User login
Belimumab Autoinjector Approved for Pediatric Lupus
The US Food and Drug Administration (FDA) has approved Benlysta (belimumab) autoinjector for patients aged 5 years or older with active systemic lupus erythematosus (SLE) on standard therapy. This is the first time that children with SLE can receive this treatment at home, according to a GSK press release.
Prior to this approval, pediatric patients aged 5 years or older could receive belimumab only intravenously via a 1-hour infusion in a hospital or clinic setting.
“Going to the doctor’s office once every 4 weeks can be a logistical hurdle for some children and their caregivers, so having the option to administer Benlysta in the comfort of their home provides much-needed flexibility,” Mary Crimmings, the interim CEO and senior vice president for marketing and communications at the Lupus Foundation of America, said in a statement.
An estimated 5000-10,000 children in the United States are living with SLE.
Belimumab is a B-lymphocyte stimulator–specific inhibitor approved for the treatment of active SLE and active lupus nephritis in patients aged 5 years or older receiving standard therapy. This approval of the subcutaneous administration of belimumab applies only to pediatric patients with SLE.
The 200-mg injection can be administered once every week for children who weigh ≥ 40 kg and should be given once every 2 weeks for children weighing between 15 and 40 kg.
The autoinjector “will be available immediately” for caregivers, the company announcement said.
“Patients are our top priority, and we are always working to innovate solutions that can improve lives and address unmet needs,” Court Horncastle, senior vice president and head of US specialty at GSK, said in the press release. “This approval for an at-home treatment is the first and only of its kind for children with lupus and is a testament to our continued commitment to the lupus community.”
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved Benlysta (belimumab) autoinjector for patients aged 5 years or older with active systemic lupus erythematosus (SLE) on standard therapy. This is the first time that children with SLE can receive this treatment at home, according to a GSK press release.
Prior to this approval, pediatric patients aged 5 years or older could receive belimumab only intravenously via a 1-hour infusion in a hospital or clinic setting.
“Going to the doctor’s office once every 4 weeks can be a logistical hurdle for some children and their caregivers, so having the option to administer Benlysta in the comfort of their home provides much-needed flexibility,” Mary Crimmings, the interim CEO and senior vice president for marketing and communications at the Lupus Foundation of America, said in a statement.
An estimated 5000-10,000 children in the United States are living with SLE.
Belimumab is a B-lymphocyte stimulator–specific inhibitor approved for the treatment of active SLE and active lupus nephritis in patients aged 5 years or older receiving standard therapy. This approval of the subcutaneous administration of belimumab applies only to pediatric patients with SLE.
The 200-mg injection can be administered once every week for children who weigh ≥ 40 kg and should be given once every 2 weeks for children weighing between 15 and 40 kg.
The autoinjector “will be available immediately” for caregivers, the company announcement said.
“Patients are our top priority, and we are always working to innovate solutions that can improve lives and address unmet needs,” Court Horncastle, senior vice president and head of US specialty at GSK, said in the press release. “This approval for an at-home treatment is the first and only of its kind for children with lupus and is a testament to our continued commitment to the lupus community.”
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved Benlysta (belimumab) autoinjector for patients aged 5 years or older with active systemic lupus erythematosus (SLE) on standard therapy. This is the first time that children with SLE can receive this treatment at home, according to a GSK press release.
Prior to this approval, pediatric patients aged 5 years or older could receive belimumab only intravenously via a 1-hour infusion in a hospital or clinic setting.
“Going to the doctor’s office once every 4 weeks can be a logistical hurdle for some children and their caregivers, so having the option to administer Benlysta in the comfort of their home provides much-needed flexibility,” Mary Crimmings, the interim CEO and senior vice president for marketing and communications at the Lupus Foundation of America, said in a statement.
An estimated 5000-10,000 children in the United States are living with SLE.
Belimumab is a B-lymphocyte stimulator–specific inhibitor approved for the treatment of active SLE and active lupus nephritis in patients aged 5 years or older receiving standard therapy. This approval of the subcutaneous administration of belimumab applies only to pediatric patients with SLE.
The 200-mg injection can be administered once every week for children who weigh ≥ 40 kg and should be given once every 2 weeks for children weighing between 15 and 40 kg.
The autoinjector “will be available immediately” for caregivers, the company announcement said.
“Patients are our top priority, and we are always working to innovate solutions that can improve lives and address unmet needs,” Court Horncastle, senior vice president and head of US specialty at GSK, said in the press release. “This approval for an at-home treatment is the first and only of its kind for children with lupus and is a testament to our continued commitment to the lupus community.”
A version of this article appeared on Medscape.com.
New British Behçet’s Disease Guidelines Emphasize Multidisciplinary Management
LIVERPOOL, ENGLAND — The British Society for Rheumatology (BSR) and the British Association of Dermatologists (BAD) have joined forces for the first time to develop the first British guidelines for the management of people living with Behçet’s disease.
The guidelines will also be the first “living guidelines” produced by either society, which means they will be regularly revised and updated when new evidence emerges that warrants inclusion.
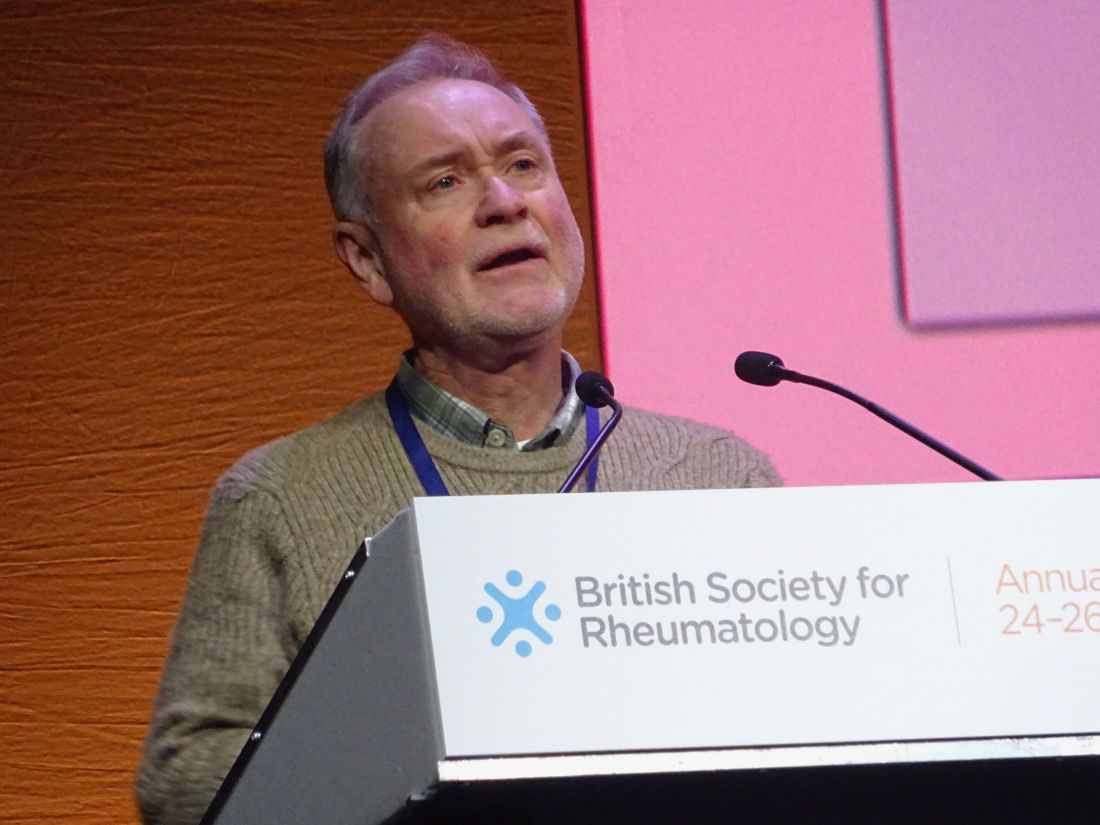
With more than 90 recommendations being made, the new guidelines promise to be the most comprehensive and most up-to-date yet for what is regarded as a rare disease. Robert Moots, MBBS, PhD, provided a “sneak peek” of the guidelines at the annual meeting of the British Society for Rheumatology.
Dr. Moots, professor of rheumatology at the University of Liverpool and a consultant rheumatologist for Liverpool University Hospitals NHS Foundation Trust in England, noted that while the European Alliance of Associations for Rheumatology has produced a guideline for Behçet’s disease, this was last updated in 2018 and is not specific for the population for patients that is seen in the United Kingdom.
The British recommendations will cover all possible manifestations of Behçet’s disease and give practical advice on how to manage everything from the most common presentations such as skin lesions, mouth ulcers, and genital ulcers, as well as the potentially more serious eye, neurological, and vascular involvement.
Importance of Raising Awareness
“Joint and musculoskeletal problems are actually one of the least complained of symptoms in people with Behçet’s, and they often can’t understand why a rheumatologist is seeing them,” Dr. Moot said. “But of course, people do get joint problems, they can get enthesitis and arthralgia.”
Dr. Moots has been leading one of the three National Health Service (NHS) Centres of Excellence for Behçet’s Syndrome in England for more than a decade and told this news organization that diagnosing patients could be challenging. It can take up to 10 years from the first symptoms appearing to getting a diagnosis, so part of the job of the NHS Centres of Excellence is to raise awareness among both the healthcare profession and the general public.
“It’s a condition that people learn about at medical school. Most doctors will have come across it, but because it was thought to be really rare in the UK, nobody perhaps really expects to see it,” Dr. Moot said.
“But we all have these patients,” he added. “In Liverpool, we’re commissioned to be looking after an anticipated 150 people with Behçet’s — we’ve got 700. With more awareness, there’s more diagnoses being made, and people are being looked after better.”
Patient Perspective
Tony Thornburn, OBE, chair of the patient advocacy group Behçet’s UK, agreed in a separate interview that raising awareness of the syndrome was key to improving its management.
“Patients have said that it is a bit like having arthritis, lupus, MS [multiple sclerosis], and Crohn’s [disease] all at once,” Mr. Thorburn said. “So what we need is a guideline to ensure that people know what they’re looking at.”
Mr. Thorburn added, “Guidelines are important for raising awareness but also providing the detailed information that clinicians and GPs [general practitioners] need to have to treat a patient when they come in with this multifaceted condition.”
Multifaceted Means Multidisciplinary Management
Because there can be so many different aspects to managing someone with Behçet’s disease, a multispecialty team that was convened to develop the guidelines agreed that multidisciplinary management should be an overarching theme.
“The guideline development group consisted of all the specialties that you would need for a complex multisystem disease like Behçet’s,” Dr. Moot said. He highlighted that working alongside the consultants in adult and pediatric rheumatology were specialists in dermatology, gastroenterology, neurology, ophthalmology, obstetrics and gynecology, and psychology.
“We’re actually looking at psychological interactions and their impact for the first time,” Dr. Moot said, noting that clinicians needed to “take it seriously, and ask about it.”
Management of Manifestations
One of the general principles of the guidelines is to assess the involvement of each organ system and target treatment accordingly.
“One of the problems is that the evidence base to tell us what to do is pretty low,” Dr. Moots acknowledged. There have been few good quality randomized trials, so “treatment tends to be eminence-based rather than evidence-based.”
The recommendation wording bears this in mind, stating whether a treatment should or should not be offered, or just considered if there is no strong evidence to back up its use.
With regard to musculoskeletal manifestations, the recommendations say that colchicine should be offered, perhaps as a first-line option, or an intraarticular steroid injection in the case of monoarthritis. An intramuscular depot steroid may also be appropriate to offer, and there was good evidence to offer azathioprine or, as an alternative in refractory cases, a tumor necrosis factor (TNF) inhibitor. Nonsteroidal anti-inflammatory drugs, methotrexate, apremilast, secukinumab, and referral to a physiotherapist could only be considered, however, based on weaker levels of evidence for their use.
To treat mucocutaneous disease, the guidelines advise offering topical steroids in the form of ointment for genital ulcers or mouthwash or ointment for oral ulcers. For skin lesions, it is recommended to offer colchicine, azathioprine, mycophenolate mofetil, or TNF inhibitor and to consider the use of apremilast, secukinumab, or dapsone.
Future Work and Revision
“One of the key things we would like to see developing is a national registry,” Dr. Moots said. This would include biobanking samples for future research and possible genomic and phenotyping studies.
More work needs to be done in conducting clinical trials in children and young people with Behçet’s disease, studies to find prognostic factors for neurological disease, and clinical trials of potential new drug approaches such as Janus kinase inhibitors. Importantly, an auditing process needs to be set up to see what effect, if any, the guidelines will actually have onpatient management.
“It’s taken 5 years to today” to develop the guidelines, Dr. Moot said. What form the process of updating them will take still has to be decided, he said in the interview. It is likely that the necessary literature searches will be performed every 6 months or so, but it will be a compromise between the ideal situation and having the staffing time to do it.
“It’s a big ask,” Dr. Moot acknowledged, adding that even if updates were only once a year, it would still be much faster than the 5- or 6-year cycle that it traditionally takes for most guidelines to be updated.
The BSR and BAD’s processes for developing guidelines are accredited by the National Institute for Health and Care Excellence in England. Dr. Moots is the chief investigator for the Secukinumab in Behçet’s trial, which is sponsored by the Liverpool University Hospitals NHS Foundation Trust via grant funding from Novartis.
A version of this article appeared on Medscape.com.
LIVERPOOL, ENGLAND — The British Society for Rheumatology (BSR) and the British Association of Dermatologists (BAD) have joined forces for the first time to develop the first British guidelines for the management of people living with Behçet’s disease.
The guidelines will also be the first “living guidelines” produced by either society, which means they will be regularly revised and updated when new evidence emerges that warrants inclusion.
With more than 90 recommendations being made, the new guidelines promise to be the most comprehensive and most up-to-date yet for what is regarded as a rare disease. Robert Moots, MBBS, PhD, provided a “sneak peek” of the guidelines at the annual meeting of the British Society for Rheumatology.
Dr. Moots, professor of rheumatology at the University of Liverpool and a consultant rheumatologist for Liverpool University Hospitals NHS Foundation Trust in England, noted that while the European Alliance of Associations for Rheumatology has produced a guideline for Behçet’s disease, this was last updated in 2018 and is not specific for the population for patients that is seen in the United Kingdom.
The British recommendations will cover all possible manifestations of Behçet’s disease and give practical advice on how to manage everything from the most common presentations such as skin lesions, mouth ulcers, and genital ulcers, as well as the potentially more serious eye, neurological, and vascular involvement.
Importance of Raising Awareness
“Joint and musculoskeletal problems are actually one of the least complained of symptoms in people with Behçet’s, and they often can’t understand why a rheumatologist is seeing them,” Dr. Moot said. “But of course, people do get joint problems, they can get enthesitis and arthralgia.”
Dr. Moots has been leading one of the three National Health Service (NHS) Centres of Excellence for Behçet’s Syndrome in England for more than a decade and told this news organization that diagnosing patients could be challenging. It can take up to 10 years from the first symptoms appearing to getting a diagnosis, so part of the job of the NHS Centres of Excellence is to raise awareness among both the healthcare profession and the general public.
“It’s a condition that people learn about at medical school. Most doctors will have come across it, but because it was thought to be really rare in the UK, nobody perhaps really expects to see it,” Dr. Moot said.
“But we all have these patients,” he added. “In Liverpool, we’re commissioned to be looking after an anticipated 150 people with Behçet’s — we’ve got 700. With more awareness, there’s more diagnoses being made, and people are being looked after better.”
Patient Perspective
Tony Thornburn, OBE, chair of the patient advocacy group Behçet’s UK, agreed in a separate interview that raising awareness of the syndrome was key to improving its management.
“Patients have said that it is a bit like having arthritis, lupus, MS [multiple sclerosis], and Crohn’s [disease] all at once,” Mr. Thorburn said. “So what we need is a guideline to ensure that people know what they’re looking at.”
Mr. Thorburn added, “Guidelines are important for raising awareness but also providing the detailed information that clinicians and GPs [general practitioners] need to have to treat a patient when they come in with this multifaceted condition.”
Multifaceted Means Multidisciplinary Management
Because there can be so many different aspects to managing someone with Behçet’s disease, a multispecialty team that was convened to develop the guidelines agreed that multidisciplinary management should be an overarching theme.
“The guideline development group consisted of all the specialties that you would need for a complex multisystem disease like Behçet’s,” Dr. Moot said. He highlighted that working alongside the consultants in adult and pediatric rheumatology were specialists in dermatology, gastroenterology, neurology, ophthalmology, obstetrics and gynecology, and psychology.
“We’re actually looking at psychological interactions and their impact for the first time,” Dr. Moot said, noting that clinicians needed to “take it seriously, and ask about it.”
Management of Manifestations
One of the general principles of the guidelines is to assess the involvement of each organ system and target treatment accordingly.
“One of the problems is that the evidence base to tell us what to do is pretty low,” Dr. Moots acknowledged. There have been few good quality randomized trials, so “treatment tends to be eminence-based rather than evidence-based.”
The recommendation wording bears this in mind, stating whether a treatment should or should not be offered, or just considered if there is no strong evidence to back up its use.
With regard to musculoskeletal manifestations, the recommendations say that colchicine should be offered, perhaps as a first-line option, or an intraarticular steroid injection in the case of monoarthritis. An intramuscular depot steroid may also be appropriate to offer, and there was good evidence to offer azathioprine or, as an alternative in refractory cases, a tumor necrosis factor (TNF) inhibitor. Nonsteroidal anti-inflammatory drugs, methotrexate, apremilast, secukinumab, and referral to a physiotherapist could only be considered, however, based on weaker levels of evidence for their use.
To treat mucocutaneous disease, the guidelines advise offering topical steroids in the form of ointment for genital ulcers or mouthwash or ointment for oral ulcers. For skin lesions, it is recommended to offer colchicine, azathioprine, mycophenolate mofetil, or TNF inhibitor and to consider the use of apremilast, secukinumab, or dapsone.
Future Work and Revision
“One of the key things we would like to see developing is a national registry,” Dr. Moots said. This would include biobanking samples for future research and possible genomic and phenotyping studies.
More work needs to be done in conducting clinical trials in children and young people with Behçet’s disease, studies to find prognostic factors for neurological disease, and clinical trials of potential new drug approaches such as Janus kinase inhibitors. Importantly, an auditing process needs to be set up to see what effect, if any, the guidelines will actually have onpatient management.
“It’s taken 5 years to today” to develop the guidelines, Dr. Moot said. What form the process of updating them will take still has to be decided, he said in the interview. It is likely that the necessary literature searches will be performed every 6 months or so, but it will be a compromise between the ideal situation and having the staffing time to do it.
“It’s a big ask,” Dr. Moot acknowledged, adding that even if updates were only once a year, it would still be much faster than the 5- or 6-year cycle that it traditionally takes for most guidelines to be updated.
The BSR and BAD’s processes for developing guidelines are accredited by the National Institute for Health and Care Excellence in England. Dr. Moots is the chief investigator for the Secukinumab in Behçet’s trial, which is sponsored by the Liverpool University Hospitals NHS Foundation Trust via grant funding from Novartis.
A version of this article appeared on Medscape.com.
LIVERPOOL, ENGLAND — The British Society for Rheumatology (BSR) and the British Association of Dermatologists (BAD) have joined forces for the first time to develop the first British guidelines for the management of people living with Behçet’s disease.
The guidelines will also be the first “living guidelines” produced by either society, which means they will be regularly revised and updated when new evidence emerges that warrants inclusion.
With more than 90 recommendations being made, the new guidelines promise to be the most comprehensive and most up-to-date yet for what is regarded as a rare disease. Robert Moots, MBBS, PhD, provided a “sneak peek” of the guidelines at the annual meeting of the British Society for Rheumatology.
Dr. Moots, professor of rheumatology at the University of Liverpool and a consultant rheumatologist for Liverpool University Hospitals NHS Foundation Trust in England, noted that while the European Alliance of Associations for Rheumatology has produced a guideline for Behçet’s disease, this was last updated in 2018 and is not specific for the population for patients that is seen in the United Kingdom.
The British recommendations will cover all possible manifestations of Behçet’s disease and give practical advice on how to manage everything from the most common presentations such as skin lesions, mouth ulcers, and genital ulcers, as well as the potentially more serious eye, neurological, and vascular involvement.
Importance of Raising Awareness
“Joint and musculoskeletal problems are actually one of the least complained of symptoms in people with Behçet’s, and they often can’t understand why a rheumatologist is seeing them,” Dr. Moot said. “But of course, people do get joint problems, they can get enthesitis and arthralgia.”
Dr. Moots has been leading one of the three National Health Service (NHS) Centres of Excellence for Behçet’s Syndrome in England for more than a decade and told this news organization that diagnosing patients could be challenging. It can take up to 10 years from the first symptoms appearing to getting a diagnosis, so part of the job of the NHS Centres of Excellence is to raise awareness among both the healthcare profession and the general public.
“It’s a condition that people learn about at medical school. Most doctors will have come across it, but because it was thought to be really rare in the UK, nobody perhaps really expects to see it,” Dr. Moot said.
“But we all have these patients,” he added. “In Liverpool, we’re commissioned to be looking after an anticipated 150 people with Behçet’s — we’ve got 700. With more awareness, there’s more diagnoses being made, and people are being looked after better.”
Patient Perspective
Tony Thornburn, OBE, chair of the patient advocacy group Behçet’s UK, agreed in a separate interview that raising awareness of the syndrome was key to improving its management.
“Patients have said that it is a bit like having arthritis, lupus, MS [multiple sclerosis], and Crohn’s [disease] all at once,” Mr. Thorburn said. “So what we need is a guideline to ensure that people know what they’re looking at.”
Mr. Thorburn added, “Guidelines are important for raising awareness but also providing the detailed information that clinicians and GPs [general practitioners] need to have to treat a patient when they come in with this multifaceted condition.”
Multifaceted Means Multidisciplinary Management
Because there can be so many different aspects to managing someone with Behçet’s disease, a multispecialty team that was convened to develop the guidelines agreed that multidisciplinary management should be an overarching theme.
“The guideline development group consisted of all the specialties that you would need for a complex multisystem disease like Behçet’s,” Dr. Moot said. He highlighted that working alongside the consultants in adult and pediatric rheumatology were specialists in dermatology, gastroenterology, neurology, ophthalmology, obstetrics and gynecology, and psychology.
“We’re actually looking at psychological interactions and their impact for the first time,” Dr. Moot said, noting that clinicians needed to “take it seriously, and ask about it.”
Management of Manifestations
One of the general principles of the guidelines is to assess the involvement of each organ system and target treatment accordingly.
“One of the problems is that the evidence base to tell us what to do is pretty low,” Dr. Moots acknowledged. There have been few good quality randomized trials, so “treatment tends to be eminence-based rather than evidence-based.”
The recommendation wording bears this in mind, stating whether a treatment should or should not be offered, or just considered if there is no strong evidence to back up its use.
With regard to musculoskeletal manifestations, the recommendations say that colchicine should be offered, perhaps as a first-line option, or an intraarticular steroid injection in the case of monoarthritis. An intramuscular depot steroid may also be appropriate to offer, and there was good evidence to offer azathioprine or, as an alternative in refractory cases, a tumor necrosis factor (TNF) inhibitor. Nonsteroidal anti-inflammatory drugs, methotrexate, apremilast, secukinumab, and referral to a physiotherapist could only be considered, however, based on weaker levels of evidence for their use.
To treat mucocutaneous disease, the guidelines advise offering topical steroids in the form of ointment for genital ulcers or mouthwash or ointment for oral ulcers. For skin lesions, it is recommended to offer colchicine, azathioprine, mycophenolate mofetil, or TNF inhibitor and to consider the use of apremilast, secukinumab, or dapsone.
Future Work and Revision
“One of the key things we would like to see developing is a national registry,” Dr. Moots said. This would include biobanking samples for future research and possible genomic and phenotyping studies.
More work needs to be done in conducting clinical trials in children and young people with Behçet’s disease, studies to find prognostic factors for neurological disease, and clinical trials of potential new drug approaches such as Janus kinase inhibitors. Importantly, an auditing process needs to be set up to see what effect, if any, the guidelines will actually have onpatient management.
“It’s taken 5 years to today” to develop the guidelines, Dr. Moot said. What form the process of updating them will take still has to be decided, he said in the interview. It is likely that the necessary literature searches will be performed every 6 months or so, but it will be a compromise between the ideal situation and having the staffing time to do it.
“It’s a big ask,” Dr. Moot acknowledged, adding that even if updates were only once a year, it would still be much faster than the 5- or 6-year cycle that it traditionally takes for most guidelines to be updated.
The BSR and BAD’s processes for developing guidelines are accredited by the National Institute for Health and Care Excellence in England. Dr. Moots is the chief investigator for the Secukinumab in Behçet’s trial, which is sponsored by the Liverpool University Hospitals NHS Foundation Trust via grant funding from Novartis.
A version of this article appeared on Medscape.com.
FROM BSR 2024
Time to Lung Disease in Patients With Dermatomyositis Subtype Estimated
TOPLINE:
The time interval between onset of interstitial lung disease (ILD) and diagnosis of anti–melanoma differentiation-associated gene 5 (MDA5) antibody-positive dermatomyositis (DM) “has not been well described,” the authors say.
METHODOLOGY:
- , with the former having a particularly high mortality rate.
- In this retrospective cohort study using electronic medical records, researchers evaluated 774 patients with DM between 2008 and 2023 to learn more about the time interval between ILD and the time of an MDA5 antibody-positive DM diagnosis, which has not been well described.
- The primary outcome was ILD diagnosis and time in days between documented ILD and MDA5 antibody-positive DM diagnoses.
TAKEAWAY:
- Overall, 14 patients with DM (1.8%) were diagnosed with MDA5 antibody-positive DM in dermatology, rheumatology, or pulmonology departments (nine women and five men; age, 24-77 years; 79% were White and 7% were Black).
- ILD was diagnosed in 9 of the 14 patients (64%); 6 of the 14 (43%) met the criteria for RPILD. Two cases were diagnosed concurrently and two prior to MDA5 antibody-positive DM diagnosis.
- The median time between ILD and MDA5 antibody-positive DM diagnoses was 163 days.
- Gottron papules/sign and midfacial erythema were the most common dermatologic findings, and no association was seen between cutaneous signs and type of ILD.
IN PRACTICE:
“Establishing an accurate timeline between MDA5 antibody-positive DM and ILD can promote urgency among dermatologists to evaluate extracutaneous manifestations in their management of patients with DM for more accurate risk stratification and appropriate treatment,” the authors wrote.
SOURCE:
This study, led by Rachel R. Lin, from the University of Miami, Miami, Florida, was published online as a research letter in JAMA Dermatology.
LIMITATIONS:
Study limitations were the study’s retrospective design and small sample size.
DISCLOSURES:
No information on study funding was provided. One author reported personal fees from argenX outside this submitted work. Other authors did not disclose any competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
The time interval between onset of interstitial lung disease (ILD) and diagnosis of anti–melanoma differentiation-associated gene 5 (MDA5) antibody-positive dermatomyositis (DM) “has not been well described,” the authors say.
METHODOLOGY:
- , with the former having a particularly high mortality rate.
- In this retrospective cohort study using electronic medical records, researchers evaluated 774 patients with DM between 2008 and 2023 to learn more about the time interval between ILD and the time of an MDA5 antibody-positive DM diagnosis, which has not been well described.
- The primary outcome was ILD diagnosis and time in days between documented ILD and MDA5 antibody-positive DM diagnoses.
TAKEAWAY:
- Overall, 14 patients with DM (1.8%) were diagnosed with MDA5 antibody-positive DM in dermatology, rheumatology, or pulmonology departments (nine women and five men; age, 24-77 years; 79% were White and 7% were Black).
- ILD was diagnosed in 9 of the 14 patients (64%); 6 of the 14 (43%) met the criteria for RPILD. Two cases were diagnosed concurrently and two prior to MDA5 antibody-positive DM diagnosis.
- The median time between ILD and MDA5 antibody-positive DM diagnoses was 163 days.
- Gottron papules/sign and midfacial erythema were the most common dermatologic findings, and no association was seen between cutaneous signs and type of ILD.
IN PRACTICE:
“Establishing an accurate timeline between MDA5 antibody-positive DM and ILD can promote urgency among dermatologists to evaluate extracutaneous manifestations in their management of patients with DM for more accurate risk stratification and appropriate treatment,” the authors wrote.
SOURCE:
This study, led by Rachel R. Lin, from the University of Miami, Miami, Florida, was published online as a research letter in JAMA Dermatology.
LIMITATIONS:
Study limitations were the study’s retrospective design and small sample size.
DISCLOSURES:
No information on study funding was provided. One author reported personal fees from argenX outside this submitted work. Other authors did not disclose any competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
The time interval between onset of interstitial lung disease (ILD) and diagnosis of anti–melanoma differentiation-associated gene 5 (MDA5) antibody-positive dermatomyositis (DM) “has not been well described,” the authors say.
METHODOLOGY:
- , with the former having a particularly high mortality rate.
- In this retrospective cohort study using electronic medical records, researchers evaluated 774 patients with DM between 2008 and 2023 to learn more about the time interval between ILD and the time of an MDA5 antibody-positive DM diagnosis, which has not been well described.
- The primary outcome was ILD diagnosis and time in days between documented ILD and MDA5 antibody-positive DM diagnoses.
TAKEAWAY:
- Overall, 14 patients with DM (1.8%) were diagnosed with MDA5 antibody-positive DM in dermatology, rheumatology, or pulmonology departments (nine women and five men; age, 24-77 years; 79% were White and 7% were Black).
- ILD was diagnosed in 9 of the 14 patients (64%); 6 of the 14 (43%) met the criteria for RPILD. Two cases were diagnosed concurrently and two prior to MDA5 antibody-positive DM diagnosis.
- The median time between ILD and MDA5 antibody-positive DM diagnoses was 163 days.
- Gottron papules/sign and midfacial erythema were the most common dermatologic findings, and no association was seen between cutaneous signs and type of ILD.
IN PRACTICE:
“Establishing an accurate timeline between MDA5 antibody-positive DM and ILD can promote urgency among dermatologists to evaluate extracutaneous manifestations in their management of patients with DM for more accurate risk stratification and appropriate treatment,” the authors wrote.
SOURCE:
This study, led by Rachel R. Lin, from the University of Miami, Miami, Florida, was published online as a research letter in JAMA Dermatology.
LIMITATIONS:
Study limitations were the study’s retrospective design and small sample size.
DISCLOSURES:
No information on study funding was provided. One author reported personal fees from argenX outside this submitted work. Other authors did not disclose any competing interests.
A version of this article appeared on Medscape.com.
Combined Pediatric Derm-Rheum Clinics Supported by Survey Respondents
TOPLINE:
.
METHODOLOGY:
- Combined pediatric dermatology-rheumatology clinics can improve patient outcomes and experiences, particularly for pediatric autoimmune conditions presenting with both cutaneous and systemic manifestations.
- The researchers surveyed 208 pediatric dermatologists working in combined pediatric dermatology-rheumatology clinics.
- A total of 13 member responses were recorded from three countries: 10 from the United States, two from Mexico, and one from Canada.
TAKEAWAY:
- Perceived benefits of combined clinics were improved patient care through coordinated treatment decisions and timely communication between providers.
- Patient satisfaction was favorable, and patients and families endorsed the combined clinic approach.
- Barriers to clinic establishment included differences in the pace between dermatology and rheumatology clinic flow, the need to generate more relative value units, resistance from colleagues, and limited time.
- Areas that needed improvement included more time for patient visits, dedicated research assistants, new patient referrals, additional patient rooms, resources for research, and patient care infrastructure.
IN PRACTICE:
The insights from this survey “will hopefully inspire further development of these combined clinics,” the authors wrote.
SOURCE:
The investigation, led by Olga S. Cherepakhin, BS, University of Washington, Seattle, Washington, was published in Pediatric Dermatology.
LIMITATIONS:
Limitations included the subjective nature, lack of some information, selection bias, and small number of respondents, and the survey reflected the perspective of the pediatric dermatologists only.
DISCLOSURES:
The study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. One author reported full-time employment at Janssen R&D, and the other authors had no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Combined pediatric dermatology-rheumatology clinics can improve patient outcomes and experiences, particularly for pediatric autoimmune conditions presenting with both cutaneous and systemic manifestations.
- The researchers surveyed 208 pediatric dermatologists working in combined pediatric dermatology-rheumatology clinics.
- A total of 13 member responses were recorded from three countries: 10 from the United States, two from Mexico, and one from Canada.
TAKEAWAY:
- Perceived benefits of combined clinics were improved patient care through coordinated treatment decisions and timely communication between providers.
- Patient satisfaction was favorable, and patients and families endorsed the combined clinic approach.
- Barriers to clinic establishment included differences in the pace between dermatology and rheumatology clinic flow, the need to generate more relative value units, resistance from colleagues, and limited time.
- Areas that needed improvement included more time for patient visits, dedicated research assistants, new patient referrals, additional patient rooms, resources for research, and patient care infrastructure.
IN PRACTICE:
The insights from this survey “will hopefully inspire further development of these combined clinics,” the authors wrote.
SOURCE:
The investigation, led by Olga S. Cherepakhin, BS, University of Washington, Seattle, Washington, was published in Pediatric Dermatology.
LIMITATIONS:
Limitations included the subjective nature, lack of some information, selection bias, and small number of respondents, and the survey reflected the perspective of the pediatric dermatologists only.
DISCLOSURES:
The study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. One author reported full-time employment at Janssen R&D, and the other authors had no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Combined pediatric dermatology-rheumatology clinics can improve patient outcomes and experiences, particularly for pediatric autoimmune conditions presenting with both cutaneous and systemic manifestations.
- The researchers surveyed 208 pediatric dermatologists working in combined pediatric dermatology-rheumatology clinics.
- A total of 13 member responses were recorded from three countries: 10 from the United States, two from Mexico, and one from Canada.
TAKEAWAY:
- Perceived benefits of combined clinics were improved patient care through coordinated treatment decisions and timely communication between providers.
- Patient satisfaction was favorable, and patients and families endorsed the combined clinic approach.
- Barriers to clinic establishment included differences in the pace between dermatology and rheumatology clinic flow, the need to generate more relative value units, resistance from colleagues, and limited time.
- Areas that needed improvement included more time for patient visits, dedicated research assistants, new patient referrals, additional patient rooms, resources for research, and patient care infrastructure.
IN PRACTICE:
The insights from this survey “will hopefully inspire further development of these combined clinics,” the authors wrote.
SOURCE:
The investigation, led by Olga S. Cherepakhin, BS, University of Washington, Seattle, Washington, was published in Pediatric Dermatology.
LIMITATIONS:
Limitations included the subjective nature, lack of some information, selection bias, and small number of respondents, and the survey reflected the perspective of the pediatric dermatologists only.
DISCLOSURES:
The study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. One author reported full-time employment at Janssen R&D, and the other authors had no disclosures.
A version of this article appeared on Medscape.com.
Autoimmunity’s Female Bias and the Mysteries of Xist
Female bias in autoimmune disease can be profound, with nine females developing lupus for every male affected, and nearly twice that ratio seen in Sjögren disease.
For years, researchers have worked to determine the reasons for sex-linked differences in immune response and autoimmunity, with environmental factors, sex hormones, and X-chromosome inactivation — the process by which a second X chromosome is silenced — all seen as having roles.
More recently, different groups of researchers have homed in on a long noncoding RNA fragment called X-inactive specific transcript, or Xist, as a potential driver of sex bias in autoimmune disease. Xist, which occurs in female mammals, has been known since the 1990s as the master regulator of X-chromosome inactivation, the process by which the second X chromosome is silenced, averting a fatal double dose of X-linked genes.
The inactivation process, which scientists liken to wrapping the extra X with a fluffy cloud of proteins, occurs early in embryonic development. After its initial work silencing the X, Xist is produced throughout the female’s life, allowing X inactivation to be maintained.
But is it possible that Xist, and the many dozens of proteins it recruits to keep that extra X chromosome silent, can also provoke autoimmunity? This is the question that several teams of researchers have been grappling with, resulting in provocative findings and opening exciting new avenues of discovery.
Xist Protein Complexes Make Male Mice Vulnerable to Lupus
In February, researchers Howard Chang, MD, PhD, and Diana Dou, PhD, of Stanford University in Stanford, California, made worldwide news when they published results from an experiment using male mice genetically engineered to carry a non-silencing form of Xist on one of their chromosomes.
Xist acts like a scaffold, recruiting multiple protein complexes to help it do its job. Dr. Dou explained in an interview that her team has been eyeing suspiciously for years the dozens of proteins Xist recruits in the process of X-chromosome inactivation, many of which are known autoantigens.
When the mice were injected with pristane, a chemical that induces lupus-like autoimmunity in mice, the Xist-producing males developed symptoms at a rate similar to that of females, while wild-type male mice did not.
By using a male model, the scientists could determine whether Xist could cause an increased vulnerability for autoimmunity absent the influence of female hormones and development. “Everything else about the animal is male,” Dr. Dou commented. “You just add the formation of the Xist ribonucleoprotein particles — Xist RNA plus the associating proteins — to male cells that would not ordinarily have these particles. Is just having the particles present in these animals sufficient to increase their autoimmunity? This is what our paper showed: That just having expression of Xist, the presence of these Xist [ribonucleoproteins], is enough in permissive genetic backgrounds to invoke higher incidence and severity of autoimmune disease development in our pristane-induced lupus model.”
The Stanford group sees the Xist protein complex, which they have studied extensively, as a key to understanding how Xist might provoke autoimmunity. Nonetheless, Dr. Dou said, “It’s important to note that there are other contributing factors, which is why not all females develop autoimmunity, and we had very different results in our autoimmune-resistant mouse strain compared to the more autoimmune-prone strain. Xist is a factor, but many factors are required to subvert the checkpoints in immune balance and allow the progression to full-blown autoimmunity.”
Faulty X Inactivation and Gene Escape
The understanding that Xist might be implicated in autoimmune disease — and explain some of its female bias — is not new.
About a decade ago, Montserrat Anguera, PhD, a biologist at the University of Pennsylvania, Philadelphia, began looking at the relationship of X-chromosome inactivation, which by definition involves Xist, and lupus.
Dr. Anguera hypothesized that imperfect X inactivation allowed for greater escape of genes associated with immunity and autoimmunity. Studying patients with lupus, Dr. Anguera found that the silencing process was abnormal, allowing more of these genes to escape the silenced X — including toll-like receptor 7 (TLR-7) and other genes implicated in the pathogenesis of lupus.
“If you get increased expression of certain genes from the [silenced] X, like TLR-7, it can result in autoimmune disease,” Dr. Anguera said. “So what we think is that in the lupus patients, because the silencing is impacted, you’re going to have more expression happening from the inactive X. And then in conjunction with the active X, that’s going to throw off the dosage [of autoimmunity-linked genes]. You’re changing the dosage of genes, and that’s what’s critical.”
Even among patients with lupus whose symptoms are well controlled with medication, “if you look at their T cells and B cells, they still have messed up X inactivation,” Dr. Anguera said. “The Xist RNA that’s supposed to be tethered to the inactive X in a fluffy cloud is not localized, and instead is dispersed all over the nucleus.”
Dr. Anguera pointed out that autoimmune diseases are complex and can result from a combination of factors. “You also have a host of hormonal and environmental contributors, such as previous viral infections,” she said. And of course men can also develop lupus, meaning that the X chromosome cannot explain everything.
Dr. Anguera said that, while the findings by the Stanford scientists do not explain the full pathogenesis of lupus and related diseases, they still support a strong role for Xist in sex-biased autoimmune diseases. “It’s sort of another take on it,” she said.
Is It the Proteins, the RNA, or Both?
The Stanford team points to the proteins recruited by Xist in the process of X-chromosome inactivation as the likely trigger of autoimmunity. However, a group of researchers at Johns Hopkins University in Baltimore, Maryland, made the case in a 2022 paper that Xist RNA itself was dangerous. They found that numerous short RNA sequences within the Xist molecule serve as ligands for TLR-7. And TLR-7 ligation causes plasmacytoid dendritic cells to overproduce type 1 interferon, a classic hallmark of lupus.
“Within rheumatology, the diseases that tend to be most female biased are the ones that are antibody positive and have this presence of upregulated interferon,” explained Brendan Antiochos, MD. “Lupus is an example of that. Sjögren’s syndrome is another. So there’s always been this quest to want to understand the mechanisms that explain why women would have more autoimmunity. And are there specific pathways which could contribute? One of the key pathways that’s been shown in humans and in mice to be important in lupus is toll-like receptor signaling.” Most convincingly, one recent study showed that people who have a gain-of-function mutation in their TLR-7 gene get a spontaneous form of lupus.
These findings led Erika Darrah, PhD, and her colleague Dr. Antiochos to begin looking more deeply into which RNAs could be triggering this signaling pathway. “We started to think: Well, there is this sex bias. Could it be that women have unique RNAs that could potentially act as triggers for TLR-7 signaling?” Dr. Darrah said.
Dr. Darrah and Dr. Antiochos looked at publicly available genetic data to identify sex-biased sources of self-RNA containing TLR-7 ligands. Xist, they found, was chock full of them. “Every time we analyzed that data, no matter what filter we applied, Xist kept popping out over and over again as the most highly female skewed RNA, the RNA most likely to contain these TLR-7 binding motifs,” Dr. Darrah said. “We started to formulate the hypothesis that Xist was actually promoting responses that were dangerous and pathogenic in lupus.”
That finding led the team to conduct in-vitro experiments that showed different fragments of Xist can activate TLR-7, resulting in higher interferon production. Finally, they looked at blood and kidney cells from women with lupus and found that higher Xist expression correlated with more interferon production, and higher disease activity. “The more Xist, the sicker people were,” Dr. Darrah said.
Xist’s Other Functions
Xist was first studied in the 1990s, and most research has centered on its primary role in X-chromosome inactivation. A research group led by Kathrin Plath, PhD, at the University of California, Los Angeles, has been occupied for years with untangling exactly how Xist does what it does. “It’s a very clever RNA, right? It can silence the whole chromosome,” Dr. Plath said in an interview.
In 2021, Dr. Plath and her colleagues established in detail how Xist executes silencing, setting down pairs of molecules in specific spots along the chromosome and building huge protein clouds around them. “We worked on learning where Xist binds and what proteins it binds, drilling down to understand how these proteins and the RNA are coming together.”
Dr. Plath has long suspected that Xist has other functions besides X inactivation, and she and her colleagues are starting to identify them. Early this year they published the surprising finding that Xist can regulate gene expression in autosomes, or non–sex-linked chromosomes, “which it might well also do in cancer cells and lymphocytes,” Dr. Plath said. “And now there is this new evidence of an autoimmune function,” she said. “It’s a super exciting time.”
The different hypotheses surrounding Xist’s role in sex-biased autoimmunity aren’t mutually exclusive, Dr. Plath said. “There’s a tremendous enrichment of proteins occurring” during X inactivation, she said, supporting the Stanford team’s hypothesis that proteins are triggering autoimmunity. As for the Johns Hopkins researchers’ understanding that Xist RNA itself is the trigger, “I’m totally open to that,” she said. “Why can’t it be an autoantigen?”
The other model in the field, Dr. Plath noted, is the one proposed by Dr. Anguera — “that there’s [gene] escape from X-inactivation — that females have more escape expression, and that Xist is more dispersed in the lymphocytes [of patients with lupus]. In fact, Xist becoming a little dispersed might make it a better antigen. So I do think everything is possible.”
The plethora of new findings related to autoimmunity has caused Dr. Plath to consider redirecting her lab’s focus toward more translational work, “because we are obviously good at studying Xist.” Among the mysteries Dr. Plath would like to solve is how some genes manage to escape the Xist cloud.
What is needed, she said, is collaboration. “Everyone will come up with different ideas. So I think it’s good to have more people look at things together. Then the field will achieve a breakthrough treatment.”
Female bias in autoimmune disease can be profound, with nine females developing lupus for every male affected, and nearly twice that ratio seen in Sjögren disease.
For years, researchers have worked to determine the reasons for sex-linked differences in immune response and autoimmunity, with environmental factors, sex hormones, and X-chromosome inactivation — the process by which a second X chromosome is silenced — all seen as having roles.
More recently, different groups of researchers have homed in on a long noncoding RNA fragment called X-inactive specific transcript, or Xist, as a potential driver of sex bias in autoimmune disease. Xist, which occurs in female mammals, has been known since the 1990s as the master regulator of X-chromosome inactivation, the process by which the second X chromosome is silenced, averting a fatal double dose of X-linked genes.
The inactivation process, which scientists liken to wrapping the extra X with a fluffy cloud of proteins, occurs early in embryonic development. After its initial work silencing the X, Xist is produced throughout the female’s life, allowing X inactivation to be maintained.
But is it possible that Xist, and the many dozens of proteins it recruits to keep that extra X chromosome silent, can also provoke autoimmunity? This is the question that several teams of researchers have been grappling with, resulting in provocative findings and opening exciting new avenues of discovery.
Xist Protein Complexes Make Male Mice Vulnerable to Lupus
In February, researchers Howard Chang, MD, PhD, and Diana Dou, PhD, of Stanford University in Stanford, California, made worldwide news when they published results from an experiment using male mice genetically engineered to carry a non-silencing form of Xist on one of their chromosomes.
Xist acts like a scaffold, recruiting multiple protein complexes to help it do its job. Dr. Dou explained in an interview that her team has been eyeing suspiciously for years the dozens of proteins Xist recruits in the process of X-chromosome inactivation, many of which are known autoantigens.
When the mice were injected with pristane, a chemical that induces lupus-like autoimmunity in mice, the Xist-producing males developed symptoms at a rate similar to that of females, while wild-type male mice did not.
By using a male model, the scientists could determine whether Xist could cause an increased vulnerability for autoimmunity absent the influence of female hormones and development. “Everything else about the animal is male,” Dr. Dou commented. “You just add the formation of the Xist ribonucleoprotein particles — Xist RNA plus the associating proteins — to male cells that would not ordinarily have these particles. Is just having the particles present in these animals sufficient to increase their autoimmunity? This is what our paper showed: That just having expression of Xist, the presence of these Xist [ribonucleoproteins], is enough in permissive genetic backgrounds to invoke higher incidence and severity of autoimmune disease development in our pristane-induced lupus model.”
The Stanford group sees the Xist protein complex, which they have studied extensively, as a key to understanding how Xist might provoke autoimmunity. Nonetheless, Dr. Dou said, “It’s important to note that there are other contributing factors, which is why not all females develop autoimmunity, and we had very different results in our autoimmune-resistant mouse strain compared to the more autoimmune-prone strain. Xist is a factor, but many factors are required to subvert the checkpoints in immune balance and allow the progression to full-blown autoimmunity.”
Faulty X Inactivation and Gene Escape
The understanding that Xist might be implicated in autoimmune disease — and explain some of its female bias — is not new.
About a decade ago, Montserrat Anguera, PhD, a biologist at the University of Pennsylvania, Philadelphia, began looking at the relationship of X-chromosome inactivation, which by definition involves Xist, and lupus.
Dr. Anguera hypothesized that imperfect X inactivation allowed for greater escape of genes associated with immunity and autoimmunity. Studying patients with lupus, Dr. Anguera found that the silencing process was abnormal, allowing more of these genes to escape the silenced X — including toll-like receptor 7 (TLR-7) and other genes implicated in the pathogenesis of lupus.
“If you get increased expression of certain genes from the [silenced] X, like TLR-7, it can result in autoimmune disease,” Dr. Anguera said. “So what we think is that in the lupus patients, because the silencing is impacted, you’re going to have more expression happening from the inactive X. And then in conjunction with the active X, that’s going to throw off the dosage [of autoimmunity-linked genes]. You’re changing the dosage of genes, and that’s what’s critical.”
Even among patients with lupus whose symptoms are well controlled with medication, “if you look at their T cells and B cells, they still have messed up X inactivation,” Dr. Anguera said. “The Xist RNA that’s supposed to be tethered to the inactive X in a fluffy cloud is not localized, and instead is dispersed all over the nucleus.”
Dr. Anguera pointed out that autoimmune diseases are complex and can result from a combination of factors. “You also have a host of hormonal and environmental contributors, such as previous viral infections,” she said. And of course men can also develop lupus, meaning that the X chromosome cannot explain everything.
Dr. Anguera said that, while the findings by the Stanford scientists do not explain the full pathogenesis of lupus and related diseases, they still support a strong role for Xist in sex-biased autoimmune diseases. “It’s sort of another take on it,” she said.
Is It the Proteins, the RNA, or Both?
The Stanford team points to the proteins recruited by Xist in the process of X-chromosome inactivation as the likely trigger of autoimmunity. However, a group of researchers at Johns Hopkins University in Baltimore, Maryland, made the case in a 2022 paper that Xist RNA itself was dangerous. They found that numerous short RNA sequences within the Xist molecule serve as ligands for TLR-7. And TLR-7 ligation causes plasmacytoid dendritic cells to overproduce type 1 interferon, a classic hallmark of lupus.
“Within rheumatology, the diseases that tend to be most female biased are the ones that are antibody positive and have this presence of upregulated interferon,” explained Brendan Antiochos, MD. “Lupus is an example of that. Sjögren’s syndrome is another. So there’s always been this quest to want to understand the mechanisms that explain why women would have more autoimmunity. And are there specific pathways which could contribute? One of the key pathways that’s been shown in humans and in mice to be important in lupus is toll-like receptor signaling.” Most convincingly, one recent study showed that people who have a gain-of-function mutation in their TLR-7 gene get a spontaneous form of lupus.
These findings led Erika Darrah, PhD, and her colleague Dr. Antiochos to begin looking more deeply into which RNAs could be triggering this signaling pathway. “We started to think: Well, there is this sex bias. Could it be that women have unique RNAs that could potentially act as triggers for TLR-7 signaling?” Dr. Darrah said.
Dr. Darrah and Dr. Antiochos looked at publicly available genetic data to identify sex-biased sources of self-RNA containing TLR-7 ligands. Xist, they found, was chock full of them. “Every time we analyzed that data, no matter what filter we applied, Xist kept popping out over and over again as the most highly female skewed RNA, the RNA most likely to contain these TLR-7 binding motifs,” Dr. Darrah said. “We started to formulate the hypothesis that Xist was actually promoting responses that were dangerous and pathogenic in lupus.”
That finding led the team to conduct in-vitro experiments that showed different fragments of Xist can activate TLR-7, resulting in higher interferon production. Finally, they looked at blood and kidney cells from women with lupus and found that higher Xist expression correlated with more interferon production, and higher disease activity. “The more Xist, the sicker people were,” Dr. Darrah said.
Xist’s Other Functions
Xist was first studied in the 1990s, and most research has centered on its primary role in X-chromosome inactivation. A research group led by Kathrin Plath, PhD, at the University of California, Los Angeles, has been occupied for years with untangling exactly how Xist does what it does. “It’s a very clever RNA, right? It can silence the whole chromosome,” Dr. Plath said in an interview.
In 2021, Dr. Plath and her colleagues established in detail how Xist executes silencing, setting down pairs of molecules in specific spots along the chromosome and building huge protein clouds around them. “We worked on learning where Xist binds and what proteins it binds, drilling down to understand how these proteins and the RNA are coming together.”
Dr. Plath has long suspected that Xist has other functions besides X inactivation, and she and her colleagues are starting to identify them. Early this year they published the surprising finding that Xist can regulate gene expression in autosomes, or non–sex-linked chromosomes, “which it might well also do in cancer cells and lymphocytes,” Dr. Plath said. “And now there is this new evidence of an autoimmune function,” she said. “It’s a super exciting time.”
The different hypotheses surrounding Xist’s role in sex-biased autoimmunity aren’t mutually exclusive, Dr. Plath said. “There’s a tremendous enrichment of proteins occurring” during X inactivation, she said, supporting the Stanford team’s hypothesis that proteins are triggering autoimmunity. As for the Johns Hopkins researchers’ understanding that Xist RNA itself is the trigger, “I’m totally open to that,” she said. “Why can’t it be an autoantigen?”
The other model in the field, Dr. Plath noted, is the one proposed by Dr. Anguera — “that there’s [gene] escape from X-inactivation — that females have more escape expression, and that Xist is more dispersed in the lymphocytes [of patients with lupus]. In fact, Xist becoming a little dispersed might make it a better antigen. So I do think everything is possible.”
The plethora of new findings related to autoimmunity has caused Dr. Plath to consider redirecting her lab’s focus toward more translational work, “because we are obviously good at studying Xist.” Among the mysteries Dr. Plath would like to solve is how some genes manage to escape the Xist cloud.
What is needed, she said, is collaboration. “Everyone will come up with different ideas. So I think it’s good to have more people look at things together. Then the field will achieve a breakthrough treatment.”
Female bias in autoimmune disease can be profound, with nine females developing lupus for every male affected, and nearly twice that ratio seen in Sjögren disease.
For years, researchers have worked to determine the reasons for sex-linked differences in immune response and autoimmunity, with environmental factors, sex hormones, and X-chromosome inactivation — the process by which a second X chromosome is silenced — all seen as having roles.
More recently, different groups of researchers have homed in on a long noncoding RNA fragment called X-inactive specific transcript, or Xist, as a potential driver of sex bias in autoimmune disease. Xist, which occurs in female mammals, has been known since the 1990s as the master regulator of X-chromosome inactivation, the process by which the second X chromosome is silenced, averting a fatal double dose of X-linked genes.
The inactivation process, which scientists liken to wrapping the extra X with a fluffy cloud of proteins, occurs early in embryonic development. After its initial work silencing the X, Xist is produced throughout the female’s life, allowing X inactivation to be maintained.
But is it possible that Xist, and the many dozens of proteins it recruits to keep that extra X chromosome silent, can also provoke autoimmunity? This is the question that several teams of researchers have been grappling with, resulting in provocative findings and opening exciting new avenues of discovery.
Xist Protein Complexes Make Male Mice Vulnerable to Lupus
In February, researchers Howard Chang, MD, PhD, and Diana Dou, PhD, of Stanford University in Stanford, California, made worldwide news when they published results from an experiment using male mice genetically engineered to carry a non-silencing form of Xist on one of their chromosomes.
Xist acts like a scaffold, recruiting multiple protein complexes to help it do its job. Dr. Dou explained in an interview that her team has been eyeing suspiciously for years the dozens of proteins Xist recruits in the process of X-chromosome inactivation, many of which are known autoantigens.
When the mice were injected with pristane, a chemical that induces lupus-like autoimmunity in mice, the Xist-producing males developed symptoms at a rate similar to that of females, while wild-type male mice did not.
By using a male model, the scientists could determine whether Xist could cause an increased vulnerability for autoimmunity absent the influence of female hormones and development. “Everything else about the animal is male,” Dr. Dou commented. “You just add the formation of the Xist ribonucleoprotein particles — Xist RNA plus the associating proteins — to male cells that would not ordinarily have these particles. Is just having the particles present in these animals sufficient to increase their autoimmunity? This is what our paper showed: That just having expression of Xist, the presence of these Xist [ribonucleoproteins], is enough in permissive genetic backgrounds to invoke higher incidence and severity of autoimmune disease development in our pristane-induced lupus model.”
The Stanford group sees the Xist protein complex, which they have studied extensively, as a key to understanding how Xist might provoke autoimmunity. Nonetheless, Dr. Dou said, “It’s important to note that there are other contributing factors, which is why not all females develop autoimmunity, and we had very different results in our autoimmune-resistant mouse strain compared to the more autoimmune-prone strain. Xist is a factor, but many factors are required to subvert the checkpoints in immune balance and allow the progression to full-blown autoimmunity.”
Faulty X Inactivation and Gene Escape
The understanding that Xist might be implicated in autoimmune disease — and explain some of its female bias — is not new.
About a decade ago, Montserrat Anguera, PhD, a biologist at the University of Pennsylvania, Philadelphia, began looking at the relationship of X-chromosome inactivation, which by definition involves Xist, and lupus.
Dr. Anguera hypothesized that imperfect X inactivation allowed for greater escape of genes associated with immunity and autoimmunity. Studying patients with lupus, Dr. Anguera found that the silencing process was abnormal, allowing more of these genes to escape the silenced X — including toll-like receptor 7 (TLR-7) and other genes implicated in the pathogenesis of lupus.
“If you get increased expression of certain genes from the [silenced] X, like TLR-7, it can result in autoimmune disease,” Dr. Anguera said. “So what we think is that in the lupus patients, because the silencing is impacted, you’re going to have more expression happening from the inactive X. And then in conjunction with the active X, that’s going to throw off the dosage [of autoimmunity-linked genes]. You’re changing the dosage of genes, and that’s what’s critical.”
Even among patients with lupus whose symptoms are well controlled with medication, “if you look at their T cells and B cells, they still have messed up X inactivation,” Dr. Anguera said. “The Xist RNA that’s supposed to be tethered to the inactive X in a fluffy cloud is not localized, and instead is dispersed all over the nucleus.”
Dr. Anguera pointed out that autoimmune diseases are complex and can result from a combination of factors. “You also have a host of hormonal and environmental contributors, such as previous viral infections,” she said. And of course men can also develop lupus, meaning that the X chromosome cannot explain everything.
Dr. Anguera said that, while the findings by the Stanford scientists do not explain the full pathogenesis of lupus and related diseases, they still support a strong role for Xist in sex-biased autoimmune diseases. “It’s sort of another take on it,” she said.
Is It the Proteins, the RNA, or Both?
The Stanford team points to the proteins recruited by Xist in the process of X-chromosome inactivation as the likely trigger of autoimmunity. However, a group of researchers at Johns Hopkins University in Baltimore, Maryland, made the case in a 2022 paper that Xist RNA itself was dangerous. They found that numerous short RNA sequences within the Xist molecule serve as ligands for TLR-7. And TLR-7 ligation causes plasmacytoid dendritic cells to overproduce type 1 interferon, a classic hallmark of lupus.
“Within rheumatology, the diseases that tend to be most female biased are the ones that are antibody positive and have this presence of upregulated interferon,” explained Brendan Antiochos, MD. “Lupus is an example of that. Sjögren’s syndrome is another. So there’s always been this quest to want to understand the mechanisms that explain why women would have more autoimmunity. And are there specific pathways which could contribute? One of the key pathways that’s been shown in humans and in mice to be important in lupus is toll-like receptor signaling.” Most convincingly, one recent study showed that people who have a gain-of-function mutation in their TLR-7 gene get a spontaneous form of lupus.
These findings led Erika Darrah, PhD, and her colleague Dr. Antiochos to begin looking more deeply into which RNAs could be triggering this signaling pathway. “We started to think: Well, there is this sex bias. Could it be that women have unique RNAs that could potentially act as triggers for TLR-7 signaling?” Dr. Darrah said.
Dr. Darrah and Dr. Antiochos looked at publicly available genetic data to identify sex-biased sources of self-RNA containing TLR-7 ligands. Xist, they found, was chock full of them. “Every time we analyzed that data, no matter what filter we applied, Xist kept popping out over and over again as the most highly female skewed RNA, the RNA most likely to contain these TLR-7 binding motifs,” Dr. Darrah said. “We started to formulate the hypothesis that Xist was actually promoting responses that were dangerous and pathogenic in lupus.”
That finding led the team to conduct in-vitro experiments that showed different fragments of Xist can activate TLR-7, resulting in higher interferon production. Finally, they looked at blood and kidney cells from women with lupus and found that higher Xist expression correlated with more interferon production, and higher disease activity. “The more Xist, the sicker people were,” Dr. Darrah said.
Xist’s Other Functions
Xist was first studied in the 1990s, and most research has centered on its primary role in X-chromosome inactivation. A research group led by Kathrin Plath, PhD, at the University of California, Los Angeles, has been occupied for years with untangling exactly how Xist does what it does. “It’s a very clever RNA, right? It can silence the whole chromosome,” Dr. Plath said in an interview.
In 2021, Dr. Plath and her colleagues established in detail how Xist executes silencing, setting down pairs of molecules in specific spots along the chromosome and building huge protein clouds around them. “We worked on learning where Xist binds and what proteins it binds, drilling down to understand how these proteins and the RNA are coming together.”
Dr. Plath has long suspected that Xist has other functions besides X inactivation, and she and her colleagues are starting to identify them. Early this year they published the surprising finding that Xist can regulate gene expression in autosomes, or non–sex-linked chromosomes, “which it might well also do in cancer cells and lymphocytes,” Dr. Plath said. “And now there is this new evidence of an autoimmune function,” she said. “It’s a super exciting time.”
The different hypotheses surrounding Xist’s role in sex-biased autoimmunity aren’t mutually exclusive, Dr. Plath said. “There’s a tremendous enrichment of proteins occurring” during X inactivation, she said, supporting the Stanford team’s hypothesis that proteins are triggering autoimmunity. As for the Johns Hopkins researchers’ understanding that Xist RNA itself is the trigger, “I’m totally open to that,” she said. “Why can’t it be an autoantigen?”
The other model in the field, Dr. Plath noted, is the one proposed by Dr. Anguera — “that there’s [gene] escape from X-inactivation — that females have more escape expression, and that Xist is more dispersed in the lymphocytes [of patients with lupus]. In fact, Xist becoming a little dispersed might make it a better antigen. So I do think everything is possible.”
The plethora of new findings related to autoimmunity has caused Dr. Plath to consider redirecting her lab’s focus toward more translational work, “because we are obviously good at studying Xist.” Among the mysteries Dr. Plath would like to solve is how some genes manage to escape the Xist cloud.
What is needed, she said, is collaboration. “Everyone will come up with different ideas. So I think it’s good to have more people look at things together. Then the field will achieve a breakthrough treatment.”
Safe Steroid Tapering in Lupus: Reducing Flares, Damage
TOPLINE:
Tapering glucocorticoids (GCs) does not increase the risk for flare in modified serologically active clinically quiescent (mSACQ) patients with systemic lupus erythematosus (SLE) with a low daily exposure to GC.
METHODOLOGY:
- Previous research has indicated that SACQ SLE is associated with an increased risk for flare after low-dose GC withdrawal.
- Researchers assessed the risk for flare and damage accrual after tapering GCs in mSACQ patients with SLE.
- They used data from the Asia Pacific Lupus Collaboration (APLC) to study 1850 patients (mean age, 40 years; 91.6% women) who met the criteria for SLE, including the definition of mSACQ at least once during observation and being followed up for 2 years after the first mSACQ visit.
- mSACQ was defined as a condition with serological activity but without clinical activity managed with ≤ 7.5 mg/d of -equivalent GCs, regardless of duration.
- The primary outcome was disease flare (both severe and overall) on the basis of the SELENA-SLEDAI flare index definitions.
TAKEAWAY:
- A total of 742 patients experienced an overall flare, 271 experienced a severe flare, and 180 experienced damage accrual.
- Reducing the prednisolone-equivalent GC dosage by 1 mg/d did not increase the risk for an overall (P = .27) or severe (P = .11) flare in patients initially on prednisolone-equivalent GC dosages of 0-7.5 mg/d.
- Antimalarial use decreased the risk for overall (hazard ratio [HR], 0.78; P = .002) and severe (HR, 0.59; P < .001) flares, and immunosuppressant use decreased the risk for severe flares (HR, 0.77; P = .043) but not overall flares.
- Reducing the GC dosage by 1 mg/d reduced the risk for damage accrual by 4% in patients who started taking prednisolone at a dose > 5 but ≤ 7.5 mg/d (P = .007).
IN PRACTICE:
“Cautious tapering of GCs is a feasible option for mSACQ-SLE with low daily exposure to GCs (≤ 7.5 mg/d of prednisolone-equivalent) and can reduce GC burden,” wrote the authors.
SOURCE:
The study, led by Yasuhiro Katsumata, Division of Rheumatology, Tokyo Women’s Medical University School of Medicine, Tokyo, Japan, was published online in Annals of the Rheumatic Diseases.
LIMITATIONS:
The data were collected retrospectively. A short follow-up duration might have prevented the demonstration of clear benefits in terms of damage accrual among patients receiving < 5 mg of GCs. Moreover, the findings may have limited generalizability as the majority of patients had Asian ancestry.
DISCLOSURES:
This work was supported by grants and funding from AstraZeneca, Bristol-Myers Squibb, Eli Lily, Janssen, Merck Serono, UCB, GlaxoSmithKline, Australia, and others to APLC. Some of the authors declared receiving honoraria, consulting fees, research grants, and research support from various sources.
A version of this article appeared on Medscape.com.
TOPLINE:
Tapering glucocorticoids (GCs) does not increase the risk for flare in modified serologically active clinically quiescent (mSACQ) patients with systemic lupus erythematosus (SLE) with a low daily exposure to GC.
METHODOLOGY:
- Previous research has indicated that SACQ SLE is associated with an increased risk for flare after low-dose GC withdrawal.
- Researchers assessed the risk for flare and damage accrual after tapering GCs in mSACQ patients with SLE.
- They used data from the Asia Pacific Lupus Collaboration (APLC) to study 1850 patients (mean age, 40 years; 91.6% women) who met the criteria for SLE, including the definition of mSACQ at least once during observation and being followed up for 2 years after the first mSACQ visit.
- mSACQ was defined as a condition with serological activity but without clinical activity managed with ≤ 7.5 mg/d of -equivalent GCs, regardless of duration.
- The primary outcome was disease flare (both severe and overall) on the basis of the SELENA-SLEDAI flare index definitions.
TAKEAWAY:
- A total of 742 patients experienced an overall flare, 271 experienced a severe flare, and 180 experienced damage accrual.
- Reducing the prednisolone-equivalent GC dosage by 1 mg/d did not increase the risk for an overall (P = .27) or severe (P = .11) flare in patients initially on prednisolone-equivalent GC dosages of 0-7.5 mg/d.
- Antimalarial use decreased the risk for overall (hazard ratio [HR], 0.78; P = .002) and severe (HR, 0.59; P < .001) flares, and immunosuppressant use decreased the risk for severe flares (HR, 0.77; P = .043) but not overall flares.
- Reducing the GC dosage by 1 mg/d reduced the risk for damage accrual by 4% in patients who started taking prednisolone at a dose > 5 but ≤ 7.5 mg/d (P = .007).
IN PRACTICE:
“Cautious tapering of GCs is a feasible option for mSACQ-SLE with low daily exposure to GCs (≤ 7.5 mg/d of prednisolone-equivalent) and can reduce GC burden,” wrote the authors.
SOURCE:
The study, led by Yasuhiro Katsumata, Division of Rheumatology, Tokyo Women’s Medical University School of Medicine, Tokyo, Japan, was published online in Annals of the Rheumatic Diseases.
LIMITATIONS:
The data were collected retrospectively. A short follow-up duration might have prevented the demonstration of clear benefits in terms of damage accrual among patients receiving < 5 mg of GCs. Moreover, the findings may have limited generalizability as the majority of patients had Asian ancestry.
DISCLOSURES:
This work was supported by grants and funding from AstraZeneca, Bristol-Myers Squibb, Eli Lily, Janssen, Merck Serono, UCB, GlaxoSmithKline, Australia, and others to APLC. Some of the authors declared receiving honoraria, consulting fees, research grants, and research support from various sources.
A version of this article appeared on Medscape.com.
TOPLINE:
Tapering glucocorticoids (GCs) does not increase the risk for flare in modified serologically active clinically quiescent (mSACQ) patients with systemic lupus erythematosus (SLE) with a low daily exposure to GC.
METHODOLOGY:
- Previous research has indicated that SACQ SLE is associated with an increased risk for flare after low-dose GC withdrawal.
- Researchers assessed the risk for flare and damage accrual after tapering GCs in mSACQ patients with SLE.
- They used data from the Asia Pacific Lupus Collaboration (APLC) to study 1850 patients (mean age, 40 years; 91.6% women) who met the criteria for SLE, including the definition of mSACQ at least once during observation and being followed up for 2 years after the first mSACQ visit.
- mSACQ was defined as a condition with serological activity but without clinical activity managed with ≤ 7.5 mg/d of -equivalent GCs, regardless of duration.
- The primary outcome was disease flare (both severe and overall) on the basis of the SELENA-SLEDAI flare index definitions.
TAKEAWAY:
- A total of 742 patients experienced an overall flare, 271 experienced a severe flare, and 180 experienced damage accrual.
- Reducing the prednisolone-equivalent GC dosage by 1 mg/d did not increase the risk for an overall (P = .27) or severe (P = .11) flare in patients initially on prednisolone-equivalent GC dosages of 0-7.5 mg/d.
- Antimalarial use decreased the risk for overall (hazard ratio [HR], 0.78; P = .002) and severe (HR, 0.59; P < .001) flares, and immunosuppressant use decreased the risk for severe flares (HR, 0.77; P = .043) but not overall flares.
- Reducing the GC dosage by 1 mg/d reduced the risk for damage accrual by 4% in patients who started taking prednisolone at a dose > 5 but ≤ 7.5 mg/d (P = .007).
IN PRACTICE:
“Cautious tapering of GCs is a feasible option for mSACQ-SLE with low daily exposure to GCs (≤ 7.5 mg/d of prednisolone-equivalent) and can reduce GC burden,” wrote the authors.
SOURCE:
The study, led by Yasuhiro Katsumata, Division of Rheumatology, Tokyo Women’s Medical University School of Medicine, Tokyo, Japan, was published online in Annals of the Rheumatic Diseases.
LIMITATIONS:
The data were collected retrospectively. A short follow-up duration might have prevented the demonstration of clear benefits in terms of damage accrual among patients receiving < 5 mg of GCs. Moreover, the findings may have limited generalizability as the majority of patients had Asian ancestry.
DISCLOSURES:
This work was supported by grants and funding from AstraZeneca, Bristol-Myers Squibb, Eli Lily, Janssen, Merck Serono, UCB, GlaxoSmithKline, Australia, and others to APLC. Some of the authors declared receiving honoraria, consulting fees, research grants, and research support from various sources.
A version of this article appeared on Medscape.com.
Autoimmune Disease Risk May Rise Following Cushing Disease Remission After Surgery
Patients with Cushing disease have an increased risk for new-onset autoimmune disease in the 3 years after surgical remission, according to a new retrospective study published on February 20 in Annals of Internal Medicine.
Outcomes for patients with Cushing disease were compared against those with nonfunctioning pituitary adenomas (NFPAs). New-onset autoimmune disease occurred in 10.4% with Cushing disease and 1.6% among patients with NFPA (hazard ratio, 7.80; 95% CI, 2.88-21.10).
“Understanding and recognizing new and recurrent autoimmune disease in this setting is important to avoid misclassifying such patients with glucocorticoid withdrawal syndrome, which could result in failure to treat underlying autoimmune disease, as well as erroneous diagnosis of steroid withdrawal cases,” wrote Dennis Delasi Nyanyo of Massachusetts General Hospital and Harvard Medical School, Boston, and colleagues.
Given the general population’s annual incidence of major autoimmune diseases, estimated at about 100 cases per 100,000 people, and the 3-year incidence of 10.4% found in this study’s cohort, “our findings suggest that Cushing disease remission may trigger development of autoimmune disease,” the authors wrote.
Monitor Patients With Family History of Autoimmune Disease?
The study results were not necessarily surprising to Anthony P. Heaney, MD, PhD, an endocrinologist and professor of medicine at the University of California, Los Angeles, because past research has raised similar questions. The authors’ suggestion that the rapid postsurgical drop in cortisol that occurs as a result of treating Cushing disease becomes some sort of autoimmune trigger is interesting but remains speculative, Dr. Heaney pointed out.
If future evidence supports that possibility, “it would suggest, in terms of managing those patients in the postoperative setting, that there may be some merit to giving them higher concentrations of glucocorticoids for a short period of time,” Dr. Heaney said, thereby bringing their levels down more gradually rather than taking them off a cliff, in a sense. Or, if more evidence bears out the authors’ hypothesis, another approach might be treating patients with medicine to bring down the cortisol before surgery, though there are challenges to that approach, Dr. Heaney said.
At the same time, those who developed new autoimmune disease remain a small subset of patients with Cushing disease, so such approaches may become only potentially appropriate to consider in patients with risk factors, such as a family history of autoimmune disease.
The researchers conducted a retrospective chart review of adult patients who underwent transsphenoidal surgery for either Cushing disease or NFPA at Massachusetts General Hospital between 2005 and 2019.
The study involved 194 patients with Cushing disease who had postsurgical remission and at least one follow-up visit with a pituitary expert and 92 patients with NFPA who were matched to patients with Cushing disease based on age and sex. The authors regarded autoimmune disease diagnosed within 36 months of the surgery to be temporally associated with Cushing disease remission. Among the autoimmune diseases considered were “rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, autoimmune thyroiditis, celiac disease, psoriasis, vitiligo, autoimmune neuropathy, multiple sclerosis, myasthenia gravis, and ulcerative colitis.”
Patients differed in average body mass index and tumor size, but family history of autoimmune disease was similar in both groups. Average BMI was 34.5 in the Cushing group and 29.5 in the NFPA group. Average tumor size was 5.7 mm in the Cushing group and 21.3 mm in the NFPA group.
Before surgery, 2.9% of patients with Cushing disease and 15.4% of patients with NFPA had central hypothyroidism, and 8% in the Cushing group and 56.8% in the NFPA group had hyperprolactinemia. Central adrenal insufficiency occurred in 11% with NFPA and in all with Cushing disease, by definition.
After surgery, 93.8% in the Cushing group and 16.5% in the NFPA group had adrenal insufficiency. In addition, patients with Cushing disease had lower postsurgical nadir serum cortisol levels (63.8 nmol/L) than those with NFPA (282.3 nmol/L).
Of the 17 patients with Cushing disease — all women — who developed autoimmune disease within 3 years, 6 had a personal history of autoimmune disease and 7 had a family history of it. In addition, 41.2% of them had adrenal insufficiency when they developed the new autoimmune disease. Among the diseases were six autoimmune thyroiditis cases, three Sjögren syndrome cases, and two autoimmune seronegative spondyloarthropathy.
Dr. Heaney said he found it interesting that more than half of the new autoimmune diseases in patients with Cushing disease were related to the thyroid. “In this kind of setting, where you have a patient who has been producing too much steroid over a period of time and then you take that away, it’s almost like you release a brake on the TSH [thyroid-stimulating hormone],” Dr. Heaney said. “So, there’s probably some rebound in TSH that occurs, and that could be driving the thyroiditis, to some extent, that we see in these patients.”
Only one patient with NFPA developed new-onset autoimmune disease, a woman who developed Graves disease 22 months after surgery. When the researchers excluded patients in both groups with central hypothyroidism, new-onset autoimmune disease was still significantly higher (11.4%) in the Cushing group than in the NFPA group (1.9%; HR, 7.02; 95% CI, 2.54-19.39).
Could Postoperative Adrenal Insufficiency Contribute to Risk?
Within the Cushing cohort, those who developed autoimmune disease had a lower BMI (31.8 vs 34.8) and larger tumor size (7.2 vs 5.6 mm) than those who didn’t develop new autoimmune disease. Patients who developed autoimmune disease also had a lower baseline urine free cortisol ratio (2.7 vs 6.3) before surgery and more family history of autoimmune disease (41.2% vs 20.9%) than those who didn’t develop one.
“The higher prevalence of adrenal insufficiency and the lower nadir serum cortisol levels in the Cushing disease group suggest that the postoperative adrenal insufficiency in the Cushing disease group might have contributed to autoimmune disease pathogenesis,” the authors wrote. “This finding is clinically significant because cortisol plays a pivotal role in modulating the immune system.”
Most postoperative management among patients with Cushing disease was similar, with all but one patient receiving 0.5 or 1 mg daily dexamethasone within the first week after surgery. (The one outlier received 5 mg daily prednisone.) However, fewer patients who developed autoimmune disease (17.6%) received supraphysiologic doses of glucocorticoid — equivalent to at least 25 mg hydrocortisone — compared with patients who didn’t develop autoimmune disease (41.8%).
“Although the daily average hydrocortisone equivalent replacement doses within the first month and during long-term follow-up were within the physiologic range in both subgroups, patients with Cushing disease who had autoimmune disease received slightly lower doses of glucocorticoid replacement within the first month after surgery,” the authors reported. “The immediate postoperative period might be a critical window where supraphysiologic glucocorticoids seem to be protective with regard to development of autoimmune disease,” they wrote, though they acknowledged the study’s retrospective design as a limitation in drawing that conclusion.
At the least, they suggested that new symptoms in patients with Cushing disease, particularly those with a family history of autoimmune disease, should prompt investigation of potential autoimmune disease.
Recordati Rare Diseases funded the study. The research was also conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center) as well as financial contributions from Harvard University and its affiliated academic healthcare centers. One author reported holding stocks in Pfizer and Amgen, and another reported receiving consulting fees from Corcept. Dr. Heaney reported receiving institutional grants for trials from Corcept, Ascendis, Crinetics, and Sparrow Pharm; serving on the advisory board for Xeris, Recordati, Corcept, Novo Nordisk, Lundbeck, and Crinetics; and serving as a speaker for Chiesi, Novo Nordisk, and Corcept.
A version of this article appeared on Medscape.com.
Patients with Cushing disease have an increased risk for new-onset autoimmune disease in the 3 years after surgical remission, according to a new retrospective study published on February 20 in Annals of Internal Medicine.
Outcomes for patients with Cushing disease were compared against those with nonfunctioning pituitary adenomas (NFPAs). New-onset autoimmune disease occurred in 10.4% with Cushing disease and 1.6% among patients with NFPA (hazard ratio, 7.80; 95% CI, 2.88-21.10).
“Understanding and recognizing new and recurrent autoimmune disease in this setting is important to avoid misclassifying such patients with glucocorticoid withdrawal syndrome, which could result in failure to treat underlying autoimmune disease, as well as erroneous diagnosis of steroid withdrawal cases,” wrote Dennis Delasi Nyanyo of Massachusetts General Hospital and Harvard Medical School, Boston, and colleagues.
Given the general population’s annual incidence of major autoimmune diseases, estimated at about 100 cases per 100,000 people, and the 3-year incidence of 10.4% found in this study’s cohort, “our findings suggest that Cushing disease remission may trigger development of autoimmune disease,” the authors wrote.
Monitor Patients With Family History of Autoimmune Disease?
The study results were not necessarily surprising to Anthony P. Heaney, MD, PhD, an endocrinologist and professor of medicine at the University of California, Los Angeles, because past research has raised similar questions. The authors’ suggestion that the rapid postsurgical drop in cortisol that occurs as a result of treating Cushing disease becomes some sort of autoimmune trigger is interesting but remains speculative, Dr. Heaney pointed out.
If future evidence supports that possibility, “it would suggest, in terms of managing those patients in the postoperative setting, that there may be some merit to giving them higher concentrations of glucocorticoids for a short period of time,” Dr. Heaney said, thereby bringing their levels down more gradually rather than taking them off a cliff, in a sense. Or, if more evidence bears out the authors’ hypothesis, another approach might be treating patients with medicine to bring down the cortisol before surgery, though there are challenges to that approach, Dr. Heaney said.
At the same time, those who developed new autoimmune disease remain a small subset of patients with Cushing disease, so such approaches may become only potentially appropriate to consider in patients with risk factors, such as a family history of autoimmune disease.
The researchers conducted a retrospective chart review of adult patients who underwent transsphenoidal surgery for either Cushing disease or NFPA at Massachusetts General Hospital between 2005 and 2019.
The study involved 194 patients with Cushing disease who had postsurgical remission and at least one follow-up visit with a pituitary expert and 92 patients with NFPA who were matched to patients with Cushing disease based on age and sex. The authors regarded autoimmune disease diagnosed within 36 months of the surgery to be temporally associated with Cushing disease remission. Among the autoimmune diseases considered were “rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, autoimmune thyroiditis, celiac disease, psoriasis, vitiligo, autoimmune neuropathy, multiple sclerosis, myasthenia gravis, and ulcerative colitis.”
Patients differed in average body mass index and tumor size, but family history of autoimmune disease was similar in both groups. Average BMI was 34.5 in the Cushing group and 29.5 in the NFPA group. Average tumor size was 5.7 mm in the Cushing group and 21.3 mm in the NFPA group.
Before surgery, 2.9% of patients with Cushing disease and 15.4% of patients with NFPA had central hypothyroidism, and 8% in the Cushing group and 56.8% in the NFPA group had hyperprolactinemia. Central adrenal insufficiency occurred in 11% with NFPA and in all with Cushing disease, by definition.
After surgery, 93.8% in the Cushing group and 16.5% in the NFPA group had adrenal insufficiency. In addition, patients with Cushing disease had lower postsurgical nadir serum cortisol levels (63.8 nmol/L) than those with NFPA (282.3 nmol/L).
Of the 17 patients with Cushing disease — all women — who developed autoimmune disease within 3 years, 6 had a personal history of autoimmune disease and 7 had a family history of it. In addition, 41.2% of them had adrenal insufficiency when they developed the new autoimmune disease. Among the diseases were six autoimmune thyroiditis cases, three Sjögren syndrome cases, and two autoimmune seronegative spondyloarthropathy.
Dr. Heaney said he found it interesting that more than half of the new autoimmune diseases in patients with Cushing disease were related to the thyroid. “In this kind of setting, where you have a patient who has been producing too much steroid over a period of time and then you take that away, it’s almost like you release a brake on the TSH [thyroid-stimulating hormone],” Dr. Heaney said. “So, there’s probably some rebound in TSH that occurs, and that could be driving the thyroiditis, to some extent, that we see in these patients.”
Only one patient with NFPA developed new-onset autoimmune disease, a woman who developed Graves disease 22 months after surgery. When the researchers excluded patients in both groups with central hypothyroidism, new-onset autoimmune disease was still significantly higher (11.4%) in the Cushing group than in the NFPA group (1.9%; HR, 7.02; 95% CI, 2.54-19.39).
Could Postoperative Adrenal Insufficiency Contribute to Risk?
Within the Cushing cohort, those who developed autoimmune disease had a lower BMI (31.8 vs 34.8) and larger tumor size (7.2 vs 5.6 mm) than those who didn’t develop new autoimmune disease. Patients who developed autoimmune disease also had a lower baseline urine free cortisol ratio (2.7 vs 6.3) before surgery and more family history of autoimmune disease (41.2% vs 20.9%) than those who didn’t develop one.
“The higher prevalence of adrenal insufficiency and the lower nadir serum cortisol levels in the Cushing disease group suggest that the postoperative adrenal insufficiency in the Cushing disease group might have contributed to autoimmune disease pathogenesis,” the authors wrote. “This finding is clinically significant because cortisol plays a pivotal role in modulating the immune system.”
Most postoperative management among patients with Cushing disease was similar, with all but one patient receiving 0.5 or 1 mg daily dexamethasone within the first week after surgery. (The one outlier received 5 mg daily prednisone.) However, fewer patients who developed autoimmune disease (17.6%) received supraphysiologic doses of glucocorticoid — equivalent to at least 25 mg hydrocortisone — compared with patients who didn’t develop autoimmune disease (41.8%).
“Although the daily average hydrocortisone equivalent replacement doses within the first month and during long-term follow-up were within the physiologic range in both subgroups, patients with Cushing disease who had autoimmune disease received slightly lower doses of glucocorticoid replacement within the first month after surgery,” the authors reported. “The immediate postoperative period might be a critical window where supraphysiologic glucocorticoids seem to be protective with regard to development of autoimmune disease,” they wrote, though they acknowledged the study’s retrospective design as a limitation in drawing that conclusion.
At the least, they suggested that new symptoms in patients with Cushing disease, particularly those with a family history of autoimmune disease, should prompt investigation of potential autoimmune disease.
Recordati Rare Diseases funded the study. The research was also conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center) as well as financial contributions from Harvard University and its affiliated academic healthcare centers. One author reported holding stocks in Pfizer and Amgen, and another reported receiving consulting fees from Corcept. Dr. Heaney reported receiving institutional grants for trials from Corcept, Ascendis, Crinetics, and Sparrow Pharm; serving on the advisory board for Xeris, Recordati, Corcept, Novo Nordisk, Lundbeck, and Crinetics; and serving as a speaker for Chiesi, Novo Nordisk, and Corcept.
A version of this article appeared on Medscape.com.
Patients with Cushing disease have an increased risk for new-onset autoimmune disease in the 3 years after surgical remission, according to a new retrospective study published on February 20 in Annals of Internal Medicine.
Outcomes for patients with Cushing disease were compared against those with nonfunctioning pituitary adenomas (NFPAs). New-onset autoimmune disease occurred in 10.4% with Cushing disease and 1.6% among patients with NFPA (hazard ratio, 7.80; 95% CI, 2.88-21.10).
“Understanding and recognizing new and recurrent autoimmune disease in this setting is important to avoid misclassifying such patients with glucocorticoid withdrawal syndrome, which could result in failure to treat underlying autoimmune disease, as well as erroneous diagnosis of steroid withdrawal cases,” wrote Dennis Delasi Nyanyo of Massachusetts General Hospital and Harvard Medical School, Boston, and colleagues.
Given the general population’s annual incidence of major autoimmune diseases, estimated at about 100 cases per 100,000 people, and the 3-year incidence of 10.4% found in this study’s cohort, “our findings suggest that Cushing disease remission may trigger development of autoimmune disease,” the authors wrote.
Monitor Patients With Family History of Autoimmune Disease?
The study results were not necessarily surprising to Anthony P. Heaney, MD, PhD, an endocrinologist and professor of medicine at the University of California, Los Angeles, because past research has raised similar questions. The authors’ suggestion that the rapid postsurgical drop in cortisol that occurs as a result of treating Cushing disease becomes some sort of autoimmune trigger is interesting but remains speculative, Dr. Heaney pointed out.
If future evidence supports that possibility, “it would suggest, in terms of managing those patients in the postoperative setting, that there may be some merit to giving them higher concentrations of glucocorticoids for a short period of time,” Dr. Heaney said, thereby bringing their levels down more gradually rather than taking them off a cliff, in a sense. Or, if more evidence bears out the authors’ hypothesis, another approach might be treating patients with medicine to bring down the cortisol before surgery, though there are challenges to that approach, Dr. Heaney said.
At the same time, those who developed new autoimmune disease remain a small subset of patients with Cushing disease, so such approaches may become only potentially appropriate to consider in patients with risk factors, such as a family history of autoimmune disease.
The researchers conducted a retrospective chart review of adult patients who underwent transsphenoidal surgery for either Cushing disease or NFPA at Massachusetts General Hospital between 2005 and 2019.
The study involved 194 patients with Cushing disease who had postsurgical remission and at least one follow-up visit with a pituitary expert and 92 patients with NFPA who were matched to patients with Cushing disease based on age and sex. The authors regarded autoimmune disease diagnosed within 36 months of the surgery to be temporally associated with Cushing disease remission. Among the autoimmune diseases considered were “rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, autoimmune thyroiditis, celiac disease, psoriasis, vitiligo, autoimmune neuropathy, multiple sclerosis, myasthenia gravis, and ulcerative colitis.”
Patients differed in average body mass index and tumor size, but family history of autoimmune disease was similar in both groups. Average BMI was 34.5 in the Cushing group and 29.5 in the NFPA group. Average tumor size was 5.7 mm in the Cushing group and 21.3 mm in the NFPA group.
Before surgery, 2.9% of patients with Cushing disease and 15.4% of patients with NFPA had central hypothyroidism, and 8% in the Cushing group and 56.8% in the NFPA group had hyperprolactinemia. Central adrenal insufficiency occurred in 11% with NFPA and in all with Cushing disease, by definition.
After surgery, 93.8% in the Cushing group and 16.5% in the NFPA group had adrenal insufficiency. In addition, patients with Cushing disease had lower postsurgical nadir serum cortisol levels (63.8 nmol/L) than those with NFPA (282.3 nmol/L).
Of the 17 patients with Cushing disease — all women — who developed autoimmune disease within 3 years, 6 had a personal history of autoimmune disease and 7 had a family history of it. In addition, 41.2% of them had adrenal insufficiency when they developed the new autoimmune disease. Among the diseases were six autoimmune thyroiditis cases, three Sjögren syndrome cases, and two autoimmune seronegative spondyloarthropathy.
Dr. Heaney said he found it interesting that more than half of the new autoimmune diseases in patients with Cushing disease were related to the thyroid. “In this kind of setting, where you have a patient who has been producing too much steroid over a period of time and then you take that away, it’s almost like you release a brake on the TSH [thyroid-stimulating hormone],” Dr. Heaney said. “So, there’s probably some rebound in TSH that occurs, and that could be driving the thyroiditis, to some extent, that we see in these patients.”
Only one patient with NFPA developed new-onset autoimmune disease, a woman who developed Graves disease 22 months after surgery. When the researchers excluded patients in both groups with central hypothyroidism, new-onset autoimmune disease was still significantly higher (11.4%) in the Cushing group than in the NFPA group (1.9%; HR, 7.02; 95% CI, 2.54-19.39).
Could Postoperative Adrenal Insufficiency Contribute to Risk?
Within the Cushing cohort, those who developed autoimmune disease had a lower BMI (31.8 vs 34.8) and larger tumor size (7.2 vs 5.6 mm) than those who didn’t develop new autoimmune disease. Patients who developed autoimmune disease also had a lower baseline urine free cortisol ratio (2.7 vs 6.3) before surgery and more family history of autoimmune disease (41.2% vs 20.9%) than those who didn’t develop one.
“The higher prevalence of adrenal insufficiency and the lower nadir serum cortisol levels in the Cushing disease group suggest that the postoperative adrenal insufficiency in the Cushing disease group might have contributed to autoimmune disease pathogenesis,” the authors wrote. “This finding is clinically significant because cortisol plays a pivotal role in modulating the immune system.”
Most postoperative management among patients with Cushing disease was similar, with all but one patient receiving 0.5 or 1 mg daily dexamethasone within the first week after surgery. (The one outlier received 5 mg daily prednisone.) However, fewer patients who developed autoimmune disease (17.6%) received supraphysiologic doses of glucocorticoid — equivalent to at least 25 mg hydrocortisone — compared with patients who didn’t develop autoimmune disease (41.8%).
“Although the daily average hydrocortisone equivalent replacement doses within the first month and during long-term follow-up were within the physiologic range in both subgroups, patients with Cushing disease who had autoimmune disease received slightly lower doses of glucocorticoid replacement within the first month after surgery,” the authors reported. “The immediate postoperative period might be a critical window where supraphysiologic glucocorticoids seem to be protective with regard to development of autoimmune disease,” they wrote, though they acknowledged the study’s retrospective design as a limitation in drawing that conclusion.
At the least, they suggested that new symptoms in patients with Cushing disease, particularly those with a family history of autoimmune disease, should prompt investigation of potential autoimmune disease.
Recordati Rare Diseases funded the study. The research was also conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center) as well as financial contributions from Harvard University and its affiliated academic healthcare centers. One author reported holding stocks in Pfizer and Amgen, and another reported receiving consulting fees from Corcept. Dr. Heaney reported receiving institutional grants for trials from Corcept, Ascendis, Crinetics, and Sparrow Pharm; serving on the advisory board for Xeris, Recordati, Corcept, Novo Nordisk, Lundbeck, and Crinetics; and serving as a speaker for Chiesi, Novo Nordisk, and Corcept.
A version of this article appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Inflammatory Arthritis Often Occurs with Systemic Sclerosis; Has Big Impact
TOPLINE:
Inflammatory arthritis (IA) occurred in one-third of patients with systemic sclerosis (SSc) in a large observational study and was significantly associated with poor quality of life and physical function, as well as diffuse disease, musculoskeletal manifestations, myositis, and sicca.
METHODOLOGY:
- Researchers reviewed data from 1717 adults with SSc who were enrolled in the Australian Cohort Study to identify those with IA, defined as the presence of synovitis in one or more joints on clinical examination documented by the treating physician.
- The primary outcome was health-related quality of life (HRQoL) based on patient reports using the Medical Outcomes Short Form 36 and Patient-Reported Outcomes Measurement Information System, and physical function measured with the Health Assessment Questionnaire.
TAKEAWAY:
- IA was identified in 33.3% of the study participants over a median of 4.3 years’ follow-up. IA occurred at a median age of about 60 years and after a median SSc disease duration of 7.9 years. No significant differences in baseline demographics appeared between patients with and without IA.
- Patients with IA had significantly increased risk for diffuse cutaneous SSc (odds ratio [OR], 1.33), concurrent musculoskeletal manifestations such as tendon friction rubs and joint contractures (OR, 1.70), myositis (OR, 2.11), and sicca symptoms (OR, 1.57), compared with those without.
- Patients with IA reported significantly lower HRQoL scores and significantly greater physical disability, compared with those who did not have IA (P < .001 for both).
- IA was significantly less common among patients with , compared with those without pulmonary arterial hypertension (7.2% vs 11.3%; P = .007).
IN PRACTICE:
“Recognizing the presence of IA in SSc is an important first step, as its treatment and monitoring may alleviate some of the associated morbidity,” the researchers wrote.
SOURCE:
The lead author of the study was Eric Schwender, a medical student at the Royal College of Surgeons in Ireland, Dublin, Ireland. The study was published online in Arthritis Care & Research.
LIMITATIONS:
The inability to assess distribution and severity of IA limited the results, as did the inability to assess the impact of disease-modifying antirheumatic drugs in patients with IA.
DISCLOSURES:
The study was supported by Scleroderma Australia, Arthritis Australia, Actelion Australia, Bayer, CSL Biotherapies, GlaxoSmithKline Australia, and Pfizer, as well as grants to several researchers from the National Health and Medical Research Council of Australia. Lead author Mr. Schwender had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
Inflammatory arthritis (IA) occurred in one-third of patients with systemic sclerosis (SSc) in a large observational study and was significantly associated with poor quality of life and physical function, as well as diffuse disease, musculoskeletal manifestations, myositis, and sicca.
METHODOLOGY:
- Researchers reviewed data from 1717 adults with SSc who were enrolled in the Australian Cohort Study to identify those with IA, defined as the presence of synovitis in one or more joints on clinical examination documented by the treating physician.
- The primary outcome was health-related quality of life (HRQoL) based on patient reports using the Medical Outcomes Short Form 36 and Patient-Reported Outcomes Measurement Information System, and physical function measured with the Health Assessment Questionnaire.
TAKEAWAY:
- IA was identified in 33.3% of the study participants over a median of 4.3 years’ follow-up. IA occurred at a median age of about 60 years and after a median SSc disease duration of 7.9 years. No significant differences in baseline demographics appeared between patients with and without IA.
- Patients with IA had significantly increased risk for diffuse cutaneous SSc (odds ratio [OR], 1.33), concurrent musculoskeletal manifestations such as tendon friction rubs and joint contractures (OR, 1.70), myositis (OR, 2.11), and sicca symptoms (OR, 1.57), compared with those without.
- Patients with IA reported significantly lower HRQoL scores and significantly greater physical disability, compared with those who did not have IA (P < .001 for both).
- IA was significantly less common among patients with , compared with those without pulmonary arterial hypertension (7.2% vs 11.3%; P = .007).
IN PRACTICE:
“Recognizing the presence of IA in SSc is an important first step, as its treatment and monitoring may alleviate some of the associated morbidity,” the researchers wrote.
SOURCE:
The lead author of the study was Eric Schwender, a medical student at the Royal College of Surgeons in Ireland, Dublin, Ireland. The study was published online in Arthritis Care & Research.
LIMITATIONS:
The inability to assess distribution and severity of IA limited the results, as did the inability to assess the impact of disease-modifying antirheumatic drugs in patients with IA.
DISCLOSURES:
The study was supported by Scleroderma Australia, Arthritis Australia, Actelion Australia, Bayer, CSL Biotherapies, GlaxoSmithKline Australia, and Pfizer, as well as grants to several researchers from the National Health and Medical Research Council of Australia. Lead author Mr. Schwender had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
Inflammatory arthritis (IA) occurred in one-third of patients with systemic sclerosis (SSc) in a large observational study and was significantly associated with poor quality of life and physical function, as well as diffuse disease, musculoskeletal manifestations, myositis, and sicca.
METHODOLOGY:
- Researchers reviewed data from 1717 adults with SSc who were enrolled in the Australian Cohort Study to identify those with IA, defined as the presence of synovitis in one or more joints on clinical examination documented by the treating physician.
- The primary outcome was health-related quality of life (HRQoL) based on patient reports using the Medical Outcomes Short Form 36 and Patient-Reported Outcomes Measurement Information System, and physical function measured with the Health Assessment Questionnaire.
TAKEAWAY:
- IA was identified in 33.3% of the study participants over a median of 4.3 years’ follow-up. IA occurred at a median age of about 60 years and after a median SSc disease duration of 7.9 years. No significant differences in baseline demographics appeared between patients with and without IA.
- Patients with IA had significantly increased risk for diffuse cutaneous SSc (odds ratio [OR], 1.33), concurrent musculoskeletal manifestations such as tendon friction rubs and joint contractures (OR, 1.70), myositis (OR, 2.11), and sicca symptoms (OR, 1.57), compared with those without.
- Patients with IA reported significantly lower HRQoL scores and significantly greater physical disability, compared with those who did not have IA (P < .001 for both).
- IA was significantly less common among patients with , compared with those without pulmonary arterial hypertension (7.2% vs 11.3%; P = .007).
IN PRACTICE:
“Recognizing the presence of IA in SSc is an important first step, as its treatment and monitoring may alleviate some of the associated morbidity,” the researchers wrote.
SOURCE:
The lead author of the study was Eric Schwender, a medical student at the Royal College of Surgeons in Ireland, Dublin, Ireland. The study was published online in Arthritis Care & Research.
LIMITATIONS:
The inability to assess distribution and severity of IA limited the results, as did the inability to assess the impact of disease-modifying antirheumatic drugs in patients with IA.
DISCLOSURES:
The study was supported by Scleroderma Australia, Arthritis Australia, Actelion Australia, Bayer, CSL Biotherapies, GlaxoSmithKline Australia, and Pfizer, as well as grants to several researchers from the National Health and Medical Research Council of Australia. Lead author Mr. Schwender had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Mixing Paxlovid With Specific Immunosuppressants Risks Serious Adverse Reactions
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA) has issued a reminder to healthcare professionals regarding the potential serious adverse reactions associated with Paxlovid when administered in combination with specific immunosuppressants.
These immunosuppressants, encompassing calcineurin inhibitors (tacrolimus and ciclosporin) and mTOR inhibitors (everolimus and sirolimus), possess a narrow safe dosage range. They are recognized for their role in diminishing the activity of the immune system and are typically prescribed for autoimmune conditions and organ transplant recipients.
The highlighted risk arises due to drug-drug interactions, which can compromise the body’s ability to eliminate these medicines effectively.
Paxlovid, also known as nirmatrelvir with ritonavir, is an antiviral medication used to treat COVID-19 in adults who do not require supplemental oxygen and who are at an increased risk of progressing to severe COVID-19. It should be administered as soon as possible after a diagnosis of COVID-19 has been made and within 5 days of symptom onset.
Conditional marketing authorization for Paxlovid was granted across the European Union (EU) on January 28, 2022, and subsequently transitioned to full marketing authorization on February 24, 2023.
Developed by Pfizer, Paxlovid exhibited an 89% reduction in the risk for hospitalization or death among unvaccinated individuals in a phase 2-3 clinical trial. This led the National Institutes of Health to prioritize Paxlovid over other COVID-19 treatments. Subsequent real-world studies have affirmed its effectiveness, even among the vaccinated.
When combining Paxlovid with tacrolimus, ciclosporin, everolimus, or sirolimus, healthcare professionals need to actively monitor their blood levels. This proactive approach is essential to mitigate the risk for drug-drug interactions and potential serious reactions. They should collaborate with a multidisciplinary team of specialists to navigate the complexities of administering these medications concurrently.
Further, Paxlovid must not be coadministered with medications highly reliant on CYP3A liver enzymes for elimination, such as the immunosuppressant voclosporin. When administered together, there is a risk for these drugs interfering with each other’s metabolism, potentially leading to altered blood levels, reduced effectiveness, or an increased risk for adverse reactions.
After a thorough review, PRAC has highlighted potential serious adverse reactions, including fatal cases, due to drug interactions between Paxlovid and specified immunosuppressants. Thus, it issued a direct healthcare professional communication (DHPC) to emphasize the recognized risk for these interactions, as previously outlined in Paxlovid’s product information.
The DHPC for Paxlovid will undergo further evaluation by EMA’s Committee for Medicinal Products for Human Use and, upon adoption, will be disseminated to healthcare professionals. The communication plan will include publication on the DHPCs page and in national registers across EU Member States.
A version of this article appeared on Medscape.com.
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA) has issued a reminder to healthcare professionals regarding the potential serious adverse reactions associated with Paxlovid when administered in combination with specific immunosuppressants.
These immunosuppressants, encompassing calcineurin inhibitors (tacrolimus and ciclosporin) and mTOR inhibitors (everolimus and sirolimus), possess a narrow safe dosage range. They are recognized for their role in diminishing the activity of the immune system and are typically prescribed for autoimmune conditions and organ transplant recipients.
The highlighted risk arises due to drug-drug interactions, which can compromise the body’s ability to eliminate these medicines effectively.
Paxlovid, also known as nirmatrelvir with ritonavir, is an antiviral medication used to treat COVID-19 in adults who do not require supplemental oxygen and who are at an increased risk of progressing to severe COVID-19. It should be administered as soon as possible after a diagnosis of COVID-19 has been made and within 5 days of symptom onset.
Conditional marketing authorization for Paxlovid was granted across the European Union (EU) on January 28, 2022, and subsequently transitioned to full marketing authorization on February 24, 2023.
Developed by Pfizer, Paxlovid exhibited an 89% reduction in the risk for hospitalization or death among unvaccinated individuals in a phase 2-3 clinical trial. This led the National Institutes of Health to prioritize Paxlovid over other COVID-19 treatments. Subsequent real-world studies have affirmed its effectiveness, even among the vaccinated.
When combining Paxlovid with tacrolimus, ciclosporin, everolimus, or sirolimus, healthcare professionals need to actively monitor their blood levels. This proactive approach is essential to mitigate the risk for drug-drug interactions and potential serious reactions. They should collaborate with a multidisciplinary team of specialists to navigate the complexities of administering these medications concurrently.
Further, Paxlovid must not be coadministered with medications highly reliant on CYP3A liver enzymes for elimination, such as the immunosuppressant voclosporin. When administered together, there is a risk for these drugs interfering with each other’s metabolism, potentially leading to altered blood levels, reduced effectiveness, or an increased risk for adverse reactions.
After a thorough review, PRAC has highlighted potential serious adverse reactions, including fatal cases, due to drug interactions between Paxlovid and specified immunosuppressants. Thus, it issued a direct healthcare professional communication (DHPC) to emphasize the recognized risk for these interactions, as previously outlined in Paxlovid’s product information.
The DHPC for Paxlovid will undergo further evaluation by EMA’s Committee for Medicinal Products for Human Use and, upon adoption, will be disseminated to healthcare professionals. The communication plan will include publication on the DHPCs page and in national registers across EU Member States.
A version of this article appeared on Medscape.com.
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA) has issued a reminder to healthcare professionals regarding the potential serious adverse reactions associated with Paxlovid when administered in combination with specific immunosuppressants.
These immunosuppressants, encompassing calcineurin inhibitors (tacrolimus and ciclosporin) and mTOR inhibitors (everolimus and sirolimus), possess a narrow safe dosage range. They are recognized for their role in diminishing the activity of the immune system and are typically prescribed for autoimmune conditions and organ transplant recipients.
The highlighted risk arises due to drug-drug interactions, which can compromise the body’s ability to eliminate these medicines effectively.
Paxlovid, also known as nirmatrelvir with ritonavir, is an antiviral medication used to treat COVID-19 in adults who do not require supplemental oxygen and who are at an increased risk of progressing to severe COVID-19. It should be administered as soon as possible after a diagnosis of COVID-19 has been made and within 5 days of symptom onset.
Conditional marketing authorization for Paxlovid was granted across the European Union (EU) on January 28, 2022, and subsequently transitioned to full marketing authorization on February 24, 2023.
Developed by Pfizer, Paxlovid exhibited an 89% reduction in the risk for hospitalization or death among unvaccinated individuals in a phase 2-3 clinical trial. This led the National Institutes of Health to prioritize Paxlovid over other COVID-19 treatments. Subsequent real-world studies have affirmed its effectiveness, even among the vaccinated.
When combining Paxlovid with tacrolimus, ciclosporin, everolimus, or sirolimus, healthcare professionals need to actively monitor their blood levels. This proactive approach is essential to mitigate the risk for drug-drug interactions and potential serious reactions. They should collaborate with a multidisciplinary team of specialists to navigate the complexities of administering these medications concurrently.
Further, Paxlovid must not be coadministered with medications highly reliant on CYP3A liver enzymes for elimination, such as the immunosuppressant voclosporin. When administered together, there is a risk for these drugs interfering with each other’s metabolism, potentially leading to altered blood levels, reduced effectiveness, or an increased risk for adverse reactions.
After a thorough review, PRAC has highlighted potential serious adverse reactions, including fatal cases, due to drug interactions between Paxlovid and specified immunosuppressants. Thus, it issued a direct healthcare professional communication (DHPC) to emphasize the recognized risk for these interactions, as previously outlined in Paxlovid’s product information.
The DHPC for Paxlovid will undergo further evaluation by EMA’s Committee for Medicinal Products for Human Use and, upon adoption, will be disseminated to healthcare professionals. The communication plan will include publication on the DHPCs page and in national registers across EU Member States.
A version of this article appeared on Medscape.com.
Patients With Stable Lupus May Be Safely Weaned Off MMF
Patients with quiescent systemic lupus erythematosus (SLE) who are on maintenance therapy with mycophenolate mofetil (MMF) may be able to be safely weaned off the drug with the understanding that disease flare may occur and may require restarting immunosuppressive therapy.
That’s the conclusion of investigators in a multicenter randomized trial conducted at 19 US centers and published in The Lancet Rheumatology. They found that among 100 patients with stable SLE who were on MMF for at least 2 years for renal indications or at least 1 year for nonrenal indications, MMF withdrawal was not significantly inferior to MMF maintenance in terms of clinically significant disease reactivation within at least 1 year.
“Our findings suggest that mycophenolate mofetil could be safely withdrawn in patients with stable SLE. However, larger studies with a longer follow-up are still needed,” wrote Eliza F. Chakravarty, MD, MS, from the University of Oklahoma College of Medicine in Oklahoma City, and colleagues.
“Our study was only for 60 weeks, so we don’t have long-term data on what happens when patients taper off, but my recommendation — and I think the data support this — is that even if you do have a history of lupus nephritis, if you had stable disease or very little to no activity for a year or 2, then I think it’s worth stopping the medication and following for any signs of disease flare,” Dr. Chakravarty said in an interview with this news organization.
She added that “in clinical practice, we would follow patients regularly no matter what they’re on, even if they’re in remission, looking for clinical signs or laboratory evidence of flare, and then if they look like they might be having flare, treat them accordingly.”
Toxicities a Concern
Although MMF is effective for inducing prolonged disease quiescence, it is a known teratogen and has significant toxicities, and it’s desirable to wean patients off the drug if it can be done safely, Dr. Chakravarty said.
The optimal duration of maintenance therapy with MMF is not known, however, which prompted the researchers to conduct the open-label study.
Patients aged 18-70 years who met the American College of Rheumatology (ACR) 1997 SLE criteria and had a clinical SLE Disease Activity Index (SLEDAI) score ≤ 4 at screening and who also had been on stable or tapering MMF therapy for 2 or more years for renal indications or 1 or more year for nonrenal indications were eligible. All patients were on a background regimen of hydroxychloroquine.
Patients were randomly assigned on an equal basis to either withdrawal with a 12-week taper or to continued maintenance at their baseline dose, ranging from 1 to 3 g/day for 60 weeks.
The investigators used an adaptive random-allocation strategy to ensure that the groups were balanced for study site, renal vs nonrenal disease, and baseline MMF dose (≥ 2 g/day vs < 2 g/day).
A total of 100 patients with an average age of 42 years were included in a modified intention-to-treat analysis: 49 were randomly assigned to maintenance and 51 to withdrawal.
Overall, 84% of patients were women, 40% were White, and 41% were Black. Most patients, 76%, had a history of lupus nephritis.
Significant disease reactivation, the primary endpoints, was defined as the need to increase prednisone to ≥ 15 mg/day for 4 weeks, the need for two or more short steroid bursts, or the need to resume MMF or start patients on another immunosuppressive therapy.
By week 60, 18% of patients in the withdrawal group had clinically significant disease reactivation compared with 10% of patients in the maintenance group.
“Although the differences were not significant, this study used an estimation-based design to determine estimated increases in clinically significant disease reactivation risk with 75%, 85%, and 95% confidence limits to assist clinicians and patients in making informed treatment decisions. We found a 6%-8% increase with upper 85% confidence limits of 11%-19% in clinically significant disease reactivation and flare risk following mycophenolate mofetil withdrawal,” the investigators wrote.
Rates of adverse events were similar between the groups, occurring in 90% of patients in the maintenance arm and 88% of those in the withdrawal arm. Infections occurred more frequently among patients in the maintenance group, at 64% vs 46%.
Encouraging Data
In an accompanying editorial, Noémie Jourde-Chiche, MD, PhD, from Aix-Marseille University in Marseille, France, and Laurent Chiche, MD, from Hopital Europeen de Marseille, wrote that the study data “were clearly encouraging.” They noted that the results show that it’s feasible to wean select patients off immunosuppressive therapy and keep SLE in check and that the quantified risk assessment strategy will allow shared decision-making for each patient.
“Overall, the prospect of a time-limited (versus lifelong) treatment may favor compliance, as observed in other disease fields, which might consolidate remission and reduce the risk of subsequent relapse, using sequentially treat-to-target and think-to-untreat strategies for a win-wean era in SLE,” they wrote.
“We’ve been awaiting the results of this trial for quite a while, and so it is nice to see it out,” commented Karen H. Costenbader, MD, MPH, professor of medicine at Harvard Medical School, and chair of the division of rheumatology and director of the Lupus Program at Brigham and Women’s Hospital in Boston, Massachusetts.
“It does provide some data to address a question that comes up in discussions with patients all the time: A person with lupus has been doing really well, in what we call low disease activity state or remission, but on mycophenolate, possibly for several years,” she said in a reply to a request for objective commentary.
“The question is how and when to taper and can MMF be safely discontinued,” she said. “Personally, I always review the severity of the underlying disease and indication for the MMF in the first place. Really active SLE with rapidly progressing kidney or other organ damage has to be treated with tremendous respect and no one wants to go back there. I also think about how long it has been, which other medications are still being taken (hydroxychloroquine, belimumab [Benlysta], etc.) and whether the labs and symptoms have really returned to completely normal. Then I have discussions about all this with my patient and we often try a long, slow, gingerly taper with a lot of interim monitoring.”
The study was funded by the National Institute of Allergy and Infectious Diseases and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Chakravarty and Dr. Costenbader report no relevant financial relationships. Dr. Jourde-Chiche declares personal consulting fees from Otsuka and AstraZeneca, personal speaking fees from GlaxoSmithKline and Otsuka, and personal payment for expert testimony from Otsuka. Dr. Chiche declares research grants paid to his institution from AstraZeneca and GlaxoSmithKline, personal consulting fees from Novartis and AstraZeneca, and personal speaking fees from GlaxoSmithKline and Novartis.
A version of this article appeared on Medscape.com .
Patients with quiescent systemic lupus erythematosus (SLE) who are on maintenance therapy with mycophenolate mofetil (MMF) may be able to be safely weaned off the drug with the understanding that disease flare may occur and may require restarting immunosuppressive therapy.
That’s the conclusion of investigators in a multicenter randomized trial conducted at 19 US centers and published in The Lancet Rheumatology. They found that among 100 patients with stable SLE who were on MMF for at least 2 years for renal indications or at least 1 year for nonrenal indications, MMF withdrawal was not significantly inferior to MMF maintenance in terms of clinically significant disease reactivation within at least 1 year.
“Our findings suggest that mycophenolate mofetil could be safely withdrawn in patients with stable SLE. However, larger studies with a longer follow-up are still needed,” wrote Eliza F. Chakravarty, MD, MS, from the University of Oklahoma College of Medicine in Oklahoma City, and colleagues.
“Our study was only for 60 weeks, so we don’t have long-term data on what happens when patients taper off, but my recommendation — and I think the data support this — is that even if you do have a history of lupus nephritis, if you had stable disease or very little to no activity for a year or 2, then I think it’s worth stopping the medication and following for any signs of disease flare,” Dr. Chakravarty said in an interview with this news organization.
She added that “in clinical practice, we would follow patients regularly no matter what they’re on, even if they’re in remission, looking for clinical signs or laboratory evidence of flare, and then if they look like they might be having flare, treat them accordingly.”
Toxicities a Concern
Although MMF is effective for inducing prolonged disease quiescence, it is a known teratogen and has significant toxicities, and it’s desirable to wean patients off the drug if it can be done safely, Dr. Chakravarty said.
The optimal duration of maintenance therapy with MMF is not known, however, which prompted the researchers to conduct the open-label study.
Patients aged 18-70 years who met the American College of Rheumatology (ACR) 1997 SLE criteria and had a clinical SLE Disease Activity Index (SLEDAI) score ≤ 4 at screening and who also had been on stable or tapering MMF therapy for 2 or more years for renal indications or 1 or more year for nonrenal indications were eligible. All patients were on a background regimen of hydroxychloroquine.
Patients were randomly assigned on an equal basis to either withdrawal with a 12-week taper or to continued maintenance at their baseline dose, ranging from 1 to 3 g/day for 60 weeks.
The investigators used an adaptive random-allocation strategy to ensure that the groups were balanced for study site, renal vs nonrenal disease, and baseline MMF dose (≥ 2 g/day vs < 2 g/day).
A total of 100 patients with an average age of 42 years were included in a modified intention-to-treat analysis: 49 were randomly assigned to maintenance and 51 to withdrawal.
Overall, 84% of patients were women, 40% were White, and 41% were Black. Most patients, 76%, had a history of lupus nephritis.
Significant disease reactivation, the primary endpoints, was defined as the need to increase prednisone to ≥ 15 mg/day for 4 weeks, the need for two or more short steroid bursts, or the need to resume MMF or start patients on another immunosuppressive therapy.
By week 60, 18% of patients in the withdrawal group had clinically significant disease reactivation compared with 10% of patients in the maintenance group.
“Although the differences were not significant, this study used an estimation-based design to determine estimated increases in clinically significant disease reactivation risk with 75%, 85%, and 95% confidence limits to assist clinicians and patients in making informed treatment decisions. We found a 6%-8% increase with upper 85% confidence limits of 11%-19% in clinically significant disease reactivation and flare risk following mycophenolate mofetil withdrawal,” the investigators wrote.
Rates of adverse events were similar between the groups, occurring in 90% of patients in the maintenance arm and 88% of those in the withdrawal arm. Infections occurred more frequently among patients in the maintenance group, at 64% vs 46%.
Encouraging Data
In an accompanying editorial, Noémie Jourde-Chiche, MD, PhD, from Aix-Marseille University in Marseille, France, and Laurent Chiche, MD, from Hopital Europeen de Marseille, wrote that the study data “were clearly encouraging.” They noted that the results show that it’s feasible to wean select patients off immunosuppressive therapy and keep SLE in check and that the quantified risk assessment strategy will allow shared decision-making for each patient.
“Overall, the prospect of a time-limited (versus lifelong) treatment may favor compliance, as observed in other disease fields, which might consolidate remission and reduce the risk of subsequent relapse, using sequentially treat-to-target and think-to-untreat strategies for a win-wean era in SLE,” they wrote.
“We’ve been awaiting the results of this trial for quite a while, and so it is nice to see it out,” commented Karen H. Costenbader, MD, MPH, professor of medicine at Harvard Medical School, and chair of the division of rheumatology and director of the Lupus Program at Brigham and Women’s Hospital in Boston, Massachusetts.
“It does provide some data to address a question that comes up in discussions with patients all the time: A person with lupus has been doing really well, in what we call low disease activity state or remission, but on mycophenolate, possibly for several years,” she said in a reply to a request for objective commentary.
“The question is how and when to taper and can MMF be safely discontinued,” she said. “Personally, I always review the severity of the underlying disease and indication for the MMF in the first place. Really active SLE with rapidly progressing kidney or other organ damage has to be treated with tremendous respect and no one wants to go back there. I also think about how long it has been, which other medications are still being taken (hydroxychloroquine, belimumab [Benlysta], etc.) and whether the labs and symptoms have really returned to completely normal. Then I have discussions about all this with my patient and we often try a long, slow, gingerly taper with a lot of interim monitoring.”
The study was funded by the National Institute of Allergy and Infectious Diseases and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Chakravarty and Dr. Costenbader report no relevant financial relationships. Dr. Jourde-Chiche declares personal consulting fees from Otsuka and AstraZeneca, personal speaking fees from GlaxoSmithKline and Otsuka, and personal payment for expert testimony from Otsuka. Dr. Chiche declares research grants paid to his institution from AstraZeneca and GlaxoSmithKline, personal consulting fees from Novartis and AstraZeneca, and personal speaking fees from GlaxoSmithKline and Novartis.
A version of this article appeared on Medscape.com .
Patients with quiescent systemic lupus erythematosus (SLE) who are on maintenance therapy with mycophenolate mofetil (MMF) may be able to be safely weaned off the drug with the understanding that disease flare may occur and may require restarting immunosuppressive therapy.
That’s the conclusion of investigators in a multicenter randomized trial conducted at 19 US centers and published in The Lancet Rheumatology. They found that among 100 patients with stable SLE who were on MMF for at least 2 years for renal indications or at least 1 year for nonrenal indications, MMF withdrawal was not significantly inferior to MMF maintenance in terms of clinically significant disease reactivation within at least 1 year.
“Our findings suggest that mycophenolate mofetil could be safely withdrawn in patients with stable SLE. However, larger studies with a longer follow-up are still needed,” wrote Eliza F. Chakravarty, MD, MS, from the University of Oklahoma College of Medicine in Oklahoma City, and colleagues.
“Our study was only for 60 weeks, so we don’t have long-term data on what happens when patients taper off, but my recommendation — and I think the data support this — is that even if you do have a history of lupus nephritis, if you had stable disease or very little to no activity for a year or 2, then I think it’s worth stopping the medication and following for any signs of disease flare,” Dr. Chakravarty said in an interview with this news organization.
She added that “in clinical practice, we would follow patients regularly no matter what they’re on, even if they’re in remission, looking for clinical signs or laboratory evidence of flare, and then if they look like they might be having flare, treat them accordingly.”
Toxicities a Concern
Although MMF is effective for inducing prolonged disease quiescence, it is a known teratogen and has significant toxicities, and it’s desirable to wean patients off the drug if it can be done safely, Dr. Chakravarty said.
The optimal duration of maintenance therapy with MMF is not known, however, which prompted the researchers to conduct the open-label study.
Patients aged 18-70 years who met the American College of Rheumatology (ACR) 1997 SLE criteria and had a clinical SLE Disease Activity Index (SLEDAI) score ≤ 4 at screening and who also had been on stable or tapering MMF therapy for 2 or more years for renal indications or 1 or more year for nonrenal indications were eligible. All patients were on a background regimen of hydroxychloroquine.
Patients were randomly assigned on an equal basis to either withdrawal with a 12-week taper or to continued maintenance at their baseline dose, ranging from 1 to 3 g/day for 60 weeks.
The investigators used an adaptive random-allocation strategy to ensure that the groups were balanced for study site, renal vs nonrenal disease, and baseline MMF dose (≥ 2 g/day vs < 2 g/day).
A total of 100 patients with an average age of 42 years were included in a modified intention-to-treat analysis: 49 were randomly assigned to maintenance and 51 to withdrawal.
Overall, 84% of patients were women, 40% were White, and 41% were Black. Most patients, 76%, had a history of lupus nephritis.
Significant disease reactivation, the primary endpoints, was defined as the need to increase prednisone to ≥ 15 mg/day for 4 weeks, the need for two or more short steroid bursts, or the need to resume MMF or start patients on another immunosuppressive therapy.
By week 60, 18% of patients in the withdrawal group had clinically significant disease reactivation compared with 10% of patients in the maintenance group.
“Although the differences were not significant, this study used an estimation-based design to determine estimated increases in clinically significant disease reactivation risk with 75%, 85%, and 95% confidence limits to assist clinicians and patients in making informed treatment decisions. We found a 6%-8% increase with upper 85% confidence limits of 11%-19% in clinically significant disease reactivation and flare risk following mycophenolate mofetil withdrawal,” the investigators wrote.
Rates of adverse events were similar between the groups, occurring in 90% of patients in the maintenance arm and 88% of those in the withdrawal arm. Infections occurred more frequently among patients in the maintenance group, at 64% vs 46%.
Encouraging Data
In an accompanying editorial, Noémie Jourde-Chiche, MD, PhD, from Aix-Marseille University in Marseille, France, and Laurent Chiche, MD, from Hopital Europeen de Marseille, wrote that the study data “were clearly encouraging.” They noted that the results show that it’s feasible to wean select patients off immunosuppressive therapy and keep SLE in check and that the quantified risk assessment strategy will allow shared decision-making for each patient.
“Overall, the prospect of a time-limited (versus lifelong) treatment may favor compliance, as observed in other disease fields, which might consolidate remission and reduce the risk of subsequent relapse, using sequentially treat-to-target and think-to-untreat strategies for a win-wean era in SLE,” they wrote.
“We’ve been awaiting the results of this trial for quite a while, and so it is nice to see it out,” commented Karen H. Costenbader, MD, MPH, professor of medicine at Harvard Medical School, and chair of the division of rheumatology and director of the Lupus Program at Brigham and Women’s Hospital in Boston, Massachusetts.
“It does provide some data to address a question that comes up in discussions with patients all the time: A person with lupus has been doing really well, in what we call low disease activity state or remission, but on mycophenolate, possibly for several years,” she said in a reply to a request for objective commentary.
“The question is how and when to taper and can MMF be safely discontinued,” she said. “Personally, I always review the severity of the underlying disease and indication for the MMF in the first place. Really active SLE with rapidly progressing kidney or other organ damage has to be treated with tremendous respect and no one wants to go back there. I also think about how long it has been, which other medications are still being taken (hydroxychloroquine, belimumab [Benlysta], etc.) and whether the labs and symptoms have really returned to completely normal. Then I have discussions about all this with my patient and we often try a long, slow, gingerly taper with a lot of interim monitoring.”
The study was funded by the National Institute of Allergy and Infectious Diseases and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Chakravarty and Dr. Costenbader report no relevant financial relationships. Dr. Jourde-Chiche declares personal consulting fees from Otsuka and AstraZeneca, personal speaking fees from GlaxoSmithKline and Otsuka, and personal payment for expert testimony from Otsuka. Dr. Chiche declares research grants paid to his institution from AstraZeneca and GlaxoSmithKline, personal consulting fees from Novartis and AstraZeneca, and personal speaking fees from GlaxoSmithKline and Novartis.
A version of this article appeared on Medscape.com .
FROM THE LANCET RHEUMATOLOGY