User login
Service Connection Expanded to Additional Cancers
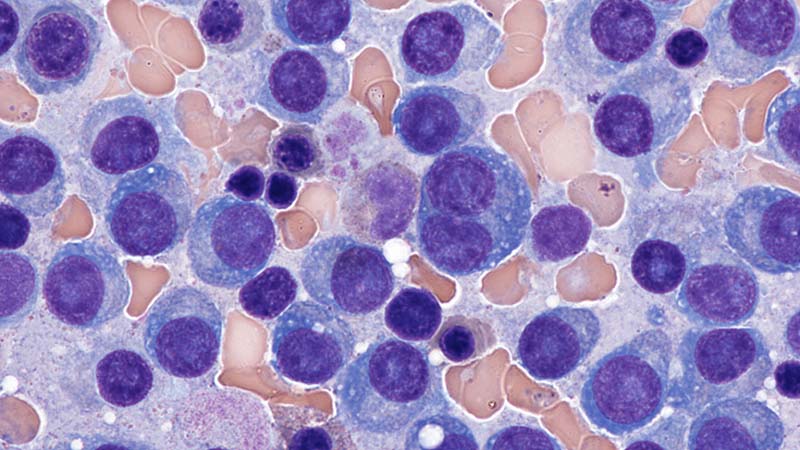
The US Department of Veterans Affairs (VA) is "lowering the burden of proof" for thousands, making acute and chronic leukemias, multiple myelomas, myelodysplastic syndromes, myelofibrosis, urinary bladder, ureter, and related genitourinary cancers presumptive for service connection.
The Jan. 8 decision included Gulf War veterans, those who served in Somalia or the Southwest Asia theater of operations during the Persian Gulf War on or after Aug. 2, 1990; and post-9/11 veterans, those who served in Afghanistan, Iraq, Djibouti, Egypt, Jordan, Lebanon, Syria, Yemen, or Uzbekistan and the airspace above these locations during the Gulf War on or after Sept. 11, 2001. It also includes veterans who served at the Karshi-Khanabad (K2) base in Uzbekistan after Sept. 11, 2001.
Veterans no longer must prove their service caused their condition to receive benefits. This landmark decision allows them access to free health care for that condition.
According to the VA, these steps are also part of a comprehensive effort to ensure that K2 veterans—and their survivors—receive the care and benefits they deserve. K2 veterans have higher claim and approval rates than any other cohort of veterans: 13,002 are enrolled in VA health care, and the average K2 veteran is service connected for 14.6 conditions.
The 2022 PACT Act was the largest expansion of veteran benefits in generations. The VA then made millions of veterans eligible for health care and benefits years earlier than called for by the law. It also launched the largest outreach campaign in the history of the VA to encourage veterans to apply.
Nearly 890,000 veterans have signed up for VA health care since the bill was signed into law, a nearly 40% increase over the previous equivalent period, and veterans have submitted > 4.8 million applications for VA benefits (a 42% increase over the previous equivalent period and an all-time record). The VA has delivered > $600 billion in earned benefits directly to veterans, their families, and survivors during that time.
The VA encourages all eligible veterans—including those with previously denied claims—to apply for benefits. To apply for benefits, veterans and survivors may visit VA.gov or call 1-800-MYVA411.
The US Department of Veterans Affairs (VA) is "lowering the burden of proof" for thousands, making acute and chronic leukemias, multiple myelomas, myelodysplastic syndromes, myelofibrosis, urinary bladder, ureter, and related genitourinary cancers presumptive for service connection.
The Jan. 8 decision included Gulf War veterans, those who served in Somalia or the Southwest Asia theater of operations during the Persian Gulf War on or after Aug. 2, 1990; and post-9/11 veterans, those who served in Afghanistan, Iraq, Djibouti, Egypt, Jordan, Lebanon, Syria, Yemen, or Uzbekistan and the airspace above these locations during the Gulf War on or after Sept. 11, 2001. It also includes veterans who served at the Karshi-Khanabad (K2) base in Uzbekistan after Sept. 11, 2001.
Veterans no longer must prove their service caused their condition to receive benefits. This landmark decision allows them access to free health care for that condition.
According to the VA, these steps are also part of a comprehensive effort to ensure that K2 veterans—and their survivors—receive the care and benefits they deserve. K2 veterans have higher claim and approval rates than any other cohort of veterans: 13,002 are enrolled in VA health care, and the average K2 veteran is service connected for 14.6 conditions.
The 2022 PACT Act was the largest expansion of veteran benefits in generations. The VA then made millions of veterans eligible for health care and benefits years earlier than called for by the law. It also launched the largest outreach campaign in the history of the VA to encourage veterans to apply.
Nearly 890,000 veterans have signed up for VA health care since the bill was signed into law, a nearly 40% increase over the previous equivalent period, and veterans have submitted > 4.8 million applications for VA benefits (a 42% increase over the previous equivalent period and an all-time record). The VA has delivered > $600 billion in earned benefits directly to veterans, their families, and survivors during that time.
The VA encourages all eligible veterans—including those with previously denied claims—to apply for benefits. To apply for benefits, veterans and survivors may visit VA.gov or call 1-800-MYVA411.
The US Department of Veterans Affairs (VA) is "lowering the burden of proof" for thousands, making acute and chronic leukemias, multiple myelomas, myelodysplastic syndromes, myelofibrosis, urinary bladder, ureter, and related genitourinary cancers presumptive for service connection.
The Jan. 8 decision included Gulf War veterans, those who served in Somalia or the Southwest Asia theater of operations during the Persian Gulf War on or after Aug. 2, 1990; and post-9/11 veterans, those who served in Afghanistan, Iraq, Djibouti, Egypt, Jordan, Lebanon, Syria, Yemen, or Uzbekistan and the airspace above these locations during the Gulf War on or after Sept. 11, 2001. It also includes veterans who served at the Karshi-Khanabad (K2) base in Uzbekistan after Sept. 11, 2001.
Veterans no longer must prove their service caused their condition to receive benefits. This landmark decision allows them access to free health care for that condition.
According to the VA, these steps are also part of a comprehensive effort to ensure that K2 veterans—and their survivors—receive the care and benefits they deserve. K2 veterans have higher claim and approval rates than any other cohort of veterans: 13,002 are enrolled in VA health care, and the average K2 veteran is service connected for 14.6 conditions.
The 2022 PACT Act was the largest expansion of veteran benefits in generations. The VA then made millions of veterans eligible for health care and benefits years earlier than called for by the law. It also launched the largest outreach campaign in the history of the VA to encourage veterans to apply.
Nearly 890,000 veterans have signed up for VA health care since the bill was signed into law, a nearly 40% increase over the previous equivalent period, and veterans have submitted > 4.8 million applications for VA benefits (a 42% increase over the previous equivalent period and an all-time record). The VA has delivered > $600 billion in earned benefits directly to veterans, their families, and survivors during that time.
The VA encourages all eligible veterans—including those with previously denied claims—to apply for benefits. To apply for benefits, veterans and survivors may visit VA.gov or call 1-800-MYVA411.
ERCC2, KDM6A, and TERT as Key Prognostic Factors in Bladder Cancer: Insights from the AACR Project GENIE Database
Background
Urothelial carcinoma (UC) is among the top 10 frequently diagnosed cancers in the world. Mutations in FGFR3, ARID1A, and TP53 are well documented as being some of the most frequent mutations found in UC. Despite advances in treatment, survival outcomes remain poor, especially in advanced stages. To promote future pharmacotherapeutic development, the molecular understanding of UC needs to be continually updated using more recently available databases.
Methods
This study utilizes the AACR Project GENIE database from the American Association for Cancer Research to explore the mutational profiles of patients with UC. Gene mutation frequencies were calculated, and two Kaplan-Meier curves were drawn for each gene, showing one curve for patients with the mutation and one for those without. Log-Rank tests were calculated with subsequent FDR (Benjamini–Hochberg) correction applied to account for multiple hypothesis testing. Data was analyzed using R 4.4.2 and statistical significance was set at α = 0.05.
Results
In this study, 4525 patients had histology consistent with UC. The 5 most common mutations were TERT (n = 1714, 37.9%), TP53 (n = 1689, 37.3%), KDM6A (n = 1091, 24.1%), ARID1A (n = 872, 19.3%), and FGFR3 (n = 762, 16.8%). Mutations associated with differential survival outcomes included ERCC2 (mutated n = 387, wild type n = 3751, p < 0.0001), KDM6A (mutated n = 1091, wild type n = 3047, p < 0.0001), TERT (mutated n = 1714, wild type n = 2424), and TP53 (mutated n = 1689, wild type n = 2449, p < 0.0001).
Conclusions
Interestingly, while mutations in TP53 and ERCC2 were associated with shorter median survival, mutations in KDM6A and TERT were associated with longer median survival.
Background
Urothelial carcinoma (UC) is among the top 10 frequently diagnosed cancers in the world. Mutations in FGFR3, ARID1A, and TP53 are well documented as being some of the most frequent mutations found in UC. Despite advances in treatment, survival outcomes remain poor, especially in advanced stages. To promote future pharmacotherapeutic development, the molecular understanding of UC needs to be continually updated using more recently available databases.
Methods
This study utilizes the AACR Project GENIE database from the American Association for Cancer Research to explore the mutational profiles of patients with UC. Gene mutation frequencies were calculated, and two Kaplan-Meier curves were drawn for each gene, showing one curve for patients with the mutation and one for those without. Log-Rank tests were calculated with subsequent FDR (Benjamini–Hochberg) correction applied to account for multiple hypothesis testing. Data was analyzed using R 4.4.2 and statistical significance was set at α = 0.05.
Results
In this study, 4525 patients had histology consistent with UC. The 5 most common mutations were TERT (n = 1714, 37.9%), TP53 (n = 1689, 37.3%), KDM6A (n = 1091, 24.1%), ARID1A (n = 872, 19.3%), and FGFR3 (n = 762, 16.8%). Mutations associated with differential survival outcomes included ERCC2 (mutated n = 387, wild type n = 3751, p < 0.0001), KDM6A (mutated n = 1091, wild type n = 3047, p < 0.0001), TERT (mutated n = 1714, wild type n = 2424), and TP53 (mutated n = 1689, wild type n = 2449, p < 0.0001).
Conclusions
Interestingly, while mutations in TP53 and ERCC2 were associated with shorter median survival, mutations in KDM6A and TERT were associated with longer median survival.
Background
Urothelial carcinoma (UC) is among the top 10 frequently diagnosed cancers in the world. Mutations in FGFR3, ARID1A, and TP53 are well documented as being some of the most frequent mutations found in UC. Despite advances in treatment, survival outcomes remain poor, especially in advanced stages. To promote future pharmacotherapeutic development, the molecular understanding of UC needs to be continually updated using more recently available databases.
Methods
This study utilizes the AACR Project GENIE database from the American Association for Cancer Research to explore the mutational profiles of patients with UC. Gene mutation frequencies were calculated, and two Kaplan-Meier curves were drawn for each gene, showing one curve for patients with the mutation and one for those without. Log-Rank tests were calculated with subsequent FDR (Benjamini–Hochberg) correction applied to account for multiple hypothesis testing. Data was analyzed using R 4.4.2 and statistical significance was set at α = 0.05.
Results
In this study, 4525 patients had histology consistent with UC. The 5 most common mutations were TERT (n = 1714, 37.9%), TP53 (n = 1689, 37.3%), KDM6A (n = 1091, 24.1%), ARID1A (n = 872, 19.3%), and FGFR3 (n = 762, 16.8%). Mutations associated with differential survival outcomes included ERCC2 (mutated n = 387, wild type n = 3751, p < 0.0001), KDM6A (mutated n = 1091, wild type n = 3047, p < 0.0001), TERT (mutated n = 1714, wild type n = 2424), and TP53 (mutated n = 1689, wild type n = 2449, p < 0.0001).
Conclusions
Interestingly, while mutations in TP53 and ERCC2 were associated with shorter median survival, mutations in KDM6A and TERT were associated with longer median survival.
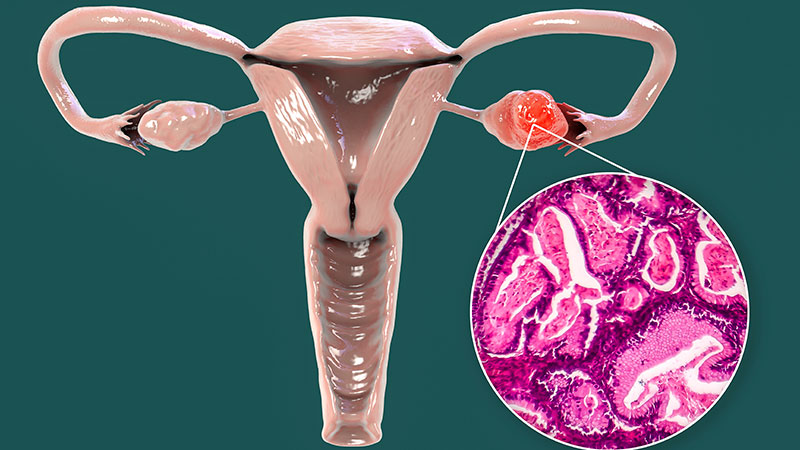
Papillary Cystadenocarcinoma: NCDB Insights on Outcomes and Socioeconomic Disparities
Background
Papillary cystadenocarcinoma is a rare, aggressive malignancy typically arising in the ovaries, often following malignant transformation of benign precursors. Characterized by local invasion and recurrence, it lacks standardized treatment protocols and comprehensive epidemiological data. Existing literature is limited to case reports and small series, leaving gaps in population-level data to guide clinical decision-making. This study uses the National Cancer Database (NCDB) to assess demographic, socioeconomic, and treatment patterns to identify disparities and inform management.
Methods
A retrospective cohort analysis of 345 patients with histologically confirmed papillary cystadenocarcinoma (ICD-O-3 code 8450) was conducted using the 2004–2020 NCDB. Demographic, treatment, and survival data were described; incidence trends were assessed via linear regression; and survival was analyzed using Kaplan-Meier curves.
Results
The cohort was predominantly female (97.1%), mean age 62.1 years (SD = 14.0), and 87.2% White. Most had private insurance (44.9%) or Medicare (40.9%). Over half (51.9%) resided in metropolitan areas >1 million. Primary tumor sites were ovarian (80.0%) and endometrial (5.2%), with 39.7% presenting at Stage III. Surgery was performed in 90.4% of cases, with 51.9% achieving negative margins. Most were treated at comprehensive community (41.0%) or academic/research programs (28.7%). Primary therapies included chemotherapy (62.3%), radiation (6.4%), and hormone therapy (1.7%). Thirty-day mortality was 1.9%, and 90-day mortality was 5.4%. Survival was 97.7% at 2 years, 94.2% at 5 years, and 88.6% at 10 years. Mean survival was 97.5 months (95% CI: 88.2–106.7).
Conclusions
This is the first NCDB-based analysis of papillary cystadenocarcinoma, offering insight into its clinical characteristics. Ovarian and endometrial origins were most common, reinforcing its gynecologic profile. High surgical rates and margin negativity suggest aggressive local treatment is central to management. Disparities emerged: patients were more likely to live in urban areas, hold private insurance, and receive care at community programs. These findings highlight the need for further investigation into socioeconomic inequities and may inform future guidelines to improve equitable care delivery across health systems, including community-based programs such as the VHA.
Background
Papillary cystadenocarcinoma is a rare, aggressive malignancy typically arising in the ovaries, often following malignant transformation of benign precursors. Characterized by local invasion and recurrence, it lacks standardized treatment protocols and comprehensive epidemiological data. Existing literature is limited to case reports and small series, leaving gaps in population-level data to guide clinical decision-making. This study uses the National Cancer Database (NCDB) to assess demographic, socioeconomic, and treatment patterns to identify disparities and inform management.
Methods
A retrospective cohort analysis of 345 patients with histologically confirmed papillary cystadenocarcinoma (ICD-O-3 code 8450) was conducted using the 2004–2020 NCDB. Demographic, treatment, and survival data were described; incidence trends were assessed via linear regression; and survival was analyzed using Kaplan-Meier curves.
Results
The cohort was predominantly female (97.1%), mean age 62.1 years (SD = 14.0), and 87.2% White. Most had private insurance (44.9%) or Medicare (40.9%). Over half (51.9%) resided in metropolitan areas >1 million. Primary tumor sites were ovarian (80.0%) and endometrial (5.2%), with 39.7% presenting at Stage III. Surgery was performed in 90.4% of cases, with 51.9% achieving negative margins. Most were treated at comprehensive community (41.0%) or academic/research programs (28.7%). Primary therapies included chemotherapy (62.3%), radiation (6.4%), and hormone therapy (1.7%). Thirty-day mortality was 1.9%, and 90-day mortality was 5.4%. Survival was 97.7% at 2 years, 94.2% at 5 years, and 88.6% at 10 years. Mean survival was 97.5 months (95% CI: 88.2–106.7).
Conclusions
This is the first NCDB-based analysis of papillary cystadenocarcinoma, offering insight into its clinical characteristics. Ovarian and endometrial origins were most common, reinforcing its gynecologic profile. High surgical rates and margin negativity suggest aggressive local treatment is central to management. Disparities emerged: patients were more likely to live in urban areas, hold private insurance, and receive care at community programs. These findings highlight the need for further investigation into socioeconomic inequities and may inform future guidelines to improve equitable care delivery across health systems, including community-based programs such as the VHA.
Background
Papillary cystadenocarcinoma is a rare, aggressive malignancy typically arising in the ovaries, often following malignant transformation of benign precursors. Characterized by local invasion and recurrence, it lacks standardized treatment protocols and comprehensive epidemiological data. Existing literature is limited to case reports and small series, leaving gaps in population-level data to guide clinical decision-making. This study uses the National Cancer Database (NCDB) to assess demographic, socioeconomic, and treatment patterns to identify disparities and inform management.
Methods
A retrospective cohort analysis of 345 patients with histologically confirmed papillary cystadenocarcinoma (ICD-O-3 code 8450) was conducted using the 2004–2020 NCDB. Demographic, treatment, and survival data were described; incidence trends were assessed via linear regression; and survival was analyzed using Kaplan-Meier curves.
Results
The cohort was predominantly female (97.1%), mean age 62.1 years (SD = 14.0), and 87.2% White. Most had private insurance (44.9%) or Medicare (40.9%). Over half (51.9%) resided in metropolitan areas >1 million. Primary tumor sites were ovarian (80.0%) and endometrial (5.2%), with 39.7% presenting at Stage III. Surgery was performed in 90.4% of cases, with 51.9% achieving negative margins. Most were treated at comprehensive community (41.0%) or academic/research programs (28.7%). Primary therapies included chemotherapy (62.3%), radiation (6.4%), and hormone therapy (1.7%). Thirty-day mortality was 1.9%, and 90-day mortality was 5.4%. Survival was 97.7% at 2 years, 94.2% at 5 years, and 88.6% at 10 years. Mean survival was 97.5 months (95% CI: 88.2–106.7).
Conclusions
This is the first NCDB-based analysis of papillary cystadenocarcinoma, offering insight into its clinical characteristics. Ovarian and endometrial origins were most common, reinforcing its gynecologic profile. High surgical rates and margin negativity suggest aggressive local treatment is central to management. Disparities emerged: patients were more likely to live in urban areas, hold private insurance, and receive care at community programs. These findings highlight the need for further investigation into socioeconomic inequities and may inform future guidelines to improve equitable care delivery across health systems, including community-based programs such as the VHA.
Can a Polygenic Risk Score Turn the Tide on Prostate Cancer Screening?
Incorporating a polygenic risk score into prostate cancer screening could enhance the detection of clinically significant prostate cancer that conventional screening may miss, according to results of the BARCODE 1 clinical trial conducted in the United Kingdom.
The study found that about 72% of participants with high polygenic risk scores were diagnosed with clinically significant prostate cancers, which would not have been detected with prostate-specific antigen (PSA) testing or MRI.
“With this test, it could be possible to turn the tide on prostate cancer,” study author Ros Eeles, PhD, professor of oncogenetics at The Institute of Cancer Research, London, England, said in a statement following the publication of the analysis in The New England Journal of Medicine.
Prostate cancer remains the second most commonly diagnosed cancer among men. As a screening tool, PSA testing has been criticized for leading to a high rate of false positive results and overdiagnosis — defined as a screen-detected cancer that would take longer to progress to clinical cancer than the patient’s lifetime. Both issues can result in overtreatment.
Given prostate cancer’s high heritability and the proliferation of genome-wide association studies identifying common genetic variants, there has been growing interest in using polygenic risk scores to improve risk stratification and guide screening.
“Building on decades of research into the genetic markers of prostate cancer, our study shows that the theory does work in practice — we can identify men at risk of aggressive cancers who need further tests and spare the men who are at lower risk from unnecessary treatments,” said Eeles.
An Adjunct to Screening?
The BARCODE 1 study, conducted in the United Kingdom, tested the clinical utility of a polygenic risk score as an adjunct to screening.
The researchers recruited men aged 55-69 years from primary care centers in the United Kingdom. Using germline DNA extracted from saliva, they derived polygenic risk scores from 130 genetic variants known to be associated with an increased risk for prostate cancer.
Among a total of 6393 men who had their scores calculated, 745 (12%) had a score in the top 10% of genetic risk (≥ 90th percentile) and were invited to undergo further screening.
Of these, 468 (63%) accepted the invite and underwent multiparametric MRI and transperineal prostate biopsy, irrespective of the PSA level. Overall, 187 (40%) were diagnosed with prostate cancer following biopsy. Of the 187 men with prostate cancer, 55% (n = 103) had disease classified as intermediate or high risk (Gleason score ≥ 7) per National Comprehensive Cancer Network criteria and therefore warranted further treatment.
Researchers then compared screening that incorporated polygenic risk scores with standard screening with PSA levels and MRI.
When participants’ risk was stratified by their polygenic risk score, 103 patients (55%) with prostate cancer could be classified as intermediate or higher risk, thus warranting treatment. Overall, 74 (71.8%) of those cancers would have been missed using the standard diagnostic pathway in the United Kingdom, which requires patients to have a high PSA level (> 3.0 μg/L) as well as a positive MRI result. These 74 patients either had PSA levels ≤ 3.0 μg/L or negative MRIs, which would mean these patients would typically fall below the action threshold for further testing.
Of the 103 participants warranting treatment, 40 of these men would have been classified as unfavorable intermediate, high, or very high risk, which would require radical treatment. Among this group, roughly 43% would have been missed using the UK diagnostic pathway.
However, the investigators estimated a rate of overdiagnosis with the use of polygenic risk scores of 16%-21%, similar to the overdiagnosis estimates in two prior PSA-based screening studies, signaling that the addition of polygenic risk scores does not necessarily reduce the risk for overdiagnosis.
Overall, “this study is the strongest evidence to date on the clinical utility of a polygenic score for prostate cancer screening,” commented Michael Inouye, professor of systems genomics & population health, University of Cambridge, Cambridge, England, in a statement from the UK nonprofit Science Media Centre (SMC).
“I suspect we will look back on this as a landmark study that really made the clinical case for polygenic scores as a new tool that moved health systems from disease management to early detection and prevention,” said Inouye, who was not involved in the study.
However, other experts were more cautious about the findings.
Dusko Ilic, MD, professor of stem cell sciences, King’s College London, London, England, said the results are “promising, especially in identifying significant cancers that would otherwise be missed,” but cautioned that “there is no direct evidence yet that using [polygenic risk scores] improves long-term outcomes such as mortality or quality-adjusted life years.”
“Modeling suggests benefit, but empirical confirmation is needed,” Ilic said in the SMC statement.
The hope is that the recently launched TRANSFORM trial will help answer some of these outstanding questions.
The current study suggests that polygenic risk scores for prostate cancer “would be a useful component of a multimodality screening program that assesses age, family history of prostate cancer, PSA, and MRI results as triage tools before biopsy is recommended,” David Hunter, MPH, ScD, with Harvard T. H. Chan School of Public Health, Boston, and University of Oxford, Oxford, England, wrote in an editorial accompanying the study.
“To make this integrated program a reality, however, changes to infrastructure would be needed to make running and analyzing a regulated genome array as easy as requesting a PSA level or ordering an MRI. Clearly, we are far from that future,” Hunter cautioned.
“A possible first step that would require less infrastructure could be to order a polygenic risk score only for men with a positive PSA result, then use the polygenic risk score to determine who should undergo an MRI, and then use all the information to determine whether biopsy is recommended,” Hunter said.
In his view, the current study is a “first step on a long road to evaluating new components of any disease screening pathway.”
The research received funding from the European Research Council, the Bob Willis Fund, Cancer Research UK, the Peacock Trust, and the National Institute for Health and Care Research Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research. Disclosures for authors and editorialists are available with the original article. Inouye and Ilic reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Incorporating a polygenic risk score into prostate cancer screening could enhance the detection of clinically significant prostate cancer that conventional screening may miss, according to results of the BARCODE 1 clinical trial conducted in the United Kingdom.
The study found that about 72% of participants with high polygenic risk scores were diagnosed with clinically significant prostate cancers, which would not have been detected with prostate-specific antigen (PSA) testing or MRI.
“With this test, it could be possible to turn the tide on prostate cancer,” study author Ros Eeles, PhD, professor of oncogenetics at The Institute of Cancer Research, London, England, said in a statement following the publication of the analysis in The New England Journal of Medicine.
Prostate cancer remains the second most commonly diagnosed cancer among men. As a screening tool, PSA testing has been criticized for leading to a high rate of false positive results and overdiagnosis — defined as a screen-detected cancer that would take longer to progress to clinical cancer than the patient’s lifetime. Both issues can result in overtreatment.
Given prostate cancer’s high heritability and the proliferation of genome-wide association studies identifying common genetic variants, there has been growing interest in using polygenic risk scores to improve risk stratification and guide screening.
“Building on decades of research into the genetic markers of prostate cancer, our study shows that the theory does work in practice — we can identify men at risk of aggressive cancers who need further tests and spare the men who are at lower risk from unnecessary treatments,” said Eeles.
An Adjunct to Screening?
The BARCODE 1 study, conducted in the United Kingdom, tested the clinical utility of a polygenic risk score as an adjunct to screening.
The researchers recruited men aged 55-69 years from primary care centers in the United Kingdom. Using germline DNA extracted from saliva, they derived polygenic risk scores from 130 genetic variants known to be associated with an increased risk for prostate cancer.
Among a total of 6393 men who had their scores calculated, 745 (12%) had a score in the top 10% of genetic risk (≥ 90th percentile) and were invited to undergo further screening.
Of these, 468 (63%) accepted the invite and underwent multiparametric MRI and transperineal prostate biopsy, irrespective of the PSA level. Overall, 187 (40%) were diagnosed with prostate cancer following biopsy. Of the 187 men with prostate cancer, 55% (n = 103) had disease classified as intermediate or high risk (Gleason score ≥ 7) per National Comprehensive Cancer Network criteria and therefore warranted further treatment.
Researchers then compared screening that incorporated polygenic risk scores with standard screening with PSA levels and MRI.
When participants’ risk was stratified by their polygenic risk score, 103 patients (55%) with prostate cancer could be classified as intermediate or higher risk, thus warranting treatment. Overall, 74 (71.8%) of those cancers would have been missed using the standard diagnostic pathway in the United Kingdom, which requires patients to have a high PSA level (> 3.0 μg/L) as well as a positive MRI result. These 74 patients either had PSA levels ≤ 3.0 μg/L or negative MRIs, which would mean these patients would typically fall below the action threshold for further testing.
Of the 103 participants warranting treatment, 40 of these men would have been classified as unfavorable intermediate, high, or very high risk, which would require radical treatment. Among this group, roughly 43% would have been missed using the UK diagnostic pathway.
However, the investigators estimated a rate of overdiagnosis with the use of polygenic risk scores of 16%-21%, similar to the overdiagnosis estimates in two prior PSA-based screening studies, signaling that the addition of polygenic risk scores does not necessarily reduce the risk for overdiagnosis.
Overall, “this study is the strongest evidence to date on the clinical utility of a polygenic score for prostate cancer screening,” commented Michael Inouye, professor of systems genomics & population health, University of Cambridge, Cambridge, England, in a statement from the UK nonprofit Science Media Centre (SMC).
“I suspect we will look back on this as a landmark study that really made the clinical case for polygenic scores as a new tool that moved health systems from disease management to early detection and prevention,” said Inouye, who was not involved in the study.
However, other experts were more cautious about the findings.
Dusko Ilic, MD, professor of stem cell sciences, King’s College London, London, England, said the results are “promising, especially in identifying significant cancers that would otherwise be missed,” but cautioned that “there is no direct evidence yet that using [polygenic risk scores] improves long-term outcomes such as mortality or quality-adjusted life years.”
“Modeling suggests benefit, but empirical confirmation is needed,” Ilic said in the SMC statement.
The hope is that the recently launched TRANSFORM trial will help answer some of these outstanding questions.
The current study suggests that polygenic risk scores for prostate cancer “would be a useful component of a multimodality screening program that assesses age, family history of prostate cancer, PSA, and MRI results as triage tools before biopsy is recommended,” David Hunter, MPH, ScD, with Harvard T. H. Chan School of Public Health, Boston, and University of Oxford, Oxford, England, wrote in an editorial accompanying the study.
“To make this integrated program a reality, however, changes to infrastructure would be needed to make running and analyzing a regulated genome array as easy as requesting a PSA level or ordering an MRI. Clearly, we are far from that future,” Hunter cautioned.
“A possible first step that would require less infrastructure could be to order a polygenic risk score only for men with a positive PSA result, then use the polygenic risk score to determine who should undergo an MRI, and then use all the information to determine whether biopsy is recommended,” Hunter said.
In his view, the current study is a “first step on a long road to evaluating new components of any disease screening pathway.”
The research received funding from the European Research Council, the Bob Willis Fund, Cancer Research UK, the Peacock Trust, and the National Institute for Health and Care Research Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research. Disclosures for authors and editorialists are available with the original article. Inouye and Ilic reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Incorporating a polygenic risk score into prostate cancer screening could enhance the detection of clinically significant prostate cancer that conventional screening may miss, according to results of the BARCODE 1 clinical trial conducted in the United Kingdom.
The study found that about 72% of participants with high polygenic risk scores were diagnosed with clinically significant prostate cancers, which would not have been detected with prostate-specific antigen (PSA) testing or MRI.
“With this test, it could be possible to turn the tide on prostate cancer,” study author Ros Eeles, PhD, professor of oncogenetics at The Institute of Cancer Research, London, England, said in a statement following the publication of the analysis in The New England Journal of Medicine.
Prostate cancer remains the second most commonly diagnosed cancer among men. As a screening tool, PSA testing has been criticized for leading to a high rate of false positive results and overdiagnosis — defined as a screen-detected cancer that would take longer to progress to clinical cancer than the patient’s lifetime. Both issues can result in overtreatment.
Given prostate cancer’s high heritability and the proliferation of genome-wide association studies identifying common genetic variants, there has been growing interest in using polygenic risk scores to improve risk stratification and guide screening.
“Building on decades of research into the genetic markers of prostate cancer, our study shows that the theory does work in practice — we can identify men at risk of aggressive cancers who need further tests and spare the men who are at lower risk from unnecessary treatments,” said Eeles.
An Adjunct to Screening?
The BARCODE 1 study, conducted in the United Kingdom, tested the clinical utility of a polygenic risk score as an adjunct to screening.
The researchers recruited men aged 55-69 years from primary care centers in the United Kingdom. Using germline DNA extracted from saliva, they derived polygenic risk scores from 130 genetic variants known to be associated with an increased risk for prostate cancer.
Among a total of 6393 men who had their scores calculated, 745 (12%) had a score in the top 10% of genetic risk (≥ 90th percentile) and were invited to undergo further screening.
Of these, 468 (63%) accepted the invite and underwent multiparametric MRI and transperineal prostate biopsy, irrespective of the PSA level. Overall, 187 (40%) were diagnosed with prostate cancer following biopsy. Of the 187 men with prostate cancer, 55% (n = 103) had disease classified as intermediate or high risk (Gleason score ≥ 7) per National Comprehensive Cancer Network criteria and therefore warranted further treatment.
Researchers then compared screening that incorporated polygenic risk scores with standard screening with PSA levels and MRI.
When participants’ risk was stratified by their polygenic risk score, 103 patients (55%) with prostate cancer could be classified as intermediate or higher risk, thus warranting treatment. Overall, 74 (71.8%) of those cancers would have been missed using the standard diagnostic pathway in the United Kingdom, which requires patients to have a high PSA level (> 3.0 μg/L) as well as a positive MRI result. These 74 patients either had PSA levels ≤ 3.0 μg/L or negative MRIs, which would mean these patients would typically fall below the action threshold for further testing.
Of the 103 participants warranting treatment, 40 of these men would have been classified as unfavorable intermediate, high, or very high risk, which would require radical treatment. Among this group, roughly 43% would have been missed using the UK diagnostic pathway.
However, the investigators estimated a rate of overdiagnosis with the use of polygenic risk scores of 16%-21%, similar to the overdiagnosis estimates in two prior PSA-based screening studies, signaling that the addition of polygenic risk scores does not necessarily reduce the risk for overdiagnosis.
Overall, “this study is the strongest evidence to date on the clinical utility of a polygenic score for prostate cancer screening,” commented Michael Inouye, professor of systems genomics & population health, University of Cambridge, Cambridge, England, in a statement from the UK nonprofit Science Media Centre (SMC).
“I suspect we will look back on this as a landmark study that really made the clinical case for polygenic scores as a new tool that moved health systems from disease management to early detection and prevention,” said Inouye, who was not involved in the study.
However, other experts were more cautious about the findings.
Dusko Ilic, MD, professor of stem cell sciences, King’s College London, London, England, said the results are “promising, especially in identifying significant cancers that would otherwise be missed,” but cautioned that “there is no direct evidence yet that using [polygenic risk scores] improves long-term outcomes such as mortality or quality-adjusted life years.”
“Modeling suggests benefit, but empirical confirmation is needed,” Ilic said in the SMC statement.
The hope is that the recently launched TRANSFORM trial will help answer some of these outstanding questions.
The current study suggests that polygenic risk scores for prostate cancer “would be a useful component of a multimodality screening program that assesses age, family history of prostate cancer, PSA, and MRI results as triage tools before biopsy is recommended,” David Hunter, MPH, ScD, with Harvard T. H. Chan School of Public Health, Boston, and University of Oxford, Oxford, England, wrote in an editorial accompanying the study.
“To make this integrated program a reality, however, changes to infrastructure would be needed to make running and analyzing a regulated genome array as easy as requesting a PSA level or ordering an MRI. Clearly, we are far from that future,” Hunter cautioned.
“A possible first step that would require less infrastructure could be to order a polygenic risk score only for men with a positive PSA result, then use the polygenic risk score to determine who should undergo an MRI, and then use all the information to determine whether biopsy is recommended,” Hunter said.
In his view, the current study is a “first step on a long road to evaluating new components of any disease screening pathway.”
The research received funding from the European Research Council, the Bob Willis Fund, Cancer Research UK, the Peacock Trust, and the National Institute for Health and Care Research Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research. Disclosures for authors and editorialists are available with the original article. Inouye and Ilic reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Do Patients With Intermediate-Risk Cervical Cancer Need Adjuvant Chemotherapy?
New findings on radiation plus adjuvant chemotherapy in patients with intermediate-risk cervical cancer seem to spell the end for the dual therapy in this group.
Results from a phase 3 clinical trial of 316 women who’d had radical hysterectomies found that adjuvant chemotherapy as treatment for their early-stage, intermediate-risk cervical carcinoma did not improve outcomes but did increase toxicity. The results were the inverse of the study’s intention.
The NRG-GOG 0263 (NCT01101451) study failed to reach its endpoint of improving recurrence-free survival through the addition of cisplatin chemotherapy, confirming instead that cisplatin chemotherapy given adjuvantly with radiotherapy is not a superior alternative in this cohort. The results were presented during a plenary session of the Society of Gynecologic Oncology Annual Meeting on Women’s Cancers in Seattle, Washington.
The current standard of care in this cohort is for radiotherapy alone, although the National Comprehensive Cancer Network (NCCN) guidelines place adjuvant chemotherapy in category 2B recommendations.
“Perhaps the NCCN guidelines will have to change what it says here,” Andrew Berchuck, MD, chief of gynecologic oncology and professor of obstetrics and gynecology at Duke University School of Medicine in Durham, North Carolina, told this news organization. Berchuck was not involved in the clinical trial.
The National Cancer Institute lists adjuvant chemotherapy first in its guidelines for this group.
Another study published online this month in JAMA Oncology concluded that morbidity in these patients could be reduced if the use of chemoradiotherapy were de-escalated.
This population-based cohort study of 1116 women, conducted by Núria Agustí Garcia, MD, postdoctoral fellow at The University of Texas MD Anderson Cancer Center in Houston, and colleagues, found no significant overall survival benefit of adjuvant chemotherapy in intermediate-risk cervical cancer, and that when it was given, patients tended to have larger tumors and nonsquamous cell history.
The 5-year survival rate in patients who received chemoradiotherapy was 87%, compared with an 87% 5-year survival rate in those who received radiotherapy alone (hazard ratio = 0.85; 95% CI, 0.59-1.23; P =.38).
If the standard of care in this cohort is radiation only, and outcomes are not better in adjuvant treatment, then why is there a controversy at all, and why are some investigators such as Agustí Garcia attempting to clarify adjuvant treatment’s effects?
Experts say it’s because of the history of adjuvant chemotherapy in more advanced cervical cancer and the extrapolations clinicians made when treating patients with intermediate risk.
What Is the History of Adjuvant Treatment in Cervical Cancer?
Concomitant therapies in intermediate-risk cervical cancer began in the late 1990s, at a time when it was found effective in more advanced disease, according to Berchuck, who also was not involved in the population study.
“Say back then, you had a stage IIIb cervical cancer. With external radiation alone, followed by brachytherapy internally, the cure rate for something like that would have been maybe 50 or 60%,” Berchuck said in an interview. “Adding cisplatin improved the cure rate by about 15%.”
That cisplatin improved survival rates in advanced disease, led to using it in less advanced cases, according to Berchuck. “The idea here was that if the pathology report indicated a larger tumor involving the lymphatics, the risk of recurrence went up to about 20%, so by adding chemo to postsurgical radiotherapy, you could improve things more than with just radiation alone,” Berchuck said.
Studies of adjuvant chemotherapy in advanced cervical cancers confused the matter, according to Agustí Garcia.
“The theoretical benefit of adding chemotherapy to radiotherapy for patients with intermediate-risk cervical cancer has been extrapolated from studies on locally advanced or high-risk cases, for example, those with parametrial or lymph node metastases,” Agustí Garcia said in an interview.
“However, before its implementation, there was no solid evidence supporting this approach in intermediate-risk patients,” she said. “The oncologic behavior of this subgroup may differ, and in the absence of parametrial or lymph node metastasis, chemotherapy may not be necessary.”
Do Both Studies Suggest That Radiotherapy Has Become More Effective Recently?
“Probably. Modern radiation techniques, such as IMRT [intensity-modulated radiation therapy] and IGRT [image-guided radiation therapy] are more effective than historical techniques,” said Amer Karam, MD, a clinical professor of obstetrics and gynecology at Stanford University in Palo Alto, California. Karam was not involved in either study mentioned previously.
Agustí Garcia said that while it’s true radiotherapy techniques have improved, these advancements primarily impact morbidity rather than survival outcomes.
“The lack of survival benefit from concomitant chemotherapy in intermediate-risk patients suggests that such benefit may never have existed in this subgroup,” she said.
What Explains Why Overall Survival Did Not Significantly Differ Between Patients Who Received Radiotherapy Alone and Those Who Received Chemoradiotherapy?
For Karam, there is a question as to whether chemosensitization mechanisms in radiation therapy, such as reactive oxygen species, inhibition of DNA repair, modulating tumor microenvironment, and cell cycle arrest — all used to induce apoptosis — are as efficacious as once thought.
“Also, systemic chemosensitization may not be as effective at controlling systemic disease beyond the pelvis and radiation field,” he said.
“Radiation is extremely effective in cervical cancer,” said Berchuck. “When you’re giving radiation in a situation like this where there is none, to only microscopic disease, it makes sense that radiation could be effective by itself.”
Why in the JAMA Oncology Study Were Larger Tumor Size and Nonsquamous Histology Associated With the Use of Chemoradiotherapy?
All experts agreed this is likely because this subgroup of patients with larger tumors is typically seen as being at higher risk for recurrence. This might be due to what Karam called an “unfavorable histology” and certain tumor characteristics, including depth of invasion.
Yet Agustí Garcia said, in her study, even after propensity score matching, adjuvant chemotherapy did not demonstrate any survival benefit in this subgroup.
“The importance of performing propensity score matching in our analysis was to ensure that populations with comparable baseline recurrence and death risks were being evaluated fairly,” she told this news organization.
Do These Findings Change Clinical Practice for Intermediate-Risk Cervical Cancer Treatment?
For Karam, the new evidence in intermediate-risk cervical cancer confirms rather than changes clinical practice. “The standard of care was radiation therapy alone, which is now confirmed, based on the results of GOG 263,” Karam said. “The standard of care for these patients will remain the same.”
Agustí Garcia said her study results can help “refine” clinical practice.
“The results suggest that adjuvant therapy could be safely de-escalated in intermediate-risk cervical cancer,” Agustí Garcia said.
“We should avoid chemotherapy when there is no evidence-based benefit, reserving its use for locally advanced or high-risk cases, refining clinical guidelines to ensure treatment recommendations are based on higher-quality evidence, thereby standardizing care and reducing overtreatment,” she continued. “Current guidelines lack consensus and rely on lower-quality evidence.”
Agustí Garcia reported grants from Fundación Alfonso Martín Escudero. Berchuck has no disclosures. Karam reported royalties from UpToDate and that he is a speaker for AstraZeneca.
A version of this article first appeared on Medscape.com.
New findings on radiation plus adjuvant chemotherapy in patients with intermediate-risk cervical cancer seem to spell the end for the dual therapy in this group.
Results from a phase 3 clinical trial of 316 women who’d had radical hysterectomies found that adjuvant chemotherapy as treatment for their early-stage, intermediate-risk cervical carcinoma did not improve outcomes but did increase toxicity. The results were the inverse of the study’s intention.
The NRG-GOG 0263 (NCT01101451) study failed to reach its endpoint of improving recurrence-free survival through the addition of cisplatin chemotherapy, confirming instead that cisplatin chemotherapy given adjuvantly with radiotherapy is not a superior alternative in this cohort. The results were presented during a plenary session of the Society of Gynecologic Oncology Annual Meeting on Women’s Cancers in Seattle, Washington.
The current standard of care in this cohort is for radiotherapy alone, although the National Comprehensive Cancer Network (NCCN) guidelines place adjuvant chemotherapy in category 2B recommendations.
“Perhaps the NCCN guidelines will have to change what it says here,” Andrew Berchuck, MD, chief of gynecologic oncology and professor of obstetrics and gynecology at Duke University School of Medicine in Durham, North Carolina, told this news organization. Berchuck was not involved in the clinical trial.
The National Cancer Institute lists adjuvant chemotherapy first in its guidelines for this group.
Another study published online this month in JAMA Oncology concluded that morbidity in these patients could be reduced if the use of chemoradiotherapy were de-escalated.
This population-based cohort study of 1116 women, conducted by Núria Agustí Garcia, MD, postdoctoral fellow at The University of Texas MD Anderson Cancer Center in Houston, and colleagues, found no significant overall survival benefit of adjuvant chemotherapy in intermediate-risk cervical cancer, and that when it was given, patients tended to have larger tumors and nonsquamous cell history.
The 5-year survival rate in patients who received chemoradiotherapy was 87%, compared with an 87% 5-year survival rate in those who received radiotherapy alone (hazard ratio = 0.85; 95% CI, 0.59-1.23; P =.38).
If the standard of care in this cohort is radiation only, and outcomes are not better in adjuvant treatment, then why is there a controversy at all, and why are some investigators such as Agustí Garcia attempting to clarify adjuvant treatment’s effects?
Experts say it’s because of the history of adjuvant chemotherapy in more advanced cervical cancer and the extrapolations clinicians made when treating patients with intermediate risk.
What Is the History of Adjuvant Treatment in Cervical Cancer?
Concomitant therapies in intermediate-risk cervical cancer began in the late 1990s, at a time when it was found effective in more advanced disease, according to Berchuck, who also was not involved in the population study.
“Say back then, you had a stage IIIb cervical cancer. With external radiation alone, followed by brachytherapy internally, the cure rate for something like that would have been maybe 50 or 60%,” Berchuck said in an interview. “Adding cisplatin improved the cure rate by about 15%.”
That cisplatin improved survival rates in advanced disease, led to using it in less advanced cases, according to Berchuck. “The idea here was that if the pathology report indicated a larger tumor involving the lymphatics, the risk of recurrence went up to about 20%, so by adding chemo to postsurgical radiotherapy, you could improve things more than with just radiation alone,” Berchuck said.
Studies of adjuvant chemotherapy in advanced cervical cancers confused the matter, according to Agustí Garcia.
“The theoretical benefit of adding chemotherapy to radiotherapy for patients with intermediate-risk cervical cancer has been extrapolated from studies on locally advanced or high-risk cases, for example, those with parametrial or lymph node metastases,” Agustí Garcia said in an interview.
“However, before its implementation, there was no solid evidence supporting this approach in intermediate-risk patients,” she said. “The oncologic behavior of this subgroup may differ, and in the absence of parametrial or lymph node metastasis, chemotherapy may not be necessary.”
Do Both Studies Suggest That Radiotherapy Has Become More Effective Recently?
“Probably. Modern radiation techniques, such as IMRT [intensity-modulated radiation therapy] and IGRT [image-guided radiation therapy] are more effective than historical techniques,” said Amer Karam, MD, a clinical professor of obstetrics and gynecology at Stanford University in Palo Alto, California. Karam was not involved in either study mentioned previously.
Agustí Garcia said that while it’s true radiotherapy techniques have improved, these advancements primarily impact morbidity rather than survival outcomes.
“The lack of survival benefit from concomitant chemotherapy in intermediate-risk patients suggests that such benefit may never have existed in this subgroup,” she said.
What Explains Why Overall Survival Did Not Significantly Differ Between Patients Who Received Radiotherapy Alone and Those Who Received Chemoradiotherapy?
For Karam, there is a question as to whether chemosensitization mechanisms in radiation therapy, such as reactive oxygen species, inhibition of DNA repair, modulating tumor microenvironment, and cell cycle arrest — all used to induce apoptosis — are as efficacious as once thought.
“Also, systemic chemosensitization may not be as effective at controlling systemic disease beyond the pelvis and radiation field,” he said.
“Radiation is extremely effective in cervical cancer,” said Berchuck. “When you’re giving radiation in a situation like this where there is none, to only microscopic disease, it makes sense that radiation could be effective by itself.”
Why in the JAMA Oncology Study Were Larger Tumor Size and Nonsquamous Histology Associated With the Use of Chemoradiotherapy?
All experts agreed this is likely because this subgroup of patients with larger tumors is typically seen as being at higher risk for recurrence. This might be due to what Karam called an “unfavorable histology” and certain tumor characteristics, including depth of invasion.
Yet Agustí Garcia said, in her study, even after propensity score matching, adjuvant chemotherapy did not demonstrate any survival benefit in this subgroup.
“The importance of performing propensity score matching in our analysis was to ensure that populations with comparable baseline recurrence and death risks were being evaluated fairly,” she told this news organization.
Do These Findings Change Clinical Practice for Intermediate-Risk Cervical Cancer Treatment?
For Karam, the new evidence in intermediate-risk cervical cancer confirms rather than changes clinical practice. “The standard of care was radiation therapy alone, which is now confirmed, based on the results of GOG 263,” Karam said. “The standard of care for these patients will remain the same.”
Agustí Garcia said her study results can help “refine” clinical practice.
“The results suggest that adjuvant therapy could be safely de-escalated in intermediate-risk cervical cancer,” Agustí Garcia said.
“We should avoid chemotherapy when there is no evidence-based benefit, reserving its use for locally advanced or high-risk cases, refining clinical guidelines to ensure treatment recommendations are based on higher-quality evidence, thereby standardizing care and reducing overtreatment,” she continued. “Current guidelines lack consensus and rely on lower-quality evidence.”
Agustí Garcia reported grants from Fundación Alfonso Martín Escudero. Berchuck has no disclosures. Karam reported royalties from UpToDate and that he is a speaker for AstraZeneca.
A version of this article first appeared on Medscape.com.
New findings on radiation plus adjuvant chemotherapy in patients with intermediate-risk cervical cancer seem to spell the end for the dual therapy in this group.
Results from a phase 3 clinical trial of 316 women who’d had radical hysterectomies found that adjuvant chemotherapy as treatment for their early-stage, intermediate-risk cervical carcinoma did not improve outcomes but did increase toxicity. The results were the inverse of the study’s intention.
The NRG-GOG 0263 (NCT01101451) study failed to reach its endpoint of improving recurrence-free survival through the addition of cisplatin chemotherapy, confirming instead that cisplatin chemotherapy given adjuvantly with radiotherapy is not a superior alternative in this cohort. The results were presented during a plenary session of the Society of Gynecologic Oncology Annual Meeting on Women’s Cancers in Seattle, Washington.
The current standard of care in this cohort is for radiotherapy alone, although the National Comprehensive Cancer Network (NCCN) guidelines place adjuvant chemotherapy in category 2B recommendations.
“Perhaps the NCCN guidelines will have to change what it says here,” Andrew Berchuck, MD, chief of gynecologic oncology and professor of obstetrics and gynecology at Duke University School of Medicine in Durham, North Carolina, told this news organization. Berchuck was not involved in the clinical trial.
The National Cancer Institute lists adjuvant chemotherapy first in its guidelines for this group.
Another study published online this month in JAMA Oncology concluded that morbidity in these patients could be reduced if the use of chemoradiotherapy were de-escalated.
This population-based cohort study of 1116 women, conducted by Núria Agustí Garcia, MD, postdoctoral fellow at The University of Texas MD Anderson Cancer Center in Houston, and colleagues, found no significant overall survival benefit of adjuvant chemotherapy in intermediate-risk cervical cancer, and that when it was given, patients tended to have larger tumors and nonsquamous cell history.
The 5-year survival rate in patients who received chemoradiotherapy was 87%, compared with an 87% 5-year survival rate in those who received radiotherapy alone (hazard ratio = 0.85; 95% CI, 0.59-1.23; P =.38).
If the standard of care in this cohort is radiation only, and outcomes are not better in adjuvant treatment, then why is there a controversy at all, and why are some investigators such as Agustí Garcia attempting to clarify adjuvant treatment’s effects?
Experts say it’s because of the history of adjuvant chemotherapy in more advanced cervical cancer and the extrapolations clinicians made when treating patients with intermediate risk.
What Is the History of Adjuvant Treatment in Cervical Cancer?
Concomitant therapies in intermediate-risk cervical cancer began in the late 1990s, at a time when it was found effective in more advanced disease, according to Berchuck, who also was not involved in the population study.
“Say back then, you had a stage IIIb cervical cancer. With external radiation alone, followed by brachytherapy internally, the cure rate for something like that would have been maybe 50 or 60%,” Berchuck said in an interview. “Adding cisplatin improved the cure rate by about 15%.”
That cisplatin improved survival rates in advanced disease, led to using it in less advanced cases, according to Berchuck. “The idea here was that if the pathology report indicated a larger tumor involving the lymphatics, the risk of recurrence went up to about 20%, so by adding chemo to postsurgical radiotherapy, you could improve things more than with just radiation alone,” Berchuck said.
Studies of adjuvant chemotherapy in advanced cervical cancers confused the matter, according to Agustí Garcia.
“The theoretical benefit of adding chemotherapy to radiotherapy for patients with intermediate-risk cervical cancer has been extrapolated from studies on locally advanced or high-risk cases, for example, those with parametrial or lymph node metastases,” Agustí Garcia said in an interview.
“However, before its implementation, there was no solid evidence supporting this approach in intermediate-risk patients,” she said. “The oncologic behavior of this subgroup may differ, and in the absence of parametrial or lymph node metastasis, chemotherapy may not be necessary.”
Do Both Studies Suggest That Radiotherapy Has Become More Effective Recently?
“Probably. Modern radiation techniques, such as IMRT [intensity-modulated radiation therapy] and IGRT [image-guided radiation therapy] are more effective than historical techniques,” said Amer Karam, MD, a clinical professor of obstetrics and gynecology at Stanford University in Palo Alto, California. Karam was not involved in either study mentioned previously.
Agustí Garcia said that while it’s true radiotherapy techniques have improved, these advancements primarily impact morbidity rather than survival outcomes.
“The lack of survival benefit from concomitant chemotherapy in intermediate-risk patients suggests that such benefit may never have existed in this subgroup,” she said.
What Explains Why Overall Survival Did Not Significantly Differ Between Patients Who Received Radiotherapy Alone and Those Who Received Chemoradiotherapy?
For Karam, there is a question as to whether chemosensitization mechanisms in radiation therapy, such as reactive oxygen species, inhibition of DNA repair, modulating tumor microenvironment, and cell cycle arrest — all used to induce apoptosis — are as efficacious as once thought.
“Also, systemic chemosensitization may not be as effective at controlling systemic disease beyond the pelvis and radiation field,” he said.
“Radiation is extremely effective in cervical cancer,” said Berchuck. “When you’re giving radiation in a situation like this where there is none, to only microscopic disease, it makes sense that radiation could be effective by itself.”
Why in the JAMA Oncology Study Were Larger Tumor Size and Nonsquamous Histology Associated With the Use of Chemoradiotherapy?
All experts agreed this is likely because this subgroup of patients with larger tumors is typically seen as being at higher risk for recurrence. This might be due to what Karam called an “unfavorable histology” and certain tumor characteristics, including depth of invasion.
Yet Agustí Garcia said, in her study, even after propensity score matching, adjuvant chemotherapy did not demonstrate any survival benefit in this subgroup.
“The importance of performing propensity score matching in our analysis was to ensure that populations with comparable baseline recurrence and death risks were being evaluated fairly,” she told this news organization.
Do These Findings Change Clinical Practice for Intermediate-Risk Cervical Cancer Treatment?
For Karam, the new evidence in intermediate-risk cervical cancer confirms rather than changes clinical practice. “The standard of care was radiation therapy alone, which is now confirmed, based on the results of GOG 263,” Karam said. “The standard of care for these patients will remain the same.”
Agustí Garcia said her study results can help “refine” clinical practice.
“The results suggest that adjuvant therapy could be safely de-escalated in intermediate-risk cervical cancer,” Agustí Garcia said.
“We should avoid chemotherapy when there is no evidence-based benefit, reserving its use for locally advanced or high-risk cases, refining clinical guidelines to ensure treatment recommendations are based on higher-quality evidence, thereby standardizing care and reducing overtreatment,” she continued. “Current guidelines lack consensus and rely on lower-quality evidence.”
Agustí Garcia reported grants from Fundación Alfonso Martín Escudero. Berchuck has no disclosures. Karam reported royalties from UpToDate and that he is a speaker for AstraZeneca.
A version of this article first appeared on Medscape.com.
OK to Skip Pelvic Lymph Node Dissection in Cervical Cancer?
Results from the PHENIX-I trial support skipping pelvic lymphadenectomy in women with early cervical cancer who have a negative sentinel lymph node biopsy.
Omitting pelvic lymphadenectomy in these patients “did not compromise disease-free survival and potentially [led to] improved overall survival,” reported lead investigator Jihong Liu, MD, gynecologic oncologist, Sun Yat-sen University Cancer Center, Guangzhou, China.
Forgoing the additional procedure also decreased the incidence of retroperitoneal lymph node recurrence and adverse events and demonstrated superior surgical outcomes including shorter operative duration, reduced blood loss, and a lower morbidity.
Liu reported the PHENIX-I results at this year’s Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025.
Pelvic lymphadenectomy has been part of standard care for early-stage cervical cancer for over a century, even though the incidence of lymph node metastasis in early-stage cervical cancer is relatively low. Overtreatment and increased morbidity have been notable drawbacks of the procedure.
It may be possible to forgo pelvic lymphadenectomy in early-stage cervical cancer when sentinel lymph node biopsy findings are negative, but evidence from randomized controlled trials are lacking, Liu explained.
The PHENIX-I trial prospectively assessed survival outcomes among patients who received pelvic lymphadenectomy and those who did not. More specifically, all patients underwent sentinel lymph node biopsy and patients with negative lymph nodes were then intraoperatively randomized (1:1) to undergo pelvic lymphadenectomy (417 patients) or not (416 patients).
The multicenter, randomized controlled trial involved patients undergoing radical hysterectomy for stage IA1 (lymphovascular invasion), IA2, IB1, IB2 or IIA1 cervical cancer with tumor size not exceeding 3 cm.
“The only difference between the two groups was that patients in the experimental arm did not have pelvic lymphadenectomy,” Liu said.
Liu and colleagues reported that 23 patients (2.8%) had a positive lymph node on postoperative pathology examination. The rate of false-negative sentinel lymph node biopsy was < 1%. About half the patients in both groups received postoperative adjuvant therapy, and there was no significant between-group difference in the rates and time to initiate adjuvant therapy.
Overall, about 3.85% of patients (n = 16) in the biopsy-only group had a recurrence compared with 6.24% (n = 26) in the pelvic lymphadenectomy group at a median follow-up of 50 months.
But no patients in the biopsy-only group had a recurrence in the retroperitoneal lymph nodes compared with 9 patients in the pelvic lymphadenectomy group.
The 3-year disease-free survival (primary endpoint) rates were similar between the two groups — 96.8% in the biopsy-only group and 94.5% in the lymphadenectomy group (hazard ratio [HR], 0.61; P = .12). However, the 3-year overall survival was significantly higher in biopsy-only group — 100% vs 97.8% in the lymphadenectomy group (HR, 0.21; P = .007). Overall, three patients (19%) in the biopsy-only group died from cervical cancer vs 14 (54%) in the lymphadenectomy group.
As for surgical complications, pelvic lymphadenectomy was associated with a higher incidence of pain (5.8% vs 1.7%), lymphocyst (22.1% vs 8.4%), and lymphedema (10.1% vs 2.4%), as well as longer operating time and more blood loss.
Offering perspective on PHENIX-I, discussant Premal Thaker, MD, noted that this is the first randomized trial to report on the use of sentinel lymph node biopsy alone vs biopsy plus pelvic lymphadenectomy after radical hysterectomy.
Key takeaways are the “equivalent” 3-year disease-free outcomes but “lower” overall survival in the pelvic lymphadenectomy group as well as more adverse events, said Thaker, gynecologic oncologist and surgeon, Siteman Cancer Center, Washington University, St Louis.
Although quality of life data was not presented in the trial, patients who skipped pelvic lymphadenectomy had fewer adverse events, “which is very important for our patients,” Thaker added.
This study had no commercial funding. Liu and Thaker had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Results from the PHENIX-I trial support skipping pelvic lymphadenectomy in women with early cervical cancer who have a negative sentinel lymph node biopsy.
Omitting pelvic lymphadenectomy in these patients “did not compromise disease-free survival and potentially [led to] improved overall survival,” reported lead investigator Jihong Liu, MD, gynecologic oncologist, Sun Yat-sen University Cancer Center, Guangzhou, China.
Forgoing the additional procedure also decreased the incidence of retroperitoneal lymph node recurrence and adverse events and demonstrated superior surgical outcomes including shorter operative duration, reduced blood loss, and a lower morbidity.
Liu reported the PHENIX-I results at this year’s Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025.
Pelvic lymphadenectomy has been part of standard care for early-stage cervical cancer for over a century, even though the incidence of lymph node metastasis in early-stage cervical cancer is relatively low. Overtreatment and increased morbidity have been notable drawbacks of the procedure.
It may be possible to forgo pelvic lymphadenectomy in early-stage cervical cancer when sentinel lymph node biopsy findings are negative, but evidence from randomized controlled trials are lacking, Liu explained.
The PHENIX-I trial prospectively assessed survival outcomes among patients who received pelvic lymphadenectomy and those who did not. More specifically, all patients underwent sentinel lymph node biopsy and patients with negative lymph nodes were then intraoperatively randomized (1:1) to undergo pelvic lymphadenectomy (417 patients) or not (416 patients).
The multicenter, randomized controlled trial involved patients undergoing radical hysterectomy for stage IA1 (lymphovascular invasion), IA2, IB1, IB2 or IIA1 cervical cancer with tumor size not exceeding 3 cm.
“The only difference between the two groups was that patients in the experimental arm did not have pelvic lymphadenectomy,” Liu said.
Liu and colleagues reported that 23 patients (2.8%) had a positive lymph node on postoperative pathology examination. The rate of false-negative sentinel lymph node biopsy was < 1%. About half the patients in both groups received postoperative adjuvant therapy, and there was no significant between-group difference in the rates and time to initiate adjuvant therapy.
Overall, about 3.85% of patients (n = 16) in the biopsy-only group had a recurrence compared with 6.24% (n = 26) in the pelvic lymphadenectomy group at a median follow-up of 50 months.
But no patients in the biopsy-only group had a recurrence in the retroperitoneal lymph nodes compared with 9 patients in the pelvic lymphadenectomy group.
The 3-year disease-free survival (primary endpoint) rates were similar between the two groups — 96.8% in the biopsy-only group and 94.5% in the lymphadenectomy group (hazard ratio [HR], 0.61; P = .12). However, the 3-year overall survival was significantly higher in biopsy-only group — 100% vs 97.8% in the lymphadenectomy group (HR, 0.21; P = .007). Overall, three patients (19%) in the biopsy-only group died from cervical cancer vs 14 (54%) in the lymphadenectomy group.
As for surgical complications, pelvic lymphadenectomy was associated with a higher incidence of pain (5.8% vs 1.7%), lymphocyst (22.1% vs 8.4%), and lymphedema (10.1% vs 2.4%), as well as longer operating time and more blood loss.
Offering perspective on PHENIX-I, discussant Premal Thaker, MD, noted that this is the first randomized trial to report on the use of sentinel lymph node biopsy alone vs biopsy plus pelvic lymphadenectomy after radical hysterectomy.
Key takeaways are the “equivalent” 3-year disease-free outcomes but “lower” overall survival in the pelvic lymphadenectomy group as well as more adverse events, said Thaker, gynecologic oncologist and surgeon, Siteman Cancer Center, Washington University, St Louis.
Although quality of life data was not presented in the trial, patients who skipped pelvic lymphadenectomy had fewer adverse events, “which is very important for our patients,” Thaker added.
This study had no commercial funding. Liu and Thaker had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Results from the PHENIX-I trial support skipping pelvic lymphadenectomy in women with early cervical cancer who have a negative sentinel lymph node biopsy.
Omitting pelvic lymphadenectomy in these patients “did not compromise disease-free survival and potentially [led to] improved overall survival,” reported lead investigator Jihong Liu, MD, gynecologic oncologist, Sun Yat-sen University Cancer Center, Guangzhou, China.
Forgoing the additional procedure also decreased the incidence of retroperitoneal lymph node recurrence and adverse events and demonstrated superior surgical outcomes including shorter operative duration, reduced blood loss, and a lower morbidity.
Liu reported the PHENIX-I results at this year’s Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025.
Pelvic lymphadenectomy has been part of standard care for early-stage cervical cancer for over a century, even though the incidence of lymph node metastasis in early-stage cervical cancer is relatively low. Overtreatment and increased morbidity have been notable drawbacks of the procedure.
It may be possible to forgo pelvic lymphadenectomy in early-stage cervical cancer when sentinel lymph node biopsy findings are negative, but evidence from randomized controlled trials are lacking, Liu explained.
The PHENIX-I trial prospectively assessed survival outcomes among patients who received pelvic lymphadenectomy and those who did not. More specifically, all patients underwent sentinel lymph node biopsy and patients with negative lymph nodes were then intraoperatively randomized (1:1) to undergo pelvic lymphadenectomy (417 patients) or not (416 patients).
The multicenter, randomized controlled trial involved patients undergoing radical hysterectomy for stage IA1 (lymphovascular invasion), IA2, IB1, IB2 or IIA1 cervical cancer with tumor size not exceeding 3 cm.
“The only difference between the two groups was that patients in the experimental arm did not have pelvic lymphadenectomy,” Liu said.
Liu and colleagues reported that 23 patients (2.8%) had a positive lymph node on postoperative pathology examination. The rate of false-negative sentinel lymph node biopsy was < 1%. About half the patients in both groups received postoperative adjuvant therapy, and there was no significant between-group difference in the rates and time to initiate adjuvant therapy.
Overall, about 3.85% of patients (n = 16) in the biopsy-only group had a recurrence compared with 6.24% (n = 26) in the pelvic lymphadenectomy group at a median follow-up of 50 months.
But no patients in the biopsy-only group had a recurrence in the retroperitoneal lymph nodes compared with 9 patients in the pelvic lymphadenectomy group.
The 3-year disease-free survival (primary endpoint) rates were similar between the two groups — 96.8% in the biopsy-only group and 94.5% in the lymphadenectomy group (hazard ratio [HR], 0.61; P = .12). However, the 3-year overall survival was significantly higher in biopsy-only group — 100% vs 97.8% in the lymphadenectomy group (HR, 0.21; P = .007). Overall, three patients (19%) in the biopsy-only group died from cervical cancer vs 14 (54%) in the lymphadenectomy group.
As for surgical complications, pelvic lymphadenectomy was associated with a higher incidence of pain (5.8% vs 1.7%), lymphocyst (22.1% vs 8.4%), and lymphedema (10.1% vs 2.4%), as well as longer operating time and more blood loss.
Offering perspective on PHENIX-I, discussant Premal Thaker, MD, noted that this is the first randomized trial to report on the use of sentinel lymph node biopsy alone vs biopsy plus pelvic lymphadenectomy after radical hysterectomy.
Key takeaways are the “equivalent” 3-year disease-free outcomes but “lower” overall survival in the pelvic lymphadenectomy group as well as more adverse events, said Thaker, gynecologic oncologist and surgeon, Siteman Cancer Center, Washington University, St Louis.
Although quality of life data was not presented in the trial, patients who skipped pelvic lymphadenectomy had fewer adverse events, “which is very important for our patients,” Thaker added.
This study had no commercial funding. Liu and Thaker had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SGO 2025
ASCO Updates Treatment Guidance for Newly Diagnosed, Advanced Ovarian Cancer
The American Society of Clinical Oncology (ASCO) has released updated guidelines for neoadjuvant chemotherapy in newly diagnosed advanced ovarian cancer, introducing changes in patient selection and treatment strategies. The changes reflect emerging evidence on racial disparities, treatment outcomes, and quality of life considerations.
The publication of the new guidance follows dramatic shifts in treatment patterns over the past decade.
“There had been a big shift in how we were treating patients in the United States,” explained Stephanie Gaillard, MD, PhD, one of the authors of the updated guidelines. “We saw a substantial drop in the number of patients undergoing primary cytoreductive surgery for ovarian cancer from about 70% of patients in 2010 to only about 37% in 2021.”
The new guidelines maintain the recommendation for platinum/taxane-based neoadjuvant chemotherapy but introduce modifications regarding timing and duration.
“It’s still a recommendation that gynecologic oncologists are involved in determining whether someone is eligible for primary cytoreductive surgery or should undergo neoadjuvant chemotherapy first,” Gaillard noted. “We emphasize that patients who are eligible for primary cytoreductive surgery should undergo surgery as opposed to receiving neoadjuvant chemotherapy.”
Alexander Melamed, MD, MPH, a gynecologic oncologist at Massachusetts General Hospital, Boston, who was not involved in authoring the updated guidelines, noted that additional evidence-based guidance is needed to individualize treatment plans. He pointed to four completed trials comparing neoadjuvant chemotherapy with cytoreductive surgery, noting: “When these trials have been pooled together in meta-analyses, there was a higher risk of mortality associated with primary cytoreductive surgery and a higher risk of severe complications.”
The updated guidelines take this higher risk for mortality with primary cytoreductive surgery into consideration, and patients who are not eligible for primary surgery would receive neoadjuvant chemotherapy, Gaillard noted.
Changes in Patient Selection
The 2025 guidelines describe a more nuanced approach for selecting patients for neoadjuvant chemotherapy vs primary cytoreductive surgery. While the 2016 ASCO guidelines primarily focused on disease burden and surgical resectability when selecting patients for neoadjuvant chemotherapy, the new recommendations incorporate additional factors.
The guidelines discuss recent findings showing that Black patients experience a 38% lower likelihood of undergoing cytoreductive surgery than non-Black patients. In addition, compared with non-Hispanic White women, Asian and Black women more frequently receive neoadjuvant chemotherapy with interval debulking surgery rather than primary cytoreductive surgery. According to the authors, these differences persist even after accounting for clinical factors, suggesting that structural barriers to healthcare access may play a role.
The guidelines discuss how affordability, availability, and accessibility mediate racial disparities in ovarian cancer care. According to the authors, structural inequities in healthcare access influence treatment quality for minority patients. Non-White patients face greater challenges in accessing gynecologic oncology consultations and standard-of-care combination therapy, leading to poorer survival outcomes, the guidelines say.
According to Melamed, the guidelines serve as an important tool for promoting healthcare equity. “Having recommendations and standards is incredibly important for achieving equity because once there is consensus on a best practice, it doesn’t matter if you’re rich, poor, or a patient of a particular racial or ethnic group — if you have the disease, you ought to have access to that standard,” he said.
The 2016 ASCO guidelines focused primarily on disease burden and surgical resectability, whereas the 2024 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for ovarian cancer focus more on oncologic outcomes and surgical considerations. Based on the NCCN guidelines, treatment selection for ovarian cancer is primarily determined by the histologic subtype, stage of disease, and whether the patient is a candidate for primary surgery. The 2025 ASCO guidelines, on the other hand, emphasize the importance of quality-of-life outcomes during treatment selection. The authors of the updated ASCO guidelines acknowledged that treatment decisions should consider both the duration and quality of life, particularly for elderly patients or those with multiple comorbidities.
Treatment Timing and Duration
The guidelines maintain the recommendations for platinum/taxane-based neoadjuvant chemotherapy described in the previous ASCO guidelines but introduce modifications regarding treatment timing and duration. The optimal window for interval cytoreductive surgery now falls after three to four chemotherapy cycles, allowing more individualized approaches based on patient response and tolerance.
In addition, postsurgical chemotherapy protocols have become more flexible. Rather than mandating a fixed number of cycles, the guidelines encourage tailoring treatment duration to individual patient factors including response assessment, performance status, and quality-of-life considerations.
The updated guidelines also emphasize the importance of genetic and molecular testing at diagnosis, which Melamed identifies as “absolutely central to treatment and deciding who receives maintenance therapy.” This is also recommended by the NCCN guidelines.
However, he highlighted the following practical challenge in molecular testing after neoadjuvant chemotherapy. “Probably 20% of patients have an exceptional response to neoadjuvant therapy, such that there is insufficient tissue at the time of their cytoreduction to do somatic testing,” he said.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
A notable difference between the 2016 and 2025 guidelines is the inclusion of HIPEC in the updated guidelines.
Commenting to this news organization, Gaillard explained the nuanced approach to HIPEC: “The committee discussed HIPEC extensively. We recognize that it may not be available at many centers and requires specially trained staff and dedicated resources. The reason for including HIPEC in the guidelines is to highlight that there have been studies that show a potential overall survival benefit.”
Melamed considers the recommendation of HIPEC to be one of the strongest aspects of the updated guidelines. “There have been two large trials and one smaller one that have shown that for patients treated with neoadjuvant chemotherapy, the addition of HIPEC appears to improve overall survival,” he explained.
Implementation Strategies
The authors acknowledged that barriers to healthcare delivery present significant challenges to the implementation of the guidelines. Limited access to gynecologic oncologists in rural areas, insurance coverage gaps, and varying surgical expertise across institutions complicate the delivery of optimal care. The guidelines also emphasize the need for solutions to ensure equitable access to recommended treatments.
Melamed noted that the decentralized structure of the healthcare system in the United States complicates the uniform adoption of guidelines, particularly in resource-limited settings, adding that “geographic region and local resources and expertise influence both access to treatment and outcomes.”
Although both the updated ASCO guidelines and NCCN guidelines emphasize the importance of evaluation by a gynecologic oncologist for determining the most appropriate treatment strategy, the scarcity of gynecologic oncologists is one of the most significant barriers to accessing optimal care, according to Gaillard. She proposes telemedicine consultations and enhanced communication between medical oncologists and gynecologic oncologists to ensure equitable access.
Gaillard also commented on the challenges in implementing a multidisciplinary treatment approach, the importance of which is emphasized in the updated guidelines.
“There can be a limited availability of the multidisciplinary team to be involved in this decision-making,” she said. “Ideally, patient assessment by a gynecologic oncologist would happen in person, but recognizing that availability is limited, it doesn’t necessarily have to. Sometimes, it can just be a conversation between a medical oncologist and a gynecologic oncologist detailing a treatment plan together.”
Looking Ahead
Gaillard noted that ovarian cancer is a very active field of research and that the guidelines may need to be updated again in the near future to incorporate novel treatment approaches.
“Newer and more effective targeted therapies based on tumor profiling are being developed,” she said. “These will hopefully move earlier in the treatment course for patients. Maybe we will not use chemotherapy in the future because we will have more directed and targeted therapies.”
She also emphasized the importance of early diagnosis in shaping future treatment guidelines for ovarian cancer.
“Neoadjuvant chemotherapy is predominantly used in situations where patients have very advanced disease and may not benefit from primary cytoreductive surgery,” she noted. “If we develop better diagnostic tools that will allow us to diagnose patients earlier, then we may not need to use neoadjuvant chemotherapy.”
All funding for the administration of the guideline development project was provided by ASCO. Gaillard reported receiving consulting or advisory fees from Verastem, Merck, AstraZeneca, and Compugen; research funding from AstraZeneca, Tesaro, Compugen, Genentech/Roche, Clovis Oncology, Tempest Therapeutics, Blueprint Pharmaceutic, Immunogen, Volastra Therapeutics, and Beigene; and patents, royalties, or other intellectual property from US Patent Nos 10,258,604 and 10,905,659, licensed by Duke University to Sermonix. Melamed reported receiving research funding from the National Cancer Institute and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
The American Society of Clinical Oncology (ASCO) has released updated guidelines for neoadjuvant chemotherapy in newly diagnosed advanced ovarian cancer, introducing changes in patient selection and treatment strategies. The changes reflect emerging evidence on racial disparities, treatment outcomes, and quality of life considerations.
The publication of the new guidance follows dramatic shifts in treatment patterns over the past decade.
“There had been a big shift in how we were treating patients in the United States,” explained Stephanie Gaillard, MD, PhD, one of the authors of the updated guidelines. “We saw a substantial drop in the number of patients undergoing primary cytoreductive surgery for ovarian cancer from about 70% of patients in 2010 to only about 37% in 2021.”
The new guidelines maintain the recommendation for platinum/taxane-based neoadjuvant chemotherapy but introduce modifications regarding timing and duration.
“It’s still a recommendation that gynecologic oncologists are involved in determining whether someone is eligible for primary cytoreductive surgery or should undergo neoadjuvant chemotherapy first,” Gaillard noted. “We emphasize that patients who are eligible for primary cytoreductive surgery should undergo surgery as opposed to receiving neoadjuvant chemotherapy.”
Alexander Melamed, MD, MPH, a gynecologic oncologist at Massachusetts General Hospital, Boston, who was not involved in authoring the updated guidelines, noted that additional evidence-based guidance is needed to individualize treatment plans. He pointed to four completed trials comparing neoadjuvant chemotherapy with cytoreductive surgery, noting: “When these trials have been pooled together in meta-analyses, there was a higher risk of mortality associated with primary cytoreductive surgery and a higher risk of severe complications.”
The updated guidelines take this higher risk for mortality with primary cytoreductive surgery into consideration, and patients who are not eligible for primary surgery would receive neoadjuvant chemotherapy, Gaillard noted.
Changes in Patient Selection
The 2025 guidelines describe a more nuanced approach for selecting patients for neoadjuvant chemotherapy vs primary cytoreductive surgery. While the 2016 ASCO guidelines primarily focused on disease burden and surgical resectability when selecting patients for neoadjuvant chemotherapy, the new recommendations incorporate additional factors.
The guidelines discuss recent findings showing that Black patients experience a 38% lower likelihood of undergoing cytoreductive surgery than non-Black patients. In addition, compared with non-Hispanic White women, Asian and Black women more frequently receive neoadjuvant chemotherapy with interval debulking surgery rather than primary cytoreductive surgery. According to the authors, these differences persist even after accounting for clinical factors, suggesting that structural barriers to healthcare access may play a role.
The guidelines discuss how affordability, availability, and accessibility mediate racial disparities in ovarian cancer care. According to the authors, structural inequities in healthcare access influence treatment quality for minority patients. Non-White patients face greater challenges in accessing gynecologic oncology consultations and standard-of-care combination therapy, leading to poorer survival outcomes, the guidelines say.
According to Melamed, the guidelines serve as an important tool for promoting healthcare equity. “Having recommendations and standards is incredibly important for achieving equity because once there is consensus on a best practice, it doesn’t matter if you’re rich, poor, or a patient of a particular racial or ethnic group — if you have the disease, you ought to have access to that standard,” he said.
The 2016 ASCO guidelines focused primarily on disease burden and surgical resectability, whereas the 2024 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for ovarian cancer focus more on oncologic outcomes and surgical considerations. Based on the NCCN guidelines, treatment selection for ovarian cancer is primarily determined by the histologic subtype, stage of disease, and whether the patient is a candidate for primary surgery. The 2025 ASCO guidelines, on the other hand, emphasize the importance of quality-of-life outcomes during treatment selection. The authors of the updated ASCO guidelines acknowledged that treatment decisions should consider both the duration and quality of life, particularly for elderly patients or those with multiple comorbidities.
Treatment Timing and Duration
The guidelines maintain the recommendations for platinum/taxane-based neoadjuvant chemotherapy described in the previous ASCO guidelines but introduce modifications regarding treatment timing and duration. The optimal window for interval cytoreductive surgery now falls after three to four chemotherapy cycles, allowing more individualized approaches based on patient response and tolerance.
In addition, postsurgical chemotherapy protocols have become more flexible. Rather than mandating a fixed number of cycles, the guidelines encourage tailoring treatment duration to individual patient factors including response assessment, performance status, and quality-of-life considerations.
The updated guidelines also emphasize the importance of genetic and molecular testing at diagnosis, which Melamed identifies as “absolutely central to treatment and deciding who receives maintenance therapy.” This is also recommended by the NCCN guidelines.
However, he highlighted the following practical challenge in molecular testing after neoadjuvant chemotherapy. “Probably 20% of patients have an exceptional response to neoadjuvant therapy, such that there is insufficient tissue at the time of their cytoreduction to do somatic testing,” he said.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
A notable difference between the 2016 and 2025 guidelines is the inclusion of HIPEC in the updated guidelines.
Commenting to this news organization, Gaillard explained the nuanced approach to HIPEC: “The committee discussed HIPEC extensively. We recognize that it may not be available at many centers and requires specially trained staff and dedicated resources. The reason for including HIPEC in the guidelines is to highlight that there have been studies that show a potential overall survival benefit.”
Melamed considers the recommendation of HIPEC to be one of the strongest aspects of the updated guidelines. “There have been two large trials and one smaller one that have shown that for patients treated with neoadjuvant chemotherapy, the addition of HIPEC appears to improve overall survival,” he explained.
Implementation Strategies
The authors acknowledged that barriers to healthcare delivery present significant challenges to the implementation of the guidelines. Limited access to gynecologic oncologists in rural areas, insurance coverage gaps, and varying surgical expertise across institutions complicate the delivery of optimal care. The guidelines also emphasize the need for solutions to ensure equitable access to recommended treatments.
Melamed noted that the decentralized structure of the healthcare system in the United States complicates the uniform adoption of guidelines, particularly in resource-limited settings, adding that “geographic region and local resources and expertise influence both access to treatment and outcomes.”
Although both the updated ASCO guidelines and NCCN guidelines emphasize the importance of evaluation by a gynecologic oncologist for determining the most appropriate treatment strategy, the scarcity of gynecologic oncologists is one of the most significant barriers to accessing optimal care, according to Gaillard. She proposes telemedicine consultations and enhanced communication between medical oncologists and gynecologic oncologists to ensure equitable access.
Gaillard also commented on the challenges in implementing a multidisciplinary treatment approach, the importance of which is emphasized in the updated guidelines.
“There can be a limited availability of the multidisciplinary team to be involved in this decision-making,” she said. “Ideally, patient assessment by a gynecologic oncologist would happen in person, but recognizing that availability is limited, it doesn’t necessarily have to. Sometimes, it can just be a conversation between a medical oncologist and a gynecologic oncologist detailing a treatment plan together.”
Looking Ahead
Gaillard noted that ovarian cancer is a very active field of research and that the guidelines may need to be updated again in the near future to incorporate novel treatment approaches.
“Newer and more effective targeted therapies based on tumor profiling are being developed,” she said. “These will hopefully move earlier in the treatment course for patients. Maybe we will not use chemotherapy in the future because we will have more directed and targeted therapies.”
She also emphasized the importance of early diagnosis in shaping future treatment guidelines for ovarian cancer.
“Neoadjuvant chemotherapy is predominantly used in situations where patients have very advanced disease and may not benefit from primary cytoreductive surgery,” she noted. “If we develop better diagnostic tools that will allow us to diagnose patients earlier, then we may not need to use neoadjuvant chemotherapy.”
All funding for the administration of the guideline development project was provided by ASCO. Gaillard reported receiving consulting or advisory fees from Verastem, Merck, AstraZeneca, and Compugen; research funding from AstraZeneca, Tesaro, Compugen, Genentech/Roche, Clovis Oncology, Tempest Therapeutics, Blueprint Pharmaceutic, Immunogen, Volastra Therapeutics, and Beigene; and patents, royalties, or other intellectual property from US Patent Nos 10,258,604 and 10,905,659, licensed by Duke University to Sermonix. Melamed reported receiving research funding from the National Cancer Institute and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
The American Society of Clinical Oncology (ASCO) has released updated guidelines for neoadjuvant chemotherapy in newly diagnosed advanced ovarian cancer, introducing changes in patient selection and treatment strategies. The changes reflect emerging evidence on racial disparities, treatment outcomes, and quality of life considerations.
The publication of the new guidance follows dramatic shifts in treatment patterns over the past decade.
“There had been a big shift in how we were treating patients in the United States,” explained Stephanie Gaillard, MD, PhD, one of the authors of the updated guidelines. “We saw a substantial drop in the number of patients undergoing primary cytoreductive surgery for ovarian cancer from about 70% of patients in 2010 to only about 37% in 2021.”
The new guidelines maintain the recommendation for platinum/taxane-based neoadjuvant chemotherapy but introduce modifications regarding timing and duration.
“It’s still a recommendation that gynecologic oncologists are involved in determining whether someone is eligible for primary cytoreductive surgery or should undergo neoadjuvant chemotherapy first,” Gaillard noted. “We emphasize that patients who are eligible for primary cytoreductive surgery should undergo surgery as opposed to receiving neoadjuvant chemotherapy.”
Alexander Melamed, MD, MPH, a gynecologic oncologist at Massachusetts General Hospital, Boston, who was not involved in authoring the updated guidelines, noted that additional evidence-based guidance is needed to individualize treatment plans. He pointed to four completed trials comparing neoadjuvant chemotherapy with cytoreductive surgery, noting: “When these trials have been pooled together in meta-analyses, there was a higher risk of mortality associated with primary cytoreductive surgery and a higher risk of severe complications.”
The updated guidelines take this higher risk for mortality with primary cytoreductive surgery into consideration, and patients who are not eligible for primary surgery would receive neoadjuvant chemotherapy, Gaillard noted.
Changes in Patient Selection
The 2025 guidelines describe a more nuanced approach for selecting patients for neoadjuvant chemotherapy vs primary cytoreductive surgery. While the 2016 ASCO guidelines primarily focused on disease burden and surgical resectability when selecting patients for neoadjuvant chemotherapy, the new recommendations incorporate additional factors.
The guidelines discuss recent findings showing that Black patients experience a 38% lower likelihood of undergoing cytoreductive surgery than non-Black patients. In addition, compared with non-Hispanic White women, Asian and Black women more frequently receive neoadjuvant chemotherapy with interval debulking surgery rather than primary cytoreductive surgery. According to the authors, these differences persist even after accounting for clinical factors, suggesting that structural barriers to healthcare access may play a role.
The guidelines discuss how affordability, availability, and accessibility mediate racial disparities in ovarian cancer care. According to the authors, structural inequities in healthcare access influence treatment quality for minority patients. Non-White patients face greater challenges in accessing gynecologic oncology consultations and standard-of-care combination therapy, leading to poorer survival outcomes, the guidelines say.
According to Melamed, the guidelines serve as an important tool for promoting healthcare equity. “Having recommendations and standards is incredibly important for achieving equity because once there is consensus on a best practice, it doesn’t matter if you’re rich, poor, or a patient of a particular racial or ethnic group — if you have the disease, you ought to have access to that standard,” he said.
The 2016 ASCO guidelines focused primarily on disease burden and surgical resectability, whereas the 2024 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for ovarian cancer focus more on oncologic outcomes and surgical considerations. Based on the NCCN guidelines, treatment selection for ovarian cancer is primarily determined by the histologic subtype, stage of disease, and whether the patient is a candidate for primary surgery. The 2025 ASCO guidelines, on the other hand, emphasize the importance of quality-of-life outcomes during treatment selection. The authors of the updated ASCO guidelines acknowledged that treatment decisions should consider both the duration and quality of life, particularly for elderly patients or those with multiple comorbidities.
Treatment Timing and Duration
The guidelines maintain the recommendations for platinum/taxane-based neoadjuvant chemotherapy described in the previous ASCO guidelines but introduce modifications regarding treatment timing and duration. The optimal window for interval cytoreductive surgery now falls after three to four chemotherapy cycles, allowing more individualized approaches based on patient response and tolerance.
In addition, postsurgical chemotherapy protocols have become more flexible. Rather than mandating a fixed number of cycles, the guidelines encourage tailoring treatment duration to individual patient factors including response assessment, performance status, and quality-of-life considerations.
The updated guidelines also emphasize the importance of genetic and molecular testing at diagnosis, which Melamed identifies as “absolutely central to treatment and deciding who receives maintenance therapy.” This is also recommended by the NCCN guidelines.
However, he highlighted the following practical challenge in molecular testing after neoadjuvant chemotherapy. “Probably 20% of patients have an exceptional response to neoadjuvant therapy, such that there is insufficient tissue at the time of their cytoreduction to do somatic testing,” he said.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
A notable difference between the 2016 and 2025 guidelines is the inclusion of HIPEC in the updated guidelines.
Commenting to this news organization, Gaillard explained the nuanced approach to HIPEC: “The committee discussed HIPEC extensively. We recognize that it may not be available at many centers and requires specially trained staff and dedicated resources. The reason for including HIPEC in the guidelines is to highlight that there have been studies that show a potential overall survival benefit.”
Melamed considers the recommendation of HIPEC to be one of the strongest aspects of the updated guidelines. “There have been two large trials and one smaller one that have shown that for patients treated with neoadjuvant chemotherapy, the addition of HIPEC appears to improve overall survival,” he explained.
Implementation Strategies
The authors acknowledged that barriers to healthcare delivery present significant challenges to the implementation of the guidelines. Limited access to gynecologic oncologists in rural areas, insurance coverage gaps, and varying surgical expertise across institutions complicate the delivery of optimal care. The guidelines also emphasize the need for solutions to ensure equitable access to recommended treatments.
Melamed noted that the decentralized structure of the healthcare system in the United States complicates the uniform adoption of guidelines, particularly in resource-limited settings, adding that “geographic region and local resources and expertise influence both access to treatment and outcomes.”
Although both the updated ASCO guidelines and NCCN guidelines emphasize the importance of evaluation by a gynecologic oncologist for determining the most appropriate treatment strategy, the scarcity of gynecologic oncologists is one of the most significant barriers to accessing optimal care, according to Gaillard. She proposes telemedicine consultations and enhanced communication between medical oncologists and gynecologic oncologists to ensure equitable access.
Gaillard also commented on the challenges in implementing a multidisciplinary treatment approach, the importance of which is emphasized in the updated guidelines.
“There can be a limited availability of the multidisciplinary team to be involved in this decision-making,” she said. “Ideally, patient assessment by a gynecologic oncologist would happen in person, but recognizing that availability is limited, it doesn’t necessarily have to. Sometimes, it can just be a conversation between a medical oncologist and a gynecologic oncologist detailing a treatment plan together.”
Looking Ahead
Gaillard noted that ovarian cancer is a very active field of research and that the guidelines may need to be updated again in the near future to incorporate novel treatment approaches.
“Newer and more effective targeted therapies based on tumor profiling are being developed,” she said. “These will hopefully move earlier in the treatment course for patients. Maybe we will not use chemotherapy in the future because we will have more directed and targeted therapies.”
She also emphasized the importance of early diagnosis in shaping future treatment guidelines for ovarian cancer.
“Neoadjuvant chemotherapy is predominantly used in situations where patients have very advanced disease and may not benefit from primary cytoreductive surgery,” she noted. “If we develop better diagnostic tools that will allow us to diagnose patients earlier, then we may not need to use neoadjuvant chemotherapy.”
All funding for the administration of the guideline development project was provided by ASCO. Gaillard reported receiving consulting or advisory fees from Verastem, Merck, AstraZeneca, and Compugen; research funding from AstraZeneca, Tesaro, Compugen, Genentech/Roche, Clovis Oncology, Tempest Therapeutics, Blueprint Pharmaceutic, Immunogen, Volastra Therapeutics, and Beigene; and patents, royalties, or other intellectual property from US Patent Nos 10,258,604 and 10,905,659, licensed by Duke University to Sermonix. Melamed reported receiving research funding from the National Cancer Institute and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Diet Changes Show Promise in Early Prostate Cancer
A diet high in omega-3 and low in omega-6 fatty acids, alongside fish oil supplements, may curb the growth of prostate cancer cells in men with early-stage disease, new data showed.
Among men on active surveillance for prostate cancer, consuming this diet for a year led to a significant decrease in the prostate cancer tissue Ki-67 index, a biomarker for prostate cancer progression, metastasis, and death, according to findings from the phase 2 CAPFISH-3 study presented at the 2025 American Society of Clinical Oncology Genitourinary Cancers Symposium.
“This data is certainly intriguing and supports studies looking at this further in prostate cancer,” Bradley Alexander McGregor, MD, from Dana-Farber Cancer Institute, Boston, Massachusetts, who wasn’t involved in the study, told this news organization. But, McGregor noted, patients were on the diet for 1 year, and the long-term implications of this diet are not known.
Growing Evidence on Diet
Diets that include fried and processed foods tend to be high in omega 6s, while those that include salmon and tuna are higher in omega 3s.
Research has shown that consuming more omega-3 fatty acids is associated with a lower risk for mortality from prostate cancer, explained study investigator William Aronson, MD, with David Geffen School of Medicine at University of California, Los Angeles (UCLA). Research suggests that ingesting more omega-6 accelerates the growth of human tumors in mice, while raising omega-3 levels lowers it. High omega-3 and low omega-6 are also known to have an inhibitory effect on M2-like macrophages, which are the predominant immune cell type in prostate cancer metastasis.
To investigate the impact of these fatty acids on early-stage prostate cancer, Aronson and colleagues conducted a single-center, phase 2, randomized, open-label study in 100 men with grade 1/2 prostate cancer who elected active surveillance.
Patients were randomly allocated 1:1 to a control group that continued their normal diet (minus fish oil) or to an intervention group that followed a low omega-6/high omega-3 diet, supplemented with fish oil (2.2 g/d), for 1 year.
The primary endpoint was the change in Ki-67 index from baseline to 1 year from same-site biopsies between the groups.
For the primary endpoint, the Ki-67 index decreased in the intervention group by 15% from baseline to 1 year and increased in the control group by 24%. The difference between groups was statistically significant (P = .043).
For the secondary endpoints, the intervention led to a reduction in triglyceride levels and macrophage colony stimulating factor but no change in tumor volume grade group, PSA level, or Decipher 22 gene score.
Aronson said the findings support future phase 3 trials incorporating this intervention among men on active surveillance for prostate cancer.
McGregor said it’s important to note that this was “an aggressive intervention with dietary changes and addition of fish oil and patients need to be highly motivated.” Four men discontinued due to adverse effects — primarily gastrointestinal adverse effects such as diarrhea and nausea — larger sample sizes will be key to better understand the tolerability.
Bottom line, said McGregor, “based on this data alone, it should not be recommended but can be considered for highly motivated patients after discussion of the limitations of available data and side effects.”
The study was funded in part by the National Cancer Institute, the UCLA Health Jonsson Comprehensive Cancer Center, Howard B. Klein, and the Seafood Industry Research Fund. Aronson disclosed relationships with AstraZeneca, Bayer, Blue Earth Diagnostics, Janssen Oncology, and Pfizer/Astellas. McGregor disclosed relationships with Arcus Biosciences, Astellas Pharma, Bristol Myers Squibb, Daiichi Sankyo/AstraZeneca, Eisai, Exelixis, Genmab, Gilead Sciences, Loxo/Lilly, Pfizer, and Seattle Genetics/Astellas.
A version of this article first appeared on Medscape.com.
A diet high in omega-3 and low in omega-6 fatty acids, alongside fish oil supplements, may curb the growth of prostate cancer cells in men with early-stage disease, new data showed.
Among men on active surveillance for prostate cancer, consuming this diet for a year led to a significant decrease in the prostate cancer tissue Ki-67 index, a biomarker for prostate cancer progression, metastasis, and death, according to findings from the phase 2 CAPFISH-3 study presented at the 2025 American Society of Clinical Oncology Genitourinary Cancers Symposium.
“This data is certainly intriguing and supports studies looking at this further in prostate cancer,” Bradley Alexander McGregor, MD, from Dana-Farber Cancer Institute, Boston, Massachusetts, who wasn’t involved in the study, told this news organization. But, McGregor noted, patients were on the diet for 1 year, and the long-term implications of this diet are not known.
Growing Evidence on Diet
Diets that include fried and processed foods tend to be high in omega 6s, while those that include salmon and tuna are higher in omega 3s.
Research has shown that consuming more omega-3 fatty acids is associated with a lower risk for mortality from prostate cancer, explained study investigator William Aronson, MD, with David Geffen School of Medicine at University of California, Los Angeles (UCLA). Research suggests that ingesting more omega-6 accelerates the growth of human tumors in mice, while raising omega-3 levels lowers it. High omega-3 and low omega-6 are also known to have an inhibitory effect on M2-like macrophages, which are the predominant immune cell type in prostate cancer metastasis.
To investigate the impact of these fatty acids on early-stage prostate cancer, Aronson and colleagues conducted a single-center, phase 2, randomized, open-label study in 100 men with grade 1/2 prostate cancer who elected active surveillance.
Patients were randomly allocated 1:1 to a control group that continued their normal diet (minus fish oil) or to an intervention group that followed a low omega-6/high omega-3 diet, supplemented with fish oil (2.2 g/d), for 1 year.
The primary endpoint was the change in Ki-67 index from baseline to 1 year from same-site biopsies between the groups.
For the primary endpoint, the Ki-67 index decreased in the intervention group by 15% from baseline to 1 year and increased in the control group by 24%. The difference between groups was statistically significant (P = .043).
For the secondary endpoints, the intervention led to a reduction in triglyceride levels and macrophage colony stimulating factor but no change in tumor volume grade group, PSA level, or Decipher 22 gene score.
Aronson said the findings support future phase 3 trials incorporating this intervention among men on active surveillance for prostate cancer.
McGregor said it’s important to note that this was “an aggressive intervention with dietary changes and addition of fish oil and patients need to be highly motivated.” Four men discontinued due to adverse effects — primarily gastrointestinal adverse effects such as diarrhea and nausea — larger sample sizes will be key to better understand the tolerability.
Bottom line, said McGregor, “based on this data alone, it should not be recommended but can be considered for highly motivated patients after discussion of the limitations of available data and side effects.”
The study was funded in part by the National Cancer Institute, the UCLA Health Jonsson Comprehensive Cancer Center, Howard B. Klein, and the Seafood Industry Research Fund. Aronson disclosed relationships with AstraZeneca, Bayer, Blue Earth Diagnostics, Janssen Oncology, and Pfizer/Astellas. McGregor disclosed relationships with Arcus Biosciences, Astellas Pharma, Bristol Myers Squibb, Daiichi Sankyo/AstraZeneca, Eisai, Exelixis, Genmab, Gilead Sciences, Loxo/Lilly, Pfizer, and Seattle Genetics/Astellas.
A version of this article first appeared on Medscape.com.
A diet high in omega-3 and low in omega-6 fatty acids, alongside fish oil supplements, may curb the growth of prostate cancer cells in men with early-stage disease, new data showed.
Among men on active surveillance for prostate cancer, consuming this diet for a year led to a significant decrease in the prostate cancer tissue Ki-67 index, a biomarker for prostate cancer progression, metastasis, and death, according to findings from the phase 2 CAPFISH-3 study presented at the 2025 American Society of Clinical Oncology Genitourinary Cancers Symposium.
“This data is certainly intriguing and supports studies looking at this further in prostate cancer,” Bradley Alexander McGregor, MD, from Dana-Farber Cancer Institute, Boston, Massachusetts, who wasn’t involved in the study, told this news organization. But, McGregor noted, patients were on the diet for 1 year, and the long-term implications of this diet are not known.
Growing Evidence on Diet
Diets that include fried and processed foods tend to be high in omega 6s, while those that include salmon and tuna are higher in omega 3s.
Research has shown that consuming more omega-3 fatty acids is associated with a lower risk for mortality from prostate cancer, explained study investigator William Aronson, MD, with David Geffen School of Medicine at University of California, Los Angeles (UCLA). Research suggests that ingesting more omega-6 accelerates the growth of human tumors in mice, while raising omega-3 levels lowers it. High omega-3 and low omega-6 are also known to have an inhibitory effect on M2-like macrophages, which are the predominant immune cell type in prostate cancer metastasis.
To investigate the impact of these fatty acids on early-stage prostate cancer, Aronson and colleagues conducted a single-center, phase 2, randomized, open-label study in 100 men with grade 1/2 prostate cancer who elected active surveillance.
Patients were randomly allocated 1:1 to a control group that continued their normal diet (minus fish oil) or to an intervention group that followed a low omega-6/high omega-3 diet, supplemented with fish oil (2.2 g/d), for 1 year.
The primary endpoint was the change in Ki-67 index from baseline to 1 year from same-site biopsies between the groups.
For the primary endpoint, the Ki-67 index decreased in the intervention group by 15% from baseline to 1 year and increased in the control group by 24%. The difference between groups was statistically significant (P = .043).
For the secondary endpoints, the intervention led to a reduction in triglyceride levels and macrophage colony stimulating factor but no change in tumor volume grade group, PSA level, or Decipher 22 gene score.
Aronson said the findings support future phase 3 trials incorporating this intervention among men on active surveillance for prostate cancer.
McGregor said it’s important to note that this was “an aggressive intervention with dietary changes and addition of fish oil and patients need to be highly motivated.” Four men discontinued due to adverse effects — primarily gastrointestinal adverse effects such as diarrhea and nausea — larger sample sizes will be key to better understand the tolerability.
Bottom line, said McGregor, “based on this data alone, it should not be recommended but can be considered for highly motivated patients after discussion of the limitations of available data and side effects.”
The study was funded in part by the National Cancer Institute, the UCLA Health Jonsson Comprehensive Cancer Center, Howard B. Klein, and the Seafood Industry Research Fund. Aronson disclosed relationships with AstraZeneca, Bayer, Blue Earth Diagnostics, Janssen Oncology, and Pfizer/Astellas. McGregor disclosed relationships with Arcus Biosciences, Astellas Pharma, Bristol Myers Squibb, Daiichi Sankyo/AstraZeneca, Eisai, Exelixis, Genmab, Gilead Sciences, Loxo/Lilly, Pfizer, and Seattle Genetics/Astellas.
A version of this article first appeared on Medscape.com.
FROM GUCS 2025
Next-Gen Sequencing Tumor Testing Remains Low in Prostate and Urothelial Cancer Cases
This article is a based on a video essay. The transcript has been edited for clarity.
I’d like to discuss what I think is a very interesting analysis that we need to see much more of. It’s perhaps not surprising, but the data, I think, are sobering. The paper was published in JAMA Network Open, entitled, “Trends and Disparities in Next-Generation Sequencing in Metastatic Prostate and Urothelial Cancers.”
As I think most of the listening audience is aware, we are in the midst of an ongoing — I would argue, accelerating — revolution in our understanding of cancer, its development and treatments, based upon our characterization at the molecular level of individual cancers.
This, of course, is changing the treatment paradigms and the drugs that we might have available in the first-, second-, and third-line settings. The question to be asked is, how are we, at a clinical level, keeping up with all of these changes, like those approved by the US Food and Drug Administration, and new diagnostic testing with a variety of molecular platforms?
This particular analysis looked at that specific question in metastatic prostate cancer and urothelial malignancies, obviously including bladder cancer. With the new approvals — including tumor agnostic testing, very specific testing, and very molecularly based drugs that are approved for particular abnormalities — they looked at the percentages of patients and the potential disparities in terms of the testing that has been performed.
There were 11,927 patients with prostate cancer. There were 6490 patients with advanced urothelial malignancies; the majority of these were male, but there were females included in this group.
The researchers looked at 2015 vs 2022 data. It’s not 2024 data, but it goes all the way to the end of 2022, so, not that long ago. In the metastatic prostate cancer group, 19% of patients had undergone molecular testing or next-generation sequencing in 2015.
By 2022, that number had increased, but only to 27%. Three out of four patients with metastatic prostate cancer had not undergone testing to know whether they were potential candidates for specific therapies. I won’t even get into the question of potential germline abnormalities that might be observed that are relevant for other discussions.
Among patients with urothelial cancer, in 2015, 14% had undergone such testing. By 2022, this number was substantially increased to 46.6%, but still, that’s less than 1 out of 2 patients. More than 50% of patients had not undergone the testing, and yet we have therapy that might be available for these populations based on such testing.
I should add that the population of Black, African American, and Hispanic patients was actually considerably lower, percentage-wise, than the numbers that I’ve quoted.
Clearly, there are explanations. There are socioeconomic explanations and insurance coverage explanations. However, the bottom line is that we have therapies available today, and we’ll have more in the future, that are based on knowledge of this testing.
Based on these data, which most recently included 2022 — we’ll see where we are in 2024 and 2025, and with other types — more than half of patients are not getting the testing to know if this is relevant for them and their care.
These are major questions that need to be addressed. Hopefully, answers will be forthcoming and we will see in the future that these percentages will be much higher for the benefit of our patients.
Dr Markman, Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix, has disclosed the following relevant financial relationships with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
This article is a based on a video essay. The transcript has been edited for clarity.
I’d like to discuss what I think is a very interesting analysis that we need to see much more of. It’s perhaps not surprising, but the data, I think, are sobering. The paper was published in JAMA Network Open, entitled, “Trends and Disparities in Next-Generation Sequencing in Metastatic Prostate and Urothelial Cancers.”
As I think most of the listening audience is aware, we are in the midst of an ongoing — I would argue, accelerating — revolution in our understanding of cancer, its development and treatments, based upon our characterization at the molecular level of individual cancers.
This, of course, is changing the treatment paradigms and the drugs that we might have available in the first-, second-, and third-line settings. The question to be asked is, how are we, at a clinical level, keeping up with all of these changes, like those approved by the US Food and Drug Administration, and new diagnostic testing with a variety of molecular platforms?
This particular analysis looked at that specific question in metastatic prostate cancer and urothelial malignancies, obviously including bladder cancer. With the new approvals — including tumor agnostic testing, very specific testing, and very molecularly based drugs that are approved for particular abnormalities — they looked at the percentages of patients and the potential disparities in terms of the testing that has been performed.
There were 11,927 patients with prostate cancer. There were 6490 patients with advanced urothelial malignancies; the majority of these were male, but there were females included in this group.
The researchers looked at 2015 vs 2022 data. It’s not 2024 data, but it goes all the way to the end of 2022, so, not that long ago. In the metastatic prostate cancer group, 19% of patients had undergone molecular testing or next-generation sequencing in 2015.
By 2022, that number had increased, but only to 27%. Three out of four patients with metastatic prostate cancer had not undergone testing to know whether they were potential candidates for specific therapies. I won’t even get into the question of potential germline abnormalities that might be observed that are relevant for other discussions.
Among patients with urothelial cancer, in 2015, 14% had undergone such testing. By 2022, this number was substantially increased to 46.6%, but still, that’s less than 1 out of 2 patients. More than 50% of patients had not undergone the testing, and yet we have therapy that might be available for these populations based on such testing.
I should add that the population of Black, African American, and Hispanic patients was actually considerably lower, percentage-wise, than the numbers that I’ve quoted.
Clearly, there are explanations. There are socioeconomic explanations and insurance coverage explanations. However, the bottom line is that we have therapies available today, and we’ll have more in the future, that are based on knowledge of this testing.
Based on these data, which most recently included 2022 — we’ll see where we are in 2024 and 2025, and with other types — more than half of patients are not getting the testing to know if this is relevant for them and their care.
These are major questions that need to be addressed. Hopefully, answers will be forthcoming and we will see in the future that these percentages will be much higher for the benefit of our patients.
Dr Markman, Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix, has disclosed the following relevant financial relationships with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
This article is a based on a video essay. The transcript has been edited for clarity.
I’d like to discuss what I think is a very interesting analysis that we need to see much more of. It’s perhaps not surprising, but the data, I think, are sobering. The paper was published in JAMA Network Open, entitled, “Trends and Disparities in Next-Generation Sequencing in Metastatic Prostate and Urothelial Cancers.”
As I think most of the listening audience is aware, we are in the midst of an ongoing — I would argue, accelerating — revolution in our understanding of cancer, its development and treatments, based upon our characterization at the molecular level of individual cancers.
This, of course, is changing the treatment paradigms and the drugs that we might have available in the first-, second-, and third-line settings. The question to be asked is, how are we, at a clinical level, keeping up with all of these changes, like those approved by the US Food and Drug Administration, and new diagnostic testing with a variety of molecular platforms?
This particular analysis looked at that specific question in metastatic prostate cancer and urothelial malignancies, obviously including bladder cancer. With the new approvals — including tumor agnostic testing, very specific testing, and very molecularly based drugs that are approved for particular abnormalities — they looked at the percentages of patients and the potential disparities in terms of the testing that has been performed.
There were 11,927 patients with prostate cancer. There were 6490 patients with advanced urothelial malignancies; the majority of these were male, but there were females included in this group.
The researchers looked at 2015 vs 2022 data. It’s not 2024 data, but it goes all the way to the end of 2022, so, not that long ago. In the metastatic prostate cancer group, 19% of patients had undergone molecular testing or next-generation sequencing in 2015.
By 2022, that number had increased, but only to 27%. Three out of four patients with metastatic prostate cancer had not undergone testing to know whether they were potential candidates for specific therapies. I won’t even get into the question of potential germline abnormalities that might be observed that are relevant for other discussions.
Among patients with urothelial cancer, in 2015, 14% had undergone such testing. By 2022, this number was substantially increased to 46.6%, but still, that’s less than 1 out of 2 patients. More than 50% of patients had not undergone the testing, and yet we have therapy that might be available for these populations based on such testing.
I should add that the population of Black, African American, and Hispanic patients was actually considerably lower, percentage-wise, than the numbers that I’ve quoted.
Clearly, there are explanations. There are socioeconomic explanations and insurance coverage explanations. However, the bottom line is that we have therapies available today, and we’ll have more in the future, that are based on knowledge of this testing.
Based on these data, which most recently included 2022 — we’ll see where we are in 2024 and 2025, and with other types — more than half of patients are not getting the testing to know if this is relevant for them and their care.
These are major questions that need to be addressed. Hopefully, answers will be forthcoming and we will see in the future that these percentages will be much higher for the benefit of our patients.
Dr Markman, Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix, has disclosed the following relevant financial relationships with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
VA Study Asks: Has Active Surveillance Solved the Problem of Overtreatment?
Overtreatment of men with prostate cancer and limited life expectancy (LE) has persisted in the era of active surveillance and worsened in some instances, according to a new study of nearly 250,000 veterans.
“Overtreatment of men with limited longevity for intermediate- and high-risk tumors has not only failed to improve but has actually worsened over the last 20 years,” Timothy Daskivich, MD, MSHPM, with Cedars-Sinai Medical Center, Los Angeles, said in an interview.
“Many doctors assume that the increase in uptake of active surveillance for low-risk prostate cancers has solved the problem of overtreatment, but this trend has not affected overtreatment of men with low likelihood of living long enough to benefit from treatment who have higher-risk tumors,” Daskivich said.
The study was published online on November 11 in JAMA Internal Medicine.
‘Concerning’ Real-World Data
For men with low- and intermediate-risk prostate cancer expected to live fewer than 10 years, prostate cancer screening and aggressive treatment are not recommended.
Daskivich and colleagues analyzed data on 243,928 men (mean age, 66 years) in the Veterans Affairs (VA) Health System with clinically localized prostate cancer diagnosed between 2000 and 2019.
About 21% had LE < 10 years, and about 4% had LE < 5 years, according to the validated age-adjusted Prostate Cancer Comorbidity Index.
Overtreatment was defined as aggressive treatment (surgery or radiation) in those with LE < 10 years and low- to intermediate-risk disease and in those with LE < 5 years and high-risk disease, in line with current guidelines.
Among men with LE < 10 years, the proportion of men overtreated with surgery or radiotherapy for low-risk disease decreased 22% but increased 22% for intermediate-risk disease during the study period.
Among men with LE < 5 years, the proportion of men treated with definitive treatment for high-risk disease increased 29%.
“While lower-risk tumors are treated less aggressively across the board, including in men with limited longevity, it seems that we are more indiscriminately treating men with higher-risk disease without considering their expected longevity,” Daskivich said, in an interview.
Is This Happening in the General US Population?
Daskivich noted that the sample included a large sample of men diagnosed with localized prostate cancer in the VA Health System.
“Rates of overtreatment are likely to be lower in the VA [Health System], so the problem may be worse in the community setting. The VA [Health System] has been exemplary in its uptake of active surveillance for low-risk cancers, leading the effort to reduce overtreatment of men with low-risk cancers. However, the problem of overtreatment of men with limited longevity persists in the VA [Health System], underscoring the pervasiveness of this problem,” he explained.
“We don’t have a perfect head-to-head comparison of overtreatment in the VA setting vs in the community. [However, one study shows] that this is not a VA-specific phenomenon and that there is an increase in overtreatment of men with limited longevity in a Medicare population as well,” Daskivich noted.
Is Overtreatment All Bad?
Overtreatment of prostate cancer, especially in cases where the cancer is unlikely to progress or cause symptoms, can lead to significant physical, psychological, and financial harms, Christopher Anderson, MD, urologist with Columbia University Irving Medical Center in New York City, who wasn’t involved in the study, noted in an interview.
In the study by Daskivich and colleagues, over three quarters of the overtreatment was radiation therapy, which carries the risk for urinary, bowel, and sexual issues.
“Overscreening, which can lead to overtreatment, is a core issue,” Anderson said. It’s easy to order a “simple” prostate-specific antigen blood test, but in an older man with limited LE, that can lead to a host of further testing, he commented.
Stopping the pipeline of overscreening that then feeds into the cascade of overtreatment is the first step in addressing the problem of prostate cancer overtreatment, Nancy Li Schoenborn, MD, MHS, with Johns Hopkins University School of Medicine, Baltimore, and Louise C. Walter, MD, with University of California San Francisco, wrote in an editorial in JAMA Internal Medicine.
Considering LE during screening decision-making is “fundamental to reducing harms of prostate cancer overdiagnosis and overtreatment” because limited LE increases the likelihood of experiencing “harms all along the diagnostic and treatment cascade following screening,” the editorial writers said.
The time spent diagnosing, monitoring, and treating asymptomatic prostate cancer in men with limited LE distracts from monitoring and treating chronic symptomatic life-limiting illnesses, they noted.
Tough to Talk About?
Anderson noted that, in general, doctors are not great at estimating and counseling patients on LE. “It’s sometimes difficult to have that conversation,” he said.
Daskivich said physicians may fail to include average LE when advising patients on treatments because they believe that the patients do not want to discuss this topic. “Yet, in interviews with patients, we found that prostate cancer patients reported they wanted this information,” he continued, in an interview.
Solving the problem of overscreening and overtreatment will require a “multifaceted approach, including improving access to life expectancy data at the point of care for providers, educating providers on how to communicate this information, and improving data sources to predict longevity,” Daskivich said.
He said it’s equally important to note that some men with prostate cancer may choose treatment even if they have a limited longevity.
“Not all patients will choose conservative management, even if it is recommended by guidelines. However, they need to be given the opportunity to make a good decision for themselves with the best possible data,” Daskivich said.
This work was supported in part by a US Department of VA Merit Review. Daskivich reported receiving personal fees from the Medical Education Speakers Network, EDAP, and RAND; research support from Lantheus and Janssen; and a patent pending for a system for healthcare visit quality assessment outside the submitted work. Schoenborn, Walter, and Anderson had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Overtreatment of men with prostate cancer and limited life expectancy (LE) has persisted in the era of active surveillance and worsened in some instances, according to a new study of nearly 250,000 veterans.
“Overtreatment of men with limited longevity for intermediate- and high-risk tumors has not only failed to improve but has actually worsened over the last 20 years,” Timothy Daskivich, MD, MSHPM, with Cedars-Sinai Medical Center, Los Angeles, said in an interview.
“Many doctors assume that the increase in uptake of active surveillance for low-risk prostate cancers has solved the problem of overtreatment, but this trend has not affected overtreatment of men with low likelihood of living long enough to benefit from treatment who have higher-risk tumors,” Daskivich said.
The study was published online on November 11 in JAMA Internal Medicine.
‘Concerning’ Real-World Data
For men with low- and intermediate-risk prostate cancer expected to live fewer than 10 years, prostate cancer screening and aggressive treatment are not recommended.
Daskivich and colleagues analyzed data on 243,928 men (mean age, 66 years) in the Veterans Affairs (VA) Health System with clinically localized prostate cancer diagnosed between 2000 and 2019.
About 21% had LE < 10 years, and about 4% had LE < 5 years, according to the validated age-adjusted Prostate Cancer Comorbidity Index.
Overtreatment was defined as aggressive treatment (surgery or radiation) in those with LE < 10 years and low- to intermediate-risk disease and in those with LE < 5 years and high-risk disease, in line with current guidelines.
Among men with LE < 10 years, the proportion of men overtreated with surgery or radiotherapy for low-risk disease decreased 22% but increased 22% for intermediate-risk disease during the study period.
Among men with LE < 5 years, the proportion of men treated with definitive treatment for high-risk disease increased 29%.
“While lower-risk tumors are treated less aggressively across the board, including in men with limited longevity, it seems that we are more indiscriminately treating men with higher-risk disease without considering their expected longevity,” Daskivich said, in an interview.
Is This Happening in the General US Population?
Daskivich noted that the sample included a large sample of men diagnosed with localized prostate cancer in the VA Health System.
“Rates of overtreatment are likely to be lower in the VA [Health System], so the problem may be worse in the community setting. The VA [Health System] has been exemplary in its uptake of active surveillance for low-risk cancers, leading the effort to reduce overtreatment of men with low-risk cancers. However, the problem of overtreatment of men with limited longevity persists in the VA [Health System], underscoring the pervasiveness of this problem,” he explained.
“We don’t have a perfect head-to-head comparison of overtreatment in the VA setting vs in the community. [However, one study shows] that this is not a VA-specific phenomenon and that there is an increase in overtreatment of men with limited longevity in a Medicare population as well,” Daskivich noted.
Is Overtreatment All Bad?
Overtreatment of prostate cancer, especially in cases where the cancer is unlikely to progress or cause symptoms, can lead to significant physical, psychological, and financial harms, Christopher Anderson, MD, urologist with Columbia University Irving Medical Center in New York City, who wasn’t involved in the study, noted in an interview.
In the study by Daskivich and colleagues, over three quarters of the overtreatment was radiation therapy, which carries the risk for urinary, bowel, and sexual issues.
“Overscreening, which can lead to overtreatment, is a core issue,” Anderson said. It’s easy to order a “simple” prostate-specific antigen blood test, but in an older man with limited LE, that can lead to a host of further testing, he commented.
Stopping the pipeline of overscreening that then feeds into the cascade of overtreatment is the first step in addressing the problem of prostate cancer overtreatment, Nancy Li Schoenborn, MD, MHS, with Johns Hopkins University School of Medicine, Baltimore, and Louise C. Walter, MD, with University of California San Francisco, wrote in an editorial in JAMA Internal Medicine.
Considering LE during screening decision-making is “fundamental to reducing harms of prostate cancer overdiagnosis and overtreatment” because limited LE increases the likelihood of experiencing “harms all along the diagnostic and treatment cascade following screening,” the editorial writers said.
The time spent diagnosing, monitoring, and treating asymptomatic prostate cancer in men with limited LE distracts from monitoring and treating chronic symptomatic life-limiting illnesses, they noted.
Tough to Talk About?
Anderson noted that, in general, doctors are not great at estimating and counseling patients on LE. “It’s sometimes difficult to have that conversation,” he said.
Daskivich said physicians may fail to include average LE when advising patients on treatments because they believe that the patients do not want to discuss this topic. “Yet, in interviews with patients, we found that prostate cancer patients reported they wanted this information,” he continued, in an interview.
Solving the problem of overscreening and overtreatment will require a “multifaceted approach, including improving access to life expectancy data at the point of care for providers, educating providers on how to communicate this information, and improving data sources to predict longevity,” Daskivich said.
He said it’s equally important to note that some men with prostate cancer may choose treatment even if they have a limited longevity.
“Not all patients will choose conservative management, even if it is recommended by guidelines. However, they need to be given the opportunity to make a good decision for themselves with the best possible data,” Daskivich said.
This work was supported in part by a US Department of VA Merit Review. Daskivich reported receiving personal fees from the Medical Education Speakers Network, EDAP, and RAND; research support from Lantheus and Janssen; and a patent pending for a system for healthcare visit quality assessment outside the submitted work. Schoenborn, Walter, and Anderson had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Overtreatment of men with prostate cancer and limited life expectancy (LE) has persisted in the era of active surveillance and worsened in some instances, according to a new study of nearly 250,000 veterans.
“Overtreatment of men with limited longevity for intermediate- and high-risk tumors has not only failed to improve but has actually worsened over the last 20 years,” Timothy Daskivich, MD, MSHPM, with Cedars-Sinai Medical Center, Los Angeles, said in an interview.
“Many doctors assume that the increase in uptake of active surveillance for low-risk prostate cancers has solved the problem of overtreatment, but this trend has not affected overtreatment of men with low likelihood of living long enough to benefit from treatment who have higher-risk tumors,” Daskivich said.
The study was published online on November 11 in JAMA Internal Medicine.
‘Concerning’ Real-World Data
For men with low- and intermediate-risk prostate cancer expected to live fewer than 10 years, prostate cancer screening and aggressive treatment are not recommended.
Daskivich and colleagues analyzed data on 243,928 men (mean age, 66 years) in the Veterans Affairs (VA) Health System with clinically localized prostate cancer diagnosed between 2000 and 2019.
About 21% had LE < 10 years, and about 4% had LE < 5 years, according to the validated age-adjusted Prostate Cancer Comorbidity Index.
Overtreatment was defined as aggressive treatment (surgery or radiation) in those with LE < 10 years and low- to intermediate-risk disease and in those with LE < 5 years and high-risk disease, in line with current guidelines.
Among men with LE < 10 years, the proportion of men overtreated with surgery or radiotherapy for low-risk disease decreased 22% but increased 22% for intermediate-risk disease during the study period.
Among men with LE < 5 years, the proportion of men treated with definitive treatment for high-risk disease increased 29%.
“While lower-risk tumors are treated less aggressively across the board, including in men with limited longevity, it seems that we are more indiscriminately treating men with higher-risk disease without considering their expected longevity,” Daskivich said, in an interview.
Is This Happening in the General US Population?
Daskivich noted that the sample included a large sample of men diagnosed with localized prostate cancer in the VA Health System.
“Rates of overtreatment are likely to be lower in the VA [Health System], so the problem may be worse in the community setting. The VA [Health System] has been exemplary in its uptake of active surveillance for low-risk cancers, leading the effort to reduce overtreatment of men with low-risk cancers. However, the problem of overtreatment of men with limited longevity persists in the VA [Health System], underscoring the pervasiveness of this problem,” he explained.
“We don’t have a perfect head-to-head comparison of overtreatment in the VA setting vs in the community. [However, one study shows] that this is not a VA-specific phenomenon and that there is an increase in overtreatment of men with limited longevity in a Medicare population as well,” Daskivich noted.
Is Overtreatment All Bad?
Overtreatment of prostate cancer, especially in cases where the cancer is unlikely to progress or cause symptoms, can lead to significant physical, psychological, and financial harms, Christopher Anderson, MD, urologist with Columbia University Irving Medical Center in New York City, who wasn’t involved in the study, noted in an interview.
In the study by Daskivich and colleagues, over three quarters of the overtreatment was radiation therapy, which carries the risk for urinary, bowel, and sexual issues.
“Overscreening, which can lead to overtreatment, is a core issue,” Anderson said. It’s easy to order a “simple” prostate-specific antigen blood test, but in an older man with limited LE, that can lead to a host of further testing, he commented.
Stopping the pipeline of overscreening that then feeds into the cascade of overtreatment is the first step in addressing the problem of prostate cancer overtreatment, Nancy Li Schoenborn, MD, MHS, with Johns Hopkins University School of Medicine, Baltimore, and Louise C. Walter, MD, with University of California San Francisco, wrote in an editorial in JAMA Internal Medicine.
Considering LE during screening decision-making is “fundamental to reducing harms of prostate cancer overdiagnosis and overtreatment” because limited LE increases the likelihood of experiencing “harms all along the diagnostic and treatment cascade following screening,” the editorial writers said.
The time spent diagnosing, monitoring, and treating asymptomatic prostate cancer in men with limited LE distracts from monitoring and treating chronic symptomatic life-limiting illnesses, they noted.
Tough to Talk About?
Anderson noted that, in general, doctors are not great at estimating and counseling patients on LE. “It’s sometimes difficult to have that conversation,” he said.
Daskivich said physicians may fail to include average LE when advising patients on treatments because they believe that the patients do not want to discuss this topic. “Yet, in interviews with patients, we found that prostate cancer patients reported they wanted this information,” he continued, in an interview.
Solving the problem of overscreening and overtreatment will require a “multifaceted approach, including improving access to life expectancy data at the point of care for providers, educating providers on how to communicate this information, and improving data sources to predict longevity,” Daskivich said.
He said it’s equally important to note that some men with prostate cancer may choose treatment even if they have a limited longevity.
“Not all patients will choose conservative management, even if it is recommended by guidelines. However, they need to be given the opportunity to make a good decision for themselves with the best possible data,” Daskivich said.
This work was supported in part by a US Department of VA Merit Review. Daskivich reported receiving personal fees from the Medical Education Speakers Network, EDAP, and RAND; research support from Lantheus and Janssen; and a patent pending for a system for healthcare visit quality assessment outside the submitted work. Schoenborn, Walter, and Anderson had no relevant disclosures.
A version of this article first appeared on Medscape.com.