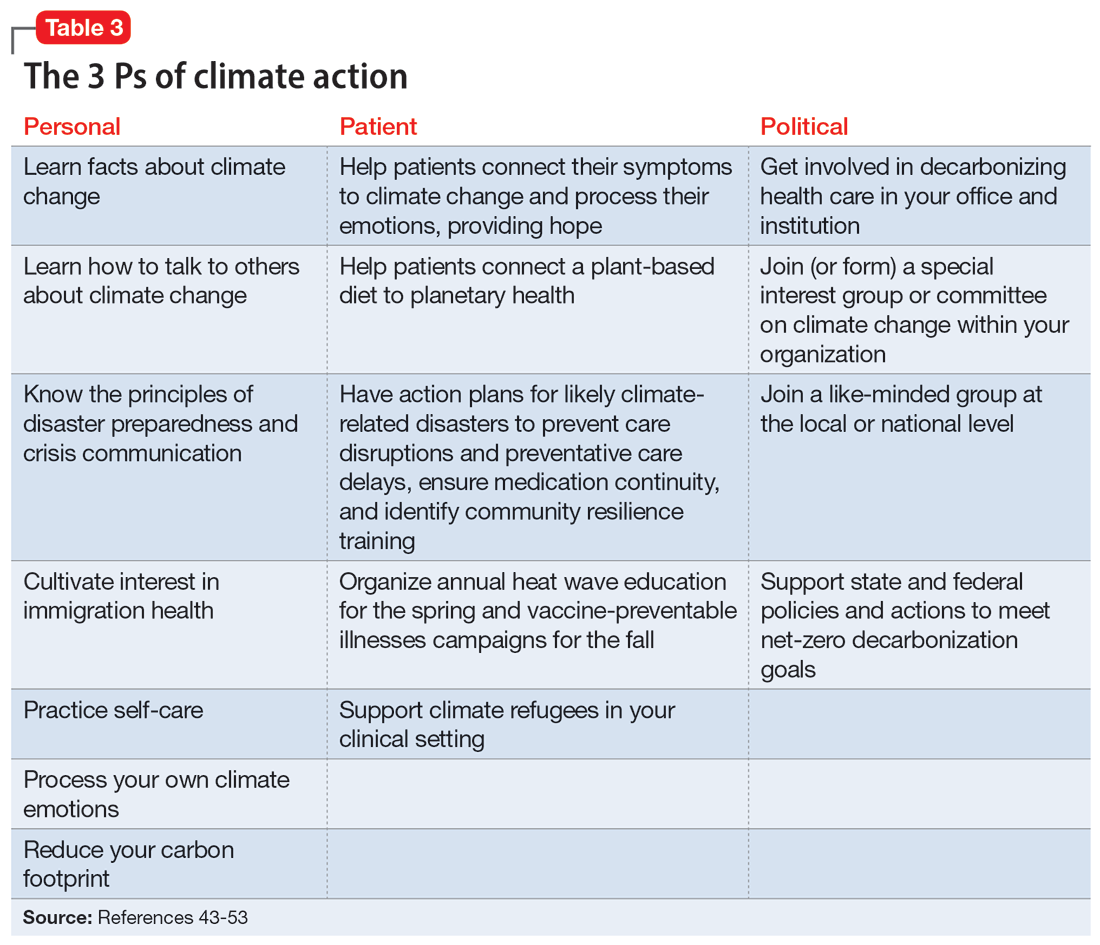
Personal
Even if clinicians believe climate change is important for their clinical work, they may still feel overwhelmed and unsure what to do in the context of competing responsibilities. A necessary first step is overcoming paralysis from the enormity of the problem, including the need to shift away from an expanding consumption model to environmental sustainability in a short period of time.
A good starting point is to get educated on the facts of climate change and how to discuss it in an office setting as well as in your personal life. A basic principle of climate change communication is that constructive hope (progress achieved despite everything) coupled with constructive doubt (the reality of the threat) can mobilize people towards action, whereas false hope or fatalistic doubt impedes action.43 The importance of optimal public health messaging cannot be overstated; well-meaning campaigns to change behavior can fail if they emphasize the wrong message. For example, in a study examining COVID-19 messaging in >80 countries, Dorison et al44 found that negatively framed messages mostly increased anxiety but had no benefit with regard to shifting people toward desired behaviors.
In addition, clinicians can learn how to confront climate disavowal and difficult emotions in themselves and even plan to shift to carbon neutrality, such as purchasing carbon offsets or green sources of energy and transportation. They may not be familiar with principles of disaster preparedness or crisis communication.46 Acquiring those professional skills may suggest next steps for action. Being familiar with the challenges and resources for immigrants, including individuals displaced due to climate change, may be necessary.47 Finally, to reduce the risk of burnout, it is important to practice self-care, including strategies to reduce feelings of being overwhelmed.
Patient
In clinical encounters, clinicians can be proactive in helping patients understand their climate-related anxieties around an uncertain future, including identifying barriers to climate action.48
Continue to: Clinics must prepare for disasters...
Clinics must prepare for disasters in their communities to prevent disruption of psychiatric care by having an action plan, including the provision of medications. Such action plans should be prioritized for the most likely scenarios in an individual’s setting (eg, heat waves, wildfires, hurricanes, or flooding).
It is important to educate clinic staff and include them in planning for emergencies, because an all-hands approach and buy-in from all team members is critical. Clinicians should review how patients would continue to receive services, particularly medications, in the event of a disaster. In some cases, providing a 90-day medication supply will suffice, while in others (eg, patients receiving long-acting antipsychotics or clozapine) more preparation is necessary. Some events are predictable and can be organized annually, such as clinicians becoming vaccine ambassadors and organizing vaccine campaigns every fall50; winter-related disaster preparation every fall; and heat wave education every spring (leaflets for patients, staff, and family members; review of safety of medications during heat waves). Plan for, monitor, and coordinate medical care and services for climate refugees and other populations that may otherwise delay medical care and impede illness prevention. Finally, support climate refugees, including connecting them to services or providing trauma-informed care.
Political
Some clinicians may feel compelled to become politically active to advocate for changes within the health care system. Two initiatives related to decarbonizing the health care sector are My Green Doctor51 and Health Care Without Harm,52 which offer help in shifting your office, clinic, or hospital towards carbon neutrality.
Climate change unevenly affects people and will continue to exacerbate inequalities in society, including individuals with mental illness.53 To work toward climate justice on behalf of their patients, clinicians could join (or form) climate committees of special interest groups in their professional organizations or setting. Joining like-minded groups working on climate change at the local or national level prevents an omission of a psychiatric voice and counteracts burnout. It is important to stay focused on the root causes of the problem during activism: doing something to reduce fossil fuel use is ultimately most important.54 The concrete goal of reaching the Paris 1.5-degree Celsius climate goal is a critical benchmark against which any other action can be measured.54
Planning for the future
Over the course of history, societies have always faced difficult periods in which they needed to rebuild after natural disasters or self-inflicted catastrophes such as terrorist attacks or wars. Since the advent of the nuclear age, people have lived under the existential threat of nuclear war. The Anthropocene is a proposed geological term that reflects the enormous and possibly disastrous impact human activity has had on our planet.55 While not yet formally adopted, this term has heuristic value, directing attention and reflection to our role and its now undisputed consequences. In the future, historians will debate if the scale of our current climate crisis has been different. It is, however, not controversial that humanity will be faced with the effects of climate change for the foreseeable future.10 Already, even “normal” weather events are fueled by energy in overcharged and altered weather systems due to global warming, leading to weather events ranging from droughts to floods and storms that are more severe, more frequent, and have longer-lasting effects on communities.56
Continue to: As physicians, we are tasked...
As physicians, we are tasked by society to create and maintain a health care system that addresses the needs of our patients and the communities in which they live. Increasingly, we are forced to contend with an addition to the traditional 5 phases of acute disaster management (prevention, mitigation, preparedness, response, and recovery) to manage prolonged or even parallel disasters, where a series of disasters occurs before the community has recovered and healed. We must grapple with a sense of an “extended period of insecurity and instability” (permacrisis) and must better prepare for and prevent the polycrisis (many simultaneous crises) or the metacrisis of our “age of turmoil”57 in which we must limit global warming, mitigate its damage, and increase community resilience to adapt.
Leading by personal example and providing hope may be what some patients need, as the reality of climate change contributes to the general uneasiness about the future and doomsday scenarios to which many fall victim. At the level of professional societies, many are calling for leadership, including from mental health organizations, to bolster the “social climate,” to help us strengthen our emotional resilience and social bonds to better withstand climate change together.58 It is becoming harder to justify standing on the sidelines,59 and it may be better for both our world and a clinician’s own sanity to be engaged in professional and private hopeful action1 to address climate change. Without ecological or planetary health, there can be no mental health.
Bottom Line
Clinicians can prepare their patients for climate-related disruptions and manage the impact climate change has on their mental health. Addressing climate change at clinical and political levels is consistent with the leadership roles and professional ethics clinicians face in daily practice.
Related Resources
- Lim C, MacLaurin S, Freudenreich O. Preparing patients with serious mental illness for extreme HEAT. Current Psychiatry. 2022;21(9):27-28. doi:10.12788/cp.0287
- My Green Doctor. https://mygreendoctor.org/
- The Climate Resilience for Frontline Clinics Toolkit from Americares. https://www.americares.org/what-we-do/community-health/climate-resilient-health-clinics
- Climate Psychiatry Alliance. https://www.climatepsychiatry.org/
Drug Brand Names
Clozapine • Clozaril
1. Kretz L. Hope in environmental philosophy. J Agricult Environ Ethics. 2013;26:925-944. doi:10.1007/s10806-012-9425-8
2. Ursano RJ, Morganstein JC, Cooper R. Position statement on mental health and climate change. American Psychiatric Association. March 2023. Accessed August 6, 2023. https://www.psychiatry.org/getattachment/0ce71f37-61a6-44d0-8fcd-c752b7e935fd/Position-Mental-Health-Climate-Change.pdf
3. Eckelman MJ, Huang K, Lagasse R, et al. Health care pollution and public health damage in the United States: an update. Health Aff (Millwood). 2020;39:2071-2079.
4. Dzau VJ, Levine R, Barrett G, et al. Decarbonizing the U.S. health sector - a call to action. N Engl J Med. 2021;385(23):2117-2119. doi:10.1056/NEJMp2115675
5. Haase E, Augustinavicius JH, K. Climate change and psychiatry. In: Tasman A, Riba MB, Alarcón RD, et al, eds. Tasman’s Psychiatry. 5th ed. Springer; 2023.
6. Belkin G. Mental health and the global race to resilience. Psychiatr Times. 2023;40(3):26.
7. Hu SR, Yang JQ. Harvard Medical School will integrate climate change into M.D. curriculum. The Harvard Crimson. February 3, 2023. Accessed August 6, 2023. https://www.thecrimson.com/article/2023/2/3/hms-climate-curriculum/#:~:text=The%20new%20climate%20change%20curriculum,in%20arriving%20at%20climate%20solutions
8. Funk C, Gramlich J. Amid coronavirus threat, Americans generally have a high level of trust in medical doctors. Pew Research Center. March 13, 2020. Accessed August 6, 2023. https://www.pewresearch.org/fact-tank/2020/03/13/amid-coronavirus-threat-americans-generally-have-a-high-level-of-trust-in-medical-doctors/
9. Coverdale J, Balon R, Beresin EV, et al. Climate change: a call to action for the psychiatric profession. Acad Psychiatry. 2018;42(3):317-323. doi:10.1007/s40596-018-0885-7
10. Intergovernmental Panel on Climate Change. AR6 synthesis report: climate change 2023. Accessed August 6, 2023. https://www.ipcc.ch/report/sixth-assessment-report-cycle/
11. Perera FP. Multiple threats to child health from fossil fuel combustion: impacts of air pollution and climate change. Environ Health Perspect. 2017;125(2):141-148. doi:10.1289/EHP299
12. Hahad O, Lelieveldz J, Birklein F, et al. Ambient air pollution increases the risk of cerebrovascular and neuropsychiatric disorders through induction of inflammation and oxidative stress. Int J Mol Sci. 2020;21(12):4306. doi:10.3390/ijms21124306
13. Brockmeyer S, D’Angiulli A. How air pollution alters brain development: the role of neuroinflammation. Translational Neurosci. 2016;7(1):24-30. doi:10.1515/tnsci-2016-0005
14. Yang T, Wang J, Huang J, et al. Long-term exposure to multiple ambient air pollutants and association with incident depression and anxiety. JAMA Psychiatry. 2023;80:305-313. doi:10.1001/jamapsychiatry.2022.4812
15. Worthington MA, Petkova E, Freudenreich O, et al. Air pollution and hippocampal atrophy in first episode schizophrenia. Schizophr Res. 2020;218:63-69. doi:10.1016/j.schres.2020.03.001
16. Dumont C, Haase E, Dolber T, et al. Climate change and risk of completed suicide. J Nerv Ment Dis. 2020;208(7):559-565. doi:10.1097/NMD.0000000000001162
17. Burke M, Gonzales F, Bayis P, et al. Higher temperatures increase suicide rates in the United States and Mexico. Nat Climate Change. 2018;8:723-729. doi:10.1038/s41558-018-0222-x
18. Frangione B, Villamizar LAR, Lang JJ, et al. Short-term changes in meteorological conditions and suicide: a systematic review and meta-analysis. Environ Res. 2022;207:112230. doi:10.1016/j.envres.2021.112230
19. Rocklov J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol. 2020;21(5):479-483. doi:10.1038/s41590-020-0648-y
20. Carlson CJ, Albery GF, Merow C, et al. Climate change increases cross-species viral transmission risk. Nature. 2022;607(7919):555-562. doi:10.1038/s41586-022-04788-w
21. Roseboom TJ, Painter RC, van Abeelen AFM, et al. Hungry in the womb: what are the consequences? Lessons from the Dutch famine. Maturitas. 2011;70(2):141-145. doi:10.1016/j.maturitas.2011.06.017
22. Liu Y, Diao L, Xu L. The impact of childhood experience of starvations on the health of older adults: evidence from China. Int J Health Plann Manage. 2021;36(2):515-531. doi:10.1002/hpm.3099
23. Rothschild J, Haase E. The mental health of women and climate change: direct neuropsychiatric impacts and associated psychological concerns. Int J Gynaecol Obstet. 2023;160(2):405-413. doi:10.1002/ijgo.14479
24. Cianconi P, Betro S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Frontiers Psychiatry. 2020;11:74. doi:10.3389/fpsyt.2020.00074
25. World Economic Forum. Climate refugees – the world’s forgotten victims. June 18, 2021. Accessed August 6, 2023. https://www.weforum.org/agenda/2021/06/climate-refugees-the-world-s-forgotten-victims
26. Climate Refugees. Accessed August 6, 2023. https://www.climate-refugees.org/why
27. Pihkala P. Anxiety and the ecological crisis: an analysis of eco-anxiety and climate anxiety. Sustainability. 2020;12(19):7836. doi:10.3390/su12197836
28. Galway LP, Beery T, Jones-Casey K, et al. Mapping the solastalgia literature: a scoping review study. Int J Environ Res Public Health. 2019;16(15):2662. doi:10.3390/ijerph16152662
29. Albrecht GA. Earth Emotions. New Words for a New World. Cornell University Press; 2019.
30. Sorensen C, Hess J. Treatment and prevention of heat-related illness. N Engl J Med. 2022;387(15):1404-1413. doi:10.1056/NEJMcp2210623
31. Chong TWH, Castle DJ. Layer upon layer: thermoregulation in schizophrenia. Schizophr Res. 2004;69(2-3):149-157. doi:10.1016/s0920-9964(03)00222-6
32. von Salis S, Ehlert U, Fischer S. Altered experienced thermoregulation in depression--no evidence for an effect of early life stress. Front Psychiatry. 2021;12:620656. doi:10.3389/fpsyt.2021.620656
33. Sarchiapone M, Gramaglia C, Iosue M, et al. The association between electrodermal activity (EDA), depression and suicidal behaviour: a systematic review and narrative synthesis. BMC Psychiatry. 2018;18(1):22. doi:10.1186/s12888-017-1551-4
34. Martin-Latry K, Goumy MP, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalisation. Eur Psychiatry. 2007;22(6):335-338. doi:10.1016/j.eurpsy.2007.03.007
35. Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. Lancet. 2021;398(10301):698-708. doi:10.1016/S0140-6736(21)01208-3
36. Lee MJ, McLean KE, Kuo M, et al. Chronic diseases associated with mortality in British Columbia, Canada during the 2021 Western North America extreme heat event. Geohealth. 2023;7(3):e2022GH000729. doi:10.1029/2022GH000729
37. Busch AB, Huskamp HA, Raja P, et al. Disruptions in care for Medicare beneficiaries with severe mental illness during the COVID-19 pandemic. JAMA Netw Open. 2022;5(1):e2145677. doi:10.1001/jamanetworkopen.2021.45677
38. Siskind D, Honer WG, Clark S, et al. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45(3):222-223. doi:10.1503/jpn.200061
39. MacLaurin SA, Mulligan C, Van Alphen MU, et al. Optimal long-acting injectable antipsychotic management during COVID-19. J Clin Psychiatry. 2021;82(1): 20l13730. doi:10.4088/JCP.20l13730
40. Bartels SJ, Baggett TP, Freudenreich O, et al. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness. Psychiatr Serv. 2020;71(10):1078-1081. doi:10.1176/appi.ps.202000244
41. Van Alphen MU, Lim C, Freudenreich O. Mobile vaccine clinics for patients with serious mental illness and health care workers in outpatient mental health clinics. Psychiatr Serv. February 8, 2023. doi:10.1176/appi.ps.20220460
42. Lim C, Van Alphen MU, Maclaurin S, et al. Increasing COVID-19 vaccination rates among patients with serious mental illness: a pilot intervention study. Psychiatr Serv. 2022;73(11):1274-1277. doi:10.1176/appi.ps.202100702
43. Marlon JR, Bloodhart B, Ballew MT, et al. How hope and doubt affect climate change mobilization. Front Commun. May 21, 2019. doi:10.3389/fcomm.2019.00020
44. Dorison CA, Lerner JS, Heller BH, et al. In COVID-19 health messaging, loss framing increases anxiety with little-to-no concomitant benefits: experimental evidence from 84 countries. Affective Sci. 2022;3(3):577-602. doi:10.1007/s42761-022-00128-3
45. Maibach E. Increasing public awareness and facilitating behavior change: two guiding heuristics. George Mason University, Center for Climate Change Communication. September 2015. Accessed August 6, 2023. https://www.climatechangecommunication.org/wp-content/uploads/2018/06/Maibach-Two-hueristics-September-2015-revised.pdf
46. Koh KA, Raviola G, Stoddard FJ Jr. Psychiatry and crisis communication during COVID-19: a view from the trenches. Psychiatr Serv. 2021;72(5):615. doi:10.1176/appi.ps.202000912
47. Velez G, Adam B, Shadid O, et al. The clock is ticking: are we prepared for mass climate migration? Psychiatr News. March 24, 2023. Accessed August 6, 2023. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2023.04.4.3
48. Ingle HE, Mikulewicz M. Mental health and climate change: tackling invisible injustice. Lancet Planet Health. 2020;4:e128-e130. doi:10.1016/S2542-5196(20)30081-4
49. Shah UA, Merlo G. Personal and planetary health--the connection with dietary choices. JAMA. 2023;329(21):1823-1824. doi:10.1001/jama.2023.6118
50. Lim C, Van Alphen MU, Freudenreich O. Becoming vaccine ambassadors: a new role for psychiatrists. Current Psychiatry. 2021;20(8):10-11,17-21,26-28,38. doi:10.12788/cp.0155
51. My Green Doctor. Accessed August 6, 2023. https://mygreendoctor.org/
52. Healthcare Without Harm. Accessed August 6, 2023. https://noharm.org/
53. Levy BS, Patz JA. Climate change, human rights, and social justice. Ann Glob Health. 2015;81:310-322.
54. Intergovernmental Panel on Climate Change. Global warming of 1.5° C 2018. Accessed August 6, 2023. https://www.ipcc.ch/sr15/
55. Steffen W, Crutzen J, McNeill JR. The Anthropocene: are humans now overwhelming the great forces of nature? Ambio. 2007;36(8):614-621. doi:10.1579/0044-7447(2007)36[614:taahno]2.0.co;2
56. American Meteorological Society. Explaining extreme events from a climate perspective. Accessed August 6, 2023. https://www.ametsoc.org/ams/index.cfm/publications/bulletin-of-the-american-meteorological-society-bams/explaining-extreme-events-from-a-climate-perspective/
57. Nierenberg AA. Coping in the age of turmoil. Psychiatr Ann. 2022;52(7):263. July 1, 2022. doi:10.3928/23258160-20220701-01
58. Belkin G. Leadership for the social climate. N Engl J Med. 2020;382(21):1975-1977. doi:10.1056/NEJMp2001507
59. Skinner JR. Doctors and climate change: first do no harm. J Paediatr Child Health. 2021;57(11):1754-1758. doi:10.1111/jpc.15658
1. Kretz L. Hope in environmental philosophy. J Agricult Environ Ethics. 2013;26:925-944. doi:10.1007/s10806-012-9425-8
2. Ursano RJ, Morganstein JC, Cooper R. Position statement on mental health and climate change. American Psychiatric Association. March 2023. Accessed August 6, 2023. https://www.psychiatry.org/getattachment/0ce71f37-61a6-44d0-8fcd-c752b7e935fd/Position-Mental-Health-Climate-Change.pdf
3. Eckelman MJ, Huang K, Lagasse R, et al. Health care pollution and public health damage in the United States: an update. Health Aff (Millwood). 2020;39:2071-2079.
4. Dzau VJ, Levine R, Barrett G, et al. Decarbonizing the U.S. health sector - a call to action. N Engl J Med. 2021;385(23):2117-2119. doi:10.1056/NEJMp2115675
5. Haase E, Augustinavicius JH, K. Climate change and psychiatry. In: Tasman A, Riba MB, Alarcón RD, et al, eds. Tasman’s Psychiatry. 5th ed. Springer; 2023.
6. Belkin G. Mental health and the global race to resilience. Psychiatr Times. 2023;40(3):26.
7. Hu SR, Yang JQ. Harvard Medical School will integrate climate change into M.D. curriculum. The Harvard Crimson. February 3, 2023. Accessed August 6, 2023. https://www.thecrimson.com/article/2023/2/3/hms-climate-curriculum/#:~:text=The%20new%20climate%20change%20curriculum,in%20arriving%20at%20climate%20solutions
8. Funk C, Gramlich J. Amid coronavirus threat, Americans generally have a high level of trust in medical doctors. Pew Research Center. March 13, 2020. Accessed August 6, 2023. https://www.pewresearch.org/fact-tank/2020/03/13/amid-coronavirus-threat-americans-generally-have-a-high-level-of-trust-in-medical-doctors/
9. Coverdale J, Balon R, Beresin EV, et al. Climate change: a call to action for the psychiatric profession. Acad Psychiatry. 2018;42(3):317-323. doi:10.1007/s40596-018-0885-7
10. Intergovernmental Panel on Climate Change. AR6 synthesis report: climate change 2023. Accessed August 6, 2023. https://www.ipcc.ch/report/sixth-assessment-report-cycle/
11. Perera FP. Multiple threats to child health from fossil fuel combustion: impacts of air pollution and climate change. Environ Health Perspect. 2017;125(2):141-148. doi:10.1289/EHP299
12. Hahad O, Lelieveldz J, Birklein F, et al. Ambient air pollution increases the risk of cerebrovascular and neuropsychiatric disorders through induction of inflammation and oxidative stress. Int J Mol Sci. 2020;21(12):4306. doi:10.3390/ijms21124306
13. Brockmeyer S, D’Angiulli A. How air pollution alters brain development: the role of neuroinflammation. Translational Neurosci. 2016;7(1):24-30. doi:10.1515/tnsci-2016-0005
14. Yang T, Wang J, Huang J, et al. Long-term exposure to multiple ambient air pollutants and association with incident depression and anxiety. JAMA Psychiatry. 2023;80:305-313. doi:10.1001/jamapsychiatry.2022.4812
15. Worthington MA, Petkova E, Freudenreich O, et al. Air pollution and hippocampal atrophy in first episode schizophrenia. Schizophr Res. 2020;218:63-69. doi:10.1016/j.schres.2020.03.001
16. Dumont C, Haase E, Dolber T, et al. Climate change and risk of completed suicide. J Nerv Ment Dis. 2020;208(7):559-565. doi:10.1097/NMD.0000000000001162
17. Burke M, Gonzales F, Bayis P, et al. Higher temperatures increase suicide rates in the United States and Mexico. Nat Climate Change. 2018;8:723-729. doi:10.1038/s41558-018-0222-x
18. Frangione B, Villamizar LAR, Lang JJ, et al. Short-term changes in meteorological conditions and suicide: a systematic review and meta-analysis. Environ Res. 2022;207:112230. doi:10.1016/j.envres.2021.112230
19. Rocklov J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol. 2020;21(5):479-483. doi:10.1038/s41590-020-0648-y
20. Carlson CJ, Albery GF, Merow C, et al. Climate change increases cross-species viral transmission risk. Nature. 2022;607(7919):555-562. doi:10.1038/s41586-022-04788-w
21. Roseboom TJ, Painter RC, van Abeelen AFM, et al. Hungry in the womb: what are the consequences? Lessons from the Dutch famine. Maturitas. 2011;70(2):141-145. doi:10.1016/j.maturitas.2011.06.017
22. Liu Y, Diao L, Xu L. The impact of childhood experience of starvations on the health of older adults: evidence from China. Int J Health Plann Manage. 2021;36(2):515-531. doi:10.1002/hpm.3099
23. Rothschild J, Haase E. The mental health of women and climate change: direct neuropsychiatric impacts and associated psychological concerns. Int J Gynaecol Obstet. 2023;160(2):405-413. doi:10.1002/ijgo.14479
24. Cianconi P, Betro S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Frontiers Psychiatry. 2020;11:74. doi:10.3389/fpsyt.2020.00074
25. World Economic Forum. Climate refugees – the world’s forgotten victims. June 18, 2021. Accessed August 6, 2023. https://www.weforum.org/agenda/2021/06/climate-refugees-the-world-s-forgotten-victims
26. Climate Refugees. Accessed August 6, 2023. https://www.climate-refugees.org/why
27. Pihkala P. Anxiety and the ecological crisis: an analysis of eco-anxiety and climate anxiety. Sustainability. 2020;12(19):7836. doi:10.3390/su12197836
28. Galway LP, Beery T, Jones-Casey K, et al. Mapping the solastalgia literature: a scoping review study. Int J Environ Res Public Health. 2019;16(15):2662. doi:10.3390/ijerph16152662
29. Albrecht GA. Earth Emotions. New Words for a New World. Cornell University Press; 2019.
30. Sorensen C, Hess J. Treatment and prevention of heat-related illness. N Engl J Med. 2022;387(15):1404-1413. doi:10.1056/NEJMcp2210623
31. Chong TWH, Castle DJ. Layer upon layer: thermoregulation in schizophrenia. Schizophr Res. 2004;69(2-3):149-157. doi:10.1016/s0920-9964(03)00222-6
32. von Salis S, Ehlert U, Fischer S. Altered experienced thermoregulation in depression--no evidence for an effect of early life stress. Front Psychiatry. 2021;12:620656. doi:10.3389/fpsyt.2021.620656
33. Sarchiapone M, Gramaglia C, Iosue M, et al. The association between electrodermal activity (EDA), depression and suicidal behaviour: a systematic review and narrative synthesis. BMC Psychiatry. 2018;18(1):22. doi:10.1186/s12888-017-1551-4
34. Martin-Latry K, Goumy MP, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalisation. Eur Psychiatry. 2007;22(6):335-338. doi:10.1016/j.eurpsy.2007.03.007
35. Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. Lancet. 2021;398(10301):698-708. doi:10.1016/S0140-6736(21)01208-3
36. Lee MJ, McLean KE, Kuo M, et al. Chronic diseases associated with mortality in British Columbia, Canada during the 2021 Western North America extreme heat event. Geohealth. 2023;7(3):e2022GH000729. doi:10.1029/2022GH000729
37. Busch AB, Huskamp HA, Raja P, et al. Disruptions in care for Medicare beneficiaries with severe mental illness during the COVID-19 pandemic. JAMA Netw Open. 2022;5(1):e2145677. doi:10.1001/jamanetworkopen.2021.45677
38. Siskind D, Honer WG, Clark S, et al. Consensus statement on the use of clozapine during the COVID-19 pandemic. J Psychiatry Neurosci. 2020;45(3):222-223. doi:10.1503/jpn.200061
39. MacLaurin SA, Mulligan C, Van Alphen MU, et al. Optimal long-acting injectable antipsychotic management during COVID-19. J Clin Psychiatry. 2021;82(1): 20l13730. doi:10.4088/JCP.20l13730
40. Bartels SJ, Baggett TP, Freudenreich O, et al. COVID-19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness. Psychiatr Serv. 2020;71(10):1078-1081. doi:10.1176/appi.ps.202000244
41. Van Alphen MU, Lim C, Freudenreich O. Mobile vaccine clinics for patients with serious mental illness and health care workers in outpatient mental health clinics. Psychiatr Serv. February 8, 2023. doi:10.1176/appi.ps.20220460
42. Lim C, Van Alphen MU, Maclaurin S, et al. Increasing COVID-19 vaccination rates among patients with serious mental illness: a pilot intervention study. Psychiatr Serv. 2022;73(11):1274-1277. doi:10.1176/appi.ps.202100702
43. Marlon JR, Bloodhart B, Ballew MT, et al. How hope and doubt affect climate change mobilization. Front Commun. May 21, 2019. doi:10.3389/fcomm.2019.00020
44. Dorison CA, Lerner JS, Heller BH, et al. In COVID-19 health messaging, loss framing increases anxiety with little-to-no concomitant benefits: experimental evidence from 84 countries. Affective Sci. 2022;3(3):577-602. doi:10.1007/s42761-022-00128-3
45. Maibach E. Increasing public awareness and facilitating behavior change: two guiding heuristics. George Mason University, Center for Climate Change Communication. September 2015. Accessed August 6, 2023. https://www.climatechangecommunication.org/wp-content/uploads/2018/06/Maibach-Two-hueristics-September-2015-revised.pdf
46. Koh KA, Raviola G, Stoddard FJ Jr. Psychiatry and crisis communication during COVID-19: a view from the trenches. Psychiatr Serv. 2021;72(5):615. doi:10.1176/appi.ps.202000912
47. Velez G, Adam B, Shadid O, et al. The clock is ticking: are we prepared for mass climate migration? Psychiatr News. March 24, 2023. Accessed August 6, 2023. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2023.04.4.3
48. Ingle HE, Mikulewicz M. Mental health and climate change: tackling invisible injustice. Lancet Planet Health. 2020;4:e128-e130. doi:10.1016/S2542-5196(20)30081-4
49. Shah UA, Merlo G. Personal and planetary health--the connection with dietary choices. JAMA. 2023;329(21):1823-1824. doi:10.1001/jama.2023.6118
50. Lim C, Van Alphen MU, Freudenreich O. Becoming vaccine ambassadors: a new role for psychiatrists. Current Psychiatry. 2021;20(8):10-11,17-21,26-28,38. doi:10.12788/cp.0155
51. My Green Doctor. Accessed August 6, 2023. https://mygreendoctor.org/
52. Healthcare Without Harm. Accessed August 6, 2023. https://noharm.org/
53. Levy BS, Patz JA. Climate change, human rights, and social justice. Ann Glob Health. 2015;81:310-322.
54. Intergovernmental Panel on Climate Change. Global warming of 1.5° C 2018. Accessed August 6, 2023. https://www.ipcc.ch/sr15/
55. Steffen W, Crutzen J, McNeill JR. The Anthropocene: are humans now overwhelming the great forces of nature? Ambio. 2007;36(8):614-621. doi:10.1579/0044-7447(2007)36[614:taahno]2.0.co;2
56. American Meteorological Society. Explaining extreme events from a climate perspective. Accessed August 6, 2023. https://www.ametsoc.org/ams/index.cfm/publications/bulletin-of-the-american-meteorological-society-bams/explaining-extreme-events-from-a-climate-perspective/
57. Nierenberg AA. Coping in the age of turmoil. Psychiatr Ann. 2022;52(7):263. July 1, 2022. doi:10.3928/23258160-20220701-01
58. Belkin G. Leadership for the social climate. N Engl J Med. 2020;382(21):1975-1977. doi:10.1056/NEJMp2001507
59. Skinner JR. Doctors and climate change: first do no harm. J Paediatr Child Health. 2021;57(11):1754-1758. doi:10.1111/jpc.15658
A toxic and fractured political system can breed angst and PTSD
As psychiatrists know, many of our severely traumatized adult patients were victims of abuse during childhood. We routinely ask every new patient about physical, emotional, or sexual abuse when they were growing up because of the well-established, serious neurobiological and mental repercussions.1,2
Perhaps one of the worst experiences for a child is to witness bitterly adversarial parents (their vital role models) who argue viciously, despise each other, and hurl insults (and even punches) at each other. Such a chronically and emotionally traumatic upbringing can haunt kids well into adulthood, disrupting their hypothalamic-pituitary-adrenal axis and triggering anxiety, depression, and even psychosis due to epigenetic changes that ultimately lead to abnormal brain development.3
It often feels that the governance of our country, or the national “political family,” is seriously fractured like a hopelessly dysfunctional family. Could that be negatively impacting the mental health of the citizenry? Having 2 antagonistic political parties expressing visceral hatred and undisguised contempt for each other 24/7 (thanks to the enabling era of cable TV, the internet, and social media) has transformed each party’s fanatic followers from fellow citizens to ideological combatants. In this poisonous societal zeitgeist of bidirectional acrimony and mutual detestation, the opposing parties and their “intellectual militias” label each other as “extremists” or “radicals.” They become completely blind to any redeeming social value in the ideas or principles of their political opponents. They spend enormous time and energy on undermining each other instead of attending to the myriad vital issues involved in the governance of a massive and complex country.
Winston Churchill said, “Democracy is the worst form of government, except for all the others that have been tried.”4 The current toxic cloud of intense “hyperpartisanship” is emblematic of the dark Machiavellian side of democracy. But those who lament the current distorted version of democracy should contemplate living in a dictatorship or totalitarian regime, where a despot would execute any dissenter or invade and destroy an adjacent country at a whim.
Churchill made that statement in 1947. The internet, social media, and smartphones were science fiction back then. Those technological advances have added fuel to the political process and significantly stoked the flames of hyperpartisanship. It’s now democracy on steroids, where freedom of expression goes to extremes, highlighting the warts and pitfalls of the democratic system. Political rivals can now communicate their ferocious disagreements to millions of their disciples instantaneously, triggering immediate rebuttals and counterattacks by their adversaries. This “virtual guerilla warfare” is mentally and emotionally exhausting to all involved, especially to the subset of neutral bystanders who are unaffiliated with either political party, which, due to the “religification” of politics, have become like secular religions.5 Chronic, unremitting, inescapable stress is a sure pathway for anxiety, depression, posttraumatic stress disorder, and even brain atrophy.
Optimists may point out that the United States has weathered and emerged stronger from many serious traumas, including the Civil War (with its lethal divisiveness), World War I, the deadly 1918 influenza pandemic, the Great Depression, Pearl Harbor, World War II, the Cold War, the Vietnam War, the Watergate political scandal, the 9/11 terrorist attacks, the banking collapse and recession, and most recently the COVID-19 pandemic, which brought society to a standstill and induced so much anxiety and uncertainty.
On the other hand, pessimists would insist those sequential crises left indelible scars that cumulatively altered the mindset of political rivals, predisposing them to extreme views of each other. Alienation inevitably leads to fanaticism. It’s perplexing but fascinating how the fierce bidirectional missives of weaponized ideas can be as virulent and destructive as a traditional physical war. Perhaps in this era, the pen is mightier than the sword after all.
Continue to: From a psychiatric perspective...
From a psychiatric perspective, the intransigent groupthink of political partisanship eerily resembles folie en masse, a psychiatric syndrome for which there is no established treatment. It has become a serious threat to our modern democracy. So I decided to ask the “know-it-all” artificial intelligence ChatGPT, whom I previously had “invited” to write a “guest editorial” about myths surrounding psychiatry,6 to answer 3 burning questions:
1. Is there toxic hyperpartisanship in the USA today? (Box 1)
Box 1
Yes, there is toxic hyperpartisanship in the United States today. Political polarization has been on the rise for several decades, and in recent years, it has become increasingly toxic and divisive. This toxic hyperpartisanship has contributed to a breakdown in civil discourse and a lack of cooperation and compromise in government.
The toxic hyperpartisanship is evident in many aspects of American society, including politics, media, and social media. Political leaders often engage in divisive rhetoric and focus on winning at all costs, rather than working towards solutions that benefit the country as a whole. Media outlets often present news in a partisan manner, further fueling political polarization. Social media platforms have also played a role in exacerbating toxic hyperpartisanship by allowing the spread of misinformation and creating echo chambers where people are only exposed to like-minded viewpoints.
The consequences of toxic hyperpartisanship are significant, as it can hinder progress on important issues and erode trust in institutions and government. It also makes it difficult for people to engage in productive dialogue and find common ground, leading to a lack of cooperation and compromise.
It is important for individuals to be aware of the impact of toxic hyperpartisanship and work towards finding ways to bridge the political divide and engage in constructive dialogue.
2. How can severe hyperpartisanship be corrected? (Supplemental Box 1)
Supplemental Box 1
Severe hyperpartisanship, characterized by intense and entrenched divisions between political parties, can be a challenging issue to address, but there are several steps that can be taken to work towards correcting it. Here are some potential approaches:
1. Promote civil discourse: Encourage respectful and constructive conversations between individuals with differing political views. This can be achieved through education programs, media campaigns, and initiatives to foster open dialogue.
2. Electoral reforms: Consider implementing electoral reforms that can reduce the influence of extreme partisanship. For example, ranked-choice voting or nonpartisan primaries may encourage candidates to appeal to a broader base of voters rather than just their party’s base.
3. Campaign finance reform: Limit the influence of money in politics, as it can exacerbate hyperpartisanship by allowing wealthy donors to have undue influence over candidates and parties.
4. Independent redistricting: Ensure that electoral district boundaries are drawn in a fair and nonpartisan manner. Gerrymandering, the manipulation of district lines to favor one party, can contribute to hyperpartisanship by creating “safe” districts where extreme candidates are more likely to be elected.
5. Promote media literacy: Encourage media literacy education to help citizens critically evaluate information sources and avoid echo chambers. A well-informed electorate is less susceptible to extreme partisanship.
6. Encourage bipartisan collaboration: Highlight and support instances of successful bipartisan collaboration. Elected officials who work across the aisle can serve as positive examples and encourage others to follow suit.
7. Address economic inequality: Tackling economic disparities can alleviate some of the underlying factors that contribute to polarization. When people feel economically secure, they may be more willing to seek common ground.
8. Civics education: Improve civics education in schools to foster a deeper understanding of democratic values, the political process, and the importance of civic engagement.
9. Leadership example: Encourage political leaders to model cooperation and compromise rather than relying on divisive rhetoric. Voters often take cues from their leaders’ behavior.
10. Promote third parties: Support and encourage the emergence of viable thirdparty candidates. A more diverse political landscape can provide alternatives to extreme partisanship.
11. Focus on common ground: Identify and prioritize issues where there is potential for bipartisan consensus and progress. Building success on these issues can create momentum for further cooperation.
12. Encourage grassroots activism: Support grassroots movements that seek to bridge divides and foster understanding between individuals and communities with different political perspectives.
It’s essential to recognize that addressing severe hyperpartisanship is a complex and long-term process that requires collective effort from citizens, political leaders, educators, and institutions. It won’t be achieved overnight, but through sustained and committed actions, progress can be made toward a more collaborative and less divisive political climate.
3. What can cause the collapse of a democracy? (Supplemental Box 2).
Supplemental Box 2
The collapse of a democracy can be a complex and multifaceted process, influenced by various factors and circumstances. Some of the common causes that can lead to the erosion or breakdown of a democratic system include:
1. Authoritarianism and power concentration: When leaders or institutions become increasingly authoritarian, centralizing power and weakening checks and balances, it can undermine democratic principles.
2. Corruption and lack of accountability: Rampant corruption among political leaders and institutions can erode public trust in the democratic system, leading to disillusionment and disengagement.
3. Economic instability: Prolonged economic crises or severe inequality can lead to social unrest, increasing the appeal of populist or extremist movements that may challenge democratic norms.
4. Weakening of rule of law: If the rule of law is weakened, and there is a lack of respect for judicial independence and constitutional principles, democratic institutions can become vulnerable to manipulation.
5. Erosion of civil liberties: Suppression of freedom of speech, media, assembly, and association can limit citizens’ ability to express their opinions and participate in the democratic process.
6. Polarization and divisive politics: Extreme political polarization and a breakdown of civil discourse can hinder cooperation and compromise essential for a functioning democracy.
7. External interference: Foreign intervention, propaganda, or cyberattacks can influence electoral processes and undermine democratic institutions.
8. Rise of populism and nationalism: Populist movements that challenge democratic norms, demonize minorities, or advocate for a strongman leadership can pose a threat to democracy.
9. Demographic and social shifts: Demographic changes and social tensions can exacerbate political divisions and weaken the fabric of democratic societies.
10. Lack of civic education and participation: A lack of civic education and low voter turnout can lead to reduced civic engagement and undermine the democratic process.
It is crucial to understand that no democracy is immune to these challenges, and the strength of a democratic system depends on the vigilance and engagement of its citizens, the integrity of its institutions, and the commitment to upholding democratic values. Safeguarding and strengthening democracy requires ongoing efforts to address these issues and protect the principles that underpin democratic governance.
Judge for yourself, but I believe the ChatGPT responses were spot-on.
1. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. 2023;180(8):548-564.
2. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892-909.
3. Zhang ZZ, Moeckel C, Mustafa M, et al. The association of epigenetic age acceleration and depressive and anxiety symptom severity among children recently exposed to substantiated maltreatment. J Psychiatr Res. 2023;165:7-13.
4. International Churchill Society. The worst form of government. Accessed August 8, 2023. https://winstonchurchill.org/resources/quotes/the-worst-form-of-government/
5. Nasrallah HA. From ideology to articles of faith: the ‘religification’ of political beliefs. Current Psychiatry. 2021;20(7):4-5,19.
6. Nasrallah HA. A ‘guest editorial’ … generated by ChatGPT? Current Psychiatry. 2023;22(4):22:6-7.
As psychiatrists know, many of our severely traumatized adult patients were victims of abuse during childhood. We routinely ask every new patient about physical, emotional, or sexual abuse when they were growing up because of the well-established, serious neurobiological and mental repercussions.1,2
Perhaps one of the worst experiences for a child is to witness bitterly adversarial parents (their vital role models) who argue viciously, despise each other, and hurl insults (and even punches) at each other. Such a chronically and emotionally traumatic upbringing can haunt kids well into adulthood, disrupting their hypothalamic-pituitary-adrenal axis and triggering anxiety, depression, and even psychosis due to epigenetic changes that ultimately lead to abnormal brain development.3
It often feels that the governance of our country, or the national “political family,” is seriously fractured like a hopelessly dysfunctional family. Could that be negatively impacting the mental health of the citizenry? Having 2 antagonistic political parties expressing visceral hatred and undisguised contempt for each other 24/7 (thanks to the enabling era of cable TV, the internet, and social media) has transformed each party’s fanatic followers from fellow citizens to ideological combatants. In this poisonous societal zeitgeist of bidirectional acrimony and mutual detestation, the opposing parties and their “intellectual militias” label each other as “extremists” or “radicals.” They become completely blind to any redeeming social value in the ideas or principles of their political opponents. They spend enormous time and energy on undermining each other instead of attending to the myriad vital issues involved in the governance of a massive and complex country.
Winston Churchill said, “Democracy is the worst form of government, except for all the others that have been tried.”4 The current toxic cloud of intense “hyperpartisanship” is emblematic of the dark Machiavellian side of democracy. But those who lament the current distorted version of democracy should contemplate living in a dictatorship or totalitarian regime, where a despot would execute any dissenter or invade and destroy an adjacent country at a whim.
Churchill made that statement in 1947. The internet, social media, and smartphones were science fiction back then. Those technological advances have added fuel to the political process and significantly stoked the flames of hyperpartisanship. It’s now democracy on steroids, where freedom of expression goes to extremes, highlighting the warts and pitfalls of the democratic system. Political rivals can now communicate their ferocious disagreements to millions of their disciples instantaneously, triggering immediate rebuttals and counterattacks by their adversaries. This “virtual guerilla warfare” is mentally and emotionally exhausting to all involved, especially to the subset of neutral bystanders who are unaffiliated with either political party, which, due to the “religification” of politics, have become like secular religions.5 Chronic, unremitting, inescapable stress is a sure pathway for anxiety, depression, posttraumatic stress disorder, and even brain atrophy.
Optimists may point out that the United States has weathered and emerged stronger from many serious traumas, including the Civil War (with its lethal divisiveness), World War I, the deadly 1918 influenza pandemic, the Great Depression, Pearl Harbor, World War II, the Cold War, the Vietnam War, the Watergate political scandal, the 9/11 terrorist attacks, the banking collapse and recession, and most recently the COVID-19 pandemic, which brought society to a standstill and induced so much anxiety and uncertainty.
On the other hand, pessimists would insist those sequential crises left indelible scars that cumulatively altered the mindset of political rivals, predisposing them to extreme views of each other. Alienation inevitably leads to fanaticism. It’s perplexing but fascinating how the fierce bidirectional missives of weaponized ideas can be as virulent and destructive as a traditional physical war. Perhaps in this era, the pen is mightier than the sword after all.
Continue to: From a psychiatric perspective...
From a psychiatric perspective, the intransigent groupthink of political partisanship eerily resembles folie en masse, a psychiatric syndrome for which there is no established treatment. It has become a serious threat to our modern democracy. So I decided to ask the “know-it-all” artificial intelligence ChatGPT, whom I previously had “invited” to write a “guest editorial” about myths surrounding psychiatry,6 to answer 3 burning questions:
1. Is there toxic hyperpartisanship in the USA today? (Box 1)
Box 1
Yes, there is toxic hyperpartisanship in the United States today. Political polarization has been on the rise for several decades, and in recent years, it has become increasingly toxic and divisive. This toxic hyperpartisanship has contributed to a breakdown in civil discourse and a lack of cooperation and compromise in government.
The toxic hyperpartisanship is evident in many aspects of American society, including politics, media, and social media. Political leaders often engage in divisive rhetoric and focus on winning at all costs, rather than working towards solutions that benefit the country as a whole. Media outlets often present news in a partisan manner, further fueling political polarization. Social media platforms have also played a role in exacerbating toxic hyperpartisanship by allowing the spread of misinformation and creating echo chambers where people are only exposed to like-minded viewpoints.
The consequences of toxic hyperpartisanship are significant, as it can hinder progress on important issues and erode trust in institutions and government. It also makes it difficult for people to engage in productive dialogue and find common ground, leading to a lack of cooperation and compromise.
It is important for individuals to be aware of the impact of toxic hyperpartisanship and work towards finding ways to bridge the political divide and engage in constructive dialogue.
2. How can severe hyperpartisanship be corrected? (Supplemental Box 1)
Supplemental Box 1
Severe hyperpartisanship, characterized by intense and entrenched divisions between political parties, can be a challenging issue to address, but there are several steps that can be taken to work towards correcting it. Here are some potential approaches:
1. Promote civil discourse: Encourage respectful and constructive conversations between individuals with differing political views. This can be achieved through education programs, media campaigns, and initiatives to foster open dialogue.
2. Electoral reforms: Consider implementing electoral reforms that can reduce the influence of extreme partisanship. For example, ranked-choice voting or nonpartisan primaries may encourage candidates to appeal to a broader base of voters rather than just their party’s base.
3. Campaign finance reform: Limit the influence of money in politics, as it can exacerbate hyperpartisanship by allowing wealthy donors to have undue influence over candidates and parties.
4. Independent redistricting: Ensure that electoral district boundaries are drawn in a fair and nonpartisan manner. Gerrymandering, the manipulation of district lines to favor one party, can contribute to hyperpartisanship by creating “safe” districts where extreme candidates are more likely to be elected.
5. Promote media literacy: Encourage media literacy education to help citizens critically evaluate information sources and avoid echo chambers. A well-informed electorate is less susceptible to extreme partisanship.
6. Encourage bipartisan collaboration: Highlight and support instances of successful bipartisan collaboration. Elected officials who work across the aisle can serve as positive examples and encourage others to follow suit.
7. Address economic inequality: Tackling economic disparities can alleviate some of the underlying factors that contribute to polarization. When people feel economically secure, they may be more willing to seek common ground.
8. Civics education: Improve civics education in schools to foster a deeper understanding of democratic values, the political process, and the importance of civic engagement.
9. Leadership example: Encourage political leaders to model cooperation and compromise rather than relying on divisive rhetoric. Voters often take cues from their leaders’ behavior.
10. Promote third parties: Support and encourage the emergence of viable thirdparty candidates. A more diverse political landscape can provide alternatives to extreme partisanship.
11. Focus on common ground: Identify and prioritize issues where there is potential for bipartisan consensus and progress. Building success on these issues can create momentum for further cooperation.
12. Encourage grassroots activism: Support grassroots movements that seek to bridge divides and foster understanding between individuals and communities with different political perspectives.
It’s essential to recognize that addressing severe hyperpartisanship is a complex and long-term process that requires collective effort from citizens, political leaders, educators, and institutions. It won’t be achieved overnight, but through sustained and committed actions, progress can be made toward a more collaborative and less divisive political climate.
3. What can cause the collapse of a democracy? (Supplemental Box 2).
Supplemental Box 2
The collapse of a democracy can be a complex and multifaceted process, influenced by various factors and circumstances. Some of the common causes that can lead to the erosion or breakdown of a democratic system include:
1. Authoritarianism and power concentration: When leaders or institutions become increasingly authoritarian, centralizing power and weakening checks and balances, it can undermine democratic principles.
2. Corruption and lack of accountability: Rampant corruption among political leaders and institutions can erode public trust in the democratic system, leading to disillusionment and disengagement.
3. Economic instability: Prolonged economic crises or severe inequality can lead to social unrest, increasing the appeal of populist or extremist movements that may challenge democratic norms.
4. Weakening of rule of law: If the rule of law is weakened, and there is a lack of respect for judicial independence and constitutional principles, democratic institutions can become vulnerable to manipulation.
5. Erosion of civil liberties: Suppression of freedom of speech, media, assembly, and association can limit citizens’ ability to express their opinions and participate in the democratic process.
6. Polarization and divisive politics: Extreme political polarization and a breakdown of civil discourse can hinder cooperation and compromise essential for a functioning democracy.
7. External interference: Foreign intervention, propaganda, or cyberattacks can influence electoral processes and undermine democratic institutions.
8. Rise of populism and nationalism: Populist movements that challenge democratic norms, demonize minorities, or advocate for a strongman leadership can pose a threat to democracy.
9. Demographic and social shifts: Demographic changes and social tensions can exacerbate political divisions and weaken the fabric of democratic societies.
10. Lack of civic education and participation: A lack of civic education and low voter turnout can lead to reduced civic engagement and undermine the democratic process.
It is crucial to understand that no democracy is immune to these challenges, and the strength of a democratic system depends on the vigilance and engagement of its citizens, the integrity of its institutions, and the commitment to upholding democratic values. Safeguarding and strengthening democracy requires ongoing efforts to address these issues and protect the principles that underpin democratic governance.
Judge for yourself, but I believe the ChatGPT responses were spot-on.
As psychiatrists know, many of our severely traumatized adult patients were victims of abuse during childhood. We routinely ask every new patient about physical, emotional, or sexual abuse when they were growing up because of the well-established, serious neurobiological and mental repercussions.1,2
Perhaps one of the worst experiences for a child is to witness bitterly adversarial parents (their vital role models) who argue viciously, despise each other, and hurl insults (and even punches) at each other. Such a chronically and emotionally traumatic upbringing can haunt kids well into adulthood, disrupting their hypothalamic-pituitary-adrenal axis and triggering anxiety, depression, and even psychosis due to epigenetic changes that ultimately lead to abnormal brain development.3
It often feels that the governance of our country, or the national “political family,” is seriously fractured like a hopelessly dysfunctional family. Could that be negatively impacting the mental health of the citizenry? Having 2 antagonistic political parties expressing visceral hatred and undisguised contempt for each other 24/7 (thanks to the enabling era of cable TV, the internet, and social media) has transformed each party’s fanatic followers from fellow citizens to ideological combatants. In this poisonous societal zeitgeist of bidirectional acrimony and mutual detestation, the opposing parties and their “intellectual militias” label each other as “extremists” or “radicals.” They become completely blind to any redeeming social value in the ideas or principles of their political opponents. They spend enormous time and energy on undermining each other instead of attending to the myriad vital issues involved in the governance of a massive and complex country.
Winston Churchill said, “Democracy is the worst form of government, except for all the others that have been tried.”4 The current toxic cloud of intense “hyperpartisanship” is emblematic of the dark Machiavellian side of democracy. But those who lament the current distorted version of democracy should contemplate living in a dictatorship or totalitarian regime, where a despot would execute any dissenter or invade and destroy an adjacent country at a whim.
Churchill made that statement in 1947. The internet, social media, and smartphones were science fiction back then. Those technological advances have added fuel to the political process and significantly stoked the flames of hyperpartisanship. It’s now democracy on steroids, where freedom of expression goes to extremes, highlighting the warts and pitfalls of the democratic system. Political rivals can now communicate their ferocious disagreements to millions of their disciples instantaneously, triggering immediate rebuttals and counterattacks by their adversaries. This “virtual guerilla warfare” is mentally and emotionally exhausting to all involved, especially to the subset of neutral bystanders who are unaffiliated with either political party, which, due to the “religification” of politics, have become like secular religions.5 Chronic, unremitting, inescapable stress is a sure pathway for anxiety, depression, posttraumatic stress disorder, and even brain atrophy.
Optimists may point out that the United States has weathered and emerged stronger from many serious traumas, including the Civil War (with its lethal divisiveness), World War I, the deadly 1918 influenza pandemic, the Great Depression, Pearl Harbor, World War II, the Cold War, the Vietnam War, the Watergate political scandal, the 9/11 terrorist attacks, the banking collapse and recession, and most recently the COVID-19 pandemic, which brought society to a standstill and induced so much anxiety and uncertainty.
On the other hand, pessimists would insist those sequential crises left indelible scars that cumulatively altered the mindset of political rivals, predisposing them to extreme views of each other. Alienation inevitably leads to fanaticism. It’s perplexing but fascinating how the fierce bidirectional missives of weaponized ideas can be as virulent and destructive as a traditional physical war. Perhaps in this era, the pen is mightier than the sword after all.
Continue to: From a psychiatric perspective...
From a psychiatric perspective, the intransigent groupthink of political partisanship eerily resembles folie en masse, a psychiatric syndrome for which there is no established treatment. It has become a serious threat to our modern democracy. So I decided to ask the “know-it-all” artificial intelligence ChatGPT, whom I previously had “invited” to write a “guest editorial” about myths surrounding psychiatry,6 to answer 3 burning questions:
1. Is there toxic hyperpartisanship in the USA today? (Box 1)
Box 1
Yes, there is toxic hyperpartisanship in the United States today. Political polarization has been on the rise for several decades, and in recent years, it has become increasingly toxic and divisive. This toxic hyperpartisanship has contributed to a breakdown in civil discourse and a lack of cooperation and compromise in government.
The toxic hyperpartisanship is evident in many aspects of American society, including politics, media, and social media. Political leaders often engage in divisive rhetoric and focus on winning at all costs, rather than working towards solutions that benefit the country as a whole. Media outlets often present news in a partisan manner, further fueling political polarization. Social media platforms have also played a role in exacerbating toxic hyperpartisanship by allowing the spread of misinformation and creating echo chambers where people are only exposed to like-minded viewpoints.
The consequences of toxic hyperpartisanship are significant, as it can hinder progress on important issues and erode trust in institutions and government. It also makes it difficult for people to engage in productive dialogue and find common ground, leading to a lack of cooperation and compromise.
It is important for individuals to be aware of the impact of toxic hyperpartisanship and work towards finding ways to bridge the political divide and engage in constructive dialogue.
2. How can severe hyperpartisanship be corrected? (Supplemental Box 1)
Supplemental Box 1
Severe hyperpartisanship, characterized by intense and entrenched divisions between political parties, can be a challenging issue to address, but there are several steps that can be taken to work towards correcting it. Here are some potential approaches:
1. Promote civil discourse: Encourage respectful and constructive conversations between individuals with differing political views. This can be achieved through education programs, media campaigns, and initiatives to foster open dialogue.
2. Electoral reforms: Consider implementing electoral reforms that can reduce the influence of extreme partisanship. For example, ranked-choice voting or nonpartisan primaries may encourage candidates to appeal to a broader base of voters rather than just their party’s base.
3. Campaign finance reform: Limit the influence of money in politics, as it can exacerbate hyperpartisanship by allowing wealthy donors to have undue influence over candidates and parties.
4. Independent redistricting: Ensure that electoral district boundaries are drawn in a fair and nonpartisan manner. Gerrymandering, the manipulation of district lines to favor one party, can contribute to hyperpartisanship by creating “safe” districts where extreme candidates are more likely to be elected.
5. Promote media literacy: Encourage media literacy education to help citizens critically evaluate information sources and avoid echo chambers. A well-informed electorate is less susceptible to extreme partisanship.
6. Encourage bipartisan collaboration: Highlight and support instances of successful bipartisan collaboration. Elected officials who work across the aisle can serve as positive examples and encourage others to follow suit.
7. Address economic inequality: Tackling economic disparities can alleviate some of the underlying factors that contribute to polarization. When people feel economically secure, they may be more willing to seek common ground.
8. Civics education: Improve civics education in schools to foster a deeper understanding of democratic values, the political process, and the importance of civic engagement.
9. Leadership example: Encourage political leaders to model cooperation and compromise rather than relying on divisive rhetoric. Voters often take cues from their leaders’ behavior.
10. Promote third parties: Support and encourage the emergence of viable thirdparty candidates. A more diverse political landscape can provide alternatives to extreme partisanship.
11. Focus on common ground: Identify and prioritize issues where there is potential for bipartisan consensus and progress. Building success on these issues can create momentum for further cooperation.
12. Encourage grassroots activism: Support grassroots movements that seek to bridge divides and foster understanding between individuals and communities with different political perspectives.
It’s essential to recognize that addressing severe hyperpartisanship is a complex and long-term process that requires collective effort from citizens, political leaders, educators, and institutions. It won’t be achieved overnight, but through sustained and committed actions, progress can be made toward a more collaborative and less divisive political climate.
3. What can cause the collapse of a democracy? (Supplemental Box 2).
Supplemental Box 2
The collapse of a democracy can be a complex and multifaceted process, influenced by various factors and circumstances. Some of the common causes that can lead to the erosion or breakdown of a democratic system include:
1. Authoritarianism and power concentration: When leaders or institutions become increasingly authoritarian, centralizing power and weakening checks and balances, it can undermine democratic principles.
2. Corruption and lack of accountability: Rampant corruption among political leaders and institutions can erode public trust in the democratic system, leading to disillusionment and disengagement.
3. Economic instability: Prolonged economic crises or severe inequality can lead to social unrest, increasing the appeal of populist or extremist movements that may challenge democratic norms.
4. Weakening of rule of law: If the rule of law is weakened, and there is a lack of respect for judicial independence and constitutional principles, democratic institutions can become vulnerable to manipulation.
5. Erosion of civil liberties: Suppression of freedom of speech, media, assembly, and association can limit citizens’ ability to express their opinions and participate in the democratic process.
6. Polarization and divisive politics: Extreme political polarization and a breakdown of civil discourse can hinder cooperation and compromise essential for a functioning democracy.
7. External interference: Foreign intervention, propaganda, or cyberattacks can influence electoral processes and undermine democratic institutions.
8. Rise of populism and nationalism: Populist movements that challenge democratic norms, demonize minorities, or advocate for a strongman leadership can pose a threat to democracy.
9. Demographic and social shifts: Demographic changes and social tensions can exacerbate political divisions and weaken the fabric of democratic societies.
10. Lack of civic education and participation: A lack of civic education and low voter turnout can lead to reduced civic engagement and undermine the democratic process.
It is crucial to understand that no democracy is immune to these challenges, and the strength of a democratic system depends on the vigilance and engagement of its citizens, the integrity of its institutions, and the commitment to upholding democratic values. Safeguarding and strengthening democracy requires ongoing efforts to address these issues and protect the principles that underpin democratic governance.
Judge for yourself, but I believe the ChatGPT responses were spot-on.
1. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. 2023;180(8):548-564.
2. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892-909.
3. Zhang ZZ, Moeckel C, Mustafa M, et al. The association of epigenetic age acceleration and depressive and anxiety symptom severity among children recently exposed to substantiated maltreatment. J Psychiatr Res. 2023;165:7-13.
4. International Churchill Society. The worst form of government. Accessed August 8, 2023. https://winstonchurchill.org/resources/quotes/the-worst-form-of-government/
5. Nasrallah HA. From ideology to articles of faith: the ‘religification’ of political beliefs. Current Psychiatry. 2021;20(7):4-5,19.
6. Nasrallah HA. A ‘guest editorial’ … generated by ChatGPT? Current Psychiatry. 2023;22(4):22:6-7.
1. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. 2023;180(8):548-564.
2. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892-909.
3. Zhang ZZ, Moeckel C, Mustafa M, et al. The association of epigenetic age acceleration and depressive and anxiety symptom severity among children recently exposed to substantiated maltreatment. J Psychiatr Res. 2023;165:7-13.
4. International Churchill Society. The worst form of government. Accessed August 8, 2023. https://winstonchurchill.org/resources/quotes/the-worst-form-of-government/
5. Nasrallah HA. From ideology to articles of faith: the ‘religification’ of political beliefs. Current Psychiatry. 2021;20(7):4-5,19.
6. Nasrallah HA. A ‘guest editorial’ … generated by ChatGPT? Current Psychiatry. 2023;22(4):22:6-7.
More on prescribing controlled substances
I was disheartened with the June 2023 issue of
The benzodiazepine pharmacology discussed in this article is interesting, but it would be helpful if it had been integrated within a much more extensive discussion of careful prescribing practices. In 2020, the FDA updated the boxed warning to alert prescribers to the serious risks of abuse, addiction, physical dependence, and withdrawal reactions associated with benzodiazepines.2 I would hope that an article on benzodiazepines would provide more discussion and guidance surrounding these important issues.
The June 2023 issue also included “High-dose stimulants for adult ADHD” (p. 34-39, doi:10.12788/cp.0366). This article provided esoteric advice on managing stimulant therapy in the setting of Roux-en-Y gastric bypass surgery, yet I would regard stimulant misuse as a far more common and pressing issue.3,4 The recent Drug Enforcement Administration investigation of telehealth stimulant prescribing is a notable example of this problem.5
The patient discussed in this article was receiving large doses of stimulants for a purported case of refractory attention-deficit/hyperactivity disorder (ADHD). The article provided a sparse differential diagnosis for the patient’s intractable symptoms. While rapid metabolism may be an explanation, I would also like to know how the authors ruled out physiological dependence and/or addiction to a controlled substance. How was misuse excluded? Was urine drug testing (UDS) performed? UDS is highly irregular among prescribers,6 which suggests that practices for detecting covert substance abuse and stimulant misuse are inadequate. Wouldn’t such investigations be fundamental to ethical stimulant prescribing?
Jeff Sanders, MD, PhD
Atlanta, Georgia
References
1. Centers for Disease Control and Prevention. Trends in nonfatal and fatal overdoses involving benzodiazepines—38 states and the District of Columbia, 2019-2020. Accessed August 9, 2023. https://www.cdc.gov/mmwr/volumes/70/wr/mm7034a2.htm
2. US Food & Drug Administration. FDA requiring boxed warning updated to improve safe use of benzodiazepine drug class. Accessed August 14, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requiring-boxed-warning-updated-improve-safe-use-benzodiazepine-drug-class
3. McCabe SE, Schulenberg JE, Wilens TE, et al. Prescription stimulant medical and nonmedical use among US secondary school students, 2005 to 2020. JAMA Netw Open. 2023;6(4):e238707. doi:10.1001/jamanetworkopen.2023.8707
4. US Food & Drug Administration. FDA updating warnings to improve safe use of prescription stimulants used to treat ADHD and other conditions. Accessed August 14, 2023. https://www.fda.gov/safety/medical-product-safety-information/fda-updating-warnings-improve-safe-use-prescription-stimulants-used-treat-adhd-and-other-conditions
5. Vaidya A. Report: telehealth company’s prescribing practices come under DEA scrutiny. September 16, 2022. Accessed August 9, 2023. https://mhealthintelligence.com/news/report-telehealth-company-dones-prescribing-practices-come-under-dea-scrutiny
6. Zionts A. Some ADHD patients are drug-tested often, while others are never asked. Kaiser Health News. March 25, 2023. Accessed August 9, 2023. https://www.nbcnews.com/news/amp/rcna76330
Continue to: Drs. Stimpfl and Strawn respond
Drs. Stimpfl and Strawn respond
We thank Dr. Sanders for highlighting the need for clinical equipoise in considering the risks and benefits of medications—something that is true for benzodiazepines, antipsychotics, antidepressants, and in fact all medications. He reminds us that the risks of misuse, dependence, and withdrawal associated with benzodiazepines led to a boxed warning in September 2020 and highlights recent trends of fatal and nonfatal benzodiazepine overdose, especially when combined with opiates.
Our article, which aimed to educate clinicians on benzodiazepine pharmacology and patient-specific factors influencing benzodiazepine selection and dosing, did not focus significantly on the risks associated with benzodiazepines. We do encourage careful and individualized benzodiazepine prescribing. However, we wish to remind our colleagues that benzodiazepines, while associated with risks, continue to have utility in acute and periprocedural settings, and remain an important treatment option for patients with panic disorder, generalized anxiety disorder (especially while waiting for other medications to take effect), catatonia, seizure disorders, and alcohol withdrawal.
We agree that patient-specific risk assessment is essential, as some patients benefit from benzodiazepines despite the risks. However, we also acknowledge that some individuals are at higher risk for adverse outcomes, including those with concurrent opiate use or who are prescribed other sedative-hypnotics; older adults and those with neurocognitive disorders; and patients susceptible to respiratory depression due to other medical reasons (eg, myasthenia gravis, sleep apnea, and chronic obstructive pulmonary disease). Further, we agree that benzodiazepine use during pregnancy is generally not advised due to the risks of neonatal hypotonia and neonatal withdrawal syndrome1 as well as a possible risk of cleft palate that has been reported in some studies.2 Finally, paradoxical reactions may be more common at the extremes of age and in patients with intellectual disability or personality disorders.3,4
Patient characteristics that have been associated with a higher risk of benzodiazepine use disorder include lower education/income, unemployment, having another substance use disorder, and severe psychopathology.5 In some studies, using benzodiazepines for prolonged periods at high doses as well as using those with a rapid onset of action was associated with an increased risk of benzodiazepine use disorder.5-7
Ultimately, we concur with Dr. Sanders on the perils of the “irresponsible use” of medication and emphasize the need for discernment when choosing treatments to avoid rashly discarding an effective remedy while attempting to mitigate all conceivable risks.
Julia Stimpfl, MD
Jeffrey R. Strawn, MD
Cincinnati, Ohio
References
1. McElhatton PR. The effects of benzodiazepine use during pregnancy and lactation. Reprod Toxicol. 1994;8(6):461-475. doi:10.1016/0890-6238(94)90029-9
2. Enato E, Moretti M, Koren G. The fetal safety of benzodiazepines: an updated meta-analysis. J Obstet Gynaecol Can. 2011;33(1):46-48. doi:10.1016/S1701-2163(16)34772-7 Erratum in: J Obstet Gynaecol Can. 2011;33(4):319.
3. Hakimi Y, Petitpain N, Pinzani V, et al. Paradoxical adverse drug reactions: descriptive analysis of French reports. Eur J Clin Pharmacol. 2020;76(8):1169-1174. doi:10.1007/s00228-020-02892-2
4. Paton C. Benzodiazepines and disinhibition: a review. Psychiatric Bulletin. 2002;26(12):460-462. doi:10.1192/pb.26.12.460
5. Fride Tvete I, Bjørner T, Skomedal T. Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway. Scand J Prim Health Care. 2015;33(4):252-259. doi:10.3109/02813432.2015.1117282
6. Griffiths RR, Johnson MW. Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds. J Clin Psychiatry. 2005;66 Suppl 9:31-41.
7. Kan CC, Hilberink SR, Breteler MH. Determination of the main risk factors for benzodiazepine dependence using a multivariate and multidimensional approach. Compr Psychiatry. 2004;45(2):88-94. doi:10.1016/j.comppsych.2003.12.007
Continue to: Drs. Sarma and Grady respond
Drs. Sarma and Grady respond
Dr. Sanders’ letter highlights the potential caveats associated with prescribing controlled substances. We agree that our short case summary includes numerous interesting elements, each of which would be worthy of further exploration and discussion. Our choice was to highlight the patient history of bariatric surgery and use this as a springboard into a review of stimulants, including the newest formulations for ADHD. For more than 1 year, many generic stimulants have been in short supply, and patients and clinicians have been seeking other therapeutic options. Given this background and with newer, branded stimulant use becoming more commonplace, we believe our article was useful and timely.
Our original intent had been to include an example of a controlled substance agreement. Regrettably, there was simply not enough space for this document or the additional discussion that its inclusion would deem necessary. Nevertheless, had the May 2023 FDA requirement for manufacturers to update the labeling of prescription stimulants1 to clarify misuse and abuse been published before our article’s final revision, we would have mentioned it and provided the appropriate link.
Subbu J. Sarma, MD, FAPA
Kansas City, Missouri
Sarah E. Grady, PharmD, BCPS, BCPP
Des Moines, Iowa
References
1. US Food & Drug Administration. FDA requires updates to clarify labeling of prescription stimulants used to treat ADHD and other conditions. Accessed August 9, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requires-updates-clarify-labeling-prescription-stimulants-used-treat-adhd-and-other-conditions
I was disheartened with the June 2023 issue of
The benzodiazepine pharmacology discussed in this article is interesting, but it would be helpful if it had been integrated within a much more extensive discussion of careful prescribing practices. In 2020, the FDA updated the boxed warning to alert prescribers to the serious risks of abuse, addiction, physical dependence, and withdrawal reactions associated with benzodiazepines.2 I would hope that an article on benzodiazepines would provide more discussion and guidance surrounding these important issues.
The June 2023 issue also included “High-dose stimulants for adult ADHD” (p. 34-39, doi:10.12788/cp.0366). This article provided esoteric advice on managing stimulant therapy in the setting of Roux-en-Y gastric bypass surgery, yet I would regard stimulant misuse as a far more common and pressing issue.3,4 The recent Drug Enforcement Administration investigation of telehealth stimulant prescribing is a notable example of this problem.5
The patient discussed in this article was receiving large doses of stimulants for a purported case of refractory attention-deficit/hyperactivity disorder (ADHD). The article provided a sparse differential diagnosis for the patient’s intractable symptoms. While rapid metabolism may be an explanation, I would also like to know how the authors ruled out physiological dependence and/or addiction to a controlled substance. How was misuse excluded? Was urine drug testing (UDS) performed? UDS is highly irregular among prescribers,6 which suggests that practices for detecting covert substance abuse and stimulant misuse are inadequate. Wouldn’t such investigations be fundamental to ethical stimulant prescribing?
Jeff Sanders, MD, PhD
Atlanta, Georgia
References
1. Centers for Disease Control and Prevention. Trends in nonfatal and fatal overdoses involving benzodiazepines—38 states and the District of Columbia, 2019-2020. Accessed August 9, 2023. https://www.cdc.gov/mmwr/volumes/70/wr/mm7034a2.htm
2. US Food & Drug Administration. FDA requiring boxed warning updated to improve safe use of benzodiazepine drug class. Accessed August 14, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requiring-boxed-warning-updated-improve-safe-use-benzodiazepine-drug-class
3. McCabe SE, Schulenberg JE, Wilens TE, et al. Prescription stimulant medical and nonmedical use among US secondary school students, 2005 to 2020. JAMA Netw Open. 2023;6(4):e238707. doi:10.1001/jamanetworkopen.2023.8707
4. US Food & Drug Administration. FDA updating warnings to improve safe use of prescription stimulants used to treat ADHD and other conditions. Accessed August 14, 2023. https://www.fda.gov/safety/medical-product-safety-information/fda-updating-warnings-improve-safe-use-prescription-stimulants-used-treat-adhd-and-other-conditions
5. Vaidya A. Report: telehealth company’s prescribing practices come under DEA scrutiny. September 16, 2022. Accessed August 9, 2023. https://mhealthintelligence.com/news/report-telehealth-company-dones-prescribing-practices-come-under-dea-scrutiny
6. Zionts A. Some ADHD patients are drug-tested often, while others are never asked. Kaiser Health News. March 25, 2023. Accessed August 9, 2023. https://www.nbcnews.com/news/amp/rcna76330
Continue to: Drs. Stimpfl and Strawn respond
Drs. Stimpfl and Strawn respond
We thank Dr. Sanders for highlighting the need for clinical equipoise in considering the risks and benefits of medications—something that is true for benzodiazepines, antipsychotics, antidepressants, and in fact all medications. He reminds us that the risks of misuse, dependence, and withdrawal associated with benzodiazepines led to a boxed warning in September 2020 and highlights recent trends of fatal and nonfatal benzodiazepine overdose, especially when combined with opiates.
Our article, which aimed to educate clinicians on benzodiazepine pharmacology and patient-specific factors influencing benzodiazepine selection and dosing, did not focus significantly on the risks associated with benzodiazepines. We do encourage careful and individualized benzodiazepine prescribing. However, we wish to remind our colleagues that benzodiazepines, while associated with risks, continue to have utility in acute and periprocedural settings, and remain an important treatment option for patients with panic disorder, generalized anxiety disorder (especially while waiting for other medications to take effect), catatonia, seizure disorders, and alcohol withdrawal.
We agree that patient-specific risk assessment is essential, as some patients benefit from benzodiazepines despite the risks. However, we also acknowledge that some individuals are at higher risk for adverse outcomes, including those with concurrent opiate use or who are prescribed other sedative-hypnotics; older adults and those with neurocognitive disorders; and patients susceptible to respiratory depression due to other medical reasons (eg, myasthenia gravis, sleep apnea, and chronic obstructive pulmonary disease). Further, we agree that benzodiazepine use during pregnancy is generally not advised due to the risks of neonatal hypotonia and neonatal withdrawal syndrome1 as well as a possible risk of cleft palate that has been reported in some studies.2 Finally, paradoxical reactions may be more common at the extremes of age and in patients with intellectual disability or personality disorders.3,4
Patient characteristics that have been associated with a higher risk of benzodiazepine use disorder include lower education/income, unemployment, having another substance use disorder, and severe psychopathology.5 In some studies, using benzodiazepines for prolonged periods at high doses as well as using those with a rapid onset of action was associated with an increased risk of benzodiazepine use disorder.5-7
Ultimately, we concur with Dr. Sanders on the perils of the “irresponsible use” of medication and emphasize the need for discernment when choosing treatments to avoid rashly discarding an effective remedy while attempting to mitigate all conceivable risks.
Julia Stimpfl, MD
Jeffrey R. Strawn, MD
Cincinnati, Ohio
References
1. McElhatton PR. The effects of benzodiazepine use during pregnancy and lactation. Reprod Toxicol. 1994;8(6):461-475. doi:10.1016/0890-6238(94)90029-9
2. Enato E, Moretti M, Koren G. The fetal safety of benzodiazepines: an updated meta-analysis. J Obstet Gynaecol Can. 2011;33(1):46-48. doi:10.1016/S1701-2163(16)34772-7 Erratum in: J Obstet Gynaecol Can. 2011;33(4):319.
3. Hakimi Y, Petitpain N, Pinzani V, et al. Paradoxical adverse drug reactions: descriptive analysis of French reports. Eur J Clin Pharmacol. 2020;76(8):1169-1174. doi:10.1007/s00228-020-02892-2
4. Paton C. Benzodiazepines and disinhibition: a review. Psychiatric Bulletin. 2002;26(12):460-462. doi:10.1192/pb.26.12.460
5. Fride Tvete I, Bjørner T, Skomedal T. Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway. Scand J Prim Health Care. 2015;33(4):252-259. doi:10.3109/02813432.2015.1117282
6. Griffiths RR, Johnson MW. Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds. J Clin Psychiatry. 2005;66 Suppl 9:31-41.
7. Kan CC, Hilberink SR, Breteler MH. Determination of the main risk factors for benzodiazepine dependence using a multivariate and multidimensional approach. Compr Psychiatry. 2004;45(2):88-94. doi:10.1016/j.comppsych.2003.12.007
Continue to: Drs. Sarma and Grady respond
Drs. Sarma and Grady respond
Dr. Sanders’ letter highlights the potential caveats associated with prescribing controlled substances. We agree that our short case summary includes numerous interesting elements, each of which would be worthy of further exploration and discussion. Our choice was to highlight the patient history of bariatric surgery and use this as a springboard into a review of stimulants, including the newest formulations for ADHD. For more than 1 year, many generic stimulants have been in short supply, and patients and clinicians have been seeking other therapeutic options. Given this background and with newer, branded stimulant use becoming more commonplace, we believe our article was useful and timely.
Our original intent had been to include an example of a controlled substance agreement. Regrettably, there was simply not enough space for this document or the additional discussion that its inclusion would deem necessary. Nevertheless, had the May 2023 FDA requirement for manufacturers to update the labeling of prescription stimulants1 to clarify misuse and abuse been published before our article’s final revision, we would have mentioned it and provided the appropriate link.
Subbu J. Sarma, MD, FAPA
Kansas City, Missouri
Sarah E. Grady, PharmD, BCPS, BCPP
Des Moines, Iowa
References
1. US Food & Drug Administration. FDA requires updates to clarify labeling of prescription stimulants used to treat ADHD and other conditions. Accessed August 9, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requires-updates-clarify-labeling-prescription-stimulants-used-treat-adhd-and-other-conditions
I was disheartened with the June 2023 issue of
The benzodiazepine pharmacology discussed in this article is interesting, but it would be helpful if it had been integrated within a much more extensive discussion of careful prescribing practices. In 2020, the FDA updated the boxed warning to alert prescribers to the serious risks of abuse, addiction, physical dependence, and withdrawal reactions associated with benzodiazepines.2 I would hope that an article on benzodiazepines would provide more discussion and guidance surrounding these important issues.
The June 2023 issue also included “High-dose stimulants for adult ADHD” (p. 34-39, doi:10.12788/cp.0366). This article provided esoteric advice on managing stimulant therapy in the setting of Roux-en-Y gastric bypass surgery, yet I would regard stimulant misuse as a far more common and pressing issue.3,4 The recent Drug Enforcement Administration investigation of telehealth stimulant prescribing is a notable example of this problem.5
The patient discussed in this article was receiving large doses of stimulants for a purported case of refractory attention-deficit/hyperactivity disorder (ADHD). The article provided a sparse differential diagnosis for the patient’s intractable symptoms. While rapid metabolism may be an explanation, I would also like to know how the authors ruled out physiological dependence and/or addiction to a controlled substance. How was misuse excluded? Was urine drug testing (UDS) performed? UDS is highly irregular among prescribers,6 which suggests that practices for detecting covert substance abuse and stimulant misuse are inadequate. Wouldn’t such investigations be fundamental to ethical stimulant prescribing?
Jeff Sanders, MD, PhD
Atlanta, Georgia
References
1. Centers for Disease Control and Prevention. Trends in nonfatal and fatal overdoses involving benzodiazepines—38 states and the District of Columbia, 2019-2020. Accessed August 9, 2023. https://www.cdc.gov/mmwr/volumes/70/wr/mm7034a2.htm
2. US Food & Drug Administration. FDA requiring boxed warning updated to improve safe use of benzodiazepine drug class. Accessed August 14, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requiring-boxed-warning-updated-improve-safe-use-benzodiazepine-drug-class
3. McCabe SE, Schulenberg JE, Wilens TE, et al. Prescription stimulant medical and nonmedical use among US secondary school students, 2005 to 2020. JAMA Netw Open. 2023;6(4):e238707. doi:10.1001/jamanetworkopen.2023.8707
4. US Food & Drug Administration. FDA updating warnings to improve safe use of prescription stimulants used to treat ADHD and other conditions. Accessed August 14, 2023. https://www.fda.gov/safety/medical-product-safety-information/fda-updating-warnings-improve-safe-use-prescription-stimulants-used-treat-adhd-and-other-conditions
5. Vaidya A. Report: telehealth company’s prescribing practices come under DEA scrutiny. September 16, 2022. Accessed August 9, 2023. https://mhealthintelligence.com/news/report-telehealth-company-dones-prescribing-practices-come-under-dea-scrutiny
6. Zionts A. Some ADHD patients are drug-tested often, while others are never asked. Kaiser Health News. March 25, 2023. Accessed August 9, 2023. https://www.nbcnews.com/news/amp/rcna76330
Continue to: Drs. Stimpfl and Strawn respond
Drs. Stimpfl and Strawn respond
We thank Dr. Sanders for highlighting the need for clinical equipoise in considering the risks and benefits of medications—something that is true for benzodiazepines, antipsychotics, antidepressants, and in fact all medications. He reminds us that the risks of misuse, dependence, and withdrawal associated with benzodiazepines led to a boxed warning in September 2020 and highlights recent trends of fatal and nonfatal benzodiazepine overdose, especially when combined with opiates.
Our article, which aimed to educate clinicians on benzodiazepine pharmacology and patient-specific factors influencing benzodiazepine selection and dosing, did not focus significantly on the risks associated with benzodiazepines. We do encourage careful and individualized benzodiazepine prescribing. However, we wish to remind our colleagues that benzodiazepines, while associated with risks, continue to have utility in acute and periprocedural settings, and remain an important treatment option for patients with panic disorder, generalized anxiety disorder (especially while waiting for other medications to take effect), catatonia, seizure disorders, and alcohol withdrawal.
We agree that patient-specific risk assessment is essential, as some patients benefit from benzodiazepines despite the risks. However, we also acknowledge that some individuals are at higher risk for adverse outcomes, including those with concurrent opiate use or who are prescribed other sedative-hypnotics; older adults and those with neurocognitive disorders; and patients susceptible to respiratory depression due to other medical reasons (eg, myasthenia gravis, sleep apnea, and chronic obstructive pulmonary disease). Further, we agree that benzodiazepine use during pregnancy is generally not advised due to the risks of neonatal hypotonia and neonatal withdrawal syndrome1 as well as a possible risk of cleft palate that has been reported in some studies.2 Finally, paradoxical reactions may be more common at the extremes of age and in patients with intellectual disability or personality disorders.3,4
Patient characteristics that have been associated with a higher risk of benzodiazepine use disorder include lower education/income, unemployment, having another substance use disorder, and severe psychopathology.5 In some studies, using benzodiazepines for prolonged periods at high doses as well as using those with a rapid onset of action was associated with an increased risk of benzodiazepine use disorder.5-7
Ultimately, we concur with Dr. Sanders on the perils of the “irresponsible use” of medication and emphasize the need for discernment when choosing treatments to avoid rashly discarding an effective remedy while attempting to mitigate all conceivable risks.
Julia Stimpfl, MD
Jeffrey R. Strawn, MD
Cincinnati, Ohio
References
1. McElhatton PR. The effects of benzodiazepine use during pregnancy and lactation. Reprod Toxicol. 1994;8(6):461-475. doi:10.1016/0890-6238(94)90029-9
2. Enato E, Moretti M, Koren G. The fetal safety of benzodiazepines: an updated meta-analysis. J Obstet Gynaecol Can. 2011;33(1):46-48. doi:10.1016/S1701-2163(16)34772-7 Erratum in: J Obstet Gynaecol Can. 2011;33(4):319.
3. Hakimi Y, Petitpain N, Pinzani V, et al. Paradoxical adverse drug reactions: descriptive analysis of French reports. Eur J Clin Pharmacol. 2020;76(8):1169-1174. doi:10.1007/s00228-020-02892-2
4. Paton C. Benzodiazepines and disinhibition: a review. Psychiatric Bulletin. 2002;26(12):460-462. doi:10.1192/pb.26.12.460
5. Fride Tvete I, Bjørner T, Skomedal T. Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway. Scand J Prim Health Care. 2015;33(4):252-259. doi:10.3109/02813432.2015.1117282
6. Griffiths RR, Johnson MW. Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds. J Clin Psychiatry. 2005;66 Suppl 9:31-41.
7. Kan CC, Hilberink SR, Breteler MH. Determination of the main risk factors for benzodiazepine dependence using a multivariate and multidimensional approach. Compr Psychiatry. 2004;45(2):88-94. doi:10.1016/j.comppsych.2003.12.007
Continue to: Drs. Sarma and Grady respond
Drs. Sarma and Grady respond
Dr. Sanders’ letter highlights the potential caveats associated with prescribing controlled substances. We agree that our short case summary includes numerous interesting elements, each of which would be worthy of further exploration and discussion. Our choice was to highlight the patient history of bariatric surgery and use this as a springboard into a review of stimulants, including the newest formulations for ADHD. For more than 1 year, many generic stimulants have been in short supply, and patients and clinicians have been seeking other therapeutic options. Given this background and with newer, branded stimulant use becoming more commonplace, we believe our article was useful and timely.
Our original intent had been to include an example of a controlled substance agreement. Regrettably, there was simply not enough space for this document or the additional discussion that its inclusion would deem necessary. Nevertheless, had the May 2023 FDA requirement for manufacturers to update the labeling of prescription stimulants1 to clarify misuse and abuse been published before our article’s final revision, we would have mentioned it and provided the appropriate link.
Subbu J. Sarma, MD, FAPA
Kansas City, Missouri
Sarah E. Grady, PharmD, BCPS, BCPP
Des Moines, Iowa
References
1. US Food & Drug Administration. FDA requires updates to clarify labeling of prescription stimulants used to treat ADHD and other conditions. Accessed August 9, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requires-updates-clarify-labeling-prescription-stimulants-used-treat-adhd-and-other-conditions
No link between most cancers and depression/anxiety: Study
from a large, individual participant data meta-analysis.
An exception was for lung and smoking-related cancers, but key covariates appeared to explain the relationship between depression, anxiety, and these cancer types, the investigators reported.
The findings challenge a common theory that depression and anxiety increase cancer risk and should “change current thinking,” they argue.
“Our results may come as a relief to many patients with cancer who believe their diagnosis is attributed to previous anxiety or depression,” first author Lonneke A. van Tuijl, PhD, of the University of Groningen and Utrecht University, the Netherlands, noted in a press release.
Analyses included data from up to nearly 320,000 individuals from the 18 prospective cohorts included in the international Psychosocial Factors and Cancer Incidence (PSY-CA) consortium. The cohorts are from studies conducted in the Netherlands, United Kingdom, Norway, and Canada, and included 25,803 patients with cancer. During follow-up of up to 26 years and more than 3.2 million person-years, depression and anxiety symptoms and diagnoses showed no association with overall breast, prostate, colorectal, and alcohol-related cancers (hazard ratios, 0.98-1.05).
For the specific cancer types, the investigators “found no evidence for an association between depression or anxiety and the incidence of colorectal cancer (HRs, 0.88-1.13), prostate cancer (HRs, 0.97-1.17), or alcohol-related cancers (HRs, 0.97-1.06).”
“For breast cancer, all pooled HRs were consistently negative but mean pooled HRs were close to 1 (HRs, 0.92-0.98) and the upper limit of the 95% confidence intervals all exceeded 1 (with the exception of anxiety symptoms),” they noted.
An increase in risk observed between depression and anxiety symptoms and diagnoses and lung cancer (HRs, 1.12-1.60) and smoking-related cancers (HRs, 1.06-1.60), in minimally adjusted models, was substantially attenuated after adjusting for known risk factors such as smoking, alcohol use, and body mass index (HRs, 1.04-1.08), the investigators reported.
The findings were published online in Cancer.
“Depression and anxiety have long been hypothesized to increase the risk for cancer. It is thought that the increased cancer risk can occur via several pathways, including health behaviors, or by influencing mutation, viral oncogenes, cell proliferation, or DNA repair,” the authors explained, noting that “[c]onclusions drawn in meta-analyses vary greatly, with some supporting an association between depression, anxiety, and cancer incidence and others finding no or a negligible association.”
The current findings “may help health professionals to alleviate feelings of guilt and self-blame in patients with cancer who attribute their diagnosis to previous depression or anxiety,” they said, noting that the findings “also underscore the importance of addressing tobacco smoking and other unhealthy behaviors – including those that may develop as a result of anxiety or depression.”
“However, further research is needed to understand exactly how depression, anxiety, health behaviors, and lung cancer are related,” said Dr. Tuijl.
Dr. Tuijl has received grants and travel support from the Dutch Cancer Society (KWF).
from a large, individual participant data meta-analysis.
An exception was for lung and smoking-related cancers, but key covariates appeared to explain the relationship between depression, anxiety, and these cancer types, the investigators reported.
The findings challenge a common theory that depression and anxiety increase cancer risk and should “change current thinking,” they argue.
“Our results may come as a relief to many patients with cancer who believe their diagnosis is attributed to previous anxiety or depression,” first author Lonneke A. van Tuijl, PhD, of the University of Groningen and Utrecht University, the Netherlands, noted in a press release.
Analyses included data from up to nearly 320,000 individuals from the 18 prospective cohorts included in the international Psychosocial Factors and Cancer Incidence (PSY-CA) consortium. The cohorts are from studies conducted in the Netherlands, United Kingdom, Norway, and Canada, and included 25,803 patients with cancer. During follow-up of up to 26 years and more than 3.2 million person-years, depression and anxiety symptoms and diagnoses showed no association with overall breast, prostate, colorectal, and alcohol-related cancers (hazard ratios, 0.98-1.05).
For the specific cancer types, the investigators “found no evidence for an association between depression or anxiety and the incidence of colorectal cancer (HRs, 0.88-1.13), prostate cancer (HRs, 0.97-1.17), or alcohol-related cancers (HRs, 0.97-1.06).”
“For breast cancer, all pooled HRs were consistently negative but mean pooled HRs were close to 1 (HRs, 0.92-0.98) and the upper limit of the 95% confidence intervals all exceeded 1 (with the exception of anxiety symptoms),” they noted.
An increase in risk observed between depression and anxiety symptoms and diagnoses and lung cancer (HRs, 1.12-1.60) and smoking-related cancers (HRs, 1.06-1.60), in minimally adjusted models, was substantially attenuated after adjusting for known risk factors such as smoking, alcohol use, and body mass index (HRs, 1.04-1.08), the investigators reported.
The findings were published online in Cancer.
“Depression and anxiety have long been hypothesized to increase the risk for cancer. It is thought that the increased cancer risk can occur via several pathways, including health behaviors, or by influencing mutation, viral oncogenes, cell proliferation, or DNA repair,” the authors explained, noting that “[c]onclusions drawn in meta-analyses vary greatly, with some supporting an association between depression, anxiety, and cancer incidence and others finding no or a negligible association.”
The current findings “may help health professionals to alleviate feelings of guilt and self-blame in patients with cancer who attribute their diagnosis to previous depression or anxiety,” they said, noting that the findings “also underscore the importance of addressing tobacco smoking and other unhealthy behaviors – including those that may develop as a result of anxiety or depression.”
“However, further research is needed to understand exactly how depression, anxiety, health behaviors, and lung cancer are related,” said Dr. Tuijl.
Dr. Tuijl has received grants and travel support from the Dutch Cancer Society (KWF).
from a large, individual participant data meta-analysis.
An exception was for lung and smoking-related cancers, but key covariates appeared to explain the relationship between depression, anxiety, and these cancer types, the investigators reported.
The findings challenge a common theory that depression and anxiety increase cancer risk and should “change current thinking,” they argue.
“Our results may come as a relief to many patients with cancer who believe their diagnosis is attributed to previous anxiety or depression,” first author Lonneke A. van Tuijl, PhD, of the University of Groningen and Utrecht University, the Netherlands, noted in a press release.
Analyses included data from up to nearly 320,000 individuals from the 18 prospective cohorts included in the international Psychosocial Factors and Cancer Incidence (PSY-CA) consortium. The cohorts are from studies conducted in the Netherlands, United Kingdom, Norway, and Canada, and included 25,803 patients with cancer. During follow-up of up to 26 years and more than 3.2 million person-years, depression and anxiety symptoms and diagnoses showed no association with overall breast, prostate, colorectal, and alcohol-related cancers (hazard ratios, 0.98-1.05).
For the specific cancer types, the investigators “found no evidence for an association between depression or anxiety and the incidence of colorectal cancer (HRs, 0.88-1.13), prostate cancer (HRs, 0.97-1.17), or alcohol-related cancers (HRs, 0.97-1.06).”
“For breast cancer, all pooled HRs were consistently negative but mean pooled HRs were close to 1 (HRs, 0.92-0.98) and the upper limit of the 95% confidence intervals all exceeded 1 (with the exception of anxiety symptoms),” they noted.
An increase in risk observed between depression and anxiety symptoms and diagnoses and lung cancer (HRs, 1.12-1.60) and smoking-related cancers (HRs, 1.06-1.60), in minimally adjusted models, was substantially attenuated after adjusting for known risk factors such as smoking, alcohol use, and body mass index (HRs, 1.04-1.08), the investigators reported.
The findings were published online in Cancer.
“Depression and anxiety have long been hypothesized to increase the risk for cancer. It is thought that the increased cancer risk can occur via several pathways, including health behaviors, or by influencing mutation, viral oncogenes, cell proliferation, or DNA repair,” the authors explained, noting that “[c]onclusions drawn in meta-analyses vary greatly, with some supporting an association between depression, anxiety, and cancer incidence and others finding no or a negligible association.”
The current findings “may help health professionals to alleviate feelings of guilt and self-blame in patients with cancer who attribute their diagnosis to previous depression or anxiety,” they said, noting that the findings “also underscore the importance of addressing tobacco smoking and other unhealthy behaviors – including those that may develop as a result of anxiety or depression.”
“However, further research is needed to understand exactly how depression, anxiety, health behaviors, and lung cancer are related,” said Dr. Tuijl.
Dr. Tuijl has received grants and travel support from the Dutch Cancer Society (KWF).
FROM CANCER
Use of mental health services soared during pandemic
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
Child assault tied to triple the risk for mental illness within 1 year
The greatest risk was found in the first year following the assault, increasing to three times the risk of being diagnosed with mental illness, compared with children not assaulted. Mood and anxiety disorders were the most common diagnoses.
“From a clinical and policy perspective, our study highlights that there is a critical opportunity for health care clinicians to support children in the first year following physical assault,” Natasha Saunders, MD, MSc, of the Hospital for Sick Children, Toronto, and colleagues wrote. “There is a need to develop and implement targeted mental illness prevention, screening, and treatment programs for assaulted children.”
The findings were published online in JAMA Network Open.
While it has been well established that children exposed to assault have an increased risk for subsequent mental illness, Dr. Saunders and coinvestigators noted that using an age-matched, population-based cohort study would enable them to obtain detailed information on the patterns and timing of subsequent psychiatric diagnoses.
To that end, the researchers used several medical databases in Ontario to find 5,487 children (infants to age 13 years) who required an ED visit or hospitalization for a physical assault in Ontario between 2006 and 2014.
These children were matched on a 1:4 basis with 21,948 children not exposed to physical assault. The children were followed until their 18th birthday or until the study ended in March 2019.
The researchers found that more than a third of the children (39%) who were exposed to assault received a mental health diagnosis, according to health records, compared with 23% of unexposed children.
Mood and anxiety disorders were the most common diagnoses among children exposed to assault (16.2% vs. 10.6%, respectively); followed by select childhood behavior disorders, such as ADHD, oppositional defiant disorder, or conduct disorder (9.9% vs. 5.2%); and substance use disorders (2.4% vs. 0.4%).
Triple risk of mental illness in first year
The researchers found that the children exposed to assault were nearly twice as likely to be diagnosed with a mental illness over a median follow-up of 7 years, compared with those not exposed to assault (adjusted hazard ratio, 1.96; 95% confidence interval, 1.85,2.08).
In the year following the assault, children exposed to assault bore three times the risk of being diagnosed with a mental illness, compared with unexposed children (aHR, 3.08; 95% CI, 2.68,3.54).
In addition, the children who had been assaulted were more likely to be diagnosed in an acute care setting than those who were not assaulted (14% vs. 2.8%).
The children who had been assaulted were an average age of 7 years and were more often boys (55% vs. 45%). Children who were assaulted were also more likely to have mothers with mental illness (35% vs. 19%).
The investigators noted that the study likely underestimated the number of children exposed to assault, as many do not end up in the ED.
In addition to highlighting the need for medical personnel to support children in the first year following assault, the investigators wrote that “our results also advocate for accessible mental health care outside of the acute setting and for care that addresses the social and health needs of mothers, who themselves have high social and health risks.”
This study received funding from the National Foundation to End Child Abuse and Neglect and the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Saunders reported receiving personal fees from The BMJ Group, Archives of Diseases in Childhood outside the submitted work.
A version of this article first appeared on Medscape.com.
The greatest risk was found in the first year following the assault, increasing to three times the risk of being diagnosed with mental illness, compared with children not assaulted. Mood and anxiety disorders were the most common diagnoses.
“From a clinical and policy perspective, our study highlights that there is a critical opportunity for health care clinicians to support children in the first year following physical assault,” Natasha Saunders, MD, MSc, of the Hospital for Sick Children, Toronto, and colleagues wrote. “There is a need to develop and implement targeted mental illness prevention, screening, and treatment programs for assaulted children.”
The findings were published online in JAMA Network Open.
While it has been well established that children exposed to assault have an increased risk for subsequent mental illness, Dr. Saunders and coinvestigators noted that using an age-matched, population-based cohort study would enable them to obtain detailed information on the patterns and timing of subsequent psychiatric diagnoses.
To that end, the researchers used several medical databases in Ontario to find 5,487 children (infants to age 13 years) who required an ED visit or hospitalization for a physical assault in Ontario between 2006 and 2014.
These children were matched on a 1:4 basis with 21,948 children not exposed to physical assault. The children were followed until their 18th birthday or until the study ended in March 2019.
The researchers found that more than a third of the children (39%) who were exposed to assault received a mental health diagnosis, according to health records, compared with 23% of unexposed children.
Mood and anxiety disorders were the most common diagnoses among children exposed to assault (16.2% vs. 10.6%, respectively); followed by select childhood behavior disorders, such as ADHD, oppositional defiant disorder, or conduct disorder (9.9% vs. 5.2%); and substance use disorders (2.4% vs. 0.4%).
Triple risk of mental illness in first year
The researchers found that the children exposed to assault were nearly twice as likely to be diagnosed with a mental illness over a median follow-up of 7 years, compared with those not exposed to assault (adjusted hazard ratio, 1.96; 95% confidence interval, 1.85,2.08).
In the year following the assault, children exposed to assault bore three times the risk of being diagnosed with a mental illness, compared with unexposed children (aHR, 3.08; 95% CI, 2.68,3.54).
In addition, the children who had been assaulted were more likely to be diagnosed in an acute care setting than those who were not assaulted (14% vs. 2.8%).
The children who had been assaulted were an average age of 7 years and were more often boys (55% vs. 45%). Children who were assaulted were also more likely to have mothers with mental illness (35% vs. 19%).
The investigators noted that the study likely underestimated the number of children exposed to assault, as many do not end up in the ED.
In addition to highlighting the need for medical personnel to support children in the first year following assault, the investigators wrote that “our results also advocate for accessible mental health care outside of the acute setting and for care that addresses the social and health needs of mothers, who themselves have high social and health risks.”
This study received funding from the National Foundation to End Child Abuse and Neglect and the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Saunders reported receiving personal fees from The BMJ Group, Archives of Diseases in Childhood outside the submitted work.
A version of this article first appeared on Medscape.com.
The greatest risk was found in the first year following the assault, increasing to three times the risk of being diagnosed with mental illness, compared with children not assaulted. Mood and anxiety disorders were the most common diagnoses.
“From a clinical and policy perspective, our study highlights that there is a critical opportunity for health care clinicians to support children in the first year following physical assault,” Natasha Saunders, MD, MSc, of the Hospital for Sick Children, Toronto, and colleagues wrote. “There is a need to develop and implement targeted mental illness prevention, screening, and treatment programs for assaulted children.”
The findings were published online in JAMA Network Open.
While it has been well established that children exposed to assault have an increased risk for subsequent mental illness, Dr. Saunders and coinvestigators noted that using an age-matched, population-based cohort study would enable them to obtain detailed information on the patterns and timing of subsequent psychiatric diagnoses.
To that end, the researchers used several medical databases in Ontario to find 5,487 children (infants to age 13 years) who required an ED visit or hospitalization for a physical assault in Ontario between 2006 and 2014.
These children were matched on a 1:4 basis with 21,948 children not exposed to physical assault. The children were followed until their 18th birthday or until the study ended in March 2019.
The researchers found that more than a third of the children (39%) who were exposed to assault received a mental health diagnosis, according to health records, compared with 23% of unexposed children.
Mood and anxiety disorders were the most common diagnoses among children exposed to assault (16.2% vs. 10.6%, respectively); followed by select childhood behavior disorders, such as ADHD, oppositional defiant disorder, or conduct disorder (9.9% vs. 5.2%); and substance use disorders (2.4% vs. 0.4%).
Triple risk of mental illness in first year
The researchers found that the children exposed to assault were nearly twice as likely to be diagnosed with a mental illness over a median follow-up of 7 years, compared with those not exposed to assault (adjusted hazard ratio, 1.96; 95% confidence interval, 1.85,2.08).
In the year following the assault, children exposed to assault bore three times the risk of being diagnosed with a mental illness, compared with unexposed children (aHR, 3.08; 95% CI, 2.68,3.54).
In addition, the children who had been assaulted were more likely to be diagnosed in an acute care setting than those who were not assaulted (14% vs. 2.8%).
The children who had been assaulted were an average age of 7 years and were more often boys (55% vs. 45%). Children who were assaulted were also more likely to have mothers with mental illness (35% vs. 19%).
The investigators noted that the study likely underestimated the number of children exposed to assault, as many do not end up in the ED.
In addition to highlighting the need for medical personnel to support children in the first year following assault, the investigators wrote that “our results also advocate for accessible mental health care outside of the acute setting and for care that addresses the social and health needs of mothers, who themselves have high social and health risks.”
This study received funding from the National Foundation to End Child Abuse and Neglect and the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Saunders reported receiving personal fees from The BMJ Group, Archives of Diseases in Childhood outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Prescribing lifestyle changes: When medicine isn’t enough
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
In psychiatry, patients come to us with their list of symptoms, often a diagnosis they’ve made themselves, and the expectation that they will be given medication to fix their problem. Their diagnoses are often right on target – people often know if they are depressed or anxious, and Doctor Google may provide useful information.
Sometimes they want a specific medication, one they saw in a TV ad, or one that helped them in the past or has helped someone they know. As psychiatrists have focused more on their strengths as psychopharmacologists and less on psychotherapy, it gets easy for both the patient and the doctor to look to medication, cocktails, and titration as the only thing we do.
“My medicine stopped working,” is a line I commonly hear. Often the patient is on a complicated regimen that has been serving them well, and it seems unlikely that the five psychotropic medications they are taking have suddenly “stopped working.” An obvious exception is the SSRI “poop out” that can occur 6-12 months or more after beginning treatment. In addition, it’s important to make sure patients are taking their medications as prescribed, and that the generic formulations have not changed.
But as rates of mental illness increase, some of it spurred on by difficult times,
This is not to devalue our medications, but to help the patient see symptoms as having multiple factors and give them some means to intervene, in addition to medications. At the beginning of therapy, it is important to “prescribe” lifestyle changes that will facilitate the best possible outcomes.
Nonpharmaceutical prescriptions
Early in my career, people with alcohol use problems were told they needed to be substance free before they were candidates for antidepressants. While we no longer do that, it is still important to emphasize abstinence from addictive substances, and to recommend specific treatment when necessary.
Patients are often reluctant to see their use of alcohol, marijuana (it’s medical! It’s part of wellness!), or their pain medications as part of the problem, and this can be difficult. There have been times, after multiple medications have failed to help their symptoms, when I have said, “If you don’t get treatment for this problem, I am not going to be able to help you feel better” and that has been motivating for the patient.
There are other “prescriptions” to write. Regular sleep is essential for people with mood disorders, and this can be difficult for many patients, especially those who do shift work, or who have regular disruptions to their sleep from noise, pets, and children. Exercise is wonderful for the cardiovascular system, calms anxiety, and maintains strength, endurance, mobility, and quality of life as people age. But it can be a hard sell to people in a mental health crisis.
Nature is healing, and sunshine helps with maintaining circadian rhythms. For those who don’t exercise, I often “prescribe” 20 to 30 minutes a day of walking, preferably outside, during daylight hours, in a park or natural setting. For people with anxiety, it is important to check their caffeine consumption and to suggest ways to moderate it – moving to decaffeinated beverages or titrating down by mixing decaf with caffeinated.
Meditation is something that many people find helpful. For anxious people, it can be very difficult, and I will prescribe a specific instructional video course that I like on the well-being app InsightTimer – Sarah Blondin’s Learn How to Meditate in Seven Days. The sessions are approximately 10 minutes long, and that seems like the right amount of time for a beginner.
When people are very ill and don’t want to go into the hospital, I talk with them about things that happen in the hospital that are helpful, things they can try to mimic at home. In the hospital, patients don’t go to work, they don’t spend hours a day on the computer, and they are given a pass from dealing with the routine stresses of daily life.
I ask them to take time off work, to avoid as much stress as possible, to spend time with loved ones who give them comfort, and to avoid the people who leave them feeling drained or distressed. I ask them to engage in activities they find healing, to eat well, exercise, and avoid social media. In the hospital, I emphasize, they wake patients up in the morning, ask them to get out of bed and engage in therapeutic activities. They are fed and kept from intoxicants.
When it comes to nutrition, we know so little about how food affects mental health. I feel like it can’t hurt to ask people to avoid fast foods, soft drinks, and processed foods, and so I do.
And what about compliance? Of course, not everyone complies; not everyone is interested in making changes and these can be hard changes. I’ve recently started to recommend the book Atomic Habits by James Clear. Sometimes a bit of motivational interviewing can also be helpful in getting people to look at slowly moving toward making changes.
In prescribing lifestyle changes, it is important to offer most of these changes as suggestions, not as things we insist on, or that will leave the patient feeling ashamed if he doesn’t follow through. They should be discussed early in treatment so that patients don’t feel blamed for their illness or relapses. As with all the things we prescribe, some of these behavior changes help some of the people some of the time. Suggesting them, however, makes the strong statement that treating psychiatric disorders can be about more than passively swallowing a pill.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She disclosed no relevant conflicts of interest.
Most Americans in favor of regulated therapeutic psychedelics
It is a surprisingly large percentage, said officials at the University of California, Berkeley, Center for the Science of Psychedelics, which conducted the online survey of 1,500 registered voters in early June.
“That is a stunning number,” said Michael Pollan, cofounder of the center, and author of “How to Change Your Mind,” a book that explored potential uses of psychedelics.
In a briefing with reporters, Mr. Pollan said that he believes the large support base, in part, reflects campaigns that have “been successful by highlighting the effectiveness of psychedelics as therapy for mental illness.”
However, the poll also showed that 61% of voters said that they do not perceive psychedelics as “good for society,” and 69% do not perceive them as “something for people like me.”
These negative sentiments “suggest a fragile kind of support – the kind of support where you’re only hearing one side of the story,” said Mr. Pollan.
Still, poll respondents supported other potential policy changes, including 56% in support of the U.S. Food and Drug Administration vetting and approving psychedelics so they could be available by prescription.
50% have tried psychedelics
Almost 80% said that it should be easier for researchers to study psychedelics, and just under one-half said that they backed removing criminal penalties for personal use and possession.
The poll results also show that almost half of respondents had heard about psychedelics recently, with 48% saying they had heard about the drugs’ use in treating mental illness.
Respondents who were most familiar with and positive about psychedelics tended to be White, male, aged 30-50 years, liberal, highly educated, living in a Western state, and have little to no religious or spiritual practice.
Overall, 52% of survey respondents said that they or someone close to them had used a psychedelic, with almost half of that use coming in the past 5 years. Some 40% said that the use had been more than a decade ago.
Almost three-quarters of psychedelic use was reported as recreational, but the second-biggest category was therapeutic use at 39%. About one-third of respondents said that they or someone close to them had microdosed.
Conservative voters had lower levels of awareness and first-degree connection use as well as the least amount of support for regulated therapeutic use, with only 45% saying they would back such a policy, compared with 80% of liberal voters and 66% of moderate voters.
Black individuals were the least likely to be familiar with psychedelics: Just 29% said that they had heard a little or a lot about the drugs, compared with 39% of Latinx individuals and 51% of White individuals. And just one-quarter reported first-degree use, compared with half of Latinx individuals and 56% of White individuals.
Who should be eligible?
When asked who should be eligible for treatment with psychedelics, 80% said that they were comfortable with its use for those with terminal illnesses. More than two-thirds expressed comfort with the drugs being used to help veterans and people with treatment-resistant depression and anxiety.
Less than one-half of respondents said that psychedelics should be available to everyone older than 21 years. And voters seemed to be less inclined to say psychedelics should be used to treat people with addiction, with just 45% indicating that they were very or somewhat comfortable with that use.
Mr. Pollan said that reflects perhaps some lack of knowledge or education.
“The story about addiction and psychedelics hasn’t gotten out,” he said. “I kind of get that intuitively the idea of using a drug to treat a drug doesn’t sound right to a lot of people. But in fact, there’s good evidence it works,” Mr. Pollan said.
Respondents said that doctors, nurses, and scientists were the most trusted source of information about psychedelics, whereas the FDA received lower confidence. Law enforcement was least trusted by liberals and most trusted by conservatives.
Mr. Pollan noted the reversal in attitudes, with Americans mostly now looking to the scientific and medical establishment for guidance on psychedelics.
“We went from a counterculture drug to something that is being taken seriously by scientists as a potential therapy,” he said.
The poll’s margin of error was ± 2.5%.
A version of this article first appeared on Medscape.com.
It is a surprisingly large percentage, said officials at the University of California, Berkeley, Center for the Science of Psychedelics, which conducted the online survey of 1,500 registered voters in early June.
“That is a stunning number,” said Michael Pollan, cofounder of the center, and author of “How to Change Your Mind,” a book that explored potential uses of psychedelics.
In a briefing with reporters, Mr. Pollan said that he believes the large support base, in part, reflects campaigns that have “been successful by highlighting the effectiveness of psychedelics as therapy for mental illness.”
However, the poll also showed that 61% of voters said that they do not perceive psychedelics as “good for society,” and 69% do not perceive them as “something for people like me.”
These negative sentiments “suggest a fragile kind of support – the kind of support where you’re only hearing one side of the story,” said Mr. Pollan.
Still, poll respondents supported other potential policy changes, including 56% in support of the U.S. Food and Drug Administration vetting and approving psychedelics so they could be available by prescription.
50% have tried psychedelics
Almost 80% said that it should be easier for researchers to study psychedelics, and just under one-half said that they backed removing criminal penalties for personal use and possession.
The poll results also show that almost half of respondents had heard about psychedelics recently, with 48% saying they had heard about the drugs’ use in treating mental illness.
Respondents who were most familiar with and positive about psychedelics tended to be White, male, aged 30-50 years, liberal, highly educated, living in a Western state, and have little to no religious or spiritual practice.
Overall, 52% of survey respondents said that they or someone close to them had used a psychedelic, with almost half of that use coming in the past 5 years. Some 40% said that the use had been more than a decade ago.
Almost three-quarters of psychedelic use was reported as recreational, but the second-biggest category was therapeutic use at 39%. About one-third of respondents said that they or someone close to them had microdosed.
Conservative voters had lower levels of awareness and first-degree connection use as well as the least amount of support for regulated therapeutic use, with only 45% saying they would back such a policy, compared with 80% of liberal voters and 66% of moderate voters.
Black individuals were the least likely to be familiar with psychedelics: Just 29% said that they had heard a little or a lot about the drugs, compared with 39% of Latinx individuals and 51% of White individuals. And just one-quarter reported first-degree use, compared with half of Latinx individuals and 56% of White individuals.
Who should be eligible?
When asked who should be eligible for treatment with psychedelics, 80% said that they were comfortable with its use for those with terminal illnesses. More than two-thirds expressed comfort with the drugs being used to help veterans and people with treatment-resistant depression and anxiety.
Less than one-half of respondents said that psychedelics should be available to everyone older than 21 years. And voters seemed to be less inclined to say psychedelics should be used to treat people with addiction, with just 45% indicating that they were very or somewhat comfortable with that use.
Mr. Pollan said that reflects perhaps some lack of knowledge or education.
“The story about addiction and psychedelics hasn’t gotten out,” he said. “I kind of get that intuitively the idea of using a drug to treat a drug doesn’t sound right to a lot of people. But in fact, there’s good evidence it works,” Mr. Pollan said.
Respondents said that doctors, nurses, and scientists were the most trusted source of information about psychedelics, whereas the FDA received lower confidence. Law enforcement was least trusted by liberals and most trusted by conservatives.
Mr. Pollan noted the reversal in attitudes, with Americans mostly now looking to the scientific and medical establishment for guidance on psychedelics.
“We went from a counterculture drug to something that is being taken seriously by scientists as a potential therapy,” he said.
The poll’s margin of error was ± 2.5%.
A version of this article first appeared on Medscape.com.
It is a surprisingly large percentage, said officials at the University of California, Berkeley, Center for the Science of Psychedelics, which conducted the online survey of 1,500 registered voters in early June.
“That is a stunning number,” said Michael Pollan, cofounder of the center, and author of “How to Change Your Mind,” a book that explored potential uses of psychedelics.
In a briefing with reporters, Mr. Pollan said that he believes the large support base, in part, reflects campaigns that have “been successful by highlighting the effectiveness of psychedelics as therapy for mental illness.”
However, the poll also showed that 61% of voters said that they do not perceive psychedelics as “good for society,” and 69% do not perceive them as “something for people like me.”
These negative sentiments “suggest a fragile kind of support – the kind of support where you’re only hearing one side of the story,” said Mr. Pollan.
Still, poll respondents supported other potential policy changes, including 56% in support of the U.S. Food and Drug Administration vetting and approving psychedelics so they could be available by prescription.
50% have tried psychedelics
Almost 80% said that it should be easier for researchers to study psychedelics, and just under one-half said that they backed removing criminal penalties for personal use and possession.
The poll results also show that almost half of respondents had heard about psychedelics recently, with 48% saying they had heard about the drugs’ use in treating mental illness.
Respondents who were most familiar with and positive about psychedelics tended to be White, male, aged 30-50 years, liberal, highly educated, living in a Western state, and have little to no religious or spiritual practice.
Overall, 52% of survey respondents said that they or someone close to them had used a psychedelic, with almost half of that use coming in the past 5 years. Some 40% said that the use had been more than a decade ago.
Almost three-quarters of psychedelic use was reported as recreational, but the second-biggest category was therapeutic use at 39%. About one-third of respondents said that they or someone close to them had microdosed.
Conservative voters had lower levels of awareness and first-degree connection use as well as the least amount of support for regulated therapeutic use, with only 45% saying they would back such a policy, compared with 80% of liberal voters and 66% of moderate voters.
Black individuals were the least likely to be familiar with psychedelics: Just 29% said that they had heard a little or a lot about the drugs, compared with 39% of Latinx individuals and 51% of White individuals. And just one-quarter reported first-degree use, compared with half of Latinx individuals and 56% of White individuals.
Who should be eligible?
When asked who should be eligible for treatment with psychedelics, 80% said that they were comfortable with its use for those with terminal illnesses. More than two-thirds expressed comfort with the drugs being used to help veterans and people with treatment-resistant depression and anxiety.
Less than one-half of respondents said that psychedelics should be available to everyone older than 21 years. And voters seemed to be less inclined to say psychedelics should be used to treat people with addiction, with just 45% indicating that they were very or somewhat comfortable with that use.
Mr. Pollan said that reflects perhaps some lack of knowledge or education.
“The story about addiction and psychedelics hasn’t gotten out,” he said. “I kind of get that intuitively the idea of using a drug to treat a drug doesn’t sound right to a lot of people. But in fact, there’s good evidence it works,” Mr. Pollan said.
Respondents said that doctors, nurses, and scientists were the most trusted source of information about psychedelics, whereas the FDA received lower confidence. Law enforcement was least trusted by liberals and most trusted by conservatives.
Mr. Pollan noted the reversal in attitudes, with Americans mostly now looking to the scientific and medical establishment for guidance on psychedelics.
“We went from a counterculture drug to something that is being taken seriously by scientists as a potential therapy,” he said.
The poll’s margin of error was ± 2.5%.
A version of this article first appeared on Medscape.com.










