User login
Artificial intelligence matches cancer genotypes to patient phenotypes
Precision medicine is driven by technologies such as rapid genome sequencing and artificial intelligence (AI), according to a presentation at the AACR virtual meeting II.
AI can be applied to the sequencing information derived from advanced cancers to make highly personalized treatment recommendations for patients, said Olivier Elemento, PhD, of Weill Cornell Medicine, New York.
Dr. Elemento described such work during the opening plenary session of the meeting.
Dr. Elemento advocated for whole-genome sequencing (WGS) of metastatic sites, as it can reveal “branched evolution” as tumors progress from localized to metastatic (Nat Genet. 2016 Dec;48[12]:1490-9).
The metastases share common mutations with the primaries from which they arise but also develop their own mutational profiles, which facilitate site-of-origin-agnostic, predictive treatment choices.
As examples, Dr. Elemento mentioned HER2 amplification found in a patient with urothelial cancer (J Natl Compr Canc Netw. 2019 Mar 1;17[3]:194-200) and a patient with uterine serous carcinoma (Gynecol Oncol Rep. 2019 Feb 21;28:54-7), both of whom experienced long-lasting remissions to HER2-targeted therapy.
Dr. Elemento also noted that WGS can reveal complex structural variants in lung adenocarcinomas that lack alterations in the RTK/RAS/RAF pathway (unpublished data).
Application of machine learning
One study suggested that microRNA expression and machine learning can be used to identify malignant thyroid lesions (Clin Cancer Res. 2012 Apr 1;18[7]:2032-8). The approach diagnosed malignant lesions with 90% accuracy, 100% sensitivity, and 86% specificity.
Dr. Elemento and colleagues used a similar approach to predict response to immunotherapy in melanoma (unpublished data).
The idea was to mine the cancer genome and transcriptome, allowing for identification of signals from neoantigens, immune gene expression, immune cell composition, and T-cell receptor repertoires, Dr. Elemento said. Integrating these signals with clinical outcome data via machine learning technology enabled the researchers to predict immunotherapy response in malignant melanoma with nearly 90% accuracy.
AI and image analysis
Studies have indicated that AI can be applied to medical images to improve diagnosis and treatment. The approach has been shown to:
- Facilitate correct diagnoses of malignant skin lesions (Nature. 2017 Feb 2;542[7639]:115-8).
- Distinguish lung adenocarcinoma from squamous cell cancer with 100% accuracy (EBioMedicine. 2018 Jan;27:317-28).
- Recognize distinct breast cancer subtypes (ductal, lobular, mucinous, papillary) and biomarkers (bioRxiv 242818. doi: 10.1101/242818; EBioMedicine. 2018 Jan;27:317-28)
- Predict mesothelioma prognosis (Nat Med. 2019 Oct;25[10]:1519-25).
- Predict prostate biopsy results (unpublished data) and calculate Gleason scores that can predict survival in prostate cancer patients (AACR 2020, Abstract 867).
Drug development through applied AI
In another study, Dr. Elemento and colleagues used a Bayesian machine learning approach to predict targets of molecules without a known mechanism of action (Nat Commun. 2019 Nov 19;10[1]:5221).
The method involved using data on gene expression profiles, cell line viability, side effects in animals, and structures of the molecules. The researchers applied this method to a large library of orphan small molecules and found it could predict targets in about 40% of cases.
Of 24 AI-predicted microtubule-targeting molecules, 14 depolymerized microtubules in the lab. Five of these molecules were effective in cell lines that were resistant to other microtubule-targeted drugs.
Dr. Elemento went on to describe how Oncoceutics was developing an antineoplastic agent called ONC201, but the company lacked information about the agent’s target. Using AI, the target was identified as dopamine receptor 2 (DRD2; Clin Cancer Res. 2019 Apr 1;25[7]:2305-13).
With that information, Oncoceutics initiated trials of ONC201 in tumors expressing high levels of DRD2, including a highly resistant glioma (J Neurooncol. 2019 Oct;145[1]:97-105). Responses were seen, and ONC201 is now being tested against other DRD2-expressing cancers.
Challenges to acknowledge
Potential benefits of AI in the clinic are exciting, but there are many bench-to-bedside challenges.
A clinically obvious example of AI’s applications is radiographic image analysis. There is no biologic rationale for our RECIST “cut values” for partial response, minimal response, and stable disease.
If AI can measure subtle changes on imaging that correlate with tumor biology (i.e., radiomics), we stand a better chance of predicting treatment outcomes than we can with conventional measurements of shrinkage of arbitrarily selected “target lesions.”
A tremendous amount of work is needed to build the required large image banks. During that time, AI will only improve – and without the human risks of fatigue, inconsistency, or burnout.
Those human frailties notwithstanding, AI cannot substitute for the key discussions between patient and clinician regarding goals of care, trade-offs of risks and benefits, and shared decision-making regarding management options.
At least initially (but painfully), complex technologies like WGS and digital image analysis via AI may further disadvantage patients who are medically disadvantaged by geography or socioeconomic circumstances.
In the discussion period, AACR President Antoni Ribas, MD, of University of California, Los Angeles, asked whether AI can simulate crosstalk between gene pathways so that unique treatment combinations can be identified. Dr. Elemento said those simulations are the subject of ongoing investigation.
The theme of the opening plenary session at the AACR virtual meeting II was “Turning Science into Life-Saving Care.” Applications of AI to optimize personalized use of genomics, digital image analysis, and drug development show great promise for being among the technologies that can help to realize AACR’s thematic vision.
Dr. Elemento disclosed relationships with Volastra Therapeutics, OneThree Biotech, Owkin, Freenome, Genetic Intelligence, Acuamark Diagnostics, Eli Lilly, Janssen, and Sanofi.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Precision medicine is driven by technologies such as rapid genome sequencing and artificial intelligence (AI), according to a presentation at the AACR virtual meeting II.
AI can be applied to the sequencing information derived from advanced cancers to make highly personalized treatment recommendations for patients, said Olivier Elemento, PhD, of Weill Cornell Medicine, New York.
Dr. Elemento described such work during the opening plenary session of the meeting.
Dr. Elemento advocated for whole-genome sequencing (WGS) of metastatic sites, as it can reveal “branched evolution” as tumors progress from localized to metastatic (Nat Genet. 2016 Dec;48[12]:1490-9).
The metastases share common mutations with the primaries from which they arise but also develop their own mutational profiles, which facilitate site-of-origin-agnostic, predictive treatment choices.
As examples, Dr. Elemento mentioned HER2 amplification found in a patient with urothelial cancer (J Natl Compr Canc Netw. 2019 Mar 1;17[3]:194-200) and a patient with uterine serous carcinoma (Gynecol Oncol Rep. 2019 Feb 21;28:54-7), both of whom experienced long-lasting remissions to HER2-targeted therapy.
Dr. Elemento also noted that WGS can reveal complex structural variants in lung adenocarcinomas that lack alterations in the RTK/RAS/RAF pathway (unpublished data).
Application of machine learning
One study suggested that microRNA expression and machine learning can be used to identify malignant thyroid lesions (Clin Cancer Res. 2012 Apr 1;18[7]:2032-8). The approach diagnosed malignant lesions with 90% accuracy, 100% sensitivity, and 86% specificity.
Dr. Elemento and colleagues used a similar approach to predict response to immunotherapy in melanoma (unpublished data).
The idea was to mine the cancer genome and transcriptome, allowing for identification of signals from neoantigens, immune gene expression, immune cell composition, and T-cell receptor repertoires, Dr. Elemento said. Integrating these signals with clinical outcome data via machine learning technology enabled the researchers to predict immunotherapy response in malignant melanoma with nearly 90% accuracy.
AI and image analysis
Studies have indicated that AI can be applied to medical images to improve diagnosis and treatment. The approach has been shown to:
- Facilitate correct diagnoses of malignant skin lesions (Nature. 2017 Feb 2;542[7639]:115-8).
- Distinguish lung adenocarcinoma from squamous cell cancer with 100% accuracy (EBioMedicine. 2018 Jan;27:317-28).
- Recognize distinct breast cancer subtypes (ductal, lobular, mucinous, papillary) and biomarkers (bioRxiv 242818. doi: 10.1101/242818; EBioMedicine. 2018 Jan;27:317-28)
- Predict mesothelioma prognosis (Nat Med. 2019 Oct;25[10]:1519-25).
- Predict prostate biopsy results (unpublished data) and calculate Gleason scores that can predict survival in prostate cancer patients (AACR 2020, Abstract 867).
Drug development through applied AI
In another study, Dr. Elemento and colleagues used a Bayesian machine learning approach to predict targets of molecules without a known mechanism of action (Nat Commun. 2019 Nov 19;10[1]:5221).
The method involved using data on gene expression profiles, cell line viability, side effects in animals, and structures of the molecules. The researchers applied this method to a large library of orphan small molecules and found it could predict targets in about 40% of cases.
Of 24 AI-predicted microtubule-targeting molecules, 14 depolymerized microtubules in the lab. Five of these molecules were effective in cell lines that were resistant to other microtubule-targeted drugs.
Dr. Elemento went on to describe how Oncoceutics was developing an antineoplastic agent called ONC201, but the company lacked information about the agent’s target. Using AI, the target was identified as dopamine receptor 2 (DRD2; Clin Cancer Res. 2019 Apr 1;25[7]:2305-13).
With that information, Oncoceutics initiated trials of ONC201 in tumors expressing high levels of DRD2, including a highly resistant glioma (J Neurooncol. 2019 Oct;145[1]:97-105). Responses were seen, and ONC201 is now being tested against other DRD2-expressing cancers.
Challenges to acknowledge
Potential benefits of AI in the clinic are exciting, but there are many bench-to-bedside challenges.
A clinically obvious example of AI’s applications is radiographic image analysis. There is no biologic rationale for our RECIST “cut values” for partial response, minimal response, and stable disease.
If AI can measure subtle changes on imaging that correlate with tumor biology (i.e., radiomics), we stand a better chance of predicting treatment outcomes than we can with conventional measurements of shrinkage of arbitrarily selected “target lesions.”
A tremendous amount of work is needed to build the required large image banks. During that time, AI will only improve – and without the human risks of fatigue, inconsistency, or burnout.
Those human frailties notwithstanding, AI cannot substitute for the key discussions between patient and clinician regarding goals of care, trade-offs of risks and benefits, and shared decision-making regarding management options.
At least initially (but painfully), complex technologies like WGS and digital image analysis via AI may further disadvantage patients who are medically disadvantaged by geography or socioeconomic circumstances.
In the discussion period, AACR President Antoni Ribas, MD, of University of California, Los Angeles, asked whether AI can simulate crosstalk between gene pathways so that unique treatment combinations can be identified. Dr. Elemento said those simulations are the subject of ongoing investigation.
The theme of the opening plenary session at the AACR virtual meeting II was “Turning Science into Life-Saving Care.” Applications of AI to optimize personalized use of genomics, digital image analysis, and drug development show great promise for being among the technologies that can help to realize AACR’s thematic vision.
Dr. Elemento disclosed relationships with Volastra Therapeutics, OneThree Biotech, Owkin, Freenome, Genetic Intelligence, Acuamark Diagnostics, Eli Lilly, Janssen, and Sanofi.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Precision medicine is driven by technologies such as rapid genome sequencing and artificial intelligence (AI), according to a presentation at the AACR virtual meeting II.
AI can be applied to the sequencing information derived from advanced cancers to make highly personalized treatment recommendations for patients, said Olivier Elemento, PhD, of Weill Cornell Medicine, New York.
Dr. Elemento described such work during the opening plenary session of the meeting.
Dr. Elemento advocated for whole-genome sequencing (WGS) of metastatic sites, as it can reveal “branched evolution” as tumors progress from localized to metastatic (Nat Genet. 2016 Dec;48[12]:1490-9).
The metastases share common mutations with the primaries from which they arise but also develop their own mutational profiles, which facilitate site-of-origin-agnostic, predictive treatment choices.
As examples, Dr. Elemento mentioned HER2 amplification found in a patient with urothelial cancer (J Natl Compr Canc Netw. 2019 Mar 1;17[3]:194-200) and a patient with uterine serous carcinoma (Gynecol Oncol Rep. 2019 Feb 21;28:54-7), both of whom experienced long-lasting remissions to HER2-targeted therapy.
Dr. Elemento also noted that WGS can reveal complex structural variants in lung adenocarcinomas that lack alterations in the RTK/RAS/RAF pathway (unpublished data).
Application of machine learning
One study suggested that microRNA expression and machine learning can be used to identify malignant thyroid lesions (Clin Cancer Res. 2012 Apr 1;18[7]:2032-8). The approach diagnosed malignant lesions with 90% accuracy, 100% sensitivity, and 86% specificity.
Dr. Elemento and colleagues used a similar approach to predict response to immunotherapy in melanoma (unpublished data).
The idea was to mine the cancer genome and transcriptome, allowing for identification of signals from neoantigens, immune gene expression, immune cell composition, and T-cell receptor repertoires, Dr. Elemento said. Integrating these signals with clinical outcome data via machine learning technology enabled the researchers to predict immunotherapy response in malignant melanoma with nearly 90% accuracy.
AI and image analysis
Studies have indicated that AI can be applied to medical images to improve diagnosis and treatment. The approach has been shown to:
- Facilitate correct diagnoses of malignant skin lesions (Nature. 2017 Feb 2;542[7639]:115-8).
- Distinguish lung adenocarcinoma from squamous cell cancer with 100% accuracy (EBioMedicine. 2018 Jan;27:317-28).
- Recognize distinct breast cancer subtypes (ductal, lobular, mucinous, papillary) and biomarkers (bioRxiv 242818. doi: 10.1101/242818; EBioMedicine. 2018 Jan;27:317-28)
- Predict mesothelioma prognosis (Nat Med. 2019 Oct;25[10]:1519-25).
- Predict prostate biopsy results (unpublished data) and calculate Gleason scores that can predict survival in prostate cancer patients (AACR 2020, Abstract 867).
Drug development through applied AI
In another study, Dr. Elemento and colleagues used a Bayesian machine learning approach to predict targets of molecules without a known mechanism of action (Nat Commun. 2019 Nov 19;10[1]:5221).
The method involved using data on gene expression profiles, cell line viability, side effects in animals, and structures of the molecules. The researchers applied this method to a large library of orphan small molecules and found it could predict targets in about 40% of cases.
Of 24 AI-predicted microtubule-targeting molecules, 14 depolymerized microtubules in the lab. Five of these molecules were effective in cell lines that were resistant to other microtubule-targeted drugs.
Dr. Elemento went on to describe how Oncoceutics was developing an antineoplastic agent called ONC201, but the company lacked information about the agent’s target. Using AI, the target was identified as dopamine receptor 2 (DRD2; Clin Cancer Res. 2019 Apr 1;25[7]:2305-13).
With that information, Oncoceutics initiated trials of ONC201 in tumors expressing high levels of DRD2, including a highly resistant glioma (J Neurooncol. 2019 Oct;145[1]:97-105). Responses were seen, and ONC201 is now being tested against other DRD2-expressing cancers.
Challenges to acknowledge
Potential benefits of AI in the clinic are exciting, but there are many bench-to-bedside challenges.
A clinically obvious example of AI’s applications is radiographic image analysis. There is no biologic rationale for our RECIST “cut values” for partial response, minimal response, and stable disease.
If AI can measure subtle changes on imaging that correlate with tumor biology (i.e., radiomics), we stand a better chance of predicting treatment outcomes than we can with conventional measurements of shrinkage of arbitrarily selected “target lesions.”
A tremendous amount of work is needed to build the required large image banks. During that time, AI will only improve – and without the human risks of fatigue, inconsistency, or burnout.
Those human frailties notwithstanding, AI cannot substitute for the key discussions between patient and clinician regarding goals of care, trade-offs of risks and benefits, and shared decision-making regarding management options.
At least initially (but painfully), complex technologies like WGS and digital image analysis via AI may further disadvantage patients who are medically disadvantaged by geography or socioeconomic circumstances.
In the discussion period, AACR President Antoni Ribas, MD, of University of California, Los Angeles, asked whether AI can simulate crosstalk between gene pathways so that unique treatment combinations can be identified. Dr. Elemento said those simulations are the subject of ongoing investigation.
The theme of the opening plenary session at the AACR virtual meeting II was “Turning Science into Life-Saving Care.” Applications of AI to optimize personalized use of genomics, digital image analysis, and drug development show great promise for being among the technologies that can help to realize AACR’s thematic vision.
Dr. Elemento disclosed relationships with Volastra Therapeutics, OneThree Biotech, Owkin, Freenome, Genetic Intelligence, Acuamark Diagnostics, Eli Lilly, Janssen, and Sanofi.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM AACR 2020
Chronicles of cancer: A history of mammography, part 1
Technological imperatives
The history of mammography provides a powerful example of the connection between social factors and the rise of a medical technology. It is also an object lesson in the profound difficulties that the medical community faces when trying to evaluate and embrace new discoveries in such a complex area as cancer diagnosis and treatment, especially when tied to issues of sex-based bias and gender identity. Given its profound ties to women’s lives and women’s bodies, mammography holds a unique place in the history of cancer. Part 1 will examine the technological imperatives driving mammography forward, and part 2 will address the social factors that promoted and inhibited the developing technology.
All that glitters
Innovations in technology have contributed so greatly to the progress of medical science in saving and improving patients’ lives that the lure of new technology and the desire to see it succeed and to embrace it has become profound.
In a debate on the adoption of new technologies, Michael Rosen, MD, a surgeon at the Cleveland Clinic, Ohio, pointed out the inherent risks in the life cycle of medical technology: “The stages of surgical innovation have been well described as moving from the generation of a hypothesis with an early promising report to being accepted conclusively as a new standard without formal testing. As the life cycle continues and comparative effectiveness data begin to emerge slowly through appropriately designed trials, the procedure or device is often ultimately abandoned.”1
The history of mammography bears out this grim warning in example after example as an object lesson, revealing not only the difficulties involved in the development of new medical technologies, but also the profound problems involved in validating the effectiveness and appropriateness of a new technology from its inception to the present.
A modern failure?
In fact, one of the more modern developments in mammography technology – digital imaging – has recently been called into question with regard to its effectiveness in saving lives, even as the technology continues to spread throughout the medical community.
A recent meta-analysis has shown that there is little or no improvement in outcomes of breast cancer screening when using digital analysis and screening mammograms vs. traditional film recording.
The meta-analysis assessed 24 studies with a combined total of 16,583,743 screening examinations (10,968,843 film and 5,614,900 digital). The study found that the difference in cancer detection rate using digital rather than film screening showed an increase of only 0.51 detections per 1,000 screens.
The researchers concluded “that while digital mammography is beneficial for medical facilities due to easier storage and handling of images, these results suggest the transition from film to digital mammography has not resulted in health benefits for screened women.”2
In fact, the researchers added that “This analysis reinforces the need to carefully evaluate effects of future changes in technology, such as tomosynthesis, to ensure new technology leads to improved health outcomes and beyond technical gains.”2
None of the nine main randomized clinical trials that were used to determine the effectiveness of mammography screening from the 1960s to the 1990s used digital or 3-D digital mammography (digital breast tomosynthesis or DBT). The earliest trial used direct-exposure film mammography and the others relied upon screen-film mammography.3 And yet the assumptions of the validity of the new digital technologies were predicated on the generalized acceptance of the validity of screening derived from these studies, and a corollary assumption that any technological improvement in the quality of the image must inherently be an improvement of the overall results of screening.
The failure of new technologies to meet expectations is a sobering corrective to the high hopes of researchers, practitioners, and patient groups alike, and is perhaps destined to contribute more to the parallel history of controversy and distrust concerning the risk/benefits of mammography that has been a media and scientific mainstay.
Too often the history of medical technology has found disappointment at the end of the road for new discoveries. But although the disappointing results of digital screening might be considered a failure in the progress of mammography, it is likely just another pause on the road of this technology, the history of which has been rocky from the start.
The need for a new way of looking
The rationale behind the original and continuing development of mammography is a simple one, common to all cancer screening methods – the belief that the earlier the detection of a cancer, the more likely it is to be treated effectively with the therapeutic regimens at hand. While there is some controversy regarding the cost-benefit ratio of screening, especially when therapies for breast cancer are not perfect and vary widely in expense and availability globally, the driving belief has been that mammography provides an outcomes benefit in allowing early surgical and chemoradiation therapy with a curative intent.
There were two main driving forces behind the early development of mammography. The first was the highly lethal nature of breast cancer, especially when it was caught too late and had spread too far to benefit from the only available option at the time – surgery. The second was the severity of the surgical treatment, the only therapeutic option at the time, and the distressing number of women who faced the radical mastectomy procedure pioneered by physicians William Stewart Halsted (1852-1922) at Johns Hopkins University, Baltimore, and Willy Meyer (1858-1932) in New York.
In 1894, in an era when the development of anesthetics and antisepsis made ever more difficult surgical procedures possible without inevitably killing the patient, both men separately published their results of a highly extensive operation that consisted of removal of the breast, chest muscles, and axillary lymph nodes.
As long as there was no presurgical method of determining the extent of a breast cancer’s spread, much less an ability to visually distinguish malignant from benign growths, this “better safe than sorry” approach became the default approach of an increasing number of surgeons, and the drastic solution of radical mastectomy was increasingly applied universally.
But in 1895, with the discovery of x-rays, medical science recognized a nearly miraculous technology for visualizing the inside of the body, and radioactive materials were also routinely used in medical therapies, by both legitimate practitioners and hucksters.
However, in the very early days, the users of x-rays were unaware that large radiation doses could have serious biological effects and had no way of determining radiation field strength and accumulating dosage.
In fact, early calibration of x-ray tubes was based on the amount of skin reddening (erythema) produced when the operator placed a hand directly in the x-ray beam.
It was in this environment that, within only a few decades, the new x-rays, especially with the development of improvements in mammography imaging, were able in many cases to identify smaller, more curable breast cancers. This eventually allowed surgeons to develop and use less extensive operations than the highly disfiguring radical mastectomy that was simultaneously dreaded for its invasiveness and embraced for its life-saving potential.4
Pioneering era
The technological history of mammography was thus driven by the quest for better imaging and reproducibility in order to further the hopes of curative surgical approaches.
In 1913, the German surgeon Albert Salomon (1883-1976) was the first to detect breast cancer using x-rays, but its clinical use was not established, as the images published in his “Beiträge zur pathologie und klinik der mammakarzinome (Contributions to the pathology and clinic of breast cancers)” were photographs of postsurgical breast specimens that illustrated the anatomy and spread of breast cancer tumors but were not adapted to presurgical screening.
After Salomon’s work was published in 1913, there was no new mammography literature published until 1927, when German surgeon Otto Kleinschmidt (1880-1948) published a report describing the world’s first authentic mammography, which he attributed to his mentor, the plastic surgeon Erwin Payr (1871-1946).5
This was followed soon after in 1930 by the work of radiologist Stafford L. Warren (1896-1981), of the University of Rochester (N.Y.), who published a paper on the use of standard roentgenograms for the in vivo preoperative assessment of breast malignancies. His technique involved the use of a stereoscopic system with a grid mechanism and intensifying screens to amplify the image. Breast compression was not involved in his mammogram technique. “Dr. Warren claimed to be correct 92% of the time when using this technique to predict malignancy.”5
His study of 119 women with a histopathologic diagnosis (61 benign and 58 malignant) demonstrated the feasibility of the technique for routine use and “created a surge of interest.”6
But the technology of the time proved difficult to use, and the results difficult to reproduce from laboratory to laboratory, and ultimately did not gain wide acceptance. Among Warren’s other claims to fame, he was a participant in the Manhattan Project and was a member of the teams sent to assess radiation damage in Hiroshima and Nagasaki after the dropping of the atomic bombs.
And in fact, future developments in mammography and all other x-ray screening techniques included attempts to minimize radiation exposure; such attempts were driven, in part, by the tragic impact of atomic bomb radiation and the medical studies carried out on the survivors.
An image more deadly than the disease
Further improvements in mammography technique occurred through the 1930s and 1940s, including better visualization of the mammary ducts based upon the pioneering studies of Emil Ries, MD, in Chicago, who, along with Nymphus Frederick Hicken, MD (1900-1998), reported on the use of contrast mammography (also known as ductography or galactography). On a side note, Dr. Hicken was responsible for introducing the terms mammogram and mammography in 1937.
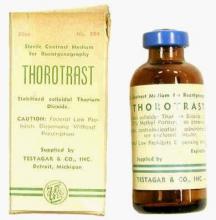
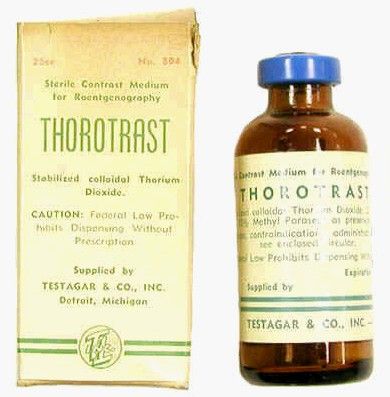
Problems with ductography, which involved the injection of a radiographically opaque contrast agent into the nipple, occurred when the early contrast agents, such as oil-based lipiodol, proved to be toxic and capable of causing abscesses.7This advance led to the development of other agents, and among the most popular at the time was one that would prove deadly to many.
Thorotrast, first used in 1928, was widely embraced because of its lack of immediately noticeable side effects and the high-quality contrast it provided. Thorotrast was a suspension of radioactive thorium dioxide particles, which gained popularity for use as a radiological imaging agent from the 1930s to 1950s throughout the world, being used in an estimated 2-10 million radiographic exams, primarily for neurosurgery.
In the 1920s and 1930s, world governments had begun to recognize the dangers of radiation exposure, especially among workers, but thorotrast was a unique case because, unbeknownst to most practitioners at the time, thorium dioxide was retained in the body for the lifetime of the patient, with 70% deposited in the liver, 20% in the spleen, and the remaining in the bony medulla and in the peripheral lymph nodes.
Nineteen years after the first use of thorotrast, the first case of a human malignant tumor attributed to its exposure was reported. “Besides the liver neoplasm cases, aplastic anemia, leukemia and an impressive incidence of chromosome aberrations were registered in exposed individuals.”8
Despite its widespread adoption elsewhere, especially in Japan, the use of thorotrast never became popular in the United States, in part because in 1932 and 1937, warnings were issued by the American Medical Association to restrict its use.9
There was a shift to the use of iodinated hydrophilic molecules as contrast agents for conventional x-ray, computed tomography, and fluoroscopy procedures.9 However, it was discovered that these agents, too, have their own risks and dangerous side effects. They can cause severe adverse effects, including allergies, cardiovascular diseases, and nephrotoxicity in some patients.
Slow adoption and limited results
Between 1930 and 1950, Dr. Warren, Jacob Gershon-Cohen, MD (1899-1971) of Philadelphia, and radiologist Raul Leborgne of Uruguay “spread the gospel of mammography as an adjunct to physical examination for the diagnosis of breast cancer.”4 The latter also developed the breast compression technique to produce better quality images and lower the radiation exposure needed, and described the differences that could be visualized between benign and malign microcalcifications.
But despite the introduction of improvements such as double-emulsion film and breast compression to produce higher-quality images, “mammographic films often remained dark and hazy. Moreover, the new techniques, while improving the images, were not easily reproduced by other investigators and clinicians,” and therefore were still not widely adopted.4
Little noticeable effect of mammography
Although the technology existed and had its popularizers, mammography had little impact on an epidemiological level.
There was no major change in the mean maximum breast cancer tumor diameter and node positivity rate detected over the 20 years from 1929 to 1948.10 However, starting in the late 1940s, the American Cancer Society began public education campaigns and early detection education, and thereafter, there was a 3% decline in mean maximum diameter of tumor size seen every 10 years until 1968.
“We have interpreted this as the effect of public education and professional education about early detection through television, print media, and professional publications that began in 1947 because no other event was known to occur that would affect cancer detection beginning in the late 1940s.”10
However, the early detection methods at the time were self-examination and clinical examination for lumps, with mammography remaining a relatively limited tool until its general acceptance broadened a few decades later.
Robert Egan, “Father of Mammography,” et al.
The broad acceptance of mammography as a screening tool and its impacts on a broad population level resulted in large part from the work of Robert L. Egan, MD (1921-2001) in the late 1950s and 1960s.
Dr. Egan’s work was inspired in 1956 by a presentation by a visiting fellow, Jean Pierre Batiani, who brought a mammogram clearly showing a breast cancer from his institution, the Curie Foundation in Paris. The image had been made using very low kilowattage, high tube currents, and fine-grain film.
Dr. Egan, then a resident in radiology, was given the task by the head of his department of reproducing the results.
In 1959, Dr. Egan, then at the University of Texas MD Anderson Cancer Center, Houston, published a combined technique that used a high-milliamperage–low-voltage technique, a fine-grain intensifying screen, and single-emulsion films for mammography, thereby decreasing the radiation exposure significantly from previous x-ray techniques and improving the visualization and reproducibility of screening.
By 1960, Dr. Egan reported on 1,000 mammography cases at MD Anderson, demonstrating the ability of proper screening to detect unsuspected cancers and to limit mastectomies on benign masses. Of 245 breast cancers ultimately confirmed by biopsy, 238 were discovered by mammography, 19 of which were in women whose physical examinations had revealed no breast pathology. One of the cancers was only 8 mm in diameter when sectioned at biopsy.
Dr. Egan’s findings prompted an investigation by the Cancer Control Program (CCP) of the U.S. Public Health Service and led to a study jointly conducted by the National Cancer Institute and MD Anderson Hospital and the CCP, which involved 24 institutions and 1,500 patients.
“The results showed a 21% false-negative rate and a 79% true-positive rate for screening studies using Egan’s technique. This was a milestone for women’s imaging in the United States. Screening mammography was off to a tentative start.”5
“Egan was the man who developed a smooth-riding automobile compared to a Model T. He put mammography on the map and made it an intelligible, reproducible study. In short, he was the father of modern mammography,” according to his professor, mentor, and fellow mammography pioneer Gerald Dodd, MD (Emory School of Medicine website biography).
In 1964 Dr. Egan published his definitive book, “Mammography,” and in 1965 he hosted a 30-minute audiovisual presentation describing in detail his technique.11
The use of mammography was further powered by improved methods of preoperative needle localization, pioneered by Richard H. Gold, MD, in 1963 at Jefferson Medical College, Philadelphia, which eased obtaining a tissue diagnosis for any suspicious lesions detected in the mammogram. Dr. Gold performed needle localization of nonpalpable, mammographically visible lesions before biopsy, which allowed surgical resection of a smaller volume of breast tissue than was possible before.
Throughout the era, there were also incremental improvements in mammography machines and an increase in the number of commercial manufacturers.
Xeroradiography, an imaging technique adapted from xerographic photocopying, was seen as a major improvement over direct film imaging, and the technology became popular throughout the 1970s based on the research of John N. Wolfe, MD (1923-1993), who worked closely with the Xerox Corporation to improve the breast imaging process.6 However, this technology had all the same problems associated with running an office copying machine, including paper jams and toner issues, and the worst aspect was the high dose of radiation required. For this reason, it would quickly be superseded by the use of screen-film mammography, which eventually completely replaced the use of both xeromammography and direct-exposure film mammography.
The march of mammography
A series of nine randomized clinical trials (RCTs) between the 1960s and 1990s formed the foundation of the clinical use of mammography. These studies enrolled more than 600,000 women in the United States, Canada, the United Kingdom, and Sweden. The nine main RCTs of breast cancer screening were the Health Insurance Plan of Greater New York (HIP) trial, the Edinburgh trial, the Canadian National Breast Screening Study, the Canadian National Breast Screening Study 2, the United Kingdom Age trial, the Stockholm trial, the Malmö Mammographic Screening Trial, the Gothenburg trial, and the Swedish Two-County Study.3
These trials incorporated improvements in the technology as it developed, as seen in the fact that the earliest, the HIP trial, used direct-exposure film mammography and the other trials used screen-film mammography.3
Meta-analyses of the major nine screening trials indicated that reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials. “Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60-69 years.”3 In addition the estimates for women aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
However, at the time, the studies had a profound influence on increasing the popularity and spread of mammography.
As mammographies became more common, standardization became an important issue and a Mammography Accreditation Program began in 1987. Originally a voluntary program, it became mandatory with the Mammography Quality Standards Act of 1992, which required all U.S. mammography facilities to become accredited and certified.
In 1986, the American College of Radiology proposed its Breast Imaging Reporting and Data System (BI-RADS) initiative to enable standardized reporting of mammography; the first report was released in 1993.
BI-RADS is now on its fifth edition and has addressed the use of mammography, breast ultrasonography, and breast magnetic resonance imaging, developing standardized auditing approaches for all three techniques of breast cancer imaging.6
The digital era and beyond
With the dawn of the 21st century, the era of digital breast cancer screening began.
The screen-film mammography (SFM) technique employed throughout the 1980s and 1990s had significant advantages over earlier x-ray films for producing more vivid images of dense breast tissues. The next technology, digital mammography, was introduced in the late 20th century, and the first system was approved by the U.S. FDA in 2000.
One of the key benefits touted for digital mammograms is the fact that the radiologist can manipulate the contrast of the images, which allows for masses to be identified that might otherwise not be visible on standard film.
However, the recent meta-analysis discussed in the introduction calls such benefits into question, and a new controversy is likely to ensue on the question of the effectiveness of digital mammography on overall clinical outcomes.
But the technology continues to evolve.
“There has been a continuous and substantial technical development from SFM to full-field digital mammography and very recently also the introduction of digital breast tomosynthesis (DBT). This technical evolution calls for new evidence regarding the performance of screening using new mammography technologies, and the evidence needed to translate new technologies into screening practice,” according to an updated assessment by the U.S. Preventive Services Task Force.12
DBT was approved by the Food and Drug Administration in 2011. The technology involves the creation of a series of images, which are assembled into a 3-D–like image of breast slices. Traditional digital mammography creates a 2-D image of a flattened breast, and the radiologist must peer through the layers to find abnormalities. DBT uses a computer algorithm to reconstruct multiple low-dose digital images of the breast that can be displayed individually or in cinematic mode.13
Early trials showed a significant benefit of DBT in detecting new and smaller breast cancers, compared with standard digital mammography.
In women in their 40s, DBT found 1.7 more cancers than digital mammography for every 1,000 exams of women with normal breast tissue. In addition, 16.3% of women in this age group who were screened using digital mammography received callbacks, versus 11.7% of those screened using DBT. For younger women with dense breasts, the advantage of DBT was even greater, with 2.27 more cancers found for every 1,000 women screened. Whether such results will lead to clinically improved outcomes remains a question. “It can still miss cancers. Also, like traditional mammography, DBT might not reduce deaths from tumors that are very aggressive and fast-growing. And some women will still be called back unnecessarily for false-positive results.”14
But such technological advances further the hopes of researchers and patients alike.
Conclusion
Medical technology is driven both by advances in science and by the demands of patients and physicians for improved outcomes. The history of mammography, for example, is tied to the scientific advancements in x-ray technology, which allowed physicians for the first time to peer inside a living body without a scalpel at hand. But mammography was also an outgrowth of the profound need of the surgeon to identify cancerous masses in the breast at an early-enough stage to attempt a cure, while simultaneously minimizing the radical nature of the surgery required.
And while seeing is believing, the need to see and verify what was seen in order to make life-and-death decisions drove the demand for improvements in the technology of mammography throughout most of the 20th century and beyond.
The tortuous path from the early and continuing snafus with contrast agents to the apparent failure of the promise of digital technology serves as a continuing reminder of the hopes and perils that developing medical technologies present. It will be interesting to see if further refinements to mammography, such as DBT, will enhance the technology enough to have a major impact on countless women’s lives, or if new developments in magnetic resonance imaging and ultrasound make traditional mammography a relic of the past.
Part 2 of this history will present the social dynamics intimately involved with the rise and promulgation of mammography and how social need and public fears and controversies affected its development and spread as much, if not more, than technological innovation.
This article could only touch upon the myriad of details and technologies involved in the history of mammography, and I urge interested readers to check out the relevant references for far more in-depth and fascinating stories from its complex and controversial past.
References
1. Felix EL, Rosen M, Earle D. “Curbing Our Enthusiasm for Surgical Innovation: Is It a Good Thing or Bad Thing?” The Great Debates, General Surgery News, 2018 Oct 17
2. J Natl Cancer Inst. 2020 Jun 23. doi: 10.1093/jnci/djaa080.
3. Nelson H et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. Evidence Synthesis No. 124. (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan, pp. 29-49)4. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography,” background paper for Patlak M et al., Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer (Washington: National Academies Press, 2001).
5. Grady I, Hansen P. Chapter 28: Mammography in “Kuerer’s Breast Surgical Oncology”(New York: McGaw-Hill Medical, 2010)
6. Radiology. 2014 Nov;273(2 Suppl):S23-44.
7. Bassett LW, Kim CH. (2003) Chapter 1: Ductography in Dershaw DD (eds) “Imaging-Guided Interventional Breast Techniques” (New York: Springer, 2003, pp. 1-30).
8. Cuperschmid EM, Ribeiro de Campos TP. 2009 International Nuclear Atlantic Conference, Rio de Janeiro, Sept 27–Oct 2, 2009
9. Bioscience Microflora. 2000;19(2):107-16.
10. Cady B. New era in breast cancer. Impact of screening on disease presentation. Surg Oncol Clin N Am. 1997 Apr;6(2):195-202.
11. Egan R. “Mammography Technique.” Audiovisual presentation. (Washington: U.S. Public Health Service, 1965).
12. Zackrisson S, Houssami N. Chapter 13: Evolution of Mammography Screening: From Film Screen to Digital Breast Tomosynthesis in “Breast Cancer Screening: An Examination of Scientific Evidence” (Cambridge, Mass.: Academic Press, 2016, pp. 323-46).13. Melnikow J et al. Screening for breast cancer with digital breast tomosynthesis. Evidence Synthesis No. 125 (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan).
14. Newer breast screening technology may spot more cancers. Harvard Women’s Health Watch online, June 2019.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Technological imperatives
Technological imperatives
The history of mammography provides a powerful example of the connection between social factors and the rise of a medical technology. It is also an object lesson in the profound difficulties that the medical community faces when trying to evaluate and embrace new discoveries in such a complex area as cancer diagnosis and treatment, especially when tied to issues of sex-based bias and gender identity. Given its profound ties to women’s lives and women’s bodies, mammography holds a unique place in the history of cancer. Part 1 will examine the technological imperatives driving mammography forward, and part 2 will address the social factors that promoted and inhibited the developing technology.
All that glitters
Innovations in technology have contributed so greatly to the progress of medical science in saving and improving patients’ lives that the lure of new technology and the desire to see it succeed and to embrace it has become profound.
In a debate on the adoption of new technologies, Michael Rosen, MD, a surgeon at the Cleveland Clinic, Ohio, pointed out the inherent risks in the life cycle of medical technology: “The stages of surgical innovation have been well described as moving from the generation of a hypothesis with an early promising report to being accepted conclusively as a new standard without formal testing. As the life cycle continues and comparative effectiveness data begin to emerge slowly through appropriately designed trials, the procedure or device is often ultimately abandoned.”1
The history of mammography bears out this grim warning in example after example as an object lesson, revealing not only the difficulties involved in the development of new medical technologies, but also the profound problems involved in validating the effectiveness and appropriateness of a new technology from its inception to the present.
A modern failure?
In fact, one of the more modern developments in mammography technology – digital imaging – has recently been called into question with regard to its effectiveness in saving lives, even as the technology continues to spread throughout the medical community.
A recent meta-analysis has shown that there is little or no improvement in outcomes of breast cancer screening when using digital analysis and screening mammograms vs. traditional film recording.
The meta-analysis assessed 24 studies with a combined total of 16,583,743 screening examinations (10,968,843 film and 5,614,900 digital). The study found that the difference in cancer detection rate using digital rather than film screening showed an increase of only 0.51 detections per 1,000 screens.
The researchers concluded “that while digital mammography is beneficial for medical facilities due to easier storage and handling of images, these results suggest the transition from film to digital mammography has not resulted in health benefits for screened women.”2
In fact, the researchers added that “This analysis reinforces the need to carefully evaluate effects of future changes in technology, such as tomosynthesis, to ensure new technology leads to improved health outcomes and beyond technical gains.”2
None of the nine main randomized clinical trials that were used to determine the effectiveness of mammography screening from the 1960s to the 1990s used digital or 3-D digital mammography (digital breast tomosynthesis or DBT). The earliest trial used direct-exposure film mammography and the others relied upon screen-film mammography.3 And yet the assumptions of the validity of the new digital technologies were predicated on the generalized acceptance of the validity of screening derived from these studies, and a corollary assumption that any technological improvement in the quality of the image must inherently be an improvement of the overall results of screening.
The failure of new technologies to meet expectations is a sobering corrective to the high hopes of researchers, practitioners, and patient groups alike, and is perhaps destined to contribute more to the parallel history of controversy and distrust concerning the risk/benefits of mammography that has been a media and scientific mainstay.
Too often the history of medical technology has found disappointment at the end of the road for new discoveries. But although the disappointing results of digital screening might be considered a failure in the progress of mammography, it is likely just another pause on the road of this technology, the history of which has been rocky from the start.
The need for a new way of looking
The rationale behind the original and continuing development of mammography is a simple one, common to all cancer screening methods – the belief that the earlier the detection of a cancer, the more likely it is to be treated effectively with the therapeutic regimens at hand. While there is some controversy regarding the cost-benefit ratio of screening, especially when therapies for breast cancer are not perfect and vary widely in expense and availability globally, the driving belief has been that mammography provides an outcomes benefit in allowing early surgical and chemoradiation therapy with a curative intent.
There were two main driving forces behind the early development of mammography. The first was the highly lethal nature of breast cancer, especially when it was caught too late and had spread too far to benefit from the only available option at the time – surgery. The second was the severity of the surgical treatment, the only therapeutic option at the time, and the distressing number of women who faced the radical mastectomy procedure pioneered by physicians William Stewart Halsted (1852-1922) at Johns Hopkins University, Baltimore, and Willy Meyer (1858-1932) in New York.
In 1894, in an era when the development of anesthetics and antisepsis made ever more difficult surgical procedures possible without inevitably killing the patient, both men separately published their results of a highly extensive operation that consisted of removal of the breast, chest muscles, and axillary lymph nodes.
As long as there was no presurgical method of determining the extent of a breast cancer’s spread, much less an ability to visually distinguish malignant from benign growths, this “better safe than sorry” approach became the default approach of an increasing number of surgeons, and the drastic solution of radical mastectomy was increasingly applied universally.
But in 1895, with the discovery of x-rays, medical science recognized a nearly miraculous technology for visualizing the inside of the body, and radioactive materials were also routinely used in medical therapies, by both legitimate practitioners and hucksters.
However, in the very early days, the users of x-rays were unaware that large radiation doses could have serious biological effects and had no way of determining radiation field strength and accumulating dosage.
In fact, early calibration of x-ray tubes was based on the amount of skin reddening (erythema) produced when the operator placed a hand directly in the x-ray beam.
It was in this environment that, within only a few decades, the new x-rays, especially with the development of improvements in mammography imaging, were able in many cases to identify smaller, more curable breast cancers. This eventually allowed surgeons to develop and use less extensive operations than the highly disfiguring radical mastectomy that was simultaneously dreaded for its invasiveness and embraced for its life-saving potential.4
Pioneering era
The technological history of mammography was thus driven by the quest for better imaging and reproducibility in order to further the hopes of curative surgical approaches.
In 1913, the German surgeon Albert Salomon (1883-1976) was the first to detect breast cancer using x-rays, but its clinical use was not established, as the images published in his “Beiträge zur pathologie und klinik der mammakarzinome (Contributions to the pathology and clinic of breast cancers)” were photographs of postsurgical breast specimens that illustrated the anatomy and spread of breast cancer tumors but were not adapted to presurgical screening.
After Salomon’s work was published in 1913, there was no new mammography literature published until 1927, when German surgeon Otto Kleinschmidt (1880-1948) published a report describing the world’s first authentic mammography, which he attributed to his mentor, the plastic surgeon Erwin Payr (1871-1946).5
This was followed soon after in 1930 by the work of radiologist Stafford L. Warren (1896-1981), of the University of Rochester (N.Y.), who published a paper on the use of standard roentgenograms for the in vivo preoperative assessment of breast malignancies. His technique involved the use of a stereoscopic system with a grid mechanism and intensifying screens to amplify the image. Breast compression was not involved in his mammogram technique. “Dr. Warren claimed to be correct 92% of the time when using this technique to predict malignancy.”5
His study of 119 women with a histopathologic diagnosis (61 benign and 58 malignant) demonstrated the feasibility of the technique for routine use and “created a surge of interest.”6
But the technology of the time proved difficult to use, and the results difficult to reproduce from laboratory to laboratory, and ultimately did not gain wide acceptance. Among Warren’s other claims to fame, he was a participant in the Manhattan Project and was a member of the teams sent to assess radiation damage in Hiroshima and Nagasaki after the dropping of the atomic bombs.
And in fact, future developments in mammography and all other x-ray screening techniques included attempts to minimize radiation exposure; such attempts were driven, in part, by the tragic impact of atomic bomb radiation and the medical studies carried out on the survivors.
An image more deadly than the disease
Further improvements in mammography technique occurred through the 1930s and 1940s, including better visualization of the mammary ducts based upon the pioneering studies of Emil Ries, MD, in Chicago, who, along with Nymphus Frederick Hicken, MD (1900-1998), reported on the use of contrast mammography (also known as ductography or galactography). On a side note, Dr. Hicken was responsible for introducing the terms mammogram and mammography in 1937.
Problems with ductography, which involved the injection of a radiographically opaque contrast agent into the nipple, occurred when the early contrast agents, such as oil-based lipiodol, proved to be toxic and capable of causing abscesses.7This advance led to the development of other agents, and among the most popular at the time was one that would prove deadly to many.
Thorotrast, first used in 1928, was widely embraced because of its lack of immediately noticeable side effects and the high-quality contrast it provided. Thorotrast was a suspension of radioactive thorium dioxide particles, which gained popularity for use as a radiological imaging agent from the 1930s to 1950s throughout the world, being used in an estimated 2-10 million radiographic exams, primarily for neurosurgery.
In the 1920s and 1930s, world governments had begun to recognize the dangers of radiation exposure, especially among workers, but thorotrast was a unique case because, unbeknownst to most practitioners at the time, thorium dioxide was retained in the body for the lifetime of the patient, with 70% deposited in the liver, 20% in the spleen, and the remaining in the bony medulla and in the peripheral lymph nodes.
Nineteen years after the first use of thorotrast, the first case of a human malignant tumor attributed to its exposure was reported. “Besides the liver neoplasm cases, aplastic anemia, leukemia and an impressive incidence of chromosome aberrations were registered in exposed individuals.”8
Despite its widespread adoption elsewhere, especially in Japan, the use of thorotrast never became popular in the United States, in part because in 1932 and 1937, warnings were issued by the American Medical Association to restrict its use.9
There was a shift to the use of iodinated hydrophilic molecules as contrast agents for conventional x-ray, computed tomography, and fluoroscopy procedures.9 However, it was discovered that these agents, too, have their own risks and dangerous side effects. They can cause severe adverse effects, including allergies, cardiovascular diseases, and nephrotoxicity in some patients.
Slow adoption and limited results
Between 1930 and 1950, Dr. Warren, Jacob Gershon-Cohen, MD (1899-1971) of Philadelphia, and radiologist Raul Leborgne of Uruguay “spread the gospel of mammography as an adjunct to physical examination for the diagnosis of breast cancer.”4 The latter also developed the breast compression technique to produce better quality images and lower the radiation exposure needed, and described the differences that could be visualized between benign and malign microcalcifications.
But despite the introduction of improvements such as double-emulsion film and breast compression to produce higher-quality images, “mammographic films often remained dark and hazy. Moreover, the new techniques, while improving the images, were not easily reproduced by other investigators and clinicians,” and therefore were still not widely adopted.4
Little noticeable effect of mammography
Although the technology existed and had its popularizers, mammography had little impact on an epidemiological level.
There was no major change in the mean maximum breast cancer tumor diameter and node positivity rate detected over the 20 years from 1929 to 1948.10 However, starting in the late 1940s, the American Cancer Society began public education campaigns and early detection education, and thereafter, there was a 3% decline in mean maximum diameter of tumor size seen every 10 years until 1968.
“We have interpreted this as the effect of public education and professional education about early detection through television, print media, and professional publications that began in 1947 because no other event was known to occur that would affect cancer detection beginning in the late 1940s.”10
However, the early detection methods at the time were self-examination and clinical examination for lumps, with mammography remaining a relatively limited tool until its general acceptance broadened a few decades later.
Robert Egan, “Father of Mammography,” et al.
The broad acceptance of mammography as a screening tool and its impacts on a broad population level resulted in large part from the work of Robert L. Egan, MD (1921-2001) in the late 1950s and 1960s.
Dr. Egan’s work was inspired in 1956 by a presentation by a visiting fellow, Jean Pierre Batiani, who brought a mammogram clearly showing a breast cancer from his institution, the Curie Foundation in Paris. The image had been made using very low kilowattage, high tube currents, and fine-grain film.
Dr. Egan, then a resident in radiology, was given the task by the head of his department of reproducing the results.
In 1959, Dr. Egan, then at the University of Texas MD Anderson Cancer Center, Houston, published a combined technique that used a high-milliamperage–low-voltage technique, a fine-grain intensifying screen, and single-emulsion films for mammography, thereby decreasing the radiation exposure significantly from previous x-ray techniques and improving the visualization and reproducibility of screening.
By 1960, Dr. Egan reported on 1,000 mammography cases at MD Anderson, demonstrating the ability of proper screening to detect unsuspected cancers and to limit mastectomies on benign masses. Of 245 breast cancers ultimately confirmed by biopsy, 238 were discovered by mammography, 19 of which were in women whose physical examinations had revealed no breast pathology. One of the cancers was only 8 mm in diameter when sectioned at biopsy.
Dr. Egan’s findings prompted an investigation by the Cancer Control Program (CCP) of the U.S. Public Health Service and led to a study jointly conducted by the National Cancer Institute and MD Anderson Hospital and the CCP, which involved 24 institutions and 1,500 patients.
“The results showed a 21% false-negative rate and a 79% true-positive rate for screening studies using Egan’s technique. This was a milestone for women’s imaging in the United States. Screening mammography was off to a tentative start.”5
“Egan was the man who developed a smooth-riding automobile compared to a Model T. He put mammography on the map and made it an intelligible, reproducible study. In short, he was the father of modern mammography,” according to his professor, mentor, and fellow mammography pioneer Gerald Dodd, MD (Emory School of Medicine website biography).
In 1964 Dr. Egan published his definitive book, “Mammography,” and in 1965 he hosted a 30-minute audiovisual presentation describing in detail his technique.11
The use of mammography was further powered by improved methods of preoperative needle localization, pioneered by Richard H. Gold, MD, in 1963 at Jefferson Medical College, Philadelphia, which eased obtaining a tissue diagnosis for any suspicious lesions detected in the mammogram. Dr. Gold performed needle localization of nonpalpable, mammographically visible lesions before biopsy, which allowed surgical resection of a smaller volume of breast tissue than was possible before.
Throughout the era, there were also incremental improvements in mammography machines and an increase in the number of commercial manufacturers.
Xeroradiography, an imaging technique adapted from xerographic photocopying, was seen as a major improvement over direct film imaging, and the technology became popular throughout the 1970s based on the research of John N. Wolfe, MD (1923-1993), who worked closely with the Xerox Corporation to improve the breast imaging process.6 However, this technology had all the same problems associated with running an office copying machine, including paper jams and toner issues, and the worst aspect was the high dose of radiation required. For this reason, it would quickly be superseded by the use of screen-film mammography, which eventually completely replaced the use of both xeromammography and direct-exposure film mammography.
The march of mammography
A series of nine randomized clinical trials (RCTs) between the 1960s and 1990s formed the foundation of the clinical use of mammography. These studies enrolled more than 600,000 women in the United States, Canada, the United Kingdom, and Sweden. The nine main RCTs of breast cancer screening were the Health Insurance Plan of Greater New York (HIP) trial, the Edinburgh trial, the Canadian National Breast Screening Study, the Canadian National Breast Screening Study 2, the United Kingdom Age trial, the Stockholm trial, the Malmö Mammographic Screening Trial, the Gothenburg trial, and the Swedish Two-County Study.3
These trials incorporated improvements in the technology as it developed, as seen in the fact that the earliest, the HIP trial, used direct-exposure film mammography and the other trials used screen-film mammography.3
Meta-analyses of the major nine screening trials indicated that reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials. “Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60-69 years.”3 In addition the estimates for women aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
However, at the time, the studies had a profound influence on increasing the popularity and spread of mammography.
As mammographies became more common, standardization became an important issue and a Mammography Accreditation Program began in 1987. Originally a voluntary program, it became mandatory with the Mammography Quality Standards Act of 1992, which required all U.S. mammography facilities to become accredited and certified.
In 1986, the American College of Radiology proposed its Breast Imaging Reporting and Data System (BI-RADS) initiative to enable standardized reporting of mammography; the first report was released in 1993.
BI-RADS is now on its fifth edition and has addressed the use of mammography, breast ultrasonography, and breast magnetic resonance imaging, developing standardized auditing approaches for all three techniques of breast cancer imaging.6
The digital era and beyond
With the dawn of the 21st century, the era of digital breast cancer screening began.
The screen-film mammography (SFM) technique employed throughout the 1980s and 1990s had significant advantages over earlier x-ray films for producing more vivid images of dense breast tissues. The next technology, digital mammography, was introduced in the late 20th century, and the first system was approved by the U.S. FDA in 2000.
One of the key benefits touted for digital mammograms is the fact that the radiologist can manipulate the contrast of the images, which allows for masses to be identified that might otherwise not be visible on standard film.
However, the recent meta-analysis discussed in the introduction calls such benefits into question, and a new controversy is likely to ensue on the question of the effectiveness of digital mammography on overall clinical outcomes.
But the technology continues to evolve.
“There has been a continuous and substantial technical development from SFM to full-field digital mammography and very recently also the introduction of digital breast tomosynthesis (DBT). This technical evolution calls for new evidence regarding the performance of screening using new mammography technologies, and the evidence needed to translate new technologies into screening practice,” according to an updated assessment by the U.S. Preventive Services Task Force.12
DBT was approved by the Food and Drug Administration in 2011. The technology involves the creation of a series of images, which are assembled into a 3-D–like image of breast slices. Traditional digital mammography creates a 2-D image of a flattened breast, and the radiologist must peer through the layers to find abnormalities. DBT uses a computer algorithm to reconstruct multiple low-dose digital images of the breast that can be displayed individually or in cinematic mode.13
Early trials showed a significant benefit of DBT in detecting new and smaller breast cancers, compared with standard digital mammography.
In women in their 40s, DBT found 1.7 more cancers than digital mammography for every 1,000 exams of women with normal breast tissue. In addition, 16.3% of women in this age group who were screened using digital mammography received callbacks, versus 11.7% of those screened using DBT. For younger women with dense breasts, the advantage of DBT was even greater, with 2.27 more cancers found for every 1,000 women screened. Whether such results will lead to clinically improved outcomes remains a question. “It can still miss cancers. Also, like traditional mammography, DBT might not reduce deaths from tumors that are very aggressive and fast-growing. And some women will still be called back unnecessarily for false-positive results.”14
But such technological advances further the hopes of researchers and patients alike.
Conclusion
Medical technology is driven both by advances in science and by the demands of patients and physicians for improved outcomes. The history of mammography, for example, is tied to the scientific advancements in x-ray technology, which allowed physicians for the first time to peer inside a living body without a scalpel at hand. But mammography was also an outgrowth of the profound need of the surgeon to identify cancerous masses in the breast at an early-enough stage to attempt a cure, while simultaneously minimizing the radical nature of the surgery required.
And while seeing is believing, the need to see and verify what was seen in order to make life-and-death decisions drove the demand for improvements in the technology of mammography throughout most of the 20th century and beyond.
The tortuous path from the early and continuing snafus with contrast agents to the apparent failure of the promise of digital technology serves as a continuing reminder of the hopes and perils that developing medical technologies present. It will be interesting to see if further refinements to mammography, such as DBT, will enhance the technology enough to have a major impact on countless women’s lives, or if new developments in magnetic resonance imaging and ultrasound make traditional mammography a relic of the past.
Part 2 of this history will present the social dynamics intimately involved with the rise and promulgation of mammography and how social need and public fears and controversies affected its development and spread as much, if not more, than technological innovation.
This article could only touch upon the myriad of details and technologies involved in the history of mammography, and I urge interested readers to check out the relevant references for far more in-depth and fascinating stories from its complex and controversial past.
References
1. Felix EL, Rosen M, Earle D. “Curbing Our Enthusiasm for Surgical Innovation: Is It a Good Thing or Bad Thing?” The Great Debates, General Surgery News, 2018 Oct 17
2. J Natl Cancer Inst. 2020 Jun 23. doi: 10.1093/jnci/djaa080.
3. Nelson H et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. Evidence Synthesis No. 124. (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan, pp. 29-49)4. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography,” background paper for Patlak M et al., Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer (Washington: National Academies Press, 2001).
5. Grady I, Hansen P. Chapter 28: Mammography in “Kuerer’s Breast Surgical Oncology”(New York: McGaw-Hill Medical, 2010)
6. Radiology. 2014 Nov;273(2 Suppl):S23-44.
7. Bassett LW, Kim CH. (2003) Chapter 1: Ductography in Dershaw DD (eds) “Imaging-Guided Interventional Breast Techniques” (New York: Springer, 2003, pp. 1-30).
8. Cuperschmid EM, Ribeiro de Campos TP. 2009 International Nuclear Atlantic Conference, Rio de Janeiro, Sept 27–Oct 2, 2009
9. Bioscience Microflora. 2000;19(2):107-16.
10. Cady B. New era in breast cancer. Impact of screening on disease presentation. Surg Oncol Clin N Am. 1997 Apr;6(2):195-202.
11. Egan R. “Mammography Technique.” Audiovisual presentation. (Washington: U.S. Public Health Service, 1965).
12. Zackrisson S, Houssami N. Chapter 13: Evolution of Mammography Screening: From Film Screen to Digital Breast Tomosynthesis in “Breast Cancer Screening: An Examination of Scientific Evidence” (Cambridge, Mass.: Academic Press, 2016, pp. 323-46).13. Melnikow J et al. Screening for breast cancer with digital breast tomosynthesis. Evidence Synthesis No. 125 (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan).
14. Newer breast screening technology may spot more cancers. Harvard Women’s Health Watch online, June 2019.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
The history of mammography provides a powerful example of the connection between social factors and the rise of a medical technology. It is also an object lesson in the profound difficulties that the medical community faces when trying to evaluate and embrace new discoveries in such a complex area as cancer diagnosis and treatment, especially when tied to issues of sex-based bias and gender identity. Given its profound ties to women’s lives and women’s bodies, mammography holds a unique place in the history of cancer. Part 1 will examine the technological imperatives driving mammography forward, and part 2 will address the social factors that promoted and inhibited the developing technology.
All that glitters
Innovations in technology have contributed so greatly to the progress of medical science in saving and improving patients’ lives that the lure of new technology and the desire to see it succeed and to embrace it has become profound.
In a debate on the adoption of new technologies, Michael Rosen, MD, a surgeon at the Cleveland Clinic, Ohio, pointed out the inherent risks in the life cycle of medical technology: “The stages of surgical innovation have been well described as moving from the generation of a hypothesis with an early promising report to being accepted conclusively as a new standard without formal testing. As the life cycle continues and comparative effectiveness data begin to emerge slowly through appropriately designed trials, the procedure or device is often ultimately abandoned.”1
The history of mammography bears out this grim warning in example after example as an object lesson, revealing not only the difficulties involved in the development of new medical technologies, but also the profound problems involved in validating the effectiveness and appropriateness of a new technology from its inception to the present.
A modern failure?
In fact, one of the more modern developments in mammography technology – digital imaging – has recently been called into question with regard to its effectiveness in saving lives, even as the technology continues to spread throughout the medical community.
A recent meta-analysis has shown that there is little or no improvement in outcomes of breast cancer screening when using digital analysis and screening mammograms vs. traditional film recording.
The meta-analysis assessed 24 studies with a combined total of 16,583,743 screening examinations (10,968,843 film and 5,614,900 digital). The study found that the difference in cancer detection rate using digital rather than film screening showed an increase of only 0.51 detections per 1,000 screens.
The researchers concluded “that while digital mammography is beneficial for medical facilities due to easier storage and handling of images, these results suggest the transition from film to digital mammography has not resulted in health benefits for screened women.”2
In fact, the researchers added that “This analysis reinforces the need to carefully evaluate effects of future changes in technology, such as tomosynthesis, to ensure new technology leads to improved health outcomes and beyond technical gains.”2
None of the nine main randomized clinical trials that were used to determine the effectiveness of mammography screening from the 1960s to the 1990s used digital or 3-D digital mammography (digital breast tomosynthesis or DBT). The earliest trial used direct-exposure film mammography and the others relied upon screen-film mammography.3 And yet the assumptions of the validity of the new digital technologies were predicated on the generalized acceptance of the validity of screening derived from these studies, and a corollary assumption that any technological improvement in the quality of the image must inherently be an improvement of the overall results of screening.
The failure of new technologies to meet expectations is a sobering corrective to the high hopes of researchers, practitioners, and patient groups alike, and is perhaps destined to contribute more to the parallel history of controversy and distrust concerning the risk/benefits of mammography that has been a media and scientific mainstay.
Too often the history of medical technology has found disappointment at the end of the road for new discoveries. But although the disappointing results of digital screening might be considered a failure in the progress of mammography, it is likely just another pause on the road of this technology, the history of which has been rocky from the start.
The need for a new way of looking
The rationale behind the original and continuing development of mammography is a simple one, common to all cancer screening methods – the belief that the earlier the detection of a cancer, the more likely it is to be treated effectively with the therapeutic regimens at hand. While there is some controversy regarding the cost-benefit ratio of screening, especially when therapies for breast cancer are not perfect and vary widely in expense and availability globally, the driving belief has been that mammography provides an outcomes benefit in allowing early surgical and chemoradiation therapy with a curative intent.
There were two main driving forces behind the early development of mammography. The first was the highly lethal nature of breast cancer, especially when it was caught too late and had spread too far to benefit from the only available option at the time – surgery. The second was the severity of the surgical treatment, the only therapeutic option at the time, and the distressing number of women who faced the radical mastectomy procedure pioneered by physicians William Stewart Halsted (1852-1922) at Johns Hopkins University, Baltimore, and Willy Meyer (1858-1932) in New York.
In 1894, in an era when the development of anesthetics and antisepsis made ever more difficult surgical procedures possible without inevitably killing the patient, both men separately published their results of a highly extensive operation that consisted of removal of the breast, chest muscles, and axillary lymph nodes.
As long as there was no presurgical method of determining the extent of a breast cancer’s spread, much less an ability to visually distinguish malignant from benign growths, this “better safe than sorry” approach became the default approach of an increasing number of surgeons, and the drastic solution of radical mastectomy was increasingly applied universally.
But in 1895, with the discovery of x-rays, medical science recognized a nearly miraculous technology for visualizing the inside of the body, and radioactive materials were also routinely used in medical therapies, by both legitimate practitioners and hucksters.
However, in the very early days, the users of x-rays were unaware that large radiation doses could have serious biological effects and had no way of determining radiation field strength and accumulating dosage.
In fact, early calibration of x-ray tubes was based on the amount of skin reddening (erythema) produced when the operator placed a hand directly in the x-ray beam.
It was in this environment that, within only a few decades, the new x-rays, especially with the development of improvements in mammography imaging, were able in many cases to identify smaller, more curable breast cancers. This eventually allowed surgeons to develop and use less extensive operations than the highly disfiguring radical mastectomy that was simultaneously dreaded for its invasiveness and embraced for its life-saving potential.4
Pioneering era
The technological history of mammography was thus driven by the quest for better imaging and reproducibility in order to further the hopes of curative surgical approaches.
In 1913, the German surgeon Albert Salomon (1883-1976) was the first to detect breast cancer using x-rays, but its clinical use was not established, as the images published in his “Beiträge zur pathologie und klinik der mammakarzinome (Contributions to the pathology and clinic of breast cancers)” were photographs of postsurgical breast specimens that illustrated the anatomy and spread of breast cancer tumors but were not adapted to presurgical screening.
After Salomon’s work was published in 1913, there was no new mammography literature published until 1927, when German surgeon Otto Kleinschmidt (1880-1948) published a report describing the world’s first authentic mammography, which he attributed to his mentor, the plastic surgeon Erwin Payr (1871-1946).5
This was followed soon after in 1930 by the work of radiologist Stafford L. Warren (1896-1981), of the University of Rochester (N.Y.), who published a paper on the use of standard roentgenograms for the in vivo preoperative assessment of breast malignancies. His technique involved the use of a stereoscopic system with a grid mechanism and intensifying screens to amplify the image. Breast compression was not involved in his mammogram technique. “Dr. Warren claimed to be correct 92% of the time when using this technique to predict malignancy.”5
His study of 119 women with a histopathologic diagnosis (61 benign and 58 malignant) demonstrated the feasibility of the technique for routine use and “created a surge of interest.”6
But the technology of the time proved difficult to use, and the results difficult to reproduce from laboratory to laboratory, and ultimately did not gain wide acceptance. Among Warren’s other claims to fame, he was a participant in the Manhattan Project and was a member of the teams sent to assess radiation damage in Hiroshima and Nagasaki after the dropping of the atomic bombs.
And in fact, future developments in mammography and all other x-ray screening techniques included attempts to minimize radiation exposure; such attempts were driven, in part, by the tragic impact of atomic bomb radiation and the medical studies carried out on the survivors.
An image more deadly than the disease
Further improvements in mammography technique occurred through the 1930s and 1940s, including better visualization of the mammary ducts based upon the pioneering studies of Emil Ries, MD, in Chicago, who, along with Nymphus Frederick Hicken, MD (1900-1998), reported on the use of contrast mammography (also known as ductography or galactography). On a side note, Dr. Hicken was responsible for introducing the terms mammogram and mammography in 1937.
Problems with ductography, which involved the injection of a radiographically opaque contrast agent into the nipple, occurred when the early contrast agents, such as oil-based lipiodol, proved to be toxic and capable of causing abscesses.7This advance led to the development of other agents, and among the most popular at the time was one that would prove deadly to many.
Thorotrast, first used in 1928, was widely embraced because of its lack of immediately noticeable side effects and the high-quality contrast it provided. Thorotrast was a suspension of radioactive thorium dioxide particles, which gained popularity for use as a radiological imaging agent from the 1930s to 1950s throughout the world, being used in an estimated 2-10 million radiographic exams, primarily for neurosurgery.
In the 1920s and 1930s, world governments had begun to recognize the dangers of radiation exposure, especially among workers, but thorotrast was a unique case because, unbeknownst to most practitioners at the time, thorium dioxide was retained in the body for the lifetime of the patient, with 70% deposited in the liver, 20% in the spleen, and the remaining in the bony medulla and in the peripheral lymph nodes.
Nineteen years after the first use of thorotrast, the first case of a human malignant tumor attributed to its exposure was reported. “Besides the liver neoplasm cases, aplastic anemia, leukemia and an impressive incidence of chromosome aberrations were registered in exposed individuals.”8
Despite its widespread adoption elsewhere, especially in Japan, the use of thorotrast never became popular in the United States, in part because in 1932 and 1937, warnings were issued by the American Medical Association to restrict its use.9
There was a shift to the use of iodinated hydrophilic molecules as contrast agents for conventional x-ray, computed tomography, and fluoroscopy procedures.9 However, it was discovered that these agents, too, have their own risks and dangerous side effects. They can cause severe adverse effects, including allergies, cardiovascular diseases, and nephrotoxicity in some patients.
Slow adoption and limited results
Between 1930 and 1950, Dr. Warren, Jacob Gershon-Cohen, MD (1899-1971) of Philadelphia, and radiologist Raul Leborgne of Uruguay “spread the gospel of mammography as an adjunct to physical examination for the diagnosis of breast cancer.”4 The latter also developed the breast compression technique to produce better quality images and lower the radiation exposure needed, and described the differences that could be visualized between benign and malign microcalcifications.
But despite the introduction of improvements such as double-emulsion film and breast compression to produce higher-quality images, “mammographic films often remained dark and hazy. Moreover, the new techniques, while improving the images, were not easily reproduced by other investigators and clinicians,” and therefore were still not widely adopted.4
Little noticeable effect of mammography
Although the technology existed and had its popularizers, mammography had little impact on an epidemiological level.
There was no major change in the mean maximum breast cancer tumor diameter and node positivity rate detected over the 20 years from 1929 to 1948.10 However, starting in the late 1940s, the American Cancer Society began public education campaigns and early detection education, and thereafter, there was a 3% decline in mean maximum diameter of tumor size seen every 10 years until 1968.
“We have interpreted this as the effect of public education and professional education about early detection through television, print media, and professional publications that began in 1947 because no other event was known to occur that would affect cancer detection beginning in the late 1940s.”10
However, the early detection methods at the time were self-examination and clinical examination for lumps, with mammography remaining a relatively limited tool until its general acceptance broadened a few decades later.
Robert Egan, “Father of Mammography,” et al.
The broad acceptance of mammography as a screening tool and its impacts on a broad population level resulted in large part from the work of Robert L. Egan, MD (1921-2001) in the late 1950s and 1960s.
Dr. Egan’s work was inspired in 1956 by a presentation by a visiting fellow, Jean Pierre Batiani, who brought a mammogram clearly showing a breast cancer from his institution, the Curie Foundation in Paris. The image had been made using very low kilowattage, high tube currents, and fine-grain film.
Dr. Egan, then a resident in radiology, was given the task by the head of his department of reproducing the results.
In 1959, Dr. Egan, then at the University of Texas MD Anderson Cancer Center, Houston, published a combined technique that used a high-milliamperage–low-voltage technique, a fine-grain intensifying screen, and single-emulsion films for mammography, thereby decreasing the radiation exposure significantly from previous x-ray techniques and improving the visualization and reproducibility of screening.
By 1960, Dr. Egan reported on 1,000 mammography cases at MD Anderson, demonstrating the ability of proper screening to detect unsuspected cancers and to limit mastectomies on benign masses. Of 245 breast cancers ultimately confirmed by biopsy, 238 were discovered by mammography, 19 of which were in women whose physical examinations had revealed no breast pathology. One of the cancers was only 8 mm in diameter when sectioned at biopsy.
Dr. Egan’s findings prompted an investigation by the Cancer Control Program (CCP) of the U.S. Public Health Service and led to a study jointly conducted by the National Cancer Institute and MD Anderson Hospital and the CCP, which involved 24 institutions and 1,500 patients.
“The results showed a 21% false-negative rate and a 79% true-positive rate for screening studies using Egan’s technique. This was a milestone for women’s imaging in the United States. Screening mammography was off to a tentative start.”5
“Egan was the man who developed a smooth-riding automobile compared to a Model T. He put mammography on the map and made it an intelligible, reproducible study. In short, he was the father of modern mammography,” according to his professor, mentor, and fellow mammography pioneer Gerald Dodd, MD (Emory School of Medicine website biography).
In 1964 Dr. Egan published his definitive book, “Mammography,” and in 1965 he hosted a 30-minute audiovisual presentation describing in detail his technique.11
The use of mammography was further powered by improved methods of preoperative needle localization, pioneered by Richard H. Gold, MD, in 1963 at Jefferson Medical College, Philadelphia, which eased obtaining a tissue diagnosis for any suspicious lesions detected in the mammogram. Dr. Gold performed needle localization of nonpalpable, mammographically visible lesions before biopsy, which allowed surgical resection of a smaller volume of breast tissue than was possible before.
Throughout the era, there were also incremental improvements in mammography machines and an increase in the number of commercial manufacturers.
Xeroradiography, an imaging technique adapted from xerographic photocopying, was seen as a major improvement over direct film imaging, and the technology became popular throughout the 1970s based on the research of John N. Wolfe, MD (1923-1993), who worked closely with the Xerox Corporation to improve the breast imaging process.6 However, this technology had all the same problems associated with running an office copying machine, including paper jams and toner issues, and the worst aspect was the high dose of radiation required. For this reason, it would quickly be superseded by the use of screen-film mammography, which eventually completely replaced the use of both xeromammography and direct-exposure film mammography.
The march of mammography
A series of nine randomized clinical trials (RCTs) between the 1960s and 1990s formed the foundation of the clinical use of mammography. These studies enrolled more than 600,000 women in the United States, Canada, the United Kingdom, and Sweden. The nine main RCTs of breast cancer screening were the Health Insurance Plan of Greater New York (HIP) trial, the Edinburgh trial, the Canadian National Breast Screening Study, the Canadian National Breast Screening Study 2, the United Kingdom Age trial, the Stockholm trial, the Malmö Mammographic Screening Trial, the Gothenburg trial, and the Swedish Two-County Study.3
These trials incorporated improvements in the technology as it developed, as seen in the fact that the earliest, the HIP trial, used direct-exposure film mammography and the other trials used screen-film mammography.3
Meta-analyses of the major nine screening trials indicated that reduced breast cancer mortality with screening was dependent on age. In particular, the results for women aged 40-49 years and 50-59 years showed only borderline statistical significance, and they varied depending on how cases were accrued in individual trials. “Assuming that differences actually exist, the absolute breast cancer mortality reduction per 10,000 women screened for 10 years ranged from 3 for age 39-49 years; 5-8 for age 50-59 years; and 12-21 for age 60-69 years.”3 In addition the estimates for women aged 70-74 years were limited by low numbers of events in trials that had smaller numbers of women in this age group.
However, at the time, the studies had a profound influence on increasing the popularity and spread of mammography.
As mammographies became more common, standardization became an important issue and a Mammography Accreditation Program began in 1987. Originally a voluntary program, it became mandatory with the Mammography Quality Standards Act of 1992, which required all U.S. mammography facilities to become accredited and certified.
In 1986, the American College of Radiology proposed its Breast Imaging Reporting and Data System (BI-RADS) initiative to enable standardized reporting of mammography; the first report was released in 1993.
BI-RADS is now on its fifth edition and has addressed the use of mammography, breast ultrasonography, and breast magnetic resonance imaging, developing standardized auditing approaches for all three techniques of breast cancer imaging.6
The digital era and beyond
With the dawn of the 21st century, the era of digital breast cancer screening began.
The screen-film mammography (SFM) technique employed throughout the 1980s and 1990s had significant advantages over earlier x-ray films for producing more vivid images of dense breast tissues. The next technology, digital mammography, was introduced in the late 20th century, and the first system was approved by the U.S. FDA in 2000.
One of the key benefits touted for digital mammograms is the fact that the radiologist can manipulate the contrast of the images, which allows for masses to be identified that might otherwise not be visible on standard film.
However, the recent meta-analysis discussed in the introduction calls such benefits into question, and a new controversy is likely to ensue on the question of the effectiveness of digital mammography on overall clinical outcomes.
But the technology continues to evolve.
“There has been a continuous and substantial technical development from SFM to full-field digital mammography and very recently also the introduction of digital breast tomosynthesis (DBT). This technical evolution calls for new evidence regarding the performance of screening using new mammography technologies, and the evidence needed to translate new technologies into screening practice,” according to an updated assessment by the U.S. Preventive Services Task Force.12
DBT was approved by the Food and Drug Administration in 2011. The technology involves the creation of a series of images, which are assembled into a 3-D–like image of breast slices. Traditional digital mammography creates a 2-D image of a flattened breast, and the radiologist must peer through the layers to find abnormalities. DBT uses a computer algorithm to reconstruct multiple low-dose digital images of the breast that can be displayed individually or in cinematic mode.13
Early trials showed a significant benefit of DBT in detecting new and smaller breast cancers, compared with standard digital mammography.
In women in their 40s, DBT found 1.7 more cancers than digital mammography for every 1,000 exams of women with normal breast tissue. In addition, 16.3% of women in this age group who were screened using digital mammography received callbacks, versus 11.7% of those screened using DBT. For younger women with dense breasts, the advantage of DBT was even greater, with 2.27 more cancers found for every 1,000 women screened. Whether such results will lead to clinically improved outcomes remains a question. “It can still miss cancers. Also, like traditional mammography, DBT might not reduce deaths from tumors that are very aggressive and fast-growing. And some women will still be called back unnecessarily for false-positive results.”14
But such technological advances further the hopes of researchers and patients alike.
Conclusion
Medical technology is driven both by advances in science and by the demands of patients and physicians for improved outcomes. The history of mammography, for example, is tied to the scientific advancements in x-ray technology, which allowed physicians for the first time to peer inside a living body without a scalpel at hand. But mammography was also an outgrowth of the profound need of the surgeon to identify cancerous masses in the breast at an early-enough stage to attempt a cure, while simultaneously minimizing the radical nature of the surgery required.
And while seeing is believing, the need to see and verify what was seen in order to make life-and-death decisions drove the demand for improvements in the technology of mammography throughout most of the 20th century and beyond.
The tortuous path from the early and continuing snafus with contrast agents to the apparent failure of the promise of digital technology serves as a continuing reminder of the hopes and perils that developing medical technologies present. It will be interesting to see if further refinements to mammography, such as DBT, will enhance the technology enough to have a major impact on countless women’s lives, or if new developments in magnetic resonance imaging and ultrasound make traditional mammography a relic of the past.
Part 2 of this history will present the social dynamics intimately involved with the rise and promulgation of mammography and how social need and public fears and controversies affected its development and spread as much, if not more, than technological innovation.
This article could only touch upon the myriad of details and technologies involved in the history of mammography, and I urge interested readers to check out the relevant references for far more in-depth and fascinating stories from its complex and controversial past.
References
1. Felix EL, Rosen M, Earle D. “Curbing Our Enthusiasm for Surgical Innovation: Is It a Good Thing or Bad Thing?” The Great Debates, General Surgery News, 2018 Oct 17
2. J Natl Cancer Inst. 2020 Jun 23. doi: 10.1093/jnci/djaa080.
3. Nelson H et al. Screening for Breast Cancer: A Systematic Review to Update the 2009 U.S. Preventive Services Task Force Recommendation. Evidence Synthesis No. 124. (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan, pp. 29-49)4. Lerner, BH. “To See Today With the Eyes of Tomorrow: A History of Screening Mammography,” background paper for Patlak M et al., Mammography and Beyond: Developing Technologies for the Early Detection of Breast Cancer (Washington: National Academies Press, 2001).
5. Grady I, Hansen P. Chapter 28: Mammography in “Kuerer’s Breast Surgical Oncology”(New York: McGaw-Hill Medical, 2010)
6. Radiology. 2014 Nov;273(2 Suppl):S23-44.
7. Bassett LW, Kim CH. (2003) Chapter 1: Ductography in Dershaw DD (eds) “Imaging-Guided Interventional Breast Techniques” (New York: Springer, 2003, pp. 1-30).
8. Cuperschmid EM, Ribeiro de Campos TP. 2009 International Nuclear Atlantic Conference, Rio de Janeiro, Sept 27–Oct 2, 2009
9. Bioscience Microflora. 2000;19(2):107-16.
10. Cady B. New era in breast cancer. Impact of screening on disease presentation. Surg Oncol Clin N Am. 1997 Apr;6(2):195-202.
11. Egan R. “Mammography Technique.” Audiovisual presentation. (Washington: U.S. Public Health Service, 1965).
12. Zackrisson S, Houssami N. Chapter 13: Evolution of Mammography Screening: From Film Screen to Digital Breast Tomosynthesis in “Breast Cancer Screening: An Examination of Scientific Evidence” (Cambridge, Mass.: Academic Press, 2016, pp. 323-46).13. Melnikow J et al. Screening for breast cancer with digital breast tomosynthesis. Evidence Synthesis No. 125 (Rockville, Md.: U.S. Agency for Healthcare Research and Quality, 2016 Jan).
14. Newer breast screening technology may spot more cancers. Harvard Women’s Health Watch online, June 2019.
Mark Lesney is the editor of Hematology News and the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has worked as a writer/editor for the American Chemical Society, and has served as an adjunct assistant professor in the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
System provides ‘faster, less invasive’ method for breast cancer detection
A system designed for resource-limited settings provides rapid cancer profiling and requires “scant” cellular specimens, according to researchers.
The automated image cytometry system is called CytoPAN. In preclinical experiments, CytoPAN provided accurate cancer detection in 1 hour using as few as 50 cells.
In a prospective study of 68 breast cancer patients, CytoPAN detected cancer with 100% accuracy. The receptor subtyping accuracy was 96% for HER2 and 93% for estrogen and progesterone receptors.
Jouha Min, PhD, of Massachusetts General Hospital, Boston, and colleagues reported these findings in Science Translational Medicine.
The authors explained that the CytoPAN system is designed to address one of the biggest cancer challenges in low- and middle-income countries (LMICs), where more than two-thirds of cancer deaths occur: providing rapid, affordable diagnostics that enable patients to obtain locally available treatments.
Unfortunately, because of bottlenecks in specimen acquisition, complex handling logistics, a lack of pathologists, and limited laboratory infrastructure, diagnosis in many LMICs frequently takes months. Cancers typically are not diagnosed until advanced symptoms such as palpable mass lesions, weight loss, and malaise have become manifest.
Lesion assessment guides management
For women with suspicion of breast cancer, the authors noted, preoperative assessment of focal lesions for receptor status, presence of invasion, histologic type, and tumor grade are crucial for planning therapeutic management. For physicians to provide, for example, tamoxifen, which is commonly available at low cost in LMICs, they must know a patients’ hormone receptor status.
While core and open surgical biopsies yield abundant tissue for embedding, sectioning, and staining for subsequent histopathological analysis, they entail lengthy work flow and call for expensive instrumentation and a trained workforce, the authors noted.
Fine needle aspirations (FNAs) can be performed by nonphysicians after minimal training with very low complication rates. The much smaller–gauge needles (20-25 gauge) used in FNAs are generally well tolerated, the authors added.
This is why CytoPAN was designed for use with specimens obtained via FNA of palpable mass lesions.
Self-contained design
The CytoPAN system was engineered as a self-contained, integrated cytometry platform enabling same-day diagnosis and treatment of breast lesions.
The system was designed to comply with the World Health Organization’s “ASSURED” criteria (affordable, sensitive, specific, user friendly, rapid and robust, equipment free, and deliverable to end users), and to be potentially operable by nonphysicians after brief training.
CytoPAN operators collect cells through minimally invasive FNAs and use lyophilized immunostaining kits with relevant antibodies (not requiring refrigeration). Operators perform imaging using the CytoPAN device, which is then subjected to an automated analysis algorithm with results displayed on a user interface.
CytoPAN classifies detected malignant cells according to four subtypes reflecting estrogen receptor (ER), progesterone receptor (PR), and HER2 status – luminal HER2-negative, luminal HER2-positive, HER2-positive, and triple-negative breast cancer. This is intended to facilitate informed treatment choices (e.g., a selective ER modulator, antiestrogen or aromatase inhibitor for ER/PR-positive patients; an anti-HER2 agent for HER2-positive patients).
The final diagnostic report from a given patient sample includes cancer cell population and molecular subtype distribution. The entire diagnostic procedure takes less than an hour. A repeat biopsy, should the sample be nondiagnostic, can be taken within an hour.
Murine, then human testing
A test of CytoPAN on FNA samples from mouse xenografts representing the spectrum of human breast cancer subtypes showed correct and reproducible molecular subtyping that matched well with flow cytometry reports derived from the same tumors.
To determine the clinical utility of CytoPAN, investigators enrolled 68 treatment-naive breast cancer patients who were referred for primary surgery at the Kyungpook National University Chilgok Hospital in Daegu, South Korea. FNA samples were obtained after visualization of breast masses by ultrasound or CT.
Surgical specimens and/or core biopsies were processed by routine pathology for “gold-standard” comparison. FNA samples had sufficient numbers of cells in 63 (93%) patients, with a mean number of cells among them of 1,308 (range, 93-11,985).
CytoPAN analysis correctly identified malignant breast cancer in 55 patients and benign lesions in 5 patients. Three cases were inconclusive because of low numbers of Quad-positive cells for further analysis. The authors pointed out that roughly 20% of biopsy samples in developed countries are deemed “nondiagnostic” because of insufficient cellular contents.
The authors’ summary underscored CytoPAN’s affordable system using cellular rather than tissue specimens, actionable results in an hour, lack of moving parts, multiplexed analysis, and user-friendly interface.
Cancer detection accuracy was 100% (no false negatives or false positives), and receptor subtyping accuracy was 97% for HER2 and 93% for ER/PR.
“Based on these results, we envision prospective clinical trials in remote, decentralized locations,” the authors wrote. The system is being tested further in Botswana.
“I find the data in this paper compelling – particularly for those patients presenting with a palpable mass on clinical exam. ... Certainly in resource-limited settings, this would have significant appeal,” William J. Gradishar, MD, of Northwestern University, Chicago, said in an interview.
Dr. Gradishar explained that, while palpable masses that lead to a diagnosis of noninvasive disease alone are uncommon in the United States because of routine screening mammography, they may still be an issue in other parts of the world.
The authors received funding from the National Institutes of Health, the MGH Scholar Fund, and Robert Wood Johnson Foundation. Some authors disclosed relationships with Akili, Accure Health, ModeRNA, Tarveda, Lumicell, and Noul. Dr. Gradishar reported having no disclosures.
SOURCE: Min J et al. Sci Transl Med. 2020 Aug 5. doi: 10.1126/scitranslmed.aaz9746.
A system designed for resource-limited settings provides rapid cancer profiling and requires “scant” cellular specimens, according to researchers.
The automated image cytometry system is called CytoPAN. In preclinical experiments, CytoPAN provided accurate cancer detection in 1 hour using as few as 50 cells.
In a prospective study of 68 breast cancer patients, CytoPAN detected cancer with 100% accuracy. The receptor subtyping accuracy was 96% for HER2 and 93% for estrogen and progesterone receptors.
Jouha Min, PhD, of Massachusetts General Hospital, Boston, and colleagues reported these findings in Science Translational Medicine.
The authors explained that the CytoPAN system is designed to address one of the biggest cancer challenges in low- and middle-income countries (LMICs), where more than two-thirds of cancer deaths occur: providing rapid, affordable diagnostics that enable patients to obtain locally available treatments.
Unfortunately, because of bottlenecks in specimen acquisition, complex handling logistics, a lack of pathologists, and limited laboratory infrastructure, diagnosis in many LMICs frequently takes months. Cancers typically are not diagnosed until advanced symptoms such as palpable mass lesions, weight loss, and malaise have become manifest.
Lesion assessment guides management
For women with suspicion of breast cancer, the authors noted, preoperative assessment of focal lesions for receptor status, presence of invasion, histologic type, and tumor grade are crucial for planning therapeutic management. For physicians to provide, for example, tamoxifen, which is commonly available at low cost in LMICs, they must know a patients’ hormone receptor status.
While core and open surgical biopsies yield abundant tissue for embedding, sectioning, and staining for subsequent histopathological analysis, they entail lengthy work flow and call for expensive instrumentation and a trained workforce, the authors noted.
Fine needle aspirations (FNAs) can be performed by nonphysicians after minimal training with very low complication rates. The much smaller–gauge needles (20-25 gauge) used in FNAs are generally well tolerated, the authors added.
This is why CytoPAN was designed for use with specimens obtained via FNA of palpable mass lesions.
Self-contained design
The CytoPAN system was engineered as a self-contained, integrated cytometry platform enabling same-day diagnosis and treatment of breast lesions.
The system was designed to comply with the World Health Organization’s “ASSURED” criteria (affordable, sensitive, specific, user friendly, rapid and robust, equipment free, and deliverable to end users), and to be potentially operable by nonphysicians after brief training.
CytoPAN operators collect cells through minimally invasive FNAs and use lyophilized immunostaining kits with relevant antibodies (not requiring refrigeration). Operators perform imaging using the CytoPAN device, which is then subjected to an automated analysis algorithm with results displayed on a user interface.
CytoPAN classifies detected malignant cells according to four subtypes reflecting estrogen receptor (ER), progesterone receptor (PR), and HER2 status – luminal HER2-negative, luminal HER2-positive, HER2-positive, and triple-negative breast cancer. This is intended to facilitate informed treatment choices (e.g., a selective ER modulator, antiestrogen or aromatase inhibitor for ER/PR-positive patients; an anti-HER2 agent for HER2-positive patients).
The final diagnostic report from a given patient sample includes cancer cell population and molecular subtype distribution. The entire diagnostic procedure takes less than an hour. A repeat biopsy, should the sample be nondiagnostic, can be taken within an hour.
Murine, then human testing
A test of CytoPAN on FNA samples from mouse xenografts representing the spectrum of human breast cancer subtypes showed correct and reproducible molecular subtyping that matched well with flow cytometry reports derived from the same tumors.
To determine the clinical utility of CytoPAN, investigators enrolled 68 treatment-naive breast cancer patients who were referred for primary surgery at the Kyungpook National University Chilgok Hospital in Daegu, South Korea. FNA samples were obtained after visualization of breast masses by ultrasound or CT.
Surgical specimens and/or core biopsies were processed by routine pathology for “gold-standard” comparison. FNA samples had sufficient numbers of cells in 63 (93%) patients, with a mean number of cells among them of 1,308 (range, 93-11,985).
CytoPAN analysis correctly identified malignant breast cancer in 55 patients and benign lesions in 5 patients. Three cases were inconclusive because of low numbers of Quad-positive cells for further analysis. The authors pointed out that roughly 20% of biopsy samples in developed countries are deemed “nondiagnostic” because of insufficient cellular contents.
The authors’ summary underscored CytoPAN’s affordable system using cellular rather than tissue specimens, actionable results in an hour, lack of moving parts, multiplexed analysis, and user-friendly interface.
Cancer detection accuracy was 100% (no false negatives or false positives), and receptor subtyping accuracy was 97% for HER2 and 93% for ER/PR.
“Based on these results, we envision prospective clinical trials in remote, decentralized locations,” the authors wrote. The system is being tested further in Botswana.
“I find the data in this paper compelling – particularly for those patients presenting with a palpable mass on clinical exam. ... Certainly in resource-limited settings, this would have significant appeal,” William J. Gradishar, MD, of Northwestern University, Chicago, said in an interview.
Dr. Gradishar explained that, while palpable masses that lead to a diagnosis of noninvasive disease alone are uncommon in the United States because of routine screening mammography, they may still be an issue in other parts of the world.
The authors received funding from the National Institutes of Health, the MGH Scholar Fund, and Robert Wood Johnson Foundation. Some authors disclosed relationships with Akili, Accure Health, ModeRNA, Tarveda, Lumicell, and Noul. Dr. Gradishar reported having no disclosures.
SOURCE: Min J et al. Sci Transl Med. 2020 Aug 5. doi: 10.1126/scitranslmed.aaz9746.
A system designed for resource-limited settings provides rapid cancer profiling and requires “scant” cellular specimens, according to researchers.
The automated image cytometry system is called CytoPAN. In preclinical experiments, CytoPAN provided accurate cancer detection in 1 hour using as few as 50 cells.
In a prospective study of 68 breast cancer patients, CytoPAN detected cancer with 100% accuracy. The receptor subtyping accuracy was 96% for HER2 and 93% for estrogen and progesterone receptors.
Jouha Min, PhD, of Massachusetts General Hospital, Boston, and colleagues reported these findings in Science Translational Medicine.
The authors explained that the CytoPAN system is designed to address one of the biggest cancer challenges in low- and middle-income countries (LMICs), where more than two-thirds of cancer deaths occur: providing rapid, affordable diagnostics that enable patients to obtain locally available treatments.
Unfortunately, because of bottlenecks in specimen acquisition, complex handling logistics, a lack of pathologists, and limited laboratory infrastructure, diagnosis in many LMICs frequently takes months. Cancers typically are not diagnosed until advanced symptoms such as palpable mass lesions, weight loss, and malaise have become manifest.
Lesion assessment guides management
For women with suspicion of breast cancer, the authors noted, preoperative assessment of focal lesions for receptor status, presence of invasion, histologic type, and tumor grade are crucial for planning therapeutic management. For physicians to provide, for example, tamoxifen, which is commonly available at low cost in LMICs, they must know a patients’ hormone receptor status.
While core and open surgical biopsies yield abundant tissue for embedding, sectioning, and staining for subsequent histopathological analysis, they entail lengthy work flow and call for expensive instrumentation and a trained workforce, the authors noted.
Fine needle aspirations (FNAs) can be performed by nonphysicians after minimal training with very low complication rates. The much smaller–gauge needles (20-25 gauge) used in FNAs are generally well tolerated, the authors added.
This is why CytoPAN was designed for use with specimens obtained via FNA of palpable mass lesions.
Self-contained design
The CytoPAN system was engineered as a self-contained, integrated cytometry platform enabling same-day diagnosis and treatment of breast lesions.
The system was designed to comply with the World Health Organization’s “ASSURED” criteria (affordable, sensitive, specific, user friendly, rapid and robust, equipment free, and deliverable to end users), and to be potentially operable by nonphysicians after brief training.
CytoPAN operators collect cells through minimally invasive FNAs and use lyophilized immunostaining kits with relevant antibodies (not requiring refrigeration). Operators perform imaging using the CytoPAN device, which is then subjected to an automated analysis algorithm with results displayed on a user interface.
CytoPAN classifies detected malignant cells according to four subtypes reflecting estrogen receptor (ER), progesterone receptor (PR), and HER2 status – luminal HER2-negative, luminal HER2-positive, HER2-positive, and triple-negative breast cancer. This is intended to facilitate informed treatment choices (e.g., a selective ER modulator, antiestrogen or aromatase inhibitor for ER/PR-positive patients; an anti-HER2 agent for HER2-positive patients).
The final diagnostic report from a given patient sample includes cancer cell population and molecular subtype distribution. The entire diagnostic procedure takes less than an hour. A repeat biopsy, should the sample be nondiagnostic, can be taken within an hour.
Murine, then human testing
A test of CytoPAN on FNA samples from mouse xenografts representing the spectrum of human breast cancer subtypes showed correct and reproducible molecular subtyping that matched well with flow cytometry reports derived from the same tumors.
To determine the clinical utility of CytoPAN, investigators enrolled 68 treatment-naive breast cancer patients who were referred for primary surgery at the Kyungpook National University Chilgok Hospital in Daegu, South Korea. FNA samples were obtained after visualization of breast masses by ultrasound or CT.
Surgical specimens and/or core biopsies were processed by routine pathology for “gold-standard” comparison. FNA samples had sufficient numbers of cells in 63 (93%) patients, with a mean number of cells among them of 1,308 (range, 93-11,985).
CytoPAN analysis correctly identified malignant breast cancer in 55 patients and benign lesions in 5 patients. Three cases were inconclusive because of low numbers of Quad-positive cells for further analysis. The authors pointed out that roughly 20% of biopsy samples in developed countries are deemed “nondiagnostic” because of insufficient cellular contents.
The authors’ summary underscored CytoPAN’s affordable system using cellular rather than tissue specimens, actionable results in an hour, lack of moving parts, multiplexed analysis, and user-friendly interface.
Cancer detection accuracy was 100% (no false negatives or false positives), and receptor subtyping accuracy was 97% for HER2 and 93% for ER/PR.
“Based on these results, we envision prospective clinical trials in remote, decentralized locations,” the authors wrote. The system is being tested further in Botswana.
“I find the data in this paper compelling – particularly for those patients presenting with a palpable mass on clinical exam. ... Certainly in resource-limited settings, this would have significant appeal,” William J. Gradishar, MD, of Northwestern University, Chicago, said in an interview.
Dr. Gradishar explained that, while palpable masses that lead to a diagnosis of noninvasive disease alone are uncommon in the United States because of routine screening mammography, they may still be an issue in other parts of the world.
The authors received funding from the National Institutes of Health, the MGH Scholar Fund, and Robert Wood Johnson Foundation. Some authors disclosed relationships with Akili, Accure Health, ModeRNA, Tarveda, Lumicell, and Noul. Dr. Gradishar reported having no disclosures.
SOURCE: Min J et al. Sci Transl Med. 2020 Aug 5. doi: 10.1126/scitranslmed.aaz9746.
FROM SCIENCE TRANSLATIONAL MEDICINE
Hepatitis screening now for all patients with cancer on therapy
All patients with cancer who are candidates for systemic anticancer therapy should be screened for hepatitis B virus (HBV) infection prior to or at the start of therapy, according to an updated provisional clinical opinion (PCO) from the American Society of Clinical Oncology.
“This is a new approach [that] will actively take system changes ... but it will ultimately be safer for patients – and that is crucial,” commented Jessica P. Hwang, MD, MPH, cochair of the American Society of Clinical Oncology HBV Screening Expert Panel and the first author of the PCO.
Uptake of this universal screening approach would streamline testing protocols and identify more patients at risk for HBV reactivation who should receive prophylactic antiviral therapy, Dr. Hwang said in an interview.
The PCO calls for antiviral prophylaxis during and for at least 12 months after therapy for those with chronic HBV infection who are receiving any systemic anticancer treatment and for those with have had HBV in the past and are receiving any therapies that pose a risk for HBV reactivation.
“Hepatitis B reactivation can cause really terrible outcomes, like organ failure and even death,” Dr. Hwang, who is also a professor at the University of Texas MD Anderson Cancer Center, Houston, commented in an interview.
“This whole [issue of] reactivation and adverse outcomes with anticancer therapies is completely preventable with good planning, good communication, comanagement with specialists, and antiviral therapy and monitoring,” she added.
The updated opinion was published online July 27 in the Journal of Clinical Oncology.
It was developed in response to new data that call into question the previously recommended risk-adaptive approach to HBV screening of cancer patients, say the authors.
ASCO PCOs are developed “to provide timely clinical guidance” on the basis of emerging practice-changing information. This is the second update to follow the initial HBV screening PCO, published in 2010. In the absence of clear consensus because of limited data, the original PCO called for a risk-based approach to screening. A 2015 update extended the recommendation for screening to patients starting anti-CD20 therapy or who are to undergo stem cell transplant and to those with risk factors for HBV exposure.
The current update provides “a clinically pragmatic approach to HBV screening and management” that is based on the latest findings, say the authors. These include findings from a multicenter prospective cohort study of more than 3000 patients. In that study, 21% of patients with chronic HBV had no known risk factors for the infection. In another large prospective observational cohort study, led by Dr. Hwang, which included more than 2100 patients with cancer, 90% had one or more significant risk factors for HBV infection, making selective screening “inefficient and impractical,” she said.
“The results of these two studies suggest that a universal screening approach, its potential harms (e.g., patient and clinician anxiety about management, financial burden associated with antiviral therapy) notwithstanding, is the most efficient, clinically pragmatic approach to HBV screening in persons anticipating systemic anticancer treatment,” the authors comment.
The screening recommended in the PCO requires three tests: hepatitis B surface antigen (HBsAg), core antibody total immunoglobulin or IgG, and antibody to HBsAg tests.
Anticancer therapy should not be delayed pending the results, they write.
Planning for monitoring and long-term prophylaxis for chronic HBV infection should involve a clinician experienced in HBV management, the authors write. Management of those with past infection should be individualized. Alternatively, patients with past infection can be carefully monitored rather than given prophylactic treatment, as long as frequent and consistent follow-up is possible to allow for rapid initiation of antiviral therapy in the event of reactivation, they say.
Hormonal therapy without systemic anticancer therapy is not likely to lead to HBV reactivation in patients with chronic or past infection; antiviral therapy and management of these patients should follow relevant national HBV guidelines, they note.
Challenges in implementing universal HBV screening
The expert panel acknowledges the challenges associated with implementation of universal HBV screening as recommended in their report and notes that electronic health record–based approaches that use alerts to prompt screening have demonstrated success. In one study of high-risk primary care patients, an EHR alert system significantly increased testing rates (odds ratio, 2.64 in comparison with a control group without alerts), and another study that used a simple “sticky-note” alert system to promote referral of HBsAg patients to hepatologists increased referrals from 28% to 73%.
In a cancer population, a “comprehensive set of multimodal interventions,” including pharmacy staff checks for screening prior to anti-CD20 therapy administration and electronic medication order reviews to assess for appropriate testing and treatment before anti-CD20 therapy, increased testing rates to greater than 90% and antiviral prophylaxis rates to more than 80%.
A study of 965 patients in Taiwan showed that a computer-assisted reminder system that prompted for testing prior to ordering anticancer therapy increased screening from 8% to 86% but was less effective for improving the rates of antiviral prophylaxis for those who tested positive for HBV, particularly among physicians treating patients with nonhematologic malignancies.
“Future studies will be needed to make universal HBV screening and linkage to care efficient and systematic, likely based in EHR systems,” the panel says. The authors note that “[o]ngoing studies of HBV tests such as ultrasensitive HBsAg, HBV RNA, and hepatitis B core antigen are being studied and may be useful in predicting risk of HBV reactivation.”
The panel also identified a research gap related to HBV reactivation risks “for the growing list of agents that deplete or modulate B cells.” It notes a need for additional research on the cost-effectiveness of HBV screening. The results of prior cost analyses have been inconsistent and vary with respect to the population studied. For example, universal screening and antiviral prophylaxis approaches have been shown to be cost-effective for patients with hematologic malignancies and high HBV reactivation risk but are less so for patients with solid tumors and lower reactivation risk, they explain.
Dr. Hwang said that not one of the more than 2100 patients in her HBV screening cohort study encountered problems with receiving insurance payment for their HBV screening.
“That’s a really strong statement that insurance payers are accepting of this kind of preventative service,” she said.
Expert panel cochair Andrew Artz, MD, commented that there is now greater acceptance of the need for HBV screening across medical specialties.
“There’s growing consensus among hepatologists, infectious disease specialists, oncologists, and HBV specialists that we need to do a better job of finding patients with hepatitis B [who are] about to receive immunocompromising treatment,” Dr. Artz said in an interview.
Dr. Artz is director of the Program for Aging and Blood Cancers and deputy director of the Center for Cancer and Aging at City of Hope Comprehensive Cancer Center, Duarte, California.
He suggested that the growing acceptance is due in part to the increasing number of anticancer therapies available and the resulting increase in the likelihood of patients receiving therapies that could cause reactivation.
More therapies – and more lines of therapy – could mean greater risk, he explained. He said that testing is easy and that universal screening is the simplest approach to determining who needs it. “There’s no question we will have to change practice,” Dr. Artz said in an interview. “But this is easier than the previous approach that essentially wasn’t being followed because it was too difficult to follow and patients were being missed.”
Most clinicians will appreciate having an approach that’s easier to follow, Dr. Artz predicted.
If there’s a challenge it will be in developing partnerships with HBV specialists, particularly in rural areas. In areas where there is a paucity of subspecialists, oncologists will have to “take some ownership of the issue,” as they often do in such settings, he said.
However, with support from pharmacists, administrators, and others in embracing this guidance, implementation can take place at a systems level rather than an individual clinician level, he added.
The recommendations in this updated PCO were all rated as “strong,” with the exception of the recommendation on hormonal therapy in the absence of systemic anticancer therapy, which was rated as “moderate.” All were based on “informal consensus,” with the exception of the key recommendation for universal HBV screening – use of three specific tests – which was “evidence based.”
The expert panel agreed that the benefits outweigh the harms for each recommendation in the update.
Dr. Hwang received research funding to her institution from Gilead Sciences and Merck Sharp & Dohme. She also has a relationship with the Asian Health Foundation. Dr. Artz received research funding from Miltenyi Biotec. All expert panel members’ disclosures are available in the PCO update.
This article first appeared on Medscape.com.
All patients with cancer who are candidates for systemic anticancer therapy should be screened for hepatitis B virus (HBV) infection prior to or at the start of therapy, according to an updated provisional clinical opinion (PCO) from the American Society of Clinical Oncology.
“This is a new approach [that] will actively take system changes ... but it will ultimately be safer for patients – and that is crucial,” commented Jessica P. Hwang, MD, MPH, cochair of the American Society of Clinical Oncology HBV Screening Expert Panel and the first author of the PCO.
Uptake of this universal screening approach would streamline testing protocols and identify more patients at risk for HBV reactivation who should receive prophylactic antiviral therapy, Dr. Hwang said in an interview.
The PCO calls for antiviral prophylaxis during and for at least 12 months after therapy for those with chronic HBV infection who are receiving any systemic anticancer treatment and for those with have had HBV in the past and are receiving any therapies that pose a risk for HBV reactivation.
“Hepatitis B reactivation can cause really terrible outcomes, like organ failure and even death,” Dr. Hwang, who is also a professor at the University of Texas MD Anderson Cancer Center, Houston, commented in an interview.
“This whole [issue of] reactivation and adverse outcomes with anticancer therapies is completely preventable with good planning, good communication, comanagement with specialists, and antiviral therapy and monitoring,” she added.
The updated opinion was published online July 27 in the Journal of Clinical Oncology.
It was developed in response to new data that call into question the previously recommended risk-adaptive approach to HBV screening of cancer patients, say the authors.
ASCO PCOs are developed “to provide timely clinical guidance” on the basis of emerging practice-changing information. This is the second update to follow the initial HBV screening PCO, published in 2010. In the absence of clear consensus because of limited data, the original PCO called for a risk-based approach to screening. A 2015 update extended the recommendation for screening to patients starting anti-CD20 therapy or who are to undergo stem cell transplant and to those with risk factors for HBV exposure.
The current update provides “a clinically pragmatic approach to HBV screening and management” that is based on the latest findings, say the authors. These include findings from a multicenter prospective cohort study of more than 3000 patients. In that study, 21% of patients with chronic HBV had no known risk factors for the infection. In another large prospective observational cohort study, led by Dr. Hwang, which included more than 2100 patients with cancer, 90% had one or more significant risk factors for HBV infection, making selective screening “inefficient and impractical,” she said.
“The results of these two studies suggest that a universal screening approach, its potential harms (e.g., patient and clinician anxiety about management, financial burden associated with antiviral therapy) notwithstanding, is the most efficient, clinically pragmatic approach to HBV screening in persons anticipating systemic anticancer treatment,” the authors comment.
The screening recommended in the PCO requires three tests: hepatitis B surface antigen (HBsAg), core antibody total immunoglobulin or IgG, and antibody to HBsAg tests.
Anticancer therapy should not be delayed pending the results, they write.
Planning for monitoring and long-term prophylaxis for chronic HBV infection should involve a clinician experienced in HBV management, the authors write. Management of those with past infection should be individualized. Alternatively, patients with past infection can be carefully monitored rather than given prophylactic treatment, as long as frequent and consistent follow-up is possible to allow for rapid initiation of antiviral therapy in the event of reactivation, they say.
Hormonal therapy without systemic anticancer therapy is not likely to lead to HBV reactivation in patients with chronic or past infection; antiviral therapy and management of these patients should follow relevant national HBV guidelines, they note.
Challenges in implementing universal HBV screening
The expert panel acknowledges the challenges associated with implementation of universal HBV screening as recommended in their report and notes that electronic health record–based approaches that use alerts to prompt screening have demonstrated success. In one study of high-risk primary care patients, an EHR alert system significantly increased testing rates (odds ratio, 2.64 in comparison with a control group without alerts), and another study that used a simple “sticky-note” alert system to promote referral of HBsAg patients to hepatologists increased referrals from 28% to 73%.
In a cancer population, a “comprehensive set of multimodal interventions,” including pharmacy staff checks for screening prior to anti-CD20 therapy administration and electronic medication order reviews to assess for appropriate testing and treatment before anti-CD20 therapy, increased testing rates to greater than 90% and antiviral prophylaxis rates to more than 80%.
A study of 965 patients in Taiwan showed that a computer-assisted reminder system that prompted for testing prior to ordering anticancer therapy increased screening from 8% to 86% but was less effective for improving the rates of antiviral prophylaxis for those who tested positive for HBV, particularly among physicians treating patients with nonhematologic malignancies.
“Future studies will be needed to make universal HBV screening and linkage to care efficient and systematic, likely based in EHR systems,” the panel says. The authors note that “[o]ngoing studies of HBV tests such as ultrasensitive HBsAg, HBV RNA, and hepatitis B core antigen are being studied and may be useful in predicting risk of HBV reactivation.”
The panel also identified a research gap related to HBV reactivation risks “for the growing list of agents that deplete or modulate B cells.” It notes a need for additional research on the cost-effectiveness of HBV screening. The results of prior cost analyses have been inconsistent and vary with respect to the population studied. For example, universal screening and antiviral prophylaxis approaches have been shown to be cost-effective for patients with hematologic malignancies and high HBV reactivation risk but are less so for patients with solid tumors and lower reactivation risk, they explain.
Dr. Hwang said that not one of the more than 2100 patients in her HBV screening cohort study encountered problems with receiving insurance payment for their HBV screening.
“That’s a really strong statement that insurance payers are accepting of this kind of preventative service,” she said.
Expert panel cochair Andrew Artz, MD, commented that there is now greater acceptance of the need for HBV screening across medical specialties.
“There’s growing consensus among hepatologists, infectious disease specialists, oncologists, and HBV specialists that we need to do a better job of finding patients with hepatitis B [who are] about to receive immunocompromising treatment,” Dr. Artz said in an interview.
Dr. Artz is director of the Program for Aging and Blood Cancers and deputy director of the Center for Cancer and Aging at City of Hope Comprehensive Cancer Center, Duarte, California.
He suggested that the growing acceptance is due in part to the increasing number of anticancer therapies available and the resulting increase in the likelihood of patients receiving therapies that could cause reactivation.
More therapies – and more lines of therapy – could mean greater risk, he explained. He said that testing is easy and that universal screening is the simplest approach to determining who needs it. “There’s no question we will have to change practice,” Dr. Artz said in an interview. “But this is easier than the previous approach that essentially wasn’t being followed because it was too difficult to follow and patients were being missed.”
Most clinicians will appreciate having an approach that’s easier to follow, Dr. Artz predicted.
If there’s a challenge it will be in developing partnerships with HBV specialists, particularly in rural areas. In areas where there is a paucity of subspecialists, oncologists will have to “take some ownership of the issue,” as they often do in such settings, he said.
However, with support from pharmacists, administrators, and others in embracing this guidance, implementation can take place at a systems level rather than an individual clinician level, he added.
The recommendations in this updated PCO were all rated as “strong,” with the exception of the recommendation on hormonal therapy in the absence of systemic anticancer therapy, which was rated as “moderate.” All were based on “informal consensus,” with the exception of the key recommendation for universal HBV screening – use of three specific tests – which was “evidence based.”
The expert panel agreed that the benefits outweigh the harms for each recommendation in the update.
Dr. Hwang received research funding to her institution from Gilead Sciences and Merck Sharp & Dohme. She also has a relationship with the Asian Health Foundation. Dr. Artz received research funding from Miltenyi Biotec. All expert panel members’ disclosures are available in the PCO update.
This article first appeared on Medscape.com.
All patients with cancer who are candidates for systemic anticancer therapy should be screened for hepatitis B virus (HBV) infection prior to or at the start of therapy, according to an updated provisional clinical opinion (PCO) from the American Society of Clinical Oncology.
“This is a new approach [that] will actively take system changes ... but it will ultimately be safer for patients – and that is crucial,” commented Jessica P. Hwang, MD, MPH, cochair of the American Society of Clinical Oncology HBV Screening Expert Panel and the first author of the PCO.
Uptake of this universal screening approach would streamline testing protocols and identify more patients at risk for HBV reactivation who should receive prophylactic antiviral therapy, Dr. Hwang said in an interview.
The PCO calls for antiviral prophylaxis during and for at least 12 months after therapy for those with chronic HBV infection who are receiving any systemic anticancer treatment and for those with have had HBV in the past and are receiving any therapies that pose a risk for HBV reactivation.
“Hepatitis B reactivation can cause really terrible outcomes, like organ failure and even death,” Dr. Hwang, who is also a professor at the University of Texas MD Anderson Cancer Center, Houston, commented in an interview.
“This whole [issue of] reactivation and adverse outcomes with anticancer therapies is completely preventable with good planning, good communication, comanagement with specialists, and antiviral therapy and monitoring,” she added.
The updated opinion was published online July 27 in the Journal of Clinical Oncology.
It was developed in response to new data that call into question the previously recommended risk-adaptive approach to HBV screening of cancer patients, say the authors.
ASCO PCOs are developed “to provide timely clinical guidance” on the basis of emerging practice-changing information. This is the second update to follow the initial HBV screening PCO, published in 2010. In the absence of clear consensus because of limited data, the original PCO called for a risk-based approach to screening. A 2015 update extended the recommendation for screening to patients starting anti-CD20 therapy or who are to undergo stem cell transplant and to those with risk factors for HBV exposure.
The current update provides “a clinically pragmatic approach to HBV screening and management” that is based on the latest findings, say the authors. These include findings from a multicenter prospective cohort study of more than 3000 patients. In that study, 21% of patients with chronic HBV had no known risk factors for the infection. In another large prospective observational cohort study, led by Dr. Hwang, which included more than 2100 patients with cancer, 90% had one or more significant risk factors for HBV infection, making selective screening “inefficient and impractical,” she said.
“The results of these two studies suggest that a universal screening approach, its potential harms (e.g., patient and clinician anxiety about management, financial burden associated with antiviral therapy) notwithstanding, is the most efficient, clinically pragmatic approach to HBV screening in persons anticipating systemic anticancer treatment,” the authors comment.
The screening recommended in the PCO requires three tests: hepatitis B surface antigen (HBsAg), core antibody total immunoglobulin or IgG, and antibody to HBsAg tests.
Anticancer therapy should not be delayed pending the results, they write.
Planning for monitoring and long-term prophylaxis for chronic HBV infection should involve a clinician experienced in HBV management, the authors write. Management of those with past infection should be individualized. Alternatively, patients with past infection can be carefully monitored rather than given prophylactic treatment, as long as frequent and consistent follow-up is possible to allow for rapid initiation of antiviral therapy in the event of reactivation, they say.
Hormonal therapy without systemic anticancer therapy is not likely to lead to HBV reactivation in patients with chronic or past infection; antiviral therapy and management of these patients should follow relevant national HBV guidelines, they note.
Challenges in implementing universal HBV screening
The expert panel acknowledges the challenges associated with implementation of universal HBV screening as recommended in their report and notes that electronic health record–based approaches that use alerts to prompt screening have demonstrated success. In one study of high-risk primary care patients, an EHR alert system significantly increased testing rates (odds ratio, 2.64 in comparison with a control group without alerts), and another study that used a simple “sticky-note” alert system to promote referral of HBsAg patients to hepatologists increased referrals from 28% to 73%.
In a cancer population, a “comprehensive set of multimodal interventions,” including pharmacy staff checks for screening prior to anti-CD20 therapy administration and electronic medication order reviews to assess for appropriate testing and treatment before anti-CD20 therapy, increased testing rates to greater than 90% and antiviral prophylaxis rates to more than 80%.
A study of 965 patients in Taiwan showed that a computer-assisted reminder system that prompted for testing prior to ordering anticancer therapy increased screening from 8% to 86% but was less effective for improving the rates of antiviral prophylaxis for those who tested positive for HBV, particularly among physicians treating patients with nonhematologic malignancies.
“Future studies will be needed to make universal HBV screening and linkage to care efficient and systematic, likely based in EHR systems,” the panel says. The authors note that “[o]ngoing studies of HBV tests such as ultrasensitive HBsAg, HBV RNA, and hepatitis B core antigen are being studied and may be useful in predicting risk of HBV reactivation.”
The panel also identified a research gap related to HBV reactivation risks “for the growing list of agents that deplete or modulate B cells.” It notes a need for additional research on the cost-effectiveness of HBV screening. The results of prior cost analyses have been inconsistent and vary with respect to the population studied. For example, universal screening and antiviral prophylaxis approaches have been shown to be cost-effective for patients with hematologic malignancies and high HBV reactivation risk but are less so for patients with solid tumors and lower reactivation risk, they explain.
Dr. Hwang said that not one of the more than 2100 patients in her HBV screening cohort study encountered problems with receiving insurance payment for their HBV screening.
“That’s a really strong statement that insurance payers are accepting of this kind of preventative service,” she said.
Expert panel cochair Andrew Artz, MD, commented that there is now greater acceptance of the need for HBV screening across medical specialties.
“There’s growing consensus among hepatologists, infectious disease specialists, oncologists, and HBV specialists that we need to do a better job of finding patients with hepatitis B [who are] about to receive immunocompromising treatment,” Dr. Artz said in an interview.
Dr. Artz is director of the Program for Aging and Blood Cancers and deputy director of the Center for Cancer and Aging at City of Hope Comprehensive Cancer Center, Duarte, California.
He suggested that the growing acceptance is due in part to the increasing number of anticancer therapies available and the resulting increase in the likelihood of patients receiving therapies that could cause reactivation.
More therapies – and more lines of therapy – could mean greater risk, he explained. He said that testing is easy and that universal screening is the simplest approach to determining who needs it. “There’s no question we will have to change practice,” Dr. Artz said in an interview. “But this is easier than the previous approach that essentially wasn’t being followed because it was too difficult to follow and patients were being missed.”
Most clinicians will appreciate having an approach that’s easier to follow, Dr. Artz predicted.
If there’s a challenge it will be in developing partnerships with HBV specialists, particularly in rural areas. In areas where there is a paucity of subspecialists, oncologists will have to “take some ownership of the issue,” as they often do in such settings, he said.
However, with support from pharmacists, administrators, and others in embracing this guidance, implementation can take place at a systems level rather than an individual clinician level, he added.
The recommendations in this updated PCO were all rated as “strong,” with the exception of the recommendation on hormonal therapy in the absence of systemic anticancer therapy, which was rated as “moderate.” All were based on “informal consensus,” with the exception of the key recommendation for universal HBV screening – use of three specific tests – which was “evidence based.”
The expert panel agreed that the benefits outweigh the harms for each recommendation in the update.
Dr. Hwang received research funding to her institution from Gilead Sciences and Merck Sharp & Dohme. She also has a relationship with the Asian Health Foundation. Dr. Artz received research funding from Miltenyi Biotec. All expert panel members’ disclosures are available in the PCO update.
This article first appeared on Medscape.com.
ASCO says ‘no’ to home infusions of cancer treatment, with exceptions
in a new policy statement issued July 31.
At the same time, it supports exceptions: namely, when individual physicians and patients, having jointly discussed risks and benefits, agree to have treatments administered in the home.
The new policy is limited to intravenous infusions of anticancer agents such as chemotherapy, monoclonal antibodies, and other drugs — administered by health care personnel. It does not refer to injections.
The policy was prompted by regulatory flexibilities from the Centers for Medicare & Medicaid Services made in response to the accelerating COVID-19 pandemic. “Among these flexibilities were new provisions that enabled providers to deliver care in a setting most appropriate – and safest – for individual patient circumstances,” which has “opened the path for potential increases in use of home infusion for anticancer therapy,” says ASCO.
“We’re not ready to endorse [chemo at home] as a general policy until we have evidence that it’s safe. At the same time, the policy gives physicians and patients autonomy to respond to whatever situation they find themselves in,” Stephen Grubbs, MD, ASCO’s senior director of clinical affairs, said in an interview.
“Antineoplastic drugs are effective at treating cancer but can be extremely toxic to normal human cells,” reads the statement, which was written by a group of about 25 professionals, including Grubbs and other ASCO staff as well as independent advisers.
“There is a paucity of evidence directly comparing the safety of chemotherapy infusions in the home and outpatient settings,” the ASCO policy explains.
ASCO’s policy acknowledges that there are data “from other countries demonstrating that ... home infusion can be safe, well-tolerated, and may be preferred by some patients.” But such data are limited and only apply “to certain circumstances and for specific agents,” it adds.
One US cancer center (in Philadelphia) already has an established chemo-at-home program and has seen an increase in its use during the pandemic, as reported by Medscape Medical News. Approached for comment, Justin Bekelman, MD, director of the Penn Center for Cancer Care Innovation in Philadelphia, interpreted the new ASCO policy in a positive light.
“Physicians at the Abramson Cancer Center of the University of Pennsylvania and ASCO agree – home-based cancer therapy with oncologist oversight and well-designed safety protocols can be a safe option for patients with cancer,” he said in a statement.
ASCO says its existing safety standards “may be difficult to satisfy in the home infusion context,” including for safely resolving life-threatening emergencies.
Grubbs said that in the worst-case scenario, such as anaphylaxis, “you can die from [it] if you don’t manage it quickly and properly.”
“When I was practicing, we always had a physician present right next to the infusion area because these are severe reactions that happen very quickly,” he said, adding that “several a year” occurred when he practiced full-time.
Also, chemotherapy spills are a “big deal” in the home, as clean-up may be complex and difficult, added Grubbs.
Data from ASCO’s PracticeNET program show that in the first months (March and April) of the COVID-19 pandemic, chemotherapy visits to infusion suites were not reduced in a dataset of 16 US practices, he noted. However, there are exceptions and variance based on location, Grubbs said, such as “hot spots” including New York City in April.
While the pandemic has no end in sight, ASCO issued a set of six recommendations for use of anticancer therapies infused in the home. First, they call for independent, publicly funded research to evaluate the safety and effectiveness of home infusion of anticancer therapy.
Next in importance, ASCO wants the current temporary regulation change from CMS due to the pandemic to end.
“CMS should not extend the temporary flexibility related to home infusion for Part B cancer drugs that was approved as part of their response to the public health emergency,” they state.
Even before the pandemic, changes were afoot. Under the 21st Century Cures Act, which was passed in 2019 and will be implemented in 2021, CMS instituted a permanent home infusion therapy services benefit, which includes anticancer therapies. It “remains to be seen what, if any, shift away from outpatient infusion facilities will occur,” observes ASCO in its policy statement.
This article first appeared on Medscape.com.
in a new policy statement issued July 31.
At the same time, it supports exceptions: namely, when individual physicians and patients, having jointly discussed risks and benefits, agree to have treatments administered in the home.
The new policy is limited to intravenous infusions of anticancer agents such as chemotherapy, monoclonal antibodies, and other drugs — administered by health care personnel. It does not refer to injections.
The policy was prompted by regulatory flexibilities from the Centers for Medicare & Medicaid Services made in response to the accelerating COVID-19 pandemic. “Among these flexibilities were new provisions that enabled providers to deliver care in a setting most appropriate – and safest – for individual patient circumstances,” which has “opened the path for potential increases in use of home infusion for anticancer therapy,” says ASCO.
“We’re not ready to endorse [chemo at home] as a general policy until we have evidence that it’s safe. At the same time, the policy gives physicians and patients autonomy to respond to whatever situation they find themselves in,” Stephen Grubbs, MD, ASCO’s senior director of clinical affairs, said in an interview.
“Antineoplastic drugs are effective at treating cancer but can be extremely toxic to normal human cells,” reads the statement, which was written by a group of about 25 professionals, including Grubbs and other ASCO staff as well as independent advisers.
“There is a paucity of evidence directly comparing the safety of chemotherapy infusions in the home and outpatient settings,” the ASCO policy explains.
ASCO’s policy acknowledges that there are data “from other countries demonstrating that ... home infusion can be safe, well-tolerated, and may be preferred by some patients.” But such data are limited and only apply “to certain circumstances and for specific agents,” it adds.
One US cancer center (in Philadelphia) already has an established chemo-at-home program and has seen an increase in its use during the pandemic, as reported by Medscape Medical News. Approached for comment, Justin Bekelman, MD, director of the Penn Center for Cancer Care Innovation in Philadelphia, interpreted the new ASCO policy in a positive light.
“Physicians at the Abramson Cancer Center of the University of Pennsylvania and ASCO agree – home-based cancer therapy with oncologist oversight and well-designed safety protocols can be a safe option for patients with cancer,” he said in a statement.
ASCO says its existing safety standards “may be difficult to satisfy in the home infusion context,” including for safely resolving life-threatening emergencies.
Grubbs said that in the worst-case scenario, such as anaphylaxis, “you can die from [it] if you don’t manage it quickly and properly.”
“When I was practicing, we always had a physician present right next to the infusion area because these are severe reactions that happen very quickly,” he said, adding that “several a year” occurred when he practiced full-time.
Also, chemotherapy spills are a “big deal” in the home, as clean-up may be complex and difficult, added Grubbs.
Data from ASCO’s PracticeNET program show that in the first months (March and April) of the COVID-19 pandemic, chemotherapy visits to infusion suites were not reduced in a dataset of 16 US practices, he noted. However, there are exceptions and variance based on location, Grubbs said, such as “hot spots” including New York City in April.
While the pandemic has no end in sight, ASCO issued a set of six recommendations for use of anticancer therapies infused in the home. First, they call for independent, publicly funded research to evaluate the safety and effectiveness of home infusion of anticancer therapy.
Next in importance, ASCO wants the current temporary regulation change from CMS due to the pandemic to end.
“CMS should not extend the temporary flexibility related to home infusion for Part B cancer drugs that was approved as part of their response to the public health emergency,” they state.
Even before the pandemic, changes were afoot. Under the 21st Century Cures Act, which was passed in 2019 and will be implemented in 2021, CMS instituted a permanent home infusion therapy services benefit, which includes anticancer therapies. It “remains to be seen what, if any, shift away from outpatient infusion facilities will occur,” observes ASCO in its policy statement.
This article first appeared on Medscape.com.
in a new policy statement issued July 31.
At the same time, it supports exceptions: namely, when individual physicians and patients, having jointly discussed risks and benefits, agree to have treatments administered in the home.
The new policy is limited to intravenous infusions of anticancer agents such as chemotherapy, monoclonal antibodies, and other drugs — administered by health care personnel. It does not refer to injections.
The policy was prompted by regulatory flexibilities from the Centers for Medicare & Medicaid Services made in response to the accelerating COVID-19 pandemic. “Among these flexibilities were new provisions that enabled providers to deliver care in a setting most appropriate – and safest – for individual patient circumstances,” which has “opened the path for potential increases in use of home infusion for anticancer therapy,” says ASCO.
“We’re not ready to endorse [chemo at home] as a general policy until we have evidence that it’s safe. At the same time, the policy gives physicians and patients autonomy to respond to whatever situation they find themselves in,” Stephen Grubbs, MD, ASCO’s senior director of clinical affairs, said in an interview.
“Antineoplastic drugs are effective at treating cancer but can be extremely toxic to normal human cells,” reads the statement, which was written by a group of about 25 professionals, including Grubbs and other ASCO staff as well as independent advisers.
“There is a paucity of evidence directly comparing the safety of chemotherapy infusions in the home and outpatient settings,” the ASCO policy explains.
ASCO’s policy acknowledges that there are data “from other countries demonstrating that ... home infusion can be safe, well-tolerated, and may be preferred by some patients.” But such data are limited and only apply “to certain circumstances and for specific agents,” it adds.
One US cancer center (in Philadelphia) already has an established chemo-at-home program and has seen an increase in its use during the pandemic, as reported by Medscape Medical News. Approached for comment, Justin Bekelman, MD, director of the Penn Center for Cancer Care Innovation in Philadelphia, interpreted the new ASCO policy in a positive light.
“Physicians at the Abramson Cancer Center of the University of Pennsylvania and ASCO agree – home-based cancer therapy with oncologist oversight and well-designed safety protocols can be a safe option for patients with cancer,” he said in a statement.
ASCO says its existing safety standards “may be difficult to satisfy in the home infusion context,” including for safely resolving life-threatening emergencies.
Grubbs said that in the worst-case scenario, such as anaphylaxis, “you can die from [it] if you don’t manage it quickly and properly.”
“When I was practicing, we always had a physician present right next to the infusion area because these are severe reactions that happen very quickly,” he said, adding that “several a year” occurred when he practiced full-time.
Also, chemotherapy spills are a “big deal” in the home, as clean-up may be complex and difficult, added Grubbs.
Data from ASCO’s PracticeNET program show that in the first months (March and April) of the COVID-19 pandemic, chemotherapy visits to infusion suites were not reduced in a dataset of 16 US practices, he noted. However, there are exceptions and variance based on location, Grubbs said, such as “hot spots” including New York City in April.
While the pandemic has no end in sight, ASCO issued a set of six recommendations for use of anticancer therapies infused in the home. First, they call for independent, publicly funded research to evaluate the safety and effectiveness of home infusion of anticancer therapy.
Next in importance, ASCO wants the current temporary regulation change from CMS due to the pandemic to end.
“CMS should not extend the temporary flexibility related to home infusion for Part B cancer drugs that was approved as part of their response to the public health emergency,” they state.
Even before the pandemic, changes were afoot. Under the 21st Century Cures Act, which was passed in 2019 and will be implemented in 2021, CMS instituted a permanent home infusion therapy services benefit, which includes anticancer therapies. It “remains to be seen what, if any, shift away from outpatient infusion facilities will occur,” observes ASCO in its policy statement.
This article first appeared on Medscape.com.
Many older adults ‘overscreened’ for cancer
Older adults are being “overscreened” for cancer, say researchers who discovered that many patients reported undergoing screening for cancer even though they were older than the upper age limit recommended.
The U.S. Preventive Services Task Force recommends an upper age limit on cancer screening that varies by cancer type – 75 years old for colorectal cancer, 74 for breast cancer, and 65 for cervical cancer.
The study found that 59.3% of men and 56.2% of women being screening for colorectal cancer were above that cut-off age, as were 45.8% of women being screened for cervical cancer and 74.1% of women being screened for breast cancer.
Overscreening was particularly high for women living in metropolitan areas.
The finding is of concern, say the researchers, because “continuing to screen patients who are older and/or who have limited life expectancy may cause more harms than benefits.”
“The development of successful interventions to address this problem are thus essential,” they write.
The study was published online July 27 in JAMA Network Open.
Clinicians, patients, and health care systems can be changed – and should be changed – to minimize overscreening,” said lead author Jennifer L. Moss, PhD, assistant professor of family and community medicine and public health sciences at Penn State University, Hershey.
“It will probably take many changes to meaningfully decrease overscreening,” she told Medscape Medical News.
One change that would help is if health insurance companies stopped reimbursing providers for screening after the recommended upper age limit, she continued. “Another change is if providers had evidence-based tools to guide conversations about stopping screening, given an individual patient’s demographics, health status, and risks and benefits of the screening test.”
Approached for comment on the study, Nancy Schoenborn, MD, MHS, an associate professor of medicine in the Division of Geriatric Medicine and Gerontology at Johns Hopkins University, Baltimore, noted that the finding of high overscreening is not surprising and is consistent with prior works that found similar results.
“One value of this paper is that the timing of the study is more recent and confirms that the issue of overscreening is one that is still ongoing,” she told Medscape Medical News. Schoenborn was not associated with the study.
As for what physicians should do about the findings in this study, Schoenborn suggested the first step is to simply recognize that overscreening is likely a problem and “to reflect if there are instances in one’s own practice where overscreening may occur.”
In her own work, Schoenborn continued, “I was recently surprised that a substantial minority of clinicians actually do not believe overscreening to be a problem in older adults, and they have a number of concerns about how overscreening is defined and about unintended consequences that can occur from efforts to reduce overscreening.”
She added that there are a number of reasons why overscreening occurs. These include guideline inconsistencies, inertia, patient request, clinician knowledge gaps, and discomfort with discussing stopping. “A lot of work is ongoing to address each of these issues, but I think the first step would be the clinician recognizing and agreeing that this is a problem that needs to be addressed,” she said.
Unnecessary screening
The authors note that the prevalence estimates for overscreening have not been reported on a national level, and it is also unclear how overscreening may vary among subgroups.
“The reason I focused on colorectal, cervical, and breast cancers is because USPSTF has very clear, age-based recommendations for these cancers in terms of who should and should not get screened routinely,” explained Moss. “This was important because it allowed me and my coauthors to clearly say, based on age alone, this person probably was screened unnecessarily, and this person was not.”
She noted that the age-based recommendations for routine screening are based on very large clinical trials to examine the effectiveness of the screening tool. “The recommendations for lung and prostate cancer screening are not so clear cut, and we would not be able to tell, based only on the available survey data, if someone was overscreened,” she said.
For their study, the team used data from the 2018 Behavioral Risk Factor Surveillance System, administered by the Centers for Disease Control and Prevention.
Overscreening was assessed in a cohort of 20,937 men and 34,244 women for colorectal cancer, 82,811 women for cervical cancer, and 38,356 women for breast cancer. Most the participants lived in a metropolitan area (about 80%) and were white (about 80%).
Being overscreened was also more common in metropolitan vs. nonmetropolitan areas for colorectal cancer in women (adjusted odds ratio, 1.23), cervical cancer (aOR, 1.20), and breast cancer (aOR, 1.36).
Overscreening for cervical and breast cancers was also associated with having a usual source of care, good/very good/excellent self-reported health, education beyond a high school diploma, and being married or living as married.
The study was carried out in 2018, and the situation is likely to have changed over recent months during the COVID-19 pandemic.
“We have already seen dramatic reductions in routine cancer screening among age-eligible adults, so part of this problem of overscreening among older adults will likely diminish,” said Moss. “State and national cancer surveillance systems will continue to monitor trends in cancer screening, including overscreening, cancer incidence, and cancer mortality.”
Johns Hopkins’ Schoenborn said one finding of particular interest was that the colorectal cancer overscreening rate was higher in those older than 80 and in those with higher mortality risk.
“It makes me wonder if this is due to the increasing use of noninvasive colorectal cancer screening modalities, such as the fecal immunochemical test FIT or Cologuard,” Schoenborn commented. “It would be important for clinicians to consider downstream effects even when the initial test is low risk, such as if the stool test screens positive, would the patient still need a colonoscopy, and is that something the patient can undergo and wants to undergo?”
The study was funded by the National Cancer Institute and American Cancer Society. Moss, study coauthors, and Schoenborn have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Older adults are being “overscreened” for cancer, say researchers who discovered that many patients reported undergoing screening for cancer even though they were older than the upper age limit recommended.
The U.S. Preventive Services Task Force recommends an upper age limit on cancer screening that varies by cancer type – 75 years old for colorectal cancer, 74 for breast cancer, and 65 for cervical cancer.
The study found that 59.3% of men and 56.2% of women being screening for colorectal cancer were above that cut-off age, as were 45.8% of women being screened for cervical cancer and 74.1% of women being screened for breast cancer.
Overscreening was particularly high for women living in metropolitan areas.
The finding is of concern, say the researchers, because “continuing to screen patients who are older and/or who have limited life expectancy may cause more harms than benefits.”
“The development of successful interventions to address this problem are thus essential,” they write.
The study was published online July 27 in JAMA Network Open.
Clinicians, patients, and health care systems can be changed – and should be changed – to minimize overscreening,” said lead author Jennifer L. Moss, PhD, assistant professor of family and community medicine and public health sciences at Penn State University, Hershey.
“It will probably take many changes to meaningfully decrease overscreening,” she told Medscape Medical News.
One change that would help is if health insurance companies stopped reimbursing providers for screening after the recommended upper age limit, she continued. “Another change is if providers had evidence-based tools to guide conversations about stopping screening, given an individual patient’s demographics, health status, and risks and benefits of the screening test.”
Approached for comment on the study, Nancy Schoenborn, MD, MHS, an associate professor of medicine in the Division of Geriatric Medicine and Gerontology at Johns Hopkins University, Baltimore, noted that the finding of high overscreening is not surprising and is consistent with prior works that found similar results.
“One value of this paper is that the timing of the study is more recent and confirms that the issue of overscreening is one that is still ongoing,” she told Medscape Medical News. Schoenborn was not associated with the study.
As for what physicians should do about the findings in this study, Schoenborn suggested the first step is to simply recognize that overscreening is likely a problem and “to reflect if there are instances in one’s own practice where overscreening may occur.”
In her own work, Schoenborn continued, “I was recently surprised that a substantial minority of clinicians actually do not believe overscreening to be a problem in older adults, and they have a number of concerns about how overscreening is defined and about unintended consequences that can occur from efforts to reduce overscreening.”
She added that there are a number of reasons why overscreening occurs. These include guideline inconsistencies, inertia, patient request, clinician knowledge gaps, and discomfort with discussing stopping. “A lot of work is ongoing to address each of these issues, but I think the first step would be the clinician recognizing and agreeing that this is a problem that needs to be addressed,” she said.
Unnecessary screening
The authors note that the prevalence estimates for overscreening have not been reported on a national level, and it is also unclear how overscreening may vary among subgroups.
“The reason I focused on colorectal, cervical, and breast cancers is because USPSTF has very clear, age-based recommendations for these cancers in terms of who should and should not get screened routinely,” explained Moss. “This was important because it allowed me and my coauthors to clearly say, based on age alone, this person probably was screened unnecessarily, and this person was not.”
She noted that the age-based recommendations for routine screening are based on very large clinical trials to examine the effectiveness of the screening tool. “The recommendations for lung and prostate cancer screening are not so clear cut, and we would not be able to tell, based only on the available survey data, if someone was overscreened,” she said.
For their study, the team used data from the 2018 Behavioral Risk Factor Surveillance System, administered by the Centers for Disease Control and Prevention.
Overscreening was assessed in a cohort of 20,937 men and 34,244 women for colorectal cancer, 82,811 women for cervical cancer, and 38,356 women for breast cancer. Most the participants lived in a metropolitan area (about 80%) and were white (about 80%).
Being overscreened was also more common in metropolitan vs. nonmetropolitan areas for colorectal cancer in women (adjusted odds ratio, 1.23), cervical cancer (aOR, 1.20), and breast cancer (aOR, 1.36).
Overscreening for cervical and breast cancers was also associated with having a usual source of care, good/very good/excellent self-reported health, education beyond a high school diploma, and being married or living as married.
The study was carried out in 2018, and the situation is likely to have changed over recent months during the COVID-19 pandemic.
“We have already seen dramatic reductions in routine cancer screening among age-eligible adults, so part of this problem of overscreening among older adults will likely diminish,” said Moss. “State and national cancer surveillance systems will continue to monitor trends in cancer screening, including overscreening, cancer incidence, and cancer mortality.”
Johns Hopkins’ Schoenborn said one finding of particular interest was that the colorectal cancer overscreening rate was higher in those older than 80 and in those with higher mortality risk.
“It makes me wonder if this is due to the increasing use of noninvasive colorectal cancer screening modalities, such as the fecal immunochemical test FIT or Cologuard,” Schoenborn commented. “It would be important for clinicians to consider downstream effects even when the initial test is low risk, such as if the stool test screens positive, would the patient still need a colonoscopy, and is that something the patient can undergo and wants to undergo?”
The study was funded by the National Cancer Institute and American Cancer Society. Moss, study coauthors, and Schoenborn have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Older adults are being “overscreened” for cancer, say researchers who discovered that many patients reported undergoing screening for cancer even though they were older than the upper age limit recommended.
The U.S. Preventive Services Task Force recommends an upper age limit on cancer screening that varies by cancer type – 75 years old for colorectal cancer, 74 for breast cancer, and 65 for cervical cancer.
The study found that 59.3% of men and 56.2% of women being screening for colorectal cancer were above that cut-off age, as were 45.8% of women being screened for cervical cancer and 74.1% of women being screened for breast cancer.
Overscreening was particularly high for women living in metropolitan areas.
The finding is of concern, say the researchers, because “continuing to screen patients who are older and/or who have limited life expectancy may cause more harms than benefits.”
“The development of successful interventions to address this problem are thus essential,” they write.
The study was published online July 27 in JAMA Network Open.
Clinicians, patients, and health care systems can be changed – and should be changed – to minimize overscreening,” said lead author Jennifer L. Moss, PhD, assistant professor of family and community medicine and public health sciences at Penn State University, Hershey.
“It will probably take many changes to meaningfully decrease overscreening,” she told Medscape Medical News.
One change that would help is if health insurance companies stopped reimbursing providers for screening after the recommended upper age limit, she continued. “Another change is if providers had evidence-based tools to guide conversations about stopping screening, given an individual patient’s demographics, health status, and risks and benefits of the screening test.”
Approached for comment on the study, Nancy Schoenborn, MD, MHS, an associate professor of medicine in the Division of Geriatric Medicine and Gerontology at Johns Hopkins University, Baltimore, noted that the finding of high overscreening is not surprising and is consistent with prior works that found similar results.
“One value of this paper is that the timing of the study is more recent and confirms that the issue of overscreening is one that is still ongoing,” she told Medscape Medical News. Schoenborn was not associated with the study.
As for what physicians should do about the findings in this study, Schoenborn suggested the first step is to simply recognize that overscreening is likely a problem and “to reflect if there are instances in one’s own practice where overscreening may occur.”
In her own work, Schoenborn continued, “I was recently surprised that a substantial minority of clinicians actually do not believe overscreening to be a problem in older adults, and they have a number of concerns about how overscreening is defined and about unintended consequences that can occur from efforts to reduce overscreening.”
She added that there are a number of reasons why overscreening occurs. These include guideline inconsistencies, inertia, patient request, clinician knowledge gaps, and discomfort with discussing stopping. “A lot of work is ongoing to address each of these issues, but I think the first step would be the clinician recognizing and agreeing that this is a problem that needs to be addressed,” she said.
Unnecessary screening
The authors note that the prevalence estimates for overscreening have not been reported on a national level, and it is also unclear how overscreening may vary among subgroups.
“The reason I focused on colorectal, cervical, and breast cancers is because USPSTF has very clear, age-based recommendations for these cancers in terms of who should and should not get screened routinely,” explained Moss. “This was important because it allowed me and my coauthors to clearly say, based on age alone, this person probably was screened unnecessarily, and this person was not.”
She noted that the age-based recommendations for routine screening are based on very large clinical trials to examine the effectiveness of the screening tool. “The recommendations for lung and prostate cancer screening are not so clear cut, and we would not be able to tell, based only on the available survey data, if someone was overscreened,” she said.
For their study, the team used data from the 2018 Behavioral Risk Factor Surveillance System, administered by the Centers for Disease Control and Prevention.
Overscreening was assessed in a cohort of 20,937 men and 34,244 women for colorectal cancer, 82,811 women for cervical cancer, and 38,356 women for breast cancer. Most the participants lived in a metropolitan area (about 80%) and were white (about 80%).
Being overscreened was also more common in metropolitan vs. nonmetropolitan areas for colorectal cancer in women (adjusted odds ratio, 1.23), cervical cancer (aOR, 1.20), and breast cancer (aOR, 1.36).
Overscreening for cervical and breast cancers was also associated with having a usual source of care, good/very good/excellent self-reported health, education beyond a high school diploma, and being married or living as married.
The study was carried out in 2018, and the situation is likely to have changed over recent months during the COVID-19 pandemic.
“We have already seen dramatic reductions in routine cancer screening among age-eligible adults, so part of this problem of overscreening among older adults will likely diminish,” said Moss. “State and national cancer surveillance systems will continue to monitor trends in cancer screening, including overscreening, cancer incidence, and cancer mortality.”
Johns Hopkins’ Schoenborn said one finding of particular interest was that the colorectal cancer overscreening rate was higher in those older than 80 and in those with higher mortality risk.
“It makes me wonder if this is due to the increasing use of noninvasive colorectal cancer screening modalities, such as the fecal immunochemical test FIT or Cologuard,” Schoenborn commented. “It would be important for clinicians to consider downstream effects even when the initial test is low risk, such as if the stool test screens positive, would the patient still need a colonoscopy, and is that something the patient can undergo and wants to undergo?”
The study was funded by the National Cancer Institute and American Cancer Society. Moss, study coauthors, and Schoenborn have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
OK to treat many cancer patients despite pandemic, says ESMO
Not all are highly vulnerable to COVID-19
Another important recommendation is to stop labeling all patients with cancer as being vulnerable to infection with the virus as it can lead to inappropriate care with potential negative outcomes.
“Although it was reasonable to adopt over-protective measures for our patients at the outbreak of a novel infective disease which was not previously observed in humans, we now need to step away from the assumption that all cancer patients are vulnerable to COVID-19,” said first author of the consensus article Giuseppe Curigliano, MD, PhD, of the European Institute of Oncology, Milan, Italy, in a statement. “The implications have been important because for some patients treatment was delayed or interrupted over the last few months, and I believe that we will see the impact of this over-precautionary approach in the...future.”
The recommendations were issued by the European Society of Medical Oncology (ESMO) to help guide physicians in “optimizing the pathway to cancer care” as well as to improve outcomes during the pandemic. The recommendations were published online July 31 in Annals of Oncology.
Studies have found that patients with cancer face a higher risk of serious complications and death if they develop COVID-19. Data from the COVID-19 and Cancer Consortium registry, for example, showed that patients with progressing cancer and COVID-19 infection had a fivefold increase in the risk of 30-day mortality compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer.
But while this may be true for some patients, Curigliano and colleagues emphasize that individuals with cancer are not a heterogeneous group and that the term “cancer” itself represents myriad different diseases. The European experts note that current evidence suggests many patients with solid tumors are not more vulnerable to serious complications than the general population.
Thus, cancer prognoses vary considerably, and addressing all patients with cancer as being “COVID-19-vulnerable is probably neither reasonable nor informative,” say the authors.
Dramatic changes were initiated in cancer management for all cancer types, nevertheless, and although these changes seemed reasonable in an acute pandemic situation, note the authors, they were made in the absence of strong supportive evidence. Attempts to define the individualized risk for a given patient, taking into account their primary tumor subtype, stage, age, and gender, have been limited.
“Based on current evidence, only patients who are elderly, with multiple comorbidities, and receiving chemotherapy are vulnerable to the infection,” explained Curigliano.
However, on a positive note, a recently published prospective cohort study looked at approximately 800 patients with cancer – who had symptomatic COVID-19 – in the United Kingdom. The analysis showed no association at all between the risk for death and receiving chemotherapy or immunotherapy, points out Medscape commentator David Kerr, MD, of the University of Oxford, UK, in a recent commentary.
Key recommendations
An international consortium was established by ESMO, and the interdisciplinary expert panel consisted of 64 experts and one voting patient advocate. They agreed on 28 statements that can be used to help with many of the current clinical and technical areas of uncertainty that range from diagnosis to treatment decisions.
The following are several of the key recommendations:
- Patients with cancer who face the highest risk of severe COVID-19 are characterized by active and progressive cancer, advanced age, poor performance status, smoking status, comorbidities, and possibly type of cancer.
- Telehealth and digital health can be excellent tools for some types of care such as primary care triage and counseling, but meeting in person may be more effective for situations that include delivery of key cancer-related information and for patients with complex cancer needs.
- Prior to hospital admission, patients with cancer should be tested for COVID-19, if feasible, and if they are considered at high risk, regardless of symptoms or chest radiological findings.
- Patients with cancer and COVID-19 have a higher risk of thromboembolic events, and prophylaxis using low molecular weight or novel oral anticoagulants is recommended.
- Immune checkpoint inhibitors should not be withheld or delayed when there is a significant survival benefit, but use should be postponed in patients who test positive for COVID-19 until they recover.
- Use of high-dose steroids in patients with cancer infected with COVID-19 could potentially increase the risk of mortality, and a switch should be made to another immunosuppressant, if possible.
- The decision to use tyrosine kinase inhibitors (TKIs) of the PI3K/AKT/mTOR or RAS/RAF/MEK axis is complex, as they interfere with critical pathways involved in innate or adaptive immune responses. Stopping or withholding therapy depends on the risk-benefit balance, and the magnitude of benefit from the TKI needs to be considered.
The authors conclude that “ultimately, this set of statements will serve as a dynamic knowledge repository that will be better informed by accumulating data on SARS-CoV-2 biology, COVID-19 pandemic characteristics, on the risk of cancer patients for COVID-19 and its modulating factors, and finally, on optimal cancer care in the presence of the virus.”
No funding was reported for the current study. Several authors have disclosed relationships with industry, which are listed in the article.
This article first appeared on Medscape.com.
Not all are highly vulnerable to COVID-19
Not all are highly vulnerable to COVID-19
Another important recommendation is to stop labeling all patients with cancer as being vulnerable to infection with the virus as it can lead to inappropriate care with potential negative outcomes.
“Although it was reasonable to adopt over-protective measures for our patients at the outbreak of a novel infective disease which was not previously observed in humans, we now need to step away from the assumption that all cancer patients are vulnerable to COVID-19,” said first author of the consensus article Giuseppe Curigliano, MD, PhD, of the European Institute of Oncology, Milan, Italy, in a statement. “The implications have been important because for some patients treatment was delayed or interrupted over the last few months, and I believe that we will see the impact of this over-precautionary approach in the...future.”
The recommendations were issued by the European Society of Medical Oncology (ESMO) to help guide physicians in “optimizing the pathway to cancer care” as well as to improve outcomes during the pandemic. The recommendations were published online July 31 in Annals of Oncology.
Studies have found that patients with cancer face a higher risk of serious complications and death if they develop COVID-19. Data from the COVID-19 and Cancer Consortium registry, for example, showed that patients with progressing cancer and COVID-19 infection had a fivefold increase in the risk of 30-day mortality compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer.
But while this may be true for some patients, Curigliano and colleagues emphasize that individuals with cancer are not a heterogeneous group and that the term “cancer” itself represents myriad different diseases. The European experts note that current evidence suggests many patients with solid tumors are not more vulnerable to serious complications than the general population.
Thus, cancer prognoses vary considerably, and addressing all patients with cancer as being “COVID-19-vulnerable is probably neither reasonable nor informative,” say the authors.
Dramatic changes were initiated in cancer management for all cancer types, nevertheless, and although these changes seemed reasonable in an acute pandemic situation, note the authors, they were made in the absence of strong supportive evidence. Attempts to define the individualized risk for a given patient, taking into account their primary tumor subtype, stage, age, and gender, have been limited.
“Based on current evidence, only patients who are elderly, with multiple comorbidities, and receiving chemotherapy are vulnerable to the infection,” explained Curigliano.
However, on a positive note, a recently published prospective cohort study looked at approximately 800 patients with cancer – who had symptomatic COVID-19 – in the United Kingdom. The analysis showed no association at all between the risk for death and receiving chemotherapy or immunotherapy, points out Medscape commentator David Kerr, MD, of the University of Oxford, UK, in a recent commentary.
Key recommendations
An international consortium was established by ESMO, and the interdisciplinary expert panel consisted of 64 experts and one voting patient advocate. They agreed on 28 statements that can be used to help with many of the current clinical and technical areas of uncertainty that range from diagnosis to treatment decisions.
The following are several of the key recommendations:
- Patients with cancer who face the highest risk of severe COVID-19 are characterized by active and progressive cancer, advanced age, poor performance status, smoking status, comorbidities, and possibly type of cancer.
- Telehealth and digital health can be excellent tools for some types of care such as primary care triage and counseling, but meeting in person may be more effective for situations that include delivery of key cancer-related information and for patients with complex cancer needs.
- Prior to hospital admission, patients with cancer should be tested for COVID-19, if feasible, and if they are considered at high risk, regardless of symptoms or chest radiological findings.
- Patients with cancer and COVID-19 have a higher risk of thromboembolic events, and prophylaxis using low molecular weight or novel oral anticoagulants is recommended.
- Immune checkpoint inhibitors should not be withheld or delayed when there is a significant survival benefit, but use should be postponed in patients who test positive for COVID-19 until they recover.
- Use of high-dose steroids in patients with cancer infected with COVID-19 could potentially increase the risk of mortality, and a switch should be made to another immunosuppressant, if possible.
- The decision to use tyrosine kinase inhibitors (TKIs) of the PI3K/AKT/mTOR or RAS/RAF/MEK axis is complex, as they interfere with critical pathways involved in innate or adaptive immune responses. Stopping or withholding therapy depends on the risk-benefit balance, and the magnitude of benefit from the TKI needs to be considered.
The authors conclude that “ultimately, this set of statements will serve as a dynamic knowledge repository that will be better informed by accumulating data on SARS-CoV-2 biology, COVID-19 pandemic characteristics, on the risk of cancer patients for COVID-19 and its modulating factors, and finally, on optimal cancer care in the presence of the virus.”
No funding was reported for the current study. Several authors have disclosed relationships with industry, which are listed in the article.
This article first appeared on Medscape.com.
Another important recommendation is to stop labeling all patients with cancer as being vulnerable to infection with the virus as it can lead to inappropriate care with potential negative outcomes.
“Although it was reasonable to adopt over-protective measures for our patients at the outbreak of a novel infective disease which was not previously observed in humans, we now need to step away from the assumption that all cancer patients are vulnerable to COVID-19,” said first author of the consensus article Giuseppe Curigliano, MD, PhD, of the European Institute of Oncology, Milan, Italy, in a statement. “The implications have been important because for some patients treatment was delayed or interrupted over the last few months, and I believe that we will see the impact of this over-precautionary approach in the...future.”
The recommendations were issued by the European Society of Medical Oncology (ESMO) to help guide physicians in “optimizing the pathway to cancer care” as well as to improve outcomes during the pandemic. The recommendations were published online July 31 in Annals of Oncology.
Studies have found that patients with cancer face a higher risk of serious complications and death if they develop COVID-19. Data from the COVID-19 and Cancer Consortium registry, for example, showed that patients with progressing cancer and COVID-19 infection had a fivefold increase in the risk of 30-day mortality compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer.
But while this may be true for some patients, Curigliano and colleagues emphasize that individuals with cancer are not a heterogeneous group and that the term “cancer” itself represents myriad different diseases. The European experts note that current evidence suggests many patients with solid tumors are not more vulnerable to serious complications than the general population.
Thus, cancer prognoses vary considerably, and addressing all patients with cancer as being “COVID-19-vulnerable is probably neither reasonable nor informative,” say the authors.
Dramatic changes were initiated in cancer management for all cancer types, nevertheless, and although these changes seemed reasonable in an acute pandemic situation, note the authors, they were made in the absence of strong supportive evidence. Attempts to define the individualized risk for a given patient, taking into account their primary tumor subtype, stage, age, and gender, have been limited.
“Based on current evidence, only patients who are elderly, with multiple comorbidities, and receiving chemotherapy are vulnerable to the infection,” explained Curigliano.
However, on a positive note, a recently published prospective cohort study looked at approximately 800 patients with cancer – who had symptomatic COVID-19 – in the United Kingdom. The analysis showed no association at all between the risk for death and receiving chemotherapy or immunotherapy, points out Medscape commentator David Kerr, MD, of the University of Oxford, UK, in a recent commentary.
Key recommendations
An international consortium was established by ESMO, and the interdisciplinary expert panel consisted of 64 experts and one voting patient advocate. They agreed on 28 statements that can be used to help with many of the current clinical and technical areas of uncertainty that range from diagnosis to treatment decisions.
The following are several of the key recommendations:
- Patients with cancer who face the highest risk of severe COVID-19 are characterized by active and progressive cancer, advanced age, poor performance status, smoking status, comorbidities, and possibly type of cancer.
- Telehealth and digital health can be excellent tools for some types of care such as primary care triage and counseling, but meeting in person may be more effective for situations that include delivery of key cancer-related information and for patients with complex cancer needs.
- Prior to hospital admission, patients with cancer should be tested for COVID-19, if feasible, and if they are considered at high risk, regardless of symptoms or chest radiological findings.
- Patients with cancer and COVID-19 have a higher risk of thromboembolic events, and prophylaxis using low molecular weight or novel oral anticoagulants is recommended.
- Immune checkpoint inhibitors should not be withheld or delayed when there is a significant survival benefit, but use should be postponed in patients who test positive for COVID-19 until they recover.
- Use of high-dose steroids in patients with cancer infected with COVID-19 could potentially increase the risk of mortality, and a switch should be made to another immunosuppressant, if possible.
- The decision to use tyrosine kinase inhibitors (TKIs) of the PI3K/AKT/mTOR or RAS/RAF/MEK axis is complex, as they interfere with critical pathways involved in innate or adaptive immune responses. Stopping or withholding therapy depends on the risk-benefit balance, and the magnitude of benefit from the TKI needs to be considered.
The authors conclude that “ultimately, this set of statements will serve as a dynamic knowledge repository that will be better informed by accumulating data on SARS-CoV-2 biology, COVID-19 pandemic characteristics, on the risk of cancer patients for COVID-19 and its modulating factors, and finally, on optimal cancer care in the presence of the virus.”
No funding was reported for the current study. Several authors have disclosed relationships with industry, which are listed in the article.
This article first appeared on Medscape.com.
Postmenopausal use of estrogen alone lowers breast cancer cases, deaths
A new follow-up study of menopausal hormone therapy found that prior use of conjugated equine estrogen (CEE) decreased both breast cancer incidence and mortality, while prior use of CEE plus medroxyprogesterone acetate (MPA) was associated with an increase in incidence.
“Prior use of CEE alone is, to our knowledge, the first pharmacologic intervention demonstrated to be associated with a statistically significantly reduction in deaths from breast cancer,” wrote Rowan T. Chlebowski, MD, PhD, of the Lundquist Institute for Biomedical Innovation in Torrance, Calif., and his coauthors. The study was published July 28 in JAMA.
To further investigate the outcomes of the Women’s Health Initiative in regard to hormone therapy and breast cancer risk, the researchers analyzed the long-term follow-up of two randomized trials that included 27,347 postmenopausal women with no prior breast cancer and negative mammograms at baseline. Their mean (SD) age was 63.4 (7.2) years. Enrollment took place from 1993 to 1998; participants were contacted for follow-up every 6 months through 2005 and annually from then on. Mortality data were gathered from follow-up and the National Death Index.
The first trial included 16,608 women with a uterus. Among these women, 8,506 received 0.625 mg/day of CEE plus 2.5 mg/day of MPA, and 8,102 received placebo. The second trial included 10,739 women who’d gotten a hysterectomy, 5,310 of whom received 0.625 mg/day of CEE alone and 5,429 of whom received placebo. The first trial ended in 2002 after a median intervention period of 5.6 years, and the second trial ended in 2004 after a period of 7.2 years.
An analysis in 2015 found that CEE alone was associated with lower risk of breast cancer and CEE plus MPA was associated with increased risk.
The current analysis confirmed that, after a median of 20.3 years of follow-up, and with mortality data now available for more than 98% of participants, CEE alone was associated with fewer cases of breast cancer (238 cases, annualized rate 0.30%), compared with placebo (296 cases, annualized rate 0.37%; hazard ratio 0.78; 95% confidence interval, 0.65-0.93; P = .005).
Furthermore, CEE alone was also associated with lower mortality (30 deaths, annualized mortality rate 0.031%), compared with placebo (46 deaths, annualized mortality rate 0.046%; HR 0.60; 95% CI, 0.37-0.97; P = .04).
By comparison, CEE plus MPA was linked with more cases of breast cancer (584 cases, annualized rate 0.45%) than placebo (447 cases, annualized rate 0.36%; HR 1.28; 95% CI, 1.13-1.45; P < .001). In regard to mortality, there was no statistically significant difference between CEE plus MPA (71 deaths, annualized mortality rate 0.045%) and placebo (53 deaths, annualized mortality rate 0.035%; HR 1.35; 95% CI, 0.94-1.95; P = .11).
“The big thing to think about is estrogen alone reducing breast cancer mortality by 40%,” said Dr. Chlebowski in an interview. “None of the other interventions, including tamoxifen, had any change on mortality. This should change the way we look at breast cancer prevention, though we might have to be a little creative about it. I think you have to be a little away from menopause for it to reduce breast cancer. But we wanted to start that debate.
“On the other hand,” he said, “a woman takes estrogen plus progestin and when you look at that curve, it’s staying about 25% increased. You take it for 5.6 years and the increase continues through 20 years, so you’re maybe buying a lifetime of increase in breast cancer by taking estrogen plus progestin for 5 years.”
He also highlighted the comprehensiveness of the mortality data, noting that “when you hook up to the National Death Index, they find 98% of all deaths in the United States. That’s really remarkable; you retain the whole power of the randomization. It means our data, between the death index and our follow-up of participants, is essentially complete.”
Use of hormone therapy, and decoding the outcomes, remains ‘complex’
Decades after the data were gathered from the Women’s Health Initiative clinical trials, they continue to assist researchers and patients alike, wrote Christina A. Minami, MD, of Brigham and Women’s Hospital in Boston and Rachel A. Freedman, MD, of the Dana-Farber Cancer Institute in Boston, in an accompanying editorial.
That said, in regard to the findings of this latest analysis, “many questions still remain on whether (and how) a hormone therapy intervention that occurred many years earlier may continue to affect breast cancer risk and mortality at 20 years,” they wrote. They noted that it’s “impossible” to isolate how exposure to certain therapies can impact long-term outcomes, and that a high percentage of patients who discontinued the drugs during each trial muddy the waters even further.
“Decisions to initiate these medications remain complex,” they added, emphasizing that breast cancer risk is just one of many factors that physicians must consider when considering hormone therapy for their patients.
Dr. Chlebowski and his coauthors acknowledged their study’s limitations, including the use of very specifically administered and formulated dosages making their findings “not necessarily generalizable to other preparations.” In addition, they noted the significant percentage of patients – 54% with CEE alone and 42% with CEE plus MPA – who discontinued drug usage during their respective trials.
The Women’s Health Initiative is supported by the National Institutes of Health and the Department of Health and Human Services. The authors reported numerous potential conflicts of interest, including receiving personal fees and grants from various government organizations, foundations, and pharmaceutical companies. The editorial’s authors reported no conflicts of interest.
SOURCE: Chlebowski RT et al. JAMA. 2020 Jul 28. doi: 10.1001/jama.2020.9482.
A new follow-up study of menopausal hormone therapy found that prior use of conjugated equine estrogen (CEE) decreased both breast cancer incidence and mortality, while prior use of CEE plus medroxyprogesterone acetate (MPA) was associated with an increase in incidence.
“Prior use of CEE alone is, to our knowledge, the first pharmacologic intervention demonstrated to be associated with a statistically significantly reduction in deaths from breast cancer,” wrote Rowan T. Chlebowski, MD, PhD, of the Lundquist Institute for Biomedical Innovation in Torrance, Calif., and his coauthors. The study was published July 28 in JAMA.
To further investigate the outcomes of the Women’s Health Initiative in regard to hormone therapy and breast cancer risk, the researchers analyzed the long-term follow-up of two randomized trials that included 27,347 postmenopausal women with no prior breast cancer and negative mammograms at baseline. Their mean (SD) age was 63.4 (7.2) years. Enrollment took place from 1993 to 1998; participants were contacted for follow-up every 6 months through 2005 and annually from then on. Mortality data were gathered from follow-up and the National Death Index.
The first trial included 16,608 women with a uterus. Among these women, 8,506 received 0.625 mg/day of CEE plus 2.5 mg/day of MPA, and 8,102 received placebo. The second trial included 10,739 women who’d gotten a hysterectomy, 5,310 of whom received 0.625 mg/day of CEE alone and 5,429 of whom received placebo. The first trial ended in 2002 after a median intervention period of 5.6 years, and the second trial ended in 2004 after a period of 7.2 years.
An analysis in 2015 found that CEE alone was associated with lower risk of breast cancer and CEE plus MPA was associated with increased risk.
The current analysis confirmed that, after a median of 20.3 years of follow-up, and with mortality data now available for more than 98% of participants, CEE alone was associated with fewer cases of breast cancer (238 cases, annualized rate 0.30%), compared with placebo (296 cases, annualized rate 0.37%; hazard ratio 0.78; 95% confidence interval, 0.65-0.93; P = .005).
Furthermore, CEE alone was also associated with lower mortality (30 deaths, annualized mortality rate 0.031%), compared with placebo (46 deaths, annualized mortality rate 0.046%; HR 0.60; 95% CI, 0.37-0.97; P = .04).
By comparison, CEE plus MPA was linked with more cases of breast cancer (584 cases, annualized rate 0.45%) than placebo (447 cases, annualized rate 0.36%; HR 1.28; 95% CI, 1.13-1.45; P < .001). In regard to mortality, there was no statistically significant difference between CEE plus MPA (71 deaths, annualized mortality rate 0.045%) and placebo (53 deaths, annualized mortality rate 0.035%; HR 1.35; 95% CI, 0.94-1.95; P = .11).
“The big thing to think about is estrogen alone reducing breast cancer mortality by 40%,” said Dr. Chlebowski in an interview. “None of the other interventions, including tamoxifen, had any change on mortality. This should change the way we look at breast cancer prevention, though we might have to be a little creative about it. I think you have to be a little away from menopause for it to reduce breast cancer. But we wanted to start that debate.
“On the other hand,” he said, “a woman takes estrogen plus progestin and when you look at that curve, it’s staying about 25% increased. You take it for 5.6 years and the increase continues through 20 years, so you’re maybe buying a lifetime of increase in breast cancer by taking estrogen plus progestin for 5 years.”
He also highlighted the comprehensiveness of the mortality data, noting that “when you hook up to the National Death Index, they find 98% of all deaths in the United States. That’s really remarkable; you retain the whole power of the randomization. It means our data, between the death index and our follow-up of participants, is essentially complete.”
Use of hormone therapy, and decoding the outcomes, remains ‘complex’
Decades after the data were gathered from the Women’s Health Initiative clinical trials, they continue to assist researchers and patients alike, wrote Christina A. Minami, MD, of Brigham and Women’s Hospital in Boston and Rachel A. Freedman, MD, of the Dana-Farber Cancer Institute in Boston, in an accompanying editorial.
That said, in regard to the findings of this latest analysis, “many questions still remain on whether (and how) a hormone therapy intervention that occurred many years earlier may continue to affect breast cancer risk and mortality at 20 years,” they wrote. They noted that it’s “impossible” to isolate how exposure to certain therapies can impact long-term outcomes, and that a high percentage of patients who discontinued the drugs during each trial muddy the waters even further.
“Decisions to initiate these medications remain complex,” they added, emphasizing that breast cancer risk is just one of many factors that physicians must consider when considering hormone therapy for their patients.
Dr. Chlebowski and his coauthors acknowledged their study’s limitations, including the use of very specifically administered and formulated dosages making their findings “not necessarily generalizable to other preparations.” In addition, they noted the significant percentage of patients – 54% with CEE alone and 42% with CEE plus MPA – who discontinued drug usage during their respective trials.
The Women’s Health Initiative is supported by the National Institutes of Health and the Department of Health and Human Services. The authors reported numerous potential conflicts of interest, including receiving personal fees and grants from various government organizations, foundations, and pharmaceutical companies. The editorial’s authors reported no conflicts of interest.
SOURCE: Chlebowski RT et al. JAMA. 2020 Jul 28. doi: 10.1001/jama.2020.9482.
A new follow-up study of menopausal hormone therapy found that prior use of conjugated equine estrogen (CEE) decreased both breast cancer incidence and mortality, while prior use of CEE plus medroxyprogesterone acetate (MPA) was associated with an increase in incidence.
“Prior use of CEE alone is, to our knowledge, the first pharmacologic intervention demonstrated to be associated with a statistically significantly reduction in deaths from breast cancer,” wrote Rowan T. Chlebowski, MD, PhD, of the Lundquist Institute for Biomedical Innovation in Torrance, Calif., and his coauthors. The study was published July 28 in JAMA.
To further investigate the outcomes of the Women’s Health Initiative in regard to hormone therapy and breast cancer risk, the researchers analyzed the long-term follow-up of two randomized trials that included 27,347 postmenopausal women with no prior breast cancer and negative mammograms at baseline. Their mean (SD) age was 63.4 (7.2) years. Enrollment took place from 1993 to 1998; participants were contacted for follow-up every 6 months through 2005 and annually from then on. Mortality data were gathered from follow-up and the National Death Index.
The first trial included 16,608 women with a uterus. Among these women, 8,506 received 0.625 mg/day of CEE plus 2.5 mg/day of MPA, and 8,102 received placebo. The second trial included 10,739 women who’d gotten a hysterectomy, 5,310 of whom received 0.625 mg/day of CEE alone and 5,429 of whom received placebo. The first trial ended in 2002 after a median intervention period of 5.6 years, and the second trial ended in 2004 after a period of 7.2 years.
An analysis in 2015 found that CEE alone was associated with lower risk of breast cancer and CEE plus MPA was associated with increased risk.
The current analysis confirmed that, after a median of 20.3 years of follow-up, and with mortality data now available for more than 98% of participants, CEE alone was associated with fewer cases of breast cancer (238 cases, annualized rate 0.30%), compared with placebo (296 cases, annualized rate 0.37%; hazard ratio 0.78; 95% confidence interval, 0.65-0.93; P = .005).
Furthermore, CEE alone was also associated with lower mortality (30 deaths, annualized mortality rate 0.031%), compared with placebo (46 deaths, annualized mortality rate 0.046%; HR 0.60; 95% CI, 0.37-0.97; P = .04).
By comparison, CEE plus MPA was linked with more cases of breast cancer (584 cases, annualized rate 0.45%) than placebo (447 cases, annualized rate 0.36%; HR 1.28; 95% CI, 1.13-1.45; P < .001). In regard to mortality, there was no statistically significant difference between CEE plus MPA (71 deaths, annualized mortality rate 0.045%) and placebo (53 deaths, annualized mortality rate 0.035%; HR 1.35; 95% CI, 0.94-1.95; P = .11).
“The big thing to think about is estrogen alone reducing breast cancer mortality by 40%,” said Dr. Chlebowski in an interview. “None of the other interventions, including tamoxifen, had any change on mortality. This should change the way we look at breast cancer prevention, though we might have to be a little creative about it. I think you have to be a little away from menopause for it to reduce breast cancer. But we wanted to start that debate.
“On the other hand,” he said, “a woman takes estrogen plus progestin and when you look at that curve, it’s staying about 25% increased. You take it for 5.6 years and the increase continues through 20 years, so you’re maybe buying a lifetime of increase in breast cancer by taking estrogen plus progestin for 5 years.”
He also highlighted the comprehensiveness of the mortality data, noting that “when you hook up to the National Death Index, they find 98% of all deaths in the United States. That’s really remarkable; you retain the whole power of the randomization. It means our data, between the death index and our follow-up of participants, is essentially complete.”
Use of hormone therapy, and decoding the outcomes, remains ‘complex’
Decades after the data were gathered from the Women’s Health Initiative clinical trials, they continue to assist researchers and patients alike, wrote Christina A. Minami, MD, of Brigham and Women’s Hospital in Boston and Rachel A. Freedman, MD, of the Dana-Farber Cancer Institute in Boston, in an accompanying editorial.
That said, in regard to the findings of this latest analysis, “many questions still remain on whether (and how) a hormone therapy intervention that occurred many years earlier may continue to affect breast cancer risk and mortality at 20 years,” they wrote. They noted that it’s “impossible” to isolate how exposure to certain therapies can impact long-term outcomes, and that a high percentage of patients who discontinued the drugs during each trial muddy the waters even further.
“Decisions to initiate these medications remain complex,” they added, emphasizing that breast cancer risk is just one of many factors that physicians must consider when considering hormone therapy for their patients.
Dr. Chlebowski and his coauthors acknowledged their study’s limitations, including the use of very specifically administered and formulated dosages making their findings “not necessarily generalizable to other preparations.” In addition, they noted the significant percentage of patients – 54% with CEE alone and 42% with CEE plus MPA – who discontinued drug usage during their respective trials.
The Women’s Health Initiative is supported by the National Institutes of Health and the Department of Health and Human Services. The authors reported numerous potential conflicts of interest, including receiving personal fees and grants from various government organizations, foundations, and pharmaceutical companies. The editorial’s authors reported no conflicts of interest.
SOURCE: Chlebowski RT et al. JAMA. 2020 Jul 28. doi: 10.1001/jama.2020.9482.
FROM JAMA
‘Knowledge is power’: Knowing BRCA1/2 status tied to survival
The study, conducted among Ashkenazi Jewish women in Israel, showed that among women who knew their carrier status before they developed breast cancer, diagnoses were made at an earlier disease stage and 5-year survival was improved compared to women who learned their carrier status only after their disease had been diagnosed.
The study was published online on July 9 in JAMA Oncology.
“I don’t want to belittle the complexities of knowing that you’re a carrier. But I think these results really show that knowledge is power,” first author Ephrat Levy-Lahad, MD, director of the medical genetics unit at Shaare Zedek Medical Center in Jerusalem, Israel, told Medscape Medical News.
Carrying a BRCA1/2 pathogenic mutation is associated with a 70% to 80% lifetime risk for breast cancer and about a 10% to 50% lifetime risk for ovarian cancer, depending on the specific mutation. Only about 10% of carriers will not develop either cancer during their lifetime.
The study provides support for genetic screening for pathogenic BRCA1/2 mutations, especially in high-risk populations, according to Levy-Lahad.
“For me, the results are part of a bigger picture.... I think we should be moving towards general population screening, certainly in high-risk populations like Ashkenazi Jews,” she said.
In Israel, that decision has already been made: a new policy, introduced in January 2020, offers testing for common BRCA1/2 mutations for all Ashkenazi Jewish women.
However, women in other countries may also benefit from testing, she argues. About half of BRCA1/2 carriers in a general population like that of the United States do not have a family history that would indicate a need for testing. That means many women who carry these mutations may not be taking advantage of recommended surveillance and prevention measures, she said.
But screening for BRCA1/2 mutations becomes more complicated when applied to more general populations, she acknowledged.
About 2.5% of women of Ashkenazi Jewish descent carry pathogenic mutations for BRCA1/2, compared to 0.5% in the general White population.
Also, screening in the Ashkenazi Jewish population is probably simpler than in the general population. Just three mutations are definitely known to cause disease and need to be tested for among Ashkenazi Jews. Screening in a larger population would require full sequencing of the gene. That increases the likelihood of finding variants of unknown significance (VUSs), which muddies the water. Knowledge is incomplete about whether some of these VUSs increase cancer risk, and physicians do not always know how to manage them in women who test positive.
Moreover, Israel has a national health system. Screening in a country without universal health insurance such as the United States raises questions about whether follow-up would be covered by insurance carriers for women who test positive.
Mehmet Copur, MD, an oncologist at Morrison Cancer Center in Hastings, Nebraska, questions how general population screening could be done in “real life.”
“These findings should be taken into consideration in the context of the patient population who would agree to genetic testing, who would agree to comply with the recommended guidelines for risk reduction, and who would have insurance coverage or resources to comply with the recommendations,” Copur told Medscape Medical News.
“If BRCA-positive patients did not or could not follow these recommendations, the results would different,” he added.
The most crucial component of screening for these mutations is genetic counselors, who are in short supply in the United States, according to Copur.
Another issue is that of cost. Genetic counseling is not always covered by insurance, especially for individuals who do not have a family history of BRCA-related cancers. Genetic testing is not cheap, and the costs of monitoring women who test positive could be prohibitive, especially in a healthcare system burdened by COVID-19.
“Whether our current healthcare system could bear the cost of such a change is up for debate. The screening itself may be feasible, but offering lifelong surveillance to every woman identified with mutations could present huge capacity issues,” Copur said. “Maybe in the future, the healthcare system can be ready for such an undertaking, but I don’t think we are there yet.”
Although she acknowledges the differences in risk between Ashkenazi Jews and the general population, Levy-Lahad thinks not having screening is like “throwing the baby out with the bath water.”
“Maybe we’re not ready for total general population screening, but I think we have to start thinking along those lines,” she said. “We have this incredible tool for cancer prevention, and we should really be using it, certainly in populations like Ashkenazi Jews.”
Researchers conducted a retrospective analysis that included 105 women diagnosed with breast cancer at Shaare Zedek Medical Center in Jerusalem between 2005 and 2016. Forty-two women knew they were carriers before their breast cancer diagnosis, and 63 learned of their carrier status only after diagnosis. Of the participants, 83% were Ashkenazi Jews. For both prediagnosis and postdiagnosis groups, the age at diagnosis was the same (50.4 years). For both groups, distributions of pathogenic mutations were similar. There were no significant differences in hormone receptor or ERBB2 status.
Among women who knew they were carriers before diagnosis, 80.9% (34/42) were diagnosed either with ductal carcinoma in situ or stage 1 disease. Only 9.5% (4/42) of these women were diagnosed with disease of stage 2 or higher.
In comparison, among women who learned their carrier status after diagnosis, 30% (19/63) had early-stage disease at diagnosis, and 52.4% (33/63) were diagnosed at stage 2 or higher (P < .001).
Compared to women who knew their carrier status before diagnosis, women who found out after diagnosis had 12 times higher odds of being diagnosed with disease of advanced clinical stage (P = .001) and eight times higher odds of being diagnosed with disease of advanced pathologic stage (P = .002).
A sentinel node biopsy was sufficient in 85.7% (36/42) of women who knew their carrier status before diagnosis; 7.2% (3/42) of these women needed a full lymph node dissection. In contrast, 3.2% (2/63) of women who learned their carrier status after diagnosis underwent sentinel node biopsy, and 34.9% (25/105) needed a full lymph node dissection (P < .001).
Among women who knew their carrier status before diagnosis, 54.8% (23/42) did not need chemotherapy at all, and none needed neoadjuvant chemotherapy. Only 4.8% (3/63) of women who learned their mutation status after diagnosis were able to forgo chemotherapy (P < .001); 22.2% (14/63) needed neoadjuvant therapy (P = .001).
These findings appeared to translate into better outcomes. Overall 5-year survival was significantly higher among women who knew their carrier status before diagnosis compared to women who found out afterward (94% [SE 4%] vs 78% [SE 5%]; P = .03). Only two of 42 women (4.8%) in the prediagnosis group died, compared to 16 of 63 (25.4%) in the postdiagnosis group.
Analyses that controlled for year at diagnosis showed that women who learned their carrier status before diagnosis had significantly lower risk for overall mortality compared with those who found out after diagnosis (hazard ratio [HR], 0.20; 95% CI, 0.04 – 0.93; P = .04). However, these results lost significance when controlled for age, socioeconomic index, family history, and gene variant (HR, 0.16; 95% CI, 0.02 – 1.4; P = .10).
Higher socioeconomic status (HR, 0.76; 95% CI, 0.6 – 0.97; P = .03), gene variant (BRCA2 vs BRCA1: HR, 0.15; 95% CI, 0.03 – 0.75; P = .02), and age at diagnosis (HR, 1.047; 95% CI, 1.003 – 1.093; P = .04) were all associated with overall mortality.
“I can’t infer causation, but we suspect that the reason for these results is the difference in follow-up,” Levy-Lahad said.
Most of the women (95.2%, 40/42) who knew their carrier status before diagnosis received their follow-up at the medical center’s high-risk carrier clinic. Twenty-seven of 42 (64.3%) of these women were diagnosed with breast MRI. By contrast, only 1.6% (1/63) of women who found out their carrier status after diagnosis were diagnosed with breast MRI. Breast MRI is not routinely used for breast cancer screening but can be more sensitive than mammography for detecting breast cancer.
The study was funded by the Breast Cancer Research Foundation and by a gift from Ellie and David Werber to ShaareZedek Medical Center.
Levy-Lahad received grants from the Breast Cancer Research Foundation and from the Israel Cancer Association during the conduct of the study and personal fees from AstraZeneca outside the submitted work. Copur has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The study, conducted among Ashkenazi Jewish women in Israel, showed that among women who knew their carrier status before they developed breast cancer, diagnoses were made at an earlier disease stage and 5-year survival was improved compared to women who learned their carrier status only after their disease had been diagnosed.
The study was published online on July 9 in JAMA Oncology.
“I don’t want to belittle the complexities of knowing that you’re a carrier. But I think these results really show that knowledge is power,” first author Ephrat Levy-Lahad, MD, director of the medical genetics unit at Shaare Zedek Medical Center in Jerusalem, Israel, told Medscape Medical News.
Carrying a BRCA1/2 pathogenic mutation is associated with a 70% to 80% lifetime risk for breast cancer and about a 10% to 50% lifetime risk for ovarian cancer, depending on the specific mutation. Only about 10% of carriers will not develop either cancer during their lifetime.
The study provides support for genetic screening for pathogenic BRCA1/2 mutations, especially in high-risk populations, according to Levy-Lahad.
“For me, the results are part of a bigger picture.... I think we should be moving towards general population screening, certainly in high-risk populations like Ashkenazi Jews,” she said.
In Israel, that decision has already been made: a new policy, introduced in January 2020, offers testing for common BRCA1/2 mutations for all Ashkenazi Jewish women.
However, women in other countries may also benefit from testing, she argues. About half of BRCA1/2 carriers in a general population like that of the United States do not have a family history that would indicate a need for testing. That means many women who carry these mutations may not be taking advantage of recommended surveillance and prevention measures, she said.
But screening for BRCA1/2 mutations becomes more complicated when applied to more general populations, she acknowledged.
About 2.5% of women of Ashkenazi Jewish descent carry pathogenic mutations for BRCA1/2, compared to 0.5% in the general White population.
Also, screening in the Ashkenazi Jewish population is probably simpler than in the general population. Just three mutations are definitely known to cause disease and need to be tested for among Ashkenazi Jews. Screening in a larger population would require full sequencing of the gene. That increases the likelihood of finding variants of unknown significance (VUSs), which muddies the water. Knowledge is incomplete about whether some of these VUSs increase cancer risk, and physicians do not always know how to manage them in women who test positive.
Moreover, Israel has a national health system. Screening in a country without universal health insurance such as the United States raises questions about whether follow-up would be covered by insurance carriers for women who test positive.
Mehmet Copur, MD, an oncologist at Morrison Cancer Center in Hastings, Nebraska, questions how general population screening could be done in “real life.”
“These findings should be taken into consideration in the context of the patient population who would agree to genetic testing, who would agree to comply with the recommended guidelines for risk reduction, and who would have insurance coverage or resources to comply with the recommendations,” Copur told Medscape Medical News.
“If BRCA-positive patients did not or could not follow these recommendations, the results would different,” he added.
The most crucial component of screening for these mutations is genetic counselors, who are in short supply in the United States, according to Copur.
Another issue is that of cost. Genetic counseling is not always covered by insurance, especially for individuals who do not have a family history of BRCA-related cancers. Genetic testing is not cheap, and the costs of monitoring women who test positive could be prohibitive, especially in a healthcare system burdened by COVID-19.
“Whether our current healthcare system could bear the cost of such a change is up for debate. The screening itself may be feasible, but offering lifelong surveillance to every woman identified with mutations could present huge capacity issues,” Copur said. “Maybe in the future, the healthcare system can be ready for such an undertaking, but I don’t think we are there yet.”
Although she acknowledges the differences in risk between Ashkenazi Jews and the general population, Levy-Lahad thinks not having screening is like “throwing the baby out with the bath water.”
“Maybe we’re not ready for total general population screening, but I think we have to start thinking along those lines,” she said. “We have this incredible tool for cancer prevention, and we should really be using it, certainly in populations like Ashkenazi Jews.”
Researchers conducted a retrospective analysis that included 105 women diagnosed with breast cancer at Shaare Zedek Medical Center in Jerusalem between 2005 and 2016. Forty-two women knew they were carriers before their breast cancer diagnosis, and 63 learned of their carrier status only after diagnosis. Of the participants, 83% were Ashkenazi Jews. For both prediagnosis and postdiagnosis groups, the age at diagnosis was the same (50.4 years). For both groups, distributions of pathogenic mutations were similar. There were no significant differences in hormone receptor or ERBB2 status.
Among women who knew they were carriers before diagnosis, 80.9% (34/42) were diagnosed either with ductal carcinoma in situ or stage 1 disease. Only 9.5% (4/42) of these women were diagnosed with disease of stage 2 or higher.
In comparison, among women who learned their carrier status after diagnosis, 30% (19/63) had early-stage disease at diagnosis, and 52.4% (33/63) were diagnosed at stage 2 or higher (P < .001).
Compared to women who knew their carrier status before diagnosis, women who found out after diagnosis had 12 times higher odds of being diagnosed with disease of advanced clinical stage (P = .001) and eight times higher odds of being diagnosed with disease of advanced pathologic stage (P = .002).
A sentinel node biopsy was sufficient in 85.7% (36/42) of women who knew their carrier status before diagnosis; 7.2% (3/42) of these women needed a full lymph node dissection. In contrast, 3.2% (2/63) of women who learned their carrier status after diagnosis underwent sentinel node biopsy, and 34.9% (25/105) needed a full lymph node dissection (P < .001).
Among women who knew their carrier status before diagnosis, 54.8% (23/42) did not need chemotherapy at all, and none needed neoadjuvant chemotherapy. Only 4.8% (3/63) of women who learned their mutation status after diagnosis were able to forgo chemotherapy (P < .001); 22.2% (14/63) needed neoadjuvant therapy (P = .001).
These findings appeared to translate into better outcomes. Overall 5-year survival was significantly higher among women who knew their carrier status before diagnosis compared to women who found out afterward (94% [SE 4%] vs 78% [SE 5%]; P = .03). Only two of 42 women (4.8%) in the prediagnosis group died, compared to 16 of 63 (25.4%) in the postdiagnosis group.
Analyses that controlled for year at diagnosis showed that women who learned their carrier status before diagnosis had significantly lower risk for overall mortality compared with those who found out after diagnosis (hazard ratio [HR], 0.20; 95% CI, 0.04 – 0.93; P = .04). However, these results lost significance when controlled for age, socioeconomic index, family history, and gene variant (HR, 0.16; 95% CI, 0.02 – 1.4; P = .10).
Higher socioeconomic status (HR, 0.76; 95% CI, 0.6 – 0.97; P = .03), gene variant (BRCA2 vs BRCA1: HR, 0.15; 95% CI, 0.03 – 0.75; P = .02), and age at diagnosis (HR, 1.047; 95% CI, 1.003 – 1.093; P = .04) were all associated with overall mortality.
“I can’t infer causation, but we suspect that the reason for these results is the difference in follow-up,” Levy-Lahad said.
Most of the women (95.2%, 40/42) who knew their carrier status before diagnosis received their follow-up at the medical center’s high-risk carrier clinic. Twenty-seven of 42 (64.3%) of these women were diagnosed with breast MRI. By contrast, only 1.6% (1/63) of women who found out their carrier status after diagnosis were diagnosed with breast MRI. Breast MRI is not routinely used for breast cancer screening but can be more sensitive than mammography for detecting breast cancer.
The study was funded by the Breast Cancer Research Foundation and by a gift from Ellie and David Werber to ShaareZedek Medical Center.
Levy-Lahad received grants from the Breast Cancer Research Foundation and from the Israel Cancer Association during the conduct of the study and personal fees from AstraZeneca outside the submitted work. Copur has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The study, conducted among Ashkenazi Jewish women in Israel, showed that among women who knew their carrier status before they developed breast cancer, diagnoses were made at an earlier disease stage and 5-year survival was improved compared to women who learned their carrier status only after their disease had been diagnosed.
The study was published online on July 9 in JAMA Oncology.
“I don’t want to belittle the complexities of knowing that you’re a carrier. But I think these results really show that knowledge is power,” first author Ephrat Levy-Lahad, MD, director of the medical genetics unit at Shaare Zedek Medical Center in Jerusalem, Israel, told Medscape Medical News.
Carrying a BRCA1/2 pathogenic mutation is associated with a 70% to 80% lifetime risk for breast cancer and about a 10% to 50% lifetime risk for ovarian cancer, depending on the specific mutation. Only about 10% of carriers will not develop either cancer during their lifetime.
The study provides support for genetic screening for pathogenic BRCA1/2 mutations, especially in high-risk populations, according to Levy-Lahad.
“For me, the results are part of a bigger picture.... I think we should be moving towards general population screening, certainly in high-risk populations like Ashkenazi Jews,” she said.
In Israel, that decision has already been made: a new policy, introduced in January 2020, offers testing for common BRCA1/2 mutations for all Ashkenazi Jewish women.
However, women in other countries may also benefit from testing, she argues. About half of BRCA1/2 carriers in a general population like that of the United States do not have a family history that would indicate a need for testing. That means many women who carry these mutations may not be taking advantage of recommended surveillance and prevention measures, she said.
But screening for BRCA1/2 mutations becomes more complicated when applied to more general populations, she acknowledged.
About 2.5% of women of Ashkenazi Jewish descent carry pathogenic mutations for BRCA1/2, compared to 0.5% in the general White population.
Also, screening in the Ashkenazi Jewish population is probably simpler than in the general population. Just three mutations are definitely known to cause disease and need to be tested for among Ashkenazi Jews. Screening in a larger population would require full sequencing of the gene. That increases the likelihood of finding variants of unknown significance (VUSs), which muddies the water. Knowledge is incomplete about whether some of these VUSs increase cancer risk, and physicians do not always know how to manage them in women who test positive.
Moreover, Israel has a national health system. Screening in a country without universal health insurance such as the United States raises questions about whether follow-up would be covered by insurance carriers for women who test positive.
Mehmet Copur, MD, an oncologist at Morrison Cancer Center in Hastings, Nebraska, questions how general population screening could be done in “real life.”
“These findings should be taken into consideration in the context of the patient population who would agree to genetic testing, who would agree to comply with the recommended guidelines for risk reduction, and who would have insurance coverage or resources to comply with the recommendations,” Copur told Medscape Medical News.
“If BRCA-positive patients did not or could not follow these recommendations, the results would different,” he added.
The most crucial component of screening for these mutations is genetic counselors, who are in short supply in the United States, according to Copur.
Another issue is that of cost. Genetic counseling is not always covered by insurance, especially for individuals who do not have a family history of BRCA-related cancers. Genetic testing is not cheap, and the costs of monitoring women who test positive could be prohibitive, especially in a healthcare system burdened by COVID-19.
“Whether our current healthcare system could bear the cost of such a change is up for debate. The screening itself may be feasible, but offering lifelong surveillance to every woman identified with mutations could present huge capacity issues,” Copur said. “Maybe in the future, the healthcare system can be ready for such an undertaking, but I don’t think we are there yet.”
Although she acknowledges the differences in risk between Ashkenazi Jews and the general population, Levy-Lahad thinks not having screening is like “throwing the baby out with the bath water.”
“Maybe we’re not ready for total general population screening, but I think we have to start thinking along those lines,” she said. “We have this incredible tool for cancer prevention, and we should really be using it, certainly in populations like Ashkenazi Jews.”
Researchers conducted a retrospective analysis that included 105 women diagnosed with breast cancer at Shaare Zedek Medical Center in Jerusalem between 2005 and 2016. Forty-two women knew they were carriers before their breast cancer diagnosis, and 63 learned of their carrier status only after diagnosis. Of the participants, 83% were Ashkenazi Jews. For both prediagnosis and postdiagnosis groups, the age at diagnosis was the same (50.4 years). For both groups, distributions of pathogenic mutations were similar. There were no significant differences in hormone receptor or ERBB2 status.
Among women who knew they were carriers before diagnosis, 80.9% (34/42) were diagnosed either with ductal carcinoma in situ or stage 1 disease. Only 9.5% (4/42) of these women were diagnosed with disease of stage 2 or higher.
In comparison, among women who learned their carrier status after diagnosis, 30% (19/63) had early-stage disease at diagnosis, and 52.4% (33/63) were diagnosed at stage 2 or higher (P < .001).
Compared to women who knew their carrier status before diagnosis, women who found out after diagnosis had 12 times higher odds of being diagnosed with disease of advanced clinical stage (P = .001) and eight times higher odds of being diagnosed with disease of advanced pathologic stage (P = .002).
A sentinel node biopsy was sufficient in 85.7% (36/42) of women who knew their carrier status before diagnosis; 7.2% (3/42) of these women needed a full lymph node dissection. In contrast, 3.2% (2/63) of women who learned their carrier status after diagnosis underwent sentinel node biopsy, and 34.9% (25/105) needed a full lymph node dissection (P < .001).
Among women who knew their carrier status before diagnosis, 54.8% (23/42) did not need chemotherapy at all, and none needed neoadjuvant chemotherapy. Only 4.8% (3/63) of women who learned their mutation status after diagnosis were able to forgo chemotherapy (P < .001); 22.2% (14/63) needed neoadjuvant therapy (P = .001).
These findings appeared to translate into better outcomes. Overall 5-year survival was significantly higher among women who knew their carrier status before diagnosis compared to women who found out afterward (94% [SE 4%] vs 78% [SE 5%]; P = .03). Only two of 42 women (4.8%) in the prediagnosis group died, compared to 16 of 63 (25.4%) in the postdiagnosis group.
Analyses that controlled for year at diagnosis showed that women who learned their carrier status before diagnosis had significantly lower risk for overall mortality compared with those who found out after diagnosis (hazard ratio [HR], 0.20; 95% CI, 0.04 – 0.93; P = .04). However, these results lost significance when controlled for age, socioeconomic index, family history, and gene variant (HR, 0.16; 95% CI, 0.02 – 1.4; P = .10).
Higher socioeconomic status (HR, 0.76; 95% CI, 0.6 – 0.97; P = .03), gene variant (BRCA2 vs BRCA1: HR, 0.15; 95% CI, 0.03 – 0.75; P = .02), and age at diagnosis (HR, 1.047; 95% CI, 1.003 – 1.093; P = .04) were all associated with overall mortality.
“I can’t infer causation, but we suspect that the reason for these results is the difference in follow-up,” Levy-Lahad said.
Most of the women (95.2%, 40/42) who knew their carrier status before diagnosis received their follow-up at the medical center’s high-risk carrier clinic. Twenty-seven of 42 (64.3%) of these women were diagnosed with breast MRI. By contrast, only 1.6% (1/63) of women who found out their carrier status after diagnosis were diagnosed with breast MRI. Breast MRI is not routinely used for breast cancer screening but can be more sensitive than mammography for detecting breast cancer.
The study was funded by the Breast Cancer Research Foundation and by a gift from Ellie and David Werber to ShaareZedek Medical Center.
Levy-Lahad received grants from the Breast Cancer Research Foundation and from the Israel Cancer Association during the conduct of the study and personal fees from AstraZeneca outside the submitted work. Copur has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Early screening may halve breast cancer mortality in childhood cancer survivors
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
FROM ANNALS OF INTERNAL MEDICINE