User login
Temper tantrums, bullying colleagues: How to avert physician misbehavior?
Daniel Freedman, DO, a pediatric neurologist in Austin, Tex., remembers being flabbergasted when a surgeon threw an instrument across the room in medical school.
“I remember thinking, ‘I can’t believe people actually do this, a grown man in his 50s having a temper tantrum,’” Dr. Freedman said in an interview. But it certainly wasn’t the last time he witnessed bad behavior by one of his peers.
The results of Medscape’s recent report, Physicians Behaving Badly: Stress and Hardship Trigger Misconduct, suggest he has plenty of company. More than 4 in 10 respondents (41%) observed inappropriate behavior in the workplace in 2022, an uptick from 35% in 2021, according to the report, which polled more than 1,500 physicians about inappropriate behavior on and off the clock.
Of course, 38% of respondents have not seen any instances of misbehavior; and many of the instances that were seen were mild or infrequent. Additionally, instances of bad behavior have declined significantly over the past 5 years.
Dr. Freedman said he learned a lesson from his mentor and program director during training that has stuck with him throughout his career. “If you couldn’t act that way at any job, whether at McDonald’s or any other possible place, you shouldn’t act that way in medicine.” But he recognizes one limitation of that advice. “A lot of the people that behave badly may not have ever worked in a different environment before,” he said.
“They only perceive that they’re at the top of the food chain, so they can behave badly without repercussions.”
What Dr. Freedman described is formally called disruptive physician behavior, one of several categories of inappropriate behavior in medicine, according to Charles Samenow, MD, MPH, an associate professor of psychiatry and behavioral sciences at George Washington University, Washington, who has studied this phenomenon for years.
“Disruptive physician behavior compromises the safety of the workplace,” Dr. Samenow explained. The behavior can occur at work, outside of work, or on social media. It can hinder operations, threaten patient and staff safety, and affect workplace morale.
“The question is trying to understand where that bad behavior is coming from and the impact of that bad behavior,” Dr. Samenow said in an interview.
One reason is fairly simple: doctors are human, and humans have a wide range of behavior. Plus, as the Medscape survey showed,
Self-selecting traits become an Achilles heel
“Any human put in a position of power over other humans has the potential to be disruptive, harass, etc, if they have certain personality traits,” said David Gorski, MD, a professor of surgery at Wayne State University, Detroit. That jibes with Dr. Samenow’s research.
Classic disruptive behavior isn’t usually associated with depression, mania, psychosis, or similar characteristics, Dr. Samenow explained. Rather, it tends to be personality driven. “Physicians are not immune to the normal problems every human being faces,” he said.
In the Medscape report, physicians cited personal arrogance as one of the leading reasons physicians engaged in inappropriate behavior (56%), followed closely by personal problems outside of work (52%), a social shift in accepting more casual behavior (50%), and job-related stress (46%). (Respondents could choose more than one answer).
One factor contributing to misbehavior that Dr. Samenow has consistently identified in his research is a history of adverse childhood experiences or family dysfunction: People who grew up in homes with physical or verbal abuse learned anger as a coping skill instead of positive, assertive communication. It’s likely that some physicians, as well as the overall population, learned anger as a coping skill for that reason.
How to help avert disruptive behavior in medical settings
Dr. Samenow said that coaching is a “wonderful tool” in teaching the interpersonal skills that medical school often doesn’t address.
In some case, interventions can be very helpful. For example, programs that teach effective communication strategies and teamwork through a combination of culturally sensitive dialectical and cognitive-behavioral therapy and other modalities have been successful, Dr. Samenow said. Although they are more about treating an illness than addressing “misbehavior,” programs for substance use that have been developed by and for doctors are very effective, too.
Fewer resources are available, however, for addressing racism, classism, misogyny, and other forms of bigotry, Dr. Samenow noted. “There’s implicit bias training, but not at the level of what exists for disruptive physicians and those with addiction. “That’s an area we need to work on.” Racist language was the third most commonly observed bad behavior cited in the Medscape survey, behind only bullying of staff and mocking or disparaging of patients. It was reported frequently outside of work as well.
The Medscape report found an increase in observed behavior at work and on social media, although it’s hard to determine prevalence trends over time, Dr. Samenow said. “The tolerance for this behavior has really gone down,” likely leading to more reporting, he said, and more systems for reporting bad behavior exist today than in the past.
However, Dr. Freedman said inadequate regulation, disciplinary action, and follow-through remain a problem.
“There are lots of limitations to our reporting system and to our follow-through with those reports,” including hospitals that, whether for fear of litigation or other reasons, allow physicians to quietly resign and move to another institution, even with positive recommendations, Dr. Freedman said.
Indeed, only a third of observed misbehavior in the Medscape report resulted in disciplinary action. Half the respondents believed a verbal warning was a necessary consequence, followed by a conversation from management and being reported to a supervisor or human resources. Though only 10% thought a report to the medical board was warranted, it likely depends on the offense and its frequency.
“I think going from paternalism to more patient-centered care and having patients involved in those conversations is a nice shift that makes doctors more human and relatable, and hopefully makes the public more forgiving, that we’re going to make mistakes and nobody’s perfect,” Freedman said. But he added that physicians should be held accountable when a mistake or two becomes a pattern.
Misinformation is professional misconduct
Sufficient accountability is especially absent, these doctors said, for a subset of professional misconduct: spreading misinformation.
While more “conventional” bad behaviors include fraud, dishonesty, abuse of underlings, and incompetence, bad behavior should also include “selling quackery and antivaccine misinformation, the way some doctors did with various nostrums for COVID-19,” said Dr. Gorski, who frequently blogs about doctors’ spreading misinformation.
Taylor Nichols, MD, an emergency medicine physician based in Sacramento, cites the desire for attention and clout as motivations. “Saying things that are wildly, provably false is professional misconduct,” Nichols said. He distinguished such statements from scientific, academic, or clinical disagreement that is necessary within medicine.
Yet there’s been a “long tradition of looking the other way or letting people with fancy titles get away with saying nonsense just because they’re respected,” Jonathan Howard, MD, an associate professor of psychiatry and neurology at New York University said in an interview.
“We have a duty to be trusted members of the community,” Dr. Howard said. “People listen when we say things, and we have an obligation to try to be accurate and humble and as honest as possible and admit mistakes when we inevitably make them.”
That extends to social media, which Dr. Nichols said has magnified the problem of promoting quackery and misinformation. He thinks medical boards and professional credentialing bodies should pay attention to what’s happening in the public conversation and understand that our professional responsibility extends beyond the walls of the hospital or clinic. Physicians must represent themselves professionally and uphold the standards that the profession expects.
On the one hand, Medscape respondents agreed: 70% said one doctor’s misbehavior taints the whole profession. Yet, at the same time, 58% of respondents believed physicians should be able to “keep their private lives private” in 2022. But that’s not the reality of the profession when the lines between private life and behavior away from work get blurred, Dr. Samenow said.
“The way a physician behaves in public represents you,” he said. “What happens in Vegas doesn’t always stay in Vegas.”
A version of this article first appeared on Medscape.com.
Daniel Freedman, DO, a pediatric neurologist in Austin, Tex., remembers being flabbergasted when a surgeon threw an instrument across the room in medical school.
“I remember thinking, ‘I can’t believe people actually do this, a grown man in his 50s having a temper tantrum,’” Dr. Freedman said in an interview. But it certainly wasn’t the last time he witnessed bad behavior by one of his peers.
The results of Medscape’s recent report, Physicians Behaving Badly: Stress and Hardship Trigger Misconduct, suggest he has plenty of company. More than 4 in 10 respondents (41%) observed inappropriate behavior in the workplace in 2022, an uptick from 35% in 2021, according to the report, which polled more than 1,500 physicians about inappropriate behavior on and off the clock.
Of course, 38% of respondents have not seen any instances of misbehavior; and many of the instances that were seen were mild or infrequent. Additionally, instances of bad behavior have declined significantly over the past 5 years.
Dr. Freedman said he learned a lesson from his mentor and program director during training that has stuck with him throughout his career. “If you couldn’t act that way at any job, whether at McDonald’s or any other possible place, you shouldn’t act that way in medicine.” But he recognizes one limitation of that advice. “A lot of the people that behave badly may not have ever worked in a different environment before,” he said.
“They only perceive that they’re at the top of the food chain, so they can behave badly without repercussions.”
What Dr. Freedman described is formally called disruptive physician behavior, one of several categories of inappropriate behavior in medicine, according to Charles Samenow, MD, MPH, an associate professor of psychiatry and behavioral sciences at George Washington University, Washington, who has studied this phenomenon for years.
“Disruptive physician behavior compromises the safety of the workplace,” Dr. Samenow explained. The behavior can occur at work, outside of work, or on social media. It can hinder operations, threaten patient and staff safety, and affect workplace morale.
“The question is trying to understand where that bad behavior is coming from and the impact of that bad behavior,” Dr. Samenow said in an interview.
One reason is fairly simple: doctors are human, and humans have a wide range of behavior. Plus, as the Medscape survey showed,
Self-selecting traits become an Achilles heel
“Any human put in a position of power over other humans has the potential to be disruptive, harass, etc, if they have certain personality traits,” said David Gorski, MD, a professor of surgery at Wayne State University, Detroit. That jibes with Dr. Samenow’s research.
Classic disruptive behavior isn’t usually associated with depression, mania, psychosis, or similar characteristics, Dr. Samenow explained. Rather, it tends to be personality driven. “Physicians are not immune to the normal problems every human being faces,” he said.
In the Medscape report, physicians cited personal arrogance as one of the leading reasons physicians engaged in inappropriate behavior (56%), followed closely by personal problems outside of work (52%), a social shift in accepting more casual behavior (50%), and job-related stress (46%). (Respondents could choose more than one answer).
One factor contributing to misbehavior that Dr. Samenow has consistently identified in his research is a history of adverse childhood experiences or family dysfunction: People who grew up in homes with physical or verbal abuse learned anger as a coping skill instead of positive, assertive communication. It’s likely that some physicians, as well as the overall population, learned anger as a coping skill for that reason.
How to help avert disruptive behavior in medical settings
Dr. Samenow said that coaching is a “wonderful tool” in teaching the interpersonal skills that medical school often doesn’t address.
In some case, interventions can be very helpful. For example, programs that teach effective communication strategies and teamwork through a combination of culturally sensitive dialectical and cognitive-behavioral therapy and other modalities have been successful, Dr. Samenow said. Although they are more about treating an illness than addressing “misbehavior,” programs for substance use that have been developed by and for doctors are very effective, too.
Fewer resources are available, however, for addressing racism, classism, misogyny, and other forms of bigotry, Dr. Samenow noted. “There’s implicit bias training, but not at the level of what exists for disruptive physicians and those with addiction. “That’s an area we need to work on.” Racist language was the third most commonly observed bad behavior cited in the Medscape survey, behind only bullying of staff and mocking or disparaging of patients. It was reported frequently outside of work as well.
The Medscape report found an increase in observed behavior at work and on social media, although it’s hard to determine prevalence trends over time, Dr. Samenow said. “The tolerance for this behavior has really gone down,” likely leading to more reporting, he said, and more systems for reporting bad behavior exist today than in the past.
However, Dr. Freedman said inadequate regulation, disciplinary action, and follow-through remain a problem.
“There are lots of limitations to our reporting system and to our follow-through with those reports,” including hospitals that, whether for fear of litigation or other reasons, allow physicians to quietly resign and move to another institution, even with positive recommendations, Dr. Freedman said.
Indeed, only a third of observed misbehavior in the Medscape report resulted in disciplinary action. Half the respondents believed a verbal warning was a necessary consequence, followed by a conversation from management and being reported to a supervisor or human resources. Though only 10% thought a report to the medical board was warranted, it likely depends on the offense and its frequency.
“I think going from paternalism to more patient-centered care and having patients involved in those conversations is a nice shift that makes doctors more human and relatable, and hopefully makes the public more forgiving, that we’re going to make mistakes and nobody’s perfect,” Freedman said. But he added that physicians should be held accountable when a mistake or two becomes a pattern.
Misinformation is professional misconduct
Sufficient accountability is especially absent, these doctors said, for a subset of professional misconduct: spreading misinformation.
While more “conventional” bad behaviors include fraud, dishonesty, abuse of underlings, and incompetence, bad behavior should also include “selling quackery and antivaccine misinformation, the way some doctors did with various nostrums for COVID-19,” said Dr. Gorski, who frequently blogs about doctors’ spreading misinformation.
Taylor Nichols, MD, an emergency medicine physician based in Sacramento, cites the desire for attention and clout as motivations. “Saying things that are wildly, provably false is professional misconduct,” Nichols said. He distinguished such statements from scientific, academic, or clinical disagreement that is necessary within medicine.
Yet there’s been a “long tradition of looking the other way or letting people with fancy titles get away with saying nonsense just because they’re respected,” Jonathan Howard, MD, an associate professor of psychiatry and neurology at New York University said in an interview.
“We have a duty to be trusted members of the community,” Dr. Howard said. “People listen when we say things, and we have an obligation to try to be accurate and humble and as honest as possible and admit mistakes when we inevitably make them.”
That extends to social media, which Dr. Nichols said has magnified the problem of promoting quackery and misinformation. He thinks medical boards and professional credentialing bodies should pay attention to what’s happening in the public conversation and understand that our professional responsibility extends beyond the walls of the hospital or clinic. Physicians must represent themselves professionally and uphold the standards that the profession expects.
On the one hand, Medscape respondents agreed: 70% said one doctor’s misbehavior taints the whole profession. Yet, at the same time, 58% of respondents believed physicians should be able to “keep their private lives private” in 2022. But that’s not the reality of the profession when the lines between private life and behavior away from work get blurred, Dr. Samenow said.
“The way a physician behaves in public represents you,” he said. “What happens in Vegas doesn’t always stay in Vegas.”
A version of this article first appeared on Medscape.com.
Daniel Freedman, DO, a pediatric neurologist in Austin, Tex., remembers being flabbergasted when a surgeon threw an instrument across the room in medical school.
“I remember thinking, ‘I can’t believe people actually do this, a grown man in his 50s having a temper tantrum,’” Dr. Freedman said in an interview. But it certainly wasn’t the last time he witnessed bad behavior by one of his peers.
The results of Medscape’s recent report, Physicians Behaving Badly: Stress and Hardship Trigger Misconduct, suggest he has plenty of company. More than 4 in 10 respondents (41%) observed inappropriate behavior in the workplace in 2022, an uptick from 35% in 2021, according to the report, which polled more than 1,500 physicians about inappropriate behavior on and off the clock.
Of course, 38% of respondents have not seen any instances of misbehavior; and many of the instances that were seen were mild or infrequent. Additionally, instances of bad behavior have declined significantly over the past 5 years.
Dr. Freedman said he learned a lesson from his mentor and program director during training that has stuck with him throughout his career. “If you couldn’t act that way at any job, whether at McDonald’s or any other possible place, you shouldn’t act that way in medicine.” But he recognizes one limitation of that advice. “A lot of the people that behave badly may not have ever worked in a different environment before,” he said.
“They only perceive that they’re at the top of the food chain, so they can behave badly without repercussions.”
What Dr. Freedman described is formally called disruptive physician behavior, one of several categories of inappropriate behavior in medicine, according to Charles Samenow, MD, MPH, an associate professor of psychiatry and behavioral sciences at George Washington University, Washington, who has studied this phenomenon for years.
“Disruptive physician behavior compromises the safety of the workplace,” Dr. Samenow explained. The behavior can occur at work, outside of work, or on social media. It can hinder operations, threaten patient and staff safety, and affect workplace morale.
“The question is trying to understand where that bad behavior is coming from and the impact of that bad behavior,” Dr. Samenow said in an interview.
One reason is fairly simple: doctors are human, and humans have a wide range of behavior. Plus, as the Medscape survey showed,
Self-selecting traits become an Achilles heel
“Any human put in a position of power over other humans has the potential to be disruptive, harass, etc, if they have certain personality traits,” said David Gorski, MD, a professor of surgery at Wayne State University, Detroit. That jibes with Dr. Samenow’s research.
Classic disruptive behavior isn’t usually associated with depression, mania, psychosis, or similar characteristics, Dr. Samenow explained. Rather, it tends to be personality driven. “Physicians are not immune to the normal problems every human being faces,” he said.
In the Medscape report, physicians cited personal arrogance as one of the leading reasons physicians engaged in inappropriate behavior (56%), followed closely by personal problems outside of work (52%), a social shift in accepting more casual behavior (50%), and job-related stress (46%). (Respondents could choose more than one answer).
One factor contributing to misbehavior that Dr. Samenow has consistently identified in his research is a history of adverse childhood experiences or family dysfunction: People who grew up in homes with physical or verbal abuse learned anger as a coping skill instead of positive, assertive communication. It’s likely that some physicians, as well as the overall population, learned anger as a coping skill for that reason.
How to help avert disruptive behavior in medical settings
Dr. Samenow said that coaching is a “wonderful tool” in teaching the interpersonal skills that medical school often doesn’t address.
In some case, interventions can be very helpful. For example, programs that teach effective communication strategies and teamwork through a combination of culturally sensitive dialectical and cognitive-behavioral therapy and other modalities have been successful, Dr. Samenow said. Although they are more about treating an illness than addressing “misbehavior,” programs for substance use that have been developed by and for doctors are very effective, too.
Fewer resources are available, however, for addressing racism, classism, misogyny, and other forms of bigotry, Dr. Samenow noted. “There’s implicit bias training, but not at the level of what exists for disruptive physicians and those with addiction. “That’s an area we need to work on.” Racist language was the third most commonly observed bad behavior cited in the Medscape survey, behind only bullying of staff and mocking or disparaging of patients. It was reported frequently outside of work as well.
The Medscape report found an increase in observed behavior at work and on social media, although it’s hard to determine prevalence trends over time, Dr. Samenow said. “The tolerance for this behavior has really gone down,” likely leading to more reporting, he said, and more systems for reporting bad behavior exist today than in the past.
However, Dr. Freedman said inadequate regulation, disciplinary action, and follow-through remain a problem.
“There are lots of limitations to our reporting system and to our follow-through with those reports,” including hospitals that, whether for fear of litigation or other reasons, allow physicians to quietly resign and move to another institution, even with positive recommendations, Dr. Freedman said.
Indeed, only a third of observed misbehavior in the Medscape report resulted in disciplinary action. Half the respondents believed a verbal warning was a necessary consequence, followed by a conversation from management and being reported to a supervisor or human resources. Though only 10% thought a report to the medical board was warranted, it likely depends on the offense and its frequency.
“I think going from paternalism to more patient-centered care and having patients involved in those conversations is a nice shift that makes doctors more human and relatable, and hopefully makes the public more forgiving, that we’re going to make mistakes and nobody’s perfect,” Freedman said. But he added that physicians should be held accountable when a mistake or two becomes a pattern.
Misinformation is professional misconduct
Sufficient accountability is especially absent, these doctors said, for a subset of professional misconduct: spreading misinformation.
While more “conventional” bad behaviors include fraud, dishonesty, abuse of underlings, and incompetence, bad behavior should also include “selling quackery and antivaccine misinformation, the way some doctors did with various nostrums for COVID-19,” said Dr. Gorski, who frequently blogs about doctors’ spreading misinformation.
Taylor Nichols, MD, an emergency medicine physician based in Sacramento, cites the desire for attention and clout as motivations. “Saying things that are wildly, provably false is professional misconduct,” Nichols said. He distinguished such statements from scientific, academic, or clinical disagreement that is necessary within medicine.
Yet there’s been a “long tradition of looking the other way or letting people with fancy titles get away with saying nonsense just because they’re respected,” Jonathan Howard, MD, an associate professor of psychiatry and neurology at New York University said in an interview.
“We have a duty to be trusted members of the community,” Dr. Howard said. “People listen when we say things, and we have an obligation to try to be accurate and humble and as honest as possible and admit mistakes when we inevitably make them.”
That extends to social media, which Dr. Nichols said has magnified the problem of promoting quackery and misinformation. He thinks medical boards and professional credentialing bodies should pay attention to what’s happening in the public conversation and understand that our professional responsibility extends beyond the walls of the hospital or clinic. Physicians must represent themselves professionally and uphold the standards that the profession expects.
On the one hand, Medscape respondents agreed: 70% said one doctor’s misbehavior taints the whole profession. Yet, at the same time, 58% of respondents believed physicians should be able to “keep their private lives private” in 2022. But that’s not the reality of the profession when the lines between private life and behavior away from work get blurred, Dr. Samenow said.
“The way a physician behaves in public represents you,” he said. “What happens in Vegas doesn’t always stay in Vegas.”
A version of this article first appeared on Medscape.com.
Med groups urge feds to protect physicians from anti-trans violence
Several leading medical groups on Oct. 3 called on U.S. Attorney General Merrick Garland to investigate and prosecute those responsible for a recent spate of threats and attacks against hospitals and physicians who are providing gender-affirming care.
In an Oct. 3 letter, the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the Children’s Hospital Association detailed the risk posed by these threats to physicians, patients, and the federally protected right to health care.
The letter comes during a campaign of intimidation and misinformation that has disrupted gender-related care in Seattle, Akron, Ohio, Nashville, Tenn., and Boston in the past few weeks. Hospitals across the country and their ambulatory sites have been forced to substantially increase protection, and “some providers have needed 24/7 security,” according to the letter.
Not only do the threats bully physicians providing gender-affirming care and the patients who receive that care, but “they have also disrupted many other services to families seeking care,” the letter claims.
According to STAT, many hospitals that provide gender-affirming care have responded to the threats by removing information about the treatment from their websites.
At one hospital, a new mother was separated from her preterm infant because the facility’s neonatal intensive care unit was locked down as the result of a bomb threat. (It’s not clear whether that incident is the same as a similar threat that led to the arrest of a 37-year-old Massachusetts woman, who is facing criminal charges in the episode.)
“The attacks are rooted in an intentional campaign of disinformation” by high-profile social media users, according to the letter. The medical organizations have also called on major tech companies, including TikTok, Twitter, and Meta, to do more to prevent the coordination of disinformation campaigns and violence against health care providers and patients.
“We now urge your office to take swift action to investigate and prosecute all organizations, individuals, and entities responsible,” the letter states.
“We cannot stand by as threats of violence against our members and their patients proliferate with little consequence. We call on the Department of Justice to investigate these attacks and social media platforms to reduce the spread of the misinformation enabling them,” AAP President Moira Szilagyi, MD, PhD, FAAP, said in a press release.
In addition to physical threats at their workplace, providers face threats on their personal social media accounts and harassment via phone and email. The letter notes that these unchecked attacks are coming after health care workers spent 3 years working on the front lines of a pandemic.
“Individuals in all workplaces have the right to a safe environment, out of harm’s way and free of intimidation or reprisal,” AMA President Jack Resneck Jr, MD, said in a statement. “The AMA will continue to work with federal, state, and local law enforcement officials to develop and implement strategies that protect hard-working, law-abiding physicians and other health care workers from senseless acts of violence, abuse, and intimidation.”
A version of this article first appeared on Medscape.com.
Several leading medical groups on Oct. 3 called on U.S. Attorney General Merrick Garland to investigate and prosecute those responsible for a recent spate of threats and attacks against hospitals and physicians who are providing gender-affirming care.
In an Oct. 3 letter, the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the Children’s Hospital Association detailed the risk posed by these threats to physicians, patients, and the federally protected right to health care.
The letter comes during a campaign of intimidation and misinformation that has disrupted gender-related care in Seattle, Akron, Ohio, Nashville, Tenn., and Boston in the past few weeks. Hospitals across the country and their ambulatory sites have been forced to substantially increase protection, and “some providers have needed 24/7 security,” according to the letter.
Not only do the threats bully physicians providing gender-affirming care and the patients who receive that care, but “they have also disrupted many other services to families seeking care,” the letter claims.
According to STAT, many hospitals that provide gender-affirming care have responded to the threats by removing information about the treatment from their websites.
At one hospital, a new mother was separated from her preterm infant because the facility’s neonatal intensive care unit was locked down as the result of a bomb threat. (It’s not clear whether that incident is the same as a similar threat that led to the arrest of a 37-year-old Massachusetts woman, who is facing criminal charges in the episode.)
“The attacks are rooted in an intentional campaign of disinformation” by high-profile social media users, according to the letter. The medical organizations have also called on major tech companies, including TikTok, Twitter, and Meta, to do more to prevent the coordination of disinformation campaigns and violence against health care providers and patients.
“We now urge your office to take swift action to investigate and prosecute all organizations, individuals, and entities responsible,” the letter states.
“We cannot stand by as threats of violence against our members and their patients proliferate with little consequence. We call on the Department of Justice to investigate these attacks and social media platforms to reduce the spread of the misinformation enabling them,” AAP President Moira Szilagyi, MD, PhD, FAAP, said in a press release.
In addition to physical threats at their workplace, providers face threats on their personal social media accounts and harassment via phone and email. The letter notes that these unchecked attacks are coming after health care workers spent 3 years working on the front lines of a pandemic.
“Individuals in all workplaces have the right to a safe environment, out of harm’s way and free of intimidation or reprisal,” AMA President Jack Resneck Jr, MD, said in a statement. “The AMA will continue to work with federal, state, and local law enforcement officials to develop and implement strategies that protect hard-working, law-abiding physicians and other health care workers from senseless acts of violence, abuse, and intimidation.”
A version of this article first appeared on Medscape.com.
Several leading medical groups on Oct. 3 called on U.S. Attorney General Merrick Garland to investigate and prosecute those responsible for a recent spate of threats and attacks against hospitals and physicians who are providing gender-affirming care.
In an Oct. 3 letter, the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the Children’s Hospital Association detailed the risk posed by these threats to physicians, patients, and the federally protected right to health care.
The letter comes during a campaign of intimidation and misinformation that has disrupted gender-related care in Seattle, Akron, Ohio, Nashville, Tenn., and Boston in the past few weeks. Hospitals across the country and their ambulatory sites have been forced to substantially increase protection, and “some providers have needed 24/7 security,” according to the letter.
Not only do the threats bully physicians providing gender-affirming care and the patients who receive that care, but “they have also disrupted many other services to families seeking care,” the letter claims.
According to STAT, many hospitals that provide gender-affirming care have responded to the threats by removing information about the treatment from their websites.
At one hospital, a new mother was separated from her preterm infant because the facility’s neonatal intensive care unit was locked down as the result of a bomb threat. (It’s not clear whether that incident is the same as a similar threat that led to the arrest of a 37-year-old Massachusetts woman, who is facing criminal charges in the episode.)
“The attacks are rooted in an intentional campaign of disinformation” by high-profile social media users, according to the letter. The medical organizations have also called on major tech companies, including TikTok, Twitter, and Meta, to do more to prevent the coordination of disinformation campaigns and violence against health care providers and patients.
“We now urge your office to take swift action to investigate and prosecute all organizations, individuals, and entities responsible,” the letter states.
“We cannot stand by as threats of violence against our members and their patients proliferate with little consequence. We call on the Department of Justice to investigate these attacks and social media platforms to reduce the spread of the misinformation enabling them,” AAP President Moira Szilagyi, MD, PhD, FAAP, said in a press release.
In addition to physical threats at their workplace, providers face threats on their personal social media accounts and harassment via phone and email. The letter notes that these unchecked attacks are coming after health care workers spent 3 years working on the front lines of a pandemic.
“Individuals in all workplaces have the right to a safe environment, out of harm’s way and free of intimidation or reprisal,” AMA President Jack Resneck Jr, MD, said in a statement. “The AMA will continue to work with federal, state, and local law enforcement officials to develop and implement strategies that protect hard-working, law-abiding physicians and other health care workers from senseless acts of violence, abuse, and intimidation.”
A version of this article first appeared on Medscape.com.
Don’t make children with head lice leave school, report says
The American Academy of Pediatrics says children with head lice don’t need to be sent home from school.
Head lice infestations aren’t really a health hazard because of low transmission rates, a new report from the academy says, and sending students home “may stigmatize children suspected of having head lice.” The group says schools should instead offer education programs to help families understand how to manage head lice.
“Head lice are an unpleasant part of the human experience, but they can be successfully managed and are no reason for a child to miss school,” Dawn Nolt, MD, lead author of the report on head lice, said in a news release.
The report advises schools to abandon “no-nit” policies, which call for a student to be lice-free before being allowed back in class.
“A child or adolescent should not be restricted from school attendance because of head lice, given the low contagion within classrooms. ‘No-nit’ policies that exclude children or adolescents until all nits are removed may violate a child’s or adolescent’s civil liberties and are best addressed with legal counsel for schools,” the report says.
The report notes that lice almost always spread through head-to-head contact, not by “jumping” from one person to another. It’s possible for lice to spread by touching the belongings of a person with lice, such as combs or sports helmets, but the chances of that happening are very low, the academy said.
“Lice found on combs are likely to be injured or dead, and a louse is not likely to leave a healthy head unless there is a heavy infestation,” the report says.
The report lists new medications for treatment and gives an algorithm for managing head lice cases.
“The ideal treatment of head lice should be safe, free of toxic chemicals, readily available, simple to apply, effective, and inexpensive,” the report says.
This is the first updated guidance on head lice from the American Academy of Pediatrics since 2015. The CDC also says students with head lice don’t need to be sent home.
“Students diagnosed with live head lice do not need to be sent home early from school; they can go home at the end of the day, be treated, and return to class after appropriate treatment has begun. Nits may persist after treatment, but successful treatment should kill crawling lice,” the CDC says.
A version of this article first appeared on WebMD.com.
The American Academy of Pediatrics says children with head lice don’t need to be sent home from school.
Head lice infestations aren’t really a health hazard because of low transmission rates, a new report from the academy says, and sending students home “may stigmatize children suspected of having head lice.” The group says schools should instead offer education programs to help families understand how to manage head lice.
“Head lice are an unpleasant part of the human experience, but they can be successfully managed and are no reason for a child to miss school,” Dawn Nolt, MD, lead author of the report on head lice, said in a news release.
The report advises schools to abandon “no-nit” policies, which call for a student to be lice-free before being allowed back in class.
“A child or adolescent should not be restricted from school attendance because of head lice, given the low contagion within classrooms. ‘No-nit’ policies that exclude children or adolescents until all nits are removed may violate a child’s or adolescent’s civil liberties and are best addressed with legal counsel for schools,” the report says.
The report notes that lice almost always spread through head-to-head contact, not by “jumping” from one person to another. It’s possible for lice to spread by touching the belongings of a person with lice, such as combs or sports helmets, but the chances of that happening are very low, the academy said.
“Lice found on combs are likely to be injured or dead, and a louse is not likely to leave a healthy head unless there is a heavy infestation,” the report says.
The report lists new medications for treatment and gives an algorithm for managing head lice cases.
“The ideal treatment of head lice should be safe, free of toxic chemicals, readily available, simple to apply, effective, and inexpensive,” the report says.
This is the first updated guidance on head lice from the American Academy of Pediatrics since 2015. The CDC also says students with head lice don’t need to be sent home.
“Students diagnosed with live head lice do not need to be sent home early from school; they can go home at the end of the day, be treated, and return to class after appropriate treatment has begun. Nits may persist after treatment, but successful treatment should kill crawling lice,” the CDC says.
A version of this article first appeared on WebMD.com.
The American Academy of Pediatrics says children with head lice don’t need to be sent home from school.
Head lice infestations aren’t really a health hazard because of low transmission rates, a new report from the academy says, and sending students home “may stigmatize children suspected of having head lice.” The group says schools should instead offer education programs to help families understand how to manage head lice.
“Head lice are an unpleasant part of the human experience, but they can be successfully managed and are no reason for a child to miss school,” Dawn Nolt, MD, lead author of the report on head lice, said in a news release.
The report advises schools to abandon “no-nit” policies, which call for a student to be lice-free before being allowed back in class.
“A child or adolescent should not be restricted from school attendance because of head lice, given the low contagion within classrooms. ‘No-nit’ policies that exclude children or adolescents until all nits are removed may violate a child’s or adolescent’s civil liberties and are best addressed with legal counsel for schools,” the report says.
The report notes that lice almost always spread through head-to-head contact, not by “jumping” from one person to another. It’s possible for lice to spread by touching the belongings of a person with lice, such as combs or sports helmets, but the chances of that happening are very low, the academy said.
“Lice found on combs are likely to be injured or dead, and a louse is not likely to leave a healthy head unless there is a heavy infestation,” the report says.
The report lists new medications for treatment and gives an algorithm for managing head lice cases.
“The ideal treatment of head lice should be safe, free of toxic chemicals, readily available, simple to apply, effective, and inexpensive,” the report says.
This is the first updated guidance on head lice from the American Academy of Pediatrics since 2015. The CDC also says students with head lice don’t need to be sent home.
“Students diagnosed with live head lice do not need to be sent home early from school; they can go home at the end of the day, be treated, and return to class after appropriate treatment has begun. Nits may persist after treatment, but successful treatment should kill crawling lice,” the CDC says.
A version of this article first appeared on WebMD.com.
Physician bias may prevent quality care for patients with disabilities
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
For Tara Lagu, MD, the realization that the health care system was broken for patients with disabilities came when a woman she had been treating seemed to keep ignoring Dr. Lagu’s request to see a urologist.
When Dr. Lagu asked the patient’s two attentive daughters about the delay, their response surprised her. The women said they couldn’t find a urologist who was willing to see a patient in a wheelchair.
Surprised and a bit doubtful, Dr. Lagu checked around. She found that, indeed, the only way to get her patient in to see the type of physician required was to send her by ambulance.
“It opened my eyes to how hard it is for patients with disabilities to navigate the health care system,” Dr. Lagu said.
Dr. Lagu, director of the Center for Health Services and Outcomes Research at Northwestern University in Chicago, decided to take a closer look at how her colleagues in medicine care for – or not, as the case proved – the roughly one in four American adults, and millions of children, with disabilities.
In a series of three focus groups, Dr. Lagu and colleagues identified a range of obstacles – including some physician attitudes – that prevent people with disabilities from getting adequate care.
For the study, published in Health Affairs, the researchers interviewed 22 physicians in three groups: Nonrural primary care physicians, rural primary care physicians, and specialists in rheumatology, neurology, obstetrics/gynecology, orthopedics, and ophthalmology.
During the interviews, conducted in the fall of 2018, participants were asked about providing care for five specific types of disabilities: mobility, hearing, vision, mental health, and intellectual limitations.
Lack of experience, logistics often cited
Some physicians admitted that limited resources and training left them without the space and necessary knowledge to properly care for patients with disabilities. They felt they lacked the expertise or exposure to care for individuals with disabilities, nor did they have enough time and space to properly accommodate these patients, according to the researchers. Some said they struggled to coordinate care for individuals with disabilities and did not know which types of accessible equipment, such as adjustable tables and chair scales, were needed or how to use them.
Several physicians also noted that they are inadequately reimbursed for the special accommodations – including additional staff, equipment, and time – required to care for these patients. One primary care physician said he hired a sign-language interpreter for a patient but the bill for the services exceeded the amount insurance reimbursed. As a result, he said, he spent $30 of his own money per visit to see the patient.
Because of these limitations, some physicians in the focus groups said they try to turn away patients with disabilities. Both specialists and general practitioners said they had told patients with disabilities that they didn’t feel they could provide the care needed, and suggested they look elsewhere. A few were surprisingly – even upsettingly – honest, Dr. Lagu said, making statements such as: “I am not the doctor for you.”
‘We really need a rewrite’
Previous work has shown that people with disabilities have worse health outcomes, such as undetected cancer, obesity, and cardiovascular disease.
But “the disability itself isn’t what leads to worse outcomes,” said Allison Kessler, MD, section chief of the Renée Crown Center for Spinal Cord Innovation and associate director of the Shirley Ryan AbilityLab in Chicago*. This study does a good job at highlighting “the need for change on multiple levels,” said Dr. Kessler, who was not a member of the study team.
“People with disabilities have all these disparities in access and outcomes. We’ve never understood why. I think the why is complicated,” Dr. Lagu added. “I think this study suggests some of the negative outcomes are due to explicit bias.”
“It’s also clear that the current framework of health care in the United States does not lend to allowing physicians and medical providers the time needed to adequately address patient issues – those with disabilities or just multiple complex problems,” Colin O’Reilly, DO, vice president and chief medical officer at Children’s Specialized Hospital, an acute rehabilitation facility affiliated with RWJBarnabas Health, in New Brunswick, N.J. “We really need a rewrite.”
However, Dr. O’Reilly said, such a small study population with no control group and no mention of physician resources makes it difficult to come to a strong conclusion about physician bias and discriminatory attitudes against individuals with disabilities.
Dr. Lagu agreed, saying this research “is not conclusive in any way.” The excuses doctors use to discharge patients with disabilities, such as “we don’t accept your insurance,” “we aren’t taking new patients,” and “we can’t provide you with the appropriate care,” could be legitimate, the study authors wrote. But the “disparities in care for people with disabilities suggest that there is a pattern of more frequently denying care to them than people without a disability,” they added.
Dr. Kessler said many of her patients have told her they experience barriers to care. Some say finding an office with the necessary equipment is a challenge or that they often don’t feel welcome.
The Americans With Disabilities Act (ADA) is a federal civil rights law that prohibits discrimination against individuals with disabilities in all public and private places that are open to the general public, including medical offices.
“It is difficult to enforce the ADA in medical settings,” the researchers noted. “Explanations physicians gave in this study could, for any single case of denying care, be legitimate.” Knowing whether a particular instance of denial of care represents discrimination related to disability is “nearly impossible,” they wrote.
All the experts agreed that the study adds valuable insight into an ongoing health disparity. And while system and policy changes are required, Dr. Kessler said, individual physicians can take steps to improve the situation.
A physician in an academic setting can look at the curriculum and the medical school and see about increasing exposure to patients with disabilities earlier in training. In a practice, physicians can retrain staff to ask every patient if an accommodation is needed. “Each one of those changes can only help us move our system in the right direction,” Dr. Kessler said.
The study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
*Correction, 10/5/22: This article includes a corrected title for Dr. Allison Kessler.
A version of this article first appeared on Medscape.com.
Turned away from urgent care – and toward a big ER bill
Frankie Cook remembers last year’s car crash only in flashes.
She was driving a friend home from high school on a winding road outside Rome, Ga. She saw standing water from a recent rain. She tried to slow down but lost control of her car on a big curve. “The car flipped about three times,” Frankie said. “We spun around and went off the side of this hill. My car was on its side, and the back end was crushed up into a tree.”
Frankie said the air bags deployed and both passengers were wearing seat belts, so she was left with just a headache when her father, Russell Cook, came to pick her up from the crash site.
Frankie, then a high school junior, worried she might have a concussion that could affect her performance on an upcoming Advanced Placement exam, so she and her father decided to stop by an urgent care center near their house to get her checked out. They didn’t make it past the front desk.
“‘We don’t take third-party insurance,’” Russell said the receptionist at Atrium Health Floyd Urgent Care Rome told him, though he wasn’t sure what she meant. “She told me, like, three times.”
The problem didn’t seem to be that the clinic lacked the medical expertise to evaluate Frankie. Rather, the Cooks seemed to be confronting a reimbursement policy that is often used by urgent care centers to avoid waiting for payments from car insurance settlements.
Russell was told to take Frankie to an emergency room, which by law must see all patients regardless of such issues. The nearest one, at Atrium Health Floyd Medical Center, was about a mile down the road and was owned by the same hospital system as the urgent care center.
There, Russell said, a doctor looked Frankie over “for just a few minutes,” did precautionary CT scans of her head and body, and sent her home with advice to “take some Tylenol” and rest. She did not have a concussion or serious head injury and was able to take her AP exam on time.
Then the bill came.
The patient: Frankie Cook, 18, now a first-year college student from Rome, Ga.
Medical services: A medical evaluation and two CT scans.
Service provider: Atrium Health Floyd, a hospital system with urgent care centers in northwestern Georgia and northeastern Alabama.
Total bill: $17,005 for an emergency room visit; it was later adjusted to $11,805 after a duplicate charge was removed.
What gives: The Cooks hit a hazard in the health care system after Frankie’s car struck that tree: More and more hospital systems own urgent care centers, which have limits on whom they treat – for both financial and medical reasons.
Russell was pretty upset after he received such a large bill, especially when he had tried to make a quick, inexpensive trip to the clinic. He said Frankie’s grandmother was seen at an urgent care center after a car wreck and walked out with a bill for just a few hundred dollars.
“That’s kind of what I was expecting,” he said. “She just really needed to be looked over.”
So why was Frankie turned away from an urgent care center?
Lou Ellen Horwitz, CEO of the Urgent Care Association, said it’s a pretty standard policy for urgent care centers not to treat injuries that result from car crashes, even minor ones. “Generally, as a rule, they do not take care of car accident victims regardless of the extent of their injuries, because it is going to go through that auto insurance claims process before the provider gets paid,” she said.
Ms. Horwitz said urgent care centers – even ones owned by big health systems – often operate on thin margins and can’t wait months and months for an auto insurance company to pay out a claim. She said “unfortunately” people tend to learn about such policies when they show up expecting care.
Fold in the complicated relationship between health and auto insurance companies and you have what Barak D. Richman, a health care policy professor at Duke University’s law school, called “the wildly complex world that we live in.”
“Each product has its own specifications about where to go and what it covers. Each one is incredibly difficult and complex to administer,” he said. “And each one imposes mistakes on the system.”
Atrium Health did not respond to repeated requests for comment on Frankie’s case.
Ms. Horwitz dismissed the idea that a health system might push people in car wrecks from urgent care centers to emergency rooms to make more money off them. Still, auto insurance generally pays more than health insurance for the same services.
Mr. Richman remained skeptical.
“At the risk of sounding a little too cynical, there are always dollar signs when a health care provider sees a patient come through the door,” Mr. Richman said.
Ateev Mehrotra, MD, professor of health care policy at Harvard Medical School, Boston, said it was likely strategic for the urgent care center to be right down the street from the ER. Part of the strategy makes sense medically, he said, “because if a bad thing happens, you want to get them to some place with more skill really quickly.”
But he also said urgent care centers are “one of the most effective ways” for a health system to generate new revenue, creating a pipeline of new patients to visit its hospitals and later see doctors for testing and follow-up.
Dr. Mehrotra said urgent care centers are not bound by the Emergency Medical Treatment and Labor Act, a federal law known as EMTALA that requires hospitals to stabilize patients regardless of their ability to pay.
At the time of Frankie’s visit, both the urgent care center and emergency room were owned by Floyd health system, which operated a handful of hospitals and clinics in northwestern Georgia and northeastern Alabama. Since then, Floyd has merged with Atrium Health – a larger, North Carolina–based company that operates dozens of hospitals across the Southeast.
Frankie got a CT scan of her head and body in the emergency room, tests KHN confirmed she couldn’t have gotten at the urgent care center regardless of whether the test was medically necessary or just part of a protocol for people in car wrecks who complain of a headache.
Resolution: Sixteen months have passed since Frankie Cook’s hospital visit, and Russell has delayed paying any of the bill on advice he got from a family friend who’s an attorney. After insurance covered its share, the Cooks’ portion came to $1,042.
Getting to that number has been a frustrating process, Russell said. He heard about the initial $17,005 bill in a letter from a lawyer representing the hospital – another unnerving wrinkle of Frankie’s care resulting from the car wreck. The Cooks then had to pursue a lengthy appeal process to get a $5,200 duplicate charge removed from the bill.
Anthem Blue Cross Blue Shield, the Cooks’ insurer, paid $4,006 of the claim. It said in a statement that it’s “committed to providing access to high-quality medical care for our members. This matter was reviewed in accordance with our clinical guidelines, and the billed claims were processed accordingly.”
“It’s not going to put us out on the street,” Russell said of the $1,042 balance, “but we’ve got expenses like everybody else.”
He added, “I would have loved a $200 urgent care visit, but that ship has sailed.”
The takeaway: It’s important to remember that urgent care centers aren’t governed by the same laws as emergency rooms and that they can be more selective about whom they treat. Sometimes their reasons are financial, not clinical.
It’s not uncommon for urgent care centers – even ones in large health systems – to turn away people who have been in car wrecks because of the complications that car insurance settlements create.
Although urgent care visits are less expensive than going to an emergency room, the clinics often can’t offer the same level of care. And you might have to pay the cost of an urgent care visit just to find out you need follow-up care in the emergency room. Then you could be stuck with two bills.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Frankie Cook remembers last year’s car crash only in flashes.
She was driving a friend home from high school on a winding road outside Rome, Ga. She saw standing water from a recent rain. She tried to slow down but lost control of her car on a big curve. “The car flipped about three times,” Frankie said. “We spun around and went off the side of this hill. My car was on its side, and the back end was crushed up into a tree.”
Frankie said the air bags deployed and both passengers were wearing seat belts, so she was left with just a headache when her father, Russell Cook, came to pick her up from the crash site.
Frankie, then a high school junior, worried she might have a concussion that could affect her performance on an upcoming Advanced Placement exam, so she and her father decided to stop by an urgent care center near their house to get her checked out. They didn’t make it past the front desk.
“‘We don’t take third-party insurance,’” Russell said the receptionist at Atrium Health Floyd Urgent Care Rome told him, though he wasn’t sure what she meant. “She told me, like, three times.”
The problem didn’t seem to be that the clinic lacked the medical expertise to evaluate Frankie. Rather, the Cooks seemed to be confronting a reimbursement policy that is often used by urgent care centers to avoid waiting for payments from car insurance settlements.
Russell was told to take Frankie to an emergency room, which by law must see all patients regardless of such issues. The nearest one, at Atrium Health Floyd Medical Center, was about a mile down the road and was owned by the same hospital system as the urgent care center.
There, Russell said, a doctor looked Frankie over “for just a few minutes,” did precautionary CT scans of her head and body, and sent her home with advice to “take some Tylenol” and rest. She did not have a concussion or serious head injury and was able to take her AP exam on time.
Then the bill came.
The patient: Frankie Cook, 18, now a first-year college student from Rome, Ga.
Medical services: A medical evaluation and two CT scans.
Service provider: Atrium Health Floyd, a hospital system with urgent care centers in northwestern Georgia and northeastern Alabama.
Total bill: $17,005 for an emergency room visit; it was later adjusted to $11,805 after a duplicate charge was removed.
What gives: The Cooks hit a hazard in the health care system after Frankie’s car struck that tree: More and more hospital systems own urgent care centers, which have limits on whom they treat – for both financial and medical reasons.
Russell was pretty upset after he received such a large bill, especially when he had tried to make a quick, inexpensive trip to the clinic. He said Frankie’s grandmother was seen at an urgent care center after a car wreck and walked out with a bill for just a few hundred dollars.
“That’s kind of what I was expecting,” he said. “She just really needed to be looked over.”
So why was Frankie turned away from an urgent care center?
Lou Ellen Horwitz, CEO of the Urgent Care Association, said it’s a pretty standard policy for urgent care centers not to treat injuries that result from car crashes, even minor ones. “Generally, as a rule, they do not take care of car accident victims regardless of the extent of their injuries, because it is going to go through that auto insurance claims process before the provider gets paid,” she said.
Ms. Horwitz said urgent care centers – even ones owned by big health systems – often operate on thin margins and can’t wait months and months for an auto insurance company to pay out a claim. She said “unfortunately” people tend to learn about such policies when they show up expecting care.
Fold in the complicated relationship between health and auto insurance companies and you have what Barak D. Richman, a health care policy professor at Duke University’s law school, called “the wildly complex world that we live in.”
“Each product has its own specifications about where to go and what it covers. Each one is incredibly difficult and complex to administer,” he said. “And each one imposes mistakes on the system.”
Atrium Health did not respond to repeated requests for comment on Frankie’s case.
Ms. Horwitz dismissed the idea that a health system might push people in car wrecks from urgent care centers to emergency rooms to make more money off them. Still, auto insurance generally pays more than health insurance for the same services.
Mr. Richman remained skeptical.
“At the risk of sounding a little too cynical, there are always dollar signs when a health care provider sees a patient come through the door,” Mr. Richman said.
Ateev Mehrotra, MD, professor of health care policy at Harvard Medical School, Boston, said it was likely strategic for the urgent care center to be right down the street from the ER. Part of the strategy makes sense medically, he said, “because if a bad thing happens, you want to get them to some place with more skill really quickly.”
But he also said urgent care centers are “one of the most effective ways” for a health system to generate new revenue, creating a pipeline of new patients to visit its hospitals and later see doctors for testing and follow-up.
Dr. Mehrotra said urgent care centers are not bound by the Emergency Medical Treatment and Labor Act, a federal law known as EMTALA that requires hospitals to stabilize patients regardless of their ability to pay.
At the time of Frankie’s visit, both the urgent care center and emergency room were owned by Floyd health system, which operated a handful of hospitals and clinics in northwestern Georgia and northeastern Alabama. Since then, Floyd has merged with Atrium Health – a larger, North Carolina–based company that operates dozens of hospitals across the Southeast.
Frankie got a CT scan of her head and body in the emergency room, tests KHN confirmed she couldn’t have gotten at the urgent care center regardless of whether the test was medically necessary or just part of a protocol for people in car wrecks who complain of a headache.
Resolution: Sixteen months have passed since Frankie Cook’s hospital visit, and Russell has delayed paying any of the bill on advice he got from a family friend who’s an attorney. After insurance covered its share, the Cooks’ portion came to $1,042.
Getting to that number has been a frustrating process, Russell said. He heard about the initial $17,005 bill in a letter from a lawyer representing the hospital – another unnerving wrinkle of Frankie’s care resulting from the car wreck. The Cooks then had to pursue a lengthy appeal process to get a $5,200 duplicate charge removed from the bill.
Anthem Blue Cross Blue Shield, the Cooks’ insurer, paid $4,006 of the claim. It said in a statement that it’s “committed to providing access to high-quality medical care for our members. This matter was reviewed in accordance with our clinical guidelines, and the billed claims were processed accordingly.”
“It’s not going to put us out on the street,” Russell said of the $1,042 balance, “but we’ve got expenses like everybody else.”
He added, “I would have loved a $200 urgent care visit, but that ship has sailed.”
The takeaway: It’s important to remember that urgent care centers aren’t governed by the same laws as emergency rooms and that they can be more selective about whom they treat. Sometimes their reasons are financial, not clinical.
It’s not uncommon for urgent care centers – even ones in large health systems – to turn away people who have been in car wrecks because of the complications that car insurance settlements create.
Although urgent care visits are less expensive than going to an emergency room, the clinics often can’t offer the same level of care. And you might have to pay the cost of an urgent care visit just to find out you need follow-up care in the emergency room. Then you could be stuck with two bills.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Frankie Cook remembers last year’s car crash only in flashes.
She was driving a friend home from high school on a winding road outside Rome, Ga. She saw standing water from a recent rain. She tried to slow down but lost control of her car on a big curve. “The car flipped about three times,” Frankie said. “We spun around and went off the side of this hill. My car was on its side, and the back end was crushed up into a tree.”
Frankie said the air bags deployed and both passengers were wearing seat belts, so she was left with just a headache when her father, Russell Cook, came to pick her up from the crash site.
Frankie, then a high school junior, worried she might have a concussion that could affect her performance on an upcoming Advanced Placement exam, so she and her father decided to stop by an urgent care center near their house to get her checked out. They didn’t make it past the front desk.
“‘We don’t take third-party insurance,’” Russell said the receptionist at Atrium Health Floyd Urgent Care Rome told him, though he wasn’t sure what she meant. “She told me, like, three times.”
The problem didn’t seem to be that the clinic lacked the medical expertise to evaluate Frankie. Rather, the Cooks seemed to be confronting a reimbursement policy that is often used by urgent care centers to avoid waiting for payments from car insurance settlements.
Russell was told to take Frankie to an emergency room, which by law must see all patients regardless of such issues. The nearest one, at Atrium Health Floyd Medical Center, was about a mile down the road and was owned by the same hospital system as the urgent care center.
There, Russell said, a doctor looked Frankie over “for just a few minutes,” did precautionary CT scans of her head and body, and sent her home with advice to “take some Tylenol” and rest. She did not have a concussion or serious head injury and was able to take her AP exam on time.
Then the bill came.
The patient: Frankie Cook, 18, now a first-year college student from Rome, Ga.
Medical services: A medical evaluation and two CT scans.
Service provider: Atrium Health Floyd, a hospital system with urgent care centers in northwestern Georgia and northeastern Alabama.
Total bill: $17,005 for an emergency room visit; it was later adjusted to $11,805 after a duplicate charge was removed.
What gives: The Cooks hit a hazard in the health care system after Frankie’s car struck that tree: More and more hospital systems own urgent care centers, which have limits on whom they treat – for both financial and medical reasons.
Russell was pretty upset after he received such a large bill, especially when he had tried to make a quick, inexpensive trip to the clinic. He said Frankie’s grandmother was seen at an urgent care center after a car wreck and walked out with a bill for just a few hundred dollars.
“That’s kind of what I was expecting,” he said. “She just really needed to be looked over.”
So why was Frankie turned away from an urgent care center?
Lou Ellen Horwitz, CEO of the Urgent Care Association, said it’s a pretty standard policy for urgent care centers not to treat injuries that result from car crashes, even minor ones. “Generally, as a rule, they do not take care of car accident victims regardless of the extent of their injuries, because it is going to go through that auto insurance claims process before the provider gets paid,” she said.
Ms. Horwitz said urgent care centers – even ones owned by big health systems – often operate on thin margins and can’t wait months and months for an auto insurance company to pay out a claim. She said “unfortunately” people tend to learn about such policies when they show up expecting care.
Fold in the complicated relationship between health and auto insurance companies and you have what Barak D. Richman, a health care policy professor at Duke University’s law school, called “the wildly complex world that we live in.”
“Each product has its own specifications about where to go and what it covers. Each one is incredibly difficult and complex to administer,” he said. “And each one imposes mistakes on the system.”
Atrium Health did not respond to repeated requests for comment on Frankie’s case.
Ms. Horwitz dismissed the idea that a health system might push people in car wrecks from urgent care centers to emergency rooms to make more money off them. Still, auto insurance generally pays more than health insurance for the same services.
Mr. Richman remained skeptical.
“At the risk of sounding a little too cynical, there are always dollar signs when a health care provider sees a patient come through the door,” Mr. Richman said.
Ateev Mehrotra, MD, professor of health care policy at Harvard Medical School, Boston, said it was likely strategic for the urgent care center to be right down the street from the ER. Part of the strategy makes sense medically, he said, “because if a bad thing happens, you want to get them to some place with more skill really quickly.”
But he also said urgent care centers are “one of the most effective ways” for a health system to generate new revenue, creating a pipeline of new patients to visit its hospitals and later see doctors for testing and follow-up.
Dr. Mehrotra said urgent care centers are not bound by the Emergency Medical Treatment and Labor Act, a federal law known as EMTALA that requires hospitals to stabilize patients regardless of their ability to pay.
At the time of Frankie’s visit, both the urgent care center and emergency room were owned by Floyd health system, which operated a handful of hospitals and clinics in northwestern Georgia and northeastern Alabama. Since then, Floyd has merged with Atrium Health – a larger, North Carolina–based company that operates dozens of hospitals across the Southeast.
Frankie got a CT scan of her head and body in the emergency room, tests KHN confirmed she couldn’t have gotten at the urgent care center regardless of whether the test was medically necessary or just part of a protocol for people in car wrecks who complain of a headache.
Resolution: Sixteen months have passed since Frankie Cook’s hospital visit, and Russell has delayed paying any of the bill on advice he got from a family friend who’s an attorney. After insurance covered its share, the Cooks’ portion came to $1,042.
Getting to that number has been a frustrating process, Russell said. He heard about the initial $17,005 bill in a letter from a lawyer representing the hospital – another unnerving wrinkle of Frankie’s care resulting from the car wreck. The Cooks then had to pursue a lengthy appeal process to get a $5,200 duplicate charge removed from the bill.
Anthem Blue Cross Blue Shield, the Cooks’ insurer, paid $4,006 of the claim. It said in a statement that it’s “committed to providing access to high-quality medical care for our members. This matter was reviewed in accordance with our clinical guidelines, and the billed claims were processed accordingly.”
“It’s not going to put us out on the street,” Russell said of the $1,042 balance, “but we’ve got expenses like everybody else.”
He added, “I would have loved a $200 urgent care visit, but that ship has sailed.”
The takeaway: It’s important to remember that urgent care centers aren’t governed by the same laws as emergency rooms and that they can be more selective about whom they treat. Sometimes their reasons are financial, not clinical.
It’s not uncommon for urgent care centers – even ones in large health systems – to turn away people who have been in car wrecks because of the complications that car insurance settlements create.
Although urgent care visits are less expensive than going to an emergency room, the clinics often can’t offer the same level of care. And you might have to pay the cost of an urgent care visit just to find out you need follow-up care in the emergency room. Then you could be stuck with two bills.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The hunt for N-acetylcysteine: Medicine or dietary supplement?
Medicine or dietary supplement? N-acetylcysteine (NAC) is marketed as both and in 2021, the supplement abruptly became difficult to find, causing distress to people who had been using it for a variety of conditions. The story behind its disappearance is one of a cat-and-mouse chase between manufacturers, advocacy agencies, and the Food and Drug Administration.
NAC is a medication that was approved by the FDA in 1963. It has two FDA-approved uses: To prevent hepatotoxicity after overdose with acetaminophen, administered intravenously or by mouth, and as a mucolytic agent – previously available as Mucomyst, now available only as a generic – given by inhaler or nebulizer for pulmonary illnesses. Since the 1990s, NAC has been labeled by manufacturers as a dietary supplement. It is a derivative of the amino acid L-cysteine and a precursor to glutathione, an antioxidant.
Studies have had small sample sizes, and the supplement has not been considered an “off label” use of an already available medication. People have purchased NAC from retail drug and big box stores, Amazon, and online companies. So what’s the problem?
In July 2020, the FDA issued a warning letter to Purple Biosciences LLC, because of claims on the company’s website that the product “Purple Tree,” sold by Amazon, could cure hangovers that result from alcohol intoxication. The letter discussed justification for why a hangover is a disease, and goes on to note:
Based on the product label on your website, it appears that you intend to market your Purple Tree® product, which contains N-acetyl-L-cysteine (NAC), as a dietary supplement. However, even if your product labeling did not have therapeutic claims that make your product an unapproved new drug, your product could not be a dietary supplement, because it does not meet the definition of dietary supplement ... products containing that article are outside the definition of a dietary supplement, unless before such approval that article was marketed as a dietary supplement or as a food. NAC was approved as a new drug under section 505 of the Act [21 U.S.C. § 355] on September 14, 1963.
The issue here is that because NAC was first approved as a drug in 1963, it cannot be marketed as a supplement. If it had been marketed as a supplement before it was approved as a drug by the FDA, then it could remain on the market. The fact that it had been sold as a supplement since the 1990s and could be classified as an “old dietary ingredient” according to the Dietary Supplement Health and Education Act of 1994 did not seem to matter. Following the warning letter, NAC was pulled from shelves and websites.
Citizen petitions allow people and organizations to request that the FDA change their policy. During summer 2021, there were two citizen petitions – one from the Council for Responsible Nutrition (CRN) and another from the Natural Products Association (NPA) – asking that the FDA look at policy around NAC. In response, in November 2021, the FDA put out a request for more information about how long NAC had been used and if there were safety concerns, to determine if making it a lawful supplement would be appropriate. CRN promptly released a response that they were “extremely dissatisfied” and felt this was an unnecessary tactic to delay a decision. Two members of Congress wrote letters to the FDA in support of leaving NAC as an available supplement. Congressman Jeff Duncan noted that there were over 1,170 products containing NAC.
The FDA continued to issue responses. On March 31, 2022, the agency formally denied the requests of the two citizen petitions, and 3 weeks later the Guidance for Industry: Policy Regarding N-acetyl-L-cysteine was released, saying that the FDA would “... exercise enforcement discretion with respect to the sale and distribution of certain products that contain NAC.” While NAC was still not considered a supplement, no safety issues had been identified to date. Thus, while the FDA investigation continues, the agency will essentially look the other way.
The agency will consider rulemaking to include NAC as a supplement, a process that may take years. In a notice of final guidance released in August 2022, the FDA reiterated, “unless we identify safety-related concerns during our ongoing review, FDA intends to exercise enforcement discretion until either of the following occurs: we complete notice-and-comment rulemaking to allow the use of NAC in or as a dietary supplement (should we move forward with such proceedings) or we deny the NPA citizen petition’s request for rulemaking.”
It’s a win for the consumer who wants the supplement, and a half-win for the supplement manufacturers and their advocacy organizations who would like NAC to be an official dietary supplement. But just to be clear, the issue is one of a technicality: If NAC had been marketed as a supplement before it was a drug, it would just be a dietary supplement without all the controversy and scrutiny. It was not pulled because of a clinical concern.
For now, NAC is again readily available.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Medicine or dietary supplement? N-acetylcysteine (NAC) is marketed as both and in 2021, the supplement abruptly became difficult to find, causing distress to people who had been using it for a variety of conditions. The story behind its disappearance is one of a cat-and-mouse chase between manufacturers, advocacy agencies, and the Food and Drug Administration.
NAC is a medication that was approved by the FDA in 1963. It has two FDA-approved uses: To prevent hepatotoxicity after overdose with acetaminophen, administered intravenously or by mouth, and as a mucolytic agent – previously available as Mucomyst, now available only as a generic – given by inhaler or nebulizer for pulmonary illnesses. Since the 1990s, NAC has been labeled by manufacturers as a dietary supplement. It is a derivative of the amino acid L-cysteine and a precursor to glutathione, an antioxidant.
Studies have had small sample sizes, and the supplement has not been considered an “off label” use of an already available medication. People have purchased NAC from retail drug and big box stores, Amazon, and online companies. So what’s the problem?
In July 2020, the FDA issued a warning letter to Purple Biosciences LLC, because of claims on the company’s website that the product “Purple Tree,” sold by Amazon, could cure hangovers that result from alcohol intoxication. The letter discussed justification for why a hangover is a disease, and goes on to note:
Based on the product label on your website, it appears that you intend to market your Purple Tree® product, which contains N-acetyl-L-cysteine (NAC), as a dietary supplement. However, even if your product labeling did not have therapeutic claims that make your product an unapproved new drug, your product could not be a dietary supplement, because it does not meet the definition of dietary supplement ... products containing that article are outside the definition of a dietary supplement, unless before such approval that article was marketed as a dietary supplement or as a food. NAC was approved as a new drug under section 505 of the Act [21 U.S.C. § 355] on September 14, 1963.
The issue here is that because NAC was first approved as a drug in 1963, it cannot be marketed as a supplement. If it had been marketed as a supplement before it was approved as a drug by the FDA, then it could remain on the market. The fact that it had been sold as a supplement since the 1990s and could be classified as an “old dietary ingredient” according to the Dietary Supplement Health and Education Act of 1994 did not seem to matter. Following the warning letter, NAC was pulled from shelves and websites.
Citizen petitions allow people and organizations to request that the FDA change their policy. During summer 2021, there were two citizen petitions – one from the Council for Responsible Nutrition (CRN) and another from the Natural Products Association (NPA) – asking that the FDA look at policy around NAC. In response, in November 2021, the FDA put out a request for more information about how long NAC had been used and if there were safety concerns, to determine if making it a lawful supplement would be appropriate. CRN promptly released a response that they were “extremely dissatisfied” and felt this was an unnecessary tactic to delay a decision. Two members of Congress wrote letters to the FDA in support of leaving NAC as an available supplement. Congressman Jeff Duncan noted that there were over 1,170 products containing NAC.
The FDA continued to issue responses. On March 31, 2022, the agency formally denied the requests of the two citizen petitions, and 3 weeks later the Guidance for Industry: Policy Regarding N-acetyl-L-cysteine was released, saying that the FDA would “... exercise enforcement discretion with respect to the sale and distribution of certain products that contain NAC.” While NAC was still not considered a supplement, no safety issues had been identified to date. Thus, while the FDA investigation continues, the agency will essentially look the other way.
The agency will consider rulemaking to include NAC as a supplement, a process that may take years. In a notice of final guidance released in August 2022, the FDA reiterated, “unless we identify safety-related concerns during our ongoing review, FDA intends to exercise enforcement discretion until either of the following occurs: we complete notice-and-comment rulemaking to allow the use of NAC in or as a dietary supplement (should we move forward with such proceedings) or we deny the NPA citizen petition’s request for rulemaking.”
It’s a win for the consumer who wants the supplement, and a half-win for the supplement manufacturers and their advocacy organizations who would like NAC to be an official dietary supplement. But just to be clear, the issue is one of a technicality: If NAC had been marketed as a supplement before it was a drug, it would just be a dietary supplement without all the controversy and scrutiny. It was not pulled because of a clinical concern.
For now, NAC is again readily available.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Medicine or dietary supplement? N-acetylcysteine (NAC) is marketed as both and in 2021, the supplement abruptly became difficult to find, causing distress to people who had been using it for a variety of conditions. The story behind its disappearance is one of a cat-and-mouse chase between manufacturers, advocacy agencies, and the Food and Drug Administration.
NAC is a medication that was approved by the FDA in 1963. It has two FDA-approved uses: To prevent hepatotoxicity after overdose with acetaminophen, administered intravenously or by mouth, and as a mucolytic agent – previously available as Mucomyst, now available only as a generic – given by inhaler or nebulizer for pulmonary illnesses. Since the 1990s, NAC has been labeled by manufacturers as a dietary supplement. It is a derivative of the amino acid L-cysteine and a precursor to glutathione, an antioxidant.
Studies have had small sample sizes, and the supplement has not been considered an “off label” use of an already available medication. People have purchased NAC from retail drug and big box stores, Amazon, and online companies. So what’s the problem?
In July 2020, the FDA issued a warning letter to Purple Biosciences LLC, because of claims on the company’s website that the product “Purple Tree,” sold by Amazon, could cure hangovers that result from alcohol intoxication. The letter discussed justification for why a hangover is a disease, and goes on to note:
Based on the product label on your website, it appears that you intend to market your Purple Tree® product, which contains N-acetyl-L-cysteine (NAC), as a dietary supplement. However, even if your product labeling did not have therapeutic claims that make your product an unapproved new drug, your product could not be a dietary supplement, because it does not meet the definition of dietary supplement ... products containing that article are outside the definition of a dietary supplement, unless before such approval that article was marketed as a dietary supplement or as a food. NAC was approved as a new drug under section 505 of the Act [21 U.S.C. § 355] on September 14, 1963.
The issue here is that because NAC was first approved as a drug in 1963, it cannot be marketed as a supplement. If it had been marketed as a supplement before it was approved as a drug by the FDA, then it could remain on the market. The fact that it had been sold as a supplement since the 1990s and could be classified as an “old dietary ingredient” according to the Dietary Supplement Health and Education Act of 1994 did not seem to matter. Following the warning letter, NAC was pulled from shelves and websites.
Citizen petitions allow people and organizations to request that the FDA change their policy. During summer 2021, there were two citizen petitions – one from the Council for Responsible Nutrition (CRN) and another from the Natural Products Association (NPA) – asking that the FDA look at policy around NAC. In response, in November 2021, the FDA put out a request for more information about how long NAC had been used and if there were safety concerns, to determine if making it a lawful supplement would be appropriate. CRN promptly released a response that they were “extremely dissatisfied” and felt this was an unnecessary tactic to delay a decision. Two members of Congress wrote letters to the FDA in support of leaving NAC as an available supplement. Congressman Jeff Duncan noted that there were over 1,170 products containing NAC.
The FDA continued to issue responses. On March 31, 2022, the agency formally denied the requests of the two citizen petitions, and 3 weeks later the Guidance for Industry: Policy Regarding N-acetyl-L-cysteine was released, saying that the FDA would “... exercise enforcement discretion with respect to the sale and distribution of certain products that contain NAC.” While NAC was still not considered a supplement, no safety issues had been identified to date. Thus, while the FDA investigation continues, the agency will essentially look the other way.
The agency will consider rulemaking to include NAC as a supplement, a process that may take years. In a notice of final guidance released in August 2022, the FDA reiterated, “unless we identify safety-related concerns during our ongoing review, FDA intends to exercise enforcement discretion until either of the following occurs: we complete notice-and-comment rulemaking to allow the use of NAC in or as a dietary supplement (should we move forward with such proceedings) or we deny the NPA citizen petition’s request for rulemaking.”
It’s a win for the consumer who wants the supplement, and a half-win for the supplement manufacturers and their advocacy organizations who would like NAC to be an official dietary supplement. But just to be clear, the issue is one of a technicality: If NAC had been marketed as a supplement before it was a drug, it would just be a dietary supplement without all the controversy and scrutiny. It was not pulled because of a clinical concern.
For now, NAC is again readily available.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Instagram: Cosmetic procedures discussed without cosmetic experts
according to an analysis of related posts on the photo-sharing service.
“Given that there is little to no oversight on social networking sites, unqualified sources can widely disseminate misinformation resulting in misguided management or unnecessary procedures,” Taryn N. Murray, MD, and associates said in Lasers in Surgery and Medicine.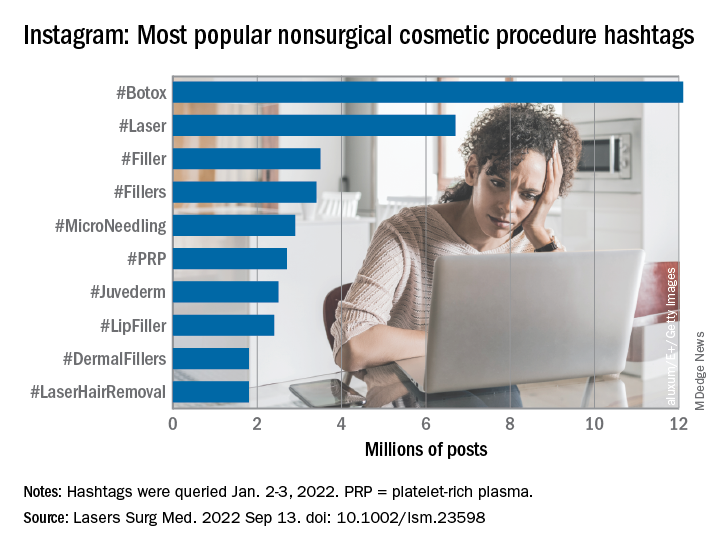
They generated a list of 25 hashtags related to nonsurgical cosmetic procedures, which were queried on Instagram on Jan. 2-3, 2022. The most popular was #Botox, with 12.1 million posts, followed by #Laser with 6.7 million, and #Filler with 3.5 million. Each of the 25 hashtags had at least 250,000 posts, they reported.
“Studies have shown that cosmetic patients and younger patients value social media when selecting a provider and patients often make treatment decisions based on social media,” they noted.
The bulk of the study involved “the first 10 posts displayed under the ‘Top’ section for each hashtag, as sorted by Instagram’s proprietary algorithm,” explained Dr. Murray and associates at the Dermatology and Laser Surgery Center in Houston. The 250 posts eventually selected for inclusion each received scrutiny in terms of content type and creator credentials.
Physicians in core cosmetic specialties – dermatology, plastic surgery, facial plastic surgery, and oculoplastic surgery – created just 12% of those 250 posts, compared with 68% for nonphysician providers, 13% for consumers/others, and 8% for other physicians, they said.
Educational content made up the largest share (38%) of posts by core cosmetic physicians, with before-and-after next at 31%, self-promotional at 21%, and personal at 10%. Nonphysician providers were the most likely to create before-and-after (49% of their total) and self-promotional (28%) content, while consumers had the largest share of promotional posts (31%) and other physicians posted the most entertainment content (25%), the researchers said.
An overall look at the content shows that the largest proportion of all 250 posts included in the analysis involved before-and-after photos (45%), with self-promotion next at 23%. Education represented just 17% of the posting total for nonsurgical cosmetic procedures, with personal, entertainment, and promotional each at 5%, Dr. Murray and associates reported.
By recognizing “the role social media plays in patients’ understanding of and desire to undergo nonsurgical cosmetic procedures” and “increasing their presence on Instagram, core cosmetic physicians can provide patient education, counteract misinformation, and raise awareness on training and qualifications,” they wrote.
The study authors did not provide any disclosures regarding funding or financial conflicts.
according to an analysis of related posts on the photo-sharing service.
“Given that there is little to no oversight on social networking sites, unqualified sources can widely disseminate misinformation resulting in misguided management or unnecessary procedures,” Taryn N. Murray, MD, and associates said in Lasers in Surgery and Medicine.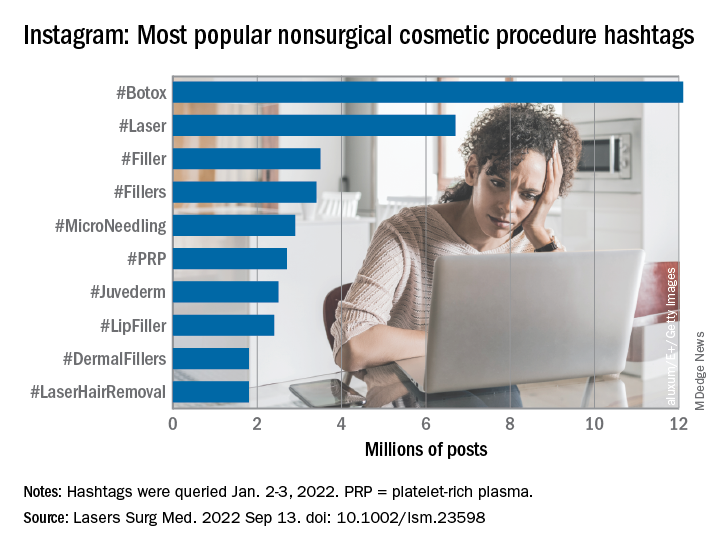
They generated a list of 25 hashtags related to nonsurgical cosmetic procedures, which were queried on Instagram on Jan. 2-3, 2022. The most popular was #Botox, with 12.1 million posts, followed by #Laser with 6.7 million, and #Filler with 3.5 million. Each of the 25 hashtags had at least 250,000 posts, they reported.
“Studies have shown that cosmetic patients and younger patients value social media when selecting a provider and patients often make treatment decisions based on social media,” they noted.
The bulk of the study involved “the first 10 posts displayed under the ‘Top’ section for each hashtag, as sorted by Instagram’s proprietary algorithm,” explained Dr. Murray and associates at the Dermatology and Laser Surgery Center in Houston. The 250 posts eventually selected for inclusion each received scrutiny in terms of content type and creator credentials.
Physicians in core cosmetic specialties – dermatology, plastic surgery, facial plastic surgery, and oculoplastic surgery – created just 12% of those 250 posts, compared with 68% for nonphysician providers, 13% for consumers/others, and 8% for other physicians, they said.
Educational content made up the largest share (38%) of posts by core cosmetic physicians, with before-and-after next at 31%, self-promotional at 21%, and personal at 10%. Nonphysician providers were the most likely to create before-and-after (49% of their total) and self-promotional (28%) content, while consumers had the largest share of promotional posts (31%) and other physicians posted the most entertainment content (25%), the researchers said.
An overall look at the content shows that the largest proportion of all 250 posts included in the analysis involved before-and-after photos (45%), with self-promotion next at 23%. Education represented just 17% of the posting total for nonsurgical cosmetic procedures, with personal, entertainment, and promotional each at 5%, Dr. Murray and associates reported.
By recognizing “the role social media plays in patients’ understanding of and desire to undergo nonsurgical cosmetic procedures” and “increasing their presence on Instagram, core cosmetic physicians can provide patient education, counteract misinformation, and raise awareness on training and qualifications,” they wrote.
The study authors did not provide any disclosures regarding funding or financial conflicts.
according to an analysis of related posts on the photo-sharing service.
“Given that there is little to no oversight on social networking sites, unqualified sources can widely disseminate misinformation resulting in misguided management or unnecessary procedures,” Taryn N. Murray, MD, and associates said in Lasers in Surgery and Medicine.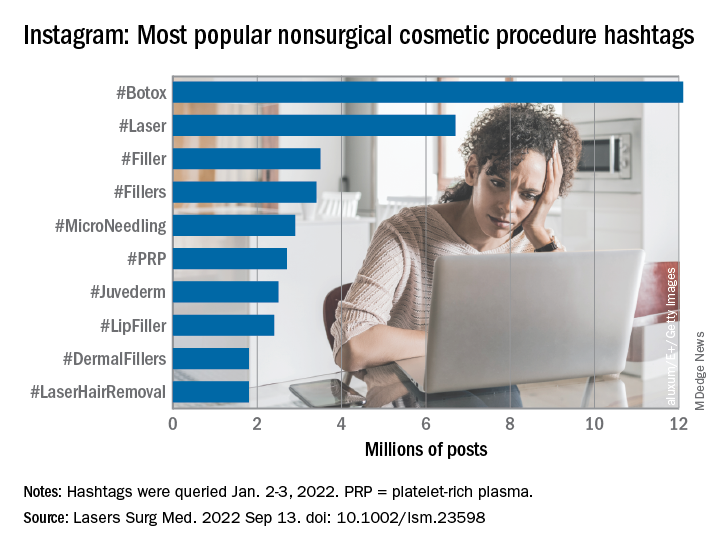
They generated a list of 25 hashtags related to nonsurgical cosmetic procedures, which were queried on Instagram on Jan. 2-3, 2022. The most popular was #Botox, with 12.1 million posts, followed by #Laser with 6.7 million, and #Filler with 3.5 million. Each of the 25 hashtags had at least 250,000 posts, they reported.
“Studies have shown that cosmetic patients and younger patients value social media when selecting a provider and patients often make treatment decisions based on social media,” they noted.
The bulk of the study involved “the first 10 posts displayed under the ‘Top’ section for each hashtag, as sorted by Instagram’s proprietary algorithm,” explained Dr. Murray and associates at the Dermatology and Laser Surgery Center in Houston. The 250 posts eventually selected for inclusion each received scrutiny in terms of content type and creator credentials.
Physicians in core cosmetic specialties – dermatology, plastic surgery, facial plastic surgery, and oculoplastic surgery – created just 12% of those 250 posts, compared with 68% for nonphysician providers, 13% for consumers/others, and 8% for other physicians, they said.
Educational content made up the largest share (38%) of posts by core cosmetic physicians, with before-and-after next at 31%, self-promotional at 21%, and personal at 10%. Nonphysician providers were the most likely to create before-and-after (49% of their total) and self-promotional (28%) content, while consumers had the largest share of promotional posts (31%) and other physicians posted the most entertainment content (25%), the researchers said.
An overall look at the content shows that the largest proportion of all 250 posts included in the analysis involved before-and-after photos (45%), with self-promotion next at 23%. Education represented just 17% of the posting total for nonsurgical cosmetic procedures, with personal, entertainment, and promotional each at 5%, Dr. Murray and associates reported.
By recognizing “the role social media plays in patients’ understanding of and desire to undergo nonsurgical cosmetic procedures” and “increasing their presence on Instagram, core cosmetic physicians can provide patient education, counteract misinformation, and raise awareness on training and qualifications,” they wrote.
The study authors did not provide any disclosures regarding funding or financial conflicts.
FROM LASERS IN SURGERY AND MEDICINE
The dubious value of online reviews
I hear other doctors talk about online reviews, both good and bad.
I recently read a piece where a practice gave doctors a bonus for getting 5-star reviews, though it doesn’t say if they were penalized for getting bad reviews. I assume the latter docs got a good “talking to” by someone in administration, or marketing, or both.
I get my share of them, too, both good and bad, scattered across at least a dozen sites that profess to offer accurate ratings.
I tend to ignore all of them.
Bad ratings mean nothing. They might be reasonable. They can also be from patients whom I fired for noncompliance, or from patients I refused to give an early narcotic refill to. They can also be from people who aren’t patients, such as a neighbor angry at the way I voted at a home owners association meeting, or a person who never saw me but was upset because I don’t take their insurance, or someone at the hospital whom I had to hang up on after being put on hold for 10 minutes.
Good reviews also don’t mean much, either. They might be from patients. They could also be from well-meaning family and friends. Or the waiter I left an extra-large tip for the other night.
One of my 1-star reviews even goes on to describe me in glowing terms (the lady called my office to apologize, saying the site confused her).
There’s also a whole cottage industry around this: Like restaurants, you can pay people to give you good reviews. They’re on Craig’s list and other sites. Some are freelancers. Others are actually well-organized companies, offering to give you X number of good reviews per month for a regular fee. I see ads for the latter online, usually describing themselves as “reputation recovery services.”
There was even a recent post on Sermo about this. A doctor noted he’d gotten a string of bad reviews from nonpatients, and shortly afterward was contacted by a reputation recovery service to help. He wondered if the crappy reviews were intentionally written by that business before they called him. He also questioned if it was an unspoken blackmail tactic – pay us or we’ll write more bad reviews.
Unlike a restaurant, we can’t respond because of patient confidentiality. Unless it’s something meaninglessly generic like “thank you” or “sorry you had a bad experience.”
A friend of mine (not in medicine) said that picking your doctor from online reviews is like selecting a wine recommended by a guy who lives at the train yard.
While there are pros and cons to the whole online review thing, in medicine there are mostly cons. Many reviews are anonymous, with no way to trace them. Unless details are provided, you don’t know if the reviewer is really a patient (or even a human in this bot era). Neither does the general public, reading them and presumably making decisions about who to see.
There are minimal (if any) rules, no law enforcement, and no one knows who the good guys and bad guys really are.
And there’s nothing we can do about it, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I hear other doctors talk about online reviews, both good and bad.
I recently read a piece where a practice gave doctors a bonus for getting 5-star reviews, though it doesn’t say if they were penalized for getting bad reviews. I assume the latter docs got a good “talking to” by someone in administration, or marketing, or both.
I get my share of them, too, both good and bad, scattered across at least a dozen sites that profess to offer accurate ratings.
I tend to ignore all of them.
Bad ratings mean nothing. They might be reasonable. They can also be from patients whom I fired for noncompliance, or from patients I refused to give an early narcotic refill to. They can also be from people who aren’t patients, such as a neighbor angry at the way I voted at a home owners association meeting, or a person who never saw me but was upset because I don’t take their insurance, or someone at the hospital whom I had to hang up on after being put on hold for 10 minutes.
Good reviews also don’t mean much, either. They might be from patients. They could also be from well-meaning family and friends. Or the waiter I left an extra-large tip for the other night.
One of my 1-star reviews even goes on to describe me in glowing terms (the lady called my office to apologize, saying the site confused her).
There’s also a whole cottage industry around this: Like restaurants, you can pay people to give you good reviews. They’re on Craig’s list and other sites. Some are freelancers. Others are actually well-organized companies, offering to give you X number of good reviews per month for a regular fee. I see ads for the latter online, usually describing themselves as “reputation recovery services.”
There was even a recent post on Sermo about this. A doctor noted he’d gotten a string of bad reviews from nonpatients, and shortly afterward was contacted by a reputation recovery service to help. He wondered if the crappy reviews were intentionally written by that business before they called him. He also questioned if it was an unspoken blackmail tactic – pay us or we’ll write more bad reviews.
Unlike a restaurant, we can’t respond because of patient confidentiality. Unless it’s something meaninglessly generic like “thank you” or “sorry you had a bad experience.”
A friend of mine (not in medicine) said that picking your doctor from online reviews is like selecting a wine recommended by a guy who lives at the train yard.
While there are pros and cons to the whole online review thing, in medicine there are mostly cons. Many reviews are anonymous, with no way to trace them. Unless details are provided, you don’t know if the reviewer is really a patient (or even a human in this bot era). Neither does the general public, reading them and presumably making decisions about who to see.
There are minimal (if any) rules, no law enforcement, and no one knows who the good guys and bad guys really are.
And there’s nothing we can do about it, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I hear other doctors talk about online reviews, both good and bad.
I recently read a piece where a practice gave doctors a bonus for getting 5-star reviews, though it doesn’t say if they were penalized for getting bad reviews. I assume the latter docs got a good “talking to” by someone in administration, or marketing, or both.
I get my share of them, too, both good and bad, scattered across at least a dozen sites that profess to offer accurate ratings.
I tend to ignore all of them.
Bad ratings mean nothing. They might be reasonable. They can also be from patients whom I fired for noncompliance, or from patients I refused to give an early narcotic refill to. They can also be from people who aren’t patients, such as a neighbor angry at the way I voted at a home owners association meeting, or a person who never saw me but was upset because I don’t take their insurance, or someone at the hospital whom I had to hang up on after being put on hold for 10 minutes.
Good reviews also don’t mean much, either. They might be from patients. They could also be from well-meaning family and friends. Or the waiter I left an extra-large tip for the other night.
One of my 1-star reviews even goes on to describe me in glowing terms (the lady called my office to apologize, saying the site confused her).
There’s also a whole cottage industry around this: Like restaurants, you can pay people to give you good reviews. They’re on Craig’s list and other sites. Some are freelancers. Others are actually well-organized companies, offering to give you X number of good reviews per month for a regular fee. I see ads for the latter online, usually describing themselves as “reputation recovery services.”
There was even a recent post on Sermo about this. A doctor noted he’d gotten a string of bad reviews from nonpatients, and shortly afterward was contacted by a reputation recovery service to help. He wondered if the crappy reviews were intentionally written by that business before they called him. He also questioned if it was an unspoken blackmail tactic – pay us or we’ll write more bad reviews.
Unlike a restaurant, we can’t respond because of patient confidentiality. Unless it’s something meaninglessly generic like “thank you” or “sorry you had a bad experience.”
A friend of mine (not in medicine) said that picking your doctor from online reviews is like selecting a wine recommended by a guy who lives at the train yard.
While there are pros and cons to the whole online review thing, in medicine there are mostly cons. Many reviews are anonymous, with no way to trace them. Unless details are provided, you don’t know if the reviewer is really a patient (or even a human in this bot era). Neither does the general public, reading them and presumably making decisions about who to see.
There are minimal (if any) rules, no law enforcement, and no one knows who the good guys and bad guys really are.
And there’s nothing we can do about it, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Racial disparities in preventive services use seen among patients with spina bifida or cerebral palsy
Black adults also had lower odds of having a bone density screening, compared with White adults. Plus, comorbidities were highest among the Black patients, according to the paper, which was published in Annals of Family Medicine.
Elham Mahmoudi, PhD, and her coauthors examined private insurance claims from 11,635 patients with cerebral palsy (CP) or spina bifida over ten years from 2007 to 2017. The researchers analyzed comorbidities and compared the rates of different psychological, cardiometabolic, and musculoskeletal conditions among these patients.
Only 23% of Hispanic participants and 18% of Black participants attended an annual wellness visit, compared with 32% of the White participants.
Only 1% of Black and 2% of White participants received any bone density screening (odds ratio = 0.54, 95% confidence interval [CI], 0.31-0.95), a service that is essential for catching a patient’s potential risk for osteoporosis and fractures.
According to the researchers, patients accessed services such as bone density scans, cholesterol assessments, diabetes screenings, and annual wellness visits less than recommended for people with those chronic conditions.
“People with spina bifida and cerebral palsy have complex care needs. We know through our work that chronic conditions are much higher among them compared with adults without disabilities,” Dr. Mahmoudi, associate professor in the department of family medicine at University of Michigan, Ann Arbor, said in an interview. “I was surprised to see even with private insurance, the rate of using preventative services is so low among White people and minority populations.”
Comorbidities highest in Black participants
Black adults had the highest comorbidity score of 2.5, and Hispanic adults had the lowest comorbidity score of 1.8. For White adults in the study, the comorbidity score was 2.0.
Osteoporosis, a common concern for people with spina bifida or cerebral palsy, was detected in around 4% of all participants. Osteoarthritis was detected in 13.38% of Black participants, versus 8.53% of Hispanic participants and 11.09% of White participants.
Diabetes and hypertension were more common among Black participants than among Hispanic and White participants. The percentages of Black patients with hypertension and diabetes were 16.5% and 39.89%, respectively. Among the Hispanic and White adults, the percentages with hypertension were 22.3% and 28.2%, respectively, according to the paper.
Disparities in access
Jamil Paden, racial and health equity manager at the Christopher and Dana Reeve Foundation, said getting access to literature, transportation, tables, chairs, weigh scales, and imaging equipment that accommodate the needs of people with disabilities are some of the biggest challenges for people with disabilities who are trying to receive care.
“It’s not a one size fits all, we have to recognize that if someone doesn’t see themselves in a particular place, then it makes it more challenging for them to feel comfortable speaking up and saying things about their health, which would prevent a person from saying something early on,” Mr. Paden said in an interview. “That particular issue will continue to grow and become more of a health risk, or health challenge down the line.”
Mr. Paden emphasized intersections between class, race, and circumstances which can, together, make health care less equitable for people with disabilities, especially in underserved communities and communities of color. He urged health care providers to distance their practices from a “one size fits all” approach to treatment and engage in their patients’ individual lives and communities.
“It’s not enough to just say, Hey, you have a disability. So let me treat your disability ... You have to recognize that although a patient may have a dire diagnosis, they also are a person of color, and they have to navigate different aspects of life from their counterparts,” he said.
Dr. Mahmoudi said patient and provider understanding of the disability is often lacking. She recommended advocating for patients, noting that giving both patients and providers the tools to further educate themselves and apply that to their regular visits is a good first step.
“Just having access to a facility doesn’t mean they will get the services they need. Preventative services that are recommended for people with disabilities differ from the general population. Providers should be educated about that and the patient needs to be educated about that,” she added.
“Patients who do not approach clinicians get lost in the system. Maybe many facilities are not disability friendly, or they need health literacy. If they don’t know they are at risk for osteoporosis, for example, then they won’t ask,” Dr. Mahmoudi said.
The study was funded by The National Institute on Disability, Independent Living, and Rehabilitation Research. Dr. Mahmoudi and Mr. Paden report no relevant financial relationships.
Black adults also had lower odds of having a bone density screening, compared with White adults. Plus, comorbidities were highest among the Black patients, according to the paper, which was published in Annals of Family Medicine.
Elham Mahmoudi, PhD, and her coauthors examined private insurance claims from 11,635 patients with cerebral palsy (CP) or spina bifida over ten years from 2007 to 2017. The researchers analyzed comorbidities and compared the rates of different psychological, cardiometabolic, and musculoskeletal conditions among these patients.
Only 23% of Hispanic participants and 18% of Black participants attended an annual wellness visit, compared with 32% of the White participants.
Only 1% of Black and 2% of White participants received any bone density screening (odds ratio = 0.54, 95% confidence interval [CI], 0.31-0.95), a service that is essential for catching a patient’s potential risk for osteoporosis and fractures.
According to the researchers, patients accessed services such as bone density scans, cholesterol assessments, diabetes screenings, and annual wellness visits less than recommended for people with those chronic conditions.
“People with spina bifida and cerebral palsy have complex care needs. We know through our work that chronic conditions are much higher among them compared with adults without disabilities,” Dr. Mahmoudi, associate professor in the department of family medicine at University of Michigan, Ann Arbor, said in an interview. “I was surprised to see even with private insurance, the rate of using preventative services is so low among White people and minority populations.”
Comorbidities highest in Black participants
Black adults had the highest comorbidity score of 2.5, and Hispanic adults had the lowest comorbidity score of 1.8. For White adults in the study, the comorbidity score was 2.0.
Osteoporosis, a common concern for people with spina bifida or cerebral palsy, was detected in around 4% of all participants. Osteoarthritis was detected in 13.38% of Black participants, versus 8.53% of Hispanic participants and 11.09% of White participants.
Diabetes and hypertension were more common among Black participants than among Hispanic and White participants. The percentages of Black patients with hypertension and diabetes were 16.5% and 39.89%, respectively. Among the Hispanic and White adults, the percentages with hypertension were 22.3% and 28.2%, respectively, according to the paper.
Disparities in access
Jamil Paden, racial and health equity manager at the Christopher and Dana Reeve Foundation, said getting access to literature, transportation, tables, chairs, weigh scales, and imaging equipment that accommodate the needs of people with disabilities are some of the biggest challenges for people with disabilities who are trying to receive care.
“It’s not a one size fits all, we have to recognize that if someone doesn’t see themselves in a particular place, then it makes it more challenging for them to feel comfortable speaking up and saying things about their health, which would prevent a person from saying something early on,” Mr. Paden said in an interview. “That particular issue will continue to grow and become more of a health risk, or health challenge down the line.”
Mr. Paden emphasized intersections between class, race, and circumstances which can, together, make health care less equitable for people with disabilities, especially in underserved communities and communities of color. He urged health care providers to distance their practices from a “one size fits all” approach to treatment and engage in their patients’ individual lives and communities.
“It’s not enough to just say, Hey, you have a disability. So let me treat your disability ... You have to recognize that although a patient may have a dire diagnosis, they also are a person of color, and they have to navigate different aspects of life from their counterparts,” he said.
Dr. Mahmoudi said patient and provider understanding of the disability is often lacking. She recommended advocating for patients, noting that giving both patients and providers the tools to further educate themselves and apply that to their regular visits is a good first step.
“Just having access to a facility doesn’t mean they will get the services they need. Preventative services that are recommended for people with disabilities differ from the general population. Providers should be educated about that and the patient needs to be educated about that,” she added.
“Patients who do not approach clinicians get lost in the system. Maybe many facilities are not disability friendly, or they need health literacy. If they don’t know they are at risk for osteoporosis, for example, then they won’t ask,” Dr. Mahmoudi said.
The study was funded by The National Institute on Disability, Independent Living, and Rehabilitation Research. Dr. Mahmoudi and Mr. Paden report no relevant financial relationships.
Black adults also had lower odds of having a bone density screening, compared with White adults. Plus, comorbidities were highest among the Black patients, according to the paper, which was published in Annals of Family Medicine.
Elham Mahmoudi, PhD, and her coauthors examined private insurance claims from 11,635 patients with cerebral palsy (CP) or spina bifida over ten years from 2007 to 2017. The researchers analyzed comorbidities and compared the rates of different psychological, cardiometabolic, and musculoskeletal conditions among these patients.
Only 23% of Hispanic participants and 18% of Black participants attended an annual wellness visit, compared with 32% of the White participants.
Only 1% of Black and 2% of White participants received any bone density screening (odds ratio = 0.54, 95% confidence interval [CI], 0.31-0.95), a service that is essential for catching a patient’s potential risk for osteoporosis and fractures.
According to the researchers, patients accessed services such as bone density scans, cholesterol assessments, diabetes screenings, and annual wellness visits less than recommended for people with those chronic conditions.
“People with spina bifida and cerebral palsy have complex care needs. We know through our work that chronic conditions are much higher among them compared with adults without disabilities,” Dr. Mahmoudi, associate professor in the department of family medicine at University of Michigan, Ann Arbor, said in an interview. “I was surprised to see even with private insurance, the rate of using preventative services is so low among White people and minority populations.”
Comorbidities highest in Black participants
Black adults had the highest comorbidity score of 2.5, and Hispanic adults had the lowest comorbidity score of 1.8. For White adults in the study, the comorbidity score was 2.0.
Osteoporosis, a common concern for people with spina bifida or cerebral palsy, was detected in around 4% of all participants. Osteoarthritis was detected in 13.38% of Black participants, versus 8.53% of Hispanic participants and 11.09% of White participants.
Diabetes and hypertension were more common among Black participants than among Hispanic and White participants. The percentages of Black patients with hypertension and diabetes were 16.5% and 39.89%, respectively. Among the Hispanic and White adults, the percentages with hypertension were 22.3% and 28.2%, respectively, according to the paper.
Disparities in access
Jamil Paden, racial and health equity manager at the Christopher and Dana Reeve Foundation, said getting access to literature, transportation, tables, chairs, weigh scales, and imaging equipment that accommodate the needs of people with disabilities are some of the biggest challenges for people with disabilities who are trying to receive care.
“It’s not a one size fits all, we have to recognize that if someone doesn’t see themselves in a particular place, then it makes it more challenging for them to feel comfortable speaking up and saying things about their health, which would prevent a person from saying something early on,” Mr. Paden said in an interview. “That particular issue will continue to grow and become more of a health risk, or health challenge down the line.”
Mr. Paden emphasized intersections between class, race, and circumstances which can, together, make health care less equitable for people with disabilities, especially in underserved communities and communities of color. He urged health care providers to distance their practices from a “one size fits all” approach to treatment and engage in their patients’ individual lives and communities.
“It’s not enough to just say, Hey, you have a disability. So let me treat your disability ... You have to recognize that although a patient may have a dire diagnosis, they also are a person of color, and they have to navigate different aspects of life from their counterparts,” he said.
Dr. Mahmoudi said patient and provider understanding of the disability is often lacking. She recommended advocating for patients, noting that giving both patients and providers the tools to further educate themselves and apply that to their regular visits is a good first step.
“Just having access to a facility doesn’t mean they will get the services they need. Preventative services that are recommended for people with disabilities differ from the general population. Providers should be educated about that and the patient needs to be educated about that,” she added.
“Patients who do not approach clinicians get lost in the system. Maybe many facilities are not disability friendly, or they need health literacy. If they don’t know they are at risk for osteoporosis, for example, then they won’t ask,” Dr. Mahmoudi said.
The study was funded by The National Institute on Disability, Independent Living, and Rehabilitation Research. Dr. Mahmoudi and Mr. Paden report no relevant financial relationships.
FROM ANNALS OF FAMILY MEDICINE
Why private practice will always survive: Seven doctors who left employment tell why
Employed physicians are often torn. Many relish the steady salary and ability to focus on being a physician rather than handle administrative duties, but they bemoan their employers’ rules and their lack of input into key decisions. And thus, many doctors are leaving employment to start a private practice. For this article,
Leaving employment is ‘an invigorating time’
On Sept. 9, Aaron Przybysz, MD, gave notice to his employer, a large academic medical center in Southern California, that he would be leaving to start a private practice.
“It’s an invigorating time,” said Dr. Przybysz, 41, an anesthesiologist and pain management physician who plans to open his new pain management practice on Dec. 1 in Orange County. He has picked out the space he will rent but has not yet hired his staff.
“I’ve been serious about doing this for at least a year,” Dr. Przybysz said. “What held me back is the concern that my business could fail. But even if that happens, what’s the worst that could occur? I’d have to find a new job as an employed physician.
“I feel comfortable with the business side of medicine,” he said. His father was an executive in the automotive industry and his father-in-law is an entrepreneur in construction and housing.
“One of the biggest reasons for moving to private practice is making sure I don’t miss my kids’ activities,” he said, referring to his children, ages 9 and 7. Recently, he said, “I had to spend the whole weekend on call in the hospital. I came home and had to sleep most of the next day.
“I love the people that I have been working with and I’ve learned and matured as a physician during that time,” he said. “But it was time to move on.”
The desire to be in charge
In Medscape’s recent Employed Physicians Report, doctors said they enjoy the steady salary and ability to focus on patients, which comes with being employed.
Other physicians feel differently. John Machata, MD, a solo family physician in the village of Wickford, R.I., 20 miles south of Providence, chose private practice because “I have total control,” he said. “I make decisions that I couldn’t have made as an employed physician, such as closing my practice to new patients.”
He can also decide on his work hours. “I see patients for 35 hours, 4 days a week and then I have a 3-day weekend.” In a large organization, “the focus is on revenue,” said Dr. Machata. “They’re always measuring your productivity. If you are slower, you won’t make enough money for them.”
When he worked for a large group practice about a decade ago, “I felt burnt out every day,” he said. “I had to see patients every 10 minutes, with no breaks for anything in between. Within a month I was devising my exit strategy.”
Dr. Machata maintains long appointments – 25 minutes for a typical follow-up visit and 55 minutes for an annual check-in – but he still earns above the state average for primary care doctors. “I have no nurse or front-office staff, which means I can save $125,000 to $150,000 a year,” he said.
In 2018, for the first time, employed physicians outnumbered self-employed physicians, according to a survey by the American Medical Association (AMA). By the end of 2021, more than half (52.1%) of U.S. physicians were employed by hospitals or health systems.
Yet the negatives of employment have begun to turn some physicians back toward private practice. Many physicians who were employed by a hospital or a large practice have become disillusioned and want to return to private practice.
His practice is the ‘best of both worlds’
Adam Bruggeman, MD, a 42-year-old spine surgeon who is CEO of Texas Spine Care Center, a solo practice in San Antonio, said he has “the best of both worlds.”
“As a solo physician, I have total control over how I practice,” he said. “But I also have access to value-based contracts and the data and staff needed to implement them.
“You need a lot of administrative overhead to take on these contracts, which a private practice normally doesn’t have,” he said. But Dr. Bruggeman gets this work done through a clinically integrated network (CIN) of private practices, Spinalytics of Texas, where he is chief medical director.
The CIN represents 150 musculoskeletal care providers and provides access to bundled networks, such as a total joint bundle with Blue Cross Blue Shield of Texas, as well as fee-for-service contracts.
He is also building a new ambulatory surgery center (ASC) that is scheduled to open in January. There, he plans to perform total joint and spine surgeries at a lower cost than at the hospital, which will be useful for value-based contracts through the CIN.
Dr. Bruggeman said it would be hard to run his private practice without the CIN and the ASC. “Private practice has changed,” he said. “The days of hanging up a shingle and immediately being successful are gone. You’ve got to be smart about business to run a successful practice.”
He started his practice while the pandemic raged
Joe Greene, MD, 42, an orthopedic surgeon in Louisville, Ky., had to open his hip and knee surgery practice when the COVID-19 pandemic was raging a year and a half ago, but that did not stop him.
“Federal financing of small bank loans completely stopped, but that only amounted to a small delay because our bank took care of it,” said Dr. Greene, who codirects his new practice with another orthopedic surgeon.
Even during the pandemic, “we could be very nimble,” he said. “For instance, when we want to institute new technology or a new patient-centric educational platform, we can do it immediately rather than going through an approval process at a health system.”
The partners, both ex-employees of a health system, also have an ASC, which allows them better control over their surgery schedules. “At a hospital, you can be bumped from the schedule by other surgeries, and you can’t be as productive as an ASC in the number of surgeries per day,” he said.
Dr. Greene attributes the practice’s success to long and careful planning. “We had to learn about business,” he said. “We did 3 to 4 years of research to find the right business model and implement it.”
As they were considering the new practice, a survey of patients showed that more than 75% chose them by word-of-mouth – because they specialize in complex and revision surgeries – rather than through referrals within their health system. This meant they could survive without their employer.
Planning for the new practice took up all his free time, but now he can relax and spend time with his three daughters, ages 12, 10, and 8. Dr. Greene currently coaches two of their teams. “We’re loving it,” he said.
Colleagues want to know how he did it
Clinton Sheets, MD, an ophthalmologist in Hudson and Clearwater, Fla., went solo in 2019 after being in a group practice for 11 years. Since he opened up, “I get phone calls from colleagues all the time, asking me about how I did it,” he said. “At least two of them followed in my footsteps.
“I tell them it’s very doable,” he said. “If you have the motivation, you can do it. Depending on your competence, you can outsource as much or as little as you want. Some management companies can do almost all of the nonclinical work for you.
“Smaller practices can streamline processes because they have a flatter organizational structure and have fewer issues with administrative bloat than larger organizations,” he said.
“Technology hinders and helps a private practice,” he said. On the one hand, he had to buy a lot of expensive equipment that otherwise would be shared by a group of doctors. On the other hand, using the cloud makes it possible to easily store practice management software and the electronic health record.
He’s opening a private practice while staying employed
In December, Dev Basu, MD, a hospitalist in Baltimore, plans to start his own private practice, seeing patients in skilled nursing homes, while still working as a nocturnist in a large health care system.
He said his employer has been supportive of his plans. “My work will not directly compete with them and it will benefit them by serving patients discharged from their hospitals,” said Dr. Basu, 38. He added, however, that he will be allowed to work only at certain facilities, and these will be subject to annual review.
“The financial risk of the new practice is low, because I haven’t had to invest much,” he said. “I won’t have a staff or an office.” He plans to maintain his full schedule as an employee, working 12 nights a month, because it will give him a great deal of time to do the new work.
“I also have no particular interest in running a business,” he said. “I come from a family of doctors, professors, and teachers who never ran a business. But I’m willing to learn so that I can practice medicine the way I want to.
“The ability to set my own schedule and deal with patients in the way I think is best is very important to me,” he said.
Private practitioners don’t have to face ‘moral distress’
One thing private practitioners typically don’t have to contend with is “moral distress,” which occurs when you have to follow institutional concerns on how much time you can spend with a patient or on the need to keep referrals in-house, according to Marie T. Brown, MD.
Dr. Brown is an internist who ran a small private practice in Oak Park, Ill., and is now the physician lead for the American Medical Association’s STEPS Forward program, which provides strategies on how to improve a medical practice.
“In my private practice, I could control the time I spent with each patient,” she said. “I also had control over my schedule. If I didn’t have the time, I just took a lower income, but that was okay.”
Dr. Brown said it is a myth that employment offers a better work-life balance. “Young physicians who take employment for this reason may find that they’re not allowed to drop off and pick up their children from school at a certain time. But you can do that in a private practice.”
She said it’s not that hard to run a practice. “Young physicians don’t think they could run a practice because they don’t have any business skills,” she said. “Yes, you do need some management skills, and you have to devote time to management. But you don’t need to have special expertise. You can outsource much of the work.”
A growing trend?
David J. Zetter, a consultant in Mechanicsburg, Pa., who helps doctors set up private practices, sees more interest in this in the past 5 years. “The overwhelming trend used to be private practices being bought up by hospitals and other entities,” he said. “Now we’re seeing the pendulum swing in the opposite direction.
“Generally, these doctors are fed up with being employed at a large organization,” he added. “Recently I got a call from a doctor who had never thought about running his own business, but he’s had it with being an employed physician.”
Switching to private practice is scary for a lot of them, but the alternative is worse. “A podiatrist I’m working with tells me she is scared to death about setting up a private practice, but she’s doing it because she doesn’t want to be employed anymore,” Mr. Zetter said.
A version of this article first appeared on Medscape.com.
Employed physicians are often torn. Many relish the steady salary and ability to focus on being a physician rather than handle administrative duties, but they bemoan their employers’ rules and their lack of input into key decisions. And thus, many doctors are leaving employment to start a private practice. For this article,
Leaving employment is ‘an invigorating time’
On Sept. 9, Aaron Przybysz, MD, gave notice to his employer, a large academic medical center in Southern California, that he would be leaving to start a private practice.
“It’s an invigorating time,” said Dr. Przybysz, 41, an anesthesiologist and pain management physician who plans to open his new pain management practice on Dec. 1 in Orange County. He has picked out the space he will rent but has not yet hired his staff.
“I’ve been serious about doing this for at least a year,” Dr. Przybysz said. “What held me back is the concern that my business could fail. But even if that happens, what’s the worst that could occur? I’d have to find a new job as an employed physician.
“I feel comfortable with the business side of medicine,” he said. His father was an executive in the automotive industry and his father-in-law is an entrepreneur in construction and housing.
“One of the biggest reasons for moving to private practice is making sure I don’t miss my kids’ activities,” he said, referring to his children, ages 9 and 7. Recently, he said, “I had to spend the whole weekend on call in the hospital. I came home and had to sleep most of the next day.
“I love the people that I have been working with and I’ve learned and matured as a physician during that time,” he said. “But it was time to move on.”
The desire to be in charge
In Medscape’s recent Employed Physicians Report, doctors said they enjoy the steady salary and ability to focus on patients, which comes with being employed.
Other physicians feel differently. John Machata, MD, a solo family physician in the village of Wickford, R.I., 20 miles south of Providence, chose private practice because “I have total control,” he said. “I make decisions that I couldn’t have made as an employed physician, such as closing my practice to new patients.”
He can also decide on his work hours. “I see patients for 35 hours, 4 days a week and then I have a 3-day weekend.” In a large organization, “the focus is on revenue,” said Dr. Machata. “They’re always measuring your productivity. If you are slower, you won’t make enough money for them.”
When he worked for a large group practice about a decade ago, “I felt burnt out every day,” he said. “I had to see patients every 10 minutes, with no breaks for anything in between. Within a month I was devising my exit strategy.”
Dr. Machata maintains long appointments – 25 minutes for a typical follow-up visit and 55 minutes for an annual check-in – but he still earns above the state average for primary care doctors. “I have no nurse or front-office staff, which means I can save $125,000 to $150,000 a year,” he said.
In 2018, for the first time, employed physicians outnumbered self-employed physicians, according to a survey by the American Medical Association (AMA). By the end of 2021, more than half (52.1%) of U.S. physicians were employed by hospitals or health systems.
Yet the negatives of employment have begun to turn some physicians back toward private practice. Many physicians who were employed by a hospital or a large practice have become disillusioned and want to return to private practice.
His practice is the ‘best of both worlds’
Adam Bruggeman, MD, a 42-year-old spine surgeon who is CEO of Texas Spine Care Center, a solo practice in San Antonio, said he has “the best of both worlds.”
“As a solo physician, I have total control over how I practice,” he said. “But I also have access to value-based contracts and the data and staff needed to implement them.
“You need a lot of administrative overhead to take on these contracts, which a private practice normally doesn’t have,” he said. But Dr. Bruggeman gets this work done through a clinically integrated network (CIN) of private practices, Spinalytics of Texas, where he is chief medical director.
The CIN represents 150 musculoskeletal care providers and provides access to bundled networks, such as a total joint bundle with Blue Cross Blue Shield of Texas, as well as fee-for-service contracts.
He is also building a new ambulatory surgery center (ASC) that is scheduled to open in January. There, he plans to perform total joint and spine surgeries at a lower cost than at the hospital, which will be useful for value-based contracts through the CIN.
Dr. Bruggeman said it would be hard to run his private practice without the CIN and the ASC. “Private practice has changed,” he said. “The days of hanging up a shingle and immediately being successful are gone. You’ve got to be smart about business to run a successful practice.”
He started his practice while the pandemic raged
Joe Greene, MD, 42, an orthopedic surgeon in Louisville, Ky., had to open his hip and knee surgery practice when the COVID-19 pandemic was raging a year and a half ago, but that did not stop him.
“Federal financing of small bank loans completely stopped, but that only amounted to a small delay because our bank took care of it,” said Dr. Greene, who codirects his new practice with another orthopedic surgeon.
Even during the pandemic, “we could be very nimble,” he said. “For instance, when we want to institute new technology or a new patient-centric educational platform, we can do it immediately rather than going through an approval process at a health system.”
The partners, both ex-employees of a health system, also have an ASC, which allows them better control over their surgery schedules. “At a hospital, you can be bumped from the schedule by other surgeries, and you can’t be as productive as an ASC in the number of surgeries per day,” he said.
Dr. Greene attributes the practice’s success to long and careful planning. “We had to learn about business,” he said. “We did 3 to 4 years of research to find the right business model and implement it.”
As they were considering the new practice, a survey of patients showed that more than 75% chose them by word-of-mouth – because they specialize in complex and revision surgeries – rather than through referrals within their health system. This meant they could survive without their employer.
Planning for the new practice took up all his free time, but now he can relax and spend time with his three daughters, ages 12, 10, and 8. Dr. Greene currently coaches two of their teams. “We’re loving it,” he said.
Colleagues want to know how he did it
Clinton Sheets, MD, an ophthalmologist in Hudson and Clearwater, Fla., went solo in 2019 after being in a group practice for 11 years. Since he opened up, “I get phone calls from colleagues all the time, asking me about how I did it,” he said. “At least two of them followed in my footsteps.
“I tell them it’s very doable,” he said. “If you have the motivation, you can do it. Depending on your competence, you can outsource as much or as little as you want. Some management companies can do almost all of the nonclinical work for you.
“Smaller practices can streamline processes because they have a flatter organizational structure and have fewer issues with administrative bloat than larger organizations,” he said.
“Technology hinders and helps a private practice,” he said. On the one hand, he had to buy a lot of expensive equipment that otherwise would be shared by a group of doctors. On the other hand, using the cloud makes it possible to easily store practice management software and the electronic health record.
He’s opening a private practice while staying employed
In December, Dev Basu, MD, a hospitalist in Baltimore, plans to start his own private practice, seeing patients in skilled nursing homes, while still working as a nocturnist in a large health care system.
He said his employer has been supportive of his plans. “My work will not directly compete with them and it will benefit them by serving patients discharged from their hospitals,” said Dr. Basu, 38. He added, however, that he will be allowed to work only at certain facilities, and these will be subject to annual review.
“The financial risk of the new practice is low, because I haven’t had to invest much,” he said. “I won’t have a staff or an office.” He plans to maintain his full schedule as an employee, working 12 nights a month, because it will give him a great deal of time to do the new work.
“I also have no particular interest in running a business,” he said. “I come from a family of doctors, professors, and teachers who never ran a business. But I’m willing to learn so that I can practice medicine the way I want to.
“The ability to set my own schedule and deal with patients in the way I think is best is very important to me,” he said.
Private practitioners don’t have to face ‘moral distress’
One thing private practitioners typically don’t have to contend with is “moral distress,” which occurs when you have to follow institutional concerns on how much time you can spend with a patient or on the need to keep referrals in-house, according to Marie T. Brown, MD.
Dr. Brown is an internist who ran a small private practice in Oak Park, Ill., and is now the physician lead for the American Medical Association’s STEPS Forward program, which provides strategies on how to improve a medical practice.
“In my private practice, I could control the time I spent with each patient,” she said. “I also had control over my schedule. If I didn’t have the time, I just took a lower income, but that was okay.”
Dr. Brown said it is a myth that employment offers a better work-life balance. “Young physicians who take employment for this reason may find that they’re not allowed to drop off and pick up their children from school at a certain time. But you can do that in a private practice.”
She said it’s not that hard to run a practice. “Young physicians don’t think they could run a practice because they don’t have any business skills,” she said. “Yes, you do need some management skills, and you have to devote time to management. But you don’t need to have special expertise. You can outsource much of the work.”
A growing trend?
David J. Zetter, a consultant in Mechanicsburg, Pa., who helps doctors set up private practices, sees more interest in this in the past 5 years. “The overwhelming trend used to be private practices being bought up by hospitals and other entities,” he said. “Now we’re seeing the pendulum swing in the opposite direction.
“Generally, these doctors are fed up with being employed at a large organization,” he added. “Recently I got a call from a doctor who had never thought about running his own business, but he’s had it with being an employed physician.”
Switching to private practice is scary for a lot of them, but the alternative is worse. “A podiatrist I’m working with tells me she is scared to death about setting up a private practice, but she’s doing it because she doesn’t want to be employed anymore,” Mr. Zetter said.
A version of this article first appeared on Medscape.com.
Employed physicians are often torn. Many relish the steady salary and ability to focus on being a physician rather than handle administrative duties, but they bemoan their employers’ rules and their lack of input into key decisions. And thus, many doctors are leaving employment to start a private practice. For this article,
Leaving employment is ‘an invigorating time’
On Sept. 9, Aaron Przybysz, MD, gave notice to his employer, a large academic medical center in Southern California, that he would be leaving to start a private practice.
“It’s an invigorating time,” said Dr. Przybysz, 41, an anesthesiologist and pain management physician who plans to open his new pain management practice on Dec. 1 in Orange County. He has picked out the space he will rent but has not yet hired his staff.
“I’ve been serious about doing this for at least a year,” Dr. Przybysz said. “What held me back is the concern that my business could fail. But even if that happens, what’s the worst that could occur? I’d have to find a new job as an employed physician.
“I feel comfortable with the business side of medicine,” he said. His father was an executive in the automotive industry and his father-in-law is an entrepreneur in construction and housing.
“One of the biggest reasons for moving to private practice is making sure I don’t miss my kids’ activities,” he said, referring to his children, ages 9 and 7. Recently, he said, “I had to spend the whole weekend on call in the hospital. I came home and had to sleep most of the next day.
“I love the people that I have been working with and I’ve learned and matured as a physician during that time,” he said. “But it was time to move on.”
The desire to be in charge
In Medscape’s recent Employed Physicians Report, doctors said they enjoy the steady salary and ability to focus on patients, which comes with being employed.
Other physicians feel differently. John Machata, MD, a solo family physician in the village of Wickford, R.I., 20 miles south of Providence, chose private practice because “I have total control,” he said. “I make decisions that I couldn’t have made as an employed physician, such as closing my practice to new patients.”
He can also decide on his work hours. “I see patients for 35 hours, 4 days a week and then I have a 3-day weekend.” In a large organization, “the focus is on revenue,” said Dr. Machata. “They’re always measuring your productivity. If you are slower, you won’t make enough money for them.”
When he worked for a large group practice about a decade ago, “I felt burnt out every day,” he said. “I had to see patients every 10 minutes, with no breaks for anything in between. Within a month I was devising my exit strategy.”
Dr. Machata maintains long appointments – 25 minutes for a typical follow-up visit and 55 minutes for an annual check-in – but he still earns above the state average for primary care doctors. “I have no nurse or front-office staff, which means I can save $125,000 to $150,000 a year,” he said.
In 2018, for the first time, employed physicians outnumbered self-employed physicians, according to a survey by the American Medical Association (AMA). By the end of 2021, more than half (52.1%) of U.S. physicians were employed by hospitals or health systems.
Yet the negatives of employment have begun to turn some physicians back toward private practice. Many physicians who were employed by a hospital or a large practice have become disillusioned and want to return to private practice.
His practice is the ‘best of both worlds’
Adam Bruggeman, MD, a 42-year-old spine surgeon who is CEO of Texas Spine Care Center, a solo practice in San Antonio, said he has “the best of both worlds.”
“As a solo physician, I have total control over how I practice,” he said. “But I also have access to value-based contracts and the data and staff needed to implement them.
“You need a lot of administrative overhead to take on these contracts, which a private practice normally doesn’t have,” he said. But Dr. Bruggeman gets this work done through a clinically integrated network (CIN) of private practices, Spinalytics of Texas, where he is chief medical director.
The CIN represents 150 musculoskeletal care providers and provides access to bundled networks, such as a total joint bundle with Blue Cross Blue Shield of Texas, as well as fee-for-service contracts.
He is also building a new ambulatory surgery center (ASC) that is scheduled to open in January. There, he plans to perform total joint and spine surgeries at a lower cost than at the hospital, which will be useful for value-based contracts through the CIN.
Dr. Bruggeman said it would be hard to run his private practice without the CIN and the ASC. “Private practice has changed,” he said. “The days of hanging up a shingle and immediately being successful are gone. You’ve got to be smart about business to run a successful practice.”
He started his practice while the pandemic raged
Joe Greene, MD, 42, an orthopedic surgeon in Louisville, Ky., had to open his hip and knee surgery practice when the COVID-19 pandemic was raging a year and a half ago, but that did not stop him.
“Federal financing of small bank loans completely stopped, but that only amounted to a small delay because our bank took care of it,” said Dr. Greene, who codirects his new practice with another orthopedic surgeon.
Even during the pandemic, “we could be very nimble,” he said. “For instance, when we want to institute new technology or a new patient-centric educational platform, we can do it immediately rather than going through an approval process at a health system.”
The partners, both ex-employees of a health system, also have an ASC, which allows them better control over their surgery schedules. “At a hospital, you can be bumped from the schedule by other surgeries, and you can’t be as productive as an ASC in the number of surgeries per day,” he said.
Dr. Greene attributes the practice’s success to long and careful planning. “We had to learn about business,” he said. “We did 3 to 4 years of research to find the right business model and implement it.”
As they were considering the new practice, a survey of patients showed that more than 75% chose them by word-of-mouth – because they specialize in complex and revision surgeries – rather than through referrals within their health system. This meant they could survive without their employer.
Planning for the new practice took up all his free time, but now he can relax and spend time with his three daughters, ages 12, 10, and 8. Dr. Greene currently coaches two of their teams. “We’re loving it,” he said.
Colleagues want to know how he did it
Clinton Sheets, MD, an ophthalmologist in Hudson and Clearwater, Fla., went solo in 2019 after being in a group practice for 11 years. Since he opened up, “I get phone calls from colleagues all the time, asking me about how I did it,” he said. “At least two of them followed in my footsteps.
“I tell them it’s very doable,” he said. “If you have the motivation, you can do it. Depending on your competence, you can outsource as much or as little as you want. Some management companies can do almost all of the nonclinical work for you.
“Smaller practices can streamline processes because they have a flatter organizational structure and have fewer issues with administrative bloat than larger organizations,” he said.
“Technology hinders and helps a private practice,” he said. On the one hand, he had to buy a lot of expensive equipment that otherwise would be shared by a group of doctors. On the other hand, using the cloud makes it possible to easily store practice management software and the electronic health record.
He’s opening a private practice while staying employed
In December, Dev Basu, MD, a hospitalist in Baltimore, plans to start his own private practice, seeing patients in skilled nursing homes, while still working as a nocturnist in a large health care system.
He said his employer has been supportive of his plans. “My work will not directly compete with them and it will benefit them by serving patients discharged from their hospitals,” said Dr. Basu, 38. He added, however, that he will be allowed to work only at certain facilities, and these will be subject to annual review.
“The financial risk of the new practice is low, because I haven’t had to invest much,” he said. “I won’t have a staff or an office.” He plans to maintain his full schedule as an employee, working 12 nights a month, because it will give him a great deal of time to do the new work.
“I also have no particular interest in running a business,” he said. “I come from a family of doctors, professors, and teachers who never ran a business. But I’m willing to learn so that I can practice medicine the way I want to.
“The ability to set my own schedule and deal with patients in the way I think is best is very important to me,” he said.
Private practitioners don’t have to face ‘moral distress’
One thing private practitioners typically don’t have to contend with is “moral distress,” which occurs when you have to follow institutional concerns on how much time you can spend with a patient or on the need to keep referrals in-house, according to Marie T. Brown, MD.
Dr. Brown is an internist who ran a small private practice in Oak Park, Ill., and is now the physician lead for the American Medical Association’s STEPS Forward program, which provides strategies on how to improve a medical practice.
“In my private practice, I could control the time I spent with each patient,” she said. “I also had control over my schedule. If I didn’t have the time, I just took a lower income, but that was okay.”
Dr. Brown said it is a myth that employment offers a better work-life balance. “Young physicians who take employment for this reason may find that they’re not allowed to drop off and pick up their children from school at a certain time. But you can do that in a private practice.”
She said it’s not that hard to run a practice. “Young physicians don’t think they could run a practice because they don’t have any business skills,” she said. “Yes, you do need some management skills, and you have to devote time to management. But you don’t need to have special expertise. You can outsource much of the work.”
A growing trend?
David J. Zetter, a consultant in Mechanicsburg, Pa., who helps doctors set up private practices, sees more interest in this in the past 5 years. “The overwhelming trend used to be private practices being bought up by hospitals and other entities,” he said. “Now we’re seeing the pendulum swing in the opposite direction.
“Generally, these doctors are fed up with being employed at a large organization,” he added. “Recently I got a call from a doctor who had never thought about running his own business, but he’s had it with being an employed physician.”
Switching to private practice is scary for a lot of them, but the alternative is worse. “A podiatrist I’m working with tells me she is scared to death about setting up a private practice, but she’s doing it because she doesn’t want to be employed anymore,” Mr. Zetter said.
A version of this article first appeared on Medscape.com.








