User login
Large percentage of psychiatrists sued for malpractice at least once
Forty-one percent of U.S. psychiatrists have been sued for malpractice at least once, findings from the newly released Medscape Psychiatrist Malpractice Report 2019 show.
The top reason for the legal action was wrongful death (31%), followed by poor outcome/disease progression (23%), failure to treat/delayed treatment (11%), errors in medication administration (10%), and complications from treatment/surgery (8%).
Only 7% of psychiatrists said failure to treat/delayed treatment was the reason for the lawsuit, whereas this was the top reason for physicians overall (33%) in the report.
Medscape surveyed 4,360 physician members in more than 25 specialties about whether they have been sued for malpractice, reasons for a lawsuit, what happened, and how the experience affected the way they practice medicine and interact with patients.
Among psychiatrists named in a lawsuit, 44% said they were very surprised to be the subject of litigation. A similar percentage reported they were somewhat surprised (41%), while 15% were not at all surprised.
The vast majority of psychiatrists (87%) believed the lawsuit was not warranted, while 11% were unsure. Only a small percentage (2%) believed that legal action was justified, the lowest percentage of all physicians (6%).
Among psychiatrists who were sued, 42% were able to identify the incident that sparked the lawsuit. A slightly higher percentage (47%) said there was no specific incident that spurred legal action; 11% couldn’t recall.
Psychological factors
“There’s a whole host of what you could call psychological factors that can contribute to the filing of a claim,” David S. Szabo, a malpractice defense attorney with Locke Lord LLP, Boston, said in an interview.
“These can occur when a patient perceives a breakdown in the doctor-patient relationship or is pretty certain that there’s been a mistake and they feel like they’ve been shut out of productive conversation with their health care provider or providers,” said Mr. Szabo.
Legal action eats up time. A total of 43% of psychiatrists reported spending more than 40 hours on their defense, which involved gathering records, meeting with attorneys, and preparing for depositions.
Forty-six percent reported that the entire process took 1-2 years to resolve, but nearly a quarter (23%) said the process dragged on for 3-5 years.
One-third of psychiatrists who were named in a malpractice lawsuit said the case was settled out of court. Of the cases that went to trial, 12% of psychiatrists reported that the verdict was in their favor; 3% reported that the outcome of the case was in the plaintiff’s favor.
Asked why they think most malpractice lawsuits occurred, 61% of psychiatrists said that patients don’t understand medical risks and blame the doctor for bad outcomes even if the doctor does everything right.
A similar percentage of psychiatrists recognized that if a true medical error has occurred, patients wanted to seek restitution and/or assign blame. Only 29% of psychiatrists felt that constant advertising by lawyers to get new clients was the reason for most malpractice cases.
The overwhelming majority of psychiatrists (93%) who responded to the survey carry malpractice insurance, about the same as physicians overall (94%).
Among those with malpractice coverage who either settled or went to trial, about half were either encouraged by their insurer to settle the case or were required by their insurer to do so.
“Generally, if a physician senses that he or she is heading toward a difference of opinion with the insurer about settlement, they probably ought to invest a little time in having personal counsel look at the case,” Mr. Szabo said.
Practice changing?
Facing a lawsuit can be devastating for any physician, but nearly half (48%) of psychiatrists surveyed said they made no changes after the case was resolved.
Just over a quarter (27%) of psychiatrists said the legal action prompted a change in their approach to patients. In addition, 8% said they left their practice setting, and 3% said they bought more malpractice insurance.
Among psychiatrist cases that resulted in a settlement or a verdict in the plaintiff’s favor, nearly half (48%) of monetary awards maxed out at $100,000, while 31% maxed out at $500,000, and 8% at $1 million.
More than half of psychiatrists (55%) named in a lawsuit believed the outcome of the case was fair; 45% felt it was unfair.
Psychiatrists reported that, in retrospect, they would have done several things differently. These included maintaining better documentation of their patient’s chart (20%) and not taking on the patient in the first place (15%), followed by spending more time with the patient and his/her family (11%), getting a second opinion from a colleague (9%), and reviewing the history/chart more carefully (7%).
About three-quarters of psychiatrists felt that saying sorry or offering an apology to the patient would not have prevented the lawsuit. This is a lower percentage than was indicated by all physicians (82%) who have been sued.
Psychiatrists believe the best ways to discourage lawsuits is through better patient communication and rapport (59%) and having a medical panel screen cases for merit (50%).
About half of psychiatrists (51%) and more than half (56%) of all physicians believe that medical organizations or state societies are not doing enough to discourage malpractice cases.
This article first appeared on Medscape.com.
Forty-one percent of U.S. psychiatrists have been sued for malpractice at least once, findings from the newly released Medscape Psychiatrist Malpractice Report 2019 show.
The top reason for the legal action was wrongful death (31%), followed by poor outcome/disease progression (23%), failure to treat/delayed treatment (11%), errors in medication administration (10%), and complications from treatment/surgery (8%).
Only 7% of psychiatrists said failure to treat/delayed treatment was the reason for the lawsuit, whereas this was the top reason for physicians overall (33%) in the report.
Medscape surveyed 4,360 physician members in more than 25 specialties about whether they have been sued for malpractice, reasons for a lawsuit, what happened, and how the experience affected the way they practice medicine and interact with patients.
Among psychiatrists named in a lawsuit, 44% said they were very surprised to be the subject of litigation. A similar percentage reported they were somewhat surprised (41%), while 15% were not at all surprised.
The vast majority of psychiatrists (87%) believed the lawsuit was not warranted, while 11% were unsure. Only a small percentage (2%) believed that legal action was justified, the lowest percentage of all physicians (6%).
Among psychiatrists who were sued, 42% were able to identify the incident that sparked the lawsuit. A slightly higher percentage (47%) said there was no specific incident that spurred legal action; 11% couldn’t recall.
Psychological factors
“There’s a whole host of what you could call psychological factors that can contribute to the filing of a claim,” David S. Szabo, a malpractice defense attorney with Locke Lord LLP, Boston, said in an interview.
“These can occur when a patient perceives a breakdown in the doctor-patient relationship or is pretty certain that there’s been a mistake and they feel like they’ve been shut out of productive conversation with their health care provider or providers,” said Mr. Szabo.
Legal action eats up time. A total of 43% of psychiatrists reported spending more than 40 hours on their defense, which involved gathering records, meeting with attorneys, and preparing for depositions.
Forty-six percent reported that the entire process took 1-2 years to resolve, but nearly a quarter (23%) said the process dragged on for 3-5 years.
One-third of psychiatrists who were named in a malpractice lawsuit said the case was settled out of court. Of the cases that went to trial, 12% of psychiatrists reported that the verdict was in their favor; 3% reported that the outcome of the case was in the plaintiff’s favor.
Asked why they think most malpractice lawsuits occurred, 61% of psychiatrists said that patients don’t understand medical risks and blame the doctor for bad outcomes even if the doctor does everything right.
A similar percentage of psychiatrists recognized that if a true medical error has occurred, patients wanted to seek restitution and/or assign blame. Only 29% of psychiatrists felt that constant advertising by lawyers to get new clients was the reason for most malpractice cases.
The overwhelming majority of psychiatrists (93%) who responded to the survey carry malpractice insurance, about the same as physicians overall (94%).
Among those with malpractice coverage who either settled or went to trial, about half were either encouraged by their insurer to settle the case or were required by their insurer to do so.
“Generally, if a physician senses that he or she is heading toward a difference of opinion with the insurer about settlement, they probably ought to invest a little time in having personal counsel look at the case,” Mr. Szabo said.
Practice changing?
Facing a lawsuit can be devastating for any physician, but nearly half (48%) of psychiatrists surveyed said they made no changes after the case was resolved.
Just over a quarter (27%) of psychiatrists said the legal action prompted a change in their approach to patients. In addition, 8% said they left their practice setting, and 3% said they bought more malpractice insurance.
Among psychiatrist cases that resulted in a settlement or a verdict in the plaintiff’s favor, nearly half (48%) of monetary awards maxed out at $100,000, while 31% maxed out at $500,000, and 8% at $1 million.
More than half of psychiatrists (55%) named in a lawsuit believed the outcome of the case was fair; 45% felt it was unfair.
Psychiatrists reported that, in retrospect, they would have done several things differently. These included maintaining better documentation of their patient’s chart (20%) and not taking on the patient in the first place (15%), followed by spending more time with the patient and his/her family (11%), getting a second opinion from a colleague (9%), and reviewing the history/chart more carefully (7%).
About three-quarters of psychiatrists felt that saying sorry or offering an apology to the patient would not have prevented the lawsuit. This is a lower percentage than was indicated by all physicians (82%) who have been sued.
Psychiatrists believe the best ways to discourage lawsuits is through better patient communication and rapport (59%) and having a medical panel screen cases for merit (50%).
About half of psychiatrists (51%) and more than half (56%) of all physicians believe that medical organizations or state societies are not doing enough to discourage malpractice cases.
This article first appeared on Medscape.com.
Forty-one percent of U.S. psychiatrists have been sued for malpractice at least once, findings from the newly released Medscape Psychiatrist Malpractice Report 2019 show.
The top reason for the legal action was wrongful death (31%), followed by poor outcome/disease progression (23%), failure to treat/delayed treatment (11%), errors in medication administration (10%), and complications from treatment/surgery (8%).
Only 7% of psychiatrists said failure to treat/delayed treatment was the reason for the lawsuit, whereas this was the top reason for physicians overall (33%) in the report.
Medscape surveyed 4,360 physician members in more than 25 specialties about whether they have been sued for malpractice, reasons for a lawsuit, what happened, and how the experience affected the way they practice medicine and interact with patients.
Among psychiatrists named in a lawsuit, 44% said they were very surprised to be the subject of litigation. A similar percentage reported they were somewhat surprised (41%), while 15% were not at all surprised.
The vast majority of psychiatrists (87%) believed the lawsuit was not warranted, while 11% were unsure. Only a small percentage (2%) believed that legal action was justified, the lowest percentage of all physicians (6%).
Among psychiatrists who were sued, 42% were able to identify the incident that sparked the lawsuit. A slightly higher percentage (47%) said there was no specific incident that spurred legal action; 11% couldn’t recall.
Psychological factors
“There’s a whole host of what you could call psychological factors that can contribute to the filing of a claim,” David S. Szabo, a malpractice defense attorney with Locke Lord LLP, Boston, said in an interview.
“These can occur when a patient perceives a breakdown in the doctor-patient relationship or is pretty certain that there’s been a mistake and they feel like they’ve been shut out of productive conversation with their health care provider or providers,” said Mr. Szabo.
Legal action eats up time. A total of 43% of psychiatrists reported spending more than 40 hours on their defense, which involved gathering records, meeting with attorneys, and preparing for depositions.
Forty-six percent reported that the entire process took 1-2 years to resolve, but nearly a quarter (23%) said the process dragged on for 3-5 years.
One-third of psychiatrists who were named in a malpractice lawsuit said the case was settled out of court. Of the cases that went to trial, 12% of psychiatrists reported that the verdict was in their favor; 3% reported that the outcome of the case was in the plaintiff’s favor.
Asked why they think most malpractice lawsuits occurred, 61% of psychiatrists said that patients don’t understand medical risks and blame the doctor for bad outcomes even if the doctor does everything right.
A similar percentage of psychiatrists recognized that if a true medical error has occurred, patients wanted to seek restitution and/or assign blame. Only 29% of psychiatrists felt that constant advertising by lawyers to get new clients was the reason for most malpractice cases.
The overwhelming majority of psychiatrists (93%) who responded to the survey carry malpractice insurance, about the same as physicians overall (94%).
Among those with malpractice coverage who either settled or went to trial, about half were either encouraged by their insurer to settle the case or were required by their insurer to do so.
“Generally, if a physician senses that he or she is heading toward a difference of opinion with the insurer about settlement, they probably ought to invest a little time in having personal counsel look at the case,” Mr. Szabo said.
Practice changing?
Facing a lawsuit can be devastating for any physician, but nearly half (48%) of psychiatrists surveyed said they made no changes after the case was resolved.
Just over a quarter (27%) of psychiatrists said the legal action prompted a change in their approach to patients. In addition, 8% said they left their practice setting, and 3% said they bought more malpractice insurance.
Among psychiatrist cases that resulted in a settlement or a verdict in the plaintiff’s favor, nearly half (48%) of monetary awards maxed out at $100,000, while 31% maxed out at $500,000, and 8% at $1 million.
More than half of psychiatrists (55%) named in a lawsuit believed the outcome of the case was fair; 45% felt it was unfair.
Psychiatrists reported that, in retrospect, they would have done several things differently. These included maintaining better documentation of their patient’s chart (20%) and not taking on the patient in the first place (15%), followed by spending more time with the patient and his/her family (11%), getting a second opinion from a colleague (9%), and reviewing the history/chart more carefully (7%).
About three-quarters of psychiatrists felt that saying sorry or offering an apology to the patient would not have prevented the lawsuit. This is a lower percentage than was indicated by all physicians (82%) who have been sued.
Psychiatrists believe the best ways to discourage lawsuits is through better patient communication and rapport (59%) and having a medical panel screen cases for merit (50%).
About half of psychiatrists (51%) and more than half (56%) of all physicians believe that medical organizations or state societies are not doing enough to discourage malpractice cases.
This article first appeared on Medscape.com.
Dermatologists are uniquely suited to help sexual-, gender-minority patients
ORLANDO – There is a these patients, Angelo Landriscina, MD, said at the ODAC Dermatology, Aesthetic, & Clinical Conference.
“Our knowledge lagging behind is really to our own detriment,” said Dr. Landriscina, chief resident of dermatology at George Washington University, Washington. “The unique comorbidities and lived experiences of queer patients can impact their dermatologic disease. In addition to that, we are in a really unique position to provide life-changing care for these patients.”
The topic of dermatologic care for SGM patients has been discussed with interest in the dermatology community, but it has not been well studied. In one of two papers recently published in Pediatric Dermatology, Markus D. Boos, MD, PhD, from the University of Washington, Seattle, and Seattle Children’s Hospital, and coauthors noted that there is a particular knowledge gap in how to care for SGM pediatric and adolescent patients (Pediatr Dermatol. 2019 Sep;36[5]:581-6; 587-93).
In his presentation, Dr. Landriscina outlined the differences between sexual orientation – an emotional, romantic, or sexual attraction to others – and gender identity, or how one perceives their own gender. Lesbian, gay, transgender, and queer/questioning are classical definitions, but SGM patients may also self-identify in any number of other ways. Some SGM patients may identify as gender-fluid or nonbinary, while genderqueer is an umbrella term for individuals who don’t identify with typical gender roles. On the topic of pronouns, asking SGM patients how they want to be referred to is ideal, but the singular they is considered a gender-neutral term that should work for most situations.
There are also terms to avoid: “Homosexual” may be acceptable to some SGM patients, but is from an era when same-sex attraction was pathologized; “sexual preference” characterizes sexuality as a choice; the term “lifestyle” perpetuates the idea that all SGM patients are the same; and referring to transgender patients as "pre-op" or "post-op" is problematic as these terms imply that transgender identity is defined by a medical transition. Using transgender or gay as a noun, or the word transsexual, is offensive and shouldn’t be used at all, according to Dr. Landriscina.
As these terms continue to change and be redefined, dermatologists are likely to encounter terms they are unfamiliar with in the clinic, but he emphasized that attendees need not know every term to care for these patients. “The easiest way to be right in all of these situations is to let your patients define themselves,” he said, but noted that “assumptions are your worst enemy. You’re going to have to ask the hard questions.”
Updating understanding of SGM patients
Much of the medical community’s understanding of SGM patients hasn’t been updated in decades, Dr. Landriscina said. For example, medical school students typically learn about SGM risk factors that only apply to men who have sex with men (MSM), but there is new interest in caring for transgender patients within dermatology. The focus on classical notions for treating MSM can be reductive, Dr. Landriscina explained. “It boils a whole community of people down to one disease process. I think that we need to expand the thought that there are other associations here. There are other risks these patients face.”
In contrast, dermatologists who strive to understand their patients can better see them as a whole person, can engage in a better differential diagnosis, are aware of the current comorbidities SGM patients face that affect dermatologic disease, and can even work with the patient toward preventative care.
“It’s been decades since we’ve had a paradigm shift about this, and I think it’s time,” he said.
Overall, SGM patients have a higher likelihood of suffering from mental illness and suicidal ideation, with 10%-20% of lesbian, gay, and bisexual patients attempting suicide. Gender-minority patients have a significantly higher rate of attempting suicide at 40%. SGM patients are also more likely to be homeless and uninsured, and have the highest rates of tobacco, alcohol, and illicit drug use. In the SGM population, there is a higher likelihood of being victimized, and discriminated against, with this risk being much higher in transgender patients.
For MSM, there is a high risk of HIV and other STIs such as herpes simplex virus type 2 (HSV2), human papillomavirus (HPV), gonorrhea, and chlamydia, Dr. Landriscina said. They are also at risk for hepatitis A, B, and C; clusters of meningococcal meningitis; and human herpes virus 8. While MSM are more likely to use sunscreen, they also are more likely to use tanning beds and not wear protective clothing outdoors, and are at a greater risk of skin cancer. The risks of body dysmorphia and eating disorders are also increased for MSM.
While there is not as much research on risk factors for women who have sex with women (WSW), they are still at risk for HIV, HSV, and HPV and are less likely to engage in safe sex practices. For women who have sex with both men and other women, there is an even greater risk of STIs. While WSW are more likely to perceive less need for screening, they should be given the same screening as all other women, and dermatologists can help by ensuring these patients are connected with primary care providers, he said.
Dermatologic sequelae for transgender patients
For patients who transition from male to female, there is little information on their sexual risk from studies, but their care should be managed similarly to MSM, Dr. Landriscina said. When seeing transgender patients, dermatologists should be aware of issues of gender dysphoria, but not offer any intervention without first having a conversation about the patient’s hopes and goals. “Not every patient will have the means or desire to have everything that you can offer,” he said.
For patients who choose to undergo a female-to-male transition, dermatological sequelae may include classical manifestations of androgen excess from hormone therapy such as acne and androgenic alopecia; acne, miliaria, tinea corporis, contact dermatitis from chest binding; and surgical scars and keloids. For acne, isotretinoin is an option if a case is severe, but dermatologists should be aware these patients may still be able to become pregnant. There is no consensus on treatment for androgenic alopecia, but use of finasteride might block wanted secondary sex characteristics, Dr. Landriscina noted.
Patients who undergo a male-to-female transition may develop melasma or asteatotic eczema while receiving estrogen therapy; unwanted facial or body hair; and complications from illicit “filler” injections that may cause foreign-body granulomas, bacterial or atypical mycobacterial infection, lymphedema, and scarring.
Transgender patients may choose to undergo aesthetic treatments that can affirm their gender and decrease their gender dysphoria, augment the effects of hormone therapy and gender-confirmation surgery, and improve their quality of life. “While this has classically fallen under the purview of plastic surgery, I feel like we’re uniquely positioned to provide really life-changing aesthetic services to these patients,” Dr. Landriscina said.
Creating an inclusive environment is key to successfully caring for SGM patients. Any practice policies should have SGM-inclusive language, employees should receive mandatory LGBTQ+ focused training, and a point person should oversee LGBTQ+ matters, according to the Joint Commission’s LGBT Guide. Practices should also begin collecting data on sexual orientation and gender identity, which may help patients who are reluctant to vocally disclose their sexual orientation and gender identity and expand understanding of SGM patients. “Before you even walk into that visit, you know what the patient’s identity is, how they want to be addressed,” said Dr. Landriscina. “It also shows patients that you value what their identities are and that you’re competent in taking care of them.”
Dr. Landriscina encouraged attendees to take the information they learned in the session and “run with it.”
“Go for it. Keep learning,” he said. “There’s more about this topic than I even had the chance to include. Your patients are going to appreciate your dedication to them.”
In an interview, Adam Friedman, MD, professor and interim chair of dermatology at George Washington University and medical director of ODAC, acknowledged the large gaps in care for SGM patients and the unique role dermatologists can play in their care, both in terms of medical and surgical procedures.
“There are specific considerations that we as dermatologists need to think about in terms of just quality of life, potentially mental disease, homelessness, access to care. I think if we consider the whole picture, we can not only provide dermatologic care, but maybe serve as a pivot point to direct them to other specialists, and other physicians, and even nonphysicians who play a role in all facets of life to really get these individuals all the care, in broader senses, that they need,” he said.
Dr. Landriscina reported no relevant conflicts of interest.
ORLANDO – There is a these patients, Angelo Landriscina, MD, said at the ODAC Dermatology, Aesthetic, & Clinical Conference.
“Our knowledge lagging behind is really to our own detriment,” said Dr. Landriscina, chief resident of dermatology at George Washington University, Washington. “The unique comorbidities and lived experiences of queer patients can impact their dermatologic disease. In addition to that, we are in a really unique position to provide life-changing care for these patients.”
The topic of dermatologic care for SGM patients has been discussed with interest in the dermatology community, but it has not been well studied. In one of two papers recently published in Pediatric Dermatology, Markus D. Boos, MD, PhD, from the University of Washington, Seattle, and Seattle Children’s Hospital, and coauthors noted that there is a particular knowledge gap in how to care for SGM pediatric and adolescent patients (Pediatr Dermatol. 2019 Sep;36[5]:581-6; 587-93).
In his presentation, Dr. Landriscina outlined the differences between sexual orientation – an emotional, romantic, or sexual attraction to others – and gender identity, or how one perceives their own gender. Lesbian, gay, transgender, and queer/questioning are classical definitions, but SGM patients may also self-identify in any number of other ways. Some SGM patients may identify as gender-fluid or nonbinary, while genderqueer is an umbrella term for individuals who don’t identify with typical gender roles. On the topic of pronouns, asking SGM patients how they want to be referred to is ideal, but the singular they is considered a gender-neutral term that should work for most situations.
There are also terms to avoid: “Homosexual” may be acceptable to some SGM patients, but is from an era when same-sex attraction was pathologized; “sexual preference” characterizes sexuality as a choice; the term “lifestyle” perpetuates the idea that all SGM patients are the same; and referring to transgender patients as "pre-op" or "post-op" is problematic as these terms imply that transgender identity is defined by a medical transition. Using transgender or gay as a noun, or the word transsexual, is offensive and shouldn’t be used at all, according to Dr. Landriscina.
As these terms continue to change and be redefined, dermatologists are likely to encounter terms they are unfamiliar with in the clinic, but he emphasized that attendees need not know every term to care for these patients. “The easiest way to be right in all of these situations is to let your patients define themselves,” he said, but noted that “assumptions are your worst enemy. You’re going to have to ask the hard questions.”
Updating understanding of SGM patients
Much of the medical community’s understanding of SGM patients hasn’t been updated in decades, Dr. Landriscina said. For example, medical school students typically learn about SGM risk factors that only apply to men who have sex with men (MSM), but there is new interest in caring for transgender patients within dermatology. The focus on classical notions for treating MSM can be reductive, Dr. Landriscina explained. “It boils a whole community of people down to one disease process. I think that we need to expand the thought that there are other associations here. There are other risks these patients face.”
In contrast, dermatologists who strive to understand their patients can better see them as a whole person, can engage in a better differential diagnosis, are aware of the current comorbidities SGM patients face that affect dermatologic disease, and can even work with the patient toward preventative care.
“It’s been decades since we’ve had a paradigm shift about this, and I think it’s time,” he said.
Overall, SGM patients have a higher likelihood of suffering from mental illness and suicidal ideation, with 10%-20% of lesbian, gay, and bisexual patients attempting suicide. Gender-minority patients have a significantly higher rate of attempting suicide at 40%. SGM patients are also more likely to be homeless and uninsured, and have the highest rates of tobacco, alcohol, and illicit drug use. In the SGM population, there is a higher likelihood of being victimized, and discriminated against, with this risk being much higher in transgender patients.
For MSM, there is a high risk of HIV and other STIs such as herpes simplex virus type 2 (HSV2), human papillomavirus (HPV), gonorrhea, and chlamydia, Dr. Landriscina said. They are also at risk for hepatitis A, B, and C; clusters of meningococcal meningitis; and human herpes virus 8. While MSM are more likely to use sunscreen, they also are more likely to use tanning beds and not wear protective clothing outdoors, and are at a greater risk of skin cancer. The risks of body dysmorphia and eating disorders are also increased for MSM.
While there is not as much research on risk factors for women who have sex with women (WSW), they are still at risk for HIV, HSV, and HPV and are less likely to engage in safe sex practices. For women who have sex with both men and other women, there is an even greater risk of STIs. While WSW are more likely to perceive less need for screening, they should be given the same screening as all other women, and dermatologists can help by ensuring these patients are connected with primary care providers, he said.
Dermatologic sequelae for transgender patients
For patients who transition from male to female, there is little information on their sexual risk from studies, but their care should be managed similarly to MSM, Dr. Landriscina said. When seeing transgender patients, dermatologists should be aware of issues of gender dysphoria, but not offer any intervention without first having a conversation about the patient’s hopes and goals. “Not every patient will have the means or desire to have everything that you can offer,” he said.
For patients who choose to undergo a female-to-male transition, dermatological sequelae may include classical manifestations of androgen excess from hormone therapy such as acne and androgenic alopecia; acne, miliaria, tinea corporis, contact dermatitis from chest binding; and surgical scars and keloids. For acne, isotretinoin is an option if a case is severe, but dermatologists should be aware these patients may still be able to become pregnant. There is no consensus on treatment for androgenic alopecia, but use of finasteride might block wanted secondary sex characteristics, Dr. Landriscina noted.
Patients who undergo a male-to-female transition may develop melasma or asteatotic eczema while receiving estrogen therapy; unwanted facial or body hair; and complications from illicit “filler” injections that may cause foreign-body granulomas, bacterial or atypical mycobacterial infection, lymphedema, and scarring.
Transgender patients may choose to undergo aesthetic treatments that can affirm their gender and decrease their gender dysphoria, augment the effects of hormone therapy and gender-confirmation surgery, and improve their quality of life. “While this has classically fallen under the purview of plastic surgery, I feel like we’re uniquely positioned to provide really life-changing aesthetic services to these patients,” Dr. Landriscina said.
Creating an inclusive environment is key to successfully caring for SGM patients. Any practice policies should have SGM-inclusive language, employees should receive mandatory LGBTQ+ focused training, and a point person should oversee LGBTQ+ matters, according to the Joint Commission’s LGBT Guide. Practices should also begin collecting data on sexual orientation and gender identity, which may help patients who are reluctant to vocally disclose their sexual orientation and gender identity and expand understanding of SGM patients. “Before you even walk into that visit, you know what the patient’s identity is, how they want to be addressed,” said Dr. Landriscina. “It also shows patients that you value what their identities are and that you’re competent in taking care of them.”
Dr. Landriscina encouraged attendees to take the information they learned in the session and “run with it.”
“Go for it. Keep learning,” he said. “There’s more about this topic than I even had the chance to include. Your patients are going to appreciate your dedication to them.”
In an interview, Adam Friedman, MD, professor and interim chair of dermatology at George Washington University and medical director of ODAC, acknowledged the large gaps in care for SGM patients and the unique role dermatologists can play in their care, both in terms of medical and surgical procedures.
“There are specific considerations that we as dermatologists need to think about in terms of just quality of life, potentially mental disease, homelessness, access to care. I think if we consider the whole picture, we can not only provide dermatologic care, but maybe serve as a pivot point to direct them to other specialists, and other physicians, and even nonphysicians who play a role in all facets of life to really get these individuals all the care, in broader senses, that they need,” he said.
Dr. Landriscina reported no relevant conflicts of interest.
ORLANDO – There is a these patients, Angelo Landriscina, MD, said at the ODAC Dermatology, Aesthetic, & Clinical Conference.
“Our knowledge lagging behind is really to our own detriment,” said Dr. Landriscina, chief resident of dermatology at George Washington University, Washington. “The unique comorbidities and lived experiences of queer patients can impact their dermatologic disease. In addition to that, we are in a really unique position to provide life-changing care for these patients.”
The topic of dermatologic care for SGM patients has been discussed with interest in the dermatology community, but it has not been well studied. In one of two papers recently published in Pediatric Dermatology, Markus D. Boos, MD, PhD, from the University of Washington, Seattle, and Seattle Children’s Hospital, and coauthors noted that there is a particular knowledge gap in how to care for SGM pediatric and adolescent patients (Pediatr Dermatol. 2019 Sep;36[5]:581-6; 587-93).
In his presentation, Dr. Landriscina outlined the differences between sexual orientation – an emotional, romantic, or sexual attraction to others – and gender identity, or how one perceives their own gender. Lesbian, gay, transgender, and queer/questioning are classical definitions, but SGM patients may also self-identify in any number of other ways. Some SGM patients may identify as gender-fluid or nonbinary, while genderqueer is an umbrella term for individuals who don’t identify with typical gender roles. On the topic of pronouns, asking SGM patients how they want to be referred to is ideal, but the singular they is considered a gender-neutral term that should work for most situations.
There are also terms to avoid: “Homosexual” may be acceptable to some SGM patients, but is from an era when same-sex attraction was pathologized; “sexual preference” characterizes sexuality as a choice; the term “lifestyle” perpetuates the idea that all SGM patients are the same; and referring to transgender patients as "pre-op" or "post-op" is problematic as these terms imply that transgender identity is defined by a medical transition. Using transgender or gay as a noun, or the word transsexual, is offensive and shouldn’t be used at all, according to Dr. Landriscina.
As these terms continue to change and be redefined, dermatologists are likely to encounter terms they are unfamiliar with in the clinic, but he emphasized that attendees need not know every term to care for these patients. “The easiest way to be right in all of these situations is to let your patients define themselves,” he said, but noted that “assumptions are your worst enemy. You’re going to have to ask the hard questions.”
Updating understanding of SGM patients
Much of the medical community’s understanding of SGM patients hasn’t been updated in decades, Dr. Landriscina said. For example, medical school students typically learn about SGM risk factors that only apply to men who have sex with men (MSM), but there is new interest in caring for transgender patients within dermatology. The focus on classical notions for treating MSM can be reductive, Dr. Landriscina explained. “It boils a whole community of people down to one disease process. I think that we need to expand the thought that there are other associations here. There are other risks these patients face.”
In contrast, dermatologists who strive to understand their patients can better see them as a whole person, can engage in a better differential diagnosis, are aware of the current comorbidities SGM patients face that affect dermatologic disease, and can even work with the patient toward preventative care.
“It’s been decades since we’ve had a paradigm shift about this, and I think it’s time,” he said.
Overall, SGM patients have a higher likelihood of suffering from mental illness and suicidal ideation, with 10%-20% of lesbian, gay, and bisexual patients attempting suicide. Gender-minority patients have a significantly higher rate of attempting suicide at 40%. SGM patients are also more likely to be homeless and uninsured, and have the highest rates of tobacco, alcohol, and illicit drug use. In the SGM population, there is a higher likelihood of being victimized, and discriminated against, with this risk being much higher in transgender patients.
For MSM, there is a high risk of HIV and other STIs such as herpes simplex virus type 2 (HSV2), human papillomavirus (HPV), gonorrhea, and chlamydia, Dr. Landriscina said. They are also at risk for hepatitis A, B, and C; clusters of meningococcal meningitis; and human herpes virus 8. While MSM are more likely to use sunscreen, they also are more likely to use tanning beds and not wear protective clothing outdoors, and are at a greater risk of skin cancer. The risks of body dysmorphia and eating disorders are also increased for MSM.
While there is not as much research on risk factors for women who have sex with women (WSW), they are still at risk for HIV, HSV, and HPV and are less likely to engage in safe sex practices. For women who have sex with both men and other women, there is an even greater risk of STIs. While WSW are more likely to perceive less need for screening, they should be given the same screening as all other women, and dermatologists can help by ensuring these patients are connected with primary care providers, he said.
Dermatologic sequelae for transgender patients
For patients who transition from male to female, there is little information on their sexual risk from studies, but their care should be managed similarly to MSM, Dr. Landriscina said. When seeing transgender patients, dermatologists should be aware of issues of gender dysphoria, but not offer any intervention without first having a conversation about the patient’s hopes and goals. “Not every patient will have the means or desire to have everything that you can offer,” he said.
For patients who choose to undergo a female-to-male transition, dermatological sequelae may include classical manifestations of androgen excess from hormone therapy such as acne and androgenic alopecia; acne, miliaria, tinea corporis, contact dermatitis from chest binding; and surgical scars and keloids. For acne, isotretinoin is an option if a case is severe, but dermatologists should be aware these patients may still be able to become pregnant. There is no consensus on treatment for androgenic alopecia, but use of finasteride might block wanted secondary sex characteristics, Dr. Landriscina noted.
Patients who undergo a male-to-female transition may develop melasma or asteatotic eczema while receiving estrogen therapy; unwanted facial or body hair; and complications from illicit “filler” injections that may cause foreign-body granulomas, bacterial or atypical mycobacterial infection, lymphedema, and scarring.
Transgender patients may choose to undergo aesthetic treatments that can affirm their gender and decrease their gender dysphoria, augment the effects of hormone therapy and gender-confirmation surgery, and improve their quality of life. “While this has classically fallen under the purview of plastic surgery, I feel like we’re uniquely positioned to provide really life-changing aesthetic services to these patients,” Dr. Landriscina said.
Creating an inclusive environment is key to successfully caring for SGM patients. Any practice policies should have SGM-inclusive language, employees should receive mandatory LGBTQ+ focused training, and a point person should oversee LGBTQ+ matters, according to the Joint Commission’s LGBT Guide. Practices should also begin collecting data on sexual orientation and gender identity, which may help patients who are reluctant to vocally disclose their sexual orientation and gender identity and expand understanding of SGM patients. “Before you even walk into that visit, you know what the patient’s identity is, how they want to be addressed,” said Dr. Landriscina. “It also shows patients that you value what their identities are and that you’re competent in taking care of them.”
Dr. Landriscina encouraged attendees to take the information they learned in the session and “run with it.”
“Go for it. Keep learning,” he said. “There’s more about this topic than I even had the chance to include. Your patients are going to appreciate your dedication to them.”
In an interview, Adam Friedman, MD, professor and interim chair of dermatology at George Washington University and medical director of ODAC, acknowledged the large gaps in care for SGM patients and the unique role dermatologists can play in their care, both in terms of medical and surgical procedures.
“There are specific considerations that we as dermatologists need to think about in terms of just quality of life, potentially mental disease, homelessness, access to care. I think if we consider the whole picture, we can not only provide dermatologic care, but maybe serve as a pivot point to direct them to other specialists, and other physicians, and even nonphysicians who play a role in all facets of life to really get these individuals all the care, in broader senses, that they need,” he said.
Dr. Landriscina reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM ODAC 2020
Is our mental health system broken? If so, can it be fixed?
Numerous articles, books, and newspaper editorials have been written about the “crisis” in mental health care in our country from various perspectives, and the phrase is often used that the mental health system is “broken.” It seems that lately, this topic is often brought up after the most recent mass shooting.1
Philip T. Yanos, PhD, correctly asked recently whether we should be talking about a “broken” system, because implicit in the phrase is the assumption that the mental health system was once “whole,” and he has pointed out2 chronic deficiencies, such as the absence of affordable housing, and the availability of services to those with chronic mental illness.
In addition, many authors have asserted that, with deinstitutionalization – which occurred starting with the Community Mental Health Act of 1963 – homelessness also became a big problem for people in our prisons and jails, which became the default treatment providers for many of those with serious mental illness.Once authors make this point, they often offer up ways to start addressing various parts of the system, and it usually comes down to asking for more funding for more outpatient treatment and services as well as more inpatient beds. Some authors make the point3 that people with mental illness often lack insight into their illness and the need for treatment. Thus, we have the quandary of people with severe mental illness not believing that they need help, and thus not even trying to access services, which can lead to homelessness and jail time.
But what of those individuals with serious mental health problems who aren’t facing those obstacles and complications? What about individuals who aren’t facing homelessness, who haven’t gotten embroiled in the legal system, who do have insurance coverage, who live in areas with sufficient numbers of outpatient mental health centers to choose from, and who have no problems finding an inpatient bed when needed? Let’s suppose that we have an individual who does have insight into his mental illness and need for treatment, and is motivated to seek treatment. How responsive is the system to such individuals? That will be the focus on my article.
In a recent report,4 the author quotes American Psychiatric Association President Bruce J. Schwartz, MD, appealing to members of the U.S. Congress to step in. According to the author, Dr. Schwartz’s position is that the crisis in American mental health begins specifically with a drastic, and growing, shortage of psychiatric beds, especially in publicly funded state and county hospital beds. From there, the crisis spreads to the nation’s city streets, and its jails and prisons, where the largest number of people with serious mental illness now reside. He also talks about a shortage of psychiatrists and child psychiatrists, and says the shortage is likely to worsen. The proposed solution to this problem, of course, is more funding from Congress to open more psychiatric beds, as well as providing more funding for mental health in general and funding to residency programs to increase the numbers of psychiatrists.
I respect the opinions of Dr. Schwartz and that of the other authors who want to talk about lack of adequate beds, outpatient clinics and services, insufficient numbers of psychiatrists, and a lack of funding by Congress. However, I would like to provide further information, from a personal perspective, which causes me to believe that the problem is even more complex than that, and that the failures of the system are compounded by a dysfunctional culture within the ranks of professional caregivers. In other words, once the pieces are in place and assembled, the mental health system still seems to be “broken” but from within. I worry about apathy and an absence of motivation to provide good or even adequate services by the very people who are or should be aware of the problems and what it takes to help our vulnerable patients lead better lives.
I have practiced psychiatry for many years in various settings. I have spent many years working as an inpatient psychiatrist in a large state hospital. I have worked in community mental health outpatient settings. I have also worked in a private practice doing both inpatient and outpatient patient care as well as significant forensic work. At the hospitals, I have witnessed and prepared internal reports about patients who are “revolving doors.” Such patients often had more than 50 psychiatric hospitalizations and no apparent solution to keep them stable enough in the community.
But mental illness is not just a career for me. In addition to being psychiatrist, I am the father of a son with severe and persistent mental illness. I have watched him struggle to find stability. He, too, has been in and out of hospitals. My wife is also in the mental health field. She and I have endlessly tried to work with our son’s local community mental health center to provide them with feedback and to get them to respond to his needs – often with great frustration. It has been our impression that clinicians have difficulty listening to us and understanding the difficulties our son is having, from my son’s case manager to the treating psychiatrist, to the director of the agency. We have tried shifting him to other programs in a neighboring county, including one known to be a “model” program, but had the same issues.
Psychiatry is more of an art than science. Our other medical colleagues can try to resolve a clinical problem, no matter their rank, by ordering the right blood test or getting certain imaging. Psychiatry has no such biomarkers, or validated tests, to rely on to resolve disputes. We have only our training and experience and, unfortunately, our biases. If we don’t agree with a colleague, we often resort to rank and argument.
Psychiatrists (just as can colleagues in other specialties) can be insufferably arrogant.
My personal experience has been that the hospital and the community often don’t communicate well. This seems to be a systems problem, as is the case for many complex unsolvable problems. I have been to discharge meetings involving hospital staff and the receiving community system. The attitude of the inpatient psychiatrist is often: “If you guys only did your job better, this patient wouldn’t keep having to be admitted. It’s your job to keep him out of the hospital.”
Alternatively, the community rejects this attitude and points to the absence of resources that prevents them from seeing patients in a timely manner and from adequately monitoring them. They say they are shackled by their resource constraints and that the endless admissions are inevitable. Further, the outpatient psychiatrists complain bitterly that all the inpatient doctors do is make a bunch of useless medication changes and then don’t keep patients in long enough to make sure the patient stays well. And on and on the arguments go with no resolution.
Sadly, and confirmed by my personal experience, when well-meaning and knowledgeable family members try to communicate with the community mental health system about their son’s mental disintegration, the community agency often doesn’t welcome the feedback. They resort to “confidentiality” concerns, often ill advised. Their opinion seems to be that the patient, (i.e. the patient who is falling apart and is becoming psychotic), should be the one calling the agency, waiting on hold forever, and not getting a call back. When my son has been in this situation, he has hung up his telephone out of frustration, then headed off to the emergency room, where he knew he would be seen.
The other area of frustration is that of the ideal of recovery. Mental health programs love to tout that their mission is “recovery,” and they list it as one of their primary areas of vision and goals. Yet, when we tried to communicate with community clinicians, they usually ignored our request to assist our son with supported employment and to help him achieve independence and a social life. When we tried to convey our recovery concerns to the psychiatrist, the usual response was also to ignore it and focus on “meds, meds, meds,” which most psychiatrists seem to view as their mission and area of expertise. Many psychiatrists have embraced the “bio-bio-bio” model of evaluation and treatment5 with only lip service paid to the “biopsychosocial” theory they like to say they advocate. When we reached out to our son’s psychiatrists and could get through, we found that they mostly failed to display much interest in paying attention to broader areas of functioning, instead focusing on symptoms, which they could observe in person.
So, I add to the chorus complaining that our mental health system is broken. Broken not only in terms of adequate funding, but also broken from within. It would require much wisdom and self-examination to even begin to address the problem. Without a better plan, throwing money at this broken system won’t improve the lives of our seriously ill and vulnerable psychiatric patients.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University in Cleveland as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
References
1. Doroshow D. “We need to stop focusing on the mental health of mass shooters.” Washington Post. 2019 May 20.
2. Yanos P. “Is the mental health system ‘broken’?” Psychology Today. 2018 Oct 11.
3. Orenstein N. “How to fix a broken mental health system.” The Atlantic. 2016 Jun 8.
4. Moran M. APA rings alarm in nation’s capitol about crisis in mental health care. Psychiatr News. 2020 Jan 1.
5. Paris J. “Psychotherapy in an Age of Neuroscience.” New York: Oxford University Press, 2017.
Numerous articles, books, and newspaper editorials have been written about the “crisis” in mental health care in our country from various perspectives, and the phrase is often used that the mental health system is “broken.” It seems that lately, this topic is often brought up after the most recent mass shooting.1
Philip T. Yanos, PhD, correctly asked recently whether we should be talking about a “broken” system, because implicit in the phrase is the assumption that the mental health system was once “whole,” and he has pointed out2 chronic deficiencies, such as the absence of affordable housing, and the availability of services to those with chronic mental illness.
In addition, many authors have asserted that, with deinstitutionalization – which occurred starting with the Community Mental Health Act of 1963 – homelessness also became a big problem for people in our prisons and jails, which became the default treatment providers for many of those with serious mental illness.Once authors make this point, they often offer up ways to start addressing various parts of the system, and it usually comes down to asking for more funding for more outpatient treatment and services as well as more inpatient beds. Some authors make the point3 that people with mental illness often lack insight into their illness and the need for treatment. Thus, we have the quandary of people with severe mental illness not believing that they need help, and thus not even trying to access services, which can lead to homelessness and jail time.
But what of those individuals with serious mental health problems who aren’t facing those obstacles and complications? What about individuals who aren’t facing homelessness, who haven’t gotten embroiled in the legal system, who do have insurance coverage, who live in areas with sufficient numbers of outpatient mental health centers to choose from, and who have no problems finding an inpatient bed when needed? Let’s suppose that we have an individual who does have insight into his mental illness and need for treatment, and is motivated to seek treatment. How responsive is the system to such individuals? That will be the focus on my article.
In a recent report,4 the author quotes American Psychiatric Association President Bruce J. Schwartz, MD, appealing to members of the U.S. Congress to step in. According to the author, Dr. Schwartz’s position is that the crisis in American mental health begins specifically with a drastic, and growing, shortage of psychiatric beds, especially in publicly funded state and county hospital beds. From there, the crisis spreads to the nation’s city streets, and its jails and prisons, where the largest number of people with serious mental illness now reside. He also talks about a shortage of psychiatrists and child psychiatrists, and says the shortage is likely to worsen. The proposed solution to this problem, of course, is more funding from Congress to open more psychiatric beds, as well as providing more funding for mental health in general and funding to residency programs to increase the numbers of psychiatrists.
I respect the opinions of Dr. Schwartz and that of the other authors who want to talk about lack of adequate beds, outpatient clinics and services, insufficient numbers of psychiatrists, and a lack of funding by Congress. However, I would like to provide further information, from a personal perspective, which causes me to believe that the problem is even more complex than that, and that the failures of the system are compounded by a dysfunctional culture within the ranks of professional caregivers. In other words, once the pieces are in place and assembled, the mental health system still seems to be “broken” but from within. I worry about apathy and an absence of motivation to provide good or even adequate services by the very people who are or should be aware of the problems and what it takes to help our vulnerable patients lead better lives.
I have practiced psychiatry for many years in various settings. I have spent many years working as an inpatient psychiatrist in a large state hospital. I have worked in community mental health outpatient settings. I have also worked in a private practice doing both inpatient and outpatient patient care as well as significant forensic work. At the hospitals, I have witnessed and prepared internal reports about patients who are “revolving doors.” Such patients often had more than 50 psychiatric hospitalizations and no apparent solution to keep them stable enough in the community.
But mental illness is not just a career for me. In addition to being psychiatrist, I am the father of a son with severe and persistent mental illness. I have watched him struggle to find stability. He, too, has been in and out of hospitals. My wife is also in the mental health field. She and I have endlessly tried to work with our son’s local community mental health center to provide them with feedback and to get them to respond to his needs – often with great frustration. It has been our impression that clinicians have difficulty listening to us and understanding the difficulties our son is having, from my son’s case manager to the treating psychiatrist, to the director of the agency. We have tried shifting him to other programs in a neighboring county, including one known to be a “model” program, but had the same issues.
Psychiatry is more of an art than science. Our other medical colleagues can try to resolve a clinical problem, no matter their rank, by ordering the right blood test or getting certain imaging. Psychiatry has no such biomarkers, or validated tests, to rely on to resolve disputes. We have only our training and experience and, unfortunately, our biases. If we don’t agree with a colleague, we often resort to rank and argument.
Psychiatrists (just as can colleagues in other specialties) can be insufferably arrogant.
My personal experience has been that the hospital and the community often don’t communicate well. This seems to be a systems problem, as is the case for many complex unsolvable problems. I have been to discharge meetings involving hospital staff and the receiving community system. The attitude of the inpatient psychiatrist is often: “If you guys only did your job better, this patient wouldn’t keep having to be admitted. It’s your job to keep him out of the hospital.”
Alternatively, the community rejects this attitude and points to the absence of resources that prevents them from seeing patients in a timely manner and from adequately monitoring them. They say they are shackled by their resource constraints and that the endless admissions are inevitable. Further, the outpatient psychiatrists complain bitterly that all the inpatient doctors do is make a bunch of useless medication changes and then don’t keep patients in long enough to make sure the patient stays well. And on and on the arguments go with no resolution.
Sadly, and confirmed by my personal experience, when well-meaning and knowledgeable family members try to communicate with the community mental health system about their son’s mental disintegration, the community agency often doesn’t welcome the feedback. They resort to “confidentiality” concerns, often ill advised. Their opinion seems to be that the patient, (i.e. the patient who is falling apart and is becoming psychotic), should be the one calling the agency, waiting on hold forever, and not getting a call back. When my son has been in this situation, he has hung up his telephone out of frustration, then headed off to the emergency room, where he knew he would be seen.
The other area of frustration is that of the ideal of recovery. Mental health programs love to tout that their mission is “recovery,” and they list it as one of their primary areas of vision and goals. Yet, when we tried to communicate with community clinicians, they usually ignored our request to assist our son with supported employment and to help him achieve independence and a social life. When we tried to convey our recovery concerns to the psychiatrist, the usual response was also to ignore it and focus on “meds, meds, meds,” which most psychiatrists seem to view as their mission and area of expertise. Many psychiatrists have embraced the “bio-bio-bio” model of evaluation and treatment5 with only lip service paid to the “biopsychosocial” theory they like to say they advocate. When we reached out to our son’s psychiatrists and could get through, we found that they mostly failed to display much interest in paying attention to broader areas of functioning, instead focusing on symptoms, which they could observe in person.
So, I add to the chorus complaining that our mental health system is broken. Broken not only in terms of adequate funding, but also broken from within. It would require much wisdom and self-examination to even begin to address the problem. Without a better plan, throwing money at this broken system won’t improve the lives of our seriously ill and vulnerable psychiatric patients.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University in Cleveland as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
References
1. Doroshow D. “We need to stop focusing on the mental health of mass shooters.” Washington Post. 2019 May 20.
2. Yanos P. “Is the mental health system ‘broken’?” Psychology Today. 2018 Oct 11.
3. Orenstein N. “How to fix a broken mental health system.” The Atlantic. 2016 Jun 8.
4. Moran M. APA rings alarm in nation’s capitol about crisis in mental health care. Psychiatr News. 2020 Jan 1.
5. Paris J. “Psychotherapy in an Age of Neuroscience.” New York: Oxford University Press, 2017.
Numerous articles, books, and newspaper editorials have been written about the “crisis” in mental health care in our country from various perspectives, and the phrase is often used that the mental health system is “broken.” It seems that lately, this topic is often brought up after the most recent mass shooting.1
Philip T. Yanos, PhD, correctly asked recently whether we should be talking about a “broken” system, because implicit in the phrase is the assumption that the mental health system was once “whole,” and he has pointed out2 chronic deficiencies, such as the absence of affordable housing, and the availability of services to those with chronic mental illness.
In addition, many authors have asserted that, with deinstitutionalization – which occurred starting with the Community Mental Health Act of 1963 – homelessness also became a big problem for people in our prisons and jails, which became the default treatment providers for many of those with serious mental illness.Once authors make this point, they often offer up ways to start addressing various parts of the system, and it usually comes down to asking for more funding for more outpatient treatment and services as well as more inpatient beds. Some authors make the point3 that people with mental illness often lack insight into their illness and the need for treatment. Thus, we have the quandary of people with severe mental illness not believing that they need help, and thus not even trying to access services, which can lead to homelessness and jail time.
But what of those individuals with serious mental health problems who aren’t facing those obstacles and complications? What about individuals who aren’t facing homelessness, who haven’t gotten embroiled in the legal system, who do have insurance coverage, who live in areas with sufficient numbers of outpatient mental health centers to choose from, and who have no problems finding an inpatient bed when needed? Let’s suppose that we have an individual who does have insight into his mental illness and need for treatment, and is motivated to seek treatment. How responsive is the system to such individuals? That will be the focus on my article.
In a recent report,4 the author quotes American Psychiatric Association President Bruce J. Schwartz, MD, appealing to members of the U.S. Congress to step in. According to the author, Dr. Schwartz’s position is that the crisis in American mental health begins specifically with a drastic, and growing, shortage of psychiatric beds, especially in publicly funded state and county hospital beds. From there, the crisis spreads to the nation’s city streets, and its jails and prisons, where the largest number of people with serious mental illness now reside. He also talks about a shortage of psychiatrists and child psychiatrists, and says the shortage is likely to worsen. The proposed solution to this problem, of course, is more funding from Congress to open more psychiatric beds, as well as providing more funding for mental health in general and funding to residency programs to increase the numbers of psychiatrists.
I respect the opinions of Dr. Schwartz and that of the other authors who want to talk about lack of adequate beds, outpatient clinics and services, insufficient numbers of psychiatrists, and a lack of funding by Congress. However, I would like to provide further information, from a personal perspective, which causes me to believe that the problem is even more complex than that, and that the failures of the system are compounded by a dysfunctional culture within the ranks of professional caregivers. In other words, once the pieces are in place and assembled, the mental health system still seems to be “broken” but from within. I worry about apathy and an absence of motivation to provide good or even adequate services by the very people who are or should be aware of the problems and what it takes to help our vulnerable patients lead better lives.
I have practiced psychiatry for many years in various settings. I have spent many years working as an inpatient psychiatrist in a large state hospital. I have worked in community mental health outpatient settings. I have also worked in a private practice doing both inpatient and outpatient patient care as well as significant forensic work. At the hospitals, I have witnessed and prepared internal reports about patients who are “revolving doors.” Such patients often had more than 50 psychiatric hospitalizations and no apparent solution to keep them stable enough in the community.
But mental illness is not just a career for me. In addition to being psychiatrist, I am the father of a son with severe and persistent mental illness. I have watched him struggle to find stability. He, too, has been in and out of hospitals. My wife is also in the mental health field. She and I have endlessly tried to work with our son’s local community mental health center to provide them with feedback and to get them to respond to his needs – often with great frustration. It has been our impression that clinicians have difficulty listening to us and understanding the difficulties our son is having, from my son’s case manager to the treating psychiatrist, to the director of the agency. We have tried shifting him to other programs in a neighboring county, including one known to be a “model” program, but had the same issues.
Psychiatry is more of an art than science. Our other medical colleagues can try to resolve a clinical problem, no matter their rank, by ordering the right blood test or getting certain imaging. Psychiatry has no such biomarkers, or validated tests, to rely on to resolve disputes. We have only our training and experience and, unfortunately, our biases. If we don’t agree with a colleague, we often resort to rank and argument.
Psychiatrists (just as can colleagues in other specialties) can be insufferably arrogant.
My personal experience has been that the hospital and the community often don’t communicate well. This seems to be a systems problem, as is the case for many complex unsolvable problems. I have been to discharge meetings involving hospital staff and the receiving community system. The attitude of the inpatient psychiatrist is often: “If you guys only did your job better, this patient wouldn’t keep having to be admitted. It’s your job to keep him out of the hospital.”
Alternatively, the community rejects this attitude and points to the absence of resources that prevents them from seeing patients in a timely manner and from adequately monitoring them. They say they are shackled by their resource constraints and that the endless admissions are inevitable. Further, the outpatient psychiatrists complain bitterly that all the inpatient doctors do is make a bunch of useless medication changes and then don’t keep patients in long enough to make sure the patient stays well. And on and on the arguments go with no resolution.
Sadly, and confirmed by my personal experience, when well-meaning and knowledgeable family members try to communicate with the community mental health system about their son’s mental disintegration, the community agency often doesn’t welcome the feedback. They resort to “confidentiality” concerns, often ill advised. Their opinion seems to be that the patient, (i.e. the patient who is falling apart and is becoming psychotic), should be the one calling the agency, waiting on hold forever, and not getting a call back. When my son has been in this situation, he has hung up his telephone out of frustration, then headed off to the emergency room, where he knew he would be seen.
The other area of frustration is that of the ideal of recovery. Mental health programs love to tout that their mission is “recovery,” and they list it as one of their primary areas of vision and goals. Yet, when we tried to communicate with community clinicians, they usually ignored our request to assist our son with supported employment and to help him achieve independence and a social life. When we tried to convey our recovery concerns to the psychiatrist, the usual response was also to ignore it and focus on “meds, meds, meds,” which most psychiatrists seem to view as their mission and area of expertise. Many psychiatrists have embraced the “bio-bio-bio” model of evaluation and treatment5 with only lip service paid to the “biopsychosocial” theory they like to say they advocate. When we reached out to our son’s psychiatrists and could get through, we found that they mostly failed to display much interest in paying attention to broader areas of functioning, instead focusing on symptoms, which they could observe in person.
So, I add to the chorus complaining that our mental health system is broken. Broken not only in terms of adequate funding, but also broken from within. It would require much wisdom and self-examination to even begin to address the problem. Without a better plan, throwing money at this broken system won’t improve the lives of our seriously ill and vulnerable psychiatric patients.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University in Cleveland as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
References
1. Doroshow D. “We need to stop focusing on the mental health of mass shooters.” Washington Post. 2019 May 20.
2. Yanos P. “Is the mental health system ‘broken’?” Psychology Today. 2018 Oct 11.
3. Orenstein N. “How to fix a broken mental health system.” The Atlantic. 2016 Jun 8.
4. Moran M. APA rings alarm in nation’s capitol about crisis in mental health care. Psychiatr News. 2020 Jan 1.
5. Paris J. “Psychotherapy in an Age of Neuroscience.” New York: Oxford University Press, 2017.
Doctor wins $4.75 million award in defamation suit against hospital
Jurors awarded Carmel, Ind.–based ob.gyn. Rebecca Denman, MD, $4.75 million in damages against St. Vincent Carmel Hospital and St. Vincent Carmel Medical Group on Jan. 16, 2020, after a 4-day trial in Indiana Commercial Court. Dr. Denman sued after the hospital and medical group took a series of actions in response to a nurse practitioner’s claim that Dr. Denman smelled of alcohol while on duty. The doctor’s lawsuit alleged the NP’s claim was unproven; that administrators failed to conduct a proper peer-review investigation; and that repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
Indianapolis attorney Kathleen DeLaney, who represented Dr. Denman in the case, said that her client was pleased with the verdict.
“Dr. Denman feels vindicated that a group of jurors spent 4 days listening to all the evidence and gave her a resounding victory,” she said in an interview.
Dr. Denman declined to comment for this story through her attorney.
In a statement, a spokesman for Ascension, the hospital’s parent company, said the hospital was disappointed by the verdict and that it was “exploring all options available to us, including appeal.” The spokesman declined to answer further questions about the case or its peer-review process.
The case stems from an NP’s claim that Dr. Denman’s breath smelled of alcohol during an evening shift on Dec. 11, 2017. Dr. Denman was not informed of the allegation on Dec. 11 and was not tested for alcohol at the time, according to Dr. Denman’s lawsuit. Under hospital policy, if a physician is suspected of being under the influence of alcohol at work, the employer must immediately assess the doctor, relieve the doctor of duty, and request the physician submit to immediate blood testing at an external facility.
The NP reported the allegation to her supervisor through an email on Dec. 12, 2017. The supervisor relayed the information to the hospital’s chief medical officer who met with other administrators and physicians to discuss the claim. During the discussions, a previous concern about Dr. Denman’s drinking was raised, according to deposition information included in court documents. In 2015, two physicians had suggested Dr. Denman consider an assistance program after expressing concerns that she was arriving late to work and missing partner meetings. At the time, Dr. Denman did not enter an assistance program, but she changed her drinking habits, began seeing a therapist, and started arriving on-time to work and to partner meetings, according to court documents. No other criticism or complaints regarding her drinking or workplace behavior had been reported since, according to court documents.
When confronted with the NP’s claim on Dec. 13, 2017, Dr. Denman denied consuming alcohol on Dec. 11, 2017, and questioned why the hospital’s substance abuse protocol was not followed.
St. Vincent Carmel Hospital conducted a preliminary review of the allegation through its peer-review process and turned the matter over to St. Vincent Medical Group for further review, according to court documents. St. Vincent Medical Group later informed Dr. Denman they had reviewed the allegation through its peer-review process and that she was suspended with partial pay until she underwent an evaluation for alcohol abuse through the Indiana State Medical Association, according to the lawsuit.
“They falsely misrepresented to her that peer review had been done,” Ms. DeLaney said in an interview. “In spite of that statement, they never offered her a hearing before a peer-review committee, they never shared with her the substance of any evidence they had against her, they never gave her an opportunity to respond to the allegations. In fact, she wasn’t interviewed at all until the deposition in the lawsuit.”
According to the Indiana Peer Review law, a health care provider under investigation is permitted to see any records accumulated by a peer-review committee pertaining to the provider’s personal practice, and the provider shall be offered the opportunity to appear before the peer-review committee with adequate representation to hear all charges and findings concerning the provider and to offer rebuttal information. The rebuttal shall be part of the record before any disclosure of the charges and before any findings can be made, according to the statute.
Dr. Denman was referred by the medical association to an addiction treatment center that evaluated Dr. Denman and diagnosed her with alcohol use disorder, according to the lawsuit. As a result of the report and as a condition of retaining her medical license, the medical association and St. Vincent Medical Group required Dr. Denman to enter a treatment program at the same addiction treatment center. Dr. Denman was also required to sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit.
“The actions had life-changing consequences,” Ms. DeLaney said. “As a result, she was required to sign a contract that mandates she do a breathalyzer test four times a day for the first year and then three times a day for 4 more years. She has to go for random drug screenings. For the first year, she had to go to four [Alcoholics Anonymous] meetings a week. Now that number has been reduced, but she’s on a 5-year monitoring contract because of all of this.”
Dr. Denman sued the hospital, the medical group, and the NP in July 2018 alleging fraud, defamation, tortuous interference with an employment relationship, and negligent misrepresentation. The NP was dismissed from the case shortly before trial.
In its response to the lawsuit, attorneys for St. Vincent wrote that Dr. Denman’s action was frivolous, vexatious, and executed in bad faith. The defendants requested that a judge dismiss the lawsuit, noting that they were entitled to immunity pursuant to Indiana state and federal laws, including protection by Indiana’s Peer Review statute. In October 2019, a judge denied the hospital’s request to dismiss the lawsuit and allowed the case to proceed.
In their verdict, jurors awarded Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
Dr. Denman remains employed by the medical group and must continue the conditions of her 5-year monitoring contract, Ms. DeLaney said. She hopes Dr. Denman’s case raises awareness about physicians’ due process rights.
“We hope that Dr. Denman’s case emboldens physicians to stand up for themselves in the face of false accusations and rushes to judgment,” she said. “We hope the verdict leads to fair, prompt, and unbiased investigations by hospital and medical practice administrators, which include due process for accused physicians.”
Jurors awarded Carmel, Ind.–based ob.gyn. Rebecca Denman, MD, $4.75 million in damages against St. Vincent Carmel Hospital and St. Vincent Carmel Medical Group on Jan. 16, 2020, after a 4-day trial in Indiana Commercial Court. Dr. Denman sued after the hospital and medical group took a series of actions in response to a nurse practitioner’s claim that Dr. Denman smelled of alcohol while on duty. The doctor’s lawsuit alleged the NP’s claim was unproven; that administrators failed to conduct a proper peer-review investigation; and that repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
Indianapolis attorney Kathleen DeLaney, who represented Dr. Denman in the case, said that her client was pleased with the verdict.
“Dr. Denman feels vindicated that a group of jurors spent 4 days listening to all the evidence and gave her a resounding victory,” she said in an interview.
Dr. Denman declined to comment for this story through her attorney.
In a statement, a spokesman for Ascension, the hospital’s parent company, said the hospital was disappointed by the verdict and that it was “exploring all options available to us, including appeal.” The spokesman declined to answer further questions about the case or its peer-review process.
The case stems from an NP’s claim that Dr. Denman’s breath smelled of alcohol during an evening shift on Dec. 11, 2017. Dr. Denman was not informed of the allegation on Dec. 11 and was not tested for alcohol at the time, according to Dr. Denman’s lawsuit. Under hospital policy, if a physician is suspected of being under the influence of alcohol at work, the employer must immediately assess the doctor, relieve the doctor of duty, and request the physician submit to immediate blood testing at an external facility.
The NP reported the allegation to her supervisor through an email on Dec. 12, 2017. The supervisor relayed the information to the hospital’s chief medical officer who met with other administrators and physicians to discuss the claim. During the discussions, a previous concern about Dr. Denman’s drinking was raised, according to deposition information included in court documents. In 2015, two physicians had suggested Dr. Denman consider an assistance program after expressing concerns that she was arriving late to work and missing partner meetings. At the time, Dr. Denman did not enter an assistance program, but she changed her drinking habits, began seeing a therapist, and started arriving on-time to work and to partner meetings, according to court documents. No other criticism or complaints regarding her drinking or workplace behavior had been reported since, according to court documents.
When confronted with the NP’s claim on Dec. 13, 2017, Dr. Denman denied consuming alcohol on Dec. 11, 2017, and questioned why the hospital’s substance abuse protocol was not followed.
St. Vincent Carmel Hospital conducted a preliminary review of the allegation through its peer-review process and turned the matter over to St. Vincent Medical Group for further review, according to court documents. St. Vincent Medical Group later informed Dr. Denman they had reviewed the allegation through its peer-review process and that she was suspended with partial pay until she underwent an evaluation for alcohol abuse through the Indiana State Medical Association, according to the lawsuit.
“They falsely misrepresented to her that peer review had been done,” Ms. DeLaney said in an interview. “In spite of that statement, they never offered her a hearing before a peer-review committee, they never shared with her the substance of any evidence they had against her, they never gave her an opportunity to respond to the allegations. In fact, she wasn’t interviewed at all until the deposition in the lawsuit.”
According to the Indiana Peer Review law, a health care provider under investigation is permitted to see any records accumulated by a peer-review committee pertaining to the provider’s personal practice, and the provider shall be offered the opportunity to appear before the peer-review committee with adequate representation to hear all charges and findings concerning the provider and to offer rebuttal information. The rebuttal shall be part of the record before any disclosure of the charges and before any findings can be made, according to the statute.
Dr. Denman was referred by the medical association to an addiction treatment center that evaluated Dr. Denman and diagnosed her with alcohol use disorder, according to the lawsuit. As a result of the report and as a condition of retaining her medical license, the medical association and St. Vincent Medical Group required Dr. Denman to enter a treatment program at the same addiction treatment center. Dr. Denman was also required to sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit.
“The actions had life-changing consequences,” Ms. DeLaney said. “As a result, she was required to sign a contract that mandates she do a breathalyzer test four times a day for the first year and then three times a day for 4 more years. She has to go for random drug screenings. For the first year, she had to go to four [Alcoholics Anonymous] meetings a week. Now that number has been reduced, but she’s on a 5-year monitoring contract because of all of this.”
Dr. Denman sued the hospital, the medical group, and the NP in July 2018 alleging fraud, defamation, tortuous interference with an employment relationship, and negligent misrepresentation. The NP was dismissed from the case shortly before trial.
In its response to the lawsuit, attorneys for St. Vincent wrote that Dr. Denman’s action was frivolous, vexatious, and executed in bad faith. The defendants requested that a judge dismiss the lawsuit, noting that they were entitled to immunity pursuant to Indiana state and federal laws, including protection by Indiana’s Peer Review statute. In October 2019, a judge denied the hospital’s request to dismiss the lawsuit and allowed the case to proceed.
In their verdict, jurors awarded Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
Dr. Denman remains employed by the medical group and must continue the conditions of her 5-year monitoring contract, Ms. DeLaney said. She hopes Dr. Denman’s case raises awareness about physicians’ due process rights.
“We hope that Dr. Denman’s case emboldens physicians to stand up for themselves in the face of false accusations and rushes to judgment,” she said. “We hope the verdict leads to fair, prompt, and unbiased investigations by hospital and medical practice administrators, which include due process for accused physicians.”
Jurors awarded Carmel, Ind.–based ob.gyn. Rebecca Denman, MD, $4.75 million in damages against St. Vincent Carmel Hospital and St. Vincent Carmel Medical Group on Jan. 16, 2020, after a 4-day trial in Indiana Commercial Court. Dr. Denman sued after the hospital and medical group took a series of actions in response to a nurse practitioner’s claim that Dr. Denman smelled of alcohol while on duty. The doctor’s lawsuit alleged the NP’s claim was unproven; that administrators failed to conduct a proper peer-review investigation; and that repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
Indianapolis attorney Kathleen DeLaney, who represented Dr. Denman in the case, said that her client was pleased with the verdict.
“Dr. Denman feels vindicated that a group of jurors spent 4 days listening to all the evidence and gave her a resounding victory,” she said in an interview.
Dr. Denman declined to comment for this story through her attorney.
In a statement, a spokesman for Ascension, the hospital’s parent company, said the hospital was disappointed by the verdict and that it was “exploring all options available to us, including appeal.” The spokesman declined to answer further questions about the case or its peer-review process.
The case stems from an NP’s claim that Dr. Denman’s breath smelled of alcohol during an evening shift on Dec. 11, 2017. Dr. Denman was not informed of the allegation on Dec. 11 and was not tested for alcohol at the time, according to Dr. Denman’s lawsuit. Under hospital policy, if a physician is suspected of being under the influence of alcohol at work, the employer must immediately assess the doctor, relieve the doctor of duty, and request the physician submit to immediate blood testing at an external facility.
The NP reported the allegation to her supervisor through an email on Dec. 12, 2017. The supervisor relayed the information to the hospital’s chief medical officer who met with other administrators and physicians to discuss the claim. During the discussions, a previous concern about Dr. Denman’s drinking was raised, according to deposition information included in court documents. In 2015, two physicians had suggested Dr. Denman consider an assistance program after expressing concerns that she was arriving late to work and missing partner meetings. At the time, Dr. Denman did not enter an assistance program, but she changed her drinking habits, began seeing a therapist, and started arriving on-time to work and to partner meetings, according to court documents. No other criticism or complaints regarding her drinking or workplace behavior had been reported since, according to court documents.
When confronted with the NP’s claim on Dec. 13, 2017, Dr. Denman denied consuming alcohol on Dec. 11, 2017, and questioned why the hospital’s substance abuse protocol was not followed.
St. Vincent Carmel Hospital conducted a preliminary review of the allegation through its peer-review process and turned the matter over to St. Vincent Medical Group for further review, according to court documents. St. Vincent Medical Group later informed Dr. Denman they had reviewed the allegation through its peer-review process and that she was suspended with partial pay until she underwent an evaluation for alcohol abuse through the Indiana State Medical Association, according to the lawsuit.
“They falsely misrepresented to her that peer review had been done,” Ms. DeLaney said in an interview. “In spite of that statement, they never offered her a hearing before a peer-review committee, they never shared with her the substance of any evidence they had against her, they never gave her an opportunity to respond to the allegations. In fact, she wasn’t interviewed at all until the deposition in the lawsuit.”
According to the Indiana Peer Review law, a health care provider under investigation is permitted to see any records accumulated by a peer-review committee pertaining to the provider’s personal practice, and the provider shall be offered the opportunity to appear before the peer-review committee with adequate representation to hear all charges and findings concerning the provider and to offer rebuttal information. The rebuttal shall be part of the record before any disclosure of the charges and before any findings can be made, according to the statute.
Dr. Denman was referred by the medical association to an addiction treatment center that evaluated Dr. Denman and diagnosed her with alcohol use disorder, according to the lawsuit. As a result of the report and as a condition of retaining her medical license, the medical association and St. Vincent Medical Group required Dr. Denman to enter a treatment program at the same addiction treatment center. Dr. Denman was also required to sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit.
“The actions had life-changing consequences,” Ms. DeLaney said. “As a result, she was required to sign a contract that mandates she do a breathalyzer test four times a day for the first year and then three times a day for 4 more years. She has to go for random drug screenings. For the first year, she had to go to four [Alcoholics Anonymous] meetings a week. Now that number has been reduced, but she’s on a 5-year monitoring contract because of all of this.”
Dr. Denman sued the hospital, the medical group, and the NP in July 2018 alleging fraud, defamation, tortuous interference with an employment relationship, and negligent misrepresentation. The NP was dismissed from the case shortly before trial.
In its response to the lawsuit, attorneys for St. Vincent wrote that Dr. Denman’s action was frivolous, vexatious, and executed in bad faith. The defendants requested that a judge dismiss the lawsuit, noting that they were entitled to immunity pursuant to Indiana state and federal laws, including protection by Indiana’s Peer Review statute. In October 2019, a judge denied the hospital’s request to dismiss the lawsuit and allowed the case to proceed.
In their verdict, jurors awarded Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
Dr. Denman remains employed by the medical group and must continue the conditions of her 5-year monitoring contract, Ms. DeLaney said. She hopes Dr. Denman’s case raises awareness about physicians’ due process rights.
“We hope that Dr. Denman’s case emboldens physicians to stand up for themselves in the face of false accusations and rushes to judgment,” she said. “We hope the verdict leads to fair, prompt, and unbiased investigations by hospital and medical practice administrators, which include due process for accused physicians.”
Clinical Psychiatry News welcomes new board member
Clinical Psychiatry News is pleased to welcome Alice W. Lee, MD, to its editorial advisory board.
Dr. Lee, who works with children, adolescents and adults, specializes in integrative and holistic psychiatry. In her private practice in Gaithersburg, Md., she integrates functional/orthomolecular medicine and mind–body/energy medicine in her work with patients.
In addition, Dr. Lee is a Reiki master who integrates the biochemistry of chemistry with the quantum physics of healing. One of her specialties is helping patients withdraw from their psychiatric medications safely.
Dr. Lee is a member of the Academy of Integrative Health & Medicine, the Association for Comprehensive Energy Psychology, the Integrative Healthcare Symposium, and the Physicians Committee for Responsible Medicine.
Clinical Psychiatry News is pleased to welcome Alice W. Lee, MD, to its editorial advisory board.
Dr. Lee, who works with children, adolescents and adults, specializes in integrative and holistic psychiatry. In her private practice in Gaithersburg, Md., she integrates functional/orthomolecular medicine and mind–body/energy medicine in her work with patients.
In addition, Dr. Lee is a Reiki master who integrates the biochemistry of chemistry with the quantum physics of healing. One of her specialties is helping patients withdraw from their psychiatric medications safely.
Dr. Lee is a member of the Academy of Integrative Health & Medicine, the Association for Comprehensive Energy Psychology, the Integrative Healthcare Symposium, and the Physicians Committee for Responsible Medicine.
Clinical Psychiatry News is pleased to welcome Alice W. Lee, MD, to its editorial advisory board.
Dr. Lee, who works with children, adolescents and adults, specializes in integrative and holistic psychiatry. In her private practice in Gaithersburg, Md., she integrates functional/orthomolecular medicine and mind–body/energy medicine in her work with patients.
In addition, Dr. Lee is a Reiki master who integrates the biochemistry of chemistry with the quantum physics of healing. One of her specialties is helping patients withdraw from their psychiatric medications safely.
Dr. Lee is a member of the Academy of Integrative Health & Medicine, the Association for Comprehensive Energy Psychology, the Integrative Healthcare Symposium, and the Physicians Committee for Responsible Medicine.
New appointments at Cleveland Clinic, Fox Chase
Melissa Walt, PsyD, a clinical psychologist, recently joined the Taussig Cancer Institute at Cleveland Clinic. In this role, Dr. Walt focuses on the psychological treatment of cancer patients, helping them adjust to their diagnosis and navigate life with cancer.
Dr. Walt was previously a staff psychologist at the outpatient behavioral health/mental health clinic at the VA Southern Nevada Healthcare System in North Las Vegas. She obtained her doctorate degree from Adler University in Chicago, completed a residency at the VA Southern Nevada Healthcare System, and completed a fellowship at Memphis VA Medical Center.
Sheela Ahmed, MD, has joined Fox Chase Cancer Center in Philadelphia and works in the department of medicine as an associate clinical professor in the division of pulmonary, sleep, and critical care medicine. She is board certified in internal, pulmonary, critical care, and sleep medicine.
Dr. Ahmed was previously a pulmonary, critical care, and sleep physician at WellSpan Health in York, Pa. She received her medical degree from Patna (India) Medical College and Hospital. Dr. Ahmed completed a residency at the Postgraduate Institute of Medical Education and Research in Chandigarh, India, and a fellowship at St. Thomas Hospital in London and North Manchester (England) General Hospital. She also completed a residency and fellowship at Oregon Health and Science University in Portland.
Usman Ali, MD, has joined Fox Chase as an assistant professor in the division of hospital medicine within the department of medicine. Dr. Ali is board certified to practice medicine in Pennsylvania and New Jersey, and he is certified by the Educational Commission for Foreign Medical Graduates.
Dr. Ali previously worked as a contracted hospitalist at Fox Chase. He obtained his medical degree from Jawaharlal Nehru Medical College in Aligarh, India, and completed a residency at the Institute of Ophthalmology in Aligarh. Dr. Ali also completed a residency at Capital Health System in Pennington, N.J., and a fellowship at Mount Sinai Beth Israel Medical Center in New York City.
Dylan R. Sherry, MD, has joined the pain and palliative care program in the department of hematology/oncology at Fox Chase as an assistant professor on the academic clinician track. Dr. Sherry is board certified in internal medicine and board eligible in hospice and palliative medicine.
Dr. Sherry was previously a hospitalist at Abington Memorial Hospital, now Abington Hospital–Jefferson Health, in Abington Township, Pa. He received his medical degree from Case Western Reserve University in Cleveland. He completed his residency and fellowship at Beth Israel Deaconess Medical Center in Boston.
Melissa Walt, PsyD, a clinical psychologist, recently joined the Taussig Cancer Institute at Cleveland Clinic. In this role, Dr. Walt focuses on the psychological treatment of cancer patients, helping them adjust to their diagnosis and navigate life with cancer.
Dr. Walt was previously a staff psychologist at the outpatient behavioral health/mental health clinic at the VA Southern Nevada Healthcare System in North Las Vegas. She obtained her doctorate degree from Adler University in Chicago, completed a residency at the VA Southern Nevada Healthcare System, and completed a fellowship at Memphis VA Medical Center.
Sheela Ahmed, MD, has joined Fox Chase Cancer Center in Philadelphia and works in the department of medicine as an associate clinical professor in the division of pulmonary, sleep, and critical care medicine. She is board certified in internal, pulmonary, critical care, and sleep medicine.
Dr. Ahmed was previously a pulmonary, critical care, and sleep physician at WellSpan Health in York, Pa. She received her medical degree from Patna (India) Medical College and Hospital. Dr. Ahmed completed a residency at the Postgraduate Institute of Medical Education and Research in Chandigarh, India, and a fellowship at St. Thomas Hospital in London and North Manchester (England) General Hospital. She also completed a residency and fellowship at Oregon Health and Science University in Portland.
Usman Ali, MD, has joined Fox Chase as an assistant professor in the division of hospital medicine within the department of medicine. Dr. Ali is board certified to practice medicine in Pennsylvania and New Jersey, and he is certified by the Educational Commission for Foreign Medical Graduates.
Dr. Ali previously worked as a contracted hospitalist at Fox Chase. He obtained his medical degree from Jawaharlal Nehru Medical College in Aligarh, India, and completed a residency at the Institute of Ophthalmology in Aligarh. Dr. Ali also completed a residency at Capital Health System in Pennington, N.J., and a fellowship at Mount Sinai Beth Israel Medical Center in New York City.
Dylan R. Sherry, MD, has joined the pain and palliative care program in the department of hematology/oncology at Fox Chase as an assistant professor on the academic clinician track. Dr. Sherry is board certified in internal medicine and board eligible in hospice and palliative medicine.
Dr. Sherry was previously a hospitalist at Abington Memorial Hospital, now Abington Hospital–Jefferson Health, in Abington Township, Pa. He received his medical degree from Case Western Reserve University in Cleveland. He completed his residency and fellowship at Beth Israel Deaconess Medical Center in Boston.
Melissa Walt, PsyD, a clinical psychologist, recently joined the Taussig Cancer Institute at Cleveland Clinic. In this role, Dr. Walt focuses on the psychological treatment of cancer patients, helping them adjust to their diagnosis and navigate life with cancer.
Dr. Walt was previously a staff psychologist at the outpatient behavioral health/mental health clinic at the VA Southern Nevada Healthcare System in North Las Vegas. She obtained her doctorate degree from Adler University in Chicago, completed a residency at the VA Southern Nevada Healthcare System, and completed a fellowship at Memphis VA Medical Center.
Sheela Ahmed, MD, has joined Fox Chase Cancer Center in Philadelphia and works in the department of medicine as an associate clinical professor in the division of pulmonary, sleep, and critical care medicine. She is board certified in internal, pulmonary, critical care, and sleep medicine.
Dr. Ahmed was previously a pulmonary, critical care, and sleep physician at WellSpan Health in York, Pa. She received her medical degree from Patna (India) Medical College and Hospital. Dr. Ahmed completed a residency at the Postgraduate Institute of Medical Education and Research in Chandigarh, India, and a fellowship at St. Thomas Hospital in London and North Manchester (England) General Hospital. She also completed a residency and fellowship at Oregon Health and Science University in Portland.
Usman Ali, MD, has joined Fox Chase as an assistant professor in the division of hospital medicine within the department of medicine. Dr. Ali is board certified to practice medicine in Pennsylvania and New Jersey, and he is certified by the Educational Commission for Foreign Medical Graduates.
Dr. Ali previously worked as a contracted hospitalist at Fox Chase. He obtained his medical degree from Jawaharlal Nehru Medical College in Aligarh, India, and completed a residency at the Institute of Ophthalmology in Aligarh. Dr. Ali also completed a residency at Capital Health System in Pennington, N.J., and a fellowship at Mount Sinai Beth Israel Medical Center in New York City.
Dylan R. Sherry, MD, has joined the pain and palliative care program in the department of hematology/oncology at Fox Chase as an assistant professor on the academic clinician track. Dr. Sherry is board certified in internal medicine and board eligible in hospice and palliative medicine.
Dr. Sherry was previously a hospitalist at Abington Memorial Hospital, now Abington Hospital–Jefferson Health, in Abington Township, Pa. He received his medical degree from Case Western Reserve University in Cleveland. He completed his residency and fellowship at Beth Israel Deaconess Medical Center in Boston.
Neurologic disease doesn’t discriminate against anyone
In 1982, I went to my first concert. It was Rush, on their “Signals” tour, and I loved it. In fact, I went back and saw them again about a year later. I bought a concert T-shirt at the first one. I still have it somewhere, though I am pretty sure it hasn’t fit me in years.
I loved their music before the concert, enjoyed it even more afterwards, and still do. Their albums are all on my computer and phone, and part of the daily soundtrack of my life when working at my desk, driving, and walking (I’m trying to fit back in the shirt).
On Jan. 7, 2020, Neil Peart, the trio’s remarkably gifted drummer, died of a neurologic disease.
According to the news, he had a glioblastoma multiforme, a tumor terrifying for its aggressiveness, difficulty of treatment, and lack of preventable risk factors.
The cost of neurologic disease is terrible. Glioblastoma multiforme, unfortunately, is far from rare, nor is it the only one. In recent times, entertainers afflicted with neurologic disease have included Neil Diamond, Linda Ronstadt, Peter Falk, Glen Campbell, Charlton Heston, Gene Siskel, Michael J. Fox, Stephen Hillenburg, Teri Garr, Annette Funicello, Robin Williams, Dudley Moore, and most recently Ozzy Osbourne.
That’s a pretty short list, too, far from all-encompassing. The majority of people with these disorders won’t be in the news. Their everyday struggles, stories, and losses are known only to family, friends, and the medical team doing its best to help.
Medical technology advances every year. In the 22 years since I began practicing, we’ve made remarkable strides in some areas – multiple sclerosis, for example. But our work in so many other areas is nowhere close. The increasing knowledge as to the mechanisms and causes of Alzheimer’s disease have, to date, failed to translate into treatment success.
That’s not to say we should give up. Far from it. Our species has gotten where we are by always wanting to get over the next hill. Initial failures will always outnumber successes. But when you’re a doctor dealing with the very real human cost of neurologic disease, that’s not much consolation. And it’s far less so for the patients and families affected who come to us for help.
We use terms like “burden” or “cost” to discuss the financial aspects of illness, but they often don’t seem adequate to describe the real effects. The emotional damages. The gifted musicians and loved family members lost. Family members struggling with the difficult role of being care givers.
Neurologic disease doesn’t discriminate against anyone, regardless of age, fame, or talent. I’ll stay here and do my best for all of them who come to me. I’m certainly not on the front line of research. That’s incredibly important, but I’ll leave it to others. My work is where the patients are every day.
Thank you for the music, Neil.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1982, I went to my first concert. It was Rush, on their “Signals” tour, and I loved it. In fact, I went back and saw them again about a year later. I bought a concert T-shirt at the first one. I still have it somewhere, though I am pretty sure it hasn’t fit me in years.
I loved their music before the concert, enjoyed it even more afterwards, and still do. Their albums are all on my computer and phone, and part of the daily soundtrack of my life when working at my desk, driving, and walking (I’m trying to fit back in the shirt).
On Jan. 7, 2020, Neil Peart, the trio’s remarkably gifted drummer, died of a neurologic disease.
According to the news, he had a glioblastoma multiforme, a tumor terrifying for its aggressiveness, difficulty of treatment, and lack of preventable risk factors.
The cost of neurologic disease is terrible. Glioblastoma multiforme, unfortunately, is far from rare, nor is it the only one. In recent times, entertainers afflicted with neurologic disease have included Neil Diamond, Linda Ronstadt, Peter Falk, Glen Campbell, Charlton Heston, Gene Siskel, Michael J. Fox, Stephen Hillenburg, Teri Garr, Annette Funicello, Robin Williams, Dudley Moore, and most recently Ozzy Osbourne.
That’s a pretty short list, too, far from all-encompassing. The majority of people with these disorders won’t be in the news. Their everyday struggles, stories, and losses are known only to family, friends, and the medical team doing its best to help.
Medical technology advances every year. In the 22 years since I began practicing, we’ve made remarkable strides in some areas – multiple sclerosis, for example. But our work in so many other areas is nowhere close. The increasing knowledge as to the mechanisms and causes of Alzheimer’s disease have, to date, failed to translate into treatment success.
That’s not to say we should give up. Far from it. Our species has gotten where we are by always wanting to get over the next hill. Initial failures will always outnumber successes. But when you’re a doctor dealing with the very real human cost of neurologic disease, that’s not much consolation. And it’s far less so for the patients and families affected who come to us for help.
We use terms like “burden” or “cost” to discuss the financial aspects of illness, but they often don’t seem adequate to describe the real effects. The emotional damages. The gifted musicians and loved family members lost. Family members struggling with the difficult role of being care givers.
Neurologic disease doesn’t discriminate against anyone, regardless of age, fame, or talent. I’ll stay here and do my best for all of them who come to me. I’m certainly not on the front line of research. That’s incredibly important, but I’ll leave it to others. My work is where the patients are every day.
Thank you for the music, Neil.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1982, I went to my first concert. It was Rush, on their “Signals” tour, and I loved it. In fact, I went back and saw them again about a year later. I bought a concert T-shirt at the first one. I still have it somewhere, though I am pretty sure it hasn’t fit me in years.
I loved their music before the concert, enjoyed it even more afterwards, and still do. Their albums are all on my computer and phone, and part of the daily soundtrack of my life when working at my desk, driving, and walking (I’m trying to fit back in the shirt).
On Jan. 7, 2020, Neil Peart, the trio’s remarkably gifted drummer, died of a neurologic disease.
According to the news, he had a glioblastoma multiforme, a tumor terrifying for its aggressiveness, difficulty of treatment, and lack of preventable risk factors.
The cost of neurologic disease is terrible. Glioblastoma multiforme, unfortunately, is far from rare, nor is it the only one. In recent times, entertainers afflicted with neurologic disease have included Neil Diamond, Linda Ronstadt, Peter Falk, Glen Campbell, Charlton Heston, Gene Siskel, Michael J. Fox, Stephen Hillenburg, Teri Garr, Annette Funicello, Robin Williams, Dudley Moore, and most recently Ozzy Osbourne.
That’s a pretty short list, too, far from all-encompassing. The majority of people with these disorders won’t be in the news. Their everyday struggles, stories, and losses are known only to family, friends, and the medical team doing its best to help.
Medical technology advances every year. In the 22 years since I began practicing, we’ve made remarkable strides in some areas – multiple sclerosis, for example. But our work in so many other areas is nowhere close. The increasing knowledge as to the mechanisms and causes of Alzheimer’s disease have, to date, failed to translate into treatment success.
That’s not to say we should give up. Far from it. Our species has gotten where we are by always wanting to get over the next hill. Initial failures will always outnumber successes. But when you’re a doctor dealing with the very real human cost of neurologic disease, that’s not much consolation. And it’s far less so for the patients and families affected who come to us for help.
We use terms like “burden” or “cost” to discuss the financial aspects of illness, but they often don’t seem adequate to describe the real effects. The emotional damages. The gifted musicians and loved family members lost. Family members struggling with the difficult role of being care givers.
Neurologic disease doesn’t discriminate against anyone, regardless of age, fame, or talent. I’ll stay here and do my best for all of them who come to me. I’m certainly not on the front line of research. That’s incredibly important, but I’ll leave it to others. My work is where the patients are every day.
Thank you for the music, Neil.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Suicide rate higher than average for female clinicians
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
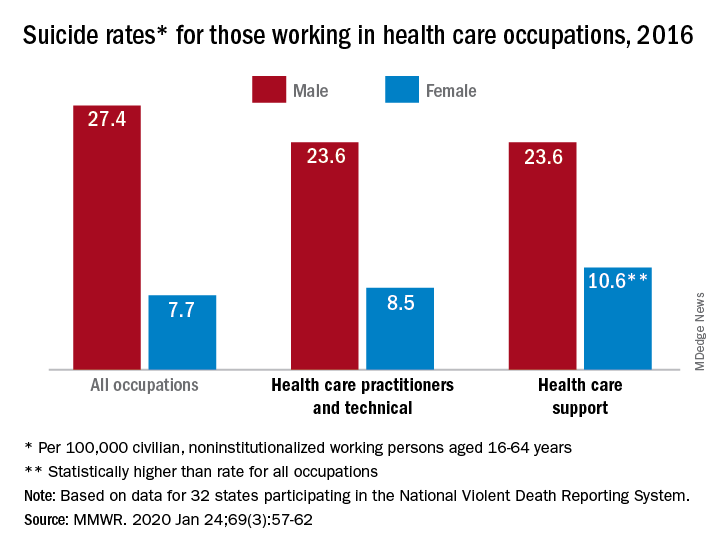
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
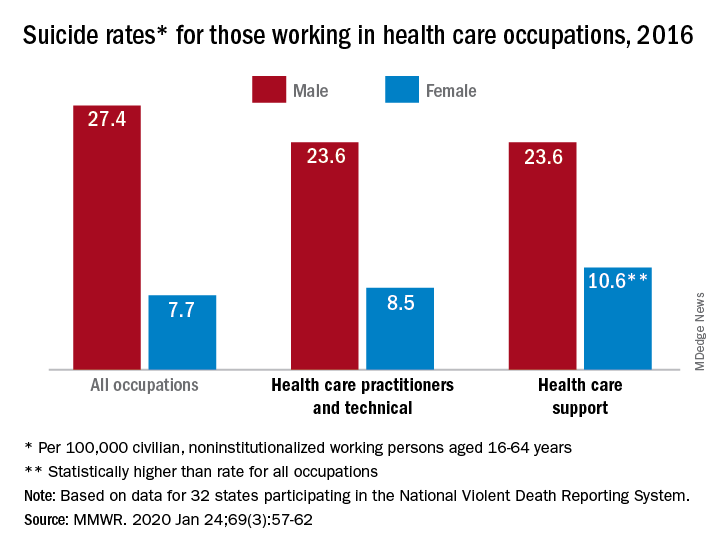
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
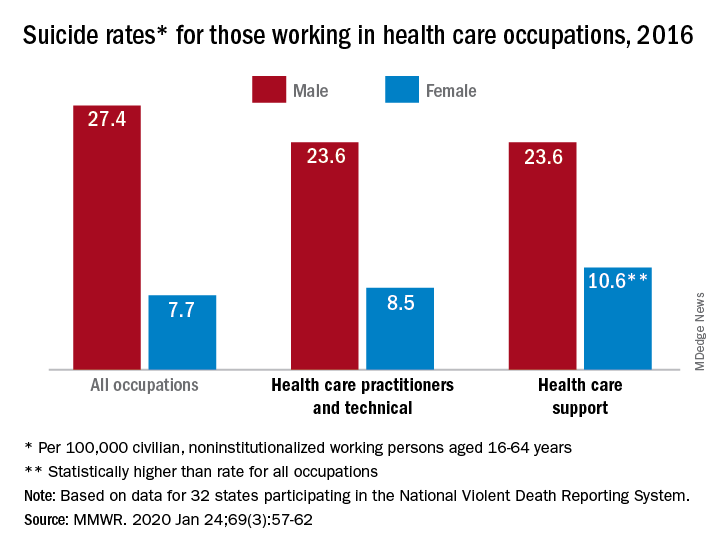
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
FROM MMWR
Actor Alan Alda discusses using empathy as an antidote to burnout
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.

“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.

“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – Physicians and other medical professionals who routinely foster empathic connections with patients may be helping themselves steer clear of burnout.
That’s what iconic actor Alan Alda suggested during a media briefing at Scripps Research on Jan. 16, 2020.

“There’s a tremendous pressure on doctors now to have shorter and shorter visits with their patients,” said the 83-year-old Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016 for his work as a champion of science. “A lot of that time is taken up with recording on a computer, which can only put pressure on the doctor.”
Practicing empathy, he continued, “kind of opens people up to one another, which inspirits them.”
Mr. Alda appeared on the research campus to announce that Scripps Research will serve as the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at Stony Brook (N.Y.) University, a nonprofit organization that Mr. Alda helped found in 2009.
“This will be a center where people can come to get training in effective communication,” Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards, told an audience of scientists and medical professionals prior to the media briefing.
“It’s an experiential kind of training,” he explained. “We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that, when you get a diagnosis, your life is over,” said Mr. Alda, who played army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H.”
“Under the burden of that belief, some people won’t tell their family or workplace colleagues,” he said. “There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
New year, old you
This column should arrive just in time. By this time in February, eighty percent of us will abort what we resolved to do this year. If this was you, it could be considered a catastrophic failure because not only is it a new year, it is a new decade. That’s right, the opportunity to fix the 10-year-imperfect you won’t come again until 2030!
I’m among you. I intended to read fiction daily (starting with “The Great Gatsby,” not “Moby Dick” – I thought I would give myself a fighting chance, but alas ...), to workout at least 5 days every week (I tore my left triangular fibrocartilage complex, so there’s that), to write at least 500 words daily (I’m typing this one-handed: I’m lucky to get 500 letters a day). So I’m out.
If you resolved to do something this year, chances are it was to make a better you: a self-improvement goal such as losing weight, saving more money, or exercising more. According to a Marist Poll, these were the most popular resolutions for 2020. At the bottom of the most-likely-resolutions list were things like “worry less” or “be kinder to others.” These are important goals we’d agree, but we don’t deem them resolution-worthy. Why?
And why do we have New Year’s resolutions in the first place? When I looked into this further, I was surprised by some of the history I discovered.
As far back as the Babylonians, once a year, we’ve tried our best to get better. At the feast of Akitu, the Babylonian new year festival (about March on our modern calendar), people resolved to do a better job of paying debts and returning favors – spin had not been invented, and yoga hadn’t caught on in the Middle East yet. This fundamental desire to be a better human seems hardwired, and long before Bullet Journals we seem to have loved “fresh start” days on the calendar. Yet, we’re doomed to fail, over and over, at least for the last 5,000 or so attempts.
We know so much more now. Put your Nike Renue Fusion shoes next to your bed so you get up and run first thing. Set SMART goals. Sign up for automatic retirement contribution and for automatic, plant-based meal delivery from Blue Apron. (I’ve no conflict of interest in these products).
Good ideas all, but I’m suggesting a different approach: Resolve to do something else this year.
Rather than try the same things we’ve attempted, how about selecting something from the bottom of the Marist Poll list – such as resolving to be more humble. Admit when you don’t know something or don’t understand what’s being discussed. Recognize and acknowledge when you’ve screwed up. Or resolve to be more selfless. Add on someone else’s patient, an extra call without expecting a favor in return, or do what you can to help a curbside consult, even if there is no reward or even a small risk to you. Repay the debt you owe your friends, family, colleagues, staff, and patients.
These things are a little trickier to track, but you can find a way to keep yourself accountable. Add a box to your weekly planner that says “Be humble and kind” and check it off for the next 42 weeks. Good news, March 1 falls on a Sunday this year – let’s call it the feast of Akitu.
Happy New Year! And good luck!
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
This column should arrive just in time. By this time in February, eighty percent of us will abort what we resolved to do this year. If this was you, it could be considered a catastrophic failure because not only is it a new year, it is a new decade. That’s right, the opportunity to fix the 10-year-imperfect you won’t come again until 2030!
I’m among you. I intended to read fiction daily (starting with “The Great Gatsby,” not “Moby Dick” – I thought I would give myself a fighting chance, but alas ...), to workout at least 5 days every week (I tore my left triangular fibrocartilage complex, so there’s that), to write at least 500 words daily (I’m typing this one-handed: I’m lucky to get 500 letters a day). So I’m out.
If you resolved to do something this year, chances are it was to make a better you: a self-improvement goal such as losing weight, saving more money, or exercising more. According to a Marist Poll, these were the most popular resolutions for 2020. At the bottom of the most-likely-resolutions list were things like “worry less” or “be kinder to others.” These are important goals we’d agree, but we don’t deem them resolution-worthy. Why?
And why do we have New Year’s resolutions in the first place? When I looked into this further, I was surprised by some of the history I discovered.
As far back as the Babylonians, once a year, we’ve tried our best to get better. At the feast of Akitu, the Babylonian new year festival (about March on our modern calendar), people resolved to do a better job of paying debts and returning favors – spin had not been invented, and yoga hadn’t caught on in the Middle East yet. This fundamental desire to be a better human seems hardwired, and long before Bullet Journals we seem to have loved “fresh start” days on the calendar. Yet, we’re doomed to fail, over and over, at least for the last 5,000 or so attempts.
We know so much more now. Put your Nike Renue Fusion shoes next to your bed so you get up and run first thing. Set SMART goals. Sign up for automatic retirement contribution and for automatic, plant-based meal delivery from Blue Apron. (I’ve no conflict of interest in these products).
Good ideas all, but I’m suggesting a different approach: Resolve to do something else this year.
Rather than try the same things we’ve attempted, how about selecting something from the bottom of the Marist Poll list – such as resolving to be more humble. Admit when you don’t know something or don’t understand what’s being discussed. Recognize and acknowledge when you’ve screwed up. Or resolve to be more selfless. Add on someone else’s patient, an extra call without expecting a favor in return, or do what you can to help a curbside consult, even if there is no reward or even a small risk to you. Repay the debt you owe your friends, family, colleagues, staff, and patients.
These things are a little trickier to track, but you can find a way to keep yourself accountable. Add a box to your weekly planner that says “Be humble and kind” and check it off for the next 42 weeks. Good news, March 1 falls on a Sunday this year – let’s call it the feast of Akitu.
Happy New Year! And good luck!
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
This column should arrive just in time. By this time in February, eighty percent of us will abort what we resolved to do this year. If this was you, it could be considered a catastrophic failure because not only is it a new year, it is a new decade. That’s right, the opportunity to fix the 10-year-imperfect you won’t come again until 2030!
I’m among you. I intended to read fiction daily (starting with “The Great Gatsby,” not “Moby Dick” – I thought I would give myself a fighting chance, but alas ...), to workout at least 5 days every week (I tore my left triangular fibrocartilage complex, so there’s that), to write at least 500 words daily (I’m typing this one-handed: I’m lucky to get 500 letters a day). So I’m out.
If you resolved to do something this year, chances are it was to make a better you: a self-improvement goal such as losing weight, saving more money, or exercising more. According to a Marist Poll, these were the most popular resolutions for 2020. At the bottom of the most-likely-resolutions list were things like “worry less” or “be kinder to others.” These are important goals we’d agree, but we don’t deem them resolution-worthy. Why?
And why do we have New Year’s resolutions in the first place? When I looked into this further, I was surprised by some of the history I discovered.
As far back as the Babylonians, once a year, we’ve tried our best to get better. At the feast of Akitu, the Babylonian new year festival (about March on our modern calendar), people resolved to do a better job of paying debts and returning favors – spin had not been invented, and yoga hadn’t caught on in the Middle East yet. This fundamental desire to be a better human seems hardwired, and long before Bullet Journals we seem to have loved “fresh start” days on the calendar. Yet, we’re doomed to fail, over and over, at least for the last 5,000 or so attempts.
We know so much more now. Put your Nike Renue Fusion shoes next to your bed so you get up and run first thing. Set SMART goals. Sign up for automatic retirement contribution and for automatic, plant-based meal delivery from Blue Apron. (I’ve no conflict of interest in these products).
Good ideas all, but I’m suggesting a different approach: Resolve to do something else this year.
Rather than try the same things we’ve attempted, how about selecting something from the bottom of the Marist Poll list – such as resolving to be more humble. Admit when you don’t know something or don’t understand what’s being discussed. Recognize and acknowledge when you’ve screwed up. Or resolve to be more selfless. Add on someone else’s patient, an extra call without expecting a favor in return, or do what you can to help a curbside consult, even if there is no reward or even a small risk to you. Repay the debt you owe your friends, family, colleagues, staff, and patients.
These things are a little trickier to track, but you can find a way to keep yourself accountable. Add a box to your weekly planner that says “Be humble and kind” and check it off for the next 42 weeks. Good news, March 1 falls on a Sunday this year – let’s call it the feast of Akitu.
Happy New Year! And good luck!
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].