User login
Medicaid expansion linked to more early cancer diagnoses
Cancer patients in states that opted to expand Medicaid insurance coverage under the Affordable Care Act saw a slightly better rate of early diagnosis, compared with patients in states that refused expansion, according to a new study. However, time to treatment was similar in states that opted for expansion and states that did not.
Samuel U. Takvorian, MD, of the University of Pennsylvania, Philadelphia, and colleagues reported these results in JAMA Network Open.
The researchers used the National Cancer Database to examine the changes in health insurance coverage and cancer health outcomes in nonelderly patients following implementation of the Affordable Care Act in January 2014. The investigators identified records for 925,543 patients who had new-onset breast (59%), colon (15%), or non–small cell lung (27%) cancer between 2011 and 2016. The patients’ mean age was 55 years (range, 40-64 years), 79% were women, 14% were black, and 6% were Hispanic.
The researchers looked at insurance status, cancer stage at diagnosis, and treatment initiation within 30 and 90 days of diagnosis. The cohort was equally divided between residents of Medicaid expansion states (48%) and nonexpansion states (52%).
Using a statistical technique that mimics a controlled experiment, the investigators found the percentage of uninsured patients decreased more in the expansion states (adjusted difference-in-differences, −0.7 percentage points; 95% confidence interval, −1.2 to −0.3; P = .001), compared with nonexpansion states. Expansion states also had a greater increase in early-stage cancer diagnoses (adjusted DID, 0.8; 95% CI 0.3-1.2; P = .001) and a greater decrease in advanced-stage cancer diagnoses (adjusted DID, −0.5; 95% CI, −0.9 to −0.2; P = .003).
Among the 848,329 patients who underwent cancer treatment within a year of diagnosis, the percentage initiating treatment within 30 days declined from 52.7% before to 48% after Medicaid expansion in states opting in (unadjusted DID, −4.7; percentage points, 95% CI; −5.1 to −4.5). States that did not expand their Medicaid programs, meanwhile, saw the share decline from 56.9% to 51.5% in the same time period (adjusted DID, −5.4; 95% CI, −5.6 to −5.1). There was no statistically significant difference in timely treatment associated with Medicaid expansion (adjusted DID, 0.6; 95% CI, −0.2 to 1.4; P = .14).
The researchers speculated that the lack of significant between-group differences in time to treatment, despite an improvement in early-stage diagnoses associated with Medicaid expansion, could reflect a cancer care system strained by a surge in insured patients, overall increases in cancer prevalence and complexity of care, a shortage of workers, or a mixture of factors.
In a related editorial, Sue Fu, MD, of Stanford (Calif.) University, and colleagues wrote that, while the findings of increased early diagnosis seen in the study are promising, the time to treatment results are “puzzling” and deserve further consideration.
Time to treatment is important in cancer, as longer times are associated with increased mortality, Dr. Fu and colleagues noted. Slowing times to cancer treatment is a systemic problem in the United States that has been documented since the mid-2000s. Paradoxically, expanded insurance coverage could contribute to increasing time to treatment even after timely diagnosis by adding administrative burdens leading to longer wait times. “Newly insured and underinsured individuals may be particularly vulnerable to this,” the editorialists wrote.
Dr. Takvorian and colleagues noted as weaknesses of their study its observational design, a limited range of ages and cancers included, and an inability to adjust for state-level effects.
This study was funded by the National Cancer Institute and the Agency for Health Research and Quality. The authors of the study and the editorial disclosed no relevant conflicts of interest.
SOURCES: Takvorian SU et al. JAMA Netw Open. 2020 Feb 5;3(2):e1921653; Fu S et al. JAMA Netw Open. 2020 Feb 5;3(2):e1921690.
Cancer patients in states that opted to expand Medicaid insurance coverage under the Affordable Care Act saw a slightly better rate of early diagnosis, compared with patients in states that refused expansion, according to a new study. However, time to treatment was similar in states that opted for expansion and states that did not.
Samuel U. Takvorian, MD, of the University of Pennsylvania, Philadelphia, and colleagues reported these results in JAMA Network Open.
The researchers used the National Cancer Database to examine the changes in health insurance coverage and cancer health outcomes in nonelderly patients following implementation of the Affordable Care Act in January 2014. The investigators identified records for 925,543 patients who had new-onset breast (59%), colon (15%), or non–small cell lung (27%) cancer between 2011 and 2016. The patients’ mean age was 55 years (range, 40-64 years), 79% were women, 14% were black, and 6% were Hispanic.
The researchers looked at insurance status, cancer stage at diagnosis, and treatment initiation within 30 and 90 days of diagnosis. The cohort was equally divided between residents of Medicaid expansion states (48%) and nonexpansion states (52%).
Using a statistical technique that mimics a controlled experiment, the investigators found the percentage of uninsured patients decreased more in the expansion states (adjusted difference-in-differences, −0.7 percentage points; 95% confidence interval, −1.2 to −0.3; P = .001), compared with nonexpansion states. Expansion states also had a greater increase in early-stage cancer diagnoses (adjusted DID, 0.8; 95% CI 0.3-1.2; P = .001) and a greater decrease in advanced-stage cancer diagnoses (adjusted DID, −0.5; 95% CI, −0.9 to −0.2; P = .003).
Among the 848,329 patients who underwent cancer treatment within a year of diagnosis, the percentage initiating treatment within 30 days declined from 52.7% before to 48% after Medicaid expansion in states opting in (unadjusted DID, −4.7; percentage points, 95% CI; −5.1 to −4.5). States that did not expand their Medicaid programs, meanwhile, saw the share decline from 56.9% to 51.5% in the same time period (adjusted DID, −5.4; 95% CI, −5.6 to −5.1). There was no statistically significant difference in timely treatment associated with Medicaid expansion (adjusted DID, 0.6; 95% CI, −0.2 to 1.4; P = .14).
The researchers speculated that the lack of significant between-group differences in time to treatment, despite an improvement in early-stage diagnoses associated with Medicaid expansion, could reflect a cancer care system strained by a surge in insured patients, overall increases in cancer prevalence and complexity of care, a shortage of workers, or a mixture of factors.
In a related editorial, Sue Fu, MD, of Stanford (Calif.) University, and colleagues wrote that, while the findings of increased early diagnosis seen in the study are promising, the time to treatment results are “puzzling” and deserve further consideration.
Time to treatment is important in cancer, as longer times are associated with increased mortality, Dr. Fu and colleagues noted. Slowing times to cancer treatment is a systemic problem in the United States that has been documented since the mid-2000s. Paradoxically, expanded insurance coverage could contribute to increasing time to treatment even after timely diagnosis by adding administrative burdens leading to longer wait times. “Newly insured and underinsured individuals may be particularly vulnerable to this,” the editorialists wrote.
Dr. Takvorian and colleagues noted as weaknesses of their study its observational design, a limited range of ages and cancers included, and an inability to adjust for state-level effects.
This study was funded by the National Cancer Institute and the Agency for Health Research and Quality. The authors of the study and the editorial disclosed no relevant conflicts of interest.
SOURCES: Takvorian SU et al. JAMA Netw Open. 2020 Feb 5;3(2):e1921653; Fu S et al. JAMA Netw Open. 2020 Feb 5;3(2):e1921690.
Cancer patients in states that opted to expand Medicaid insurance coverage under the Affordable Care Act saw a slightly better rate of early diagnosis, compared with patients in states that refused expansion, according to a new study. However, time to treatment was similar in states that opted for expansion and states that did not.
Samuel U. Takvorian, MD, of the University of Pennsylvania, Philadelphia, and colleagues reported these results in JAMA Network Open.
The researchers used the National Cancer Database to examine the changes in health insurance coverage and cancer health outcomes in nonelderly patients following implementation of the Affordable Care Act in January 2014. The investigators identified records for 925,543 patients who had new-onset breast (59%), colon (15%), or non–small cell lung (27%) cancer between 2011 and 2016. The patients’ mean age was 55 years (range, 40-64 years), 79% were women, 14% were black, and 6% were Hispanic.
The researchers looked at insurance status, cancer stage at diagnosis, and treatment initiation within 30 and 90 days of diagnosis. The cohort was equally divided between residents of Medicaid expansion states (48%) and nonexpansion states (52%).
Using a statistical technique that mimics a controlled experiment, the investigators found the percentage of uninsured patients decreased more in the expansion states (adjusted difference-in-differences, −0.7 percentage points; 95% confidence interval, −1.2 to −0.3; P = .001), compared with nonexpansion states. Expansion states also had a greater increase in early-stage cancer diagnoses (adjusted DID, 0.8; 95% CI 0.3-1.2; P = .001) and a greater decrease in advanced-stage cancer diagnoses (adjusted DID, −0.5; 95% CI, −0.9 to −0.2; P = .003).
Among the 848,329 patients who underwent cancer treatment within a year of diagnosis, the percentage initiating treatment within 30 days declined from 52.7% before to 48% after Medicaid expansion in states opting in (unadjusted DID, −4.7; percentage points, 95% CI; −5.1 to −4.5). States that did not expand their Medicaid programs, meanwhile, saw the share decline from 56.9% to 51.5% in the same time period (adjusted DID, −5.4; 95% CI, −5.6 to −5.1). There was no statistically significant difference in timely treatment associated with Medicaid expansion (adjusted DID, 0.6; 95% CI, −0.2 to 1.4; P = .14).
The researchers speculated that the lack of significant between-group differences in time to treatment, despite an improvement in early-stage diagnoses associated with Medicaid expansion, could reflect a cancer care system strained by a surge in insured patients, overall increases in cancer prevalence and complexity of care, a shortage of workers, or a mixture of factors.
In a related editorial, Sue Fu, MD, of Stanford (Calif.) University, and colleagues wrote that, while the findings of increased early diagnosis seen in the study are promising, the time to treatment results are “puzzling” and deserve further consideration.
Time to treatment is important in cancer, as longer times are associated with increased mortality, Dr. Fu and colleagues noted. Slowing times to cancer treatment is a systemic problem in the United States that has been documented since the mid-2000s. Paradoxically, expanded insurance coverage could contribute to increasing time to treatment even after timely diagnosis by adding administrative burdens leading to longer wait times. “Newly insured and underinsured individuals may be particularly vulnerable to this,” the editorialists wrote.
Dr. Takvorian and colleagues noted as weaknesses of their study its observational design, a limited range of ages and cancers included, and an inability to adjust for state-level effects.
This study was funded by the National Cancer Institute and the Agency for Health Research and Quality. The authors of the study and the editorial disclosed no relevant conflicts of interest.
SOURCES: Takvorian SU et al. JAMA Netw Open. 2020 Feb 5;3(2):e1921653; Fu S et al. JAMA Netw Open. 2020 Feb 5;3(2):e1921690.
FROM JAMA NETWORK OPEN
Irinotecan shows promise for triple-negative breast cancer
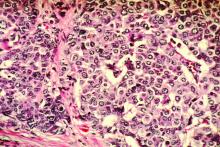
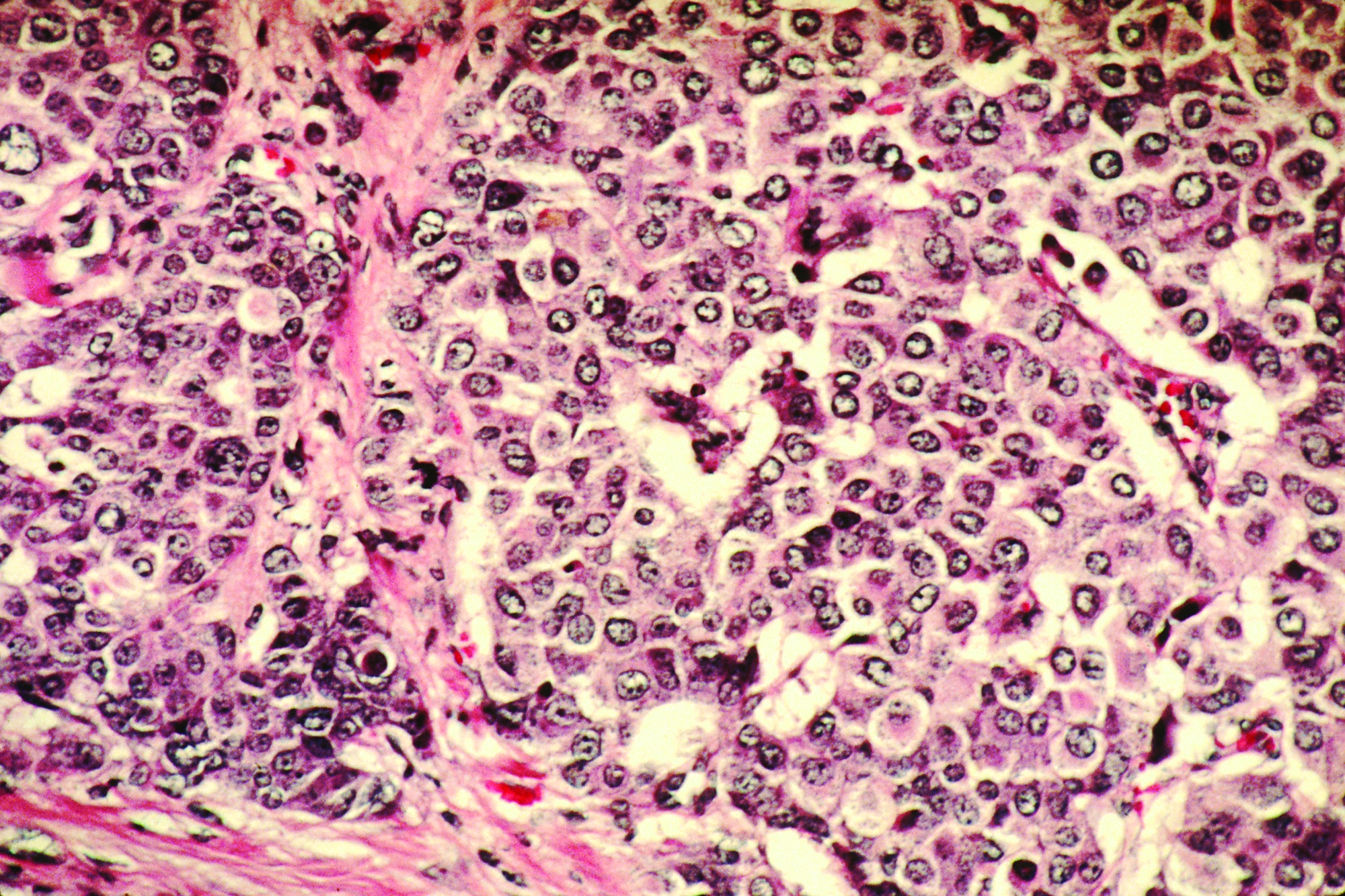
The topoisomerase I (TOP1) inhibitor irinotecan could be effective in treating triple-negative breast cancer (TNBC), according to results from a preclinical study published in Science Translational Medicine.
Florence Coussy, MD, PhD, of Institut Curie, Paris, and colleagues evaluated the antitumor activity of the Food and Drug Administration–approved TOP1 inhibitor irinotecan in 40 patient-derived xenografts (PDXs) of TNBC.
Other treatments, such as noncamptothecin TOP1 inhibitors (indotecan and indimitecan) and irinotecan plus VE-822 (an ataxia telangiectasia and Rad3-related protein [ATR] inhibitor), were also evaluated in the PDX models.
Tumor samples were collected from patients with primary breast cancer at the time of surgery (55%), residual breast cancer after neoadjuvant treatment (40%), or axillary lymph node metastases (5%). The patients had a mean age of 56 years (range, 29-89 years).
The researchers assessed BRCAness using the homologous recombination deficiency–large-scale state transition assay. Additional potential markers of response, including expression of retinoblastoma transcriptional corepressor 1 (RB1) and Schlafen family member 11 (SLFN11), were detected on transcriptomic analysis and validated using immunohistochemistry analyses.
The researchers found that 37.5% (n = 15) of TNBC PDX models achieved a partial or complete response to irinotecan therapy, while 22.5% (n = 9) of models had stable disease. BRCAness, RB1 loss, and high SLFN11 expression were deemed potential markers of response to irinotecan and other clinical TOP1 inhibitors.
The researchers then evaluated 250 breast cancer patients treated with anthracycline-based chemotherapy and found that lower expression of SLFN11 was associated with worse survival.
“We also [found] that, in the absence of SLFN11, response to irinotecan can be increased by adding an ATR inhibitor and that the clinical TOP1 inhibitors are highly efficient in BRCA1-mutant and BRCAness-positive TNBC PDXs,” the researchers reported.
They acknowledged that a key limitation of this study was the absence of tumor samples from patients who had received a TOP1 inhibitor.
“Overall, our findings are in line with the notion that concomitant defects in DNA repair and checkpoints render cancer cells highly vulnerable to TOP1 inhibitors,” the researchers concluded.
The study was funded by the National Cancer Institute, PIC3i NCI-Curie, and Site de Recherche Intégrée sur le Cancer. One author is an inventor of indotecan and indimitecan. Two authors are coinventors of the method used to detect inactivation of the homologous recombination pathway, which is licensed to Myriad Genetics.
SOURCE: Coussy F et al. Sci Transl Med. 2020 Feb 19. doi: 10.1126/scitranslmed.aax2625.
The topoisomerase I (TOP1) inhibitor irinotecan could be effective in treating triple-negative breast cancer (TNBC), according to results from a preclinical study published in Science Translational Medicine.
Florence Coussy, MD, PhD, of Institut Curie, Paris, and colleagues evaluated the antitumor activity of the Food and Drug Administration–approved TOP1 inhibitor irinotecan in 40 patient-derived xenografts (PDXs) of TNBC.
Other treatments, such as noncamptothecin TOP1 inhibitors (indotecan and indimitecan) and irinotecan plus VE-822 (an ataxia telangiectasia and Rad3-related protein [ATR] inhibitor), were also evaluated in the PDX models.
Tumor samples were collected from patients with primary breast cancer at the time of surgery (55%), residual breast cancer after neoadjuvant treatment (40%), or axillary lymph node metastases (5%). The patients had a mean age of 56 years (range, 29-89 years).
The researchers assessed BRCAness using the homologous recombination deficiency–large-scale state transition assay. Additional potential markers of response, including expression of retinoblastoma transcriptional corepressor 1 (RB1) and Schlafen family member 11 (SLFN11), were detected on transcriptomic analysis and validated using immunohistochemistry analyses.
The researchers found that 37.5% (n = 15) of TNBC PDX models achieved a partial or complete response to irinotecan therapy, while 22.5% (n = 9) of models had stable disease. BRCAness, RB1 loss, and high SLFN11 expression were deemed potential markers of response to irinotecan and other clinical TOP1 inhibitors.
The researchers then evaluated 250 breast cancer patients treated with anthracycline-based chemotherapy and found that lower expression of SLFN11 was associated with worse survival.
“We also [found] that, in the absence of SLFN11, response to irinotecan can be increased by adding an ATR inhibitor and that the clinical TOP1 inhibitors are highly efficient in BRCA1-mutant and BRCAness-positive TNBC PDXs,” the researchers reported.
They acknowledged that a key limitation of this study was the absence of tumor samples from patients who had received a TOP1 inhibitor.
“Overall, our findings are in line with the notion that concomitant defects in DNA repair and checkpoints render cancer cells highly vulnerable to TOP1 inhibitors,” the researchers concluded.
The study was funded by the National Cancer Institute, PIC3i NCI-Curie, and Site de Recherche Intégrée sur le Cancer. One author is an inventor of indotecan and indimitecan. Two authors are coinventors of the method used to detect inactivation of the homologous recombination pathway, which is licensed to Myriad Genetics.
SOURCE: Coussy F et al. Sci Transl Med. 2020 Feb 19. doi: 10.1126/scitranslmed.aax2625.
The topoisomerase I (TOP1) inhibitor irinotecan could be effective in treating triple-negative breast cancer (TNBC), according to results from a preclinical study published in Science Translational Medicine.
Florence Coussy, MD, PhD, of Institut Curie, Paris, and colleagues evaluated the antitumor activity of the Food and Drug Administration–approved TOP1 inhibitor irinotecan in 40 patient-derived xenografts (PDXs) of TNBC.
Other treatments, such as noncamptothecin TOP1 inhibitors (indotecan and indimitecan) and irinotecan plus VE-822 (an ataxia telangiectasia and Rad3-related protein [ATR] inhibitor), were also evaluated in the PDX models.
Tumor samples were collected from patients with primary breast cancer at the time of surgery (55%), residual breast cancer after neoadjuvant treatment (40%), or axillary lymph node metastases (5%). The patients had a mean age of 56 years (range, 29-89 years).
The researchers assessed BRCAness using the homologous recombination deficiency–large-scale state transition assay. Additional potential markers of response, including expression of retinoblastoma transcriptional corepressor 1 (RB1) and Schlafen family member 11 (SLFN11), were detected on transcriptomic analysis and validated using immunohistochemistry analyses.
The researchers found that 37.5% (n = 15) of TNBC PDX models achieved a partial or complete response to irinotecan therapy, while 22.5% (n = 9) of models had stable disease. BRCAness, RB1 loss, and high SLFN11 expression were deemed potential markers of response to irinotecan and other clinical TOP1 inhibitors.
The researchers then evaluated 250 breast cancer patients treated with anthracycline-based chemotherapy and found that lower expression of SLFN11 was associated with worse survival.
“We also [found] that, in the absence of SLFN11, response to irinotecan can be increased by adding an ATR inhibitor and that the clinical TOP1 inhibitors are highly efficient in BRCA1-mutant and BRCAness-positive TNBC PDXs,” the researchers reported.
They acknowledged that a key limitation of this study was the absence of tumor samples from patients who had received a TOP1 inhibitor.
“Overall, our findings are in line with the notion that concomitant defects in DNA repair and checkpoints render cancer cells highly vulnerable to TOP1 inhibitors,” the researchers concluded.
The study was funded by the National Cancer Institute, PIC3i NCI-Curie, and Site de Recherche Intégrée sur le Cancer. One author is an inventor of indotecan and indimitecan. Two authors are coinventors of the method used to detect inactivation of the homologous recombination pathway, which is licensed to Myriad Genetics.
SOURCE: Coussy F et al. Sci Transl Med. 2020 Feb 19. doi: 10.1126/scitranslmed.aax2625.
FROM SCIENCE TRANSLATIONAL MEDICINE
First robot for supermicrosurgery, used for lymphedema
The first trial of robot-assisted, high-precision supermicrosurgery in humans has shown that the technique was safe for treating breast cancer–related lymphedema.
Although results were preliminary – only 20 patients participated, and a single highly skilled surgeon performed the supermicrosurgery – additional trials are underway to test the new robotic technique at other centers.
The pilot study was published online Feb. 11 in Nature Communications.
The new device, known as MUSA, was supplied by MicroSure.
MUSA allowed surgeons to connect tiny vessels, as small as 0.3-0.8 mm across, a technique referred to as supermicrosurgery. This technique can be used to connect blocked lymph vessels to veins, which can reestablish flow of lymphatic fluid and decrease arm swelling in women with breast cancer–related lymphedema, the researchers explain.
Only a few highly skilled surgeons worldwide can conduct supermicrosurgery using current surgical techniques, the authors comment.
“The success of supermicrosurgery is limited by the precision and stability of the surgeon’s hands. Robot-assisted supermicrosurgery has the potential to overcome this obstacle because more refined and subtle movements can be performed. Before now, no robots were able to perform this type of surgery,” coauthor Rutger M. Schols, MD, PhD, of Maastricht (the Netherlands) University Medical Center, said in an interview.
Robot-assisted surgery is not new – the Da Vinci system was the first robotic surgery device to be approved by the Food and Drug Administration. It was approved in 2000. However, Da Vinci was developed for minimally invasive surgery and is not precise enough for supermicrosurgery. And despite its $2 million price tag, Da Vinci has yet to show that it performs better than traditional surgery.
Designed specifically for supermicrosurgery
The MUSA robot was designed by surgeons at the Maastricht University Medical Center, engineers at the Eindhoven University of Technology, and the medical technology company Microsure specifically for reconstructive supermicrosurgery; all are located in the Netherlands. Two of the authors of the article hold positions and are shareholders in the company.
Surgeons activate MUSA using foot pedals and operate forceps-like joysticks to control high-precision surgical instruments that filter out hand tremors and scale down motions. For example, moving the joystick 1 cm causes the robot to move 0.10 mm. MUSA also works with standard microscopes found in most operating rooms.
To test MUSA, Dr. Schols and colleagues conducted a prospective, randomized trial that included 20 women with breast cancer–related lymphedema. The team randomly assigned eight women to undergo supermicrosurgery with MUSA and 12 women to undergo manual supermicrosurgery performed by a single surgeon. Two microsurgeons who were blinded to treatment groups evaluated the quality of the surgery using standardized scoring methods.
The results, which were adjusted for baseline factors, showed no significant differences in upper-limb lymphedema between the two groups 1 and 3 months after surgery, nor were there significant differences between the two groups in quality of life.
A slightly higher percentage of women in the MUSA group were able to discontinue daily use of a compressive garment to treat arm swelling at 3 months, compared with the group that underwent manual supermicrosurgery (87.5% vs. 83.3%). Participants reported no serious adverse events.
For the group that underwent manual surgery, the quality of anastomosis was significantly better, compared with the MUSA group. Surgical competency also was significantly higher in the group that underwent manual surgery.
The MUSA group experienced a longer total surgery time (mean, 115 min), compared with the group that underwent manual surgery (mean, 81 min). But the authors note that duration of surgery declined steeply over time for the MUSA group, suggesting a learning curve in using the robot.
The researchers caution that the study may have been too small to detect significant differences between groups. Larger studies are needed to test MUSA with other surgeons operating in other centers, the authors note.
“With respect to treatment of breast cancer–related lymphedema, we are continuing trials with more patients, more surgeons, and more centers,” Dr. Schols said in an interview.
“We expect that other centers – both national and international – are willing to test the MUSA,” he added.
Dr. Schols and several coauthors have disclosed no relevant financial relationships. Two coauthors are shareholders and hold positions at MicroSure.
This article first appeared on Medscape.com.
The first trial of robot-assisted, high-precision supermicrosurgery in humans has shown that the technique was safe for treating breast cancer–related lymphedema.
Although results were preliminary – only 20 patients participated, and a single highly skilled surgeon performed the supermicrosurgery – additional trials are underway to test the new robotic technique at other centers.
The pilot study was published online Feb. 11 in Nature Communications.
The new device, known as MUSA, was supplied by MicroSure.
MUSA allowed surgeons to connect tiny vessels, as small as 0.3-0.8 mm across, a technique referred to as supermicrosurgery. This technique can be used to connect blocked lymph vessels to veins, which can reestablish flow of lymphatic fluid and decrease arm swelling in women with breast cancer–related lymphedema, the researchers explain.
Only a few highly skilled surgeons worldwide can conduct supermicrosurgery using current surgical techniques, the authors comment.
“The success of supermicrosurgery is limited by the precision and stability of the surgeon’s hands. Robot-assisted supermicrosurgery has the potential to overcome this obstacle because more refined and subtle movements can be performed. Before now, no robots were able to perform this type of surgery,” coauthor Rutger M. Schols, MD, PhD, of Maastricht (the Netherlands) University Medical Center, said in an interview.
Robot-assisted surgery is not new – the Da Vinci system was the first robotic surgery device to be approved by the Food and Drug Administration. It was approved in 2000. However, Da Vinci was developed for minimally invasive surgery and is not precise enough for supermicrosurgery. And despite its $2 million price tag, Da Vinci has yet to show that it performs better than traditional surgery.
Designed specifically for supermicrosurgery
The MUSA robot was designed by surgeons at the Maastricht University Medical Center, engineers at the Eindhoven University of Technology, and the medical technology company Microsure specifically for reconstructive supermicrosurgery; all are located in the Netherlands. Two of the authors of the article hold positions and are shareholders in the company.
Surgeons activate MUSA using foot pedals and operate forceps-like joysticks to control high-precision surgical instruments that filter out hand tremors and scale down motions. For example, moving the joystick 1 cm causes the robot to move 0.10 mm. MUSA also works with standard microscopes found in most operating rooms.
To test MUSA, Dr. Schols and colleagues conducted a prospective, randomized trial that included 20 women with breast cancer–related lymphedema. The team randomly assigned eight women to undergo supermicrosurgery with MUSA and 12 women to undergo manual supermicrosurgery performed by a single surgeon. Two microsurgeons who were blinded to treatment groups evaluated the quality of the surgery using standardized scoring methods.
The results, which were adjusted for baseline factors, showed no significant differences in upper-limb lymphedema between the two groups 1 and 3 months after surgery, nor were there significant differences between the two groups in quality of life.
A slightly higher percentage of women in the MUSA group were able to discontinue daily use of a compressive garment to treat arm swelling at 3 months, compared with the group that underwent manual supermicrosurgery (87.5% vs. 83.3%). Participants reported no serious adverse events.
For the group that underwent manual surgery, the quality of anastomosis was significantly better, compared with the MUSA group. Surgical competency also was significantly higher in the group that underwent manual surgery.
The MUSA group experienced a longer total surgery time (mean, 115 min), compared with the group that underwent manual surgery (mean, 81 min). But the authors note that duration of surgery declined steeply over time for the MUSA group, suggesting a learning curve in using the robot.
The researchers caution that the study may have been too small to detect significant differences between groups. Larger studies are needed to test MUSA with other surgeons operating in other centers, the authors note.
“With respect to treatment of breast cancer–related lymphedema, we are continuing trials with more patients, more surgeons, and more centers,” Dr. Schols said in an interview.
“We expect that other centers – both national and international – are willing to test the MUSA,” he added.
Dr. Schols and several coauthors have disclosed no relevant financial relationships. Two coauthors are shareholders and hold positions at MicroSure.
This article first appeared on Medscape.com.
The first trial of robot-assisted, high-precision supermicrosurgery in humans has shown that the technique was safe for treating breast cancer–related lymphedema.
Although results were preliminary – only 20 patients participated, and a single highly skilled surgeon performed the supermicrosurgery – additional trials are underway to test the new robotic technique at other centers.
The pilot study was published online Feb. 11 in Nature Communications.
The new device, known as MUSA, was supplied by MicroSure.
MUSA allowed surgeons to connect tiny vessels, as small as 0.3-0.8 mm across, a technique referred to as supermicrosurgery. This technique can be used to connect blocked lymph vessels to veins, which can reestablish flow of lymphatic fluid and decrease arm swelling in women with breast cancer–related lymphedema, the researchers explain.
Only a few highly skilled surgeons worldwide can conduct supermicrosurgery using current surgical techniques, the authors comment.
“The success of supermicrosurgery is limited by the precision and stability of the surgeon’s hands. Robot-assisted supermicrosurgery has the potential to overcome this obstacle because more refined and subtle movements can be performed. Before now, no robots were able to perform this type of surgery,” coauthor Rutger M. Schols, MD, PhD, of Maastricht (the Netherlands) University Medical Center, said in an interview.
Robot-assisted surgery is not new – the Da Vinci system was the first robotic surgery device to be approved by the Food and Drug Administration. It was approved in 2000. However, Da Vinci was developed for minimally invasive surgery and is not precise enough for supermicrosurgery. And despite its $2 million price tag, Da Vinci has yet to show that it performs better than traditional surgery.
Designed specifically for supermicrosurgery
The MUSA robot was designed by surgeons at the Maastricht University Medical Center, engineers at the Eindhoven University of Technology, and the medical technology company Microsure specifically for reconstructive supermicrosurgery; all are located in the Netherlands. Two of the authors of the article hold positions and are shareholders in the company.
Surgeons activate MUSA using foot pedals and operate forceps-like joysticks to control high-precision surgical instruments that filter out hand tremors and scale down motions. For example, moving the joystick 1 cm causes the robot to move 0.10 mm. MUSA also works with standard microscopes found in most operating rooms.
To test MUSA, Dr. Schols and colleagues conducted a prospective, randomized trial that included 20 women with breast cancer–related lymphedema. The team randomly assigned eight women to undergo supermicrosurgery with MUSA and 12 women to undergo manual supermicrosurgery performed by a single surgeon. Two microsurgeons who were blinded to treatment groups evaluated the quality of the surgery using standardized scoring methods.
The results, which were adjusted for baseline factors, showed no significant differences in upper-limb lymphedema between the two groups 1 and 3 months after surgery, nor were there significant differences between the two groups in quality of life.
A slightly higher percentage of women in the MUSA group were able to discontinue daily use of a compressive garment to treat arm swelling at 3 months, compared with the group that underwent manual supermicrosurgery (87.5% vs. 83.3%). Participants reported no serious adverse events.
For the group that underwent manual surgery, the quality of anastomosis was significantly better, compared with the MUSA group. Surgical competency also was significantly higher in the group that underwent manual surgery.
The MUSA group experienced a longer total surgery time (mean, 115 min), compared with the group that underwent manual surgery (mean, 81 min). But the authors note that duration of surgery declined steeply over time for the MUSA group, suggesting a learning curve in using the robot.
The researchers caution that the study may have been too small to detect significant differences between groups. Larger studies are needed to test MUSA with other surgeons operating in other centers, the authors note.
“With respect to treatment of breast cancer–related lymphedema, we are continuing trials with more patients, more surgeons, and more centers,” Dr. Schols said in an interview.
“We expect that other centers – both national and international – are willing to test the MUSA,” he added.
Dr. Schols and several coauthors have disclosed no relevant financial relationships. Two coauthors are shareholders and hold positions at MicroSure.
This article first appeared on Medscape.com.
Adding pembrolizumab to chemo doubled pCR rates in early-stage breast cancer
Adding pembrolizumab to neoadjuvant chemotherapy more than doubled the rate of pathologic complete response, compared with chemotherapy alone, in women with early-stage breast cancer enrolled in the phase 2 I-SPY2 trial.
Pathologic complete response (pCR) rates up to 60% were reported for patients with high-risk, stage II/III breast cancer who received pembrolizumab plus chemotherapy in I-SPY2, an ongoing platform trial designed to rapidly screen multiple agents and pinpoint those with a high probability of success.
The doubling of pCR rates was seen in all three biomarker signatures studied, including ERBB2(HER2)-negative, hormone receptor (HR)-positive/ERBB2-negative, or triple-negative breast cancer.
These results mean that pembrolizumab can “graduate” from I-SPY2 and suggest a greater than 99% predictive probability that the pembrolizumab-plus-chemotherapy approach will be superior to chemotherapy alone in a phase 3 trial, according to Rita Nanda, MD, of the University of Chicago, and colleagues.
“Notably, pembrolizumab was the first agent of 10 studied to graduate in the HR-positive/ERBB2-negative signature since I-SPY2 opened in 2010,” Dr. Nanda and colleagues wrote in JAMA Oncology.
The I-SPY2 study has enrolled adult women with stage II/III breast cancer at high risk of recurrence. The control arm included 181 patients randomized to receive standard neoadjuvant paclitaxel followed by doxorubicin plus cyclophosphamide. The pembrolizumab arm included 69 patients who received the same chemotherapy regimen plus pembrolizumab given concurrently with paclitaxel.
In ERBB2-negative patients, the estimated pCR rates were 44% in the pembrolizumab arm and 17% in the control arm. In HR-positive/ERBB2-negative patients, the estimated pCR rates were 30% and 13%, respectively. In triple-negative patients, the estimated pCR rates were 60% and 22%, respectively.
Residual cancer burden classified as extensive was less often seen in the pembrolizumab-treated patients, the investigators noted.
Event-free survival was qualitatively similar between the pembrolizumab and control arms, although the investigators cautioned against drawing conclusions based on this exploratory analysis in a small number of patients.
“Patients who achieved pCR had excellent outcomes regardless of arm,” the investigators wrote.
Immune-related adverse events (irAEs) were seen in the pembrolizumab-treated patients, although most were grade 1 or 2 and managed with dose interruption or corticosteroid therapy.
The most common irAE was thyroid dysfunction in 13% of patients, which was on par with what was seen in previously published reports. By contrast, adrenal insufficiency was observed in about 9% of patients, which is higher than in published reports for reasons that are unclear.
“Future work to characterize the risk factors for developing irAEs is warranted to improve the therapeutic index of these agents,” Dr. Nanda and colleagues wrote.
Pembrolizumab plus standard neoadjuvant chemotherapy is being evaluated in two ongoing, randomized phase 3 trials – KEYNOTE 522, which is evaluating patients with triple-negative breast cancer, and KEYNOTE 756, which is focused on high-risk, HR-positive/ERBB2-negative breast cancer.
The ongoing I-SPY2 study is supported by a grant from the National Cancer Institute as well as funding from charitable organizations, pharmaceutical companies, and private individuals. The investigators disclosed relationships with a range of pharmaceutical companies.
SOURCE: Nanda R et al. JAMA Oncol. 2020 Feb 13. doi: 10.1001/jamaoncol.2019.6650.
Adding pembrolizumab to neoadjuvant chemotherapy more than doubled the rate of pathologic complete response, compared with chemotherapy alone, in women with early-stage breast cancer enrolled in the phase 2 I-SPY2 trial.
Pathologic complete response (pCR) rates up to 60% were reported for patients with high-risk, stage II/III breast cancer who received pembrolizumab plus chemotherapy in I-SPY2, an ongoing platform trial designed to rapidly screen multiple agents and pinpoint those with a high probability of success.
The doubling of pCR rates was seen in all three biomarker signatures studied, including ERBB2(HER2)-negative, hormone receptor (HR)-positive/ERBB2-negative, or triple-negative breast cancer.
These results mean that pembrolizumab can “graduate” from I-SPY2 and suggest a greater than 99% predictive probability that the pembrolizumab-plus-chemotherapy approach will be superior to chemotherapy alone in a phase 3 trial, according to Rita Nanda, MD, of the University of Chicago, and colleagues.
“Notably, pembrolizumab was the first agent of 10 studied to graduate in the HR-positive/ERBB2-negative signature since I-SPY2 opened in 2010,” Dr. Nanda and colleagues wrote in JAMA Oncology.
The I-SPY2 study has enrolled adult women with stage II/III breast cancer at high risk of recurrence. The control arm included 181 patients randomized to receive standard neoadjuvant paclitaxel followed by doxorubicin plus cyclophosphamide. The pembrolizumab arm included 69 patients who received the same chemotherapy regimen plus pembrolizumab given concurrently with paclitaxel.
In ERBB2-negative patients, the estimated pCR rates were 44% in the pembrolizumab arm and 17% in the control arm. In HR-positive/ERBB2-negative patients, the estimated pCR rates were 30% and 13%, respectively. In triple-negative patients, the estimated pCR rates were 60% and 22%, respectively.
Residual cancer burden classified as extensive was less often seen in the pembrolizumab-treated patients, the investigators noted.
Event-free survival was qualitatively similar between the pembrolizumab and control arms, although the investigators cautioned against drawing conclusions based on this exploratory analysis in a small number of patients.
“Patients who achieved pCR had excellent outcomes regardless of arm,” the investigators wrote.
Immune-related adverse events (irAEs) were seen in the pembrolizumab-treated patients, although most were grade 1 or 2 and managed with dose interruption or corticosteroid therapy.
The most common irAE was thyroid dysfunction in 13% of patients, which was on par with what was seen in previously published reports. By contrast, adrenal insufficiency was observed in about 9% of patients, which is higher than in published reports for reasons that are unclear.
“Future work to characterize the risk factors for developing irAEs is warranted to improve the therapeutic index of these agents,” Dr. Nanda and colleagues wrote.
Pembrolizumab plus standard neoadjuvant chemotherapy is being evaluated in two ongoing, randomized phase 3 trials – KEYNOTE 522, which is evaluating patients with triple-negative breast cancer, and KEYNOTE 756, which is focused on high-risk, HR-positive/ERBB2-negative breast cancer.
The ongoing I-SPY2 study is supported by a grant from the National Cancer Institute as well as funding from charitable organizations, pharmaceutical companies, and private individuals. The investigators disclosed relationships with a range of pharmaceutical companies.
SOURCE: Nanda R et al. JAMA Oncol. 2020 Feb 13. doi: 10.1001/jamaoncol.2019.6650.
Adding pembrolizumab to neoadjuvant chemotherapy more than doubled the rate of pathologic complete response, compared with chemotherapy alone, in women with early-stage breast cancer enrolled in the phase 2 I-SPY2 trial.
Pathologic complete response (pCR) rates up to 60% were reported for patients with high-risk, stage II/III breast cancer who received pembrolizumab plus chemotherapy in I-SPY2, an ongoing platform trial designed to rapidly screen multiple agents and pinpoint those with a high probability of success.
The doubling of pCR rates was seen in all three biomarker signatures studied, including ERBB2(HER2)-negative, hormone receptor (HR)-positive/ERBB2-negative, or triple-negative breast cancer.
These results mean that pembrolizumab can “graduate” from I-SPY2 and suggest a greater than 99% predictive probability that the pembrolizumab-plus-chemotherapy approach will be superior to chemotherapy alone in a phase 3 trial, according to Rita Nanda, MD, of the University of Chicago, and colleagues.
“Notably, pembrolizumab was the first agent of 10 studied to graduate in the HR-positive/ERBB2-negative signature since I-SPY2 opened in 2010,” Dr. Nanda and colleagues wrote in JAMA Oncology.
The I-SPY2 study has enrolled adult women with stage II/III breast cancer at high risk of recurrence. The control arm included 181 patients randomized to receive standard neoadjuvant paclitaxel followed by doxorubicin plus cyclophosphamide. The pembrolizumab arm included 69 patients who received the same chemotherapy regimen plus pembrolizumab given concurrently with paclitaxel.
In ERBB2-negative patients, the estimated pCR rates were 44% in the pembrolizumab arm and 17% in the control arm. In HR-positive/ERBB2-negative patients, the estimated pCR rates were 30% and 13%, respectively. In triple-negative patients, the estimated pCR rates were 60% and 22%, respectively.
Residual cancer burden classified as extensive was less often seen in the pembrolizumab-treated patients, the investigators noted.
Event-free survival was qualitatively similar between the pembrolizumab and control arms, although the investigators cautioned against drawing conclusions based on this exploratory analysis in a small number of patients.
“Patients who achieved pCR had excellent outcomes regardless of arm,” the investigators wrote.
Immune-related adverse events (irAEs) were seen in the pembrolizumab-treated patients, although most were grade 1 or 2 and managed with dose interruption or corticosteroid therapy.
The most common irAE was thyroid dysfunction in 13% of patients, which was on par with what was seen in previously published reports. By contrast, adrenal insufficiency was observed in about 9% of patients, which is higher than in published reports for reasons that are unclear.
“Future work to characterize the risk factors for developing irAEs is warranted to improve the therapeutic index of these agents,” Dr. Nanda and colleagues wrote.
Pembrolizumab plus standard neoadjuvant chemotherapy is being evaluated in two ongoing, randomized phase 3 trials – KEYNOTE 522, which is evaluating patients with triple-negative breast cancer, and KEYNOTE 756, which is focused on high-risk, HR-positive/ERBB2-negative breast cancer.
The ongoing I-SPY2 study is supported by a grant from the National Cancer Institute as well as funding from charitable organizations, pharmaceutical companies, and private individuals. The investigators disclosed relationships with a range of pharmaceutical companies.
SOURCE: Nanda R et al. JAMA Oncol. 2020 Feb 13. doi: 10.1001/jamaoncol.2019.6650.
FROM JAMA ONCOLOGY
Key clinical point: Adding pembrolizumab to neoadjuvant chemotherapy more than doubled the rate of pathologic complete response (pCR) in women with early-stage breast cancer.
Major finding: In ERBB2-negative patients, the estimated pCR rates were 44% in the pembrolizumab arm and 17% in the control arm. In HR-positive/ERBB2-negative patients, the estimated pCR rates were 30% and 13%, respectively. In triple-negative patients, the estimated pCR rates were 60% and 22%, respectively.
Study details: Phase 2 trial of 69 patients treated with pembrolizumab and chemotherapy, compared with 181 chemotherapy-treated control subjects.
Disclosures: The trial is supported by a grant from the National Cancer Institute as well as funding from charitable organizations, pharmaceutical companies, and private individuals. The investigators disclosed relationships with a range of pharmaceutical companies.
Source: Nanda R et al. JAMA Oncol. 2020 Feb 13.
Glaring gap in CV event reporting in pivotal cancer trials
Clinical trials supporting Food and Drug Adminstration approval of contemporary cancer therapies frequently failed to capture major adverse cardiovascular events (MACE) and, when they did, reported rates 2.6-fold lower than noncancer trials, new research shows.
Overall, 51.3% of trials did not report MACE, with that number reaching 57.6% in trials enrolling patients with baseline cardiovascular disease (CVD).
Nearly 40% of trials did not report any CVD events in follow-up, the authors reported online Feb. 10, 2020, in the Journal of the American College of Cardiology (2020;75:620-8).
“Even in drug classes where there were established or emerging associations with cardiotoxic events, often there were no reported heart events or cardiovascular events across years of follow-up in trials that examined hundreds or even thousands of patients. That was actually pretty surprising,” senior author Daniel Addison, MD, codirector of the cardio-oncology program at the Ohio State University Medical Center, Columbus, said in an interview.
The study was prompted by a series of events that crescendoed when his team was called to the ICU to determine whether a novel targeted agent played a role in the heart decline of a patient with acute myeloid leukemia. “I had a resident ask me a very important question: ‘How do we really know for sure that the trial actually reflects the true risk of heart events?’ to which I told him, ‘it’s difficult to know,’ ” he said.
“I think many of us rely heavily on what we see in the trials, particularly when they make it to the top journals, and quite frankly, we generally take it at face value,” Dr. Addison observed.
Lower Rate of Reported Events
The investigators reviewed CV events reported in 97,365 patients (median age, 61 years; 46% female) enrolled in 189 phase 2 and 3 trials supporting FDA approval of 123 anticancer drugs from 1998 to 2018. Biologic, targeted, or immune-based therapies accounted for 72.5% of drug approvals.
Over 148,138 person-years of follow-up (median trial duration, 30 months), there were 1,148 incidents of MACE (375 heart failure, 253 MIs, 180 strokes, 65 atrial fibrillation, 29 coronary revascularizations, and 246 CVD deaths). MACE rates were higher in the intervention group than in the control group (792 vs. 356; P less than .01). Among the 64 trials that excluded patients with baseline CVD, there were 269 incidents of MACE.
To put this finding in context, the researchers examined the reported incidence of MACE among some 6,000 similarly aged participants in the Multi-Ethnic Study of Atherosclerosis (MESA). The overall weighted-average incidence rate was 1,408 per 100,000 person-years among MESA participants, compared with 542 events per 100,000 person-years among oncology trial participants (716 per 100,000 in the intervention arm). This represents a reported-to-expected ratio of 0.38 – a 2.6-fold lower rate of reported events (P less than .001) – and a risk difference of 866.
Further, MACE reporting was lower by a factor of 1.7 among all cancer trial participants irrespective of baseline CVD status (reported-to-expected ratio, 0.56; risk difference, 613; P less than .001).
There was no significant difference in MACE reporting between independent or industry-sponsored trials, the authors report.
No malicious intent
“There are likely some that might lean toward not wanting to attribute blame to a new drug when the drug is in a study, but I really think that the leading factor is lack of awareness,” Dr. Addison said. “I’ve talked with several cancer collaborators around the country who run large clinical trials, and I think often, when an event may be brought to someone’s attention, there is a tendency to just write it off as kind of a generic expected event due to age, or just something that’s not really pertinent to the study. So they don’t really focus on it as much.”
“Closer collaboration between cardiologists and cancer physicians is needed to better determine true cardiac risks among patients treated with these drugs.”
Breast cancer oncologist Marc E. Lippman, MD, of Georgetown University Medical Center and Georgetown Lombardi Comprehensive Cancer Center, Washington, D.C., isn’t convinced a lack of awareness is the culprit.
“I don’t agree with that at all,” he said in an interview. “I think there are very, very clear rules and guidelines these days for adverse-event reporting. I think that’s not a very likely explanation – that it’s not on the radar.”
Part of the problem may be that some of the toxicities, particularly cardiovascular, may not emerge for years, he said. Participant screening for the trials also likely removed patients with high cardiovascular risk. “It’s very understandable to me – I’m not saying it’s good particularly – but I think it’s very understandable that, if you’re trying to develop a drug, the last thing you’d want to have is a lot of toxicity that you might have avoided by just being restrictive in who you let into the study,” Dr. Lippman said.
The underreported CVD events may also reflect the rapidly changing profile of cardiovascular toxicities associated with novel anticancer therapies.
“Providers, both cancer and noncancer, generally put cardiotoxicity in the box of anthracyclines and radiation, but particularly over the last decade, we’ve begun to understand it’s well beyond any one class of drugs,” Dr. Addison said.
“I agree completely,” Dr. Lippman said. For example, “the checkpoint inhibitors are so unbelievably different in terms of their toxicities that many people simply didn’t even know what they were getting into at first.”
One size does not fit all
Javid Moslehi, MD, director of the cardio-oncology program at Vanderbilt University, Nashville, Tenn., said echocardiography – recommended to detect changes in left ventricular function in patients exposed to anthracyclines or targeted agents like trastuzumab (Herceptin) – isn’t enough to address today’s cancer therapy–related CVD events.
“Initial drugs like anthracyclines or Herceptin in cardio-oncology were associated with systolic cardiac dysfunction, whereas the majority of issues we see in the cardio-oncology clinics today are vascular, metabolic, arrhythmogenic, and inflammatory,” he said in an interview. “Echocardiography misses the big and increasingly complex picture.”
His group, for example, has been studying myocarditis associated with immunotherapies, but none of the clinical trials require screening or surveillance for myocarditis with a cardiac biomarker like troponin.
The group also recently identified 303 deaths in patients exposed to ibrutinib, a drug that revolutionized the treatment of several B-cell malignancies but is associated with higher rates of atrial fibrillation, which is also associated with increased bleeding risk. “So there’s a little bit of a double whammy there, given that we often treat atrial fibrillation with anticoagulation and where we can cause complications in patients,” Dr. Moslehi noted.
Although there needs to be closer collaboration between cardiologists and oncologists on individual trials, cardiologists also have to realize that oncology care has become very personalized, he suggested.
“What’s probably relevant for the breast cancer patient may not be relevant for the prostate cancer patient and their respective treatments,” Dr. Moslehi said. “So if we were to say, ‘every person should get an echo,’ that may be less relevant to the prostate cancer patient where treatments can cause vascular and metabolic perturbations or to the patient treated with immunotherapy who may have myocarditis, where many of the echos can be normal. There’s no one-size-fits-all for these things.”
Wearable technologies like smartwatches could play a role in improving the reporting of CVD events with novel therapies but a lot more research needs to be done to validate these tools, Dr. Addison said. “But as we continue on into the 21st century, this is going to expand and may potentially help us,” he added.
In the interim, better standardization is needed of the cardiovascular events reported in oncology trials, particularly the Common Terminology Criteria for Adverse Events (CTCAE), said Dr. Moslehi, who also serves as chair of the American Heart Association’s subcommittee on cardio-oncology.
“Cardiovascular definitions are not exactly uniform and are not consistent with what we in cardiology consider to be important or relevant,” he said. “So I think there needs to be better standardization of these definitions, specifically within the CTCAE, which is what the oncologists use to identify adverse events.”
In a linked editorial (J Am Coll Cardiol. 2020;75:629-31), Dr. Lippman and cardiologist Nanette Bishopric, MD, of the Medstar Heart and Vascular Institute in Washington, D.C., suggested it may also be time to organize a consortium that can carry out “rigorous multicenter clinical investigations to evaluate the cardiotoxicity of emerging cancer treatments,” similar to the Thrombosis in Myocardial Infarction Study Group.
“The success of this consortium in pioneering and targeting multiple generations of drugs for the treatment of MI, involving tens of thousands of patients and thousands of collaborations across multiple national borders, is a model for how to move forward in providing the new hope of cancer cure without the trade-off of years lost to heart disease,” the editorialists concluded.
The study was supported in part by National Institutes of Health grants, including a K12-CA133250 grant to Dr. Addison. Dr. Bishopric reported being on the scientific board of C&C Biopharma. Dr. Lippman reports being on the board of directors of and holding stock in Seattle Genetics. Dr. Moslehi reported having served on advisory boards for Pfizer, Novartis, Bristol-Myers Squibb, Deciphera, Audentes Pharmaceuticals, Nektar, Takeda, Ipsen, Myokardia, AstraZeneca, GlaxoSmithKline, Intrexon, and Regeneron.
This article first appeared on Medscape.com.
Clinical trials supporting Food and Drug Adminstration approval of contemporary cancer therapies frequently failed to capture major adverse cardiovascular events (MACE) and, when they did, reported rates 2.6-fold lower than noncancer trials, new research shows.
Overall, 51.3% of trials did not report MACE, with that number reaching 57.6% in trials enrolling patients with baseline cardiovascular disease (CVD).
Nearly 40% of trials did not report any CVD events in follow-up, the authors reported online Feb. 10, 2020, in the Journal of the American College of Cardiology (2020;75:620-8).
“Even in drug classes where there were established or emerging associations with cardiotoxic events, often there were no reported heart events or cardiovascular events across years of follow-up in trials that examined hundreds or even thousands of patients. That was actually pretty surprising,” senior author Daniel Addison, MD, codirector of the cardio-oncology program at the Ohio State University Medical Center, Columbus, said in an interview.
The study was prompted by a series of events that crescendoed when his team was called to the ICU to determine whether a novel targeted agent played a role in the heart decline of a patient with acute myeloid leukemia. “I had a resident ask me a very important question: ‘How do we really know for sure that the trial actually reflects the true risk of heart events?’ to which I told him, ‘it’s difficult to know,’ ” he said.
“I think many of us rely heavily on what we see in the trials, particularly when they make it to the top journals, and quite frankly, we generally take it at face value,” Dr. Addison observed.
Lower Rate of Reported Events
The investigators reviewed CV events reported in 97,365 patients (median age, 61 years; 46% female) enrolled in 189 phase 2 and 3 trials supporting FDA approval of 123 anticancer drugs from 1998 to 2018. Biologic, targeted, or immune-based therapies accounted for 72.5% of drug approvals.
Over 148,138 person-years of follow-up (median trial duration, 30 months), there were 1,148 incidents of MACE (375 heart failure, 253 MIs, 180 strokes, 65 atrial fibrillation, 29 coronary revascularizations, and 246 CVD deaths). MACE rates were higher in the intervention group than in the control group (792 vs. 356; P less than .01). Among the 64 trials that excluded patients with baseline CVD, there were 269 incidents of MACE.
To put this finding in context, the researchers examined the reported incidence of MACE among some 6,000 similarly aged participants in the Multi-Ethnic Study of Atherosclerosis (MESA). The overall weighted-average incidence rate was 1,408 per 100,000 person-years among MESA participants, compared with 542 events per 100,000 person-years among oncology trial participants (716 per 100,000 in the intervention arm). This represents a reported-to-expected ratio of 0.38 – a 2.6-fold lower rate of reported events (P less than .001) – and a risk difference of 866.
Further, MACE reporting was lower by a factor of 1.7 among all cancer trial participants irrespective of baseline CVD status (reported-to-expected ratio, 0.56; risk difference, 613; P less than .001).
There was no significant difference in MACE reporting between independent or industry-sponsored trials, the authors report.
No malicious intent
“There are likely some that might lean toward not wanting to attribute blame to a new drug when the drug is in a study, but I really think that the leading factor is lack of awareness,” Dr. Addison said. “I’ve talked with several cancer collaborators around the country who run large clinical trials, and I think often, when an event may be brought to someone’s attention, there is a tendency to just write it off as kind of a generic expected event due to age, or just something that’s not really pertinent to the study. So they don’t really focus on it as much.”
“Closer collaboration between cardiologists and cancer physicians is needed to better determine true cardiac risks among patients treated with these drugs.”
Breast cancer oncologist Marc E. Lippman, MD, of Georgetown University Medical Center and Georgetown Lombardi Comprehensive Cancer Center, Washington, D.C., isn’t convinced a lack of awareness is the culprit.
“I don’t agree with that at all,” he said in an interview. “I think there are very, very clear rules and guidelines these days for adverse-event reporting. I think that’s not a very likely explanation – that it’s not on the radar.”
Part of the problem may be that some of the toxicities, particularly cardiovascular, may not emerge for years, he said. Participant screening for the trials also likely removed patients with high cardiovascular risk. “It’s very understandable to me – I’m not saying it’s good particularly – but I think it’s very understandable that, if you’re trying to develop a drug, the last thing you’d want to have is a lot of toxicity that you might have avoided by just being restrictive in who you let into the study,” Dr. Lippman said.
The underreported CVD events may also reflect the rapidly changing profile of cardiovascular toxicities associated with novel anticancer therapies.
“Providers, both cancer and noncancer, generally put cardiotoxicity in the box of anthracyclines and radiation, but particularly over the last decade, we’ve begun to understand it’s well beyond any one class of drugs,” Dr. Addison said.
“I agree completely,” Dr. Lippman said. For example, “the checkpoint inhibitors are so unbelievably different in terms of their toxicities that many people simply didn’t even know what they were getting into at first.”
One size does not fit all
Javid Moslehi, MD, director of the cardio-oncology program at Vanderbilt University, Nashville, Tenn., said echocardiography – recommended to detect changes in left ventricular function in patients exposed to anthracyclines or targeted agents like trastuzumab (Herceptin) – isn’t enough to address today’s cancer therapy–related CVD events.
“Initial drugs like anthracyclines or Herceptin in cardio-oncology were associated with systolic cardiac dysfunction, whereas the majority of issues we see in the cardio-oncology clinics today are vascular, metabolic, arrhythmogenic, and inflammatory,” he said in an interview. “Echocardiography misses the big and increasingly complex picture.”
His group, for example, has been studying myocarditis associated with immunotherapies, but none of the clinical trials require screening or surveillance for myocarditis with a cardiac biomarker like troponin.
The group also recently identified 303 deaths in patients exposed to ibrutinib, a drug that revolutionized the treatment of several B-cell malignancies but is associated with higher rates of atrial fibrillation, which is also associated with increased bleeding risk. “So there’s a little bit of a double whammy there, given that we often treat atrial fibrillation with anticoagulation and where we can cause complications in patients,” Dr. Moslehi noted.
Although there needs to be closer collaboration between cardiologists and oncologists on individual trials, cardiologists also have to realize that oncology care has become very personalized, he suggested.
“What’s probably relevant for the breast cancer patient may not be relevant for the prostate cancer patient and their respective treatments,” Dr. Moslehi said. “So if we were to say, ‘every person should get an echo,’ that may be less relevant to the prostate cancer patient where treatments can cause vascular and metabolic perturbations or to the patient treated with immunotherapy who may have myocarditis, where many of the echos can be normal. There’s no one-size-fits-all for these things.”
Wearable technologies like smartwatches could play a role in improving the reporting of CVD events with novel therapies but a lot more research needs to be done to validate these tools, Dr. Addison said. “But as we continue on into the 21st century, this is going to expand and may potentially help us,” he added.
In the interim, better standardization is needed of the cardiovascular events reported in oncology trials, particularly the Common Terminology Criteria for Adverse Events (CTCAE), said Dr. Moslehi, who also serves as chair of the American Heart Association’s subcommittee on cardio-oncology.
“Cardiovascular definitions are not exactly uniform and are not consistent with what we in cardiology consider to be important or relevant,” he said. “So I think there needs to be better standardization of these definitions, specifically within the CTCAE, which is what the oncologists use to identify adverse events.”
In a linked editorial (J Am Coll Cardiol. 2020;75:629-31), Dr. Lippman and cardiologist Nanette Bishopric, MD, of the Medstar Heart and Vascular Institute in Washington, D.C., suggested it may also be time to organize a consortium that can carry out “rigorous multicenter clinical investigations to evaluate the cardiotoxicity of emerging cancer treatments,” similar to the Thrombosis in Myocardial Infarction Study Group.
“The success of this consortium in pioneering and targeting multiple generations of drugs for the treatment of MI, involving tens of thousands of patients and thousands of collaborations across multiple national borders, is a model for how to move forward in providing the new hope of cancer cure without the trade-off of years lost to heart disease,” the editorialists concluded.
The study was supported in part by National Institutes of Health grants, including a K12-CA133250 grant to Dr. Addison. Dr. Bishopric reported being on the scientific board of C&C Biopharma. Dr. Lippman reports being on the board of directors of and holding stock in Seattle Genetics. Dr. Moslehi reported having served on advisory boards for Pfizer, Novartis, Bristol-Myers Squibb, Deciphera, Audentes Pharmaceuticals, Nektar, Takeda, Ipsen, Myokardia, AstraZeneca, GlaxoSmithKline, Intrexon, and Regeneron.
This article first appeared on Medscape.com.
Clinical trials supporting Food and Drug Adminstration approval of contemporary cancer therapies frequently failed to capture major adverse cardiovascular events (MACE) and, when they did, reported rates 2.6-fold lower than noncancer trials, new research shows.
Overall, 51.3% of trials did not report MACE, with that number reaching 57.6% in trials enrolling patients with baseline cardiovascular disease (CVD).
Nearly 40% of trials did not report any CVD events in follow-up, the authors reported online Feb. 10, 2020, in the Journal of the American College of Cardiology (2020;75:620-8).
“Even in drug classes where there were established or emerging associations with cardiotoxic events, often there were no reported heart events or cardiovascular events across years of follow-up in trials that examined hundreds or even thousands of patients. That was actually pretty surprising,” senior author Daniel Addison, MD, codirector of the cardio-oncology program at the Ohio State University Medical Center, Columbus, said in an interview.
The study was prompted by a series of events that crescendoed when his team was called to the ICU to determine whether a novel targeted agent played a role in the heart decline of a patient with acute myeloid leukemia. “I had a resident ask me a very important question: ‘How do we really know for sure that the trial actually reflects the true risk of heart events?’ to which I told him, ‘it’s difficult to know,’ ” he said.
“I think many of us rely heavily on what we see in the trials, particularly when they make it to the top journals, and quite frankly, we generally take it at face value,” Dr. Addison observed.
Lower Rate of Reported Events
The investigators reviewed CV events reported in 97,365 patients (median age, 61 years; 46% female) enrolled in 189 phase 2 and 3 trials supporting FDA approval of 123 anticancer drugs from 1998 to 2018. Biologic, targeted, or immune-based therapies accounted for 72.5% of drug approvals.
Over 148,138 person-years of follow-up (median trial duration, 30 months), there were 1,148 incidents of MACE (375 heart failure, 253 MIs, 180 strokes, 65 atrial fibrillation, 29 coronary revascularizations, and 246 CVD deaths). MACE rates were higher in the intervention group than in the control group (792 vs. 356; P less than .01). Among the 64 trials that excluded patients with baseline CVD, there were 269 incidents of MACE.
To put this finding in context, the researchers examined the reported incidence of MACE among some 6,000 similarly aged participants in the Multi-Ethnic Study of Atherosclerosis (MESA). The overall weighted-average incidence rate was 1,408 per 100,000 person-years among MESA participants, compared with 542 events per 100,000 person-years among oncology trial participants (716 per 100,000 in the intervention arm). This represents a reported-to-expected ratio of 0.38 – a 2.6-fold lower rate of reported events (P less than .001) – and a risk difference of 866.
Further, MACE reporting was lower by a factor of 1.7 among all cancer trial participants irrespective of baseline CVD status (reported-to-expected ratio, 0.56; risk difference, 613; P less than .001).
There was no significant difference in MACE reporting between independent or industry-sponsored trials, the authors report.
No malicious intent
“There are likely some that might lean toward not wanting to attribute blame to a new drug when the drug is in a study, but I really think that the leading factor is lack of awareness,” Dr. Addison said. “I’ve talked with several cancer collaborators around the country who run large clinical trials, and I think often, when an event may be brought to someone’s attention, there is a tendency to just write it off as kind of a generic expected event due to age, or just something that’s not really pertinent to the study. So they don’t really focus on it as much.”
“Closer collaboration between cardiologists and cancer physicians is needed to better determine true cardiac risks among patients treated with these drugs.”
Breast cancer oncologist Marc E. Lippman, MD, of Georgetown University Medical Center and Georgetown Lombardi Comprehensive Cancer Center, Washington, D.C., isn’t convinced a lack of awareness is the culprit.
“I don’t agree with that at all,” he said in an interview. “I think there are very, very clear rules and guidelines these days for adverse-event reporting. I think that’s not a very likely explanation – that it’s not on the radar.”
Part of the problem may be that some of the toxicities, particularly cardiovascular, may not emerge for years, he said. Participant screening for the trials also likely removed patients with high cardiovascular risk. “It’s very understandable to me – I’m not saying it’s good particularly – but I think it’s very understandable that, if you’re trying to develop a drug, the last thing you’d want to have is a lot of toxicity that you might have avoided by just being restrictive in who you let into the study,” Dr. Lippman said.
The underreported CVD events may also reflect the rapidly changing profile of cardiovascular toxicities associated with novel anticancer therapies.
“Providers, both cancer and noncancer, generally put cardiotoxicity in the box of anthracyclines and radiation, but particularly over the last decade, we’ve begun to understand it’s well beyond any one class of drugs,” Dr. Addison said.
“I agree completely,” Dr. Lippman said. For example, “the checkpoint inhibitors are so unbelievably different in terms of their toxicities that many people simply didn’t even know what they were getting into at first.”
One size does not fit all
Javid Moslehi, MD, director of the cardio-oncology program at Vanderbilt University, Nashville, Tenn., said echocardiography – recommended to detect changes in left ventricular function in patients exposed to anthracyclines or targeted agents like trastuzumab (Herceptin) – isn’t enough to address today’s cancer therapy–related CVD events.
“Initial drugs like anthracyclines or Herceptin in cardio-oncology were associated with systolic cardiac dysfunction, whereas the majority of issues we see in the cardio-oncology clinics today are vascular, metabolic, arrhythmogenic, and inflammatory,” he said in an interview. “Echocardiography misses the big and increasingly complex picture.”
His group, for example, has been studying myocarditis associated with immunotherapies, but none of the clinical trials require screening or surveillance for myocarditis with a cardiac biomarker like troponin.
The group also recently identified 303 deaths in patients exposed to ibrutinib, a drug that revolutionized the treatment of several B-cell malignancies but is associated with higher rates of atrial fibrillation, which is also associated with increased bleeding risk. “So there’s a little bit of a double whammy there, given that we often treat atrial fibrillation with anticoagulation and where we can cause complications in patients,” Dr. Moslehi noted.
Although there needs to be closer collaboration between cardiologists and oncologists on individual trials, cardiologists also have to realize that oncology care has become very personalized, he suggested.
“What’s probably relevant for the breast cancer patient may not be relevant for the prostate cancer patient and their respective treatments,” Dr. Moslehi said. “So if we were to say, ‘every person should get an echo,’ that may be less relevant to the prostate cancer patient where treatments can cause vascular and metabolic perturbations or to the patient treated with immunotherapy who may have myocarditis, where many of the echos can be normal. There’s no one-size-fits-all for these things.”
Wearable technologies like smartwatches could play a role in improving the reporting of CVD events with novel therapies but a lot more research needs to be done to validate these tools, Dr. Addison said. “But as we continue on into the 21st century, this is going to expand and may potentially help us,” he added.
In the interim, better standardization is needed of the cardiovascular events reported in oncology trials, particularly the Common Terminology Criteria for Adverse Events (CTCAE), said Dr. Moslehi, who also serves as chair of the American Heart Association’s subcommittee on cardio-oncology.
“Cardiovascular definitions are not exactly uniform and are not consistent with what we in cardiology consider to be important or relevant,” he said. “So I think there needs to be better standardization of these definitions, specifically within the CTCAE, which is what the oncologists use to identify adverse events.”
In a linked editorial (J Am Coll Cardiol. 2020;75:629-31), Dr. Lippman and cardiologist Nanette Bishopric, MD, of the Medstar Heart and Vascular Institute in Washington, D.C., suggested it may also be time to organize a consortium that can carry out “rigorous multicenter clinical investigations to evaluate the cardiotoxicity of emerging cancer treatments,” similar to the Thrombosis in Myocardial Infarction Study Group.
“The success of this consortium in pioneering and targeting multiple generations of drugs for the treatment of MI, involving tens of thousands of patients and thousands of collaborations across multiple national borders, is a model for how to move forward in providing the new hope of cancer cure without the trade-off of years lost to heart disease,” the editorialists concluded.
The study was supported in part by National Institutes of Health grants, including a K12-CA133250 grant to Dr. Addison. Dr. Bishopric reported being on the scientific board of C&C Biopharma. Dr. Lippman reports being on the board of directors of and holding stock in Seattle Genetics. Dr. Moslehi reported having served on advisory boards for Pfizer, Novartis, Bristol-Myers Squibb, Deciphera, Audentes Pharmaceuticals, Nektar, Takeda, Ipsen, Myokardia, AstraZeneca, GlaxoSmithKline, Intrexon, and Regeneron.
This article first appeared on Medscape.com.
Model reveals genes associated with prognosis in ER+, HER2– breast cancer
ORLANDO – , according to new research.
Yara Abdou, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and colleagues presented this work in a poster at the ASCO-SITC Clinical Immuno-Oncology Symposium.
The model used 50 cycles of machine learning to cluster 98 patients from The Cancer Genome Atlas Program into high- and low-risk groups based on mRNA expression of 26 gene groups.
The gene groups consisted of 191 genes enriched in cellular and noncellular elements of the tumor microenvironment. Mutational burden and clinical outcomes data for the patients also were considered, Dr. Abdou explained in an interview.
Kaplan-Meier curves were created for each group by K-means clustering, survival differences between the two groups were assessed, and correlations among the various gene groups were analyzed.
Five identified genes were associated with poor prognosis: LOXL2, PHEX, ACTA2, MEGF9, and TNFSF4. Fifteen genes were associated with good prognosis: CD8A, CD8B, FCRL3, GZMK, CD3E, CCL5, TP53, ICAM3, CD247, IFNG, IFNGR1, ICAM4, SHH, HLA-DOB, and CXCR3.
The Kaplan-Meier curves showed a significant difference in survival between the two groups (hazard ratio, 2.878; P = .05), confirming the validity of the risk score modeling, Dr. Abdou said.
Immune profiling showed that expression of genes associated with desmoplastic reaction, neutrophils, and immunosuppressive cytokines were higher in the high-risk group, whereas expression of genes related to immune system activation were higher in the low-risk group (P less than .05).
Stroma in the tumor microenvironment is known to affect prognosis and response to therapy in patients with breast cancer, but few mathematical models exist to determine prognosis based on mRNA expressivity in the tumor microenvironment, Dr. Abdou said, explaining the rationale for the study.
The findings suggest that when genomic profile information is available for a given patient in the clinic, this machine learning–assisted risk scoring approach could have prognostic value, she said, noting that the model also will be assessed in patients with other types of breast cancer.
Dr. Abdou reported having no disclosures.
SOURCE: Abdou Y et al. ASCO-SITC. Poster A3.
ORLANDO – , according to new research.
Yara Abdou, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and colleagues presented this work in a poster at the ASCO-SITC Clinical Immuno-Oncology Symposium.
The model used 50 cycles of machine learning to cluster 98 patients from The Cancer Genome Atlas Program into high- and low-risk groups based on mRNA expression of 26 gene groups.
The gene groups consisted of 191 genes enriched in cellular and noncellular elements of the tumor microenvironment. Mutational burden and clinical outcomes data for the patients also were considered, Dr. Abdou explained in an interview.
Kaplan-Meier curves were created for each group by K-means clustering, survival differences between the two groups were assessed, and correlations among the various gene groups were analyzed.
Five identified genes were associated with poor prognosis: LOXL2, PHEX, ACTA2, MEGF9, and TNFSF4. Fifteen genes were associated with good prognosis: CD8A, CD8B, FCRL3, GZMK, CD3E, CCL5, TP53, ICAM3, CD247, IFNG, IFNGR1, ICAM4, SHH, HLA-DOB, and CXCR3.
The Kaplan-Meier curves showed a significant difference in survival between the two groups (hazard ratio, 2.878; P = .05), confirming the validity of the risk score modeling, Dr. Abdou said.
Immune profiling showed that expression of genes associated with desmoplastic reaction, neutrophils, and immunosuppressive cytokines were higher in the high-risk group, whereas expression of genes related to immune system activation were higher in the low-risk group (P less than .05).
Stroma in the tumor microenvironment is known to affect prognosis and response to therapy in patients with breast cancer, but few mathematical models exist to determine prognosis based on mRNA expressivity in the tumor microenvironment, Dr. Abdou said, explaining the rationale for the study.
The findings suggest that when genomic profile information is available for a given patient in the clinic, this machine learning–assisted risk scoring approach could have prognostic value, she said, noting that the model also will be assessed in patients with other types of breast cancer.
Dr. Abdou reported having no disclosures.
SOURCE: Abdou Y et al. ASCO-SITC. Poster A3.
ORLANDO – , according to new research.
Yara Abdou, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and colleagues presented this work in a poster at the ASCO-SITC Clinical Immuno-Oncology Symposium.
The model used 50 cycles of machine learning to cluster 98 patients from The Cancer Genome Atlas Program into high- and low-risk groups based on mRNA expression of 26 gene groups.
The gene groups consisted of 191 genes enriched in cellular and noncellular elements of the tumor microenvironment. Mutational burden and clinical outcomes data for the patients also were considered, Dr. Abdou explained in an interview.
Kaplan-Meier curves were created for each group by K-means clustering, survival differences between the two groups were assessed, and correlations among the various gene groups were analyzed.
Five identified genes were associated with poor prognosis: LOXL2, PHEX, ACTA2, MEGF9, and TNFSF4. Fifteen genes were associated with good prognosis: CD8A, CD8B, FCRL3, GZMK, CD3E, CCL5, TP53, ICAM3, CD247, IFNG, IFNGR1, ICAM4, SHH, HLA-DOB, and CXCR3.
The Kaplan-Meier curves showed a significant difference in survival between the two groups (hazard ratio, 2.878; P = .05), confirming the validity of the risk score modeling, Dr. Abdou said.
Immune profiling showed that expression of genes associated with desmoplastic reaction, neutrophils, and immunosuppressive cytokines were higher in the high-risk group, whereas expression of genes related to immune system activation were higher in the low-risk group (P less than .05).
Stroma in the tumor microenvironment is known to affect prognosis and response to therapy in patients with breast cancer, but few mathematical models exist to determine prognosis based on mRNA expressivity in the tumor microenvironment, Dr. Abdou said, explaining the rationale for the study.
The findings suggest that when genomic profile information is available for a given patient in the clinic, this machine learning–assisted risk scoring approach could have prognostic value, she said, noting that the model also will be assessed in patients with other types of breast cancer.
Dr. Abdou reported having no disclosures.
SOURCE: Abdou Y et al. ASCO-SITC. Poster A3.
REPORTING FROM THE CLINICAL IMMUNO-ONCOLOGY SYMPOSIUM
FDA: Cell phones still look safe
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
Breast cancer treatments veer from guidelines
Women with breast cancer may be receiving treatments that are discordant with guideline recommendations for genetic subtypes of disease, based on a retrospective analysis of more than 20,000 patients.
Radiotherapy and chemotherapy practices were particularly out of alignment with guidelines, reported lead author Allison W. Kurian, MD, of Stanford (Calif.) University, and colleagues.
“Integrating genetic testing into breast cancer care has been complex and challenging,” the investigators wrote in JAMA Oncology. “There is wide variability in which clinicians order testing and disclose results, in the clinical significance of results, and in how clinicians interpret results to patients.”
According to the investigators, while germline testing is on the rise, little is known about how these test results are translating to clinical care.
To learn more, the investigators evaluated data from 20,568 women with stage 0-III breast cancer who entered the Surveillance, Epidemiology, and End Results registries of Georgia and California between 2014 and 2016.
Three treatment types were evaluated: surgery (bilateral vs. unilateral mastectomy), radiotherapy after lumpectomy, and chemotherapy. Treatment selection was compared with test results for breast cancer–associated genes, such as BRCA1/2, TP53, PTEN, and others. Associations were then compared with guideline recommendations.
Data analysis suggested that many clinicians were correctly using genetic test results to guide surgical decisions. For example, almost two-thirds (61.7%) of women with a BRCA mutation underwent bilateral mastectomy, compared with one-quarter (24.3%) who were BRCA negative (odds ratio, 5.52). For other pathogenic variants, the rate of bilateral mastectomy was still elevated, albeit to a lesser degree (OR, 2.41).
Generally, these practices align with recommendations, the investigators wrote, noting that research supports bilateral mastectomy with BRCA1/2, TP53, and PTEN variants, while data are lacking for other genetic subtypes.
Radiotherapy and chemotherapy practices were more discordant with guidelines. For example, women with a BRCA mutation were 78% less likely to receive radiotherapy after lumpectomy (OR, 0.22) and 76% more likely to receive chemotherapy for early-stage, hormone-positive disease (OR, 1.76). According to investigators, these findings suggest possible trends in undertreatment and overtreatment, respectively.
“We believe more research is needed to confirm our results and to evaluate long-term outcomes of pathogenic variant carriers to understand treatment decision making and consequences,” the investigators concluded.
The study was funded by the National Institutes of Health and the California Department of Public Health. The investigators reported relationships with Myriad Genetics, Genomic Health, Roche, and other companies.
SOURCE: Kurian AW et al. JAMA Oncol. 2020 Feb 6. doi: 10.1001/jamaoncol.2019.6400.
Women with breast cancer may be receiving treatments that are discordant with guideline recommendations for genetic subtypes of disease, based on a retrospective analysis of more than 20,000 patients.
Radiotherapy and chemotherapy practices were particularly out of alignment with guidelines, reported lead author Allison W. Kurian, MD, of Stanford (Calif.) University, and colleagues.
“Integrating genetic testing into breast cancer care has been complex and challenging,” the investigators wrote in JAMA Oncology. “There is wide variability in which clinicians order testing and disclose results, in the clinical significance of results, and in how clinicians interpret results to patients.”
According to the investigators, while germline testing is on the rise, little is known about how these test results are translating to clinical care.
To learn more, the investigators evaluated data from 20,568 women with stage 0-III breast cancer who entered the Surveillance, Epidemiology, and End Results registries of Georgia and California between 2014 and 2016.
Three treatment types were evaluated: surgery (bilateral vs. unilateral mastectomy), radiotherapy after lumpectomy, and chemotherapy. Treatment selection was compared with test results for breast cancer–associated genes, such as BRCA1/2, TP53, PTEN, and others. Associations were then compared with guideline recommendations.
Data analysis suggested that many clinicians were correctly using genetic test results to guide surgical decisions. For example, almost two-thirds (61.7%) of women with a BRCA mutation underwent bilateral mastectomy, compared with one-quarter (24.3%) who were BRCA negative (odds ratio, 5.52). For other pathogenic variants, the rate of bilateral mastectomy was still elevated, albeit to a lesser degree (OR, 2.41).
Generally, these practices align with recommendations, the investigators wrote, noting that research supports bilateral mastectomy with BRCA1/2, TP53, and PTEN variants, while data are lacking for other genetic subtypes.
Radiotherapy and chemotherapy practices were more discordant with guidelines. For example, women with a BRCA mutation were 78% less likely to receive radiotherapy after lumpectomy (OR, 0.22) and 76% more likely to receive chemotherapy for early-stage, hormone-positive disease (OR, 1.76). According to investigators, these findings suggest possible trends in undertreatment and overtreatment, respectively.
“We believe more research is needed to confirm our results and to evaluate long-term outcomes of pathogenic variant carriers to understand treatment decision making and consequences,” the investigators concluded.
The study was funded by the National Institutes of Health and the California Department of Public Health. The investigators reported relationships with Myriad Genetics, Genomic Health, Roche, and other companies.
SOURCE: Kurian AW et al. JAMA Oncol. 2020 Feb 6. doi: 10.1001/jamaoncol.2019.6400.
Women with breast cancer may be receiving treatments that are discordant with guideline recommendations for genetic subtypes of disease, based on a retrospective analysis of more than 20,000 patients.
Radiotherapy and chemotherapy practices were particularly out of alignment with guidelines, reported lead author Allison W. Kurian, MD, of Stanford (Calif.) University, and colleagues.
“Integrating genetic testing into breast cancer care has been complex and challenging,” the investigators wrote in JAMA Oncology. “There is wide variability in which clinicians order testing and disclose results, in the clinical significance of results, and in how clinicians interpret results to patients.”
According to the investigators, while germline testing is on the rise, little is known about how these test results are translating to clinical care.
To learn more, the investigators evaluated data from 20,568 women with stage 0-III breast cancer who entered the Surveillance, Epidemiology, and End Results registries of Georgia and California between 2014 and 2016.
Three treatment types were evaluated: surgery (bilateral vs. unilateral mastectomy), radiotherapy after lumpectomy, and chemotherapy. Treatment selection was compared with test results for breast cancer–associated genes, such as BRCA1/2, TP53, PTEN, and others. Associations were then compared with guideline recommendations.
Data analysis suggested that many clinicians were correctly using genetic test results to guide surgical decisions. For example, almost two-thirds (61.7%) of women with a BRCA mutation underwent bilateral mastectomy, compared with one-quarter (24.3%) who were BRCA negative (odds ratio, 5.52). For other pathogenic variants, the rate of bilateral mastectomy was still elevated, albeit to a lesser degree (OR, 2.41).
Generally, these practices align with recommendations, the investigators wrote, noting that research supports bilateral mastectomy with BRCA1/2, TP53, and PTEN variants, while data are lacking for other genetic subtypes.
Radiotherapy and chemotherapy practices were more discordant with guidelines. For example, women with a BRCA mutation were 78% less likely to receive radiotherapy after lumpectomy (OR, 0.22) and 76% more likely to receive chemotherapy for early-stage, hormone-positive disease (OR, 1.76). According to investigators, these findings suggest possible trends in undertreatment and overtreatment, respectively.
“We believe more research is needed to confirm our results and to evaluate long-term outcomes of pathogenic variant carriers to understand treatment decision making and consequences,” the investigators concluded.
The study was funded by the National Institutes of Health and the California Department of Public Health. The investigators reported relationships with Myriad Genetics, Genomic Health, Roche, and other companies.
SOURCE: Kurian AW et al. JAMA Oncol. 2020 Feb 6. doi: 10.1001/jamaoncol.2019.6400.
FROM JAMA ONCOLOGY
Abbreviated MRI equals standard protocol for high-risk breast cancer screens
CHICAGO – An abbreviated magnetic resonance imaging (MRI) protocol for screening individuals at high risk for breast cancer performed as well as a standard protocol, in about half the time and with greater patient satisfaction.
The abbreviated protocol also resulted in fewer false positive findings, with 5% fewer patients receiving biopsies for benign lesions than with a standard protocol (8.4% versus 13.7%, P less than .001).
Findings from the prospective 10-month trial conducted in the province of Ontario were presented by Jean Seely, MD, professor of radiology at the University of Ottawa, at the annual meeting of the Radiological Society of North America.
“The abbreviated protocol was shown to be as effective as the standard protocol in high-risk screening breast MRI, supporting previous studies,” said Dr. Seely. The shorter protocol took 16.3 minutes on average, compared with 27 minutes for the standard MRI protocol. This difference resulted in a 50% increase in institutional capacity, or a jump from two to three patients screened per hour.
In the province of Ontario, said Dr. Seely, women assessed at being at a 25% or greater lifetime risk of breast cancer receive MRIs as part of the Ontario Breast Screening Program (OBSP), which calculates risk by using the International Breast Cancer Intervention Study model.
For high-risk patients, the OBSP model provides annual mammography and an MRI for women between the ages of 30 and 60 years. Not only is the half-hour duration of the standard protocol resource-intensive, especially in regions with limited scanner availability, but patients may either be reluctant to undergo a half-hour scan, or not tolerate a lengthy scan very well.
Dr. Seely cited previous work (J Clin Oncol. 2014 Aug 1;32[22]:2304-10) showing that an abbreviated MRI protocol has similar accuracy as the full standard protocol. With the foundation of evidence from this study, Dr. Seely and her collaborators compared outcomes for high-risk patients who were screened with an abbreviated versus a standard protocol.
The abbreviated protocol, approved by the American College of Radiology, omits a final round of image acquisition sequences at the 9-minute mark after gadolinium administration, instead performing acquisition at 1, 2, 3, and 4 minutes after contrast delivery. Total time required for this protocol is just over 13 minutes, said Dr. Seely, and additional diagnostic MRIs were not required.
The trial was constructed so that the abbreviated protocol was used for the entire OBSP cohort for 10 months in 2018. Results were compared with those from the 12 previous months, when OBSP patients’ MRIs were performed using the standard protocol.
A total of 881 patients received standard-protocol MRIs; about three quarters (651) of those patients had previous MRI screening, while the remaining 230 patients had a baseline screen via the standard protocol.
Of the 658 patients in the abbreviated protocol group, 135, or about 20%, received the briefer scans as a baseline screen; the remast of the patients in this arm had received earlier MRI screening.
In addition to tracking scanning times, Dr. Seely and her collaborators also compared cancer detection rates, Breast Imaging Reporting and Data System (BI-RADS) assessment categories, positive predictive values, and the abnormal interpretation rate – that is, how many scans fell into BI-RADS categories 0, 4, and 5.
No significant difference was found between the rates of BI-RADs 0, 3, or 5 studies between the groups. Significantly fewer abbreviated scans fell into the BI-RADS 4 category, however (9.3% vs. 14.9%; P less than .001).
Similarly, the abnormal interpretation rate was 12.5% for the abbreviated protocol, compared with 17.5% for the standard protocol (P less than .007), with a correspondingly lower biopsy rate of 8.4% for the abbreviated protocol, compared with 13.7% for the standard protocol (P less than .001). The overall cancer detection rate did not differ between groups.
She and her colleagues will continue to track outcomes for those receiving abbreviated screening within the province of Ontario to track performance over time.
Dr. Seely reported that she had no relevant conflicts of interest. She reported no funding source beyond the province of Ontario.
SOURCE: Seely J et al. RSNA 2019, Session RC-215-04.
CHICAGO – An abbreviated magnetic resonance imaging (MRI) protocol for screening individuals at high risk for breast cancer performed as well as a standard protocol, in about half the time and with greater patient satisfaction.
The abbreviated protocol also resulted in fewer false positive findings, with 5% fewer patients receiving biopsies for benign lesions than with a standard protocol (8.4% versus 13.7%, P less than .001).
Findings from the prospective 10-month trial conducted in the province of Ontario were presented by Jean Seely, MD, professor of radiology at the University of Ottawa, at the annual meeting of the Radiological Society of North America.
“The abbreviated protocol was shown to be as effective as the standard protocol in high-risk screening breast MRI, supporting previous studies,” said Dr. Seely. The shorter protocol took 16.3 minutes on average, compared with 27 minutes for the standard MRI protocol. This difference resulted in a 50% increase in institutional capacity, or a jump from two to three patients screened per hour.
In the province of Ontario, said Dr. Seely, women assessed at being at a 25% or greater lifetime risk of breast cancer receive MRIs as part of the Ontario Breast Screening Program (OBSP), which calculates risk by using the International Breast Cancer Intervention Study model.
For high-risk patients, the OBSP model provides annual mammography and an MRI for women between the ages of 30 and 60 years. Not only is the half-hour duration of the standard protocol resource-intensive, especially in regions with limited scanner availability, but patients may either be reluctant to undergo a half-hour scan, or not tolerate a lengthy scan very well.
Dr. Seely cited previous work (J Clin Oncol. 2014 Aug 1;32[22]:2304-10) showing that an abbreviated MRI protocol has similar accuracy as the full standard protocol. With the foundation of evidence from this study, Dr. Seely and her collaborators compared outcomes for high-risk patients who were screened with an abbreviated versus a standard protocol.
The abbreviated protocol, approved by the American College of Radiology, omits a final round of image acquisition sequences at the 9-minute mark after gadolinium administration, instead performing acquisition at 1, 2, 3, and 4 minutes after contrast delivery. Total time required for this protocol is just over 13 minutes, said Dr. Seely, and additional diagnostic MRIs were not required.
The trial was constructed so that the abbreviated protocol was used for the entire OBSP cohort for 10 months in 2018. Results were compared with those from the 12 previous months, when OBSP patients’ MRIs were performed using the standard protocol.
A total of 881 patients received standard-protocol MRIs; about three quarters (651) of those patients had previous MRI screening, while the remaining 230 patients had a baseline screen via the standard protocol.
Of the 658 patients in the abbreviated protocol group, 135, or about 20%, received the briefer scans as a baseline screen; the remast of the patients in this arm had received earlier MRI screening.
In addition to tracking scanning times, Dr. Seely and her collaborators also compared cancer detection rates, Breast Imaging Reporting and Data System (BI-RADS) assessment categories, positive predictive values, and the abnormal interpretation rate – that is, how many scans fell into BI-RADS categories 0, 4, and 5.
No significant difference was found between the rates of BI-RADs 0, 3, or 5 studies between the groups. Significantly fewer abbreviated scans fell into the BI-RADS 4 category, however (9.3% vs. 14.9%; P less than .001).
Similarly, the abnormal interpretation rate was 12.5% for the abbreviated protocol, compared with 17.5% for the standard protocol (P less than .007), with a correspondingly lower biopsy rate of 8.4% for the abbreviated protocol, compared with 13.7% for the standard protocol (P less than .001). The overall cancer detection rate did not differ between groups.
She and her colleagues will continue to track outcomes for those receiving abbreviated screening within the province of Ontario to track performance over time.
Dr. Seely reported that she had no relevant conflicts of interest. She reported no funding source beyond the province of Ontario.
SOURCE: Seely J et al. RSNA 2019, Session RC-215-04.
CHICAGO – An abbreviated magnetic resonance imaging (MRI) protocol for screening individuals at high risk for breast cancer performed as well as a standard protocol, in about half the time and with greater patient satisfaction.
The abbreviated protocol also resulted in fewer false positive findings, with 5% fewer patients receiving biopsies for benign lesions than with a standard protocol (8.4% versus 13.7%, P less than .001).
Findings from the prospective 10-month trial conducted in the province of Ontario were presented by Jean Seely, MD, professor of radiology at the University of Ottawa, at the annual meeting of the Radiological Society of North America.
“The abbreviated protocol was shown to be as effective as the standard protocol in high-risk screening breast MRI, supporting previous studies,” said Dr. Seely. The shorter protocol took 16.3 minutes on average, compared with 27 minutes for the standard MRI protocol. This difference resulted in a 50% increase in institutional capacity, or a jump from two to three patients screened per hour.
In the province of Ontario, said Dr. Seely, women assessed at being at a 25% or greater lifetime risk of breast cancer receive MRIs as part of the Ontario Breast Screening Program (OBSP), which calculates risk by using the International Breast Cancer Intervention Study model.
For high-risk patients, the OBSP model provides annual mammography and an MRI for women between the ages of 30 and 60 years. Not only is the half-hour duration of the standard protocol resource-intensive, especially in regions with limited scanner availability, but patients may either be reluctant to undergo a half-hour scan, or not tolerate a lengthy scan very well.
Dr. Seely cited previous work (J Clin Oncol. 2014 Aug 1;32[22]:2304-10) showing that an abbreviated MRI protocol has similar accuracy as the full standard protocol. With the foundation of evidence from this study, Dr. Seely and her collaborators compared outcomes for high-risk patients who were screened with an abbreviated versus a standard protocol.
The abbreviated protocol, approved by the American College of Radiology, omits a final round of image acquisition sequences at the 9-minute mark after gadolinium administration, instead performing acquisition at 1, 2, 3, and 4 minutes after contrast delivery. Total time required for this protocol is just over 13 minutes, said Dr. Seely, and additional diagnostic MRIs were not required.
The trial was constructed so that the abbreviated protocol was used for the entire OBSP cohort for 10 months in 2018. Results were compared with those from the 12 previous months, when OBSP patients’ MRIs were performed using the standard protocol.
A total of 881 patients received standard-protocol MRIs; about three quarters (651) of those patients had previous MRI screening, while the remaining 230 patients had a baseline screen via the standard protocol.
Of the 658 patients in the abbreviated protocol group, 135, or about 20%, received the briefer scans as a baseline screen; the remast of the patients in this arm had received earlier MRI screening.
In addition to tracking scanning times, Dr. Seely and her collaborators also compared cancer detection rates, Breast Imaging Reporting and Data System (BI-RADS) assessment categories, positive predictive values, and the abnormal interpretation rate – that is, how many scans fell into BI-RADS categories 0, 4, and 5.
No significant difference was found between the rates of BI-RADs 0, 3, or 5 studies between the groups. Significantly fewer abbreviated scans fell into the BI-RADS 4 category, however (9.3% vs. 14.9%; P less than .001).
Similarly, the abnormal interpretation rate was 12.5% for the abbreviated protocol, compared with 17.5% for the standard protocol (P less than .007), with a correspondingly lower biopsy rate of 8.4% for the abbreviated protocol, compared with 13.7% for the standard protocol (P less than .001). The overall cancer detection rate did not differ between groups.
She and her colleagues will continue to track outcomes for those receiving abbreviated screening within the province of Ontario to track performance over time.
Dr. Seely reported that she had no relevant conflicts of interest. She reported no funding source beyond the province of Ontario.
SOURCE: Seely J et al. RSNA 2019, Session RC-215-04.
REPORTING FROM RSNA 2019
Data emerging to support personalized nutrition in oncology
SAN DIEGO – When Dawn Lemanne, MD, MPH, meets with cancer patients and their families, the question invariably comes up: “What should I eat?”
“The answer always is, ‘It depends,’” Dr. Lemanne, an oncologist who founded Oregon Integrative Oncology in Ashland, said at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine. “The answers are not the same for each of these patients.”
According to Dr. Lemanne, targeted nutrition is evolving as a key component of cancer care. One of the goals of this approach is to decrease mTOR signaling. Normally, mTOR signaling promotes cell proliferation and metabolism; aberrant mTOR signaling can contribute to cancer initiation and progression.
“When mTOR speaks it says, ‘grow,’” said Dr. Lemanne, who is also an assistant professor of clinical medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona in Tucson. This message is meant to be heard by normal tissues, to stimulate normal tissue proliferation, such as in growing children or when a wound needs to be healed.
“However, cancer cells can hear and respond to mTOR’s message,” she said. “Normal cells may listen to mTOR’s ‘grow’ message or not, depending on the task they perform. Once we reach adulthood, we all likely have some precancerous or cancerous cells around, but they’re usually dormant. That’s why once you’re an adult, however, you don’t want too much mTOR signaling, because that might stimulate growth of things you definitely don’t want to grow.”
Having excessive levels of the growth hormone insulin-like growth factor-1 (IGF-1) also appears to play a role in cancer risk. Researchers studying members of a South American clan with Laron dwarfism – an inherited IGF-1 deficiency – found that besides being very short, affected members of this family rarely develop cancer (Cells. 2019;8[6]:596). “They also don’t get diabetes,” Dr. Lemanne said. “What we see in those with Laron dwarfism is that mTOR signaling is missing.”
She went on to note that studying type 2 diabetes gives physicians “a clue as to what dietary measures we might offer our patients in terms of decreasing their risk of dying from cancer or getting cancer.” The most common types of cancer are indeed more common in patients with type 2 diabetes. In addition, once someone with type 2 diabetes is diagnosed with cancer, their prognosis is poorer, compared with a cancer patient without diabetes.
“Metformin is often prescribed to patients with type 2 diabetes because it helps keep blood sugar low,” she said. “What’s fascinating is that diabetics on metformin develop cancer less frequently than diabetics not taking this drug. And also interesting, those diabetics who do develop cancer seem to do better if they’re on metformin before and after diagnosis.”
On the other hand, exogenous insulin therapy given to people with type 2 diabetes doubles the risk of cancer. Consistent with this is the two-decades-old finding that an elevated fasting insulin level also is associated with a poor breast cancer prognosis (J Clin Oncol. 2002 Jan 1;20[1]:42-51). “It’s really important to understand that, in a person destined to become a type 2 diabetic, the level of fasting insulin rises long before fasting glucose becomes abnormally high,” Dr. Lemanne explained. “A normal fasting glucose doesn’t let you off the hook in terms of checking your patient for insulin resistance.
“We will miss diagnosing many patients with dangerous insulin resistance and prediabetes if we don’t check the fasting glucose and the fasting insulin levels together. If the fasting insulin level is high, it’s important to limit carbohydrate intake enough to bring it down permanently, even when the fasting glucose is normal, or the patient is likely at increased risk for developing cancer.”
Two large, prospective randomized trials have examined breast cancer and diet: the Women’s Intervention Study (WINS) and the Women’s Health Eating and Living Study (WHEL). Patients in both trials had early stage breast cancer and were put on low-fat diets. In the end, there was a weak to negligible connection between breast cancer survival and dietary fat restriction. “That kind of shook up the oncology world,” Dr. Lemanne said, “because before these two studies, everyone ‘knew’ that dietary fat was related to breast cancer risk. These studies showed that wasn’t the case at all.”
According to Dr. Lemanne, unexpectedly, moderate carbohydrate restriction has been associated with lower risk of breast cancer recurrence in patients with postmenopausal hormone-receptor expressing breast cancer. Researchers at the University of California, San Diego, conducted a subanalysis of 265 postmenopausal patients with estrogen receptor positive breast cancer from the WHEL cohort (Cancer Epidemiol Biomarkers Prev. 2014 23[7]:1273-9). The recurrence risk was halved in those who cut their carbohydrate intake after diagnosis. The amount of decrease was modest, only 27 grams per day – the equivalent of one banana. “That is on par with a lot of our drugs, and maybe a little bit better,” she said. The effect was strongest if the breast tumor expressed IGF-1 receptor. Dr. Lemanne pointed out that decreasing dietary carbohydrate load was not the only treatment. These patients also had appropriate conventional cancer treatments, including surgery, radiation, and chemotherapy. “If we cut just some of the daily carb load in these patients, they might have a better cancer prognosis,” she said.
Overweight or obese patients with colon cancer also may benefit from moderate carbohydrate restriction. The CALGB 89803 study assessed 1,011 subjects with stage III colon cancer. It found that the subjects in the highest quintile of daily glycemic load and total carbohydrate intake had an increased risk of cancer recurrence and mortality (hazard ratio, 2.26; J Nat Cancer Inst. 2012;104[22]:1702-11). “This is pretty strong evidence that glycemic load and total carbohydrate intake play a role in colon cancer recurrence, but there’s a caveat here,” she said. “The effect was seen only in patients who were overweight or obese.” There was no association between carbohydrate intake and colon cancer recurrence in the absence of overweight or obesity.
Based on existing evidence, she said,
“That’s pretty modest; that’s 400 calories of carbohydrates per day,” Dr. Lemanne said. “I tell patients that they can have fruit, starchy vegetables, and even very small amounts of healthy whole grains, although I’m not a fan of grains due to the heavy carbohydrate load. All those things are OK. We’re not talking about jelly beans and white sugar.
“I also have them measure their fasting glucose each day, because different people have different blood glucose responses to the same food.” The goals she aims for with many of her patients are a fasting morning glucose between 79 and 83 mg/dL consistently, an HbA1c of 5.4 or less, and a BMI of 24.9 kg/m2 or less. “This set of goals, however, has to be individualized,” she said.
The ketogenic diet is another form of carb restriction, “but it’s much more drastic,” Dr. Lemanne said. “Most people require a carbohydrate load below 30 grams a day to enter a state of ketosis. But ketosis lowers the blood sugar and dampens the mTOR signaling.”
Evidence is emerging to support the use of a ketogenic diet as an adjunct to radiation therapy and as part of a complete course of treatment for glioblastoma multiforme and cancer cachexia. As an adjunct to radiation, a ketogenic diet decreases insulin and IGF-1 signaling. “This causes normal cells to enter dormancy, decreasing oxidative damage in normal cells,” Dr. Lemanne said. “There is also suppression of tumor angiogenesis, and thus poor DNA repair of radiation damage in tumor cells (Cancer Metastasis Rev. 2014;33[1]:217-29). Being in ketosis widens the therapeutic window. There are many animal studies which show that the ketogenic diet is helpful in cancer, mainly when combined with other anticancer treatments, such as radiation. Unfortunately, the evidence in humans is very anecdotal.”
One study found that if you feed mice with cancer ketogenic chow versus standard chow, they have a modestly improved survival (a mean of 43 days vs. 33 days; PLoS ONE. 2012;7[5]:e36197). However, when radiation was added to the keto diet, there was a dramatic improvement in survival (P less than 0.001). In fact, 75% survived to 250 days. “That’s pretty spectacular,” Dr. Lemanne said.
A ketogenic diet is standard therapy for several nonmalignant conditions, including glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency syndrome, and refractory infantile epilepsy. The three major ketone bodies involved in human nutrition are acetoacetate, beta hydroxybutyrate, and acetone. Dr. Lemanne said beta hydroxybutyrate decreases inflammation and inhibits hexadecynoic acids (which induces apoptosis in cancer cells). Beta hydroxybutyrate also increases sirtuins, innate immunity, and seizure threshold; modulates circadian rhythm; and decreases insulin levels, she said.
In one case report from the scientific literature, a 38-year-old male with glioblastoma multiforme was placed on a hypocaloric ketogenic diet (Front Nutr. 2018 Mar 29;5:20). The patient had surgery, radiation, chemotherapy, and hyperbaric oxygen, and was given high doses of green tea extract in an attempt to antagonize glutamine metabolism. Two years after the beginning of his treatment, he was alive and had maintained a good level of tumor regression.
“We’ll see how he does,” said Dr. Lemanne, who was not involved in the report. “In my experience, I have a patient right now with a diagnosis of glioblastoma multiforme. She’s getting a keto diet in combo with intensive chemo, radiation, and surgery. She’s also had some hyperbaric oxygen and IV ozone therapy and is taking repurposed drugs. She has exceeded her expected survival, but she continues to have disease and symptoms. We are by no means out of the woods with this patient. But the keto diet has been quite feasible for her, because she has a lot of family and outside support.”
A ketogenic diet also may benefit patients with cancer cachexia, which is a loss of lean tissue. “Cancer cachexia is not completely understood,” Dr. Lemanne said. “What we know is that it is caused by inflammation created by the tumor itself, and this, in turn results in severe insulin resistance. Therefore, giving more calories as carbohydrate makes the cancer cachexia situation worse. Animal models of cancer cachexia have shown that the ketogenic diet normalizes metabolism and prevents lean tissue loss. Human studies are underway; we’ll see how they turn out.”
She closed her presentation by noting that in copious amounts of animal studies, fasting has been linked to improvements in chemotherapy efficacy and decreased side effects. In one study carried out at the University of Southern California in Los Angeles, volunteers fasted up to 140 hours before chemotherapy and an additional 156 hours afterward (Aging. 2009;1[12]:988-1007). The researchers found that the fasting was well-tolerated.
“The patients had some mild light-headedness, but there were no adverse effects on tumor volume or serum tumor markers,” Dr. Lemanne said. A more recent study of patients on cisplatin found that acaloric fasting led to decreased DNA damage in white blood cells, decreased IFG-1, and better white blood cell counts (BMC Cancer. 2016 Jun 10;16:360). “The benefits are immediate, and the optimal fasting time appears to be 48 hours,” Dr. Lemanne said.
One of her patients is a 64-year-old man on adjuvant cisplatin-based chemotherapy for cholangiocarcinoma. He fasts 24 hours before and 24 hours after each infusion, and has experienced no emesis or nausea. “His immune suppression and anemia are much milder than we expected, and he has not required any treatment for chemotherapy-related side effects,” Dr. Lemanne said. “That’s a big monetary value.”
Fasting 13 hours overnight has been associated with fewer breast cancer-related problems in patients already diagnosed with the disease. Chronic caloric restriction, just cutting calories by 25%-40% daily, has been shown to delay all diseases of aging, including cancer, and is associated with increased longevity in many species. “Chronic caloric restriction is difficult, however, because it results in chronic hunger and weight loss,” she said. “Occasional fasting is superior to chronic caloric restriction because it maintains normal weight, preserves lean muscle mass, enhances tumor sensitivity to chemotherapy and radiotherapy, and diminishes the side effects of chemotherapy.”
Dr. Lemanne reported having no financial disclosures.
SAN DIEGO – When Dawn Lemanne, MD, MPH, meets with cancer patients and their families, the question invariably comes up: “What should I eat?”
“The answer always is, ‘It depends,’” Dr. Lemanne, an oncologist who founded Oregon Integrative Oncology in Ashland, said at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine. “The answers are not the same for each of these patients.”
According to Dr. Lemanne, targeted nutrition is evolving as a key component of cancer care. One of the goals of this approach is to decrease mTOR signaling. Normally, mTOR signaling promotes cell proliferation and metabolism; aberrant mTOR signaling can contribute to cancer initiation and progression.
“When mTOR speaks it says, ‘grow,’” said Dr. Lemanne, who is also an assistant professor of clinical medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona in Tucson. This message is meant to be heard by normal tissues, to stimulate normal tissue proliferation, such as in growing children or when a wound needs to be healed.
“However, cancer cells can hear and respond to mTOR’s message,” she said. “Normal cells may listen to mTOR’s ‘grow’ message or not, depending on the task they perform. Once we reach adulthood, we all likely have some precancerous or cancerous cells around, but they’re usually dormant. That’s why once you’re an adult, however, you don’t want too much mTOR signaling, because that might stimulate growth of things you definitely don’t want to grow.”
Having excessive levels of the growth hormone insulin-like growth factor-1 (IGF-1) also appears to play a role in cancer risk. Researchers studying members of a South American clan with Laron dwarfism – an inherited IGF-1 deficiency – found that besides being very short, affected members of this family rarely develop cancer (Cells. 2019;8[6]:596). “They also don’t get diabetes,” Dr. Lemanne said. “What we see in those with Laron dwarfism is that mTOR signaling is missing.”
She went on to note that studying type 2 diabetes gives physicians “a clue as to what dietary measures we might offer our patients in terms of decreasing their risk of dying from cancer or getting cancer.” The most common types of cancer are indeed more common in patients with type 2 diabetes. In addition, once someone with type 2 diabetes is diagnosed with cancer, their prognosis is poorer, compared with a cancer patient without diabetes.
“Metformin is often prescribed to patients with type 2 diabetes because it helps keep blood sugar low,” she said. “What’s fascinating is that diabetics on metformin develop cancer less frequently than diabetics not taking this drug. And also interesting, those diabetics who do develop cancer seem to do better if they’re on metformin before and after diagnosis.”
On the other hand, exogenous insulin therapy given to people with type 2 diabetes doubles the risk of cancer. Consistent with this is the two-decades-old finding that an elevated fasting insulin level also is associated with a poor breast cancer prognosis (J Clin Oncol. 2002 Jan 1;20[1]:42-51). “It’s really important to understand that, in a person destined to become a type 2 diabetic, the level of fasting insulin rises long before fasting glucose becomes abnormally high,” Dr. Lemanne explained. “A normal fasting glucose doesn’t let you off the hook in terms of checking your patient for insulin resistance.
“We will miss diagnosing many patients with dangerous insulin resistance and prediabetes if we don’t check the fasting glucose and the fasting insulin levels together. If the fasting insulin level is high, it’s important to limit carbohydrate intake enough to bring it down permanently, even when the fasting glucose is normal, or the patient is likely at increased risk for developing cancer.”
Two large, prospective randomized trials have examined breast cancer and diet: the Women’s Intervention Study (WINS) and the Women’s Health Eating and Living Study (WHEL). Patients in both trials had early stage breast cancer and were put on low-fat diets. In the end, there was a weak to negligible connection between breast cancer survival and dietary fat restriction. “That kind of shook up the oncology world,” Dr. Lemanne said, “because before these two studies, everyone ‘knew’ that dietary fat was related to breast cancer risk. These studies showed that wasn’t the case at all.”
According to Dr. Lemanne, unexpectedly, moderate carbohydrate restriction has been associated with lower risk of breast cancer recurrence in patients with postmenopausal hormone-receptor expressing breast cancer. Researchers at the University of California, San Diego, conducted a subanalysis of 265 postmenopausal patients with estrogen receptor positive breast cancer from the WHEL cohort (Cancer Epidemiol Biomarkers Prev. 2014 23[7]:1273-9). The recurrence risk was halved in those who cut their carbohydrate intake after diagnosis. The amount of decrease was modest, only 27 grams per day – the equivalent of one banana. “That is on par with a lot of our drugs, and maybe a little bit better,” she said. The effect was strongest if the breast tumor expressed IGF-1 receptor. Dr. Lemanne pointed out that decreasing dietary carbohydrate load was not the only treatment. These patients also had appropriate conventional cancer treatments, including surgery, radiation, and chemotherapy. “If we cut just some of the daily carb load in these patients, they might have a better cancer prognosis,” she said.
Overweight or obese patients with colon cancer also may benefit from moderate carbohydrate restriction. The CALGB 89803 study assessed 1,011 subjects with stage III colon cancer. It found that the subjects in the highest quintile of daily glycemic load and total carbohydrate intake had an increased risk of cancer recurrence and mortality (hazard ratio, 2.26; J Nat Cancer Inst. 2012;104[22]:1702-11). “This is pretty strong evidence that glycemic load and total carbohydrate intake play a role in colon cancer recurrence, but there’s a caveat here,” she said. “The effect was seen only in patients who were overweight or obese.” There was no association between carbohydrate intake and colon cancer recurrence in the absence of overweight or obesity.
Based on existing evidence, she said,
“That’s pretty modest; that’s 400 calories of carbohydrates per day,” Dr. Lemanne said. “I tell patients that they can have fruit, starchy vegetables, and even very small amounts of healthy whole grains, although I’m not a fan of grains due to the heavy carbohydrate load. All those things are OK. We’re not talking about jelly beans and white sugar.
“I also have them measure their fasting glucose each day, because different people have different blood glucose responses to the same food.” The goals she aims for with many of her patients are a fasting morning glucose between 79 and 83 mg/dL consistently, an HbA1c of 5.4 or less, and a BMI of 24.9 kg/m2 or less. “This set of goals, however, has to be individualized,” she said.
The ketogenic diet is another form of carb restriction, “but it’s much more drastic,” Dr. Lemanne said. “Most people require a carbohydrate load below 30 grams a day to enter a state of ketosis. But ketosis lowers the blood sugar and dampens the mTOR signaling.”
Evidence is emerging to support the use of a ketogenic diet as an adjunct to radiation therapy and as part of a complete course of treatment for glioblastoma multiforme and cancer cachexia. As an adjunct to radiation, a ketogenic diet decreases insulin and IGF-1 signaling. “This causes normal cells to enter dormancy, decreasing oxidative damage in normal cells,” Dr. Lemanne said. “There is also suppression of tumor angiogenesis, and thus poor DNA repair of radiation damage in tumor cells (Cancer Metastasis Rev. 2014;33[1]:217-29). Being in ketosis widens the therapeutic window. There are many animal studies which show that the ketogenic diet is helpful in cancer, mainly when combined with other anticancer treatments, such as radiation. Unfortunately, the evidence in humans is very anecdotal.”
One study found that if you feed mice with cancer ketogenic chow versus standard chow, they have a modestly improved survival (a mean of 43 days vs. 33 days; PLoS ONE. 2012;7[5]:e36197). However, when radiation was added to the keto diet, there was a dramatic improvement in survival (P less than 0.001). In fact, 75% survived to 250 days. “That’s pretty spectacular,” Dr. Lemanne said.
A ketogenic diet is standard therapy for several nonmalignant conditions, including glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency syndrome, and refractory infantile epilepsy. The three major ketone bodies involved in human nutrition are acetoacetate, beta hydroxybutyrate, and acetone. Dr. Lemanne said beta hydroxybutyrate decreases inflammation and inhibits hexadecynoic acids (which induces apoptosis in cancer cells). Beta hydroxybutyrate also increases sirtuins, innate immunity, and seizure threshold; modulates circadian rhythm; and decreases insulin levels, she said.
In one case report from the scientific literature, a 38-year-old male with glioblastoma multiforme was placed on a hypocaloric ketogenic diet (Front Nutr. 2018 Mar 29;5:20). The patient had surgery, radiation, chemotherapy, and hyperbaric oxygen, and was given high doses of green tea extract in an attempt to antagonize glutamine metabolism. Two years after the beginning of his treatment, he was alive and had maintained a good level of tumor regression.
“We’ll see how he does,” said Dr. Lemanne, who was not involved in the report. “In my experience, I have a patient right now with a diagnosis of glioblastoma multiforme. She’s getting a keto diet in combo with intensive chemo, radiation, and surgery. She’s also had some hyperbaric oxygen and IV ozone therapy and is taking repurposed drugs. She has exceeded her expected survival, but she continues to have disease and symptoms. We are by no means out of the woods with this patient. But the keto diet has been quite feasible for her, because she has a lot of family and outside support.”
A ketogenic diet also may benefit patients with cancer cachexia, which is a loss of lean tissue. “Cancer cachexia is not completely understood,” Dr. Lemanne said. “What we know is that it is caused by inflammation created by the tumor itself, and this, in turn results in severe insulin resistance. Therefore, giving more calories as carbohydrate makes the cancer cachexia situation worse. Animal models of cancer cachexia have shown that the ketogenic diet normalizes metabolism and prevents lean tissue loss. Human studies are underway; we’ll see how they turn out.”
She closed her presentation by noting that in copious amounts of animal studies, fasting has been linked to improvements in chemotherapy efficacy and decreased side effects. In one study carried out at the University of Southern California in Los Angeles, volunteers fasted up to 140 hours before chemotherapy and an additional 156 hours afterward (Aging. 2009;1[12]:988-1007). The researchers found that the fasting was well-tolerated.
“The patients had some mild light-headedness, but there were no adverse effects on tumor volume or serum tumor markers,” Dr. Lemanne said. A more recent study of patients on cisplatin found that acaloric fasting led to decreased DNA damage in white blood cells, decreased IFG-1, and better white blood cell counts (BMC Cancer. 2016 Jun 10;16:360). “The benefits are immediate, and the optimal fasting time appears to be 48 hours,” Dr. Lemanne said.
One of her patients is a 64-year-old man on adjuvant cisplatin-based chemotherapy for cholangiocarcinoma. He fasts 24 hours before and 24 hours after each infusion, and has experienced no emesis or nausea. “His immune suppression and anemia are much milder than we expected, and he has not required any treatment for chemotherapy-related side effects,” Dr. Lemanne said. “That’s a big monetary value.”
Fasting 13 hours overnight has been associated with fewer breast cancer-related problems in patients already diagnosed with the disease. Chronic caloric restriction, just cutting calories by 25%-40% daily, has been shown to delay all diseases of aging, including cancer, and is associated with increased longevity in many species. “Chronic caloric restriction is difficult, however, because it results in chronic hunger and weight loss,” she said. “Occasional fasting is superior to chronic caloric restriction because it maintains normal weight, preserves lean muscle mass, enhances tumor sensitivity to chemotherapy and radiotherapy, and diminishes the side effects of chemotherapy.”
Dr. Lemanne reported having no financial disclosures.
SAN DIEGO – When Dawn Lemanne, MD, MPH, meets with cancer patients and their families, the question invariably comes up: “What should I eat?”
“The answer always is, ‘It depends,’” Dr. Lemanne, an oncologist who founded Oregon Integrative Oncology in Ashland, said at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine. “The answers are not the same for each of these patients.”
According to Dr. Lemanne, targeted nutrition is evolving as a key component of cancer care. One of the goals of this approach is to decrease mTOR signaling. Normally, mTOR signaling promotes cell proliferation and metabolism; aberrant mTOR signaling can contribute to cancer initiation and progression.
“When mTOR speaks it says, ‘grow,’” said Dr. Lemanne, who is also an assistant professor of clinical medicine at the Andrew Weil Center for Integrative Medicine at the University of Arizona in Tucson. This message is meant to be heard by normal tissues, to stimulate normal tissue proliferation, such as in growing children or when a wound needs to be healed.
“However, cancer cells can hear and respond to mTOR’s message,” she said. “Normal cells may listen to mTOR’s ‘grow’ message or not, depending on the task they perform. Once we reach adulthood, we all likely have some precancerous or cancerous cells around, but they’re usually dormant. That’s why once you’re an adult, however, you don’t want too much mTOR signaling, because that might stimulate growth of things you definitely don’t want to grow.”
Having excessive levels of the growth hormone insulin-like growth factor-1 (IGF-1) also appears to play a role in cancer risk. Researchers studying members of a South American clan with Laron dwarfism – an inherited IGF-1 deficiency – found that besides being very short, affected members of this family rarely develop cancer (Cells. 2019;8[6]:596). “They also don’t get diabetes,” Dr. Lemanne said. “What we see in those with Laron dwarfism is that mTOR signaling is missing.”
She went on to note that studying type 2 diabetes gives physicians “a clue as to what dietary measures we might offer our patients in terms of decreasing their risk of dying from cancer or getting cancer.” The most common types of cancer are indeed more common in patients with type 2 diabetes. In addition, once someone with type 2 diabetes is diagnosed with cancer, their prognosis is poorer, compared with a cancer patient without diabetes.
“Metformin is often prescribed to patients with type 2 diabetes because it helps keep blood sugar low,” she said. “What’s fascinating is that diabetics on metformin develop cancer less frequently than diabetics not taking this drug. And also interesting, those diabetics who do develop cancer seem to do better if they’re on metformin before and after diagnosis.”
On the other hand, exogenous insulin therapy given to people with type 2 diabetes doubles the risk of cancer. Consistent with this is the two-decades-old finding that an elevated fasting insulin level also is associated with a poor breast cancer prognosis (J Clin Oncol. 2002 Jan 1;20[1]:42-51). “It’s really important to understand that, in a person destined to become a type 2 diabetic, the level of fasting insulin rises long before fasting glucose becomes abnormally high,” Dr. Lemanne explained. “A normal fasting glucose doesn’t let you off the hook in terms of checking your patient for insulin resistance.
“We will miss diagnosing many patients with dangerous insulin resistance and prediabetes if we don’t check the fasting glucose and the fasting insulin levels together. If the fasting insulin level is high, it’s important to limit carbohydrate intake enough to bring it down permanently, even when the fasting glucose is normal, or the patient is likely at increased risk for developing cancer.”
Two large, prospective randomized trials have examined breast cancer and diet: the Women’s Intervention Study (WINS) and the Women’s Health Eating and Living Study (WHEL). Patients in both trials had early stage breast cancer and were put on low-fat diets. In the end, there was a weak to negligible connection between breast cancer survival and dietary fat restriction. “That kind of shook up the oncology world,” Dr. Lemanne said, “because before these two studies, everyone ‘knew’ that dietary fat was related to breast cancer risk. These studies showed that wasn’t the case at all.”
According to Dr. Lemanne, unexpectedly, moderate carbohydrate restriction has been associated with lower risk of breast cancer recurrence in patients with postmenopausal hormone-receptor expressing breast cancer. Researchers at the University of California, San Diego, conducted a subanalysis of 265 postmenopausal patients with estrogen receptor positive breast cancer from the WHEL cohort (Cancer Epidemiol Biomarkers Prev. 2014 23[7]:1273-9). The recurrence risk was halved in those who cut their carbohydrate intake after diagnosis. The amount of decrease was modest, only 27 grams per day – the equivalent of one banana. “That is on par with a lot of our drugs, and maybe a little bit better,” she said. The effect was strongest if the breast tumor expressed IGF-1 receptor. Dr. Lemanne pointed out that decreasing dietary carbohydrate load was not the only treatment. These patients also had appropriate conventional cancer treatments, including surgery, radiation, and chemotherapy. “If we cut just some of the daily carb load in these patients, they might have a better cancer prognosis,” she said.
Overweight or obese patients with colon cancer also may benefit from moderate carbohydrate restriction. The CALGB 89803 study assessed 1,011 subjects with stage III colon cancer. It found that the subjects in the highest quintile of daily glycemic load and total carbohydrate intake had an increased risk of cancer recurrence and mortality (hazard ratio, 2.26; J Nat Cancer Inst. 2012;104[22]:1702-11). “This is pretty strong evidence that glycemic load and total carbohydrate intake play a role in colon cancer recurrence, but there’s a caveat here,” she said. “The effect was seen only in patients who were overweight or obese.” There was no association between carbohydrate intake and colon cancer recurrence in the absence of overweight or obesity.
Based on existing evidence, she said,
“That’s pretty modest; that’s 400 calories of carbohydrates per day,” Dr. Lemanne said. “I tell patients that they can have fruit, starchy vegetables, and even very small amounts of healthy whole grains, although I’m not a fan of grains due to the heavy carbohydrate load. All those things are OK. We’re not talking about jelly beans and white sugar.
“I also have them measure their fasting glucose each day, because different people have different blood glucose responses to the same food.” The goals she aims for with many of her patients are a fasting morning glucose between 79 and 83 mg/dL consistently, an HbA1c of 5.4 or less, and a BMI of 24.9 kg/m2 or less. “This set of goals, however, has to be individualized,” she said.
The ketogenic diet is another form of carb restriction, “but it’s much more drastic,” Dr. Lemanne said. “Most people require a carbohydrate load below 30 grams a day to enter a state of ketosis. But ketosis lowers the blood sugar and dampens the mTOR signaling.”
Evidence is emerging to support the use of a ketogenic diet as an adjunct to radiation therapy and as part of a complete course of treatment for glioblastoma multiforme and cancer cachexia. As an adjunct to radiation, a ketogenic diet decreases insulin and IGF-1 signaling. “This causes normal cells to enter dormancy, decreasing oxidative damage in normal cells,” Dr. Lemanne said. “There is also suppression of tumor angiogenesis, and thus poor DNA repair of radiation damage in tumor cells (Cancer Metastasis Rev. 2014;33[1]:217-29). Being in ketosis widens the therapeutic window. There are many animal studies which show that the ketogenic diet is helpful in cancer, mainly when combined with other anticancer treatments, such as radiation. Unfortunately, the evidence in humans is very anecdotal.”
One study found that if you feed mice with cancer ketogenic chow versus standard chow, they have a modestly improved survival (a mean of 43 days vs. 33 days; PLoS ONE. 2012;7[5]:e36197). However, when radiation was added to the keto diet, there was a dramatic improvement in survival (P less than 0.001). In fact, 75% survived to 250 days. “That’s pretty spectacular,” Dr. Lemanne said.
A ketogenic diet is standard therapy for several nonmalignant conditions, including glucose transporter 1 deficiency syndrome, pyruvate dehydrogenase deficiency syndrome, and refractory infantile epilepsy. The three major ketone bodies involved in human nutrition are acetoacetate, beta hydroxybutyrate, and acetone. Dr. Lemanne said beta hydroxybutyrate decreases inflammation and inhibits hexadecynoic acids (which induces apoptosis in cancer cells). Beta hydroxybutyrate also increases sirtuins, innate immunity, and seizure threshold; modulates circadian rhythm; and decreases insulin levels, she said.
In one case report from the scientific literature, a 38-year-old male with glioblastoma multiforme was placed on a hypocaloric ketogenic diet (Front Nutr. 2018 Mar 29;5:20). The patient had surgery, radiation, chemotherapy, and hyperbaric oxygen, and was given high doses of green tea extract in an attempt to antagonize glutamine metabolism. Two years after the beginning of his treatment, he was alive and had maintained a good level of tumor regression.
“We’ll see how he does,” said Dr. Lemanne, who was not involved in the report. “In my experience, I have a patient right now with a diagnosis of glioblastoma multiforme. She’s getting a keto diet in combo with intensive chemo, radiation, and surgery. She’s also had some hyperbaric oxygen and IV ozone therapy and is taking repurposed drugs. She has exceeded her expected survival, but she continues to have disease and symptoms. We are by no means out of the woods with this patient. But the keto diet has been quite feasible for her, because she has a lot of family and outside support.”
A ketogenic diet also may benefit patients with cancer cachexia, which is a loss of lean tissue. “Cancer cachexia is not completely understood,” Dr. Lemanne said. “What we know is that it is caused by inflammation created by the tumor itself, and this, in turn results in severe insulin resistance. Therefore, giving more calories as carbohydrate makes the cancer cachexia situation worse. Animal models of cancer cachexia have shown that the ketogenic diet normalizes metabolism and prevents lean tissue loss. Human studies are underway; we’ll see how they turn out.”
She closed her presentation by noting that in copious amounts of animal studies, fasting has been linked to improvements in chemotherapy efficacy and decreased side effects. In one study carried out at the University of Southern California in Los Angeles, volunteers fasted up to 140 hours before chemotherapy and an additional 156 hours afterward (Aging. 2009;1[12]:988-1007). The researchers found that the fasting was well-tolerated.
“The patients had some mild light-headedness, but there were no adverse effects on tumor volume or serum tumor markers,” Dr. Lemanne said. A more recent study of patients on cisplatin found that acaloric fasting led to decreased DNA damage in white blood cells, decreased IFG-1, and better white blood cell counts (BMC Cancer. 2016 Jun 10;16:360). “The benefits are immediate, and the optimal fasting time appears to be 48 hours,” Dr. Lemanne said.
One of her patients is a 64-year-old man on adjuvant cisplatin-based chemotherapy for cholangiocarcinoma. He fasts 24 hours before and 24 hours after each infusion, and has experienced no emesis or nausea. “His immune suppression and anemia are much milder than we expected, and he has not required any treatment for chemotherapy-related side effects,” Dr. Lemanne said. “That’s a big monetary value.”
Fasting 13 hours overnight has been associated with fewer breast cancer-related problems in patients already diagnosed with the disease. Chronic caloric restriction, just cutting calories by 25%-40% daily, has been shown to delay all diseases of aging, including cancer, and is associated with increased longevity in many species. “Chronic caloric restriction is difficult, however, because it results in chronic hunger and weight loss,” she said. “Occasional fasting is superior to chronic caloric restriction because it maintains normal weight, preserves lean muscle mass, enhances tumor sensitivity to chemotherapy and radiotherapy, and diminishes the side effects of chemotherapy.”
Dr. Lemanne reported having no financial disclosures.
REPORTING FROM A NATURAL SUPPLEMENTS UPDATE